Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alzeer A, Wu R. Benign metastasizing leiomyoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorb9metastasizingleio.html. Accessed December 25th, 2024.
Definition / general
- Rare, benign appearing smooth muscle tumor in lung
- Generally thought to represent hematogenous spread from a uterine leiomyoma, given evidence of clonal derivation / similarities in cytogenetic abnormalities (Mod Pathol 2006;19:130, Am J Surg Pathol 2007;31:737)
Essential features
- Benign smooth muscle tumor in lung
- Arises from hematogenous spread of uterine leiomyoma, usually years following surgical manipulation
- Hormonally responsive
- Multifocal; metastasis from leiomyosarcoma must be ruled out
Terminology
- Metastasizing leiomyoma
- First described by Steiner in 1939 as metastasizing fibroleiomyoma of the uterus
- Older term was multiple fibroleiomyomatous hamartomas, when thought to originate in lung
Epidemiology
- Women of reproductive or postmenopausal age following a procedure for leiomyoma (Am J Med Sci 2009;338:72)
- Median age at diagnosis of 46 years (range: 36 - 62) (Ann Thorac Surg 2016;101:253, Ann Palliat Med 2021;10:5831)
- No ethnic predisposition
Sites
- Lung, most common site (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Other reported sites of metastasis include heart, breasts, bone, soft tissue of pelvis, liver, esophagus, lymph nodes, trachea, appendix, central nervous system, skin and scars
Pathophysiology
- Exact pathophysiology is unclear
- Most accepted hypothesis in the literature is that lesions are clonally derived from uterine leiomyomas (Mod Pathol 2006;19:130, Am J Surg Pathol 2007;31:737)
- Hormonally dependent; there is evidence of disease progression in pregnancy and regression after menopause
Etiology
- Hematogenous spread (metastasis) from benign uterine leiomyoma, often after surgical manipulation (myomectomy or hysterectomy)
Clinical features
- Asymptomatic; incidentally discovered on imaging
- 30% of patients present with symptoms including chest pain, back pain, cough, dyspnea, hemoptysis, pneumothorax and respiratory failure
- Lesions develop months to years after myomectomy; mean duration between hysterectomy and appearance of lung lesions is 23 years (Clin Chest Med 2016;37:589, Ann Thorac Surg 2016;101:253)
Diagnosis
- Clinical history of surgical removal of uterine leiomyomas (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Imaging; computed tomography (CT) scan of the thorax
- Microscopic examination of biopsy / excision of pulmonary lesion
Radiology description
- Chest Xray: multiple bilateral opacities
- CT: multiple bilateral, well circumscribed nodules (Radiol Case Rep 2020;15:2120)
- Lesions may have a cavitary or cystic appearance, radiographically mimicking lymphangiomyomatosis (LAM)
- Lesions can have a miliary pattern (Am J Respir Crit Care Med 2021;203:906)
- PET / CT: nodules have low or no fluorodeoxyglucose (FDG) uptake
- Less commonly present as a solitary nodule (Clin Chest Med 2016;37:589)
- References: Ann Palliat Med 2021;10:5831, Clin Chest Med 2016;37:589
Prognostic factors
- Prognosis is overall favorable (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Lesions follow an indolent course
- Large tumors may lead to emboli, pulmonary infarction or symptomatic disease
Case reports
- 26 year old woman with spontaneous regression of miliary pattern after delivery (Am J Respir Crit Care Med 2021;203:906)
- 37 year old woman with pulmonary benign metastasizing leiomyoma, simultaneously diagnosed with uterine leiomyoma before hysteromyomectomy (Transl Cancer Res 2021;10:567)
- 43 year old woman benign metastasizing leiomyoma in multiple organs (J Obstet Gynaecol Res 2019;45:2132)
- 45 year old woman with a benign metastasizing leiomyoma in the heart (Tex Heart Inst J 2021;48:e197066)
- 76 year old woman with pulmonary benign metastasizing leiomyoma presenting as acute respiratory distress (Respirol Case Rep 2017;5:e00216)
Treatment
- No specific guidelines for management
- Watchful management for asymptomatic patients
- Surgical resection of symptomatic lesions or lesions with interval growth
- Medical hormonal suppression (J Clin Endocrinol Metab 2004;89:3183)
- Oophorectomy for premenopausal women
Gross description
- Tan-white, well circumscribed, rounded, rubbery to firm, with a whorled cut surface
Frozen section description
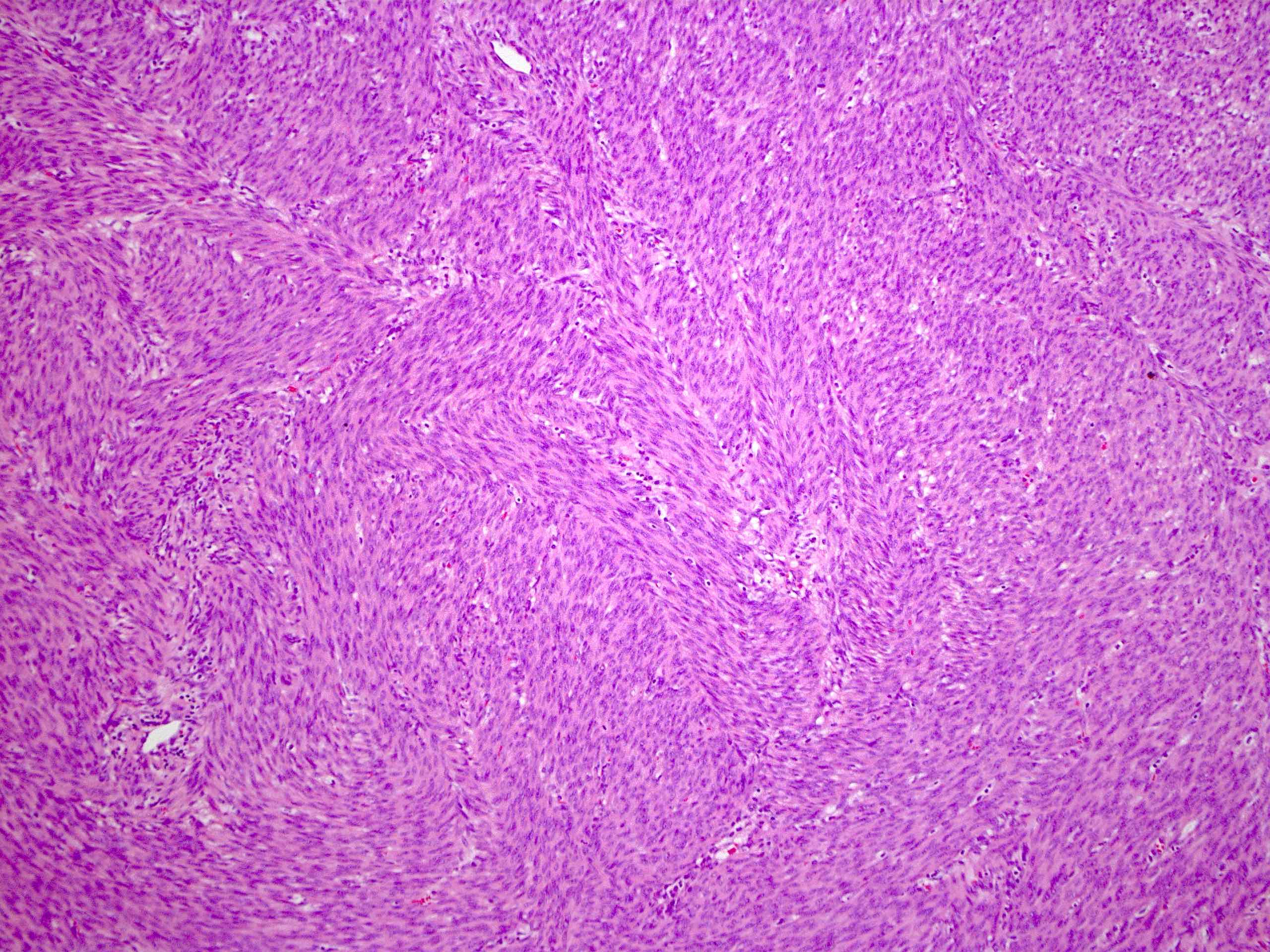
- Bland spindle cell proliferation, arranged in fascicles
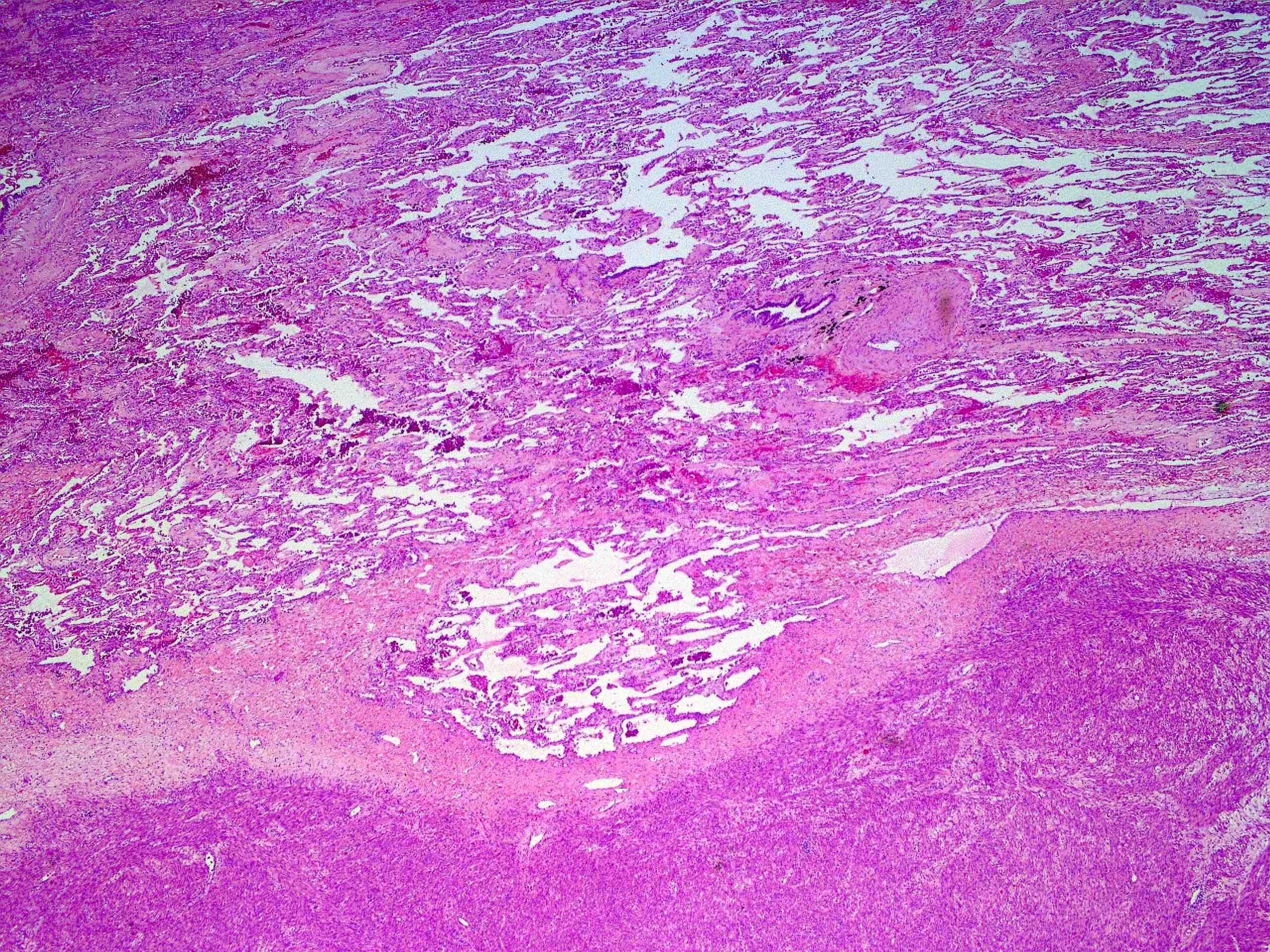
Microscopic (histologic) description
- Well circumscribed, solitary or multiple nodules of smooth muscle, similar to uterine counterparts (BMC Pulm Med 2020;20:292, Case Rep Oncol Med 2014;2014:842801)
- Whorled to intersecting fascicles of ovoid to elongated spindled cells with abundant eosinophilic cytoplasm, oval to cigar or boxcar shaped nuclei, inconspicuous nucleoli
- Large, irregular, thick walled vessels
- May contain cysts or entrapped epithelium
- No atypia, no necrosis, no vascular invasion, no mitotic figures
Microscopic (histologic) images
Cytology description
- Generally acellular or paucicellular on fine needle aspiration
- Nonspecific cytologic findings: clusters of uniform, bland, cohesive spindle cells with no mitoses, no necrosis and no significant atypia
Positive stains
Negative stains
Electron microscopy description
- Spindle cells show basal lamina material, pinocytotic vesicles, intracytoplasmic microfilaments with focal densities
Molecular / cytogenetics description
- Genetically distinct entity with consistent chromosomal aberrations (19q and 22q terminal deletion in all cases) (Am J Surg Pathol 2007;31:737)
- Similar genetic findings when comparing benign metastasizing leiomyoma and uterine leiomyoma (Mod Pathol 2006;19:130, Hum Pathol 2000;31:126, Int J Gynecol Pathol 2008;27:340, Cancer Genet 2012;205:249, Diagn Mol Pathol 2008;17:145)
Molecular / cytogenetics images
Videos
Benign metastasizing leiomyoma
Sample pathology report
- Lung, left upper lobe, mass, wedge resection:
- Low grade spindle cell neoplasm, consistent with benign metastasizing leiomyoma (see comment)
- Comment: Patient’s history of uterine leiomyoma is noted. Immunohistochemical studies were performed with adequate controls on block (A1). The tumor cells are positive for SMA, actin, desmin, ER and PR. The tumor cells are negative for pankeratin, TTF1, HMB45, STAT6 and chromogranin. The morphology and immunohistochemical profile supports the above diagnosis.
Differential diagnosis
- Metastatic low grade leiomyosarcoma (Diagn Mol Pathol 2008;17:145):
- Atypia, nuclear pleomorphism, necrosis, high mitotic activity favor malignancy
- miRNA expression differentiates leiomyosarcoma from benign metastasizing leiomyoma
- Solitary fibrous tumor:
- Schwannoma:
- S100 positive
Board review style question #1
A 45 year old woman presents with multiple incidentally discovered, well circumscribed, bilateral lung nodules on CT scan. She is asymptomatic and her history is only notable for a myomectomy, 10 years ago. A biopsy of one of the nodules is performed (see figure above). On immunohistochemical staining, the lesion is negative for STAT6 and the Ki67 proliferative index is low. What is the most likely diagnosis?
- Benign metastasizing leiomyoma
- Leiomyosarcoma
- Pulmonary hamartoma
- Solitary fibrous tumor
Board review style answer #1
Board review style question #2
A 45 year old woman presents with multiple incidentally discovered, well circumscribed, bilateral lung nodules on CT scan. She is asymptomatic and her history is only notable for a myomectomy 10 years ago. A biopsy of one of the nodules is performed (see figure above). On immunohistochemical staining, the lesion is negative for STAT6 and the Ki67 proliferative index is low. Based on this specific clinical presentation, what is the best choice for treatment?
- Chemotherapy
- Follow up imaging
- Hormonal therapy
- Surgical resection
Board review style answer #2