Table of Contents
Fixed drug reaction | Interstitial granulomatous drug reaction | Morbiliform drug reaction (pending)Cite this page: Hamodat M. Lichenoid drug reaction. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumordrugreaction.html. Accessed April 1st, 2025.
Fixed drug reaction
Definition / general
Sites
Treatment
Clinical images
Contributed by Mark R. Wick, M.D.
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Differential diagnosis
Additional references
- May cause urticaria, erythema multiforme, erythema nodosum, folliculitis, pustules, purpura, hyperpigmentation or vasculitis
- Procainamide may induce SLE-like disease
- Anti-cancer drugs may cause acute necrotizing changes in sweat glands (neutrophilic eccrine hidradenitis or syringosquamous metaplasia)
- Drug induced coma may cause necrosis of eccrine sweat coils and other adnexae, also epidermis
- Other drugs causing cutaneous reactions include gold salts, thiazides, antimalarial drugs, color film developers, tetracycline, barbiturates, phenolphthalein
- Fixed drug reaction: repeated administration causes recurrence of red-brown patch in same location, variable bullae
Sites
- Genitalia and face
Treatment
- Discontinue drug
Clinical images
Contributed by Mark R. Wick, M.D.
Images hosted on other servers:
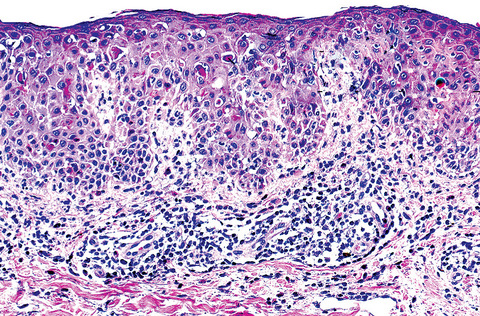
Microscopic (histologic) description
- Eosinophils and marked vascular wall thickening
- May cause granulomatous infiltrate
- Also vacuolar interface changes and often lymphocytic exocytosis, dyskeratotic keratinocytes, parakeratosis with eosinophils and plasma cells in dermis
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Differential diagnosis
- Lichen planus :
- Different sites (flexor arms / legs, glans penis and mucous membranes), lasts 1 - 2 years, not associated with drug administration, no prominent eosinophils (Indian J Dermatol Venereol Leprol 2011;77:418)
Additional references
Interstitial granulomatous drug reaction
Definition / general
Clinical features
Case reports
Microscopic (histologic) description
Differential diagnosis
- Reaction due to beta blockers, calcium channel blockers, lipid lowering agents, ACE inhibitors, diuretics, NSAIDs, antihistamines, antidepressants and oral hypoglycemic agents; often more than one of the above
- Mean duration of 5 years before onset of eruptions
- Resolves a mean 8 weeks (range 1 - 40) after drug is stopped
- May be due to exaggerated immune response to drugs
Clinical features
- Violaceous to erythematous, nonpruritic plaques with bizarre shapes or annular morphology on skin folds (axilla, inner arms, groin, medial thighs and popliteal fossa)
Case reports
- 74 year old woman with violaceous / erythematous nonpruritic plaques for 18 months (Arch Pathol Lab Med 2004;128:e129)
- Delayed cutaneous hypersensitivity reaction to hirudin (Arch Pathol Lab Med 2001;125:1585)
Microscopic (histologic) description
- Diffuse granulomatous dermatitis with interstitial histiocytes and giant cells near collagen and elastic fibers, often with piecemeal fragmentation of collagen, giant cell engulfment of elastic fibers and variable interstitial mucin (J Cutan Pathol 1998;25:72)
- Usually interface dermatitis with basilar vacuolopathy and focal dyskeratosis with lymphocytes at dermoepidermal junction
- Usually tissue eosinophilia, lymphoid atypia with hyperchromatic nuclei, convoluted nuclear contours (including a few cerebriform nuclei in dermis), variable involvement of hair follicles and acrosyringia
- Rare collagen necrobiosis
- Usually no fibrin deposition within vessels or vasculitis
Differential diagnosis
- Cutaneous T cell lymphoma:
- Similar due to cerebriform nuclei in epidermis
- Erythema annulare centrifugal
- Granuloma annulare:
- Vasculitis or vasculopathy present
- Necrobiosis
- Usually no eosinophils and no interface change
- Subacute cutaneous SLE
Morbiliform drug reaction (pending)
[Pending]