- In 2002, Beasley et al. first described a progressive variant of lung injury with organizing pneumonia and intra-alveolar fibrin, which does not fit the histologic pattern of diffuse alveolar damage (DAD), organizing pneumonia (OP) or eosinophilic pneumonia (Arch Pathol Lab Med 2002;126:1064)
- It is a newly proposed subacute interstitial pneumonia similar to organizing pneumonia or organizing diffuse alveolar damage
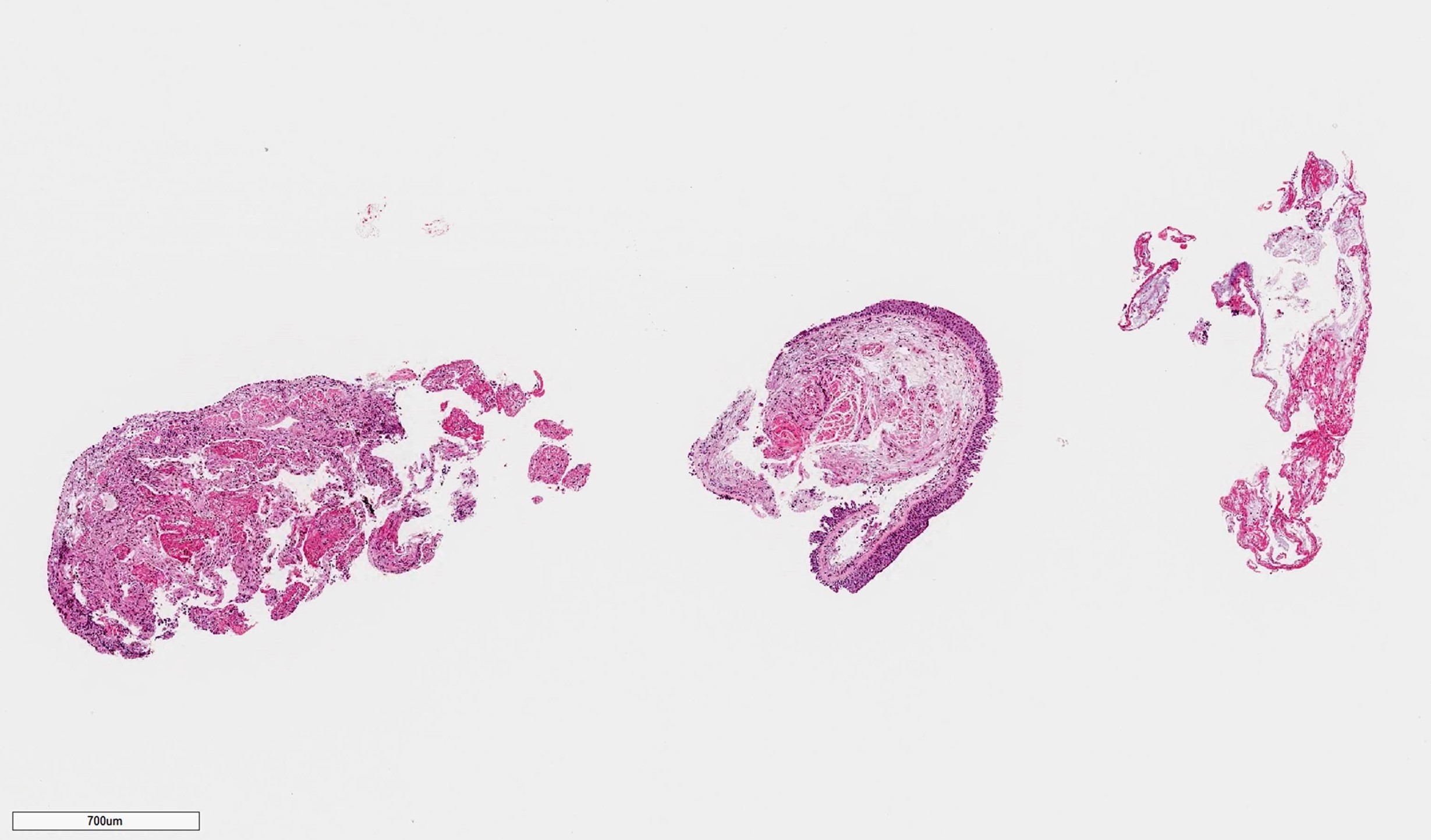
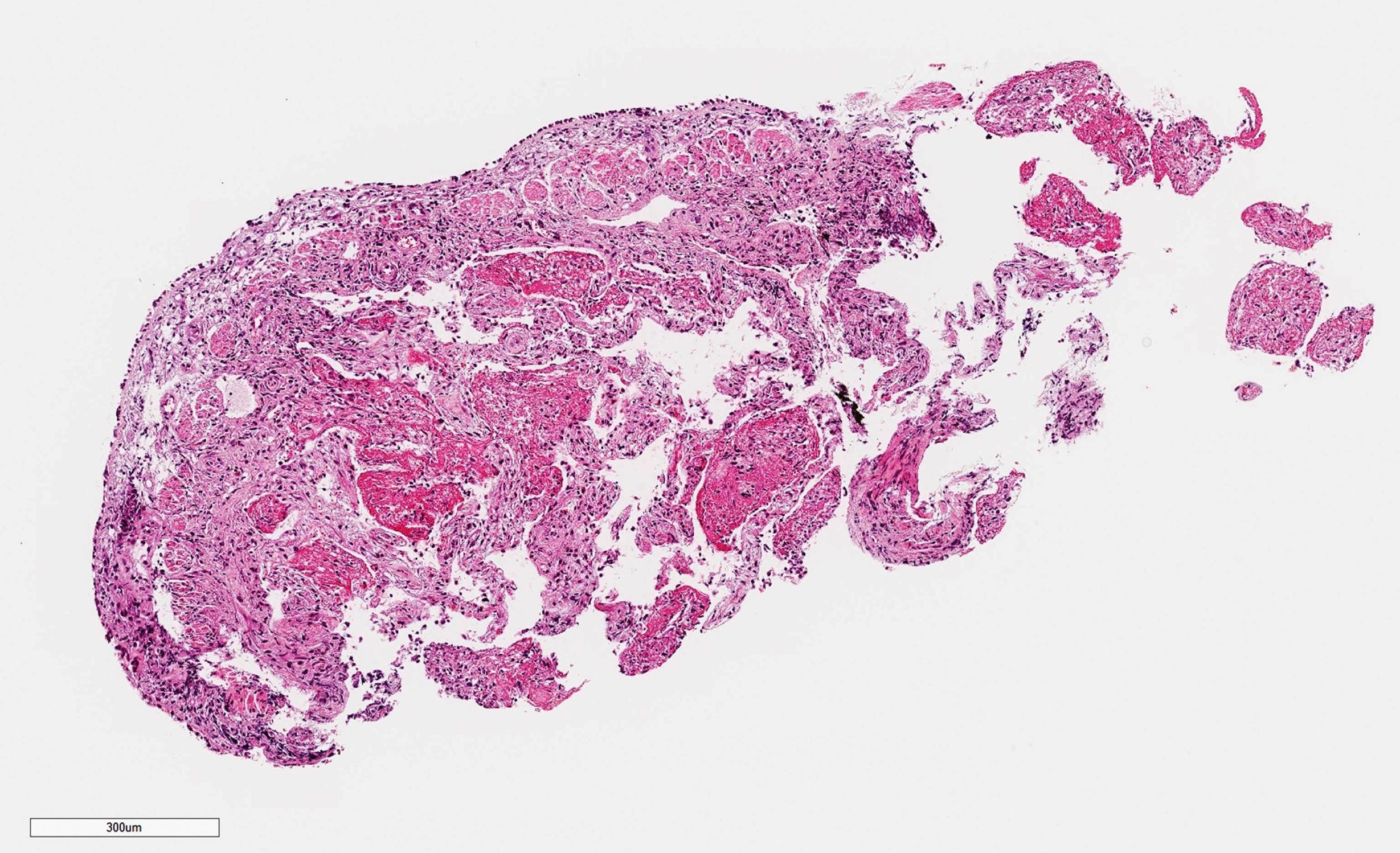
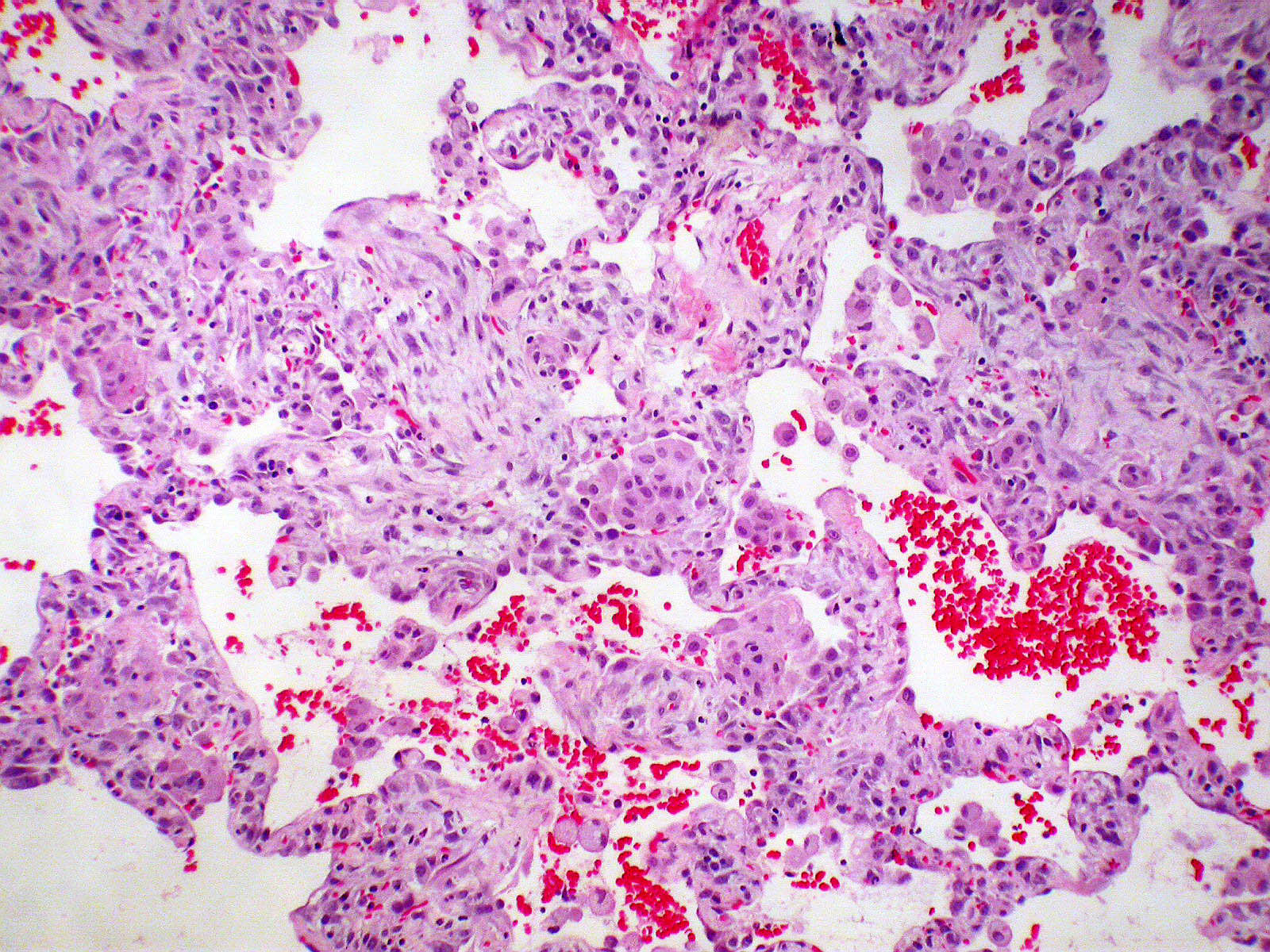
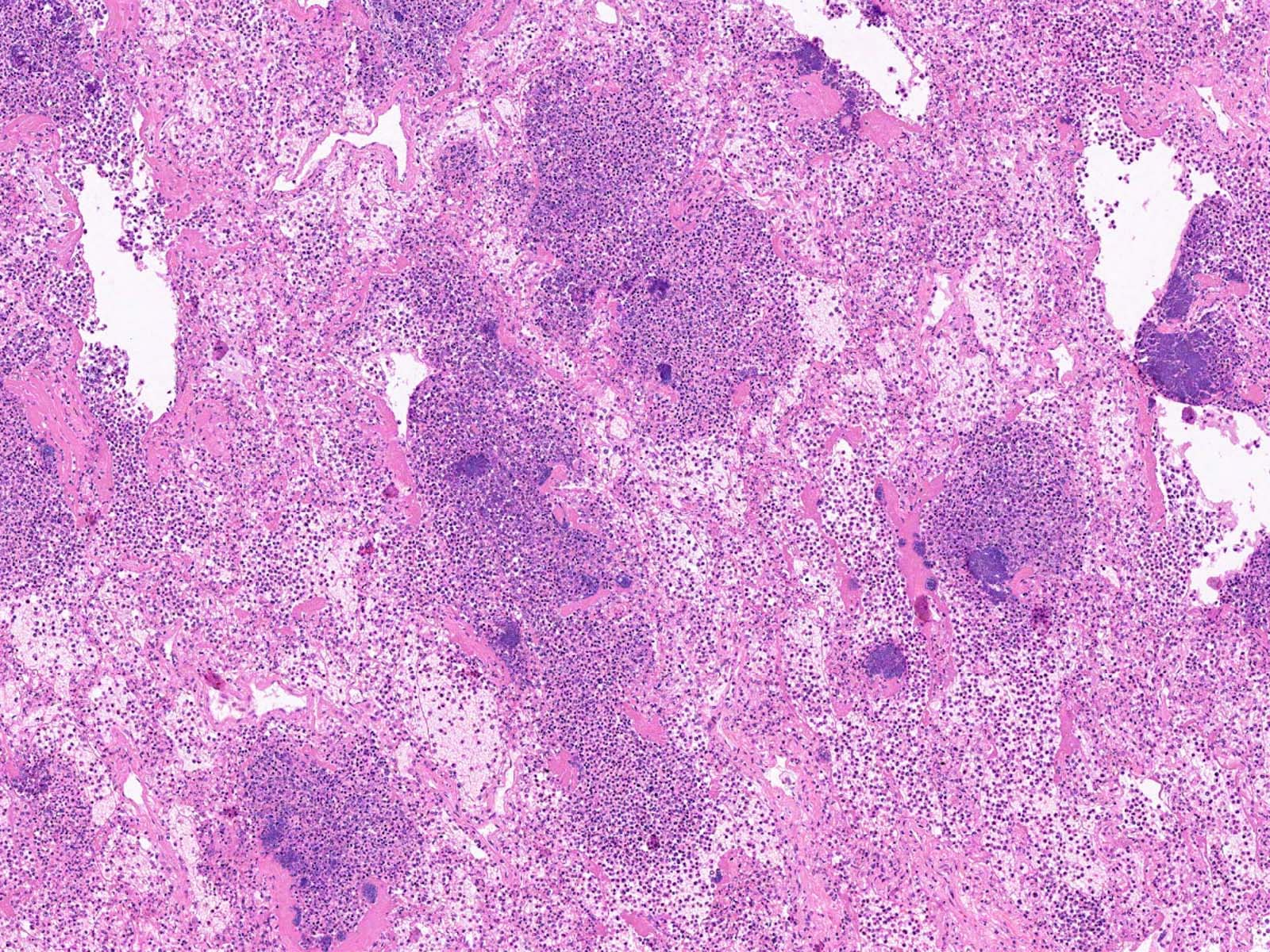
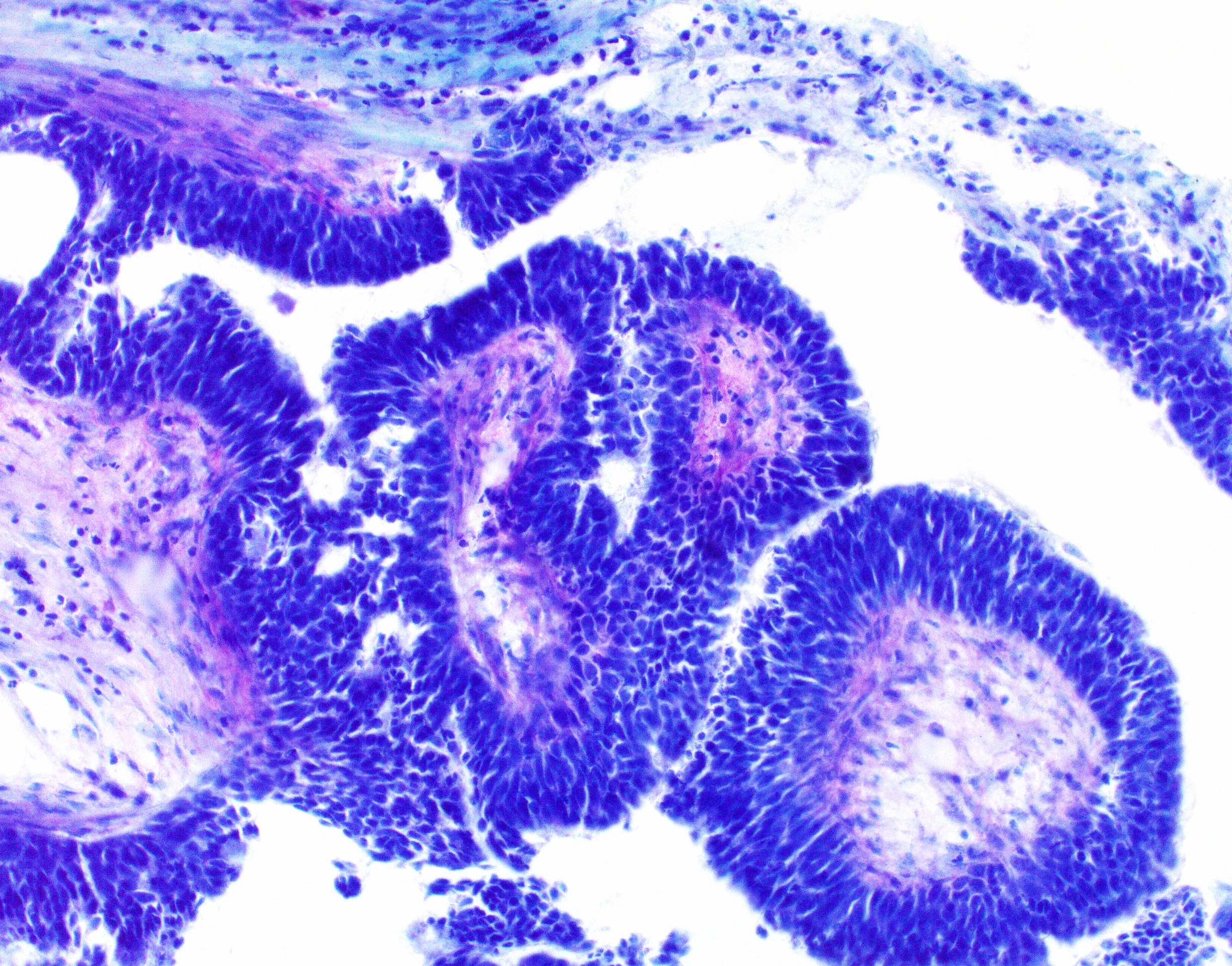
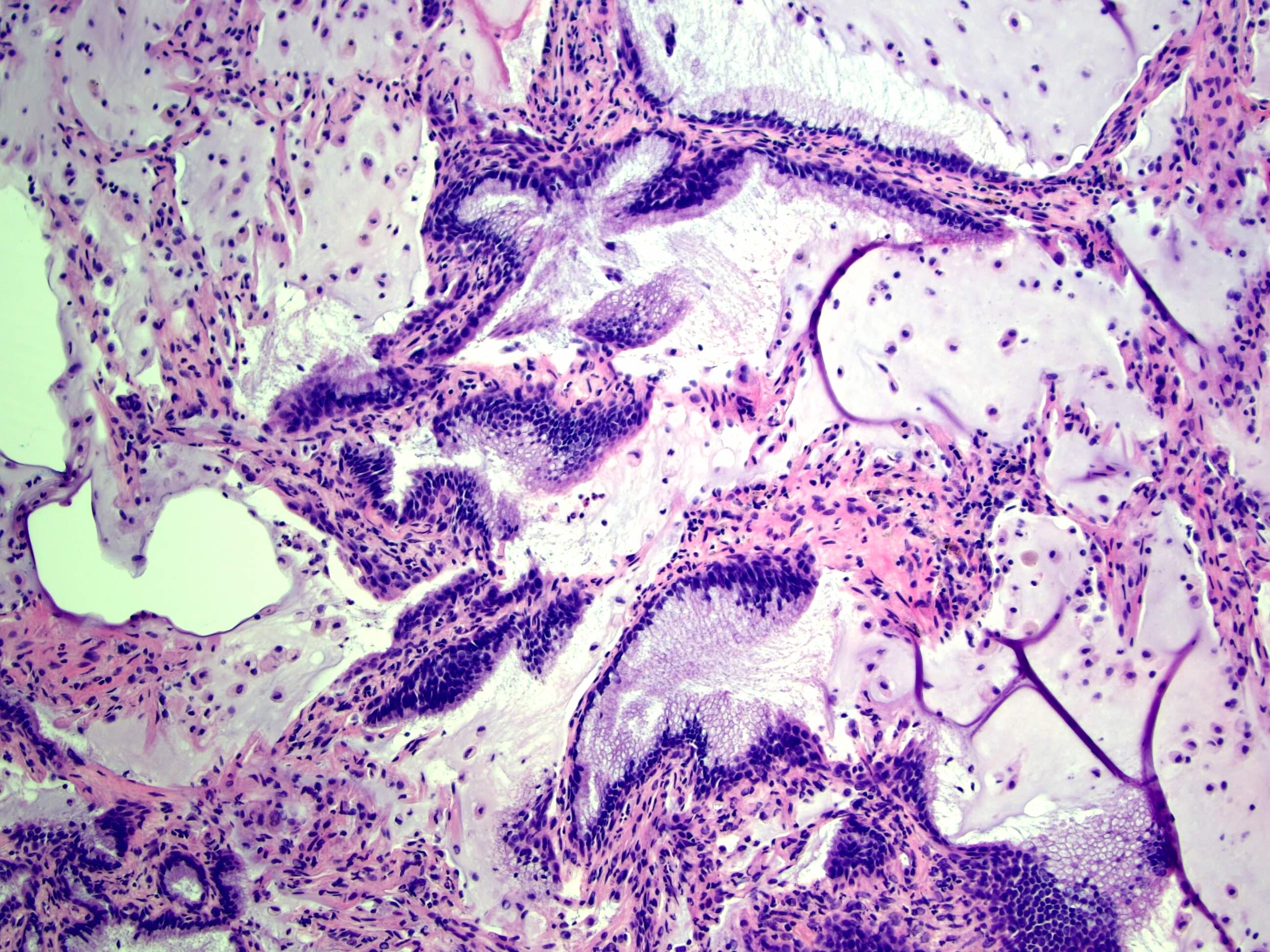
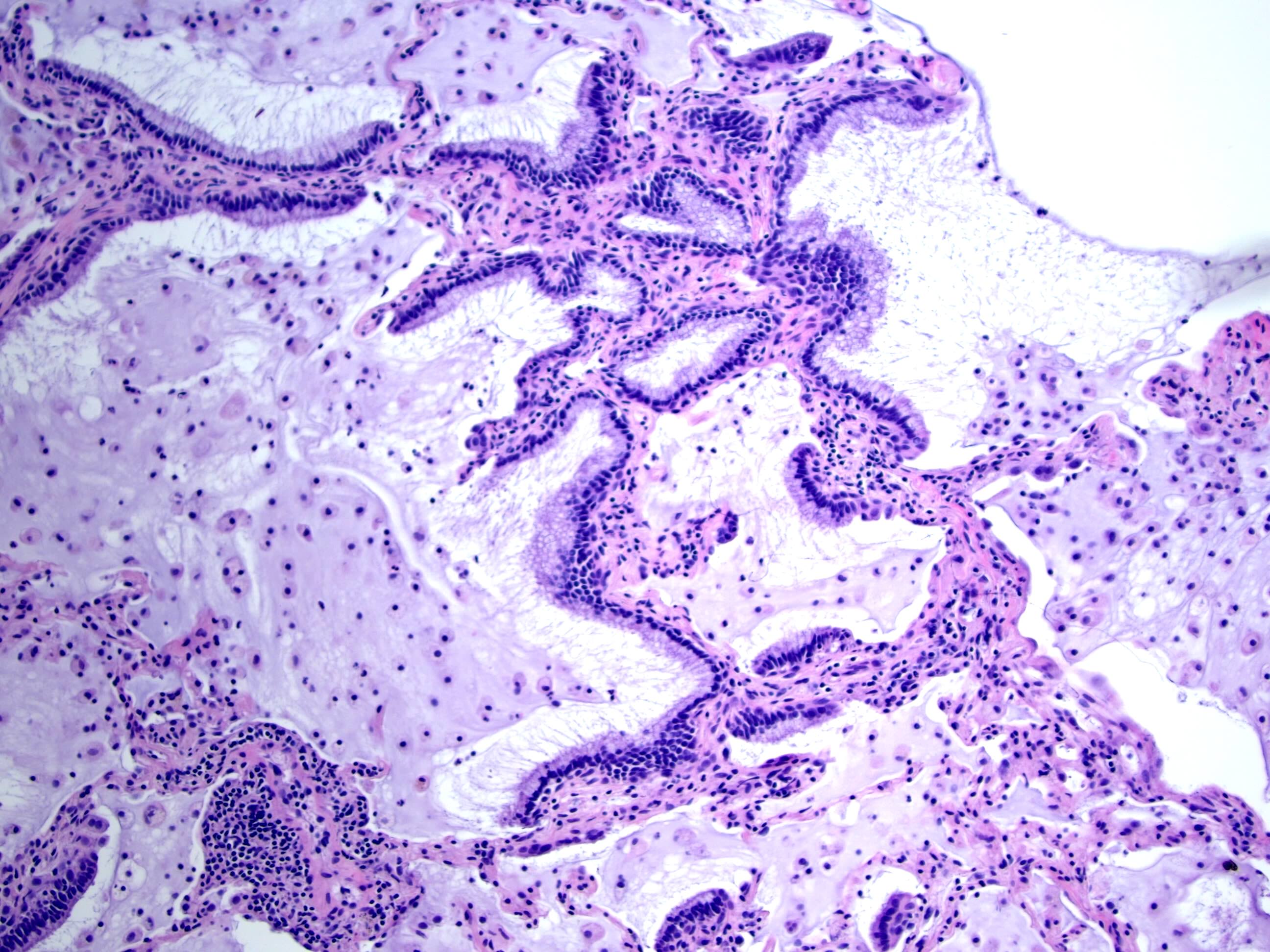
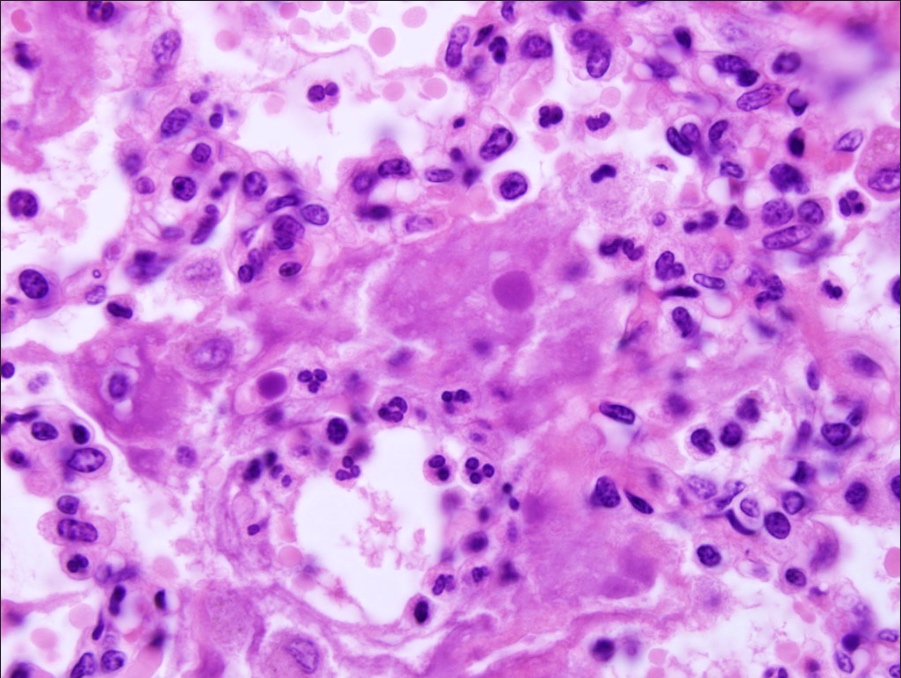
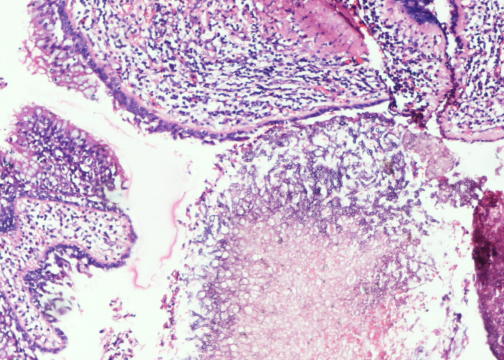
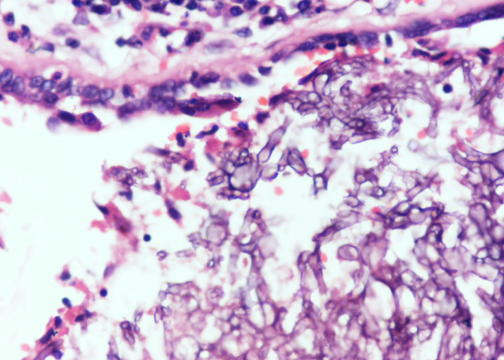
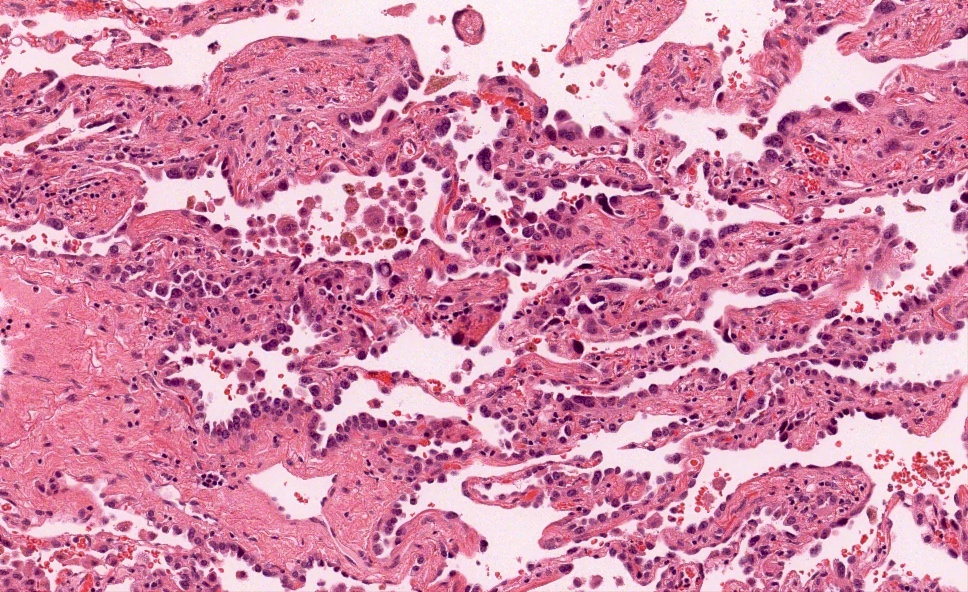
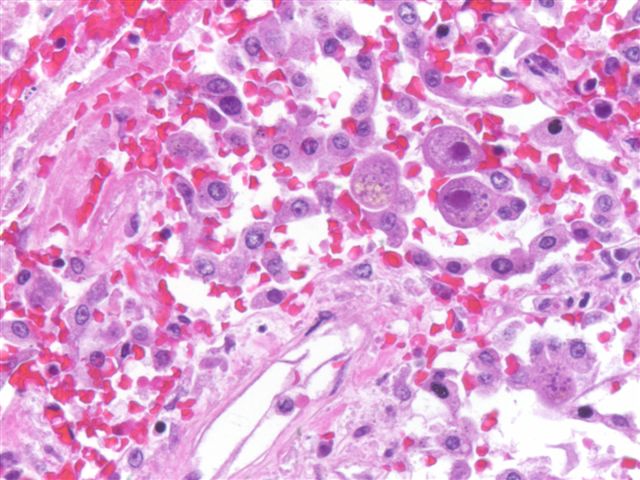
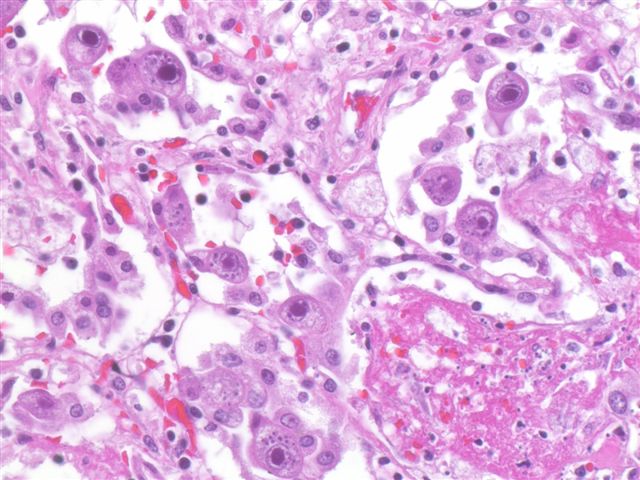
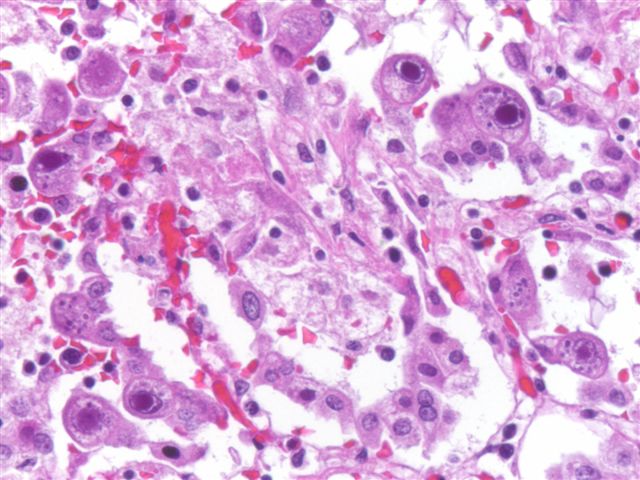
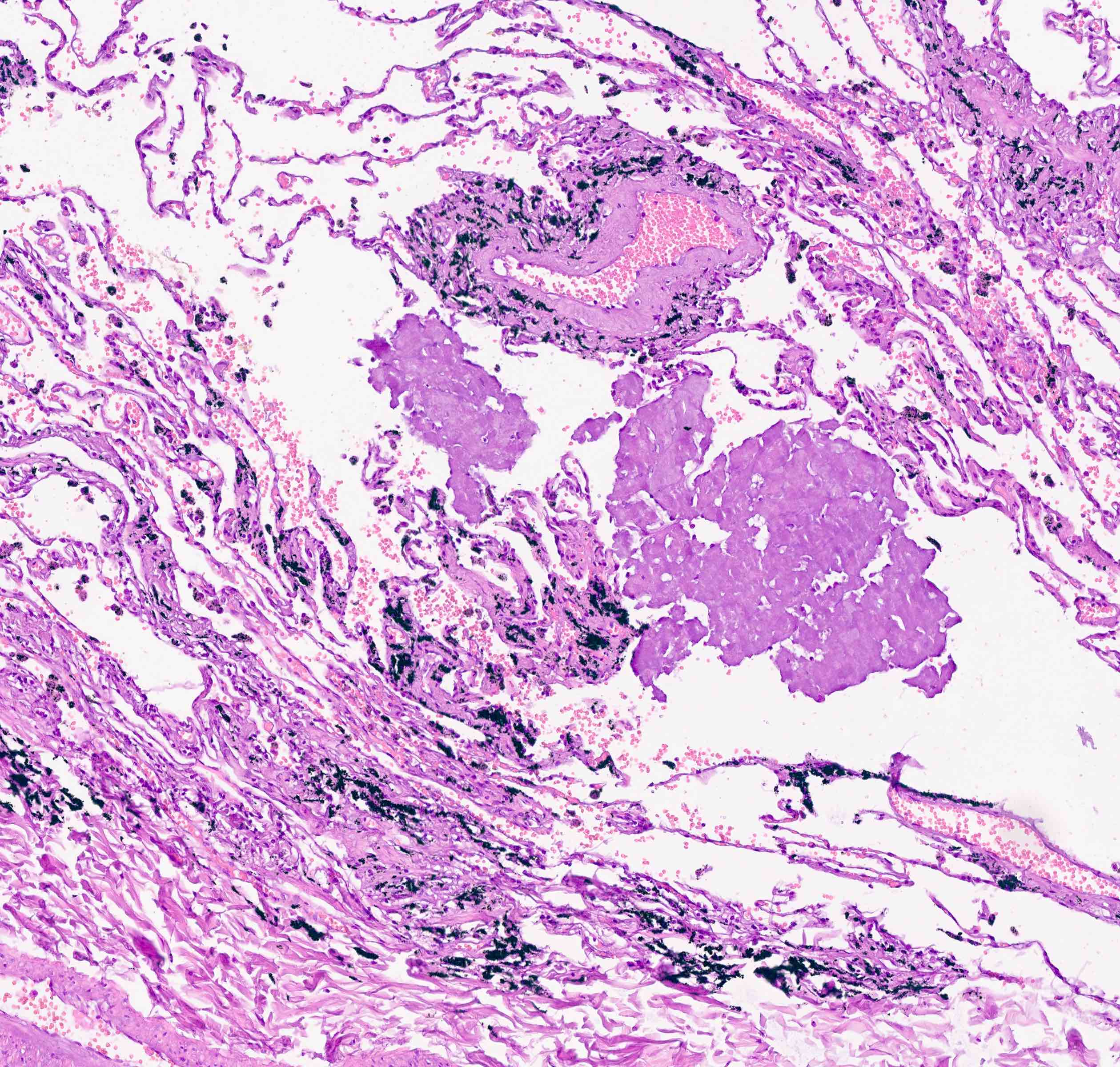
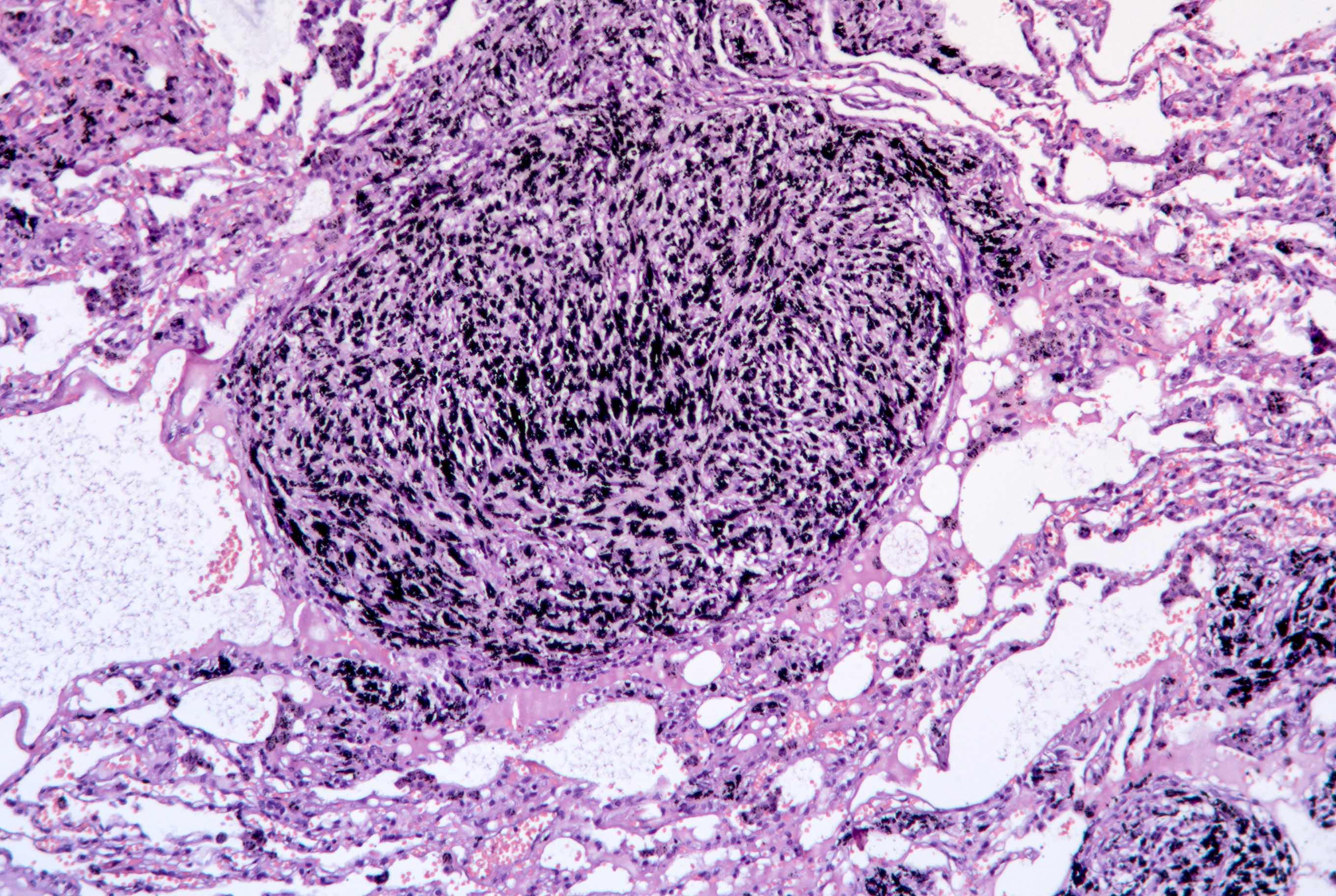
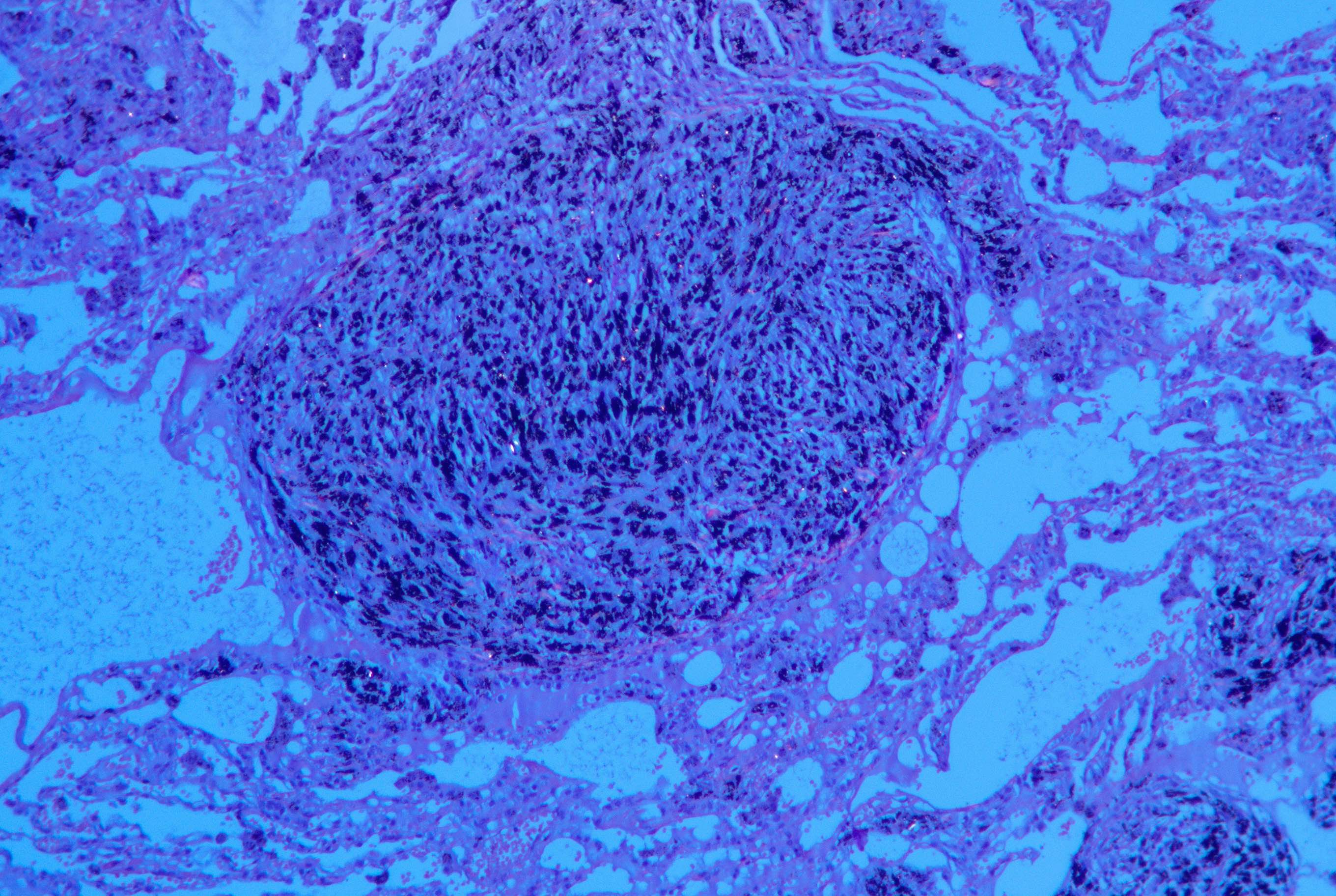
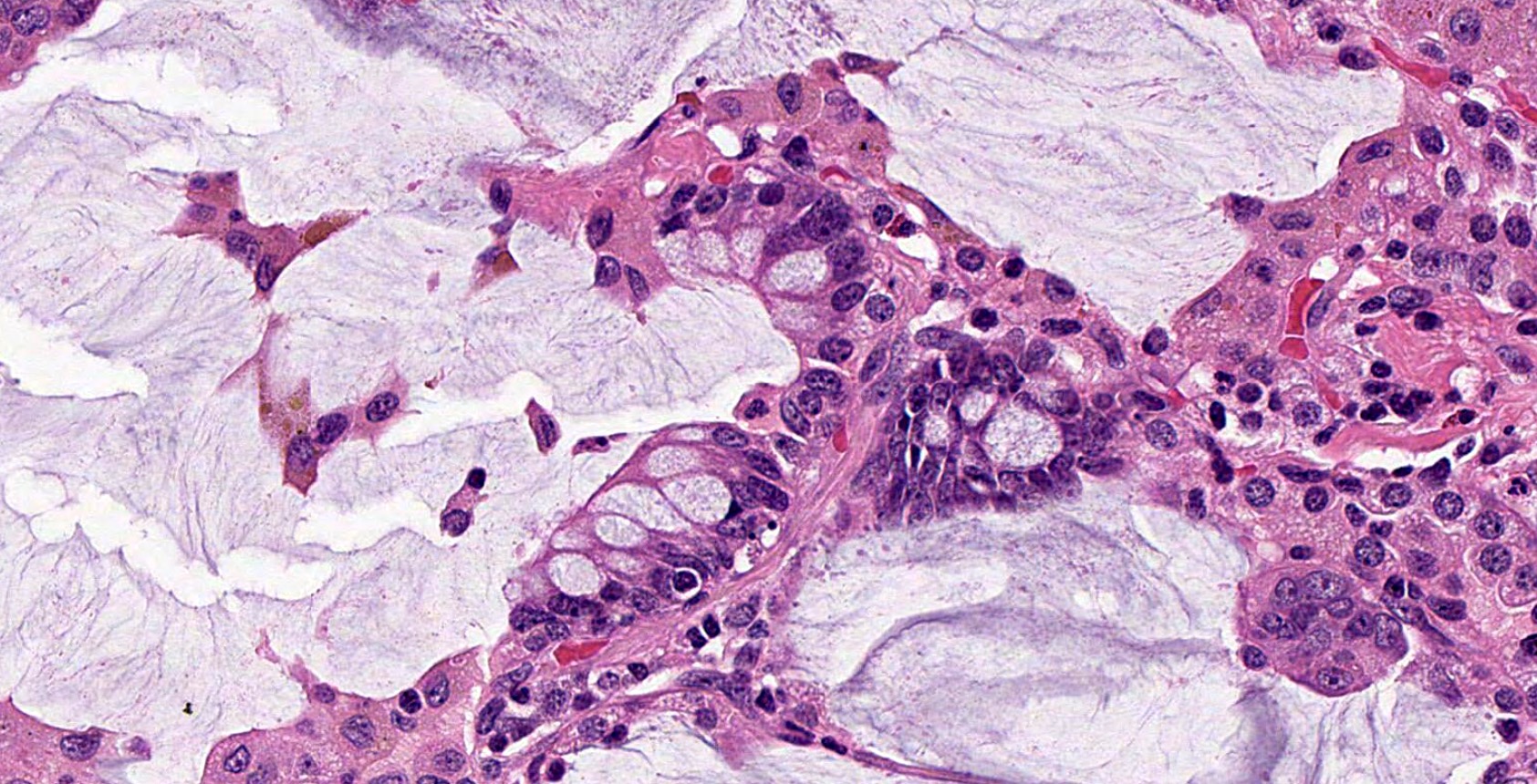
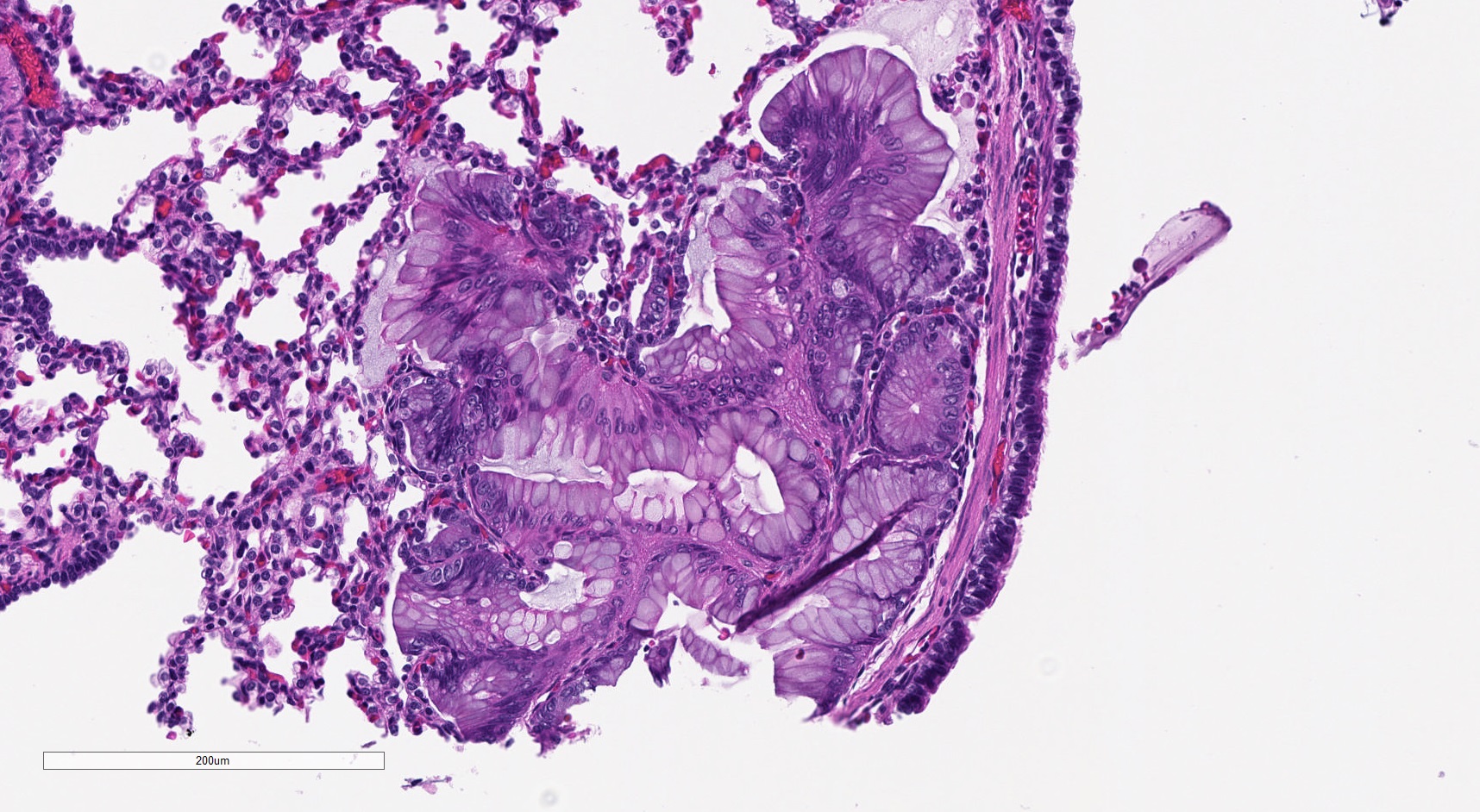
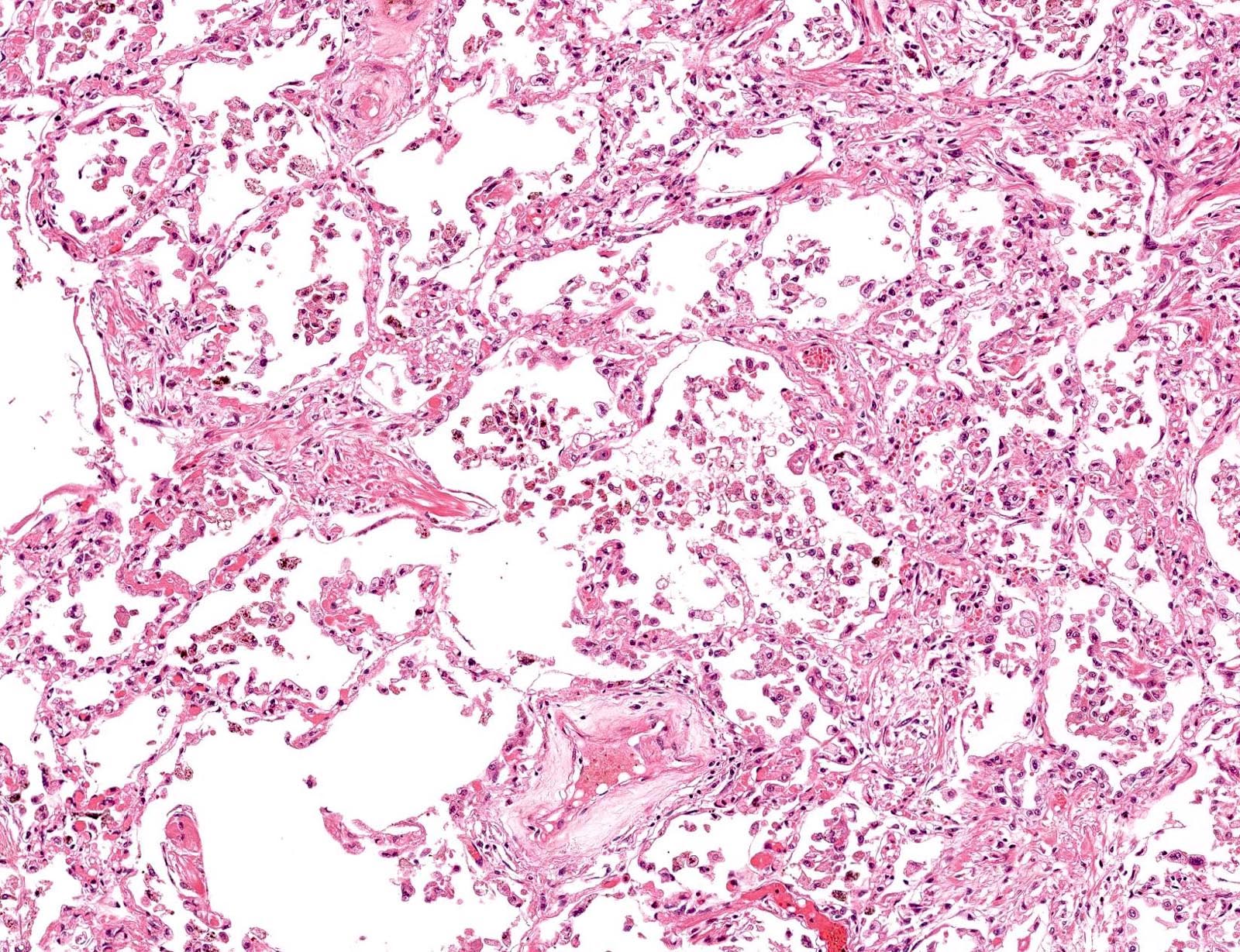
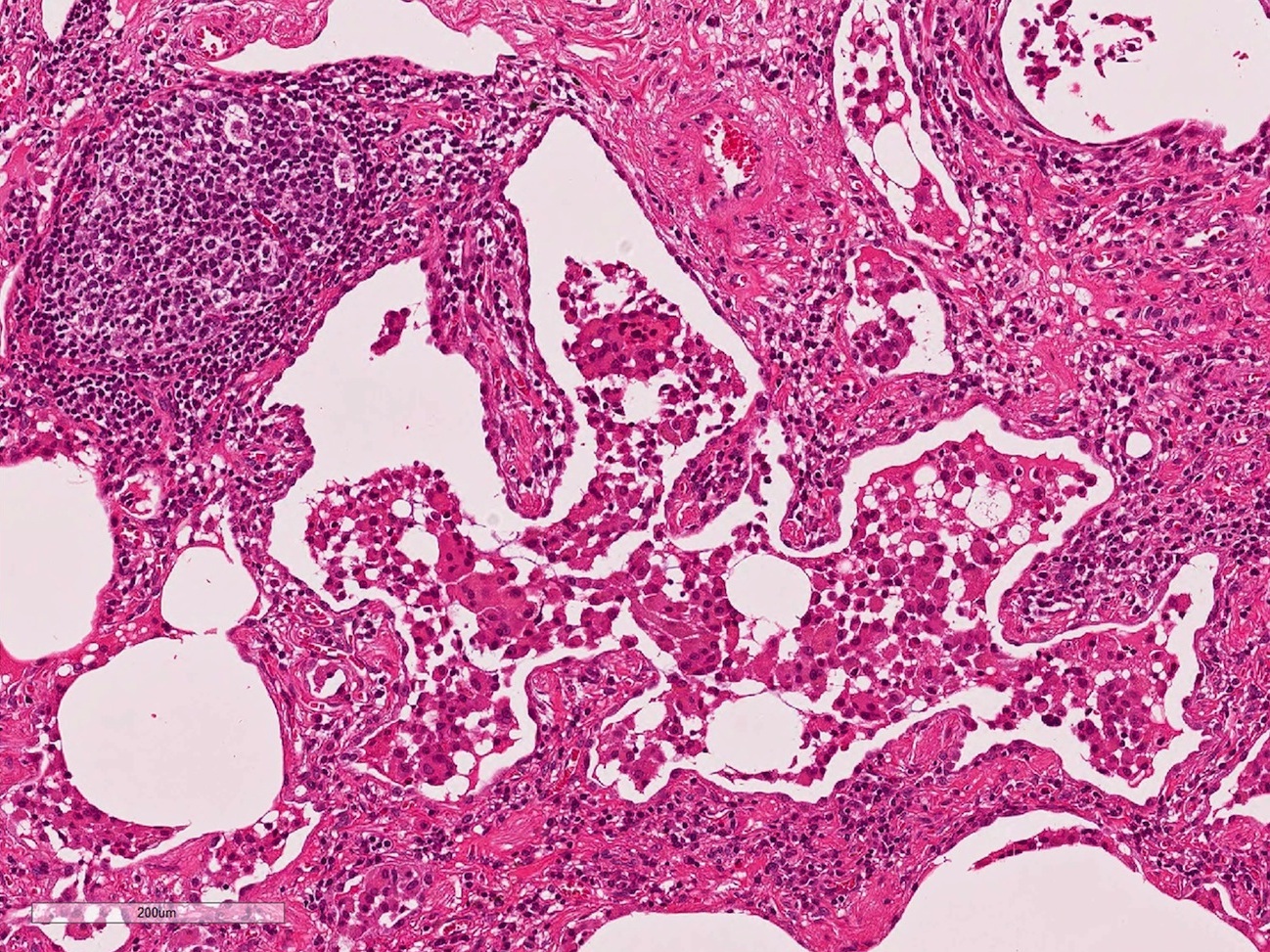
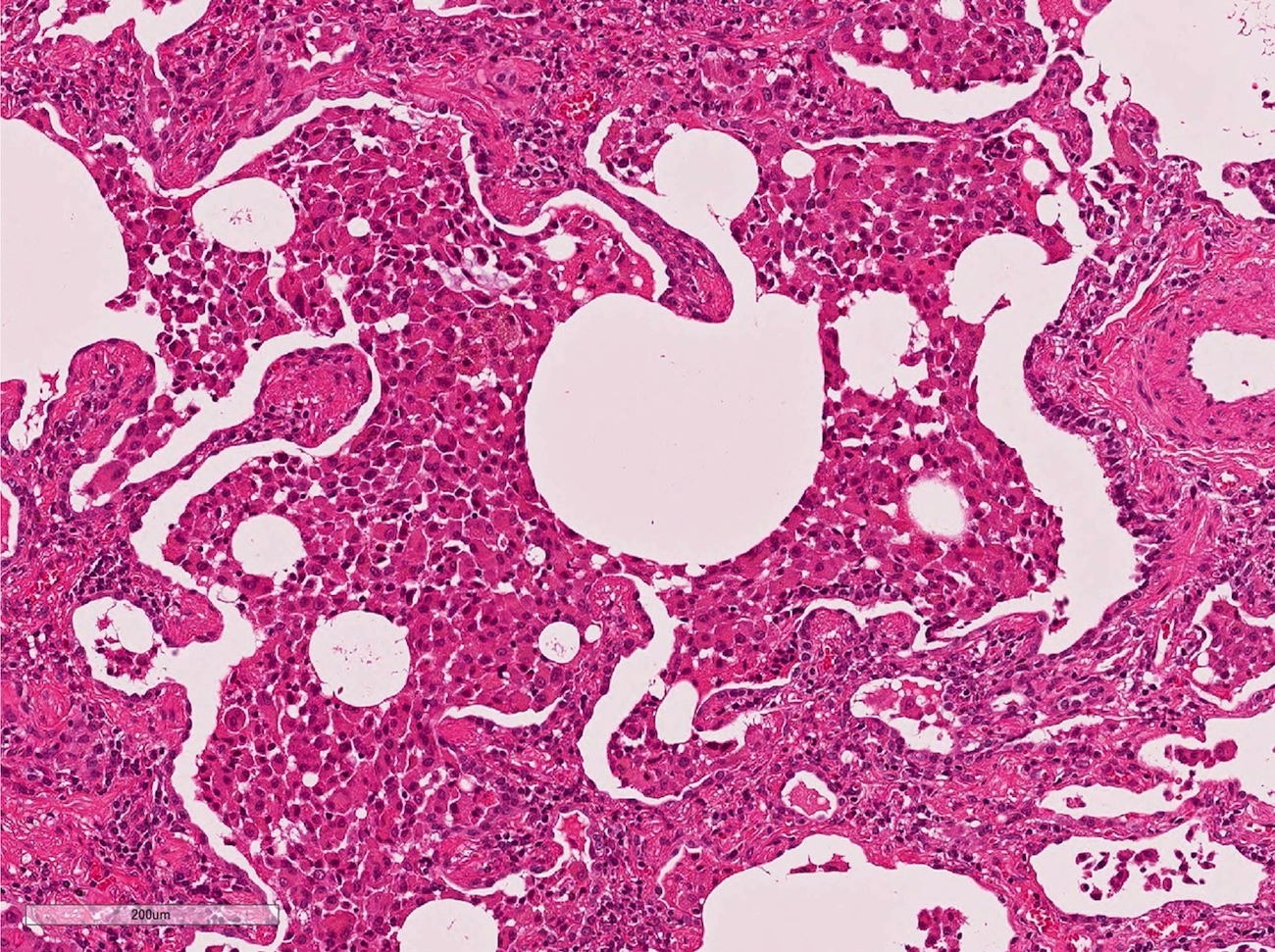
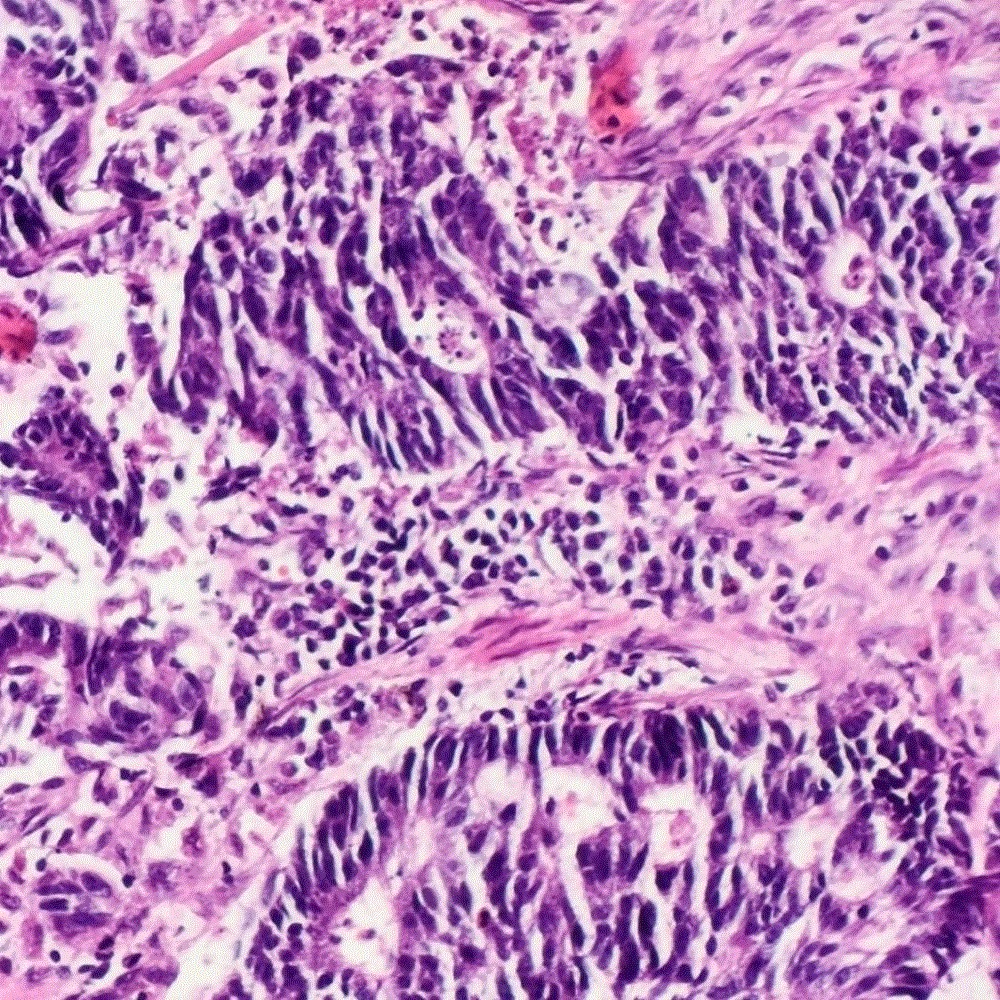
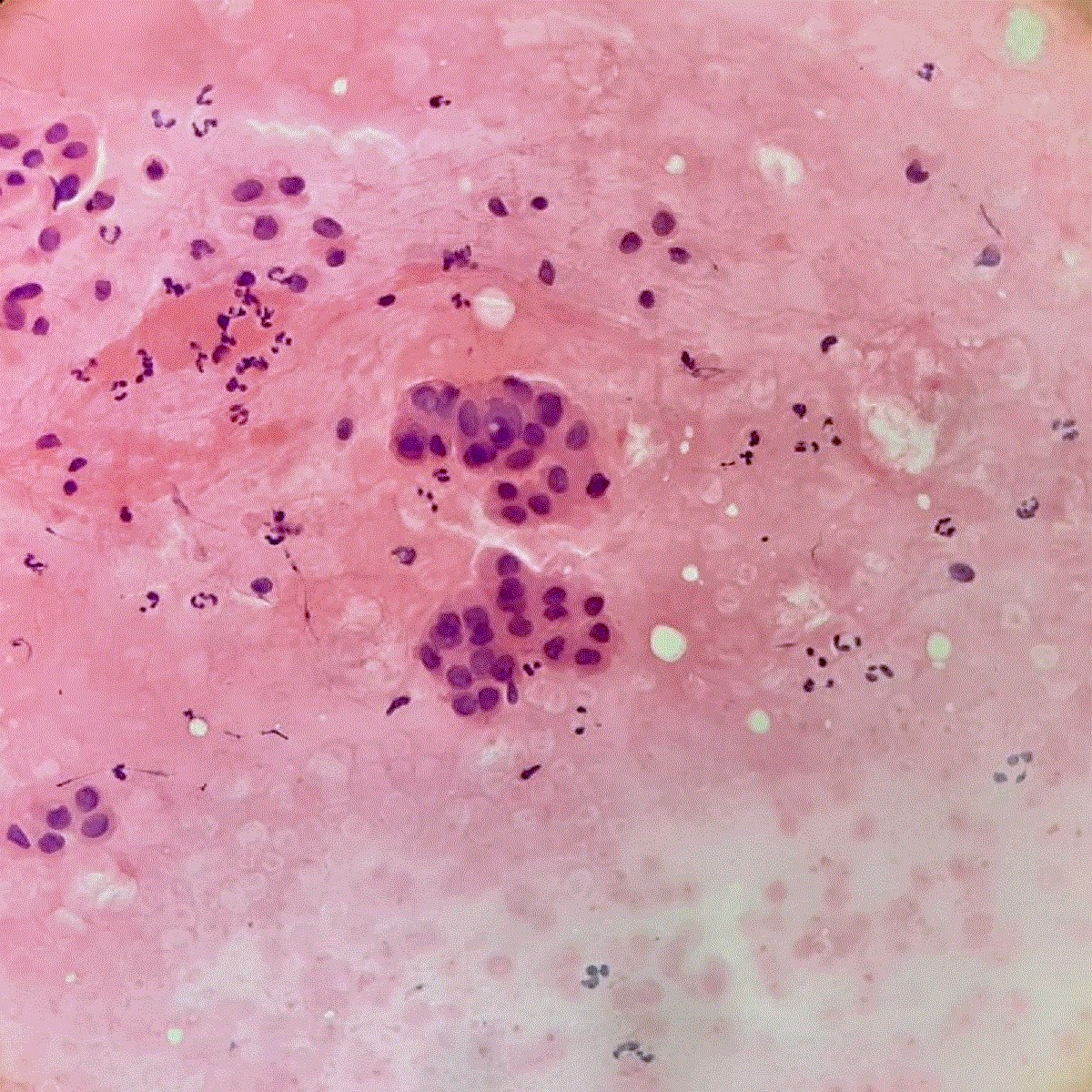
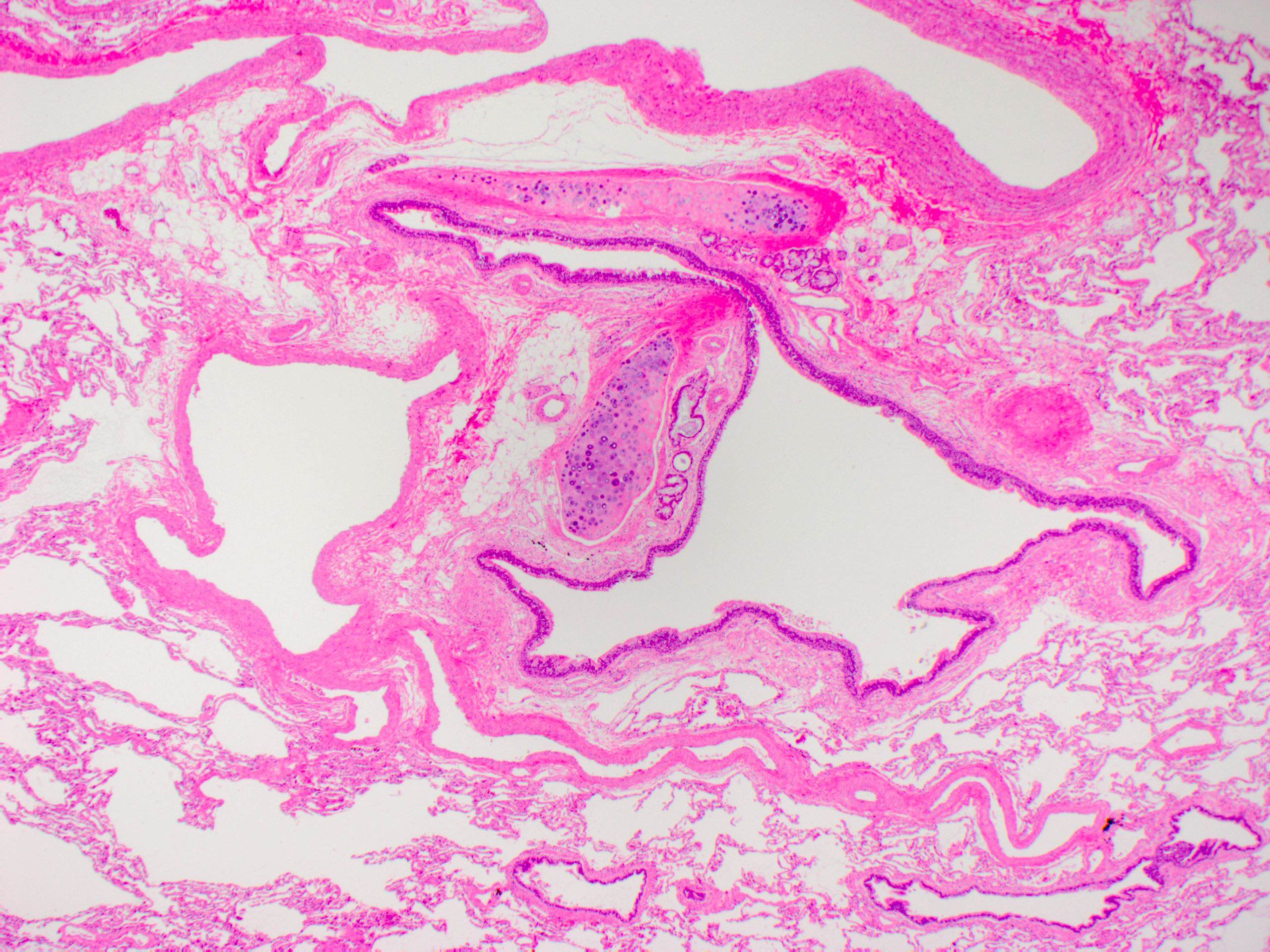
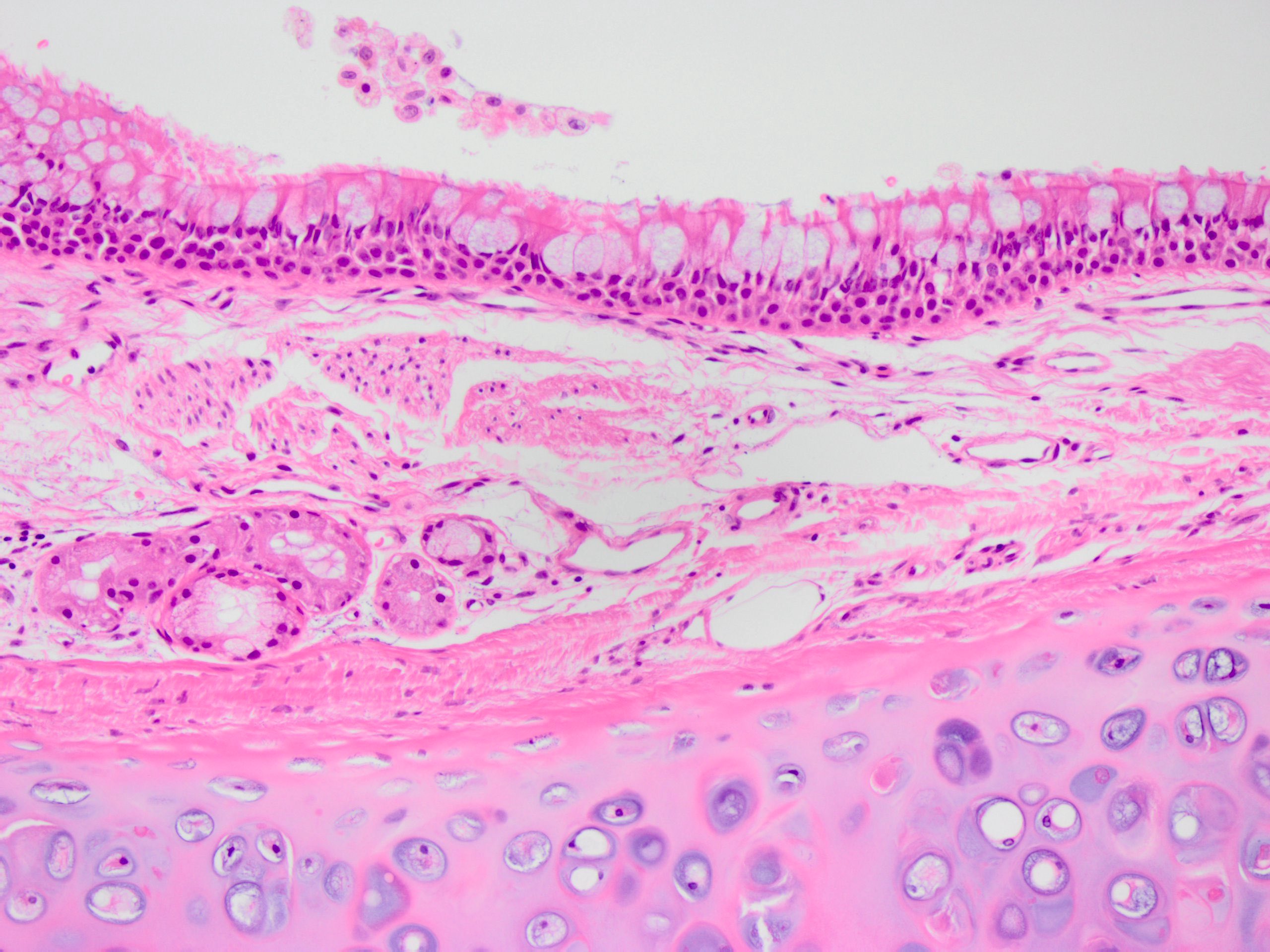
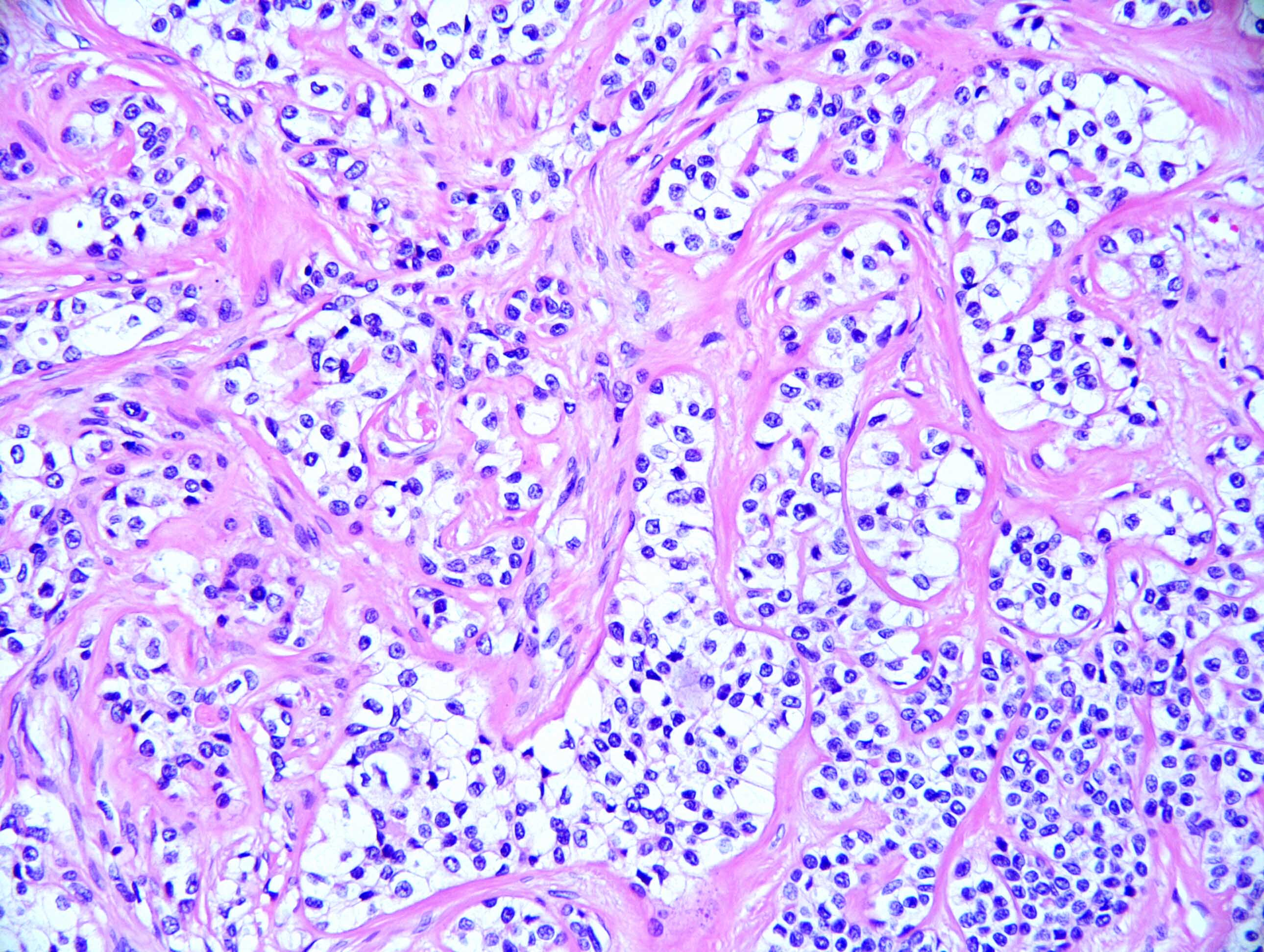
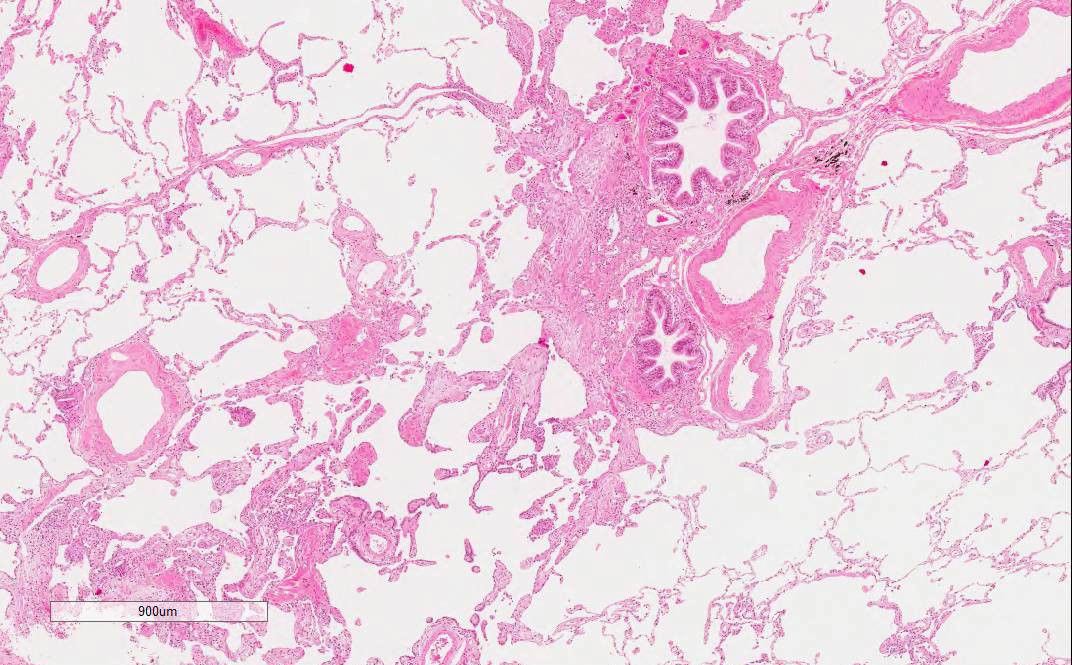
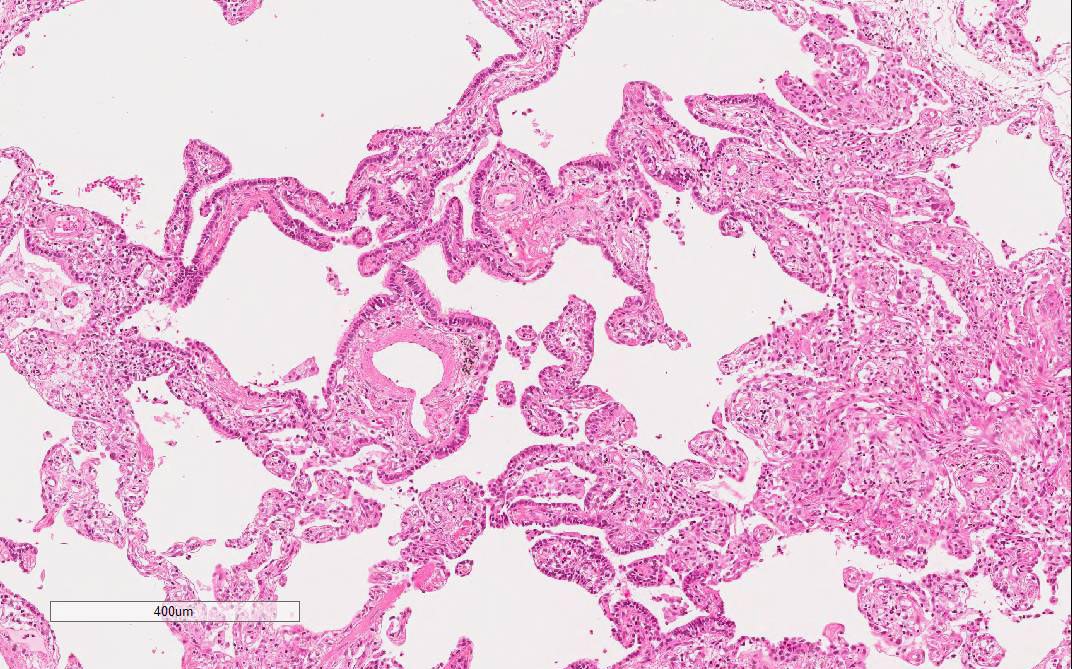
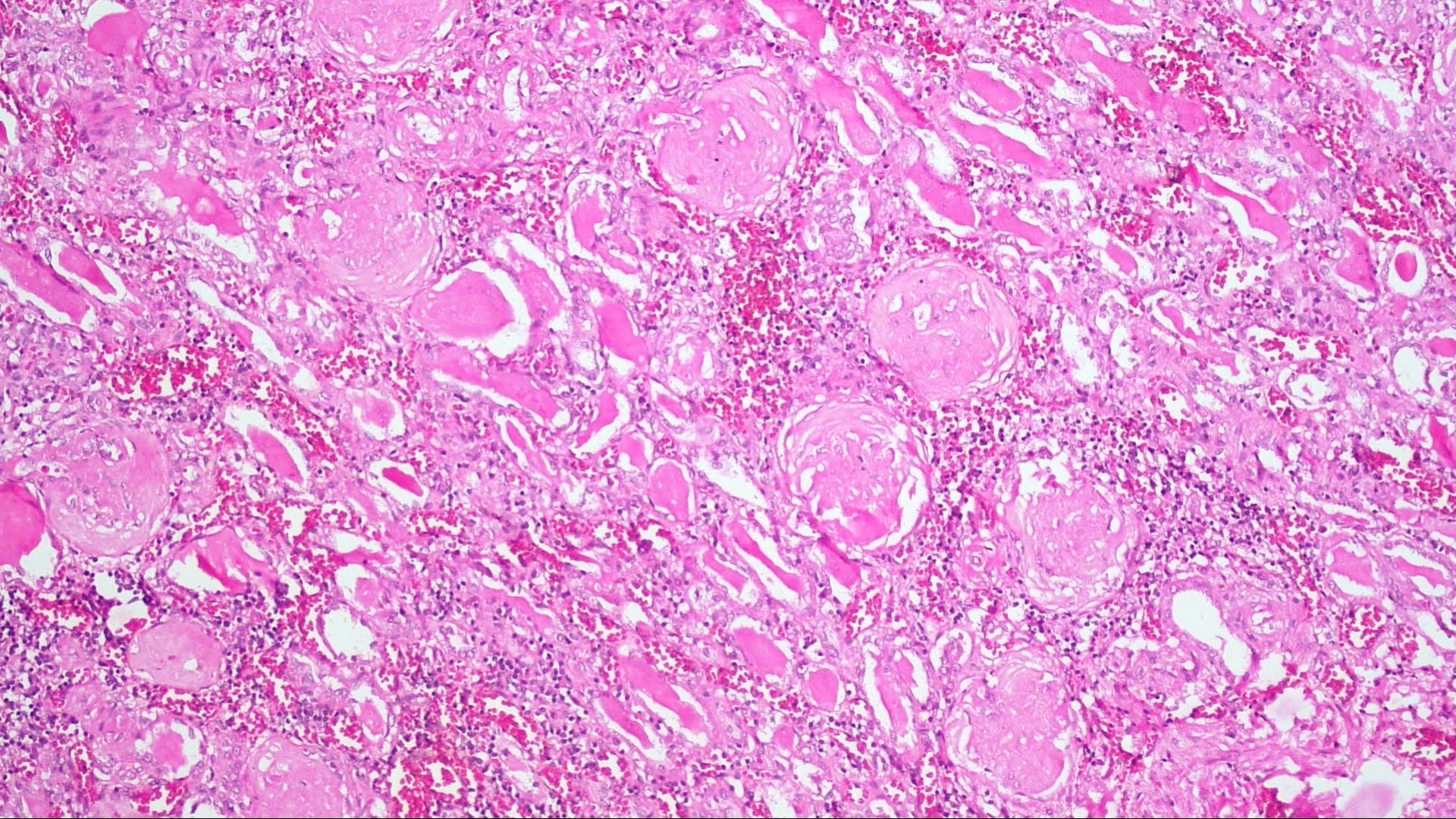
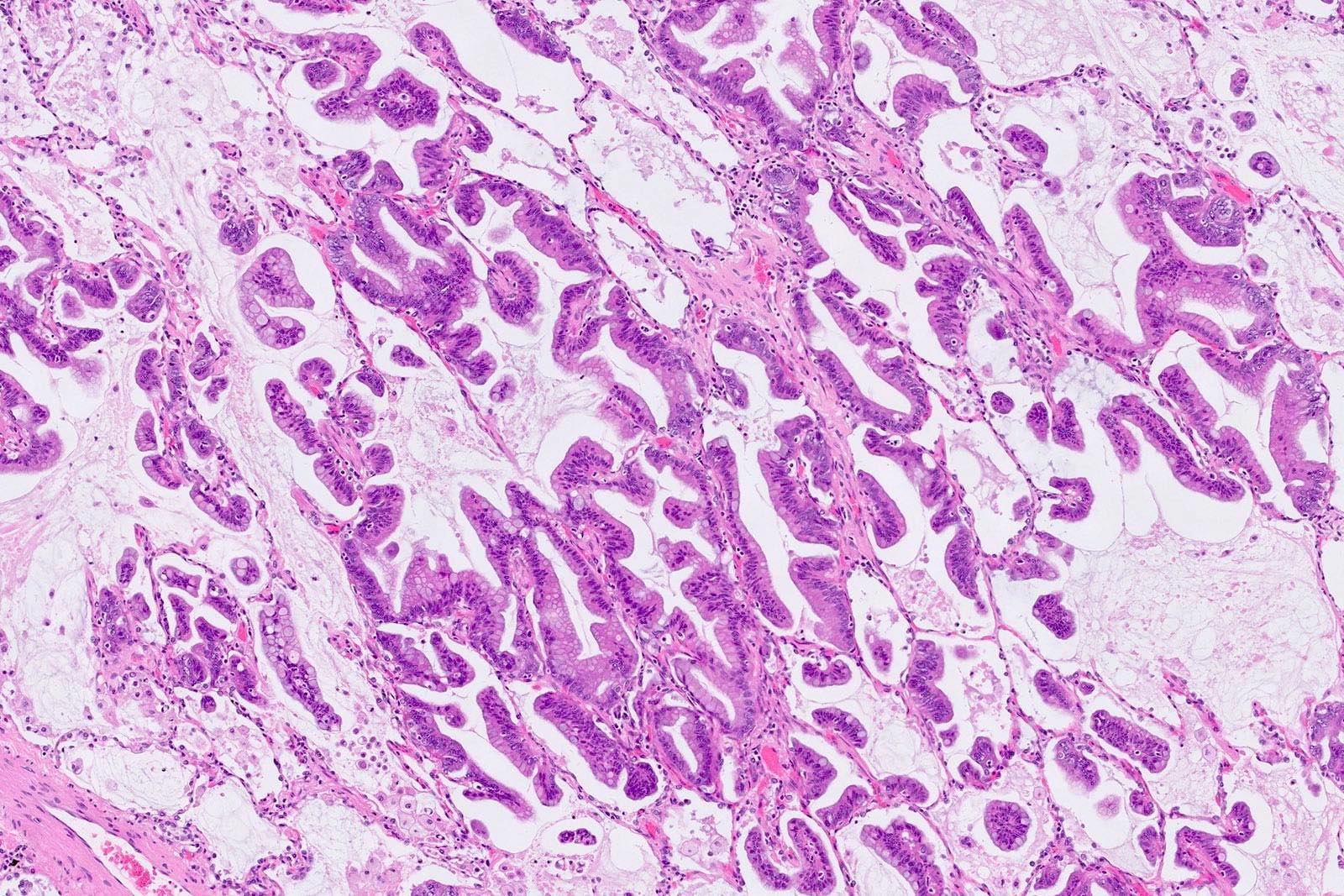
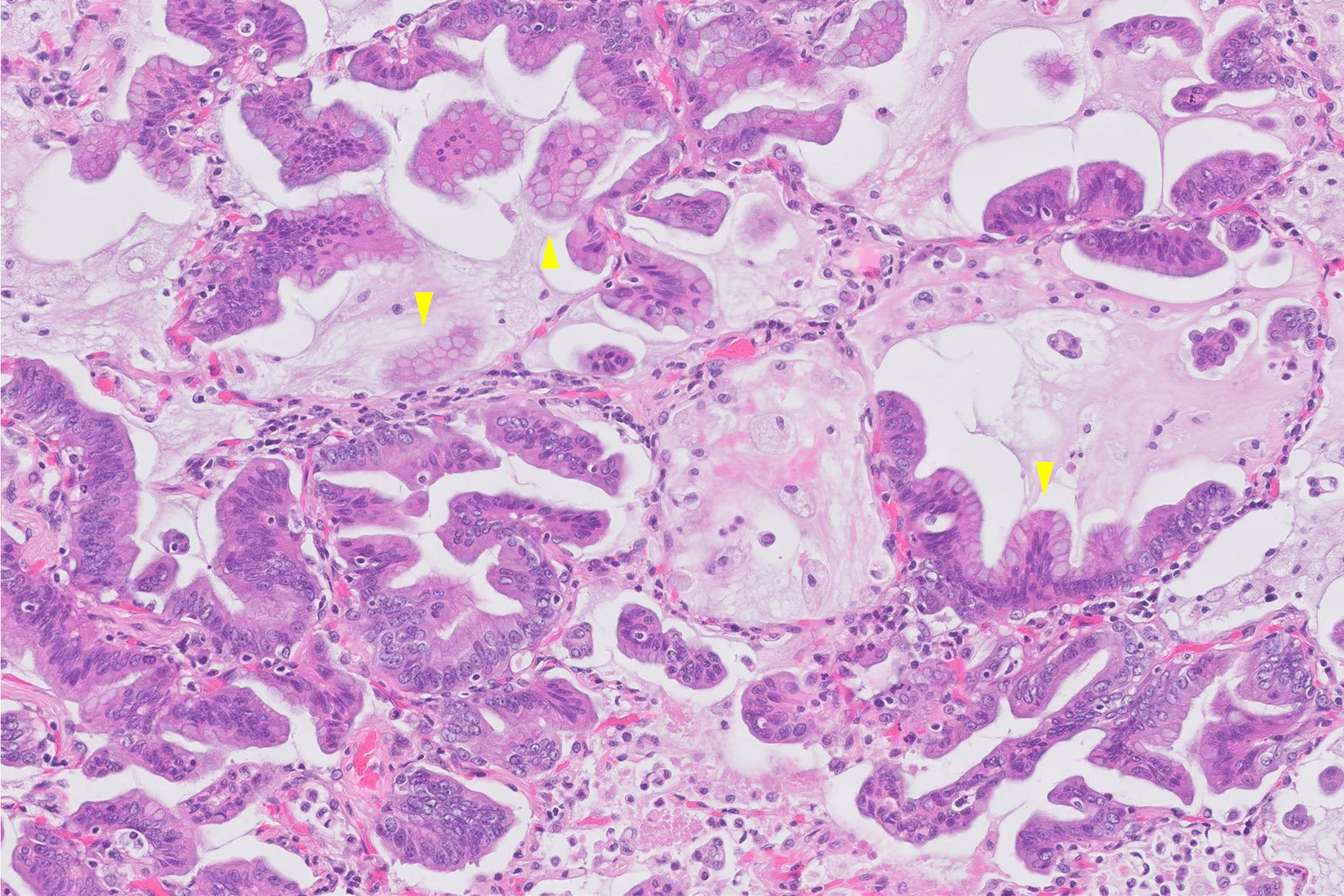
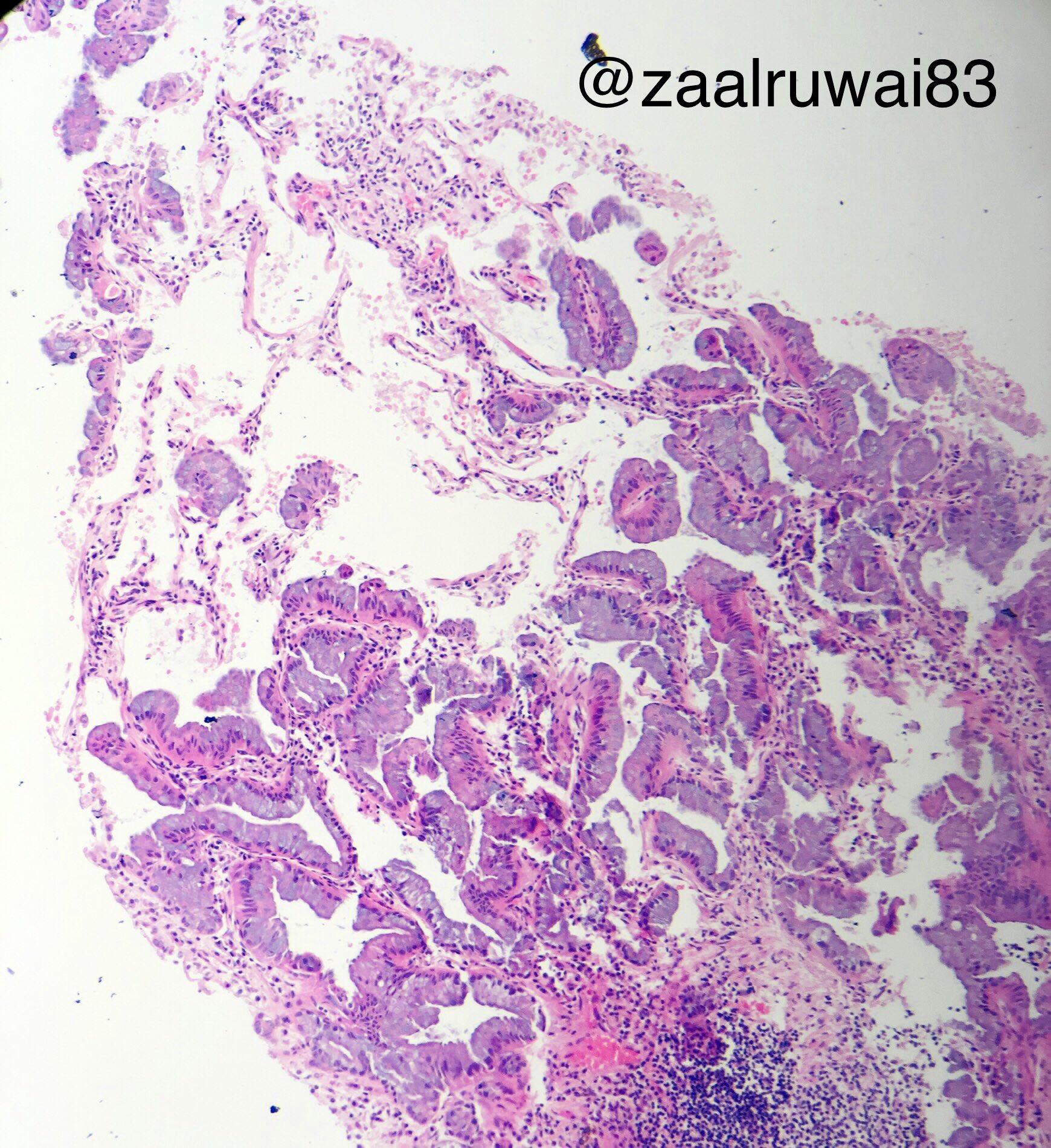
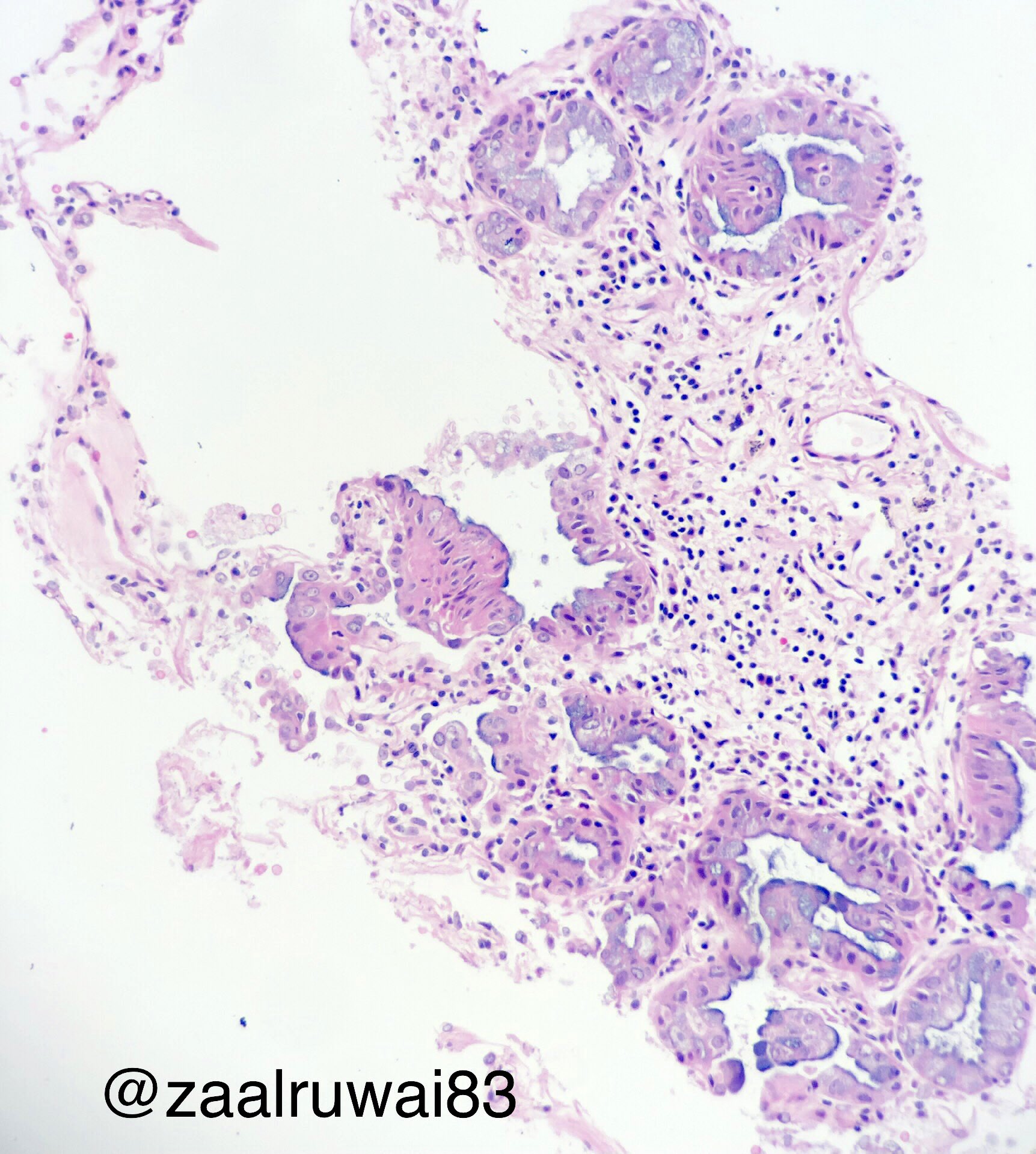
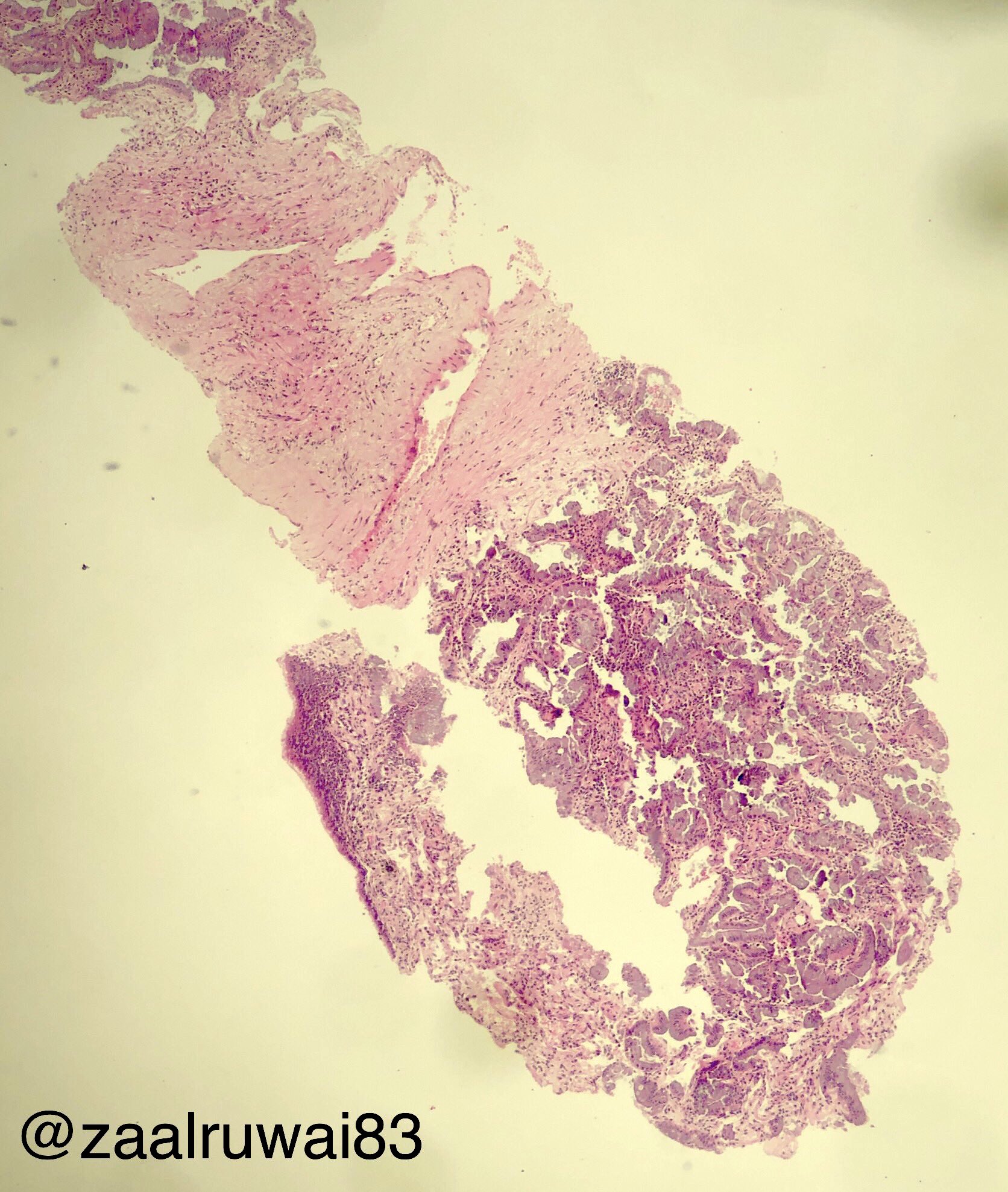
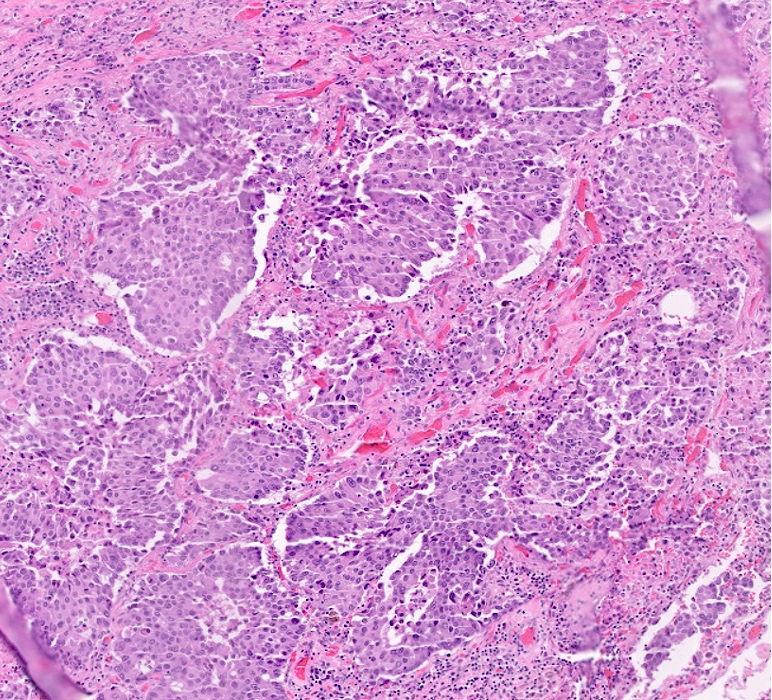
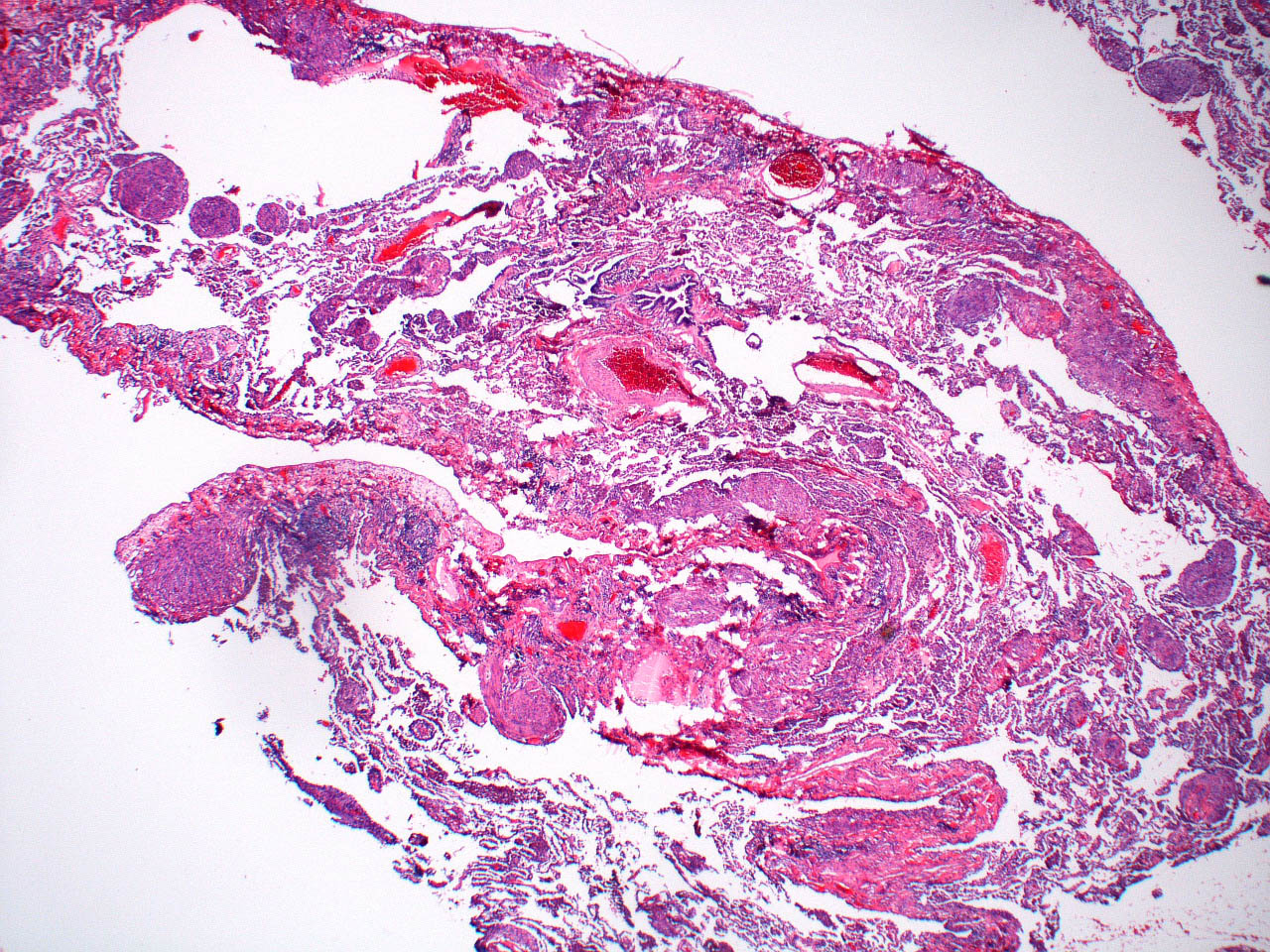
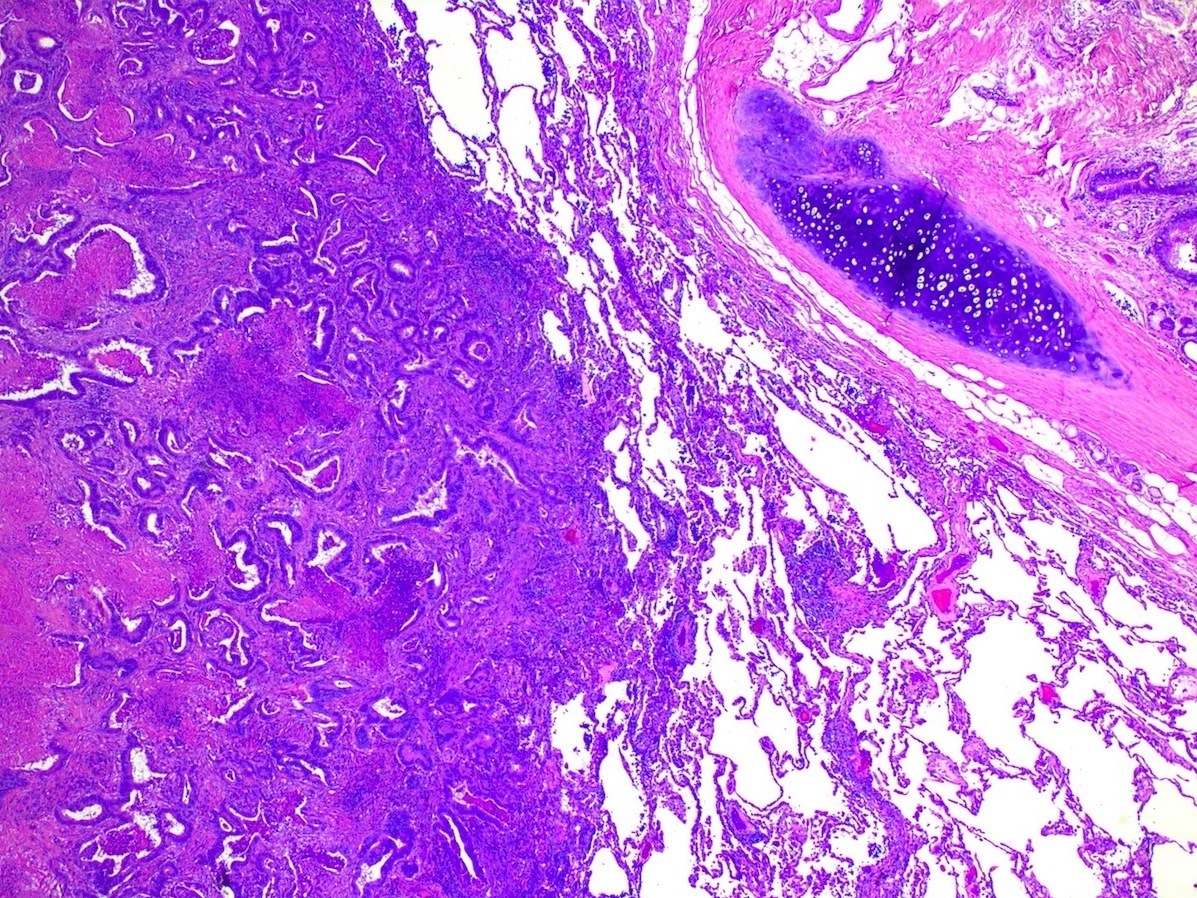
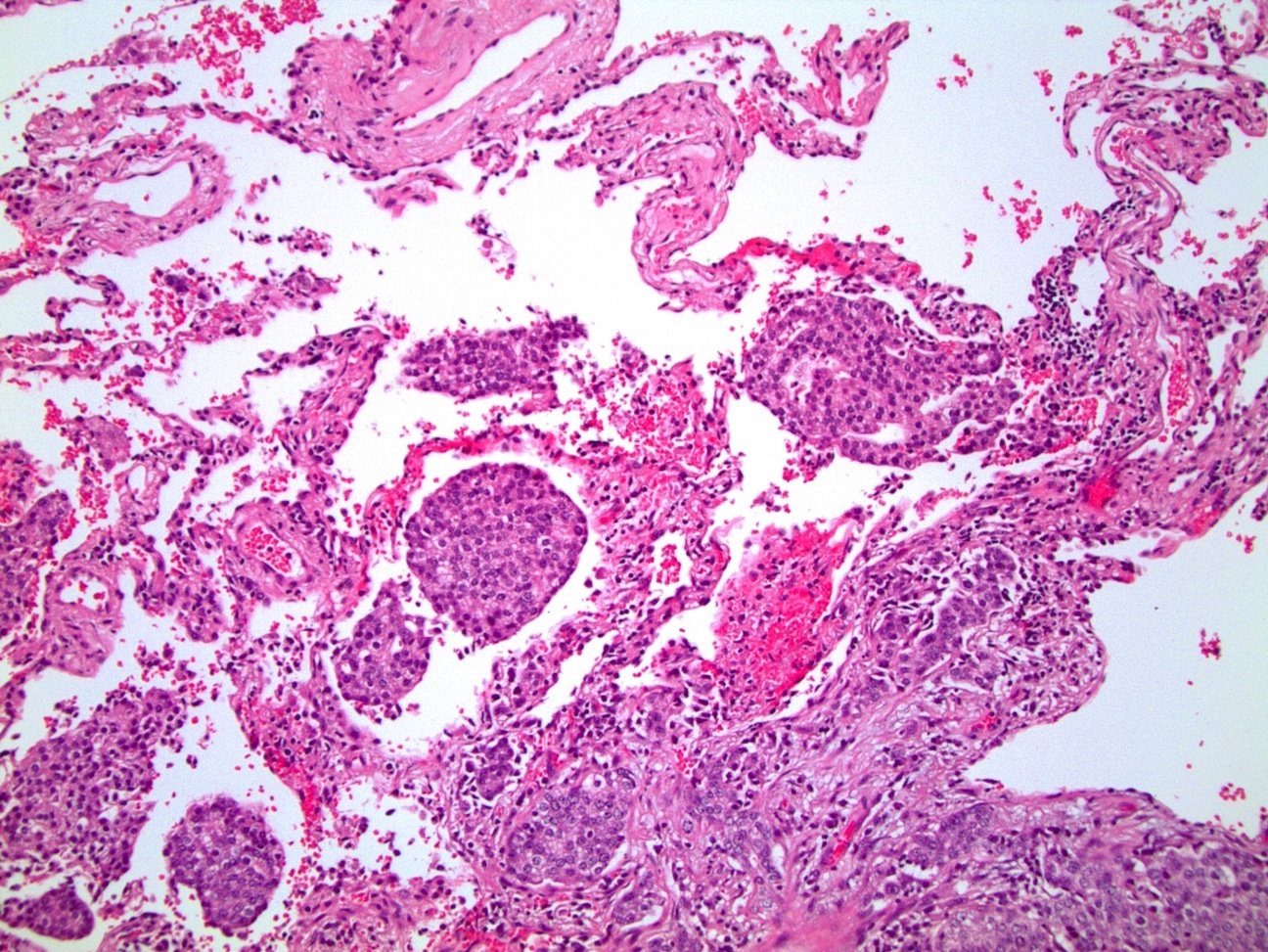
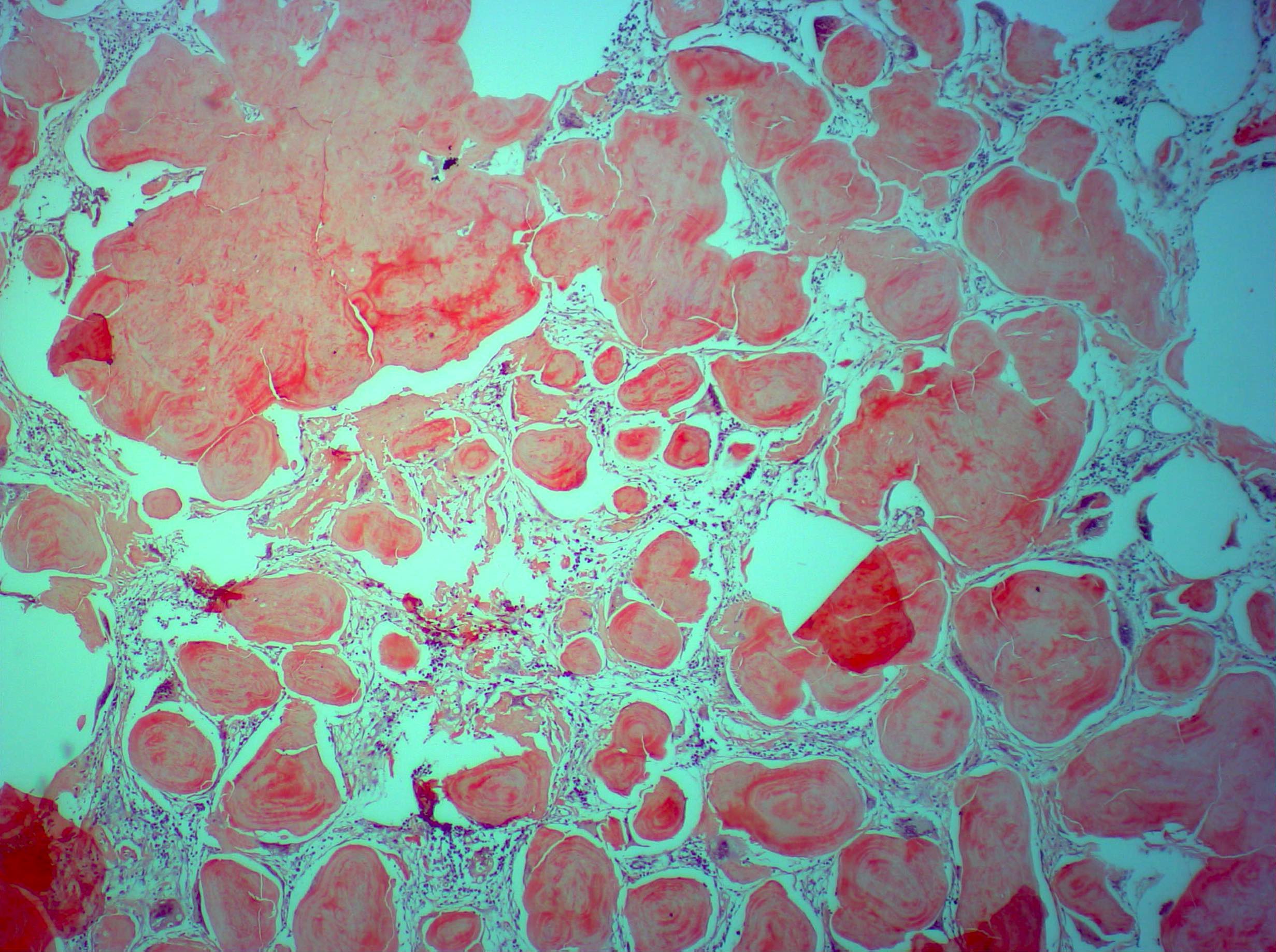
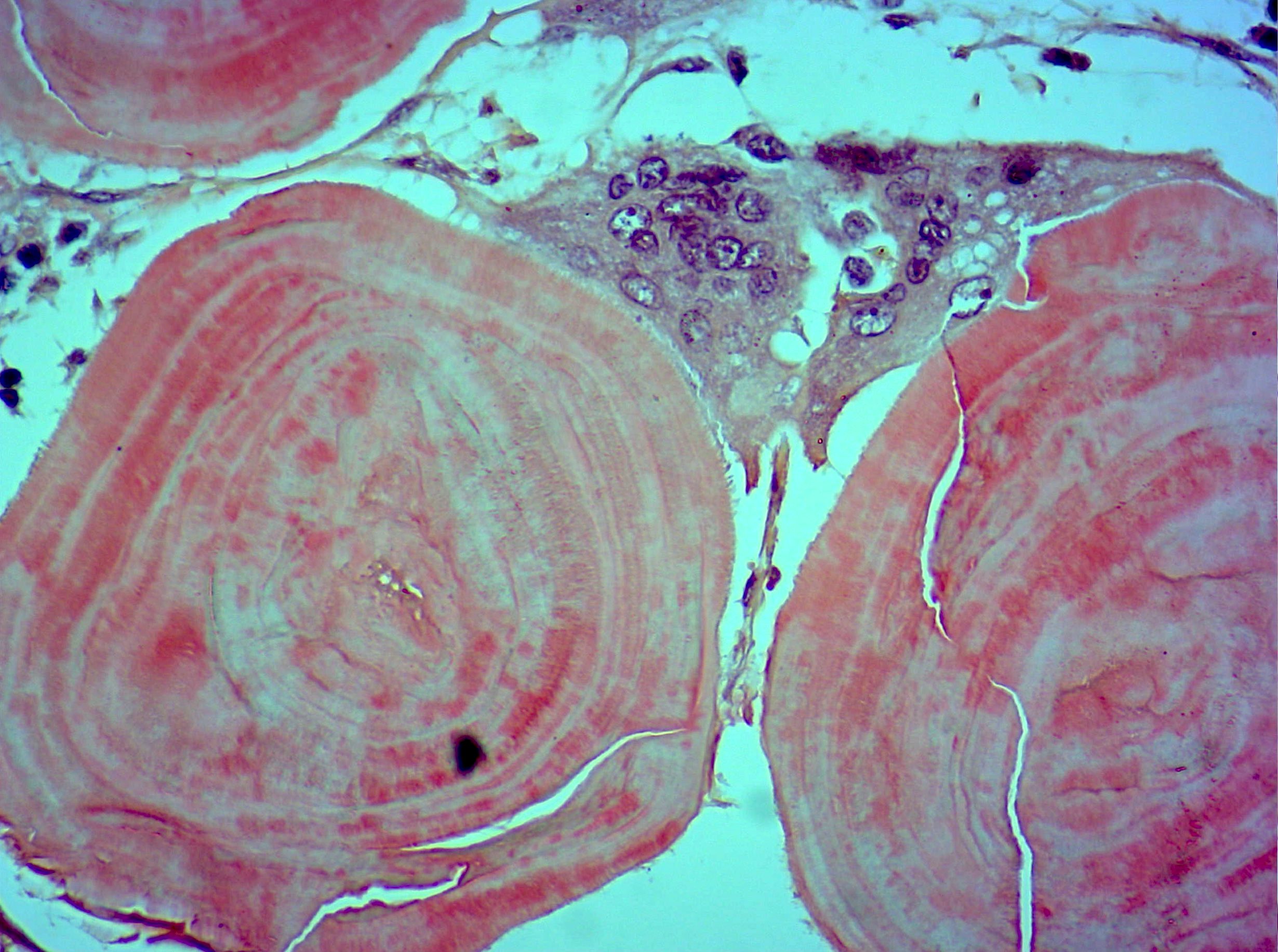
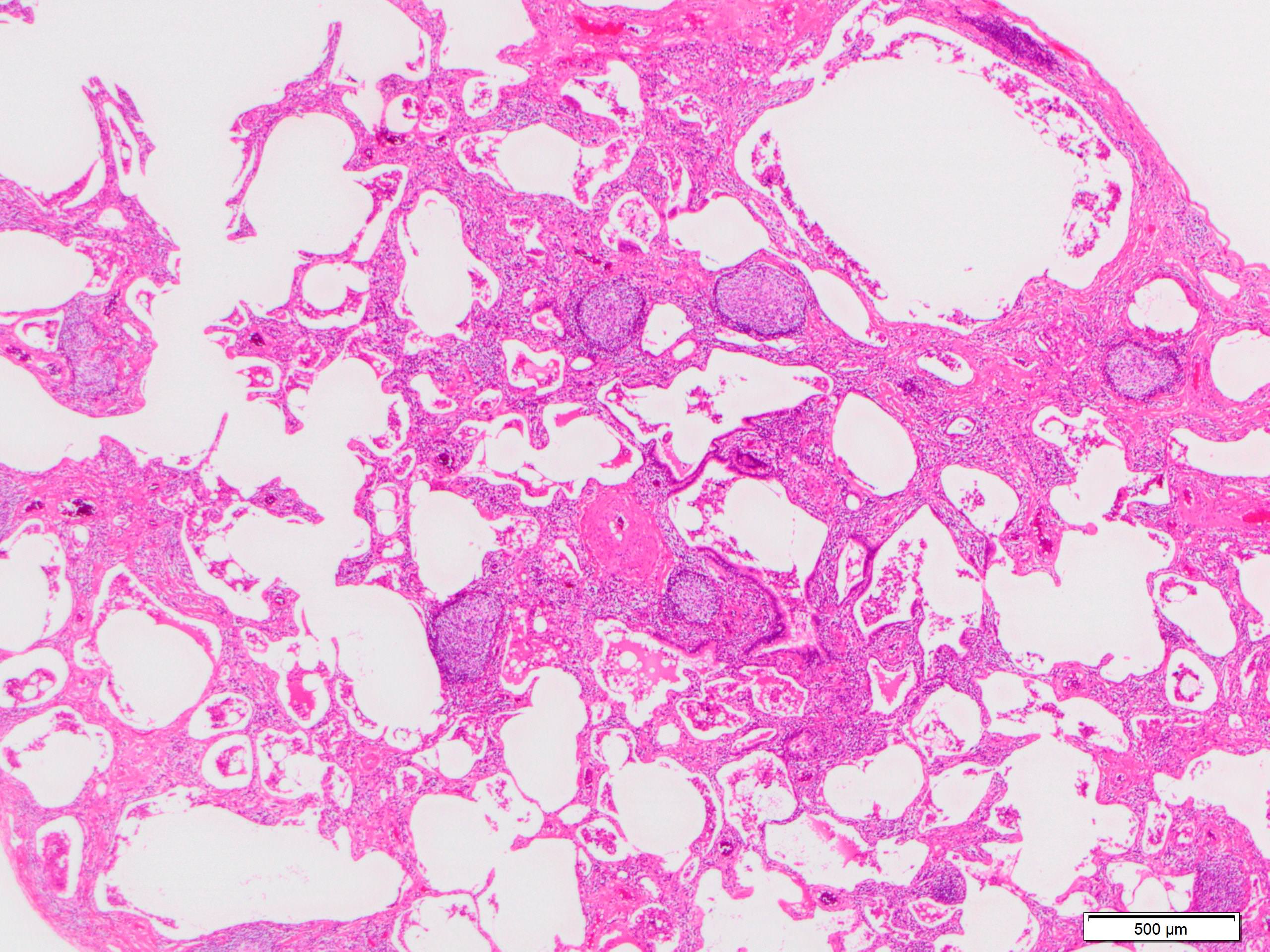
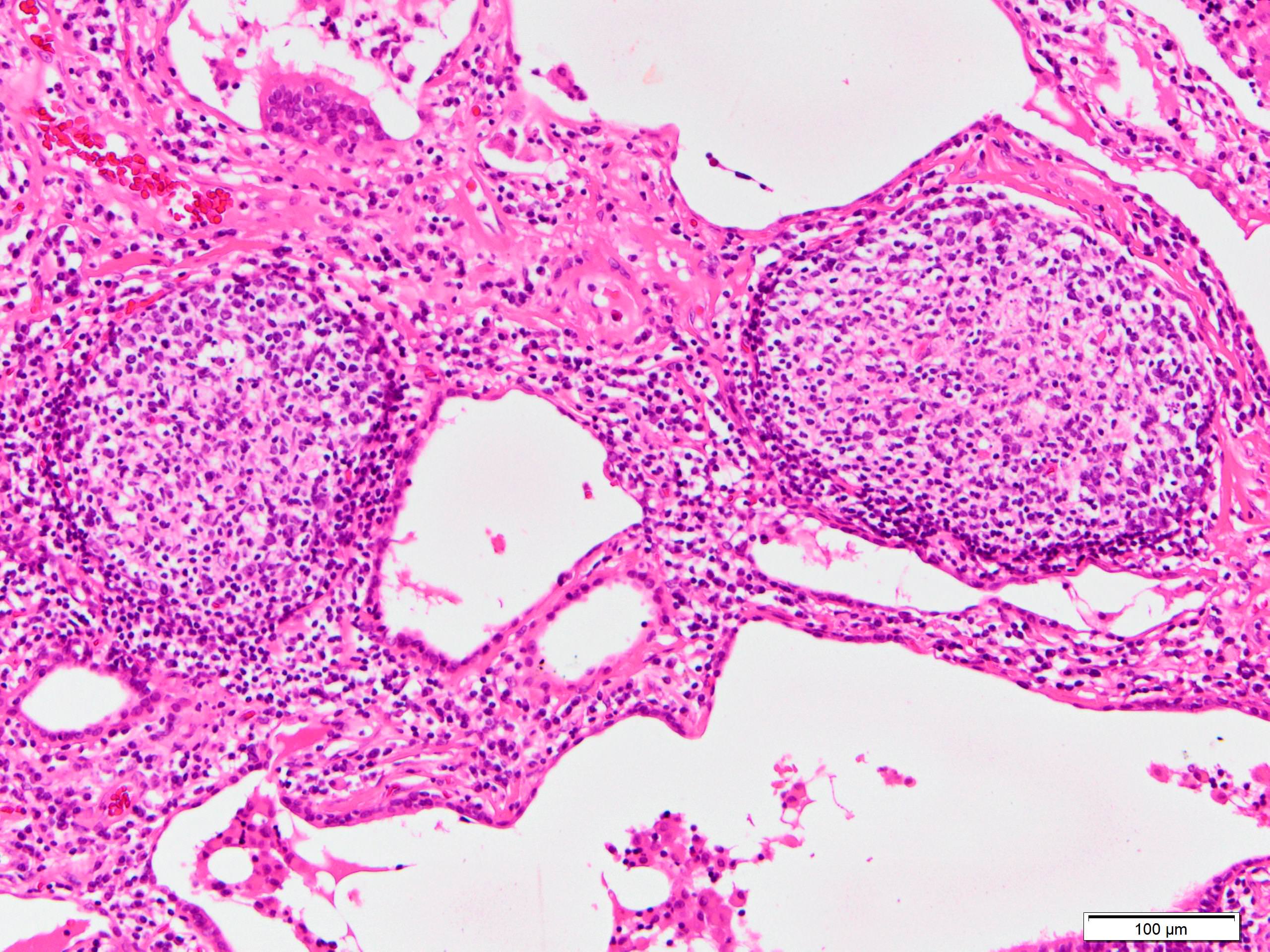
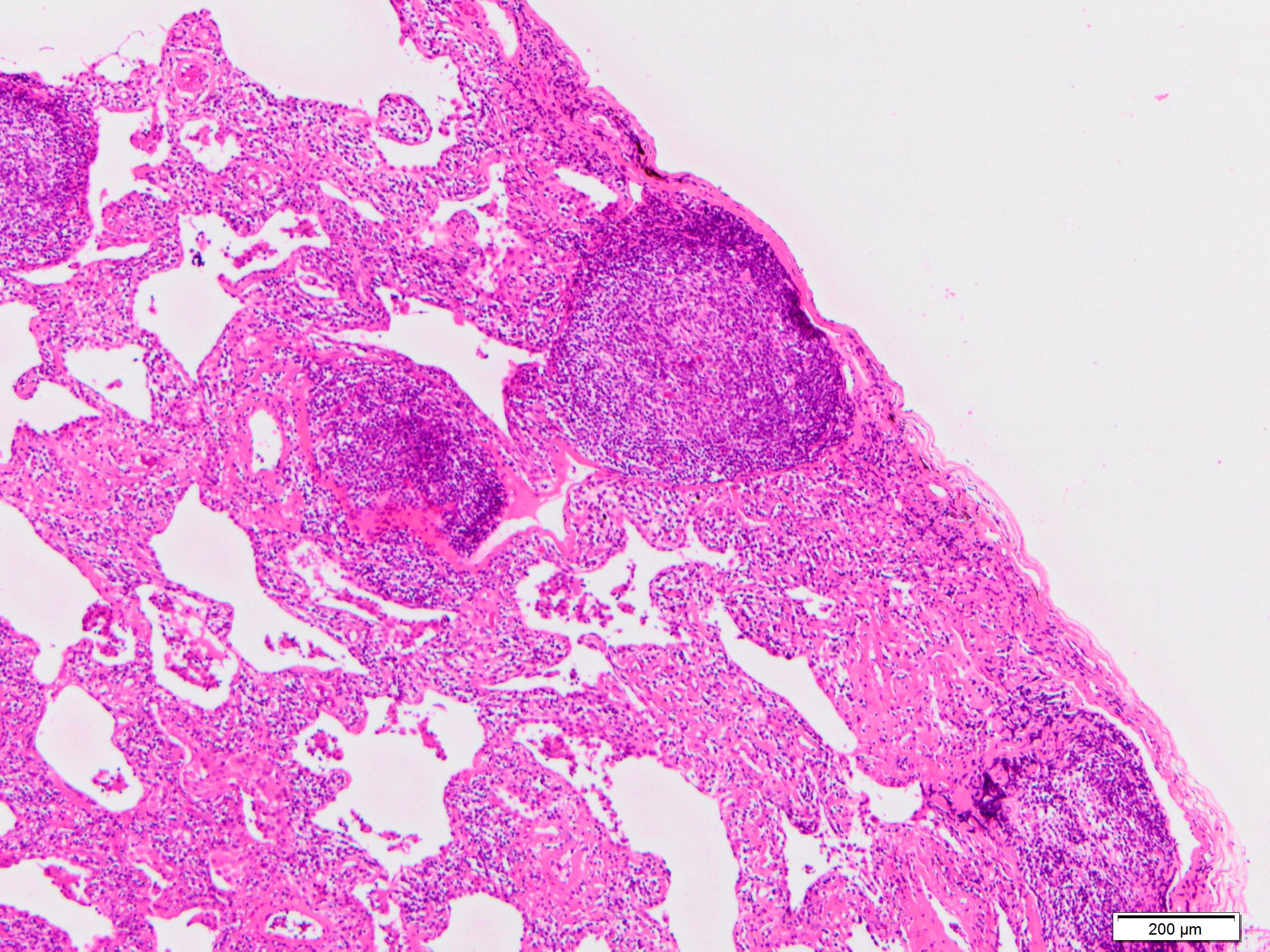
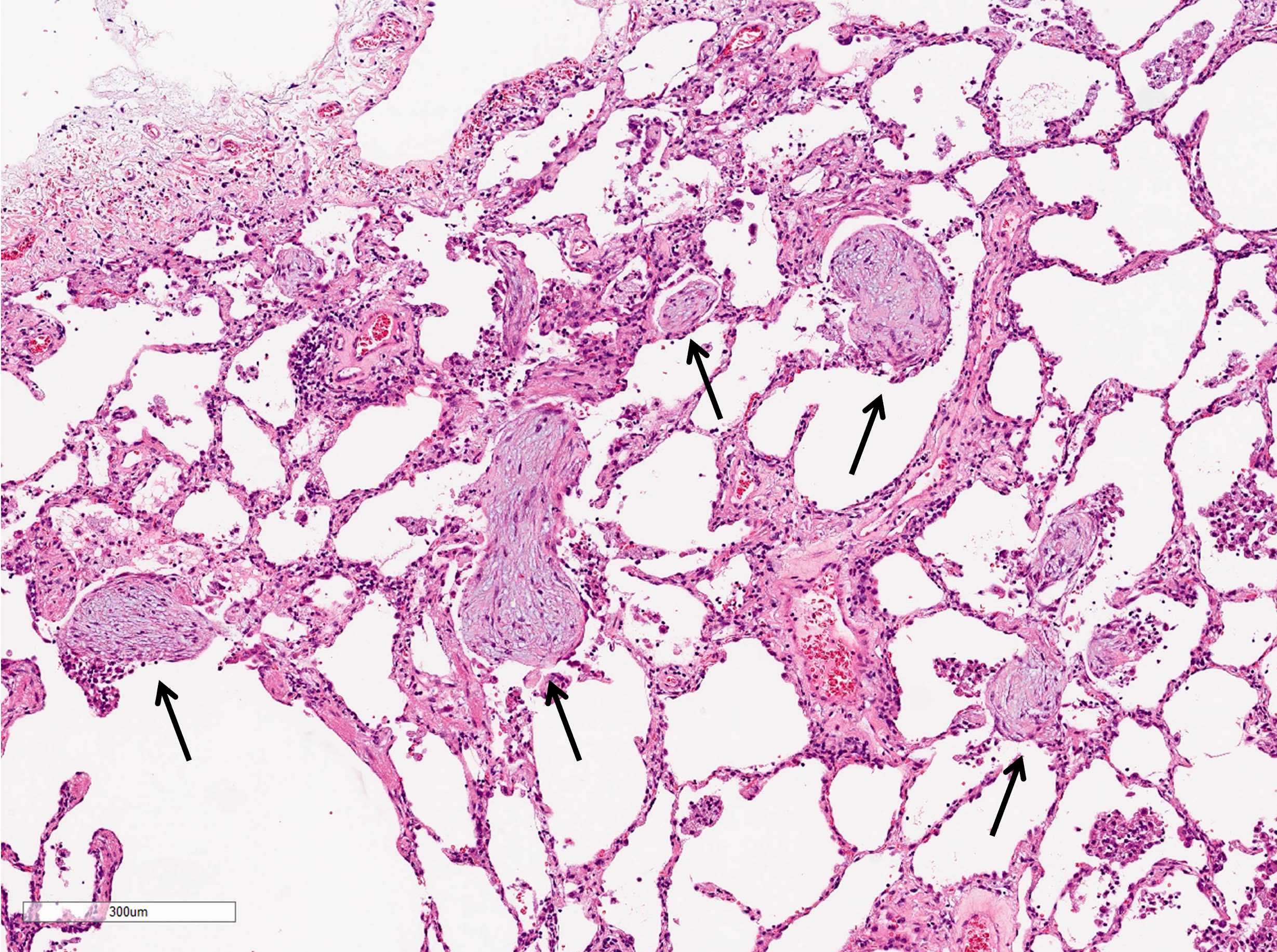
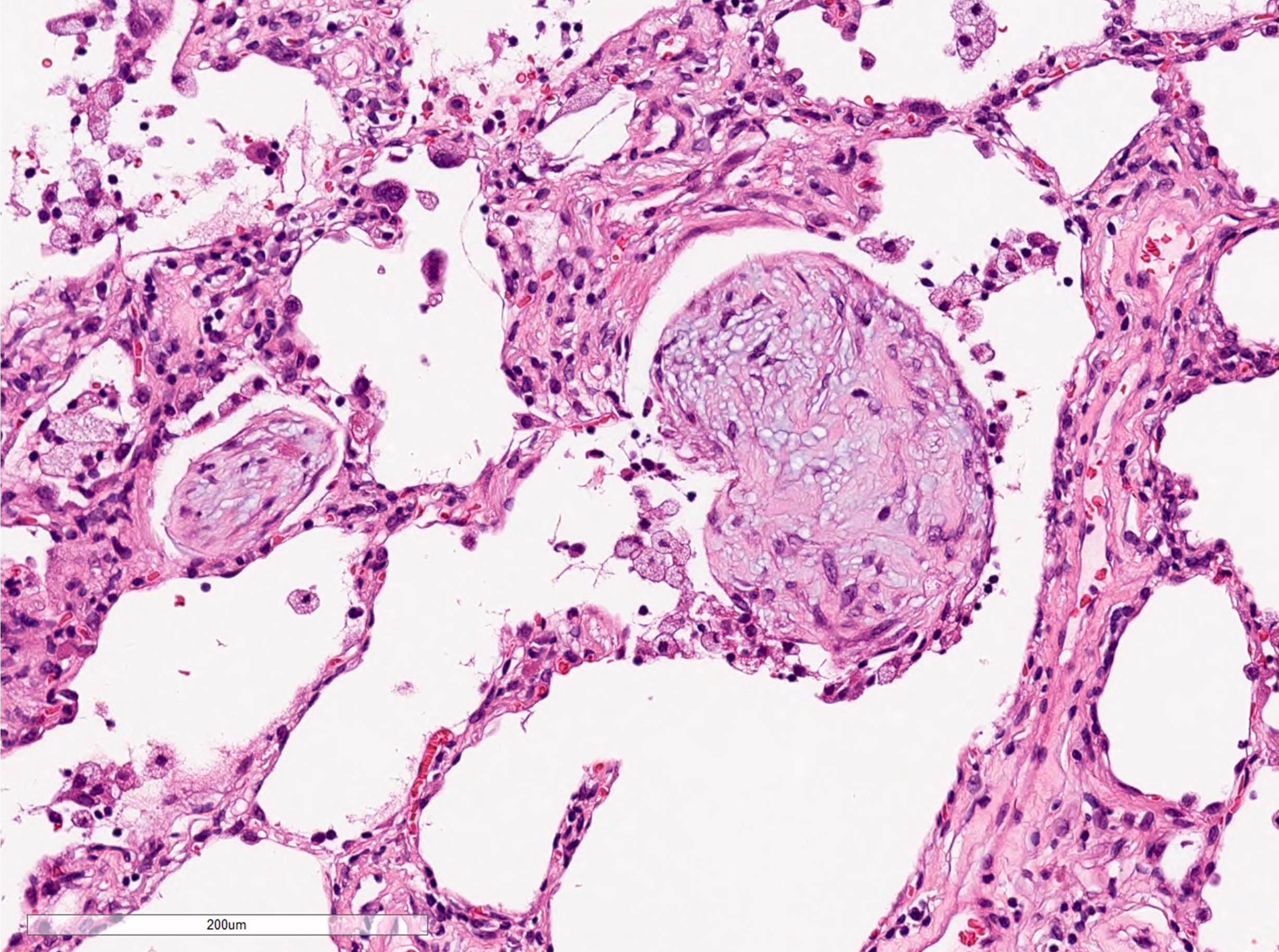
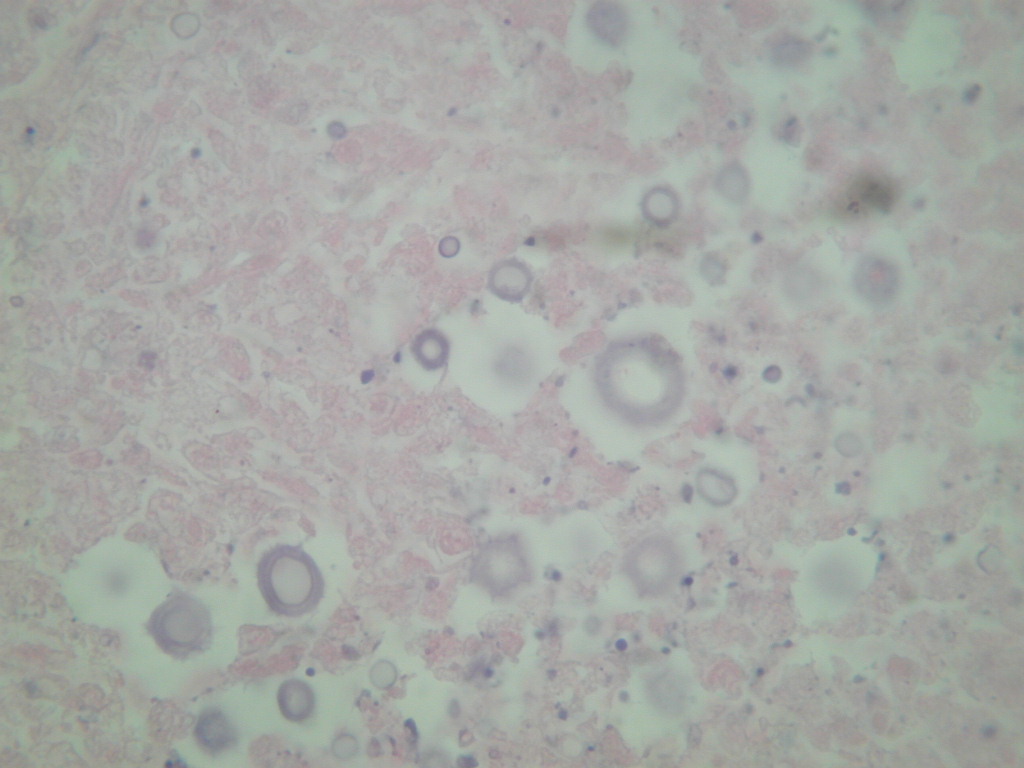
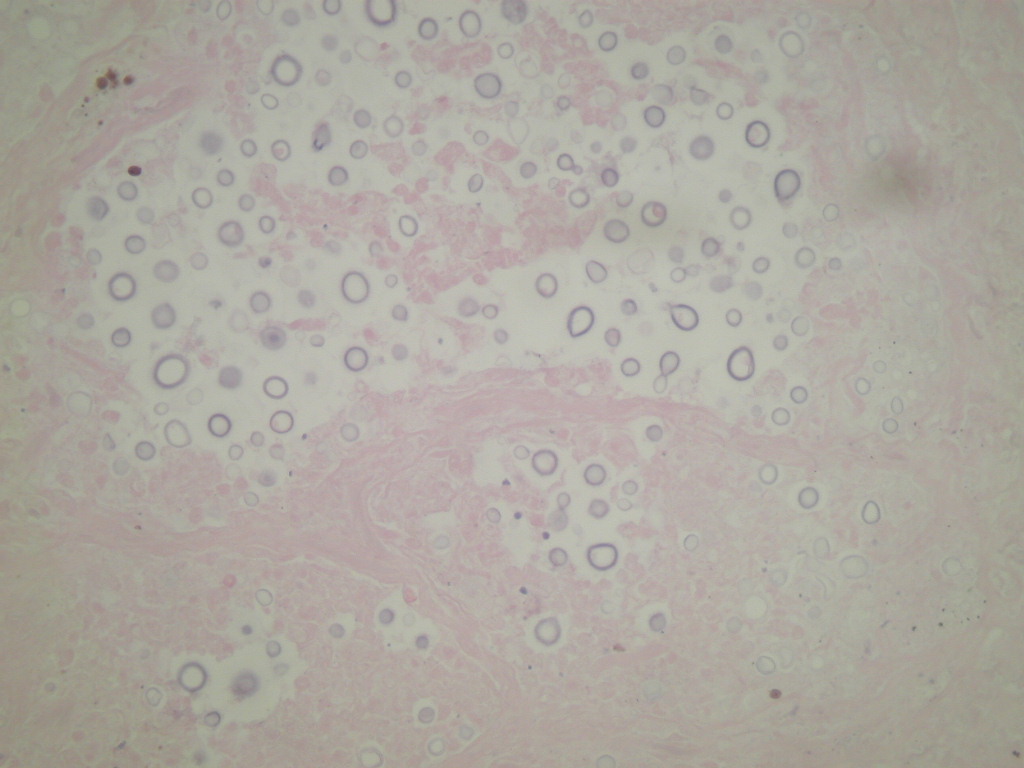
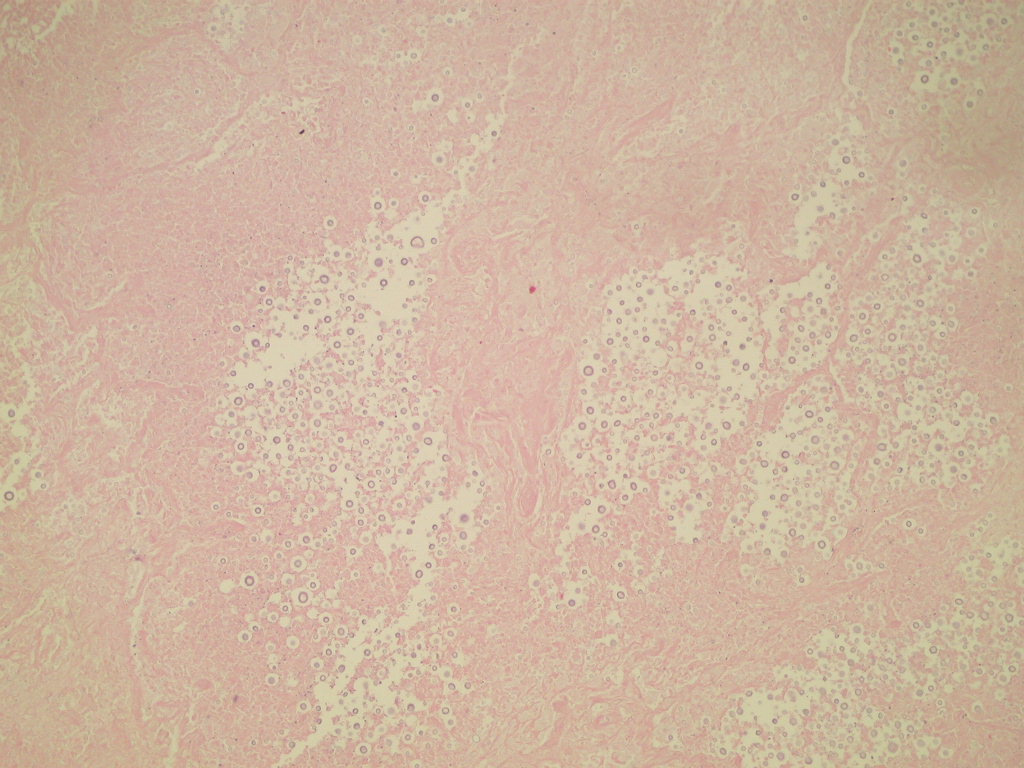
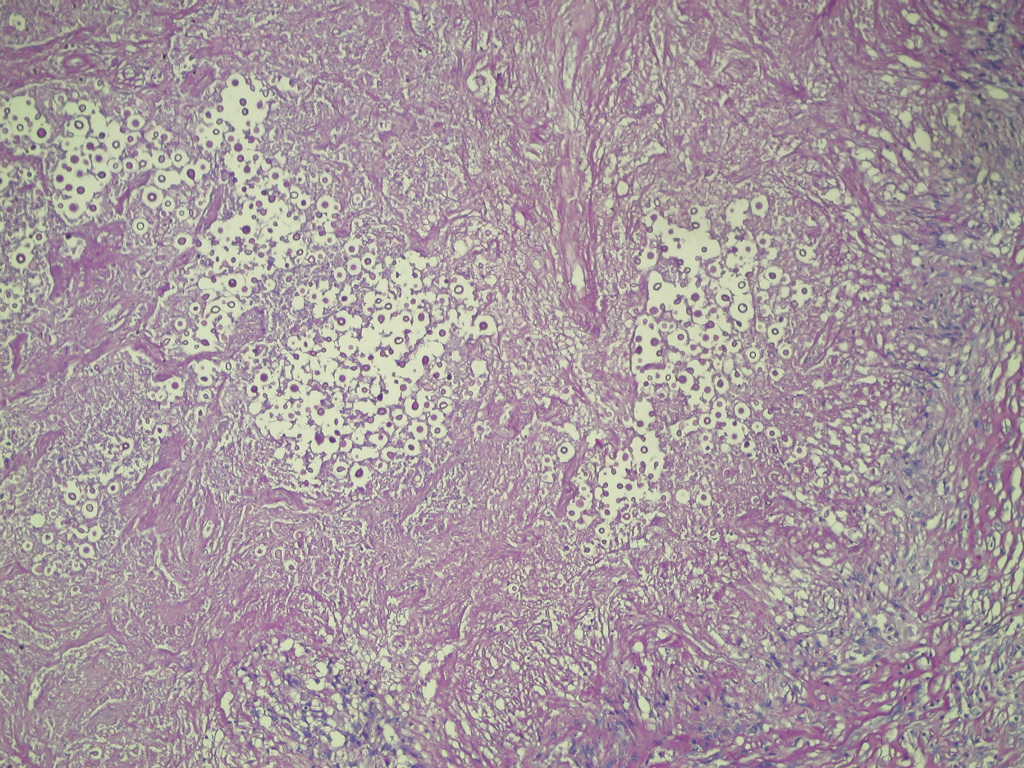
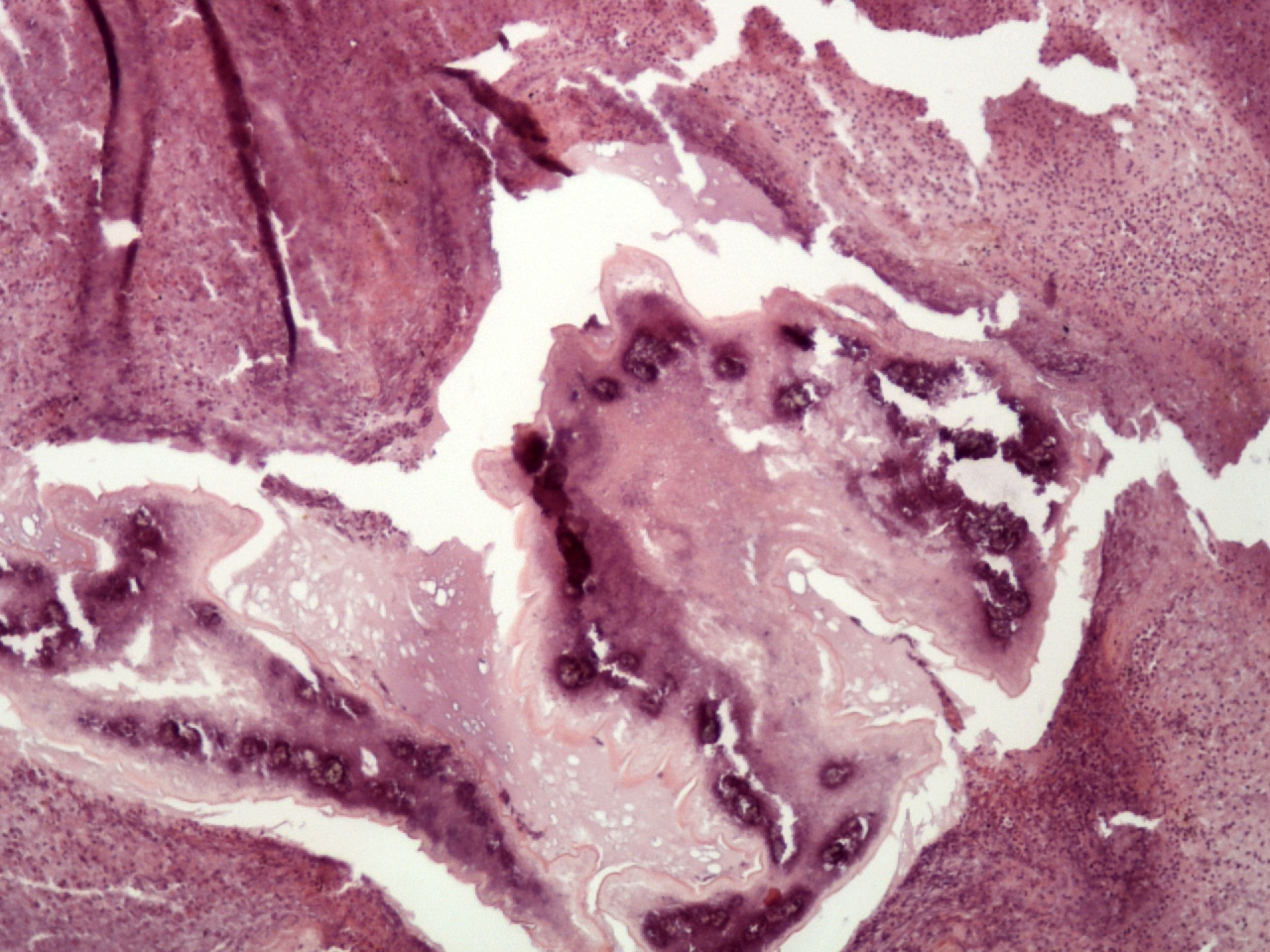
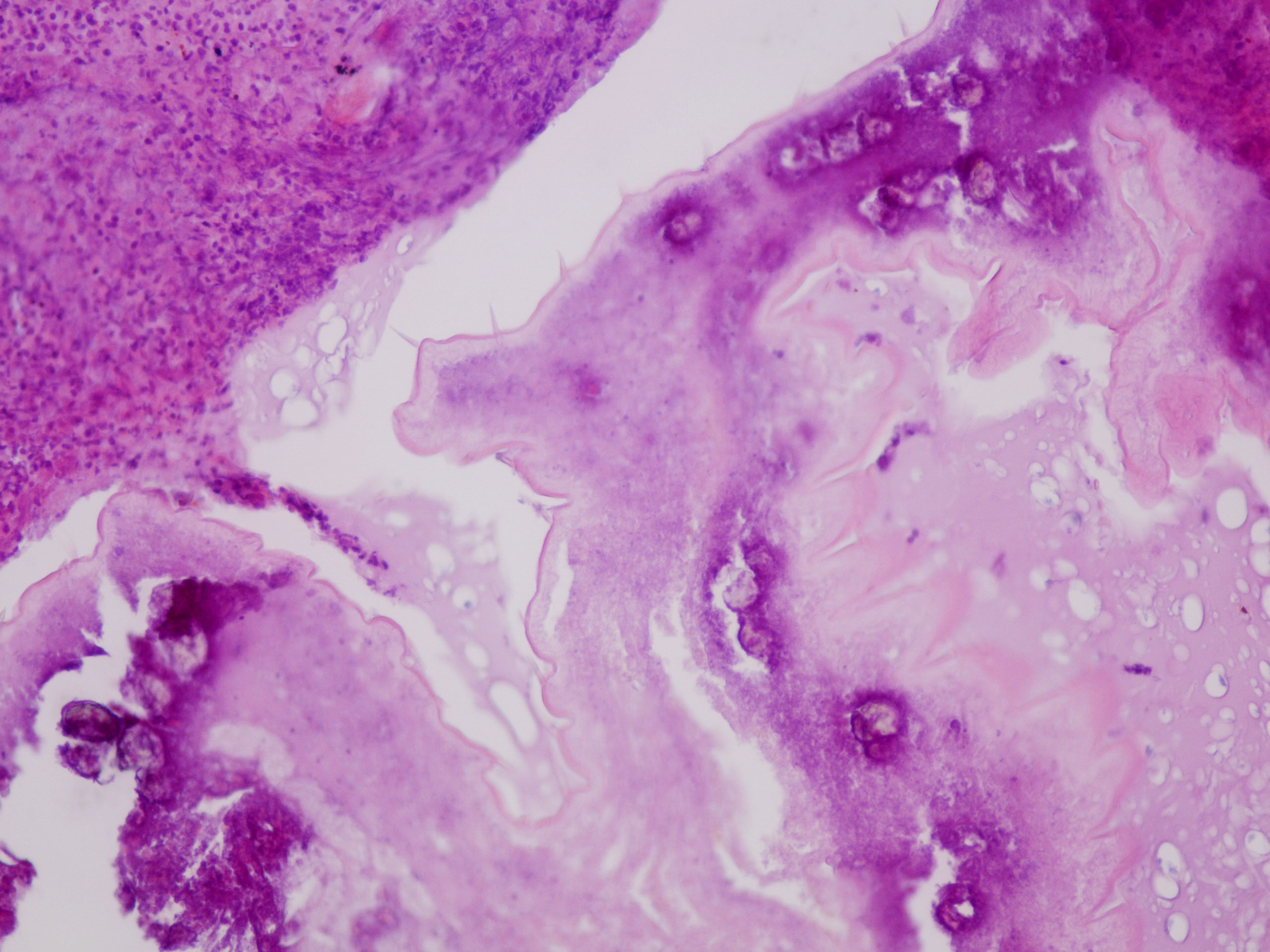
- Histologically, remarkable fibrin deposition (or "fibrin balls") along with plugs of organizing pneumonia in air spaces are characteristic
- Also called acute fibrinous organizing pneumonia
- Rare disease (no data on prevalence available so far)
- Mean age at onset is about 60 years old, with a wide age range (Arch Pathol Lab Med 2002;126:1064, J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701, Medicine (Baltimore) 2016;95:e4073)
- No gender predominance
- No association with smoking history
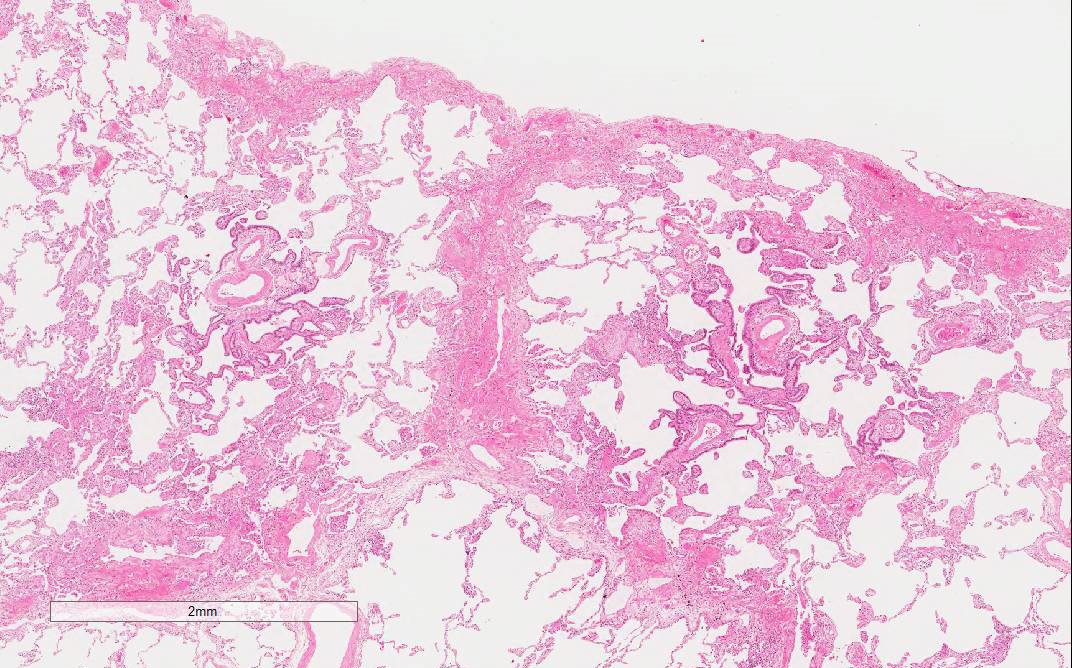
- Usually bilateral or sometimes unilateral lobes of the lung
- In the initial study, acute fibrinous and organizing pneumonia (AFOP) was described as a possible variant of diffuse alveolar damage because of its similar aggressive behavior and mortality rate (Arch Pathol Lab Med 2002;126:1064)
- However, recent studies and case reports have found that the clinical course and prognosis of AFOP is better and closer to that of organizing pneumonia (J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Nowadays, AFOP is considered a histological variant of organizing pneumonia or a different type of lung disease similar to organizing pneumonia, which sometimes follows an aggressive course
- Some idiopathic AFOP may be due to infection of undiagnosed bacteria
- Variety of possible causes and associated conditions have been reported (Arch Pathol Lab Med 2002;126:1064, J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701, Medicine (Baltimore) 2016;95:e4073):
- Idiopathic
- Infection: H. influenzae, A. baumannii, P. jirovecii, C. pneumoniae
- Autoimmune disease: polymyositis / dermatomyositis, ankylosing spondylitis, antisynthetase syndrome
- Particle exposure: animal antigens, coal dust, wood dust, hairspray
- Neoplasm: cancer, lymphoma, leukemia, myelodysplastic syndrome
- Immunosuppression: diabetes mellitus, long term corticosteroid therapy
- Drugs
- Hematopoietic stem cell transplantation (J Investig Med High Impact Case Rep 2016;4:2324709616643990)
- Lung transplantation
- Most patients present with mild to moderate subacute respiratory failure (J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Fever, fatigue and malaise
- Cough
- Dyspnea
- Sputum or sometimes hemoptysis
- Duration of symptoms before diagnosis is 1 - 4 weeks
- Some patients may follow fulminant course, need mechanical ventilation and die of the disease, similar to diffuse alveolar damage (Arch Pathol Lab Med 2002;126:1064, Medicine (Baltimore) 2016;95:e4073)
- Abnormal chest auscultation
- End inspiratory fine crackles in affected lobes
- Mild to moderate restrictive or obstructive pattern in pulmonary function tests (Chin Med J (Engl) 2015;128:2701)
- Decreased total lung capacity (TLC)
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- Based on clinical features, radiology and histology
- No unique clinical or radiological findings have been identified to date
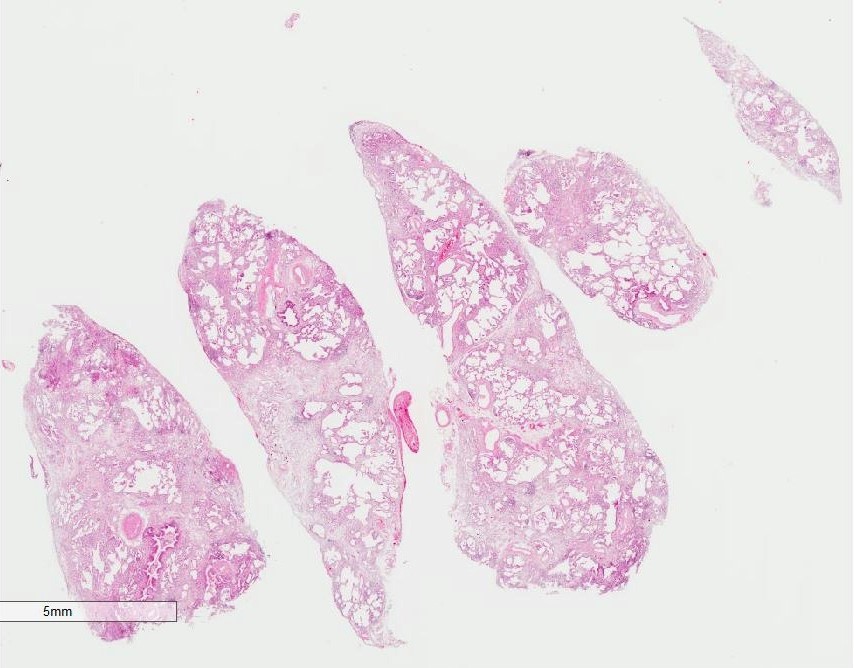
- Open chest lung biopsy is recommended
- Transbronchial lung biopsy or computed tomography guided needle lung biopsy may be diagnostic if clinical and radiological features are suggestive enough
- Acute fibrinous and organizing pneumonia can be a background pattern with other disease present
- If the specimen is too small and the main lesion is not included, acute fibrinous and organizing pneumonia can be underdiagnosed (Int J Clin Exp Pathol 2014;7:4493)
- Increased C reactive protein
- Increased serum surfactant proteins A and D
- Increased serum ferritin may predict prognosis
- Occasional positive sputum bacterial culture
- Negative serum antibodies of connective tissue diseases and hypersensitivity pneumonitis
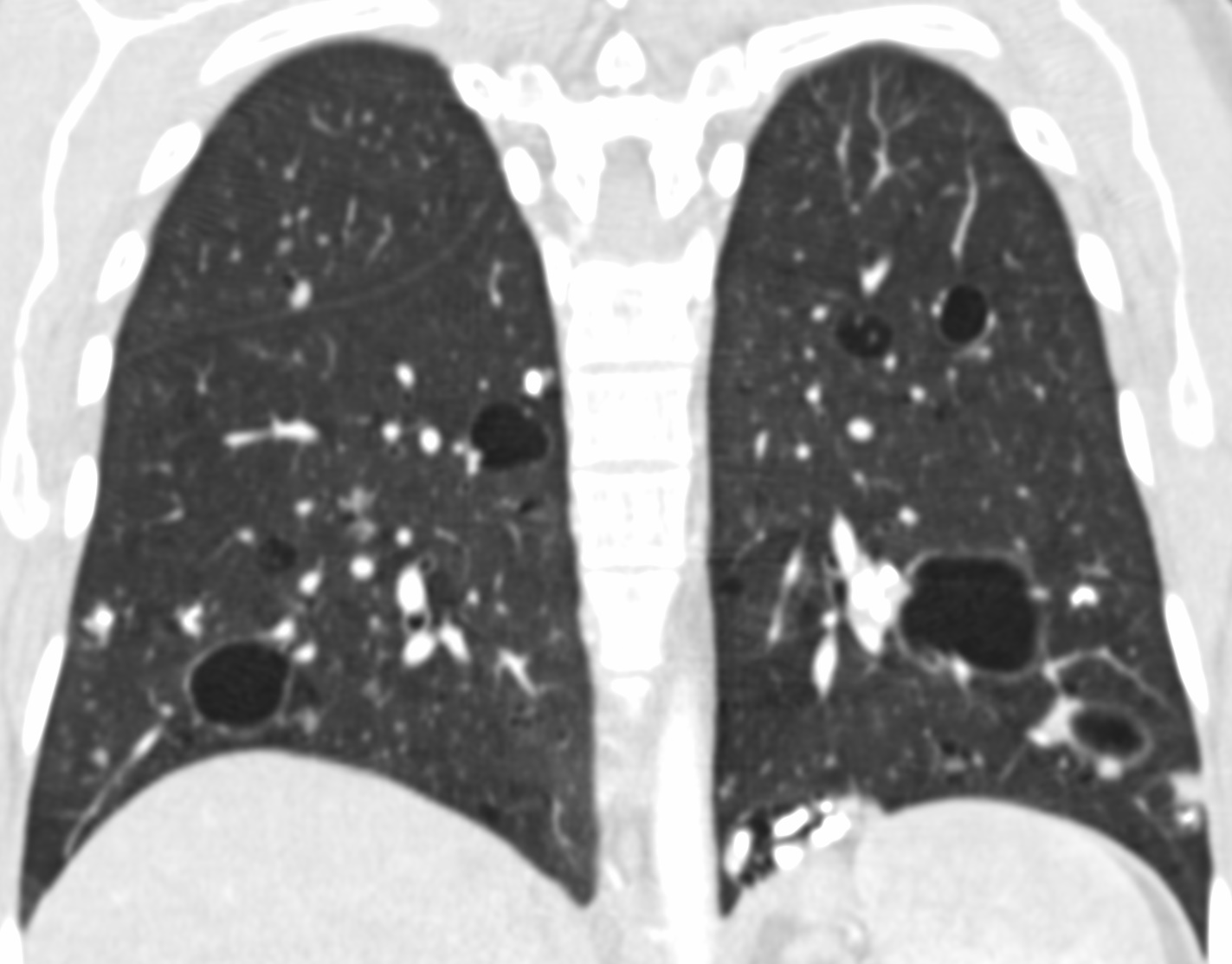
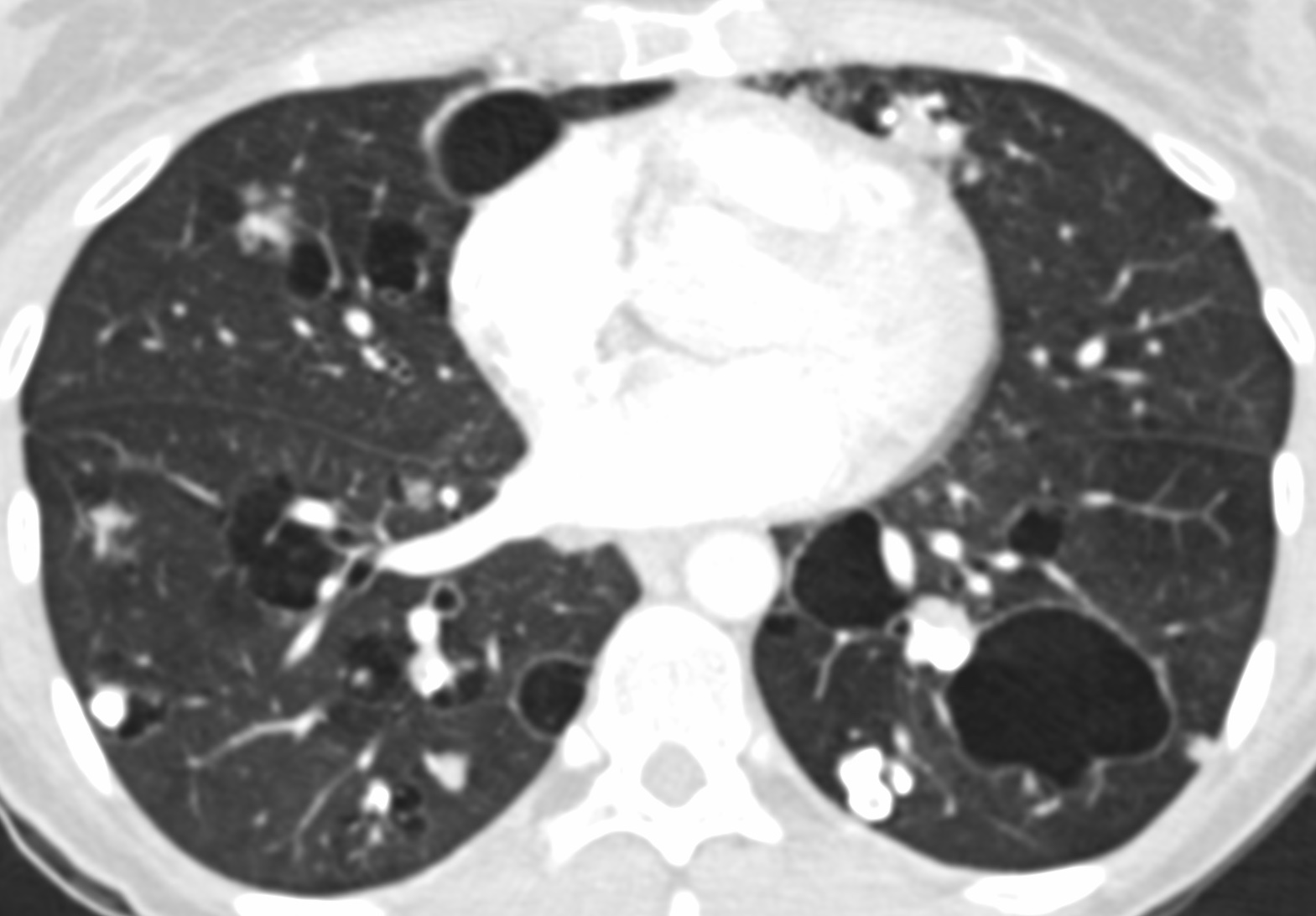
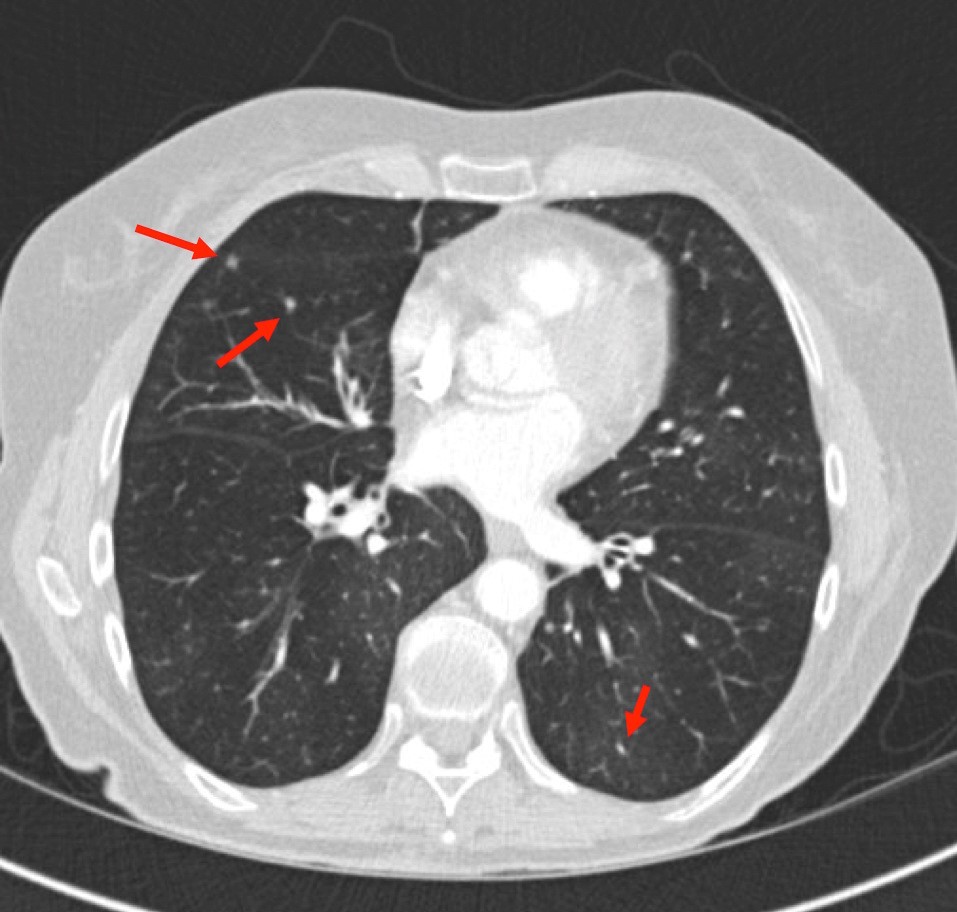
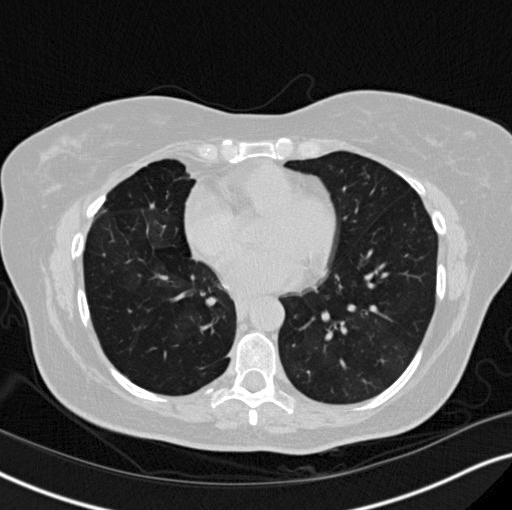
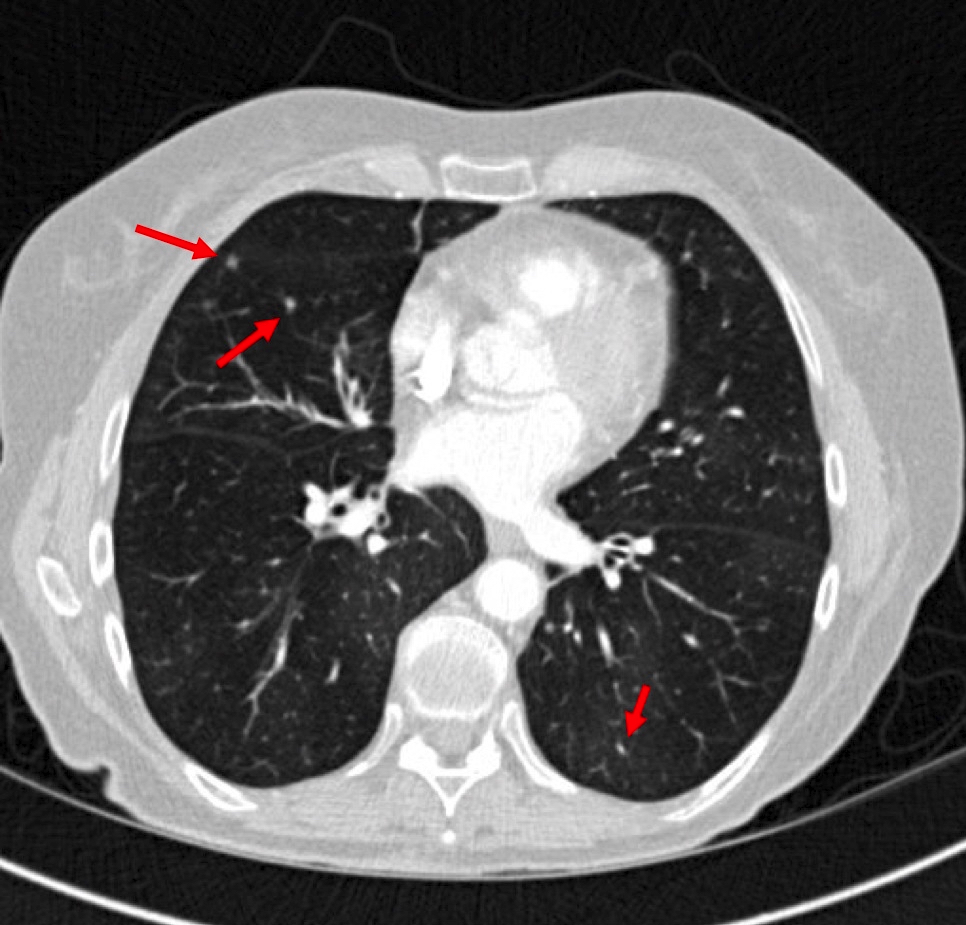
- Simple chest radiography
- Bilateral or unilateral ground glass opacity and consolidation
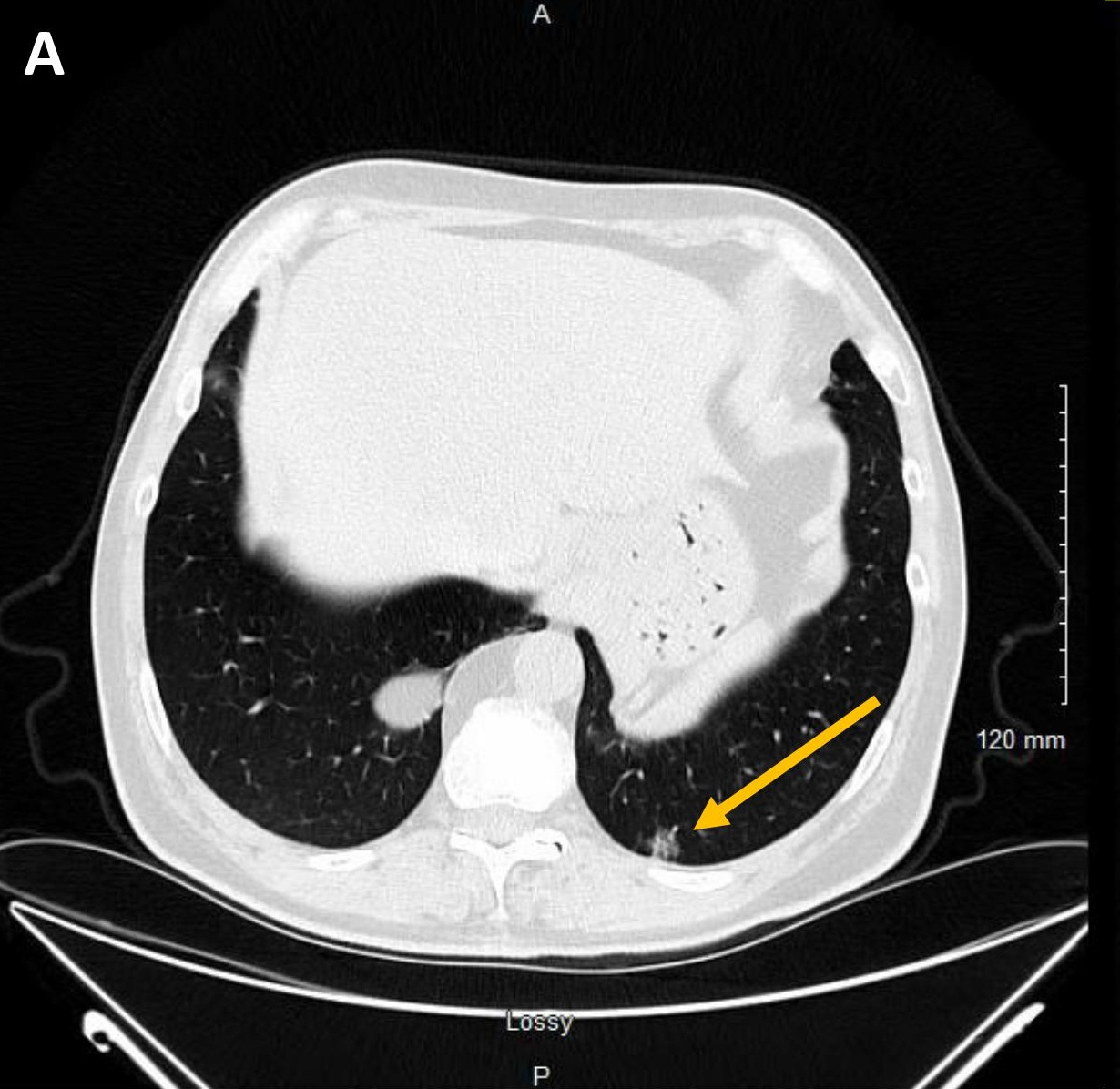
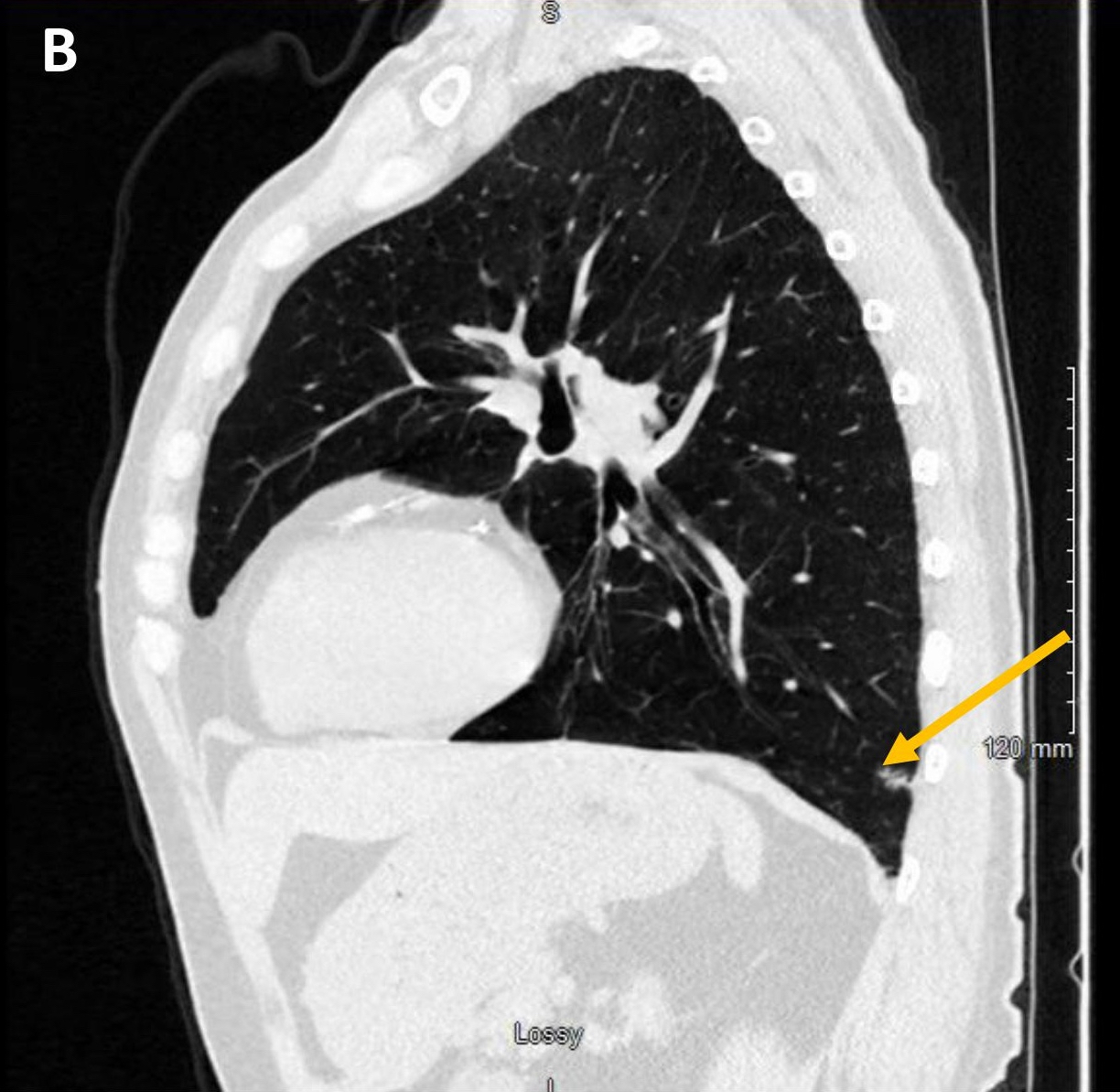
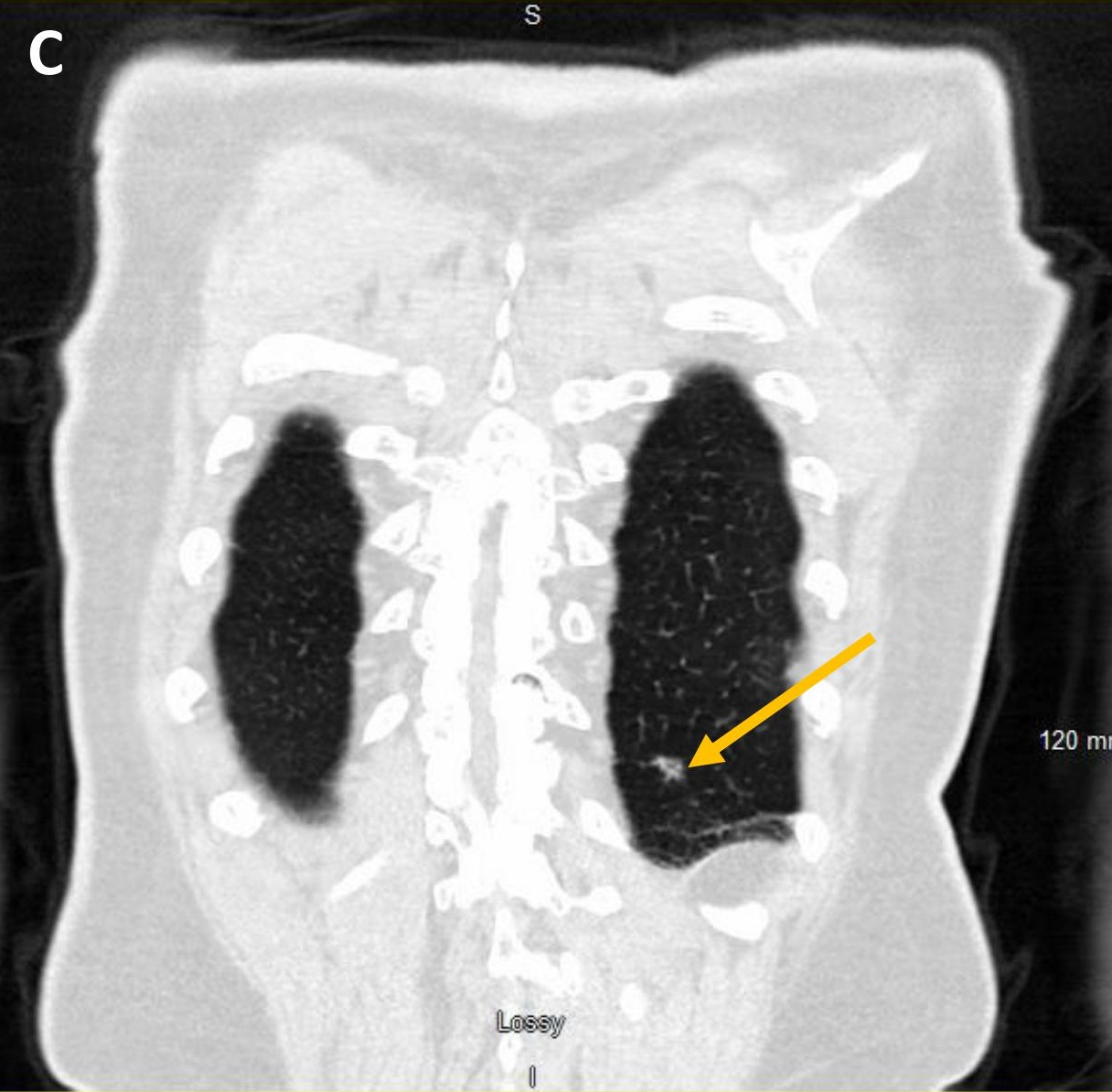
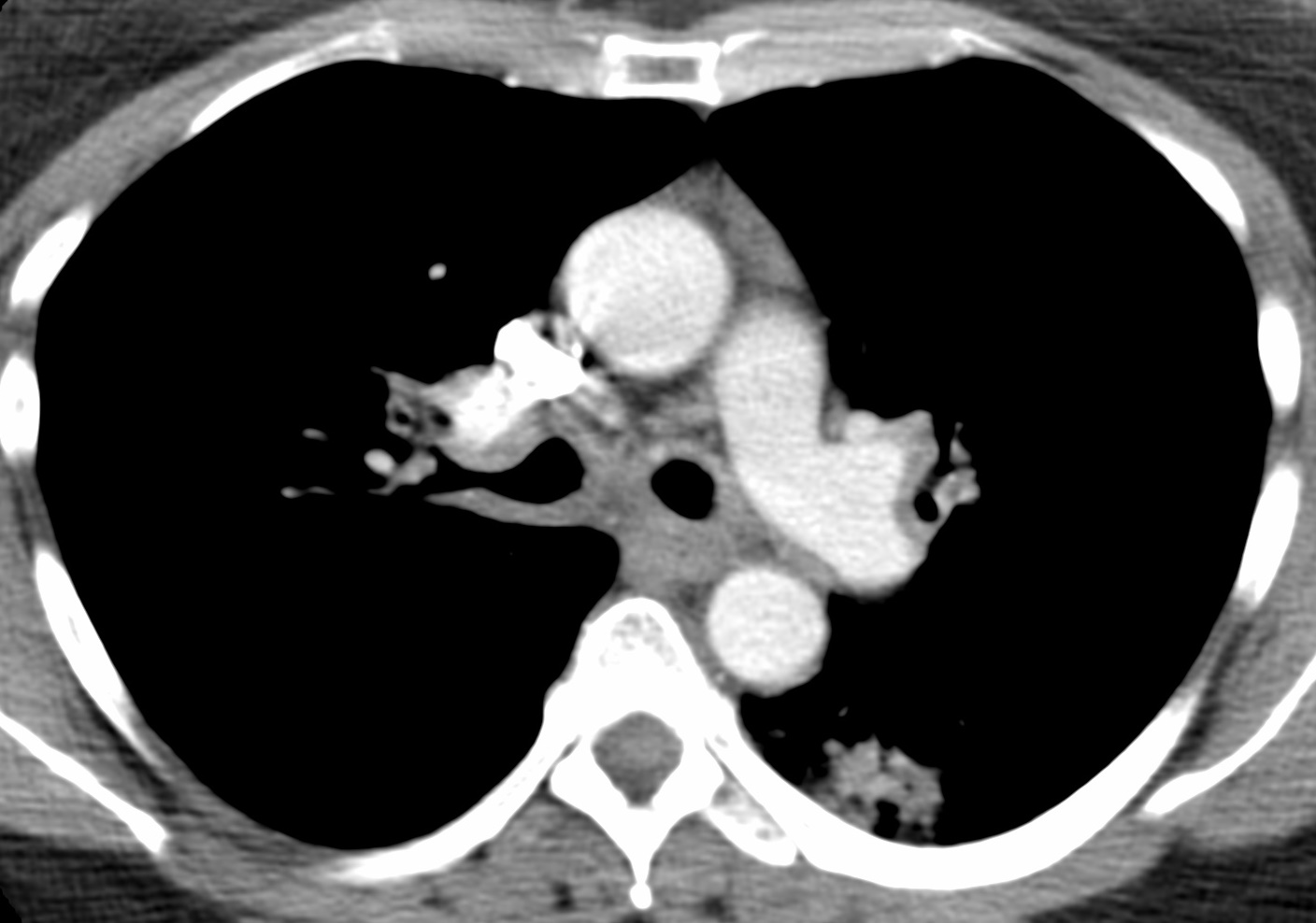
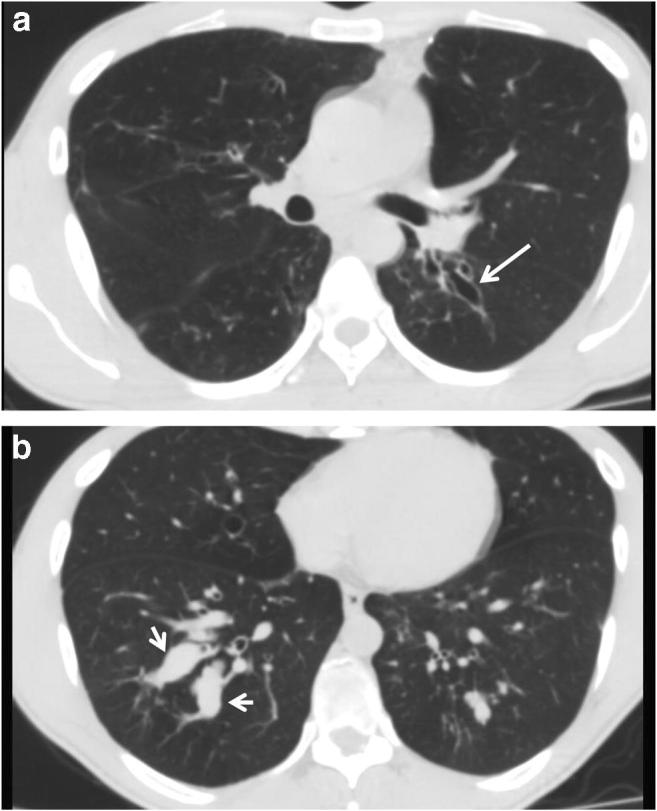
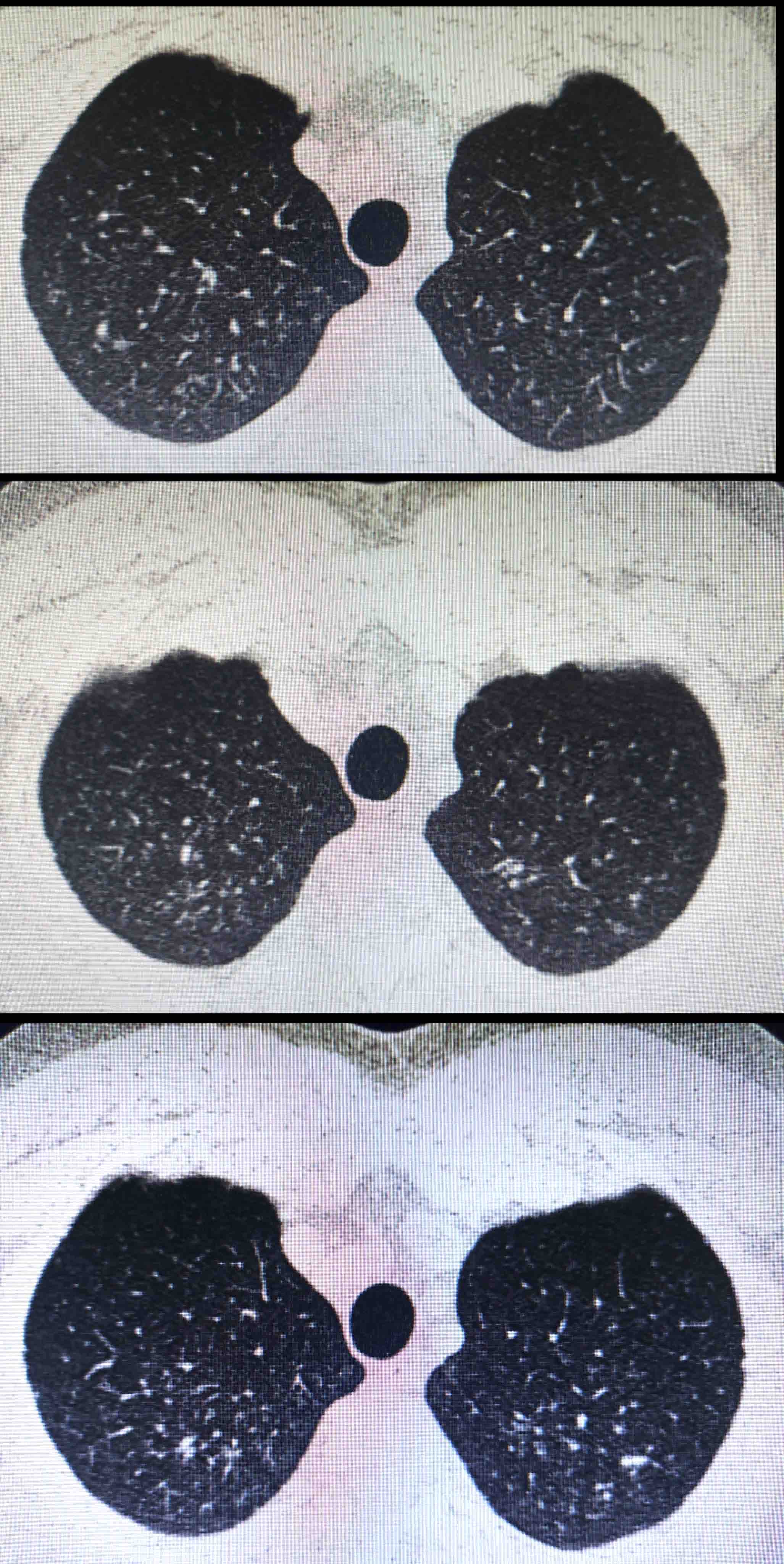
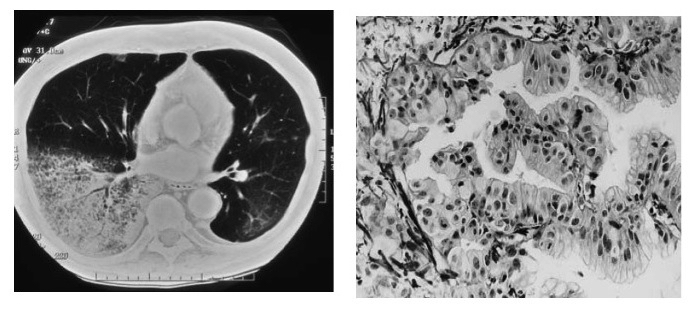
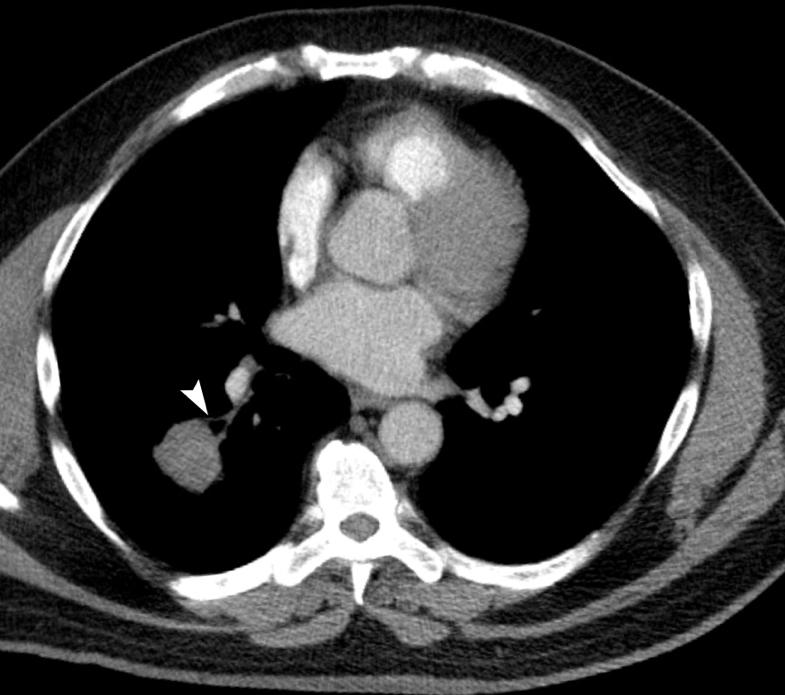
- High resolution computed tomography (Radiographics 2013;33:1951):
- Variable images, similar to organizing pneumonia
- Typically, patchy mixture of ground glass opacity and consolidation
- Size varies from a few centimeters to a whole lobe
- Rapidly progressive variant may show bilateral diffuse opacity, similar to diffuse alveolar damage
- Variable images, similar to organizing pneumonia
- Most cases achieve remission with treatment (J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Some patients die of rapidly progressive disease (Arch Pathol Lab Med 2002;126:1064, Medicine (Baltimore) 2016;95:e4073)
- Idiopathic acute fibrinous and organizing pneumonia (AFOP):
- 42 year old woman with AFOP in whole lobes (Indian J Crit Care Med 2016;20:245)
- 45 year old man with flu-like symptoms (Ann Saudi Med 2013;33:301)
- 46 year old man with rapidly progressive respiratory failure (Curr Probl Diagn Radiol 2015;44:469)
- 68 year old woman with AFOP mimicking pneumonia (BMC Res Notes 2015;8:38)
- 22 year old man who presented with AFOP after lung transplantation and underwent retransplantation (Transplant Proc 2015;47:182)
- 39 year old woman with AFOP associated with undifferentiated connective tissue disease (Case Rep Rheumatol 2012;2012:549298)
- 48 year old woman with AFOP after lung transplantation and good response to corticosteroid pulse therapy (Transplant Proc 2015;47:836)
- 62 year old man with AFOP associated with myelodysplastic syndrome (Intern Med 2016;55:3155)
- 66 year old woman died of AFOP associated with influenza A / H1N1 after lung transplantation (BMC Pulm Med 2013;13:30)
- 68 year old man with AFOP induced by nivolumab (Intern Med 2017;56:2311)
- 78 year old man with AFOP associated with amiodarone (Am J Respir Crit Care Med 2015;191:104)
- In general, corticosteroid pulse therapy with / without cyclophosphamide improves the symptoms and prognosis (Arch Pathol Lab Med 2002;126:1064, J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Treatment for underlying cause is also important for secondary acute fibrinous and organizing pneumonia
- Antibiotics are effective for acute fibrinous and organizing pneumonia induced by bacterial infection
- It is questionable if antibiotics can be a general therapeutic choice or not
- Mechanical ventilation may be necessary for aggressive type
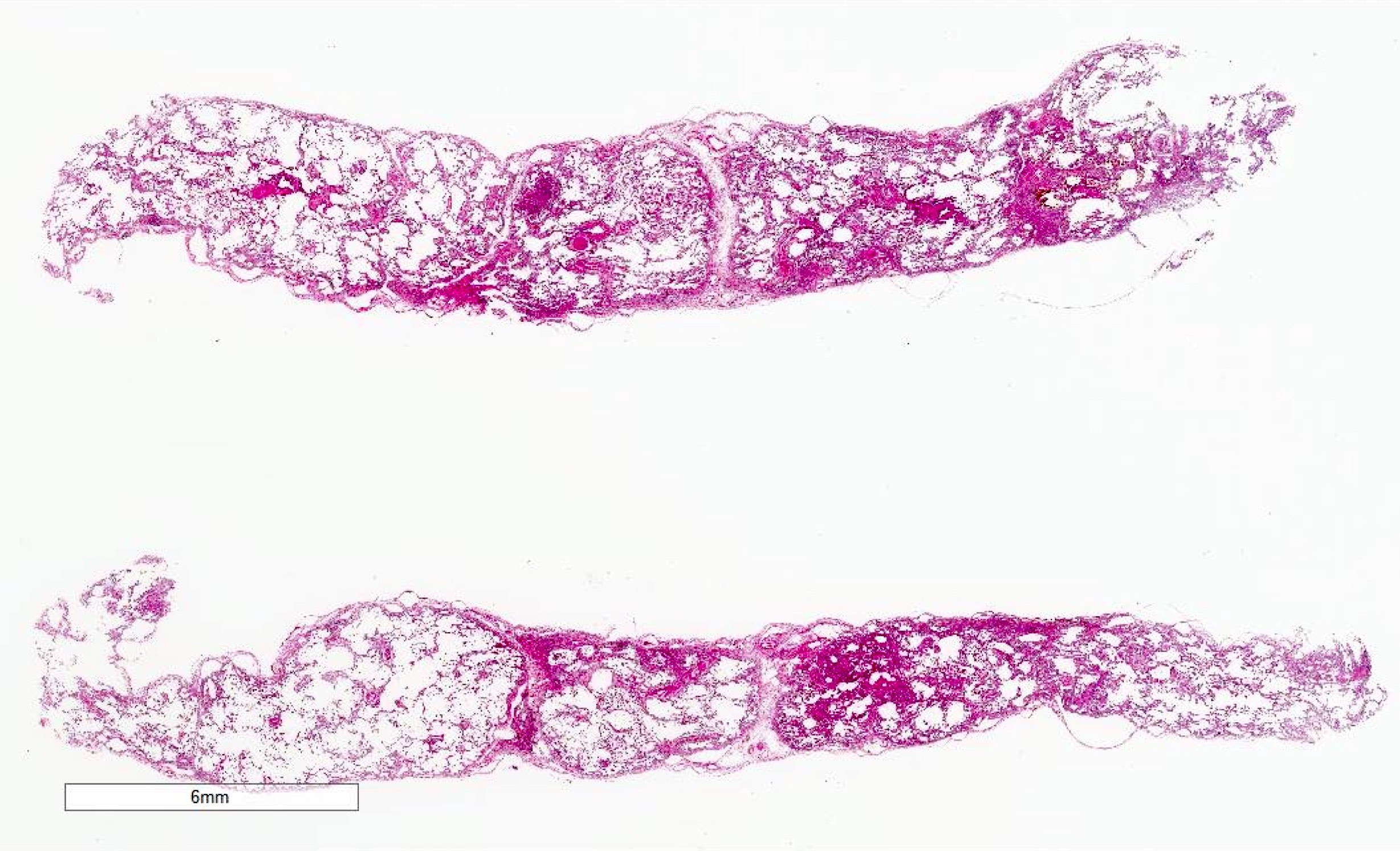
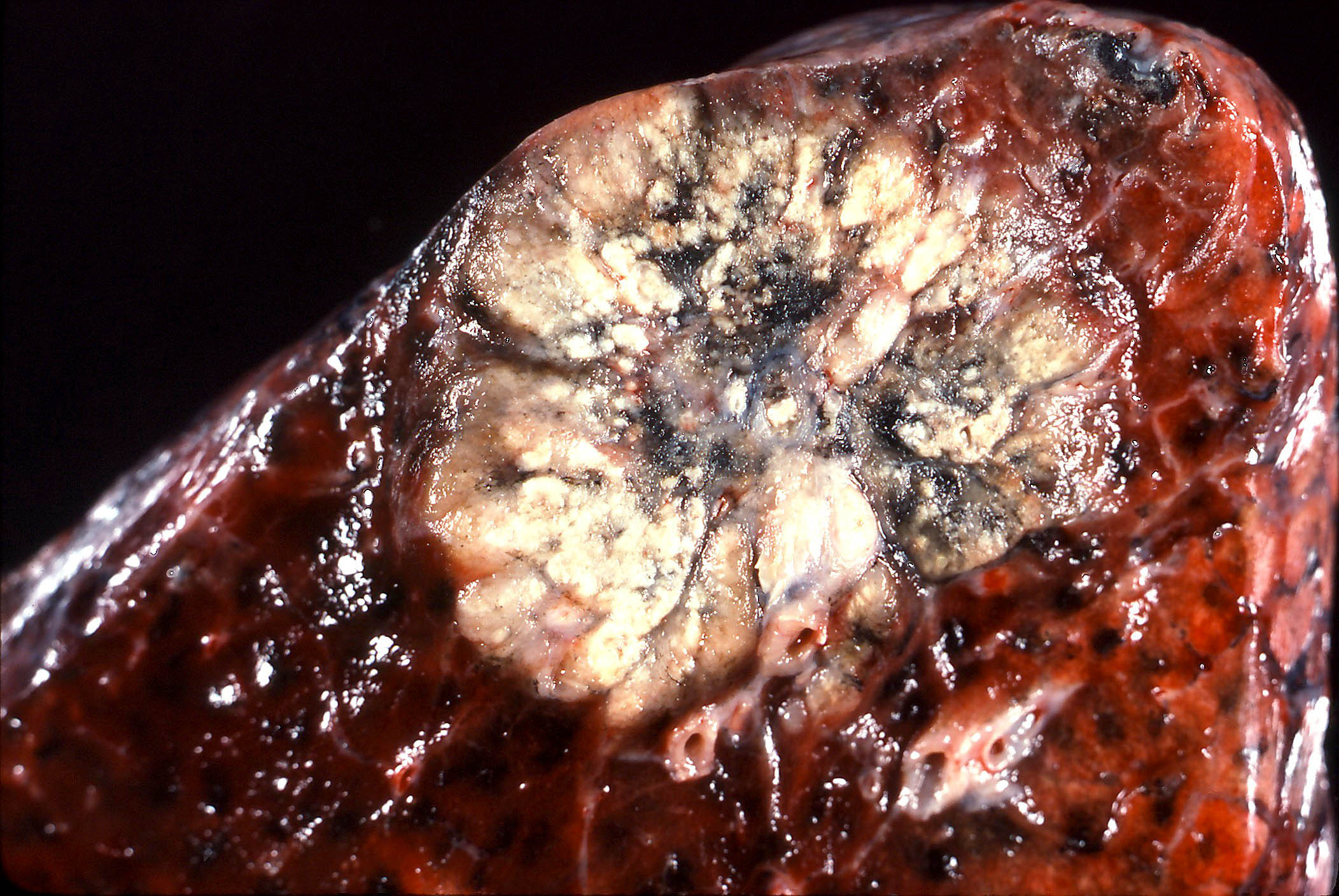
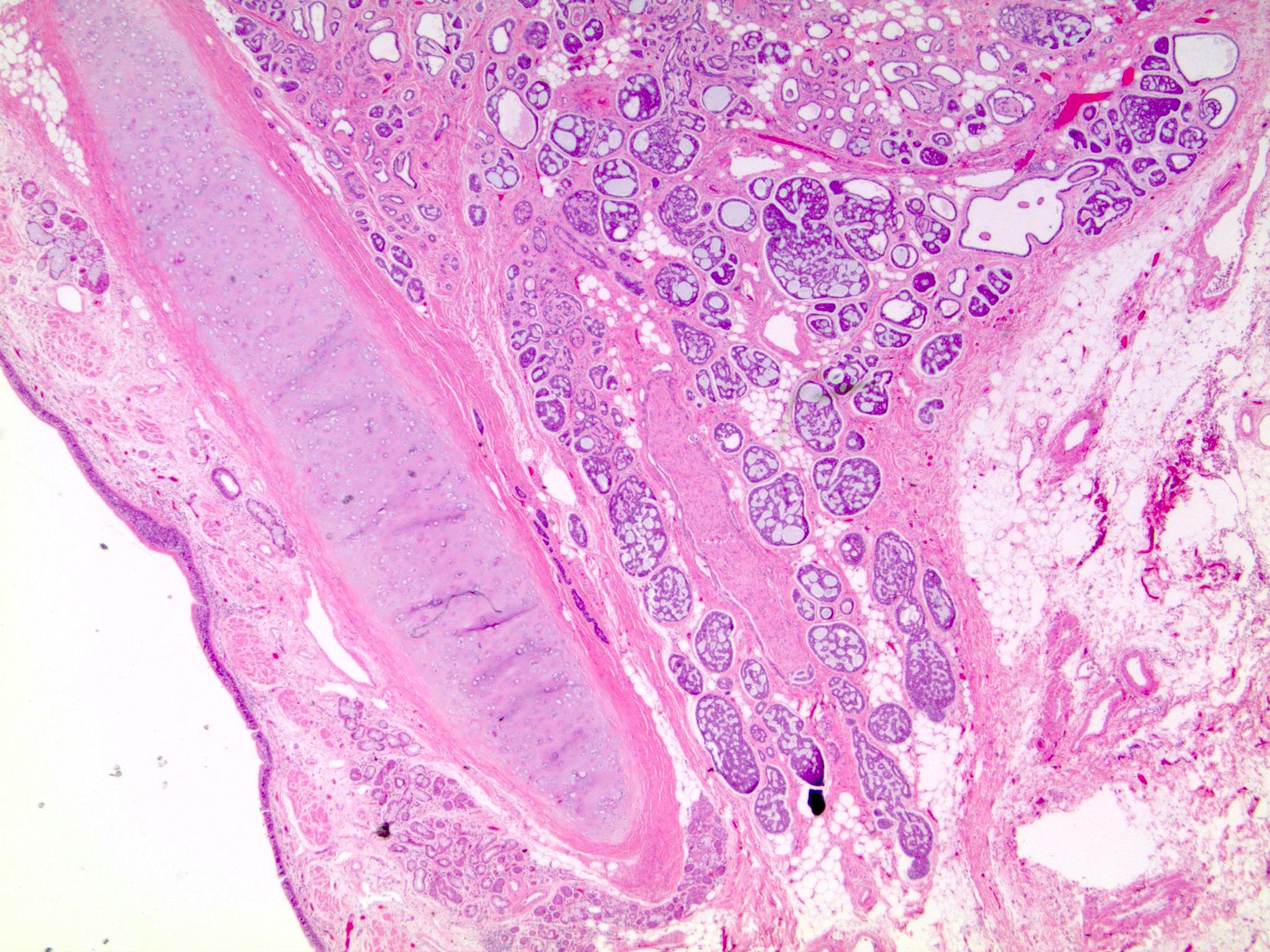
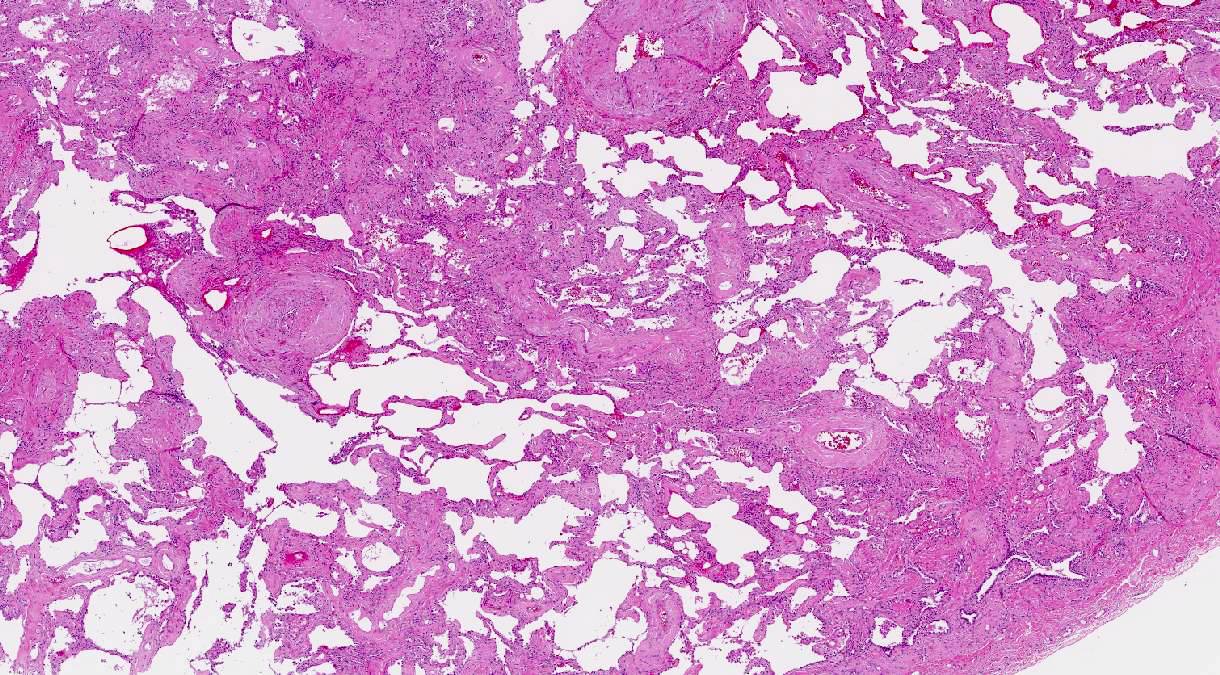
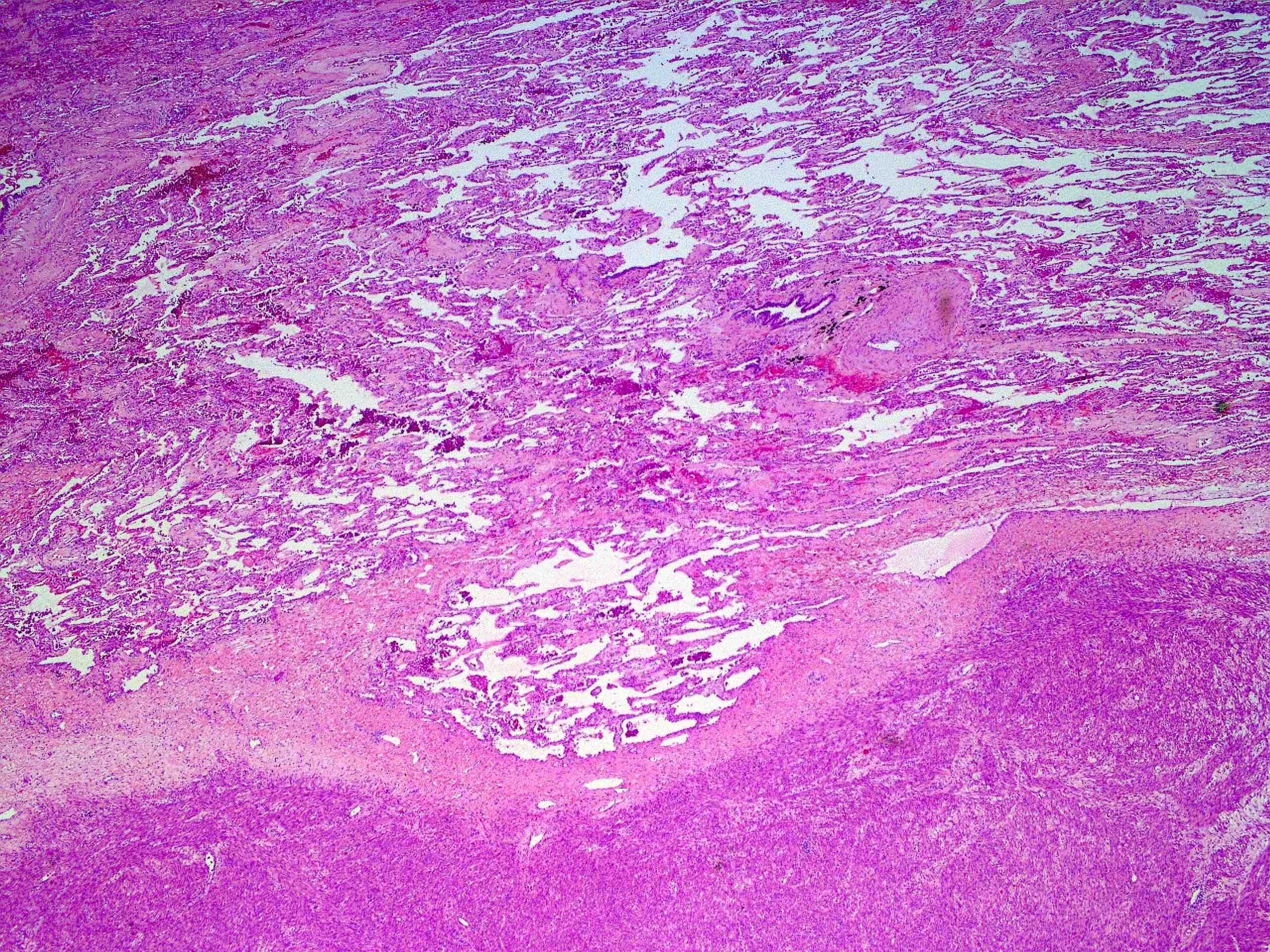
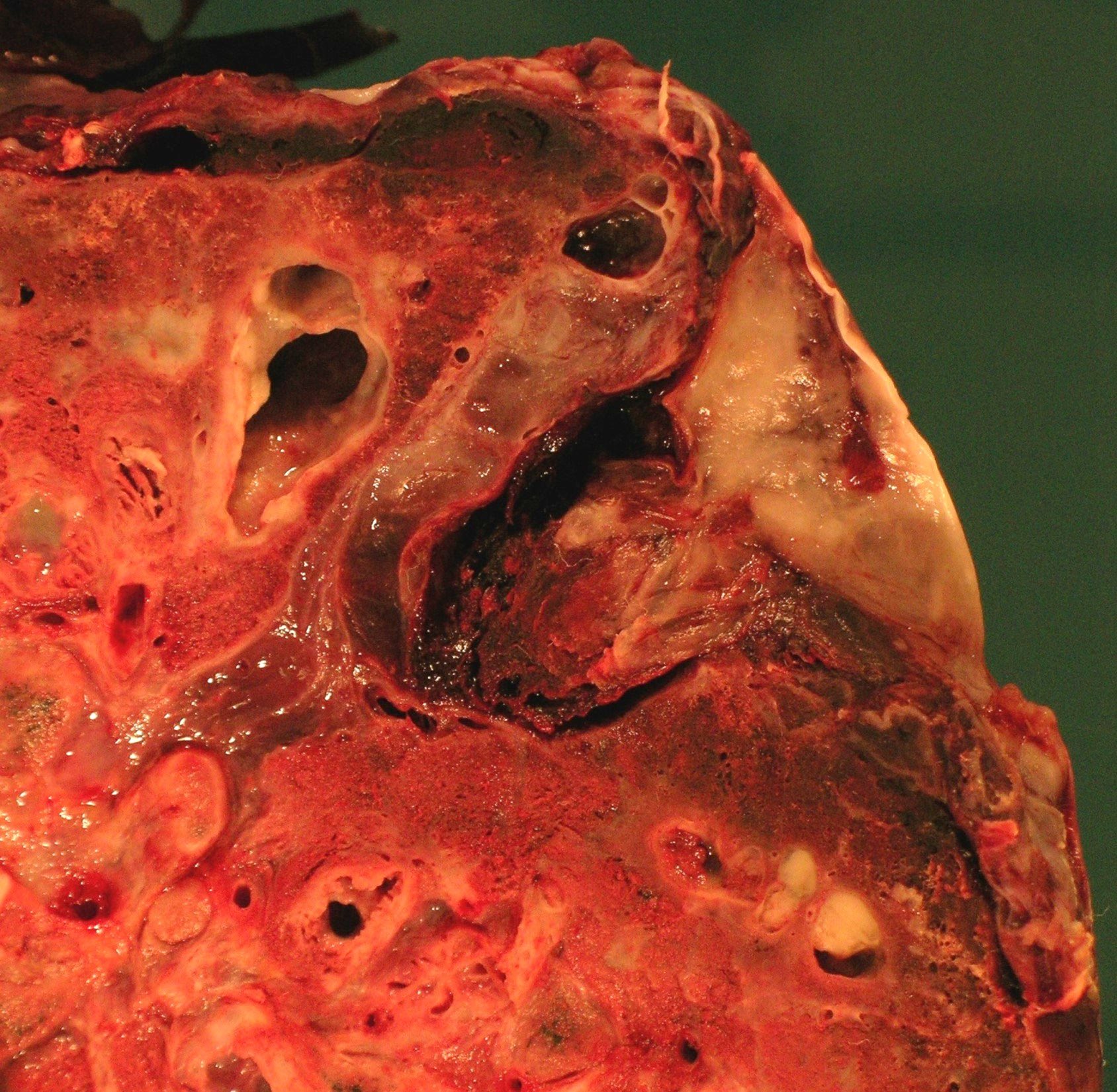
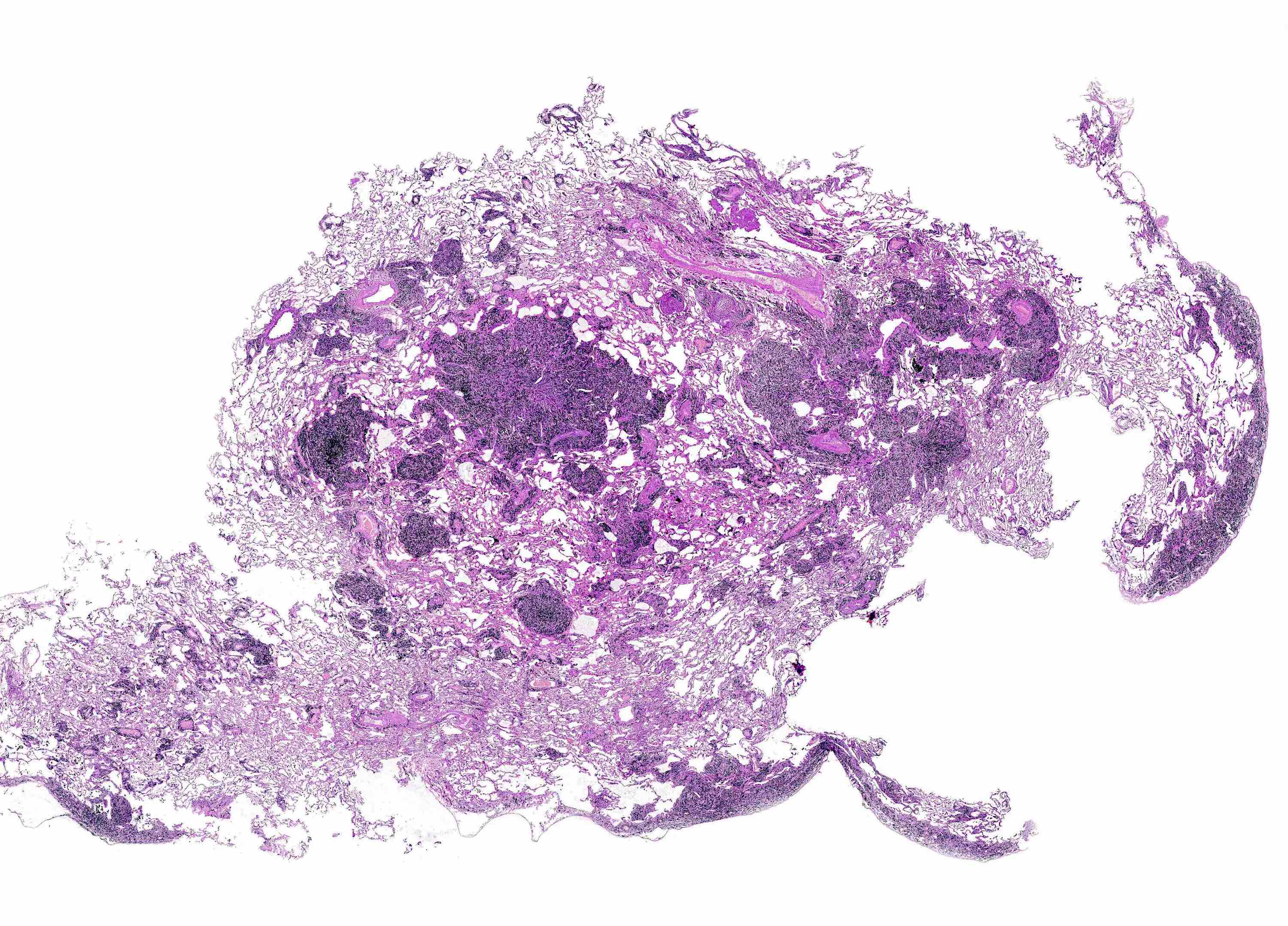
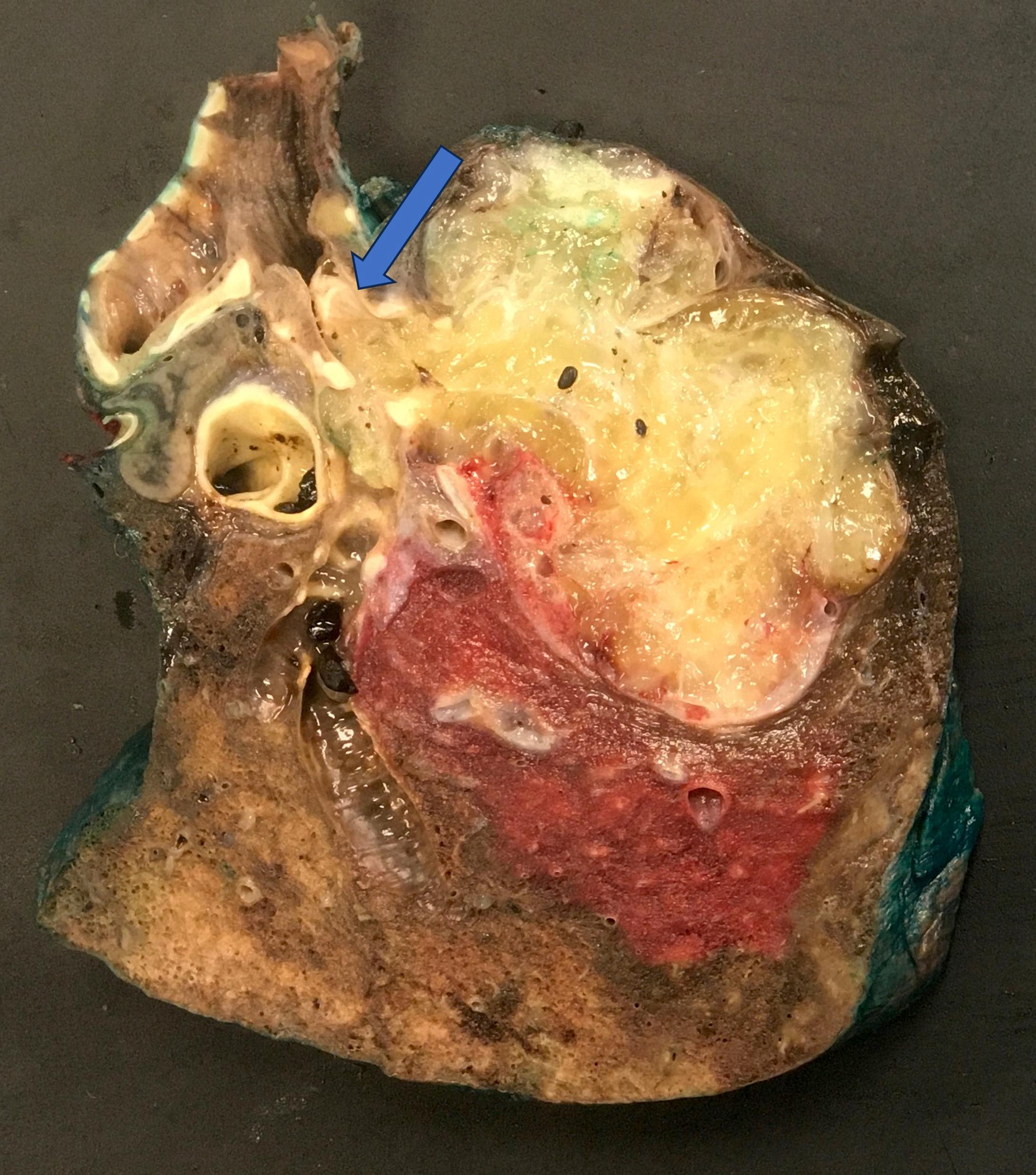
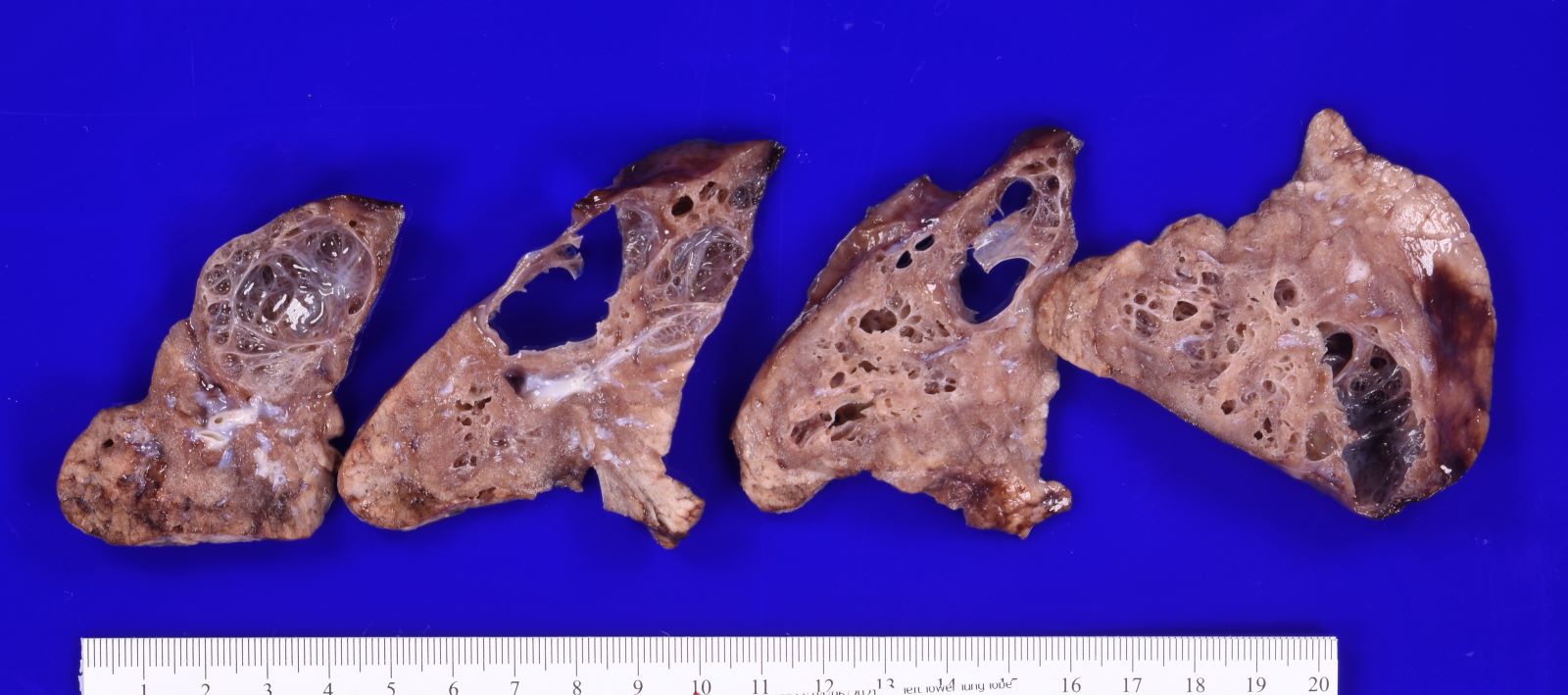
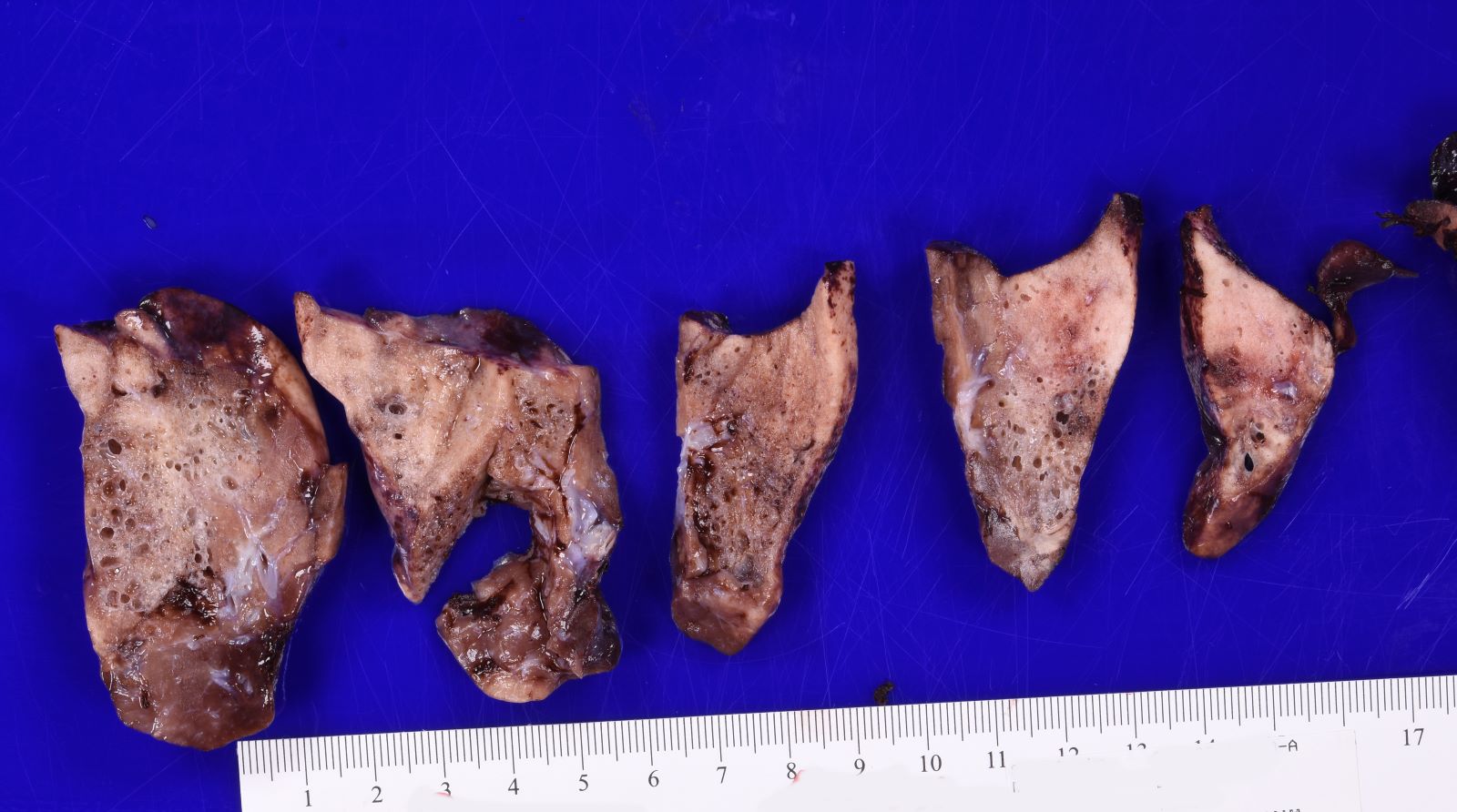
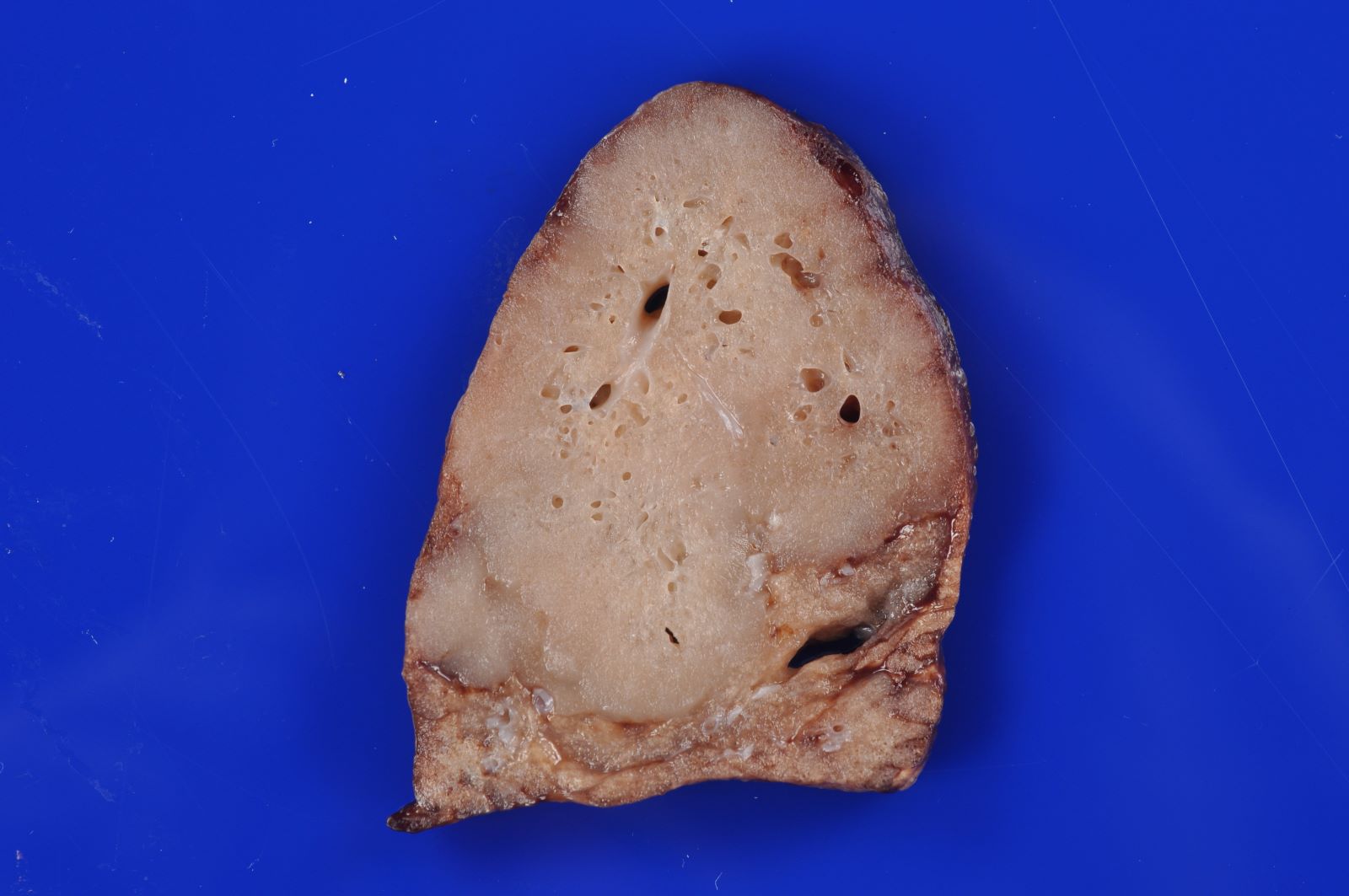
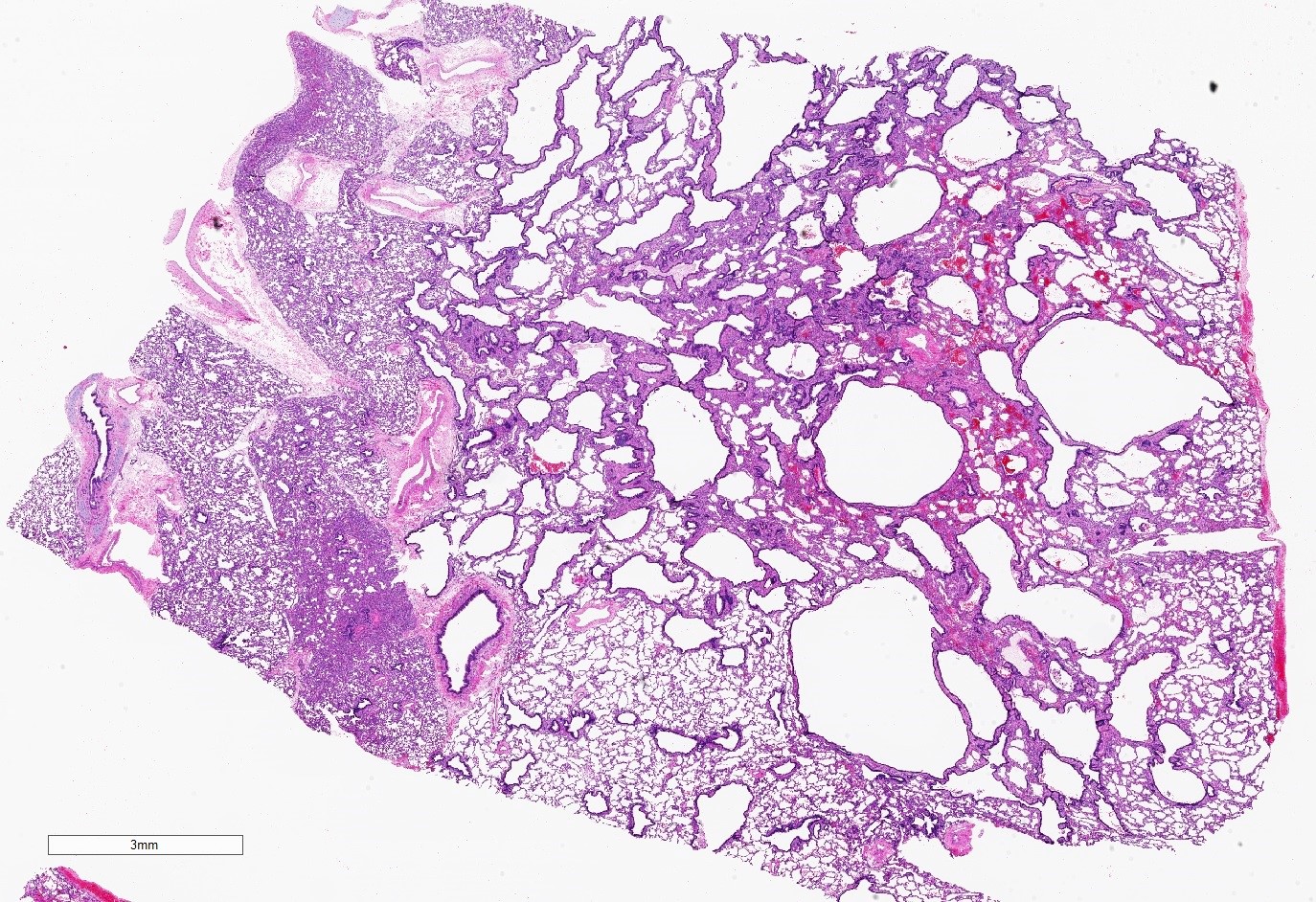
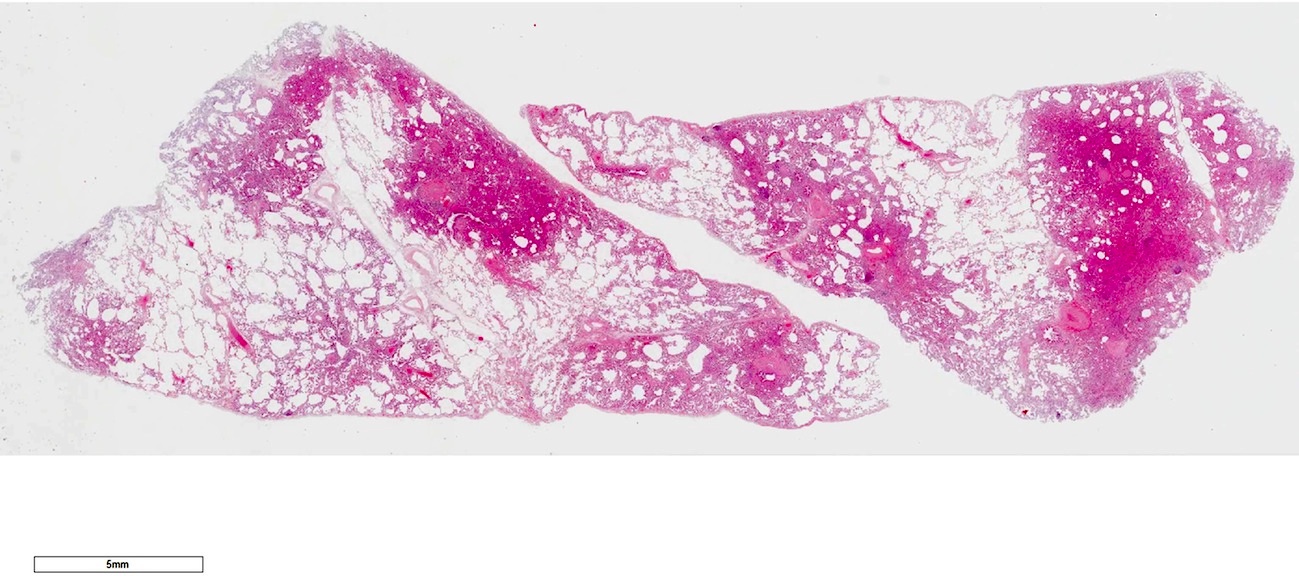
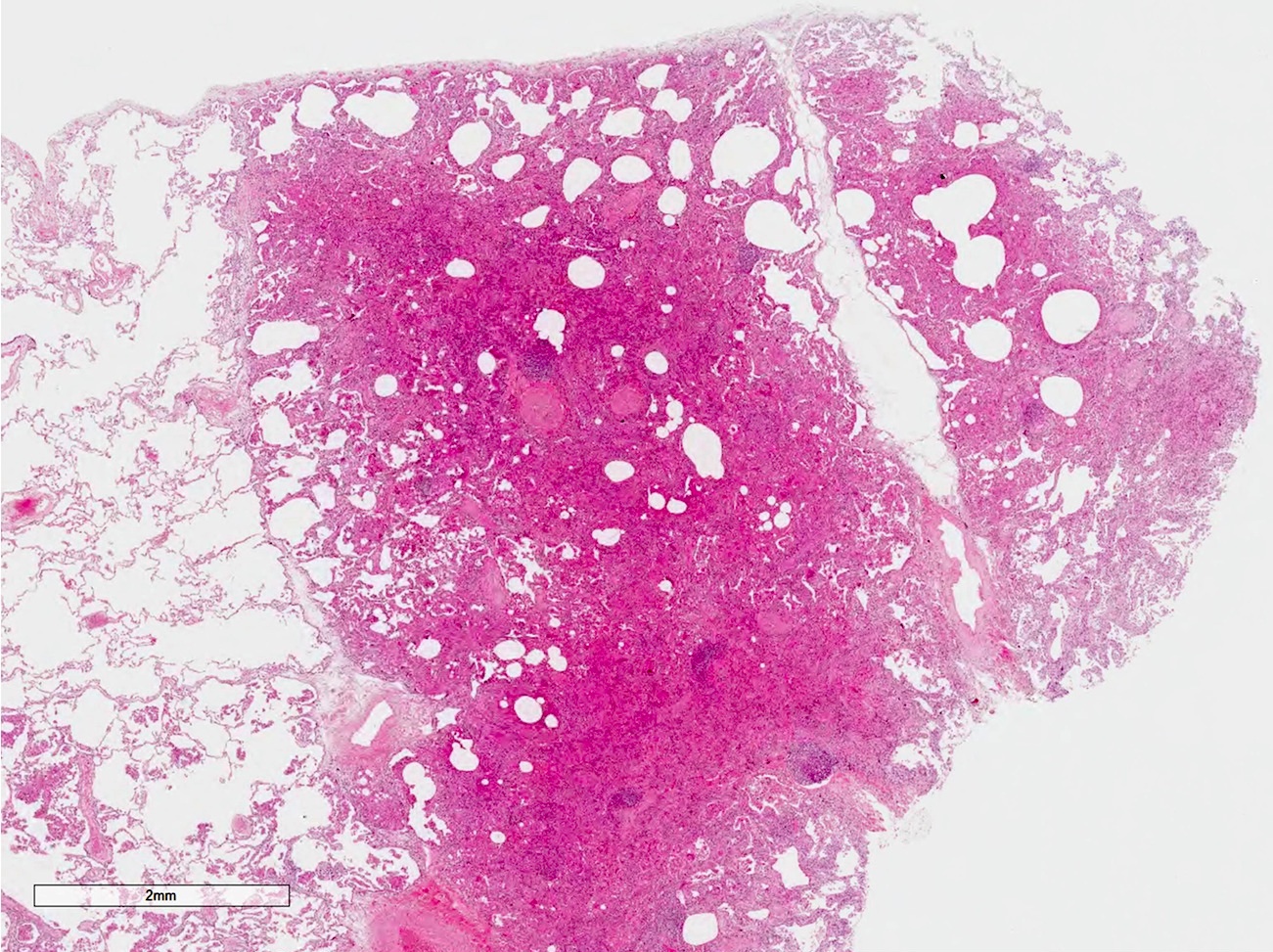
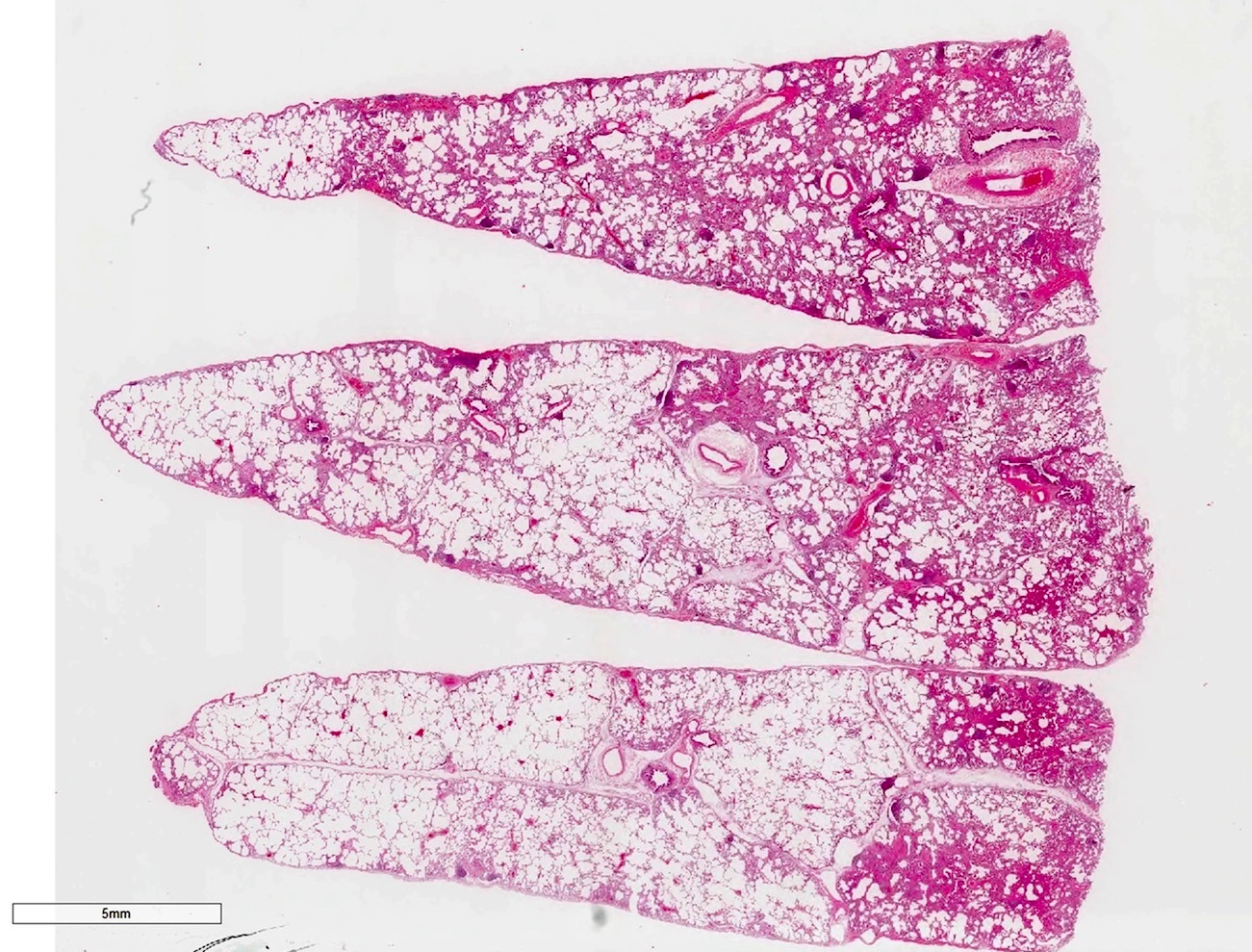
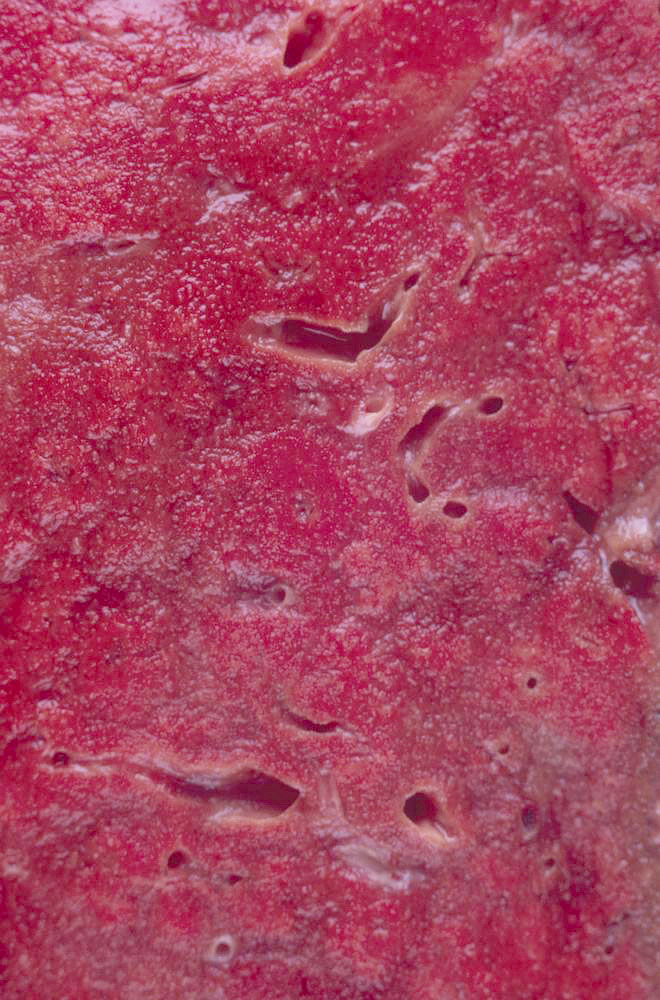
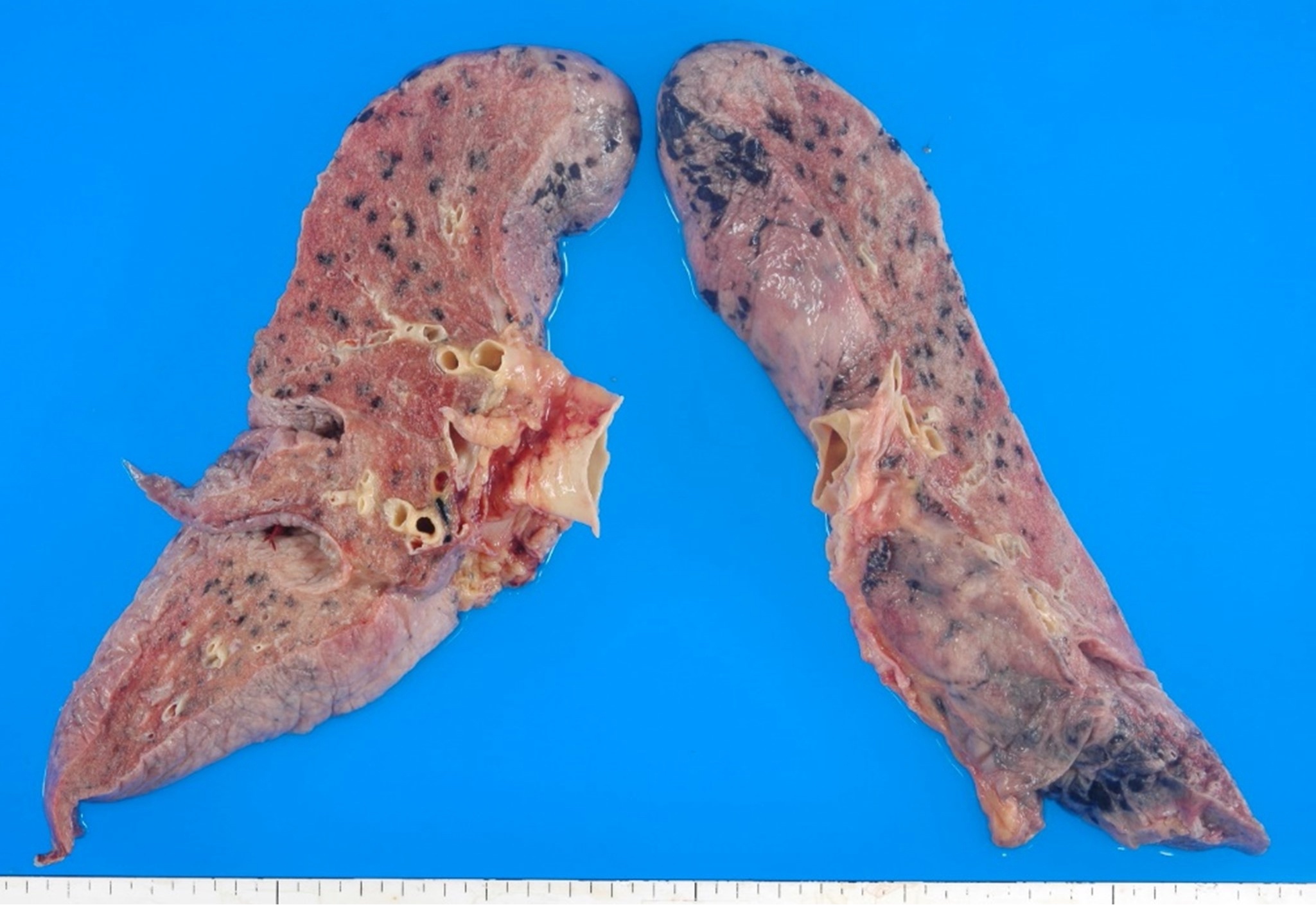
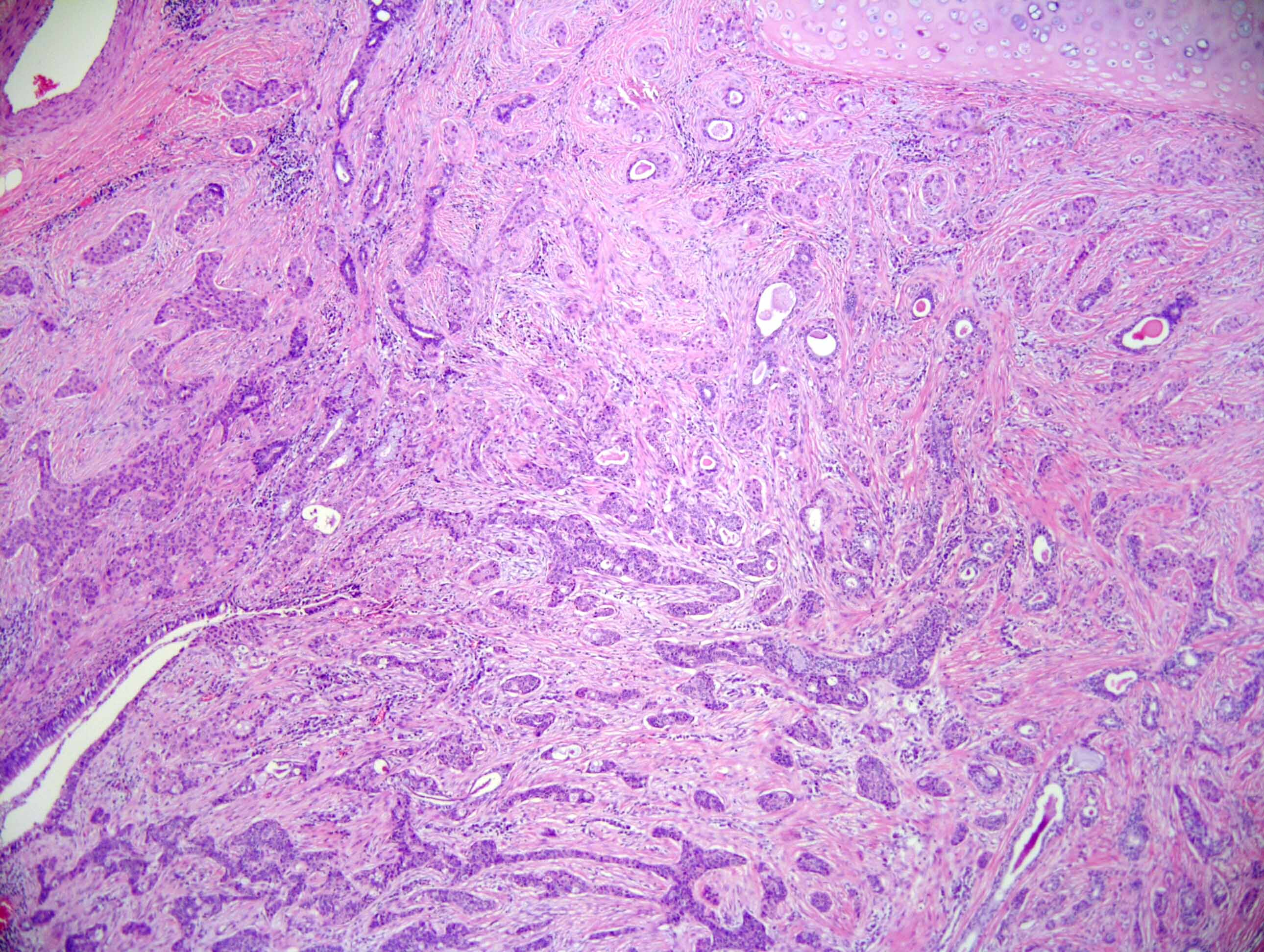
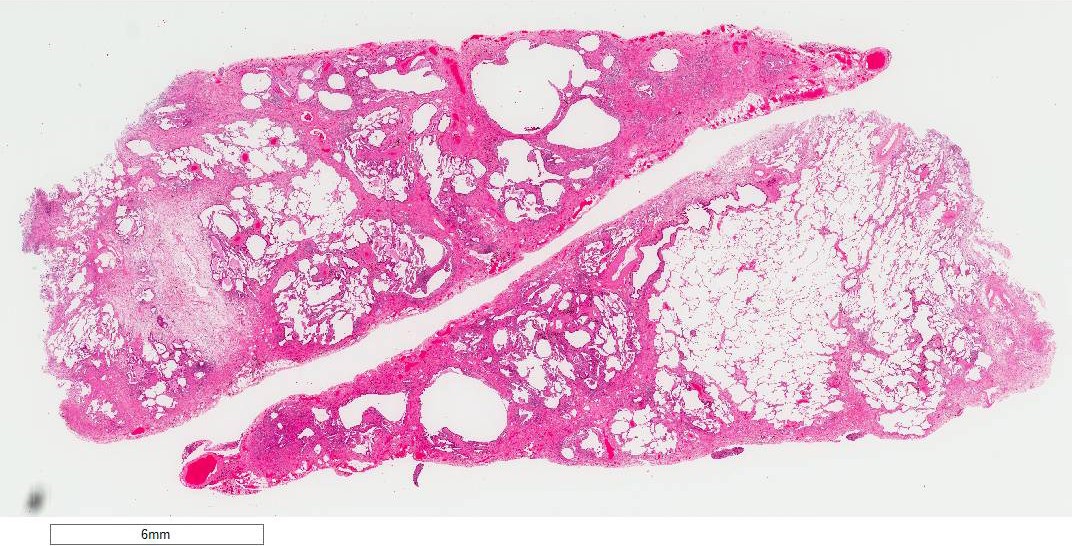
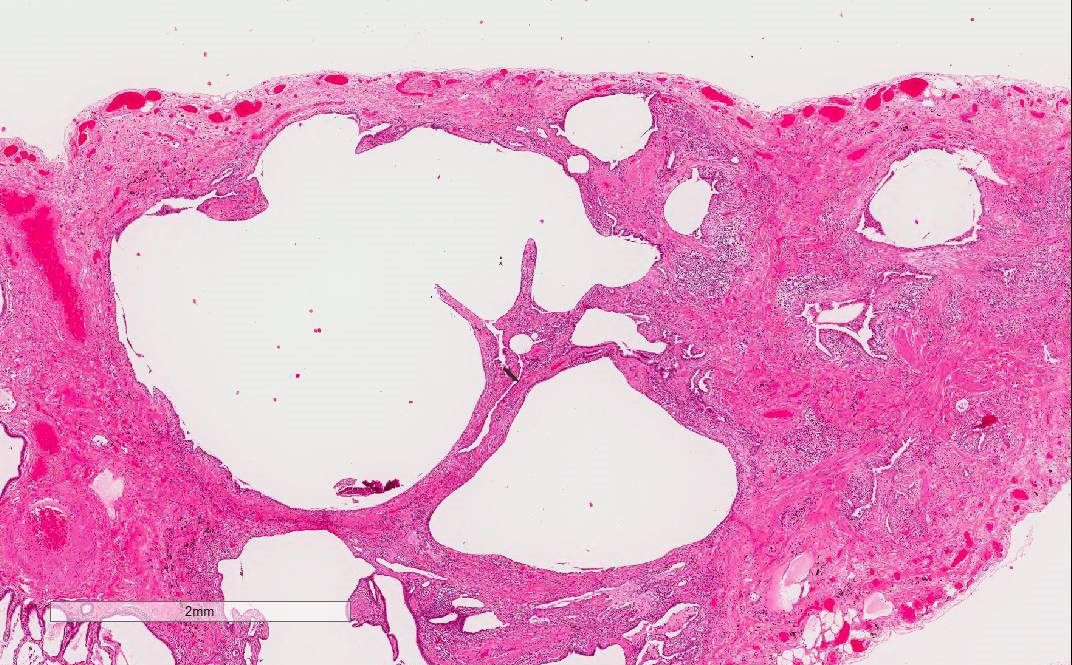
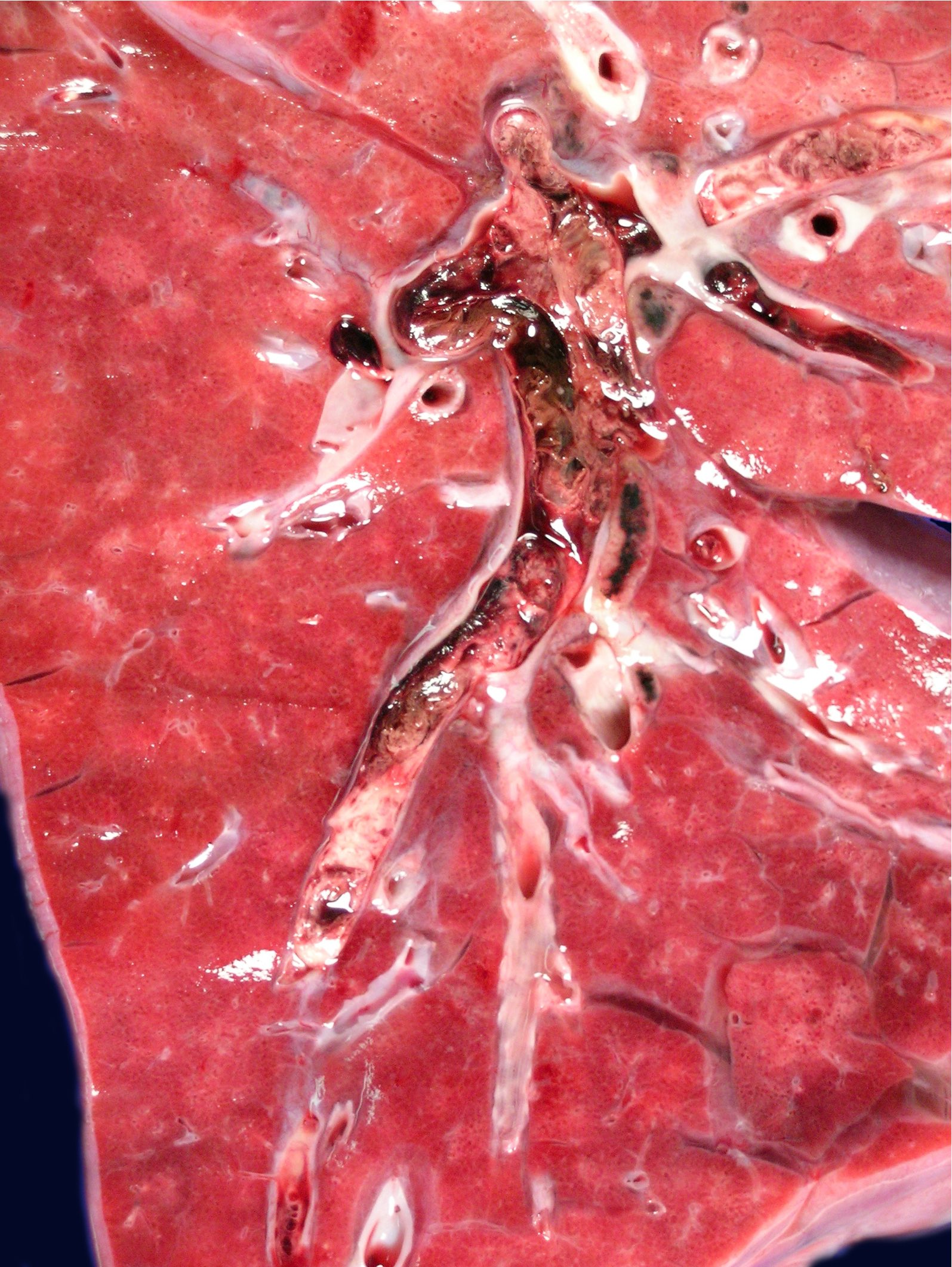
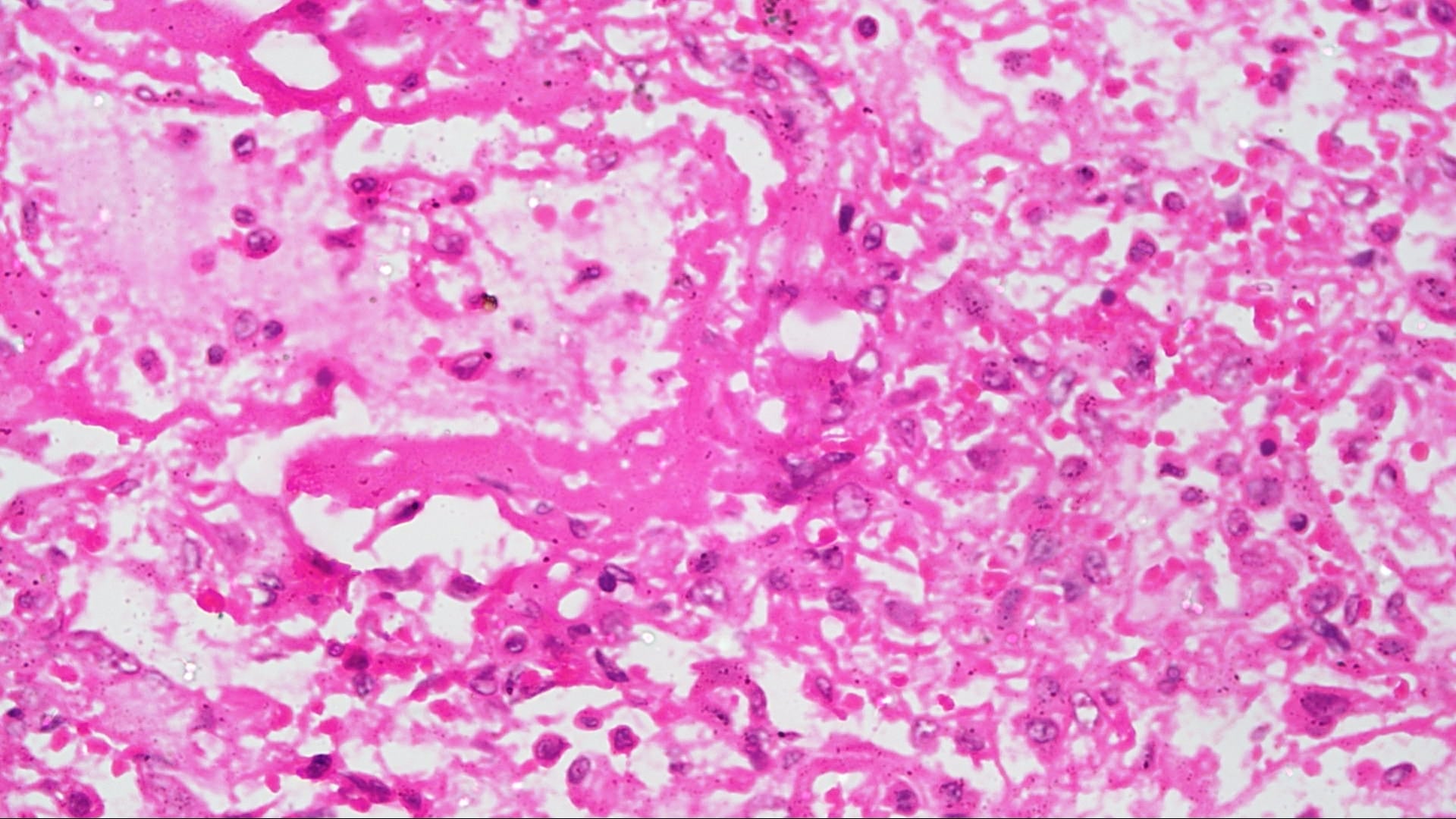
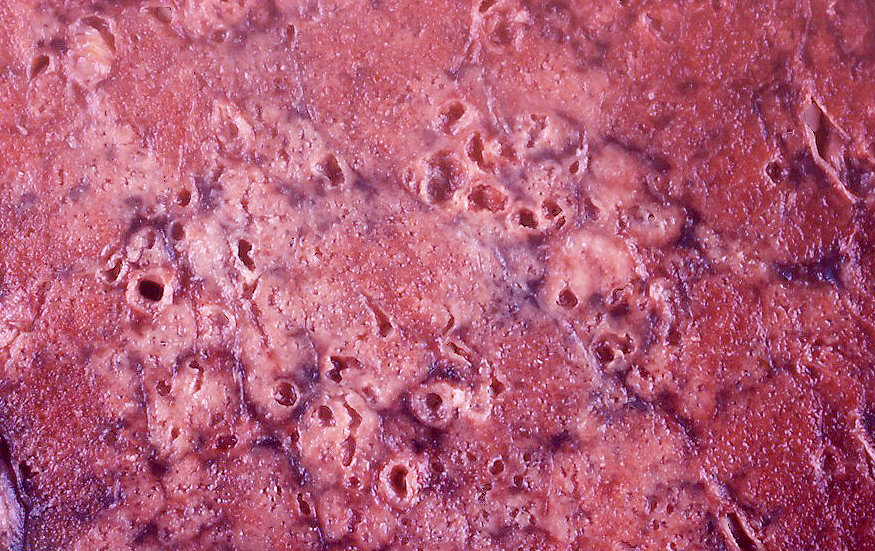
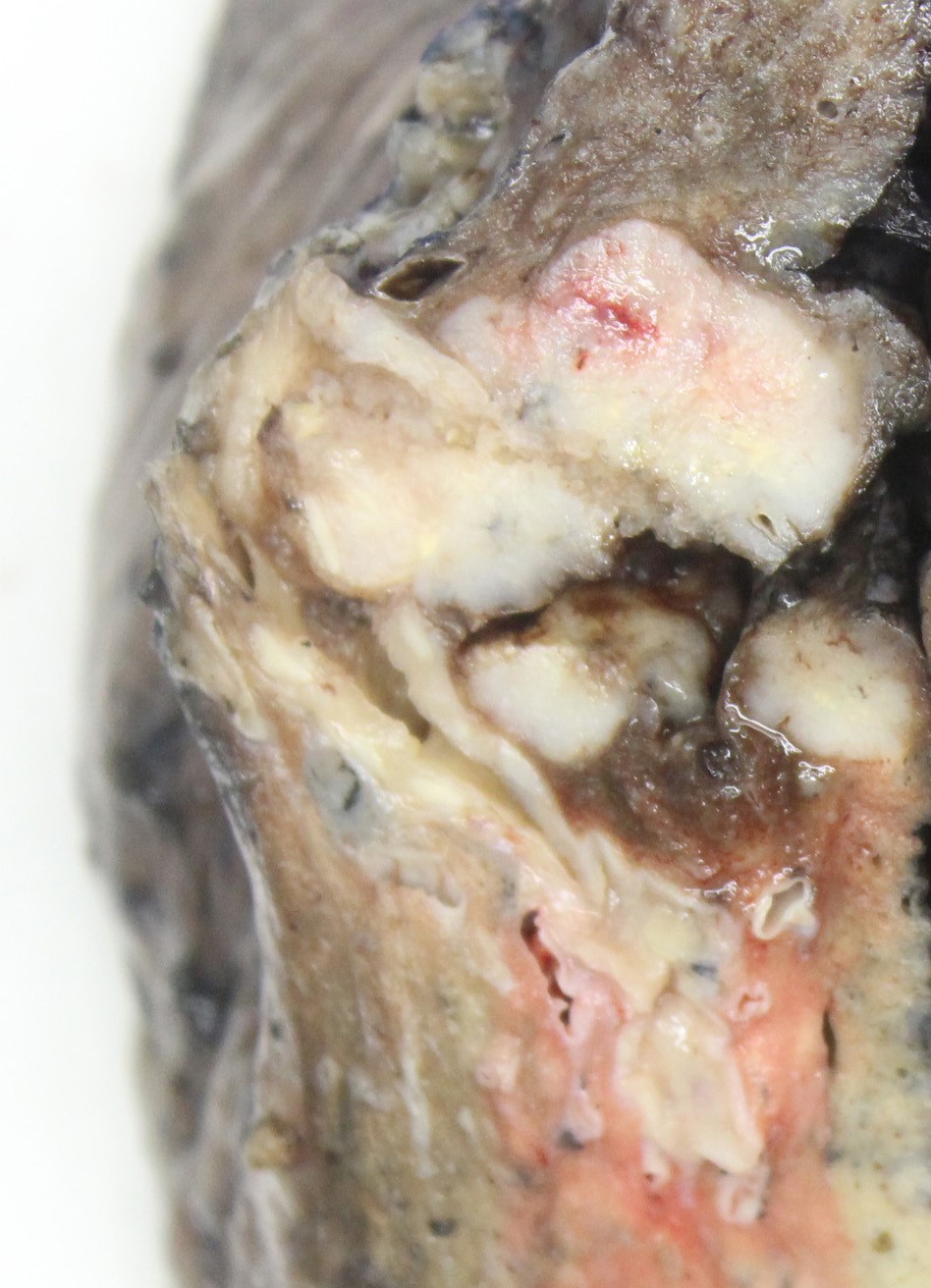
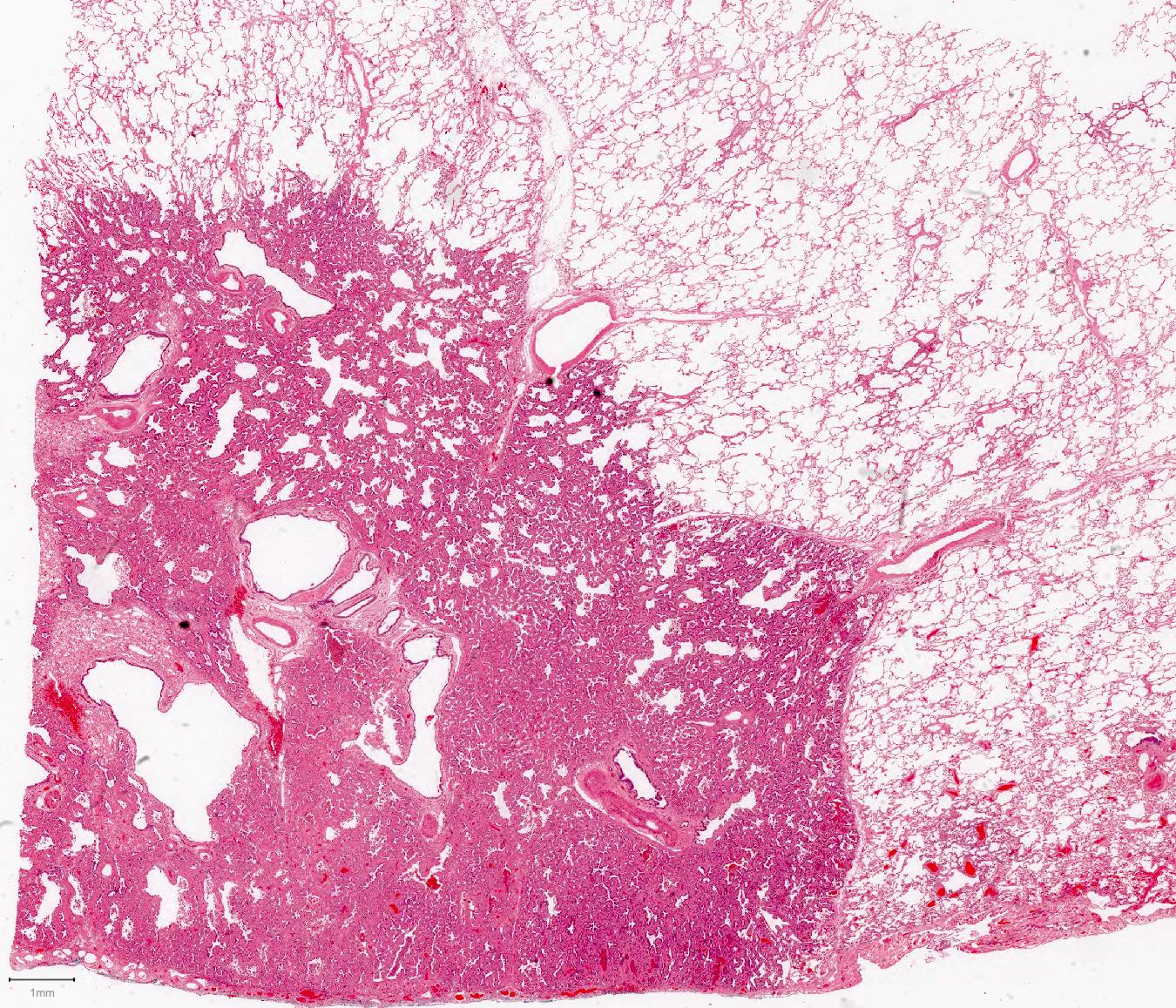
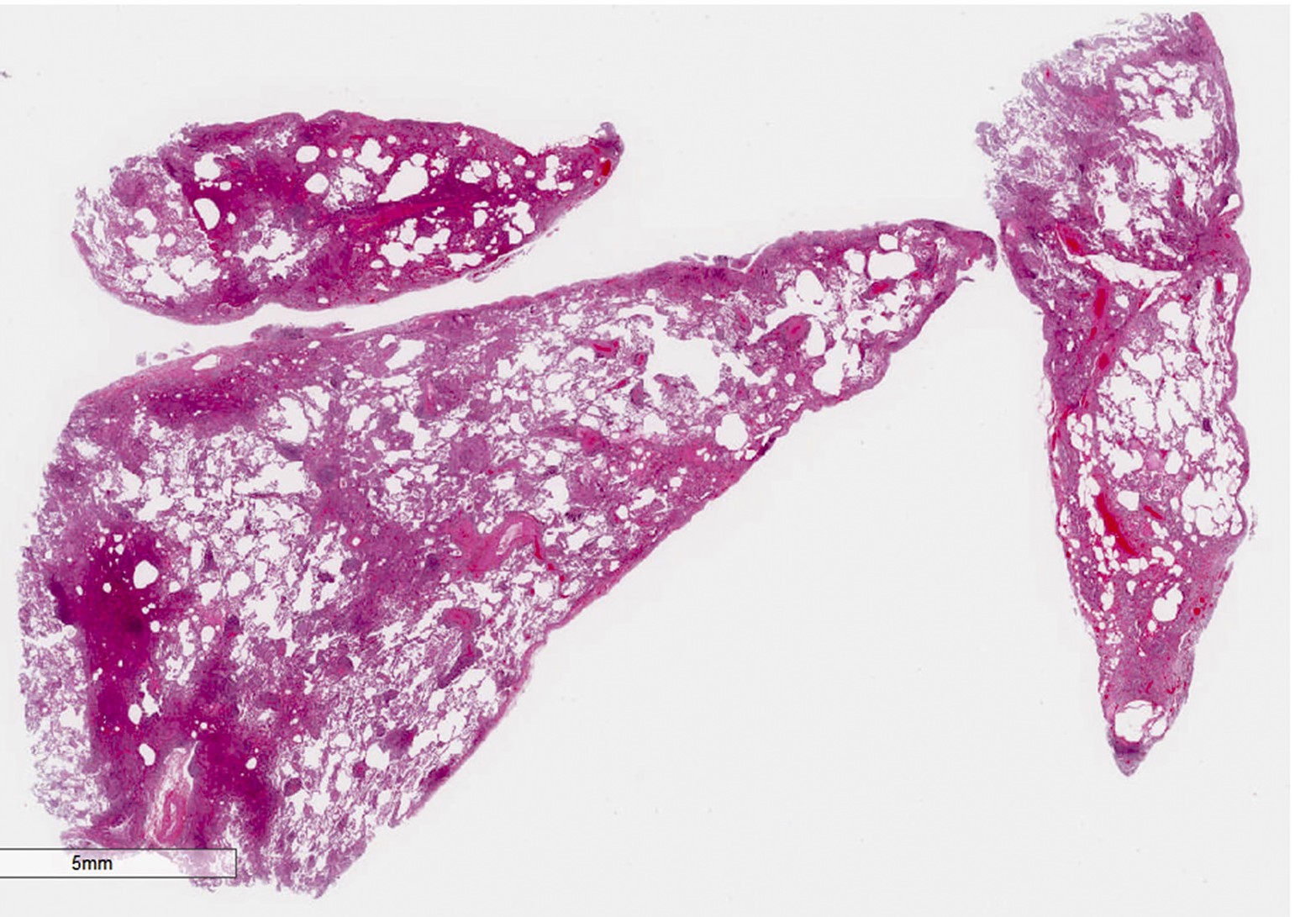
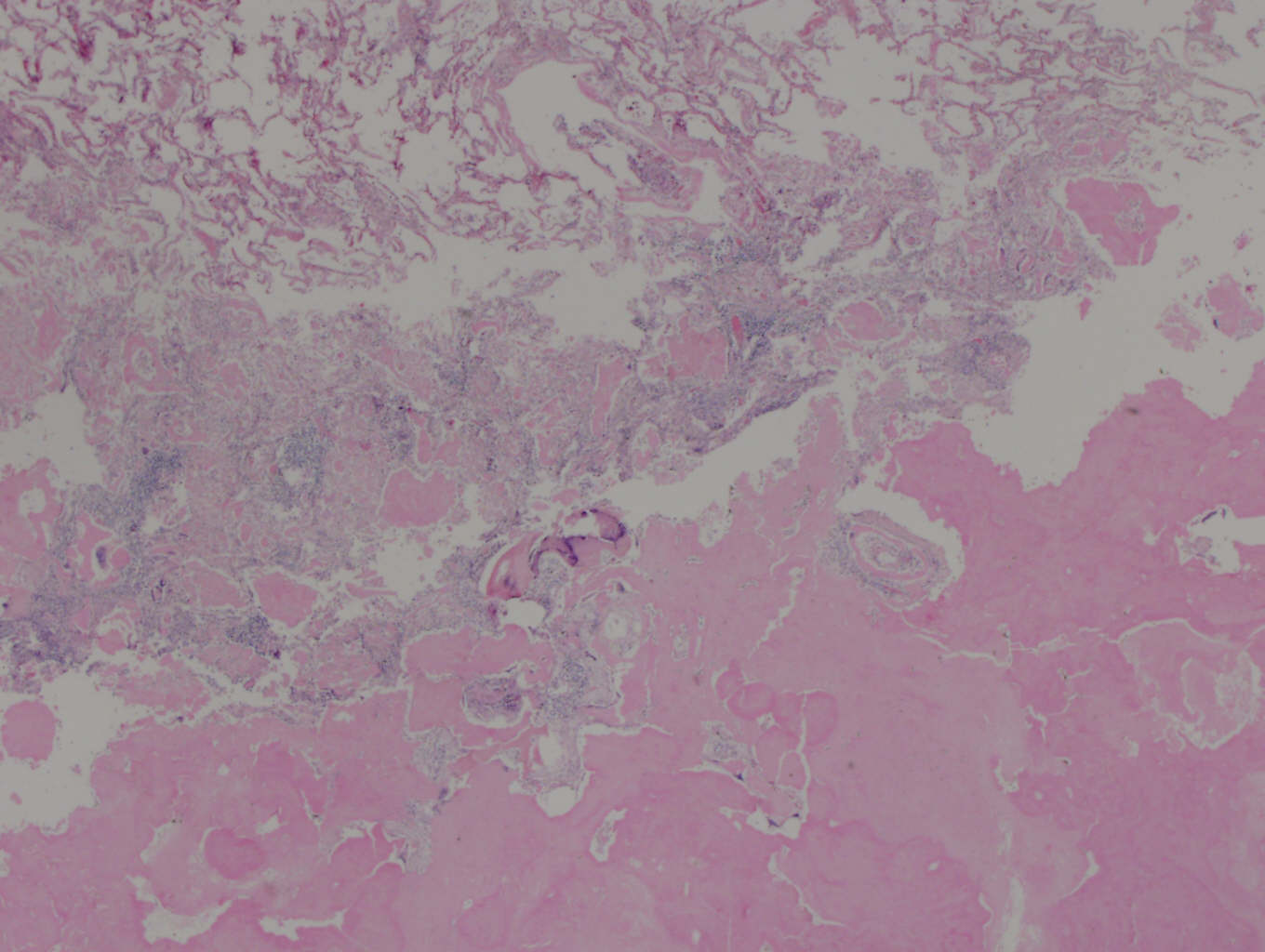
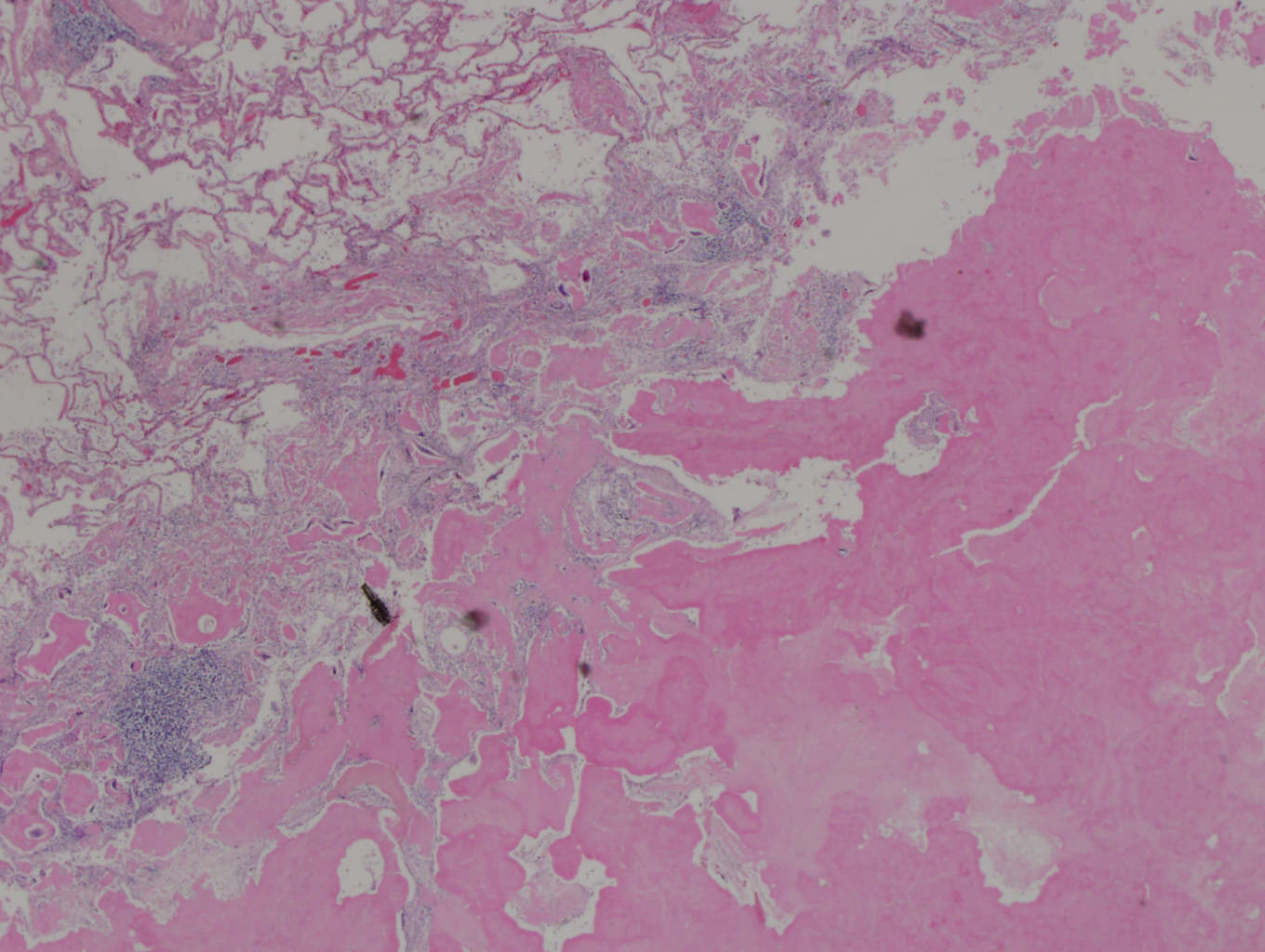
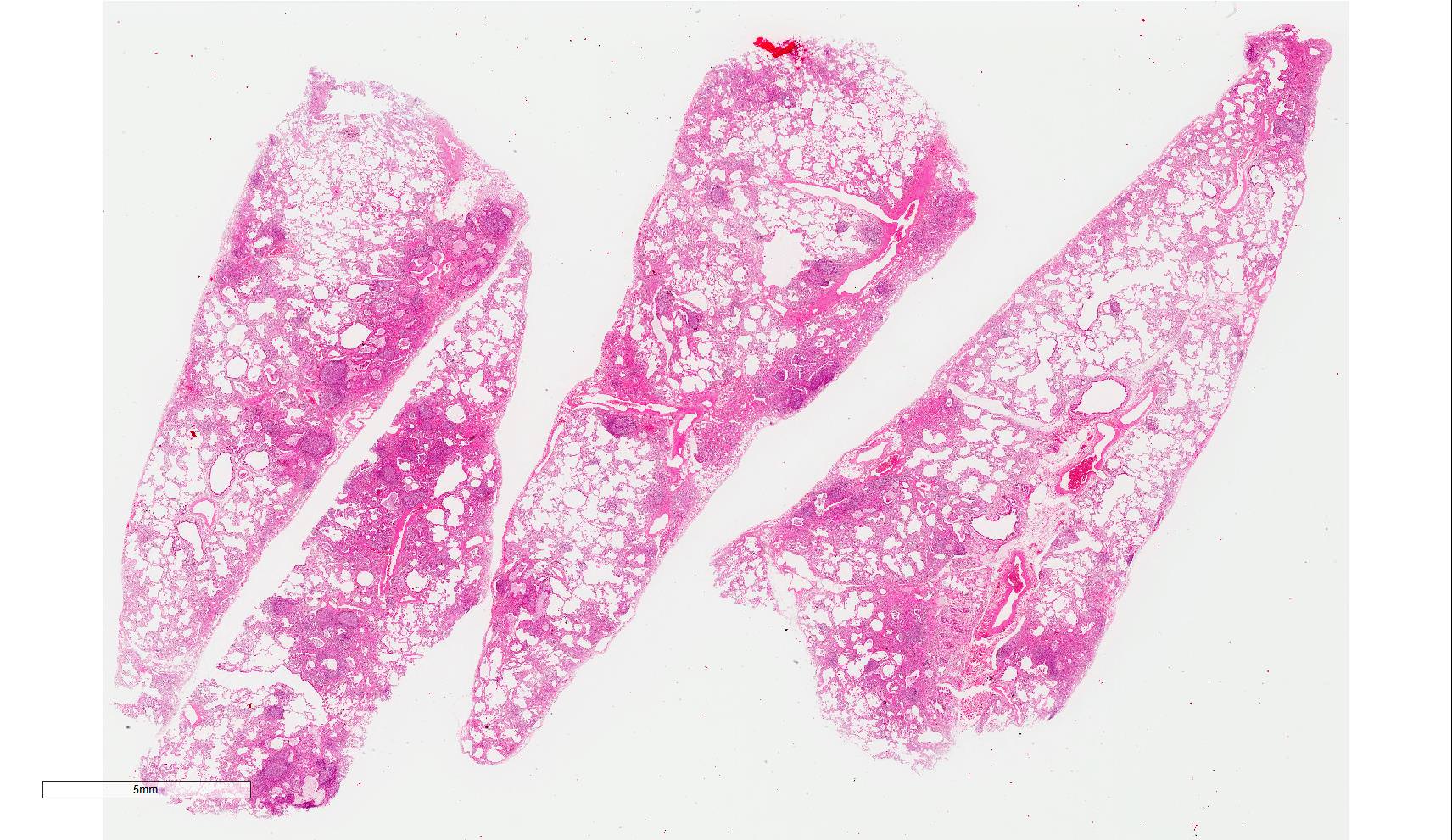
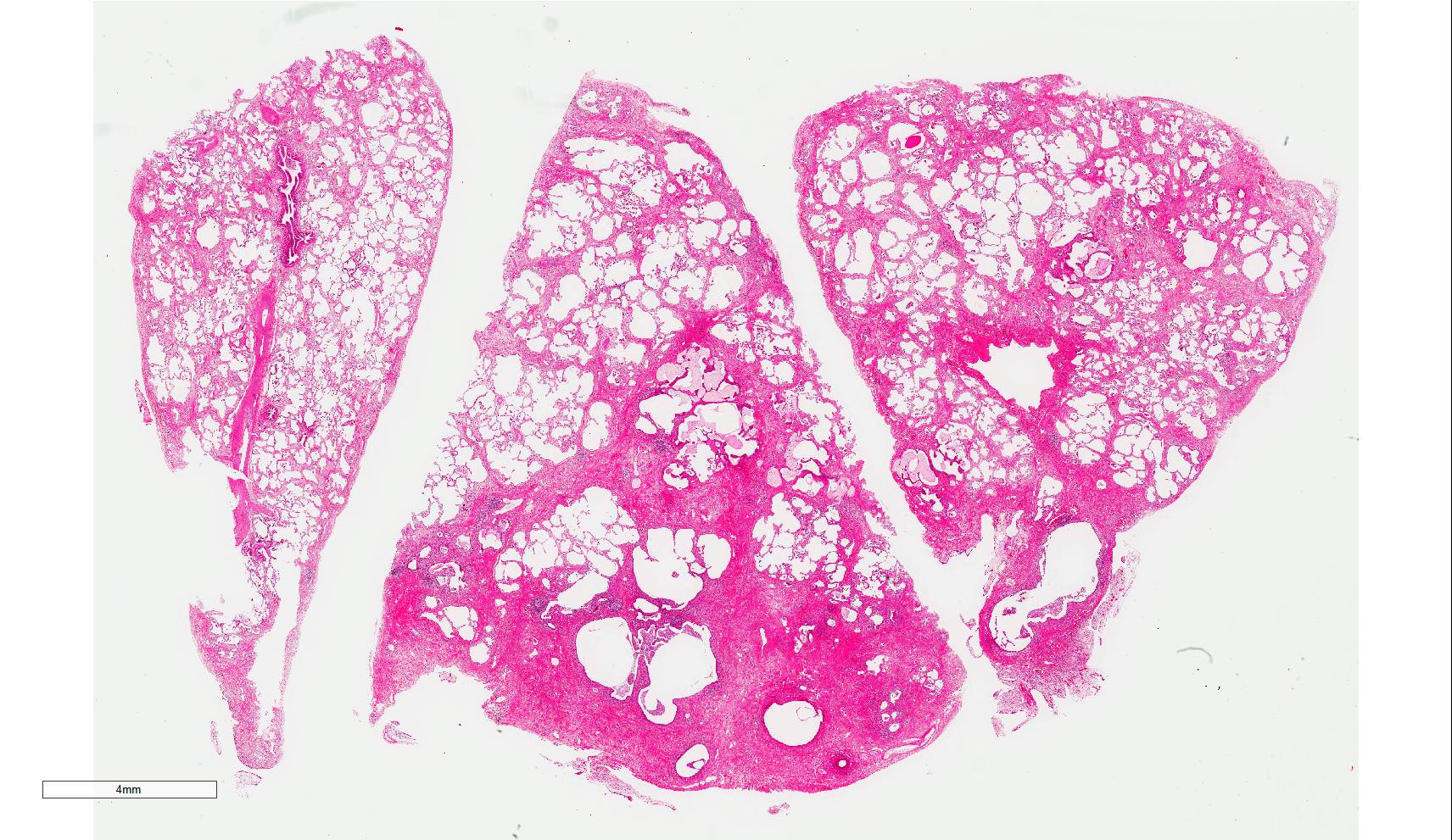
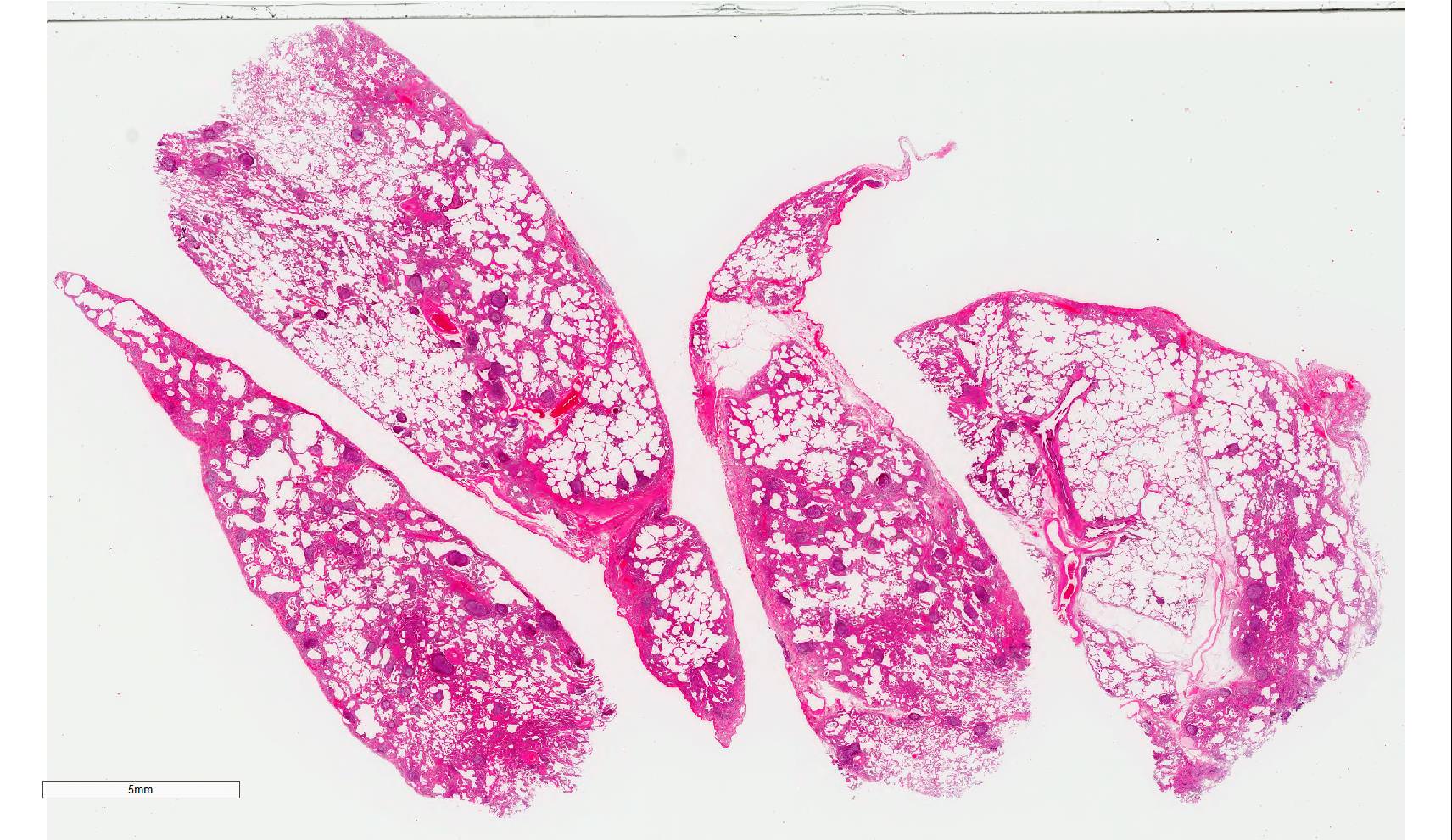
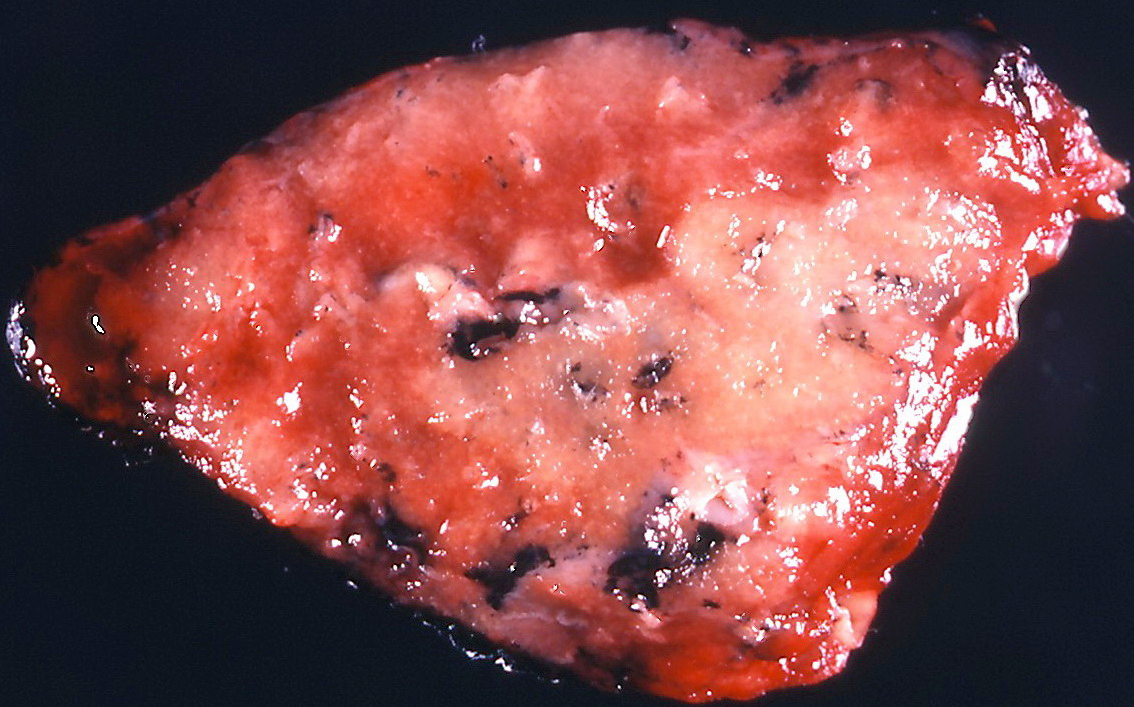
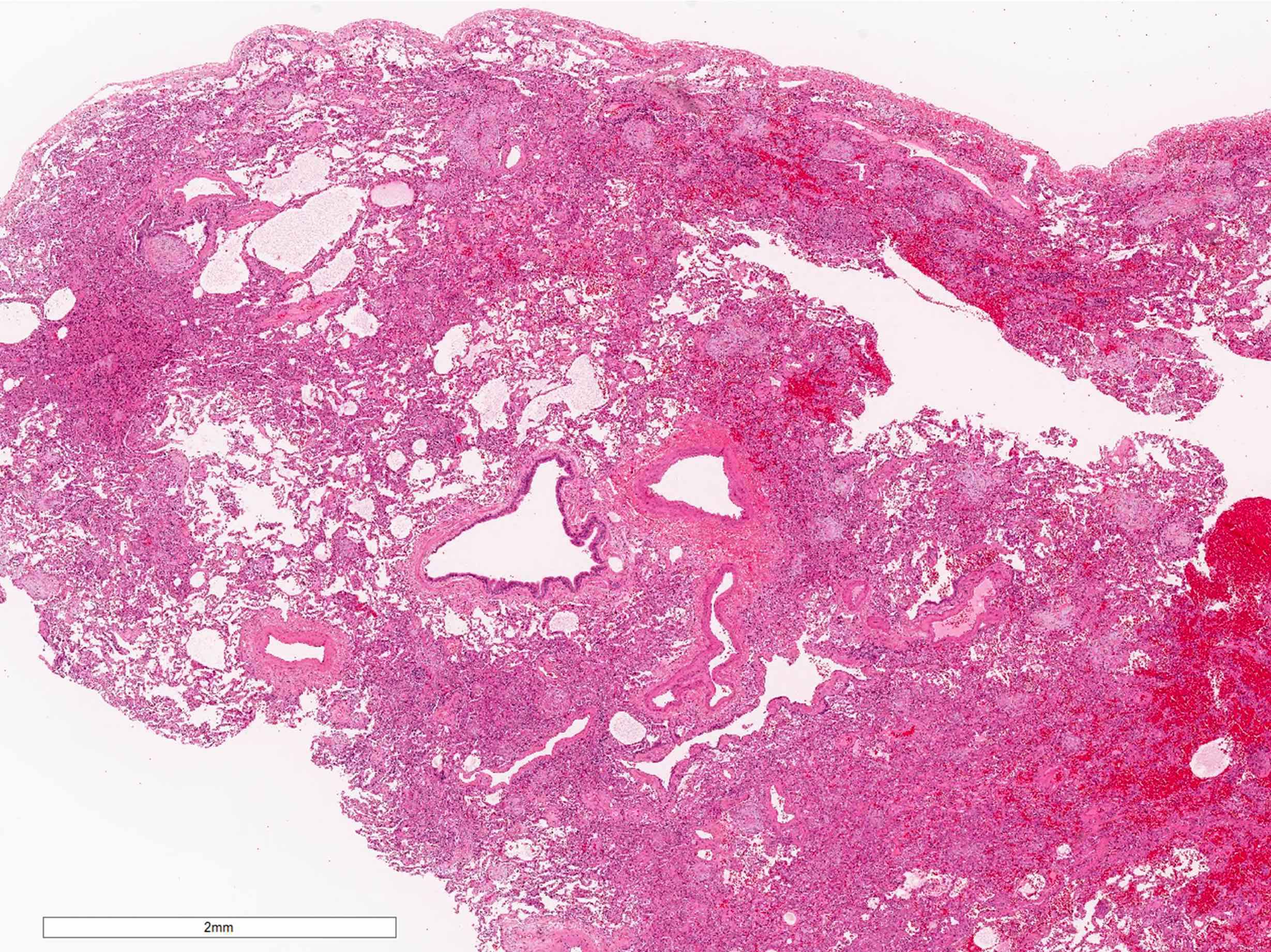
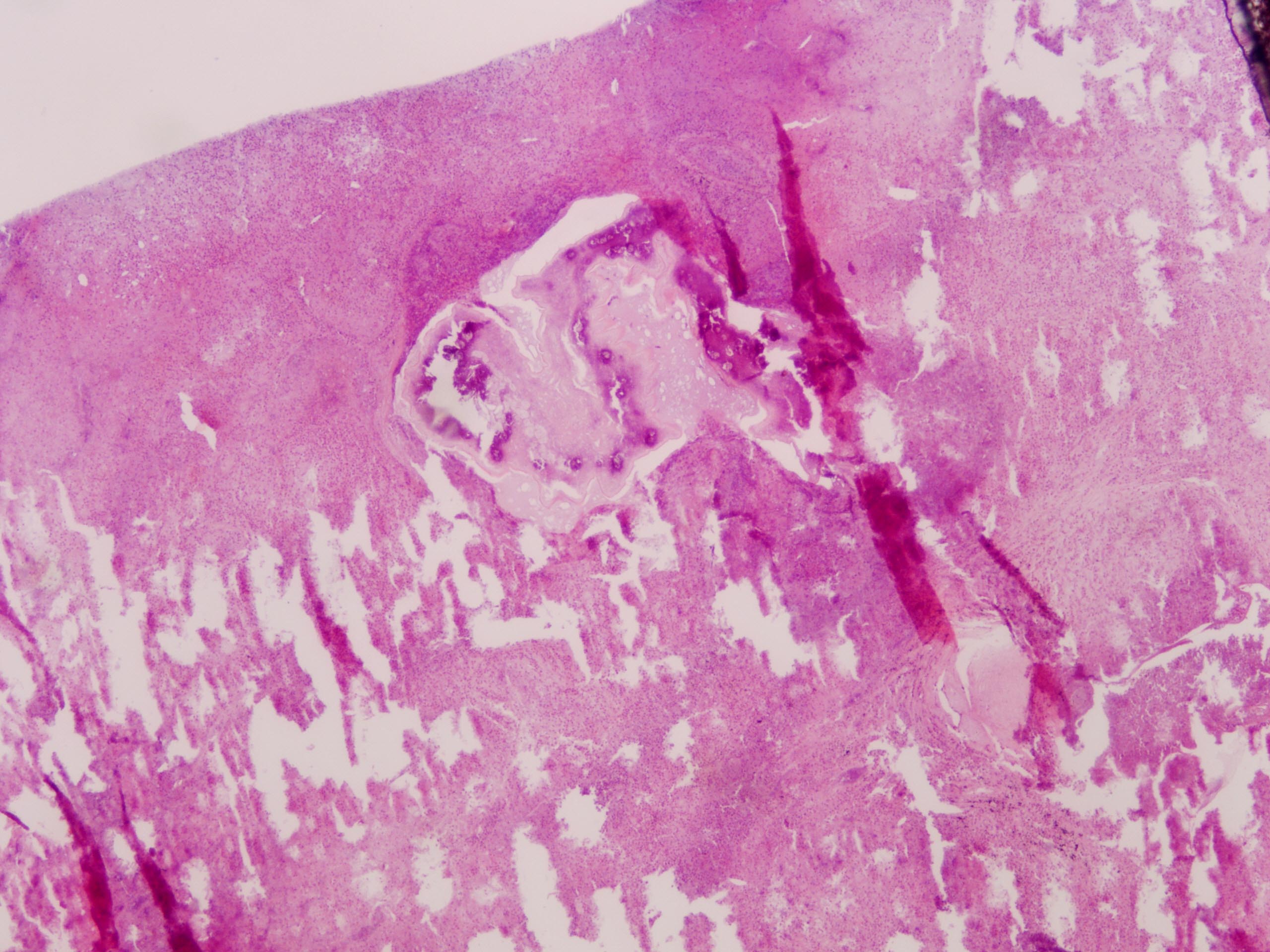
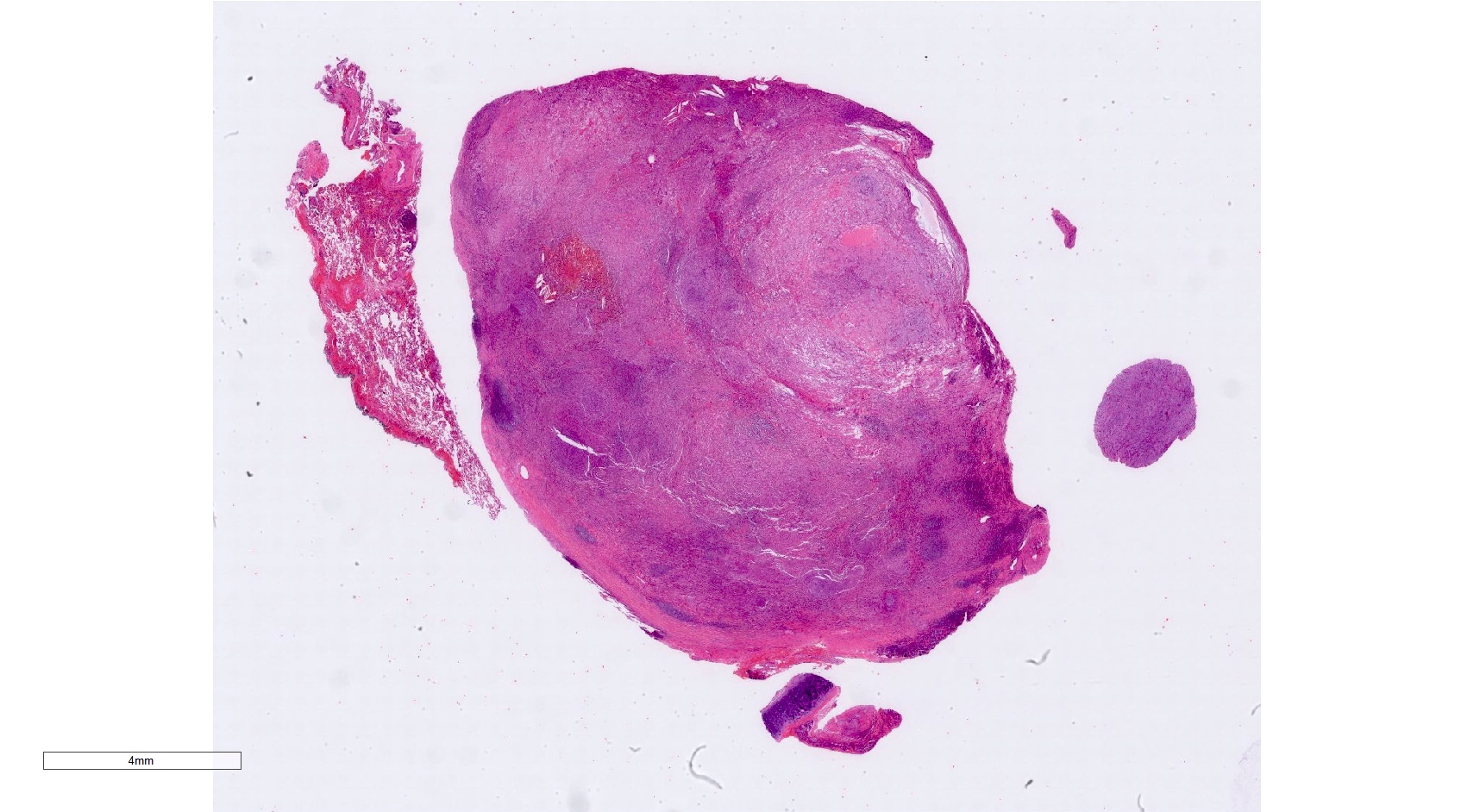
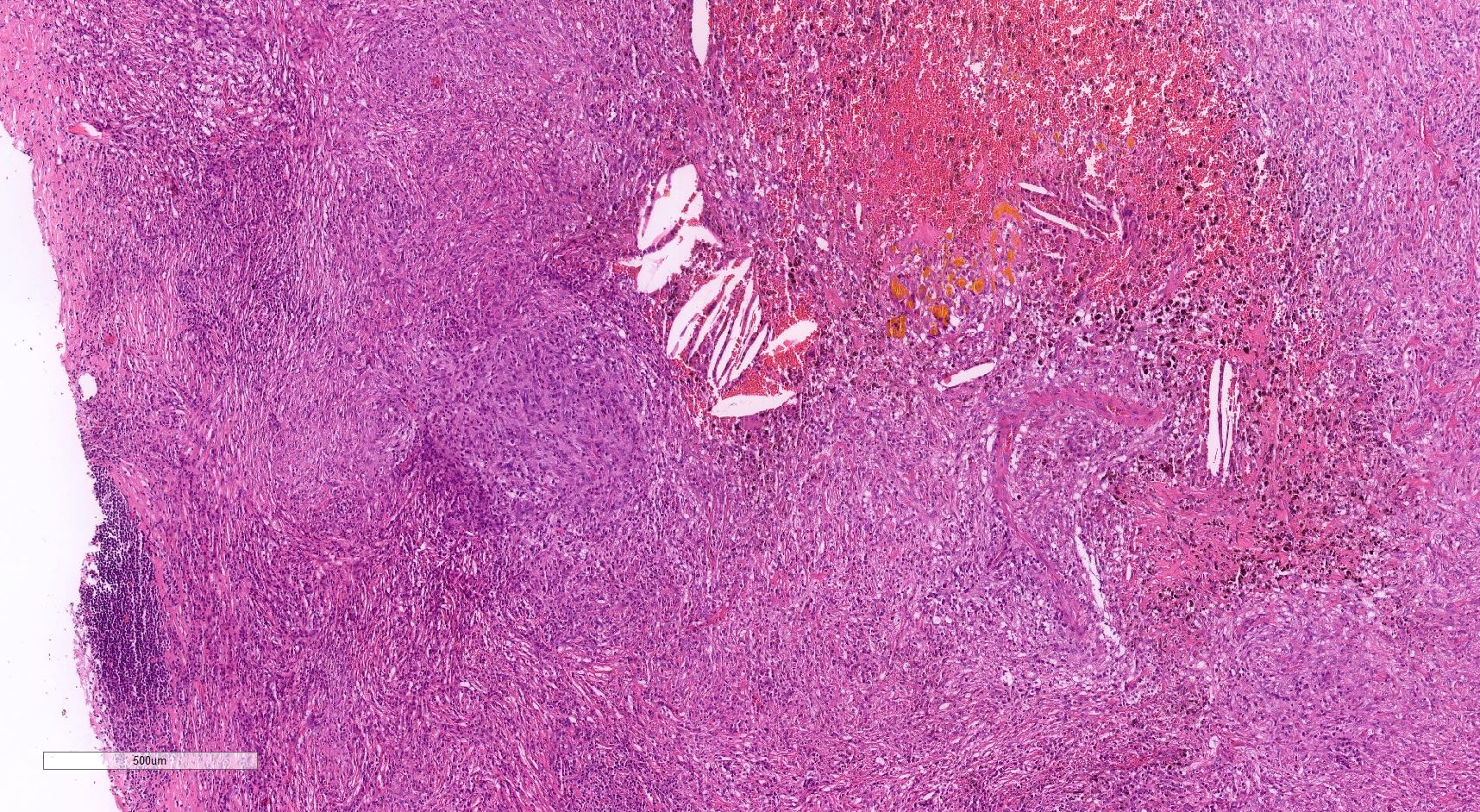
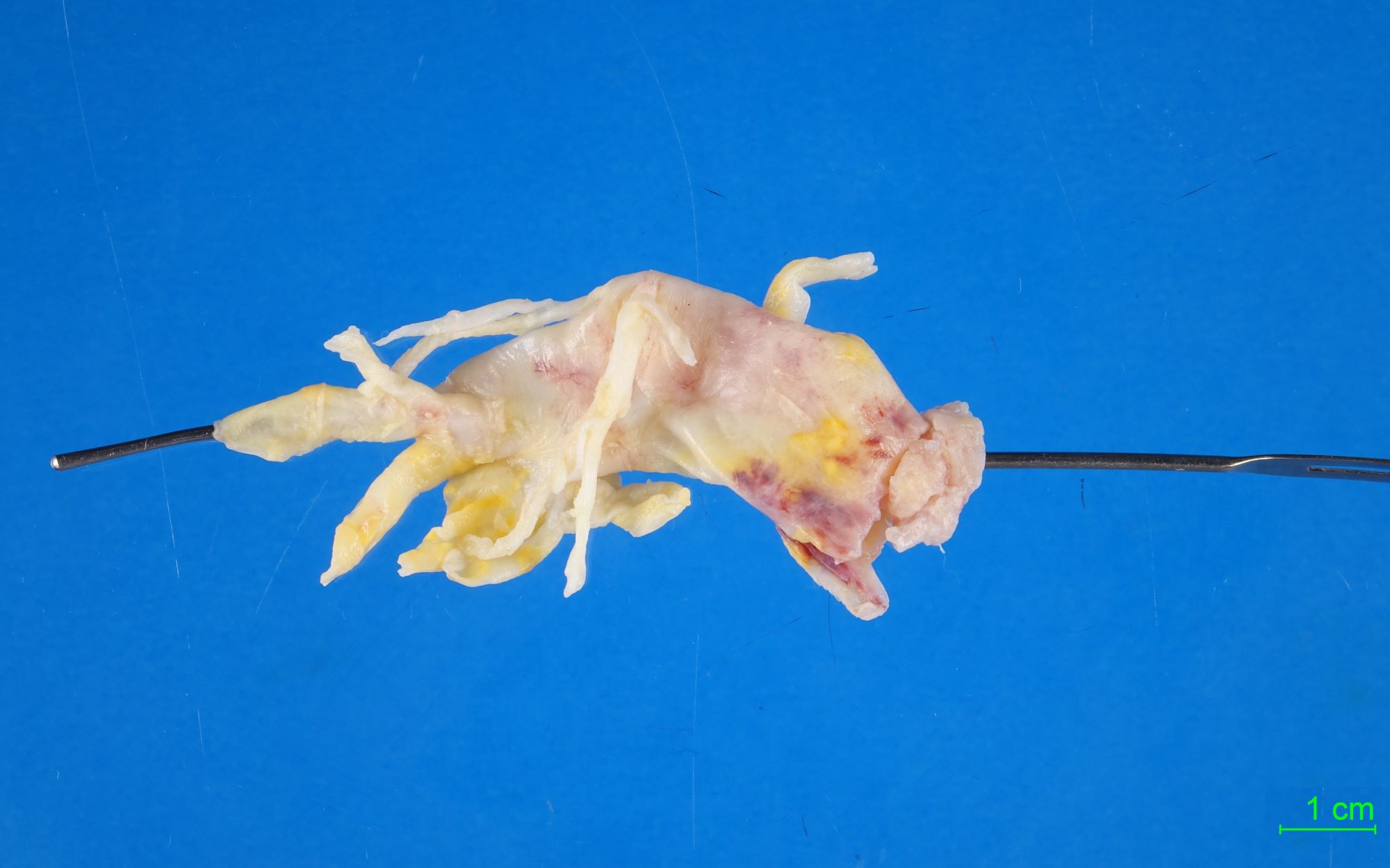
- Multiple patchy consolidated lesions
- Ill defined, soft to firm gray areas
- Mild increase in weight
- Alveoli are filled with reddish fibrinous exudates
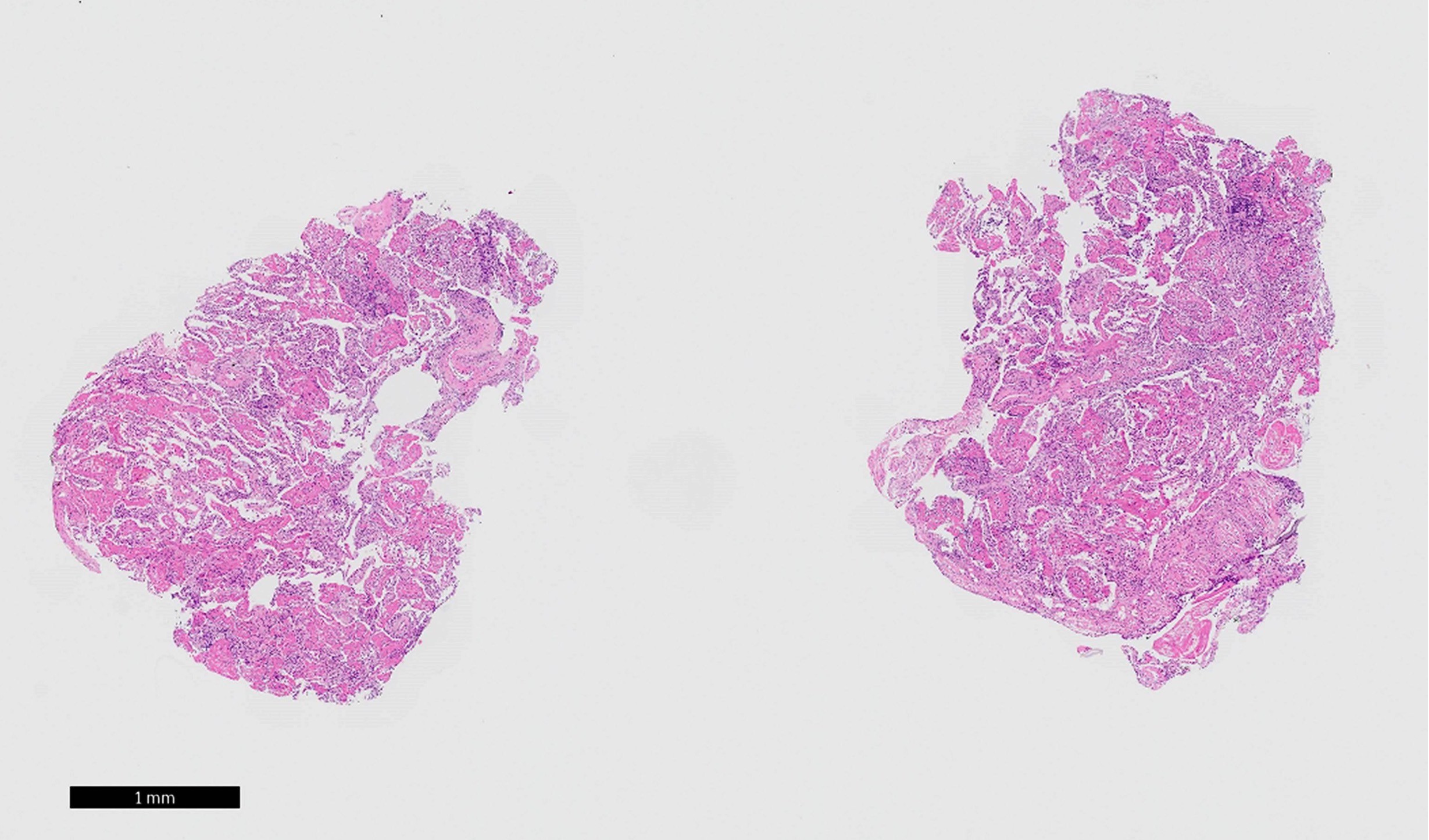
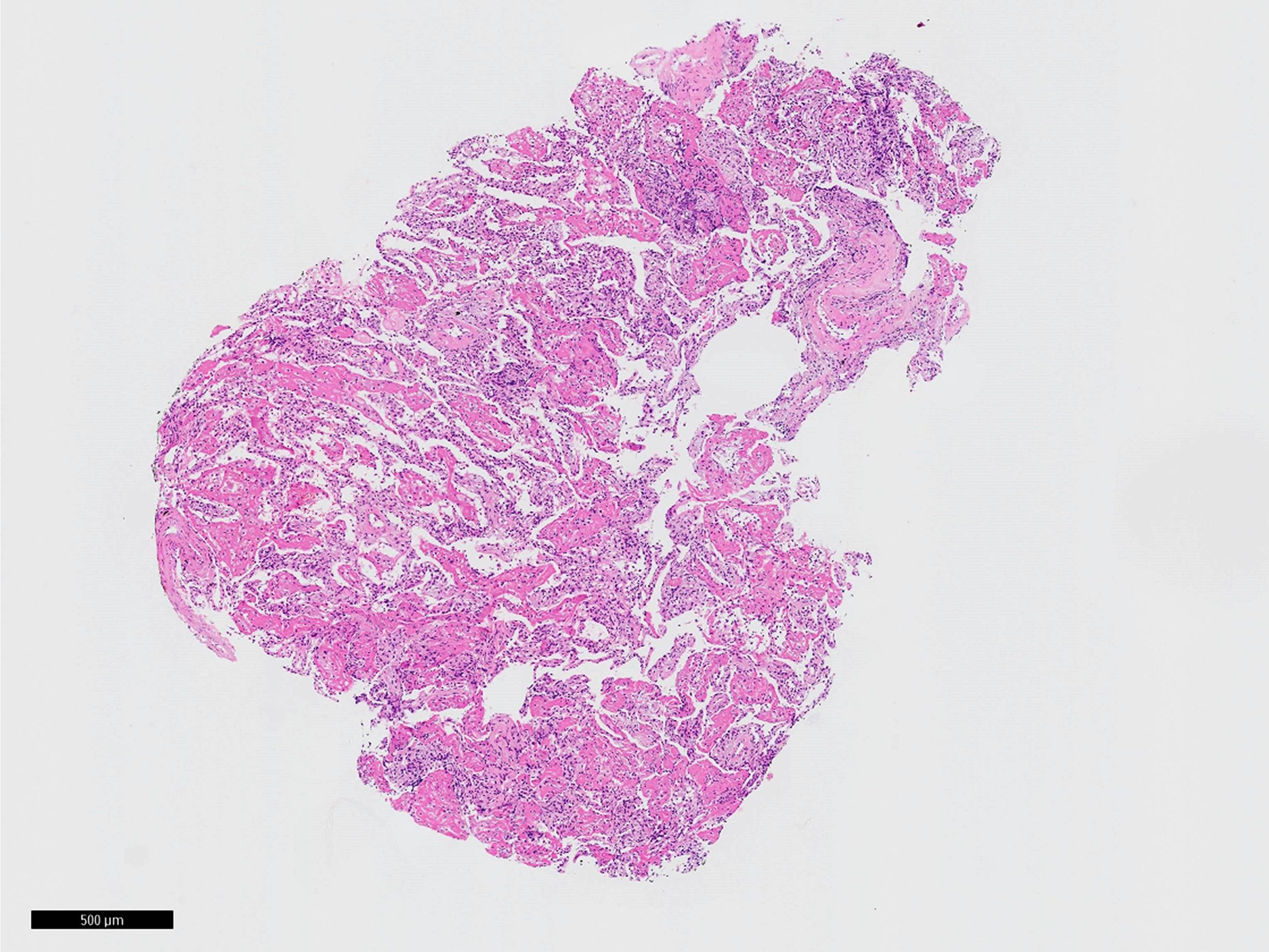
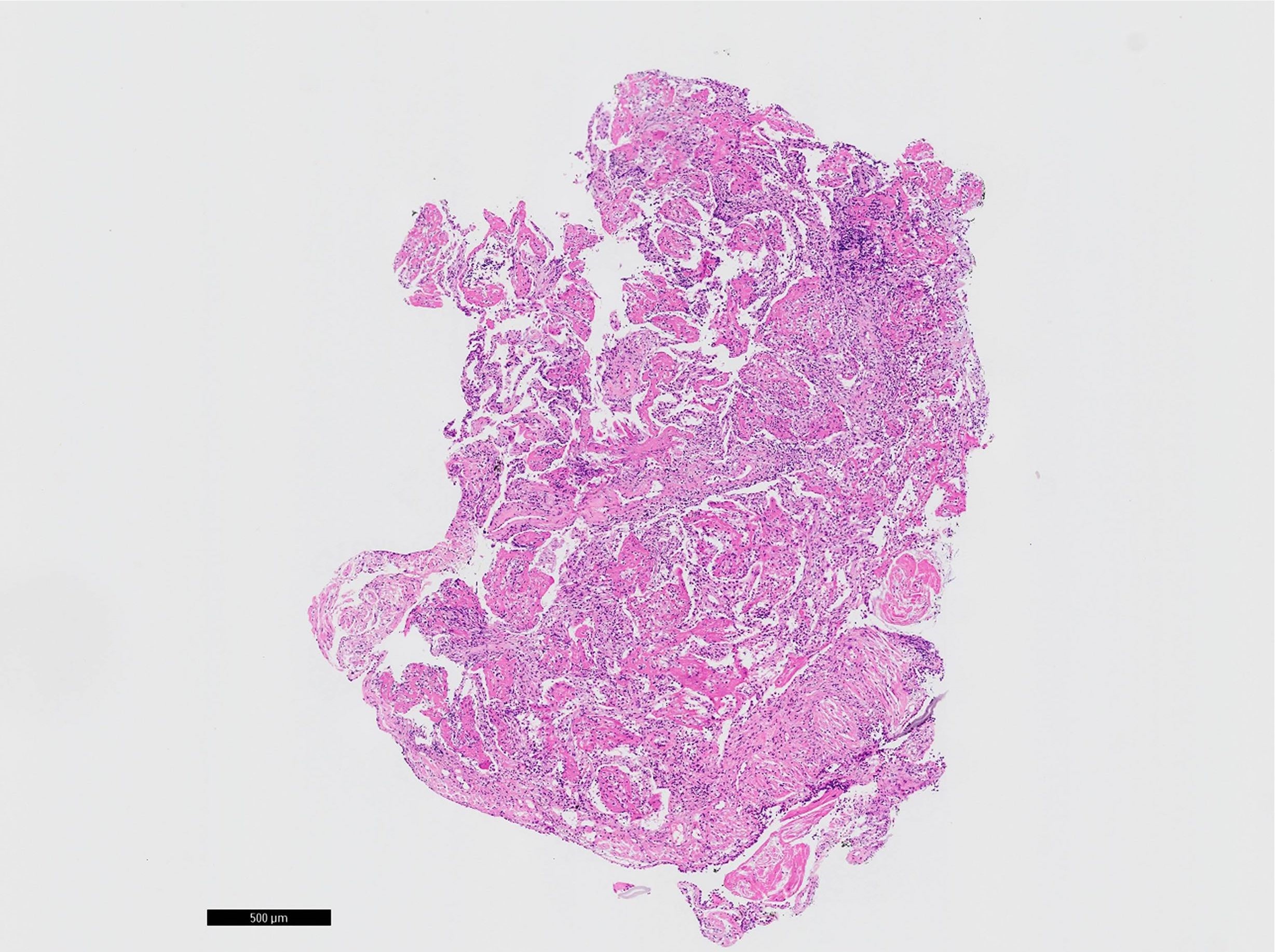
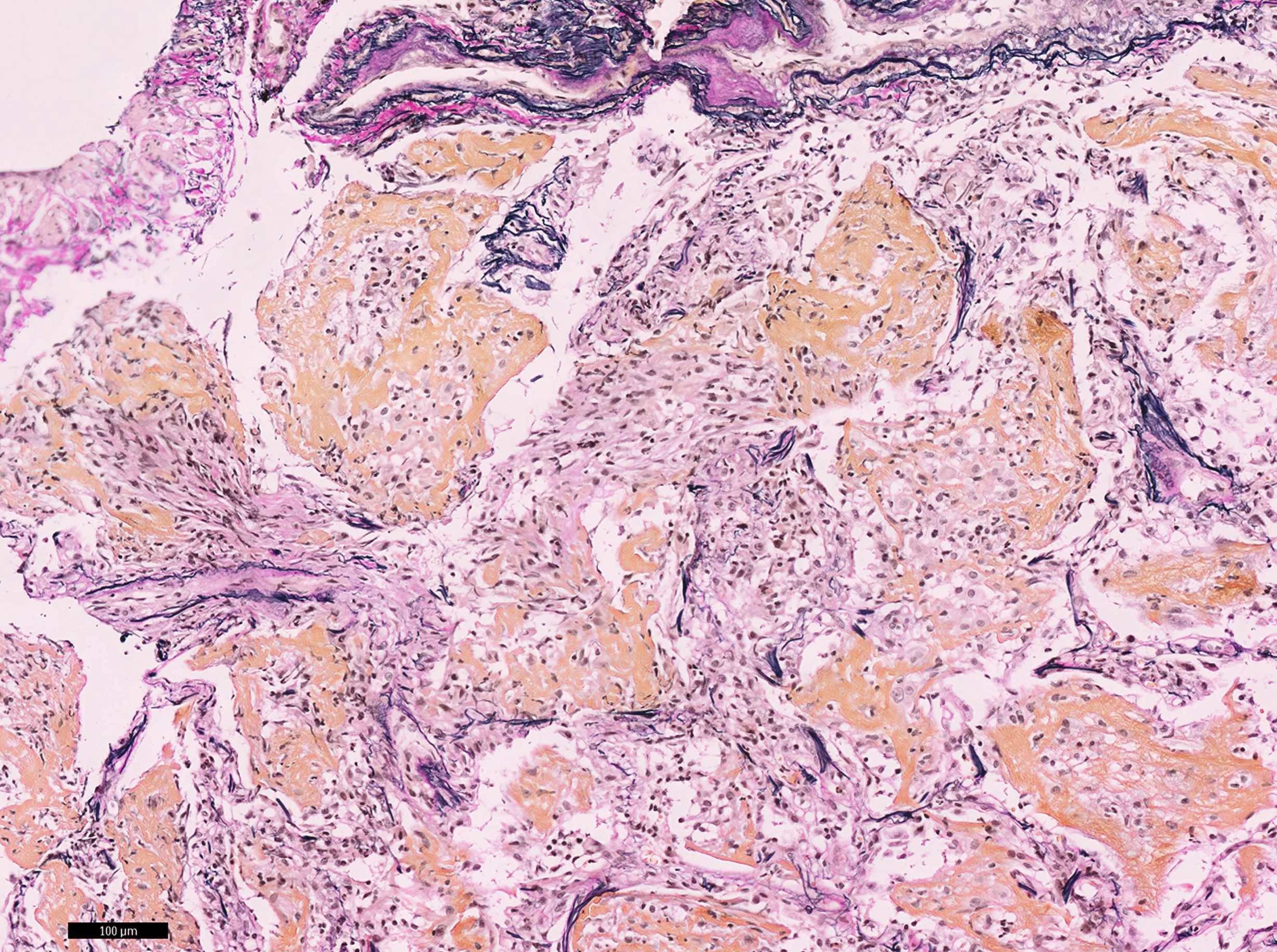
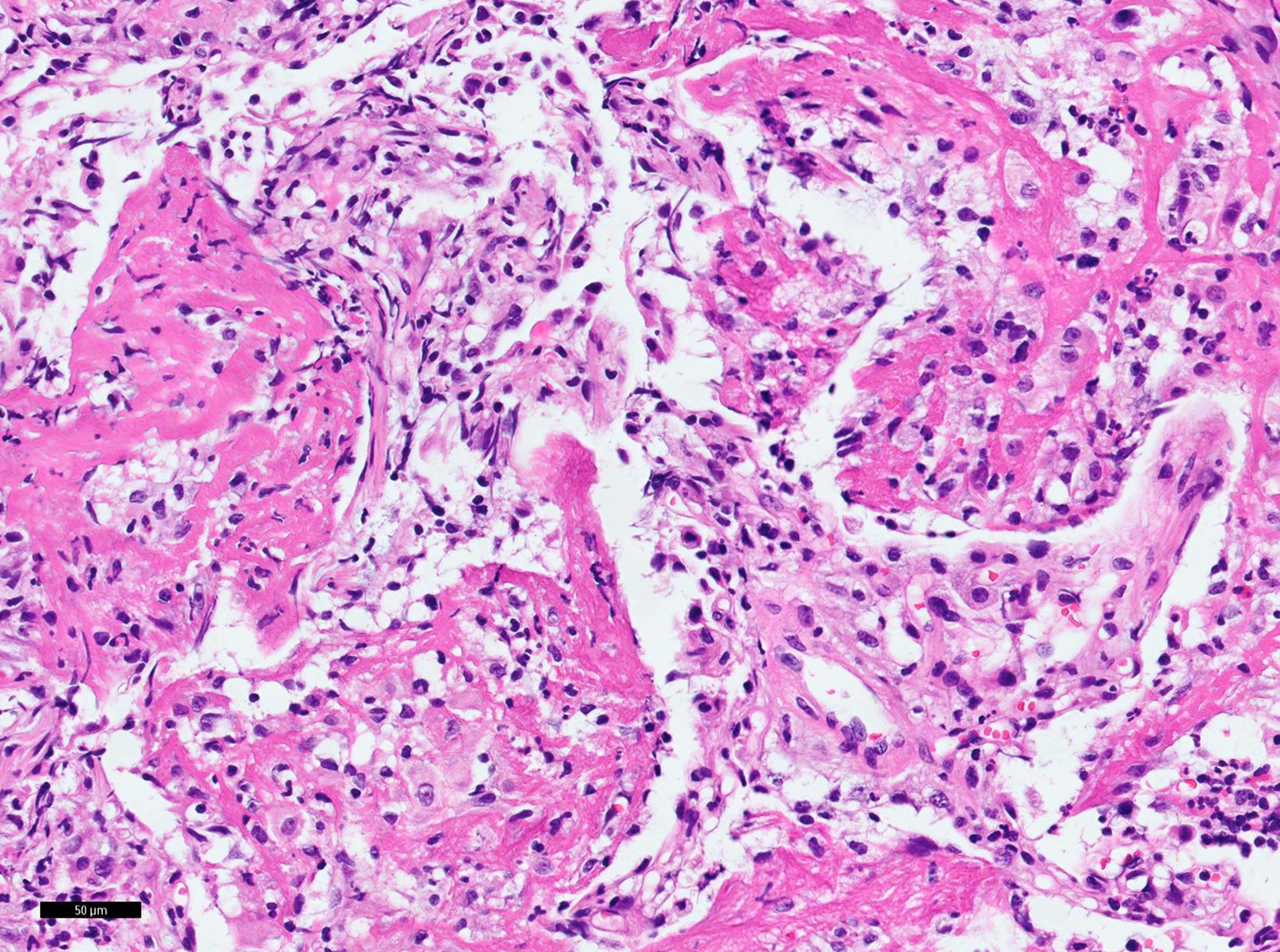
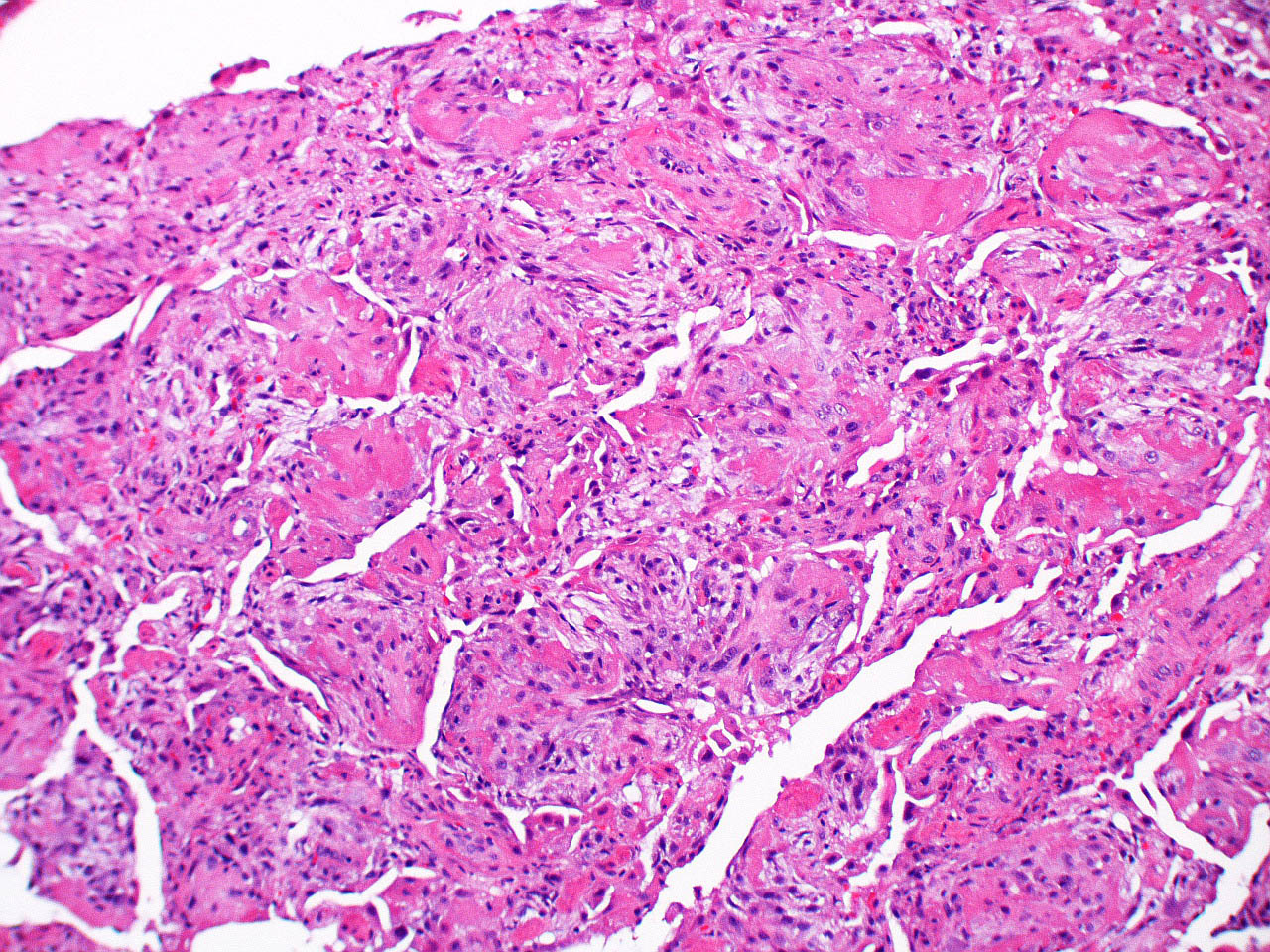
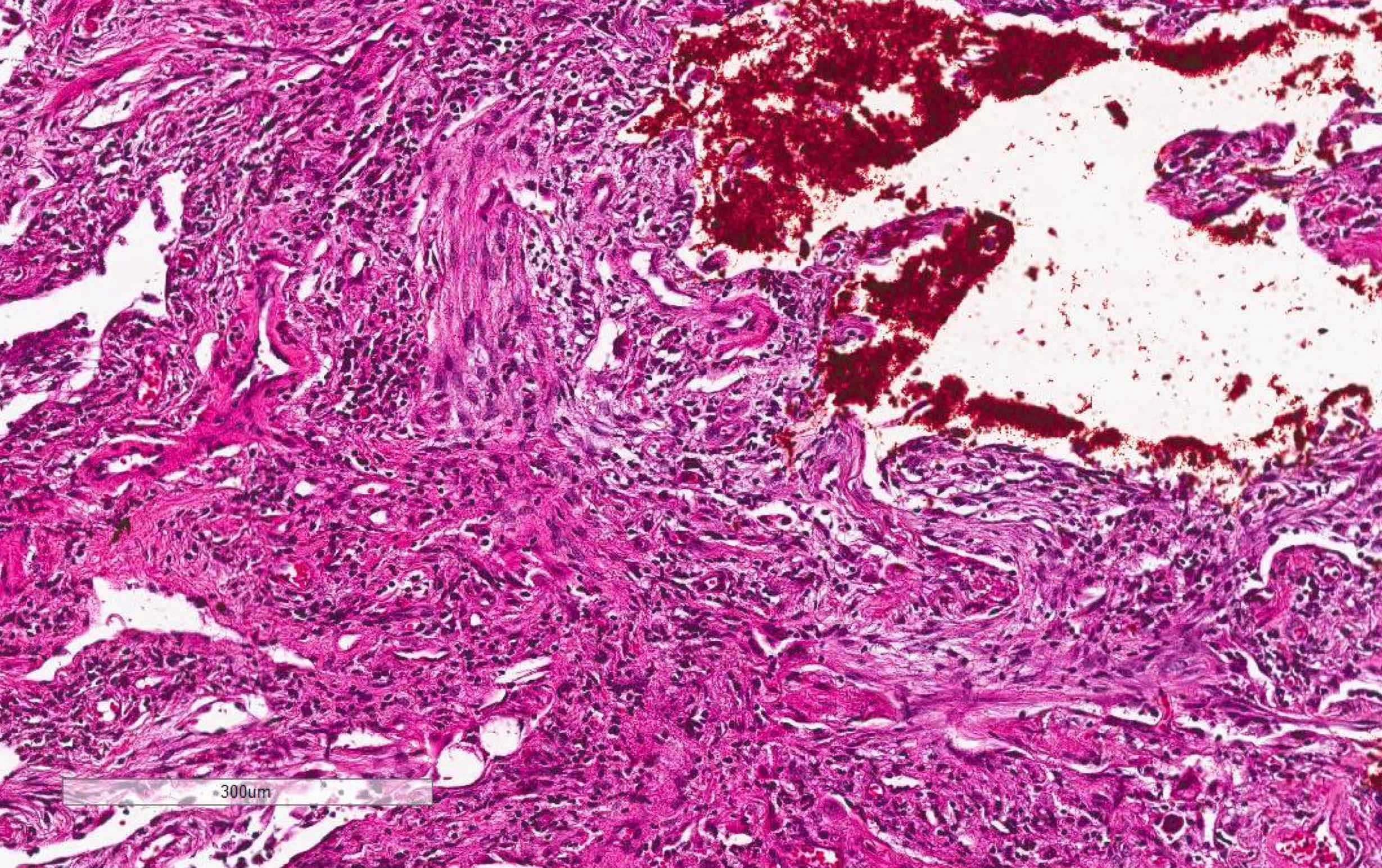
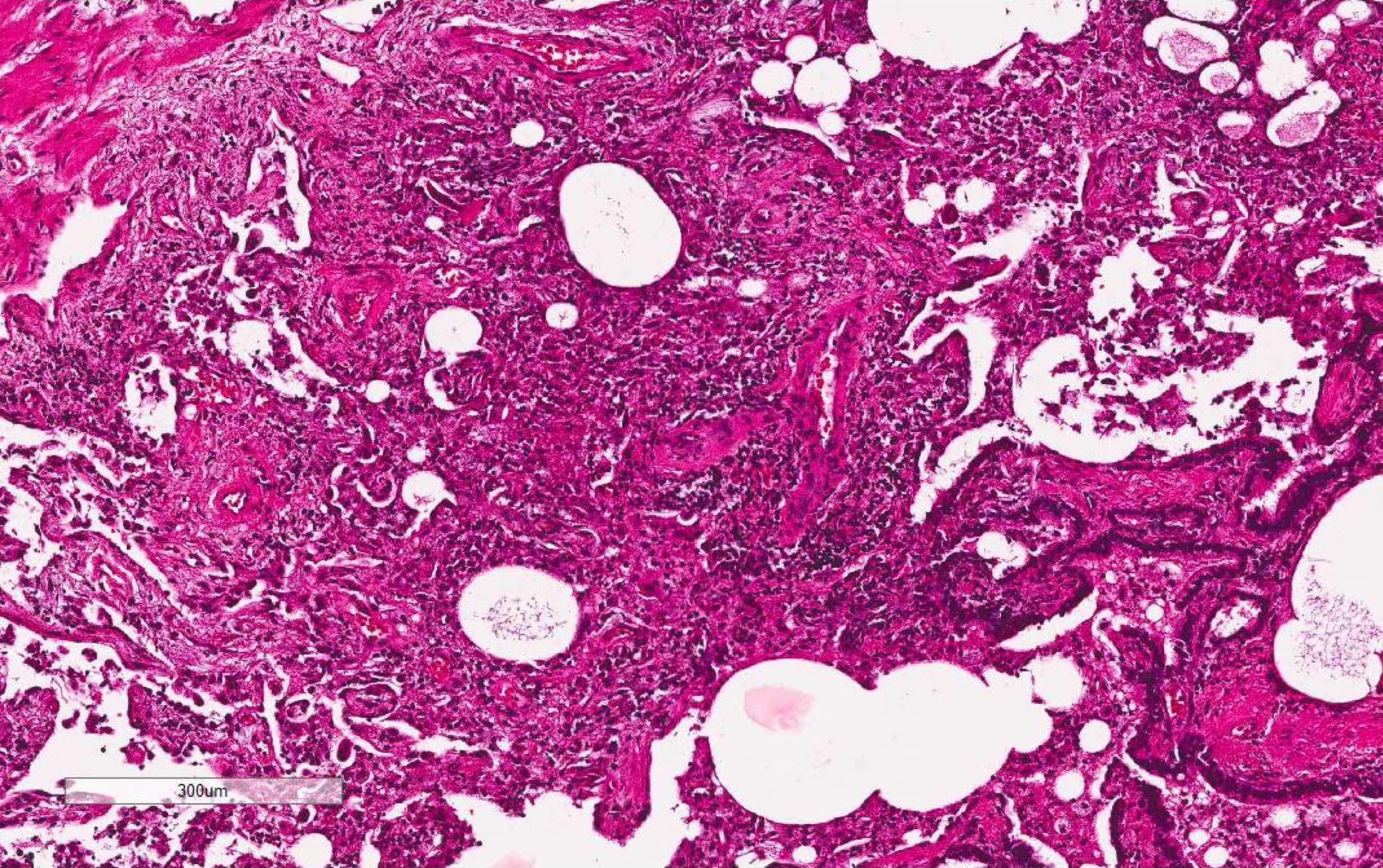
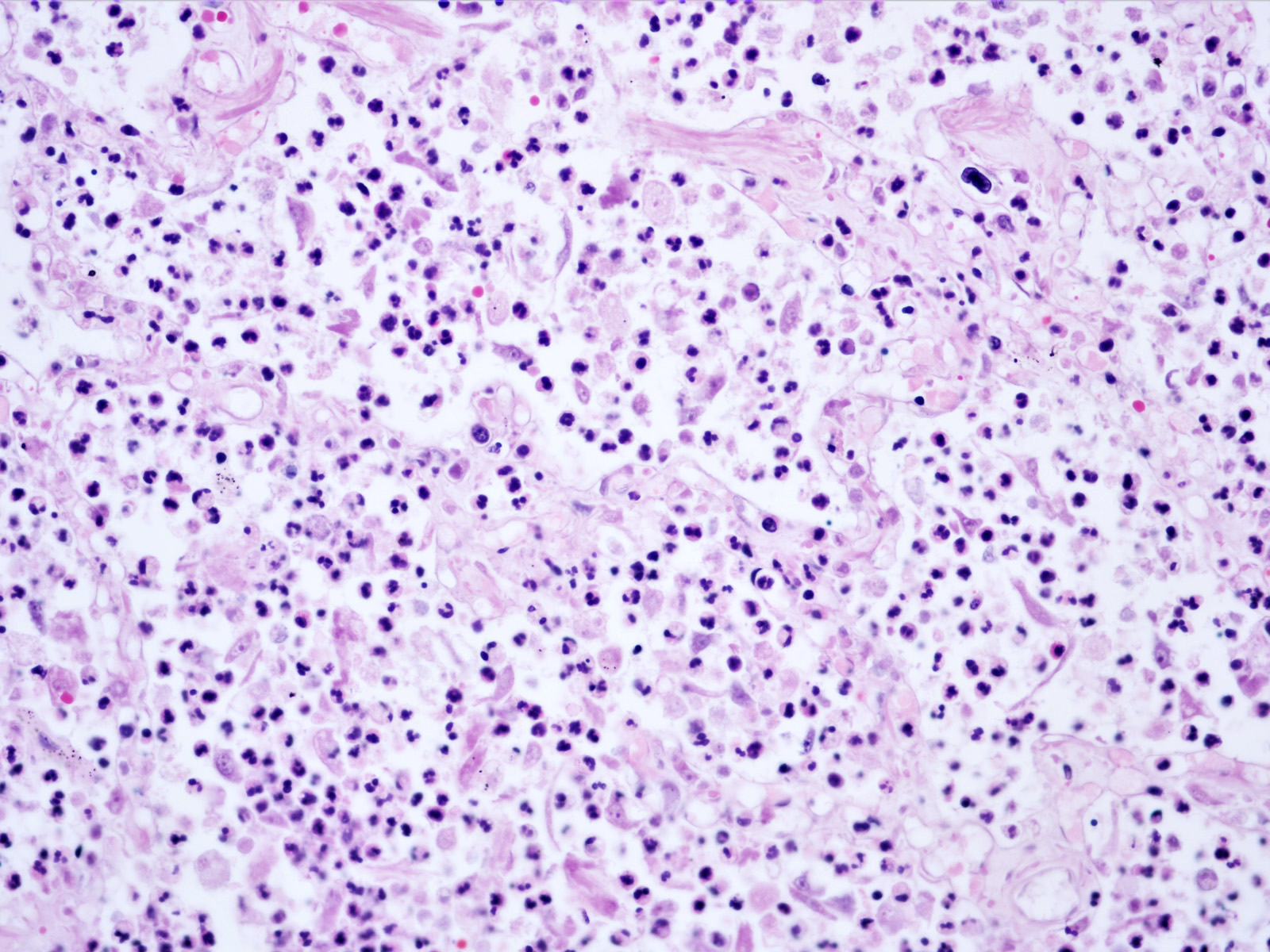
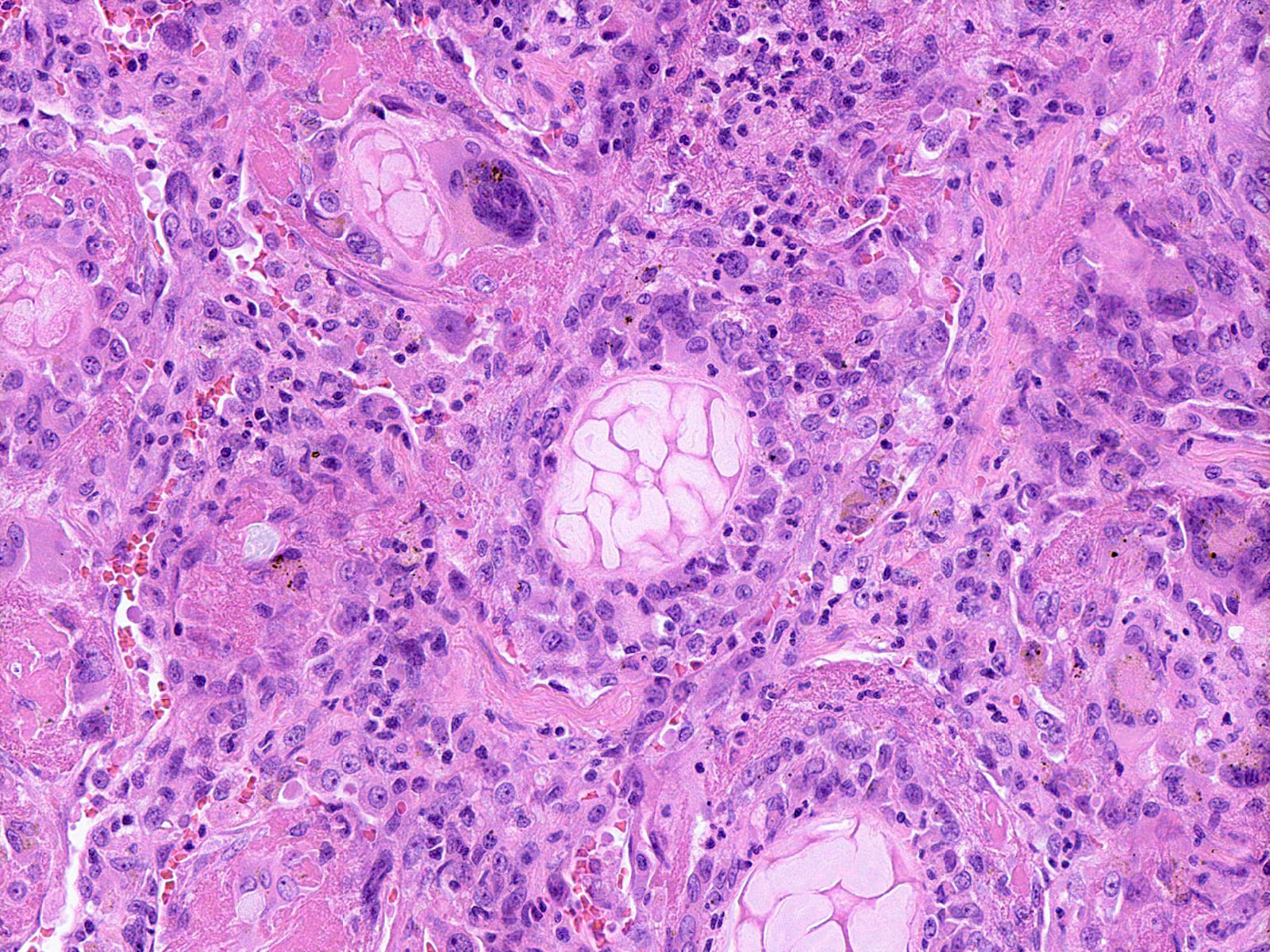
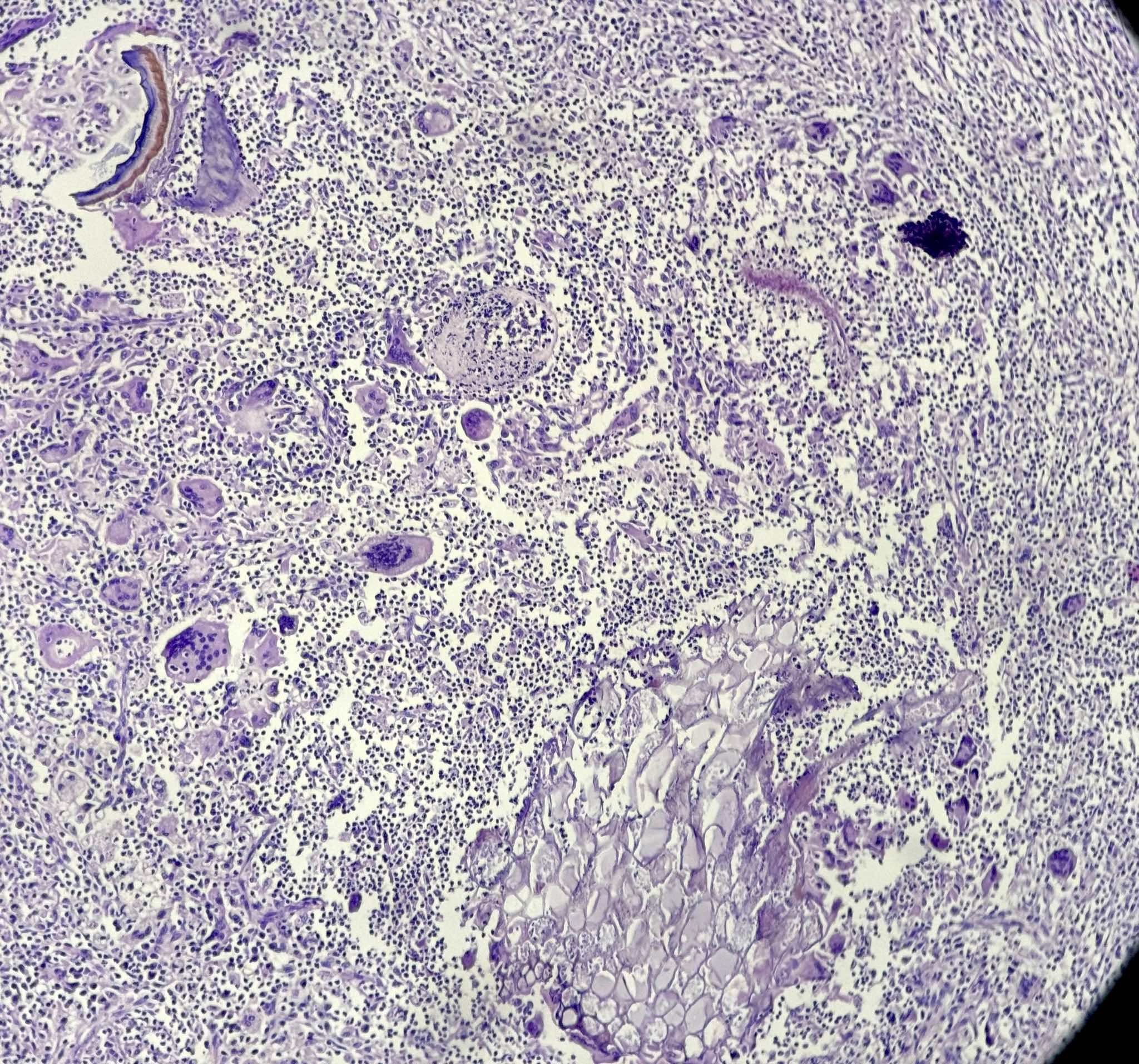
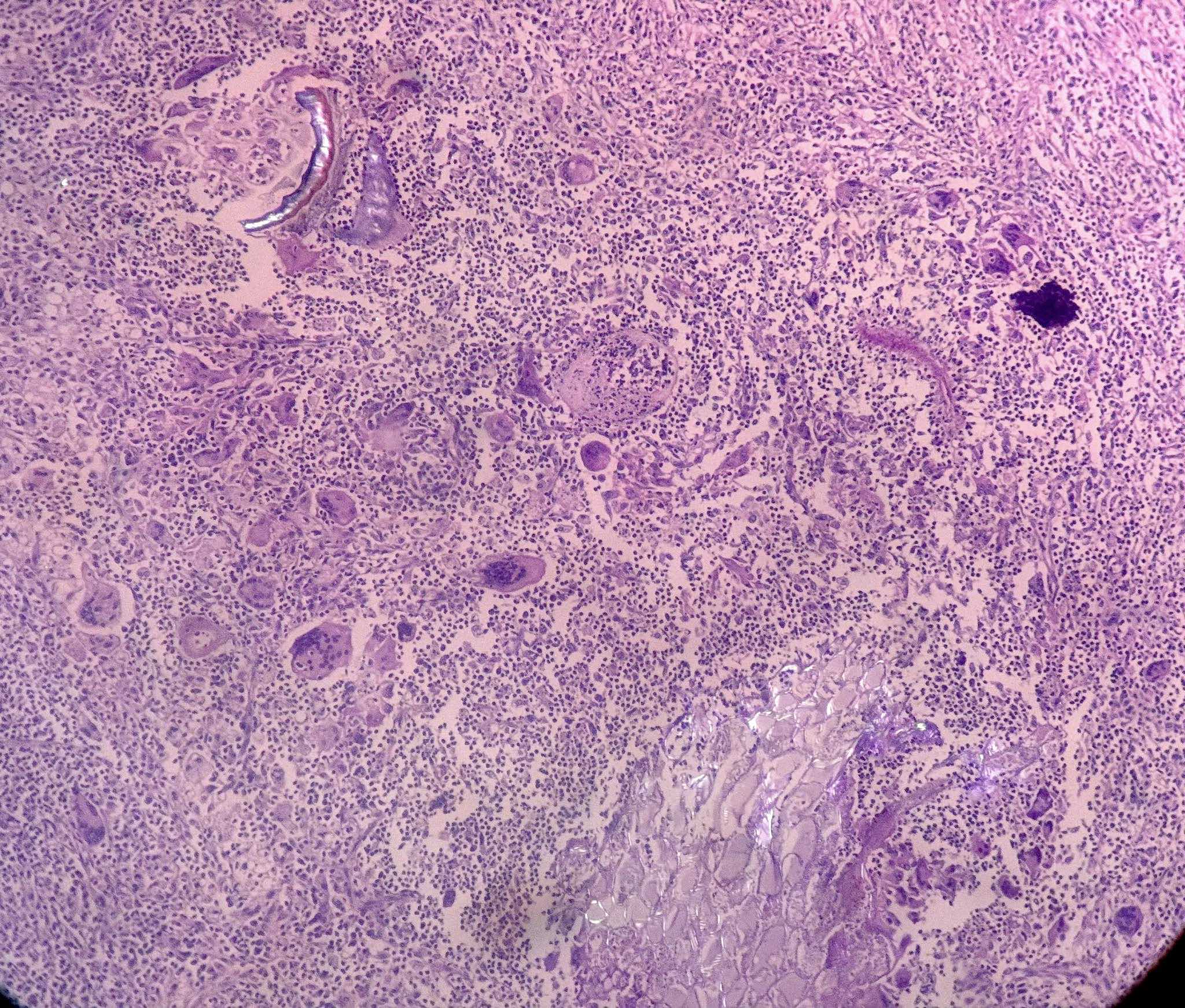
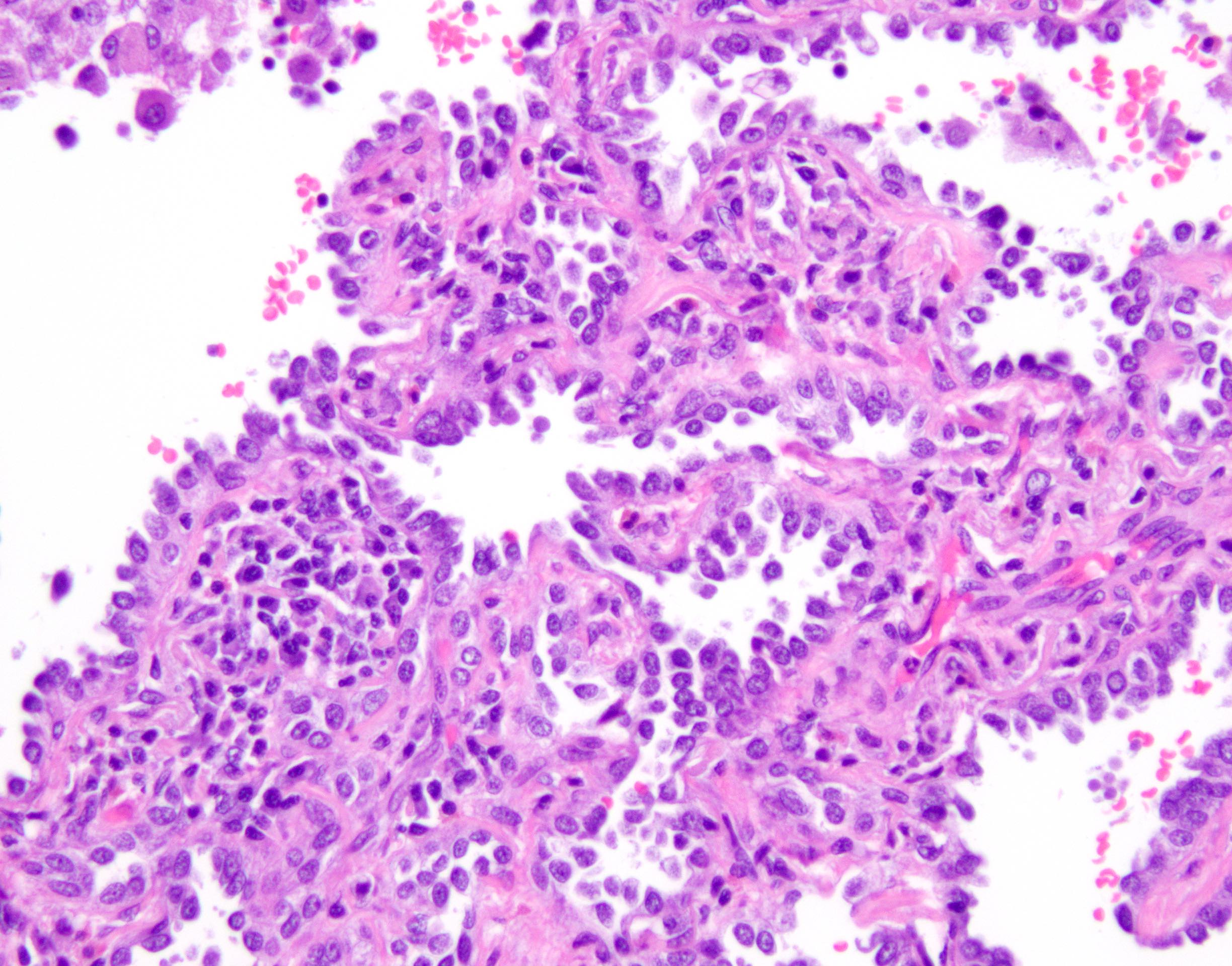
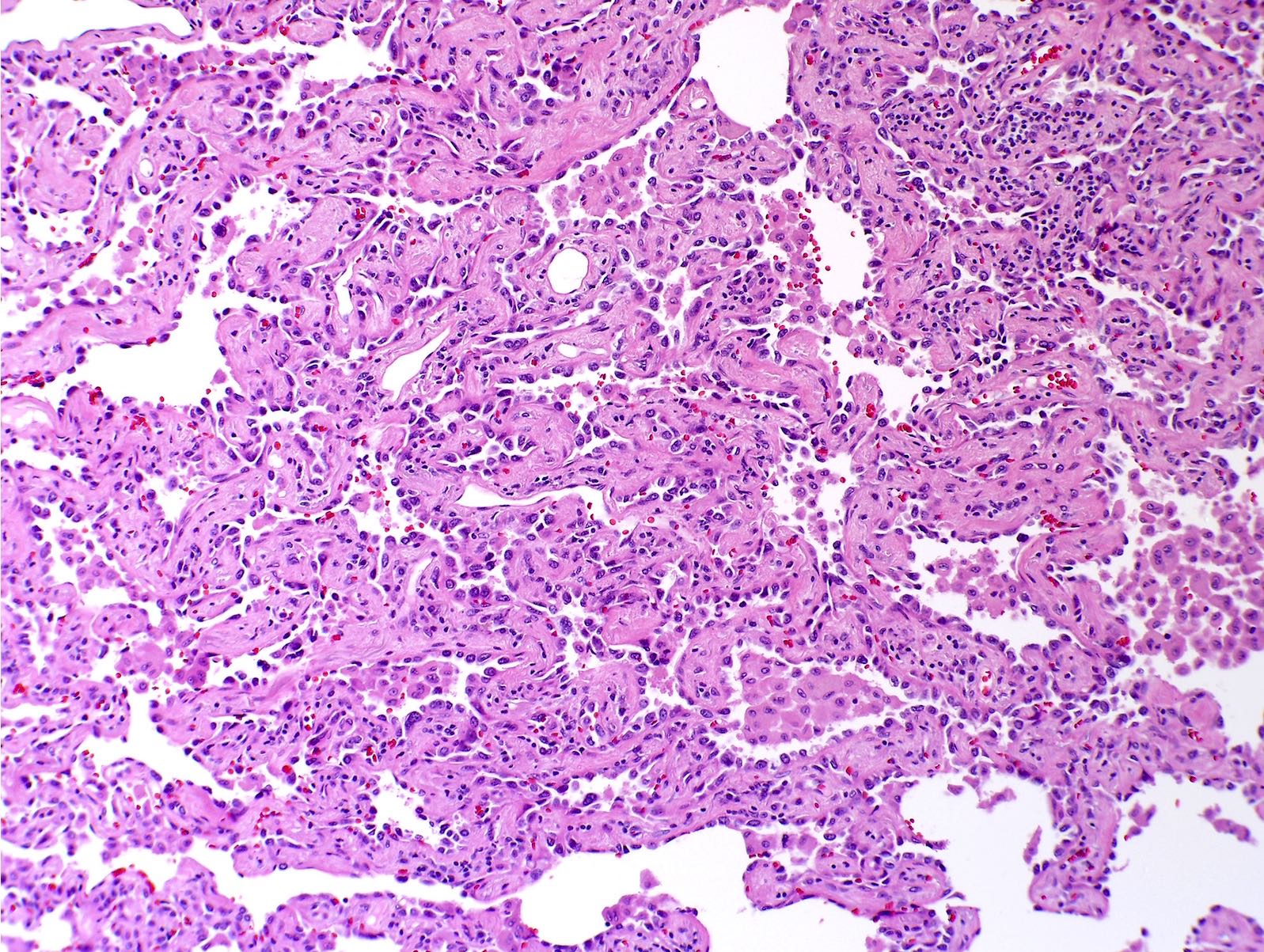
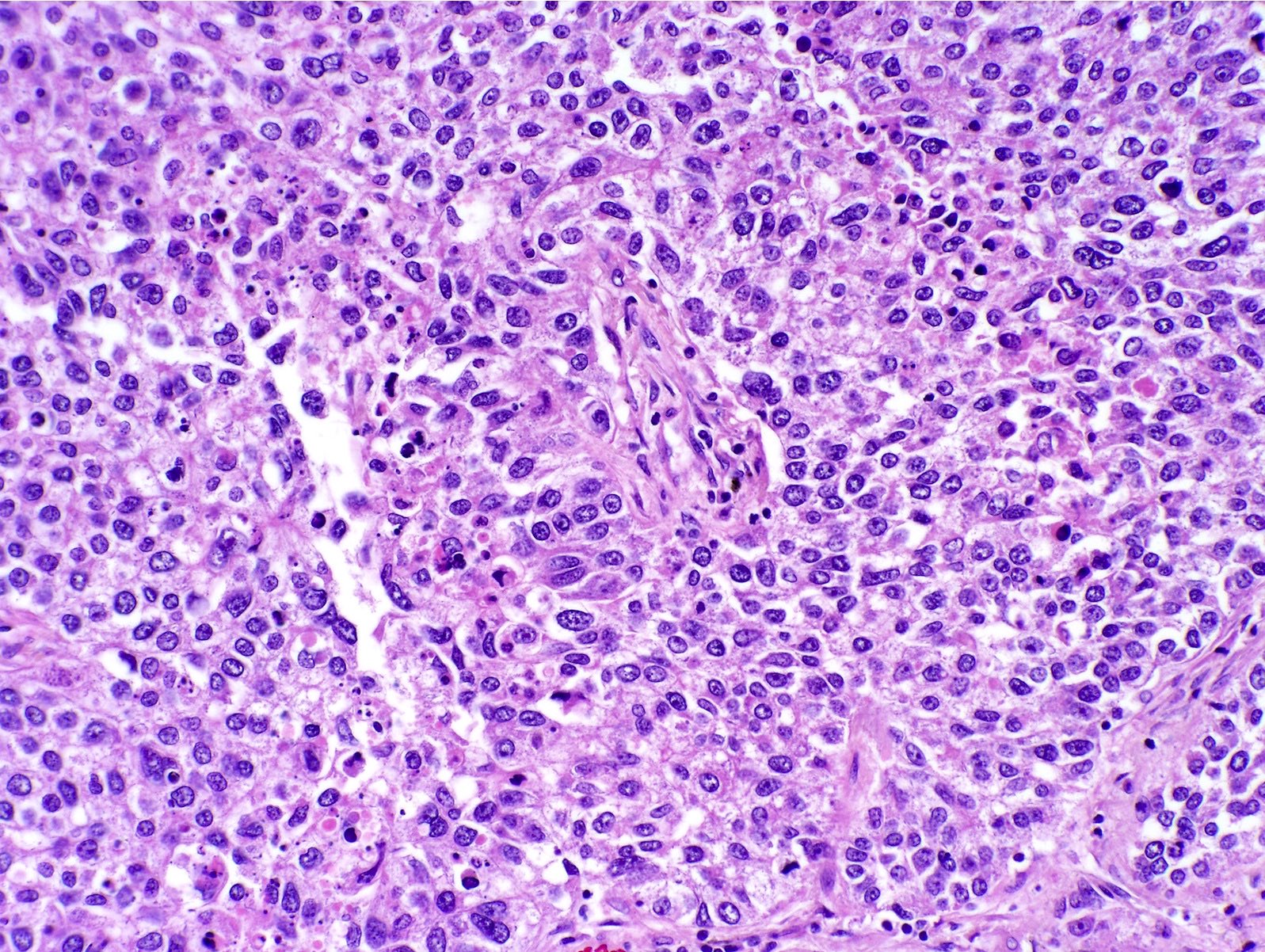
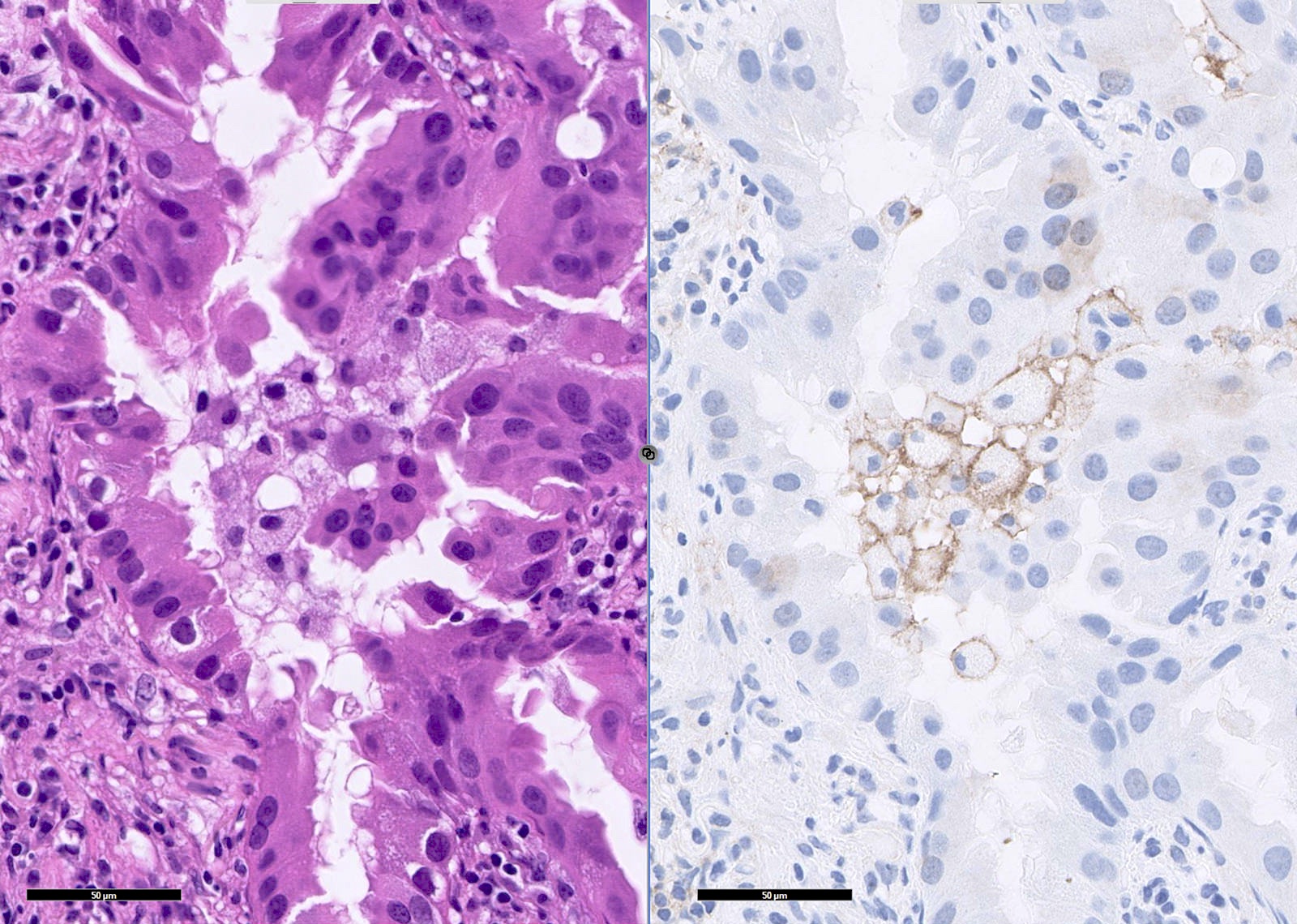
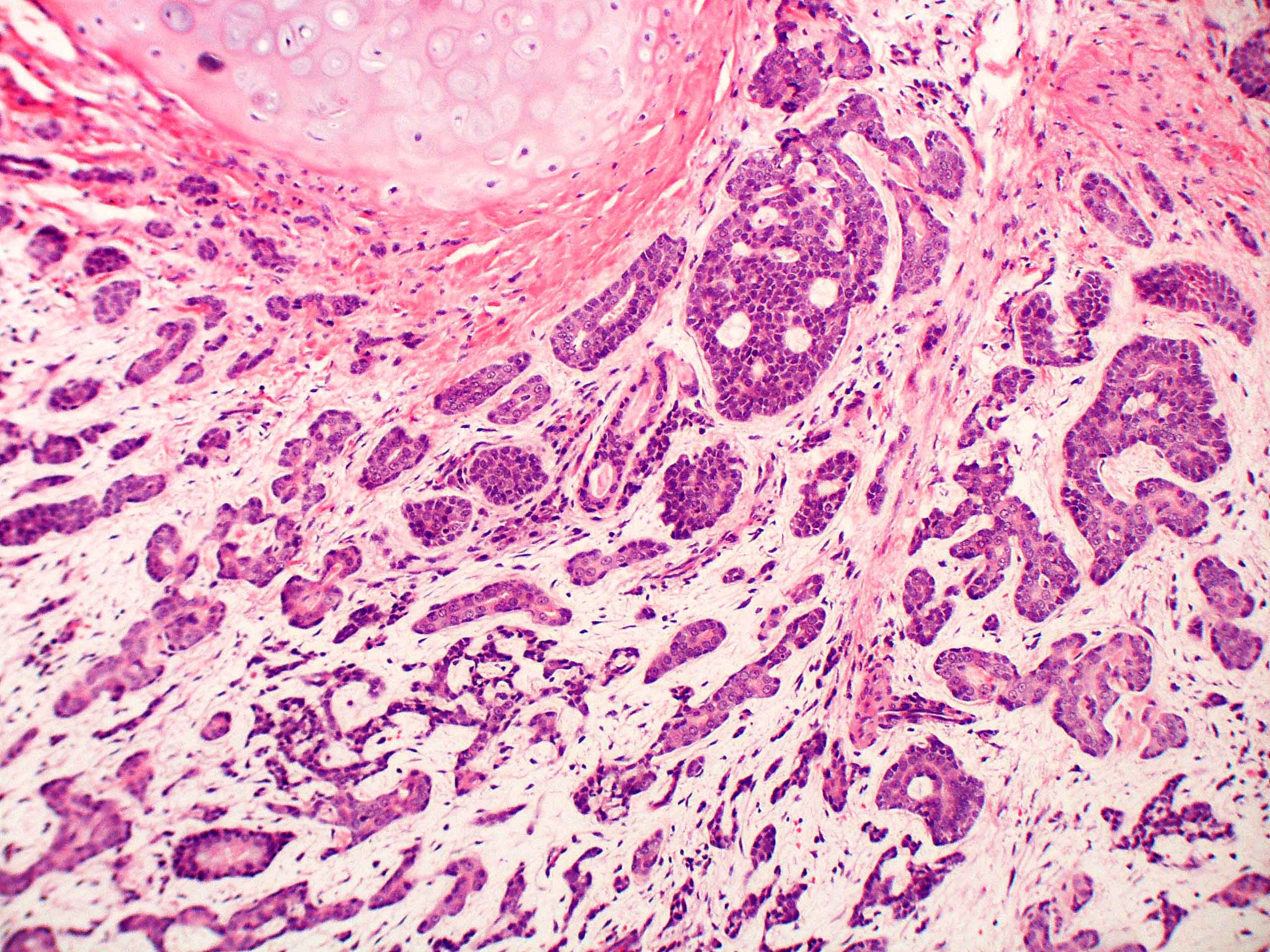
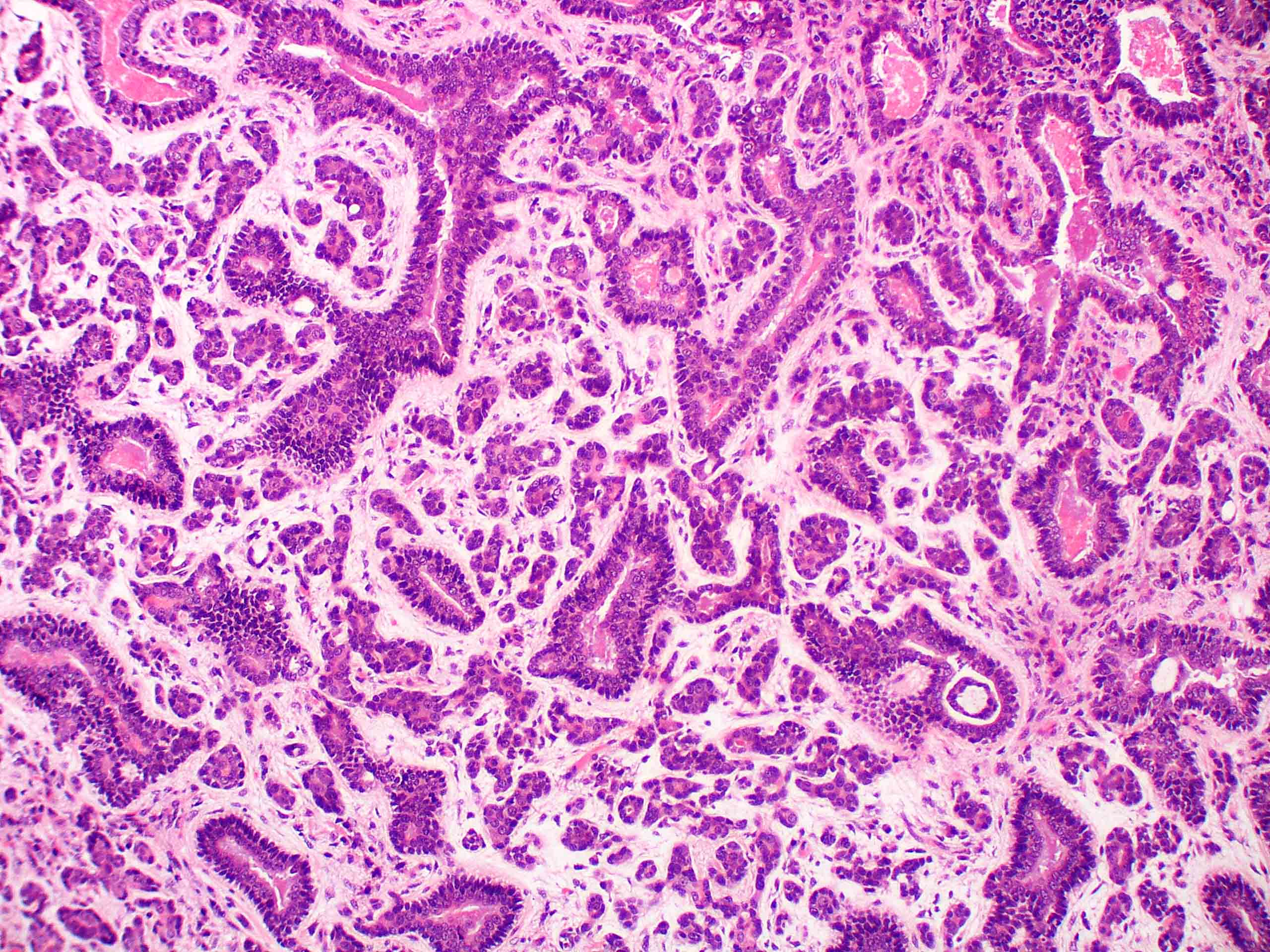
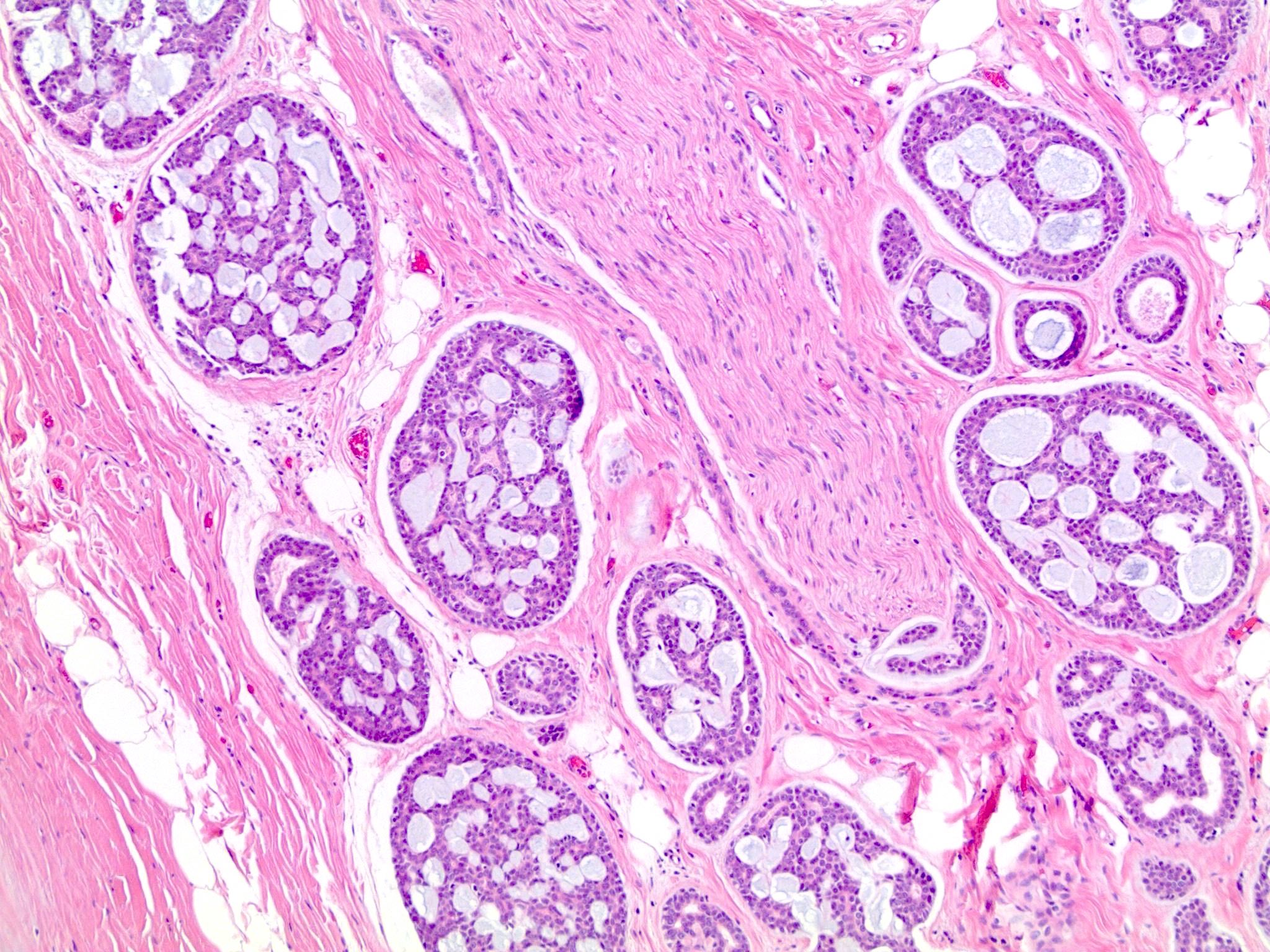
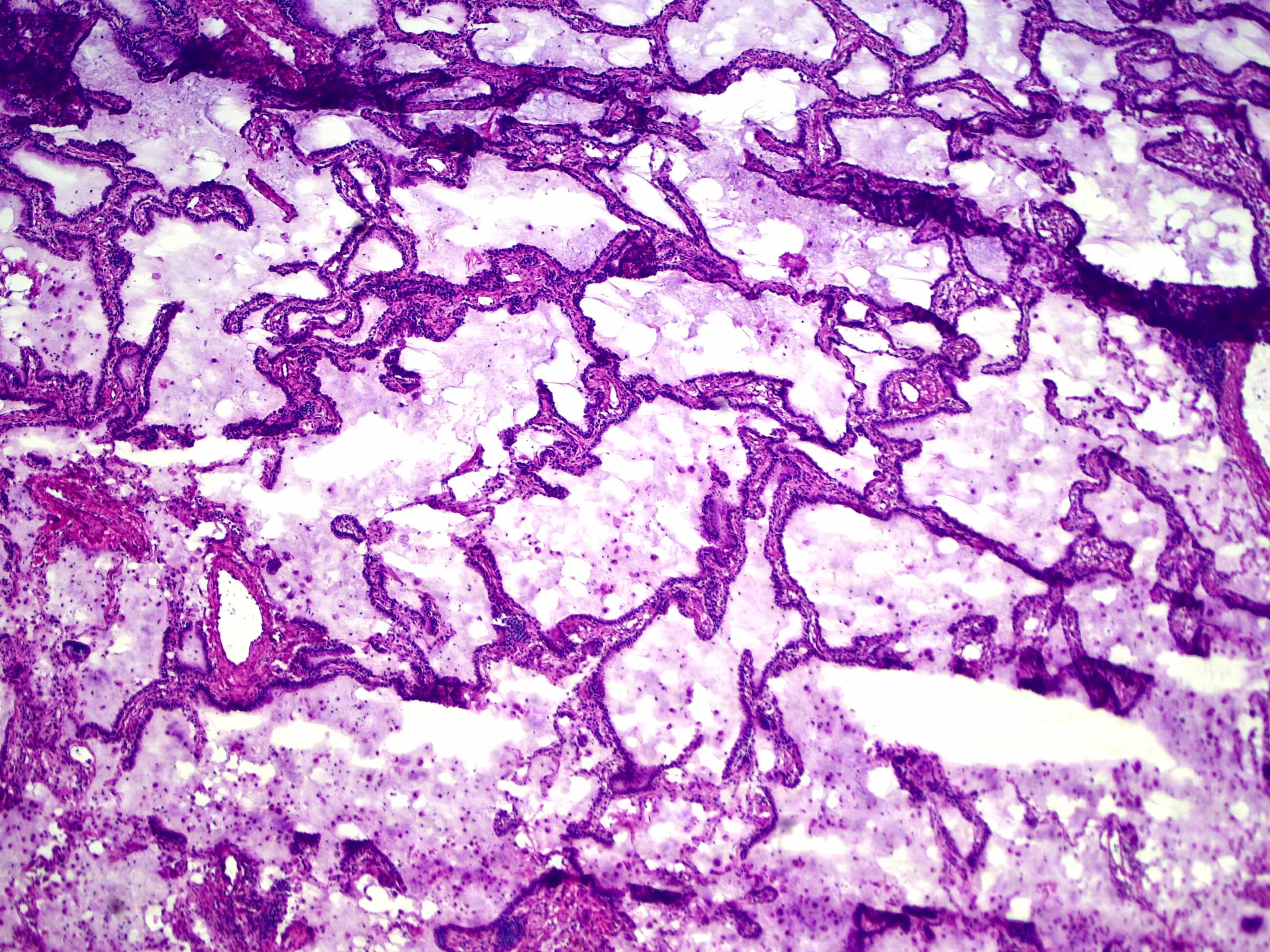
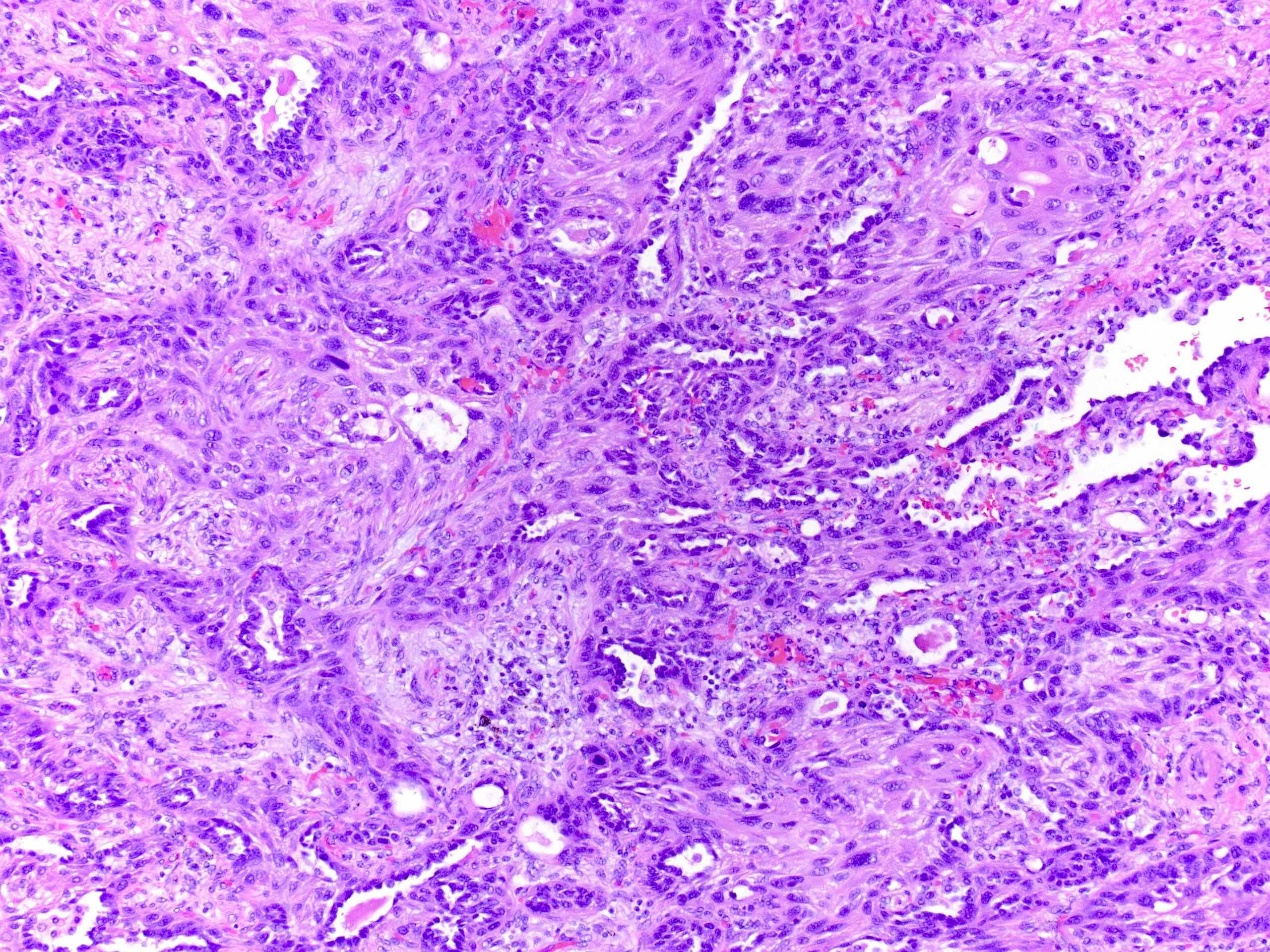
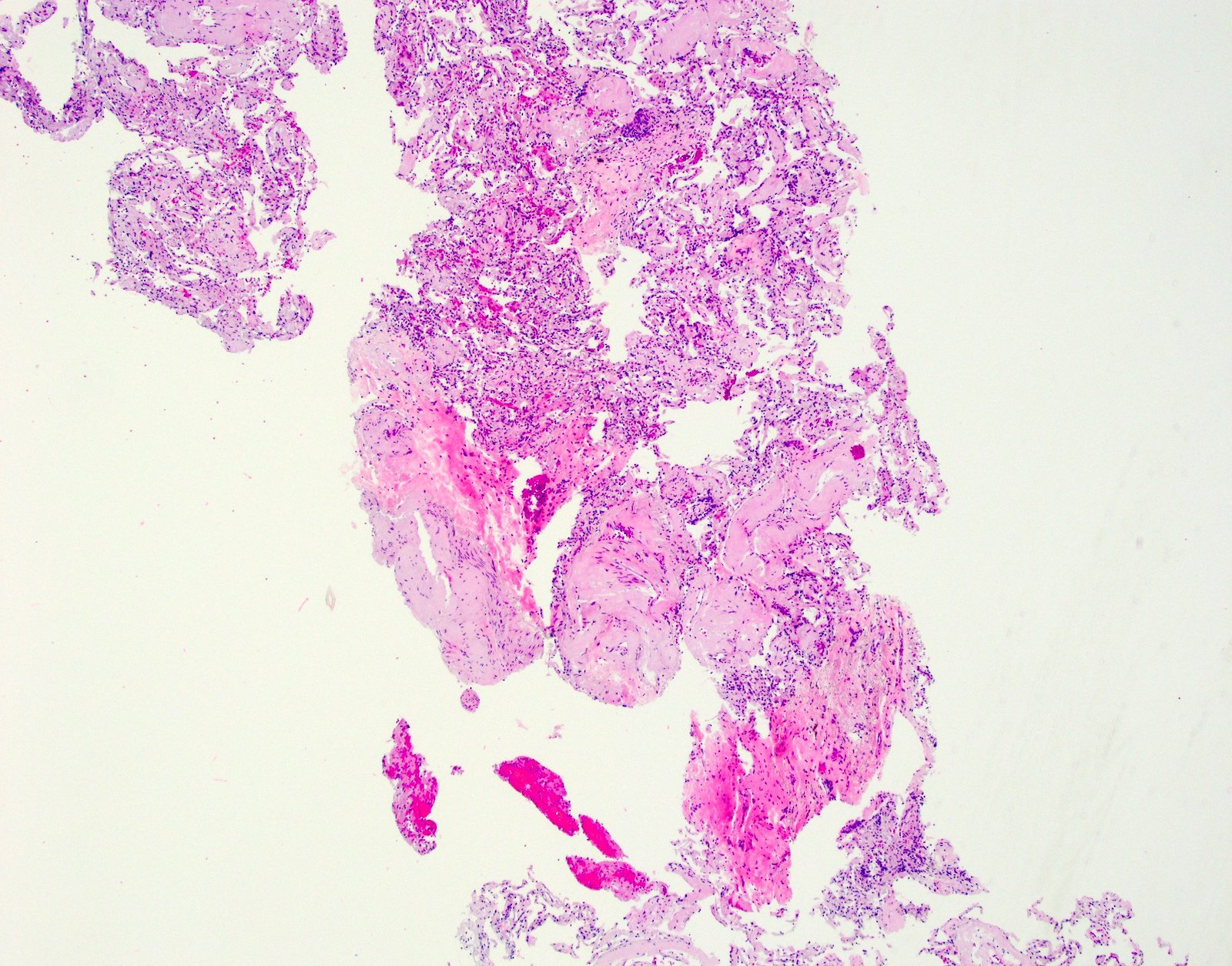
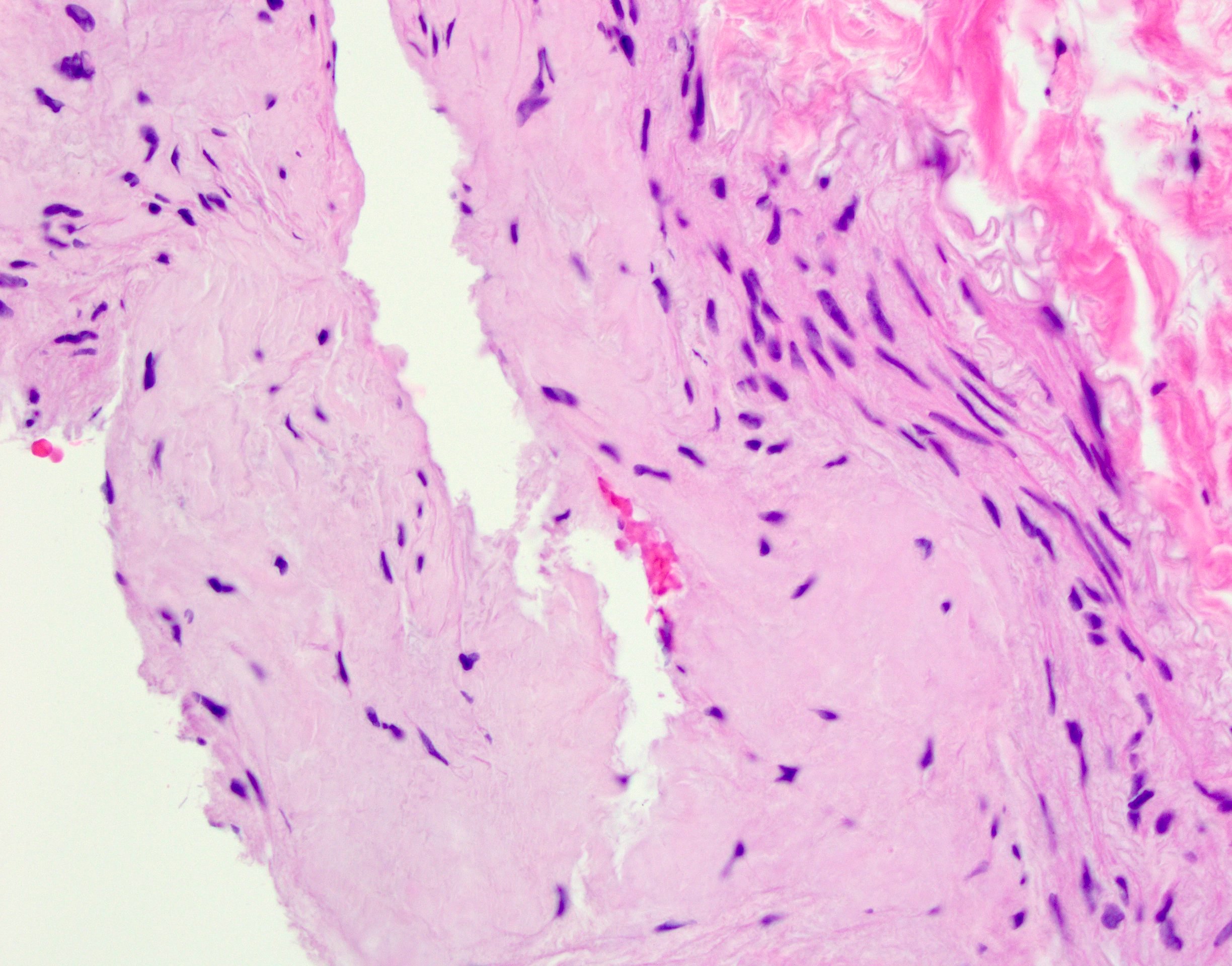
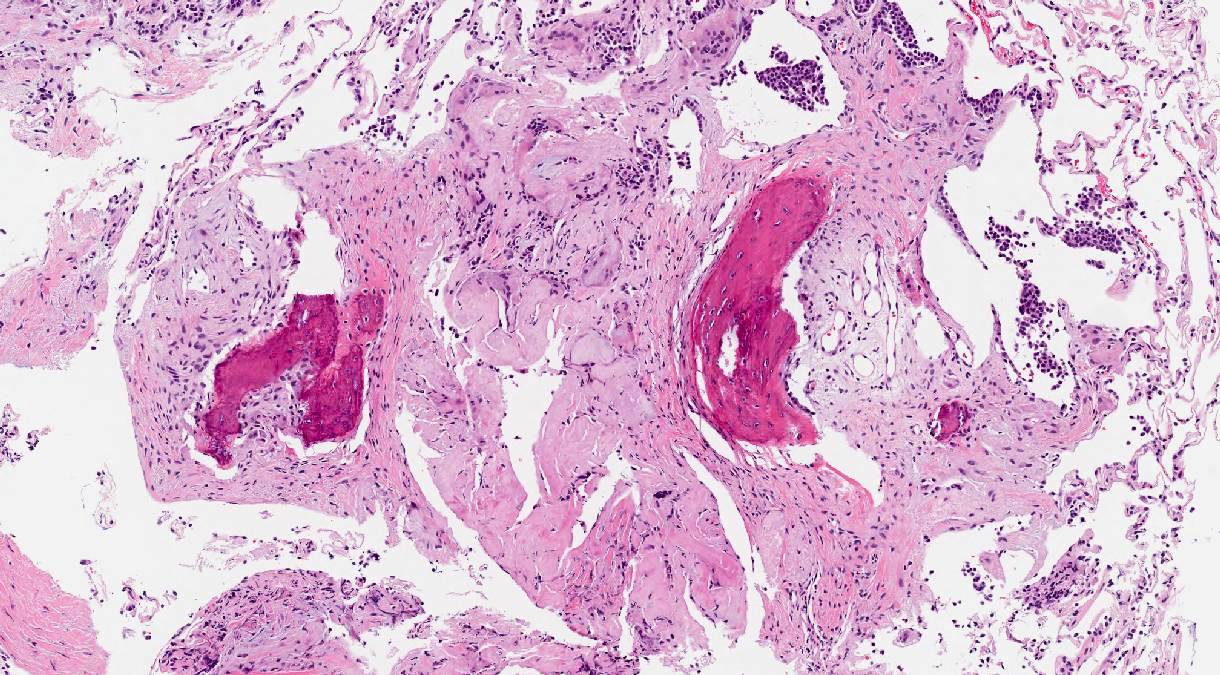
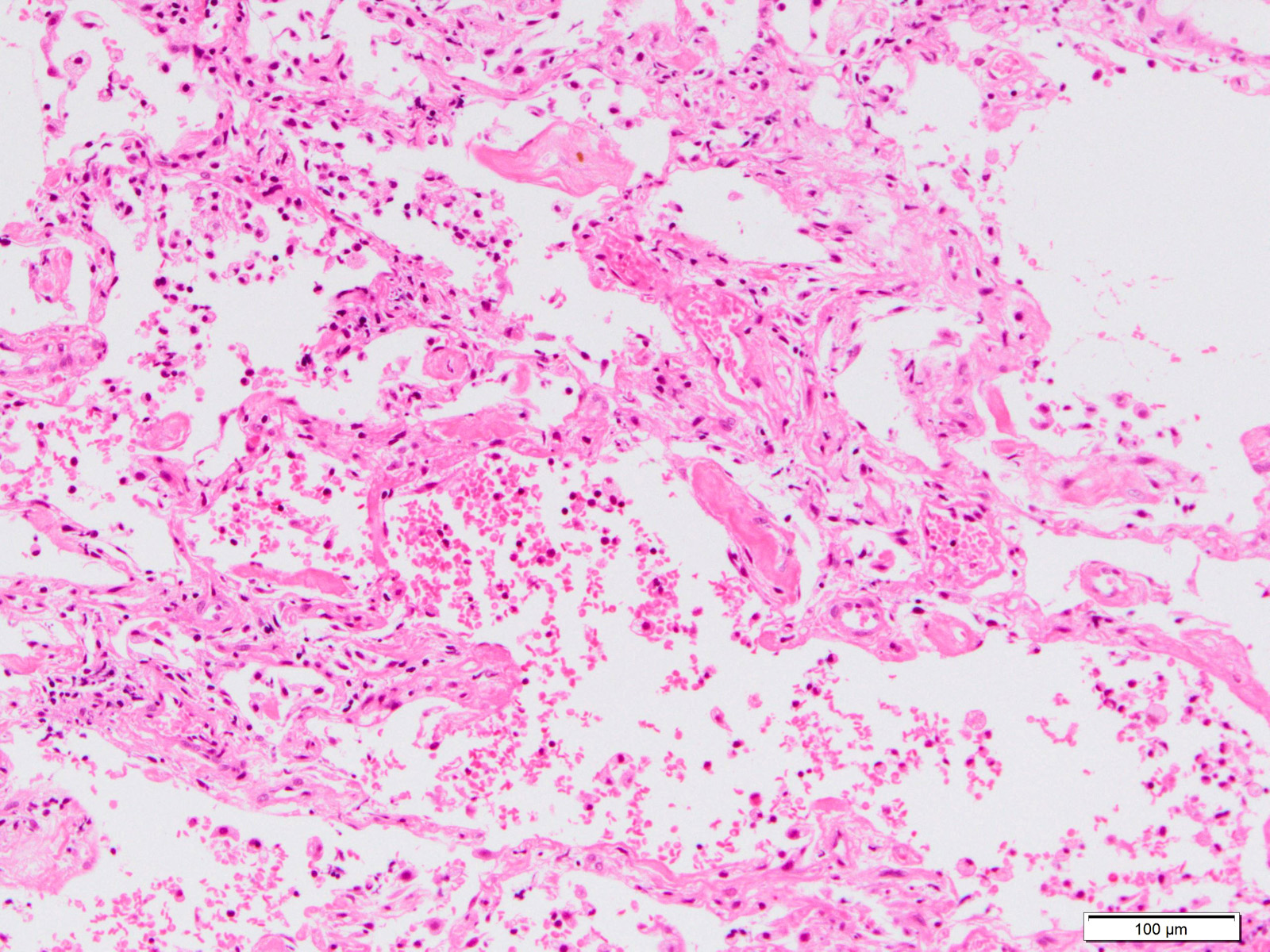
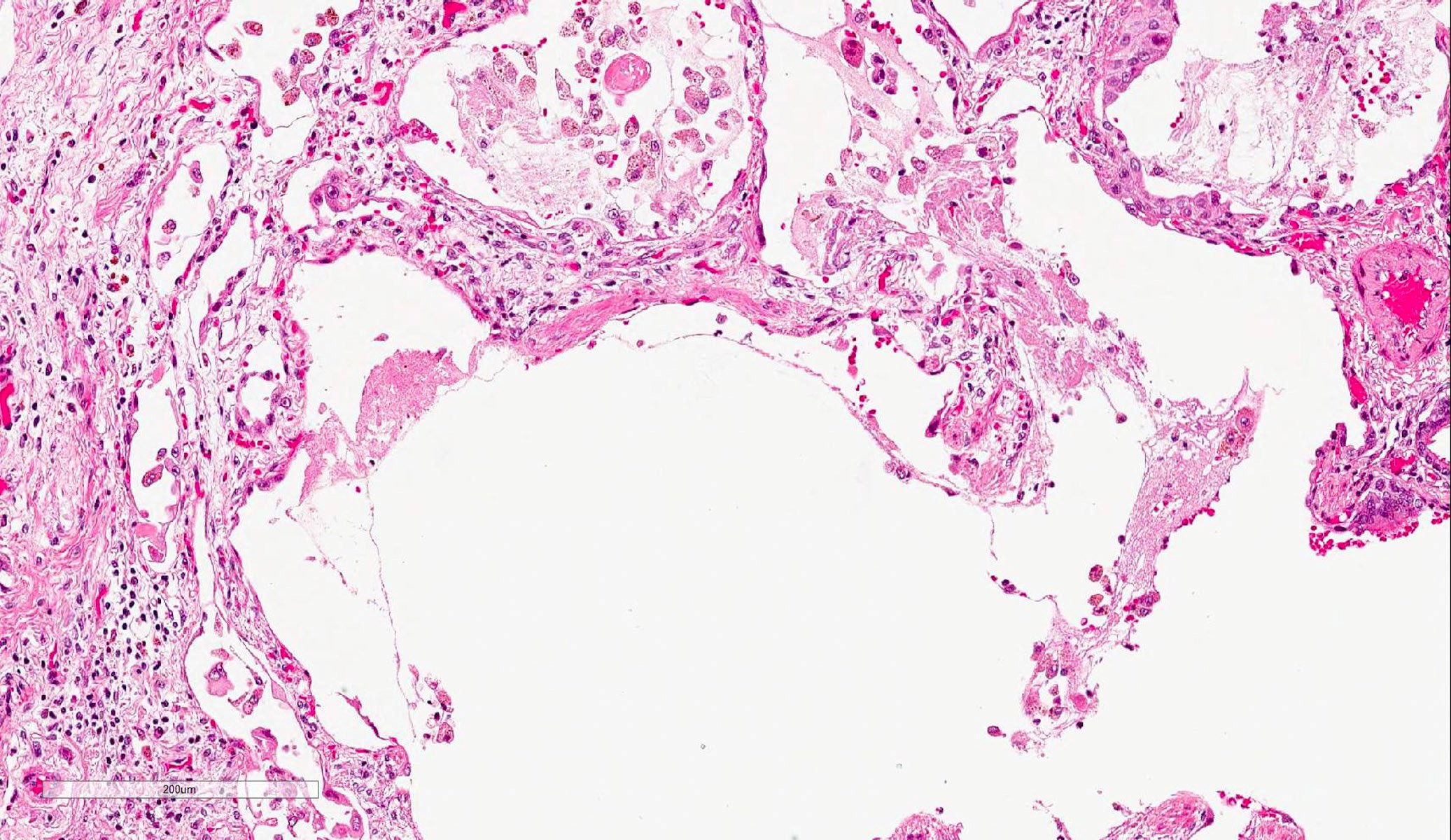
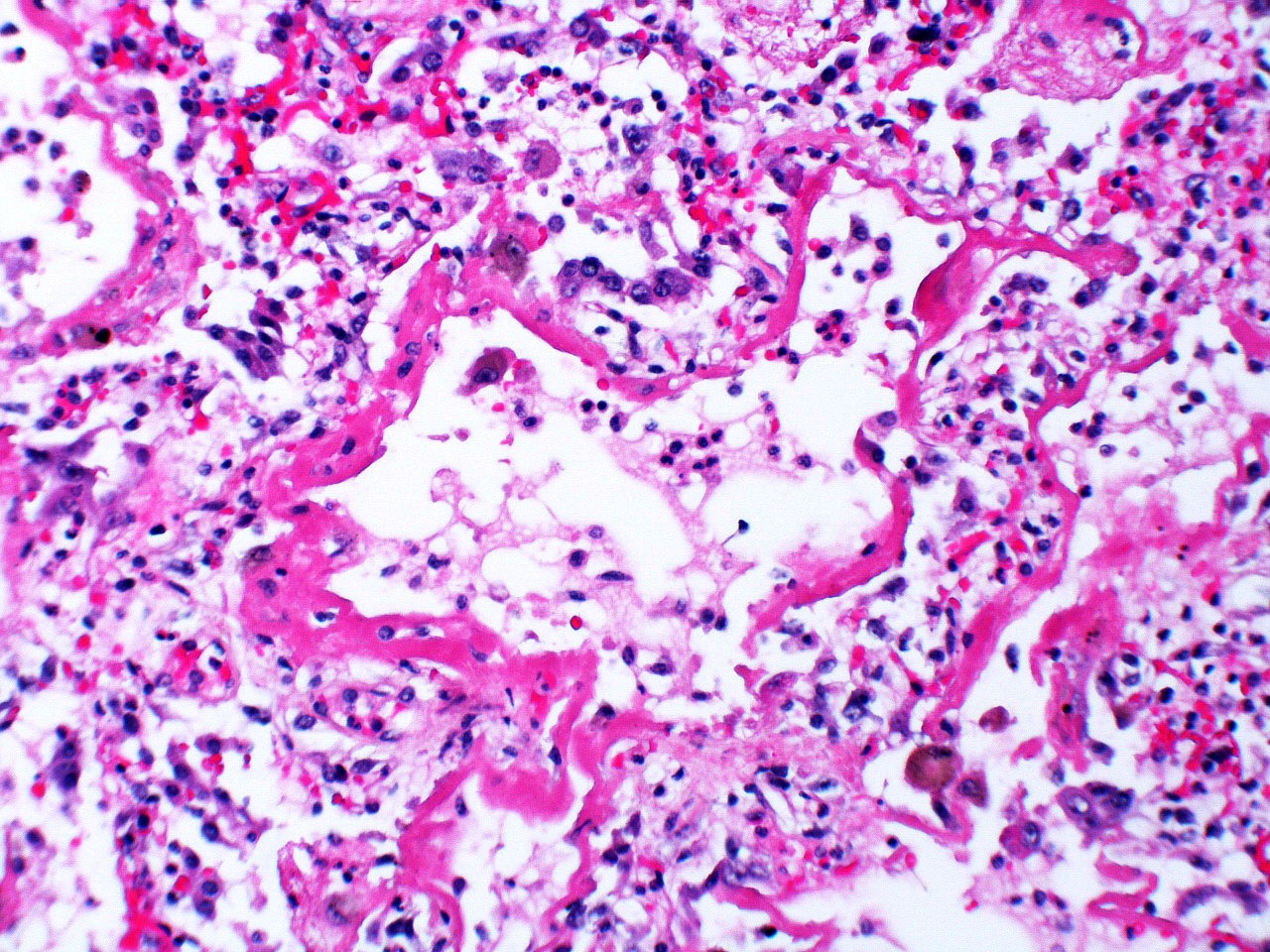
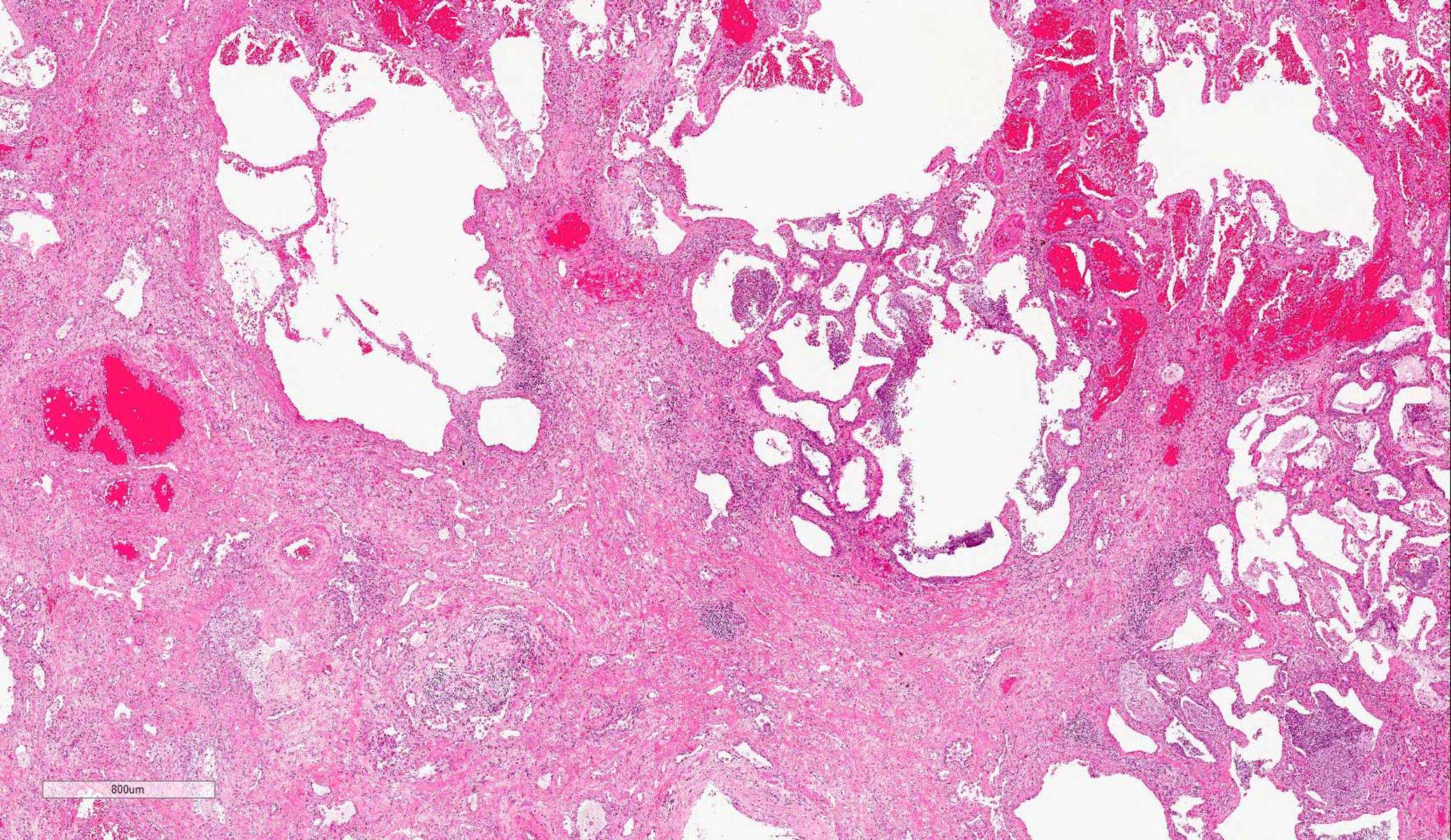
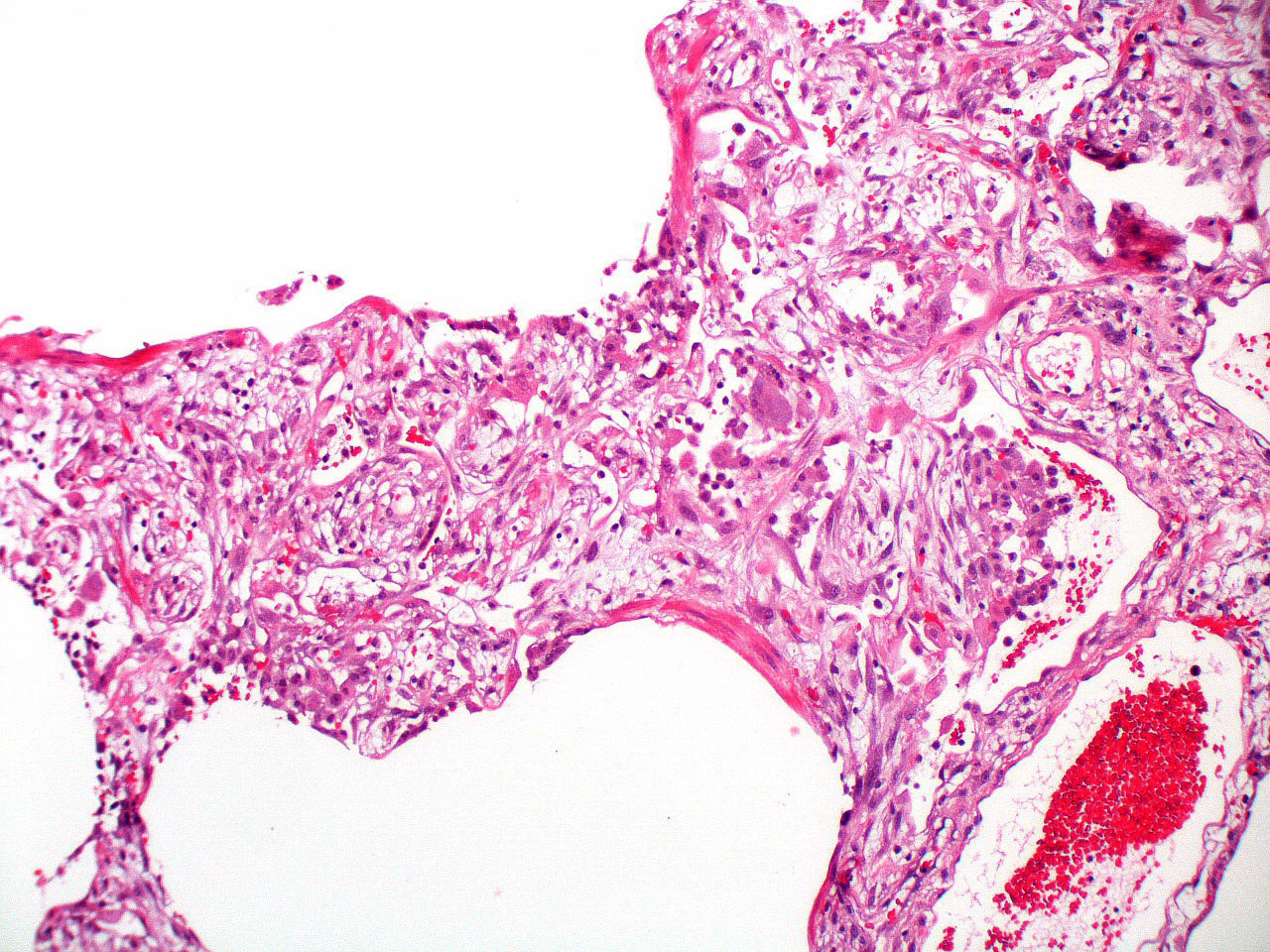
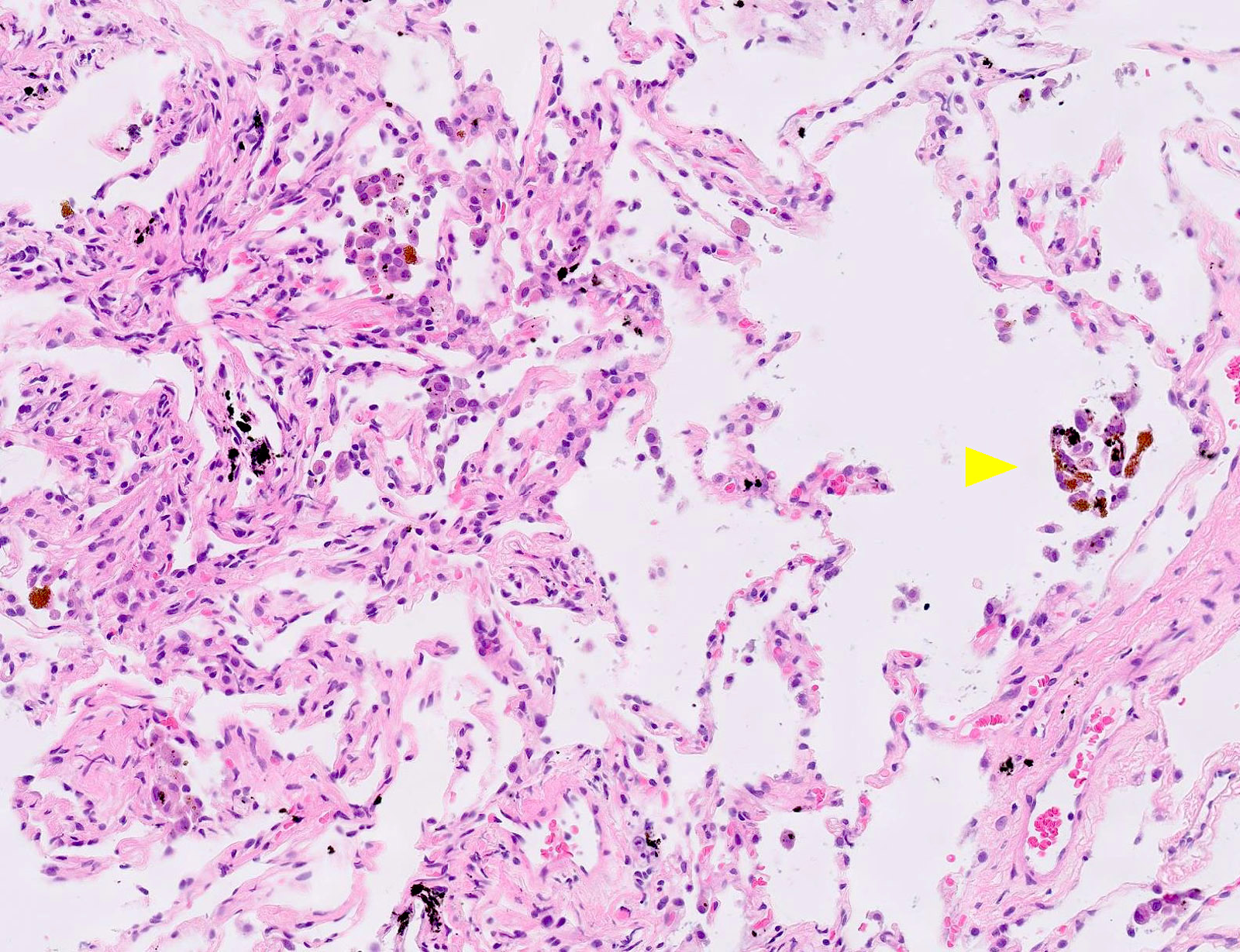
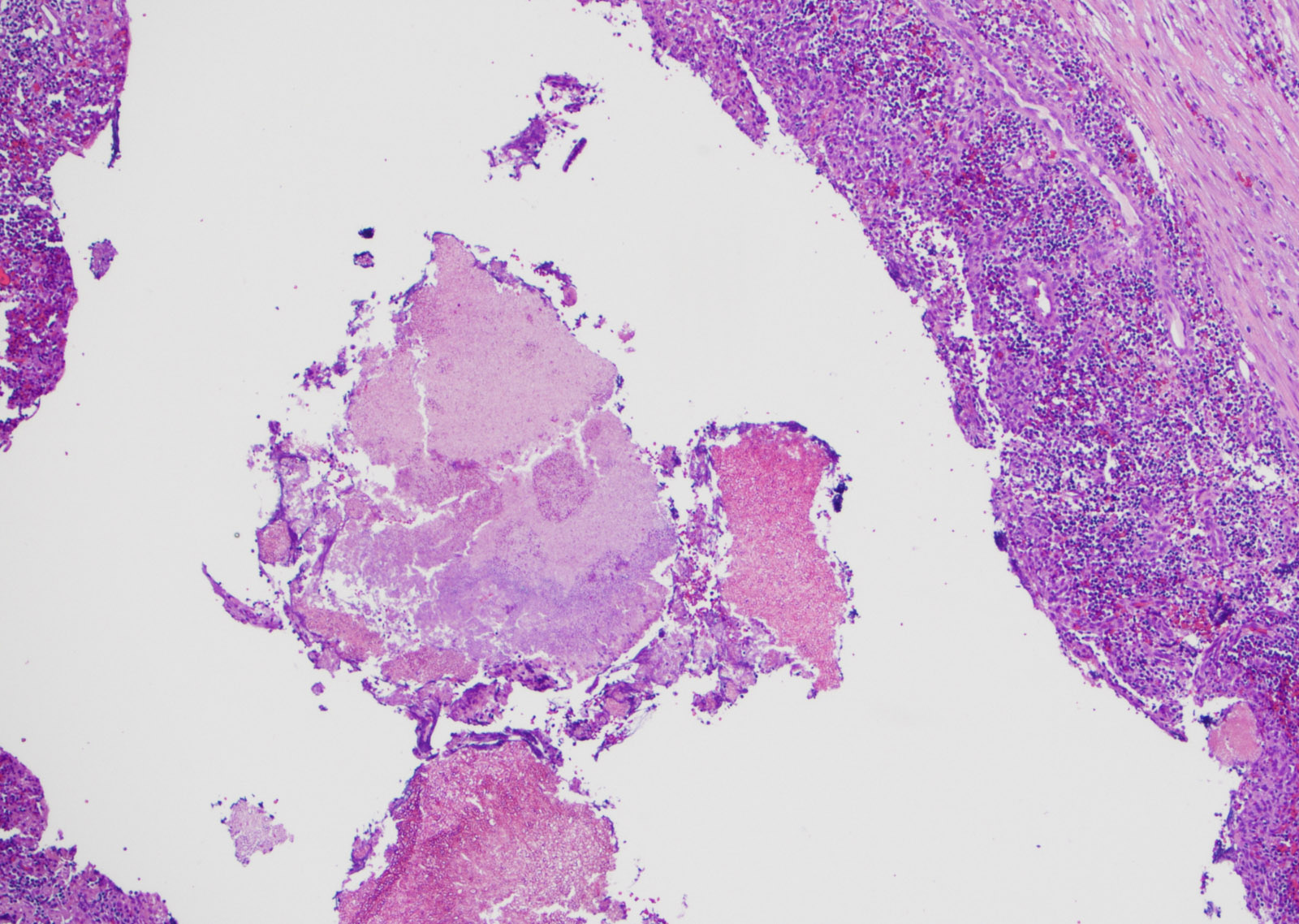
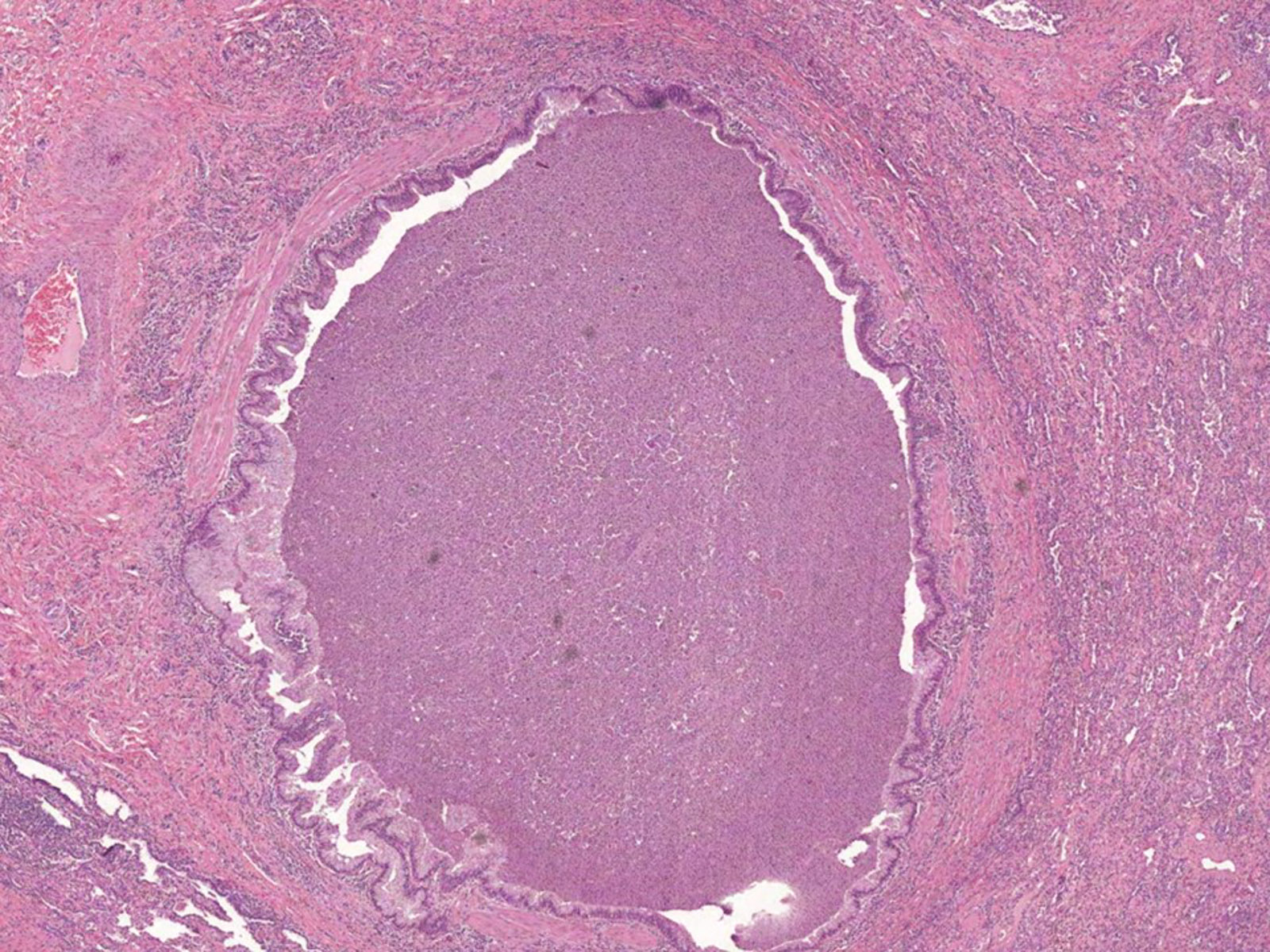
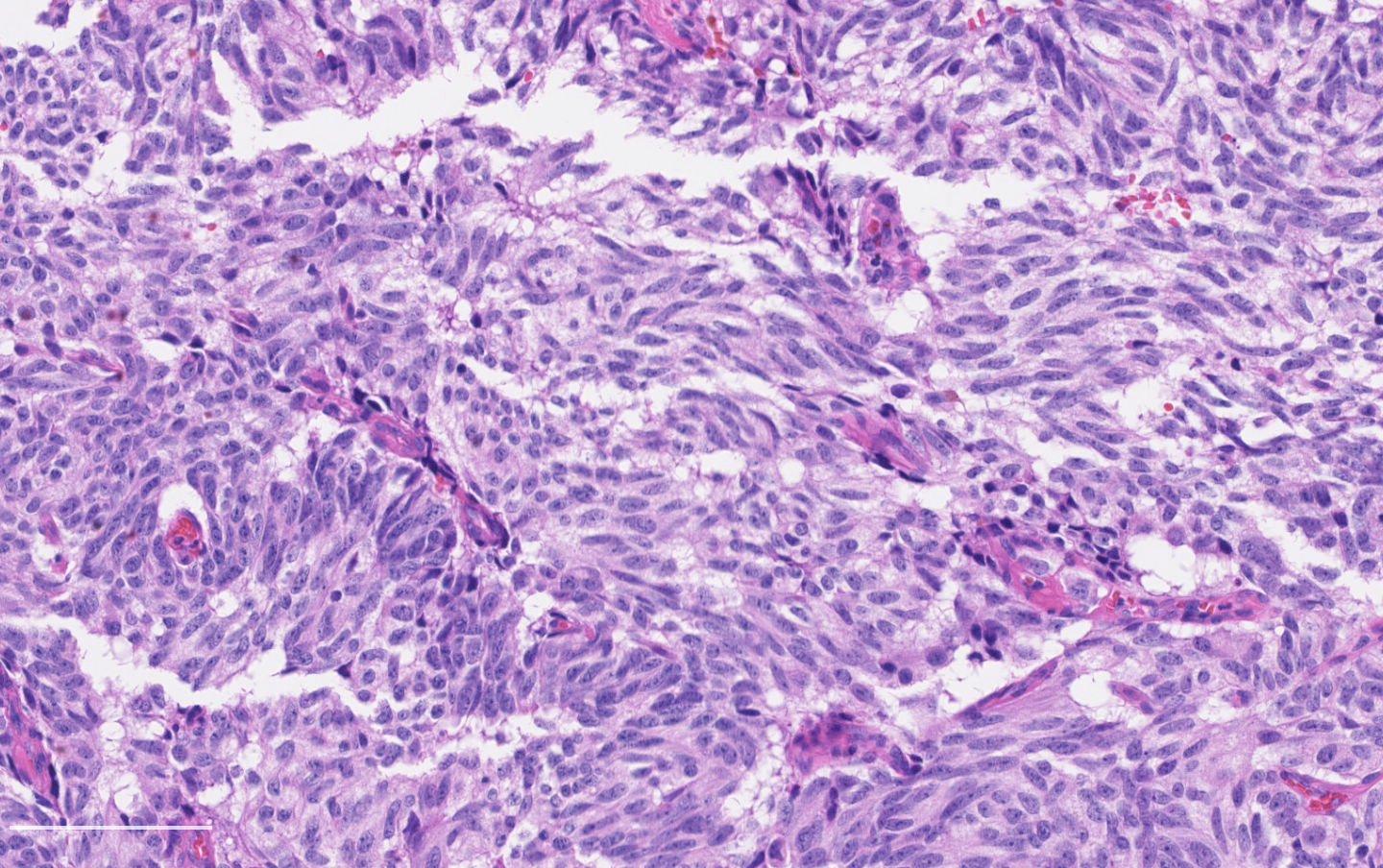
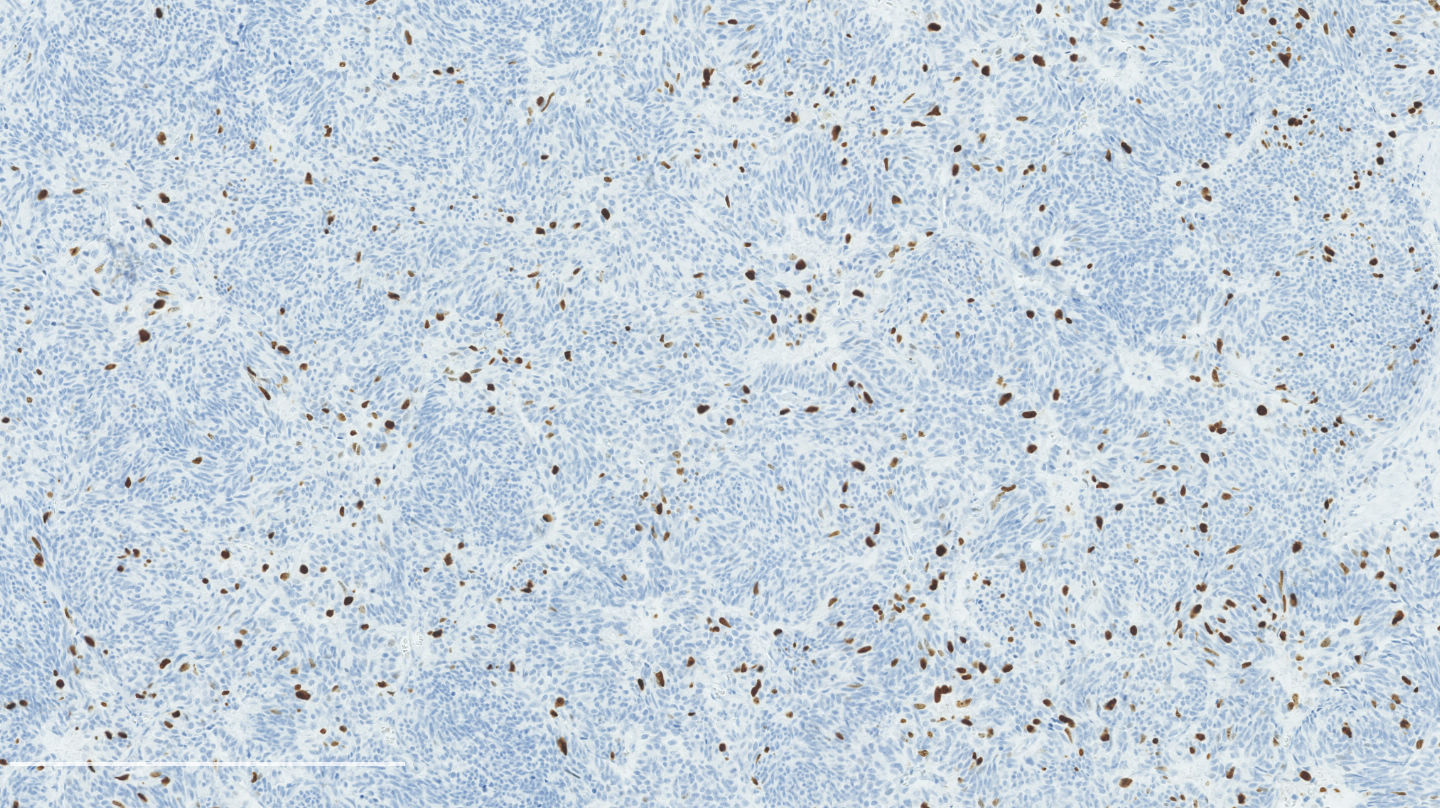
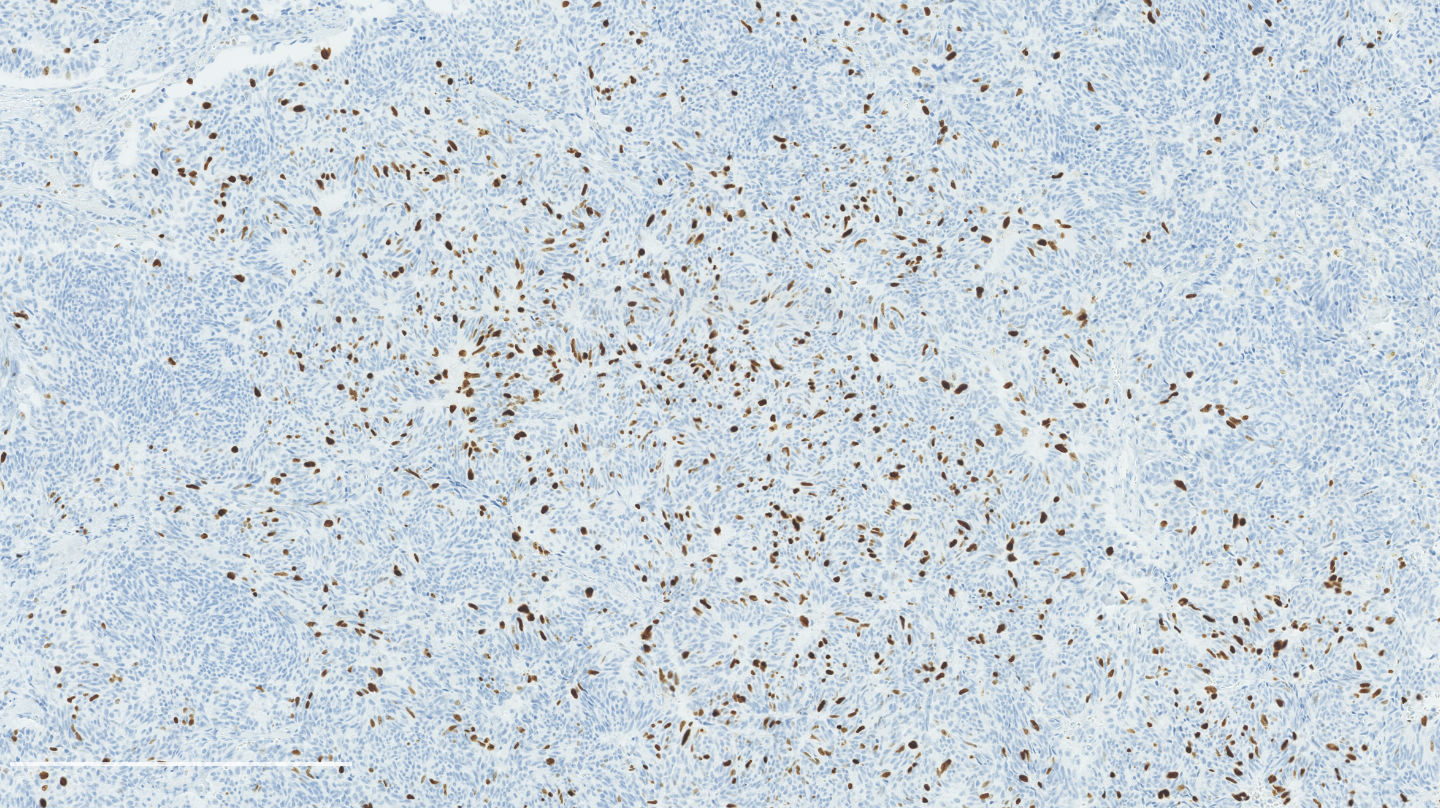
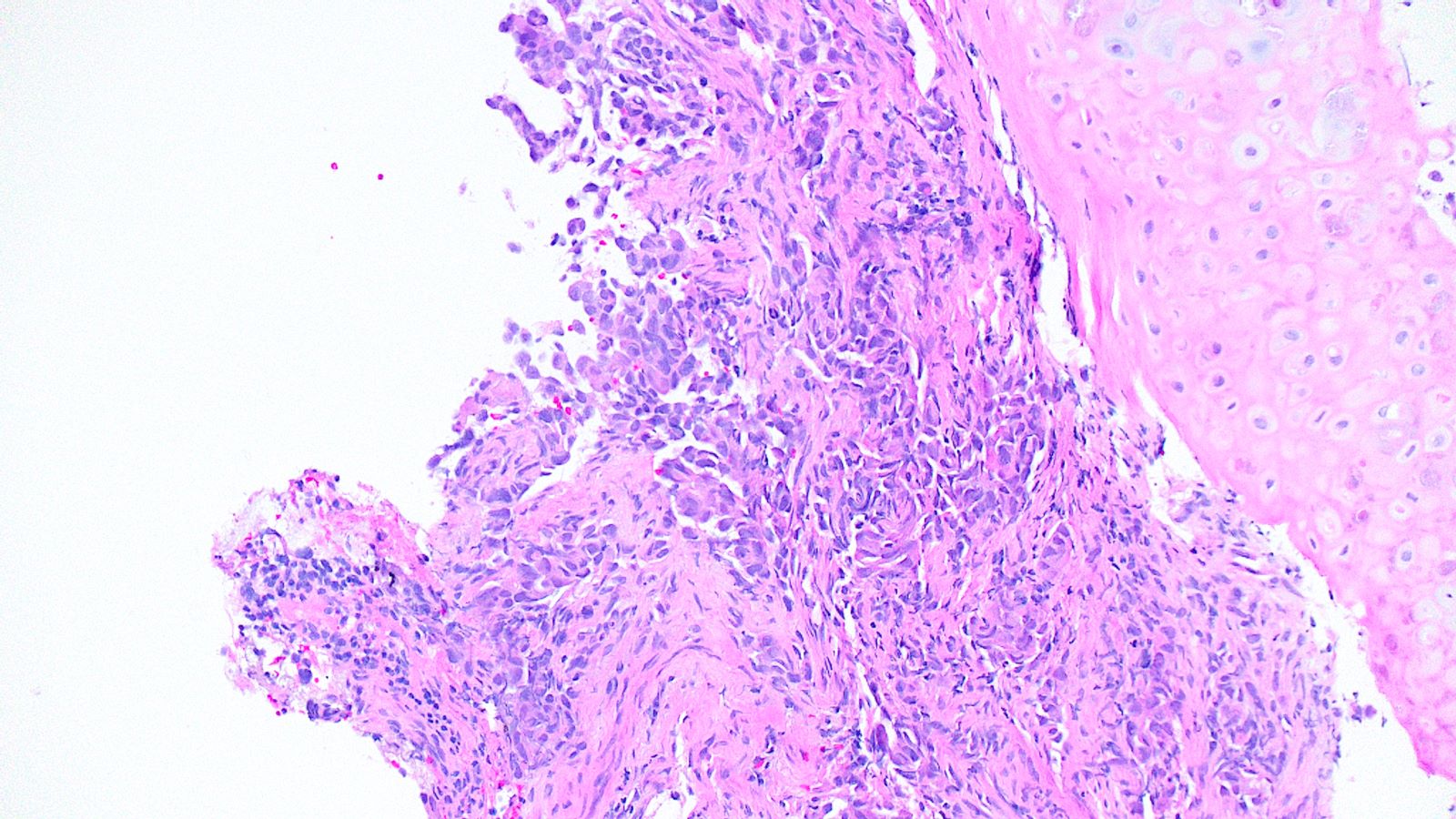
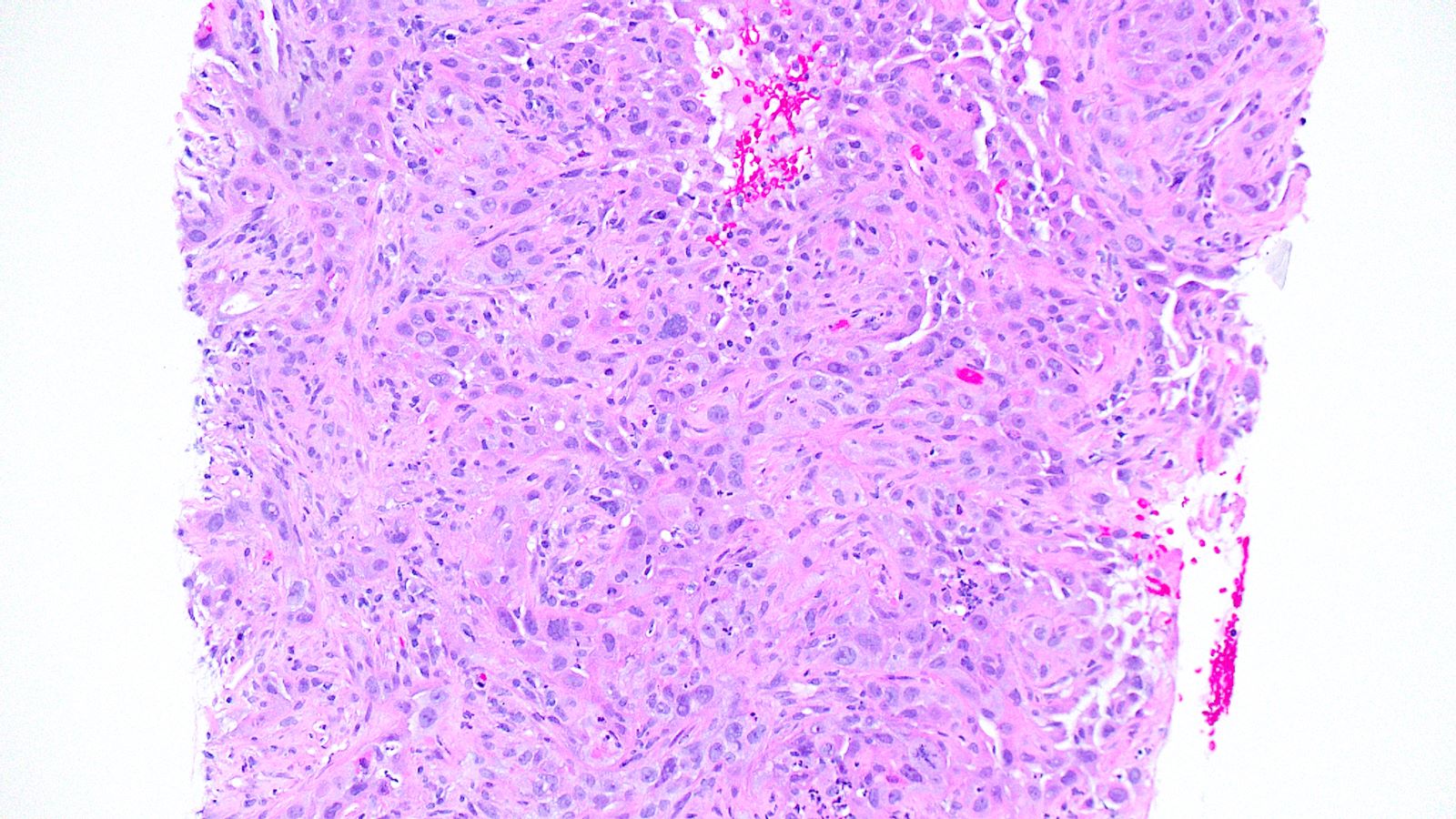
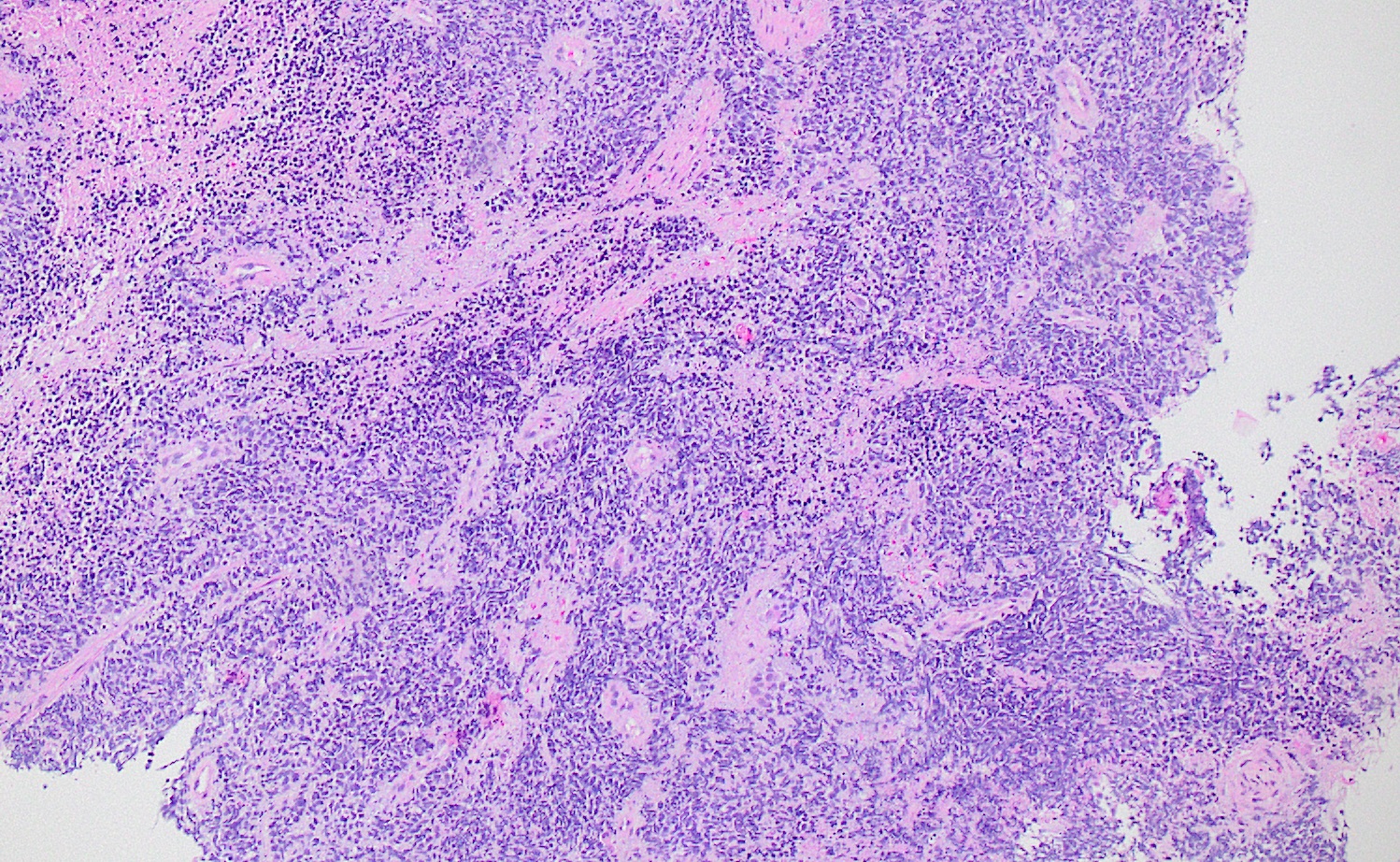
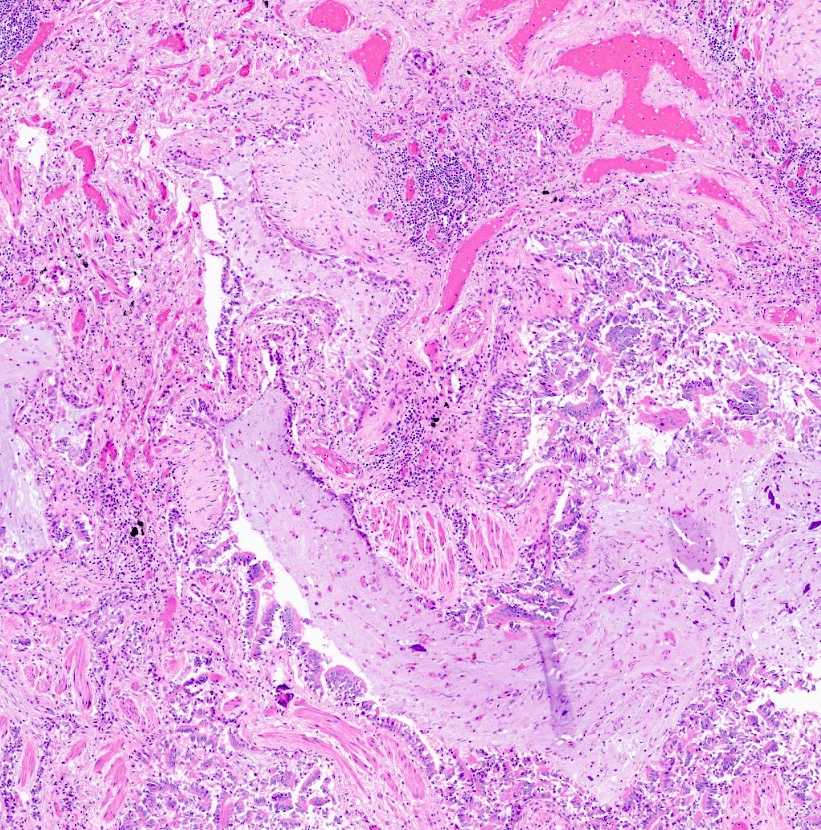
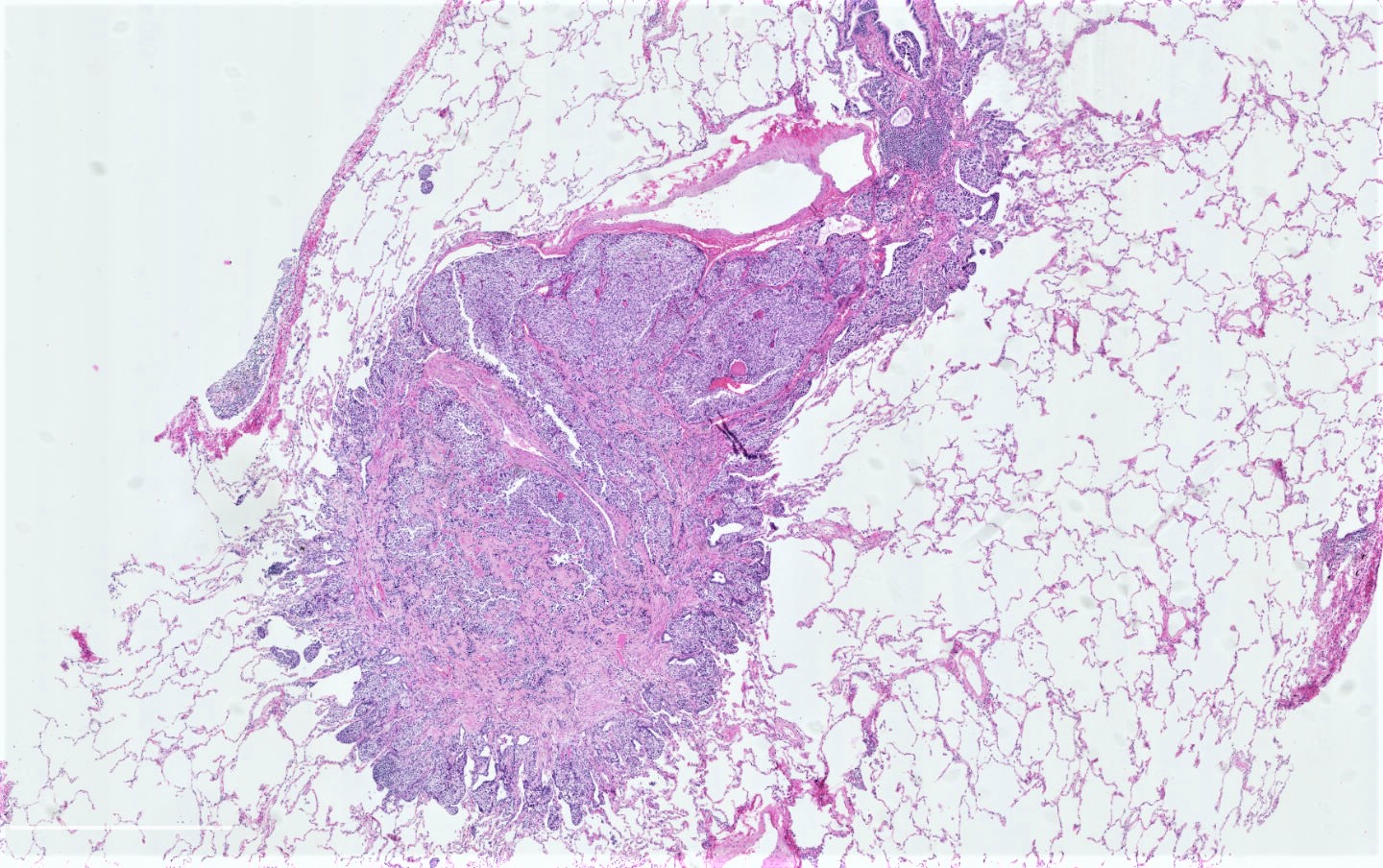
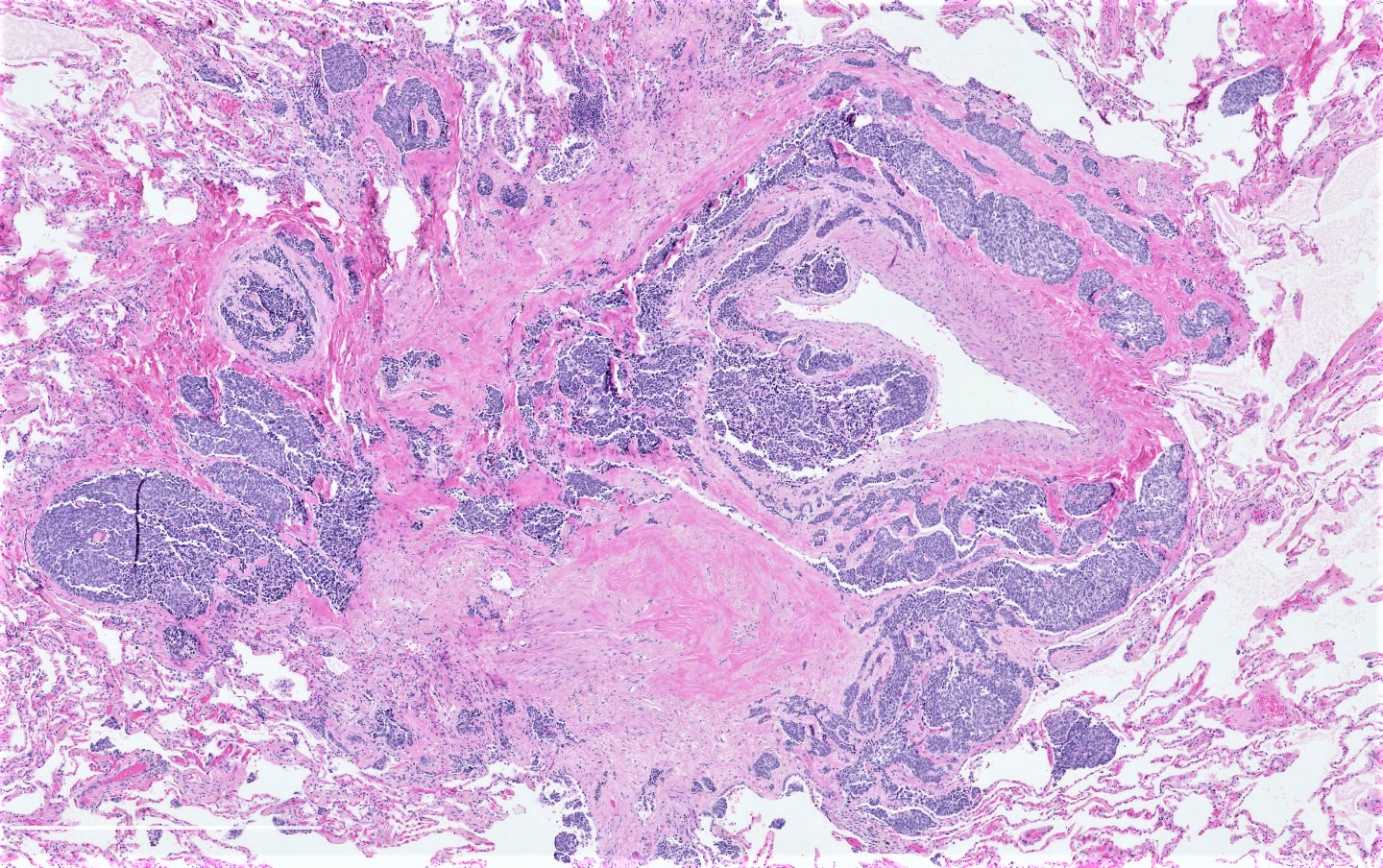
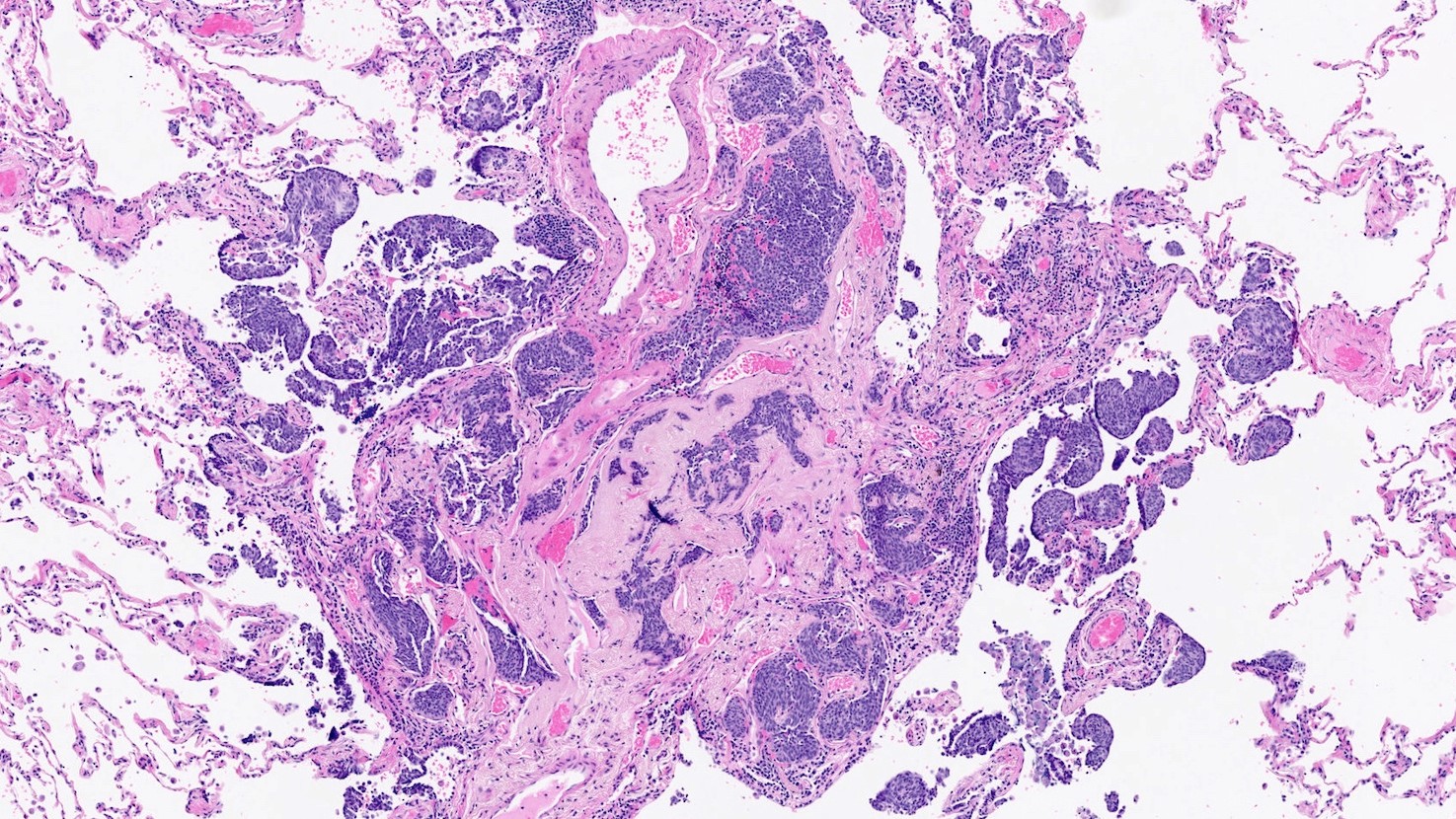
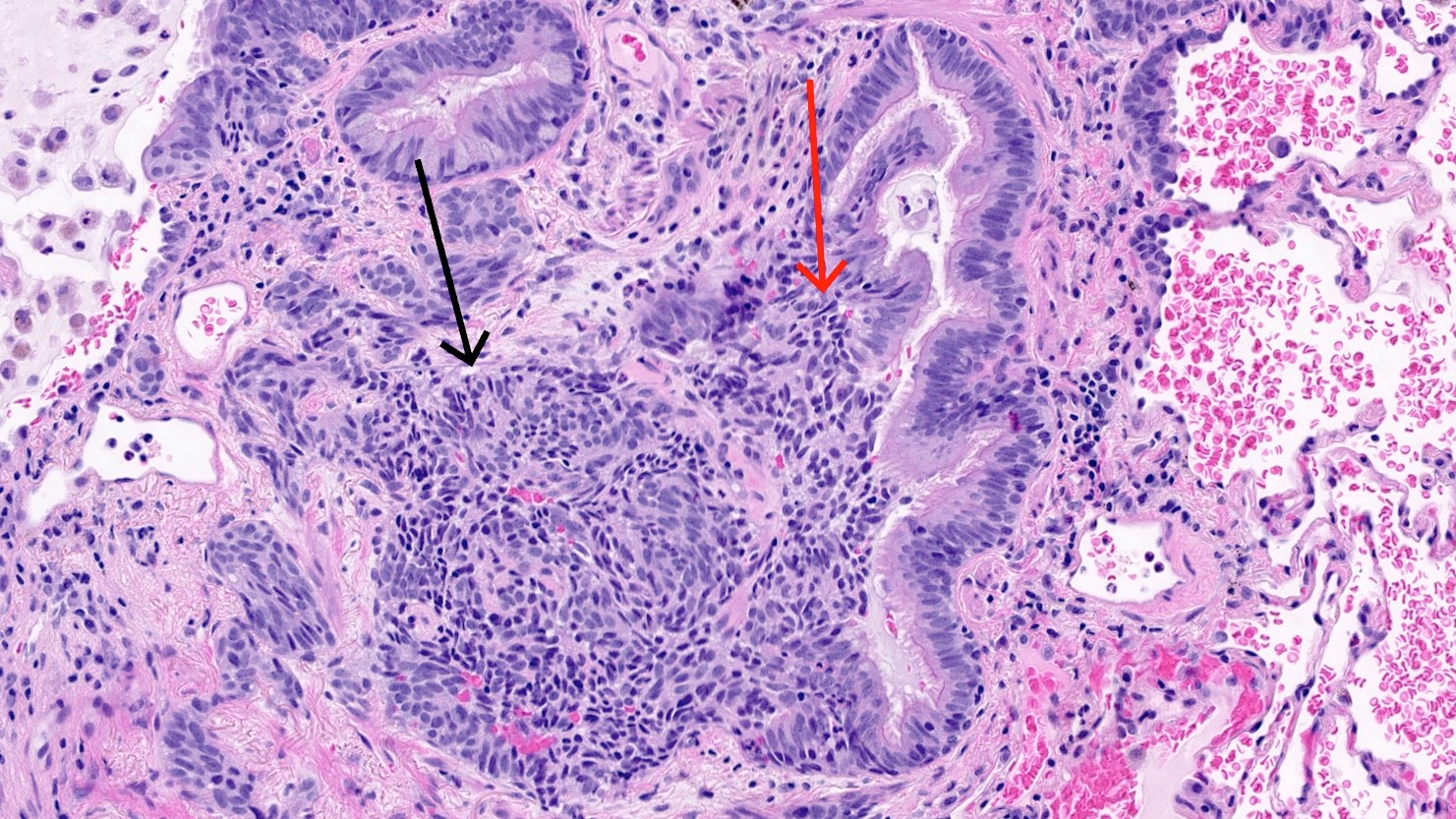
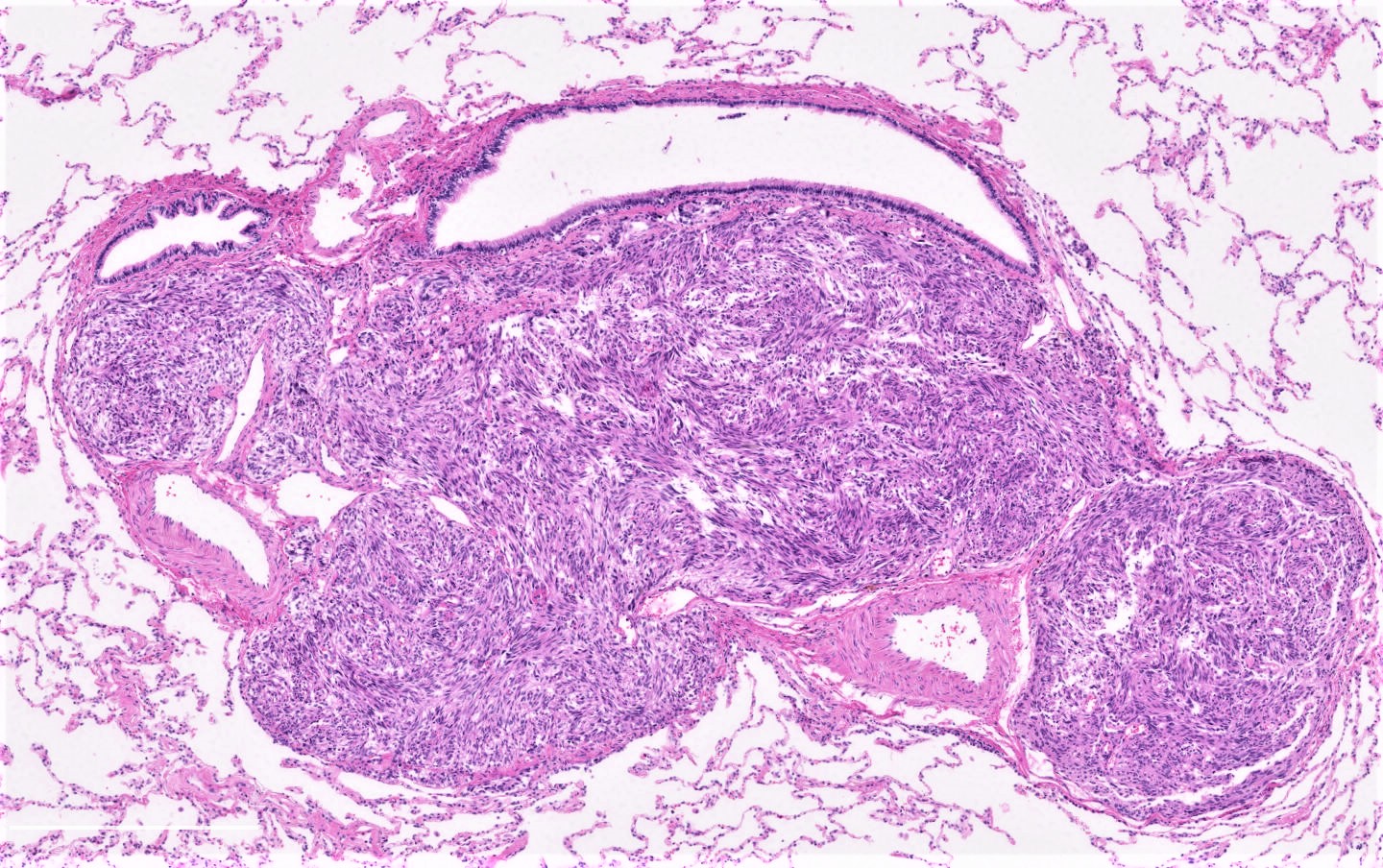
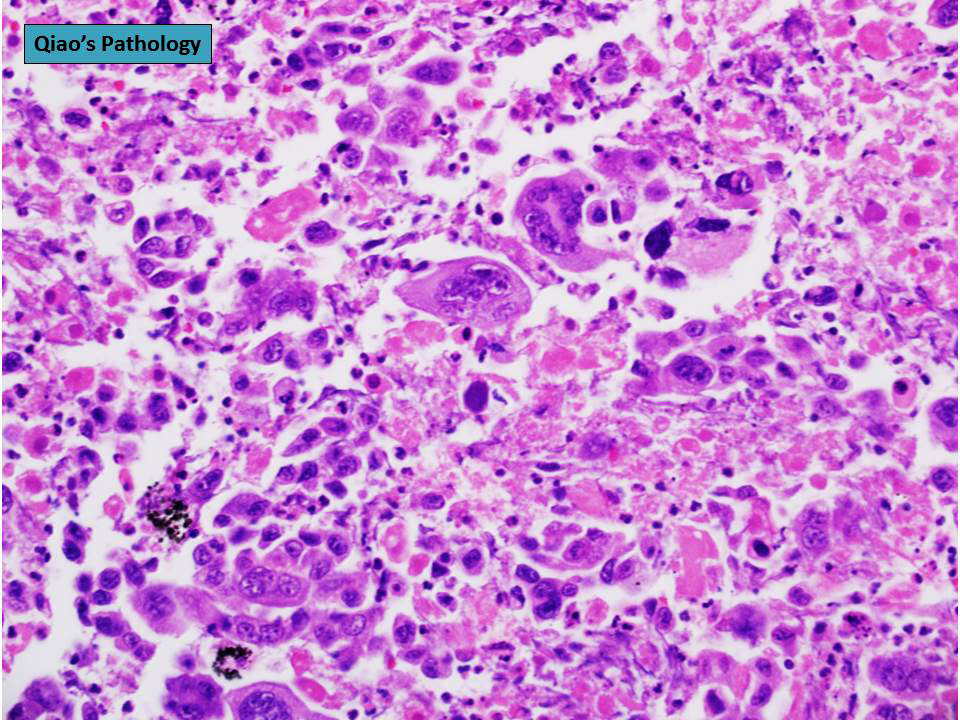
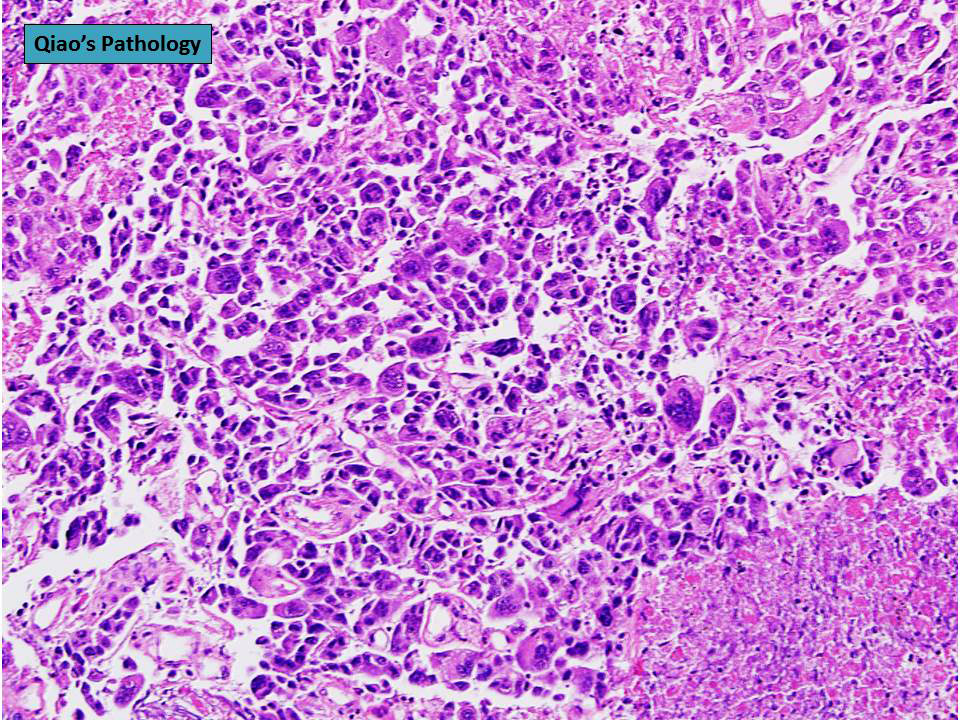
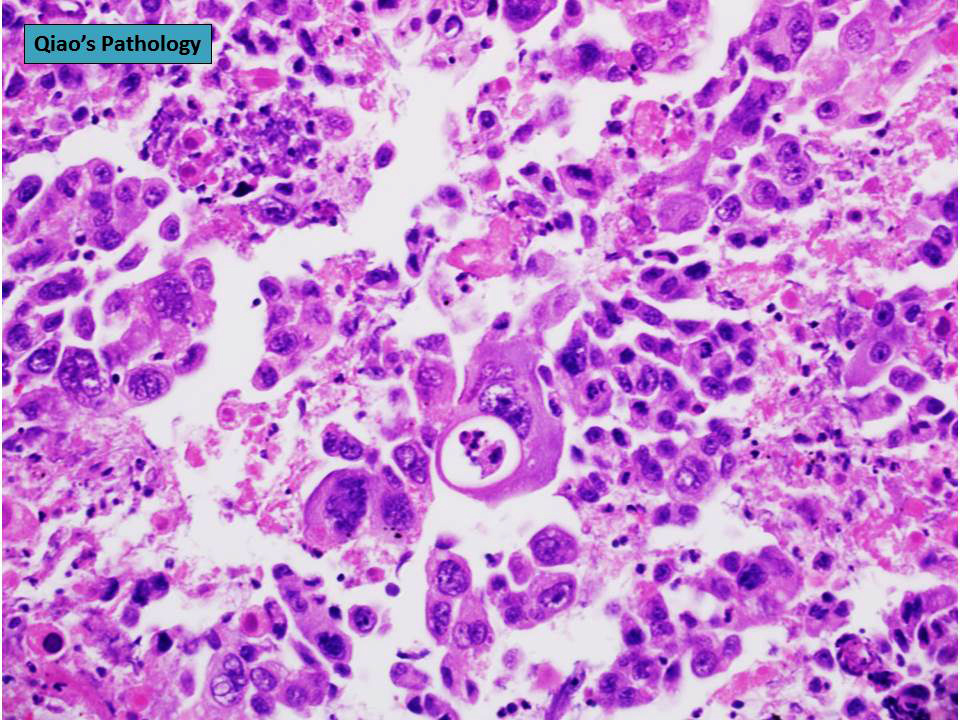
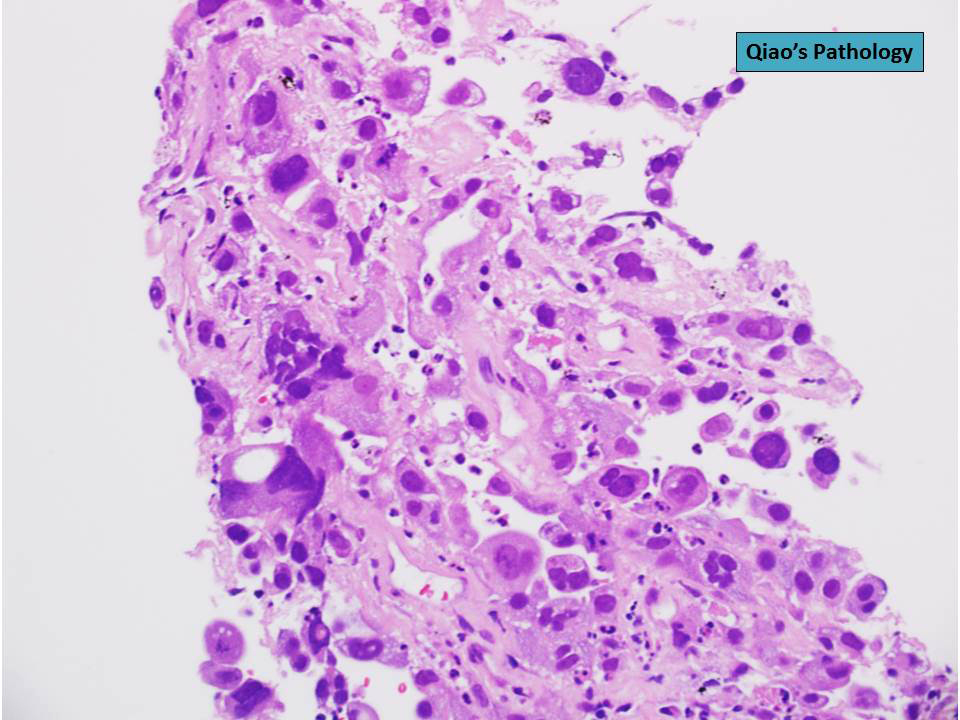
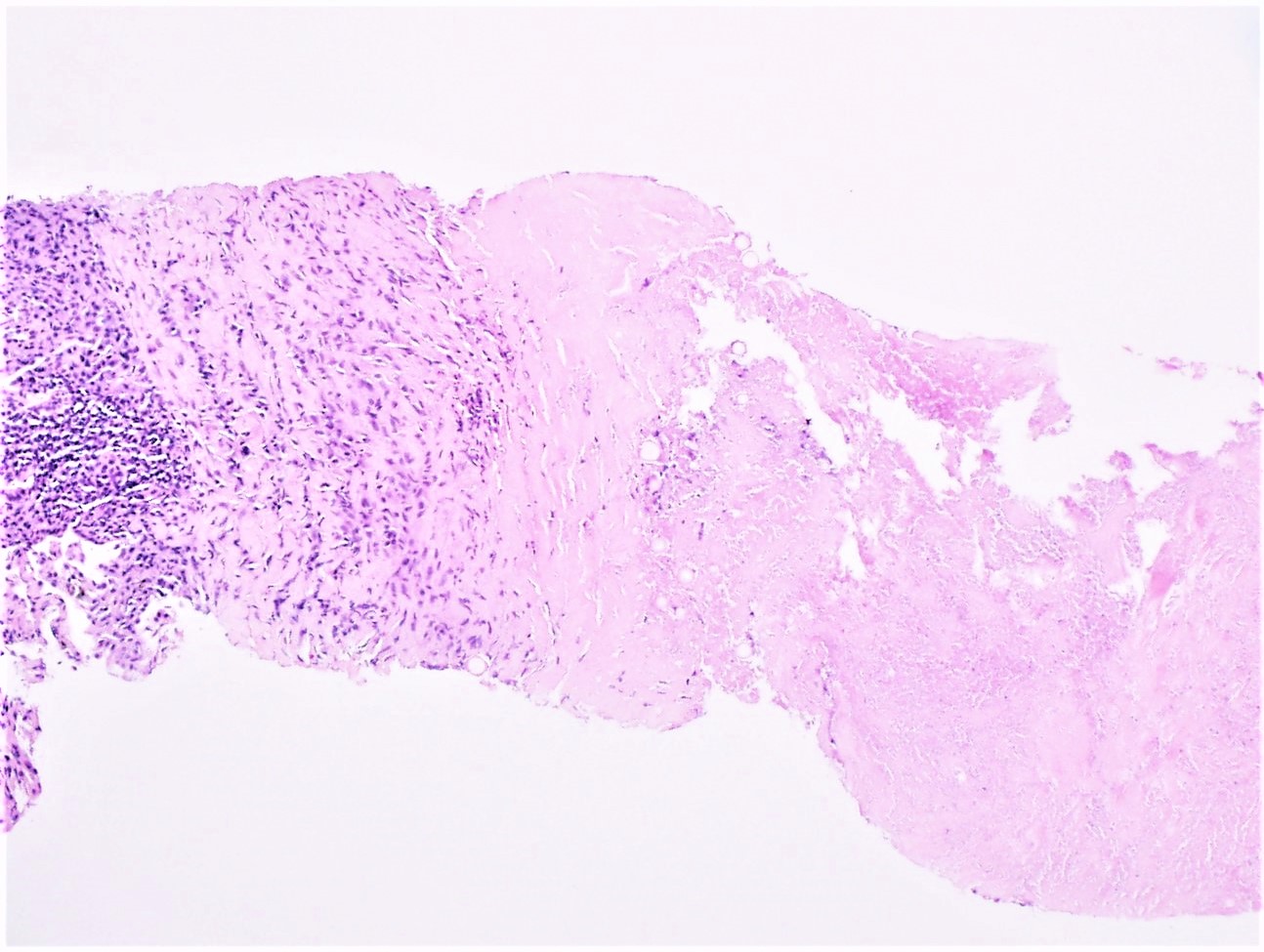
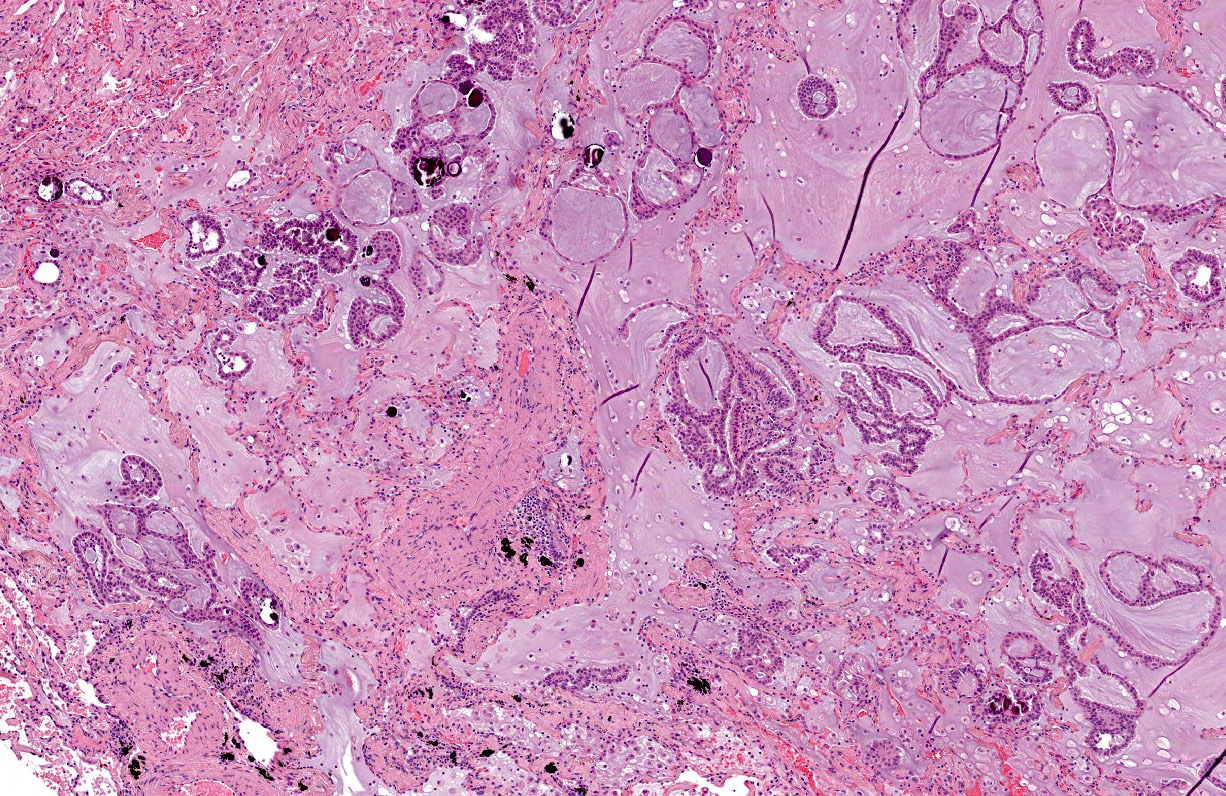
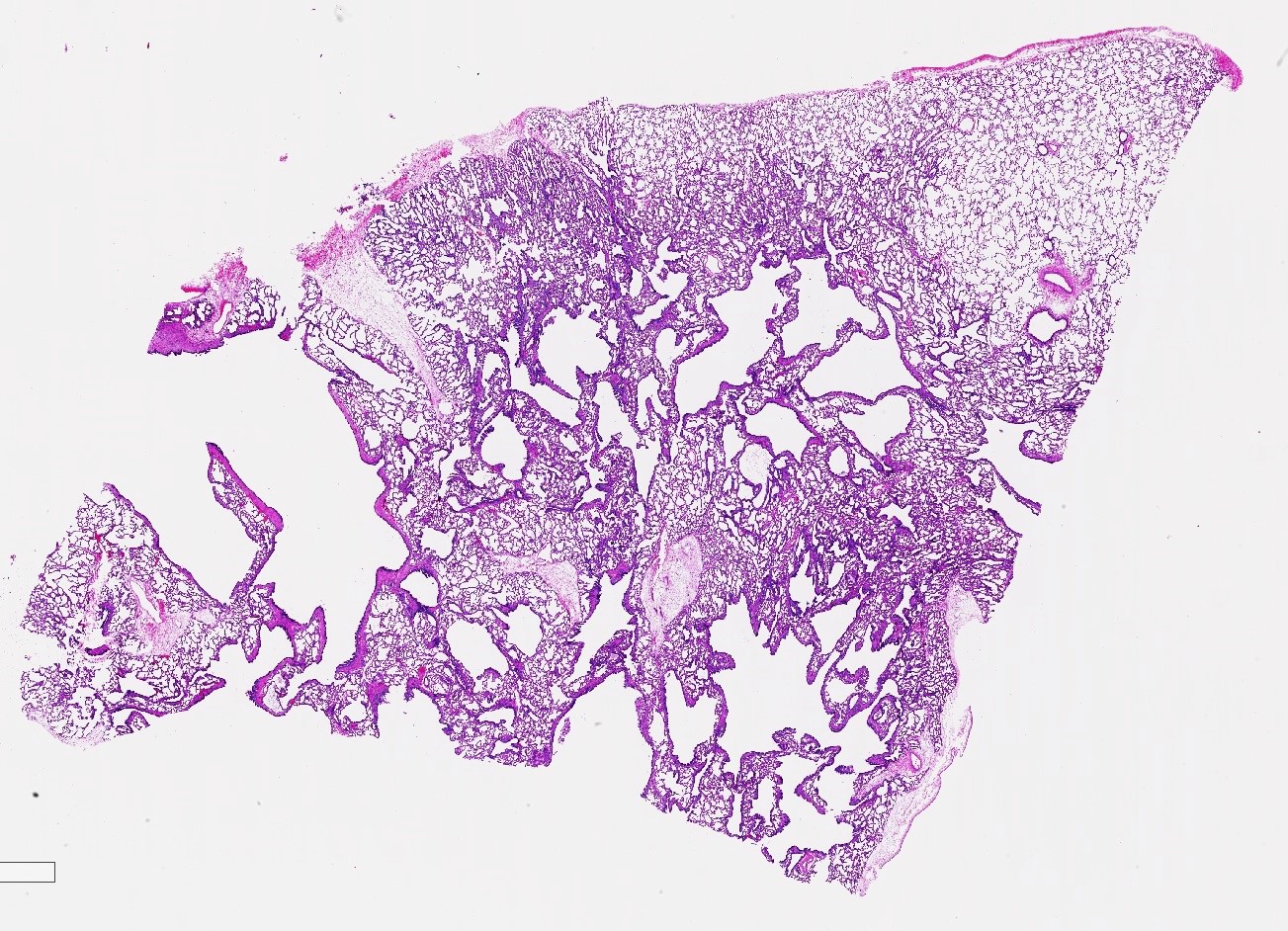
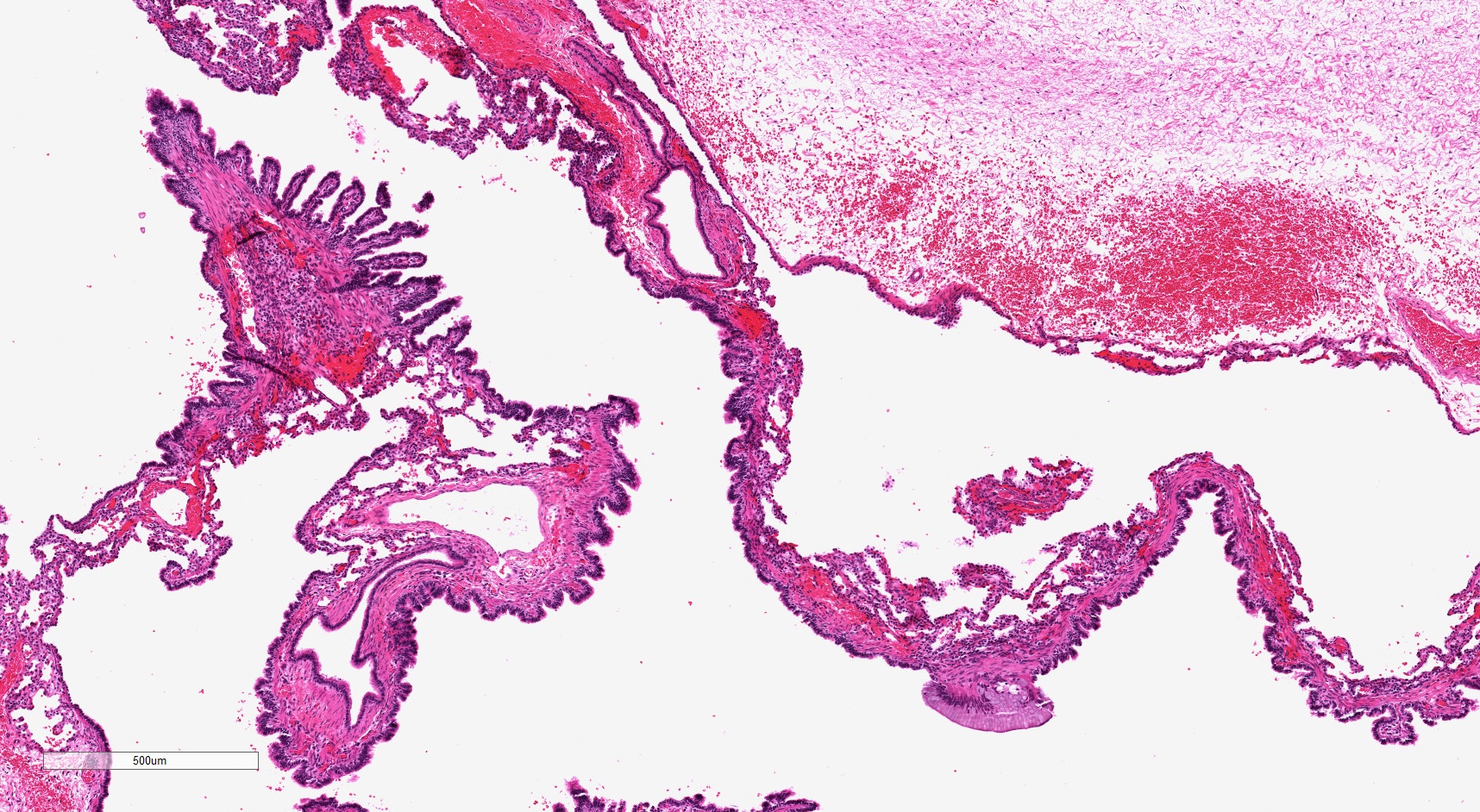
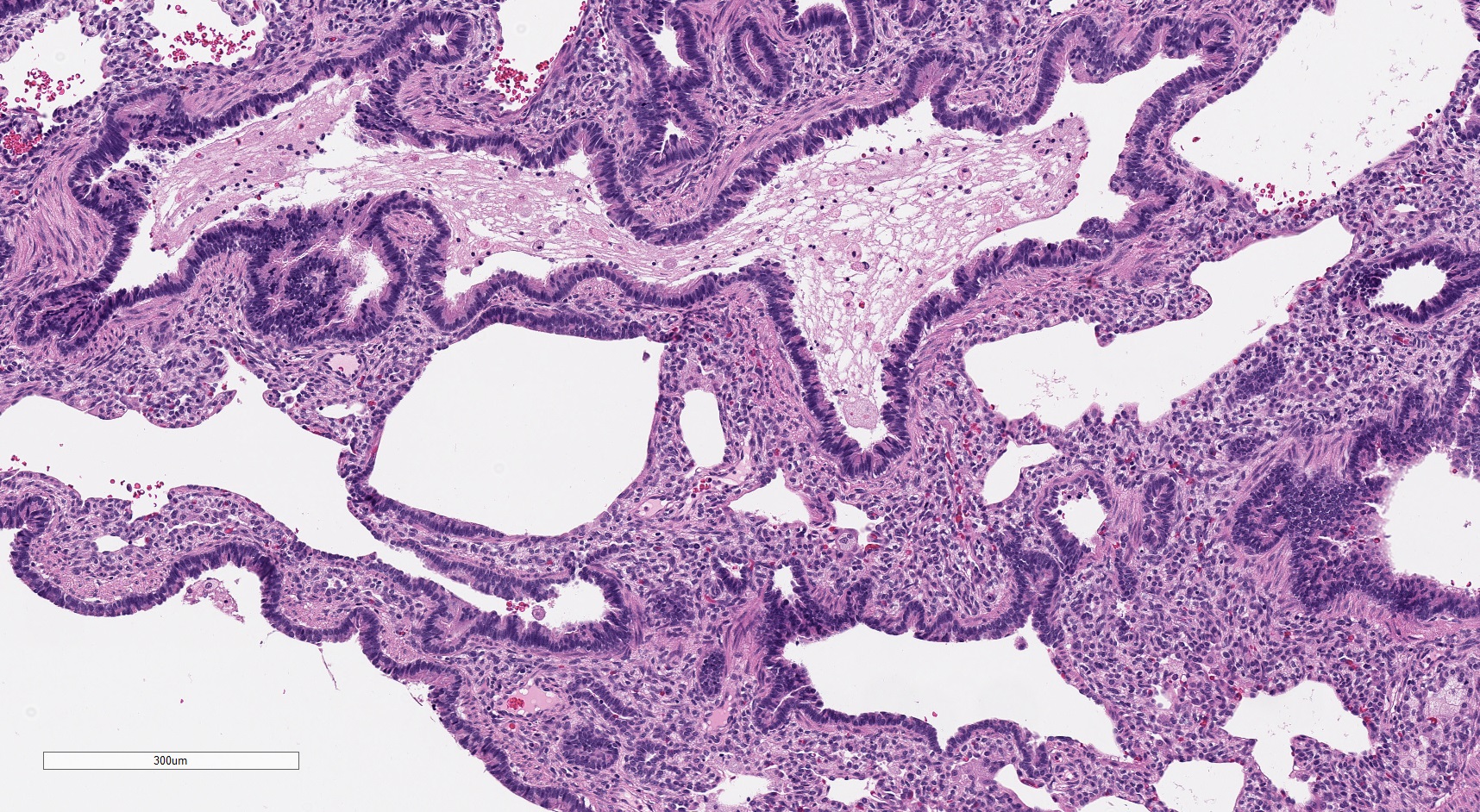
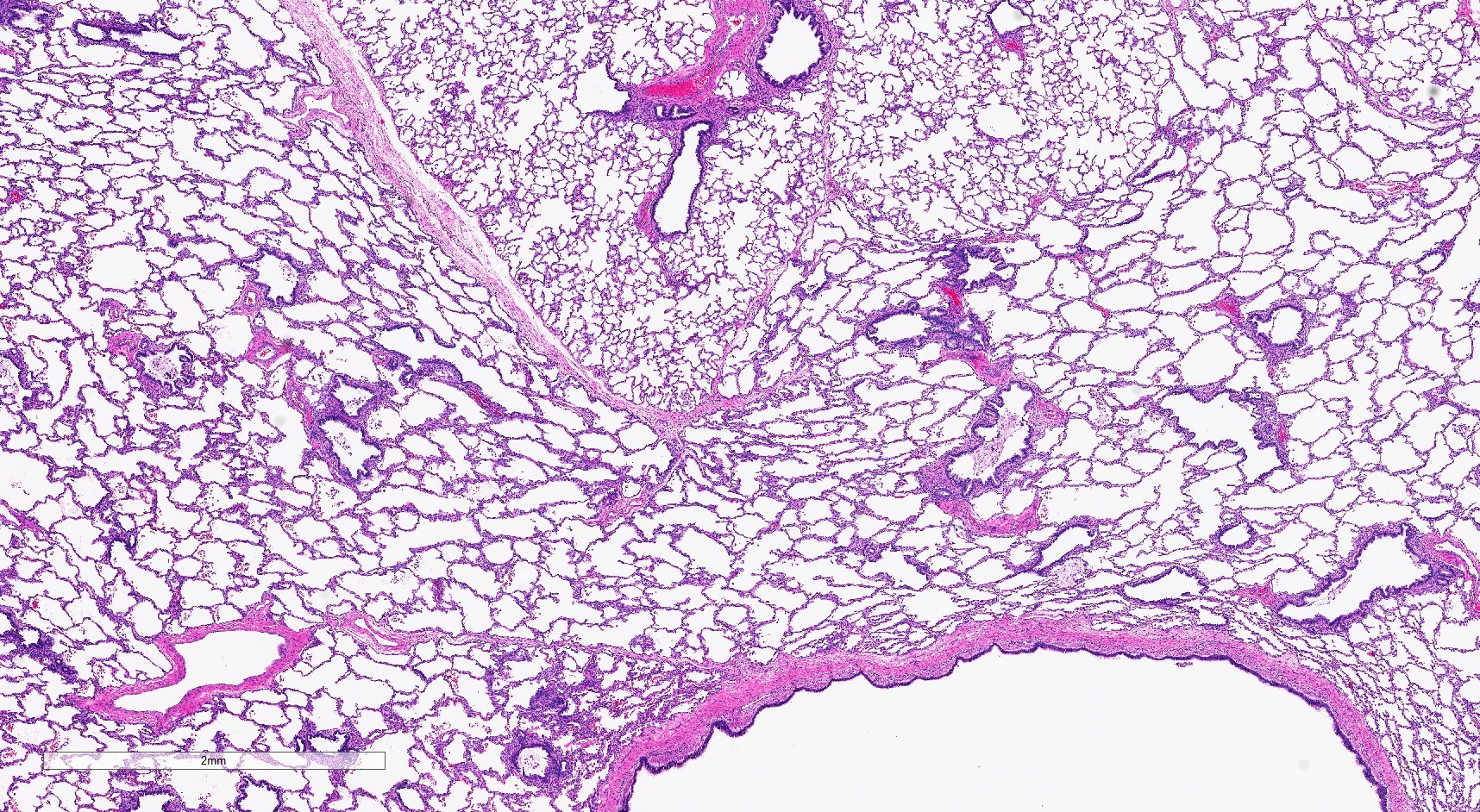
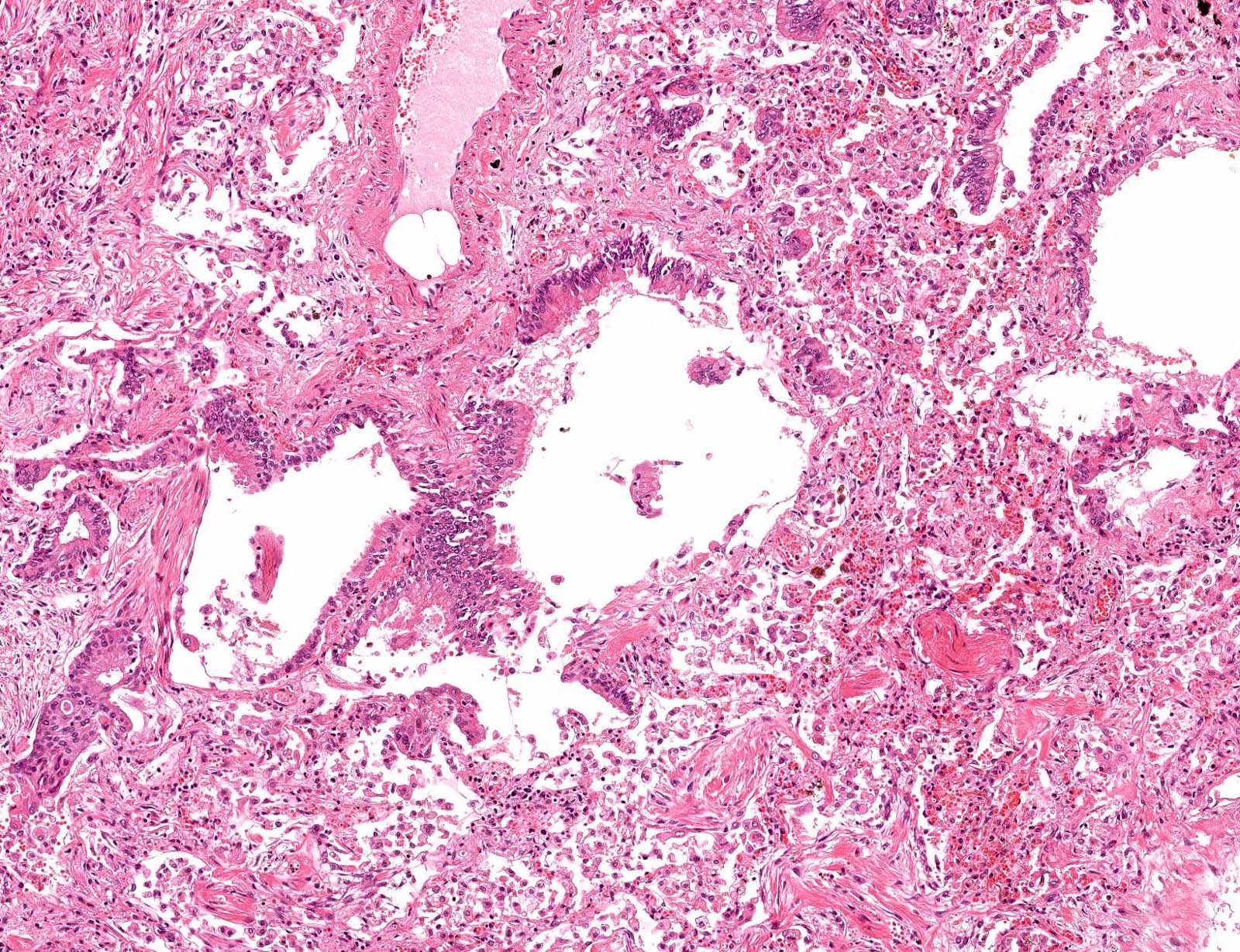
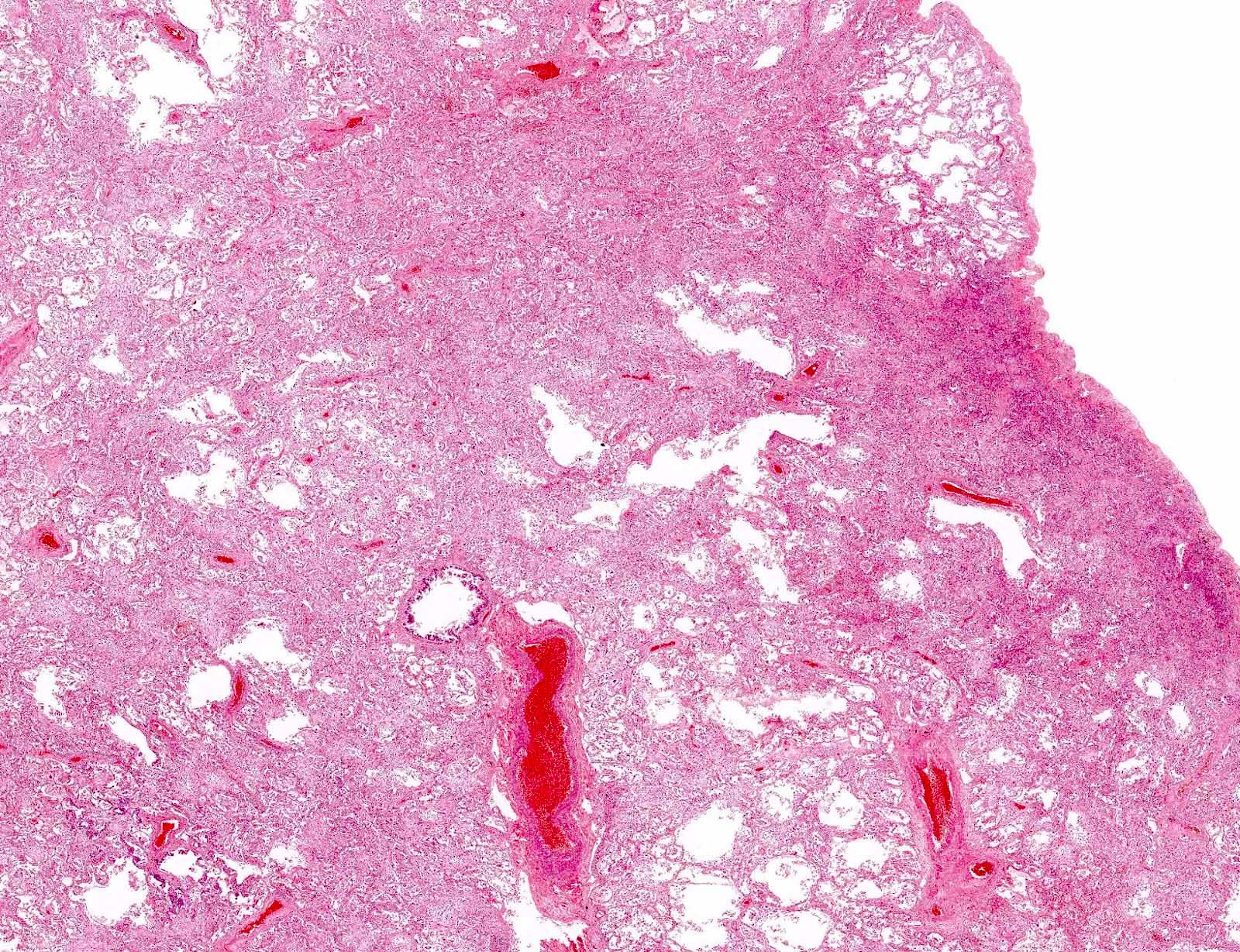
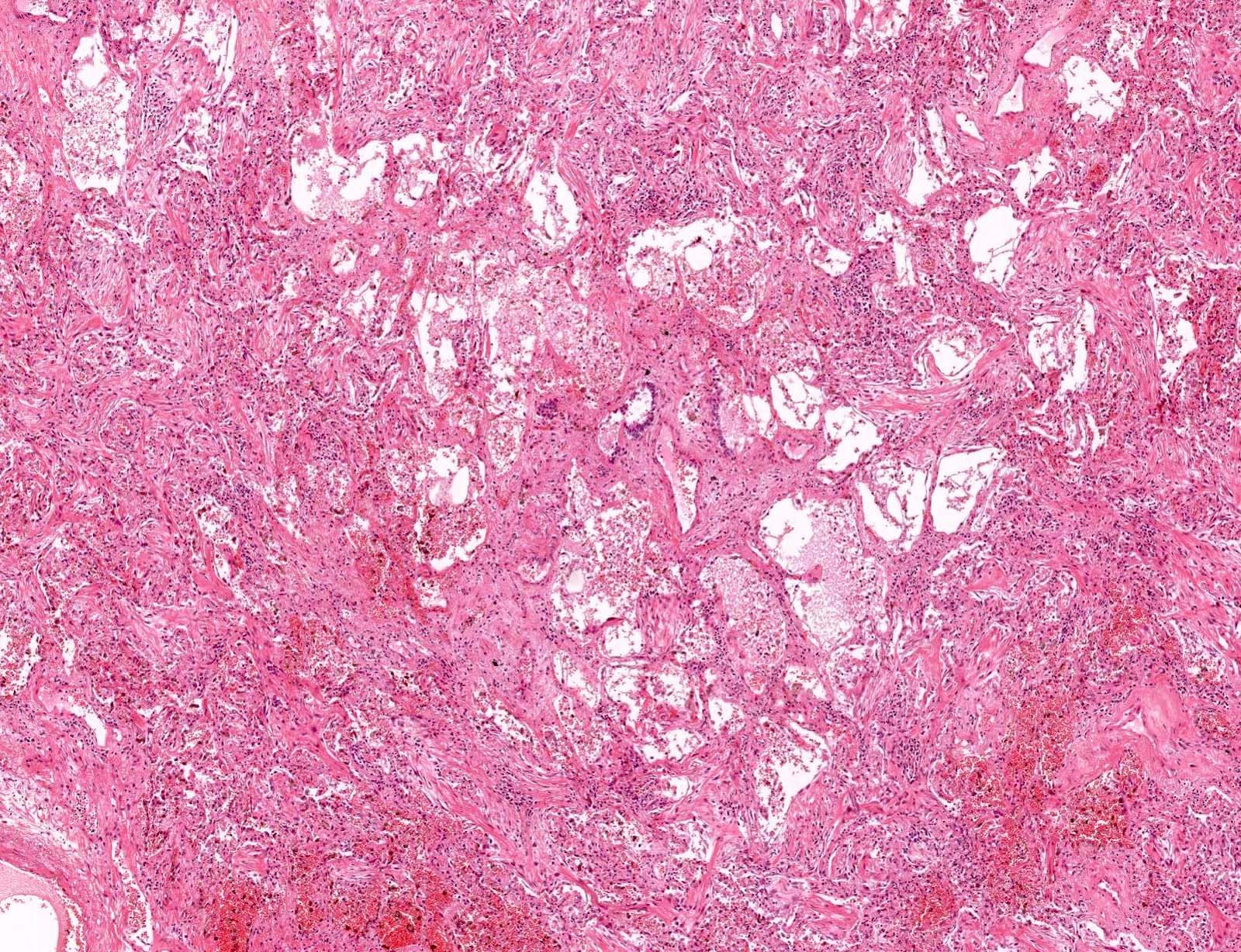
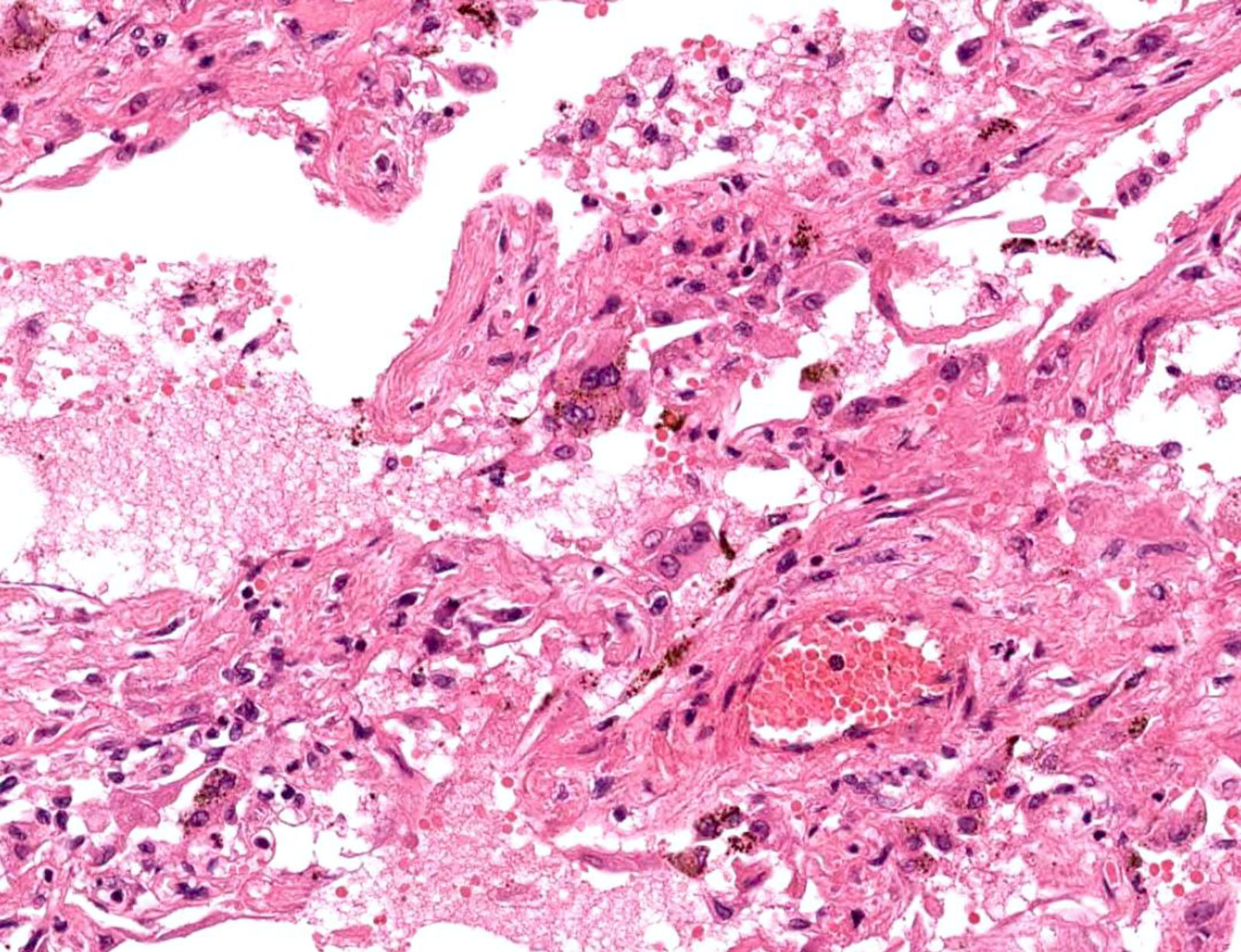
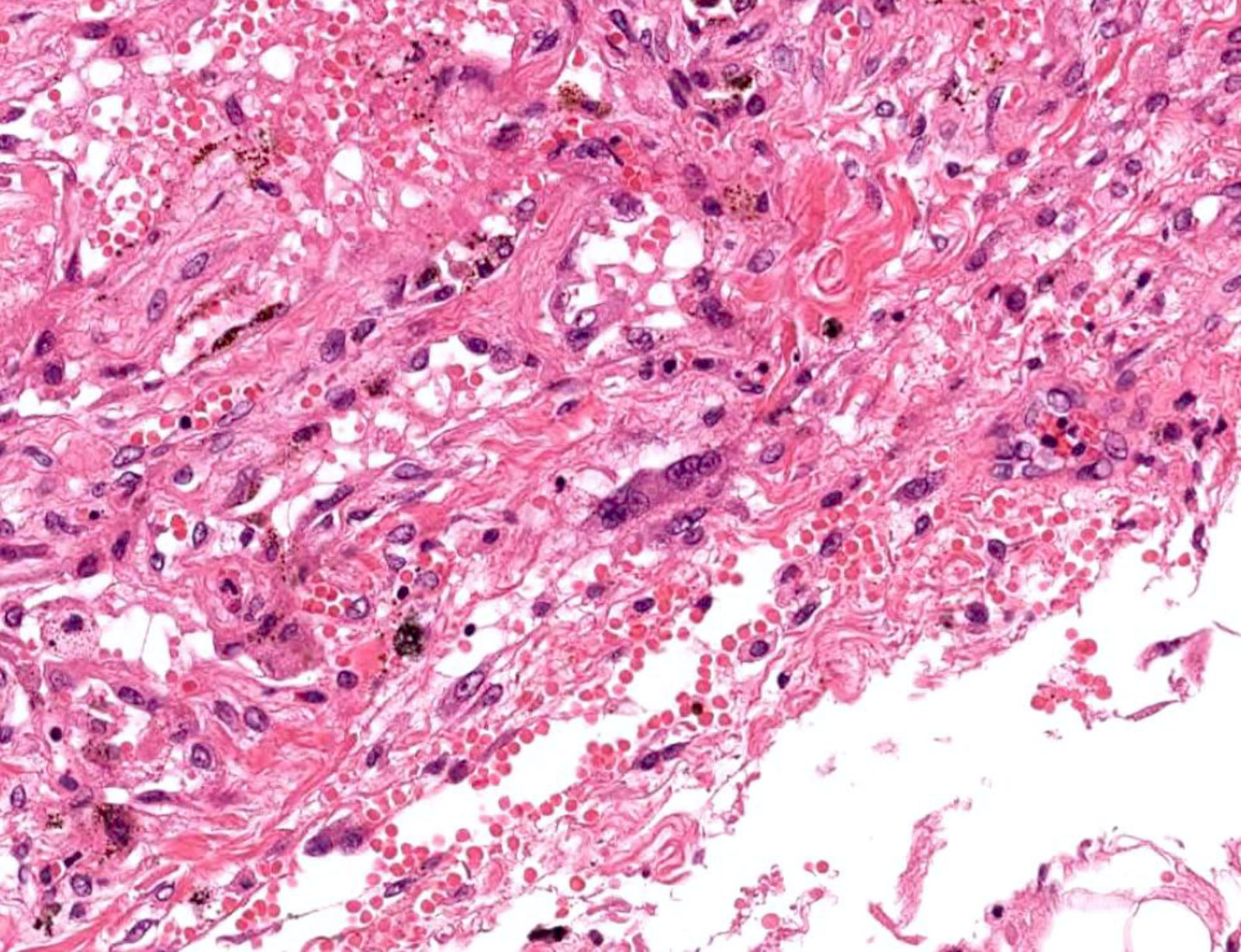
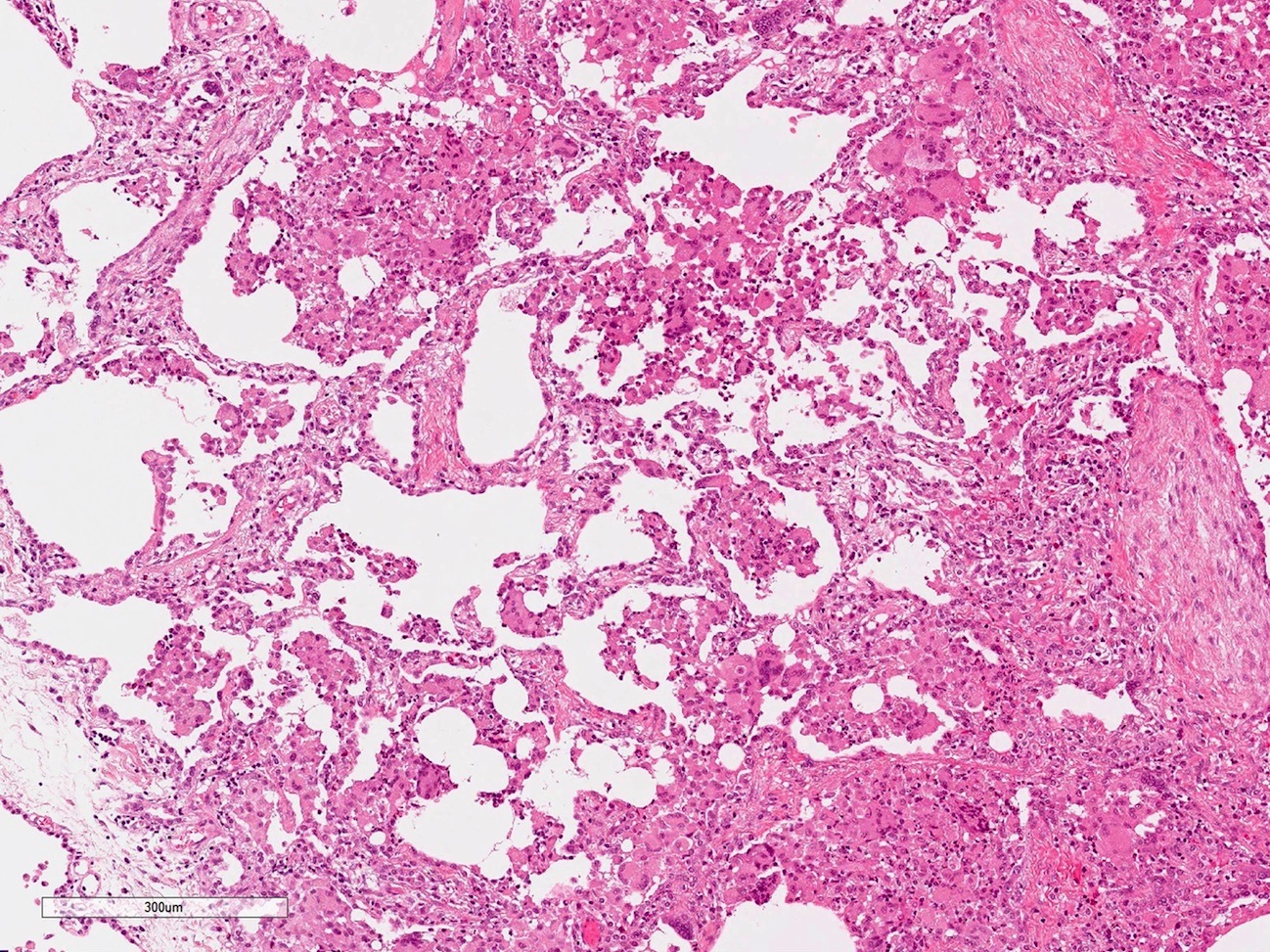
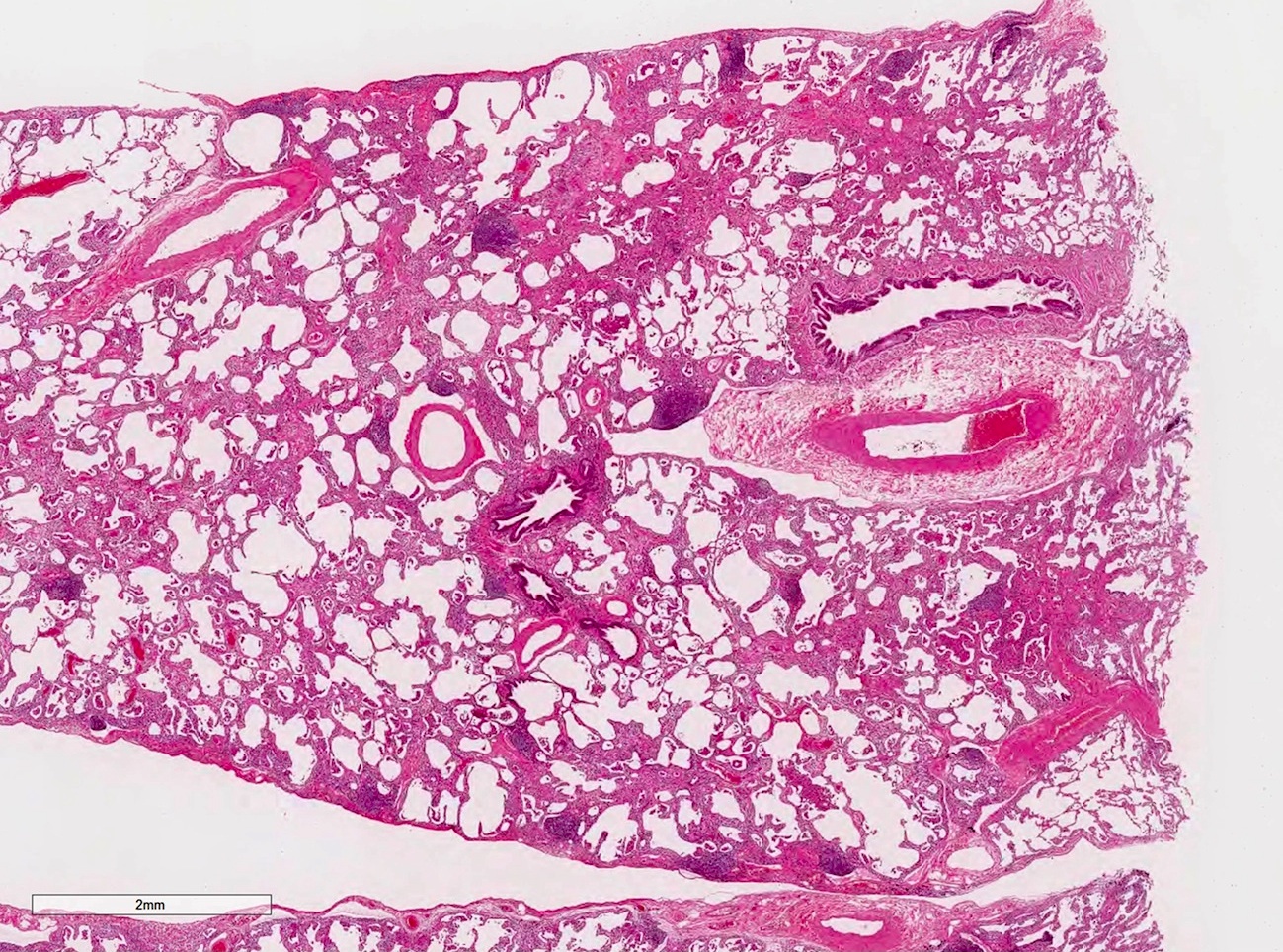
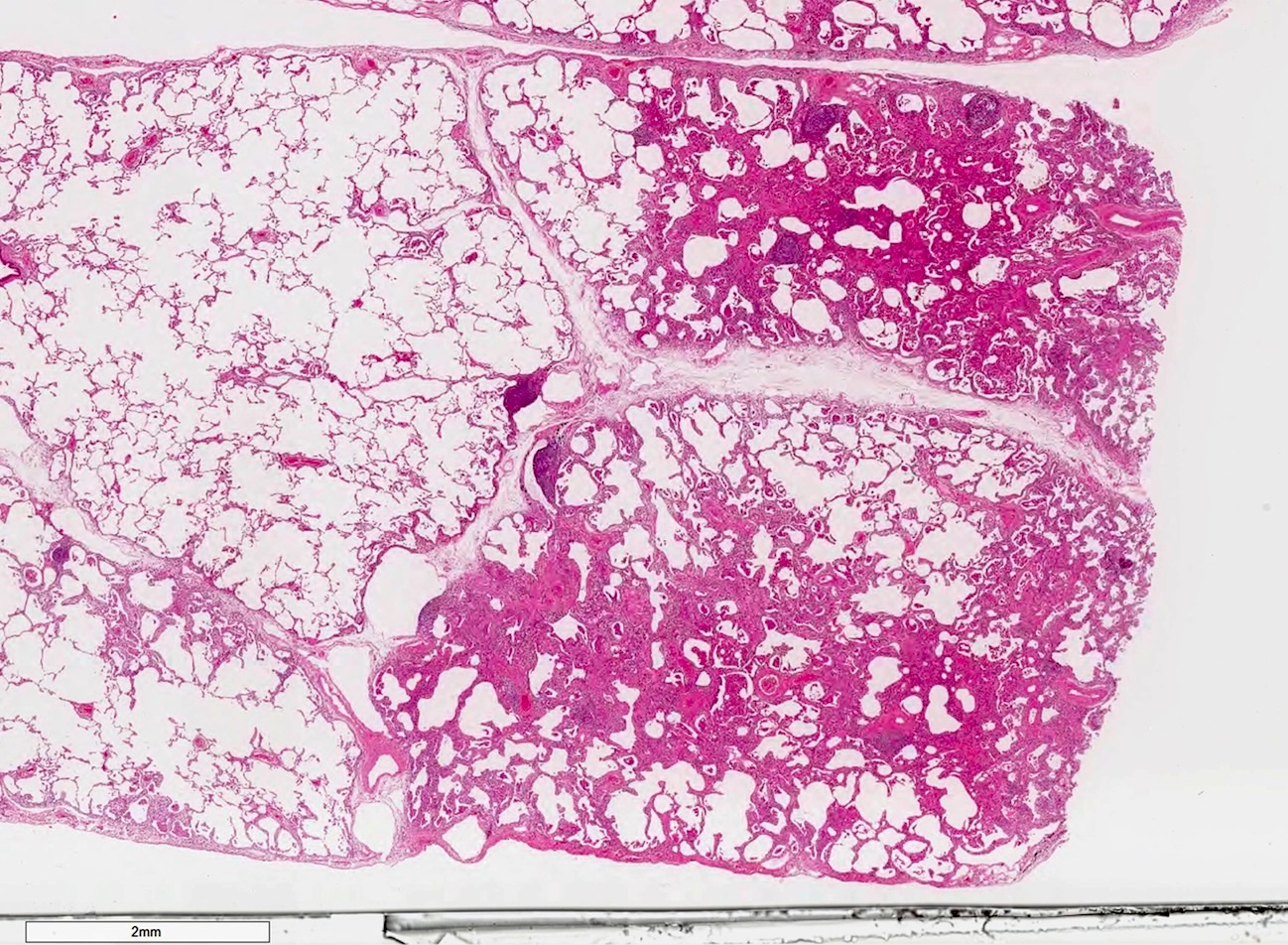
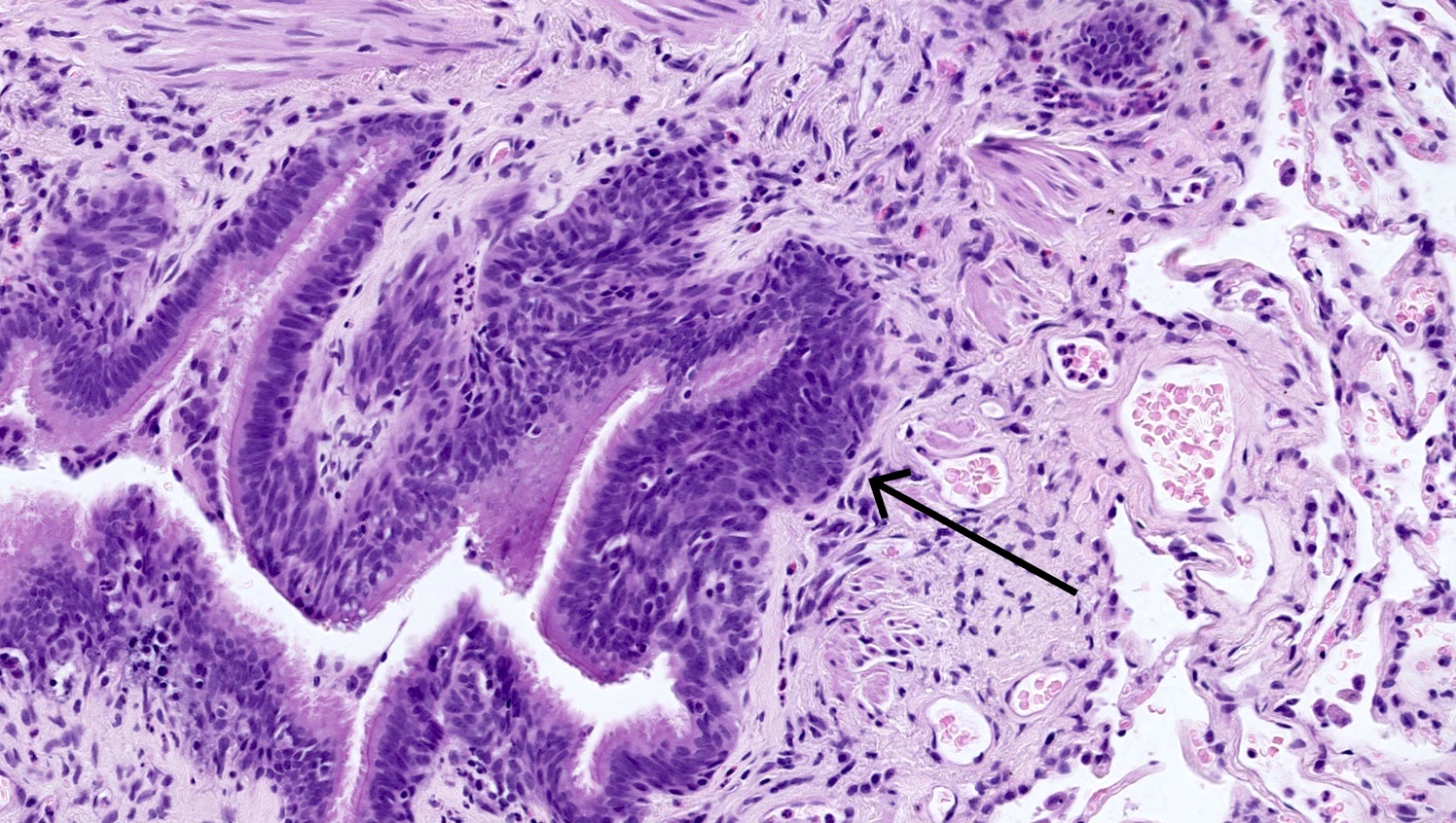
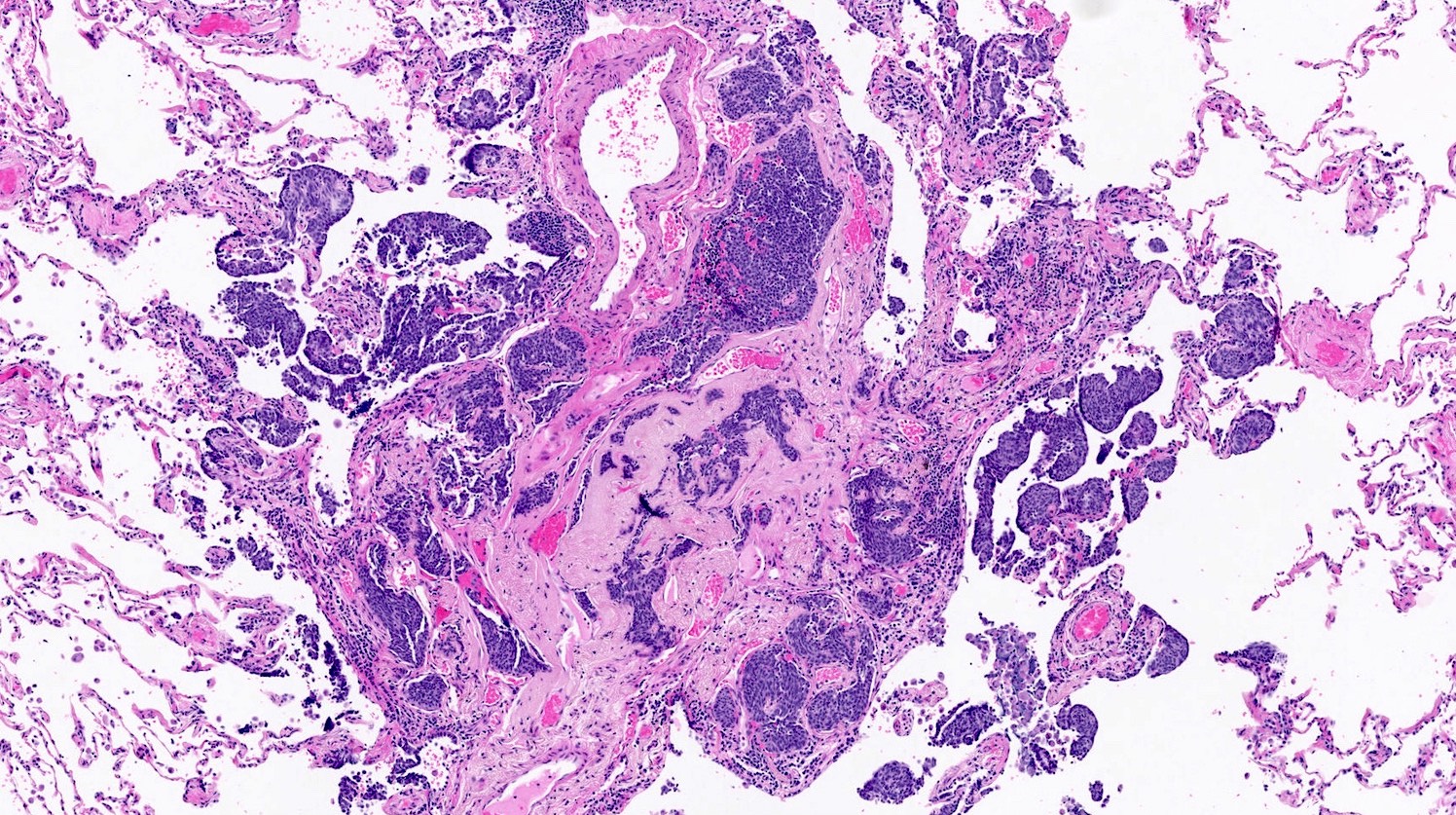
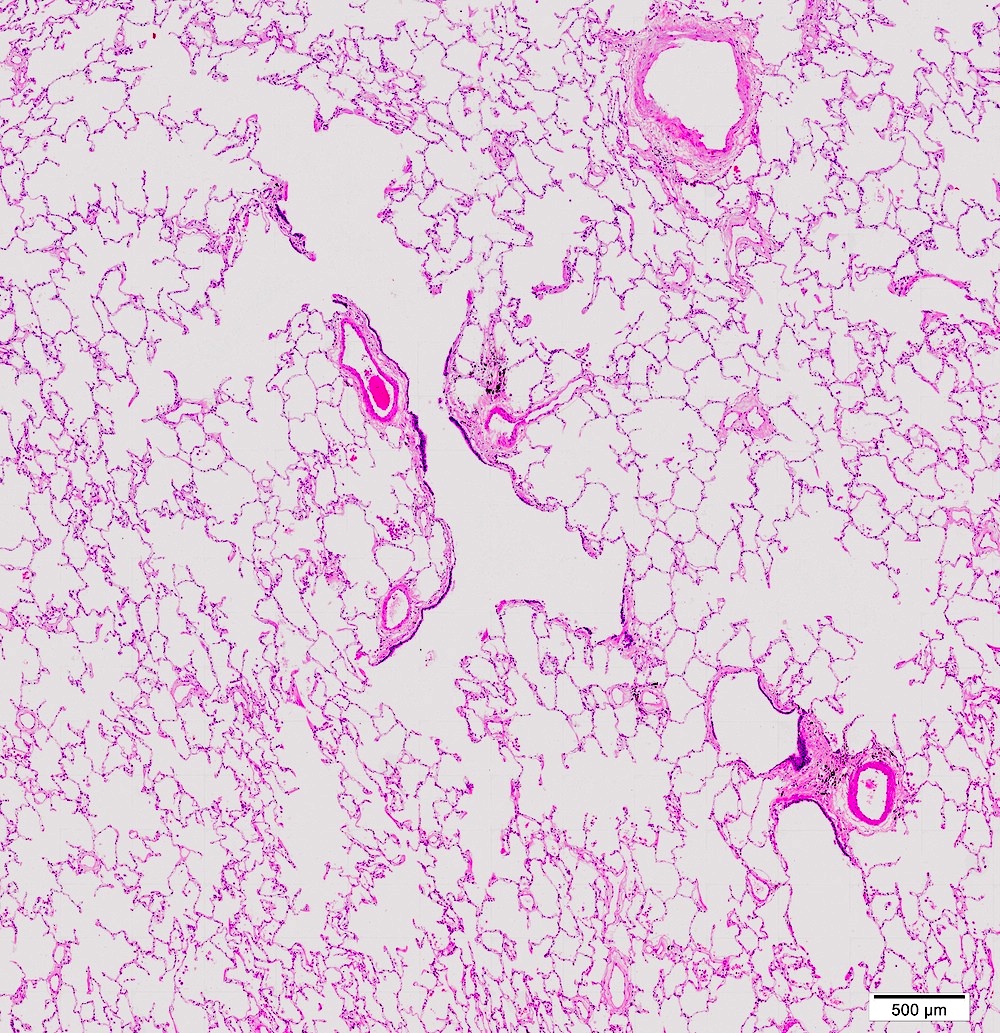
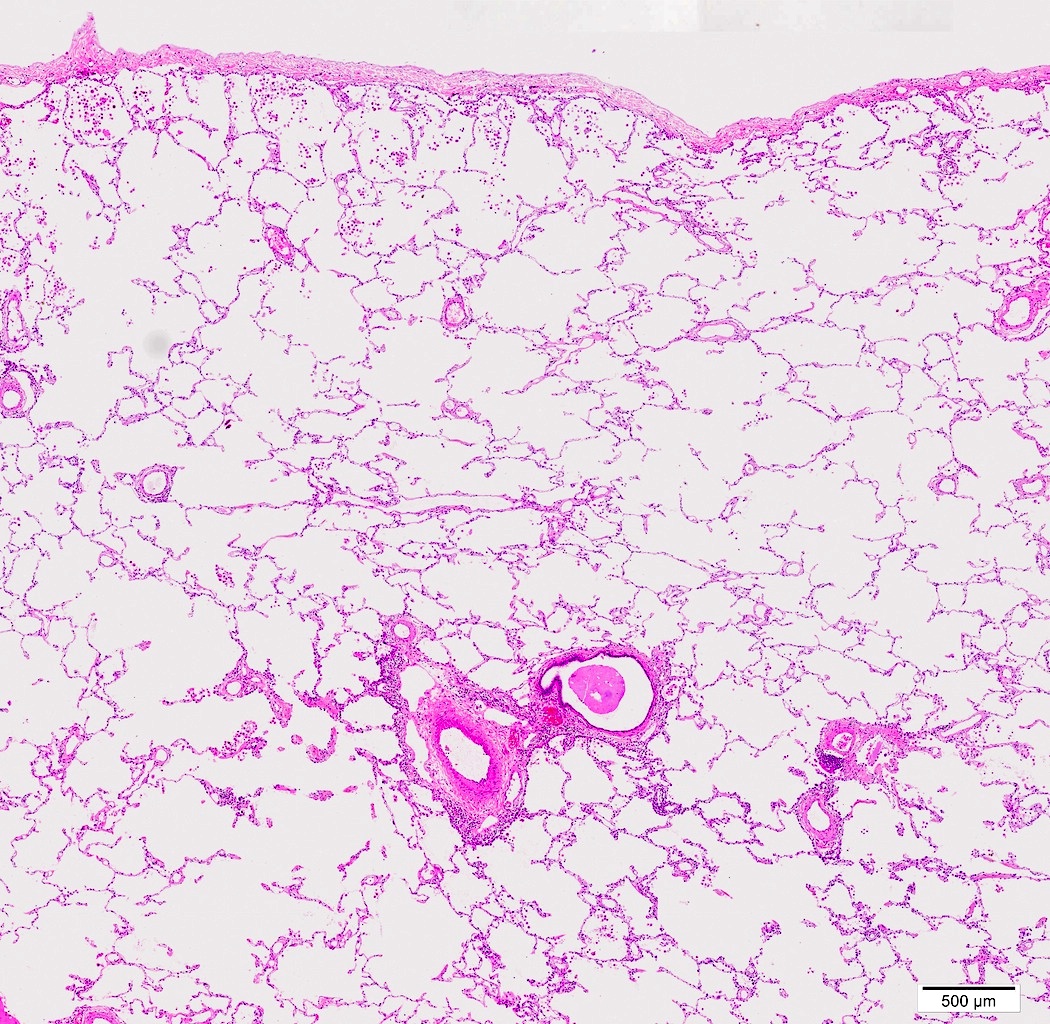
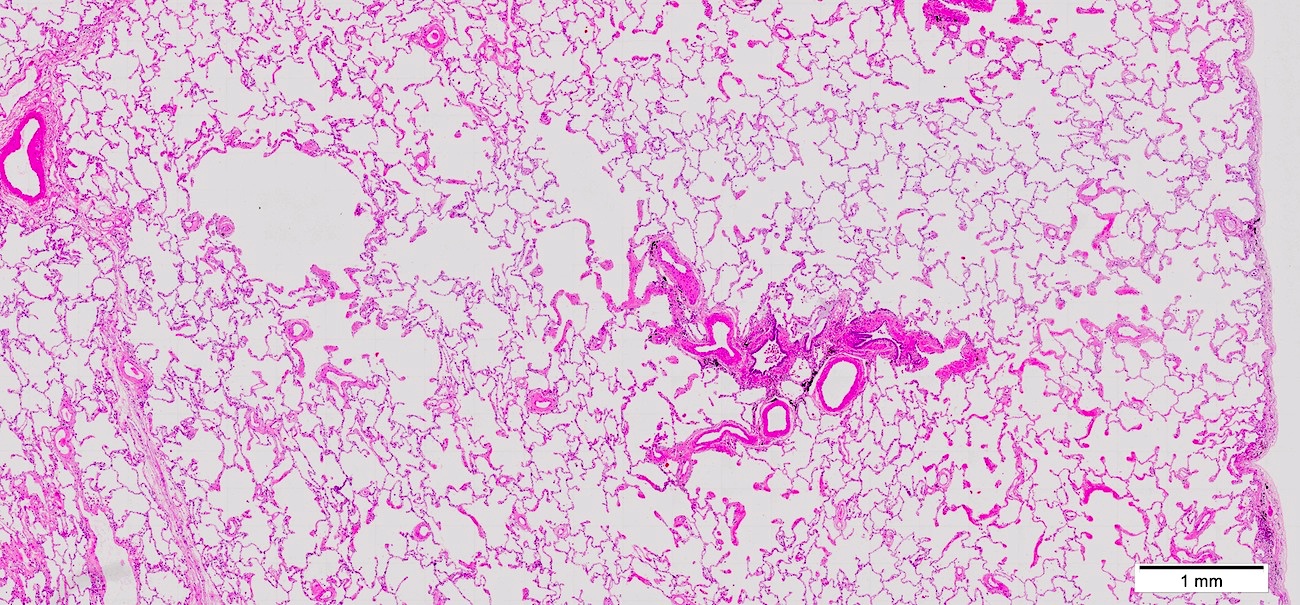
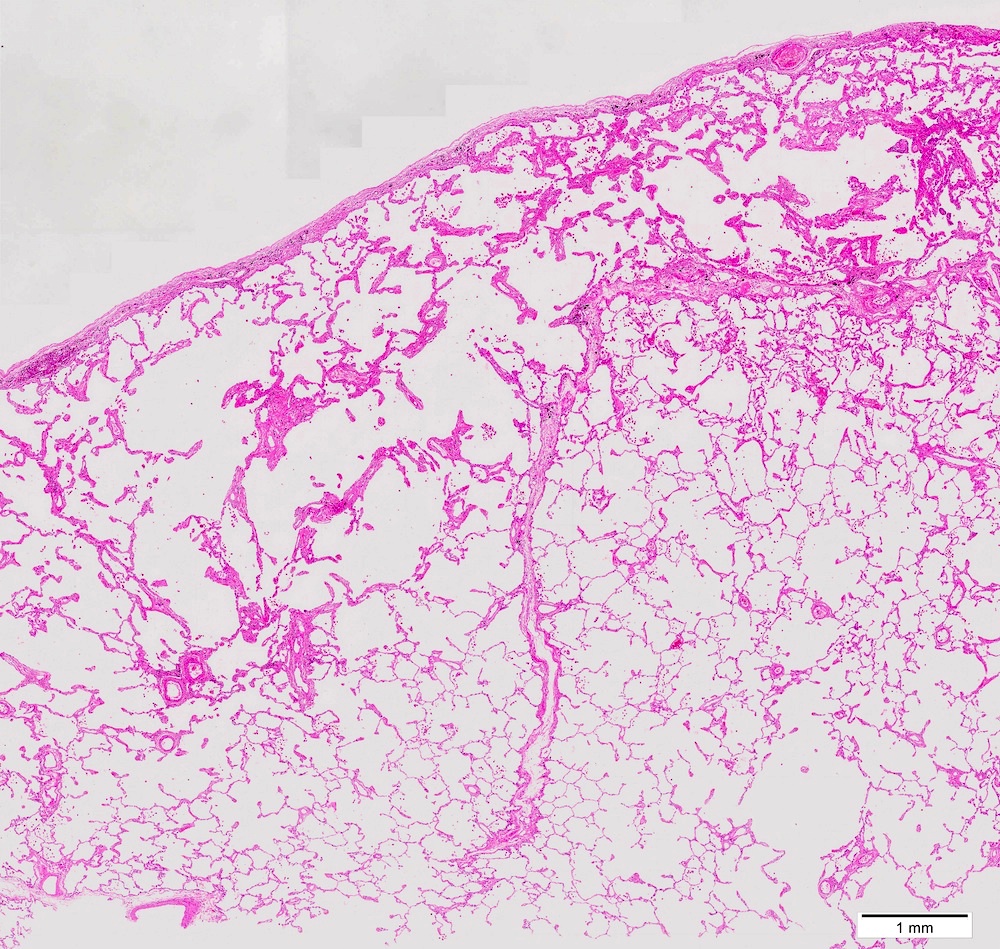
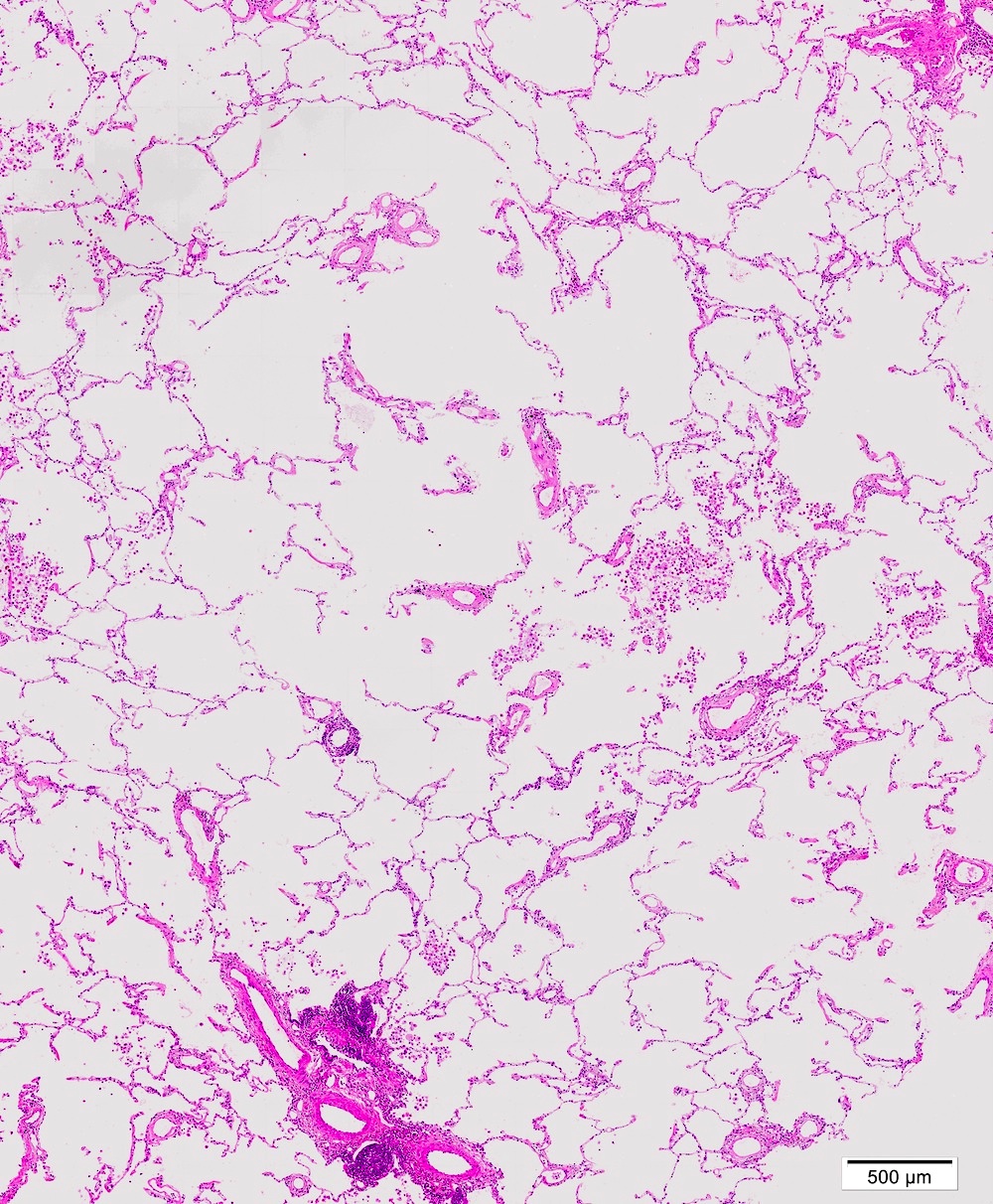
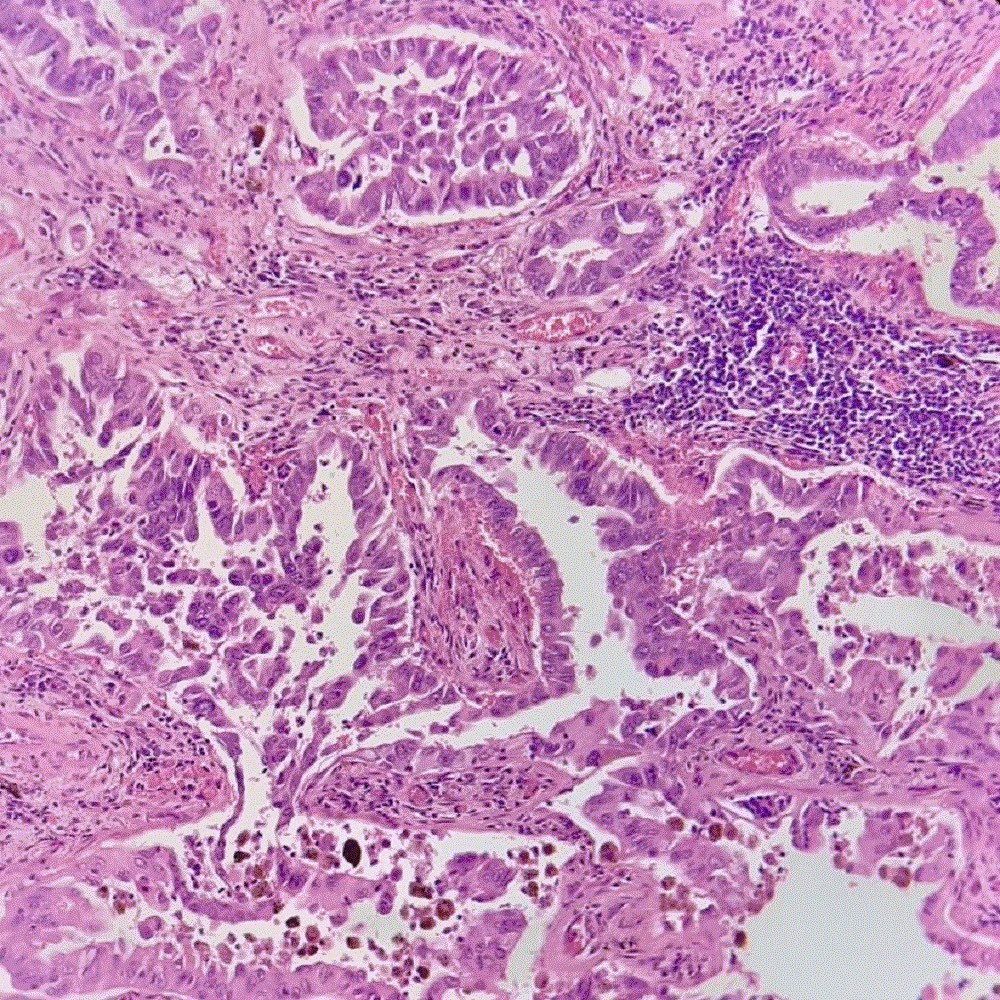
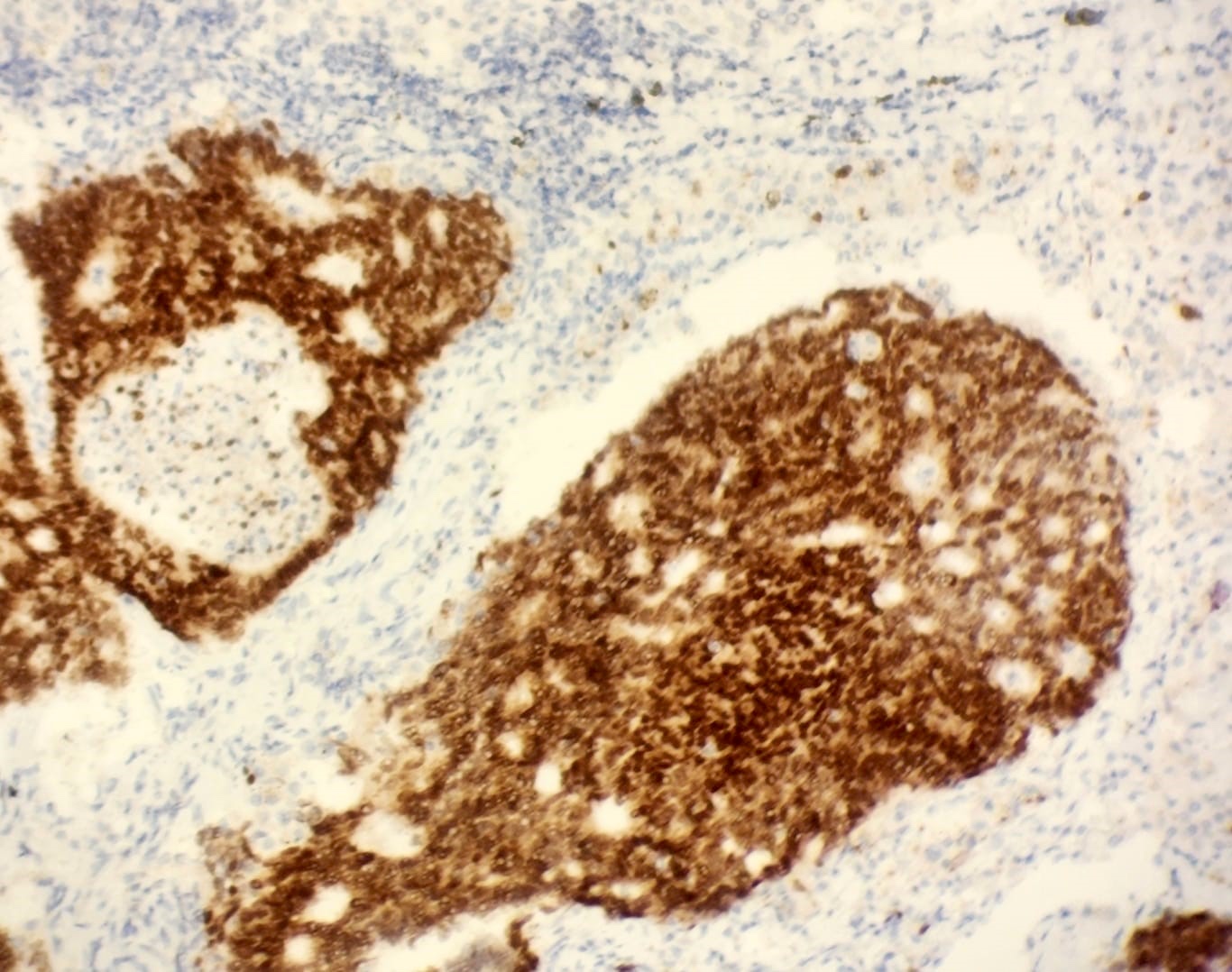
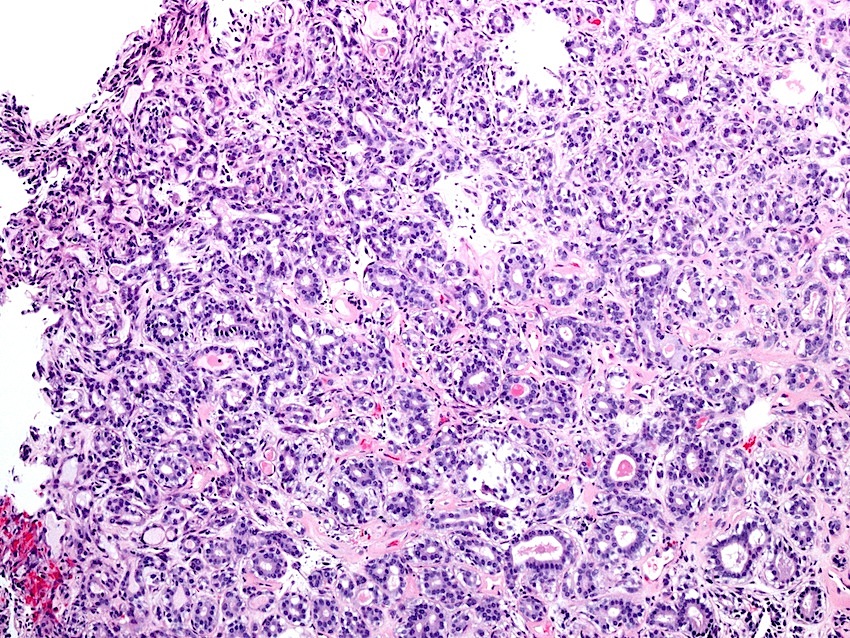
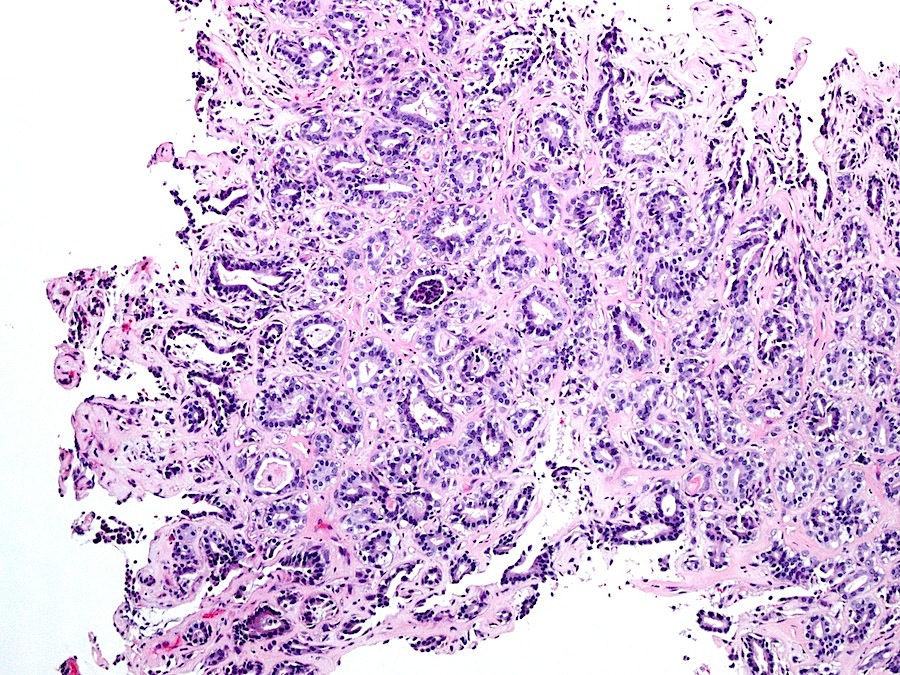
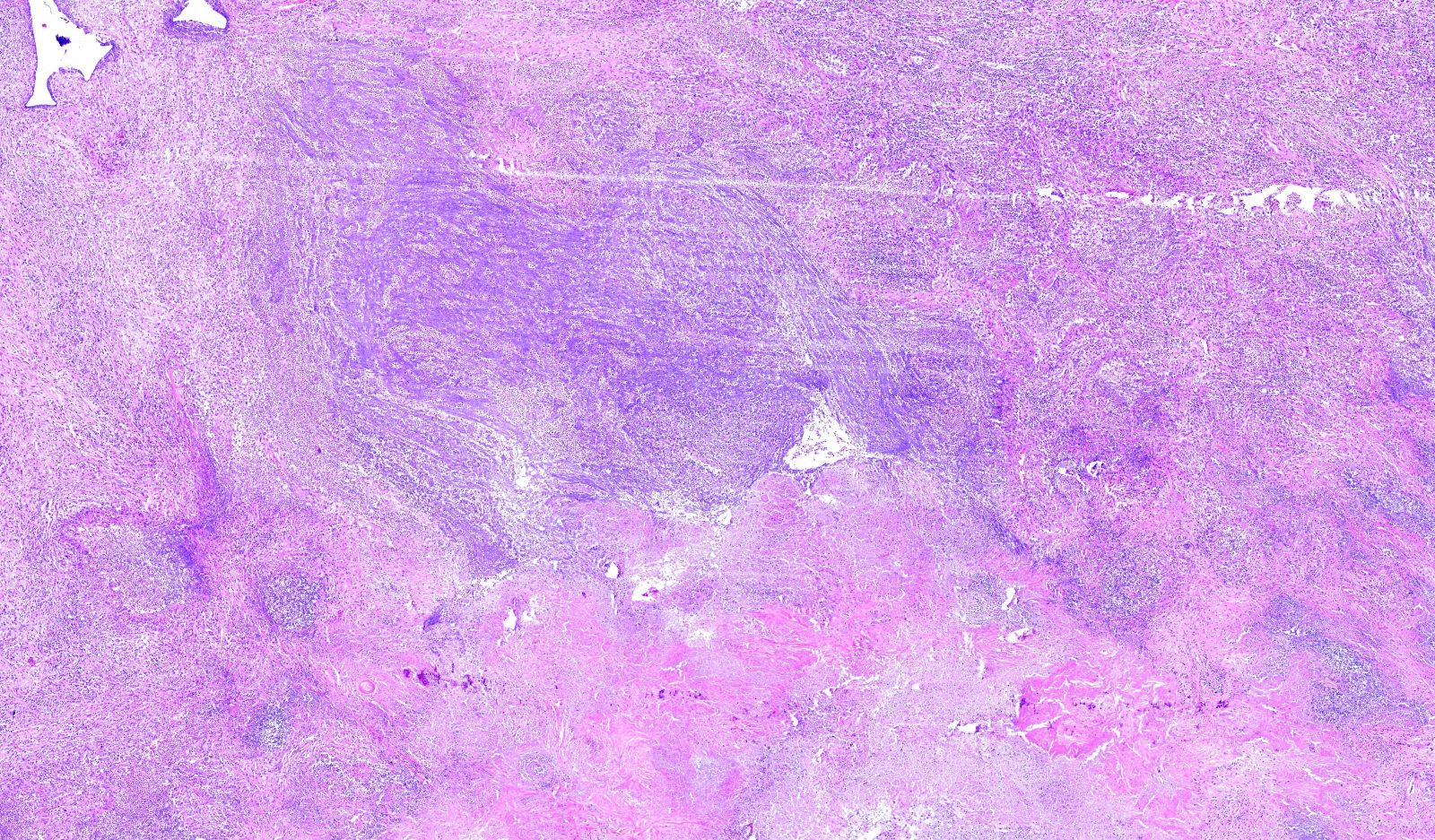
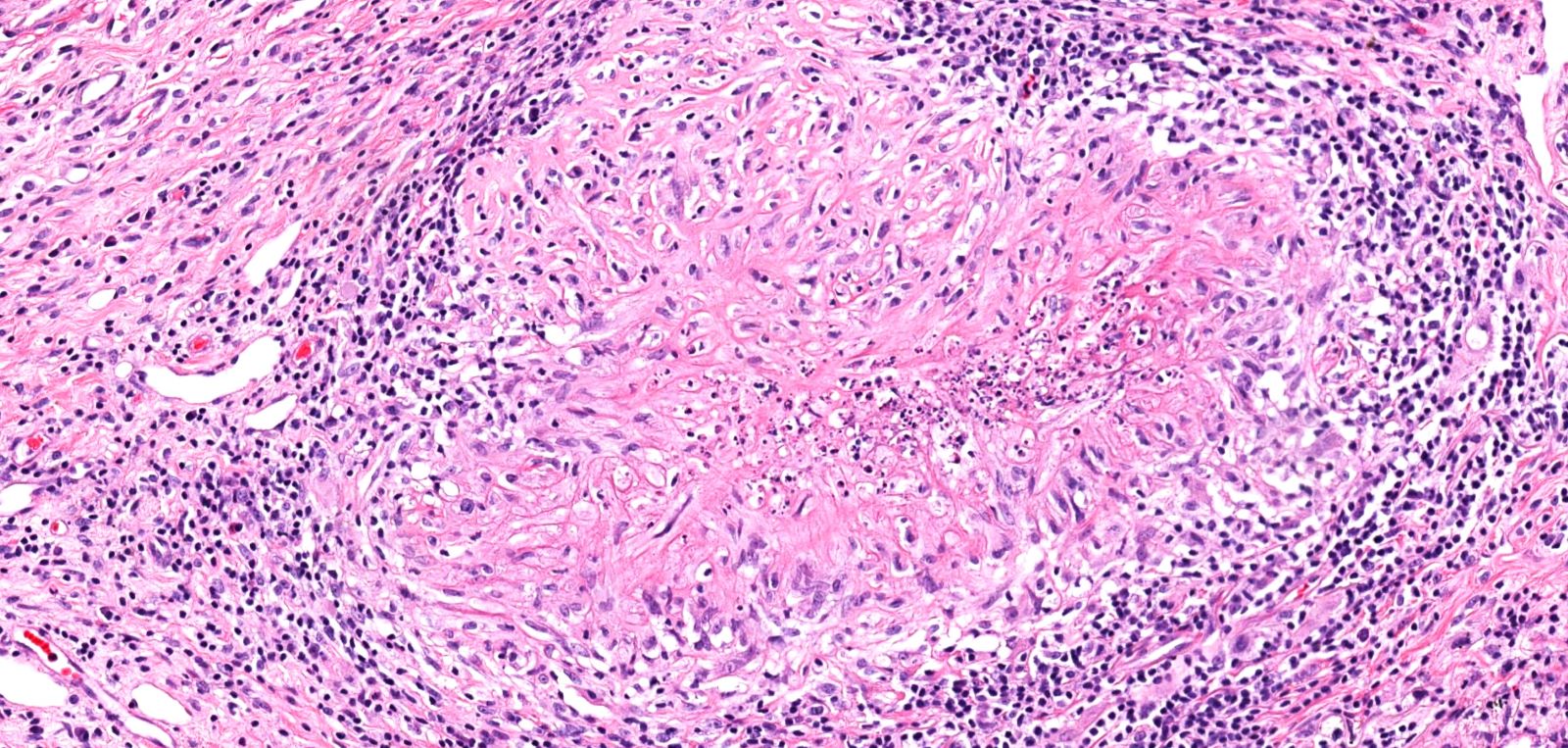
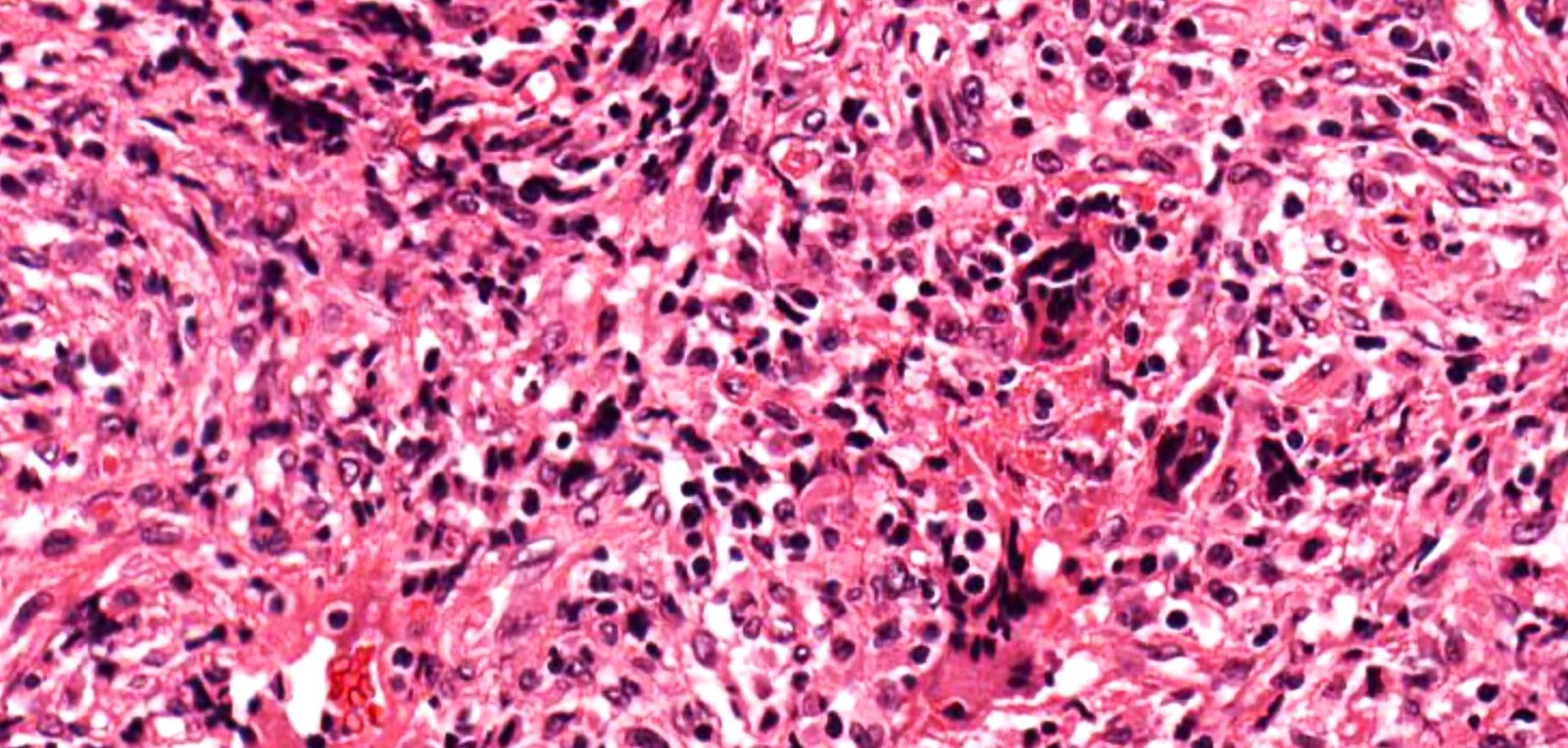
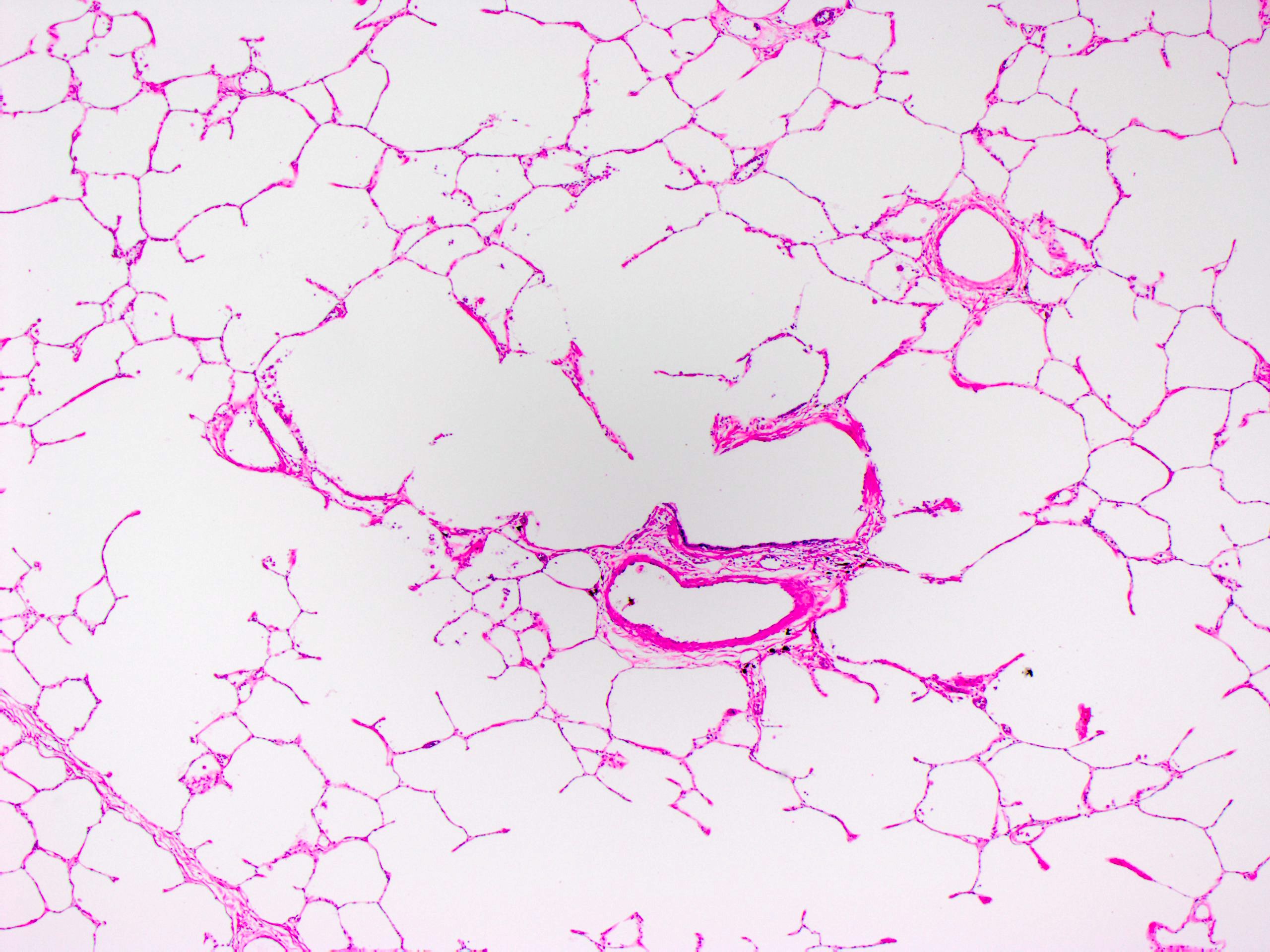
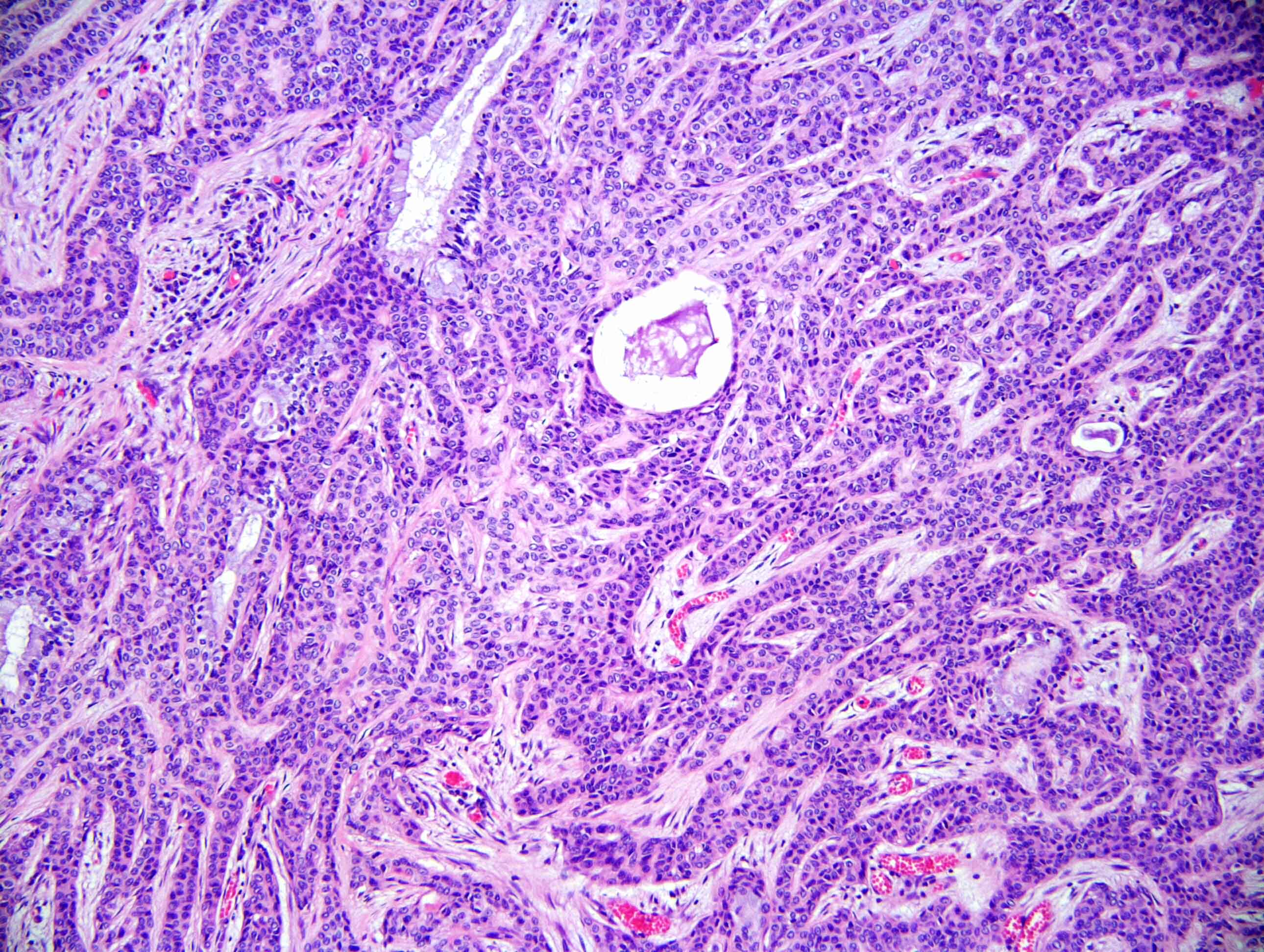
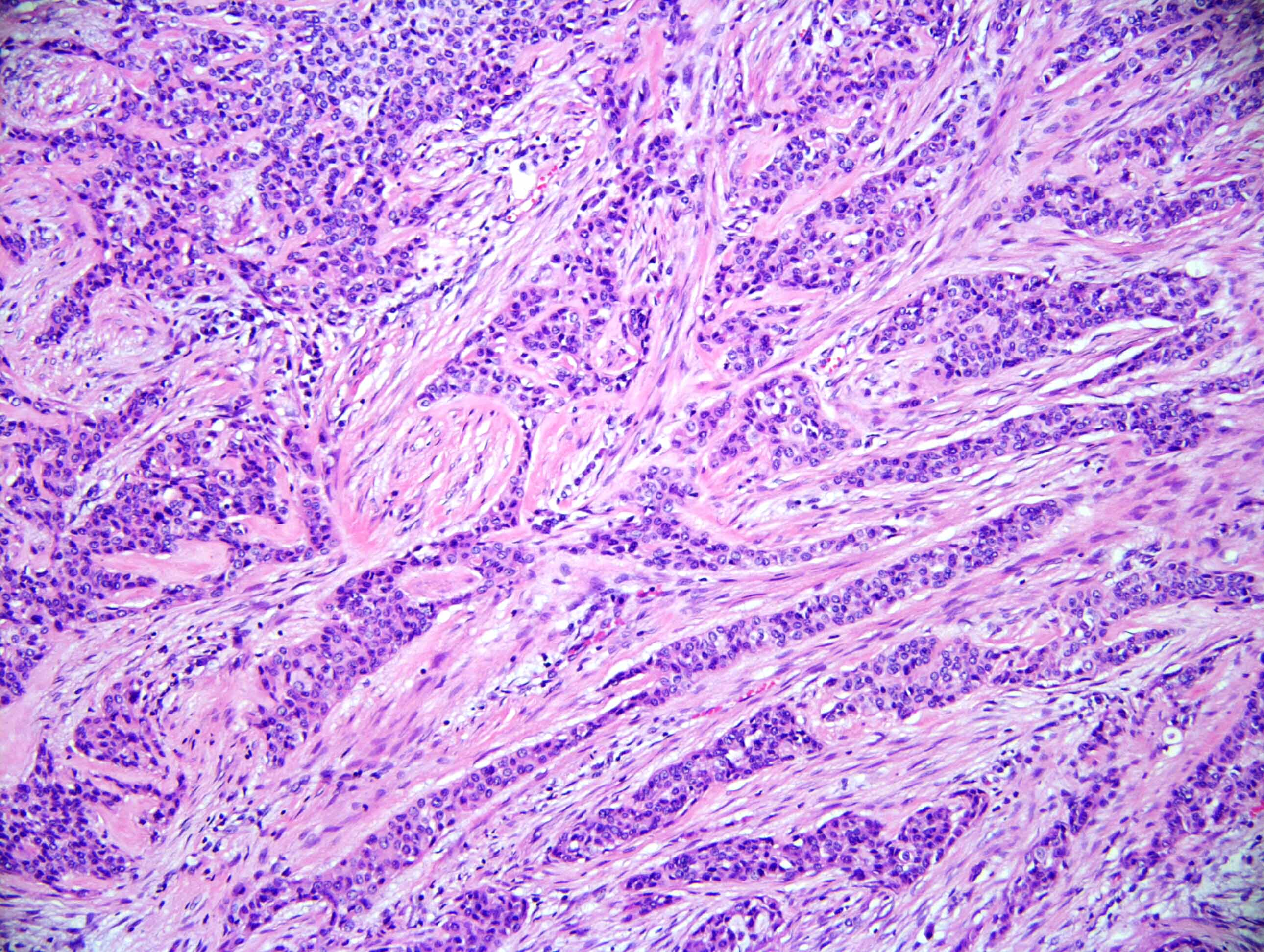
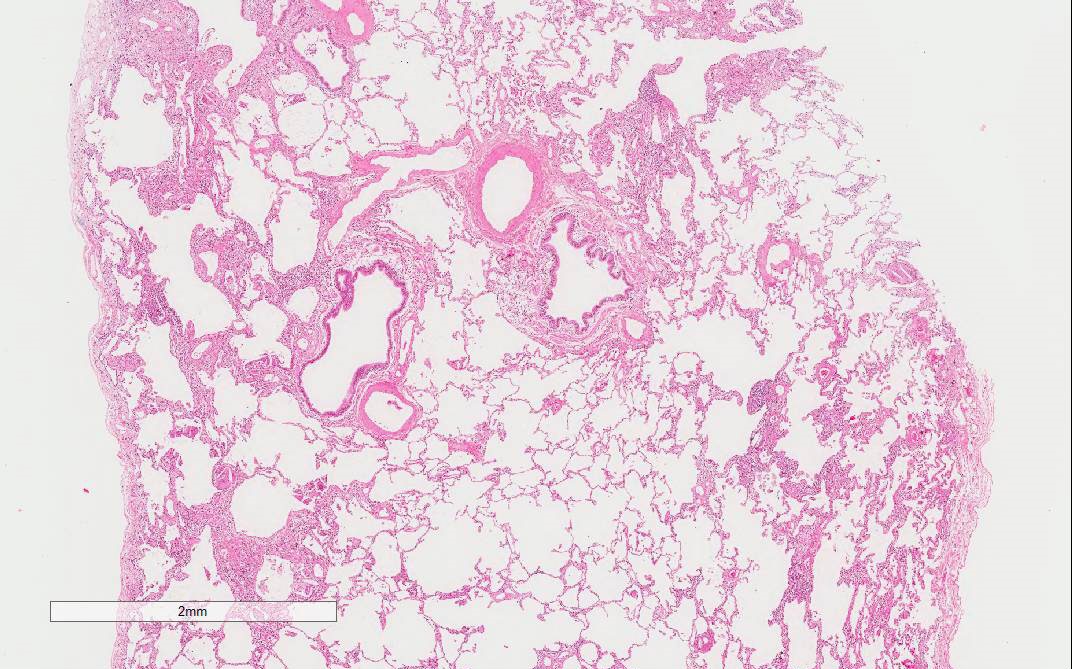
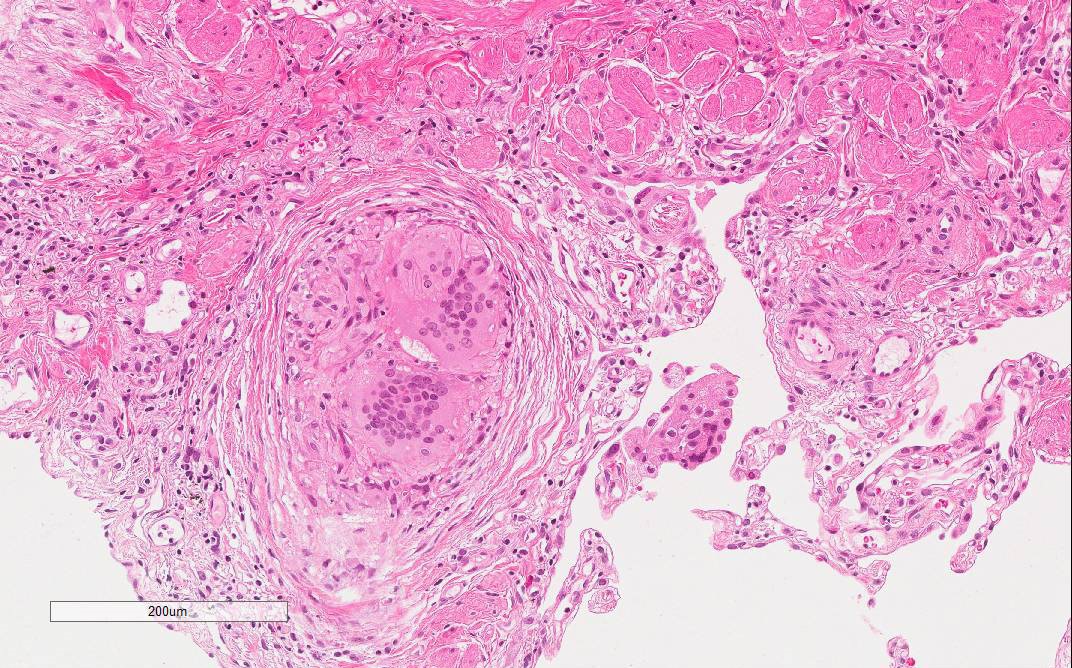
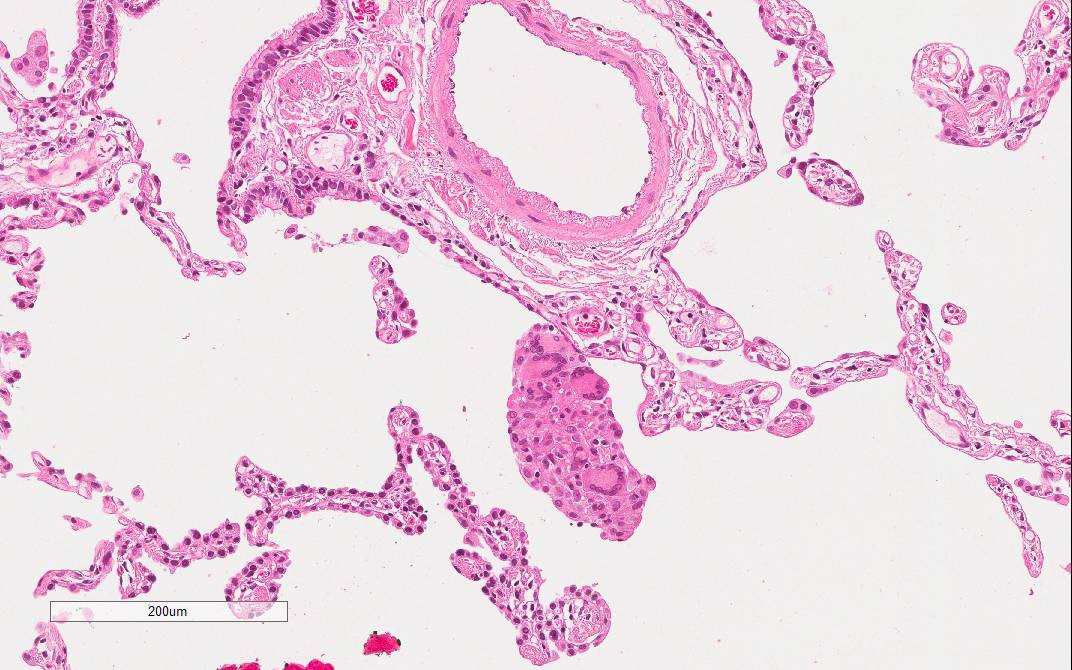
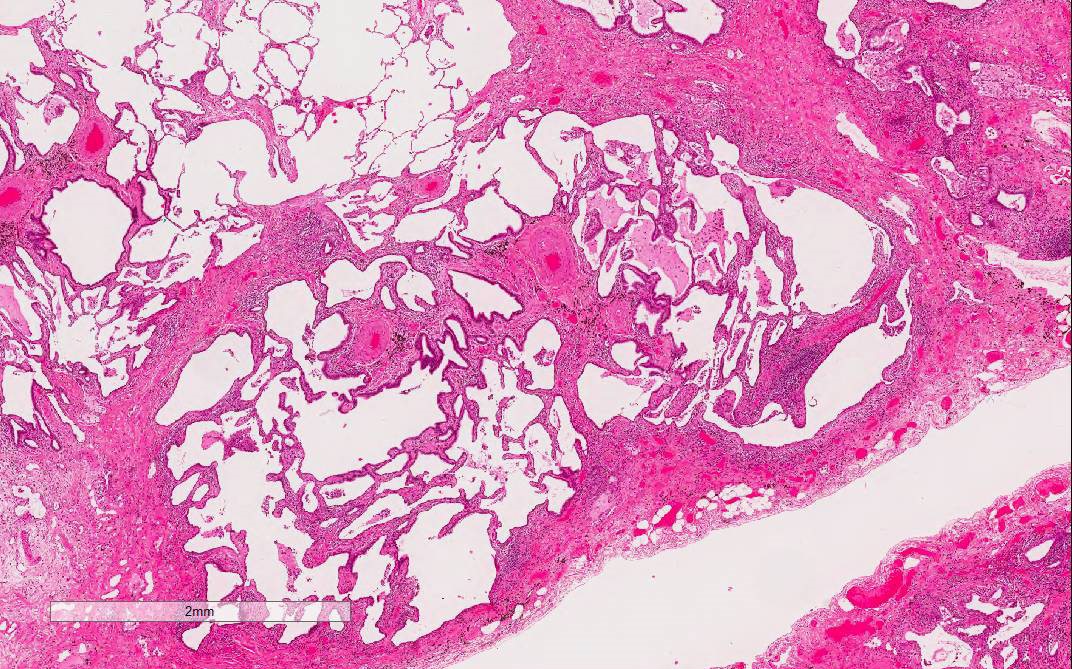
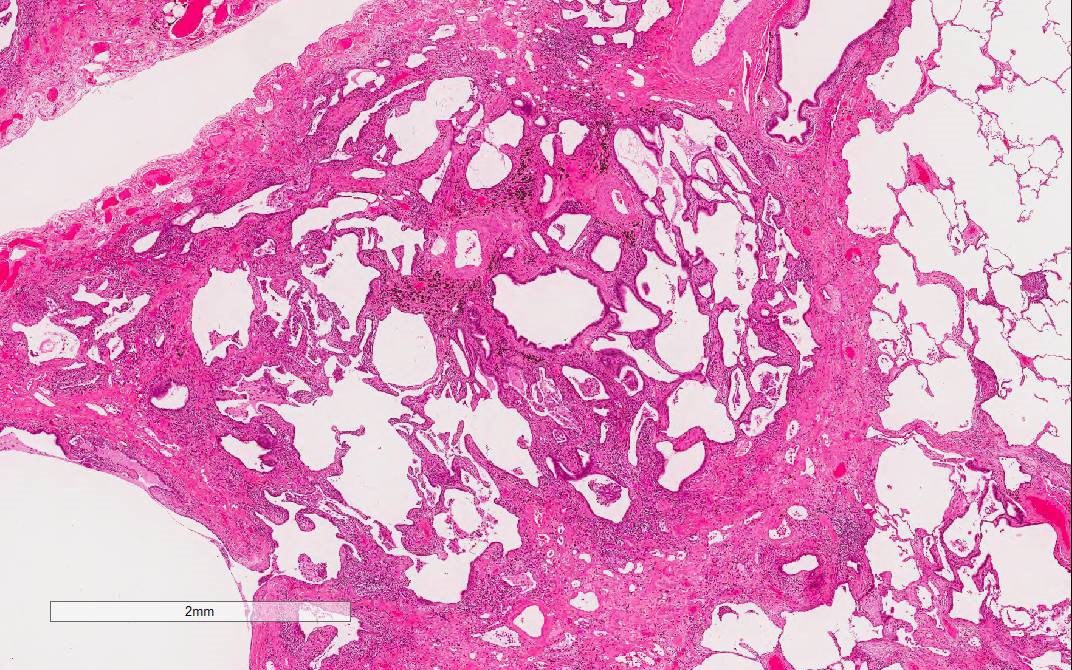
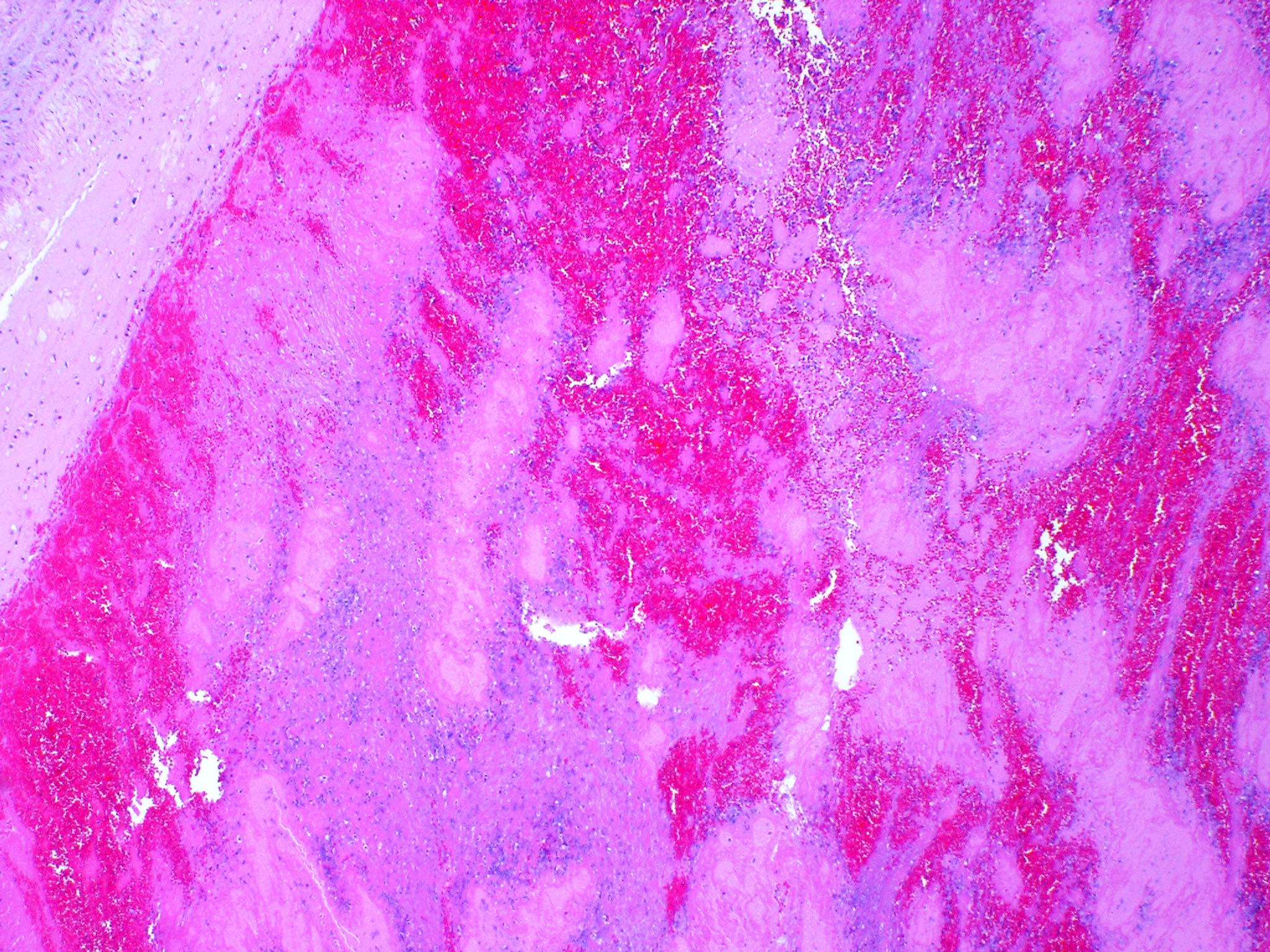
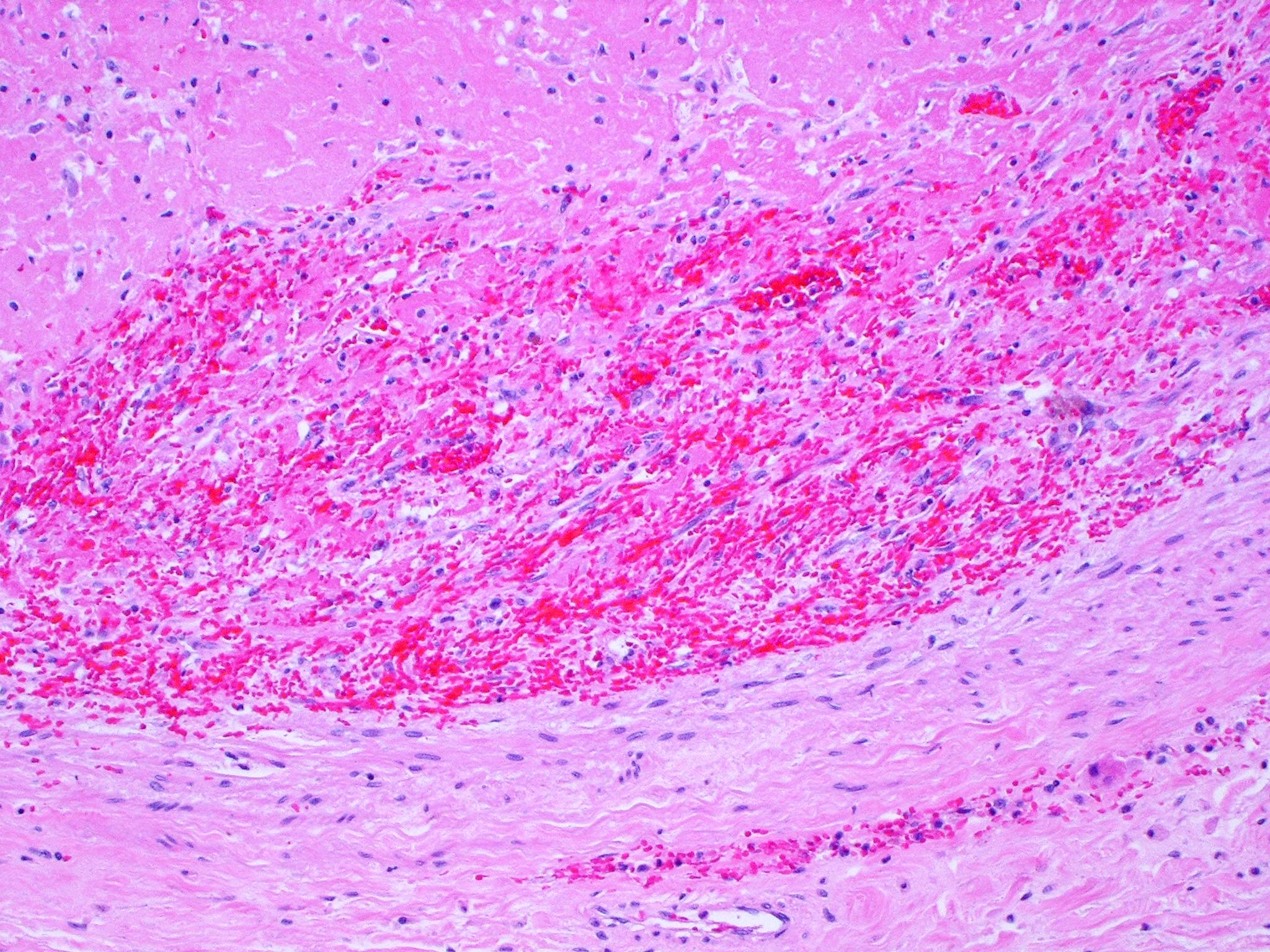
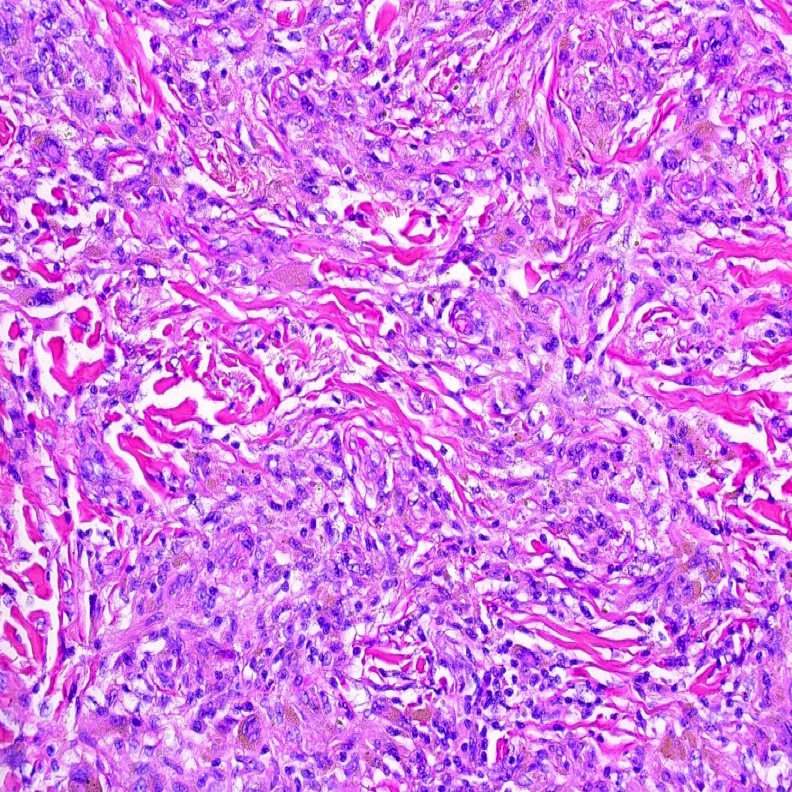
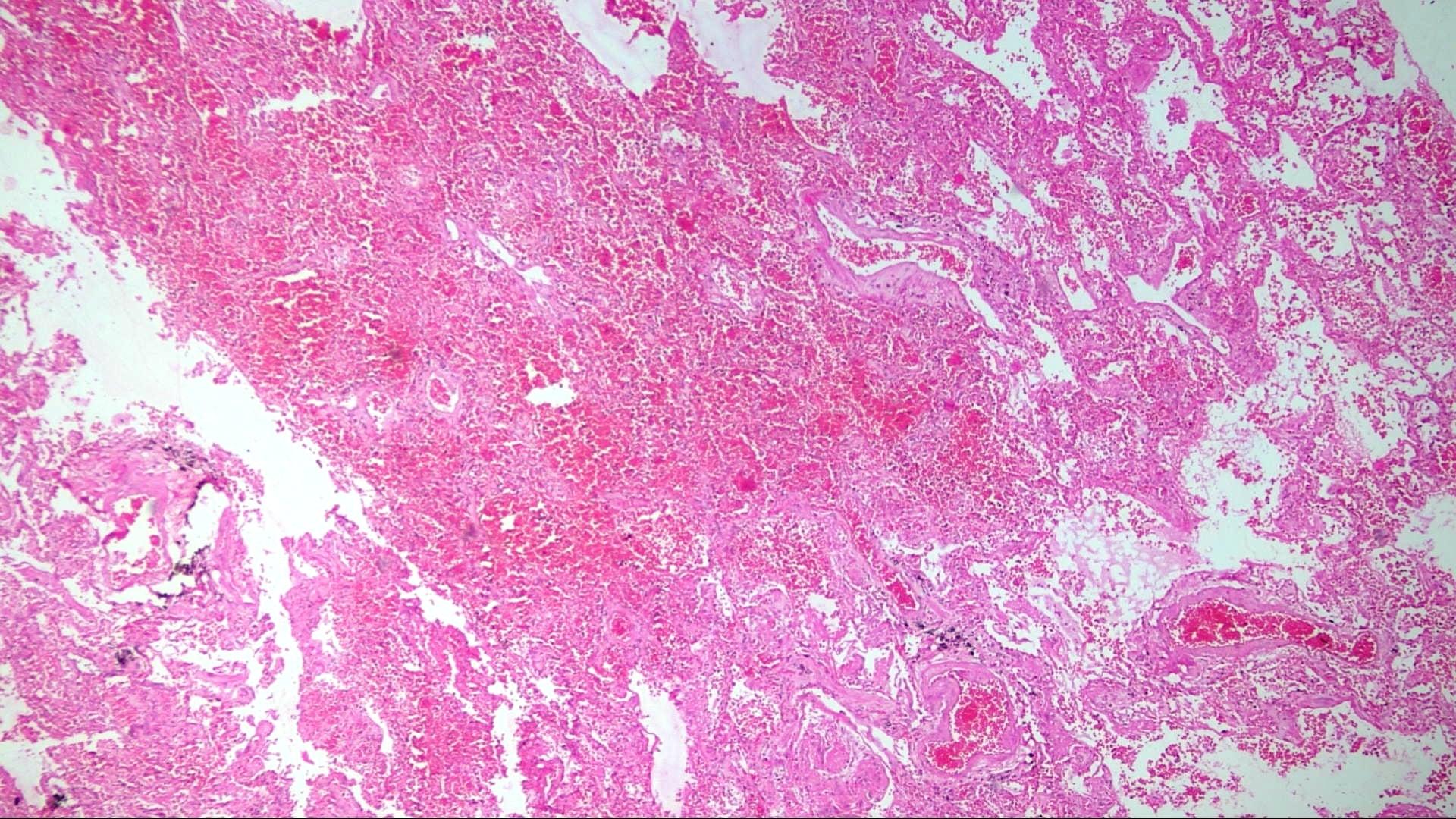
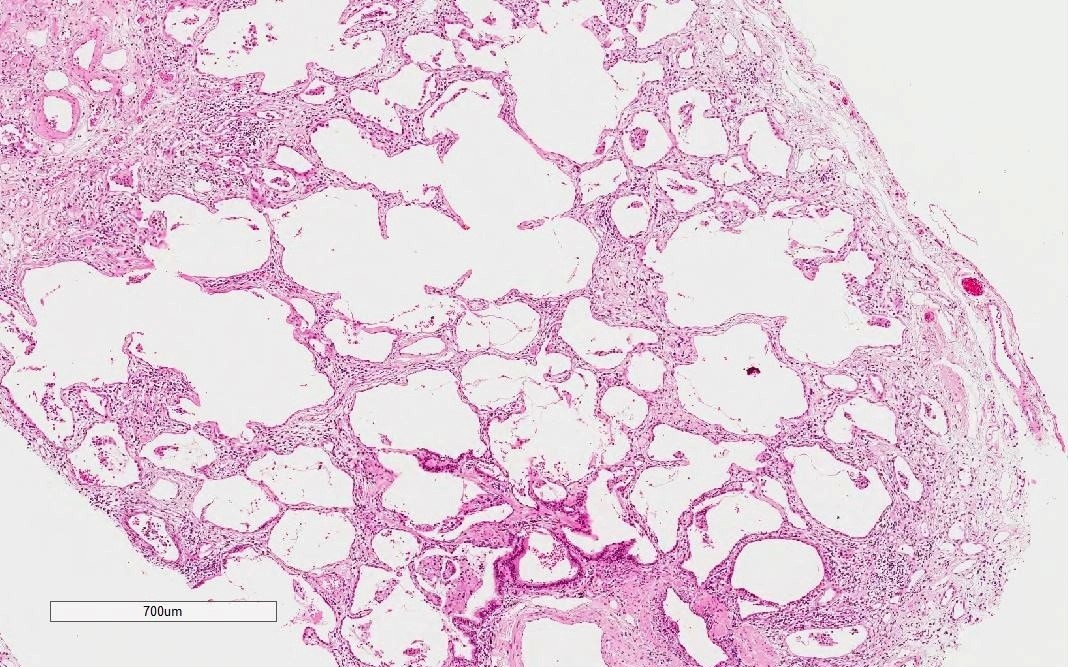
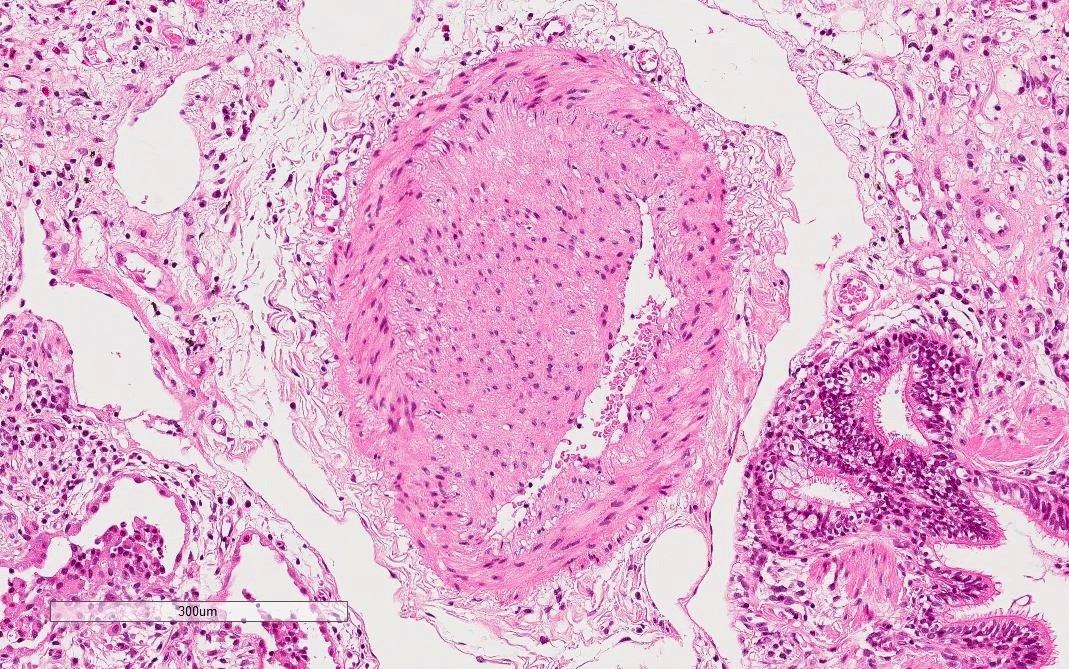
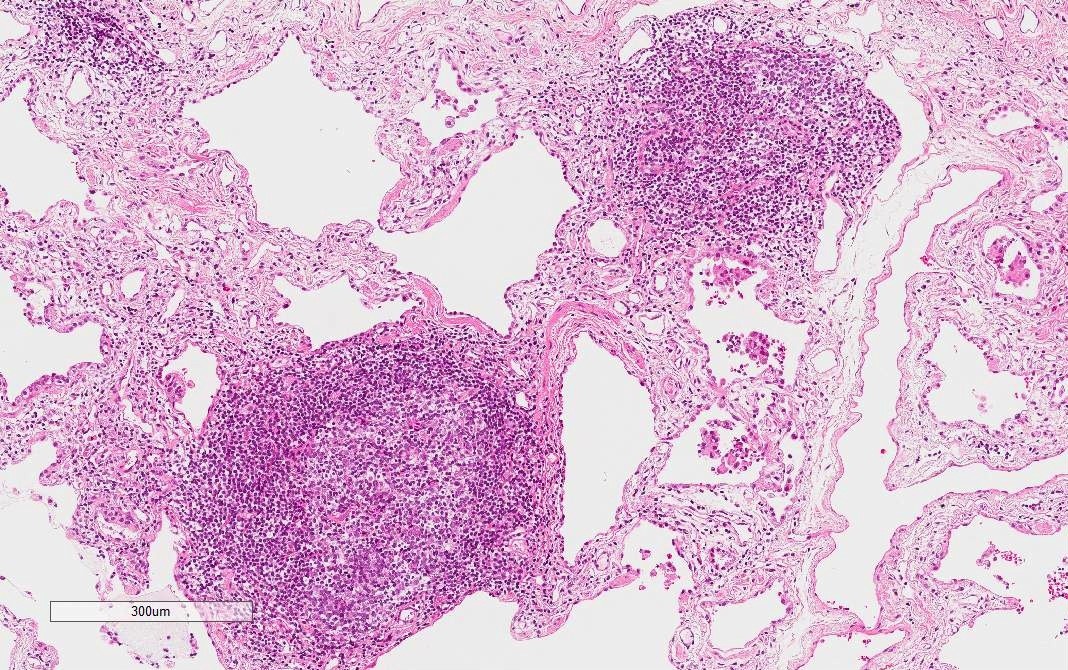
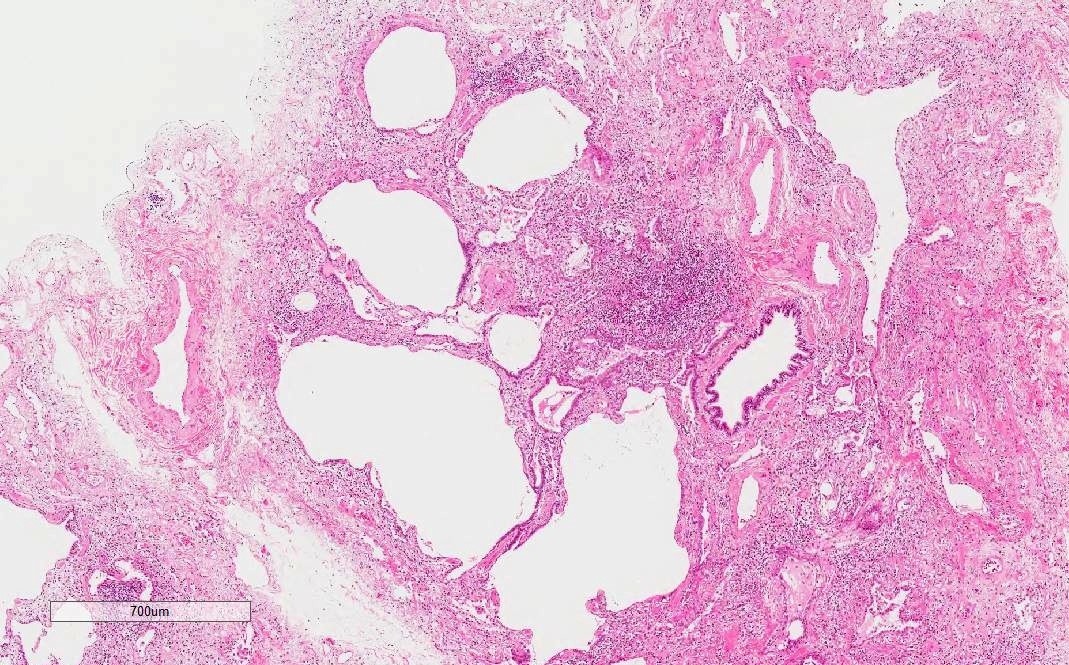
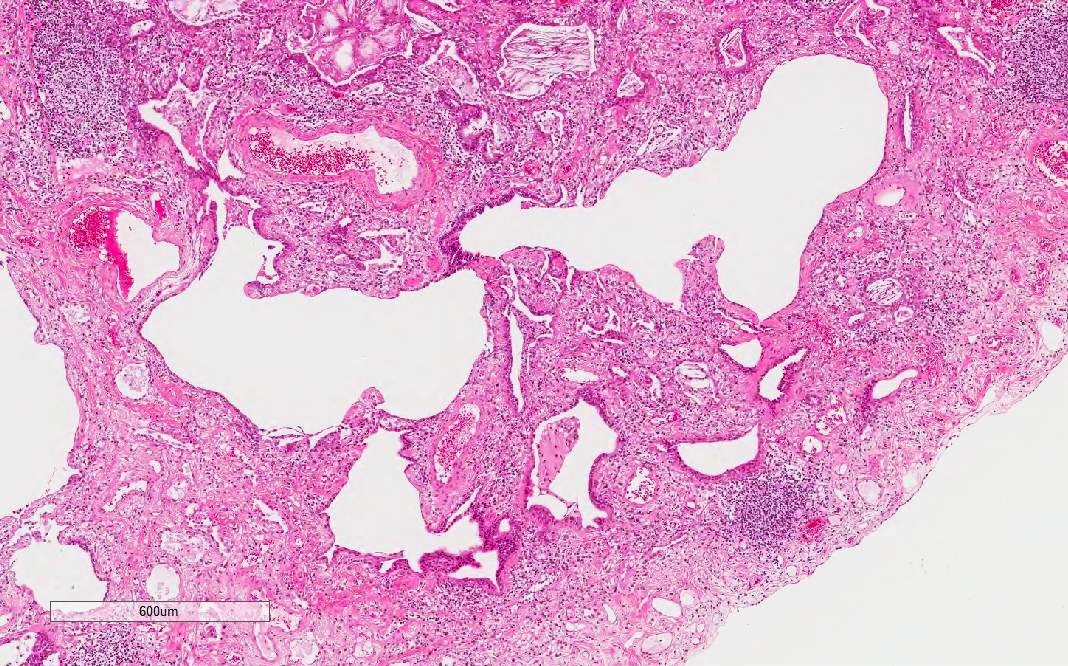
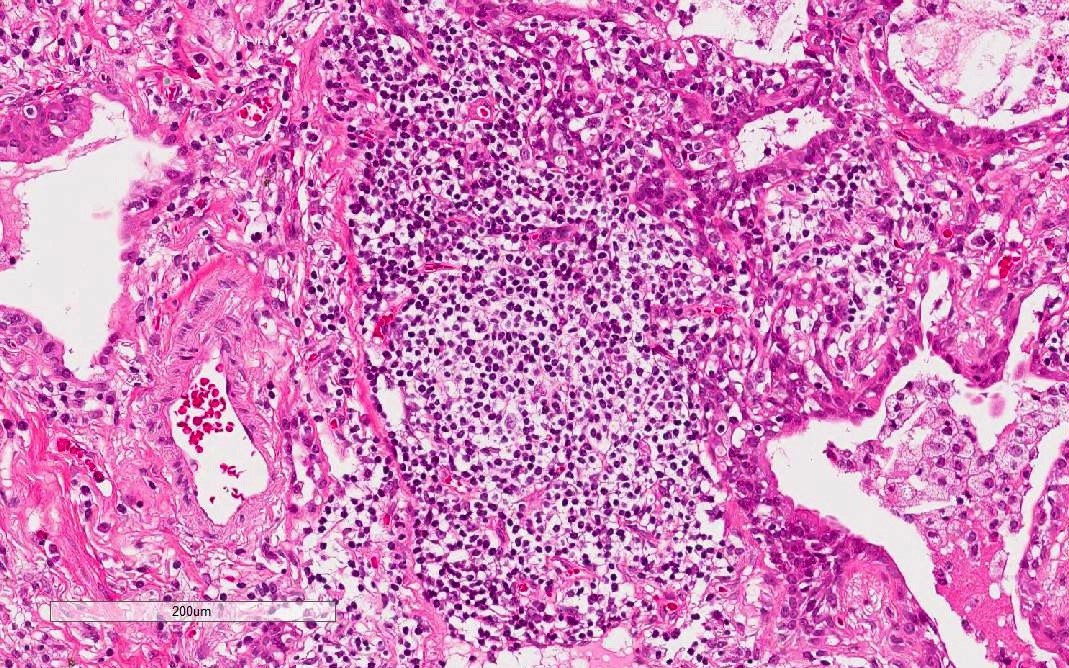
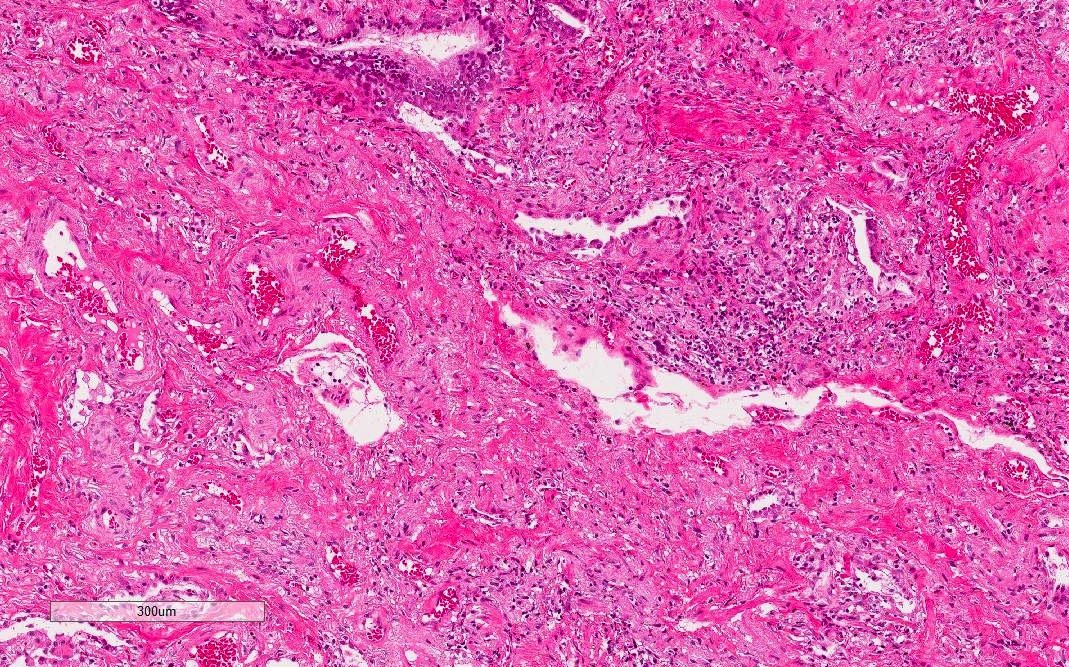
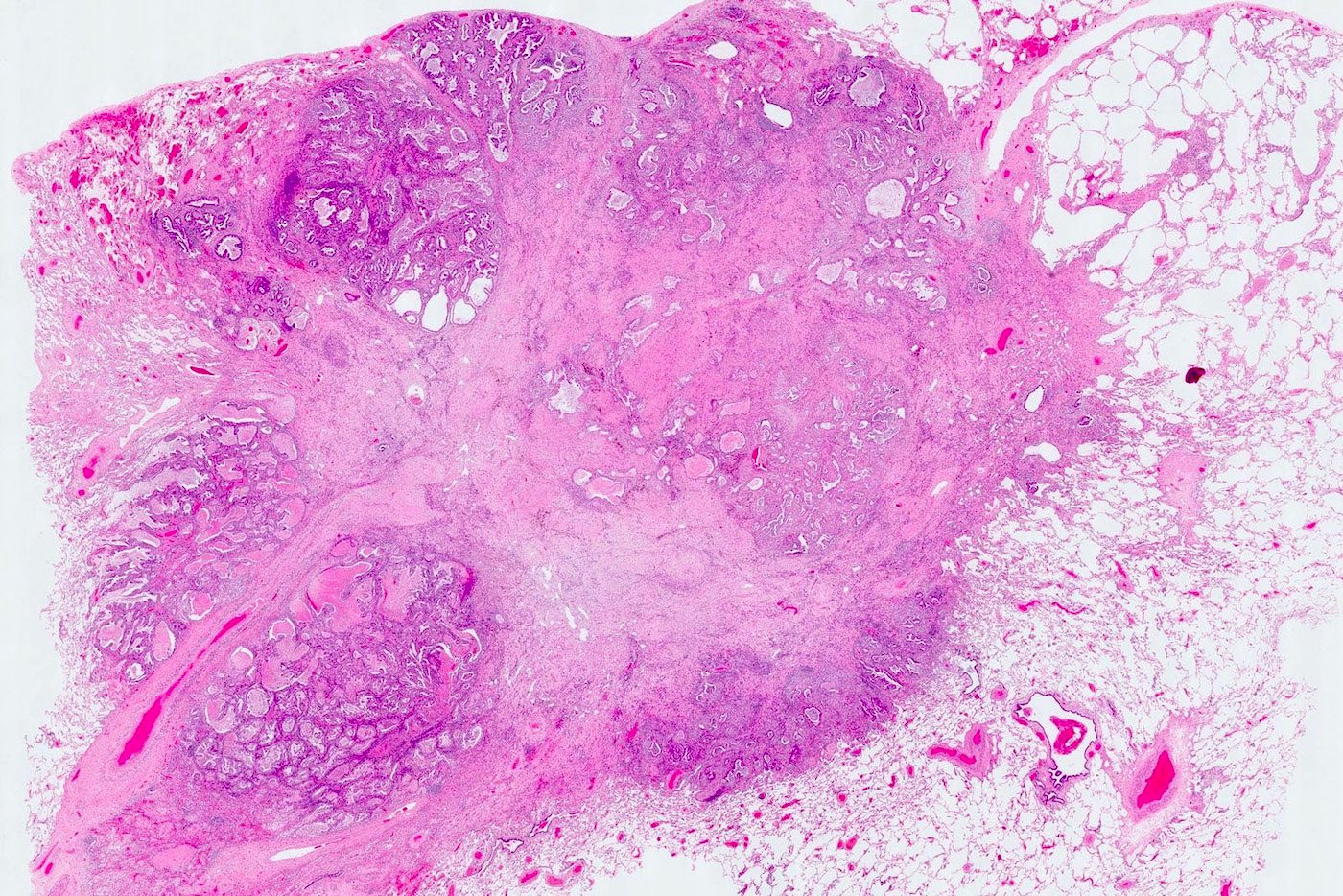
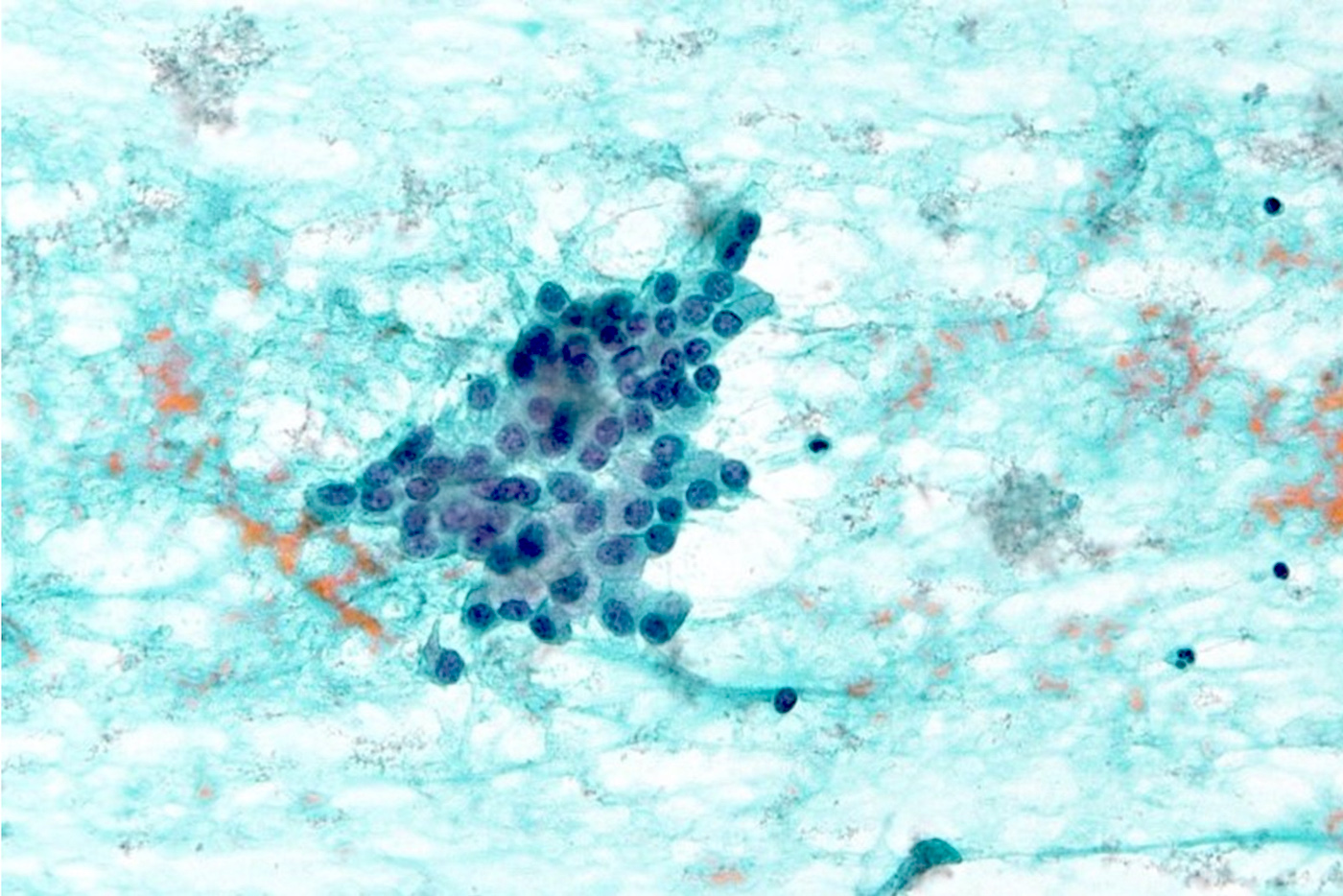
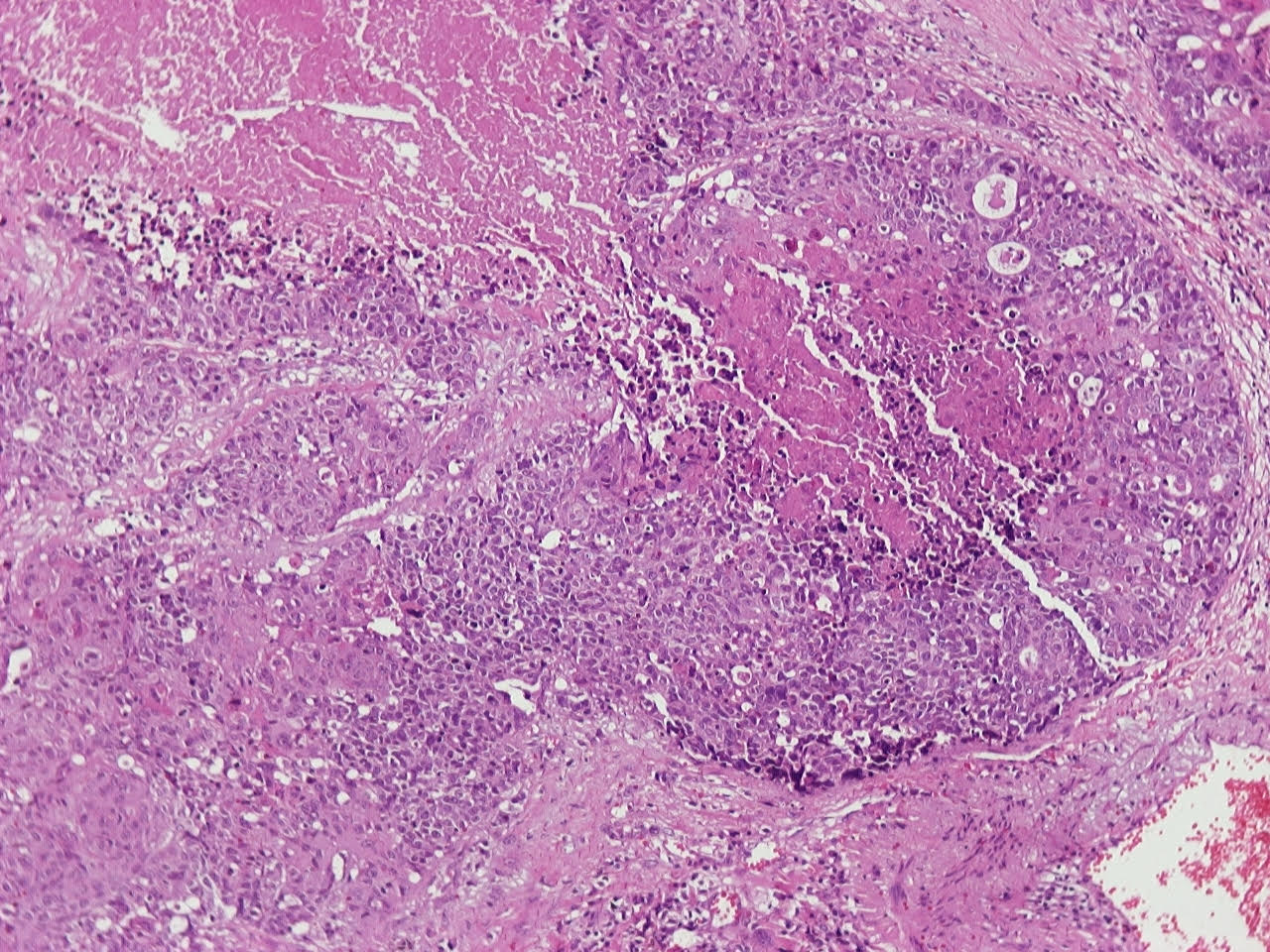
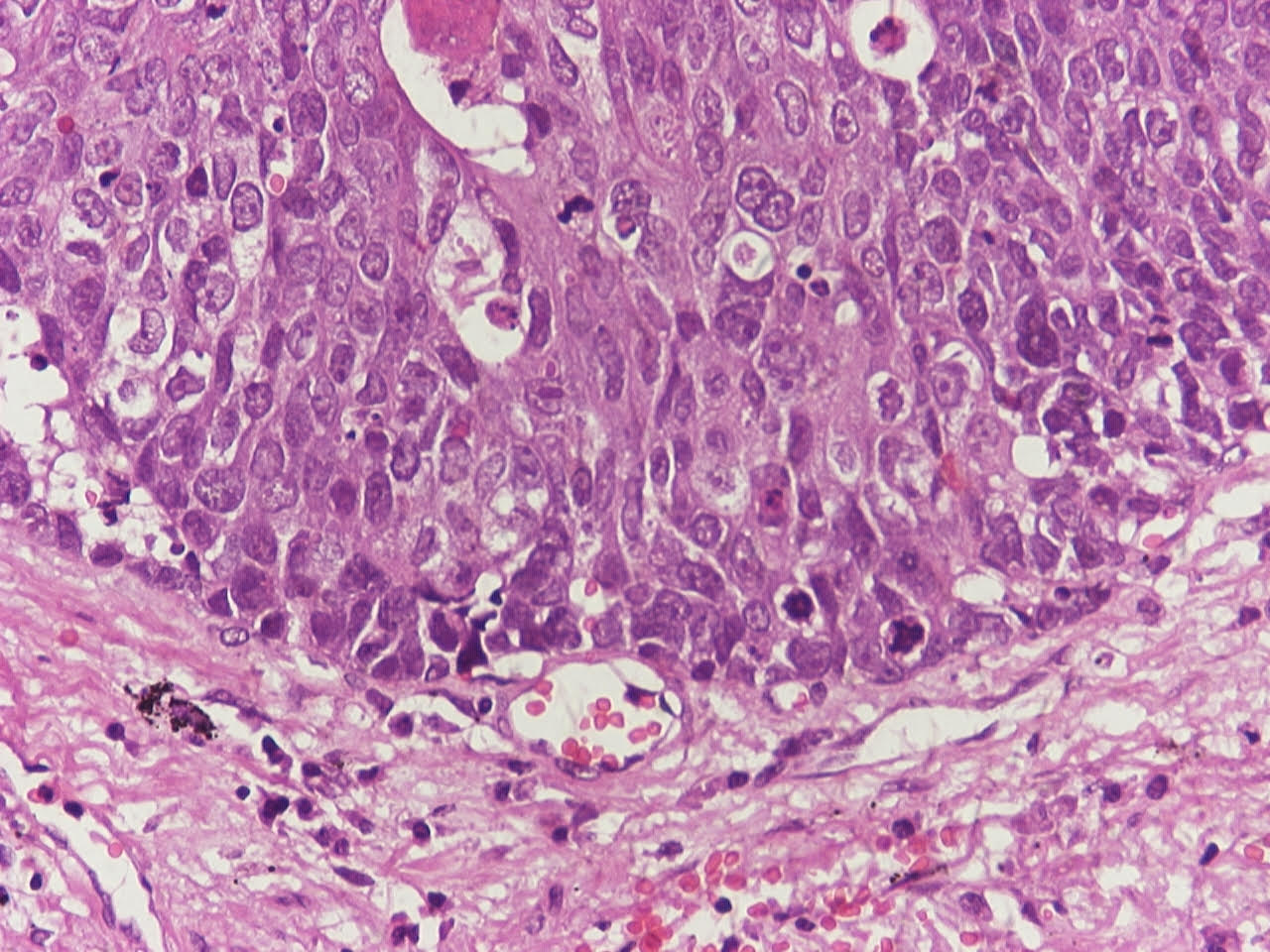
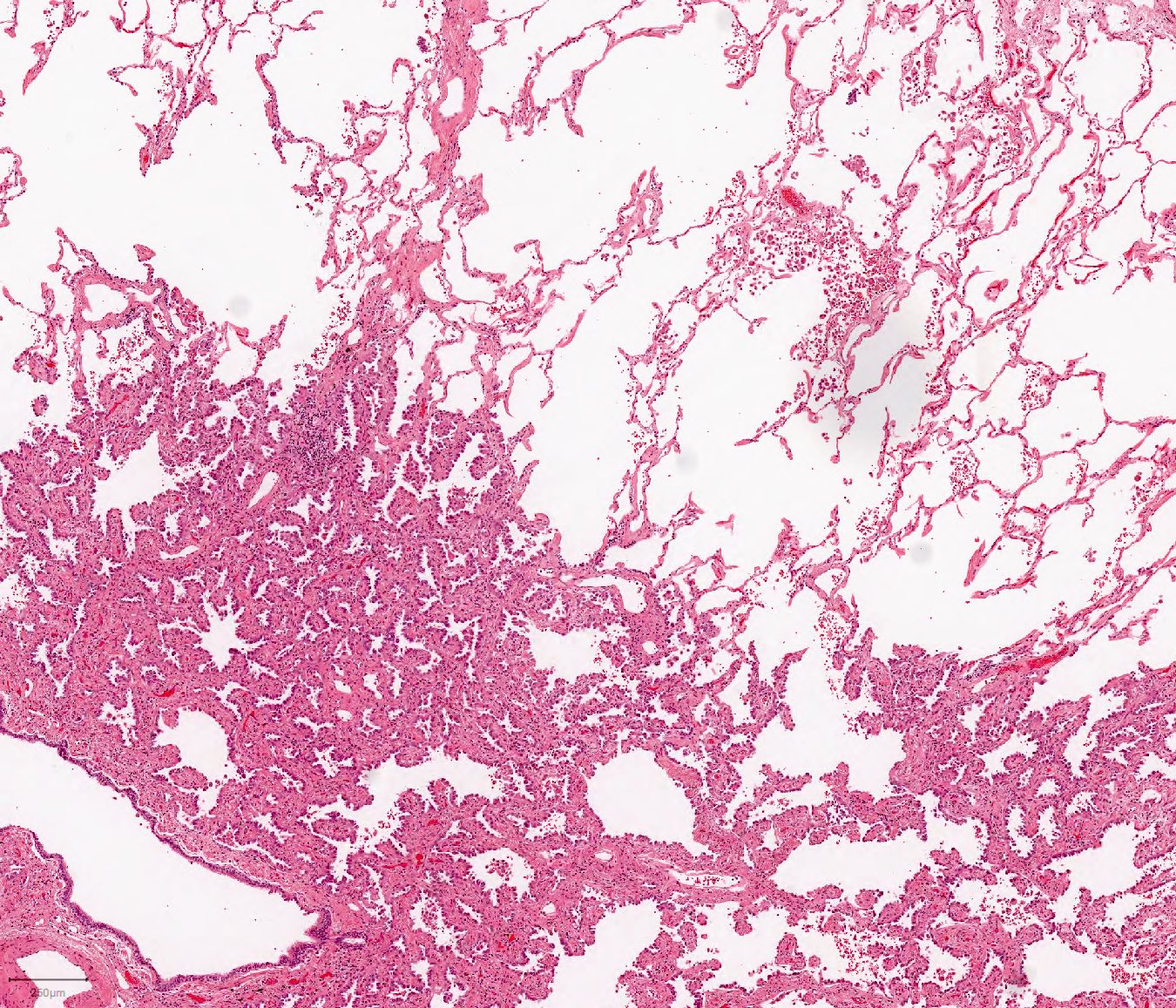
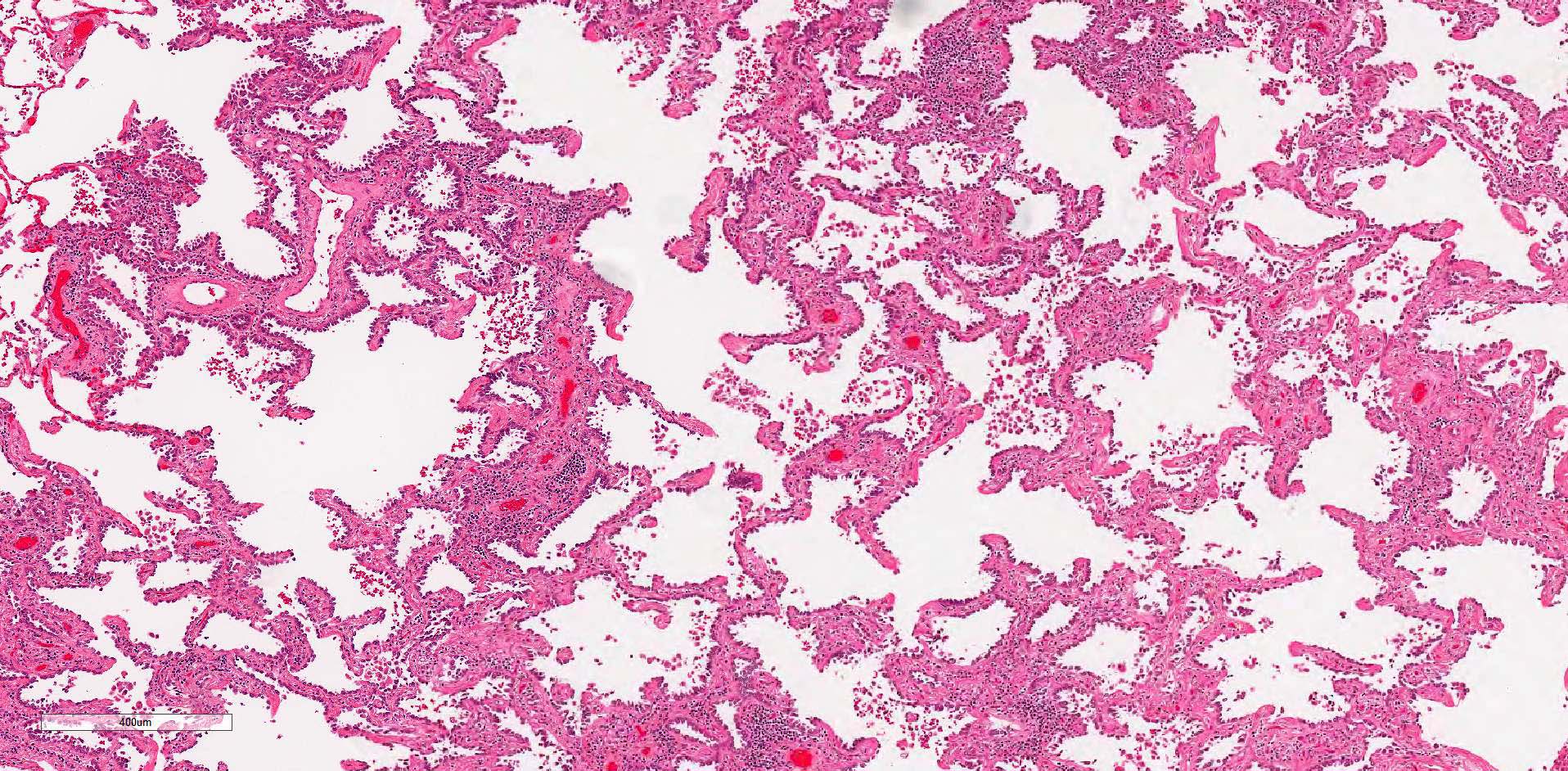
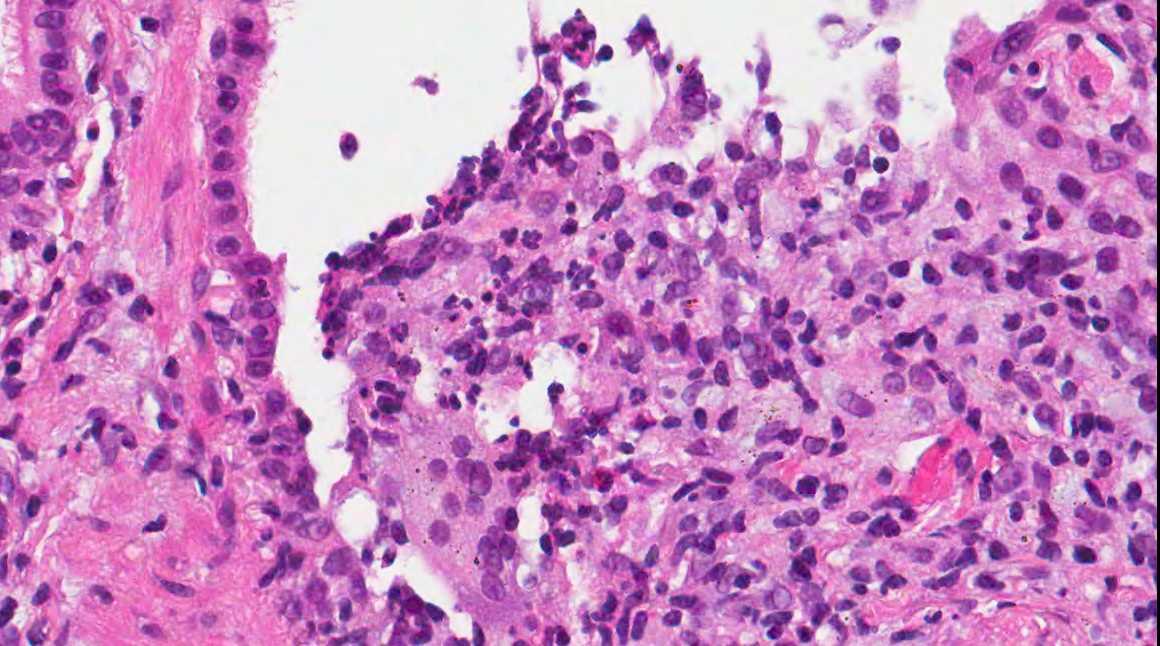
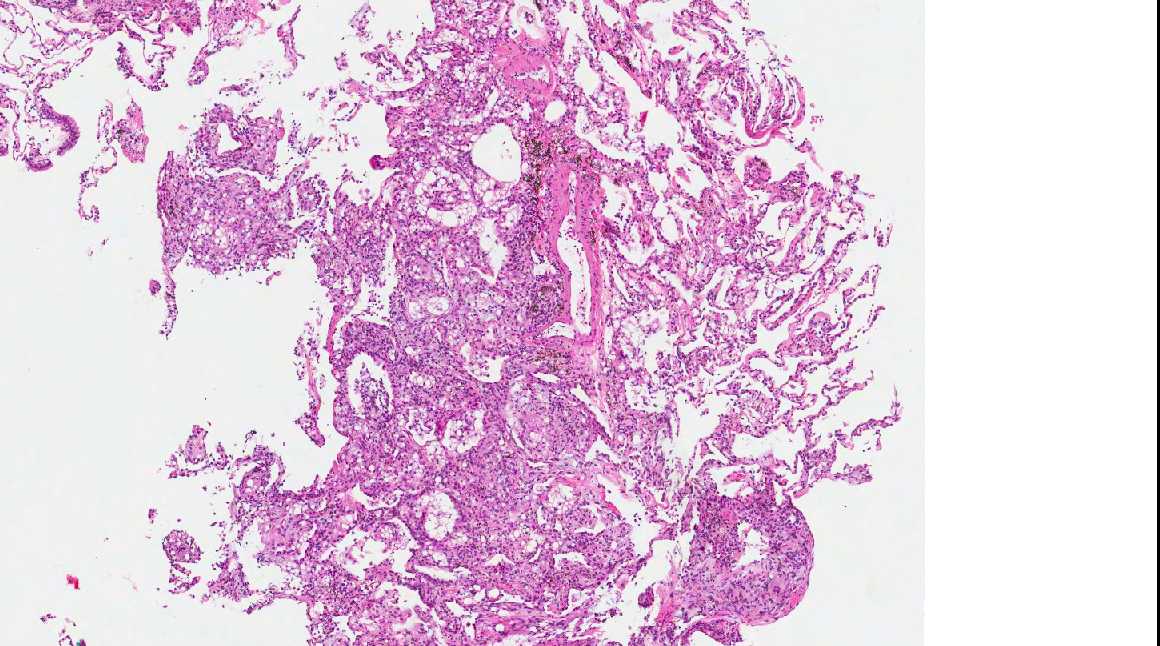
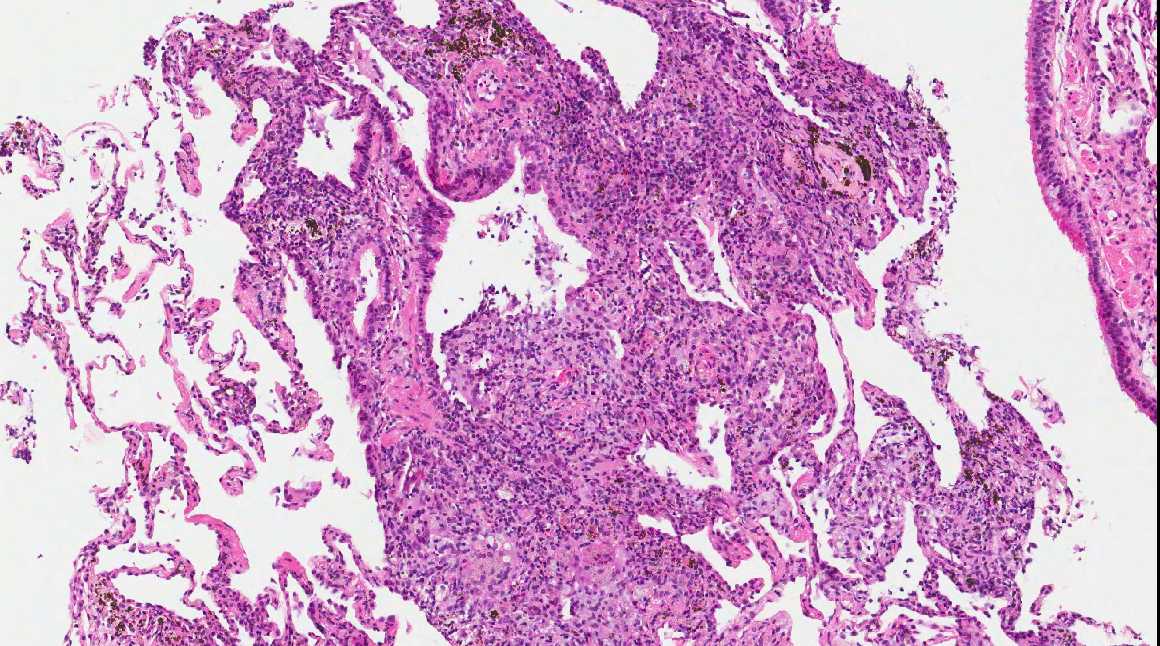
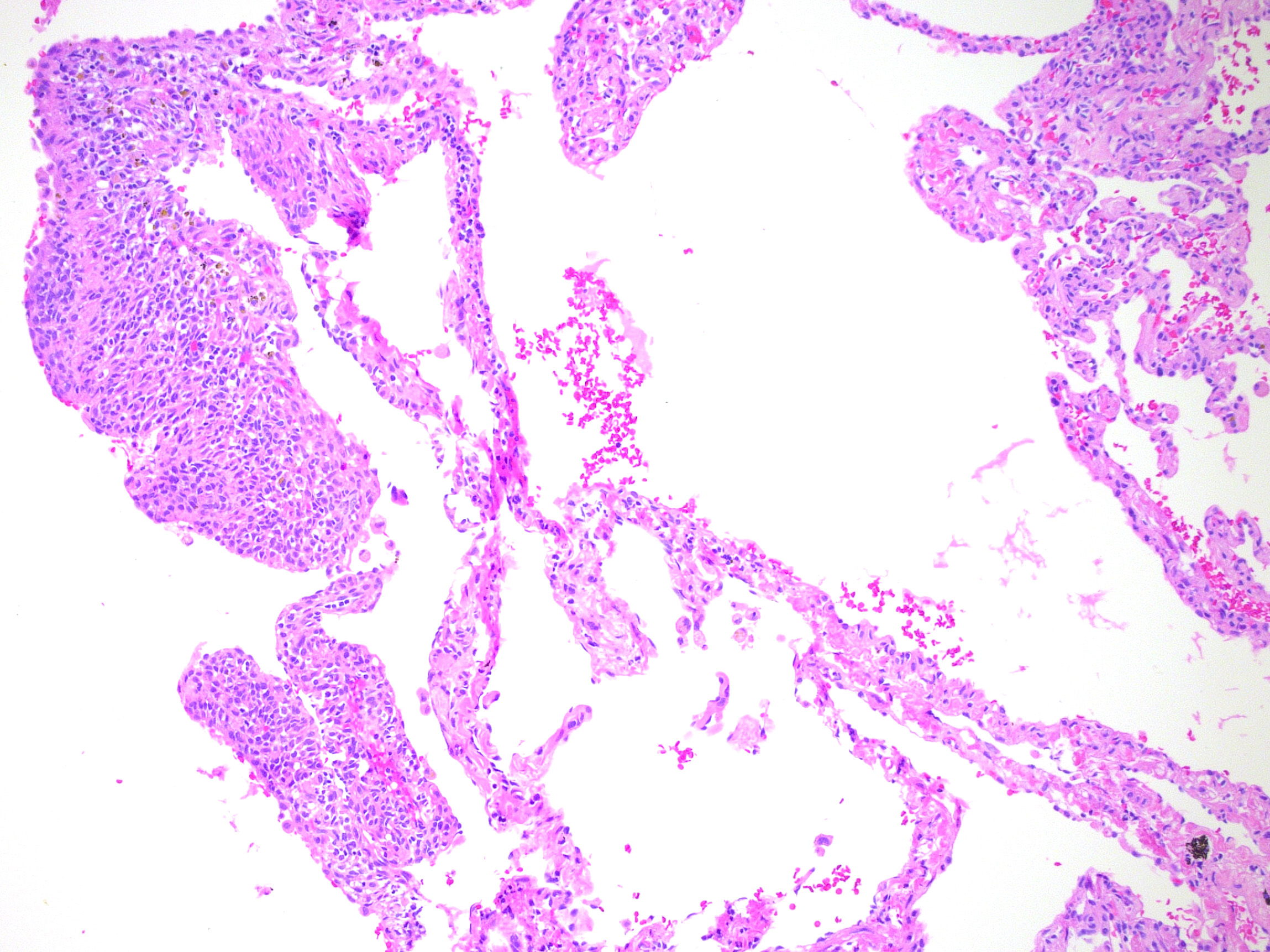
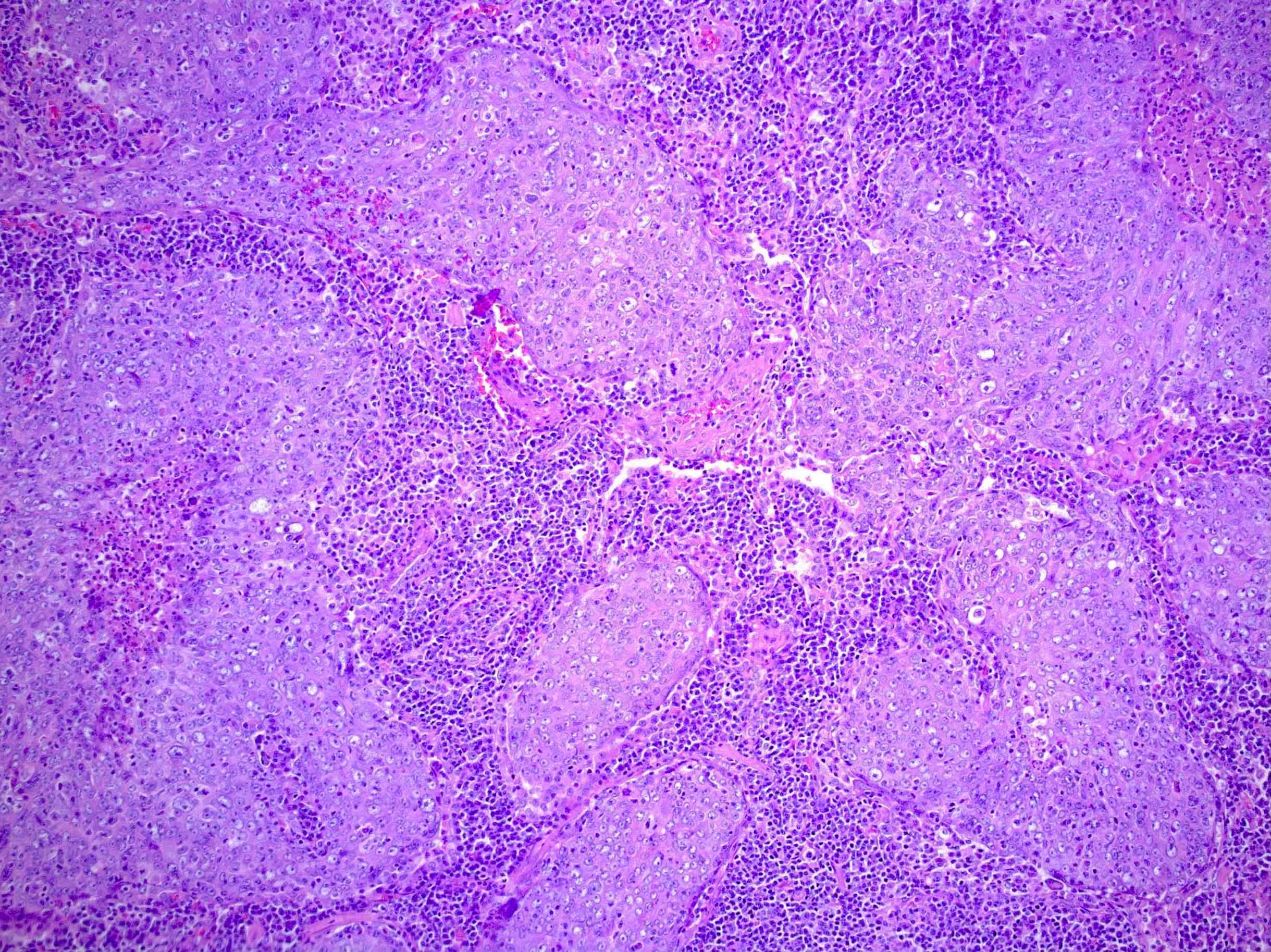
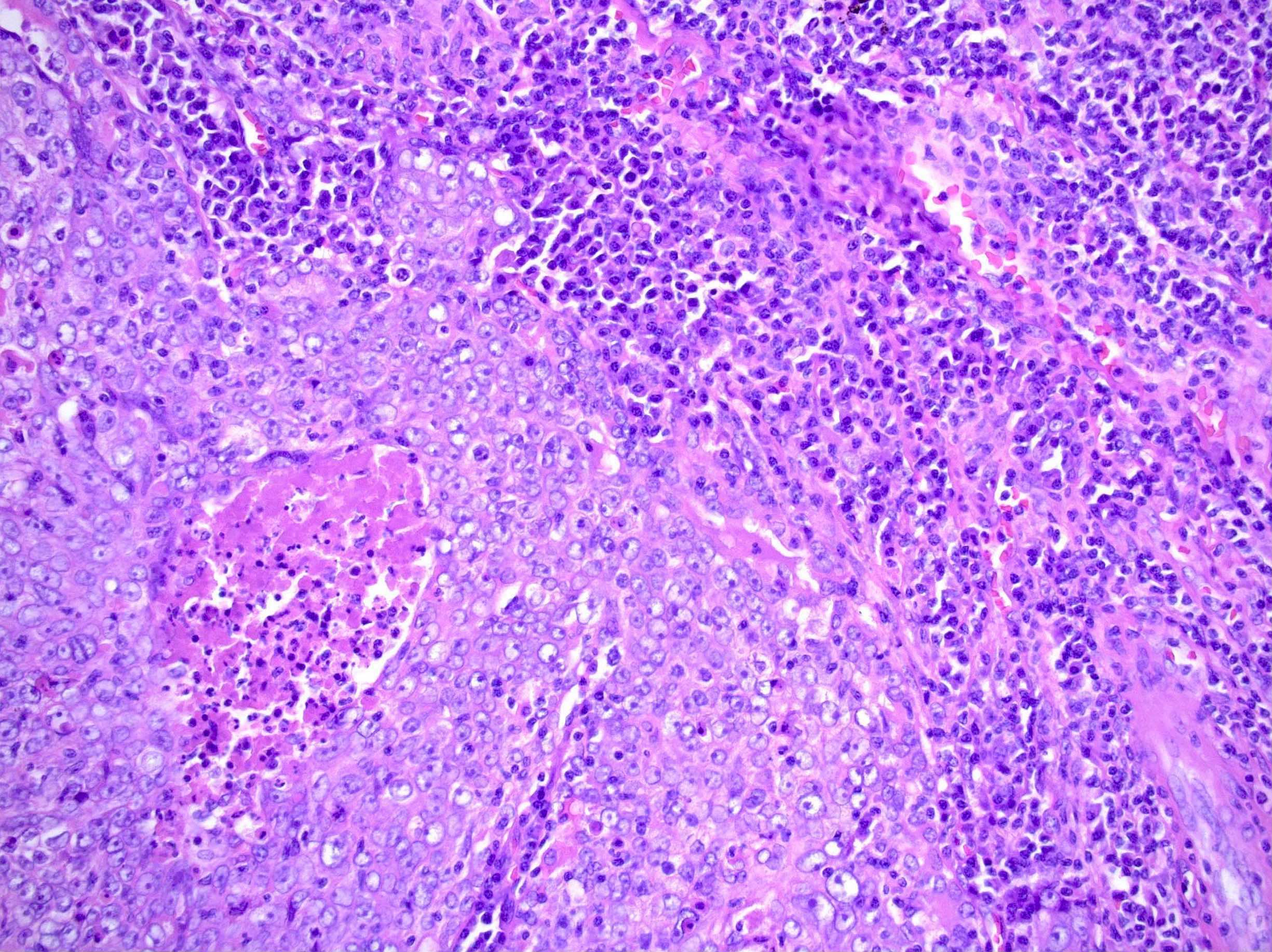
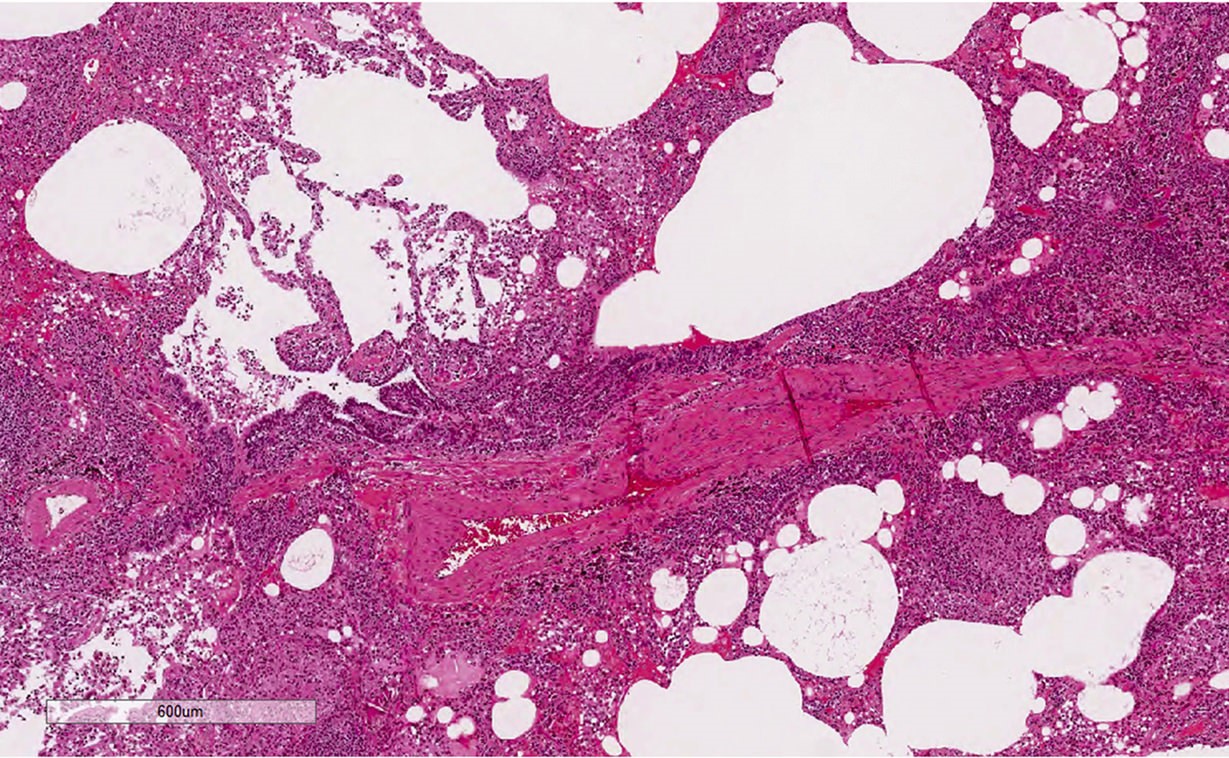
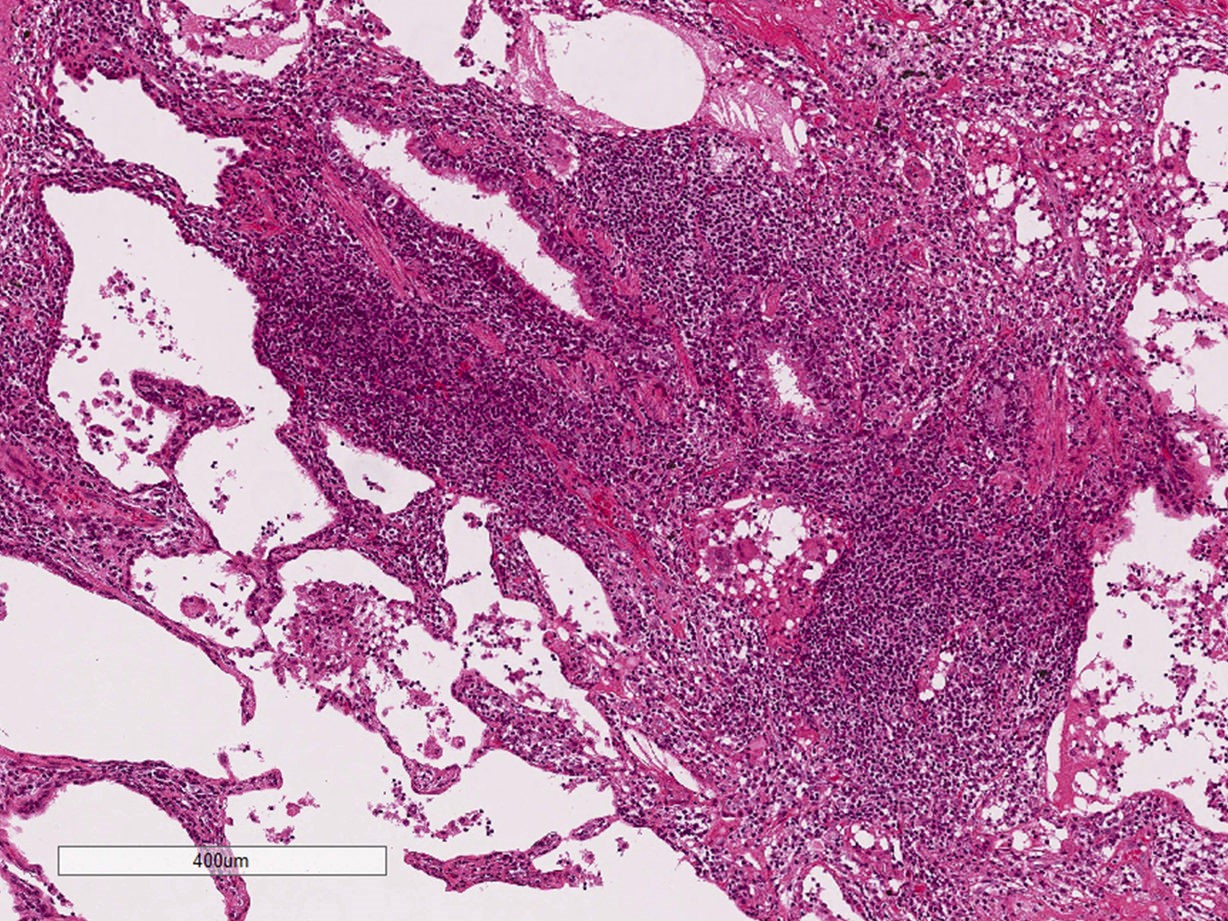
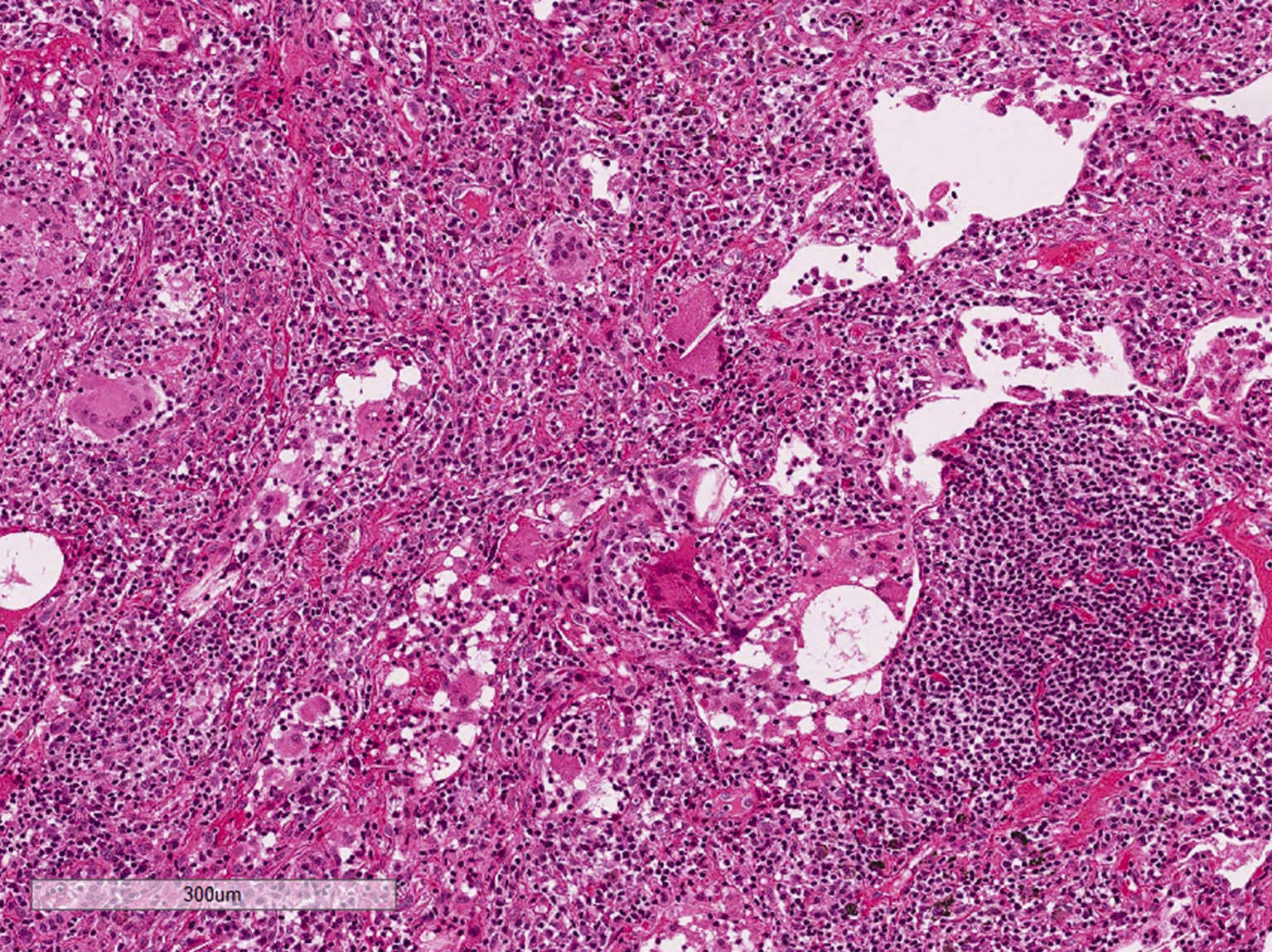
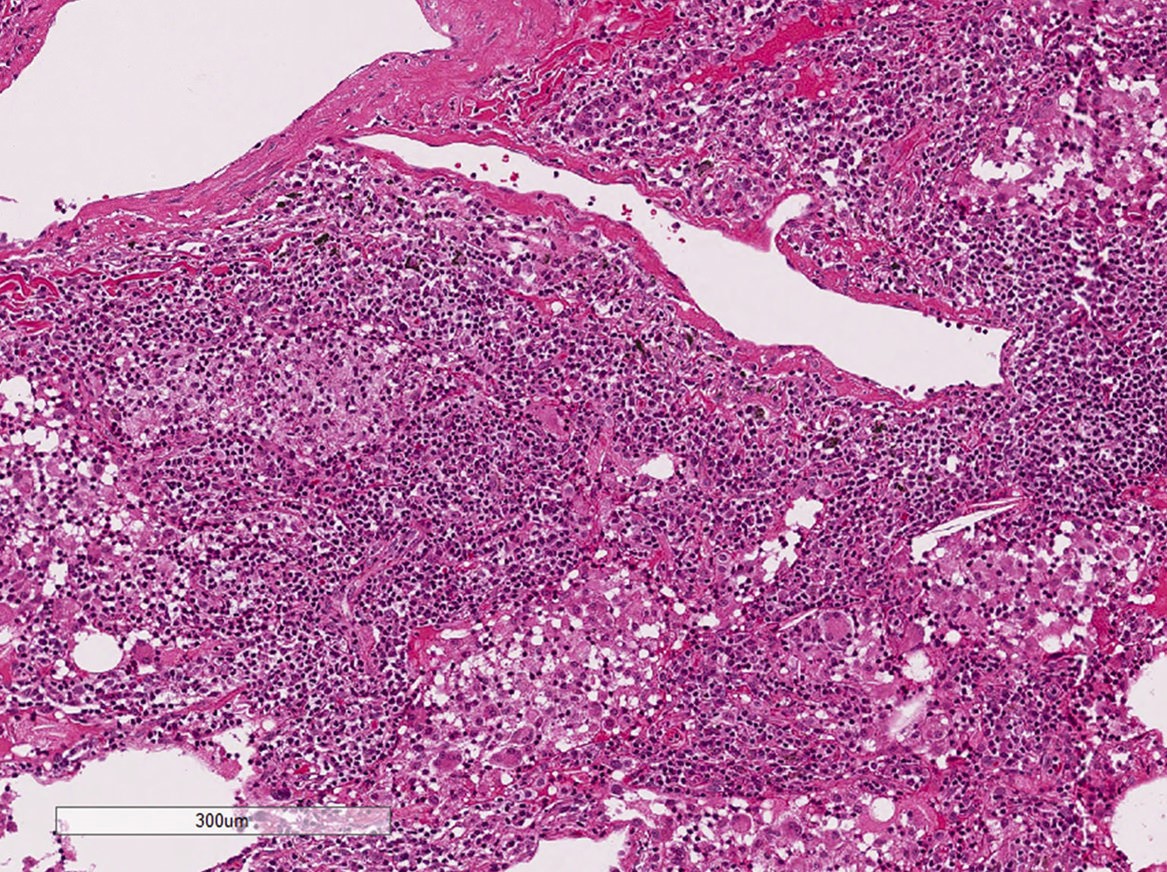
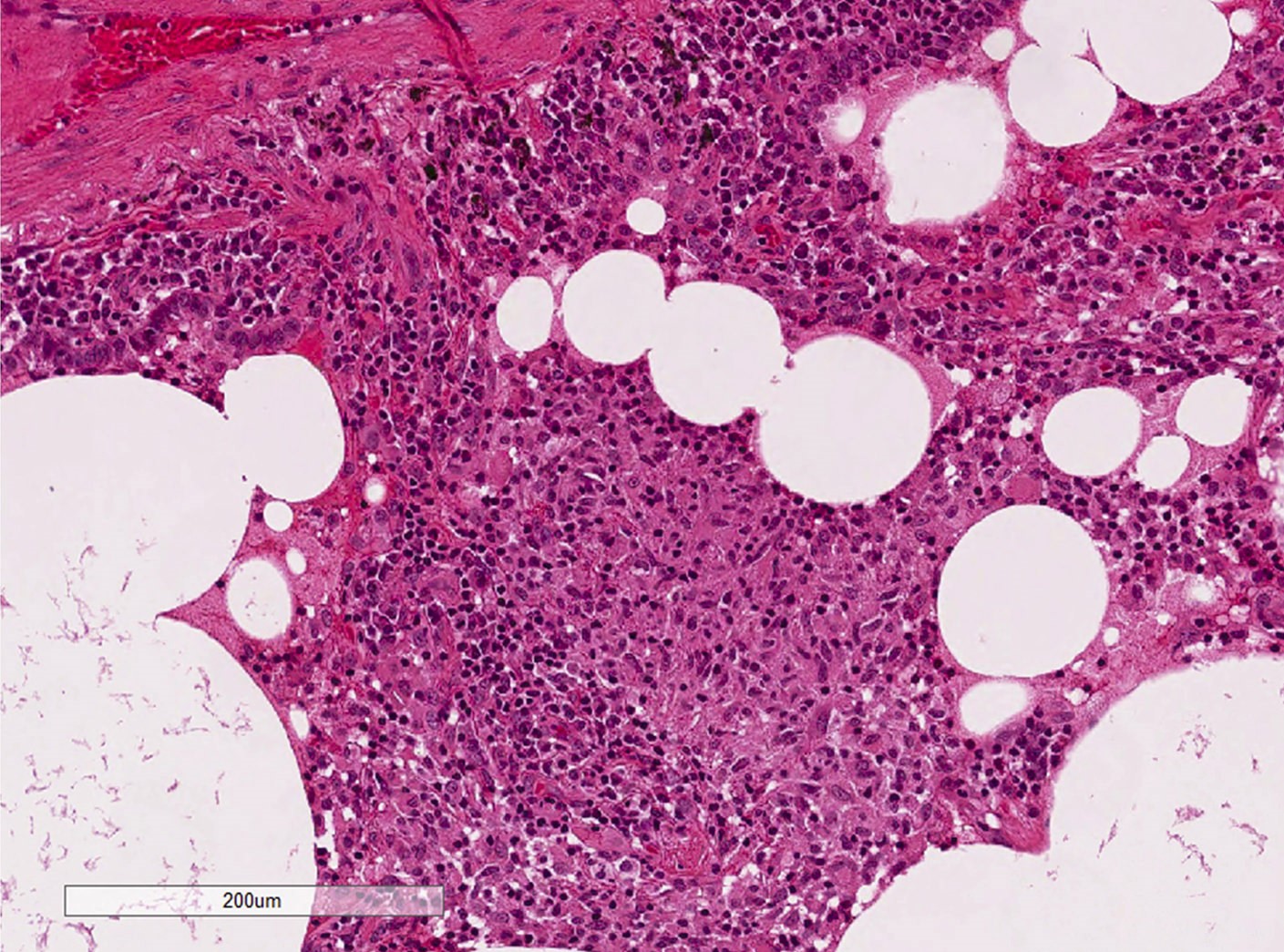
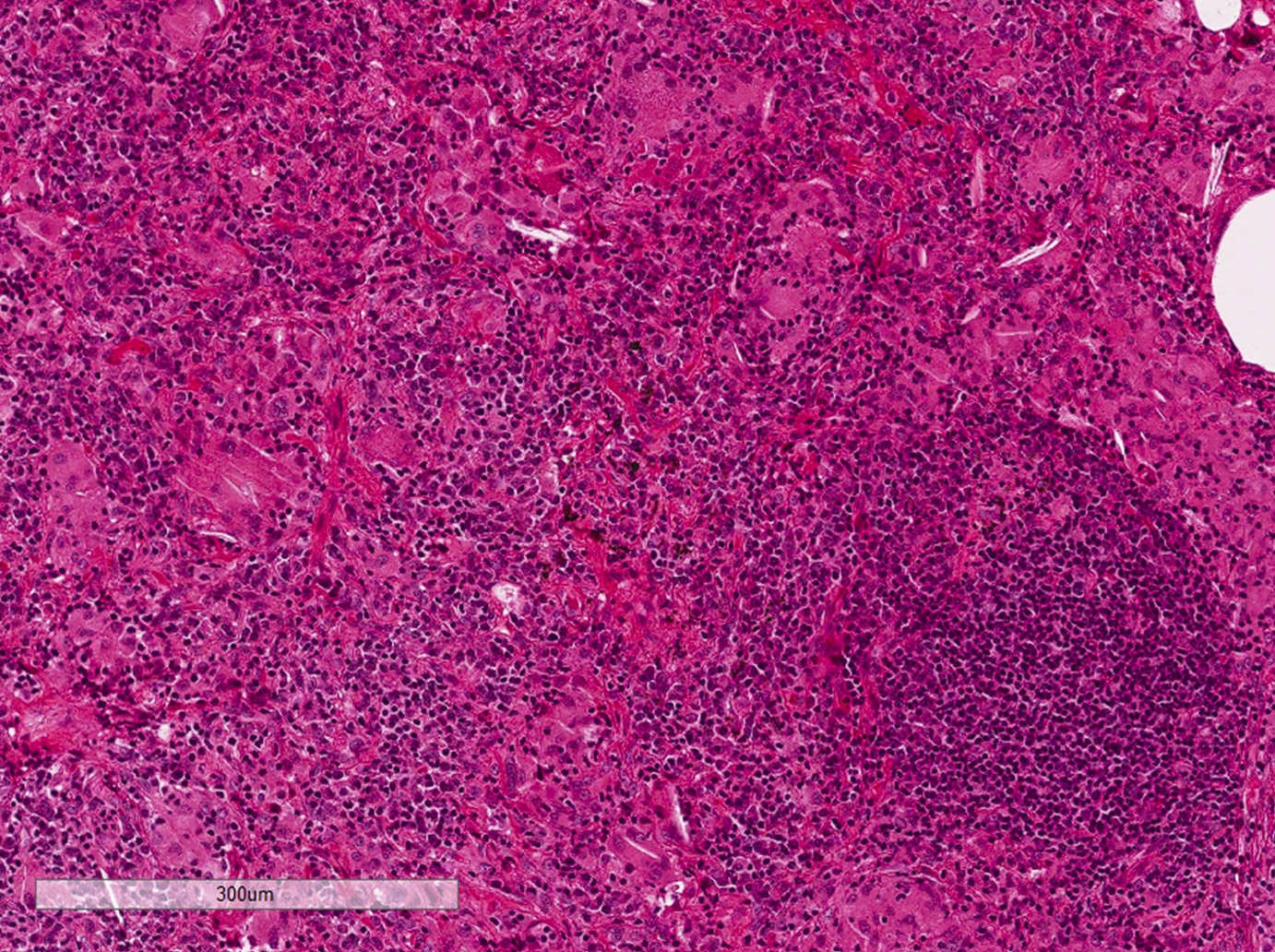
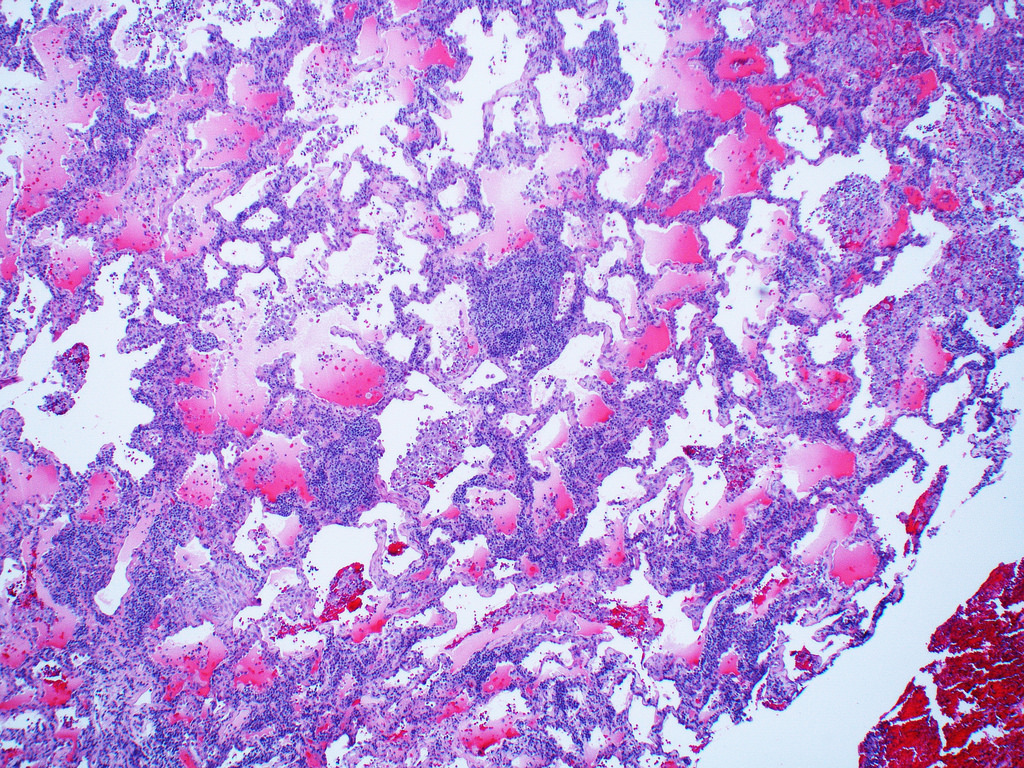
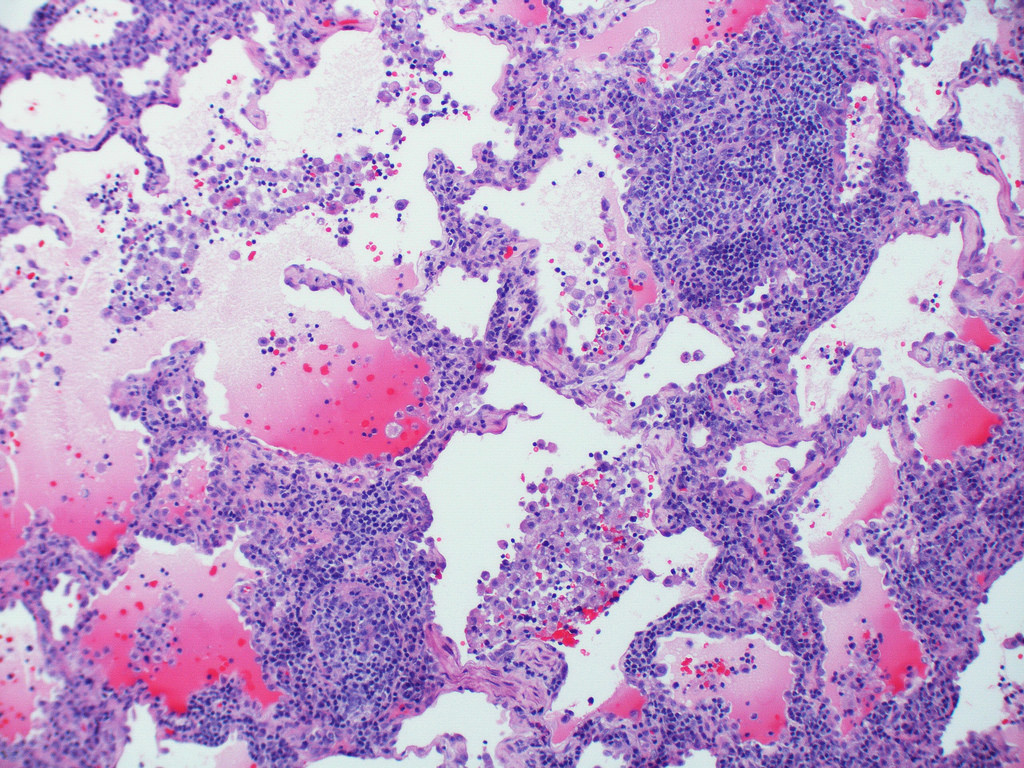
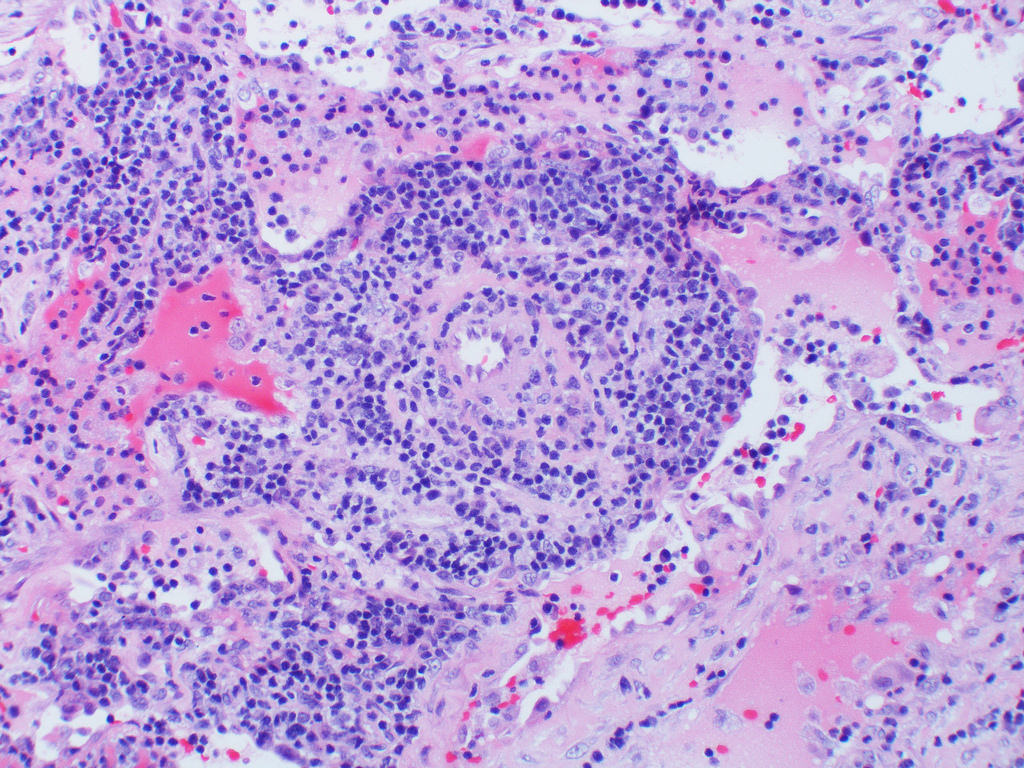
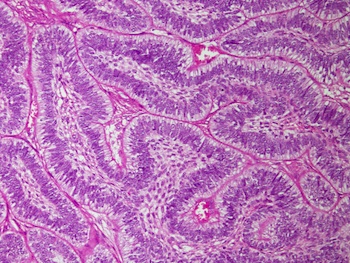
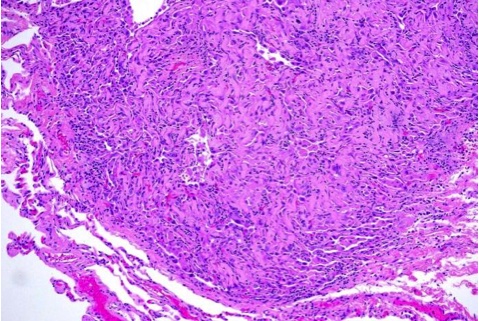
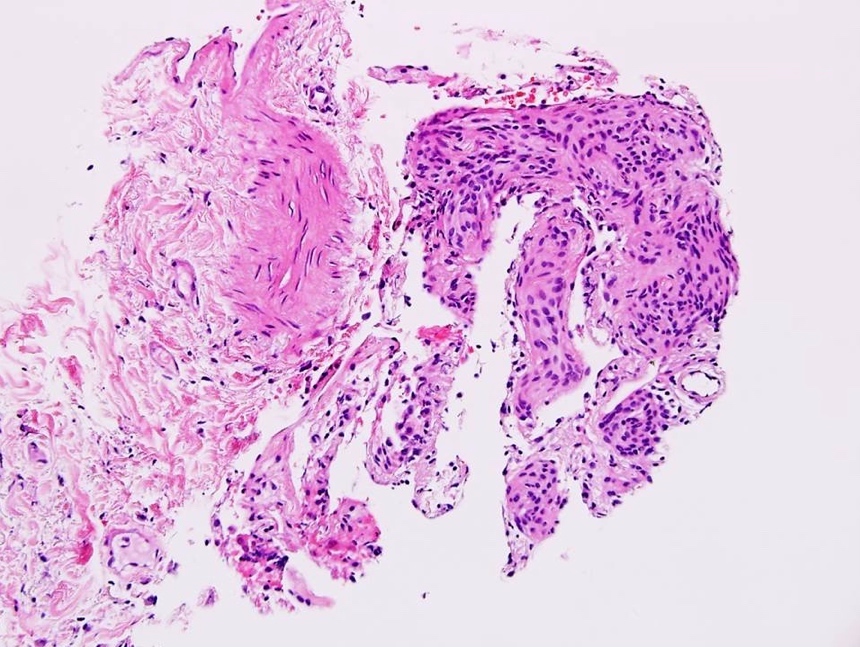
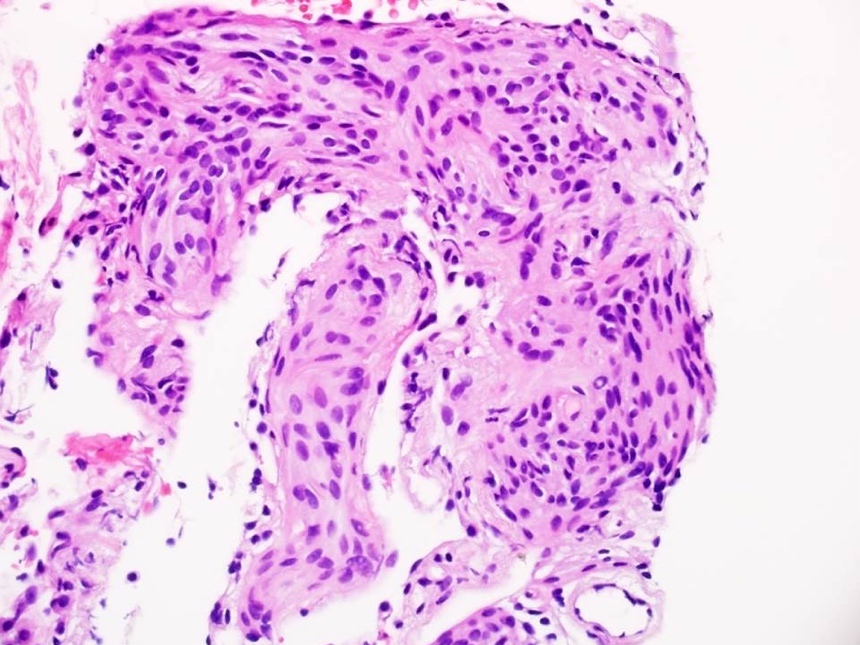
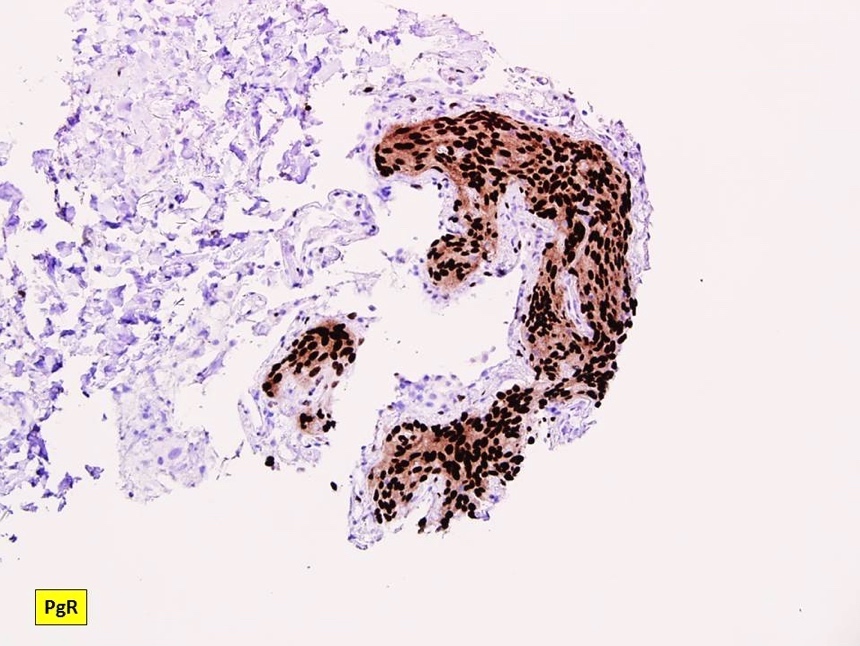
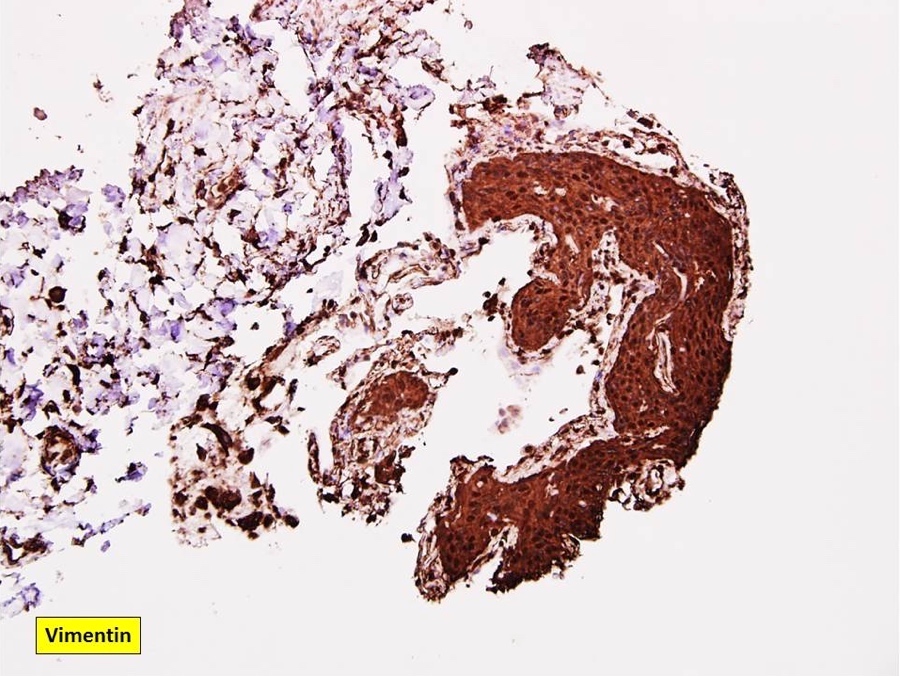
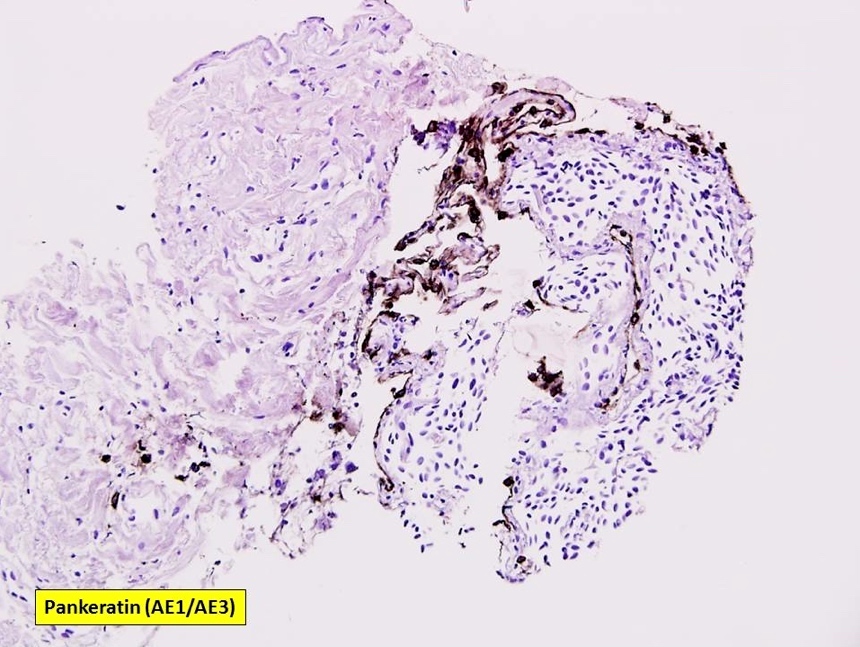
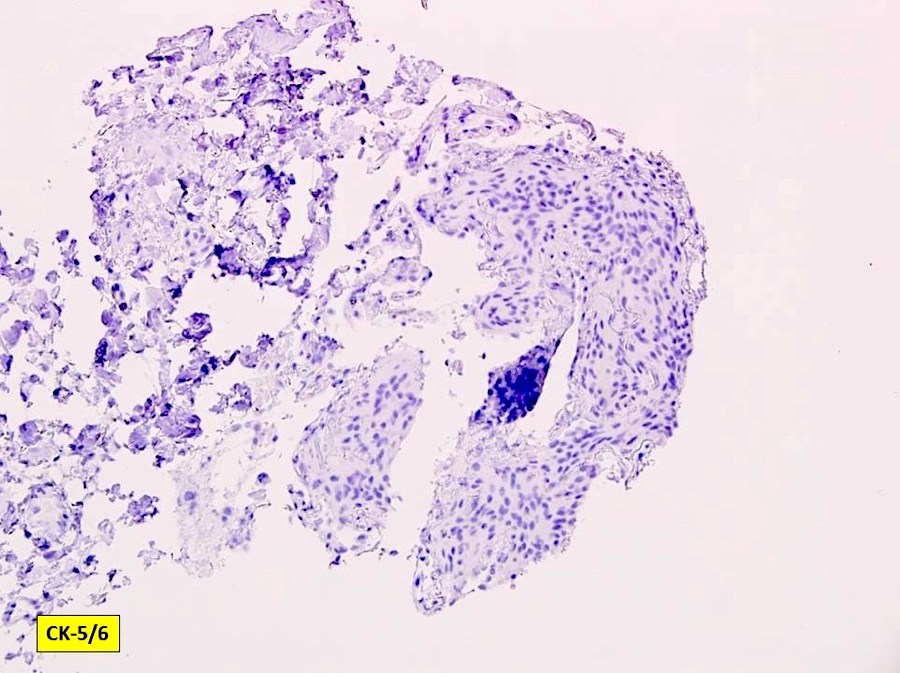
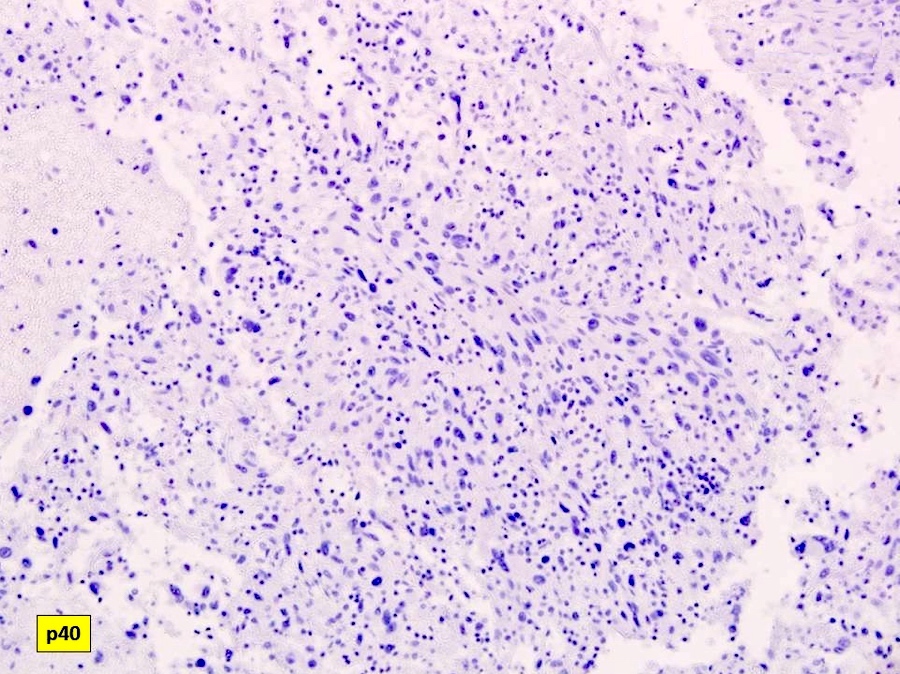
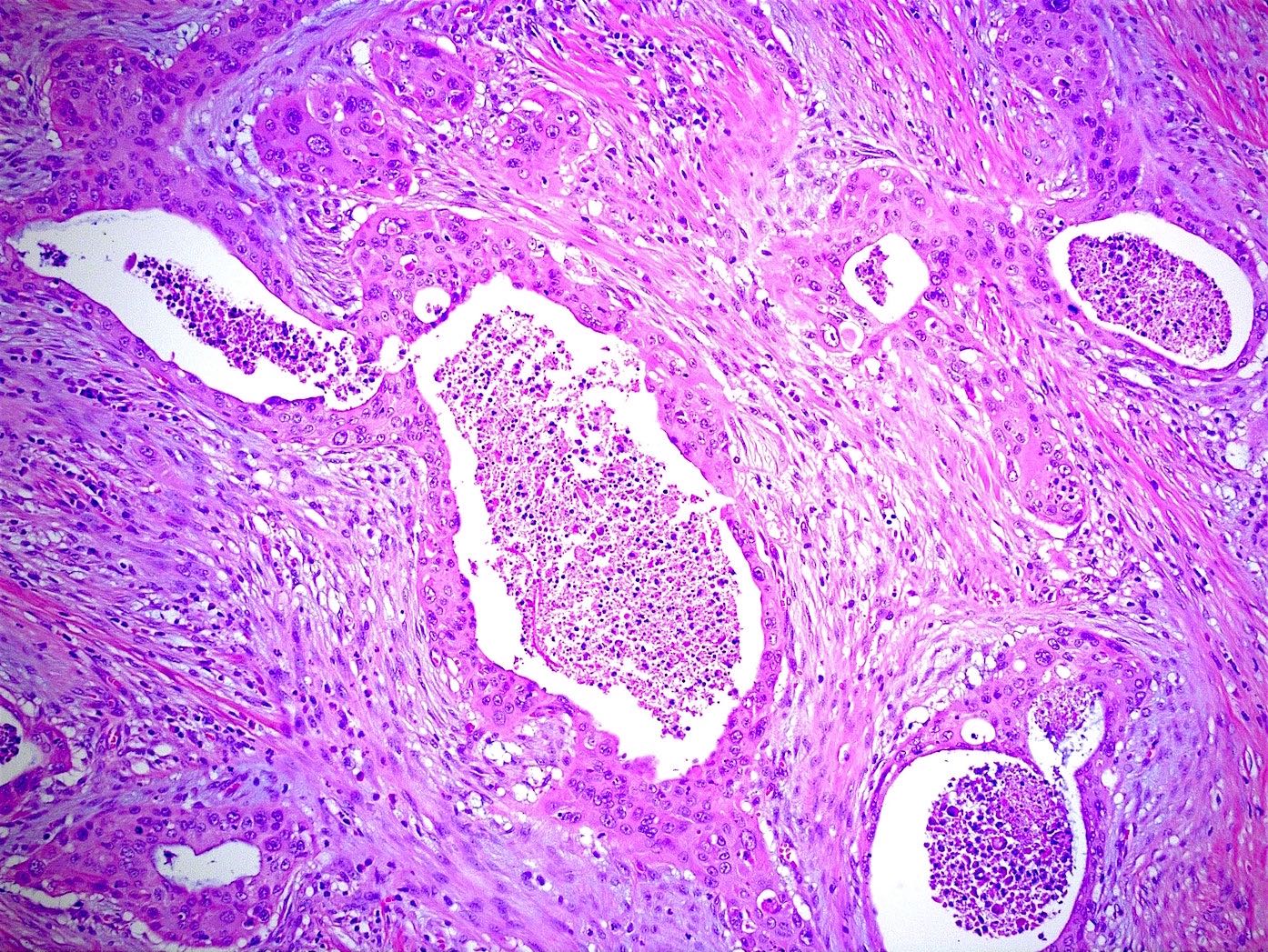
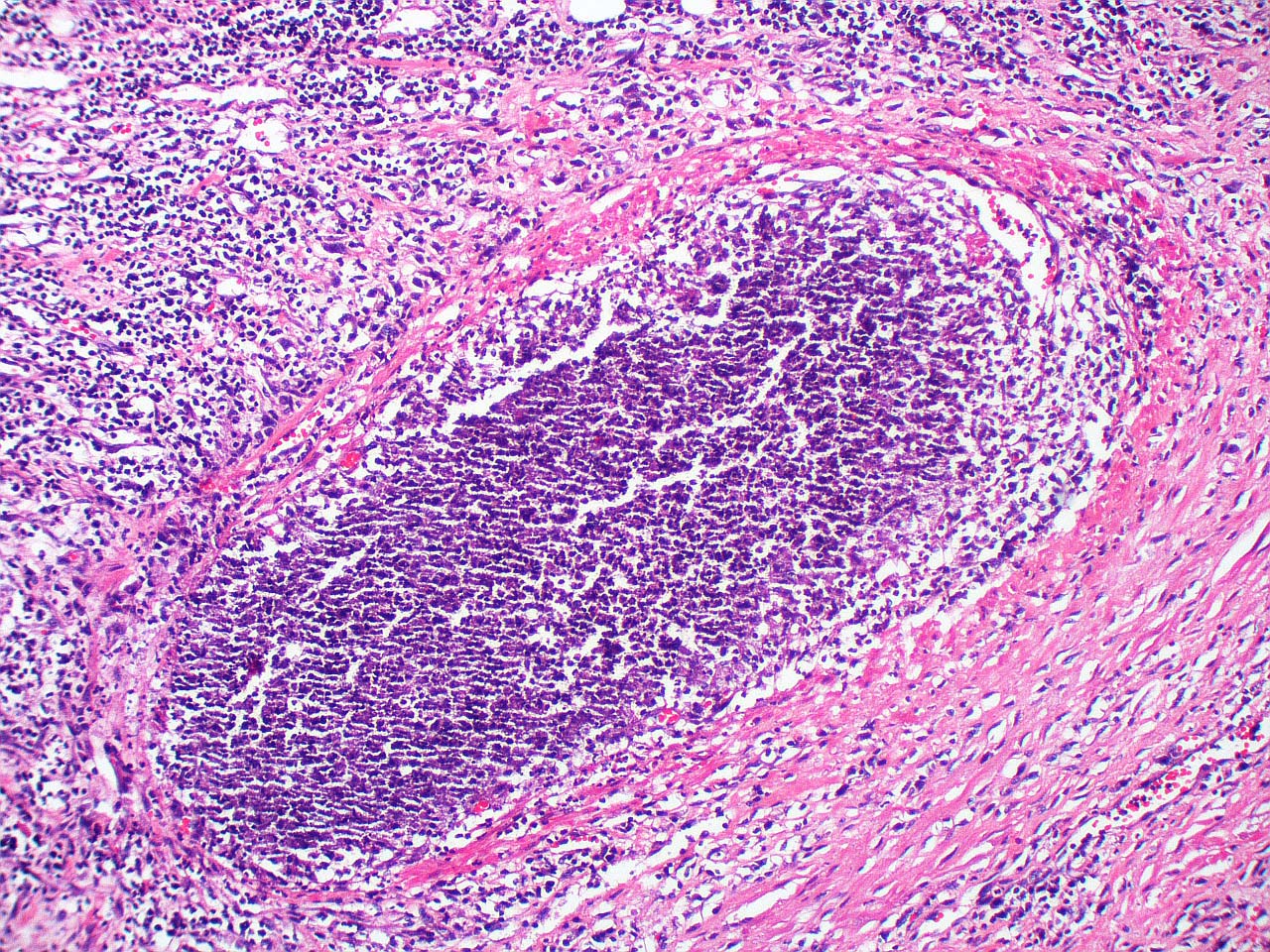
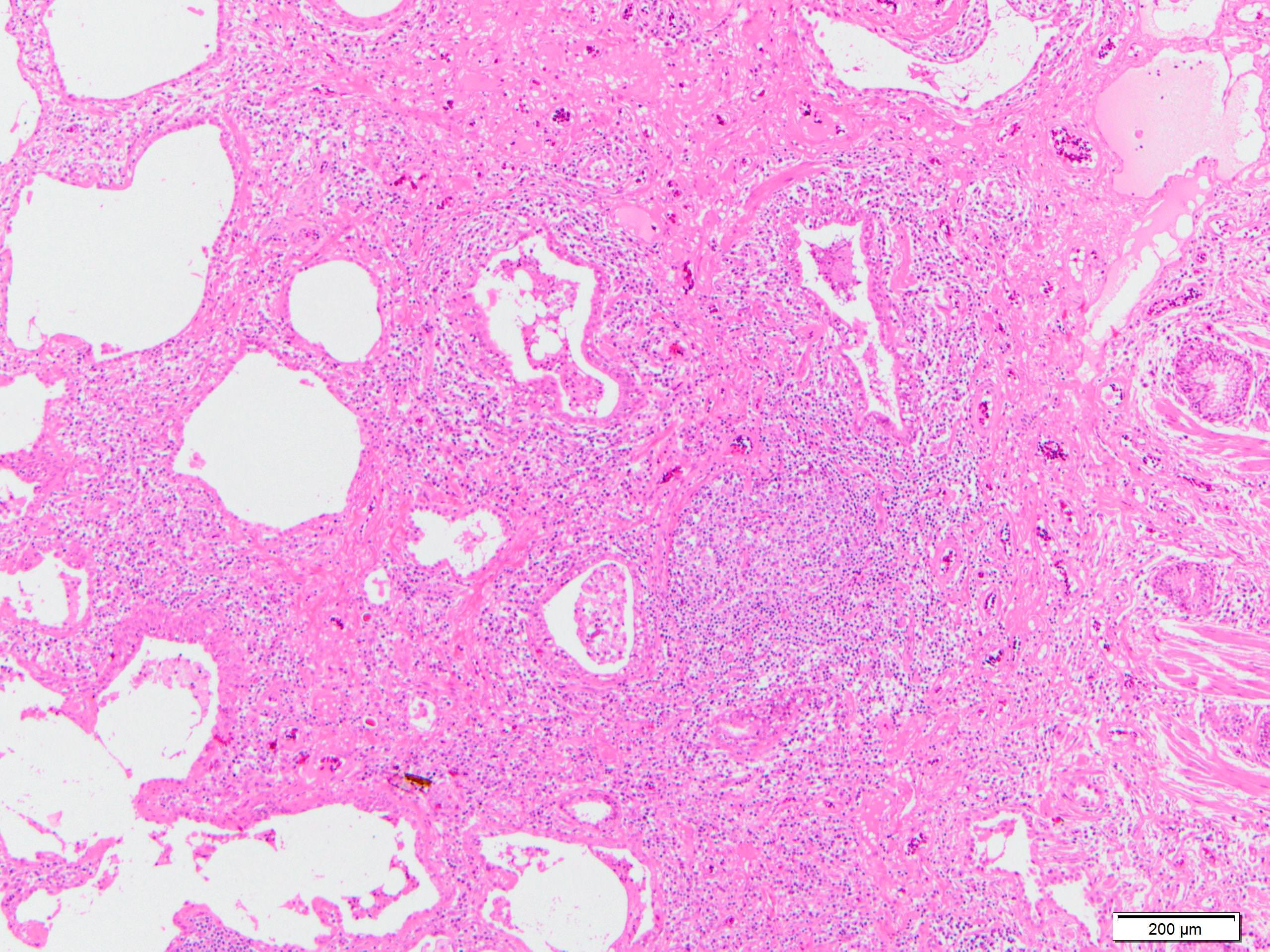
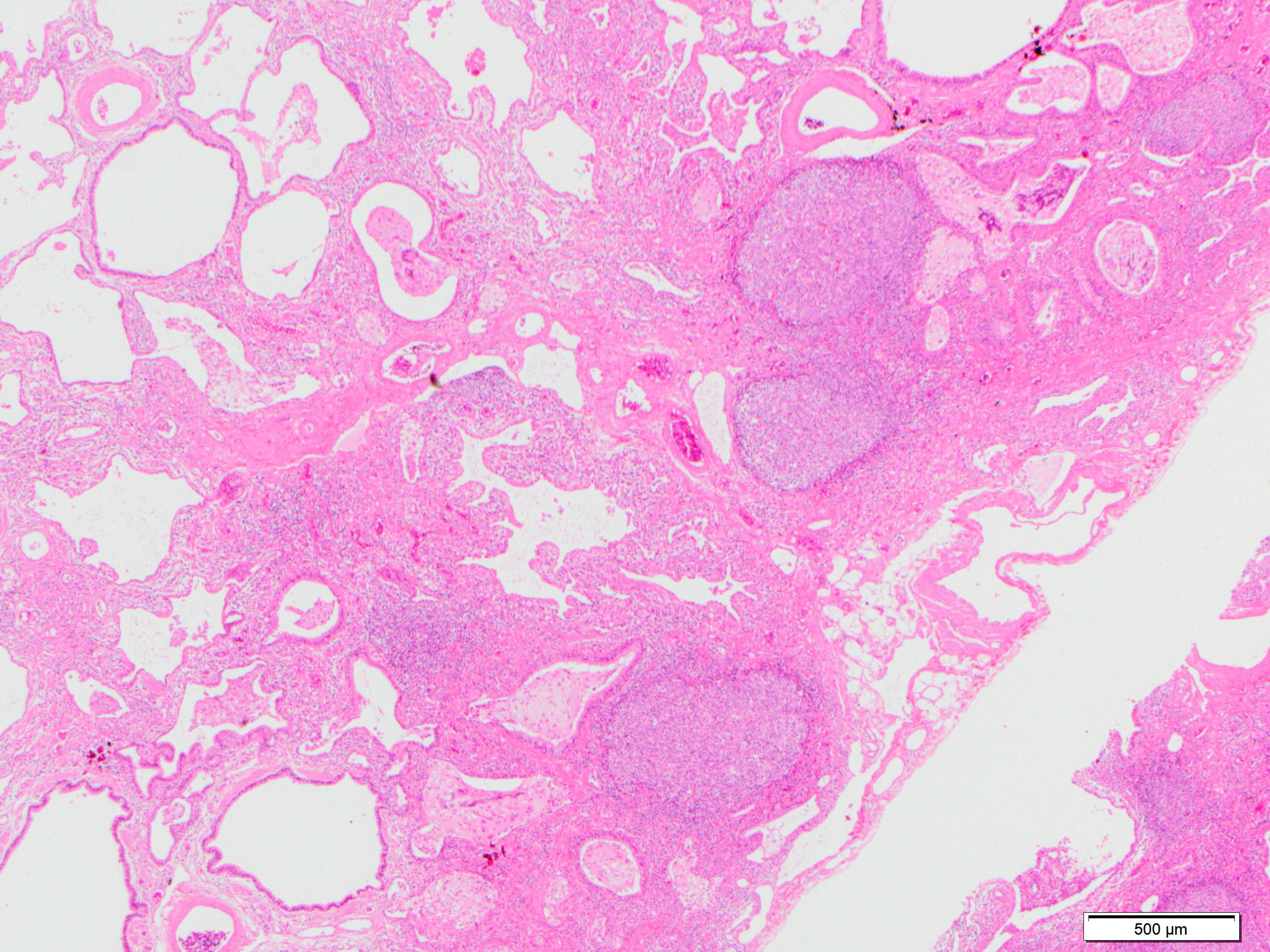
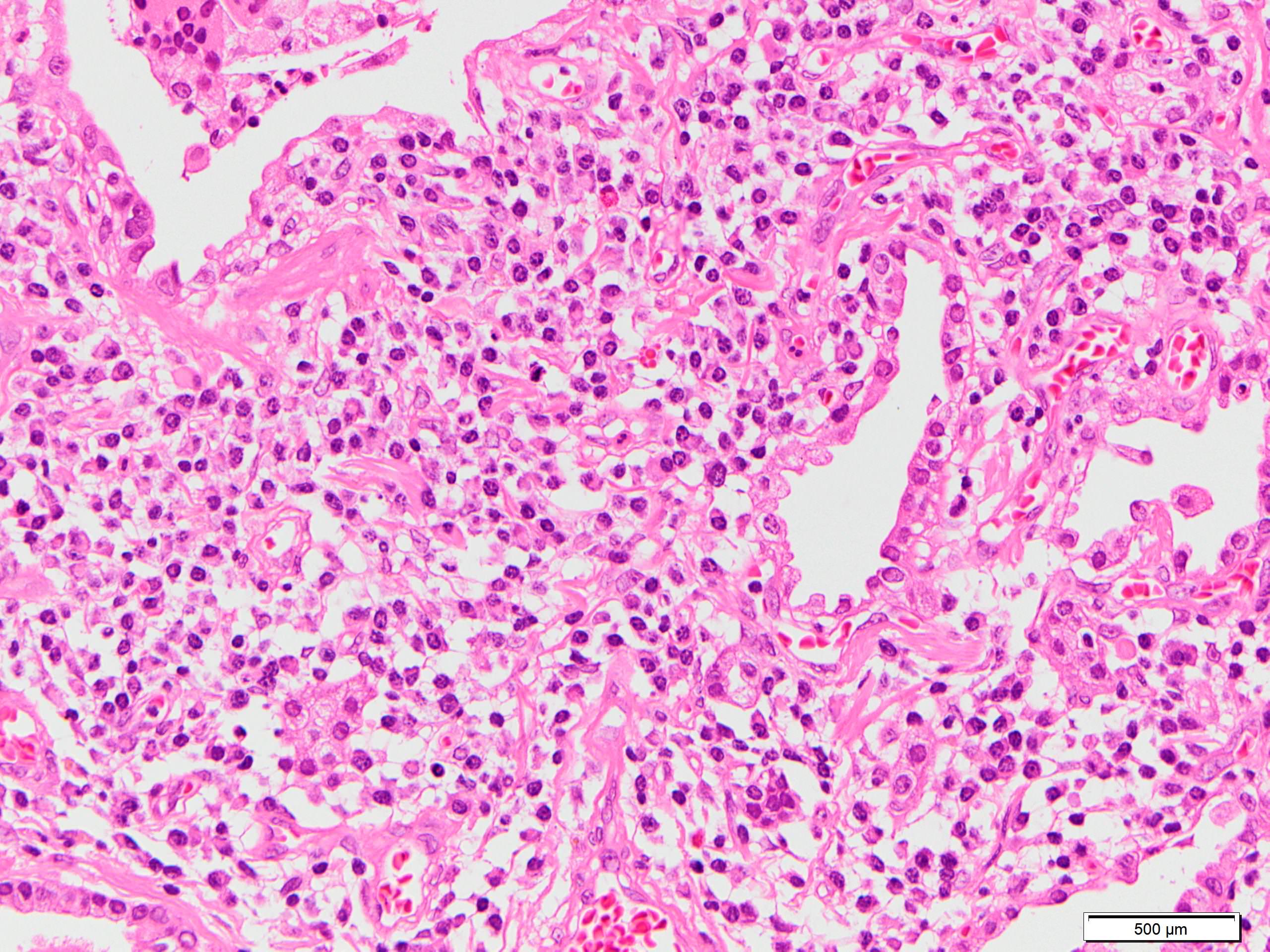
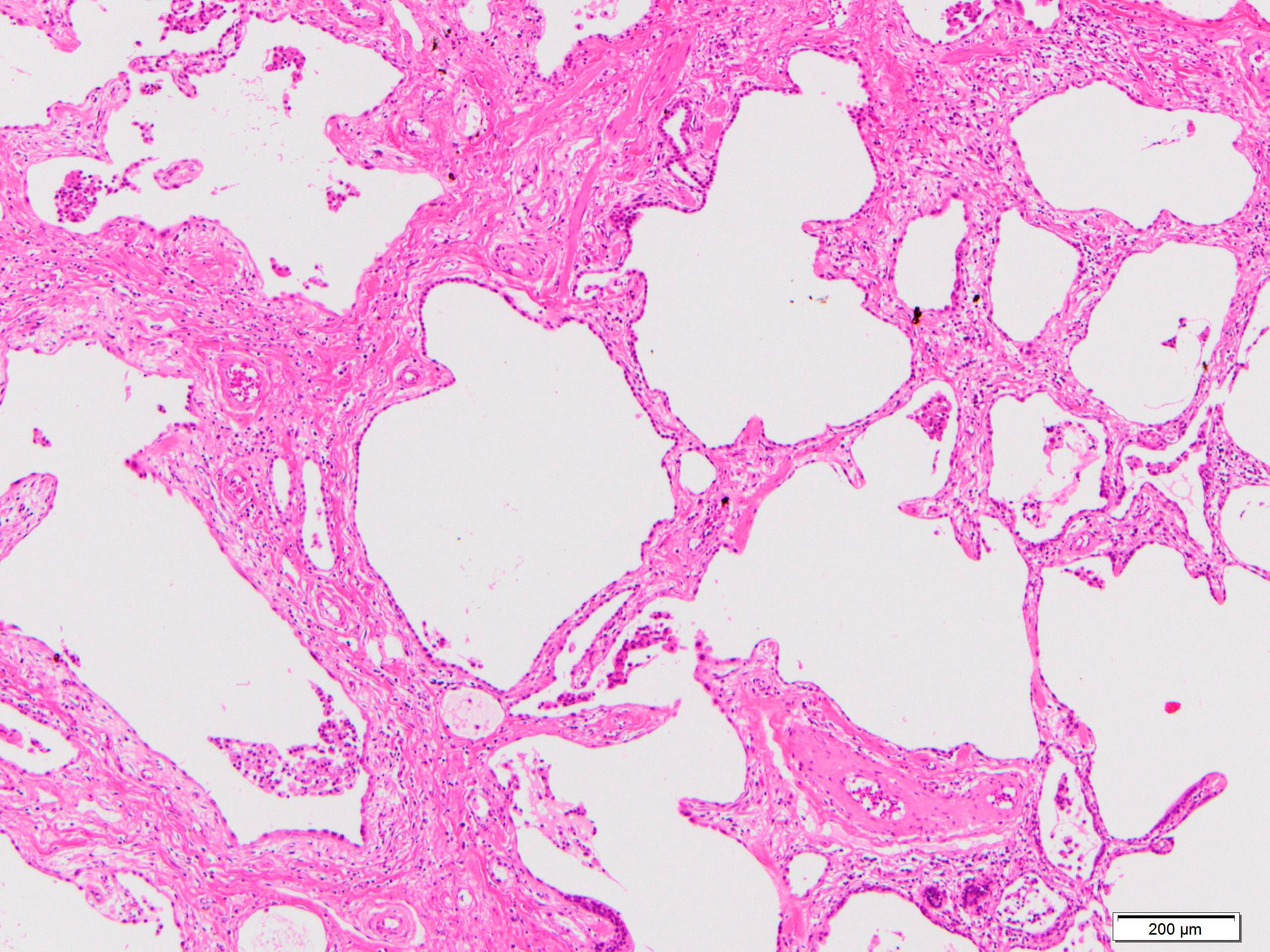
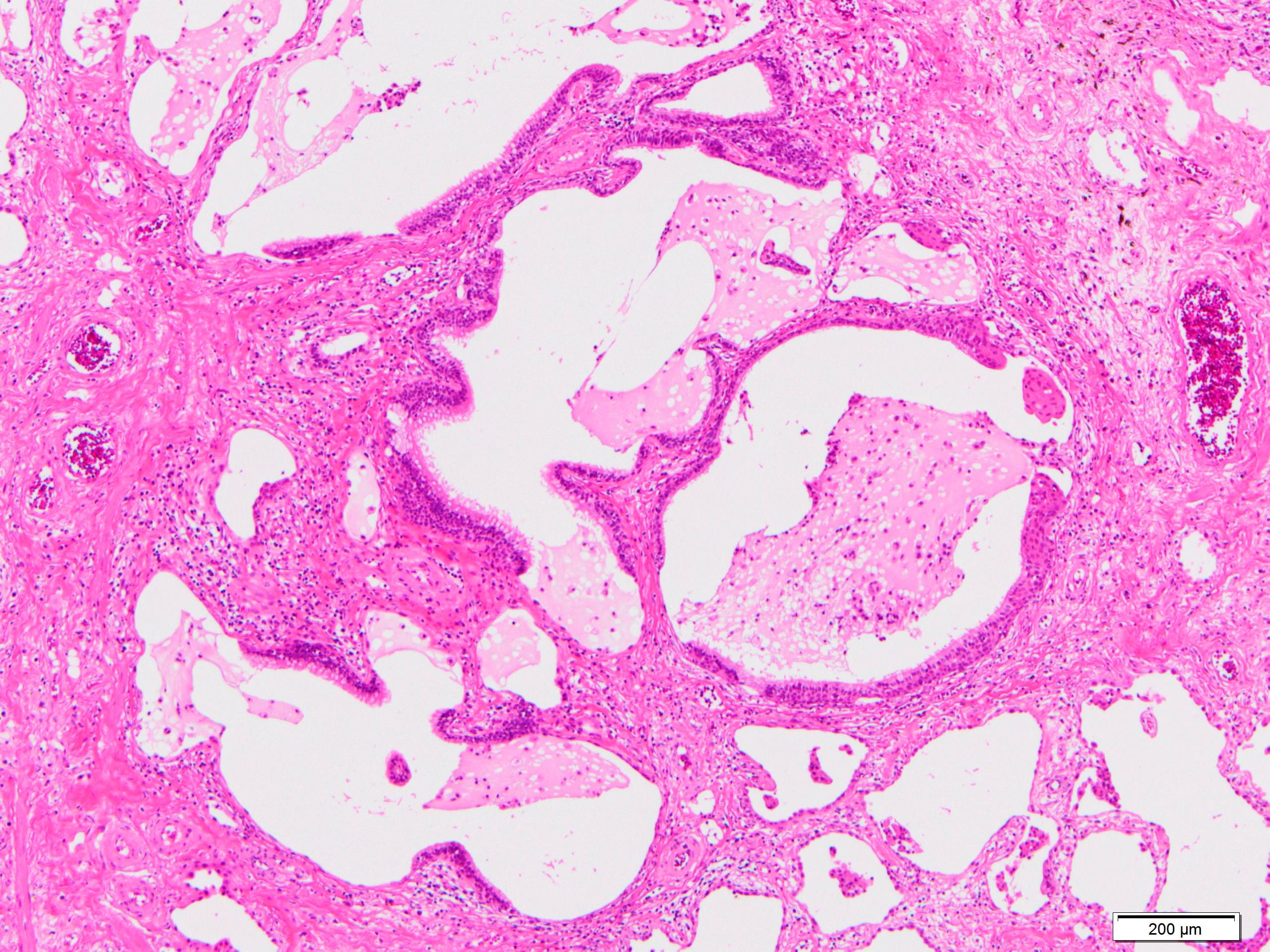
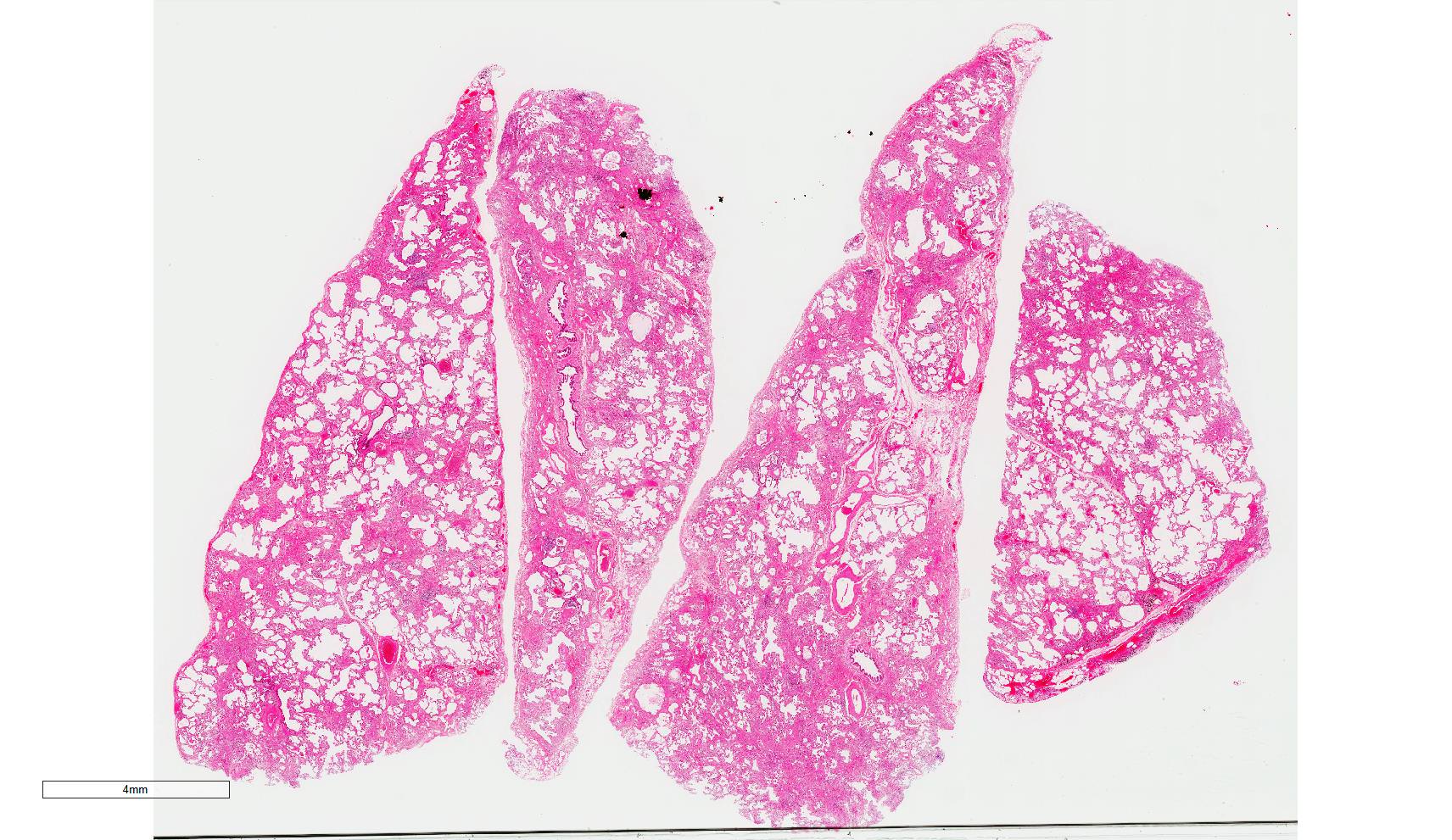
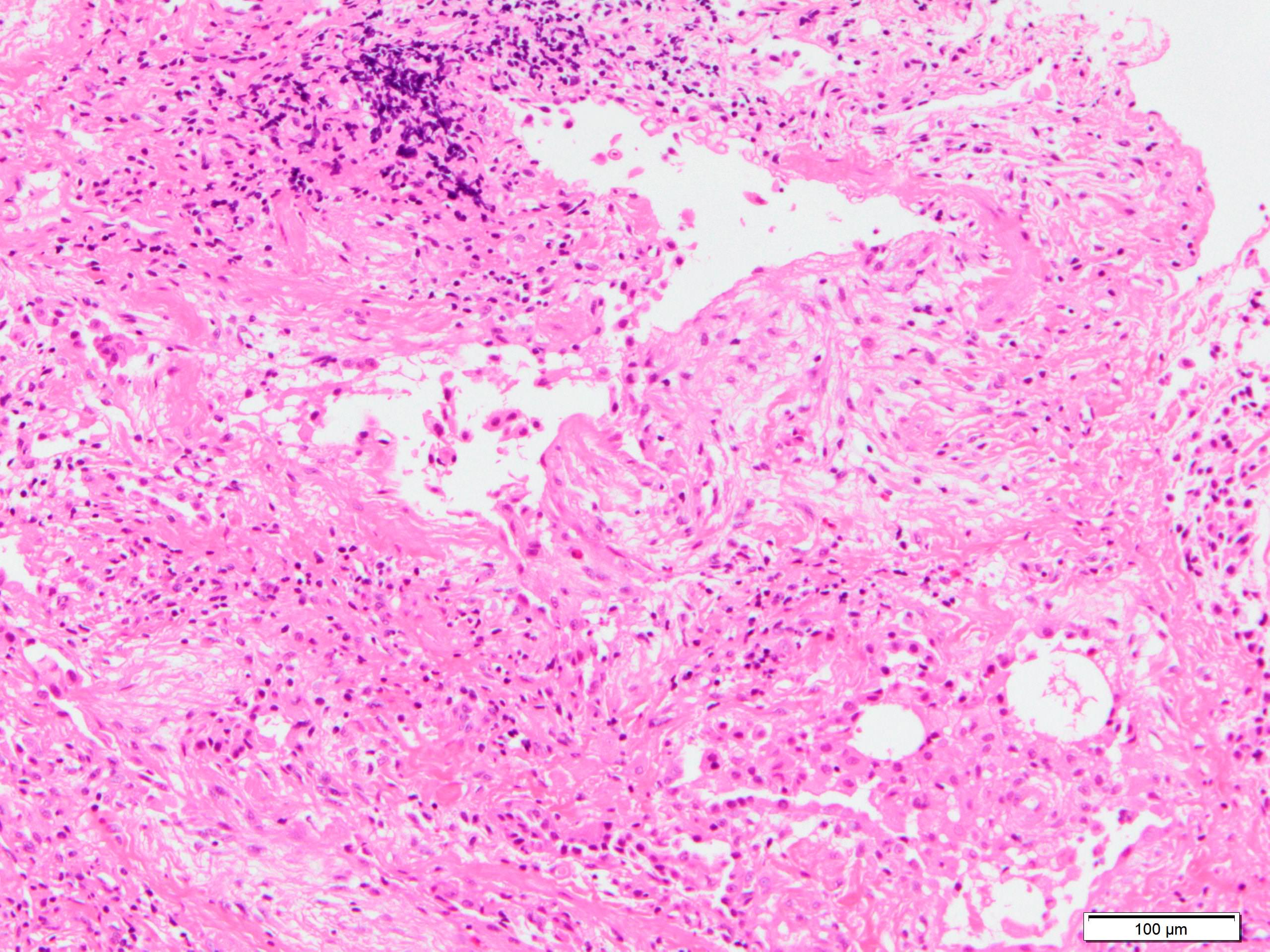
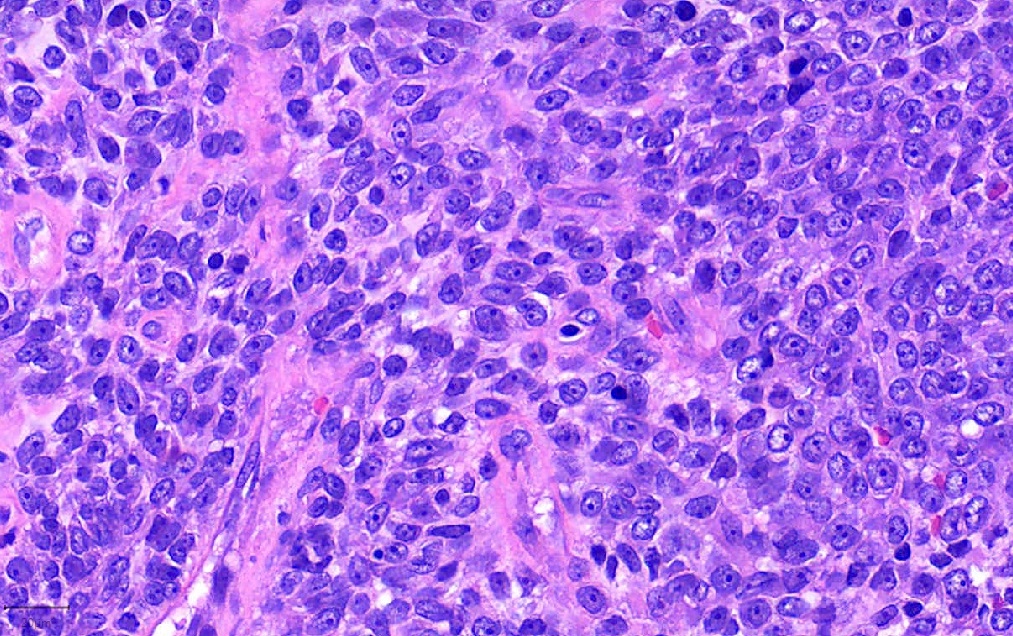
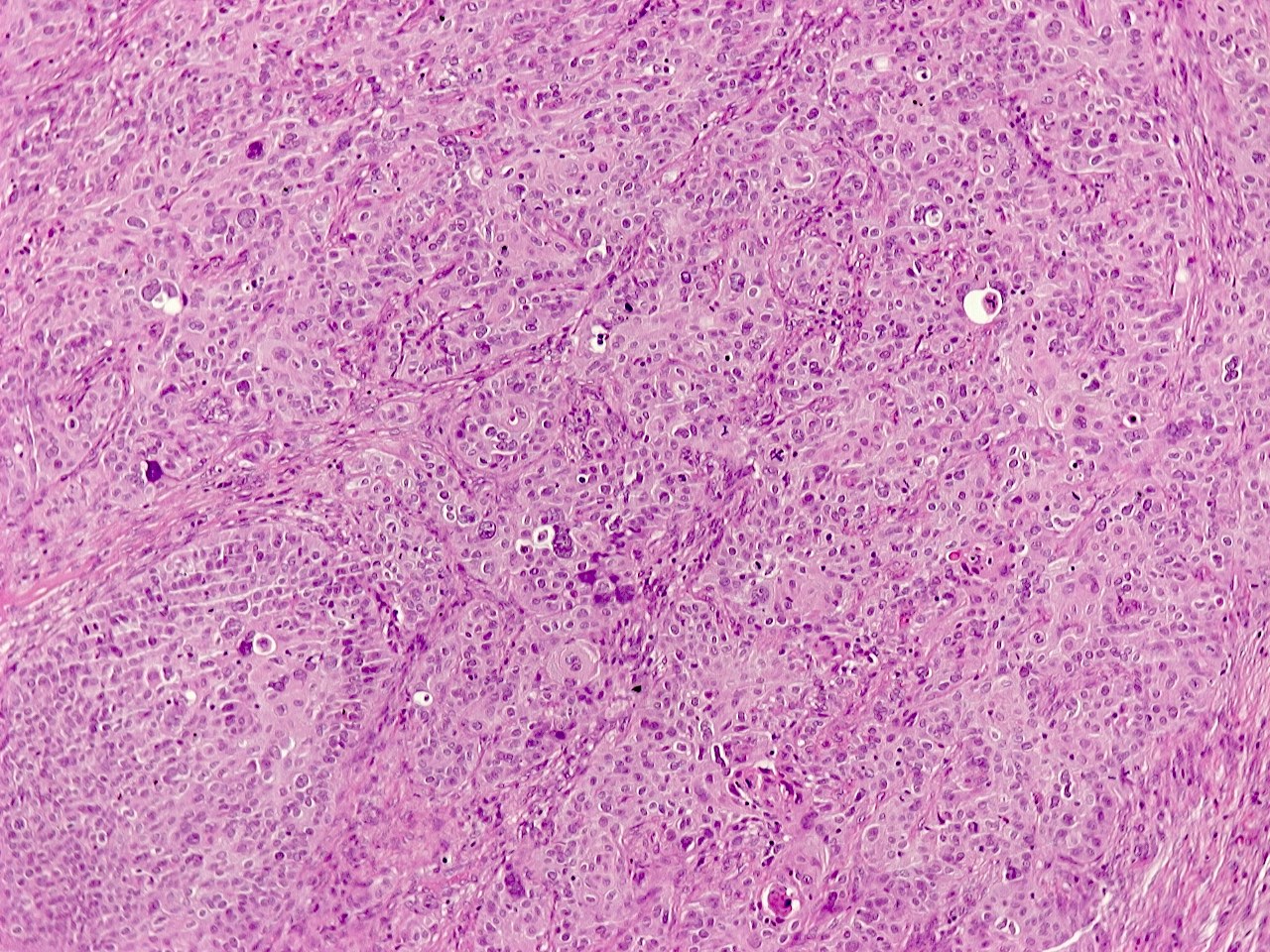
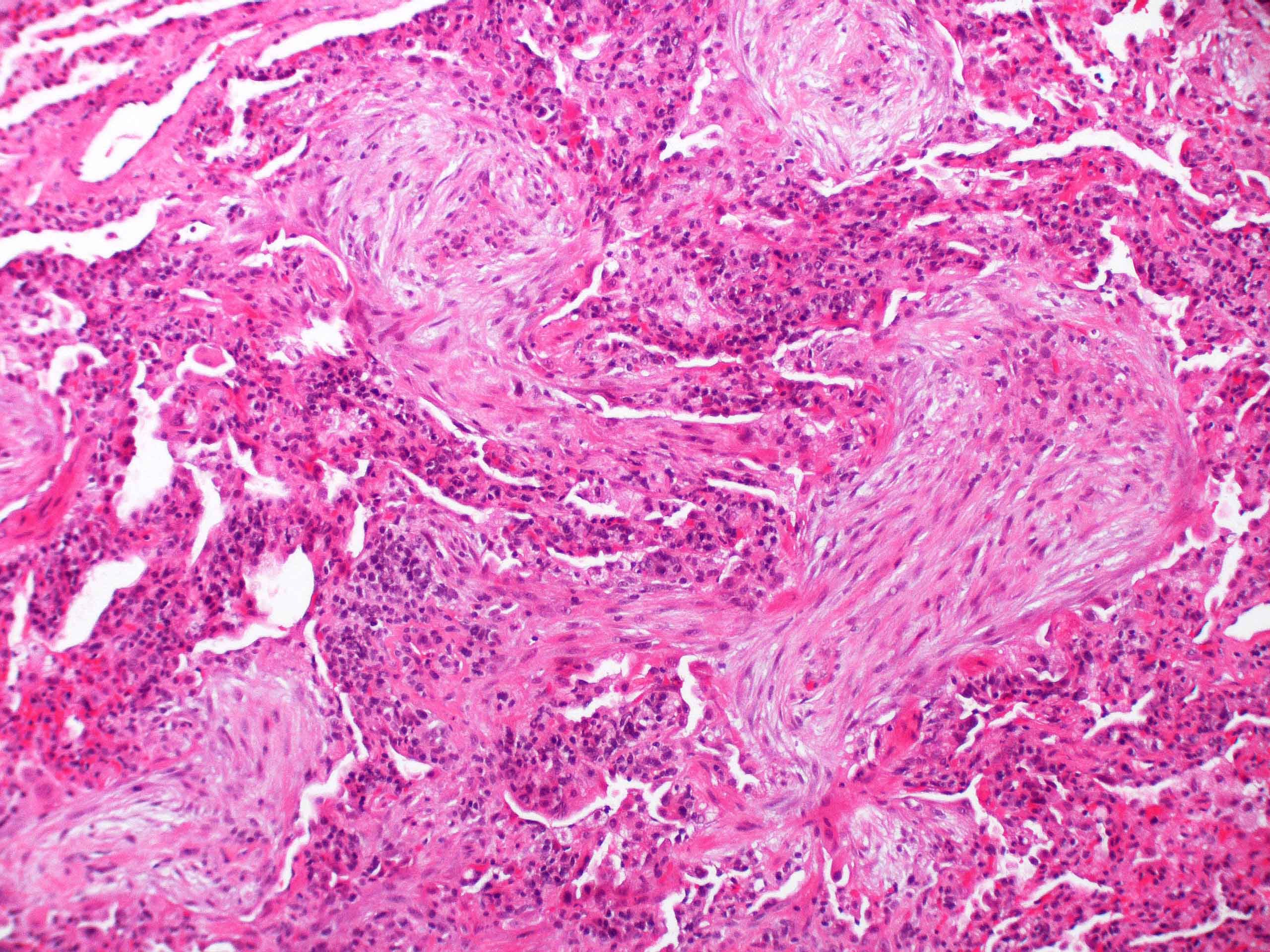
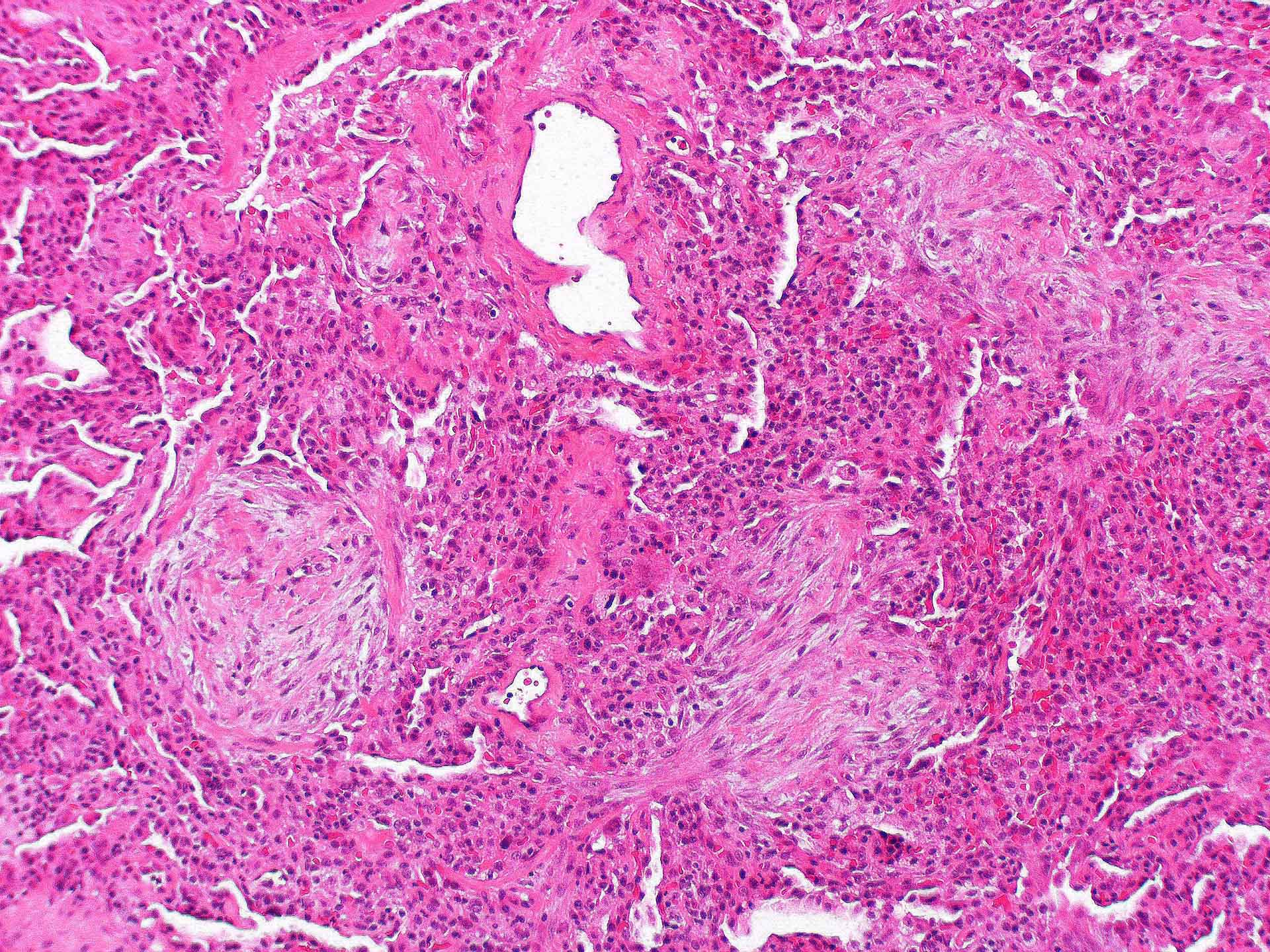
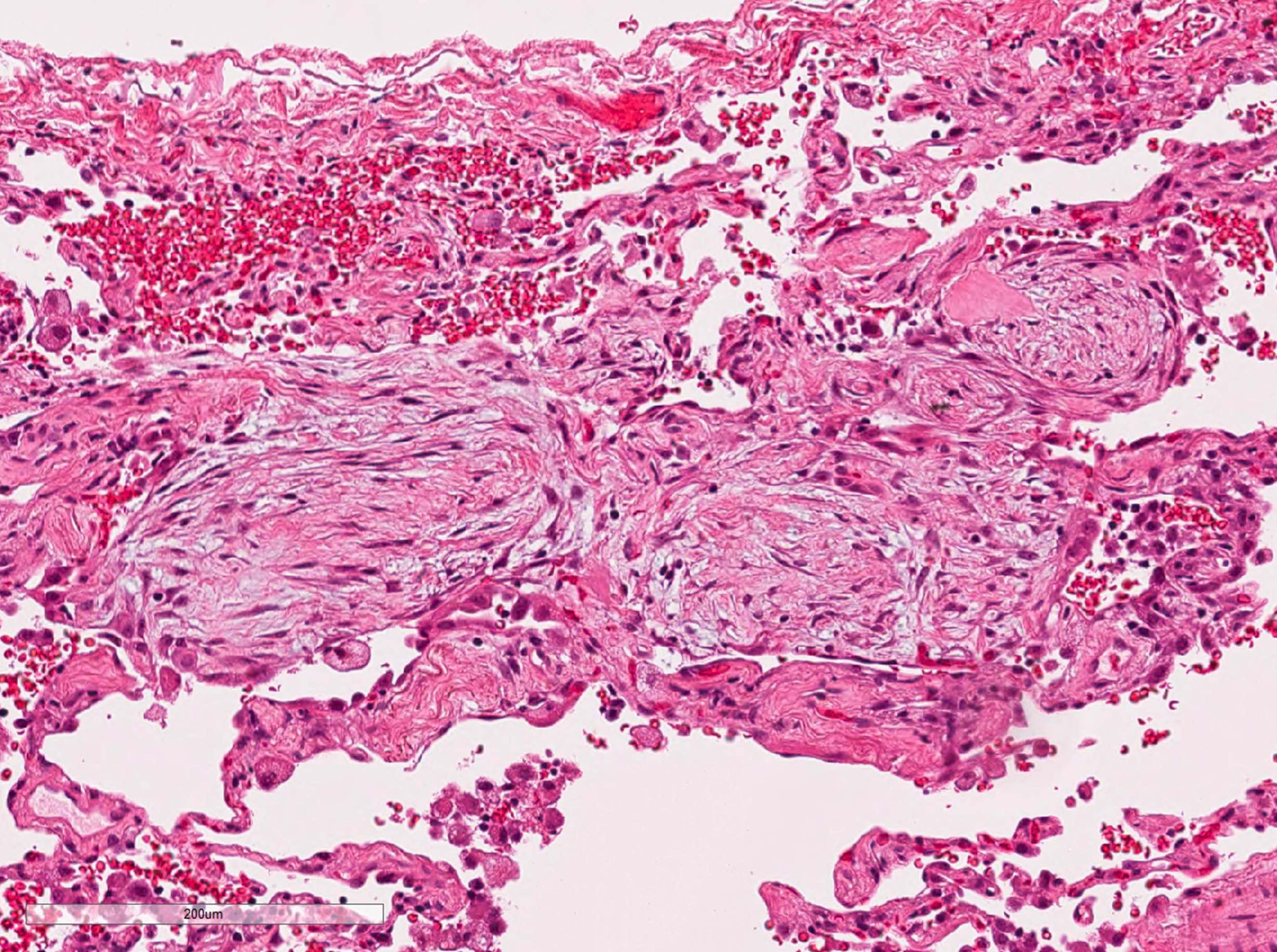
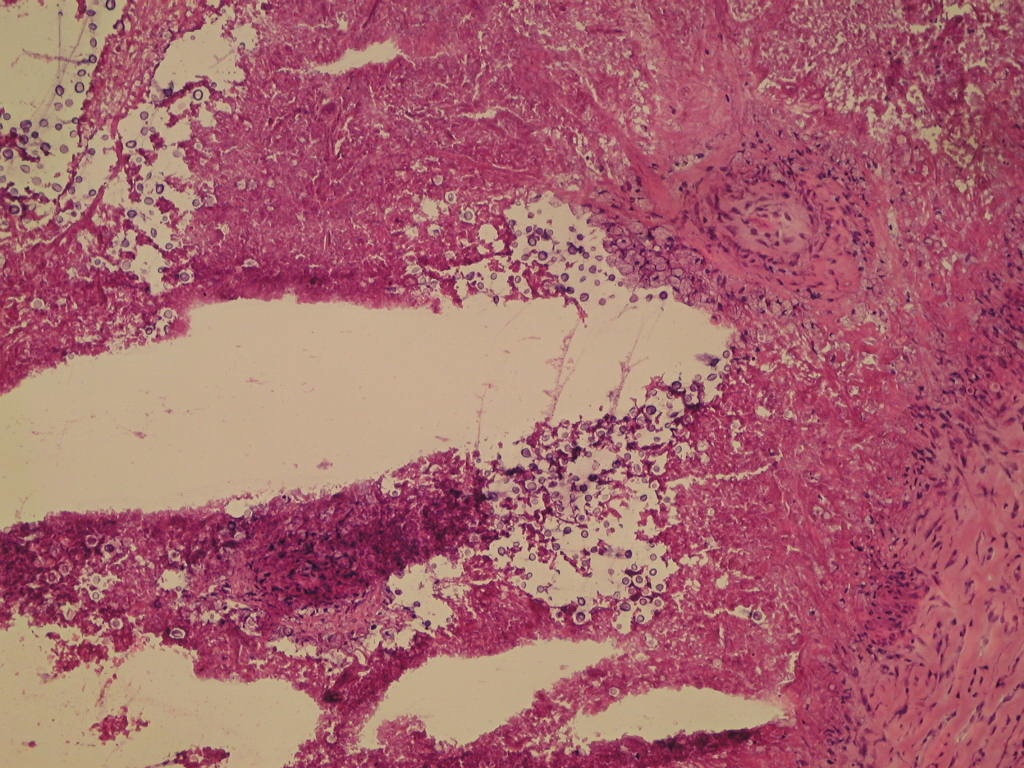
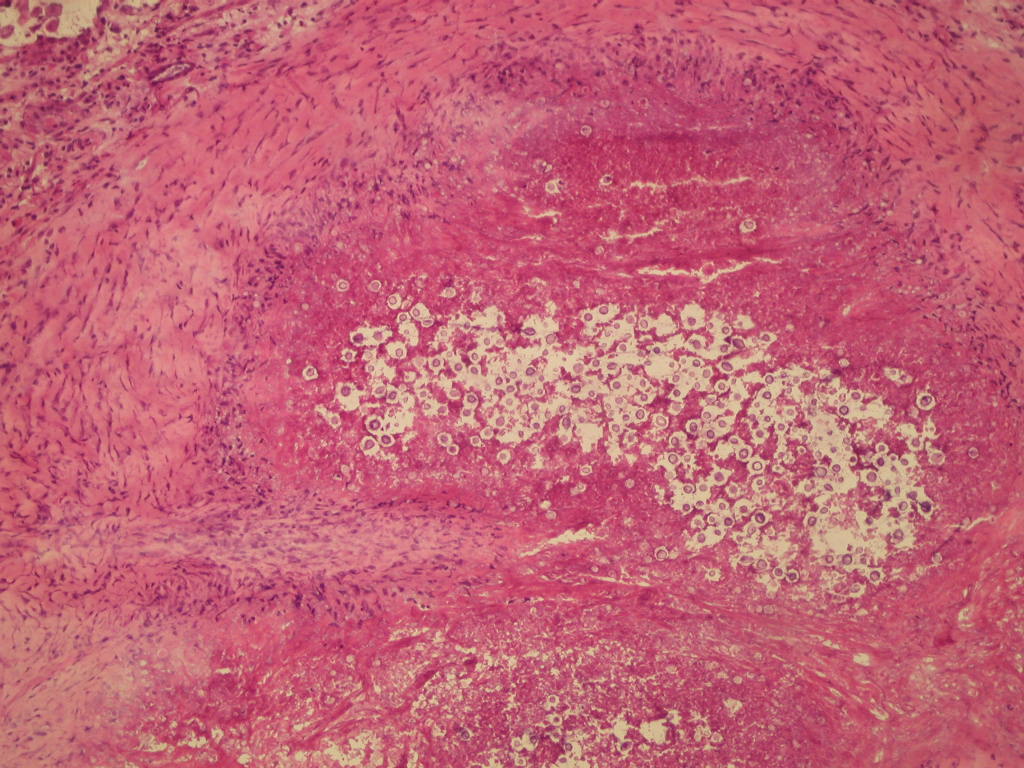
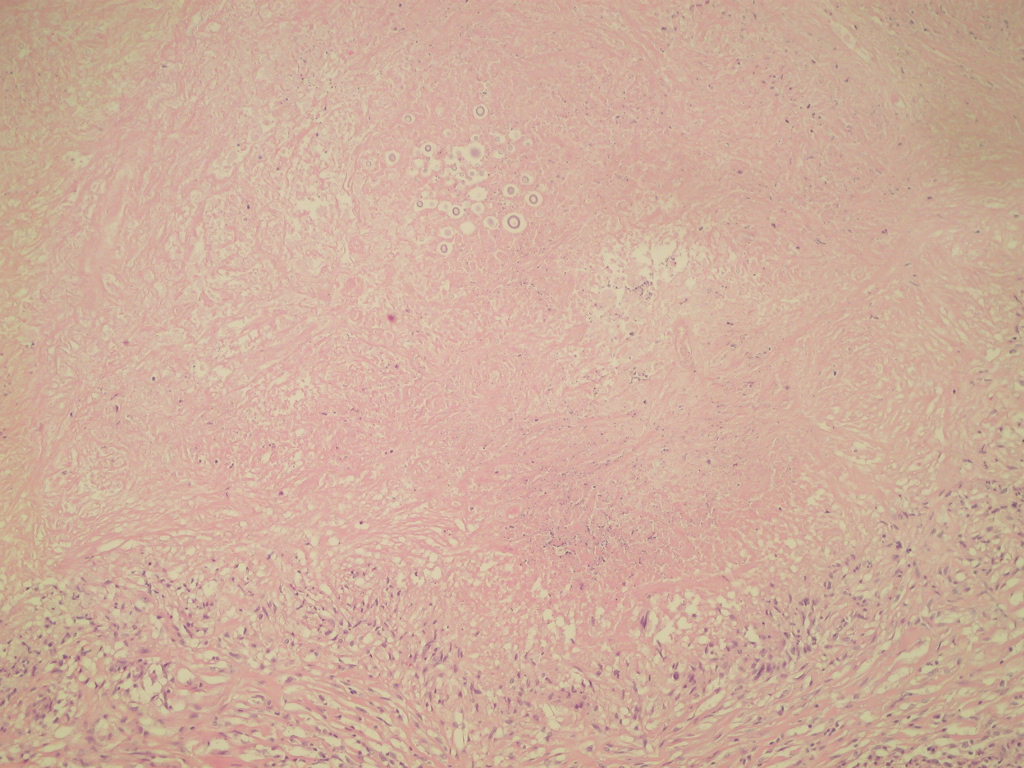
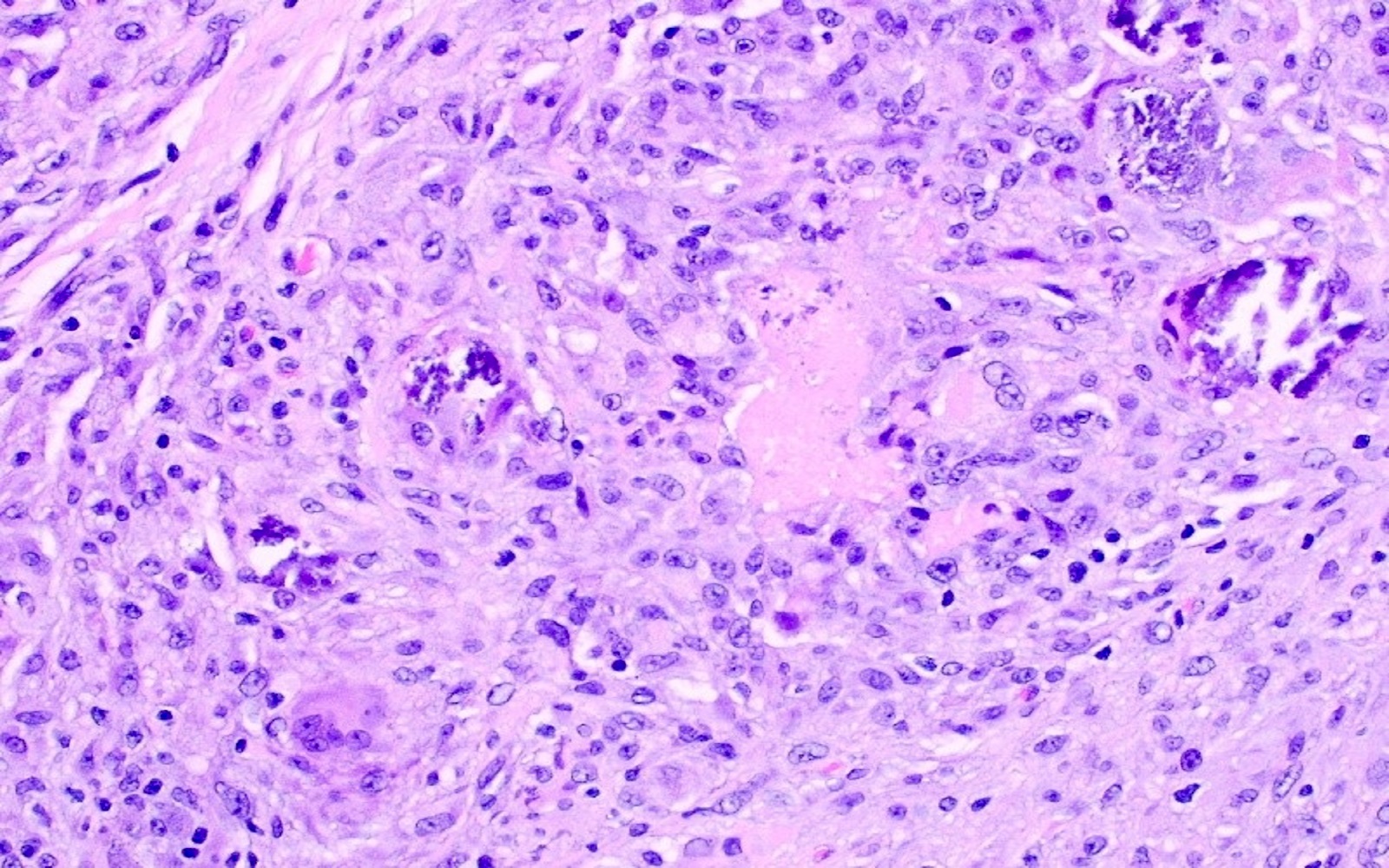
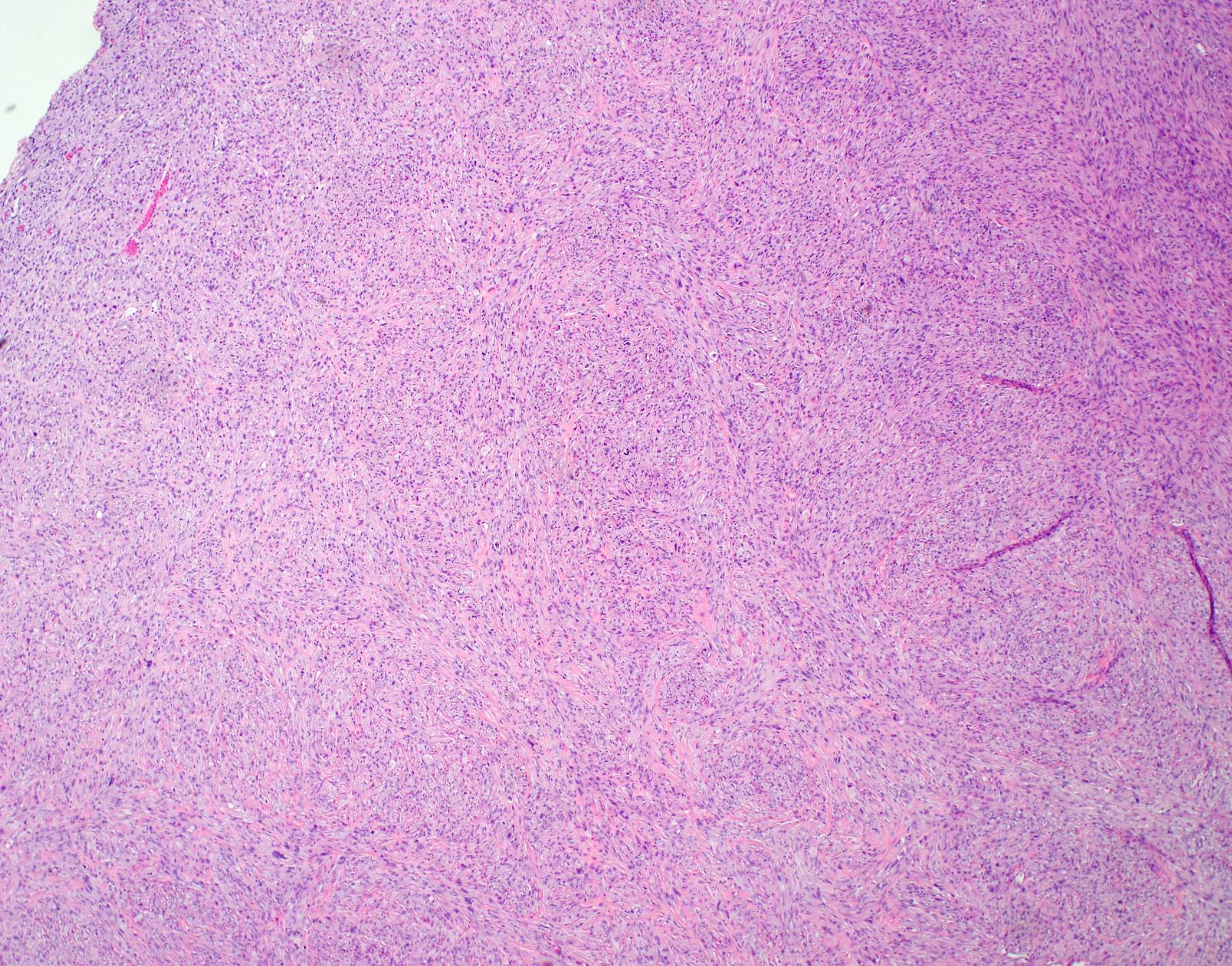
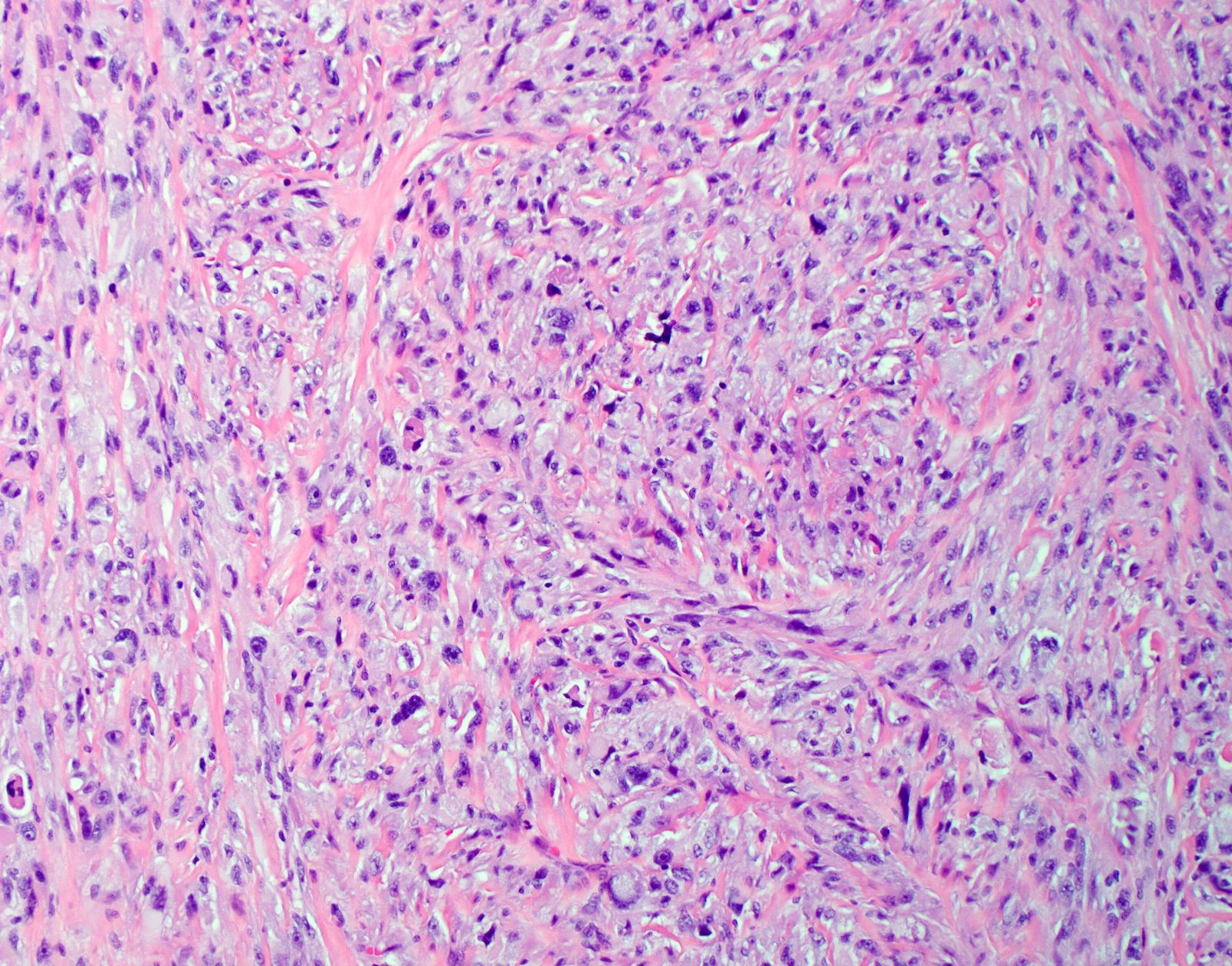
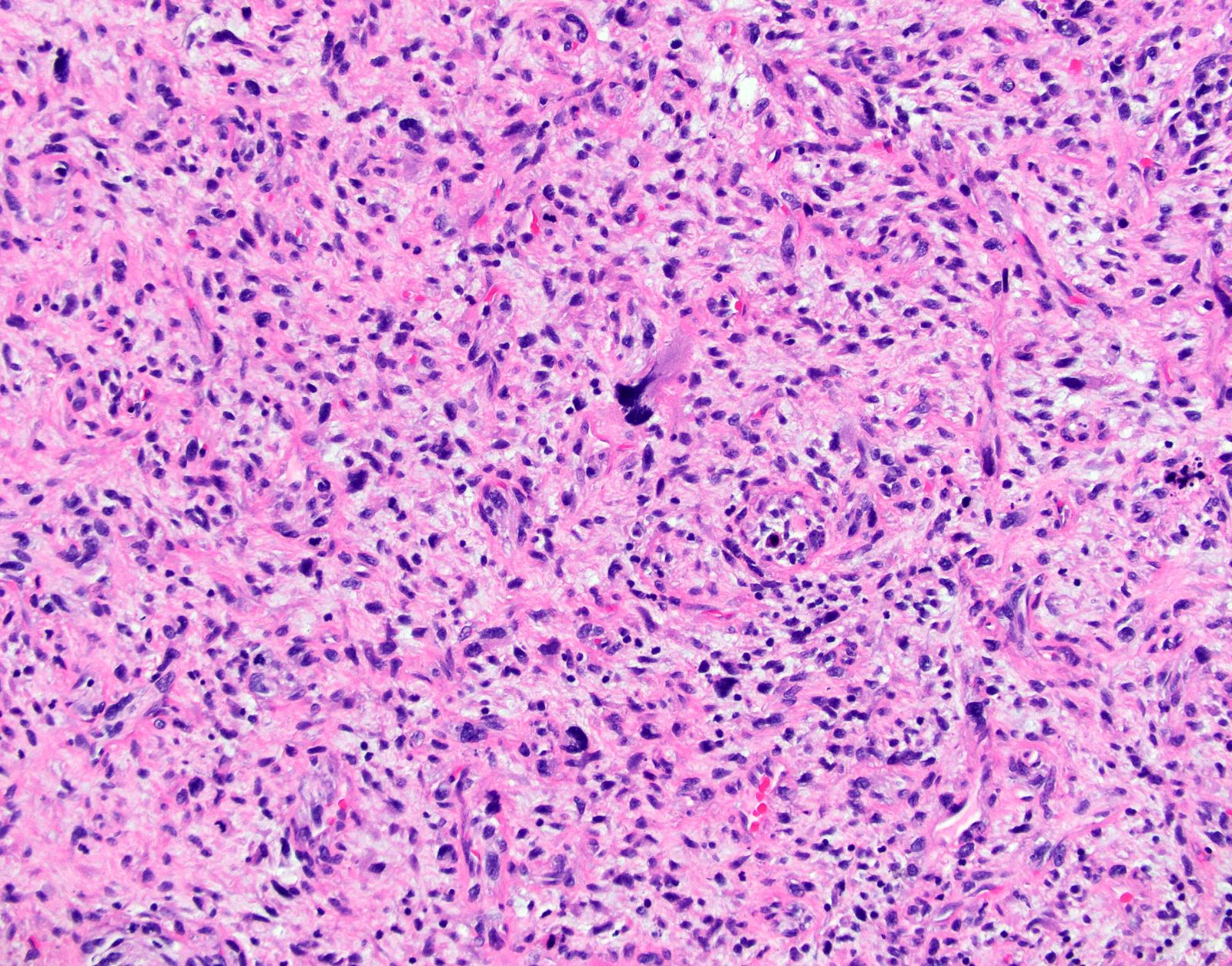
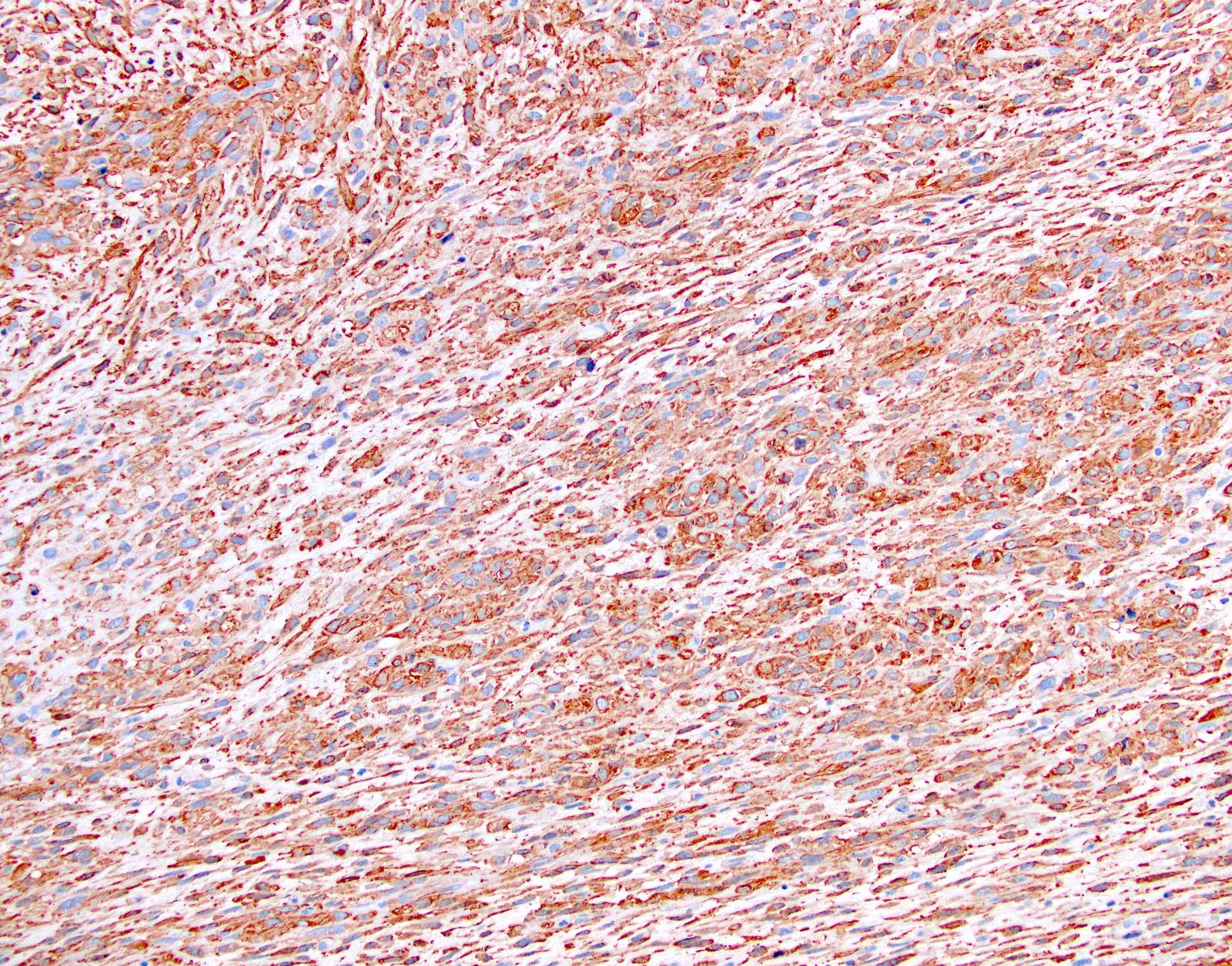
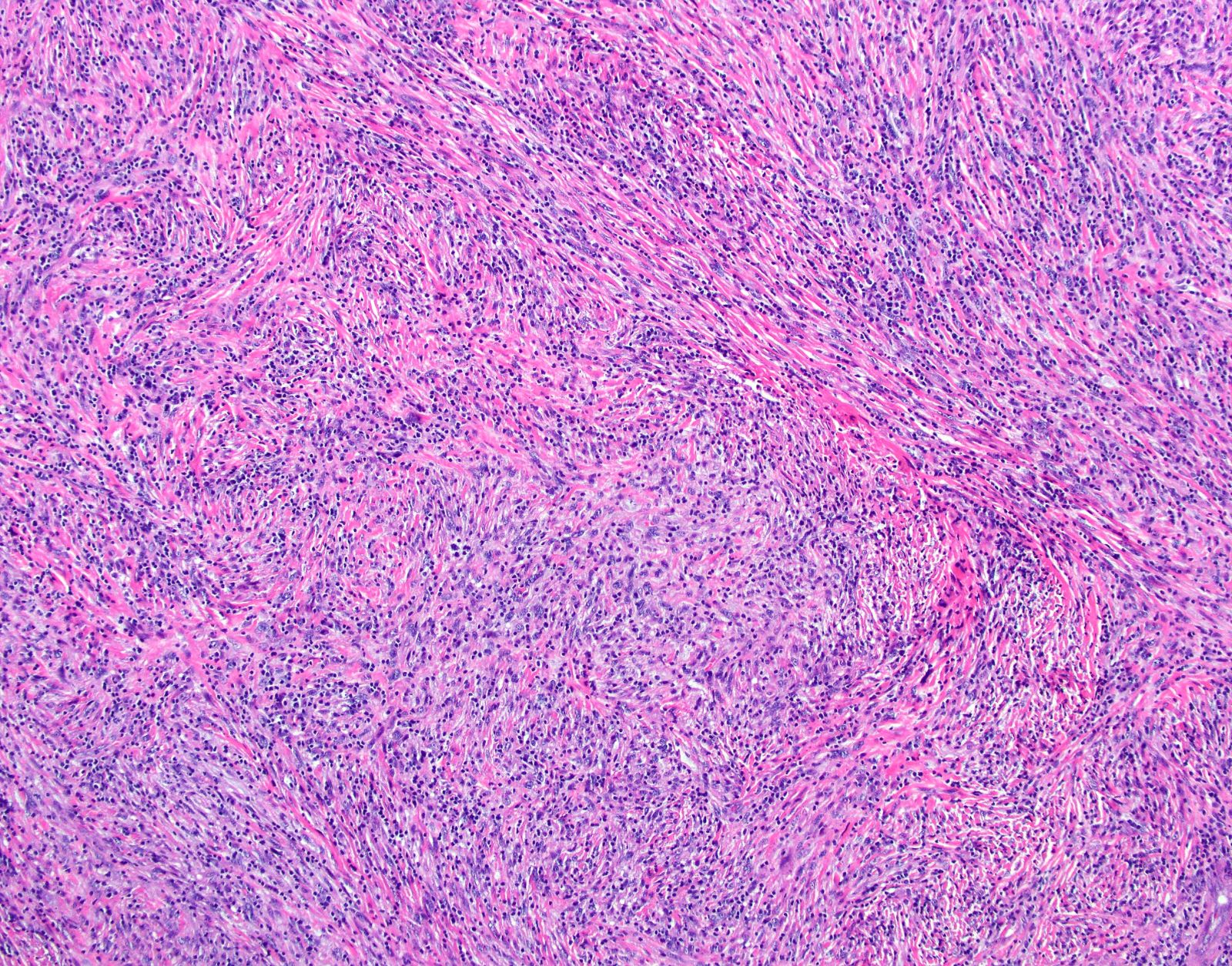
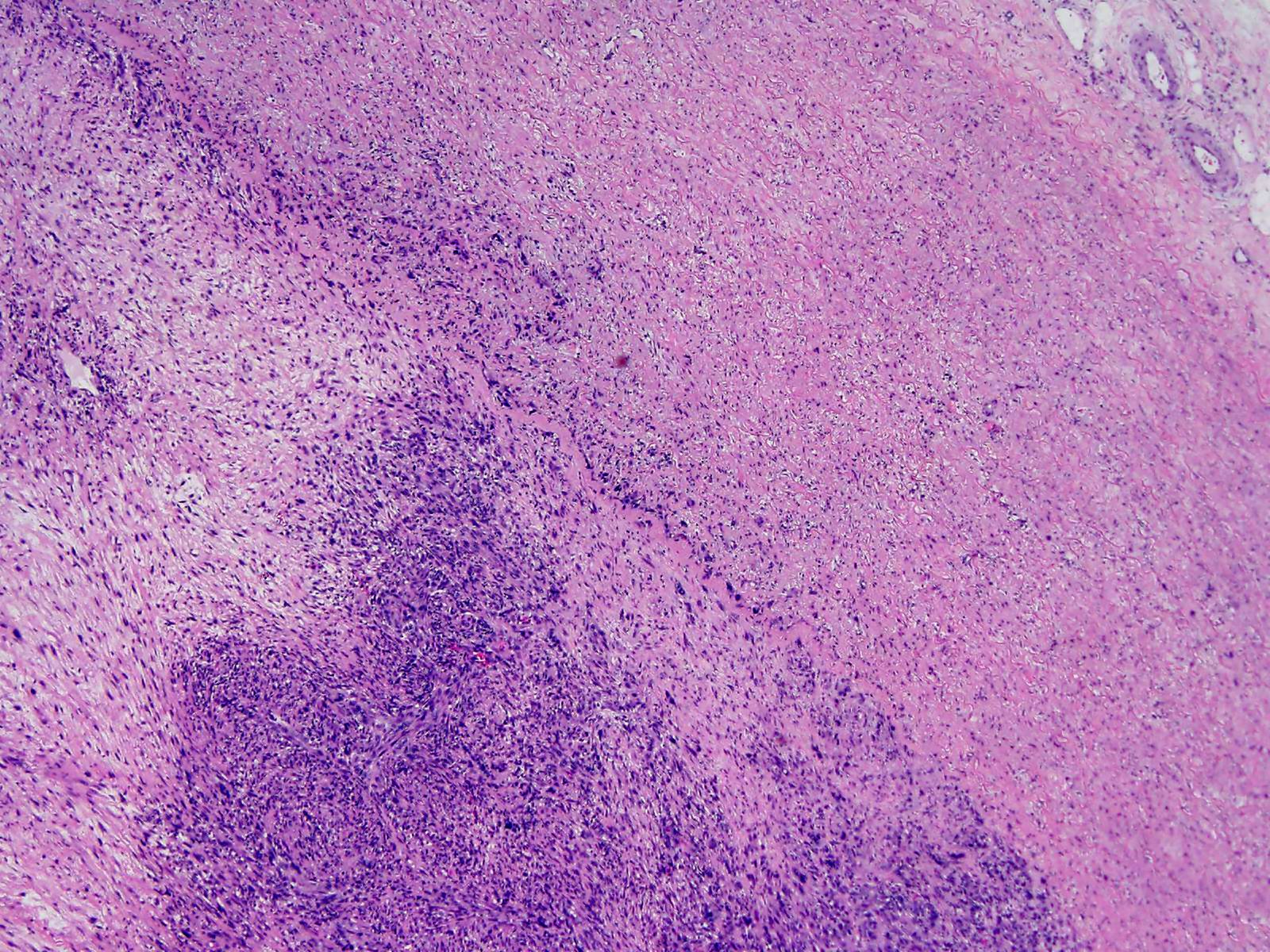
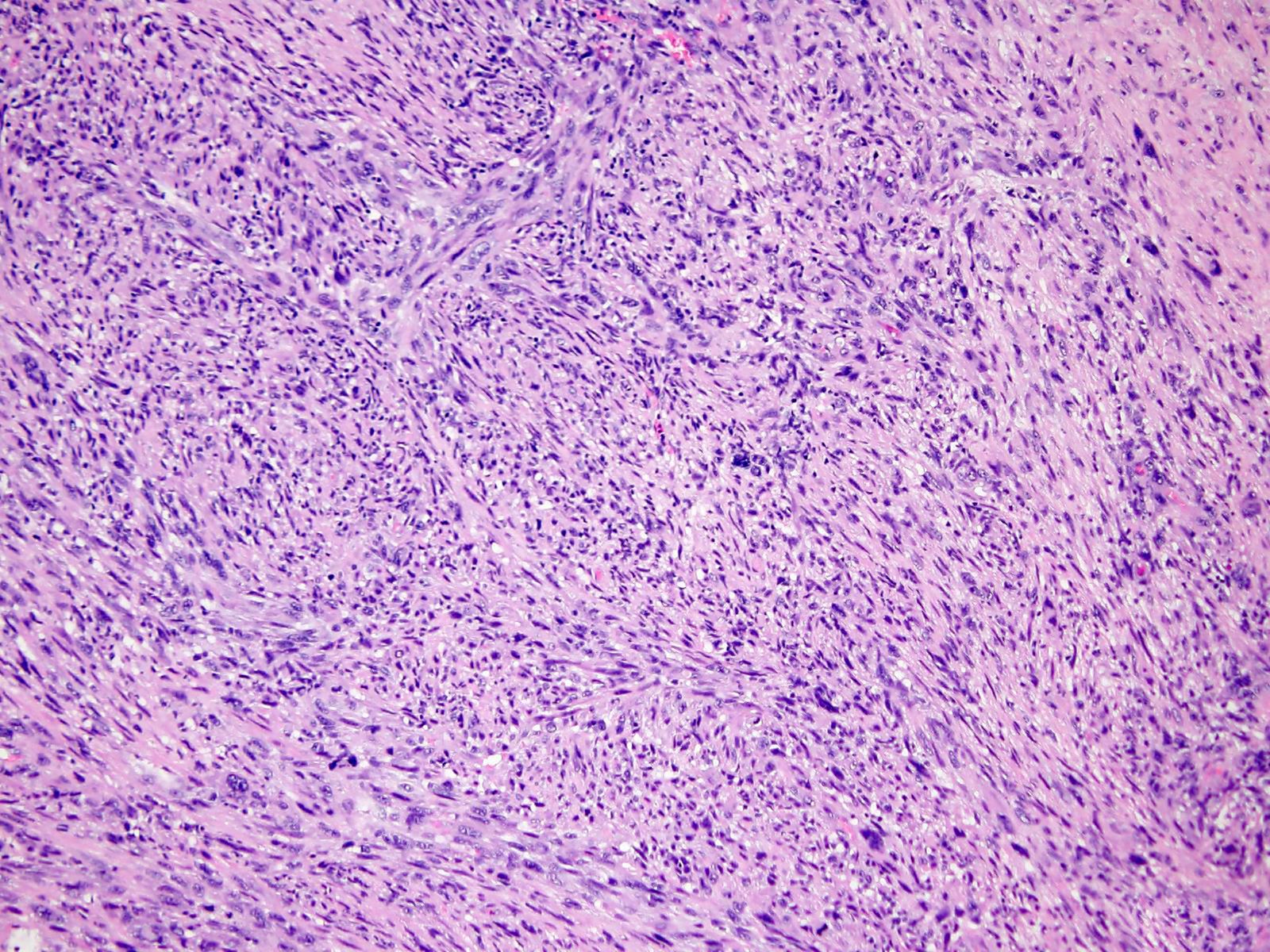
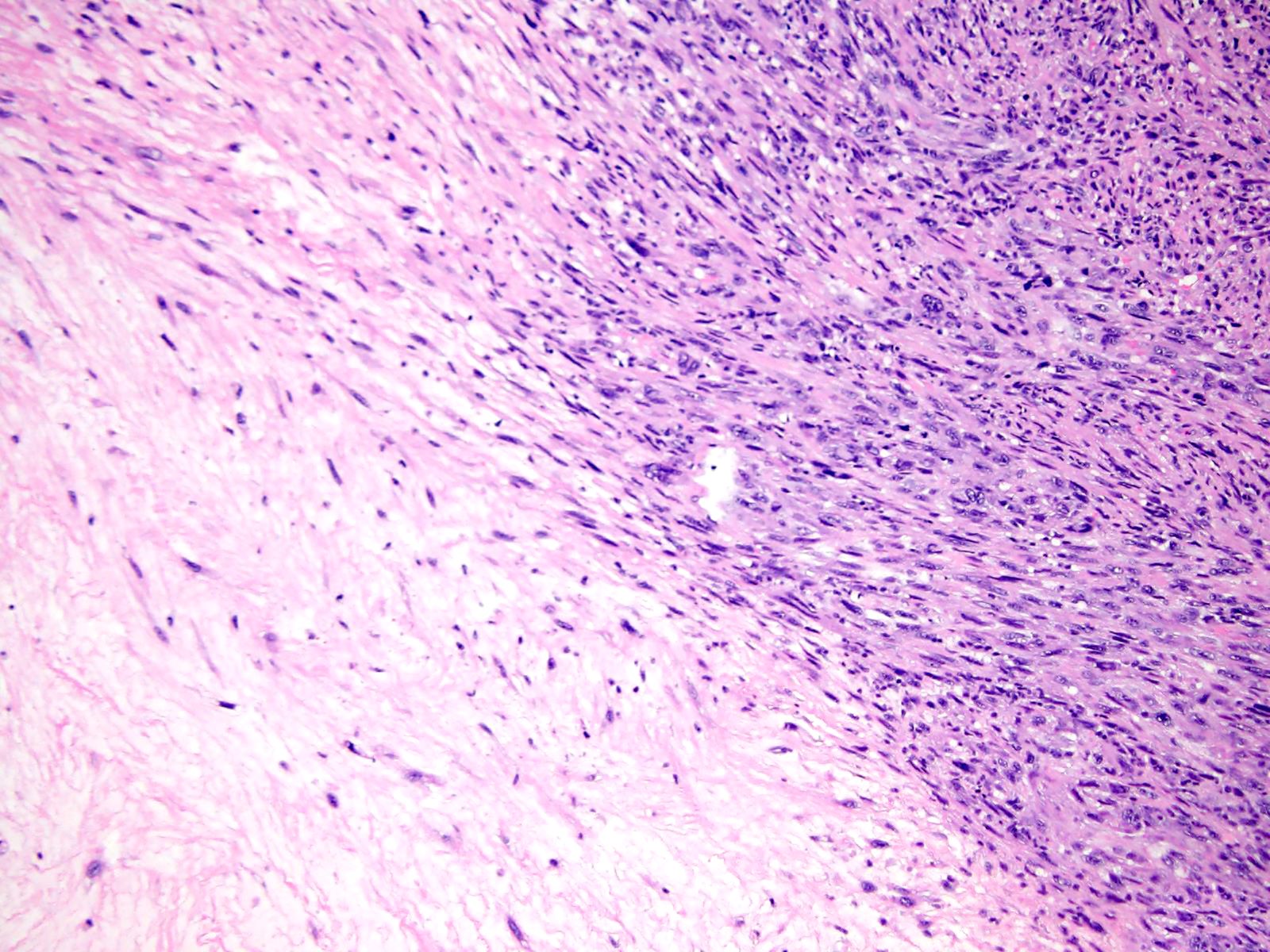
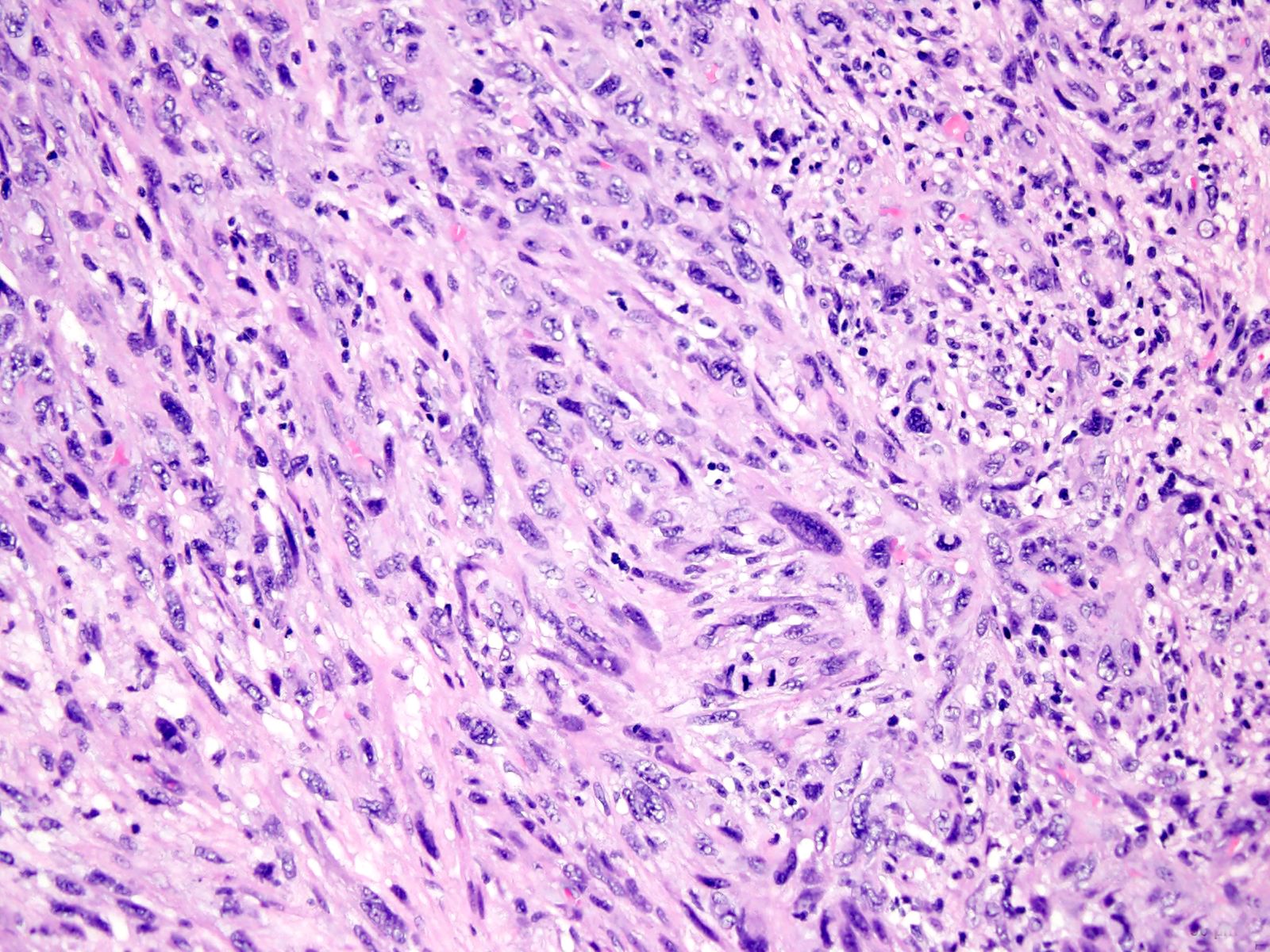
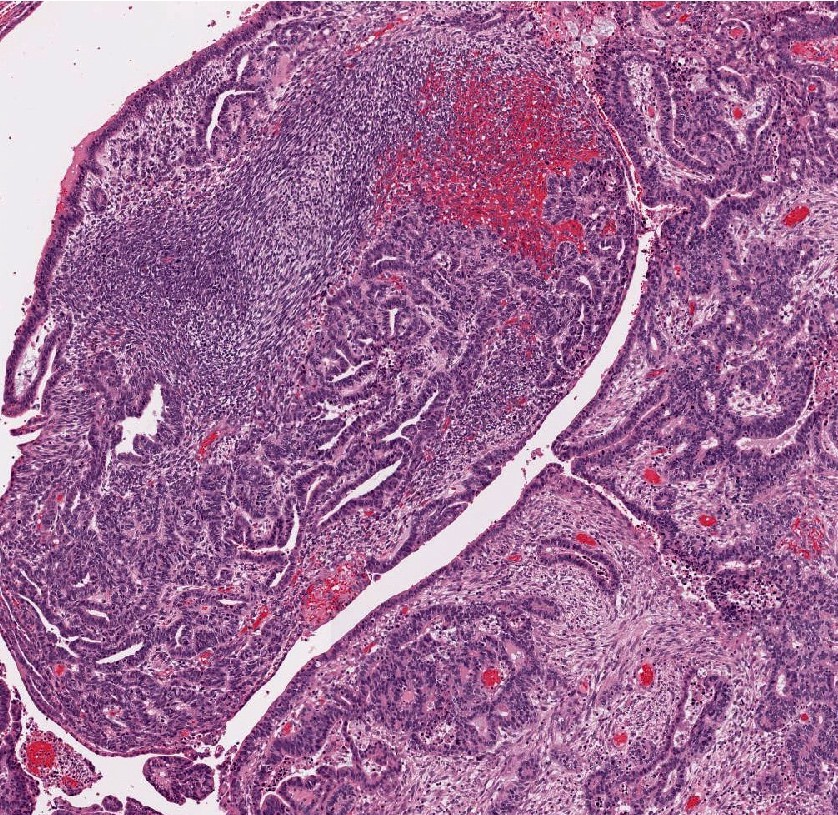
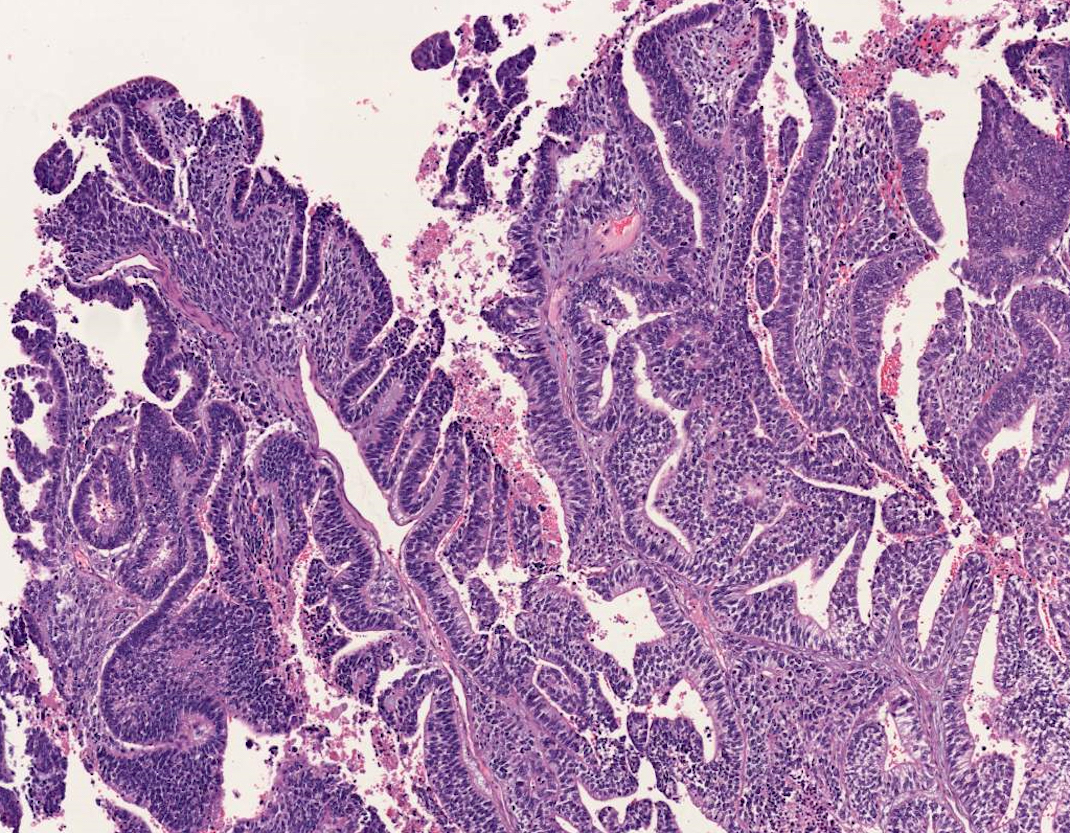
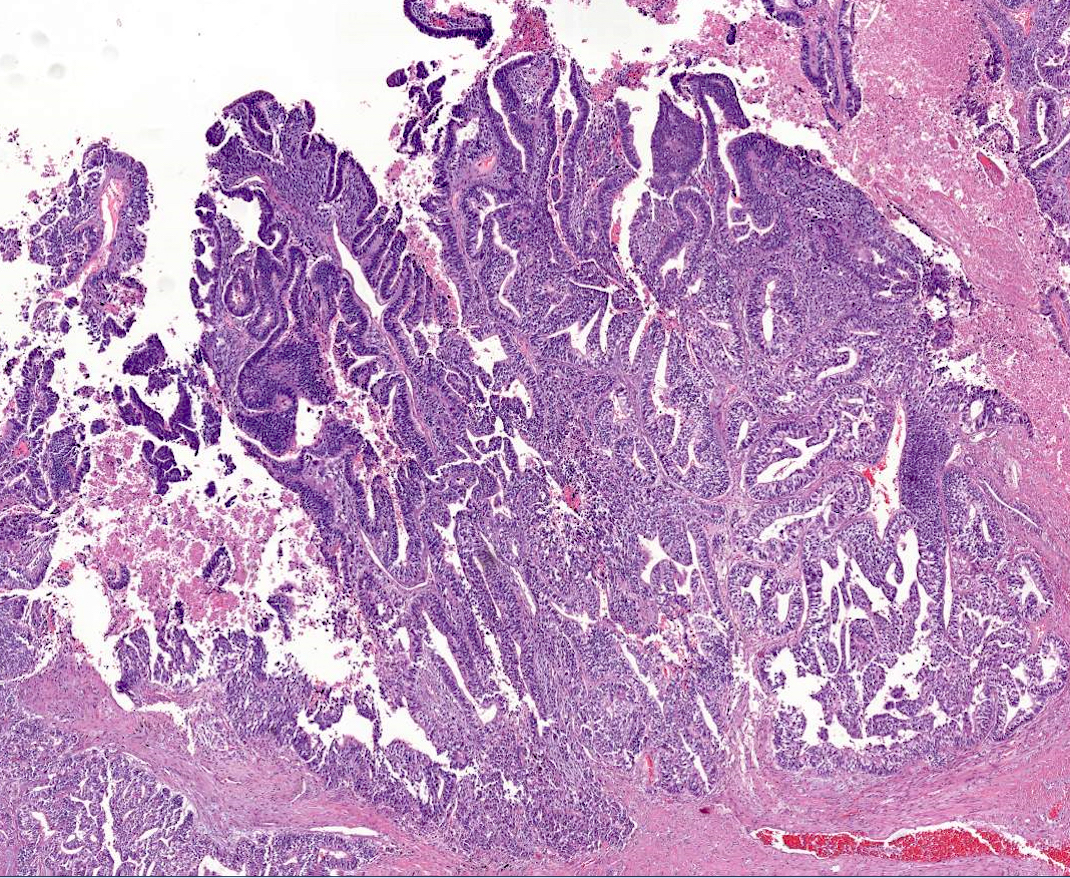
- Major findings
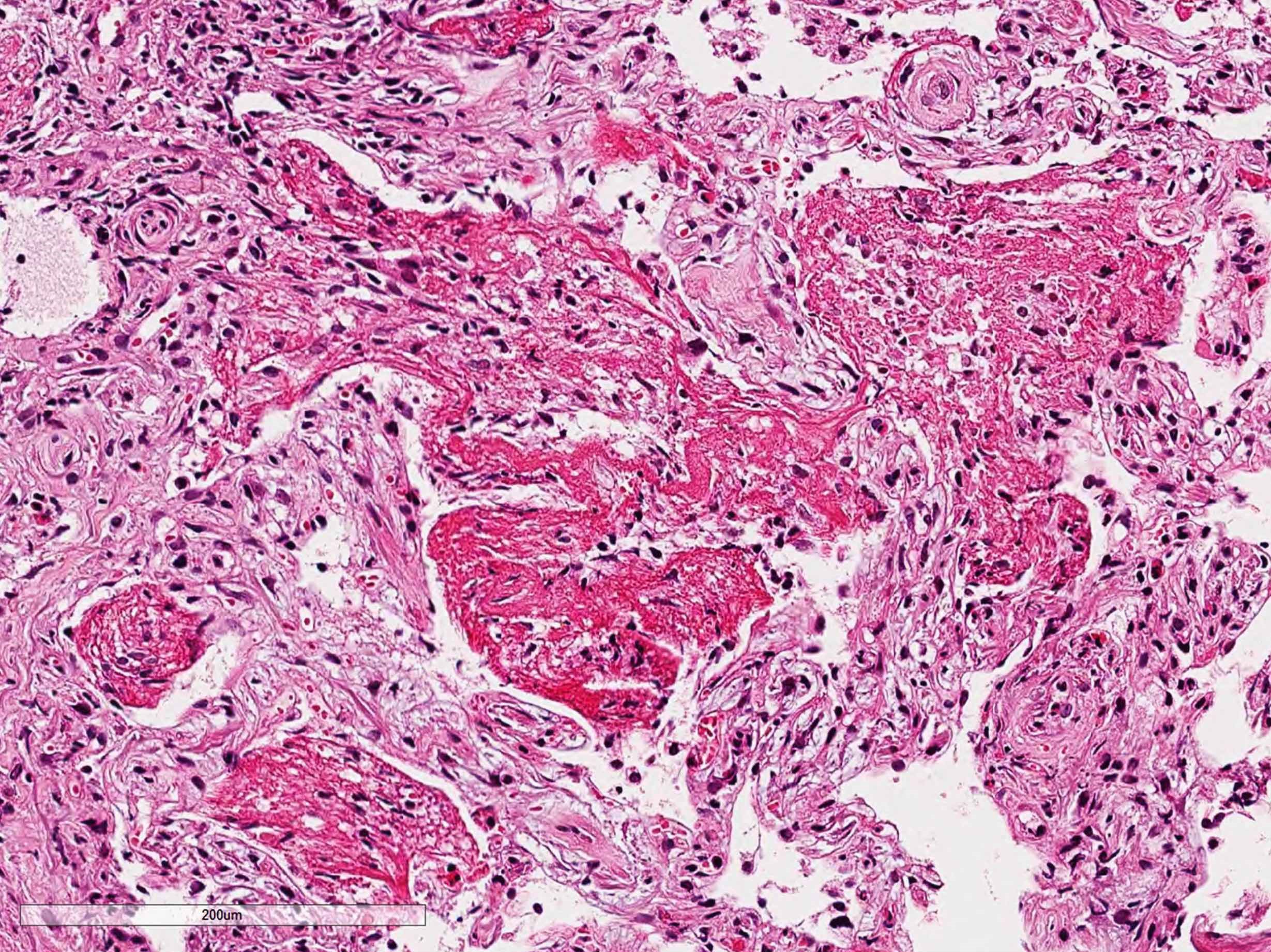
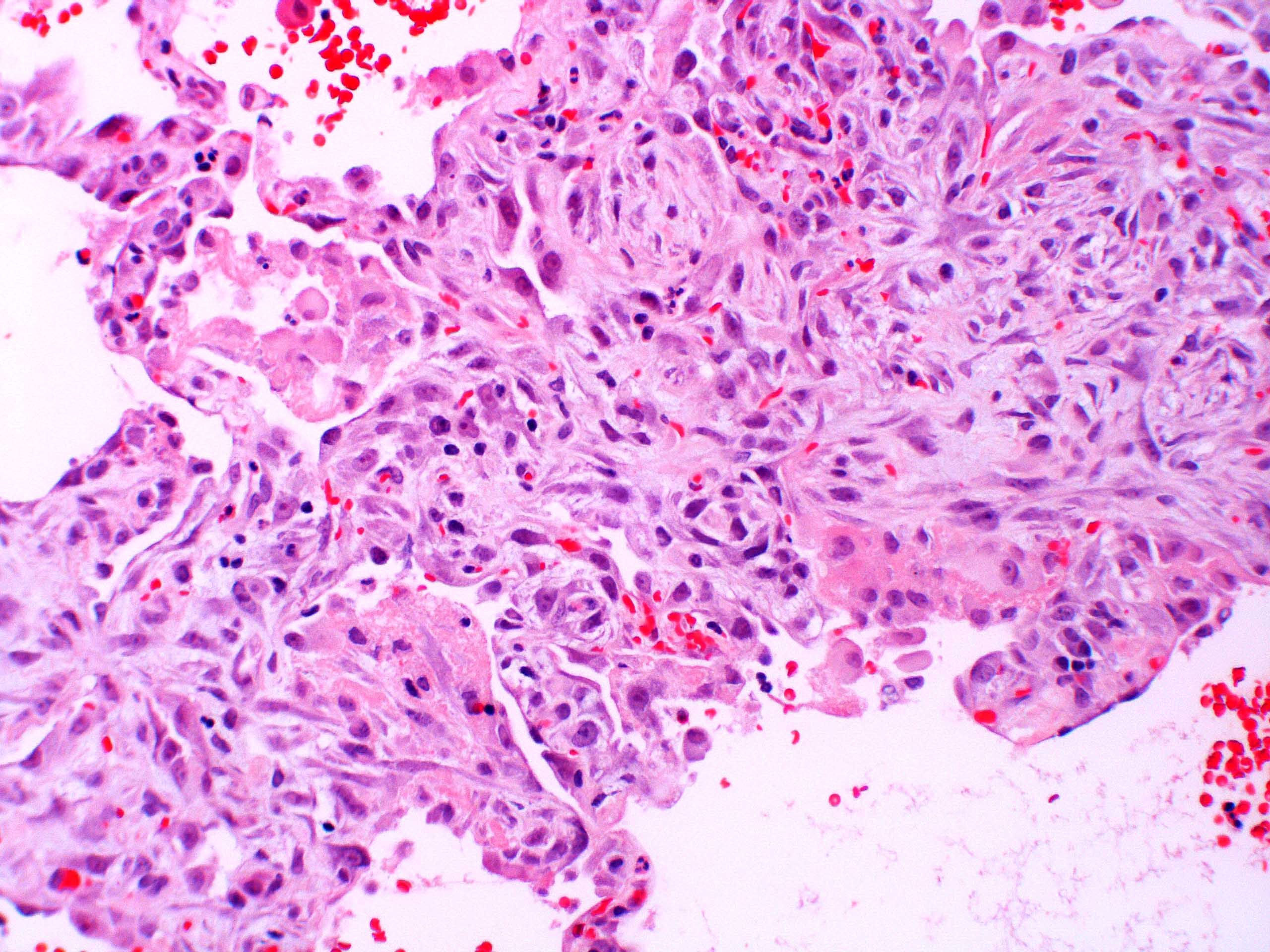
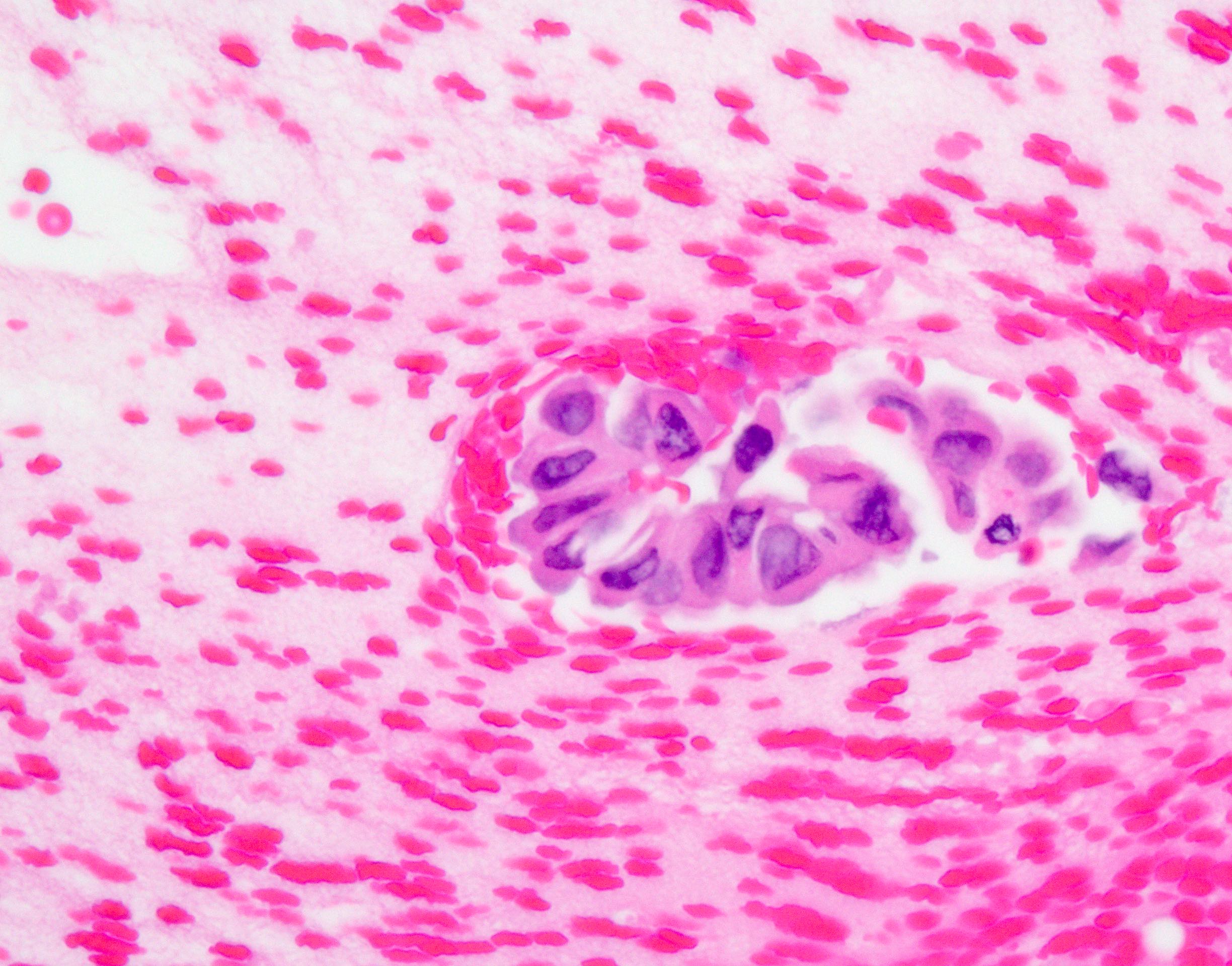
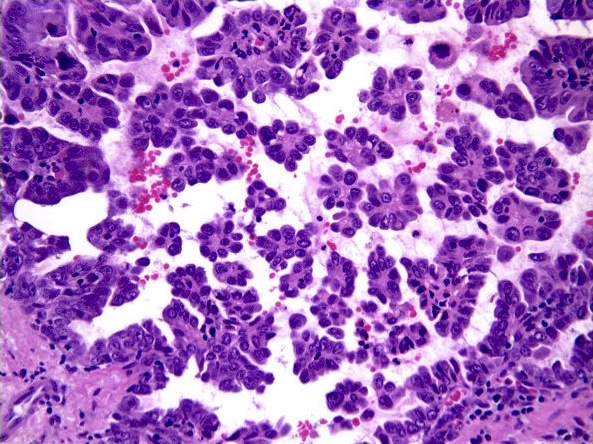
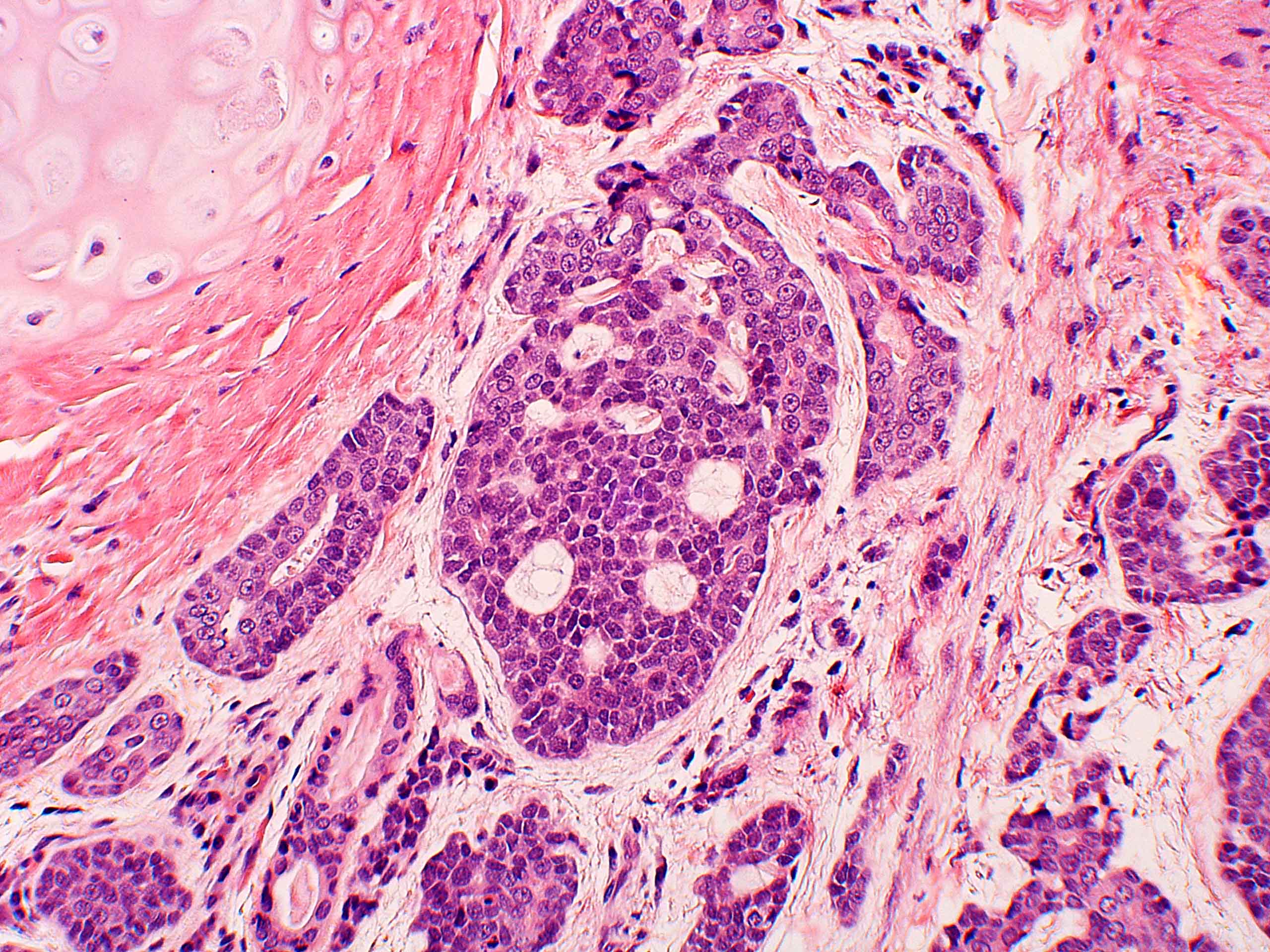
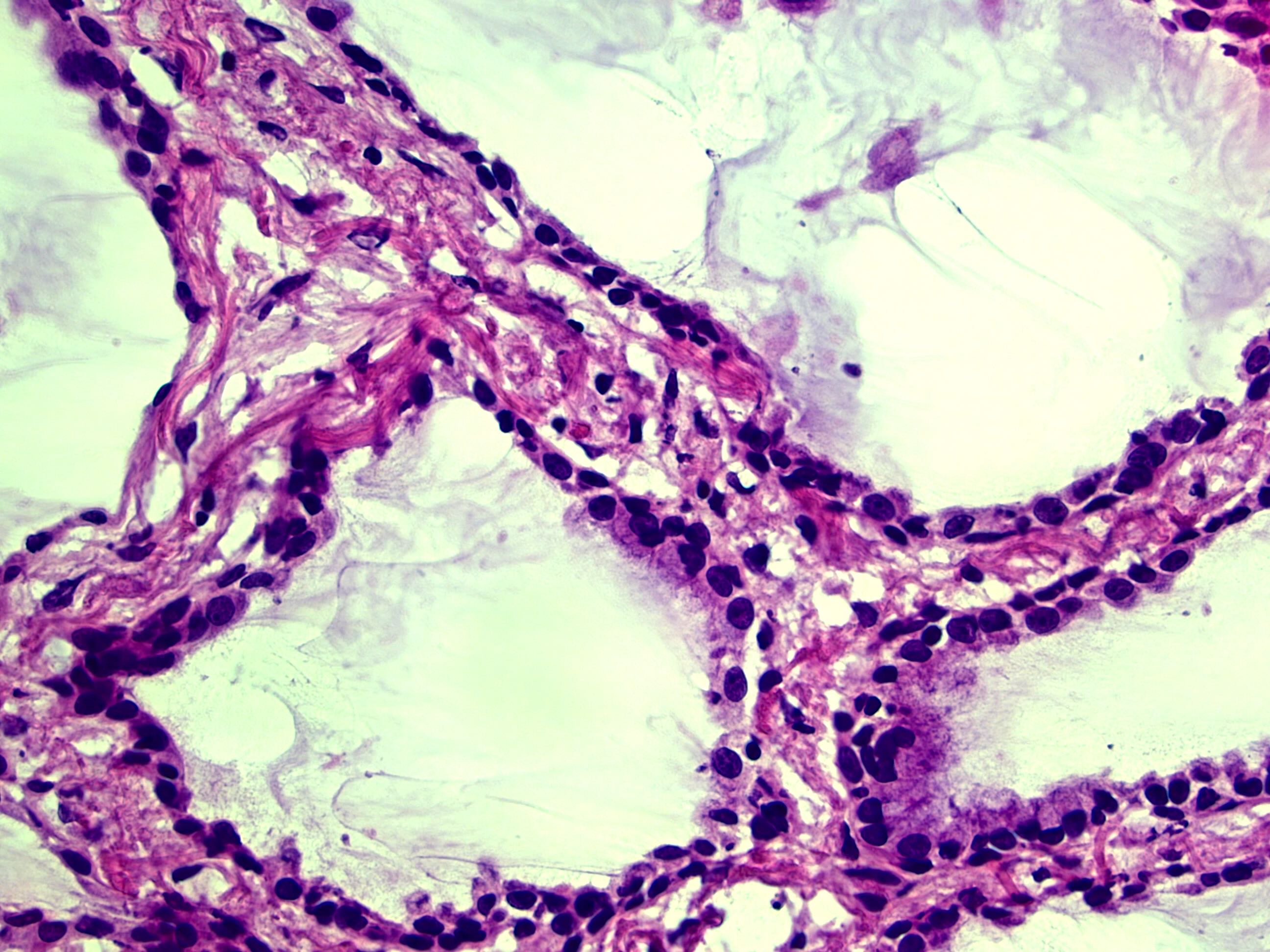
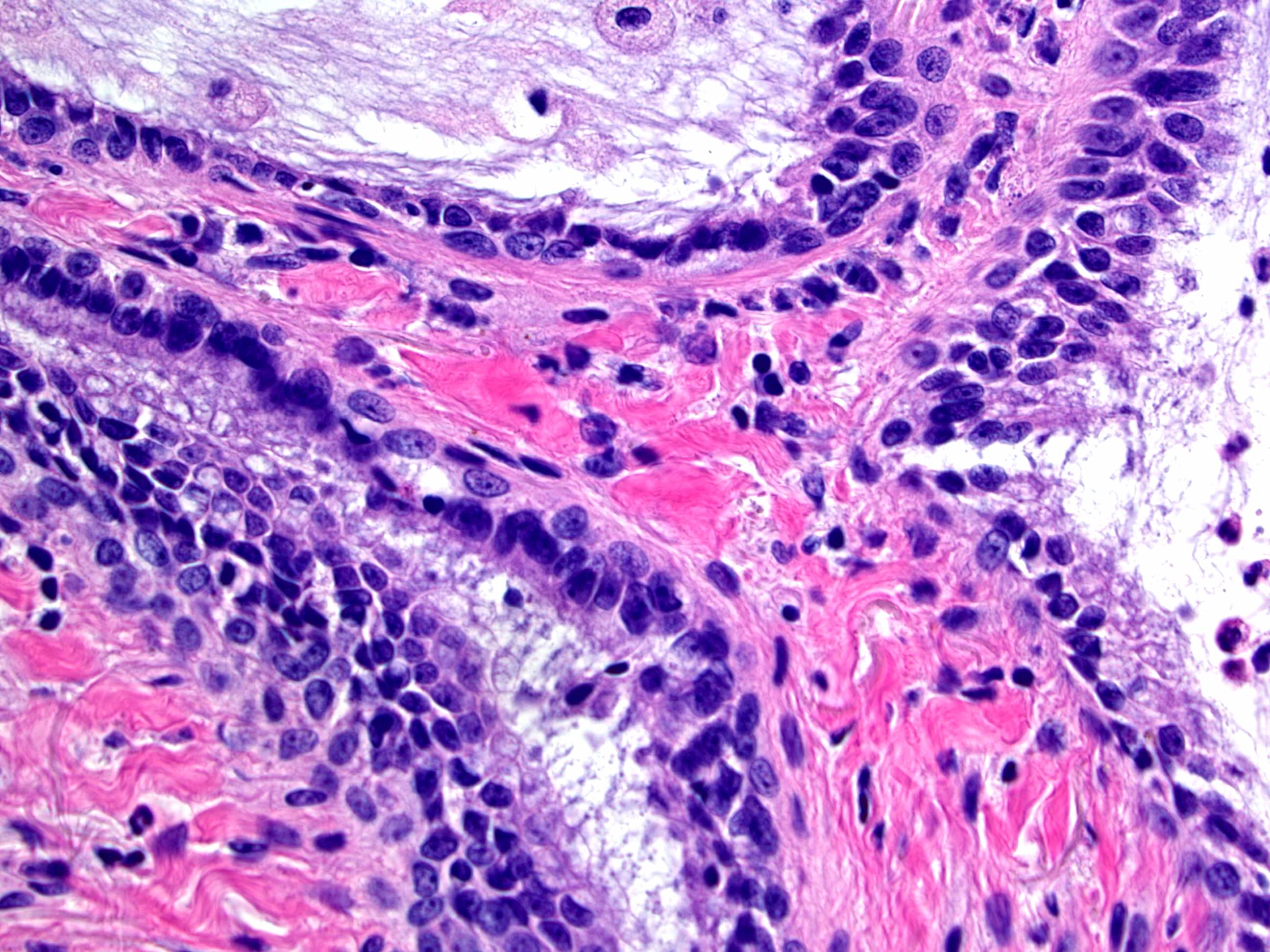
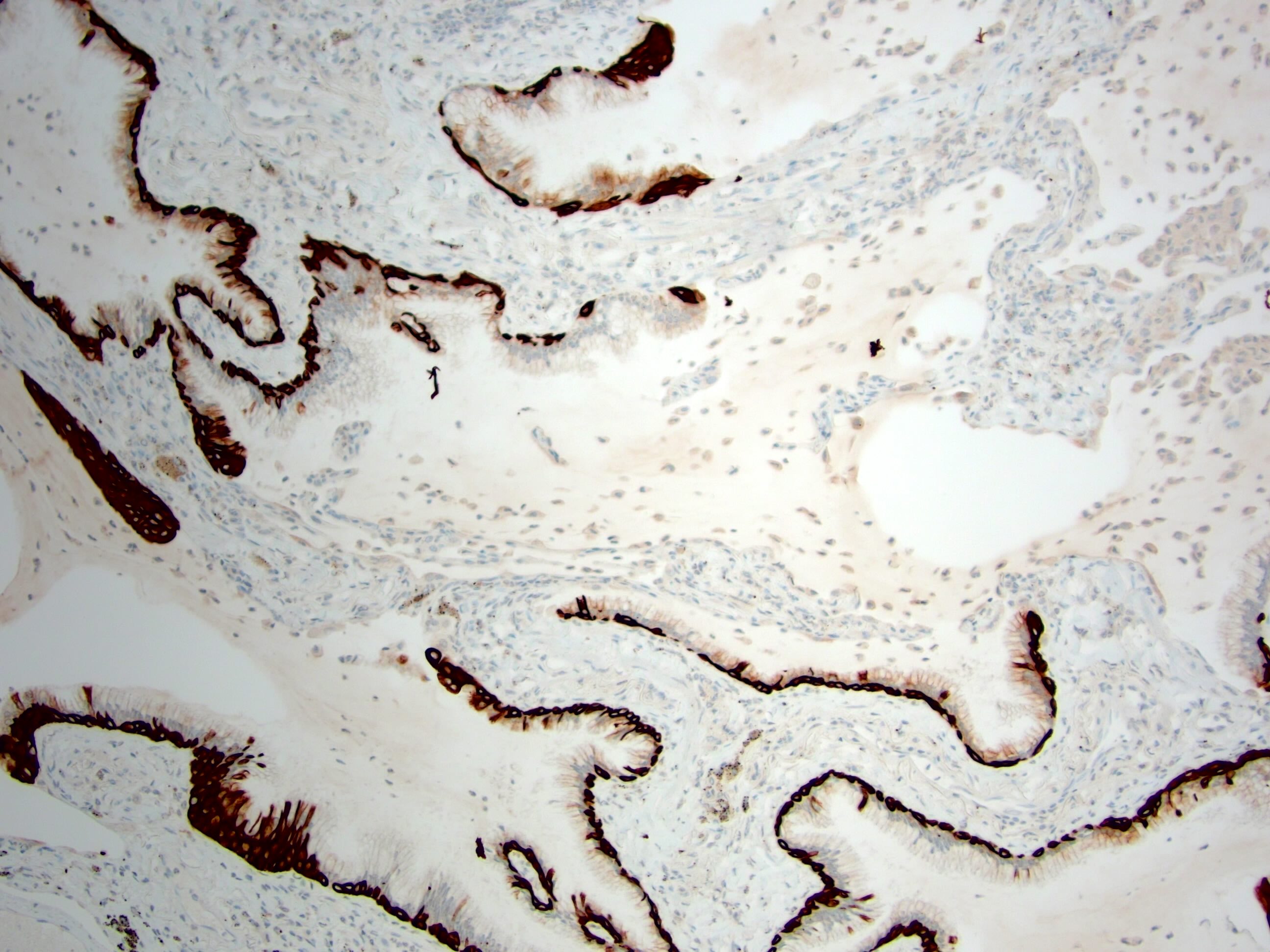
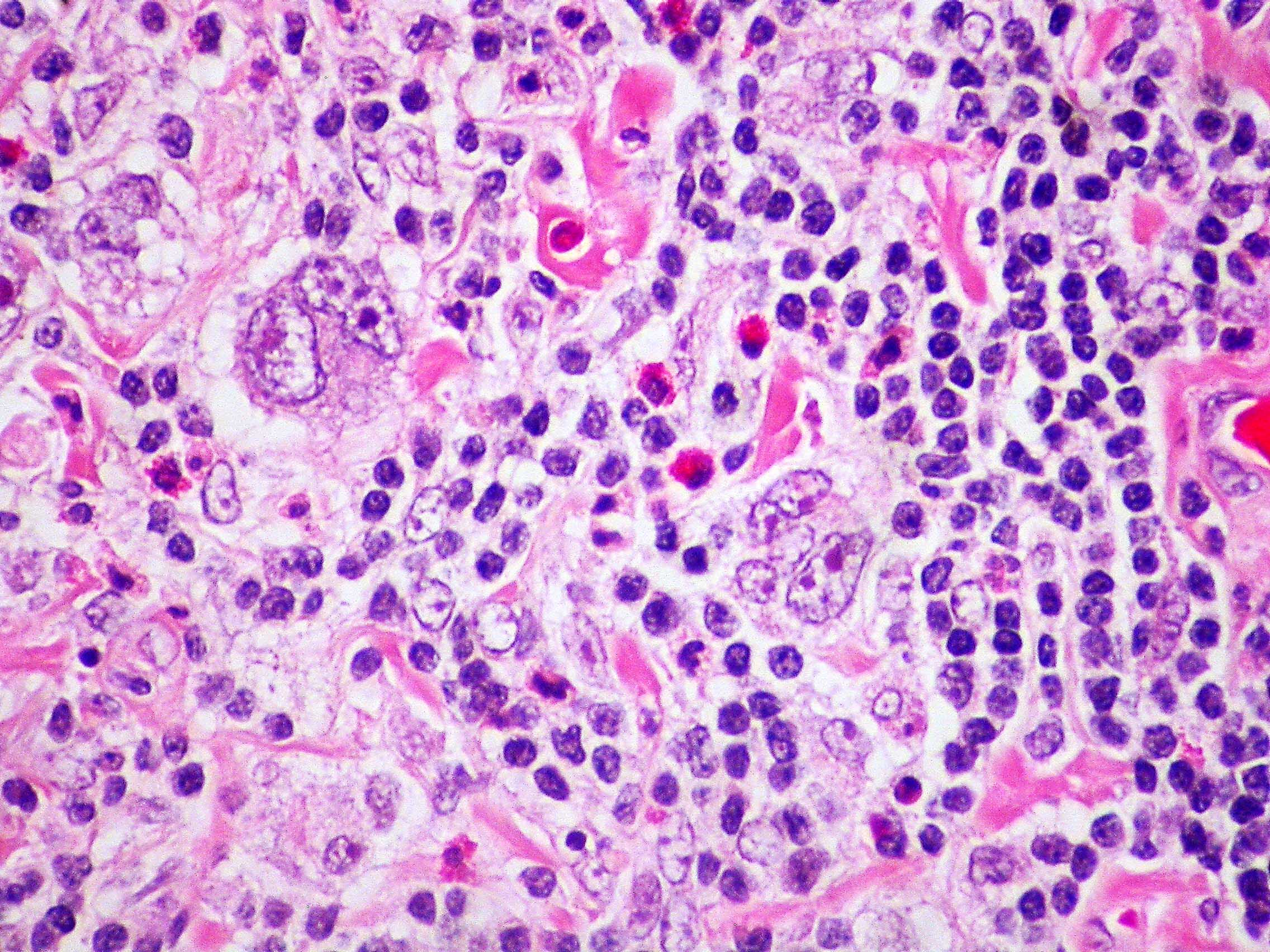
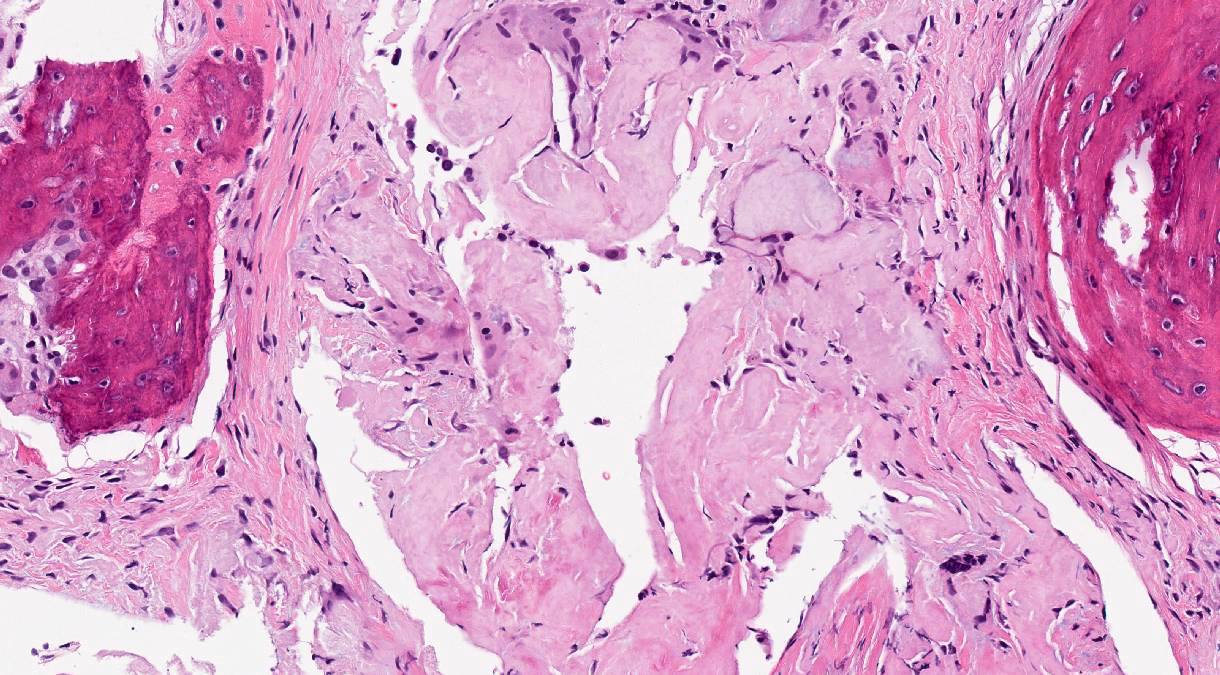
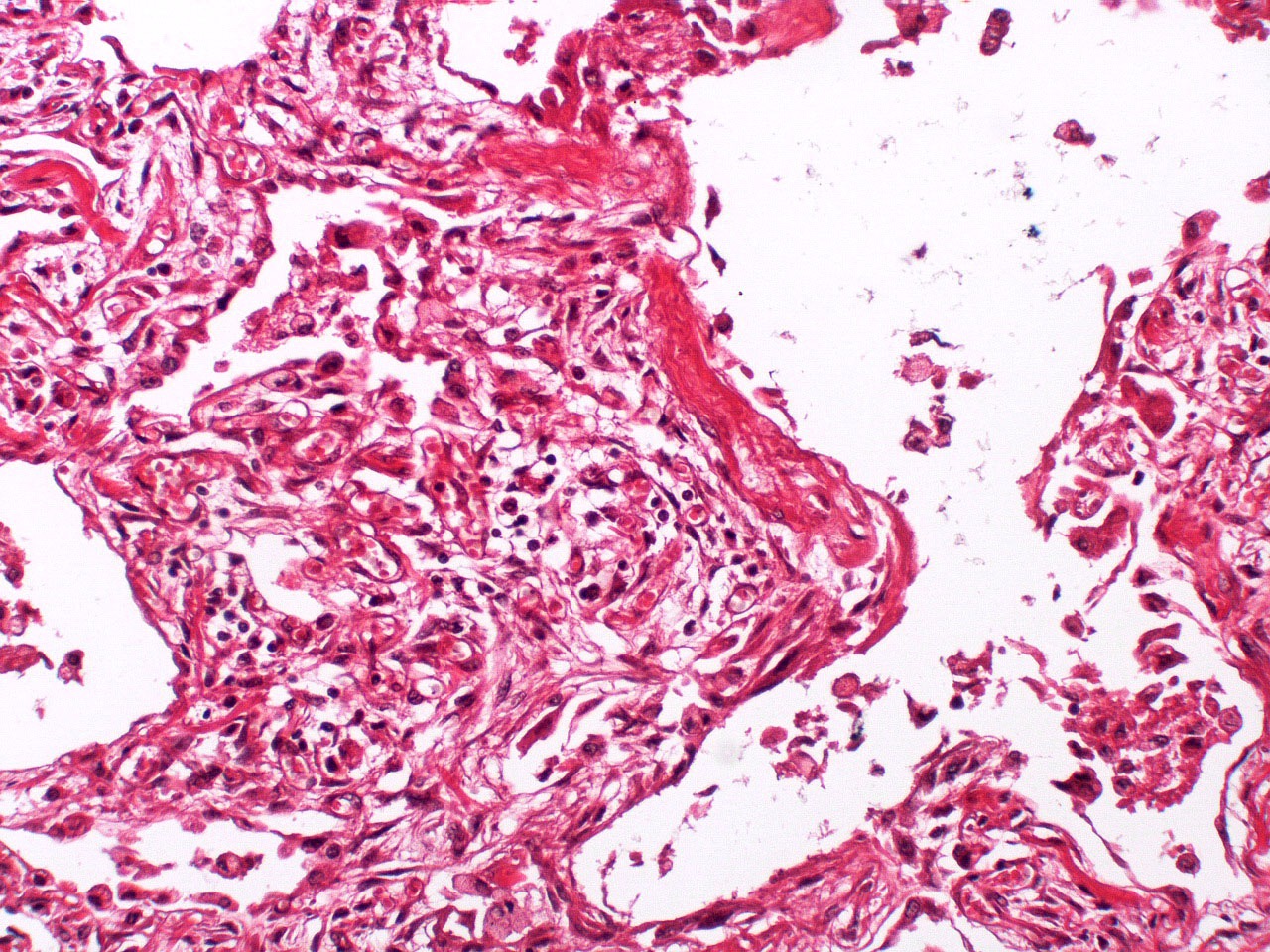
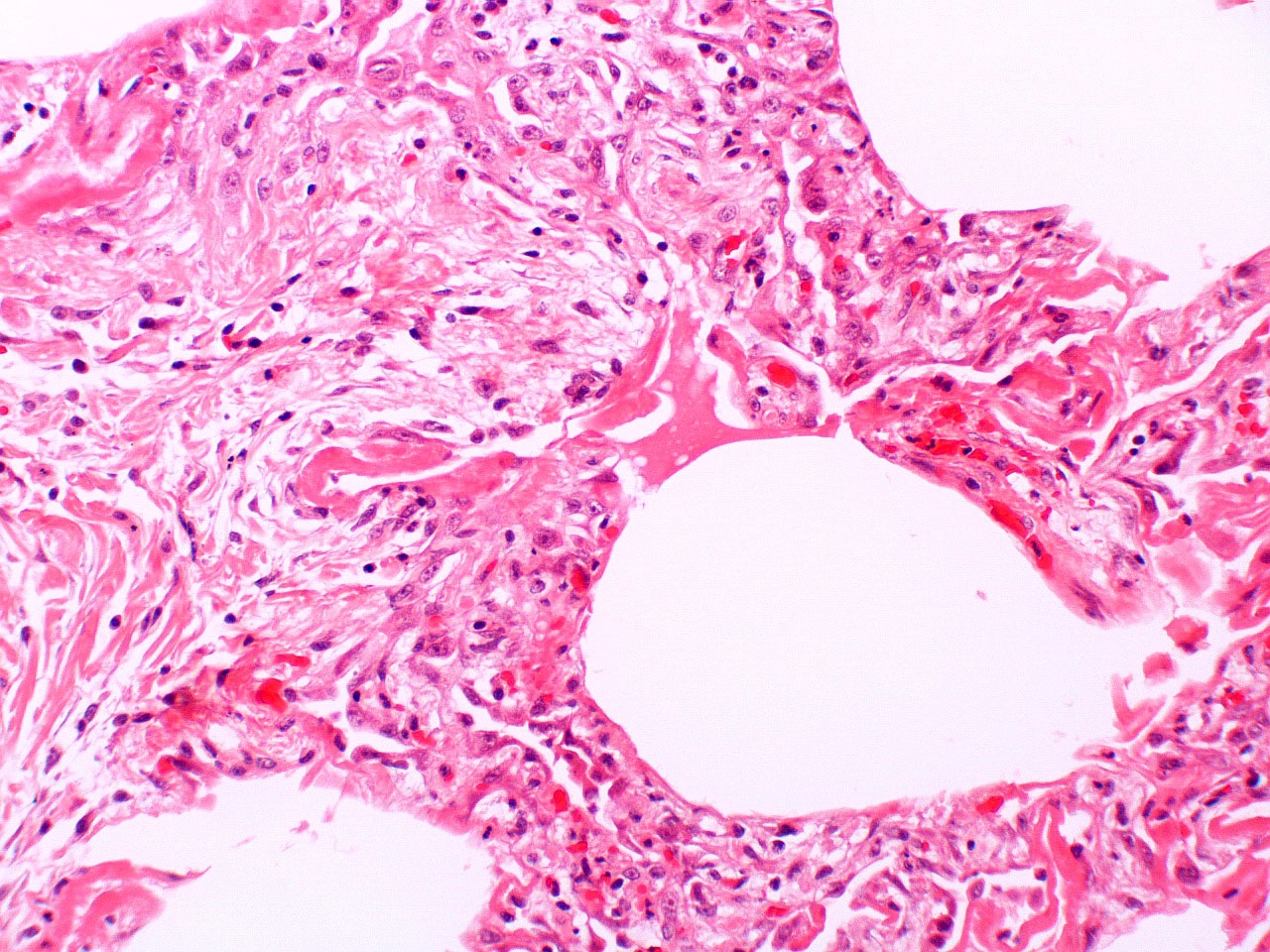
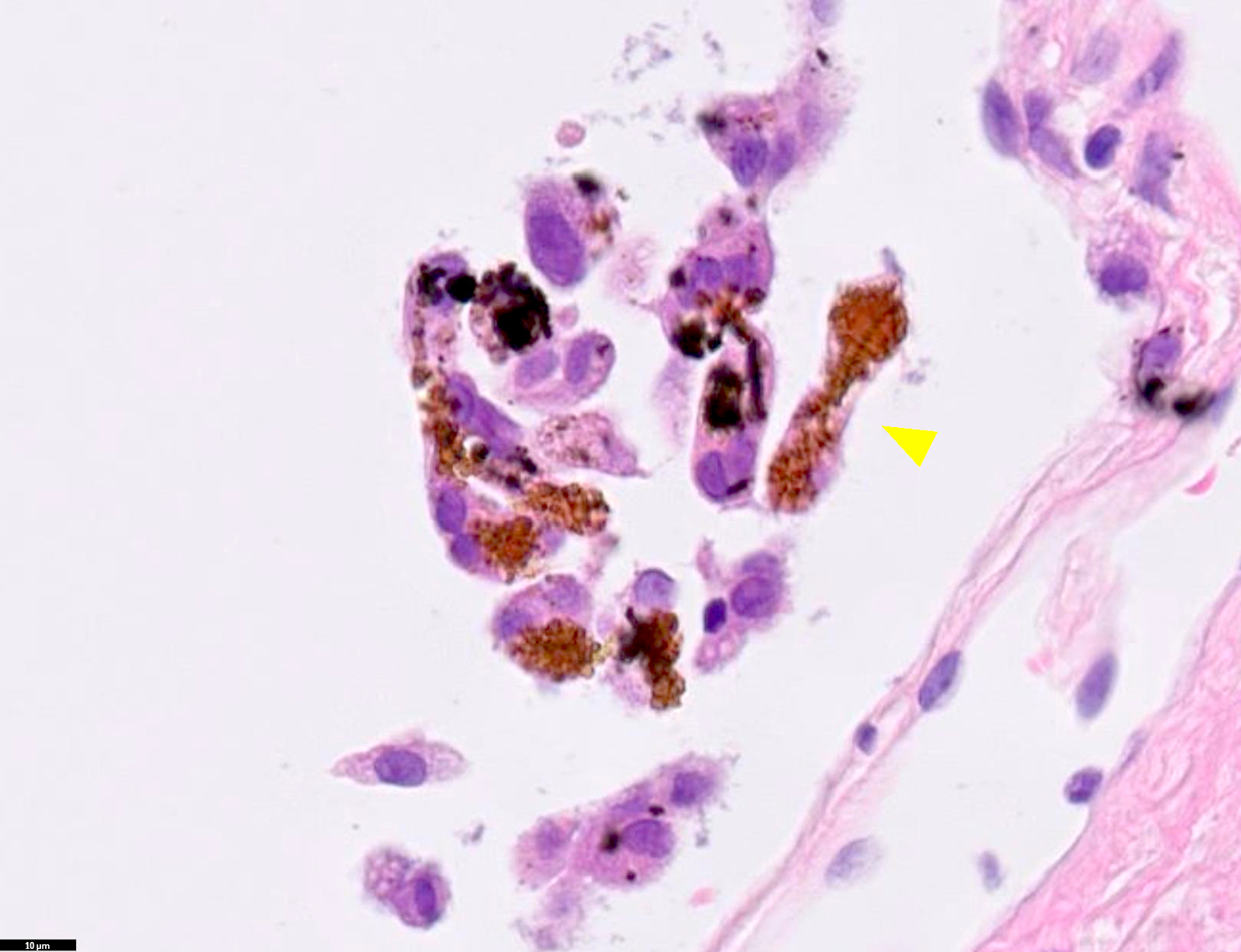
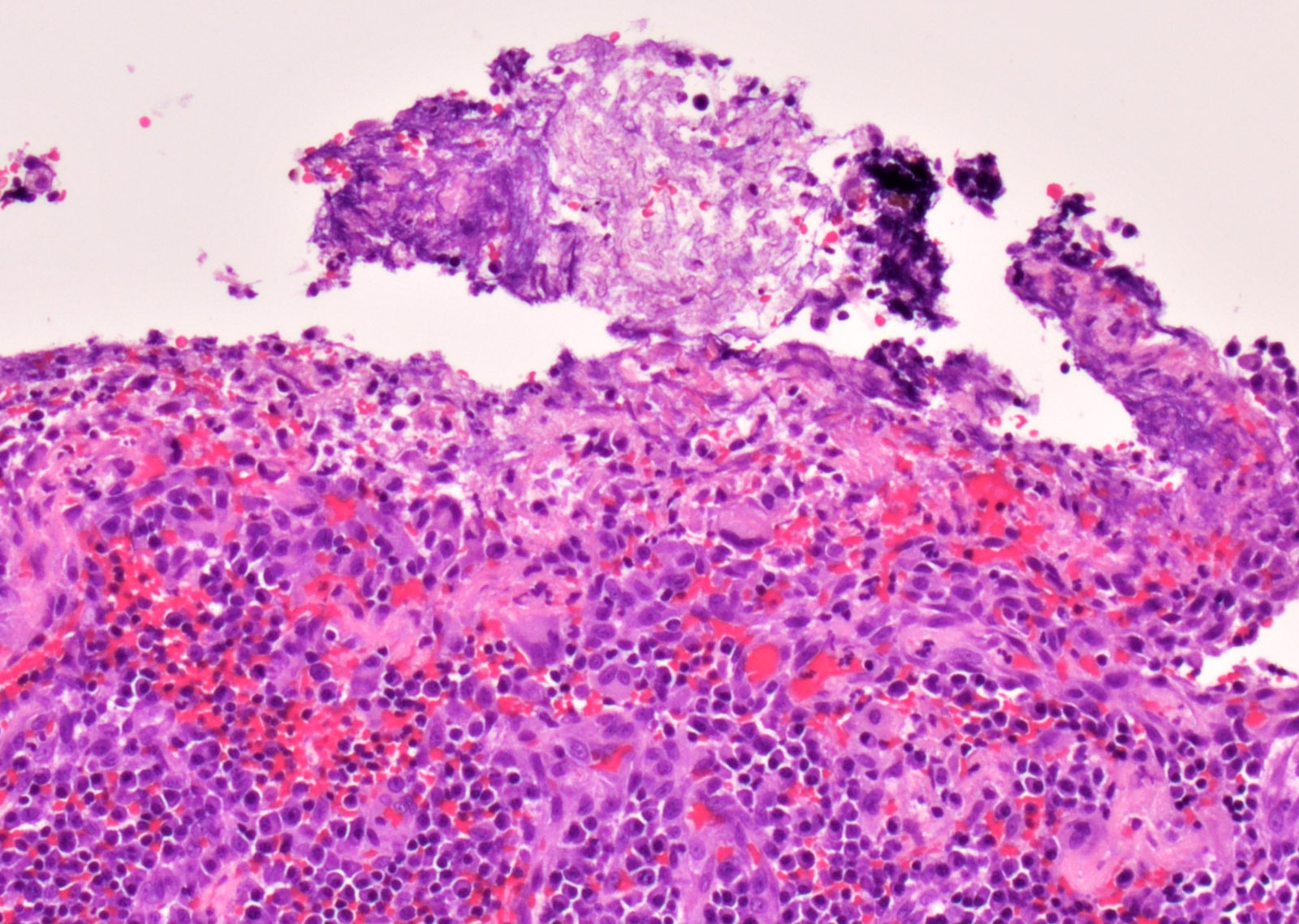
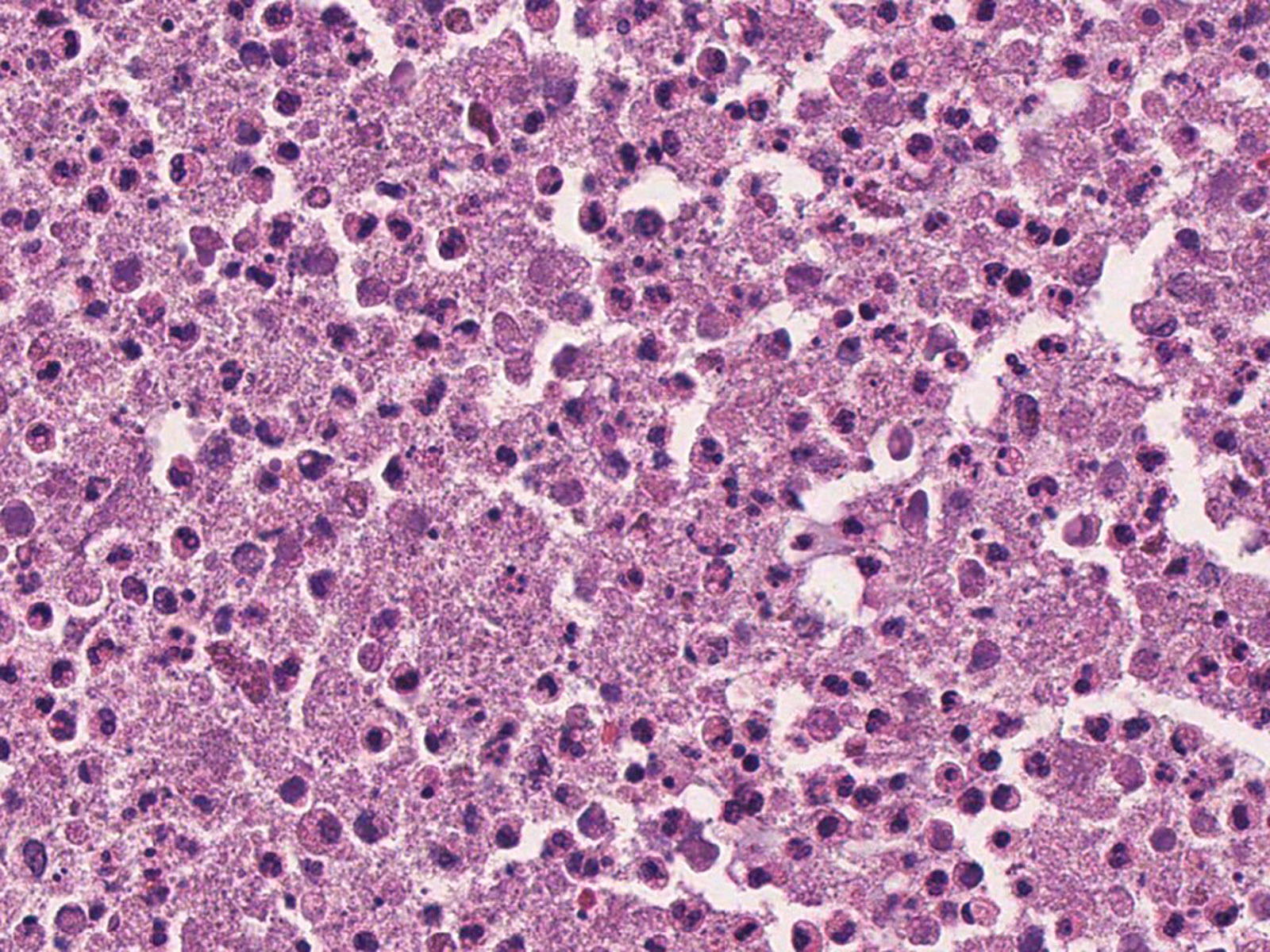
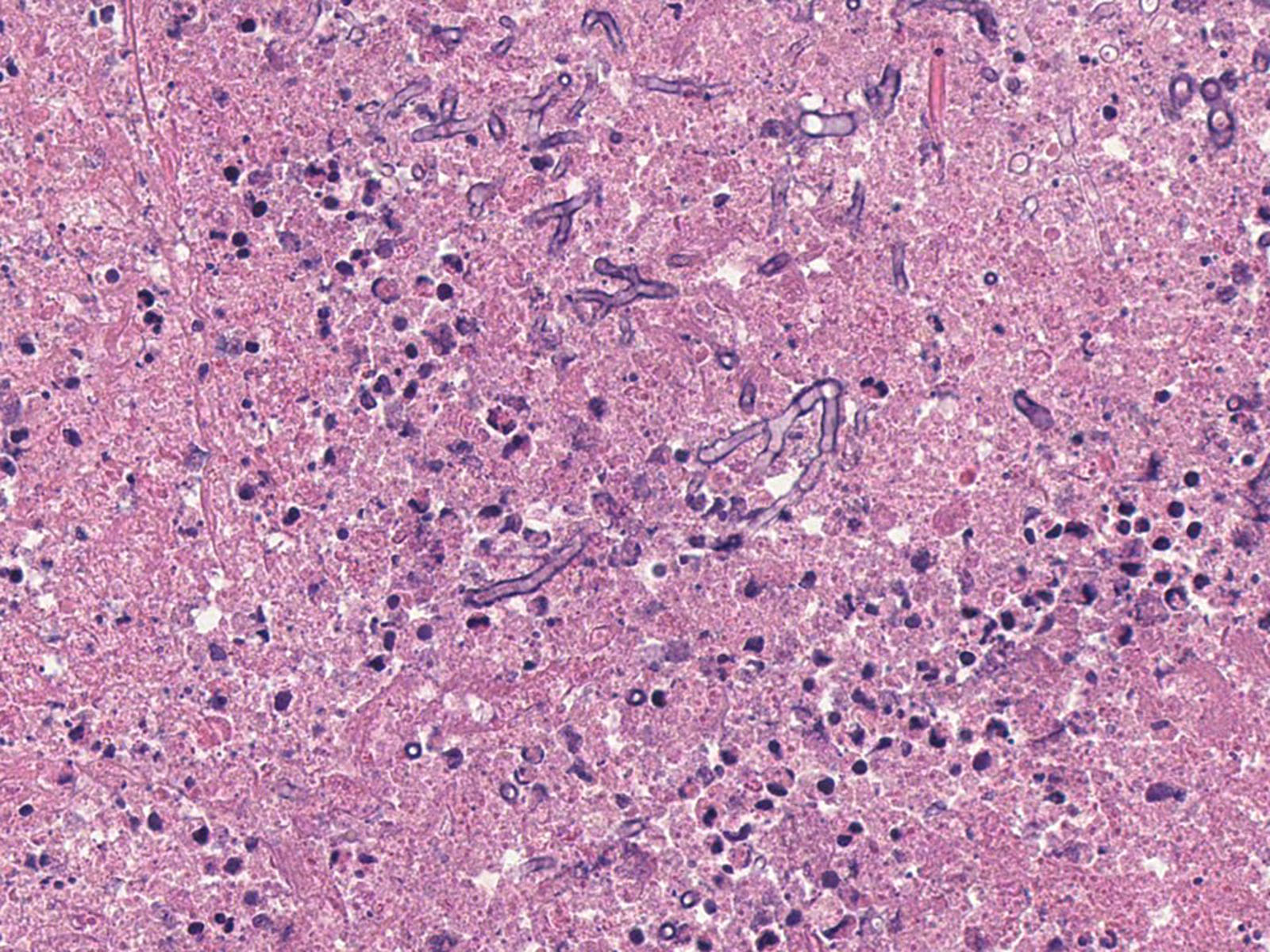
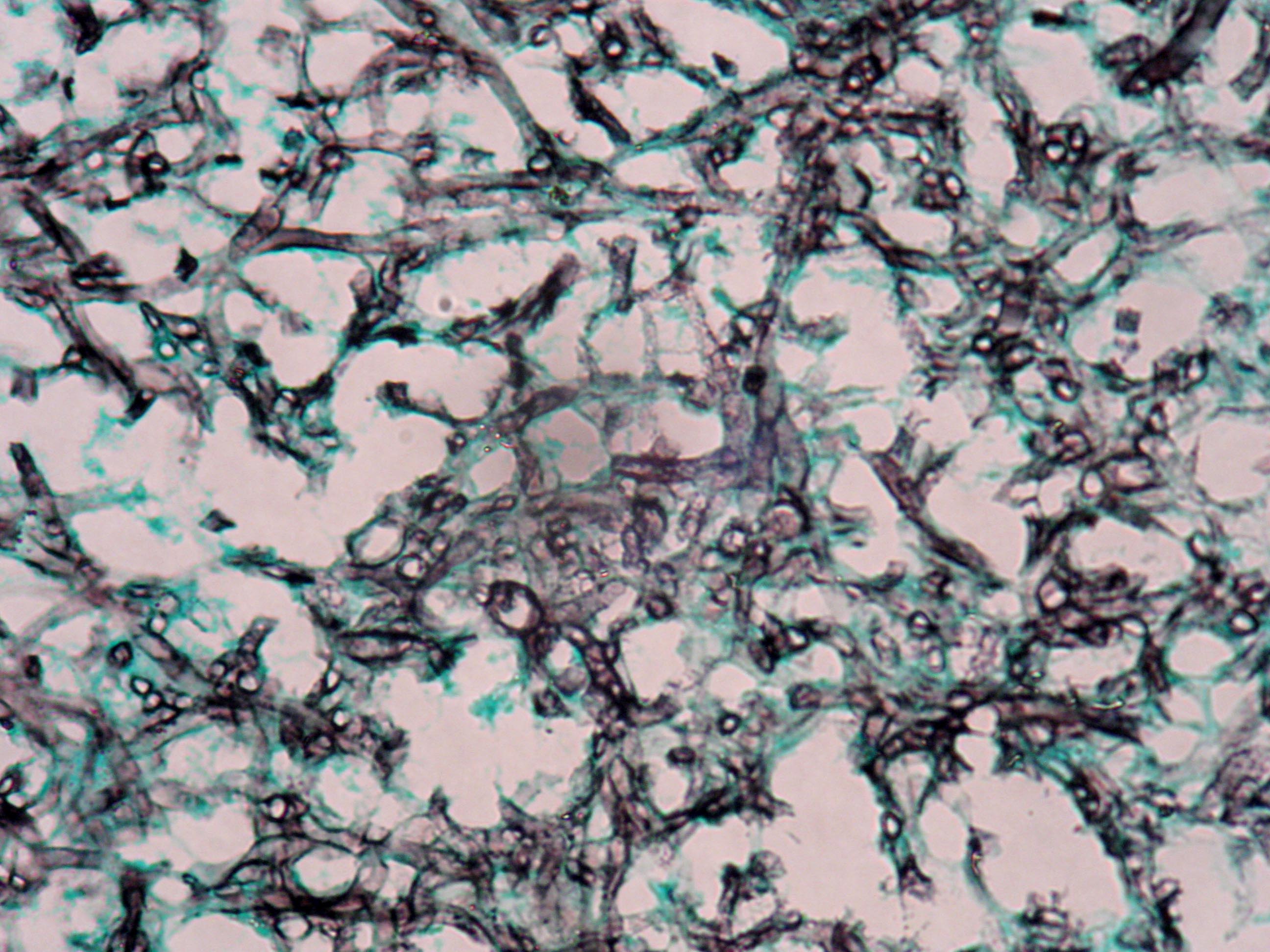
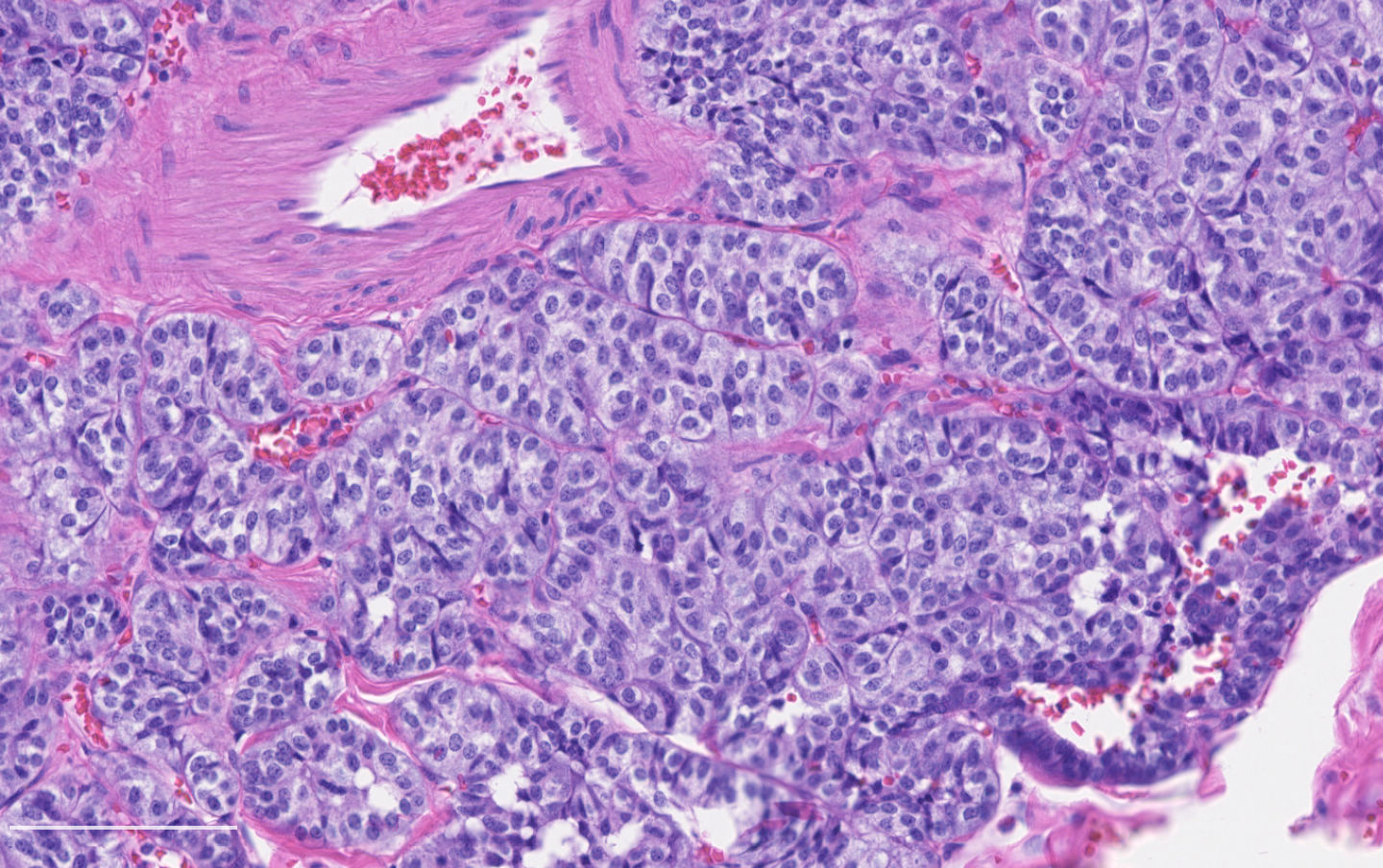
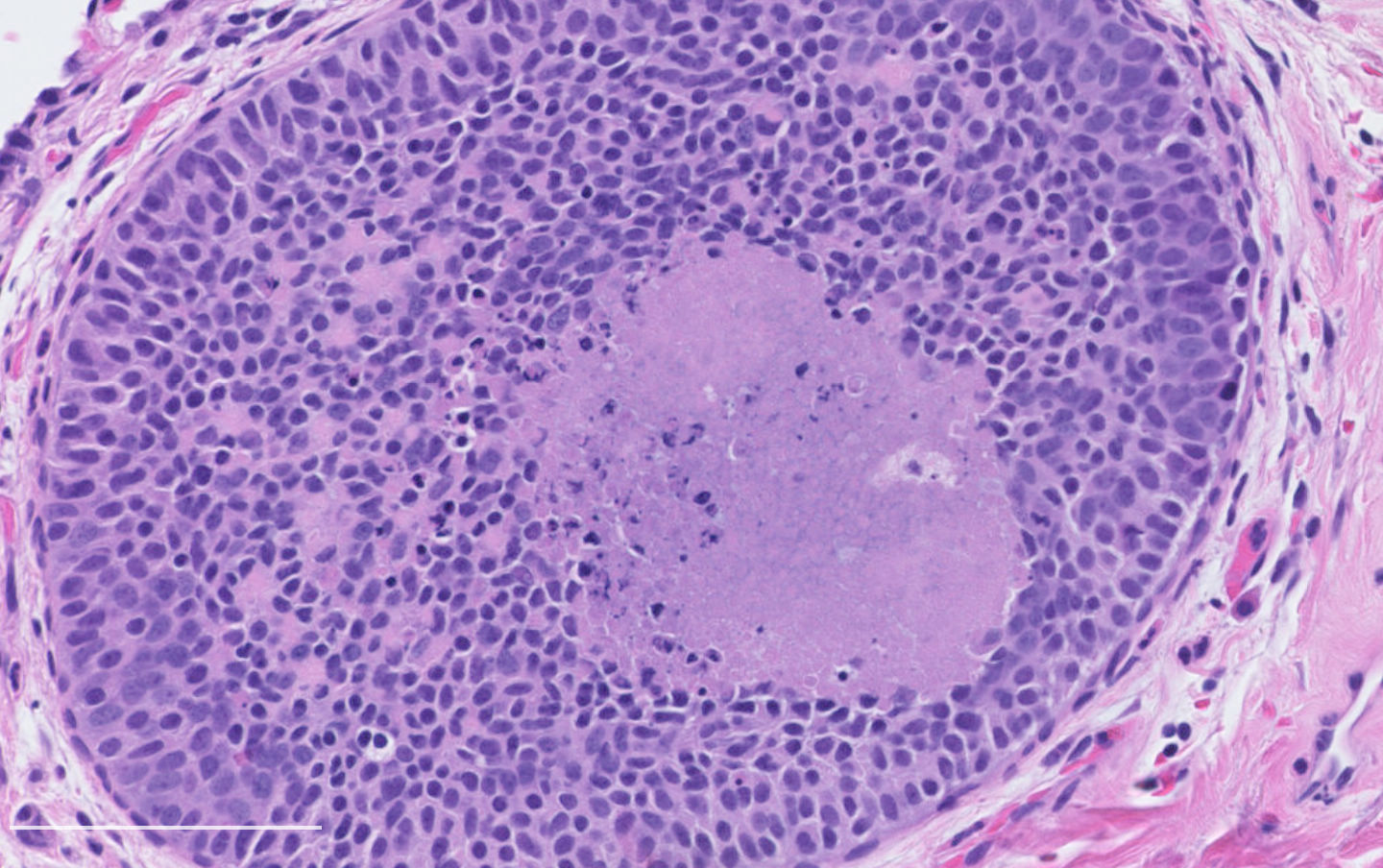
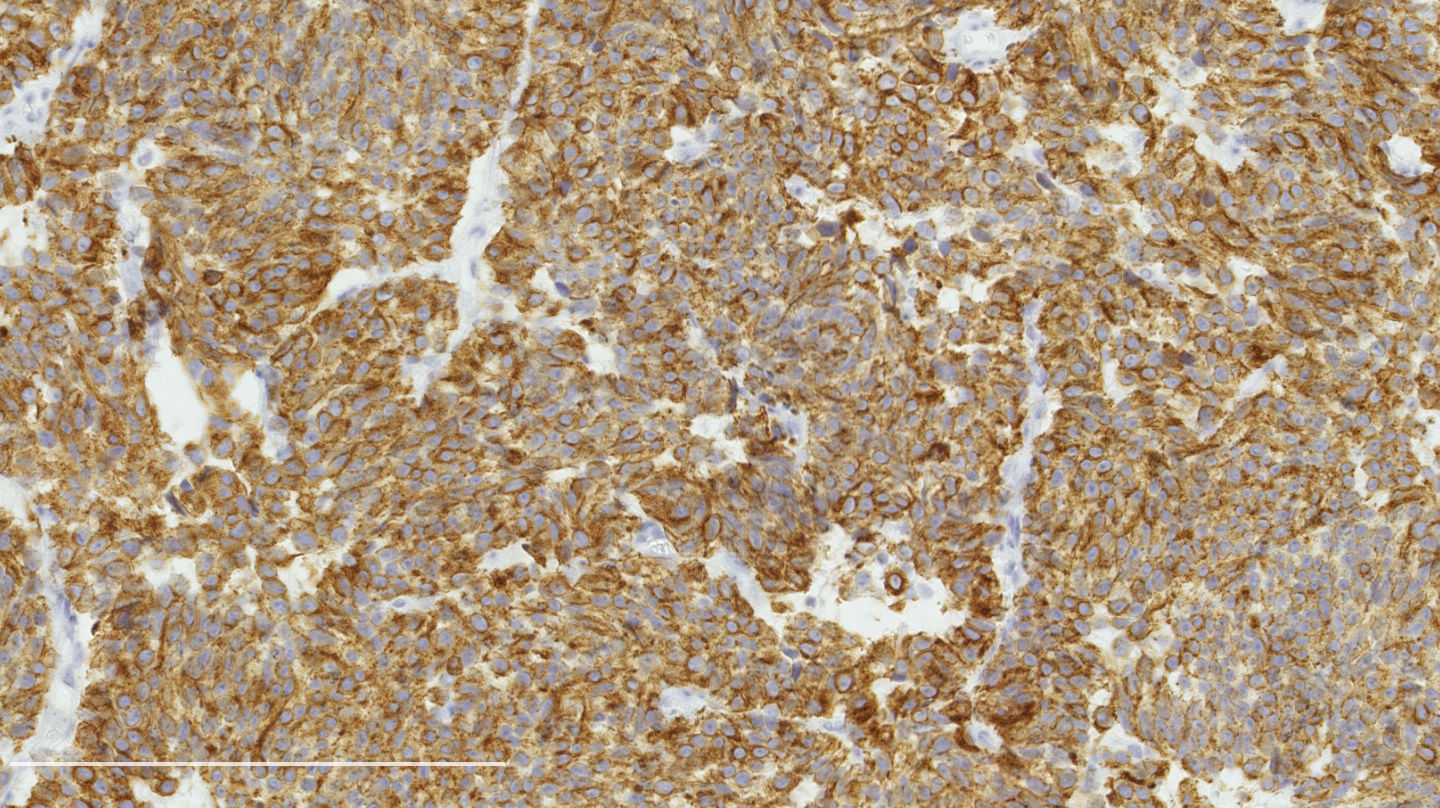
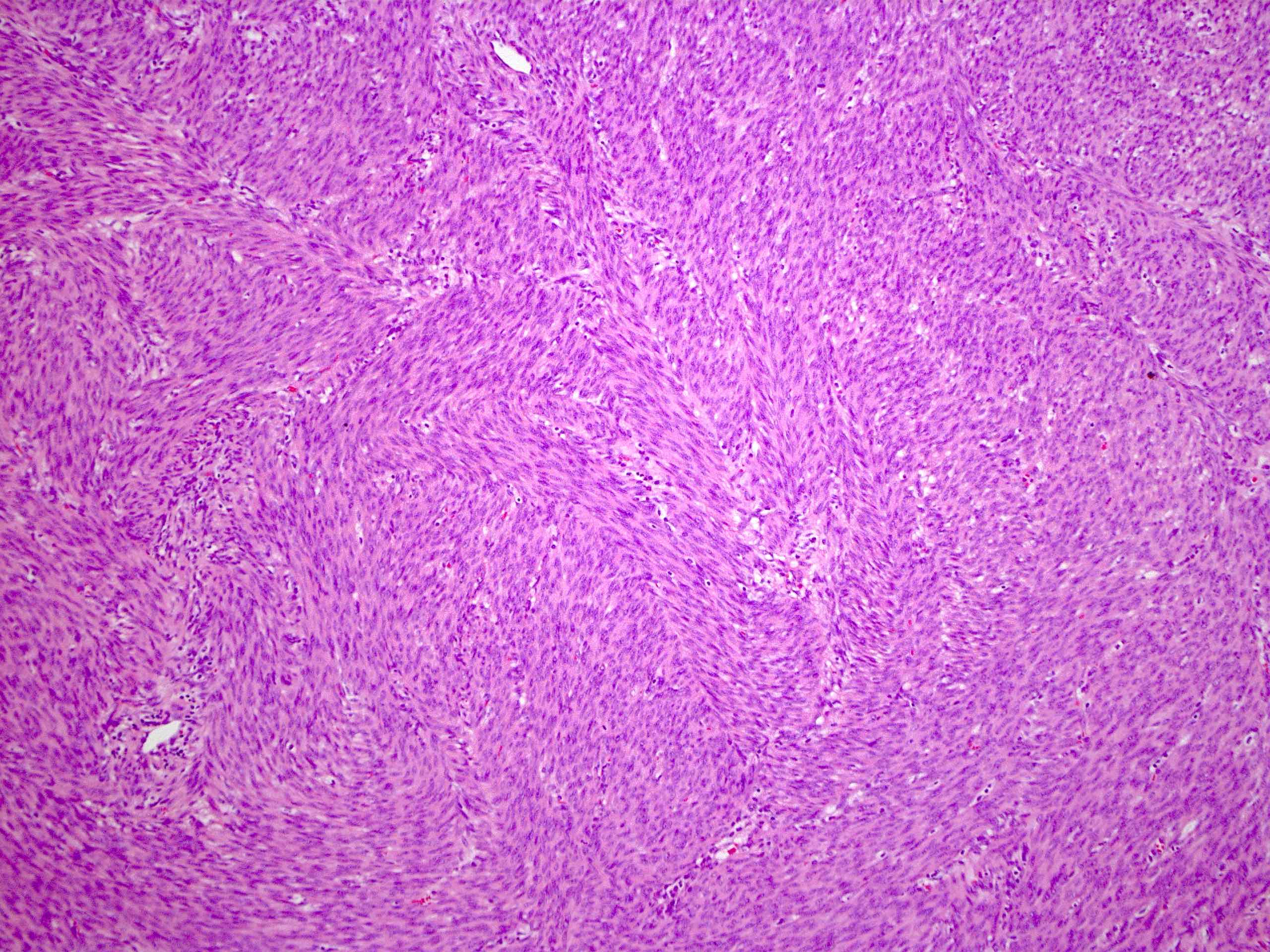
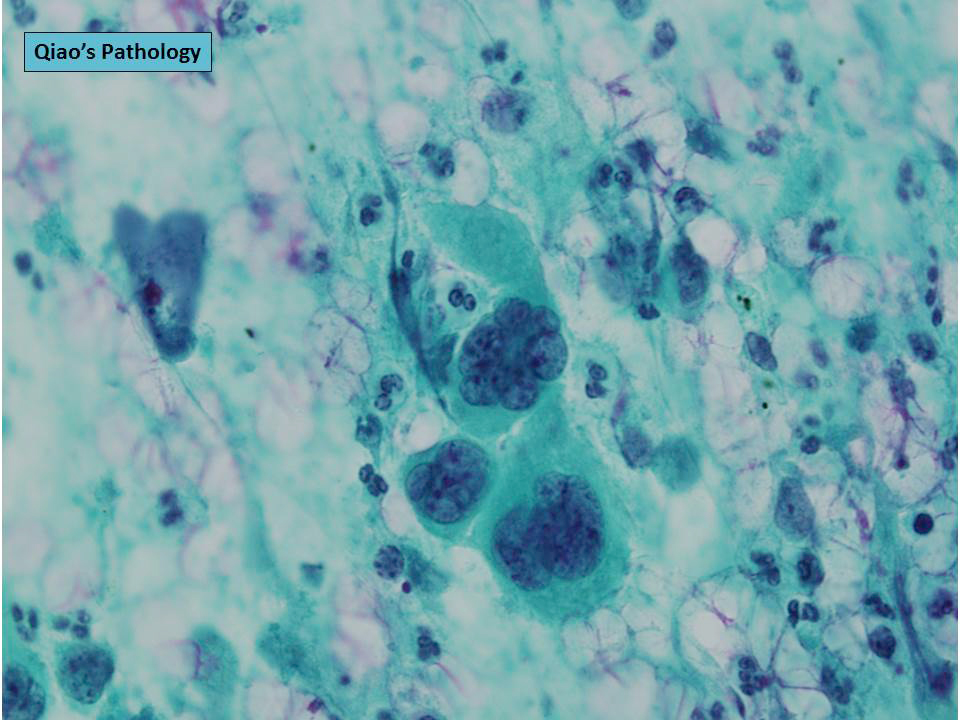
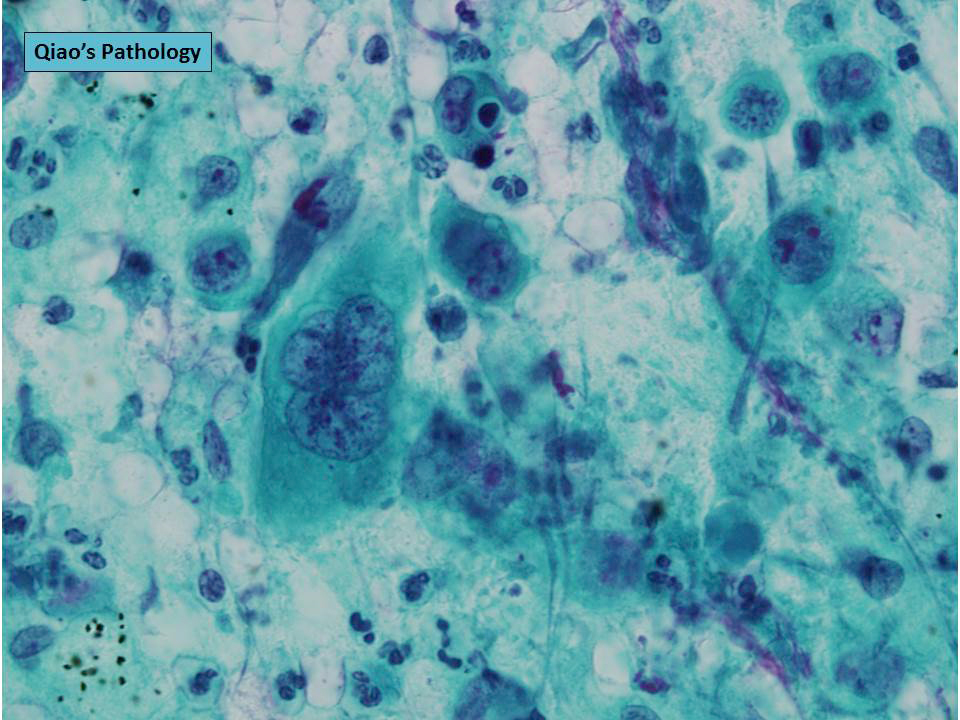
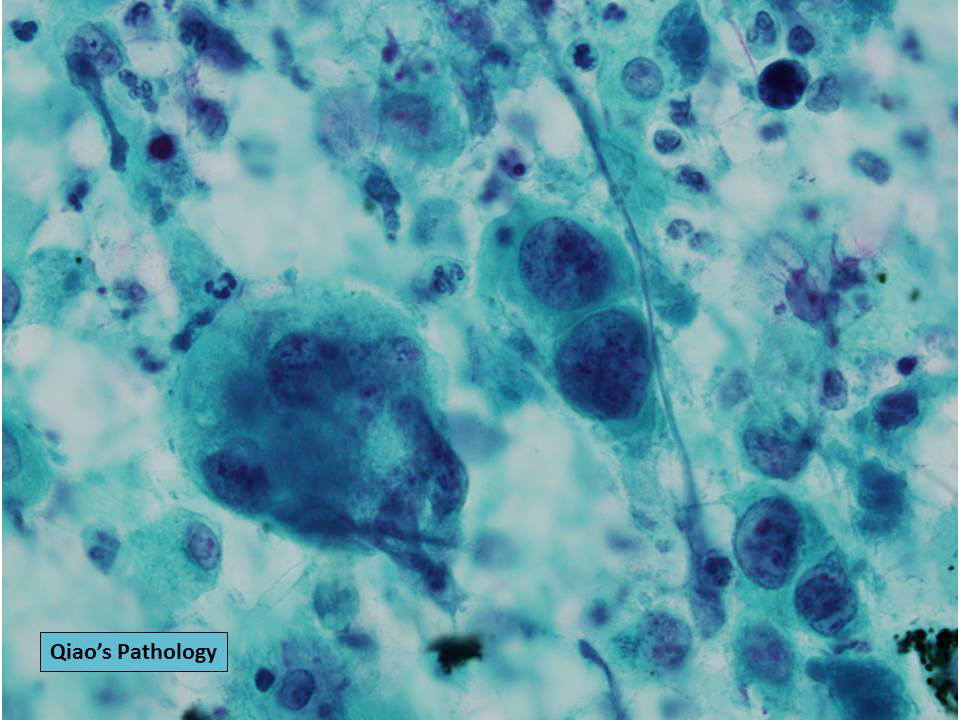
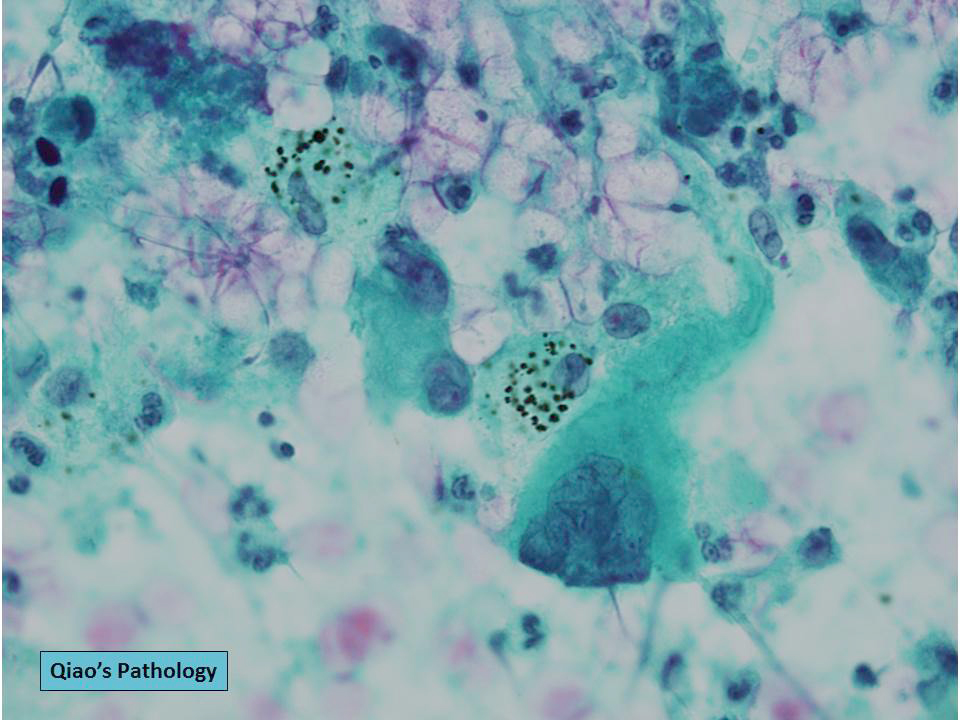
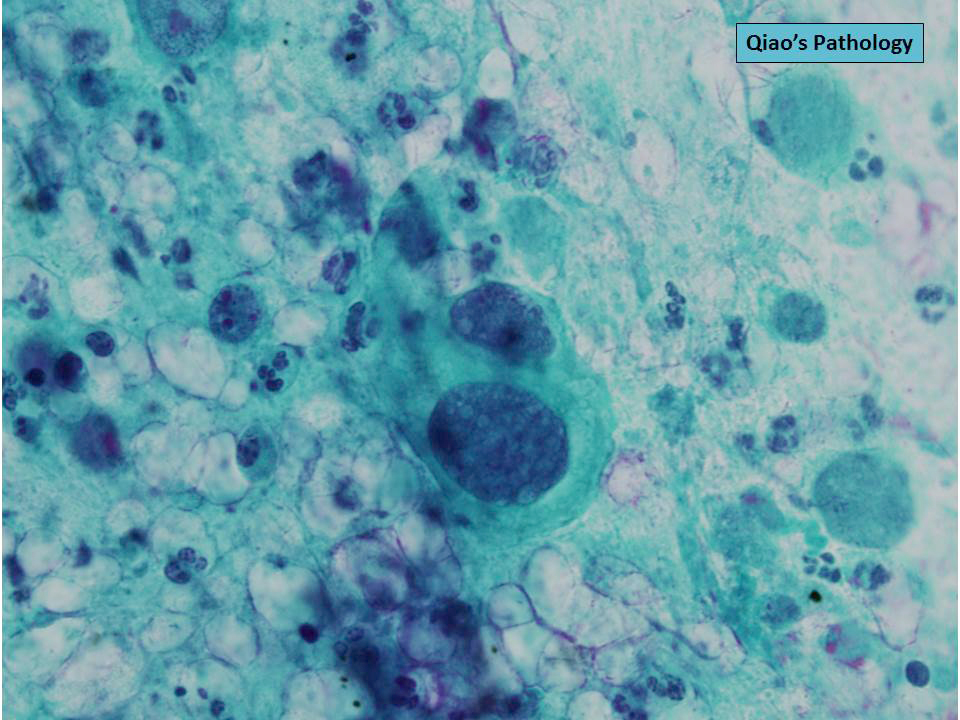
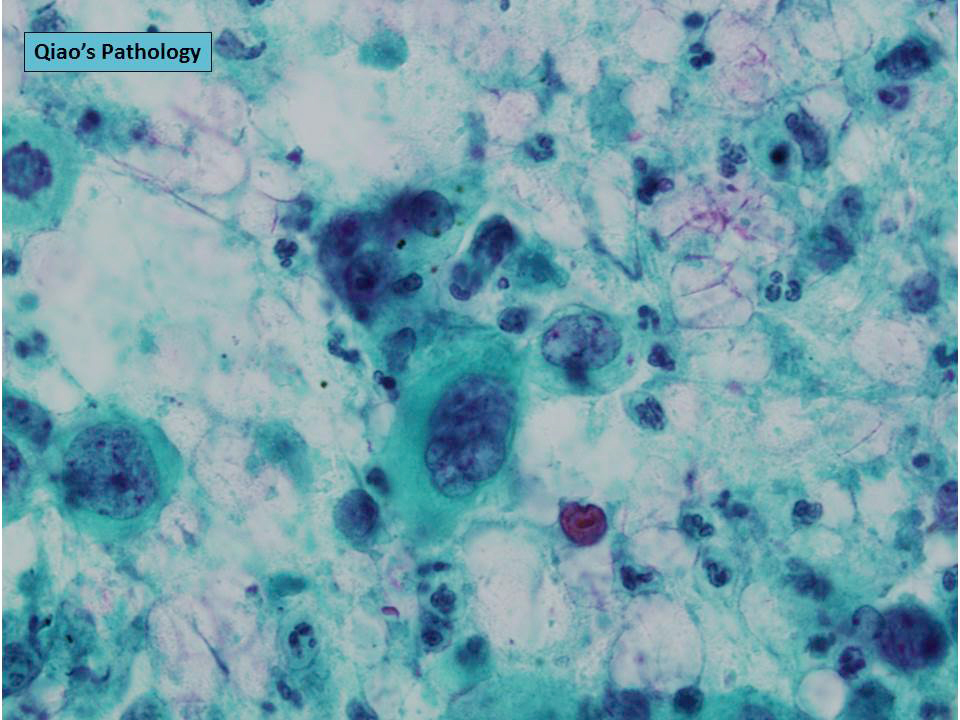
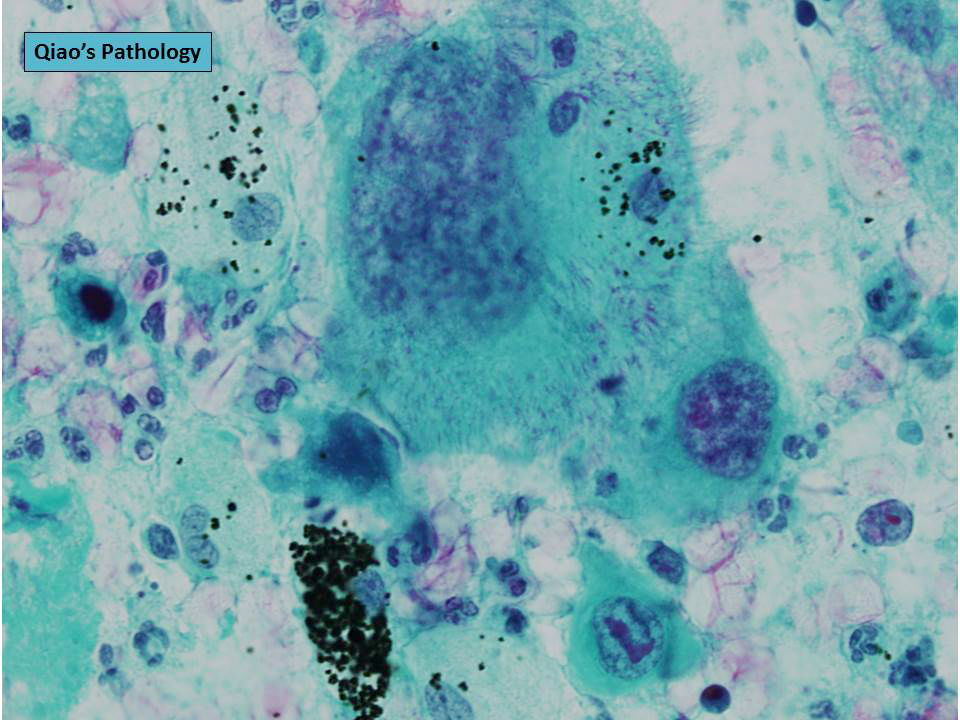
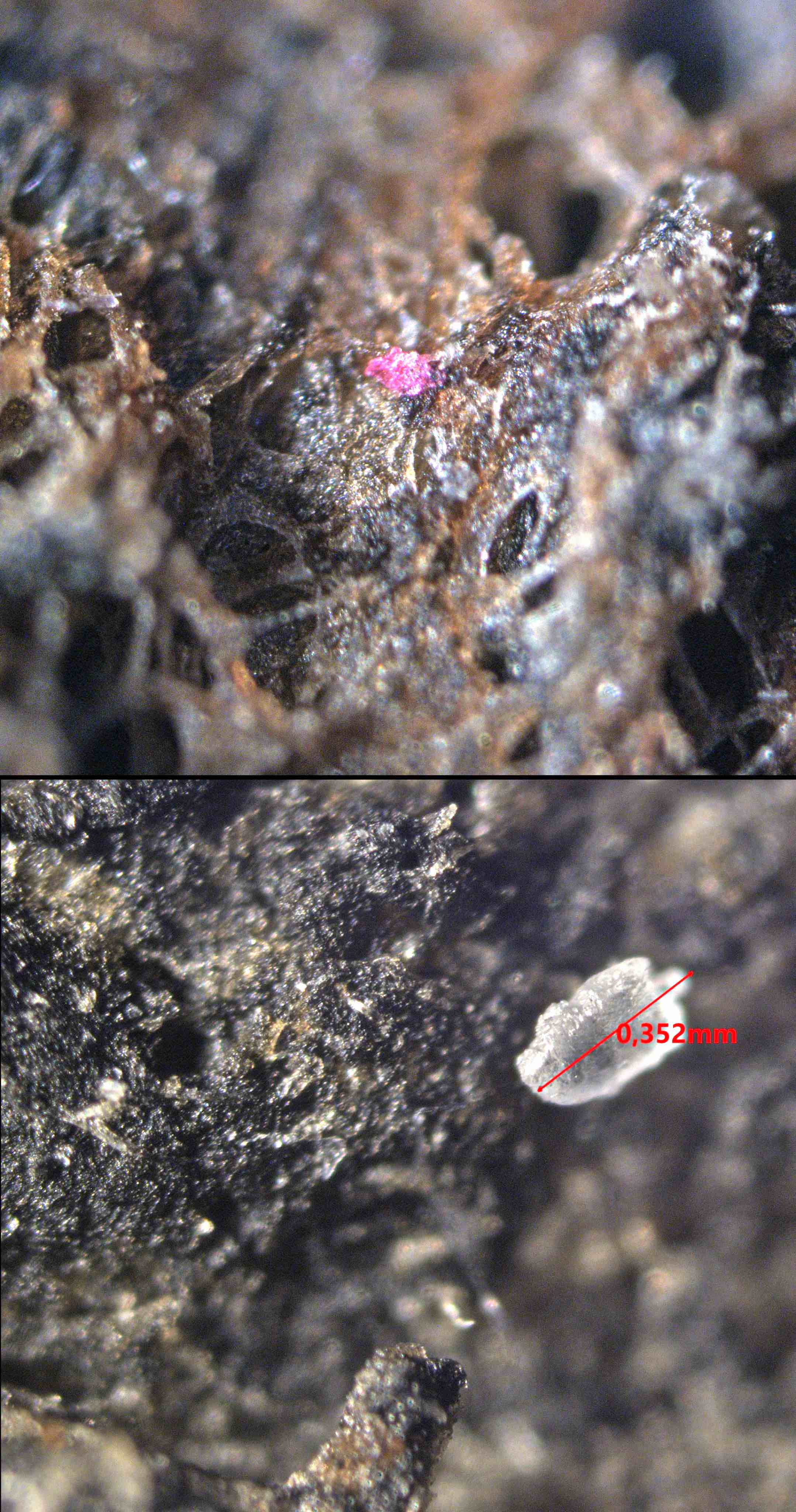
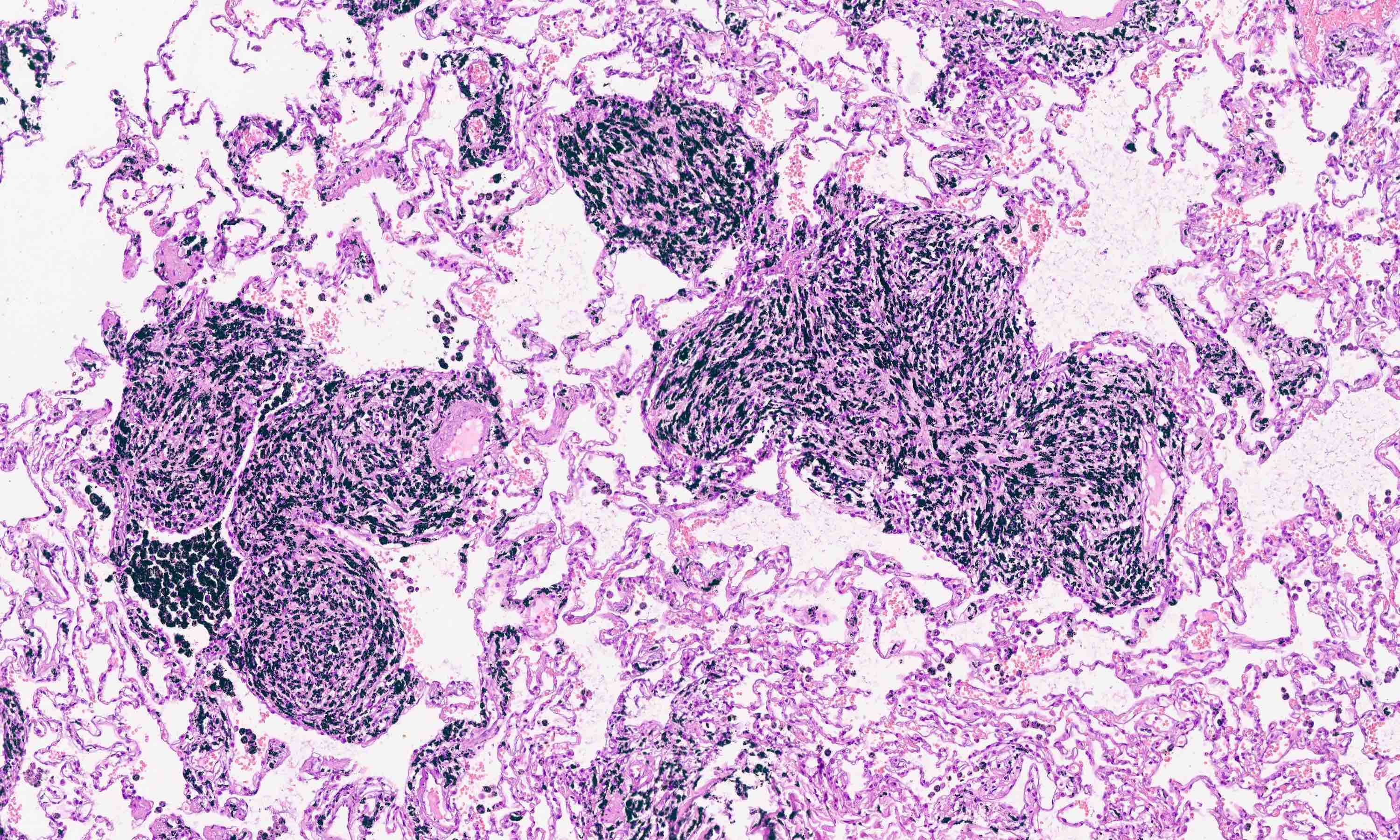
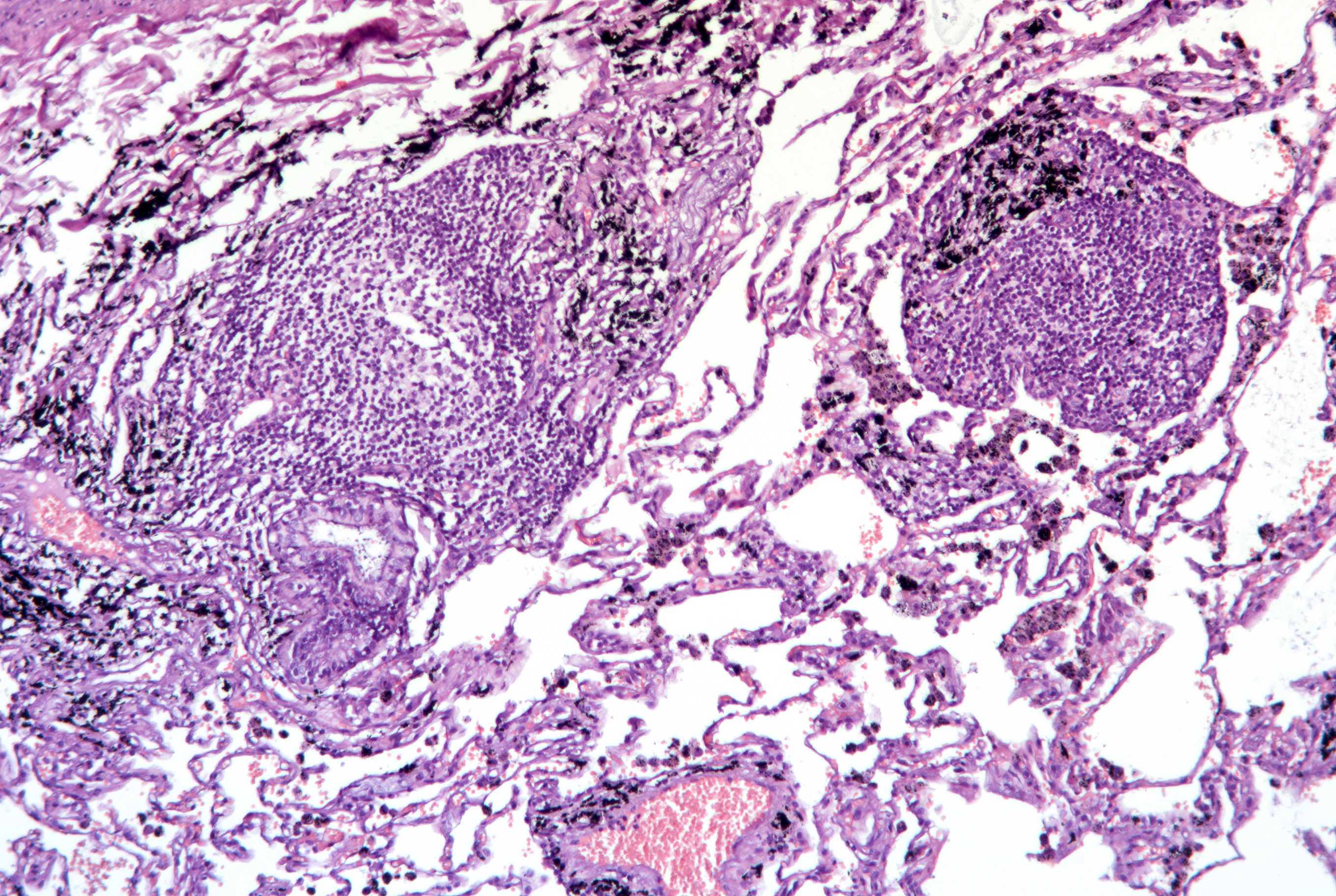
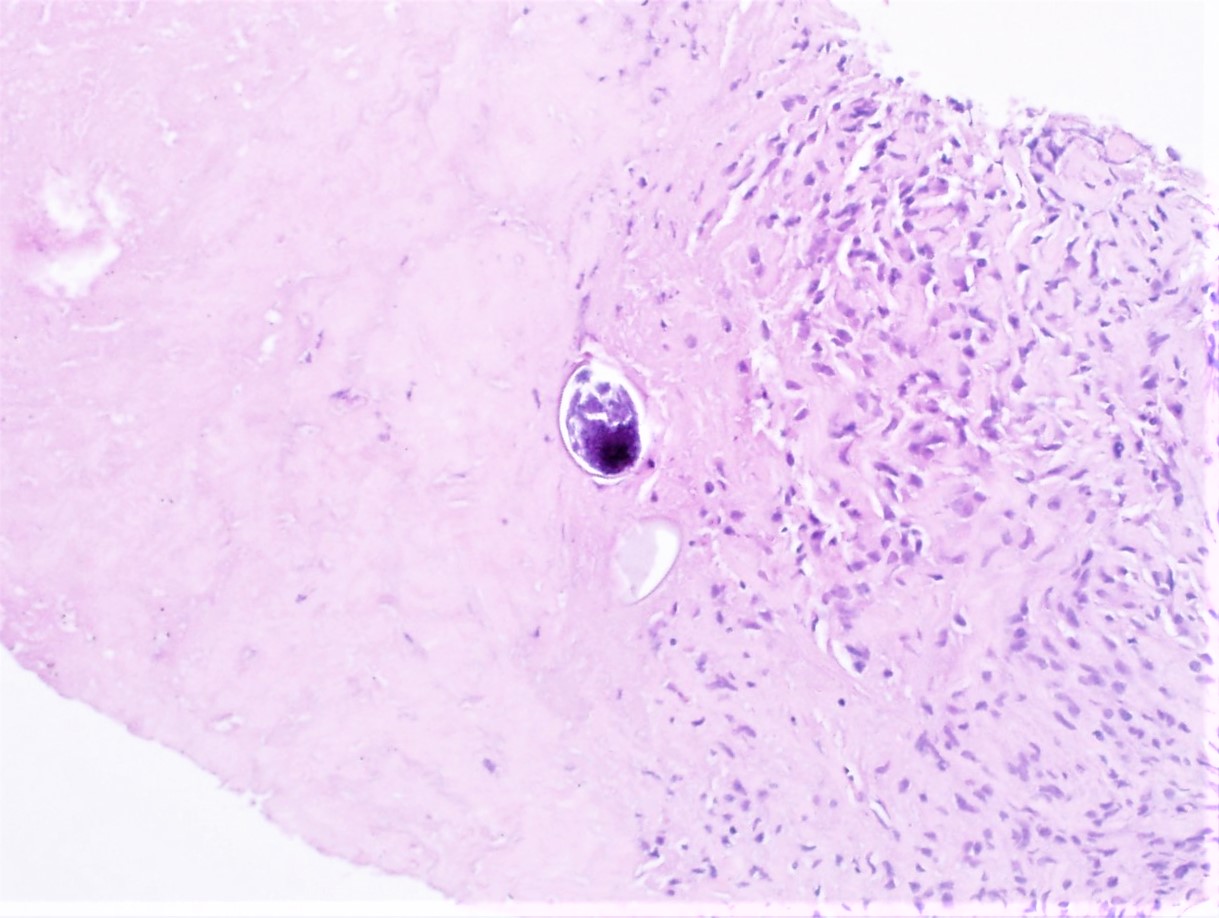
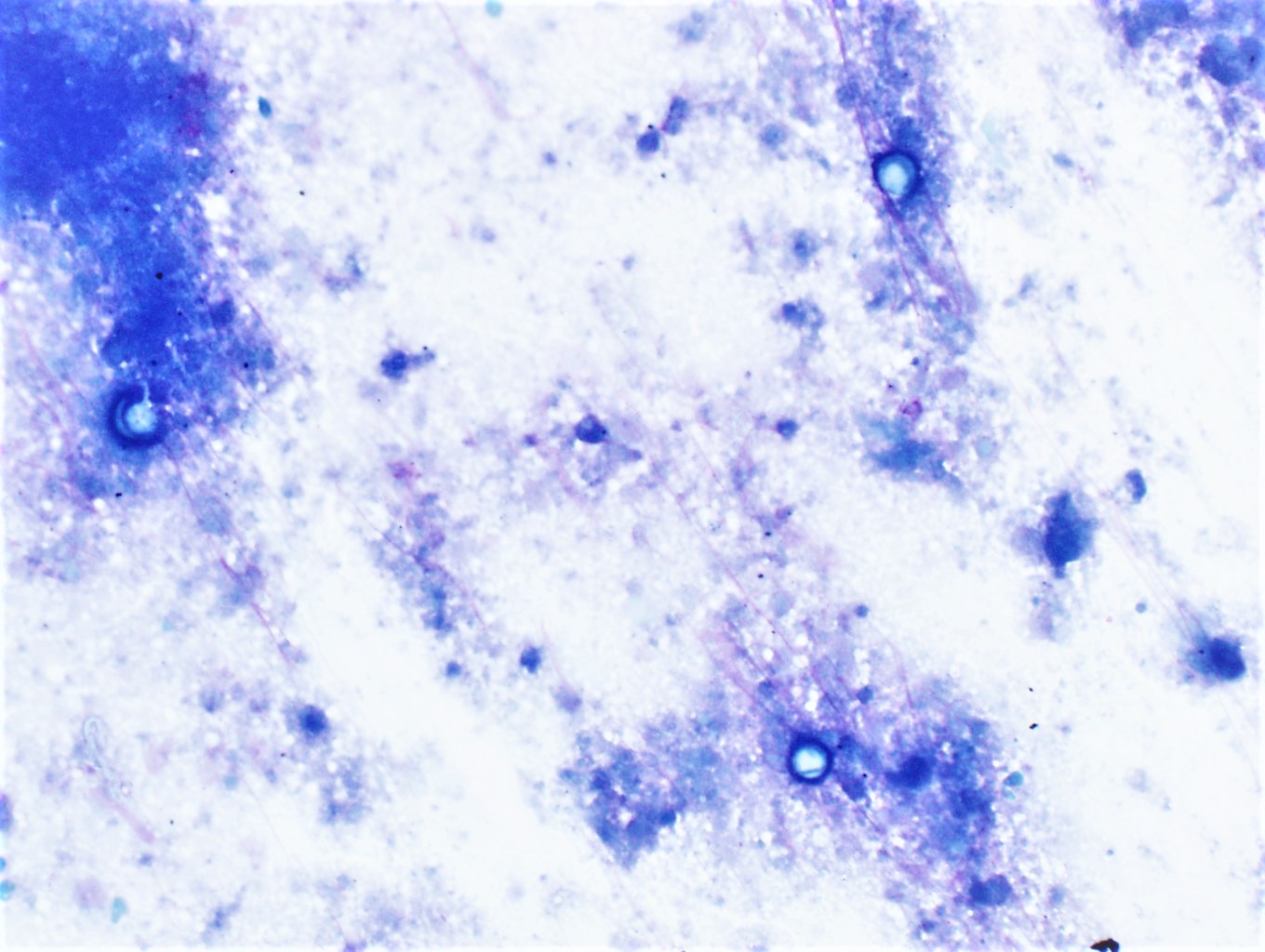
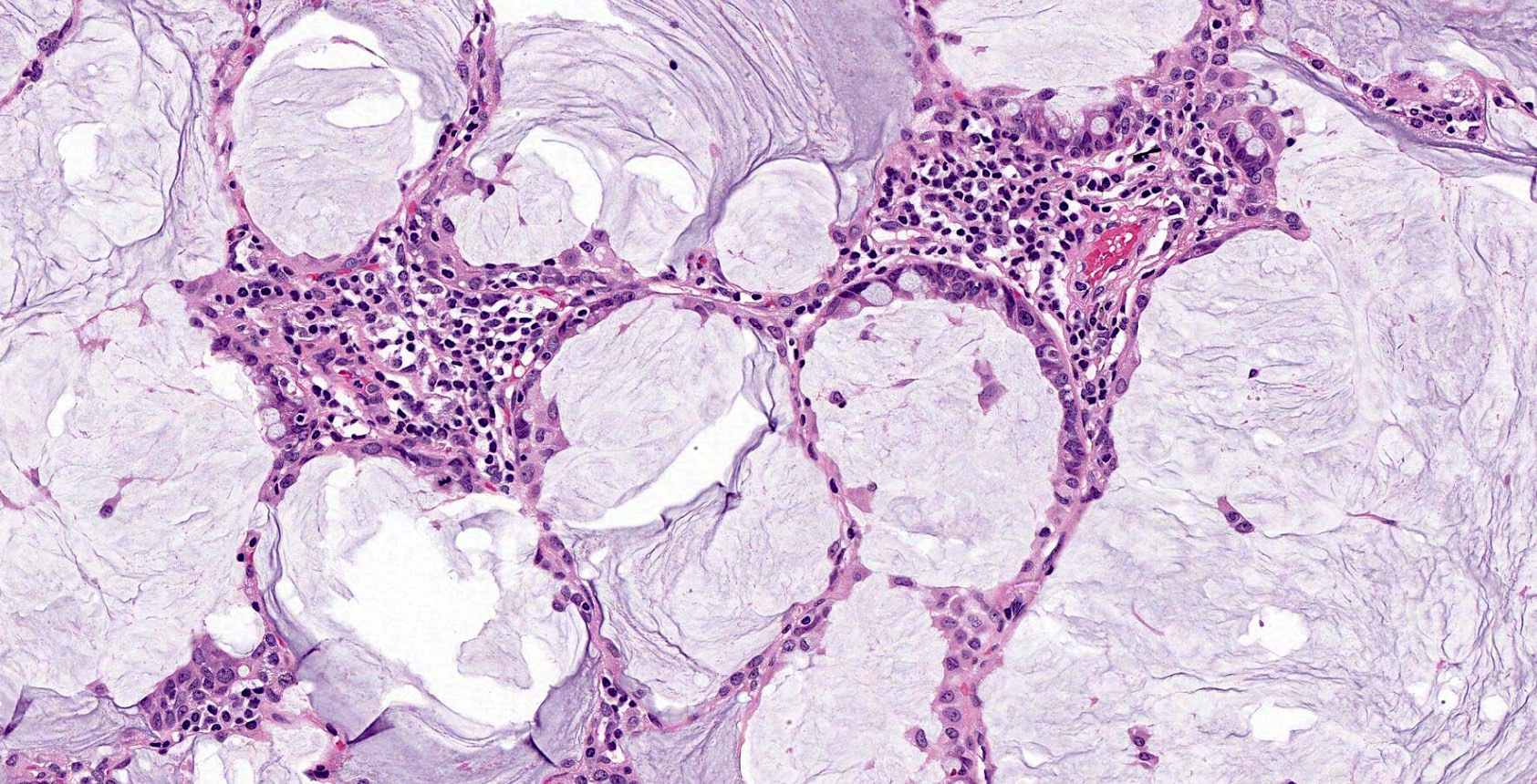
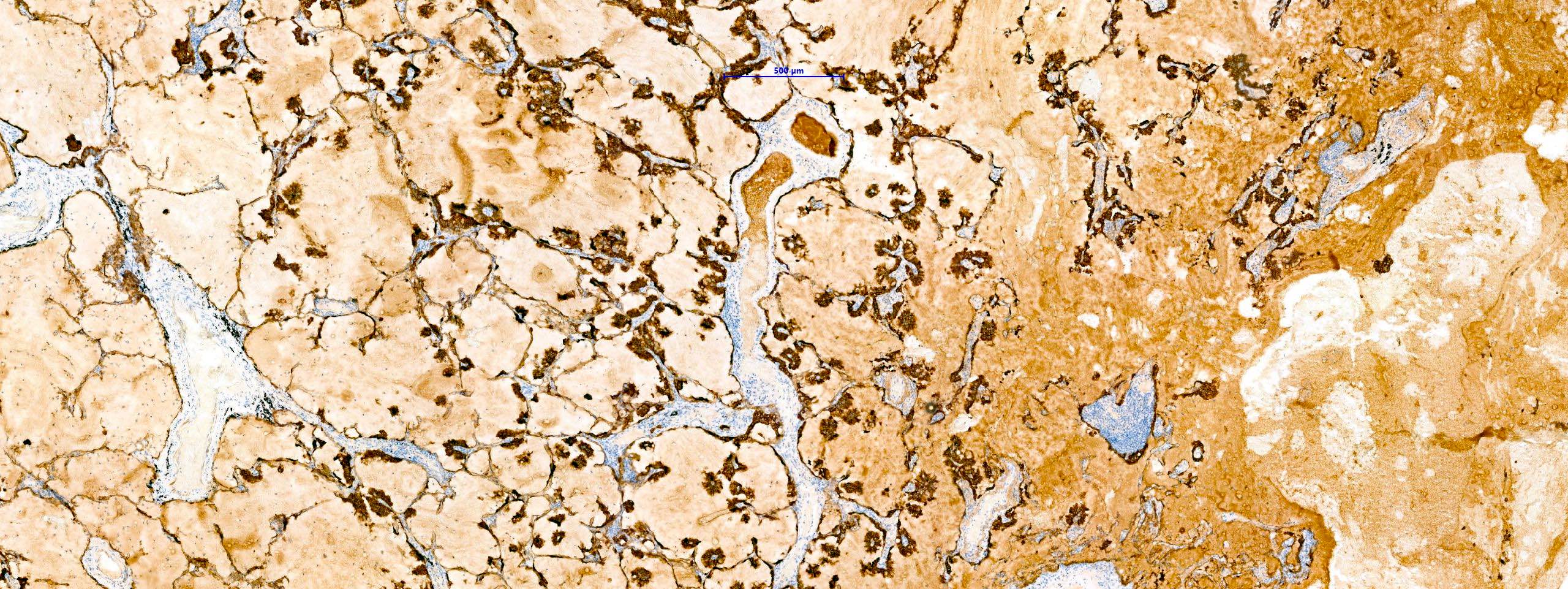
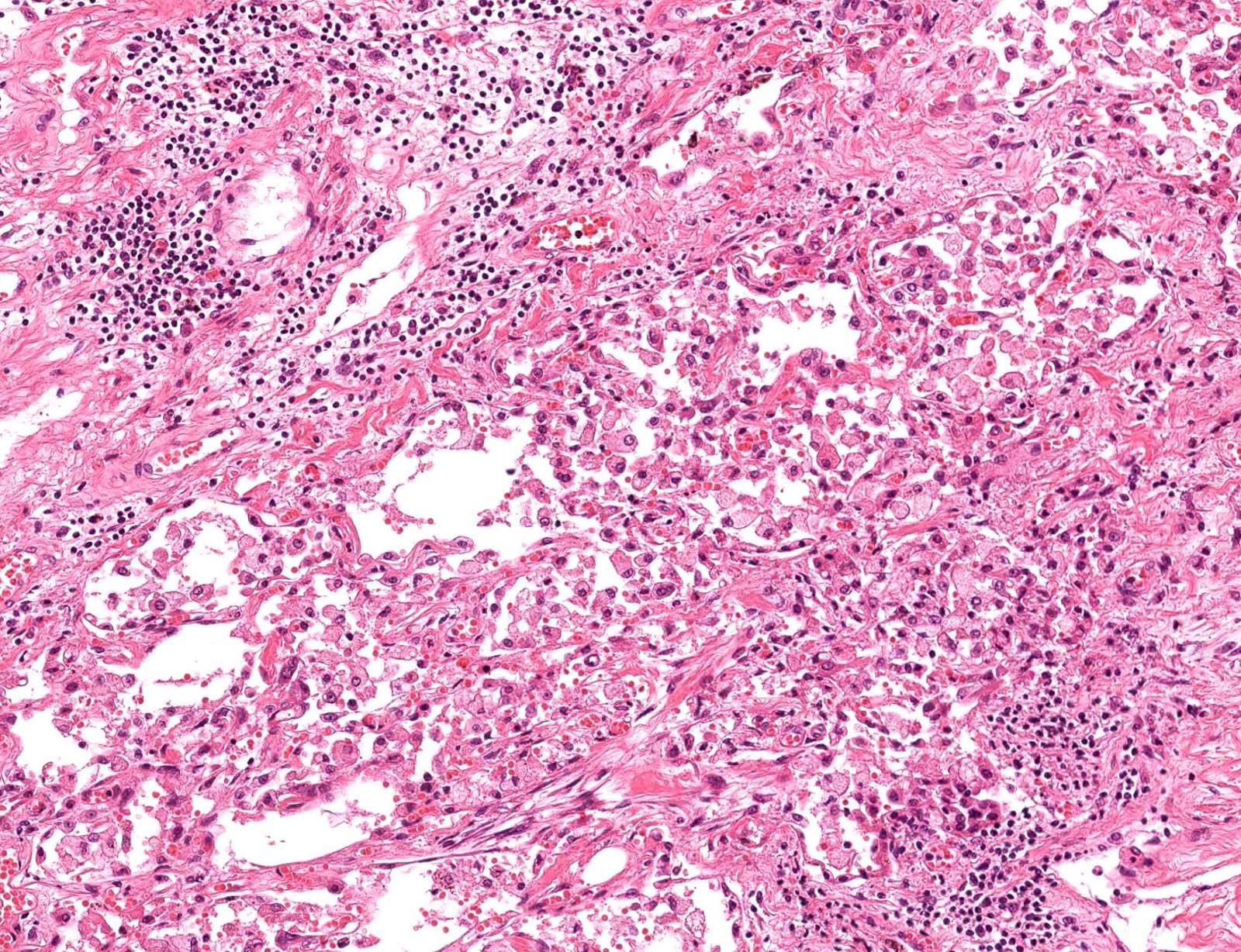
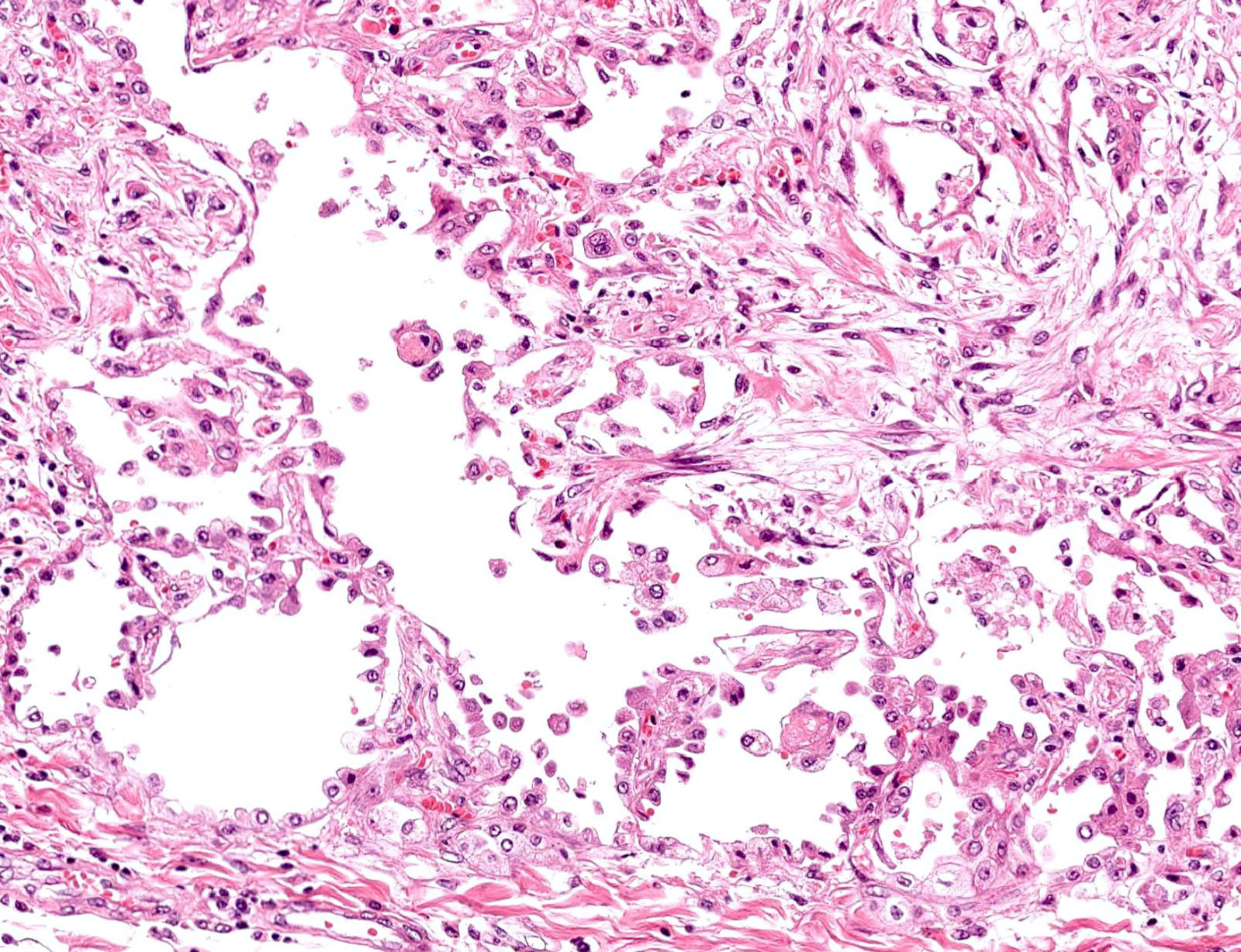
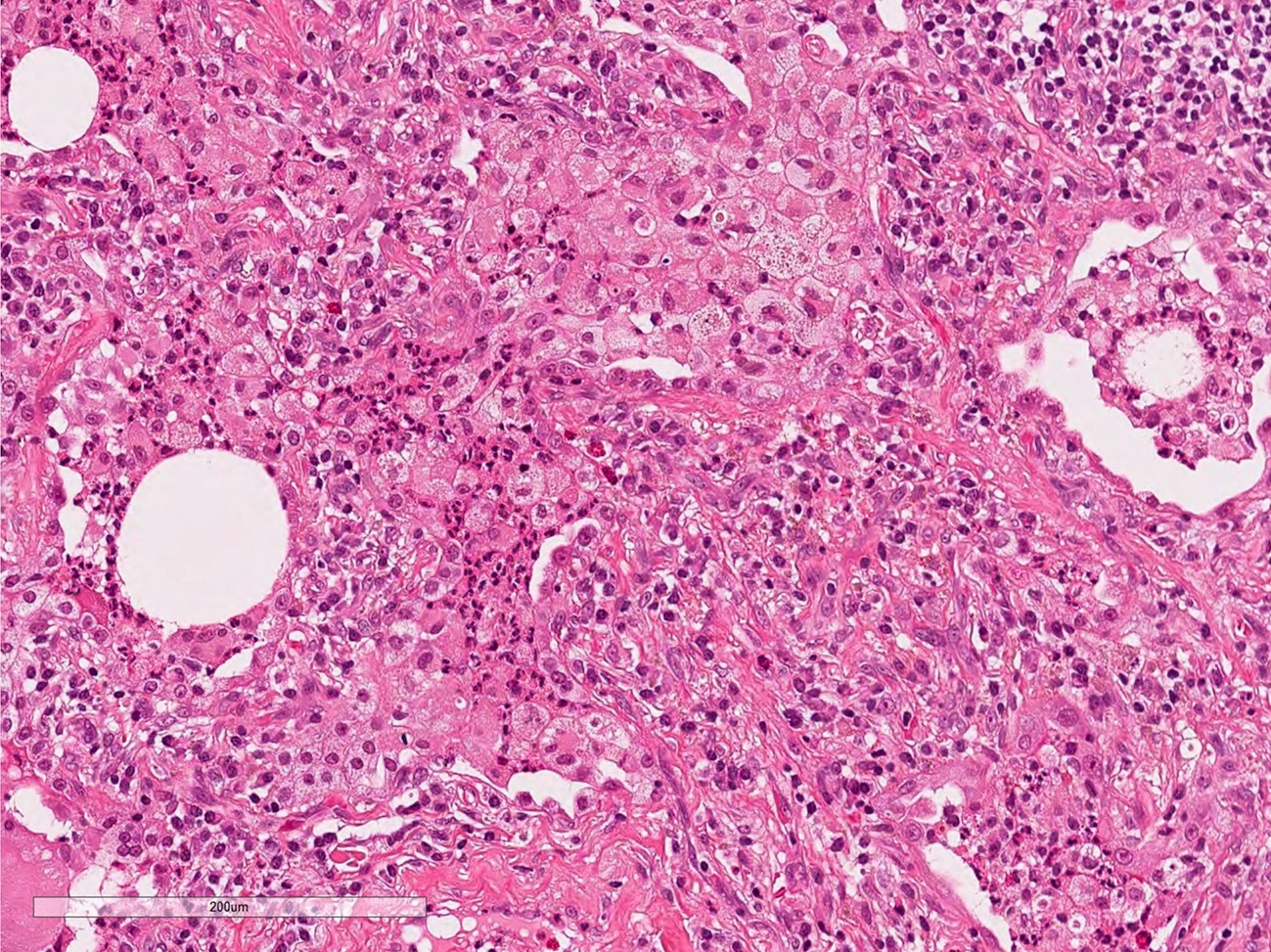
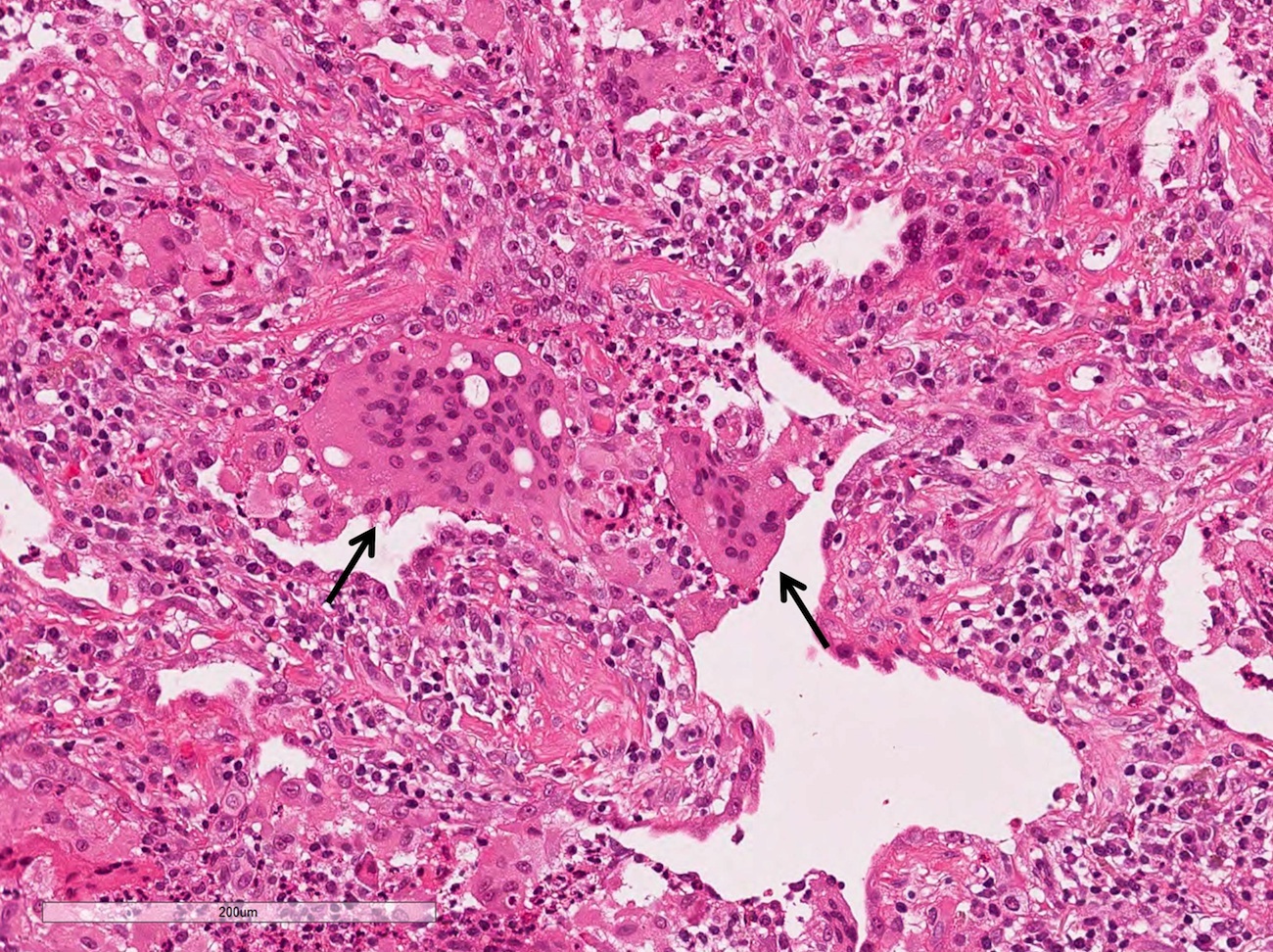
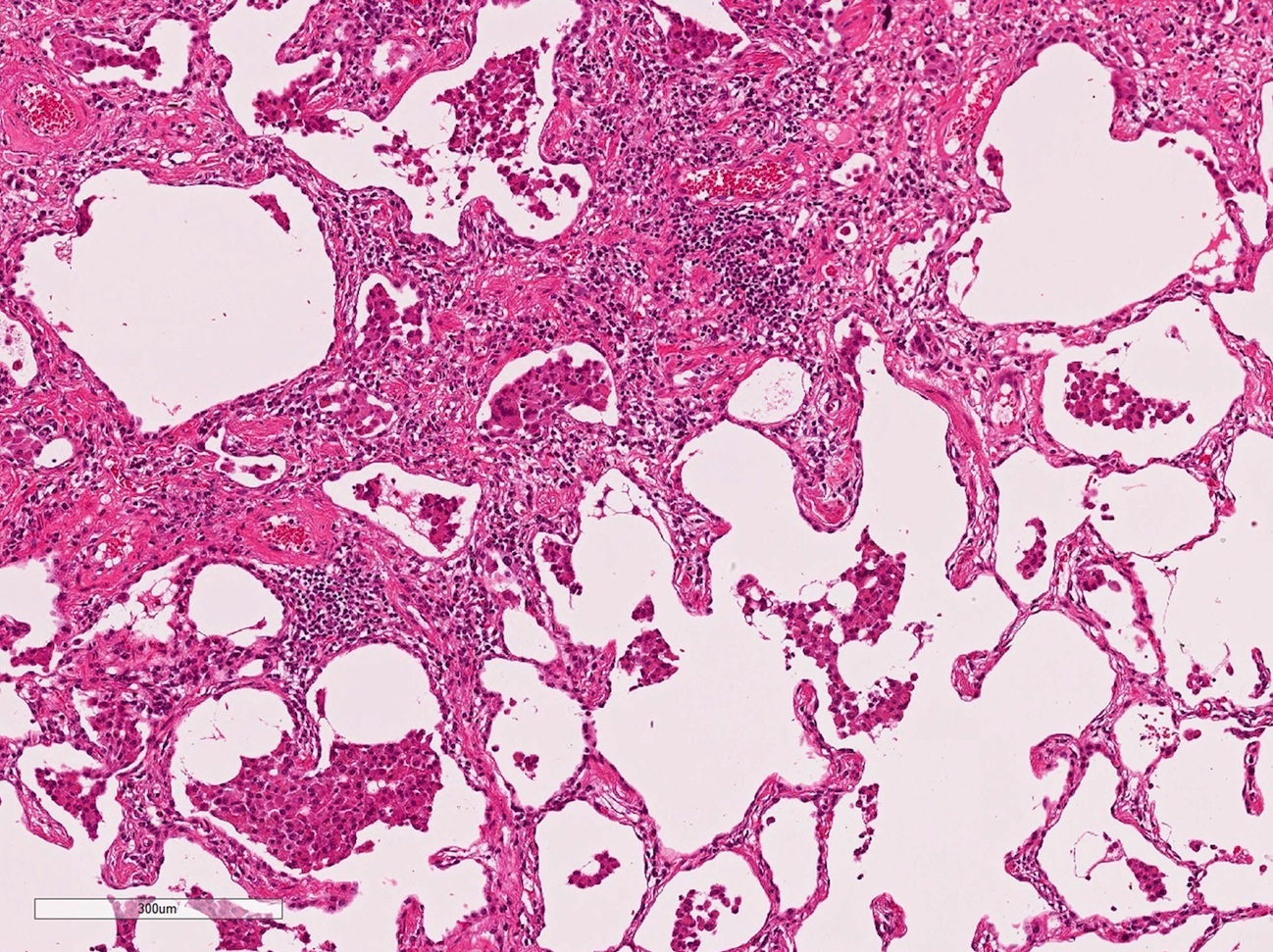
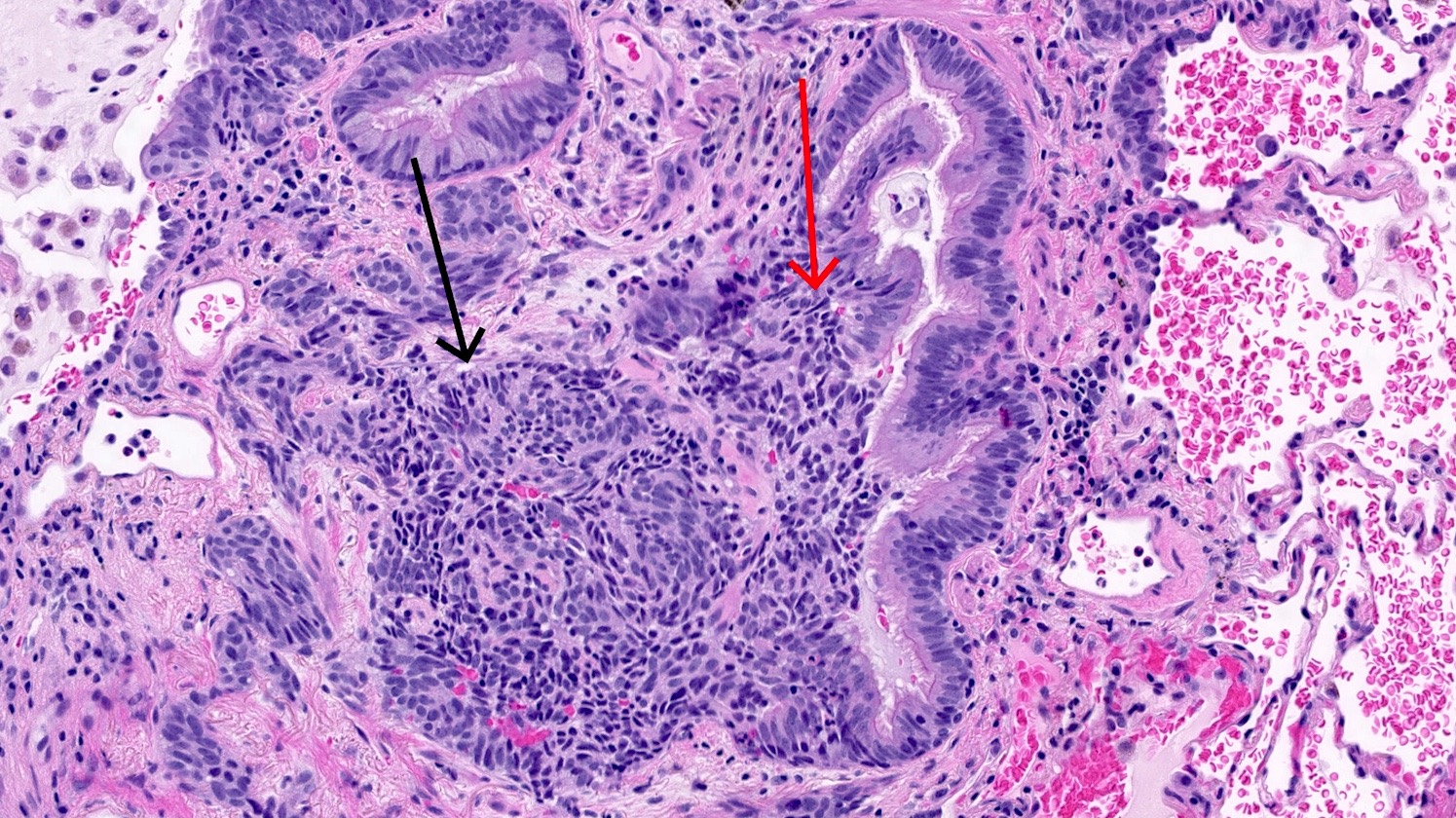
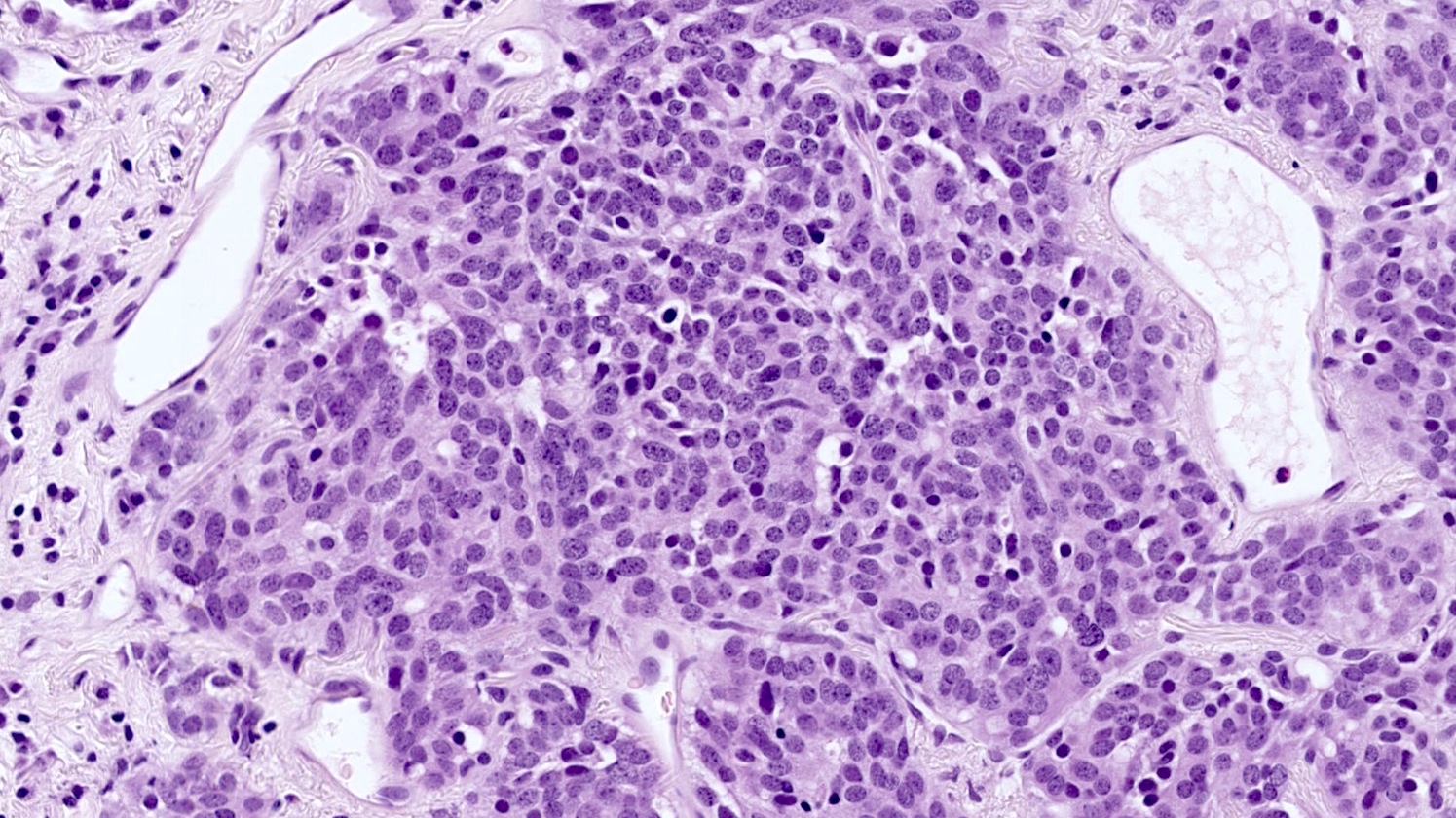
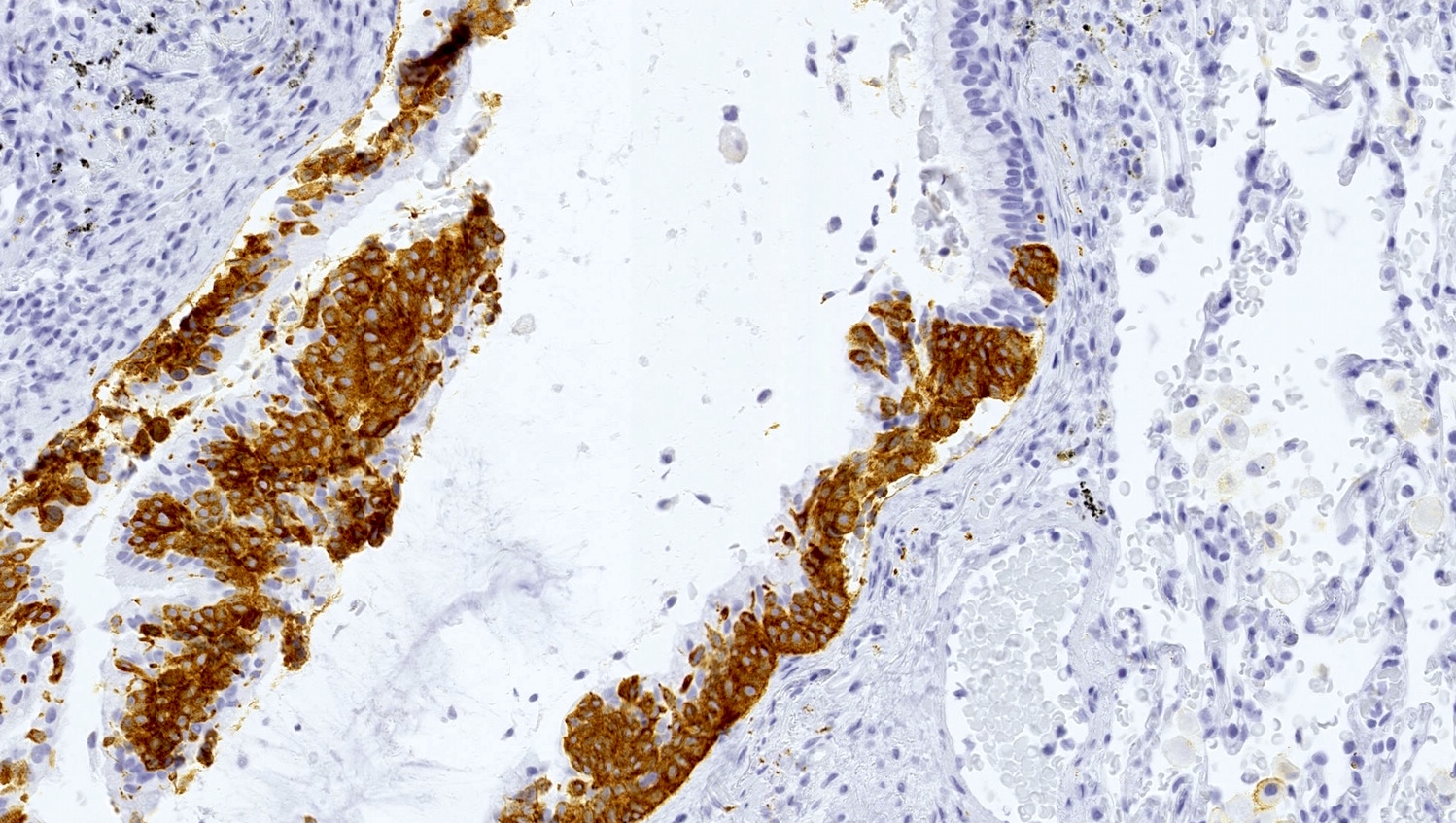
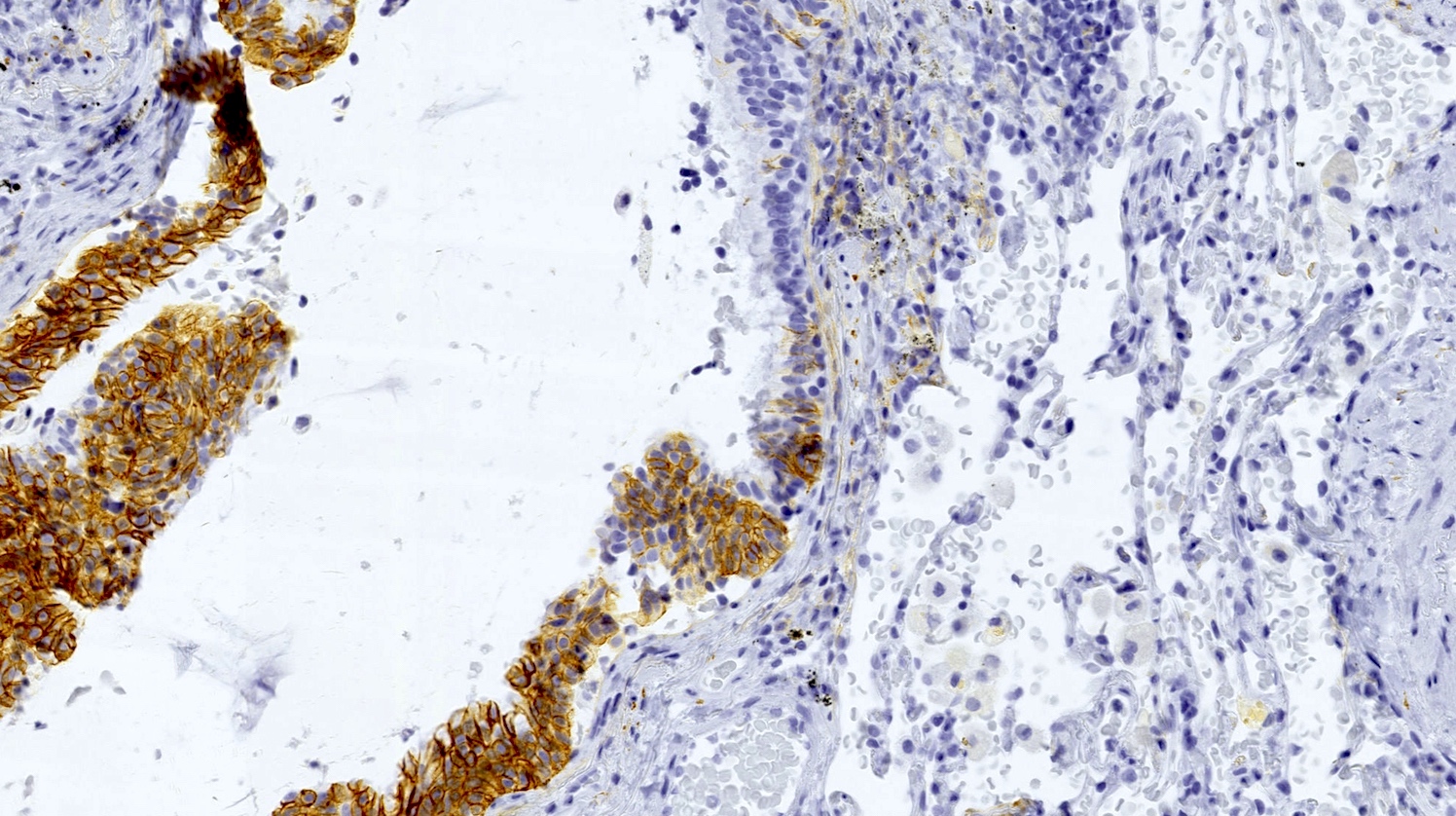
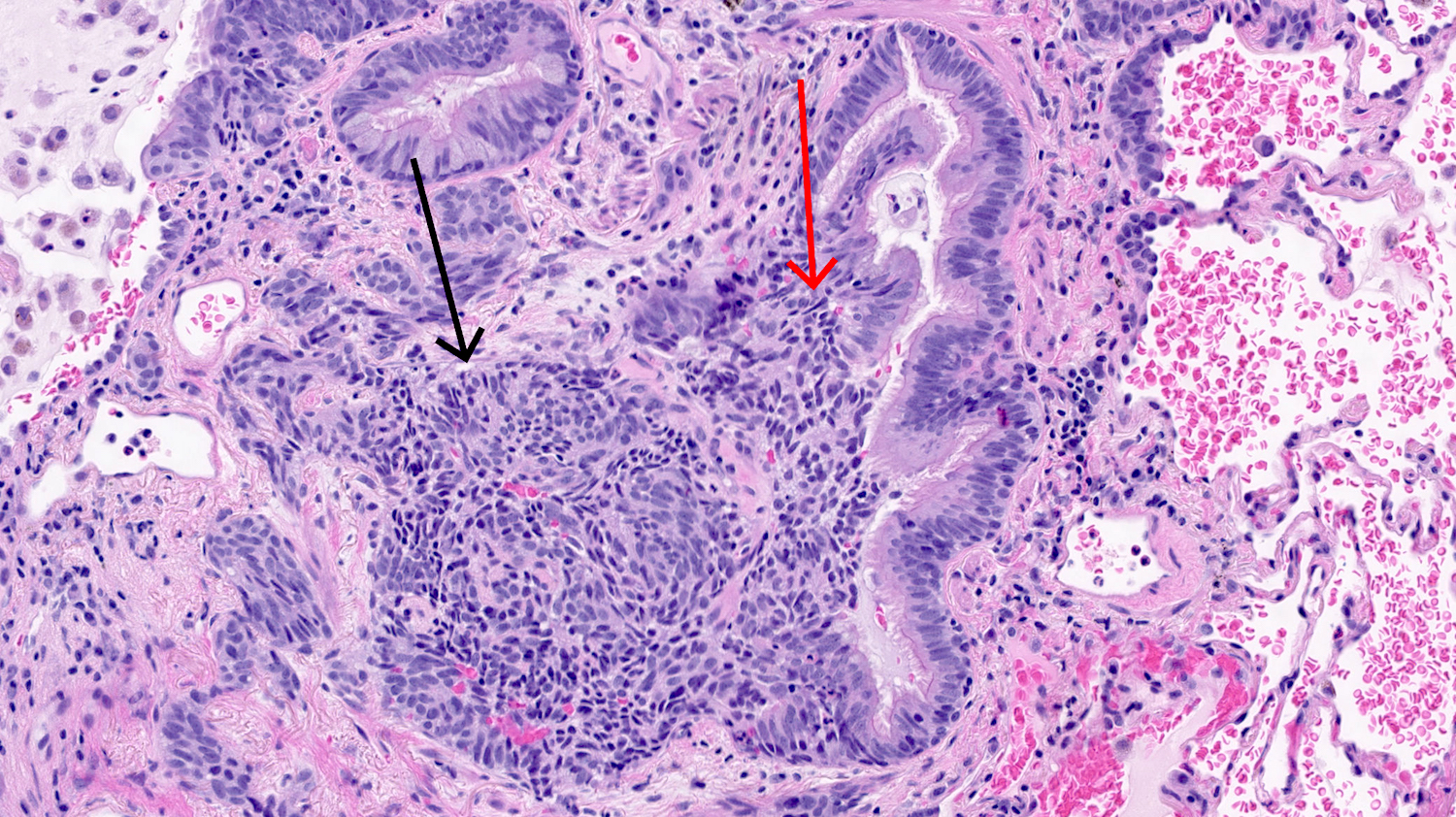
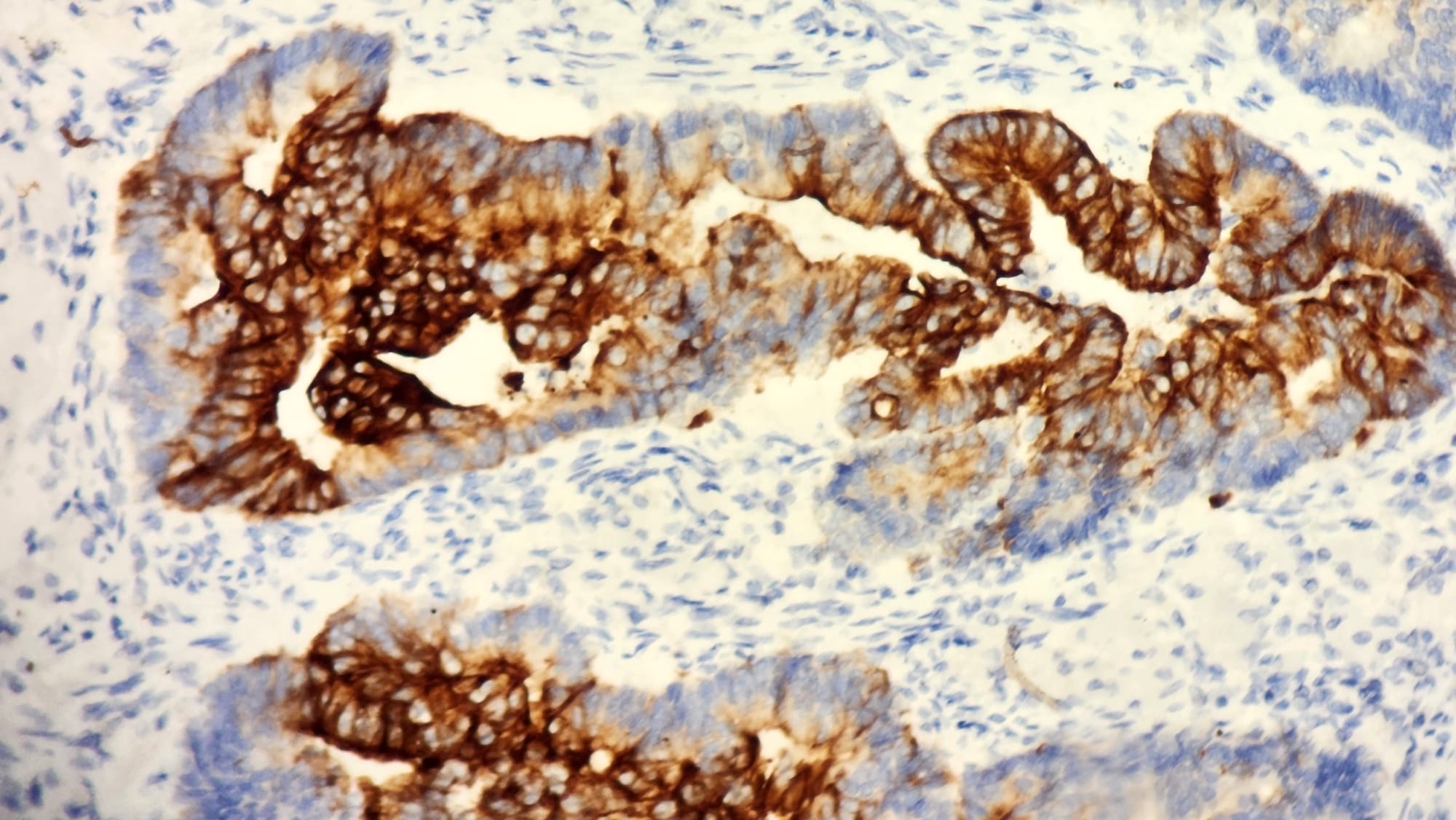
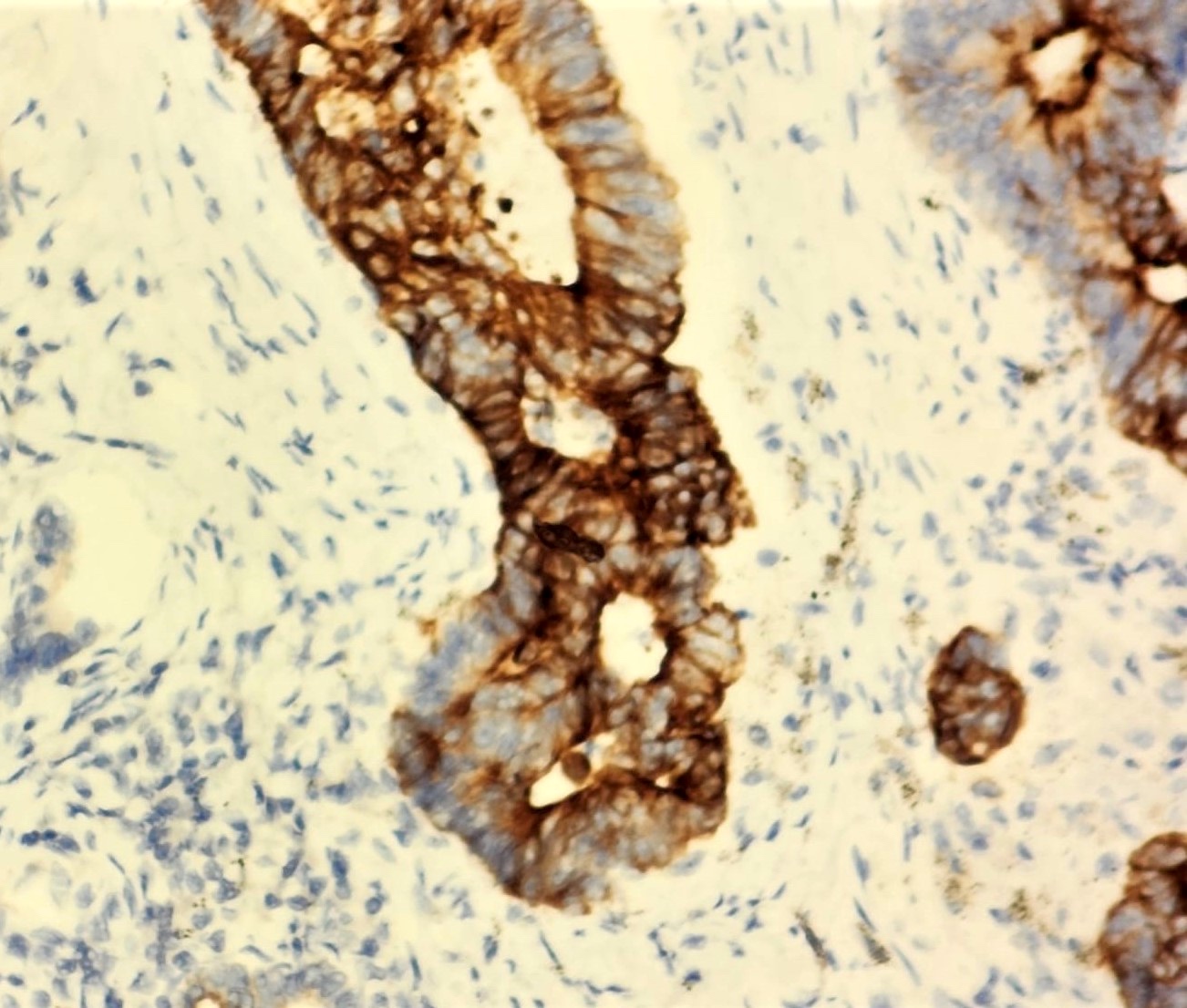
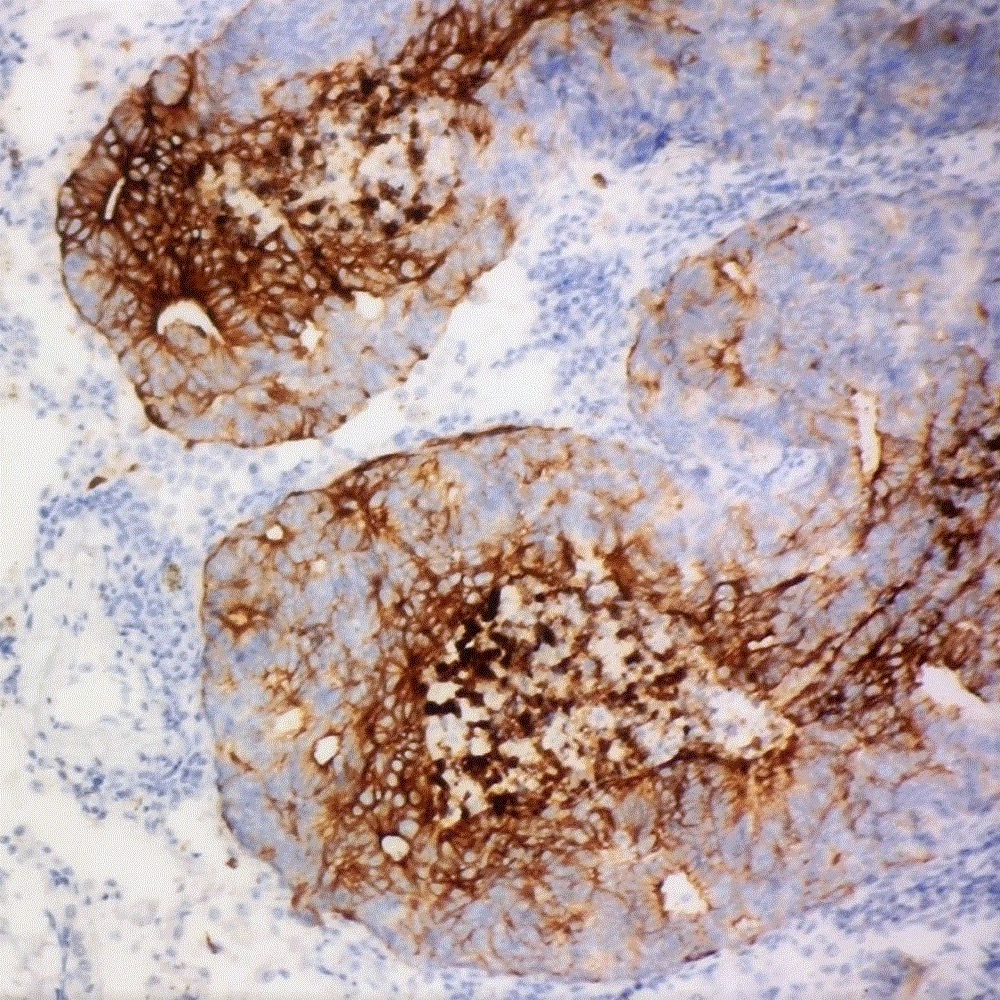
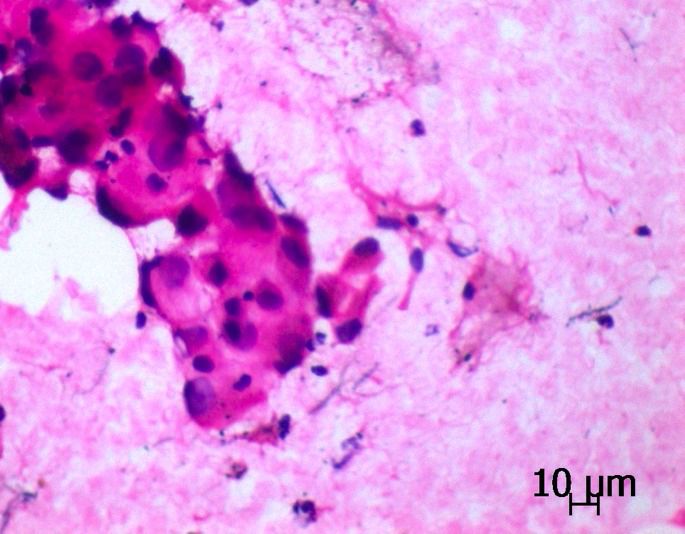
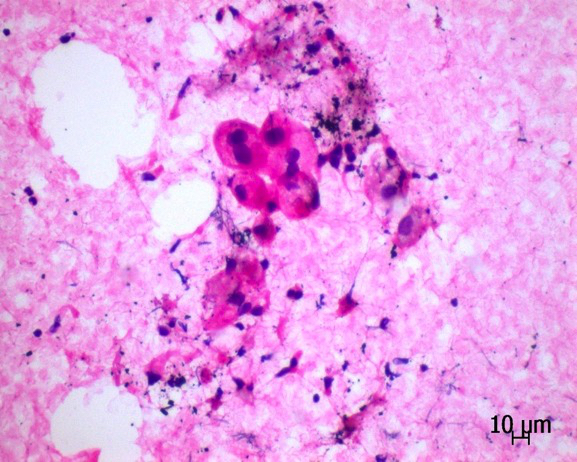
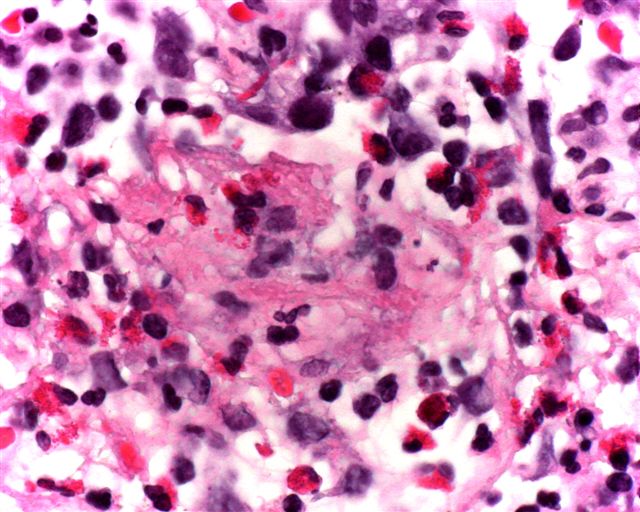
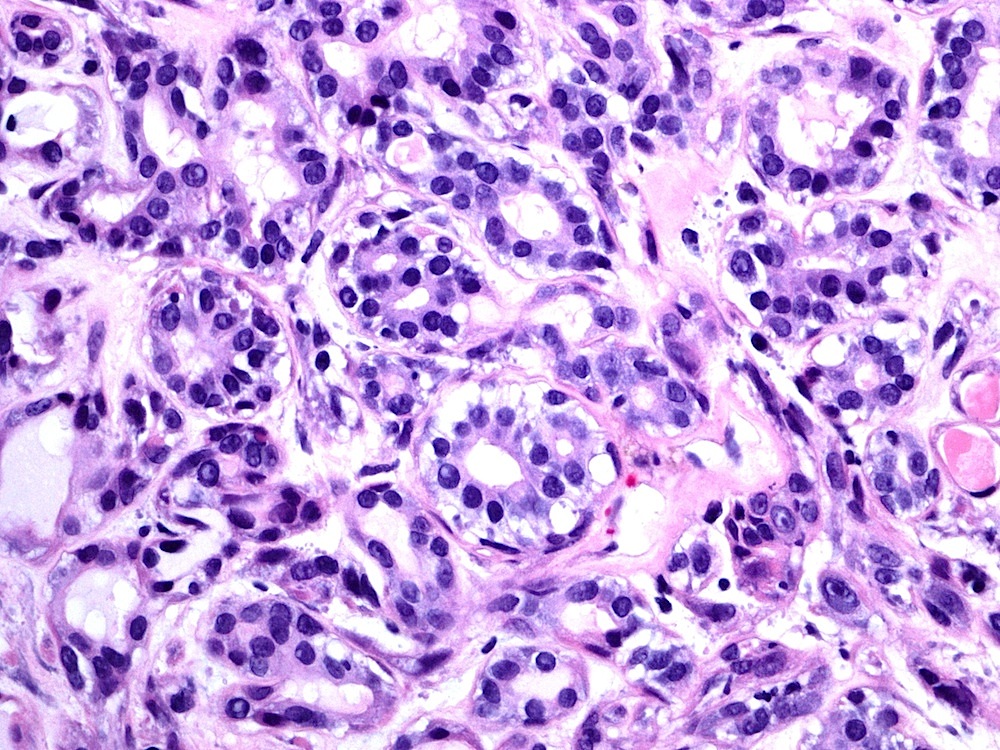
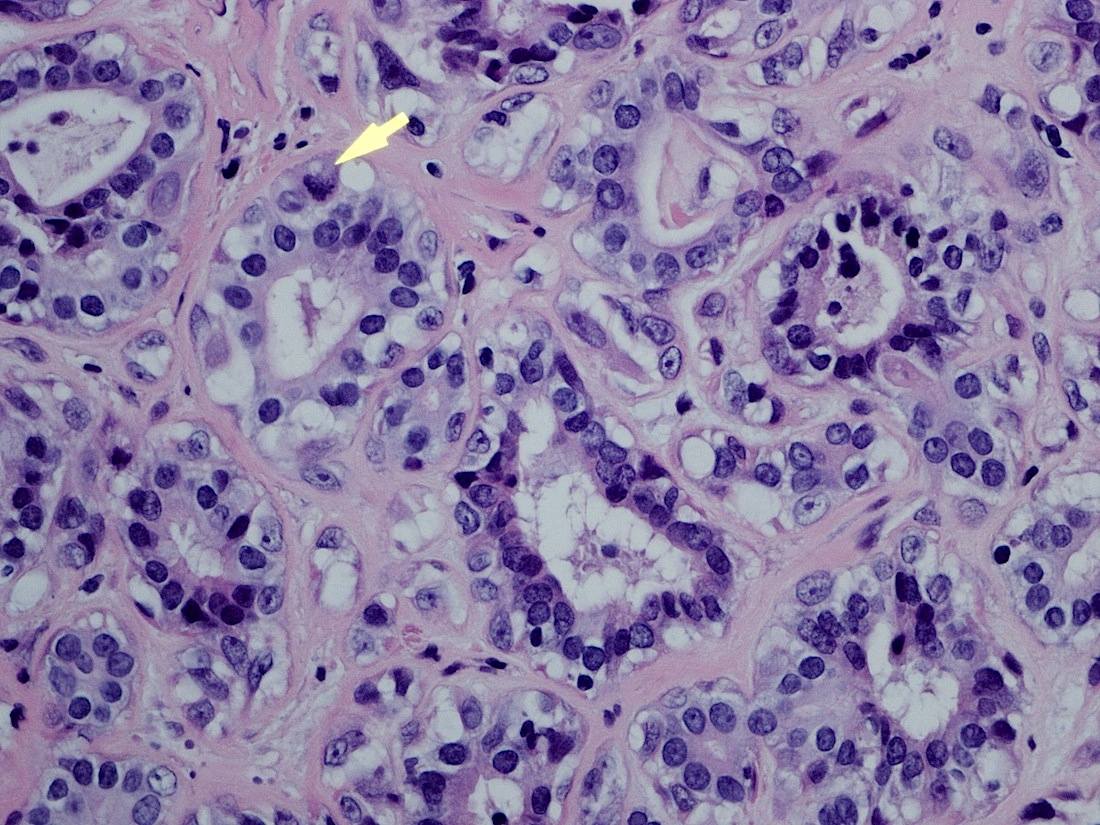
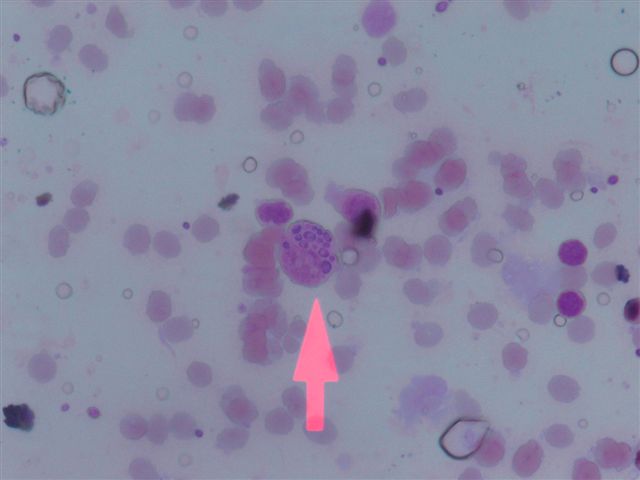
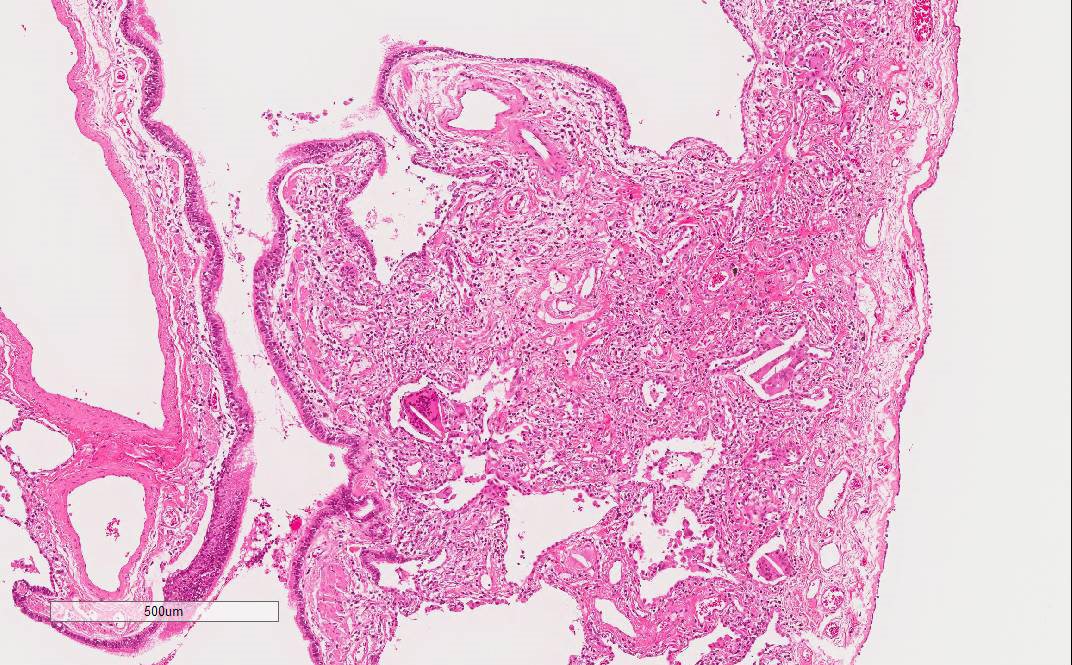
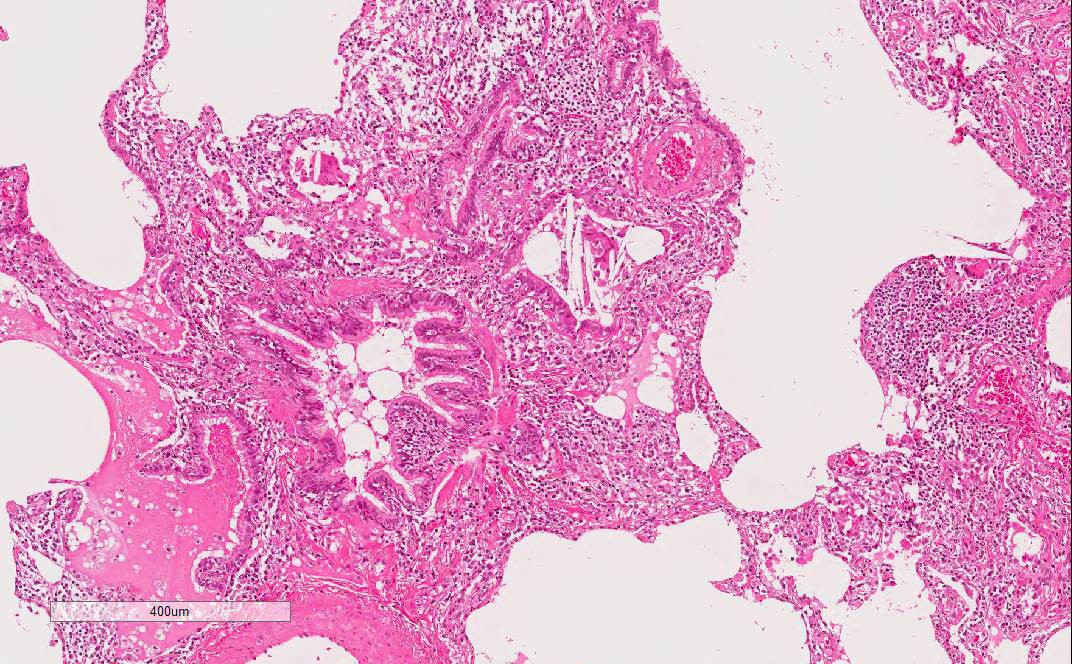
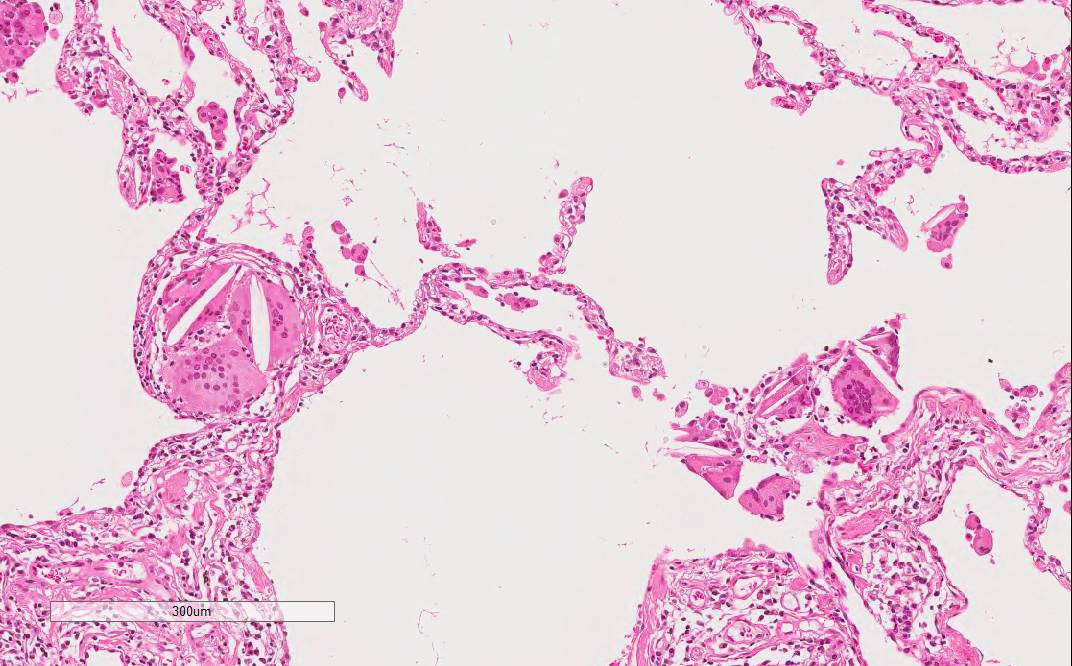
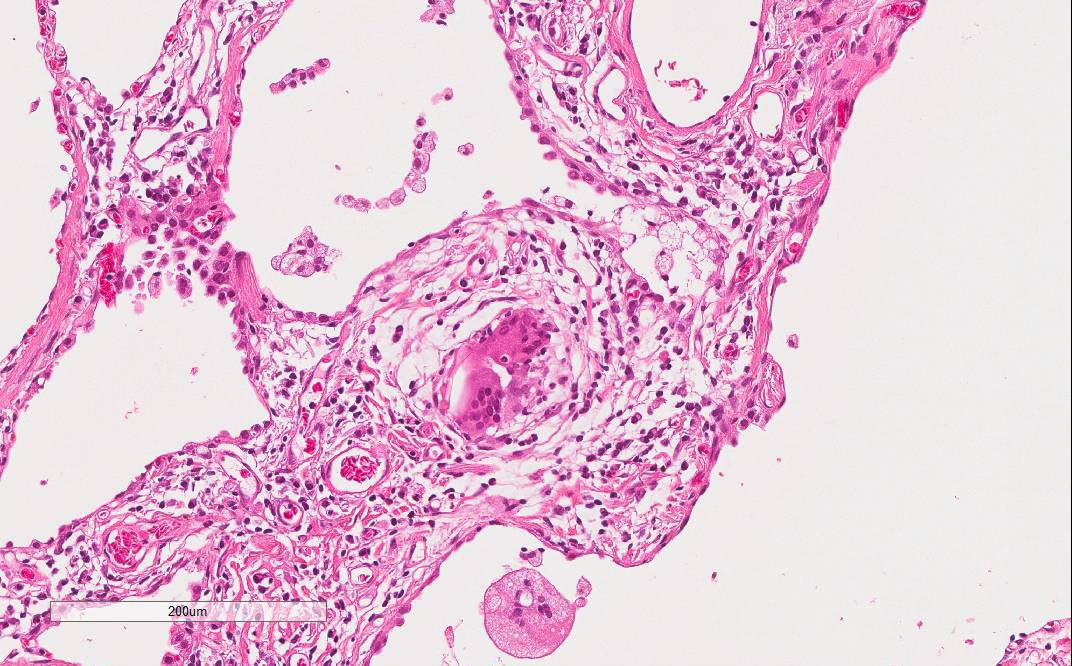
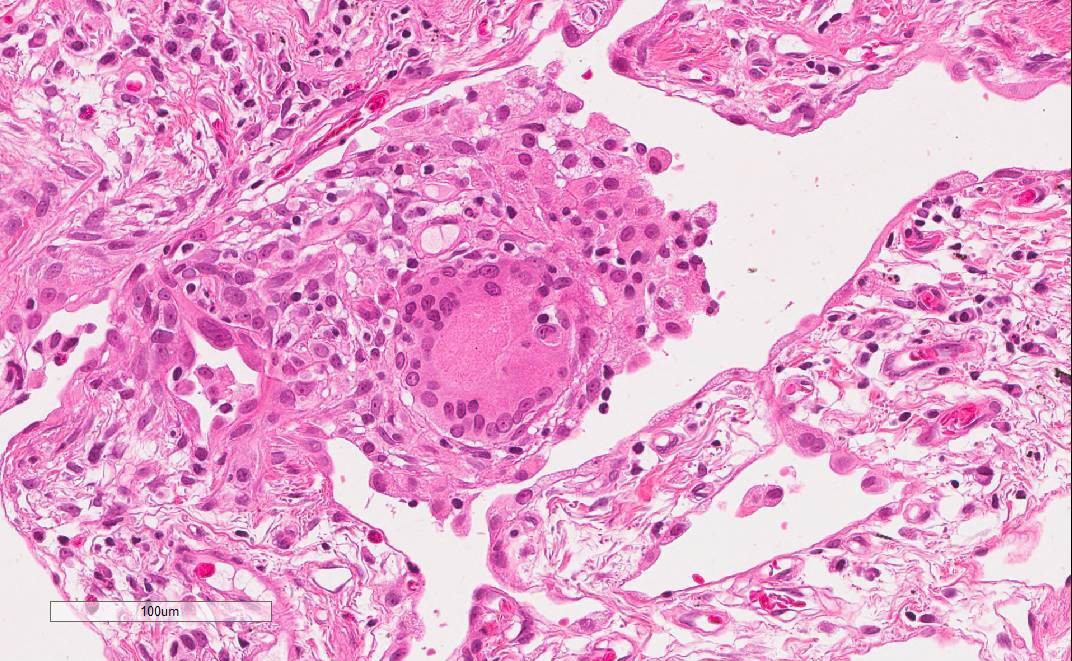
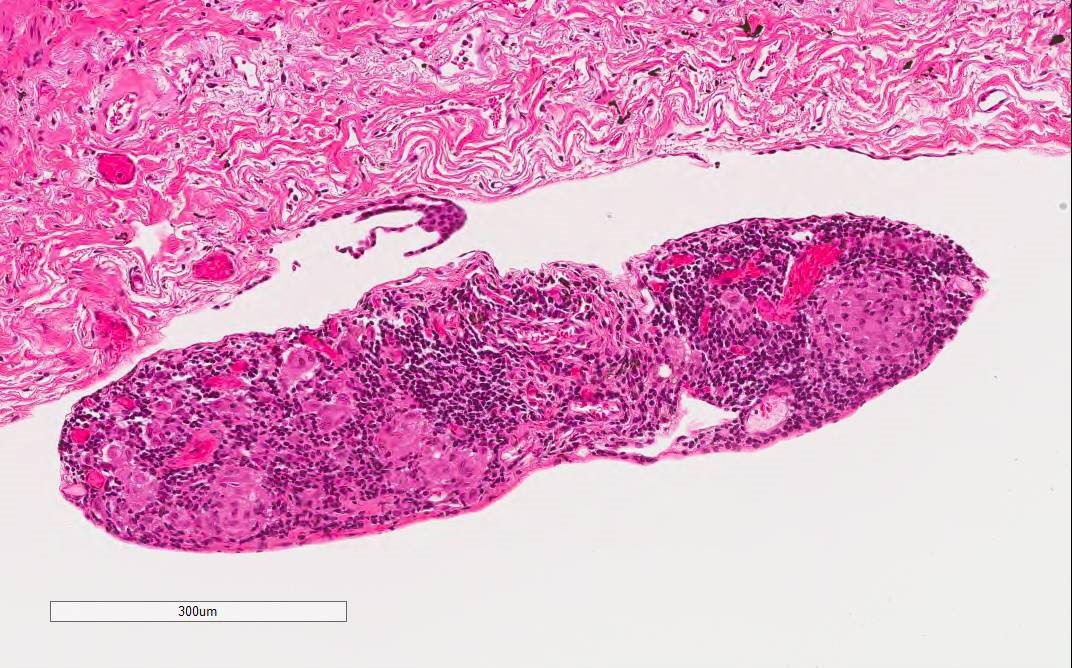
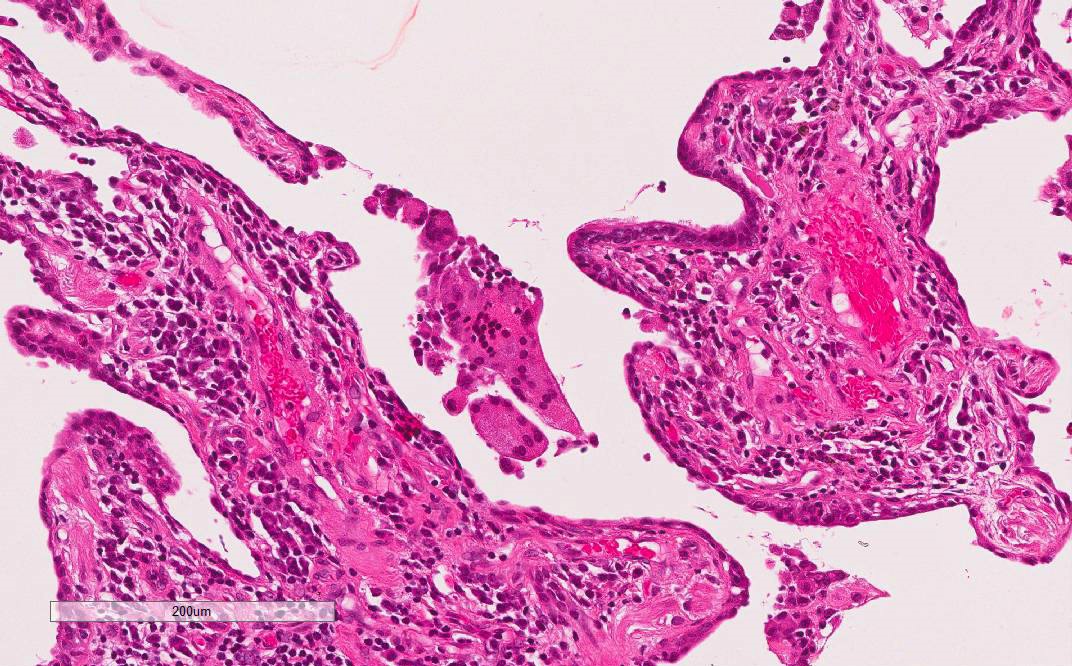
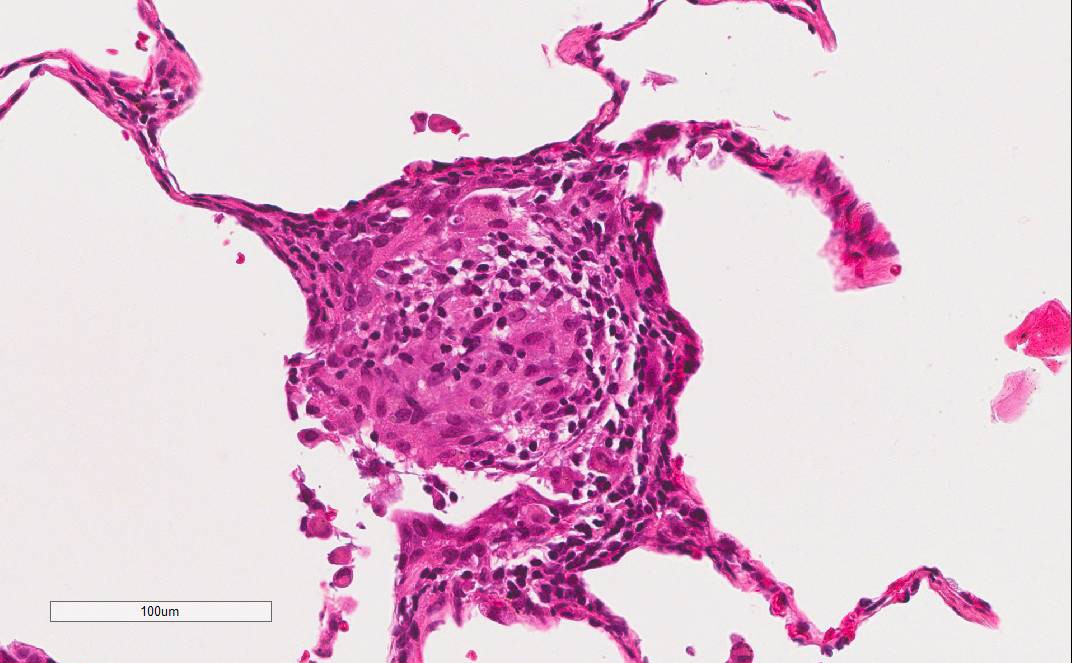
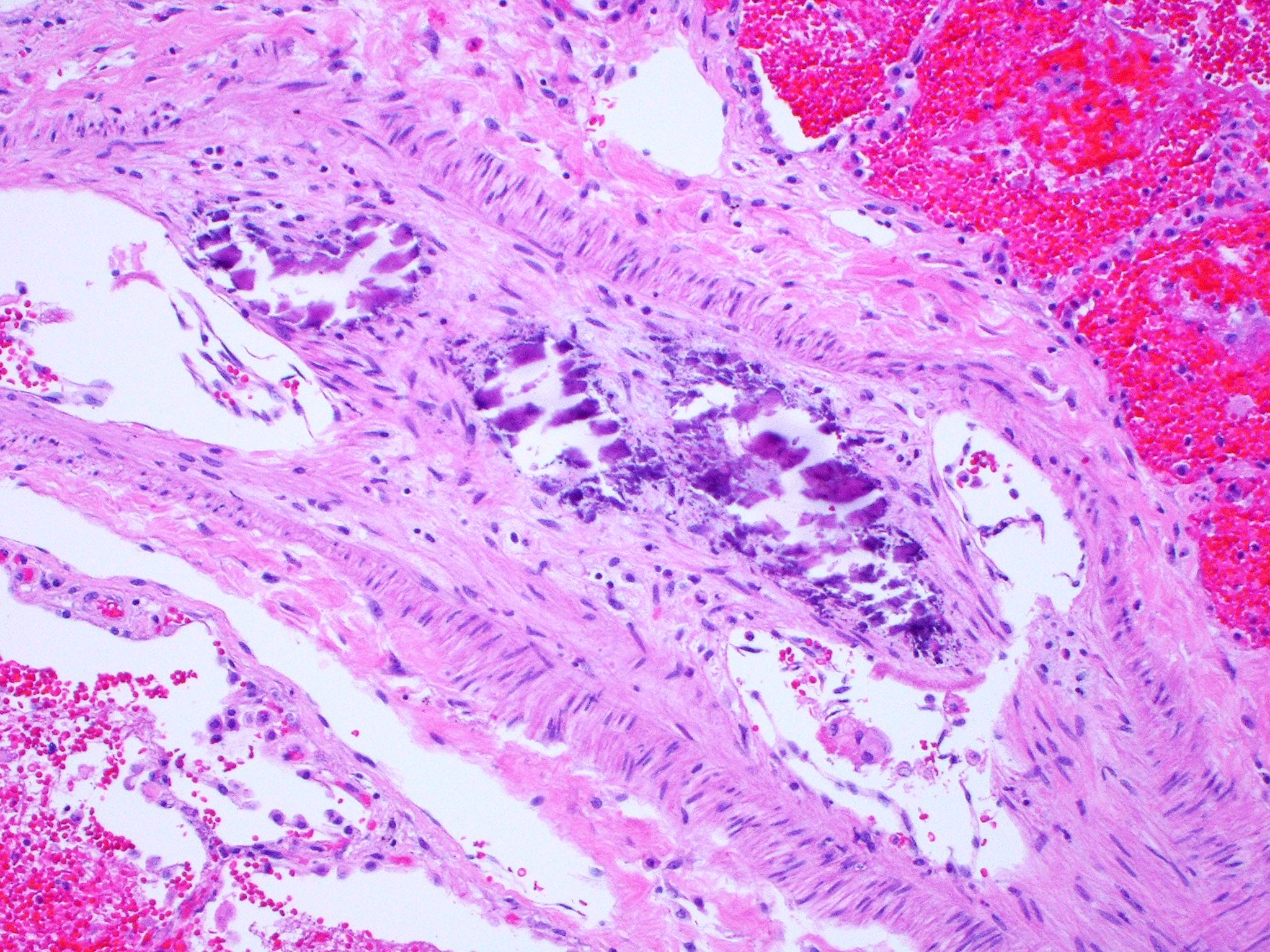
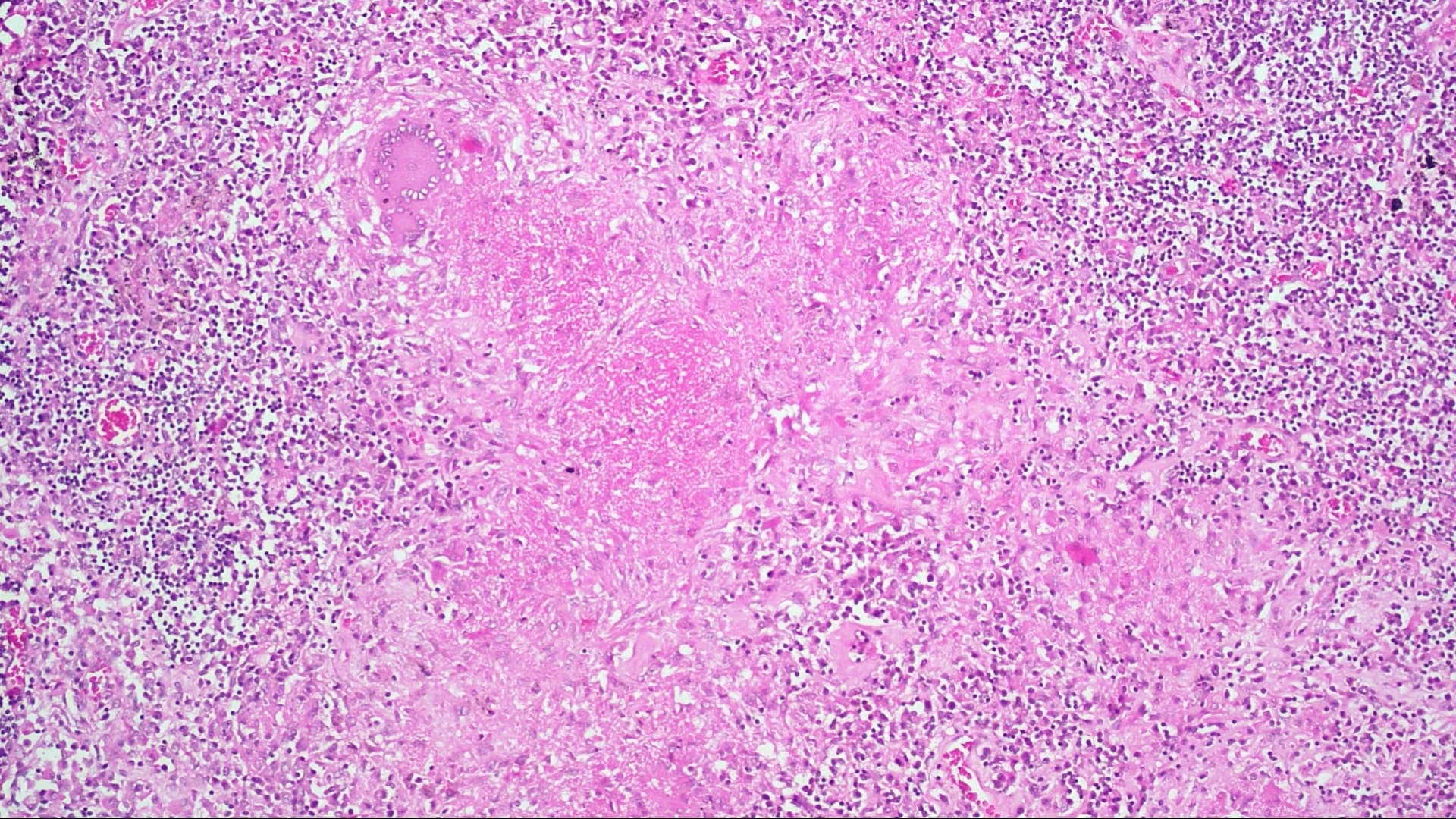
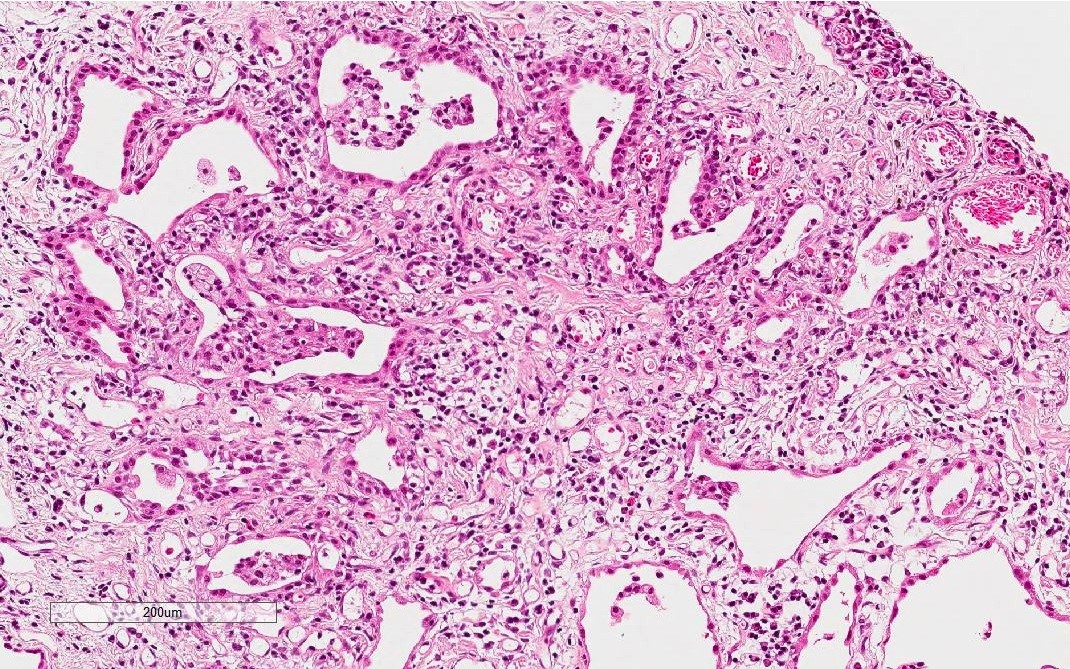
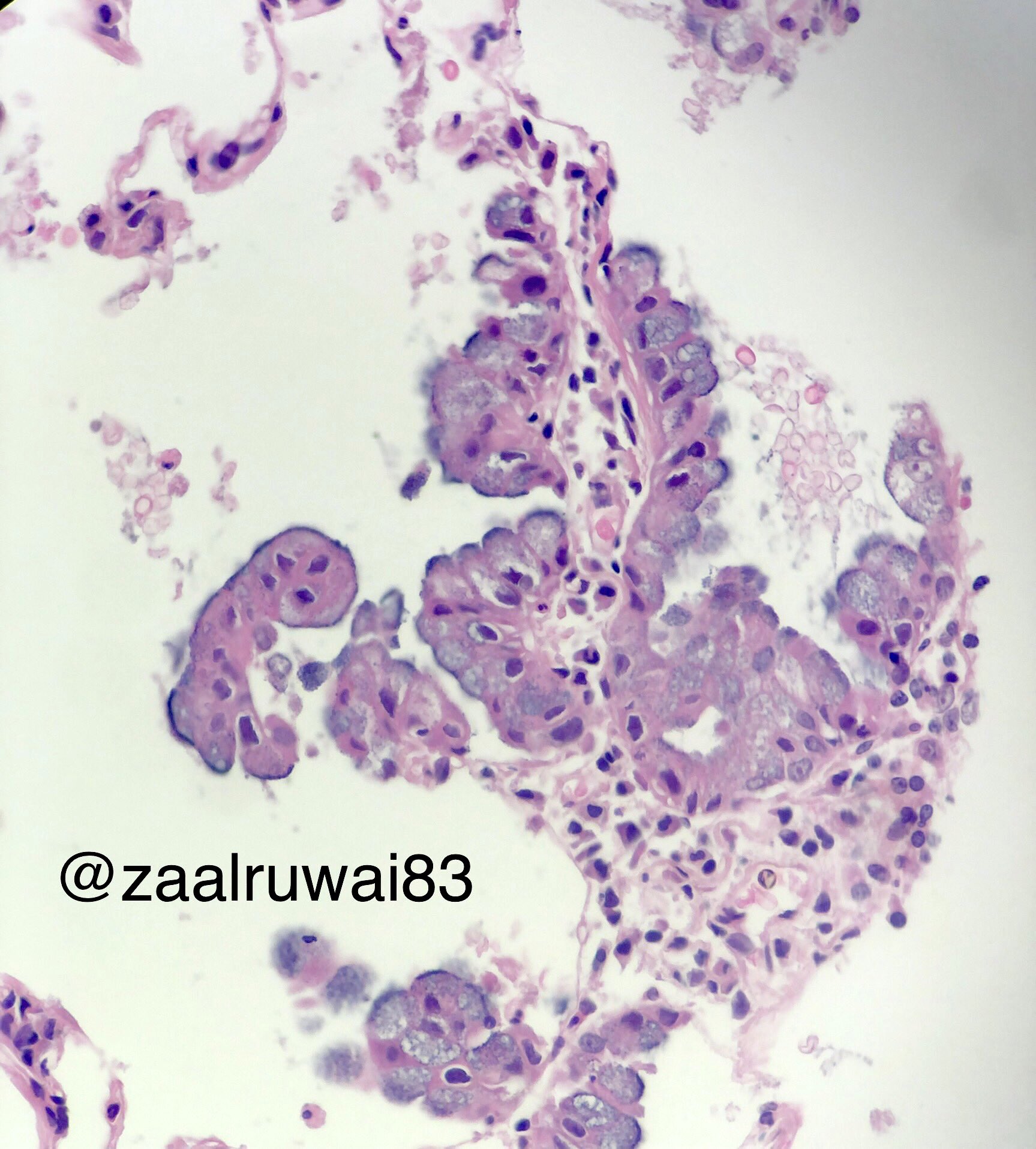
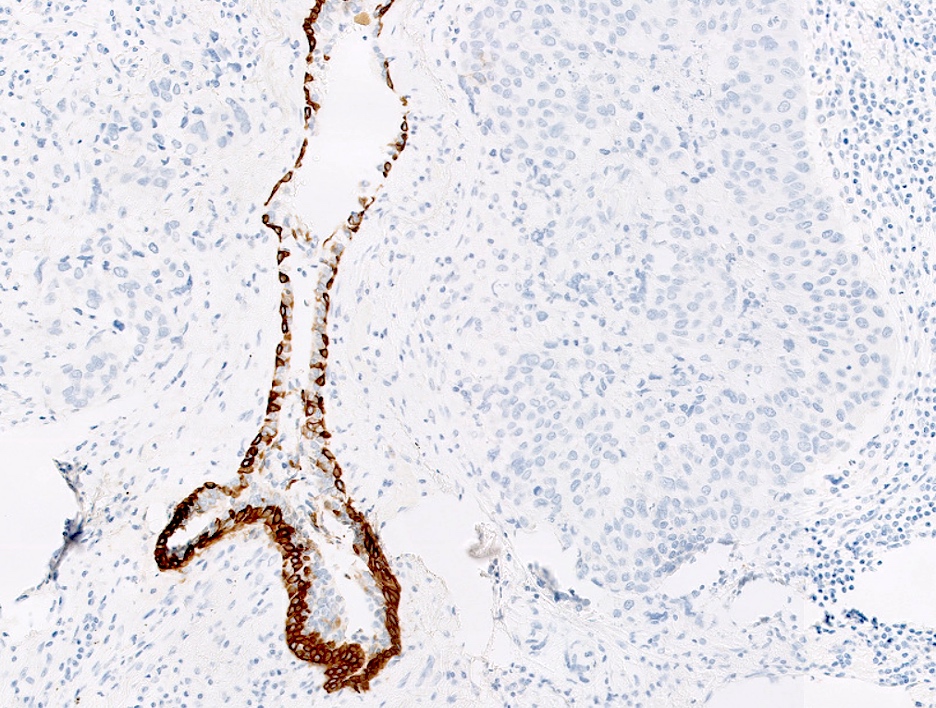
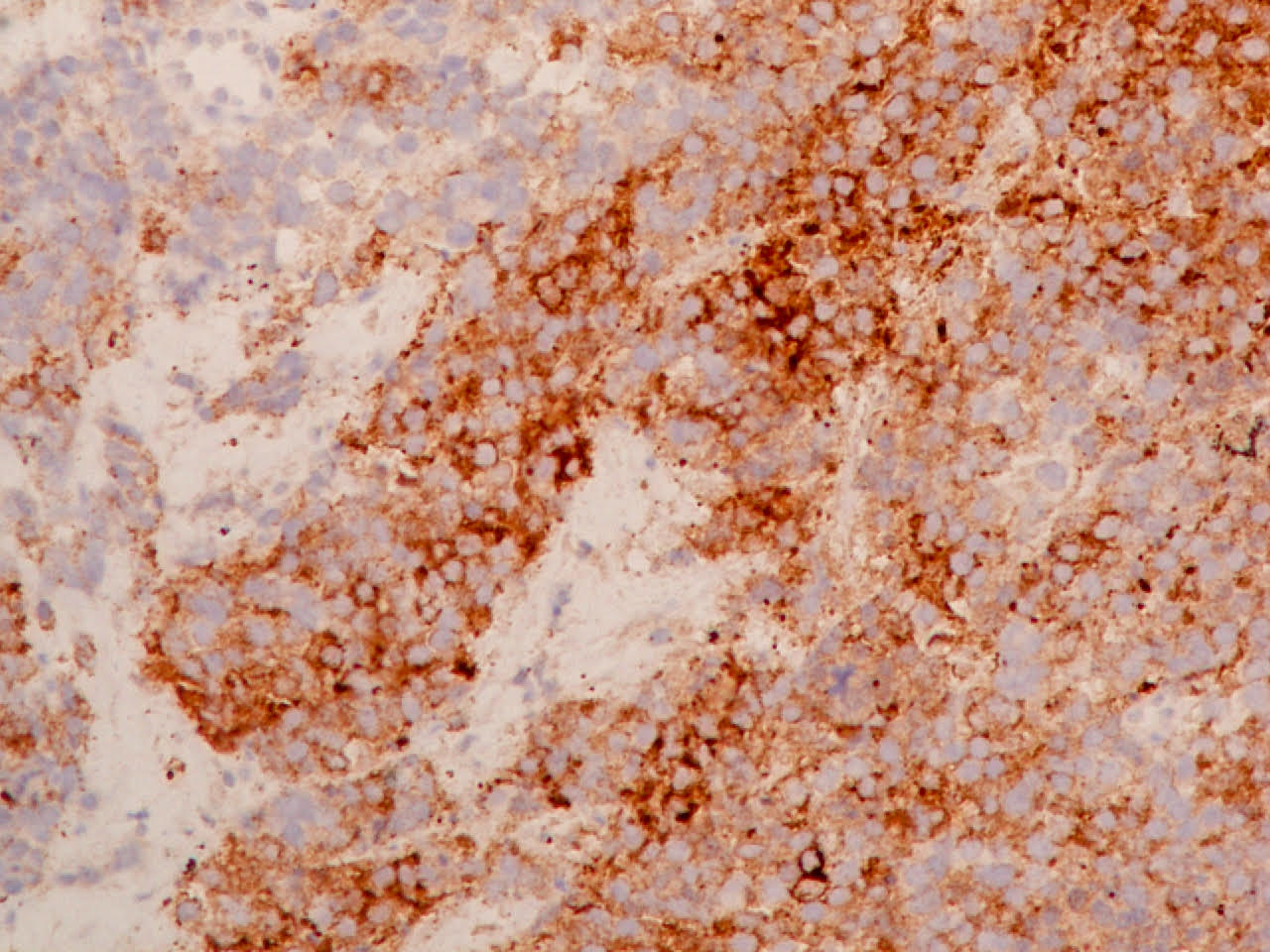
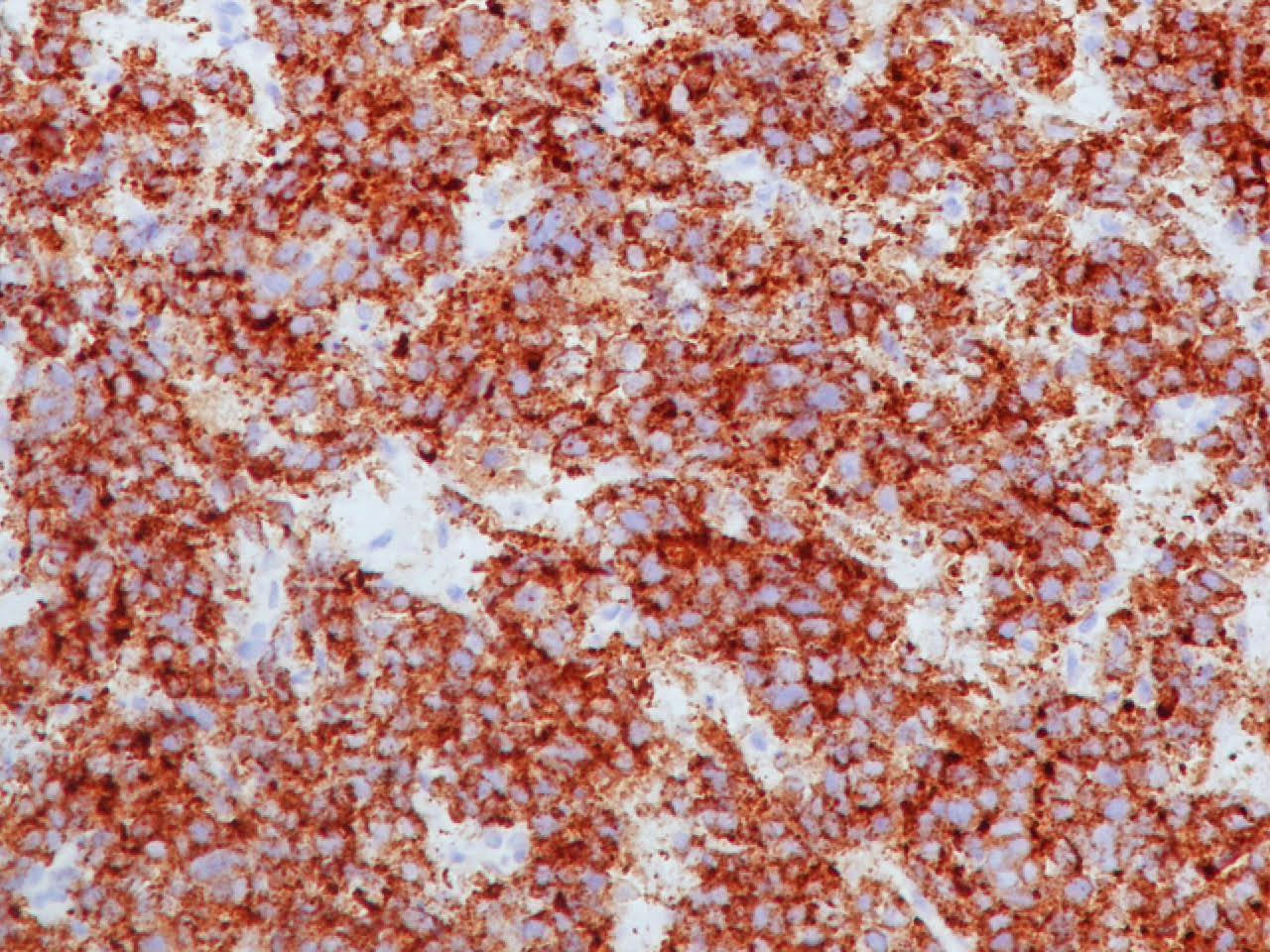
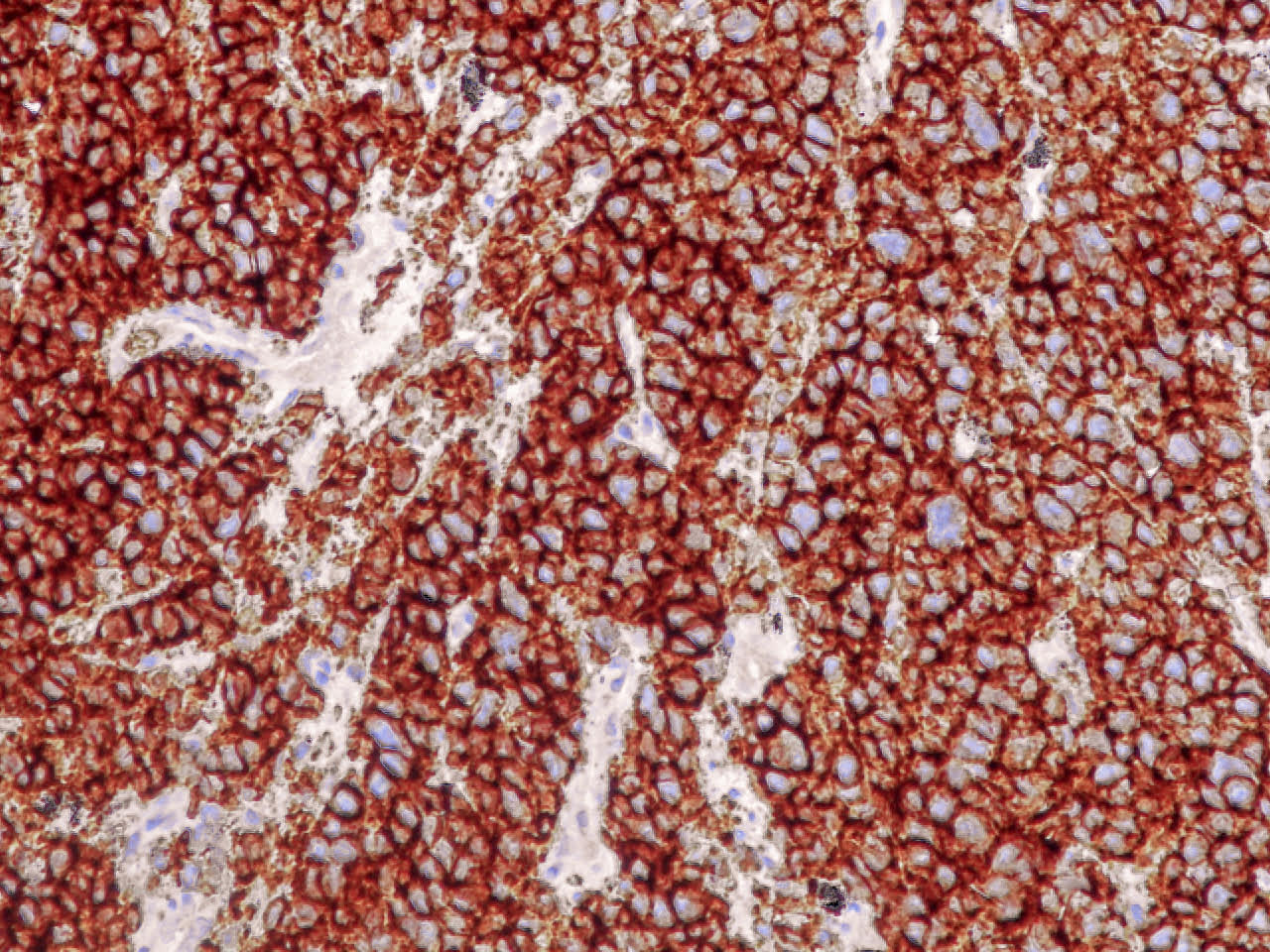
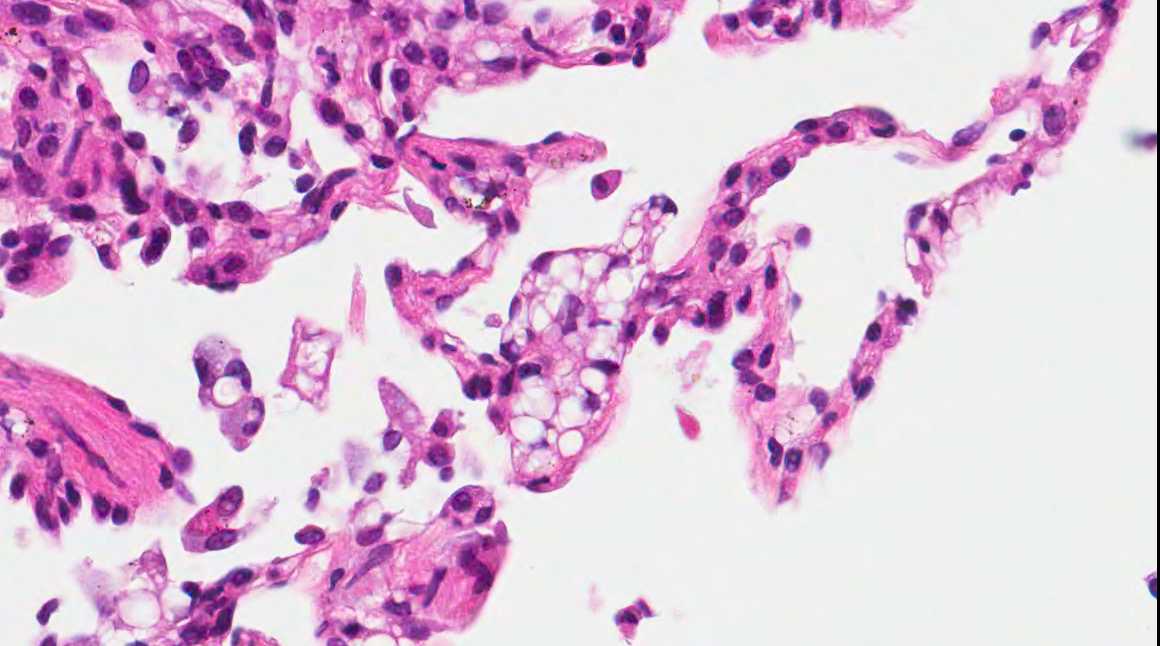
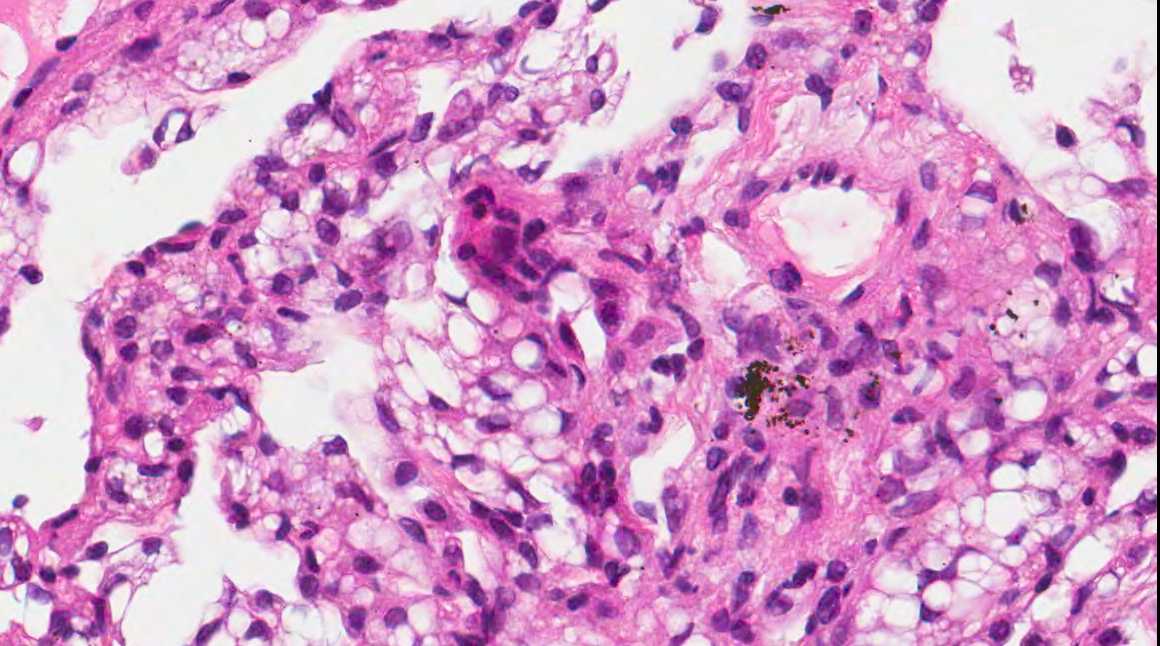
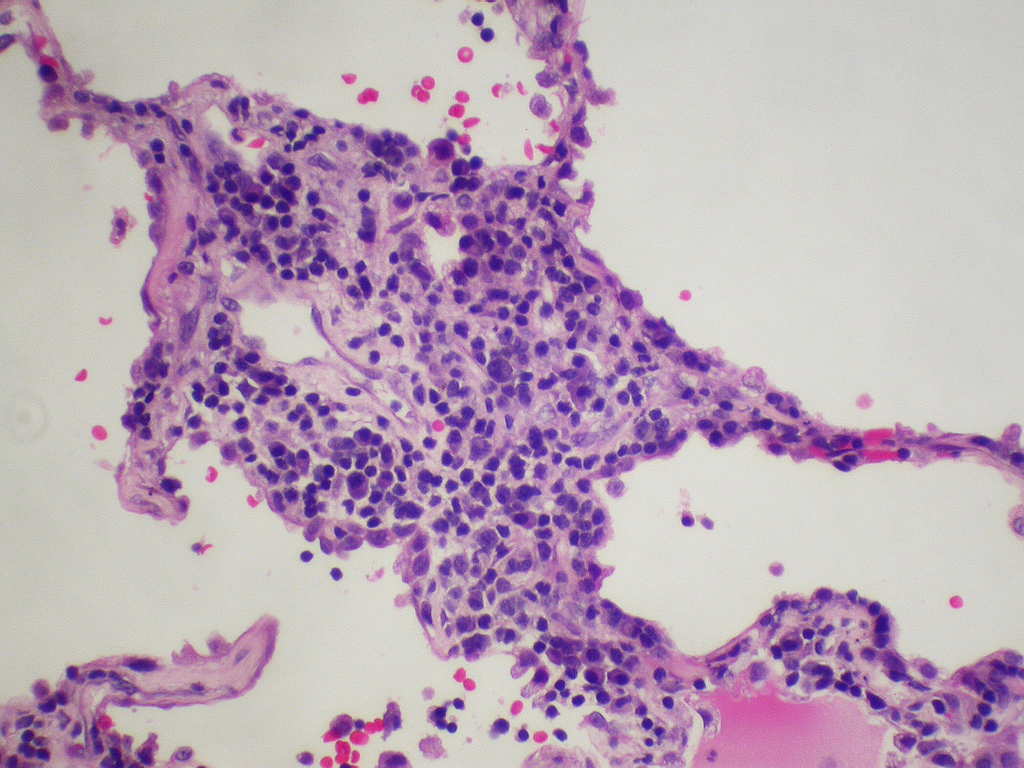
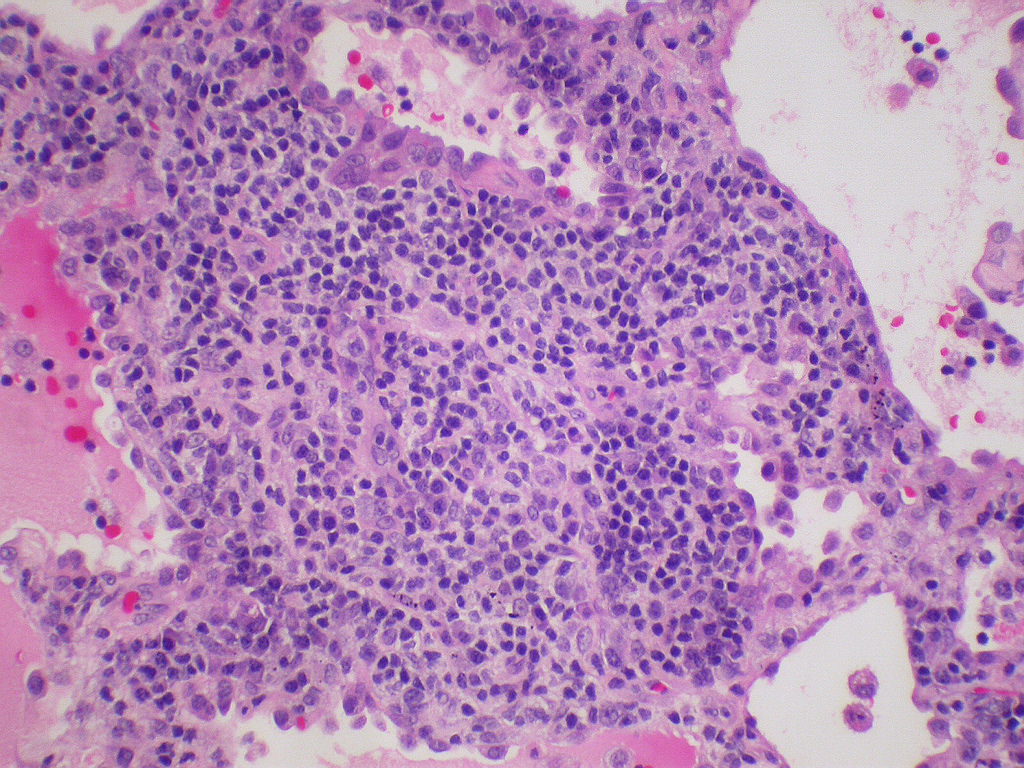
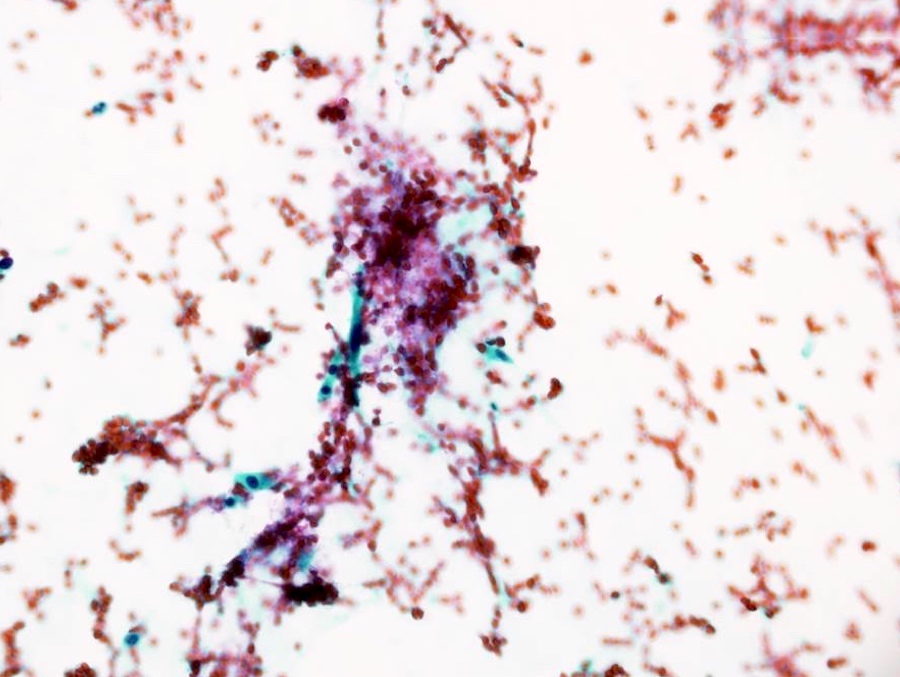
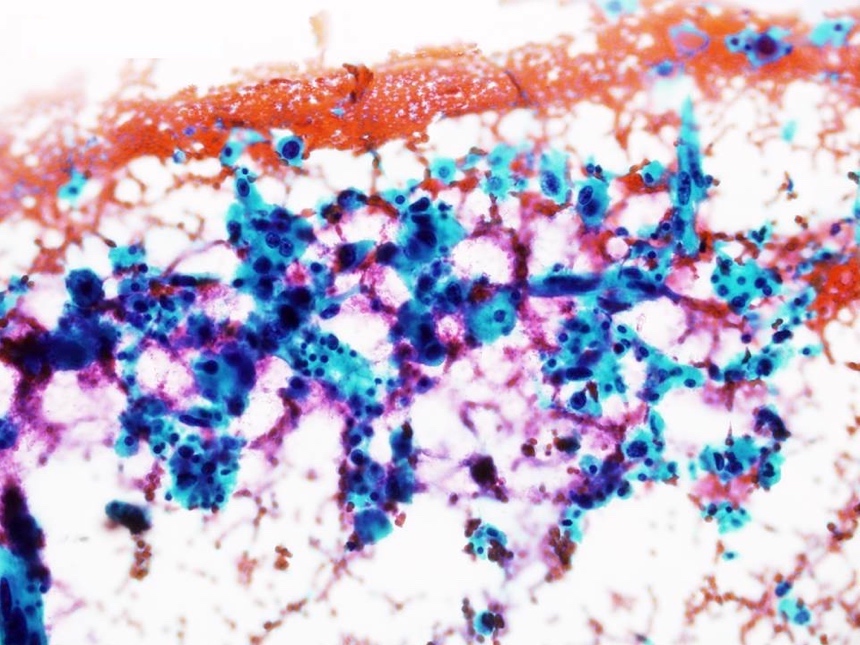
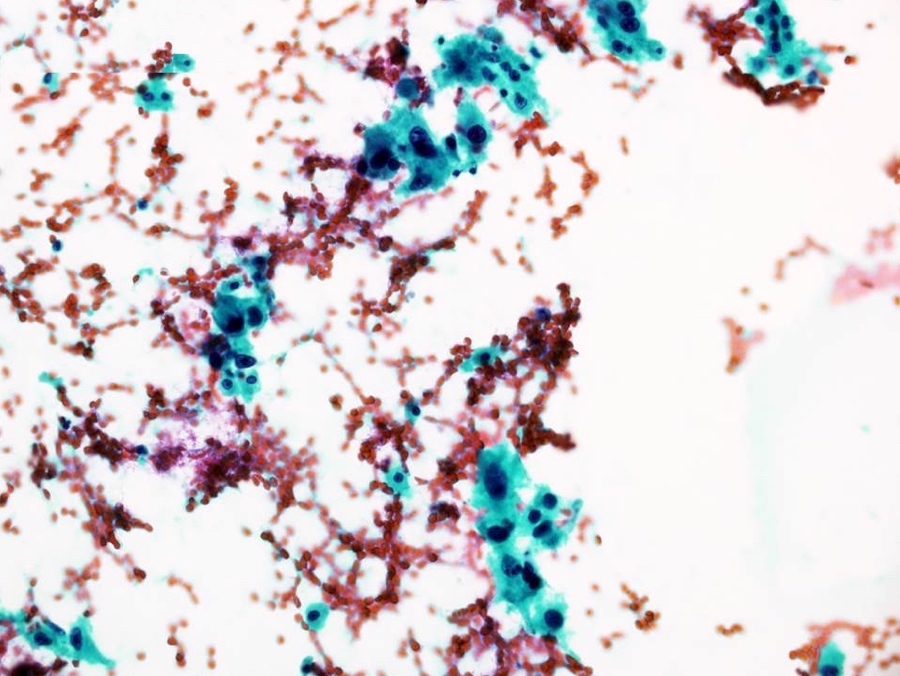
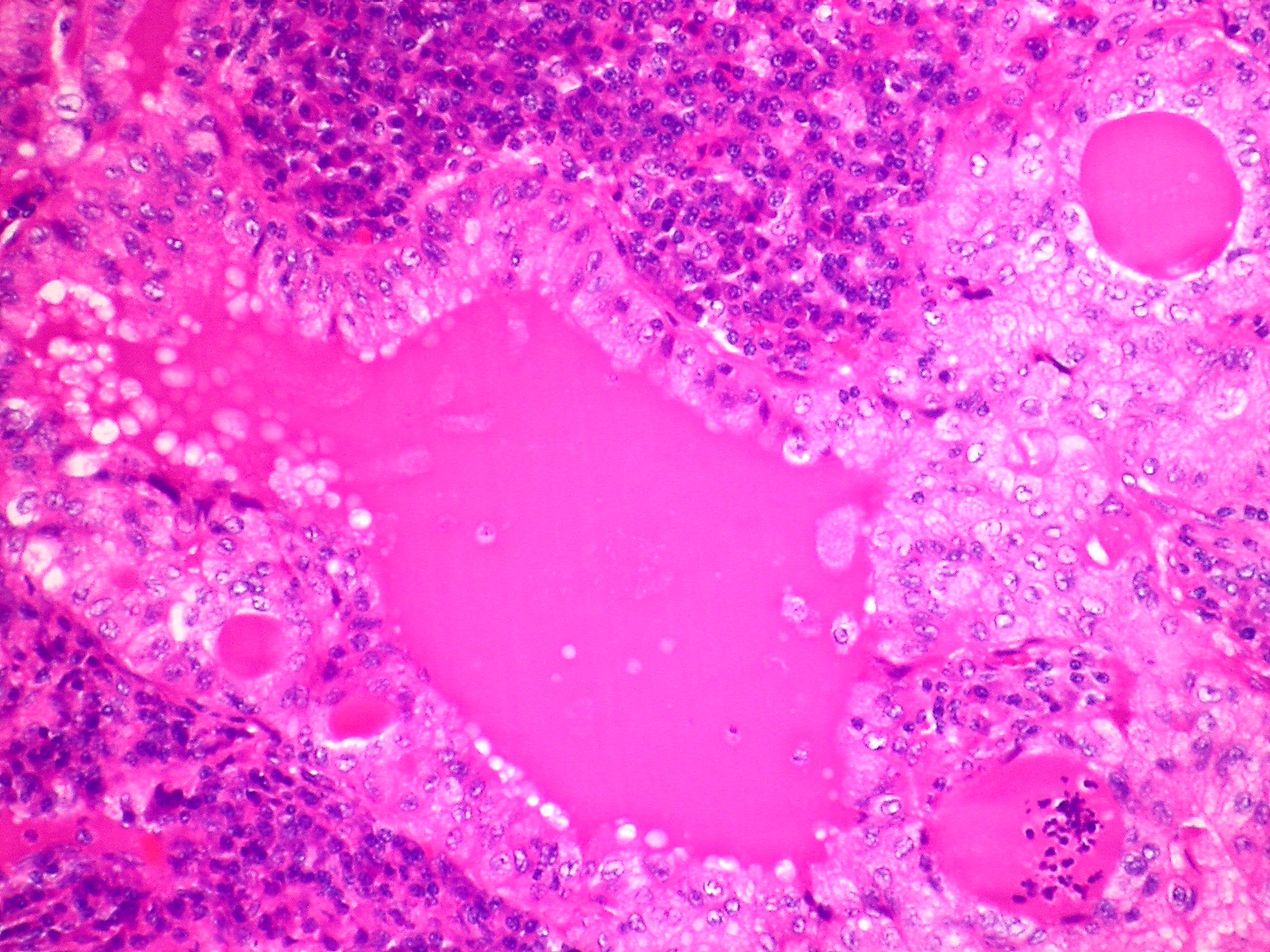
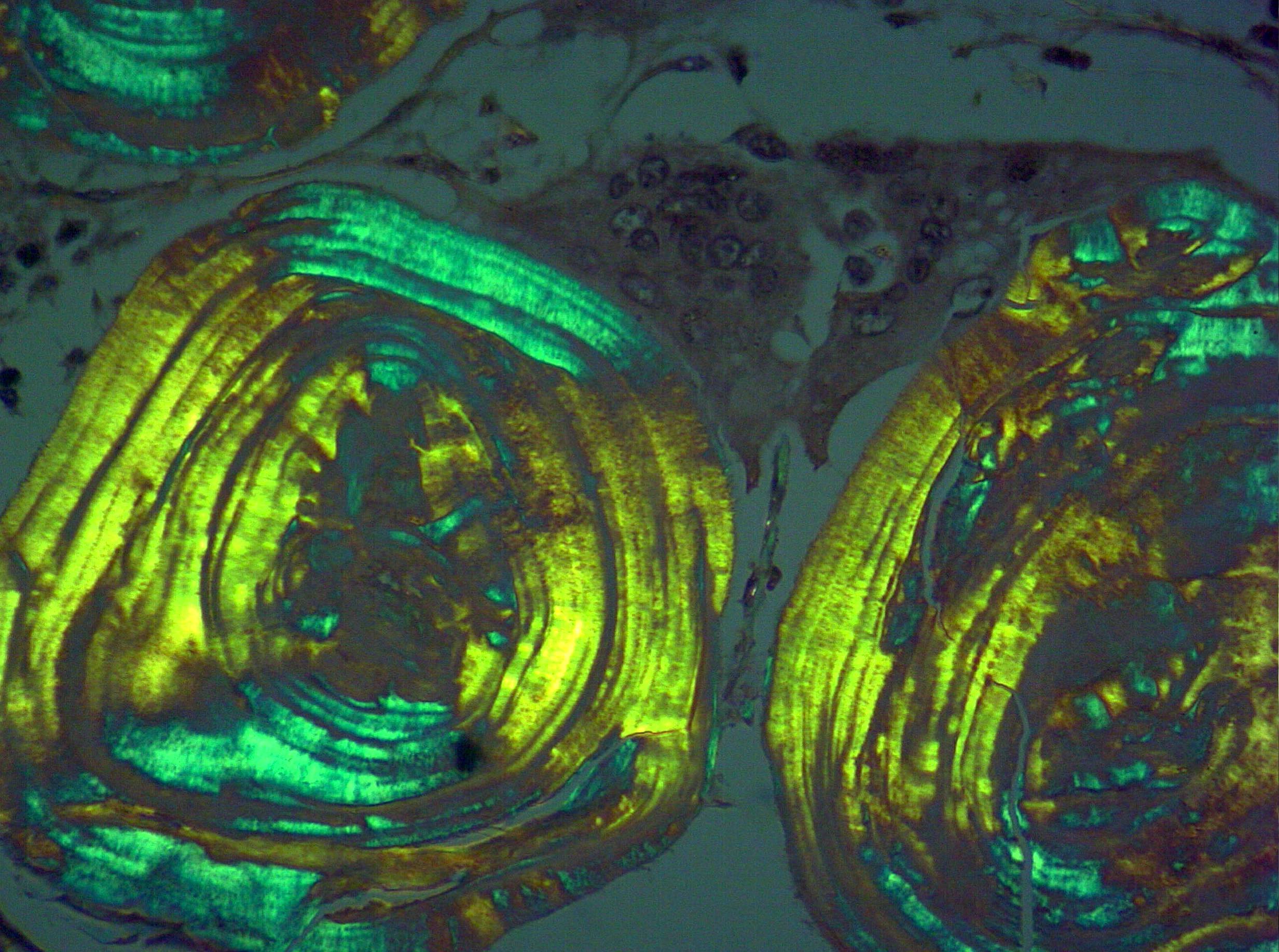
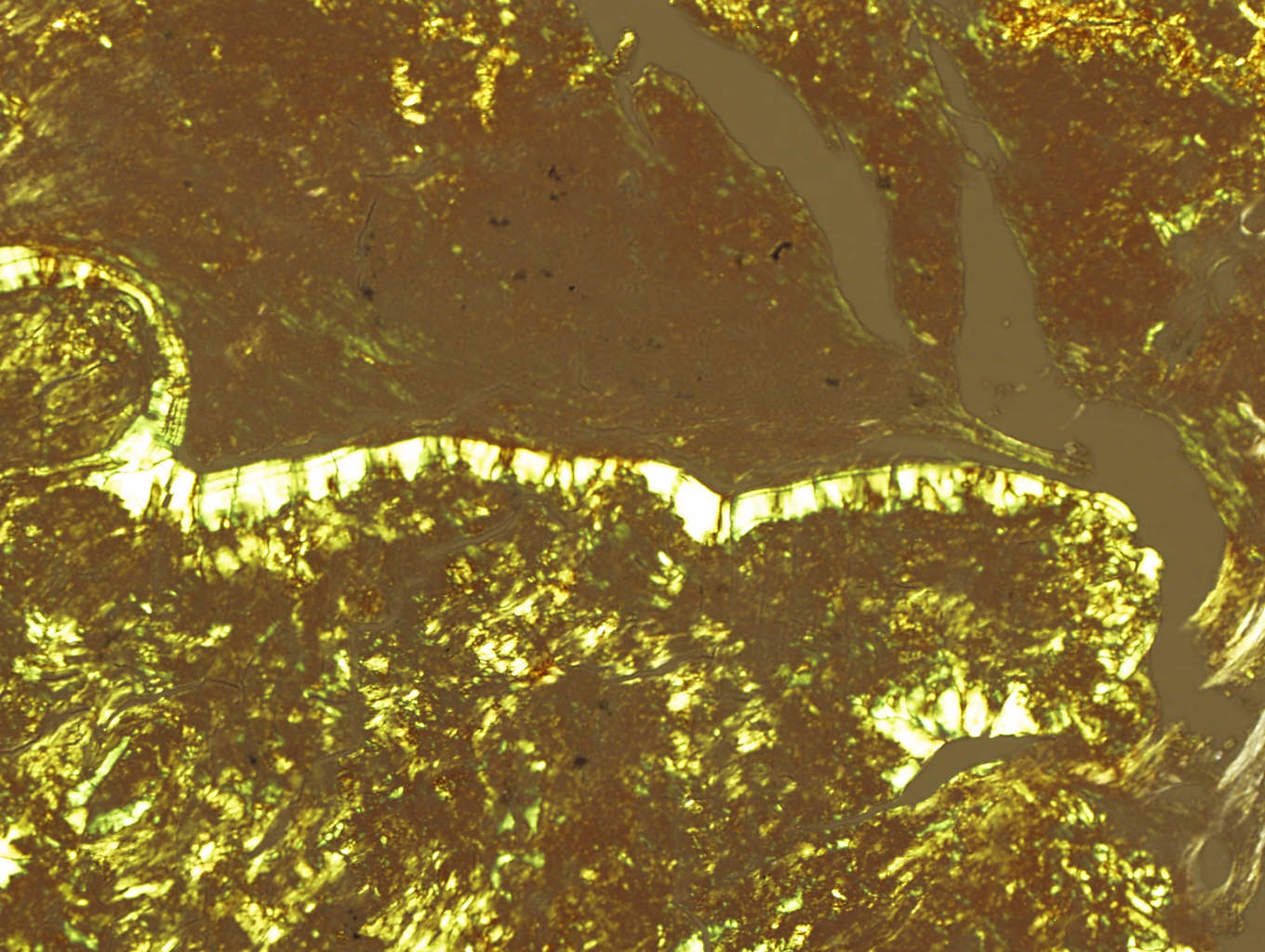
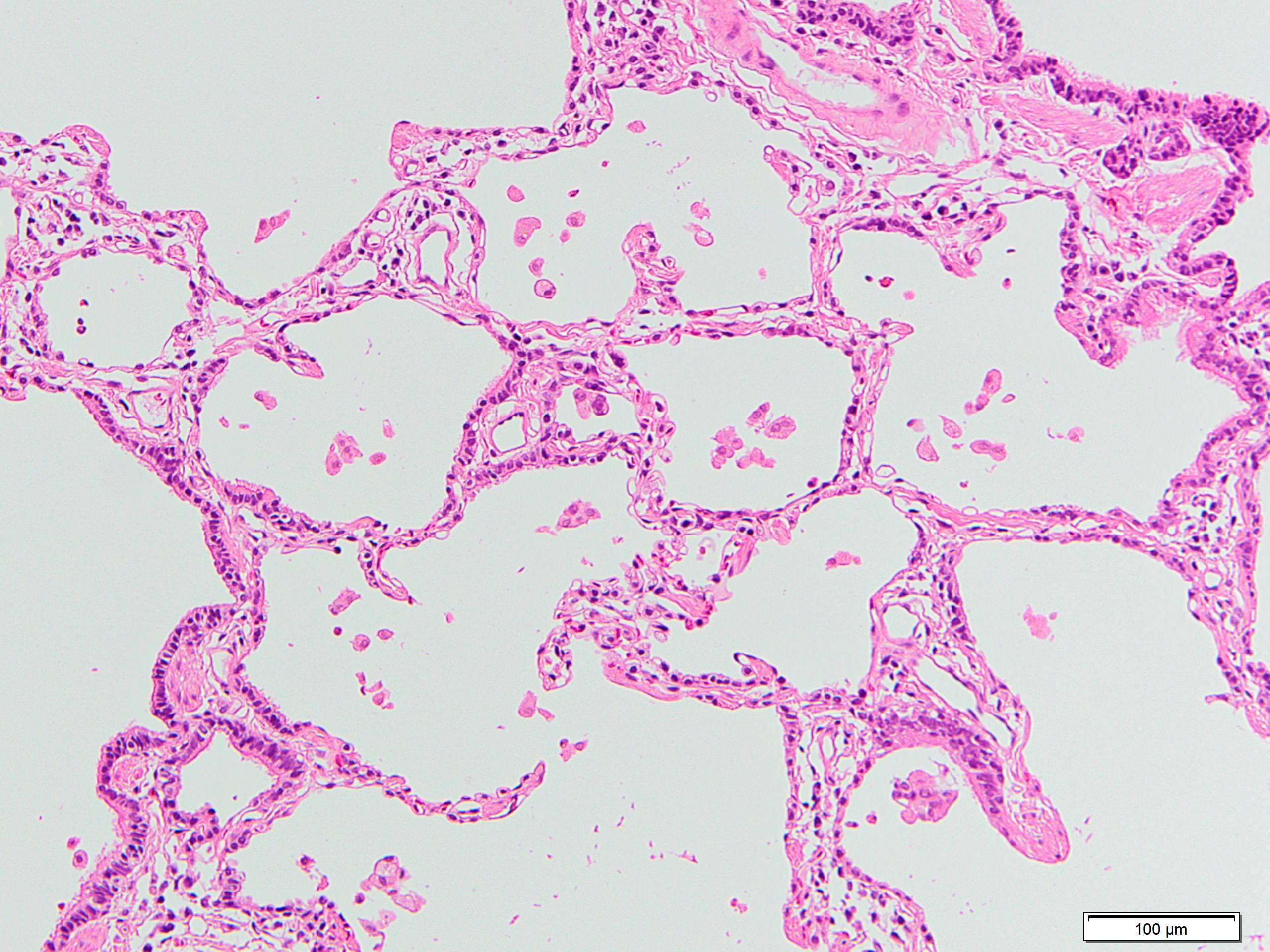
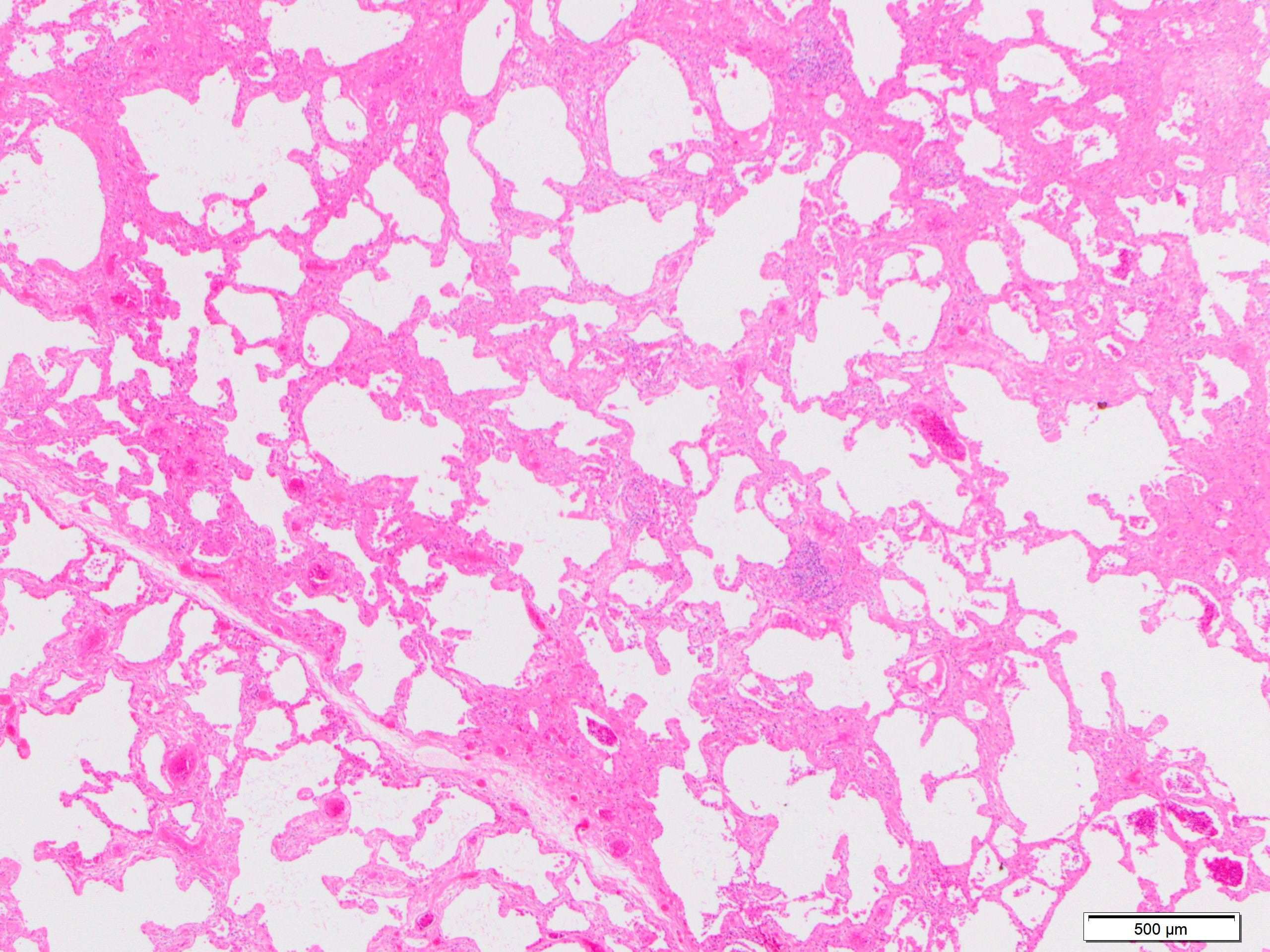
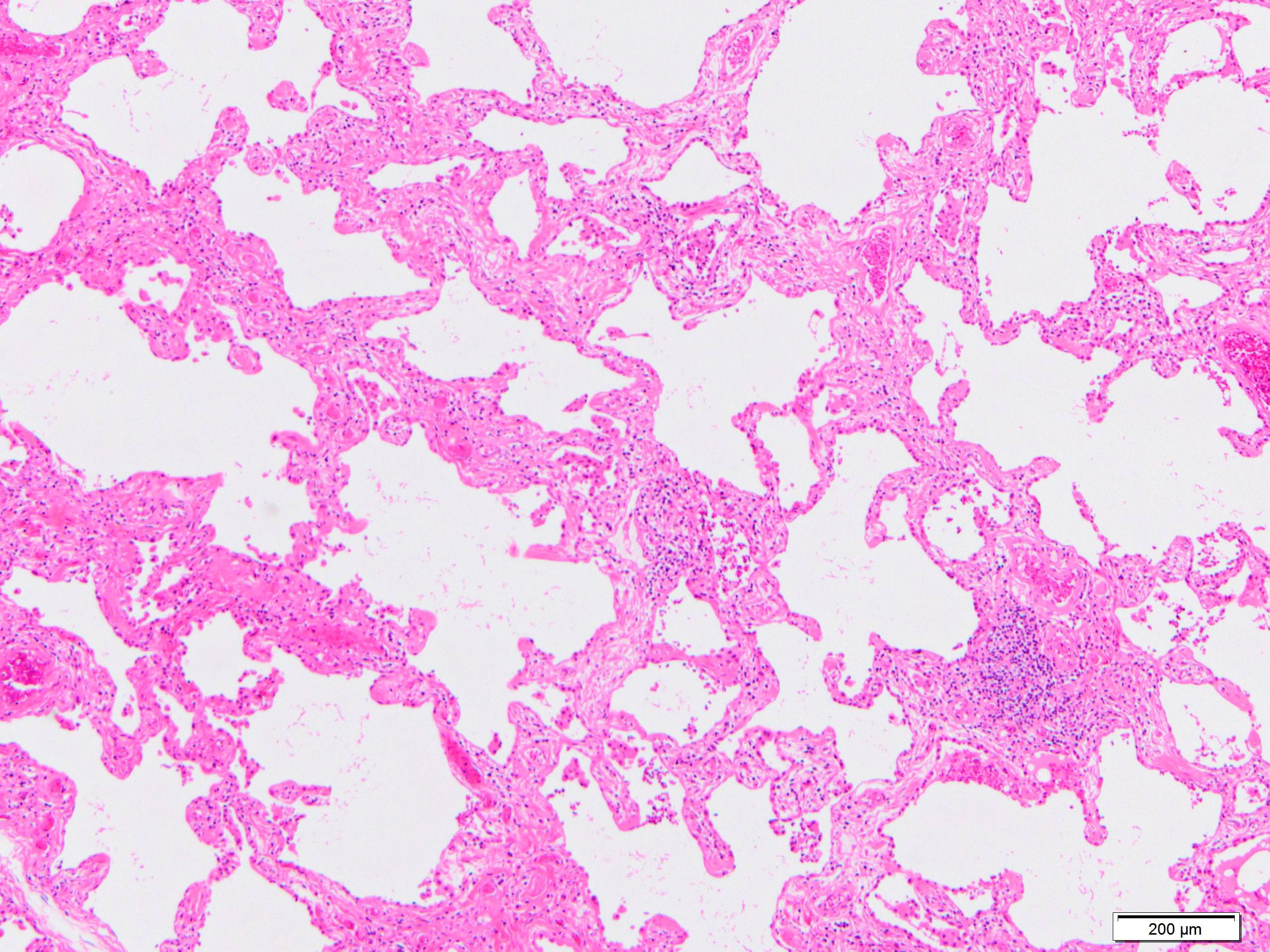
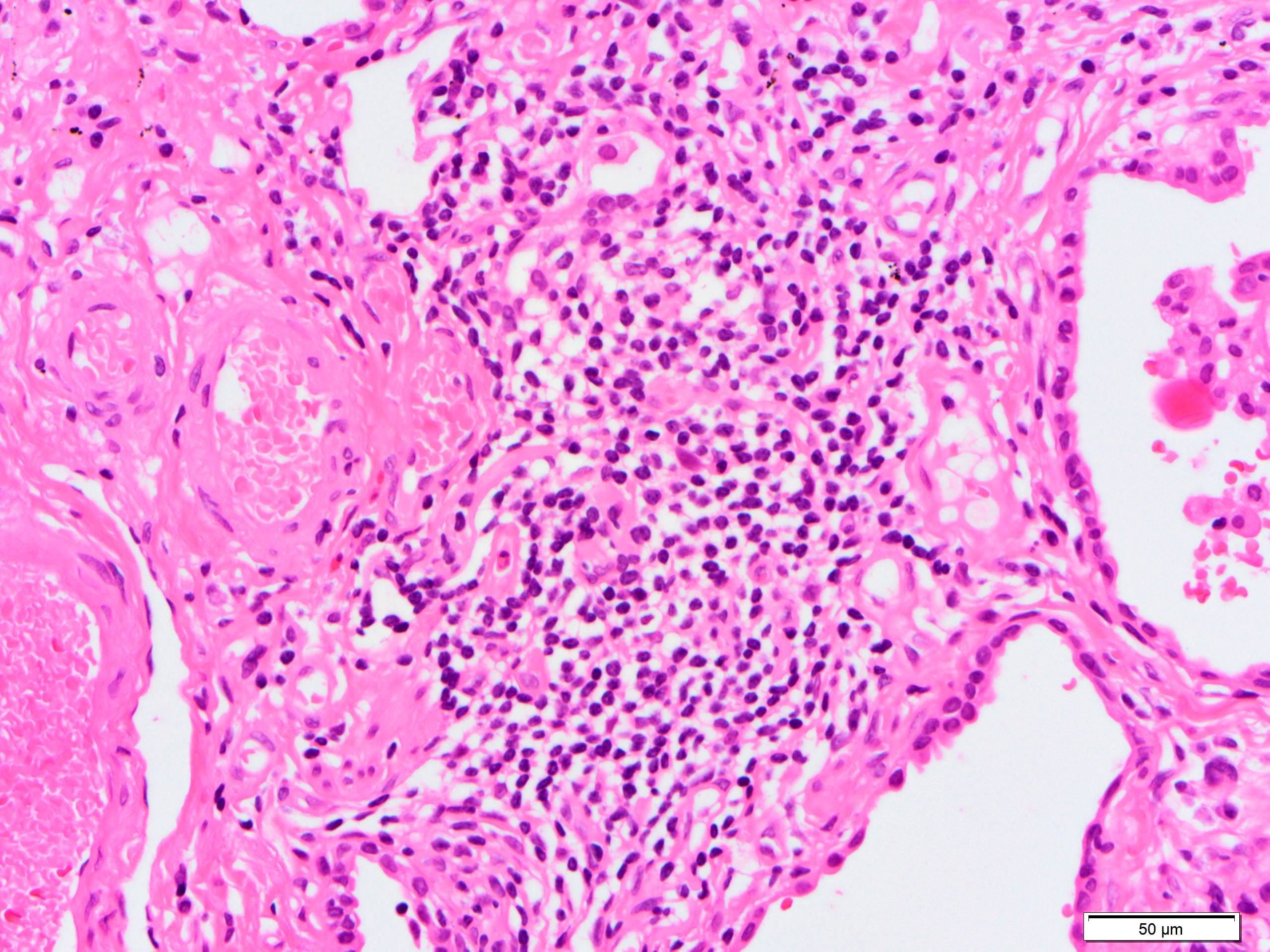
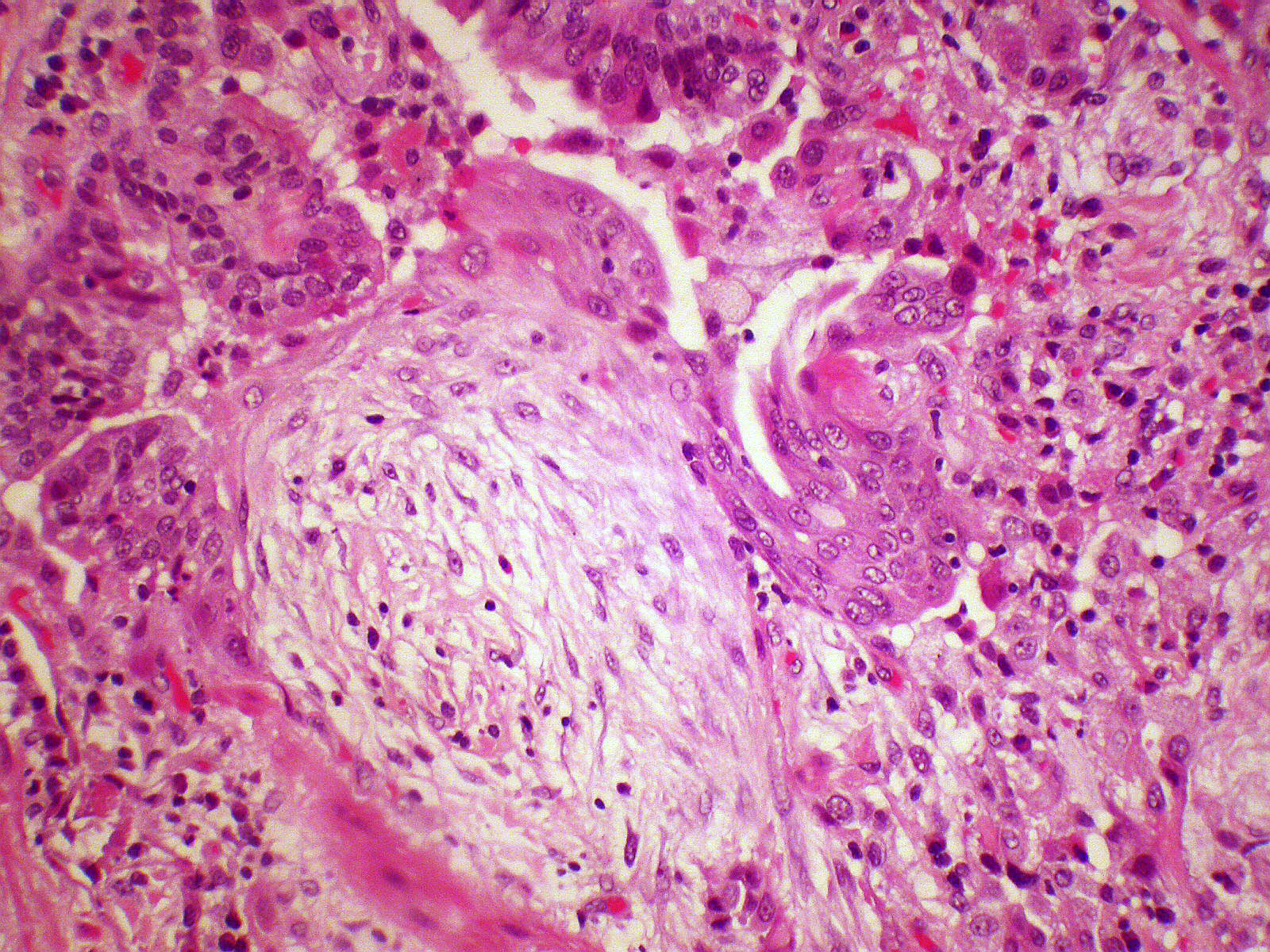
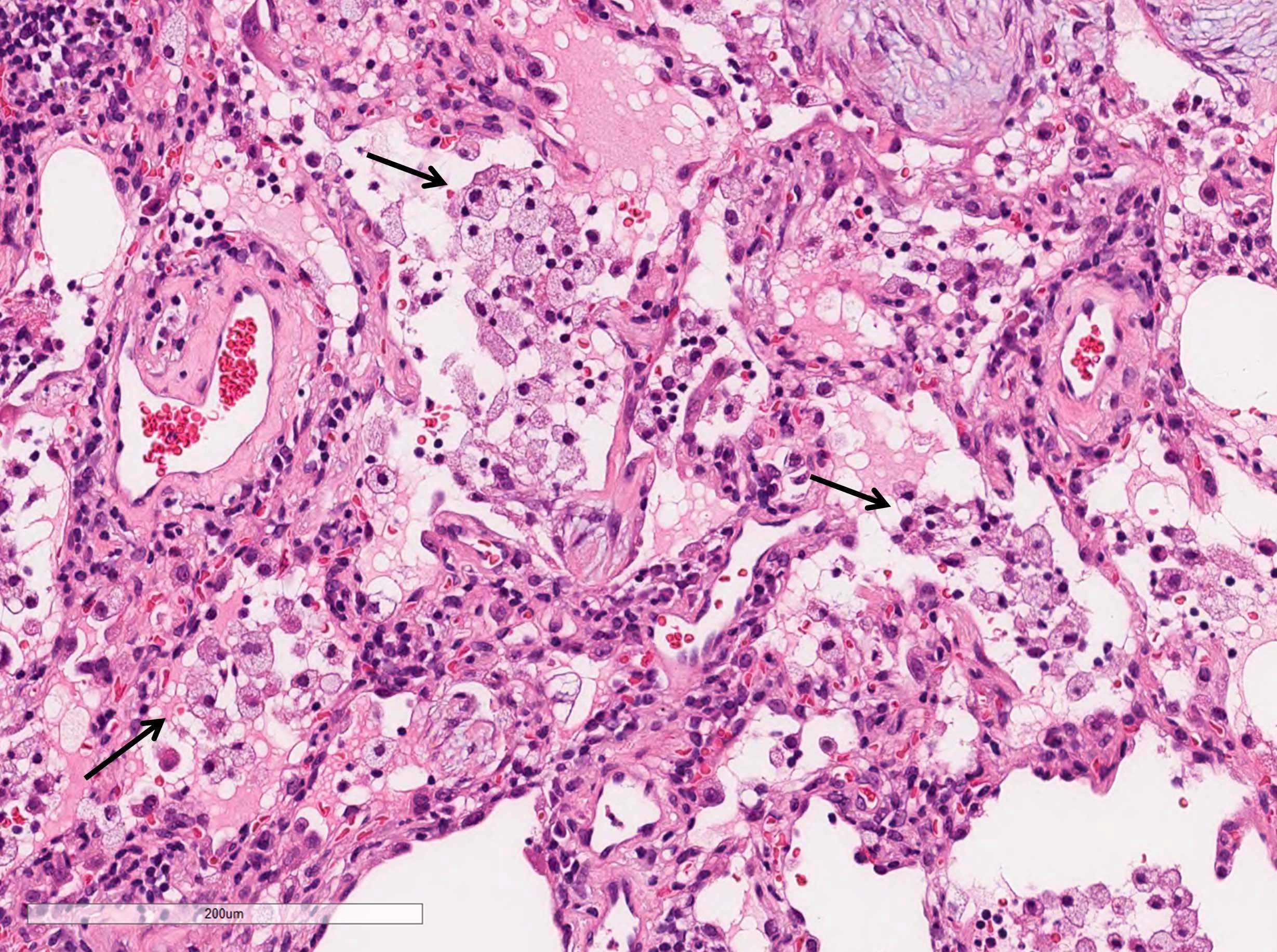
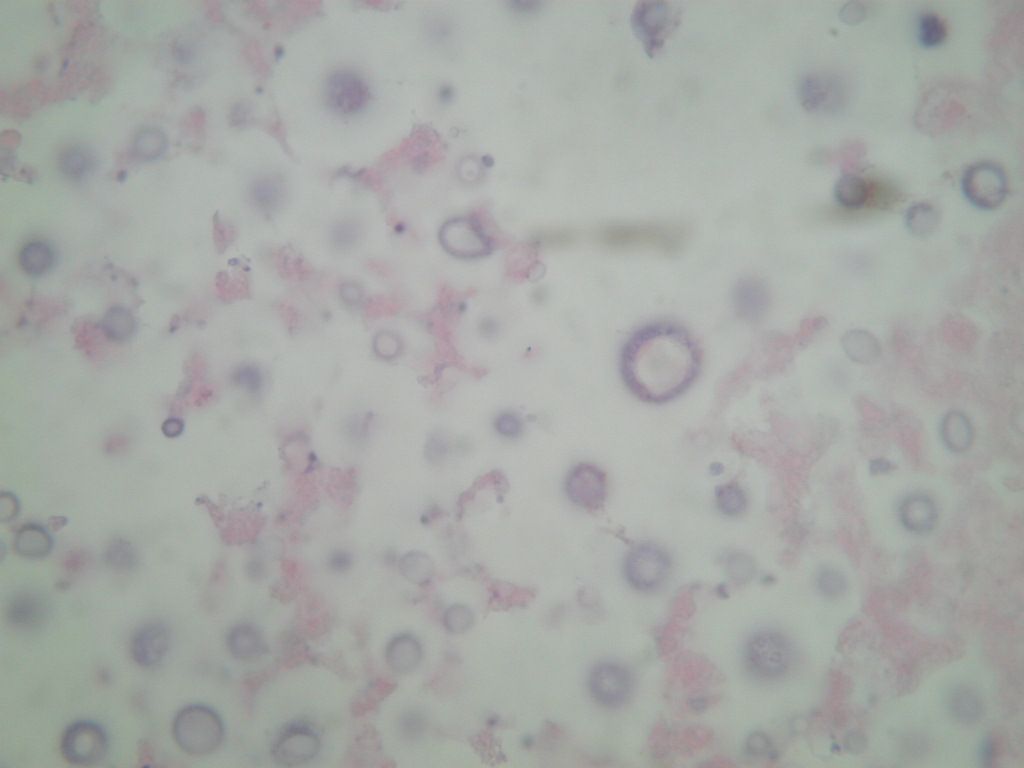
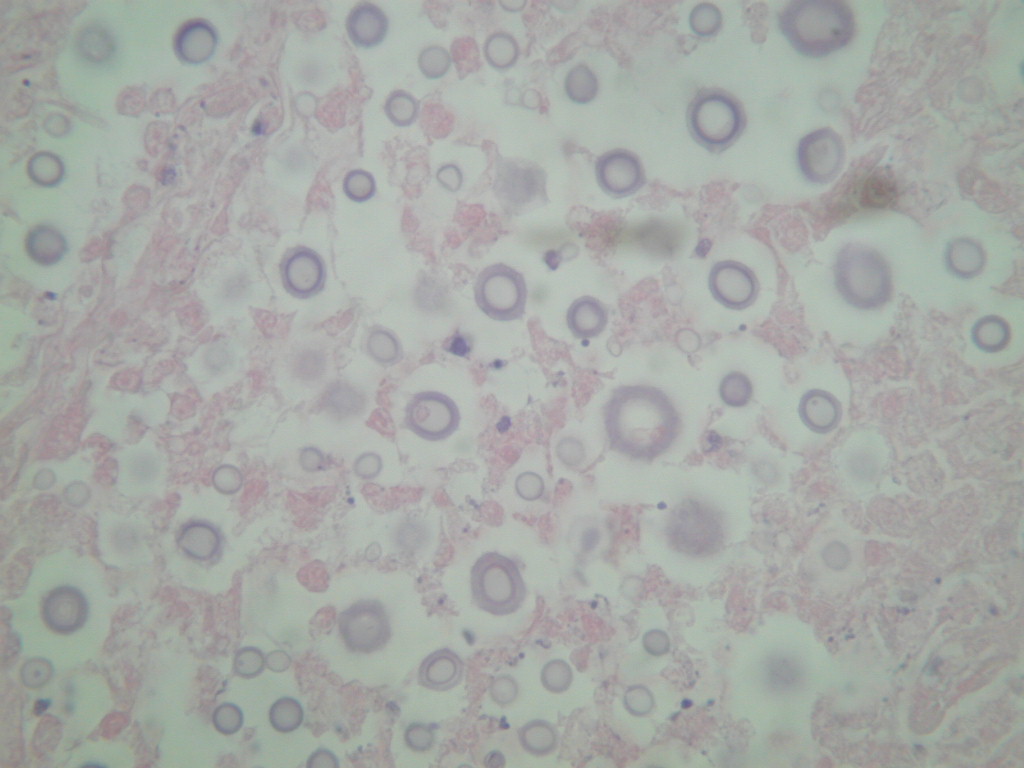
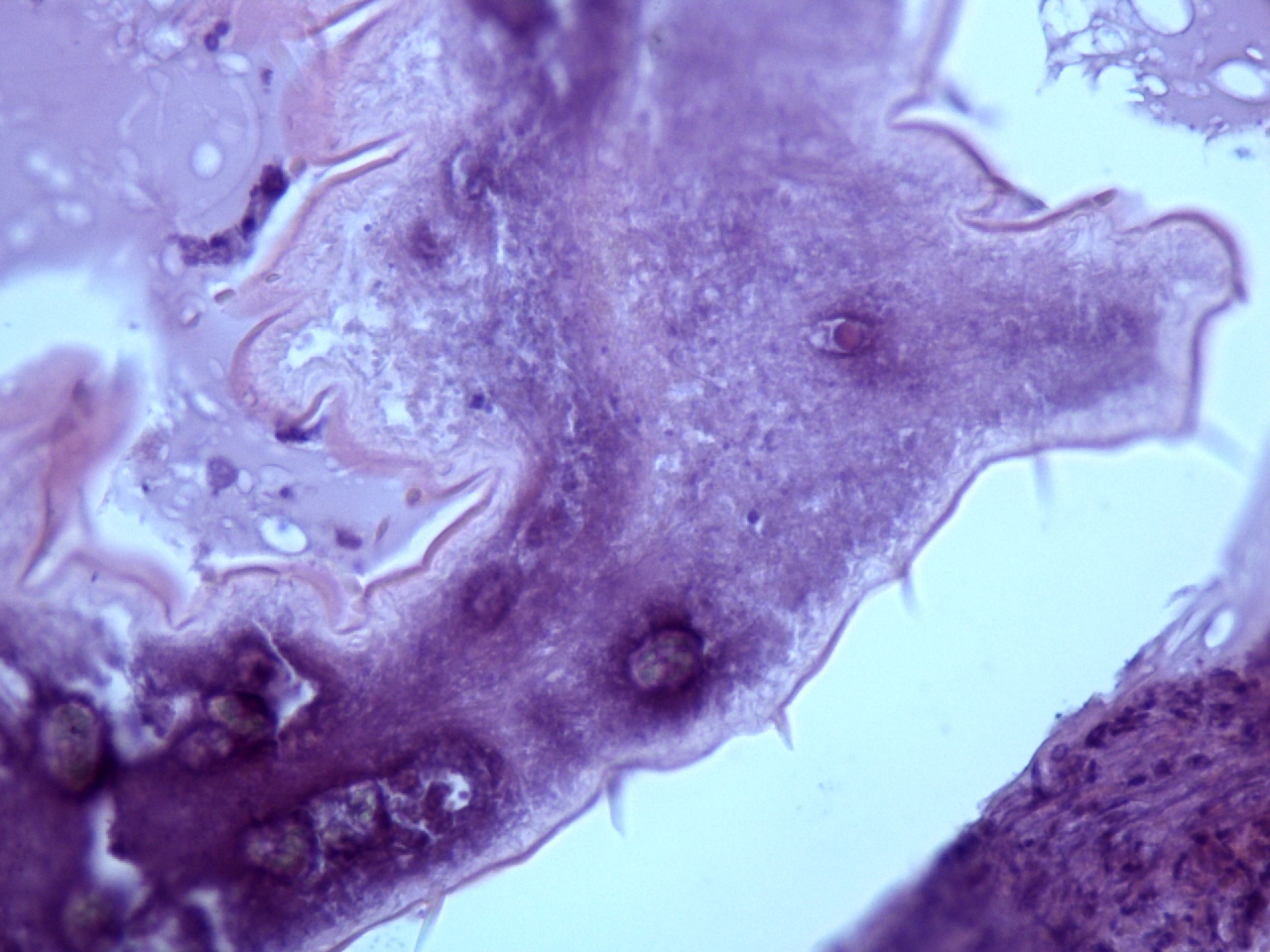
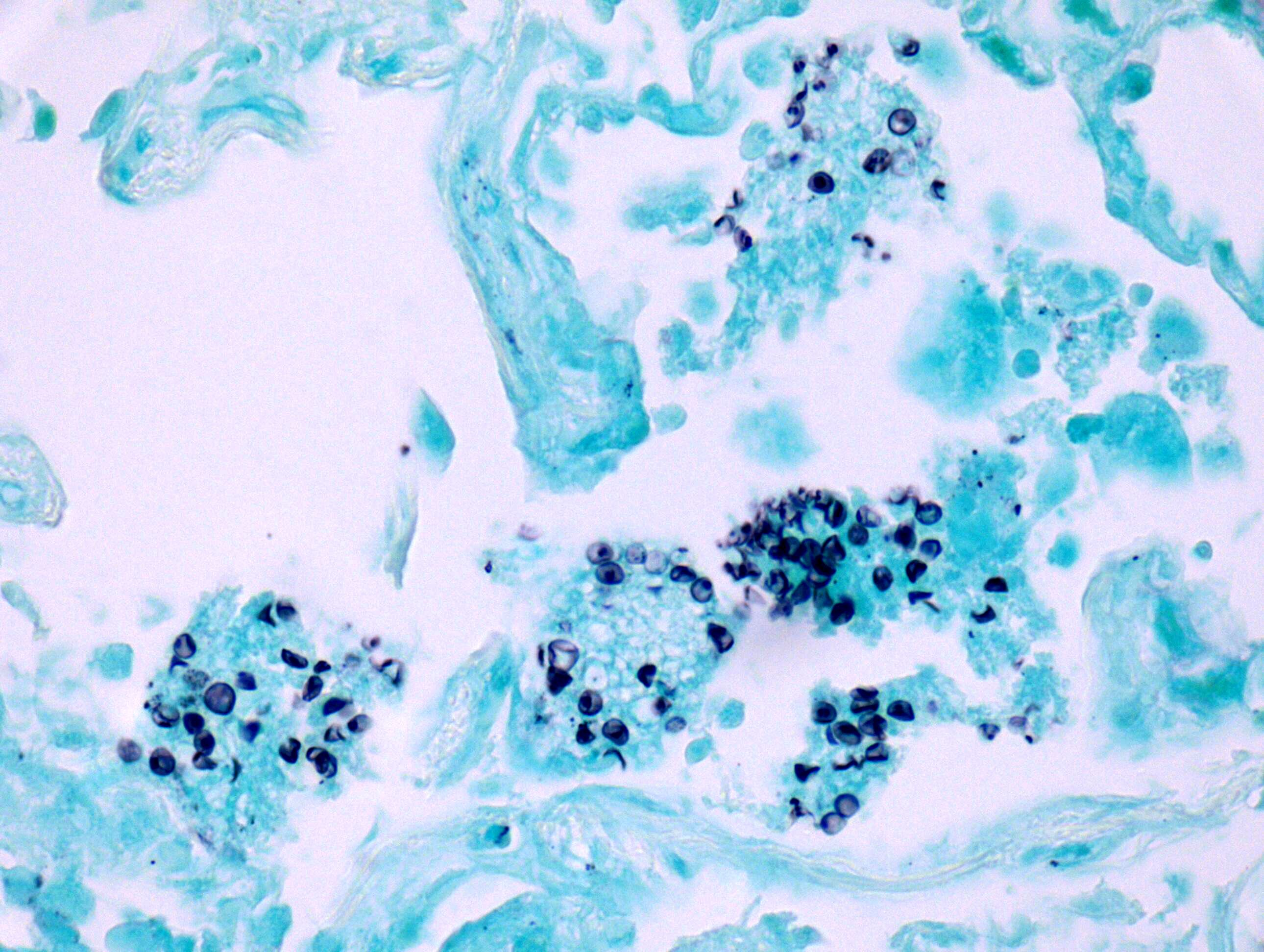
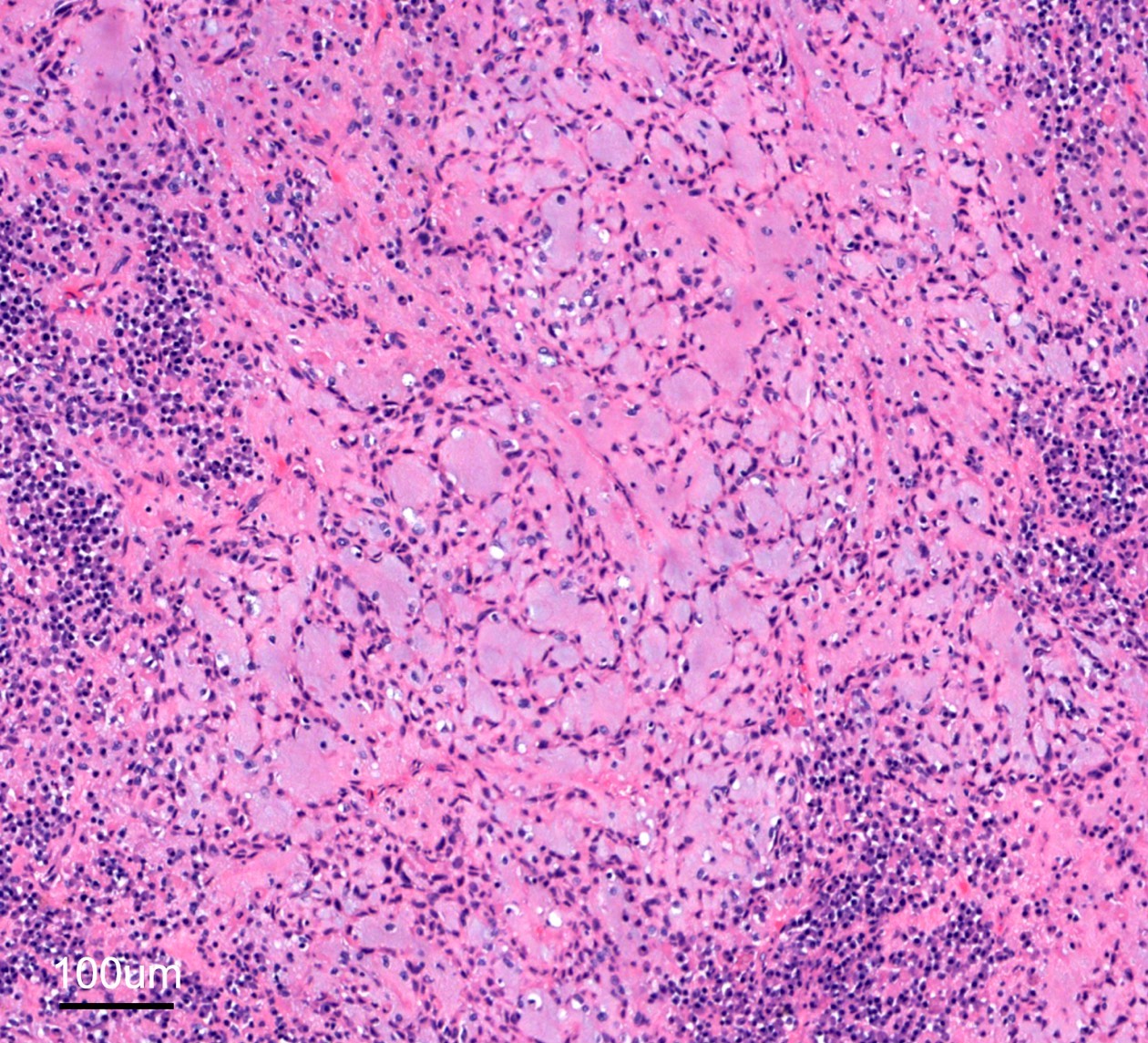
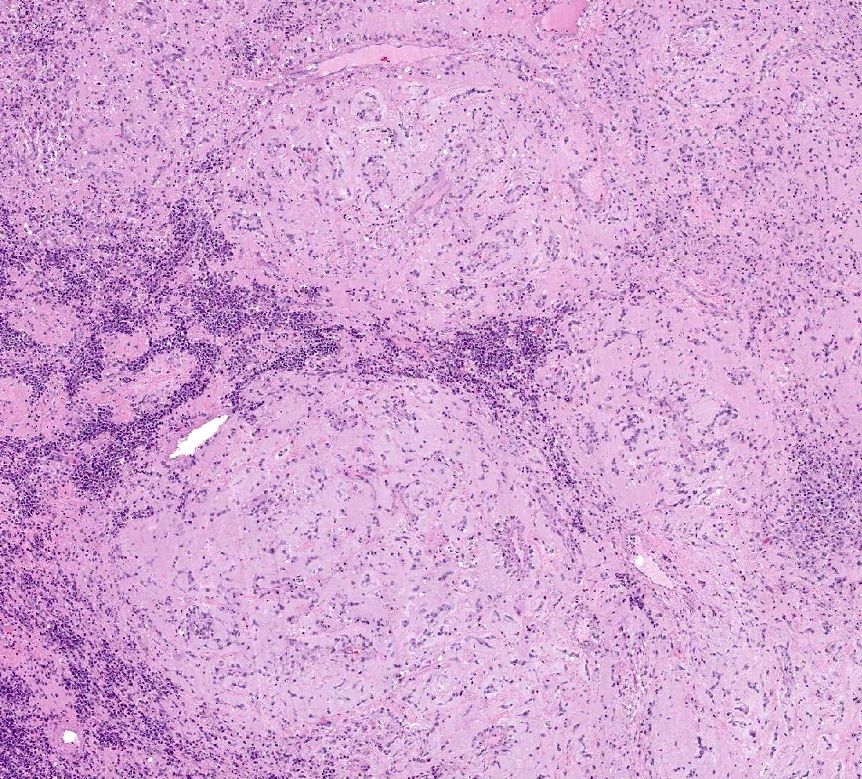
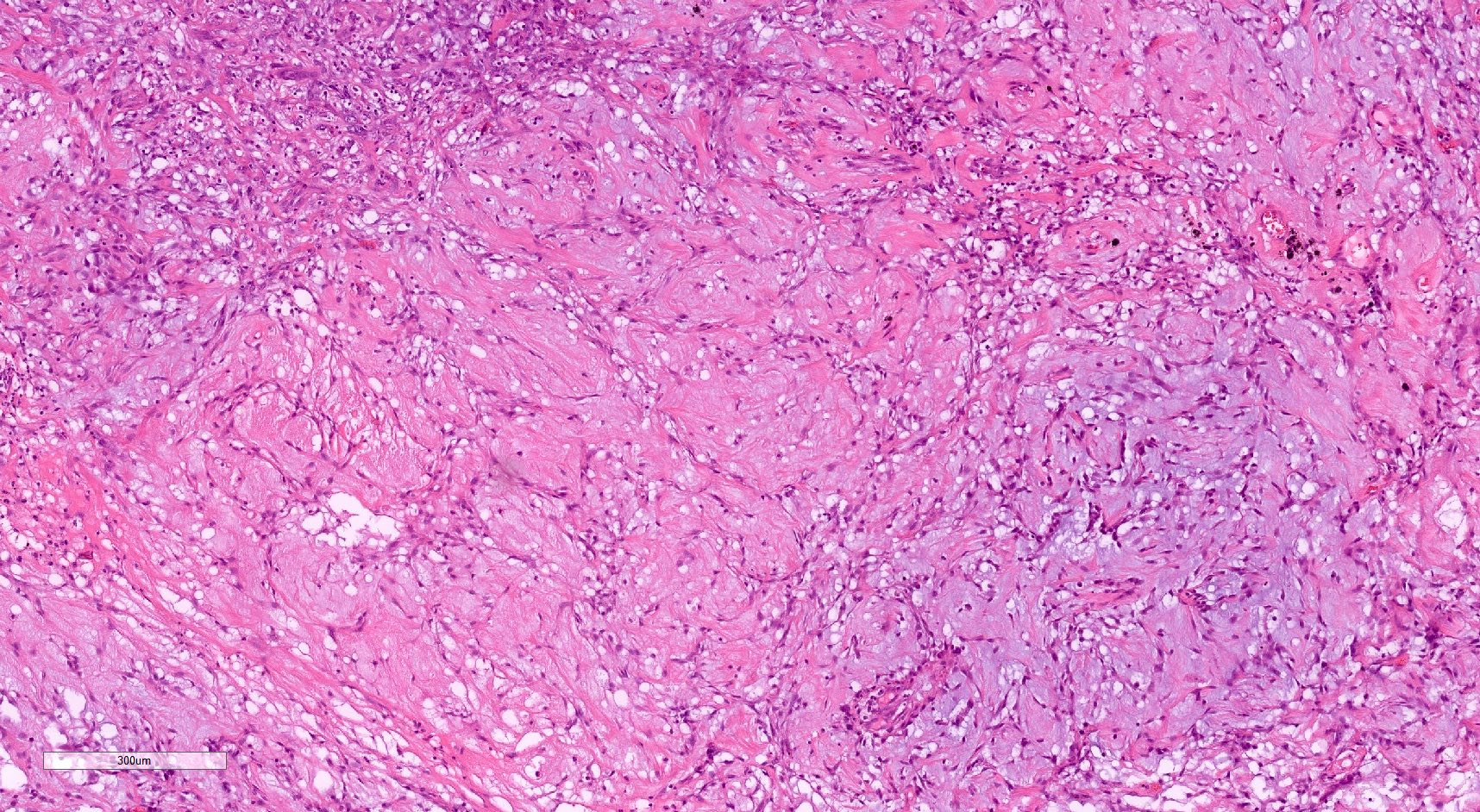
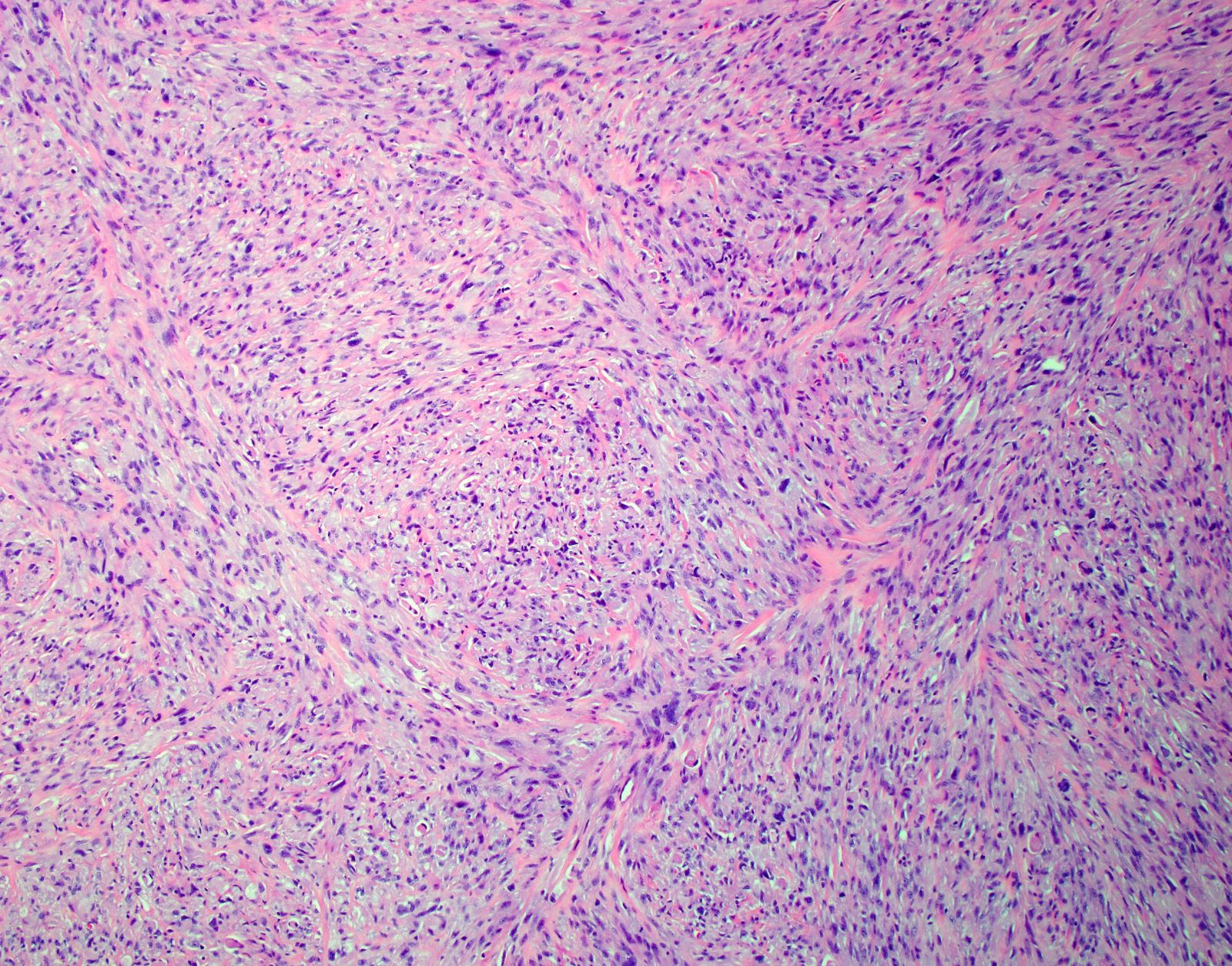
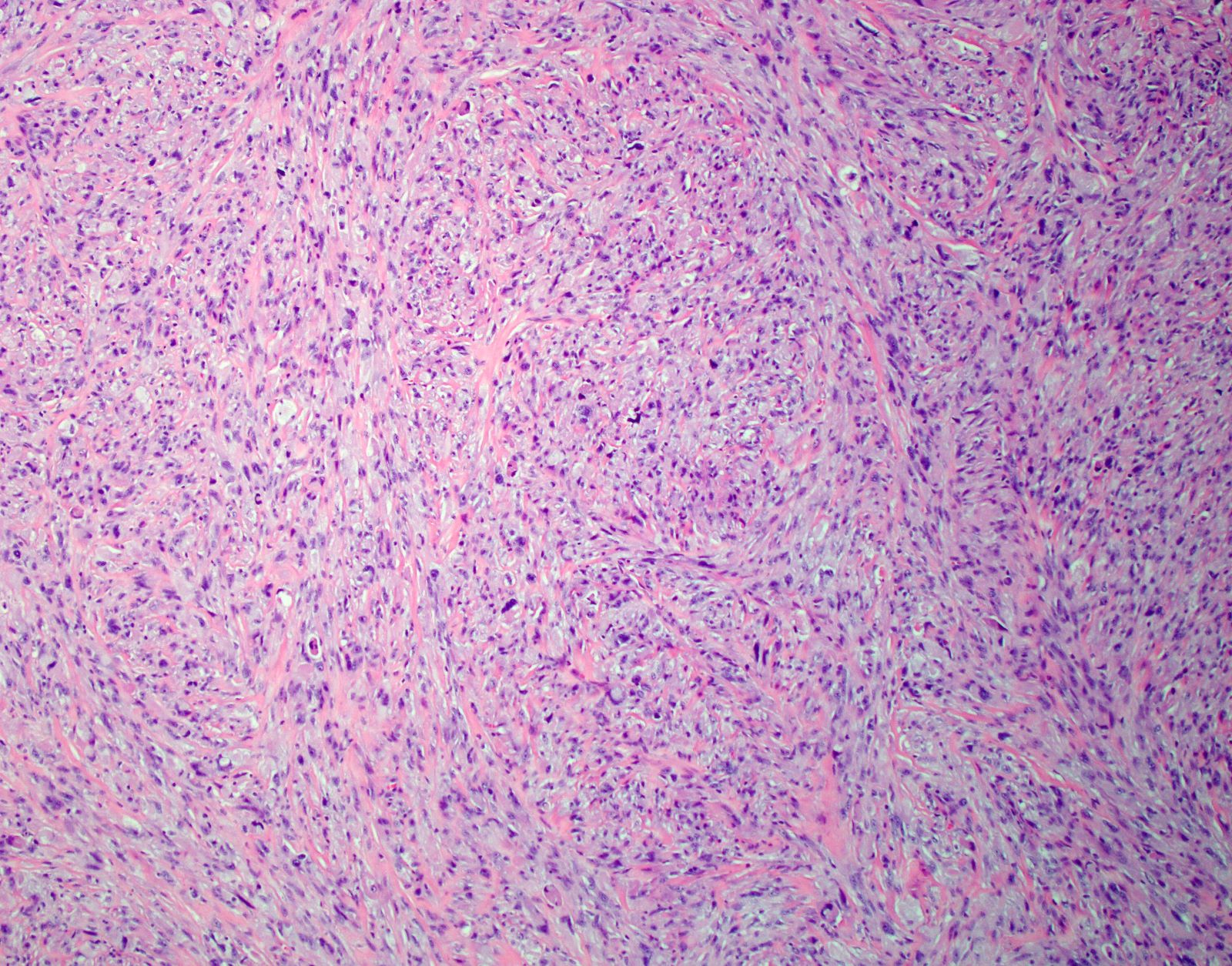
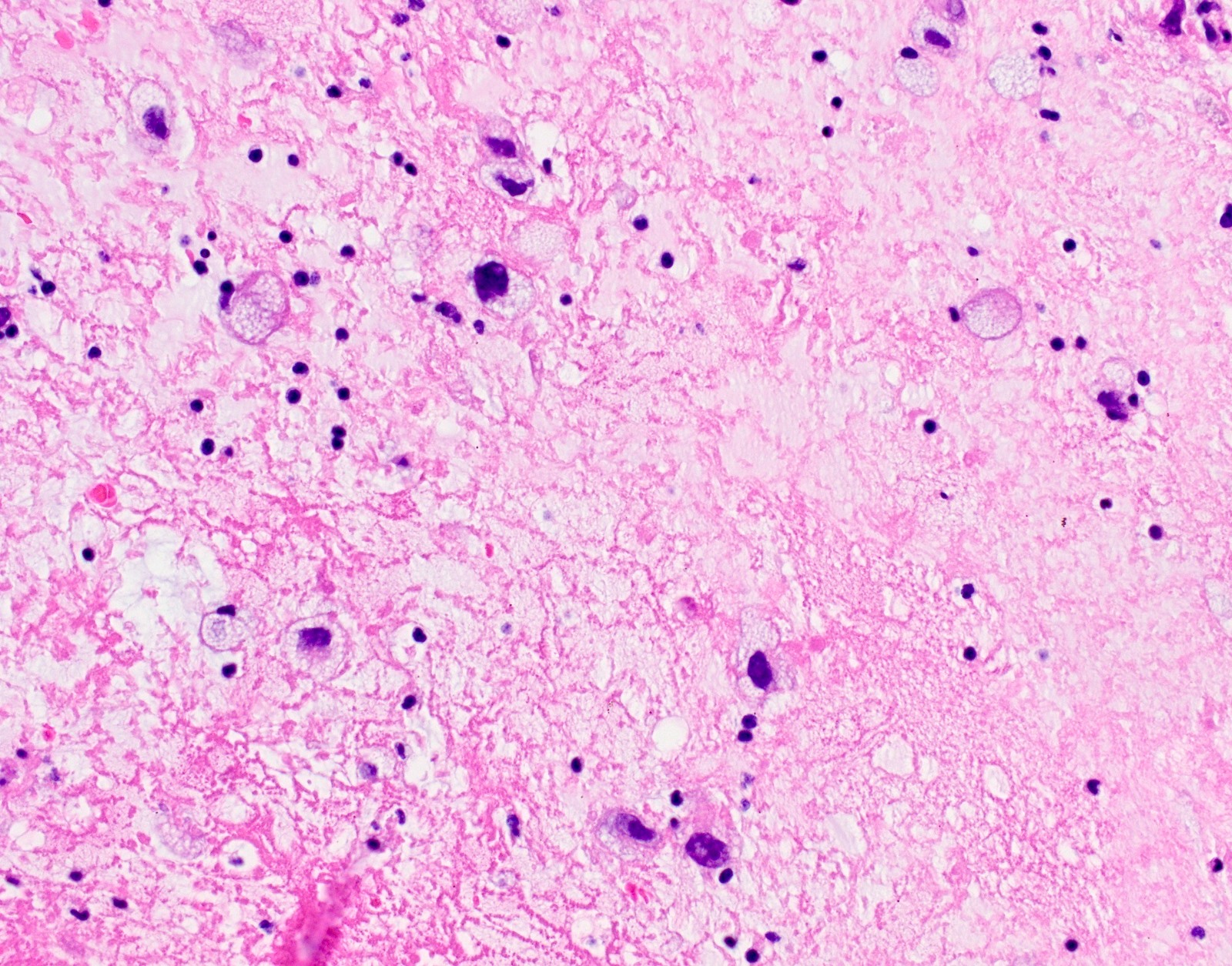
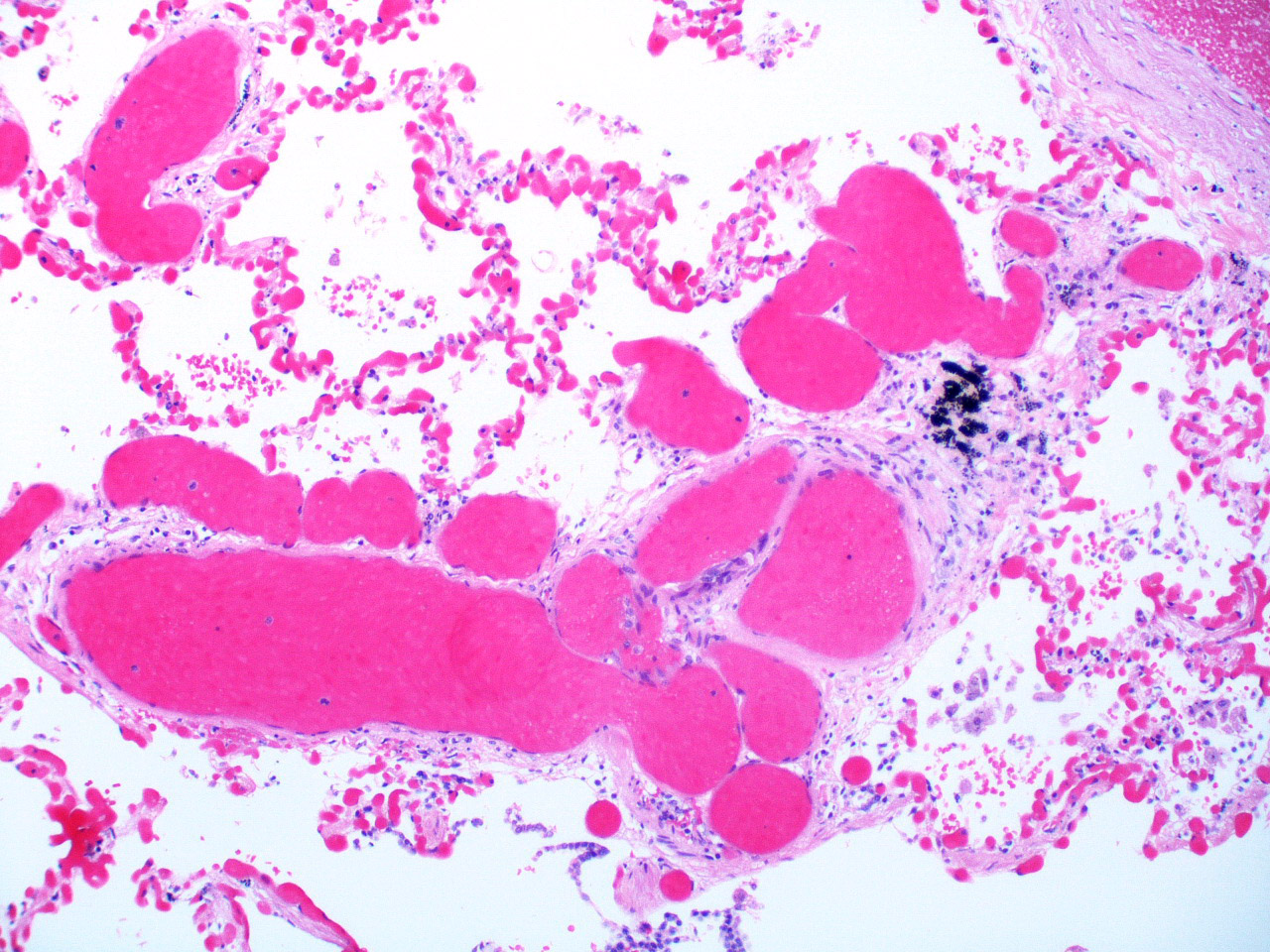
- Dominant findings of intra-alveolar fibrin, so called "fibrin ball"
- Involves more than 20% of the alveolar spaces in the lesion
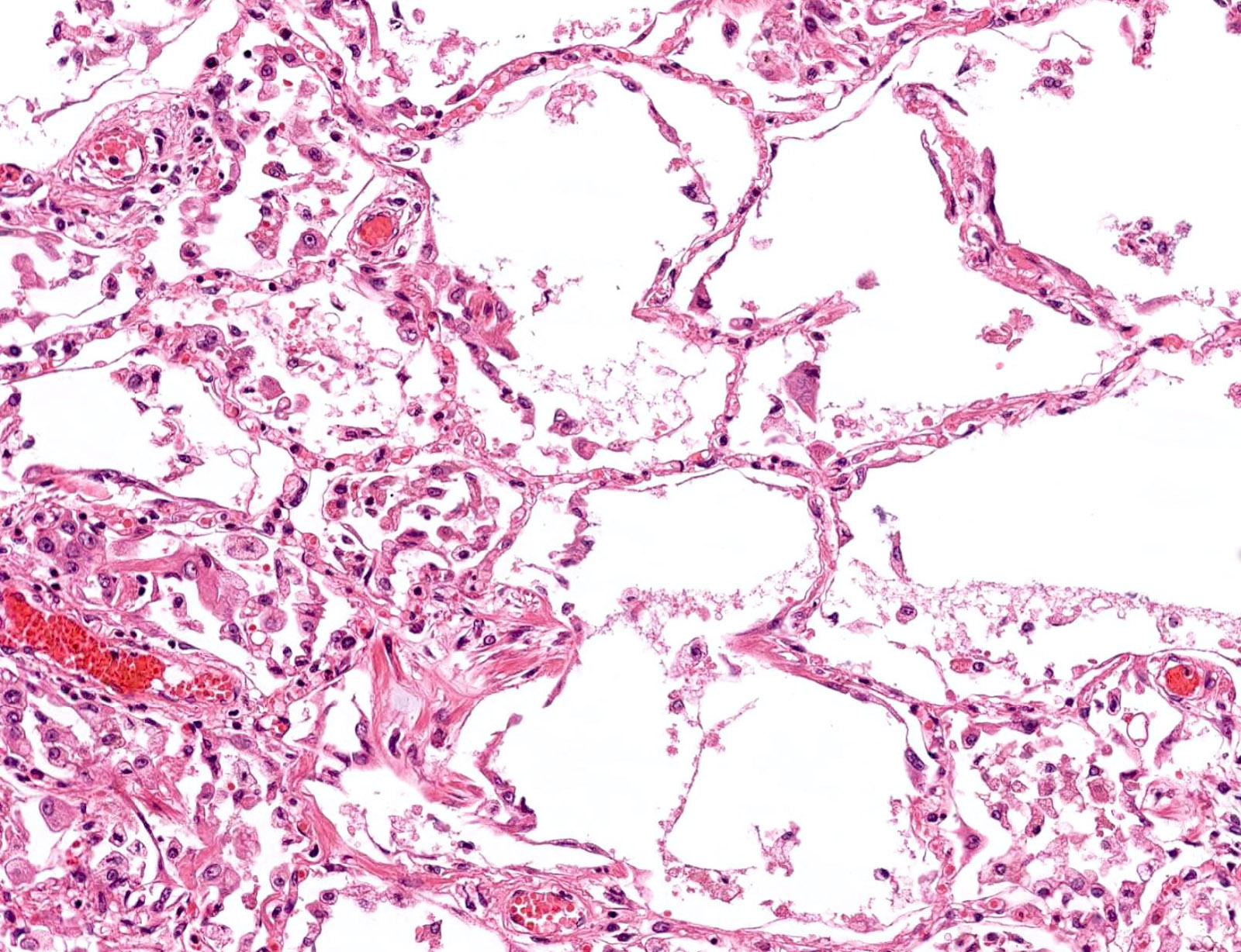
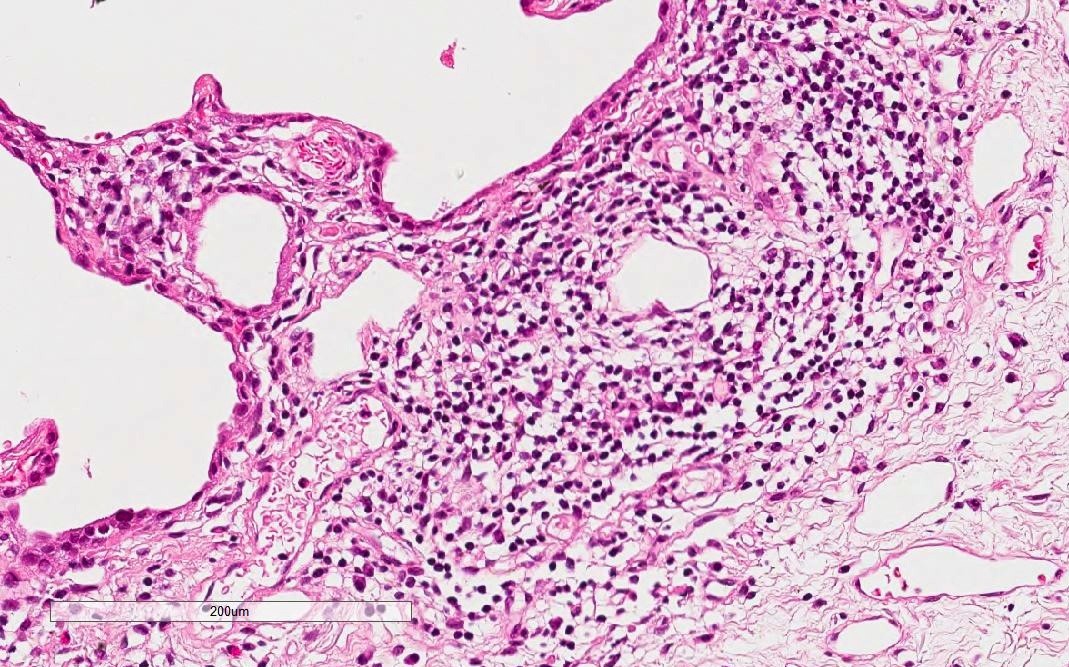
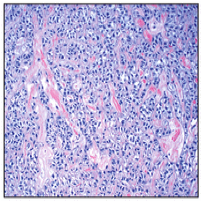
- Neutrophils are usually scanty or absent
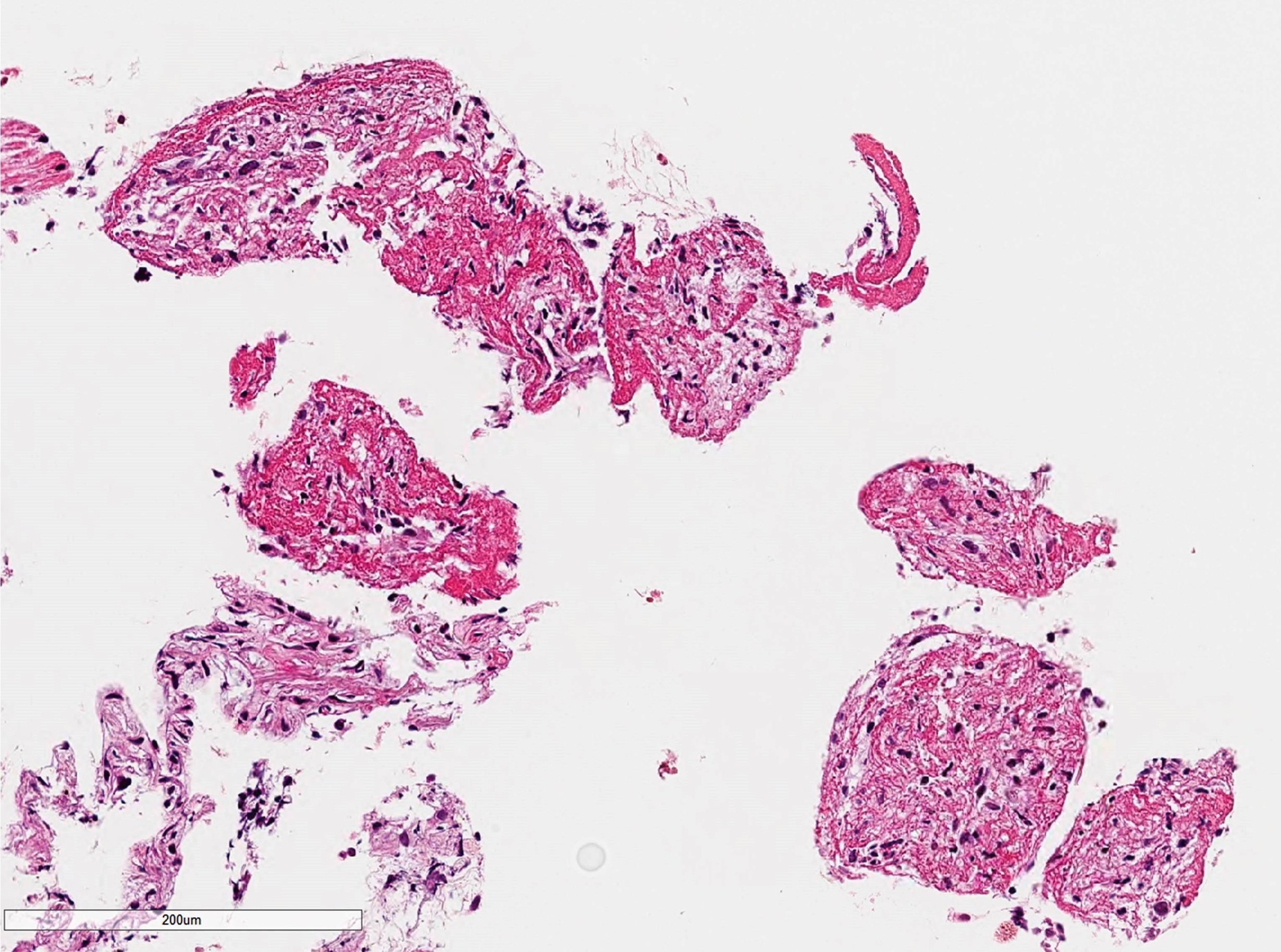
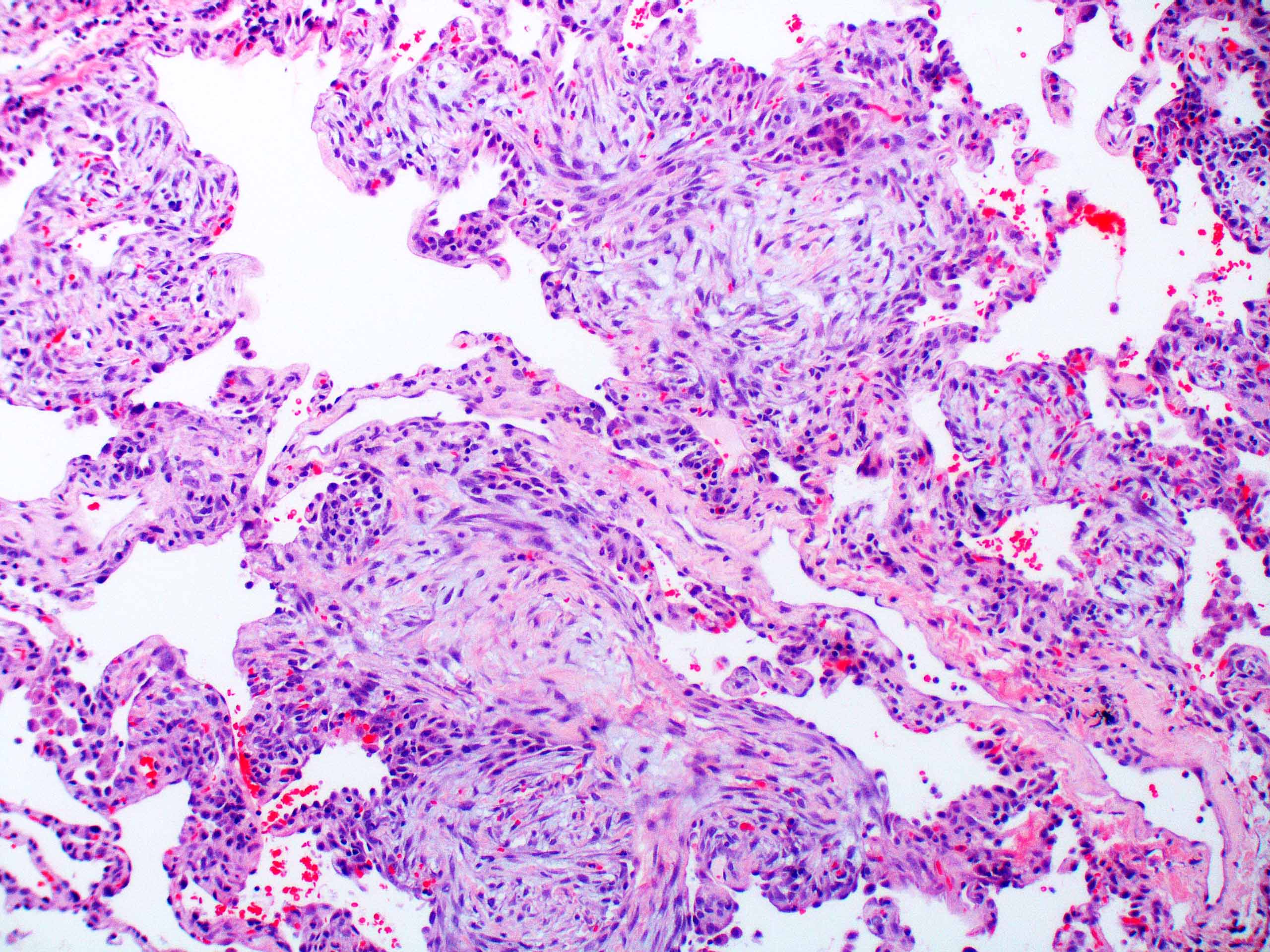
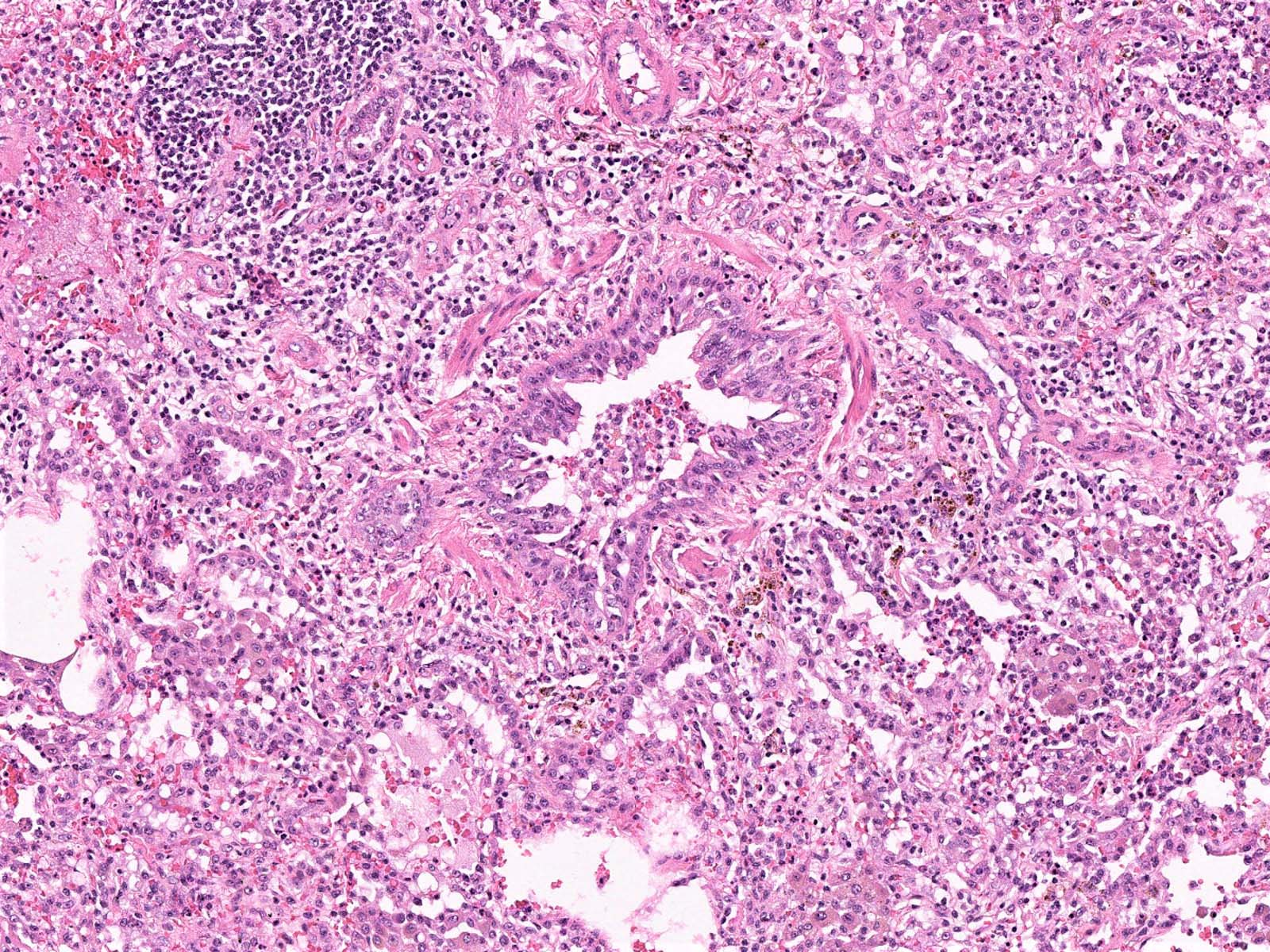
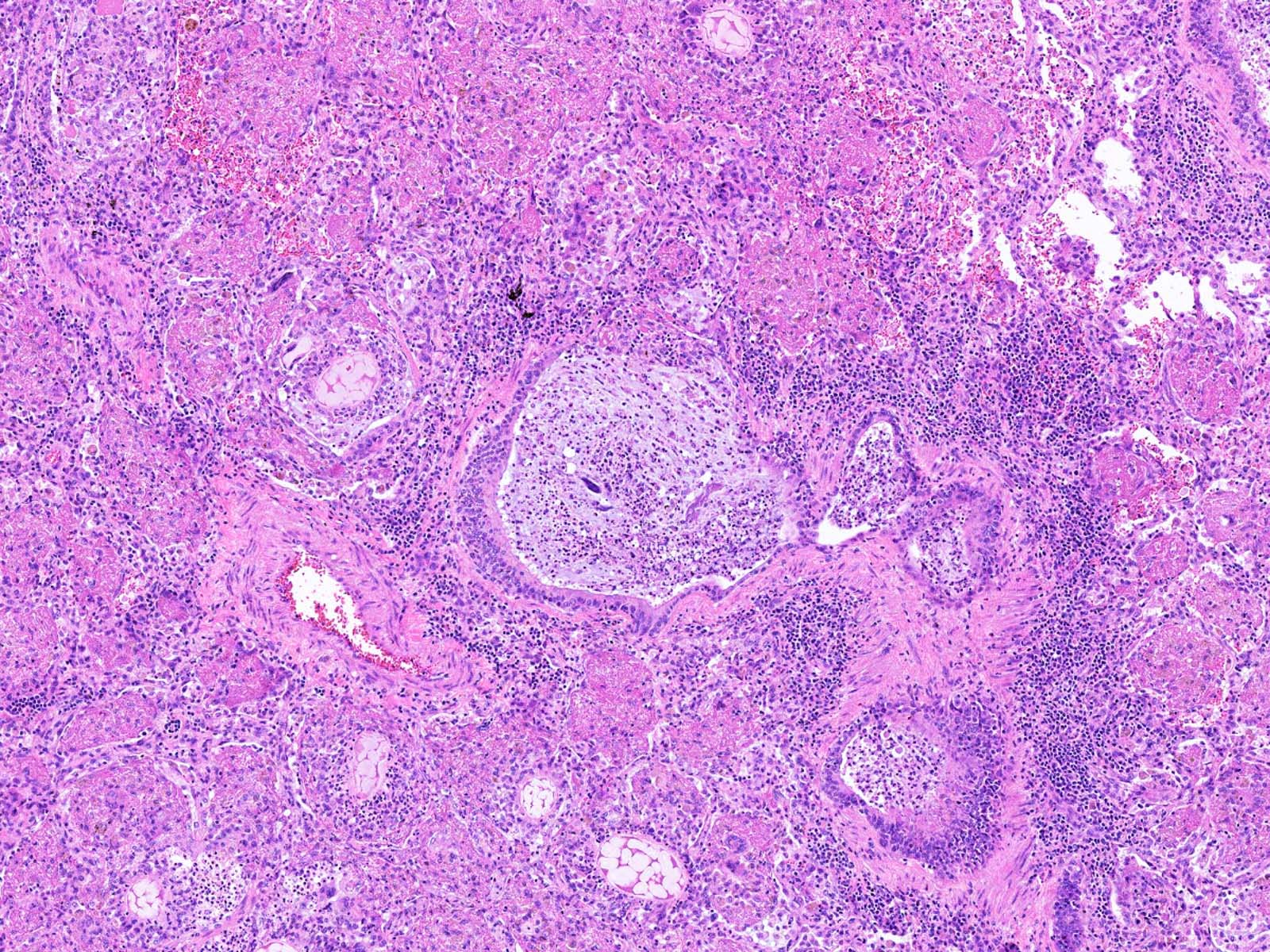
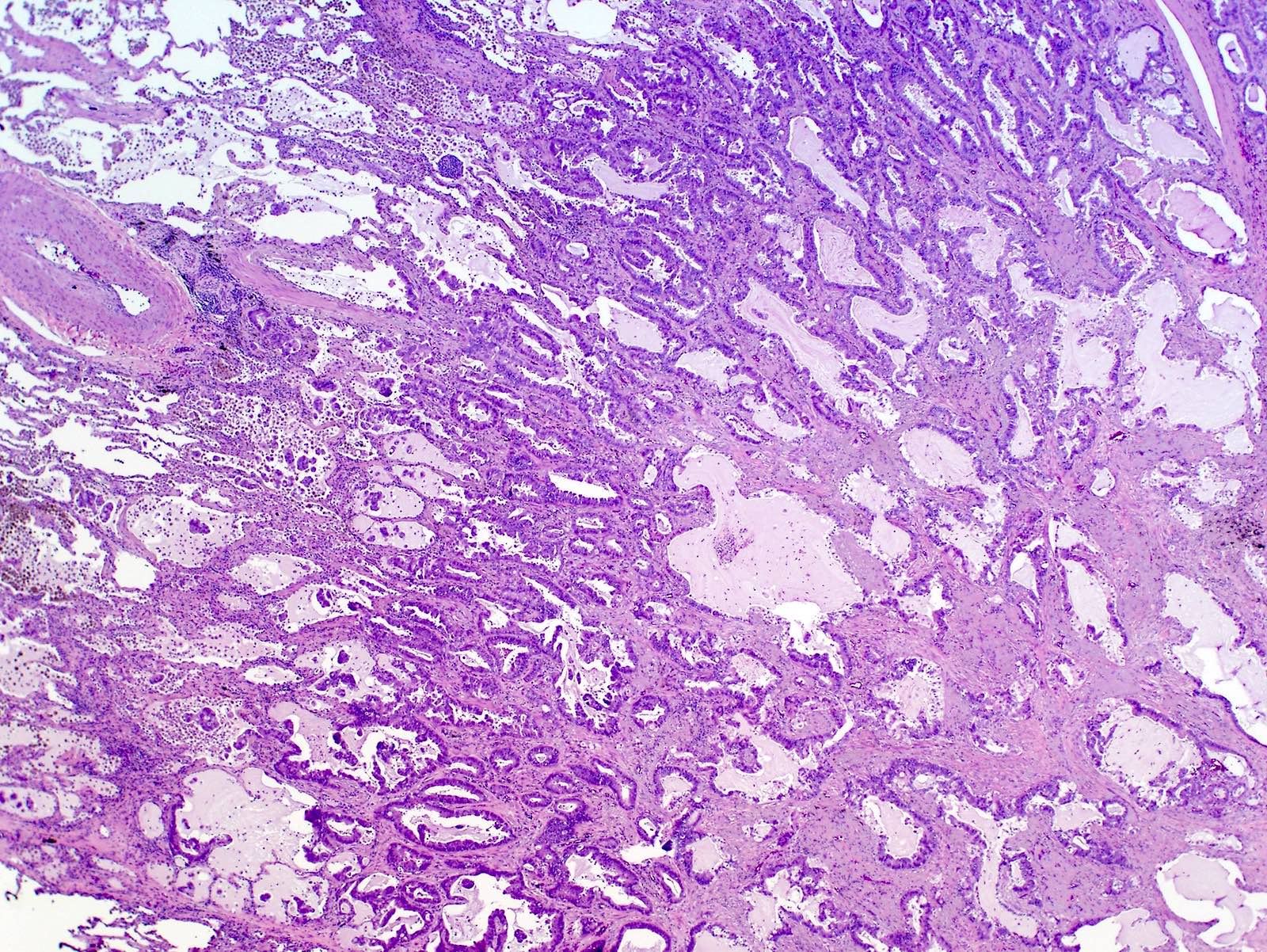
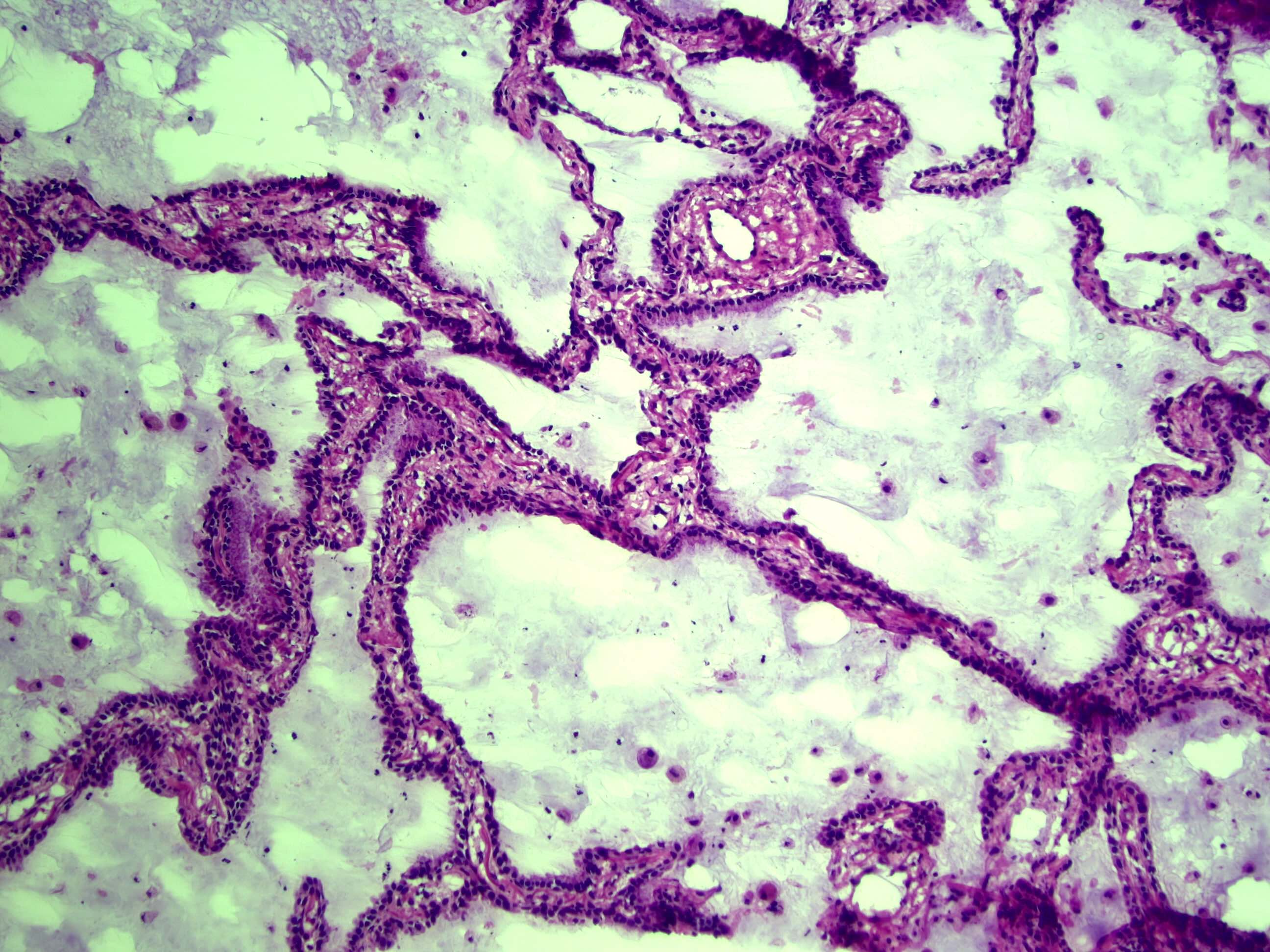
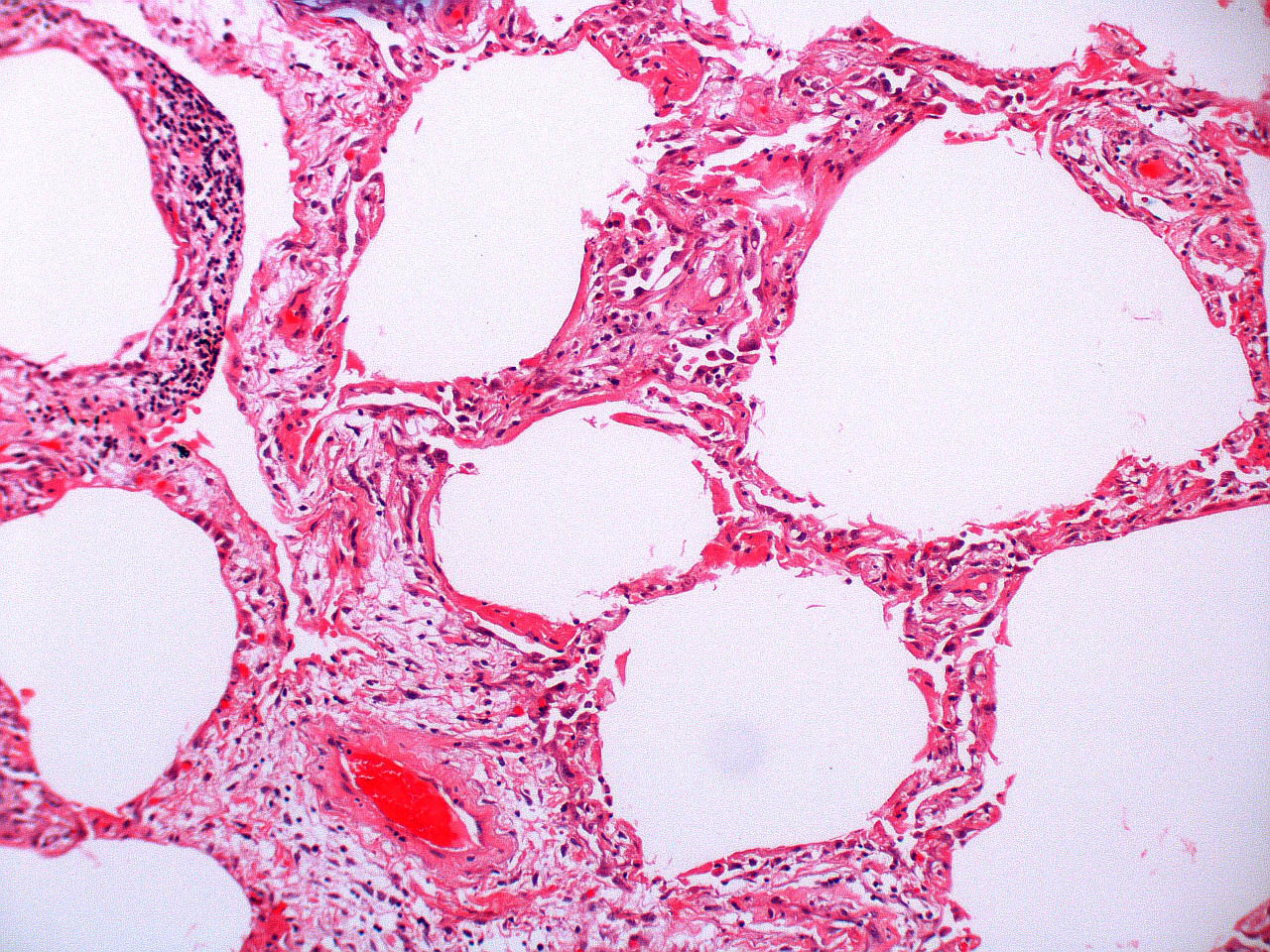
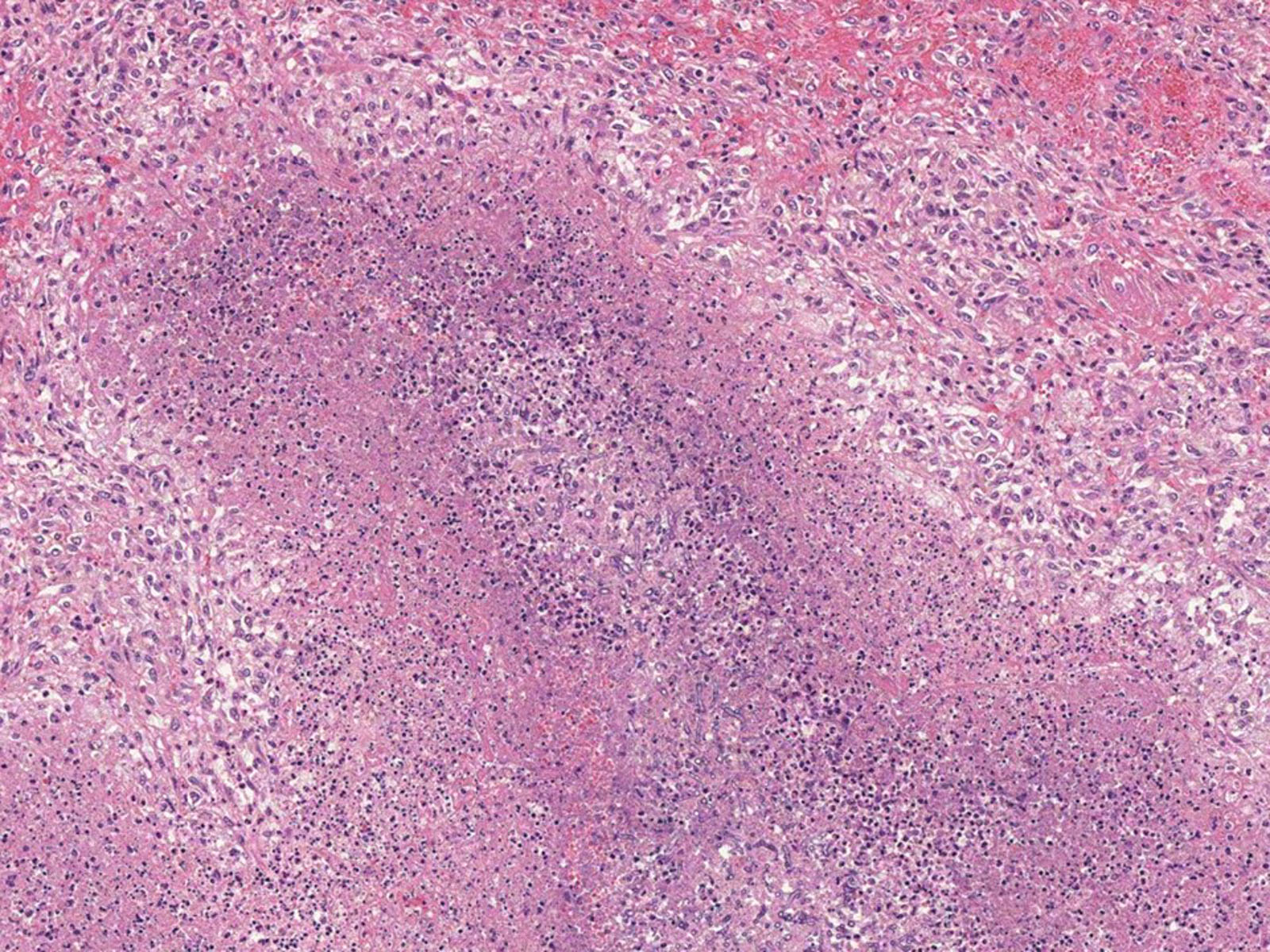
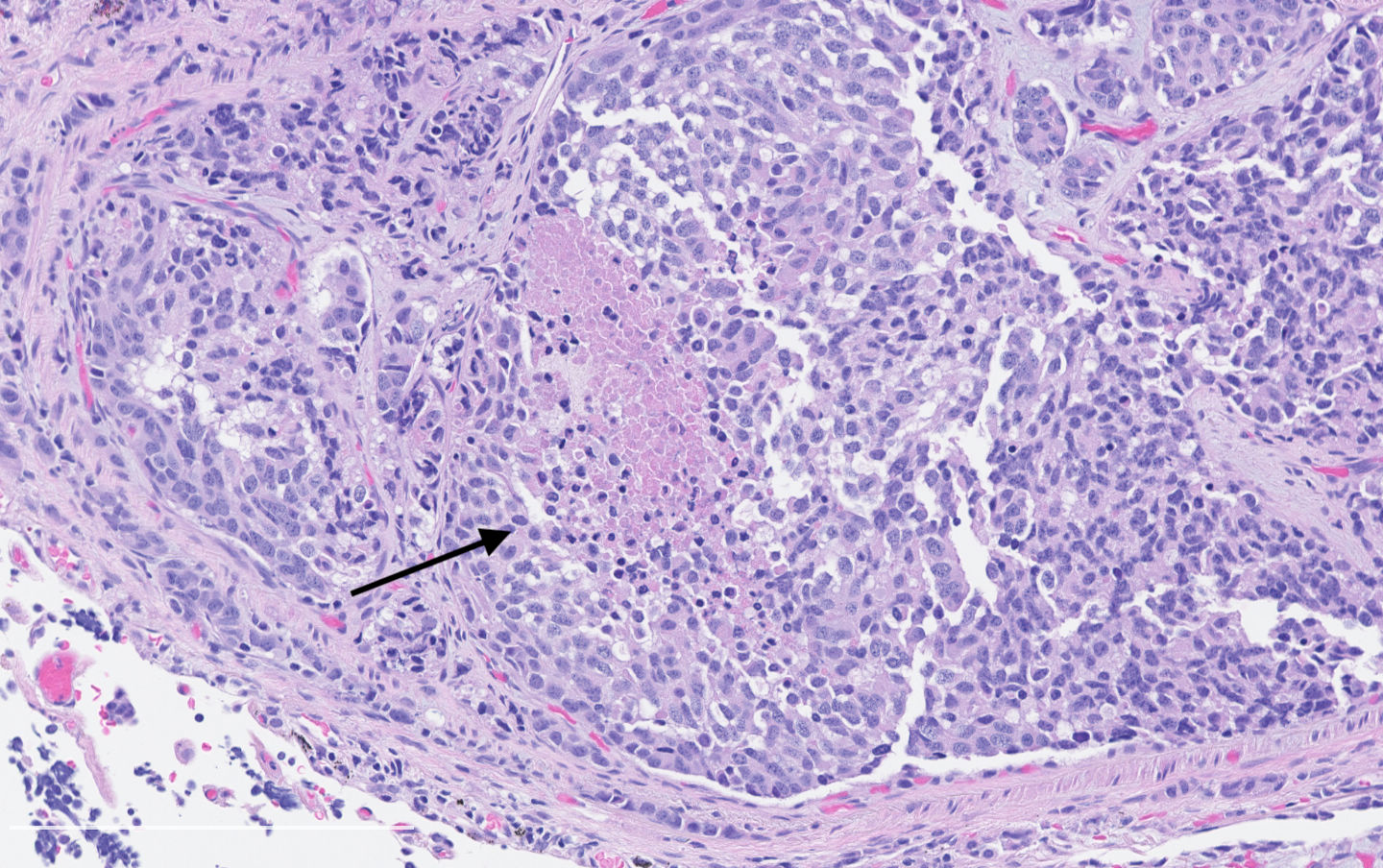
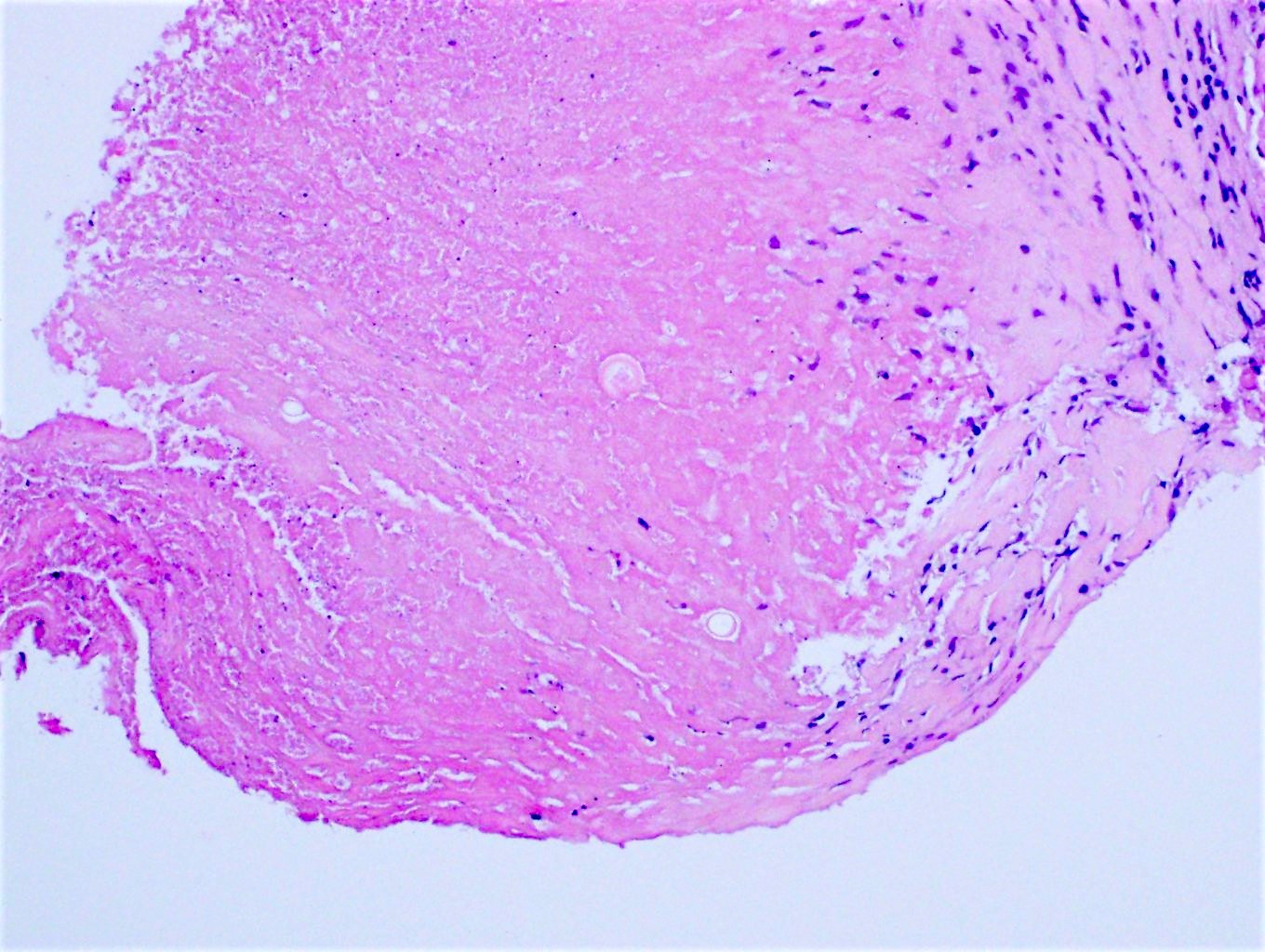
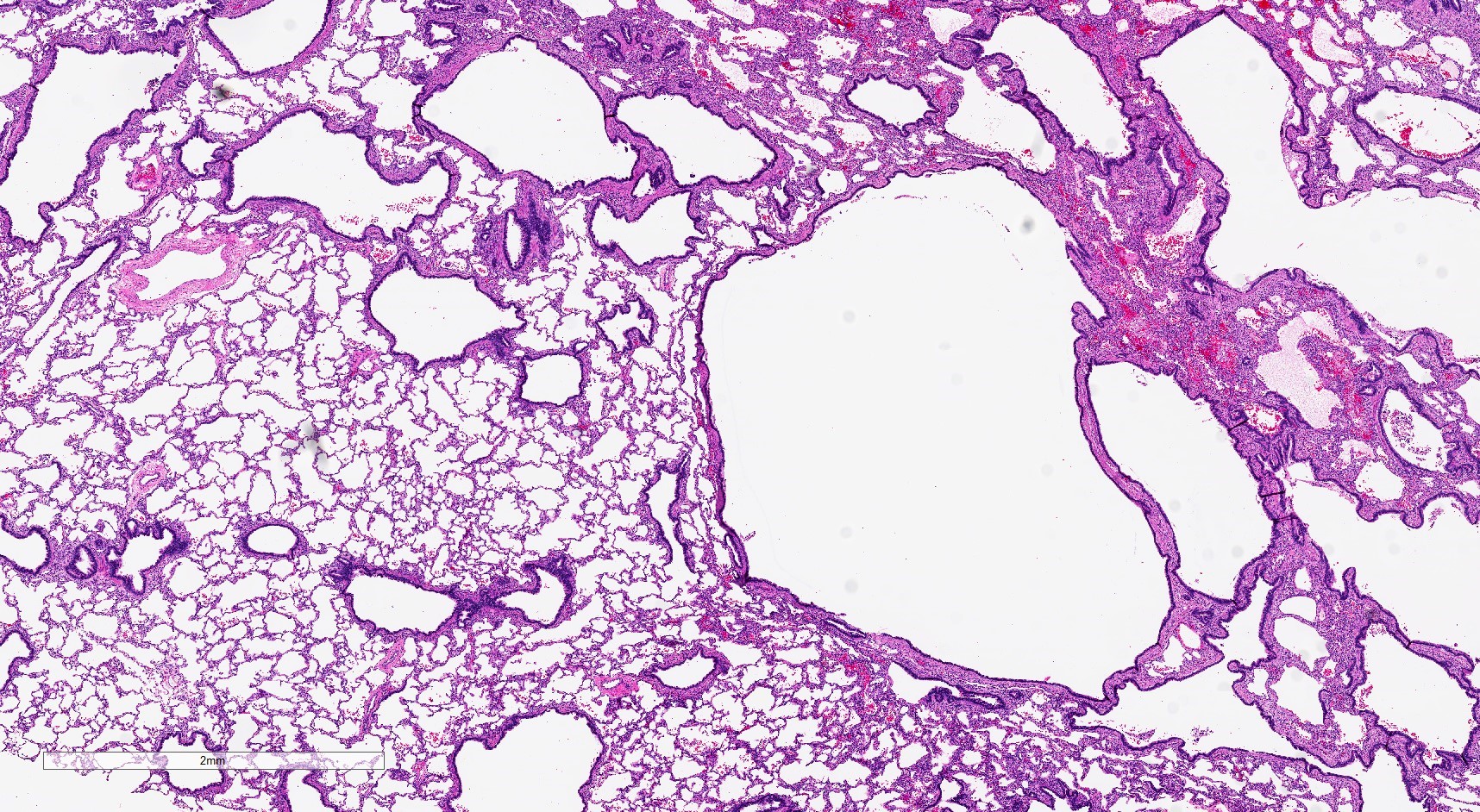
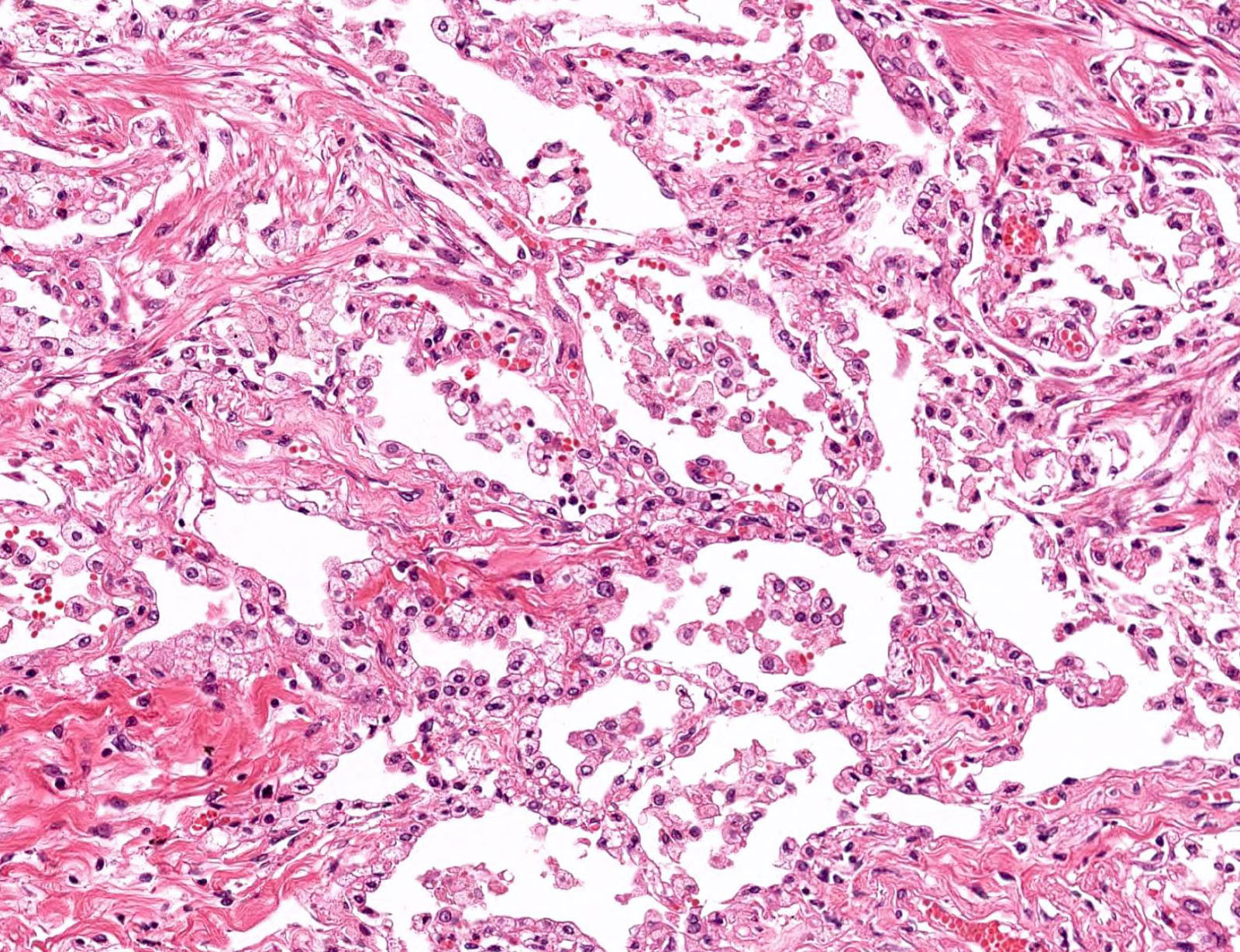
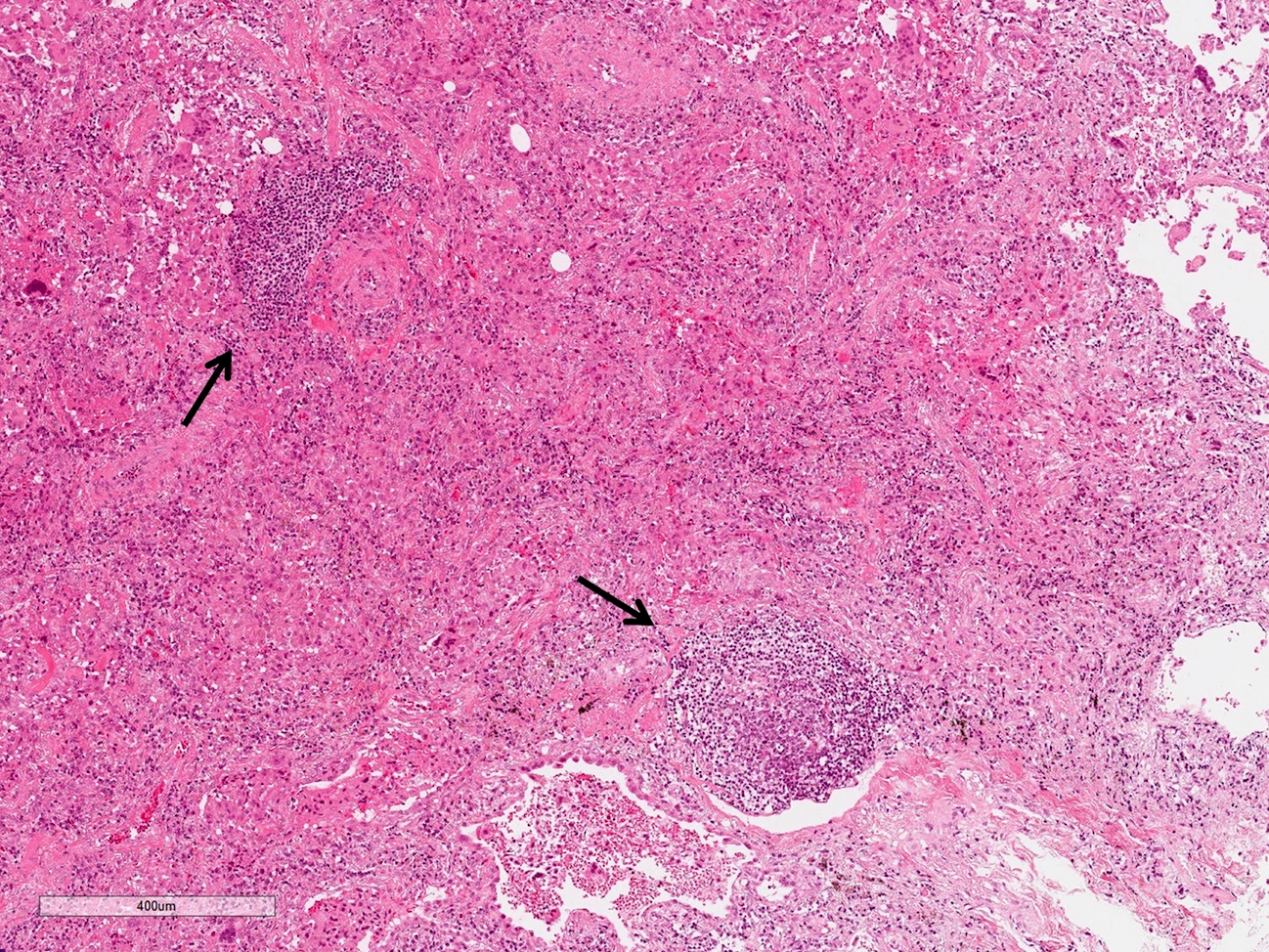
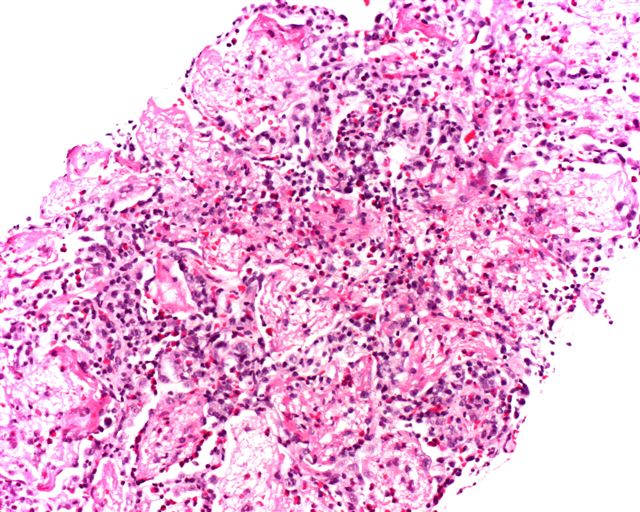
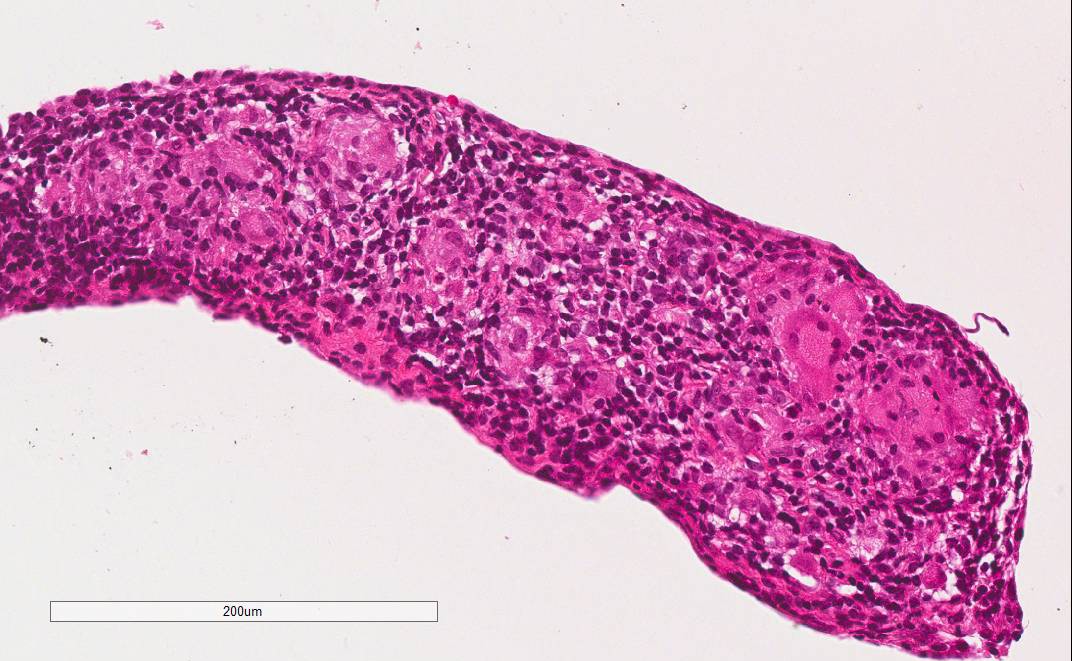
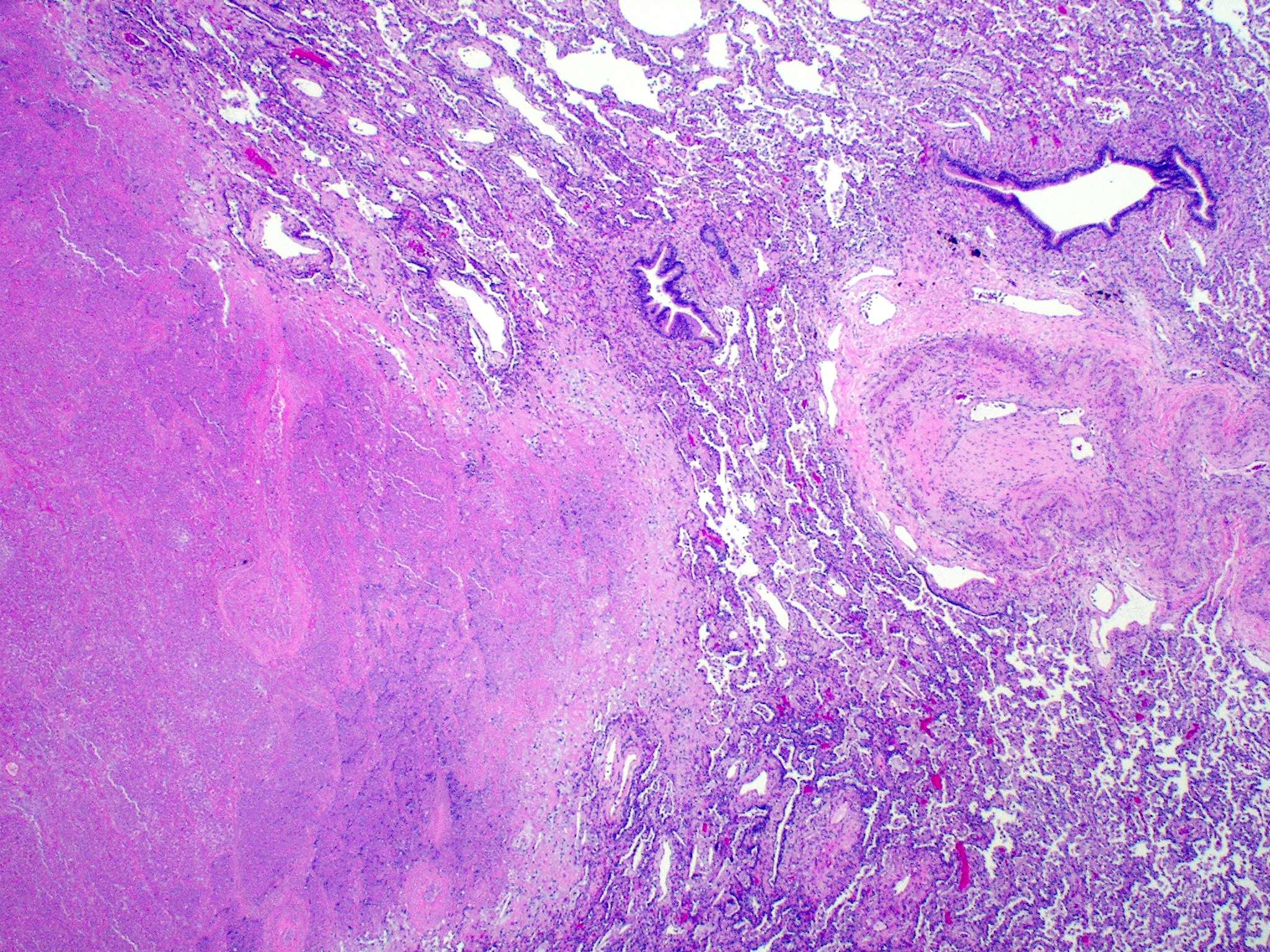
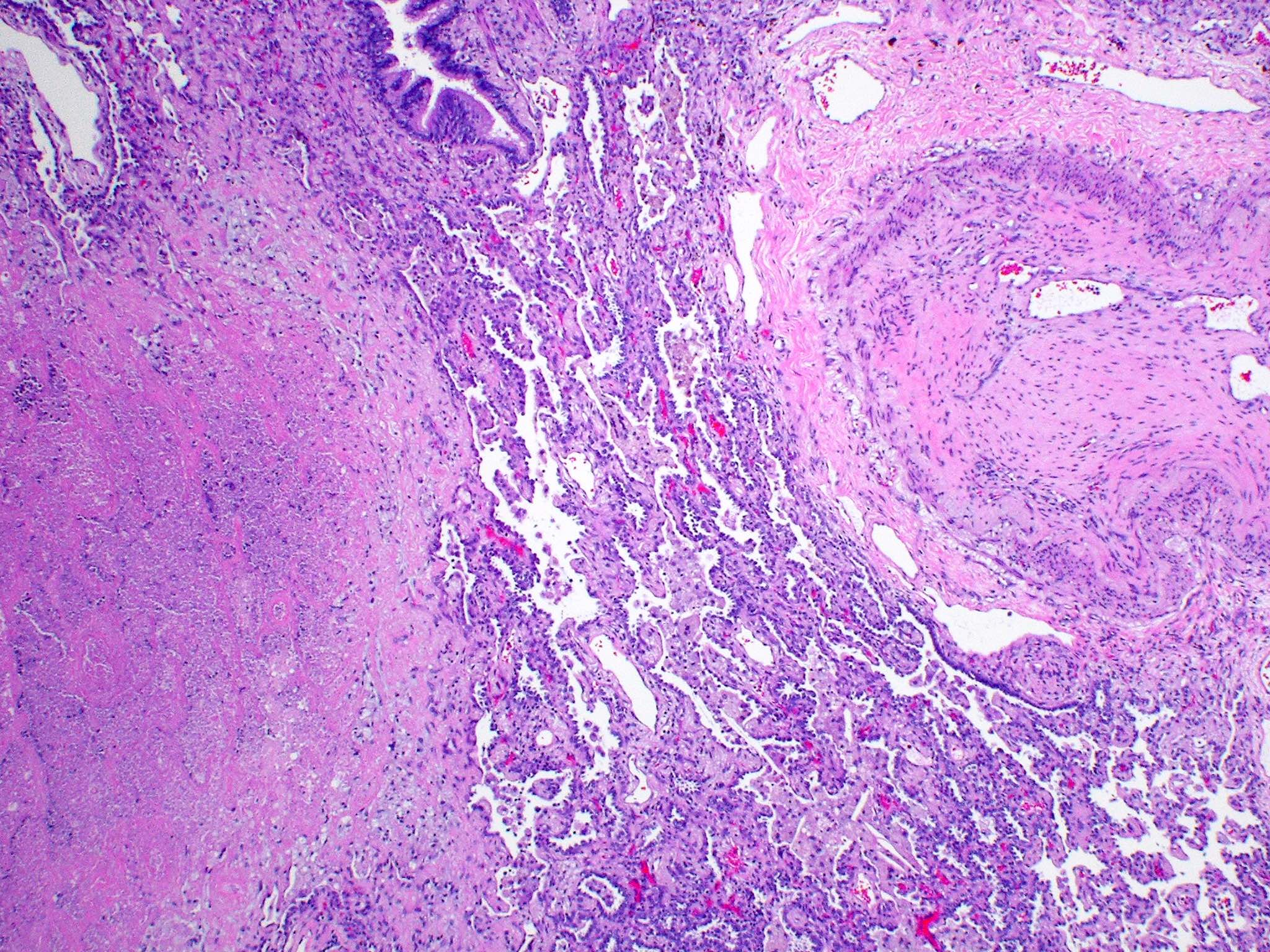
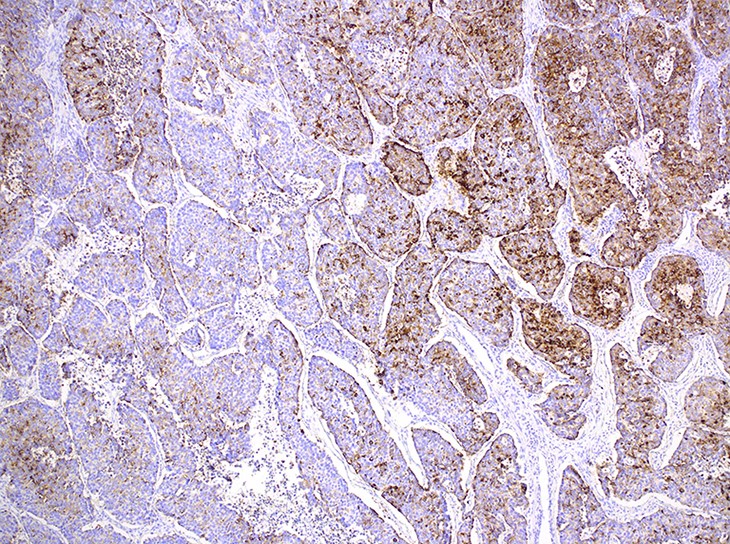
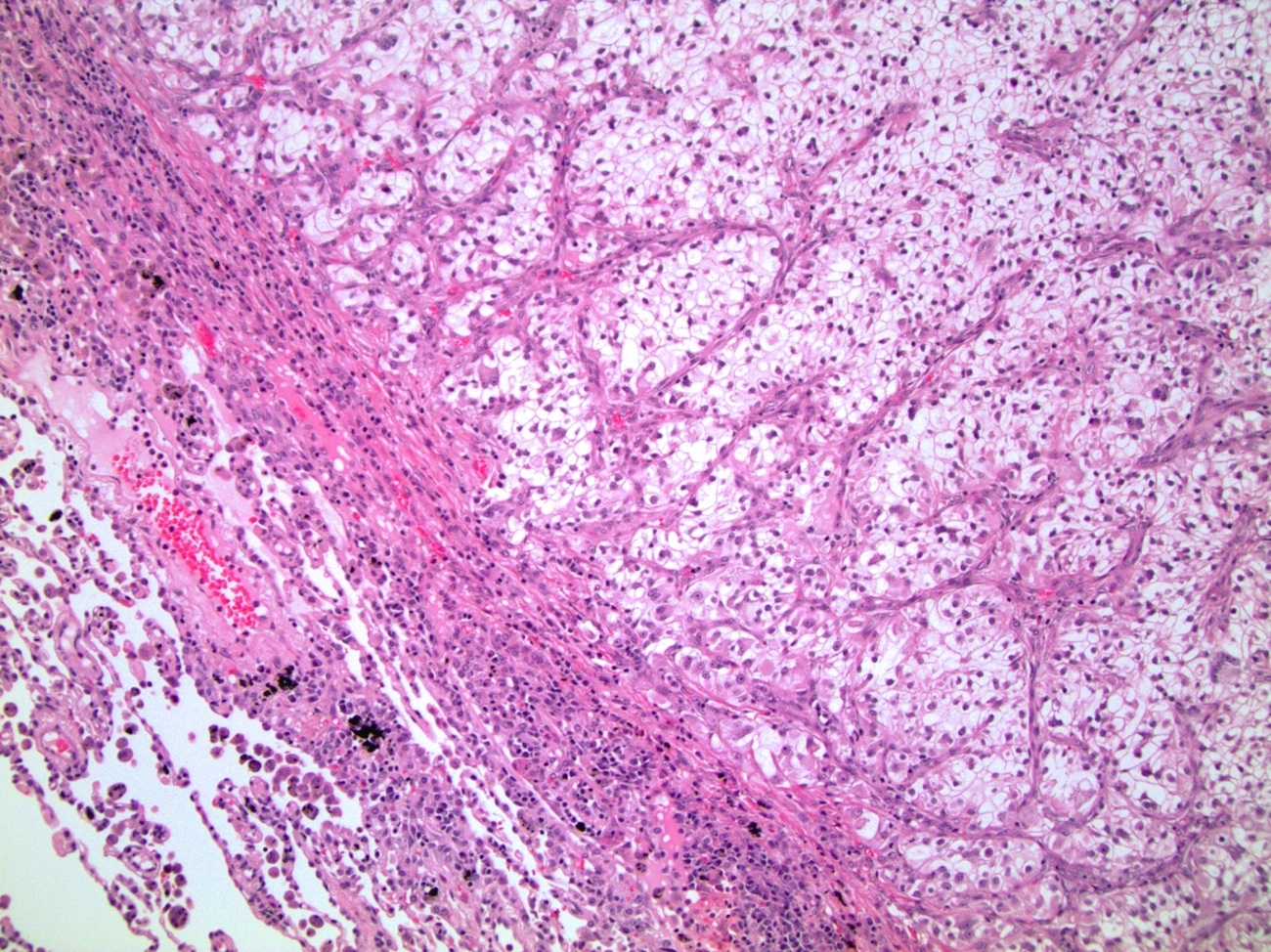
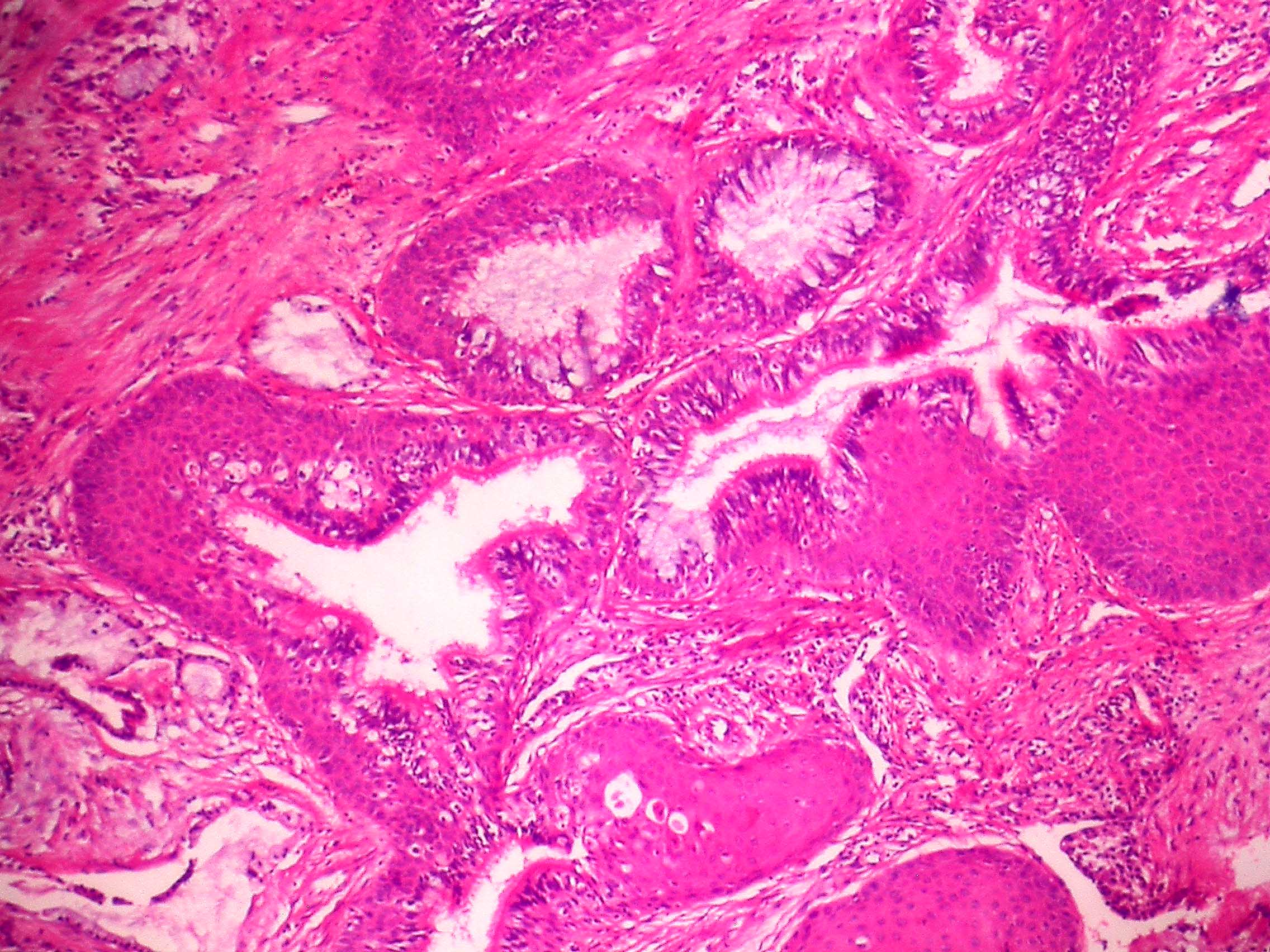
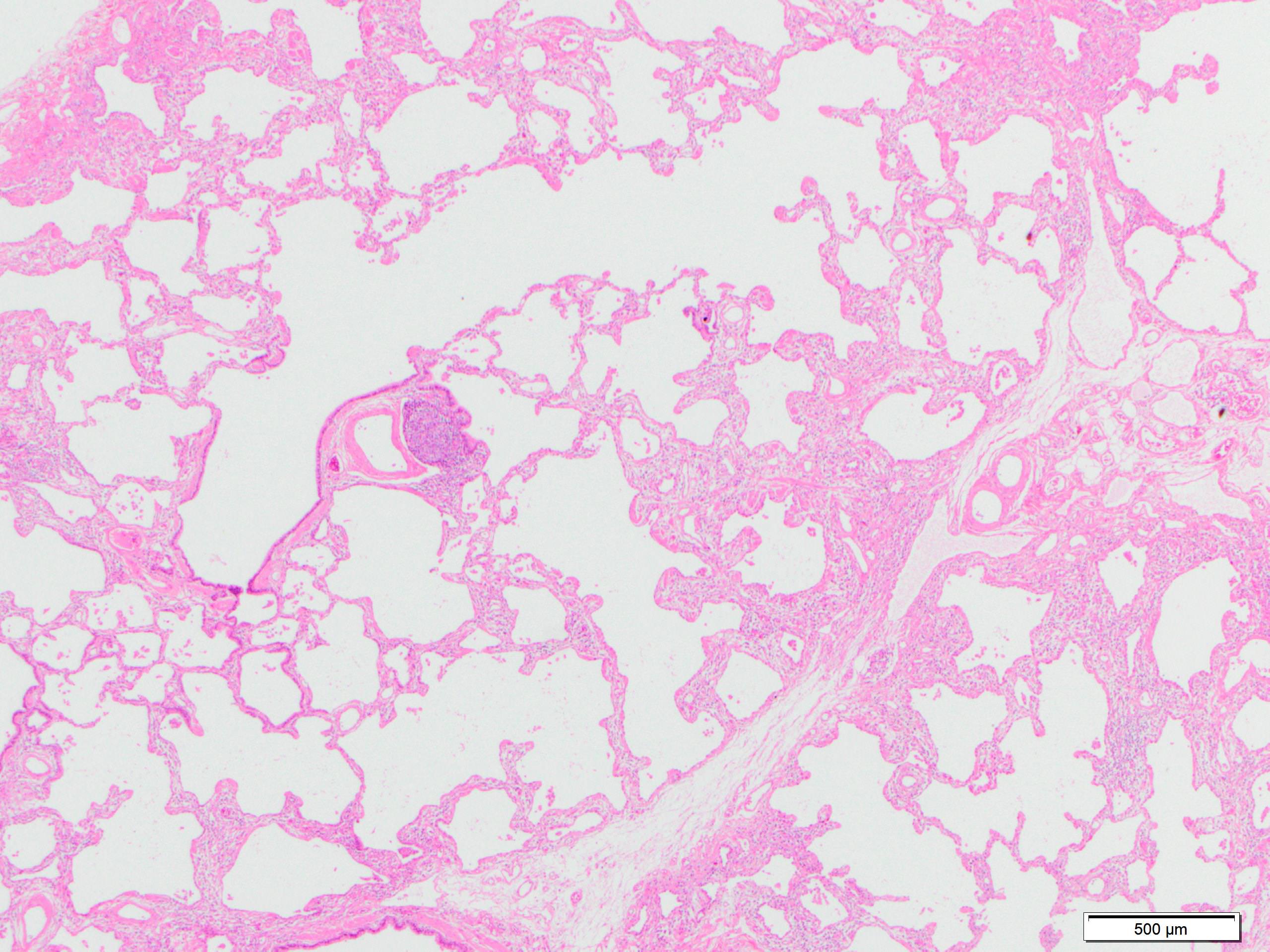
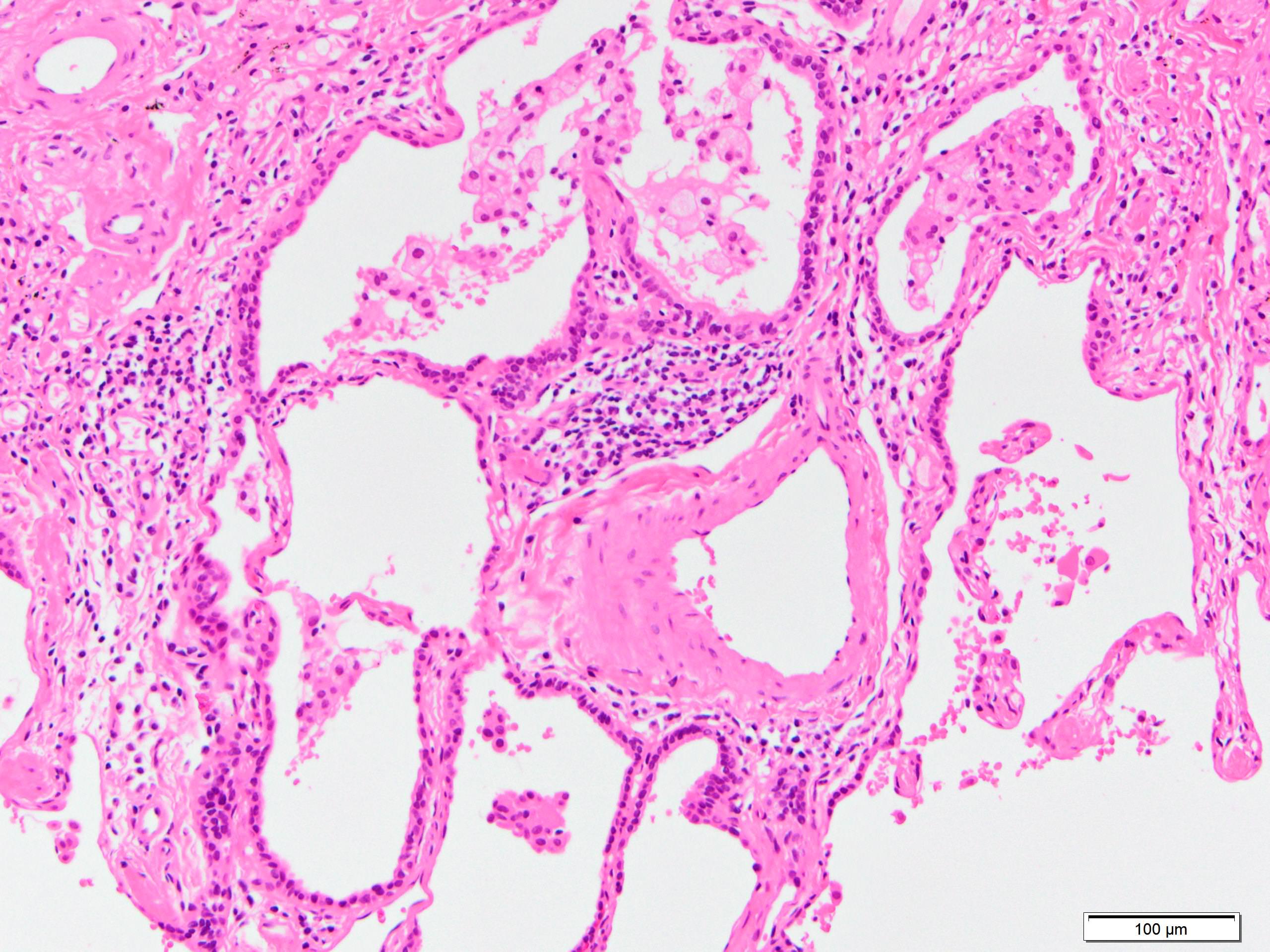
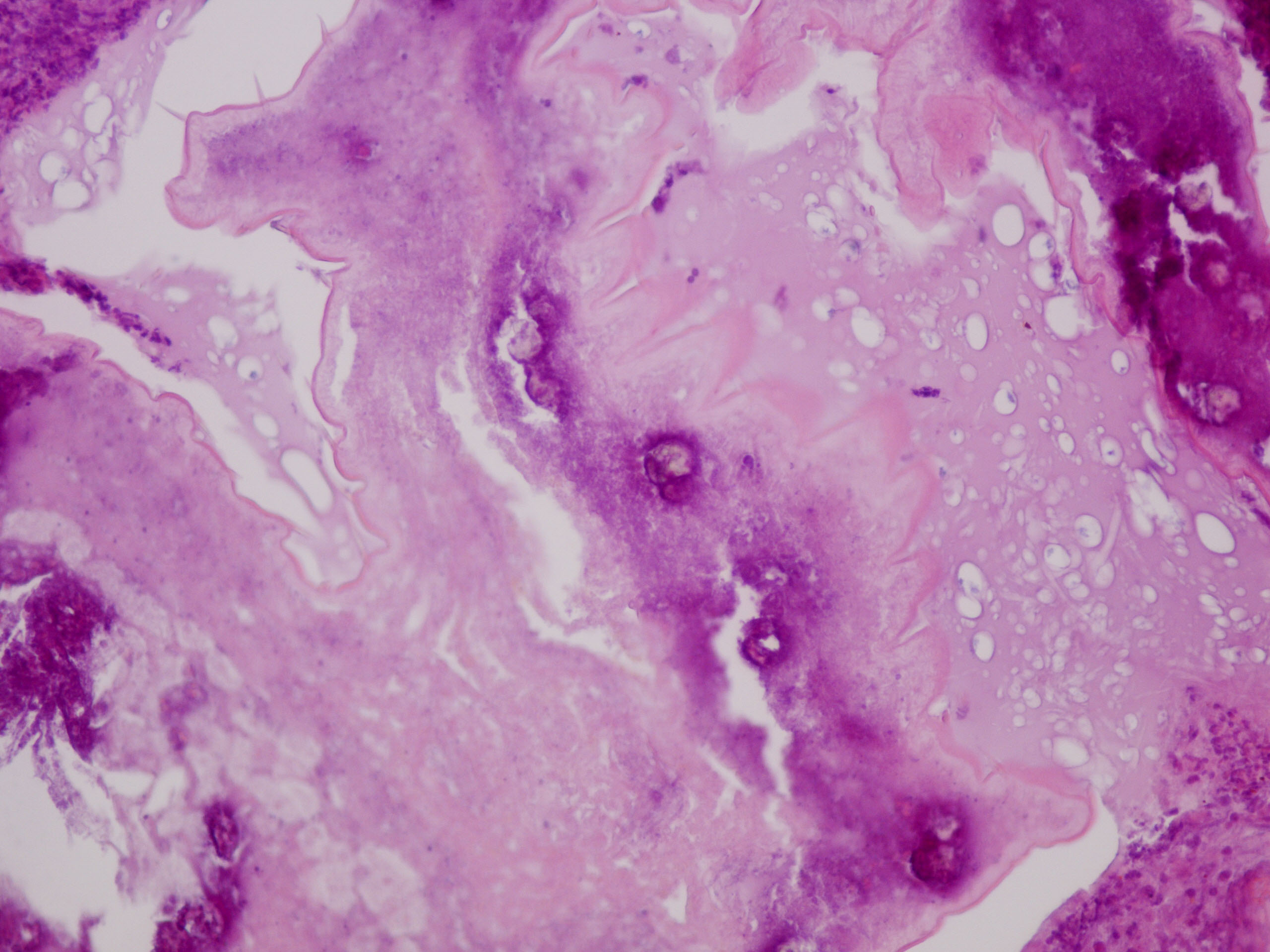
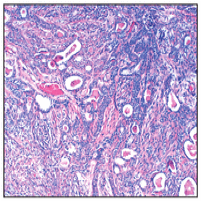
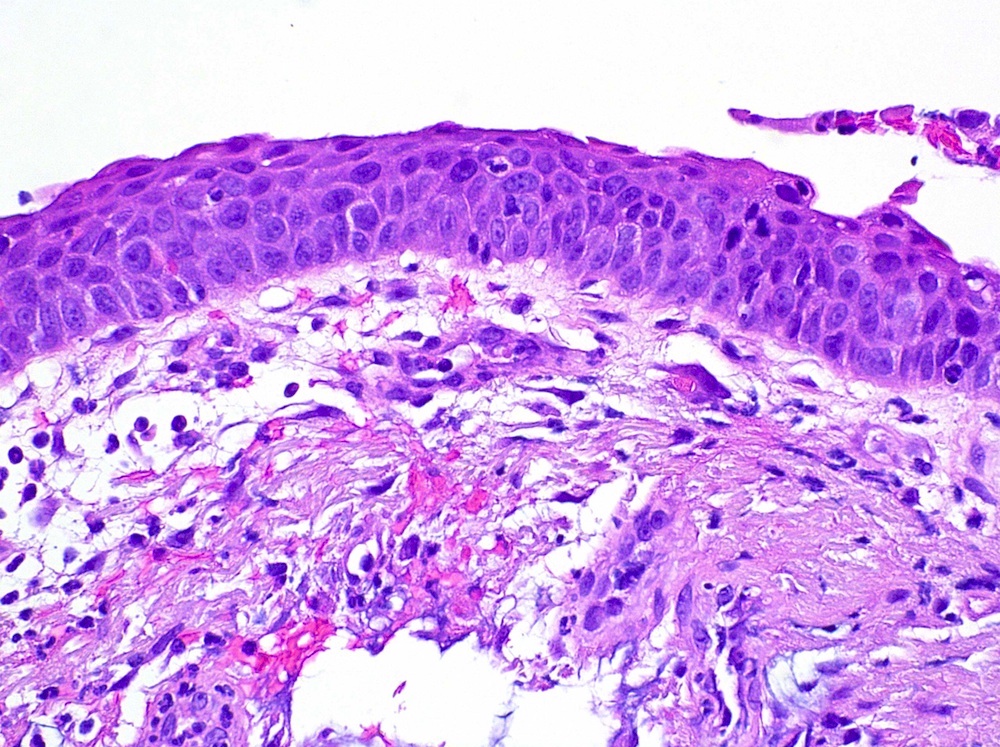
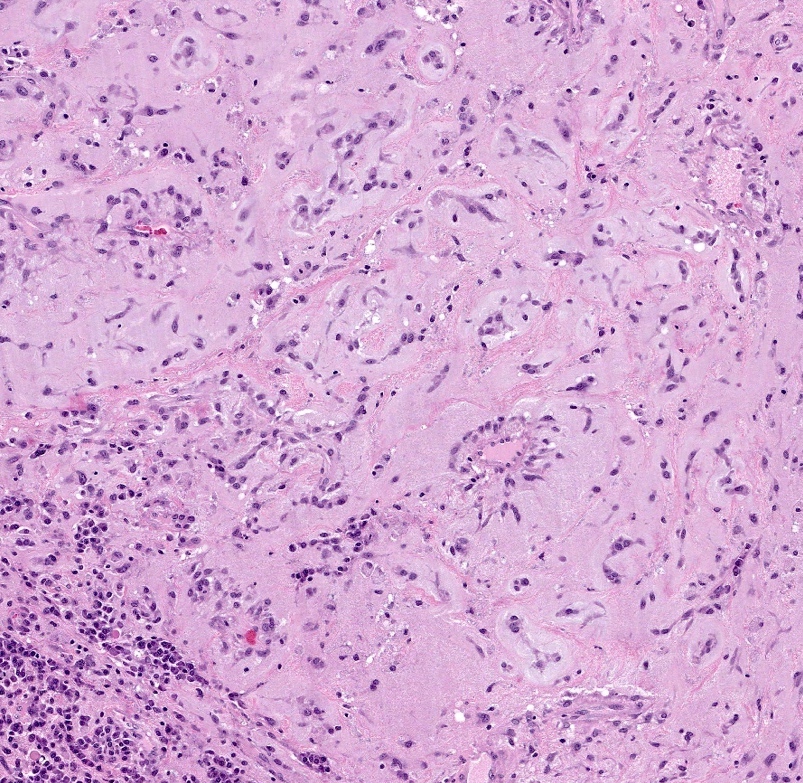
- Organizing pneumonia: fibroblastic plugs in alveolar sacs and ducts with loose collagen matrix
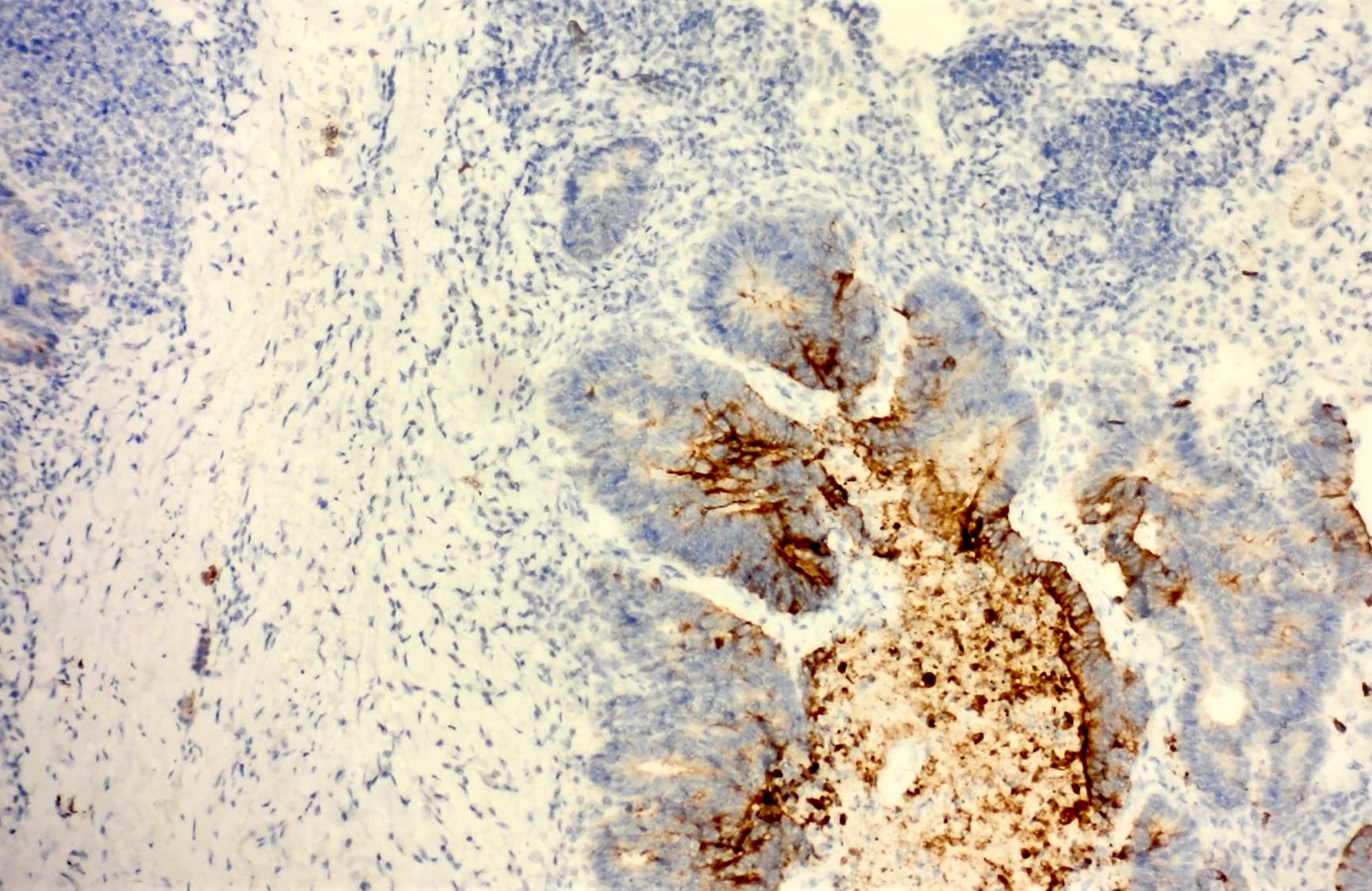
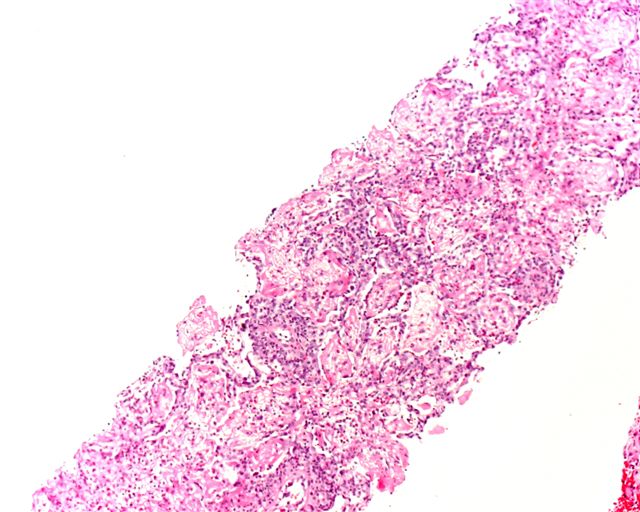
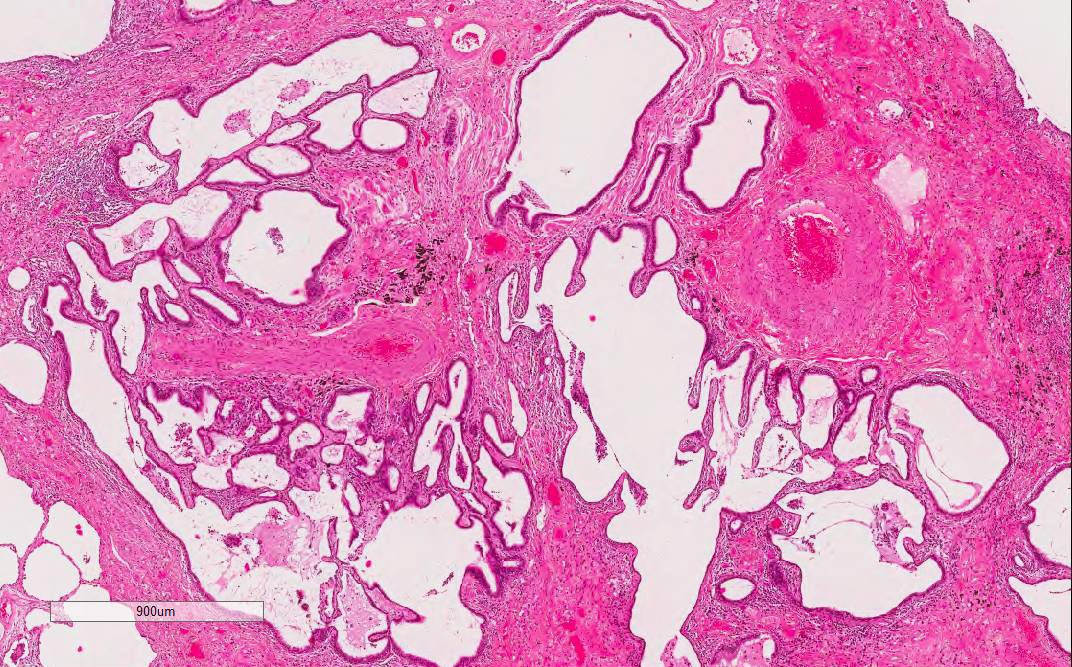
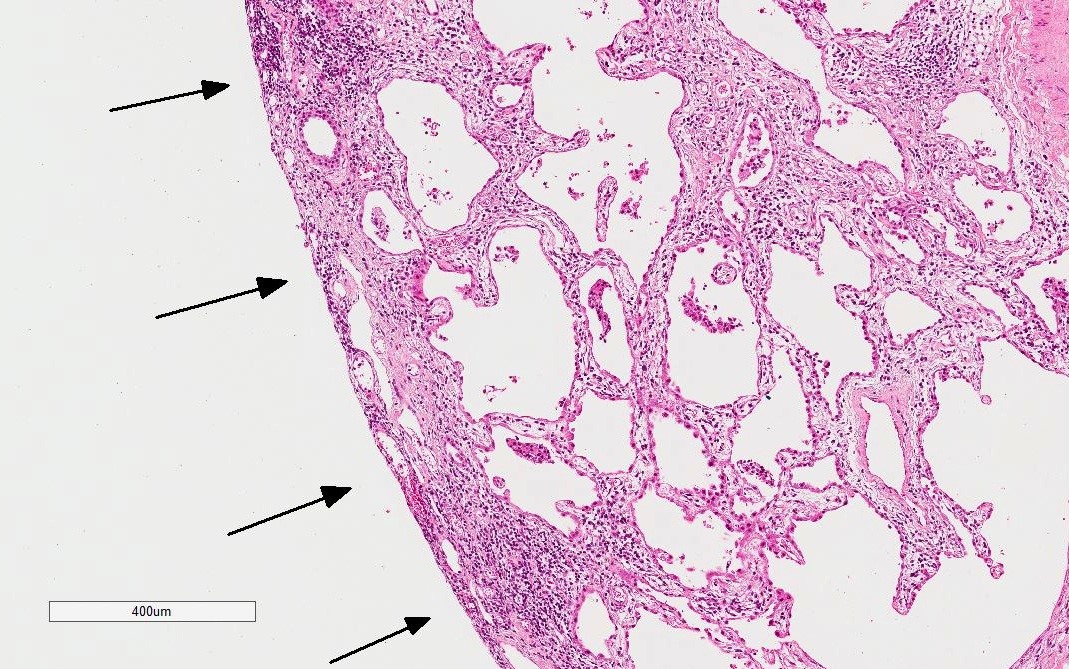
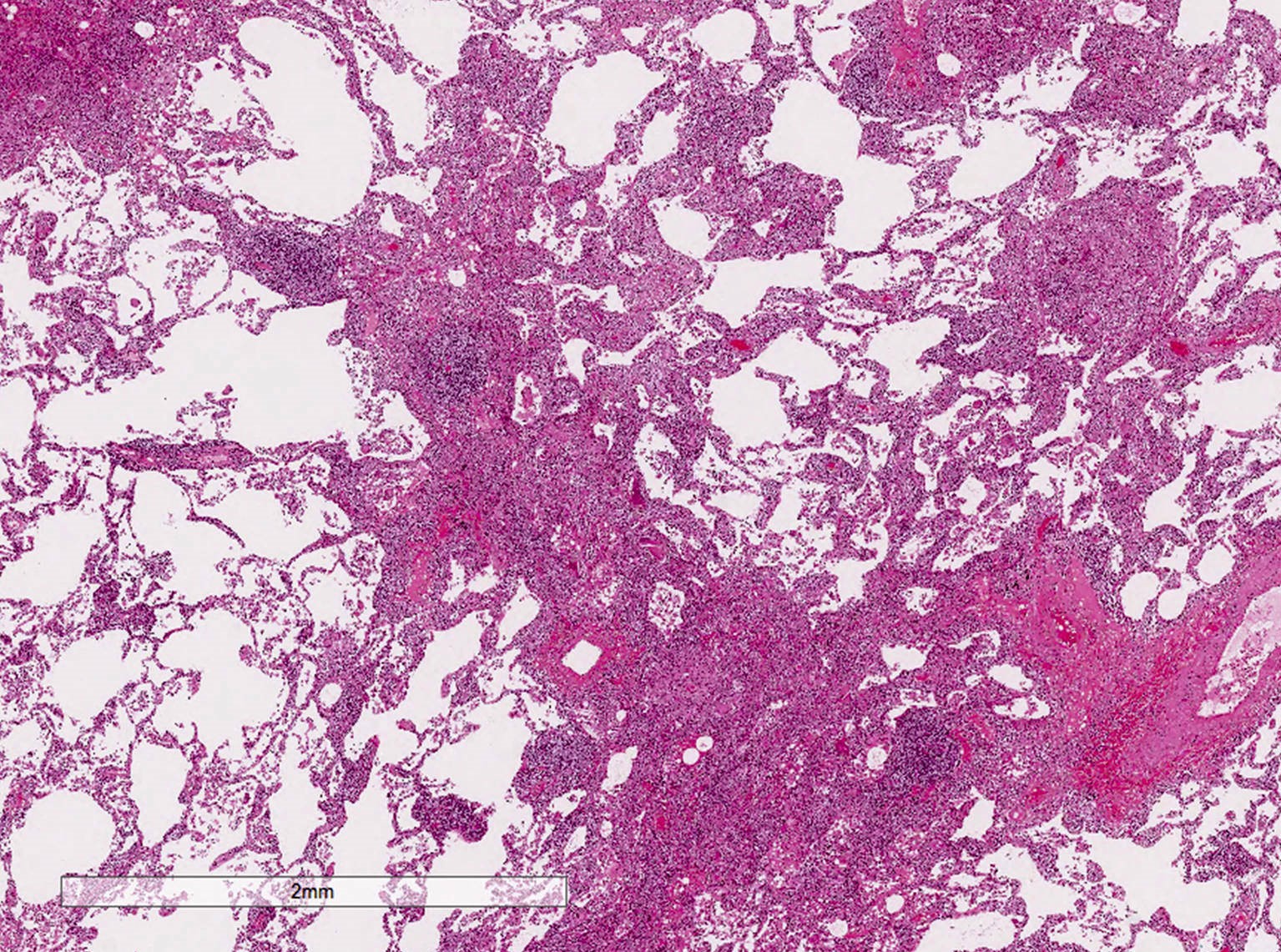
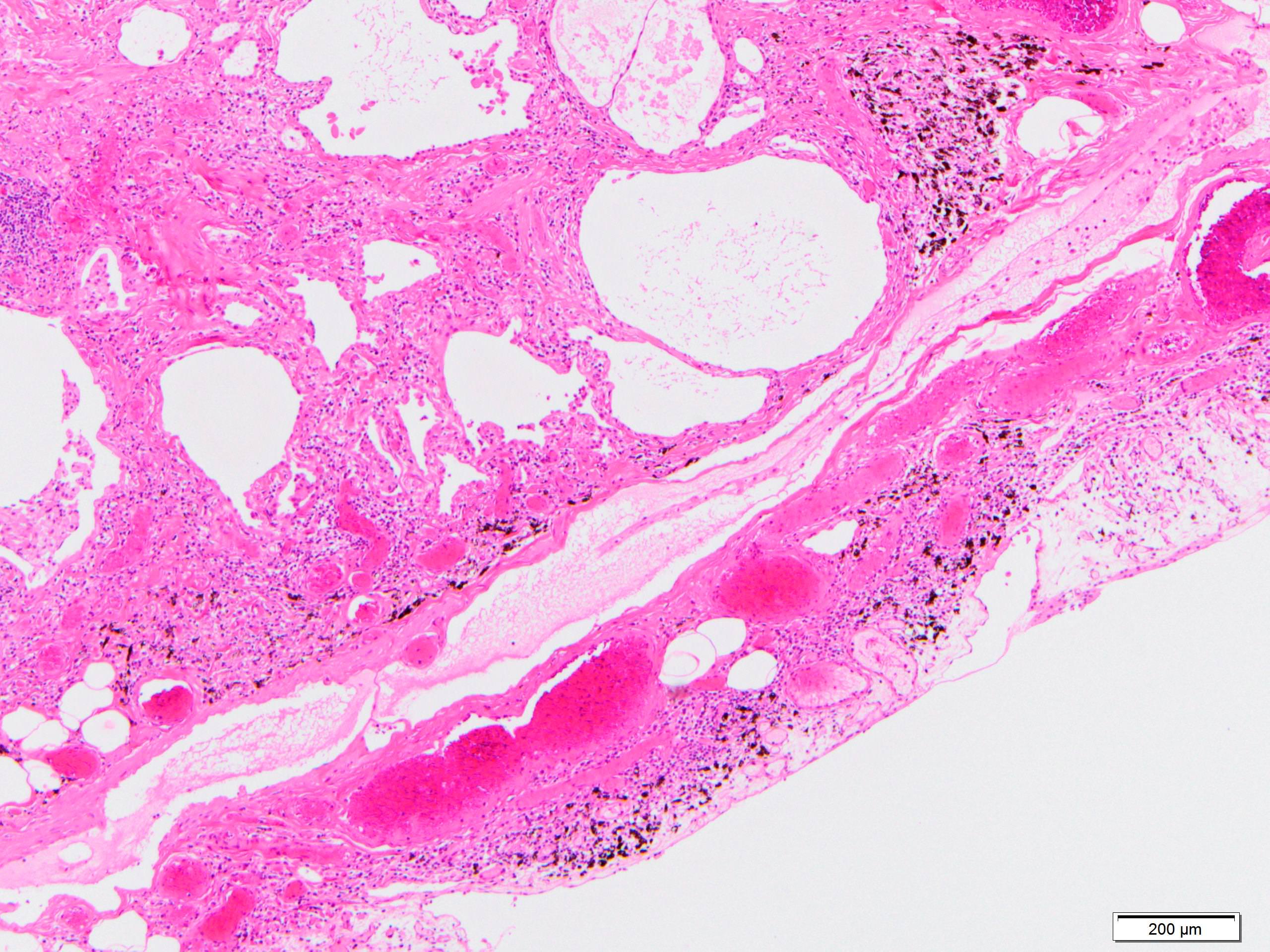
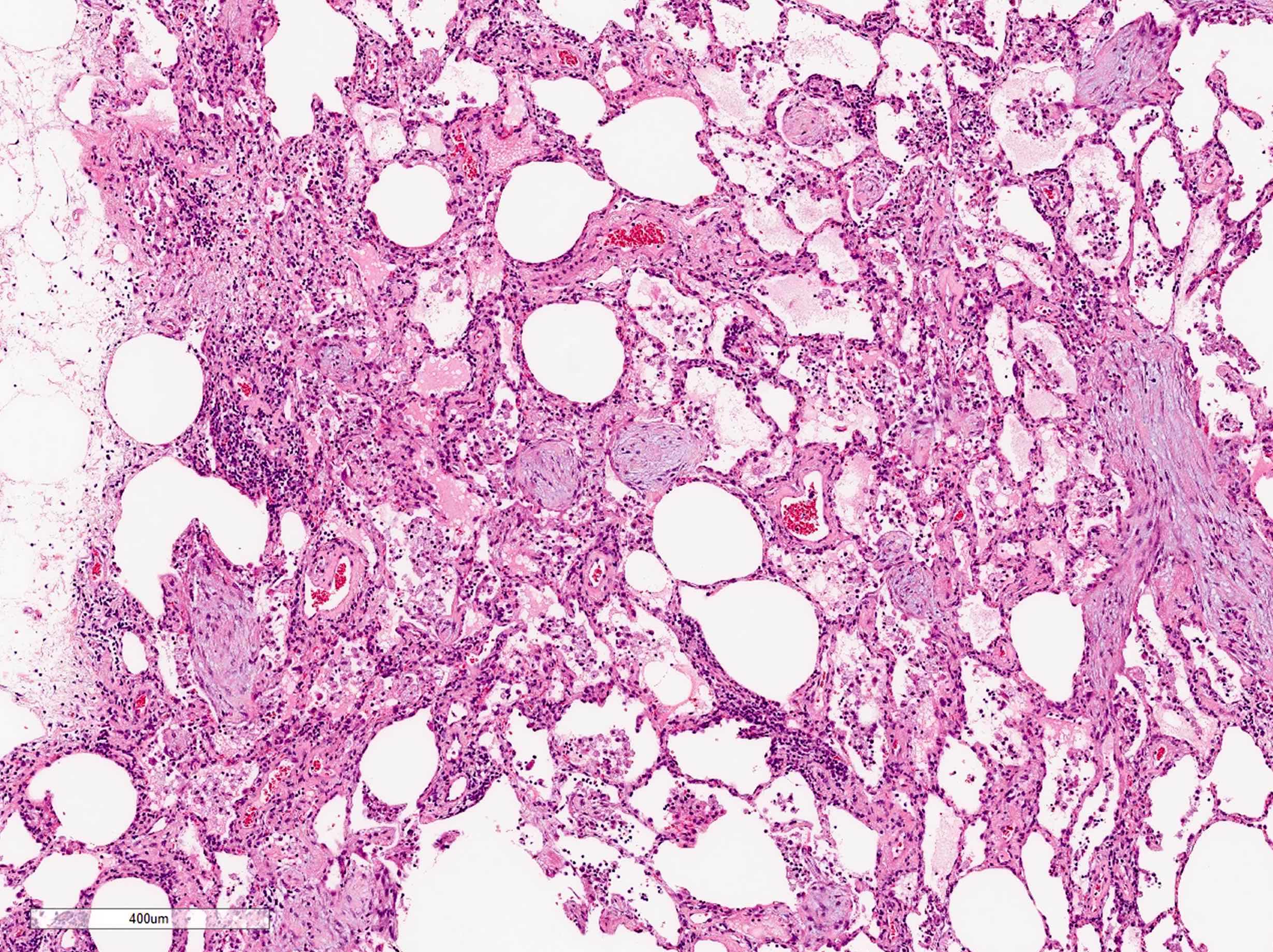
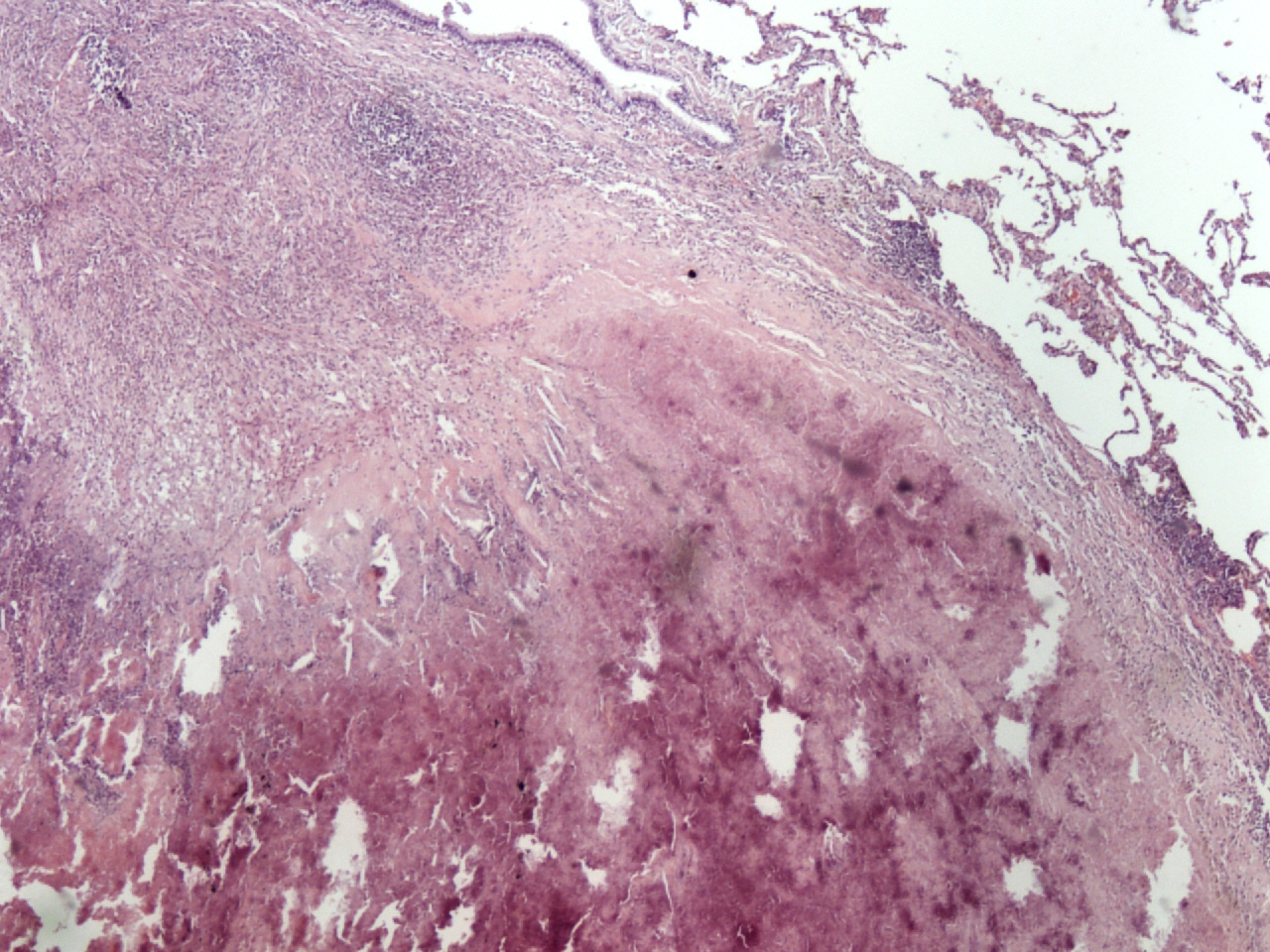
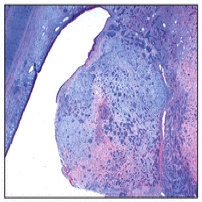
- Diffuse and patchy distribution
- Dominant findings of intra-alveolar fibrin, so called "fibrin ball"
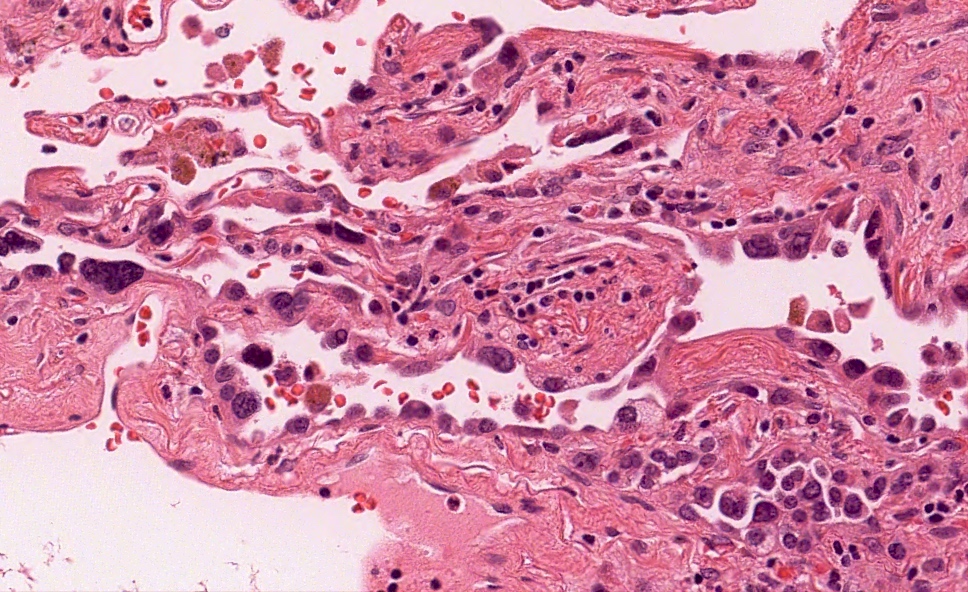
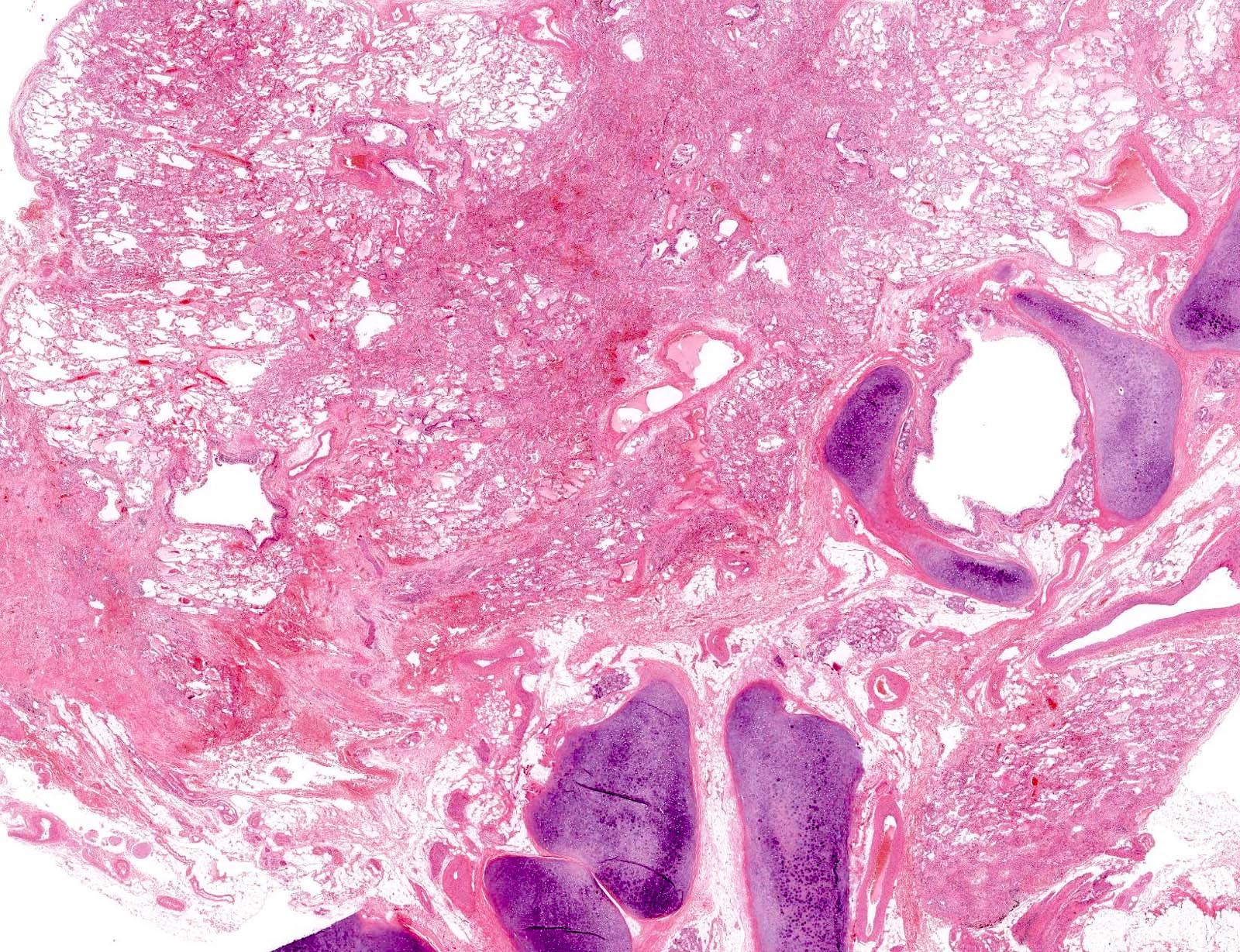
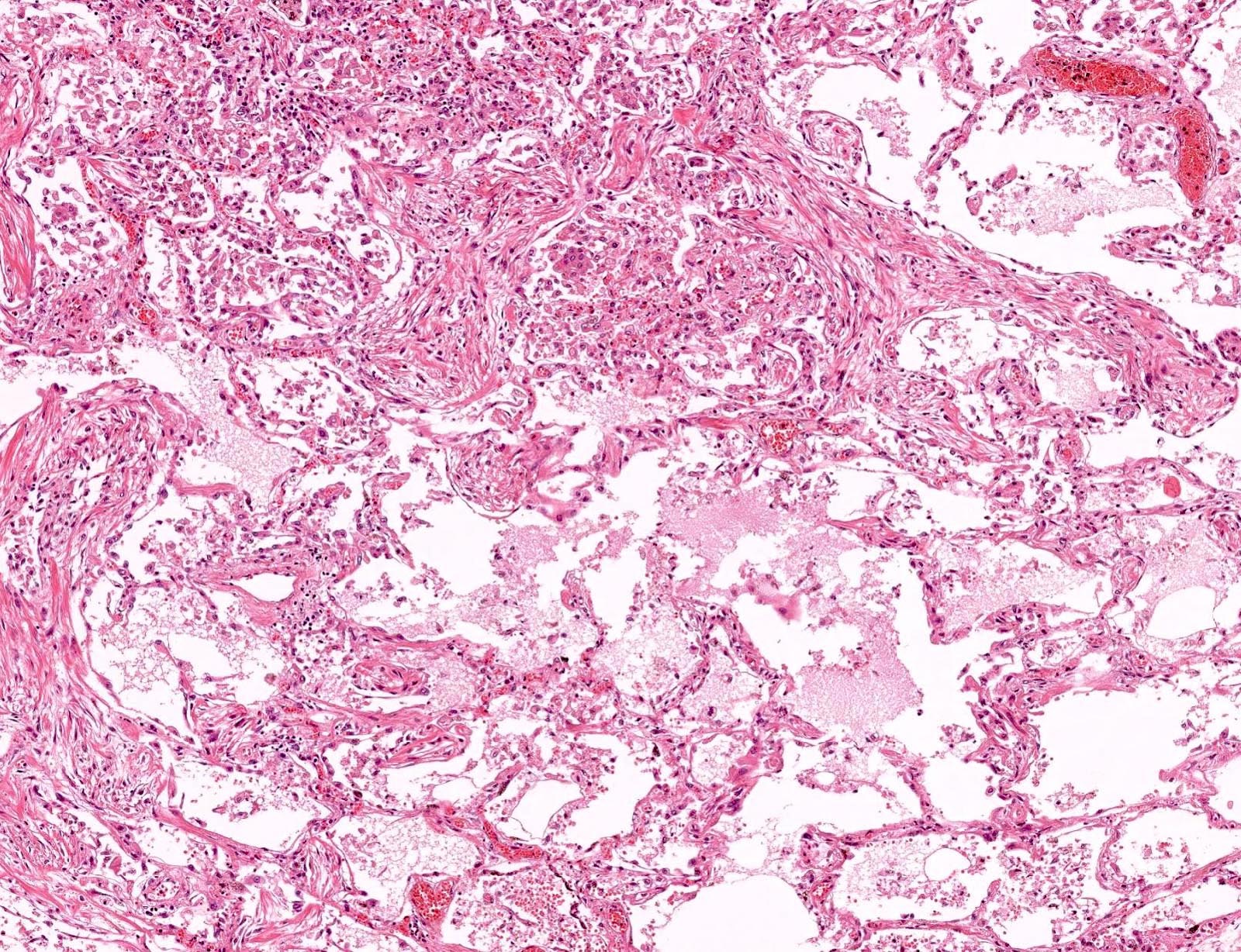
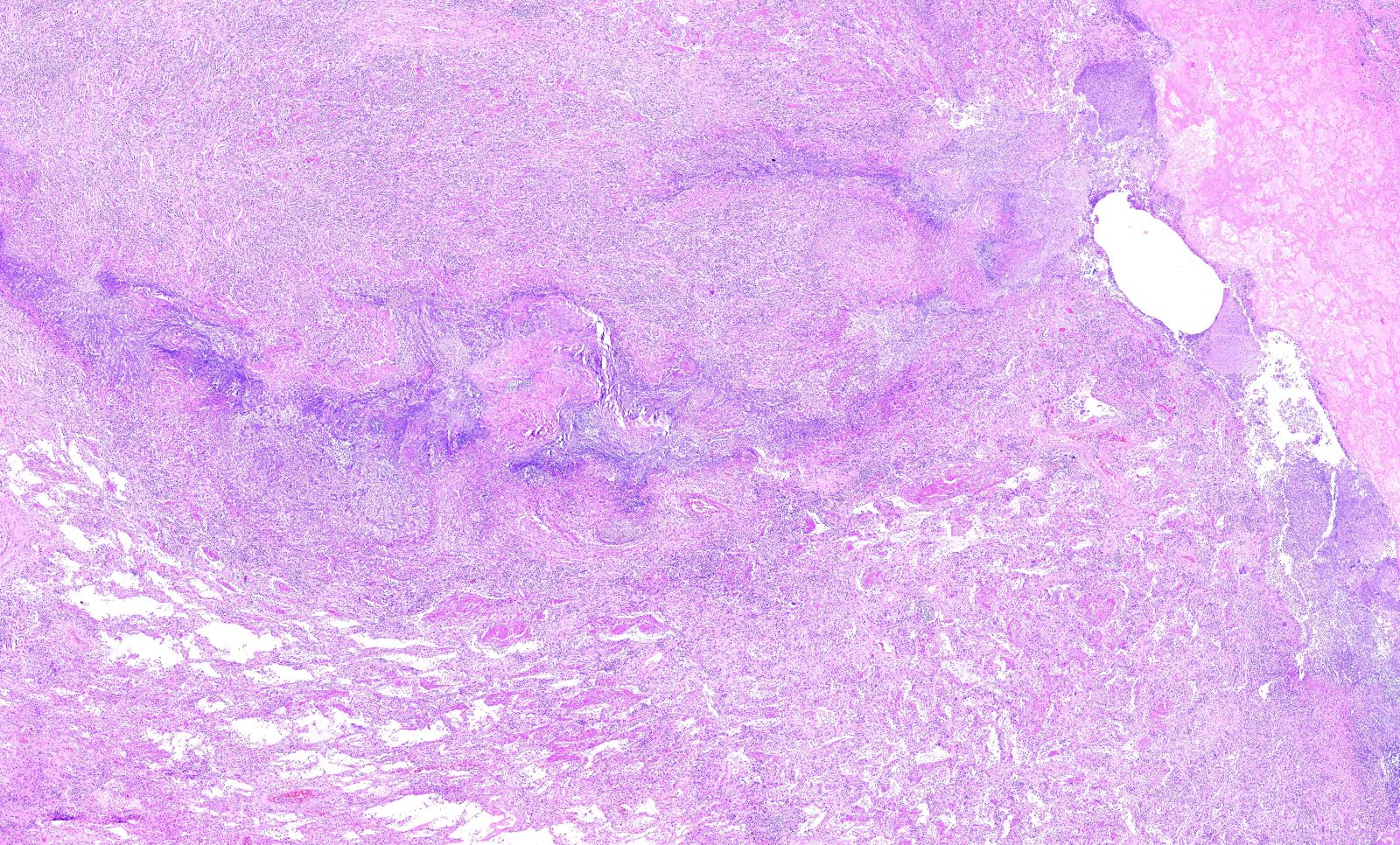
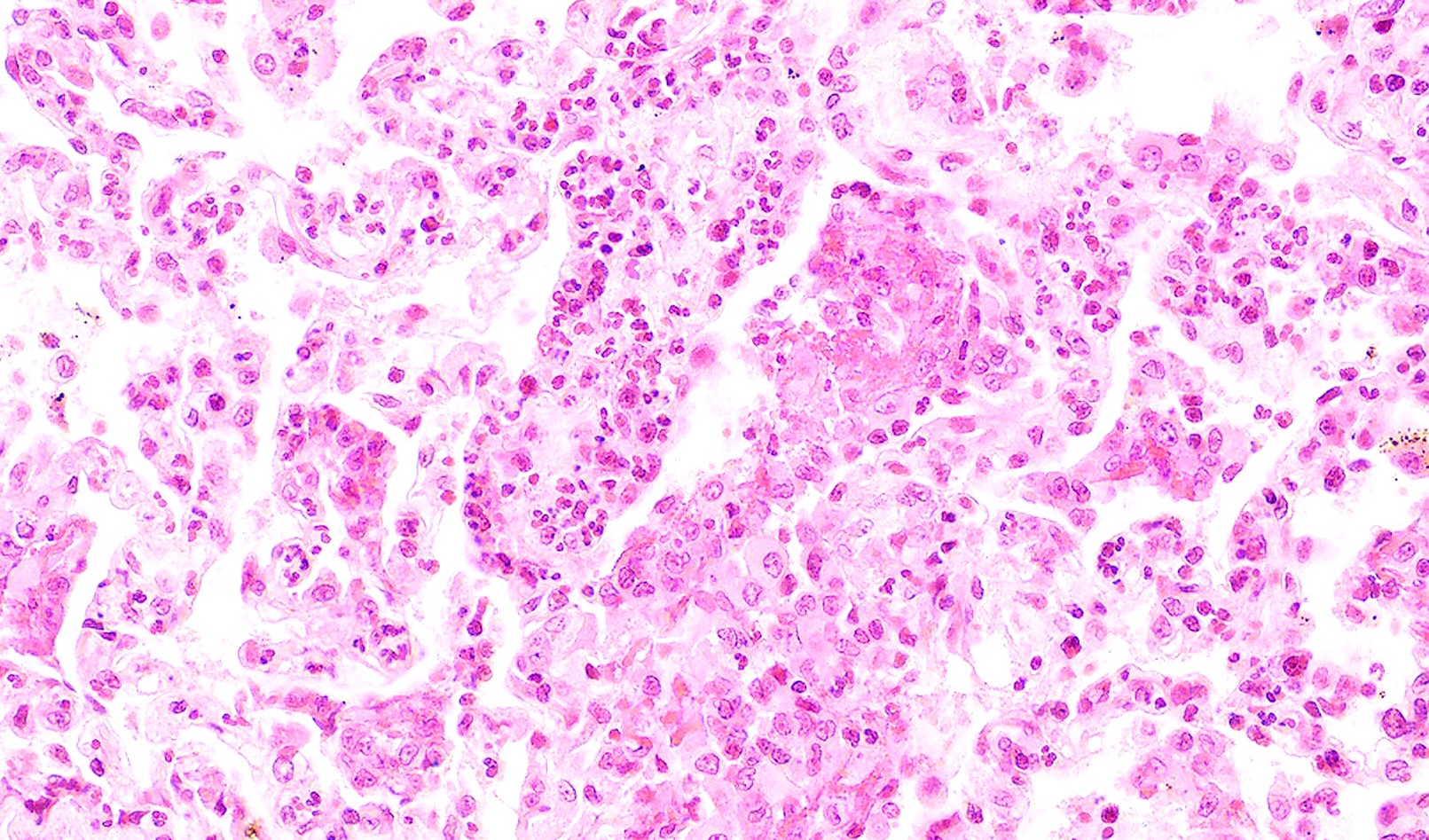
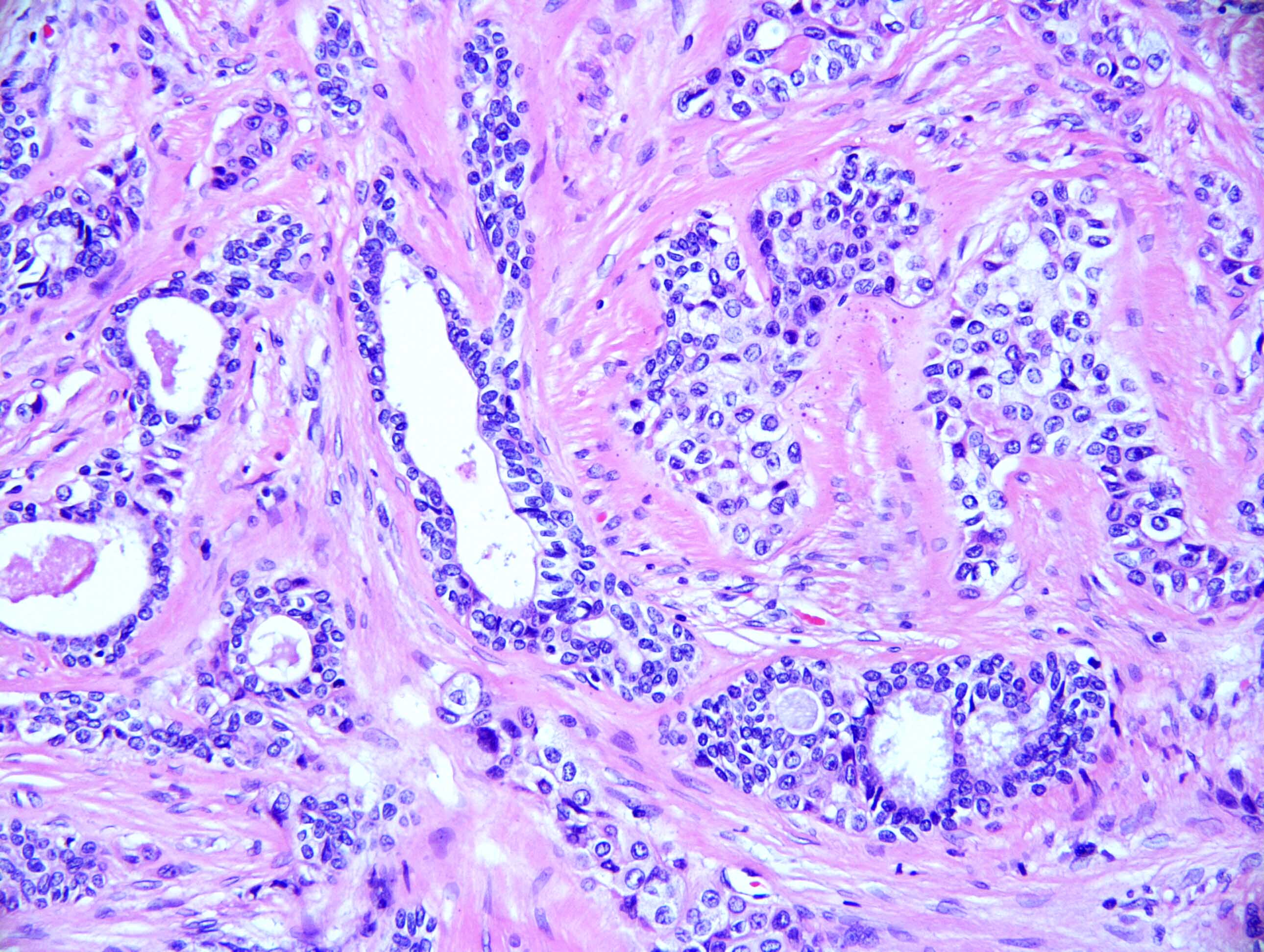
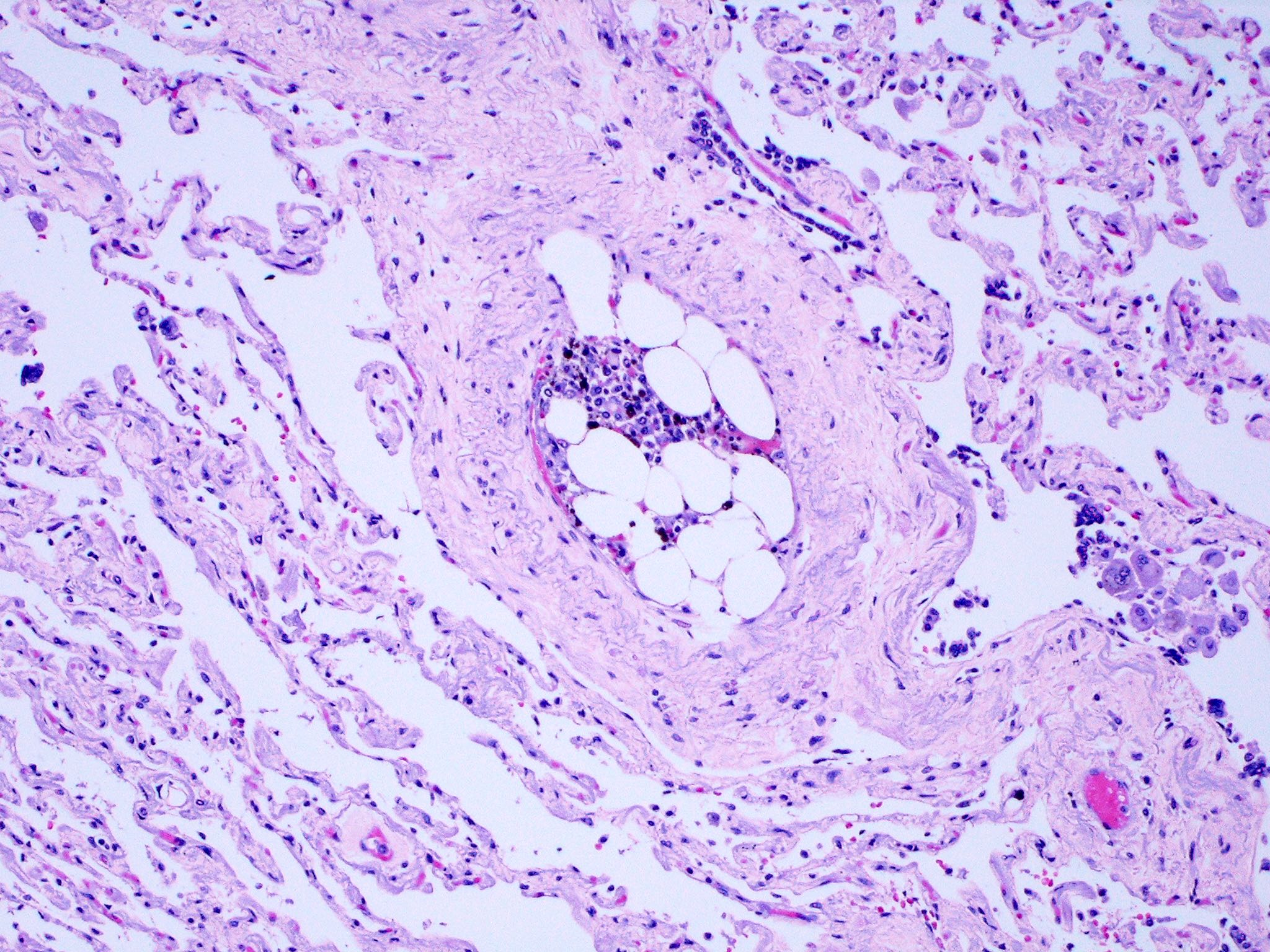
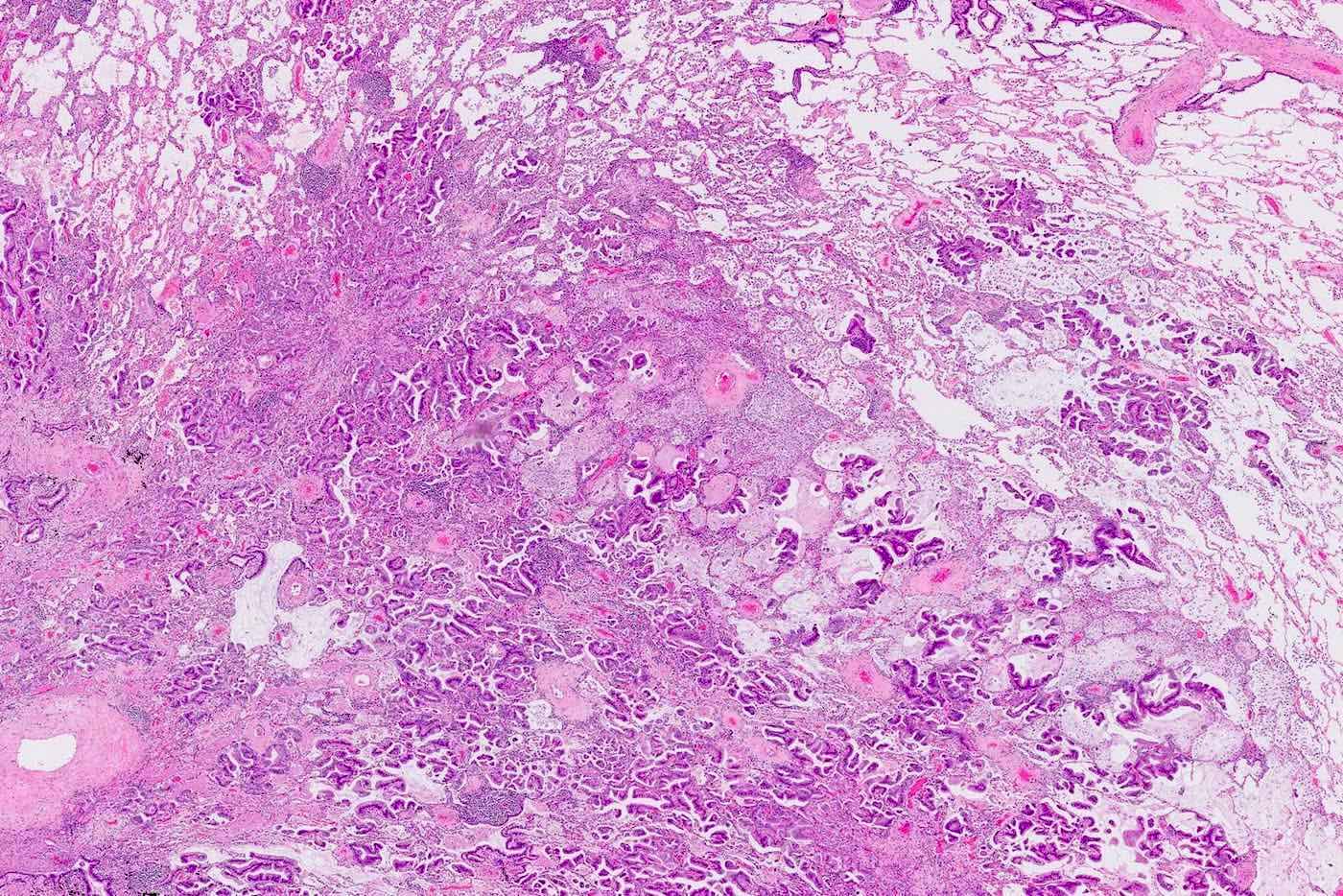
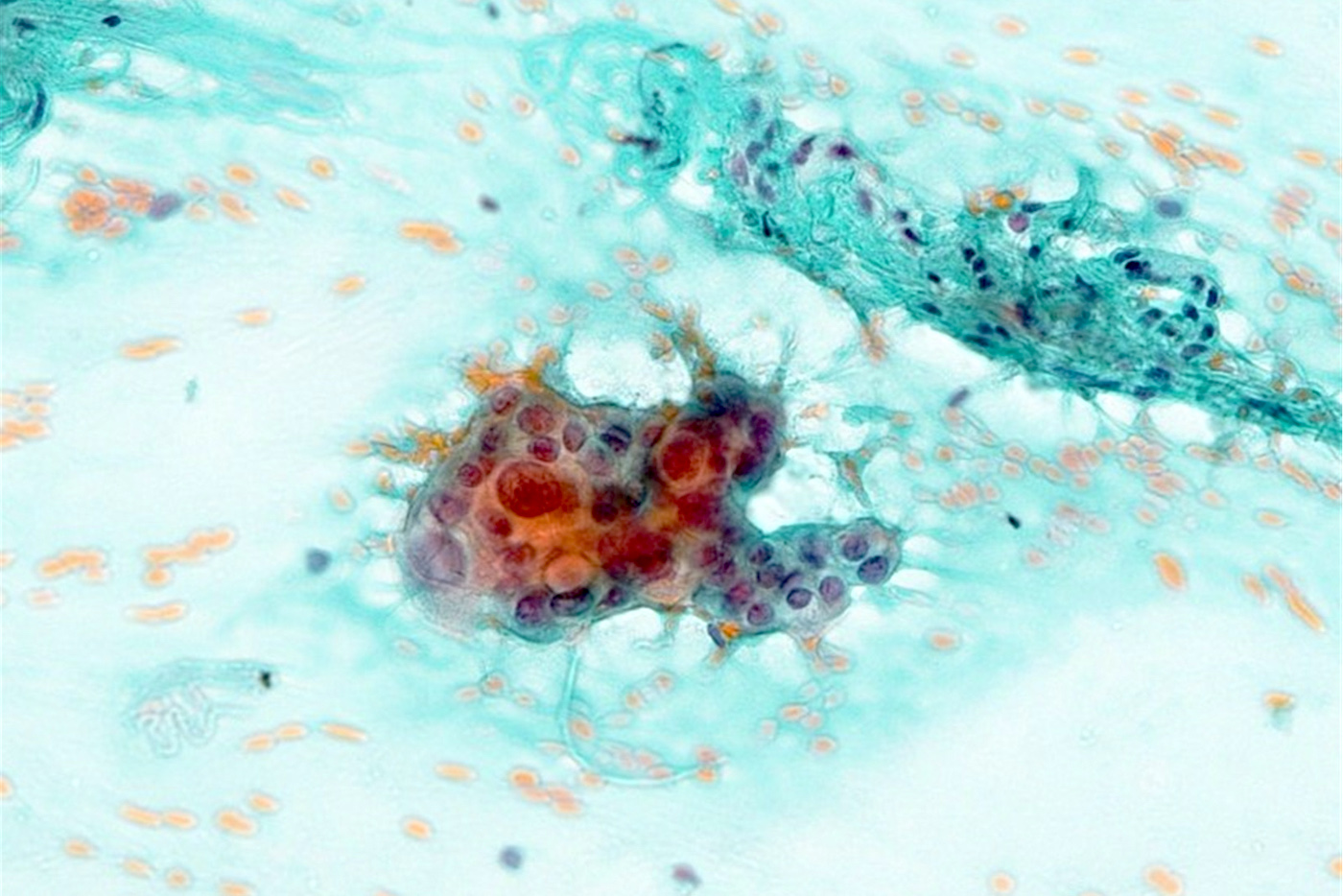
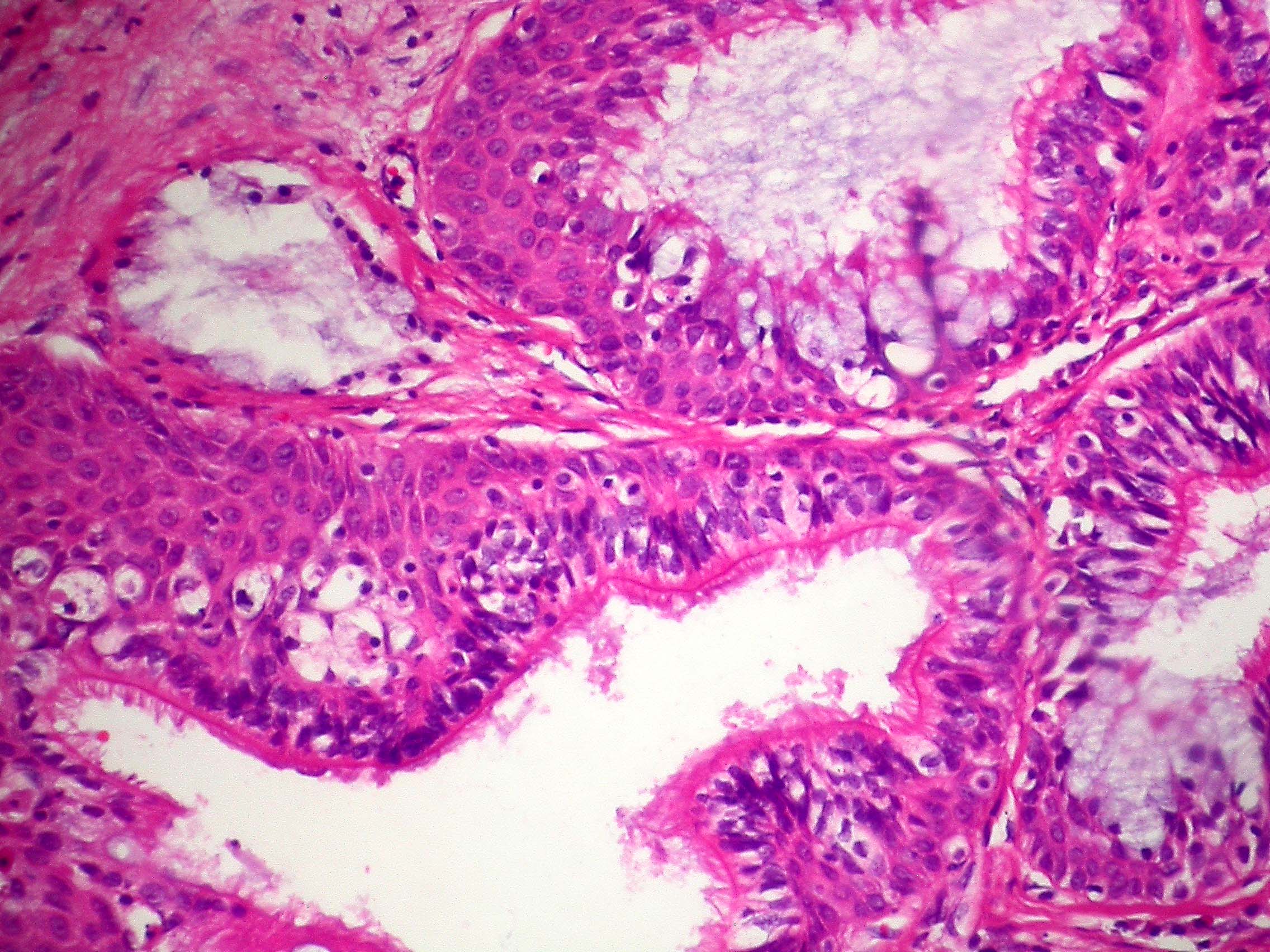
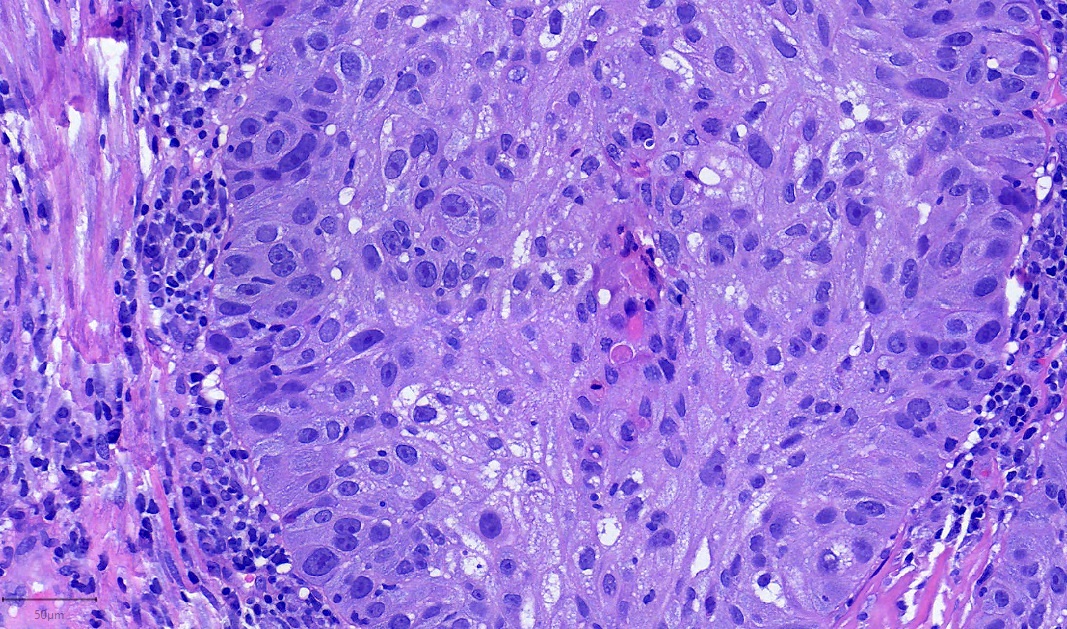
- Minor findings
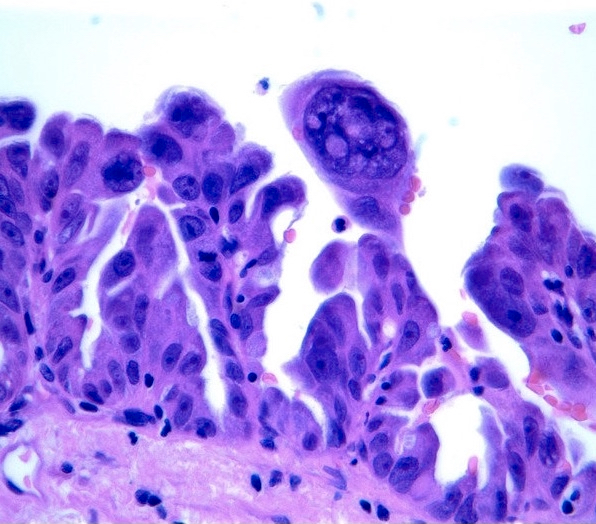
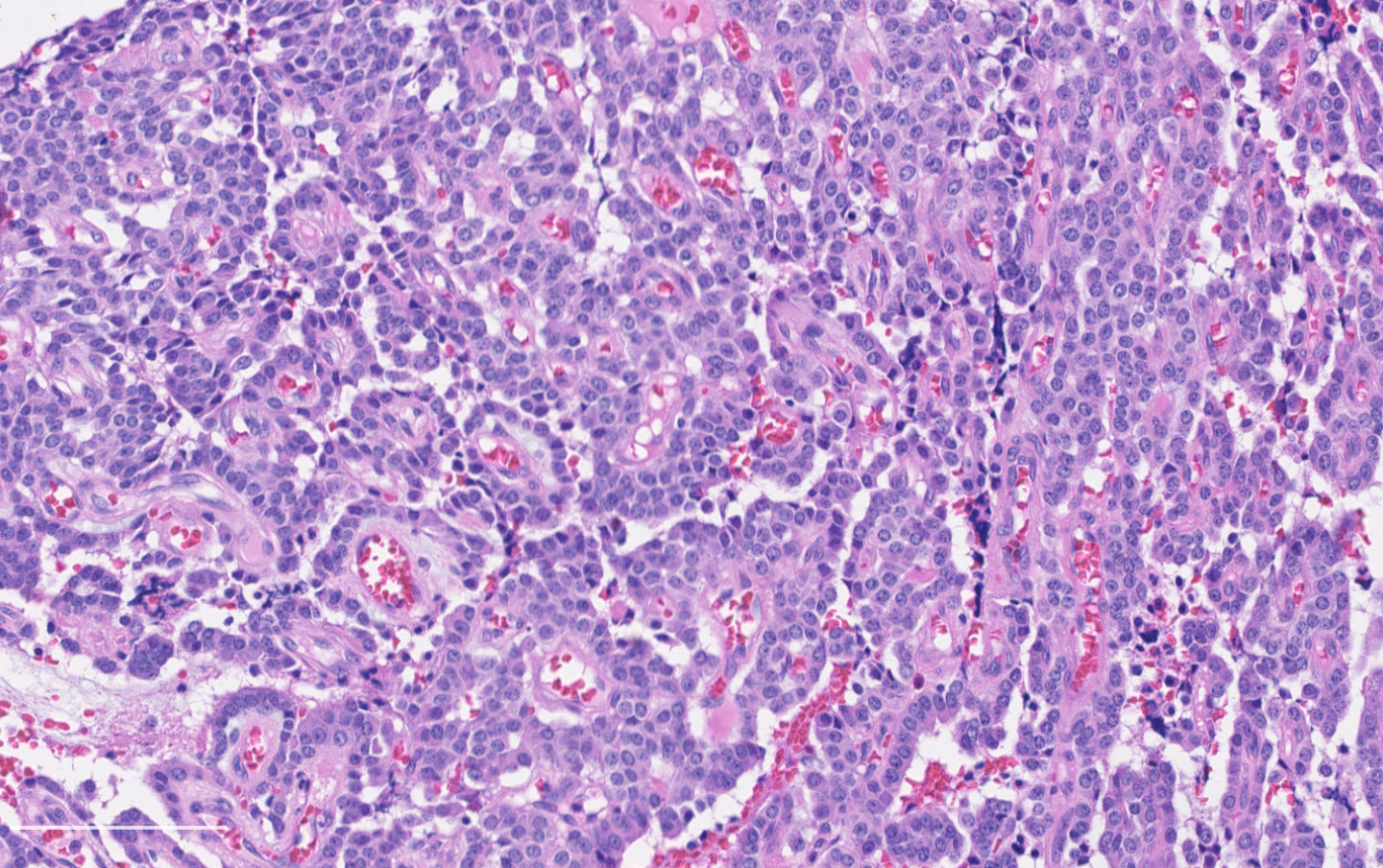
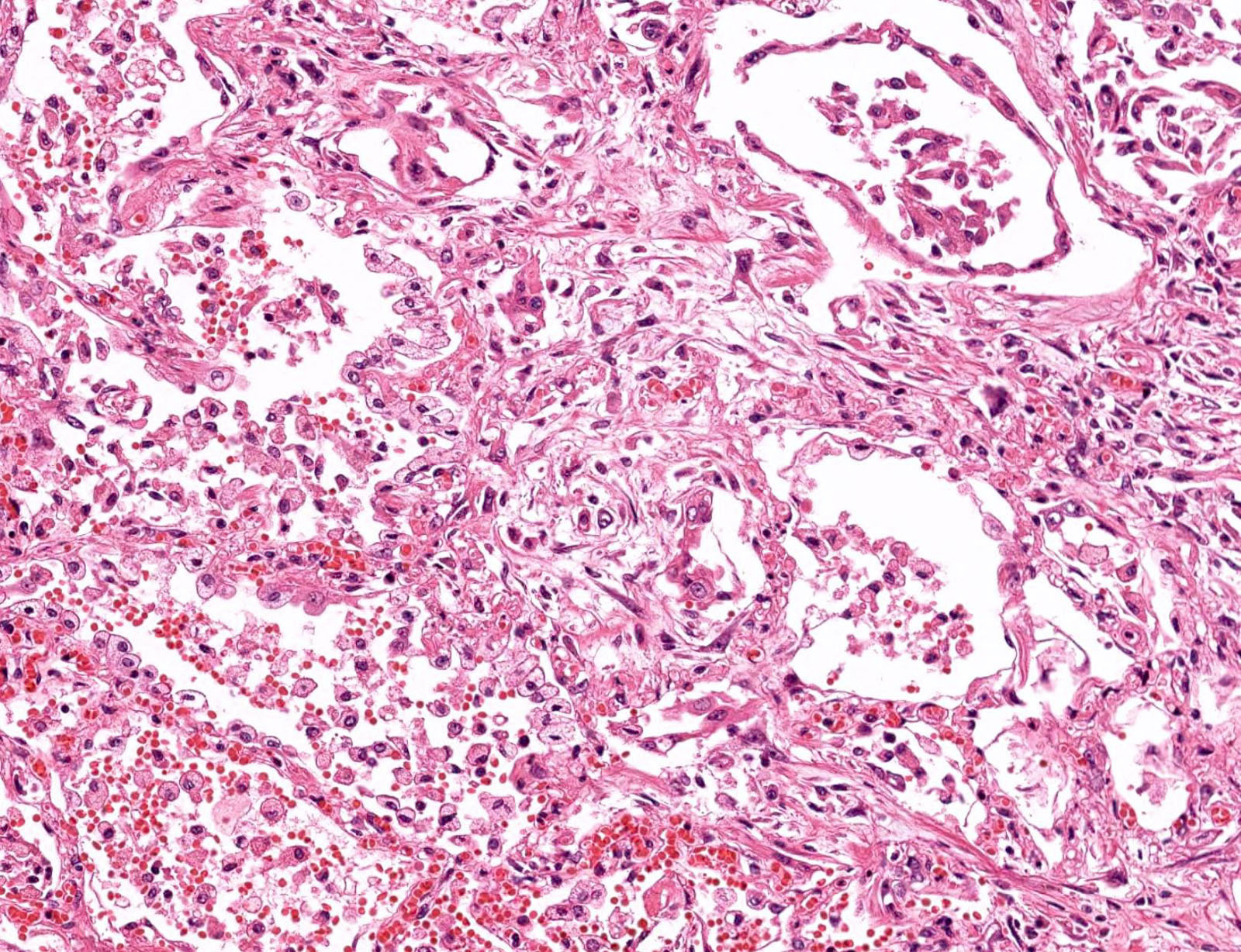
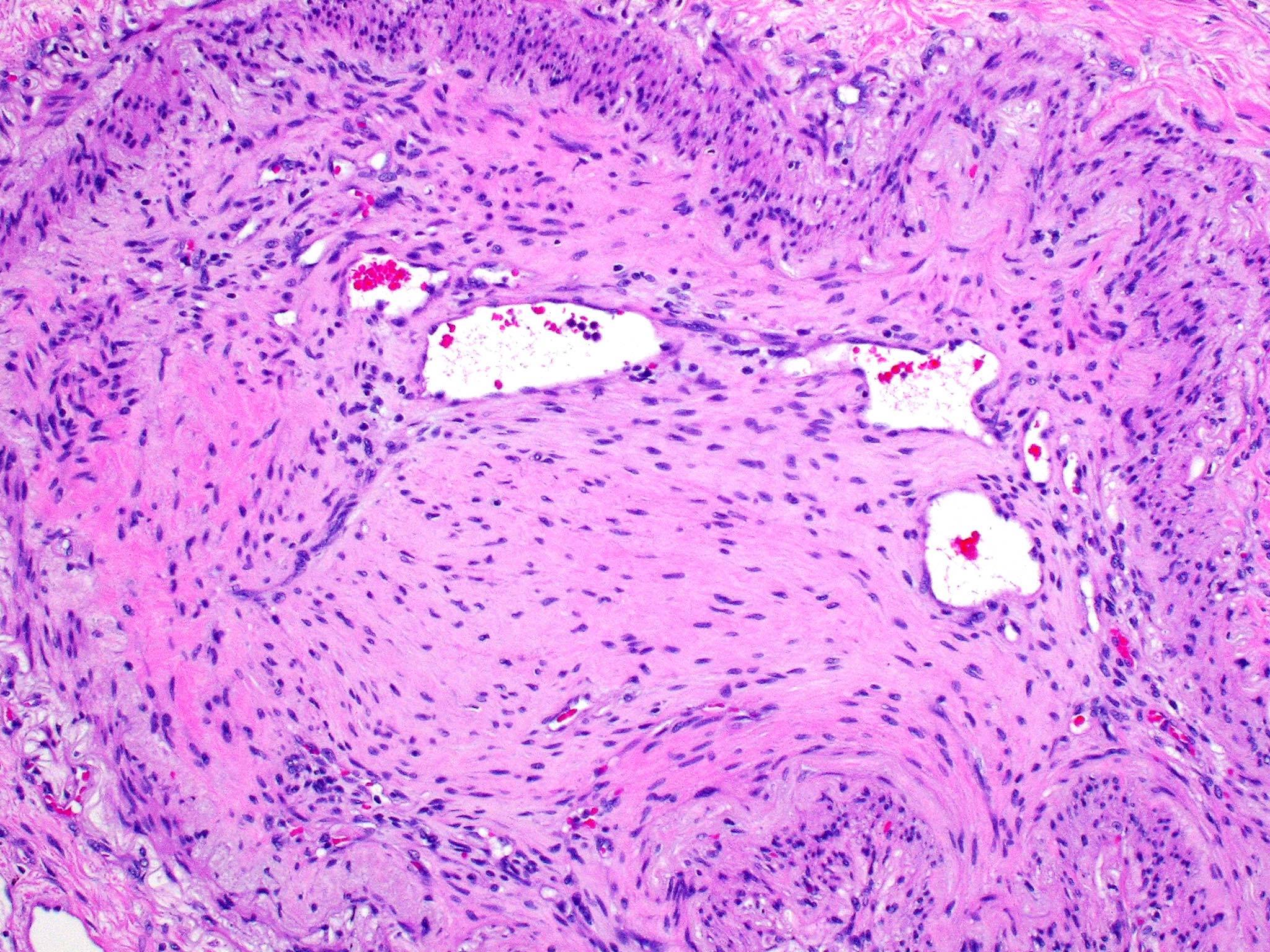
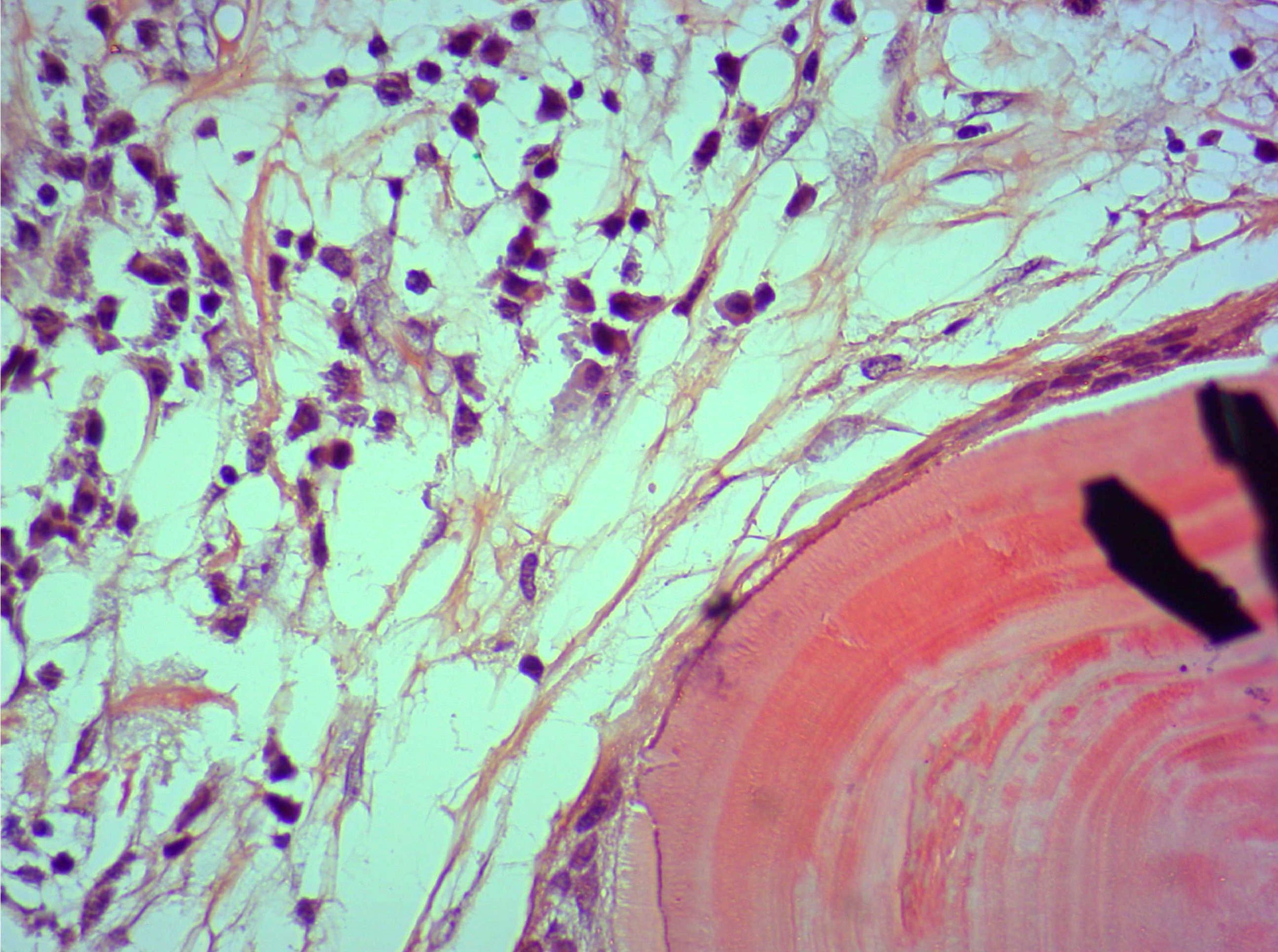
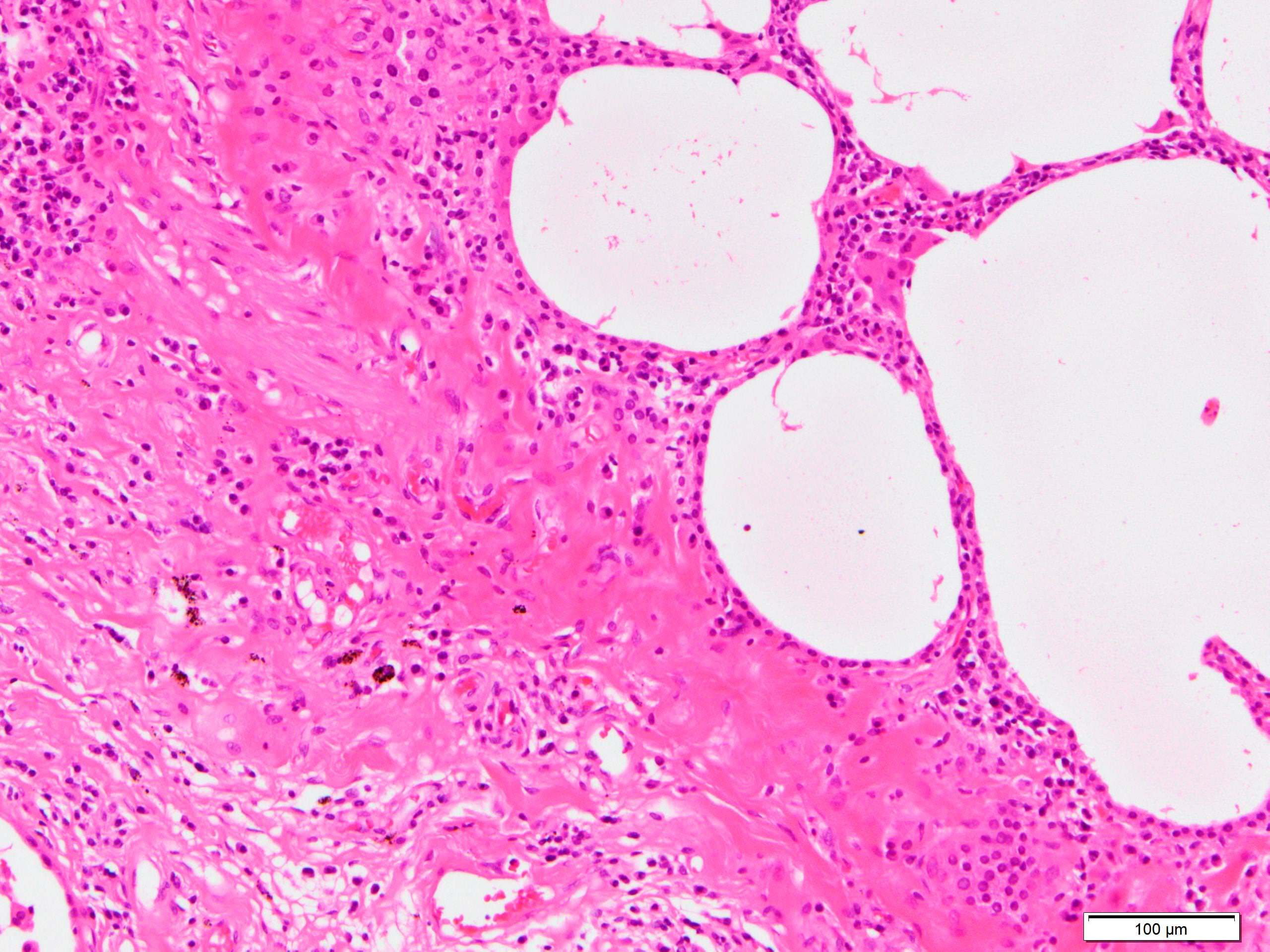
- Mild to moderate interstitial changes
- Lymphoplasmacytic infiltrate
- Alveolar septal expansion with myxoid connective tissue
- Limited within areas of fibrinous lesion
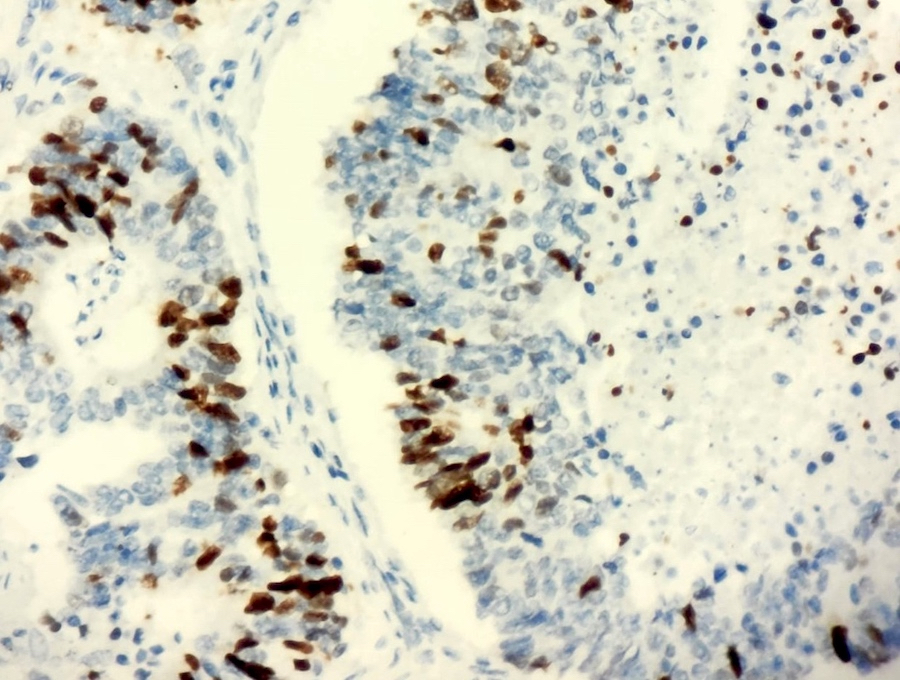
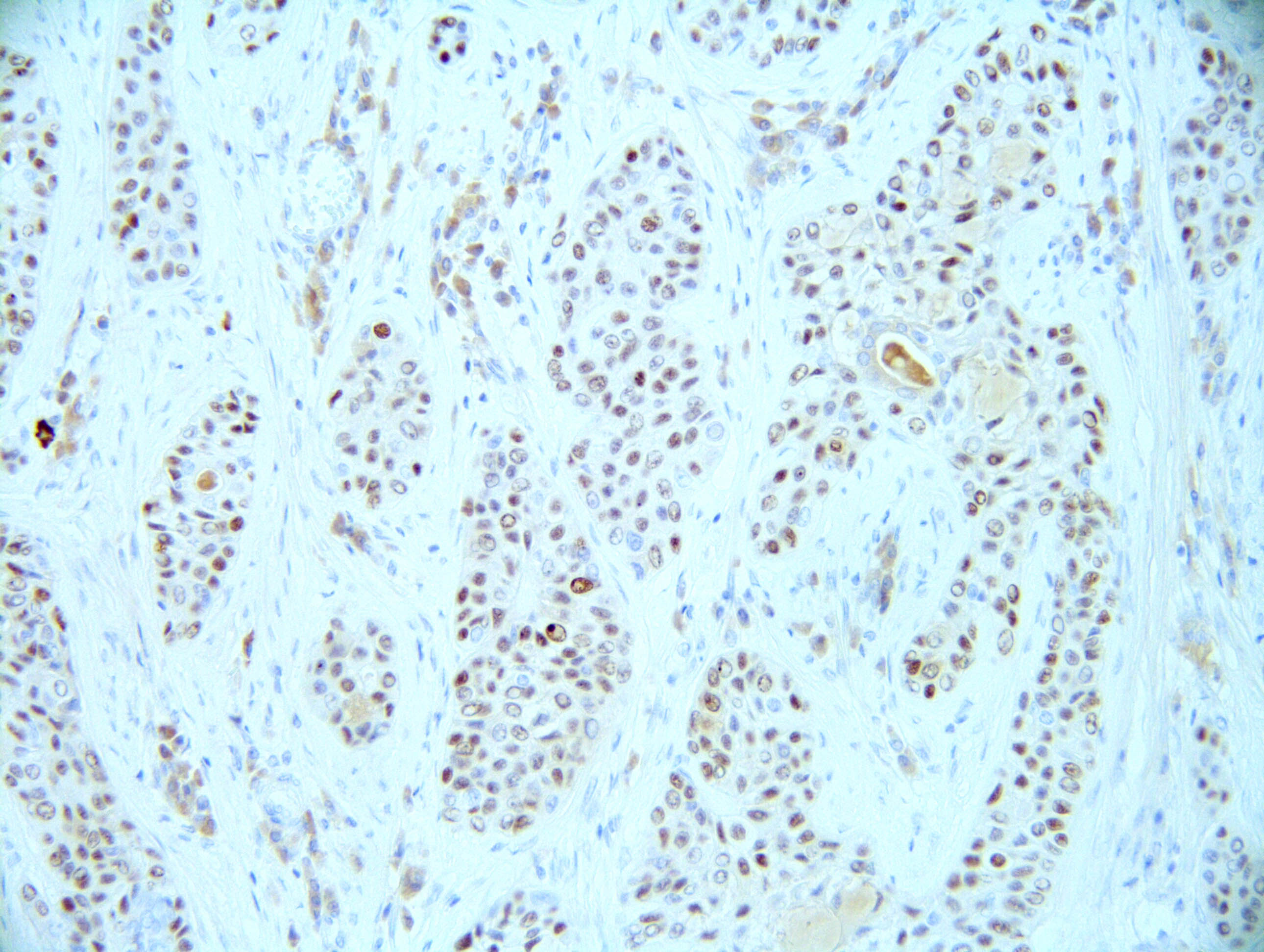
- Type 2 pneumocyte hyperplasia
- Mild to moderate interstitial changes
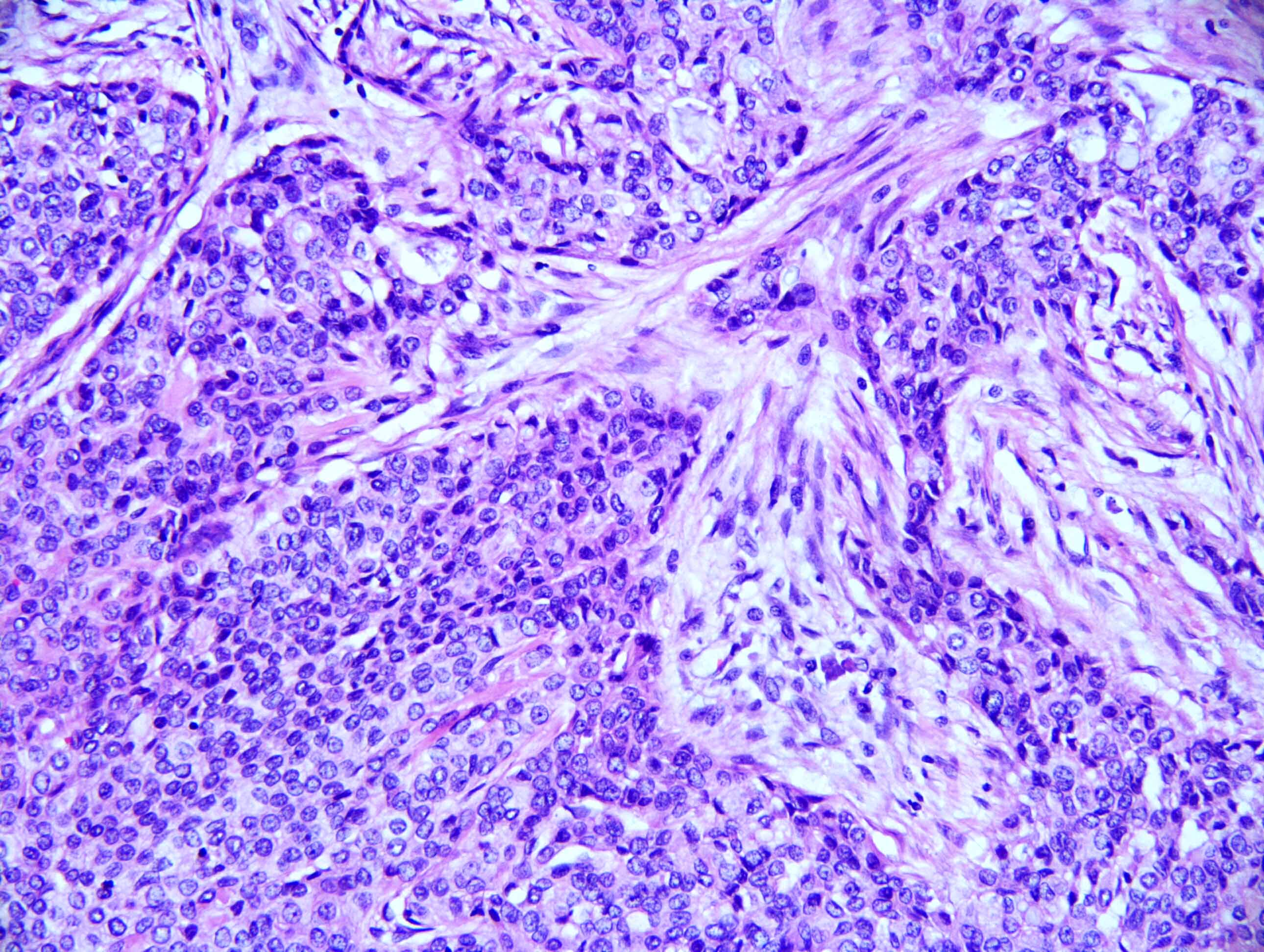
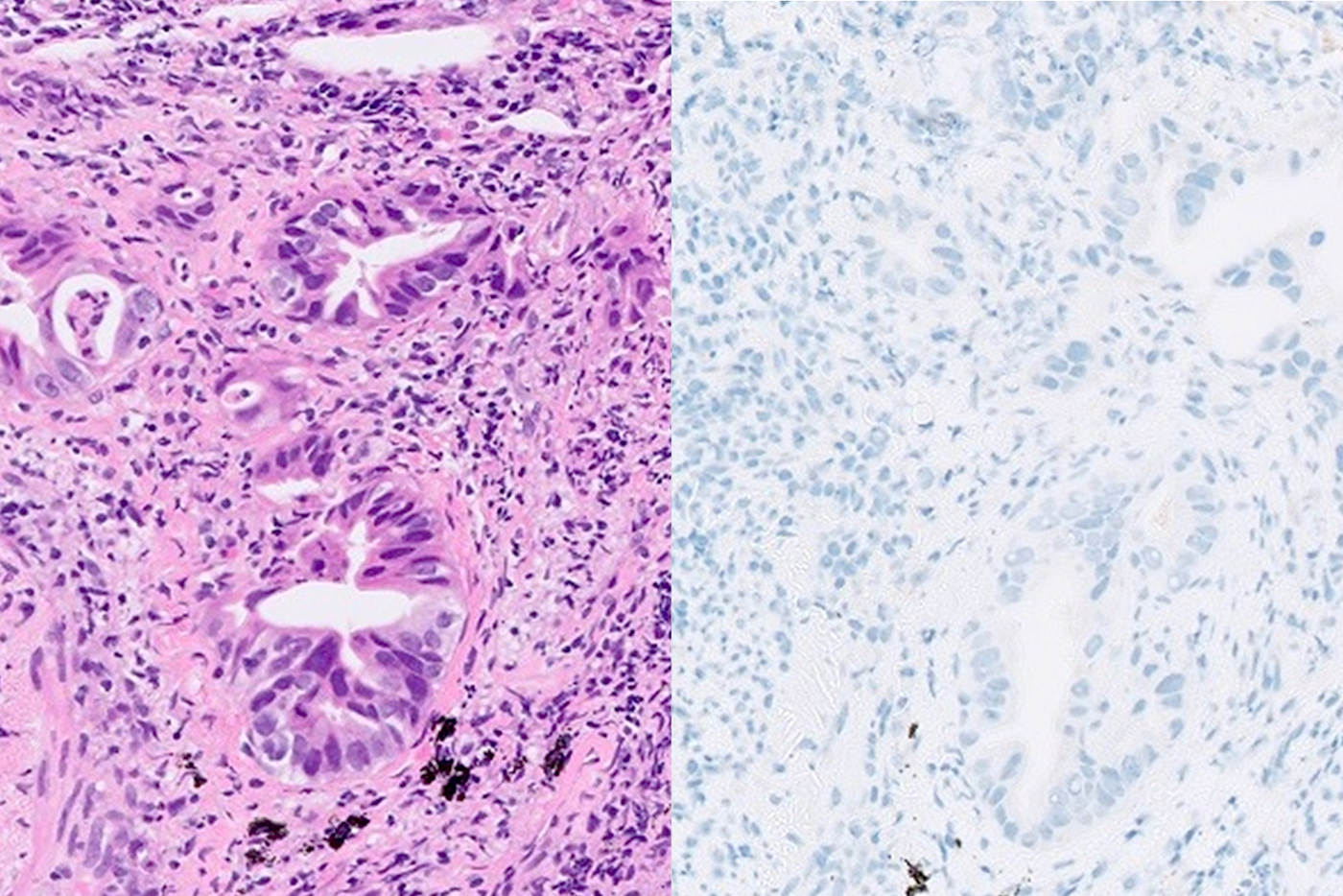
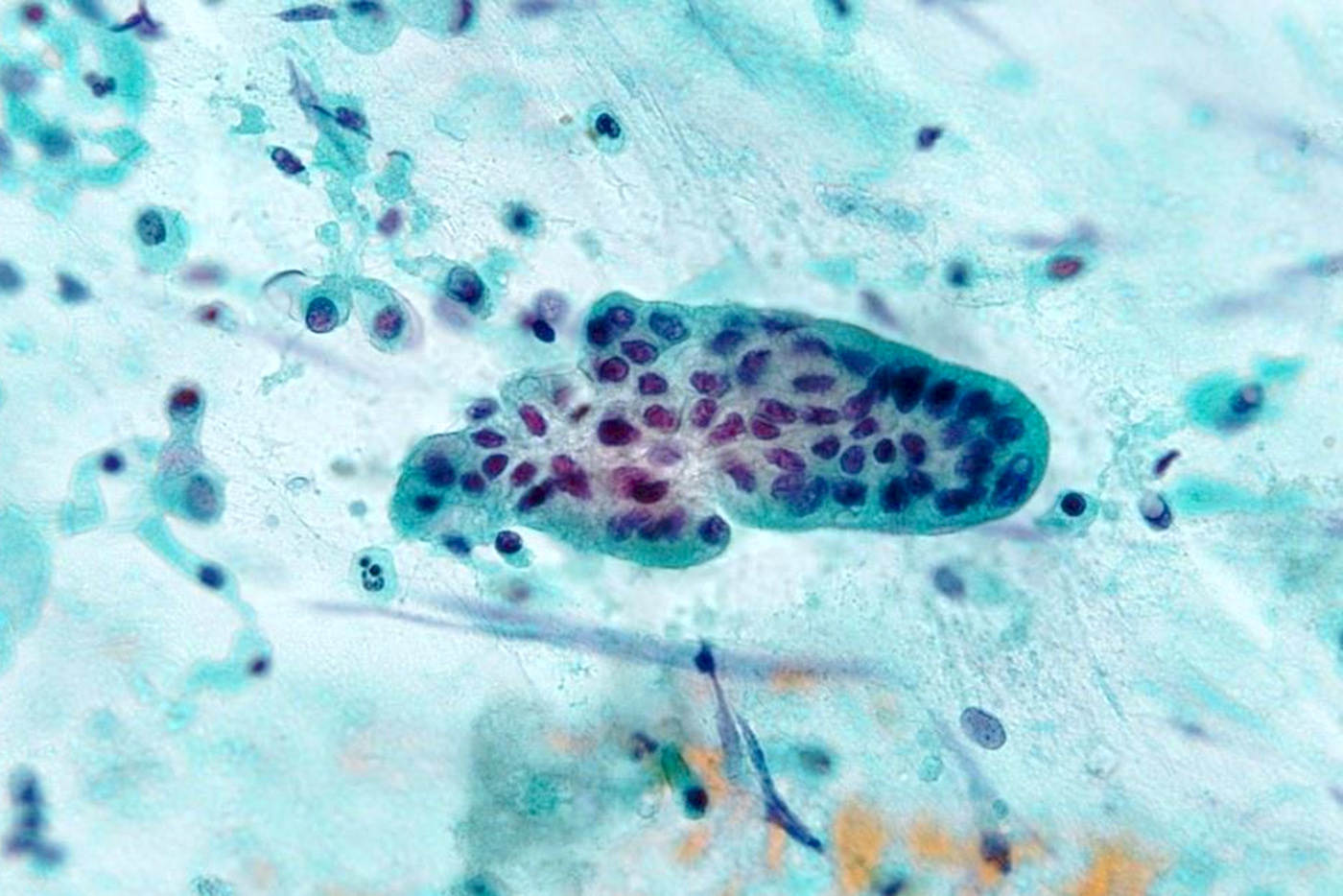
- Pertinent negative findings; need to rule out secondary causes and other lung disease if present
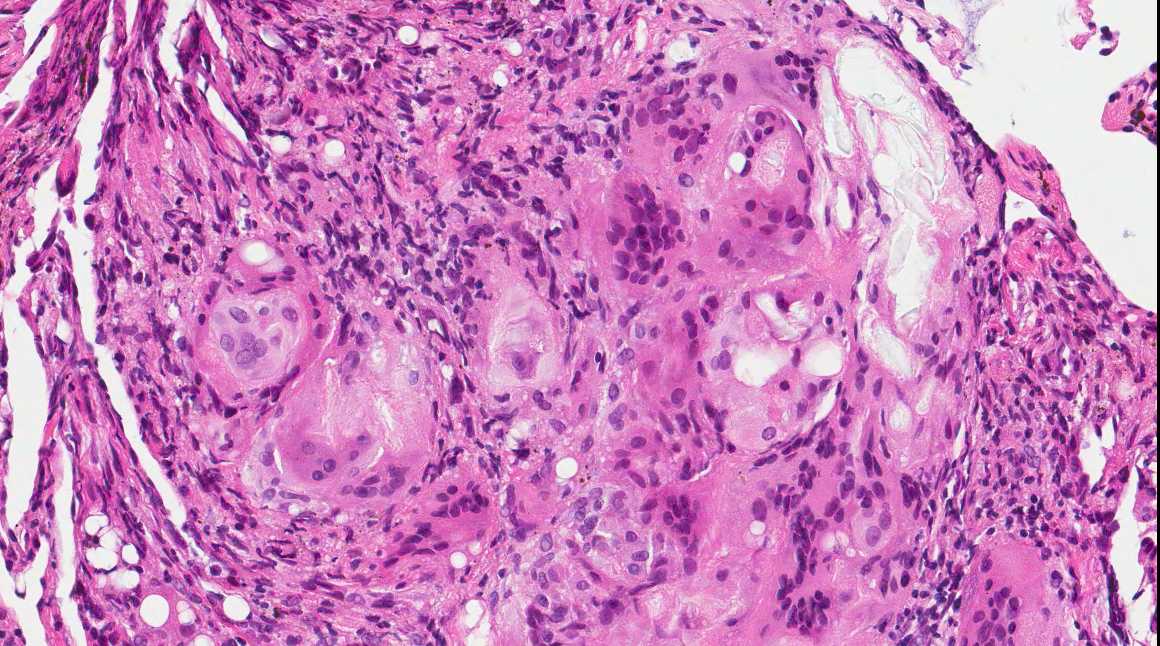
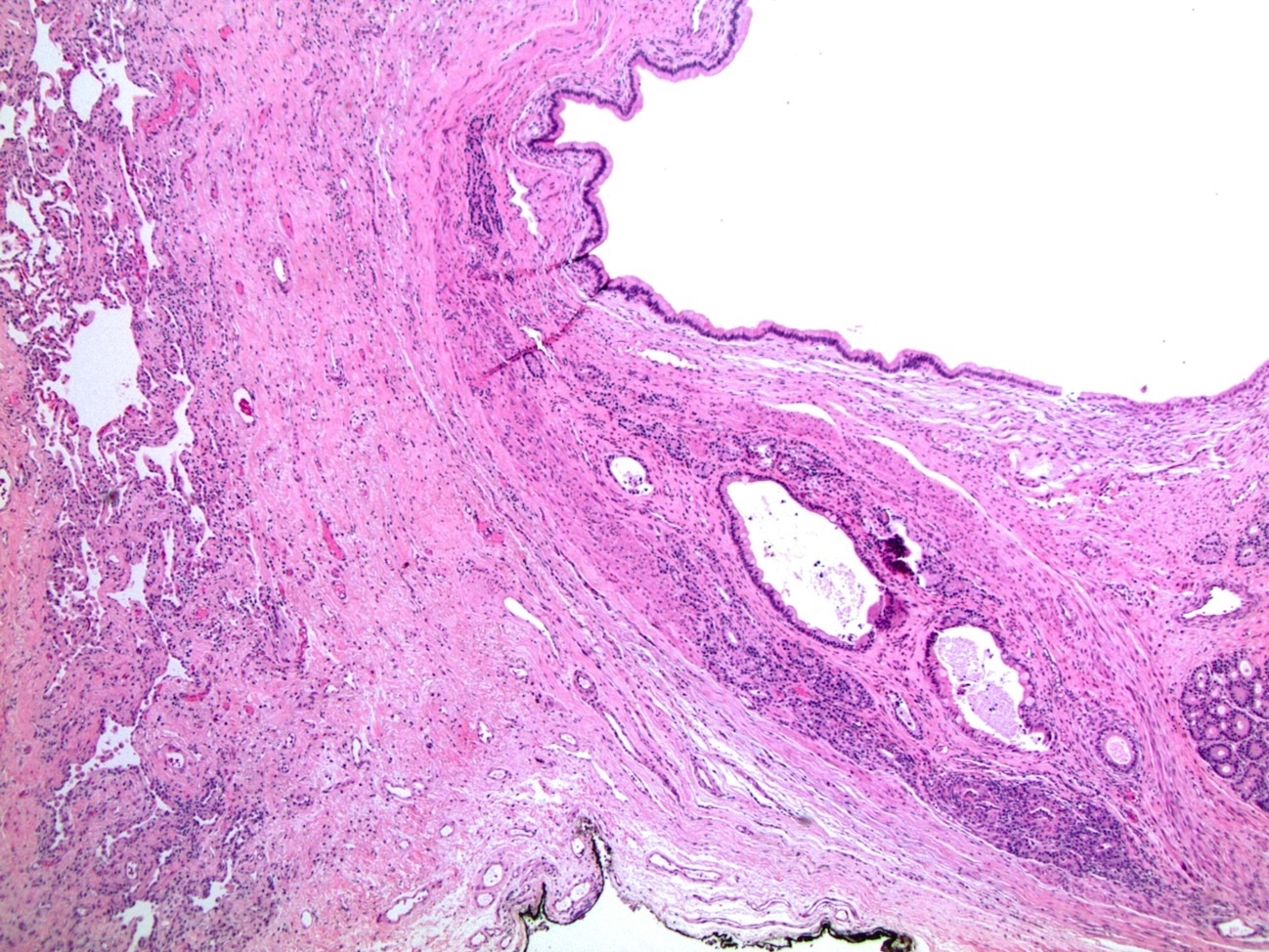
- Hyaline membranes
- Eosinophilic inflammation
- Extensive bronchopneumonia or abscess
- Granulomatous inflammation
- Vasculitis including capillaritis
- Areas of necrosis
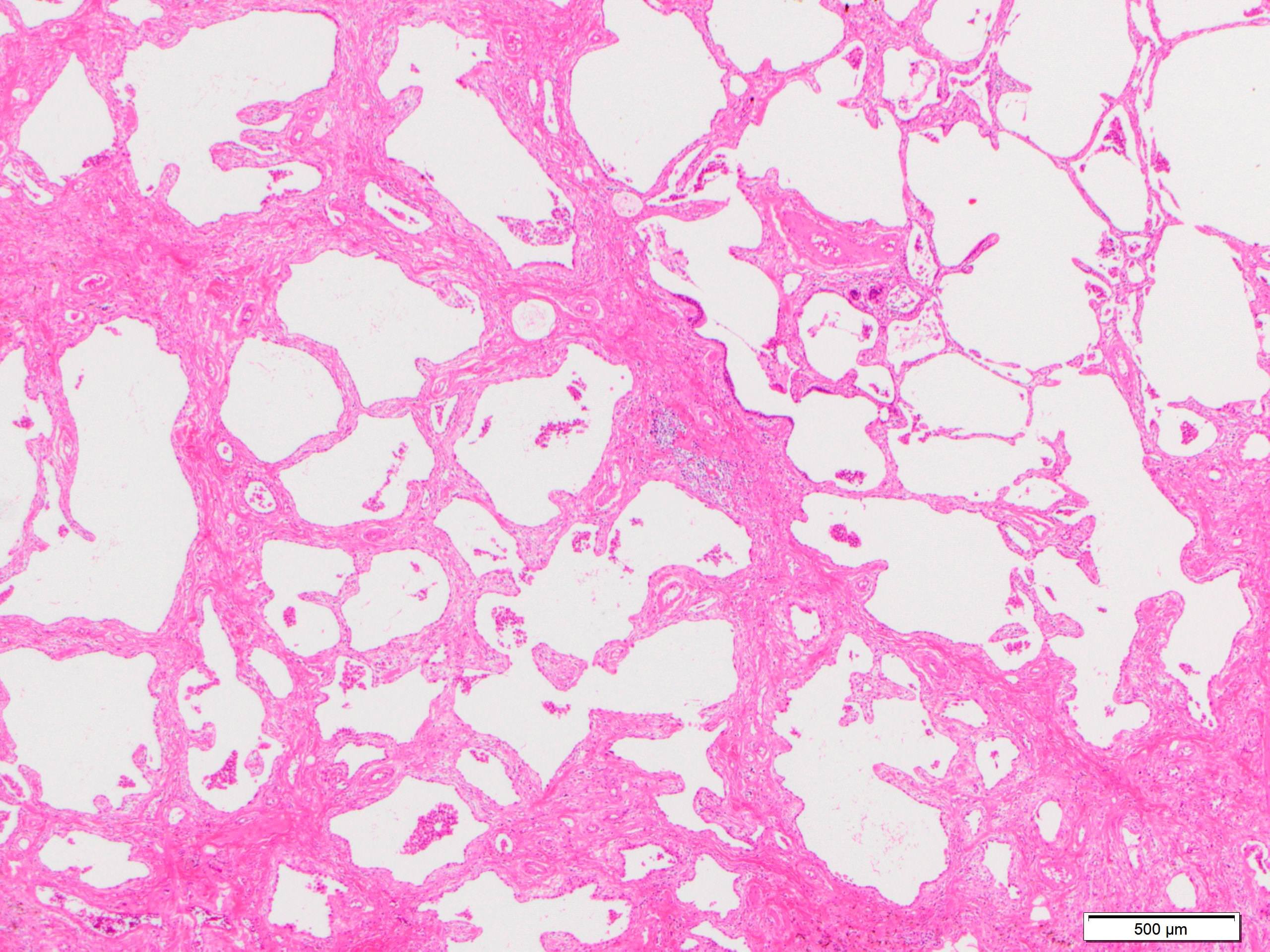
- Marked dense fibrosis or honeycombing
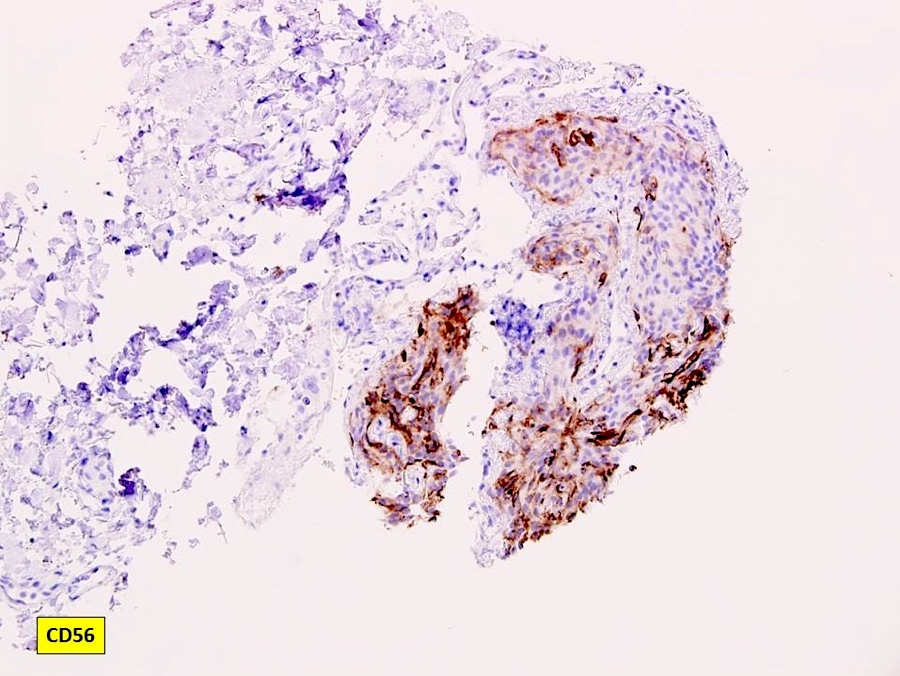
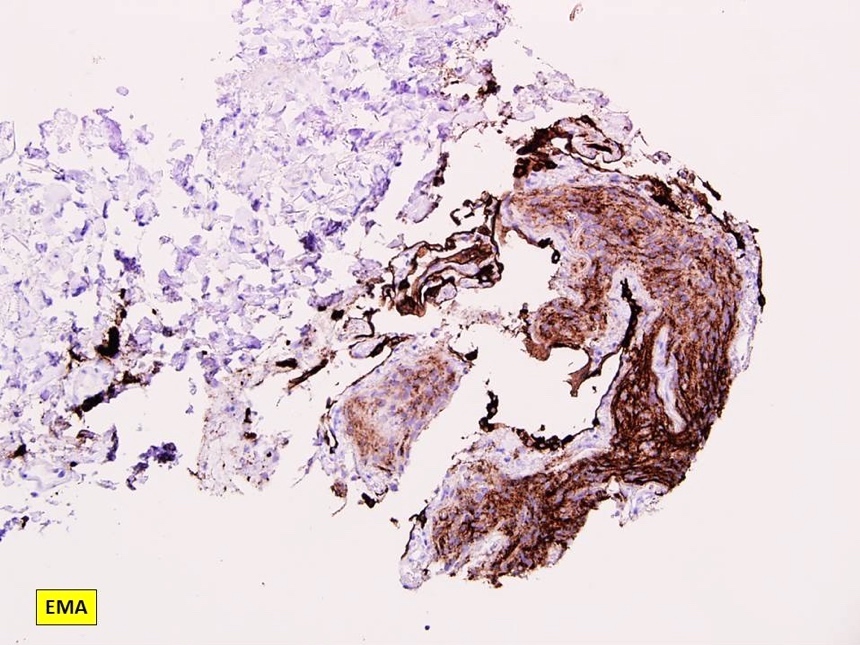
- See J Clin Pathol 2015;68:441
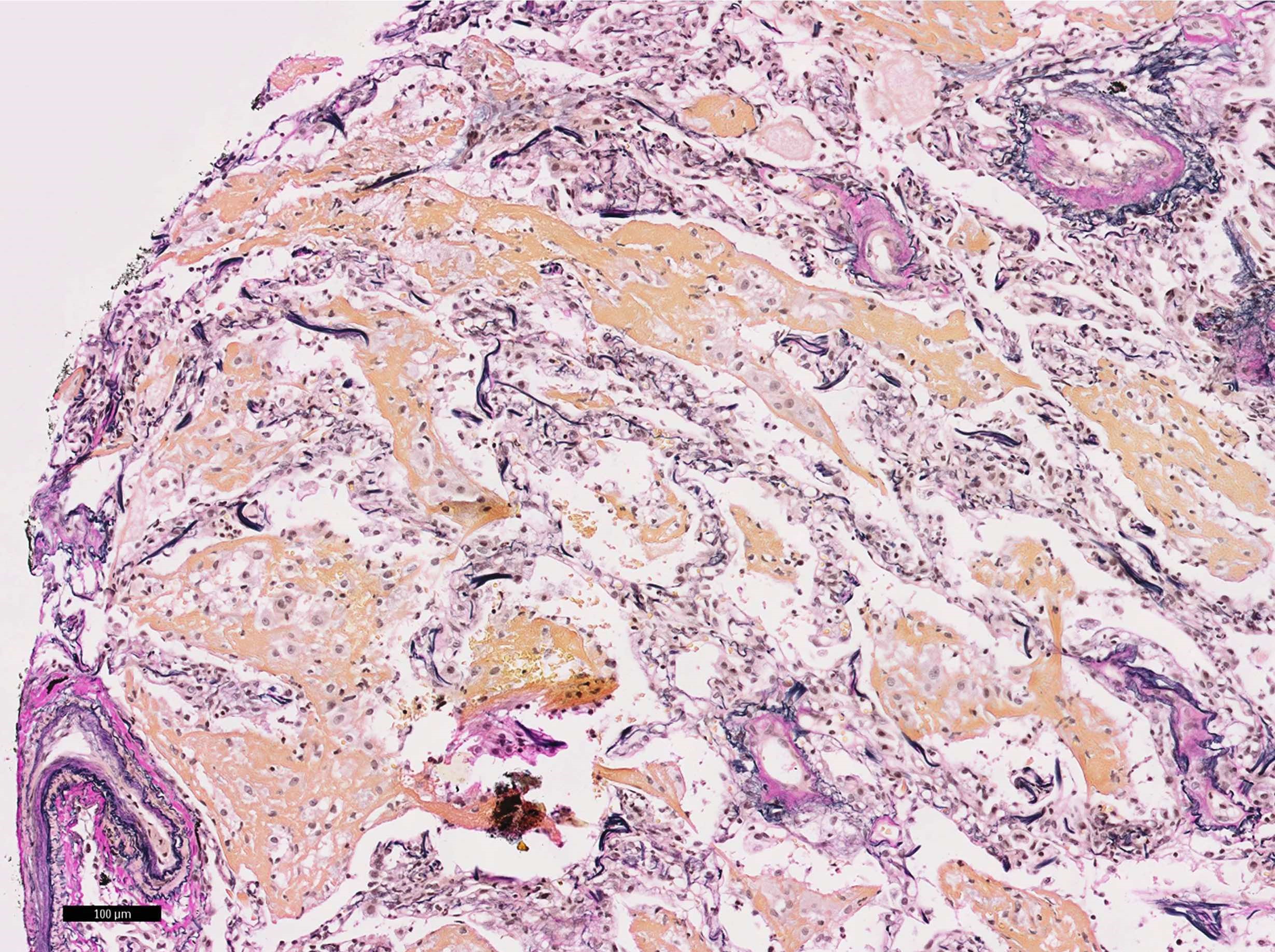
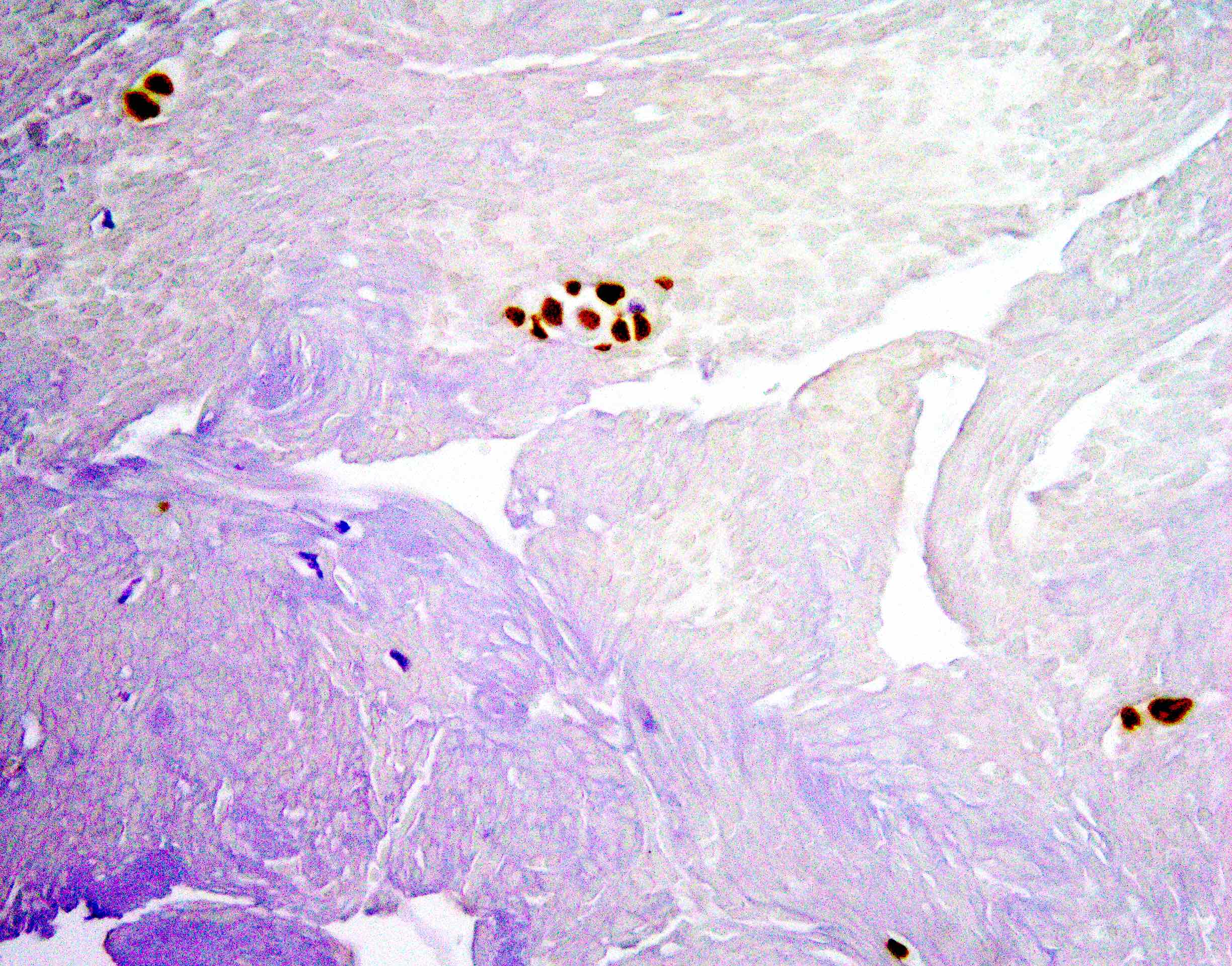
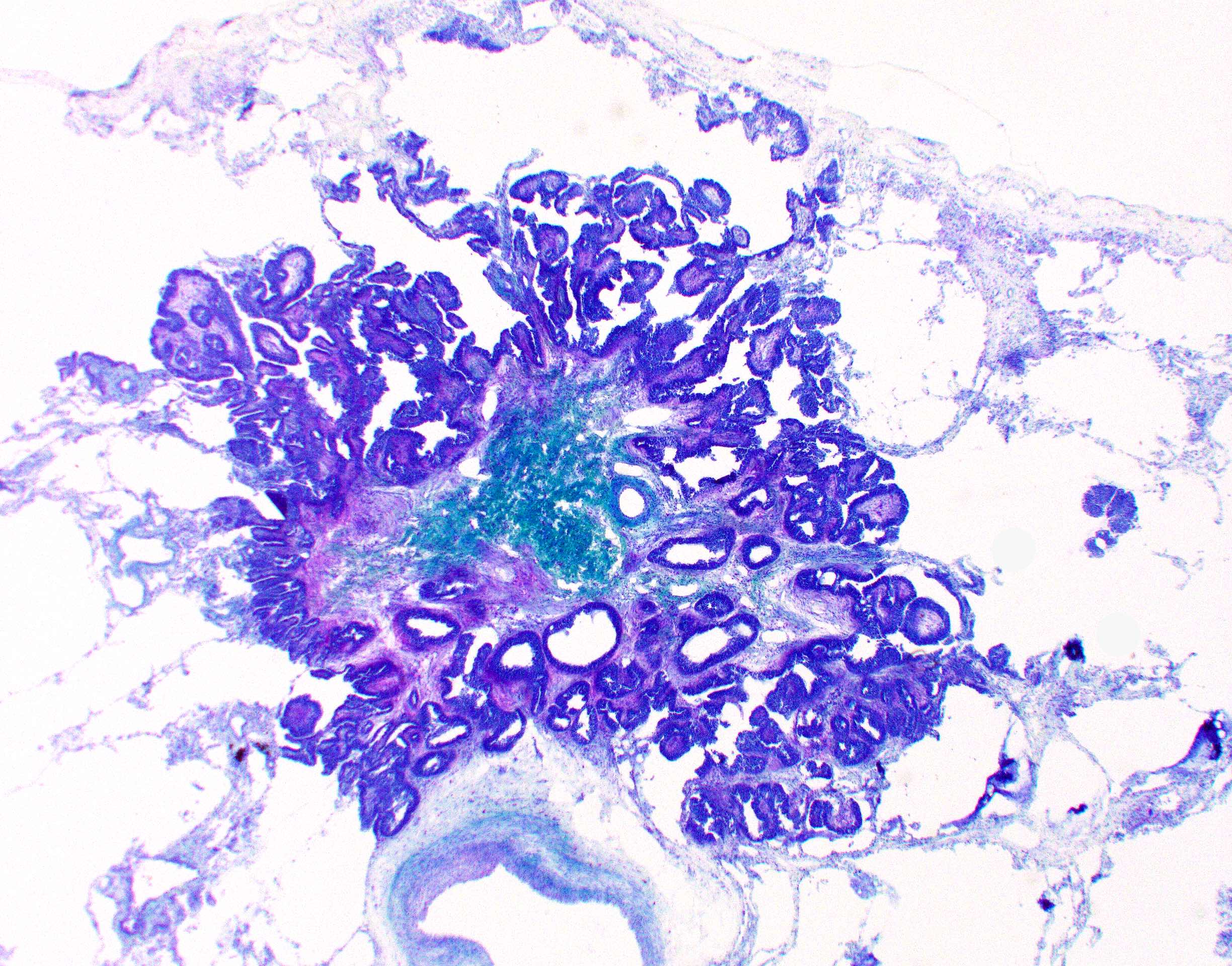
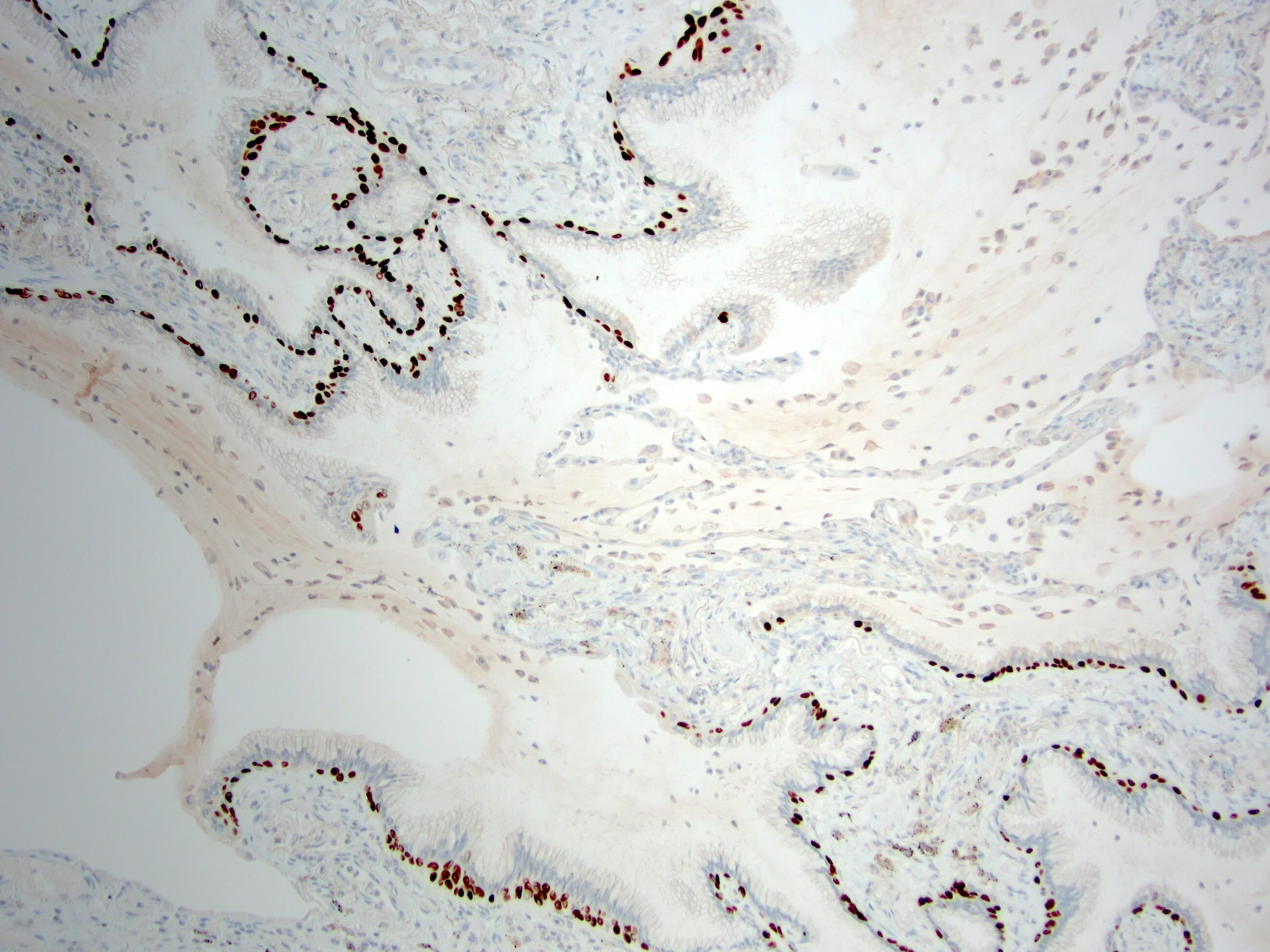
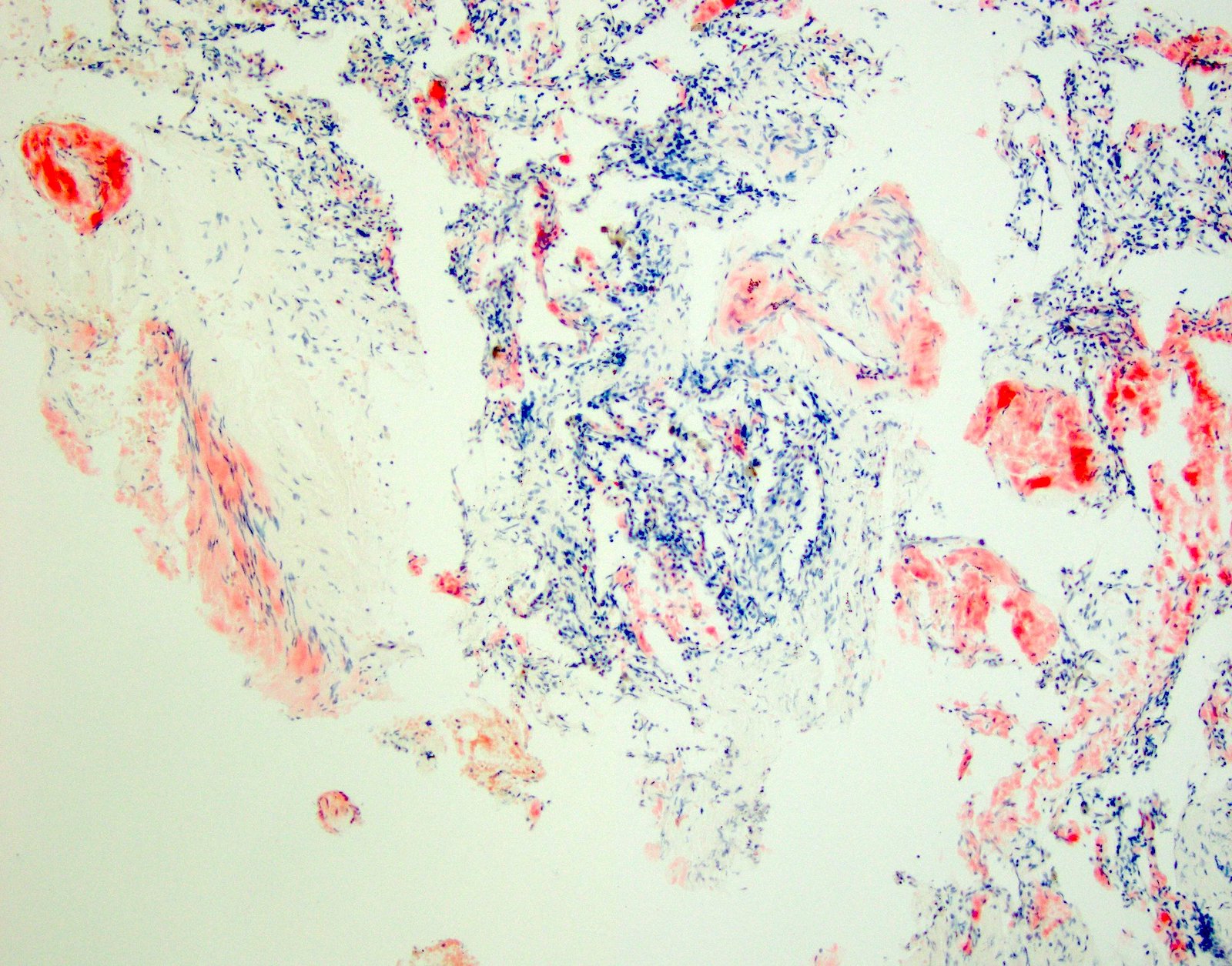
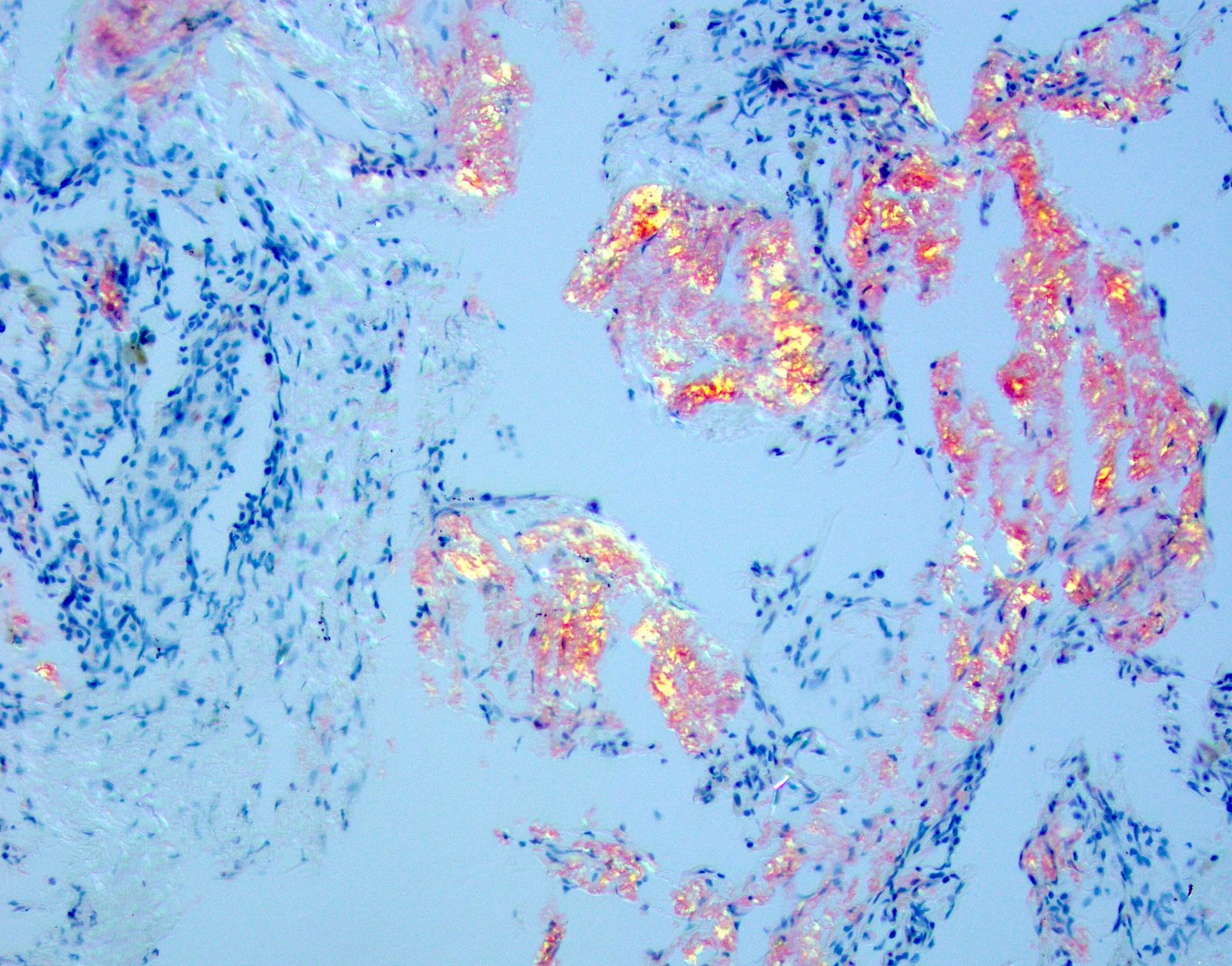
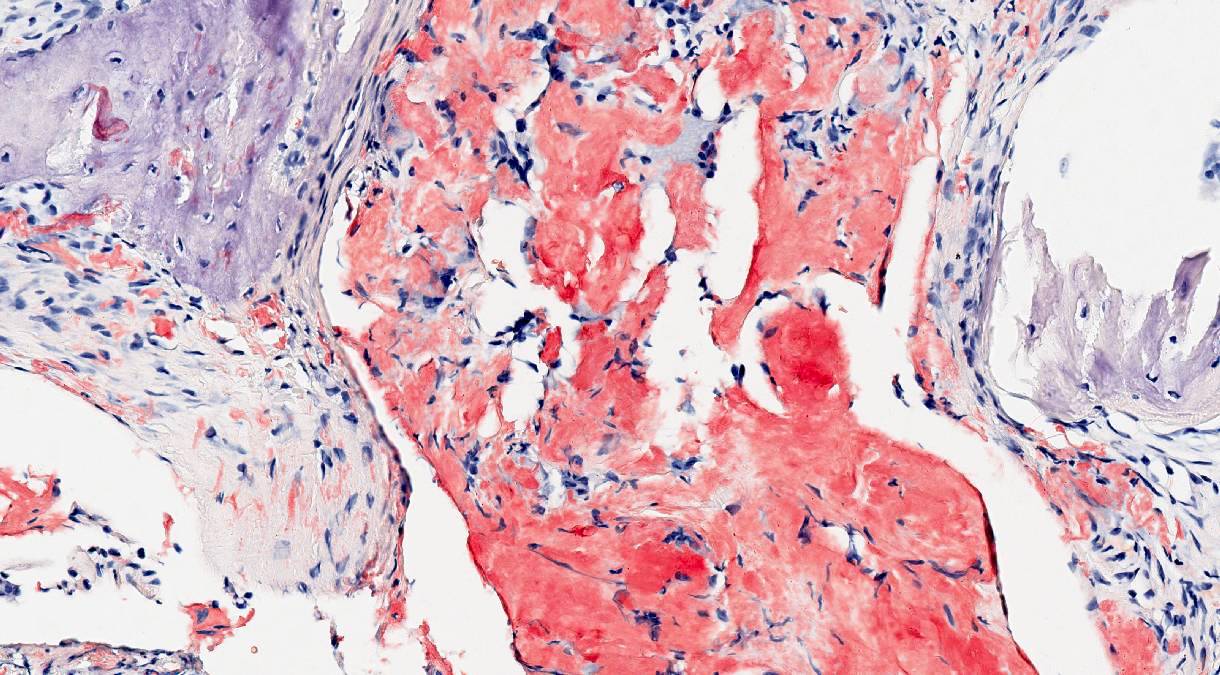
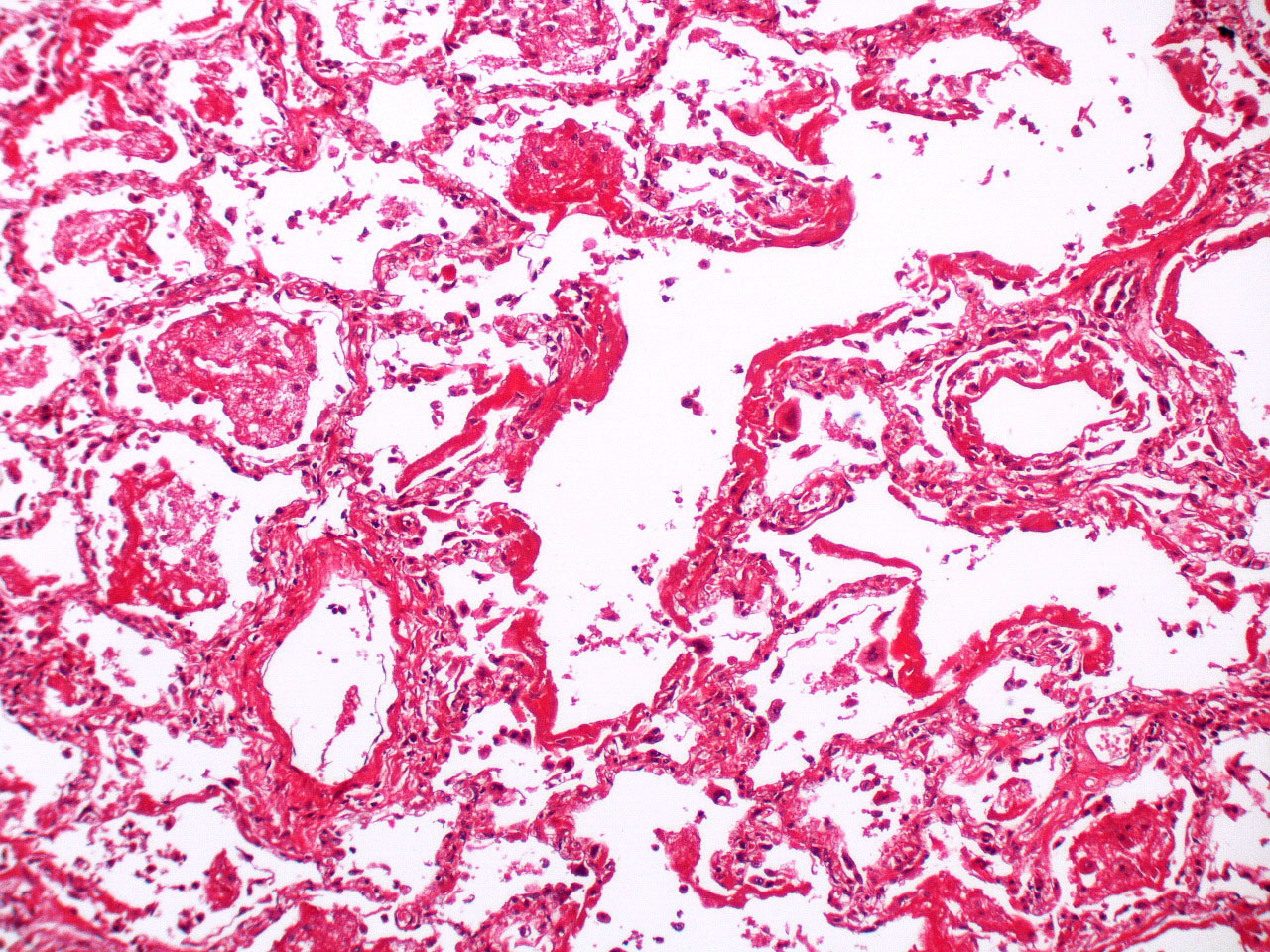
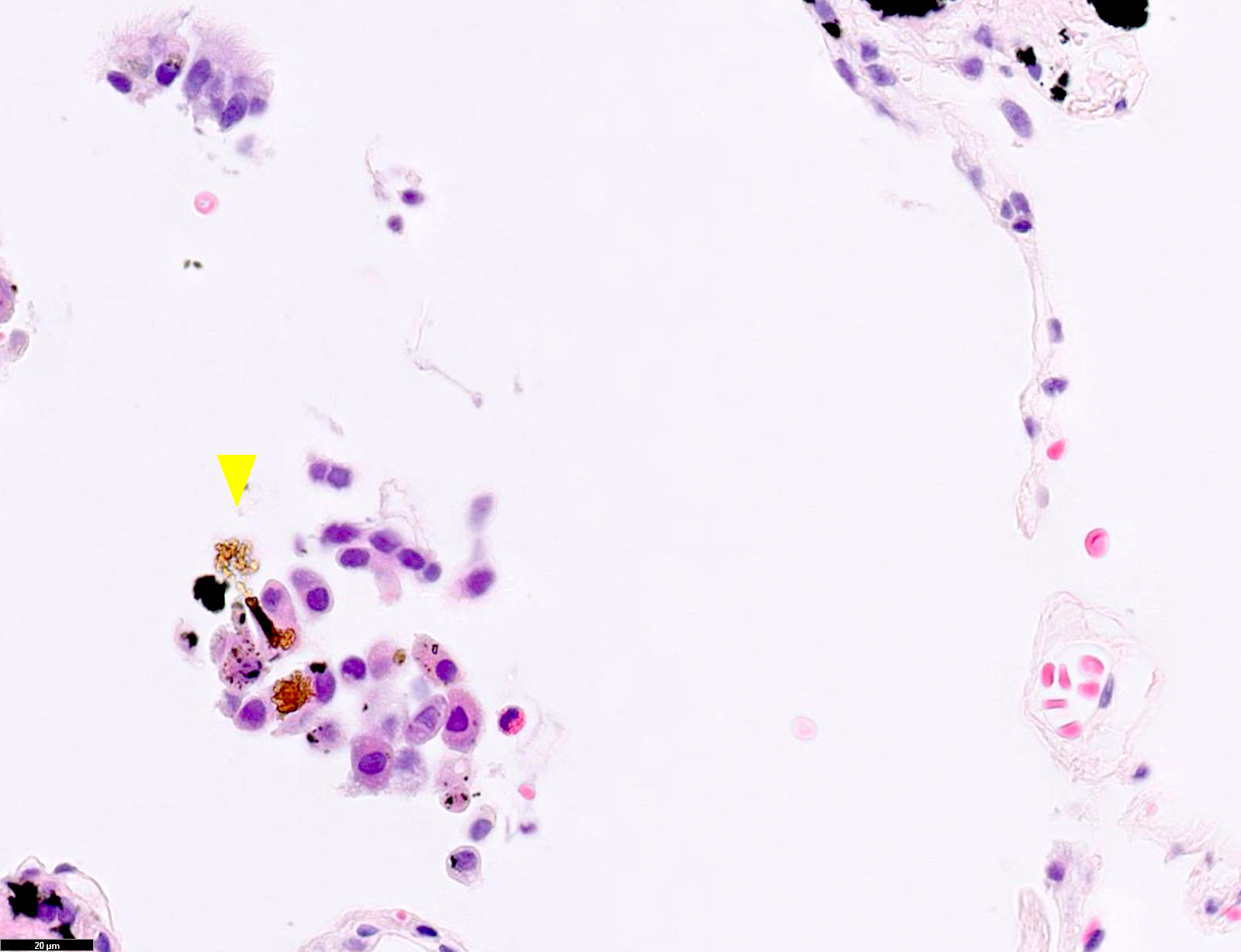
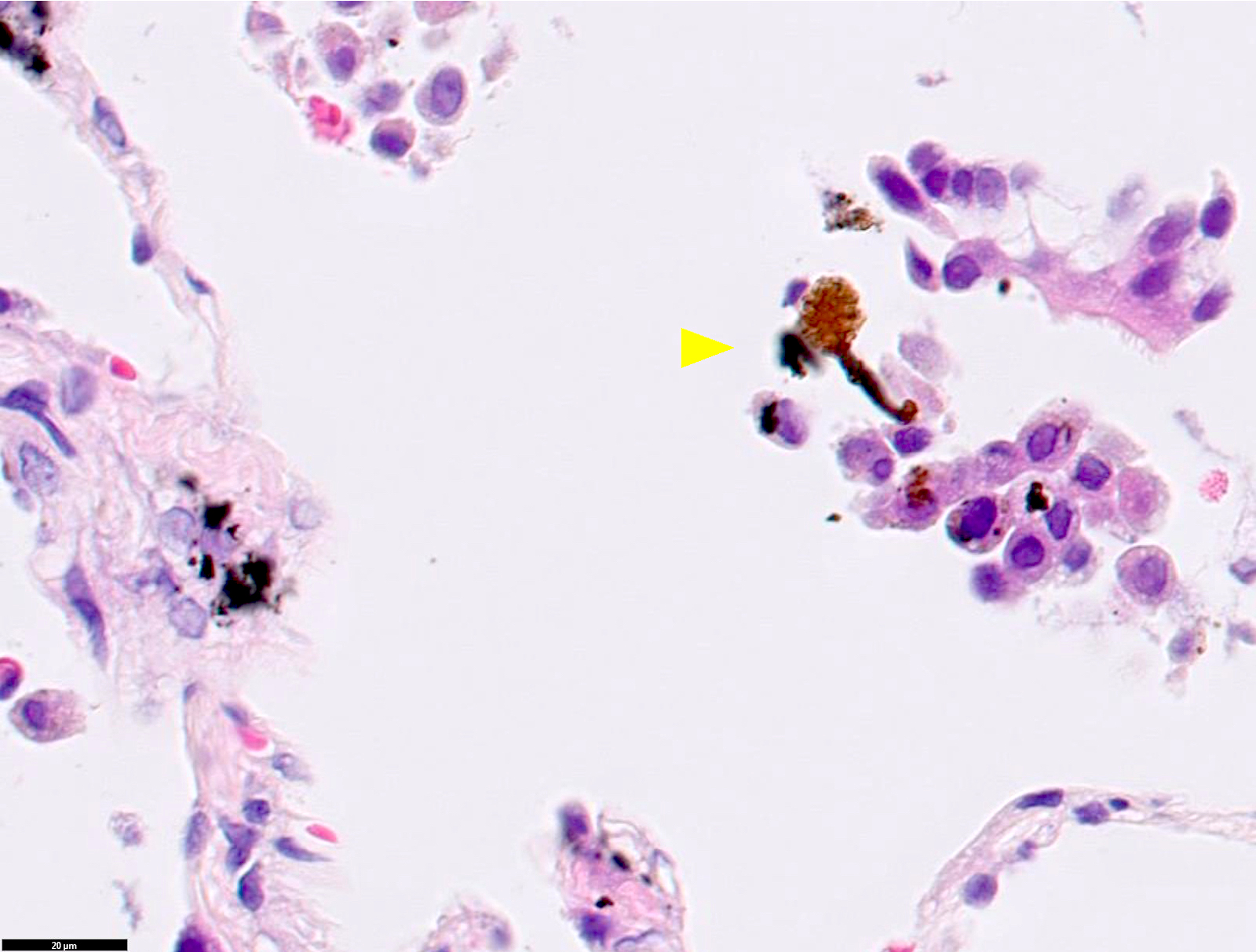
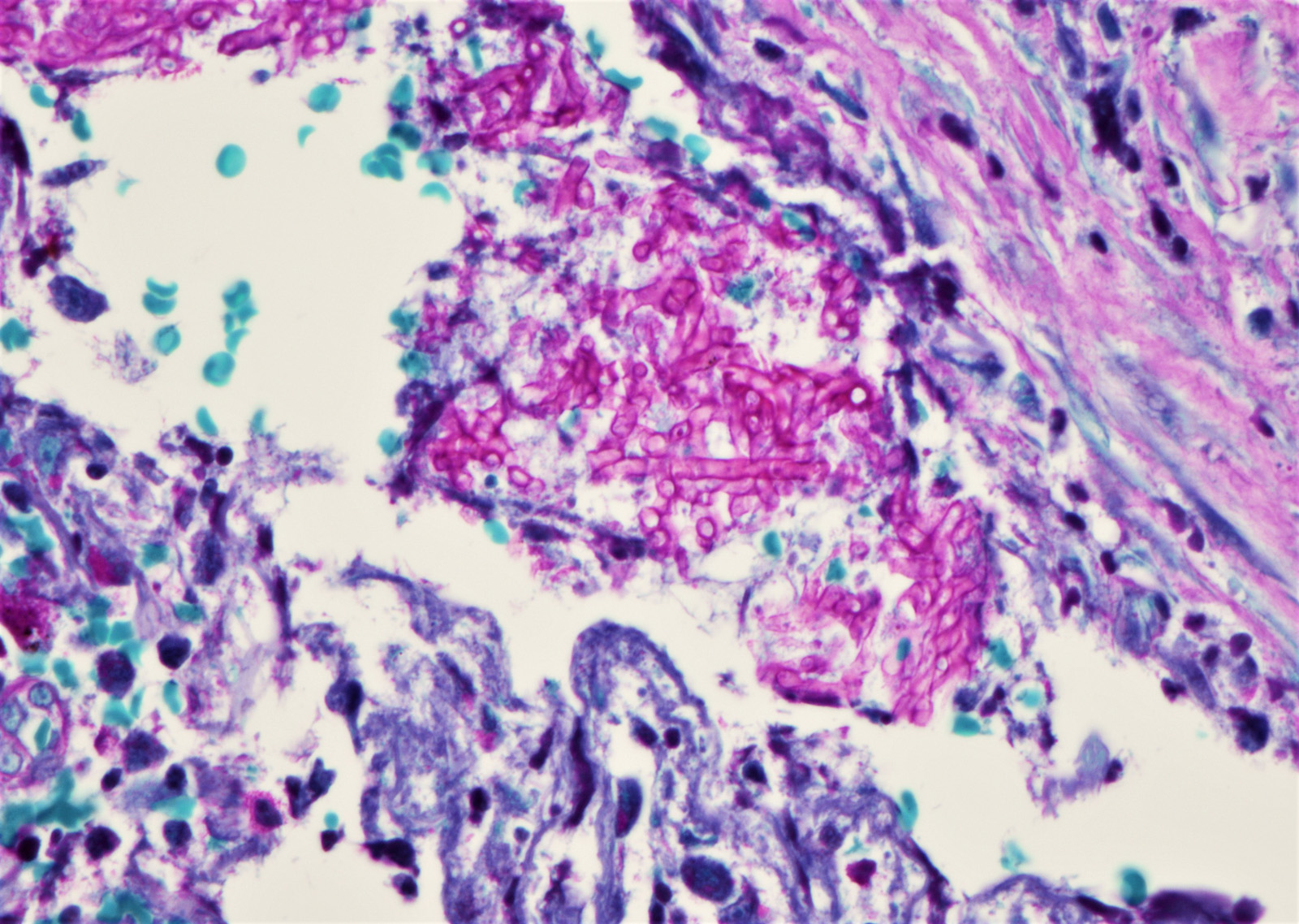
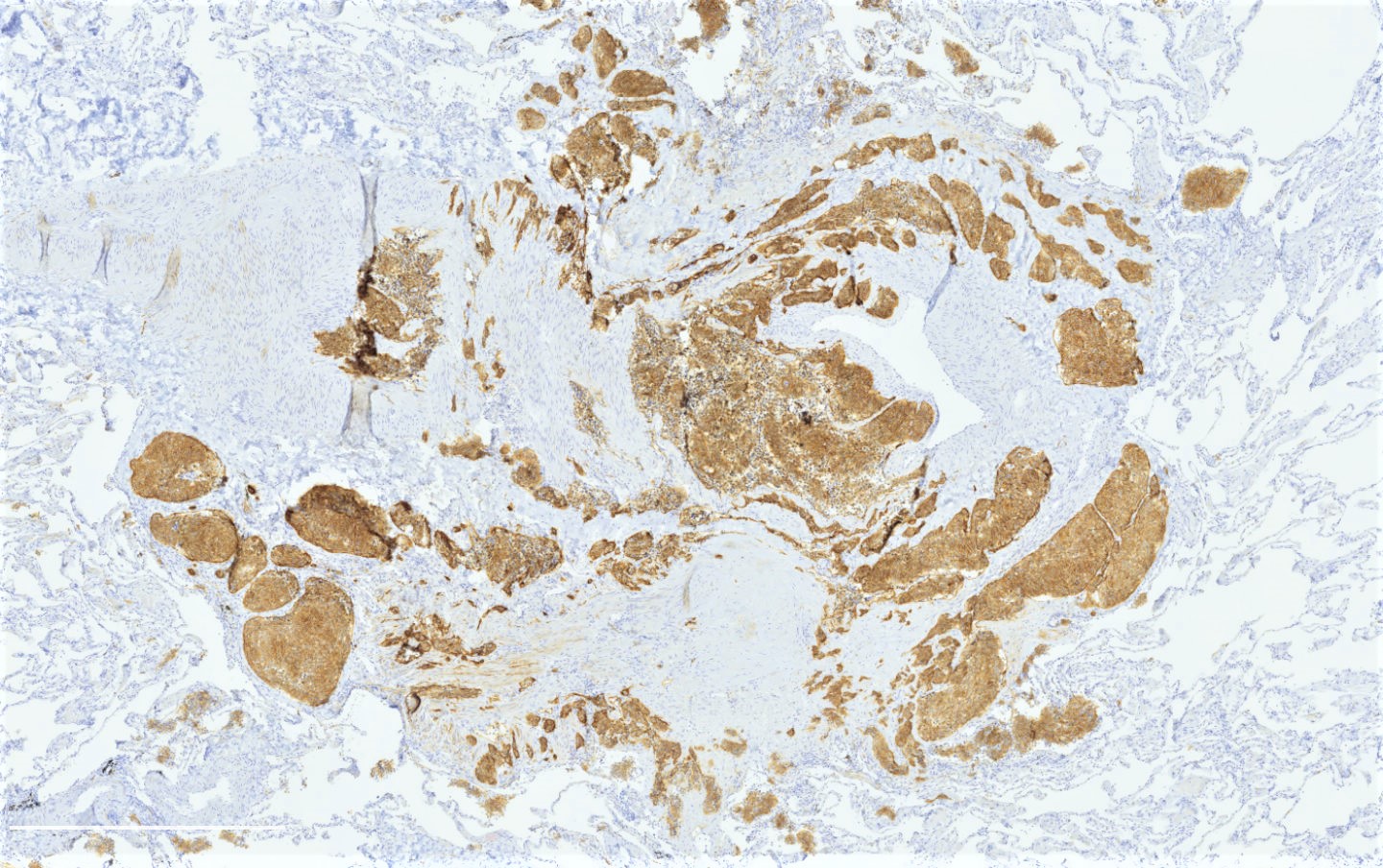
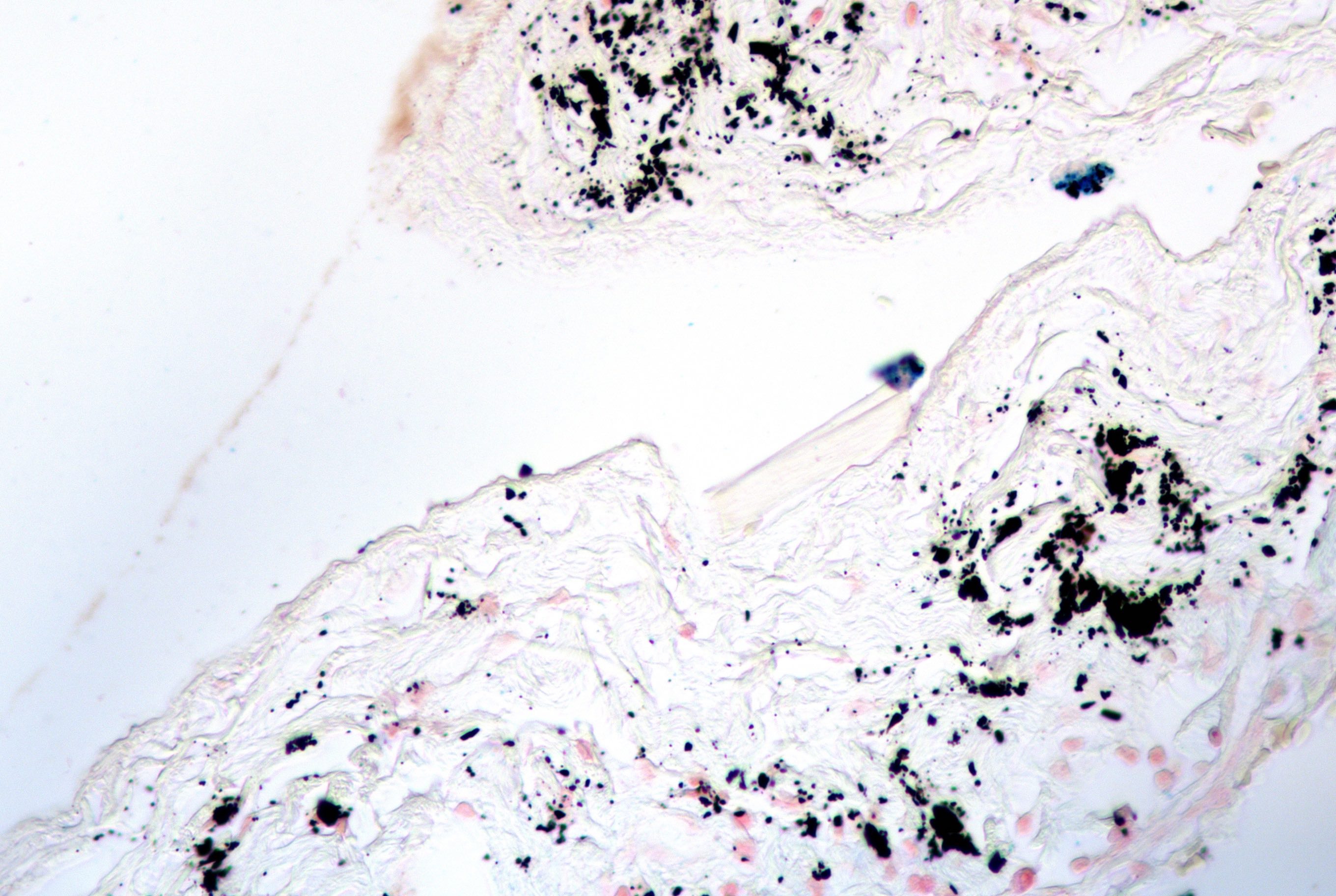
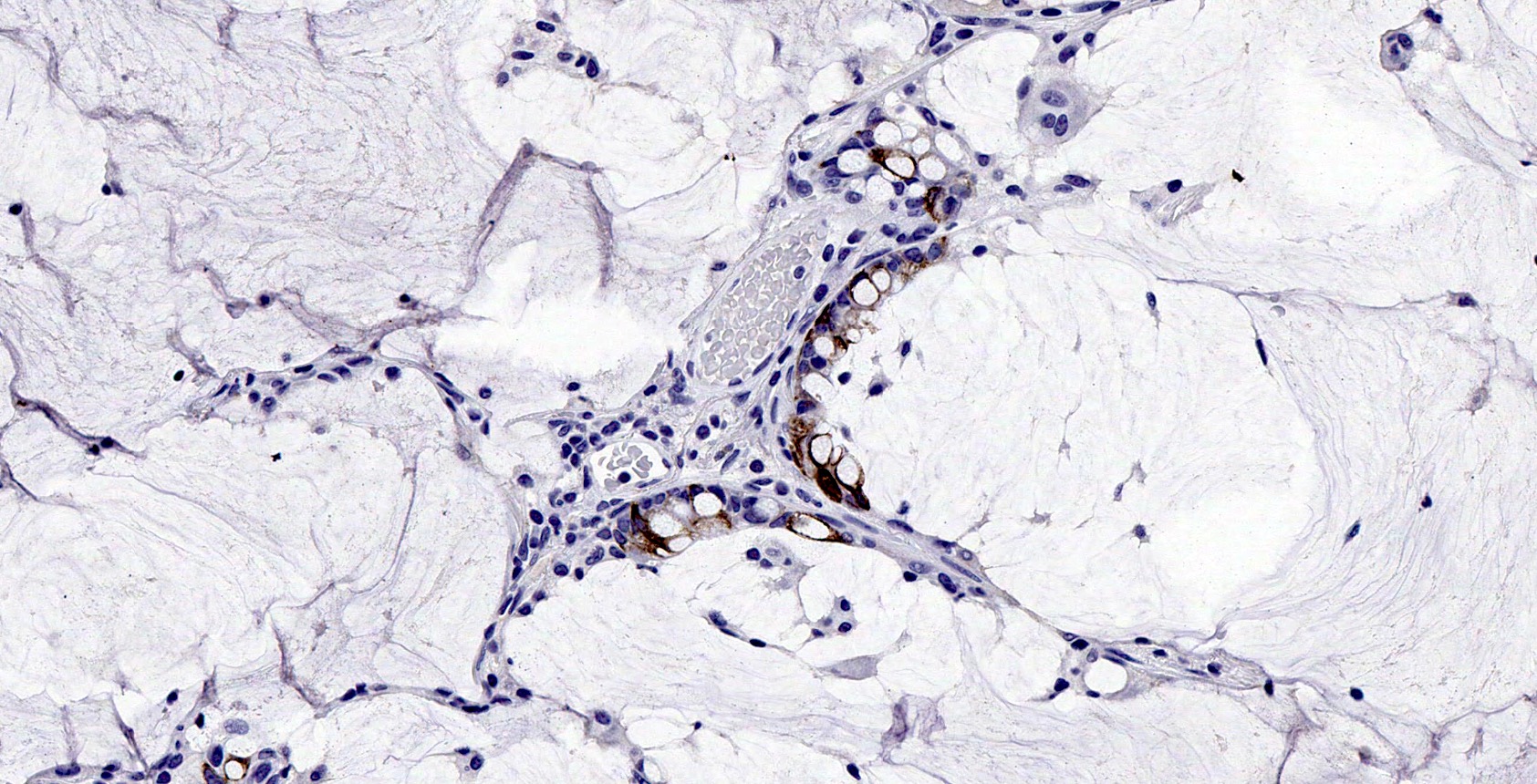
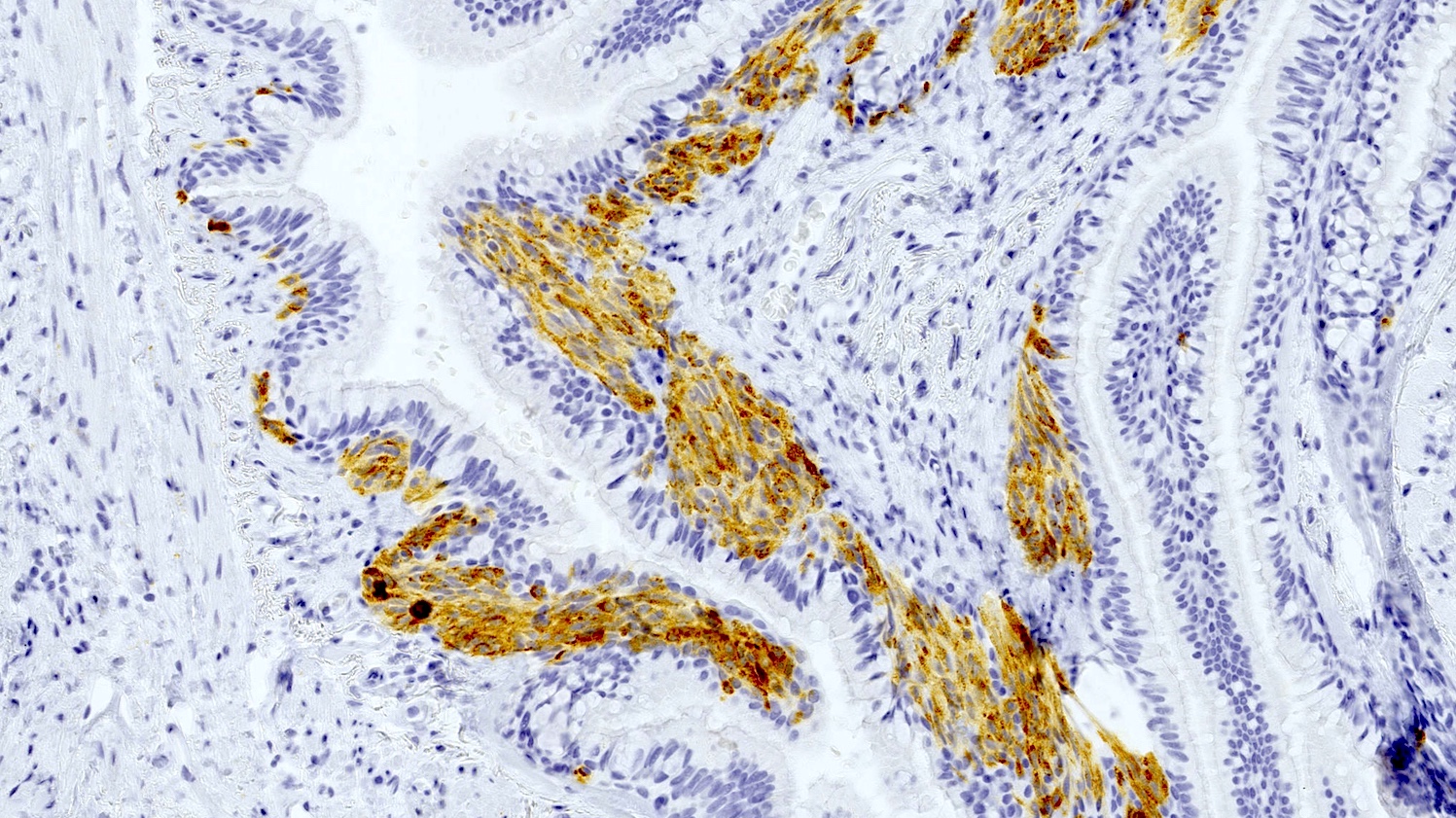
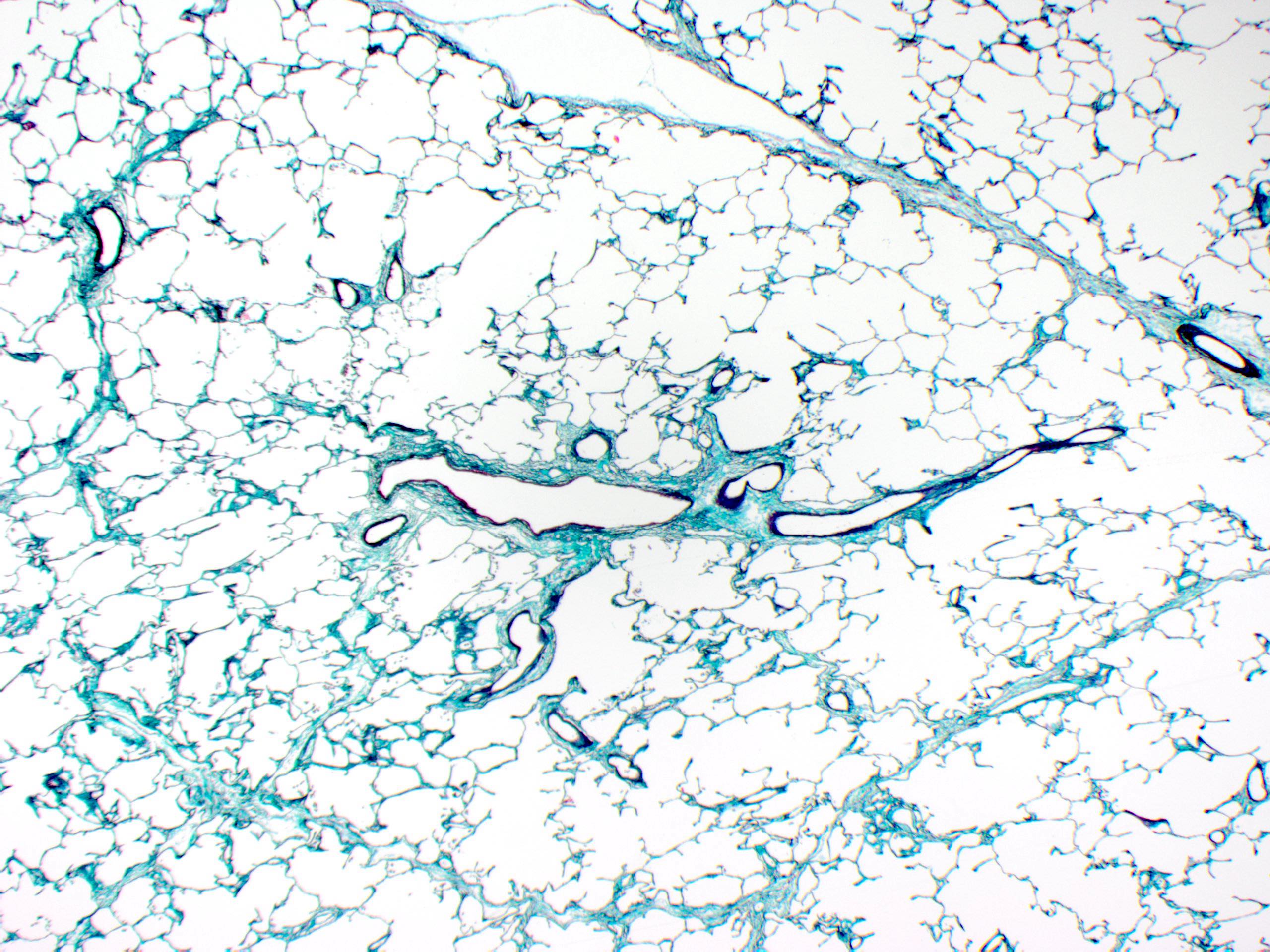
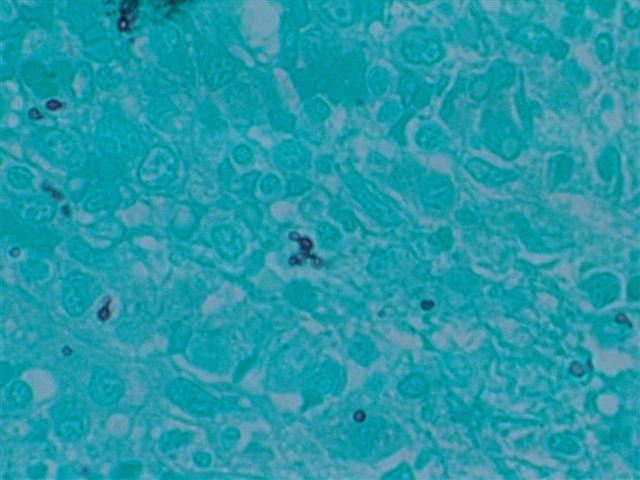
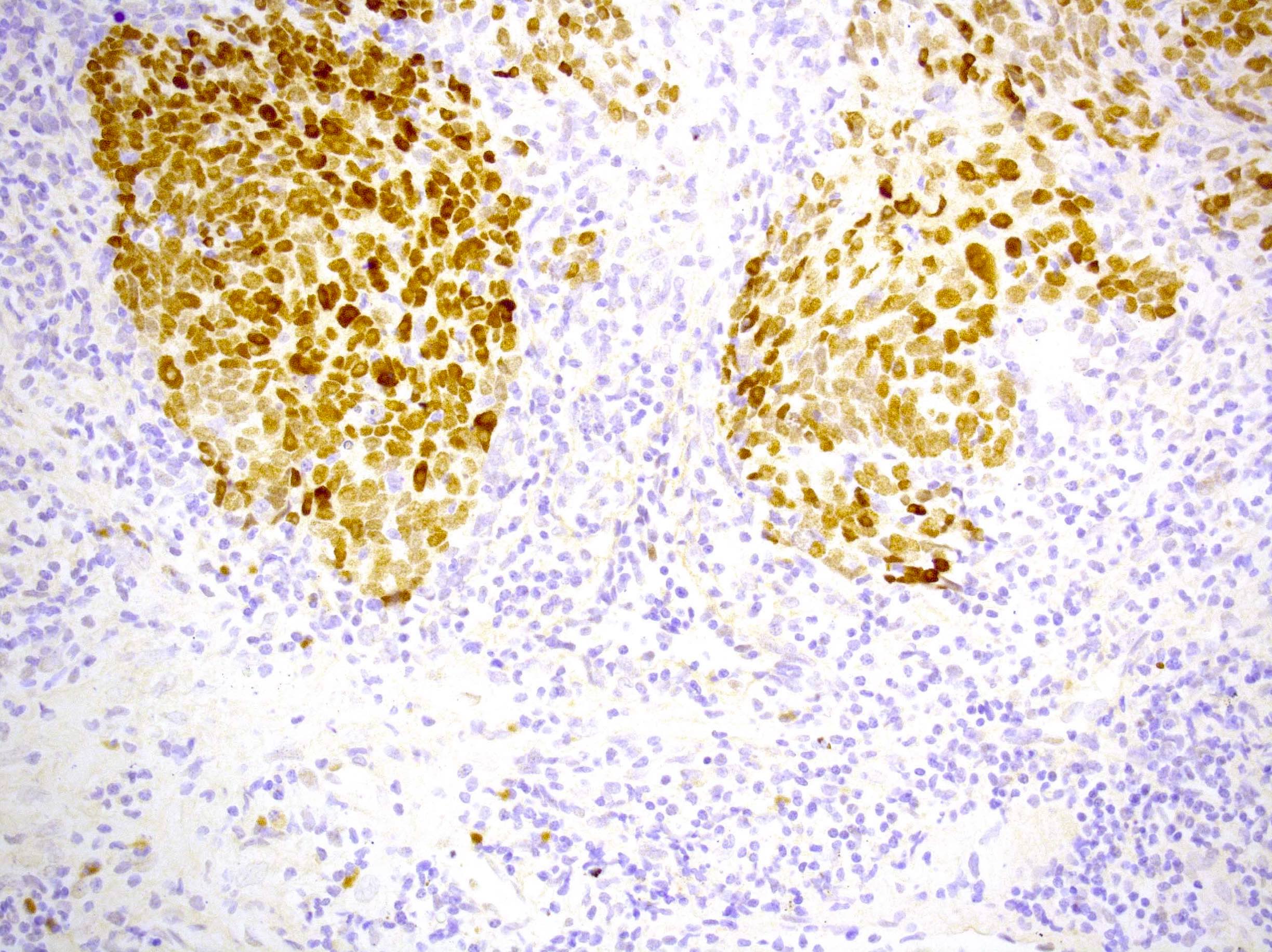
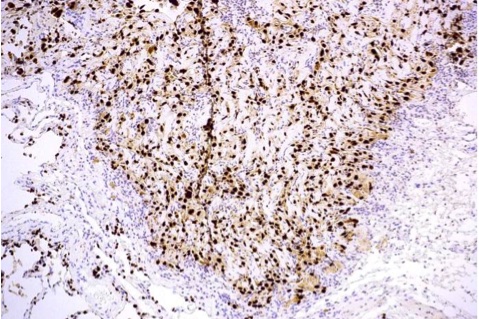
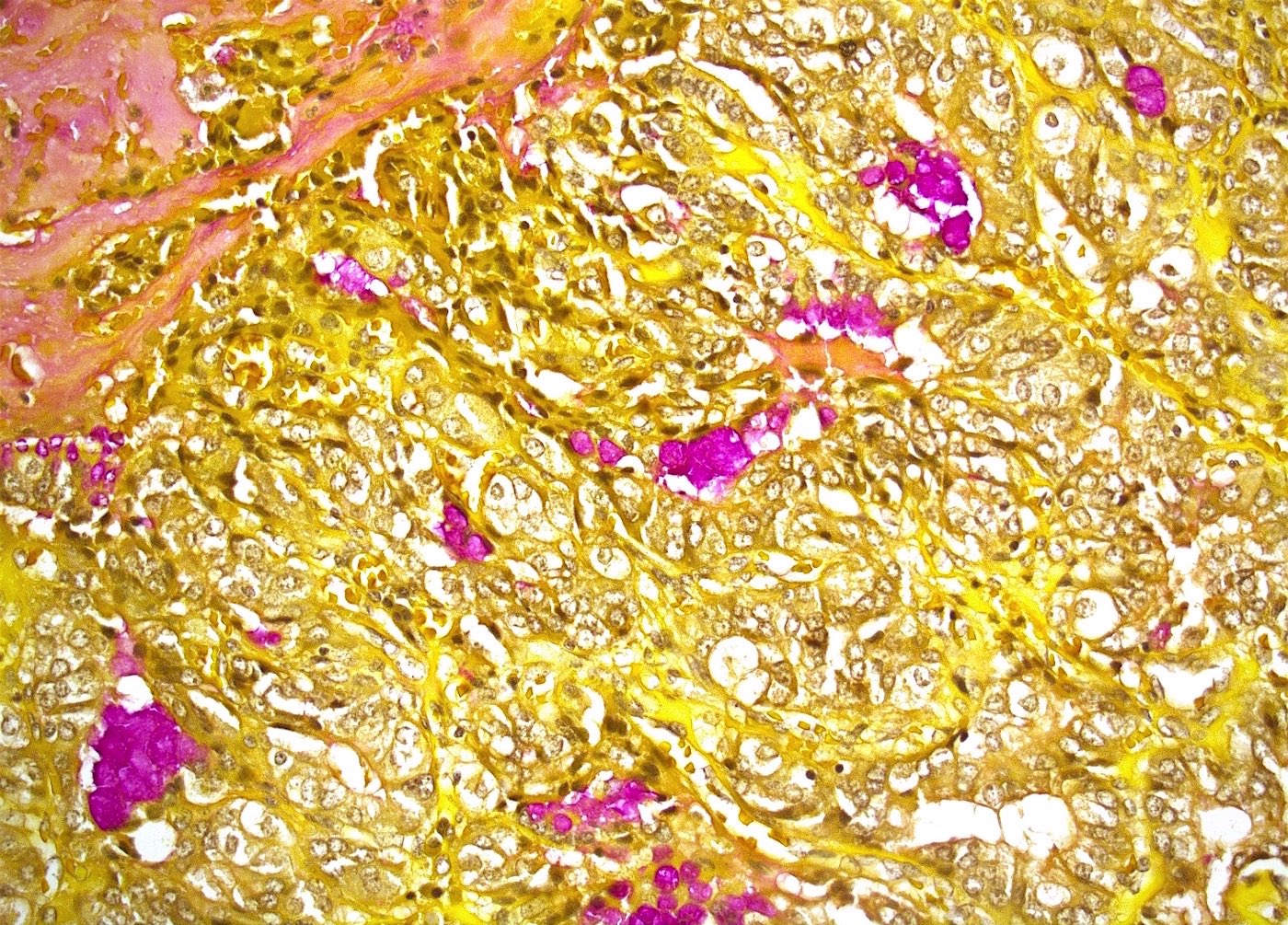
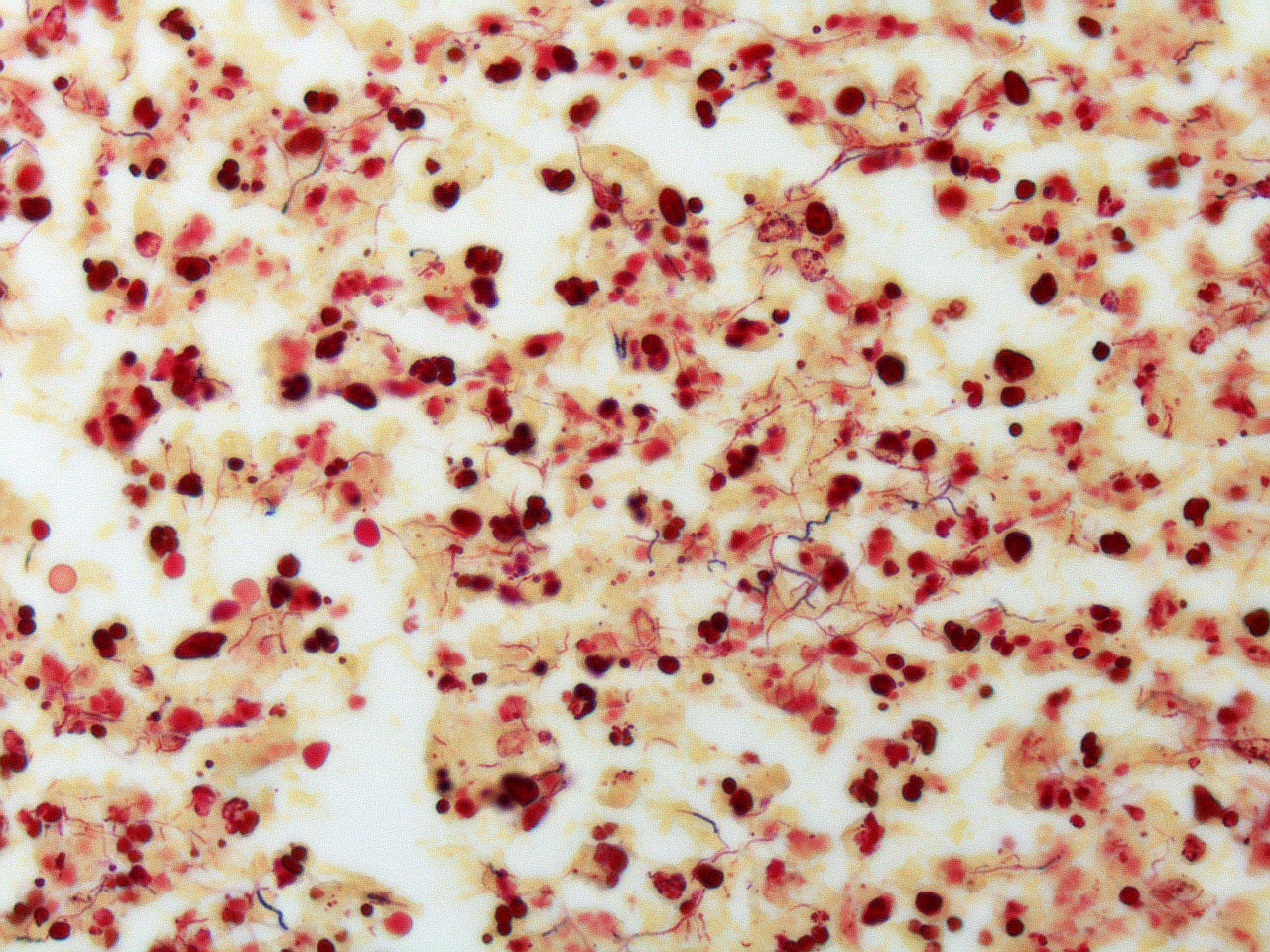
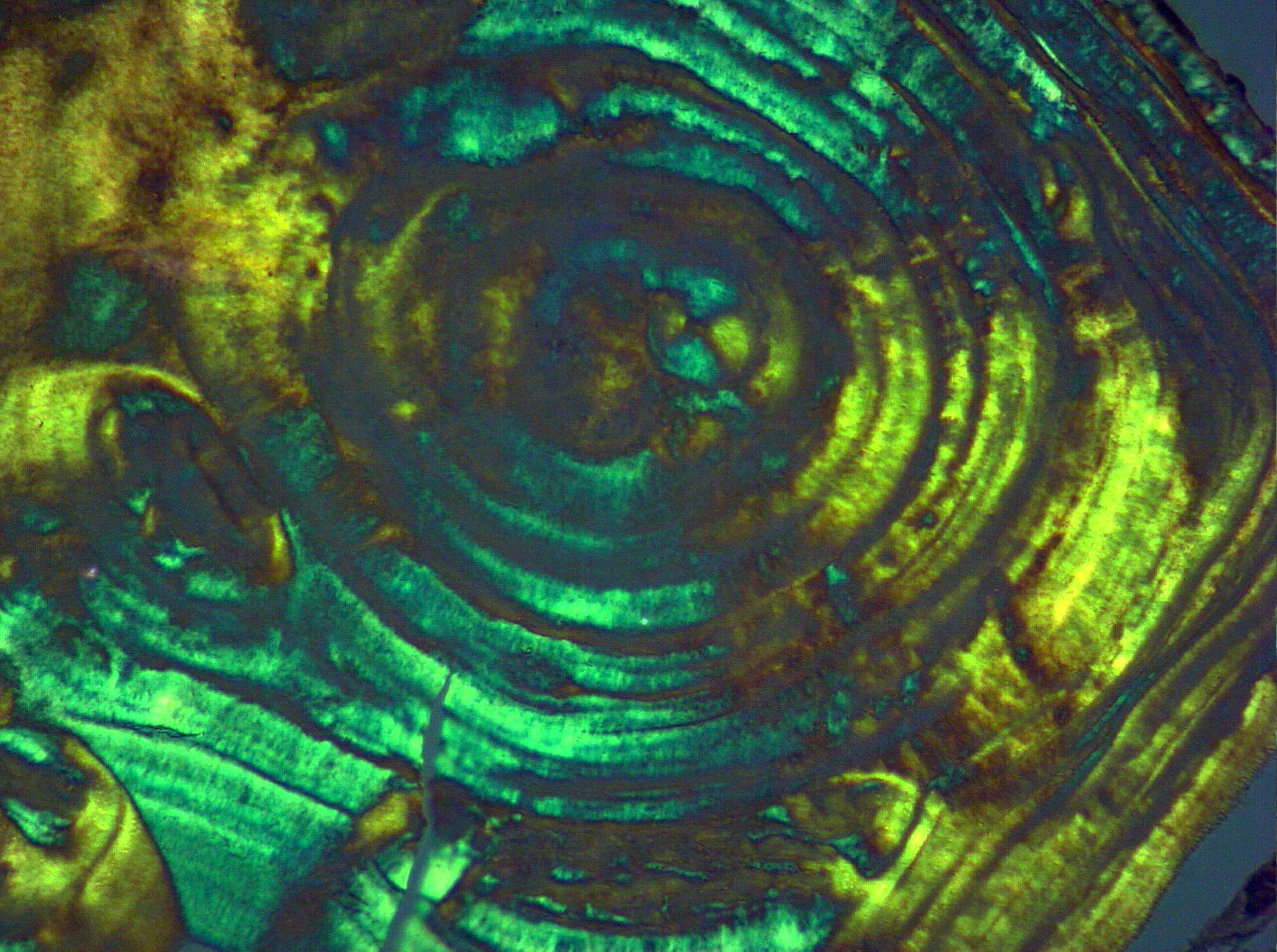
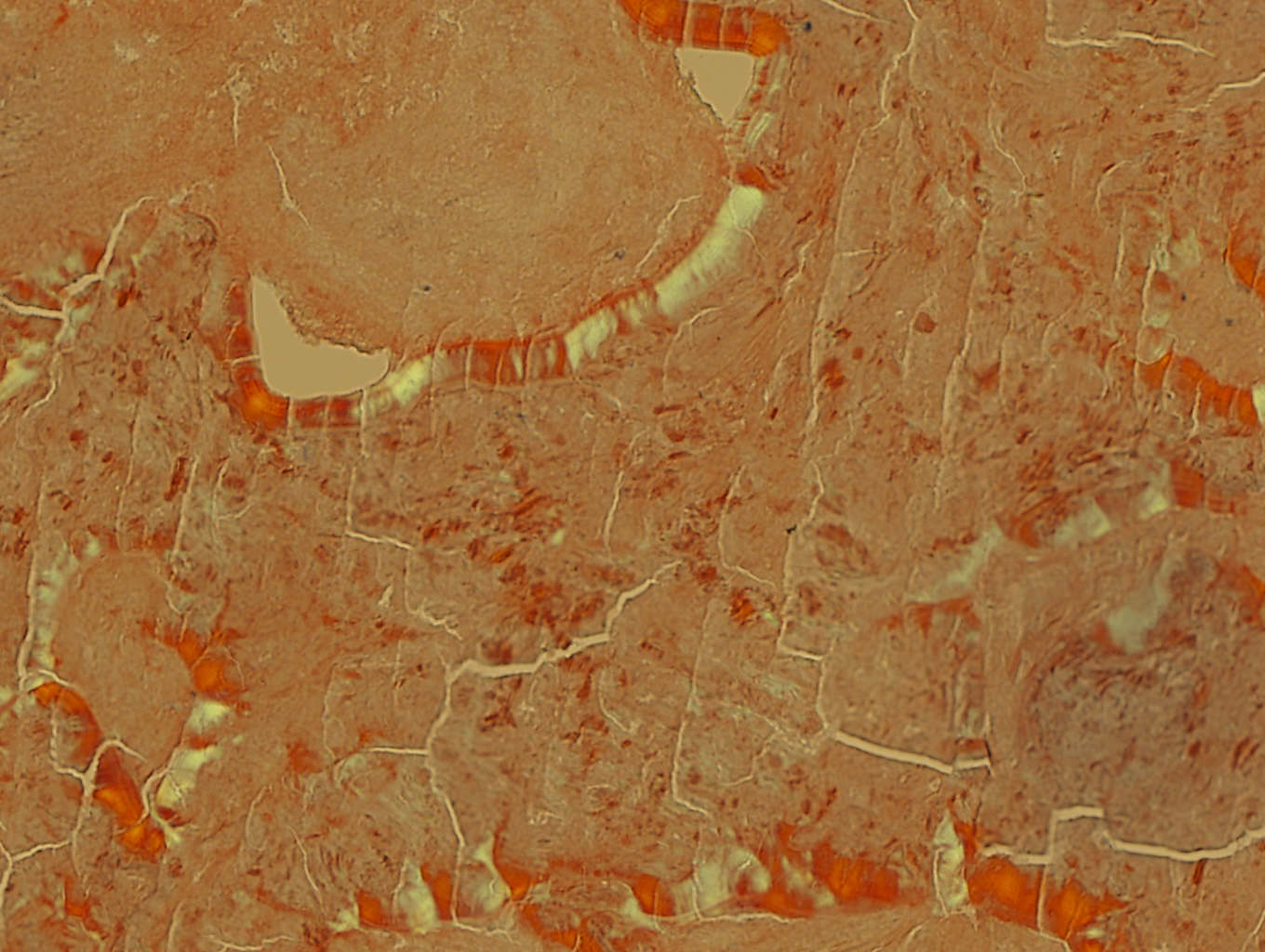
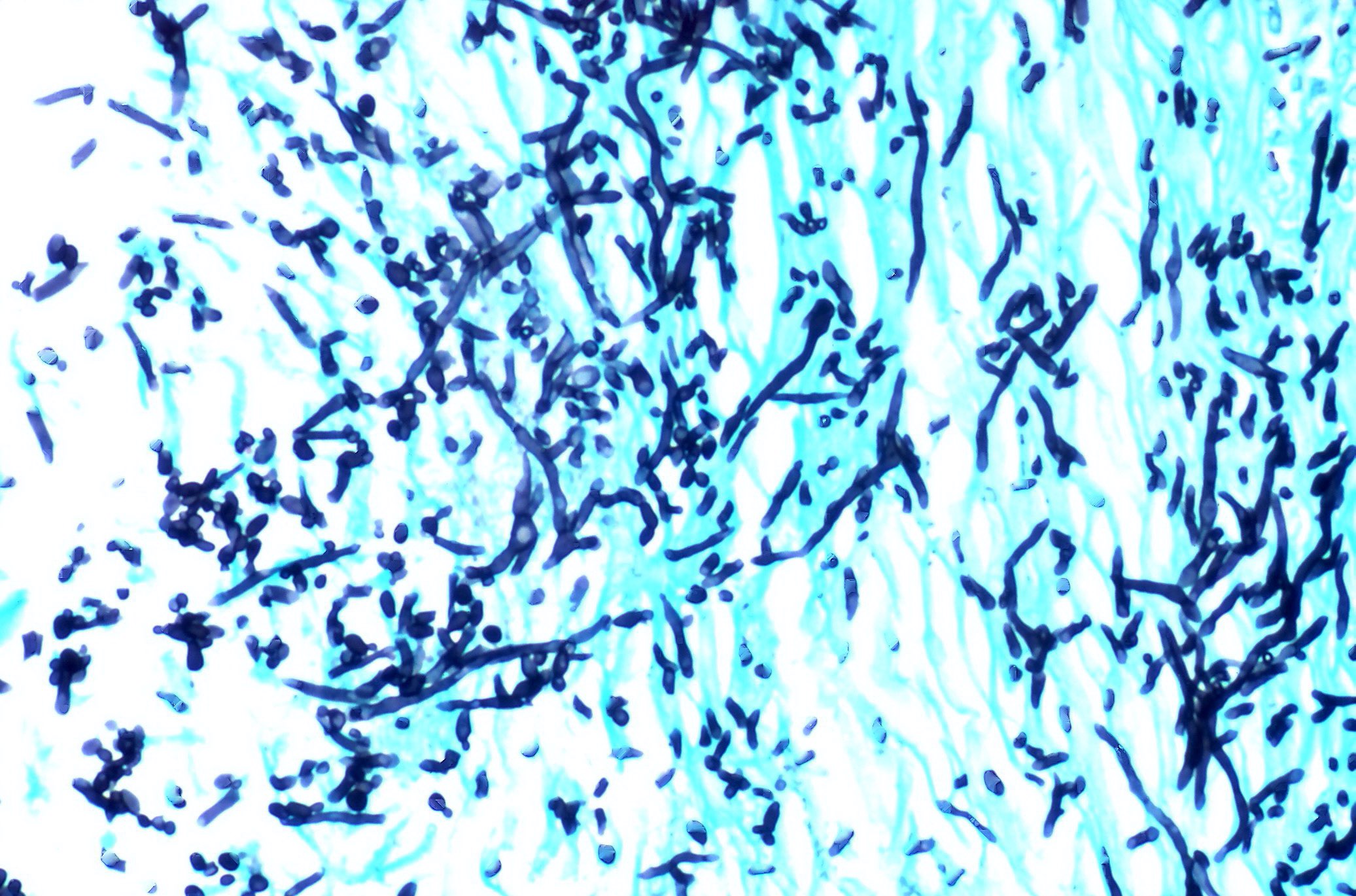
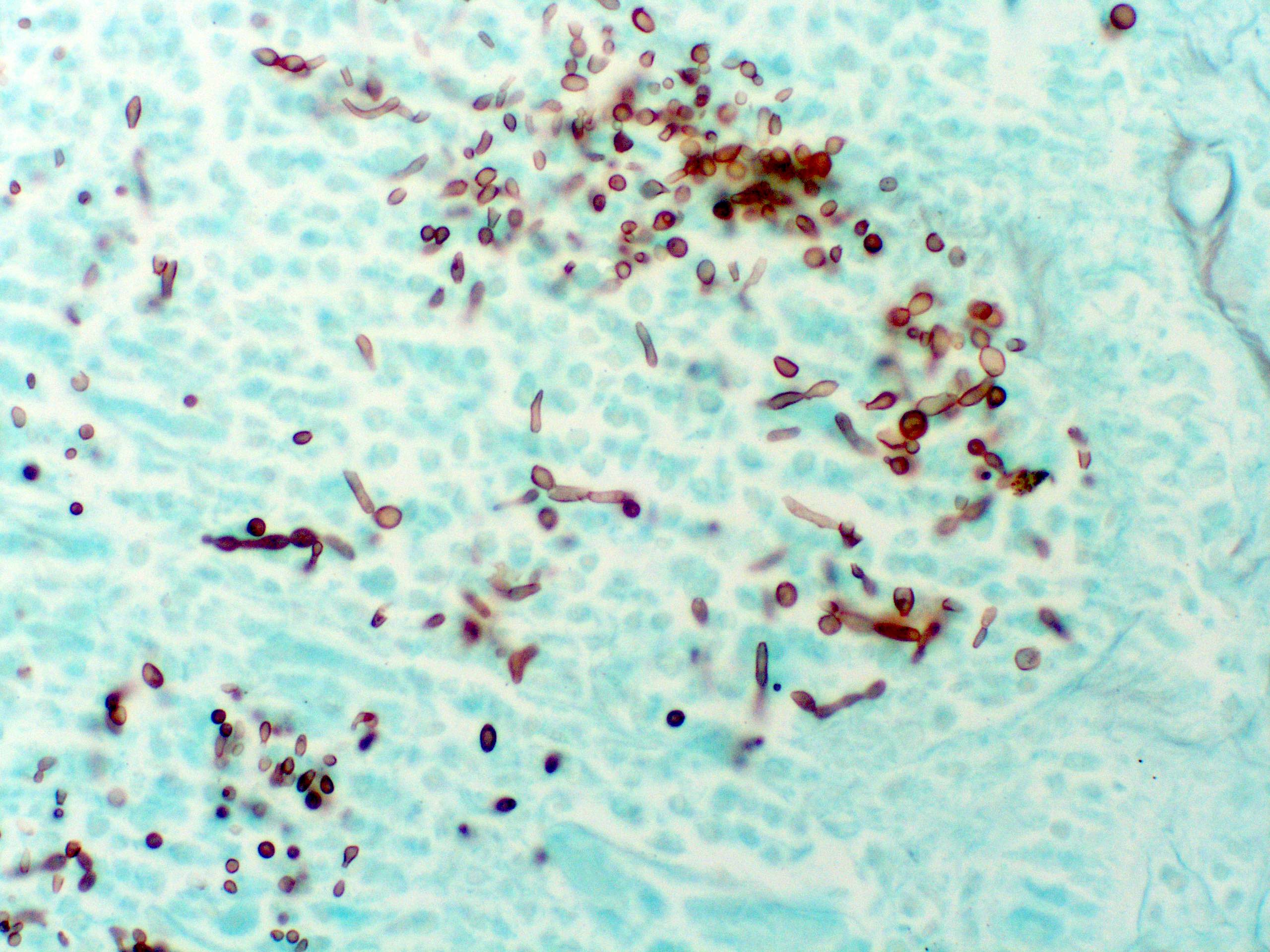
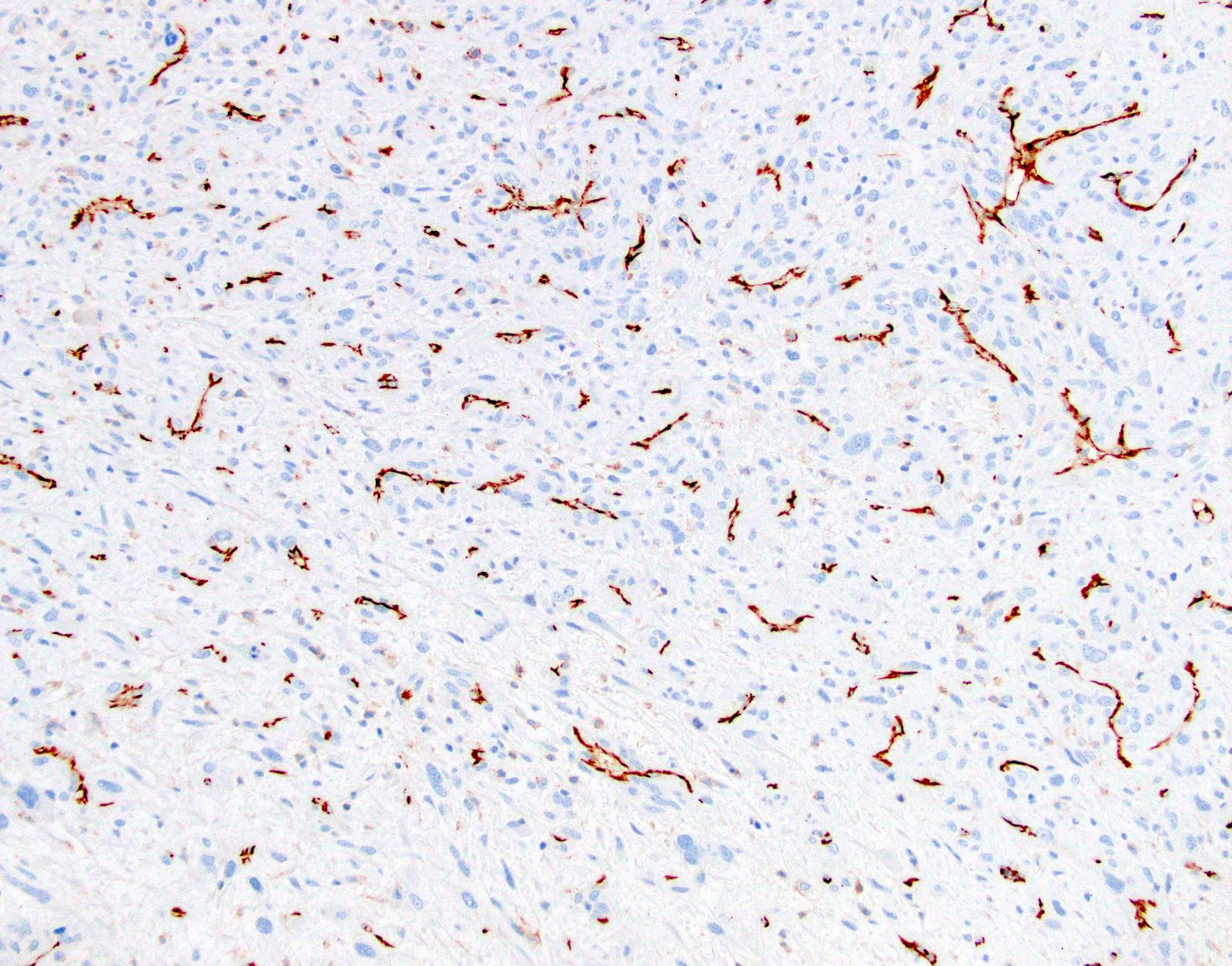
- Elastica van Gieson stains fibrin yellow
- Martius scarlet blue trichrome and picro Mallory staining are positive for fibrin
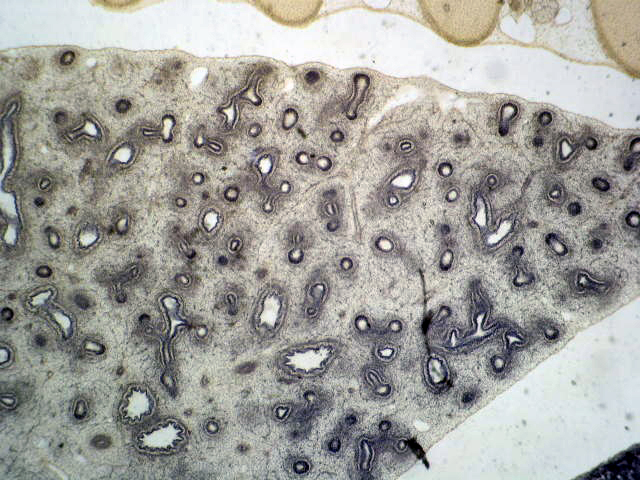
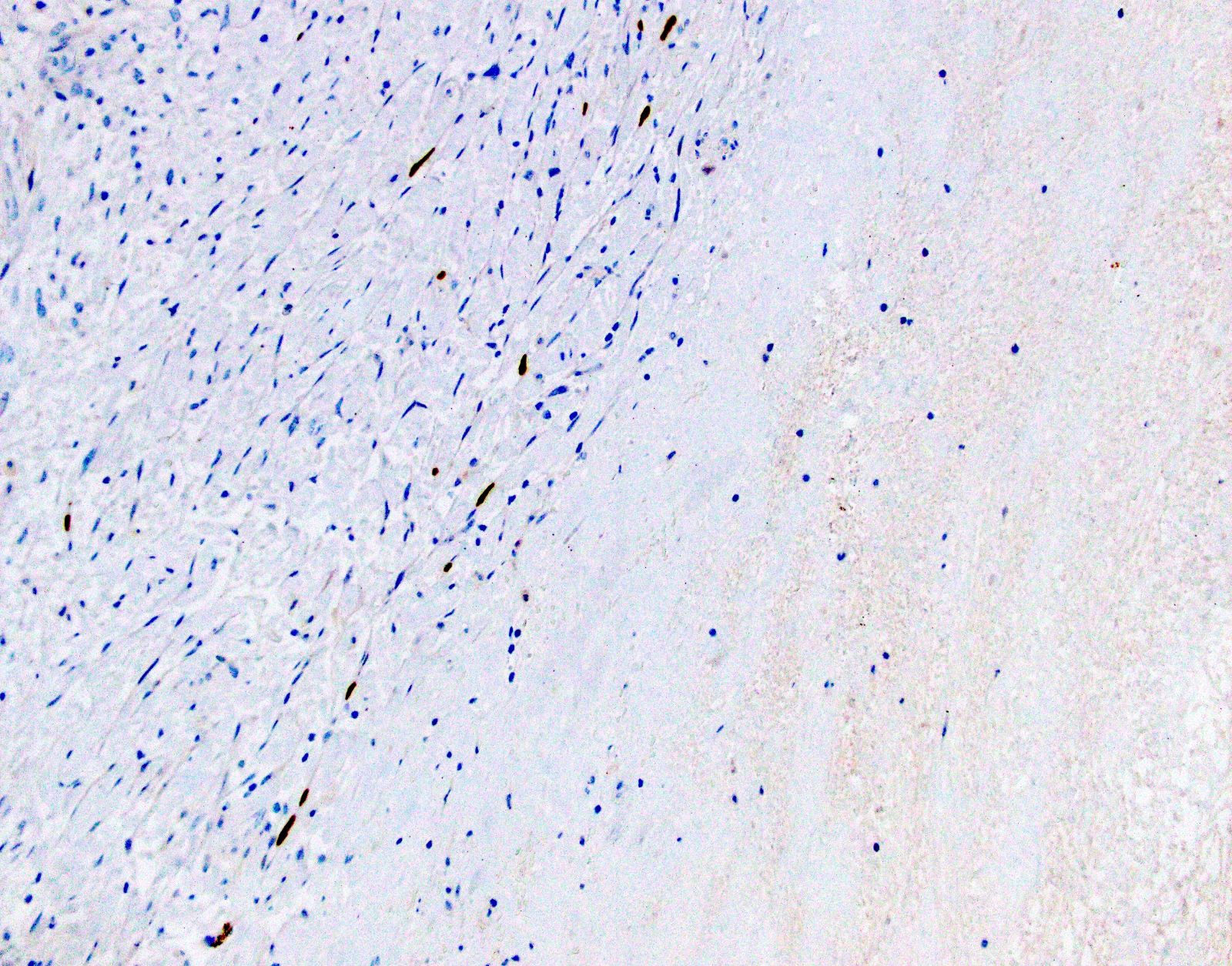
- Organizing pneumonia foci are free from elastic fiber and collagen fiber, easily confirmed by elastica van Gieson staining
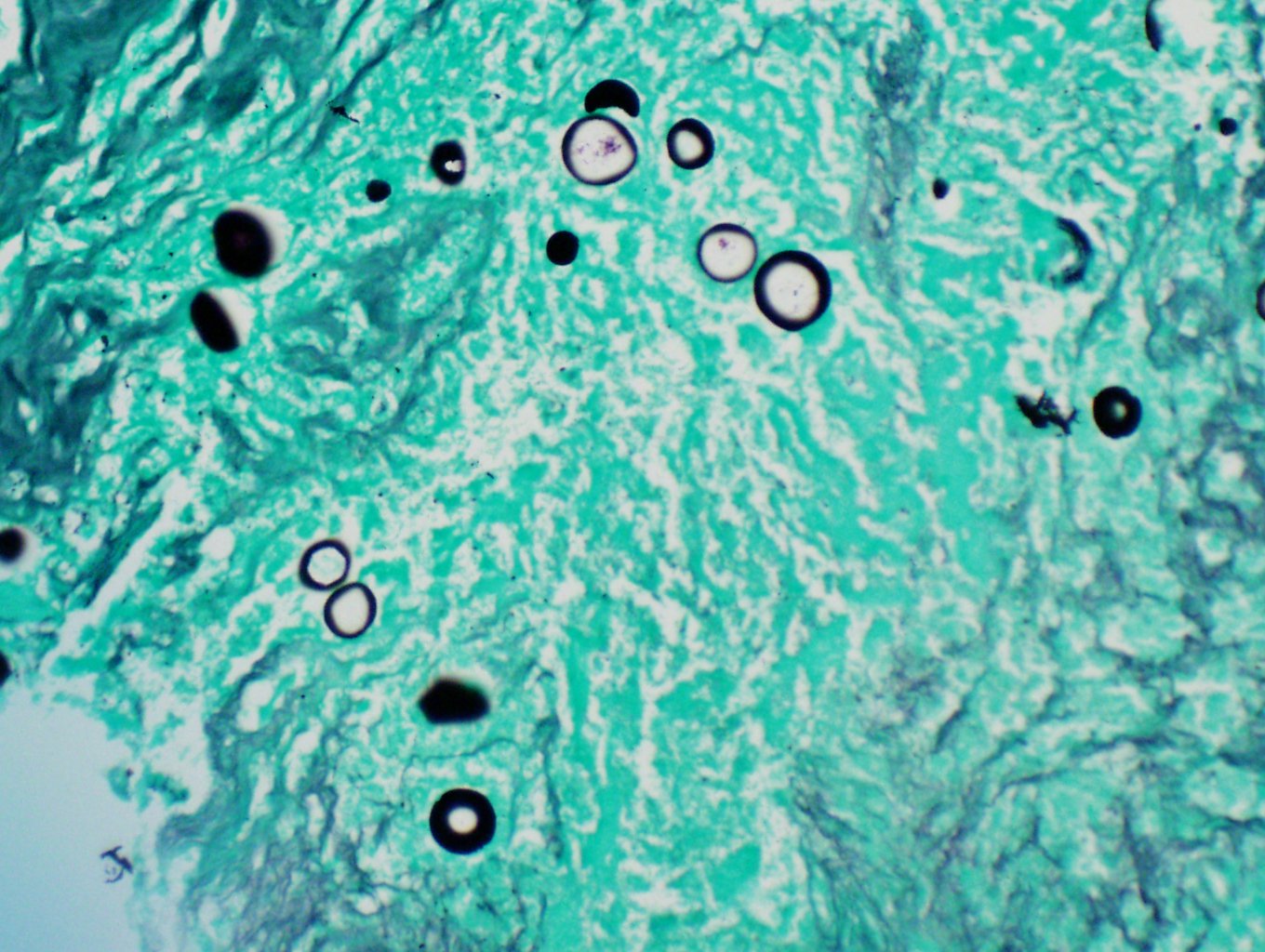
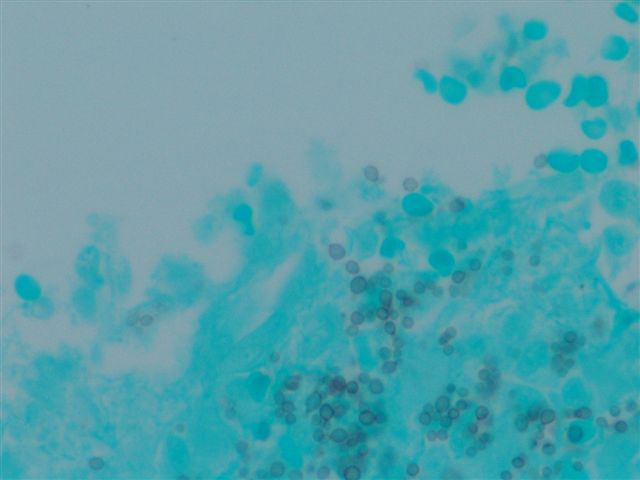
- Giemsa, Grocott and Ziehl-Neelsen stains are usually mandatory to rule out infectious diseases
- Acute exacerbation of chronic lung disease, especially hypersensitivity pneumonitis (Hum Pathol 2012;43:660)
- Cryptogenic organizing pneumonia: scanty or absent fibrin deposition
- Diffuse alveolar damage (acute interstitial pneumonia / acute respiratory distress syndrome): hyaline membranes, architectural destruction and myofibroblastic aggregation
- Eosinophilic pneumonia: prominent eosinophilic infiltrate, pink macrophages (not foamy)
- Granulomatosis with polyangiitis: geographic necrosis, alveolar hemorrhage, capillaritis, granuloma, eosinophils
- Infection: especially, fungal infection is often challenging to differentiate
- Microscopic polyangiitis: small vessel vasculitis and capillaritis with neutrophils, extravasation of neutrophils in alveolar space, alveolar hemorrhage
- Eosinophilic infiltration
- Hyaline membranes
- Lymphocytic infiltration
- Organizing pneumonia
- Type 2 pneumocyte hyperplasia
Comment Here
Reference: Acute fibrinous and organizing pneumonia
- In 1935, Hamman and Rich first reported autopsy cases of initially healthy individuals who developed a rapidly progressive and fatal type of interstitial lung disease, which differed from other interstitial pneumonia clinically and pathologically (Trans Am Clin Climatol Assoc 1935;51:154)
- Katzenstein et al. coined the term "acute interstitial pneumonia (AIP)" (Am J Surg Pathol 1986;10:256)
- In the multidisciplinary classification of idiopathic interstitial pneumonias by American Thoracic Society / European Respiratory Society, acute interstitial pneumonia is categorized as "acute / subacute interstitial pneumonia" (Am J Respir Crit Care Med 2013;188:733)
- Rare and aggressive type of idiopathic interstitial pneumonia with diffuse alveolar damage (DAD), characterized by diffuse inflammation with hyaline membrane and fibroblastic proliferation
- Acute interstitial pneumonia shares common features with acute respiratory distress syndrome (ARDS) clinically and morphologically
- Also called Hamman-Rich syndrome and idiopathic diffuse alveolar damage
- Extremely rare (no conclusive epidemiological data available)
- Mean age 50 years but can occur at any age (7 - 83 years) (Eur Respir J 2000;15:412)
- No sex predilection
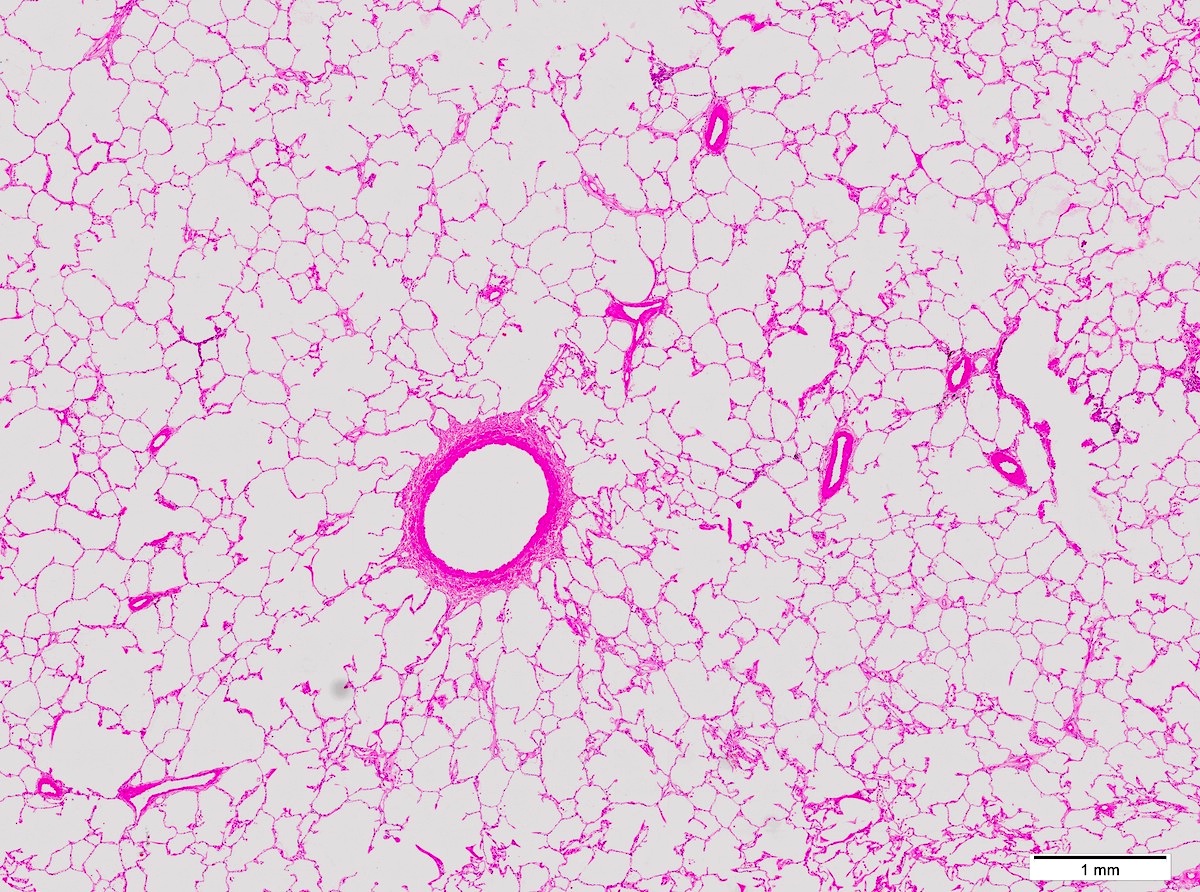
- Bilateral lung, usually in all five lobes of the lung
- Both endothelial and epithelial injury result in decreased integrity of the alveolar capillary membrane
- Imbalance of proinflammatory and anti-inflammatory mediators
- Neutrophils increase in alveoli and interstitium and release metabolites leading to lung injury
- Alveolar epithelial cells may go through epithelial - mesenchymal transition to become myofibroblasts, resulting in interstitial organization and fibrosis (BMC Pulm Med 2014;14:67)
- No definite cause; no risk factors have been identified
- Influenza-like illness, followed by progressive shortness of breath (Am J Surg Pathol 1986;10:256)
- Vast majority of patients are previously healthy and lack history of lung disease
- Many clinical characteristics of acute interstitial pneumonia are similar to acute respiratory distress syndrome (Chest 2003;124:554)
- Acute interstitial pneumonia can progress to respiratory failure as profound as severe acute respiratory distress syndrome (PaO2/FIO2 ≤ 100 mm Hg) and almost all patients need mechanical ventilation and hospital care
- Respiratory failure usually appears 1 - 3 weeks from the onset, later than acute respiratory distress syndrome (16.8 days vs. 2.2 days)
- Multiple organ failure is less common in acute interstitial pneumonia
- Diagnostic requirements
- Exclusion of any other causes of respiratory failure
- Histological diagnosis of diffuse alveolar damage
- Open lung biopsy, if possible, is recommended to reach the accurate diagnosis and to guide prompt treatment (Crit Care 2006;10:423)
- Transbronchial lung biopsy may be also helpful to find hyaline membranes of diffuse alveolar damage but it needs to be carefully distinguished from artifacts
- Hypoxia
- Increased serum ferritin, D dimer and C reactive protein
- KL-6 may increase slightly
- Heterogeneous bilateral ground glass opacity due to pulmonary edema
- Chest radiograph
- Ground glass opacity
- Consolidation with air bronchogram
- Chest CT
- Ground glass opacity
- Airspace consolidation
- Bronchiolectasis / bronchiectasis; related to worse prognosis (Am J Respir Crit Care Med 2002;165:1551)
- Volume reduction
- Most patients die within 2 months unless appropriate treatment is provided (Eur Respir J 2000;15:412)
- High dose steroid therapy drastically improves the prognosis with long term survival of more than 80% (Chest 2006;129:753, Chest 2003;124:554)
- Survivors may suffer recurrences or develop chronic lung injury
- 3 year old girl died of acute interstitial pneumonia (J Korean Med Sci 2008;23:529)
- 51 year old woman died of acute interstitial pneumonia (Case Rep Pulmonol 2012;2012:678249)
- Oxygen therapy for respiratory failure
- Mechanical ventilation with positive end expiratory pressure
- High dose steroid pulse (Chest 2006;129:753)
- Direct hemoperfusion using polymyxin B immobilized fiber column was recently found to effectively improve the prognosis of acute interstitial pneumonia patients (Ther Adv Respir Dis 2017;11:261)
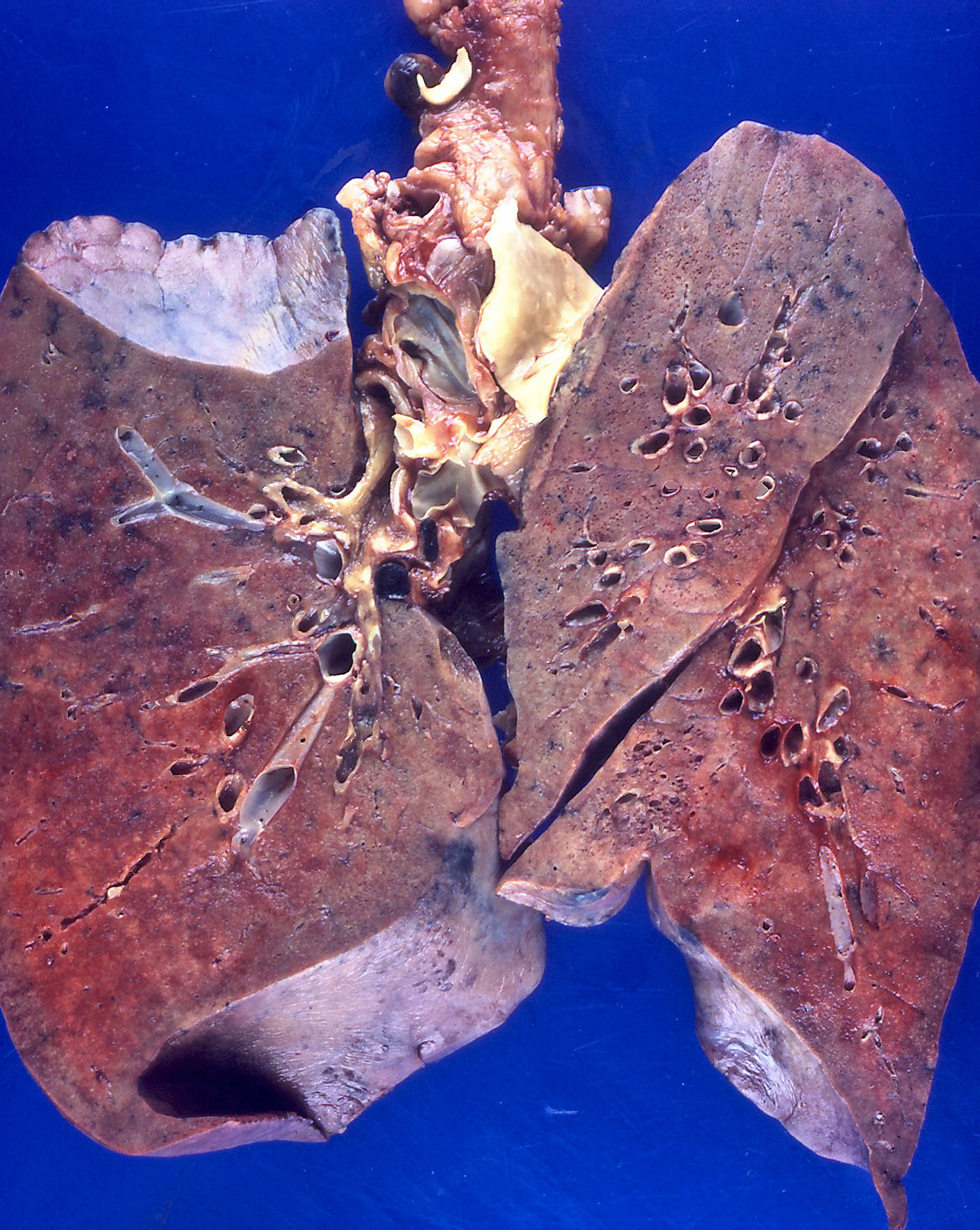
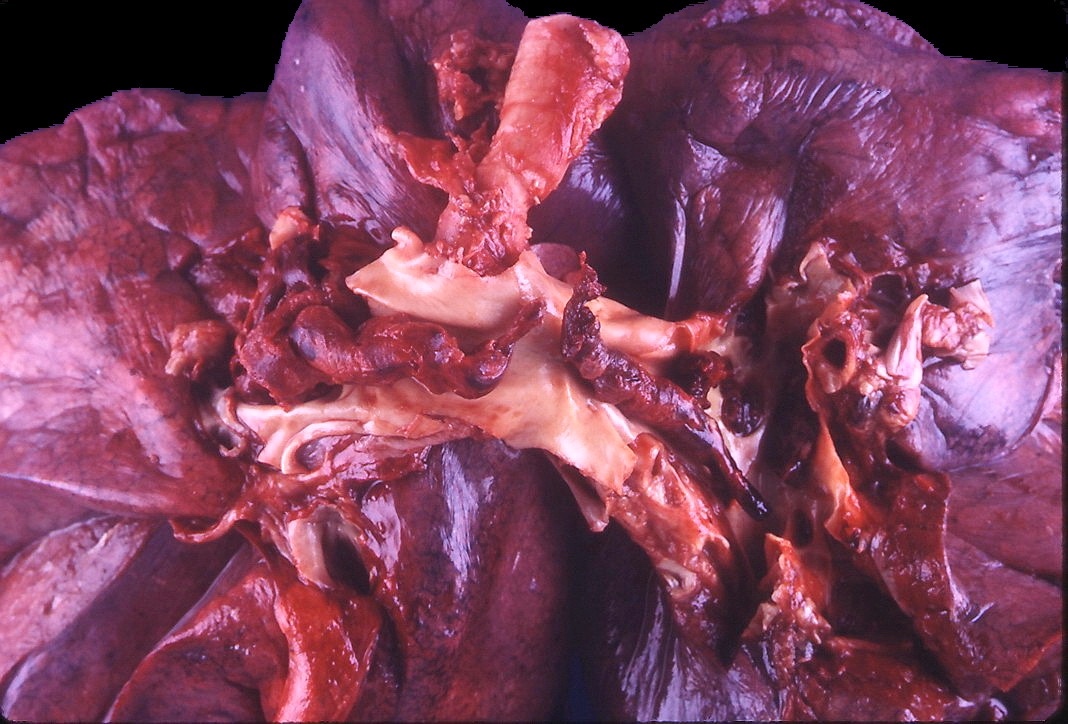
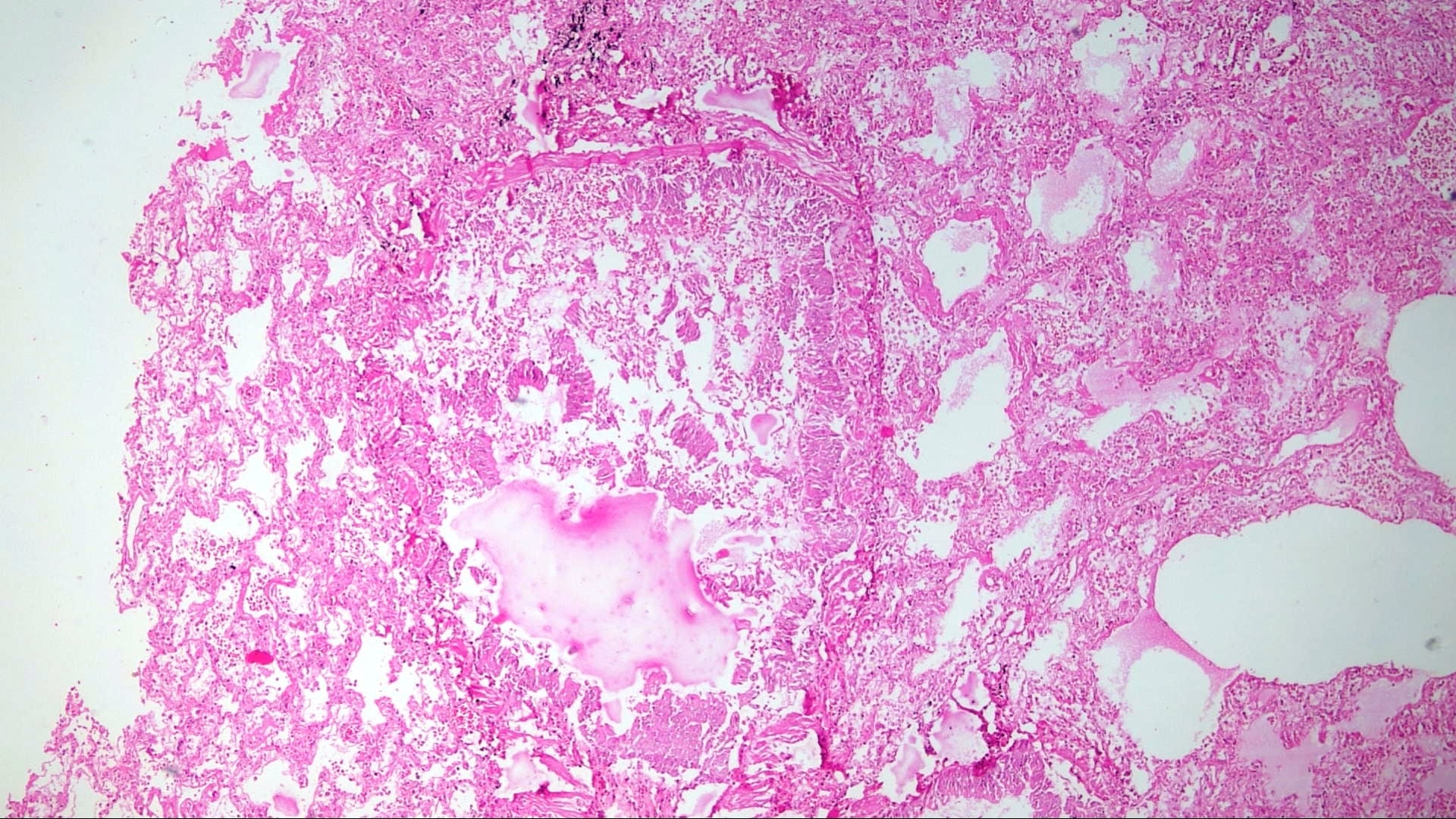
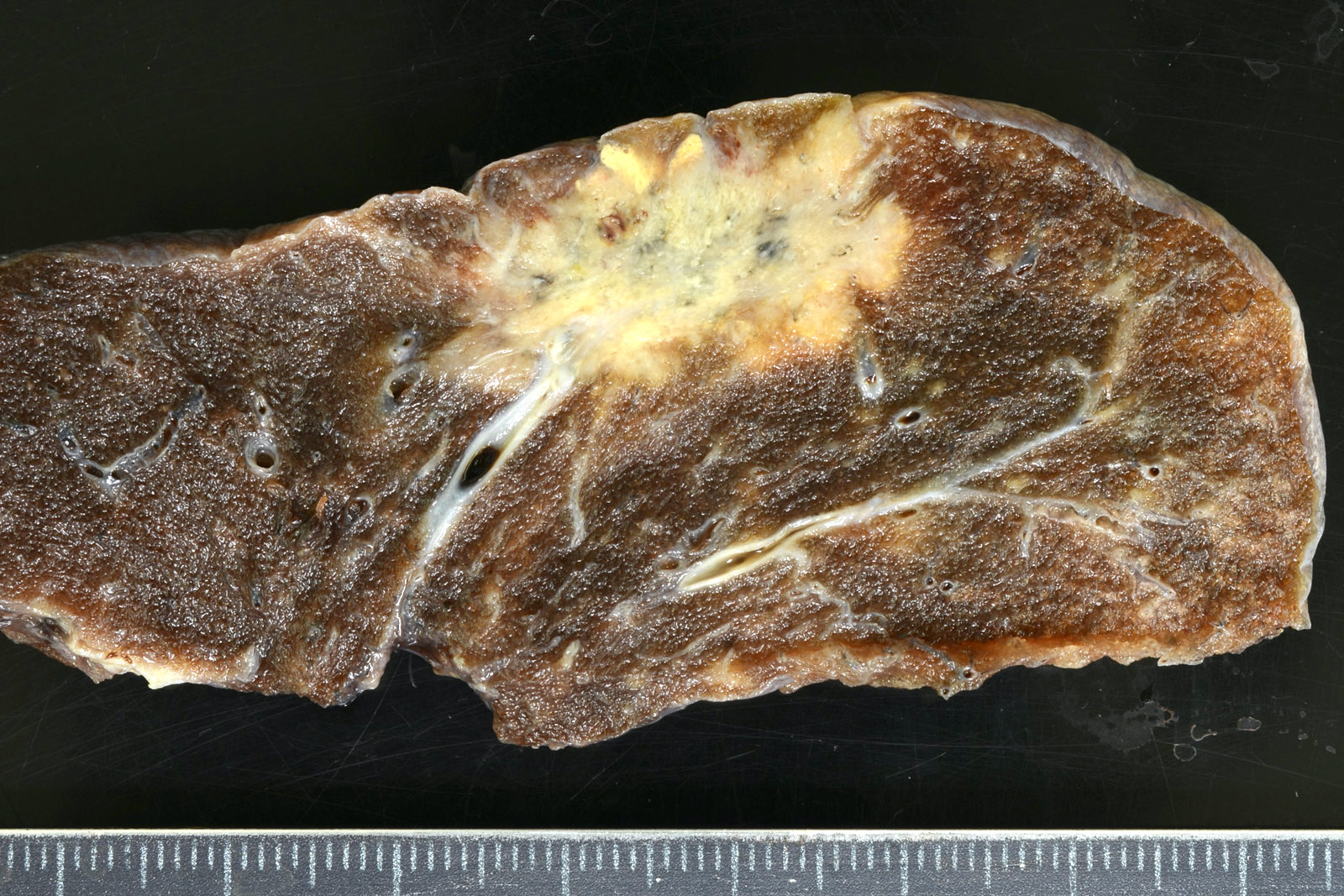
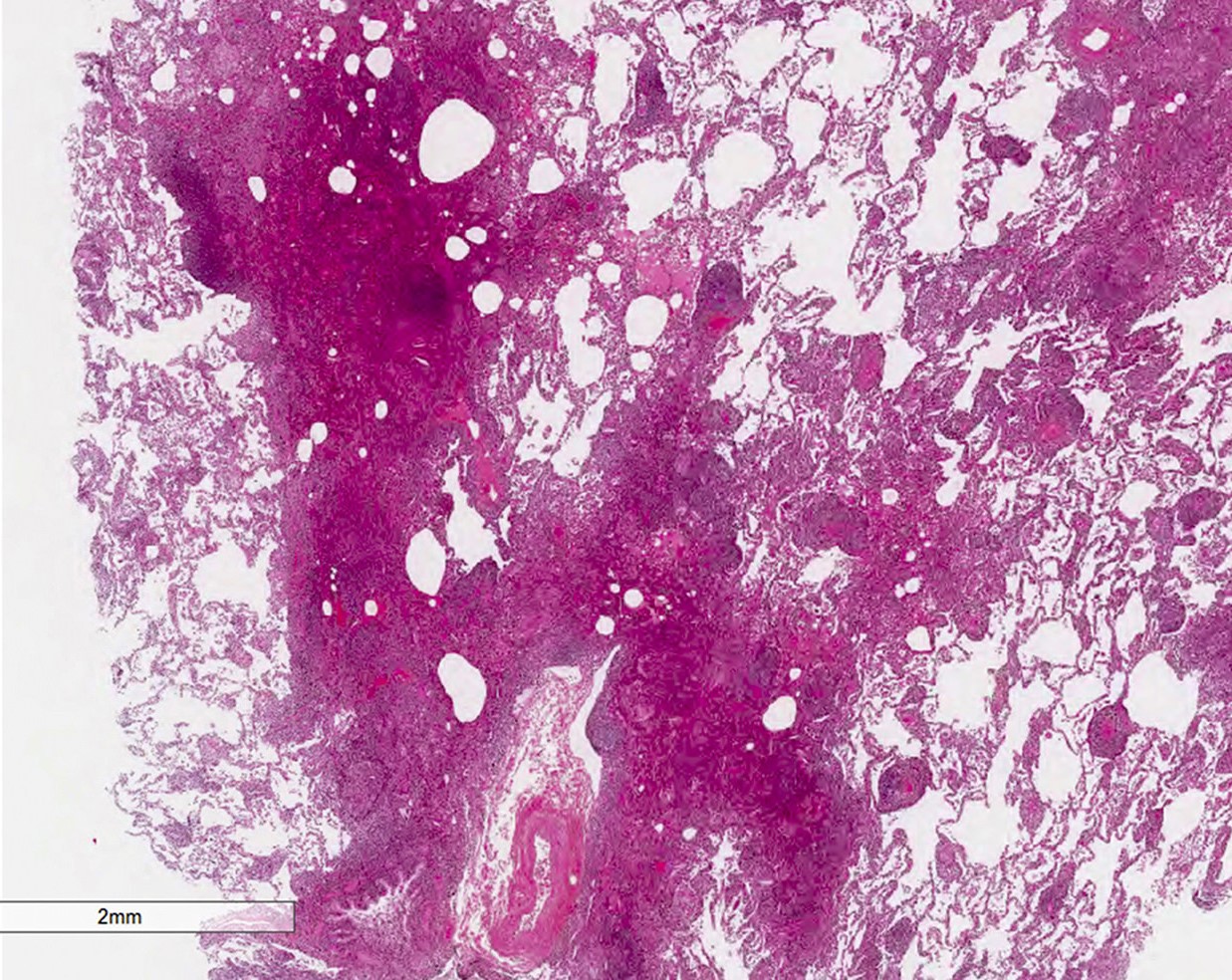
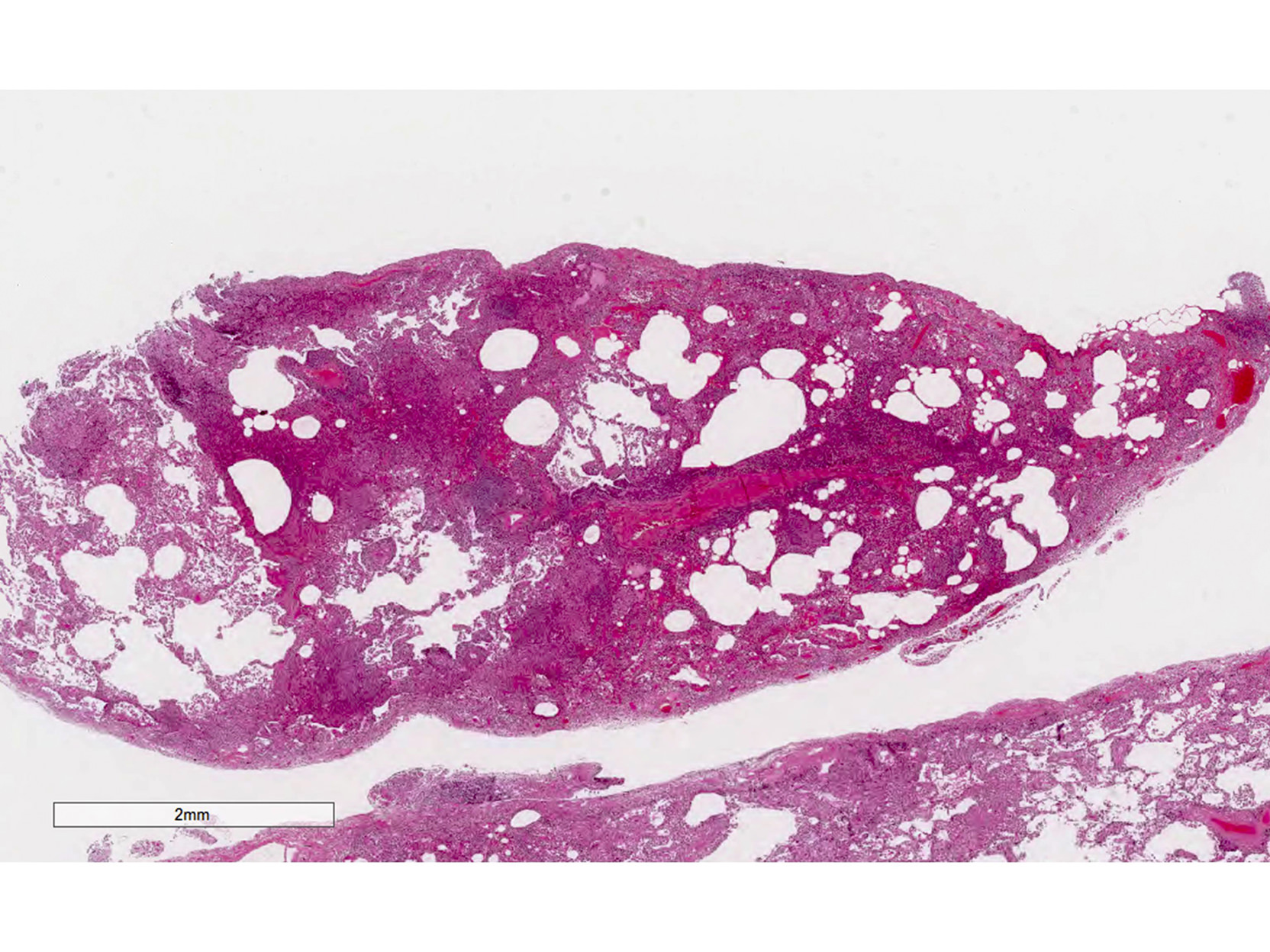
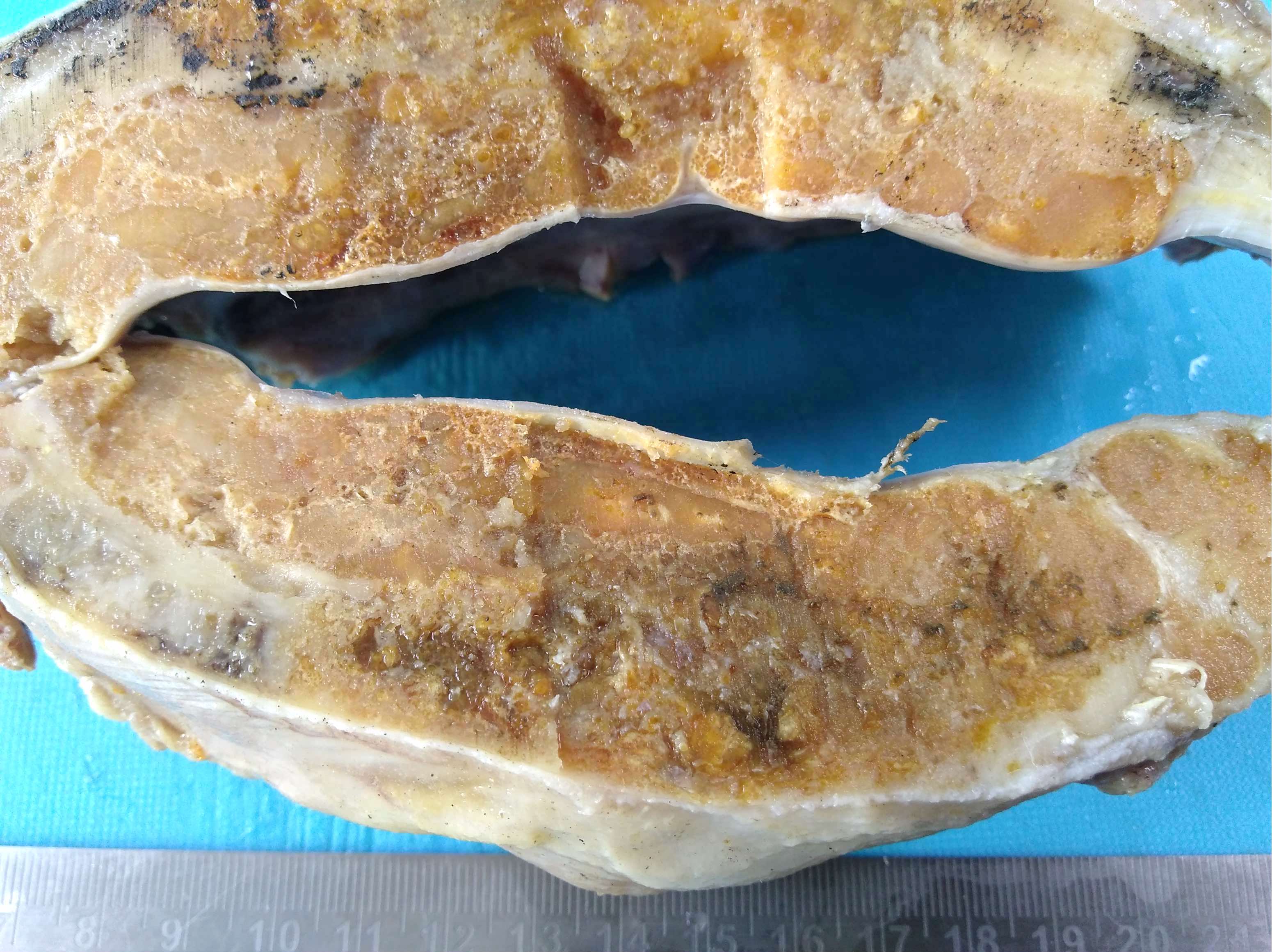
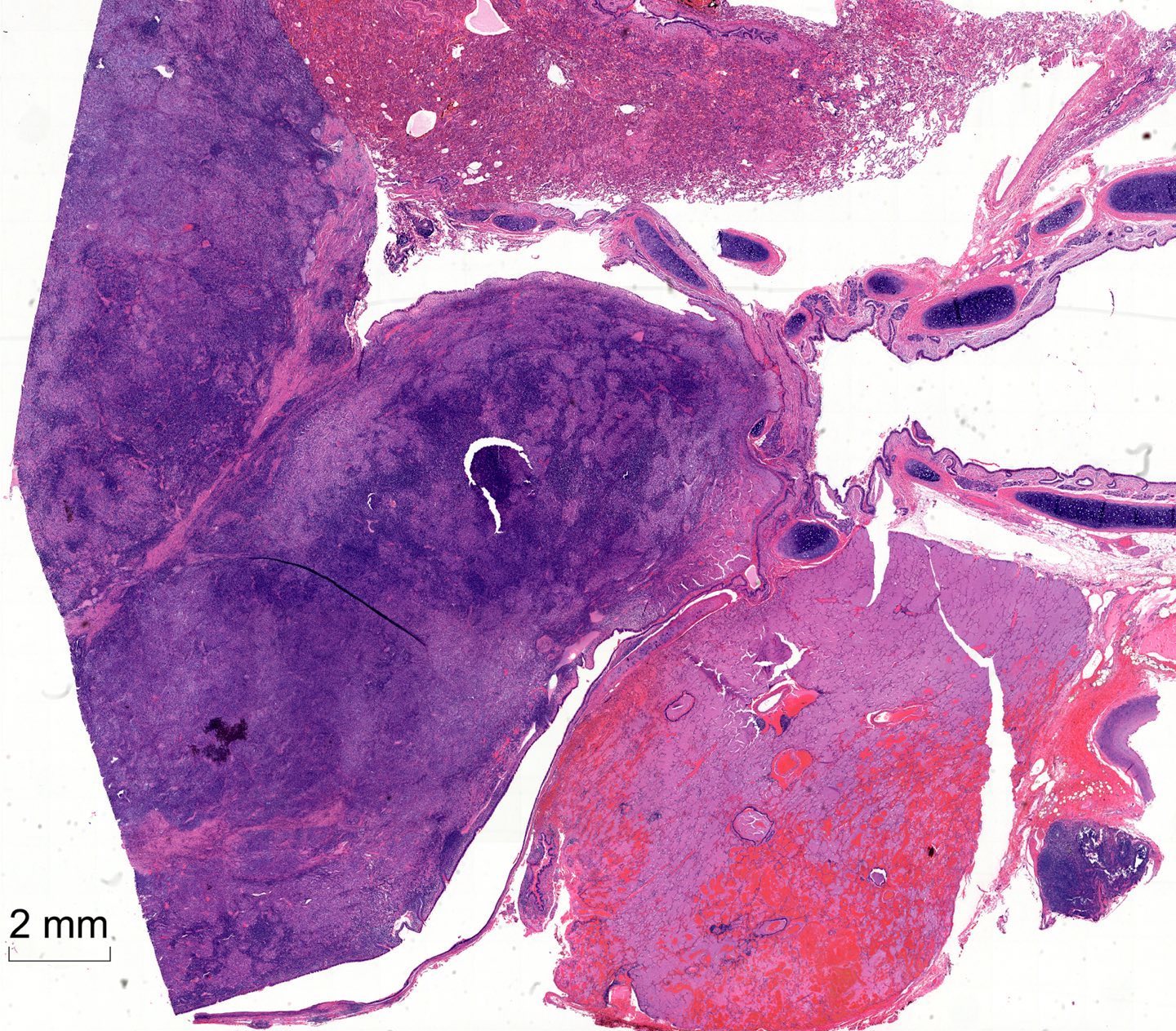
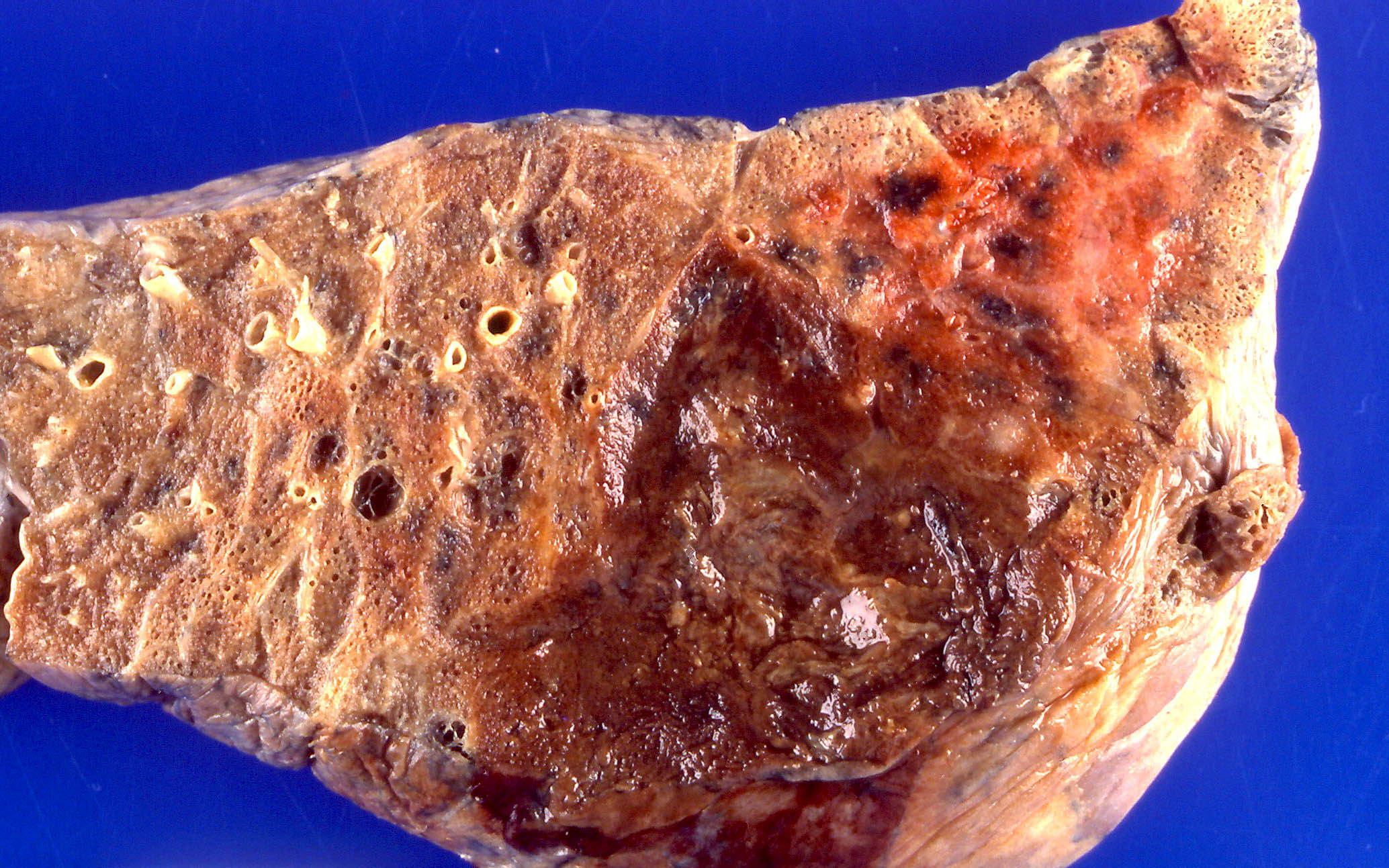
- Dark blue lungs with hemorrhagic dots on pleural surface
- Heavy and firm due to edema and fibrosis
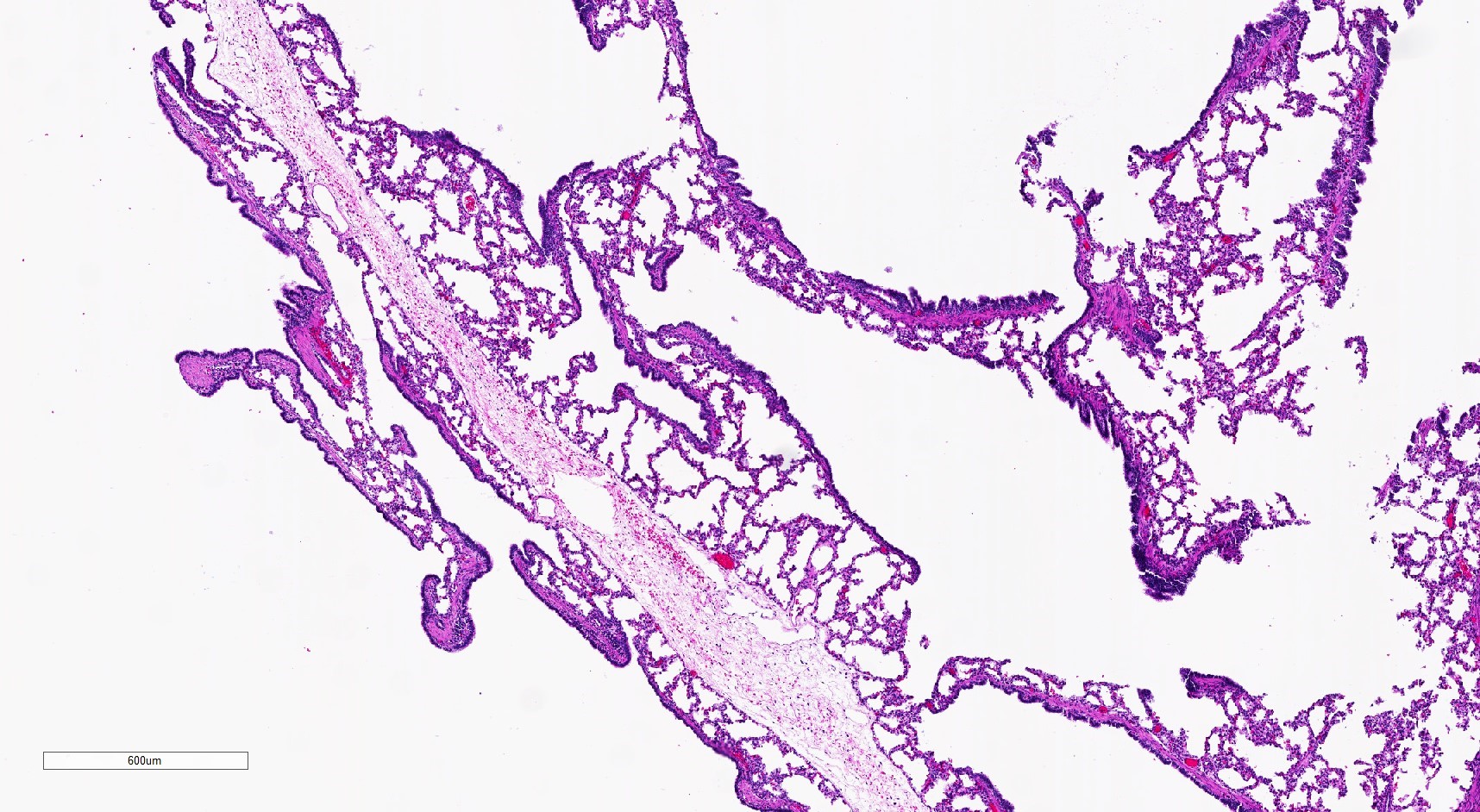
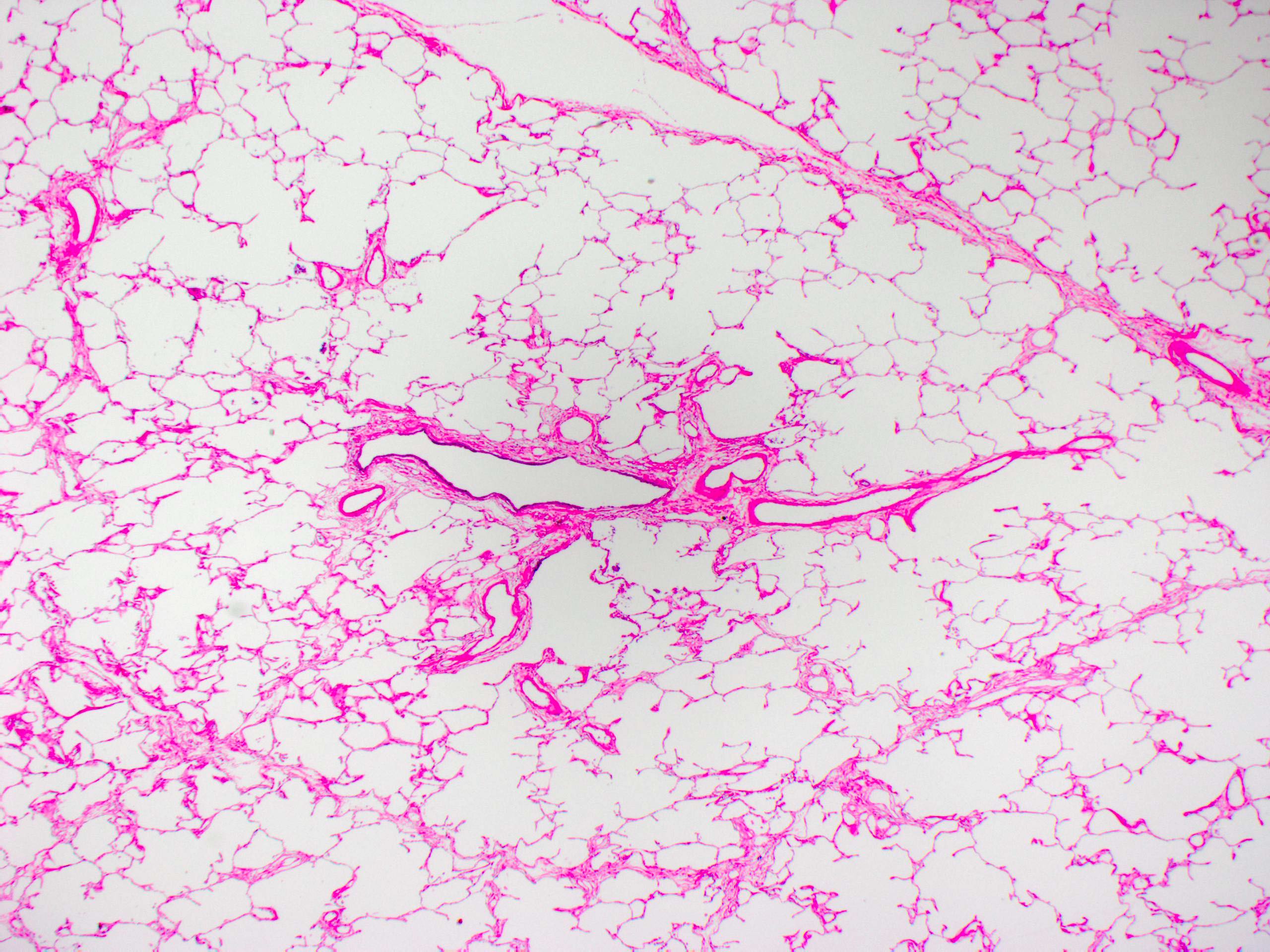
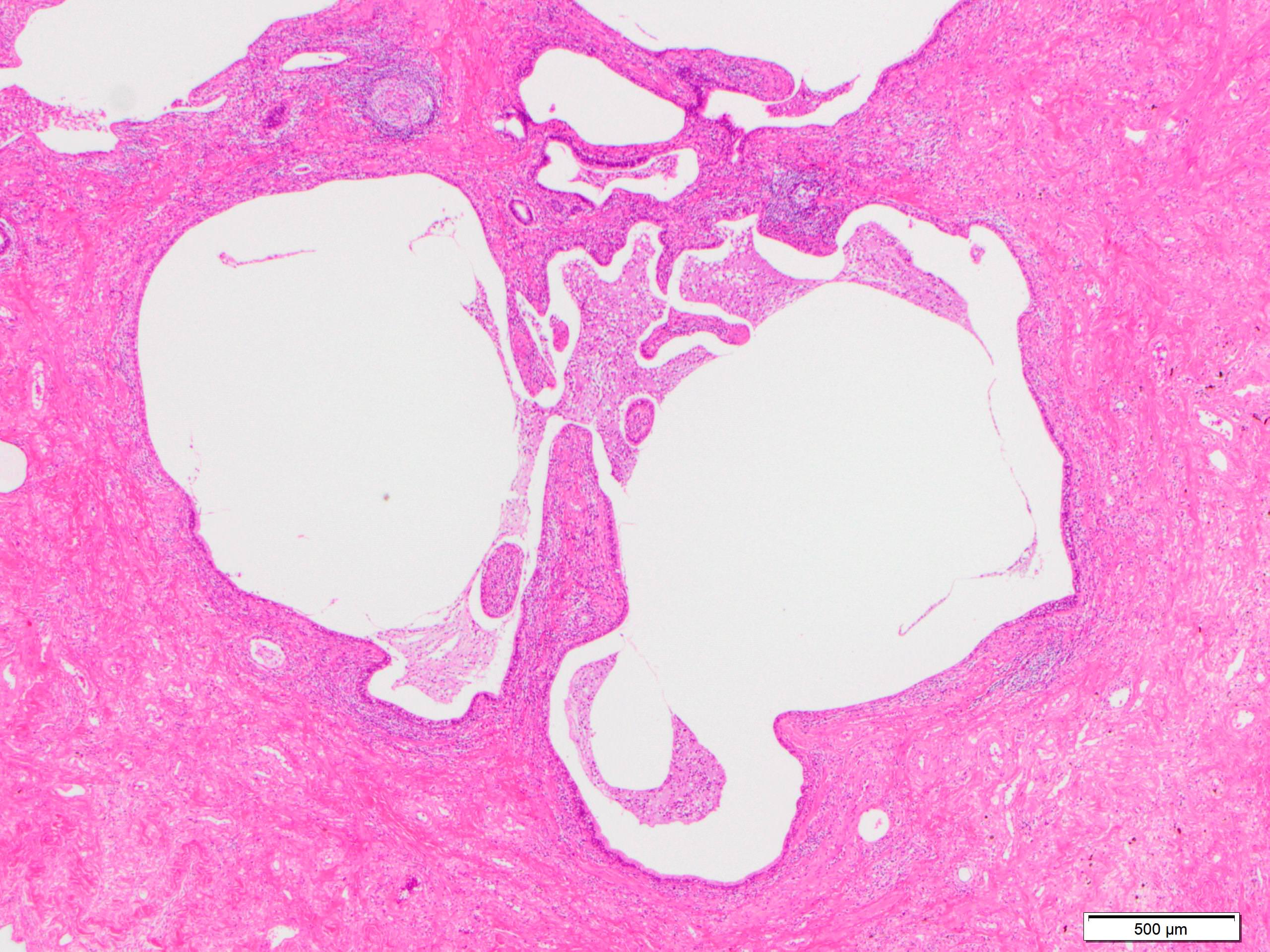
- Dilatation of alveolar ducts
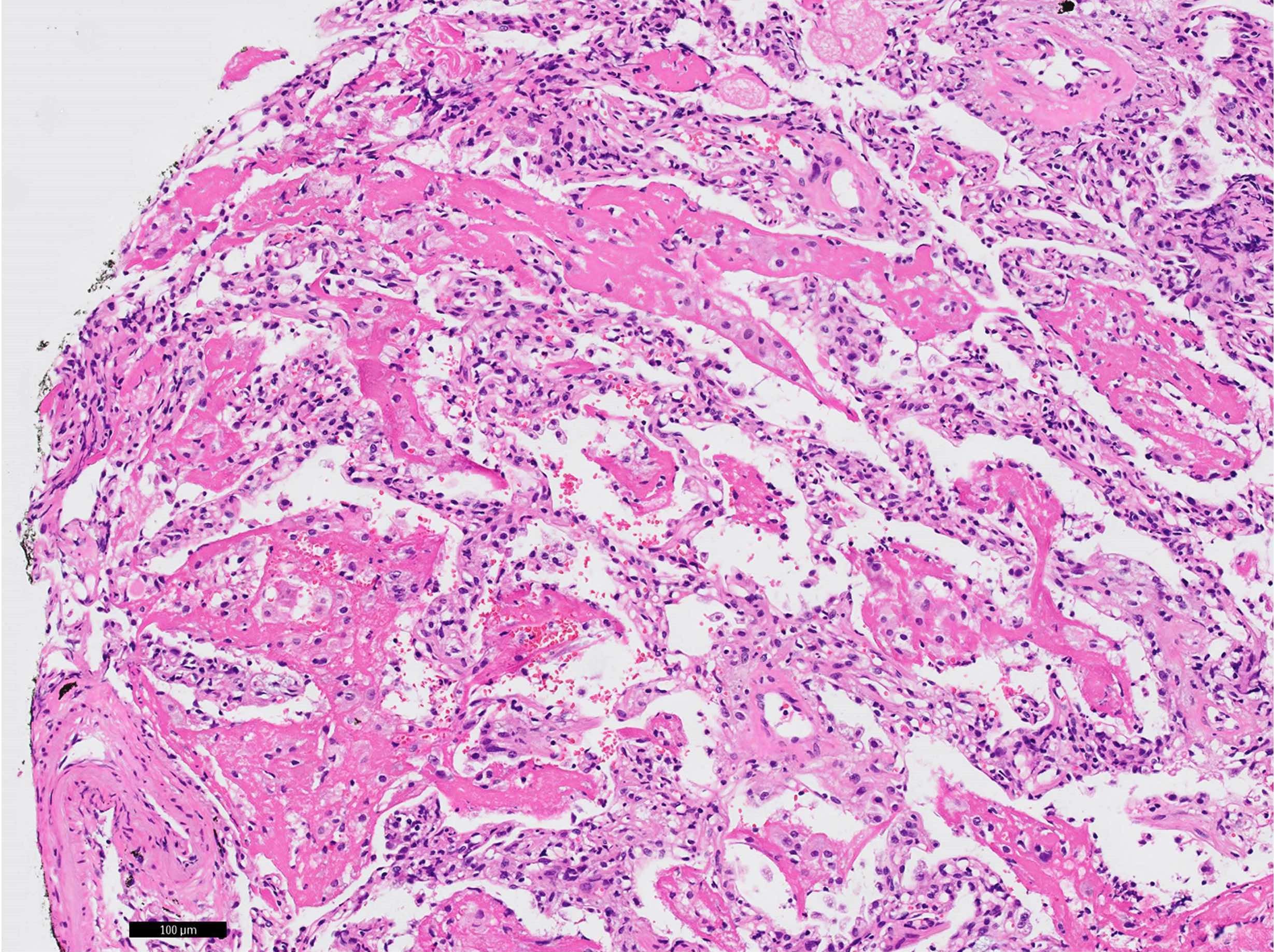
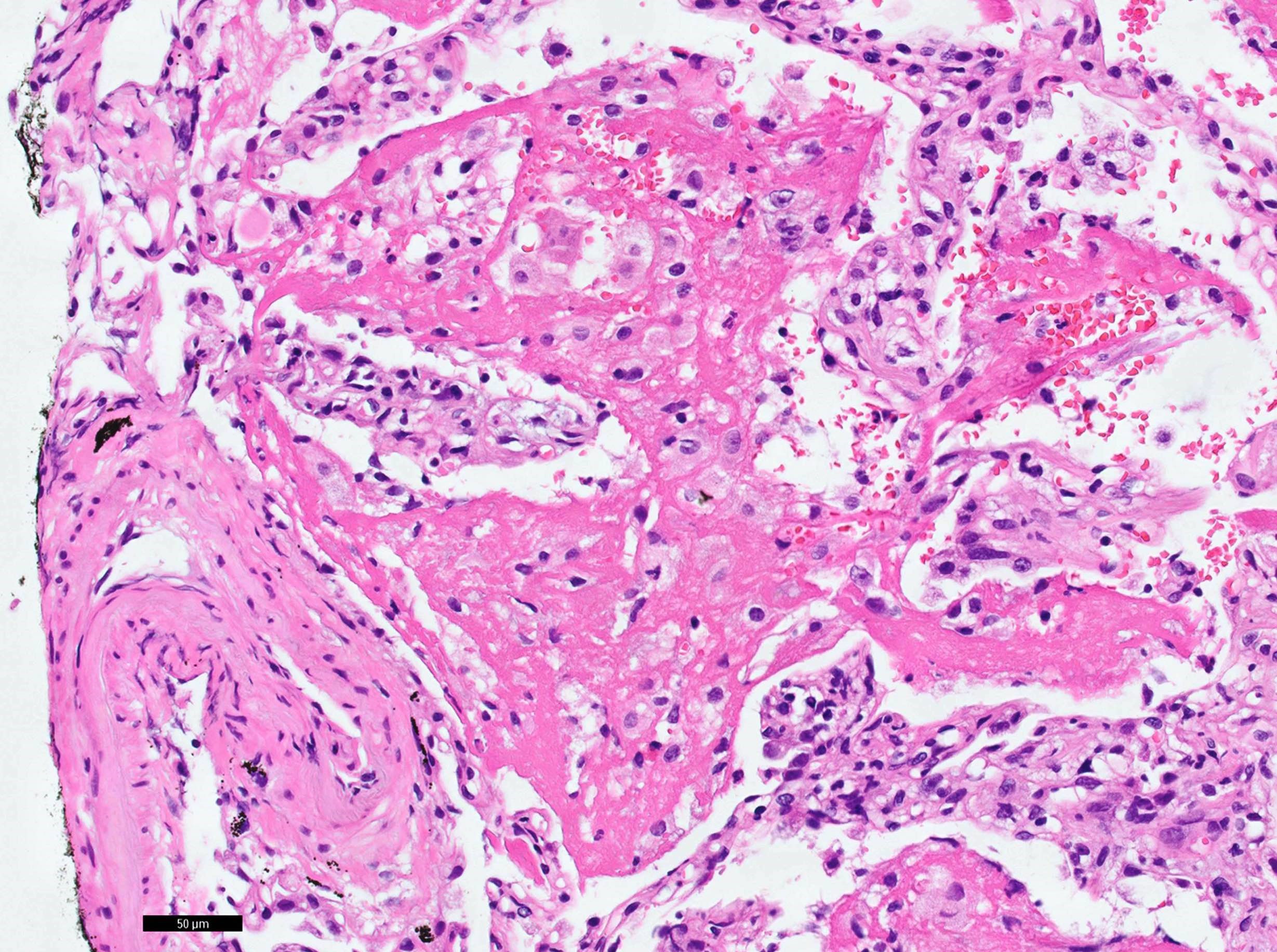
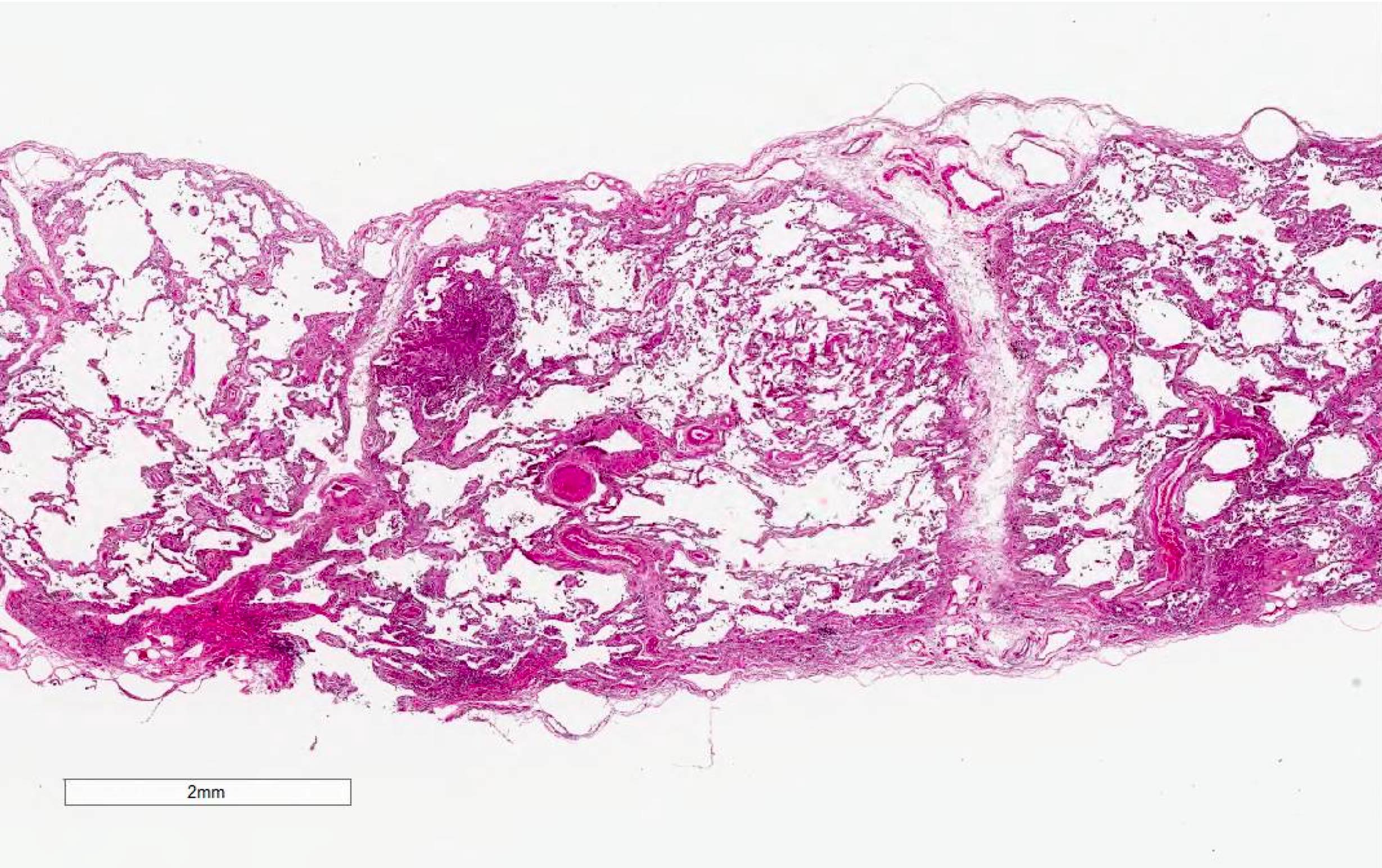
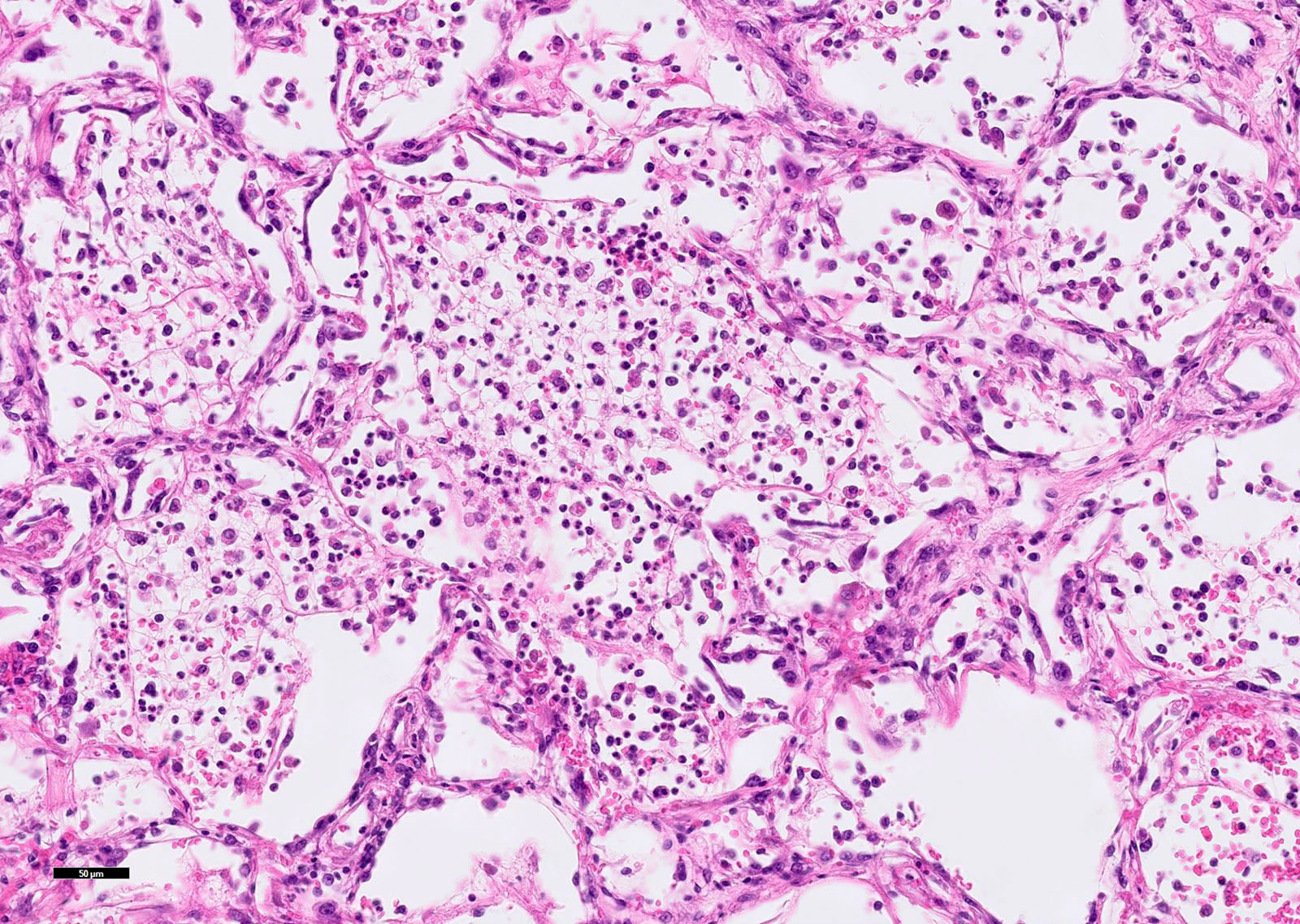
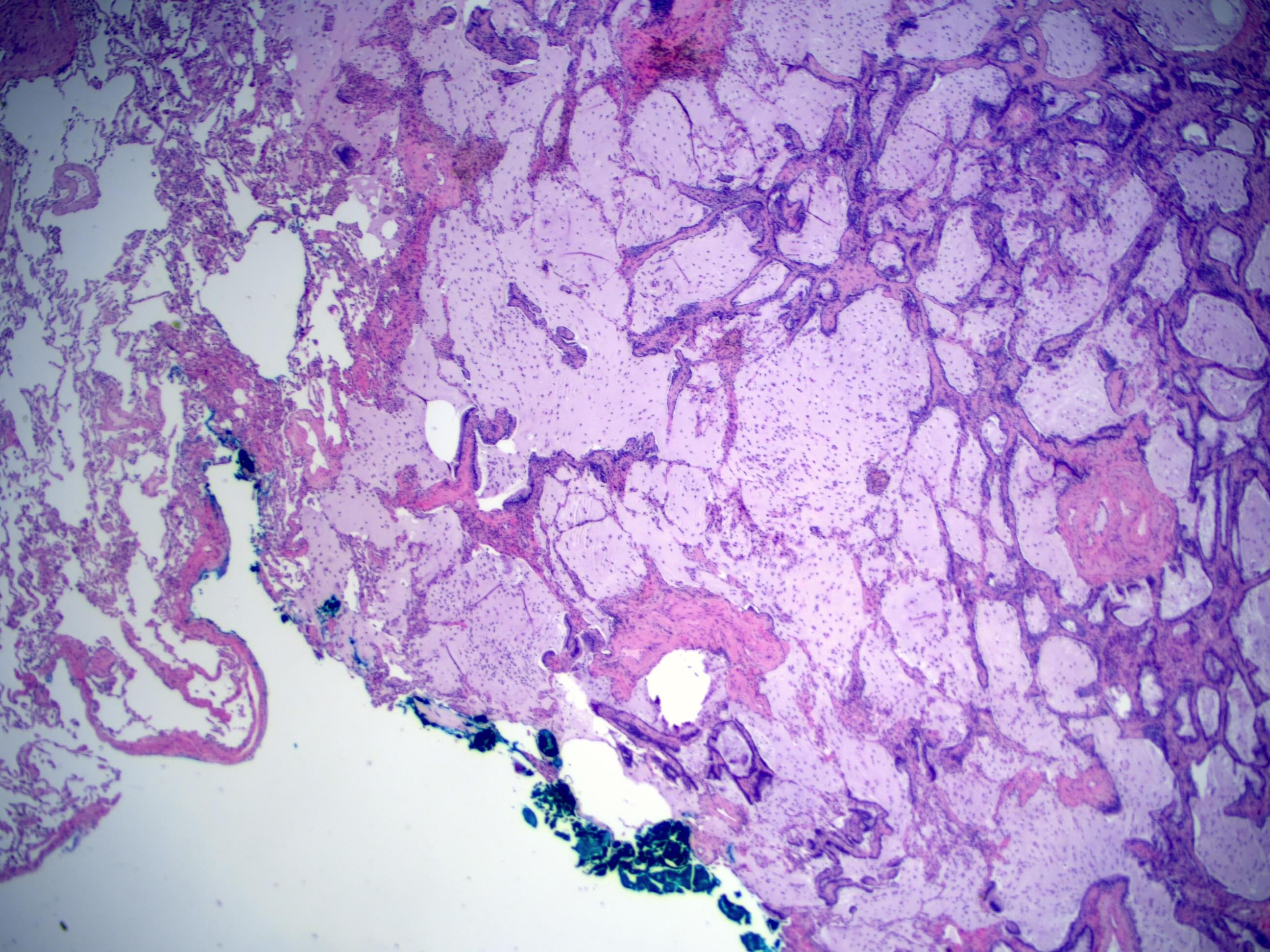
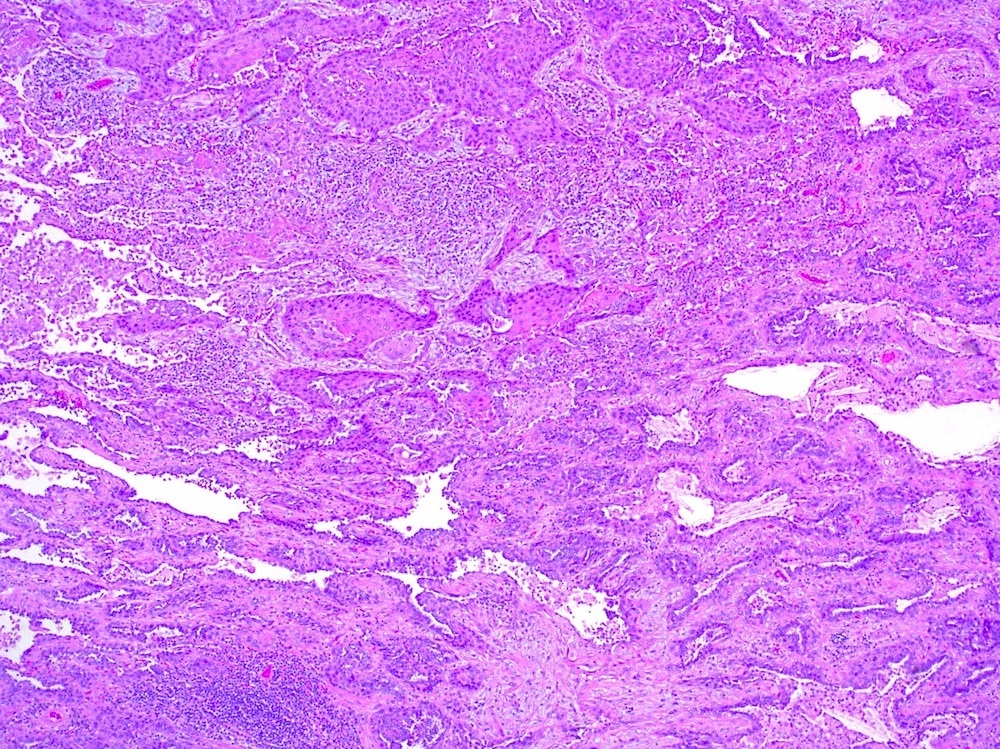
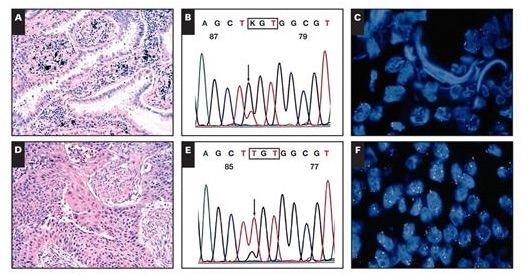
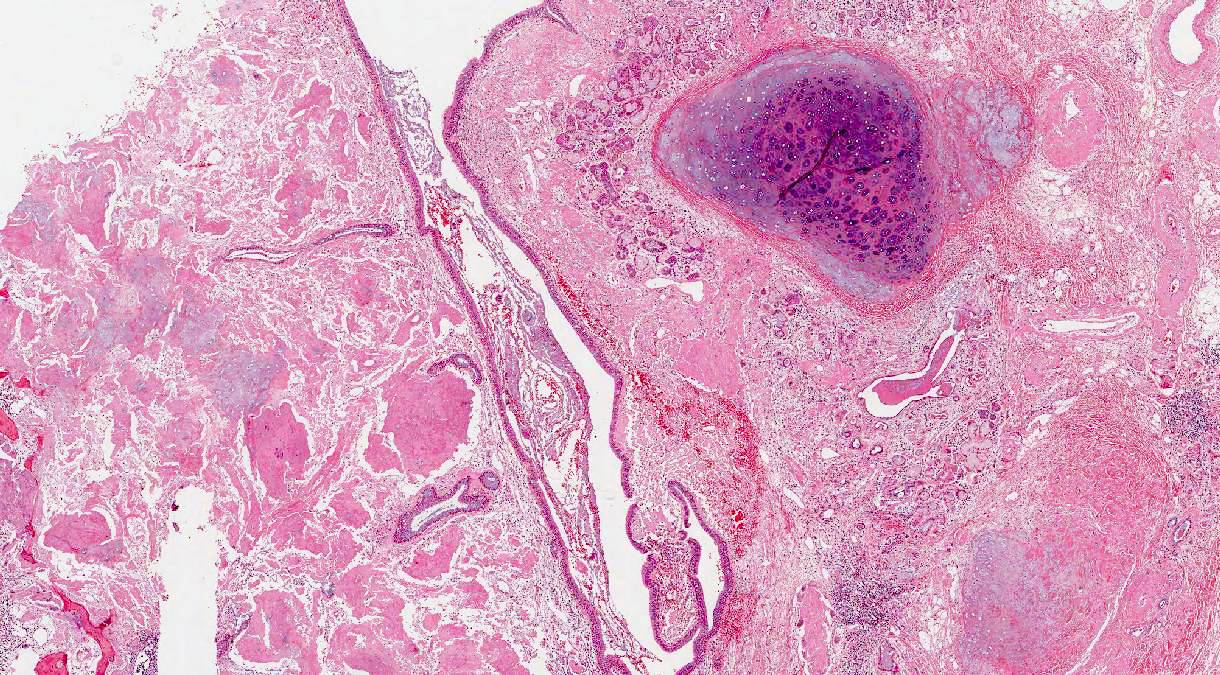
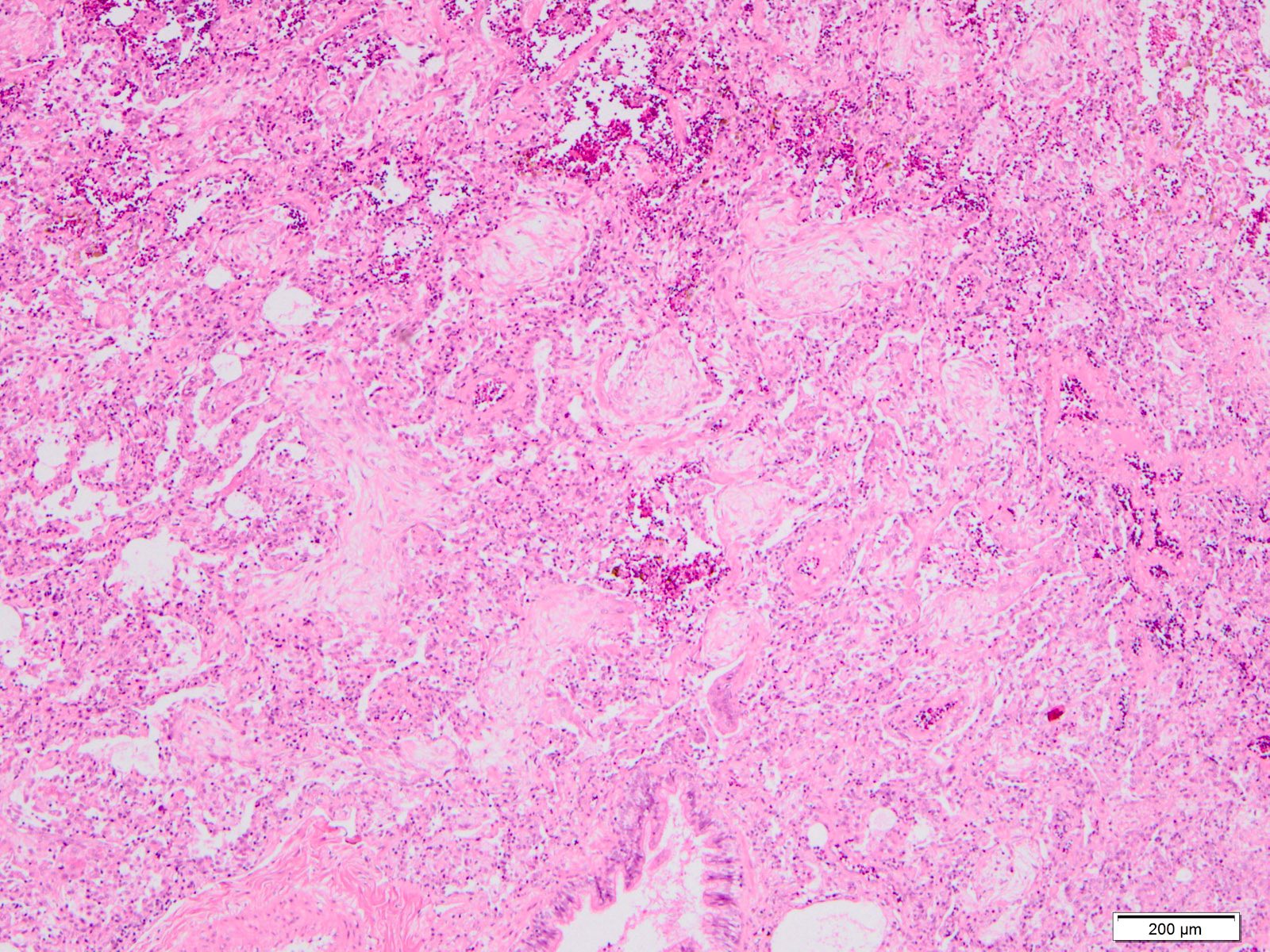
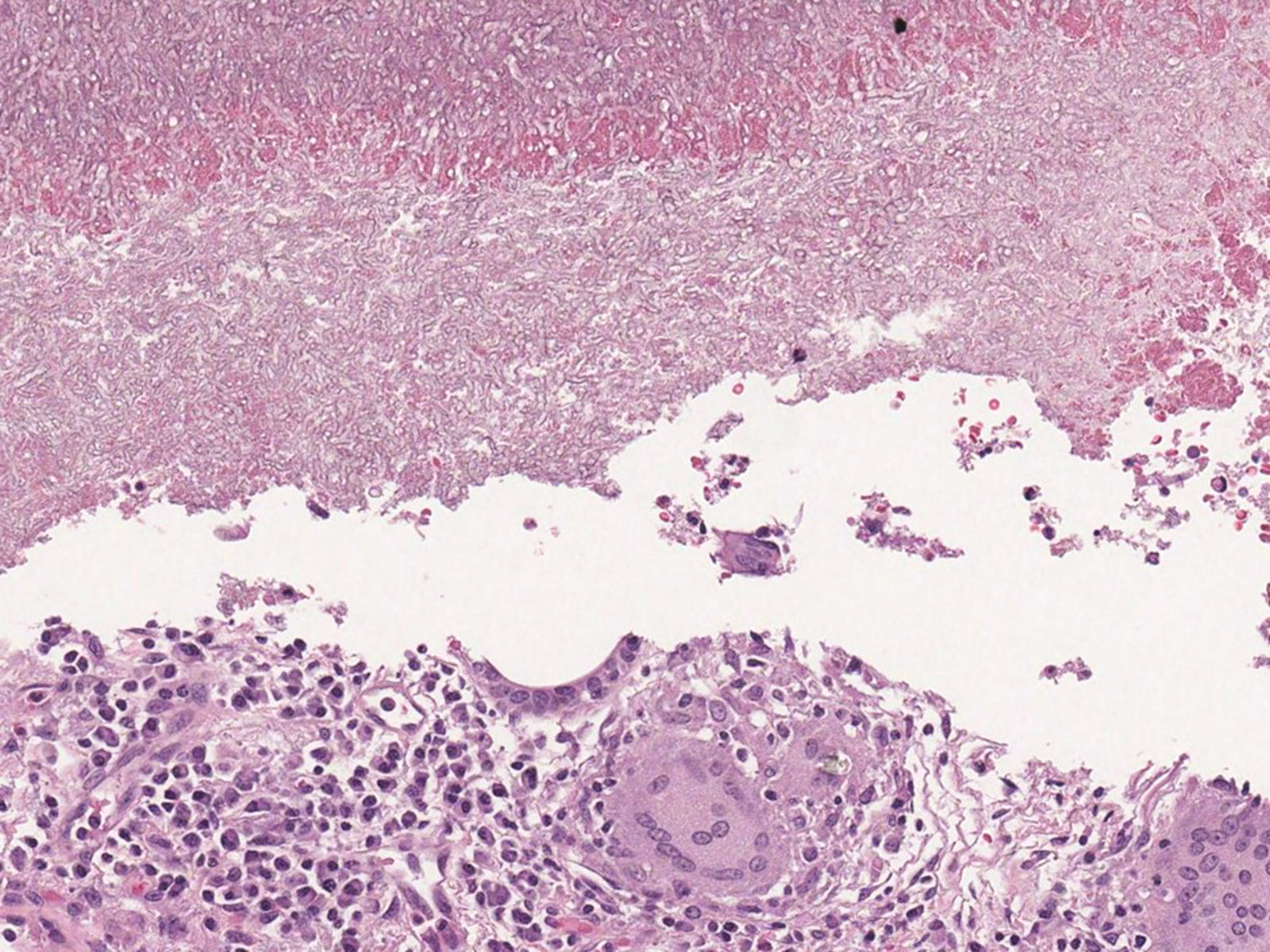
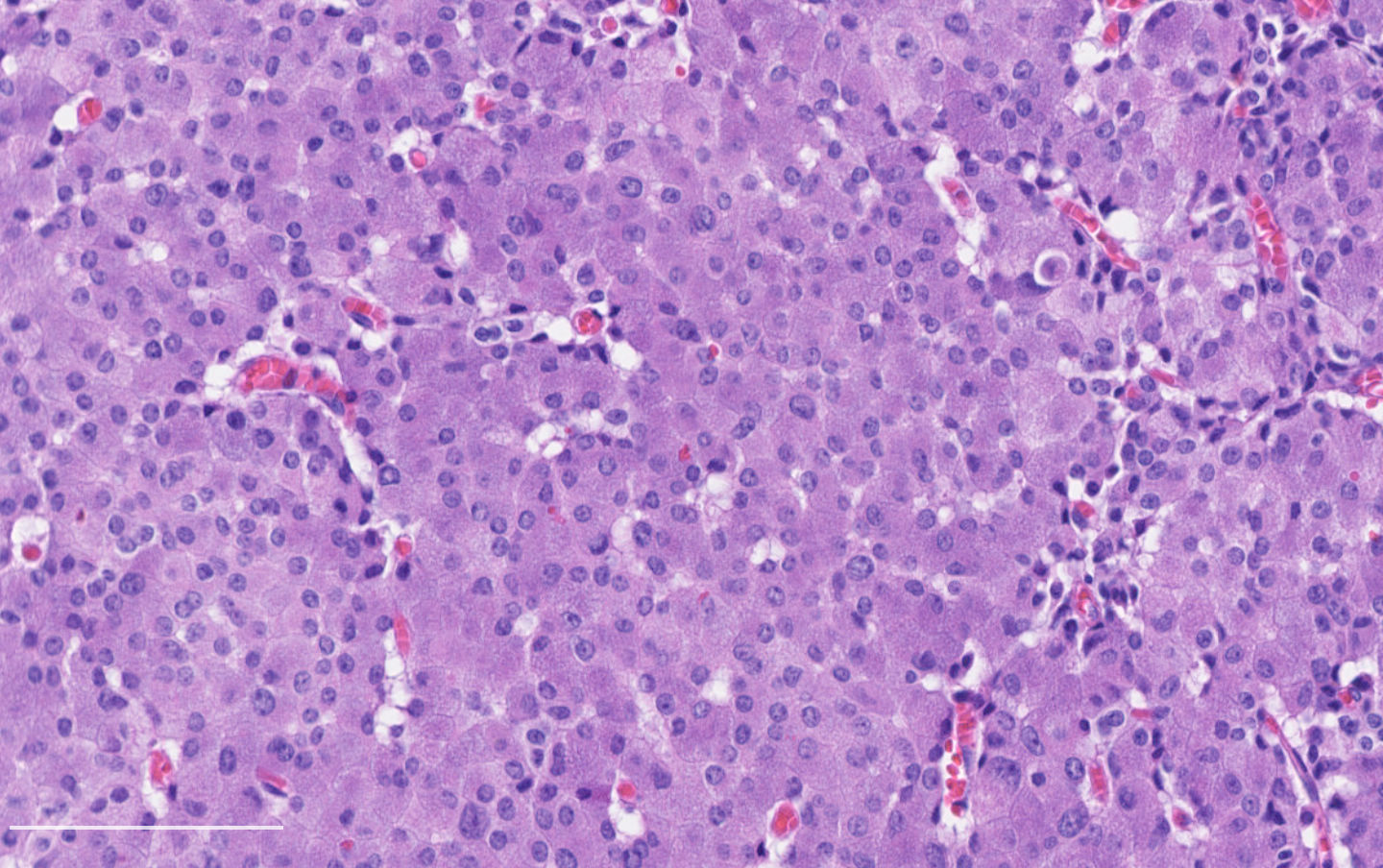
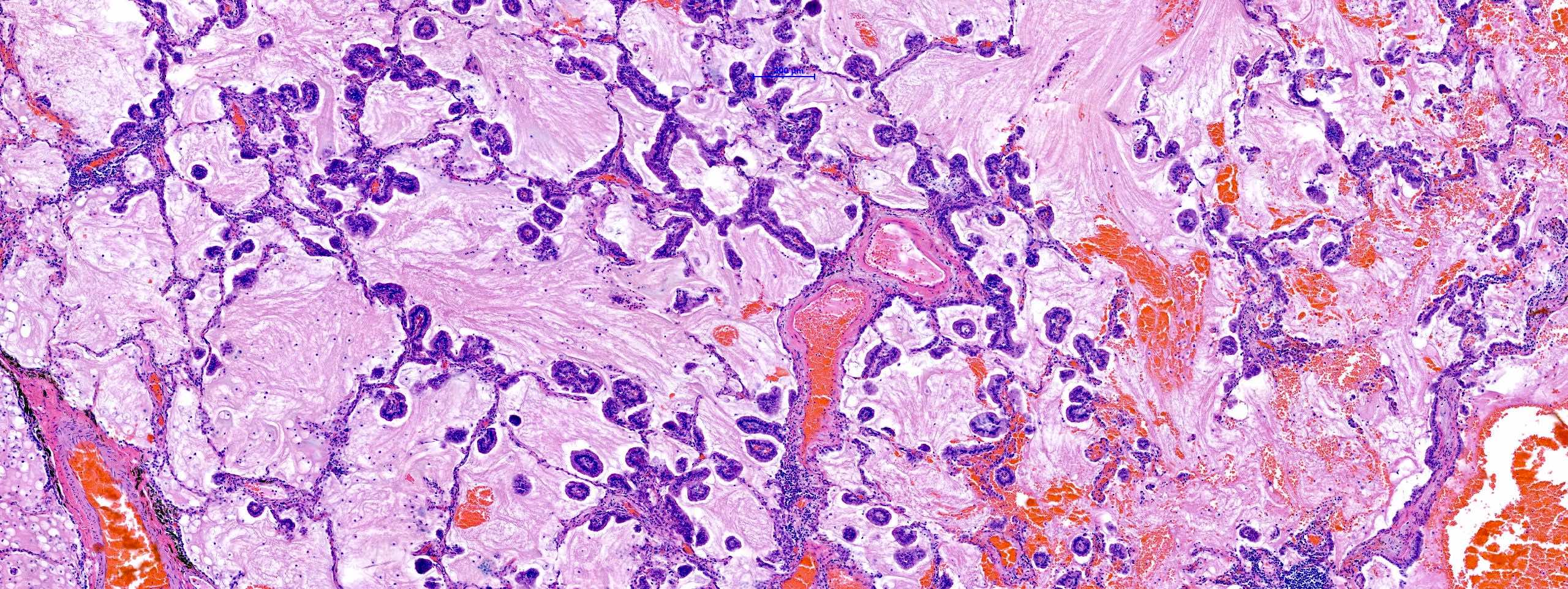
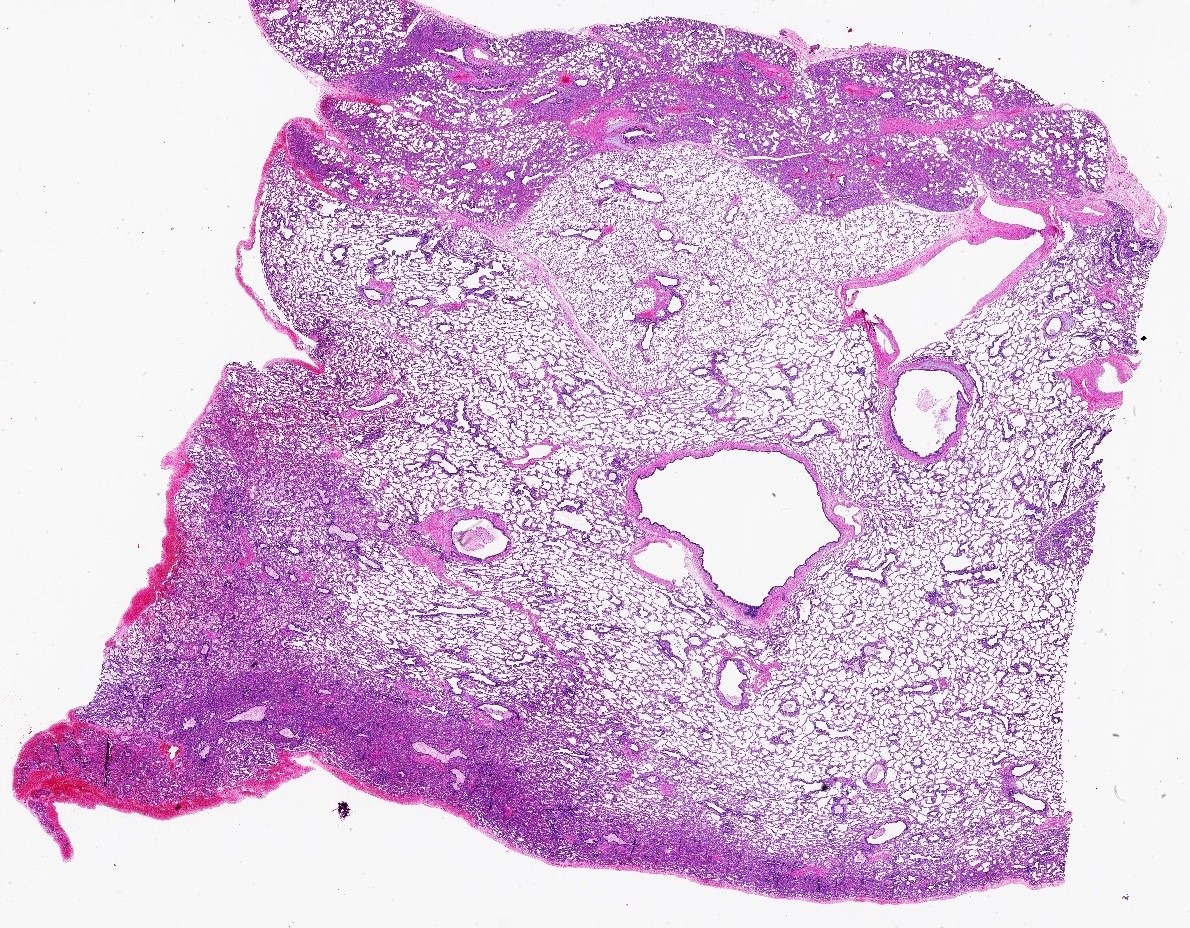
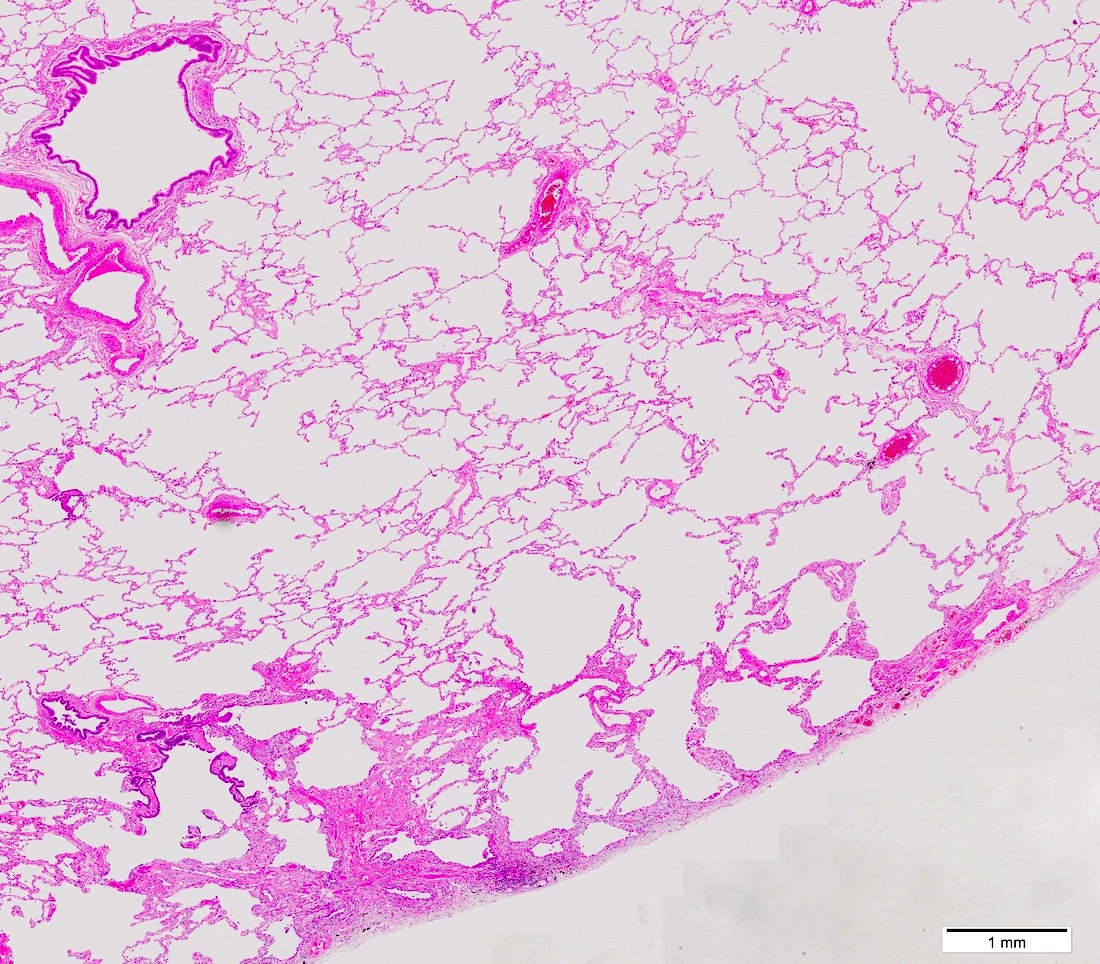
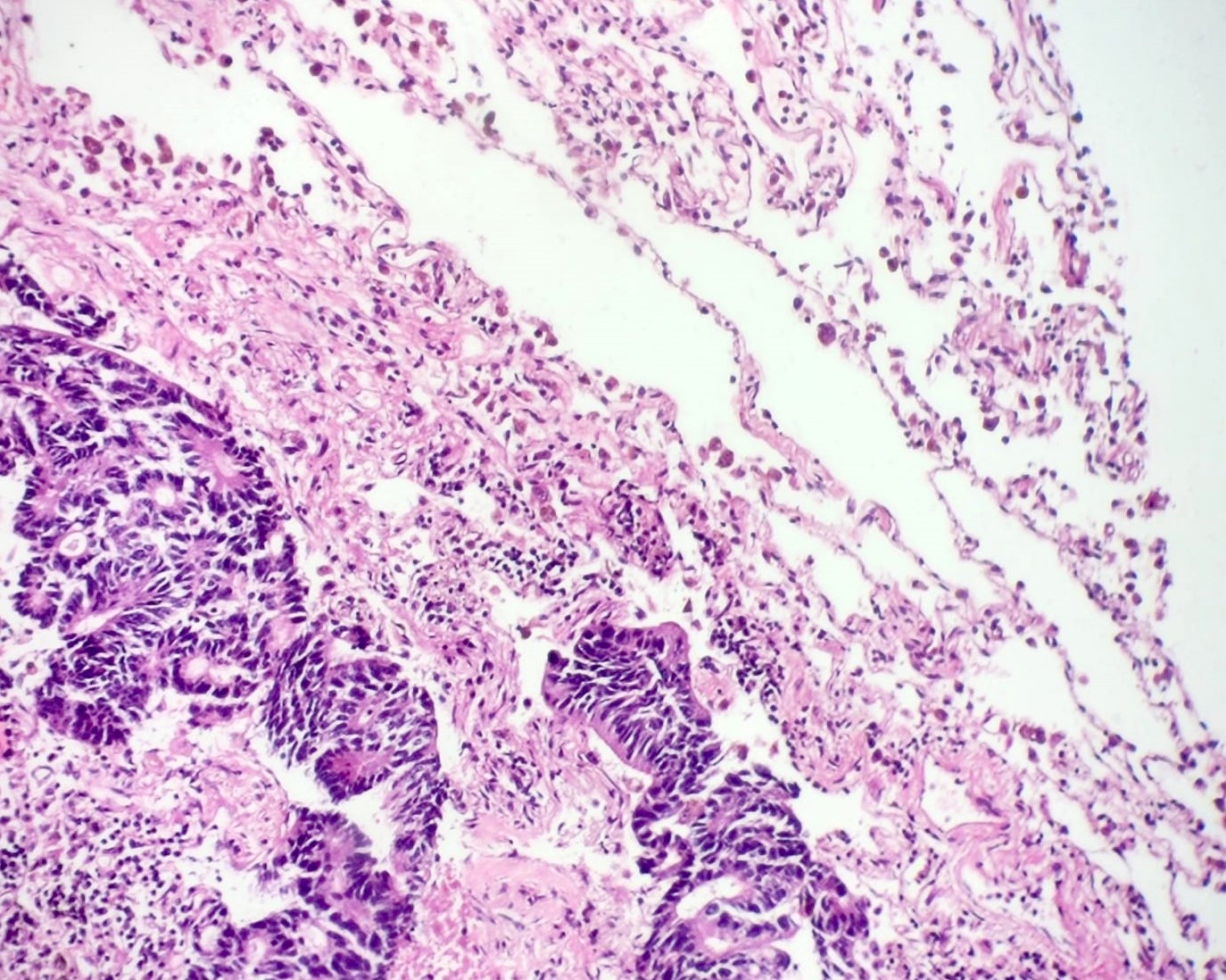
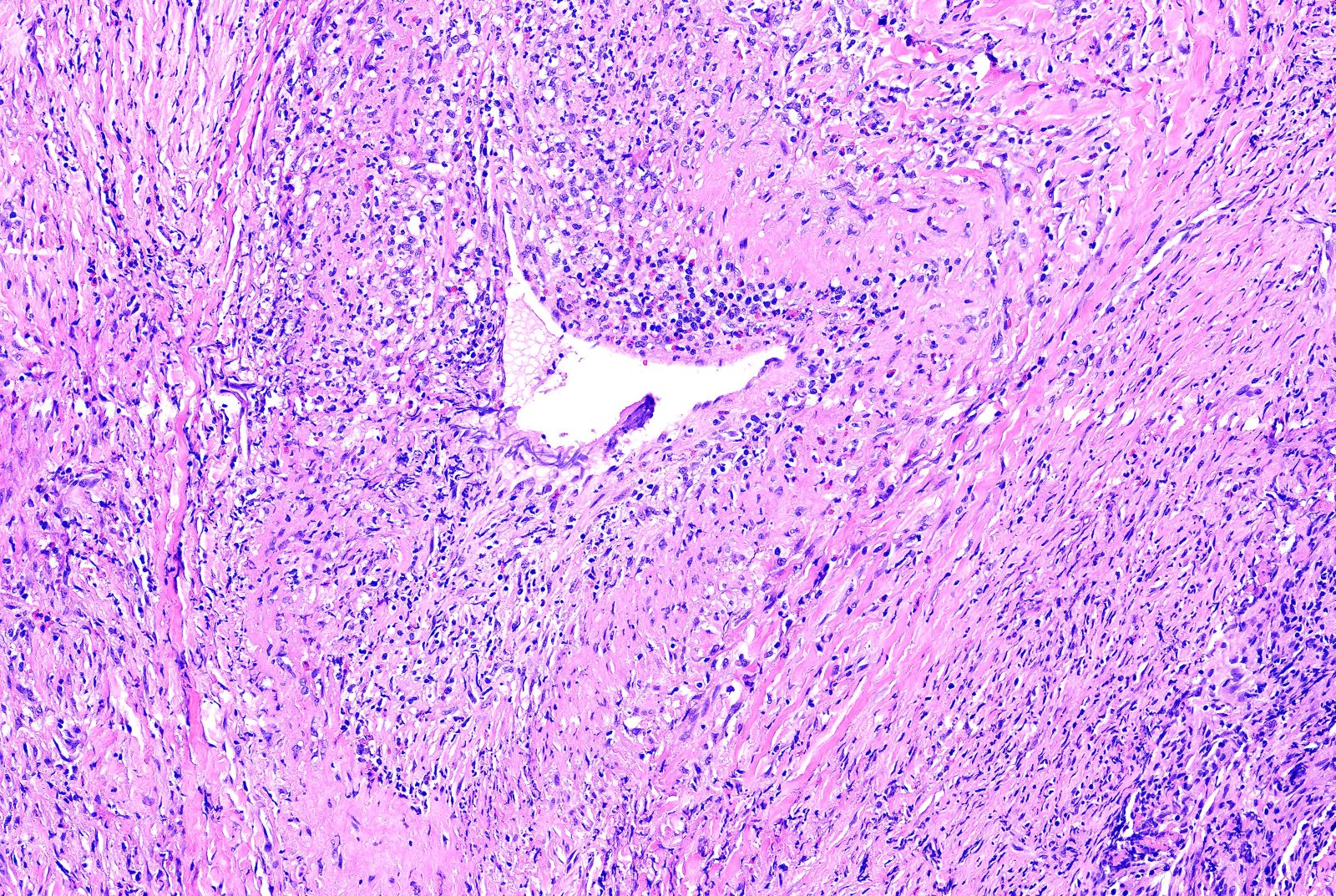
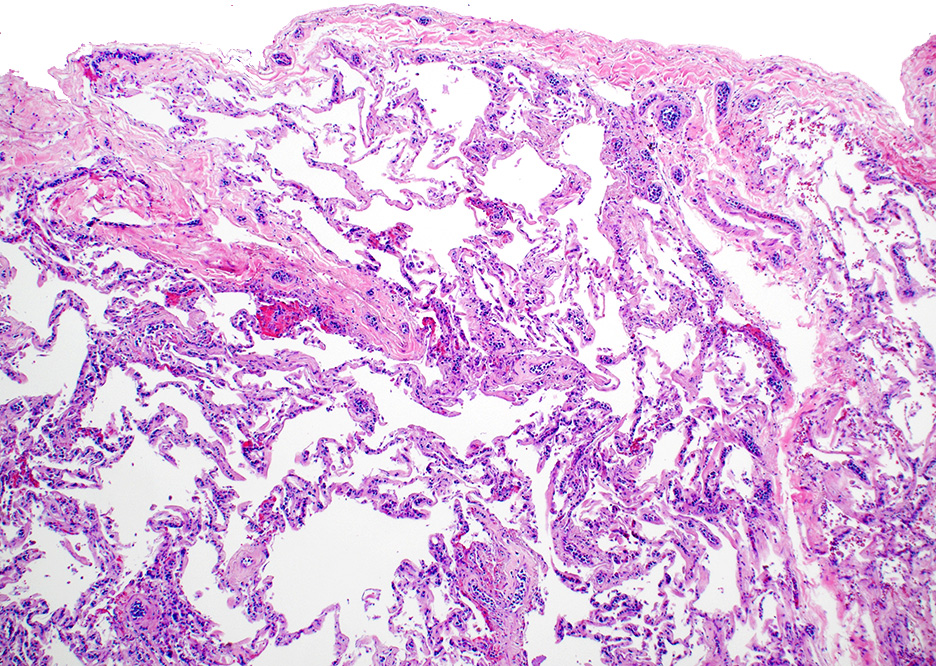
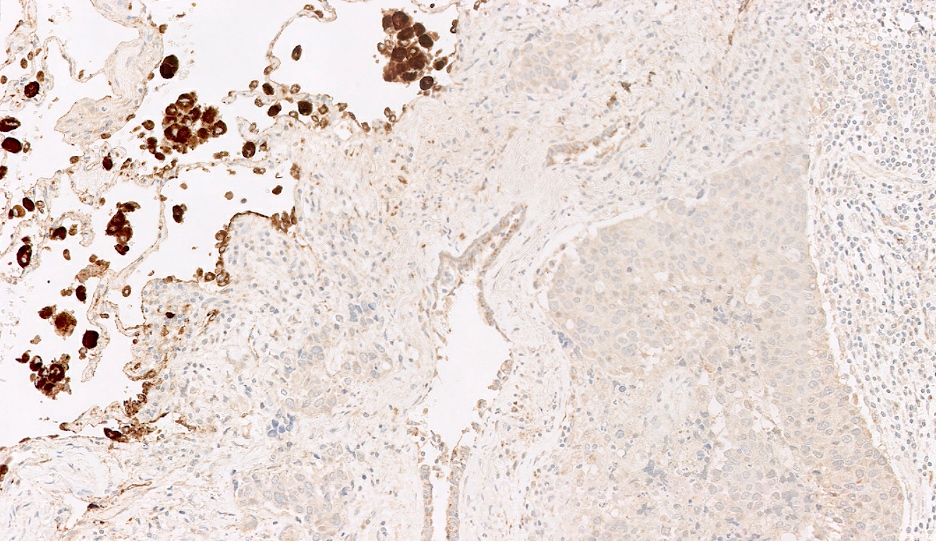
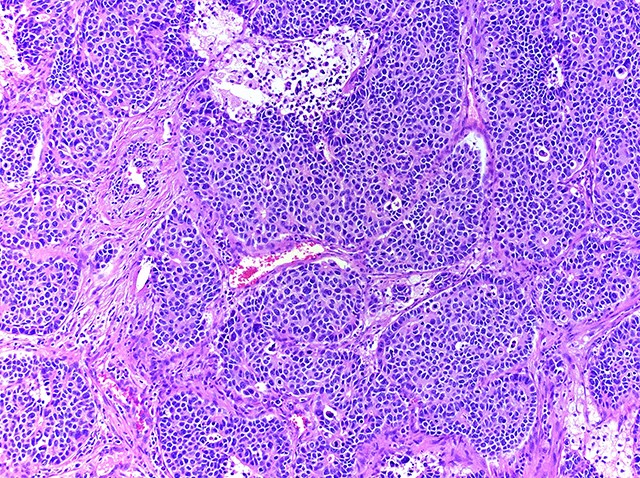
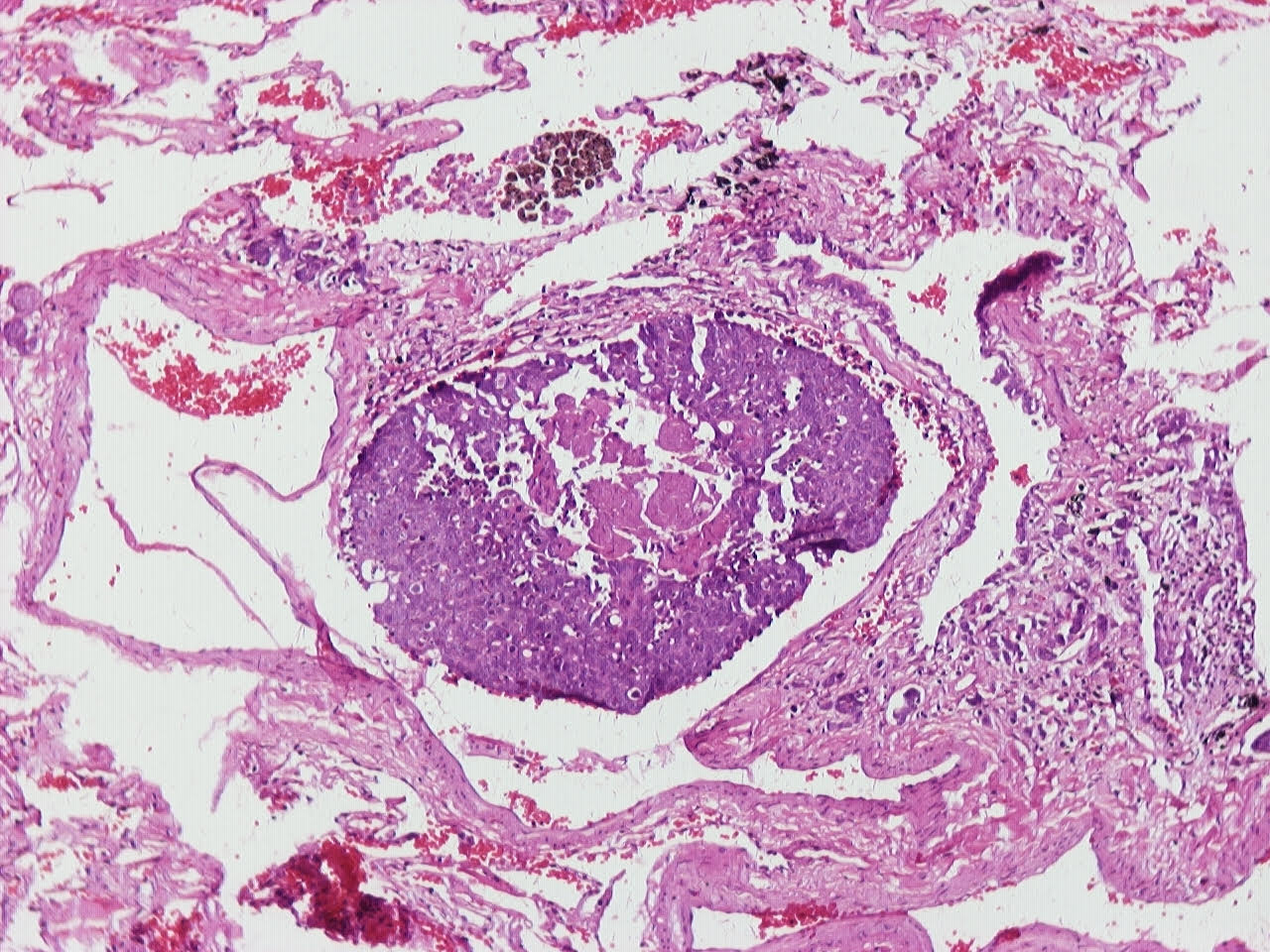
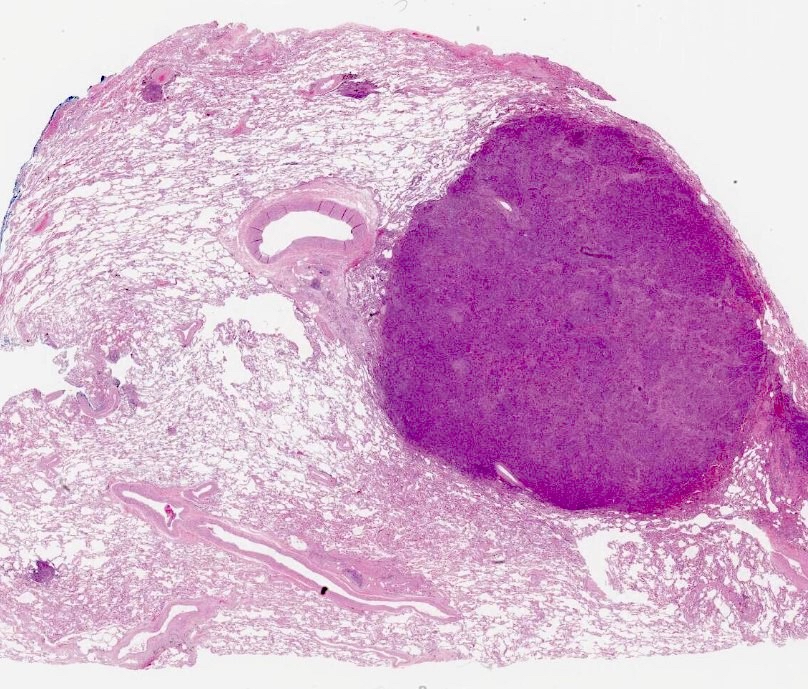
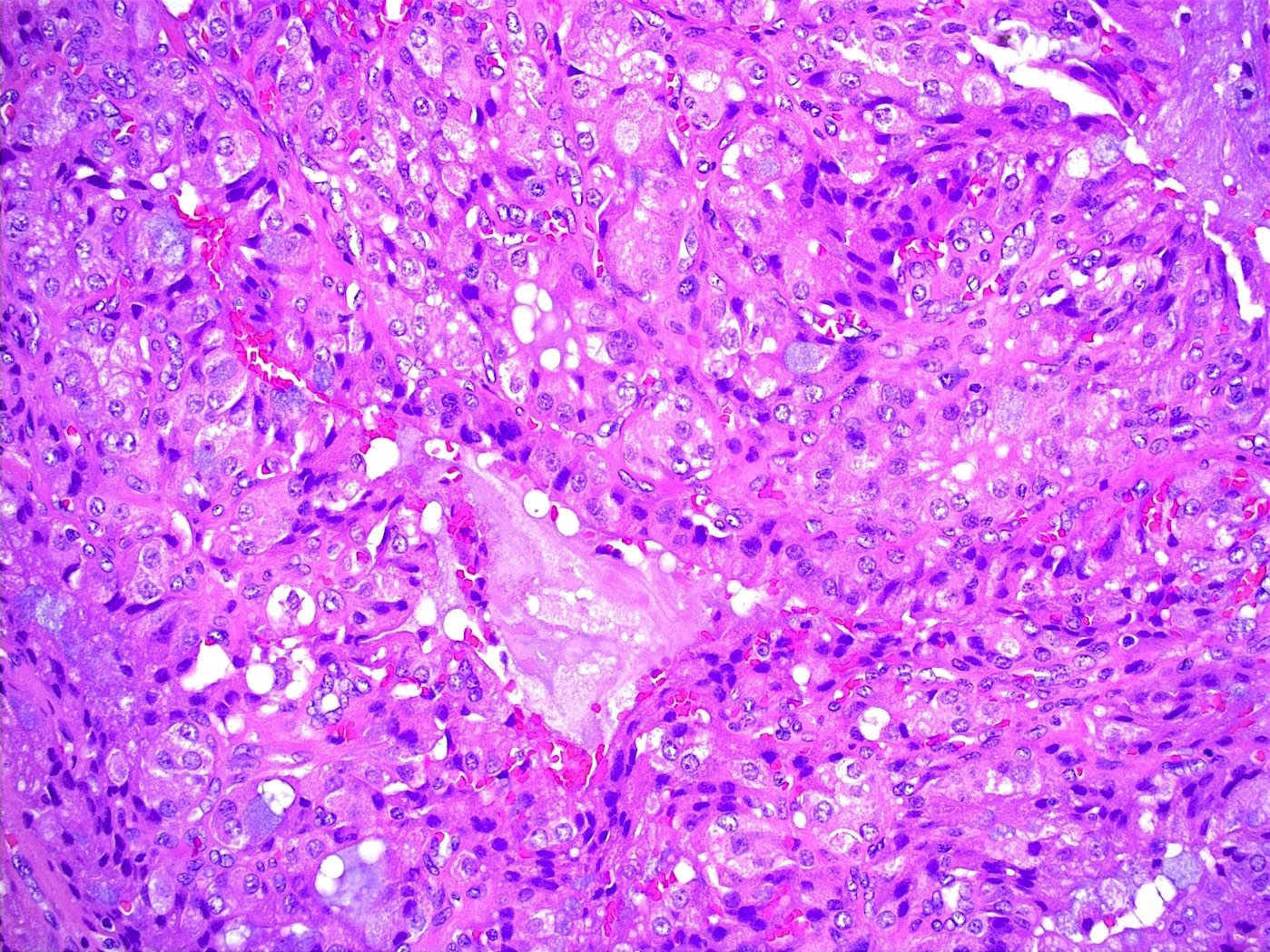
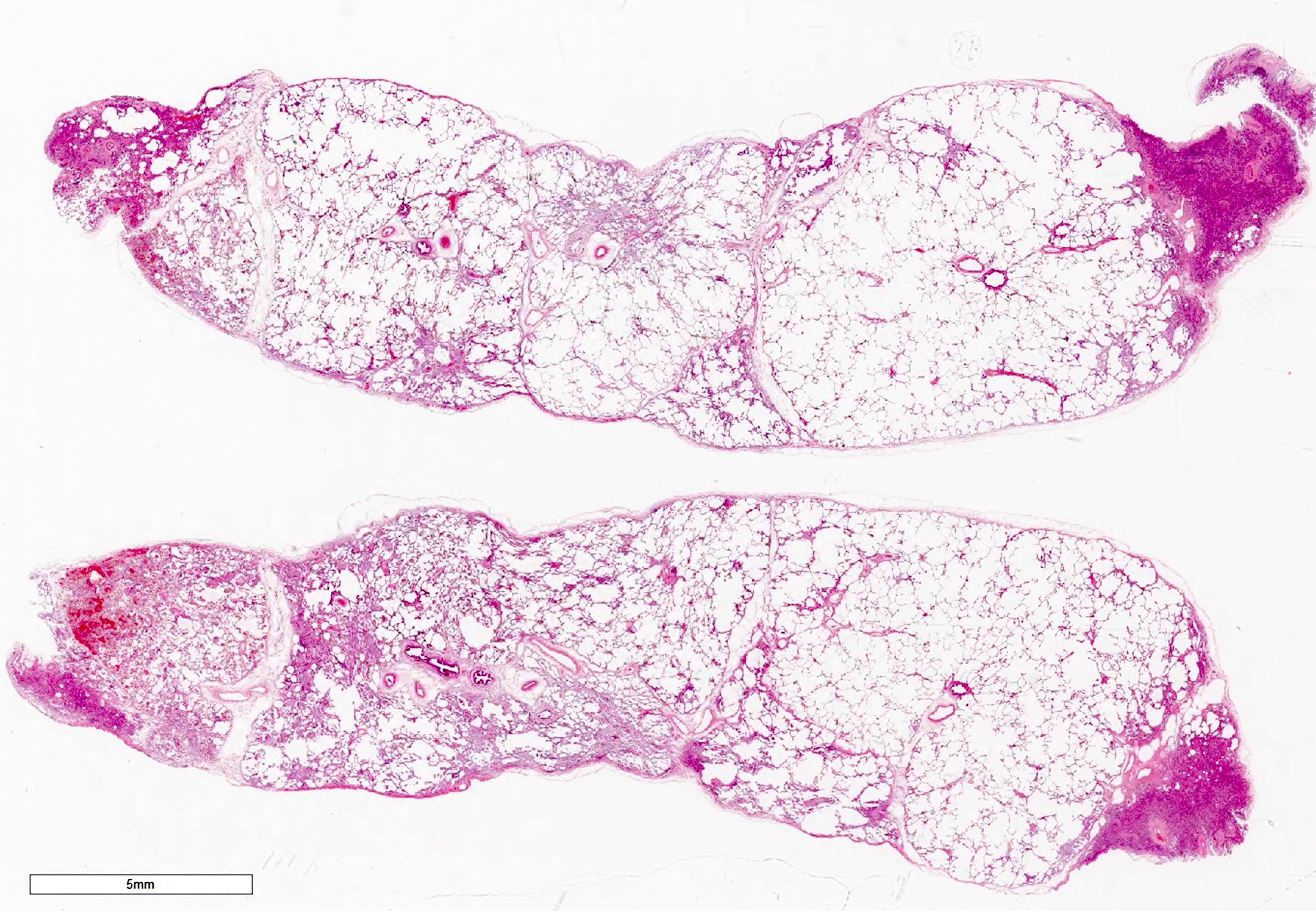
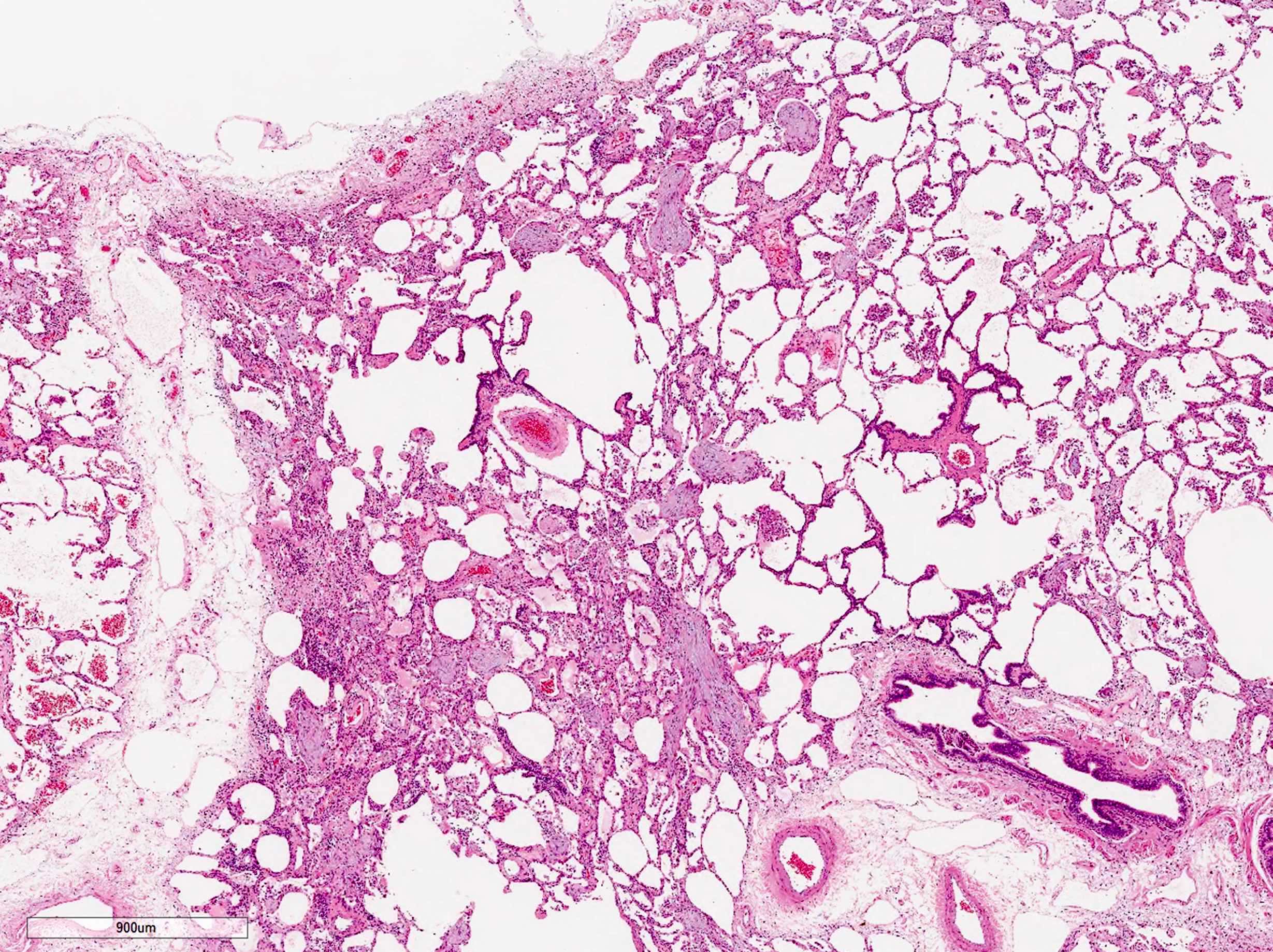
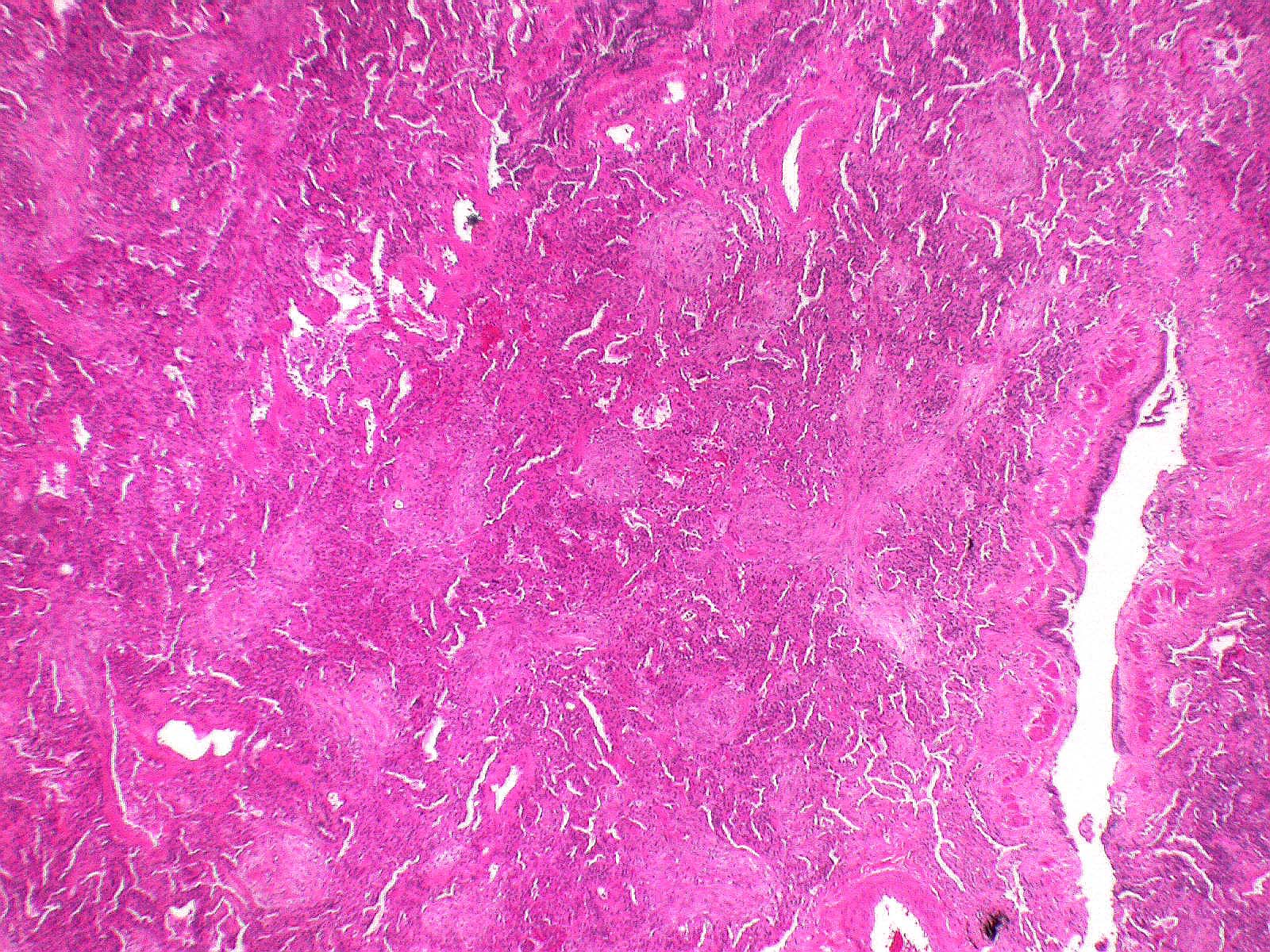
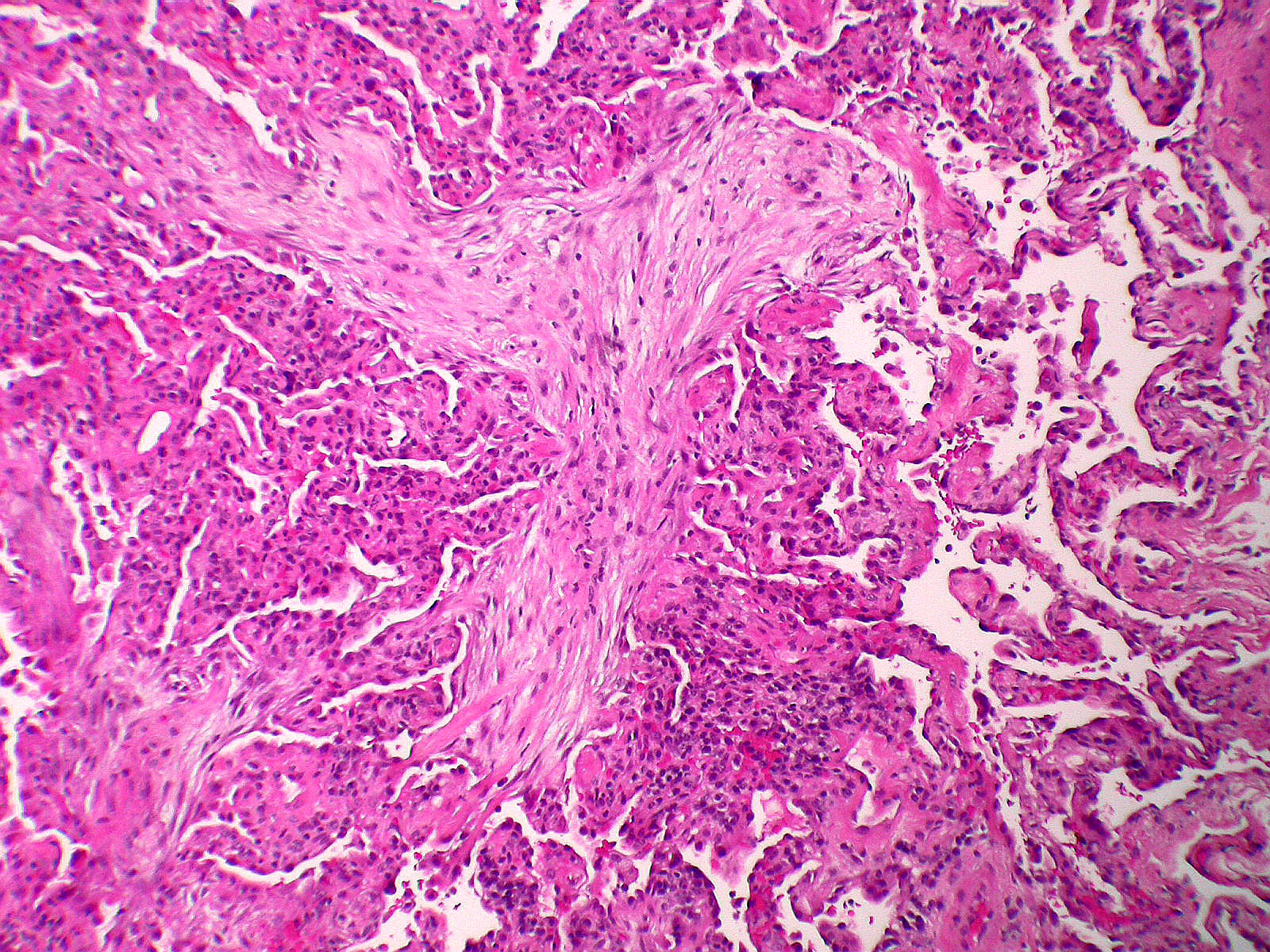
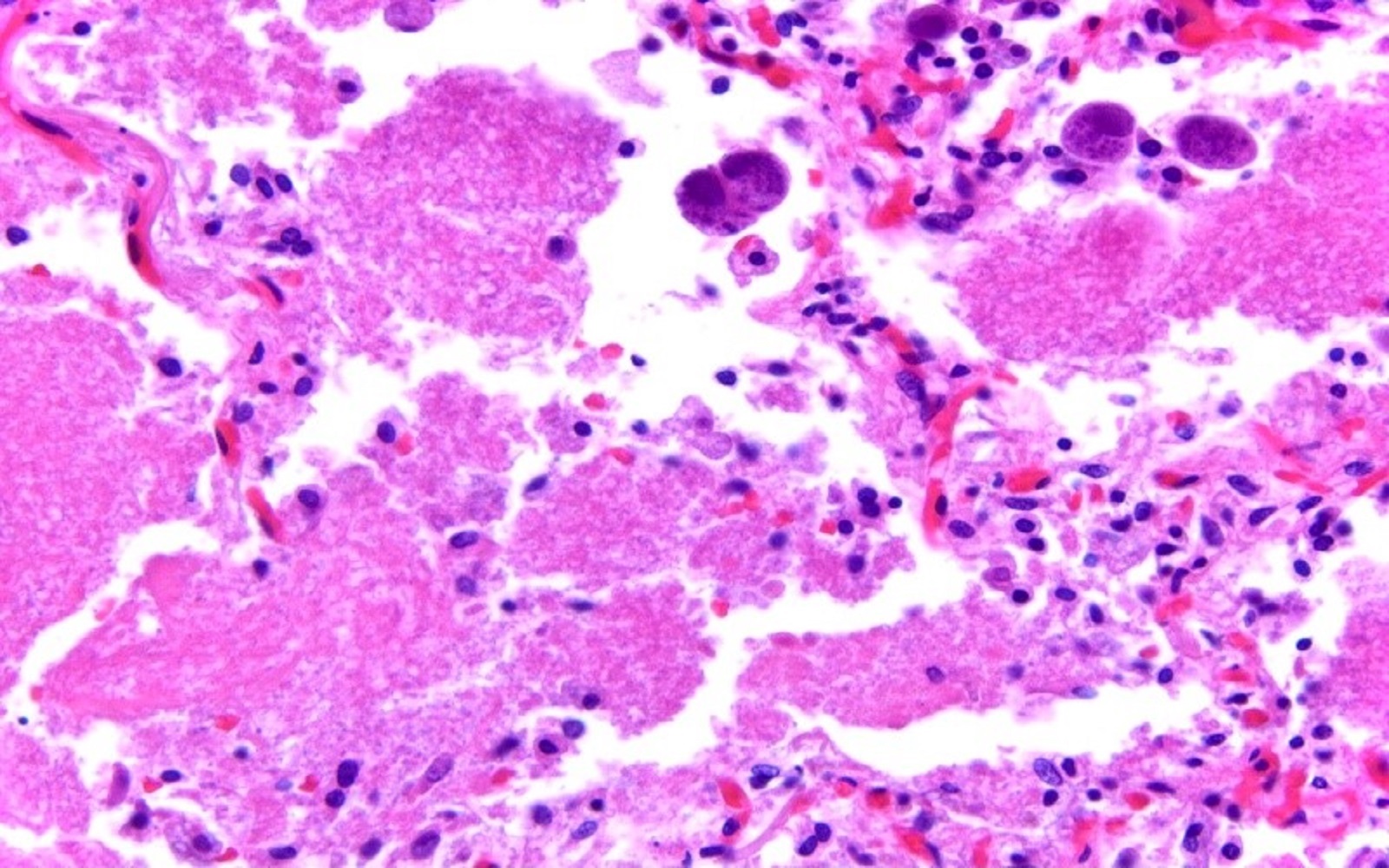
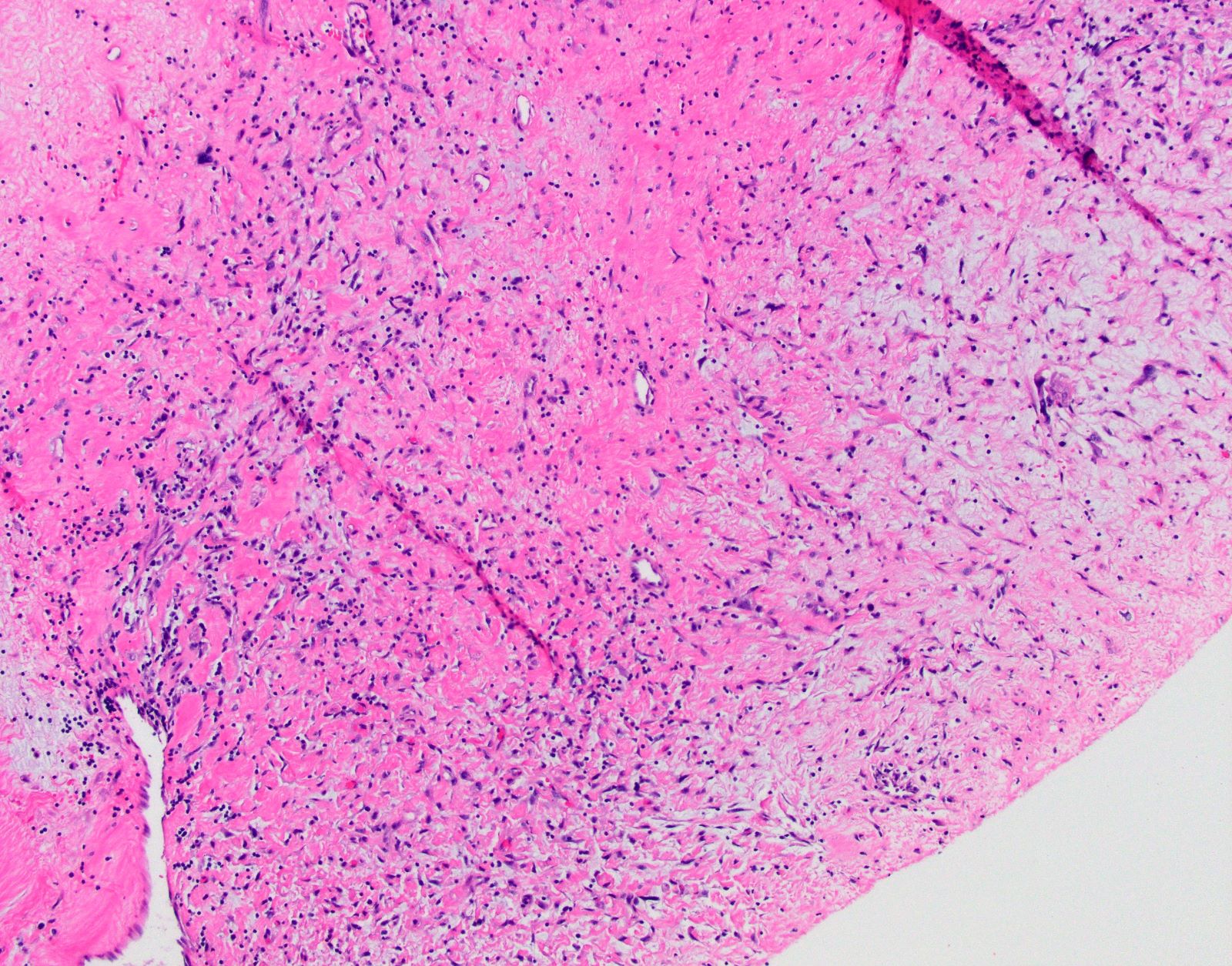
- Acute interstitial pneumonia shows diffuse alveolar damage, which is almost completely identical to acute respiratory distress syndrome / diffuse alveolar damage morphologically (Eur Respir J 2000;15:412)
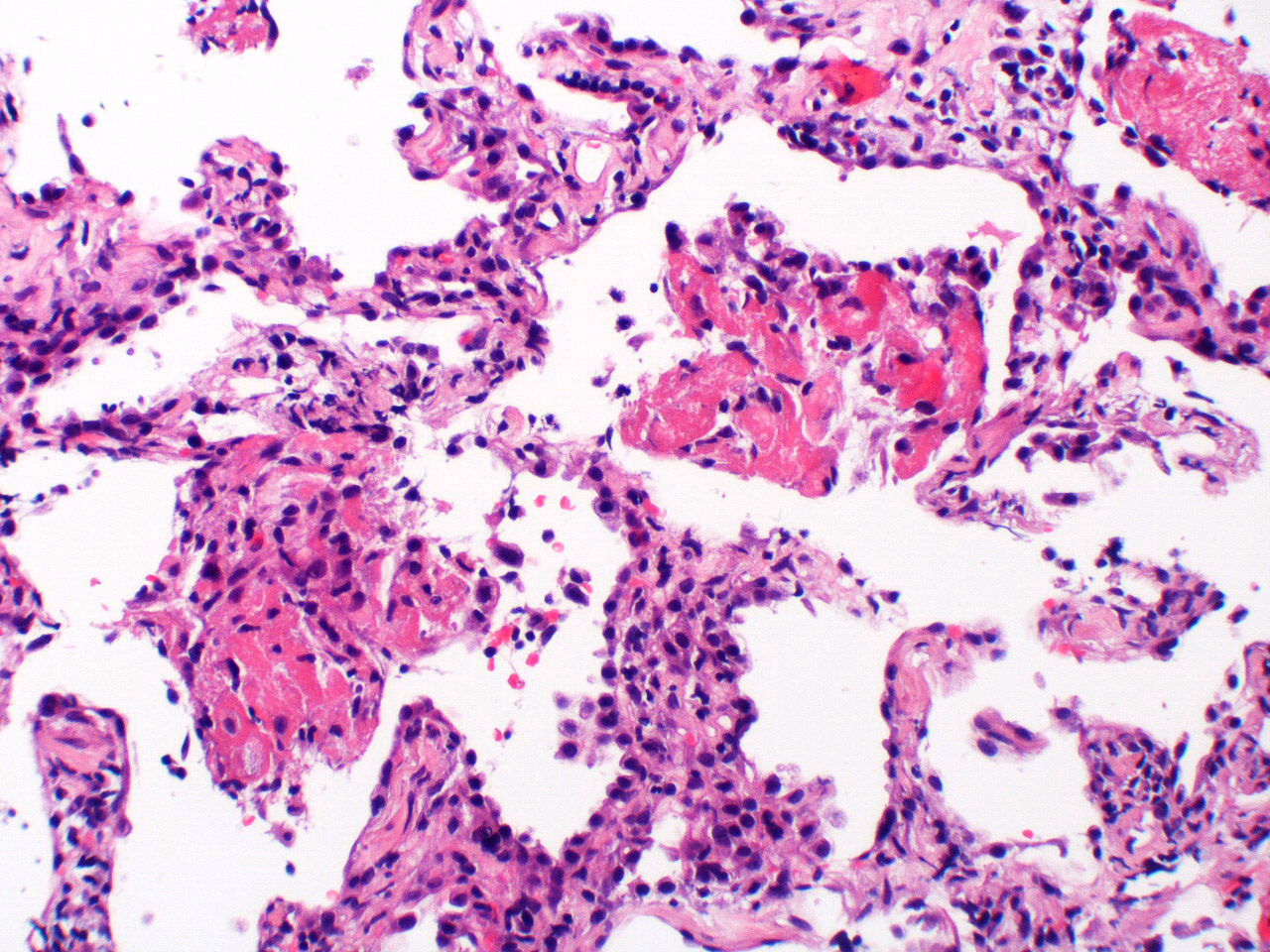
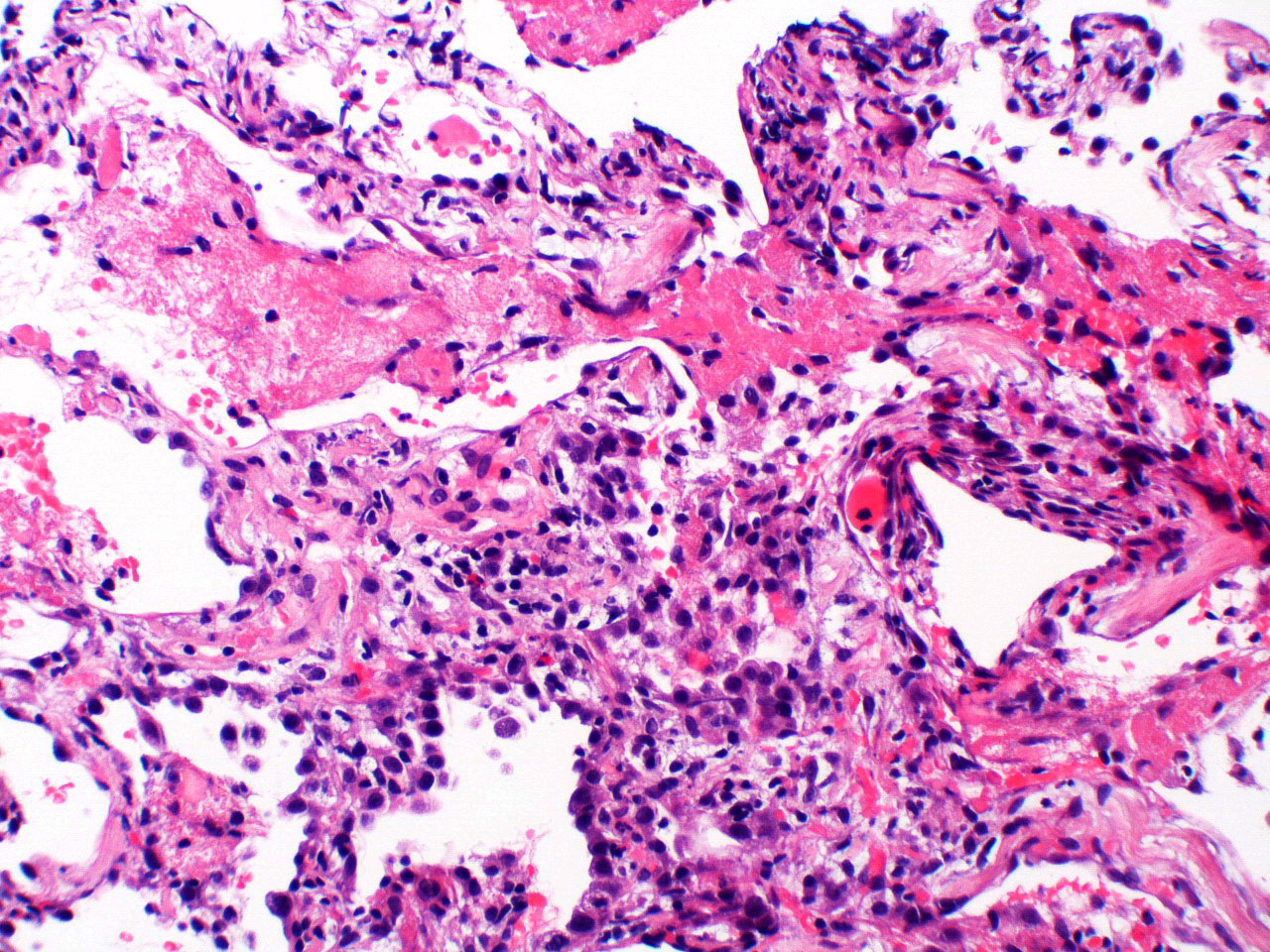
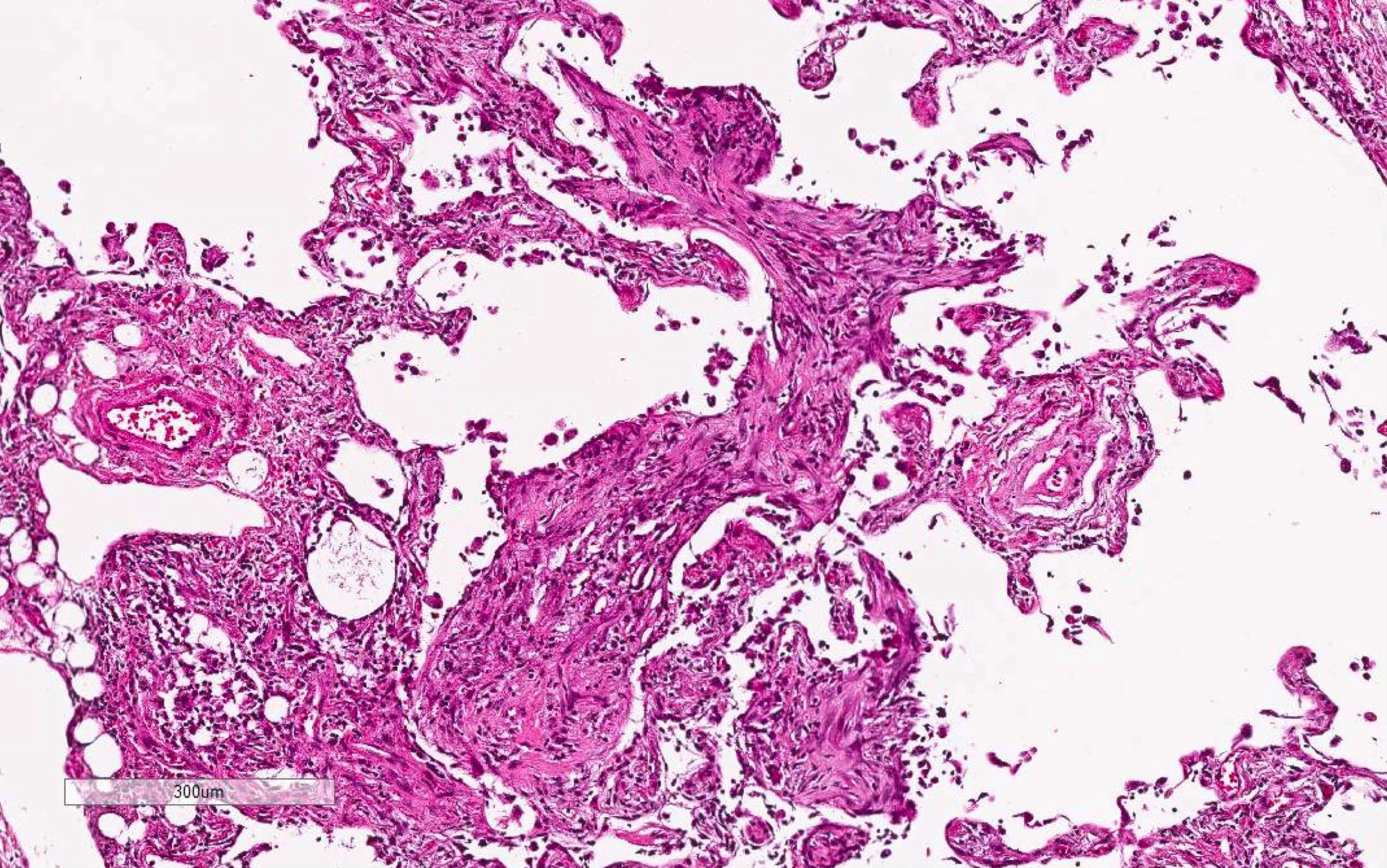
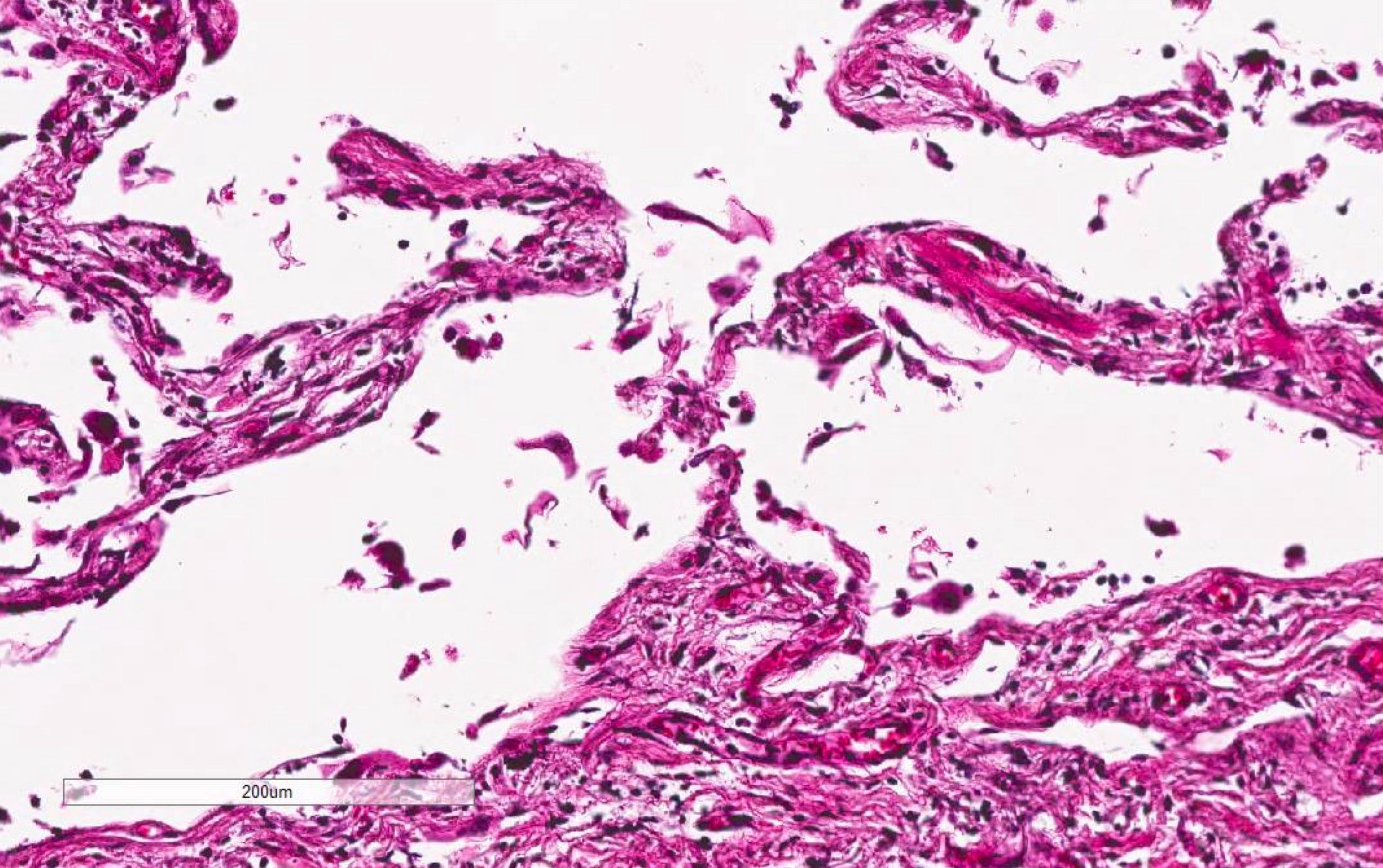
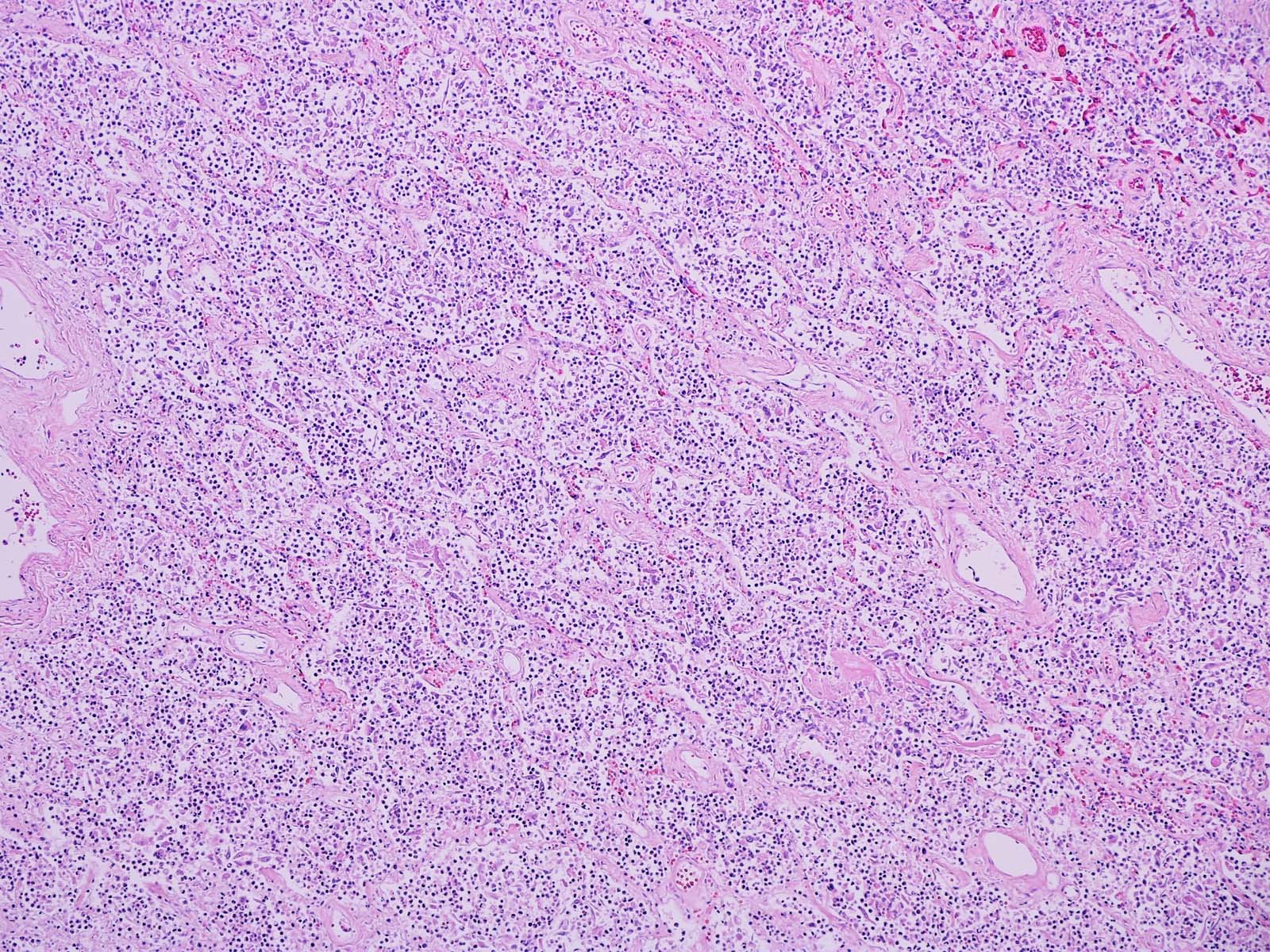
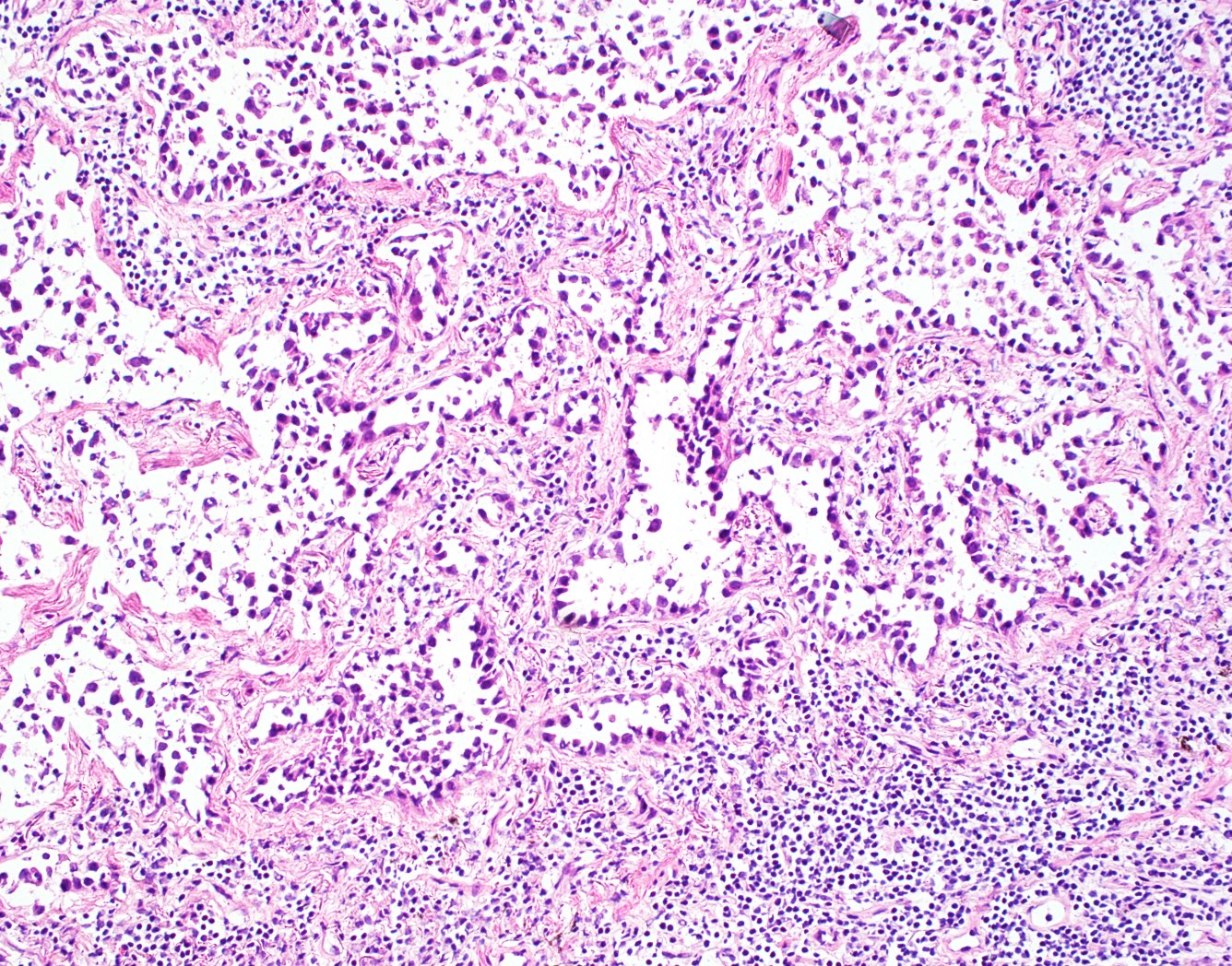
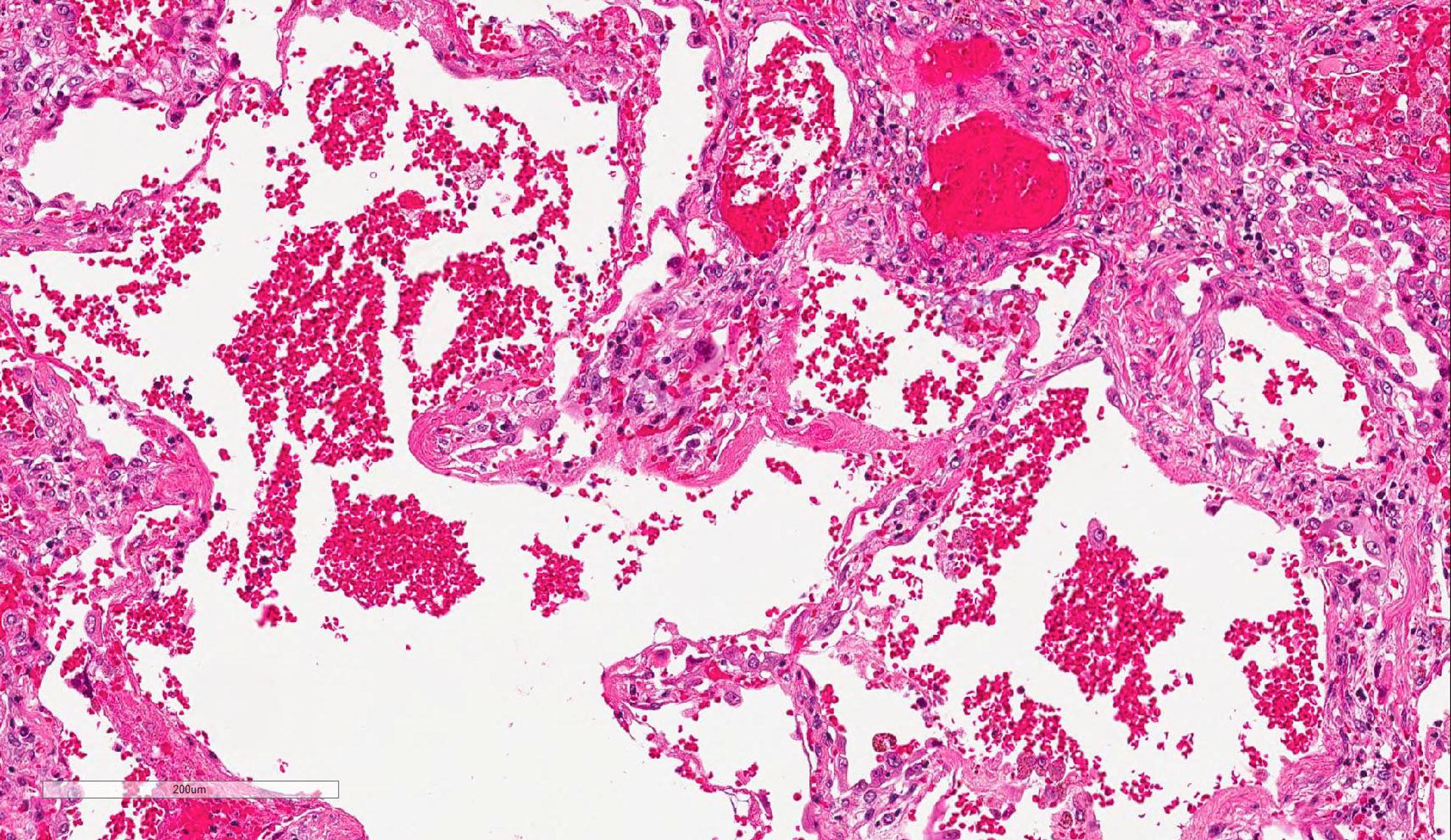
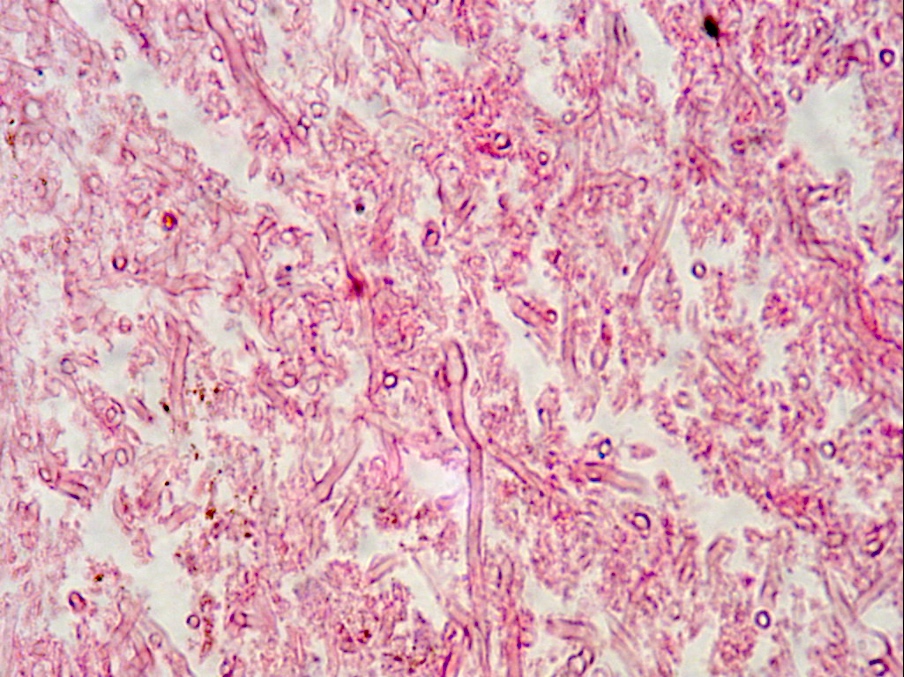
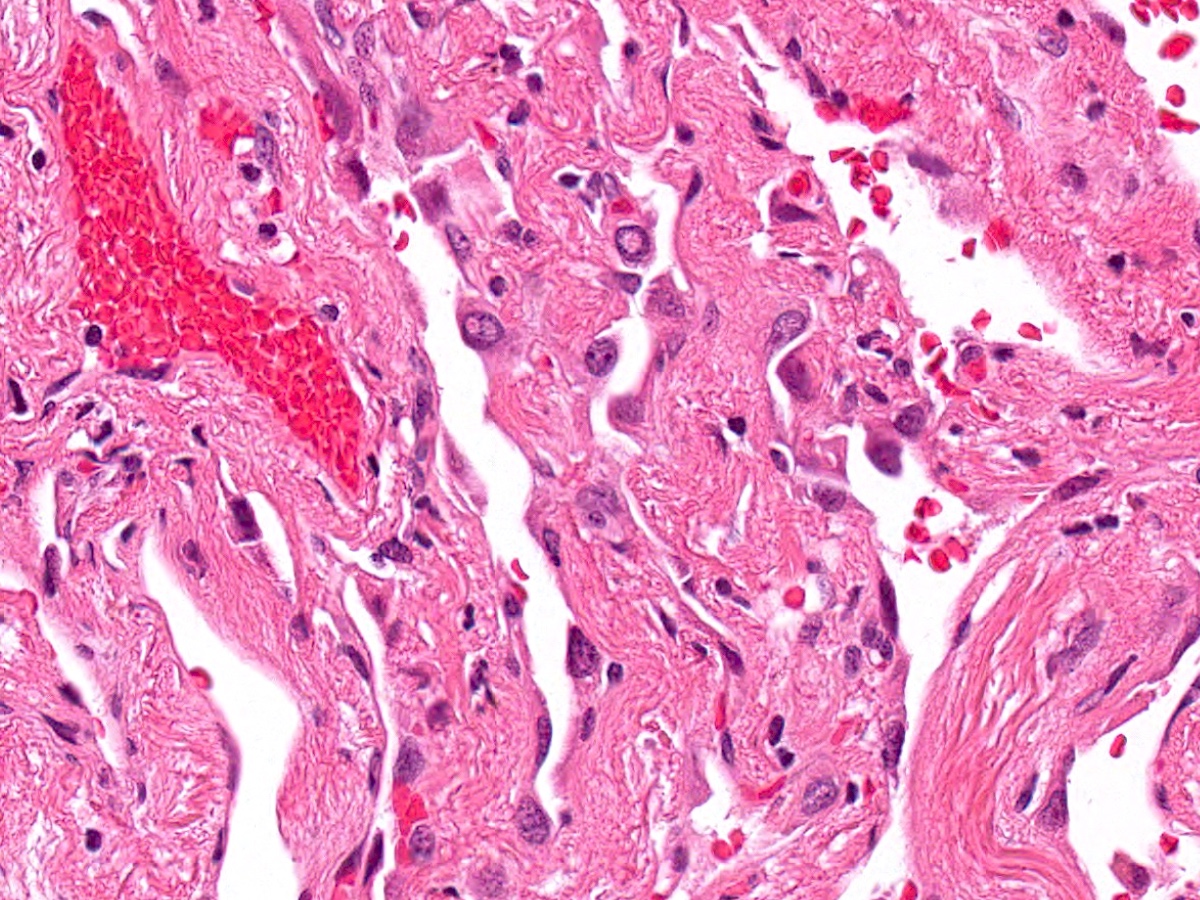
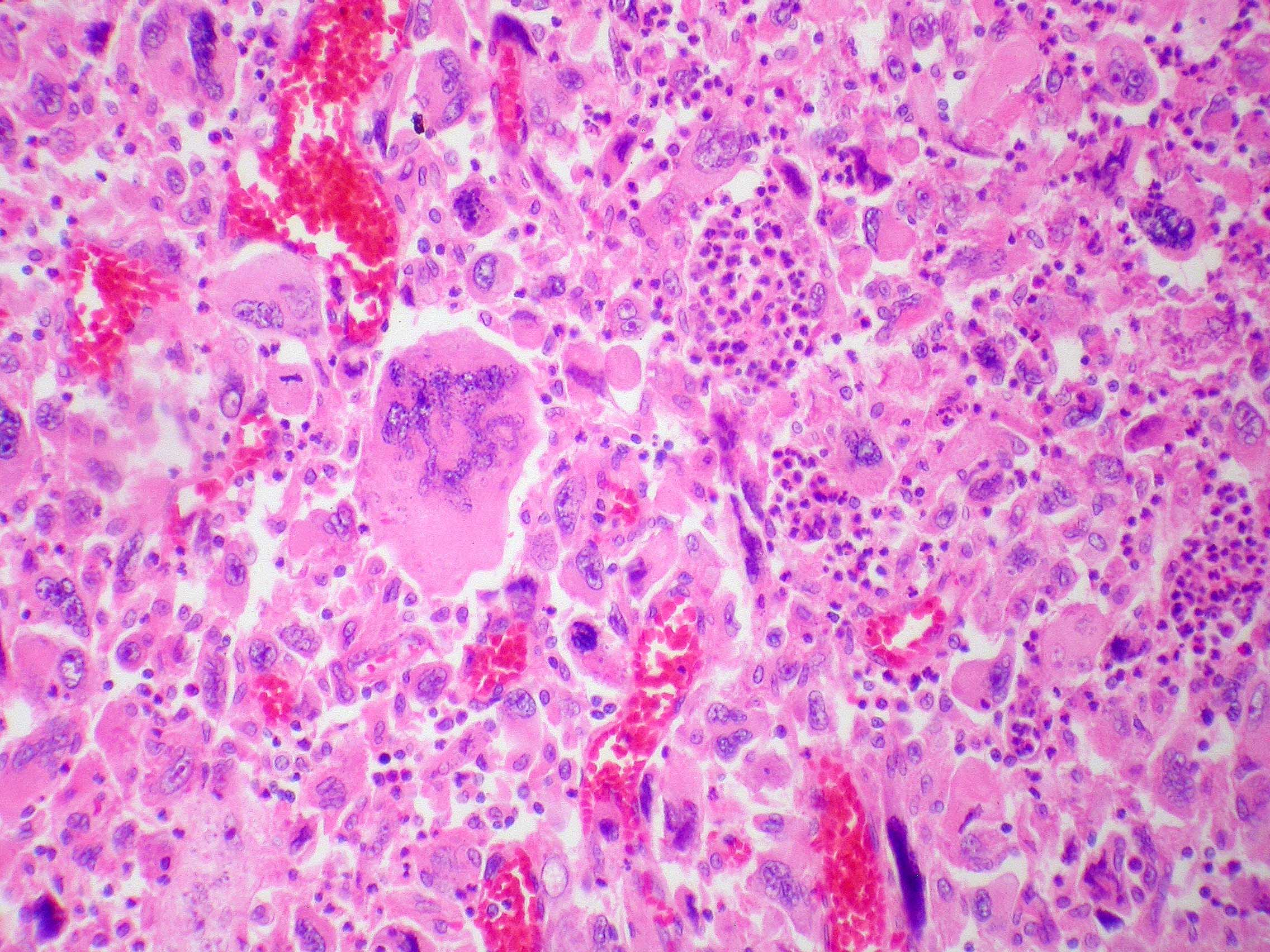
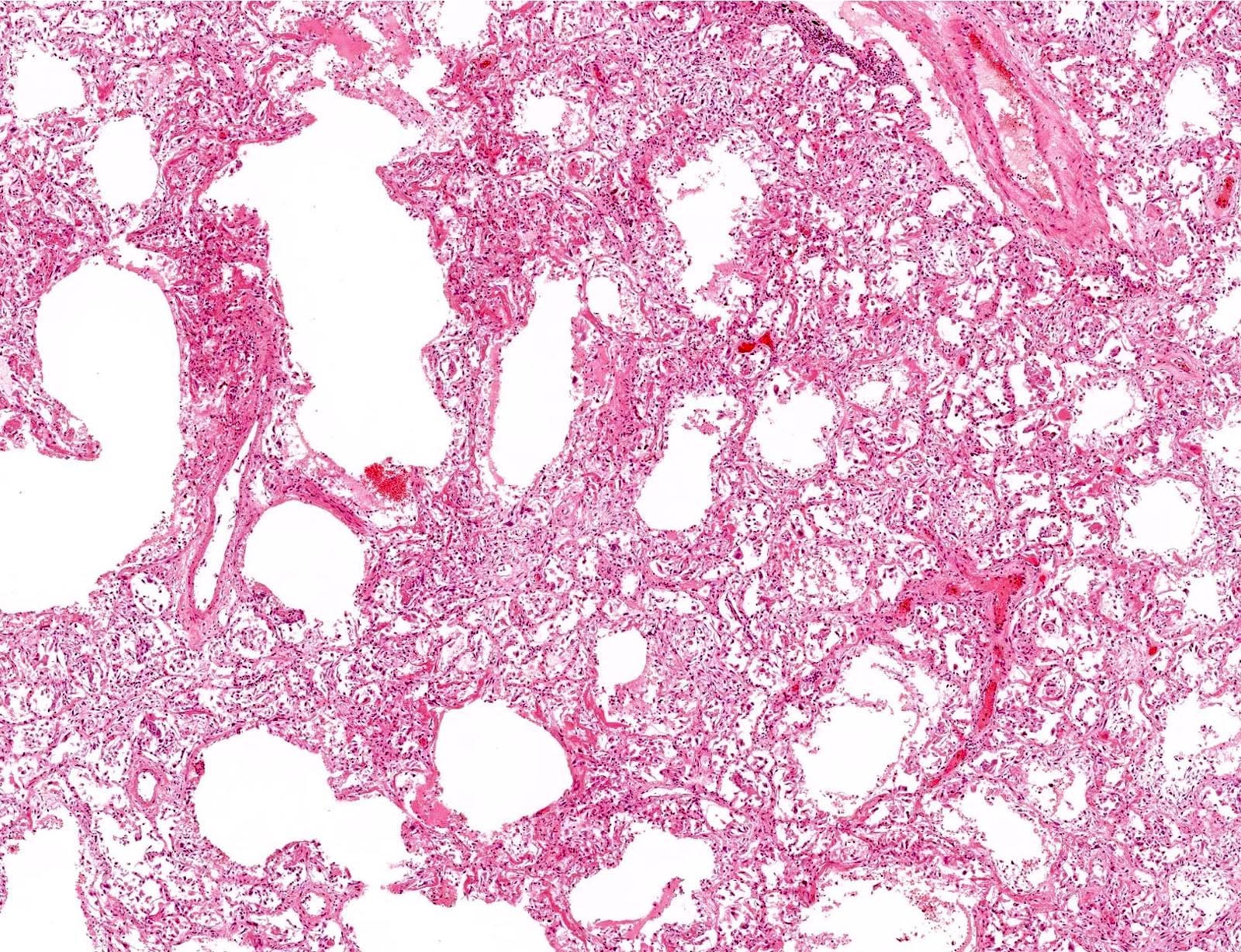
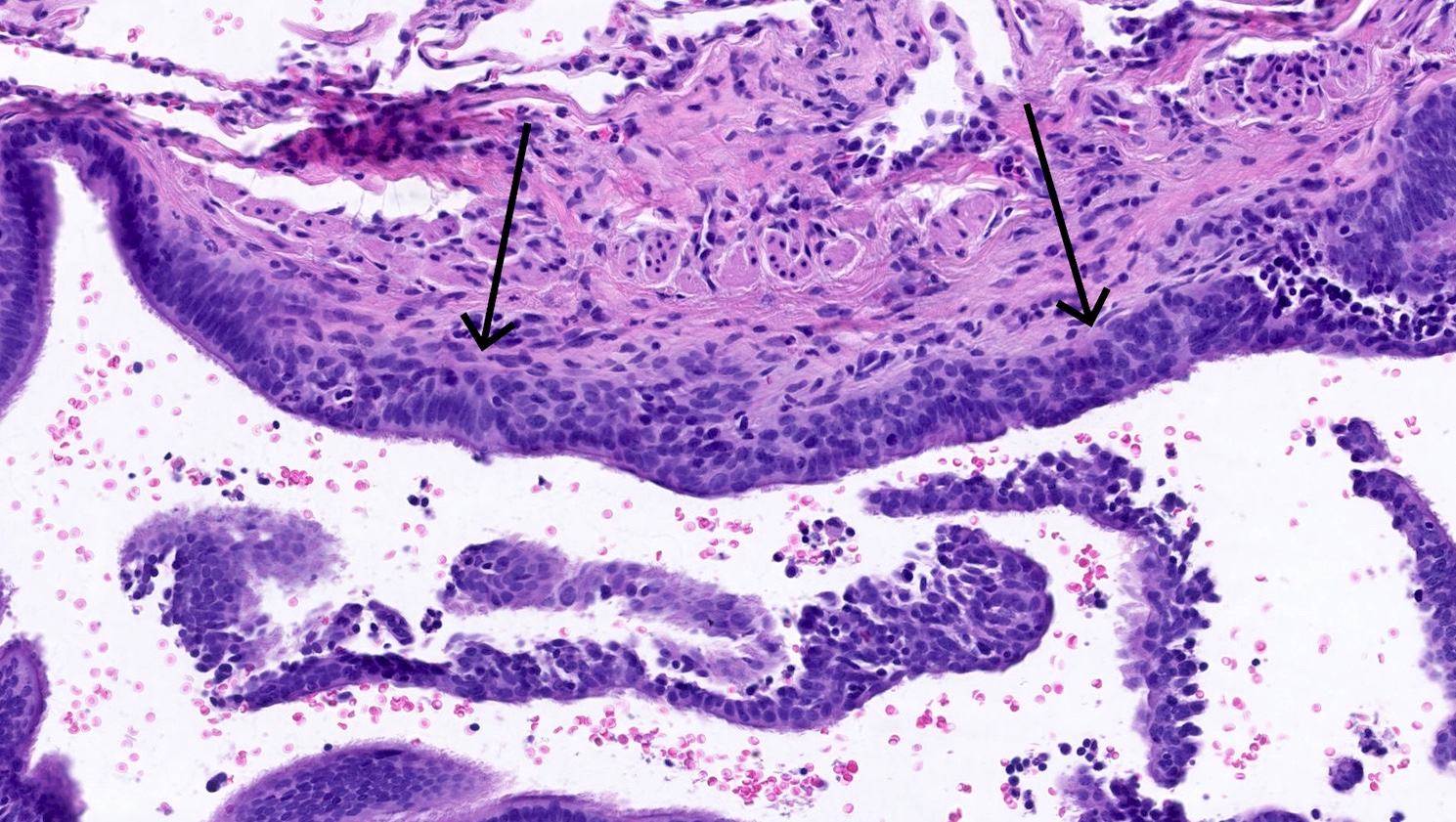
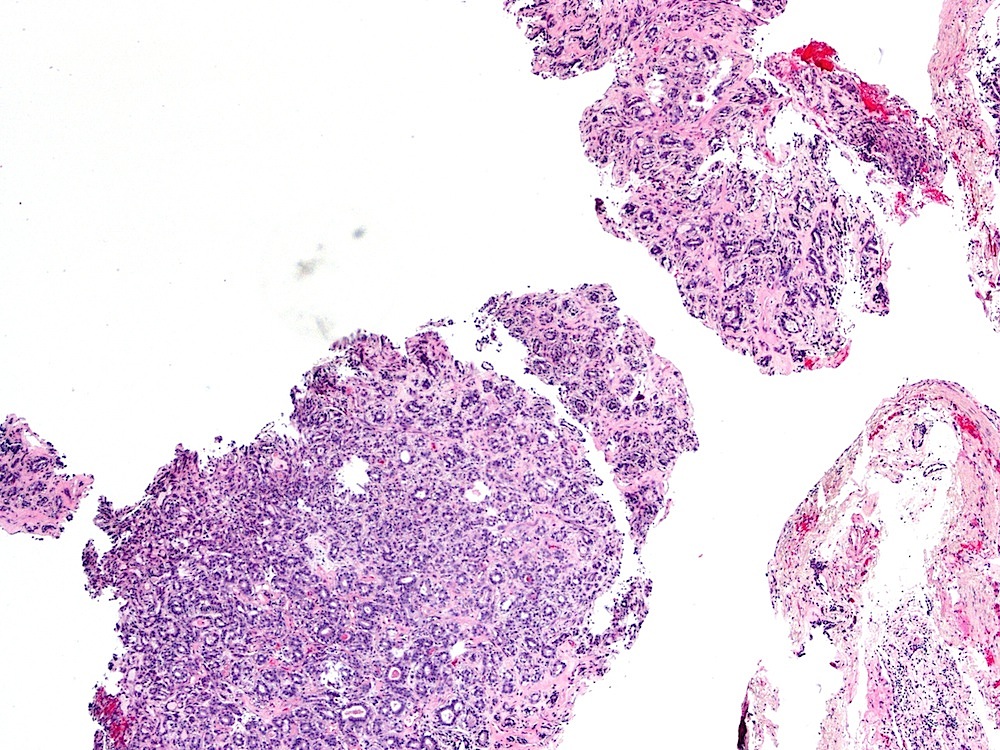
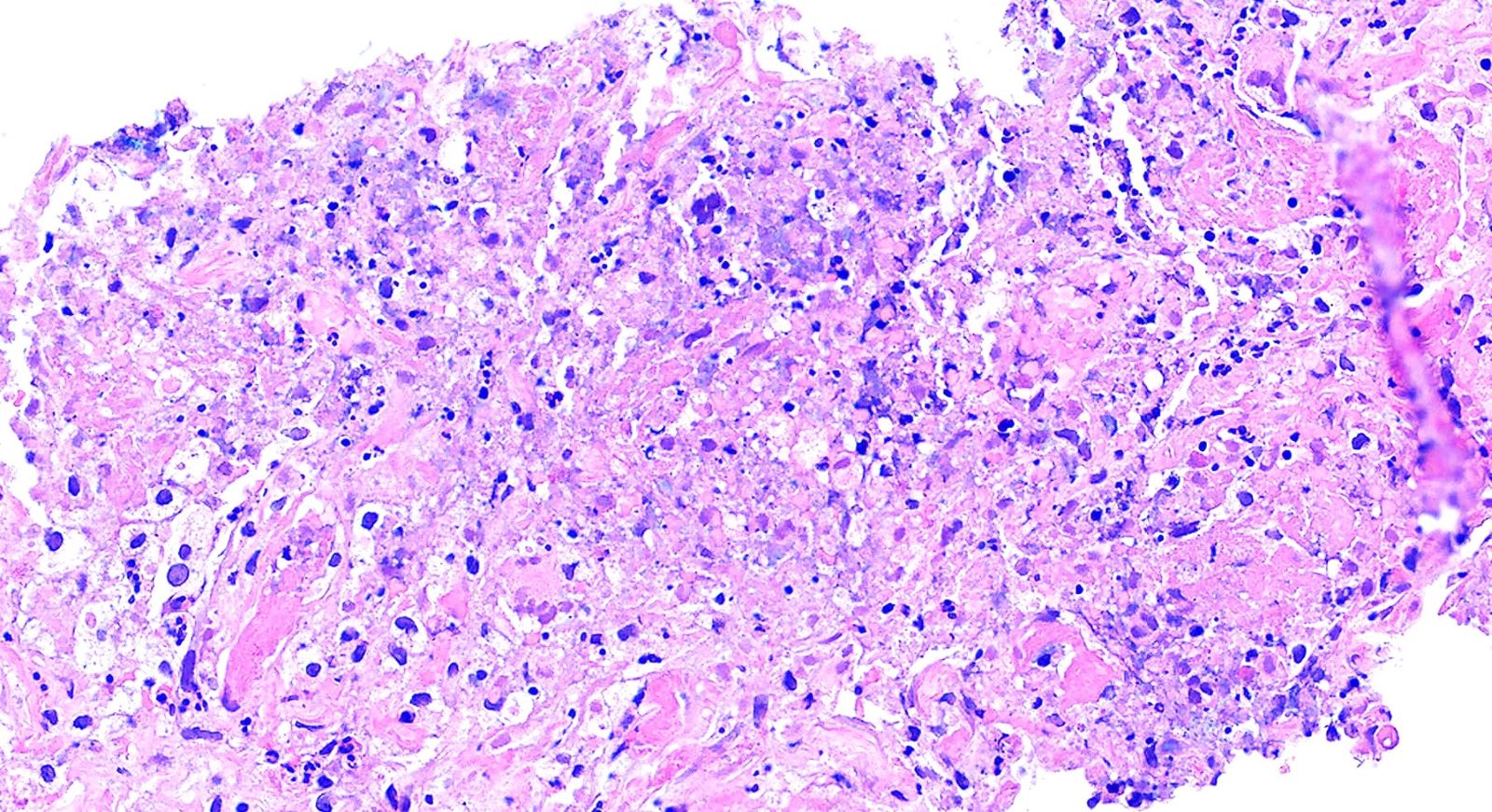
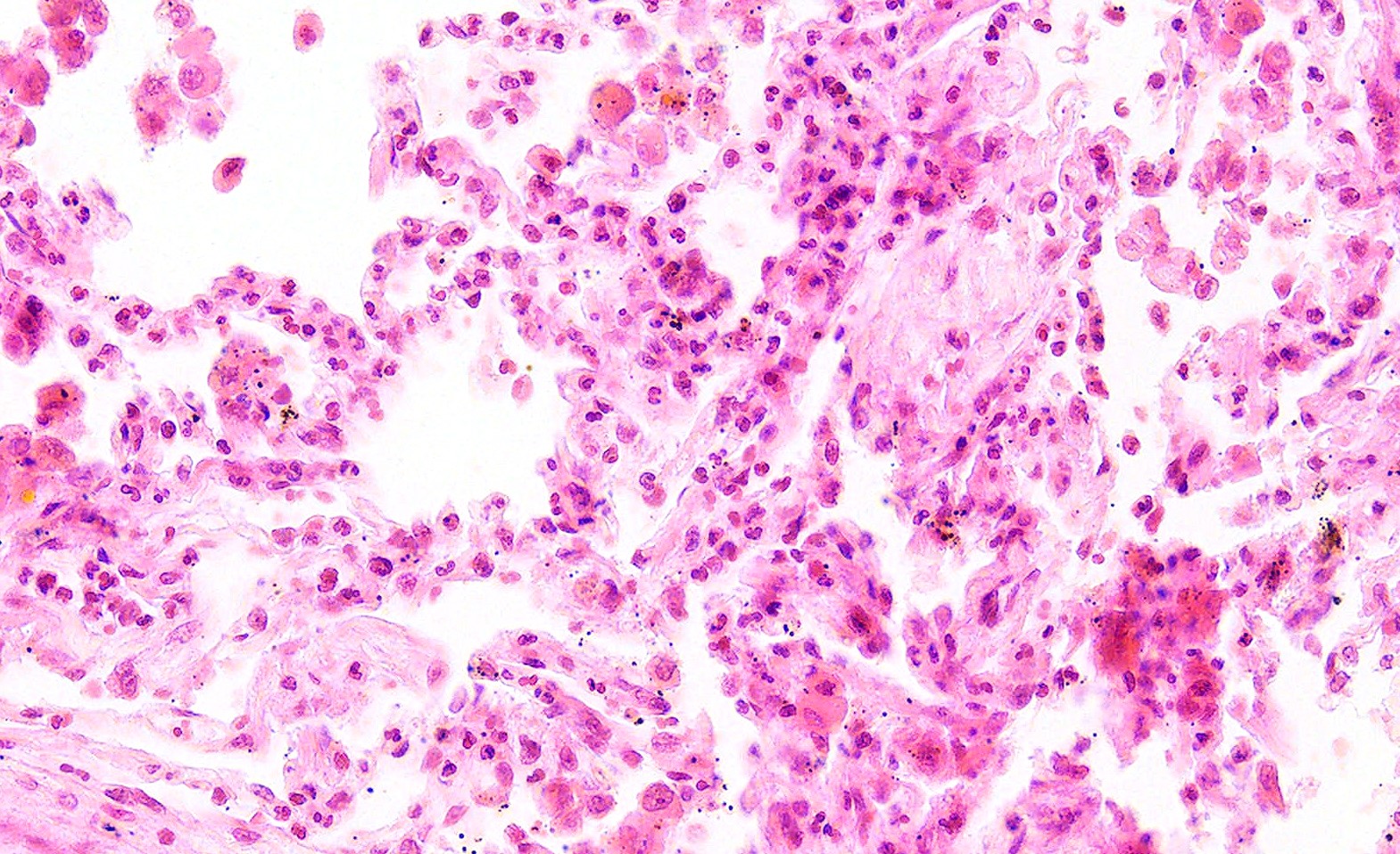
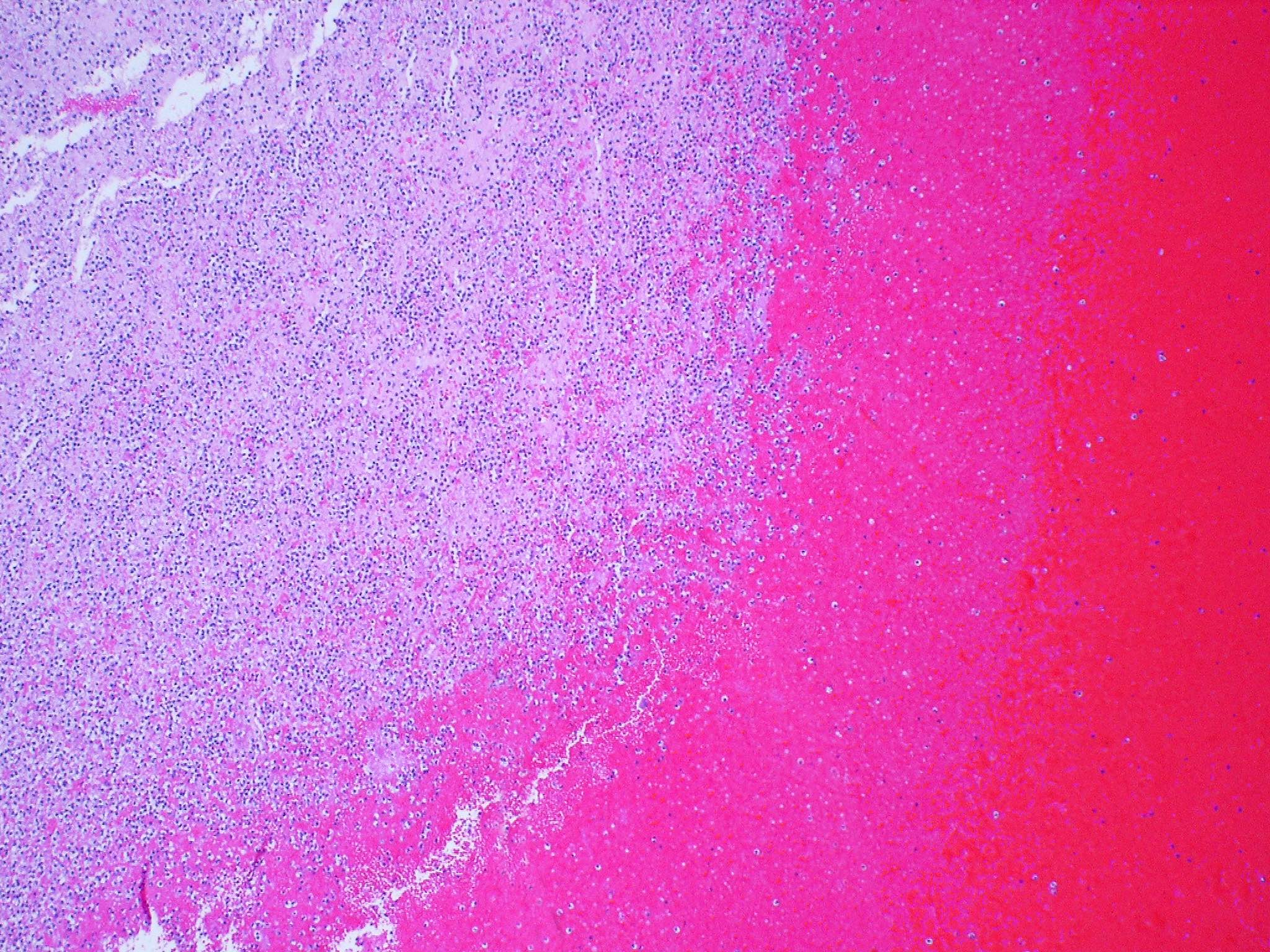
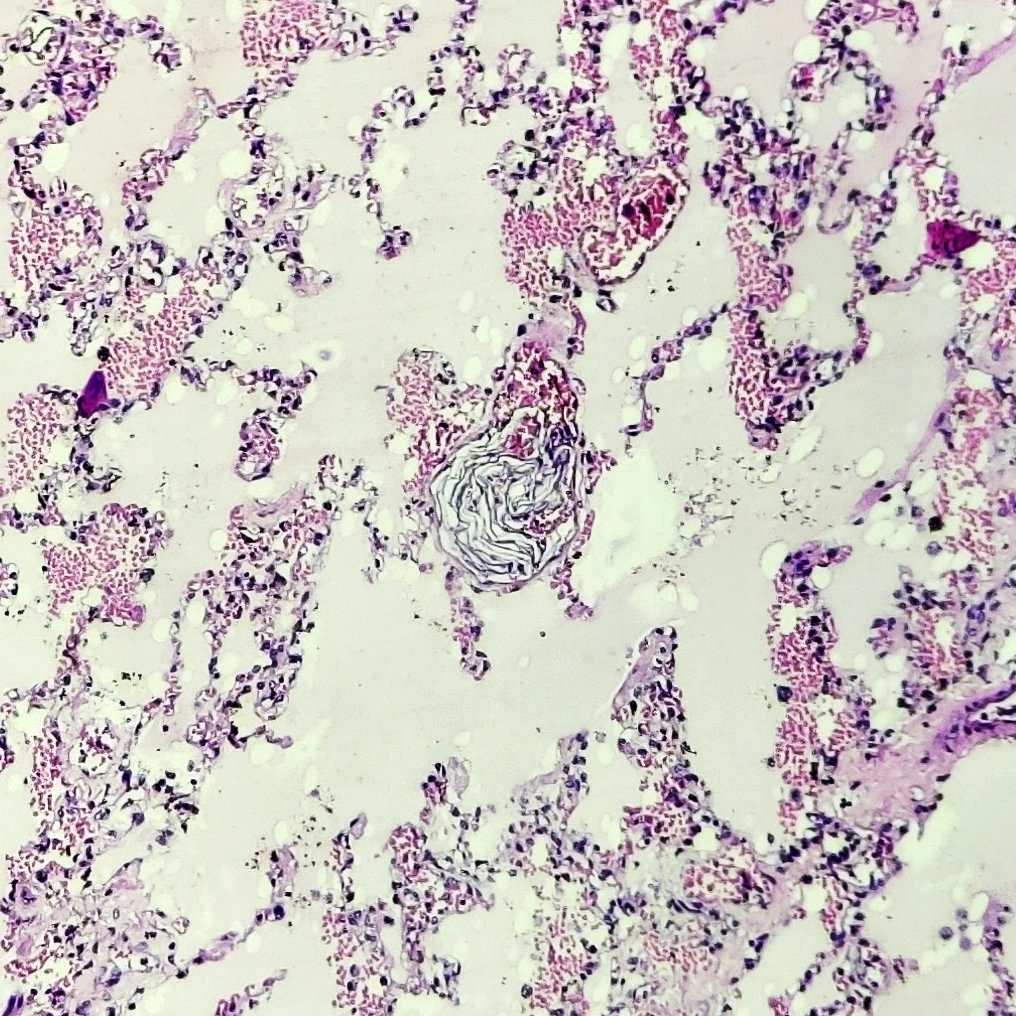
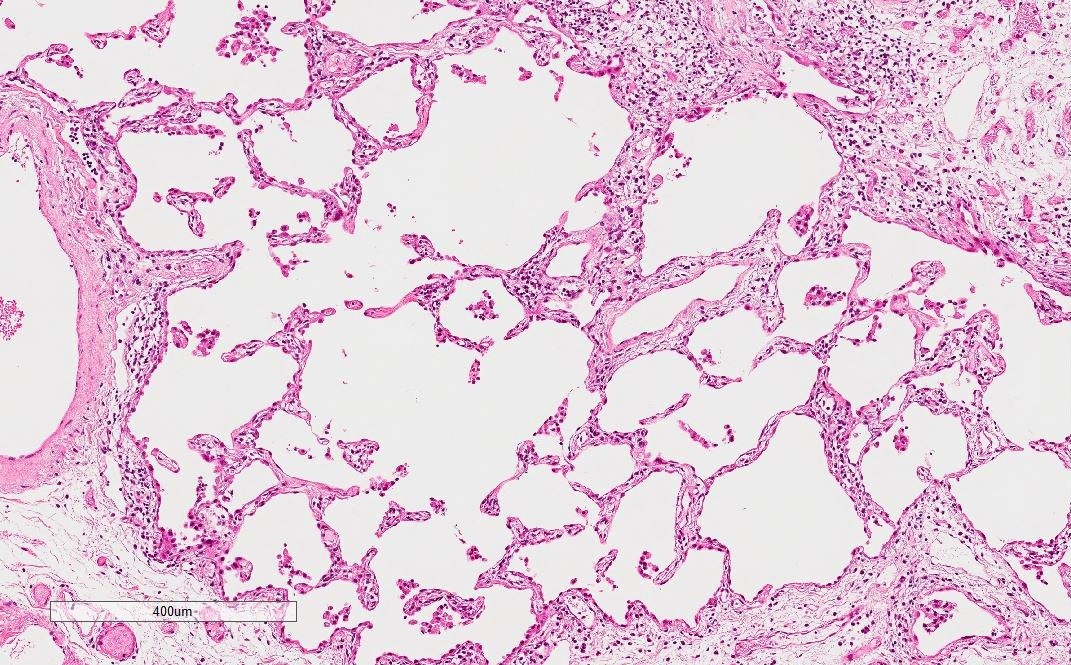
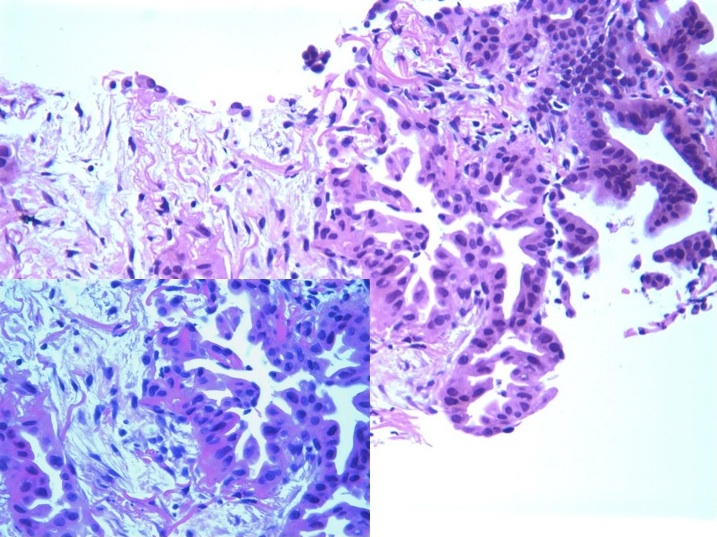
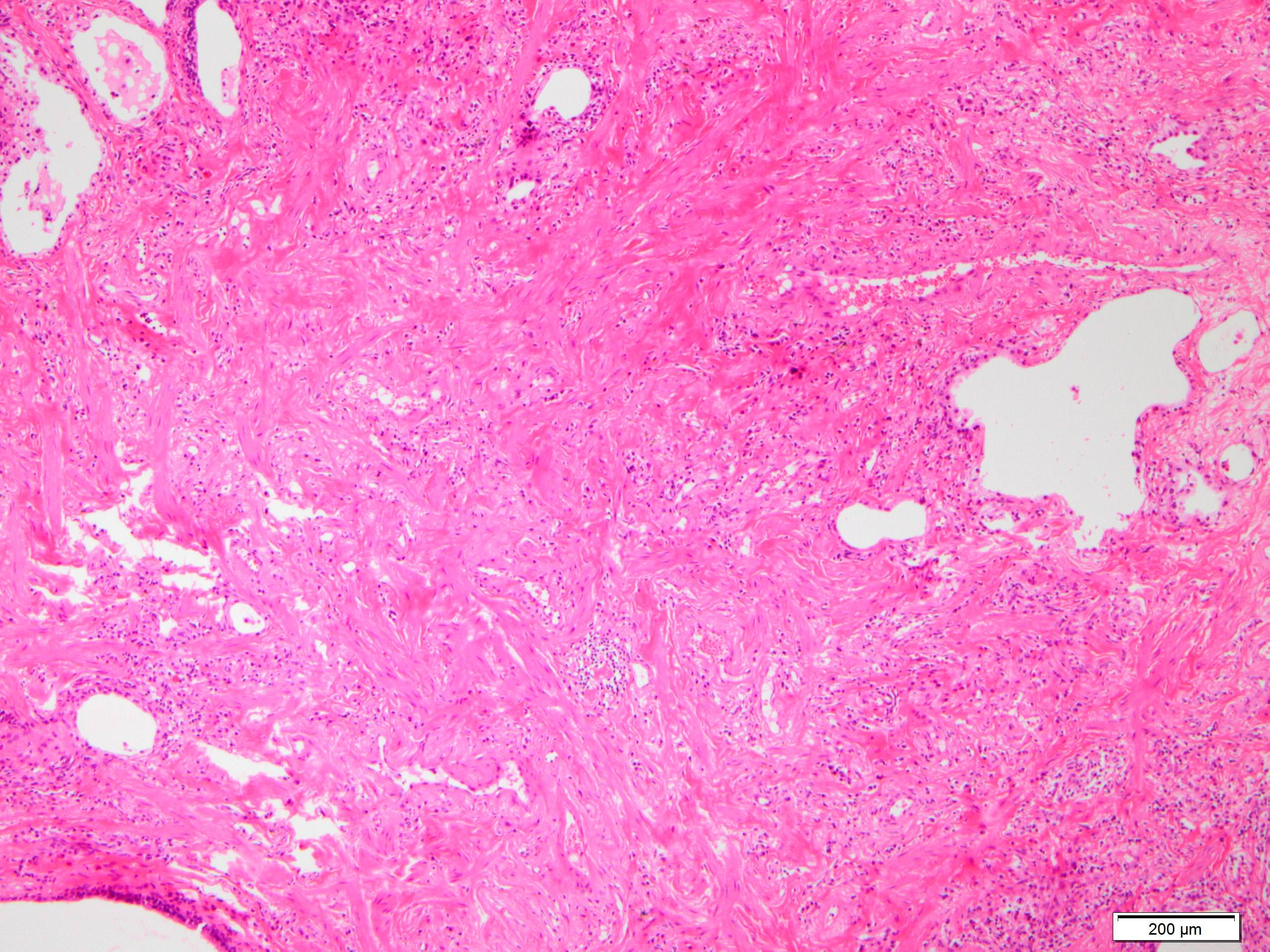
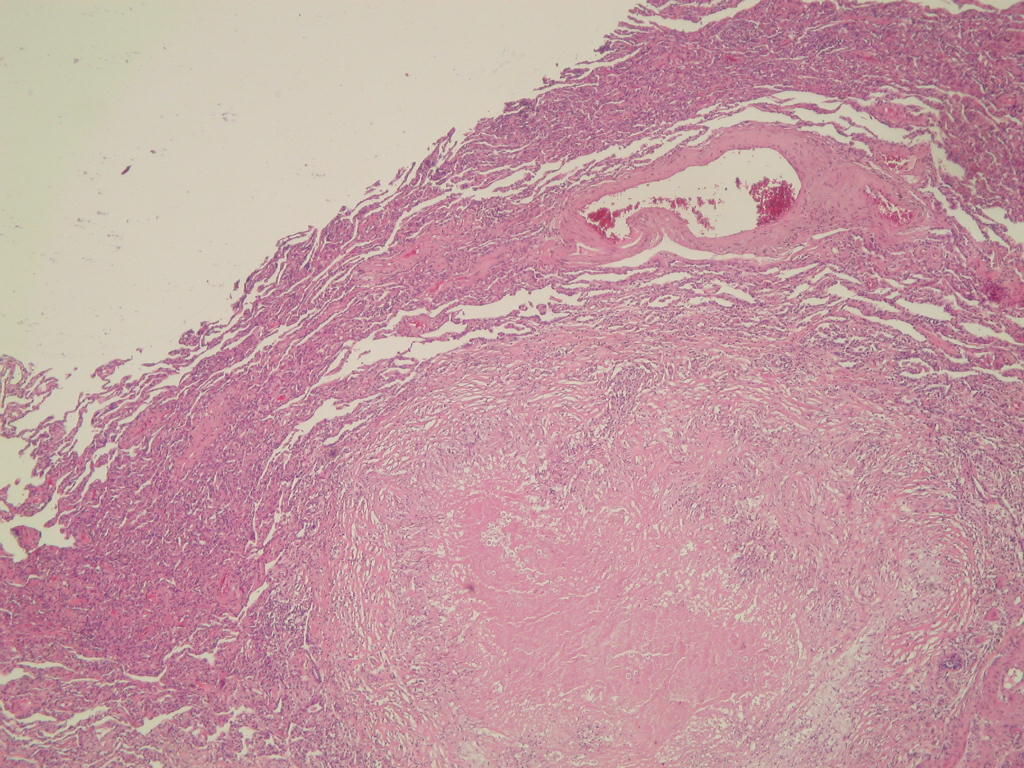
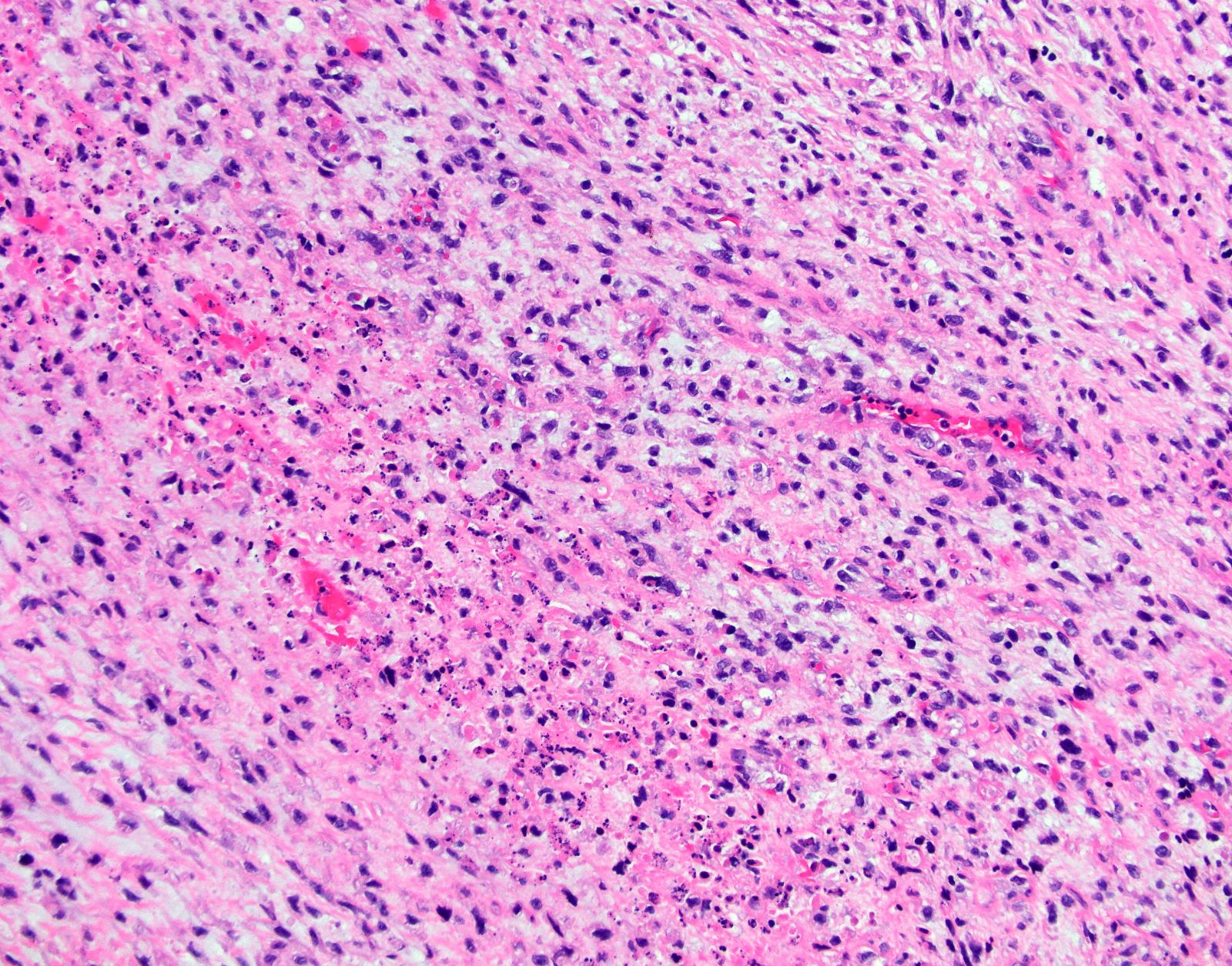
- Proliferative / organizing (subacute) phase of diffuse alveolar damage is most common in acute interstitial pneumonia but also exudative (acute) phase and fibrotic (chronic) phase can be seen
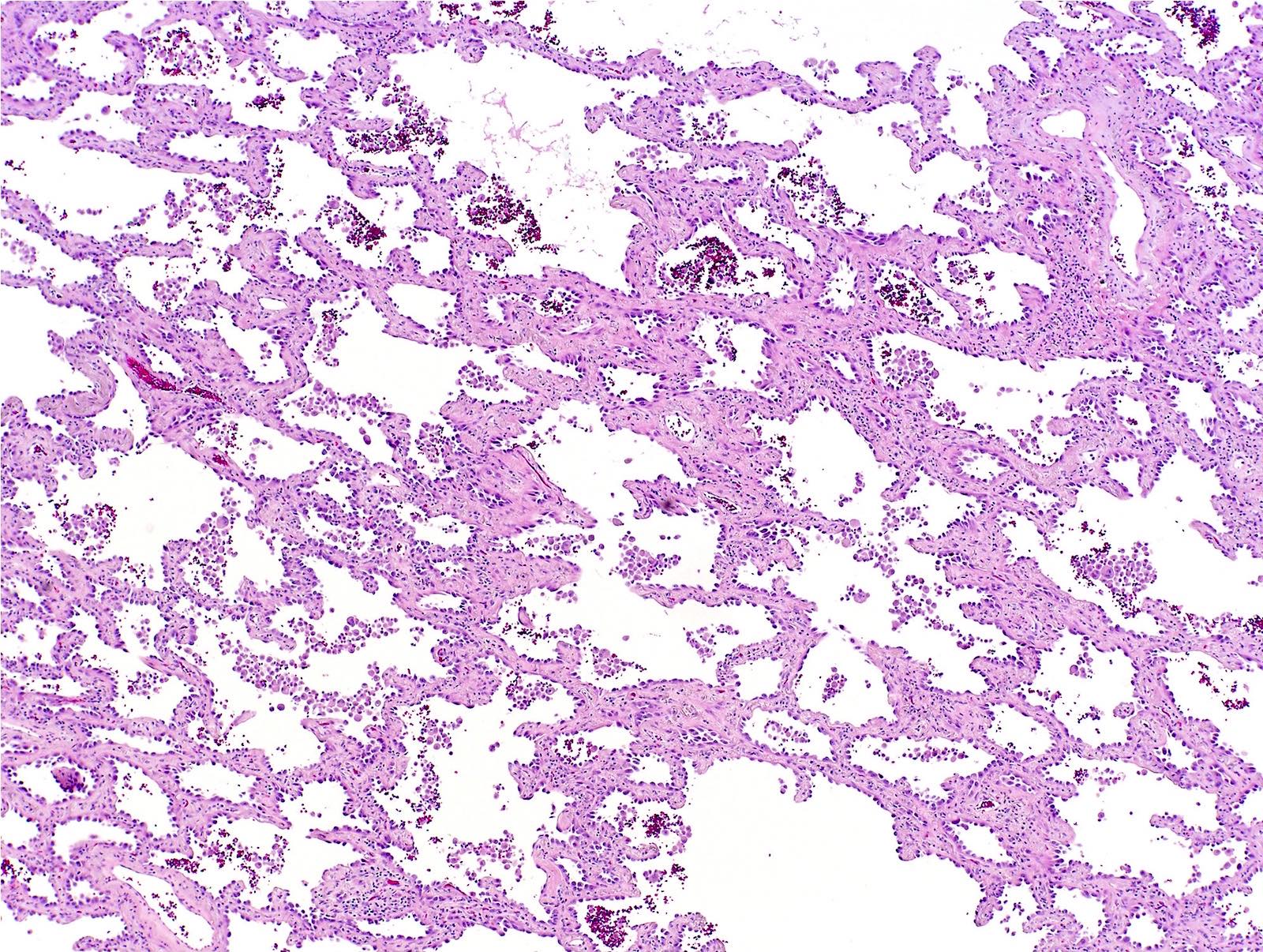
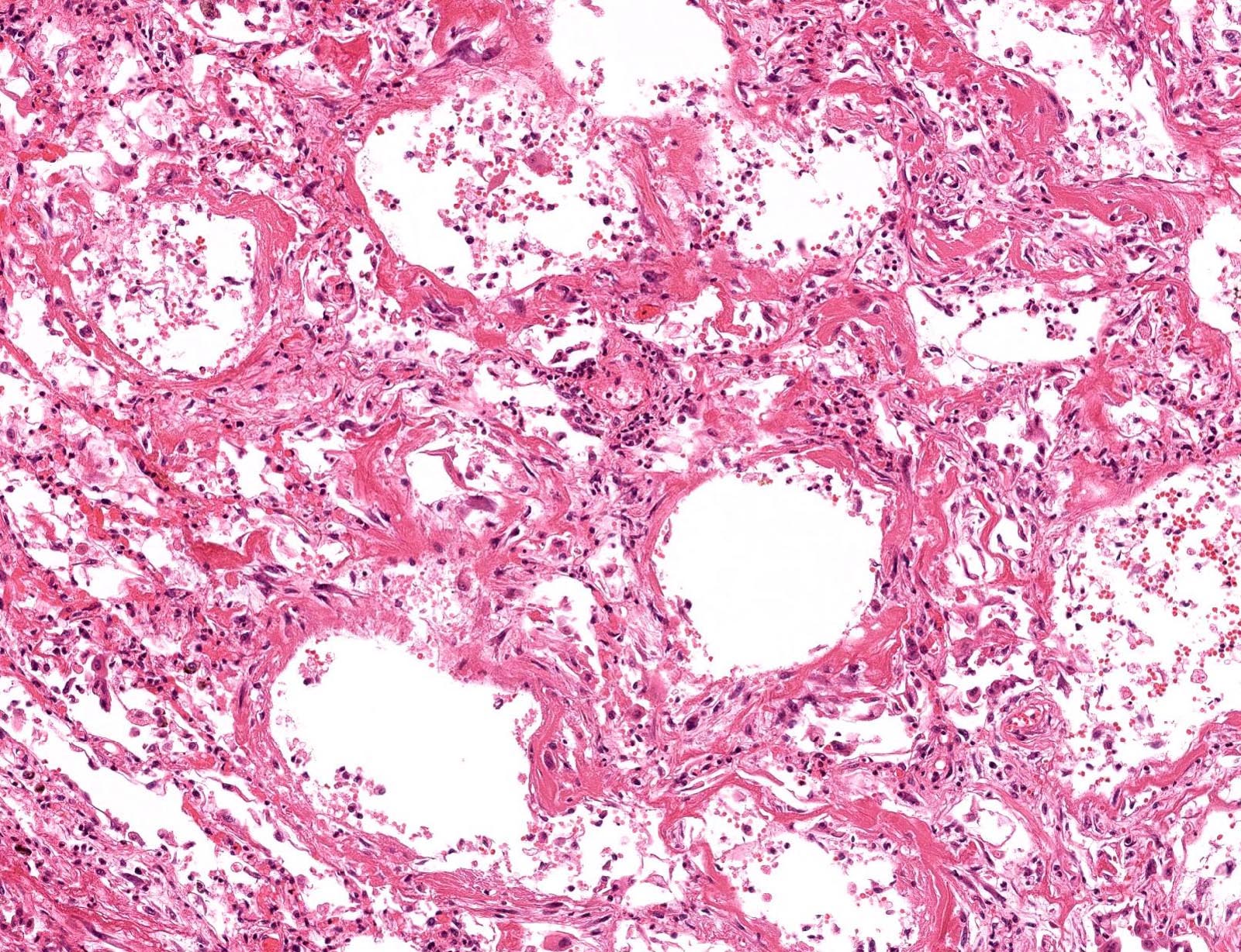
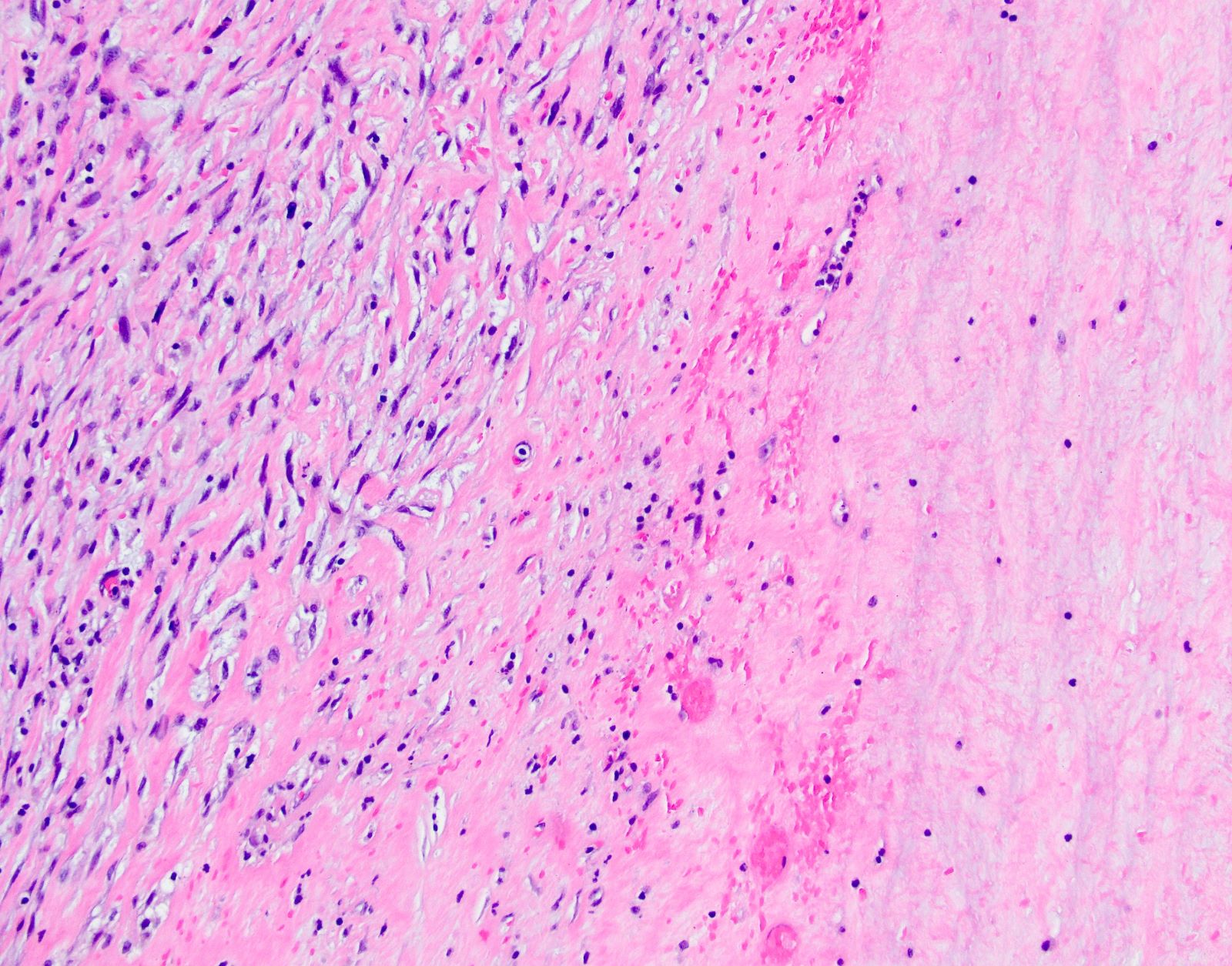
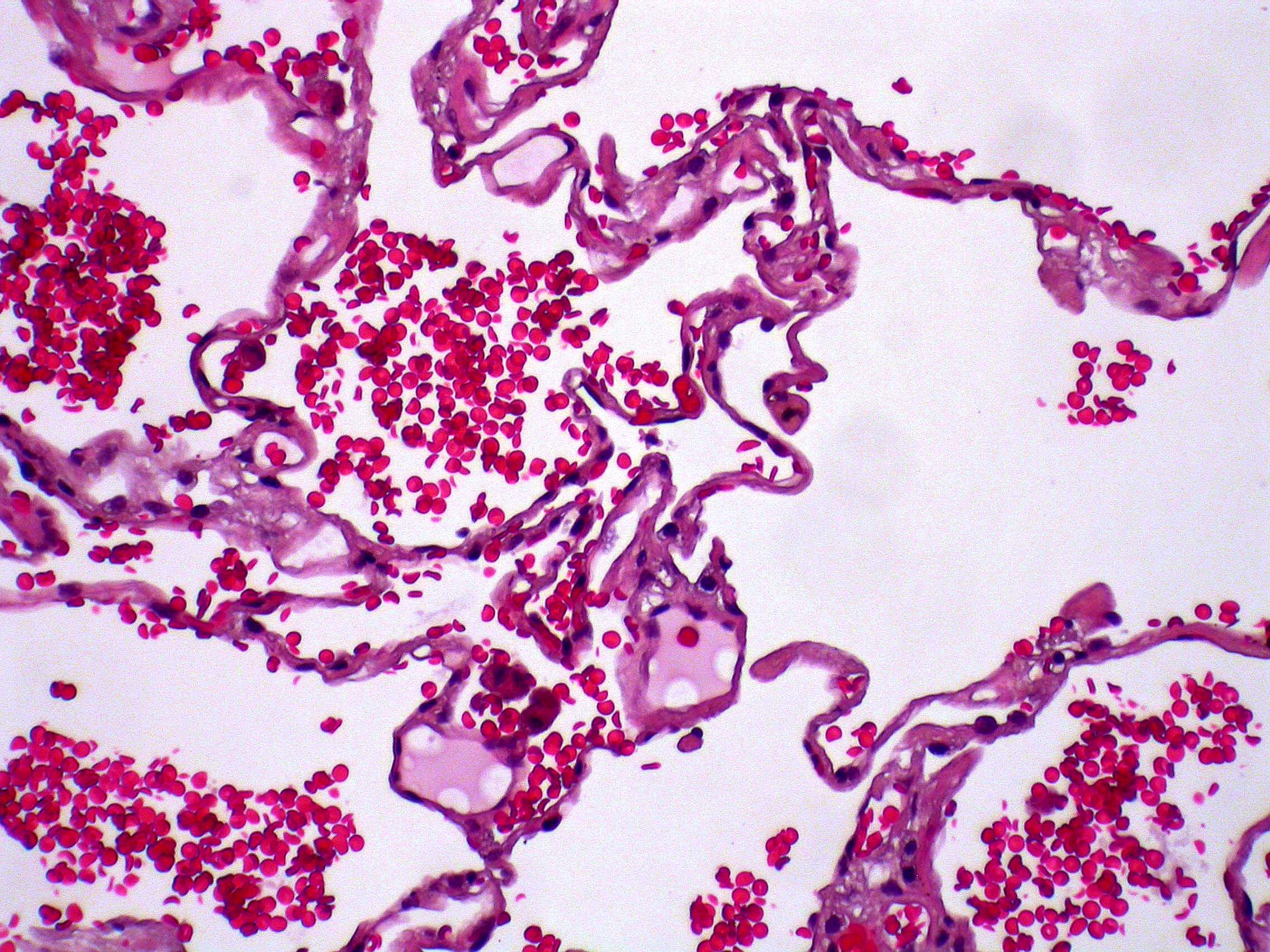
- Exudative phase
- Hyaline membranes in alveolar duct or sacs; scattered or not apparent, unlike in acute respiratory distress syndrome
- Interstitial and intra-alveolar edema
- Collapsed alveoli
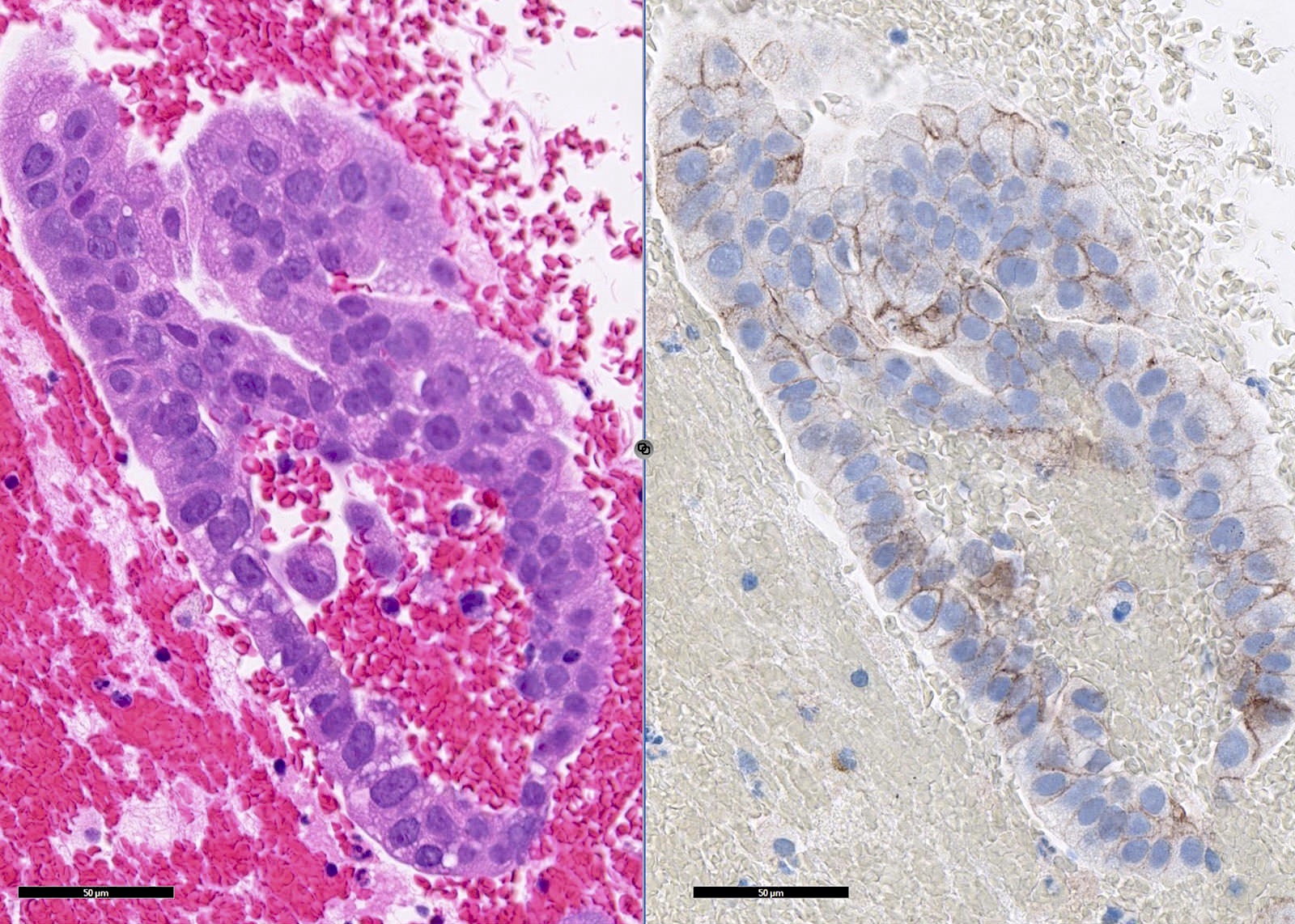
- Denudation and necrosis of type I pneumocytes
- Hemorrhage, usually mild
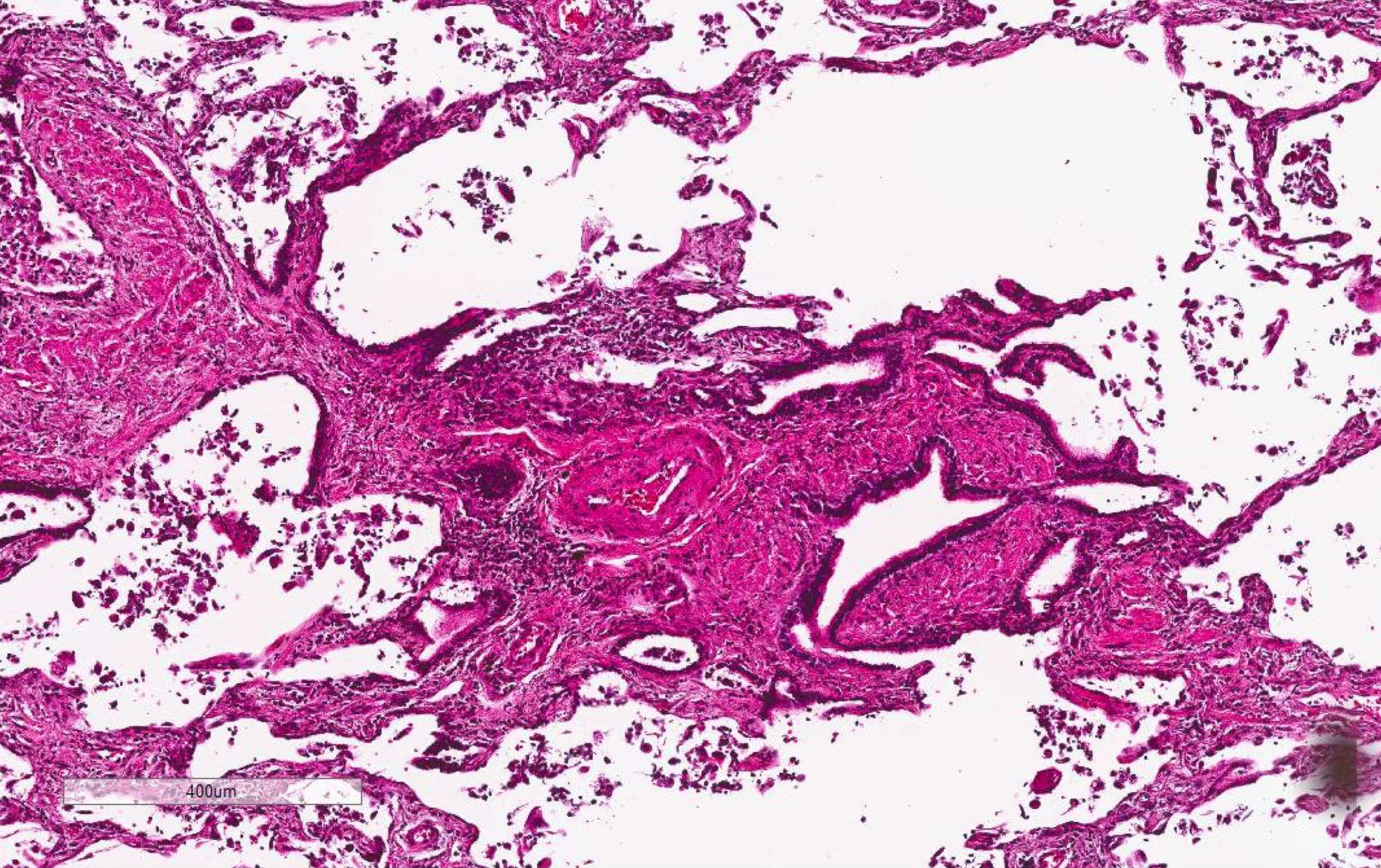
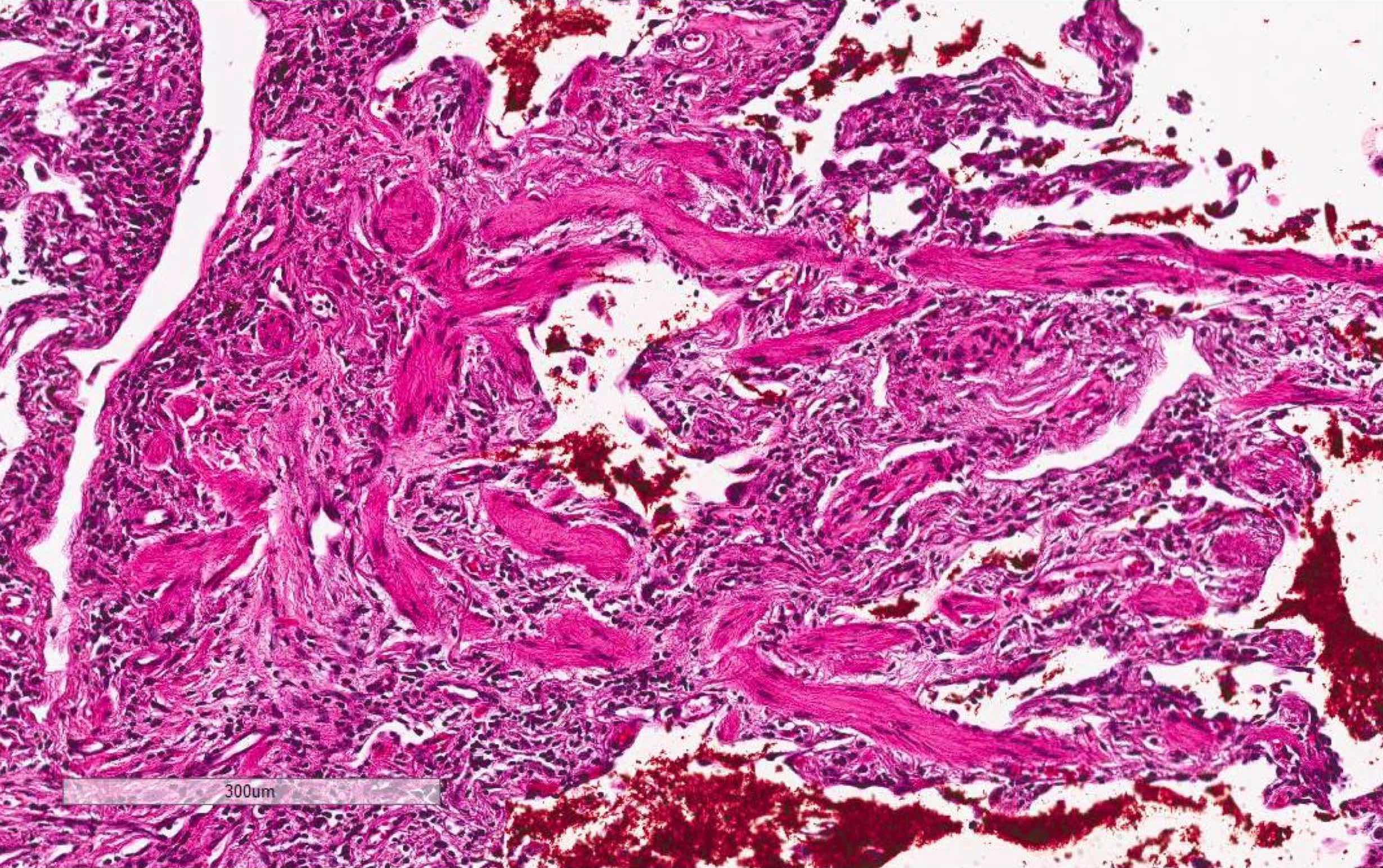
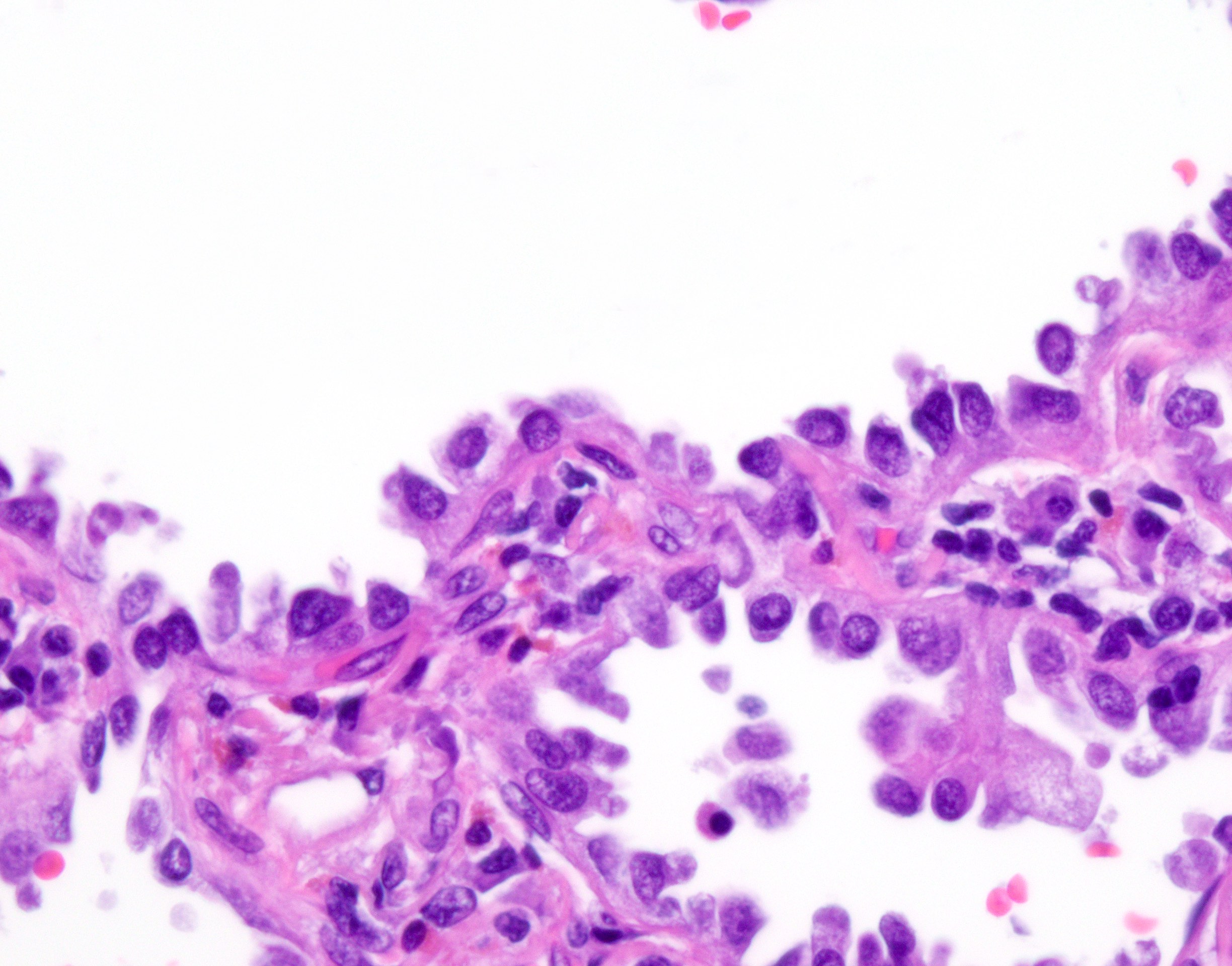
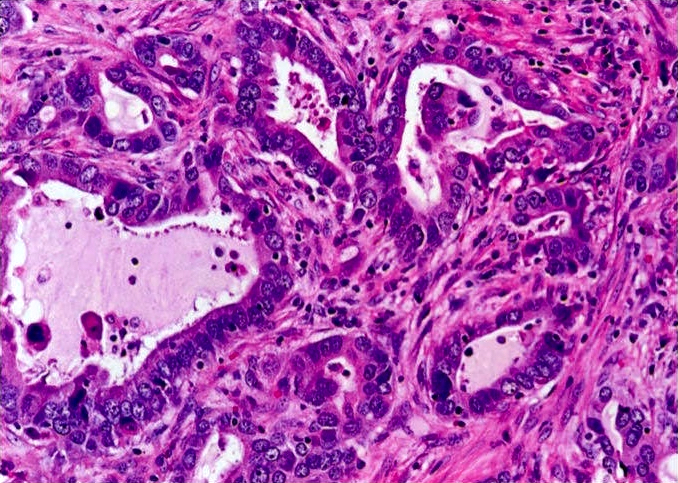
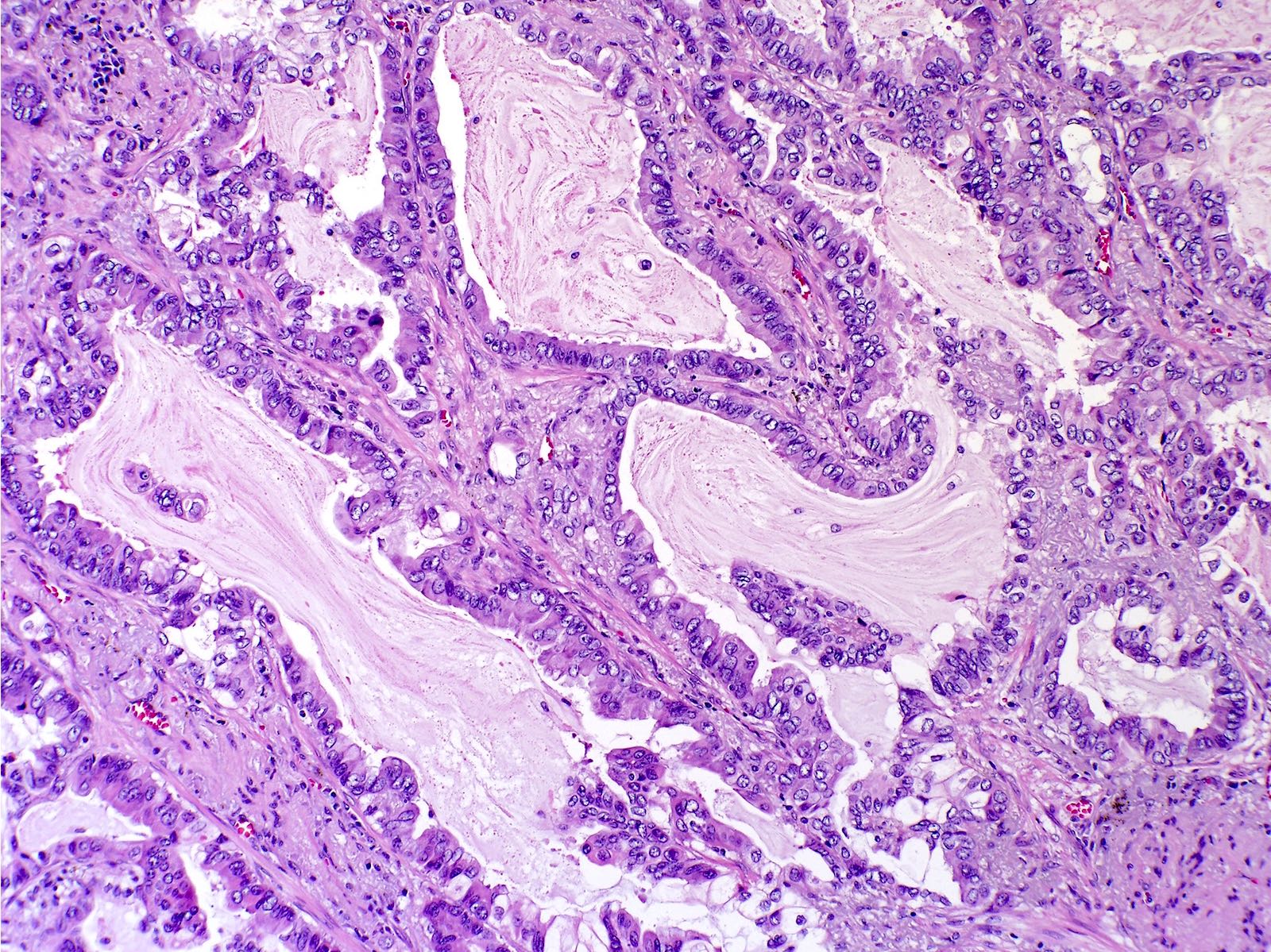
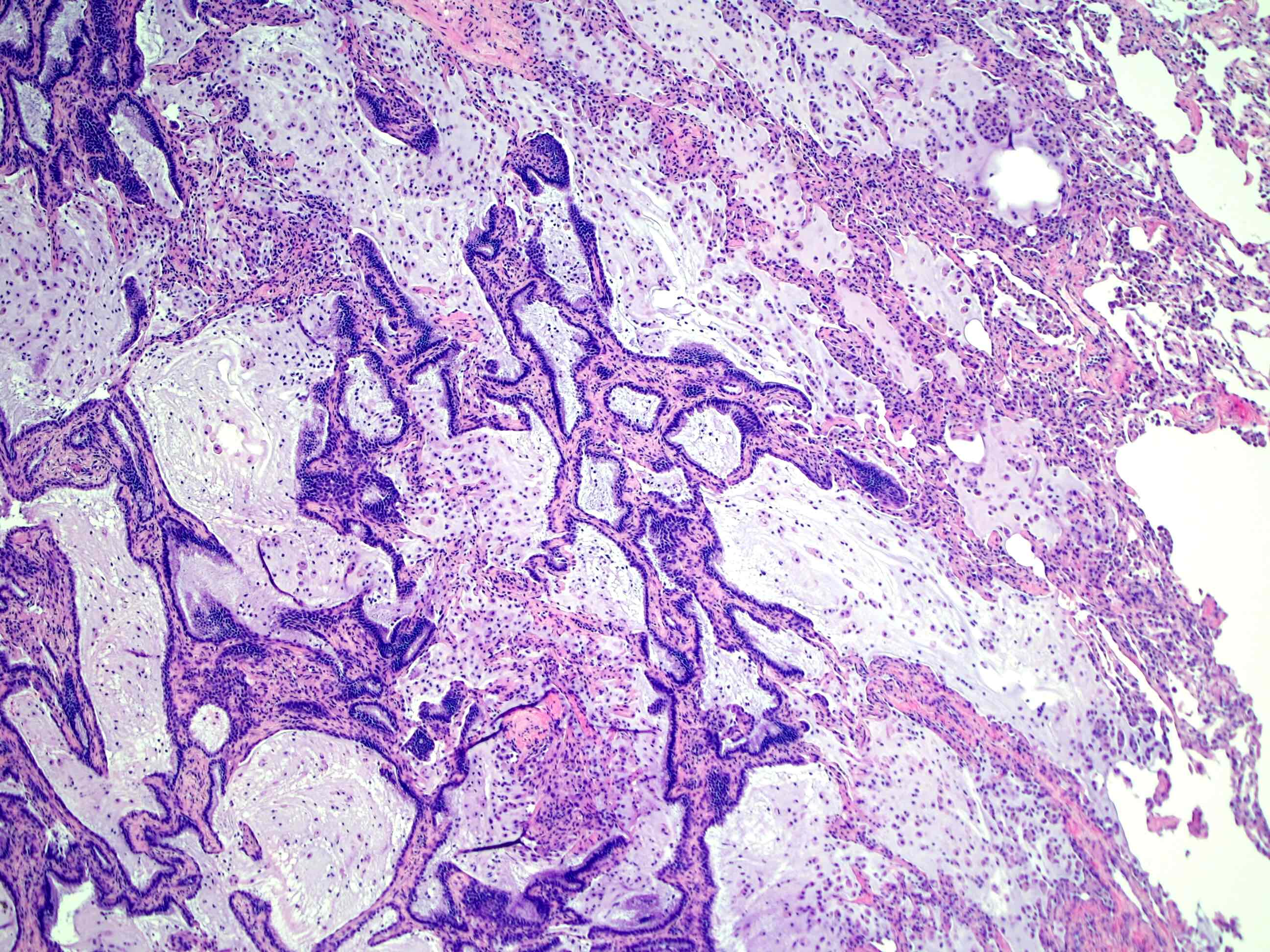
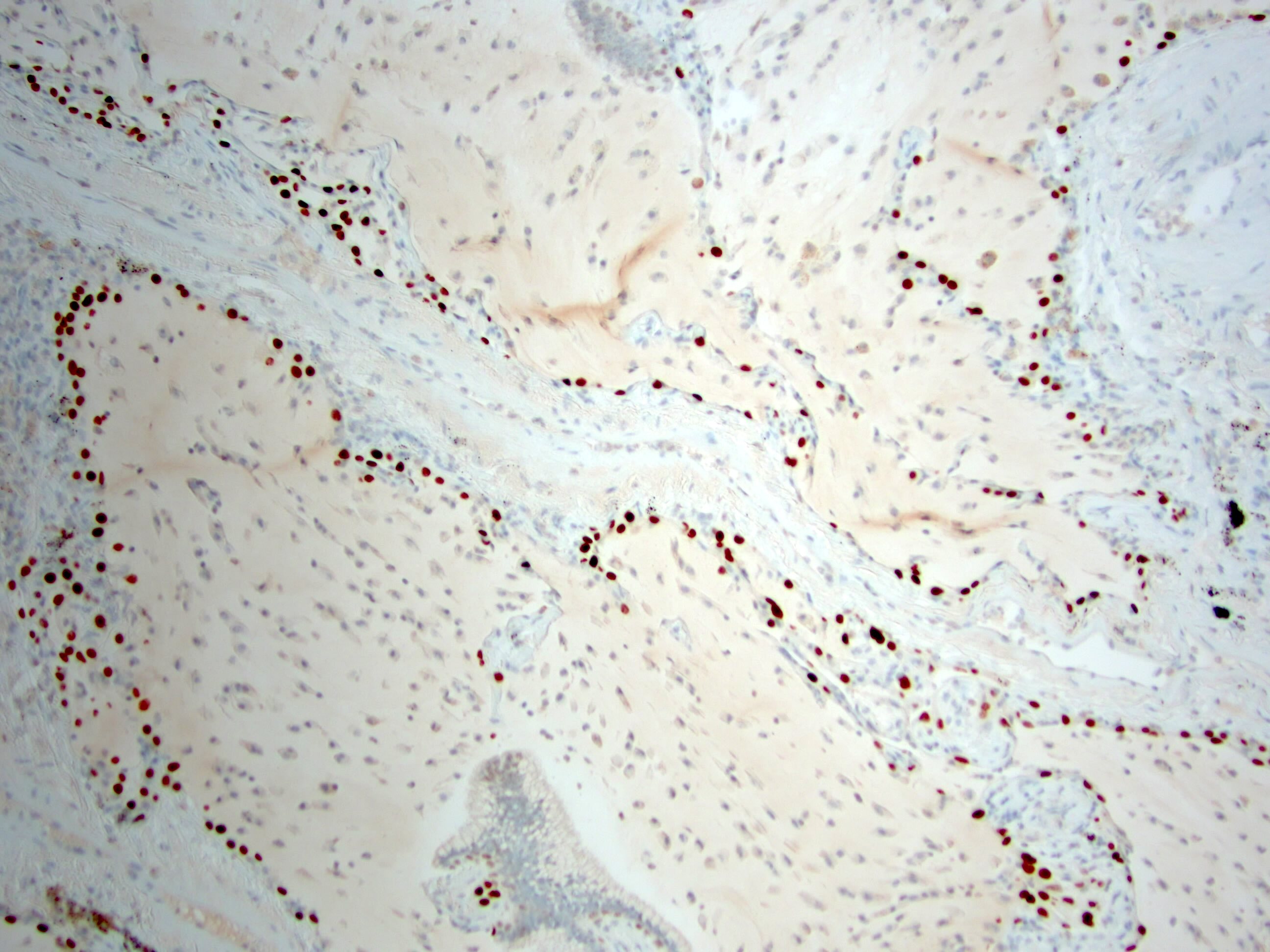
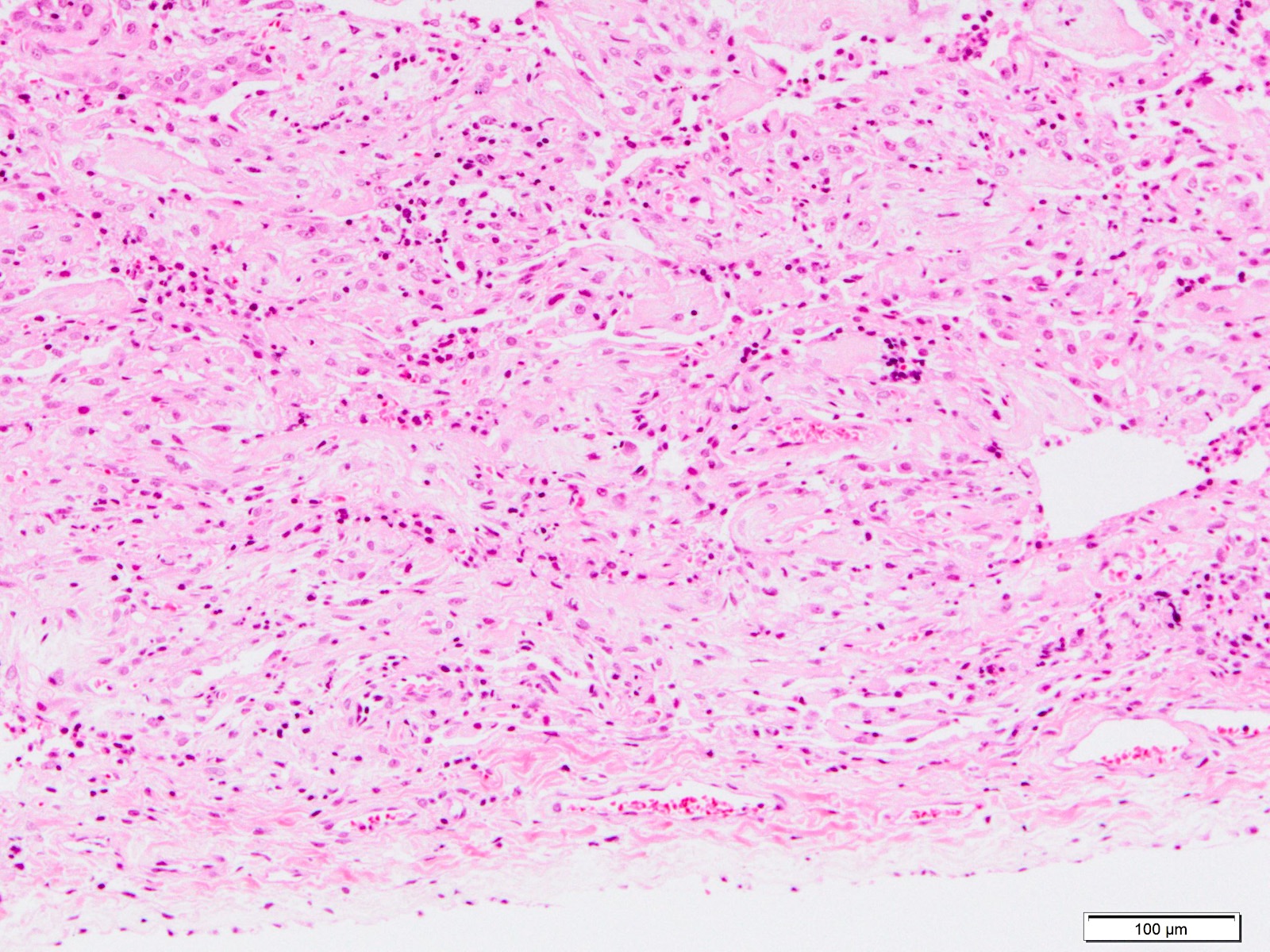
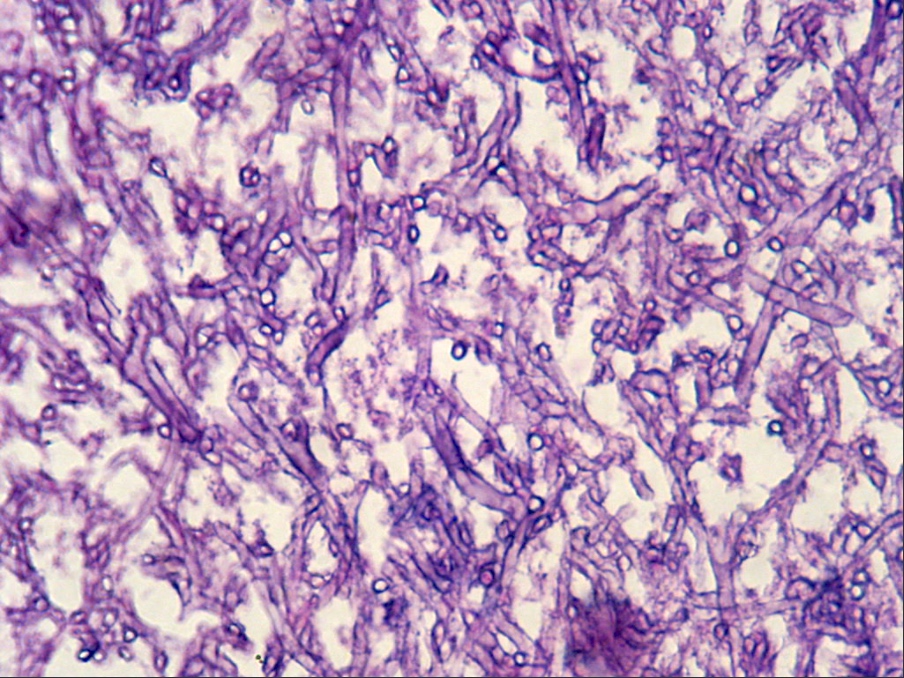
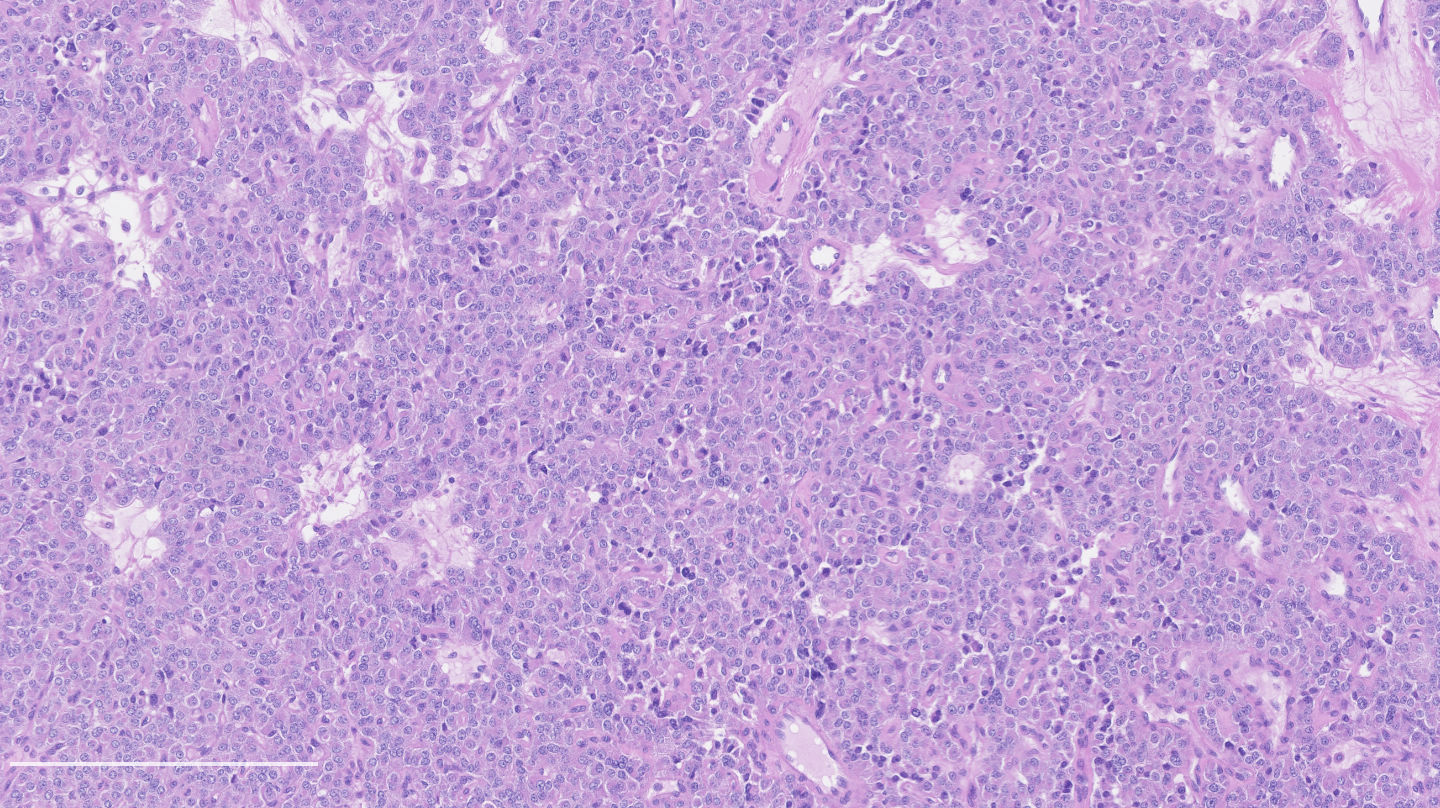
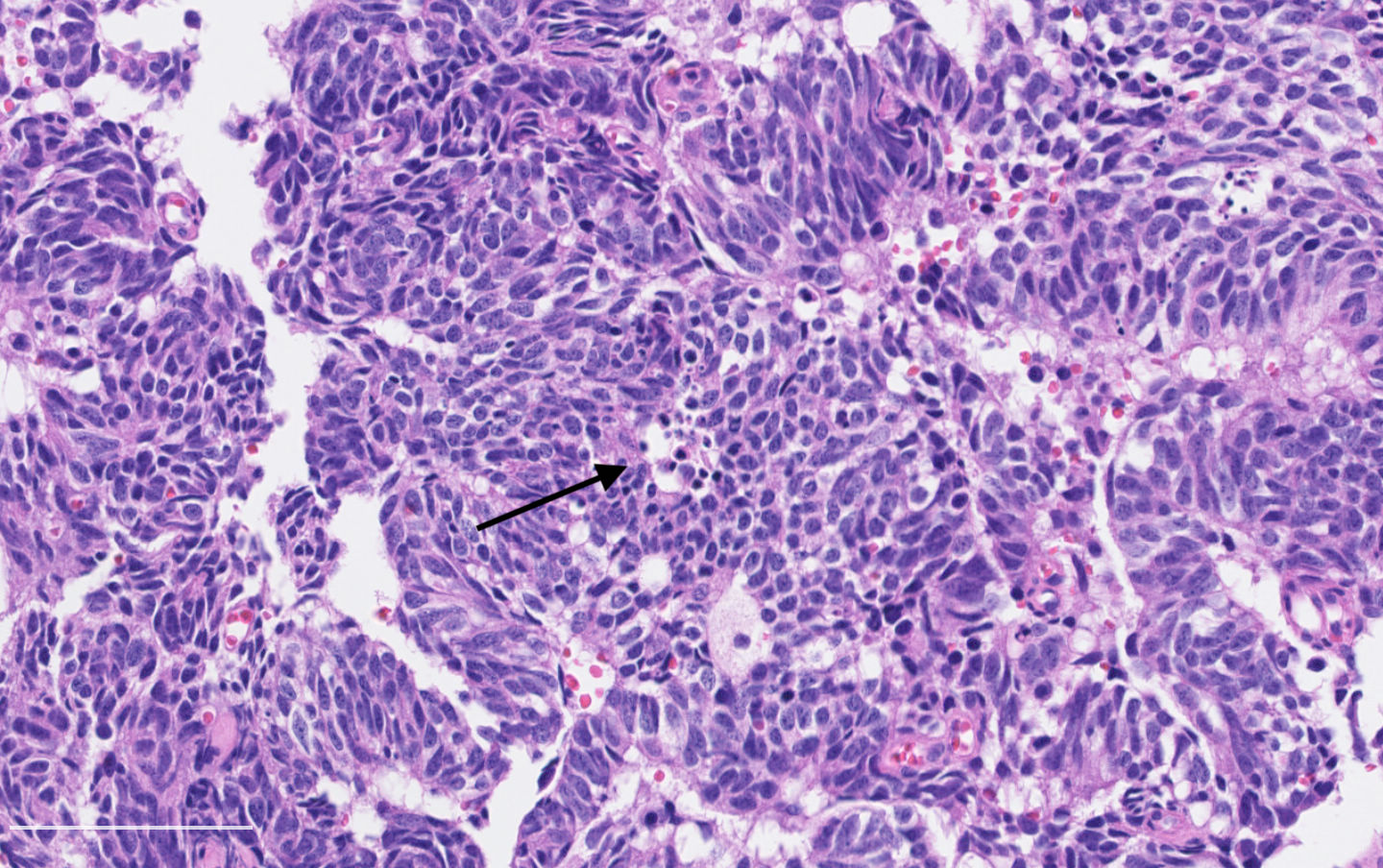
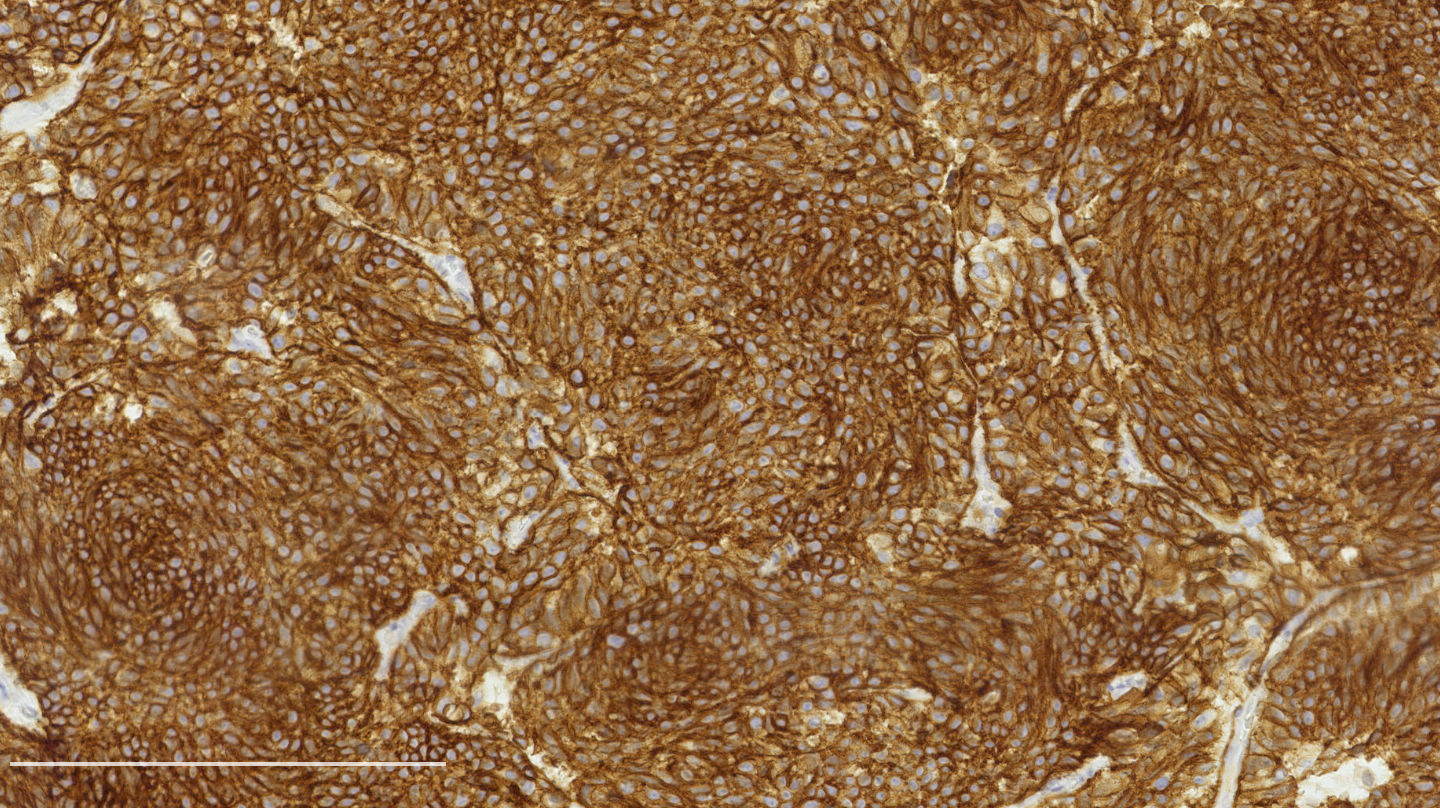
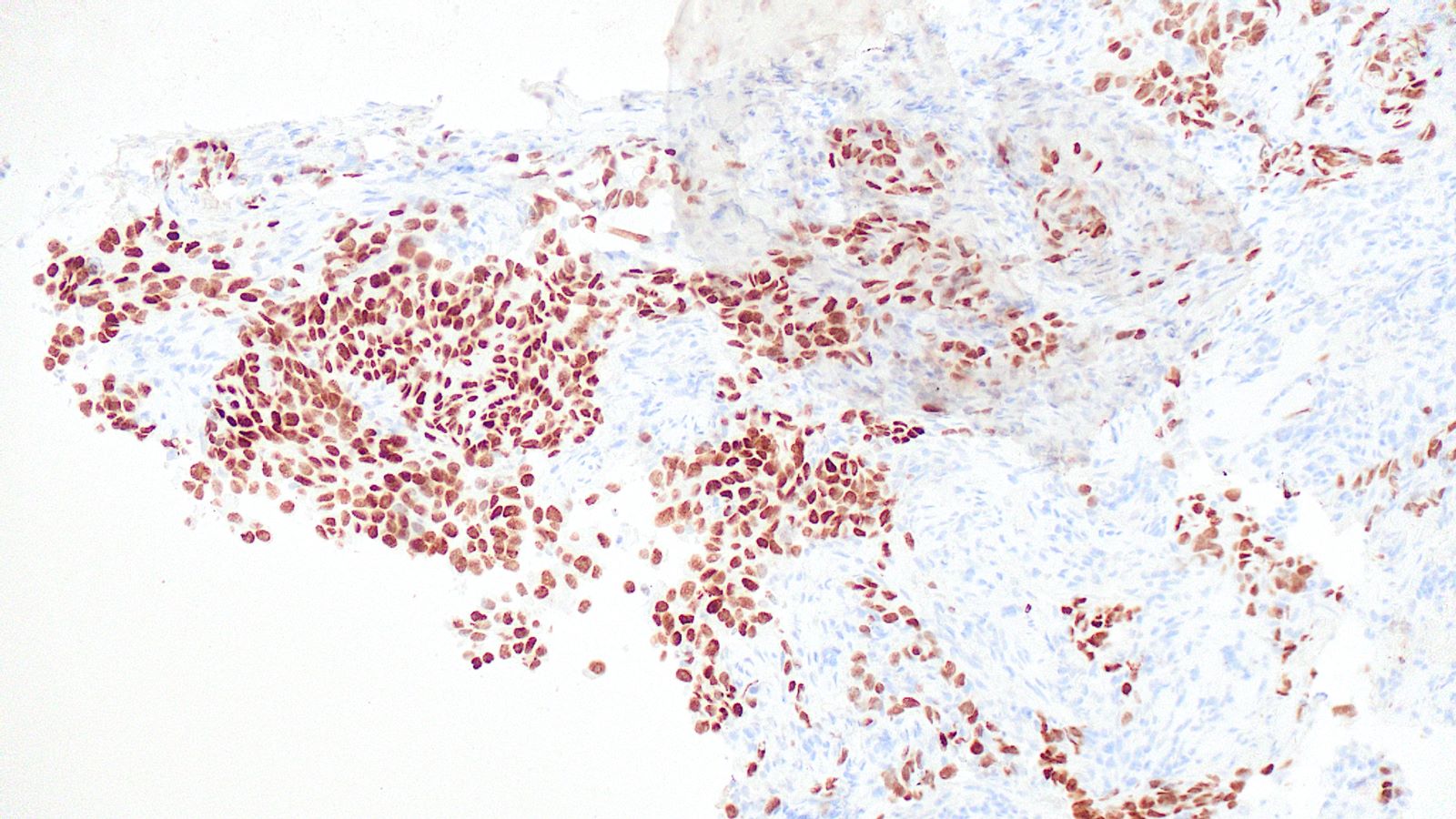
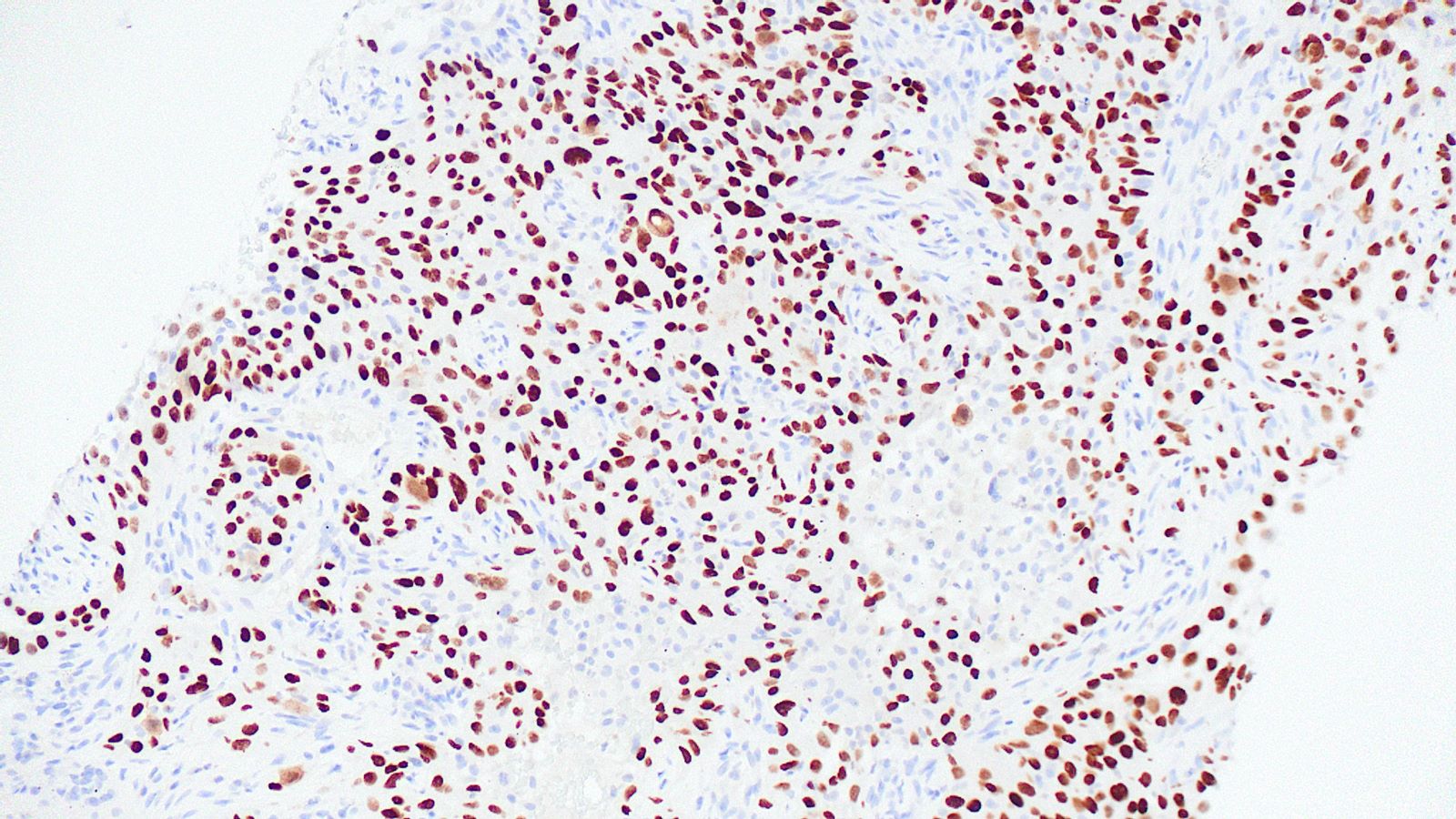
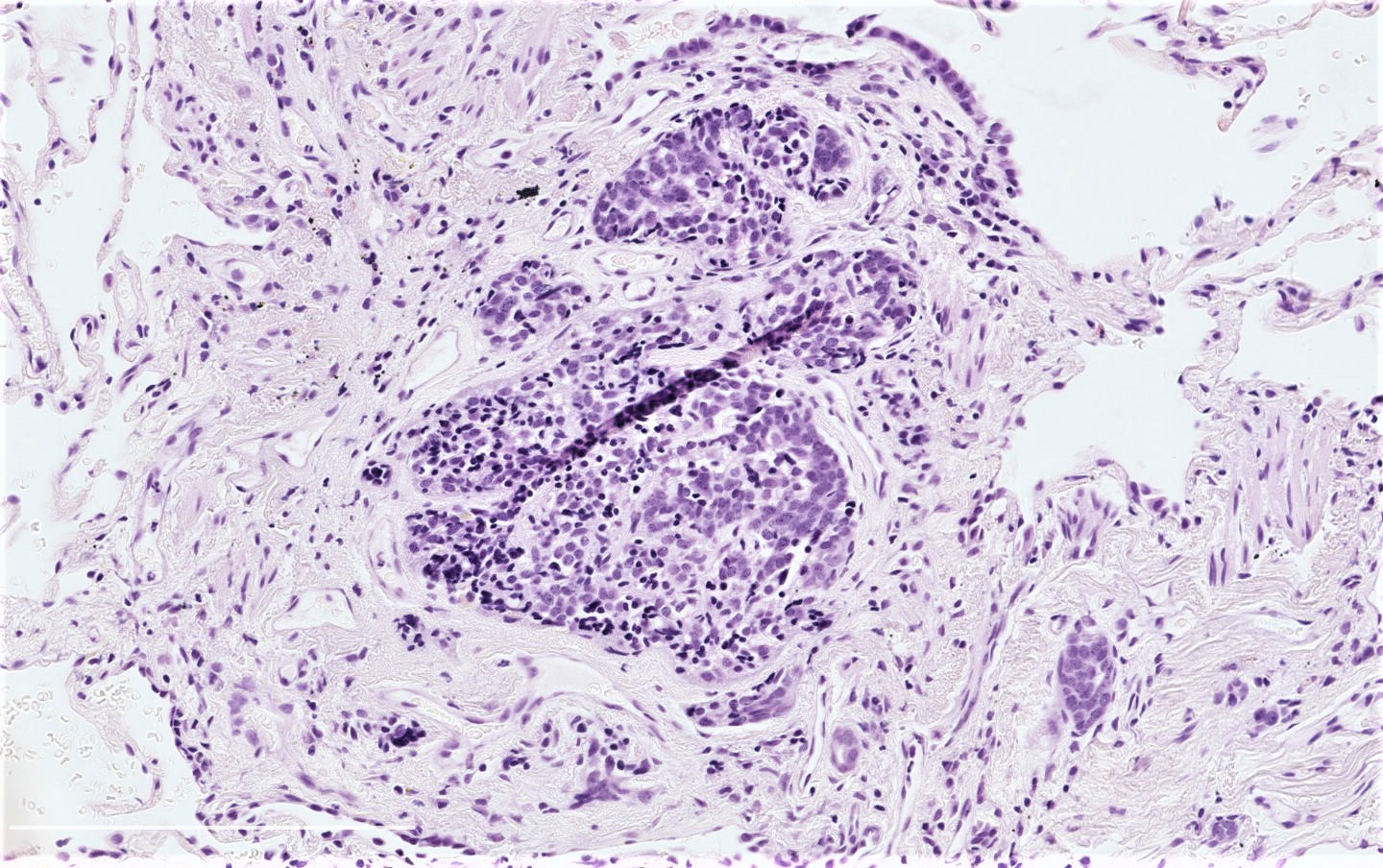
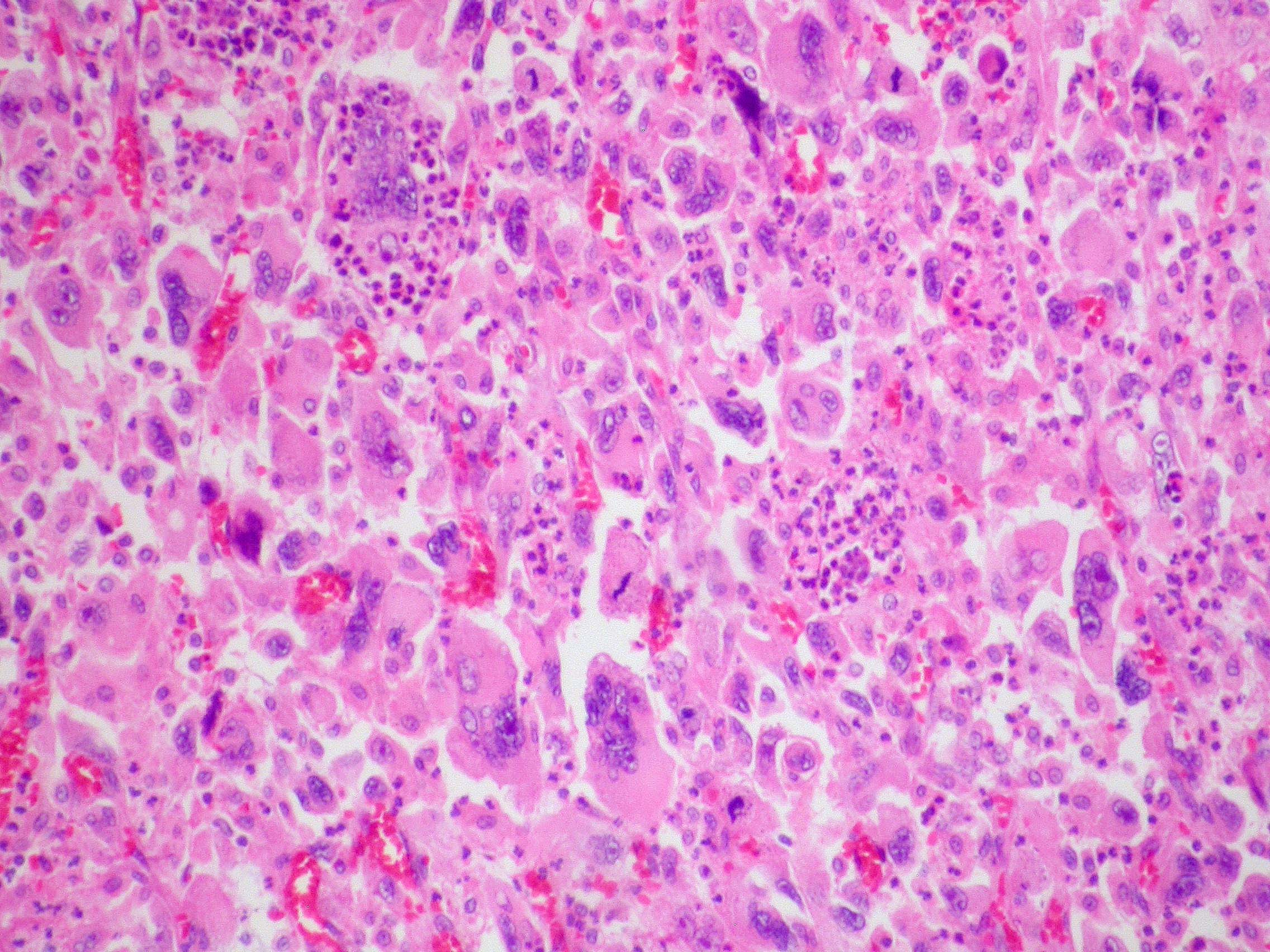
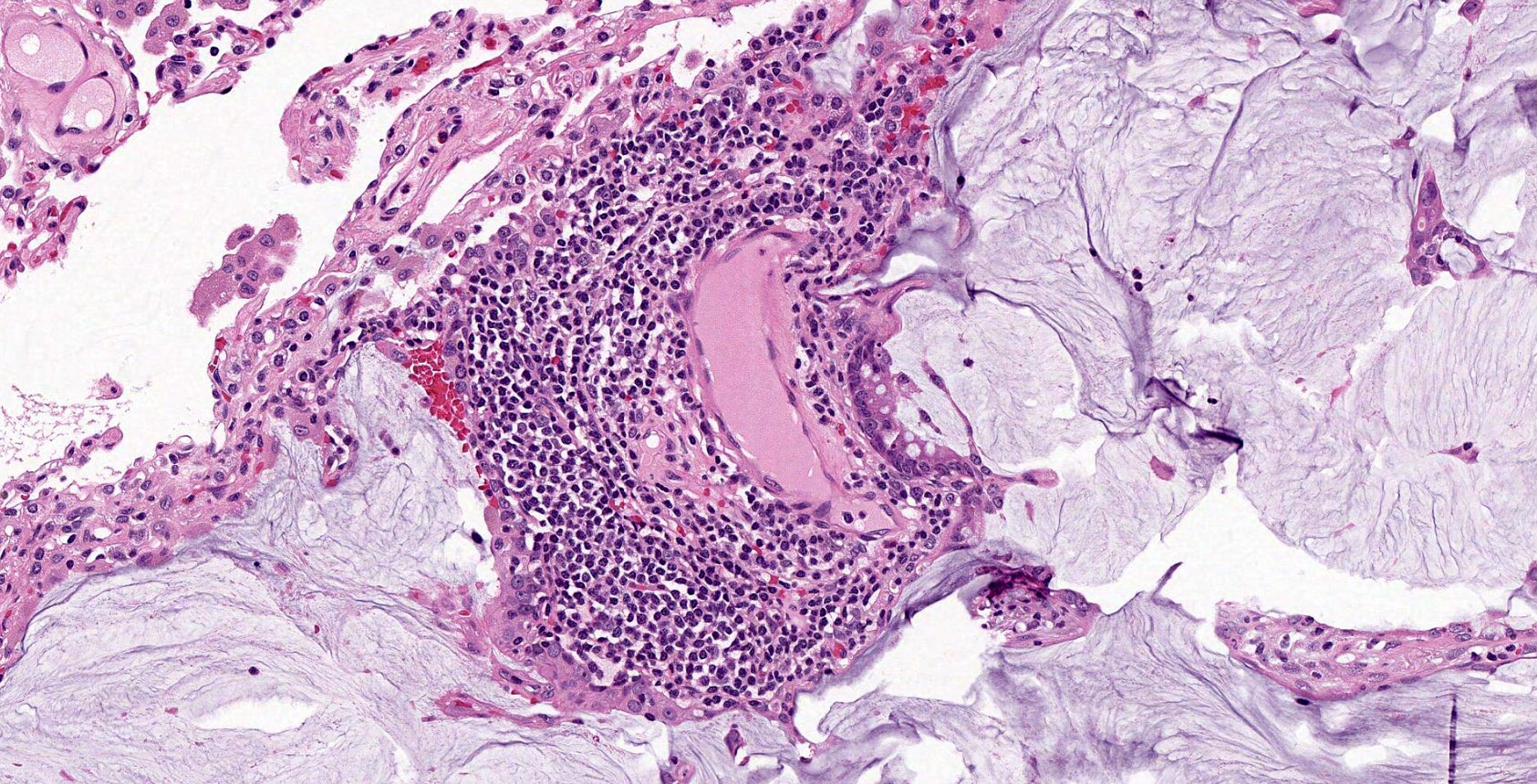
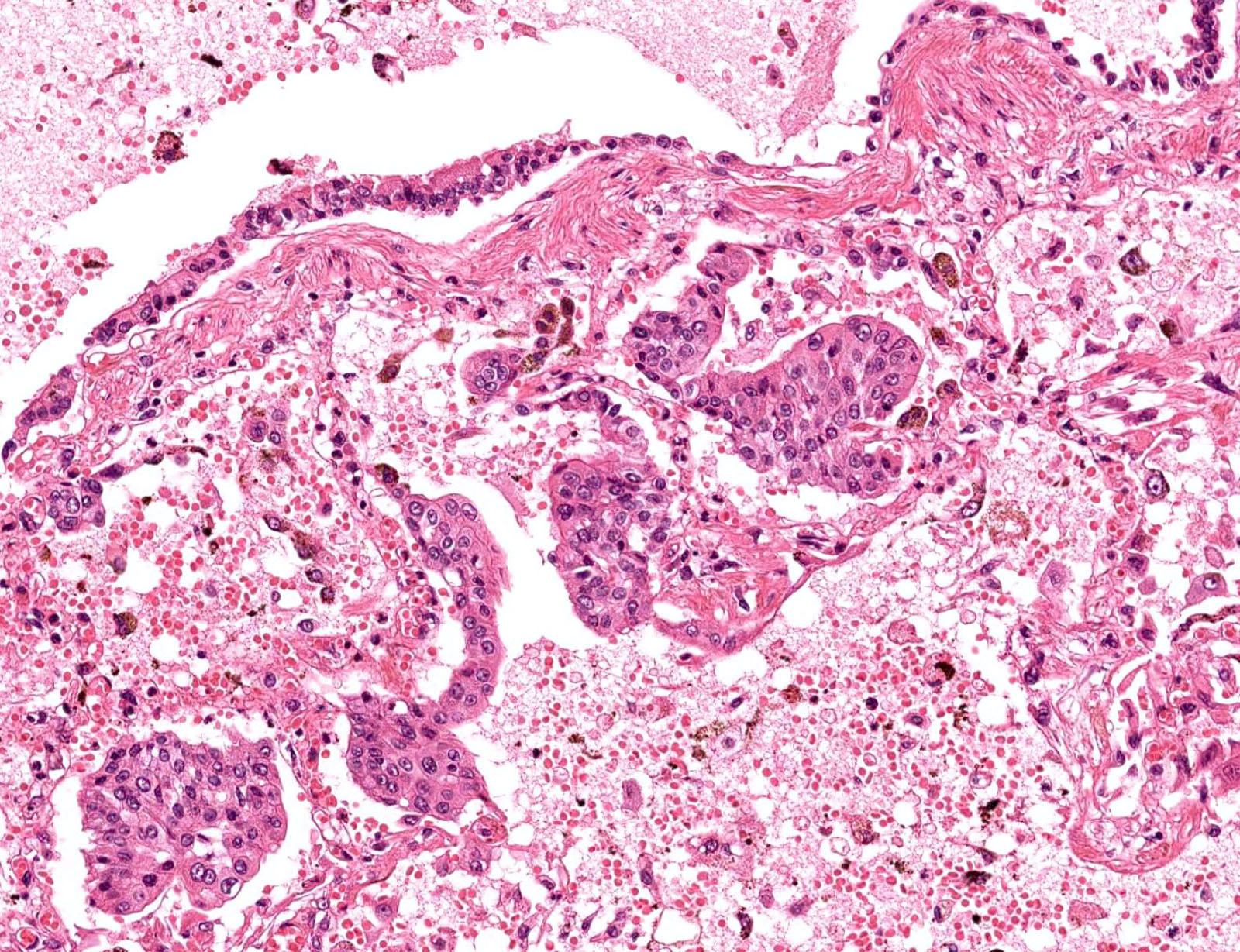
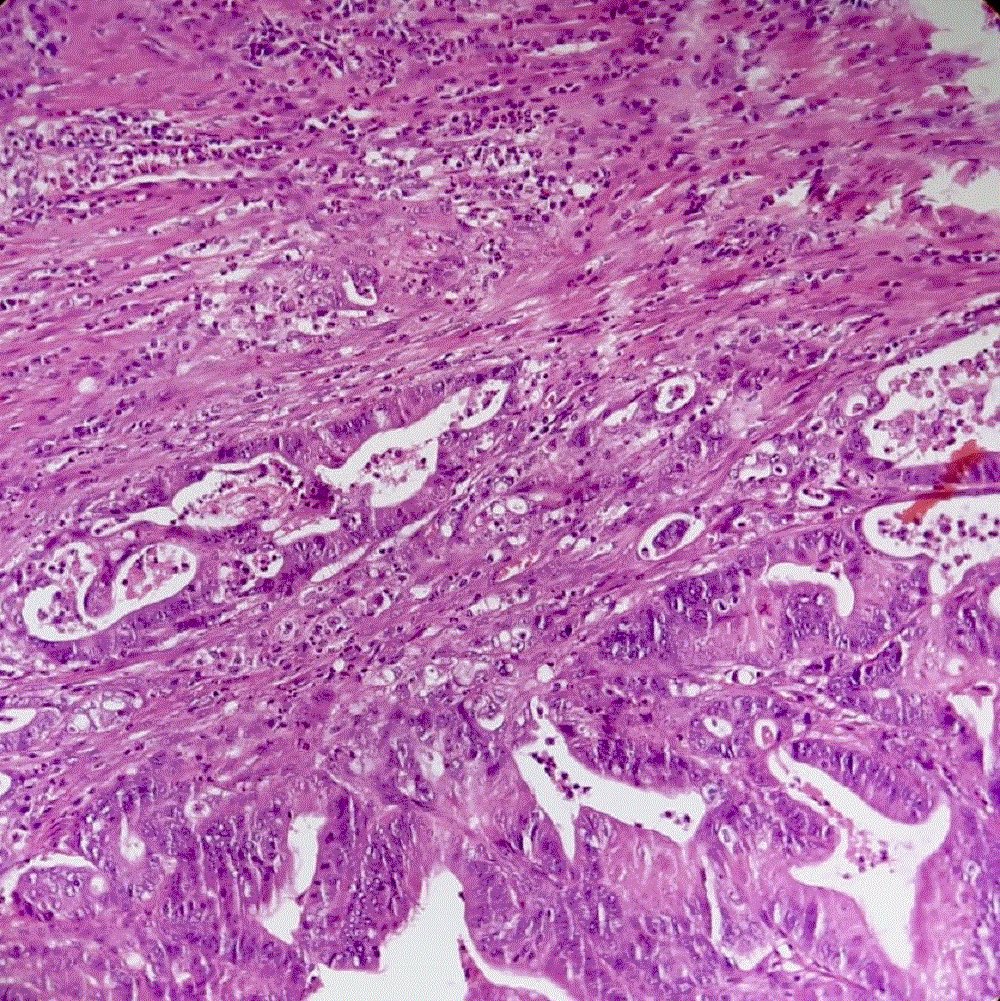
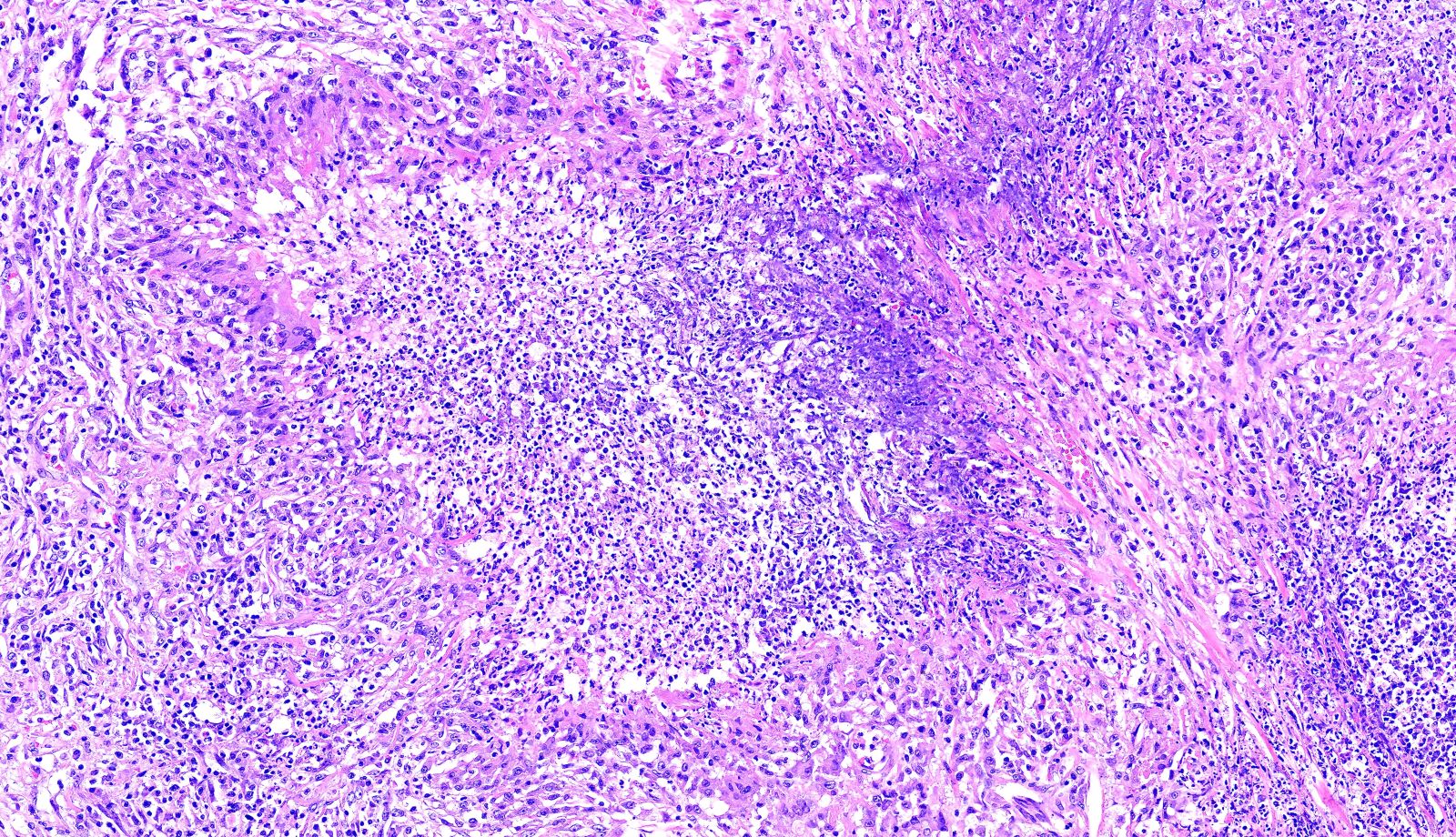
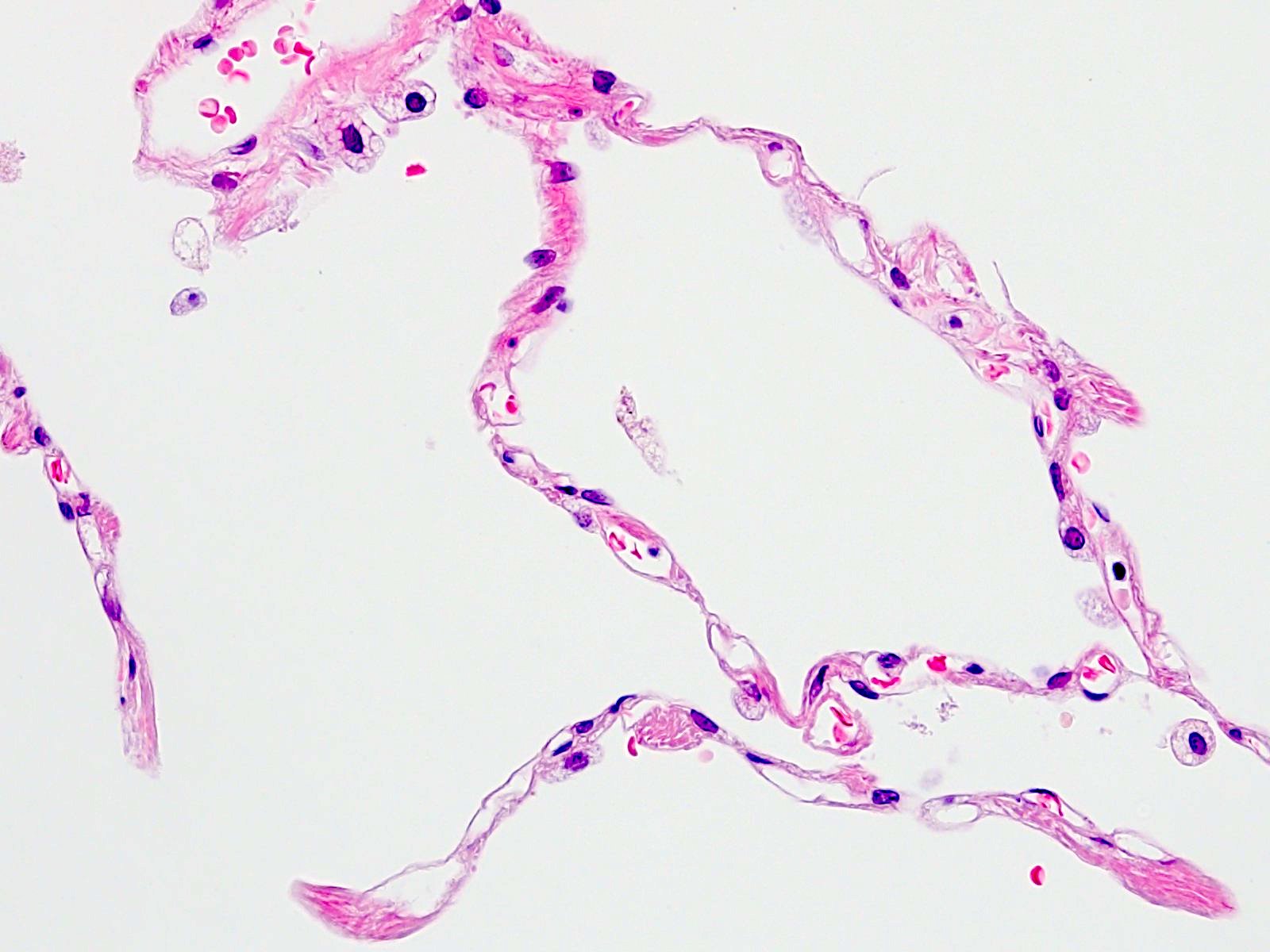
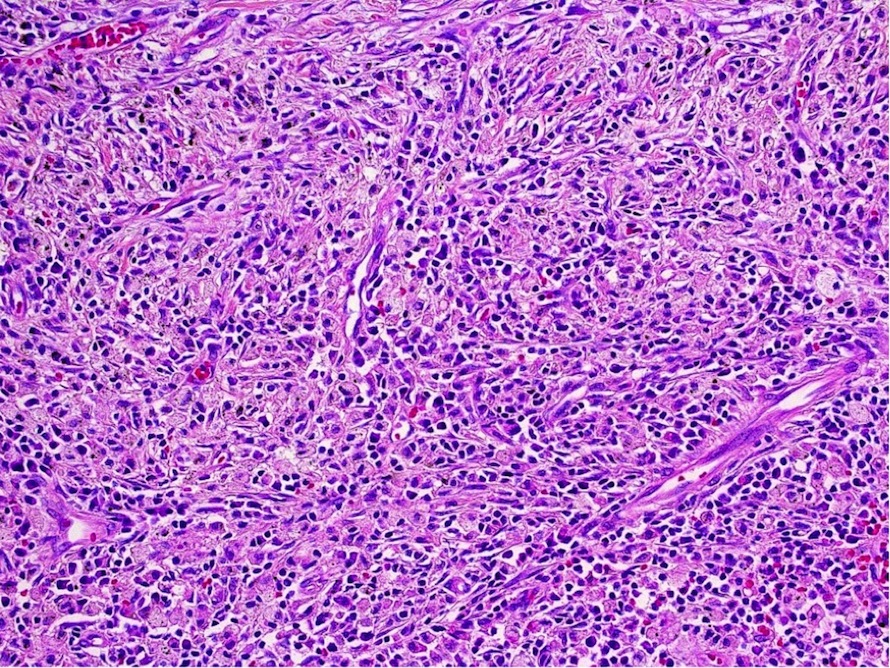
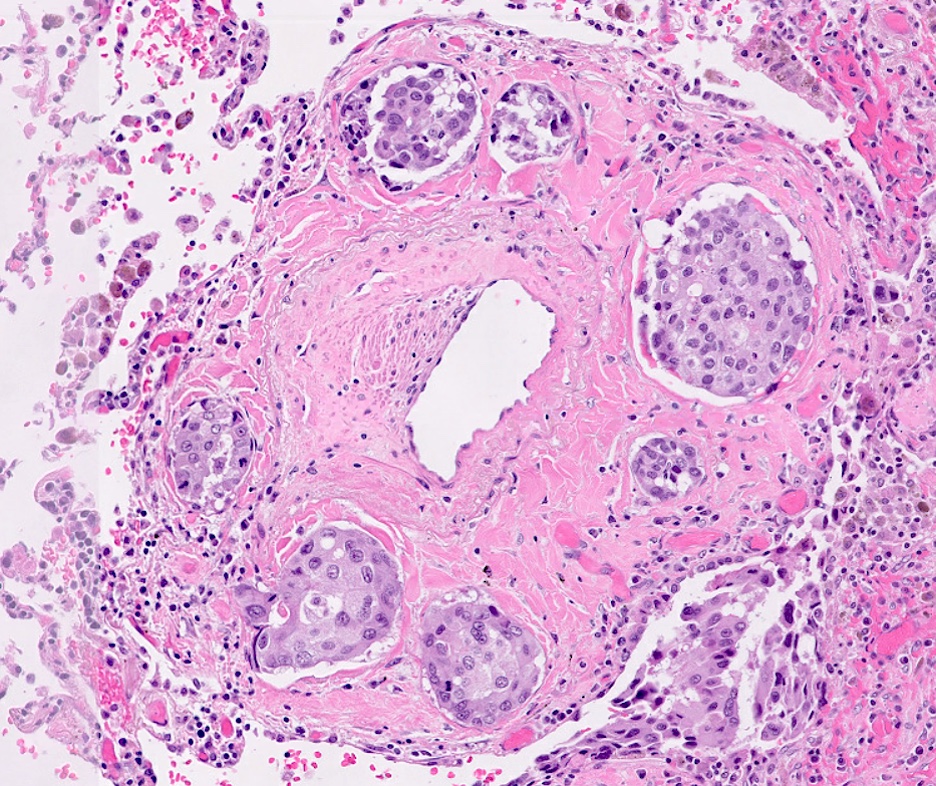
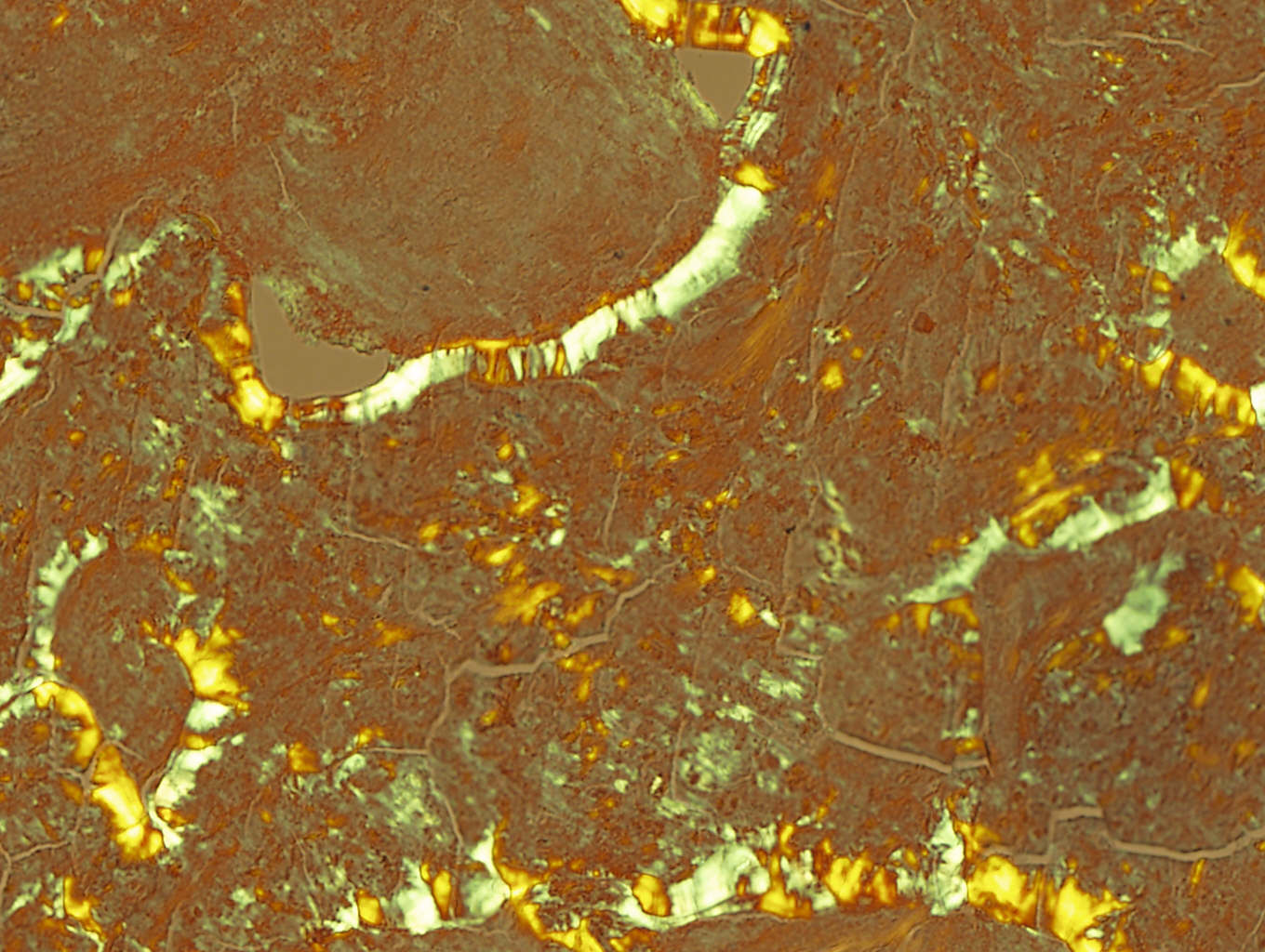
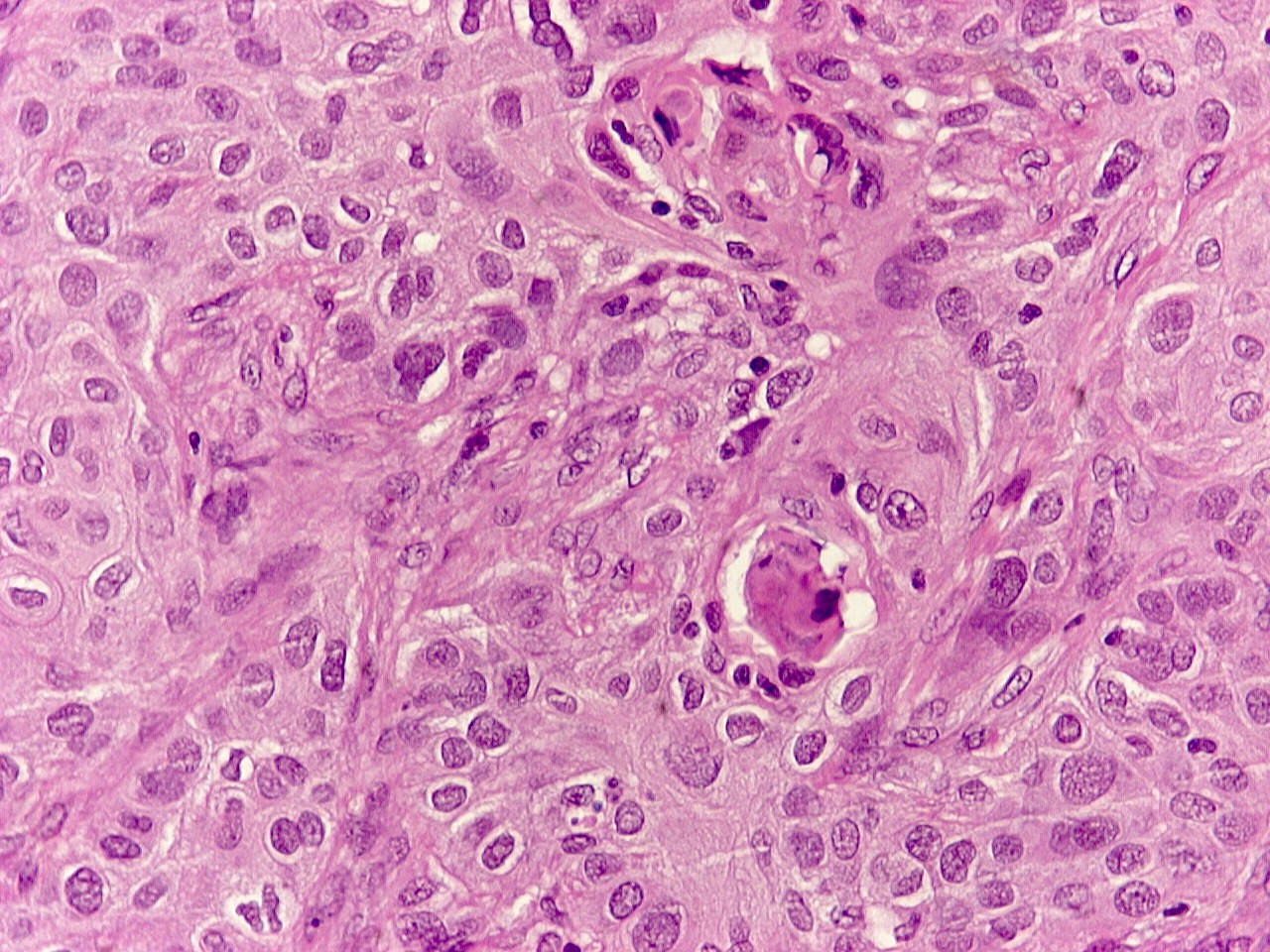
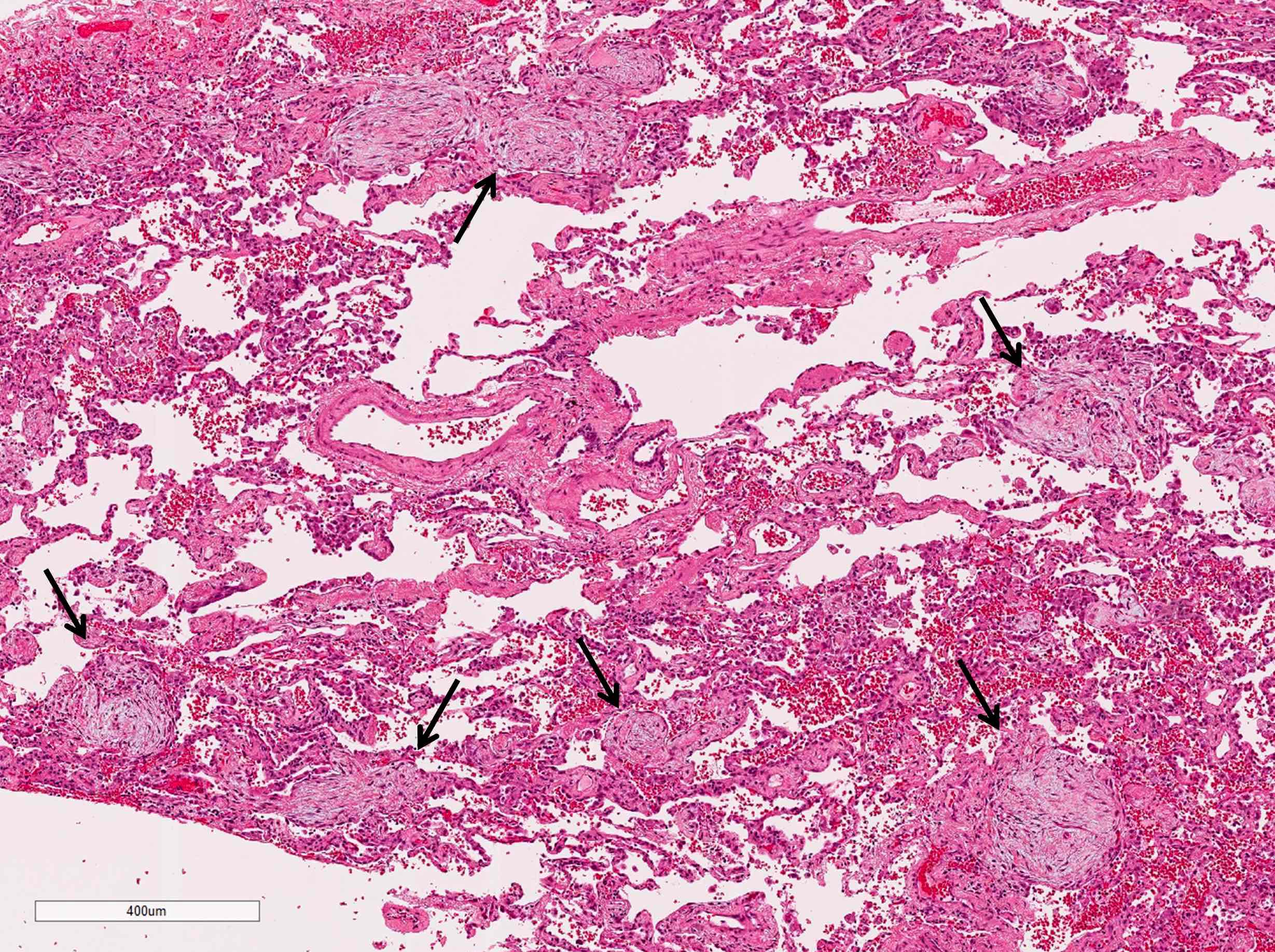
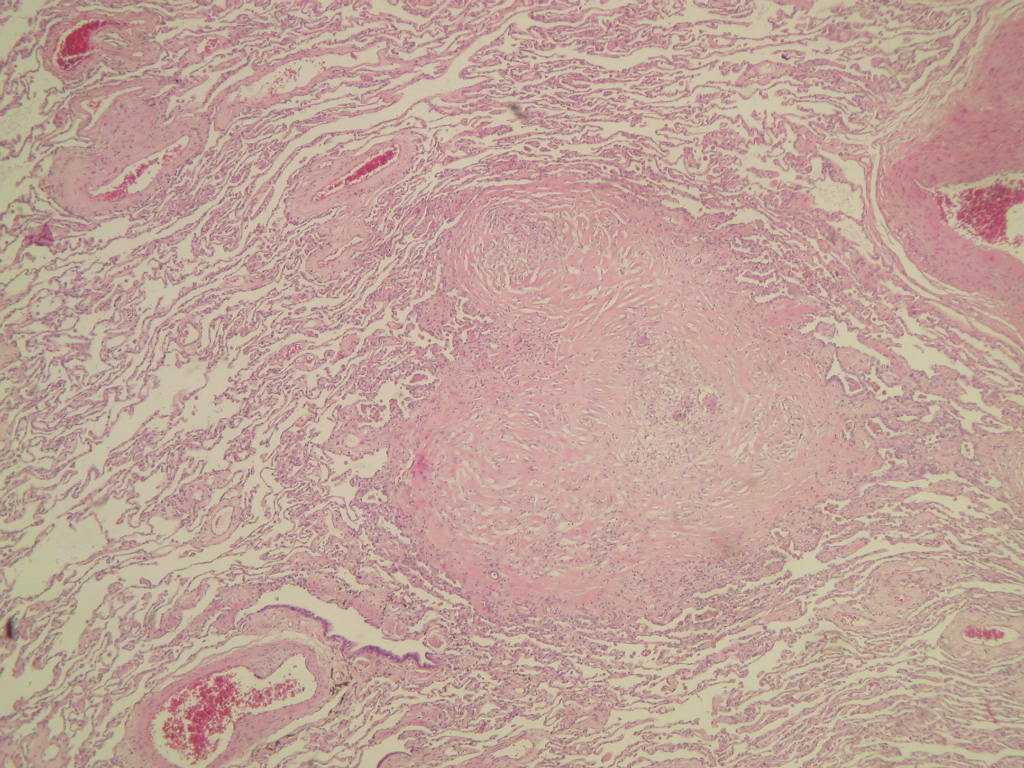
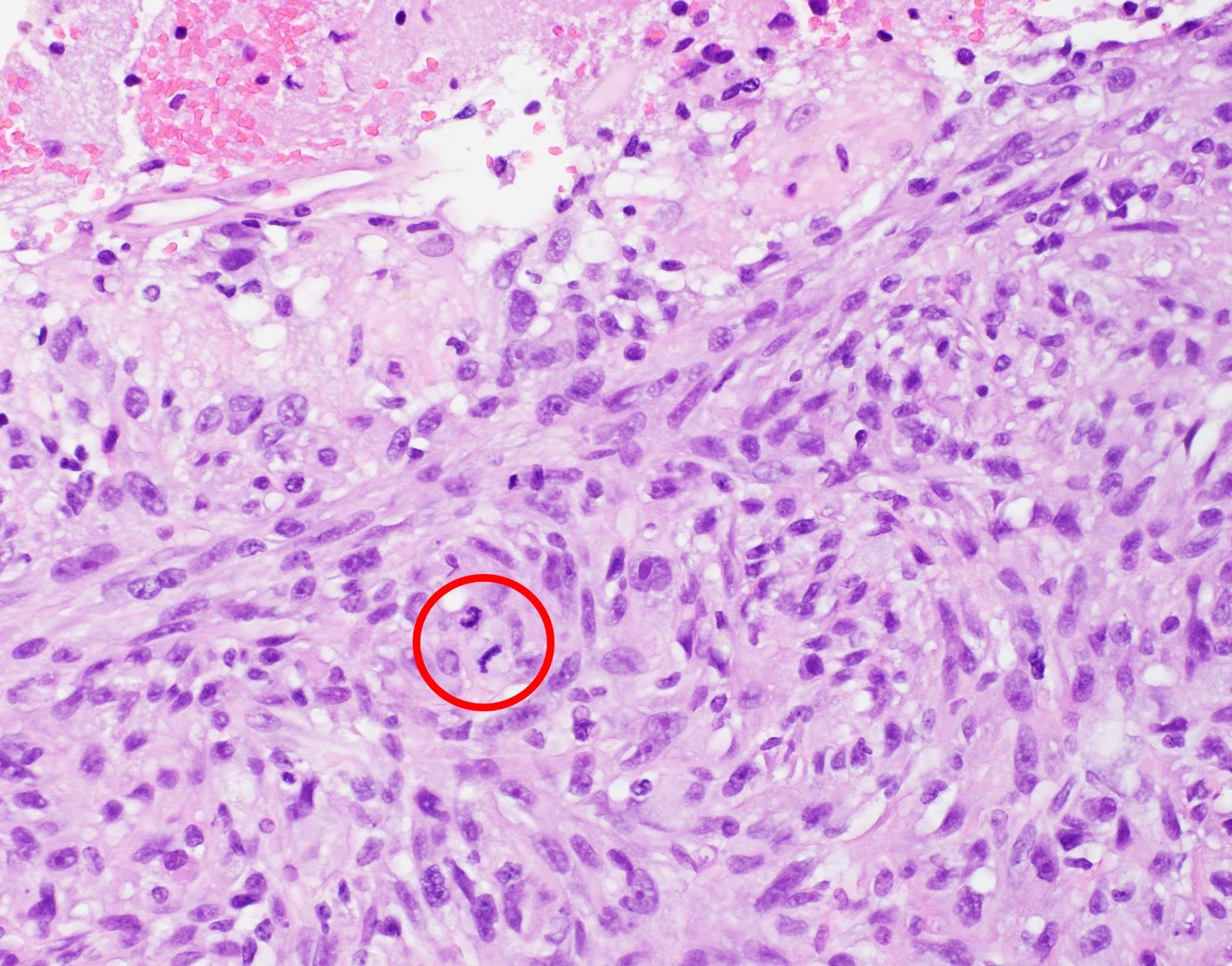
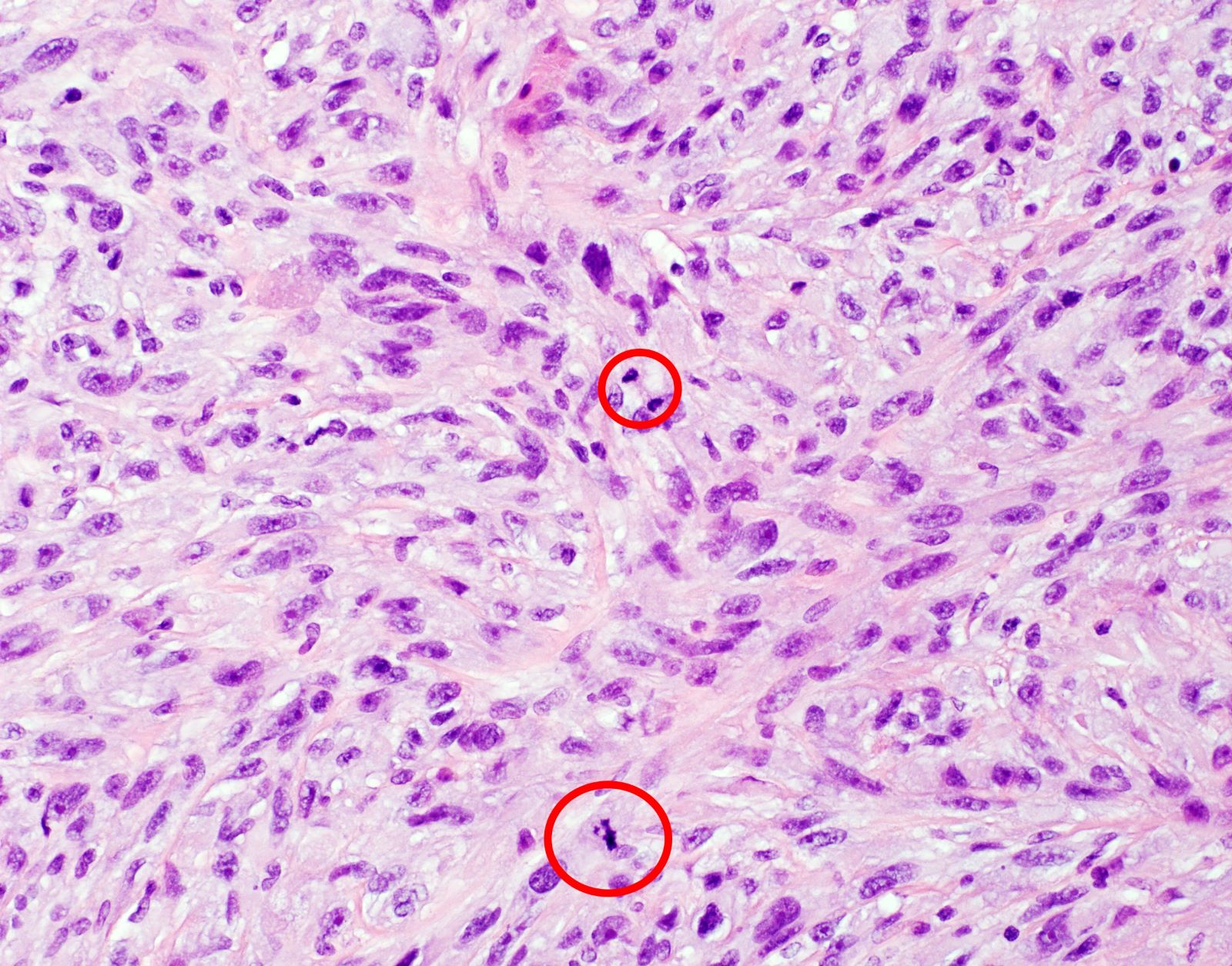
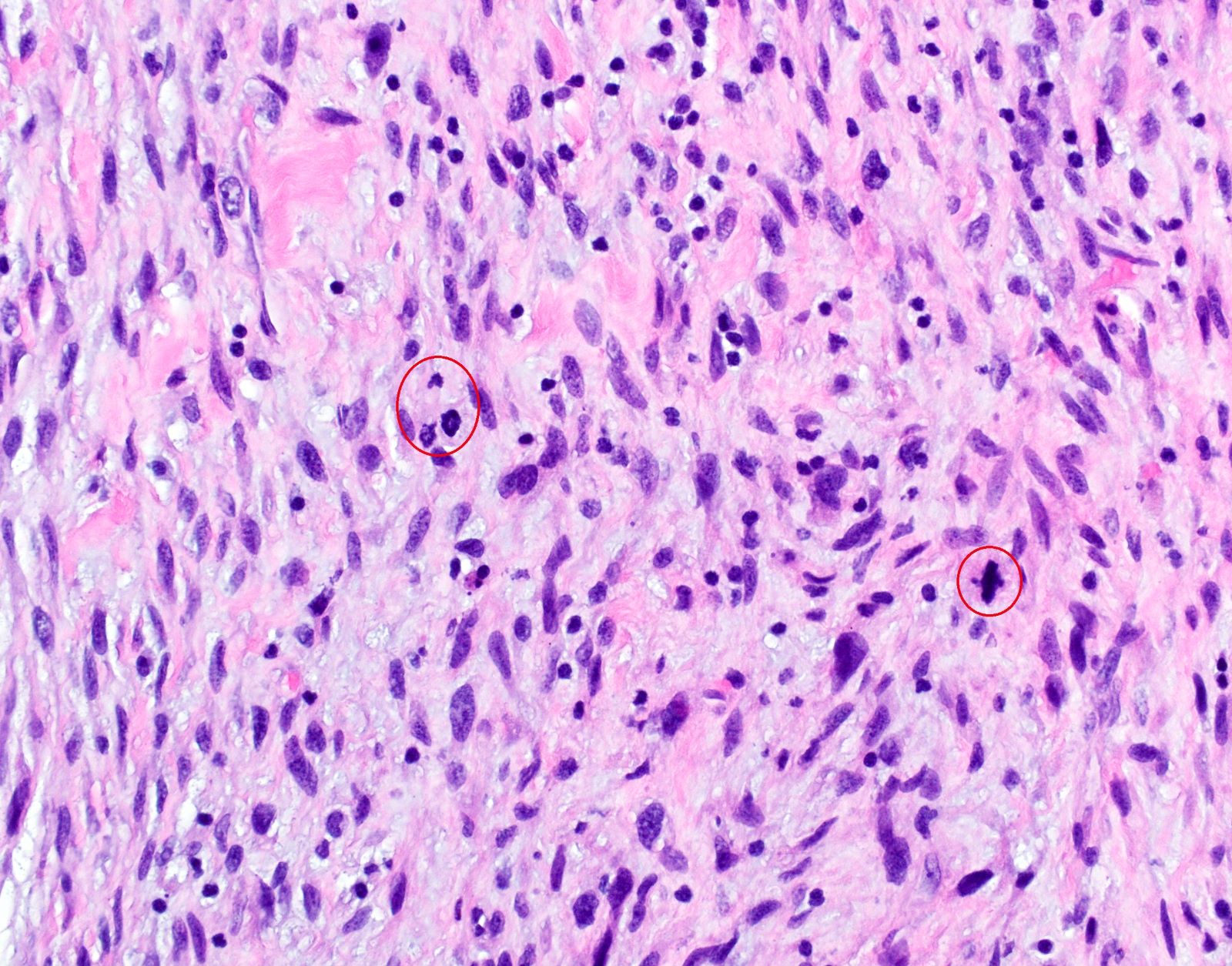
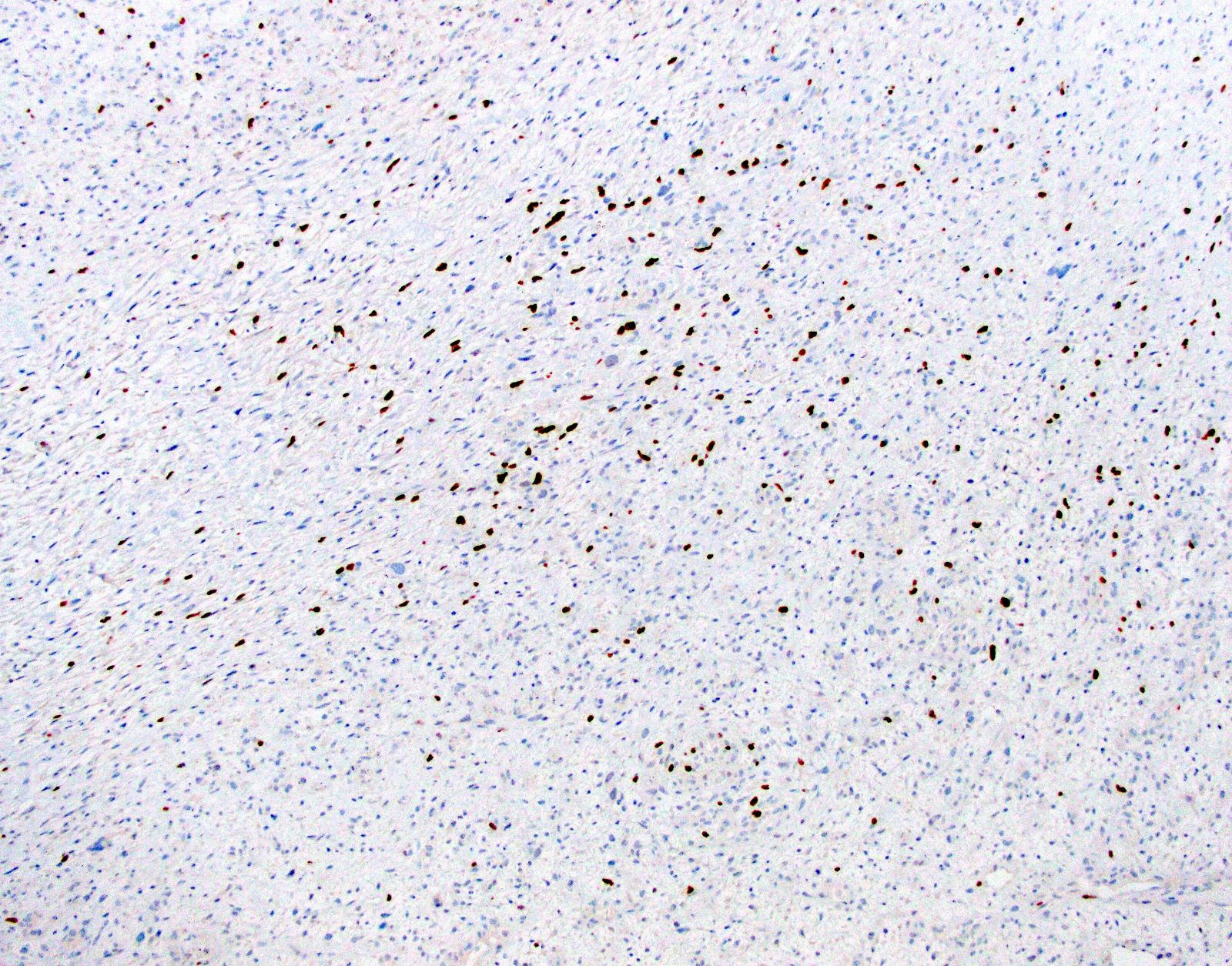
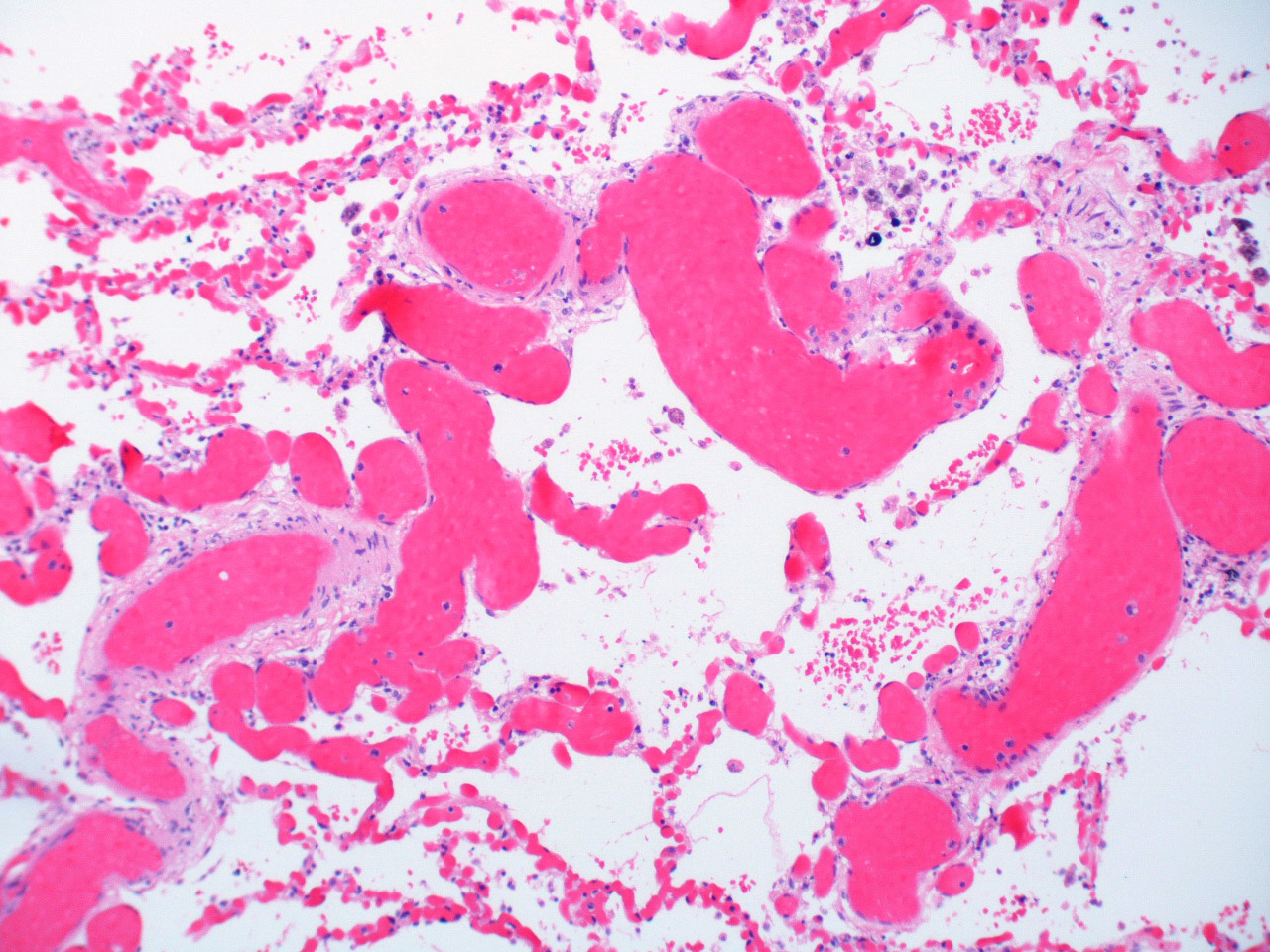
- Proliferative / organizing phase (Am J Surg Pathol 1986;10:256, Eur Respir J 2003;21:187)
- Organizing pneumonia with / without remnants of hyaline membrane
- Interstitial and intra-alveolar proliferation of fibroblasts / myofibroblasts
- Lymphocytic infiltration; usually more prominent than in acute respiratory distress syndrome
- Proliferation of type II pneumocytes with occasional cellular atypia
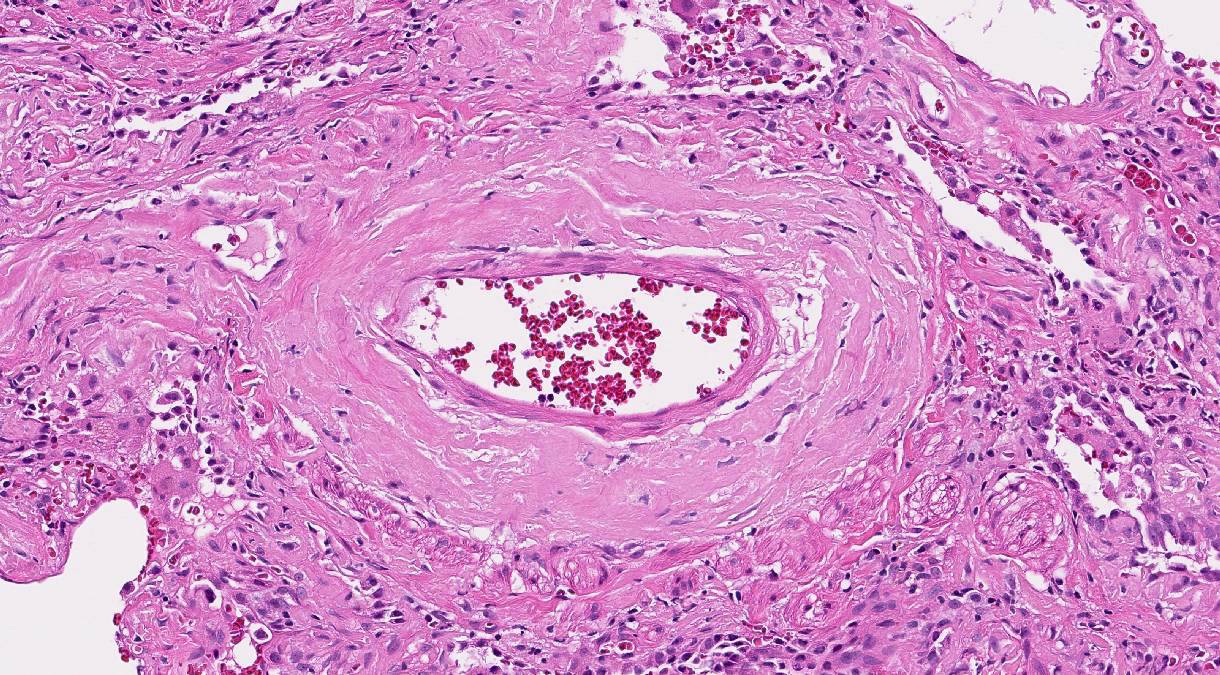
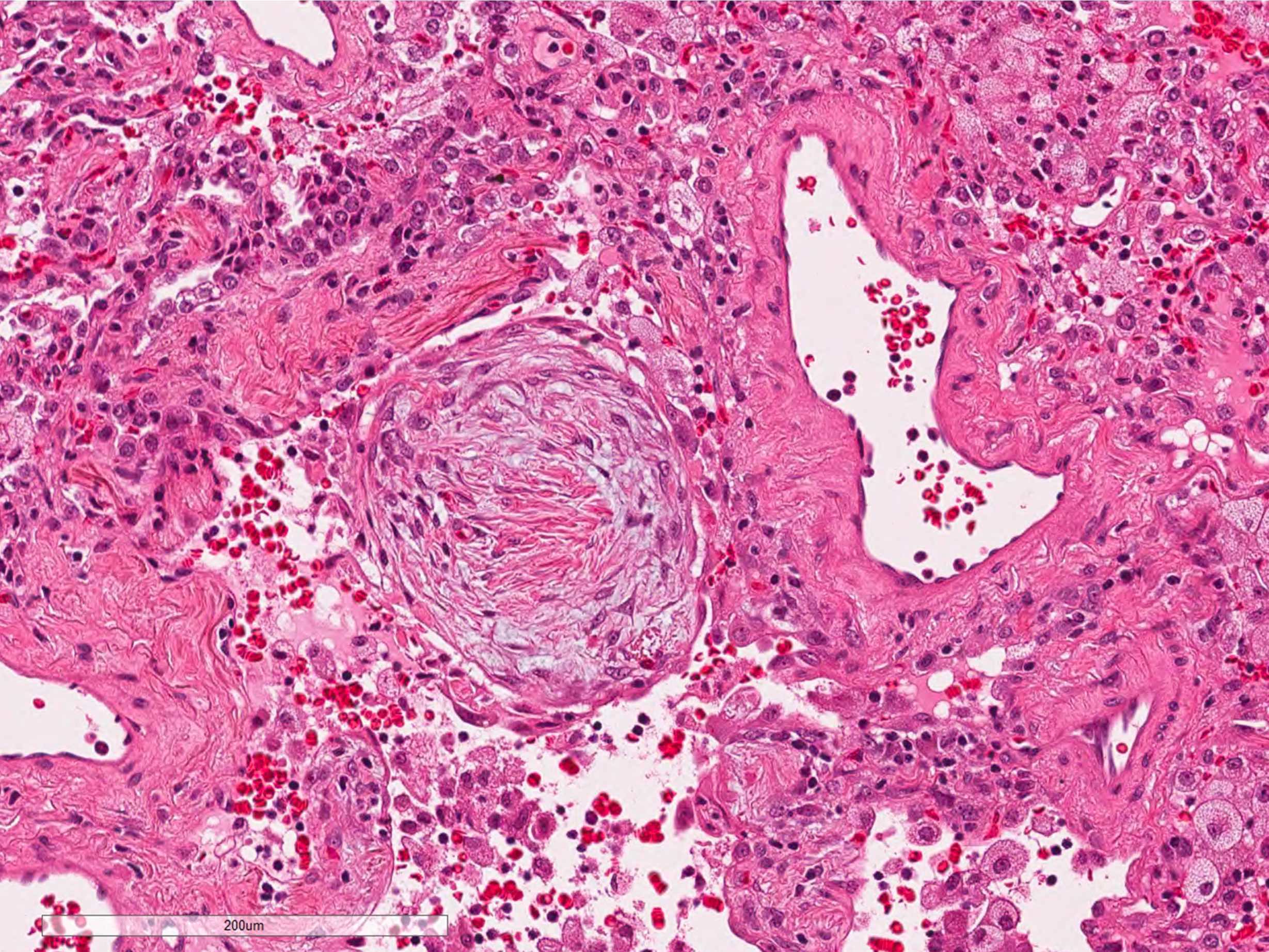
- Endothelial injury and fibrinous thromboembolism in arterioles / arteries
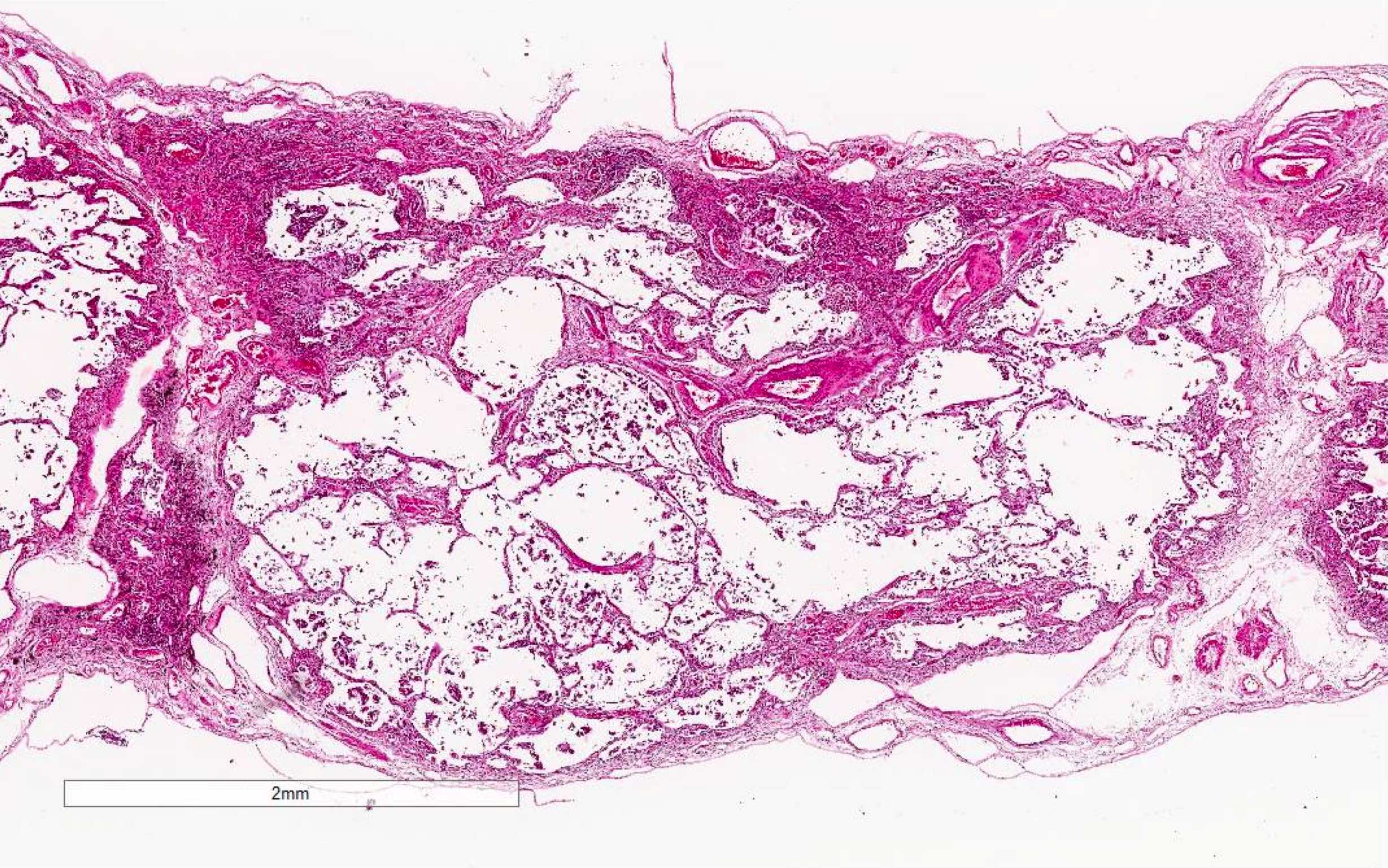
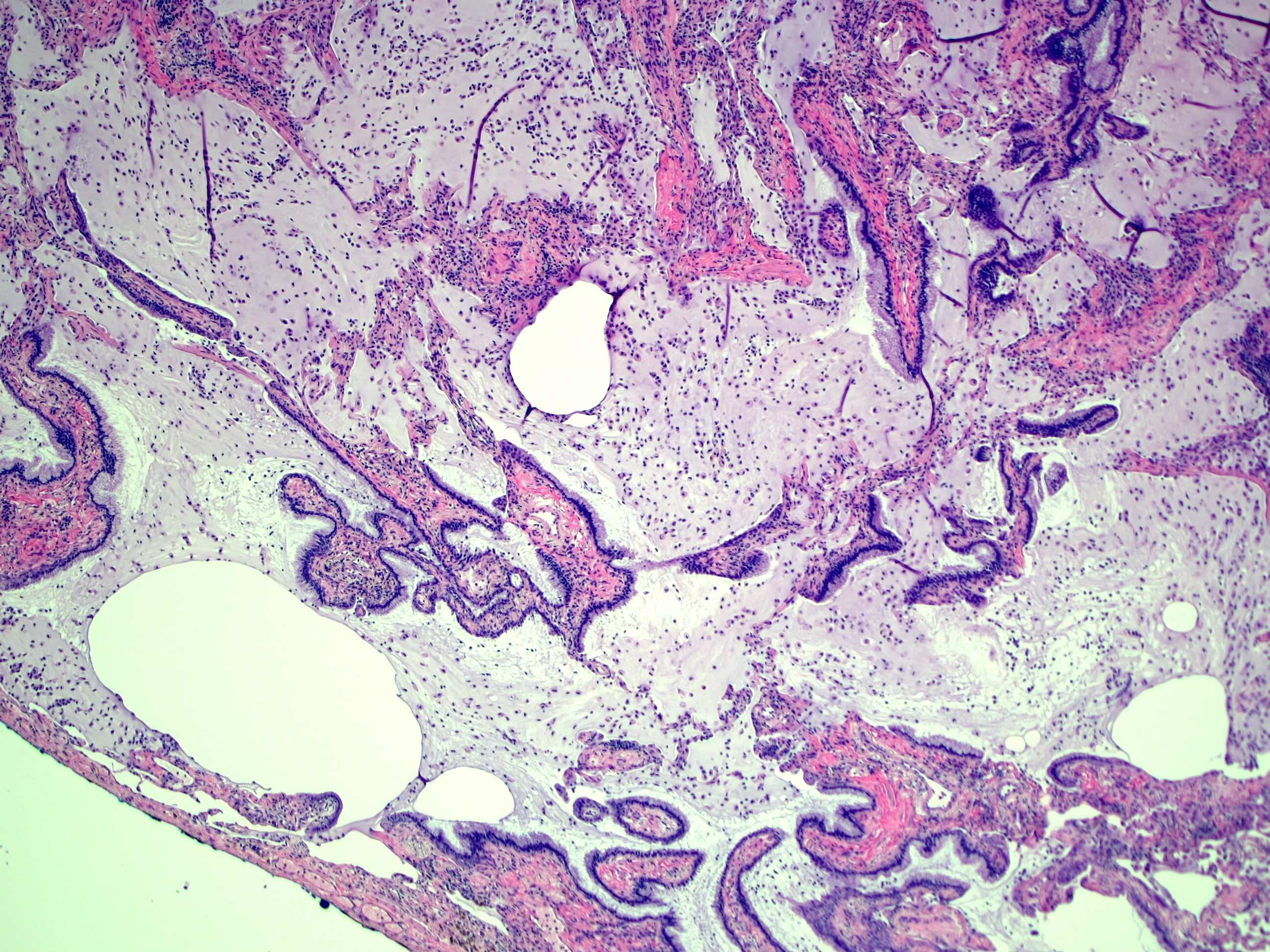
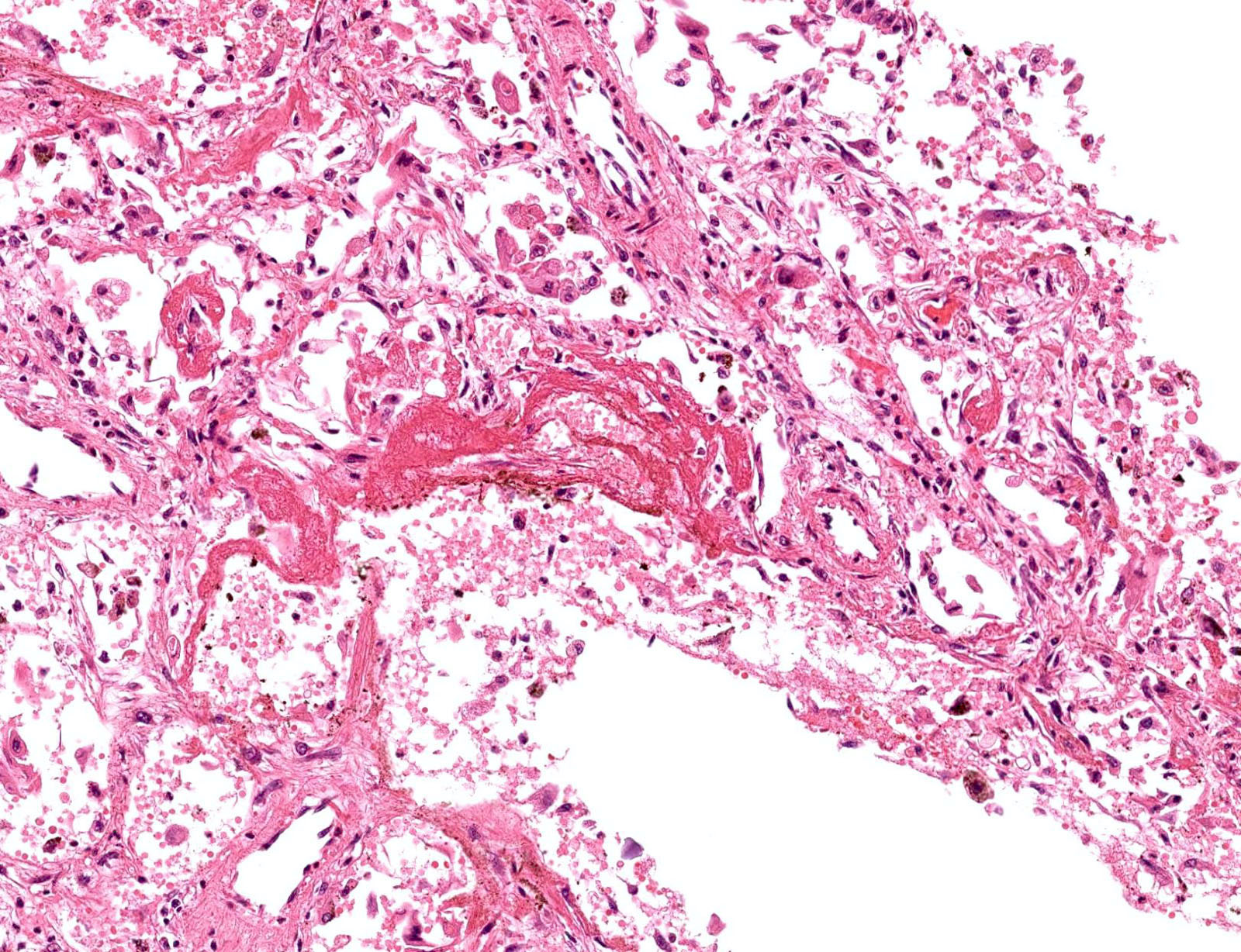
- Fibrosis phase
- Diffuse collagenous fibrosis
- Microscopic honeycomb-like change
- Traction bronchiolectasis
- Squamous metaplasia
- Organized thrombus
- Thickening of pleura with dilatation of lymphatic / blood vessels
Contributed by Akira Yoshikawa, M.D. and Yale Rosen, M.D.
Images hosted on other servers:
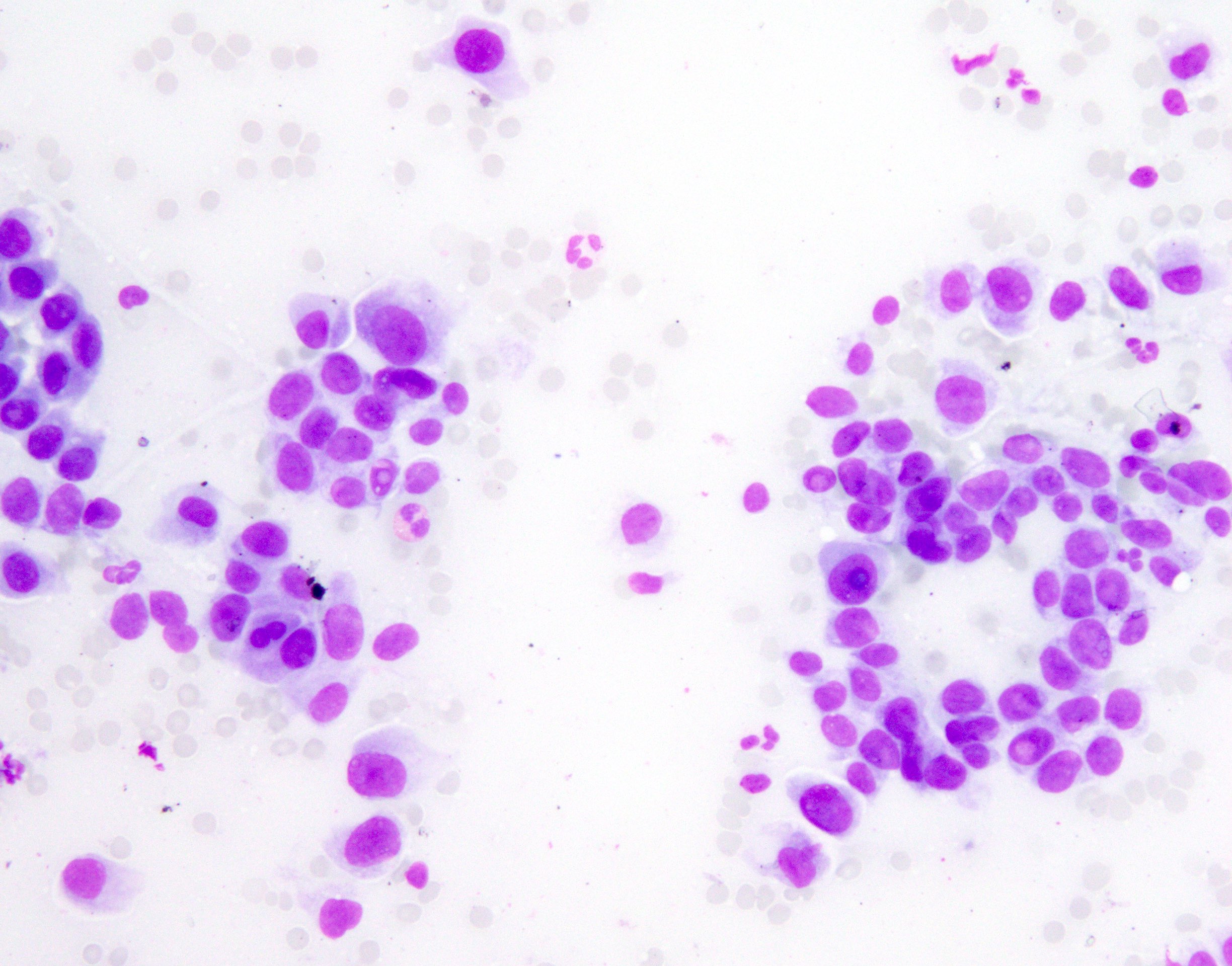
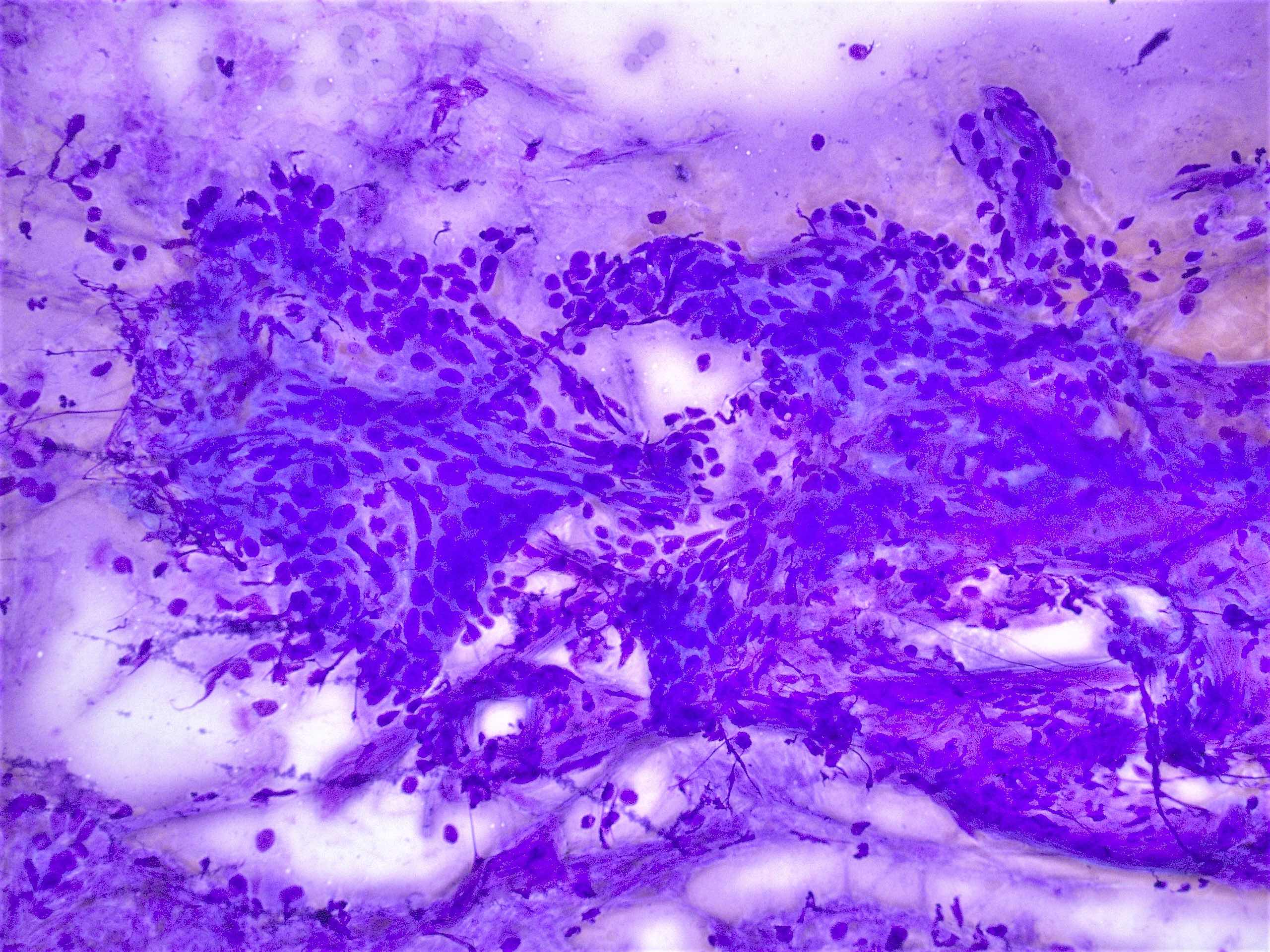
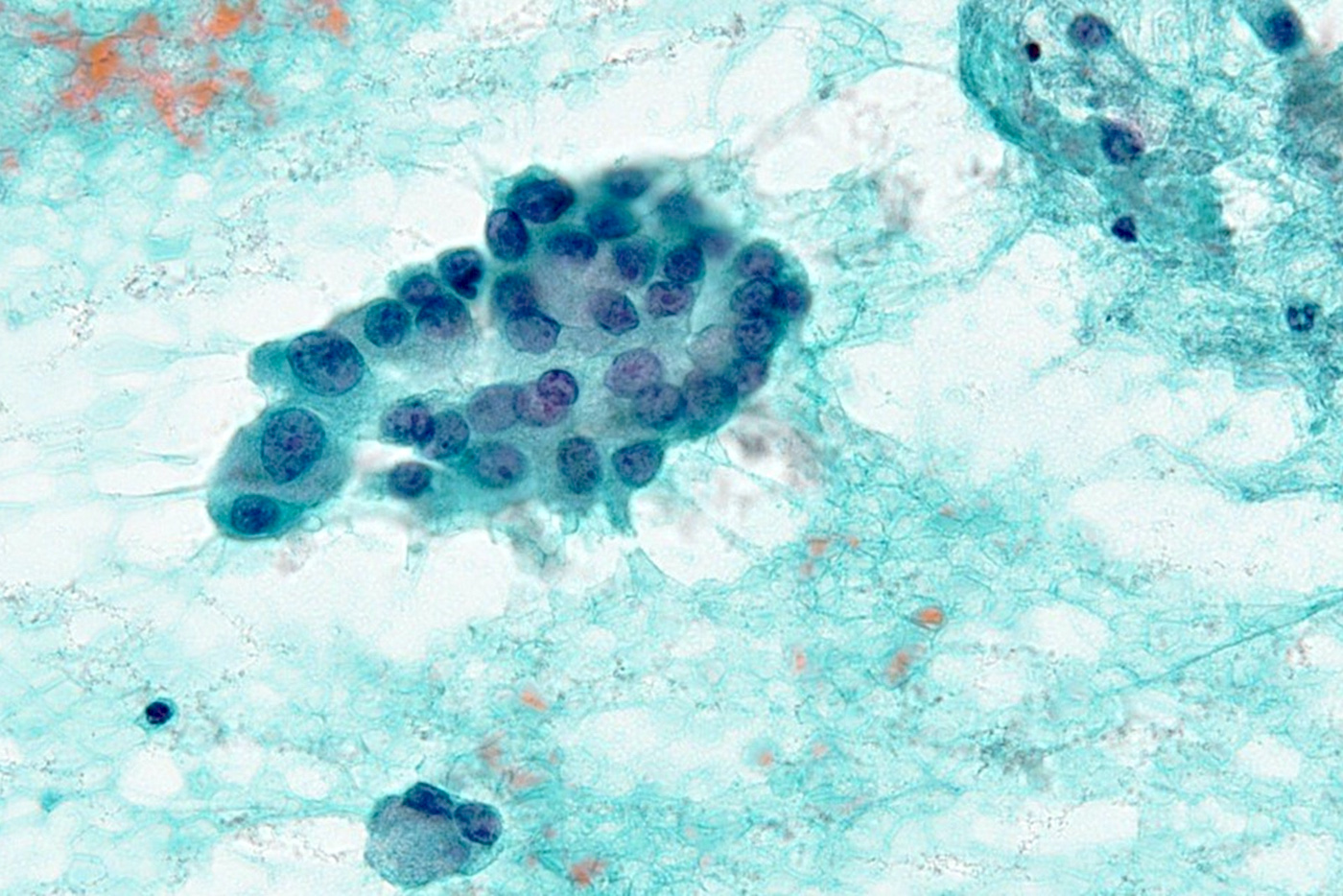
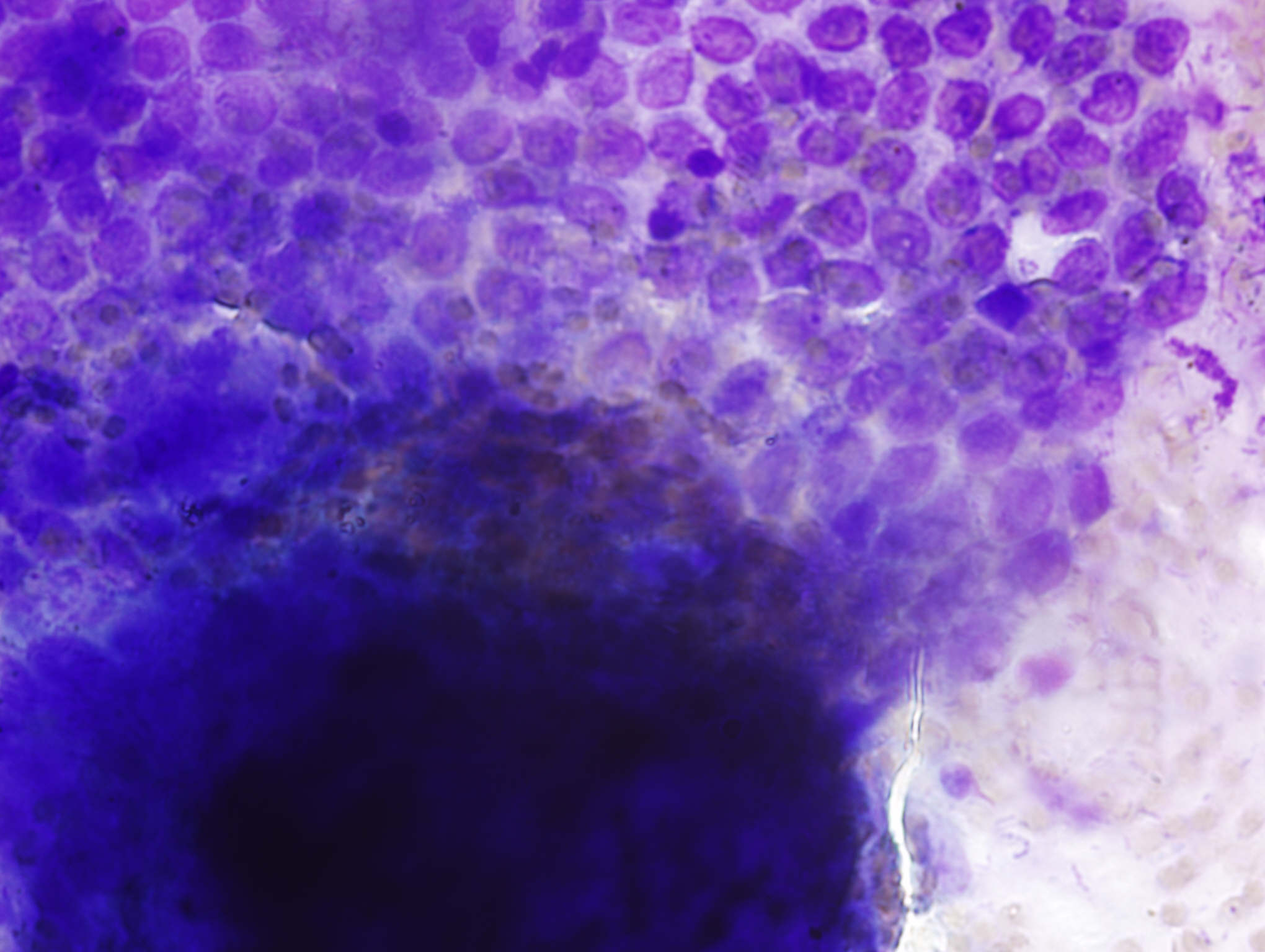
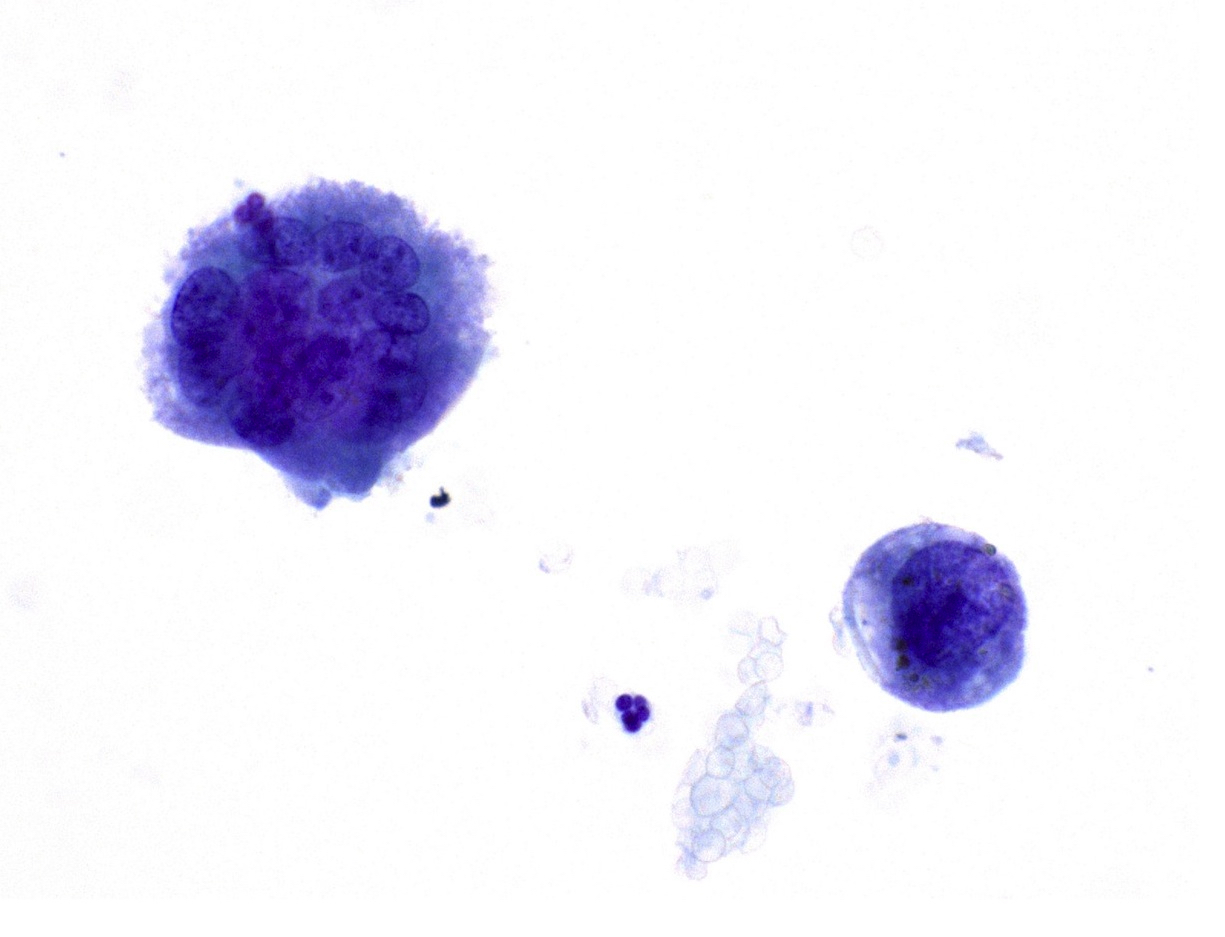
- Bronchoalveolar lavage (BAL) fluid
- Increased neutrophils (Eur Respir J 2000;15:412)
- Atypical epithelial cells are rarely present (Eur Respir J 2003;21:187)
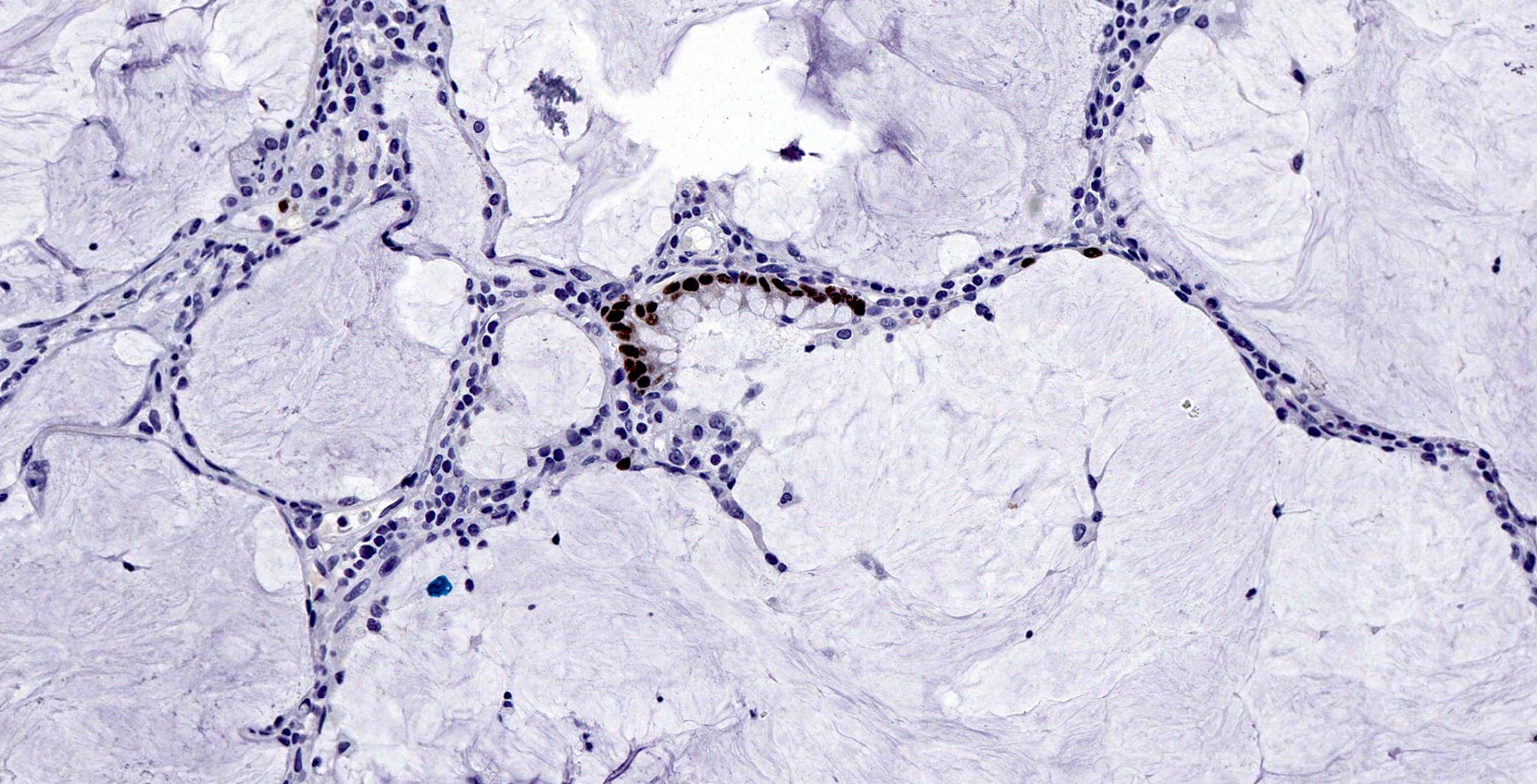
- Elastica van Gieson (fiber staining) is helpful to evaluate architectural destruction of alveoli
- Proliferation of type II pneumocyte with cytoplasmic projection into alveolar septa, abnormally large lamellar bodies or denudation from basement membrane (Am J Surg Pathol 1986;10:256)
- Acute exacerbation of interstitial lung disease, especially idiopathic pulmonary fibrosis (IPF): history of IPF, background of dense fibrosis and honeycombing
- Acute hypersensitivity pneumonitis: history of exposure to causative antigens, remission of symptoms after antigen removal, lymphocytosis ( > 30%) in bronchoalveolar lavage, nonnecrotizing granulomas, strong bronchocentric accentuation
- Acute respiratory distress syndrome: predisposition of pulmonary or systemic insult, an onset within 7 days, PaO2/FIO2 ≤ 300 mm Hg
- Collagen tissue disease associated interstitial lung disease
- Several collagen tissue disease are known to rarely present with acute interstitial pneumonia-like symptoms and diffuse alveolar damage (Mod Rheumatol 2012;22:243, Chest 2006;130:553)
- Clinical manifestation and serum autoantibody tests are helpful for the diagnosis
- Drug induced lung injury: history of causative drug, remission of symptoms after drug withdrawal, marked eosinophils, foamy changes in type II cells
- Eosinophilic pneumonia: smoking history, eosinophilia ( > 25%) in bronchoalveolar lavage, degranulation of eosinophils in the lung tissue, pink macrophages, marked gumball airspace fibrin rather than hyaline membranes
- Organizing pneumonia: exposure to causative particles, migratory shadows on radiology, preservation of alveolar architecture
- Absence of exposure to causative factors of respiratory failure
- Absence of prior history of lung disease
- Bilateral shadows on chest radiograph
- Diffuse alveolar damage on histology
- PaO2/FIO2 ≤ 300 mm Hg
Comment Here
Reference: Acute interstitial pneumonia
- Broadly defined as acute inflammation of the lung parenchyma
- Clinically characterized by fever, purulent sputum, leukocytosis and decline in oxygenation
- Caused by bacteria and other microorganisms (virus and fungus)
- Classically divided by gross morphology into lobar and bronchopneumonia
- Intra-alveolar fibrinopurulent exudate with neutrophils
- Streptococcus pneumoniae is the most common bacteria causing community acquired pneumonia
- Gram negative bacilli and Staphylococcus aureus are important causes of hospital acquired pneumonia and ventilator associated pneumonia
- Classification principles:
- Pathogens: bacterial, viral, fungal
- Clinical setting: community acquired pneumonia (CAP), hospital acquired pneumonia (HAP), ventilator associated pneumonia (VAP)
- Extent:
- Lobar pneumonia: involvement of the entire lung lobe
- Bronchopneumonia: patchy involvement of the lung parenchyma, originating from the airway
- Community acquired pneumonia (CAP):
- Lung infection that is acquired from the normal environment
- Hospital acquired pneumonia (HAP) (Clin Infect Dis 2016;63:e61):
- Pneumonia not incubating at the time of hospital admission and occurring > 48 hours after admission
- Ventilator associated pneumonia (VAP):
- Pneumonia occurring > 48 hours after endotracheal intubation
- Healthcare associated pneumonia (HCAP):
- American Thoracic Society (ATS) / Infectious Diseases Society of America (IDSA) recommend abandoning this term in the most recent HAP / VAP guideline
- ICD-10:
- J13 - pneumonia due to Streptococcus pneumoniae
- J14 - pneumonia due to Hemophilus influenzae
- J15.0 - pneumonia due to Klebsiella pneumoniae
- J15.1 - pneumonia due to Pseudomonas
- J15.2 - pneumonia due to Staphylococcus
- J15.3 - pneumonia due to streptococcus, group B
- J15.4 - pneumonia due to other streptococci
- J15.5 - pneumonia due to Escherichia coli
- J15.6 - pneumonia due to other aerobic gram negative bacteria
- J15.8 - other bacterial pneumonia
- J15.9 - bacterial pneumonia, unspecified
- ICD-11:
- CA40.0 - bacterial pneumonia
- CA40.01 - pneumonia due to Escherichia coli
- CA40.02 - pneumonia due to Hemophilus influenza
- CA40.03 - pneumonia due to Klebsiella pneumoniae
- CA40.05 - pneumonia due to Pseudomonas aeruginosa
- CA40.06 - pneumonia due to Staphylococcus
- CA40.07 - pneumonia due to Streptococcus pneumoniae
- CA40.08 - pneumonia due to beta hemolytic Streptococcus
- CA40.0Y - pneumonia due to other specified bacteria
- CA40.0Z - bacterial pneumonia, unspecified
- Leading cause of adult hospital admissions in the U.S. (Healthcare Cost and Utilization Project (HCUP) Statistical Briefs: Most Frequent Conditions in U.S. Hospitals, 2011):
- Lower respiratory tract infection accounted for 78.8% of infectious deaths (JAMA 2018;319:1248)
- HAP and VAP accounted for 22% of hospital acquired infections in a U.S. 2014 survey (N Engl J Med 2014;370:1198)
- About 10% of patients put on mechanical ventilation develop VAP (N Engl J Med 2014;370:341)
- For most cases of CAP (62%), a causative organism is not identified (N Engl J Med 2015;373:415)
- Bacterial pneumonia accounts for 11% of CAP in the U.S.
- Remainder: virus 23%, bacterial and viral pathogens 3%, fungus or mycobacterium 1%
- Risk factors related to specific pathogens in CAP (Clin Infect Dis 2007;44:S27):
- Alcohol use disorder: S. pneumoniae, oral anaerobes, Klebsiella pneumoniae, Acinetobacter species
- Chronic obstructive pulmonary disease or smoking: Haemophilus influenzae, Pseudomonas aeruginosa, S. pneumoniae, Moraxella cararrhalis
- Structural lung disease (e.g., bronchiectasis): P. aeruginosa, Burkholderia cepacia, S. aureus
- Injection drug use: S. aureus, anaerobes, S. pneumoniae
- Endobronchial obstruction: anaerobes, S. pneumoniae, H. influenzae, S. aureus
- Risk factors for multidrug resistant pathogens in HAP / VAP (Clin Infect Dis 2016;63:e61):
- Prior intravenous antibiotic use within 90 days
- Septic shock at time of VAP
- Acute respiratory distress syndrome preceding VAP
- 5 or more days of hospitalization prior to the occurrence of VAP
- Acute renal replacement therapy prior to VAP onset
- Lungs, ranging from several acini to segments and lobes (up to total involvement)
- Predilection
- K. pneumoniae has a predilection for upper lobes (South Med J 1991;84:200)
- Aspiration pneumonia tends to involve dependent areas of the lung; posterior segments of the upper lobes and apical segments of the lower lobes (Br J Radiol 2010;83:998)
- Bacteria can reach the lungs in several ways (Semin Diagn Pathol 2017;34:498)
- Airborne droplet spread
- Microaspiration of pathogens that have colonized the oropharynx is a common mechanism in bronchopneumonia
- Spread to the lungs via the pulmonary or systemic blood supply
- Exudative spread throughout the lung via the pores of Kohn, potential channels between adjacent alveoli
- Development of lobar pneumonia entails 4 stages (Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020)
- Congestion: vascular engorgement, intra-alveolar fluid with few neutrophils, red cells and fibrin
- Red hepatization: massive confluent exudation (neutrophils, red cells and fibrin), resulting in liver-like consistency
- Gray hepatization: progressive disintegration of red cells, while fibrosuppurative exudate persists
- Resolution: exudate broken down by enzymatic process, resulting in cellular debris, macrophages infiltrate and fibroblast proliferation
- 5 - 15% of CAP are aspiration pneumonia (N Engl J Med 2001;344:665)
- Pneumonia from hematogenous spread can be a result of:
- Lemierre syndrome: infection and thrombosis of the internal jugular veins following throat and tonsillar infections by Fusobacterium necrophilum (N Engl J Med 2019;380:e16)
- Infective endocarditis at the tricuspid and pulmonic valves
- Survey data in hospitalized patients from CAP in the U.S. (N Engl J Med 2015;373:415, Am J Respir Crit Care Med 2019;200:e45)
- Most common: Streptococcus pneumoniae
- Followed by Mycoplasma pneumoniae, Staphylococcus aureus, Legionella species and Enterobacteriaceae
- Recent survey data in hospitalized patients from CAP in the U.S. (N Engl J Med 2015;373:415)
- Most common bacteria: Streptococcus pneumoniae, followed by Mycoplasma pneumoniae, Staphylococcus aureus, Legionella species and Enterobacteriaceae
- Causative organisms in HAP / CAP
- Data from the U.S. Center for Disease Control and Prevention in 2009 - 2010: S. aureus (24.1%), P. aeruginosa (16.6%), Klebsiella species (10.1%), Enterobacter species (8.6%), Acinetobacter baumannii (6.6%) and E. coli (5.9%) (Infect Control Hosp Epidemiol 2013;34:1)
- Streptococcus pneumoniae
- Gram positive, diplococci, lancet shaped, facultative anaerobe
- 100 known serotypes
- Vaccine containing capsular polysaccharide available for common serotypes
- Haemophilus influenza
- Gram negative coccobacillus, can be encapsulated (typeable) or unencapsulated (nontypeable)
- 6 serotypes based on capsular polysaccharide
- Vaccine available for H. influenzae type b (Hib), the most virulent serotype
- Staphylococcus aureus
- Gram positive cocci
- Important pathogen in HAP / VAP
- Emerging cause of CAP over the past 2 decades (Semin Respir Crit Care Med 2020;41:470)
- Panton-Valentine leukocidin (PVL): important virulence factor identified in community associated methicillin resistant S. aureus
- Toxin causing lysis of leukocytes and necrosis of epithelial cells
- Common coinfection with influenza virus
- Klebsiella pneumoniae
- Gram negative bacilli, facultative anaerobic, member of Enterobacteriaceae family
- Thick, mucoid appearing sputum is characteristic
- Pseudomonas aeruginosa
- Gram negative bacilli, strictly aerobic
- Important pathogen in cystic fibrosis patients and HAP / VAP
- Moraxella catarrhalis
- Gram negative, aerobic diplococcus
- Common cause of pneumonia in children under 5 years old (Recent Pat Inflamm Allergy Drug Discov 2018;12:136)
- Common signs and symptoms in CAP: dyspnea, cough, fever, chills and pleuritis (Lancet 2015;386:1097)
- Elderly people: less evident symptoms (e.g., an altered state of consciousness, gastrointestinal discomfort and fever can be absent)
- HAP / VAP presentation: increasing oxygen requirements, leukocytosis and secretions in the intensive care unit (Cleve Clin J Med 2020;87:633)
- Suggestive scenarios: respiratory decline accompanied by fever and a productive cough, respiratory decline after a witnessed or suspected aspiration event in the hospital
- CAP (Am J Respir Crit Care Med 2019;200:e45):
- Suggestive clinical features and compatible chest radiograph or other imaging technique
- Microbiological data is not required for the diagnosis of pneumonia
- Specific pathogens should be investigated when the testing result would significantly alter standard (empirical) management decisions
- HAP / VAP (Clin Infect Dis 2016;63:e61):
- Noninvasive sampling in suspected HAP: spontaneous expectoration, sputum induction, nasotracheal suctioning (uncooperative patient) and endotracheal aspiration (subsequent mechanical ventilation)
- VAP should be diagnosed by noninvasive sampling (i.e., endotracheal aspiration) with semiquantitative cultures, rather than invasive sampling (i.e., bronchoscopy, blind bronchial sampling) with quantitative cultures and noninvasive sampling with quantitative cultures
- Pneumonia in tissue specimens:
- Occasionally diagnosed in surgical specimens as an accompanying disease
- Much more commonly diagnosed at autopsy
- Rarely diagnosed on biopsy tissue sampling
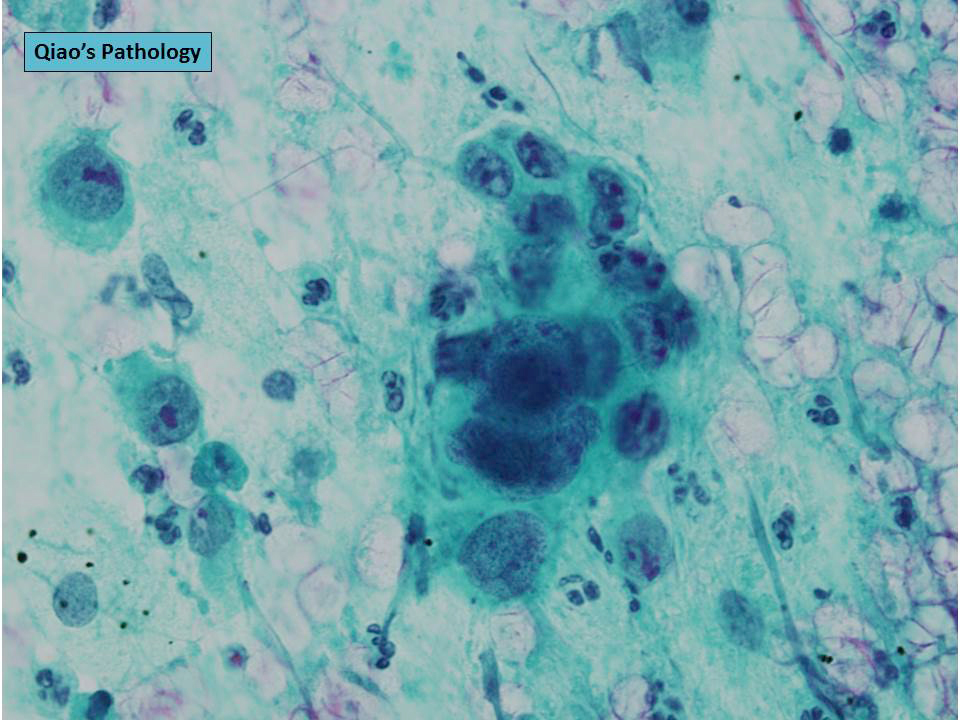
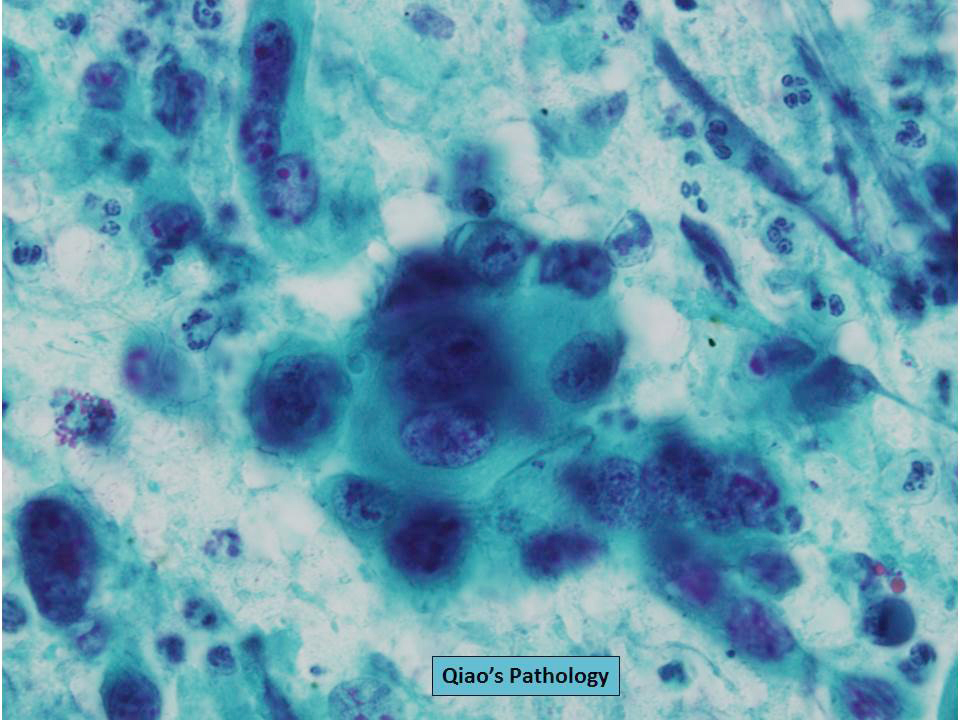
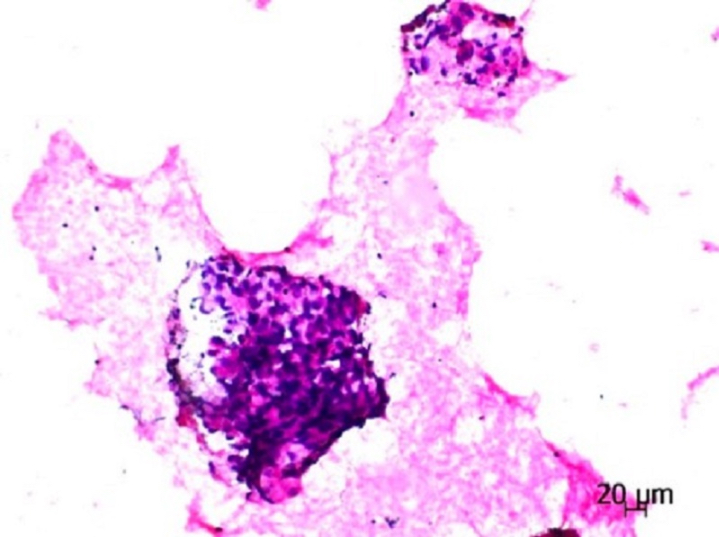
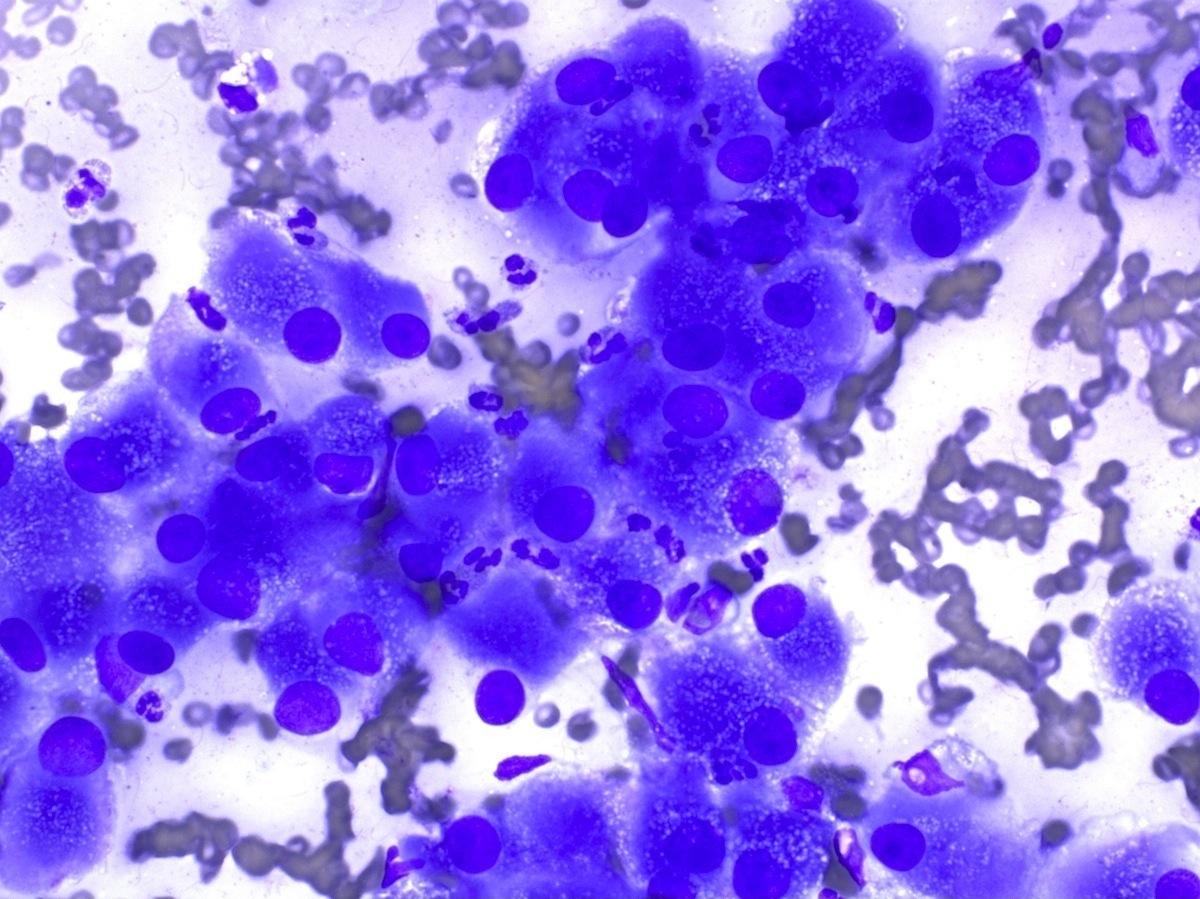
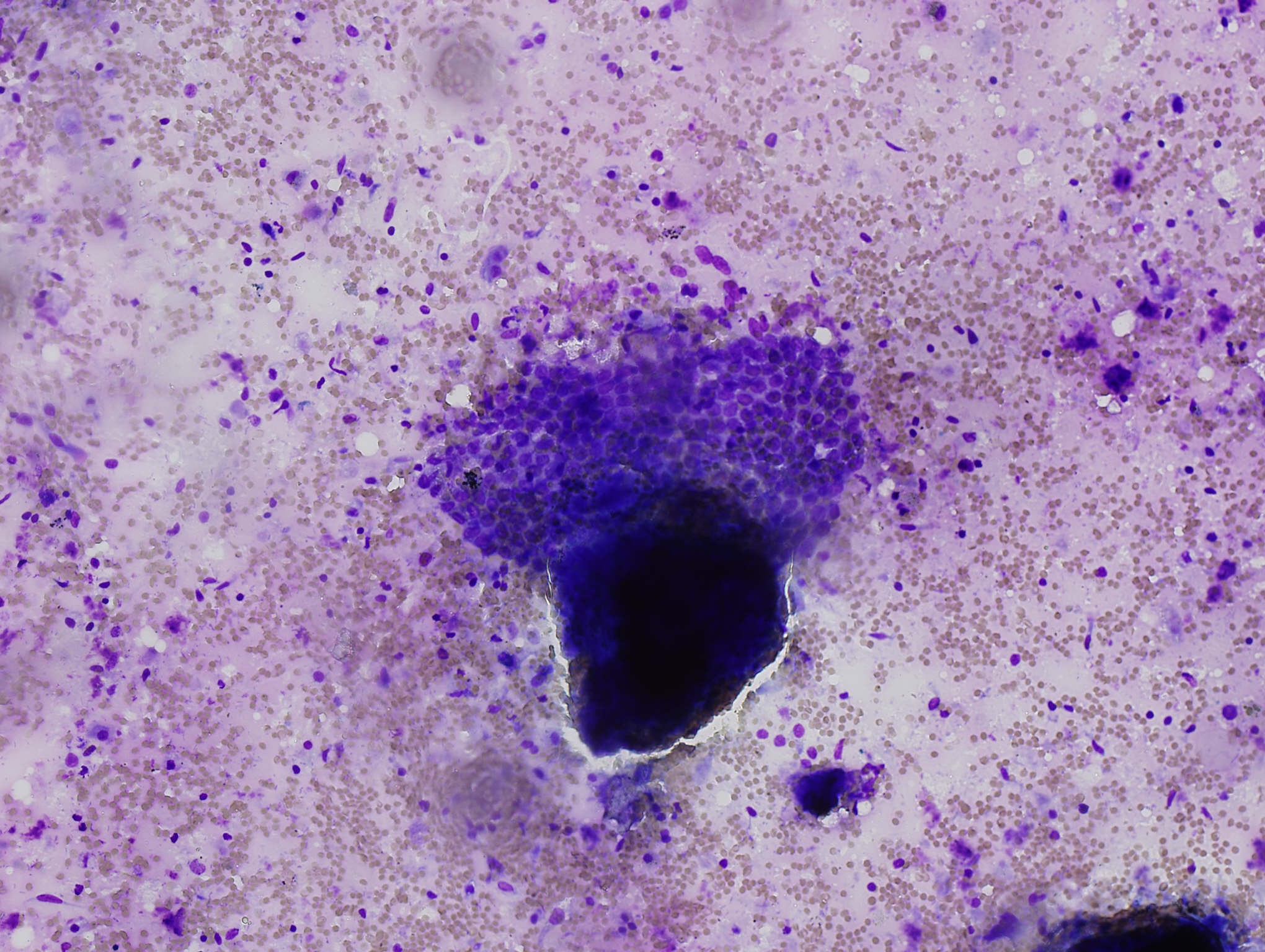
- Purulent inflammation in respiratory cytology specimen (e.g., bronchoalveolar lavage [BAL], pleural effusion) is suggestive of bacterial pneumonia
- Bacterial culture from respiratory specimens is required for proper treatment and epidemiological data (nosocomial infection):
- Sputum
- Invasive respiratory tract sample: bronchoalveolar lavage
- Others: pleural fluid, lung tissue
- Multiplex polymerase chain reaction (PCR) is commercially available for detection of common respiratory pathogens, including virus and bacteria (J Microbiol Immunol Infect 2019;52:920)
- Rapid nasal swab for methicillin resistant Staphylococcus aureus (MRSA) PCR can be used to guide therapy (Antimicrob Agents Chemother 2014;58:859)
- Tissue culture at autopsy (J Clin Microbiol 2014;52:1028):
- Specimen should be obtained with sterile forceps and scalpel to avoid contamination and within 24 - 48 hours of death
- Lung tissue specimens should be obtained with the organs being in situ and the organ surface should be sterilized
- Even with the above precautions, cultures obtained during the autopsy procedure have limited value because of the high possibility of contamination and postmortem bacterial transmigration
- Contamination is likely to occur from flora in upper respiratory tract migrating through bronchial secretion
- Up to 50% tested positive for some organism(s), despite the lack of any further pathological evidence of infection
- Blood culture:
- 15% of patients with VAP are bacteremic (Surg Infect (Larchmt) 2014;15:77)
- Complete blood count: leukocytosis (white cells > 10,000/uL)
- Urinary antigen for Streptococcus pneumoniae:
- Should only be performed in adults with severe CAP (Am J Respir Crit Care Med 2019;200:e45)
- Sensitivities: 86 - 90%, specificity: 71 - 94% (Clin Lab Med 2014;34:219)
- Not recommended on individuals vaccinated against pneumococcus in the last 5 days
- Common signs of bacterial pneumonia (AJR Am J Roentgenol 2014;202:479):
- Consolidation:
- Alveolar filling process that replaces air within the affected airspaces
- Increasing in pulmonary attenuation and obscuring the margins of adjacent airways and vessels
- Air bronchogram:
- Visible air filled bronchi surrounded by dense, consolidated lung parenchyma
- Normal lung: air filled bronchi are not visible because they are surrounded by aerated lung parenchyma
- Differential diagnosis: nonobstructive atelectasis, aspiration and neoplasms
- Silhouette sign:
- Loss of a normal lung - soft tissue interface (loss of silhouette)
- Commonly applied to the interface between the lungs and the heart, mediastinum, chest wall and diaphragm
- Caused by any pathologic mechanism that replaces or displaces air within the lung parenchyma
- Tree in bud opacity:
- Visible small airways or terminal bronchioles filled with mucus, pus, fluid or cells, forming impactions that resemble a budding tree with branching nodular V and Y shaped opacities
- Split pleura sign:
- Visible thickened visceral and parietal pleura with fluid collection in between
- Suggests the presence of empyema
- Consolidation:
- Typical appearance of pneumonia on chest radiograph and CT scan (Diagn Interv Imaging 2012;93:431):
- Lobar pneumonia: subpleural area of alveolar consolidation with blurred margins, which is restricted to the area next to the fissures, then progresses to a systematized segmental opacity affecting 1 or several contiguous segments or a lobe
- Bronchopneumonia: centrilobular micronodules with blurred margin, areas of ground glass opacity or peribronchiolar consolidation with an acinar pattern and later progress to lobular, segmental or lobar consolidation
- Accompanied by pleural effusions (20 - 60% of bacterial pneumonia)
- Aspiration pneumonia (J Crit Care 2015;30:40):
- New chest radiograph infiltrate in a dependent pulmonary segment
- Bed bound patient: posterior segments of the upper lobes and the superior segments of the lower lobes
- Ambulatory patient: lower lobes, especially the right lung
- ATS / IDSA criteria for severe CAP patients who require admission to an intensive care unit (Am J Respir Crit Care Med 2019;200:e45):
- Major criteria:
- Septic shock with need for vasopressor
- Respiratory failure requiring mechanical ventilation
- Minor criteria - at least 3 of the following:
- Altered mental status
- Hypotension requiring fluid support
- Temperature: < 36 °C (96.8 °F)
- Respiratory rate: ≥ 30 breaths/minute
- PaO2/FiO2 ratio: ≤ 250
- Blood urea nitrogen: ≥ 20 mg/dL (blood urea 7 mmol/L)
- Leukocyte count: < 4,000/uL
- Platelet count: < 100,000/uL
- Multilobar infiltrates
- Major criteria:
- Pneumonia severity index (PSI): prognostic tool for the evaluation of immunocompetent patients with CAP (N Engl J Med 1997;336:243)
- CURB-65 score is a prognostic tool based on 5 factors (Thorax 2003;58:377):
- Confusion (disorientation to person, place or time)
- Blood urea nitrogen: > 7 mmol/L (20 mg/dL)
- Respiratory rate: ≥ 30/minute
- Blood pressure: systolic < 90 mmHg or diastolic ≤ 60 mmHg
- Age: ≥ 65 years
- Risk factors associated with increased mortality rate in HAP / VAP (Clin Infect Dis 2016;63:e61):
- Multidrug resistant pathogen
- Bacteremia
- Inadequate / inappropriate antibiotic therapy
- 44 year old man with hemoptysis and back pain (Autops Case Rep 2014;4:31)
- 48 year old man with progressive dyspnea (Autops Case Rep 2019;9:e2019106)
- 62 year old man with fatigue (Intern Med 2012;51:2463)
- 63 year old woman with chronic lymphocytic leukemia and respiratory failure (Autops Case Rep 2016;6:11)
- 64 year old man with fever, sore throat and arthralgia (BMC Infect Dis 2020;20:892)
- 73 year old man with ischemic heart disease (BMJ Case Rep 2014;2014:bcr2014205907)
- 74 year old man with respiratory symptoms and large pulmonary valve vegetation (J Med Case Rep 2019;13:97)
- Antibiotics for CAP (Am J Respir Crit Care Med 2019;200:e45):
- Healthy outpatient adults: amoxicillin, doxycycline or macrolide (azithromycin, clarithromycin)
- Outpatient adults with comorbidities:
- Combination therapy (amoxicillin / clavulanate, cefpodoxime or cefuroxime and macrolide)
- Monotherapy (levofloxacin, moxifloxacin or gemifloxacin)
- Inpatient:
- Combination therapy (ampicillin + sulbactam, cefotaxime, ceftriaxone or ceftaroline and macrolide)
- Monotherapy (levofloxacin or moxifloxacin)
- Antibiotics for HAP / VAP (Clin Infect Dis 2016;63:e61):
- Piperacillin / tazobactam, cefepime, levofloxacin or imipenem + meropenem
- Plus vancomycin of linezolid if methicillin resistant S. aureus is likely
- VAP: consider antibiotics coverage for S. aureus, P. aeruginosa and other gram negative bacilli
- Piperacillin / tazobactam, cefepime, levofloxacin or imipenem + meropenem
- Respiratory support
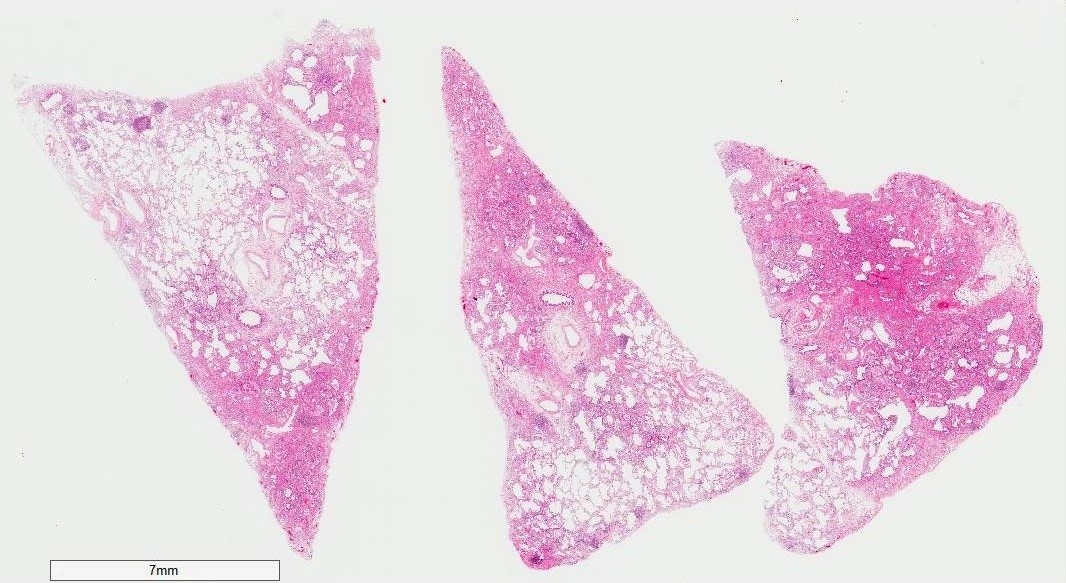
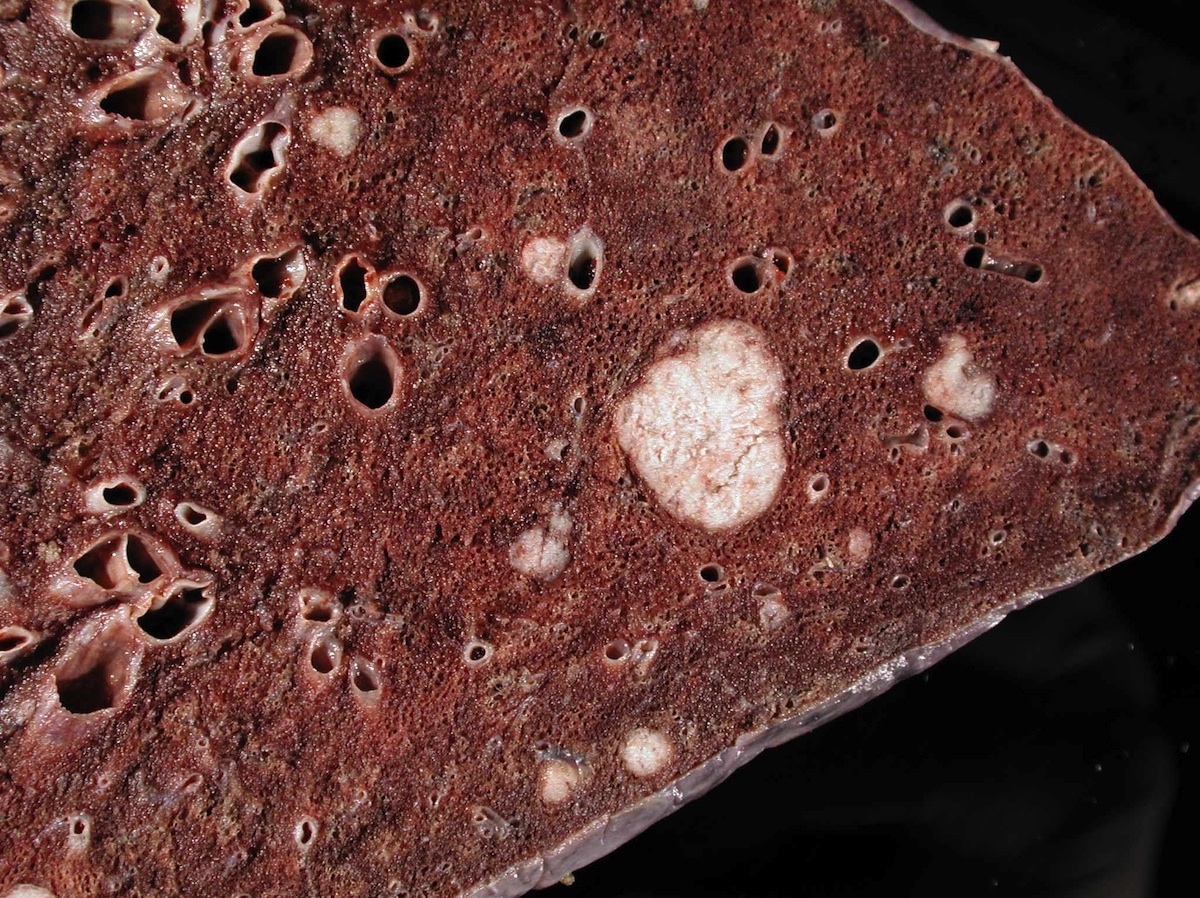
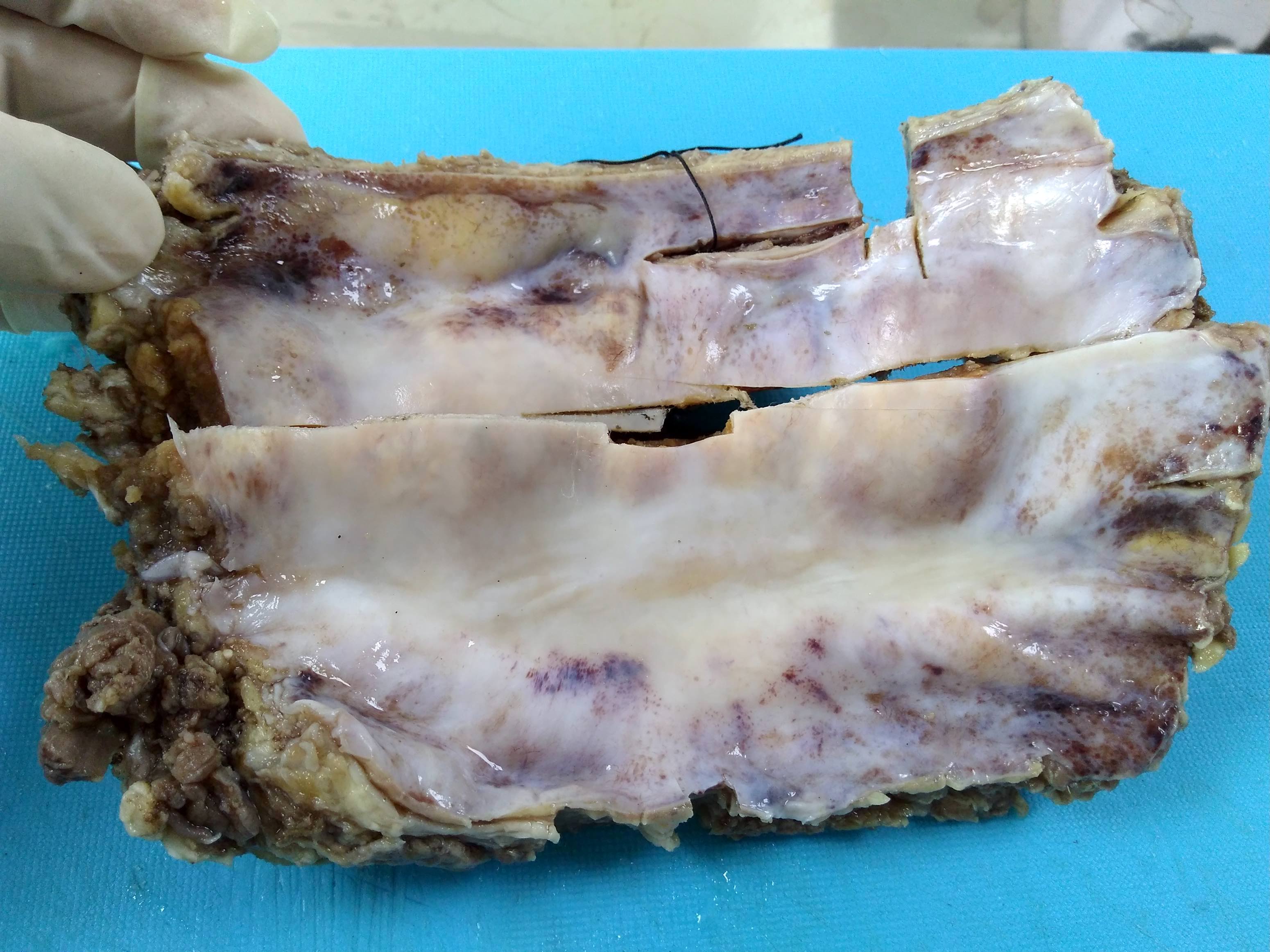
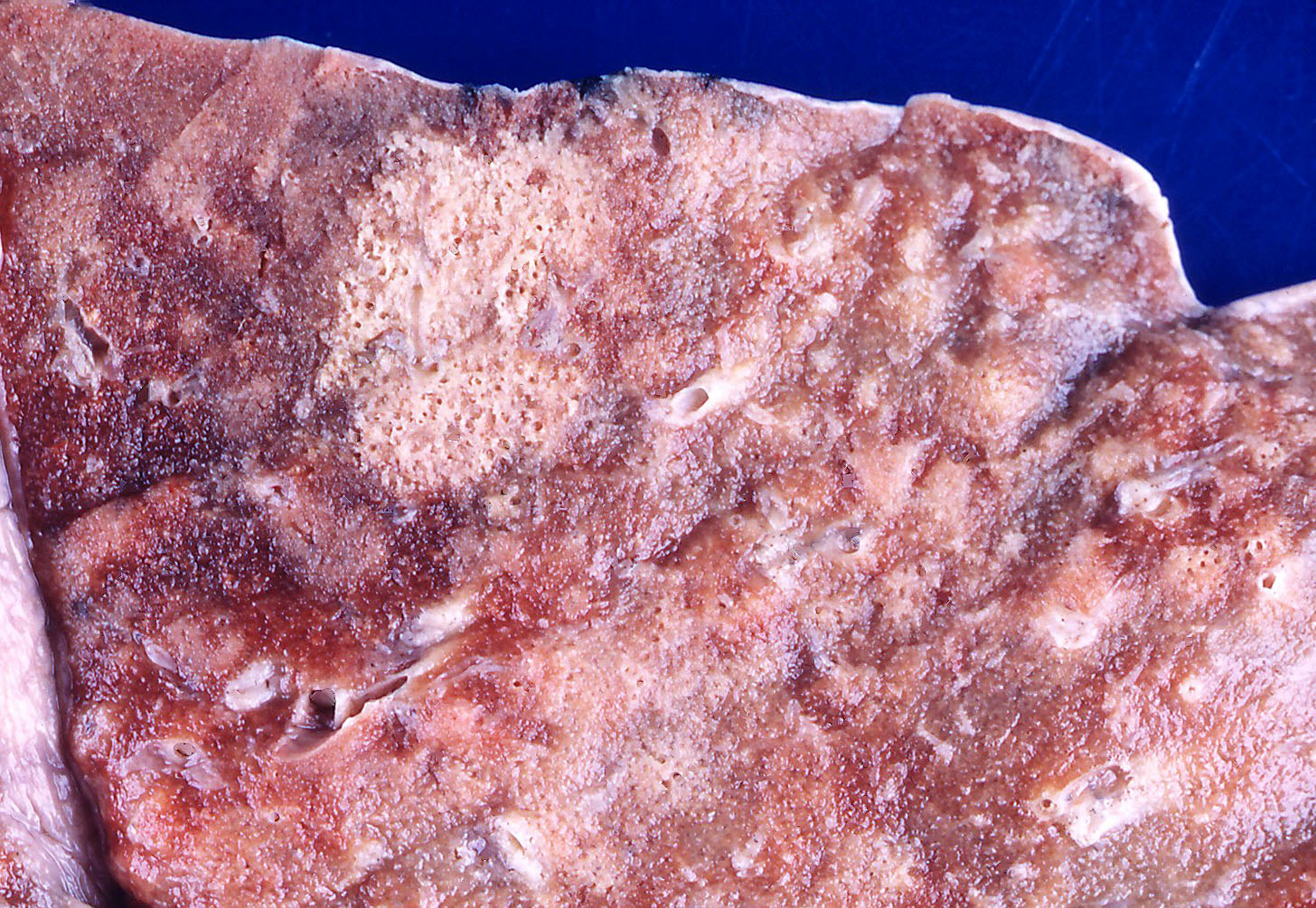
- Lobar pneumonia:
- Characteristic for S. pneumoniae and K. pneumoniae
- Uniform involvement of the whole lobe
- Increased weight of the lung
- 4 stages of inflammatory response (Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020):
- Congestion: heavy, boggy, red lung
- Red hepatization: red, firm and airless, with liver-like consistency
- Gray hepatization: grayish brown color on cut
- Resolution
- Slimy mucoid appearance is characteristic for Klebsiella spp.
- Bronchopneumonia:
- Consolidation may be confined to 1 lobe or involve multiple lobes, poorly defined, gray-red to yellow in color
- Cavitary lesion
- Common in S. aureus, P. aeruginosa
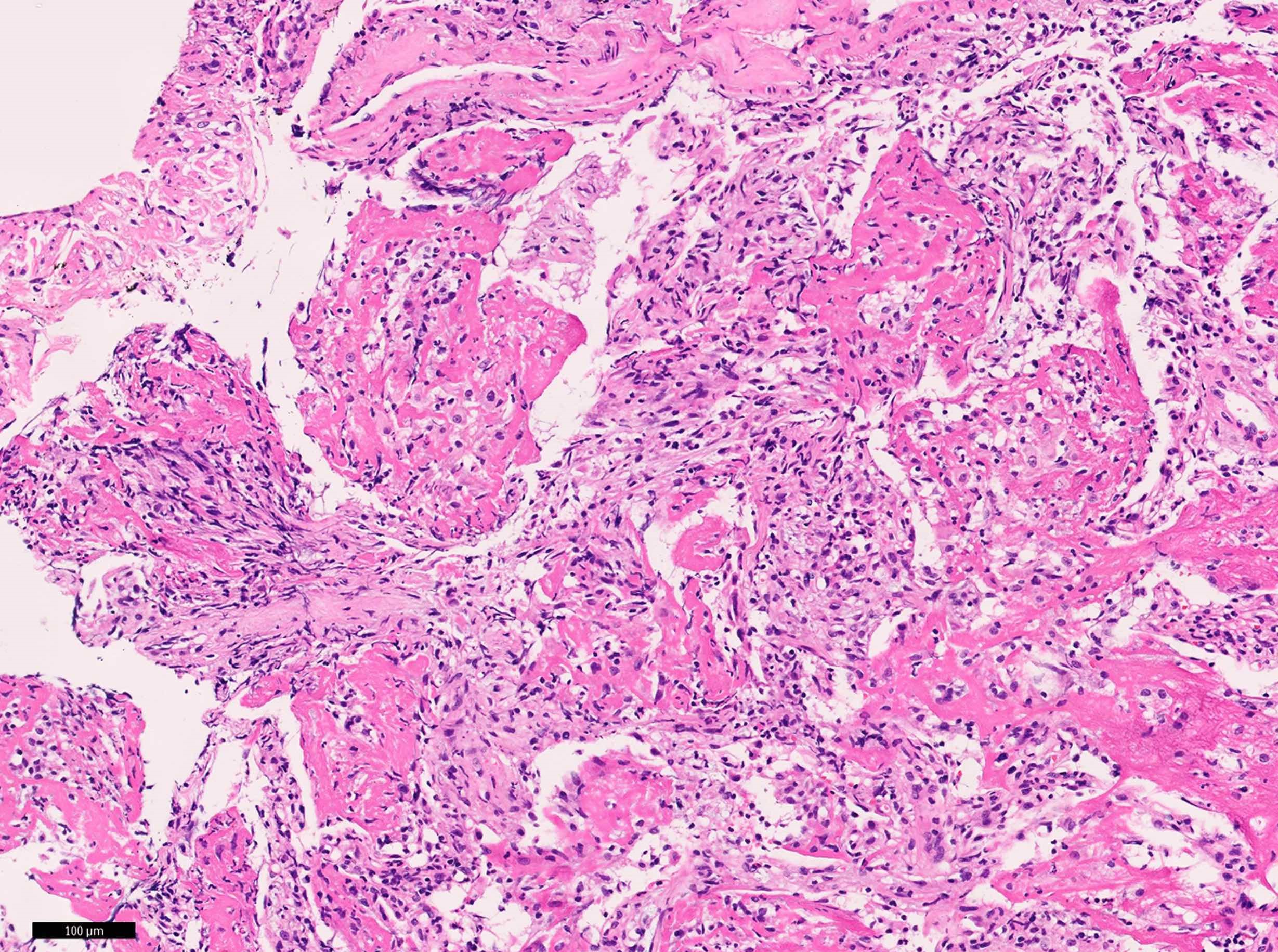
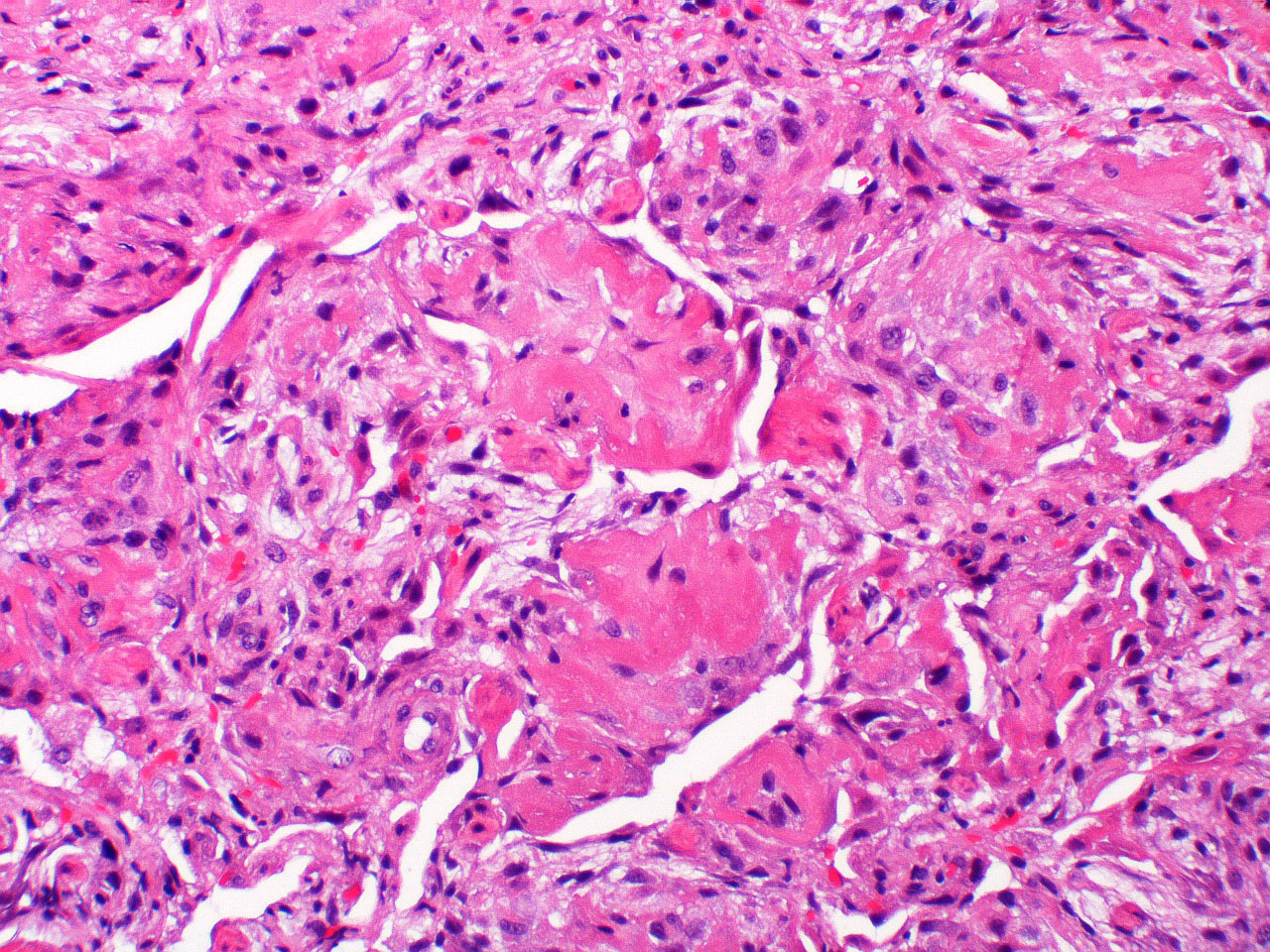
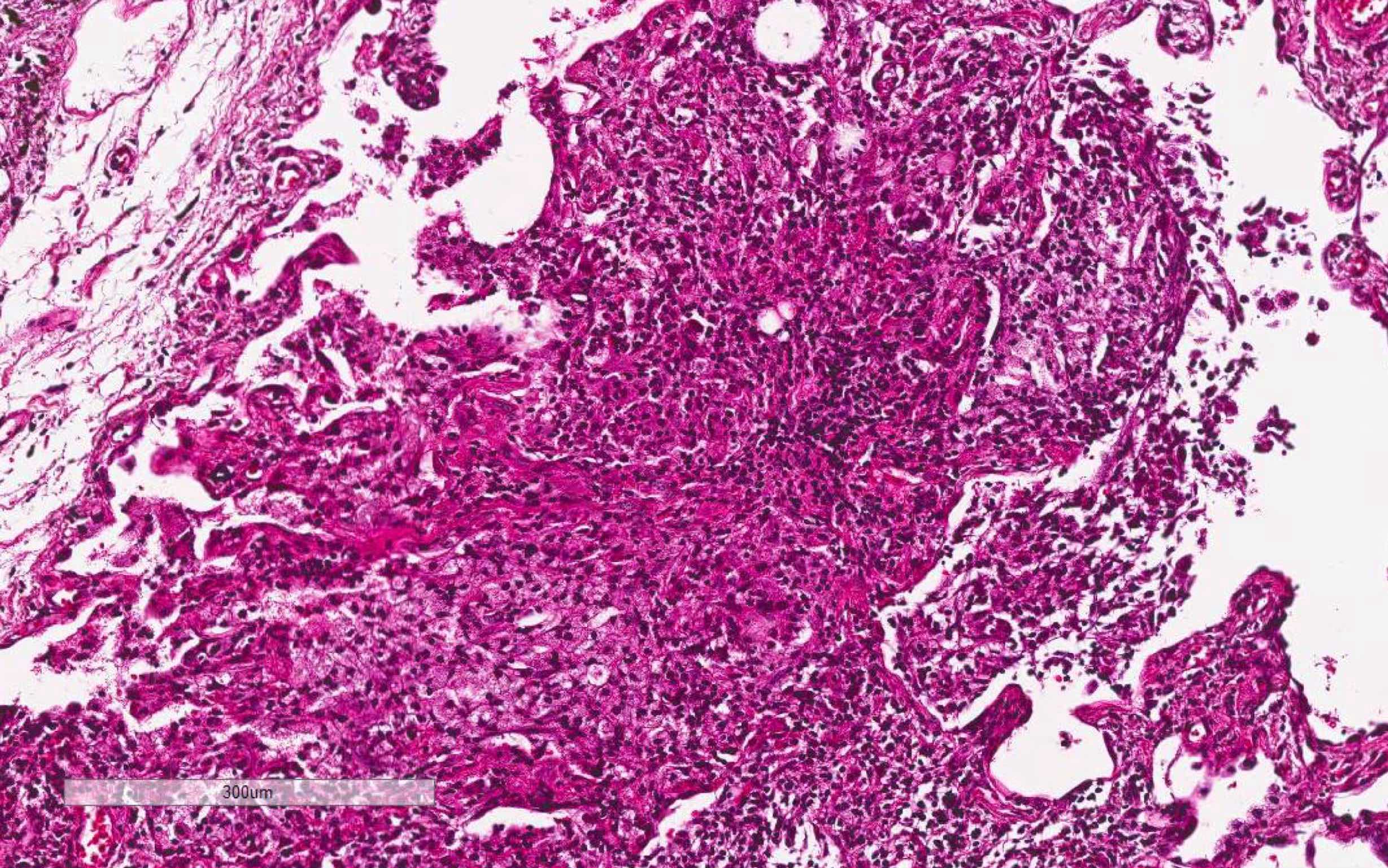
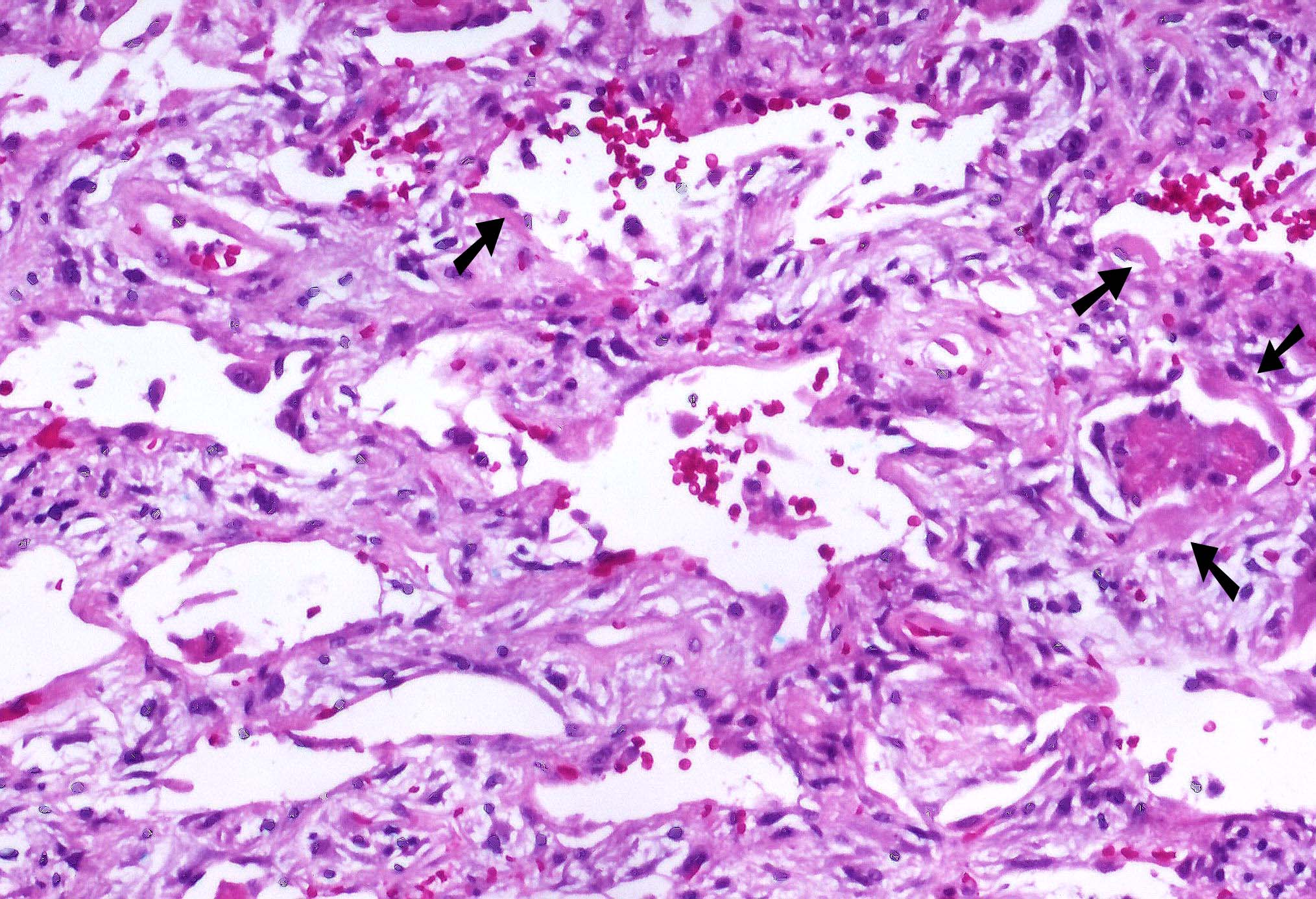
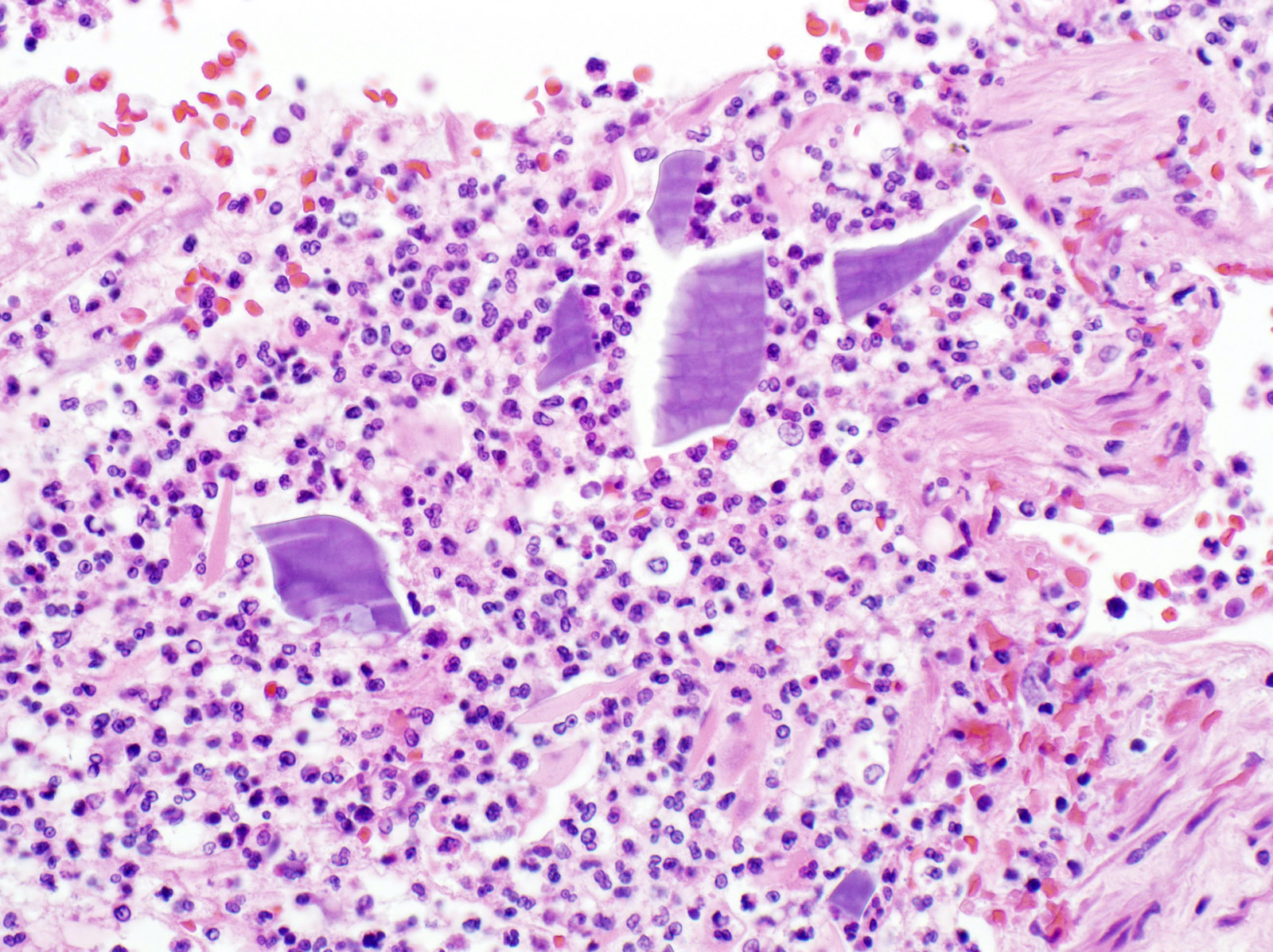
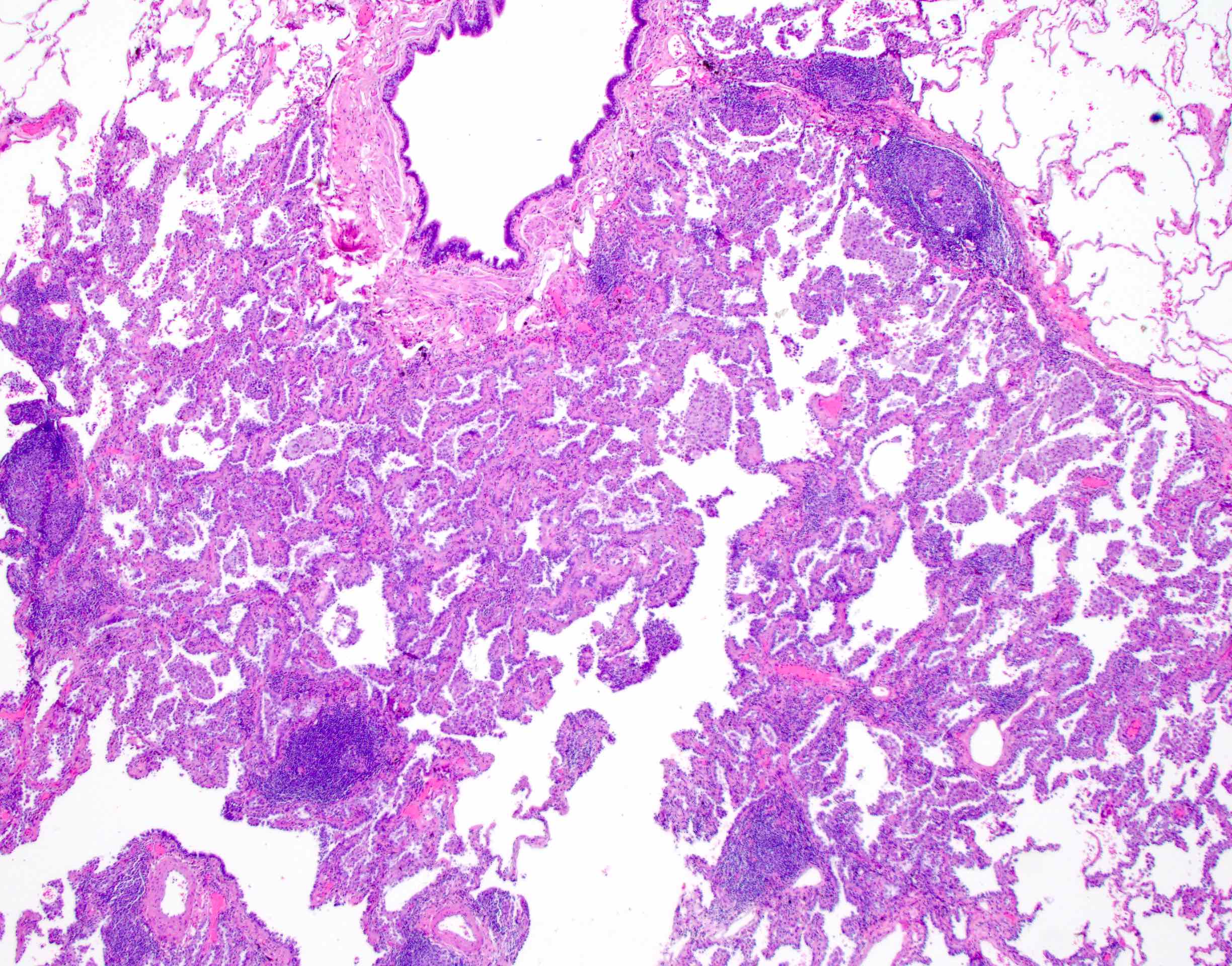
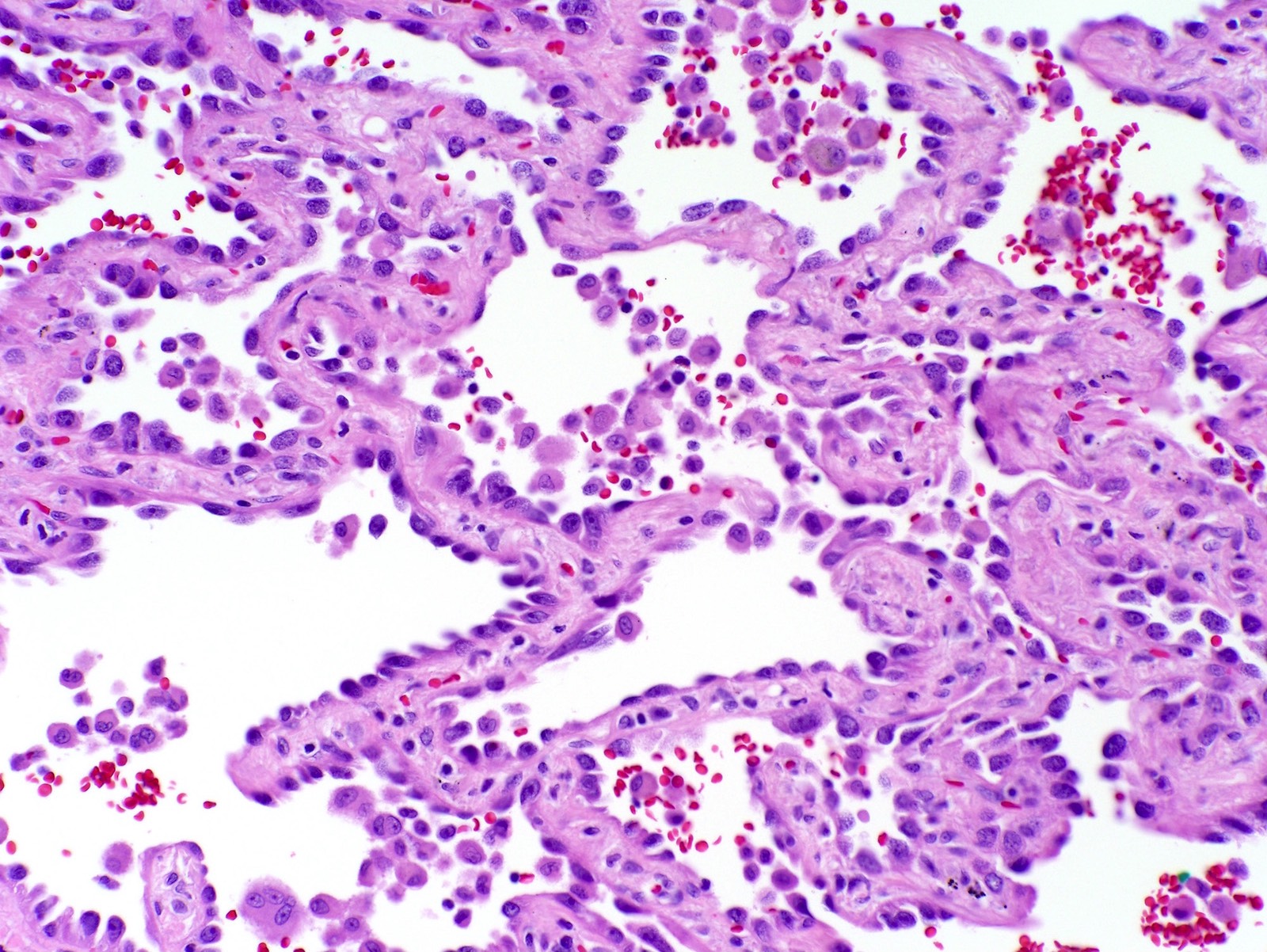
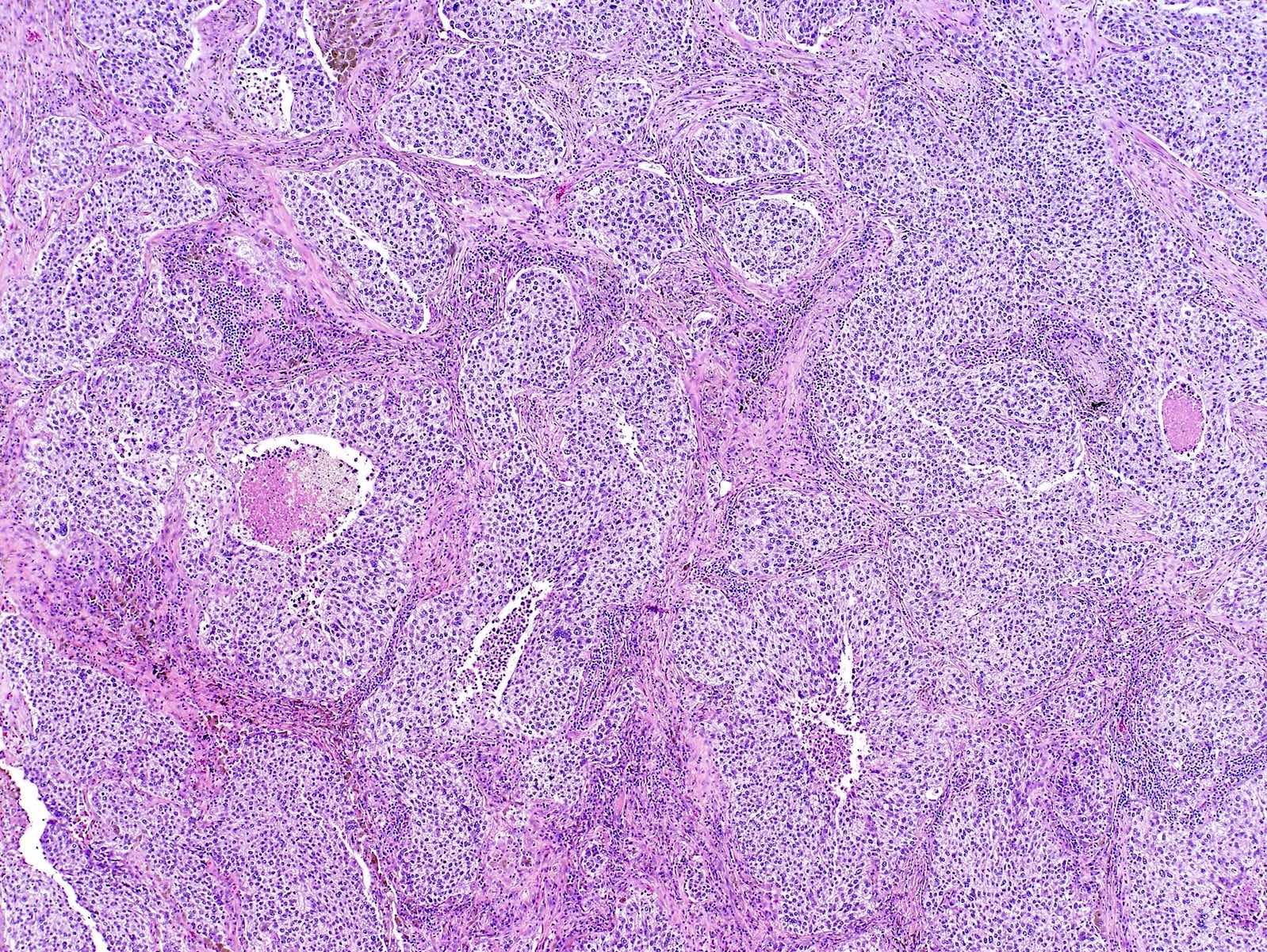
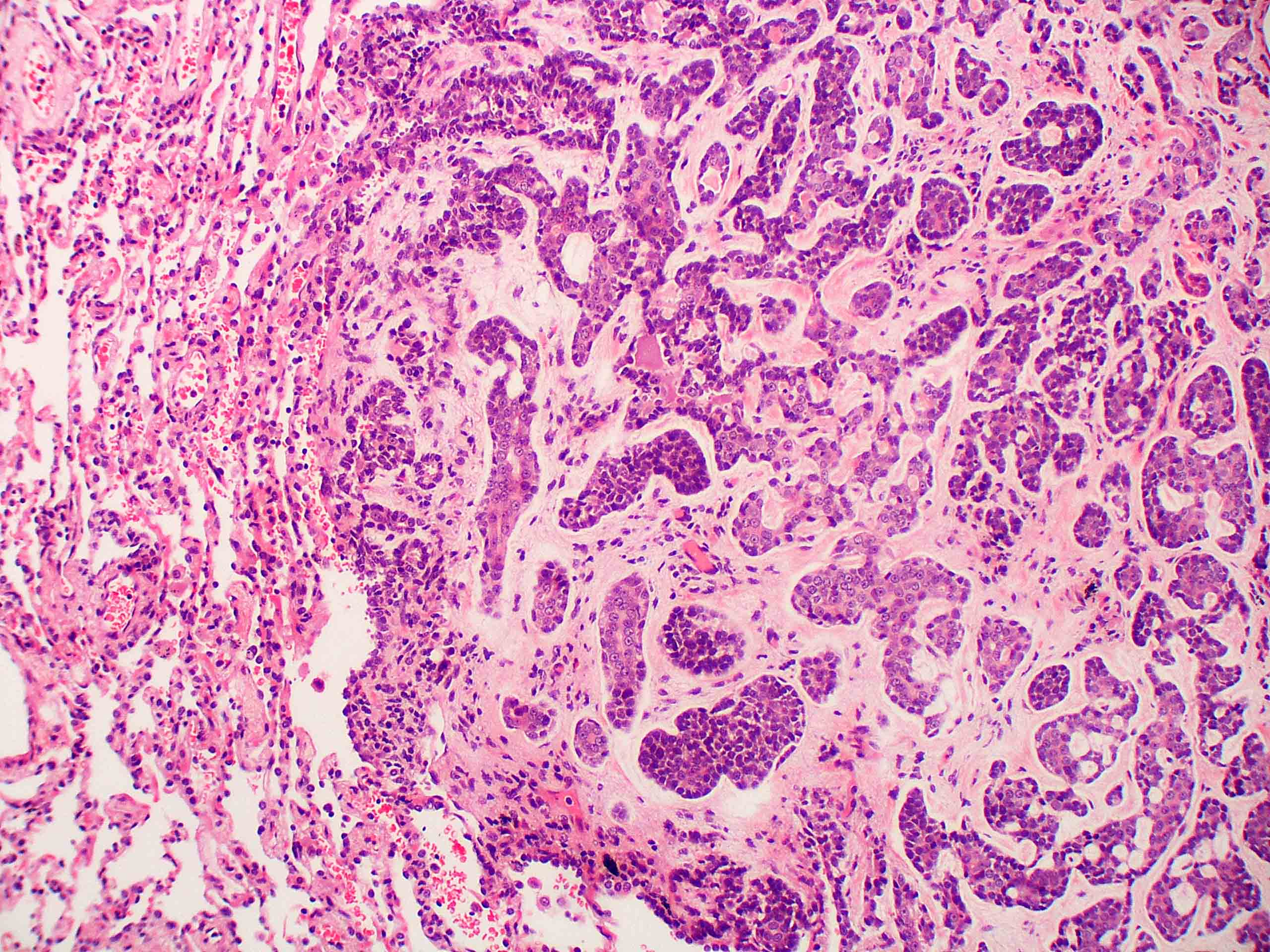
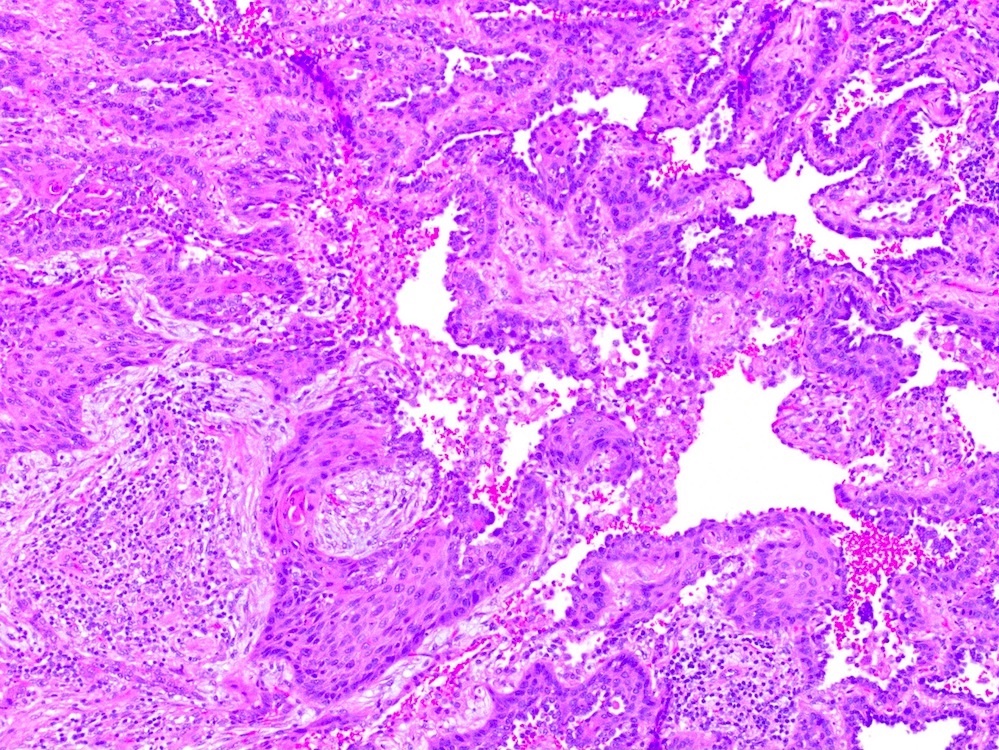
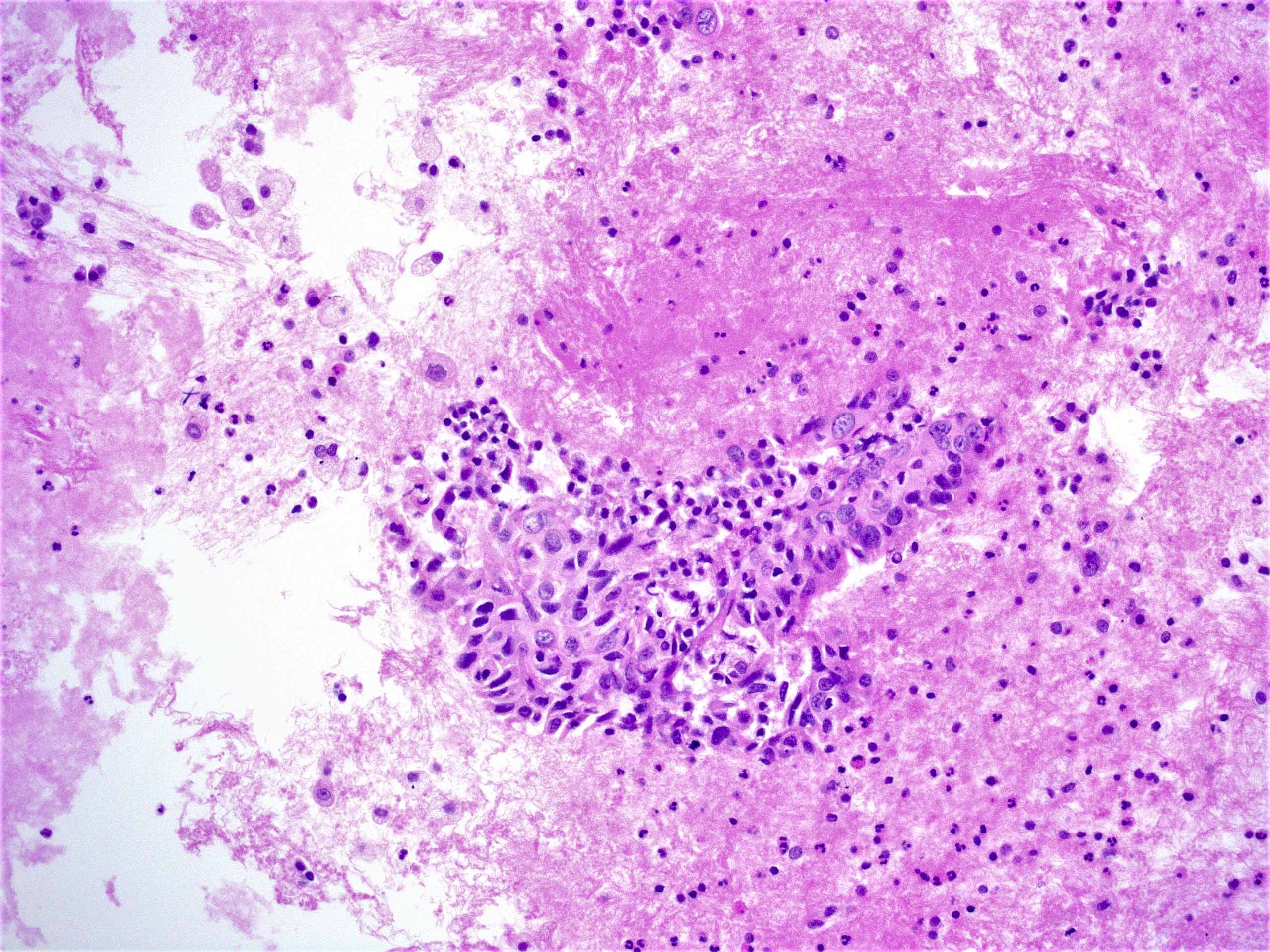
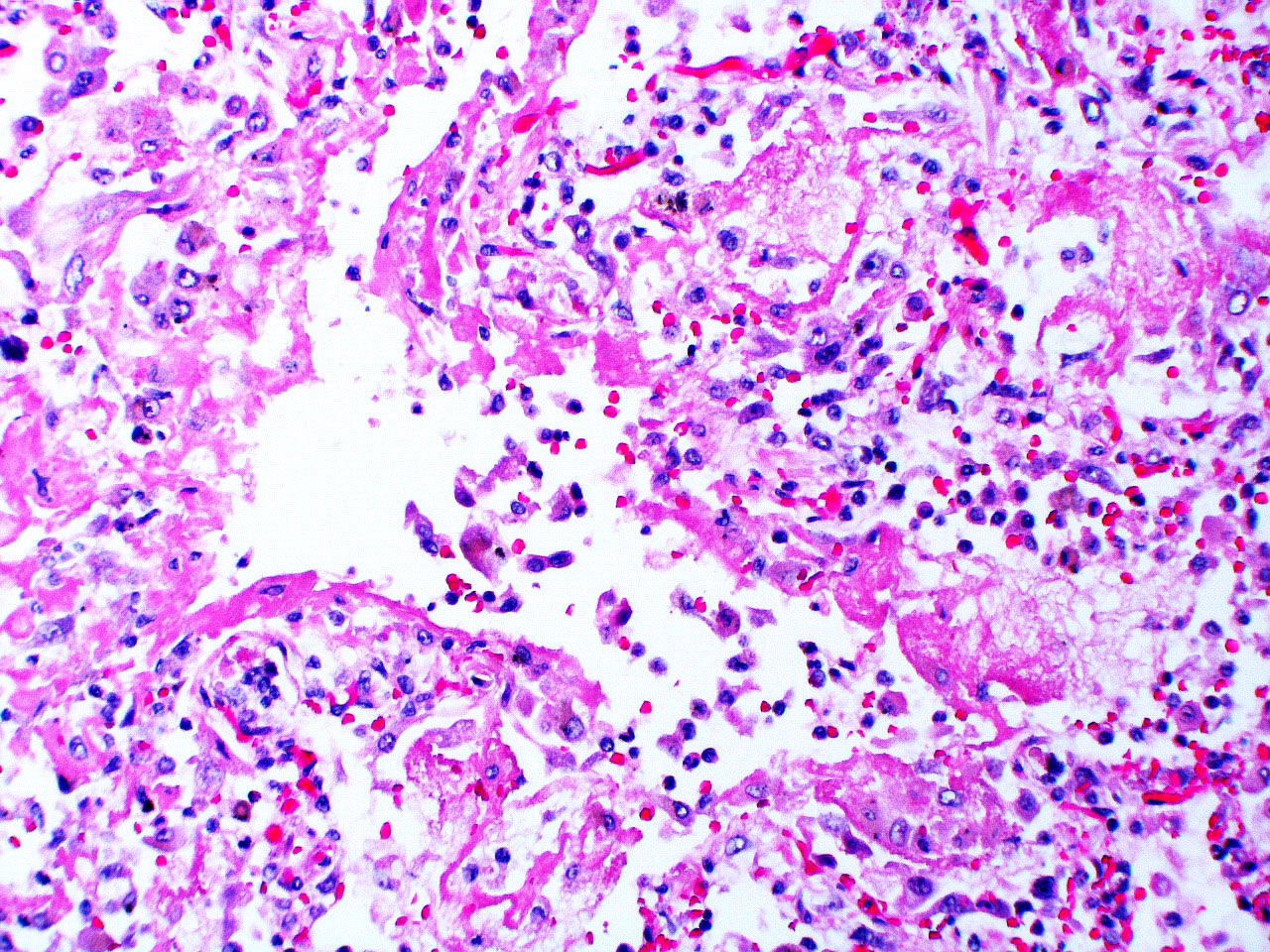
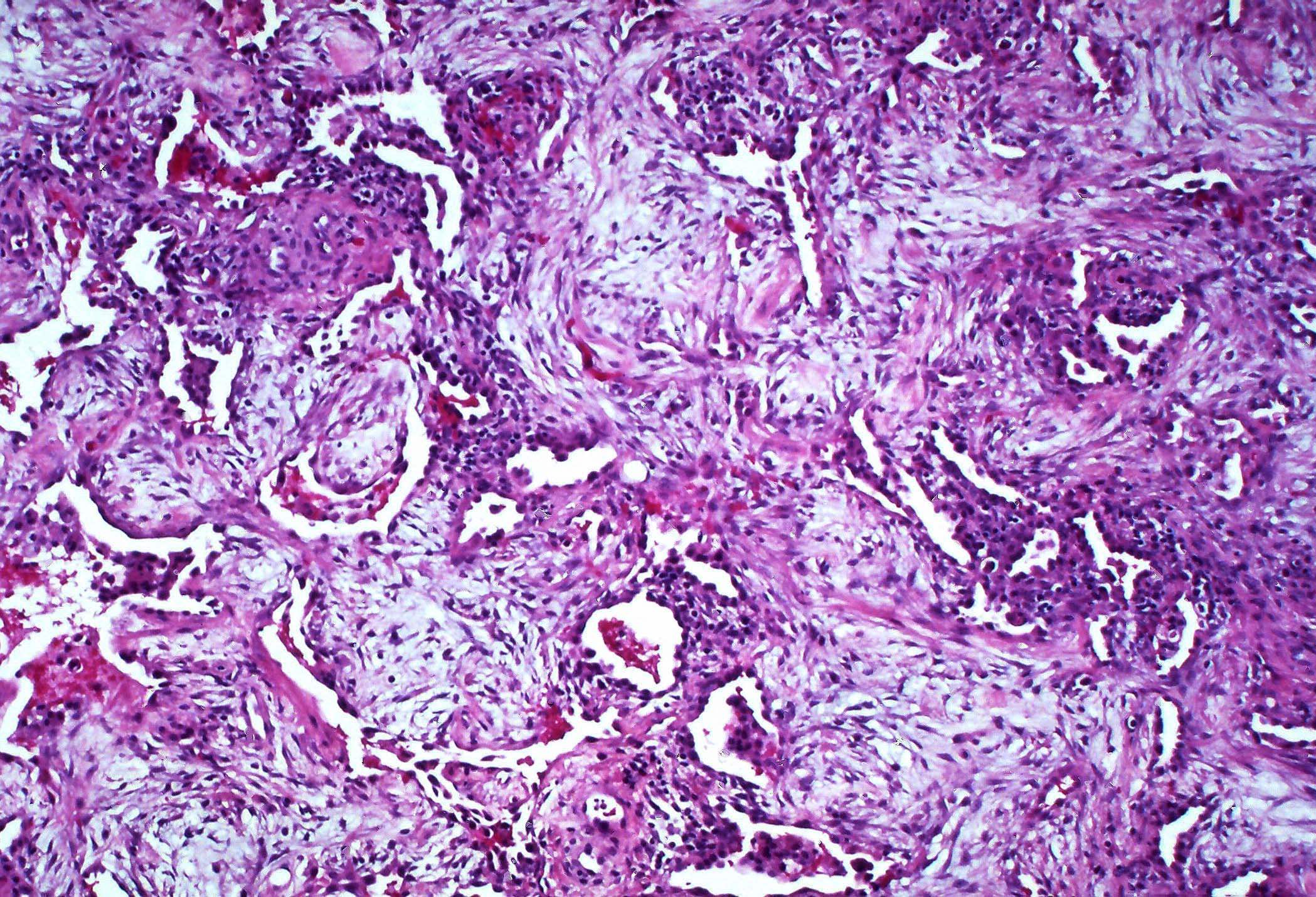
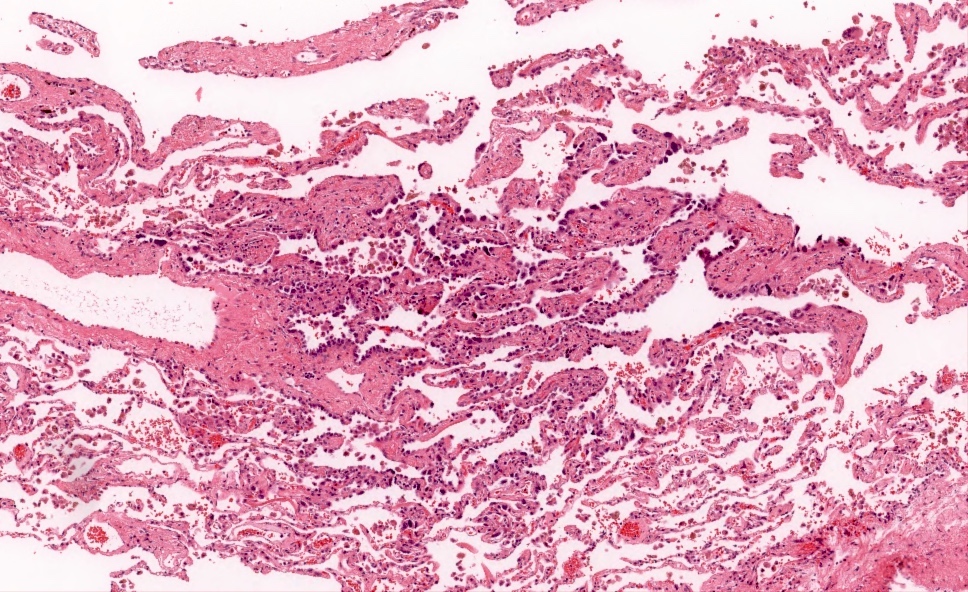
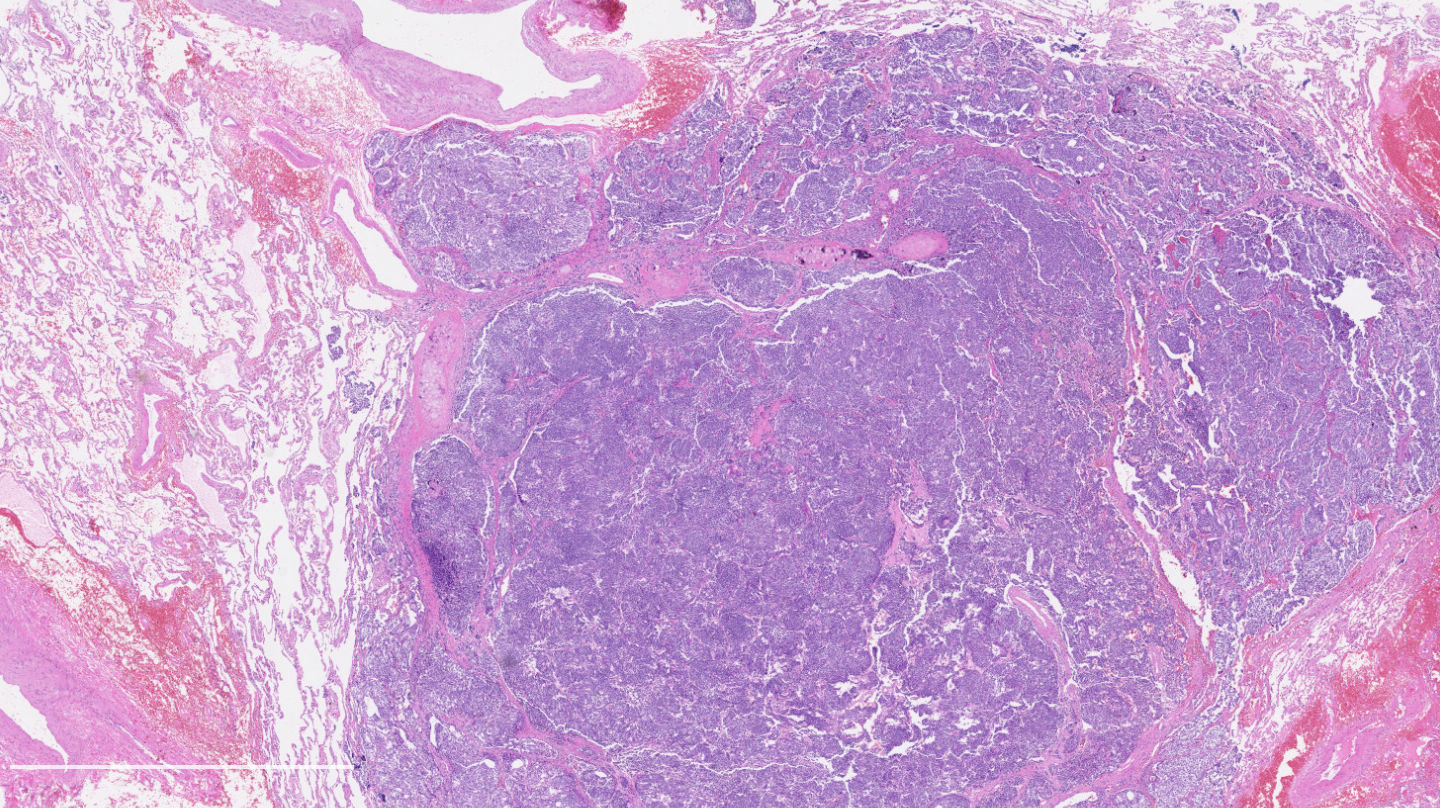
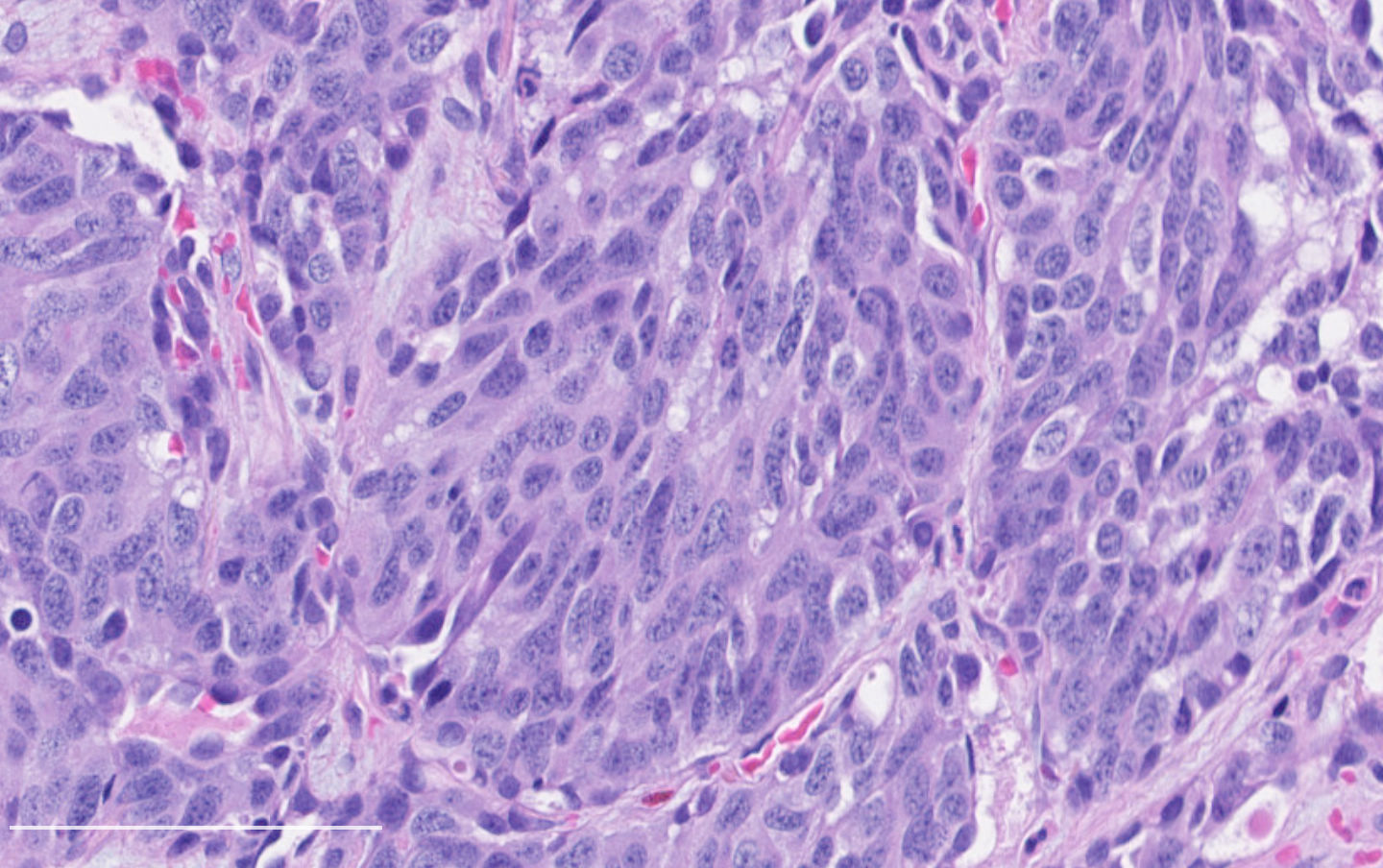
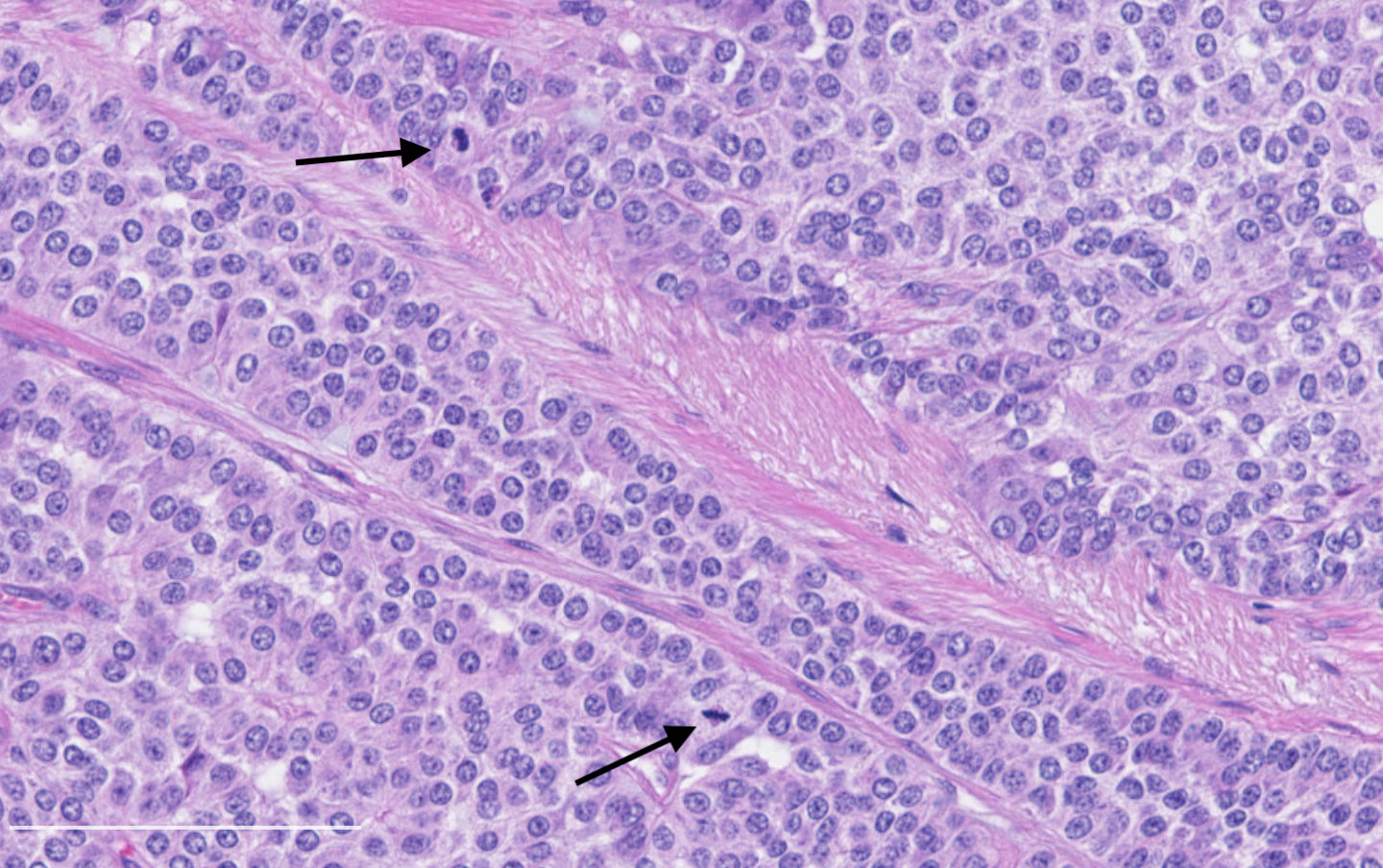
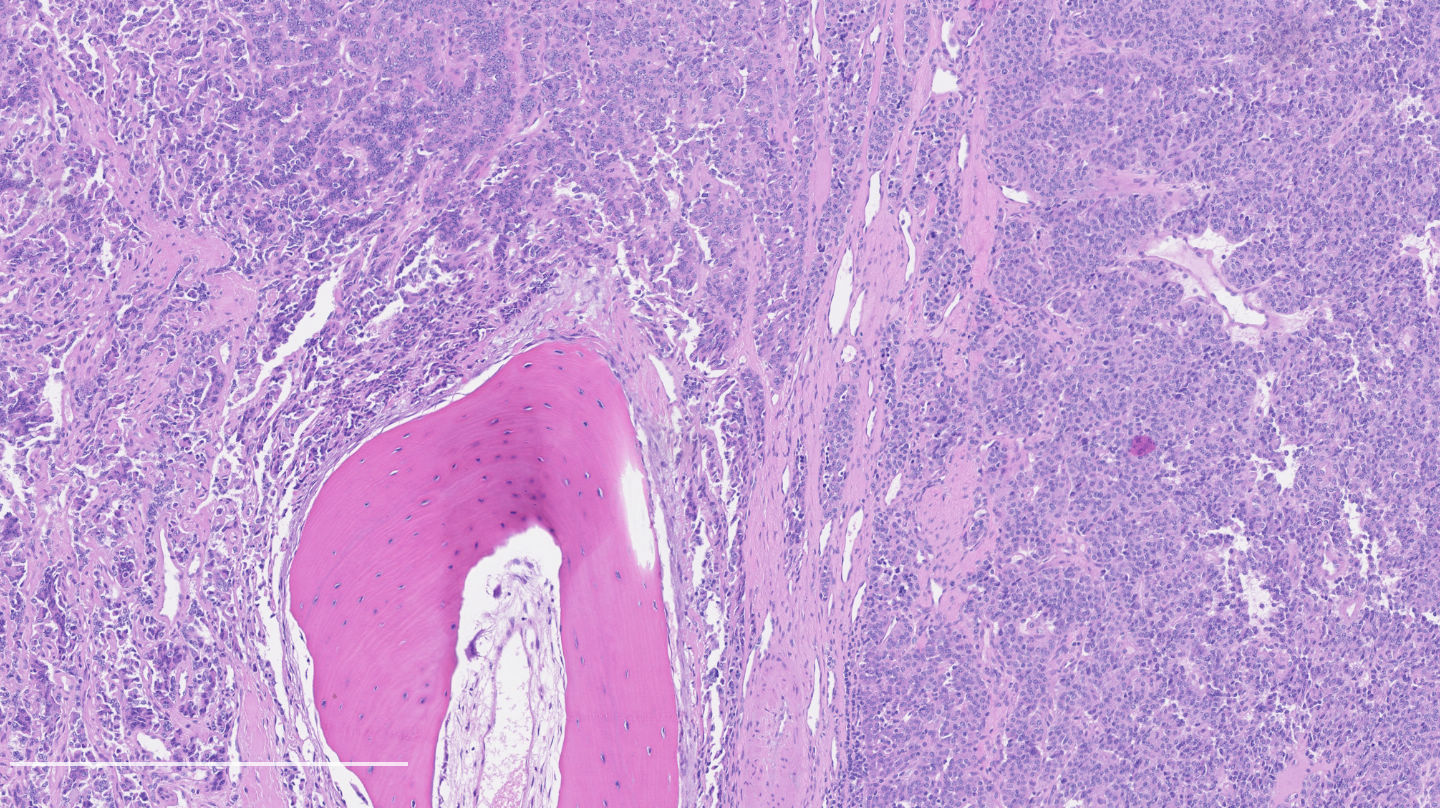
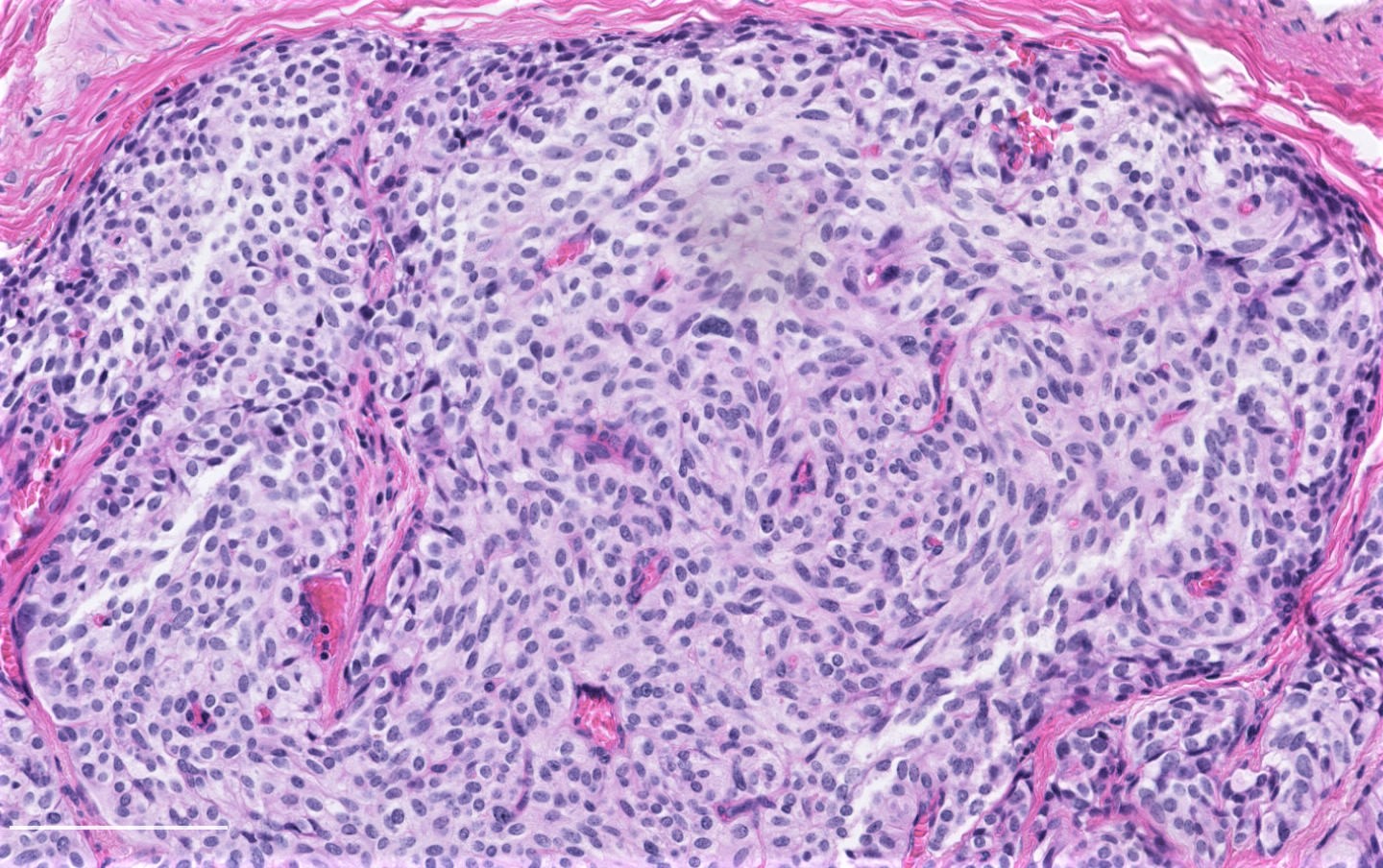
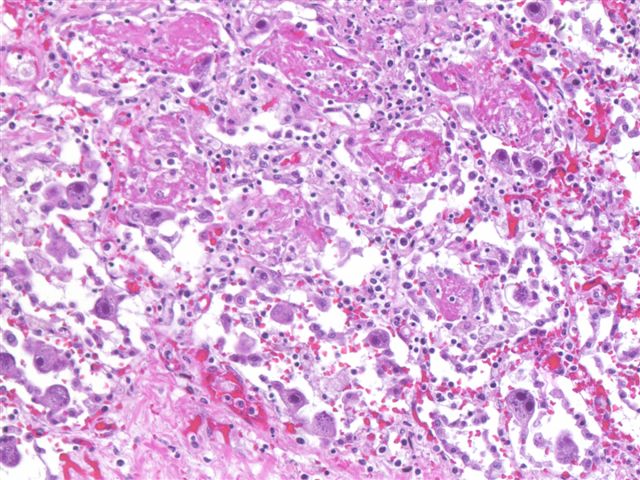
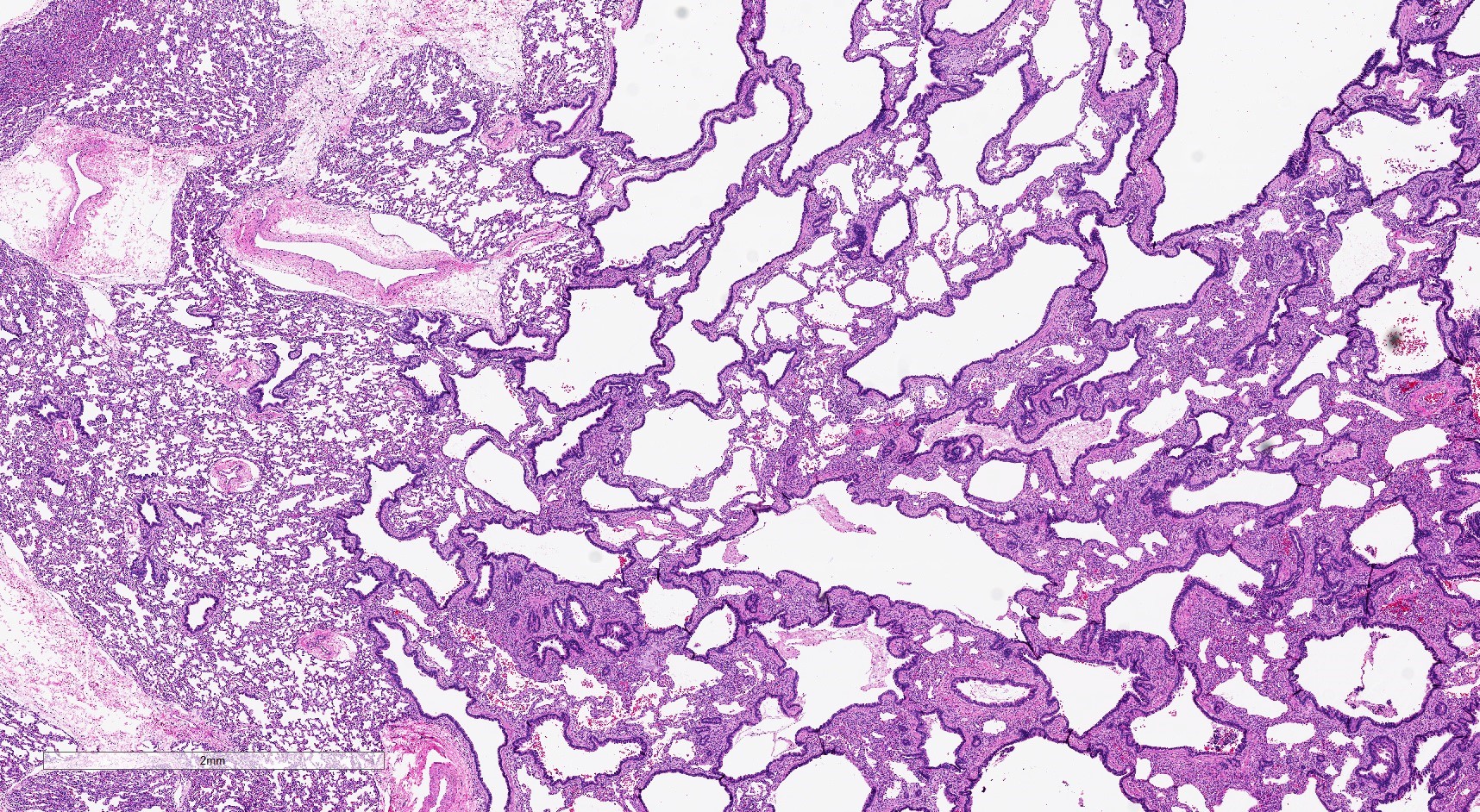
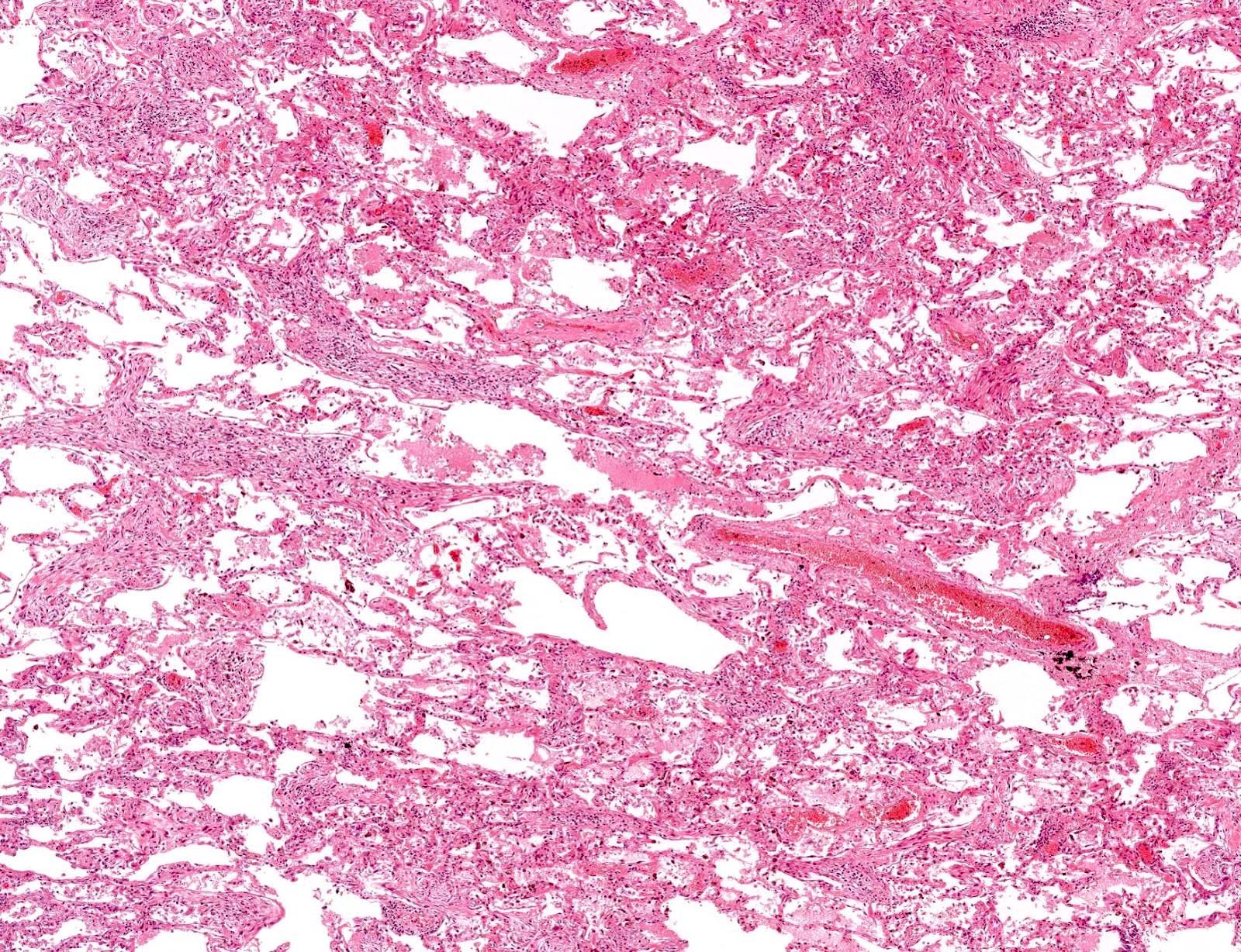
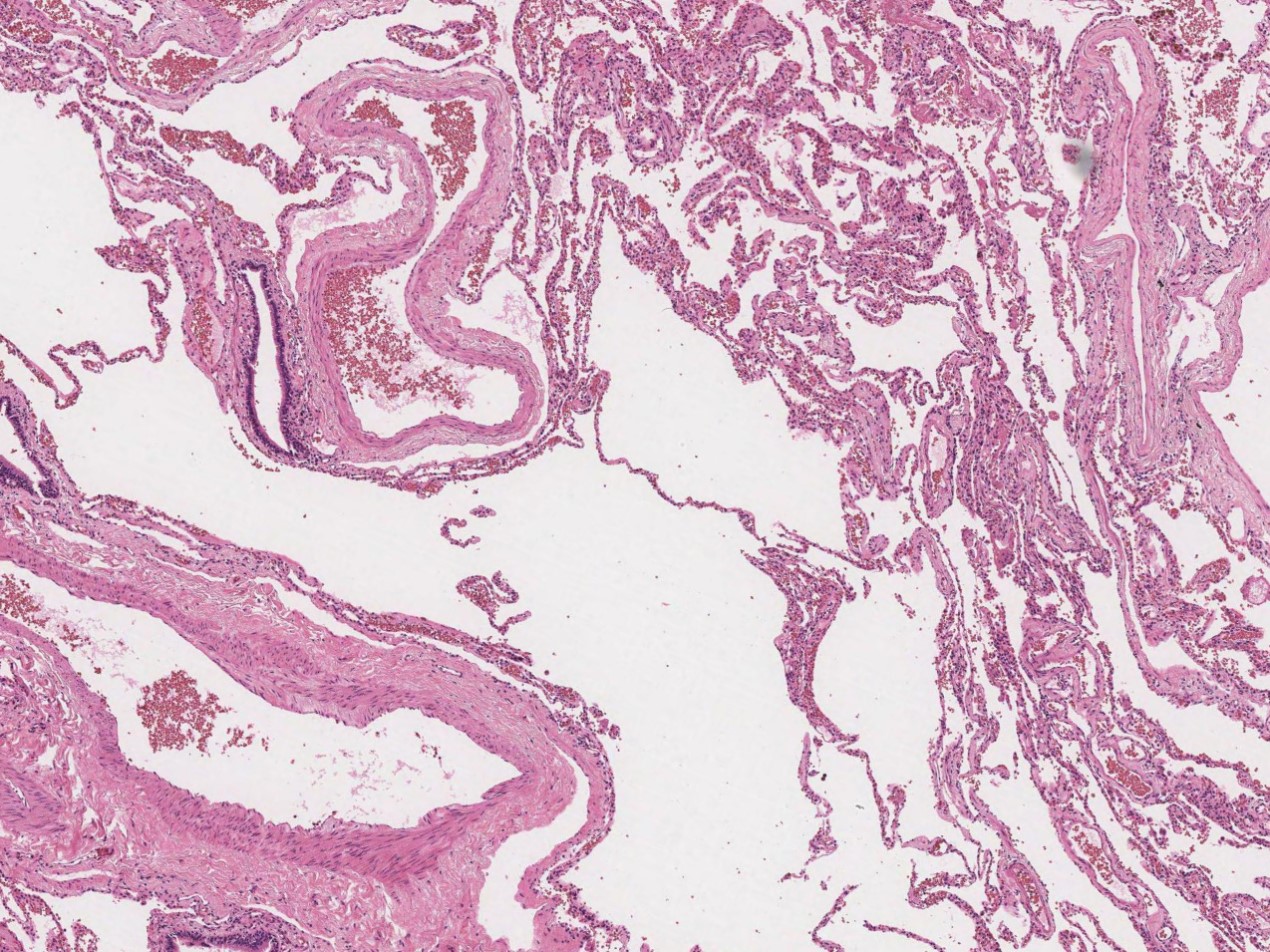
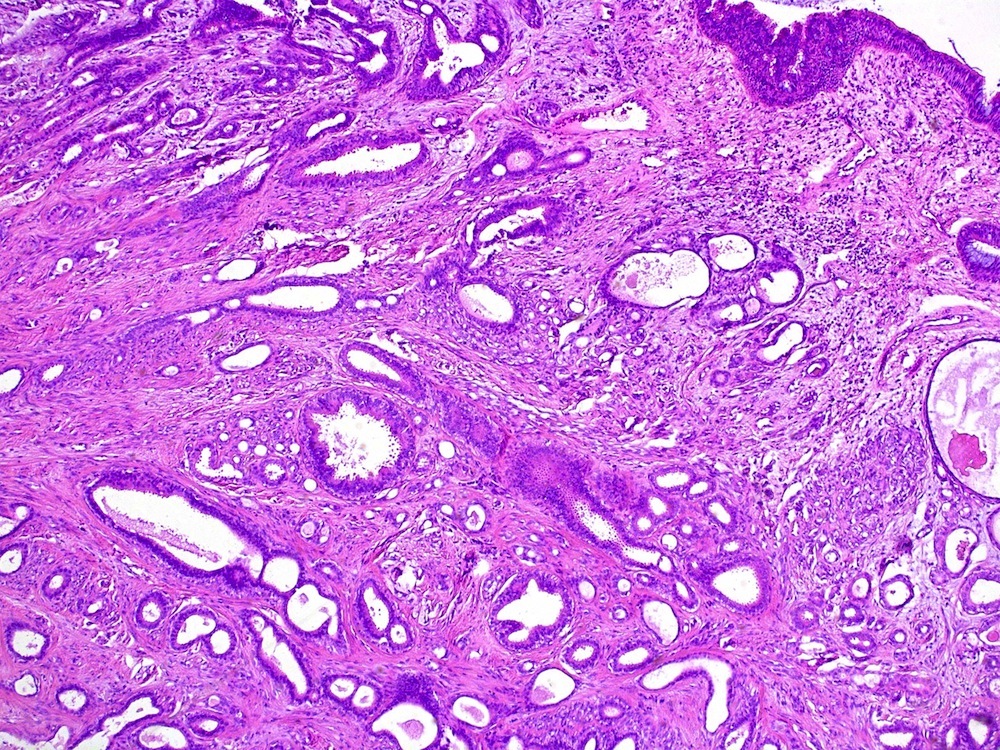
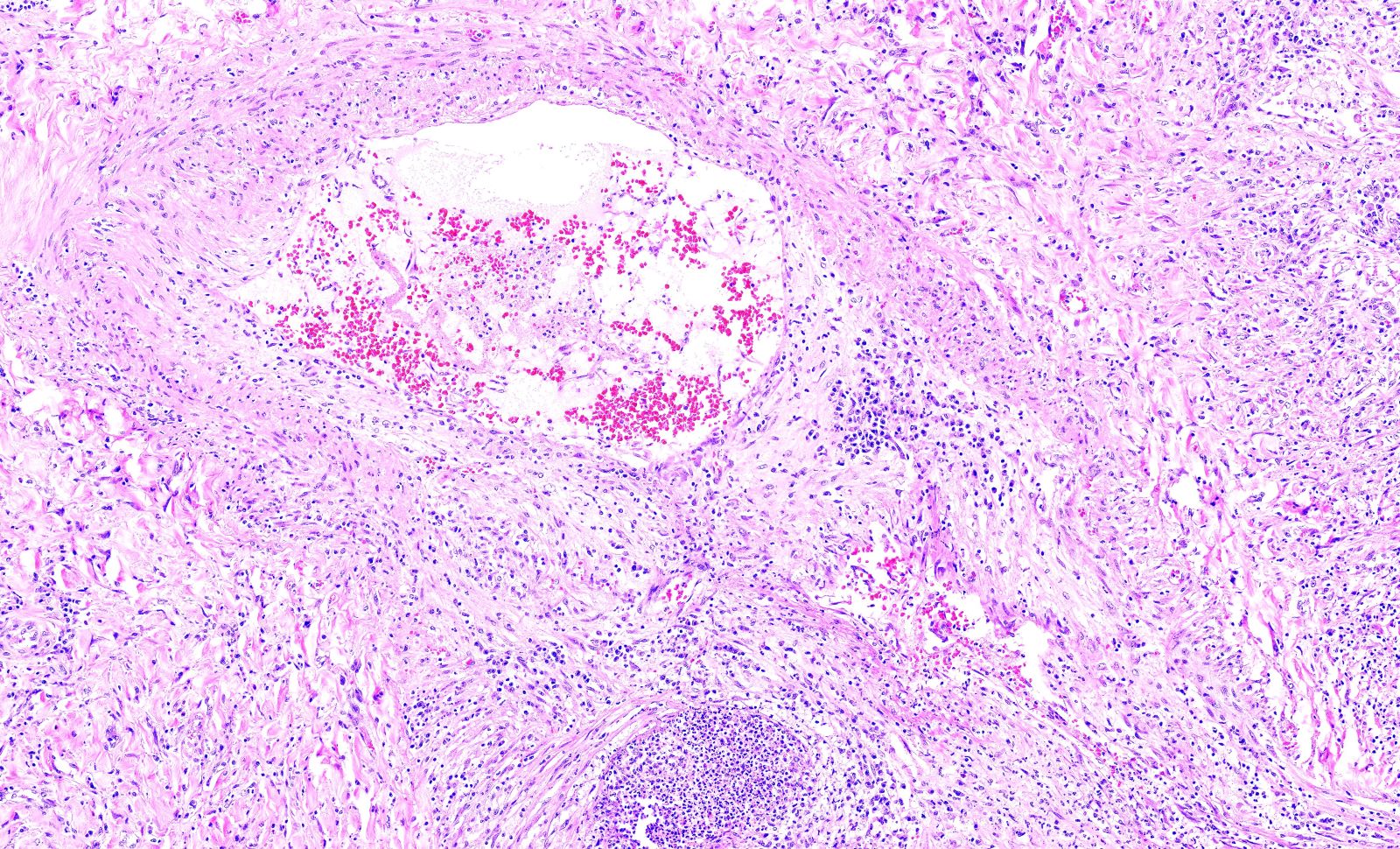
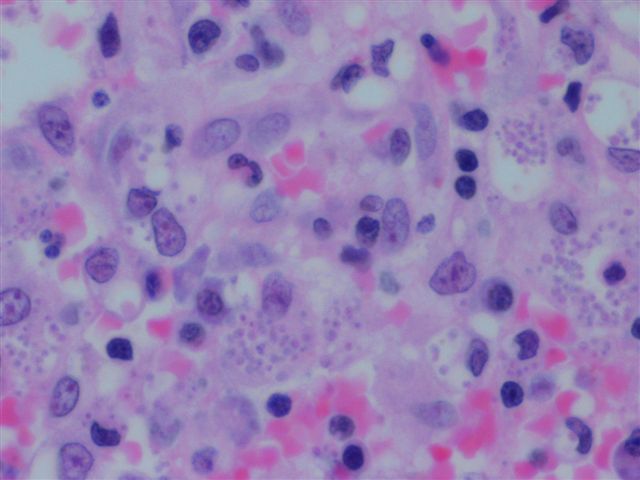
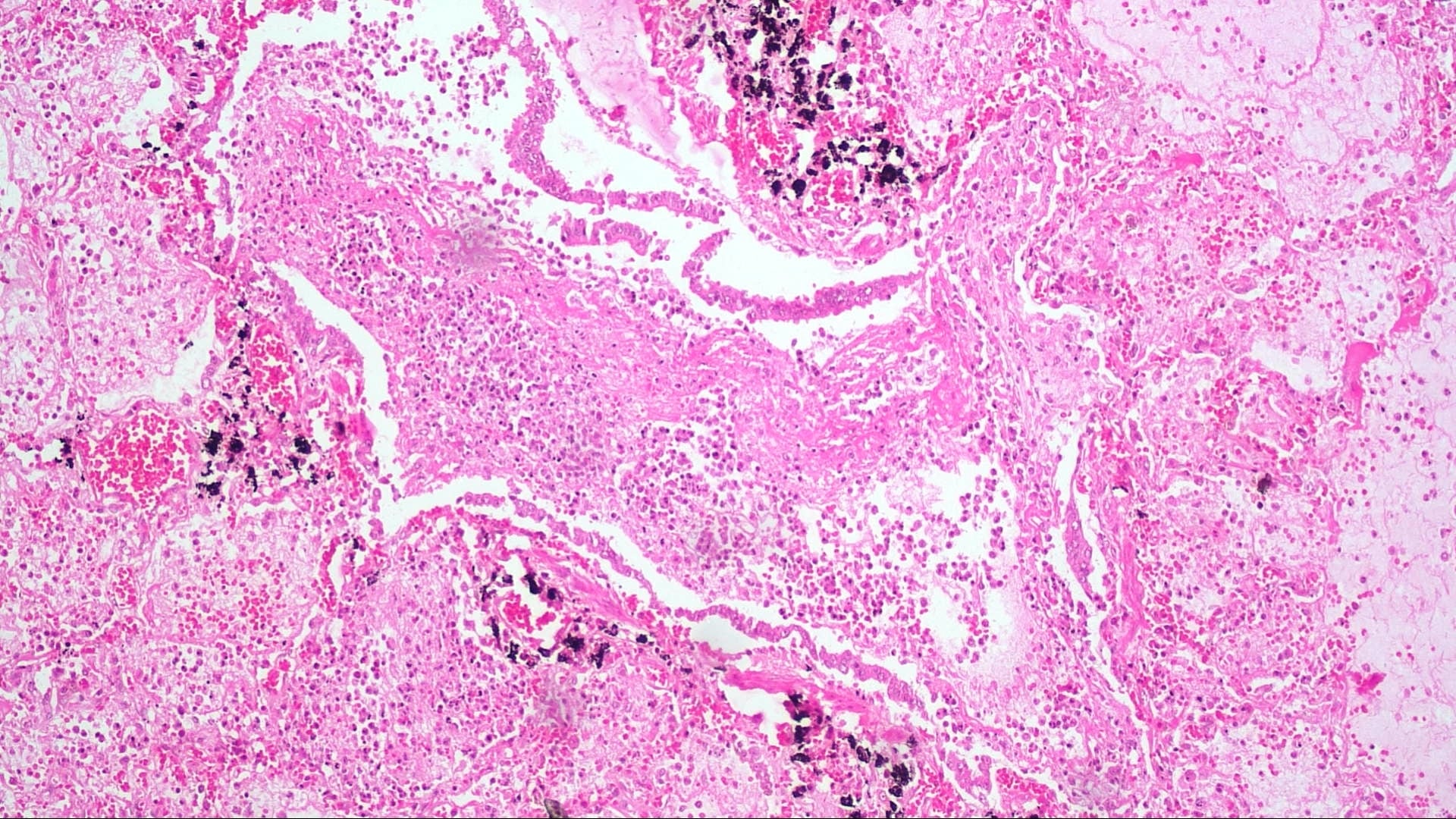
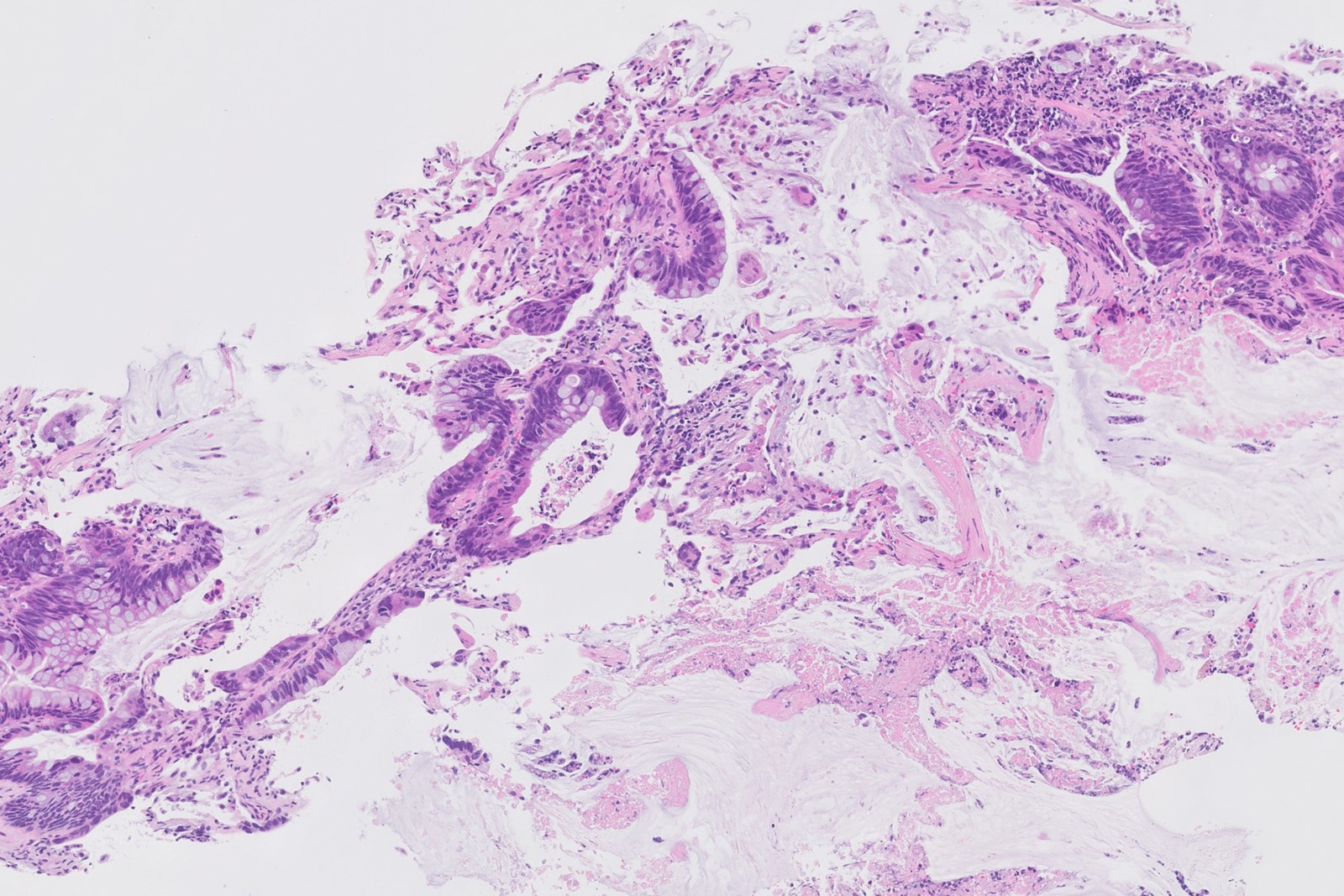
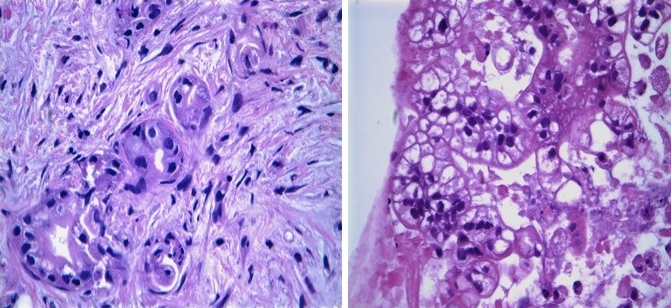
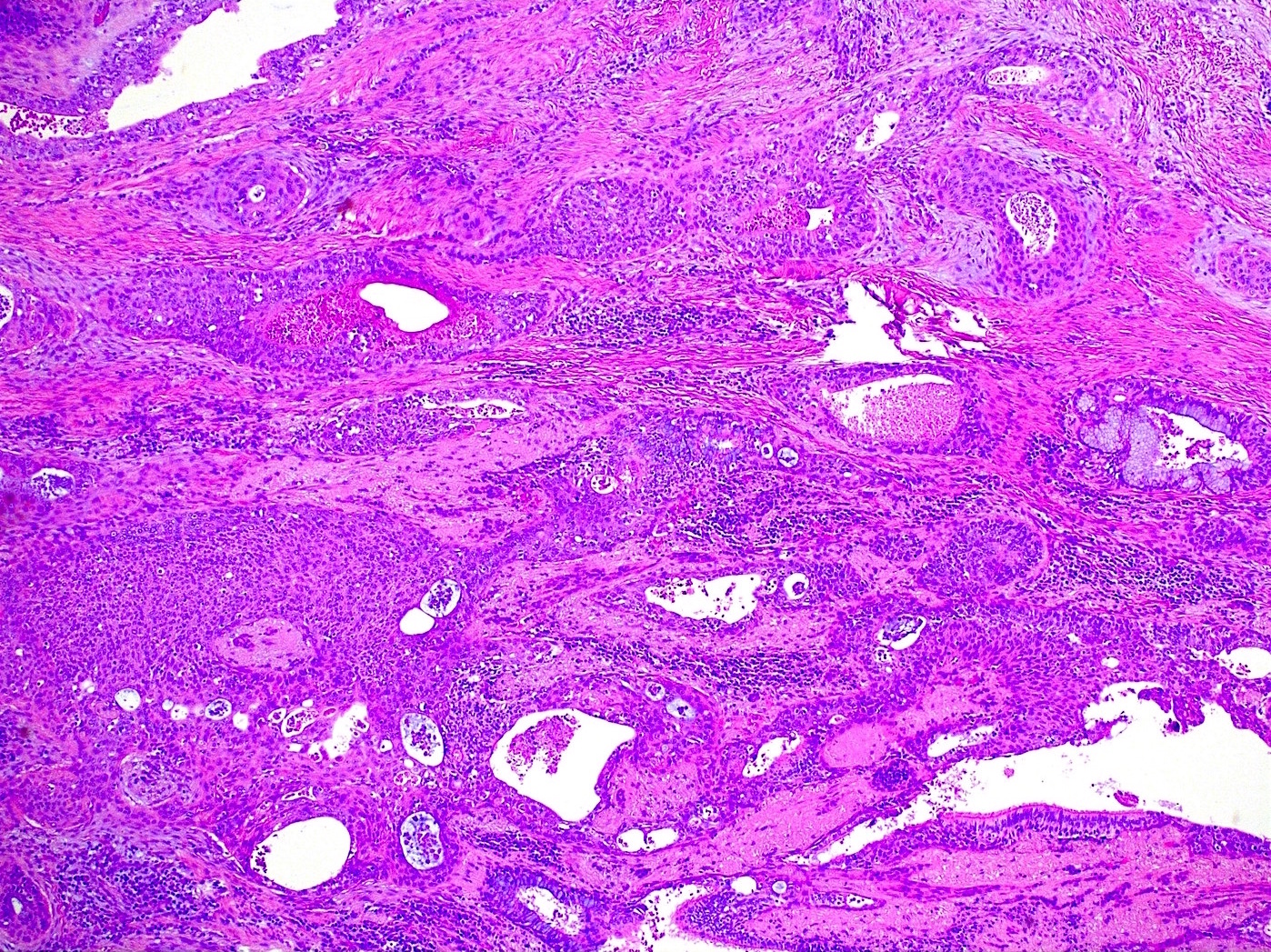
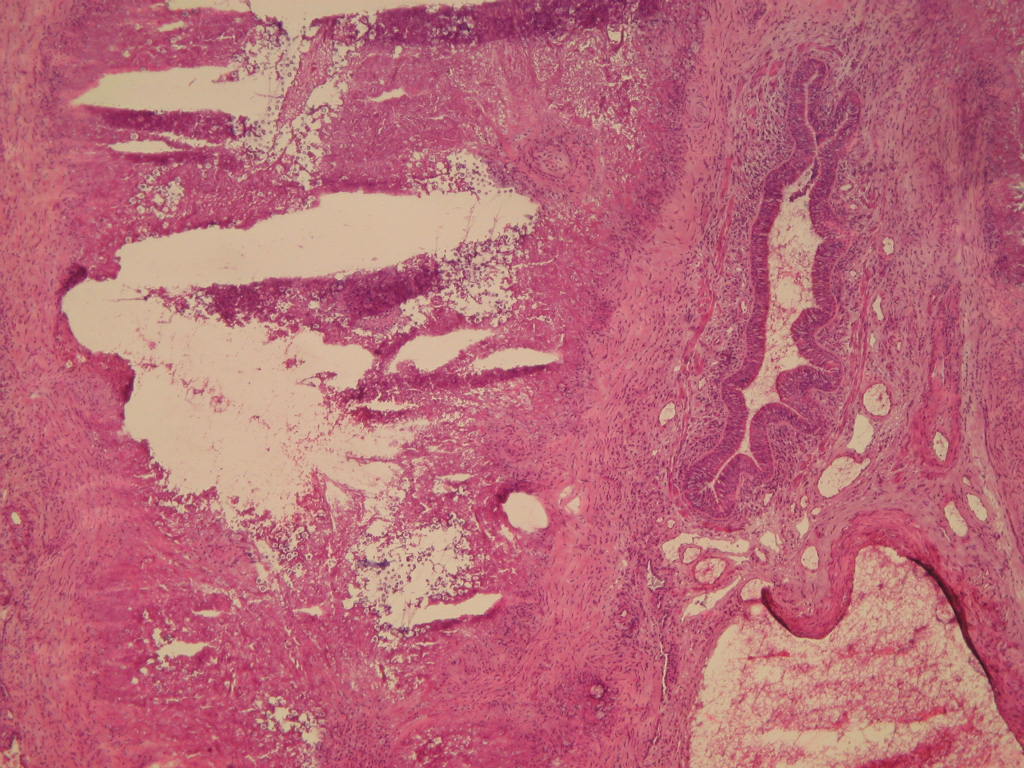
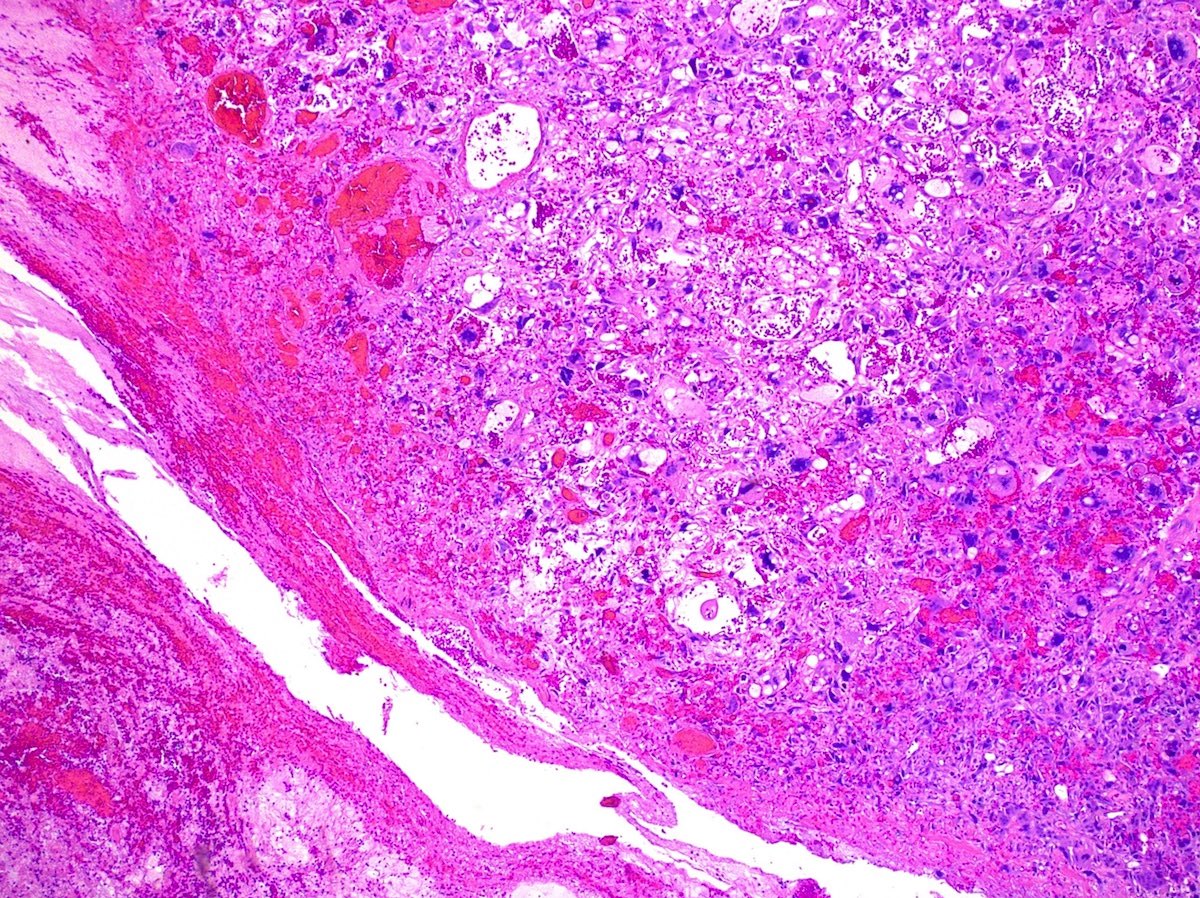
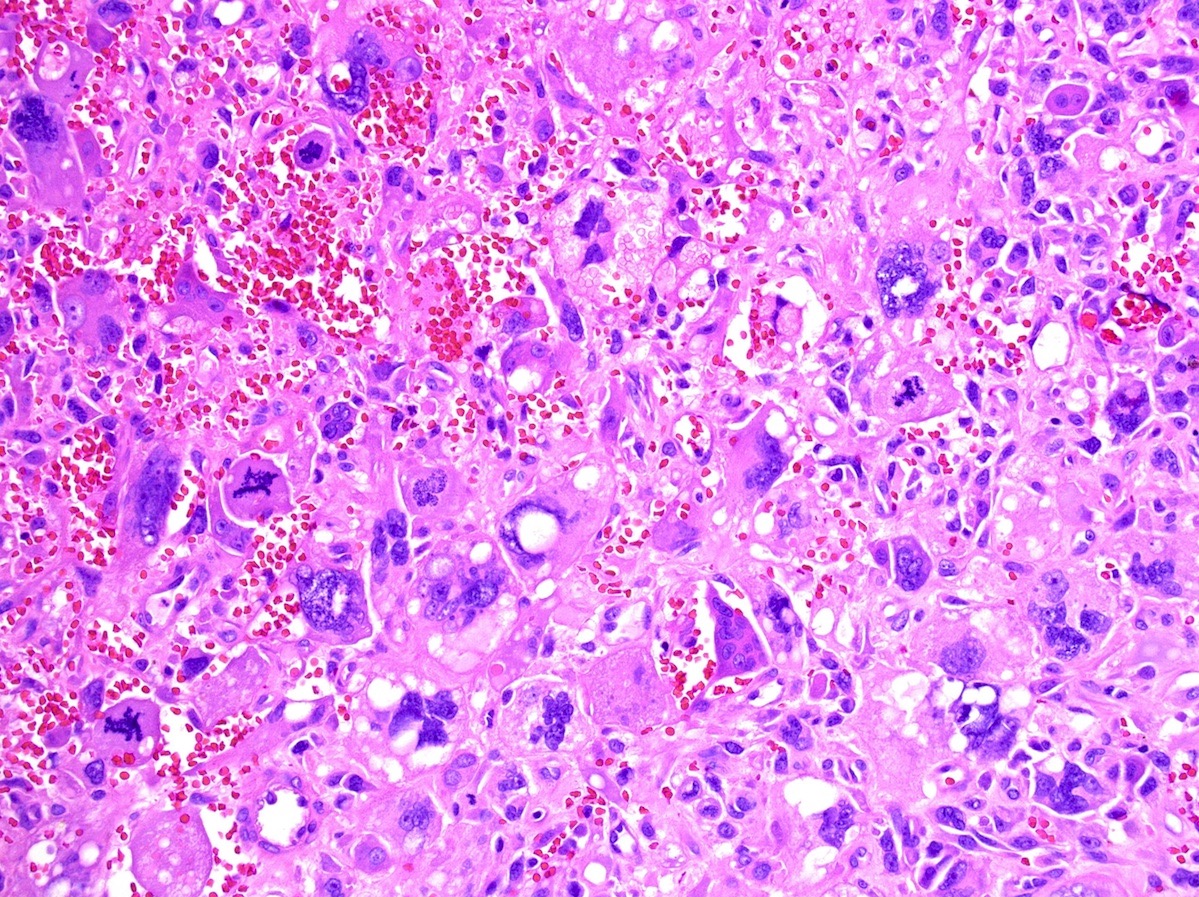
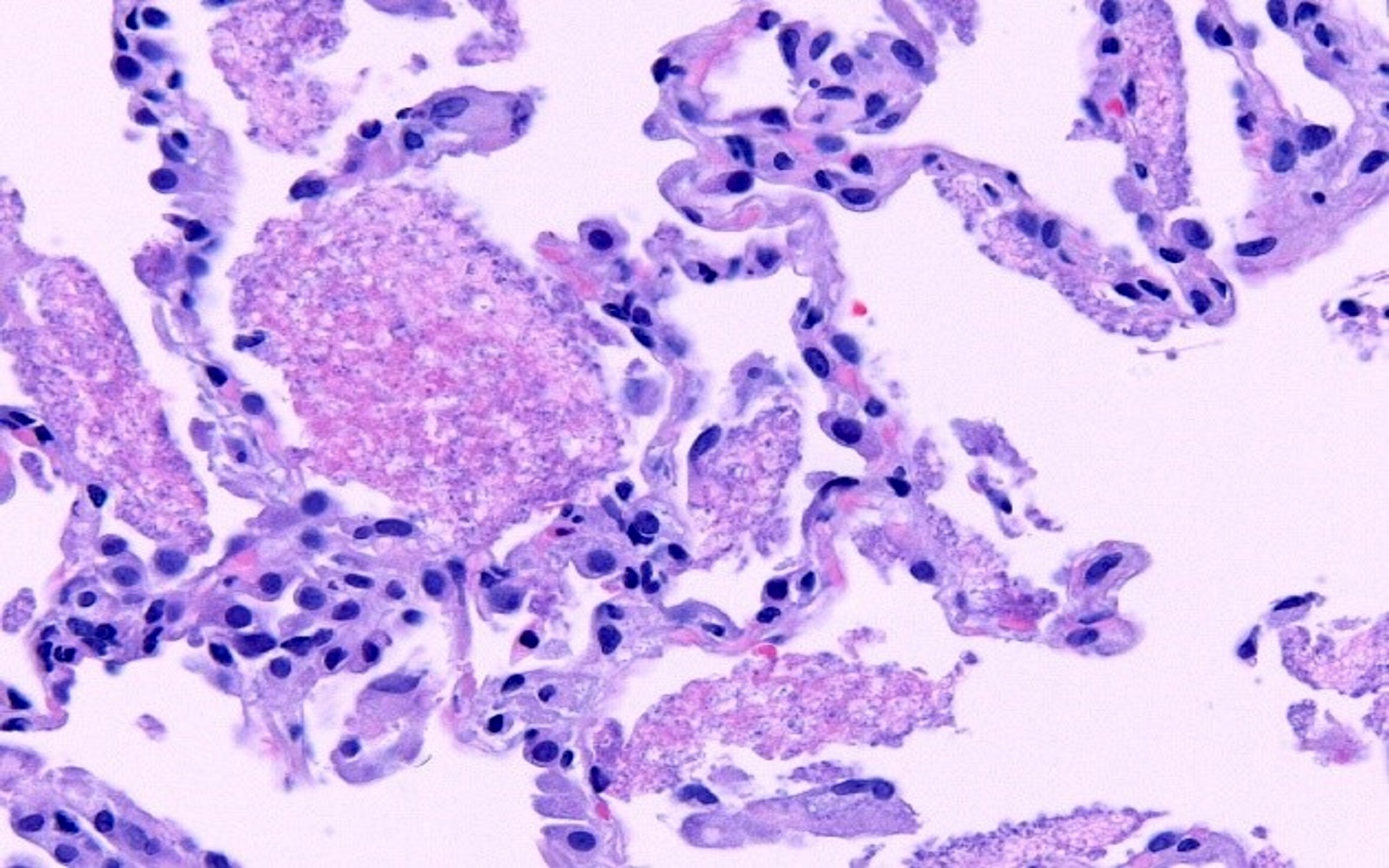
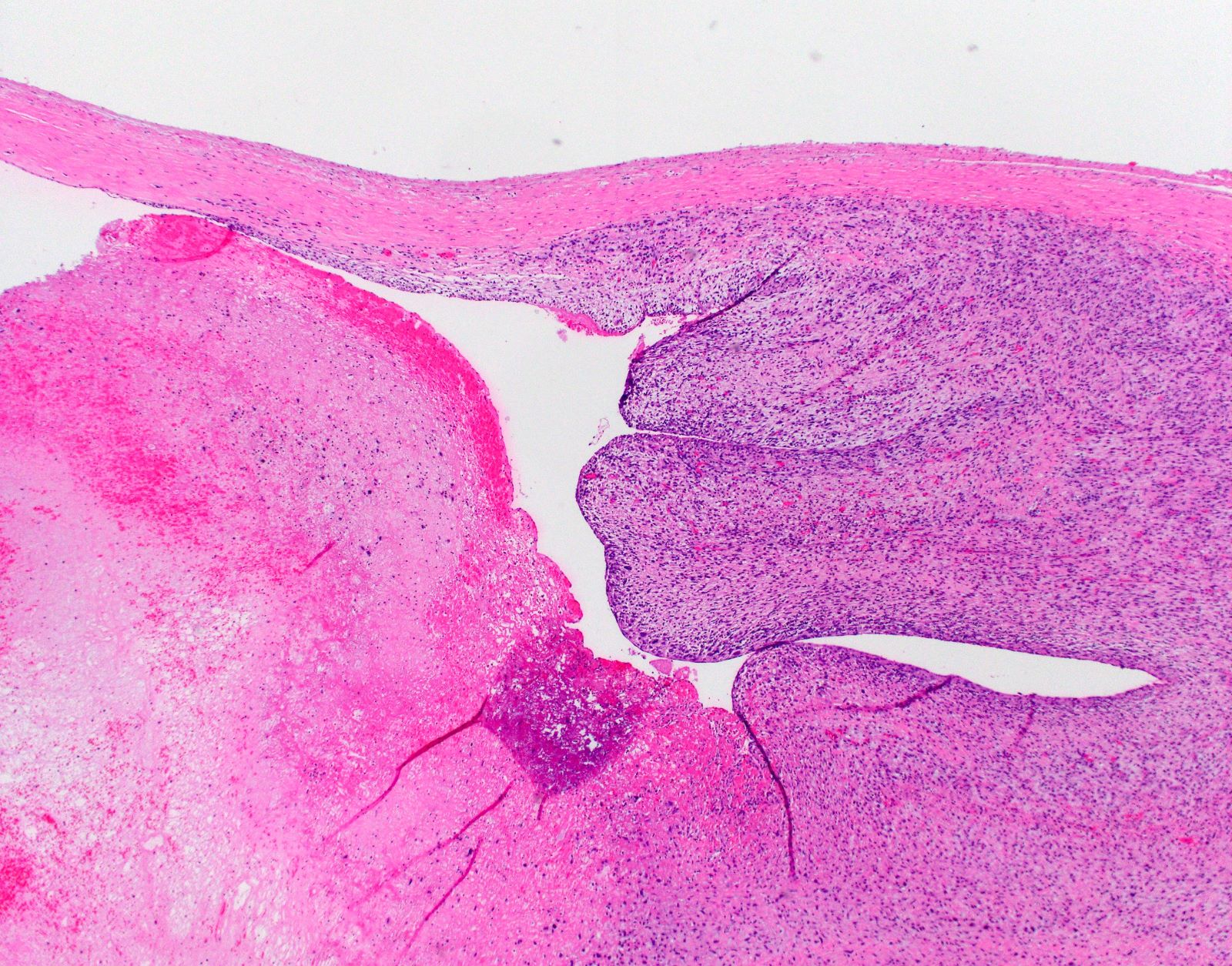
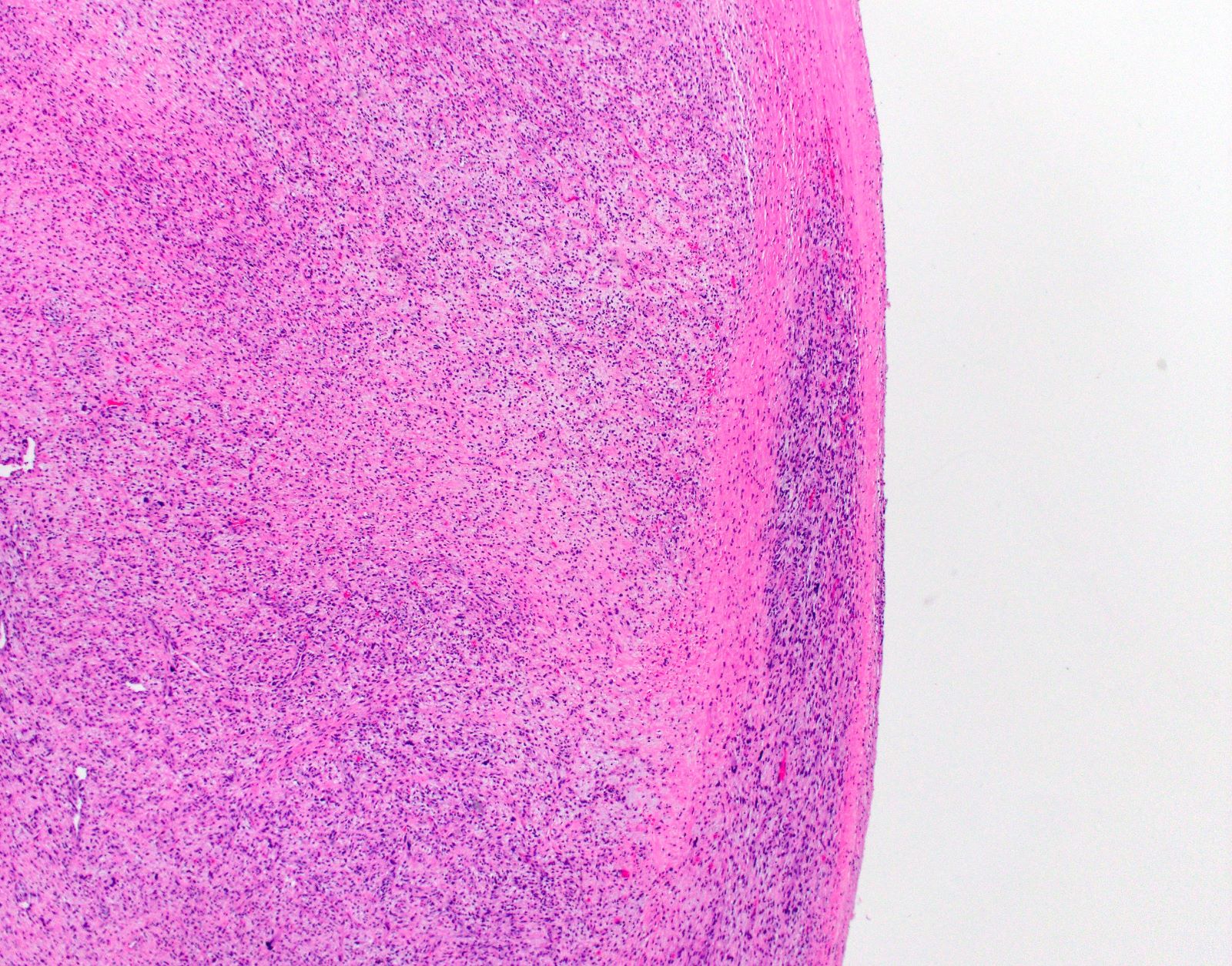
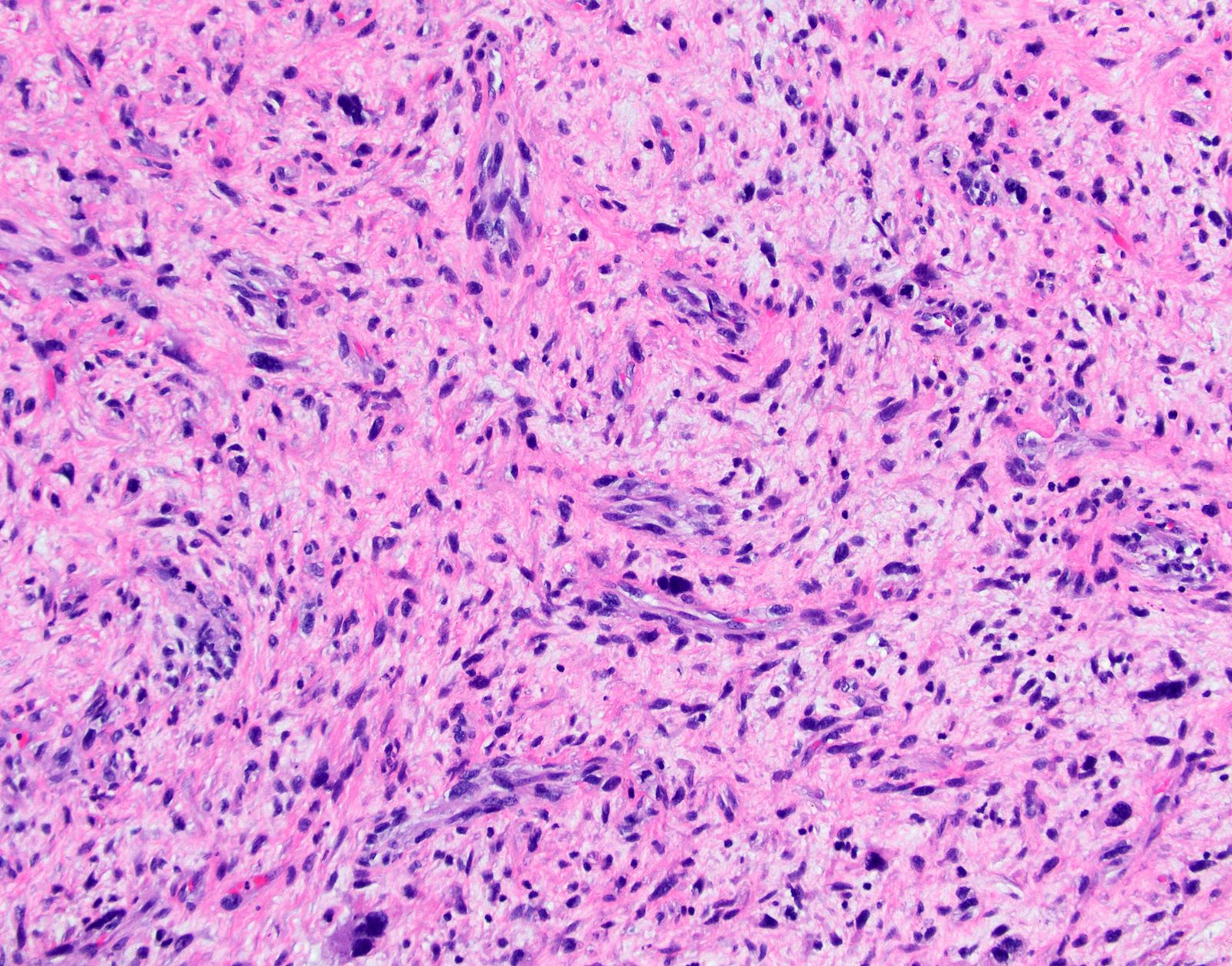
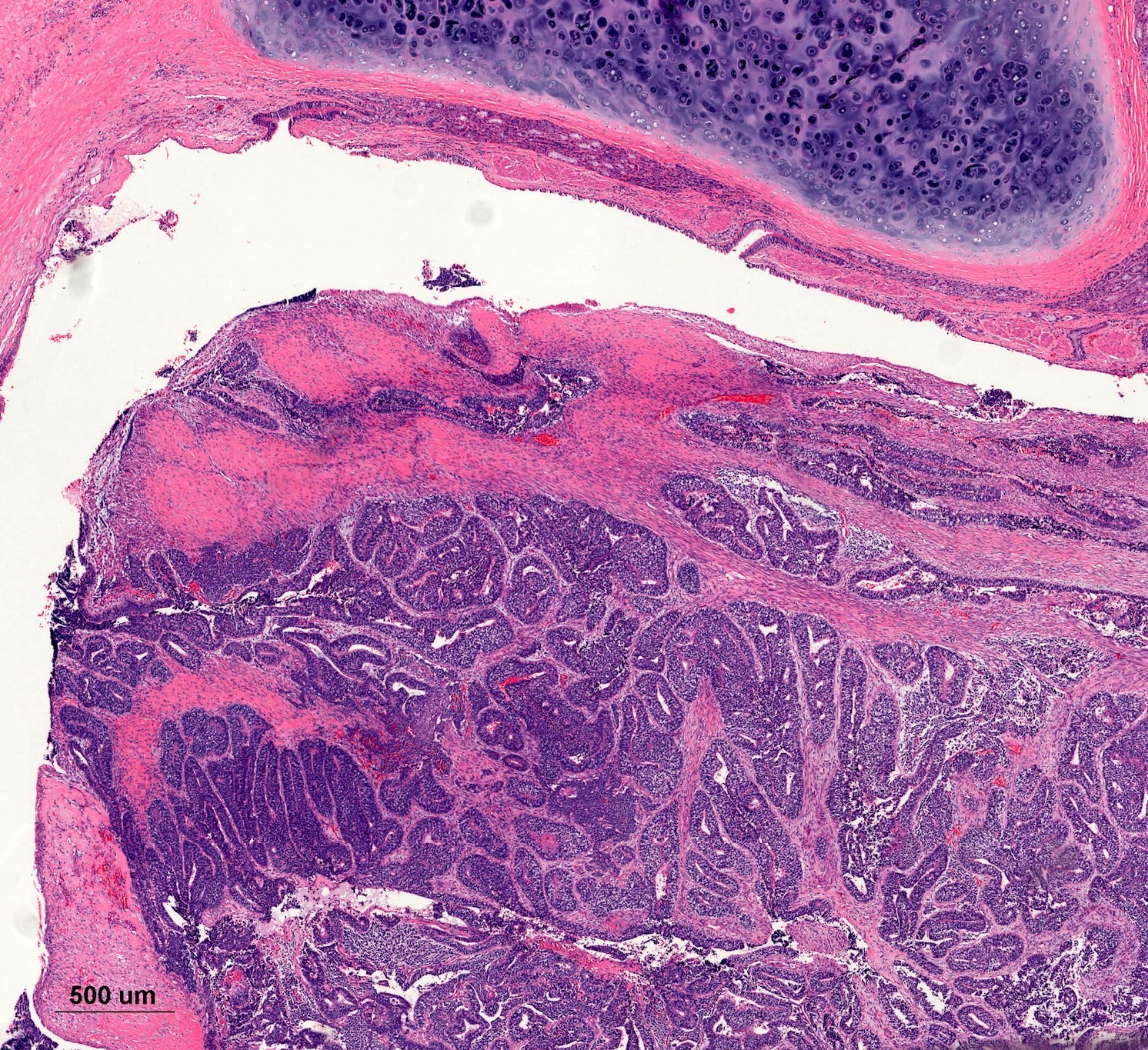
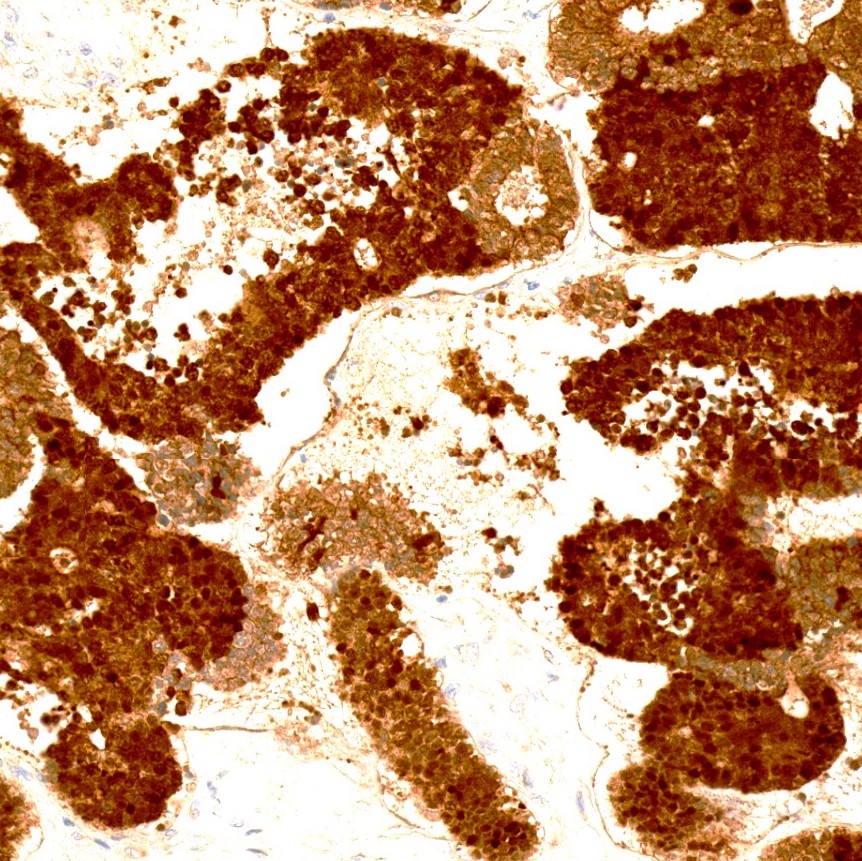
- Lobar pneumonia (Semin Diagn Pathol 2017;34:498):
- Uniform inflammatory infiltrate, the changes are at the same stage throughout the entire lobe
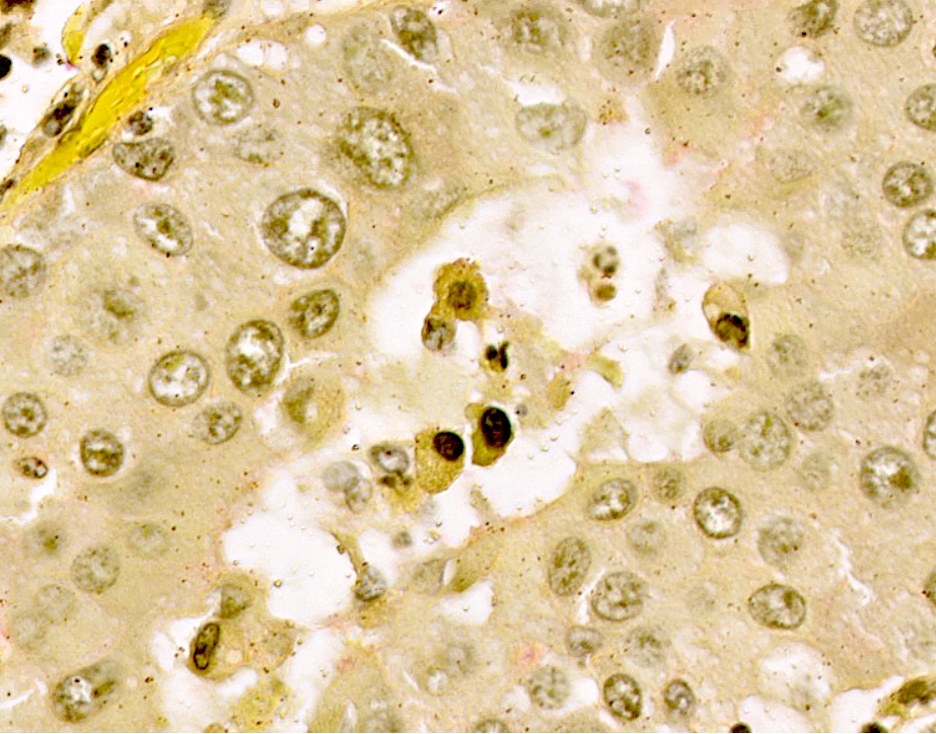
- Early stage: vascular engorgement, intra-alveolar fluid with few neutrophils and often bacterial colonies
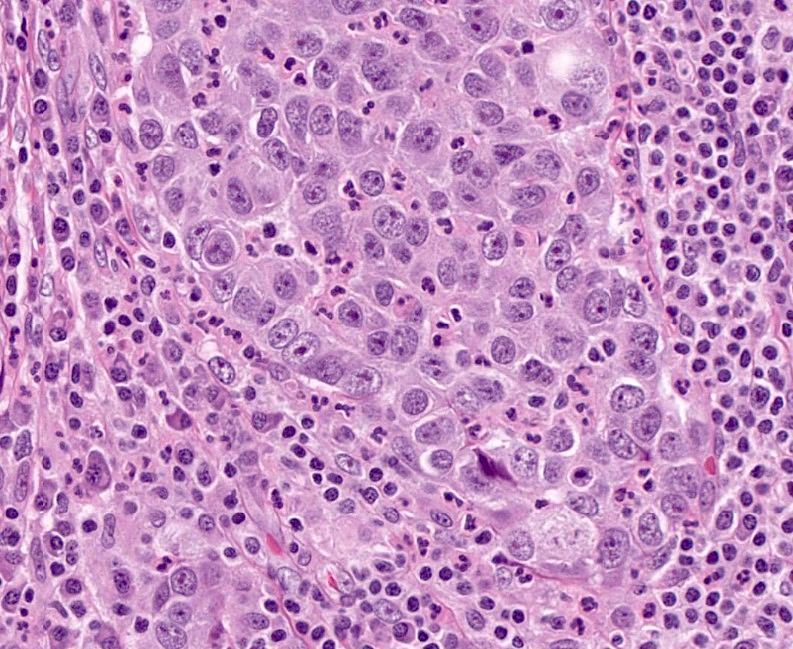
- Massive confluent exudate with intra-alveolar neutrophils, red cells and fibrin, correlates with red hepatization on gross exam
- Progressive disintegration of red cells and the persistence of a fibrinosuppurative exudate, correlates with gray hepatization on gross exam
- Resolution phase: exudates converted to fibromyxoid masses rich in macrophages and fibroblasts
- Usually resolves with minimal fibrosis
- Pleuritis can be seen
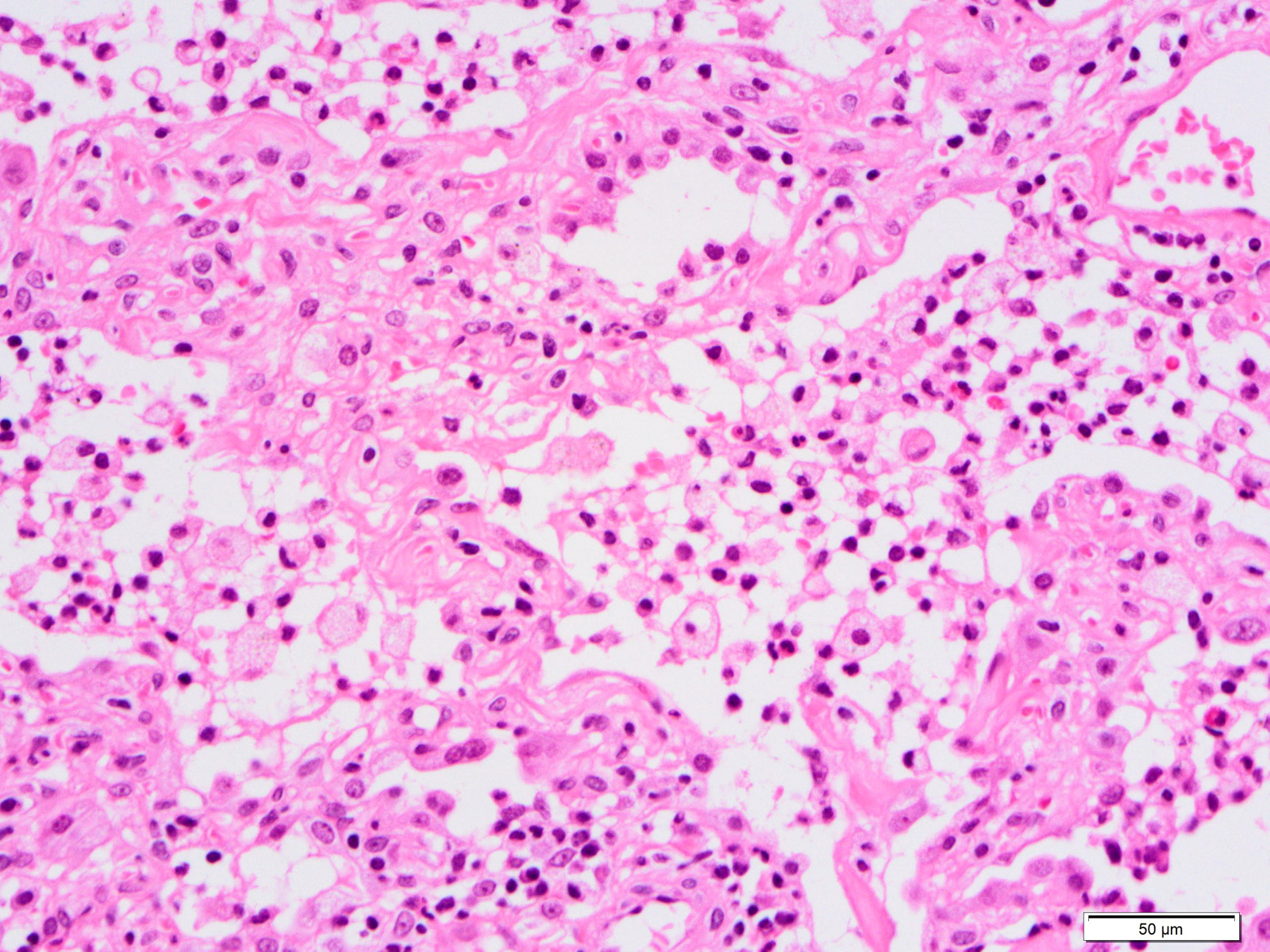
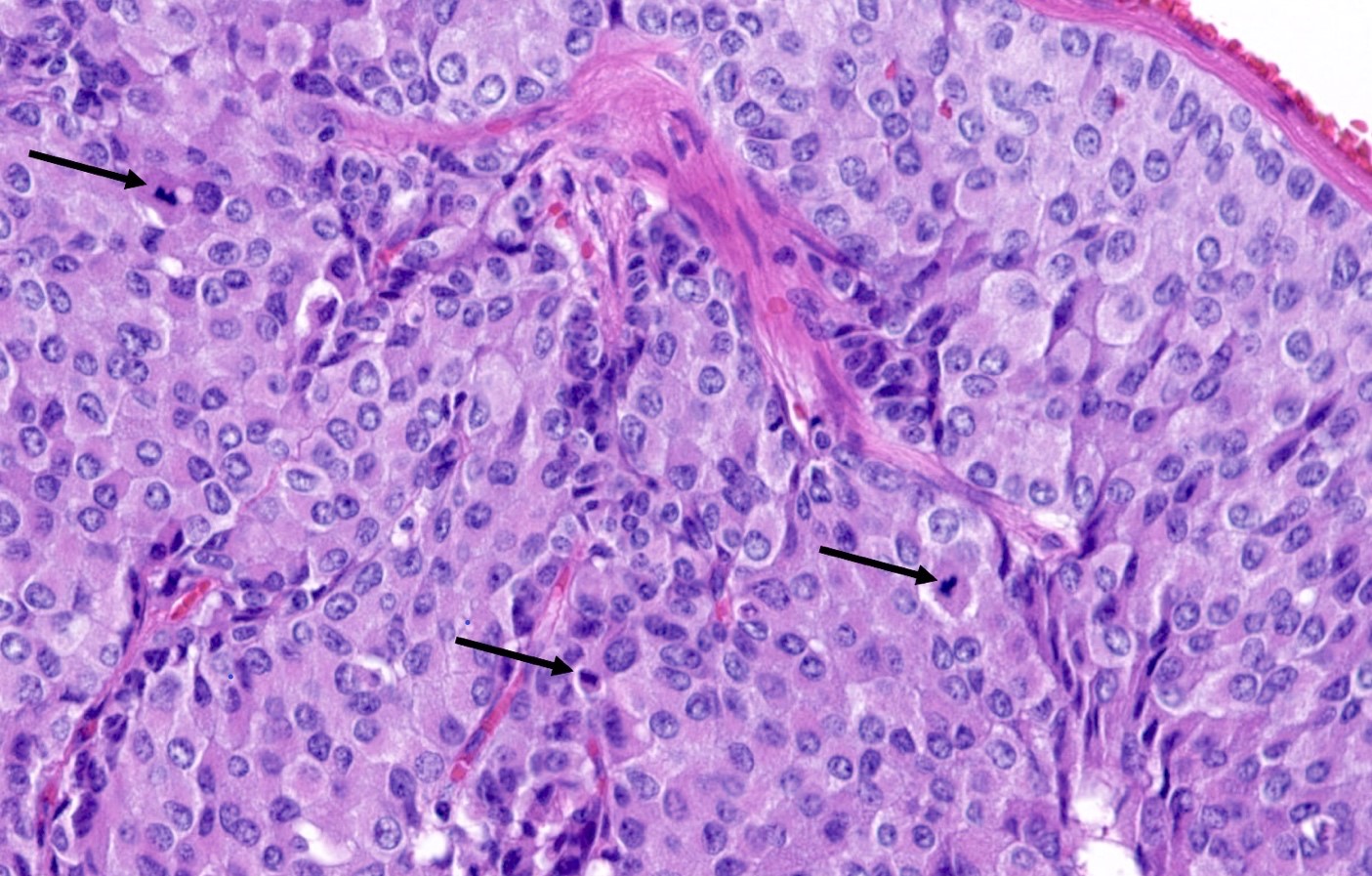
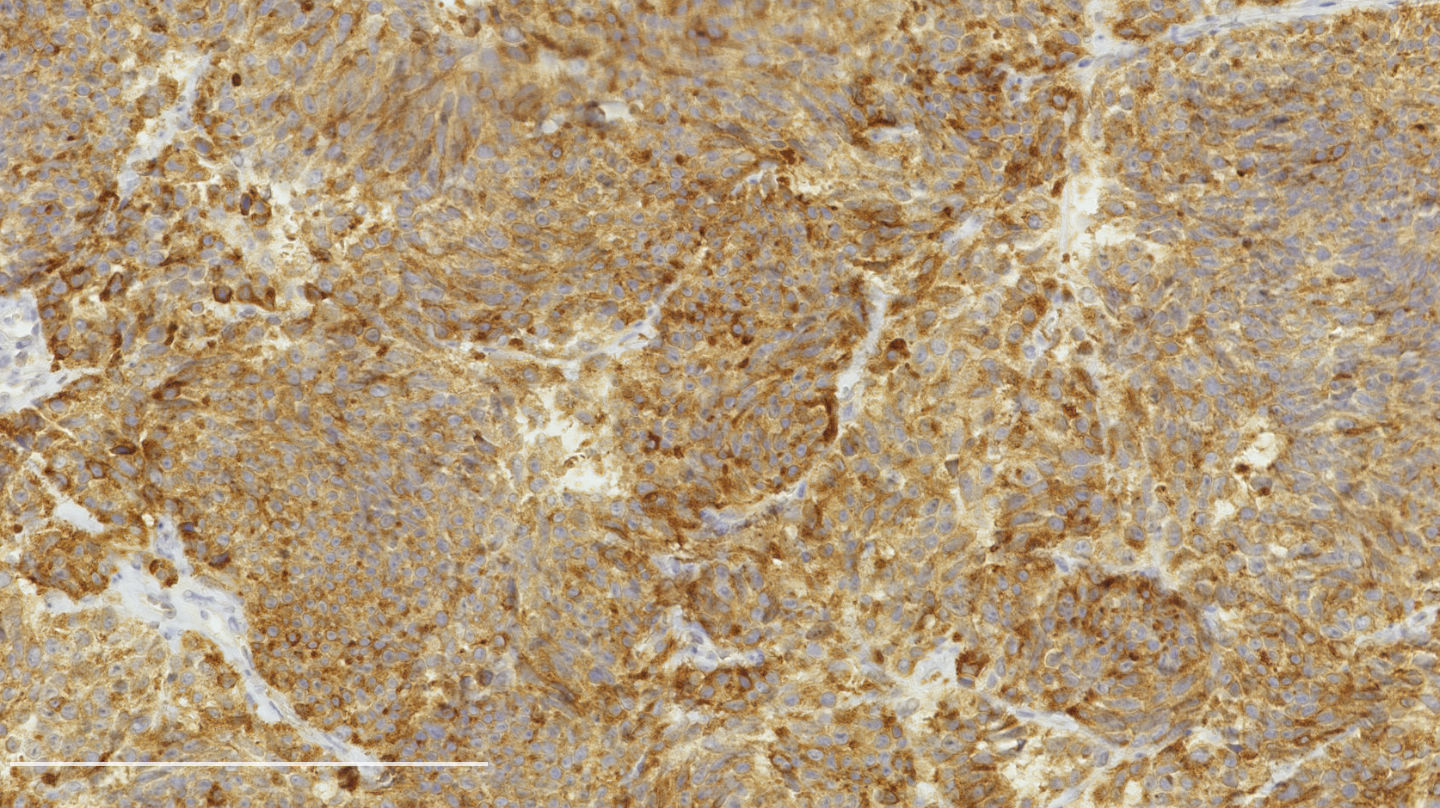
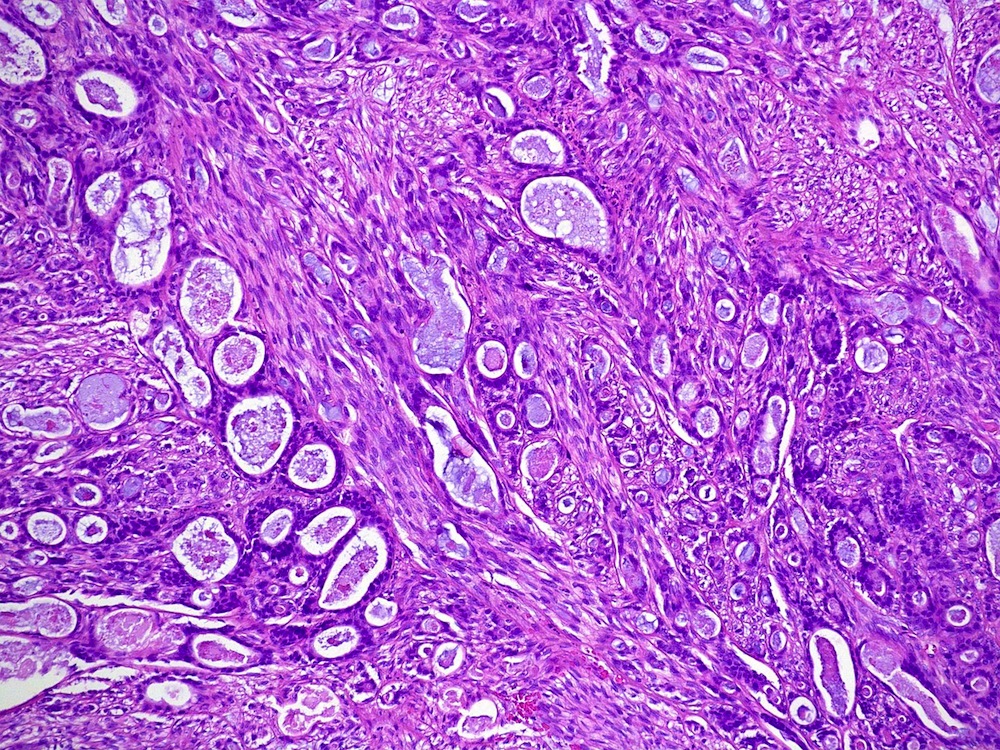
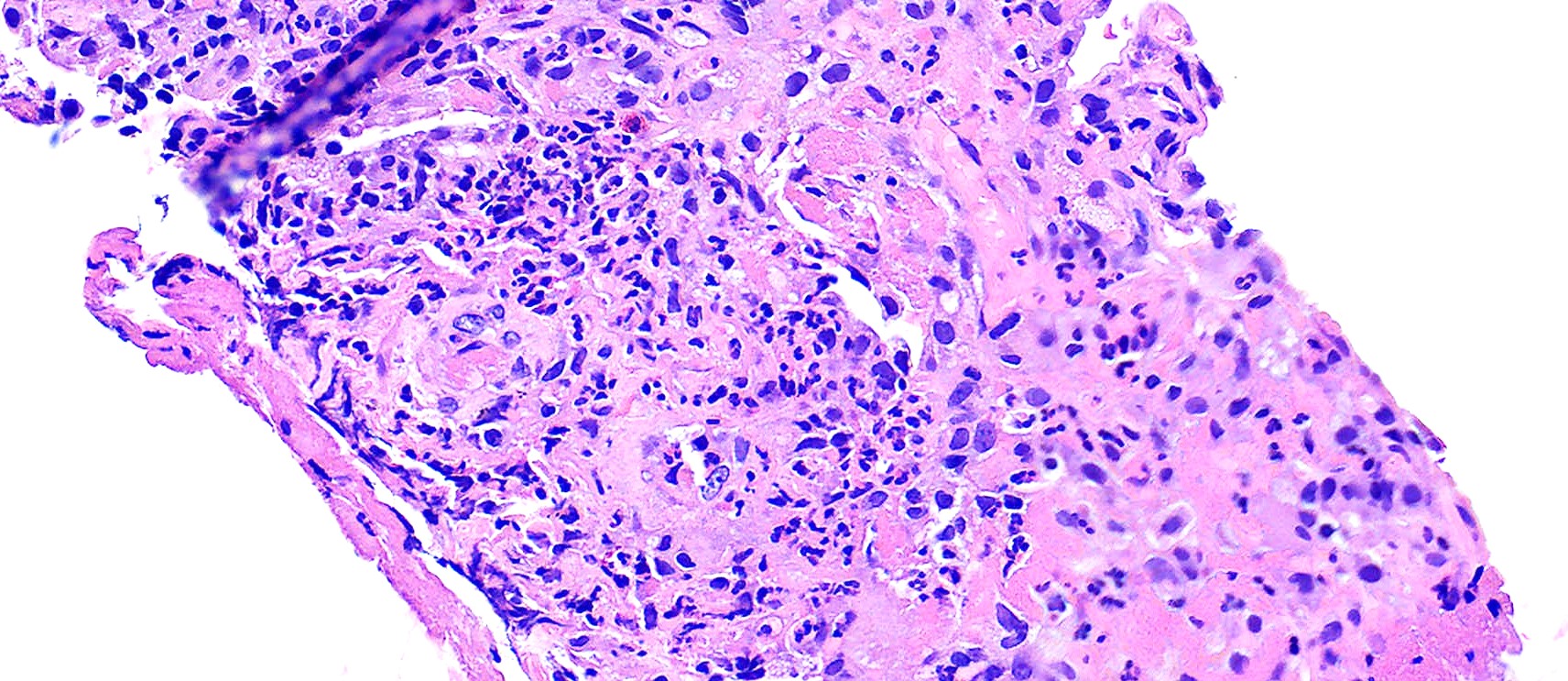
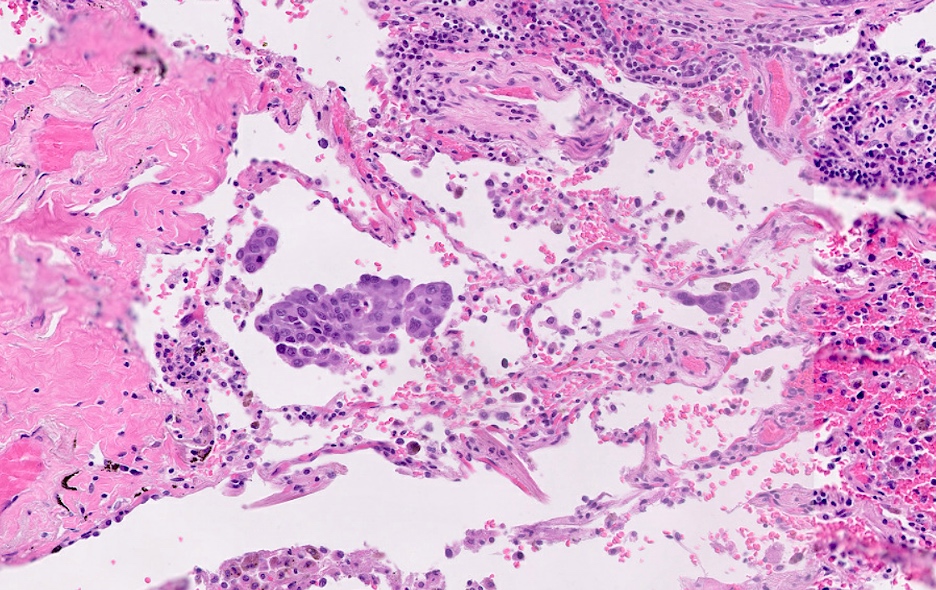
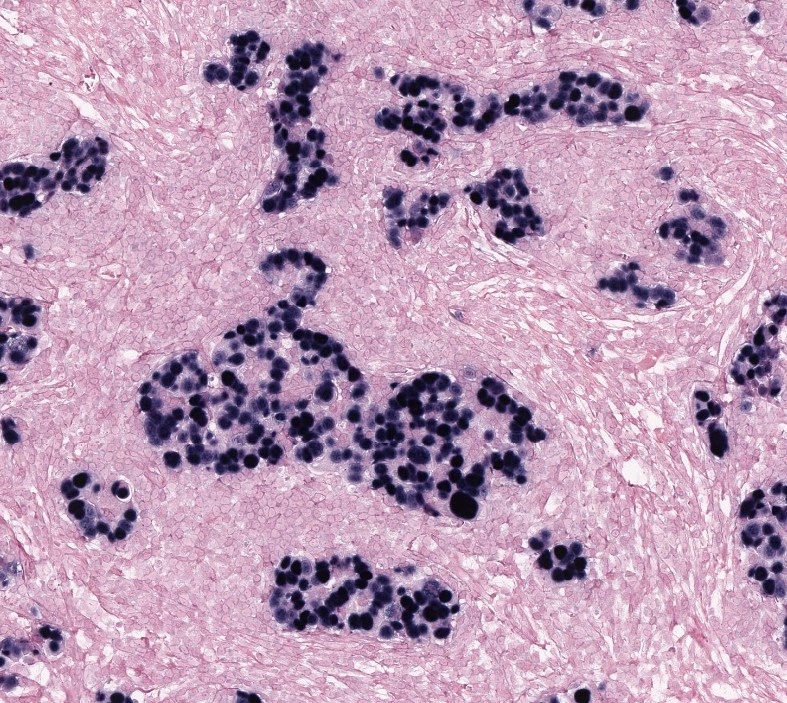
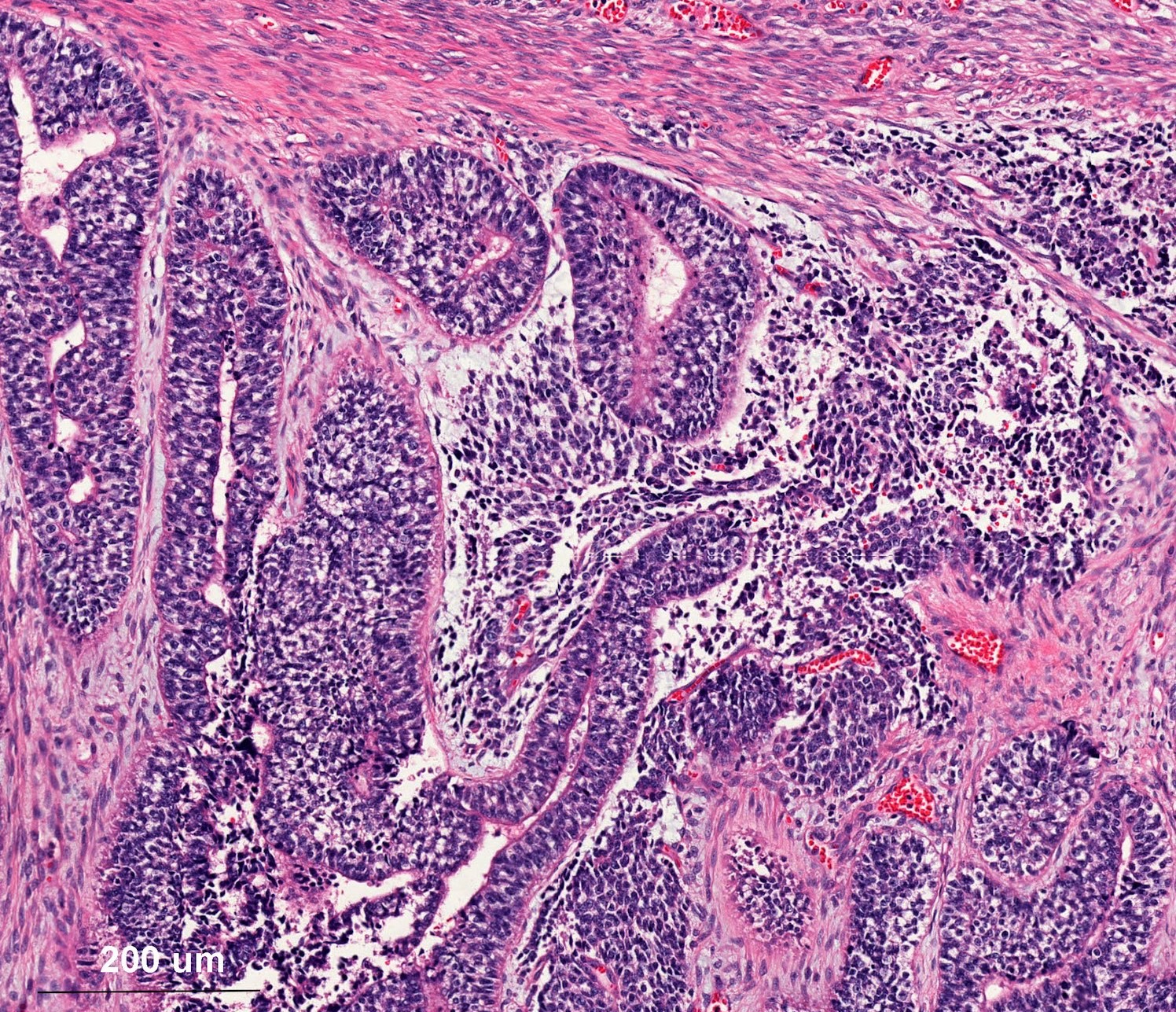
- Bronchopneumonia:
- Most common pattern of pulmonary infection
- Different stages in the different areas
- Patchy intra-alveolar fibrinopurulent exudate with neutrophils
- Acute lung injury pattern:
- Diffuse alveolar damage (DAD): hyaline membrane formation
- Organizing pneumonia (OP): fibrohistiocytic proliferation with obliteration of small airways (fibroblast plug, Masson body), accompanied by inflamed surrounding alveolar interstitium
- Necrotizing pneumonia (Can Respir J 2014;21:239):
- Characterized by necrotizing inflammation, leading to alveolar septa disruption and cavity formation
- Common organisms: Staphylococcus aureus, Streptococcus pyogenes, S. pneumoniae (certain serotypes), Klebsiella, Acinetobacter, Pseudomonas and Burkhodoria
- Aspiration pneumonia:
- Foreign body giant cell reaction, characterized by multinucleated giant cells, granulomatous inflammation
- Often necrotizing, abscess formation is common
- Presence of food particles (e.g., lentils, vegetables, pill fragments)
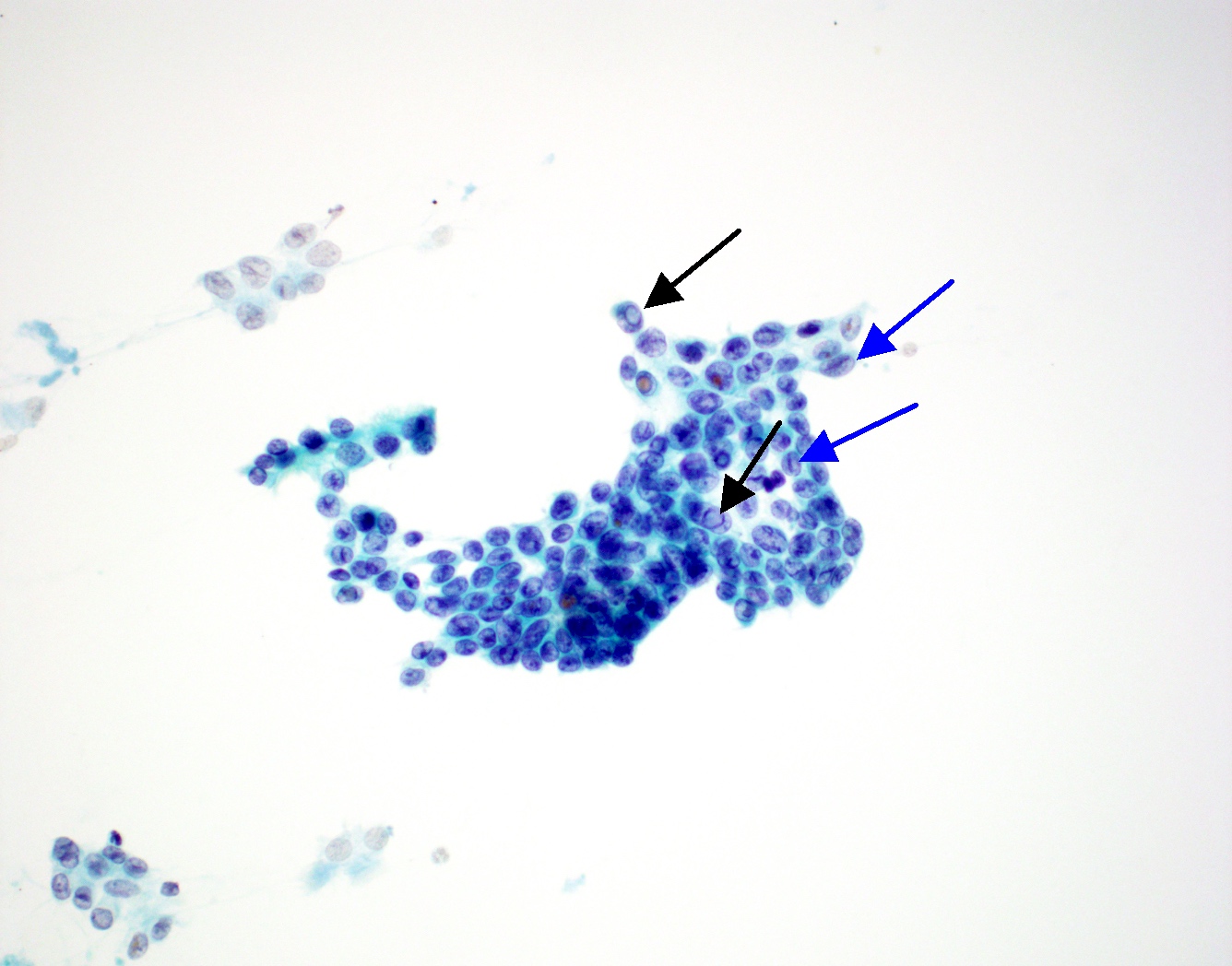
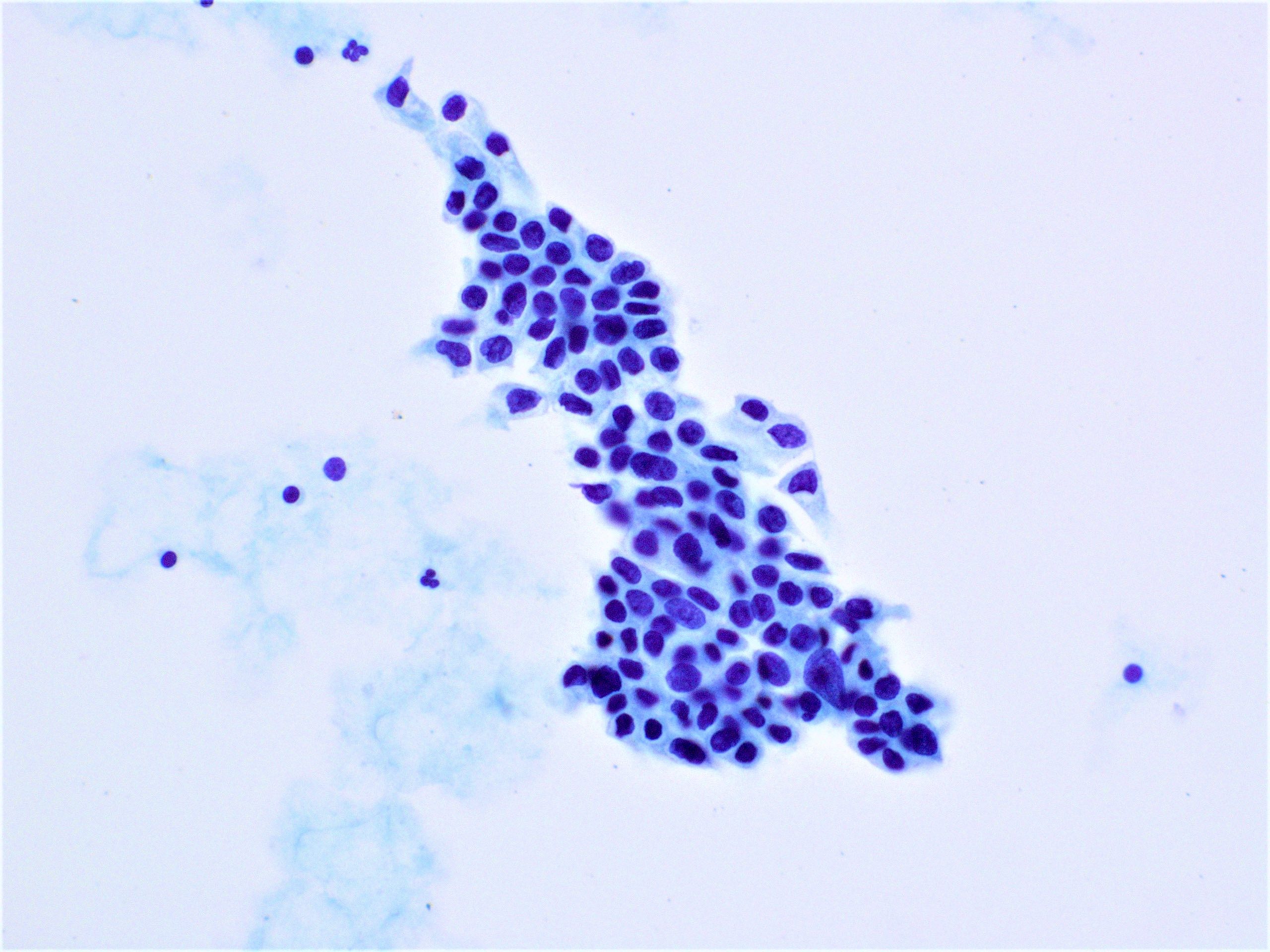
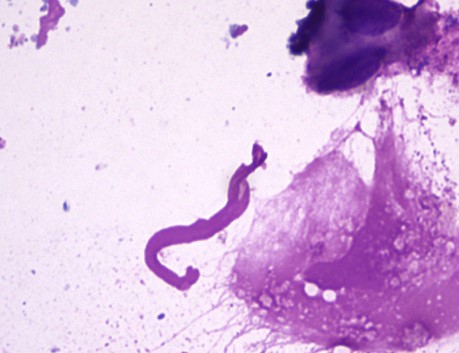
- Bacterial pneumonia is rarely diagnosed by cytology alone
- Sources of specimens: sputum, bronchoalveolar lavage, fine needle aspirate (FNA), pleural fluid
- Acute purulent inflammation, with predominant neutrophils (Practical Pulmonary Pathology 2018;147)
- Reactive pneumocytes can be mistaken for malignant cells
- Bacteria can be seen with Diff-Quik preparation
- Colonization must be differentiated from true infection
- Grocott-Gomori methenamine silver (GMS):
- Primarily for fungus detection
- Bacteria may also occasionally stain with GMS
- Silver accretion on the surface tends to make the organisms appear larger and should not be confused with yeast (Semin Diagn Pathol 2017;34:498)
- PAS: positive in fungal infections
- Mucicarmine: positive for Cryptococcus neoformans
Bronchopneumonia
Lobar pneumonia
- Lung, right middle lobe, transbronchial biopsy:
- Acute bronchopneumonia (see comment)
- Diffuse alveolar damage
- Comment: Special stains for microorganisms (AFB and GMS) are negative.
- Autopsy report
- Final pathologic diagnosis
- Acute bronchopneumonia involving right upper lobe
- Diffuse alveolar damage
- Microscopic description
- Lungs: Sections of the lungs show intra-alveolar neutrophilic infiltrate with marked congestion. Alveolar septa are widened with mixed inflammatory cells. Reactive pneumocytes and hyaline membrane can be seen throughout the lung tissue.
- Final pathologic diagnosis
- Viral pneumonia:
- Characterized by interstitial mononuclear inflammatory infiltrate, including lymphocytes, macrophages and occasional plasma cells (Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020)
- Cannot be differentiated by clinical findings
- Viruses cause up to 20% of cases of HAP and VAP (PLoS One 2014;9:e95865)
- Bacterial pneumonia can occur concurrently with influenza virus infection
- Bacterial infection was found 30% of deaths from the 2009 H1N1 influenza pandemic (Am J Pathol 2010;177:166)
- Most common: S. aureus, followed by S. pneumoniae, H. influenzae and group A Streptococcus (Am J Respir Crit Care Med 2019;200:e45)
- Fungal pneumonia:
- Likely to affect immunocompromised host
- Yeast or fungal hyphae are identified with the aid of GMS stain
- Acute interstitial pneumonia:
- Idiopathic interstitial pneumonia characterized by diffuse alveolar damage
- Bilateral lungs are involved
- No microorganism identified
- Invasive mucinous adenocarcinoma:
- Can present with pulmonary infiltrate resembling pneumonia (Cancer Imaging 2019;19:47)
- Characteristic malignant cells can be identified
An 80 year old man presented with dyspnea, altered mental status and evidence of urinary tract infection. He was hospitalized in an intensive care unit for 2 weeks. The patient later developed fever, hypoxemia and new infiltrate on chest radiograph. An autopsy was performed and the lung showed the above histomorphology. What is the likely diagnosis?
- Bronchopneumonia
- Mycoplasma pneumonia
- Pulmonary tuberculosis
- Respiratory bronchiolitis
- Usual interstitial pneumonia
- Aspergillus fumigatus
- Escherichia coli
- Influenza virus
- Staphylococcus aureus
- Streptococcus pneumoniae
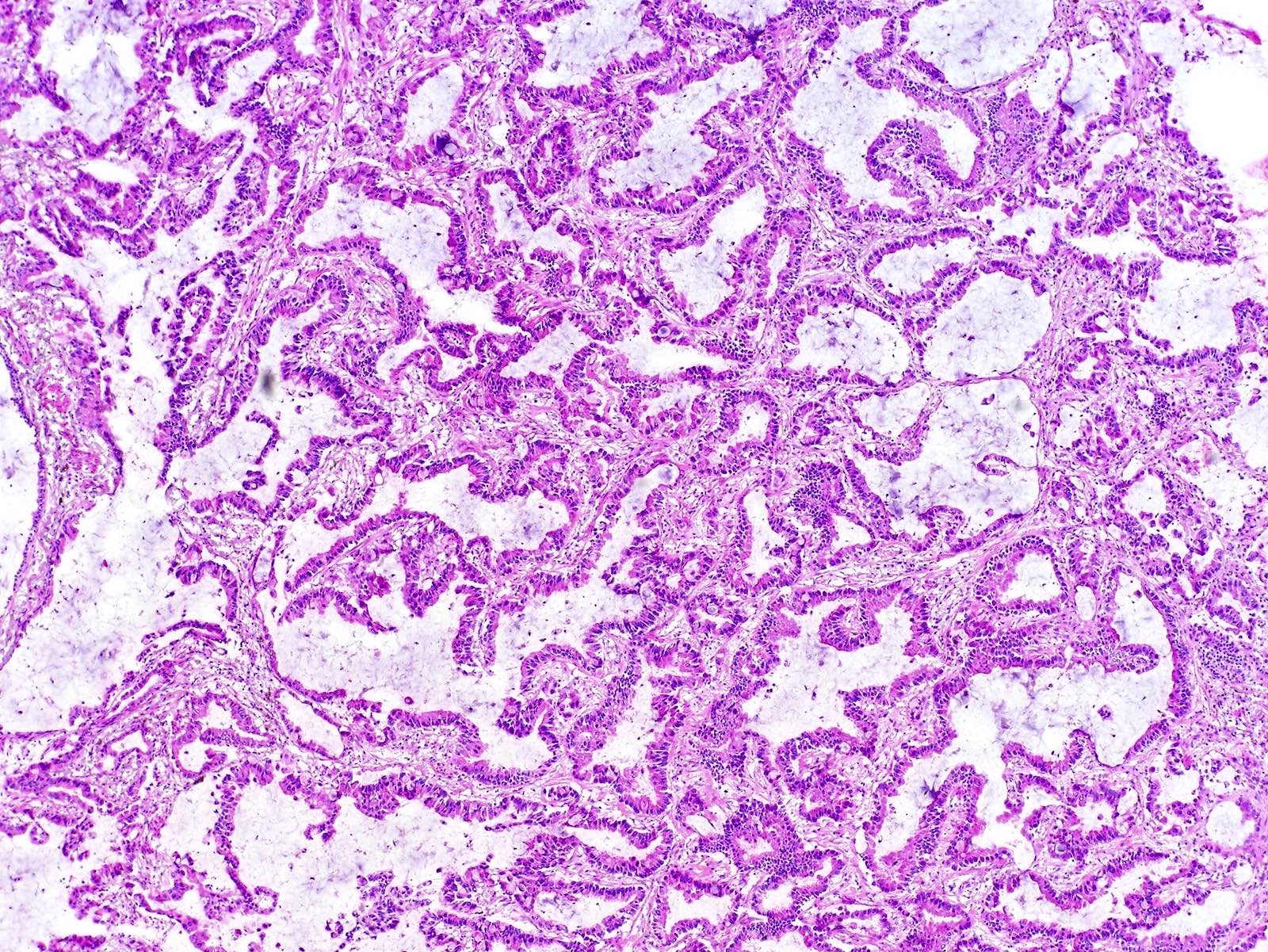
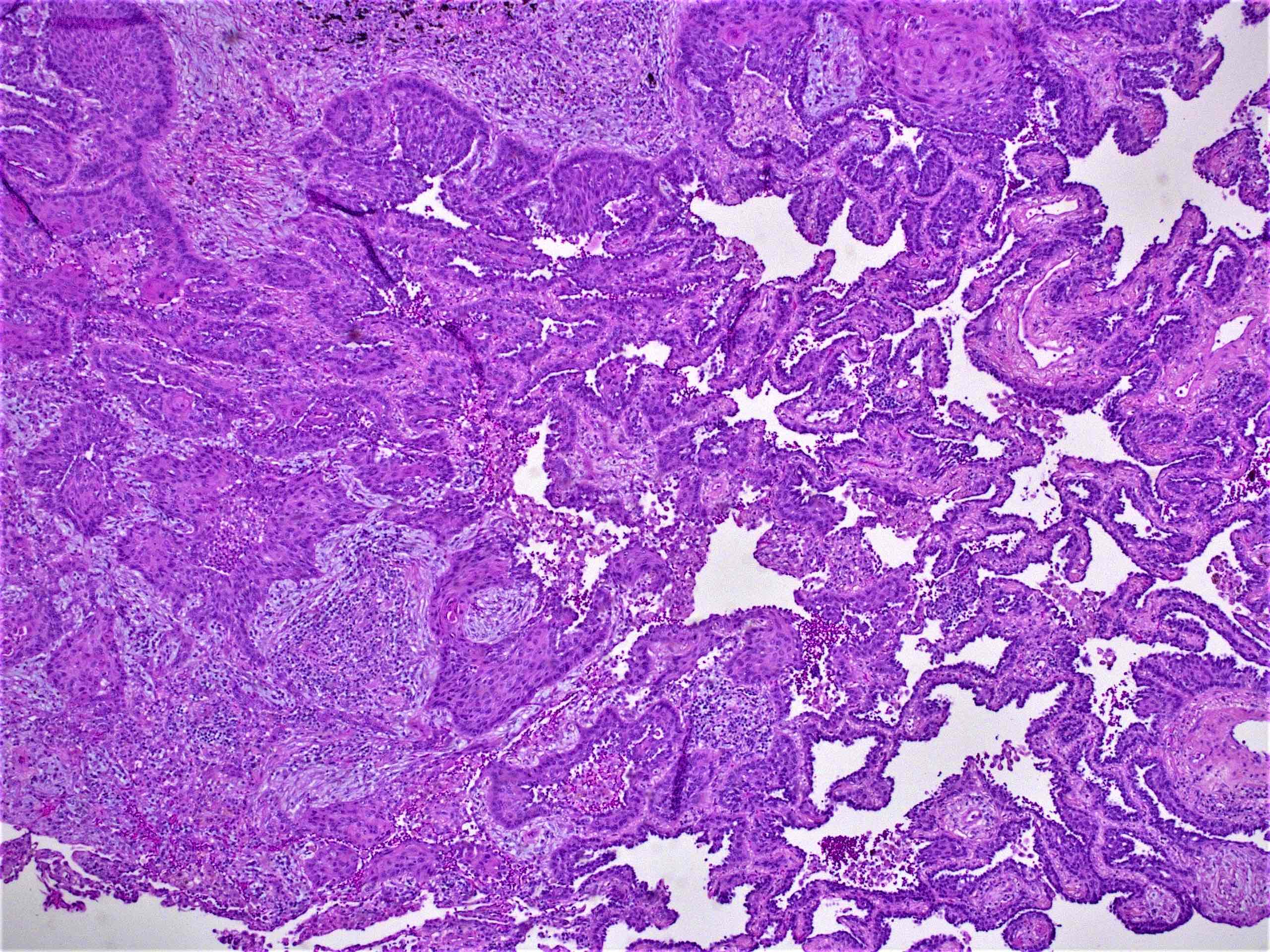
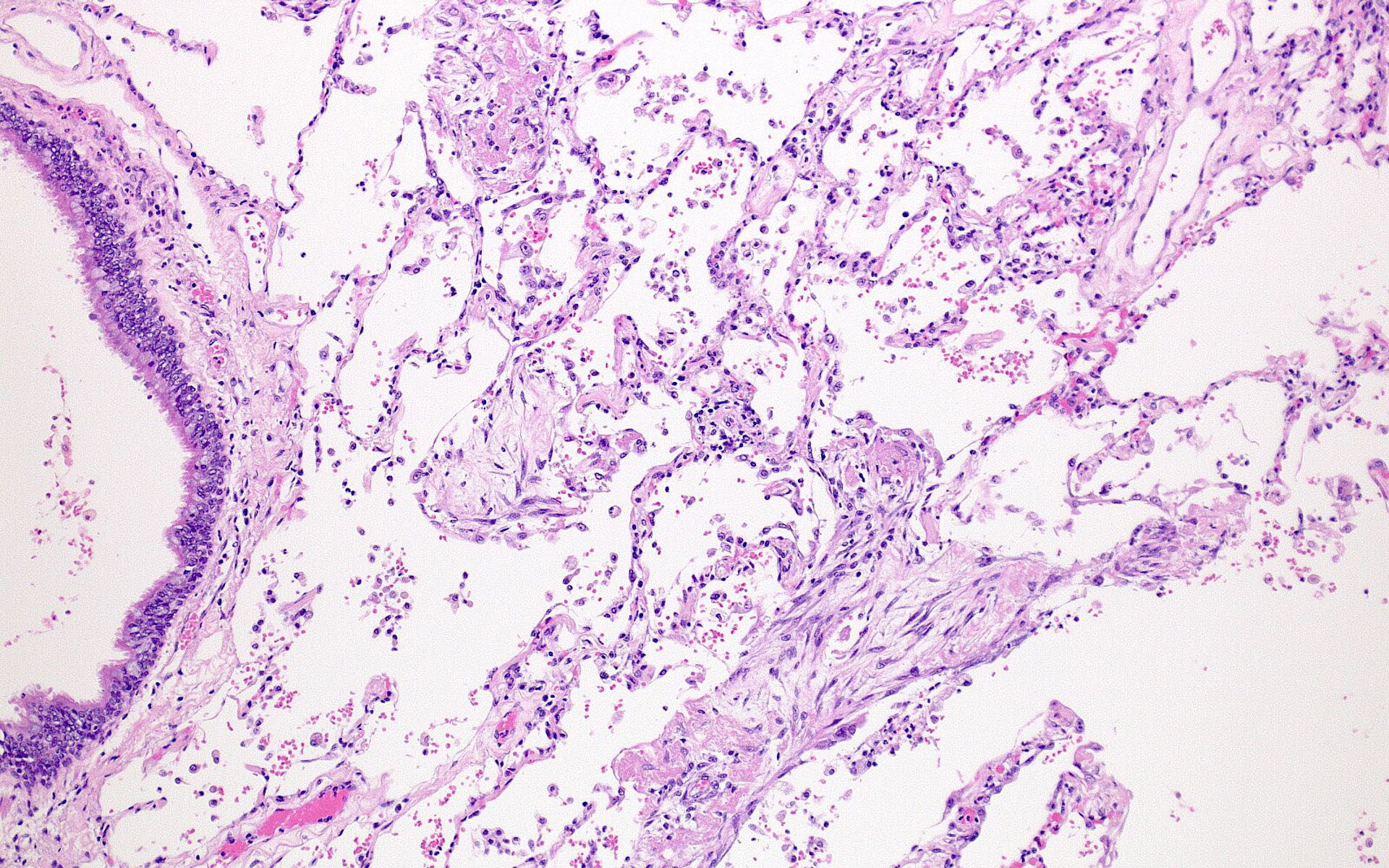
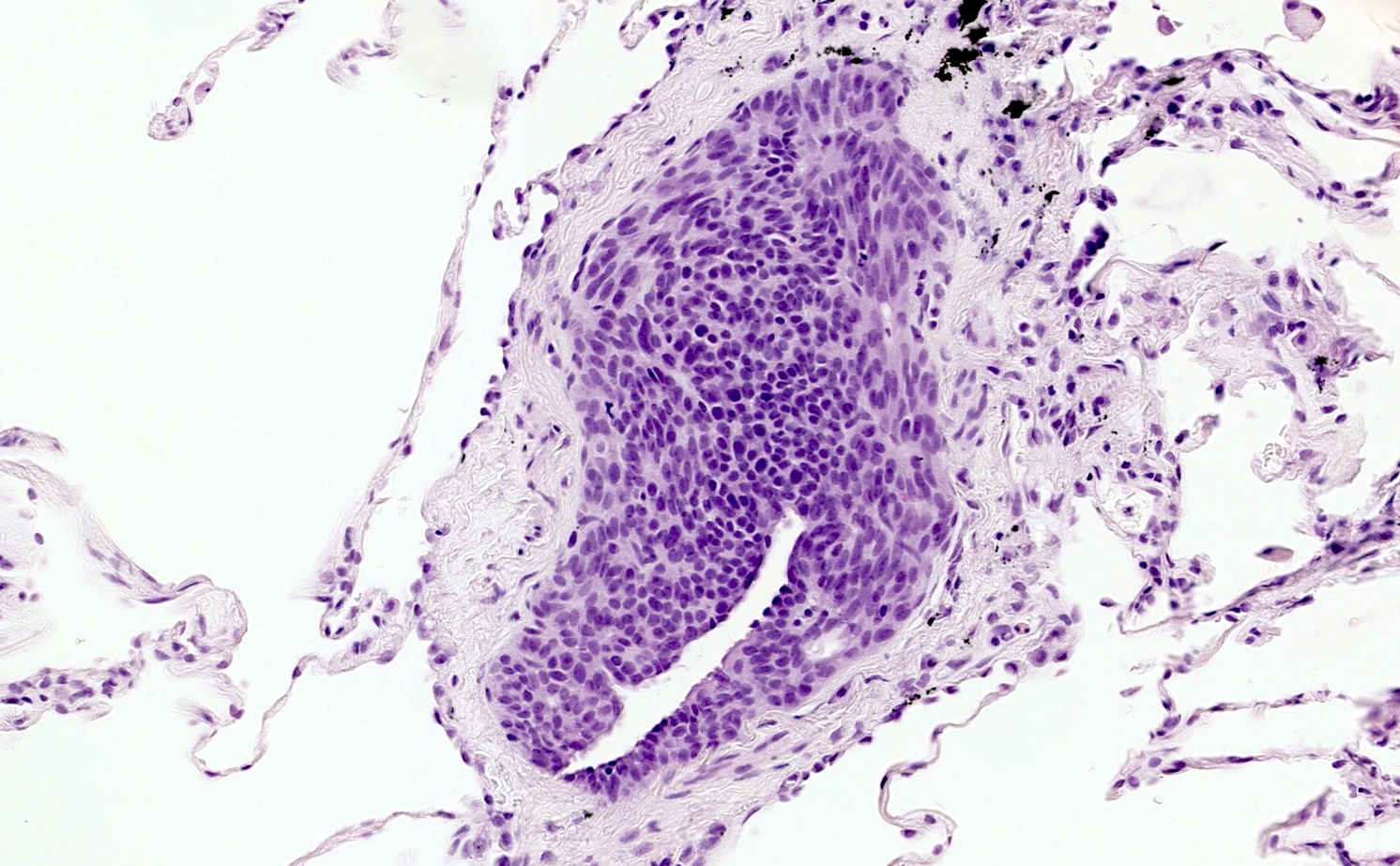
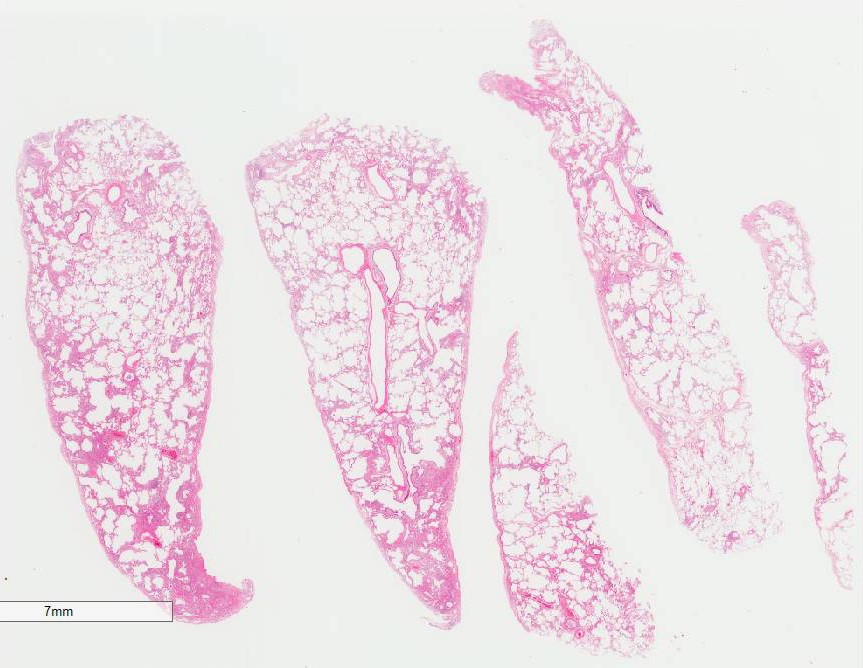
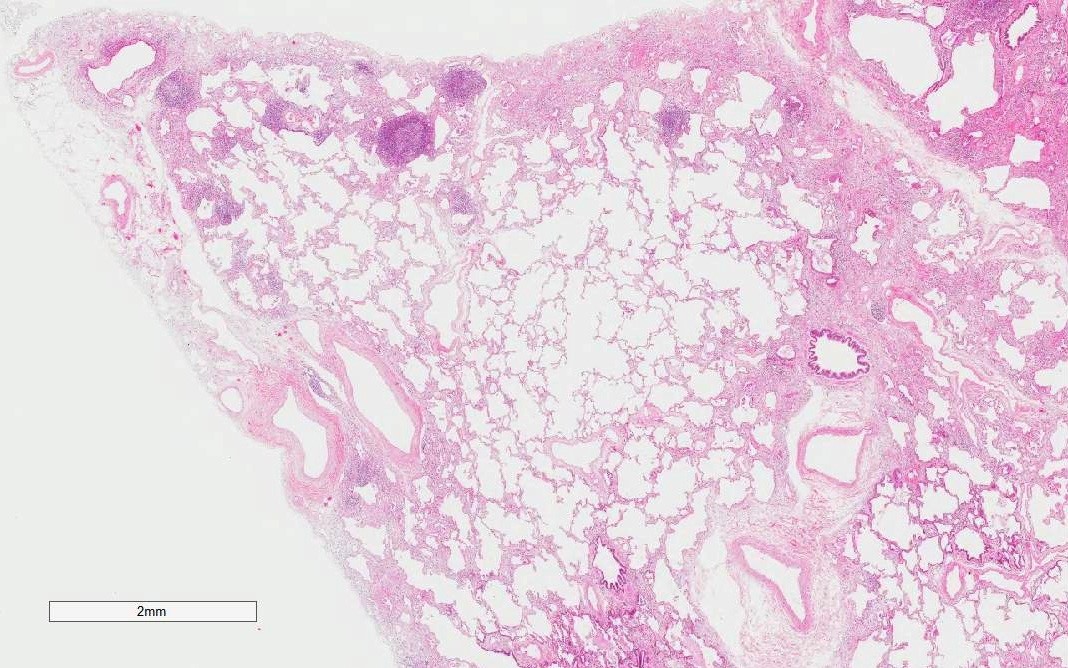
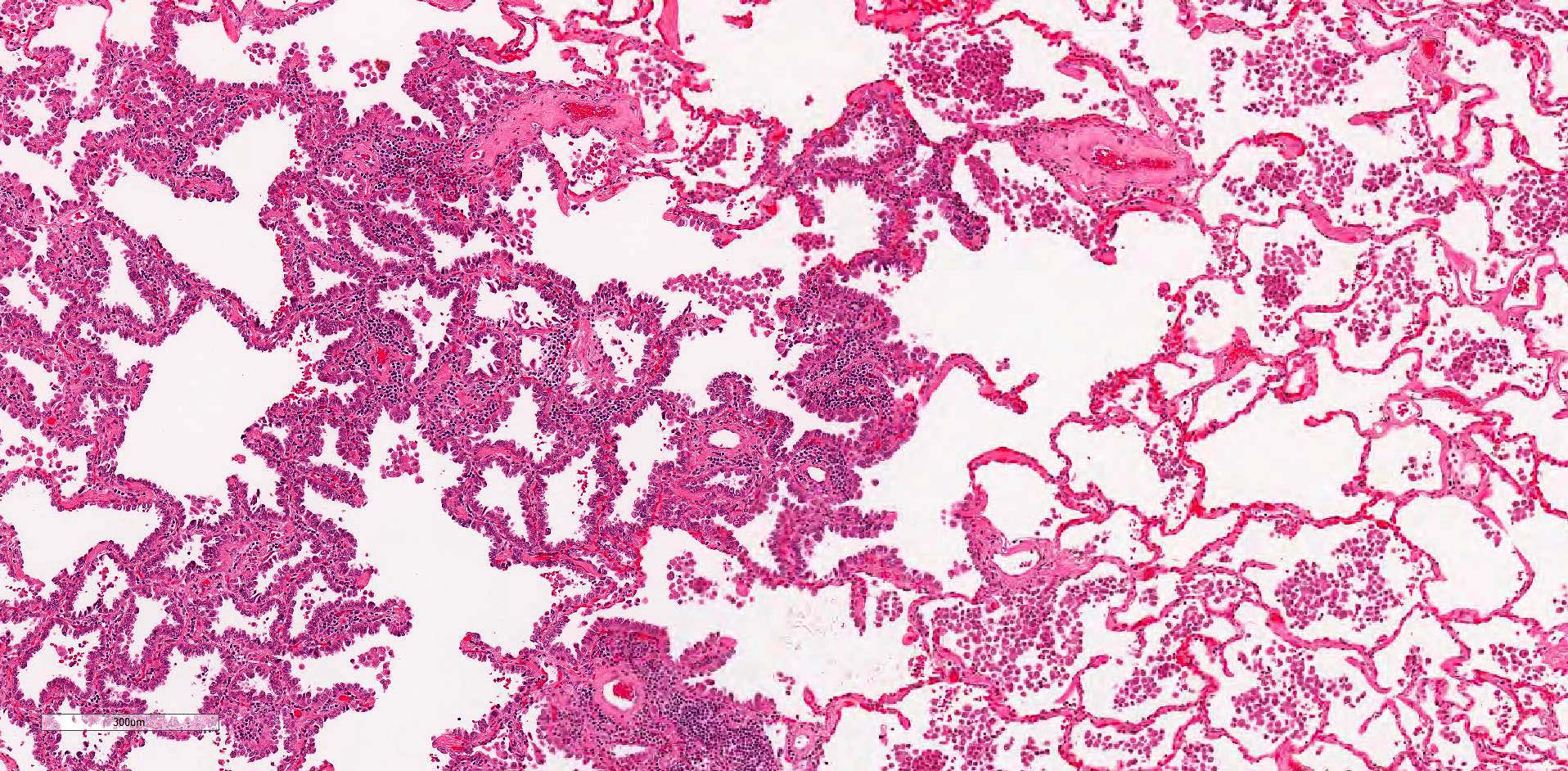
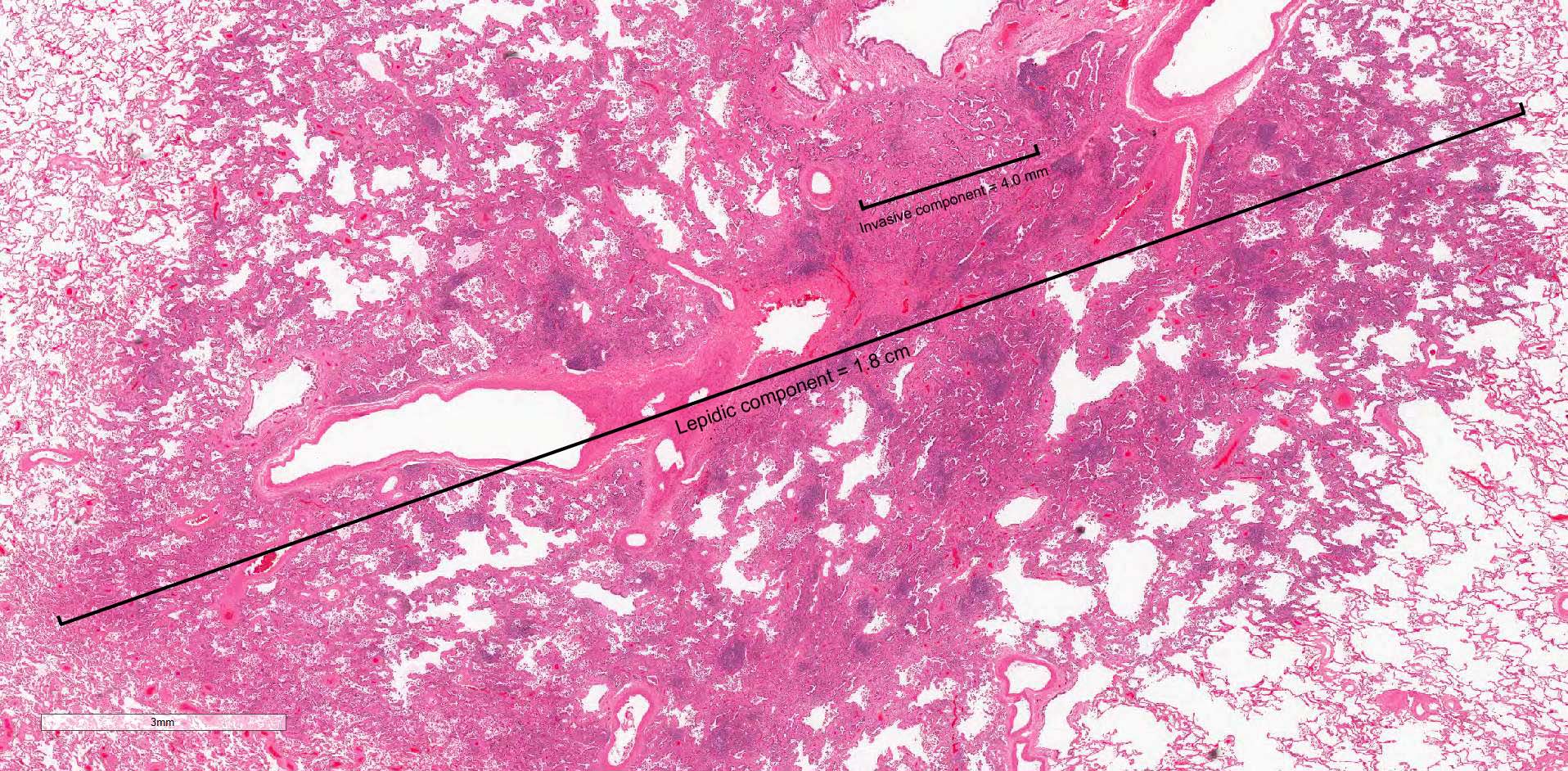
- Preinvasive lung adenocarcinoma
- Size: ≤ 30.0 mm
- Pure lepidic growth pattern with no invasion (neoplastic cells along pre-existing alveolar structures)
- Diagnosed only when all tumor has been sampled
- Diagnosis cannot be made in small biopsy or cytology specimen
- Lepidic growth with no stromal, vascular or pleural invasion
- Size: ≤ 30.0 mm
- Diagnosed only after complete sampling of a resected lesion
- Bronchioloalveolar carcinoma (historical term, obsolete)
- ~5% of nonsmall cell lung carcinomas (NSCLC)
- F = M (F slightly higher, in contrast to other NSCLC)
- References: J Clin Oncol 2005;23:8396, Lung Cancer 2004;45:137
- Peripheral lung (Cancer 1995;75:2844)
- Multistep progression model (Ann Oncol 2015;26:156, Int J Mol Sci 2018;19:1259)
- Adenocarcinoma in situ (AIS) is the step between atypical adenomatous hyperplasia (AAH) and minimally invasive carcinoma (MIA)
- Incidence of EGFR mutations increases from atypical adenomatous hyperplasia → adenocarcinoma in situ → minimally invasive carcinoma
- KRAS and BRAF mutations do not show same progression, suggesting other molecular alterations are also involved in tumor evolution
- EPPK1, KMT2C, KMT2D, NOTCH3 and NF1 mutations may present as early events in the progression of lung adenocarcinoma (Am J Respir Crit Care Med 2020;201:697)
- Same as invasive lung adenocarcinoma
- #1 risk factor is tobacco smoking
- Possible risk factors in never smokers: secondhand smoke, radon, occupational exposures, air pollution
- Most cases of lung cancer in never smokers are idiopathic, with different mutational profile than smoking related lung cancer
- Reference: J Thorac Oncol 2012;7:1352
- Often incidental
- May occur alone or along with invasive adenocarcinoma as a separate focus
- Slow growing
- May or may not be seen on CT or MRI, depending on size and association with scar
- Radiologic features that suggest indolence (Ann Am Thorac Soc 2015;12:1193):
- Small size
- Longer volumetric doubling time (> 400 days)
- Maximum standardized uptake value (SUV) < 1
- Definitive diagnosis requires excision and histopathologic evaluation
- Usually nonsolid
- May be partly solid or even solid (if tumor is mucinous or contains scar)
- References: Eur Respir J 2018;51:1800190, J Thorac Oncol 2016;11:1204
- Complete resection = 100% disease free and recurrence free survival rates (Am J Surg Pathol 2014;38:448, Lung Cancer 2019;129:16)
- If not resected, factors associated with growth of the lesions are initial tumor size, smoking and mutational status
- Reference: J Thorac Oncol 2012;7:1352
- 39 year old nonsmoking woman with adenocarcinoma in situ coexisting with low grade fetal lung adenocarcinoma (Onco Targets Ther 2020;13:6675)
- 44 year old woman with papillary thyroid carcinoma metastasizing to adenocarcinoma in situ of lung (Korean J Pathol 2012;46:282)
- 72 year old man with adenocarcinoma in situ, detected on a thin walled lung cavity (Surg Case Rep 2022;8:60)
- Complete resection is diagnostic and curative
- No adjuvant therapy
- Reference: Am J Surg Pathol 2014;38:448, Lung Cancer 2019;129:16
- Ill defined nodule
- May appear grossly solid if collapsed, compressed or associated with scar
- Size: ≤ 30.0 mm
- References: J Thorac Oncol 2016;11:1204, Int J Mol Sci 2018;19:1259
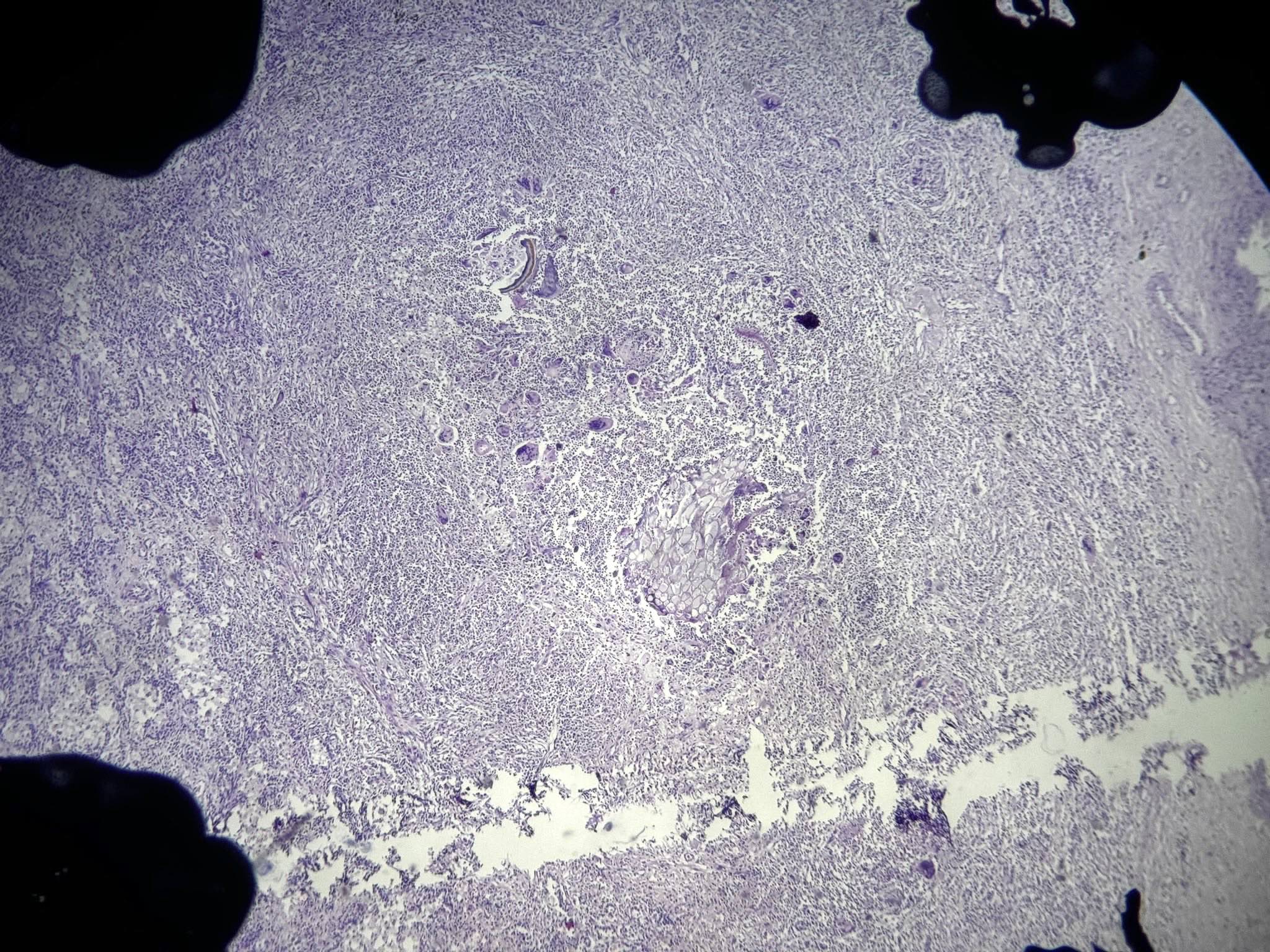
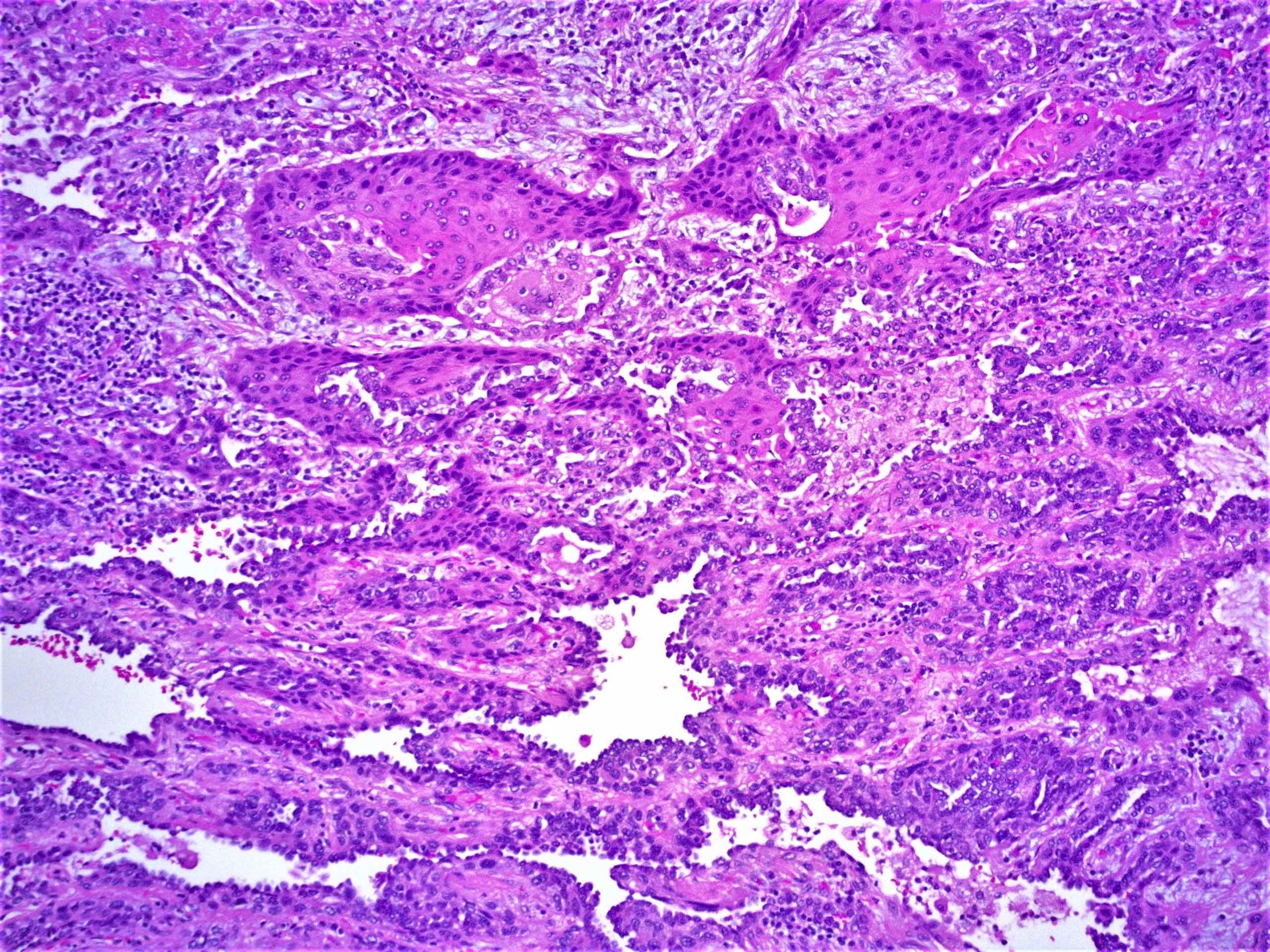
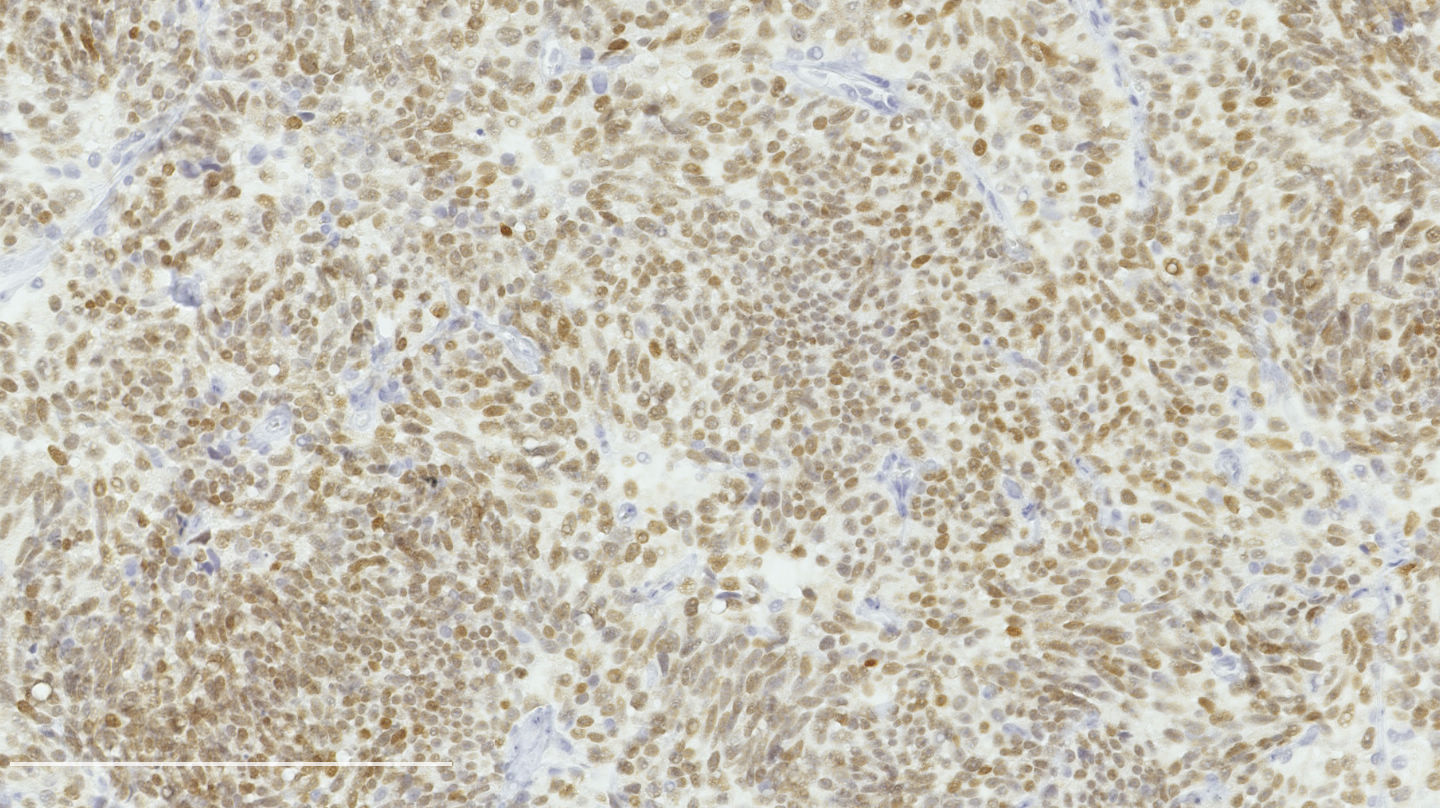
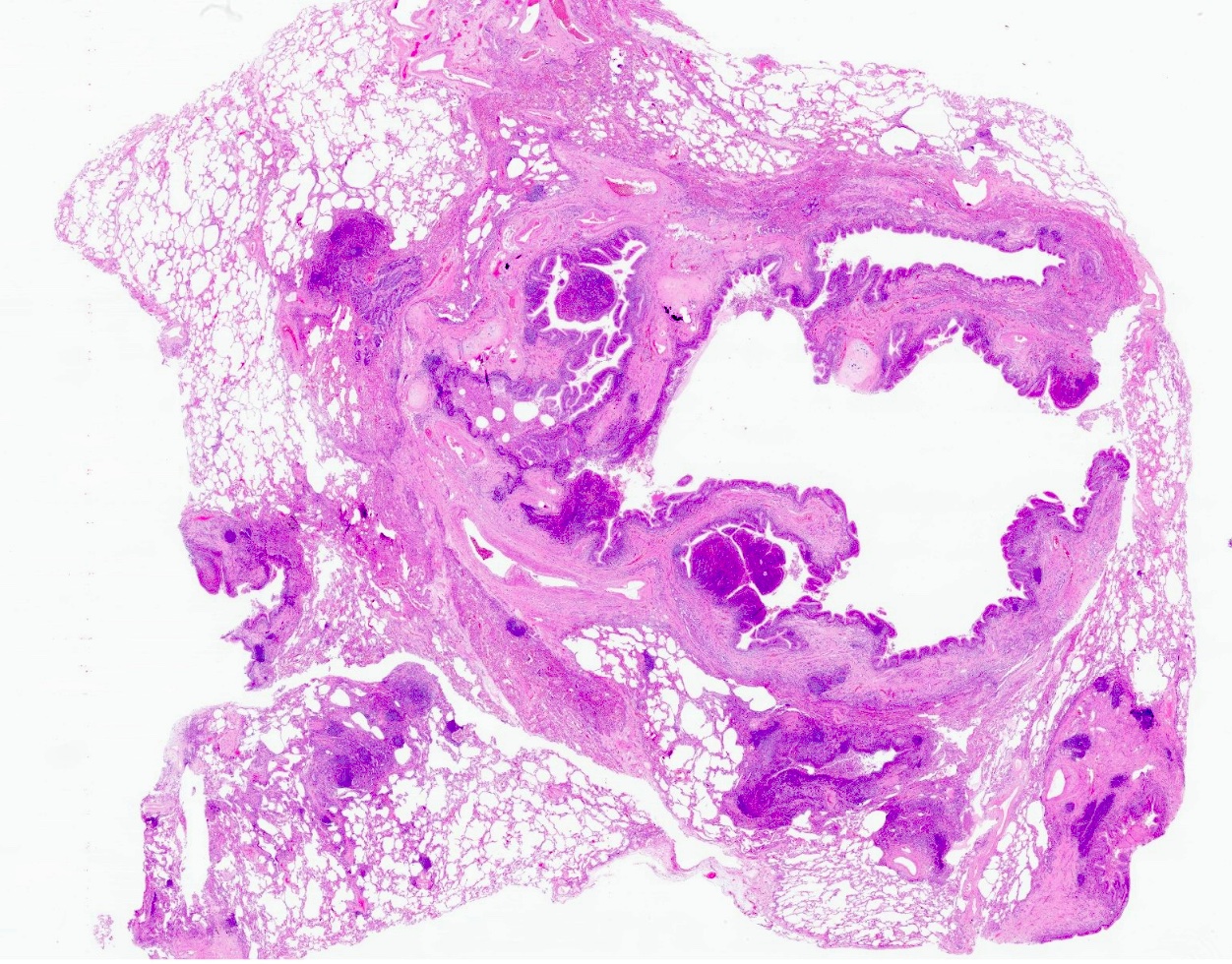
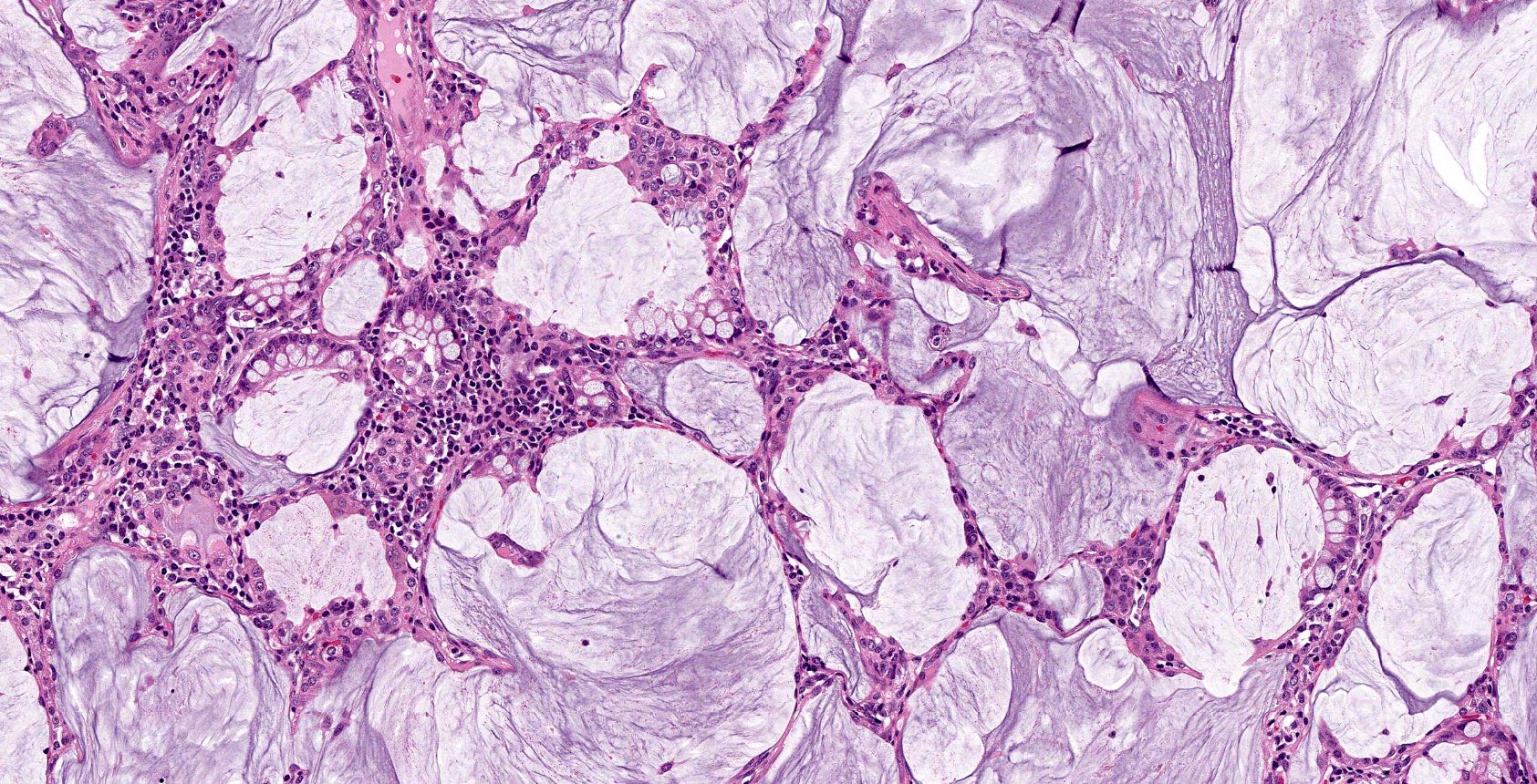
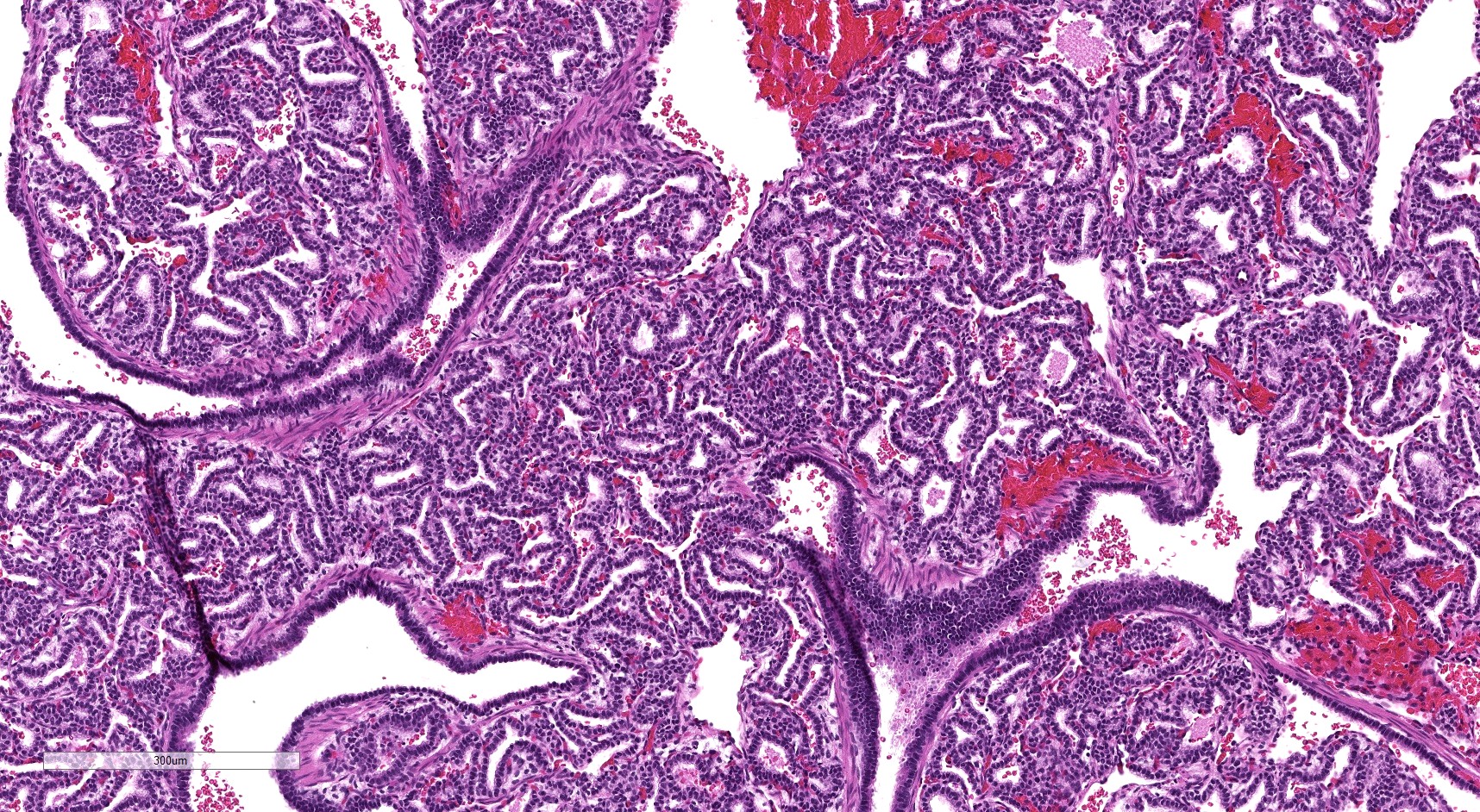
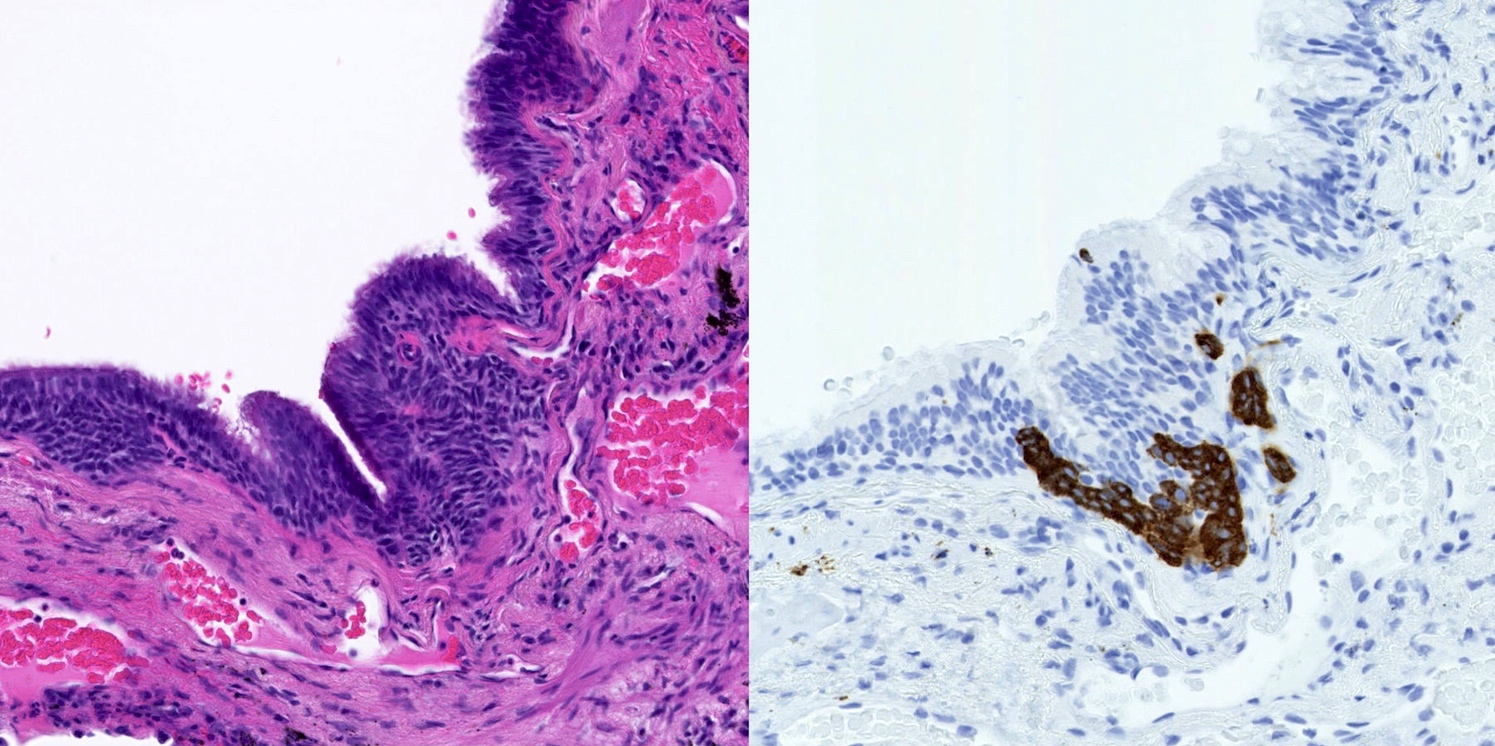
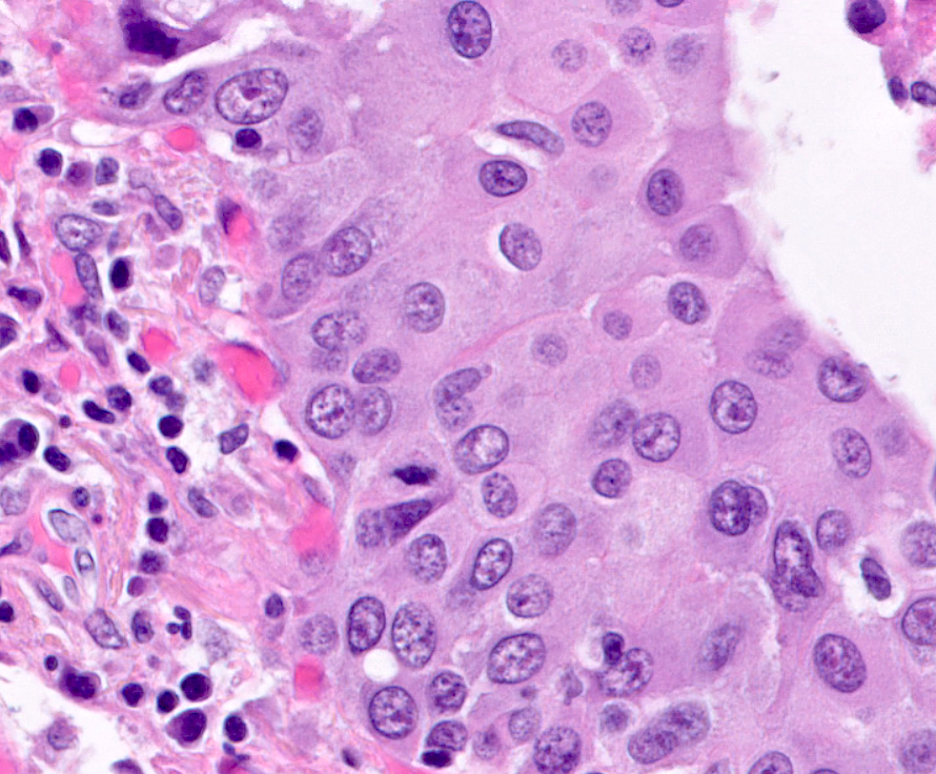
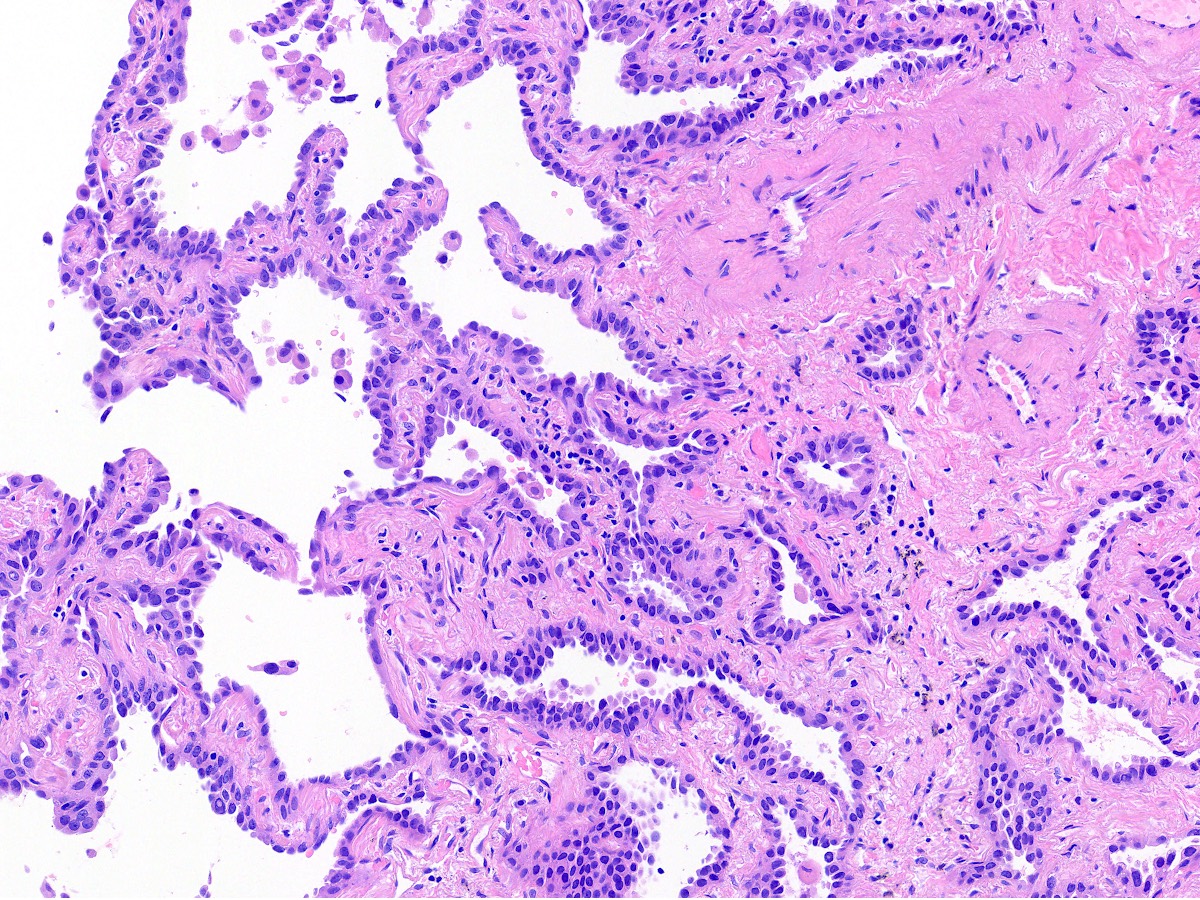
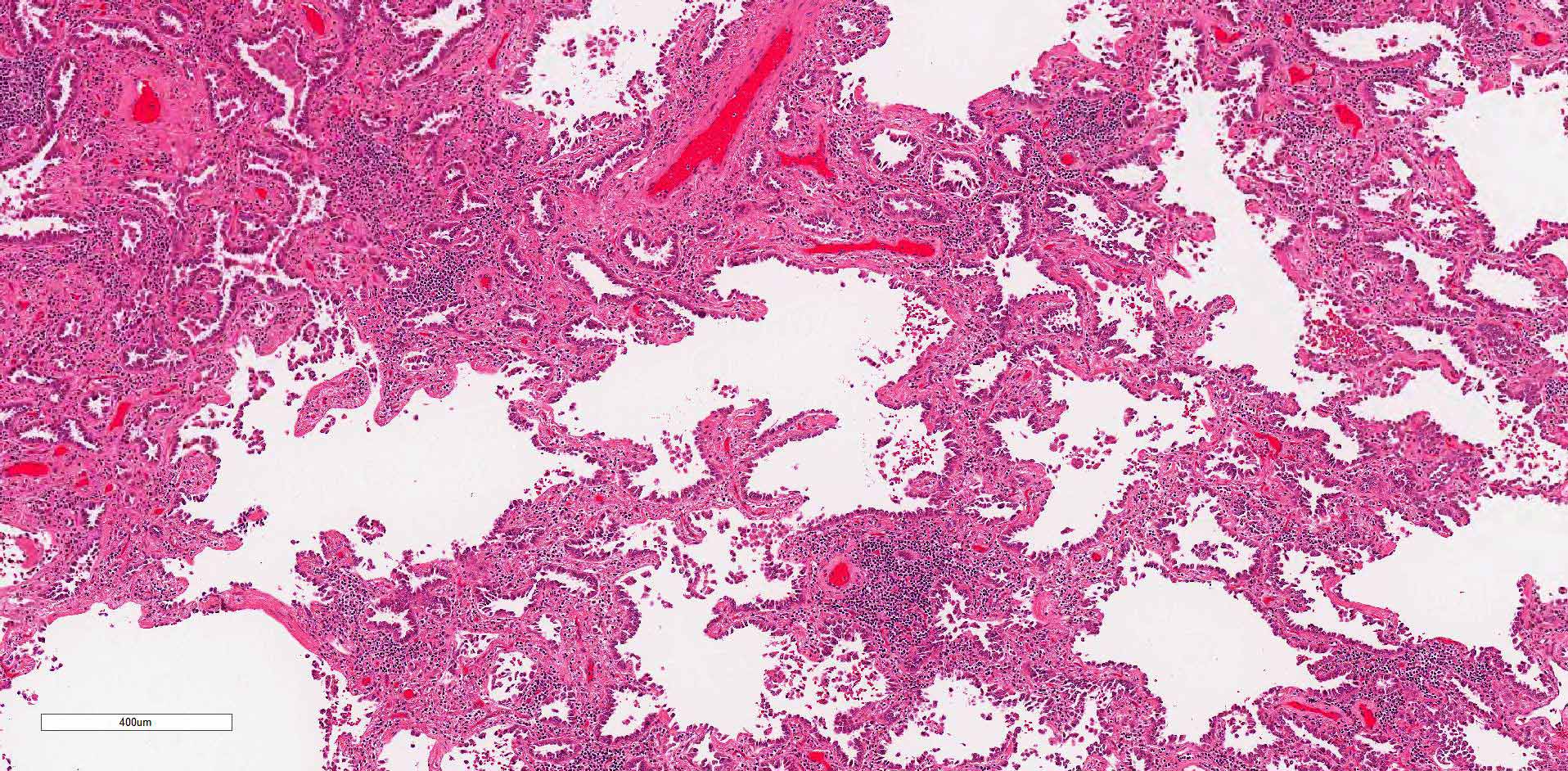
- Lepidic pattern adenocarcinoma with mild to moderate cytologic atypia
- Do not diagnose as adenocarcinoma in situ on frozen section; invasion may be present on deeper levels or in the remainder of the tumor that was not submitted for frozen section
- If no invasion is seen on frozen, one may call it adenocarcinoma with the lepidic pattern on 1 representative section, pending evaluation of permanent sections (or the remainder of the tumor)
- Reference: J Clin Pathol 2016;69:1076
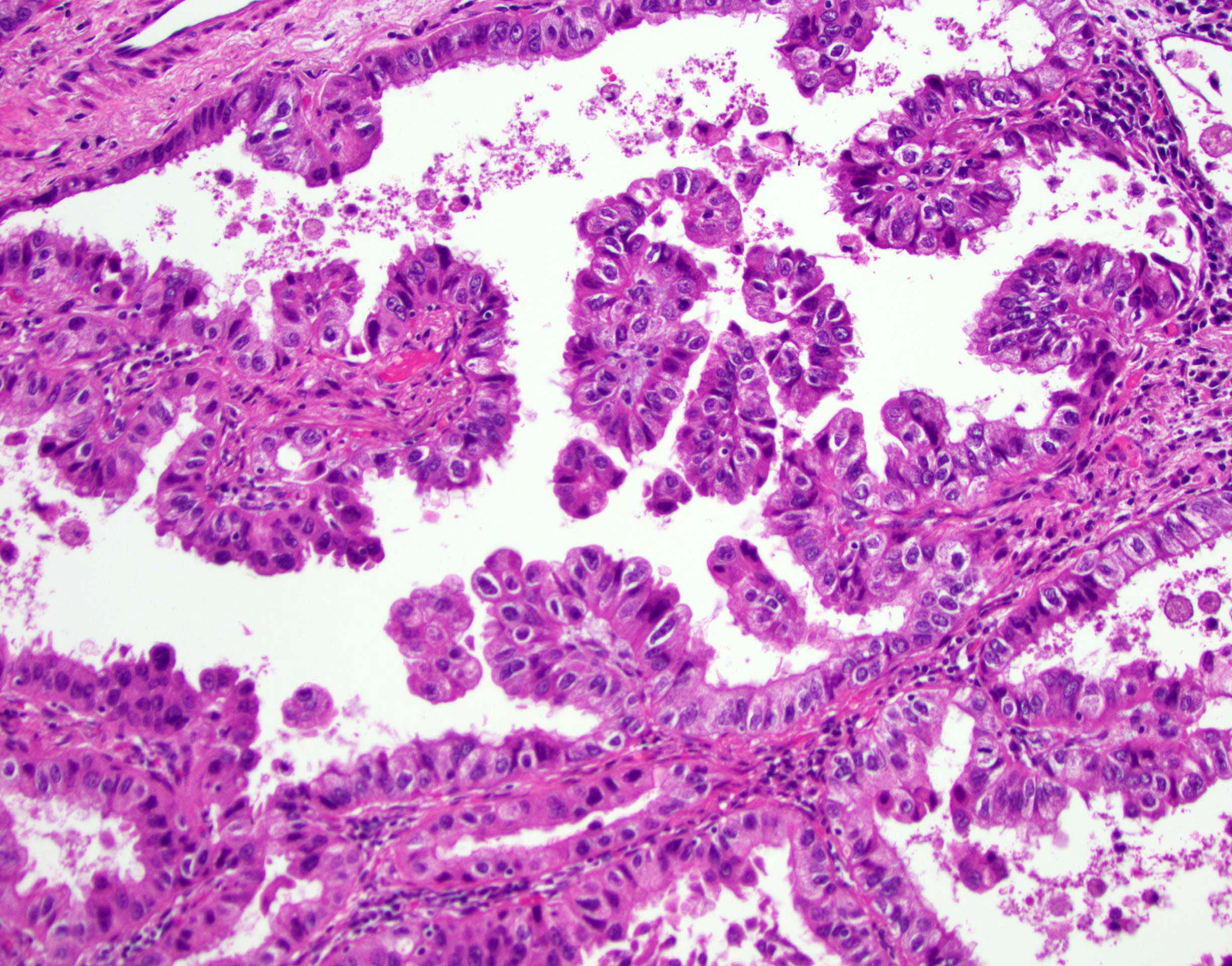
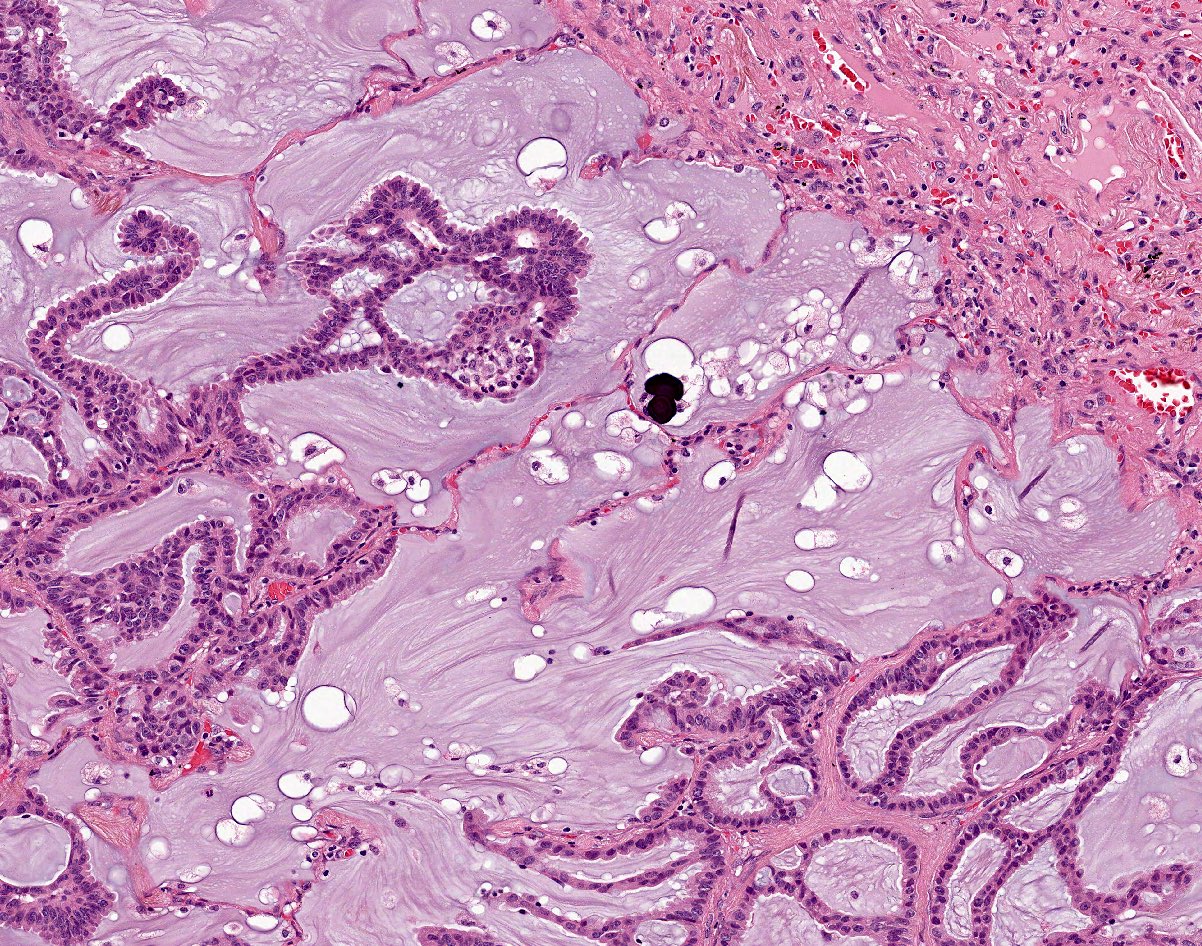
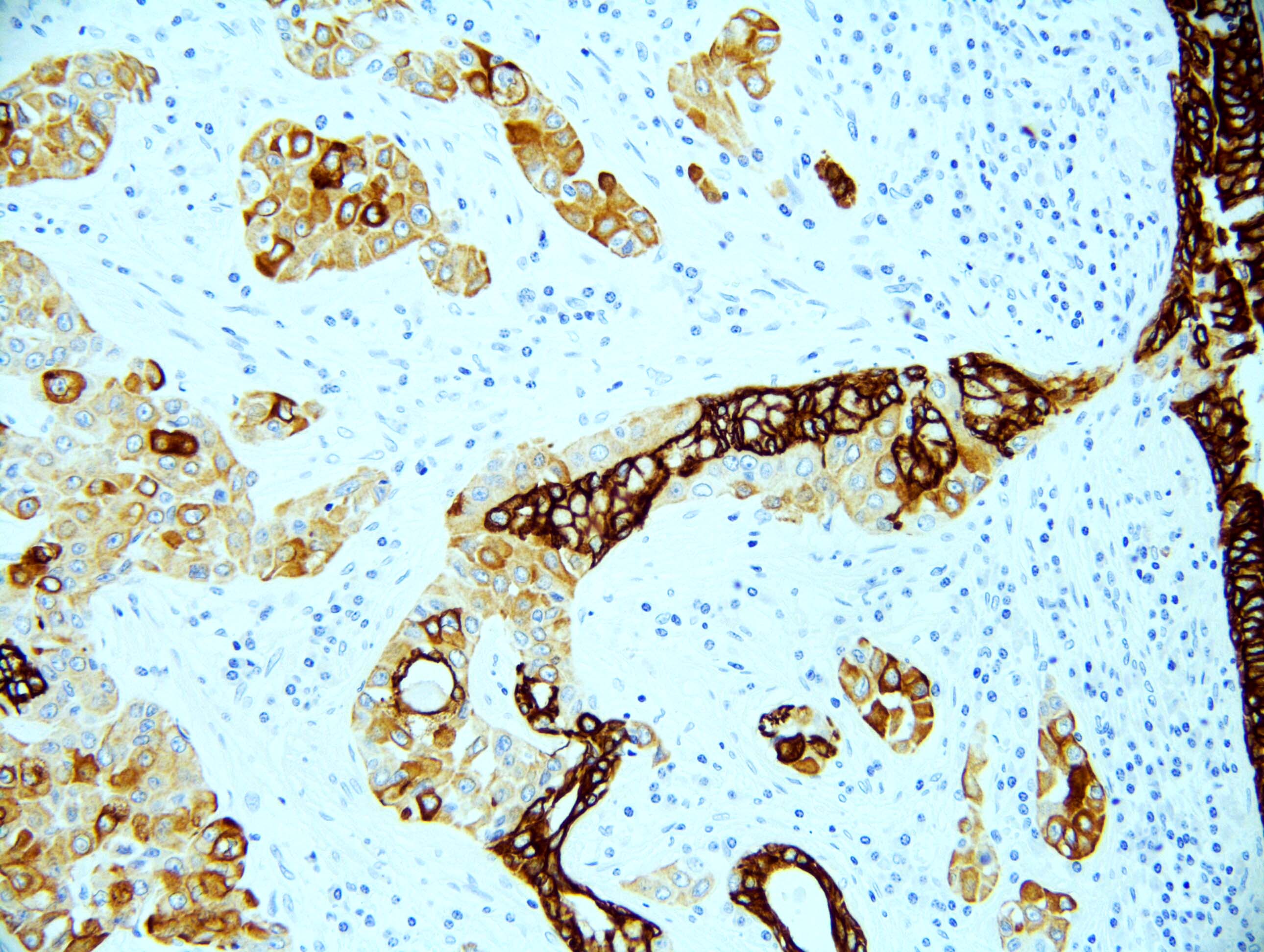
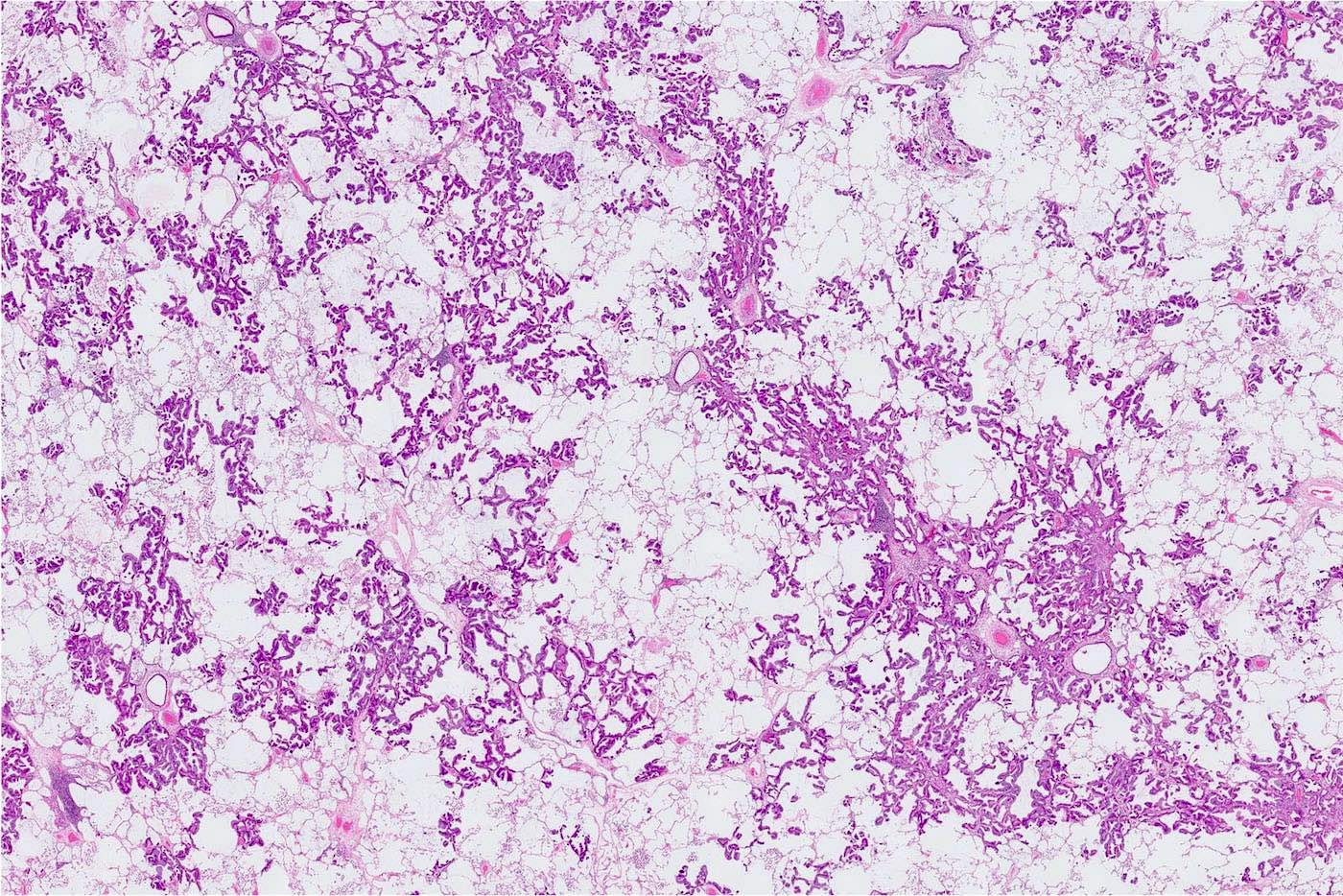
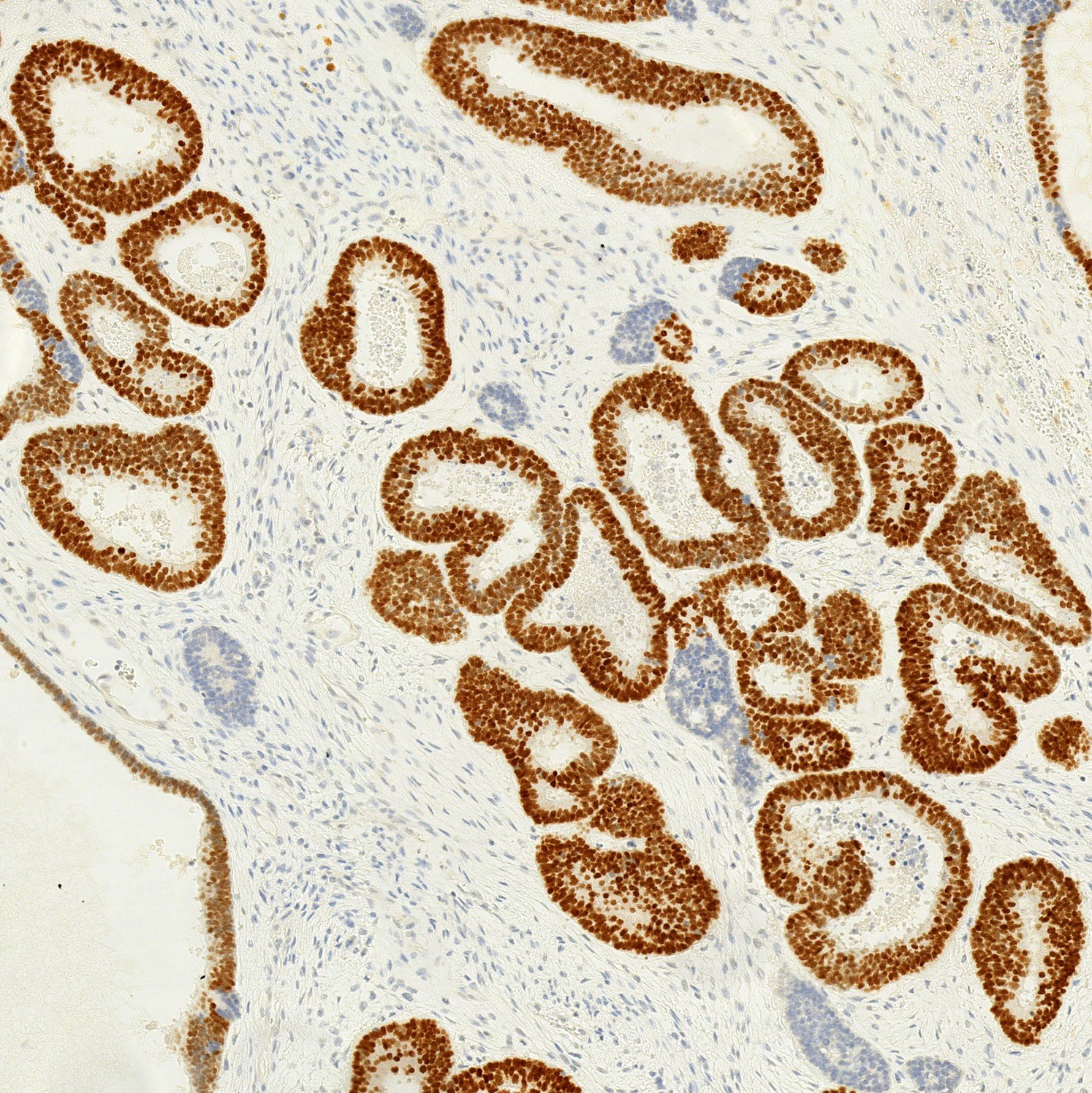
- Lepidic growth pattern only: back to back neoplastic cells growing along pre-existing alveolar structures only
- No stromal, vascular or pleural invasion; no necrosis
- Diagnosed only in resections after complete sampling
- Cannot be diagnosed in small biopsies, cytology or frozen sections (differential diagnosis minimally invasive carcinoma and invasive adenocarcinoma)
- Size: ≤ 30.0 mm
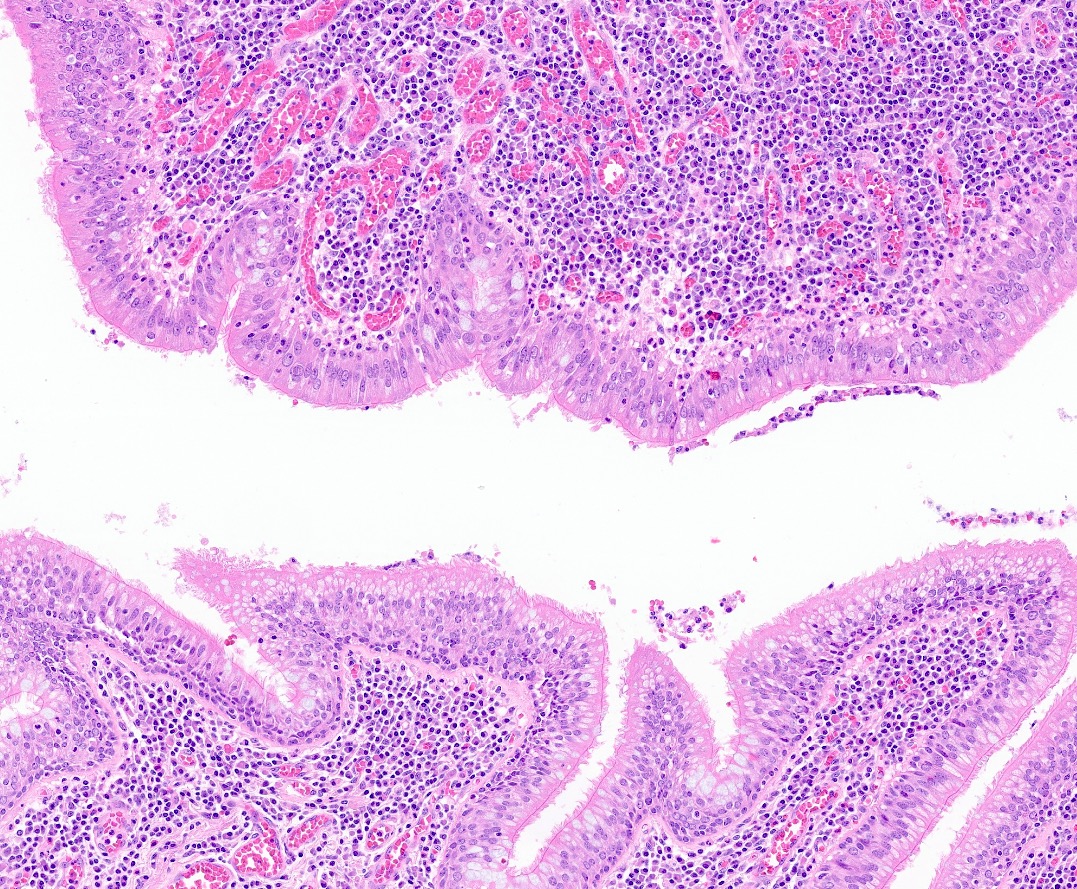
- Nonmucinous adenocarcinoma in situ = mild to moderate cytologic atypia, consisting of various combinations of the following features: nuclear membrane irregularity, intranuclear pseudoinclusions, nuclear grooves, hyperchromasia, anisocytosis, small nucleoli, increased nuclear to cytoplasmic ratio, hobnailing
- Not all features may be present
- Mucinous type adenocarcinoma in situ = extremely rare; mucinous tumors are usually associated with invasion
- Mucinous cells show minimal atypia with abundant intracellular mucin and basally oriented nuclei
- References: J Thorac Oncol 2016;11:1204, Int J Mol Sci 2018;19:1259
- Mild to moderate cytologic atypia
- Nuclear membrane irregularity, nuclear grooves and intranuclear pseudoinclusions (resembles papillary thyroid carcinoma cytology)
- Definitive diagnosis requires excision
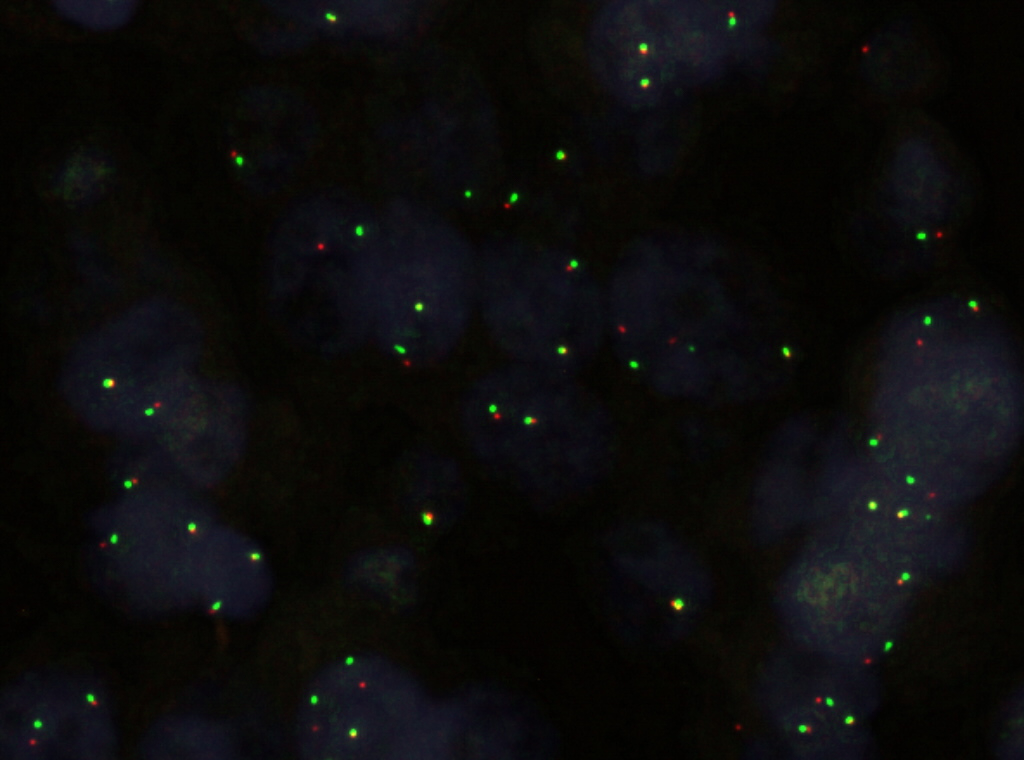
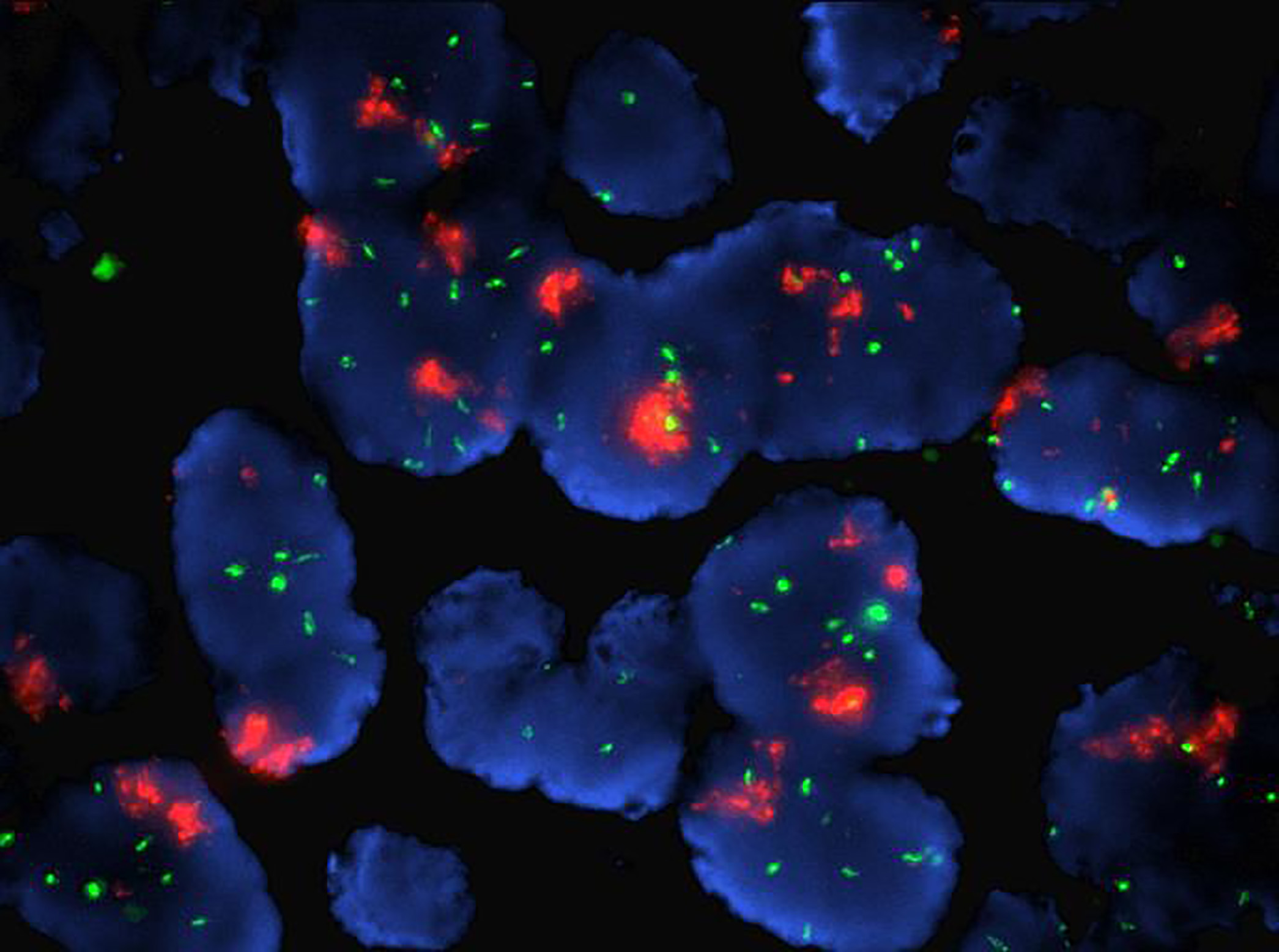
- About half of adenocarcinoma in situ cases harbor EGFR mutations (Ann Oncol 2015;26:156)
- EGFR mutation incidence is higher in Asian patients and KRAS mutation is seen more often in North American patients
- Ethnicity should not be considered in decision making; broad panel molecular testing is recommended for all patients who may benefit from targeted therapy (NCCN: NCCN Guidelines - Non-Small Cell Lung Cancer [Accessed 10 January 2022])
- Mutations of TP53 and NF1 were found to increase in frequency in adenocarcinoma in situ and minimally invasive adenocarcinoma (Am J Respir Crit Care Med 2020;201:697)
- More copy number loss was observed in adenocarcinoma in situ and minimally invasive adenocarcinoma rather than deleterious mutation burden, which was significantly greater in invasive adenocarcinoma (Am J Respir Crit Care Med 2020;201:697)
Adenocarcinoma in situ
by Dr. Thomas Colby
- Lung, middle lobe, right, lobectomy:
- Adenocarcinoma in situ (pTis) (see synoptic report)
- Tumor size: 25.0 mm
- Bronchial and vascular margins are negative for carcinoma
- Lung, right upper lobe; biopsy:
- Adenocarcinoma with lepidic pattern
- Note: Adenocarcinoma in situ cannot be definitely diagnosed until the entire tumor is examined and invasive adenocarcinoma ruled out. Thus, on small biopsy specimens, potential cases of adenocarcinoma in situ are signed out as above.
- Atypical adenomatous hyperplasia (AAH):
- Atypical cells are not back to back
- Less cytologic atypia
- Size:
- Minimally invasive adenocarcinoma:
- ≤ 30.0 mm overall size and ≤ 5.0 mm focus of invasion
- Adenocarcinoma, lepidic predominant:
- > 30.0 mm overall size (see table 1) or > 5.0 mm focus of invasion
- Bronchiolar adenoma:
- Papillary growth pattern
- Has basal layer, ciliated cells and mucus cells
- Glandular papilloma:
- Usually central, endobronchial
- Papillary growth pattern
- Papillary adenoma:
- Papillary architecture, bland cytology
- Peribronchiolar metaplasia:
- Peribronchiolar ciliated cells are seen along alveolar septa
- Has basal layer
- Does not form mass
Table 1: Differential diagnosis of lepidic predominant lung tumors
Overall size ≤ 30.0 mm Overall size > 30.0 mm
Lepidic pattern only
Adenocarcinoma in situAdenocarcinoma, lepidic predominant
(stage as pT1a)Invasion ≤ 5.0 mm Minimally invasive adenocarcinoma Adenocarcinoma, lepidic predominant Invasion > 5.0 mm Adenocarcinoma, lepidic predominant Adenocarcinoma, lepidic predominant
- Acinar predominant with lepidic adenocarcinoma
- Adenocarcinoma in situ
- Lepidic predominant with acinar adenocarcinoma
- Minimally invasive carcinoma
- Non-small cell lung carcinoma with glandular differentiation, mucin production or pneumocyte marker expression
- Most prevalent non-small cell lung carcinoma
- 5 main histologic patterns (acinar, papillary, micropapillary, lepidic, solid); mucinous and nonmucinous subtypes
- Positive for TTF1
- Terminology of lung adenocarcinoma was significantly revised in the 2015 WHO classification (J Thorac Oncol 2015;10:1243)
- Discontinuation of the terms bronchioloalveolar carcinoma (BAC) and mixed subtype adenocarcinoma
- Addition of adenocarcinoma in situ (AIS) as a preinvasive lesion to join atypical adenomatous hyperplasia
- Addition of minimally invasive adenocarcinoma
- Use of the term lepidic for a noninvasive component (previously classified as BAC) of an invasive adenocarcinoma
- Introduction of the term invasive mucinous adenocarcinoma for adenocarcinomas formerly classified as mucinous BAC, excluding tumors that meet criteria for AIS or minimally invasive adenocarcinoma (MIA)
- Discontinuation of the subtypes of clear cell and signet ring adenocarcinoma
- Discontinuation of the term mucinous cystadenocarcinoma and inclusion of these under the category of colloid adenocarcinoma
- Most prevalent non-small cell lung carcinoma (PLoS One 2015;10:e0121323)
- F > M (PLoS One 2015;10:e0121323)
- Most common type of lung cancer in male nonsmokers (PLoS One 2015;10:e0121323)
- African Americans > Caucasians (PLoS One 2015;10:e0121323)
- Age 60 - 70 (PLoS One 2015;10:e0121323)
- Upper lobe > lower lobe (Lung Cancer 2018;126:139)
- Peripheral > central (Diagn Interv Imaging 2016;97:955)
- Metastasis: brain (often only site) > bone > liver > adrenal (Cancer Biol Ther 2016;17:272)
- Risk for brain metastasis increases with tumor size and lymph node stage (Radiology 2007;242:882)
- Toxic cellular exposures → genetic mutations → proliferation of endobronchial cells (PLoS Med 2016;13:e1002162, J Transl Med 2017;15:26)
- Genetic events were characterized by TCGA project, described in Molecular / cytogenetics description (Nature 2014;511:543)
- Smoking is the greatest risk factor, including secondhand smoke (Transl Lung Cancer Res 2018;7:220)
- Radon from soil, usually in residential areas (Transl Lung Cancer Res 2018;7:220)
- Cooking oil fumes, particularly in Asia (Int J Cancer 1987;40:604, Onco Targets Ther 2016;9:2987, Transl Lung Cancer Res 2018;7:220)
- Asbestos exposure, usually occupational (ship building, construction) (Mol Clin Oncol 2017;7:135)
- Cough (productive if mucinous adenocarcinoma), hemoptysis, dyspnea, weight loss, chest pain (Chest 2012;142:1338)
- Paraneoplastic / endocrine syndromes are much less common than in small cell lung carcinoma
- Hypertrophic pulmonary osteoarthropathy with clubbing of the fingers, symmetric polyarthritis, periostitis of the long bones (World J Clin Oncol 2014;5:197)
- Histological, based on morphology and staining pattern
- Well defined borders, lobulated or spiculated, presence of air bronchograms (Diagn Interv Imaging 2016;97:955)
- Solid, dense areas have solid or acinar patterns (Diagn Interv Imaging 2016;97:955)
- Ground glass opacities are mucinous subtype or lepidic pattern (Diagn Interv Imaging 2016;97:955)
- Favorable: lepidic (J Thorac Oncol 2022;17:362)
- Unfavorable: spread through air spaces, size > 2.5 cm, visceral pleural invasion, micropapillary or solid type (Mod Pathol 2021;34:549, J Thorac Oncol 2013;8:37, Mod Pathol 2011;24:653, Sci Rep 2018;8:4743, Chest 2014;146:1619)
- 36 year old woman at 33 weeks gestation presenting with orthopnea caused by lepidic predominant lung adenocarcinoma (Case Rep Oncol 2018;11:822)
- 38 year old man with EGFR mutant lung adenocarcinoma with small cell transformation (Cancer Biol Ther 2018;19:445)
- 60 year old man with fast growing lung micropapillary predominant adenocarcinoma (Respir Med Case Rep 2017;20:125)
- 60 year old woman with EGFR wild type lung adenocarcinoma complicated by ovarian metastasis (BMC Womens Health 2021;21:152)
- 63 year old man presenting with Lambert-Eaton myasthenic syndrome caused by advanced lung adenocarcinoma (Thorac Cancer 2020;11:1334)
- For stages I, II, IIA and IIB without invasion: surgical resection + adjuvant radiation therapy
- For stages IIB with invasion, IIIA and IIIB without invasion: surgical resection + chemoradiation
- Inoperable or metastatic: molecular dependent chemotherapy + radiation
- Reference: NCCN: NCCN Guidelines - Non-Small Cell Lung Cancer [Accessed 6 July 2022]
- Adenocarcinoma (Am J Clin Pathol 2017;147:641):
- Tan-white cut surface
- May have central area of scar or necrosis
- Usually well defined but nonencapsulated
- Minimally invasive adenocarcinoma (Diagn Interv Imaging 2016;97:955):
- Focal (Usually solitary
- Diagnosis given to surgeon: non-small cell lung carcinoma or adenocarcinoma
- 85% accurately diagnosed on frozen section (J Clin Oncol 2016;34:307)
- Sampling error is the main reason for inaccurate diagnosis (Histopathology 2015;66:922)
- High grade patterns more difficult to diagnose (Histopathology 2015;66:922)
- Invasive mucinous adenocarcinoma: invasion > 5 mm, composed of goblet or columnar cells with abundant mucin (J Thorac Oncol 2022;17:362)
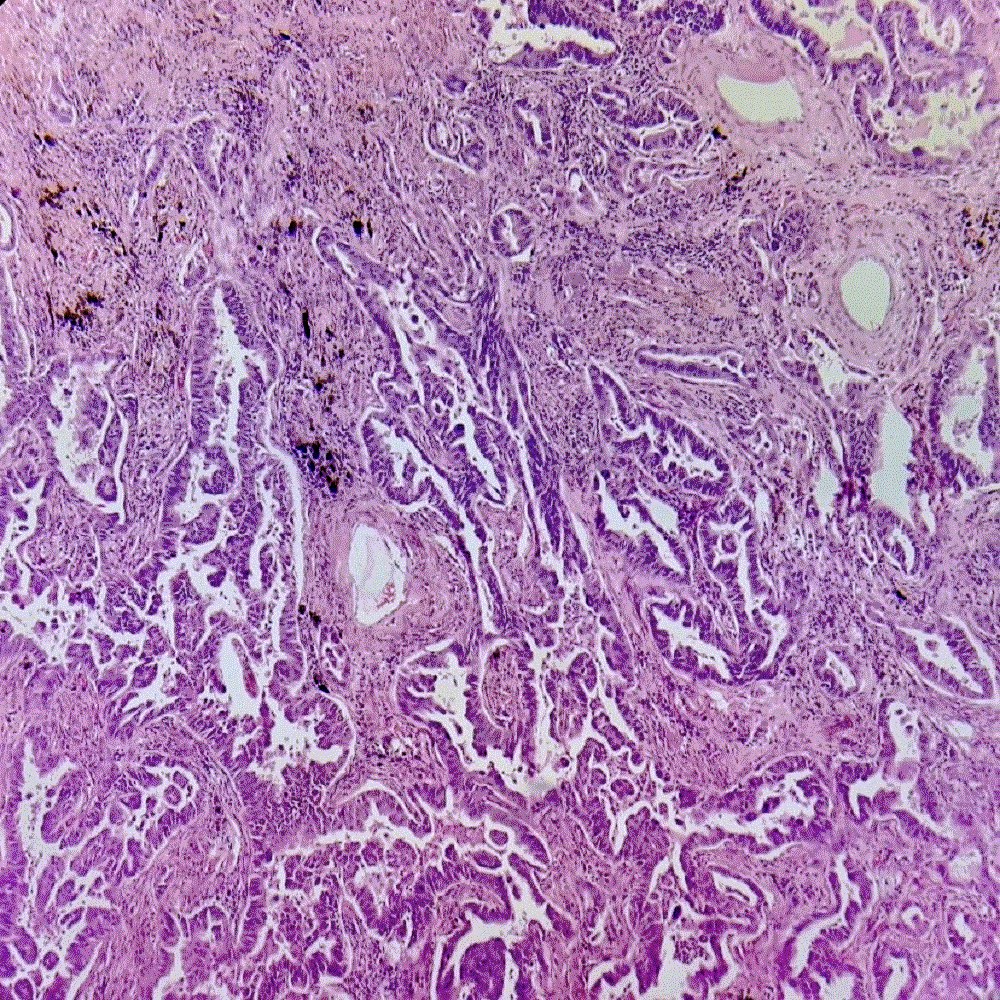
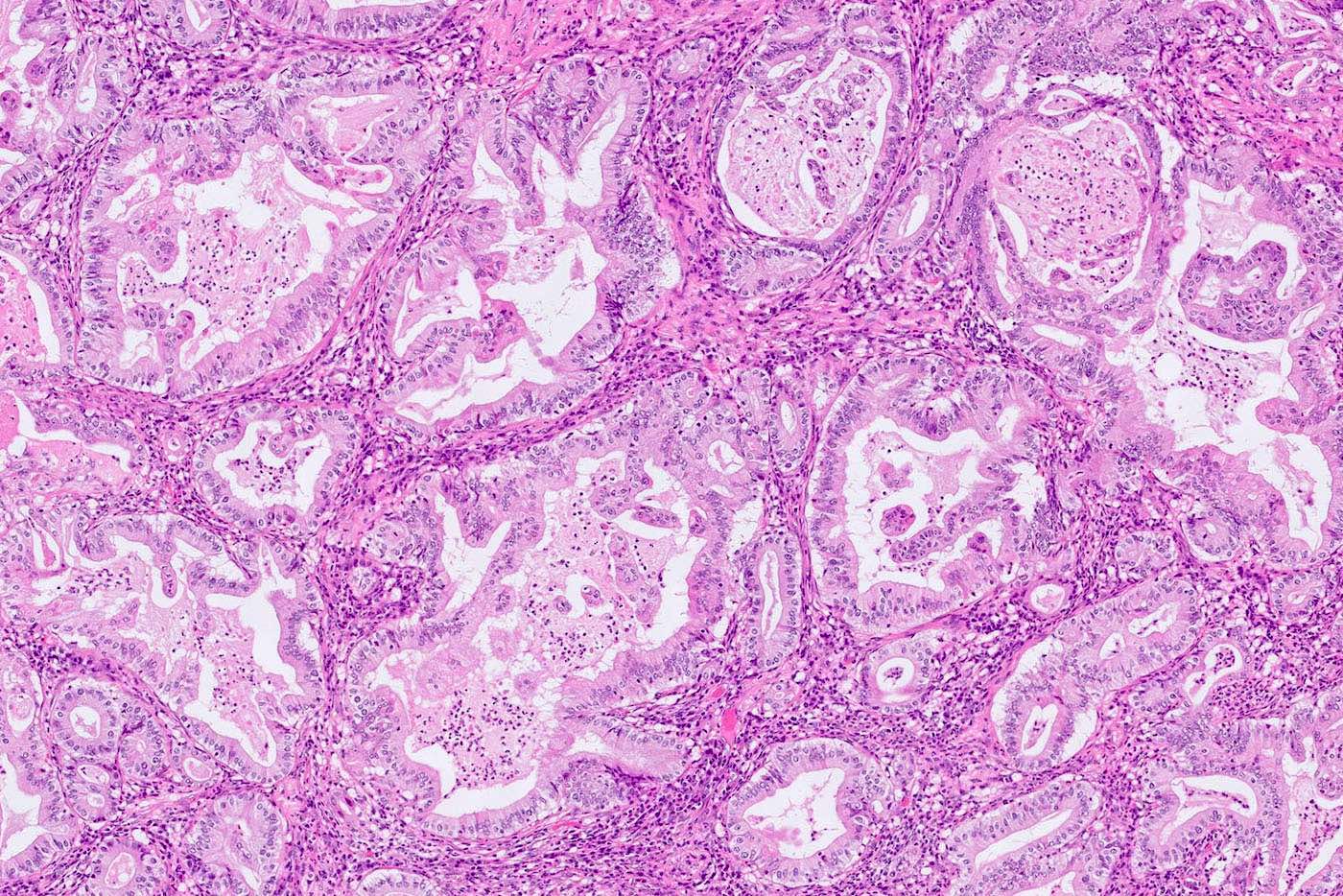
- Invasive nonmucinous adenocarcinoma: invasion > 5 mm, glandular differentiation, named by predominant pattern (J Thorac Oncol 2011;6:244)
- 5 main histologic patterns:
- Lepidic: type II pneumocytes and club cells proliferate to line alveolar walls; lacks architectural complexity; no lymphovascular or perineural invasion (J Thorac Dis 2017;9:2142, J Thorac Oncol 2011;6:244)
- Acinar: gland forming; round / oval glands invading the stroma (usually fibrous); includes high grade complex glandular subtypes (J Thorac Oncol 2020;15:1599, J Thorac Oncol 2011;6:244)
- Papillary: malignant cuboidal / columnar cells replace alveolar lining; contains fibrovascular cores (J Thorac Oncol 2011;6:244)
- Micropapillary: ill defined projection / tufting that lacks fibrovascular cores (J Thorac Oncol 2011;6:244)
- Solid: sheets of neoplastic cells (J Thorac Oncol 2011;6:244)
- Tumor grade dependent on combination of histologic patterns (J Thorac Oncol 2022;17:362, J Thorac Oncol 2020;15:1599)
- Each pattern should be recorded in 5 - 10% increments
- Grading: (J Thorac Oncol 2022;17:362)
- Grade 1 (well differentiated): lepidic, predominant, with no or Grade 2 (moderately differentiated): acinar or papillary predominant, with no or Grade 3 (poorly differentiated): any pattern with 20% or more high grade pattern
- Less common subtypes:
- Colloid: cuboidal or columnar cells with abundant pools of extracellular mucin that distort alveolar spaces (J Thorac Oncol 2022;17:362)
- Fetal: resembles pseudoglandular fetal epithelium; can be mildly atypical and low grade or severely atypical and high grade (J Thorac Oncol 2022;17:362)
- Enteric type: resembles colorectal adenocarcinoma and has at least 1 intestinal marker (J Thorac Oncol 2022;17:362)
- Minimally invasive adenocarcinoma: focal (≤ 30 mm), predominantly lepidic pattern, ≤ 5 mm area of invasion (any subtype) (J Thorac Oncol 2022;17:362, Diagn Interv Imaging 2016;97:955)
- Spread through air spaces is more commonly associated with adenocarcinomas (versus squamous cell carcinoma) (Mod Pathol 2021;34:549)
Contributed by Caroline I.M. Underwood, M.D., Andrey Bychkov, M.D., Ph.D., Fulvio Lonardo, M.D. and Negar Rassaei, M.D.
- 3D clusters of cohesive cells, foamy / vacuolated cytoplasm, fine chromatin, variable prominent nucleoli (J Thorac Oncol 2011;6:244)
- Usually on pleural effusions or needle washes
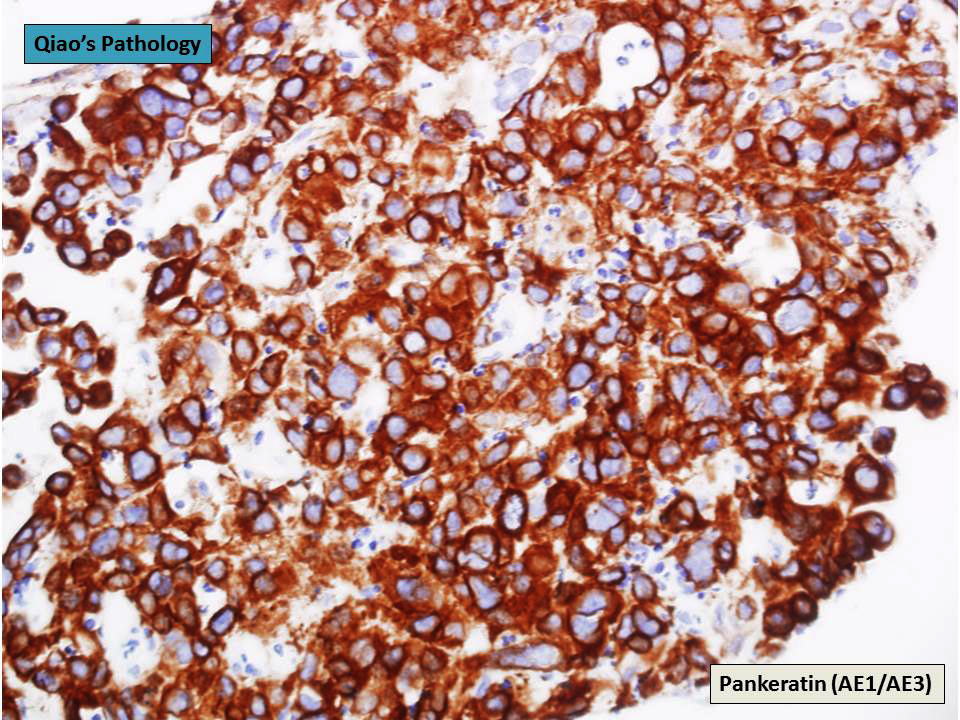
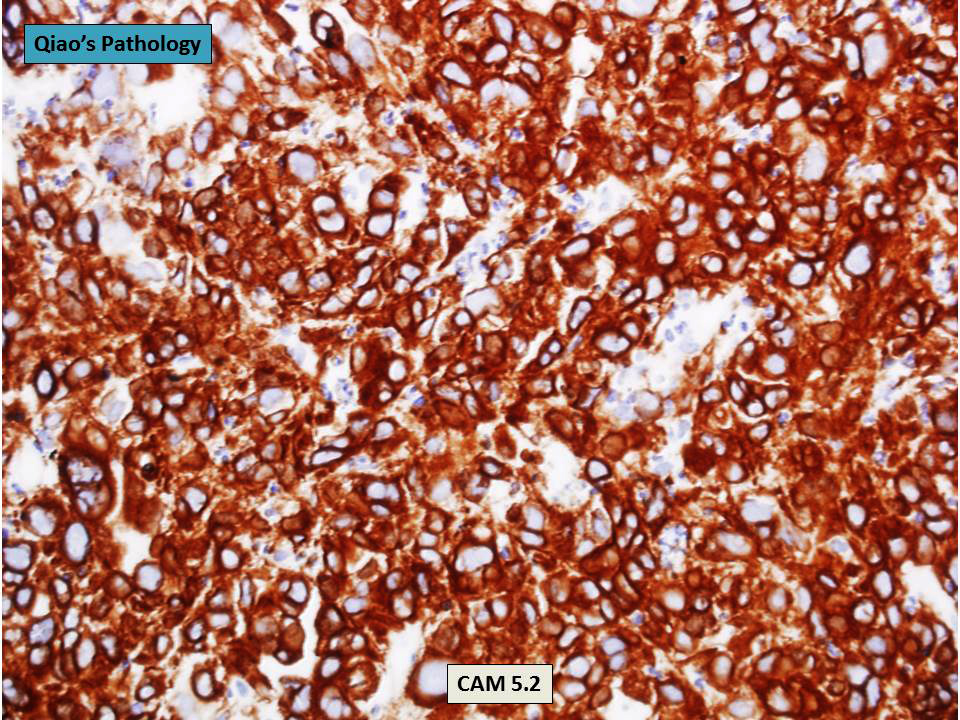
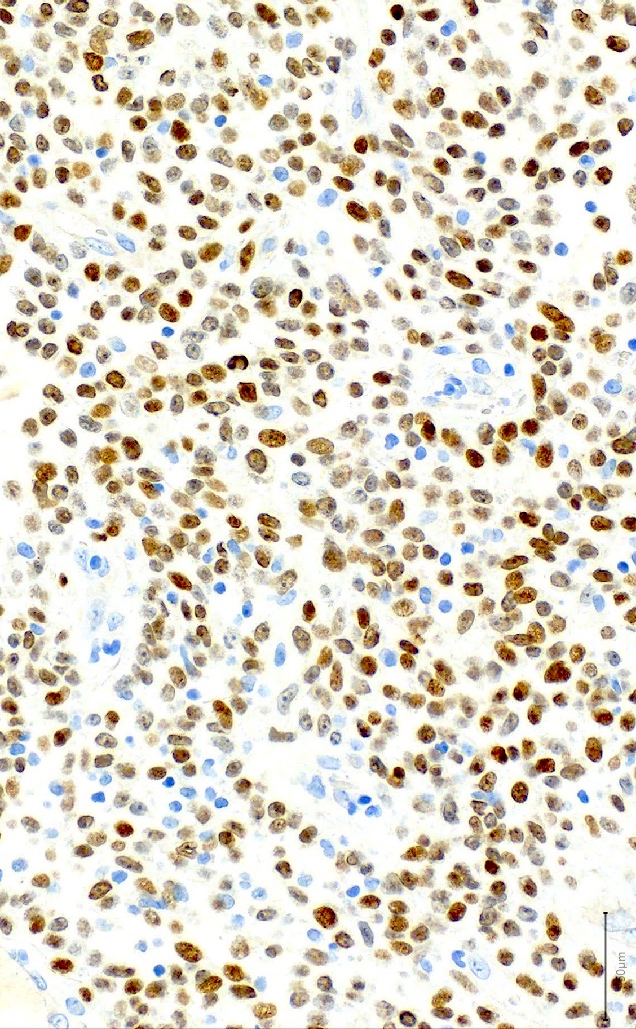
- TTF1, AE1 / AE3, CK7, beta catenin, Napsin A (Indian J Med Res 2017;146:42)
- TTF1 clone 8G7G3/1 is more specific but less sensitive compared with SPT24 and SP141 (Am J Clin Pathol 2018;150:533)
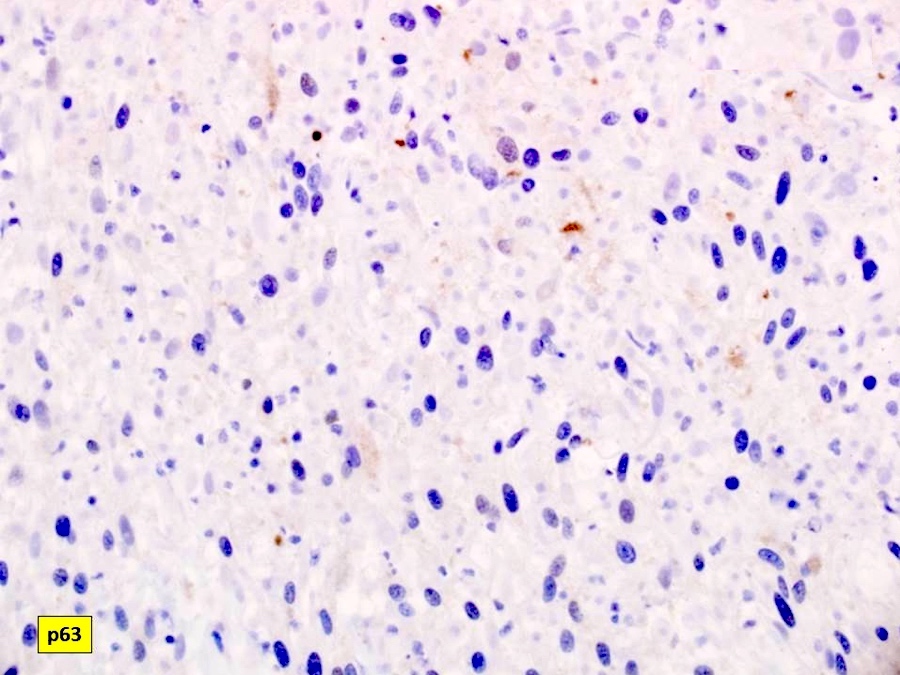
- p53, p40, p63, CK5/6, WT1, D2-40, calretinin, EGFR (positive in 33%) (Ann Am Thorac Soc 2015;12:429, Indian J Med Res 2017;146:42)
- Short microvilli (Ultrastruct Pathol 2016;40:254)
- Tumor cells lack cytoplasmic cytosomes (Ultrastruct Pathol 2016;40:254)
- EGFR mutation: 10 - 15% overall, 49% in Asia, rare in mucinous subtype (Front Pharmacol 2019;10:230, Diagn Interv Imaging 2016;97:955)
- KRAS mutation: 20 - 25% overall, 76% of mucinous subtype (Diagn Interv Imaging 2016;97:955)
- ALK rearrangement: 4% (J Thorac Dis 2019;11:S3)
- ROS1 gene fusions: 1 - 2%
- BRAF mutation: 1.5 - 3.5%, V600E most common (J Thorac Dis 2019;11:S3)
- NTRK mutation: 2 - 3% (J Thorac Dis 2019;11:S3)
- RET fusion: 0.4 - 2% (J Thorac Dis 2019;11:S3)
- HER2 amplification: 13 - 22.8% (J Thorac Dis 2019;11:S3)
- MET amplification: 2 - 4% (J Thorac Dis 2017;9:2142)
- SMARCA4 loss of function: 5% (Ann Diagn Pathol 2017;26:47)
- Lung, left upper lobe, wedge resection:
- Invasive adenocarcinoma, grade 2, acinar predominant with secondary solid growth pattern (see synoptic report)
- Squamous cell lung carcinoma:
- Small cell lung carcinoma:
- Positive for neuroendocrine markers
- Small round blue cells, usually in sheets or nests
- High grade neuroendocrine tumor:
- Increased mitotic activity (> 10/high power field), necrosis
- Positive for neuroendocrine markers and stathmin 1, nuclear chromatin is clumped / salt and pepper appearance (Ann Thorac Surg 2019;108:235)
- Metastatic adenocarcinoma:
- Negative for TTF1 (unless thyroid)
- Positive for markers from primary site
- Atypical adenomatous hyperplasia:
- > 5 mm in size
- Atypical type II pneumocytes, noninvasive (Diagn Interv Imaging 2016;97:955)
- Adenocarcinoma in situ:
- ≤ 30 mm in size, atypical type II pneumocytes, purely lepidic type, noninvasive (Diagn Interv Imaging 2016;97:955)
- Bronchial adenoma / ciliated muconodular papillary tumor (Am J Surg Pathol 2018;42:1010, Pathol Int 2017;67:99):
- Adenoid cystic carcinoma:
- Cribriform architecture and pseudocysts
- PAS positive
- Metastatic papillary thyroid carcinoma:
- Clinical history of thyroid cancer, psammoma bodies, nuclear features of PTC (orphan Annie)
- PAX8 and thyroglobulin positive
A 59 year old man presents with cough, hemoptysis and shortness of breath. A mass in his left lung was biopsied. Which of the following statements about this disease is true?
- Exposure to benzene is an important risk factor in the development of this disease
- Masses are most frequently found in central / hilar regions of both lungs
- The growth pattern indicated in the patient's biopsy above is a poor prognostic factor
- The most common site of metastasis is the liver
- This disease has a higher incidence in men than in women
Comment Here
Reference: Adenocarcinoma overview
- ALK rearrangement
- BRAF
- EGFR
- HER2 amplification
- KRAS
Comment Here
Reference: Adenocarcinoma overview
- #2 most common salivary gland-type carcinoma of lung
- Usually in large bronchi, may involve the trachea
- Prolonged course, but overall prognosis is poor
- See also Salivary glands - Adenoid cystic carcinoma
- Primary pulmonary adenoid cystic carcinoma is rare, and metastasis from salivary glands must be excluded
- Morphology is similar to adenoid cystic carcinomas in other sites, with cribriform, tubular and solid patterns
- These tumors tend to arise in association with central airways and spread along neurovascular bundles
- Formally called bronchial adenoma, but now considered malignant
- Use code specific for location of tumor
- C34.90 Malignant neoplasm of unspecified part of unspecified bronchus or lung
- Primary pulmonary adenoid cystic carcinoma is very rare, < 0.2% of lung cancers
- Typically adults
- Usually central / endobronchial but may be peripheral
- Slow growing but persistent, with recurrences over years, potentially with metastasis to lymph nodes and distant sites
- Unclear, probably arise from submucosal bronchial glands
- Obstructive symptoms, i.e., pneumonia, dyspnea, cough, wheeze, hemoptysis
- Peripheral lesions asymptomatic
- Exclude metastasis from salivary glands
- Variable by tumor stage
- 14 year old girl with large lung mass (BMJ Case Rep 2010 Nov 29;2010)
- 29 year old man with liver metastasis (J Thorac Oncol 2014;9:e67)
- 46 year old woman diagnosed by FNA cytology (Diagn Cytopathol 2011;39:283)
- 75 year old woman with peripheral adenoid cystic carcinoma (World J Surg Oncol 2010;8:74)
- Complete surgical excision
- Radiation therapy (Ann Thorac Surg 2016;101:294)
- Large, centrally located, polypoid, intrabronchial mass
- May grow along bronchi (subepithelial) causing thickened bronchial wall
- Circumscribed, soft, yellowish white
- Propensity for tracking along nerves and cartilaginous plates → bronchial margins more often positive than in other lung cancers
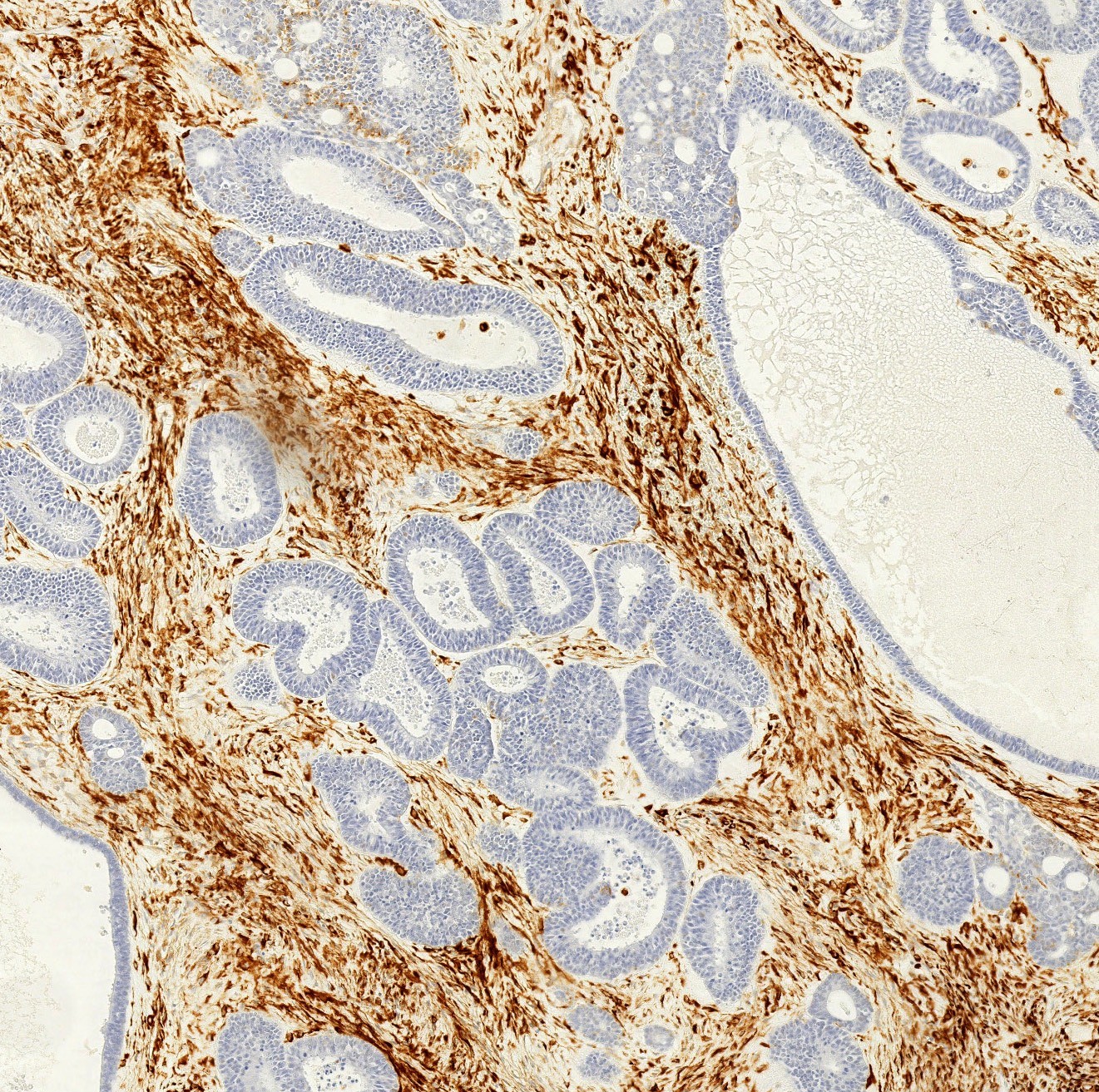
- Infiltrative growth, cribriform / cylindromatous (islands and nests, with luminal matrix), tubular (gland-like spaces) or solid (insular, with scant matrix) - usually a mix of patterns are seen
- Defining features are pseudocysts (rounded extracellular space containing basal lamina), intercellular spaces, basal lamina and true glandular lumens (Hum Pathol 1982;13:916)
- Monotonous, polygonal, basaloid cells
- Absence of mitoses, nuclear pleomorphism, necrosis and hemorrhage in most cases; solid type may show more mitoses
- Cylinders or spheres of myxochondroid matrix within epithelial groups
- Diagnosis more difficult if matrix is scarce, as in solid type
- Cellular uniformity, distinct nucleolus, granular cytoplasm, distinct cell border, organoid cluster, hyaline globule and hyaline basement membrane material (J Pathol Transl Med 2015;49:511)
- Usually not necessary for diagnosis
- Luminal cells: c-kit/CD117+, p63-, actin-
- Basal (myoepithelial) cells: c-kit/CD117-, p63+, actin+
- Tumor cells are usually positive for keratin and S100, and negative for neuroendocrine markers
- Basement membrane material is positive for collagen type IV or laminin
- May show evidence of partial myoepithelial differentiation
- t(6;9) MYB rearrangement in 41% of pulmonary adenoid cystic carcinomas, not associated with clinical features or prognosis (J Thorac Oncol 2015;10:1570)
- Generally do not have similar mutations as primary adenocarcinoma (Diagn Pathol 2015;10:161)
- Basal cell adenocarcinoma: distinction from solid adenoid cystic carcinoma may be impossible
- Basaloid squamous cell carcinoma: may have adenoid cystic carcinoma-like pattern of microcystic spaces containing mucin, surrounded by small tumor cells
- Epithelial-myoepithelial carcinoma
- Metastatic disease
- Well differentiated adenocarcinoma of the lung: larger cells with more prominent nucleoli
- Lung adenomas are benign epithelial pulmonary neoplasms
- Lung adenomas include bronchial adenoma (BA) / ciliated muconodular papillary tumor (CMPT), alveolar adenoma, papillary adenoma, mucinous cystadenoma of the lung, mucous gland adenoma of the lung and sclerosing pneumocytoma
- Well circumscribed nodules and usually found incidentally
- Benign looking cells with no cytological atypia or proliferation
- Full excision is curative
- Bronchiolar adenoma / ciliated muconodular papillary tumor: although not recommended, terminology used in the literature is peripheral papilloma; solitary peripheral ciliated glandular papilloma
- Alveolar adenoma: not recommended
- Papillary adenoma of lung: not recommended
- Mucinous cystadenoma of lung: not recommended
- Mucous gland adenoma of lung: not recommended
- Lung adenomas affect a wide range of ages (2 months to 80 years), with a slight female predominance in alveolar adenoma and mucinous cystadenoma; male predominance in papillary adenoma of the lung (Hum Pathol 1999;30:158, Cancer 1980;45:1486, J Bronchology Interv Pulmonol 2013;20:52)
- In bronchial adenoma, it usually affects mostly middle to elderly age patients with median age in early 70s without any sex predilection
- Mucous gland adenoma is a very rare entity; it has no sex predilection and has a wide age range (25 - 67 years) (Am J Surg Pathol 1995;19:887)
- All the adenomas are typically solitary tumors of the peripheral lung
- Rarely, can be located in the hilum, visceral pleura or mediastinum, except for mucous gland adenoma, which arises from proximal bronchus, although very few could be peripheral (J Comput Assist Tomogr 2002;26:358, Respiration 2012;84:142, Hum Pathol 1986;17:1066, Cancer 1980;45:1486, Am J Surg Pathol 2015;39:753, Case Rep Pathol 2013;2013:239173)
- Lung adenomas are derived from primitive respiratory epithelium
- BRAF, EGFR, KRAS, HRAS, ALK mutations are reported in bronchiolar adenoma / ciliated muconodular papillary tumor; BRAF is the most common mutation, with other mutually exclusive driver alterations (Pathol Int 2017;67:99, Diagn Pathol 2017;12:62, J Thorac Oncol 2016;11:261, Am J Surg Pathol 2018;42:1010)
- Microsatellite instabilities, diploid DNA pattern and nonbalanced translocation t(10;16) have been described in alveolar adenomas (Int J Surg Pathol 2004;12:155, APMIS 2007;115:1443, Cancer Genet Cytogenet 1996;89:34)
- See Diagrams / tables
- No predisposing factors are known
- Lung adenomas are typically incidental findings
- Mucous gland adenomas can present with dyspnea, cough, hemoptysis and recurrent pneumonia (Am J Surg Pathol 1995;19:887)
- They may appear as solid or ground glass nodules on computed tomography (CT), with some showing cavitation or cystic spaces (Am J Surg Pathol 2015;39:753, J Thorac Imaging 2002;17:163, Am J Surg Pathol 2018;42:1010)
- Definitive diagnosis requires excision and histopathologic evaluation
- Bronchial adenoma / ciliated muconodular papillary tumor
- Well circumscribed peripherally located nodules with papillary architecture
- Double layered cells, basal cells (p40 and CK5/6 positive) and luminal cells (TTF1: positive in distal type and negative or focal positive in proximal type)
- Lack of nuclear atypia and low proliferative index
- Associated with BRAF mutation
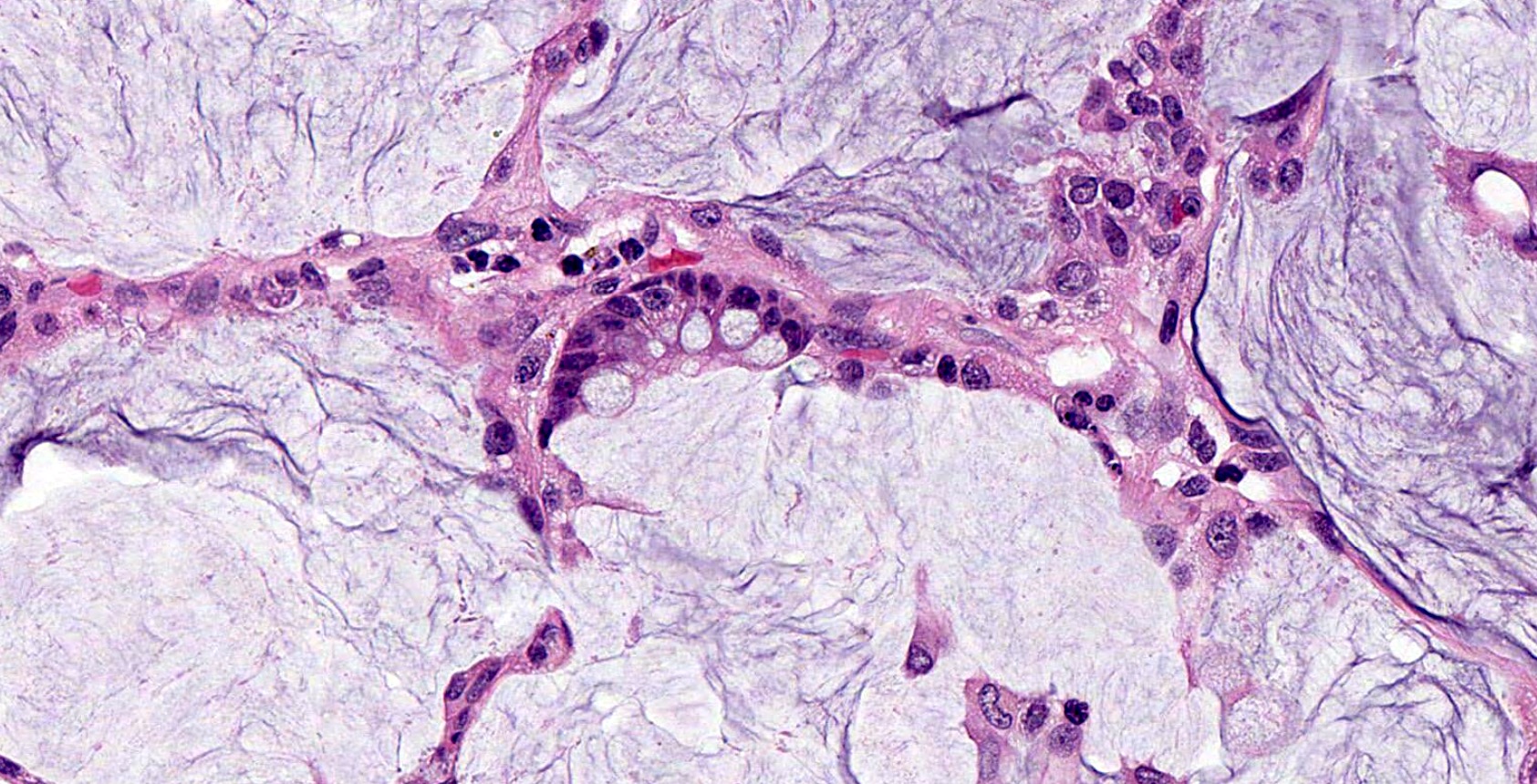
- Alveolar adenoma
- Multicystic mass with alveolus-like spaces
- Cysts are lined by a single layer of type II pneumocytes with bland cytology
- Mesenchymal stroma
- Papillary adenoma
- Circumscribed and not capsulated
- Papillary tumor with a single layer
- No cytological atypia / mitosis / necrosis / complex branching architecture
- TTF1 positive
- Mucinous cystadenoma of the lung
- Cystic mass with mucus contents
- Benign proliferation of mucous producing epithelial cells
- Mucous gland adenoma of the lung
- Well circumscribed endobronchial mass
- Acinar, tubular or papillary proliferation of cytologically bland mucous secreting cells
- Usually a solid, solitary, well circumscribed mass, which may rarely be calcified, cystic or cavitary (J Comput Assist Tomogr 2002;26:358, Respiration 2012;84:142, Radiat Med 2004;22:123, Clin Radiol 2011;66:708, Medicine (Baltimore) 2015;94:e498)
- Depending on the type of adenoma, the location would be central or peripheral
- Lung adenomas are mostly benign and surgical excision is curative (Arch Pathol Lab Med 2003;127:321, Am J Surg Pathol 2015;39:753, Hum Pathol 1999;30:158)
- Good prognosis, with no reported recurrence and metastasis (Am J Surg Pathol 2015;39:753, Am J Surg Pathol 2018;42:1010, Hum Pathol 2018;82:193)
- 51 year old woman with 1.1 cm bronchial adenoma in the right upper lobe (Asian J Surg 2023;46:4090)
- 52 year old woman with incidental finding of a 1.2 cm subpleural alveolar adenoma in the right upper lobe, consisting of multiple cystic spaces filled with eosinophilic granular material and lined by flattened to cuboid epithelial cells without significant atypia (Pathologica 2022;114:326)
- 66 year old nonsmoking woman with a 3.7 cm lobulated irregular papillary adenoma in the posterior basal segment of the right lower lobe of the lung (Diagn Pathol 2022;17:81)
- Surgical resection
- Bronchial adenoma is usually a well circumscribed white-gray nodule measuring 7 - 70 mm; cut surfaces can be solid, cystic or mucoid (Hum Pathol 1986;17:1066, Hum Pathol 1999;30:158, APMIS 2007;115:1443)
- Alveolar adenoma is a well circumscribed mass, which can have lobulated, multicystic pale yellow to tan cut surfaces
- Papillary adenoma may lack gross papillae or necrosis (J Bronchology Interv Pulmonol 2013;20:52, Am J Clin Pathol 1992;97:393)
- Although size range varies from 2 to 45 mm, these are most commonly 5 - 15 mm
- Mucinous cystadenoma usually consists of a mucin filled cyst, not associated with an airway; generally, cyst walls do not have a mural nodule
- Mucous gland adenomas are well circumscribed and majority of them arise within main, lobar or segmental bronchi; the cut surface is usually tan to gray with mucoid material (Am J Surg Pathol 1995;19:887)
- Bronchiolar adenoma on frozen sections is a mucinous neoplasm with 2 layers of basal and luminal cells
- There is minimal nuclear atypia present with no mitosis, necrosis or pleomorphism
- Presence of cilia in the luminal cells could be an important diagnostic clue for adenoma
- Multilayering can occasionally happen in proximal type bronchiolar adenoma along with basal cell hyperplasia (see Frozen section images), which can be confused for malignancy (Am J Surg Pathol 2023;47:431, Am J Surg Pathol 2015;39:753)
- Bronchiolar adenomas / ciliated muconodular papillary tumors are papillary or flat nodules, involving peribronchiolar lung tissue and composed of bilayer of continuous basal cells and luminal cells (comprising varying proportions of mucinous cells, ciliated cells, Clara cells or type II alveolar epithelial cells) (J Cardiothorac Surg 2019;14:143)
- Alveolar adenoma is comprised of multicystic spaces, filled with pulmonary eosinophilic surfactant; the cysts are lined by flattened to cuboidal epithelial cells, which correspond to type II pneumocytes
- Papillary adenomas are well defined papillary nodules with a fibrovascular core, lined by a single layer of cuboidal or ciliated epithelium (Acta Pathol Jpn 1992;42:56)
- Mucinous cystadenoma is a cyst lined by a discontinuous single layer of low cuboidal to tall columnar mucin secreting epithelial cells and mucinous contents
- Mucous gland adenoma is comprised of mucin filled cystic spaces, lined with bland columnar, cuboidal or flattened mucous secreting cells
- Bronchiolar adenoma / ciliated muconodular papillary tumor
- Columnar cells with cilia and mucous and extracellular mucin (Diagn Cytopathol 2019;47:716)
- Lacks nuclear atypia
- Papillary adenoma: papilla with bland epithelial cells with no nuclear atypia or pleomorphism (Diagn Cytopathol 2016;44:543)
- Bronchiolar adenoma / ciliated muconodular papillary tumor
- Alveolar adenoma
- Cyst lining epithelial cells are positive for cytokeratin, TTF1, Napsin A and surfactant protein
- Papillary adenoma: surface epithelial cells, positive for TTF1, CK7, pancytokeratin, surfactant protein and EMA
- Mucinous cystadenoma
- Epithelial cells positive for pancytokeratin
- Mucous gland adenoma: the epithelial cells are positive for EMA, keratin and CEA
- Neuroendocrine markers (chromogranin, synaptophysin) are negative
- Alveolar adenoma: stromal cells show focal staining for SMA and MSA and rare staining for S100 and CD34
- Alveolar adenoma and papillary adenoma: stromal cells are negative for keratin, TTF1
- Mucinous cystadenoma
- Rarely positive for CEA (Arch Pathol Lab Med 1990;114:1053)
- Epithelial cells negative for TTF1 and surfactant protein (Gen Thorac Cardiovasc Surg 2010;58:287, Arch Pathol Lab Med 1990;114:1053)
- Mucous gland adenoma: the epithelial cells are negative for TTF1
- Lung, left lower lobe, lobectomy:
- Benign bronchiolar adenoma / ciliated muconodular papillary tumor (BA / CMPT) (see comment)
- Size: 1.5 x 1.1 x 0.7 cm
- Resection margins: negative for tumor
- Comment: On histology, sections show papillary architecture and are composed of bilayered cells, luminal epithelial cells and continuous basal cells. The luminal cells consist of mucous cells and focal ciliated cells. Luminal cells are predominantly negative for TTF1 and CDX2. Immunostain for CK5/6 and p63 shows a continuous basal cell layer in the lesion. These features support the diagnosis.
- Lung, right upper lobe, biopsy:
- Papillary neoplasm of lung, favor papillary adenoma (see comment)
- Comment: Sections show fragments of papillae with fibrovascular cores, lined with a single layer of cuboidal epithelium without nuclear atypia, pleomorphism or prominent nucleoli. The lesional cells express TTF1 and have a low Ki67 proliferative index (< 1%). The definitive diagnosis is deferred to the complete excisional specimen.
- Bronchiolar adenoma / ciliated muconodular papillary tumor:
- Mucinous adenocarcinoma:
- Peribronchiolar metaplasia:
- Ill defined borders and is usually a multifocal process, often in the setting of interstitial lung disease or small airway injury
- Alveolar adenoma:
- Adenocarcinoma in situ:
- No continuous basal cell layer or ciliated cells
- Presence of nuclear atypia
- Very difficult to differentiate on frozen sections or small biopsies (Am J Clin Pathol 2021;155:832)
- Lymphangioma:
- Cytokeratin and TTF1 staining of the pneumocytes differentiates alveolar adenoma from lymphangioma, where the endothelial cells are keratin negative and D2-40 positive
- Adenocarcinoma in situ:
- Mucinous cystadenoma:
- Colloid carcinoma of the lung:
- Invasive adenocarcinoma with large pools of mucin destroying alveolar walls, which must be present in at least 50% of the tumor
- Metastatic carcinoma from the gastrointestinal tract or ovary:
- Generally multiple, well circumscribed and tend to grow rapidly
- A history of and a panel of immunohistochemical stains can help support the diagnosis
- Bronchogenic cysts:
- Unilocular cyst lined by respiratory type epithelium
- Cyst wall recapitulates bronchial wall with variable amounts of seromucinous glands, cartilage and smooth muscle
- Colloid carcinoma of the lung:
- Mucous gland adenoma:
- Endobronchial metastasis:
- Lesional cells with atypia
- Invasive mucinous adenocarcinoma:
- Involves the alveolar parenchyma
- No exclusive endobronchial growth
- Low grade mucoepidermoid carcinoma:
- Mixture of mucous cells, squamous cells and intermediate cells
- MAML mutation
- Endobronchial metastasis:
Comment Here
Reference: Adenoma
- ALK
- BRAF
- ERG
- RB1
Comment Here
Reference: Adenoma
- Substantial amounts of malignant squamous and glandular differentiation (at least 10% of each component within tumor)
- 90% peripheral, often associated with scars, with clinical / imaging features similar to adenocarcinoma
- Poorer prognosis than either component alone
- WHO classification as non-small cell lung carcinoma with at least 10% components of both adenocarcinoma and squamous cell carcinoma by histomorphology
- Diagnosis made on resection specimens, although it may be suspected on biopsy or cytology
- May harbor targetable molecular alterations seen in adenocarcinomas
- By WHO classification, adenosquamous carcinoma contains at least 10% each of malignant squamous and glandular components
- Differentiate from adenocarcinoma with squamoid features / squamous metaplasia as well as squamous cell carcinoma with pseudoglandular features
- Use code specific for location of tumor
- C34.90 Malignant neoplasm of unspecified part of unspecified bronchus or lung
- Uncommon, 1 - 5% of lung cancers
- Similar age and sex distribution to other lung cancers (Am J Clin Oncol 1992;15:356)
- Tends to arise peripherally but may be central
- More aggressive than "pure" carcinomas when matched for stage
- Association with smoking, similar to other lung cancers
- Similar to lung adenocarcinoma
- Diagnosis made on resection specimens, though can be suggested in biopsy or cytology as follows:
- Non-small cell carcinoma, see note
- Note: Glandular and squamous components are present; the findings could represent adenosquamous carcinoma
- Peripheral tumor, averages 3 - 4 cm
- Lobulated to spiculated, ill defined borders (Clin Nucl Med 2014;39:107)
- Worse than "pure" adenocarcinoma or squamous cell carcinoma; associated with larger size, visceral pleural invasion, lymphatic invasion, ipsilateral second nodules (Ann Thorac Surg 2013;95:1189)
- EGFR mutated adenosquamous carcinomas appear to have better prognosis (Pathol Int 2013;63:77)
- 57 year old man with metastasis of lung adenosquamous carcinoma to meningioma (Int J Clin Exp Pathol 2013;6:2625)
- 58 year old man with ALK rearranged adenosquamous cancer masquerading as pure squamous cell carcinoma (J Thorac Oncol 2012;7:768)
- 60 year old man with cutaneous leukocytoclastic vasculitis presenting as the first symptom of adenosquamous carcinoma of the lung (J Korean Rheum Assoc 2010;17:272)
- 60 year old woman with EGFR mutated adenosquamous carcinoma with micropapillary pattern (Respirol Case Rep 2016;4:e00179)
- 65 year old man who received chemoradiation therapy for limited stage small cell lung carcinoma (SCLC) (Haigan 2011;3:182)
- 66 year old woman with adenosquamous cell lung cancer successfully treated with gefitinib (Mol Clin Oncol 2014;2:282)
- 68 year old man presenting with a solitary pulmonary nodule at the right lower lobe (Korean J of Path 2004;15:101)
- 69 year old woman with EGFR mutated adenosquamous lung carcinoma (Soonchunhyang Med Sci 2013;19:123)
- 71 year old man with cytology consistent with adenosquamous carcinoma (Diagn Cytopathol 2012;40:830)
- 76 year old man with lung cancer and multiple metastases (CEN Case Rep 2013;2:158)
- Surgical resection
- EGFR tyrosine kinase inhibitors may be considered for those harboring this mutation (J Cancer Res Clin Oncol 2016;142:1325)
- Similar to adenocarcinoma but may show more aggressive features, i.e. larger size, pleural invasion
- Malignant cells with squamous or glandular differentiation with variable degree of admixture
- Squamous component may show keratin, intercellular bridges, squamous pearls
- Glandular components may show lumens with mucin; may have papillary, lepidic, acinar or tubular patterns
- Metastasis in lymph node tend to be same histologic type as the major component (Cancer 1991;67:649) but not necessarily
- Variable depending on squamous or glandular components and degree of differentiation
- Neuroendocrine markers
- EGFR and KRAS mutations detected in some cases; mutation profile shared by both glandular and squamous components (Am J Clin Pathol 2011;135:783; Histopathology 2015;66:939)
- Tumors with even minor adenocarcinoma component can still show KRAS and EGFR mutations (Chest 2014;145:473)
- Adenocarcinoma with "squamoid" features or foci of benign squamous metaplasia
- Collision tumor
- High grade mucoepidermoid carcinoma: central airways
- Squamous cell carcinoma with pseudoglandular features or entrapped epithelium
- Has a better prognosis than pure adenocarcinoma or squamous cell carcinoma
- Always shows both components in metastases
- Requires immunohistochemistry for diagnosis
- May harbor EGFR or Kras mutations
- Shows a benign squamous component
Comment Here
Reference: Adenosquamous carcinoma
- Malignant neoplasm showing components of both squamous cell carcinoma and adenocarcinoma (each comprising at least 10% of the tumor)
- WHO classification as non-small cell lung carcinoma with at least 10% components of both adenocarcinoma and squamous cell carcinoma by histomorphology that may be separate or intermingled
- Diagnosis made on resection specimens, although it may be suspected on biopsy or cytology
- May harbor targetable molecular alterations seen in adenocarcinomas
- Rare incidence; 0.4 - 4% of all lung cancers
- Clinical presentation frequently resembles other non-small cell carcinomas but it appears to have an adverse prognosis (Oncotarget 2017;9:8133)
- Computed tomography (CT) scan shows central or peripheral location
- Centrally located tumors commonly show postobstructive inflammatory changes
- Peripheral tumors (90%) appear as ground glass opacities, often associated with scars
- By WHO classification, adenosquamous carcinoma contains at least 10% each of malignant squamous and glandular components
- Differentiate from adenocarcinoma with squamoid features / squamous metaplasia as well as squamous cell carcinoma with pseudoglandular features
- Use code specific for location of tumor
- ICD-10: C34.90 - malignant neoplasm of unspecified part of unspecified bronchus or lung
- Uncommon; 0.4 - 4% of lung cancers
- Similar age and sex distribution to other lung cancers (Am J Clin Oncol 1992;15:356)
- Tends to arise peripherally but may be central
- More aggressive than pure carcinomas when matched for stage
- Molecular mechanisms are not fully understood
- Environmental factors are possible contributing factors
- Chronic inflammation may influence pathogenesis
- Aggressive behavior: more aggressive than adenocarcinoma or squamous cell carcinoma, leading to poorer prognosis
- Metastatic potential: high risk of spreading to lymph nodes and distant organs
- Association with smoking, similar to other lung cancers
- Similar to lung adenocarcinoma
- Diagnosis made on resection specimens, though can be suggested in biopsy or cytology as follows
- Non-small cell carcinoma (see note)
- Note: glandular and squamous components are present; the findings could represent adenosquamous carcinoma
- Peripheral tumor, averages 3 - 4 cm
- Lobulated to spiculated, ill defined borders (Am J Clin Oncol 1992;15:356)
- Resectable adenosquamous carcinoma patients had higher pleural invasion incidence, poorer differentiation and worse survival compared with squamous cell carcinoma and adenocarcinoma patients (Jpn J Clin Oncol 2022;52:1456)
- EGFR mutated adenosquamous carcinomas appear to have better prognosis (Pathol Int 2013;63:77)
- Adenosquamous carcinomas without EGFR mutations show a moderate response to immune checkpoint inhibitor (ICI) based immunotherapy (Front Immunol 2022;13:944812)
- High CXCR4 expression predicts a poor prognosis in resected lung adenosquamous carcinoma (J Cancer 2020;11:810)
- Adenocarcinomatous predominant subtype of adenosquamous carcinoma of the lung (ASC) is associated with a better prognosis than the squamous cell carcinoma predominant subtype (J Cancer 2020;11:810)
- 42 year old man with right upper lung adenosquamous carcinoma resection following neoadjuvant targeted therapy (Ann Palliat Med 2021;10:4987)
- 60 year old man with adenosquamous lung carcinoma presenting as an ulceroproliferative growth (J Cancer Res Ther 2020;16:922)
- 60 year old woman with EGFR mutated adenosquamous carcinoma with micropapillary pattern (Respirol Case Rep 2016;4:e00179)
- 66 year old man with adenosquamous carcinoma arising in the background of IgG4 related lung disease (J Pathol Transl Med 2019;53:188)
- 66 year old woman with adenosquamous cell lung cancer successfully treated with gefitinib (Mol Clin Oncol 2014;2:282)
- 71 year old man with cytology consistent with adenosquamous carcinoma (Diagn Cytopathol 2012;40:830)
- Surgical resection
- EGFR tyrosine kinase inhibitors may be considered for those harboring this mutation (Cancer Manag Res 2018;10:2401)
- Malignant cells with squamous or glandular differentiation with variable degree of admixture
- Squamous component may show intercellular bridges or keratin pearls
- Glandular components may show lumens with mucin; may have papillary, lepidic, acinar or tubular patterns
- Metastasis in lymph node tends to be same histologic type as the major component but not necessarily (Cancer 1991;67:649)
- Variable depending on squamous or glandular components and degree of differentiation (see lung adenocarcinoma and lung squamous cell carcinoma)
- Neuroendocrine markers (chromogranin, synaptophysin and CD56)
- Features of both squamous cell carcinoma and adenocarcinoma (ADC) are present in adenosquamous carcinoma
- Adenocarcinoma features include intracellular and intercellular lumina and short, stubby microvilli
- Squamous cell carcinoma features include well formed desmosomes with tonofilaments and intercellular bridges
- Proportion of primitive cells (without ultrastructural features of glandular or squamous differentiation) may be present
- EGFR and KRAS mutations, both characteristic of adenocarcinoma, have been reported in adenosquamous carcinoma
- EGFR amplification is frequent in adenosquamous carcinoma
- References: J Clin Med 2024;13:5711, Am J Transl Res 2024;16:126
Metastatic adenosquamous carcinoma of the lung to wrist with squamous histology
- Lung, right lower lobe, biopsy:
- Compatible with adenosquamous carcinoma (see comment)
- Comment: The tumor displays both glandular and squamous differentiation, characteristic of adenosquamous carcinoma. This is a rare and aggressive subtype of non-small cell lung carcinoma. The patient's clinical presentation and radiological findings support the pathological diagnosis. Further molecular testing and staging studies may be necessary for appropriate treatment planning. Immunohistochemical staining shows positivity for thyroid transcription factor 1 (TTF1) in the adenocarcinoma component, confirming its pulmonary origin. Positivity for p40 and p63 is observed in the squamous component, confirming its squamous differentiation.
- Adenocarcinoma with squamoid features or foci of benign squamous metaplasia:
- Malignant features are present only in areas of glandular differentiation
- Lacks malignant features in the foci of squamoid differentiation
- High grade mucoepidermoid carcinoma:
- Central airways
- Typical morphology shows varying proportions of epidermoid cells, intermediate cells and mucocytes
- Overt keratinization is rare
- Mucous cells embedded in epidermoid cell nests or lining cystic spaces
- Intermediate cells found within epidermoid cell nests or forming separate nests
- MAML2 rearrangement detected by FISH (helpful if present)
- Squamous cell carcinoma with pseudoglandular features or entrapped epithelium:
- Collision tumor:
- In a collision tumor, the 2 tumor components should be clearly separated, with distinct histological features for each
- In adenosquamous carcinoma, the glandular and squamous components are typically intermingled within the same tumor mass
- Always shows both components in metastases
- Has a better prognosis than pure adenocarcinoma or squamous cell carcinoma
- May harbor EGFR or KRAS mutations
- Requires immunohistochemistry for diagnosis
- Shows a benign squamous component
Comment Here
Reference: Adenosquamous carcinoma
- Always benign and does not exhibit metastatic potential
- Characterized by a glandular and squamous differentiation
- Commonly presents as a purely neuroendocrine tumor
- Exclusively composed of squamous cell carcinoma elements
- Primarily affects the bronchial cartilage and not the epithelial cells
Comment Here
Reference: Adenosquamous carcinoma
- Limited association with smoking history
- Overexpression of the ALK gene fusion
- Paraneoplastic production of PTH related peptide
- Peripheral, cavitary lesions on chest imaging
- Strong female predominance among affected patients
Comment Here
Reference: Adenosquamous carcinoma
- Lung disease caused by infection with adenovirus, a nonenveloped, lytic, double stranded DNA virus
- At least 51 serotypes of adenovirus have been associated with clinical syndromes; not well understood why specific sterotypes are associated with specific syndromes, but differences in mode of transmission and virus tropism are likely to play a role
- Seven species are known (groups A - G); respiratory disease is caused by groups C, E and some members of group B
- Infection is ubiquitous; most individuals have had several infections during childhood
- In addition to lung, also occurs in the upper respiratory tract (tonsils, adenoids), liver, GI tract, CNS, heart, kidneys, urinary bladder, ear, eyes
- Half of infections are subclinical
- Represent 5% - 10% of febrile illness in infants and young children
- Transmission is through respiratory droplets, fomites, or fecal-oral
- In children, causes 5% of upper respiratory tract infections and 10% of cases of pneumonia; adult infection is less common
- Can persist as a latent infection for years after primary disease; tonsils and adenoids are likely reservoirs
- Outbreaks among military recruits have caused epidemics of serious disease at military training centers
- Certain subgroups are associated with severe pneumonia, especially young children
- Virulent strains have led to fatalities in previously healthy young adults (Clin Infect Dis 2003;37:e142)
- Serious disease has occurred in immunocompromised hosts, especially patients with solid organ and hematopoietic stem cell transplants, although infection may be associated only with asymptomatic shedding
- Adenovirus infections are only rare causes of significant disease in AIDS patients
- When symptomatic, upper respiratory tract infection causes fever, sore throat, cough, hoarseness, rhinorrhea
- Disease may mimic tonsillitis with group A streptococcal infection, due to exudative pharyngitis and enlarged cervical lymph nodes
- Otitis media may occur children under age 1 year
- Upper respiratory tract infection may progress to involve lower respiratory tract with cough and shortness of breath; often with systemic symptoms of fever, headache, myalgias; abdominal pain may occur
- May cause a pertussis-like syndrome
- Chest Xray: bilateral, patchy, ground glass opacities consistent with viral pneumonia
- In hematopoietic stem cell transplants, the GI tract is more commonly affected than lungs; cold agglutinins are present in 20% of patients with adenovirus pneumonia
- In solid organ transplants, usually the transplanted organ affected is by adenovirus
- In lung transplant patients, disease usually occurs in early post-transplant period and is associated with graft failure, bronchiolitis obliterans, and often death
- Disease in transplant patients may be due to primary infection or reactivation
- Diagnosis: rountine tissue culture, PCR, serology, or antigen specific assays; in tissue samples, use immunostains
- In transplant patients, increasing viral load by PCR and greater immunosuppression increases the risk of serious disease
- Other risk factors are young patient age, graft vs. host disease, unrelated stem cell donor, T cell depletion of graft, cord stem cell transplant, low T cell counts post transplant, total body irradiation, use of antilymphocyte antibodies
- Only supportive care is known to be effective
- Some studies have shown benefit of ribavirin therapy, but this is not universal
- Immunotherapy is being investigated
- Appropriate hand hygiene can reduce transmission
- In the United States, military recruits formerly received vaccinations against some strains of adenovirus; production of this vaccine stopped, however, efforts to resume production are ongoing
- Epithelial cells contain smudged nuclei with brick-like, intranuclear inclusions; start as small, eosinophilic inclusions, then briefly appear as basophilic inclusions with a thin halo; then enlarge to obscure the nuclear membrane to take on the typical smudgy appearance
- Two patterns of disease are commonly encountered that may occur concurrently: diffuse alveolar damage like pattern with interstitial edema, mononuclear cell infiltrates and exudative fluid accumulation in alveoli with hyaline membranes; second pattern is necrosis of bronchi, bronchioles, and alveoli with neutrophilic and histiocytic infiltrates, with interstitial fibrosis and obliterative bronchiolitis as potential sequelae
- Adenovirus immunohistochemistry
- 60 - 90 nm, icosahedral particles in crystalline array
- The diagnosis can be made by rountine tissue culture, PCR, serology, or antigen specific assays
- In tissue samples, immunohistochemistry can confirm the diagnosis
- Alectinib is a therapeutic agent that inhibits the activity of anaplastic lymphoma kinase (ALK)
- Developed by Hoffmann-La Roche, Inc. and Genentech, Inc.
- Alecensa®
- To treat patients with advanced or recurrent ALK positive non small cell lung cancer (NSCLC) or who could not tolerate crizotinib (Xalkori®) - approved by U.S. Food and Drug Administration (FDA) in December 2015
- First line treatment of patients with ALK positive metastatic NSCLC - approved by U.S. FDA in November 2017
- In normal cells, ALK is activated by dimerization of extracellular ligands and autophosphorylation of intracellular tyrosine kinase, mostly involved in the neurodevelopment of CNS, gut and testes (Figure 1)
- ALK has been found to fuse with other genes in NSCLC, more commonly with EML4 gene; the resulting EML4-ALK fusion gene occurred in 3 - 6% of lung adenocarcinoma
- ALK is activated by the 5' fusion partner (e.g. EML4) that serves as a functional promotor and expresses a domain in the fusion protein for dimerization (Figure 1)
- Dimerized ALK rearranged fusion proteins activate downstream signaling pathways including STAT3, mTOR, PI3K, Ras and MEK to enhance cell survival, angiogenesis and cell cycle progression (Figure 1)
- Alectinib inhibits ALK tyrosine kinase by binding to its ATP binding site and blocking autophosphorylation of the EML4-ALK fusion protein, thereby inhibiting downstream STAT3, Ras and PI3K signaling pathways (Figure 2)
- Reference: Semin Cancer Biol 2017;42:81
- Hepatotoxicity: monitor liver function tests every 2 weeks for first 3 months, then monthly
- Not recommended in patients with moderate to severe hepatic impairment
- Withhold the drug if patients develop interstitial lung disease
- Withhold the drug if patients develop renal impairment
- Bradycardia: monitor heart rate and blood pressure regularly
- Myalgia: monitor creatine phosphokinase (CPK) every 2 weeks in first month
- Embryo fetal toxicity: advise females to use elective contraception
- Pharmacokinetics (Drug Saf 2019;42:199)
- Bioavailability: 37% (taken with a meal)
- Protein binding: > 99%
- Metabolism: CYP3A4 and other CYP enzymes and aldehyde dehydrogenase
- Plasma half life: 32.5 hours
- Excretion: mainly via feces (98%), minor fraction in urine (< 1%)
- Steady states: reached within 7 days
- Reference: FDA: Highlights of Prescribing Information [Accessed 8 October 2020]
- ALK immunohistochemistry: cytoplasmic staining for altered ALK protein expression (N Engl J Med 2010;363:1693, Mod Pathol 2013;26:1545)
- Clone ALK1, Dako mouse monoclonal ALK1 antibody CD246, sensitivity 100%, specificity 99%
- Clone 5A4, Novocastra mouse monoclonal antibody p80 ALK, sensitivity 100%, specificity 98%
- Clone D5F3, Cell Signaling Technology rabbit monoclonal ALK XP, sensitivity 100%, specificity 99%
- Clone 1A4, Zeta mouse monoclonal anti-ALK antibody
- ALK FISH: gold standard for evaluating ALK rearrangement
- ALK 2p23 dual color break apart FISH probe for detecting ALK gene rearrangement (Figure 3)
- ALK / EML4 tricolor FISH probe for detecting EML4-ALK gene fusion
- ALK RT-PCR and next generation sequencing
- Detecting point mutations, usually occur within tyrosine kinase domain
- Detecting gene amplifications (gene copy gain)
- Detecting rearranged ALK fusion genes and identifying fusion gene partners in chromosomal translocations, which include the following:
Chromosomal translocation Fusion gene References inv(2)(p21;p23)del(2)(p21;p23) EML4-ALK Nature 2007;448:561 t(2;2)(p23;p22) STRN-ALK J Pathol 2013;230:270 t(2;3)(p23;q12) TFG-ALK Cell 2007;131:1190 t(2;9)(p23;q31) PTPN3-ALK Genes Chromosomes Cancer 2012;51:590 t(2;10)(p23;p11) KIF5B-ALK Nat Med 2012;18:378 t(2;14)(p23;q32) KLC1-ALK PLoS One 2012;7:e31323 t(1;2)(q31;p23) TPR-ALK J Thorac Oncol 2014;9:563 t(2;7)(p23;q11) HIP1-ALK J Thorac Oncol 2014;9:419
- Fatigue (> 20%)
- Constipation (> 20%)
- Anemia (20%)
- Peripheral edema (17%)
- Myalgia (16%)
- Increased blood bilirubin (15%)
- Increased ALT (15%)
- Increased AST (14%)
- Nausea (14%)
- Diarrhea (12%)
- Increased weight (10%)
- Dizziness (8%)
- Musculoskeletal pain (7%)
- Vomiting (7%)
- Photosensitivity reaction (5%)
- Dysgeusia (3%)
- Blurred vision (2%)
- Visual impairment (1%)
- Alopecia (1%)
- Increased γ glutamyltransferase (1%)
- References: N Engl J Med 2017;377:829, FDA: Highlights of Prescribing Information [Accessed 8 October 2020]
- 600 mg po bid with food
- 450 mg po bid with food for patients with severe hepatic impairment
- Discontinue if patients cannot tolerate 300 mg po bid
- Reference: ALECENSA: Dosing and Administration [Accessed 8 October 2020]
- ALK is located at chromosome 2p21 and EML4 at 2p23.1-23.2
- EML4-ALK fusion gene can be caused by chromosomal inversion or a complicated chromosomal translocation (chromothripsis) (Figure 4) (J Thorac Oncol 2014;9:1638)
- Alectinib weakly interacts with the P loop of rearranged ALK protein shown in the cocrystal structures (Figure 5) (Lung Cancer 2017;110:32)
- Adenocarcinoma with ALK rearrangement
- Adenocarcinoma with c-MET rearrangement
- Adenocarcinoma with EGFR mutations
- Small cell carcinoma with MYC rearrangement
- Rare disease with accumulation of acellular surfactant presumedly due to impaired clearance, likely due to dysfunction of alveolar macrophages
- Considered a response to alveolar injury, not a specific entity
- Congenital (2% of cases), primary (idiopathic) or secondary forms
- Congenital cases are usually due to mutation in surfactant protein or GM-CSF receptor genes
- Secondary (most common), associated with silica dust, aluminum, fiberglass, chemicals, immunosuppression, leukemia / lymphoma, Nocardia, Mycobacteria and Aspergillosis
- Usually adults (more common in smokers), also children
- Sputum contains chunks of gelatinous material; no inflammation
- Usually does NOT progress to chronic fibrosis
- Xray: resembles pulmonary edema; diffuse pulmonary opacification
- Whole lung lavage (also diagnostic)
- Alveoli contain amorphous, eosinophilic and PAS+ material in lumina consisting of type II pneumocytes, lamellar bodies and necrotic alveolar macrophages
- Variable fibrosis
- Mild / no lymphocytic infiltration
- Exudate contains lamellar bodies, lipid particles and cellular debris
- Oral antiarrythmic drug, usually used long term
- 5% - 10% of patients develop lung injury
- Risk factors are: advanced age, higher dose therapy, lung surgery, oxygen therapy and underlying pulmonary disease; disease may occur without risk factors or at lower doses
- Drug inhibits phospholipid degradation by lysosomes, resulting in phospholipid accumulation within cells, especially alveolar macrophages
- 68 year old man with amiodarone induced pulmonary toxicity (Arch Pathol Lab Med 2002;126:745)
- Drug withdrawal or dose reduction, corticosteroid therapy
- May have 50% mortality if diffuse alveolar damage is present
- Intra-alveolar exudate of finely vacuolated foamy macrophages, also present within alveolar septa
- May have diffuse alveolar damage, cryptogenic organizing pneumonia type changes or changes of nonspecific interstitial pneumonia or desquamative interstitial pneumonia
- Finely vacuolated, foamy macrophages; variable neutrophils
- Membrane bound cytoplasmic lamellar inclusions due to drug accumulation in the lungs
- Morphologic findings are not specific and must be interpreted in conjunction with the clinical history
- Amyloidosis in the lung can present in three distinct manners: diffuse alveolar septal amyloidosis, nodular pulmonary amyloidosis and tracheobronchial amyloidosis
- Different types are distinguished by the pattern of deposition within the lung tissue; however, they are all characterized by deposition of an eosinophilic amorphous material that stains bright red with Congo red and shows an apple green birefringence upon polarization
- Ultrastructurally, it is composed of haphazardly arranged nonbranching fibrils that measure 8 to 10 nm in diameter
- Heterogenous group of entities caused by deposition of amyloid, an abnormal protein with a beta pleated structure composed of haphazardly arranged nonbranching fibrils measuring 8 to 10 nm in diameter
- Light microscopy shows amorphous eosinophilic deposits that show apple green birefringence under polarized light
- Main pulmonary forms are diffuse alveolar septal, nodular and tracheobronchial
- Most commonly caused by AL amyloidosis: the deposition of light chains due to a monoclonal hematologic process
- AL is associated with hematologic malignancies, commonly multiple myeloma
- Subtyping should be performed with mass spectrometry
- Amyloidosis in general (not organ / lung specific)
- Primary amyloidosis (now systemic AL amyloidosis)
- Secondary amyloidosis (now systemic AA amyloidosis)
- Age related or senile systemic amyloidosis (now systemic wild type ATTR amyloidosis)
- Familial amyloid polyneuropathy (now systemic hereditary ATTR amyloidosis) (Amyloid 2014;21:221)
- Pulmonary amyloidosis subtypes
- Diffuse alveolar septal amyloidosis
- Diffuse parenchymal amyloidosis
- Nodular pulmonary amyloidosis
- Nodular parenchymal amyloidosis, nodular amyloidoma
- Tracheobronchial amyloidosis
- Diffuse alveolar septal amyloidosis
- ICD-10:
- ICD-11:
- 5D00 - Amyloidosis
- 5D00.1 - AA amyloidosis
- 5D00.2 - Hereditary amyloidosis
- 5D00.20 - Hereditary ATTR amyloidosis
- 5D00.21 - Nonneuropathic heredofamilial amyloidosis
- 5D00.2Y - Other specified hereditary amyloidosis
- 5D00.2Z - Hereditary amyloidosis, unspecified
- 5D00.3 - Dialysis associated amyloidosis
- 2A83.5 - Monoclonal immunoglobulin deposition disease
- 2A83.50 - Heavy chain deposition disease
- 2A83.51 - Light and heavy chain deposition disease
- 2A83.52 - Light chain deposition disease
- 5D00.Y - Other specified amyloidosis
- 5D00.Z - Amyloidosis, unspecified
- Systemic AL amyloidosis
- Elderly men (Mayo Clin Proc 1983;58:665)
- Systemic AA amyloidosis
- Those with chronic inflammatory conditions
- Systemic wild type ATTR amyloidosis
- Elderly (Amyloid 2003;10:48, Arch Intern Med 2005;165:1425)
- Diffuse alveolar septal amyloidosis
- Dependent on the type of amyloid (see above)
- Nodular pulmonary amyloidosis
- Mean age 67
- M:F = 3:2
- Tracheobronchial amyloidosis
- Rare, ~ 100 cases reported
- Mean age 48 - 57 (Medicine (Baltimore) 2000;79:69, Mayo Clin Proc 2000;75:1148)
- M = F
- Systemic or localized
- Systemic AL amyloid
- May present with nephrotic syndrome, restrictive cardiomyopathy, peripheral neuropathy, hepatomegaly, macroglossia, purpura and bleeding diathesis
- Localized AL amyloidosis
- Larynx, bladder, colon (Mol Immunol 1982;19:447, Urol Int 1992;48:228, Amyloid 2003;10:36)
- Systemic AA amyloidosis
- Nephrotic syndrome
- Systemic wild type ATTR amyloidosis
- Myocardium
- Significant involvement of kidney is rare
- Systemic AL amyloid
- Tracheobronchial amyloidosis
- Laryngeal and tracheal colocalization described (Otolaryngol Head Neck Surg 1992;106:372, Int J Clin Exp Pathol 2014;7:7088)
- ~ 95% composed of fibril proteins
- 31 human fibril proteins have met the criteria from the International Society of Amyloidosis (ISA) Nomenclature Committee (Amyloid 2014;21:221)
- Insoluble fibril proteins from improper folding of soluble precursors
- When produced in excessive amounts:
- Immunoglobulin light chains
- Serum amyloid A
- Wild type transthyretin
- Abnormal amino acid sequence (i.e., transthyretin variants)
- When produced in excessive amounts:
- ~ 5% serum amyloid P component and other glycoproteins
- Systemic AL amyloidosis
- Monoclonal plasma cell proliferative disorder
- Monoclonal immunoglobulin light chains deposit in tissues
- Can follow monoclonal gammopathy of undetermined significance (MGUS), multiple myeloma and Waldenström macroglobulinemia (N Engl J Med 2002;346:564)
- Systemic AA amyloidosis
- Deposition of serum amyloid A (Apo), an acute phase reactant produced in the liver
- Usually secondary to a chronic inflammatory condition
- Systemic wild type ATTR amyloidosis
- Deposition of unmutated transthyretin (prealbumin) in tissues that accumulates with age
- Systemic hereditary ATTR amyloidosis
- Mutations in the transthyretin gene
- Most common in the U.S. and U.K. is Thr60Ala (T60A) (Amyloid 2015;22:123)
- Mutations in the transthyretin gene
- Acquired or hereditary
- Diffuse alveolar septal amyloidosis
- Manifestation of systemic amyloidosis
- Most commonly AL amyloid
- Rare cases without systemic manifestations (Arch Pathol Lab Med 1986;110:212, Curr Opin Pulm Med 2009;15:517, Respirology 2010;15:860)
- Manifestation of systemic amyloidosis
- Nodular pulmonary amyloidosis
- Usually localized AL amyloidosis or mixed Ig light chain / heavy chain (AL / AH) (Am J Surg Pathol 2013;37:406, Virchows Arch 2005;447:756)
- Tracheobronchial amyloidosis
- Most represent AL amyloidosis
- Diffuse alveolar septal amyloidosis
- Rarely symptomatic from a pulmonary standpoint (Semin Respir Crit Care Med 2005;26:502, Semin Respir Crit Care Med 2002;23:155)
- Impairment of other organs dominants clinical picture
- If pleura involved, may present with pleural effusions (Diagn Cytopathol 2018;46:522)
- Rarely, if vasculature involvement is extensive, can present with pulmonary hypertension or hemorrhage (Chest 2001;120:1735)
- Usually seen as autopsy findings
- Nodular pulmonary amyloidosis
- Nodules usually asymptomatic and discovered incidentally on chest imaging
- Some associated with autoimmune disorders such as Sjögren syndrome (Pathol Res Pract 2013;209:62)
- Tracheobronchial amyloidosis
- Dyspnea, cough, hoarseness
- Diffuse alveolar septal amyloidosis
- Usually incidental
- Symptoms due to amyloid deposition in other organs
- Pulmonary involvement usually made at autopsy
- Nodular pulmonary amyloidosis
- Chest imaging
- Tracheobronchial amyloidosis
- Bronchoscopy with transbronchial biopsy
- CT to determine extent (Medicine (Baltimore) 2000;79:69)
- DNA sequencing may be needed to distinguish between wild type and hereditary ATTR amyloidosis when a family history is not apparent (J Am Coll Cardiol 2015;66:2451)
- Diffuse alveolar septal amyloidosis
- Restrictive pattern pulmonary function tests in rare patients without extrapulmonary involvement (Curr Opin Pulm Med 2009;15:517)
- Tracheobronchial amyloidosis
- Decreased airflow with proximal airway involvement on pulmonary function tests
- Normal airflow if just distal involvement
- Diffuse alveolar septal amyloidosis (Hodler: Diseases of the Chest, Breast, Heart and Vessels 2019-2022 - Diagnostic and Interventional Imaging, 2019)
- Small nodules (typically in a perilymphatic distribution), consolidation, ground glass opacity and reticulations
- Widespread throughout the lungs
- Nodular pulmonary amyloidosis
- One or more solid lung nodules:
- May have spiculated borders and be confused with malignancy
- May have calcifications
- Cystic features have been described (Eur Respir J 2007;30:589)
- One or more solid lung nodules:
- Tracheobronchial amyloidosis
- Extensive thickening of the trachea or bronchi with or without calcification
- May show postobstructive changes (atelectasis, pneumonia or long term bronchiectasis) (J Thorac Imaging 2005;20:41)
Contributed by Tan-Lucien H. Mohammed, M.D.
- Systemic AL amyloidosis
- Depends on the organs affected
- Systemic AA amyloidosis
- High mortality due to end stage renal disease, infection, heart failure, bowel perforation or GI bleeding if left untreated
- Systemic wild type ATTR amyloidosis
- Survival is better than AL amyloidosis
- 45 year old woman with multiple pulmonary nodules and Sjögren syndrome (Chest 2019;155:e51)
- 59 year old man with newly diagnosed multiple myeloma and pulmonary amyloidosis diagnosed on cytology of pleural fluid (Diagn Cytopathol 2018;46:522)
- 61 year old with progressive dyspnea and dry cough without fever found to have diffuse alveolar septal amyloidosis (Int J Surg Pathol 2018;26:334)
- 65 year old man with shortness of breath and primary endobronchial amyloidosis (Respir Med Case Rep 2018;23:163)
- Japanese man in his late 70s with diffuse alveolar septal amyloidosis (Ann Thorac Surg 2019;107:e131)
- 82 year old woman with innumerable pulmonary nodules incidentally found on chest CT workup for chest pain (BMJ Case Rep 2019;12:e229718)
- Typing of the amyloid is essential because treatment depends on the form
- Systemic AL amyloidosis
- Chemotherapy followed by autologous stem cell transplantation (Lancet 2016;387:2641)
- Systemic AA amyloidosis
- Colchicine both prophylactically and therapeutically (Semin Arthritis Rheum 1993;23:206)
- Treatment of underlying condition
- Systemic wild type ATTR amyloidosis
- Chemotherapy and stem cell transplant contraindicated
- Systemic hereditary ATTR amyloidosis
- Liver transplant (J Am Coll Cardiol 2015;66:2451)
- No role for chemotherapy or stem cell transplant
- Systemic AL amyloidosis
- Diffuse alveolar septal amyloidosis
- Prognosis worse with primary amyloidosis compared to other types
- Death usually due to cardiac involvement or less often pulmonary hypertension
- Prognosis worse with primary amyloidosis compared to other types
- Nodular pulmonary amyloidosis
- Conservative excision usually curative
- Long term prognosis excellent
- Tracheobronchial amyloidosis
- Laser or forceps debridement
- External beam radiation (Chest 2007;132:262, Medicine (Baltimore) 2000;79:69)
- Diffuse alveolar septal amyloidosis
- Lungs are rubbery
- Cut surface with uniform sponge-like appearance involving all lobes
- Nodular pulmonary amyloidosis
- 1 (rarely more) nodules, 0.4 - 5 cm in diameter (Ann Intern Med 1996;124:407)
- Cut surface is waxy, gray-tan (Arch Pathol Lab Med 2017;141:247)
- Tracheobronchial amyloidosis
- Thickened airway walls with a narrowed lumen
- Deposits may be seen in the submucosa (Arch Pathol Lab Med 2017;141:247)
- General: amyloid appears as glassy amorphous eosinophilic material
- Diffuse alveolar septal amyloidosis
- Low magnification: well preserved pulmonary architecture
- Higher magnification
- Alveolar septae thickened amyloid
- Vessel walls involved and may form small nodules
- Amyloid may be seen in visceral pleura
- May see scant plasma cells
- Nodular pulmonary amyloidosis
- Well circumscribed nodules
- Homogenous, densely eosinophilic material with associated small aggregates of lymphocytes and plasma cells
- May see foreign body type giant cells, calcification, ossification and cartilage (Arch Pathol Lab Med 2017;141:247)
- Tracheobronchial amyloidosis
- Deposits of homogeneous eosinophilic material around seromucinous glands and cartilage
- Involvement of submucosal vessels
- Plasma cells, foreign body type giant cells, calcification, ossification (Arch Pathol Lab Med 1986;110:212)
- Limited value in routine smears
- Cell block of pleural fluid may show amorphous waxy material with a rim of reactive mesothelial cells (Diagn Cytopathol 2018;46:522)
- Thioflavin T is a fluorescent dye and is viewed under a fluorescent microscope
- Binds to the beta pleated sheet of amyloid
- Less specific than Congo red and should be confirmed (Biochim Biophys Acta 2010;1804:1405)
- Special stains
- Congo red
- Performed on 10 μm sections
- Apple green birefringence
- Often best appreciated with the ambient room lights off (Arch Pathol Lab Med 2017;141:247)
- Thioflavin T (see above)
- Crystal violet
- Congo red
- Immunohistochemistry for subtypes
- Kappa and lambda light chains
- Serum amyloid A
- Transthyretin (prealbumin)
- Trichrome (does not stain blue)
- Haphazardly arranged nonbranching fibrils that measure 8 - 10 nm in diameter (J Struct Biol 2000;130:88)
- Mass spectrometry based proteomic analysis
- Performed on formalin fixed, paraffin embedded tissue after microdissection
- Considered the preferred method for amyloid subtyping (Blood 2009;114:4957)
Definition, historical aspects and properties
Pathogenesis and classification
Pathology, clinical features and prognosis
- Lung, right lower lobe, transbronchial biopsy:
- Nodular pulmonary amyloidosis (see comment)
- Comment: Sections show bronchial wall and alveolated lung parenchyma with nodular deposits of eosinophilic amorphous material deposited mostly within the vascular walls. Congo red special stain shows apple green birefringence upon polarization, supporting the diagnosis. The specimen will be sent for mass spectrometry for amyloid typing and these results will be issued as an addendum.
- Diffuse alveolar septal amyloidosis:
- Fibrosing interstitial pneumonias (i.e., usual interstitial pneumonia and fibrosing nonspecific interstitial pneumonia):
- No perivascular deposition and negative Congo red
- Light chain deposition disease (Am J Surg Pathol 2007;31:267):
- Diffuse form indistinguishable on histology
- Congo red negative
- Electron microscopy shows granular material
- Kappa light chains as opposed to lambda (Am J Surg Pathol 1988;12:405, Clin Radiol 2015;70:5155)
- Fibrosing interstitial pneumonias (i.e., usual interstitial pneumonia and fibrosing nonspecific interstitial pneumonia):
- Nodular pulmonary amyloidosis:
- Clinically granulomatous or metastatic process
- Pulmonary hyalinizing granuloma
- Amyloid-like nodules
- Light chain deposition disease (Am J Clin Pathol 2004;121:200)
- Tracheobronchial amyloidosis:
The process demonstrated in the two photomicrographs of a transbronchial biopsy is most commonly caused by which of the following?
- Uric acid crystal deposition
- Deposition of improperly folded fibril proteins
- Calcium pyrophosphate crystal deposition
- Increased collagen production
- Microscopic thromboemboli
Comment Here
Reference: Amyloidosis
- Destruction of the pulmonary architecture
- Emphysematous changes
- Diffuse alveolar damage
- Thickened vascular walls
- Acute inflammatory reaction
- Main function of lungs is gas exchange
- Trachea divides into right and left mainstem bronchi
- Right lung has 3 lobes (upper, middle and lower); left lung has 2 lobes (upper and lower) lobes; lingual is part of left upper lobe and is somewhat analogous to right middle lobe
- Right bronchus is more vertical and in line with trachea than left; thus aspirated material tends to enter right lung
- Each main bronchus divides into lobar bronchi, then into segmental bronchi
- Lobar bronchi are usually called secondary bronchi and segmental bronchi are called tertiary bronchi, except in Japan, where they are called first order and second order, respectively
- Bronchial walls contain cartilage and submucosal glands
- Bronchioles are generally < 3 mm in diameter and lack cartilage and submucosal glands in their walls; their diameter varies
- Bronchioles are generally divided into nonrespiratory bronchioles (all bronchioles proximal to respiratory bronchioles, including terminal bronchioles that are proximal to respiratory bronchioles) and respiratory bronchioles (airways with alveoli budding from their walls)
- Alveoli are "dead ends" of airways; their walls are composed only of alveoli, where gas exchange takes place
- Lung has double arterial supply - pulmonary and bronchial arteries that accompany airways; in general, diameter of airway is similar to that of accompanying pulmonary artery
- Lungs are surrounded by visceral pleural membrane; inner chest cavity is lined by parietal pleural membrane; these membranes define pleural space, which normally has minimal volume
- Regional lymph nodes: paratracheal, pre- and retrotracheal, aortic, subcarinal, periesophageal, inferior pulmonary ligament, hilar, peribronchial and intrapulmonary
- The lungs develop from the ventral wall of the foregut
- The midline trachea develops two lateral outpouchings, the right and left lung buds
- The lung buds extend into primitive thoracic mesenchyme that becomes bronchial cartilage and other connective tissue
- The right lung bud develops three branches that become mainstem bronchi, the left lung bud develops two branches that become mainstem bronchi
- The phases of lung development are embryonic (3 1/2 to 6 weeks), pseudoglandular (6 to 16 weeks), canalicular (16 to 28 weeks), saccular (28 to 36 weeks) and alveolar (36 weeks to term)
- In 1994, the American European Consensus Conference (AECC) defined acute respiratory distress syndrome (ARDS) as the acute onset of hypoxemia with bilateral infiltrates on frontal chest radiograph, with no evidence of left atrial hypertension (Am J Respir Crit Care Med 1994;149:818)
- In 2012, the ARDS Task Force revised the new definition (see Diagnosis) (JAMA 2012;307:2526)
- Diffuse alveolar damage (DAD) is manifested by injury to alveolar lining and endothelial cells, pulmonary edema, hyaline membrane formation and later by proliferative changes involving alveolar and bronchiolar lining cells and interstitial cells (Am J Pathol 1976;85:209)
- Acute and rapidly progressive hypoxia with bilateral pulmonary edema due to alveolar injury caused by pulmonary or systemic insults
- 40% die within 28 days from onset of ARDS, mainly due to infection / sepsis and multiple organ dysfunction syndrome
- Although DAD is the typical morphology of ARDS, clinical syndrome of ARDS is not synonymous with the pathologic diagnosis of DAD
- DAD pattern is often characterized by hyaline membranes in acute phase but shows a wide variety of findings that makes the diagnosis challenging
- Previously known as adult respiratory distress syndrome
- Acute lung injury, an overlapping entity suggested in AECC definition, was removed from Berlin definition; the AECC definition of acute lung injury non-ARDS is compatible with Berlin definition of mild ARDS (JAMA 2012;307:2526)
- ICD-10: J80 - acute respiratory distress syndrome
- Mean age: 60 years old; from children to elderly
- M:F = 3:2
- Incidence of 10.6 - 78.9 per 100,000 person years (N Engl J Med 2005;353:1685, Intensive Care Med 2009;35:1352)
- Incidence of ARDS in intensive care unit (ICU) (JAMA 2016;315:788):
- 10.4% of all ICU patients
- 67.2% of patients with acute hypoxemic respiratory failure
- ARDS is frequently undiagnosed (60.2% recognized by clinician) or late diagnosed (34.0% recognized at the time of criteria fulfillment)
- Diffusely involves bilateral lobes of the lung without upper or lower lobe predominance
- Distribution can be regional, depending on the degree and cause of the inflammation
- Pathogenesis (N Engl J Med 2000;342:1334, Lancet 2016;388:2416)
- Exudative (acute) phase: 1 - 7 days
- Neutrophil mediated inflammation destroys the alveolar capillary barrier (alveolar epithelium and endothelium), increases its permeability and causes intra-alveolar hemorrhage and edema
- Protein rich edema interacts with alveolar surfactants, resulting in decreased pulmonary compliance
- Hyaline membranes develop on alveolar wall where epithelium is denudated and disrupted
- Proliferative / organizing (subacute) phase: 1 - 3 weeks
- Proliferation of type II pneumocytes and subsequent differentiation into type I pneumocytes
- Proliferation of myofibroblasts
- Drainage of alveolar edema by restored type II pneumocytes
- Fibrotic (chronic) phase: after 3 weeks
- Collagenous fibrosis in alveolar spaces and interstitium
- Refractory rigidity of alveoli due to architectural remodeling
- Exudative (acute) phase: 1 - 7 days
- Pathophysiology of hypoxia
- Collapse of alveoli
- Increased right to left intrapulmonary shunt
- Decreased pulmonary compliance
- Surfactant malfunction
- Fibrosis
- Decreased diffusing capacity due to pulmonary edema
- Increased ventilation perfusion mismatch
- Increased pulmonary vascular resistance
- Mechanism of ARDS to cause multiple organ dysfunction syndrome is not clear
- Ventilator induced lung injury may play a critical role for upregulation of cytokines and eventual development of multiple organ dysfunction syndrome (Curr Opin Crit Care 2011;17:1, Respir Care 2014;59:1422)
- Pulmonary and extrapulmonary origin (N Engl J Med 2000;342:1334)
| Direct lung injury | Indirect lung injury |
|---|---|
|
|
|
|
- Infection
- Bacterial: mycoplasma, mycobacteria, legionella, rickettsia
- Viral: influenza virus, herpes virus, cytomegalovirus, hantavirus, SARS-CoV-2 (coronavirus disease 2019, COVID-19) (Histopathology 2020;77:570)
- Fungal: Pneumocystis jirovecii
- Drug (N Engl J Med 2000;342:1334)
- Chemotherapeutic drugs: methotrexate, bleomycin, azathioprine, busulfan
- Molecular targeted drugs
- Gold based
- Amiodarone
- Penicillamine
- Nitrofurantoin
- Autoimmune disease
- Polymyositis / dermatomyositis
- Especially in clinically amyopathic dermatomyositis
- Systemic lupus erythematosus
- Scleroderma
- Rheumatoid arthritis
- Polyarteritis nodosa
- Undifferentiated (subclinical) connective tissue disease
- Often positive for serum anti-MDA-5 antibody or anti-ARS antibody (Medicine (Baltimore) 2012;91:220, BMJ Case Rep 2016;2016:bcr2016217624, Tuberc Respir Dis (Seoul) 2016;79:188)
- Polymyositis / dermatomyositis
- Inhalation
- Smoke
- Sulfur dioxide
- Oxygen
- Nitrogen dioxide
- Acute and progressive respiratory failure
- Usually starts 12 - 48 hours after the initial insult
- Shortness of breath; dyspnea on exertion followed by dyspnea at rest
- Hypoxia; PaO2 / FiO2 ≤ 300 mm Hg
- Often followed by sepsis and multiple organ dysfunction syndrome (JAMA 2016;315:788)
- Respiratory dysfunction and physical disability may persist for months after remission of ARDS, with gradual improvement (N Engl J Med 2003;348:683)
- Diagnosis of ARDS is based on clinical manifestation and its severity is evaluated with ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2 / FiO2)
- Berlin definition (JAMA 2012;307:2526)
- Timing
- Within 1 week of a known clinical insult or new or worsening respiratory symptoms
- Chest imaging
- Assessed by chest Xray or CT
- Bilateral opacities; not fully explained by effusions, lobar / lung collapse or nodules
- Origin of edema
- Respiratory failure not fully explained by cardiac failure or fluid overload
- Need objective assessment (e.g. echocardiography) to exclude hydrostatic edema if no risk factor present
- Oxygenation (with positive end expiratory pressure [PEEP] or continuous positive airway pressure [CPAP] ≥ 5 cm H2O)
- Mild: 200 < PaO2 / FiO2 ≤ 300 mm Hg
- Moderate: 100 < PaO2 / FIO2 ≤ 200 mm Hg
- Severe: PaO2 / FiO2 ≤ 100 mm Hg
- Timing
- Not all ARDS show DAD pattern
- ARDS can present with organizing DAD and acute fibrinous organizing pneumonia as well
- DAD can be seen as a nonspecific manifestation of the agonal phase and shock
- Although rarely performed, lung biopsy can be helpful for critical care and prognosis estimation in patients with ARDS
- Open lung biopsy provided a specific diagnosis for 56 - 84% of ARDS patients and an alternative treatment for 73% of cases (Ann Thorac Surg 2014;98:1254, Crit Care 2015;19:228, Intensive Care Med 2015;41:222)
- ARDS with DAD is related to worse prognosis (see Prognostic factors)
- Carefully consider biopsy if there is a high prediction for beneficial result and the risk of empirical therapy is not suitable or unsuccessful (Chest 2015;148:1073)
- Arterial blood gas test
- Hypoxemia
- Ratio of pulse oximetric oxygen saturation to FIO2 (SpO2 / FiO2) may be helpful for instant follow up (Chest 2007;132:410)
- SpO2 / FiO2 of 235 ≈ PaO2 / FiO2 of 200 (sensitivity: 85%, specificity: 85%)
- SpO2 / FiO2 of 315 ≈ PaO2 / FiO2 of 300 (sensitivity: 91%, specificity: 56%)
- Other blood tests
- Increased C reactive protein
- Increased procalcitonin in septic ARDS
- Increased ferritin (Am J Respir Crit Care Med 1999;159:1506)
- Increased KL-6
- Brain natriuretic peptide (BNP) test may helpful to distinguish ARDS and cardiogenic pulmonary edema (Chest 2007;131:964)
- BNP ≤ 200 pg/mL is suggestive for ARDS (sensitivity: 40%, specificity: 91%)
- BNP ≥ 1,200 pg/mL is suggestive for cardiogenic pulmonary edema (sensitivity: 52%, specificity: 92%)
- General
- Heterogeneous bilateral shadows due to pulmonary edema
- Rule out atelectasis, pleural effusion and mass
- Takes 12 - 24 hours from onset to be apparent
- Chest Xray
- Exudative phase: ground glass opacity and consolidation with air bronchogram
- Proliferative / organizing and fibrotic phases: reticular shadow and volume reduction
- Chest CT (Radiology 1999;211:859)
- Exudative phase
- Patchy to diffuse ground glass opacity, with or without interlobular septal thickening
- Dorsal consolidation due to infiltrate
- Proliferative / organizing phase
- Ground glass opacity with bronchiolectasis and bronchiectasis
- Volume reduction
- Fibrotic phase
- Septal thickening and reticular shadow in ground glass opacity
- Peripheral cystic and honeycomb-like lesions due to fibrosis
- Exudative phase
- Septic shock and multiple organ dysfunction syndrome account for about 50% of deaths in patients with ARDS, while respiratory failure is responsible for 10 - 20% of deaths (Am J Respir Crit Care Med 2013;187:761, Chest 2005;128:525, Chest 1989;96:885, Clin Chest Med 2006;27:725)
- First 7 - 10 days are the most relevant for the prognosis of ARDS (JAMA 2016;315:788)
- Of all ARDS patients, 93.1% developed ARDS in the first 48 hours
- Mortality rate at day 28 and at hospital discharge was 29.6% and 34.9% for mild ARDS, 35.2% and 40.3% for moderate and 40.9% and 46.1% for severe, respectively
- Mortality is higher for ARDS with DAD (71.9%) than ARDS without DAD (45.5%) (Crit Care 2015;19:228, PLoS One 2017;12:e0180018, Chest 2016;149:1155)
- Prognosis of ARDS patients improved over the last decades (Chest 2008;133:1120)
- 31 year old man with ARDS / DAD and eosinophilic pneumonia due to amphetamine smoking (Chin J Physiol 2014;57:295)
- 41 year old woman died of ARDS / DAD due to influenza A virus infection (Jpn J Infect Dis 2010;63:72)
- 43 year old man died of ARDS due to clinically amyopathic dermatomyositis (Case Rep Crit Care 2016;2016:7379829)
- 45 year old woman died of ARDS / DAD due to rabies (Kaohsiung J Med Sci 2006;22:94)
- 49 year old man died of ARDS / DAD due to EBV positive diffuse large B cell lymphoma (Int J Clin Exp Pathol 2014;7:1742)
- 72 year old woman died of ARDS / DAD due to scrub typhus (J Korean Med Sci 2000;15:343)
- 72 year old man died of ARDS / DAD due to influenza B virus infection (Respirol Case Rep 2015;3:61)
- 75 year old man died of ARDS / DAD due to gemcitabine chemotoxicity (Intern Med 2003;42:1022)
- 77 year old woman died of ARDS / DAD due to acute interstitial pneumonia (Case Rep Med 2011;2011:628743)
- 93 year old woman with segmented DAD due to COVID-19 (Pathol Int 2020;70:820)
- Removal of the original insult
- Oxygen therapy for respiratory failure (Lancet 2016;388:2416)
- Mechanical ventilation
- PEEP or CPAP ≥ 5 cm H2O
- With or without neuromuscular blockade, prone position and extracorporeal membrane oxygenation
- Mechanical ventilation
- Other supportive care
- Fluid management
- Pharmacotherapy
- Glucocorticoid
- Anticoagulant
- Since no treatment drastically improves the respiratory failure of ARDS, respiratory and systemic supportive care is needed until the patient survives from ARDS
- Brown to gray consolidative lesion with indistinct borders, diffusely involving bilateral lobes
- Elastic hard and greasy due to transudate within alveolar spaces and interstitial edema
- Heavy and shrunken due to fibrosis and collapse of the tissue
- Dots of hemorrhage on pleural surface
- Histopathology of DAD progresses from exudative (acute) phase through proliferative / organizing (subacute) phase to chronic fibrotic phase roughly corresponding to the period of ARDS (Am J Pathol 1976;85:209, Arch Pathol Lab Med 2010;134:719, Clin Chest Med 2000;21:435, N Engl J Med 2000;342:1334)
- Phase of the disease is almost synchronous throughout the lung
- Features of different phases may be combined in the transitional period or with repeated bouts of lung injury
- Exudative (acute) phase
- Alveolar change
- Hyaline membranes on alveolar duct or sacs
- Interstitial and intra-alveolar edema
- Collapsed alveoli
- Epithelial change
- Denudation and necrosis of type I pneumocytes
- Vascular change
- Necrosis of endothelial cells
- Neutrophil aggregation
- Microthromboemboli
- Hemorrhage
- Alveolar change
- Proliferative / organizing (subacute) phase
- Alveolar change
- Remnants of hyaline membrane with or without organization
- Interstitial and intra-alveolar proliferation of myofibroblasts
- Lymphocytic infiltration
- Epithelial change
- Proliferation / hyperplasia of type II pneumocytes
- Vascular change
- Endothelial injury and thromboemboli in arterioles
- Alveolar change
- Fibrosis phase
- Alveolar change
- Collagenous fibrosis
- Microscopic honeycomb-like change
- Traction bronchiolectasis
- Epithelial change
- Squamous metaplasia / hyperplasia
- Vascular change
- Remodeling of arteries
- Intimal fibrosis
- Thickening of media
- Alveolar change
- Others
- May have superimposed pneumonia
- Fibrin deposition
- DAD with prominent organizing pneumonia is also called organizing DAD
Contributed by Akira Yoshikawa, M.D. and Yale Rosen, M.D.
- Bronchoalveolar lavage (BAL) fluid
- Increased neutrophils in ARDS
- Can be helpful for the diagnosis of underlying disease
- Fiber staining (e.g. elastica van Gieson) is helpful to evaluate fibrosis and to evaluate the destruction of the alveolar architecture
- Giemsa, Grocott and Ziehl-Neelsen stains are helpful to identify pathogens
- Immunohistochemistry (not of practical utility):
- Cytokeratin highlights collapsed alveoli and lung architecture
- Changes in epithelium, endothelium and interstitium (N Engl J Med 2000;342:1334)
- Exudative phase
- Vacuolization in damaged endothelial cells
- Replacement of epithelial cells by hyaline membrane on the basement membrane
- Proliferative / organizing and fibrotic phases
- Reepithelialization of type II pneumocytes with microvilli and lamellar bodies with surfactant
- Flattening of cytoplasm and loss of lamellar bodies and microvilli of type II pneumocyte, indicating transformation to type I pneumocyte
- Collagen deposition
- Exudative phase
Histology of DAD
- Lung, autopsy:
- Diffuse alveolar damage (see comment)
- Comment: Histologic sections reveal diffuse alveolar damage in subacute and chronic phases involving bilateral lobes; the former is represented by fibrin deposition, organizing pneumonia and focal hyaline membranes and the latter by interstitial fibrosis, fibroblastic foci and the destruction of alveolar architecture. Acute bacterial pneumonia is also superimposed.
- Major entities:
- Acute exacerbation of usual interstitial pneumonia / idiopathic pulmonary fibrosis (UIP / IPF):
- Acute exacerbation of IPF and DAD are clinically and morphologically similar
- IPF shows chronic and dense collagen fibrosis with smooth muscle hyperplasia, while fibrosis in DAD is not so dense and usually lacks smooth muscle hyperplasia
- Acute interstitial pneumonia:
- So called Hamman-Rich syndrome or idiopathic DAD
- Lack of clinical criteria of ARDS
- Cardiogenic pulmonary edema:
- BNP ≥ 1,200 pg/mL
- Congestive heart failure on echocardiograph
- Right heart catheterization is now not recommended due to negative influence to prognosis
- Drug induced lung injury:
- History of causative drug
- Remission of symptoms after withdrawal of the responsible drug
- Acute exacerbation of usual interstitial pneumonia / idiopathic pulmonary fibrosis (UIP / IPF):
- Minor entities:
- Organizing pneumonia:
- Migratory sign on imaging
- Good response to corticosteroid
- Eosinophilic pneumonitis:
- Current smoker or history of particle inhalation
- Eosinophilia (> 25%) in bronchoalveolar lavage
- Good response to corticosteroid
- Hypersensitivity pneumonitis:
- History of antigen exposure
- Remission of symptoms after removal of the causative antigen
- Lymphocytosis (> 30%) in bronchoalveolar lavage
- Diffuse centrilobular nodular shadow with ground glass opacity, usually in upper lobes
- Miliary tuberculosis:
- Diffuse nodular shadow (≤ 3 mm) involving whole lobes
- Mycobacterium tuberculosis in bronchoalveolar lavage or biopsy specimen
- Lymphangitic carcinomatosis:
- Known malignancy
- Tumor cells in bronchoalveolar lavage or biopsy specimen
- Organizing pneumonia:
Comment Here
Reference: ARDS / DAD
- Bacterial pneumonia
- Diffuse collagenous fibrosis
- Hyaline membranes
- Organizing pneumonia
- Proliferation of atypical pneumocytes
Comment Here
Reference: ARDS / DAD
- Similar to other pneumoconiosis
- Initial injury is at bifurcations of small airways and ducts; macrophages ingest fibers, release chemotactic factors and fibrogenic mediators, causing interstitial fibrosis similar to other fibrosing lung diseases such as UIP
- Begins around respiratory bronchioles and alveolar ducts, extends distally; eventually causes honeycomb lungs
- Begins in lower lobes and subpleurally (in contrast to coal workers' pneumoconiosisP and silicosis), progresses to middle and upper lobes
- Visceral pleura becomes fibrotic, may bind lung to chest wall; may have associated Caplan syndrome
- Symptoms: usually begin after 10 years of exposure, initially shortness of breath with exertion and later at rest; may progress to heart failure
- Pleural plaques: well circumscribed plaques of dense collagen, often with calcium; on parietal pleura and dome of diaphragm; do not contain asbestos bodies, but rare if no asbestos history; may induce pleural effusions, usually no symptoms
- Asbestos fiber detection: H&E, Prussian blue, incineration and EM
- Crystalline hydrated silicates that form fibers
- Causes localized fibrous plaques, pleural effusions, parenchymal interstitial fibrosis (asbestosis), bronchogenic carcinoma, mesothelioma, laryngeal carcinoma and possibly colon carcinoma
- Increased incidence of mesothelioma in families of asbestos workers
- Exists in serpentine / chrysotile (curly, flexible) and amphibole (straight, stiff, brittle) forms; most asbestos in industry are serpentine, but amphiboles are more pathogenic; link with mesothelioma is almost always with amphibole form
- Chrysotiles usually are caught in upper respiratory passages, removed by mucociliary elevator; they are soluble and leached from tissue if they reach alveoli
- Amphiboles (straight, stiff) go deeper into lungs; fibers > 8 mm and thinner than 0.5 mm are more injurious
- Both types are fibrogenic; act as tumor initiator and promoter; generate free radicals; toxic chemicals (tobacco smoke) may also be adsorbed to asbestos fibers
- Asbestos may act by countering antioxidant effect of Vitamin C (ascorbic acid) (Hum Pathol 2003;34:737)
- Relative risks compared to normal population: asbestos and bronchogenic carcinoma has RR of 5; with tobacco use, RR is 55
- Asbestos and mesothelioma (pleural, pericardial, peritoneal) has RR of 1000; no increased risk with smoking
- Incidence of mesothelioma expected to increase until 2020 - 2025 due to lag time between exposure and diagnosis
- Note: asbestos related tumors have no special histologic features
- Early: interstitial pneumonia with desquamative features, hyperplastic alveolar cells with intracytoplasmic Mallory's hyaline tissue
- Later: diffuse interstitial fibrosis with honeycombing (silicosis is nodular), asbestos bodies (golden brown, fusiform or beaded rods with translucent center; asbestos fibers coated with iron-containing proteinaceous material); iron from phagocyte ferritin
- Asbestos fibers may have oxalate crystal deposition (Hum Pathol 2003;34:737)
- Ferruginous bodies: inorganic particulates coated with phagocyte ferritin
- Infection of the lung by a hyaline mold in genus Aspergillus, with various manifestation based on host immune status
- Word origin: aspergillum, a ritual liturgical implement used in Roman Catholic ceremonies to sprinkle holy water (Arch Pathol Lab Med 2008;132:606)
- Aspergillus histomorphology: acute angle, dichotomous branching, septate hyphae; however, fungal culture is required for definite identification
- Noninvasive form in immunocompetent host: cavitary lesion with fungal ball and surrounding chronic inflammation
- Invasive form in immunocompromised host: necrotizing pneumonia with angioinvasion and infarct
- Allergic bronchopulmonary aspergillosis (ABPA)
- Chronic pulmonary aspergillosis (CPA)
- Simple / single aspergilloma
- Aspergillus nodule
- Chronic cavitary pulmonary aspergillosis (CCPA)
- Chronic fibrosing pulmonary aspergillosis (CFPA)
- Subacute invasive aspergillosis (formerly known as chronic necrotizing pulmonary aspergillosis)
- Invasive pulmonary aspergillosis (IPA)
- ICD-10:
- ICD-11:
- Causes a wide spectrum of diseases in humans, depending on the underlying immune status of the host (Clin Microbiol Rev 2019;33:e00140)
- One of the most common causes of infectious death in severely immunocompromised patients
- Mortality rate = 50% in neutropenic patients, 90% in hematopoietic stem cell transplantation (HSCT) recipients (QJM 2007;100:317)
- Colonization in asymptomatic patient is common
- Aspergillus DNA has been found in 37% of lung biopsy specimens of healthy adults (Clin Infect Dis 2011;52:1123)
- Culture proven colonization occurs in up to 30% of chronic obstructive pulmonary disease (COPD) patients (Med Mycol 2012;50:433)
- Lung
- Upper lobes are more frequently affected in chronic pulmonary aspergillosis (Respir Med 2018;141:121)
- Other commonly affected organs: central nervous system, eye, paranasal sinus, middle ear, heart, bone and soft tissue, skin, gastrointestinal tract (Clin Infect Dis 2016;63:e1)
- Disseminated infection
- Acquired by inhalation of airborne conidia
- Virulence factors: endotoxins, heparin-like factors and oxalic acid (Arch Pathol Lab Med 2008;132:606)
- Saprophytic fungi in genus Aspergillus, ubiquitous in environment, can be isolated from soil, household, hospital environment, food, etc.
- 300 species, only 8 species are responsible for infection in humans (Arch Pathol Lab Med 2008;132:606)
- Aspergillus fumigatus (most common), followed by A. niger
- Other: A. nidulans, A. terreus, A. clavatus, A. flavus, A. niveus and A. ustus
- 3 broad categories of clinical manifestation in pulmonary aspergillosis (Respir Med 2018;141:121)
- Allergic bronchopulmonary aspergillosis (ABPA)
- Chronic pulmonary aspergillosis (CPA)
- Invasive pulmonary aspergillosis (IPA)
- Allergic bronchopulmonary aspergillosis (ABPA)
- Immunologic pulmonary disorder caused by hypersensitivity to Aspergillus fumigatus
- Pre-existing airway disease is present
- 1 - 2% of asthma patients (Arch Pathol Lab Med 2005;129:924)
- 10.5% of cystic fibrosis patients (Eur Ann Allergy Clin Immunol 2020;52:104)
- Other predisposing conditions: hyper IgE syndrome, chronic granulomatous disease (J Allergy Clin Immunol 1999;104:1265)
- Clinically: worsening asthma symptoms, chronic productive cough and wheezing (Respir Med 2018;141:121)
- Characteristic: golden brownish mucus plugs, found in 50% of patients (Chest 2009;135:805)
- Chronic pulmonary aspergillosis (CPA)
- A spectrum of diseases in immunocompetent patients with a pre-existing pulmonary condition, including tuberculous and nontuberculous mycobacterial infections (most common), ABPA, COPD, treated lung cancer, asthma, pneumonia and fibrocavitary sarcoidosis (Respir Med 2018;141:121)
- Aspergilloma (Respir Med 2018;141:121)
- Fungal ball consisting of Aspergillus hyphae, fibrin and other debris
- Present in almost all forms of CPA
- Simple / single aspergilloma
- Single pulmonary cavity containing a fungal ball (Eur Respir J 2016;47:45)
- Chronic cavitary pulmonary aspergillosis (CCPA)
- Most common form of CPA
- Can progress to chronic fibrosing pulmonary aspergillosis (CFPA) if untreated
- Aspergillus nodule
- Unusual form of CPA, mimicking malignancy, tuberculoma or coccidioidomycosis
- Frequent necrosis but no tissue invasion
- Subacute invasive aspergillosis
- Commonly grouped under CPA but diagnosed and treated similarly to IPA (Respir Med 2018;141:121)
- Formerly known as chronic necrotizing pulmonary aspergillosis
- Mildly immunocompromised or severely debilitated patients
- Similar clinical and radiological features to CCPA but progresses rapidly (Eur Respir J 2016;47:45)
- Most common symptom is cough (> 90%) (Medicine (Baltimore) 2017;96:e8315)
- Other symptoms: shortness of breath, chest pain, hemoptysis, fever, weight loss and night sweats
- Invasive pulmonary aspergillosis (IPA)
- Most serious form of pulmonary aspergillosis in immunocompromised patients (Respir Med 2018;141:121)
- Common in HSCT and solid organ transplant (SOT) recipients, hematologic malignancy, rare in HIV infection (Arch Pathol Lab Med 2008;132:606)
- Presence of tissue invasion by Aspergillus hyphae
- Prolonged neutropenia is the most significant risk factor (Clin Infect Dis 2016;63:e1)
- Aspergillus tracheobronchitis: unique form of IPA where infection is confined in the tracheobronchial tree (Medicine (Baltimore) 2012;91:261)
- Commonly found at the anastomotic site in lung transplant patient (Semin Diagn Pathol 2017;34:530)
- Most serious form of pulmonary aspergillosis in immunocompromised patients (Respir Med 2018;141:121)
- Allergic bronchopulmonary aspergillosis (ABPA)
- Lung biopsy not routinely performed
- International Society for Human and Animal Mycology (ISHAM) diagnostic criteria (Clin Exp Allergy 2013;43:850)
- Predisposing conditions:
- Asthma
- Cystic fibrosis
- Obligatory criteria (both required):
- Type I aspergillus skin test positive or elevated IgE levels against A. fumigatus
- Elevated total IgE levels > 1,000 IU/mL (unless all other criteria are met, then total IgE levels can be
- Other criteria (at least 2 out of 3):
- Presence of IgG antibodies against A. fumigatus or precipitating antibodies
- Presence of fleeting or fixed pulmonary opacities on chest radiograph consistent with ABPA
- Eosinophils > 500/μL in steroid naive patient (may be a historical value)
- Chronic cavitary pulmonary aspergillosis (CCPA)
- Diagnostic criteria from Infectious Diseases Society of America (IDSA) guidelines (Clin Infect Dis 2016;63:e1)
- 3 months of chronic pulmonary symptoms or chronic illness or progressive radiographic abnormalities, with cavitation, pleural thickening, pericavitary infiltrates and sometimes a fungal ball
- Aspergillus IgG antibody elevated or other microbiological data
- No or minimal immunocompromise, usually with 1 or more underlying pulmonary disorders
- Diagnostic criteria from Infectious Diseases Society of America (IDSA) guidelines (Clin Infect Dis 2016;63:e1)
- Invasive pulmonary aspergillosis (IPA)
- Histopathological examination of lung tissue is the gold standard (Respir Med 2018;141:121)
- Flexible bronchoscopy with bronchoalveolar lavage (BAL) fluid for cytology and culture can be performed if biopsy is not advised (Clin Infect Dis 2016;63:e1)
- Clinical or radiological findings consistent with infection also required (Eur Respir Rev 2011;20:156)
- Standard fungal culture and identification
- Species differentiation by fruiting body (conidial heads) morphology
- Galactomannan (GM)
- Polysaccharide cell wall component of Aspergillus spp., which is released during growth (Clin Infect Dis 2006;42:1417)
- Can be measured in serum and bronchoalveolar lavage (BAL) fluid, using double sandwich ELISA technique
- Marker of invasive aspergillosis in certain subpopulation (e.g. hematologic malignancy and HSCT recipient) (Clin Infect Dis 2016;63:e1)
- Not recommended for screening in solid organ transplant (SOT) recipients (Scand J Infect Dis 2012;44:600)
- Serum 1,3-beta-D glucan
- Major cell wall components in various fungi (e.g., Aspergillus spp., Candida spp. and Pneumocystis jiroveccii) (J Clin Microbiol 2012;50:7)
- Protease zymogen based colorimetric assay, commercially available as Fungitell®, an FDA cleared in vitro diagnostic rapid screening test
- Marker of invasive fungal infection, not specific for genus Aspergillus
- Allergic bronchopulmonary aspergillosis (ABPA)
- Chest Xray (Indian J Radiol Imaging 2011;21:242)
- May be normal in early stage
- Tram line shadows, band-like (toothpaste) shadows, finger in glove opacities; represents mucoid impaction in dilated bronchi with occlusion of the distal end
- High resolution computed tomography (HRCT) (J Clin Diagn Res 2014;8:RC05)
- Centrilobular nodules, tree in bud pattern, mosaic attenuation and mucus impaction
- High attenuation mucus (HAM) (J Clin Diagn Res 2014;8:RC05)
- Pathognomonic for ABPA
- Mucus that appears denser than the skeletal muscles on HRCT (70 - 90 Hounsfield units)
- Chest Xray (Indian J Radiol Imaging 2011;21:242)
- Chronic cavitary pulmonary aspergillosis (CCPA)
- New or expanding pre-existing cavities of variable wall thickness in the setting of chronic lung disease, with or without fungal ball, often with pleural thickening and marked parenchymal destruction or fibrosis (Eur Respir J 2016;47:45)
- Fungal ball: upper lobe, solid, round or oval, intracavitary mass, partially surrounded by a crescent of air (air crescent or Monad sign) (Eur Respir J 2016;47:45)
- Invasive pulmonary aspergillosis (IPA)
- HRCT is the imaging of choice when IPA is suspected (Clin Microbiol Infect 2018;24:e1)
- Classical HRCT findings: macronodules (> 1 cm), surrounded by a halo of ground glass attenuation (halo sign)
- Other findings: pleural based wedge shaped areas of consolidation, alveolar consolidations, mass-like lesion, ground glass opacities and pleural effusion
- Delayed findings: cavity or air crescent sign
- Prognosis of ABPA is not well characterized (Mayo Clin Proc 2001;76:930)
- If ABPA is detected early and is treated promptly, the prognosis is good (Clin Dev Immunol 2011;2011:843763)
- Unfavorable prognosis can be seen in untreated patients with irreversible lung fibrosis, cor pulmonale and respiratory failure (Clin Pharm 1993;12:24)
- Poor prognostic factors in CPA (Eur Respir J 2017;49:1601062)
- History of a nontuberculous mycobacterial infection or COPD
- Low body mass index (BMI)
- Low serum albumin
- Old age
- Elevated inflammatory markers
- Lower activity
- Bilateral aspergillomas
- Risk factor for developing IPA (Eur Respir Rev 2011;20:156)
- Prolonged neutropenia (3 for > 10 days)
- Solid organ transplantation (highest risk is with lung transplantation and HSCT)
- Prolonged (> 3 weeks) and high dose corticosteroid therapy
- Hematological malignancy (risk is higher with leukemia)
- Chemotherapy
- AIDS
- Chronic granulomatous disease
- Baseline factors that predict treatment outcome in patients with invasive aspergillosis (Mycoses 2019;62:651)
- Kidney and liver failure
- ICU admission
- Uncontrolled underlying disease
- Prolonged neutropenia
- Imaging results associated with negative outcome
- Multiple consolidations
- Bilateral pulmonary lesions
- Pleural effusion
- 45 year old woman status post lung transplant with hemoptysis (Kobe J Med Sci 2020;65:E114)
- 61 year old man with hypertension, severe fever and thrombocytopenia (Viruses 2021;13:1086)
- 62 year old man with COPD and acute respiratory failure (Med Mycol Case Rep 2018;20:39)
- 64 year old man with chills and mild dyspnea on exertion after chemotherapy (Clin Case Rep 2018;6:2475)
- 68 year old man smoker with COPD and pseudomembranous lesion in the bronchus (Indian J Pathol Microbiol 2017;60:285)
- 69 year old man with fever and cavitary lung lesion after chemotherapy (Respirol Case Rep 2020;8:e00523)
- 75 year old with near drowning (Int Med Case Rep J 2020;13:77)
- 78 year old man with a recent diagnosis of nonspecific interstitial pneumonia (Intern Med 2018;57:3619)
- 79 year old man with COVID-19 and respiratory failure (J Fungi (Basel) 2021;7:230)
- 82 year old woman with wheezing, shortness of breath and productive cough (Cureus 2020;12:e11736)
- Based on guidelines from the Infectious Diseases Society of America (IDSA), endorsed by the Pediatric Infectious Diseases Society (PIDS) (Clin Infect Dis 2016;63:e1)
- Allergic bronchopulmonary aspergillosis (ABPA)
- Itraconazole
- Alternative: oral voriconazole, posaconazole
- Corticosteroids for exacerbation
- Aspergilloma
- Observation
- Surgical resection in symptomatic patient (e.g., hemoptysis)
- Alternative: itraconazole, voriconazole
- Chronic cavitary pulmonary aspergillosis (CCPA), invasive pulmonary aspergillosis (IPA), tracheobronchial aspergillosis; same treatment
- Voriconazole
- Alternative: amphotericin B, isavuconazole, caspofungin, micafungin, posaconazole, itraconazole
- Allergic bronchopulmonary aspergillosis (ABPA)
- Bronchiectasis from mucus impaction
- Airway occlusion by mucus
- Chronic cavitary pulmonary aspergillosis (CCPA)
- Corresponds with the imaging finding of cavitary lesion, with or without fungal ball
- Invasive pulmonary aspergillosis (IPA) (Arch Pathol Lab Med 2008;132:606)
- Targetoid necrosis: central thrombosed vessels secondary to angioinvasion
- Confluent bronchopneumonia or dense lobar consolidation may be seen
- Foci of infarcted lung yields an infected pulmonary sequestrum
- Organism: acute angle (
- Aspergillus has a genus specific fruiting body (Arch Pathol Lab Med 2008;132:606)
- Develops from mycelia in areas of high oxygen tension (e.g. lung, sinus cavities)
- Does not develop in tissue
- Composed of a vesicle and either 1 or 2 layers of phialides that produce conidia
- Since histomorphology alone is not accurate in identification, definite classification should be based on microbiologic culture
- Mucoid impaction of bronchi, composed of mucus and inflammatory cells (predominantly eosinophils), AKA allergic mucin
- Bronchocentric granulomatosis
- Airway centric necrotizing granulomatous inflammation with destruction of the airway wall
- Dense inflammatory infiltrate with prominent eosinophils
- May be seen in other conditions: nonfungal infection, malignancy, autoimmune disease
- Eosinophilic pneumonia
- Chronic or exudative bronchiolitis
- Fungal hyphae are rarely identified, usually fragmented
- Characteristic cavitary lesion with fungal ball (Arch Pathol Lab Med 2008;132:606)
- Cavity wall: superficial ulceration with granulation tissue, granulomatous inflammation or metaplastic squamous epithelium
- Wall must be carefully examined, to exclude subacute invasive aspergillosis (chronic necrotizing pulmonary aspergillosis) which shows invasion of lung parenchyma but no angioinvasion
- A. niger fungus ball can be associated with chronic pulmonary oxalosis (Arch Pathol Lab Med 2008;132:606)
- Oxalic acid is produced by A. niger
- Prothrombotic effect by oxalate leads to extensive ischemic necrosis
- Resection of the fungus ball is definitive treatment
- Splendore-Hoeppli phenomenon: deposition of antigen antibody complexes and debris from host inflammatory cells, resulting in amorphous eosinophilic material coating the mycelia (J Oral Maxillofac Pathol 2018;22:161)
- Necrotizing pneumonia with areas of hemorrhage and acute and granulomatous inflammation (Arch Pathol Lab Med 2008;132:606)
- Fungal hyphae occlude the lumen of the pulmonary artery with associated infarcted area (Semin Diagn Pathol 2017;34:530)
Contributed by Sakda Sathirareuangchai, M.D., Venna Maheshwar, M.D., Kiran Alam, M.D., Anshu Jain and Claudia Mendez, M.D.
- Relatively large (3 - 6 μm), septate, fungal hyphae, with regular, progressive dichotomous branching at a 45° angle (Clin Microbiol Rev 1998;11:341)
- Fine needle aspiration (FNA) of the lung shows granulomatous process (Orell & Sterret's Fine Needle Aspiration Cytology, 5th Edition, 2011)
- Epithelioid histiocytes in cohesive clusters
- Few nonpigmented multinucleate histiocytes
- Granular, calcific, mucoid or acute inflammatory debris
- Lymphocytes
- Severely reactive pneumocytes may mimic carcinoma (Clin Microbiol Rev 1998;11:341)
- Sputum cytology might show calcium oxalate crystal (Arch Pathol Lab Med 1986;110:1176)
- Grocott and Gomori methenamine silver (GMS)
- Hyphae wall stains black or dark brown
- PAS (Periodic Acid-Schiff)
- Hyphae wall stains pink to purple
- Immunohistochemistry
- Not routinely used
- Sensitivity 85%, specificity 100% (Mycoses 2019;62:1006)
- Polyclonal antibody is preferred over monoclonal antibody (Appl Immunohistochem Mol Morphol 2009;17:524)
- Mucicarmine
- Stains the capsule of Cryptococcus (Semin Diagn Pathol 2017;34:530)
- Fontana-Masson (melanin stain)
- Stain black to dark brown color in Cryptococcus and the dematiaceous fungi (Hum Pathol 2012;43:898)
Pulmonary aspergillosis
- Lung, left upper lobe, wedge resection:
- Cavitary lesion with chronic inflammation
- Fungal hyphae identified (see comment)
- Comment: Fungal hyphae is septate dichotomous branching. GMS stain is positive. The differential diagnosis includes Aspergillus spp., Fusarium and spp.
- Mucormycosis:
- Previously known as zygomycosis
- Nonseptate, broad hyphae with right angle (90°) branching, well stained by standard H&E
- Less common than aspergillosis
- Affects only immunocompromised host, especially diabetics
- Pseudallescheria boydii (anamorph Scedosporium apiospermum):
- Same histomorphology as Aspergillus
- Culture is required for definite identification (Respirology 2008;13:478)
- Fusarium spp.:
- An opportunistic mold with the same histomorphology as Aspergillus
- Culture is required for definite identification (J Clin Diagn Res 2017;11:ED04)
- Pulmonary tuberculosis:
- Also has necrotizing granulomatous inflammation
- Can coexist with chronic pulmonary aspergillosis
- AFB stain positive
- Non small cell lung carcinoma:
- Can present with cavitary and mass lesion
- Reactive pneumocytes from the surrounding tissue in aspergillosis may mimic carcinoma
A 65 year old man presented with a mass lesion in his left lung. He underwent a wedge biopsy, which showed benign lung parenchyma with chronic inflammation and an organism shown in the image. What is the most likely causative organism?
- Actinomyces israelii
- Aspergillus spp.
- Candida albicans
- Cryptococcus neoformans
- Mucor spp.
- Allergic bronchopulmonary aspergillosis
- Aspergillus nodule
- Chronic cavitary pulmonary aspergillosis
- Invasive pulmonary aspergillosis
- Tracheobronchial aspergillosis
- Isolation of Aspergillus fumigatus is not required for diagnosis
- Lung biopsy is essential for diagnosis
- Mucous plug is rarely found in the airway
- Patients are immunocompromised host
- Serologic workup is not necessary
Comment Here
Reference: Aspergillus
- Defined by the National Asthma Education and Prevention Program as a "chronic inflammatory disorder of the airways" in which many cells and cellular elements play a role - in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils and epithelial cells
- In susceptible individuals, causes episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or early morning
- Episodes are usually associated with widespread but variable airflow obstruction that is often reversible, either spontaneously or with treatment
- Inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli
- Very common, affects 14 - 15 million Americans
- Causes 3,000 US deaths annually (American Academy of Allergy, Asthma & Immunology)
- Has increased in Western hemisphere over past 40 years
- Atopic or Extrinsic: initial sensitization affects T helper 2 cells, which release IL4 / 5, which promote IgE release by B cells, mast cells, and eosinophils
- Re-exposure to allergen leads to mediator release from mucosal mast cells
- Acute / intermediate response is bronchoconstriction, edema, mucus secretion and vasodilation with increased vascular permeability
- Late phase reaction is due to influx of other inflammatory cells stimulated by chemokines released by mast cells, epithelial cells, T lymphocytes and other cytokines; includes release of major basic protein from eosinophils, which causes epithelial damage and airway constriction
- Putative mediators are leukotrienes C4, D4, E4 and acetylcholine; minor mediators are histamine, prostaglandin D2; associated with serum eosinophilia, sputum eosinophils
- Atopic or Extrinsic: Type I hypersensitivity, generally due to allergens; begins in childhood, triggered by environmental allergens (dander, dust, pollen, food), often positive family history; more common in African American children; evidence of allergen sensitization; skin test causes wheel and flare reaction (CMAJ 2009;181:E181)
- Noneosinophilic ("neutrophilic") asthma: a subgroup of atopic asthma not associated with eosinophilia; IL8 recruiting neutrophils are an important mechanism; patients tend to be less responsive to corticosteroids (Thorax 2011;66:942)
- Nonatopic or Intrinsic: nonimmune; due to aspirin ingestion, pneumonia, cold, stress, exercise; follows respiratory infection (rhinovirus, parainfluenza virus); usually not familial; no evidence of allergen sensitization; normal serum IgE, negative skin tests; viral induced inflammation may lower threshold of subepithelial vagal receptors to irritants
- Occupational asthma: due to repeated exposure to fumes, dusts, gases, chemicals, often in minute quantities; varying mechanisms of disease depending upon the stimulus
- Drug induced asthma: associated with several drugs, but most noteworthy is aspirin use; rare, aspirin related cases are associated with recurrent rhinitis, nasal polyps and urticaria; patients are sensitive to small doses of aspirin; may be due to direct effects of aspirin on cyclooxygenase pathway
- Status asthmaticus: unremitting attacks due to exposure to previously sensitized antigen; may be fatal, usually in patients with a long history of asthma
- Overdistended lungs, small areas of atelectasis, thick mucus plugs in proximal bronchi containing whorls of shed epithelium
- Curschmann spirals, eosinophils, extracellular Charcot-Leyden crystals (crystalloids composed of galectin-10, an eosinophil lysophopholipase), increased mucosal goblet cells and submucosal glands, thickened basement membrane, bronchial smooth muscle hypertrophy, airway wall edema
- Allergic bronchopulmonary aspergillosis: important complication of asthma and cystic fibrosis
- Bronchocentric granulomatosis without the granulomatous inflammation
- Incomplete expansion of lung or collapse of previously inflated lung, due to obstruction / resorption, compression or contraction
- Obstruction: resorption of oxygen causes collapse and mediastinal shifts towards affected lung; due to mucus plugs, asthma, chronic bronchitis, bronchiectasis, postoperative changes, foreign bodies, but not usually due to tumors, which cause only subtotal obstruction
- Compression: due to fluid (congestive heart failure), air (pneumothorax), tumor and blood; causes mediastinal shifts away from affected lung
- Contraction: due to fibrosis (restrictive lung disease)
- Patchy: due to loss of surfactant in acute respiratory distress syndrome
- Rounded: Localized area of subpleural lung collapse with associated pleural fibrosis; patients usually asymptomatic with occupational exposure to asbestos; usually posterior portion of a lower lobe
- Rounded: lung shows ill defined atelectasis with deeply invaginated pleural folds, which may disappear during grossing
- Rounded: pleural fibrosis and invagination (use elastic stains to highlight) and atelectasis
- Atypical adenomatous hyperplasia (AAH) is a small, localized proliferation of atypical pneumocytes (usually ≤ 5 mm) that line intact alveolar spaces
- AAH is recognized as a precursor lesion to invasive adenocarcinoma (Cancer Metastasis Rev 2010;29:15)
- Small, localized lesion (usually ≤ 5 mm)
- Discrete from alveolar parenchyma with proliferation of atypical pneumocytes
- Forms a discontinuous monolayer of cells
- Surrounding parenchyma should be devoid of substantial inflammation or fibrosis
- Obsolete terms (not recommended): atypical alveolar epithelial hyperplasia, atypical bronchoalveolar cell hyperplasia, atypical alveolar cell hyperplasia, bronchoalveolar cell adenoma, bronchial adenoma
- ICD-O: 8250/0 - atypical adenomatous hyperplasia
- ICD-11: 2F0Z & XH5QL3 - benign neoplasms of unspecified respiratory and intrathoracic organs & atypical adenomatous hyperplasia
- Commonly seen in lung resections as an incidental finding
- In some series, AAH has been reported in ≤ 30.2% of female patients undergoing a resection for adenocarcinoma (Br J Cancer 2000;83:632)
- In autopsy series, AAH has been reported in 2 - 4% of cases without cancer (Mod Pathol 1997;10:469, Lung Cancer 2000;29:125)
- F > M (Br J Cancer 2000;83:632)
- Associated CYP19A1 polymorphisms have been reported (Carcinogenesis 2010;31:1794)
- More common in the upper lobes (Thorax 2001;56:302)
- Conceptualized as the earliest morphologically recognizable lesion in the proposed stepwise progression of lung adenocarcinoma (Int J Mol Sci 2018;19:1259)
- Unknown; some series suggest that AAH is not correlated with smoking (Thorax 2001;56:302)
- AAH is usually undetectable by imaging techniques and is typically found incidentally in surgical pathology specimens
- Larger lesions may be present on high resolution CT imaging (Eur Radiol 2001;11:811)
- Typically diagnosed in lung resection specimens (often incidentally)
- Usually not diagnosed on small core needle or transbronchial biopsies since the lesion should be examined in its entirety
- Not typically assessed in AAH
- Present as faint, not solid, nodules on CT scans (J Thorac Dis 2018;10:S790)
- Patients are cured upon resection
- 12 year old girl presenting with incidental AAH upon bulla surgical resection (Korean J Thorac Cardiovasc Surg 2016;49:141)
- 50 year old woman with 3 ground glass nodules showing coexistence of atypical adenomatous hyperplasia, minimally invasive adenocarcinoma and invasive adenocarcinoma (Thorac Cancer 2021;12:693)
- 73 year old woman with AAH nodule progressing to semisolid lesion (Cureus 2019;11:e6079)
- CT surveillance; frequency and duration dependent on size of nodule (JAMA 2022;327:264)
- Patients are cured with resection
- Gray, tan-yellow, ill defined area
- Can be multifocal
- Localization: peripheral lung parenchyma, near pleura
- Size: measures ≤ 5 mm
- Diagnosis is not typically made on frozen section, given the subtle changes associated with this lesion
- Some cases with subtle atypia on frozen section, may turn out to be classified as AAH based on permanent sections
- Proliferation of atypical pneumocytes
- Mild to moderate atypia with increased cell size and nuclear to cytoplasmic ratio; nuclei are hyperchromatic and can have intranuclear eosinophilic inclusions
- Cells are present along intact alveolar spaces
- Atypical cells form a discontinuous monolayer of cells
- Mitotic activity is typically minimal
- Lesion is composed of a mixture of club cells and type II pneumocytes
- Club cells can be recognized as columnar cells with eosinophilic and cytoplasmic snouts
- Type II pneumocytes are cuboidal with finely vacuolated to clear cytoplasm
- Absence of significant parenchymal inflammation or fibrosis
- Positive for TTF1 but is not commonly required or recommended (Virchows Arch 1997;431:415)
- Lesional cells have been shown to be clonal in nature
- Degree of copy number change and mutations has been shown in some studies to be less than in adenocarcinoma in situ (Nat Commun 2019;10:2978)
- AAH has been found to have driver mutations such as KRAS, EGFR and BRAF (J Thorac Oncol 2018;13:1776)
- Given that these lesions are cured with resection, molecular testing is not typically indicated in most clinical settings
- Right lung, middle lobe, wedge resection:
- Atypical adenomatous hyperplasia (AAH) (see comment)
- 3 mm in greatest dimension
- Comment: Atypical adenomatous hyperplasia (AAH) is a preinvasive lesion in the adenocarcinoma spectrum and is regarded as a precursor to adenocarcinoma in situ. No invasive or in situ malignancy is present.
- Nonmucinous (adenocarcinoma in situ):
- Adenocarcinoma in situ (AIS) is typically > 5 mm
- More cellular cuboidal / columnar cells forming a continuous monolayer
- AIS typically has a sharper (abrupt) cutoff with the background lung parenchyma
- Distinguishing between AIS and AAH can be challenging in some cases since there is overlap in morphology; however, this is of limited clinical relevance in most cases as both lesions are cured by resection
- Reactive pneumocyte hyperplasia:
- In reactive hyperplasia, the atypical pneumocytes tend to be more diffuse and do not form well defined nodular areas
- There is often a background of inflammation, fibrosis or features of acute lung injury seen admixed with the atypical cells
Which of the following histologic features seen in the image above, best supports the classification of this sample as atypical adenomatous hyperplasia (AAH) over adenocarcinoma in situ (AIS)?
- Absence of significant inflammation
- Architectural changes
- Discontinuous nature of the atypical cells
- Loss of polarity
- Mild to moderate atypia
Comment Here
Reference: Atypical adenomatous hyperplasia
- After workup for hemoptysis
- As an incidental solid lesion on CT scan
- Based on PET scan
- Incidental finding in resected lung tissue
Comment Here
Reference: Atypical adenomatous hyperplasia
- Well differentiated neuroendocrine carcinoma with atypical features
- Defined as tumor displaying 2 - 10 mitoses per 2 mm² or foci of necrosis (Travis: WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart, 4th Edition, 2015)
- Atypical carcinoids are defined as neuroendocrine tumors with 2 - 10 mitoses per 2 mm² or foci of necrosis
- Tumors with morphologic features of carcinoid and > 10 mitoses per 2 mm² have been reported and are the focus of active research
- Histologic features include neuroendocrine differentiation, with neuroendocrine growth patterns, salt and pepper chromatin with an inconspicuous nucleolus and moderate to abundant cytoplasm
- Differentiation from typical carcinoid is crucial as they have a poorer prognosis and are more likely to metastasize
- Not recommended: moderately differentiated lung neuroendocrine carcinoma, grade 2 neuroendocrine carcinomas
- Well differentiated neuroendocrine tumors G1 to G3 nomenclature is not currently applied in pulmonary carcinoids (Mod Pathol 2018;31:1770)
- ICD-O: 8249/3 - atypical carcinoid tumor
- ICD-10: C7A.090 - malignant carcinoid tumor of the bronchus and lung
- ICD-11: 2C25.4 & XH51K1 - carcinoid or other malignant neuroendocrine neoplasms of bronchus or lung and neuroendocrine tumor, grade 2
- Rare tumors (Arch Pathol Lab Med 2010;134:1628, Ann Oncol 2015;26:1604):
- All pulmonary carcinoids account for less than 2% of all primary lung tumors
- Atypical carcinoids represent only 10% of all lung carcinoids
- Exact incidence reported as around 0.05% (J Thorac Oncol 2015;10:479)
- More frequent (J Thorac Oncol 2015;10:479, Eur J Cardiothorac Surg 2011;39:565, Ann Oncol 2015;26:1604):
- Females (69%)
- Caucasian
- Mean age at diagnosis: 65, 5 - 10 years older than typical carcinoid
- Less likely to be associated to MEN1 syndrome than typical carcinoid (Ann Oncol 2015;26:1604)
- Unrelated to smoking status
- Can be found anywhere from the trachea to the distal bronchioles (Cancer 2008;113:5)
- More likely to be peripherally located than typical carcinoids (J Thorac Oncol 2017;12:425, Eur J Cardiothorac Surg 2011;39:565)
- Unknown
- Can arise in the context of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia and tumorlets (Thorax 2007;62:248)
- Even if a diagnosis of carcinoid tumor can be made with confidence on a biopsy or cytology sample, the definitive diagnosis of atypical carcinoid can only be made on a surgical resection, unless necrosis or increased mitotic activity is seen (Ann Oncol 2015;26:1604)
- Similar to Typical carcinoid
- Standardized uptake value (SUV) is generally higher in atypical carcinoid than in typical carcinoid (Ann Oncol 2015;26:1604)
- 5 year survival: 60% (Arch Pathol Lab Med 2010;134:1628)
- Lymph node metastasis: 50%
- Distant metastasis: 20% (late metastasis can occur up to 10 years following the initial diagnosis)
- Recurrence
- Prognosis related to (Lung Cancer 2020;139:94):
- TNM stage (J Thorac Oncol 2019;14:184)
- More likely to present at a higher stage disease than typical carcinoid (Eur J Cardiothorac Surg 2011;39:565)
- Complete surgical resection: associated with a better prognosis
- Spread through air spaces (STAS): identified as a factor of poor prognosis (J Thorac Oncol 2019;14:1583, Virchows Arch 2019;475:325)
- TNM stage (J Thorac Oncol 2019;14:184)
- 25 year old woman with a postpneumonectomy-like syndrome due to a bronchial atypical carcinoid tumor (BMC Pulm Med 2019;19:44)
- 30 year old woman with a subcutaneous metastasis of a lung atypical carcinoid tumor (Medicine (Baltimore) 2018;97:e9415)
- 45 year old woman with an endobronchial atypical carcinoid tumor with postobstructive mycobacterial infection (BMC Pulm Med 2019;19:41)
- 77 year old woman with a bronchial typical carcinoid lung tumor and diffuse idiopathic neuroendocrine cell hyperplasia in the distal lung (J Thorac Dis 2017;9:E774)
- Complete surgical resection is the most efficient treatment for localized disease and has a significant impact on prognosis (Lung Cancer 2020;139:94, Chest 2017;151:1141, NCCN: NCCN Guidelines - Neuroendocrine and Adrenal Tumors [Accessed 11 November 2020])
- Chemotherapy should be considered for stage IIIA resectable tumors
- Absence of consensus for nonresectable and metastatic tumors; options include combinations of chemotherapy and radiotherapy, octreotide or lanreotide or everolimus
- Recent clinical trial explored the role of a combination of anti-CTLA4 (ipilimumab) and anti-PD1 (nivolumab) for advanced stage atypical tumors with promising results (JAMA Oncol 2020;6:1405)
- Can be similar to typical carcinoids, as they are well circumscribed and round / ovoid tumors but differ in certain points (Cancer 2008;113:5)
- On average, atypical carcinoids are larger
- Cut surface is white-gray or tan like typical carcinoids but can be less homogeneous with pink or yellow-brown or red areas
- Diagnostic criteria:
- Neuroendocrine morphology with 2 - 10 mitoses per 2 mm² or presence of necrosis
- Necrosis can be in large zones but is usually punctate
- Mitotic rate should be counted in the area with the highest proliferation rate (hot spot)
- If mitotic rate is near cutoffs, assessment should be made on three sets of 2 mm² and their mean should count as the final mitotic rate
- Rare tumors with morphologic features of carcinoid and > 10 mitoses per 2 mm² have been reported (Virchows Arch 2017;471:713, Am J Surg Pathol 2017;41:263, Diagn Pathol 2019;14:104)
- According to WHO classification, these tumors should be classified as large cell neuroendocrine carcinomas
- However, recent clinical and molecular data support a relationship with carcinoid for some of those tumors and they are the focus of active research (Clin Cancer Res 2016;22:3618, Mod Pathol 2019;32:1106, Mod Pathol 2020;33:1712, Nat Commun 2019;10:3407)
- Neuroendocrine morphology with 2 - 10 mitoses per 2 mm² or presence of necrosis
- Neuroendocrine histologic patterns similar to typical carcinoids: organoid, trabecular, rosette formation, papillary, pseudoglandular, follicular
- Tumor cells are as typical carcinoid: uniform with a polygonal shape, round to oval nuclei with salt and pepper chromatin and inconspicuous nucleoli, along with moderate to abundant eosinophilic cytoplasm
- Greater pleomorphism than for typical carcinoid is common (Arch Pathol Lab Med 2010;134:1628)
- Spindle cells and clear cell features can be seen
- Stroma is fine and highly vascularized; hyalinization, cartilage or bone formation are possible
Contributed by Philippe Joubert, M.D., Ph.D.
- Cells and architecture similar to typical carcinoid tumors but can differ in several ways (Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 4th edition, 2014)
- Groups of cells tend to be looser, with more isolated cells; rosette structures might be seen
- Population of tumor cells can be less uniform with slight pleomorphism
- Focal necrosis can be seen
- Mitoses can be seen but should be rare
- Even though the diagnosis can be suggested, a thorough examination of the surgical resection remains necessary to classify the tumor
- Chromogranin, synaptophysin, CD56: diffusely and strongly positive; can be negative in a small number of atypical carcinoids (Hum Pathol 2000;31:1255)
- Pancytokeratins: positive but up to 20% can be negative
- TTF1: useful to establish a pulmonary lineage but positive in only 50% of tumors
- Ki67: should not be used as a diagnostic criterion (J Thorac Oncol 2019;14:377)
- Mostly useful to differentiate lung carcinoids from high grade neuroendocrine carcinomas, in particular in small biopsies or cytology samples (Arch Pathol Lab Med 2018;142:947, J Thorac Oncol 2014;9:273)
- Usually 30% cutoff has been proposed (Virchows Arch 2017;470:153, J Thorac Oncol 2014;9:273)
- Reported to be higher than typical carcinoid (2 - 5% versus 9 - 18%) but not proven to be a reliable marker
- Rare tumors with > 10 mitoses per 2 mm² can have a > 30% proliferation rate (Neuroendocrinology 2019;108:109)
- Mostly useful to differentiate lung carcinoids from high grade neuroendocrine carcinomas, in particular in small biopsies or cytology samples (Arch Pathol Lab Med 2018;142:947, J Thorac Oncol 2014;9:273)
- CDX2: useful to differentiate from a metastatic gastrointestinal or pancreatic neuroendocrine tumor (Appl Immunohistochem Mol Morphol 2007;15:407)
- Mutations in the chromatin remodeling genes, including MEN1 and SWI/SNF complex (Transl Lung Cancer Res 2017;6:513)
- RB1 and TP53 are uncommon
- Low number of chromosomal imbalances
- Right lung, superior lobe, transbronchial biopsy:
- Carcinoid tumor, not further classified (see comment)
- Comment: The presence of focal necrosis or increased mitotic activity on this biopsy combined with the classic morphology of a carcinoid tumor favors a diagnosis of atypical carcinoid. However, the definitive diagnosis will be made on the resection specimen.
- A patient undergoes a lobectomy for a well circumscribed nodule. On H&E slide, the tumor exhibits a well differentiated neuroendocrine morphology and you observe the histologic features presented in the image. Which of the following statements is true?
- A Ki67 proliferation rate of > 10% is diagnostic
- It is defined as a well differentiated neuroendocrine tumor with 2 - 10 mitoses per 2 mm² or foci of necrosis
- It is defined as a well differentiated neuroendocrine tumor with 2 - 10 mitoses in 1 high power field or foci of necrosis
- This diagnosis can be made with certainty on small samples (biopsies and cytology)
While Ki67 proliferation rate is frequently > 10% in atypical carcinoids, this feature is not part of the diagnosis (A). C is nearly exact but mitotic count is not made on 1 high power field. Finally, the diagnosis can be suggested on small samples but a thorough examination of a resection specimen is necessary to confirm an atypical carcinoid diagnosis (D).
Comment Here
Reference: Atypical carcinoid
- Regarding pulmonary atypical carcinoids, which of the following statements is true?
- Differentiating them from typical carcinoid is crucial as they have a poorer prognosis and are more likely to metastasize
- Neuroendocrine immunohistochemical markers (chromogranin, synaptophysin and CD56) are systematically positive
- They are less likely to be peripherally located than typical carcinoids
- They frequently harbor ALK-ELM4 fusions
Comment Here
Reference: Atypical carcinoid
- Rare, benign appearing smooth muscle tumor in lung
- Generally thought to represent hematogenous spread from a uterine leiomyoma, given evidence of clonal derivation / similarities in cytogenetic abnormalities (Mod Pathol 2006;19:130, Am J Surg Pathol 2007;31:737)
- Benign smooth muscle tumor in lung
- Arises from hematogenous spread of uterine leiomyoma, usually years following surgical manipulation
- Hormonally responsive
- Multifocal; metastasis from leiomyosarcoma must be ruled out
- Metastasizing leiomyoma
- First described by Steiner in 1939 as metastasizing fibroleiomyoma of the uterus
- Older term was multiple fibroleiomyomatous hamartomas, when thought to originate in lung
- Women of reproductive or postmenopausal age following a procedure for leiomyoma (Am J Med Sci 2009;338:72)
- Median age at diagnosis of 46 years (range: 36 - 62) (Ann Thorac Surg 2016;101:253, Ann Palliat Med 2021;10:5831)
- No ethnic predisposition
- Lung, most common site (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Other reported sites of metastasis include heart, breasts, bone, soft tissue of pelvis, liver, esophagus, lymph nodes, trachea, appendix, central nervous system, skin and scars
- Exact pathophysiology is unclear
- Most accepted hypothesis in the literature is that lesions are clonally derived from uterine leiomyomas (Mod Pathol 2006;19:130, Am J Surg Pathol 2007;31:737)
- Hormonally dependent; there is evidence of disease progression in pregnancy and regression after menopause
- Hematogenous spread (metastasis) from benign uterine leiomyoma, often after surgical manipulation (myomectomy or hysterectomy)
- Asymptomatic; incidentally discovered on imaging
- 30% of patients present with symptoms including chest pain, back pain, cough, dyspnea, hemoptysis, pneumothorax and respiratory failure
- Lesions develop months to years after myomectomy; mean duration between hysterectomy and appearance of lung lesions is 23 years (Clin Chest Med 2016;37:589, Ann Thorac Surg 2016;101:253)
- Clinical history of surgical removal of uterine leiomyomas (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Imaging; computed tomography (CT) scan of the thorax
- Microscopic examination of biopsy / excision of pulmonary lesion
- Chest Xray: multiple bilateral opacities
- CT: multiple bilateral, well circumscribed nodules (Radiol Case Rep 2020;15:2120)
- Lesions may have a cavitary or cystic appearance, radiographically mimicking lymphangiomyomatosis (LAM)
- Lesions can have a miliary pattern (Am J Respir Crit Care Med 2021;203:906)
- PET / CT: nodules have low or no fluorodeoxyglucose (FDG) uptake
- Less commonly present as a solitary nodule (Clin Chest Med 2016;37:589)
- References: Ann Palliat Med 2021;10:5831, Clin Chest Med 2016;37:589
- Prognosis is overall favorable (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Lesions follow an indolent course
- Large tumors may lead to emboli, pulmonary infarction or symptomatic disease
- 26 year old woman with spontaneous regression of miliary pattern after delivery (Am J Respir Crit Care Med 2021;203:906)
- 37 year old woman with pulmonary benign metastasizing leiomyoma, simultaneously diagnosed with uterine leiomyoma before hysteromyomectomy (Transl Cancer Res 2021;10:567)
- 43 year old woman benign metastasizing leiomyoma in multiple organs (J Obstet Gynaecol Res 2019;45:2132)
- 45 year old woman with a benign metastasizing leiomyoma in the heart (Tex Heart Inst J 2021;48:e197066)
- 76 year old woman with pulmonary benign metastasizing leiomyoma presenting as acute respiratory distress (Respirol Case Rep 2017;5:e00216)
- No specific guidelines for management
- Watchful management for asymptomatic patients
- Surgical resection of symptomatic lesions or lesions with interval growth
- Medical hormonal suppression (J Clin Endocrinol Metab 2004;89:3183)
- Oophorectomy for premenopausal women
- Tan-white, well circumscribed, rounded, rubbery to firm, with a whorled cut surface
- Bland spindle cell proliferation, arranged in fascicles
- Well circumscribed, solitary or multiple nodules of smooth muscle, similar to uterine counterparts (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Whorled to intersecting fascicles of ovoid to elongated spindled cells with abundant eosinophilic cytoplasm, oval to cigar or boxcar shaped nuclei, inconspicuous nucleoli
- Large, irregular, thick walled vessels
- May contain cysts or entrapped epithelium
- No atypia, no necrosis, no vascular invasion, no mitotic figures
- Generally acellular or paucicellular on fine needle aspiration
- Nonspecific cytologic findings: clusters of uniform, bland, cohesive spindle cells with no mitoses, no necrosis and no significant atypia
- Spindle cells show basal lamina material, pinocytotic vesicles, intracytoplasmic microfilaments with focal densities
- Genetically distinct entity with consistent chromosomal aberrations (19q and 22q terminal deletion in all cases) (Am J Surg Pathol 2007;31:737)
- Similar genetic findings when comparing benign metastasizing leiomyoma and uterine leiomyoma (Mod Pathol 2006;19:130, Hum Pathol 2000;31:126, Int J Gynecol Pathol 2008;27:340, Cancer Genet 2012;205:249, Diagn Mol Pathol 2008;17:145)
Benign metastasizing leiomyoma
- Lung, left upper lobe, mass, wedge resection:
- Low grade spindle cell neoplasm, consistent with benign metastasizing leiomyoma (see comment)
- Comment: Patient’s history of uterine leiomyoma is noted. Immunohistochemical studies were performed with adequate controls on block (A1). The tumor cells are positive for SMA, actin, desmin, ER and PR. The tumor cells are negative for pankeratin, TTF1, HMB45, STAT6 and chromogranin. The morphology and immunohistochemical profile supports the above diagnosis.
- Metastatic low grade leiomyosarcoma (Diagn Mol Pathol 2008;17:145):
- Atypia, nuclear pleomorphism, necrosis, high mitotic activity favor malignancy
- miRNA expression differentiates leiomyosarcoma from benign metastasizing leiomyoma
- Solitary fibrous tumor:
- Schwannoma:
- S100 positive
A 45 year old woman presents with multiple incidentally discovered, well circumscribed, bilateral lung nodules on CT scan. She is asymptomatic and her history is only notable for a myomectomy, 10 years ago. A biopsy of one of the nodules is performed (see figure above). On immunohistochemical staining, the lesion is negative for STAT6 and the Ki67 proliferative index is low. What is the most likely diagnosis?
- Benign metastasizing leiomyoma
- Leiomyosarcoma
- Pulmonary hamartoma
- Solitary fibrous tumor
A 45 year old woman presents with multiple incidentally discovered, well circumscribed, bilateral lung nodules on CT scan. She is asymptomatic and her history is only notable for a myomectomy 10 years ago. A biopsy of one of the nodules is performed (see figure above). On immunohistochemical staining, the lesion is negative for STAT6 and the Ki67 proliferative index is low. Based on this specific clinical presentation, what is the best choice for treatment?
- Chemotherapy
- Follow up imaging
- Hormonal therapy
- Surgical resection
- Precise histologic classification of lung cancer is essential due to advances in tailored therapies for specific subtypes
- Biopsy is the initial step for the classification of advanced or metastatic disease and for obtaining tissue for molecular / biomarker testing
- Obtaining multiple biopsy specimens to allow for both IHC and molecular / biomarker testing is optimal
- Diagnosis in small biopsies utilizes morphologic features and judicial immunohistochemical / special stain evaluation in cases with ambiguous morphologies
- Biopsy materials should be preserved as much as possible for molecular / biomarker testing
- Diagnostic terminology can differ between small biopsies and resection specimens
- Up to 90% of lung cancers are directly attributable to smoking (Transl Lung Cancer Res 2018;7:220)
- 10 - 15% of lung cancers occur in never smokers (Transl Lung Cancer Res 2018;7:220)
- These are often associated with driver mutations (such as EGFR mutations and ALK fusions)
- Majority of cases present with advanced stage where diagnosis is often limited to small biopsies (CA Cancer J Clin 2018;68:7)
- Biopsies may be obtained from either primary or metastatic sites
| Morphology / stains | Terminology for small biopsies and cytology specimens | Terminology for resection specimens |
| Morphologic squamous cell patterns clearly present | Squamous cell carcinoma | Squamous cell carcinoma |
| Morphologic adenocarcinoma patterns clearly present | Adenocarcinoma (list patterns in the diagnosis) | Adenocarcinoma predominant patterns: Lepidic Acinar Papillary Solid Micropapillary |
| Adenocarcinoma with lepidic pattern (if pure, list the differential diagnosis on the right and add a comment that an invasive component cannot be excluded) | Minimally invasive adenocarcinoma, adenocarcinoma in situ or an invasive adenocarcinoma with a lepidic component | |
| Invasive mucinous adenocarcinoma (list the patterns; use the term mucinous adenocarcinoma with lepidic pattern if pure lepidic pattern and mention the differential diagnosis listed on the right) | Invasive mucinous adenocarcinoma, minimally invasive adenocarcinoma or adenocarcinoma in situ, mucinous type | |
| Adenocarcinoma with colloid features | Colloid adenocarcinoma | |
| Adenocarcinoma with fetal features | Fetal adenocarcinoma | |
| Adenocarcinoma with enteric features a | Enteric adenocarcinoma | |
| Morphologic squamous cell patterns not present but supported by stains (i.e., p40+) | Non-small cell carcinoma, favor squamous cell carcinoma b | Squamous cell carcinoma (nonkeratinizing pattern may be a component of the tumor) |
| Morphologic adenocarcinoma patterns not present but supported by special stains (i.e., TTF1+) | Non-small cell carcinoma, favor adenocarcinoma b | Adenocarcinoma (solid pattern may just be one component of the tumor) |
| No clear adenocarcinoma, squamous or neuroendocrine morphology or staining pattern | Non-small cell carcinoma, NOS c | Large cell carcinoma |
- Metastatic carcinomas should be carefully excluded with clinical and appropriate but judicious immunohistochemical examination
- Categories do not always correspond to solid predominant adenocarcinoma or nonkeratinizing squamous cell carcinoma, respectively; poorly differentiated components in adenocarcinoma or squamous cell carcinoma may be sampled
- Non-small cell carcinoma, NOS pattern can be seen not only in large cell carcinomas but also when the solid, poorly differentiated component of adenocarcinomas or squamous cell carcinomas is sampled but does not express immunohistochemical markers or mucin
Terminology for small biopsies and cytology versus resection specimens for small cell carcinoma, large cell neuroendocrine carcinoma, adenosquamous carcinoma and pleomorphic carcinoma (adapted from Table 4, J Thorac Oncol 2022;17:362)
| Terminology for small biopsies and cytology specimens | Terminology for resection specimens |
| Small cell carcinoma | Small cell carcinoma |
| Non-small cell carcinoma with neuroendocrine morphology and positive neuroendocrine markers, possible large cell neuroendocrine carcinoma | Large cell neuroendocrine carcinoma |
| Morphologic squamous cell and adenocarcinoma patterns both present: non-small cell carcinoma, NOS
(Comment that adenocarcinoma and squamous components are present and that this could represent adenosquamous carcinoma) | Adenosquamous carcinoma (if both components ≥ 10%) |
| Morphologic squamous cell or adenocarcinoma patterns not present but immunohistochemical stains favor separate squamous and adenocarcinoma components: non-small cell carcinoma, NOS
(Specify the results of the immunohistochemical stains and the interpretation and comment that this could represent adenosquamous carcinoma but that diagnosis requires a resection specimen) | Adenocarcinoma, squamous cell carcinoma, adenosquamous carcinoma or large cell carcinoma with unclear immunohistochemical features |
| Non-small cell carcinoma with spindle cell or giant cell carcinoma (Mention if adenocarcinoma or squamous carcinoma is present and comment that this could represent a pleomorphic carcinoma; however, that diagnosis requires a resection specimen) | Pleomorphic, spindle cell or giant cell carcinoma |
Guidelines for good practice of small biopsies and cytologic preparations (adapted / reprinted from J Thorac Oncol 2022;17:362):
- For small biopsies and cytology, NSCC should be further classified into a more specific type, such as ADC or SQCC
- The term non-small cell lung carcinoma, NOS (NSCLC, NOS) should be used as little as possible
- When a diagnosis is made in a small biopsy or cytology specimen in conjunction with special studies, it should be clarified whether the diagnosis was established on the basis of light microscopy alone or if special stains were required
- The term nonsquamous cell carcinoma (non-SQCC) should not be used by pathologists
- Terminology in above tables should be used in routine diagnosis, future research and clinical trials, in order to ensure a uniform classification of disease cohorts in relation to tumor subtypes
- When paired cytology and biopsy specimens exist, they should be reviewed together to achieve the most specific and concordant diagnosis
- The terms AIS and minimally invasive ADC should not be used for diagnosis of small biopsies or cytology specimens (a noninvasive pattern is present in a small biopsy should be referred to as a lepidic growth pattern)
- The term large cell carcinoma should not be used for diagnosis in small biopsy or cytology specimens and should be restricted to resection specimens where the tumor is thoroughly sampled to exclude a differentiated component
- Tumors exhibiting sarcomatoid features (marked nuclear pleomorphism, malignant giant cells or spindle cell morphology) should be classified as specifically as possible (i.e., ADC; NSCC, favor ADC; SQCC; or NSCC favor SQCC) with an additional statement that giant or spindle cell features are present (note: if diagnosis specific features are not present, the term NSCC, NOS should be used, again with comment on the sarcomatoid features)
- Neuroendocrine immunohistochemical markers should be performed only in cases where there is suspected neuroendocrine morphology
(Abbreviations: ADC, adenocarcinoma; AIS, adenocarcinoma in situ; NOS, not otherwise specified; NSCC, non-small cell carcinoma; SQCC, squamous cell carcinoma)
- Identification of targetable mutations has led to overall decrease in NSCLC mortality disproportionate to the decrease in incidence (N Engl J Med 2020;383:640)
- PDL1 evaluation recommended for all nonneuroendocrine carcinomas (J Thorac Oncol 2022;17:362)
- Adenocarcinoma: gland formation, mucin production and variety of architectural patterns
- Squamous cell carcinoma: intracellular bridges, keratinization
- Adenosquamous carcinoma: mixed adenocarcinomatous and squamous differentiation or solid proliferation without obvious differentiation but with immunophenotypic evidence of both squamous and glandular differentiation; can only be diagnosed on resection specimens
- Non-small cell carcinoma: carcinoma without obvious glandular or squamous differentiation further characterized by immunostaining
- Neuroendocrine tumors: salt and pepper chromatin, organoid / trabecular / nested growth
- Small cell carcinoma: fine chromatin, nuclear molding, marked mitotic activity, necrosis
- Adenocarcinoma: TTF1, napsin A, mucicarmine
- Squamous cell carcinoma: p40, CK5/6, p63 (less specific)
- Neuroendocrine tumors: keratins, TTF1 (~50% depending on location), synaptophysin, chromogranin, CD56
- Small cell carcinoma: pancytokeratin, TTF1 (~80%), neuroendocrine markers may be absent, Ki67 useful in crushed / distorted biopsies
- CAP / IASLC / AMP guidelines for molecular testing of lung cancer (Arch Pathol Lab Med 2018;142:321):
- EGFR, ALK and ROS1 are “must test” genes
- BRAF, MET, ERBB2 (HER2) and RET are recommended for patients suitable for clinical trials
- KRAS sequencing may be helpful to exclude KRAS mutant patients from extended panel testing
- While these recommendations are primarily regarding pulmonary adenocarcinoma, physicians may utilize molecular testing in nonadenocarcinomatous tumors when there are clinical features that may indicate the presence of an oncogenic driver
- Right lung, upper lobe, transbronchial biopsies:
- Non-small cell carcinoma, favor adenocarcinoma (see comment)
- Comment: The tumor cells lack morphologic evidence of squamous or glandular differentiation. Immunohistochemical studies performed with appropriate controls reveal the tumor cells are positive for TTF1 and negative for p40. The results support the rendered diagnosis and favor adenocarcinoma of lung origin.
- Non-small cell carcinoma, favor adenocarcinoma
- Non-small cell carcinoma, favor squamous cell carcinoma
- Non-small cell carcinoma, not otherwise specified
- Squamous cell carcinoma
- Squamous cell carcinoma, nonkeratinizing
Comment Here
Reference: Lung - Biopsies
- Adenocarcinoma, solid pattern
- Non-small cell carcinoma, favor adenocarcinoma
- Non-small cell carcinoma, favor large cell carcinoma
- Non-small cell carcinoma, not otherwise specified
- Squamous cell carcinoma, nonkeratinizing
Comment Here
Reference: Lung - Biopsies
A 75 year old man with a 100 pack year smoking history presents with hemoptysis and is found to have a hilar mass and lymphadenopathy. Biopsy of one of the lymph nodes reveals the proliferation seen in the above images. Mitotic activity is approximately 35 mitoses per 2 mm2 and necrosis is present. Immunophenotyping is attempted; however, the block was inadvertently exhausted and stains are not available. What is the best diagnosis that can be rendered?
- Atypical carcinoid tumor
- Carcinoid tumor, not otherwise specified
- Epithelial neoplasm, not further classifiable
- No diagnosis can be rendered, rebiopsy is needed
- Small cell carcinoma
Comment Here
Reference: Lung - Biopsies
- Portion of bronchial tree with normal branching pattern, but without any demonstrable connection to the central bronchial tree
- Congenital abnormality due to focal interruption of lobar, segmental or subsegmental bronchus with associated peripheral mucus impaction (bronchocele, mucocele) and hyperinflation of obstructed lung segment; most commonly affects apicoposterior segmental bronchus of left upper lobe, then segmental bronchi of right upper, middle and lower lobes
- Cause unknown, but appears to occur before birth
- Lobar bronchial atresia can mimic mainstem bronchial atresia on mid trimester ultrasound (Ultrasound Obstet Gynecol 2011;37:110)
- 22 year old woman with pneumothorax and bronchial atresia (Radiographics 2009;29:1531)
- Permanent dilation of bronchi and bronchioles caused by the destruction of mucosal and elastic tissues; often caused by or associated with chronic necrotizing infection of bronchi and bronchioles
- Gross pathology shows markedly distended peripheral bronchi, often with mucoid impaction and possible mucosal ulcerations
- Histology shows a range of findings in the acute setting that include luminal dilation, mucostasis, acute inflammation and inflammatory debris
- Usual respiratory type epithelium may be ulcerated and replaced by granulation tissue or squamous metaplasia
- Chronic inflammation may be variably dense and include prominent lymphoid follicles and granulomas
- Chronic findings include loss of smooth muscle, cartilage and elastic fibers with replacement fibrosis
- Can mimic squamous cell carcinoma on frozen section; on histology, need to distinguish from other lung diseases, such as chronic obstructive pulmonary disease (COPD), emphysema, cystic fibrosis and asthma
- About 350,000 to 500,000 adults in the United States have bronchiectasis (Chron Respir Dis 2017:14:377)
- Increased risk of noncystic fibrosis bronchiectasis with extremes of ages (< 5 years, adults > 75 years)
- Associated with underserved populations
- Increased incidence of childhood bronchiectasis in Maori, Pacific Islanders of New Zealand, Australian aboriginal and Alaskan native children (Expert Rev Respir Med 2017;11:517)
- Bronchi walls in lungs
- Obstruction (i.e., due to tumor, foreign body, inspissated mucus) (Int J Chron Obstruct Pulmon Dis 2009;4:411)
- Causes resorption of air distal to the obstruction
- Causes atelectasis and accumulation of intraluminal secretions
- Nonobstructive bronchiectasis (i.e., due to pneumonia and atelectasis) (Int J Chron Obstruct Pulmon Dis 2009;4:411)
- Increased negative intrapleural pressure creates a force on bronchial walls, leading to dilation
- Infectious bronchiectasis (N Engl J Med 2002;346:1383)
- Enhanced cellular and mediator responses lead to destruction of tissue
- Biopsies have shown infiltration by neutrophils and T lymphocytes
- Chemoattractants have been detected (IL8, TNFα, prostanoids)
- Idiopathic (Paediatr Respir Rev 2011;12:104)
- Congenital
- Cystic fibrosis: most common cause in children
- Primary ciliary dyskinesia and other mucociliary disorders
- Immune deficiencies (hypogammaglobulinemia, MHC1 deficiency, TAP1 deficiency, IFNγ receptor deficiency)
- Alpha-1 antitrypsin deficiency
- Williams-Campbell syndrome
- Infection
- Mycobacterial infection: most common cause globally
- Viral infection
- Allergic bronchopulmonary aspergillosis
- Postinfection sequelae (pneumonia, measles, whooping cough): most common, known noncystic fibrosis cause in adults
- Autoimmune
- Rheumatoid arthritis
- Other causes
- Chronic obstructive pulmonary disease / smoking
- Aspiration
- Extremes of age
- Immune dysfunction: HIV
- Foreign body / obstruction (i.e., tumor)
- Malnutrition
- Cough and chronic sputum production (Thorax 2019;74:1)
- Sputum is typically mucoid to mucopurulent, thick
- Can be bloody due to erosive airway damage
- Dyspnea and wheezing
- Pleuritic chest pain
- Physical exam (Thorax 2019;74:1)
- Abnormal breath sounds: crackles, wheezing, rhonchi
- Digital clubbing
- CT scan to differentiate between bronchiectasis and COPD (can overlap)
- CBC with differential
- Elevated blood platelets (> 400 x 109/L in stable state) are associated with increased mortality (Ann Am Thorac Soc 2021;18:1316)
- Depends on cause of bronchiectasis
- If infectious: sputum culture positive for infectious etiology
- If congenital: positive sweat chloride test, positive for genetic mutations, etc.
- Immunoglobulin quantitation
- Xray (Radiopaedia: Bronchiectasis [Accessed 25 August 2022]):
- Tram track opacities
- Air fluid levels
- Increase in bronchovascular markings
- CT:
- Tram track sign: thickened nontapering bronchial walls
- Signet ring sign: dilated bronchus with pulmonary artery branch seen in cross section looks like a signet ring; bronchus and artery should be the same size
- String of pearls sign
- Bunch of grapes sign: closely apposed dilated bronchi appear to look like a bunch of grapes
- Bronchus visualized within 1 cm of pleural surface
- Lack of tapering
- Increased bronchoarterial ratio
- Bronchial wall thickening
- Mucoid impaction, air trapping
- Bronchiectasis severity index
- Endorsed by the Thoracic Society of Australia and New Zealand
- Uses clinical, radiological and microbiological features to predict morbidity and mortality in noncystic fibrosis bronchiectasis
- Point system on a scale from 0 - 9
- 0 - 4: mild bronchiectasis
- 5 - 8: moderate bronchiectasis
- 9+: severe bronchiectasis
- Calculator: University of Dundee: Bronchiectasis Prediction Tools [Accessed 25 August 2022]
- FACED score (Open Respir Med J 2015;9:46)
- Uses a 0 - 7 point scale to determine the severity of bronchiectasis in noncystic fibrosis patients
- FACED stands for different metrics
- F: forced expiratory volume in 1 second (FEV1) (≥ 50% = 0 points, < 50% = 2 points)
- A: age (< 70 years = 0 points, ≥ 70 years = 2 points)
- C: chronic colonization (no Pseudomonas = 0 points, presence of Pseudomonas = 1 point)
- E: extension (1 - 2 lobes affected = 0 points, > 2 lobes affected= 1 point)
- D: dyspnea; modified Medical Research Council scale (mMRC) (0 - 2 = 0 points, 3 - 4 = 1 point)
- 42 year old man, a gardener with recurrent respiratory infections (Hosp Pract (Off Ed) 1985;20:97)
- 49 year old man who developed bronchiectasis after bronchial thermoplasty (J Thorac Dis 2018;10:E721)
- 52 year old man who developed COVID-19 associated bronchiectasis (Cureus 2021;13:e15051)
- Nonpharmacologic therapies (UpToDate: Bronchiectasis in Adults [Accessed 25 August 2022]):
- Avoid lung irritant
- Physiotherapy to clear airways
- Mucolytics
- Airway hydration
- Pulmonary rehabilitation for severe cases
- Antibiotics to prevent exacerbations:
- Macrolides: especially for Pseudomonas aeruginosa
- Other pharmacologic treatments:
- Bronchodilators
- NSAIDs
- Glucocorticoids
- Markedly distended peripheral bronchi, usually in lower lobes; can be traced up to pleura (Zander: Pulmonary Pathology, 2nd Edition, 2017)
- Variety of shapes present: saccular, cystic, cylindrical
- Ulcerations of mucosal surfaces
- Irregularly thickened bronchial walls
- Honeycomb appearance on cut surface
- Can have thick mucoid or mucopurulent secretions present in the bronchi
- Can be challenging on frozen section to distinguish from carcinoma (Int J Clin Exp Pathol 2015;8:7961)
- Bronchial epithelial shedding
- Epithelial squamous metaplasia: can be confused for carcinoma in situ
- Bronchial mural destruction
- Inflammatory cells along airways (Zander: Pulmonary Pathology, 2nd Edition, 2017)
- Prominent chronic inflammation with lymphoid follicles and germinal centers
- Varying degrees of neutrophilic inflammation
- Can have eosinophils depending on the cause or if the patient has superimposed diseases
- Epithelial ulceration
- Over time
- Loss of smooth muscle, elastic fibers, cartilage
- Replacement fibrosis
- Coexisting findings
- Organizing pneumonia
- Pulmonary hypertension
- Seen in bronchial brushings and washings (Diagn Cytopathol 2008;36:13)
- Mixed inflammation
- Cellular debris
- Mucus
- Reactive bronchial cells
- Squamous metaplasia
Histopathology: lung bronchiectasis
- Bilateral lungs, explant:
- Severe acute and chronic bronchiolitis with patchy fibrosis, consistent with bronchiectasis. Acute bronchopneumonia involving the left lower lobe.
- Bilateral lungs, explant:
- Bronchiectasis with severe and necrotizing acute and chronic bronchitis and bronchiolitis consistent with cystic fibrosis.
- Many things can mimic or be superimposed with bronchiectasis but key findings can differentiate other diseases from it
- Bronchitis:
- Increased goblet cells, thickened bronchial walls
- Asthma:
- More eosinophils, goblet cell hyperplasia and metaplasia, Charcot-Leyden crystals, smooth muscle hypertrophy
- Aspiration pneumonia:
- More neutrophils, abscesses, vegetable matter
- Tuberculosis:
- Necrotizing granulomas
- Emphysema:
- Gross findings with bullae
- Alveolar wall destruction versus bronchiole destruction
- Lymphoid malignancies:
- Monotonous lymphoid populations with abnormal germinal centers
- Bronchitis:
Comment Here
Reference: Bronchiectasis
Comment Here
Reference: Bronchiectasis
- Granulomatous disease of lungs in which almost all granulomas are centered in bronchi or bronchioles causing their destruction
- Immunologic reaction related to chronic eosinophilic pneumonia and allergic bronchopulmonary aspergillosis
- A histologic pattern of disease, not a specific diagnosis
- Usually adults, often with asthma history and limited to lungs, may be asymptomatic
- Usually solitary lesions that appear on chest Xray as atelectasis or consolidation, not nodules
- Generally favorable prognosis
- Viscous material in involved bronchi
- Large and medium bronchi infiltrated by neutrophils, eosinophils and necrotic debris surrounded by foreign body giant cells
- Fragmented elastic tissue (with elastic stain)
- Also bronchiolitis obliterans
- No fibrinoid necrosis of vessels
- Granulomatosis with polyangiitis (Wegener's): kidney involvement, may also have bronchocentric granulomas
- Rheumatoid arthritis
- Tuberculosis
- Fungi: can identify orgqanisms with silver stain
- Cystic fibrosis: different clinical history
- Complication of mechanical ventilation and oxygen therapy for treatment of neonatal respiratory distress syndrome
- Infants almost always < 1200 gram birth weight and < 30 weeks gestation
- Definition: requirement for supplemental oxygen for longer than 28 days of age, and a postmenstrual age of at least 36 weeks (eMedicine)
- Due to decreased alveolar septation and capillary derangement, secondary to arrested septation of lungs, due to therapy in the saccular stage of lung development
- Free radicals generated by oxygen therapy and inflammatory cytokines play a role in pathogenesis
- Incidence has fallen with use of surfactant therapy in premature infants for neonatal respiratory distress syndrome (Semin Perinatol 2006;30:171)
- Respiratory distress continues for months
- Patients have limited pulmonary reserve, develop repeated infections, often have pulmonary hypertension and develop cor pulmonale
- Bronchiolar and interstitial fibrosis, compensatory emphysema of less damaged acini
- Inadequate alveolar development causes fewer but larger alveoli
- Tumor of neuroendocrine differentiation, defined by size < 5 mm in diameter, mitotic count < 2 mitoses/2 mm² and absence of necrosis
- Can be found incidentally in lung resections but can arise in the context of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH)
- Defined as a proliferation of neuroendocrine cells < 5 mm in diameter that extend through the bronchial basement membrane with < 2 mitoses/2 mm² and no necrosis
- Progression to typical carcinoid tumors is possible
- Typically affects middle aged women (Ann Oncol 2010;21:vii65, Chest 2007;131:1635):
- Frequent incidental finding in lung resection specimens or can be found in the context of DIPNECH
- Real incidence and prevalence unknown:
- Often missed on imaging and can be easily overlooked during grossing because of their small size (J Thorac Oncol 2009;4:383, Med Sci Monit 2020;26:e926014)
- Can be found in lung specimens resected for typical (8%) or atypical (4.3%) carcinoids (J Thorac Oncol 2009;4:383)
- Can be found in patients with multiple endocrine neoplasia type 1 (MEN1) (Neuroendocrinology 2016;103:240)
- Tumorlets are located in the same region as inflammatory or fibrous lung disease (AJR Am J Roentgenol 2004;183:293)
- When arising in the context of DIPNECH, they are typically located in the terminal bronchioles
- Not well described
- Incidental finding in lung resection specimens, accompanying inflammatory or fibrous conditions (J Thorac Dis 2012;4:655, Med Sci Monit 2020;26:e926014, Int J Surg Pathol 2018;26:660, Respirol Case Rep 2018;6:e00373t)
- Presence of multiple carcinoids more likely to be part of DIPNECH
- It is believed that some tumorlets may progress into carcinoid tumors, mostly typical carcinoids (AJR Am J Roentgenol 2010;195:661)
- Unknown
- Frequently asymptomatic, as it can be an incidental finding (AJR Am J Roentgenol 2010;195:661)
- Clinical features of DIPNECH can be seen in patients with tumorlets arising in this context
- See DIPNECH for details on diagnosis for tumorlets arising in this setting
- CT scan: can present as a bronchial wall thickening that can appear nodular or show multiple peribronchiolar spherical to ovoid solid or ground glass nodules (Clin Radiol 2015;70:317)
- Images are similar to the ones for DIPNECH when arising in this context
- When tumorlets arise in a context of chronic pulmonary lung disease, they can be subtle and masked by the underlying process (Med Sci Monit 2020;26:e926014)
- Most tumorlets are benign incidental findings for which surgical resection is curative and prognosis is excellent (Chest 2007;131:1635)
- See DIPNECH for details on prognosis of tumorlets arising in this setting
- 18 year old man with multiple sclerosing pneumocytomas and carcinoid tumorlets (J Endocr Soc 2019;3:937)
- 73 year old woman with pulmonary hypoplasia and carcinoid tumorlets (Respirol Case Rep 2018;6:e00373t)
- 73 year old woman with a lung fungus and a carcinoid tumorlet (Intern Med 2018;57:3485)
- See DIPNECH for details on tumorlets arising in this setting
- Difficult to identify but when visible, they are seen as small gray-white nodules < 5 mm in diameter, intimately associated with bronchioles
- Poorly defined nodule of neuroendocrine cells that cross the mucosal basal membrane in a fibrotic stroma:
- Size < 5 mm with < 2 mitoses/2 mm² and absence of necrosis
- Usually found in association with an airway
- Composed of neuroendocrine cells that are oval to round or spindle shaped; cells have round to oval nuclei with salt and pepper chromatin and a moderate amount of eosinophilic cytoplasm
- Complete features of DIPNECH or an underlying lung disease can be seen
- Neuroendocrine markers: chromogranin A, synaptophysin, CD56, INSM1 (Chest 2007;131:1635, Histopathology 2018;72:1067)
- TTF1: 70% of cases (Chest 2007;131:1635)
- To date, molecular alterations of tumorlets are poorly described
- See DIPNECH for an example of a report when tumorlets arise in this setting
- Minute pulmonary meningothelial-like nodules:
- Randomly distributed nodules in the lung that are positive for EMA and CD56, negative for other neuroendocrine markers (chromogranin, synaptophysin and INSM1) and pankeratin (Histopathology 2018;72:1067, Am J Surg Pathol 2009;33:487)
- Typical carcinoid:
- Tumor size ≥ 5 mm with < 2 mitoses/2 mm² and absence of necrosis
- Atypical carcinoid:
- > 2 mitoses/2 mm² or presence of necrosis
Regarding the lung nodule (tumor size < 5 mm without necrosis and mitoses) presented in the image, which of the following is true?
- EMA and CD56 stains are positive
- Many of them have EGFR mutations
- Their prognosis is poor
- They can be seen in the context of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH)
Comment Here
Reference: Carcinoid tumorlet
- More than 2 mitoses/2 mm² can be seen
- Rare tumorlets of more than 1 cm have been reported
- They are confined to bronchial mucosa, without crossing the bronchial basal membrane
- They are frequently found in association with an airway
Comment Here
Reference: Carcinoid tumorlet
- Subtype of sarcomatoid carcinoma, consisting of a mixture of nonsmall cell lung cancer (typically squamous cell carcinoma or adenocarcinoma) and sarcomatous heterologous elements
- Monoclonal tumor with divergent lines of differentiation, leading to mixture of carcinomatous and sarcomatous elements (Am J Surg Pathol 2002;26:510)
- Biphasic tumor consisting of a nonsmall cell carcinoma with heterologous sarcomatoid differentiation
- Rare tumor with poor prognosis
- Recommend molecular testing according to associated histologic components; i.e. tumors with adenocarcinoma component should be tested for EGFR and ALK (J Thorac Oncol 2015;10:1243)
- Use specific term "carcinosarcoma" rather than general term "sarcomatoid carcinoma" whenever possible to avoid confusion (J Thorac Oncol 2015;10:1243)
- "Biphasic sarcomatoid carcinoma" has been proposed as replacement term
- Use code specific for location of tumor
- C34.90 malignant neoplasm of unspecified part of unspecified bronchus or lung
- Rare, 0.1% of all lung cancers
- M > F, most with smoking history, average age 60
- Large airways and peripheral lung
- Primary lung carcinoma undergoes sarcomatoid change
- Epithelial malignancy with divergent differentiation
- Dependent on location: endobronchial lesions have pneumonia, cough, shortness of breath, hemoptysis; peripheral lesions may have no symptoms
- Difficult to diagnose on small biopsy / cytology but possible
- Poor prognosis overall; increased tumor size appears related to reduced survival (Am J Surg Pathol 1999;23:1514)
- Better prognosis for smaller or endobronchial lesions
- 49 year old woman with a SBO secondary to small bowel metastases (Acta Chir Belg 2015;115:49)
- 50 year old woman with a 45 pack year smoking history (Surg Case Rep 2017;3:52)
- 50 year old man with complaint of pain in back radiating to right lower limb and chest pain for 3 months (J Cytol 2015r;32:28)
- 64 year old man with a seven-month history of shortness of breath (Contemp Oncol (Pozn) 2015;19:163)
- 65 year old man with bronchial carcinosarcoma (J Radiol Case Rep 2012;6:26)
- 65 year old man with tumor including chest wall invasion (Int J Clin Oncol 2010;15:319)
- 75 year old woman with diabetes, hypertension, chronic kidney disease, and coronary disease (Ochsner J 2015;15:196)
- 77 year old man with pulmonary carcinosarcoma and idiopathic pulmonary fibrosis (Lung 2016;194:171)
- 83 year old woman with glandular and lipoblastic carcinosarcoma (Case Rep Pulmonol 2016;2016:2020146)
- Cytology case report (Diagn Cytopathol 1988;4:239)
- Surgical resection in majority of cases (Surg Today 2014;44:175), followed by radiation
- Chemotherapy for cases with metastases
- Tumors with EGFR mutation can be considered for targeted therapy (Oncotarget 2017;8:25323)
- May show central necrosis and hemorrhage if larger tumor
- Irregular borders, tan to yellow
- Mixture of carcinomatous and sarcomatous elements
- Carcinoma component usually squamous but may be glandular or neuroendocrine
- Heterologous sarcomatoid component, such as rhabdomyosarcoma, osteosarcoma, chondrosarcoma
- Metastases may show carcinomatous or sarcomatous component or both
Contributed by Yale Rosen, M.D. and Jian-Hua Qiao, M.D.
Images hosted on other servers:
- May only show epithelial component, i.e. squamous cell carcinoma
- Dependent on specific components of tumor
- Dependent on specific components of tumor
- TP53 mutations often seen, Kras less frequent, EGFR mutations very uncommon (J Thorac Oncol 2015;10:1243)
- Equivalent allelic loss between the two components, supporting monoclonal origin (Am J Surg Pathol 2002;26:510)
- Other subtypes of sarcomatoid carcinoma
- Sarcomatoid mesothelioma
- True sarcomas, such as synovial sarcoma
- Other types of sarcomatoid carcinoma such as pulmonary blastoma (younger ages)
- Review of 6 patients with pulmonary carcinosarcoma (ScientificWorldJournal 2012;2012:167317)
- Adenocarcinoma
- Adenosquamous carcinoma
- Large cell carcinoma
- Small cell carcinoma
- Squamous cell carcinoma
- Diagnosis: persistent cough with sputum for 3 months in 2 consecutive years without other apparent explanation (eMedicine)
- Chronic disease of large airways, variable inflammation
- Simple chronic bronchitis: cough but no physiologic evidence of airway obstruction
- Chronic asthmatic bronchitis: hyperreactive airways with intermittent bronchospasm and wheezing
- Obstructive bronchitis: often have associated emphysema, small airway disease
- Causes: 4× - 10× more common in smokers, chronic irritation and infections may contribute
- Other causes and contributors are air pollution including passive cigarette smoke, marijuana smoke and occupational dust exposure
- Tobacco interferes with ciliary action, directly damages airway epithelium and inhibits ability of white blood cells to clear bacteria; infections maintain but do not initiate chronic bronchitis
- Often diagnosed at time of acute respiratory illness (Prim Care Respir J 2010;19:371)
- More infections, purulent sputum, hypercapnia, hypoxia than emphysema; clinically called "blue bloaters"
- May cause secondary pulmonary vascular hypertension, cor pulmonale, congestive heart failure, death due to respiratory acidosis and coma, congestive heart failure and pneumothorax
- Reid index: ratio of thickness of mucus gland layer to thickness of wall between epithelium and cartilage; normal is 0.4, increased in chronic bronchitis
- Boggy mucosa with excessive mucinous secretions, pus, prominence of bronchial mucosal pits overlying the orifices of bronchial mucous glands
- Early: hypersecretion of mucus in large airways with hypertrophy of submucosal glands in tracheobronchial tree
- Later: increase in goblet cells in small airways contributes to excessive mucus production and airway obstruction
- Increased percentage of bronchial wall is occupied by submucosal mucous glands, as measured by Reid index; this directly correlates with sputum production, variable dysplasia, squamous metaplasia, bronchiolitis obliterans
- Chronic inflammatory infiltrates range from absent to prominent
- Lung injury caused by infection by CMV, a β herpes virus
- Usually immunocompromised patients
- Often associated with pneumocystis and other infections
- Xray: 2 - 4 cm peripheral nodules, miliary pattern, diffuse interstitial process
- 70% of Americans in large cities have latent infection
- In immunocompetent individuals, primary infection is generally asymptomatic, but mononucleosis-like illness may occur; rarely, self limiting CMV pneumonia may occur during mononucleosis-like illness (eMedicine)
- In organ transplant recipients, infection may occur when the donor organ is latently infected with CMV
- When infection occurs in immunosuppressed patients, the risk of organ damage is higher the greater the immunosuppression
- In AIDS patients, CMV disease generally occurs when the CD4+ cell count < 50/mm3
- CMV is the most common life threatening infection in hematopoietic stem cell transplant recipients and is the most common opportunistic viral infection in AIDS
- Prophylactic therapy and preemptive therapy, where CMV DNA levels are monitored by PCR and antiviral therapy against CMV is given prior to end organ damage, has greatly reduced the incidence of CMV induced disease in vulnerable patients
- Highly active antiretrovirus therapy has reduced the incidence of end organ damage by 80% in HIV positive patients
- In addition to lung, CMV causes severe disease in retina, brain, kidneys, GI
- Disease may occur with primary infection or secondarily when latent disease is reactivated
- Virus can be spread transplacentally; neonatal disease can occur through exposure to cervical or vaginal secretions or from breast milk when active infection is present
- In children and adults, infection is spread through saliva, respiratory droplets or sexual activity
- Fecal oral transmission has also been documented
- CMV causes down regulation of expression of MHC class I and II molecules, which helps it elude host immune responses
- In immunocompetent patients, cough with interstitial infiltrates on chest xray
- Immunosuppressed patients present with cough, fever, fatigue, shortness of breath, malaise, night sweats, muscle and joint pain
- Note: positive culture, serology or PCR may not represent evidence of illness
- Diagnosis is based on identification of viral inclusions in biopsy material
- Acute CMV infection leads to transient but severe immunosupression
- Prevention is key as CMV pneumonia has high mortality rate even with aggressive antiviral therapy
- Ganciclovir, valganciclovir, foscarnet, cidofovir, maribavir
- Lung is firm (similar to interstitial lung disease) with hemorrhagic nodules that may become confluent
- Mononuclear infiltrates, usually mild edema and pneumocyte hyperplasia
- Infected cells are generally large with a prominent basophilic nuclear inclusion, often with a clear halo, and smaller basophilic cytoplasmic inclusions are also present
- Hemorrhagic necrosis may be present
- In lung, usually infects endothelial and epithelial cells and alveolar histiocytes
- Diagnostic inclusions may be seen in brochiolalveolar lavage fluid, but diagnostic yield is very low
- Particles are 150 - 200 nm with round core and double membrane
- Herpes simplex virus and herpes varicella zoster produce similar lung disease, but characteristic CMV inclusions are not present
- Drug induced injury, particularly in bone marrow transplant recipients, may cause changes similar to CMV; in problematic cases, immunohistochemical studies are useful
- Incidence declining due to dust reduction measures
Simple coal workers' pneumoconiosis (CWP):
- Patients have coal macules (1 - 2 mm collections of carbon laden macrophages) and coal nodules (coal macules and fibrosis) scattered throughout lung, more in upper lobe and upper lower lobe, near respiratory bronchioles
- Usually minimal symptoms but 10% develop progressive massive fibrosis
Progressive massive fibrosis:
- Also called complicated coal workers' pneumoconiosis
- Intensely blackened scars > 2 cm, multiple and containing dense collagen and pigment
- Center of lesion may be necrotic due to ischemia
- Associated with pulmonary hypertension and cor pulmonale
- May progress even if dust exposure ceases
- Due to any pneumoconiosis, although most common in CWP and silicosis
- Associated with increased incidence of clinical tuberculosis, chronic bronchitis and emphysema and independent of smoking
- In isolation, not appear to increase the risk of lung cancer
Caplan syndrome:
- Rheumatoid arthritis and pneumoconiosis cause rapidly developing nodular pulmonary lesions showing central necrosis surrounded by collagen, fibroblasts and macrophages (similar to rheumatoid nodules)
- Associated with exposure to coal, asbestosis and silica dust
- Lung infection caused by dimorphic fungi, Coccidioides spp.
- Highly prevalent in the endemic areas (southwest U.S., Central and South America)
- Lower respiratory tract symptoms resembling bacterial pneumonia; mass lesion with cavity formation in chronic infection
- Necrotizing granulomatous inflammation with characteristic spherules
- Pulmonary coccidioidomycosis
- San Joaquin Valley fever, valley fever
- Endemic areas
- Southwest U.S.: California, Arizona, New Mexico, Texas
- Central and South America: northern Mexico, Argentina, Brazil (Ann N Y Acad Sci 2007;1111:19)
- Men: higher incidence of symptomatic and severe infection (Clin Microbiol Rev 2013;26:505)
- African Americans: higher risk of disseminated disease (Clin Microbiol Rev 2013;26:505)
- Primary lung infection
- Common extrathoracic sites: skin, joints, bones and meninges (Clin Microbiol Rev 2013;26:505)
- Acquired via inhalation of aerosolized arthroconidia (3 - 5 microns) from the soil
- A specialized structure called a spherule forms in the lung
- Endospores are released from the ruptured spherule and develop into new spherules
- Disseminate via hematogenous route
- Dimorphic fungi in the genus Coccidioides, which contain 2 species
- Coccidioides immitis (central and southern California, San Joaquin Valley)
- Coccidioides posadasii (isolated outside California)
- No difference in clinical course and microscopic morphology between the 2 species
- Most infected individuals are asymptomatic or minimally symptomatic
- Symptoms include cough, fever, dyspnea, pleuritic chest pain
- Can be disseminated in 1 - 5% of cases, especially immunocompromised patients (Medicine (Baltimore) 2004;83:149)
- Desert rheumatism refers to the immunologic phenomena triad, including fever, arthralgia and erythema nodosum
- Traveling history or residence in the endemic areas
- Fungal organism identification by histology, culture or serology
- Standard fungal culture: no specific plate morphology; lactophenol cotton blue stains shows septate hyphae with alternating barrel shaped arthroconidia
- Biosafety level 3 pathogen: laboratory personnel should be aware of the diagnosis
- Serologic testing for anticoccidioidal IgG, IgM
- Increased serum (1→3)-β-D-glucan can be used to indicate invasive fungal disease, although not specific for coccidioidomycosis (J Clin Microbiol 2012;50:3060)
- Complete blood count: eosinophilia found in 27% of cases (West J Med 1993;159:153)
- Chest Xray and CT chest in acute infection: nonspecific, resembling acute bacterial pneumonia, including consolidation (75%), nodular opacities (20%), hilar adenopathy (20%), pleural effusion (15 - 20%); solitary pulmonary nodule may be seen (Radiographics 2014;34:912)
- Disseminated infection: miliary nodules from hematogenous spread (Radiographics 2014;34:912)
- Chronic cavitary lesion can be seen radiographically in 2% of cases, up to 11% by CT scan (Radiographics 2014;34:912)
- Grape skin sign: classic finding in chronic pulmonary coccidioidomycosis (AJR Am J Roentgenol 2014;202:479)
- Very thin walled cavitary lesion that develops in lung parenchyma previously affected by consolidation followed by central necrosis
- 34 year old man with left upper lobe pneumonia and cutaneous nodule (Am J Trop Med Hyg 2019;100:5)
- 42 year old man with cavitary lesion and fungal ball (Lab Med 2020;51:e12)
- 49 year old man with left upper lobe cavitary lesion (Hum Pathol 2018;71:55)
- 64 year old man with fever and respiratory failure (N Engl J Med 2020;382:276)
- Oral azole antifungal
- Amphotericin B
- Surgical resection of the cavitary lesion if (Clin Infect Dis 2016;63:e112)
- Cavities are persistently symptomatic despite antifungal treatment
- Cavities have been present for more than 2 years and if symptoms recur whenever antifungal treatment is stopped
- Mass lesion can be seen in chronic infection, usually well demarcated, often with central cavitation
- Fungus ball (mycetoma) was found in 28% of cases with cavity lesion (Hum Pathol 2014;45:153)
- Necrotizing, often suppurative, granulomatous inflammation
- Large (20 - 200 microns) thick walled spherules, with or without granular basophilic endospores (2 - 4 microns)
- Eosinophilic infiltrate is common
- Thin, septate hyphae with arthroconidia formation may be seen, more often in diabetes mellitus patients (Eur J Clin Microbiol Infect Dis 2008;27:813)
- Cavitary lesion features (Hum Pathol 2014;45:153)
- Palisading fibroblasts and fibrosis with chronic inflammation
- Granuloma not seen in the cavity wall, while multinucleated giant cells occasionally present
- Squamous metaplasia in the lining of the cavity wall
- Hyphal forms identified in 62% of cases
- Blood vessel lesion: arteritis with fibrinoid necrosis and rupture, thrombus and mural chronic inflammation
- Surrounding lung parenchyma (Hum Pathol 2014;45:153)
- Lymphoid hyperplasia
- Chronic bronchiolitis
- Organizing pneumonia
- Bronchoalveolar lavage (BAL) cytology (Diagn Cytopathol 2016;44:195)
- Various forms of spherules with associated acute inflammatory response
- Spherules can be immature (not adsorb any stains), smaller, larger, empty or fractured
- Granulomas were rare and mostly seen in lymph nodes and extra pulmonary sites (Diagn Cytopathol 2016;44:195)
- Mycelial form in BAL is uncommon but has been reported (Diagn Cytopathol 2007;35:535)
- Real time PCR assay is available for various types of specimen (e.g., bronchoalveolar lavage, sputum, lung tissue, etc.)
- In situ hybridization for C. immitis ribosomal RNA has been described (Diagn Mol Pathol 2010;19:99)
Dimorphic fungi: coccidioidomycosis by Glenn D. Roberts, Ph.D.
- Left lung, core needle biopsy:
- Necrotizing granulomatous inflammation (see comment)
- Comment: Fungal organism identified on H&E and GMS stain, consistent with Coccidioides spp.
- Histoplasmosis:
- Endemic in the central and eastern U.S. (Ohio and Mississippi River valleys)
- Small (2 - 5 microns) budding yeast within the histiocytes
- Blastomycosis:
- Endemic in the eastern U.S. (Ohio, Mississippi River valleys, Great Lakes region)
- Broad based budding yeast, smaller (8 - 15 microns) than Coccidioides sp.
- Paracoccidioidomycosis:
- Endemic in South America
- Large (10 - 60 microns) spherical yeast with circumferential budding, resembling mariner’s wheel
- Cryptococcosis:
- No specific endemic area
- Round, medium sized (4 - 7 microns), yeast with thick mucoid capsule
- Tuberculosis:
- Acid fast positive bacilli
A 40 year old man presents with chronic cough, low grade fever and mild dyspnea for several months. CT scan of the chest shows a 3 cm mass lesion in the right upper lobe of the lung. The H&E image of the core needle biopsy is shown. Which one of the followings is the most likely exposure history?
- Cave diving in Ohio
- Military training in Arizona
- Parakeet breeder
- Traveling to Africa
- Camping in Colorado
Comment Here
Reference: Coccidioides immitis
- Broad based budding yeast
- Round yeast with large mucoid capsule
- Acute angle, branching septate hyphae
- Large spherule with numerous endospores
- Oval yeast with pseudohyphae budding
- Colloid adenocarcinoma is a type of invasive lung cancer characterized by extracellular mucin accumulation that distends alveolar spaces and destroys lung tissue
- It is important to differentiate colloid adenocarcinoma from metastases of mucinous carcinoma originating in other organs and from invasive mucinous adenocarcinoma of the lung by identifying key characteristics, such as large pools of mucin destroying alveolar walls, which must be present in at least 50% of the tumor
- Invasive adenocarcinoma with extensive extracellular mucin pools distending alveolar spaces and destroying alveolar walls
- Tumor cells are mucin filled, cuboidal to columnar, floating in mucin pools or lining fibrous walls of mucin filled spaces
- Predominantly found in the peripheral lung parenchyma
- Immunohistochemistry: positive for CK7 and CDX2 and CK20; weak or negative for TTF1, napsin A and EMA (MUC1)
- Mostly indolent clinical course with a relatively favorable prognosis after complete surgical resection
- Recommended: colloid adenocarcinoma
- Not recommended: mucinous cystadenocarcinoma; mucinous cystic tumor of borderline malignancy
- ICD-O: 8480/3 - colloid adenocarcinoma
- ICD-11: 2C25.Z & XH7GY6 - malignant neoplasms of bronchus or lung, unspecified & adenocarcinoma of lung, mucinous
- Epidemiology of colloid adenocarcinoma is like that of other lung adenocarcinomas (J Surg Oncol 2016;114:211)
- Colloid adenocarcinoma typically occurs in the peripheral lung parenchyma (Intern Med 2018;57:3637, J Surg Oncol 2016;114:211)
- Pathogenesis of mucinous lung tumors, which may share similarities with mucinous / colloid gastrointestinal adenocarcinomas, could be attributed to gastrointestinal differentiation, as both types of tumors exhibit predominant extracellular accumulation of mucin
- Colloid adenocarcinomas are generally negative for predictive biomarkers such as EGFR mutations and ALK rearrangements, while KRAS mutations are found in ~50% of these tumors
- References: Virchows Arch 2015;467:675, Hum Pathol 2015;46:836
- Etiology of colloid adenocarcinoma is like that of other lung adenocarcinomas (J Surg Oncol 2016;114:211)
- In most cases, it is asymptomatic (J Surg Oncol 2016;114:211)
- Incidental findings during routine radiographic evaluation or with no specific symptoms (i.e., cough, shortness of breath and unresolved pneumonia) (Hum Pathol 2015;46:836)
- Usually diagnosed in light of incidental findings on CT scans (Hum Pathol 2015;46:836)
- Pathological diagnosis following lobectomy or wedge resection (J Surg Oncol 2016;114:211)
- On CT, colloid adenocarcinoma usually presents as an intrapulmonary mass with poor contrast enhancement (Intern Med 2018;57:3637)
- On MRI on T1 weighted imaging (WI), colloid adenocarcinoma is characterized by low intensity and high intensity on T2WI, probably from the mucus component of the tumor (Intern Med 2018;57:3637)
- On 18F fluorodeoxyglucose positron emission tomography (18F FDG PET), the majority of tumors show intense accumulation of 18F FDG (median standardized uptake value of 6.25, ranging from 3.0 to 8.6) (J Surg Oncol 2016;114:211)
- Estimated 5 year survival of 51% in patients who benefit from surgical resection (J Thorac Oncol 2011;6:1496)
- Apparent better prognosis for tumors that are CDX2 and MUC2 positive compared with tumors that are CDX2 and MUC2 negative (Am J Surg Pathol 2004;28:442)
- Clinical progression is generally slow; after comprehensive surgical removal, the prognosis is relatively favorable (Am J Surg Pathol 2004;28:442)
- Poorer prognosis, involving recurrence and metastasis, is indicated by the existence of signet ring cells and a noncolloid component (Am J Surg Pathol 2004;28:442)
- 66 year old woman with a history of ovarian cancer (Respirol Case Rep 2023;11:e01109)
- 69 year old woman with a giant lung mass detected on chest radiograph (Case Rep Oncol 2020;13:1097)
- 76 year old asymptomatic man with a mass in the right lower lung (Intern Med 2018;57:3637)
- Complete surgical resection is the treatment of choice (Respirol Case Rep 2023;11:e01109)
- KRAS mutations are the most common
- Targetable alterations in EGFR and ALK are typically absent in colloid adenocarcinoma (i.e., EGFR mutations and ALK rearrangements) (Hum Pathol 2015;46:836)
- Tumors appear as diverse, nonencapsulated, single, soft, jelly-like nodules with a mucoid appearance and protruding when cut; their sizes range from 5 to 100 mm (Mod Pathol 1992;5:634)
- In rare instances, these tumors may display a notably cystic appearance (Hum Pathol 2015;46:836)
- Abundant extracellular mucin
- Distended and destroyed alveolar spaces
- Invasive growth pattern
- Mucin laden cuboidal / columnar cells
- Possible signet ring morphology
- Inconspicuous, well differentiated cells
- Low mitotic count, no necrosis
- Inflammatory infiltrate possible
- Reference: Hum Pathol 2015;46:836
Contributed by Gheorghe-Emilian Olteanu, M.D., Ph.D., Ana Mataić, M.D. and Luka Brčić, M.D., Ph.D.
- Low cellularity
- Tumor cells in tissue fragments
- Single cells resembling histiocytes
- Thick extracellular mucin pools
- Reference: Cancer Cytopathol 2015;123:306
- CK7, CK20 and CDX2 are diffusely and strongly positive (Hum Pathol 2015;46:836)
- TTF1 can be focally positive in a percentage of cases (Hum Pathol 2015;46:836)
- KRAS mutations are more common (mutations in codons 12 and 13 have been seen)
- No EGFR mutations or ALK rearrangements
- Reference: Hum Pathol 2015;46:836
- Lung, lobectomy:
- Colloid adenocarcinoma (see comment)
- Comment: Abundant extracellular mucin pools with distended and destroyed alveolar spaces. Tumor cells are bland, mucin laden and cuboidal to columnar. Overall, the tumor has an invasive growth pattern.
- Imaging and history is often needed given the overlapping immunoprofiles of metastatic mucinous adenocarcinomas with colloid adenocarcinoma
- Metastatic carcinoma:
- Positive markers dependent on site of origin (e.g., SATB2 if colorectal, GATA3 if breast, S100P if pancreatic) (Hum Pathol 2015;46:836, Int J Surg Case Rep 2018;42:242, Am J Surg Pathol 2001;25:26, J Cytol 2018;35:247)
- Absence of smoking as a risk factor
- Invasive lung cancer characterized by large pools of mucin destroying alveolar walls, with > 50% of the tumor demonstrating these characteristics
- Positive markers for CK7 and CDX2
- Presence of KRAS mutations
Answer D is incorrect as KRAS mutations are not unique to invasive colloid adenocarcinoma; they are one of the most commonly found mutations in all types of lung adenocarcinomas. Answer C is also incorrect since positive immunohistochemistry for CK7 and CDX2 is not exclusive to invasive colloid adenocarcinoma but is also found in mucinous lung adenocarcinoma and adenocarcinoma with enteric differentiation. Answer A is incorrect because smoking is a risk factor for all lung cancers, including colloid adenocarcinoma, and is not absent as a risk factor.
Comment Here
Reference: Colloid
- Negative for CK7 and TTF1
- Positive for CDX2 and SATB2
- Positive for CK7 and CDX2
- Typically presents EGFR mutations or ALK rearrangements
Comment Here
Reference: Colloid
A 67 year old man presented with difficulty breathing, cough and expectoration. A chest CT reveals a mass in the lower right portion of the lung measuring 53 mm in diameter. A biopsy finds abundant mucin but no atypical cells. Following a lobectomy, immunohistochemistry of tumor cells indicates expression of CK7, CK20 and CDX2 but not TTF1 or SATB2. The patient has no history of previous tumors and no malignancy in the gastrointestinal tract is currently detected. Given the image and the provided information, what is your pathological diagnosis?
- Adenocarcinoma with enteric differentiation
- Invasive colloid adenocarcinoma of the lung
- Invasive mucinous adenocarcinoma of the lung
- Metastatic adenocarcinoma of the gastrointestinal tract
Comment Here
Reference: Colloid
- Congenital pulmonary airway malformations encompass a spectrum of cystic and noncystic lung malformations that develop in utero
- Cysts are interconnected with each other and with alveolar spaces and typically lined by ciliated columnar epithelium; there is substantial overlap in cyst size between type 1 and 2 CPAMs
- Type 1 and 3 CPAMs are associated with mosaic activating KRAS mutations and an increased risk of metastatic mucinous adenocarcinoma if incompletely resected (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Type 2 CPAMs are associated with bronchial atresia and do not have KRAS mutations (Semin Pediatr Surg 2003;12:17, Mod Pathol 2022;35:1404)
- Terms type 0 and type 4 CPAM are now obsolete (see Terminology below)
- Previously called congenital cystic adenomatoid malformation (CCAM) (Hum Pathol 1977;8:155)
- Most commonly used classification systems are the Stocker and Langston classification systems (Hum Pathol 1977;8:155, Semin Pediatr Surg 2003;12:17)
- Stocker type 0 and type 4 CPAMs are now recognized to represent other lung abnormalities; these terms are no longer in use
- Acinar dysplasia is the preferred term for the diffuse malformation previously described as type 0 CPAM (Am J Med Genet A 2016;170:2440, Am J Respir Crit Care Med 2019;200:1093)
- Type 4 CPAMs are now known to represent cystic pleuropulmonary blastomas and should be diagnosed as such (Pediatr Dev Pathol 2015;18:504)
- Congenital lobar emphysema due to bronchial atresia is thought to be on a spectrum with type 2 CPAMs; these findings often co-occur
- ICD-10: Q33.9 - congenital malformation of lung, unspecified
- Congenital lung lesion
- Type 2 CPAMs are the most common but are usually asymptomatic (Am J Surg Pathol 2019;43:47)
- Clinical course is dependent upon the size of the lesion and timing of resection
- Nearly all type 1 CPAMs and some type 3 CPAMs are caused by mosaic activating KRAS mutations; these are usually symptomatic (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Most commonly involve a single lobe of the lung
- Rarely, 1 lesion may involve multiple lobes or a patient may have 2 distinct lesions
- Type 1 CPAMs and many type 3 CPAMs result from mosaic activating KRAS mutations (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Mosaic mutations in other genes have been rarely reported in type 3 CPAMs (Mod Pathol 2022 Jul 6 [Epub ahead of print], Am J Med Genet A 2020;182:746)
- Type 2 CPAMs are believed to arise secondary to bronchial atresia and do not have KRAS mutations (Semin Pediatr Surg 2003;12:17, Arch Pathol Lab Med 2002;126:934, J Pediatr Surg 2006;41:61, Pediatr Dev Pathol 2006;9:361, Mod Pathol 2022;35:1404)
- Type 2 CPAMS are rarely associated with other congenital anomalies, including congenital diaphragmatic hernias (Front Pediatr 2020;8:446)
- Type 1 and 3 CPAMs have been described in patients with nevus comedonicus syndrome and Schimmelpenning syndrome (Mod Pathol 2022 Jul 6 [Epub ahead of print], Am J Med Genet A 2020;182:746)
- Lesions are typically detected on prenatal ultrasound
- Definitive diagnosis requires pathologic examination following resection
- Ultrasound: multiple hypoechoic lung cysts (Neonatology 2016;110:101)
- Fetal MRI: T2 hyperintense lesion with cystic spaces
- Type 1 and type 3 CPAMs:
- Incomplete resection in infancy or resection later in childhood is associated with an increased risk of developing metastatic mucinous adenocarcinoma (Am J Surg Pathol 2020;44:1118)
- There are no reports of metastatic mucinous adenocarcinoma arising in CPAMs that are completely resected in infancy or early childhood
- Neonate born at 32 weeks gestational age who developed respiratory failure and died shortly after birth (Autops Case Rep 2018;8:e2018022)
- 14 year old boy with shortness of breath and exercise intolerance (Am J Clin Pathol 2021;156:313)
- 14 year old boy with spontaneous pneumothorax (Ann Med Surg (Lond) 2021;68:102692)
- Complete surgical resection
- Thoracoamniotic shunts may be placed to decompress type 1 CPAMs in utero until resection can be performed after birth
- Maternal steroids may be given for symptomatic patients whose cysts are too small for shunt
- Reference: Eur J Pediatr 2017;176:1559
- Type 1 (large cyst) CPAM
- Grossly cystic lung lesion
- Largest cyst size is highly variable and ranges from 7 cm in greatest dimension (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Cysts are interspersed with relatively normal appearing lung parenchyma (alveoli are enlarged and simplified)
- No mucocele
- Type 2 (small cyst) CPAM
- Variable gross appearance
- In cystic specimens, cysts can measure up to 2.5 cm in greatest dimension and cysts are interspersed with normal appearing lung parenchyma
- Some specimens may have no grossly identifiable lesion
- May have a mucocele or grossly evident bronchial atresia
- Type 3 CPAM
- Solid / dense appearing lesion, often with a lobulated appearance
- Lesion is distinct from the uninvolved lung parenchyma
- May have very small interspersed cysts (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Type 1 (large cyst) CPAM
- Readily identifiable cysts lined by ciliated cuboidal to stratified columnar epithelium with interspersed alveolar type spaces (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Cysts connect with adjacent alveoli with frequent transitions from thick cyst wall to adjacent alveolar wall
- Often has epithelial complexity - papillary projections, irregularly shaped small cystic spaces
- May have solid appearing areas with features of both type 1 and type 3 CPAM
- Mucinous cell clusters are seen in ~75% (when carefully searched for)
- Presence of mucinous cell clusters is specific but not entirely sensitive for a KRAS mutation
- Mucinous cell clusters in infants are often multifocal and have papillary or acinar architecture when they lepidically cover a small alveolus (Am J Surg Pathol 2020;44:1118)
- Most pediatric pathologists do not diagnose mucinous adenocarcinoma in specimens from infants when only these small clusters are present
- May have foci of cartilage within the large cyst walls or foamy appearing pneumocytes with vacuolated cytoplasm (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Thoracoamniotic shunt placement may result in reactive changes, such as squamous metaplasia
- Type 2 (small cyst) CPAM
- Spectrum of histologic changes ranging from readily identifiable cysts to mildly malformed alveolar type spaces
- Cysts may be focal with the majority of the malformation having only mild changes
- Cysts are typically round and lined by ciliated columnar epithelium
- Epithelial complexity is rare
- Often with prominent evidence of mucostasis, including pools of mucin and foamy intra-alveolar macrophages
- Transitions from cystic spaces into adjacent alveolar type spaces are rare
- Cases that are clinically considered to be CPAMs but do not have cysts show milder parenchymal maldevelopment with enlarged and simplified alveoli (formerly congenital lobar emphysema)
- Striated skeletal muscle may occasionally be seen in the septa between cysts
- Type 3 CPAM
- Consist predominantly of small irregularly shaped airway spaces lined by ciliated cuboidal to columnar epithelium (Mod Pathol 2022 Jul 6 [Epub ahead of print])
- Surrounding septa often appear thickened, with prominent mesenchyme and cuboidal epithelium
- Interspersed alveolar type spaces (with thin walls and flat pneumocytes) are rare / absent in most type 3 CPAMs
- Mucinous cell clusters are seen in ~45%
- Mucinous cell clusters are often multifocal and have papillary or acinar architecture (Am J Surg Pathol 2020;44:1118)
- Most pediatric pathologists do not diagnose mucinous adenocarcinoma in specimens from infants when only these small clusters are present
- Nearly all classic type 1 CPAMs (> 98%) have an activating KRAS mutation in the mucinous and nonmucinous epithelium
- KRAS p.G12D is the most common mutation reported in type 1 CPAMs
- Type 3 CPAMs are associated with activating KRAS mutations or mutations in other genes involved in cell cycle regulation and growth
- 50% have a KRAS mutation and p.G12V is the most common variant
- 2 reported cases with mutations in other genes (FGFR2 and NEK9)
- Presence of mucinous cell clusters is highly specific but not entirely sensitive for a KRAS mutation
- Reference: Mod Pathol 2022 Jul 6 [Epub ahead of print]
- Lung, right upper lobe, lobectomy:
- Type 1 (large cyst) congenital pulmonary airway malformation, with atypical mucinous cells (see comment)
- Comment: Sections throughout the lobe demonstrate numerous, variably enlarged and cystically dilated airspaces lined by ciliated respiratory epithelium. Foci of epithelial complexity, including scattered foci of mucinous cells (1 - 2 mm each) and branching papillae are seen. The mucinous cells are seen in association with the epithelium of the cysts and in the adjacent alveoli. Children and young adults with unresected or incompletely resected type 1 CPAMs have rarely developed metastatic mucinous adenocarcinoma. While the mucinous cells in this lesion are histologically indistinguishable from mucinous adenocarcinoma in situ, recurrence / metastasis has not been reported following complete resection by lobectomy in infancy. Type 1 CPAMs are associated with mosaic activating KRAS mutations throughout the epithelium and should be entirely resected (Mod Pathol 2022 Jul 6 [Epub ahead of print]).
- Type 2 (small cyst) congenital pulmonary airway malformation (see comment)
- Comment: The epithelium is flat and simple with prominent mucostasis, consistent with bronchial atresia sequence.
- Type I pleuropulmonary blastoma:
- Gross: peripherally located multiseptated cyst
- Back to back cysts without intervening alveoli
- Septa may have primitive CD56+ round cells but may be regressed
- Associated with DICER1 mutations
- Intrapulmonary bronchogenic cyst:
- Gross: single thick walled cyst
- Single cyst wall does not connect to adjacent alveolar spaces
- Usually cartilage or submucosal glands in wall
- May have type 2 CPAM changes adjacent (due to obstruction during development)
- Intrapulmonary sequestration:
- Gross: systemic feeding vessel entering away from the hilum
- Large cartilage containing airway paired with the feeding vessel (aberrant hilum)
- Parenchymal maldevelopment is similar to type 2 CPAMs ranging from mild alveolar enlargement to type 2 CPAM-like change
- Pulmonary hypertensive changes may be present in older patients
Routine prenatal imaging revealed a cystic lung lesion. The pregnancy was otherwise uncomplicated and the lesion was resected at 3 weeks of age following a term delivery. What is the most appropriate diagnosis?
- Type 1 (large cyst) CPAM
- Type 2 (small cyst) CPAM
- Type 3 CPAM
- Type I pleuropulmonary blastoma
Comment Here
Reference: Congenital pulmonary airway malformation (CPAM)
A right upper lobe resection is performed in a 2 month old baby for an asymptomatic cystic lesion identified on routine prenatal ultrasound. It is most likely associated with which of the following?
- An aberrant systemic feeding vessel
- Bronchial atresia
- DICER1 syndrome
- Mosaic activating KRAS mutations
Comment Here
Reference: Congenital pulmonary airway malformation (CPAM)
- Coronavirus disease 2019 (COVID-19) is an infectious respiratory disease caused by novel coronavirus SARS-CoV-2 that emerged in Wuhan, China at the end of 2019, resulting in a worldwide pandemic
- Infection control guidance for healthcare professionals:
- CDC (CDC: Infection Control Guidance for Healthcare Professionals About Coronavirus (COVID-19) [Accessed 20 March 2023])
- Personal protective equipment (PPE) basics (CDC: Using Personal Protective Equipment (PPE) [Accessed 20 March 2023])
- Autopsy guidelines:
- Personal protective equipment (Pathol Res Pract 2020;216:153039)
- CAP (CAP: Amended COVID-19 Autopsy Guideline Statement from the CAP Autopsy Committee [Accessed 20 March 2023])
- CDC (CDC: Collection and Submission of Postmortem Specimens from Deceased Persons with Known or Suspected COVID-19 [Accessed 20 March 2023])
- Health and Safety Executive (HSE: Handling the Deceased with Suspected or Confirmed COVID-19 [Accessed 28 March 2023])
- Italian experience (Virchows Arch 2020;476:821)
- COVID-19 is a viral infection caused by coronavirus SARS-CoV-2 that can progress to severe acute respiratory syndrome with pneumonia and acute respiratory distress syndrome
- The disease spread rapidly and became a pandemic with > 100 million confirmed cases and over 2 million deaths worldwide by end of January 2021
- Histologically, COVID-19 shows diffuse alveolar damage corresponding to the phase of the disease (acute to fibrotic), divided into 3 main injury patterns: epithelial, vascular and fibrotic
- Definite diagnosis is based on detection of viral RNA by RT-PCR
- COVID-19 is also called novel coronavirus pneumonia
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is also called 2019 novel coronavirus (2019-nCoV)
- COVID-19 pandemic
- In December 2019, cases of pneumonia with unknown etiology were reported from Wuhan, Hubei Province, China to WHO (WHO: Novel Coronavirus (2019-nCoV) Situation Report - 1 [Accessed 20 March 2023])
- In January 2020, the Chinese authorities identified a novel type of coronavirus, which was later named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
- At the beginning of February 2020, almost 10,000 cases of COVID-19 were confirmed in China and 100+ cases were detected outside of China (WHO: Novel Coronavirus (2019-nCoV) Situation Report - 11 [Accessed 20 March 2023])
- The disease spread rapidly and became a pandemic with > 100 million confirmed cases and over 2 million deaths worldwide by end of January 2021
- By late September 2022, confirmed cases approached 580+ million with over 6.5 million deaths worldwide
- The United States now has the most confirmed cases (> 89 million) and confirmed deaths (> 1,000,000) worldwide (WHO: Coronavirus (COVID-19) Dashboard - Table [Accessed 20 March 2023])
- Coronavirus maps:
- An early mutated variant of SARS-CoV-2, B.1.1.7 (Alpha) was identified in September 2020, followed by B.1.351 variant (Beta), first identified in South Africa, the P.1 variant (Gamma), first identified in Brazil, and the Delta strain, first reported in India (Immunotherapy 2022;14:351)
- In November 2021, the latest Omicron SARS-CoV-2 variant was designated by WHO and it had been identified in 149 countries by January 2022; the variant is currently the dominant variant circulating globally (WHO: Statement on Omicron Sublineage BA.2 [Accessed 20 March 2023])
- Person to person transmission is suspected to occur via respiratory droplets (cough, sneeze)
- The key to slowing the spread of this disease is widespread testing so that patients can be quickly identified / isolated and vaccination
- COVID-19 (SARS-CoV-2) testing
- By 2022, there are 11 WHO approved vaccines and the most commonly used ones are (Immunotherapy 2022;14:351, Front Immunol 2022;13:872683, COVID19 Vaccine Tracker: World Health Organization (WHO) [Accessed 20 March 2023])
- BNT162b2 (BioNTech / Pfizer)
- mRNA-1273 (Moderna)
- ChAdOx1 (AstraZeneca)
- Ad26.COV2.S (Janssen)
- BBIBP-CorV (Sinopharm)
- By mid 2022, approximately 66% of the world population had received at least one dose of a COVID-19 vaccine, 12.3 billion doses have been given globally and ~27 million new doses are administered daily (Our World in Data: Coronavirus (COVID-19) Vaccinations [Accessed 20 March 2023])
- Upper respiratory tract in mild disease
- Bilateral lobes of the lung in more severe disease
- Spike surface glycoprotein of the virus binds to the host via receptor binding domains of the angiotensin converting enzyme 2 (ACE2), which is most abundant in type II alveolar cells (J Virol 2020;94:e00127-20)
- 10 - 20 times higher binding affinity as compared with the SARS-CoV-1 virus (J Pathol 2020;251:228)
- After a SARS-CoV-2 attaches to a target cell, the virion releases RNA into the cell, initiating replication of the virus which further disseminates to infect more cells (Cell 2020;181:271)
- SARS-CoV-2 produces several virulence factors that promote shedding of new virions from host cells and inhibit immune response
- Virus independent immunopathology in fatal COVID-19 (Am J Respir Crit Care Med 2021;203:192)
- Organ injury and death in COVID-19 is immune mediated rather than pathogen mediated
- Tissue inflammation and organ dysfunction in fatal COVID-19 do not correlate with the tissue and cellular distribution of SARS-CoV-2
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a positive sense, single stranded RNA virus having close genetic similarity to bat coronaviruses (Nature 2020;579:270)
- Average time from exposure to symptom onset is 5 days (Ann Intern Med 2020;172:577)
- 97.5% of people who develop symptoms do so within 11.5 days (JAMA 2020;324:782)
- Asymptomatic infection rate is 46% (J Med Virol 2020;92:2543)
- Rare in children, about ~2 - 5% of confirmed cases, with milder symptoms and very low hospitalization rate (JAMA 2020;324:782)
- Common symptoms in hospitalized patients (JAMA 2020;324:782):
- Fever (70 - 90%)
- Dry cough (60 - 86%)
- Shortness of breath (53 - 80%)
- Fatigue (38%)
- Myalgias (15 - 44%)
- Nausea / vomiting or diarrhea (15 - 39%)
- Headache, weakness (25%)
- Patients can present with nonclassical symptoms (JAMA 2020;324:782):
- Isolated gastrointestinal symptoms
- Isolated anosmia or ageusia (3%)
- COVID-19 can progress to severe acute respiratory syndrome and its major clinicopathological phenotypes include pneumonia and acute respiratory distress syndrome
- Distribution of severity (JAMA 2020;323:1239):
- Mild or no disease: 81%
- Severe disease: 14%
- Critical disease: 5%
- Overall case fatality rate: 2.3%
- 20 - 42% of hospitalized patients developed acute respiratory distress syndrome (JAMA Intern Med 2020;180:934, JAMA 2020;323:1061)
- Distribution of severity (JAMA 2020;323:1239):
- Patients who required ICU supportive care presented with acute respiratory distress syndrome, acute cardiac injury, acute kidney injury and shock; up to 15% of them had fatal outcomes (Travel Med Infect Dis 2020;34:101623)
- Common complications among hospitalized patients (JAMA 2020;324:782):
- Pneumonia (75%)
- Acute respiratory distress syndrome (15%)
- Acute liver injury (19%)
- Cardiac injury (7 - 17%): troponin elevation, acute heart failure, dysrhythmias, myocarditis (JAMA 2020;324:782)
- Prothrombotic coagulopathy resulting in venous and arterial thromboembolic events (10 - 25%)
- Acute kidney injury (9%)
- Acute cerebrovascular disease (3%)
- Shock (6%)
- A rare multisystem inflammatory syndrome similar to Kawasaki disease has recently been described in children (2 per 100,000 persons aged < 21 years) (JAMA 2020;324:782)
- Post acute COVID-19 syndrome: persistent symptoms, delayed or long term complications beyond 4 weeks
- Persistent ≥ 1 symptom was reported in 32.6 - 87.4% of cases (fatigue, joint pain, chest pain, dyspnea, cough, loss of taste / smell, headache, diarrhea) (Nat Med 2021;27:601)
- Diagnostic testing of SARS-CoV-2 (COVID-19)
- Nasopharyngeal swab is recommended for the PCR specimen; oropharyngeal swab, sputum and bronchoalveolar lavage may be used alternatively based on the manufacturer's instructions (CDC: Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-19) [Accessed 20 March 2023])
- Positive rates of SARS-CoV-2 PCR testing by specimen types: bronchoalveolar lavage fluid (93%), sputum (72%), nasal swabs (63%), pharyngeal swabs (32%) (JAMA 2020;324:782)
- Definite diagnosis is based on detection of viral RNA by real time RT-PCR via many available laboratory tests (CDC: Information for Laboratories [Accessed 20 March 2023])
- False negative test results may occur in up to 20 - 67% of patients depending on the quality and timing of testing
- A modeling study estimated sensitivity at 33% 4 days after exposure, 62% on the day of symptom onset and 80% 3 days after symptom onset (JAMA 2020;323:1843)
- Number of SARS-CoV-2 antigen (rapid) tests are currently in use for point of care and at home test settings (FDA: In Vitro Diagnostics EUAs - Antigen Diagnostic Tests for SARS-CoV-2 | FDA [Accessed 20 March 2023])
- Meta analysis data (Travel Med Infect Dis 2020;34:101623):
- Decreased albumin
- High C reactive protein
- High lactate dehydrogenase (LDH)
- Lymphopenia
- High erythrocyte sedimentation rate (ESR)
- D dimer elevation (J Pathol 2020;251:228)
- Ground glass opacities, crazy paving pattern and consolidation in bilateral lobes are common findings (Radiology 2020;295:715)
- 15% of CT and 40% of chest radiograph findings are normal early in the disease (JAMA 2020;324:782)
- Evolution of abnormalities occurs in the first 2 weeks after onset
- Risks of acute respiratory distress syndrome development include age (> 65 years), underlying diseases (diabetes mellitus) and secondary infection (JAMA Intern Med 2020;180:934, Intensive Care Med 2020;46:846)
- Risk factors for disease progression: male, old age (> 65 years) and smoking (J Infect 2020;81:e16)
- Risk factors for critical / mortal states, in order of strength of association (Lancet 2020;395:1054):
- Cardiovascular disease
- Respiratory disease
- Diabetes
- Hypertension
- Infant girl with COVID-19 hepatitis (Arch Pathol Lab Med 2020 Apr 17 [Epub ahead of print])
- 44 year old man and 62 year old woman with COVID-19 pneumonia (Diagn Pathol 2020;15:73)
- 65 year old man with multiorgan failure (Hum Pathol 2020;101:82)
- 71 year old man with COVID-19 acute respiratory failure; real time correlation with transbronchial biopsy (Virchows Arch 2021;479:827)
- 73 year old man and 84 year old woman with lung cancer and coincidental COVID-19 (J Thorac Oncol 2020;15:700)
- 76 year old woman with COVID-19 pneumonia (N Engl J Med 2020;383:380)
- 79 year old woman with residual SARS-CoV-2 in pulmonary tissues (Cell Res 2020;30:541)
- Autopsy case series (Lancet Respir Med 2020;8:420, Mod Pathol 2020;33:1007)
- Autopsy case series in COVID-19 vaccinees, high viral loads in organ systems in vaccinees with accentuation in incomplete vaccination (Mod Pathol 2022;35:1013)
- Biopsy proven myocarditis case series after COVID-19 vaccination (Int J Mol Sci 2022;23:6940, Clin Res Cardiol 2021;110:1855)
- Home management is recommended for patients with mild symptoms
- Optimal duration of home isolation is under investigation but in hospitalized patients the virus is shed for an average of approximately 20 days after disease onset (Lancet 2020;395:1054)
- Antiviral drugs are recommended to patients who are at high risk of progressing to severe COVID-19 (paxlovid, remdesivir, molnupiravir) (NIH: Therapeutic Management of Nonhospitalized Adults with COVID-19 [Accessed 20 March 2023])
- Patients with severe disease require hospital care
- May need oxygenation support, ranging from low dose oxygen supplement to invasive ventilation and extracorporeal membrane oxygenation (ECMO)
- Among the antiviral drugs (ribavirin, favipiravir, remdesivir) undergoing clinical testing, remdesivir seems to be most promising (JAMA 2020;324:782)
- NIH COVID-19 Treatment Guidelines Panel recommends using dexamethasone in patients on ventilators and in those that require supplemental oxygen but not in other patients (Lancet 2020;395:1054, CDC: Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) [Accessed 20 March 2023], WHO: Coronavirus disease (COVID-19) Technical Guidance - Patient Management [Accessed 20 March 2023], NIH: COVID-19 Treatment Guidelines - Corticosteroids [Accessed 20 March 2023])
- From pulmonary edema to lung consolidation (J Clin Pathol 2020;73:239)
- Increased lung weight
- Hemorrhagic changes (Mod Pathol 2020;33:2128)
- Macroscopic pulmonary emboli (Mod Pathol 2020;33:2128)
- Pleural inflammation with or without effusion may be seen
- Purulent inflammation, if secondary infection superimposed
- Pulmonary changes are the most significant, although nonspecific (Lancet Respir Med 2020;8:420, J Thorac Oncol 2020;15:700, Mod Pathol 2020;33:1007)
- Findings of diffuse alveolar damage (DAD) corresponding to the phase of disease:
- Exudative phase: hyaline membrane formation, desquamation of pneumocytes, cellular or proteinaceous exudates, alveolar hemorrhage, fibrinoid necrosis of small vessels
- Organizing phase: interstitial and intra-alveolar proliferation of fibroblasts, lymphocytic infiltration, type II pneumocyte hyperplasia, fibrin deposition
- Fibrotic phase: dense collagenous fibrosis, architectural remodeling
- Lung injury patterns (Mod Pathol 2020;33:2128, Eur J Clin Invest 2020;50:e13259):
- Epithelial (85%): DAD with varying degrees of organization, denudation, hyperplasia of pneumocytes
- DAD in COVID-19 is as frequent as in SARS and H1N1 Influenza (Chest 2021;159:73)
- Vascular (59%): diffuse intra-alveolar fibrin, microvascular damage, (micro) thrombi, acute fibrinous and organizing pneumonia
- More vascular changes (hemangiomatosis-like changes, thromboemboli, pulmonary infarcts, perivascular inflammation) in fatal COVID-19 cases compared to DAD of other causes (Am J Respir Crit Care Med 2022;206:857)
- Fibrotic (22%): fibrotic DAD, interstitial fibrosis
- Prominent ongoing fibrosis in explanted lungs, accompanied by abundant macrophage infiltration, neoangiogenesis and persistent microvascular thrombosis (Am J Clin Pathol 2022;157:908)
- Epithelial (85%): DAD with varying degrees of organization, denudation, hyperplasia of pneumocytes
- Viral infection changes:
- Multinucleated enlarged pneumocytes with large nuclei, amphophilic cytoplasm and prominent nucleoli in alveolar spaces
- Intranuclear inclusions
- Bacterial pneumonia may be superimposed
- Findings of diffuse alveolar damage (DAD) corresponding to the phase of disease:
- Extrapulmonary changes (Mod Pathol 2020;33:2128):
- Cardiovascular: mild pericardial edema, some serosanguinous pericardial effusion, mild myocardial edema, low grade interstitial infiltration of mononuclear cells, endotheliitis
- Widespread systemic vasculitis with associated thromboemboli is not as common as initially thought (Lancet 2020;396:320)
- Hepatobiliary: hepatic congestion, mild steatosis, patchy hepatic necrosis, Kupffer cell hyperplasia, increased number of lymphocyte predominant inflammatory cells in the portal tracts and sinusoids, endotheliitis
- Renal: varying degrees of acute tubular injury, lymphocytic tubule interstitial infiltration, fibrin or hyaline thrombi in blood vessel, glomerular capillary dilatation, lymphocytic endotheliitis (Kidney Int 2020;98:219)
- Gastrointestinal: epithelial damage, prominent endotheliitis, ischemic enterocolitis
- Spleen: reduced number of lymphocytes with necrosis, atrophy, congestion, hemorrhage, infarction
- Bone marrow: histiocytic hyperplasia, hemophagocytosis (Mod Pathol 2020;33:2139)
- Other: cutaneous, prostatic manifestations, inflammation and clots in placenta with funisitis
- Cardiovascular: mild pericardial edema, some serosanguinous pericardial effusion, mild myocardial edema, low grade interstitial infiltration of mononuclear cells, endotheliitis
Contributed by Toru Igari, M.D., Jin Takahashi, M.D. and Shinyu Izumi, M.D.
Images hosted on other servers:
- Bronchoalveolar lavage (BAL):
- Inflammatory background (lymphohistiocytic, histiocytic, neutrophil predominant), virus related changes (atypical nuclei, nuclear cytoplasmic inclusion, multinucleation), nonspecific reactive changes (bronchial, alveolar, reserve cell hyperplasia) (Acta Cytol 2022;66:532)
- Abundant activated plasma cells, as per a single case report (J Thorac Oncol 2020;15:e65)
- Alveolar macrophages may feature nuclear clearing or intranuclear cytopathic inclusions
- High neutrophil proportions in mechanically ventilated critically ill patients (Clin Respir J 2022;16:329)
- IHC positive for SARS-CoV-2 antigen detected in pneumocytes, ciliated airway cells and upper airway epithelium in the acute phase (Mod Pathol 2020;33:2104)
- Spherical particles sized 60 - 140 nm
- Distinctive spikes on the surface (9 - 12 nm) giving virions the appearance of a solar corona, consistent with the Coronaviridae family
- Inclusion bodies filled with virus particles in membrane bound vesicles in cytoplasm of the respiratory epithelium (N Engl J Med 2020;382:727)
- ISH, including RISH and FISH positive for SARS-CoV-2 antigen detected in pneumocytes, ciliated airway cells and upper airway epithelium in the acute phase (Lab Invest 2020;100:1485, JCI Insight 2020;5:139042)
- Guidelines from CDC (CDC: Information for Laboratories [Accessed 20 March 2023])
- Diagnostic testing of SARS-CoV-2 (COVID-19)
Pathology of COVID-19: a pulmonary pathologist explains
Sample management
Autopsy
SARS-CoV-2 detection in tissues
Pulmonary pathology
Cardiovascular pathology
COVID-19 autopsy pathology findings
Histology of acute respiratory distress syndrome
- Usually reported as part of autopsy findings:
- Diffuse alveolar damage due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection
- Diffuse alveolar damage with changes compatible with viral infection
- Diffuse alveolar damage due to COVID-19 is morphologically indistinguishable from other DAD causes, including other viral pneumonias:
- Severe acute respiratory syndrome:
- Detection of SARS virus
- Acute respiratory distress syndrome of other etiology
- Acute interstitial pneumonia:
- Idiopathic by definition
- WHO: Coronavirus Disease (COVID-19) Pandemic [Accessed 20 March 2023], CDC: Coronavirus (COVID-19) [Accessed 20 March 2023]
- General biosafety guideline protocol for histological and cytological samples from patients with suspected or proven COVID-19 infection (Cancer Cytopathol 2020;128:317)
- Alveolar hemorrhage
- Fibrin deposition
- Neutrophilic aggregation
- Nuclear inclusions
- Type II pneumocyte hyperplasia
- Autosomal recessive disorder
- 1 in 20 Caucasians in US are carriers; much lower incidence in African Americans, Asians, Hispanics
- In US, approximately 1 in 2500 live births have disease
- Over 1300 known mutations of cystic fibrosis transmembrane conductance regulator / CFTR, most common mutation (seen in 70% in UK) is #508 (Eur J Hum Genet 2002;10:583)
- Mutations cause reduced chloride ion in secretions and thicker respiratory secretions
- Primary defect is abnormal function, deficiency or absence of cystic fibrosis transmembrane conductance regulator / CFTR that regulates chloride channel in epithelial cells
- Allelic variation correlates with some aspects of disease, but lung function, neonatal intestinal obstruction, diabetes and anthropometry display strong genetic control independent of CFTR, and candidate gene studies have revealed genetic modifiers underlying these traits (Ann NY Acad Sci 2010;1214:57)
- Allergic bronchopulmonary aspergillosis: increased incidence
- Burkholderia cepacia: unique to cystic fibrosis, seen in 20% of patients; causes rapid deterioration of pulmonary status and death; transmitted person to person, has marked social impact as those infected are excluded from social functions (camps) and ineligible for transplant; treat with chloramphenicol and trimethoprim-sulfamethoxazole
- Hemophilus influenza: common
- Mycobacteria (atypical): common
- Pseudomonas aeruginosa: bacteria produces alginate, a capsular protein that mediates adherence; mucoid phenotype is unique to cystic fibrosis; bacteria is never eradicated from lung; treat with ceftazidime (BMC Med 2011 Apr 4;9:32)
- Staphylococcus aureus: infection persists despite treatment
- Stenotrophomonus maltophilia: aerobic Gram-negative rod, multidrug resistant, smells like onions; treat with trimethoprim-sulfamethoxazole, resistant to imipenim
- Also anaerobes, although difficult to detect (New Microbiol 2010;33:185)
- Note: many taxonomic changes have occured (Clin Microbiol Rev 2010;23:299)
- Disease usually manifests in young children, but also prenatally or in adolescents
- Recurrent infections cause chronic lung disease, the most severe manifestation of the disease; recurrent upper respiratory infections occur, late sequela are pancreatic insufficiency, steatorrhea, malnutrition, cirrhosis
- Mutations also cause defective cilia and infertility
- Meconium ileus seen in 5% - 10% of patients; also intussusception
- Heterozygotes (carriers) also have higher incidence of respiratory and pancreatic disease than general population
- Emphysema, bronchiectasis, abscess, fibrosis
- Kartegeners (defective cilia syndrome)
- Sputum or bronchial brushings are 80 - 90% sensitive for lung carcinoma if examine 5+ sputum samples
- Fine needle aspirate is superior to bronchoalveolar lavage for diagnosis of pathologic pathology (Mod Pathol 2002;15:1259)
- False positives: due to misidentification of macrophages or pneumocytes - includes bronchiectasis, fungal infections, infarct, lipoid pneumonia, postradiation changes, viral pneumonia
- False negatives: often due to sampling (Diagn Cytopathol 2012;40:556); pleural fluid cytology is often falsely negative for small cell carcinoma
- Also useful for mutation analysis (Acta Cytol 2012;56:661)
- In 1965, Liebow et al reported a series of cases with interstitial pneumonia characterized by massive proliferation and desquamation of epithelial cells and coined the term "desquamative interstitial pneumonia" (DIP) (Am J Med 1965;39:369)
- In 1977, Tubbs et al determined, based on electron microscopy, that most cells within alveolar spaces were macrophages (Chest 1977;72:159)
- In 2013, American Thoracic Society / European Respiratory Society (ATS / ERS) categorized DIP as a smoking related interstitial pneumonia, as well as respiratory bronchiolitis related interstitial lung disease (Am J Respir Crit Care Med 2002;165:277, Am J Respir Crit Care Med 2013;188:733)
- A rare but characteristic type of smoking related lung disease
- Histologically, massive accumulation of intra-alveolar macrophages is the key finding
- Although “desquamated cells” are now recognized as intra-alveolar macrophages and ATS / ERS once considered to change the name of this entity to “alveolar macrophage pneumonia”, it is still officially called “desquamative interstitial pneumonia” (Am J Respir Crit Care Med 2002;165:277)
- Desquamative interstitial pneumonia: J84.117
- Rare, Common age at onset is 40 - 60 years (Eur Respir Rev 2013;22:117)
- Rarely occurs in neonates or children due to ABCA3 mutations (N Engl J Med 2004;350:1296, Am J Respir Crit Care Med 2005;172:1026, Mod Pathol 2007;20:1009, Thorax 2008;63:366)
- M:F = 2:1 (Eur Respir Rev 2013;22:117)
- Bilateral (or sometimes unilateral) lobes of the lung
- Respiratory bronchiolitis, respiratory bronchiolitis associated interstitial lung disease (RB-ILD) and DIP are now considered on a spectrum and it can be difficult in some cases to separate these diseases clearly (Histopathology 2011;58:509)
- Deaths are somewhat common in DIP (6 - 30%) but rare in respiratory bronchiolitis and RB-ILD
- Studies with mouse models suggest a two hit development (Chest 2015;148:1307, Antiviral Res 2011;92:319)
- Primary smoking exposure induces GM-CSF secretion from airway epithelial cells
- Subsequent infection provokes macrophage activation and accumulation
- Majority (60 - 90%) of adult patients are current or ex smokers (Eur Respir Rev 2013;22:117, Histopathology 2011;58:509, Chest 2017;3692:33197)
- Nonsmoking patients often have a history of exposure to dust, fumes or second hand smoke (passive smoking)
- Mutation related to surfactant protein causes pediatric DIP
- Surfactant protein C (Pediatr Pulmonol 2014;49:1097, N Engl J Med 2001;344:573)
- ATP-binding cassette protein A3 (ABCA3) (Am J Respir Crit Care Med 2005;172:1026, Mod Pathol 2007;20:1009, Thorax 2008;63:366)
- Other causes
- Idiopathic
- Drugs (Respiration 2007;74:237, Pediatr Infect Dis J 2011;30:363)
- Connective tissue disease (rheumatoid arthritis, systemic sclerosis, systemic lupus erythematosus) (Intern Med 2009;48:827, Can Respir J 2012;19:50, J Clin Rheumatol 2010;16:284)
- Infection (Cytomegalovirus, aspergillus, hepatitis C virus) (Nephrol Dial Transplant 2005;20:635)
- Slight to mild chronic respiratory failure
- Dyspnea on exertion
- Dry cough
- Digital clubbing
- Abnormal chest auscultation
- End inspiratory fine crackles in bibasilar lung
- Mild systemic symptoms may accompany
- Fever
- Fatigue
- Weight loss
- Normal or slightly abnormal pulmonary function tests (restrictive, obstructive or mixed pattern)
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- See details in review (Eur Respir Rev 2013;22:117, Histopathology 2011;58:509, Chest 2017;3692:33197)
- Based on clinical features, radiology and histopathology (Am J Respir Crit Care Med 2002;165:277)
- Lung biopsy is required to establish a firm diagnosis since the clinical and radiological findings are often not specific
- However, a biopsy may not be necessary if the clinical and radiological features are suggestive enough (Radiology 1999;211:555)
- Increased serum KL-6
- Simple chest radiograph (Clin Radiol 2003;58:259)
- Variable and nonspecific, including ground glass opacity and reticulonodular shadow
- High resolution CT (Clin Radiol 2003;58:259, Chest 2017;3692:33197)
- Bilateral and subpleural ground glass opacity
- Middle to lower zones are affected predominantly; however, the upper zone can be involved
- Linear shadow, cystic spaces, emphysema, traction bronchiectasis and honeycombing can be accompanied
- Generally a favorable prognosis with good response to treatment: overall survival rate is 70 - 90% at 10 years (Am J Respir Crit Care Med 2005;172:268, Chest 2017;S0012:33197, Histopathology 2011;58:509)
- Disease can be persistent, especially in cases with marked fibrosis (Chest 1977;72:159)
- Female infant with DIP related to ABCA3 and hydroxychloroquine treatment for 10 years (Pediatr Pulmonol 2014;49:299)
- 30 month old girl with DIP and multiple organ disorders (BMC Res Notes 2014;7:383)
- 8 year old boy with DIP due to passive smoking (Pediatr Pulmonol 2014;49:E56)
- 45 year old man with DIP due to waterproofing spray (Intern Med 2014;53:2107)
- 65 year old man with DIP and IgG4-related lung disease (Intern Med 2017;56:1553)
- Smoking cessation or avoidance of etiological factors (including passive smoking) often improves the symptoms and prognosis (Histopathology 2011;58:509, Chest 2017;3692:33197, Eur Respir Rev 2013;22:117)
- Long term corticosteroid therapy is also effective
- Lung transplantation may be performed for progressive disease but recurrence of the disease was reported (Am J Respir Crit Care Med 1998;157:1349)
- Treatment for pediatric DIP includes corticosteroids, immunosuppressors (hydroxychloroquine) and lung transplantation (Pediatr Pulmonol 2014;49:1097, N Engl J Med 1993;329:1797, Pediatr Pulmonol 2014;49:299)
- Diffuse bronchocentric multinodular change with lower lobe predominance
- Firm and consolidated
- Pale gray to white
- Mild to moderate increase in weight of the lung
- Honeycomb change can be seen but sparsely
- Diffuse and massive accumulation of intra-alveolar macrophages (smoker's macrophages)
- Brown pigments, more finely granular than hemosiderin, are seen in the eosinophilic cytoplasm (smoker's pigments)
- Giant cells can be also seen
- Mild to moderate interstitial fibrosis or cellular change
- Diffuse and homogeneous involvement (similar to NSIP) along with alveolar macrophages
- Lymphoid follicles and eosinophils are often present
- Marked dense fibrosis, architectural distortion, fibroblastic focus or presence of intact alveolar walls in the area of accumulated macrophages should suggest another diagnosis
- See details (Histopathology 2011;58:509, Chest 2017;3692:33197, Chest 2015;148:1307, Eur Respir Rev 2013;22:117)
- Increased eosinophil or neutrophil ratio in bronchoalveolar lavage fluid
- Prussian blue stains iron pigments in smoker’s macrophages
- Macrophages are positive for CD68 (Histopathology 1998;33:129)
Histopathology Lung - Desquamative interstitial pneumonia
- Alveolar hemorrhage
- Hemosiderin laden macrophages are seen
- Hemosiderin is positive for Prussian blue but more coarse and larger
- Eosinophilic pneumonia
- Marked interstitial eosinophils and edema, organizing pneumonia, mucus plugs and fibrin deposition are seen
- Hypersensitivity pneumonitis
- Clinically, smoking history is less common
- Patinets have a history of exposure to antigens such as spores of fungi, animal proteins and chemicals
- Positive for serum antibody to causative antigens
- Airway centered change, interstitial cellular infiltration and granuloma are seen
- Nonspecific interstitial pneumonias
- Accumulation of intra-alveolar macrophages may be seen but focal or mild (DIP-like reaction)
- Clinically, patients with NSIP often associated with collagen tissue disease
- Pneumoconiosis
- Clinically, the patients usually have a history of occupational exposure
- Macrophages, giant cells and causative particles (e.g. asbestos body, anthrosilicotic dust) are seen especially in interstitium
- Pulmonary Langerhans cell histiocytosis
- Bronchocentric nodules of Langerhans cells
- Positive for CD1a, S100 and Langerin
- Respiratory bronchiolitis
- Most common lung disease in smokers
- Clinical manifestation is slight or absent
- Macrophage accumulation in bronchocentric predominance is seen on histology
- Interstitial pneumonia, lymphoid follicles, giant cells and eosinophils are absent
- Respiratory bronchiolitis-associated interstitial lung disease
- Less common lung disease in smokers
- Physical deterioration, including respiratory symptoms and abnormal pulmonary function, is significant enough to diagnose as interstitial lung disease
- Almost identical to respiratory bronchiolitis on histology
- Usual interstitial pneumonia
- Marked dense fibrosis, architectural distortion and fibroblastic focus are seen
- Clinically, UIP / IPF is more progressive and not responding to corticosteroid therapy
- Which clinical and morphological finding is NOT suggestive for DIP?
- A history of passive smoking
- Bilateral ground glass opacity
- Intra-alveolar cells positive for M. tuberculosis
- Intra-alveolar cells positive for Prussian blue
- Intra-alveolar giant cells
Comment Here
Reference: Desquamative interstitial pneumonitis
- Generalized proliferation of pulmonary neuroendocrine cells that can be limited to the respiratory mucosa or invade locally to form tumorlets and carcinoid tumors
- Diffuse idiopathic pulmonary neuroendocrine hyperplasia (DIPNECH) is considered a preinvasive lesion that may progress into tumorlets or carcinoid tumors (usually typical carcinoid)
- Histologic features comprise a generalized intramucosal proliferation of pulmonary neuroendocrine cells in monolayers or small groups that can penetrate through the bronchial basement membrane to form tumorlets
- Diagnostic criteria are still debated; the latest WHO edition separates diffuse idiopathic pulmonary neuroendocrine hyperplasia into a pathological diagnosis based on histologic features and a clinical diagnosis
- Some authors consider it a syndrome with a distinctive clinical presentation, typical radiological findings and a pathological demonstration
- Must be differentiated from secondary DIPNECH, which is a localized neuroendocrine proliferation secondary to another chronic lung disease
- Symptomatic patients present with insidious onset of a nonproductive chronic cough with dyspnea and wheezing that mimics asthma, chronic obstructive pulmonary disease or gastroesophageal reflux
- Description of the disease based on a few case series (approximately 200 reported cases) (Hum Pathol 2015;46:176, Eur Respir J 2016;47:1829)
- Exact prevalence unknown, since it is a rare underrecognized disease
- Can be found in 5.4% of lung resections for typical or atypical carcinoid (Eur J Cardiothorac Surg 2004;26:165)
- F:M, > 10:1 (Eur Respir J 2016;47:1829, Am J Respir Crit Care Med 2011;184:8)
- Mean age: 58 years (Lung 2016;194:243)
- Can be found in patients with multiple endocrine neoplasia type 1 (MEN1) (Thorax 2007;62:248)
- Proliferation of neuroendocrine cells arise from terminal bronchioles
- Not well described
- Idiopathic by definition
- Secondary DIPNECH is caused by other chronic lung diseases
- Considered a preneoplastic proliferation as neuroendocrine cells can cross the basement membrane to form tumorlets and carcinoid tumors (Histopathology 2011;59:751)
- Clinical symptoms are thought to be caused by the production of peptides by the neuroendocrine cells, which leads to a peribronchiolar fibrosis and an obstructive respiratory defect (Chest 2015;147:415)
- Unknown
- Mostly nonsmoker patients (Chest 2015;147:415, Clin Imaging 2015;39:243)
- Symptomatic patients present with insidious onset of a nonproductive chronic cough with dyspnea and wheezing that mimics asthma, chronic obstructive pulmonary disease or gastroesophageal reflux (Eur Respir J 2016;47:1829, Chest 2015;147:415, Am J Respir Crit Care Med 2011;184:8)
- Mean duration of symptoms before diagnosis: 10 years
- May be asymptomatic and an incidental finding during investigation for another disease (Lung 2016;194:243)
- Associated with tumorlets (67% of cases) and lung carcinoids, mostly typical carcinoids (40% of cases) (Am J Respir Crit Care Med 2011;184:8)
- Can also be found in association with lung adenocarcinoma (Pathol Res Pract 2013;209:578, J Med Case Rep 2008;2:21)
- Lung function tests may be normal or show an obstructive or a mixed obstructive and restrictive respiratory defect (Lung 2016;194:243, Lung 2018;196:577)
- Diagnostic criteria are still debated
- WHO classification of tumors and some authors use only microscopic findings to define (Hum Pathol 2015;46:176)
- Some authors consider DIPNECH a syndrome with a distinctive clinical presentation, typical radiological findings and a pathological demonstration; Carr et al. proposed diagnostic criteria but a minimum set of findings to confirm diagnosis has yet to be established (N Engl J Med 1992;327:1285, Clin Radiol 2015;70:317, Am J Surg Pathol 2018;42:646, Chest 2015;147:415)
- Serum chromogranin A may be elevated (Chest 2015;147:415)
- CT scan:
- Bilateral mosaic perfusion with air trapping is the most important feature (Clin Radiol 2015;70:317, Clin Imaging 2015;39:243)
- Better evaluated on expiratory CT scan
- Secondary to a disturbed airflow caused by the proliferation of tumor cells within small airways and constrictive bronchiolitis
- Multiple bronchiolocentric parenchymal nodules of a solid or ground glass appearance (Clin Radiol 2015;70:317)
- Represents aggregates of neuroendocrine cells, tumorlets or carcinoid tumors
- Bilateral mosaic perfusion with air trapping is the most important feature (Clin Radiol 2015;70:317, Clin Imaging 2015;39:243)
- Poorly understood
- Prognosis is mostly linked to the progressive worsening of pulmonary function (Chest 2015;147:415)
- Progression can be rapid (within 2 years) or over a long period
- Presence of constrictive bronchiolitis on histology is not a prognostic factor
- 39 year old woman with a history of chronic cough (BMJ Case Rep 2018;11:e226203)
- 55 year old woman with a coexisting thymoma and Crohn's disease (Ann Thorac Med 2019;14:161)
- Woman in her 60s with a history of unexplained dry cough with metastatic carcinoid tumors to the liver has radiological findings compatible with diffuse idiopathic pulmonary neuroendocrine hyperplasia (BMJ Case Rep 2019;12:e228536)
- 77 year old woman with an atypical carcinoid (J Thorac Dis 2017;9:E774)
- 4 patients with DIPNECH (Medicine (Baltimore) 2018;97:e13806)
- Guidelines for treatment do not exist and no treatment has been shown to be superior (Lung 2015;193:659)
- Patients have been treated with somatostatin analogs / octreotide, sirolimus, everolimus, corticosteroids and transplantation (Lung 2018;196:577, Ann Intern Med 2018;169:197, Lung 2015;193:659)
- Not visible macroscopically
- Generalized intramucosal proliferation of pulmonary neuroendocrine cells forming monolayers or small groups that can protrude into bronchial lumen
- Cells do not cross the mucosal basal lamina
- Cells are round, oval or spindle shaped, have a moderate amount of eosinophilic cytoplasm and have round to oval nuclei with a salt and pepper chromatin
- If neuroendocrine cells cross the mucosal basal lamina = tumorlet
- Poorly defined nodules with infiltrative margins in a fibrotic stroma, usually found in relation to an airway
- Size < 5 mm with < 2 mitoses/2 mm² and absence of necrosis
- A minimum number of foci of proliferating neuroendocrine cells and tumorlets has been proposed but no consensus exists (Hum Pathol 2015;46:176):
- Presence of ≥ 5 neuroendocrine cells distributed in a linear fashion or in clusters within the basement membrane in ≥ 3 bronchioles
- Combined with an association to ≥ 3 tumorlets
- Must be differentiated from secondary DIPNECH, which is a localized neuroendocrine proliferation associated to an underlying lung pathology
- Can be associated with constrictive bronchiolitis (44% of patients) (Chest 2015;147:415)
- Neuroendocrine markers (chromogranin A, synaptophysin, CD56) can be helpful to identify foci of hyperplasia (Histopathology 2011;59:751, Am J Surg Pathol 2018;42:646)
- No specific molecular alteration described (Histopathology 2018;72:142)
- Screening of targetable genes like EGFR, KRAS, c-KIT, PDGFRs, c-MET and ALK did not show any alterations (Am J Surg Pathol 2018;42:646)
- Lung, left upper lobe, wedge resection:
- Multiple foci of neuroendocrine proliferation (neuroendocrine hyperplasia and neuroendocrine tumorlet) (see comment)
- Comment: The presence of foci of neuroendocrine proliferation raises the possibility of a diffuse idiopathic pulmonary neuroendocrine cells hyperplasia (DIPNECH). Correlation with clinical symptoms, pulmonary function tests and high resolution chest CT scan with an expiratory phase is recommended to confirm this diagnosis.
- Meningothelial nodules:
- Perivascular localization instead of bronchiolar proliferation
- Neuroendocrine markers are negative but CD56 is positive (Am J Surg Pathol 2009;33:487)
A 55 year old woman with a long history of chronic cough and asthma undergoes an upper right lobectomy for a lung nodule. The final diagnosis is a typical carcinoid tumor. The adjacent lung parenchyma presents numerous lesions diffusely throughout the lobectomy as depicted in the image. Concerning this diagnosis, which of the following is true?
- Diagnostic criteria are well defined and combine histological, radiological and clinical findings
- EGFR mutations are frequently found
- Constrictive bronchiolitis can be found
- Most patients are men
Comment Here
Reference: Diffuse idiopathic pulmonary neuroendocrine hyperplasia
- There is a generalized intramucosal proliferation of pulmonary neuroendocrine cells
- There is a localized intramucosal proliferation of pulmonary neuroendocrine cells around bronchiectasis
- Tumorlets can have a size of > 5 mm
- A tumorlet is a nodule of neuroendocrine cells that is limited to the bronchial mucosa
Comment Here
Reference: Diffuse idiopathic pulmonary neuroendocrine hyperplasia
- Diffuse proliferation of abnormal, complex lymphatic channels (lymphangiomas) that may involve lung or other organs (Lymphat Res Biol 2011;9:191)
- Pulmonary involvement often accompanied by chylous pleural effusions
- May be progressive and fatal from respiratory failure
- Lymphangioma if proliferation is focal
- Rare condition, typically presents in children and young adults
- No sex predilection
- Localized to lung / chest or can also involve multiple organs, including bone, spleen, soft tissue, liver
- Progressive disease with recurrent effusions and respiratory failure secondary to infections and chylous accumulation
- Congenital, possibly from abnormal lymphatic development
- Generally presents with dyspnea, wheezing, cough and may be confused with asthma
- Occasionally with chyloptysis or hemoptysis
- Clinical presentation and imaging findings may suggest diagnosis, particularly if bone involvement is noted
- Most cases diagnosed with open lung biopsy
- Transbronchial biopsy may confirm disease if vesicles seen on bronchoscopy (Clin Radiol 2005;60:921)
- Thoracocentesis may reveal chylous effusion (elevated triglycerides)
- Xray: nonspecific findings, including pleural effusion, diffuse pulmonary opacities, interstitial thickening
- CT: bilateral ground glass opacities, smooth thickening of interlobular septa, bronchovascular bundles, pleura; may show infiltration of the mediastinal soft tissue by cystic fluid densities
- Children have a worse prognosis than older patients; pleural and lung involvement is adverse prognostic factor (J Pediatr Hematol Oncol 2004;26:136)
- 4 year old girl with recurrent hemorrhagic pericardial effusion due to diffuse lymphangiohemangiomatosis (J Med Case Rep 2010;4:62)
- 35 year old man with diffuse pulmonary lymphangiomatosis (Basic Appl Pathol 2012;5:63)
- Diffuse pulmonary lymphatic disease presenting as interstitial lung disease in adulthood (Am J Surg Pathol 2012;36:1548)
- Kaposiform lymphangiomatosis (Pediatr Blood Cancer 2015;62:901)
- Supportive, including observation and medical management
- Surgical resection for localized disease; pleurocentesis, pleurodesis, pleurodectomy, ligation of thoracic duct (J Thorac Cardiovasc Surg 2007;133:1664)
- Successful lung transplantation has been reported (Am J Transplant 2008;8:1946)
- Subpleural and septal thickening
- Diffuse proliferation of complex, anastomotic lymphatic channels without significant dilatation, lined by benign appearing, flattened endothelial cells
- Prominence of lymphatic channels in visceral pleura, interlobular septa, and bronchovascular bundles with surrounding bundles of spindle cells, interspersed collagen, vessels
- Lymphatic channels may contain acellular, eosinophilic, proteinaceous material
- May show hemorrhagic kaposiform component, with compressed vascular channels, plump spindle cells, hemosiderin
- Kaposiform hemangioendothelioma
- Kaposi sarcoma: HHV8 positive
- Lymphangiectasis: dilation of existing lymphatics in normal distribution
- Lymphangioleiomyomatosis: HMB45 positive, more smooth muscle cells
- Pulmonary capillary hemangiomatosis
- Hundred of drugs are associated with lung injury, including pulmonary edema, pulmonary hemorrhage, airway disease, pleural changes and vascular changes
- Bleomycin and amiodarone (5% - 15% of patients) causes pneumonitis and fibrosis
- Methotrexate, nitrofurantoin causes hypersensitivity pneumonitis
- Abnormal enlargement of air spaces distal to the terminal bronchioles characterized by destruction of the alveolar septa with little or no fibrosis
- Destruction of acinar structure and airspace enlargement
- Affects multiple pulmonary functions and causes chronic respiratory symptoms
- By the Global Initiative for Chronic Obstructive Lung Disease (GOLD), an international organization launched by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. and the World Health Organization (WHO)
- Chronic obstructive pulmonary disease (COPD) (Global Initiative for Chronic Obstructive Lung Disease: 2021 GOLD Reports [Accessed 20 December 2021])
- Common progressive disease that is characterized by persistent respiratory symptoms and usually associated with the prolonged exposure to noxious particles or gases, especially smoking
- Airflow limitation is caused by a combination of airways disease (chronic bronchitis) and lung parenchymal destruction (emphysema)
- Major types of emphysema (Lancet 2004;364:709, Int J Chron Obstruct Pulmon Dis 2008;3:193):
- Centriacinar, centrilobular or proximal acinar emphysema (mostly associated with smoking and COPD)
- Panacinar or panlobular emphysema
- Paraseptal or distal acinar emphysema
- Minor types of emphysema:
- Combined pulmonary fibrosis and emphysema (CPFE)
- Interstitial emphysema
- Bullous emphysema
- Senile emphysema
- Irregular emphysema
- Congenital lobar emphysema
- ICD-10:
- ICD-11:
- Globally, COPD is the third leading cause of death (Lancet 2012;380:2095)
- Affects 1.4% of adults in the U.S. (CDC: Chronic Obstructive Pulmonary Disease (COPD) Includes - Chronic Bronchitis and Emphysema [Accessed 20 December 2021], American Lung Association: Trends in COPD (Chronic Bronchitis and Emphysema) - Morbidity and Mortality [Accessed 13 January 2022])
- M:F = 1:0.9
- Usually older than 45 years old
- Centriacinar emphysema
- Upper lobe predominant
- Respiratory bronchioles and surrounding lung parenchyma
- Panacinar emphysema
- Lower lobe predominant
- Entire acinus
- Paraseptal emphysema
- Upper lung
- Distal part of acinus in subpleural area
- Destruction of lung parenchymal tissue due to chronic inflammation
- Protease mediated destruction of elastin is an important feature (Thorax 2016;71:105)
- Morphological progression (Int J Chron Obstruct Pulmon Dis 2016;11:2287, Clin Anat 2015;28:227)
- Increase in size and number of small fenestrae in alveolar walls (pores of Kohn), which leads to loss of elastic recoil
- Breakdown and merging of fibrovascular trabeculae (framework)
- Remodeling of acini results in airspace enlargement
- Inhalation
- Cigarette smoking and environmental pollutants, especially for centriacinar emphysema
- However, there is individual susceptibility (Annu Rev Physiol 2014;76:493)
- Infections
- Genetic factors
- Alpha-1 antitrypsin deficiency is well known risk factor, especially for panacinar emphysema (Eur Respir J 2017;49:1600154, Lancet 2004;364:709)
- Telomerase mutations, especially for CPFE (J Clin Invest 2015;125:563)
- Polymorphism of serpin family genes (BMC Med Genet 2010;11:159)
- Dyspnea; chronic, progressive and usually irreversible
- Chest inflation
- Combined pulmonary fibrosis and emphysema (CPFE) (Chest 2012;141:222, Eur Respir J 2005;26:586)
- Coexistence of interstitial fibrosis and emphysema of unknown causes
- Patients with CPFE have different pulmonary function tests and outcomes compared to patients with pure emphysema or pure fibrosis
- Interstitial emphysema (Am J Surg Pathol 2014;38:339)
- Air gains access to the pulmonary interstitium to cause air leak and pneumothorax
- Common in premature infants
- Adults: commonly in usual interstitial pneumonia but can occur in any interstitial lung diseases
- Bullous emphysema
- Formation of multiple bullae > 1 cm with thin wall
- Can cause bullae inflation and pneumothorax
- Senile emphysema
- Due to age related alteration of acini
- Irregular emphysema
- Occurs in relation to scars
- Congenital lobar emphysema (Pediatr Clin North Am 1994;41:453)
- Hyperinflation of one or more lobes due to malformation of bronchioles
- Causes respiratory distress
- Can be sporadic or caused by autosomal dominant inheritance
- Primarily diagnosed by imaging studies with compatible clinical manifestation
- Rarely diagnosed solely in biopsy specimens
- More commonly diagnosed in autopsy specimens or as a background finding in resection specimens
- Screening for alpha-1 antitrypsin deficiency (AATD) is recommended by some experts in all patients with COPD (Chronic Obstr Pulm Dis 2016;3:668)
- Alpha-1 antitrypsin (AAT) serum level and genotype
- Xray: overinflation of the lung but it may not be seen in early stages
- Chest CT: emphysematous regions are represented by low attenuation areas (Eur Respir J 2016;48:216)
- Based on exacerbation risk of COPD (Global Initiative for Chronic Obstructive Lung Disease: About GOLD [Accessed 27 December 2021])
- GOLD score 3 or 4 (severe or very severe airflow limitation)
- Previous history of exacerbation and hospitalization
- Faster loss of forced expiratory volume in 1 sec
- COPD assessment test score ≥ 10 (CAT: COPD Assessment Test [Accessed 27 December 2021], Eur Respir J 2009;34:648)
- 31 year old woman with congenital lobar emphysema (Surg Today 2013;43:539)
- 32 year old woman with severe bullous emphysema (Asian Cardiovasc Thorac Ann 2016;24:597)
- 38 year old man with COVID-19, complicated by mediastinal emphysema and pneumothorax (Korean J Radiol 2020;21:541)
- 52 year old man with emphysema from diffuse parenchymal pulmonary amyloidosis (Thorax 2021;76:421)
- 61 year old man with metastatic carcinoma mimicking emphysema (Medicine (Baltimore) 2017;96:e8927)
- 63 year old man with CPFE and severe pulmonary hypertension (Autops Case Rep 2017;7:15)
- 65 year old woman with severe emphysema (Clin Respir J 2017;11:1091)
- 83 year old man died of CPFE (Int J Chron Obstruct Pulmon Dis 2015;10:1299)
- Based on treatment of COPD (Global Initiative for Chronic Obstructive Lung Disease: About GOLD [Accessed 27 December 2021])
- Smoking cessation
- Medications: bronchodilators, antimuscarinic drugs, steroids, etc.
- Ventilatory support
- Surgical interventions: lung volume reduction surgery, bullectomy, lung transplant
- Augmentation therapy for alpha-1 antitrypsin deficiency (Eur Respir Rev 2015;24:46)
- Hyperinflation or ballooning due to entrapment of the air from airway obstruction
- Lungs may be overlapping the heart
- Upper lobes are more involved
- Centriacinar: sparse empty spaces with pigmentation (anthracosis) corresponding enlarged airspaces
- Panacinar: airspaces are more or less evenly inflated throughout the secondary lobules
- Paraseptal: inflated subpleural airspaces with thin walls
- Bullous emphysema
- Descriptive term regarding emphysematous lung with visible bullae upon gross examination
- Bulla: an air filled space of 1 cm in diameter within the lung which has developed because of emphysematous destruction of the lung parenchyma (StatPearls: Bullous Emphysema [Accessed 5 January 2022])
Images hosted on other servers:
- General findings
- Airspace enlargement; the size of airspace in the background parenchyma serves as a reference; although exact microscopic criteria have not been established
- Fragmented alveolar walls
- If the acinar arrangement is maintained, it is representing pores of Kohn
- If not, it is representing acinar destruction
- Mild fibrotic change can be seen
- Any degrees of inflammation can accompany
- Subtype is determined with histological landmarks, although exact classification is better appreciated at gross exam:
- Bronchovascular bundle of terminal bronchiole and arteriole is in the center of acinus
- Connective tissue septa (secondary lobule of Miller) are the periphery of acinus, which is often ambiguous in less inflamed lung
- Note: similar appearance can be seen due to inadequate inflation or fixation of specimen
- Combined pulmonary fibrosis and emphysema (CPFE)
- Centrilobular emphysema in upper lobes
- Usual interstitial pneumonia in lower lobes
- Interstitial emphysema
- Elongated or angulated spaces in fibrotic interstitium
- Surrounded by dense fibrosis and lining of multiple giant cells but not epithelium
- Most commonly around bronchovascular bundles
- Elastic stains, such as elastic van Gieson and elastica Masson
- Elastic fibers are less organized and appear unraveled and loose in emphysematous lung (Eur Respir J 2008;31:998)
- Not required for diagnosis
Emphysema histology
Emphysema classification
- Lung, right upper lobe, wedge resection:
- Squamous cell carcinoma (see comment)
- Comment: Background lung parenchyma with emphysema, respiratory bronchiolitis and smoking related interstitial fibrosis.
- Usual interstitial pneumonia:
- Interstitial emphysema versus honeycomb change: honeycomb is the air space surrounded by bronchiolar epithelium on fibrotic wall
- Lymphangiomyomatosis:
- Cystic air spaces, proliferation of spindle to epithelioid cells (HMB45+)
- Pulmonary Langerhans cell histiocytosis:
- Stellate nodules with fibrosis and Langerhans cells (CD1a+)
Comment Here
Reference: Emphysema
- Bronchiolitis
- Centriacinar emphysema
- Interstitial emphysema
- Panacinar emphysema
- Usual interstitial pneumonia
Comment Here
Reference: Emphysema
- Pulmonary enteric adenocarcinoma (PEAC) is an extremely rare subtype of non-small cell lung cancer that is characterized by pathological features similar to those of colorectal adenocarcinoma
- Morphologically similar to colorectal adenocarcinoma
- Enteric pattern may coexist with other adenocarcinoma patterns
- Diagnosis of enteric adenocarcinoma should be made when the enteric component is > 50% of the tumor (Medicine (Baltimore) 2017;96:e8153, Int J Clin Exp Pathol 2014;7:1266)
- Adenocarcinoma, enteric type
- Primary lung enteric adenocarcinoma
- Pulmonary intestinal type adenocarcinoma (not recommended)
- Pulmonary adenocarcinomas showing enteric differentiation (not recommended)
- ICD-O: 8144/3 - adenocarcinoma, intestinal type
- ICD-10: C34 - malignant neoplasm of bronchus and lung
- ICD-11: 2C25.0 & XH0349 - adenocarcinoma of bronchus or lung & adenocarcinoma, intestinal type
- Overall prevalence in non-small cell lung carcinoma and primary pulmonary adenocarcinoma is 0.5% and 0.68%, respectively (Transl Oncol 2021;14:101123)
- Large proportion of patients are elderly (Oncotarget 2017;8:63442, J Transl Med 2018;16:81)
- Youngest patients in the literature are a 24 year old man and 26 year old woman (Case Rep Pulmonol 2014;2014:282196)
- Recent epidemiological studies have revealed that it usually occurs in ex smokers or nonsmokers; in previous studies, 45.6% of patients with PEAC reported smoking (Transl Oncol 2021;14:101123)
- M:F = 4:5 (Int J Clin Exp Pathol 2014;7:1266)
- Generally located in the right upper lobe (Transl Oncol 2021;14:101123, Int J Clin Exp Pathol 2014;7:1266)
- PEAC is mostly located peripherally (Medicine (Baltimore) 2017;96:e8153)
- High ERBB2, MMR and KRAS mutation rates; low EGFR and BRAF mutation rates (Transl Oncol 2021;14:101123)
- Many studies have reported that 45.6% of patients with PEAC are smokers (Transl Oncol 2021;14:101123)
- Clinical features are not substantially different from those of other lung adenocarcinomas
- Most patients are elderly men and smokers with advanced stage disease (Hum Pathol 2017;64:179, Exp Ther Med 2016;11:201, Medicine (Baltimore) 2017;96:e8153)
- Nonproductive cough and chest pain, fever, hemoptysis (Int J Clin Exp Pathol 2014;7:1266)
- Compared with primary pulmonary invasive adenocarcinoma, patients with PEAC are older and have larger lesions at more advanced stages (Medicine (Baltimore) 2017;96:e8153)
- Coughing is the most common but nonspecific symptom (Chin Med J (Engl) 2019;132:1368, Oncol Lett 2017;13:4651)
- Other symptoms include expectoration, hemoptysis, chest tightness, chest pain, shortness of breath, fever, night sweats, throat discomfort, headache, fatigue and enlarged cervical lymph nodes (Chin Med J (Engl) 2019;132:1368)
- lt is crucial to exclude metastatic colorectal carcinoma, which is more common than primary enteric type adenocarcinoma in the lung, by careful clinical evaluation (Am J Surg Pathol 2005;29:660)
- No gastrointestinal symptoms (e.g., hematochezia, nonproductive abdominal pain, diarrhea and ventosity) (Transl Oncol 2021;14:101123, ScienceDirect: Gastrointestinal Distress [Accessed 21 March 2023], ScienceDirect: Rectal Bleeding [Accessed 21 March 2023])
- Tumor with enteric morphology and expression of intestinal markers (CDX2, CK20, HNF4a or MUC2) and coexpression of TTF1 or CK7
- Considering the common clinical features with other adenocarcinomas, a combination of clinical signs, histopathology, IHC and molecular features is required for a definitive diagnosis
- Colorectal adenocarcinoma should be ruled out by endoscopy and radiology, even if the pathological results correspond to primary enteric adenocarcinoma of the lung
- Pathology and immunohistochemistry results are mostly used in the diagnosis of PEAC (World J Clin Cases 2021;9:9236)
- The patient can finally be diagnosed with PEAC when primary PEAC consists mainly of tissue with > 50% intestinal differentiation, tumor cells are positive for at least 1 immunohistochemical marker associated with colorectal cancer (e.g., CK20, CDX2, MUC2, villin, etc.) and tumors of gastrointestinal origin are excluded
- CK7 is important for pulmonary origin
- Consistent overexpression of CEA and CA199 appears to be closely associated with advanced pathological stage in primary PEAC (J Transl Med 2018;16:81, World J Clin Cases 2021;9:9236)
- Solid nodules (Medicine (Baltimore) 2017;96:e8153)
- On CT, patients with PEAC had larger lesions than patients with primary pulmonary invasive adenocarcinoma (Medicine (Baltimore) 2017;96:e8153)
- Aggressive cancer characterized by rapid growth and early metastatic behavior (Oncol Lett 2017;13:4651)
- 24 year old man and 26 year old woman with enteric type lung adenocarcinoma in resected lung mass (Case Rep Pulmonol 2014;2014:282196)
- 53 year old woman presented with a mass around the right sternoclavicular joint and cough (Exp Ther Med 2016;11:201)
- 62 year old man with pancreatic metastases (Oncol Lett 2017;13:4651)
- Current treatment strategy is the same as for primary adenocarcinoma
- A comprehensive treatment supported by surgical treatment, chemotherapy, radiotherapy or targeted therapy is selected according to clinical stage (Transl Oncol 2021;14:101123, World J Clin Cases 2021;9:9236)
- Patients may benefit from anti-HER2 therapy and immune checkpoint inhibitors (Transl Oncol 2021;14:101123)
- EGFR tyrosine kinase inhibitor in PEAC is unreasonable and inefficient (J Transl Med 2018;16:81)
- Patients may be more likely to benefit from checkpoint blocking immunotherapy (J Transl Med 2018;16:81)
- Although only limited data are available, alterations eligible for tyrosine kinase inhibitor therapy seem to be less common than in other non-small cell lung cancer subtypes (Mod Pathol 2019;32:855)
- Enteric type adenocarcinomas are well circumscribed tumors; section surface may include areas of focal bleeding and necrosis (Int J Clin Exp Pathol 2014;7:1266)
- Often includes geographic necrosis (Transl Oncol 2021;14:101123)
- Tumors are ~10 - 115 mm (Transl Oncol 2021;14:101123)
- Cross sectional surface is gray-white or gray-yellow; some tumors contain hard or necrotic areas (Transl Oncol 2021;14:101123)
- An adenocarcinoma with enteric morphology may be said to be present on frozen sections but without immunohistochemical study and radiological and clinical correlation, it cannot be determined whether the malignancy in the lung is primary or secondary
- Enteric pattern exhibits the features of colorectal adenocarcinoma, which has glandular, papillary or cribriform structures with luminal necrosis, tall columnar cells with pseudostratified and atypical nuclei, and eosinophilic cytoplasm (Oncol Lett 2017;13:4651, Int J Clin Exp Pathol 2014;7:1266)
- Enteric pattern can be admixed with other patterns of adenocarcinoma
- Mitotic figures are often found
- Stroma is often desmoplastic and associated with prominent inflammatory cell infiltrates
- Histologically, PEAC has features of intermediate differentiation and sometimes forms a cribriform pattern with tall columnar cells arranged in irregular acini or with extensive central necrosis (Oncotarget 2017;8:63442)
Contributed by Sevilay Özmen, M.D. and Pembe Oltulu, M.D.
- Sheets or papillary clusters of high columnar cells
- Intracytoplasmic mucin
- CK7 / CK20 (J Transl Med 2018;16:81)
- CK7 expression in > 80% of tumor cells helps differential diagnosis from colorectal adenocarcinoma
- CDX2 (J Transl Med 2018;16:81, Chin Med J (Engl) 2019;132:1368, Front Oncol 2022;12:988625, Medicine (Baltimore) 2017;96:e8153)
- MUC2 positive in pulmonary intestinal type adenocarcinoma (J Transl Med 2018;16:81)
- Villin (Chin Med J (Engl) 2019;132:1368, Transl Oncol 2021;14:101123)
- HNF4a (Cancer Sci 2017;108:1888)
- TTF1, Napsin A: can be very weakly or focally positive (Mod Pathol 2019;32:855)
- MUC1 (Masui 1992;41:369)
- CDH17, only very rare expression (Mod Pathol 2008;21:1379, Adv Anat Pathol 2014;21:131, Am J Clin Pathol 2012;138:211, J Transl Med 2018;16:81, Oncotarget 2017;8:63442)
- SATB2, only very rare expression (Hum Pathol 2017;64:179, J Transl Med 2018;16:81, Oncotarget 2017;8:63442)
- Beta catenin (Hum Pathol 2017;64:179)
- KRAS mutations are more frequent in enteric adenocarcinoma than in nonenteric pulmonary adenocarcinoma (J Transl Med 2018;16:81, Mod Pathol 2019;32:855)
- Higher nonsynonymous tumor mutation burden and more frequent MMR mutation (J Transl Med 2018;16:81)
- ERBB2 (HER2) amplification / mutation and MMR gene mutation can also occur (J Transl Med 2018;16:81)
- PIK3CA mutations and ALK rearrangement can also occur
- KRAS, HER2, MMR mutation rates are higher while EGFR is much lower (Transl Oncol 2021;14:101123)
- No ALK, MET, EGFR or ROS1 alterations (Mod Pathol 2019;32:855)
- EGFR mutation is common in primary lung adenocarcinoma but is rarely reported in PEAC (Front Oncol 2022;12:988625)
- Comutations of EGFR, KRAS and TP53 are possible (Front Oncol 2022;12:988625)
- Lung, right upper lobe, resection:
- Pulmonary enteric adenocarcinoma (see synoptic report)
- Lung, biopsy:
- Adenocarcinoma with enteric differentiation (see comment)
- Comment: In the case where malignancy in the gastrointestinal tract was excluded, the findings are consistent with enteric differentiated adenocarcinoma of the lung.
- Metastatic colorectal adenocarcinoma:
- BRCA
- EGFR
- KRAS
- NRAS
- PIK3CA
Comment Here
Reference: Enteric adenocarcinoma
A 60 year old man presented with complaints of cough, chest tightness and shortness of breath. He was a former smoker with 20 pack years. Chest tomography showed a 6 cm mass in the periphery of the lung. A biopsy was performed. Tumor cells immunohistochemically express CK7, CK20, CDX2 and TTF1 and the patient does not show malignancy in the gastrointestinal tract. According to the image above, what is the pathological diagnosis?
- Adenocarcinoma with enteric differentiation
- Invasive mucinous adenocarcinoma of the lung
- Large cell carcinoma of the lung
- Small cell lung cancer
- Squamous cell lung cancer
- Also called Churg-Strauss syndrome
- Very rare
- Systemic vasculitis resembling polyarteritis nodosa or microscopic polyangiitis; associated with asthma, peripheral eosinophilia, pulmonary involvement and fever
- Rarely presents without pulmonary disease as fever of unknown origin
- < 50% have positive ANCA, often antimyeloperoxidase
- Steroids: effective, but patients may relapse
- Lung and extrapulmonary sites (skin, heart, nervous system, GI) have prominent eosinophilic infiltrate, granulomatous reaction around necrotic foci with radially arranged histiocytes and pallisading giant cells near small arteries or arterioles, eosinophilic vasculitis
- May have fibrin rich edema, lymphocytes, sarcoid-like granulomas, focal fibrosis and eosinophilic microabscesses
- Granulomatosis with polyangiitis (Wegener's): kidney involvement, no asthma, no tissue or serum eosinophilia
- Rheumatoid nodules: no tissue or serum eosinophilia, no asthma
- Acute eosinophilic pneumonia:
- Diagnosis of exclusion
- Lung disease associated with eosinophils in alveolar and interstitial spaces, usually with peripheral eosinophilia but excluding Langerhans cell histiocytosis
- Must exclude drug reactions (antibiotics, cytotoxic or anti-inflammatory drugs), immune disorders (Churg-Strauss syndrome, collagen vascular disease, asthma, hypereosinophilic syndrome, chronic eosinophilic leukemia NOS, myeloid and lymphoid neoplasms with eosinophilia and rheumatoid arthritis), infections (bacteria, Aspergillus, HIV, parasites - helminths, Dirofiliaria and filarial) or tobacco (flavored cigars, new onset of smoking (Chest 2007;131:1234, JAMA 2004;292:2997)
- Chronic eosinophilic pneumonia:
- Reaction to drugs, Aspergillus or other fungi, occurs with some malignancies and connective tissue diseases
- Prolonged (months) febrile illness with cough, weight loss, generalized fatigue, drenching night sweats and peripheral eosinophilia
- Associated with chronic asthma, usually in setting of allergic bronchopulmonary aspergillosis
- Xray: patchy infiltrates in peripheral lungs with central sparing
- Symptoms: fever, weight loss and shortness of breath
- Xray: peripheral infiltrate
- Classified as simple, acute or chronic
- Simple eosinophilic pneumonia (see Loeffler syndrome)
- Acute eosinophilic pneumonia: onset in 1 - 4 days, accompanied by fever, cough, dyspnea and chest pain; unknown cause, prominent eosinophils in bronchoalveolar lavage fluid and diffuse alveolar damage at biopsy (Am J Respir Crit Care Med 2002;166:1235)
- 6 year old boy post chemotherapy for neuroblastoma with bilateral pulmonary infiltrates (Case #105)
- Steroids cause dramatic response / complete resolution to acute or chronic forms
- Chronic eosinophilic pneumonia: consolidation, mucus plugs in distal bronchi or bronchioles
- Acute eosinophilic pneumonia:
- Acute form has diffuse alveolar damage
- Alveolar and interstitial infiltration by eosinophils, also plasma cells and histiocytes
- May have Charcot-Leyden crystals
- Variable angiitis, granulomatosis, fibrosis, mucus plugging and bronchiolitis with necrosis
- Chronic eosinophilic pneumonia:
- Patchy intraalveolar edema, interstitial inflammation with giant cells and eosinophils with scattered histiocytes and plasma cells
- Mucus plugs composed of inflammatory cells and cellular debris
- Charcot-Leyden crystals may be present
- Often bronchiolitis obliterans
- Blood vessel infiltration by inflammatory cells is common but no vascular necrosis
- No diffuse alveolar damage
- Desquamative interstitial pneumonitis (DIP):
- If extensive intra-alveolar macrophages
- Langerhans cell histiocytosis:
- Interstitial infiltrate, Langerhans cells
- Extrinsic allergic alveolitis:
- Less edema, more interstitial inflammation
- Parasites
- Fungal allergies
- Other causes of pulmonary eosinophilia must be excluded
- Low grade malignancy that arises from submucosal bronchial glands, mimics similar salivary gland tumor
- Very rare in lung, only case reports and small series
- Long interval to recurrence or metastasis
- Rare, low grade, primary salivary gland-type carcinoma of the lung
- Typically arises in bronchial tree from submucosal glands
- Characterized by biphasic proliferation of duct-like epithelial cells with surrounding myoepithelial cells
- Previous designations include adenomyoepithelioma, epithelial myoepithelial tumor, epithelial myoepithelial tumor of unknown malignant potential, pneumocytic adenomyoepithelioma (Hum Pathol 2009;40:366, Mod Pathol 2001;14:521)
- C33 Malignant neoplasm of trachea
- C34.00 Malignant neoplasm of unspecified main bronchus
- C34.01 Malignant neoplasm of right main bronchus
- C34.02 Malignant neoplasm of left main bronchus
- Code more peripheral lesions depending on specific lobe, laterality and extent
- Extremely rare in lung, case reports mostly in adults, rare case report in child (J Pediatr Hematol Oncol 2009;31:206)
- No clear sex predominance
- Bronchial tree, usually endobronchial but a few cases peripheral / parenchymal
- Low grade malignancy with rare cases of metastasis to chest wall (Lung Cancer 2014;83:416), skull (Case Rep Oncol Med 2011;2011:610383) and lymph nodes (Hum Pathol 2009;40:366)
- Arises from submucosal bronchial glands, the lung counterpart of the intercalated duct of the salivary gland (Oncol Lett 2015;10:175)
- Cough, hemoptysis, dyspnea or obstructive symptoms if endobronchial location
- Peripheral lesions may be asymptomatic
- Challenging to diagnose with small biopsy specimens
- Exclude metastasis from salivary gland
- Complete surgical resection generally curative
- High mitotic rate, tumor necrosis and nuclear pleomorphism appear to be adverse prognostic factors (Am J Surg Pathol 2001;25:1508)
- 34 year old man with tracheal tumor (J Thorac Dis 2014;1:S194)
- 52 year old woman with progressive cough, dyspnea and wheezing (Case of the Week #357)
- 53 year old woman with tumor showing lobular solid growth and lymph node metastases (Tuberc Respir Dis (Seoul) 2015;78:428)
- 57 year old man with incidental endobronchial tumor (Case Rep Pathol 2012;2012:319434)
- 72 year old woman with tumor showing high grade transformation (Oncol Lett 2015;10:175)
- 73 year old man with bronchial tumor (Arch Pathol Lab Med. 2003 Apr;127:e177)
- Complete surgical resection
- May recur after local therapy or incomplete excision (Clin Lung Cancer 2007;8:386)
- Intraluminal polypoid mass in bronchus; may invade parenchyma
- Well circumscribed, unencapsulated, tan, firm
- Variable size averaging a few centimeters
- Well circumscribed mass with pushing margin
- Thin fibrous septa with variable hyalinization or sclerosis
- Biphasic proliferation of inner epithelial and outer myoepithelial cells with formation of bilayered, duct-like structures
- Appearance and proportion of two cell types may be variable
- Epithelial cells flattened, cuboidal or columnar with somewhat clear to eosinophilic cytoplasm
- Myoepithelial cells may be indistinct, flattened, spindled or clear
- Lumens may contain pale to eosinophilic amorphous material or debris
- Scant inflammatory infiltrate may be present
- Mitoses, significant nuclear atypia, necrosis and hemorrhage typically absent
Contributed by Roseann Wu, M.D., M.P.H. and Case #357
Images hosted on other servers:
- Epithelial cells: CK7, pankeratin, EMA
- Myoepithelial cells: S100, muscle specific actin, p63, CK5/6
- Potential role of p27 kip-1 protein (Diagn Pathol 2011;6:71)
- Acinic cell carcinoma
- Adenoid cystic carcinoma with a tubular pattern
- Adenocarcinoma
- Clear cell ("sugar") tumor
- Metastatic clear cell carcinoma
- Metastatic epithelial myoepithelial carcinoma (usually parenchymal, not endobronchial)
- Mucoepidermoid carcinoma
- Myoepithelial carcinoma
- Myoepithelioma
- Pleomorphic adenoma
- Pneumocytic adenomyoepithelioma: has bronchial minor salivary gland origin; shows myoepithelial and pneumocytic differentiation (Am J Surg Pathol 2007;31:562)
- Clinicopathological analysis of primary salivary gland type lung cancer (J Thorac Oncol 2013;8:1578)
- Epithelial myoepithelial carcinoma primary to the lung is believed to arise from what cell type(s)?
- Club cells
- Ciliated columnar cells
- Submucosal bronchial glands
- Type 1 pneumocytes
- Type 2 pneumocytes
- Formerly called intravascular bronchioloalveolar tumor (see also Soft tissue topic)
- 80% women, usually young adults
- Neoplastic, but usually not metastatic
- Progressive growth, usually remains within thoracic cavity, may cause death from respiratory insufficiency
- Other sites: liver, bone
- 10% have peripheral eosinophilia
- Poor prognosis if vascular spread, pleural involvement, severe symptoms
- 54 year old man with multiple pulmonary nodules (Arch Pathol Lab Med 2003;127:e319)
- Multiple round, well demarcated nodules < 2 cm, often in lower lung, with a gray-white peripheral rim and chondroid appearance
- Resembles metastasis, granulomatous disease or interstitial lung disease
- May spread along pleura or pericardium and resemble mesothelioma
- Central hyalinized stroma, eosinophilic amorphous material or coagulative necrosis with variable calcification surrounded by thin rim of plump eosinophilic endothelial cells
- Clusters fill alveoli, apparently through pores of Kohn, and occasionally bronchioles, arteries, veins
- Nuclei are bland, round / oval, may have cytoplasmic vacuoles
- No / minimal mitoses
- Lung architecture preserved
- CD10 (Arch Pathol Lab Med 2009;133:1965), factor VIII, CD31, CD34
- Variable ER and PR
- Endothelial features: well developed basal lamina, pinocytotic vesicles, occasional Weibel-Palade bodies
- Metastatic tumor from liver or other sites: destroy lung architecture, high mitotic rate
- Sclerosing hemangioma: destroys lung architecture, negative for vascular markers
- Rare tumor resembling fetal lung in pseudoglandular stage
- Either high grade or low grade
- May be a variant of pulmonary blastoma without malignant mesenchymal components
- Low grade tumors associated with upregulation of Wnt signaling pathway (Mod Pathol 2002;15:617)
- High grade variant is very aggressive
- Irregular tubular structures of columnar epithelial cells with clear cytoplasm and oval nuclei, optically clear nuclei rich in biotin
- Resembles fetal lung in pseudoglandular stage
- High grade: disorganized glands, large vesicular nuclei, prominent nucleoli, pronounced anisonucleosis, transition to conventional adenocarcinoma, broad areas of necrosis, desmoplastic stroma, p53+, AFP+, no morules (Am J Surg Pathol 1998;22:399)
- Low grade tumors: subnuclear vacuoles with tigroid features, small, uniform, round nuclei, morules, neuroendocrine differentiation in glandular epithelial cells (Am J Clin Pathol 2010;134:894)
- Rare; currently not considered a form of idiopathic interstitial pneumonia
- Intra-alveolar multinucleated giant cells and other inflammatory cells
- Giant cells often phagocytose other histiocytes
- Autoimmune disease affecting men > women, usually ages 15 - 29 years, with simultaneous sometimes massive hemorrhagic interstitial pneumonitis and rapidly progressive (crescentic) glomerulonephritis
- Sometimes preceded by chemical or drug exposure, viral infection or malignancy
- Genetic predisposition, higher incidence with some HLA subtypes
- Death common due to uremia
- Due to IgG antibodies to basement membrane of alveoli and glomeruli
- Plasma exchange (removes antibodies and chemical mediators)
- Immunosuppressive therapy (prevents further antibody production)
- Lungs: heavy, focal necrosis of alveolar wall, fibrous thickening of septa with mild hyperplasia of alveolar lining cells, organization of blood in alveolar space and hemosiderin laden macrophages; linear deposits of immunoglobulin along basement membrane
- Kidney: focal proliferative to crescentic glomerulonephritis with linear deposits of immunoglobulin and complement along basement membrane, similar to lung
- Mitral stenosis, periarteritis nodosa, SLE and systemic vasculitis all cause secondary pulmonary alveolar bleeding and hemosiderosis
- Immune complex glomerulonephritis: granular pattern of immunofluorescence
- Idiopathic pulmonary hemosiderosis: no antibodies
- Granulomatosis with polyangiitis (GPA) is a systemic autoimmune vasculitis syndrome commonly involving the lower respiratory tract, the upper respiratory tract and the kidney
- Characterized by a necrotizing vasculitis and a systemic granulomatous inflammatory process which replaces the involved tissues
- Classic GPA clinicopathological triad
- Vascular, respiratory and renal involvement
- Histopathological features
- Necrotizing vasculitis of small to medium sized arteries and veins
- Eosinophilic palisading granulomas
- Glomerulonephritis
- Association with antineutrophil cytoplasmic antibodies (ANCA) positivity
- C-ANCA is more specific for GPA
- Obsolete term (not recommended): Wegener granulomatosis (WG), name changed due to Wegener's Nazi association in the 1930s (Lancet 2006;367:1362)
- ICD-11: 4A44.A1 - granulomatosis with polyangiitis
- Incidence
- M = F (slight male predominance)
- Mean age: 50 years (Int J Immunopathol Pharmacol 2016;29:151)
- Rare in children and young adults
- Caucasian population of European descent is most commonly affected
- Risk factors
- Infectious, environmental and drug induced triggers
- First degree relatives with GPA
- HLA-DPB1*0401 variant as genetic risk factor (Ann Rheum Dis 2011;70:707)
- Thyroid disease: Graves disease and Hashimoto thyroiditis (Arthritis Rheum 2003;48:2299)
- Systemic vasculitis may manifest in a classic triad involving
- Head and neck region (upper respiratory tract)
- Lower respiratory tract
- Kidney
- Can also occur in a combination of 1 or 2 of the classic sites, along with additional sites
- Skin, joints, middle ear, eye and nervous system
- Solitary lung involvement can occur and is difficult to diagnose for the pathologist
- Reference: Autoimmun Rev 2014;13:1121
- Exact pathophysiology is unclear and pathogenesis is likely multifactorial
- Exact mechanism is unclear
- Thought to be a result of exposure to infectious, environmental or drug induced triggers in patients with predisposing genetic background
- Recent discoveries suggest excessive activation of neutrophils that form neutrophil extracellular traps (NETs) (Front Immunol 2019;10:2617)
- Excessive NET formation is involved in ANCA mediated vascular injury and production of ANCA themselves
- Viscous cycle of NET formation and ANCA production is thought to drive GPA pathogenesis
- Typically manifest in upper / lower respiratory tract and kidney; pulmonary symptoms / signs in the absence of upper respiratory symptoms / signs are unusual
- Most common presenting symptoms / signs (local): rhinorrhea, purulent / bloody nasal discharge, oral or nasal ulcers, sinus pain, cough, hemoptysis and chest pain
- Most common presenting symptoms / signs (systemic): polyarthralgias, myalgias, fever, malaise, weight loss
- Reference: Arthritis Rheum 1990;33:1101
- Clinical setting: corresponding sites of pathology, symptoms, radiological findings and patient demographics
- Positive ELISA serum C-ANCA test or less commonly P-ANCA test
- Biopsy or resection shows characteristic histologic findings consistent with GPA
- Special stains and cultures exclude infections
- Reference: Arthritis Rheum 1990;33:1101
- ELISA test for serum antineutrophil cytoplasmic antibodies (ANCA) serotypes
- Cytoplasmic (C) [PR3]-ANCA (proteinase 3); highly specific for GPA
- Perinuclear (P) [MPO]-ANCA (myeloperoxidase); less specific for GPA
- C-ANCA found in 90% with active generalized disease and 60% with limited disease
- Positive test in an appropriate clinical setting supports GPA diagnosis
- Negative test does not exclude the diagnosis, especially with characteristic histopathology
- ANCA positivity strongly related to relapse in GPA with renal involvement (J Am Soc Nephrol 2015;26:537)
- Upper respiratory tract involvement: sinonasal mucosal thickening with bony / cartilaginous erosion
- Lower respiratory tract involvement: 4 patterns of involvement (Chest 1990;97:906, J Thorac Imaging 1988;3:33, Clin Radiol 1982;33:545)
- Nodules with or without cavitation, often around bronchovascular bundles or in a subpleural distribution
- Pulmonary hemorrhage, which can occur with nodules but in some cases the consolidation associated with the hemorrhage predominates
- Reticulonodular pattern can be the first pattern and is often asymptomatic
- Peripheral wedge-like consolidation
- Renal involvement: typically a hypovascular mass with unclear margins; in some cases, opacity of the perirenal fat and para-aortic lymph nodes can be seen
- Can be fatal without treatment
- Excellent prognosis with treatment; 5 year survival is > 80%
- Increased incidence of infection with higher disease burden, long term exposure to glucocorticoids and kidney involvement
- Reference: Nat Rev Dis Primers 2020;6:71
- 15 year old girl with granulomatosis with polyangiitis with cardiac involvement (AME Case Rep 2022;7:8)
- 16 year old girl with granulomatosis with polyangiitis masquerading as tuberculosis (Pan Afr Med 2021;38:285)
- 25 year old man with granulomatosis with polyangiitis presented with pulmonary, cutaneous and neurological manifestations (Cureus 2022;14:e31753)
- 25 year old woman with granulomatosis with polyangiitis diagnosed during the postpartum period (Matern Health Neonatol Perinatol 2023;9:2)
- 25 year old woman with granulomatosis with polyangiitis presented with thrombotic vasculopathy (Cureus 2023;15:e34479)
- 32 year old woman with granulomatosis with polyangiitis related pancolitis and stricturing small bowel disease (Case Rep Gastroenterol 2023;17:155)
- 36 year old man with granulomatosis with polyangiitis presented with recurrent myocardial infarction (Clin Exp Emerg Med 2023;10:246)
- 44 year old woman with granulomatosis with polyangiitis presented with oral involvement (J Dent Sci 2023;18:451)
- 48 year old woman with granulomatosis with polyangiitis presented with acute pancreatitis (ACG Case Rep J 2023;10:e00986)
- Man in his 60s with granulomatosis with polyangiitis presented with multiple renal masses (Radiol Case Rep 2023;18:1292)
- 65 year old man with obstructive pneumonia progressing to hypertrophic pachymeningitis (Medicine (Baltimore) 2021;100:e24028)
- 66 year old woman with rare initial presentation of pancreatic disease (BMJ Case Rep 2021;14:e241033)
- 71 year old woman with spontaneously regressed granulomatosis with polyangiitis (Respir Investig 2021;59:372)
- 72 year old woman with ANCA negative granulomatosis with polyangiitis, complicated with peripheral neuropathy; the patient underwent remission induction with mepolizumab monotherapy (Intern Med 2023 Feb 1 [Epub ahead of print])
- 75 year old woman with refractory granulomatosis with polyangiitis complicated with IgG4 related disease (Intern Med 2023 Feb 22 [Epub ahead of print])
- 77 year old woman with ANCA negative granulomatosis with polyangiitis with multiple brain infarctions and endomyocarditis (Heliyon 2023;9:e12881)
- Usually treated with corticosteroids and cyclophosphamide with excellent prognosis
- Recent addition of rituximab (monoclonal antibody) for poorly responding cases or relapses suggested (N Engl J Med 2010;363:221)
- Methotrexate serves as effective maintenance therapy for mild / limited GPA (Am J Med 2003;114:463)
- Multiple bilateral pulmonary nodules with frequent cavitation; rarely manifests as solitary lung lesion
- Necrotizing granulomatous inflammation, reactive changes in the background lung should not be interpreted as malignancy
- Necrotizing granulomatous inflammation
- Deeply basophilic necrosis due to the presence of nuclear debris derived from necrosis and karyorrhexis; this type of blue necrosis is referred to as dirty necrosis
- Necrosis is often described as suppurative given the large number of neutrophils that are often present
- Necrosis is often described as geographic, which is best appreciated at low magnification and refers to the irregular contours of the necrosis that resemble the outlines of countries on a map (Am J Surg Pathol 1991;15:315)
- Multinucleated giant cells in the granulomatous inflammation often have strikingly hyperchromatic nuclei
- Medium to small arteries and veins are heavily inflamed in GPA, the inflammatory cells being neutrophils, histiocytes and lymphocytes
- Necrotizing vasculitis is one of the diagnostic features and consists of necrosis of the vessel wall by an inflammatory infiltrate; this is best recognized when the vasculitis focally involves the vessel and the remainder of the vessel is intact (Hum Pathol 1988;19:1065)
- Elastic stains can help identify blood vessels; however, this may present a pitfall since completely necrotic blood vessels within zones of necrosis can be present that do not qualify for true necrotizing vasculitis
- GPA can also present as diffuse alveolar hemorrhage due to the destruction of capillaries in the alveolar septa
- This produces an inflammatory infiltrate that is rich in neutrophils and karyorrhectic debris that produces a histologic picture similar to leukocytoclastic vasculitis of the skin
- This histologic finding is typically classified as capillaritis (Semin Respir Crit Care Med 2004;25:475)
- In these cases, the adjacent alveoli are filled with hemosiderin laden macrophages, red blood cells and neutrophils
- Elastic stains can aid in the identification of areas of vasculitis
- Fungal stains (GMS and PASD) are negative for fungal organisms
- Acid fast stains (ZN) are negative for acid fast organisms
Granulomatosis with polyangiitis (pathophysiology, symptoms, treatment)
GPA symptoms, diagnosis, treatment
GPA review
GPA discussion at 5:01
- Lung, right, lower lobe, wedge biopsy:
- Necrotizing granulomatous inflammation and vasculitis, most consistent with granulomatosis with polyangiitis (GPA) (see comment)
- Comment: In this specimen, there is prominent granulomatous inflammation and vasculitis. Histochemical stains for fungal and acid fast organisms are negative. The features are most consistent with a diagnosis of granulomatosis with polyangiitis (GPA). Correlation with the clinical findings and serology is recommended for definitive classification.
- Granulomatous infection:
- Cultures or special stains are positive
- Eosinophilic granulomatosis with polyangiitis:
- P-ANCA positive
- Eosinophil rich inflammation
- Microscopic polyangiitis:
- Absence of granulomatous inflammation
- Acute lupus pneumonitis:
- Nonspecific findings with alveolar wall damage, inflammation, edema and features of acute lung injury including hyaline membranes
- Idiopathic pulmonary hemosiderosis:
- Absence of vasculitis and granulomatous inflammation
- ANA
- C-ANCA
- CRP
- ESR
- P-ANCA
Comment Here
Reference: Granulomatosis with polyangiitis (GPA)
Comment Here
Reference: Granulomatosis with polyangiitis (GPA)
- 1 section per cm of tumor diameter, representative of grossly distinct areas
- Margins (bronchial, pulmonary artery / vein, visceral pleura, other surgical margins)
- Tumor and adjacent lung
- Tumor and bronchial wall
- Tumor and pleura
- Bronchial mucosa proximal to tumor
- May be difficult to distinguish:
- In situ and invasive carcinoma of bronchial mucosa (Arch Pathol Lab Med 2012;136:1515)
- Bronchioloalveolar hyperplasia and carcinoma
- Primary and metastatic disease
- Touch preparation cytology recommended to supplement frozen section findings (J Clin Pathol 2010;63:675)
- Herpes simplex virus (HSV), serotypes HSV-1 and HSV-2, cause acute infection followed by latent phase that may reactivate to infectious form
- See also Skin - nontumor chapter
- HSV-1 and HSV-2 are alpha group herpes viruses with similar genotypes but serologic differences; may both infect the lung
- HSV-1 usually affects oral pharynx; HSV-2 usually causes genital infection
- Virus spreads via sensory neurons where latent infection is established
- Reactivation may be symptomatic or asymptomatic, virus spreads via nerves to mucus membranes or skin, where it replicates
- Newborns (see below), patients with impaired mucosal defenses, burn patients, trauma patients, and severely immunocompromised patients are at greatest risk
- Also associated with coexisting bacterial pneumonia (J Crit Care 2011;26:432.e1)
- Also be caused by intubation of patient with active oral disease
- Immunostains, PCR, culture or electron microscopy can confirm the diagnosis if necessary
- Diffusely firm lungs with small yellow / red necrotic areas
- Interstitial pneumonia with necrosis of bronchial and alveolar epithelium and acute and chronic inflammatory infiltrate
- Occasional intranuclear viral inclusions at edge of necrotic areas
- Neutrophilic infiltrates may resemble bacterial bronchopneumonia, but Cowdry type A or B nuclear inclusions are generally diagnostic
- Lung: organ participating in and in charge of respiration, namely, gas exchange
- Lung histology: basic microscopic structures of the unaffected lung (i.e. nonneoplastic, noninflammatory and nondegenerated lung tissue)
- Bronchus has cartilage and bronchial glands, while bronchiole lacks them (Mills: Histology for Pathologists, 5th Edition, 2019)
- Bronchi and bronchioles up to terminal bronchioles are pure conducting airways, while respiratory bronchioles and alveoli play a role in gas exchange
- There are 2 different definitions of a lobule (secondary lobule), namely, Miller's definition and Reid's definition (Radiology 2006;239:322)
- Miller: small lung units separated by interlobular septa and pulmonary veins, according to lung anatomy (Radiology 2006;239:322)
- Reid: an approximately equal sized unit (about 10 mm in diameter) of areas containing 3 to 5 acini, regardless of the interlobular septum, on the basis of bronchography (Radiology 2006;239:322)
- The term "primary pulmonary lobule," which indicates alveolar structures distal to respiratory bronchioles, is not commonly used; therefore, a lobule usually means a secondary lobule (Radiology 2006;239:322)
- Pulmonary acinus is defined as the largest unit participating in gas exchange, although there are different definitions of acinus (Radiology 2006;239:322)
- One definition of the acinus is a lung unit supplied by a single terminal bronchiole; the other is a lung unit supplied by a respiratory bronchiole
- Ciliated cell: transports foreign bodies and mucous stream from the bronchus or bronchiole toward the proximal airway (Mills: Histology for Pathologists, 5th Edition, 2019)
- Mucous cell (goblet cell): secretes sulfomucin
- Basal cell: acts as a stem cell differentiating into other cells
- Neuroendocrine cell (Kulchitsky cell): secretes hormones (e.g. catecholamine, serotonin and gastrin releasing peptide) (Lowe: Stevens & Lowe's Human Histology, 4th Edition, 2014)
- Club cell (formerly Clara cell): plays a key role in lung remodeling, secretes surfactant and repairs airway epithelium
- Type I alveolar epithelium: responsible for respiration; namely, taking oxygen from the outside into the body and transporting carbon dioxide in the opposite direction
- Type II alveolar epithelium: secretes surfactant and plays a role as a precursor cell of type I alveolar epithelium (Lung Cancer 1994;10:S53)
- Pulmonary artery: supplies hypooxgenic blood into the lung in order to exchange the gas between airway and blood
- Bronchial artery: feeds bronchial wall, bronchiole wall and other connective tissue except alveolar septum with oxygen rich blood (Pawlina: Histology - A Text and Atlas, 8th Edition, 2018)
- Pulmonary vein: transports oxygen rich blood from the lungs to the left atrium
- Lymphatics: dual system, namely, flow along bronchovascular bundle from hilum and flow along interlobular septum from visceral pleura
- Location: periphery of the pulmonary hilum
- Lungs consist of the branched bronchus (airways) and vasculatures
- Broncho (bronchiolo) vascular bundle: includes bronchus (bronchiole) and pulmonary artery (peripheral branch) located in the center of pulmonary lobe (or lobule)
- Pulmonary vein: located in the interlobular septum (Katzenstein: Diagnostic Atlas of Non-Neoplastic Lung Disease, 1st Edition, 2016)
- Peripheral lung: shows sponge-like appearance with fine wall reflecting the microscopic appearance of alveoli
- Bronchus:
- Airway lined by pseudostratified ciliated epithelium
- Mucosal and submucosal layer are separated by elastic membrane confirmed by elastic staining (e.g. elastica Masson staining and elastica van Gieson staining), although it is not clearly observed by H&E staining alone
- Bronchial glands exist in the submucosa; cartilage and annular muscular layer exist in the wall between submucosa and adventitia
- References: Pawlina: Histology - A Text and Atlas, 8th Edition, 2018, Lowe: Stevens & Lowe's Human Histology, 4th Edition, 2014
- Bronchiole:
- Small airway, usually 1 mm in diameter or less, lined by single layer of ciliated epithelium
- Lacks bronchial glands and cartilage
- Ciliated cell:
- Tall columnar epithelium, with cilia on the edge of airway side
- Height becomes shorter as bronchiole heads toward periphery
- Reference: Mills: Histology for Pathologists, 5th Edition, 2019
- Mucous cell (goblet cell):
- Tall columnar epithelium with clear cytoplasm containing mucin, lacking cilia
- Basal cell:
- Laying on the basal membrane of bronchus or bronchiole with high nucleocytoplasmic ratio (Lung Cancer 1994;10:S53)
- Neuroendocrine cell (Kulchitsky cell):
- Laying scattered on the basal membrane with granular scant cytoplasm and relatively high nucleocytoplasmic ratio
- Usually difficult to distinguish from basal cell only by H&E staining
- Club cell (formerly Clara cell):
- Toll epithelial cell, no cytoplasmic mucin, no cilia
- Number of club cells increase as bronchiole heads toward periphery
- Bronchial gland:
- Mixed gland composed of both serous and mucinous epithelium
- Its duct opens to bronchial lumen
- Interlobular septum:
- Fibrous tissue separating Miller's secondary lung lobule, which contains pulmonary vein and lymphatic vessel
- Note that not every secondary lobule is separated by this septum
- Bronchovascular bundle:
- Fibrous tissue connecting from pulmonary hilum, which contains bronchus, pulmonary artery, bronchial artery and lymphatic vessel
- Alveolar duct:
- Terminal airway opening to alveolus, of which alveolar entrance rings constitute the walls
- Alveolar entrance rings contain elastic fibers and smooth muscles
- Alveolus:
- Sac-like structure lined by alveolar epithelium
- Alveolar septum contains pulmonary capillaries
- Strictly speaking, alveolar structure is not sac shaped but is a polyhedral architecture
- Type I alveolar epithelium (pneumocyte):
- Thin flat epithelium covering about 90 - 95% of alveolar lumen in area, about 40% of all alveolar epithelia in number
- Type II alveolar epithelium (pneumocyte):
- Cuboid epithelium covering 5 - 10% of the alveolar lumen in area, about 60% of all alveolar epithelia in number
- Pulmonary artery:
- Elastic artery in the central (hilar) side and muscular artery in the peripheral (alveolar) side
- Runs in the bronchovascular bundle along bronchus
- Lumen size is almost similar to bronchus beside it
- This muscular artery often contains abundant elastic fiber in the tunica media
- Reference: Katzenstein: Diagnostic Atlas of Non-Neoplastic Lung Disease, 1st Edition, 2016
- Pulmonary vein:
- Vein composed of collagenous fiber, smooth muscle and elastic fiber in various rates
- The central part contains a lot of elastic fiber but there is less in the periphery
- Runs in the interlobular septum or periphery of Miller's secondary lung lobule
- Bronchial artery:
- Muscular artery supplied by thoracic aorta or costal artery
- Size is far smaller than bronchus beside it
- Lymphatic vessel:
- Thin vasculature lined by endothelia
- Runs with bronchovascular bundle or interlobular septum
- Anthracotic pigment:
- Black pigment, which usually is deposited in the bronchovascular (or bronchiolovascular) bundle and pleura
- Mucous cell (goblet cell): MUC2 and MUC5AC
- Basal cell: cytokeratin 5/6, cytokeratin 34 beta E12, p63 and p40
- Neuroendocrine cell (Kulchitsky cell): CD56, synaptophysin and chromogranin A (Mills: Histology for Pathologists, 5th Edition, 2019)
- Alveolar epithelium: cytokeratin 7
- Type II alveolar epithelium: TTF1, surfactant apoprotein A (SP-A) and napsin A
- Mucous cell (goblet cell): MUC6
- Basal cell: TTF1
- Alveolar epithelium: cytokeratin 20, cytokeratin 5/6, cytokeratin 34 beta E12 and p40
- Club cell (formerly Clara cell): elevated higher than ciliated cells nearby (Lowe: Stevens & Lowe's Human Histology, 4th Edition, 2014)
- Type I alveolar epithelium: fewer organelles
- Type II alveolar epithelium: lamellar body and electron dense vesicles in the cytoplasm; microvilli on the alveolar surface
- Cytokeratin 5/6
- Cytokeratin 7
- Cytokeratin 20
- p40
Comment Here
Reference: Lung nontumor - Normal histology
Comment Here
Reference: Lung nontumor - Normal histology
- Deep fungal infection indigenous to Ohio and Missouri River valleys and the Caribbean basin (eMedicine)
- See also Skin - nontumor topic
- Fungi are thermally dimorphic; spore producing hyphae outside body, but yeast at body temperature
- Infection due to inhaling dust or soil particles contaminated with bird or bat droppings
- "Capsulatum" is incorrect - no capsule is present
- In immunocompetent, generally causes a self limited or latent infection, but chronic pneumonia preferentially involving lung apices associated with systemic symptoms and cough can occur; localized lung lesions, with or without lymph node involvement, are common; also localized lesions, often calcified, in adrenal, lymph nodes, liver, spleen, meninges; resembles tuberculosis with epitheliod granulomas with caseous necrosis; necrotic foci may coalesce to produce large areas of necrosis; with drug therapy or endogenous control, fibrosis and calcification occur, causing "tree bark" lesion
- In immunocompromised, disease is often virulent and widely disseminated
- If necessary, microbiologic studies, serology, or molecular studies are confirmatory
- Infection is incompletely understood, but is usually controlled by helper T cells and heat shock protein that activate macrophages to kill yeast
- Resembles tuberculosis, may see "tree bark" appearance (due to fibrosis and calcification) or coin lesion
- Diagnosis based on identifying small, budding, intracellular yeast in tissue, 2 - 5 microns
- Yeasts usually visible with H&E, but may need special stains; GMS more sensitive than PAS, but microcalcifications may create false positives
- No / minimal granulomas in immunosuppressed or neonates; yeasts fill histiocytes and are widely disseminated
- Lung disease is most common cause of morbidity and mortality in AIDS patients
- Diagnose infection or mimickers with bronchoalveolar lavage, transbronchial biopsy or open lung biopsy
- Nonspecific features resemble DIP or lymphocytic interstitial pneumonia
- Patients often have multiple infections
- Lung biopsies in AIDS patients should routinely be stained for pneumocystis, fungi and mycobacteria
- Characteristically cavitary lesions: Staphylococcus, fungi (Candida, Aspergillus, Cryptococcus [J Acquir Immune Defic Syndr 2010;54:269], Histoplasma, Blastomyces), Mycobacterium tuberculosis, Mycobacterium avium complex, other nontuberculous mycobacteria; Rhodococcus equi, Fusarium, Pseudallescheria
- AIDS patients also have infections from CMV, Pneumocystis jeroveci (formerly Pneumocystis carinii), toxoplasma, microsporidia, herpesvirus types 1 and 2, adenovirus, Strep. pneumonia, H. influenza, Gram negative rods, Legionella pneumophilia, cryptosporidium, zygomycetes, herpes varicella zoster, Penicillium marneffei (patients from Southeast Asia) and bartonella
- Rarely pulmonary alveolar proteinosis (J Med Case Reports 2011;5:46)
- Noninfectious causes of pulmonary infiltrates: Kaposi sarcoma, drug reaction, primary lung cancer, non Hodgkin lymphoma
- Multiple infections and infections with concurrent malignancy are common in AIDS patients
- Low grade and indolent malignant neoplasm rarely seen in lung
- Head and neck is the most common location of this neoplasm
- Rare, malignant, low grade neoplasm that arises in the bronchial glands of the middle aged population but is more common in salivary glands of the oral cavity
- Composed of trabeculae and solid areas separated by dense hyalinizing stroma
- Keratin and p40 positive
- Most important differential diagnosis is squamous cell carcinoma, which also stains positively with the same immunohistochemical markers but is much more aggressive
- Diagnosis can be confirmed by demonstrating EWSR1::ATF1 fusion
- Hyalinizing clear cell carcinoma of lung (HCCC)
- ICD-O: 8310/3 - clear cell adenocarcinoma, NOS
- Commonly seen in middle aged group (32 - 75 years), nonsmokers, with a M:F ratio of 2:3 (Int J Surg Pathol 2023;31:1187)
- These tumors are commonly located in the oral cavity, followed by uncommon locations, such as trachea, bronchi and nasopharynx (Int J Surg Pathol 2023;31:1187)
- Chimeric gene EWSR1::ATF1 transcripts have been seen in soft tissue sarcomas (including hyalinizing clear cell carcinoma of salivary glands) (Hum Pathol 2015;46:471, Am J Clin Pathol 2017;148:73, Genes Chromosomes Cancer 2011;50:559)
- Although rare, hyalinizing clear cell carcinomas have also been identified in submucosal bronchial glands
- Etiology of this neoplasm remains unclear
- Most cases are detected incidentally during regular physical examination and a few present with dyspnea, chest pain and hemoptysis (Front Oncol 2023;13:1175279)
- These tumors are identified as masses incidentally on radiological imaging and on tumor cells with demonstration of EWSR1::ATF1 gene rearrangement being used as a confirmatory test (Am J Clin Pathol 2017;148:73)
- Cytogenetic or molecular study: Ewing sarcoma breakpoint region 1 (EWSR1) fluorescence in situ hybridization is a helpful ancillary test in diagnosing pulmonary hyalinizing clear cell carcinoma; most of these tumors demonstrate EWSR1::ATF1 fusion transcript (Am J Clin Pathol 2017;148:73)
- Solitary, solid, well circumscribed / lobulated and noncalcified (Malays J Pathol 2022;44:509, Front Oncol 2023;13:1175279, Am J Clin Pathol 2017;148:73)
- Excellent prognosis
- Long term follow up may be helpful in cases having lymph node metastasis, perineural invasion and tumor necrosis, as there is limited data on the prognosis of these cases (Int J Surg Pathol 2023;31:1187)
- 54 year old woman with 2.5 cm right lung hyalinizing clear cell carcinoma, which demonstrated EWSR1::ATF1 gene fusion (Medicine (Baltimore) 2023;102:e34101)
- 58 year old male smoker with right upper lobe mass, which was diagnosed to be pulmonary hyalinizing clear cell carcinoma of salivary gland type (PPS: May 2020 Case of the Month [Accessed 11 March 2024])
- 70 year old man with pulmonary hyalinizing clear cell carcinoma harboring EWSR1::CREM fusion combined with a previously unreported IRF2::NTRK3 fusion (Front Oncol 2023;13:1175279)
- 81 year old man with synchronous existence of squamous cell carcinoma of right vocal cord and 2.9 cm hyalinizing clear cell carcinoma in the right upper lung (Diagn Pathol 2023;18:90)
- 81 year old female smoker with left upper lobe hyalinizing clear cell carcinoma (PPS: December 2022 Case of the Month [Accessed 11 March 2024])
- Surgical resection is curative
- Solitary, solid, well circumscribed / lobulated and creamy white
- Neoplasm with well demarcated borders composed of tumor cells arranged in nests, trabeculae and occasional glands
- Background stroma is composed of hyalinized collagen bands
- Tumor cells have clear or eosinophilic cytoplasm, round to oval nuclei with inconspicuous nucleoli (Mod Pathol 2018;31:923)
- Neural invasion is commonly seen in this neoplasm when compared with mucoepidermoid carcinoma (Mod Pathol 2018;31:923)
- TTF1, HMB45, PAX8, myoepithelial markers (smooth muscle actin, SOX10, smooth muscle myosin heavy chain, calponin, S100), neuroendocrine markers (chromogranin and synaptophysin) and markers for metastatic clear cell renal cell carcinoma (RCC, CD10)
- References: Mod Pathol 2018;31:923, Am J Clin Pathol 2017;148:73, Malays J Pathol 2022;44:509
- Fluorescence in situ hybridization (FISH) assay using EWSR1 gene break apart probe was performed in all cases as a specific diagnostic ancillary technique; all cases harbored the characteristic EWSR1 gene rearrangement
- Lung, left, CT guided biopsy:
- Malignant neoplasm with clear cell features (see comment)
- Comment: Immunohistochemical studies (done with appropriate controls) showed that the tumor cells are immunoreactive for AE1 / AE3, p63 and negative for PAX8, TTF1, S100, SOX10 and HMB45. The morphology and staining pattern are most consistent with hyalinizing clear cell carcinoma. Fluorescence in situ hybridization assay using EWSR1 gene break apart probe to demonstrate presence of EWSR1 gene rearrangement can be used to confirm the diagnosis.
- Mucoepidermoid carcinoma:
- Only occasional cells in hyalinizing clear cell carcinoma may have intracellular mucin in contrast to mucoepidermoid carcinoma, which has abundant mucin cells (Mod Pathol 2018;31:923)
- Gene testing helps in difficult cases (Malays J Pathol 2022;44:509)
- Squamous cell carcinoma with prominent clear cell feature:
- These tumors have keratinization, high grade features, apparent dysplasia and high mitotic activity (Mod Pathol 2018;31:923)
- Metastatic clear cell renal cell carcinoma:
- PAX8 positivity
- Lung adenocarcinoma with clear cells:
- PEComa:
- Myoepithelial carcinoma:
Comment Here
Reference: Hyalinizing clear cell carcinoma
- Rare, nodular lung lesion
- Usually multiple, bilateral and cause unknown
- Inflammatory reaction of unknown stimulus
- Patients often have a history of autoimmune disease, exposure to fungal or mycobacterial antigens
- Associated with sclerosing mediastinitis, retroperitoneal fibrosis and lymphoma
- May be progressive, but does not cause death
- Central keloid-like collagen, arranged in whorls, surrounded by foreign body giant cells simulating nodular amyloidosis
- May have plasma cells and lymphocytes between collagenous bands
- Usually no epithelioid granulomas, no necrosis
- Amyloidosis (localized), rheumatoid arthritis, silicosis
- Also infection, foreign body granuloma
- Also known as extrinsic allergic alveolitis
- A complex health syndrome of varying intensity, clinical presentation and natural history
- Due to immunologically induced inflammation of lung parenchyma in response to inhalation of a large variety of antigens (Am J Respir Crit Care Med 2005;171:792)
- An interstitial pneumonia with acute to chronic respiratory failure caused by inhalation exposure to a variety of natural or chemical antigens
- Histologically characterized by airway centered inflammation with fibrosis and poorly formed nonnecrotizing granulomas
- Also called extrinsic allergic alveolitis
- J67.8
- 4 - 15% of interstitial lung diseases (Eur Respir J Suppl 2001;32:114s)
- Prevalence and incidence vary by climate, geographical condition, living environment and agricultural practice
- UK incidence is 0.9 per 100,000 person per year (QJM 2007;100:233)
- Higher prevalence and mortality rate in farmers and agricultural industries (Am J Ind Med 2006;49:997)
- Mean age is 50 - 60 years old
- No sexual predominance
- Smoking is related to lower prevalence but worse prognosis (Intern Med 1995;34:966)
- Predominant in middle to upper lobes of the lung; usually bilateral
- Gene polymorphisms related to the acquired immune response may predispose to HP (Am J Respir Crit Care Med 2012;186:314):
- Major histocompatibility complex class 2 (MHC class II)
- Proteasome subunit beta type 8 (PSMB8)
- Transporter associated with Antigen Processing 1 (TAP1)
- Malfunction of regulatory T cells (Eur Respir J 2011;37:632)
- Antigen exposure results in early formation of type III immune complexes, followed by type IV delayed hypersensitivity
- HP is developed through inhalation and exposure to a causative antigen
- Causative agents: spores of bacteria, fungi, mycobacteria, animal proteins and chemicals from hay, grain, sugar cane, bark, cheese, cork and animal feces (J Investig Allergol Clin Immunol 2015;25:237)
- According to the causative antigen, HP may have different names:
- Air conditioner lung: due to thermophilic bacteria
- Byssinosis: in textile workers due to fibers from cotton, linen and hemp
- Resembles asthma clinically
- Disease mechanism may not be immune mediated, endotoxin from bacterial contamination of cotton may play a role
- Farmer's lung: from moldy hay containing spores of thermophilic actinomycetes
- Maple bark stripper’s lung: fungal spores
- Pigeon breeder's lung: also called bird fancier's disease; proteins from serum, feathers excreta
- Hot tub lung: nontuberculous Mycobacterium
- HP is classified into acute, subacute and chronic, however there is a lack of consensus for the criteria
- Acute hypersensitivity pneumonitis
- Influenza-like syndrome a few hours after exposure to an antigen: fever, dyspnea, cough, crackles may be detected on chest auscultation
- Symptoms resolve several hours after antigen removal
- Repeated acute episodes of farmer’s lung leads to centriacinar emphysema (Eur Radiol 2003;13:2212)
- Subacute hypersensitivity pneumonitis
- Slowly progressive respiratory failure over weeks to months
- Fever, dyspnea, cough, fatigue, crackles may be detected on chest auscultation
- Pulmonary function may be normal
- Probably results from continuous low level exposure to the antigen
- Chronic hypersensitivity pneumonitis
- Slowly progressive and insidious respiratory failure; often without acute episodes
- Dyspnea, cough, fatigue, weight loss, fine crackles on chest auscultation
- Restrictive pattern on pulmonary function tests
- Decreased total lung capacity (TLC)
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- Often associated with bird antigen exposure
- Acute exacerbation followed by respiratory deterioration within 1 - 2 months can occur; usually without further antigen exposure (Chest 2008;134:844, Chest 2008;134:1265)
- Diagnosis is based on clinical, radiological (high resolution computed tomography, HRCT) and pathological examination
- Surgical lung biopsy is often necessary to differentiate subacute and chronic hypersensitivity pneumonitis from other interstitial lung disease; however, it is rare for acute hypersensitivity pneumonitis to be biopsied
- Although several diagnostic criteria have been proposed, none are widely accepted
- A large cohort study by HP Study Group suggested clinical predictors for the diagnosis of HP (Am J Respir Crit Care Med 2003;168:952)
- Exposure to a known offending antigen
- Positive precipitating antibodies
- Recurrent episodes of symptoms
- Inspiratory crackles
- Symptoms 4 - 8 hours after exposure
- Weight loss
- Bronchoalveolar lavage is supportive in the diagnosis but lacks standardization (Chest 2012;142:208, Am J Respir Crit Care Med 2012;186:314)
- Increased total cell count
- Increased lymphocyte percentage ≥ 30% for nonsmokers or exsmokers or ≥ 20% for current smokers; a normal lavage rules out the presence of active HP (Am Rev Respir Dis 1990;141:S169, Br J Ind Med 1986;43:401)
- CD4 / CD8 ratiois usually decreased in HP but can be increased as high as in sarcoidosis; CD4 / CD8 ratio is now considered to vary by clinical conditions such as causative antigen and smoking status
- Inhalation challenge is supportive but lacks standardization (Chest 2012;142:208, Am J Respir Crit Care Med 2012;186:314, Eur Respir J 2014;44:1658)
- Antigen exposure at the workplace or home or direct inhalation of the specific antigen after a period of avoidance provokes symptoms of HP and decreases FVC in 8 - 12 hours
- The patient should be monitored at least for 24 hours after the inhalation in case of severe attack of HP
- Serum IgG antibody to causative antigens may be increased; however, serum antibody could be positive in 31% of non HP subjects (Am J Respir Crit Care Med 2003;168:952)
- Avian antigens: pigeon, parakeet, budgerigar, chicken
- Fungus: trichosporon, aspergillus
- Bacteria: actinomycete
- Mycobacteria: Mycobacterium avium-intracellulare
- Chemicals
- Increased serum KL-6, often over 1000 IU (normal limit is < 500 IU)
- Findings on the chest X-ray vary from nonspecific change, especially in acute and subacute hypersensitivity pneumonitis, to upper lobe predominant fibrosis of chronic HP
- Typically, HRCT shows ground glass opacity and centrilobular nodular opacity with / without emphysema and fibrosis
- It is often challenging to differential HP from other interstitial lung diseases on HRCT such as nonspecific interstitial pneumonia (NSIP) and usual interstitial pneumonia (UIP) (Am J Surg Pathol 1994;18:136, AJR Am J Roentgenol 1995;165:807)
- HRCT features to differentiate chronic HP from NSIP and UIP (Radiology 2008;246:288):
- Lobular areas with decreased attenuation and vascularity
- Centrilobular nodules
- Absence of lower zone predominance of abnormalities
- Many patients show favorable prognosis compared to other interstitial lung diseases and improve with appropriate treatment (QJM 2007;100:233, Respir Med 2014;108:793, Am J Ind Med 2006;49:997)
- Interstitial fibrosis and emphysema are associated with worse prognosis, and once developed, may remain or progress despite treatment (Am J Med 2004;116:662, Radiology 2007;244:591)
- Smoking is also associated with worse prognosis (Intern Med 1995;34:966)
- 12 year old boy with HP due to feather duvet (BMJ Case Rep 2015 Jun 25;2015)
- 30 year old woman with HP (Chest 2014;145:856)
- 37 year old man with HP due to shiitake mushroom spores (Med Mycol 2012;50:654)
- 37 year old man who died of HP due to Fusarium vasinfectum (Int Arch Allergy Immunol 2015;166:150)
- 45 year old man with HP due to metalworking fluid (Occup Med (Lond) 2015;65:598)
- 45 year old man with pneumomediastinum as a primary manifestation of chronic HP (Med Sci Monit 2011;17:CS152)
- 72 year old woman with HP and combined pulmonary fibrosis and emphysema (BMJ Case Rep 2015 Dec 21;2015)
- Avoidance of antigen is the key of HP management
- Oral or systemic corticosteroids are considered for severe case or when the antigen is not removable; however, steroids do not change long term outcome and are not standardized (Chest 2013;144:1644)
- Diffuse involvement with mild to moderate increase in lung weight
- Bronchocentric fibrotic changes may be seen
- Common findings(J Clin Pathol 2013;66:888, Am J Respir Crit Care Med 2012;186:314, J Investig Allergol Clin Immunol 2015;25:237, Arch Pathol Lab Med 2008;132:199):
- Airway centered (peribronchiolar) change
- Interstitial cellular infiltration
- Poorly formed nonnecrotizing granulomas or interstitial giant cells with cholesterol clefts
- Well formed granulomas can be found but may raise differential diagnosis with sarcoidosis if the granulomas are numerous and predominant
- Acute HP
- Airway centered inflammation with little fibrosis
- Neutrophilic infiltration with / without capillaritis
- Intra-alveolar fibrin deposition
- Subacute HP
- Airway centered infiltration with fibrosis
- Lymphocytic infiltration with granulomas or giant cells
- Chronic HP
- Predominantly airway centered inflammation with diffuse fibrotic change
- Lymphocytic infiltration with granulomas or giant cells
- Often overlaps with NSIP, UIP, organizing pneumonia and airway centered interstitial fibrosis
- Bridging fibrosis (fibrotic band connecting bronchioles with each other and with lobular septa) and peribronchiolar metaplasia can be a diagnostic clue to differentiate HP from IPF (J Clin Pathol 2013;66:888, Histopathology 2012;61:1026)
- Additional findings
- Byssinosis bodies (hemosiderin coated strands of fiber within fibrous tissue) can be found in byssinosis
- Foamy macrophages in alveolar spaces
- Organizing pneumonia
Scroll to see all images:
Images hosted on other servers:
- Bronchoalveolar lavage fluid shows lymphocytosis (see Diagnosis)
- Staining for cathepsin K and CD68 may be helpful to detect small granulomas
- Giemsa, Grocott and Ziehl-Neelsen stains rule out infectious diseases, if suspected
- Airway centered interstitial fibrosis: absence of antigen exposure
- Connective tissue disease related interstitial pneumonia
- Idiopathic nonspecific interstitial pneumonia
- Organizing pneumonia
- Respiratory bronchiolitis related interstitial lung disease
- Sarcoidosis
- Smoking related interstitial fibrosis: smoking history, acellular fibrosis
- Usual interstitial pneumonia / idiopathic pulmonary fibrosis
- Intra-alveolar fibrin deposition
- Monocytosis in bronchoalveolar lavage
- Necrotizing granuloma
- Organizing pneumonia
- Weight loss
Comments:
- Intra-alveolar fibrin deposition is suggestive for acute HP, also for acute fibrinous and organizing pneumonia
- Typical bronchoalveolar lavage of HP shows lymphocytosis
- Necrotizing granuloma is more suggestive for tuberculosis
- Organizing pneumonia can be seen in HP but it is not specific
- Weight loss is suggestive for HP according to the large cohort study (see Diagnosis)
Comment Here
Reference: Hypersensitivity pneumonitis
- Incomplete development of lung; lung usually weighs less than normal with fewer alveoli than expected for gestational age
- Bilateral hypoplastic disease is fatal
- Causes: oligohydramnios (renal agenesis, fetal membrane rupture), decreased intrathoracic space (renal cystic disease, diaphragmatic hernia), reduced breathing (anencephaly, musculoskeletal disorders, brainstem hypodevelopment, Virchows Arch 2009;454:451)
- References: eMedicine
- Rare, usually children or teenagers with hemoptysis, hypoxemia, dypsnea and iron deficiency anemia similar to Goodpasture’s disease, but no antibodies in serum or tissue, no renal disease
- Clinical triad of hemoptysis, iron deficiency and diffuse pulmonary infiltrates
- May be related to consanguinity or environmental factors
- Fever, lymph node, liver and spleen enlargement may occur
- Usually fatal after several years
- Diagnosis of exclusion
- Hemosiderin laden macrophages in alveolar lumina, shedding and hyperplasia of alveolar epithelial cells and marked alveolar capillary congestion
- Varying interstitial fibrosis, intra-alveolar hemorrhage
- No necrosis, no vasculitis, no granulomas and no lymphoid follicles
- Note: these disorders all cause secondary pulmonary alveolar bleeding and hemosiderosis
- Mitral stenosis
- Periarteritis nodosa
- SLE (neutrophils in alveolar septal capillaries)
- Systemic vasculitis
- Also called congenital lobar emphysema
- Infants or young children
- Abnormal bronchial development resulting in air trapping, perhaps due to hypoplasia of bronchial cartilage; associated with other cardiopulmonary anomalies
- Affects left or right upper lobe or right middle lobe
- May cause severe compression of other pulmonary lobes
- Not emphysema since no tissue destruction
- 28 day old baby boy (Indian J Anaesth 2009;53:482)
- Massive distention of alveolar spaces, but no tissue destruction
- Pulmonary embolus (PE) is a blockage of the pulmonary artery or one of its branches due to material (solid, gaseous or liquid) that has traveled through the circulation from elsewhere in the body (StatPearls: Acute Pulmonary Embolism [Accessed 5 October 2022])
- Pulmonary embolism is the third most common acute cardiovascular condition worldwide, after myocardial infarction and stroke
- True antemortem clots and emboli display alternating darker and lighter striations due to erythrocyte and fibrin / platelet rich layers (lines of Zahn)
- Thromboembolism is then organized by migrating fibroblasts and myofibroblasts if thrombolysis does not occur within 1 to 2 days
- Pulmonary infarct, venous thromboembolism (VTE), pulmonary embolism
- ICD-10: I26.99 - other pulmonary embolism without acute cor pulmonale
- Third most common acute cardiovascular condition worldwide, trailing only myocardial infarction and stroke (Arterioscler Thromb Vasc Biol 2014;34:2363)
- Responsible for ~100,000 fatalities in the United States annually (Arch Intern Med 2003;163:1711)
- M > F (Arch Intern Med 2003;163:1711)
- Increased incidence with age, particularly in women, to the point that it has an incidence of > 500 per 100,000 after the age of 75 (Am J Med 2013;126:832.e13)
- Risk factors can be divided into genetic versus acquired
- Genetic factors include hypercoagulable conditions, such as factor V Leiden mutation, protein C and S deficiency, prothrombin mutations, antiphospholipid syndrome, etc.
- Acquired risk factors include but are not limited to pregnancy, hospitalization, obesity, oral contraceptive use, malignancy, long bone fracture, stroke, indwelling central venous lines, acute spinal cord injury and patients who have had joint arthroplasty or repair
- Pulmonary arteries or any of its branches
- Pathogenesis of pulmonary embolism is similar to that of thrombus formation (i.e., Virchow's triad)
- Virchow's triad includes venous stasis, endothelial damage and hypercoagulability
- Range of pathophysiologic reactions can occur when an embolus lodges in the lung:
- Pulmonary infarction due to tiny thrombi that lodge distally in segmental and subsegmental arteries in ~10% of people (Chest 1991;100:598)
- Ventilation perfusion mismatch (V/Q mismatch) in the lung is caused by insufficient perfusion, resulting in hypoxemia
- Hypotension due to increased pulmonary vascular resistance (PVR) (Clin Chest Med 1984;5:403)
- PVR increases due to the presence of thrombi and hypoxic vasoconstriction of lung capillaries
- Increased PVR, in turn, obstructs right ventricular outflow, resulting in right ventricular dilatation and flattening or bending of the intraventricular septum
- Both decreased right ventricular flow and right ventricular dilation decrease left ventricular preload, reducing cardiac output
- Most emboli originate in the proximal veins of the lower extremities (iliac, femoral and popliteal)
- At the time of presentation, more than half of patients with proximal deep vein thrombosis have concurrent pulmonary embolism (Am J Respir Crit Care Med 2001;164:1033)
- Most thrombi form in lower extremity veins at regions of diminished flow, such as valve cusps or bifurcations
- Common symptoms at presentation include (Chest 1991;100:598)
- Dyspnea at rest or with exertion
- Pleuritic pain
- Cough
- Orthopnea
- Wheezing
- Hemoptysis
- Calf or thigh pain or swelling
- Common presenting symptoms found on examination include (Am J Med 2007;120:871)
- Tachypnea
- Tachycardia
- Calf or thigh swelling, erythema, edema, tenderness, palpable cords
- Rales
- Accentuated pulmonic component of the second heart sound
- Decreased breath sounds
- Jugular venous distension
- Fever, mimicking pneumonia
- Pretest probability for pulmonary embolism should always be calculated using a validated pretest probability score or approximated clinically if pulmonary embolism is suspected (e.g., Wells score, modified Wells score or modified Geneva score)
- Criteria for Wells and modified Wells score (JAMA 2006;295:172):
- Clinical signs and symptoms of deep vein thrombosis = 3
- Alternative diagnosis is less likely than pulmonary embolism = 3
- Heart rate > 100 = 1.5
- Immobilization for ≥ consecutive days or surgery in the previous 4 weeks = 1.5
- Previously diagnosed with pulmonary embolism or deep vein thrombosis = 1.5
- Hemoptysis = 1
- Malignancy (on treatment, treatment in the last 6 months or palliative) = 1
- Interpretation of Wells and modified Wells score:
3 tier 2 tier - 0 - 1: low risk
- 2 - 6: moderate risk
- > 6: high risk
- ≤ 4: unlikely
- ≥ 4.5: likely
- Computed tomographic pulmonary angiography (CTPA) or magnetic resonance pulmonary angiography (MRPA): a filling defect in any branch of the pulmonary artery (main, lobar, segmental, subsegmental) that becomes evident after contrast enhancement is diagnostic of pulmonary embolism
- CTPA, MRPA: very sensitive and specific, fast and readily available imaging study to rule pulmonary embolism in or out; has essentially replaced conventional angiography
- Chest Xray: wedge shaped infarct after 12 - 36 hours
- Nuclear scan: macroaggregates of labeled albumin with perfusion lung scanning; angiography is the most definitive diagnostic test
- D dimer testing is an excellent validated screening test for thromboembolic disease; a negative result essentially rules out pulmonary embolism
- Laboratory tests are not diagnostic but they can raise clinical suspicion for pulmonary embolism, confirm the presence of other illnesses and offer prognostic information if pulmonary embolism is diagnosed
- These include a complete blood count and serum chemistries, arterial blood gases and D dimer
- Electrocardiogram (ECG) abnormalities are common but nonspecific in those with suspected pulmonary embolism
- The most prevalent findings are tachycardia and nonspecific ST segment and T wave changes (70%) (Eur Respir J 2005;25:843)
- CT scan findings (Insights Imaging 2019;10:114):
- Polo mint sign: the appearance of the polo mint sign inside the pulmonary artery refers to a blood clot surrounded by contrast material
- Railway sign: the railway track sign is used in chest radiography or CT to refer to the presence of contrast in the pulmonary artery surrounding a partial filling defect in the setting of acute pulmonary embolism
- Radiograph findings (Radiopaedia: Pulmonary Embolism [Accessed 5 October 2022]):
- Fleischner sign: enlarged pulmonary artery
- Hampton hump: peripheral wedge of airspace opacity and implies lung infarction
- Westermark sign: regional oligemia and the highest positive predictive value
- Pleural effusion
- Palla sign: enlarged right descending pulmonary artery
- Chang sign: dilated right descending pulmonary artery with sudden cutoff
- Knuckle sign: abrupt tapering or cutoff of a pulmonary artery secondary to a pulmonary embolus
- Pulmonary embolism fatalities decreased from 12.8 per 100,000 to 6.6 per 100,000 between 2000 and 2015, as per research that used data from the World Health Organization (WHO) mortality database (Lancet Respir Med 2020;8:277)
- The first 7 days have the highest risk of events; mortality and morbidity are usually caused by shock and recurrent pulmonary embolism during this time
- Variables that predict poor prognosis for individuals with pulmonary embolism:
- Shock and right ventricular dysfunction (Am J Cardiol 1959;4:611)
- Right ventricle thrombus (J Am Coll Cardiol 2003;41:2245)
- Deep vein thrombosis (Am J Respir Crit Care Med 2010;181:983)
- Hyponatremia (< 130 mmol/L) and indicators of renal dysfunction (Heart 2012;98:1221)
- Older age ≥ 65 years (Am J Cardiol 2015;115:681)
- Right heart thrombus (Chest 2017;151:409)
- Poor adherence to guidelines (Eur Respir J 2018;51:1800445)
- 37 year old woman with no previous medical history presented with chest discomfort, acute coronary syndrome was suspected and was later determined to be a case of pulmonary embolism (BMC Pulm Med 2019;19:44)
- 40 year old woman developed pulmonary embolism following a 1.5 meter stair fall with a craniothoracic impact point (Ann Med Surg (Lond) 2022;78:103868)
- 51 year old woman with progressive pain in her left shoulder for 6 months developed an asymptomatic pulmonary embolism after shoulder arthroscopy (Orthop Surg 2021;13:1119)
- 55 year old woman was admitted to the acute medical unit with fluctuations in consciousness and in a septic state (BMJ Case Rep 2014;2014:bcr2013201320)
- 61 year old man presented with chest pain, difficulty breathing, hemoptysis and general discomfort and was found to have a massive pulmonary embolism along with S1Q3T3 ECG findings (BMC Cardiovasc Disord 2021;21:224)
- Stabilize the patient until a clinical examination and conclusive diagnostic tests are performed
- Start anticoagulation even before establishing the diagnosis of pulmonary embolism if the risk/benefit ratio between the suspicion of pulmonary embolism and the risk of bleeding appears favorable
- Inferior vena cava (IVC) filters should be placed in most pulmonary embolism patients for whom anticoagulation is contraindicated or when the risk of bleeding is high
- For patients who present with hemodynamic instability, thrombolytic therapy, embolectomy and catheter directed modalities like ultrasound assisted thrombolysis are potentially acceptable treatment options
- Elastic graded compression stockings, frequent ambulation and IVC filters are adjunct therapies that can be used in addition to anticoagulation in patients with pulmonary embolism
- References: Am J Cardiol 1959;4:611, Circulation 2005;112:e28
- Early stages of pulmonary infarct are often red-blue and have a raised appearance
- Fibrinous exudate covers the apposed pleural surface
- Within 48 hours, the infarct grows paler and finally red-brown as hemosiderin is produced
- Fibrous replacement begins at the margins as a gray-white peripheral zone and gradually transforms the infarct into a contracted scar
- Saddle embolus arises when a large emboli lodges in the main pulmonary artery or one of its major branches or at the bifurcation
- Smaller emboli can induce bleeding or infarction in more peripheral arteries
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012
- Antemortem clots display erythrocyte and fibrin layering
- Because of erythrocyte and fibrin / platelet rich layers, true ante mortem clots and emboli exhibit alternating darker and lighter striations (lines of Zahn)
- Thromboembolus is then organized by migrating fibroblasts and myofibroblasts if thrombolysis does not take place within 1 to 2 days
- Clot organization develops from the periphery to the center
- These migratory cells combine with granulation tissue in large arteries and cause clot contraction to one side, resulting in an eccentric thickening of the affected vessel
- Hemorrhagic area exhibits ischemic necrosis of the alveolar walls, bronchioles and arteries
- Infarction results in the loss of alveolar nuclei and eventual fibrosis
- Infected embolus causes a septic infarct with a significant neutrophilic response
- Fat embolism / bone marrow embolus: the presence of fat cells with or without marrow elements in the pulmonary circulation
- Most cases are due to long bone and pelvic fractures
- Rounded clear cells can be observed in the pulmonary vessel
- Pulmonary infarcts may present in several ways:
- Typical textbook description is a wedge shaped subpleural zone of hemorrhage with coagulative necrosis
- However, it is essential to remember that various configurations, such as geographical, spherical and mixed forms, can be seen at low magnification
- All of them have coagulative necrosis and significant hemorrhage in the lung parenchyma
- Geographic form is marked by coagulative necrosis in the subpleural region with a serpentine distribution and patches of healthy lung parenchyma frequently encircled by large areas of eosinophilic necrosis
- Round configuration has a thick fibrous capsule that encases a nearly spherical zone of necrosis, while the mixed pattern has segments with both rounded and geographical arrangements
- Granulation tissue covers the airspaces around the necrotic zone and is bordered by thicker interstitium
- Foamy macrophages and histiocytes may also surround the coagulative necrosis
- Squamous metaplasia is also commonly found in pulmonary infarcts and frequently demonstrates substantial reactive changes that lead to a differential diagnosis of cancer
- It may also manifest with vascular inflammation, frequently leading to a differential diagnosis of vasculitis
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012, Mod Pathol 2009;22:679
- On frozen sections, oil red O or Sudan black stains help to highlight fat emboli
- Elastic stains demonstrate collapsed, intertwined elastic fibers inside a collagenous stroma in organized infarcts
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012
- Lung, left lower lobe, wedge biopsy:
- Organized pulmonary artery thromboembolism with associated infarct (see comment)
- Comment: An irregular intimal plaque with fibrosis is evident within the artery, along with recanalization of the vessel and the presence of small lumina, suggesting a previous clot. Areas of calcification are present within the fibrosis in the pulmonary artery. In addition, necrosis of alveolar walls with loss of nuclei in the neighboring alveoli represents an area of infarction.
- Plexiform lesions of primary pulmonary arterial hypertension
- Postmortem blood clot:
- Weak or no attachment to the wall
- Rubbery and gelatinous
- Appearance of currant jelly on chicken fat
- Absence of lines of Zahn: red blood cells and coagulated serum are mixed in 2 separate layers
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012
A 78 year old man was brought to the emergency room with complaints of shortness of breath, chest discomfort and cough. He died as the medical team was attempting to revive him. The family requested a postmortem examination to determine the cause of death. On investigation, a clot was found lodged in the right main pulmonary artery. Which one of the following characteristics of the clot will help identify if it formed antemortem and contributed to his death?
- Appearance of currant jelly on chicken fat
- Gelatinous, soft and rubbery appearance on gross examination
- Presence of lines of Zahn
- Red blood cells and coagulated serum mixed in 2 separate layers
Comment Here
Reference: Infarct / pulmonary emboli
A 62 year old woman presents to the emergency room with a right femoral fracture. 3 hours later, she develops sudden shortness of breath and altered mental status. On physical examination, she is tachycardic and a red petechial rash can be observed on her chest. A Doppler ultrasound is performed and there are no signs of a deep venous thrombosis. Which of the following best describes what the pulmonary artery histology would demonstrate?
- Atypical cells with a high N:C ratio
- Foamy macrophages and fibrin deposits
- Presence of neutrophils in a clot
- Rounded clear cells with hematopoietic elements are observed in the pulmonary vessel
Comment Here
Reference: Infarct / pulmonary emboli
- Vast majority of patients with lung disease have history of IBD in GI tract, but lung disease may occur without GI disease
- Lung involvement more common with ulcerative colitis than Crohn's disease
- Acute or chronic bronchiolitis with nonnecrotizing granulomas, bronchopneumonia, interstitial pneumonia and organizing pneumonia
- May be due to mesalamine (anti-inflammatory component of sulfasalazine, used to treat IBD)
- May have CMV or atypical mycobacteria infections
- Sarcoidosis: lymphangitic distribution, no interstitial pneumonia and no chronic bronchiolitis
- Hypersensitivity pneumonia: different history
- Category used to designate a variety of benign proliferative lesions forming a lung mass, including neoplastic and nonneoplastic entities
- Neoplastic: renamed inflammatory myofibroblastic tumor (IMT), may show clonal cytogenetic abnormalities involving 2p23 that encodes ALK gene, typically occurs in children and young adults, well demarcated but non encapsulated, usually solitary mass that replaces underlying lung tissue
- Nonneoplastic: older age, ill defined or irregular contour due to prominent organizing pneumonia component and fibrosis at edge (Arch Pathol Lab Med 2010;134:417)
- Inflammatory pseudotumor is a heterogeneous group of benign lesions that may occur in the lung, with a variable mix of inflammatory cells and fibroblasts / myofibroblasts
- Inflammatory myofibroblastic tumor is recognized as a neoplastic subset that can be associated with ALK gene rearrangement and is typically seen in the younger age group
- The differential diagnosis is broad, and diagnosis typically requires surgical excision
- Variable definitions in use of "inflammatory pseudotumor"; some use term to describe any circumscribed or irregular inflammatory nodule, mass or consolidation; others favor a more descriptive diagnosis
- Inflammatory myofibroblastic tumor means neoplastic, fibrohistiocytic, associated with ALK rearrangement
- Other names used in nonneoplastic lesions: plasma cell granuloma, hyalinizing granuloma, plasma cell pseudotumor, inflammatory myofibrohistiocytic proliferation
- Incidence unclear since terminology / definition varies
- M = F, broad age range but usually < 30 if IMT
- 3% bilateral
- Typically parenchymal, but may involve pleura
- Rarely intrabronchial
- Unknown, but may be autoimmune (IgG4) related or due to an infectious process
- 50% with cough, shortness of breath, chest pain, hemoptysis
- Surgical excision with histologic examination
- Xray: single, well defined, round or oval mass
- CT: may show pleural retraction if lesion involves pleura, may show cavitation or calcification
- Usually remains stable or grows very slowly, may spontaneously resolve
- Poor prognostic factors for IMT: metastases, necrosis > 15% of surface area examined, local recurrence, bizarre giant cells, > 3 mitotic figures / 50 HPF, advanced stage, high cellularity, poor circumscription
- 27 year old man with IMT invading into GE junction (Ann Thorac Surg 2010;89:1659)
- 45 year old man with IMT and progressive dyspnea, cough, wheezing (J Cardiothorac Surg 2010;5:55)
- 58 year old man with inflammatory pseudotumor from Coxiella burnetti (Microbes Infect 2015;17:795)
- Complete excision
- Rarely causes death due to local extension
- Variable size from < 1 cm to very large (> 30 cm)
- Well circumscribed, non encapsulated, usually solitary, white to gray, firm, fleshy parenchymal nodule
- May be yellow and friable or show hemorrhage, necrosis, calcification
- Variable patterns, e.g. fibrohistiocytic, plasma cell granuloma, largely sclerosed, compact spindle cells, hypocellular fibrous, myxoid / vascular, fibroxanthomatous
- Generally fibroinflammatory with variable numbers of plasma cells, lymphocytes, histiocytes and myofibroblasts
- May show mast cells, eosinophils, neutrophils, multinucleated cells, hemosiderin, calcification
- May resemble nodular fasciitis, fibrous histiocytoma or fibromatosis
- May show features of organizing pneumonia including lymphohistiocytic inflammation and fibrosis with preservation of alveolar architecture in early lesions; also bordering alveoli with foamy macrophages and hyperplastic pneumocytes
- Lymphoplasmacytic variant with mostly plasma cells and lymphocytes, germinal centers, paucicellular collagen, endothelialitis, fibrinous pleuritis
- Spindle cells: vimentin, smooth muscle actin
- ALK1 staining in 40% of IMTs
- Polyclonal kappa and lamda light chain Ig in plasma cells
- Elongated cytoplasmic processes with pinocytotic vesicles, subplasmalemmal plaques, thin filaments, abundant endoplasmic reticulum
- ~50% of inflammatory myofibroblastic tumor have t(2;17) translocation
- ROS1 or RET gene rearrangements reported (Am J Surg Pathol 2015;39:957)
- Amyloid tumor
- Benign fibrous histiocytoma, malignant fibrous histiocytoma
- Carcinoid tumor
- Histoplasmosis: see Am J Clin Pathol 2011;136:410
- Lipoid pneumonia
- Lymphoma
- Lymphoid hyperplasia
- Metastatic carcinoma
- Mycobacterial pseudotumor
- Organizing pneumonia
- Plasmacytoma
- Solitary fibrous tumor
- Tuberculosis: immunosuppressed patients
- Other spindle cell tumors
- Most common isolated lung lesion in children, usually asymptomatic
- Mostly neoplastic with frequent ALK gene rearrangements (in inflammatory myofibroblastic tumor)
- Benign, although rare cases of malignant behavior have been reported
Essential features
- Inflammatory myofibroblastic tumor (IMT) occurs more often in childhood and in young adults and shows morphology similar to the adult form
- IMT in children is more often associated with ALK gene rearrangement than in adults
Terminology
- Renamed inflammatory myofibroblastic tumor (formerly inflammatory pseudotumor)
Epidemiology
- Most common lung tumor in children age 16 and younger
Sites
- Lung, mediastinum, trachea, bronchus, abdomen, orbit
Radiology description
- Solid masses with homogeneous or heterogeneous enhancement, may contain calcification (Pediatr Radiol 2015;45:1672)
Case reports
- 3 year old child with cough and recurrent respiratory infections (Diagn Pathol 2012;7:83)
- 5 year old girl with recurrent pyrexia, dry cough and shortness of breath (Interact Cardiovasc Thorac Surg 2010;10:805)
Treatment
- Excision or radiation therapy
Gross description
- Solitary, small peripheral nodules, yellow, firm, covered by intact pleura or polypoid bronchial mass
Gross images
Images hosted on other servers:
Microscopic (histologic) description
- Plasma cells (often abundant), lymphocytes, histiocytes and myofibroblasts
- May have vascular proliferation, collagenous or hyalinized stroma, myxoid change, xanthoma cells, hemosiderin
- May resemble nodular fasciitis, fibrous histiocytoma or fibromatosis
Microscopic (histologic) images
Images hosted on other servers:
Molecular / cytogenetics description
- More often associated with ALK rearrangement than adult cases
- Most common cause of viral pneumonia
- RNA virus, nucleoprotein determines type of virus: A, B or C (Virol J 2009 Mar 13;6:30)
- Envelope contains the viral hemagglutinin and neuraminidase that establish the viral subtype, e.g., H1N1 (Wikipedia)
- Preexisting antibodies to specific hemagglutinins and neuraminidases prevent or amerliorate future infections
- Type A: causes most severe disease; major cause of epidemics and pandemics; also infects pigs, horses, birds; one subtype predominates at any given time
- Antigenic drift leading to epidemics is caused by small mutations in hemagglutinins and neuraminidases, which allow the virus to evade most host antibodies
- Antigenic shift leads to pandemics, and is caused by recombination of hemagglutinin and neuraminidase RNA with animal influenza RNA, leading to absence of human immunity
- Antigenic drift and shift do NOT occur with influenza types B and C, which usually cause mild, self limited illness in children
- References: World Health Organization Influenza update
- 43 year old man in India with with fever for 3 days and sudden onset of shortness of breath (Case of the Week #459)
- Cause mild acute lung injury to necrotizing pneumonia to BOOP-like changes
- May cause bronchiolitis or diffuse alveolar damage
- Viral cytopathic changes do NOT occur
- Airways show mucosal hyperemia with infiltrate of lymphocytes, histiocytes, plasma cells
- Swelling and increased mucus production impair bronchociliary elevator, and may lead to secondary bacterial infection; small airways may become occluded causing focal atelectasis; in severe disease, this is more widespread with distal airways plugged by fibrinopurulent debris
- If process is prolonged, obliterative bronchiolitis with irreversible lung damage may occur
- Histologic findings are nonspecific; the diagnosis can be confirmed with molecular testing, viral culture, DFA, IHC, serology, antigen detection assays
- Neutrophilic aggregation
- Organizing pneumonia
- Alveolar hemorrhage
- All of the above
- None of the above
Comment Here
Reference: Influenza
- Interstitial pneumonia is one of the common clinical manifestation of connective tissue disease (CTD); this entity is called CTD associated interstitial lung disease (CTD-ILD)
- Some patients initially diagnosed with idiopathic interstitial pneumonias (IIPs) eventually present with systemic autoimmune symptoms and develop a complete form of CTD; thus, it is often difficult to distinguish CTD-ILD from IIPs before the symptoms appear (Respiration 1995;62:248)
- IIP cases with certain features suggesting an underlying autoimmune process but insufficient to fulfill the diagnostic requirements of any specific CTD were previously categorized as an idiopathic or unclassifiable interstitial pneumonia (Am J Respir Crit Care Med 2013;188:733)
- In 2015, ATS / ERS working group proposed the term "interstitial pneumonia with autoimmune features (IPAF)" as a possible spectrum of CTD-ILD along with its provisional criteria (Eur Respir J 2015;46:976)
- An interstitial lung disease with clinical, serologic or histologic features suggestive of CTD which does not conclusively meet current rheumatologic criteria
- Histologically, nonspecific interstitial pneumonia (NSIP) and organizing pneumonia (OP) patterns are prevalent; lymphocytic inflammation is suggestive of IPAF
- Before the proposal from ATS / ERS, studies used nomenclature of:
- Lung dominant connective tissue disease (lung dominant CTD)
- Undifferentiated connective tissue disease associated interstitial lung disease (UCTD-ILD)
- Autoimmune featured interstitial lung disease (autoimmune featured ILD)
- Mean age 50 - 60 years old
- Female predominant
- No correlation with smoking status
- Unilateral or bilateral lower lobes of the lungs
- Although interstitial pneumonia had not been accepted as the sole manifestation of CTD in the current rheumatologic criteria, several studies suggested that interstitial pneumonia may appear as one of the preliminary manifestation of subclinical or undifferentiated CTD (Autoimmun Rev 2016;15:61, Respir Med 2005;99:234, Am J Respir Crit Care Med 2007;176:691)
- Mild to moderate chronic respiratory failure
- Shortness of breath
- Dyspnea on exertion
- Cough
- Fatigue
- Weight loss
- Abnormal chest auscultation
- End inspiratory fine crackles in lower lobes of the lungs
- Restrictive pattern in pulmonary function tests:
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- Extrathoracic autoimmune manifestation or serologic abnormality accompanythe respiratory symptoms (See Diagnosis)
- The proposed criteria consists of a priori requirements and three domains: clinical, serologic and morphologic, as below (Eur Respir J 2015;46:976)
- Findings of "multi compartment involvement" are detected by various modalities such as simple chest X ray, high resolution computed tomography (HRCT), surgical lung biopsy, pulmonary function tests and right heart catheterization
|
|
|
|
- Not included in the IPAF criteria because of their low specificity for CTD: low titer ANA, low titer RF, erythrocyte sedimentation rate, C reactive protein, creatine phosphokinase (Eur Respir J 2015;46:976)
- NSIP pattern
- Diffuse ground glass opacity
- Reticular opacity
- Traction bronchiectasis
- Often difficult to make a definite diagnosis without histopathological examination
- OP pattern
- Patchy and migratory consolidation in a subpleural and peribronchial area
- Band-like pattern
- LIP pattern
- Reticular opacity
- Air space opacity
- Often difficult to make a definite diagnosis without histopathological examination
- UIP and other radiological patterns can also be seen
- Limited data are currently available
- Retrospective studies observed different prognosis of IPAF, either better (Eur Respir J 2016;47:1767, Respir Med 2015;109:1326, Respir Med 2016;119:150) or similar (Respir Med 2017;123:56) than that of IIPs (IPF)
- Corticosteroids or immunosuppression drugs may improve the prognosis and stabilize pulmonary function deterioration (Respir Med 2016;119:150, Eur Respir J 2016;47:1767, Chest 2017 Mar 11 [Epub ahead of print], Respir Med 2015;109:1326), but evidence is limited to date
- Diffuse involvement with mild to moderate increase in weight
- Shrunken lung due to fibrotic changes in lower lobes
- Pleural thickening
- Histological NSIP pattern is the most common (about 50%) in IPAF cases, followed by NSIP with OP overlap pattern (Respir Med 2016;119:150, Eur Respir J 2016;47:1767)
- NSIP pattern
- Diffuse and uniform inflammation in alveolar walls
- Cellular or fibrotic changes
- OP pattern
- Polyps of fibroblastic organization obstructing alveolar ducts
- LIP pattern
- Marked and extensive infiltration of lymphocytes in alveolar wall
- Other findings suggestive of IPAF
- Lymphoid aggregates with germinal centers
- Diffuse lymphoplasmacytic infiltration
- Additional supportive findings (Chest 2010;138:251)
- Extensive pleuritis
- Dense perivascular collagen
- Other histological patterns, such as UIP pattern and respiratory bronchiolitis interstitial lung disease (RB-ILD) pattern, can be seen with lesser frequency
- UIP pattern may be related to poorer prognosis than NSIP pattern (Chest 2015;147:165)
- Connective tissue disease associated interstitial lung disease (CTD-ILD): clinical and serologic manifestations conclusive to meet rheumatologic criteria
- Cryptogenic organizing pneumonia (COP): no clinical or serologic autoimmune features
- Hypersensitivity pneumonitis: history of exposure to causative antigens, airway centered change, granuloma or interstitial giant cells
- Idiopathic NSIP: no clinical or serologic autoimmune features
- LIP: no clinical or serologic autoimmune features
- UIP / IPF: no or only one autoimmune features
- A current smoker with Raynaud’s phenomenon and a histological OP pattern. No serological abnormality is detected.
- Patient hospitalized for shortness of breath during the past 3 weeks, now improving over the past week. High titer ANA and radiological NSIP patterns are detected.
- Patient with swelling in both wrists for the past year, high titer anti-CCP antibody, high titer CRP, NSIP pattern on CT.
- Patient with digital tip ulceration for 6 months, high titer Scl-70 histological UIP pattern with little cellular inflammation.
- Patient with 2 year history of pulmonary hypertension who died of acute exacerbation. Histology shows NSIP with OP overlap pattern, diffuse lymphocytic infiltration and pleural thickening.
- Comments:
- IPAF. This case meets clinical and morphologic criteria of IPAF and meets no rheumatologic criteria.
- Acute hypersensitivity pneumonitis. This case shows the IPAF findings of serologic and morphologic domain. However, the clinical course is more suggestive for hypersensitivity pneumonitis. NSIP pattern is also common in hypersensitivity pneumonitis.
- CTD-ILD. This case meets the classification criteria for rheumatoid arthritis (Ann Rheum Dis 2010;62:2569).
- IPAF. This case is suspicious for systemic sclerosis, but does not fulfill the rheumatologic criteria (Ann Rheum Dis 2013;72:1747).
- Idiopathic NSIP (with OP). This case shows the findings of morphologic domain only.
Comment Here
Reference: Interstitial pneumonia with autoimmune features
- Rare and aggressive subtype of large B cell lymphoma with a predilection for intravascular spaces, absence of mass forming lesions and few to no circulating lymphoma cells
- 3 subtypes: cutaneous, classic and hemophagocytic; lung involvement is seen in the classic and hemophagocytic subtypes
- Lung involvement is seen in the classic and hemophagocytic subtypes
- On histology, large lymphoid cells with a B cell immunophenotype mostly present in alveolar capillaries; a minimal extravascular component is acceptable
- Diagnosis is often delayed and made at autopsy
- If detected in a timely manner, chemotherapy with rituximab (R-CHOP) may result in improved survival (Mol Clin Oncol 2016;5:689)
- Lung intravascular large B cell lymphoma (IVLBCL)
- Not recommended: angiotrophic lymphoma, angiotropic large cell lymphoma, angioendotheliotrophic lymphoma, intravascular lymphomatosis, malignant angioendotheliomatosis
- ICD-O: 9712/3 - intravascular large B cell lymphoma
- ICD-10: C83.8 - other nonfollicular lymphoma: intravascular large B cell lymphoma
- ICD-11: 2A81.1 & XH50S7 - intravascular large B cell lymphoma
- Rare; incidence of IVLBCL is 0.095 per million (Blood 2018;132:1561)
- Skin and central nervous system are the most affected sites (30 - 40% of cases) (Br J Haematol 2019;186:255)
- Specific incidence of IVLBCL involvement at other sites (i.e., lung, kidney, endocrine organs) is not well established
- Lung involvement is seen in the classic and hemophagocytic subtypes, with most examples documented as case reports or as case series
- Classic subtype
- Adults; median age of 70 years
- No sex predilection
- Most cases reported in North America and Western countries
- Hemophagocytic subtype
- Same age and sex distribution as classic subtype
- Most cases reported in Asia
- Intravascular spaces of the lung parenchyma, particularly alveolar capillaries
- Intravascular proliferation of lymphoma cells, leading to occlusion of small and medium sized blood vessels, leading to pulmonary dysfunction
- Lymphoma cells lack adhesion molecules required for proper migration across the endothelium
- CD29 (integrin beta 1)
- CD54 (ICAM1) (Hum Pathol 2000;31:220)
- Chemokine receptors needed for tumor migration beyond vascular lumen are decreased or absent
- CCR6, CCR7, CXCR5
- Currently unknown
- Chest pain, dyspnea, hypoxia, cough, pulmonary embolism, pulmonary hypertension (Oncol Lett 2023;25:234)
- B symptoms (systemic symptoms): fever of unknown origin (50 - 70%), weight loss, night sweats
- Lung involvement is seen in the classic and hemophagocytic subtypes
- Involvement of more common organs: skin with cutaneous lesions and central nervous system with altered mental status and strokes (Br J Haematol 2019;186:255)
- Hemophagocytic subtype presents with hemophagocytic syndrome, hepatosplenomegaly and cytopenia(s) (Blood 2018;132:1561)
- Few to rare lymphoma cells found in peripheral blood in 5 - 10% of cases
- Transbronchial biopsy, lung wedge biopsy, lung cryobiopsy or lung tissue obtained at autopsy (Am J Med 2021;134:926, Sarcoidosis Vasc Diffuse Lung Dis 2015;31:354)
- WHO classification of hematolymphoid tumors (5th edition) criteria
- Essential: large lymphoid cells restricted to intravascular spaces, especially capillaries (a minimal extravascular component is acceptable); pan-B cell markers positive
- Desirable: negative immunohistochemistry for human herpesvirus 8 (HHV8) latency associated nuclear antigen (LANA); negative in situ hybridization for Epstein-Barr virus (EBV) encoded small RNA (EBER)
- Hypoxemia, pulmonary hypertension (J Clin Oncol 2007;25:2137, Intern Med 2010;49:51)
- Anemia, leukopenia or thrombocytopenia
- Decreased albumin, elevated LDH, elevated erythrocyte sedimentation rate and C reactive protein (Oncol Lett 2023;25:234)
- Markers of disseminated intravascular coagulation (increased D dimer, prothrombin time [PT], partial thromboplastin time [PTT]) in the hemophagocytic subtype
- Chest Xray and computed tomography (CT) scan may be normal in a substantial number of cases, leading to a delayed diagnosis
- CT scan findings (if present): ground glass opacities, multiple small pulmonary nodules, interlobular septal thickening (Blood 2018;132:1561, Intern Med 2024;63:559, Oncol Lett 2023;25:234)
- Positron emission tomography (PET) / CT scan may or may not demonstrate increased radiotracer uptake
- Variable detection of defects in pulmonary blood flow scintigraphy secondary to embolisms
- Usually no mediastinal adenopathy
- Poor prognosis (Oncol Lett 2023;25:234)
- Most rapid and aggressive course with hemophagocytic subtype
- Diagnosis often delayed and made at autopsy
- 41 year old man with normal chest Xray, multiple ground glass opacities and recurrent strokes (Cureus 2024;16:e66112)
- 56 year old man with respiratory failure treated with prednisolone and R-CHOP chemotherapy (Respir Med Case Rep 2022;37:101625)
- 68 year old man with fever of unknown origin, multiple nodules and ground glass opacities on imaging, diagnosed by transbronchial cryobiopsy (Transl Cancer Res 2021;10:4571)
- 73 year old man with pneumonia, bilateral ground glass opacities and adenocarcinoma (J Clin Exp Hematop 2019;59:140)
- 75 year old woman with severe respiratory failure, high lactase dehydrogenase (LDH) and normal imaging studies (Am J Case Rep 2019;20:1199)
- Chemotherapy with rituximab may result in improved survival, if diagnosed in a timely manner (Mol Clin Oncol 2016;5:689)
- Lung may be normal or may show focal or diffuse congestion with no mass forming lesions
- Large lymphoid cells identified within the lumina of pulmonary alveolar capillaries
- Lymphoma cells may or may not be admixed with intravascular fibrin or a thrombus
- Minimal extravascular tumor cells are accepted
- Lymphoma cells may distend alveolar septa producing septal thickening
- Challenging diagnosis when scant intravascular lymphoma cells are present
- Tumor cells have centroblastic or immunoblastic morphology (multiple nucleoli or a central prominent nucleolus, vesicular chromatin and moderate amount of basophilic cytoplasm) (Arch Pathol Lab Med 2022;146:1160, J Clin Oncol 2007;25:3168)
- Lymphoma cells rarely show anaplastic morphology
- Intravascular mitotic figures may be seen
- 4 different patterns of vascular involvement (single or combined)
- Noncohesive: lymphoma cells float freely in the vascular lumen
- Cohesive: lymphoma cells fill the entire vascular lumen
- Marginated: lymphoma cells attached to vascular endothelium without fibrin or thrombus
- Tumor associated: intravascular lymphoma cells seen within a solid tumor (i.e., adenocarcinoma) but not in the adjacent normal tissue
- CD45 / LCA
- Pan-B cell markers: CD20, CD79a, CD19, PAX5
- BCL2 (Blood 2018;132:1561)
- MUM1 / IRF4 in 75 - 80% of cases with a nongerminal center / activated B cell-like immunophenotype (Arch Pathol Lab Med 2012;136:333)
- Ki67 proliferation index: high (> 60%)
- T cell markers
- Cyclin D1, CD30 (Blood 2018;132:1561)
- Cytokeratins and melanoma markers
- HHV8 LANA: rare positive cases have been described; desirable negative marker in the WHO classification of hematolymphoid tumors (5th edition)
- EBV by EBV encoded small RNA (EBER) in situ hybridization: rare cases have been described; desirable negative marker in the WHO classification of hematolymphoid tumors (5th edition)
- CD5 (positive in 20 - 40% of cases) (Mod Pathol 1998;11:983, Blood 2007;109:478)
- CD10 and BCL6 (positive in 10 - 15% of cases) (Arch Pathol Lab Med 2012;136:333)
- PDL1 (positive in up to 40% of cases) (Histopathology 2019;75:282)
- In general, IVLBCL exhibits a range of reported cytogenetic alterations but they are not diagnostic or specific for this type of lymphoma
- Reported mutations in MYD88 L265P (40 - 60%), CD79B Y196 (30 - 70%), HLA-B (~60%), SETD1B (~60%) and rearrangements in PDL1 (CD274) / PDL2 (PDCD1LG2) (~40%) (Blood 2018;131:2086, Blood 2021;137:1491)
- Lung, left, wedge biopsy:
- Intravascular large B cell lymphoma (see comment)
- Comment: The lung parenchyma contains a variable number of large, atypical lymphoid cells confined to the lumen of alveolar septal capillaries. In some areas, the alveolar septa are mildly expanded. The atypical lymphoid cells are positive for CD45, CD20, CD5 and MUM1 / IRF4 and are negative for pancytokeratin, S100, CD3, CD10, HHV8 and EBER in situ hybridization. These findings support the diagnosis of IVLBCL.
- Lymphangitic carcinomatosis or lymphangitic spread by other solid tumors:
- Lymphangitic carcinoma:
- Most common: carcinomas from lung, breast and gastric origin (Postgrad Med 2019;131:309)
- Positive cytokeratins and lineage specific markers depending on primary site (TTF1, GATA3, CDX2, others)
- Negative for CD45 and pan-B cell markers
- Lymphangitic spread of melanoma:
- Lymphangitic carcinoma:
- Intravascular leukemic infiltrates seen in hyperleukocytosis or leukostasis:
- Severe leukocytosis in the CBC and blasts / left shifted myeloid cells in peripheral blood smear
- In tissue sections, intravascular acute myeloid leukemia may be morphologically indistinguishable from lymphoma cells
- Intravascular infiltrates in chronic myeloid leukemias composed of a spectrum of immature and maturing myeloid cells
- Other intravascular lymphomas:
- Rarely, NK / T cell lymphomas may present with an intravascular component (Cancers (Basel) 2022;14:5458)
- Positive for CD3, CD8, CD56 and EBER by in situ hybridization
- Negative for pan-B cell markers
- Alveolar capillary angiomatosis:
- Interstitial organizing pneumonia:
- At low magnification, secondary to alveolar septal expansion
- At high magnification, the interstitial alveolar fibrosis lacks atypical intravascular cells
- Negative for CD45 and pan-B cell markers
- Lymphomatoid granulomatosis:
- Clinical and imaging presentation with multiple pulmonary nodules
- Angiodestructive and angiocentric; no intravascular proliferation
- Positive for pan-B cell markers and EBER in situ hybridization
A 62 year old woman with multiple comorbidities presents to the emergency department with sepsis and multiorgan system failure. After a difficult hospital course and despite aggressive measures, the patient died and an autopsy is performed. The above is seen on histologic evaluation of the lungs. Which of the following is true about this entity?
- Neoplastic cells are positive for T cell markers, such as CD3, CD5 and CD7
- Neoplastic cells confined to intravascular spaces are a diagnostic requirement
- Prognosis for this entity is excellent
- This entity has a very characteristic clinical and radiographic presentation
Comment Here
Reference: Intravascular large B cell lymphoma
- CD20-, CD3+, CD56+, EBER+
- CD20+, CD3-, MUM1+, EBER-
- CD34-, CD13+, CD33+, CD11c+
- CD34+, CD117+, MPO+, CD11c+
Comment Here
Reference: Intravascular large B cell lymphoma
- Often incidental findings at autopsy or biopsy
- Lesions due to injection of insoluble fillers of oral mediation, which lodge in small pulmonary arteries; may include crospovidone, talc, cornstarch or microcrystalline cellulose with characteristic findings
- All but cornstarch persist indefinitely
- Patients may have dyspnea or hypoxia; due to related infection, pulmonary edema, diffuse alveolar damage, vasculopathy leading to pulmonary hypertension or interstitial fibrosis
- Chest xray usually shows a micronodular pattern
- Fresh or organizing arterial thrombi with foreign material
- Perivascular foreign body granulomas contain birefringent foreign material resembling starch, talc or other materials
- May be associated with acute vasculitis, interstitial inflammation and fibrosis
- Distinct variant of lung adenocarcinoma with a goblet or columnar morphology and abundant intracytoplasmic mucin
- Rare variant of lung adenocarcinoma with a goblet or columnar morphology and abundant intracytoplasmic mucin
- No criteria regarding percentage of cells with mucin but typically homogeneous and not admixed with nonmucinous glands
- Aggressive clinical behavior often associated with intrapulmonary metastasis and recurrence
- Colloid adenocarcinoma is currently thought to be in a separate entity according to molecular and genetic differences (J Pathol Clin Res 2017;3:139, J Thorac Oncol 2011;6:244, Transl Lung Cancer Res 2017;6:234, Am J Surg Pathol 2014;38:1118)
- 0.2% of primary lung cancer (J Thorac Dis 2018;10:3595)
- 3 - 10% of all lung adenocarcinoma (J Thorac Oncol 2016;11:1064, Hum Pathol 2018;71:8, Histopathology 2018;73:38, Am J Surg Pathol 2014;38:1118)
- M:F = 1:2
- Lung; lower lobe predominant (J Thorac Dis 2018;10:3595)
- Associated with Ras-Raf-MEK-ERK pathway (Hum Pathol 2018;71:8, Am J Surg Pathol 2014;38:1118)
- KRAS mutation in 57 - 73%
- ALK rearrangement in minor cases
- Rare EGFR mutation
- Less associated with smoking than other subtypes of lung adenocarcinoma
- Frequent intrapulmonary metastasis and recurrence
- Rare extrapulmonary and distant metastasis (J Thorac Dis 2018;10:3595)
- 80% are N0 at the time of diagnosis (versus 55% in nonmucinous adenocarcinoma)
- 80% are M0 at the time of diagnosis (versus 55% in nonmucinous adenocarcinoma)
- Larger size and higher T category at presentation
- Based on histological and immunohistochemical features
- Even if pathological results correspond to primary invasive mucinous adenocarcinoma of lung, colorectal adenocarcinoma must be ruled out by endoscopy and radiology
- Consolidation with various appearance (Eur J Radiol 2015;84:993, Cancer Imaging 2019;19:47)
- Solid lesion similar to other lung cancers
- Mixed solid and gland glass opacity lesion similar to pneumonia
- Air bronchogram is common
- Often multifocal with multilobar involvement
- FDG-PET often demonstrates relatively low accumulation to the lesion
- Intermediate to poor prognosis compared with nonmucinous adenocarcinoma (Hum Pathol 2018;71:8, J Thorac Dis 2018;10:3595, Lung Cancer 2017;109:14, J Thorac Oncol 2016;11:1064, J Thorac Oncol 2015;10:1156)
- Approximately 70% spread through air space, which is associated with higher recurrence
- 19 year old woman with invasive mucinous adenocarcinoma (Asian Cardiovasc Thorac Ann 2018;26:635)
- 50 year old woman with invasive mucinous adenocarcinoma treated by radioablation (J Radiol Case Rep 2013;7:15)
- 62 year old woman with invasive mucinous adenocarcinoma having targetable NRG1 fusion (J Thorac Oncol 2017;12:e200)
- 68 year old man with invasive mucinous adenocarcinoma arising in a type 1 congenital pulmonary airway malformation (Acta Chir Belg 2019;1)
- 81 year old man with invasive mucinous adenocarcinoma harboring EGFR mutation (Surg Today 2015;45:1330)
- Same as nonmucinous adenocarcinoma
- NCCN Guidelines 3.2018
- For stages I, II, IIA: surgical resection (preferred) + adjuvant chemotherapy (platinum based) and radiation
- Inoperable or metastatic: chemotherapy variable radiation
- Gray to yellowish appearance
- Solid lesion with a gradational and ill defined border
- Mucus production inside and around the lesion
- Reference: Leslie: Practical Pulmonary Pathology - A Diagnostic Approach, 3rd edition, 2017
- Goblet cells or GI tract type columnar cells
- No criteria regarding percentage of cells with mucin but typically homogeneous and not admixed with nonmucinous glands
- Abundant intracytoplasmic mucin
- Basally oriented nuclei with minimal atypia
- Adjacent alveolar lumens are often filled with mucin (not specific for invasive mucinous adenocarcinoma)
- Tend to be well differentiated (J Thorac Dis 2018;10:3595)
- Often predominantly lepidic growth with slight distortion / destruction of alveolar architecture
- Admixed with minor papillary, acinar or micropapillary component
- Spread through air space is common
- Sheets or papillary clusters of high columnar cells (Bibbo: Comprehensive Cytopathology, 4th edition, 2014)
- Abundant intracytoplasmic mucin ("gold mucin")
- Relatively small nuclei with minimal atypia
- PAS: intracellular and extracellular mucin
- HNF4α: > 90% (but also in adenocarcinoma of other origins like stomach, intestine, pancreas, ovary, uterus, cervix) (Am J Surg Pathol 2013;37:211)
- MUC2 (but also positive in adenocarcinoma of other origins like GI tract) (Am J Surg Pathol 2004;28:442)
- CK7
- TTF1, Napsin A: can be very weakly or focally positive in rare cases
- CDX2: variable results from different reports; per own experience, negative or rarely faintly positive (J Thorac Oncol 2011;6:244, Am J Surg Pathol 2004;28:442, Am J Surg Pathol 2013;37:211)
- CK20: equivocal, variable results from different institutions
- HNF4α positive mucinous adenocarcinoma is often associated with KRAS or EGFR (Am J Surg Pathol 2013;37:211)
- Some cases with HNF4α negative mucinous adenocarcinoma is associated with ALK fusion (Am J Surg Pathol 2013;37:211)
- Other mutations in KRAS negative cases include NRG1, ERBB4 and BRAF fusions (Clin Cancer Res 2014;20:3087)
- Lung, right upper lobe, resection:
- Invasive mucinous adenocarcinoma (see synoptic report)
- Metastatic colorectal adenocarcinoma:
- Colloid adenocarcinoma (Hum Pathol 2015;46:836):
- Marked mucin pool replacing normal parenchyma
- Neoplastic epithelium floating in the mucin
- Fragments of displaced alveolar walls
- Minimal nuclear atypia
- Fibrotic encapsulation in minor cases (formerly called cystadenocarcinoma)
Comment Here
Reference: Invasive mucinous adenocarcinoma
- Abundant mucin in air spaces
- Abundant intracytoplasmic mucin
- TTF1 positive
- Napsin A positive
- p40 positive
- Proliferative disease or disorder of Langerhans cells involving lung, highly associated with smoking
- Pulmonary Langerhans cell histiocytosis (PLCH) is thought to be distinct from systemic Langerhans cell histiocytosis (LCH)
- Most common pulmonary histiocytic lesion (Arch Pathol Lab Med 2008;132:1171)
- Almost exclusively seen in young to middle aged smokers
- Stellate nodules centered around small airways, with early cellular phase and later fibrotic phase
- Langerhans cells stain for CD1a, Langerin, and S100
- Eosinophilic granuloma, Langerhans cell granulomatosis, histiocytosis X ("H-X")
- Multisystem diseases: Letterer-Siwi disease, Hand-Schüller-Christian disease, Hashimoto-Pritzker syndrome, where lung involvement is histologically indistinguishable from cellular phase of PLCH
- Uncommon, encompassing 3 - 5% of lung biopsies for interstitial lung disease
- >90% of cases associated with smoking - considered a smoking related disease
- Usually ages 20 - 50 years
- More common in Caucasian than African Americans or Asians
- 50% of cases only involve lung
- 20% of those with multicentric disease (i.e. bone, skin, lymph nodes, spleen, CNS, pituitary, rarely thyroid and thymus) have lung involvement
- Debatable as reactive versus neoplastic, could arise from smoking related and immunomodulatory processes (Arch Pathol Lab Med 2016;140:230)
- PLCH may be a reactive process with a subset showing clonality, but extrapulmonary forms of Langerhans cell histiocytosis are thought to be neoplastic
- Unpredictable course, even with smoking cessation: some spontaneously resolve, others remain stable, some progress to honeycomb fibrosis
- Disorder of cells with Langerhans cell phenotype
- Many patients asymptomatic
- Chronic cough and exertional dyspnea typical (Eur J Intern Med 2015;26:351)
- Rarely can present with hemoptysis
- Recurrent spontaneous pneumothorax in 15 - 25% of cases
- Pulmonary hypertension and vasculopathy frequent in advanced cases
- Diabetes insipidus in 15% of patients from pituitary involvement
- Generally restrictive features in early disease, obstructive features in late disease
- Secondary malignant and non-malignant neoplasms
- Lung biopsy is necessary for a definitive diagnosis, although may not be required if imaging findings are highly characteristic (Orphanet J Rare Dis 2012;7:16)
- Transbronchial biopsy may be diagnostic; otherwise, requires surgical lung biopsy
- Normal peripheral eosinophil blood count
- Upper / middle lung predominance
- X-ray: small nodules generally up to 1 cm and variably sized cysts
- High resolution CT: bronchiolocentric stellate nodules possibly with surrounding ground glass opacities, some with faint lucent cavity
- Advanced disease with cysts, emphysema adjacent to scarring, reticular and nodular opacities, honeycombing, can mimic IPF
- FDG-PET may show increased uptake, especially in early nodular disease
- 10 - 20% may progress to respiratory failure
- Median survival 12 years, 5 year survival 70%, 10 year survival 60%
- Worse prognosis in cases with pulmonary hypertension
- Worse prognosis for those with baseline poor respiratory function and those with concurrent neoplasms
- Worse prognosis with extremes of age, prolonged constitutional symptoms, multiorgan involvement, extensive cysts, honeycomb changes
- 22 year old man with PLCH and tuberculosis (Int J Clin Exp Pathol 2015;8:2146)
- 40 year old woman with Stage IV diffuse large B cell lymphoma (Arch Pathol Lab Med 2002;126:747)
- 42 year old man with bilateral axillary ulcerated masses (Am J Med 2015;128:e7)
- Smoking cessation most effective
- Corticosteroids +/- chemotherapeutic agents show mixed results
- Lung transplantation in advanced cases
- Upper lobe predominance, fine nodular infiltrate, with nodules up to 1.5 cm
- Advanced disease with cysts, cavitary lesions, and honeycombing
- Early cellular phase and older fibrotic lesions may be intermixed, but one pattern typically predominates
- Scattered, variably sized stellate nodules ("star fish-like" or "Medusa head-like") with interstitial scarring and aggregates of Langerhans cells
- Layered appearance of nodules, bronchiolocentric distribution with pleural/subpleural sparing
- Confluence of nodules → serpentine sheath around small airways
- Langerhans cells are relatively large with abundant, granular, mildly eosinophilic and indistinct cytoplasm, grooved nuclei with indented nuclear membranes / grooves, "crumpled tissue paper" nuclear outlines, pale basophilic nucleus, one or two small nucleoli
- Also prominent eosinophils, lymphocytes, plasma cells, activated macrophages, multinucleated giant cells
- Variably sized cystic spaces at periphery of nodules lacking lining cells, secondary to traction on surrounding alveolar walls or airways
- Frequent hemosiderin, necrosis, alveolar lining cell hyperplasia, pigmented alveolar macrophages ("smoker's macrophages")
- Variable vasculitis, patchy organization, other smoking related changes such as emphysema, respiratory bronchiolitis, desquamative interstitial pneumonia
- Older fibrotic lesions have fewer Langerhans cells and eosinophils, more fibrosis
- May show pulmonary hypertension
- Sarcomatous variant has significant atypia and mitotic figures
- Langerhans cells with abundant cytoplasm and grooved nuclei with background eosinophils and lymphocytes
- Bronchioalveolar lavage may show increased numbers (>5%) of CD1a+ Langerhans cells but test with low sensitivity (Respir Med 2012;106:1286)
- Birbeck's granules (pentilaminar intracytoplasmic structures, tennis racket shaped)
- Subset of PLCH cases show BRAF V600E mutation (Am J Surg Pathol 2014;38:548)
- Mutations in other MAPK genes have been identified
- Desquamative interstitial pneumonitis
- Eosinophilic pleuritis: no Langerhans cells, although mesothelial cells may appear similar
- Eosinophilic pneumonia
- Erdheim-Chester disease
- Hypersensitivity pneumonitis
- Lymphangioleiomyomatosis (LAM): HMB45 and actin positive
- Respiratory bronchiolitis
- Resected tumors that lack morphologic or immunohistochemical differentiation toward small cell carcinoma, adenocarcinoma or squamous cell carcinoma (J Thorac Oncol 2015;10:1240)
- Null or unclear immunophenotype based on IHC analysis with TTF1, p40 and neuroendocrine markers (J Thorac Oncol 2019;14:1213)
- Malignant, poorly differentiated epithelial neoplasm of lung composed of large, atypical cells
- No morphologic or immunohistochemical evidence of glandular, squamous or neuroendocrine differentiation
- Diagnosis of exclusion; diagnosis can only be made on resected tumors
- Synonymous with large cell undifferentiated carcinoma and large cell anaplastic carcinoma
- Previously, large cell carcinoma included variants such as basaloid carcinoma, large cell neuroendocrine carcinoma, lymphoepithelioma-like carcinoma, clear cell carcinoma and large cell carcinoma with rhabdoid phenotype
- As of the 2015 WHO classification, large cell carcinoma is a diagnosis of exclusion, with reclassification of the former large cell carcinoma subtypes into different categories (J Thorac Oncol 2015;10:1243)
- M > F
- Average age of 65 years
- Associated with cigarette smoking
- Becoming increasingly rare due to immunohistochemical and molecular studies that support the reclassification of entities formerly diagnosed as large cell carcinoma (Sci Transl Med 2013;5:209ra153)
- Peripheral lung
- 50% with connection to large airways
- Cough, chest pain, shortness of breath
- Typically larger than 5 cm
- Diagnosis of exclusion
- Small biopsy specimens and cytology specimens should not be used for diagnosis
- According to the 2021 WHO, only resection specimens with exclusion of a differentiated component, via thorough sampling, can be classified as large cell carcinoma (J Thorac Oncol 2022;17:362)
- NSCC, NOS (nonsmall cell carcinoma, not otherwise specified) should be used in small biopsies or cytology specimens
- Usually large, lobulated or well marginated, peripheral, heterogeneously enhancing mass, often containing central necrosis (Ghosh: Handbook of Imaging in Pulmonary Disease, 1st Edition, 2021)
- Rapid growth is common with metastasis (chest wall, thoracic lymph nodes, distant) at presentation
- PET CT preferred over CT for identification of full extent of disease and metastases
- Generally poor prognosis with limited treatment options (J Thorac Oncol 2019;14:1213)
- 52 year old man with respiratory failure and obstructing endobronchial mass (Cureus 2018;10:e2202)
- 58 year old man with prolonged cough and hemoptysis (Thorac Cancer 2021;12:1141)
- 80 year old woman with shoulder pain and vertebral compression fracture (Respir Med Case Rep 2020;31:101197)
- Dependent on stage
- Surgical excision, chemotherapy or radiation therapy
- Usually peripheral lung and unifocal; large, circumscribed with well defined borders and bulging, lobulated, homogeneous gray-white "fish flesh" cut surface
- Internal necrosis and hemorrhage are common (Fletcher: Diagnostic Histopathology of Tumors, 5th Edition, 2020)
- Sheets or solid nests of round to polygonal cells
- Moderately abundant cytoplasm, well defined cell borders
- Vesicular nuclei, prominent nucleoli
- Foci of central necrosis and hemorrhage may be present
- No glandular, squamous or neuroendocrine differentiation is present (Fletcher: Diagnostic Histopathology of Tumors, 5th Edition, 2020)
- Reference: Clin Chest Med 2020;41:67
- Large pleomorphic cells with a moderate to abundant amount of cytoplasm, vesicular nuclei, prominent nucleoli
- Broad spectrum and low molecular weight cytokeratins, such as CAM5.2
- TTF1, Napsin, mucicarmine, p40, p63, synaptophysin, chromogranin, CD56
- Molecular studies show that some null phenotype large cell carcinomas contain mutations seen in conventional adenocarcinoma (e.g., KRAS, NRAS, MET, STK11) and squamous cell carcinoma (e.g., PIK3CA amplification and mutation); this indicates that tumors classified as large cell carcinomas could represent poorly / undifferentiated nonsmall cell lung cancer (NSCLC) (J Thorac Oncol 2019;14:1213, Sci Transl Med 2013;5:209ra153)
- Lung, left, resection:
- Large cell carcinoma (1.1 cm) (see comment)
- Comment: Immunohistochemical studies are performed with appropriate controls. The tumor is negative for TTF1, Napsin A, CK5/6 and p40. There is no morphologic evidence of differentiation to adenocarcinoma or squamous cell carcinoma. The histologic features are not those of neuroendocrine carcinoma. Given these findings, the tumor is best classified as large cell carcinoma. PDL1 immunostain shows weak expression in 20% of tumor cells.
- Basaloid squamous cell carcinoma:
- Expresses squamous markers (i.e., p40)
- Large cell neuroendocrine carcinoma:
- Expresses neuroendocrine markers (i.e., chromogranin, synaptophysin, CD56)
- Solid adenocarcinoma:
- Metastatic carcinoma:
- CAM5.2
- Chromogranin
- p40
- SOX10
- TTF1
Comment Here
Reference: Large cell carcinoma
- Aggressive, poorly differentiated carcinoma composed of large cells with neuroendocrine architecture, prominent nucleoli, high mitotic activity and necrosis
- Grouped with other neuroendocrine tumors in the 2021 WHO classification of thoracic tumors (J Thorac Oncol 2022;17:362)
- More likely to recur and has shorter patient survival than other types of non-small cell lung carcinoma, even in stage I disease (Cancer Control 2006;13:270)
- May coexist with other lung cancers such as adenocarcinoma and squamous cell carcinoma
- High grade non-small cell carcinoma with neuroendocrine architecture and immunohistochemical markers, characterized by > 10 mitoses/2 mm2, prominent nucleoli and extensive necrosis (J Thorac Oncol 2022;17:362)
- Poor overall prognosis
- Should be distinguished from atypical carcinoid, basaloid squamous cell carcinoma and poorly differentiated adenocarcinoma, although diagnosis can be difficult on small biopsies or cytology specimens
- Large cell neuroendocrine carcinoma (LCNEC): proposed by Travis et al. in 1991 as distinct from small cell carcinoma (Am J Surg Pathol 1991;15:529)
- Combined LCNEC: also has components of adenocarcinoma (most common), squamous cell carcinoma, giant cell carcinoma or spindle cell carcinoma (Thorac Surg Clin 2014;24:257)
- Incidence varies between 0.3% and 3% of all lung tumors (Pathol Oncol Res 2022;28:1610730, J Clin Med 2022;11:1461)
- Older age and male sex predominance (Pathol Oncol Res 2022;28:1610730)
- Strong association with heavy smoking (Cancers (Basel) 2012;4:777)
- Thorax: lung, anterior mediastinum, thymus (Mod Pathol 2022;35:36, J Clin Med 2022;11:1461, Mol Clin Oncol 2021;14:34, BMJ Case Rep 2021;14:e240453, Int J Surg Case Rep 2019;60:53, J Med Case Rep 2017;11:155, Surg Case Rep 2018;4:133)
- Head and neck: parotid and submandibular gland, nasopharynx, hypopharynx, oral cavity, larynx (Auris Nasus Larynx 2005;32:89, Auris Nasus Larynx 2014;41:105, J Pediatr Hematol Oncol 2015;37:474, BMJ Case Rep 2015;2015:bcr2015211908, Int J Oral Maxillofac Surg 2022;51:1520, Head Neck Pathol 2010;4:198)
- Gastrointestinal tract: esophagus, esophagogastric junction, colon and rectum, ampulla (Int J Surg Case Rep 2019;60:291, Pathol Int 2019;69:481, Clin Colorectal Cancer 2020;19:61, Cureus 2022;14:e20949, Med Oncol 2010;27:1144)
- Pancreatobiliary: liver, extrahepatic biliary tract, gallbladder, pancreas (Int J Surg Pathol 2019;27:893, Surg Case Rep 2016;2:141, Jpn J Clin Oncol 2013;43:571, J Laparoendosc Adv Surg Tech A 2022;32:639)
- Genitourinary tract: kidney, urinary bladder, prostate (J Med Case Rep 2017;11:297, Cureus 2022;14:e20949, IJU Case Rep 2022;5:505)
- Gynecologic: ovary, uterus and uterine cervix (Gulf J Oncolog 2021;1:82, Eur J Gynaecol Oncol 2004;25:109, Case Rep Oncol 2018;11:665)
- Skin (J Cutan Pathol 2016;43:1067)
- Breast (Mod Pathol 2022;35:1494)
- Proposed model of histogenesis of lung neuroendocrine carcinomas, in view of similarities in the expression of primitive neural / neuroendocrine cell specific transcription factors (Pathol Int 2015;65:277)
- Strong association with heavy smoking (Cancers (Basel) 2012;4:777)
- Unclear association with preneoplastic lesions, such as neuroendocrine cell hyperplasia and carcinoid tumorlets (Endocrine 2015;50:315)
- Symptoms vary according to anatomic localization
- Centrally located tumors present with cough, hemoptysis, bronchial obstruction or recurrent pneumonia (J Thorac Dis 2020;12:466)
- Peripherally located tumors can be asymptomatic and identified incidentally (Ann Thorac Surg 1998;65:1410)
- Paraneoplastic syndromes are uncommon but may include Cushing syndrome, carcinoid syndrome or Lambert-Eaton myasthenic syndrome (J Bronchology Interv Pulmonol 2015;22:267, Clin Pathol 2021;14:2632010X211051741)
- Difficult to make specific diagnosis on small biopsy and cytology specimens
- Frequently recognized in cytology as non-small cell lung cancer (NSCLC), not otherwise specified or as adenocarcinoma
- Neuroendocrine features by light microscopy and confirmation by immunohistochemical staining for neuroendocrine markers
- Serum AFP levels can be elevated (Mol Clin Oncol 2021;14:34)
- Nonspecific findings, indistinguishable from other NSCLC
- CT findings: peripherally located tumors, expansively growing with irregular margins, with or without calcification and infrequent cavitation (Clin Imaging 2007;31:379)
- Poor prognosis with median overall survival 17.9 months and 3 year survival rate of 1.8% (Bull Cancer 2021;108:981)
- Worse prognosis than stage equivalent non-small cell lung carcinoma (Semin Thorac Cardiovasc Surg 2006;18:206)
- Adverse prognosticators (Bull Cancer 2021;108:981, Ann Thorac Surg 2015;99:983)
- Male sex
- History of smoking
- Obstructive atelectasis
- Advanced nodal stage
- Coexpression of chromogranin A and CD56
- 38 year old pregnant woman with a 5 cm left lung lower lobe mass with brain and adrenal metastases (Front Oncol 2022;12:823813)
- 64 year old man with hemoptysis and a 3 cm left lung upper lobe mass (Ann Palliat Med 2020;9:3705)
- 69 year old man with progressive weakness and a 2.5 cm right lung lower lobe mass (Clin Pathol 2021;14:2632010X211051741)
- 76 year old woman with a 2.4 cm left lung upper lobe mass, multiple liver masses and carcinoid syndrome (Intern Med 2022 Oct 5 [Epub ahead of print])
- Surgical resection in patients with stage I - IIIA disease with adjuvant chemotherapy (J Thorac Oncol 2019;14:2143, Br J Cancer 2021;125:1210)
- Chemotherapy in patients with advanced stage disease (Eur Respir J 2017;50:1701658)
- Immunotherapy is currently in clinical trials (Front Oncol 2021;11:655752)
- Gross appearance is indistinguishable from other lung malignancies
- Most tumors tumors are located peripherally and are usually nodular and circumscribed with tan-red, necrotic cut surface (Am J Clin Pathol 2004;122:884, AJR Am J Roentgenol 2004;182:87)
- Size range: 0.9 - 12 cm, with average size 3 - 4 cm (Cancer 2001;91:1992)
- Neuroendocrine organoid architecture, prominent nucleoli, abundant necrosis
- Neuroendocrine organoid architecture may include nesting with peripheral palisading, anastomosing trabeculae and rosette-like structures (Mod Pathol 2022;35:36)
- > 10 mitoses/2 mm2, extensive / geographic necrosis
- Large cells (~3x size of small cell carcinoma) with abundant amphophilic cytoplasm, intercellular membranes, nuclear pleomorphism, variably coarse, granular or vesicular chromatin with prominent nucleoli (Transl Lung Cancer Res 2020;9:860, Mod Pathol 2022;35:36)
- Occasional rhabdoid features (Pathol Int 2019;69:481, J Cancer Res Ther 2015;11:657)
- Larger tumor cells than atypical carcinoid, high nuclear grade, increased mitotic activity and necrosis (Arch Pathol Lab Med 2010;134:1628)
Contributed by Ioanna Abba Nteka, M.D., Aggeliki Cheva, M.D., Ph.D., Antonia Loukousia, M.D., Roseann Wu, M.D., M.P.H. and Kyriakos Chatzopoulos, M.D., Ph.D.
- Hypercellular, with numerous, single medium to large cells
- 3 dimensional and variably sized groups
- Large, pleomorphic cells with irregular vesicular chromatin, prominent nucleoli, abundant cytoplasm, sharp cellular borders
- Naked nuclei are abundant but with a variable subset of cells showing evident cytoplasm
- Molding, mitoses, necrotic background
- Peripheral nuclear palisading; rosette-like structures (Cancer 2008;114:180, Diagn Cytopathol 2001;24:58)
- Neuroendocrine markers, usually at least 2 focal to diffuse (chromogranin, synaptophysin, CD56), caution if CD56 is the only neuroendocrine marker expressed
- ISNM1: panneuroendocrine marker; nuclear positivity in 91.3% of large cell neuroendocrine carcinomas (Am J Surg Pathol 2017;41:1561)
- ASCL1: nuclear expression in 72.7%; neurogenic / neuroendocrine transcription factor (Hum Pathol 2016;48:142)
- Cytokeratins AE1 / AE3, CAM5.2
- Variable CK7 and 34 beta E12 (Hum Pathol 2000;31:980)
- pRb and cyclin D1 (Histopathology 2022;81:205)
- High Ki67 (40 - 80%) helpful to differentiate from carcinoid tumors, especially in small biopsies (Semin Diagn Pathol 2015;32:469)
- NKX6.1 in 80% (Diagn Cytopathol 2018;46:1010)
- CD117 in 77% (Virchows Arch 2004;445:449)
- GLUT1 in 74% (Mod Pathol 2009;22:633)
- SATB2 in 70% (Int J Surg Pathol 2022;30:151)
- TTF1 in 50% (Mod Pathol 2018;31:111)\
- p63 and p40 (Am J Clin Pathol 2014;142:320)
- Napsin A (can be focally positive in 15%) (Mod Pathol 2018;31:111)
- Loss of YAP1 in 60% (Cancer Sci 2016;107:1527)
- PDL1 in 10% (Lung Cancer 2017;108:115)
- Neurosecretory granules, occasional evidence of granular differentiation and intercellular junctions suggestive of squamous differentiation (Am J Surg Pathol 1991;15:529)
- 3 molecular subsets identified by next generation sequencing; no statistically significant differences in clinicopathologic parameters or survival among subsets:
- Small cell carcinoma-like: TP53 and RB1 comutation and MYCL amplification
- Non-small cell carcinoma-like: STK11, KRAS, KEAP1 mutations, no TP53 / RB1 comutation, molecular profile resembling adenocarcinoma, with additional NOTCH family mutations
- Carcinoid-like: MEN1 mutations, low mutation burden (Clin Cancer Res 2016;22:3618)
- Other less commonly mutated genes: PIK3CA, PTEN, AKT2, FGFR1, KIT, ERBB2, HRAS, EGFR, NTRK2 and NTRK3 (Clin Cancer Res 2017;23:757, Hum Mutat 2008;29:609)
- Case reports of tumors harboring an EML4::ALK fusion (Cold Spring Harb Mol Case Stud 2022;8:a00623, Front Oncol 2022;12:823813)
- BRAF alterations including mutations, amplifications reported in small case series (JCO Precis Oncol 2018;2:1)
- Lung, left upper lobe, CT guided needle core biopsy:
- Large cell neuroendocrine carcinoma (see comment)
- Comment: Multiple sections from the biopsy material reveal an infiltrative malignant tumor consisting of large cells with abundant amphophilic cytoplasm and large, ovoid or round nuclei with prominent nucleoli and increased mitotic activity. Tumor cells form solid nests with peripheral palisading and central necrosis. Immunostains performed on paraffin sections show diffuse and strong expression of keratins AE1 / AE3, synaptophysin, chromogranin, CD56 and nuclear expression of TTF1 and ISNM1. No expression of p40 or napsin A is seen. These findings support the diagnosis.
- Small cell carcinoma:
- Sheet-like growth, nuclear molding, round oval or spindle cells, crushing artifact, Azzopardi effect, scant cytoplasm, finely granular chromatin, no nucleoli, extensive necrosis, high mitotic count (Am J Surg Pathol 2002;26:1184, Hum Pathol 1998;29:272)
- Atypical carcinoid:
- Lack of prominent nucleoli, monotonous cells with nesting and salt and pepper chromatin distribution, mitotic count between 2 - 10/2 mm2 (Transl Lung Cancer Res 2020;9:860)
- Basaloid squamous cell carcinoma:
- Immunopositivity for p40 and CK5/6, lack of neuroendocrine granules in electron microscopy (Transl Lung Cancer Res 2017;6:530)
- Adenocarcinoma, solid pattern:
- Absence of neuroendocrine markers by immunohistochemistry, lack of peripheral palisading (Transl Lung Cancer Res 2017;6:530)
- NUT carcinoma:
- Can occasionally be positive for synaptophysin (pitfall), presence of abrupt keratinization, NUT immunopositivity (Virchows Arch 2021;478:21)
- SMARCA4 deficient undifferentiated tumor:
- Discohesive cells with occasional rhabdoid features in an otherwise diffuse and monotonous cellular population, BRG1 loss by immunohistochemistry (Virchows Arch 2021;478:21)
A 76 year old man with a history of heavy smoking is diagnosed with a large pulmonary mass and undergoes lobectomy. The histologic features of the mass can be seen in the photograph above. Which initial panel of immunostains is more likely to be helpful in the differential diagnosis of this pulmonary malignancy from its most frequent counterparts?
- BRG1, INI1 and NUT
- Chromogranin, synaptophysin and cytokeratin 8/18
- ISNM1, p40 and napsin A
- p63, TTF1 and CD56
Comment Here
Reference: Large cell neuroendocrine carcinoma
- Extensive necrosis
- Mitotic count > 10/2 mm2
- Organoid nesting
- Prominent nucleoli
Comment Here
Reference: Large cell neuroendocrine carcinoma
- Lung adenocarcinoma with primarily lepidic growth pattern with at least one of the following (Arch Pathol Lab Med 2013;137:685, J Thorac Oncol 2011;6:244):
- > 0.5 cm of stromal invasion
- Measuring > 3 cm in greatest dimension with ≤ 0.5 cm of stromal invasion
- Lymphatic, vascular or pleural invasion
- Tumor necrosis
- Spread through airspaces
- Tumor with noninvasive (lepidic) and invasive components
- Invasive component should total > 0.5 cm
- Invasive component can be defined as stromal invasion or the presence of any subtype other than lepidic
- Presence of lymphovascular invasion, tumor necrosis or pleural invasion also meets the criteria of an invasive component
- Tumors measuring > 3 cm with < 0.5 cm of invasive or nonlepidic components are also classified as lepidic adenocarcinoma
- In rare cases, a lepidic carcinoma with < 0.5 cm of invasion that has high risk features (lymphatic, vascular or pleural invasion, tumor necrosis or spread through airspaces) should also be classified as lepidic adenocarcinoma and not minimally invasive adenocarcinoma
- Lepidic adenocarcinoma
- Lepidic predominant adenocarcinoma (for mixed patterns where lepidic growth pattern predominates)
- Older terminology was bronchoalveolar carcinoma; however, this is obsolete and should no longer be utilized
- More common in Asian populations and not as strongly associated with smoking as other subtypes of adenocarcinoma (Am J Surg Pathol 2014;38:448)
- Generally peripherally located lung lesions (Lung Cancer 2000;29:179)
- Hypothesized to form after a multistep progression from atypical adenomatous hyperplasia to adenocarcinoma in situ to lepidic adenocarcinoma (J Thorac Oncol 2008;3:340)
- Generally asymptomatic, discovered as incidental mixed solid and ground glass lesions on CT scans (N Engl J Med 2013;368:1980)
- Slow growing ground glass opacity (see radiology description)
- Biopsies will show adenocarcinoma with lepidic growth pattern
- Diagnosis can only be made on the resection specimen and cannot be made with limited tissue sampling (Arch Pathol Lab Med 2013;137:668, Arch Pathol Lab Med 2007;131:1027)
- Ground glass opacity dominant, with foci of invasion represented by solid areas (Lung Cancer 2018;125:14, Hum Pathol 2016;51:41, Ann Oncol 2015;26:156)
- Early lepidic adenocarcinomas (pT1a) have a more favorable prognosis than other subtypes of adenocarcinoma (J Clin Oncol 2012;30:1438, J Thorac Oncol 2011;6:1496, Mod Pathol 2011;24:653)
- 26 year old woman with a lepidic adenocarcinoma demonstrating aerogenous spread of mucin without evidence of invasion (Exp Mol Pathol 2014;96:400)
- 36 year old woman with a 33 week pregnancy in acute respiratory failure from a lepidic pulmonary adenocarcinoma (Case Rep Oncol 2018;11:822)
- Associated with a lower risk of recurrence than other subtypes of adenocarcinoma; surgical excision with close follow up may be sufficient for early stage disease (Am J Surg Pathol 2014;38:448)
- Peripheral ill defined firm white tumor with solid areas; ill defined areas correspond to lepidic growth pattern and the solid areas correspond to invasive component (Hum Pathol 2016;51:41)
- In rare cases, necrosis and frank pleural invasion may be present
- Primary lung adenocarcinoma with lepidic growth pattern measuring ≤ 3 cm in greatest dimension with > 0.5 cm area of stromal invasion or presence of necrosis, lymphovascular invasion, pleural invasion or spread through air spaces
- Lepidic growth pattern: neoplastic cells resembling bland type II pneumocytes growing along the surface of the alveolar air spaces
- Foci of stromal invasion characterized by angulated glands, desmoplastic stroma and increased cytologic atypia (Cancer 1995;75:2844)
- Size of invasion should be measured as the largest focus of invasion (Am J Surg Pathol 2014;38:448, Arch Pathol Lab Med 2013;137:685)
- If there are multiple foci of invasion, the invasive size can be measured as a sum of the percentage of the invasive components in each section multiplied against the greatest tumor dimension (Am J Surg Pathol 2014;38:448, Surg Today 2019;49:828)
- Invasion may also be defined as presence of nonlepidic growth pattern (acinar, micropapillary, papillary, solid, colloid or fetal patterns) or the presence of necrosis, lymphovascular invasion, pleural invasion or spread through air spaces
- For the uncommon occurrence of a lepidic predominant tumor > 3.0 cm with either no invasion or ≤ 0.5 cm of invasion, it is recommended that such tumors be classified as lepidic predominant adenocarcinoma and staged as pT1a, since there is insufficient data to conclude they have the same prognostic features as ≤ 3.0 cm tumors meeting criteria for adenocarcinoma in situ or minimally invasive adenocarcinoma (J Thorac Oncol 2016;11:1204)
- Mucinous carcinoma can often display a prominent lepidic growth pattern; however, the majority of cases will have areas of invasion and should be classified as an invasive mucinous adenocarcinoma
- Lung, right lower lobe, lobectomy:
- Invasive adenocarcinoma, lepidic predominant, pT1a NX MX (see synoptic report)
- Minimally invasive adenocarcinoma:
- < 3.0 cm in greatest dimension
- Invasive foci must be < 0.5 cm in aggregate
- No other high risk features
- Adenocarcinoma in situ / atypical adenomatous hyperplasia:
- < 3.0 cm in greatest dimension
- No invasive component
Comment Here
Reference: Lepidic adenocarcinoma
- Acinar predominant adenocarcinoma
- Adenocarcinoma in situ
- Lepidic predominant adenocarcinoma
- Minimally invasive adenocarcinoma
Comment Here
Reference: Lepidic adenocarcinoma
- Usually incidental post mortem finding associated with debilitating disease
- Lipid either exogenous (from nasal sprays or inhalation of other lipid containing substances) or endogenous (bronchial obstruction)
- 1 year old man with recent history of meningitis with recurrent episodes of pneumonia (Case of the Week #287)
- Well circumscribed, firm with prominent lymphatics on lung surface in exogenous type
- Lipoid material (or empty spaces), inflammatory cells and young fibroblasts
- Reactive endarteritis, marked alveolar lining cell hyperplasia and lipid laden foamy macrophages
- Very rare; usually endobronchial, usually men ages 50+ (Chest 2003;123:293)
- Benign neoplasm composed of mature adipose tissue
- Treatment of choice is bronchoscopic removal
- Endobronchial lipomas may show focal cytologic atypia and fibrosis but molecular evidence suggests similarity to lipomas of other sites
- Endobronchial lipomas clinically mimic other tumors and may cause obstructive symptoms
- Pulmonary lipomas lack the cartilage, myxoid matrix, entrapped bronchial epithelium, or other mesenchymal components seen in pulmonary hamartomas
- Very rare, 0.1 to 0.5% of all lung tumors
- Older men, mean age 65, majority with smoking history
- May be associated with obesity
- Usually endobronchial (large bronchi), very rarely parenchymal
- More common in right lung
- Typically sporadic
- Endobronchial lesions may arise from peribronchial or submucosal adipocytes
- Parenchymal lesions may arise from adipocytes of subsegmental bronchi or subpleural fatty tissue
- Slow growing, indolent
- Discovered incidentally by imaging or during bronchoscopy for other reasons
- Larger endobronchial lesions may present with cough, pneumonia, bronchiectasis, empyema, hemoptysis
- May mimic endobronchial carcinoid, malignancy or asthma / COPD
- CT or MRI can suggest diagnosis
- Bronchoscopic biopsy or excision for endobronchial lesions
- High signal intensity of fat in all MRI sequences
- CT shows smooth, non-enhancing, homogenous mass with fat density
- May see peripheral air trapping on CT with obstructive endobronchial lesions
- Benign, but large lesions may cause obstructive complications
- 26 year old woman with peripheral intrapulmonary lipoma (Pol J Pathol 2011;62:113)
- 52 year old man with endobronchial lipoma mimicking asthma and malignancy (Prim Care Respir J 2010;19:281)
- 54 year old woman with peripheral intrapulmonary lipoma (Tuberk Toraks 2006;54:374)
- Peripheral intrapulmonary lipoma (Br J Radiol 2004;77:60)
- Endobronchial lipoma (Ther Adv Respir Dis 2014;8:162)
- Intraparenchymal pulmonary lipoma (Ann Diagn Pathol 2014;18:244)
- Resection is curative
- Endobronchial tumors are generally Well circumscribed, polypoid or sessile, yellowish mass on bronchoscopy
- Yellow-grey mass with firm capsule
- Intraparenchymal lesions are well circumscribed, soft, lobulated, yellow
- Mature adipose tissue underlying respiratory epithelium, with scattered lymphocytes and histiocytes
- May show fibrosis and hyperchromatic stromal cells
- Rarely has osteocartilaginous metaplasia
- HMGA1 or HMGA2 rearrangements seen in endobronchial lipomas (Am J Surg Pathol 2013;37:1715)
- Acute eosinophilic pneumonia with transient diffuse pulmonary infiltrates composed primarily of eosinophils and serum eosinophilia
- Characteristic imaging findings, so biopsy is rarely performed
- Eosinophils may be present in sputum
- Often associated with ascaris infection
- Self limited - lasts only up to 1 month
- Lung mesenchymal neoplasm that arises from abnormal smooth muscle cells around lymphatic vessels and causes parenchymal damage
- Rare cystic lung disease that causes progressive lung damage; mainly affects young females with tuberous sclerosis complex (TSC)
- LAM
- Overall rare (5 cases per 1 million) (QJM 2011;104:971)
- Almost exclusively seen in women of reproductive age (Semin Respir Crit Care Med 2020;41:256)
- Extremely rare in males; reported in males with tuberous sclerosis complex (Clin Radiol 2011;66:625)
- Associated with tuberous sclerosis complex; incidence increases with age in women with tuberous sclerosis complex (Chest 2013;144:578)
- Mainly lungs; usually in a bilateral fashion
- Can be found in retroperitoneal lymph nodes (Am J Respir Crit Care Med 2006;173:105)
- Proliferation of smooth muscle-like cells due to activation of the mTOR signaling pathway as a result of biallelic inactivation, loss of heterozygosity or somatic mutations in TSC1 or TSC2 genes (Lymphat Res Biol 2010;8:33, Am J Hum Genet 1998;62:810, Proc Natl Acad Sci U S A 2000;97:6085)
- Estrogen (ER) and progesterone (PR) receptors may have a role in disease development (Endocr Relat Cancer 2016;23:265)
- Sporadic (Semin Respir Crit Care Med 2020;41:256)
- Associated with tuberous sclerosis complex (Semin Respir Crit Care Med 2020;41:256)
- Progressive exertional dyspnea is the most common symptom (Semin Respir Crit Care Med 2020;41:256)
- Pneumothorax (Semin Respir Crit Care Med 2020;41:256)
- Chylous pleural effusion (Am J Respir Crit Care Med 2016;194:748)
- Hemoptysis
- Extrapulmonary involvement of retroperitoneal lymph nodes or abdominal angiomyolipoma (AML) (Am J Respir Crit Care Med 2006;173:105)
- Usually a clinical diagnosis
- Multiple bilateral round lung cysts on high resolution computed tomography (CT) scan
- Screening CT scans are recommended for females with tuberous sclerosis complex (Am J Respir Crit Care Med 2006;173:105)
- Vascular endothelial growth factor (VEGF) D level of ≥ 800 pg/mL helps distinguish lymphangioleiomyomatosis from other cystic lung diseases (Semin Respir Crit Care Med 2020;41:256)
- Multiple bilateral round thin walled cysts on high resolution CT scan (Semin Respir Crit Care Med 2020;41:256, Am J Med Genet C Semin Med Genet 2018;178:326)
- Lung cysts vary in size (2 mm to > 2 cm) (Clin Radiol 2011;66:625)
- Discrete solid and ground glass nodules, typically ranging between 2 and 14 mm in size (Am J Med Genet C Semin Med Genet 2018;178:326)
- Pneumothorax or effusion (Semin Respir Crit Care Med 2020;41:256)
- Additional findings in other organs: abdominal mass (angiomyolipoma) (Am J Respir Crit Care Med 2006;173:105)
- VEGFD levels correlate with disease progression, severity and response to therapy (Semin Respir Crit Care Med 2020;41:256)
- Monitoring through periodic pulmonary function test (PFT) can be used as a tool to assess disease progression, severity and response to therapy (Semin Respir Crit Care Med 2020;41:256, Chest 2019;155:288)
- Respiratory decline slows with menopause and is accelerated by pregnancy or exogenous estrogen (Lymphat Res Biol 2010;8:9)
- 22 year old man with sporadic lymphangioleiomyomatosis with multiple atypical features (Indian J Pathol Microbiol 2018;61:94)
- 29 year old woman with acute respiratory failure with gross hemoptysis and lymphangioleiomyomatosis as part of tuberous sclerosis complex (Intern Med 2004;43:755)
- 37 and 45 year old women with pelvic lymphangioleiomyomatosis treated successfully with everolimus (Medicine (Baltimore) 2017;96:e4562)
- 48 year old man with sporadic lymphangioleiomyomatosis as a result of extreme mosaicism for a TSC2 mutation (Ann Am Thorac Soc 2017;14:1227)
- Relies on degree of lung function and extent of lung damage
- Supportive therapy with bronchodilators or oxygen therapy (Thorax 2019;74:999)
- Observation for patients with mild function impairment
- mTOR inhibitors (sirolimus, everolimus): for symptomatic patients with severe lung damage and disease progression (N Engl J Med 2011;364:1595)
- Lung transplantation for cases refractory to medical treatment
- Multiple thin walled cysts (Semin Respir Crit Care Med 2020;41:256)
- Multiple thin walled cysts
- Cysts are lined or surrounded by nodules of rounded or spindled smooth muscle-like cells with mixed eosinophilic or clear cytoplasm, without cytologic atypia or mitoses
- Hemosiderin laden macrophages may be present as a clue to organized hemorrhage resulting from cysts infiltrating nearby vessels
- Multinodular pneumocyte hyperplasia around cysts (found in TSC LAM more than sporadic lymphangioleiomyomatosis)
- References: Semin Respir Crit Care Med 2020;41:256, Endocrinology 2016;157:3374
- Well organized, globular cluster consisting of lymphangioleiomyomatosis cells enveloped by lymphatic endothelial cells (Acta Cytol 2009;53:402)
- Lymphangioleiomyomatosis cells show strong reaction to matrix metalloproteinase 2 (MMP2) in research studies (Arch Pathol Lab Med 2000;124:1642)
- Lymphangioleiomyomatosis nodules are lined by type II pneumocytes with short microvilli and electron dense cytoplasmic lamellar bodies (Arch Pathol Lab Med 2000;124:1642)
- See Pathophysiology
Virtual slide review of a case of lymphangioleiomyomatosis
Overview of radiographic features of lymphangioleiomyomatosis
- Lung, right upper lobe, wedge biopsy:
- Lymphangioleiomyomatosis (see comment)
- Comment: Sections show cystic spaces replacing normal parenchyma. Some of the cystic spaces have mural nodules consisting of epithelioid and spindled cell proliferation. Lesional cells are immunoreactive with ER, SMA and MelanA. Control stains are satisfactory. The clinical presentation, morphology and immunohistochemical stains support the diagnosis above.
- Langerhans cell histiocytosis:
- Birt-Hogg-Dubé syndrome:
- Localized cystic lesions; lesional cells may show atypia
- Lack of immunoreactivity to melanocytic markers
- Lymphocytic interstitial pneumonia:
- Multiple cyst lesions in middle aged women
- Cysts are surrounded by lymphoplasmacytic inflammatory infiltrate
- Emphysema:
- History of smoking
- More localized process on imaging
A 44 year old woman who is a nonsmoker presented to the emergency department with acute chest pain after several months of progressive dyspnea. Physical examination was notable for diminished breath sounds on the right side. Computed tomography of the chest revealed a large pneumothorax and diffuse, intraparenchymal pulmonary cysts. The patient underwent mechanical pleurodesis and a wedge biopsy was performed. The biopsy specimens contained numerous thin walled cysts lined with spindle cells; on immunohistochemistry, the spindle cells coexpressed smooth muscle and melanocytic markers. What is the most likely diagnosis?
- Emphysema
- Lymphangioleiomyomatosis
- Metastasizing pulmonary leiomyoma
- Sarcoidosis
Comment Here
Reference: Lymphangioleiomyomatosis
- Characteristic skin changes
- Fever
- Lower extremity swelling
- Tobacco stains
Comment Here
Reference: Lymphangioleiomyomatosis
- According to the 2021 WHO classification update, lymphoepithelial carcinoma is the currently designated name and is defined as a type of poorly differentiated squamous cell carcinoma associated with variable amount of lymphoplasmacytic infiltrate and frequent association with Epstein-Barr virus (EBV)
- In the 2015 WHO classification, the preferred name was lymphoepithelioma-like carcinoma and it was in the category of other and unclassified carcinomas
- Characterized by distinct syncytial growth pattern, vesicular nuclei, prominent eosinophilic nucleoli and variable lymphoplasmacytic infiltrate
- Immunohistochemical (IHC) staining is the same as that for conventional squamous cell carcinoma (diffusely positive for CK5/6, p40 and p63)
- With complete surgical resection it has a favorable prognosis when compared with conventional squamous cell carcinoma
- Formerly known as lymphoepithelioma-like carcinoma
- Rare; 0.9% of all primary lung cancers (Oncol Lett 2017;14:3110)
- Predominately in Asian populations (Am J Surg Pathol 2002;26:715)
- M = F
- Median age: 51 - 57 years (Cancer Sci 2011;102:282)
- Lung parenchyma has an even distribution between central and peripheral (Clin Lung Cancer 2019;20:e329)
- Not typically associated with bronchi
- EBV induced carcinogenesis (Nat Commun 2019;10:3108)
- Driven by dysregulated NFkB pathway, loss of type I IFN genes, APOBEC family gene signature
- Strongly associated with EBV infection (J Thorac Disc 2021;13:5683)
- Not associated with smoking history (Oncol Lett 2017;14:3110)
- No specific clinical manifestations
- Most common respiratory symptoms (Comput Math Methods Med 2022;2022:1086697)
- Cough
- Expectoration
- Chest pain
- ~33% of patients have no symptoms (J Thorac Imaging 2014;29:246)
- CT images of the thorax and fiberoptic bronchoscopy with tissue biopsy
- FNA cytology with IHC studies may assist
- Can be limited by sampling errors
- Endoscopic examination with or without radiographic imaging of nasopharynx performed to rule out metastatic lymphoepithelial carcinoma
- Reference: Respirology 2006;11:539
- Well defined, solitary, lobulated mass > 1 cm (Clin Radiol 2022;77:e201)
- Homogeneous density
- Vascular enhancement
- High 18F-FDG uptake
- Has better outcomes than conventional squamous cell carcinoma (Respir Res 2019;20:262)
- Favorable prognostic factors (Cancer 2012;118:4748)
- Early tumor stage
- Absence of lymph node metastasis
- Complete resection
- High PDL1 or wild type p53 expression (Signal Transduct Target Ther 2021;6:6)
- Unfavorable prognostic factors
- Tumor recurrence and necrosis (Am J Clin Pathol 2001;155:841)
- High serum EBV viral capsid antigen
- 30 and 64 year old women with pulmonary masses (Medicine (Baltimore) 2018;97:e9976)
- 52 year old Asian woman with a mass (J Thorac Oncol 2018;13:e75)
- 59 year old woman with fever and cough (Clin Respir J 2017;11:1052)
- 60 year old Japanese woman with nodule on CT (Int J Surg Case Rep 2021;79:431)
- Stage I: surgery is the primary form of treatment (Med Oncol 2020;37:20)
- Complete resection is curative at stage I or II
- Stage II or higher: surgery + postoperative radiology or chemotherapy
- Potential options: PDL1 inhibitors
- Tends to be peripherally located versus central (Front Surg 2021;8:757085)
- Well circumscribed with irregular borders
- Not associated with bronchi
- Similar pitfalls to those found with lymphoepithelioma-like carcinomas in other sites (Int J Surg Pathol 2020;28:872)
- Can resemble lymphoid tissue on low power
- Epithelial component can look histiocytic
- Syncytial growth pattern
- Large polygonal cells with vesicular nuclei, prominent eosinophilic nucleoli and variably abundant eosinophilic cytoplasm
- Variable mitosis
- Variable lymphoplasmacytic infiltrate
- Infiltrate can be scant and morphologically resemble nonkeratinizing squamous cell carcinoma (Am J Surg Pathol 2019;43:211)
- Reported to also have granulomatous inflammation, focal keratinization and lepidic spreading pattern (Am J Surg Pathol 2019;43:211)
- Spindle cells are arranged in large cohesive clusters with admixed small lymphocytes (Cytopathology 2019;30:653)
- Nuclei: pleomorphic, oval, prominent nucleoli
- Can mimic melanoma, synovial sarcoma
- Squamous markers: CK5/6, p40, p63 (Front Surg 2021;8:757085)
- EBER ISH: desirable diagnostic criteria (Respir Res 2019;20:262)
- TRAF3 makes up ~80% of deletion mutations in lymphoepithelial carcinoma and 5% of simple somatic mutations (Nat Commun 2019;10:3108)
- Does not show C:G to A:T transversions from tobacco smoking
- High PDL1 expression (Oncotarget 2015;6:33019)
- Rarely shows the typical driver mutation for conventional non-small cell lung cancer, such as TP53, KRAS, EGFR mutations or ALK and ROS1 translocations
- Lung, right lower lobe, lobectomy:
- Lymphoepithelial carcinoma, 2.3 cm (see synoptic report)
- Poorly differentiated adenocarcinoma (Am J Clin Pathol 1995;103:35):
- NUT carcinoma:
- Both lymphoepithelial carcinoma and NUT carcinoma have areas of round blue cells with focal areas of abrupt squamous differentiation and extensive p63 / p40 expression
- NUT carcinoma is negative for EBER ISH
- NUT carcinoma is positive for NUT1 by IHC or has translocations involving the NUT gene; most common fusion is BRD4::NUT from a t(15;19) translocation (J Thorac Oncol 2015;10:951)
- Malignant melanoma:
- Lymphomas:
- Scant cytoplasm, stippled, fine chromatin
- Do not form sheets, clusters, nests
- Positive for lymphoid markers and negative for epithelial / squamous markers
- Metastatic undifferentiated carcinoma of nasopharynx (AJR Am J Roentgenol 2006;186:1294):
- Histologically similar, can also be EBV positive
- Requires clinical and imaging correlation
- Metastatic medullary carcinoma of breast or colon (Virchows Arch 2000;437:198, Int J Clin Exp Pathol 2012;5:105):
- Will also have strong lymphocytic infiltration
- No syncytial growth pattern, nuclear pleomorphism, high mitotic rate
- EBV negative
Comment Here
Reference: Lymphoepithelial carcinoma
- Morphologically similar to undifferentiated nasopharyngeal carcinoma
- Rare tumor in lung; more common in Asians
- Associated with Epstein-Barr virus (EBV) in Asian populations (Cancer 1998;82:2334)
- In Caucasians, usually EBV-
- Pulmonary lymphoepithelioma-like carcinoma (LELC) is an epithelial malignancy characterized by large, syncytial cells with vesicular nuclei and prominent nucleoli, with a prominent lymphocytic infiltrate
- LELC has a strong association with Epstein-Barr virus (EBV) and is more common in Asian populations
- LELC shows similar morphologic features to nasopharyngeal carcinoma and may be mistaken for lymphoma due to prominent inflammatory infiltrate
- Lymphoepithelioma-like carcinoma (LELC) primary to lung first described in 1987 by Bégin et al. (J Surg Oncol 1987;36:280)
- Previously considered subtype of large cell undifferentiated carcinoma
- By 2015 WHO, now classified under epithelial tumor, "other and unclassified carcinomas" (J Thorac Oncol 2015;10:1243)
- Use code specific for location of tumor
- C34.90 Malignant neoplasm of unspecified part of unspecified bronchus or lung
- Very rare, mostly seen in younger adults
- In Asians, usually women, nonsmokers, with EBV+ tumors (Am J Surg Pathol 2002;26:715)
- Intrapulmonary, either peripheral or central
- Better prognosis than other non small cell carcinomas of lung (Cancer 2012;118:4748, Ann Thorac Surg 2014;98:1013)
- Some association with EBV infection (Mod Pathol 1991;4:264)
- Nonspecific: cough, dyspnea, chest pain, weight loss
- Exclude metastatic nasopharyngeal carcinoma and other non small cell carcinomas
- Presence of prominent inflammatory infiltrate helpful
- Ancillary studies for EBV infection
- EBV serology often reveals prior infection, with higher titers associated with larger tumor size and higher stage (Am J Surg Pathol 2002;26:715)
- Similar to imaging characteristics of other primary lung cancers
- Solitary, peripheral pulmonary nodule with direct contact with pleura (J Thorac Imaging 2014;29:246)
- FDG PET / CT with strong FDG uptake
- Good prognosis: early tumor stage, normal serum lactate dehydrogenase level, normal serum albumin level, no lymph node metastasis
- Those who underwent complete resection had better overall survival (Cancer 2012;118:4748)
- Tumor recurrence and necrosis (5% or more of tumor) associated with poor prognosis (Am J Clin Pathol 2001;115:841)
- 25 year old Italian man with EBV+ tumor (Hum Pathol 2003;34:623)
- 53 year old woman with thin walled cavity (Ann Thorac Surg 2013;96:1857)
- 58 year old woman initially diagnosed as squamous metaplasia (Oncol Lett 2015;9:1767)
- 60 year old woman initially diagnosed as adenocarcinoma (Tuberc Respir Dis (Seoul) 2013;75:170)
- 70 year old man with partially regressed tumor (Ann Thorac Surg 2015;99:2197)
- 83 year old man with FDG avid lung lesion (Clin Nucl Med 2015;40:134)
- Complete surgical resection for early stage disease, with adjuvant chemotherapy and radiotherapy in advanced cases (J Thorac Dis 2017;9:123)
- Variable size, can be > 10 cm
- Well circumscribed, lobulated, solid nodule
- Necrosis common
- Anastamosing islands, nests, cords or diffuse sheets of tumor cells
- Syncytial growth of monomorphous, polygonal epithelial cells with large vesicular nuclei, prominent eosinophilic nucleoli, accompanied by marked CD8+ lymphocytic infiltration
- Admixed lymphocytes, plasma cells, histiocytes, occasional neutrophils or eosinophils
- Predominantly pushing borders, permeative interface with adjacent lung
- Intratumoral amyloid deposition in a few cases (Am J Surg Pathol 2002;26:715)
- Large clusters of neoplastic cells with scant cytoplasm, large hyperchromatic nuclei, irregular nuclear contours, prominent nucleoli, brisk mitotic figures and prominent intratumoral lymphoid infiltration (Diagn Cytopathol 2012;40:820)
- Stripped, naked tumor nuclei
- Interspersed lymphocytes, some with crush artifact
- Mostly TTF1 negative
- Napsin, neuroendocrine markers
- CD45 / LCA (except in stromal lymphocytes)
- High PDL1 expression and infrequent driver mutations (Oncotarget 2015;6:33019, Lung Cancer 2015;88:254)
- Microsatellite instability is uncommon (Am J Clin Pathol 2007;127:282)
- Inflammatory pseudotumor
- Lymphoma
- Melanoma
- Metastatic nasopharyngeal carcinoma
- Other non small cell lung carcinomas
- Epstein-Barr virus (EBV)
- Human immunodeficiency virus (HIV)
- Human papillomavirus (HPV)
- Human T lymphotropic virus (HTLV)
- Respiratory syncytial virus (RSV)
- In 1969, Leibow and Carrinton first described lymphoid interstitial pneumonia (LIP) as interstitial lung disease with diffuse and dense lymphocytic infiltration (Simon: Frontiers of Pulmonary Radiology, 1st Edition, 1969)
- In American Thoracic Society / European Respiratory Society classification of the idiopathic interstitial pneumonia, idiopathic LIP is categorized as a rare idiopathic interstitial pneumonia (Am J Respir Crit Care Med 2002;165:277, Am J Respir Crit Care Med 2013;188:733)
- Rare type of interstitial lung disease due to different diseases including Sjögren syndrome, rheumatoid arthritis and human immunodeficiency virus (HIV) infection
- On histology, diffuse infiltration of polyclonal lymphocytes with scant interstitial fibrosis is characteristic
- Also called lymphocytic interstitial pneumonia
- J84.2: lymphoid interstitial pneumonia
- Rare
- Typical onset at ages 40 - 70 years old but can occur at any age (Chest 2002;122:2150)
- More common in women
- No association with smoking history
- Bilateral lower lobes of the lung
- Pathogenic mechanisms of LIP are still unclear
- Has aspects of lymphoproliferative disease and lymphoid hyperplasia of polyclonal T or B cells (Chest 2002;122:2150)
- Although it may transform to lymphoma, especially MALT, the risk is lower than initially reported (Eur Respir J 2006;28:364)
- Associated with several systemic diseases and conditions (Chest 2002;122:2150,
Respirology 2016;21:600, Eur Respir J 2006;28:364)
- Autoimmune (most common)
- Sjögren syndrome (SjS); 25% of LIP cases have SjS and 1% of SjS cases present with LIP
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Polymyositis / dermatomyositis
- Hashimoto disease
- Hypothyroidism
- Castleman disease
- Myasthenia gravis
- Autoimmune hemolytic anemia
- Pernicious anemia
- Primary biliary cirrhosis
- Infection
- Human immunodeficiency virus (HIV)
- Epstein-Barr virus
- Human T cell lymphotropic virus type 1
- Legionella pneumonia
- Mycoplasma
- Chlamydia
- Tuberculosis
- Immunodeficiency
- Acquired immunodeficiency syndrome (AIDS); especially in children
- Monoclonal or polyclonal gammopathy
- Common variable immunodeficiency
- Idiopathic LIP accounts for 20% of cases (Eur Respir J 2006;28:364)
- Autoimmune (most common)
- Very slowly progressive respiratory symptoms
- Dyspnea on exertion
- Dry cough
- Systemic symptoms such as malaise, fever and weight loss
- Duration of the symptoms prior to diagnosis can exceed a year
- Bibasilar inspiratory crackles on chest auscultation
- Based on clinical, radiological and pathological findings (multidisciplinary diagnosis)
- No firm diagnostic criteria currently exist
- Dysproteinemia is often present
- Hypergammaglobulinemia is more common than hypogammaglobulinemia
- Restrictive pattern on pulmonary function tests
- Reduced forced vital capacity (FVC)
- Reduced diffusing capacity of the lung for carbon monoxide (DLCO)
- Chest radiography
- Bibasilar opacities with lower lobe predominance
- High resolution computed tomography (Eur J Radiol 2015;84:542,
Respirology 2016;21:600)
- Ground glass opacity with / without consolidation with lower lobe predominance
- Cyst formation and thickening of bronchovascular bundle and interlobular septa are often present
- Cysts often remain even after resolution of symptoms
- Prognosis varies from resolution without treatment to progression to end stage (Respirology 2016;21:600)
- Median survival: 11.5 years (Eur Respir J 2006;28:364)
- No characteristic prognostic factor has been found so far
- 30 year old woman with LIP related to common variable immunoglobulin deficiency (Intern Med 2008;47:763)
- 35 year old man with HIV related LIP treated with antiretroviral therapy (Int J STD AIDS 2000;11:119)
- 35 year old woman with idiopathic LIP and good response to mycophenolate mofetil (Respir Med Case Rep 2013;9:27)
- 47 year old woman with LIP related to systemic lupus erythematosus and secondary Sjögren syndrome (BMJ Case Rep 2013 Aug 2;2013)
- 52 year old man with HIV related LIP treated with highly active antiretroviral therapy (Sex Transm Infect 2004;80:417)
- No treatment data from a controlled study is available so far (Respirology 2016;21:600)
- Corticosteroid therapy is commonly used as a first line treatment and improves the symptoms in most cases
- Immunosuppression (eg, cyclophosphamide, azathioprine, cyclosporine A) may be used as a second line
- Treatment for underlying disease is also essential for secondary LIP
- Antiretroviral therapy can resolve HIV related LIP and its symptoms (Int J STD AIDS 2000;11:119, Sex Transm Infect 2004;80:417)
- Ill defined lesion
- Mild increase in lung weight
- Diffuse interstitial infiltration of polymorphous lymphocytes and plasma cells
- Lymphoid follicles with germinal centers, histiocytes and macrophages are often present
- Bronchovascular bundles and interlobular septa are usually involved
- Alveolar structure is often inflated and disrupted
- Typically CD8+ or CD4+ T cells or B cells predominate, with an admixture of other lymphocytes
- Immunohistochemistry or molecular testing are necessary to confirm polyclonality
- Additional findings
- Loose ill defined epithelioid granulomas
- Interstitial or intra-alveolar giant cells
- Intra-alveolar macrophages
- Type II pneumocyte hyperplasia
- Cyst formation without marked fibrosis
- Pertinent negative findings
- Loose and dense fibrosis (more common in fibrotic / cellular nonspecific interstitial pneumonia (NSIP))
- Fibroblastic focus (more common in usual interstitial pneumonia or fibrotic NSIP)
- Honeycomb change (more common in usual interstitial pneumonia or fibrotic NSIP)
- Organizing pneumonia (more common in hypersensitivity pneumonitis)
- See: Respirology 2016;21:600, Chest 2002;122:2150, Am J Respir Crit Care Med 2002;165:277
Contributed by Akira Yoshikawa M.D. and Yale Rosen, M.D.
Images hosted on other servers:
- Increase in the number of lymphocytes (especially CD8 positive) of bronchoalveolar lavage, without clonality (Eur Respir J 2006;28:364)
- Follicular bronchitis / bronchiolitis
- Lymphocytic infiltration into bronchial / bronchiolar walls with multiple lymphoid follicles
- No or slight lymphocytic aggregation in intralobular septa
- Hypersensitivity pneumonitis (HP)
- History of an antigen exposure such as animals, birds and chemicals
- Less diffuse but bronchocentric distribution
- Loose ill defined granuloma and giant cells can be seen in both LIP and HP
- Lymphoma, especially mucosa (bronchus) associated lymphoid tissue lymphoma
- Monomorphous infiltration of lymphocytes, distortion of alveolar architecture, Dutcher bodies, pleural infiltration are more common in lymphoma
- Immunohistochemistry is often helpful
- Nonspecific interstitial pneumonia
- Lymphoplasmacytic infiltration is also seen in NSIP but less severe
- Alveolar structure is usually preserved compared with LIP
Comment Here
Reference: Lymphoid interstitial pneumonia
- Also called angioimmunoproliferative lesion
- Lymphoproliferative disorder that is malignant per se, or likely to become malignant, resembles post-transplant lymphoproliferative disorders
- Middle aged men and women with well defined, bilateral rounded mass densities on chest X-ray
- Associated with transplant-related immunosuppression, Sjogren's syndrome, HIV
- 80% of cases have extrapulmonary involvement (skin, CNS, kidneys, liver, spleen, adrenal glands, heart, GI tract); rarely, there is only extrapulmonary involvement
- Usually no hilar or mediastinal lymph node involvement
- May be an EBV related, B-cell proliferation; T-cells present are usually reactive; may have reversal of T-helper / suppressor ratio
- Large number of atypical lymphoid cells is a poor prognostic factor
- Median survival 14 months; death due to sepsis, destruction of lung tissue
- Chemotherapy
- Nodular inflammatory infiltrate of large atypical lymphoid cells (prominent nuclei, mitotic activity), plasma cells, immunoblasts, involving walls of pulmonary vessels (angioinvasive, angiocentric, angiodestructive)
- No multinucleated giant cells
- Similar infiltrates found in other organs
- EBV (50 - 70%)
- Granulomatosis with polyangiitis (Wegener's): giant cells, necrosis
- Usually in urinary tract; very rare in lung, usually in immunocompromised patients
- Caused by macrophage dysfunction involving intracellular lysosomal mediated killing of bacteria
- In AIDS patients, usually due to Rhodococcus equi, an animal pathogen causing opportunistic infections (Chest 1999;115:889)
- Two cases in immunocompetent patients (Indian J Pathol Microbiol 2011;54:133)
- Antibiotics
- Nodular masses or infiltrates with cavitation
- Intraalveolar histiocytes with pink or foamy cytoplasm (von Hansemann’s histiocytes) that fill and destroy alveoli, not interstitium
- Histiocytes contain PAS+ bacteria, also Michaelis-Gutmann bodies (round / oval structures, usually intracellular, 5 - 20 microns, with laminated or targetoid appearance that stain deeply with H&E, iron and calcium stains)
- Also lymphocytes, plasma cells and neutrophils
- Atypical mycobacteria: blue histiocytes, positive acid fast stain
- Also Whipple disease, Gaucher disease, endogenous lipid pneumonia, amiodorone toxicity
- Also called rubeola
- Infectious acute febrile illness characterized by upper respiratory infection symptoms and maculopapular rash
- Spread by aerosols and droplets from respiratory secretions or rarely fomites
- Significant public health problem in United States prior to the development of an effective vaccine; still common in some nonindustrialized countries
- Recently, recrudescence has occurred in developed world due to some parents refusing to vaccinate their children and importation (Cleve Clin J Med 2010;77:207)
- Highly infectious, affecting up to 90% of individuals in nonimmune populations
- Also occurs in adults (MMWR Morb Mortal Wkly Rep 2011;60:666)
- Pneumonia is serious complication of childhood exanthema
- May cause bronchiolitis or diffuse alveolar damage
- Secondary bacterial pneumonia may occur
- Epithelial giant cells with viral inclusions
- Nuclei may contain a single large Cowdry type A inclusion
- Reticuloendothelial (Warthin-Finkeldey) giant cells may be found in lymphoid tissue
Histopathology Lung - Measles pneumonia
- Other giant cell pneumonias, RSV, parainfluenza, pneumoconioses
- Lung is a common site of metastases; usually multiple, bilateral, sharply outlined, rapidly growing, more pleomorphic and necrotic than lung primaries
- May appear as multiple discrete nodules in periphery of lung or as lymphangitic carcinomatosis (peribronchial and perivascular patterns via lymphatics)
- Rarely appear as intralymphatic microscopic foci that cause pulmonary hypertension
- Metastases can also be from other lung primaries (Am J Surg Pathol 2009;33:1752)
- Lung is a common site of metastatic disease and may be the first or only site of metastatic involvement
- Lung metastases are generally multiple, well circumscribed and tend to grow rapidly
- A history of malignancy is helpful in determining the primary site but a panel of immunohistochemical stains can help support the diagnosis
- In autopsy studies, 20 - 50% of patients with malignancy had lung metastasis (Cancer 1981;47:2595)
- Generally peripheral lung but can also be endobronchial
- Five year overall survival for all lung metastases is 36% (J Thorac Cardiovasc Surg 1997;113:37)
- Mostly hematogenous or lymphogenous spread from primary site
- Usually asymptomatic or may present with nonspecific cough, chest pain, hemoptysis, spontaneous pneumothorax (J Surg Oncol 2014;109:42)
- Typically detected by imaging, specifically CT scans
- Confirmation by cytologic or histologic sampling
- CT scans are preferred modality
- Single or multiple, peripheral, well circumscribed nodule(s)
- Limited detection of subcentimeter disease
- Clinical variables associated with prolonged survival after lung metastasectomy in colorectal cancer patients
- Prolonged disease free interval between primary tumor and metastasis, normal prethoracotomy carcinoembryonic antigen, absence of thoracic node involvement and single pulmonary lesion (Ann Surg Oncol 2013;20:572)
- Complete resection and longer disease free interval > 6 months associated with better survival (Surg Oncol 2012;21:237)
- 48 year old man with lymphangitic spread of hepatocellular carcinoma (Arch Pathol Lab Med 2003;127:e11)
- 50 year old man with ameloblastoma of jaw metastatic to lung (Case of the Week #318)
- 51 year old man with metastatic melanoma showing ground glass opacities (Am J Respir Crit Care Med 2015;191:954)
- 59 year old man with cavitary lung metastasis from urothelial carcinoma, diagnosed by FNA (Can Respir J 2011;18:e46)
- 65 year old woman with parotid gland acinic cell carcinoma metastatic to lung (Arch Pathol Lab Med 2007;131:970)
- 83 year old man with epithelioid tumor of lungs (Arch Pathol Lab Med 2005;129:e7)
- Chemotherapy, immunotherapy, other systemic therapy
- Criteria for pulmonary metastasectomy: primary site of disease controlled, complete resection of lung metastasis feasible, patient able to tolerate procedure, no better alternative treatments (J Surg Oncol 2014;109:42)
- Stereotactic body radiation therapy (SBRT) and radiofrequency ablation (RFA) may be considered for small, solitary, peripheral tumors
-
Patterns associated with specific primaries
- Central cavitation: colonic adenocarcinoma, leiomyosarcoma, squamous cell carcinoma of upper aerodigestive tract
- Intrabronchial masses: breast, colon, kidney
- Lymphangitic carcinomatosis: breast, choriocarcinoma, pancreas, prostate, stomach
- Nodular metastases: breast, GI, kidney, melanoma, sarcoma
- Tumor emboli: breast, choriocarcinoma, liver, stomach
- Dependent on site of origin (colorectal cancer, bone and soft tissue sarcoma, renal cell carcinoma, melanoma, head and neck tumors, germ cell tumors and many others)
- Evidence for breast metastasis over lung primary: comedonecrosis, solid nests, trabecular architecture, cribriform growth pattern (Am J Clin Pathol 2009;131:122)
Contributed by Roseann Wu, M.D., M.P.H., Debra Zynger, M.D., Case #318 and Fulvio Lonardo, M.D.
- CDX2 suggests colorectal carcinoma (Am J Surg Pathol 2003;27:141)
- Pankeratin to prove epithelial origin, CK7 / CK20 to help differentiate
- Lineage specific markers variable depending on site of origin, see Table 2 for suggested stains (Arch Pathol Lab Med 2016;140:508)
- Primary lung carcinoma: acini, lepidic growth, nuclear pseudoinclusions, central scar (Am J Clin Pathol 2009;131:122)
- Inflammatory nodule or benign neoplasm
- For which malignancy is pulmonary metastasectomy most commonly performed and reported?
- Colorectal cancer
- Germ cell tumors
- Melanoma
- Osteosarcoma
- Renal cell carcinoma
- First recognized in 1991 by HH Popper (Histopathology 1991;18:347)
- Benign, hamartomatous, multinodular proliferation of type II pneumocytes
- Often associated with tuberous sclerosis complex
- May coexist with lymphangioleiomyomatosis (LAM)
- Rare pulmonary manifestation of tuberous sclerosis complex that may occur in conjunction with LAM
- Composed of multiple nodules of enlarged but benign type II pneumocytes that may mimic atypical adenomatous hyperplasia
- Positive for cytokeratins and TTF1 by immunohistochemical stains, while negative for SMA
- Also called multifocal micronodular pneumocyte hyperplasia (MMPH)
- Older terminology: acinar atypical adenomatoid proliferation of epithelium, multiple adenomatoid lesions, micronodular hyperplasia of type II pneumocytes
- Young and middle aged adults, predominantly women
- Often associated with tuberous sclerosis complex but may be sporadic
- Functional loss of TSC 1 or TSC2 and hyperphosphorylation of mTOR related protein may cause this benign neoplastic proliferation of pneumocytes (Mod Pathol 2010;23:1251)
- Non-specific; may present with pneumothorax, shortness of breath, cough
- Histologic examination
- Xray: multiple pulmonary nodules
- CT: multiple diffuse, small, solid and ground glass pulmonary nodules that remain stable in short term follow-up (J Comput Assist Tomogr 2012;36:518)
- Imaging may mimic miliary tuberculosis (Int J Clin Exp Pathol 2015;8:2165)
- Typically indolent with no clinical significance
- Rare case studies report respiratory failure
- 13 year old girl with tuberous sclerosis, renal cell carcinoma, angiomyolipomas and multifocal micronodular pneumocyte hyperplasia (Chem Pharm Bull (Tokyo) 1990;38:498)
- 16 year old girl with respiratory failure (Histopathology 2002;41:263)
- 51 year old woman with tuberous sclerosis complex but no classical clinical findings (J Med Case Rep 2012 Oct 16;6:352)
- Small (1 - 10 mm), well-demarcated, randomly distributed parenchymal lung nodules
- Multiple, sharply demarcated or circumscribed nodules
- Tubulopapillary proliferation of type II pneumocytes lining fibrotic and thickened alveolar septa, moderate lymphocytic infiltration, no nuclear atypia (Int J Surg Pathol 2010;18:522)
- Enlarged type II pneumocytes with abundant eosinophilic cytoplasm, vesicular nuclei, distinct nucleoli, occasional eosinophilic inclusions
- Increased alveolar macrophages
- Osmiophilic lamellar inclusions and surface microvilli of type II pneumocytes
- Associated with loss of heterozygosity on TSC1 or TSC2 (Mod Pathol 2010;23:1251)
- Atypical adenomatous hyperplasia
- Lymphangioleiomyomatosis
- Metastases
- Resolving miliary inflammatory / infectious processes
- Primary lung adenocarcinoma measuring ≤ 3 cm in greatest dimension, with ≤ 0.5 cm area of either stromal invasion or nonlepidic growth pattern (Arch Pathol Lab Med 2013;137:685, J Thorac Oncol 2011;6:244)
- Tumor with noninvasive (lepidic) and invasive components
- Total tumor size must be less than 3 cm
- Invasive or nonlepidic components must be less than 0.5 cm
- Invasive component can be of any subtype other than lepidic
- No lymphovascular invasion, tumor necrosis or pleural invasion is present
- Usually nonmucinous but can rarely occur in mucinous tumors
- Minimally invasive adenocarcinoma (MIA)
- Microinvasive adenocarcinoma
- Older terminology used: bronchoalveolar carcinoma; however, this is obsolete and should no longer be utilized
- ICD-O: 8250/2 - minimally invasive adenocarcinoma, nonmucinous (international code)
- ICD-O: 8257/3 - minimally invasive adenocarcinoma, mucinous (international code)
- ICD-10: C34.9 - malignant neoplasm of unspecified part of unspecified bronchus or lung
- ICD-11: XH3QM0 - minimally invasive adenocarcinoma, nonmucinous
- ICD-11: XH2098 - minimally invasive adenocarcinoma, mucinous
- F > M (Cancer 2014;120:2883)
- More common in Asian populations (Am J Surg Pathol 2014;38:448)
- Usually located in the peripheral lung parenchyma (Ann Thorac Surg 2000;69:893, Lung Cancer 2000;29:179)
- Hypothesized to form after a multistep progression from atypical adenomatous hyperplasia to adenocarcinoma in situ to minimally invasive adenocarcinoma (J Thorac Oncol 2008;3:340)
- Tobacco smoking (Cancer Epidemiol Biomarkers Prev 2015;24:1902; Gen Thorac Cardiovasc Surg 2015;63:608)
- However, minimally invasive adenocarcinoma is not as strongly associated with smoking as other subtypes of adenocarcinoma (Int J Mol Sci 2018;19:1259)
- Generally asymptomatic, discovered as incidental mixed solid and ground glass lesions on CT scans (N Engl J Med 2013;368:1980)
- Slow growing, ground glass opacity (see Radiology description)
- Biopsies will show adenocarcinoma with lepidic growth pattern
- Diagnosis can only be made on the resection specimen and cannot be made with limited tissue sampling (Arch Pathol Lab Med 2013;137:668, Arch Pathol Lab Med 2007;131:1027)
- Early lesions may present as a ground glass opacity rather than a solid nodule (J Thorac Oncol 2011;6:244)
- Foci of invasion are generally solid, surrounded by areas with a ground glass opacity (Hum Pathol 2016;51:41, Ann Oncol 2015;26:156)
- Minimally invasive adenocarcinoma (pT1mi) has a more favorable prognosis than early stage invasive adenocarcinoma (pT1a) and should be distinguished accordingly (J Clin Oncol 2012;30:1438, J Thorac Cardiovasc Surg 2013;146:17)
- Since tumor growth is often indolent, a 100% disease free survival may be achieved if completely resected (Am J Surg Pathol 2014;38:448)
- 12 year old girl in posttreatment for a rhabdomyosarcoma developed a minimally invasive adenocarcinoma (Pediatr Blood Cancer 2016;63:344)
- 13 year old boy in posttreatment for osteosarcoma developed a minimally invasive adenocarcinoma (Pediatr Dev Pathol 2013;16:387)
- 64 year old woman with a resected minimally invasive adenocarcinoma and adenocarcinoma in situ (Asian Cardiovasc Thorac Ann 2019;27:45)
- Surgical excision with close followup (Am J Surg Pathol 2014;38:448, Clin Lung Cancer 2016;17:e57)
- Adjuvant therapies are generally not indicated (J Thorac Cardiovasc Surg 2017;154:1100, Surg Today 2015;45:1341)
- Peripheral, ill defined, firm, white tumor with solid areas; ill defined areas correspond to lepidic growth pattern and solid areas correspond to invasive component (Hum Pathol 2016;51:41)
- Necrosis and frank pleural invasion should be absent
- Primary lung adenocarcinoma measuring ≤ 3 cm in greatest dimension, with ≤ 0.5 cm area of either stromal invasion or nonlepidic growth pattern (acinar, micropapillary, papillary, solid, colloid, fetal or invasive mucinous patterns)
- Foci of stromal invasion characterized by angulated glands, desmoplastic stroma and increased cytologic atypia (Cancer 1995;75:2844)
- Size of invasion should be measured as the largest focus of invasion (Am J Surg Pathol 2014;38:448, Arch Pathol Lab Med 2013;137:685)
- If there are multiple foci of invasion, the invasive size can be measured as a sum of the percentage of the invasive components in each section multiplied against the greatest tumor dimension (the aggregate invasive size should be ≤ 0.5 cm to render the diagnosis of a minimally invasive adenocarcinoma) (Am J Surg Pathol 2014;38:448, Surg Today 2019;49:828)
- Necrosis, lymphovascular invasion, pleural invasion and spread through air spaces must be absent
- CK7
- TTF1, Napsin A
- References: J Clin Pathol 1997;50:30, Am J Clin Pathol 1994;102:764
- Lung, right lower lobe, lobectomy:
- Minimally invasive adenocarcinoma, pT1mi NX MX (see synoptic report)
- Invasive adenocarcinoma, lepidic predominant pattern:
- Invasive foci must total 0.5 cm or more in aggregate
- Adenocarcinoma in situ / atypical adenomatous hyperplasia:
- No invasive component
- 2 cm lepidic predominant tumor with a 0.8 cm invasive component
- 2 cm lepidic predominant tumor with a 0.4 cm invasive component
- 2 cm lepidic predominant tumor with a 0.4 cm invasive component with pleural and lymphovascular invasion
- 5 cm lepidic predominant tumor with a 0.4 cm invasive component
Comment Here
Reference: Adenocarcinoma - minimally invasive
- Uncommon incidental pulmonary nodules composed of interstitial nodular proliferation of small oval or spindle shaped cells arranged in a zellballen nesting pattern (J Thorac Imaging 2002;17:227)
- Generally detected incidentally in resected lung specimens (Hum Pathol 2009;40:678)
- Occasionally detected on thin section computed tomography (Hum Pathol 2009;40:678)
- More common in patients with malignant pulmonary tumors, especially lung adenocarcinoma, than benign disease (Hum Pathol 2009;40:678)
- No significant difference in clinicopathologic factors between patients with single and multiple nodules, except for the size of each nodule (Hum Pathol 2009;40:678)
- Pulmonary chemodectomas were first described by Korn et al. in 1960 (Am J Pathol 1960;37:641)
- In 1988, Gaffey et al. proposed to change the name of pulmonary chemodectomas to minute meningothelial-like nodules (Am J Surg Pathol 1988;12:167)
- Terminology includes
- Pulmonary meningothelial-like nodules (PMLNs)
- Minute pulmonary meningothelial-like nodules (MPMNs)
- Pulmonary chemodectoma
- MPMN-omatosis syndrome
- Diffuse pulmonary meningotheliomatosis (DPM)
- ICD-10: R91.1 - solitary pulmonary nodule
- F > M (10.7% versus 4.5%) (Hum Pathol 2009;40:678)
- Most frequent in the sixth decade
- Absent in fetuses, infants and children, indicating that they do not represent congenital rests
- Reported incidence is 0.3 to 9.5% at autopsy or in surgical specimens (Korean J Pathol 2012;46:87)
- Present in all lobes; incidence is not different between lobes (Hum Pathol 2009;40:678)
- Usually asymptomatic but can occasionally manifest as mild restrictive lung disease (Respiration 2013;86:145)
- Although recognized for decades, their nature and significance remain uncertain (Am J Surg Pathol 2009;33:487)
- Patients are usually asymptomatic, as the behavior is benign (Tuberc Respir Dis (Seoul) 2013;75:67)
- Often identified as incidental findings in histopathological lung sections or in high resolution CT scans conducted for unrelated causes (Korean J Pathol 2012;46:87)
- Thin section chest CT reveals randomly distributed, well defined ground glass appearance micronodules, which may simulate metastatic disease (J Comput Assist Tomogr 2001;25:311)
- Found more often in patients with malignant pulmonary tumors, especially lung adenocarcinoma (Korean J Pathol 2012;46:87)
- 52 year old man with 1 cm nodule in the left lower lobe discovered on CT scan (Tuberc Respir Dis (Seoul) 2013;75:67)
- 56 year old woman with left mastectomy for breast cancer (Nihon Kokyuki Gakkai Zasshi 2002;40:499)
- 65 year old diabetic woman with breast cancer and smoking history (Korean J Pathol 2012;46:87)
- 74 year old asymptomatic woman with incidentally detected diffuse bilateral pulmonary nodules (Respirol Case Rep 2017;5:e00238)
- 75 year old woman with a history of invasive rectal adenocarcinoma (Ann Saudi Med 2013;33:400)
- Multiple incidentally detected, randomly distributed, cavitating micronodules (J Comput Assist Tomogr 2010;34:780)
- Although curative surgical excision is sometimes needed, these usually run a benign course and conservative treatment is favored (Tuberc Respir Dis (Seoul) 2013;75:67)
- 1 - 3 mm, tan to yellow, pleural or parenchymal nodules (Am J Surg Pathol 1988;12:167)
- Characteristic nests of bland spindle cells with pale eosinophilic cytoplasm expand alveolar septa
- Larger lesions connected by intervening collagen, often imparting a stellate configuration
- Smaller lesions have closely apposed nests with mildly thickened alveolar septa (Am J Surg Pathol 1988;12:167)
- Single as well as clusters of bland spindle cells are present in aspirate smears
- However, marked cellular atypia is often seen with cytology diagnosis of atypical / suspicious for malignancy / positive for malignancy
- Immunohistochemistry of cell block will rule out the possibility of carcinoma or squamous cell carcinoma since the spindle cells are negative for pankeratin (AE1 / AE3), p63 and p40
- Pankeratin (AE1 / AE3), CK5 / 6, estrogen receptor / ER, HER2 nonbreast, GCDFP-15, p63, p40, synaptophysin
- Ultrastructural features include interdigitating cellular junctions, desmosomes and scattered intracytoplasmic filaments (Korean J Pathol 2012;46:87)
- Mutational analyses were performed on microdissected tissue using 20 polymorphic microsatellite markers targeting 11 genomic regions in an effort to identify genetic similarities of MPMN and meningioma (Am J Surg Pathol 2004;28:207)
- Loss of heterozygosity was identified in 25% of single MPMN affecting 3 genomic loci
- No solitary MPMN had > 1 loss of heterozygosity event
- Multiple loss of heterozygosity were seen only in diffuse pulmonary meningotheliomatosis (MPMN-omatosis syndrome), where 33.3% of MPMNs showed loss of heterozygosity affecting 7 genomic loci
- Meningioma showed the highest frequency of loss of heterozygosity with major events seen at 22q (60%), 14q (42.8%) and 1p (44.4%) that were not shared by MPMN
- MPMNs are different from meningioma based on the major molecular genetic events seen in their formation and progression
- NF2 deletion similar to meningioma found in a limited series (Oncotarget 2018;9:36012)
- Left lung, mass, CT guided needle core biopsy:
- Minute pulmonary meningothelial-like nodule
- Negative for malignancy
- Adjacent lung parenchyma with mild interstitial fibrosis
- Metastatic carcinoma: usually positive for pankeratin (AE1 / AE3)
- Pulmonary carcinoid tumors (or pulmonary tumorlets for lesions < 5 mm): positive for pankeratin (AE1 / AE3), synaptophysin and INSM1 (Histopathology 2018;72:1067)
- Paraganglioma: positive for neuron specific enolase, chromogranin, synaptophysin, CD57 and GFAP
- Pulmonary meningiomas: clonal neoplastic lesions, which usually present as lung masses rather than minute nodules
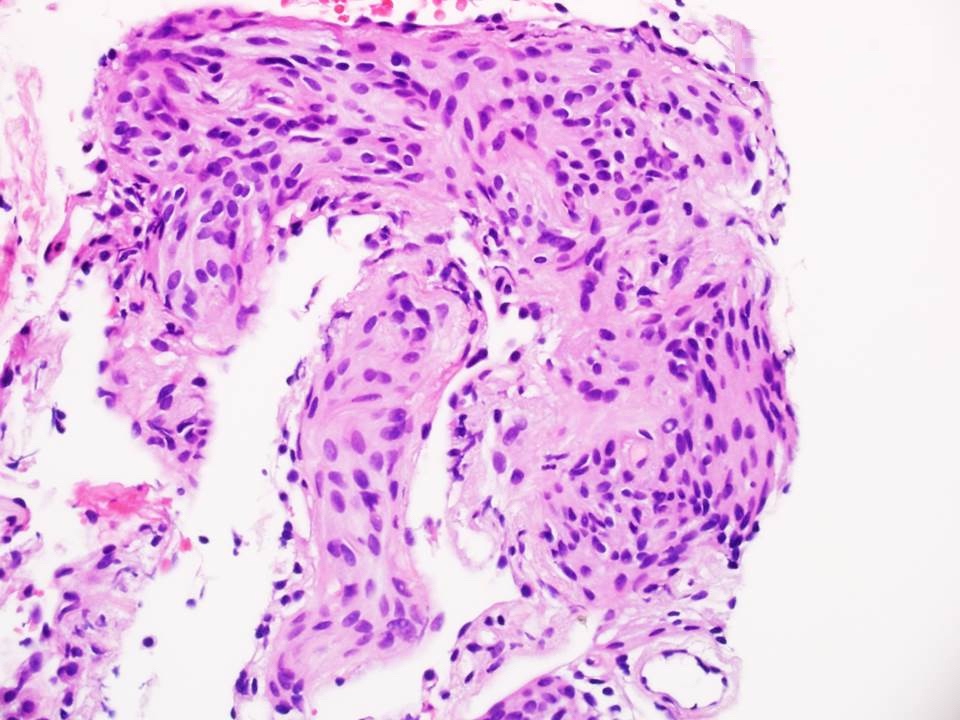
- Metastatic thyroid papillary carcinoma
- Minute pulmonary meningothelial-like nodule
- Pulmonary carcinoid tumor
- Pulmonary meningioma
- Pulmonary paraganglioma
Comment Here
Reference: Minute pulmonary meningothelial-like nodules
- CD56
- CK5 / 6
- ER
- Pankeratin (AE1 / AE3)
- Synaptophysin
Comment Here
Reference: Minute pulmonary meningothelial-like nodules
- Low grade or high grade salivary gland type tumor with mucous secreting cells, squamous cells and intermediate cells
- Distinguished from other lung cancers by central or peribronchial location, mucous cells, lack of keratinization, expression of p63 and MAML2 rearrangement (Mod Pathol 2014;27:1479)
- Most common salivary gland type tumor in the lung, tends to arise centrally
- Similar morphology to mucoepidermoid carcinoma arising in the head and neck with a mixture of mucous cells, squamous cells and intermediate cells; must exclude metastasis
- Strong association with t(11;19)(q21;p13) and MAML2 rearrangement by fluorescence in situ hybridization (FISH)
- Squamous component stains with p63 and p40
- Same diagnostic terminology as used in the salivary gland
- 0.1 - 0.2% of primary lung tumors (J Thorac Cardiovasc Surg 1978;76:431) and 9 - 18% in the pediatric population (J Surg Res 2009;156:224, J Pediatr Surg 2015;50:1004)
- May occur in any age group; many cases reported in pediatric population
- Most common of the primary salivary gland type tumors of the lung but still rare
- Any lung lobe, usually in relation to large bronchi
- Usually considered to have low malignant potential with recurrences; more aggressive when high grade (Int J Clin Exp Pathol 2014;7:6792)
- Most tumors are low stage and low to intermediate grade rather than high grade (J Thorac Oncol 2013;8:1578)
- May arise from submucosal bronchial glands
- Large central tumors cause obstructive symptoms such as dyspnea, cough, hemoptysis or pneumonia
- Peripheral lesions may be asymptomatic
- Bronchoscopy may be used to directly visualize and sample an endobronchial tumor
- Diagnosis may be difficult in small biopsies; may mimic primary non small cell lung carcinoma
- Can be difficult to detect on imaging due to small size of tumor, endobronchial location, association with pneumonia or atelectasis (Arch Pathol Lab Med 2007;131:1400)
- On CT, markedly enhanced homogeneous central bronchial nodule / mass suggests low grade mucoepidermoid carcinoma (MEC); high grade MEC tends to be peripheral with poorly defined margins, lobular, heterogeneous with less enhancement (AJR Am J Roentgenol 2015;205:1160)
- Uncommon findings included cavitation, diffuse thickening or spiculation (Clin Imaging 2012;36:8)
- Excellent prognosis after surgical removal (Thorac Cardiovasc Surg 2014;62:140, Asian Cardiovasc Thorac Ann 2016;24:257)
- Age, stage, margin status and pathological grade related to overall survival and disease free survival (J Thorac Oncol 2013;8:1578 , Int J Clin Exp Pathol 2014;7:6792)
- 22 year old man with tumor in the medial segment of the right lower lobe (Diagn Pathol 2012;7:137)
- 26 year old man with chronic cough and an endobronchial lesion (Respir Med Case Rep 2013;9:18)
- 38 year old woman with mild fever and dry cough (Oxf Med Case Reports 2015;2015:203)
- 40 year old man with dry cough (Asian Cardiovasc Thorac Ann 2015;23:988)
- 46 year old woman with dyspnea on exertion (Case Rep Oncol Med 2013;2013:625243)
- 58 year old man with shortness of breath, dysphagia and weight loss (Ann Clin Lab Sci 2015;45:219)
- 58 year old woman with mixed adenocarcinoma and mucoepidermoid carcinoma (Ann Thorac Surg 2014;98:695)
- Complete surgical excision (Int J Clin Exp Pathol 2014;7:6792)
- High grade tumors may require additional treatment, although chemotherapy and radiation controversial (World J Surg Oncol 2014;12:33)
- Polypoid, exophytic growth or sessile tumor in major bronchi, may be > 5 cm
- Generally well circumscribed and smooth with tan to yellow cut surface
- May be solid or cystic and potentially show glistening mucoid material
- Low grade has more cysts and mucous cells; high grade has more solid or nested growth, atypia, mitotic activity, necrosis, hemorrhage
- Mucus secreting cells, squamoid cells without significant keratinization, intermediate type cells
- Mucus secreting cells usually large with light blue-gray mucinous cytoplasm; variants include columnar, goblet, cuboidal, clear or oncocytic cells (Arch Pathol Lab Med 2007;131:1400)
- Squamous cells show intercellular bridges but no keratin whorls or pearls; intermediate cells usually polygonal with bland nucleus (Arch Pathol Lab Med 2007;131:1400)
- May show areas of papillary growth or spindled cells
- May have dense lymphoplasmacytic infiltrate (Am J Surg Pathol 2005;29:407)
- Lack in situ carcinoma of overlying epithelium
Contributed by Roseann Wu, M.D., M.P.H. and Yale Rosen, M.D.
Images hosted on other servers:
- Mixture of squamoid cells, mucous cells and intermediate cells
- Diff-Quik with numerous tight clusters of relatively small and bland cells with well defined but scant cytoplasm, central round and uniform nuclei with small nucleoli; second population of glandular appearing cells with cytoplasmic vacuoles with mucin, focal extracellular metachromatic mucinous material (Diagn Cytopathol 2013;41:1096)
- MAML2 rearrangement most common molecular genetic event, found more in low grade tumors (PLoS One 2015;10:e0143169)
- May stain with epidermal growth factor receptor (EGFR) but does not show the mutation or alterations in copy number (Mod Pathol 2008;21:1168)
- Reciprocal translocations, including t(1;11)(p22;q13) with overexpression of cyclin D1, t(11;19)(q14-21;p12) and t(11;19)(q21;p13) which encodes MECT1-MAML2 (MECT1 also known as CRTC1) (Arch Pathol Lab Med 2007;131:1400)
- Adenocarcinoma: lacks squamous and intermediate cells; TTF1+
- Adenosquamous carcinoma: usually peripheral in lung, not centered on bronchi; large tumors, no intermediate cells, contains adenocarcinoma component
- Metastatic renal cell carcinoma: more monotonous with foamy or eosinophilic cytoplasm; CK7-
- Mucous gland adenoma: confined to luminal aspect and not invasive; TTF1+
- PEComa: lacks mucin as well as squamous and intermediate cells; HMB45+
- Squamous cell carcinoma: may show more keratinization and lacks mucin
- Cytomorphology of salivary gland type tumors in the lung and mediastinum (Diagn Cytopathol 2012;40:1062)
- Rearrangement of which gene would support the diagnosis of mucoepidermoid carcinoma of the lung?
- APC
- BRAF
- MAML2
- PIK3CA
- PLAG1
- Proliferation of multiple smooth muscle nodules in the lung parenchyma
- Multiple, small, unencapsulated nodules of smooth muscle in fascicles
- Extremely rare, with controversial relationship to benign metastasizing leiomyoma or leiomyosarcoma
- Controversial whether are true hamartomas or represent metastasizing leiomyoma or leiomyosarcoma
- Extremely rare, almost always asymptomatic middle aged women
- Throughout lung parenchyma, occasionally bronchovascular distribution
- Possible origin from contractile system of the lung acini (contractile interstitial cell)
- Usually incidental
- Biopsy of nodules
- Xray: abnormal nodular shadows
- CT: multiple small pulmonary nodules
- Potential clonal expansion in long term follow-up (Pathol Int 2009;59:828)
- 31 year old woman whose tumors had secondary ossification (Pathol Int 1999;49:222)
- 46 year old man associated with bronchogenic cyst (Arch Pathol Lab Med 2003;127:e194)
- Surveillance, enucleation or surgical removal
- 2 - 15 mm white, firm, solid, well demarcated nodules
- Excessive smooth muscle bundles in fascicles, not associated with tumor
- Spindle cells with eosinophilic, fibrillary cytoplasm and blunt, elongated nuclei
- Scattered glands and duct-like spaces may be seen
- No mitoses, no nuclear atypia
- Benign metastasizing leiomyoma
- Lymphangioleiomyomatosis
- Native pulmonary muscle proliferation
- Strict aerobe that lacks a true cell wall, 0.2 - 0.8 μm and among the smallest free living bacterias
- Formerly called atypical pneumonia (atypical due to moderate sputum production and consolidation and only minimal leukocytosis)
- Common in children and young adults, but may occur in older age groups
- Causes community acquired pneumonia (eMedicine), either interstitial (usually) or bronchopneumonia (rare)
- Often asymptomatic
- Superimposed bacterial infection may occur
- Diagnosis: rarely biopsied, diagnose with complement fixation antigen assays; cold agglutinins present in 50% of cases
- Macrolides (erythromycin), although may be resistance (J Infect Chemother 2011;17:114)
- Reddish blue, congested, patchy lungs; usually no pleuritis
- Bronchiolitis, interstitial and minimal intra-alveolar involvement with widened alveolar septa due to lymphoplasmacytic inflammatory cells
- Intra-alveolar proteinaceous material
- Neutrophilic infiltrate in bronchioles acutely, bronchiolar metaplasia, lymphoplasmacytic infiltrate in bronchial wall and pneumocyte hyperplasia
Gliding phase
- Respiratory syncytial virus, rhinovirus, rubeola, varicella, Chlamydia psittacosis, Coxiella burnetti (Q fever)
- Ubiquitous saphrophyte; disease caused by inhalation or direct implantation into skin
- More than 30 species with clinical significance (Clin Microbiol Rev 2006;19:259)
- Opportunistic lung infection associated with transplantation, chemotherapy, immunosuppression, steroids
- Disease is relatively uncommon in HIV likely due to sulfonamide prophylaxis directed against P. jeroveci; HAART treatment may be effective (Can J Infect Dis Med Microbiol 2009;20:e103)
- Complication of alveolar proteinosis
- Focal bronchopneumonia with microabscesses, variable histiocytic response and ill defined granulomas
- If identified by anatomic pathologist, clinical microbiology laboratory should be notified as routine culture may not isolate the organism
- Modified acid fast, Fite, Gram stain and GMS
- Gram stain: slender, slightly beaded, branching filamentous bacilli
- Rare, presents as asymptomatic nodule
- Usually in asymptomatic elderly with nodule on chest Xray, but no evidence of systemic disease
- Good prognosis; typically doesn't progress to lymphoproliferative disorders
- Nodular involvement may be associated with systemic involvement
- 85 year old woman with asymptomatic pulmonary nodules (Case #197)
- Well circumscribed amyloid, often with lymphocytes (T cells) and plasma cells
- Granulomatous reaction to amyloid common, often calcification and ossification
Contributed by Dr. Sajna V.M. Kutty, MVR Cancer Centre and Research Institute, Kozhikode, Kerala, India
Case #197
- Congo red staining: glassy, salmon pink amorphous material with apple green birefringence under polarized microscopy
- Clonal restriction of plasma cells (kappa or lambda staining, not both)
- Amyloid fibrils
- Primary pulmonary lymphomas with amyloid production: < 1% of pulmonary lymphomas have amyloid deposits, usually age 70+ years with marginal zone or SLL / CLL subtypes, often with lymphatic tracking and reactive lymphoid follicles; the presence of evenly distributed lymphocytes in the nodule and invasion of the pleura is specific for lymphoma
- Hyalinizing granuloma: history of exposure to Histoplasma or TB, collagen is Congo red negative
- #2 most common type of interstitial pneumonia
- Katzenstein et al. in 1994 first proposed the idea of NSIP, as not fitting any known pattern of idiopathic interstitial pneumonia (Am J Surg Pathol 1994;18:136)
- NSIP initially was a "provisional disease" in the 2002 ATS / ERS classification (Am J Respir Crit Care Med 2002;165:277); then a statement of idiopathic NSIP was published from an ATS / ERS working group (Am J Respir Crit Care Med 2008;177:1338); finally idiopathic NSIP was considered a defined disease in the 2013 ATS / ERS classification (Am J Respir Crit Care Med 2013;188:733)
- An interstitial lung disease with a histologic NSIP pattern, due to a variety of etiologies
- The NSIP pattern is the second most common pattern, and always part of the differential diagnosis of the usual interstitial pneumonia (UIP) pattern, but NSIP has a better prognosis than UIP
- Multidisciplinary discussion is necessary to make the diagnosis and decide treatment direction
- NSIP is the name of the morphologic (histologic) pattern
- When no specific cause is identified, the clinical, radiological and pathological diagnosis of "idiopathic NSIP" is rendered
- Idiopathic nonspecific interstitial pneumonia: J84.113
- Idiopathic NSIP is the second most common idiopathic interstitial pneumonia, following idiopathic pulmonary fibrosis
- The mean onset is 50 - 60 years old
- Female predominant
- No clear association with tobacco use
- Bottom of lower lobes of bilateral (or "bibasilar") lung
- NSIP pattern is often present in connective tissue diseases, hypersensitivity pneumonitis, drug induced injury and infectious diseases
- Idiopathic form of NSIP is rare; most idiopathic NSIP appear to be an early manifestation of undifferentiated connective tissue disease (Am J Resp Crit Care Med 2007;176:691, Chest 2015;147:165, Eur Respir J 2011;38:384)
- Neovascularization promoted by the expression of VEGF-A and MMP-2 may play a role in fibrosis of NSIP (Pathol Int 2013;63:237)
- Chronic and slowly progressive respiratory failure
- Shortness of breath
- Dyspnea on exertion
- Cough
- Fatigue
- Weight loss
- Abnormal chest auscultation
- End inspiratory fine crackles in bibasilar lung
- Restrictive pattern in pulmonary function tests:
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- It is often challenging to make the diagnosis for cases with an NSIP pattern, since it includes a variety of diseases
- Therefore, two levels of diagnosis are recommended: histological diagnosis of NSIP pattern and multidisciplinary (clinical-radiological-pathological) diagnosis for its etiology (i.e. idiopathic, connective tissue, etc.), based on:
- Clinical features, including laboratory tests
- High resolution computed tomography (HRCT)
- Surgical lung biopsy
- The guidelines suggest multidisciplinary discussion by experienced physicians, radiologists and pathologists, especially when they disagree (Am J Respir Crit Care Med 2011;183:788, Am J Respir Crit Care Med 2004;170:904, Thorax 2003;58:143)
- Some NSIP cases with inconclusive autoimmune features may fit the criteria for idiopathic NSIP under current guidelines, or be classified as interstitial pneumonia with autoimmune features (IPAF) (Eur Respir J 2015;46:976)
- Some cases with NSIP pattern may be included in the newly described category of "Unclassifiable interstitial pneumonia (UCIP)" (Respirology 2016;21:51)
- Serological autoantibody tests: can be positive but not conclusive for connective tissue disease
- Antinuclear antibody
- Rheumatoid factor
- Anti-CCP antibody
- Anti-SS-A, B antibody
- Anti-Sm antibody
- Anti-Scl-70 antibody
- Anti-ARS antibody
- Antibodies tests of hypersensitivity pneumonitis: pertinent negative for idiopathic NSIP (Am J Respir Crit Care Med 2012;186:314)
- Avian antigens: pigeon, parakeet, budgerigar, chicken
- Fungus: trichosporon, aspergillus
- Bacteria: actinomycete
- Mycobacteria: Mycobacterium avium-intracellulare
- Chemicals
- Increased serum KL-6 (normal limit is < 500 IU)
- Chest xray and HRCT can detect lesions: however, it is usually not sensitive enough to render the diagnosis (PLoS One 2016;11:e0166168, Thorax 2003;58:143)
- HRCT findings suggestive for NSIP pattern:
- Diffuse ground glass opacity
- Reticular opacity
- Traction bronchiectasis
- Not suggestive findings:
- Irregular linear opacity
- Honeycombing
- Nodular opacity
- Better prognosis than UIP / IPF, with a 5 year survival of ~ 70% for all NSIP (Am J Respir Crit Care Med 1998;157:199)
- Survival rate depends on the background etiology (Eur Respir J 2015;45:746)
- 5 year survival of 61% for idiopathic NSIP
- 5 year survival of 42% for NSIP with chronic hypersensitivity pneumonitis
- 5 year survival of 77% for autoimmune NSIP
- 11 year old boy with NSIP after peripheral blood stem cell transplantation (J Thorac Imaging 2009;24:59)
- 24 year old woman and 38 year old man with connective tissue diseases and NSIP overlapping organizing pneumonia (Int J Clin Exp Pathol 2015;8:11230)
- 29 year old man and 41 year old woman with NSIP and amyopathic dermatomyositis (Clin Rheumatol 2007:26;436)
- 58 year old man with NSIP overlapping UIP (Diagn Pathol 2012;7:167)
- 64 year old woman with NSIP who developed Kaposi sarcoma after steroid therapy (Pathol Res Pract 2006;202:113)
- 66 year old man with NSIP and emphysema, which improved after smoking cessation (Respir Med Case Rep 2014;14:7)
- 73 year old woman with NSIP and bullous pemphigoid (Chest 2012;141:795)
- There is no standard treatment for idiopathic NSIP, although 80% of cases could be improved or stabilized by glucocorticoids with / without other immunosuppressive drugs such as azathioprine and cyclophosphamide (Am J Respir Crit Care Med 1998;158:1286, Respir Med 1999;93:113)
- Treat background diseases, including autoimmune diseases
- Remove suspicious drugs; reduce inhalation exposure to possible disease promoters
- Diffuse involvement with mild to moderate increase in lung weight
- Fibrotic changes in lower lobes
- Homogeneous and diffuse compared to UIP
- Shrunken lung
- Traction bronchiectasis can be seen
- Honeycomb change can be seen but limited
- Since there are few specific findings for NSIP pattern, it is essential to exclude other lung diseases on histology (Am J Respir Crit Care Med 2008;177:1338)
- Characteristic findings of NSIP pattern
- Diffuse and uniform inflammation ("temporal homogeneity") on low power of alveolar wall, bronchovascular bundles and pleura
- There are usually no normal alveolar walls in the affected lobules
- Cellular or fibrotic change
- Lymphocytic or plasmacytic infiltration
- Loose fibrosis
- Lung architecture is frequently preserved
- "Cellular NSIP" or "fibrotic NSIP" can be stated specifically in pathologist report
- Diffuse and uniform inflammation ("temporal homogeneity") on low power of alveolar wall, bronchovascular bundles and pleura
- Features of interstitial pneumonia with autoimmune features (IPAF) (Chest 2010;138:251):
- Lymphoid aggregates with germinal center
- Extensive pleuritis
- Prominent plasmacytic infiltration
- Dense perivascular collagen
- It is quite rare to see pure NSIP on histology - typically there are focal findings of other interstitial lung disease (Histopathology 2014;65:549)
- Pertinent negative findings (Am J Respir Crit Care Med 2008;177:1338)
- UIP-like change
- Marked architectural distortion
- Dense fibrosis with smooth muscle hyperplasia or elastosis
- Fibroblastic foci
- Honeycomb change
- Hypersensitivity pneumonitis-like change
- Airway centered change
- Peribronchiolar metaplasia
- Granulomas or interstitial giant cells with cholesterol cleft
- Extensive organizing pneumonia (areas more than 20% of disease)
- Desquamative interstitial pneumonia-like change
- Aggregation of respiratory bronchiolitis macrophages in alveolar sacs and respiratory bronchioles
- Diffuse alveolar damage-like change
- Hyaline membrane
- Alveolar hemorrhage
- Lymphoid interstitial pneumonia-like change
- Marked and extensive infiltration of lymphocytes in alveolar wall
- Light chain restriction
- Smoking related interstitial fibrosis (J Clin Pathol 2013;66:882)
- Alveolar hyalinized septal thickening with little cellular infiltration
- Centriacinar emphysema
- UIP-like change
Contributed by Akira Yoshikawa, M.D.
Images hosted on other servers:
- Elastica van Gieson staining highlights the relative preservation of lung architecture
- Giemsa, Grocott and Ziehl-Neelsen stains rule out infectious diseases, if suspected
- Desquamative interstitial pneumonia: smoking history, aggregates of alveolar macrophages
- Diffuse alveolar damage: hyaline membrane, alveolar hemorrhage
- Hypersensitivity pneumonitis: exposure to antigens, airway centered change
- Infectious disease (TB, fungal)
- Interstitial pneumonia with autoimmune features (IPAF): lymphoid aggregates with germinal center, extensive pleuritis, prominent plasmacytic infiltration, dense perivascular collagen
- Lymphoid interstitial pneumonia: viral infection such as HIV, CMV and HTLV1
- Organizing pneumonia: marked organizing pneumonia on histology
- Smoking related interstitial fibrosis: smoking history, acellular fibrosis
- UIP / IPF: patchy and peripheral involvement, fibroblastic focus, honeycomb change
- NUT carcinoma is an aggressive malignancy characterized by NUT gene rearrangements
- Monotonous, poorly differentiated morphology with foci of abrupt keratinization
- NUT carcinoma is an aggressive malignancy more frequently arising in the thorax or aerodigestive tract, affecting patients of any age with equal gender distribution
- Morphologically it shows diffuse architecture and consists of monotonous cells with frequent cytoplasmic clearing, large nuclei with prominent nucleoli and foci of abrupt keratinization
- Due to its largely nonspecific morphology, the differential diagnosis is broad
- Speckled nuclear immunohistochemical expression of NUT protein in ≥ 50% of cells is a diagnostic hallmark
- NUT gene rearrangements are present and can be detected by FISH
- NUT midline carcinoma (no longer recommended)
- ICD-O: 8023/3 - NUT carcinoma
- M = F (Clin Cancer Res 2012;18:5773)
- Initially thought to affect younger patients; later proven to affect patients of any age (Clin Cancer Res 2012;18:5773)
- Mediastinum (Clin Cancer Res 2012;18:5773)
- Upper aerodigestive tract (Clin Cancer Res 2012;18:5773)
- Occasionally: salivary glands, retroperitoneum, pancreas, urinary bladder (Cancer Genet Cytogenet 2010;203:16)
- Somatic NUT reciprocal translocation leading to expression of an oncogenic NUT fusion gene (Cancer Genet Cytogenet 2010;203:16)
- See Molecular / cytogenetics description
- Definitive environmental or infectious etiology is lacking (Cancer Genet Cytogenet 2010;203:16)
- Symptoms depend on anatomic location and extent of tumor
- Thoracic cases present with cough, shortness of breath, hemoptysis, pericardial or pleural effusion (Lung Cancer 2015;90:484, Diagn Cytopathol 2019;47:594)
- Very aggressive clinical course, leading to death within a few months (Eur Arch Otorhinolaryngol 2018;275:815)
- Diagnosis of NUT carcinoma can be challenging because of nonspecific morphologic features
- Features may not be uniformly present in small biopsy specimens
- A combination of subtle morphologic changes with NUT immunohistochemistry can aid in the diagnosis (Virchows Arch 2021;478:21)
- Occasional elevation of serum alpha fetoprotein in mediastinal cases (Cancer Res 2003;63:304)
- Poor prognosis, with median survival from initial diagnosis ranging 1 - 6.7 months (Clin Cancer Res 2012;18:5773, Eur Arch Otorhinolaryngol 2018;275:815, J Thorac Oncol 2015;10:951)
- 26 year old man with a 3 cm sublingual gland mass (Head Neck Pathol 2017;11:460)
- 28 year old man with a tracheal mass, false negative FISH results and long term survival (Head Neck Pathol 2021;15:698)
- 32 year old woman with a 7.6 cm perihilar mass (Int J Surg Pathol 2016;24:85)
- 34 year old pregnant woman with a right pulmonary mass (World J Surg Oncol 2020;18:290)
- Surgery, chemotherapy and radiation (Eur Arch Otorhinolaryngol 2018;275:815)
- Surgical options may be limited because of surgical inaccessibility of tumors, particularly those with thoracic anatomic localization (Pathol Int 2018;68:583)
- Radiotherapy seems to produce superior outcomes compared with conventional chemotherapy (Clin Cancer Res 2012;18:5773)
- Because of the advanced stage at diagnosis, examination of complete resection specimens is rare
- Tumor can be deceivingly well demarcated from adjacent structures (Int J Surg Pathol 2016;24:85)
- Primitive looking, monotonous, medium sized cells with frequent cytoplasmic clearing (Cancer Genet Cytogenet 2010;203:16)
- Scattered foci of abrupt keratinization (J Thorac Oncol 2015;10:951)
- Large nuclei with prominent nucleoli (Ultrastruct Pathol 2012;36:280)
- Diffuse architecture with occasional spacing and discohesion of tumor cells (Cancer Cytopathol 2016;124:901)
- Background of necrosis with prominent neutrophils (Cancer Cytopathol 2016;124:901)
- Occasionally, pseudoglandular formations; mucoid stroma, crushing artifact (Int J Surg Pathol 2019;27:225, J Thorac Oncol 2015;10:951)
- Hard to diagnose on cytology because of frequent lack of overt squamous differentiation (Cancer Cytopathol 2016;124:901)
- Scattered dyskeratotic cells may be diagnostically helpful (J Pathol Transl Med 2018;52:349)
- NUT speckled nuclear positivity (sensitivity 87%, specificity 100%) (Am J Surg Pathol 2009;33:984)
- Keratins, particularly high molecular weight (Thorac Cancer 2020;11:1724)
- p63 and p40 (J Thorac Oncol 2015;10:951)
- MYC strongly expressed in primitive component, attenuated in squamoid foci (Oncologist 2019;24:e740)
- p16 can be strongly expressed, without relationship with HPV infection (Appl Immunohistochem Mol Morphol 2014;22:262)
- Negative most of the time but with occasional positive cases (diagnostic pitfalls): CD99, synaptophysin, FLI1, EGFR, HER2, focal TTF1 (Oncologist 2019;24:e740, Biomed Res Int 2020;2020:9791208, J Thorac Oncol 2015;10:951)
- Tumor cells with short microvillous apex, intracellular desmosomes and junctional complexes (Ultrastruct Pathol 2012;36:280)
- Cytoplasmic tonofilaments, polyparticulate glycogen, lipid droplets and electron dense granules (Ultrastruct Pathol 2012;36:280)
- Reciprocal translocation t(15;19) leading to BRD4::NUT fusion in 70% of cases (Cancer Genet Cytogenet 2010;203:16)
- BRD3::NUT fusion in remaining cases (Cancer Genet Cytogenet 2010;203:16)
- Rare NUT fusion counterpart genes: NSD3, ZNF532, ZNF592 (Cancer Genet Cytogenet 2010;203:16)
- FISH for NUT rearrangements in combination with NUT immunohistochemistry has 100% sensitivity and specificity (Am J Surg Pathol 2009;33:984)
- Next generation sequencing (NGS) or reverse transcription PCR can detect rare NUT fusions nondetectable by FISH (Lung Cancer 2015;90:484)
- TP53 and PIK3CA are frequently mutated genes (Cancer Med 2021;10:5757)
- Mediastinum, anterior, excisional biopsy:
- NUT carcinoma (see comment)
- Comment: Infiltrative, poorly differentiated carcinoma, with extensive necrosis and focal keratinization. Immunohistochemically, tumor cells express p63, p40, keratins 5/6 and NUT. Break apart FISH is positive for NUT rearrangement. These findings support the diagnosis.
- Focally keratinizing or basaloid squamous cell carcinoma (Oncologist 2019;24:e740):
- NUT immunohistochemistry is important in differentiating those tumors (Am J Surg Pathol 2009;33:984, Virchows Arch 2021;478:21)
- Thymic carcinoma (Cancer Res 1991;51:3327):
- Thymic carcinomas usually express all of CD5, GLUT1 and CD117 (Am J Surg Pathol 2011;35:1296)
- Small cell carcinoma:
- Occasional positivity for synaptophysin and nuclear molding in NUT carcinoma is a diagnostic pitfall (J Thorac Oncol 2015;10:951)
- NUT immunohistochemistry can help differentiate (Virchows Arch 2021;478:21)
- Ewing sarcoma:
- Occasional positivity for CD99 in NUT carcinoma is a pitfall (Cancer Biol Ther 2019;20:150)
- Ewing sarcomas express NKX2.2 by immunohistochemistry and harbor EWSR1 gene rearrangements (Am J Surg Pathol 2012;36:993, Cancer Genet 2011;204:351)
- Adamantinoma of bone:
- Caution needed when assessing skeletal metastatic lesions (J Clin Oncol 2014;32:e57)
- Adamantinoma of bone almost exclusively arises in the tibia and contains fibro-osseous stroma in addition to epithelial elements; tumor cells harbor EPHB4::MARCH10 gene fusion (Am J Surg Pathol 2019;43:965)
- Mediastinal germ cell tumor:
- Elevated serum alpha fetoprotein is a potential pitfall (BMC Cancer 2016;16:895)
- NUT carcinoma with germ cell-like phenotype has been described in case with ZNF532::NUTM1 gene fusion (Am J Surg Pathol 2022;46:281)
- Immunohistochemistry for NUT protein and molecular pathology for NUT fusions can aid in the differential diagnosis from germ cell tumors (Am J Surg Pathol 2022;46:281)
- Desmoplastic round cell tumor (Lung Cancer 2015;90:484):
- Positive for desmin and WT1 C terminus (Arch Pathol Lab Med 2006;130:728, Am J Surg Pathol 2014;38:1220)
- Harbors EWSR1::WT1 gene fusion (Semin Cancer Biol 2005;15:197)
- Diffuse large B cell lymphoma (Lung Cancer 2015;90:484):
- Positive immunostains for B cell markers and further subclassification by the Hans algorithm (Blood 2004;103:275)
- Porocarcinoma:
- Porocarcinomas may show NUT immunopositivity because of underlying YAP1::NUT fusion (J Cutan Pathol 2021;48:403)
A 36 year old man presents with cough and shortness of breath and is diagnosed with a large mediastinal mass and undergoes open surgical biopsy. A low power hematoxylin and eosin microscopic picture is shown above. If the mass undergoes genetic testing, which of the following is the most likely finding?
- BRD4::NUT fusion transcript
- Isochromosome 12p
- MYC amplification
- SMARCA4 point mutation
BRD4::NUT fusion transcript is detected in 70% of NUT carcinomas. Answer B is incorrect because isochromosome 12p is a common finding in mediastinal germ cell tumors. Answer C is incorrect: although MYC is overexpressed in NUT carcinoma, this is because it is downstream in the BRD4::NUT fusion transcript cascade and not because of gene amplification. Answer D is incorrect because SMARCA4 point mutations are frequent in SMARCA4 deficient thoracic tumors (Cancer Genet Cytogenet 2010;203:16, Histopathology 2021;78:593, Oncogene 2014;33:1736, Virchows Arch 2021;478:21).
Comment Here
Reference: NUT carcinoma
- Detection of YAP1::NUT fusion transcript
- Positive break apart NUT FISH
- Presence of a complex karyotype
- Wild type TP53 gene
Although rare NUT fusions are nondetectable by FISH, the combination of this finding with a positive NUT immunostain has high sensitivity and specificity for diagnosing NUT carcinoma. Answer A is incorrect because a YAP1::NUT fusion, along with the patients reported history of facial nodule would be consistent with the diagnosis of porocarcinoma rather than NUT carcinoma. Answer C is incorrect because most NUT carcinomas have noncomplex karyotypes, with the only finding being a t(15;19) reciprocal translocation. Answer D is incorrect because TP53 is frequently mutated in NUT carcinoma (Lung Cancer 2015;90:484, J Cutan Pathol 2021;48:403, Pathol Int 2018;68:583, Cancer Med 2021;10:5757).
Comment Here
Reference: NUT carcinoma
- Organizing pneumonia (OP) can be defined as either clinicopathological diagnosis, histological pattern or microscopic findings
- Histologic features include polypoid fibroblastic aggregations, which plug alveolar sacs, ducts and bronchioles
- Organizing pneumonia is one of the most commonly seen lung lesions and is associated with a variety of diseases, such as infections and systemic diseases
- Cryptogenic organizing pneumonia is a relatively rare disease but often needs to be considered, since its clinical and radiological manifestations are often varied and nonspecific
- Cryptogenic organizing pneumonia is a diagnosis that is not made by a pathologist; rather, it is a diagnosis of exclusion made by the multidisciplinary care team
- Histologically, both cryptogenic organizing pneumonia and secondary organizing pneumonia are characterized by polypoid fibroblastic aggregations, which plug alveolar sacs, ducts and bronchioles
- Organizing pneumonia (OP):
- Can be either clinicopathological diagnosis (cryptogenic organizing pneumonia and secondary organizing pneumonia), histological pattern (organizing pneumonia pattern), or microscopic findings (e.g., Masson body)
- Since 1901, organizing pneumonia has been described with the name bronchiolitis obliterans as an interstitial lung disease with granulation tissue plugs within alveolar ducts and small airways secondary to a variety of causes, including infection, fume exposure, drugs, collagen vascular disease, allergic reactions and obstruction (Chest 1983;83:161)
- Davison et al. (1983) and Epler et al. (1985) reported a series of cases with organizing pneumonia and no evidence of infection or other aetiological agents; after that, the term bronchiolitis obliterans organizing pneumonia (BOOP) was commonly used for a while (Q J Med 1983;52:382, N Engl J Med 1985;312:152)
- Cryptogenic organizing pneumonia (COP):
- Idiopathic form of organizing pneumonia
- In 2002, the American Thoracic Society / European Respiratory Society suggested the term cryptogenic organizing pneumonia (COP) to avoid confusion with airway disease (such as constrictive bronchiolitis obliterans) and categorized cryptogenic organizing pneumonia into acute / subacute interstitial pneumonia (Am J Respir Crit Care Med 2002;165:277, Am J Respir Crit Care Med 2013;188:733)
- Cicatricial organizing pneumonia (ciOP) (Histopathology 2022;80:279):
- Also known as collagenized organizing pneumonia, cicatricial variant of organizing pneumonia, fibrosing organizing pneumonia, scarred organizing pneumonia
- Chronic fibrotic changes of conventional organizing pneumonia with formation of dense collagen fibers within the alveolar space, with no architectural destruction
- Incidence of cryptogenic organizing pneumonia is 6 - 9 per 100,000 (Medicine (Baltimore) 1995;74:201)
- No sex predominance
- Median age at onset is 50 - 60 years old (N Engl J Med 1985;312:152, Chest 2011;139:893, Int J Tuberc Lung Dis 2007;11:689)
- No association with smoking history
- Most patients are previously healthy individuals and lack history of lung disease
- Bilateral or unilateral lobes of the lung
- Organizing pneumonia is a repair process (wound healing) of the lung in response to preceding alveolar injury (Thorax 2000;55:318, Eur Respir J 2006;28:422)
- Injury to capillary endothelial cells and alveolar epithelial cells results in the leakage of plasma protein, especially coagulation factors
- Intra-alveolar coagulation of proteins and coagulation factors generate fibrin clotting on alveolar surfaces
- Fibroblasts / myofibroblasts migrate into the damaged area, proliferate and generate loose fibrosis in the form of a small polyp
- IL6, IL8 and TGFβ1 may play an important role in pathogenesis (Adv Exp Med Biol 2016;911:77)
- Galectin 9 and regulatory T cells are increased in the lung with cryptogenic organizing pneumonia (Lung 2015;193:683)
- Organizing pneumonia can be a complication or lung manifestation of other diseases (Thorax 2000;55:318, Chest 2011;139:893, Int J Tuberc Lung Dis 2007;11:689, J Thorac Imaging 2006;21:22)
- Idiopathic: cryptogenic organizing pneumonia
- Infection: bacterium / fungus / virus / parasite, pneumonia, lung abscess, empyema
- Other interstitial lung disease: nonspecific interstitial pneumonia, hypersensitivity pneumonitis, eosinophilic pneumonia, diffuse alveolar damage
- Autoimmune disease: rheumatoid arthritis, Sjögren syndrome, polymyositis / dermatomyositis, Sweet disease, etc.
- Aspiration
- Drug reaction, fume and toxic exposure
- Radiation
- Inflammatory bowel disease: Crohn's disease, ulcerative colitis
- Neoplasm: primary or metastatic lung cancer, lymphoma / leukemia, myelodysplastic syndrome (MDS)
- Lung infarction
- Secondary organizing pneumonia is much more common than cryptogenic organizing pneumonia; 6.5:1 (Ann Transl Med 2020;8:763)
- Mild and slowly progressive respiratory failure (Chest 2011;139:893, N Engl J Med 1985;312:152, Int J Tuberc Lung Dis 2007;11:689)
- Dry cough
- Dyspnea
- Malaise, fatigue and fever
- Duration of symptoms more than 3 months
- Abnormal chest auscultation
- End inspiratory fine crackles in affected lobes
- Restrictive pattern is often observed in pulmonary function tests; however, the abnormality is slight or within the normal range in 30% of cases (Chest 2011;139:893, N Engl J Med 1985;312:152)
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- Based on clinical features, radiology and histopathology (Am J Respir Crit Care Med 2002;165:277):
- Clinical investigation for a possible cause of the disease is necessary
- Surgical lung biopsy or transbronchial lung biopsy is required to establish a firm diagnosis since the clinical and radiological findings are often not specific
- However, a biopsy may not be necessary if the clinical and radiological features are suggestive enough
- Increased serum surfactant proteins A and D
- Negative serum antibodies of connective tissue diseases and hypersensitivity pneumonitis
- Reference: Respiration 2019;98:534
- Simple chest radiography
- Bilateral or unilateral ground glass opacity and consolidation
- High resolution computed tomography (Respirology 2016;21:810, Chest 2017;151:1356)
- Typical pattern:
- Patchy ground glass opacity and consolidation with / without air bronchogram
- Often bilateral and asymmetrical
- Often peripheral and migratory
- Size varies from a few centimeters to a whole lobe
- Typical organizing pneumonia sometimes looks similar to eosinophilic pneumonia, pulmonary lymphoma and lepidic adenocarcinoma
- Less common patterns:
- Focal organizing pneumonia: nodular or mass-like consolidation mimicking lung cancer (Int J Clin Exp Pathol 2015;8:511)
- Infiltrative organizing pneumonia: diffuse infiltrative opacity
- Reversed halo sign: central ground glass opacity surrounded by round consolidation
- Crazy paving pattern: areas of ground glass opacities superimposed to focal thickening of pulmonary parenchyma
- Progressive fibrosis pattern: subpleural basal reticulations and architectural distortion, mimicking nonspecific interstitial pneumonia and usual interstitial pneumonia
- Perilobular pattern: curved or arcade-like bands of parenchymal consolidation with blurred borders and thickening of the interlobular septa, resembling a Roman arch
- Linear and band-like opacities: thick radial bands of consolidation containing an air bronchogram or subpleural curvilinear bands, parallel to the pleura
- Typical pattern:
- Good prognosis but frequent relapse; 20 - 58% with both cryptogenic organizing pneumonia and secondary organizing pneumonia relapse (Chest 2011;139:893, N Engl J Med 1985;312:152, Int J Tuberc Lung Dis 2007;11:689)
- Relapse predictors (Respiration 2007;74:624, Tuberc Respir Dis (Seoul) 2015;78:190, Am J Respir Crit Care Med 2000;162:571, Chest 1998;114:1599):
- Delay of corticosteroid administration
- Shorter maintenance of corticosteroid dose
- Hypoxemia: lower PaO2, lower PaO2/FiO2 ratio
- Lower serum total protein
- Lower forced vital capacity (FVC)
- Multifocal opacity on radiology
- Relapse predictors (Respiration 2007;74:624, Tuberc Respir Dis (Seoul) 2015;78:190, Am J Respir Crit Care Med 2000;162:571, Chest 1998;114:1599):
- Rarely progresses to severe respiratory failure and death
- Myelodysplastic syndrome (MDS) related organizing pneumonia may be associated with worse prognosis
- Cicatricial form of cryptogenic organizing pneumonia is more progressive or persistent and resistant to treatment (Hum Pathol 2017;64:76)
- 23 year old woman with organizing pneumonia following influenza B (BMC Infect Dis 2017;17:572)
- 43 year old woman with organizing pneumonia related to trastuzumab (Springerplus 2016;5:1964)
- 57 year old man with severe organizing pneumonia following COVID-19 (Thorax 2021;76:201)
- 64 year old woman with organizing pneumonia related to pembrolizumab (Drug Target Insights 2016;10:9)
- 66 year old man with cryptogenic organizing pneumonia and atypical imaging findings (Case Rep Pulmonol 2020;2020:2094625)
- 70 year old man with cryptogenic organizing pneumonia presenting with mass-like lesion (J Int Med Res 2020;48:300060520920068)
- 74 year old woman with rapidly progressive cryptogenic organizing pneumonia (Intern Med 2017;56:1185)
- Most with cryptogenic organizing pneumonia and secondary organizing pneumonia completely recover with oral corticosteroids (N Engl J Med 1985;312:152, Chest 2011;139:893)
- Multiple patchy fibrotic lesions
- Ill defined, soft to firm gray areas
- Volume of the lung is usually normal
- Other changes overlap with secondary organizing pneumonia
- Organizing pneumonia (Semin Respir Crit Care Med 2012;33:462):
- Fibroblastic plugs in alveolar sacs and ducts (organizing pneumonia) and bronchiolar lumen
- Formed by spindled fibroblasts in pale staining matrix of immature loose collagen with polypoid shape (Masson body) or serpiginous or elongated form
- Organizing pneumonia sometimes extends from one alveolus to the next through interalveolar fenestrae (butterfly pattern)
- Mild to moderate cellular infiltrate in background (Eur Respir J 2006;28:422, Clin Med Insights Circ Respir Pulm Med 2016;9:123):
- Thickened alveolar septa with lymphocytes, plasma cells and histiocytes
- Alveolar architecture is usually preserved in cryptogenic organizing pneumonia
- Because interstitial dense fibrosis, architectural destruction and honeycomb change are not components of cryptogenic organizing pneumonia, the organizing pneumonia lesion is likely to be secondary to other lung disease if these findings are mixed or overlap (J Clin Pathol 2009;62:387)
- Airspace changes (Thorax 2000;55:318):
- Foamy macrophage accumulation in surrounding airspace may be present
- Occasional fibrin deposition
- If prominent, the lesion is more likely to be an infection, eosinophilic pneumonia (especially after corticosteroids), vasculitis (e.g., granulomatosis with polyangiitis) or acute fibrinous organizing pneumonia (AFOP)
- Cicatricial form of cryptogenic organizing pneumonia (Hum Pathol 2017;64:76):
- Organizing granulation tissue is collagenized or hyalinized and harbors eosinophilic, lamellar and dense fibers
- Airspaces can be filled with collagenized organizing pneumonia but alveolar architecture is mostly preserved
- Elastica van Gieson staining is helpful to evaluate if architecture of alveoli is preserved or not
- Organizing polyps are negative for elastica van Gieson staining except in cicatricial variant
- Type I pneumocyte necrosis in the early phase (Thorax 2000;55:318)
Cryptogenic organizing pneumonia
Focal organizing pneumonia
Fibrosing organizing pneumonia
- Lung, right middle lobe, transbronchial biopsy:
- Organizing pneumonia (see comment)
- Negative for granuloma, vasculitis and malignancy
- Comment: Based on the provided patient information, the diagnosis of cryptogenic organizing pneumonia is favored. However, secondary organizing pneumonia from various causes (infection, drug toxicity, autoimmune disease, malignancy, etc.) needs to be excluded clinically.
- Acute interstitial pneumonia (AIP) / acute respiratory distress syndrome (ARDS):
- Diffuse alveolar damage (DAD) of AIP or ARDS may have a prominent organizing pneumonia (organizing DAD) radiologic pattern
- If organizing pneumonia is so diffusely distributed that it almost completely occupies the surgical sample, organizing DAD should be favored
- Hyaline membranes, architectural destruction and myofibroblastic aggregation with less extracellular matrix are other clues of DAD pattern
- Eosinophilic pneumonia:
- Intra-alveolar eosinophils
- Pink macrophages (not foamy), more fibrin, frequent type II pneumocyte atypia
- Granulomatosis with polyangiitis:
- Geographic necrosis, hemorrhage, capillaritis
- More eosinophils
- More fibrin deposition
- Inflammatory myofibroblastic tumor:
- Inflammatory pseudotumor (IgG4 related / NOS):
- Nonspecific interstitial pneumonia (NSIP):
- Organizing pneumonia is often seen in NSIP pattern but it does not exceed more than 20% of area
- Interstitial change (cellular or fibrotic) is more predominant
- Spindle cell carcinoma (sarcomatoid carcinoma):
- Nodule / mass of atypical spindle cells
- Usual interstitial pneumonia (UIP):
- Fibroblastic focus in UIP pattern is another type of myofibroblastic aggregation but usually adjacent to dense fibrotic lesion, unlike in organizing pneumonia
- Dense interstitial fibrosis, architectural destruction and honeycomb change are other clues of UIP
- Interstitial mononuclear infiltrate
- Fibrin deposition
- Fibroblastic focus
- Foamy macrophage accumulation
- Masson body
Comment Here
Reference: Organizing pneumonia
A 70 year old woman presented with cough, chest tightness and dyspnea. She was a former smoker with 20 pack years. High resolution CT scan of the chest showed bilateral patchy ground glass opacities in the lungs. A transbronchial biopsy was performed. What is the pathologic diagnosis based on the image provided?
- Bronchial asthma
- Desquamative interstitial pneumonia
- Diffuse alveolar damage
- Organizing pneumonia
- Respiratory bronchiolitis
Comment Here
Reference: Organizing pneumonia
Clinical features
- See also Skin - nontumor chapter
- Dimorphic fungus found in soil in Central and Southeastern United States and Canada (bordering Great Lakes, St. Lawrence River, Mississippi River and Ohio River basins), Mexico, Africa, India, Middle East
- More common in males
- Due to inhalation of soil containing microfoci of mycelia (Clin Microbiol Rev 2010;23:367)
- Difficult to isolate in clinical microbiology laboratory
- May present as consolidative pneumonia, ARDS or nodules resembling carcinoma; prefers upper lobes
- May also infect skin and bone
- Grossly often resembles tuberculosis
Microscopic (histologic) description
- Mixed acute and granulomatous inflammation caused by large budding yeasts (15 - 10 μm) with broad based buds and refractile walls
- Easily seen with H&E
Microscopic (histologic) images
Images hosted on other servers:
Definition / general
- See also Skin - nontumor chapter
- Normal flora of mouth, GI tract, vagina
- May be commensal or pathogen
- Commonly present in upper airways
- Often present in aspiration pneumonia or pulmonary abscess due to colonization but invasive disease due to candida is rare in lung except in setting of candidal sepsis
- Candida pneumonia associated with malignancy or immunosuppression (West J Med 1979;131:196)
Microscopic (histologic) description
- Pseudohyphae, occasionally true hyphae and budding yeasts
- In some cases, only yeast may be present
Microscopic (histologic) images
Contributed by Yale Rosen, M.D.
Images hosted on other servers:
Positive stains
Clinical features
- Yeast, mostly encapsulated, found in pigeon droppings, that may cause mild infection after inhalation; usually confluent bronchopneumonia with "yeast lakes" of microorganisms and possibly coin lesions but no evident host response (eMedicine: Cryptococcosis [Accessed 22 March 2021])
- May also cause meningitis
- Latent infections can reactivate in immunosuppressed
- CNS disease is a major concern in immunocompromised
- Most commonly an opportunistic infection but disease may occur in immunocompetent patients
- Major virulence factor is capsular polysaccharide glucuronoxylomannin, which hinders phagocytosis by alveolar histiocytes and inflammatory cell recruitment and migration
- Other virulence factors include melanin production (Fontana-Masson stain may be positive; melanin may have antioxidant properties) and enzymes that increase invasiveness
Case reports
- 65 year old woman with arthritis and lung mass (Case of the Week #298)
Microscopic (histologic) description
- Somewhat pleomorphic, round / oval yeast, 4 - 10 microns
- Thick, mucinous capsule stains bright red with mucicarmine; some are unencapsulated
- Narrow necked budding takes place
- Smaller, unencapsulated forms resemble Histoplasma capsulatum
Microscopic (histologic) images
Case #298
Images hosted on other servers:
Definition / general
- Also known as zygomycosis or mucormycosis
- Ubiquitous fungi of class Zygomycetes, includes Mucor, Rhizopus, Absidia and Cunninghamella
- Opportunistic infection especially associated with diabetes; other predisposing factors are neutropenia, corticosteroid therapy, iron overload and mucocutaneous trauma
- Pulmonary and sinusoidal infection caused by inhaled spores or secondary to rhinocerebral mucormycosis
Case reports
- 39 year old man with necrotizing pneumonia (University of Pittsburgh: Case 181 [Accessed 22 March 2021])
Microscopic (histologic) description
- Large, nonsepta hyphae with 90 degree angle branching and nonparallel walls, angioinvasive causing tissue necrosis and hemorrhage
Microscopic (histologic) images
Images hosted on other servers:
Definition / general
- Waterborne protozoal infection that mostly infects intestinal epithelium causing diarrhea or malabsorption
- Often causes self limited illness in immunocompetent patients
- In HIV / AIDS, may spread to hepatobiliary tree or airways
Treatment
- Highly active antiretroviral therapy / HAART, paromomycin and azithromycin may be useful (Int J STD AIDS 2005;16:515)
Microscopic (histologic) description
- Characteristic spores on luminal epithelial cells
- Mucosa with mild lymphocytic infiltrate
Cytology images
Images hosted on other servers:
Clinical features
- Dog heartworm; may infect humans as secondary end stage host, particularly in southern coastal states in US
- Adult worms die in right ventricle, embolize in pulmonary arterial circulation
- Embolization of dead worms may be clinically silent or cause chest pain, fever, chills, hemoptysis or blood eosinophilia
- Evokes necrotizing granulomatous response with vasculitis in lung tissue
- Rarely see dead worms
- Usually self limited in humans but may cause lung infarct
- Usually diagnosed after resection of a nodule to exclude malignancy
- Chest Xray: solitary peripheral pulmonary nodule or coin lesion (Int J Immunopathol Pharmacol 2010;23:345)
Case reports
- 15 year old girl with solitary pulmonary nodule (Arch Pathol Lab Med 2002;126:227)
Microscopic (histologic) description
- Rounded infarct with coagulative necrosis, well demarcated from surrounding normal lung by epithelioid histiocytes and fibrous connective tissue
- Focal calcifications and lymphoid aggregates
- Necrotic nematode has homogenous cuticle without external ridges
- Longitudinal muscle layer just internal to cuticle and internal cuticular ridges
Microscopic (histologic) images
Contributed by Dr. Vladimir Zaitsev
Clinical features
- Also called hydatid cyst
- Humans become infected by eating food contaminated with tapeworm eggs, becoming intermediate hosts
- Eggs from dog tapeworm Echinococcus granulosus or E. multilocularis where foxes are the most common definitive hosts; other species rarely cause hydatid diseae in humans
- For E. granulosus, sheep are most important intermediate hosts; for E. multilocularis, rodents are most important intermediate hosts
- E. granulosus is more common in humans and is most common cestode infection of the lung
- Eggs hatch in duodenum and spread to liver, lung, bone or elsewhere
- E. granulosus cysts are most common in liver, 5 - 15% occur in lung; pulmonary disease is often secondary to hepatic disease (World J Surg 2001;25:46)
- Larvae lodge in capillaries and incite a mononuclear and eosinophilic inflammatory cell response
- Many larvae die, some encyst
- Pulmonary cysts may be asymptomatic or cause respiratory compromise by compressing airways or lung parenchyma; rarely complicated by Aspergilloma (Br J Radiol 2008;81:e279)
- Cyst rupture may cause fatal anaphylactic shock or pneumonia with consequent development of numerous new cysts throughout lung
Case reports
- 52 year old woman with solid nodule resembling malignancy (Cytojournal 2012;9:13)
Microscopic (histologic) description
- Cysts gradually enlarge and years later may be several centimeters in diameter
- Cyst is bilayered and surrounded by fibroblasts, mononuclear cells, eosinophils, multinucleated giant cells
- Daughter cysts usually develop in large mother cyst
- Daughter cysts develop as projections from a germinative layer and form brood capsules
- Degenerating scolices of developing worms produce sediment so called "hydatid sand"
Microscopic (histologic) images
Contributed by Hanni Gulwani, M.B.B.S.
Cytology images
Images hosted on other servers:
Definition / general
- Due to microfilaria of Wuchereria bancrofti or Brugia malayi, which circulate in pulmonary capillaries and cause an immediate type of eosinophilic hypersensitivity reaction
- Patients have high levels of IgE and high titers of filarial antibodies
- Adult worms not seen in lungs
- Restricted to tropical regions
- Tropical eosinophilia may occur from filaria in lymph nodes or spleen (Meyers-Kouwenaar syndrome)
- Symptoms and signs: cough, typically nocturnal, dypsnea, chest tightness, wheezing, fevers, weight loss and eosinophilia
Microscopic (histologic) description
- Rare microfilaria within pulmonary capillaries with marked eosinophilic infiltrate
- Eosinophilic abscesses develop into granulomata
Clinical features
- Freshwater trematode (lung fluke) found in North America that infects crayfish and crabs as intermediate hosts (MMWR Morb Mortal Wkly Rep 2010;59:1573)
- Humans acquire infection by ingesting raw or undercooked infected shellfish; rarely contaminated seaweed or watercress
- Larvae mature in gut and migrate through diaphragm to infect lungs
- Most cases in Asia due to P. westermani; schistosomiasis may also involve the lung
- May mimic lung tumor (Korean J Parasitol 2011;49:69)
- May require serology to confirm diagnosis
Case reports
- 35 year old man with recurrent pneumothorax and cavitary lesion (Am J Surg Pathol 2003;27:1157)
Microscopic (histologic) description
- Necrotizing or non-necrotizing granulomas with giant cells containing eggs with operculum; also organizing pneumonia (Am J Surg Pathol 2011;35:707)
- Variable vasculitis and pleuritis; also lymphocytes, plasma cells, eosinophils
- Egg is birefringent
Cytology images
Images hosted on other servers:
Definition / general
- Associated with AIDS, immunosuppression including therapy and hematologic malignancy
- May be transmitted in utero
- Ubiquitous intracellular coccidian parasite that causes focal parenchymal necrosis, diffuse interstitial pneumonia
- Cats are definitive hosts, humans are intermediate
- Very high prevalence in France; in US, from 3% to 20% depending on geography, ethnic group
- Humans acquire transmission from ingestion of material contaminated with cat feces or cysts contained in undercooked meat (pork, beef, mutton); infection may be acquired in utero
- Most disease in CNS, eye and heart; pulmonary involvement is in 70% of disseminated cases
- Pulmonary involvement is indicative of disseminated disease and risk of death from CNS disease or bronchopneumonia
- May cause severe morbidity or death in affected neonates
Gross description
- Lungs heavily congested, combined weight approximately 2000 grams
Microscopic (histologic) description
- Organisms present in histiocytes, alveolar lining cells, endothelial cells and pseudocytes abundant in necrotic areas
Positive stains
- Chronic exposure to high concentrations of fumes during aluminum arc welding causes severe pneumoconiosis with diffuse pulmonary accumulation of aluminum metal and reduction in lung function (distinct from siderosis or welder's pneumoconiosis)
- Disease also described in manufacturers of aluminum abrasives (Shaver's disease), aluminum smelters and polishers
- Due to heavy exposure to dusts or fumes of beryllium, more common in nuclear and aerospace industries
- Acute disease has disappeared due to exposure standards
- Low dose exposure may cause granulomatous lesions that mimic sarcoidosis
- Chronic berylliosis due to cell mediated immunity
- 2% of those exposed develop disease; delayed hypersensitivity leads to noncaseating granulomas in lungs and hilar nodes, which become progressively fibrotic; no symptoms until late
- Heavy beryllium exposure is linked to lung cancer
- Associated with iron workers and welders
- Welders exposed to fumes with metal oxide particles 0.1 to 1.0 μm in diameter (iron, titanium, manganese and aluminum)
- Lungs usually heavily pigmented without significant fibrosis
- Aluminum (separate topic) has higher risk for significant pulmonary disease
- Concurrent cigarette smoking, asbestos exposure may complicate clinical and pathologic findings
- Micro: dust within interstitium, usually iron predominates
- 2 aluminum welders who died of complications (Hum Pathol 2002;33:819)
- Aluminum: slate gray metallic appearance in scarred areas and peribronchial lymph nodes
- Aluminum: patchy pleural thickening, emphysematous blebs, pneumothorax and considerable fibrous replacement of lung tissue with aluminum containing macrophages; granulomatous disease has been described
- Very rare neuroendocrine tumor in lung
- Usually benign
- Metastases to lung are more common than a lung primary
- Classic "zellballen" / organoid pattern with S100+ sustentacular cells, similar to pheochromocytoma
- Primary pulmonary paraganglioma is extremely rare and requires ancillary studies to differentiate from carcinoid tumor
- Considered malignant if metastasis is demonstrated
- Extra-adrenal pheochromocytoma
- Historical names have included glomus tumor, carotid body-like tumor, chemodectoma (Thorac Cardiovasc Surg 2009;57:375)
- Extremely rare (Thoracic paragangliomas comprise 1 - 2% of all paragangliomas (including pheochromocytomas)
- Middle aged males predominate in sporadic cases, but middle aged females predominate in MEN 2 syndromes and present earlier
- Various organs
- Thoracic paragangliomas mostly in mediastinal compartment but can also be primary intrapulmonary mass
- Rarely may be endobronchial
- Arise from paraganglion cells; neural crest origin
- Intrapulmonary paragangliomas may arise from paraganglia-like structures in interstitium
- Mostly asymptomatic or non-specific symptoms
- Obstructive symptoms if endobronchial
- May show symptoms depending on specific neuropeptide production, if functional (i.e. hypertension from elevated norepinephrine)
- May invade bronchus and metastasize to lymph nodes
- Usually solitary nodules discovered incidentally
- Diagnosis requires histologic examination with ancillary studies
- May show elevated serum levels of specific neuropeptide
- Xray: abnormal lung shadow
- CT: well circumscribed to slightly irregular, solid mass
- PET scan: may show FDG avid mass
- Mostly benign behavior
- If metastases, call "malignant paraganglioma", which may show reduced sustentacular cells and decreased neuropeptide markers
- Features most predictive of malignancy: extra-adrenal location, coarse nodularity of tumor, confluent tumor necrosis, absence of hyaline globules (Hum Pathol 1990;21:1168)
- 37 year old woman with pulmonary paraganglioma manifesting as an endobronchial mass (Korean J Radiol 2008;9:87)
- 38 year old woman with primary paraganglioma of the lung (J Int Med Res 2012;40:1617)
- 69 year old woman with pulmonary metastases in a bilateral carotid body paraganglioma (Interact Cardiovasc Thorac Surg 2004;3:578)
- Middle mediastinal paraganglioma mimicking metastatic neuroendocrine tumor (Ann Thorac Surg 2015;100:702)
- Surgical resection (local excision or lobectomy)
- Solitary or multiple, usually peripheral mass, often microscopic but may be several centimeters
- Round to lobulated, well circumscribed but may show infiltrating border
- Grey, pink, tan to orange color, may show areas of hemorrhage
- Organoid, trabecular and alveolar patterns, variable "zellballen"
- Zellballen pattern (nested islands of chief cells) with inconspicuous sustentacular cells and capillary network at periphery (Am J Surg Pathol 2004;28:825)
- Variable nuclear size, some cells with pleomorphism or hyperchromasia
- Round to oval nuclei, prominent nucleoli, clear to eosinophilic and finely granular cytoplasm
- Nuclear pseudoinclusions, intercellular hyaline globules, spindle cell or oncocytic changes may be seen
- Presence of mitoses and vascular invasion not helpful for distinguishing benign and malignant
- Necrotic foci may be seen
- May show partly infiltrating border of lymphocytes
- Papillary-like clusters of epithelioid cells with round to oval nuclei, evenly dispersed chromatin, micronucleoli, occasional anisonucleosis (Acta Cytol 2001;45:459)
- Abundant cells with round or oval nuclei and marked anisokaryosis with tendency to form acini or follicular structures
- Binucleation and intranuclear cytoplasmic inclusions (Acta Cytol 1988;32:386)
- CD56, synaptophysin, chromogranin, NSE, some neurofilament (chief cells)
- S100 (sustentacular cells)
- Dense core granules with internal, submembranous, eccentric halo emanating in a bubble-like fashion ("norepinephrine-type" granules)
- Mutations in RET gene on chromosome 10
- Carcinoid tumor: cytokeratin+, TTF1+; ribbons, festoons, rosettes
- Metastatic tumors
- Pulmonary gangliocytic paraganglioma: cytokeratin+, 3 cell types (endocrine, ganglion-like, spindle-shaped)
- Major categories of interstitial lung disease
- Fibrosing: UIP, NSIP, COP, lung disease with connective tissue disease, pneumoconiosis, drug reaction, radiation pneumonitis
- Granulomatous: sarcoidosis, hypersensitivity pneumonitis
- Eosinophilic
- Smoking related: DIP, respiratory bronchiolitis-associated interstitial lung disease
- Other: pulmonary alveolar proteinosis
- Source: Kumar et al.: Robbins and Cotran Pathologic Basis of Disease, 8th Edition, 2009
- Intraalveolar reaction: DIP, pulmonary alveolar proteinosis, infection, extrinsic allergic alveolitis, chronic eosinophilic pneumonia
- Small airway disease: bronchiolitis obliterans, respiratory bronchiolitis, mycoplasma infection, viral infection, extrinsic allergic alveolitis, eosinophilic pneumonia
- Large airway disease: allergic bronchopulmonary aspergillosis, bronchocentric granulomatosis, TB, fungi, Granulomatosis with polyangiitis (Wegener's)
- Granulomatous vasculitis: Granulomatosis with polyangiitis (Wegener's), sarcoidosis, Churg-Strauss, bronchocentric granulomatosis, fungi, TB
- Small vessel disease: primary pulmonary hypertension, thromboembolism, polyarteritis nodosa, veno-occlusive disease, Churg-Strauss syndrome
- Hemorrhage: Goodpasture's, SLE, immune complex glomerulonephritis, idiopathic pulmonary hemosiderosis, Granulomatosis with polyangiitis (Wegener's)
- Lymphoid infiltrates: lymphocytic interstitial pneumonia, lymphoma, lymphoid aggregates, extrinsic allergic alveolitis
- Eosinophils: chronic eosinophilic pneumonia, Churg-Strauss syndrome, bronchocentric granulomatosis, Langerhans cell histiocytosis
- Benign/borderline peripheral lung neoplasm derived from perivascular epithelioid cells
- Member of perivascular epithelioid cell tumor (PEComa) or "myomelanocytoma" family, which includes angiomyolipoma, lymphangioleiomyomatosis (LAM)
- Grouped with LAM under PEComatous tumors in 2015 WHO Classification of Lung Tumors (J Thorac Oncol 2015;10:1243)
- Sheets of large cells with clear to eosinophilic granular cytoplasm and PAS+ glycogen granules
- Extremely rare, benign pulmonary tumor derived from perivascular epithelioid cells (PEComa family of tumors)
- Clear to eosinophilic, finely granular cytoplasm containing abundant PAS+ glycogen
- Stains with melanocytic and smooth muscle markers by immunohistochemistry
- First described as clear cell tumor of lung but also known as sugar tumor due to intracytoplasmic glycogen (Yale J Biol Med 1971;43:213)
- Considered a benign PEComa in the lung, as opposed to malignant PEComa
- D14.31 Benign neoplasm of right bronchus and lung
- D14.32 Benign neoplasm of left bronchus and lung
- D14.30 Benign neoplasm of unspecified bronchus and lung
- Extremely rare, case reports and small case series
- Generally older adults >40 years old, may occur in children
- No clear gender predilection
- Generally arises in peripheral lung, rarely in trachea or bronchi
- May rarely arise in patients with tuberous sclerosis along with lymphangioleiomyomatosis (LAM) and micronodular pneumocyte hyperplasia (MMPH) (Am J Surg Pathol 1997;21:1242)
- Mesenchymal perivascular epithelioid cells (PEComa family)
- Generally asymptomatic or nonspecific pulmonary symptoms
- Generally incidental finding on imaging
- Requires tissue diagnosis with immunohistochemistry
- Solitary, homogenous, rounded, circumscribed, peripheral lung mass
- Hyperintense due to vascularity
- May show FDG uptake on PET (Interact Cardiovasc Thorac Surg 2007;6:676)
- Rare case reports of malignant features and visceral metastasis
- Aggressive features may include nuclear pleomorphism, >5 cm size, increased mitoses, necrosis (consider malignant PEComa)
- 38 year old man with clear cell tumor of lung and liver AML (Ann Thorac Cardiovasc Surg 2014;20 Suppl:453)
- 41 year old man with rapidly growing coin lesion (Ann Thorac Surg 2011;91:588)
- 51 year old man with benign sclerosing PEComa (J Pathol Transl Med 2016;50:238)
- 60 year old man with clear cell tumor of lung with CD1a expression (Pathol Int. 2006;56:453)
- 64 year old man presenting with round pulmonary nodule (J Korean Med Sci 2008;23:1121)
- 65 year old woman with clear cell tumor of lung adjacent to visceral pleura (Gen Thorac Cardiovasc Surg 2010;58:243)
- Simple surgical excision
- Small ( Uniform cut surface, though may have foci of necrosis
- Organoid (thick cords and rounded nests with sinusoid-type vascular network) or sheets of epithelioid cells
- Clear to eosinophilic granular cytoplasm, well defined cell borders, numerous PAS+ glycogen granules
- Small, uniform, rounded nuclei with small nucleoli, variably prominent sclerotic vasculature, may have extracellular amorphous eosinophilic material with variable calcification
- Occasionally “spider cells” with nuclear condensation of eosinophilic cytoplasm with extensions to the cell membrane
- May show entrapped small airways, necrosis, sparse lymphocytes
- No fat, no / rare mitoses
- Rarely malignant features (J Clin Oncol 2010;28:e626, Histopathology 2011;58:498)
- Small and large cohesive clusters of bland epithelioid to spindle cells with oval or elongated nuclei, indistinct nucleoli, finely vacuolated cytoplasm, delicate transgressing vessels, background naked nuclei, rare intranuclear pseudoinclusion (Diagn Cytopathol 2008;36:89)
Images hosted on other servers:

(A) Large, irregular, cohesive clusters of columnar and spindle-shaped cells in background of single naked nuclei (Pap)
(B) several large clusters with open cribriform-like spaces (Pap)
(C) spindle-shaped and polygonal cells with round to oval nuclei and vacuolated ill-defined cytoplasm (Pap)
(D) cell block shows neoplastic cells arranged in a nested and insular pattern surrounding sinusoid-like vessels; inset shows sinusoid-like vessel amidst tumor
- HMB45, MART1/MelanA, MITF, SMA, desmin, variable S100
- CD1a (Pathol Int 2008;58:169)
- Hybrid features of pericytes, melanocytes, and neuroendocrine cells (Ultrastruct Pathol 2001;25:479)
- Interdigitating cell processes, primitive cell junctions, intracytoplasmic glycogen (Am J Surg Pathol 1990;14:248)
- TSC2 loss of heterozygosity when arises in patient with tuberous sclerosis
- Primary or metastatic carcinomas with clear cell pattern, e.g. renal cell carcinoma
- Metastatic clear cell sarcoma
- Metastatic melanoma
- Paraganglioma
- Pulmonary adenoma includes bronchial adenoma, alveolar adenoma, papillary adenoma
- Pleomorphic adenoma could be considered a type of bronchial adenoma
- Benign tumor with biphasic growth, resembling counterpart in salivary glands; need to exclude metastasis from salivary glands
- Related entities:
- Alveolar adenoma:
- Benign tumor in asymptomatic patients
- Presents as coin lesion, usually in peripheral lung, consisting of small cystic spaces lined by type II pneumocytes and containing fluid
- Interstitial cellular component consists of epithelioid and spindle shaped cells
- Bronchial gland adenoma:
- Includes oncocytoma and mucus gland adenoma, a rare, solitary, benign, well circumscribed, multicystic, predominately exophytic bronchial tumor
- Carcinoma ex pleomorphic adenoma:
- Malignant cases arising from pleomorphic adenoma (Am J Clin Pathol 2011;136:793)
- Intracapsular carcinoma ex pleomorphic adenoma:
- Malignant component does not breach the capsule of the parent tumor, no metastatic potential
- Papillary adenoma:
- Arises in peripheral lung, composed of type II pneumocytes (club cells), TTF1+
- Rarely has infiltrative features (Virchows Arch 2000;436:289)
- Alveolar adenoma:
- Primary pulmonary pleomorphic adenoma is a very rare benign tumor that tends to arise in the large airways
- Tumors tend to show small, branching, double layered ductules rather than ducts and less cartilaginous stroma as compared to pleomorphic adenomas arising in the salivary gland
- Keratin and vimentin staining of the epithelial component supports diagnosis of primary pulmonary tumor as opposed to only keratin staining in salivary gland tumors (Arch Pathol Lab Med 2003;127:621)
- Prognosis is generally good, but cases of carcinoma ex pleomorphic adenom have been reported
- Pleomorphic adenoma is also known as mixed tumor
- Overlaps with “myoepithelioma”, which could be used for lesions with less cartilaginous and ductal differentiation
- Very rare ( Possibly shows slight F > M
- Usually in trachea and major bronchi, rarely in distal bronchi
- Controversial, possibly from tracheal and bronchial submucosal glands or primitive stem cells
- Frequently asymptomatic but can present with dyspnea, hemoptysis, fever, weight loss or effusion
- Depending on location, may cause obstruction of airway
- Broader differential diagnosis on biopsy specimens but generally straightforward on resection specimen
- Generally indolent; no features to predict rare cases of metastasis
- 8 year old boy with severe respiratory distress and tracheal mass (J Pediatr Surg 2006;41:e23)
- 34 year old woman with dyspnea on exertion and mainstem bronchus mass (Gen Thorac Cardiovasc Surg 2009;57:43)
- 56 year old woman with incidental lesion (Arch Pathol Lab Med 2003;127:621)
- 65 year old man with stridor and mainstem bronchus mass (Ann Thorac Surg 2008;86:1025)
- Complete conservative surgical excision, but may recur many years later
- Endobronchial resection may be an option in some cases (Intern Med 2008;47:1117)
- Bronchial lesions are typically polypoid
- Peripheral lesions are usually attached to bronchi, well circumscribed, no capsule, 1 - 16 cm, gray - white, soft, rubbery with chondroid cut surface, may have tumor tongues outside circumscribed margin
- Generally less cartilaginous stroma than salivary gland counterpart, with small branching ductules rather than ducts
- Nests, tubules, trabeculae
- Mixture of round or oval epithelial cells and myoepithelial cells in chondromyxoid or fibromyxoid stroma with focal hyalinization
- Generally nuclear atypia / necrosis / hemorrhage / mitoses, occasional multinucleated giant cells
- May show myoepitheliomatous, plasmacytoid, squamous features
- Lumina may contain PAS+ eosinophilic secretions
- Fibrillary stroma mixed with bland basaloid epithelial cells
- Primary salivary gland tumors: have ducts with single layer of cells, no PAS+ material in lumens, no S100+ / vimentin+ myoepithelial layer
- In biopsy specimens: hamartoma / chondroma, squamous cell carcinoma (in cases of pleomorphic adenoma with squamous metaplasia), or biphasic malignancies could be considered
- Pleomorphic carcinoma:
- Subtype of sarcomatoid carcinoma; usually aggressive, malignant epithelial neoplasm composed of cells with significant cytologic atypia and nuclear pleomorphism
- Contains at least 10% spindle cells and / or giant cells
- Included under recent WHO classification of "carcinomas with pleomorphic, sarcomatoid or sarcomatous elements"
- Giant cell carcinoma:
- Subtype of sarcomatoid carcinoma consisting of purely giant, pleomorphic tumor cells
- Should not show differentiated non small cell components
- Tumor stains for cytokeratins
- Spindle cell carcinoma:
- Subtype of sarcomatoid carcinoma (WHO)
- < 1% of all primary lung carcinomas
- Giant cell carcinoma:
- Classified as a subtype of sarcomatoid carcinoma that is composed almost entirely of tumor giant cells with no differentiated carcinomatous elements
- Tumor giant cells may or may not stain for human chorionic gonadotrophin
- Metastatic sarcoma or germ cell tumor should be excluded
- Giant cell carcinoma:
- First described and characterized in 1958 (Cancer 1958;11:369)
- Use specific term giant cell carcinoma rather than general term sarcomatoid carcinoma whenever possible to avoid confusion (J Thorac Oncol 2015;10:1243)
- Giant cells can be a component of pleomorphic carcinoma; if tumor shows giant cells along with differentiated non small cell component, classify as pleomorphic carcinoma (Arch Pathol Lab Med 2010;134:1645)
- Large cell carcinoma is a different entity
- Giant cell carcinoma:
- Use code specific for location of tumor
- ICD-10: C34.90 - malignant neoplasm of unspecified part of unspecified bronchus or lung
- Pure giant cell carcinoma is rare, 0.3 - 2% of lung cancers
- Mean age: 65 years, range: 42 - 81 years
- > 90% men, 92% smokers
- Giant cell carcinoma:
- May show predilection for upper lobes
- Giant cell tumors frequently metastasize to small intestine
- Giant cell carcinoma: may have increased incidence of gastrointestinal tract involvement (Cancer 1992;70:606)
- Giant cell carcinoma: appears to be a morphologic phenotype expressed by a heterogeneous group of tumors (Histopathology 1998;32:225)
- Pleomorphic carcinoma:
- < 1% of all carcinomas
- Presumed epithelial origin, although epithelial and sarcomatous components express common markers differently (Am J Surg Pathol 2003;27:1203)
- Classified as carcinomas despite presence of sarcomatoid features (Arch Pathol Lab Med 2010;134:1645)
- Nodal metastases common
- Giant cell carcinoma:
- Cough, chest pain, dyspnea, malaise (varies by location)
- Giant cell carcinoma: cannot be made on small biopsies or cytology; definite diagnosis only on resected tumor
- Giant cell carcinoma:
- Related to stage
- Extent of giant cells or trophoblastic differentiation does not affect prognosis (Histopathology 1998;32:225)
- Pleomorphic carcinoma:
- Stage 1 tumors have same prognosis as other stage 1 non small cell carcinomas; at higher stages, may have worse prognosis than other non small cell carcinomas of similar stage (Am J Surg Pathol 2003;27:311)
- 51 year old man with small intestinal metastases (World J Surg Oncol 2005;3:32)
- 55 year old woman with jejunal intussusception from metastatic giant cell carcinoma of lung (BMJ Case Rep 2016;2016:bcr2016216030)
- 56 year old man with hemoptysis (J Cancer Res Ther 2011;7:363)
- 60 year old woman with pulmonary giant cell carcinoma associated with pseudomyxoma peritonei (J Bronchology Interv Pulmonol 2012;19:50)
- 66 year old man with giant cell lung carcinoma and HIV (Med Oncol 2009;26:167)
- Giant cell carcinoma: not usually surgical since metastatic at diagnosis but resection and radiation may prolong survival
- Pleomorphic carcinoma:
- 2 - 17 cm, necrosis and hemorrhage common
- Giant cell carcinoma:
- Solid, well demarcated, tan, peripheral mass with areas of necrosis and hemorrhage
- Pleomorphic carcinoma:
- Non small cell lung carcinoma with at least 10% neoplastic spindle or giant cells, usually with epithelial cells
- Epithelial component 10 - 85%, usually adenocarcinoma or large cell carcinoma, also squamous cell carcinoma (Am J Surg Pathol 2008;32:1727)
- Usually poorly differentiated
- Spindle cells resemble MPNST, MFH or fibrosarcoma
- Giant cells usually bizarre with multilobulated nuclei, abundant eosinophilic cytoplasm accompanied by heavy neutrophilic infiltrate with occasional ingested white blood cells
- Stroma often myxoid, frequent inflammatory infiltrate, collagen fibers
- Numerous mitotic figures
- Massive necrosis common
- Vascular invasion in 58%
- Giant cell carcinoma:
- Dyscohesive, polygonal, mono and multinucleated giant cells with abundant cytoplasm and prominent nucleoli
- Neoplastic, highly pleomorphic giant cells, often in inflammatory stroma with emperipolesis (Arch Pathol Lab Med 2010;134:1645)
- Giant cells are multinucleated, may resemble syncytiotrophoblasts and produce human chorionic gonadotropin but are usually fewer than in primary choriocarcinoma of lung (Histopathology 2000;36:17)
- 2 types of giant cells: βHCG positive syncytiotrophoblast-like giant cells with smudged nuclei and coarse chromatin with nuclear molding and βHCG negative giant cells with admixed neutrophils and cell in cell features (Histopathology 2016;68:680)
- Spindle cell carcinoma:
- Carcinoma composed exclusively of spindle shaped tumor cells
- Tumor cells often obliterate vessels
- Giant cell carcinoma:
- Pleomorphic cells in flat loose clusters, with abundant, thick, well demarcated cytoplasm, multinucleation (Acta Cytol 2011;55:173)
- Sharp clear nuclear membranes, acidophilic cytoplasm with finely granular or foamy appearance, irregular coarse chromatin, bizarre mitoses, neutrophil engulfment (Diagn Cytopathol 2007;35:555)
- Pleomorphic carcinoma:
- Giant cell carcinoma:
- Calretinin (67%)
- Pancytokeratin, TTF1 variable
- Pleomorphic carcinoma: CK20
- Giant cell carcinoma: chromogranin, synaptophysin, CD68, desmin
- Spindle cell carcinoma: surfactant apoprotein A
- Metastatic germ cell tumor (e.g., choriocarcinoma)
- Other subtypes of sarcomatoid carcinoma
- True sarcomas, such as undifferentiated pleomorphic sarcoma
- Adenocarcinoma
- Adenosquamous carcinoma
- Large cell carcinoma
- Squamous cell carcinoma
- None of the above
Comment Here
Reference: Pleomorphic carcinoma
- Pleuropulmonary blastoma (PPB) is a rare malignant tumor of mesenchymal origin that arises in the lungs, pleura or mediastinum of children (J Clin Med 2023;12:1918)
- International registry was established in 1987 (The International Pleuropulmonary Blastoma / DICER1 Registry [Accessed 4 June 2024])
- There are 4 morphologic subtypes of PPB: I, IR, II and III
- Type I: cystic tumor lined by benign nonneoplastic epithelial cells with a varying amount of malignant mesenchymal cells in the wall (no solid component) (Cancer 2023;129:600)
- Type IR (R stands for regressed or regressing): similar to the cystic type I tumor but the population of malignant mesenchymal cells is not found; only benign nonneoplastic epithelium forming cysts with some immature mesenchyme in the wall (Cancer 2023;129:600)
- Type II: combination of multicystic tumor and solid sarcomatous tumor (Children (Basel) 2019;6:86)
- Type III: entirely solid sarcomatous tumor without cystic foci; can be necrotic or calcified (Children (Basel) 2019;6:86)
- Older terms not currently used (StatPearls: Pleuropulmonary Blastoma [Accessed 4 June 2024])
- Pediatric pulmonary blastoma
- Pneumoblastoma
- Pulmonary rhabdomyosarcoma
- Rhabdomyosarcoma in lung cyst
- ICD-10
- C34.1 - malignant neoplasm of upper lobe, bronchus or lung
- C34.2 - malignant neoplasm of middle lobe, bronchus or lung
- C34.3 - malignant neoplasm of lower lobe, bronchus or lung
- C34.8 - malignant neoplasm of overlapping sites of bronchus and lung
- C34.9 - malignant neoplasm of unspecified part of bronchus or lung
- ICD-11: 2C25.Y & XH2FY9 - other specified malignant neoplasms of bronchus or lung & pleuropulmonary blastoma
- Primarily occurs in children under 4; median age of diagnosis differs with morphologic classification
- Type I: median 7 months (Cancer 2023;129:600)
- Type IR: median 31.2 months (Cancer 2023;129:600)
- Type II: median 35 months (Children (Basel) 2019;6:86)
- Type III: median 41 months (Children (Basel) 2019;6:86)
- Primarily arises from peripheral lung and pleura
- Metastasis is more common in type II and III PPB (Children (Basel) 2019;6:86)
- Common site for metastasis: brain (most common), liver, bone, lymph nodes, kidney, pancreas and adrenal glands (Children (Basel) 2019;6:86)
- Proliferation of malignant mesenchymal cells with nonneoplastic epithelial components (Clin Cancer Res 2018;24:2251)
- Evidence shows that PPB type I can progress to type II and then to type III but does not have to (Clin Cancer Res 2018;24:2251, Cancer 2015;121:276)
- Germline loss of function mutations of DICER1 have been found in familial PPB and somatic mutations have been identified in others (Mod Pathol 2022;35:4)
- DICER1 is involved in microRNA production, which helps regulate gene expression
- With a DICER1 mutation, the dicer protein is unable to help with microRNA production, leading to abnormal gene expression (Mod Pathol 2022;35:4)
- Currently estimated that 70% of patients with PPB have a DICER1 mutation (Mod Pathol 2022;35:4)
- Often nonspecific cough, chest pain, dyspnea or abdominal pain (J Clin Med 2023;12:1918)
- Can present with pneumothorax or pleural effusion (J Clin Med 2023;12:1918)
- In individuals with DICER1 mutations, can see features such as macrocephaly, renal structural anomalies, retinal abnormalities, dental abnormalities and the GLOW syndrome (global developmental delay, lung cysts, overgrowth and Wilms tumor) (Mod Pathol 2022;35:4)
- DICER1 mutations have been associated with several extrapulmonary neoplasms, such as Sertoli-Leydig cell tumor of the ovary, Wilms tumor, cystic nephroma, renal sarcoma, nasal chondromesenchymal hamartoma, nodular hyperplasia and carcinoma of the thyroid gland, pituitary blastoma, pineoblastoma and others (Clin Cancer Res 2018;24:2251)
- Chest radiograph, CT or MRI can aid in diagnosis (Children (Basel) 2019;6:86)
- Histological analysis via biopsy or resection is gold standard for diagnosis
- Radiograph: unilateral whiteout of lung with mediastinal shift away from whiteout (Radiopaedia: Pleuropulmonary Blastoma [Accessed 4 June 2024])
- CT scan (Children (Basel) 2019;6:86, Radiopaedia: Pleuropulmonary Blastoma [Accessed 4 June 2024])
- Type I: unilateral cystic to multicystic lesion in the thorax
- Type II: unilateral mass consisting of cystic (often air filled; can be fluid filled) components as well as solid foci
- Type III: unilateral solid mass with homogeneous or heterogeneous enhancement
- 5 year overall survival varies based on type
- Type I: 98% (Cancer 2023;129:600)
- Type IR: 100% (Cancer 2023;129:600)
- Type II: 71% (Cancer 2015;121:276)
- Type III: 53% (Cancer 2015;121:276)
- 2 year old with chest pain, difficulty breathing and low grade fever for past 2 months; 4 year old boy with difficulty in breathing and on and off fever for past 1 month; and 5 year old girl with difficulty breathing and cough for 3 months (Radiol Case Rep 2021;16:2862)
- 3 year old girl with nonimproving respiratory tract infections (Int J Surg Case Rep 2023;106:108261)
- 13 year old girl with nonproductive cough for 1 month (J Pediatr Surg Case Rep 2020;59:101482)
- Type I: surgical resection; radiation is not used (Children (Basel) 2019;6:86)
- Adjuvant therapy is not typically utilized unless there is local invasion, tumor spill during operation or positive margins (Children (Basel) 2019;6:86)
- Type IR: surgical resection; radiation is not used (Children (Basel) 2019;6:86)
- Types II and III: surgical resection if possible and adjuvant chemotherapy (Children (Basel) 2019;6:86)
- Neoadjuvant therapy may be utilized if surgical resection is not possible or puts the patient at an unreasonable level of risk (Children (Basel) 2019;6:86)
- Radiation can be used if needed (Cancer 2015;121:276)
- Type I: composed of thin walled, cystic structures
- Type II: composed of thin walled, cystic structures in addition to grossly visible solid foci in the cystic lesion (Mod Pathol 2022;35:4)
- Type III: composed of solid, noncystic tissue and may have areas of necrosis or calcification (Children (Basel) 2019;6:86)
- Type I: thin walled cysts lined by benign respiratory epithelium with small malignant mesenchymal cells in the walls of the cysts (Cancer 2023;129:600)
- These primitive cells may have rhabdomyosarcomatous differentiation
- Type IR: thin walled cysts lined by benign respiratory epithelium without the malignant cell population mentioned above (Cancer 2023;129:600)
- Type II: areas of thin walled cysts lined by respiratory epithelium with areas of solid sheets of malignant mesenchymal cells that can appear as a spindled sarcoma, embryonal rhabdomyosarcoma or have no apparent differentiation (Children (Basel) 2019;6:86)
- Type III: heterogeneous solid tumor that can contain several different patterns (Children (Basel) 2019;6:86, Cancer 2015;121:276)
- Blastema-like area with hyperchromatic nuclei, high N:C ratio and mitotic bodies
- Larger malignant sarcoma cells in myxoid background
- Can have rhabdomyosarcomatoid, chrondrosarcomatoid or liposarcomatoid features (Cancer 1988;62:1516)
- Foci of anaplastic cells with pleomorphic nuclei, mitotic bodies and hyaline inclusions
- Some microscopic areas of benign nonneoplastic respiratory epithelium
Contributed by Aliya N. Husain, M.D.
- Small ovoid cells with granular chromatin, inconspicuous nucleoli and scant eosinophilic cytoplasm with poorly defined cellular borders (Diagn Cytopathol 1997;16:336, Lung India 2015;32:281)
- Sheets of oval to spindle shaped cells with poor differentiation (Lung India 2015;32:281)
- Tumor cells with granular chromatin and a high N:C ratio (Lung India 2015;32:281)
- Oval to spindle shaped cells that can have perivascular arrangement (Lung India 2015;32:281)
- Vimentin (stains all differentiations), MSA (weak), CD56 (Mod Pathol 2022;35:4, Indian J Pathol Microbiol 2023;66:632, The International Pleuropulmonary Blastoma / DICER1 Registry [Accessed 4 June 2024])
- Depending on type of differentiation
- Rhabdomyosarcomatoid: desmin, myogenin, SMA (Indian J Pathol Microbiol 2023;66:632)
- Chondromatoid: S100 (Indian J Pathol Microbiol 2023;66:632)
- Cytokeratin, EMA: negative in malignant areas but positive in benign nonneoplastic epithelial regions (Indian J Pathol Microbiol 2023;66:632)
- NSE (can be weakly positive on rare occasions) (Indian J Pathol Microbiol 2023;66:632, The International Pleuropulmonary Blastoma / DICER1 Registry [Accessed 4 June 2024])
- Patients with PPB should undergo testing for DICER1 mutation
- Right lung, lobectomy:
- Pleuropulmonary blastoma, type IR (see comment)
- Comment: The tumor is composed of a multicystic lesion with no solid component. It is lined by benign nonneoplastic epithelium and focally has small areas of immature mesenchymal cells in the wall of the cysts.
- Embryonal rhabdomyosarcoma (Lung India 2015;32:281):
- Composed only of rhabdomyoblastic mesenchyme without chondroid differentiation
- Synovial sarcoma (Radiol Case Rep 2015;2:82):
- Metastasis of synovial sarcoma to the lung is much more common than a primary lung synovial sarcoma so history of synovial sarcoma elsewhere would favor this diagnosis
- Histologically divided into monophasic and biphasic
- Monophasic: composed entirely of spindle cells
- Biphasic: composed of spindle and epithelial cells
- Primary sarcoma:
- Lacks undifferentiated blastemic cells
- Pulmonary blastoma:
- In addition to the malignant mesenchyme, the epithelial lining is also malignant
- Seen in adults
- Metastatic Wilms tumor:
- Clinical history of primary Wilms tumor should be present
- Has fibroblastoid stroma with some epithelial components
- WT1 positive
- Fetal lung interstitial tumor (Children (Basel) 2023;10:828):
- Congenital pulmonary airway malformation (CPAM) (for types IR and I) (Children (Basel) 2019;6:86):
- PPB more likely if the patient has a family history of PPB (Cancer 2015;121:276)
- Prenatal detection is more common in CPAM (J Pediatr Surg 2016;51:33)
- Can contain clusters of mucinous cells (Mod Pathol 2022;35:1870)
- Negative for desmin or myogenin due to lack of malignant rhabdomyoblasts
- Can metastasize to the brain
- Composed of both solid and cystic foci
- Contains a population of malignant mesenchymal cells in addition to benign nonneoplastic epithelium
- Does not contain any malignant mesenchymal cells
- Often progresses to type III PPB
Comment Here
Reference: Pleuropulmonary blastoma
A 2 year old patient with no past medical history presented to the clinic with a cough that persisted for 1 month. On CT scan, a solid tumor occupying the lung was seen. After resection, the tumor was sent to pathology where the diagnosis of PPB type III was made. It was noted that the tumor had rhabdomyosarcomatoid differentiation and no chondromatoid differentiation. A picture of the tumor with an immunostain is shown above. Which staining pattern would you expect to see in this tumor?
- Positive desmin and S100, negative vimentin
- Positive MSA and S100, negative SMA
- Positive SMA and desmin, negative vimentin
- Positive vimentin and desmin, negative S100
- Positive vimentin and S100, negative desmin
Comment Here
Reference: Pleuropulmonary blastoma
- Historical term based on lesions induced by congenital heart disease
- Heath and Edwards Classification from 1958 (modified below) still in widespread use
- Open lung biopsy in patients with congenital heart disease may be performed to determine if corrective vascular surgery will be beneficial
- Muscularization and media hypertrophy (> 7% of lumen) of pulmonary arteries
Grade II:
- Intimal hyperplasia causing attenuation of vascular lumen
Grade III:
- Subintimal fibrosis with onion ring appearance
- Marked reduplication of internal elastic membrane
- Arteries and arterioles resemble pipes
Grade IV to V:
- Dilation and plexiform lesions, aneurysmal dilation of small pulmonary arteries, plexiform and glomeruloid nodules
- Fibrin thrombi within plexiform lesion, old / new hemorrhage present
Grade VI:
- Uncommon, acute necrotizing arteritis with fibrinoid necrosis and acute inflammation of vessel wall, similar to polyarteritis nodosa
- Associated with extreme pulmonary hypertension
- Secondary pulmonary hypertension: similar histology, different history
- Pneumocystis pneumonia (PCP) is a serious infection caused by the fungus Pneumocystis jirovecii in immunocompromised patients
- One of the most common AIDS defining diseases in HIV infected patients
- Substantial mortality and morbidity
- Direct microscopic examination of bronchoalveolar lavage, sputum and lung biopsy are the gold standard methods of diagnosis
- Cup shaped organisms with a central dot-like density
- Pneumocystis jirovecii pneumonia (PJP)
- Formerly known as Pneumocystis carinii
- ICD-10: B59 - pneumocystosis
- Incidence of Pneumocystis pneumonia has declined substantially with widespread use of Pneumocystis pneumonia prophylaxis and antiretroviral therapy
- Recent incidence among patients with AIDS in Western Europe and the United States is < 1 case per 100 person years
- Commonly seen in HIV and immunocompromised patients (hematologic malignancies followed by autoimmune diseases) (Int J Infect Dis 2022;121:172)
- Lung and rarely extrapulmonary sites, which include lymph nodes, spleen, liver, bone marrow, adrenal glands, gastrointestinal tract, kidneys, thyroid gland, heart, pancreas, eyes, ears, lumina of blood vessels, perivascular involvement and lymphatic invasion (Arch Intern Med 1991;151:1205)
- Lung injury during infection is mostly due to host inflammatory response mediated by CD4+ T cells, alveolar macrophages, neutrophils and the soluble mediators
- Inflammatory response is primarily responsible for the damage of the alveolar capillary interface activity (N Engl J Med 2004;350:2487)
- Immunocompromised conditions (e.g., cancer, HIV, transplant recipients on immunosuppressant therapies) (N Engl J Med 2004;350:2487)
- Symptoms include fever, nonproductive cough, difficulty breathing, chest pain, fatigue and chills (Respiration 2018;96:52)
- These symptoms develop over several days to weeks
- Sputum, bronchoalveolar lavage or lung biopsy
- Direct microscopic examination, polymerase chain reaction (PCR, highly sensitive but less specific), blood test to detect beta D glucan (Med Mycol 2020;58:1015)
- In direct microscopy, Grocott-Gomori methenamine silver (GMS) stain should be performed on tissue biopsy and lavage specimens; immunofluorescence may be performed
- Papanicolaou (Pap) and Romanowsky (Giemsa, Diff-Quik) barely stain the cyst wall of the organisms and infection can easily be missed
- Hypoxemia is the most characteristic laboratory abnormality
- Elevation of lactate dehydrogenase levels to > 500 mg/dL is common but also nonspecific
- Chest radiograph typically demonstrates diffuse, bilateral, symmetrical ground glass interstitial infiltrates emanating from the hila in a butterfly pattern (AIDS 1998;12:885)
- In early disease, a chest radiograph may be normal
- Atypical radiographic presentations also occur, e.g., nodules, blebs / cysts, asymmetric disease, upper lobe localization, intrathoracic adenopathy and pneumothorax
- Spontaneous pneumothorax in a patient with HIV infection should raise the suspicion of PCP
- Cavitation and pleural effusion are uncommon in the absence of other pulmonary pathogens or malignancy and their presence may indicate an alternative diagnosis or an additional pathology such as tuberculosis (TB), Kaposi sarcoma or bacterial pneumonia
- Treatment changes course of disease
- 45 year old woman presented with dyspnea on exertion and significant weight loss within the preceding 4 months (BMC Infect Dis 2023;23:185)
- 50 year old man presented with hypoxia, 1 week history of pleuritic chest pain and fever (Turk Patoloji Derg 2020;1:246)
- 59 year old man presented with Pneumocystis jirovecii associated pneumonia and hypercalcemia due to ectopic production of 1,25 dihydroxyvitamin D, 6 years after renal transplantation (Acta Clin Belg 2021;76:75)
- Trimethoprim and sulfamethoxazole
- Lungs are heavy, firm and gray-brown
- There is fine porosity due to trapped pockets of air
- There may be small yellow indurated areas in the lung parenchyma and occasional emphysematous subpleural blebs (Can Med Assoc J 1969;100:846)
- Lung nodules with or without cavitation have been demonstrated in response to granulomatous inflammation (Thorax 2002;57:435)
- Touch preparations with Giemsa stain of fresh frozen lung infected with Pneumocystis is preferred over histologic sections as morphologic features are more apparent in the former (Can Med Assoc J 1969;100:846)
- Alveolar spaces filled with pink, foamy amorphous material composed of proliferating fungi and cell debris
- Pneumocystis organisms can be identified in the GMS (Grocott-Gomori methenamine silver) stained tissue sections within airspaces
- They are thin walled, oval, round and crescentic forms about the size of red blood cells (7 microns) (Can Med Assoc J 1969;100:846)
- Granulomas, although rare, are mostly necrotizing and multiple
- More than 1 infection, such as coexisting cytomegalovirus infection, may be present in these patients so it is important to look for other infectious organisms
- Characteristic morphological finding is round to oval and cup shaped dark black (GMS stain) cysts with central dot-like density
- Direct immunofluorescence testing on sputum and bronchoalveolar lavage specimens
- Periodic acid-Schiff stain
- Trophic forms are 1 - 4 microns and have simple plasma membrane with filopodial projections (Clin Chest Med 2009;30:265)
- Cyst forms are 8 - 10 microns with rigid cell walls and up to 8 intracystic bodies (Clin Chest Med 2009;30:265)
- Polymerase chain reaction is sensitive and rapid in detecting the presence of Pneumocystis jirovecii in bronchoalveolar lavage specimens (J Mycol Med 2022;32:101241)
- Lung, transbronchial biopsy:
- Organisms consistent with Pneumocystis jirovecii infection (see comment)
- Comment: Grocott-Gomori methenamine silver (fungal) stain is positive for organisms morphologically consistent with Pneumocystis jirovecii (control is appropriate).
- Pneumocystis jirovecii lack budding and have a central dark dot-like density that is not seen in the following organisms: Candida, Histoplasma and Cryptococcus
- Alveolar proteinosis:
- Anti-GBM disease:
- Necrotizing, hemorrhagic, interstitial pneumonitis; associated with rapidly proliferative glomerulonephritis, linear immunoglobulin deposits on basement membranes of alveolar septal walls
- Also, intra-alveolar hemorrhage, septal thickening and hypertrophy, organization of blood in alveolar spaces
- Organizing pneumonia:
- Bronchiolar and alveolar plugs of loose fibrous tissue (Masson bodies)
Comment Here
Reference: Pneumocystis
A 60 year old woman with dry cough, fever and shortness of breath revealed bilateral pulmonary nodules on imaging. Biopsy revealed features as shown in the figure above. What is the diagnosis?
- Blastomyces and respiratory syncytial virus (RSV)
- Cryptococcus neoformans and herpes virus
- Histoplasma capsulatum and adenovirus
- Pneumocystis pneumonia and cytomegalovirus (CMV)
Comment Here
Reference: Pneumocystis
-
Pulmonary preneoplastic changes include (Respir Res 2002;3:20):
- Bronchial squamous dysplasia and in situ carcinoma preceding invasive squamous cell carcinoma and basaloid carcinoma
- Atypical adenomatous hyperplasia preceding bronchioloalveolar carcinoma
- Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia, a proposed precursor for carcinoid tumor
- Squamous dysplasia / CIS is a multifocal and clonal condition strongly associated with cigarette smoking i.e. “field cancerization”
- High grade squamous dysplasia / CIS is associated with an increased risk of invasive squamous cell carcinoma
- Squamous dysplasia / CIS tends to arise in large central airways
- “Dysplasia” usually used for squamous bronchial lesions
- Angiogenic squamous dysplasia = capillary blood vessels closely juxtaposed to and projecting into metaplastic or dysplastic squamous bronchial epithelium (Clin Cancer Res 2000;6:1616)
- D02.20: Carcinoma in situ of unspecified bronchus and lung
- D02.21: Carcinoma in situ of right bronchus and lung
- D02.22: Carcinoma in situ of left bronchus and lung
- Males appear to have higher prevalence of squamous dysplasia than females (J Natl Cancer Inst 1999;91:691)
- Squamous dysplasia / CIS with propensity for large central airways, usually around bifurcations, less commonly in trachea
- May precede mass by many years
- Pre invasive lesions and subsequent cancers are clonally related (J Pathol 2011;224:153)
- Evidence for stepwise progression relatively weak, but concept of field carcinogenesis is strongly supported (Cancer Metastasis Rev 2010;29:5)
- Associated with smoking
- Possible progression from basal cells or metaplastic goblet cells to squamous metaplasia, dysplasia, CIS
- Usually not symptomatic on its own
- Image enhanced endoscopy i.e. autofluorescence bronchoscopy (AFB), high magnification bronchovideoscopy (HMS), narrow band imaging (NBI), endobronchial ultrasonography (EBUS), optical coherence tomography (OCT) (Clin Chest Med 2013;34:373)
- Frequently encountered in resection specimens, but not often on endoscopic biopsy specimens
- Some preneoplastic lesions regress, while others progress
- No difference in progression rate and time to progression based on initial histologic grading; cannot differentiate the potentially more malignant lesions (Clin Cancer Res 2005;11:537)
- Persistence of dysplasia associated with development of invasive carcinoma (Cancer Prev Res 2016;9:96)
- Squamous dysplasia with high telomerase activity, increased Ki67 and p53 positivity tend to persist and might progress to carcinoma (Lung Cancer 2004;46:187)
- CIS is strong predictor of progression to invasive squamous cell carcinoma (Cancer Metastasis Rev 2010;29:5)
- Three men ages 63, 65 and 71 years old with dysplastic lesions in bronchi which progressed to squamous cell carcinoma (Br J Cancer 1997;75:678)
- Bronchoscopic followup of severe dysplasia and CIS, endobronchial or surgical techniques (Chest 2007;132:221S)
- Either unremarkable mucosa or papillary and granular with loss of folds
- Histological patterns of bronchial epithelial dysplasia: basal cell dysplasia, columnar cell dysplasia, bronchial epithelial dysplasia with transitional differentiation and squamous dysplasia (Mod Pathol 2006;19:429)
- Squamous dysplasia: focal to full thickness replacement of epithelium by squamous cells with increased nuclear to cytoplasmic ratio, nuclear pleomorphism, mitotic activity but intact basement membrane
- No invasive growth although may extend into ducts of submucosal glands
- Graded with a 4 tier (mild / moderate / severe / CIS) or 2 tier system (low grade / high grade) (J Clin Pathol 2001;54:257)
- Mild dysplasia: minimal abnormalities with basal expansion, increased cellularity, vertically oriented nuclei, limited to bottom third of epithelium, mitoses absent or rare, maturation present
- Moderate dysplasia: more abnormalities, partial maturation, extending to lower two thirds of epithelium, mitoses limited to lower two thirds
- Severe dysplasia: cellular pleomorphism, coarse chromatin, frequent nucleoli, basal zone to upper third, mitoses confined to lower two thirds, superficial cell flattening
- CIS: lack of maturation, significant cytologic abnormalities, coarse chromatin, inconsistent nuclear orientation, mitoses present in full thickness
- Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH): preinvasive proliferation of pulmonary neuroendocrine cells
- Proposed criteria for diagnosis on lung resection is multifocal neuroendocrine cell hyperplasia as defined by 5 or more pulmonary neuroendocrine cells in at least 3 separate small airways combined with 3 or more carcinoid tumorlets (Semin Diagn Pathol 2015;32:438, Lung 2015;193:659)
- Some cases of bronchial dysplasia show patchy or scattered staining for p53 and Ki67 (Mod Pathol 2006;19:429)
- Ki67 index significantly higher in severe dysplasia than in mild / moderate dysplasia (Pol J Pathol 2015;66:38)
- Sequential changes in lung cancer pathogenesis include LOH, microsatellite alterations, telomerase dysregulation (Clin Cancer Res 2001;7:5, Histopathology 2009;54:43)
- Discordant genetics changes can exist in the same carcinogen exposed bronchial tissues (Clin Cancer Res 2001;7:259)
- Squamous metaplasia and reactive / reparative atypia
- Basal cell hyperplasia
- Squamous papilloma
- Concise Review: Preinvasive Lesions of the Bronchus (J Thorac Oncol 2009;4:545)
- Low grade tumor
- Typically in (or close to) large airways
- Lobulated tumor with spindle and stellate cells arranged in lace-like strands and cords within prominent myxoid stroma
- Endobronchial nodular mass with reticular / lace-like growth pattern and abundant myxoid stroma
- Expresses EMA and vimentin, negative for most other markers
- FISH positive for EWSR1 rearrangement (85%)
- Primary pulmonary myxoid sarcoma
- Mean age = 46.3 years; F:M = 1.4:1 (24 cases)
- 40% with cough, hemoptysis, chest pain; 20% present as incidental lung mass (Am J Surg Pathol 2011;35:1722)
- Bilateral lungs, 76% within or close to a large bronchus (Int J Surg Pathol 2017;25:518)
- Probably originates from primitive mesenchymal cells with myofibroblastic or fibroblastic differentiation (Virchows Arch 2014;465:453)
- Controversial relationship to myxoid angiomatoid fibrous histiocytoma with similar EWSR1 fusion genes (Histopathology 2014;65:144)
- Primary pulmonary myxoid sarcoma (PPMS) and myxoid variant of angiomatoid fibrous histiocytoma may represent a continuum with overlapping histologic, immunohistochemical and genetic features (Histopathology 2014;65:144, Am J Surg Pathol 2020;44:1535)
- Smoking history in 80% (Am J Surg Pathol 2011;35:1722)
- Relies on histology, immunohistochemistry and FISH in biopsy or surgical resection
- Mass related to bronchus, predominantly endobronchial
- Patients with EWSR1 rearrangement have favorable prognosis; wild type EWSR1 portends poor clinical outcome (Pol J Pathol 2017;68:261)
- 28 year old men and 66 year old woman with features overlapping with angiomatoid fibrous histiocytoma (Histopathology 2014;65:144)
- 29 year old woman with mass in a major fissure of the left lung without parenchymal invasion (Thorac Cancer 2017;8:535)
- 32 year old woman with tumor adjacent to the right main bronchus (Pathology 2017;49:792)
- 44 and 49 year old men with both components of PPMS and angiomatoid fibrous histiocytoma (Am J Surg Pathol 2020;44:1535)
- 48 year old man with a huge mass extending into the right main bronchus (Pol J Pathol 2017;68:261)
- 80 year old woman with an endobronchial mass in the left main bronchus (Int J Surg Pathol 2017;25:518)
- Surgical resection (Am J Surg Pathol 2011;35:1722)
- Generally < 4 cm, well circumscribed or nodular
- Glistening or gelatinous cut surface, white-gray to yellow (Am J Surg Pathol 2011;35:1722)
- Lobulated architecture, reticular or lace-like pattern with anastomosing cords and strands, abundant myxoid stroma, often lightly basophilic (Am J Surg Pathol 2011;35:1722)
- Oval, spindle to polygonal cells with minimal to moderate atypia, infrequent mitotic figures with the majority < 5/10 high power fields
- Admixed lymphoplasmacytic infiltrate
- Some cells are chondrocyte-like or mimicking physaliferous cells in chordoma (Diagn Pathol 2020;15:15)
- Vimentin, EMA, CD99 (weak focal) (Pol J Pathol 2017;68:261)
- Stroma is positive for Alcian blue stain, which is sensitive to hyaluronidase treatment (Am J Surg Pathol 2011;35:1722)
- S100, cytokeratin, p63, CD34, CD31, SMA, MSA, desmin (rarely positive), TTF1, calretinin
- Focal dense plaques present in the plasma membrane, external lamina and intermediate junctions are rarely observed (Virchows Arch 2014;465:453)
- ~85% of tumors showed t(2;22)(q33;q12) with EWSR1::CREB1 fusion gene detected by FISH or PCR (Int J Surg Pathol 2017;25:518)
- First report of a case with EWSR1::ATF1 fusion gene (Am J Surg Pathol 2020;44:1535)
- Second case (Int J Surg Pathol 2022 Apr 24 [Epub ahead of print])
- Lung, right lower lobe, lobectomy:
- Primary pulmonary myxoid sarcoma (see comment)
- Comment: H&E sections demonstrate a well circumscribed endobronchial tumor composed of lobules of spindled and stellate cells arranged in a reticular pattern within a myxoid background. A chronic inflammatory infiltrate is seen throughout the tumor. Immunohistochemically, the tumor cells are positive for EMA and negative for AE1 / AE3, CAM 5.2, pancytokeratin, p40, desmin, SMA, CD34, TTF1, KIT, vimentin, CD1a and S100. A FISH test for EWSR1 was positive for rearrangement in the tumor cells. The morphology in combination with the FISH test result confirm the above diagnosis.
- Extraskeletal myxoid chondrosarcoma:
- History of soft tissue primary, rarely arising intrathoracic as a primary
- S100+
- FISH positive for EWSR1::NR4A3 fusion or others
- Myxoid angiomatoid fibrous histiocytoma:
- Peripheral lymphoid cuff
- Whorled or storiform growth patterns common
- 50% desmin+
- FISH positive for EWSR1::ATF1 (more common), EWSR1::CREB1 and FUS::ATF1
- Inflammatory myofibroblastic tumor:
- Myoepithelioma:
- Clear and plasmacytoid cells
- Positive for myoepithelial markers (cytokeratins, p63, S100, calponin and SMA)
Comment Here
Reference: Primary pulmonary myxoid sarcoma with EWSR1::CREB1 fusion
- Epithelioid hemangioendothelioma
- Extraskeletal myxoid chondrosarcoma
- Inflammatory myofibroblastic tumor
- Myoepithelioma
- Myxoid angiomatoid fibrous histiocytoma
Comment Here
Reference: Primary pulmonary myxoid sarcoma with EWSR1::CREB1 fusion
- Aerobic, mobile, flagellated Gram negative bacillus that survives in water, soil and vegetation
- Worldwide distribution (eMedicine)
- Resistant to many disinfectants, common in hospital environment, common cause of hospital acquired infections
- Commonly colonizes humans, but rarely causes disease in healthy subjects
- Affects primarily infants, cystic fibrosis, immunocompromise, critically ill, neutropenia and burns / on ventilators
- Immunocompromised usually have paucicellular pattern, rapidly progressive course with bronchopneumonia and bacteremia
- Immunocompetent have a cellular pneumonia, more protracted course
- Perivascular bacterial infiltration is somewhat specific for pseudomonas
Infants:
- Rare: 0.3% of neonatal ICU admissions
- Usually low birth weight (1.2% of low birth weight admissions)
- Mortality 32% - 87% with death within 1 - 2 days
- Diagnosis made by culture
- 49 year old woman with fatal pneumonia likely associated with contaminated hot tub (Infection 2011;39:265)
- Necrotizing pneumonia with 2 patterns: paucicellular coagulative confluent bronchopneumonia with perivascular bacillary infiltration (bacteremic) or cellular pneumonia without evidence of perivascular organisms (nonbactermic)
- Nonbacteremic: often occurs in debilitated patients with chronic lung or heart disease through aspiration
- Malignant mesenchymal tumor arising from large pulmonary blood vessels
- Predominantly intraluminal growth in pulmonary arterial circulation
- Arises from intimal layer of elastic arteries, usually sparing media
- Causes obstruction of the vessel lumen leading to pulmonary embolism (PE) or pulmonary hypertension
- Causes embolic seeding to peripheral organs
- Microscopy: spindle cells with variable smooth muscle expression and variable atypia; however, may be completely undifferentiated with or without heterologous elements (osteosarcoma, chondrosarcoma)
- > 70% cases are positive for MDM2 (mouse double minute 2) amplification
- References: J Thorac Dis 2019;11:S9, Pathol Res Pract 2021;224:153548
- ICD-O: 9137/3 - intimal sarcoma
- ICD-11: 2C25.Y & XH36H7 - other specified malignant neoplasms of bronchus or lung & intimal sarcoma
- Rare tumor
- Estimated prevalence: 0.001 - 0.003% (maybe be underestimated due to similar presentation as pulmonary thromboembolism)
- Found in 1 - 4% of pulmonary endarterectomy specimens in patients with clinical features of chronic thromboembolic pulmonary hypertension
- Females affected more than males (M:F = 0.7:1)
- Median age at diagnosis: 48 years
- References: CJC Open 2020;2:711, Aorta (Stamford) 2016;4:142, Korean J Radiol 2018;19:792, Cancer 1993;71:1761
- Pulmonary arteries
- Anywhere from pulmonary valve to lobar branches
- Bilateral or unilateral
- Can also grow backwards into heart
- Rare reports of intimal sarcoma arising from other vessels and the heart
- Larger vessels: aorta (known as aortic intimal sarcoma, which is even rarer)
- Peripheral arteries: iliac and femoral arteries; or even more rarely, may arise from the renal arteries, carotid arteries or inferior vena cava
- Heart: undifferentiated pleomorphic sarcomas (UPS) of the heart is suggested to represent the cardiac analog of intimal sarcoma
- References: Case Rep Oncol 2016;9:267, Radiographics 2021;41:361, Cancer 1993;71:1761, J Thorac Oncol 2016;11:441 Mod Pathol 2021;34:2122
- Originates from subendothelial pluripotent cells within intimal lining
- Frequent amplifications and gains as well as other alterations, in 12q12-15, 4q12, 7p12 and others, where several genes, including MDM2, CDK4, PDGFRA, EGFR and other genes, are located
- References: Pathol Res Pract 2021;224:153548, Radiographics 2021;41:361
- Not known
- Mimics pulmonary embolism and pulmonary hypertension
- Most common presentation: breathlessness
- Other symptoms: chest / back pain, cough, hemoptysis, fatigue, syncope, fever
- Clues to diagnosis:
- Absence of risk factors for pulmonary embolism (but half of patients with pulmonary embolism also have no risk factors)
- Patient fails anticoagulation therapy
- References: Radiographics 2021;41:361, Case Rep Oncol 2021;14:318, Intern Med 2019;58:3599
- Diagnostic imaging modalities: CT angiography, fluorine 18-fluorodeoxyglucose PET (18F-FDG PET), MRI and echocardiography
- Biopsies are typically not performed
- Diagnosis is usually made on resection and histopathologic exam
- Reference: Radiographics 2021;41:361
- D dimer might be elevated (mimics thromboembolism) (Radiographics 2021;41:361)
- Heterogenous lobulated mass in an elastic artery (most often a pulmonary artery)
- Forms acute angle with vessel wall (versus pulmonary embolism)
- Possible imaging features:
- Tumor typically enlarges and molds to fill the central vascular lumen and its branches
- Can also grow backwards across the pulmonary valve, into the right ventricle, even into the right atrium and vena cava = continuous or multifocal appearance
- May occlude vascular lumen
- May invade through the vascular wall into surrounding tissue
- Intralesional blood flow suggests neoplasia
- CT: scan with contrast demonstrates a large filling defect
- PET: most intimal sarcomas are F-FDG avid
- MRI, T1 weighted: isointense to mildly hyperintense
- MRI, T2 weighted: isointense to highly intense
- Imaging differential diagnosis = more common cardiovascular lesions: thrombus, tumor embolism, valvular vegetation
- References: Case Rep Oncol 2016;9:267, Radiographics 2021;41:361
Contributed by Andre L. Moreira, M.D., Ph.D.
Images hosted on other servers:
- Generally poor survival
- Median survival, untreated: as a low as 1.5 months (range 1.5 - 5.5 months)
- Median survival, if resected: 10 months
- References: CJC Open 2020;2:711, Radiographics 2021;41:361
- 25 year old Japanese woman presented with dyspnea and palpitations on exertion (Case Rep Oncol 2021;14:318)
- 36 year old man presented with chest pain and mild shortness of breath on exertion (CJC Open 2020;2:711)
- 37 year old Chinese woman presented with chest tightness and dyspnea (Medicine (Baltimore) 2021;100:e24699)
- 39 year old man experienced chest pain (World J Clin Cases 2021;9:3960)
- 42 year old woman with progressive shortness of breath and palpitation, pitting edema and fatigue (Respirol Case Rep 2020;8:e00530)
- 64 year old woman was referred to another hospital for syncope (Intern Med 2019;58:3599)
- 72 year old woman presented with a 2 month history of mild dyspnea on exertion (Case Rep Pulmonol 2021;2021:5573869)
- 79 year old patient with pulmonary arterial mass (Case of the month #535)
- Surgical resection:
- Pulmonary endarterectomy (PEA)
- Full thickness resection
- Pneumonectomy
- Full thickness resection = complete excision of affected pulmonary artery depending on extent of tumor
- Neoadjuvant or adjuvant chemotherapy or radiation therapy may be considered
- Possible chemotherapy regimens: anthracyclines, ifosfamide, gemcitabine, taxanes, platinum based antineoplastic drugs
- Immunotherapy (not yet standardized)
- Reference: Radiographics 2021;41:361
- Polypoid intraluminal masses attached to the arterial wall
- White to yellow solid mass
- Can resemble mucoid or gelatinous clots in vessel lumen
- Sometimes shows hemorrhage and necrosis
- References: Radiographics 2021;41:361, Case Rep Pulmonol 2021;2021:5573869
- Mesenchymal spindle cell neoplasm
- Variable atypia
- Variable cellularity
- Hyperchromatic nuclei
- Irregular nuclear membranes
- High grade component: high mitotic count, necrosis and more severe nuclear pleomorphism
- Low grade component: lower cellularity and myxoid areas
- With or without epithelioid morphology
- With or without heterologous element: osteosarcoma, chondrosarcoma, rarely rhabdomyosarcoma or angiosarcoma
- References: Case Rep Oncol 2016;9:267, CJC Open 2020;2:711, World J Clin Cases 2021;9:3960, Respirol Case Rep 2020;8:e00530, Case Rep Oncol 2021;14:318, Radiographics 2021;41:361, Medicine (Baltimore) 2021;100:e24699, Intern Med 2019;58:3599, Case Rep Pulmonol 2021;2021:5573869
- Pleomorphic malignant spindle cells
- Loosely cohesive clusters of tumor cells
- Reference: Cytojournal 2015;12:3
- Diagnosis does not require immunohistochemistry
- Variable expression:
- Elastic stain is helpful to identify invasion through arterial wall
- References: Case Rep Oncol 2016;9:267, CJC Open 2020;2:711, Respirol Case Rep 2020;8:e00530, Case Rep Pulmonol 2021;2021:5573869
- Keratin (AE1 / AE3, CAM5.2)
- S100
- Desmin
- CD68
- STAT6
- CD34
- Beta catenin
- ALK
- References: Medicine (Baltimore) 2021;100:e24699, Case Rep Pulmonol 2021;2021:5573869
- MDM2 gene amplification: most important in diagnosis
- Alterations have been reported in 12q12–15, 4q12, 7p12, 9p21, leading to changes or amplification of MDM2, CDK4, SAS, PDGFRA, EGFR, TERT, KIT, KDR, NOTCH2, ERBB3, GLI, VEGFR2, FBXW7, FAT3 or FANCM
- In one study, by FISH, 81% of intimal sarcomas had PDGFRA amplification, 65% had MDM2 amplification and 76% had EGFR amplification
- Cardiac intimal sarcomas from the left atrium tends to show MDM4 and CDK6 amplifications; they lack MDM2 amplification
- References: Mod Pathol 2021;34:2122, Pathol Res Pract 2021;224:153548, Zhonghua Bing Li Xue Za Zhi 2020;49:816, J Thorac Dis 2019;11:S9
- Mass, pulmonary artery, excision:
- Intimal sarcoma (see comment)
- Comment: The sections show a spindle cell proliferation arranged in fascicles, with hyperchromatic pleomorphic nuclei. The lesion invades the media of the artery (supported by elastic stain). The sections also reveal areas of necrosis, consisting of > 50% of the submitted specimen. The mitotic activity is 12 mitoses/10 high power fields. The tumor cells are positive for SMA, vimentin and CD31; negative for cytokeratin, desmin, myogenin, CD34, beta catenin and STAT6. MDM2 immunohistochemistry shows positivity in the tumor nuclei. FISH study shows MDM2 and CDK4 amplification. The histologic, immunohistochemical and molecular findings are consistent with a diagnosis of intimal sarcoma.
- Lung thromboemboli:
- Fibrin with or without organization, platelets (CD61+)
- Lines of Zahn
- History of risk factors for thromboembolism
- No atypical spindle cells, mitosis or necrosis
- Lung infarct:
- Gross: wedge shaped area of hemorrhagic or tan lung parenchyma
- Histology: no atypical spindle cells or mitosis
- Sarcomatoid carcinoma:
- Atypical spindle cells with mitoses or necrosis
- Epithelioid cells may be present
- Cytokeratin positive (may be focal)
- Metastatic sarcoma from another organ:
- Atypical spindle cells with mitoses or necrosis
- History, immunohistochemical stains, molecular studies and previous pathology are helpful to differentiate
A 50 year old woman, who completed a long distance flight the previous week, came to the ER with chest pain and breathlessness. D dimer level was elevated. CT scan with contrast showed a large filling defect in the left pulmonary artery. She was started on anticoagulation therapy but did not improve. PET / CT showed that the left pulmonary artery mass was FDG avid. The lesion was resected and the pathology revealed the findings shown above. Immunostains showed that the cells were positive for SMA and CD31 and negative for AE1 / AE3. What is the diagnosis?
- High grade sarcoma, consistent with intimal sarcoma
- Metastatic carcinoma
- Sarcomatoid carcinoma
- Thromboembolus
Comment Here
Reference: Pulmonary artery intimal sarcoma
- ETV6::NTRK3
- EWSR1::FLI1
- FUS::CREB3L2
- MDM2 amplification
- Rare lung malignancy, 0.25 - 1% of lung cancers
- Biphasic components with admixed epithelium and primitive stroma
- Highly aggressive type of sarcomatoid carcinomas (BMC Res Notes 2014;7:294)
- Peripheral solitary large mass, well circumscribed, unencapsulated
- Well differentiated glandular component and blastematous stroma
- Separated from fetal adenocarcinoma (epithelium only) and pleuropulmonary blastoma (mesenchymal only)
- ICD-O: 8972/3 - pulmonary blastoma
- Most common in fifth decade
- M:F = 1:1
- References: Lung Cancer 2011;73:127, Adv Respir Med 2021;89:511
- All lobes can be affected with upper lobe predominance (Lung Cancer 2011;73:127)
- Both components derived from single pluripotent cell clone (Lung Cancer 2011;73:127)
- TP53 and CTNNB1 mutations detected (Hum Pathol 1996;27:1117, Am J Surg Pathol 2004;28:921)
- Rare mutations such as EGFR, MET, BRAF and DICER1 mutation detected (Onco Targets Ther 2016;9:6915, Eur Respir J 2016;47:1879)
- 80% associated with smoking (BMC Res Notes 2014;7:294)
- Nonspecific, 40% asymptomatic (Cancer 1991;67:2368)
- Relies on tissue histology and IHC on biopsy or surgical resection
- Preoperative biopsy shows cytology of 2 cell patterns
- References: Lung Cancer 2011;73:127, Adv Respir Med 2021;89:511
- Large solitary peripheral mass with variable enhancement and necrosis (Lung Cancer 2011;73:127)
- 25% endobronchial growth (Respir Med 2006;100:1174)
- Poor prognosis, 5 year survival 16% (Lung Cancer 2011;73:127)
- Poor prognostic factors: tumor recurrence, metastasis at initial presentation and size > 5 cm (Lung Cancer 2011;73:127)
- 16 year old girl with a large, well defined, heterogeneously enhancing mass measuring 11 cm in right upper lobe (Case Rep Med 2012;2012:471613)
- 66 year old woman with smoking history presented with a mass in the posteromedial left hemithorax measuring 16 cm (Ann Thorac Surg 2019;107:e345)
- 67 year old male smoker with 9 cm necrotic mass from apical segments of right lower lobe (BMC Res Notes 2014;7:294)
- 68 year old man with tumor of 5.5 cm in the left upper lobe of the lung (Case Rep Oncol Med 2015;2015:842621)
- 71 year old female past smoker with 7 cm tumor in lower lobe (Crit Rev Oncol Hematol 2018;125:48)
- Surgical resection (Lung Cancer 2011;73:127)
- Chemoradiation and neoadjuvant therapy have limited responses in a few cases (Lung Cancer 2011;73:127)
- Adjuvant chemotherapy cisplatin combined with etoposide may improve survival (Cureus 2018;10:e3586, Cancer 1998;82:462)
- Multikinase inhibitor reported having good response in case report (J Int Med Res 2020;48:300060520962394)
- Mostly peripheral, large, well circumscribed, unencapsulated mass, average 9.1 cm (Lung Cancer 2011;73:127)
- Lobulated with cystic, necrotic and hemorrhagic degeneration
- Glandular branching tubules resembling fetal lung, lined by pseudostratified columnar cells with subnuclear and supranuclear glycogen vacuoles and little nuclear atypia (Lung Cancer 2011;73:127)
- Loose undifferentiated mesenchymal stroma with variable cellular atypia, possible heterologous differentiation (skeletal muscle, cartilage and bone) (Lung Cancer 2011;73:127)
- Morules and neuroendocrine cells in 67% of cases (Cancer 1991;67:2368)
- May have germ cell tumor or melanoma component (J Thorac Oncol 2008;3:1185, Arch Pathol Lab Med 1990;114:1076)
- Glandular component: beta catenin (nuclear), CK7, AE1 / AE3, TTF1, CEA, synaptophysin, focal chromogranin (BMC Res Notes 2014;7:294, Lung Cancer 2011;73:127)
- Blastemal stromal component: beta catenin (nuclear), vimentin, SMA (BMC Res Notes 2014;7:294)
- Glandular component: vimentin (BMC Res Notes 2014;7:294)
- Blastemal stromal component: CAM 5.2, TTF1 (BMC Res Notes 2014;7:294)
- Nuclear filaments and biotin rich products contribute to nuclear clearing (Ultrastruct Pathol 1995;19:501)
- Exon 3 of CTNNB1 missense mutations, associated with morule formation (Am J Surg Pathol 2004;28:921, J Pathol 2003;200:214)
- 42% with TP53 mutation (Hum Pathol 1996;27:1117)
- Lung, right lower lobe, lobectomy:
- Pulmonary blastoma, 9 cm, margins negative for tumor (see comment)
- Comment: H&E sections demonstrate an admixture of malignant epithelial and mesenchymal components. Immunostains performed with adequate controls reveal that the glandular cells are strongly positive for pancytokeratin and TTF1. The stromal cells are vimentin positive. Beta catenin reveals nuclear staining in both epithelial and stromal components. The findings are consistent with the diagnosis of pulmonary blastoma, a subgroup of sarcomatoid carcinoma.
- Fetal type adenocarcinoma:
- Epithelial component only, no blastematous stroma
- Pleuropulmonary blastoma:
- Pediatric tumor, most diagnosed before 4 years of age
- No epithelial component; admixture of blastematous and sarcomatoid components
- Epithelium (if seen) is benign entrapped respiratory type
- 40% with DICER1 mutation
- Biphasic synovial sarcoma:
- Glandular component lacks TTF1
- Focal cytokeratin, TLE1 positive, SS18::SSX fusion present
- Carcinosarcoma:
- Non-small cell carcinoma (squamous cell carcinoma or adenocarcinoma) and heterologous sarcomatous component
- Older age
- Absence of morules and no nuclear staining of beta catenin
| CTNNB1 mutation | P53 mutation | DICER1 mutation | |
| Fetal adenocarcinoma | + | - | - |
| Pulmonary blastoma | + | + | Rare |
| Carcinosarcoma | - | + | - |
| Pleuropulmonary blastoma | - | + | + |
- Which of the following is true for pulmonary blastoma?
- Associated with smoking
- Low to moderate grade tumor
- Lung counterpart of Wilms tumor
- Most common in young patients
- Mostly in a central location
Comment Here
Reference: Pulmonary blastoma
- Proliferation of benign appearing capillaries in alveolar septa that appear to compress pulmonary veins
- May represent a secondary angioproliferative process of veno-occlusive disease caused by postcapillary obstruction rather than a distinct entity (Am J Surg Pathol 2006;30:850)
- Poor prognosis, median survival after symptom onset is 3 years
- Disordered proliferation of capillaries within interstitial tissue, including involvement of larger pulmonary vessel walls and airways
- Closely related to pulmonary veno-occlusive disease (PVOD) and could be secondary process, manifests as pulmonary hypertension
- CD31 and CD34 immunohistochemistry can help distinguish capillary proliferation from congestion
- Controversial whether a distinct entity from pulmonary veno-occlusive disease (PVOD)
- Consider diagnosis of "secondary PCH" or PCH-like changes for proliferations seen in association with other disorders, reserving "primary PCH" for extremely rare cases without recognizable causative background disease (Am J Surg Pathol 2006;30:850)
- Very rare, mostly in adults
- Mean age 30 years, range 2-71 years
- Vascular transformation of sinuses in lobar, hilar and mediastinal lymph nodes is common, with intra-sinusal hemorrhage, erythrophagocytosis, lymphoid follicular hyperplasia (Virchows Arch 2008;453:171)
- Capillaries less frequently invade pericardium, pleura and mediastinal lymph nodes
- Chronic passive congestion may lead to capillary proliferation
- Not known; thought to be neoplastic but not entirely clear
- Clinically mimics PVOD or atypical interstitial lung disease due to presence of pulmonary hypertension
- Nonspecific symptoms: progressive dyspnea, cough, chest pain, fatigue, small amount of hemoptysis
- Pulmonary function tests show normal FVC and FEV with reduced diffusion capacity
- Clinically and radiographically indistinguishable from PVOD; diagnosis requires microscopic diagnosis by lung biopsy
- Diagnosis frequently made on explant specimen or after death
- Findings seen in pulmonary hypertension; i.e. cardiomegaly, enlarged pulmonary arteries
- Chest Xray: interstitial infiltrates, thick interlobular septa, bibasilar reticulonodular or micronodular areas of opacity, lymphoadenopathy
- HRCT: diffuse centrilobular ground glass opacity (Cardiovasc Pathol 2013;22:287), peripheral sparing
- Prostacyclin therapy (used in pulmonary hypertension) may cause sudden respiratory distress and death in these patients
- 47 year old man with coexisting pulmonary fibrosis (Pathol Int 2011;61:306)
- 60 year old woman with PCH incidentally discovered in lobectomy for metastatic colon cancer (Pathol Int 2006;56:350)
- Lung transplantation is only definitive treatment but recurrence has been reported
- Drugs for other causes of pulmonary hypertension are relatively ineffective
- Case reports suggest Interferon α-2a or doxycycline may be effective
- Multiple, red-brown, ill defined, nodular lesions
- Congested, edematous, without significant fibrosis
- Preserved architecture with areas of involvement admixed with areas of normal lung
- Proliferation of benign appearing capillaries expanding alveolar septa that appear to compress pulmonary veins
- Proliferation around bronchovascular bundles creating nodular appearance
- At least 2 layers of aberrant capillaries within alveolar wall (Arch Pathol Lab Med 2015;139:274)
- Bland endothelial cells, no mitoses
- Intra-alveolar hemosiderin-laden macrophages, small areas of acute or old hemorrhage, hemosiderosis
- Small pulmonary arteries with intimal thickening/medial hypertrophy
- Alveolar lavage often with increased hemosiderin-laden macrophages
- Mutations in EIF2AK4 described in some cases of familial and sporadic PCH; encodes for a translation initiation factor (Chest 2014;145:231, Appl Clin Genet 2015;8:181)
- Case of 16q deletion in FOXF1 enhancer leading to neonatal PCH (BMC Med Genet 2015;16:94)
- Capillary congestion
- Veno-occlusive disease: associated with PCH; eccentric intimal thickening of venules in lobular septa with some septal veins completely occluded, increased elastic fibers in venous media (highlighted with elastin stain); intimal fibrosis narrows and occludes the pulmonary veins, causing dilatation of capillaries
- Due to hemodynamic disturbances (cardiogenic) or local microvascular injury
Hemodynamic disturbances:
- Due to increased hydrostatic pressure from congestive heart failure
- Lungs are wet and heavy, fluid initially at base of lower lobes because hydrostatic pressure is greater here
- Congestion, fluid and hemosiderin laden macrophages (heart failure cells) are present
- Later fibrosis and thickening of alveolar walls (brown induration of lung)
Local microvascular injury:
- Injury causes leakage of fluids and proteins into interstitial space, eventually into alveoli
- When diffuse, contributes to acute respiratory distress syndrome