Superpage
Superpage Topics
Acute cellular rejection
Amyloidosis
Anomalous coronary artery
Antibody mediated rejection (pending)
Aortic aneurysms
Arrhythmogenic right ventricular cardiomyopathy
Atherosclerotic coronary artery disease
Cardiac fibroma
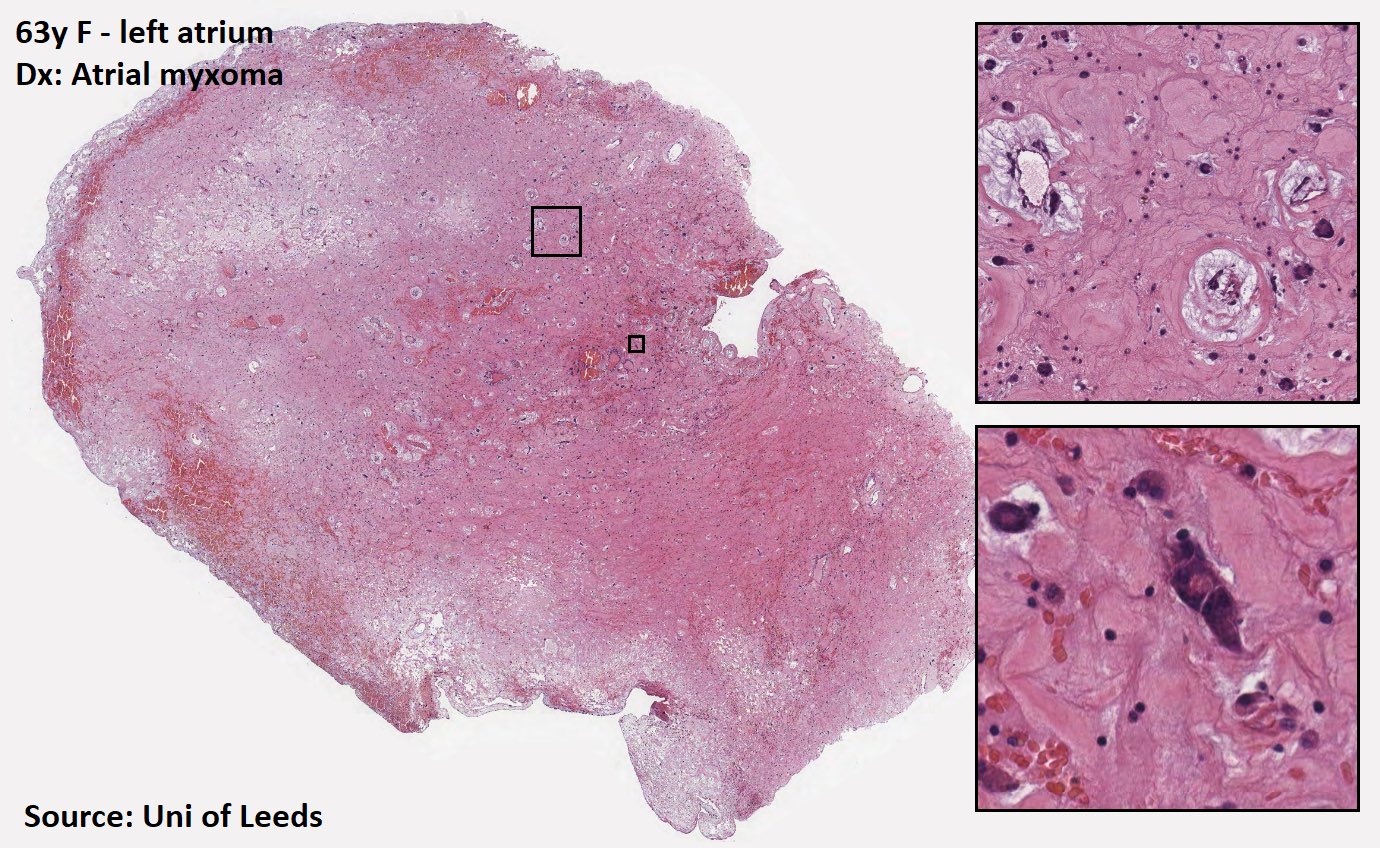
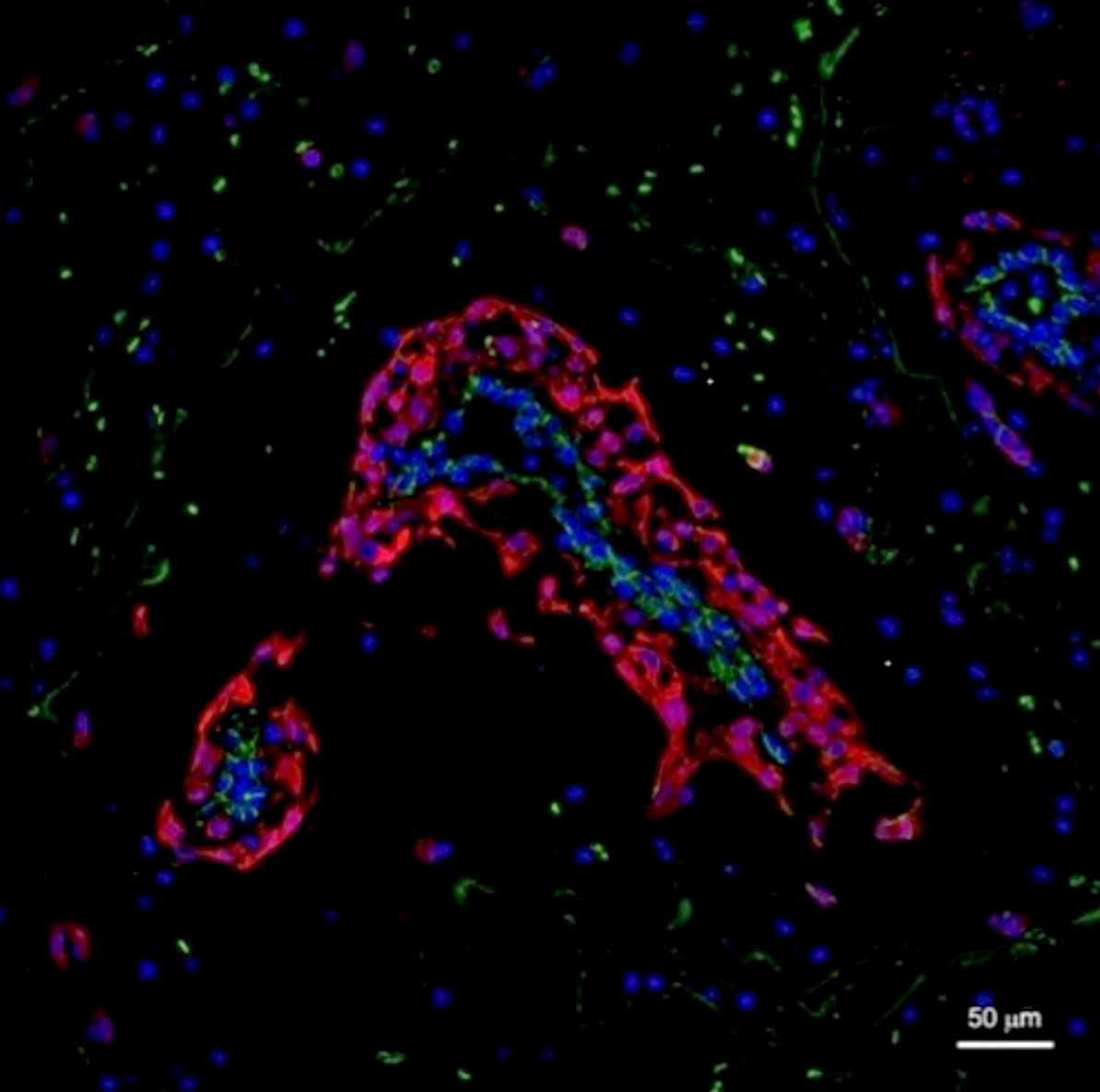
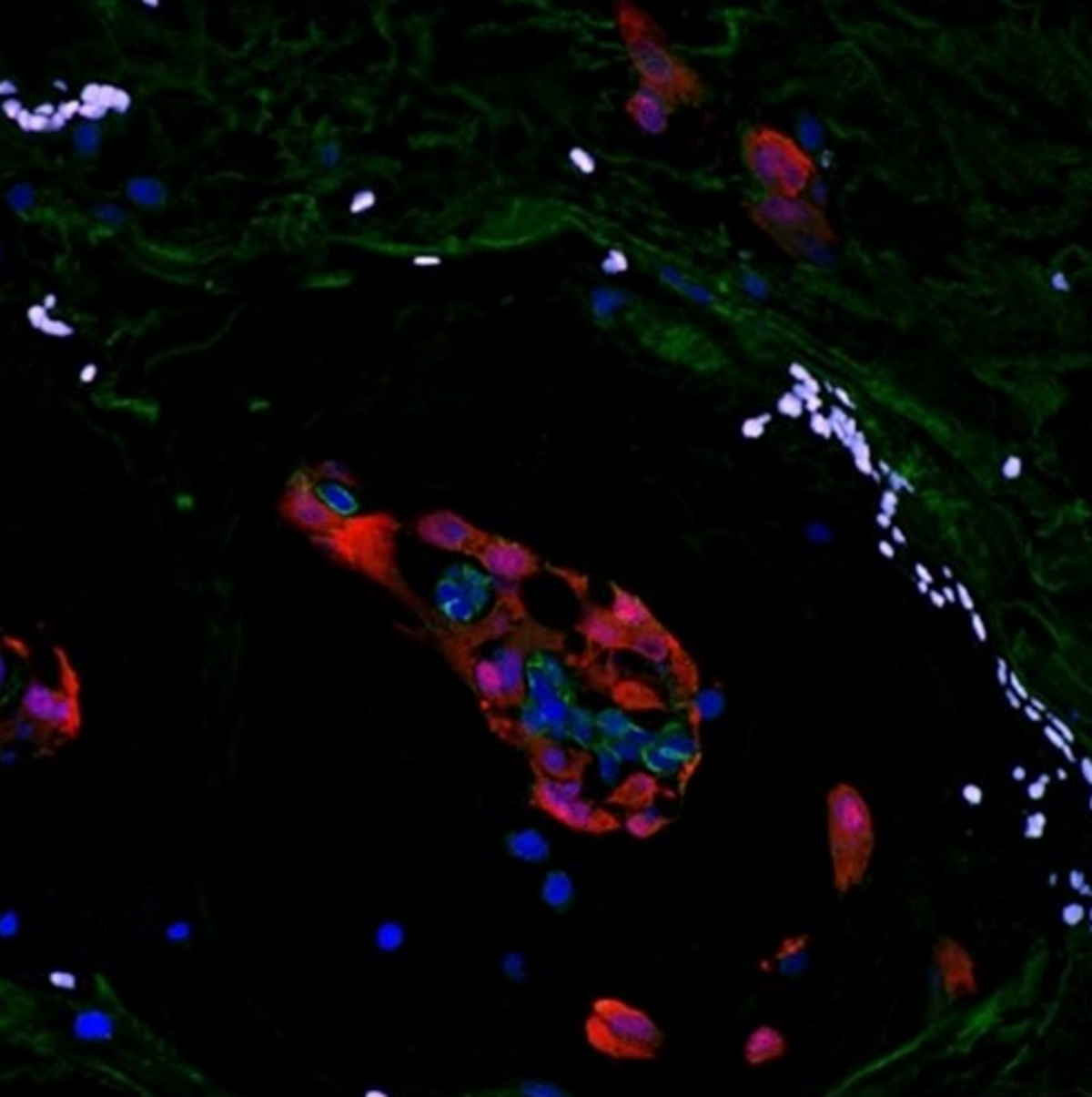
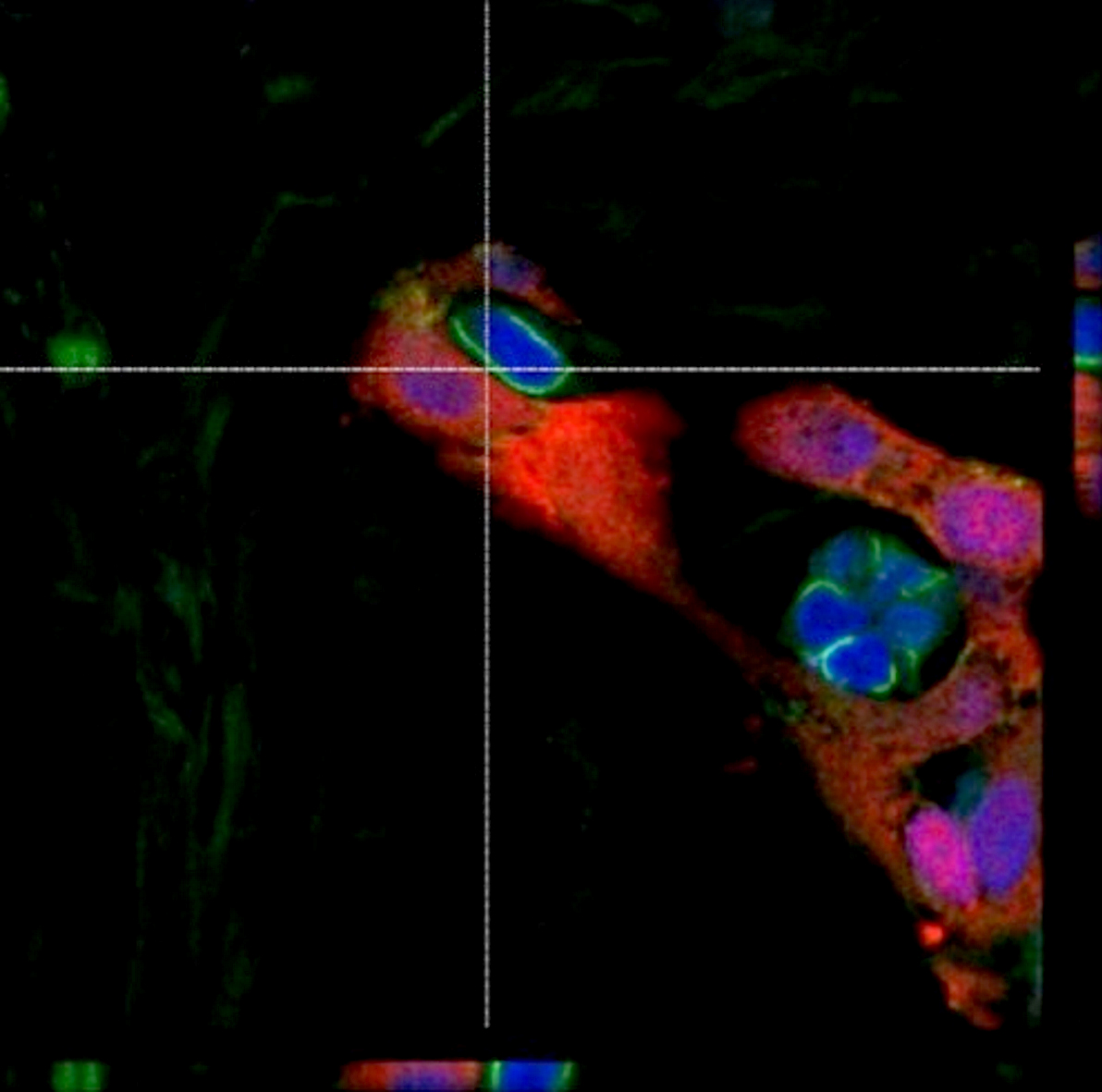
Cardiac myxoma
Chambers
Chronic allograft vasculopathy
Conduction tissue
Connective tissue diseases
Coronary vessels
COVID myocarditis (pending)
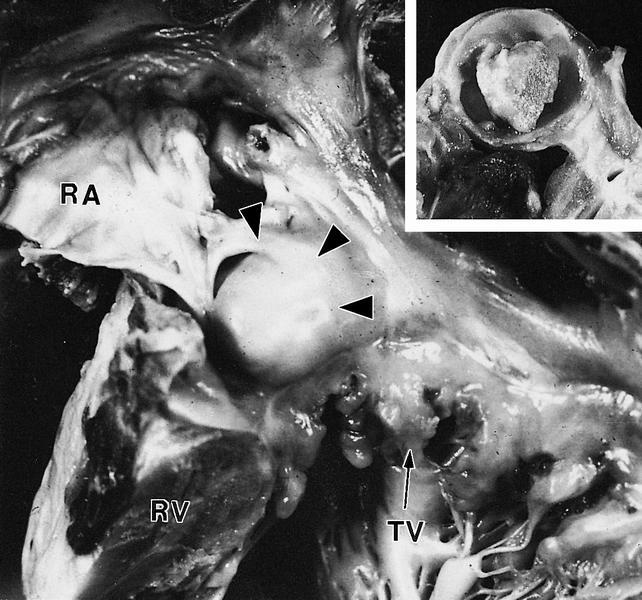
Cystic tumor of the atrioventricular node
Degenerative valve disease
Drug induced valvular heart disease
Embryology
Features to report
Fibromuscular dysplasia
General (transplant)
Giant cell arteritis
Histology
Hypertrophic cardiomyopathy
Idiopathic restrictive cardiomyopathy
Infective endocarditis
Infective myocarditis
Lambl excrescence
Left ventricular assist device (LVAD)
Nonatherosclerotic coronary artery disease
Noninfective endocarditis
Noninfective myocarditis
Noninfective pericarditis
Papillary fibroelastoma
Primary and secondary dilated cardiomyopathy
Prosthetic valves
Rhabdomyoma
Sarcoidosis
Syphilis
Takotsubo cardiomyopathy
Tetralogy of Fallot (pending)
VACTERL association
ValvesAcute cellular rejection
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Lymphocyte predominant infiltration of the perivascular and interstitial myocardial compartments after orthotopic heart transplantation resulting in myocyte damage and necrosis, distorted myocardial architecture and allograft dysfunction
Essential features
- Early complication after heart transplantation (first 3 - 6 months)
- Endomyocardial biopsy is diagnostic
- Host T cell mediated inflammatory response to allograft differences in histocompatibility antigens, precipitating myocyte damage and myocardial dysfunction
Terminology
- Acute allograft rejection
ICD coding
Epidemiology
- Early complication after orthotopic heart transplant causing less than 10% of 1 year mortality and 9% of 3 year mortality (Transl Res 2012;159:238)
- Highest incidence within first 3 years after transplant, most frequently within first 3 - 6 months (Cagle: Atlas Of Transplant Pathology, 2015)
- Up to 60% experience at least one episode within the first 6 postoperative months
- Increased incidence / risk:
- Donor factors: female, < 18 years old, longer ischemic time (Circulation 1992;86:II236)
- Recipient factors: female, black, younger age, cytomegalovirus infection, higher levels of circulating donor specific antibodies to human leukocyte antigen before transplantation, greater number of previous rejection episodes (JAMA 1989;261:3561, Ann Thorac Surg 2007;84:1556)
- Greater number of donor recipient human leukocyte antigen mismatches or sex mismatched transplantation (Transpl Int 2014;27:482)
- Decreased risk if the transplant was received in the last 15 years
Sites
- Inflammatory infiltrate associated with interstitial and/or perivascular compartments of allograft myocardium
- Severe cases may involve transmural inflammation of distal coronary arteries (Cagle: Atlas Of Transplant Pathology, 2015)
Pathophysiology
- Host allorecognition of donor major and minor histocompatibility antigens on the allograft → T cell activation → myocardial infiltration of host T cells and macrophages → myocyte damage and necrosis (Transl Res 2012;159:238)
- More severe episodes associated with polymorphonuclear leukocyte infiltration, B cell presence and greater numbers of macrophages and dendritic cells (Cagle: Atlas Of Transplant Pathology, 2015)
- CD4 T cells more abundant in mild / early rejection and CD8 T cells in moderate rejection (Arch Pathol Lab Med 2007;131:1169)
- Ratio of memory (CD45RO+) to naive (CD45RA+) T cells is higher in moderate rejection than in mild rejection
- Rejection mediated by IL-2, TNF beta and IFN gamma (Ludhwani: StatPearls, 2019)
Etiology
- Interplay between immunologic (cellular mediated rejection and human leukocyte antigen matching) and nonimmunologic (e.g., recipient cytomegalovirus infection, pediatric donor) factors
Diagrams / tables
Clinical features
- Presents with dyspnea orthopnea, paroxysmal nocturnal dyspnea, syncope, palpitations and arrhythmias (notably atrial flutter), nausea and weight gain
- Gastrointestinal symptoms due to secondary hepatic congestion can confuse the clinical picture and lead to delays in diagnosis (UpToDate: Acute Cardiac Allograft Rejection - Diagnosis [Accessed 7 October 2019])
- If severe, may present with cardiogenic shock (Cagle: Atlas Of Transplant Pathology, 2015)
- Signs: jugular vein distention, extra heart sounds, peripheral edema, hypotension and oliguria (Ludhwani: StatPearls, 2019)
Diagnosis
- Surveillance endomyocardial biopsies (J Heart Lung Transplant 2005;24:1710)
- In biopsy negative rejection (20%), utilize troponin, Doppler echocardiography, cardiovascular MRI, antimyosin scintigraphy, annexin V imaging or gene expression profiling (Ludhwani: StatPearls, 2019)
- Can screen for but not diagnose rejection via noninvasive methodologies: Doppler echocardiography, cardiovascular MRI and gene expression profiling (Transl Res 2012;159:238)
- Cannot be used as a diagnostic tool due to insufficient sensitivity and specificity
- Gene expression profiling of peripheral blood mononuclear cells distinguished moderate severe rejection from quiescence (Am J Transplant 2006;6:150)
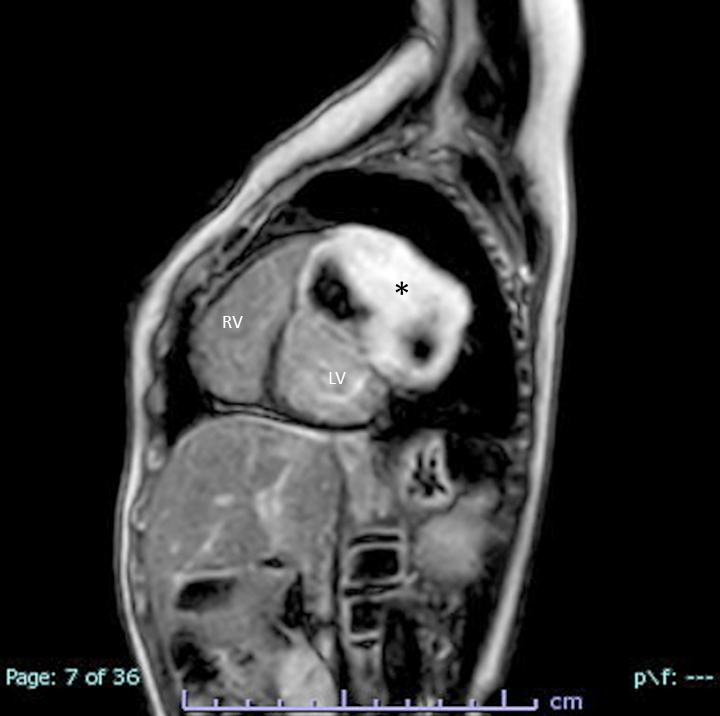
Radiology description
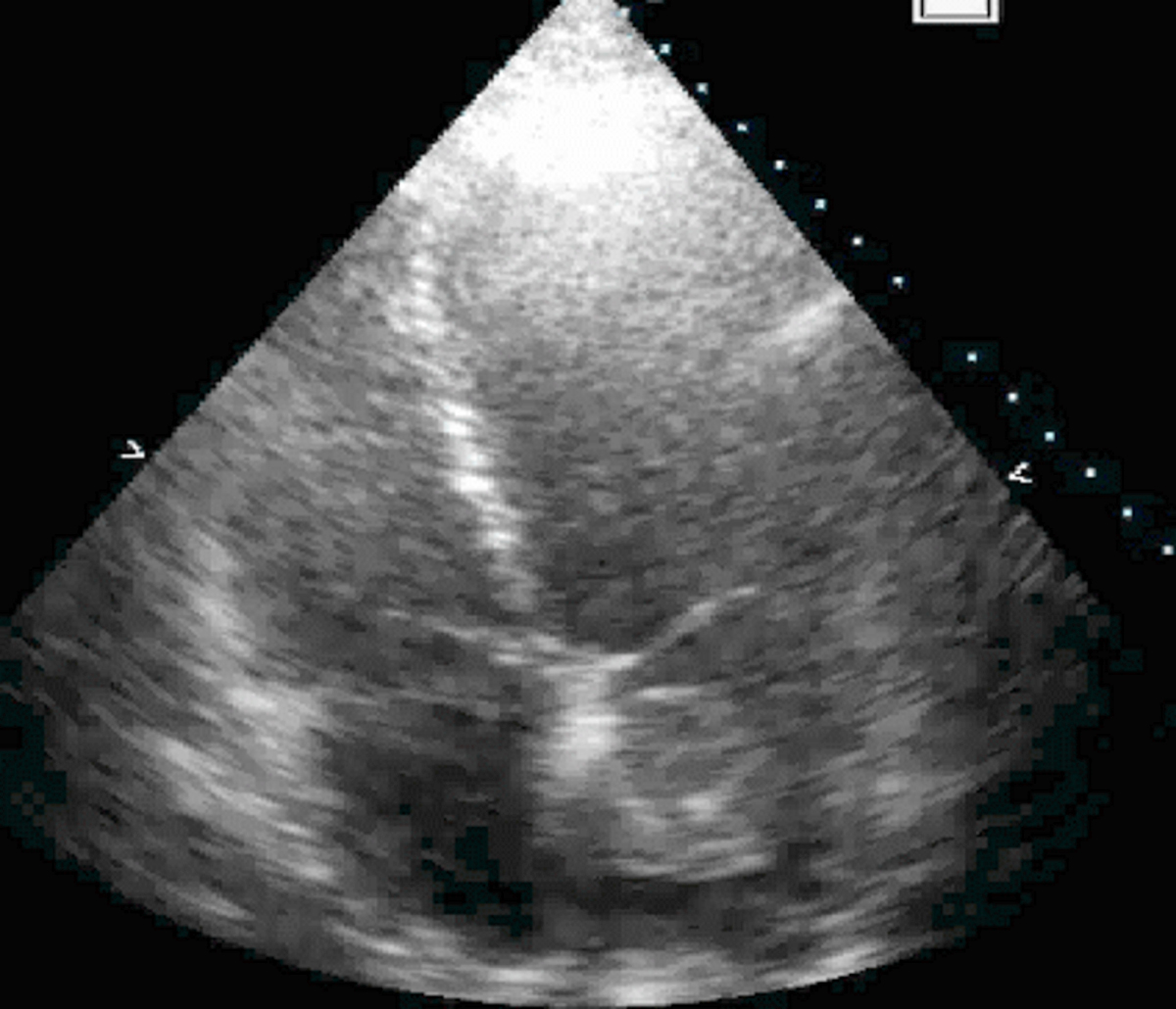
- Doppler echocardiography: decreased isovolumic relaxation time, decreased pressure half time and disturbed early diastolic wall motion velocity (J Am Coll Cardiol 1988;12:63, Circulation 2001;104:I184)
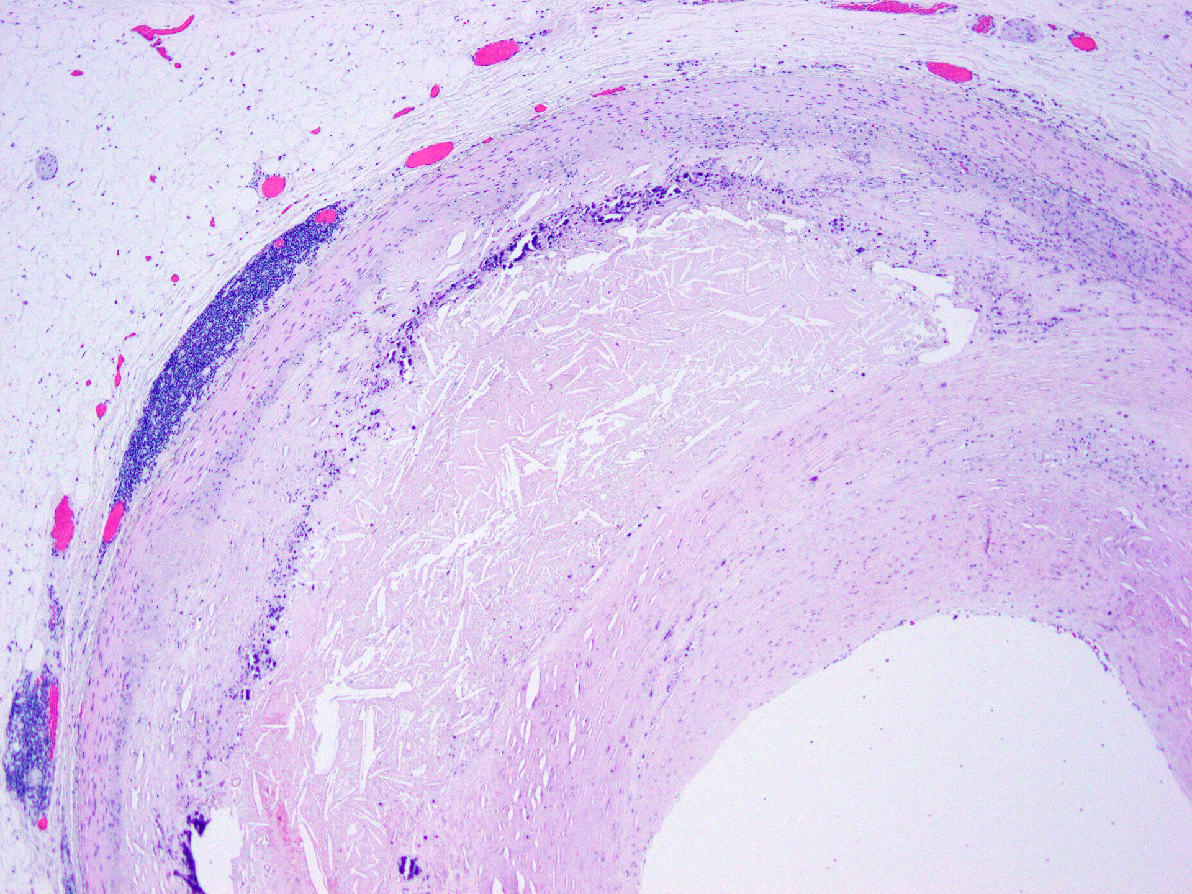
- Cardiovascular MRI: long T2 relaxation times due to myocardial edema (J Cardiovasc Magn Reson 2009;11:7, J Am Coll Cardiol 2001;37:825)
Radiology images
Prognostic factors
- Favorable:
- Use of tacrolimus based immunosuppression versus cyclosporine (Am J Transplant 2006;6:1377)
- Unfavorable:
- Sex mismatched transplantation (Clin Transplant 2017;31)
- Occurrence within the first postoperative year
- Greater numbers of rejection episodes or higher grades of rejection severity (Best Pract Res Clin Anaesthesiol 2017;31:201)
- Higher numbers of CD8 T cells on endomyocardial biopsy (J Heart Lung Transplant 1991;10:235)
- Quilty positive biopsies (Transpl Immunol 2008;19:209)
- Use of extracorporeal membrane oxygenation support before transplantation (Ludhwani: StatPearls, 2019)
Case reports
- 24 year old woman with fatal mixed humoral and cellular rejection not detected on surveillance biopsies or circulating antibodies (J Transplant 2011;2011:351950)
- 43 year old man with asymptomatic acute cellular rejection demonstrated on cardiovascular MRI (Ann Transplant 2014;19:447)
- 53 year old woman with fulminant mixed humoral and cellular rejection presenting with coronary pan-ischemia (Int Heart J 2015;56:679)
- 60 year old woman with recurrent asymptomatic acute cellular rejection monitored with speckle tracing echocardiography (Pol Arch Med Wewn 2016;126:700)
- 74 year old man with mixed humoral and cellular rejection presenting with sinus tachycardia segment elevation in leads I and aVL (Circ Heart Fail 2015;8:836)
Treatment
- Preventative therapy: posttransplantation immunosuppressants
- Treat with oral / intravenous steroids, antithymocyte globulin and Murine monoclonal antibodies OKT3 based on patient hemodynamic status and histological severity of disease (Ludhwani: StatPearls, 2019)
- First line: high-dose IV corticosteroids (J Heart Lung Transplant 2010;29:914)
- Grades ≥ 2R are considered clinically relevant and are treated even if asymptomatic (Cagle: Atlas Of Transplant Pathology, 2015)
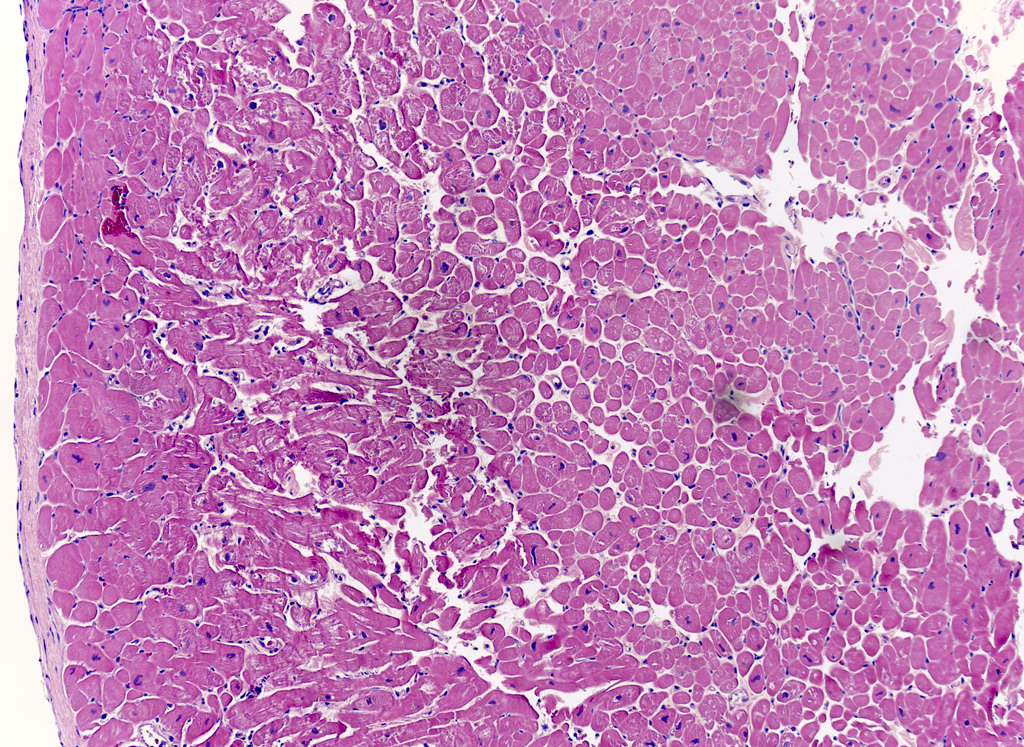
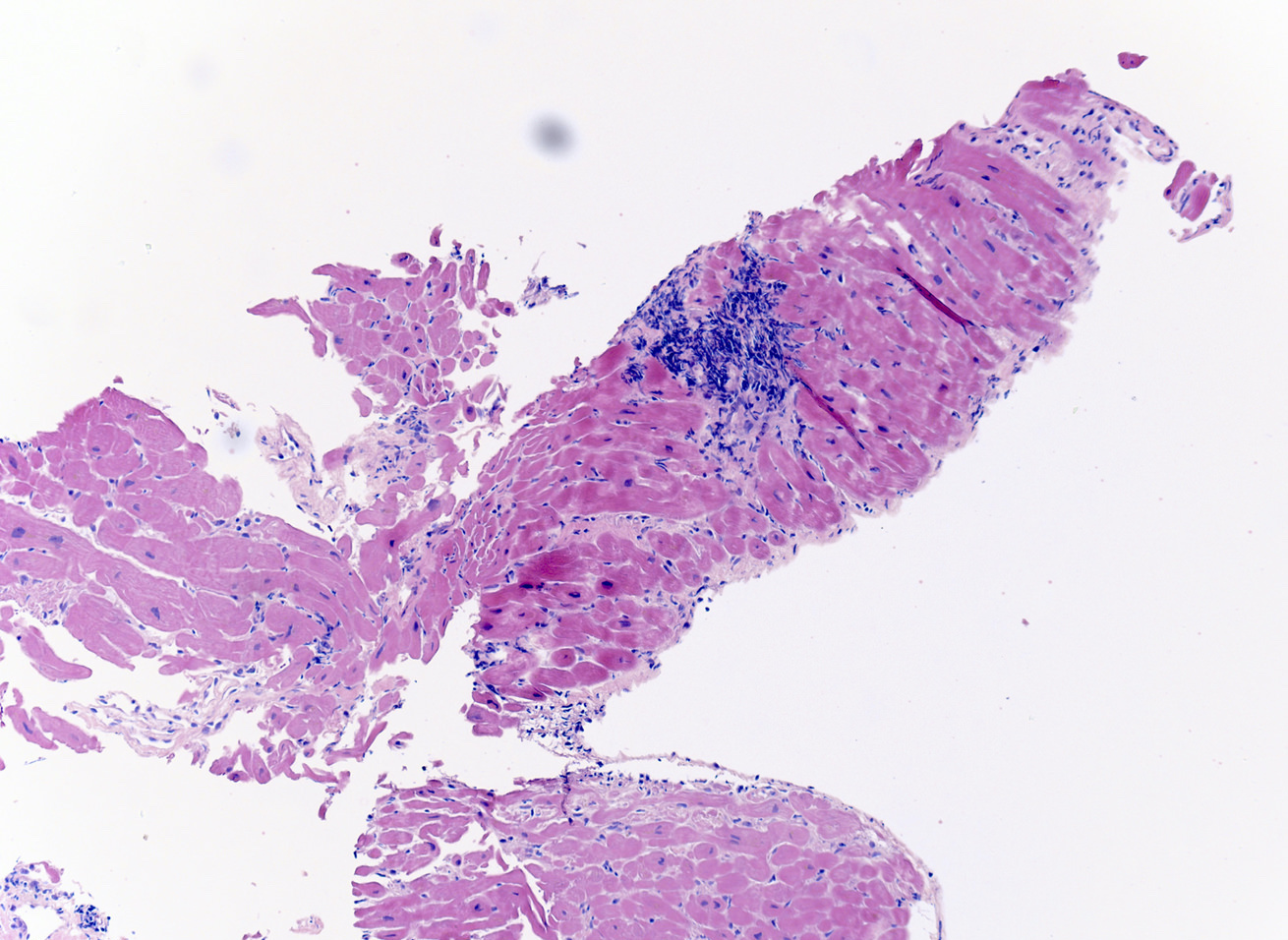
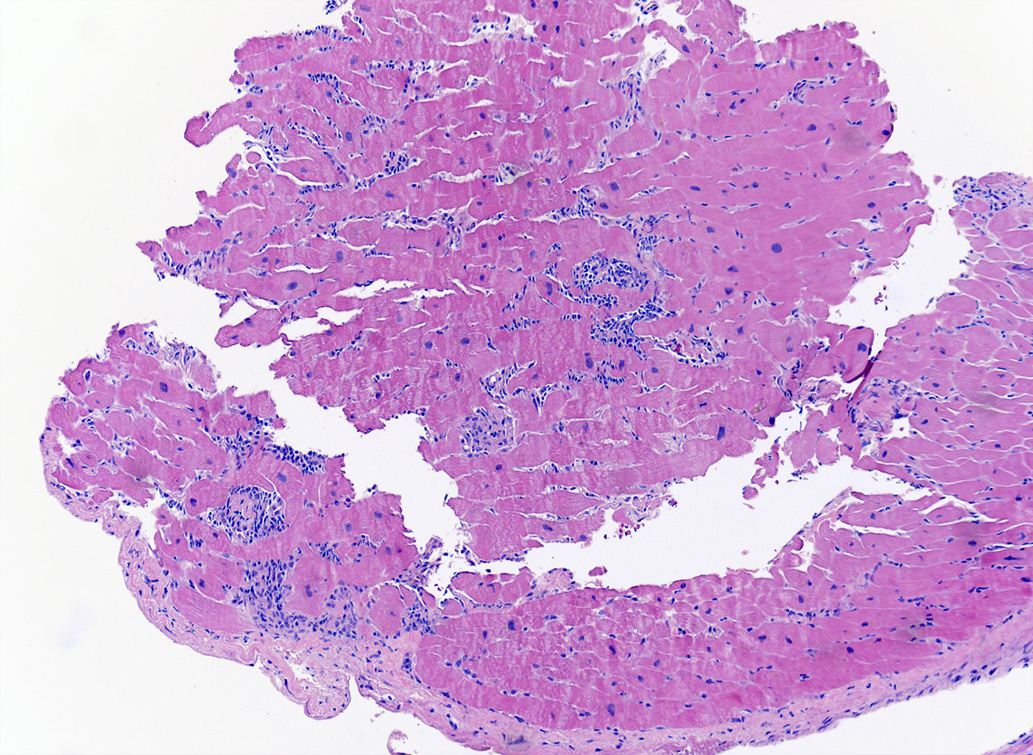
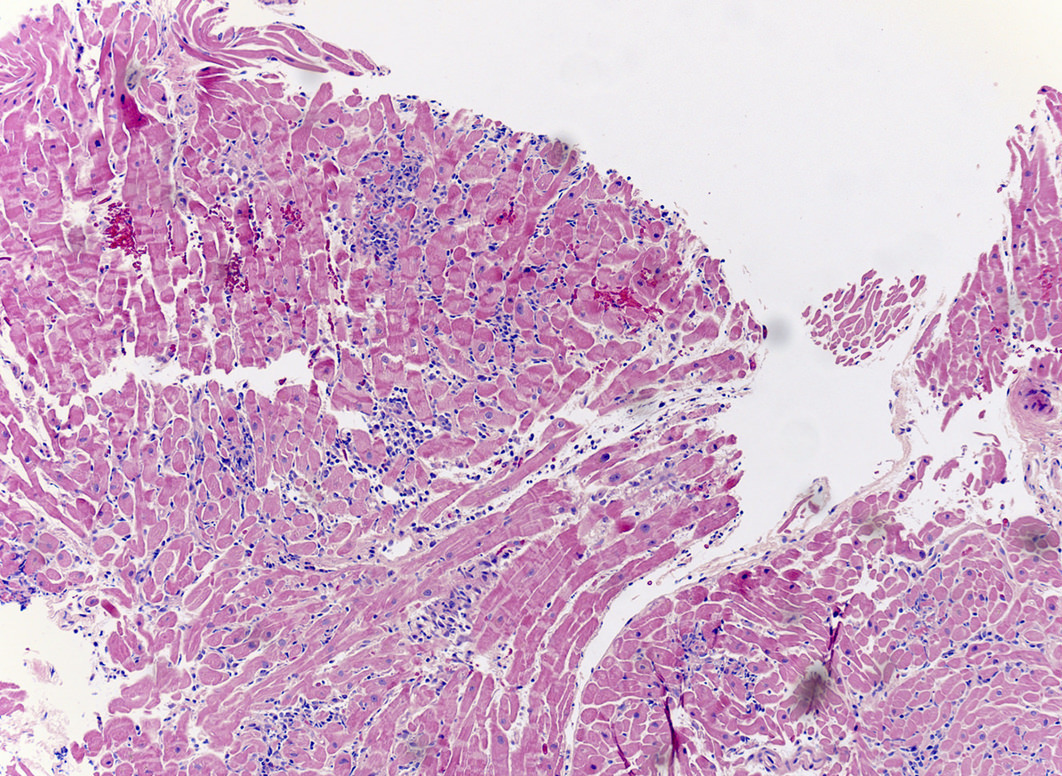
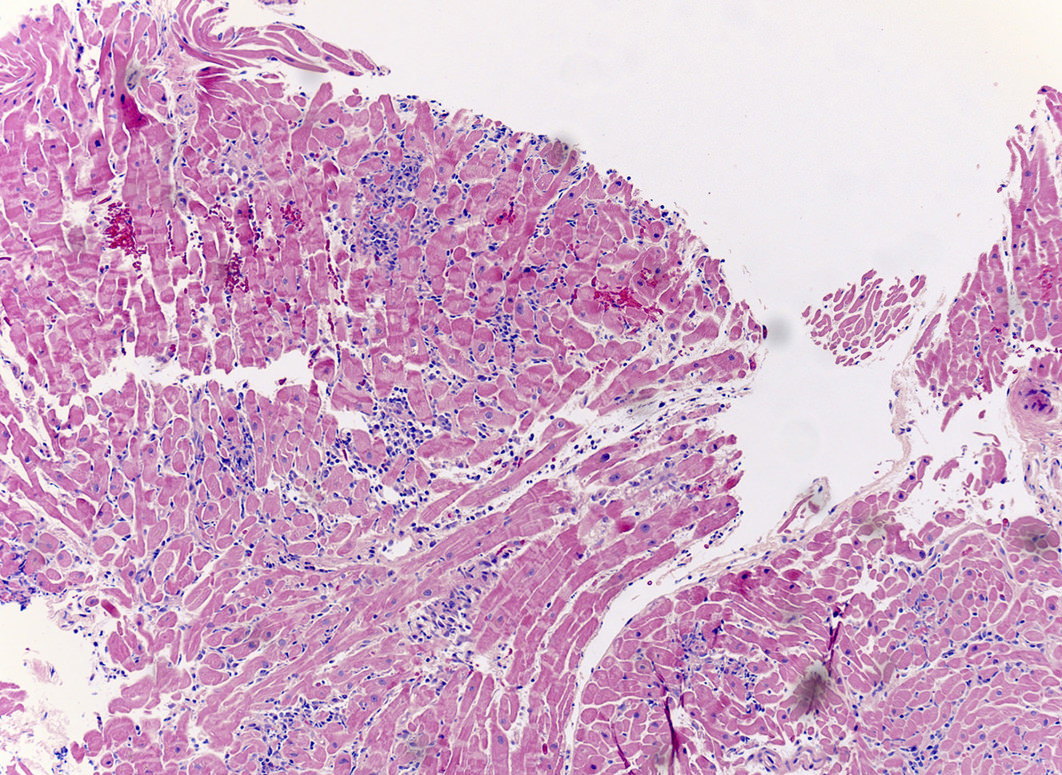
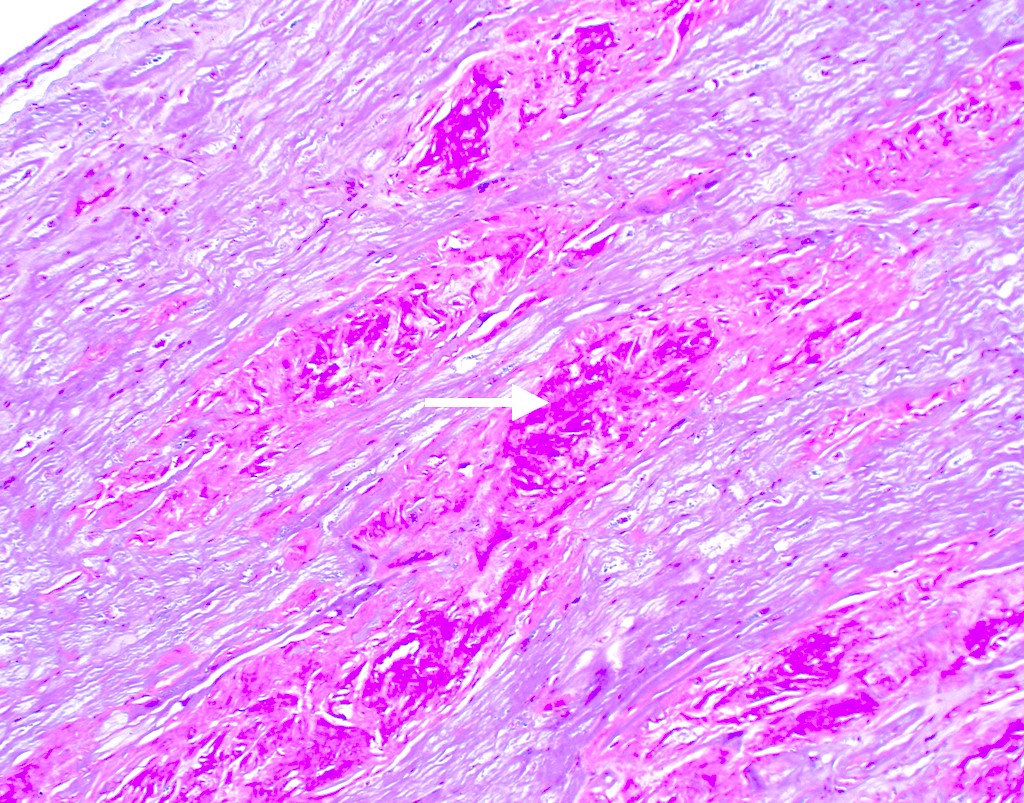
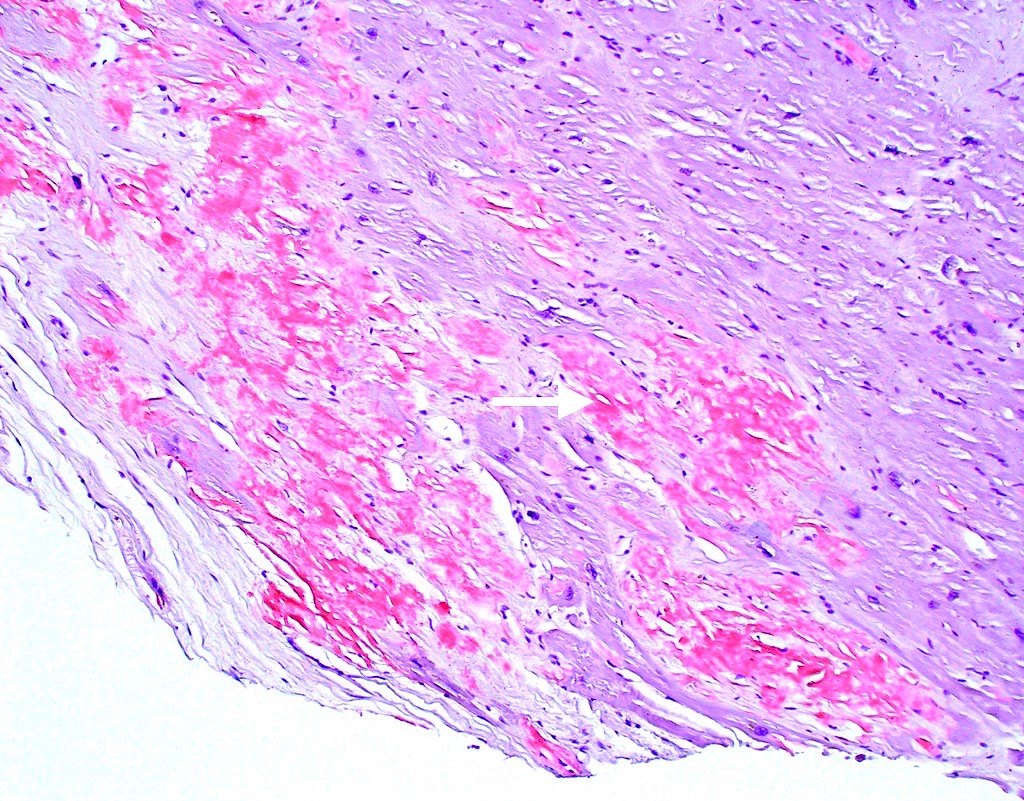
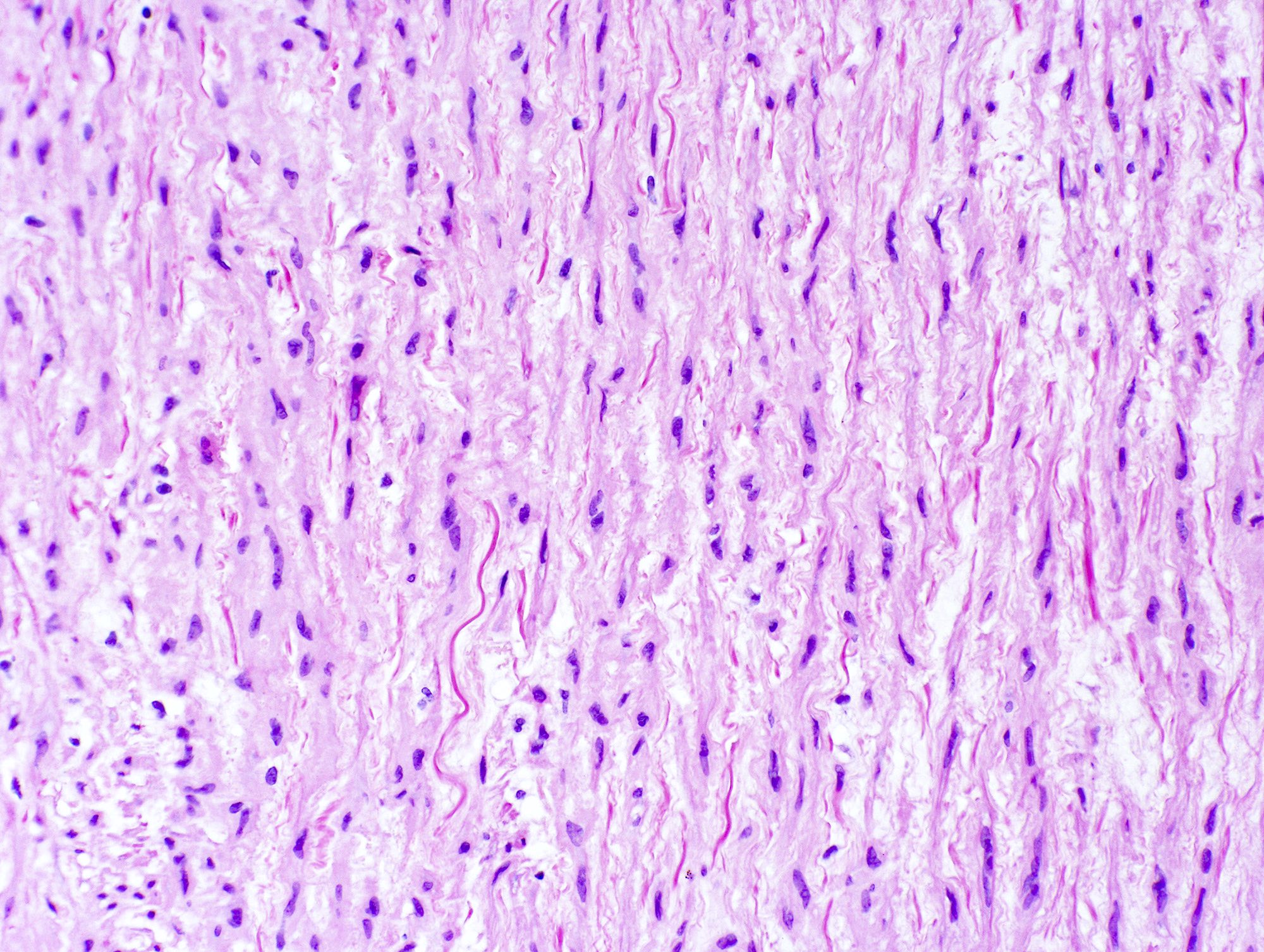
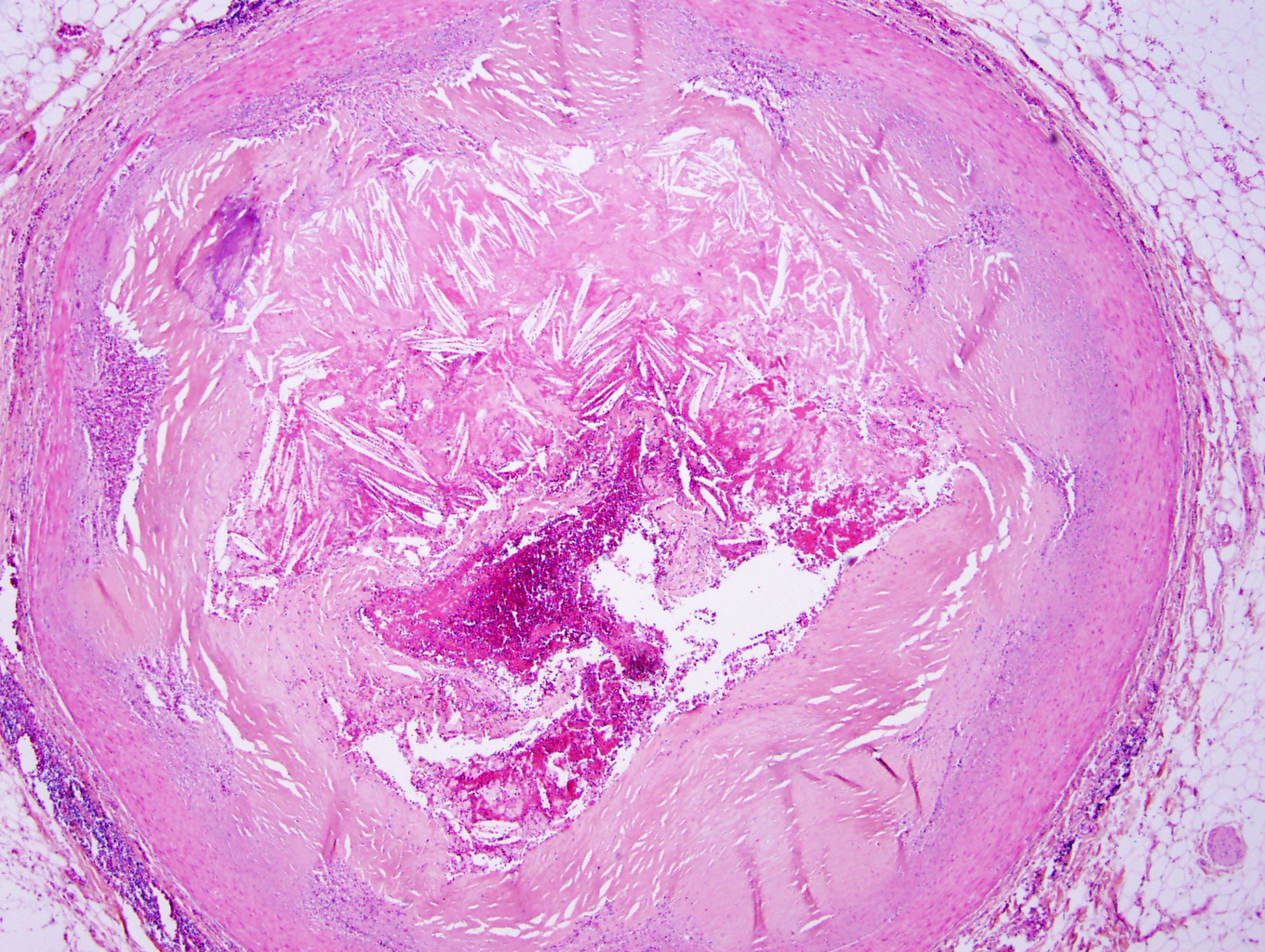
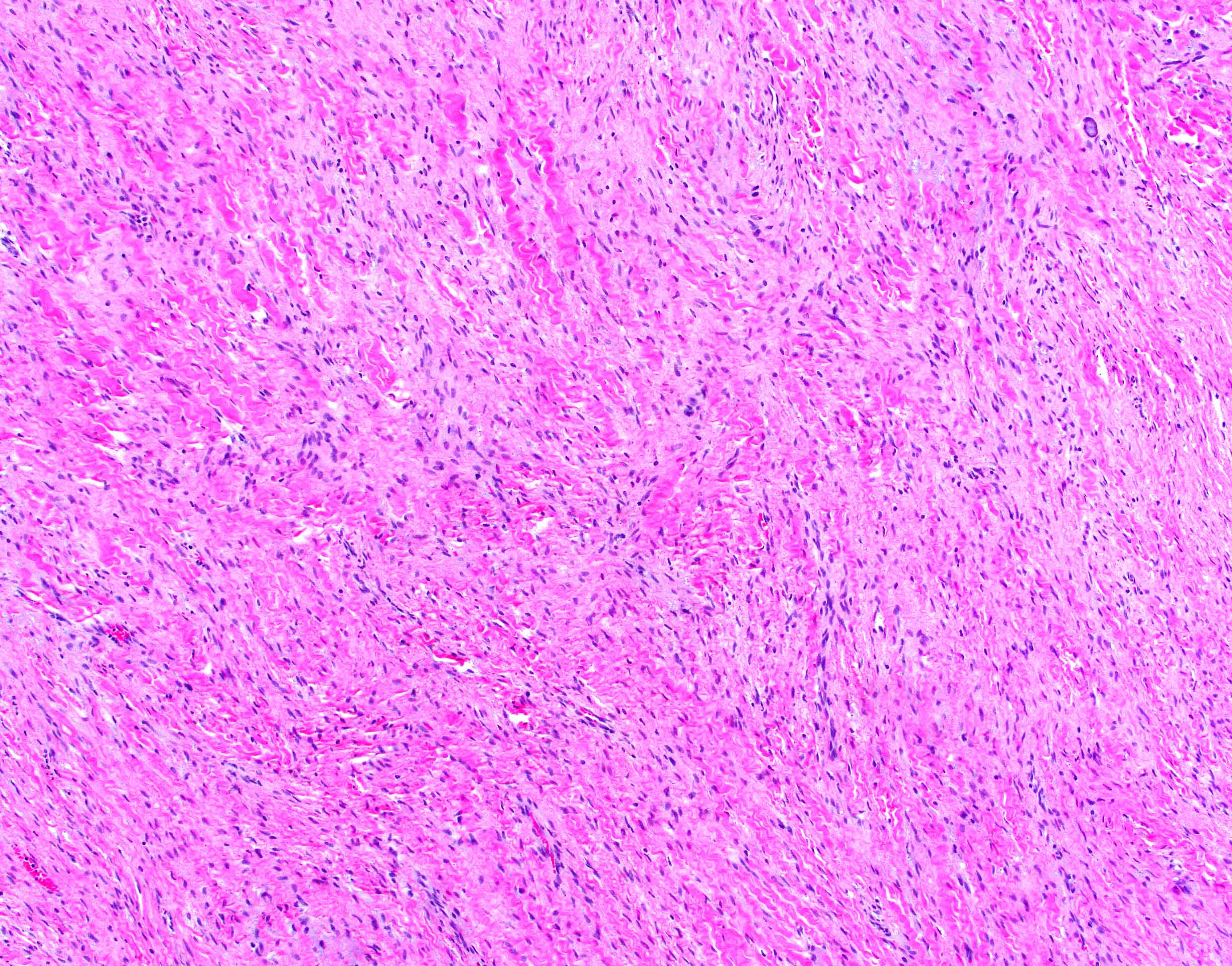
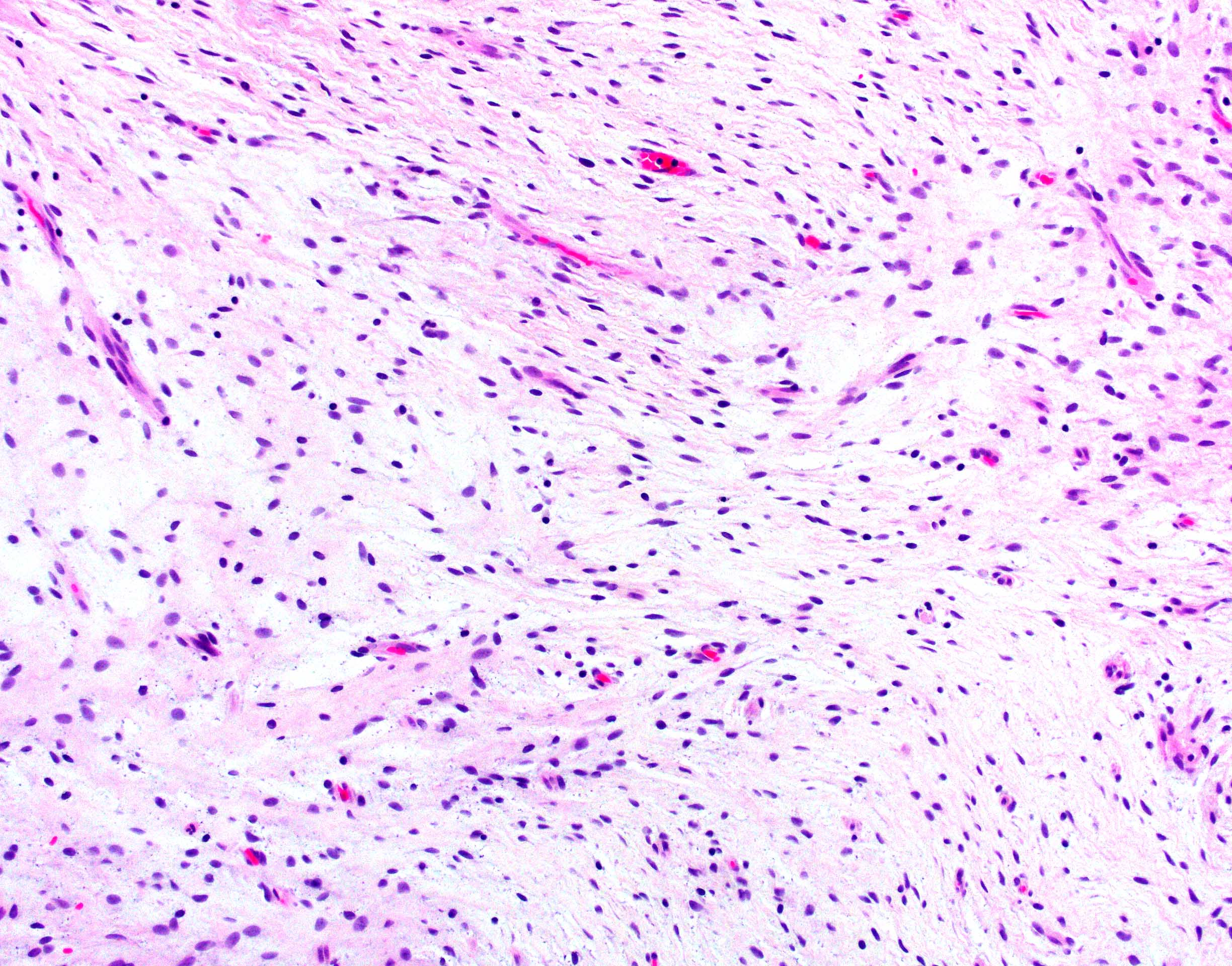
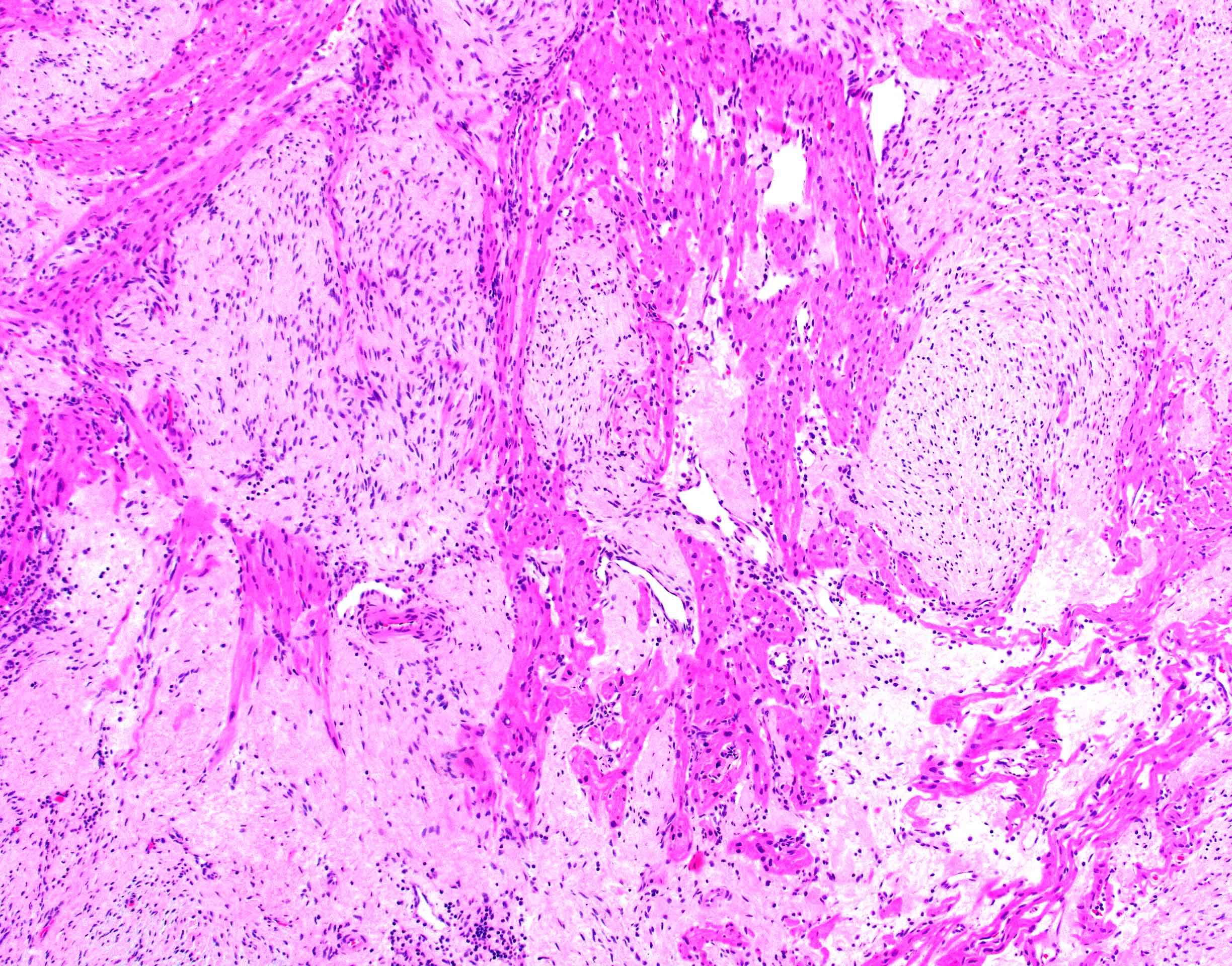
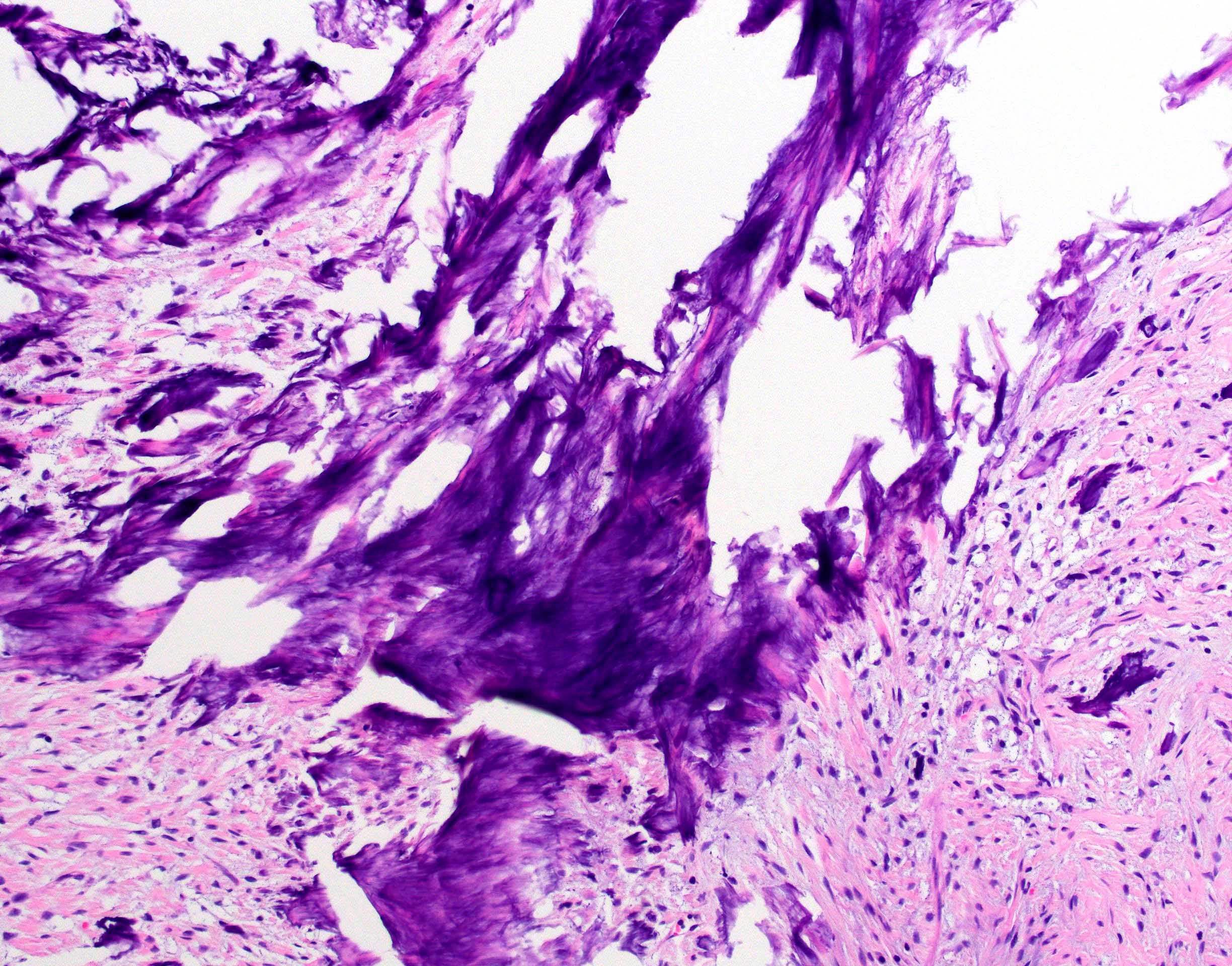
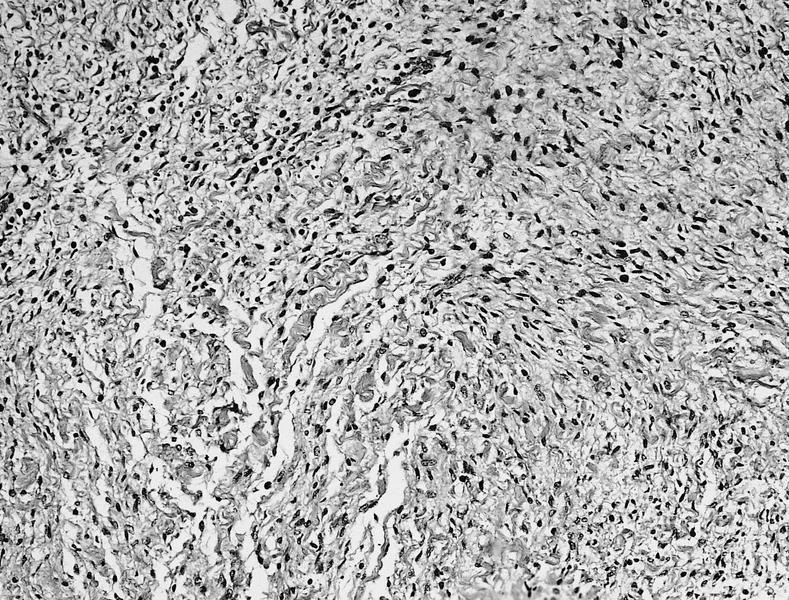
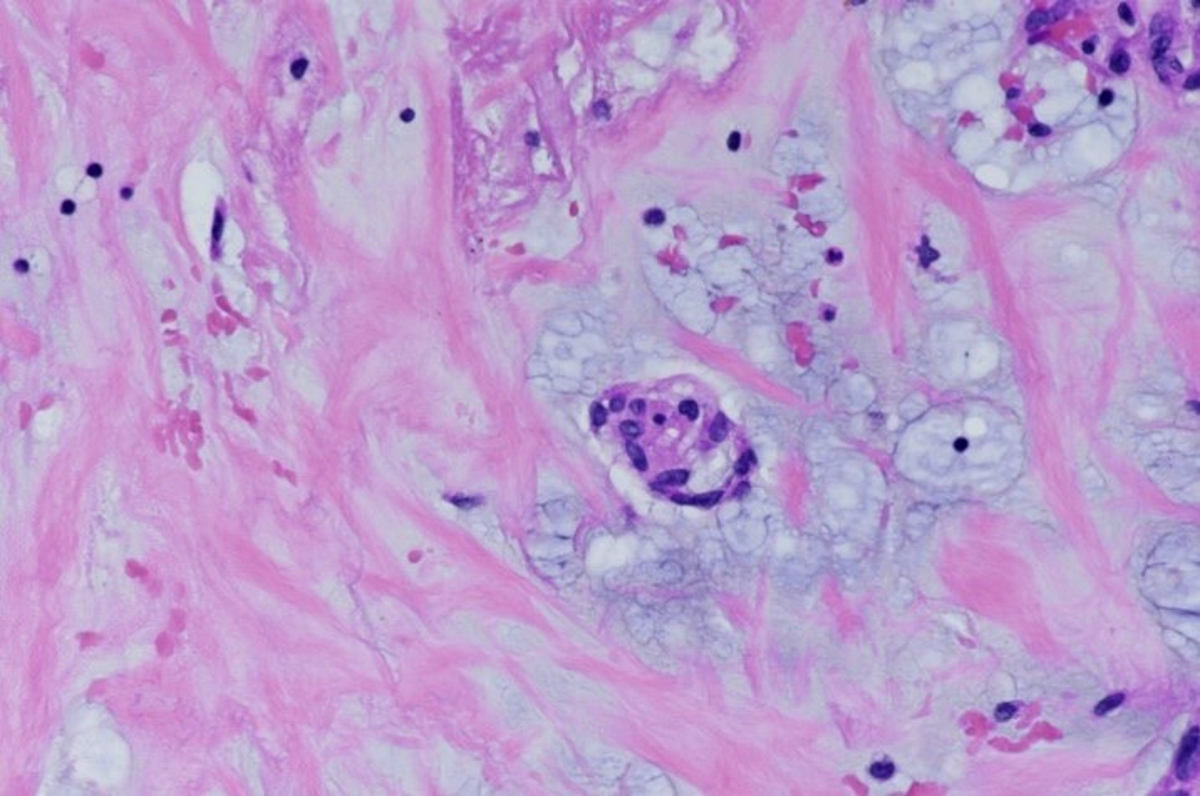
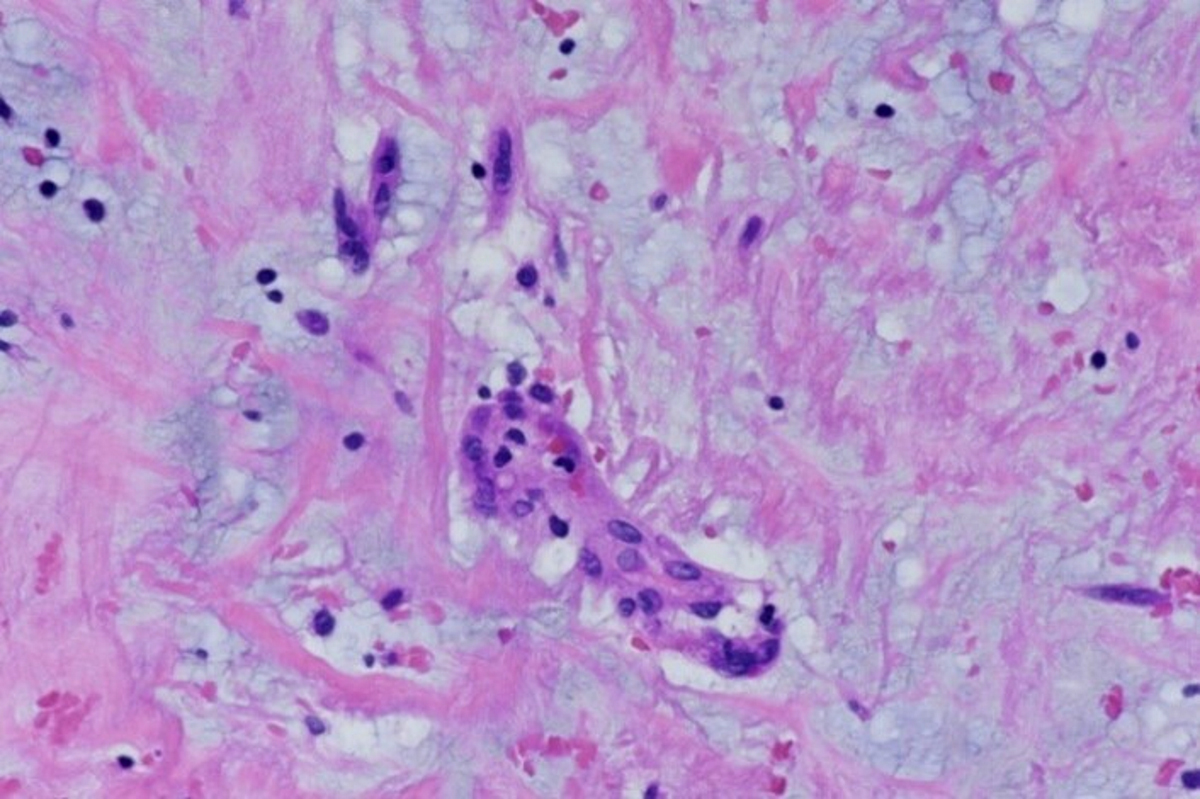
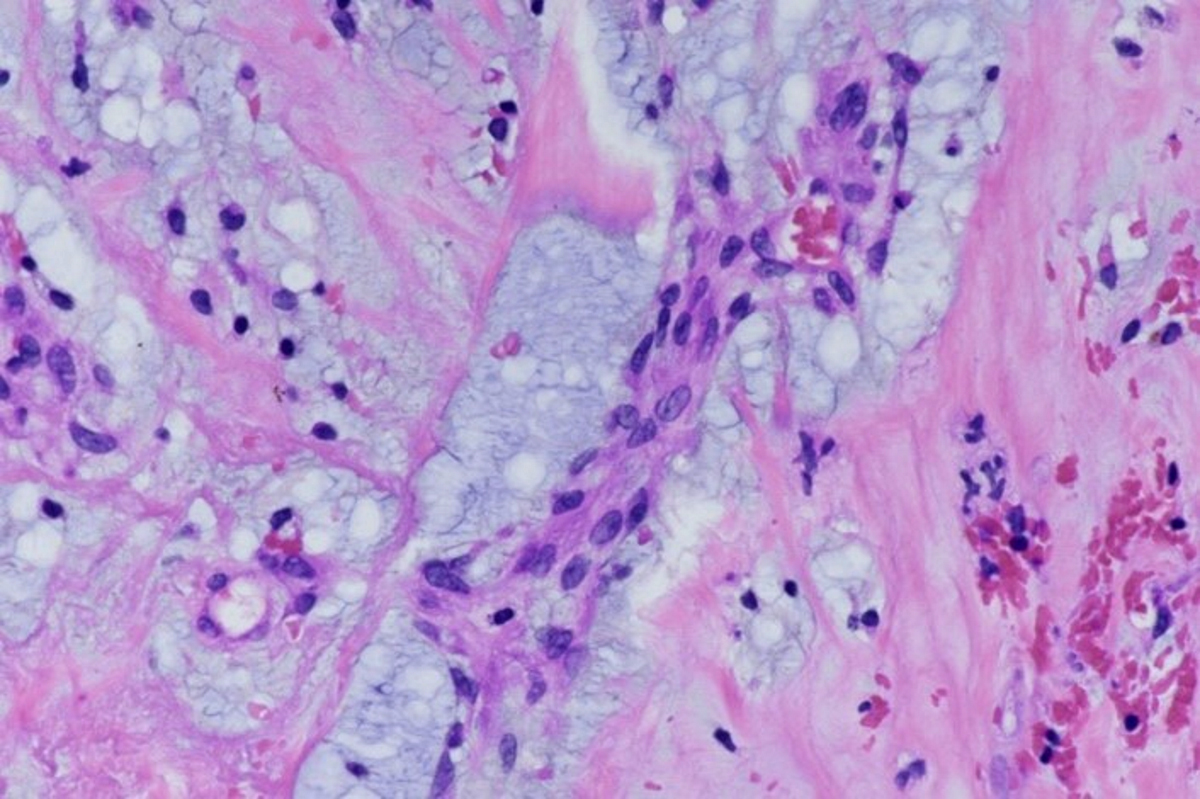
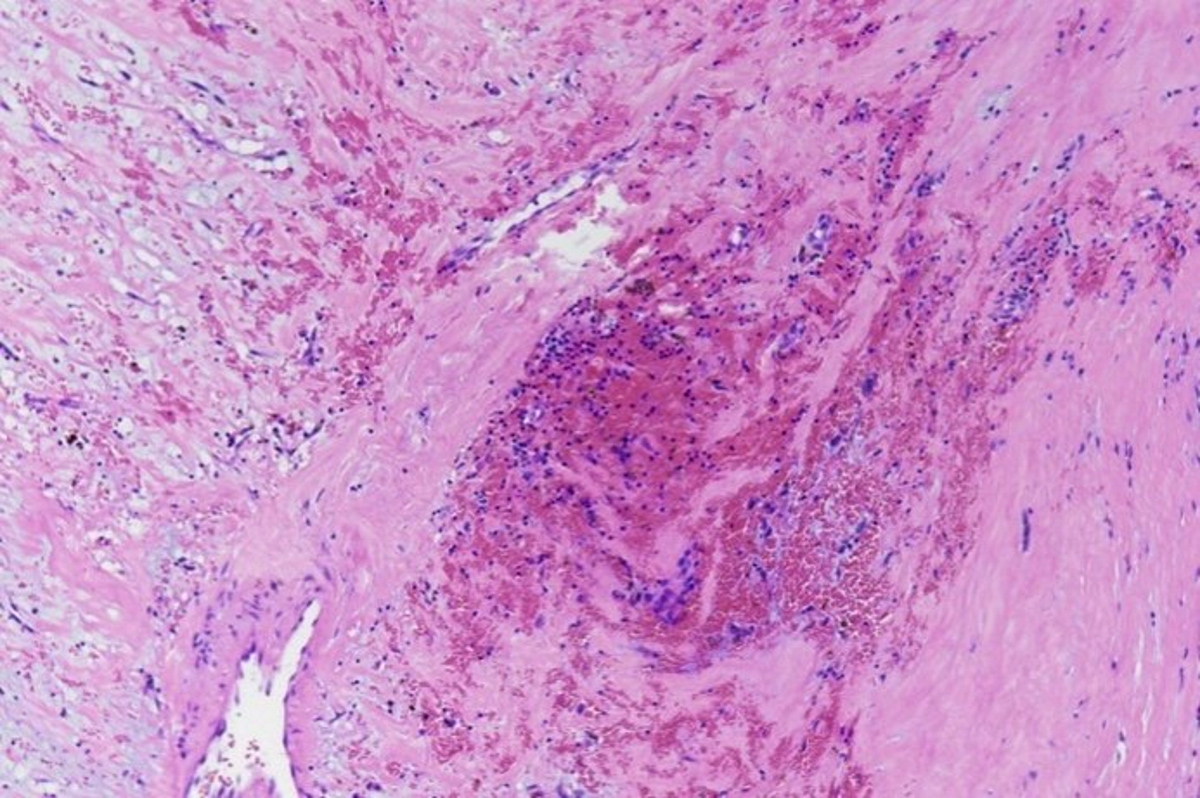
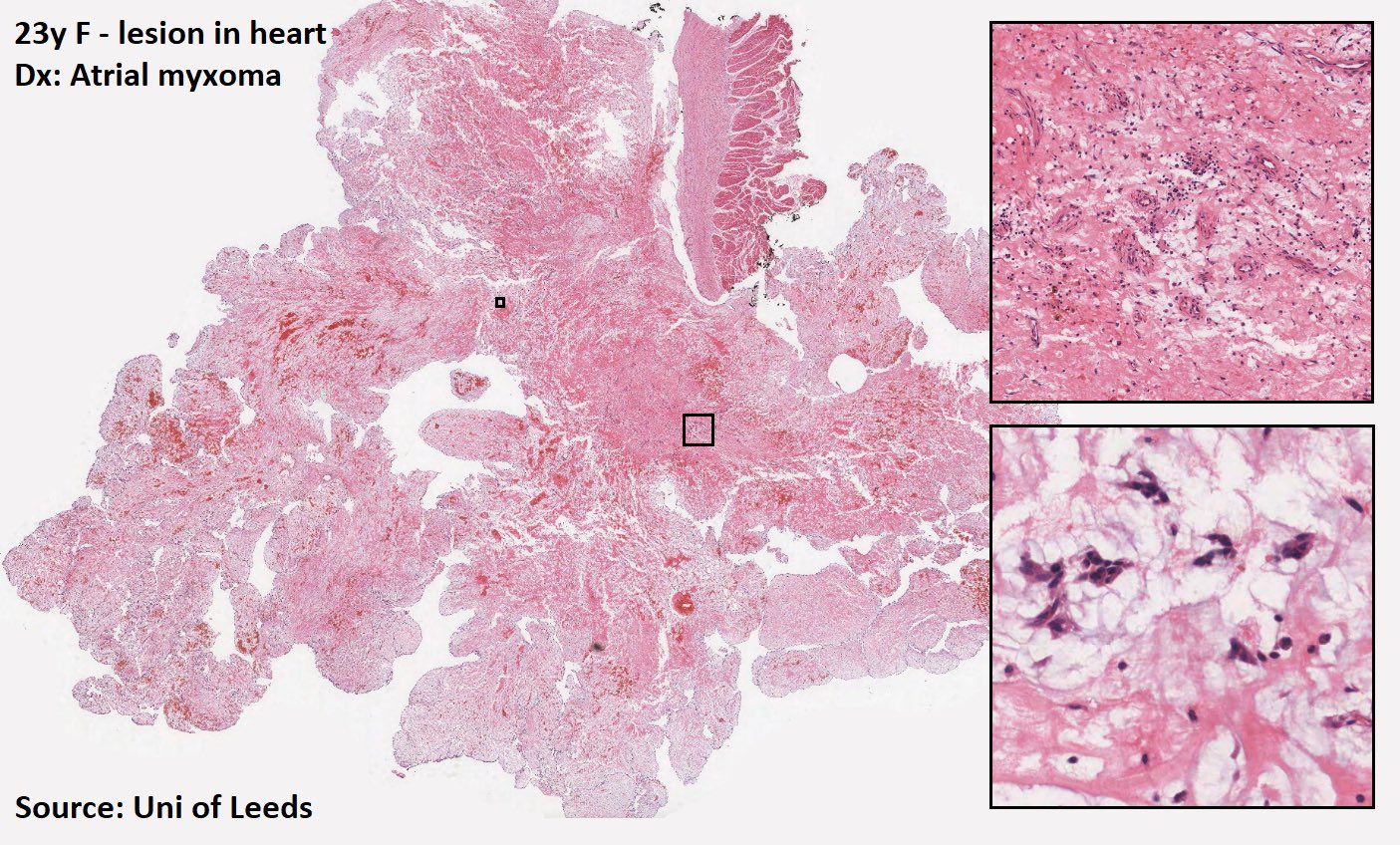
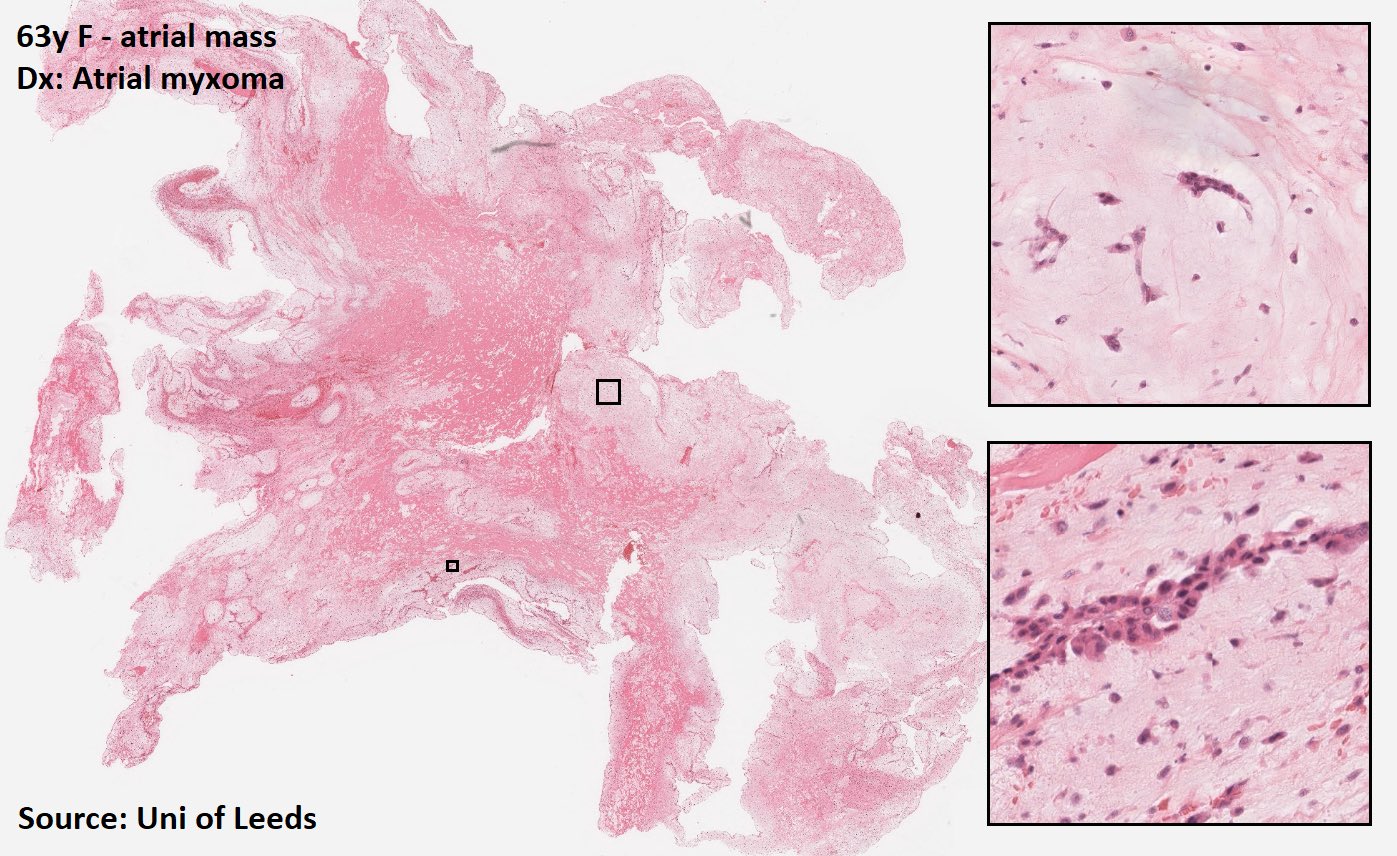
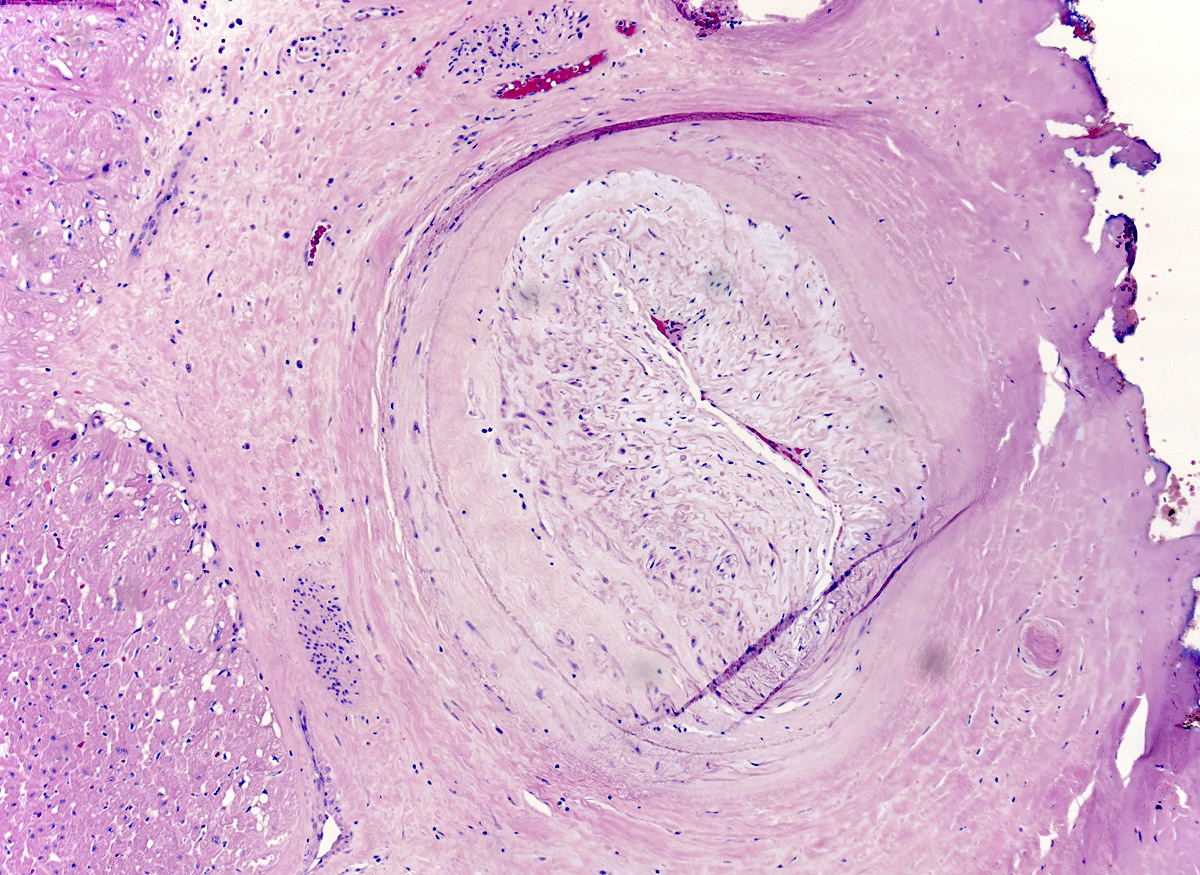
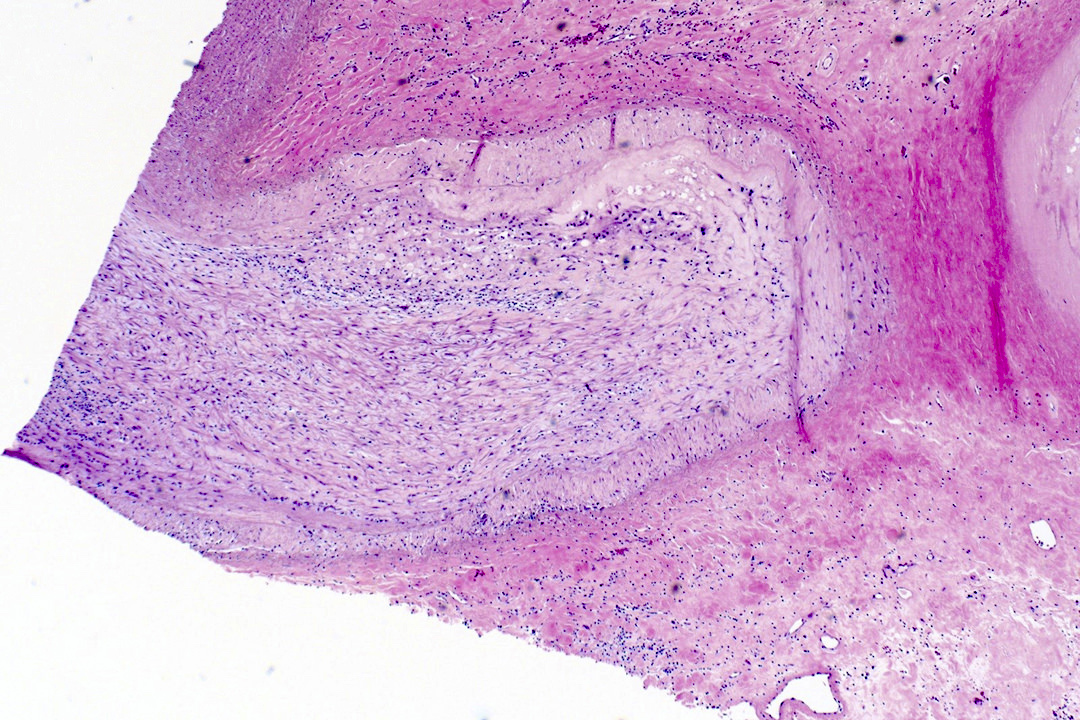
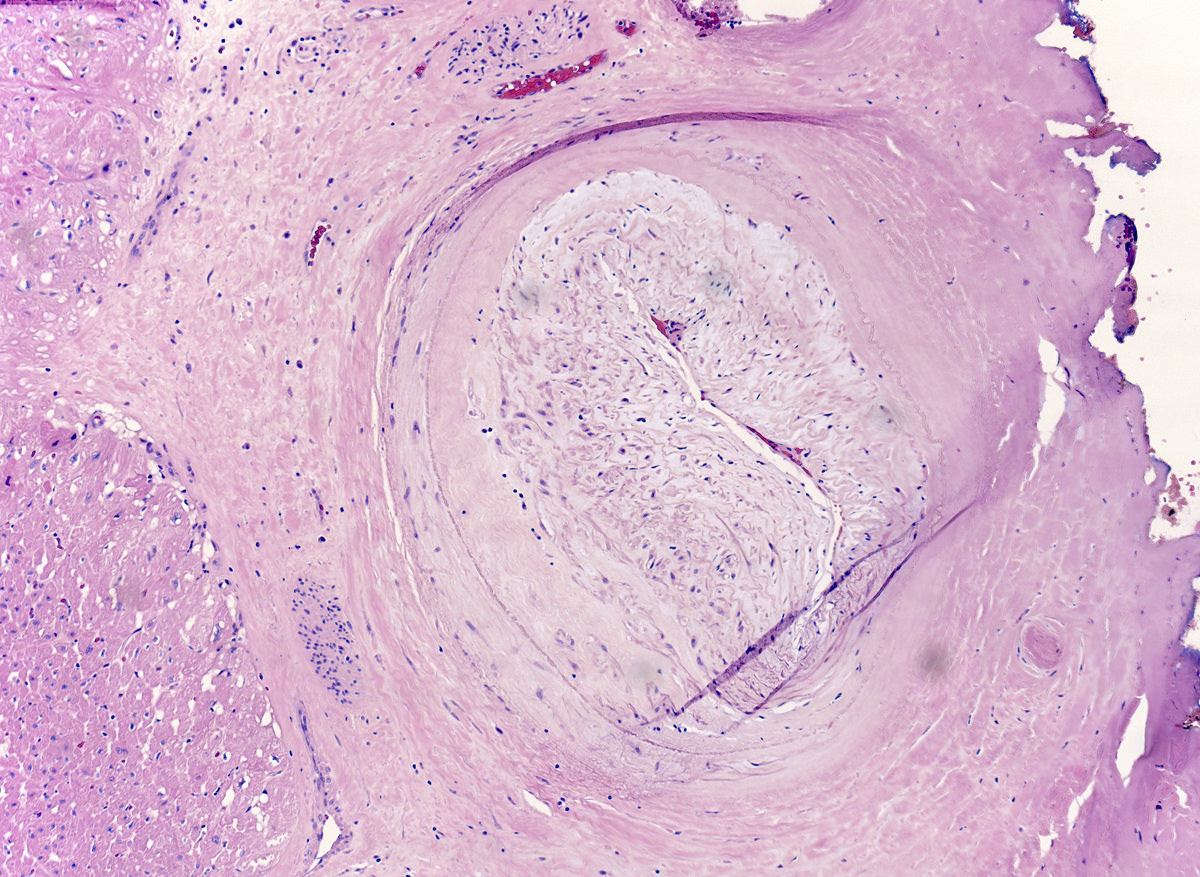
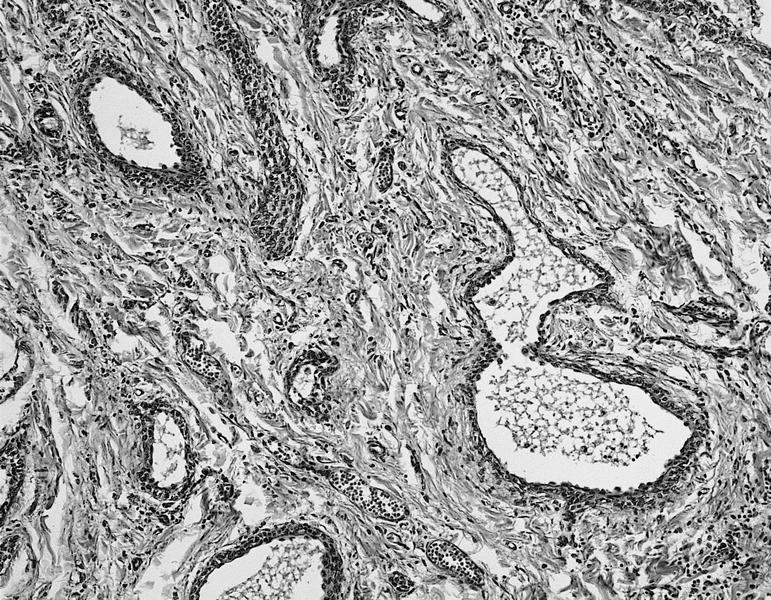
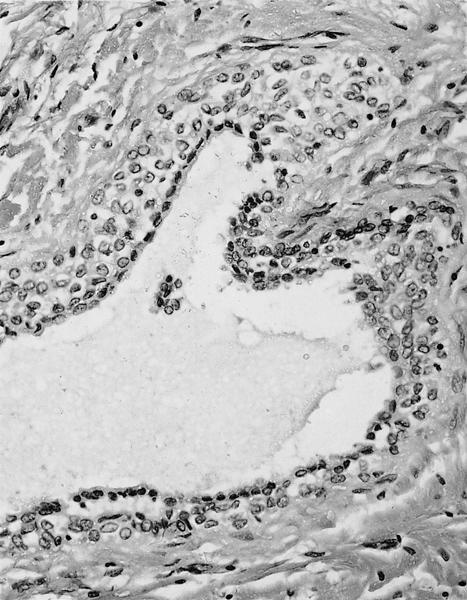
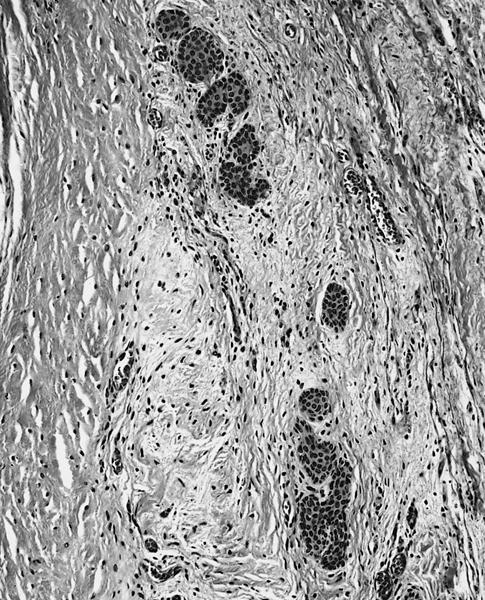
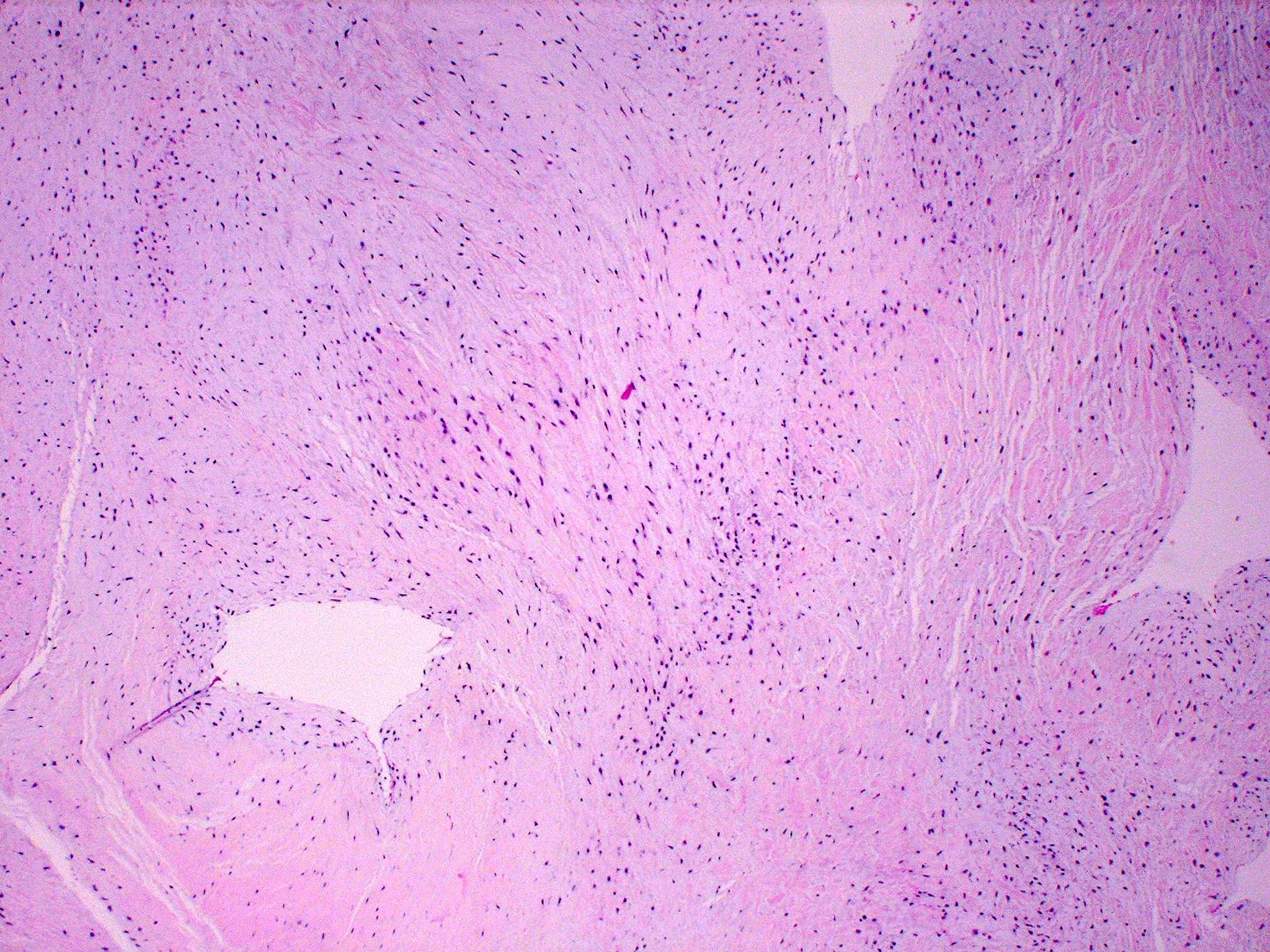
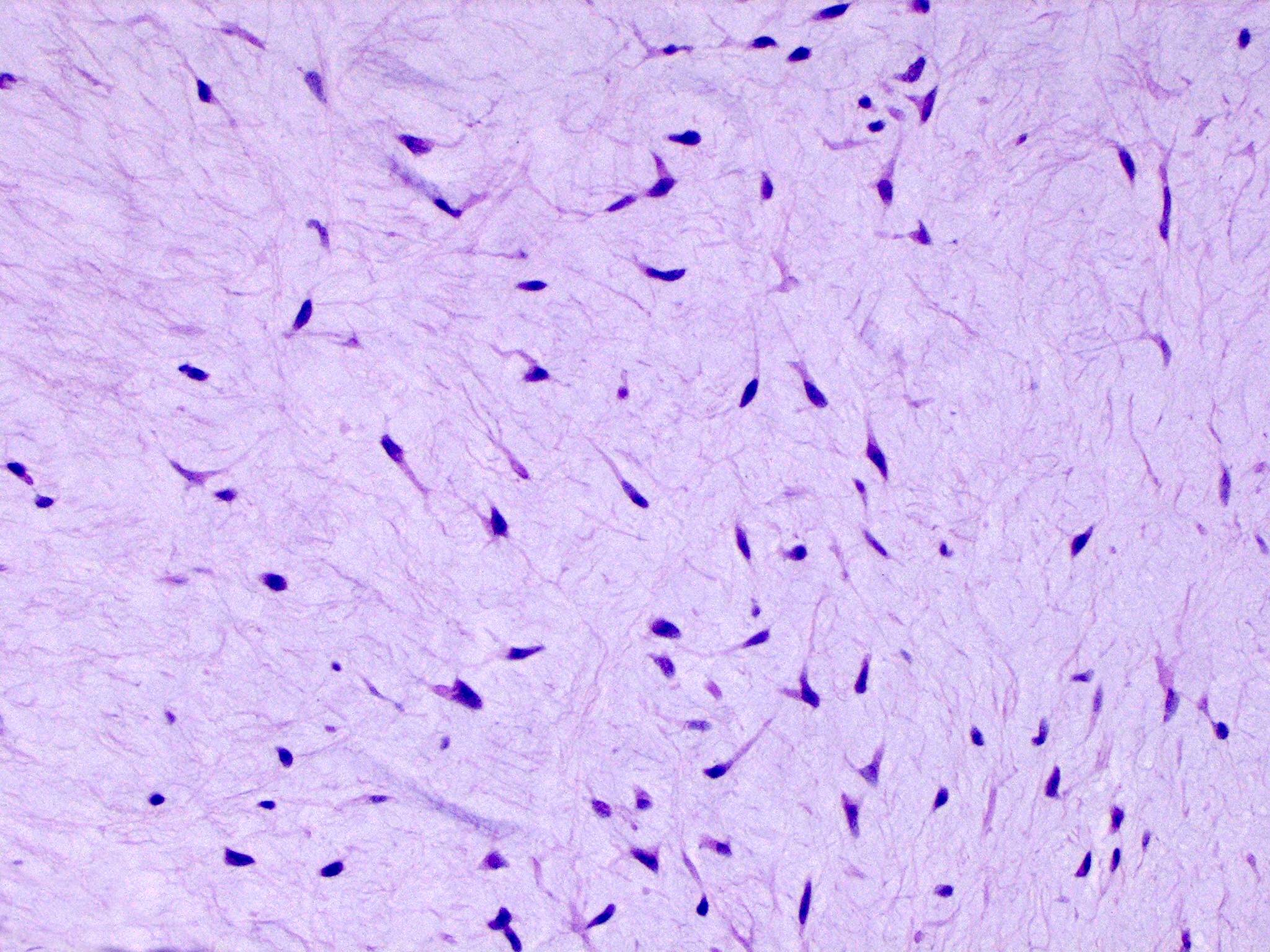
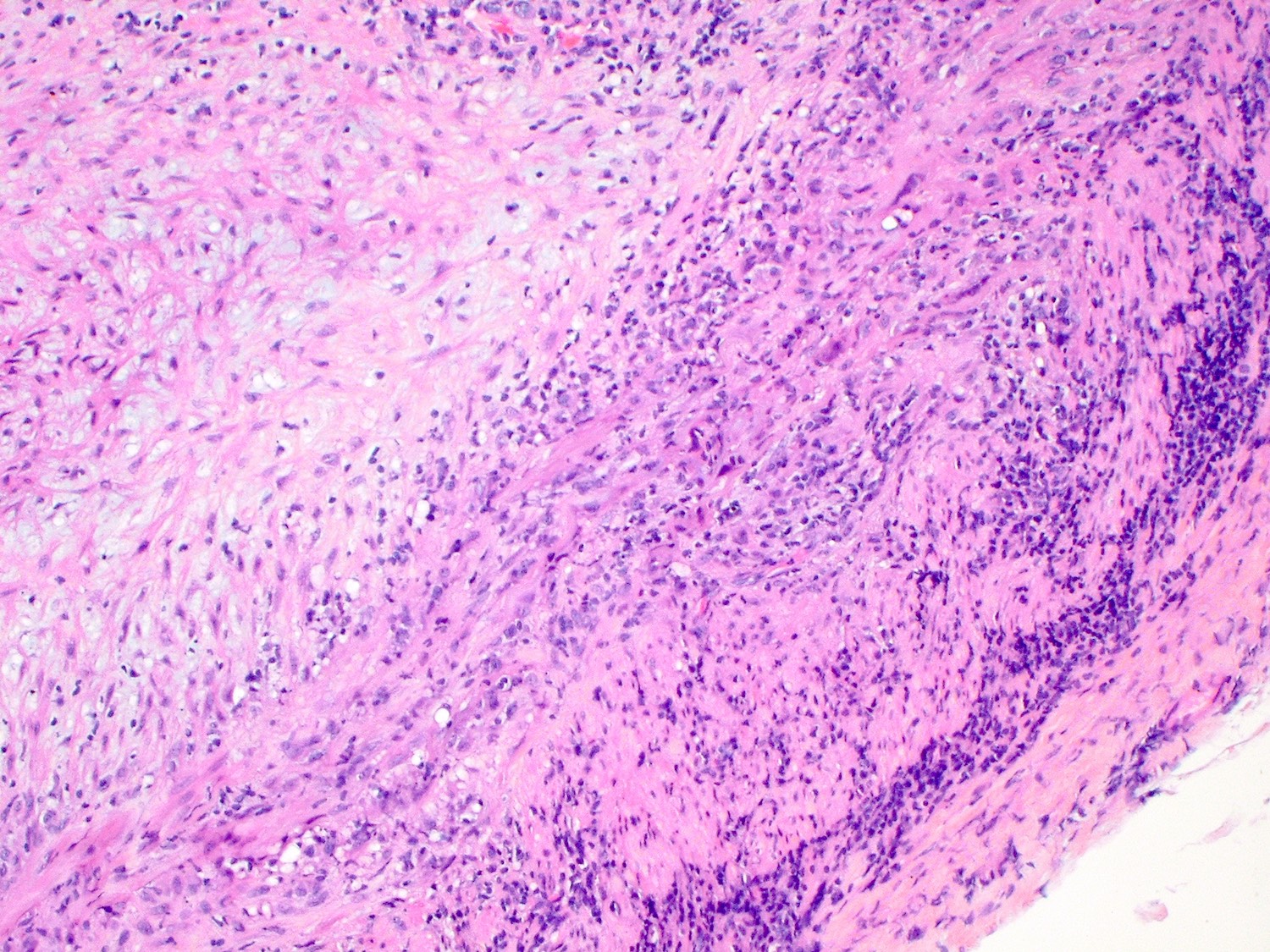
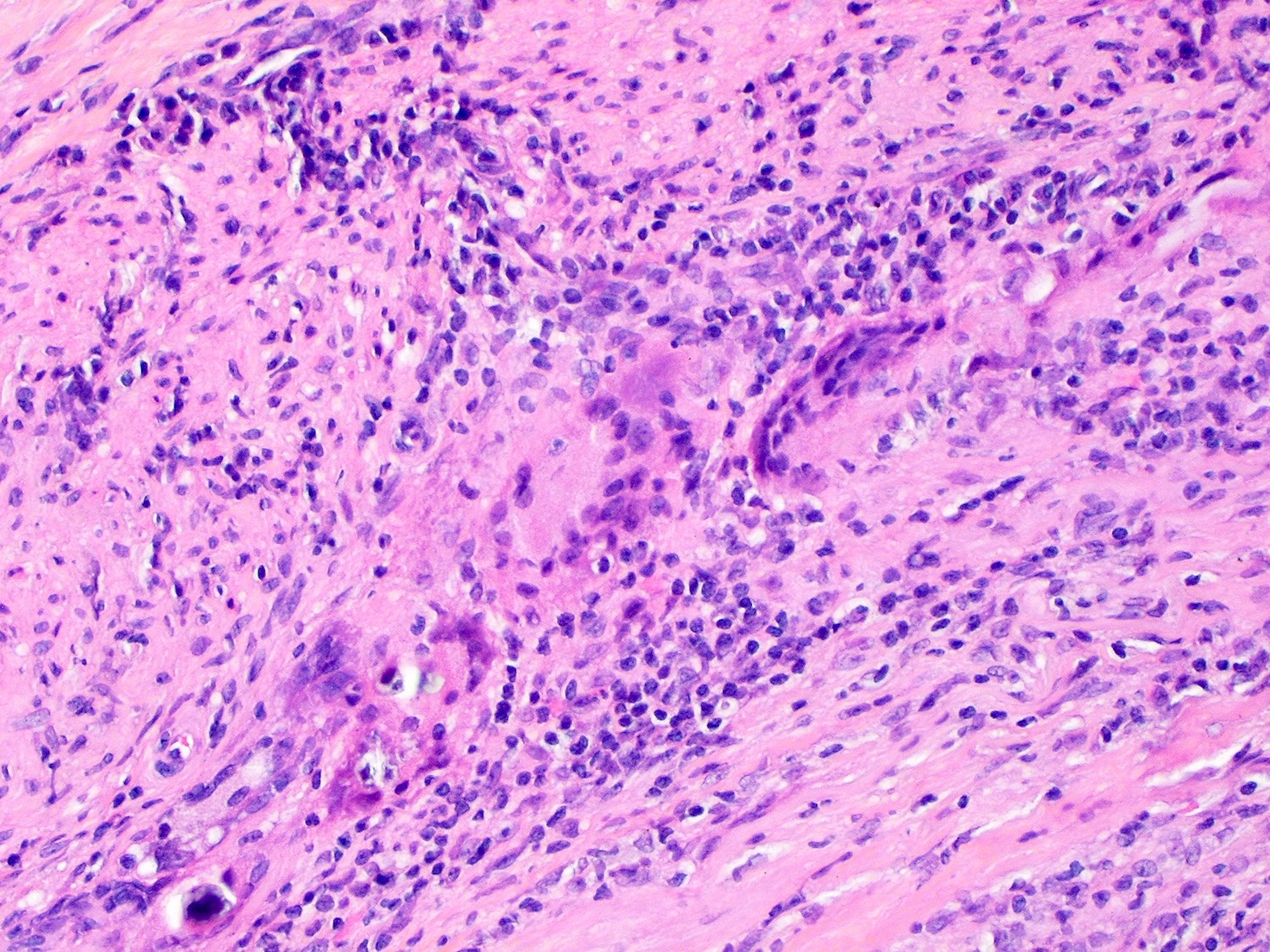
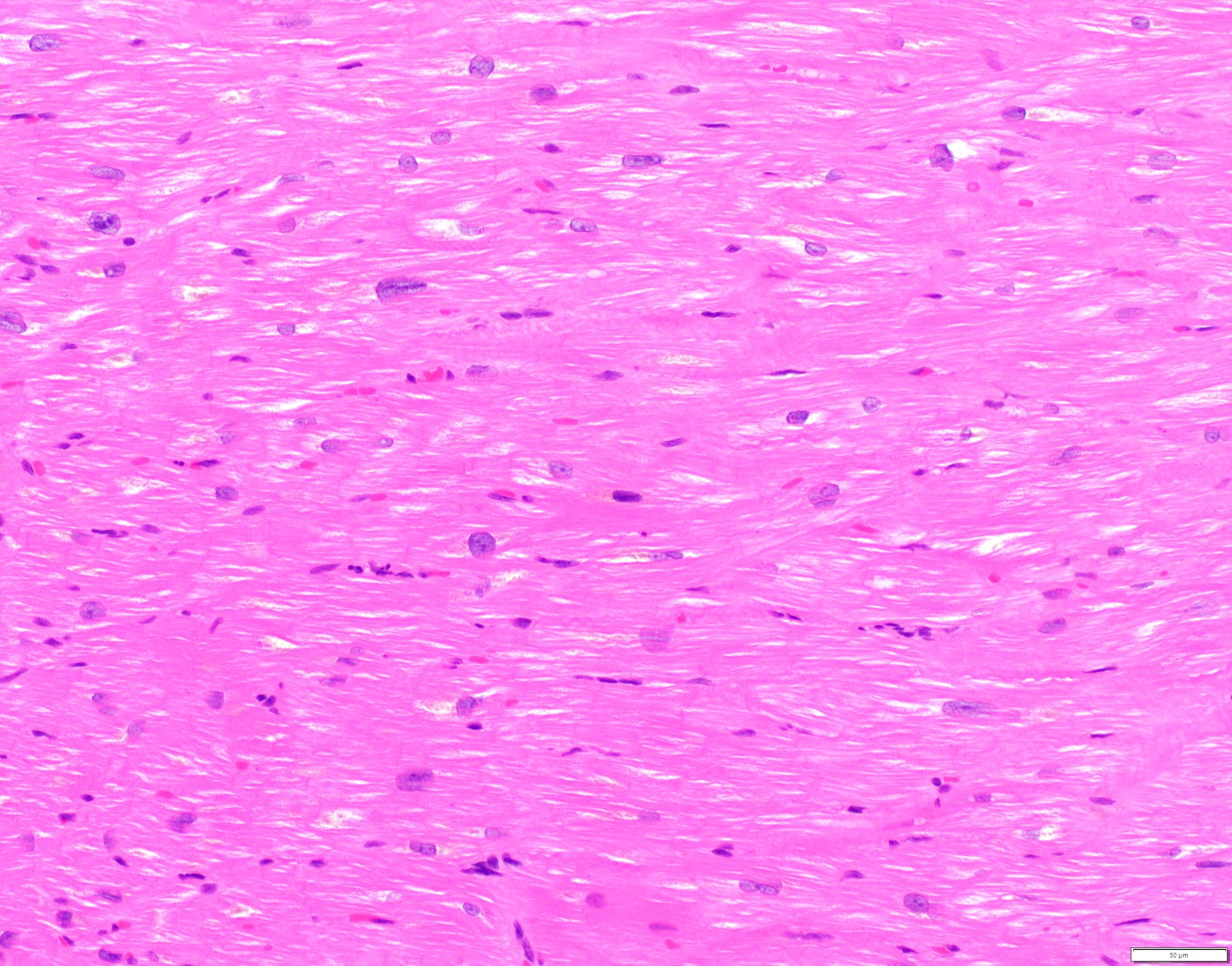
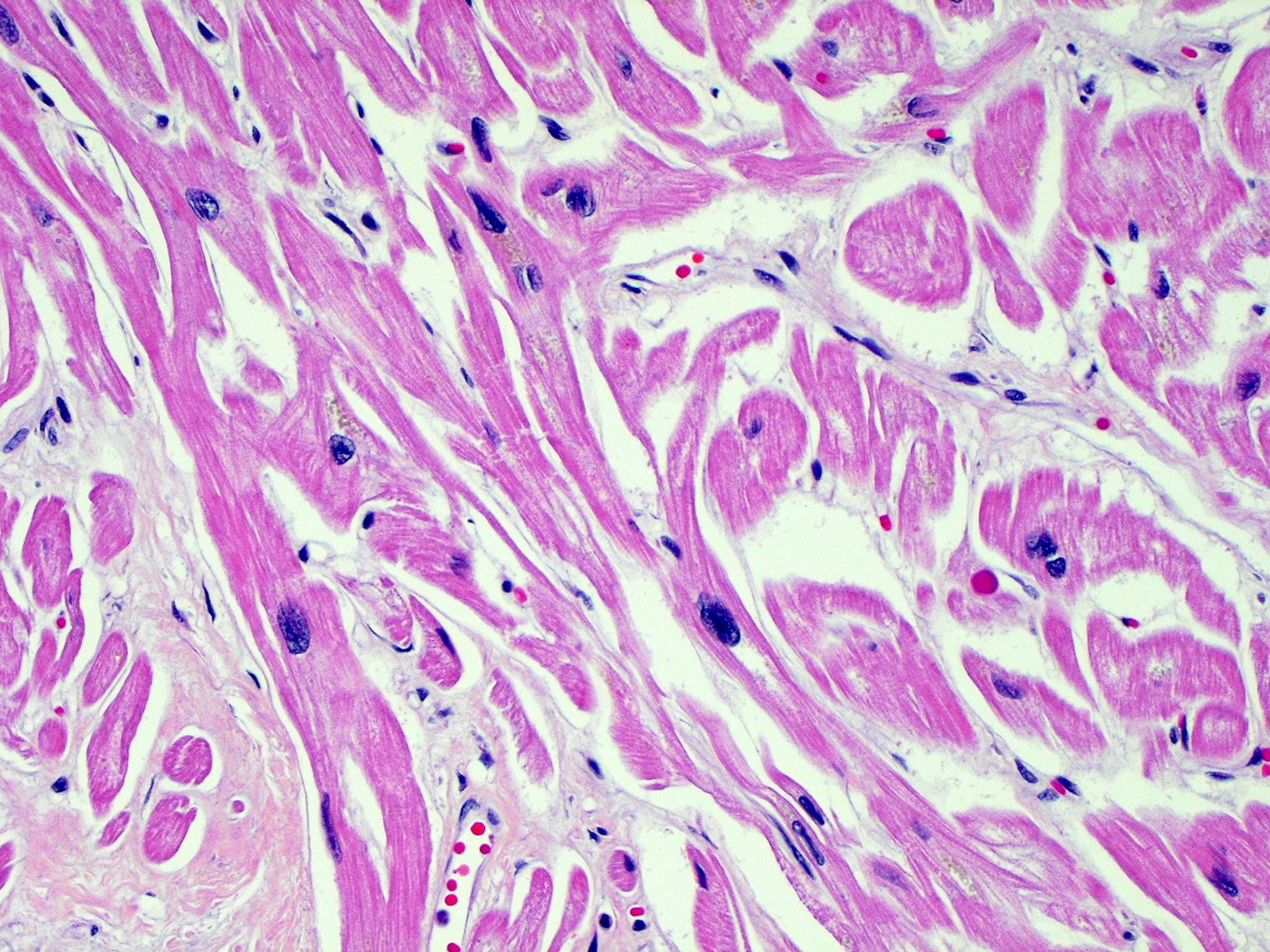
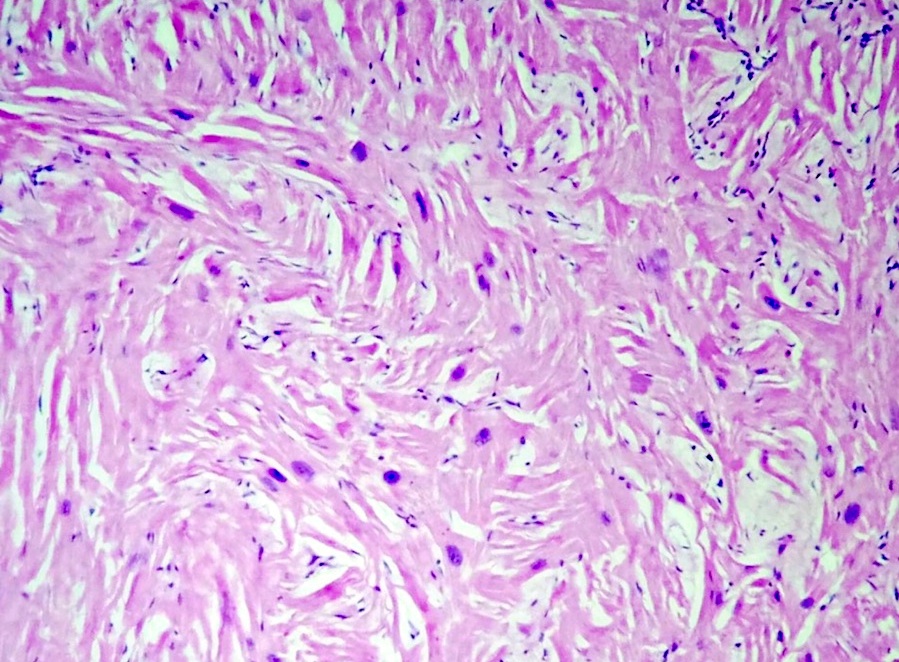
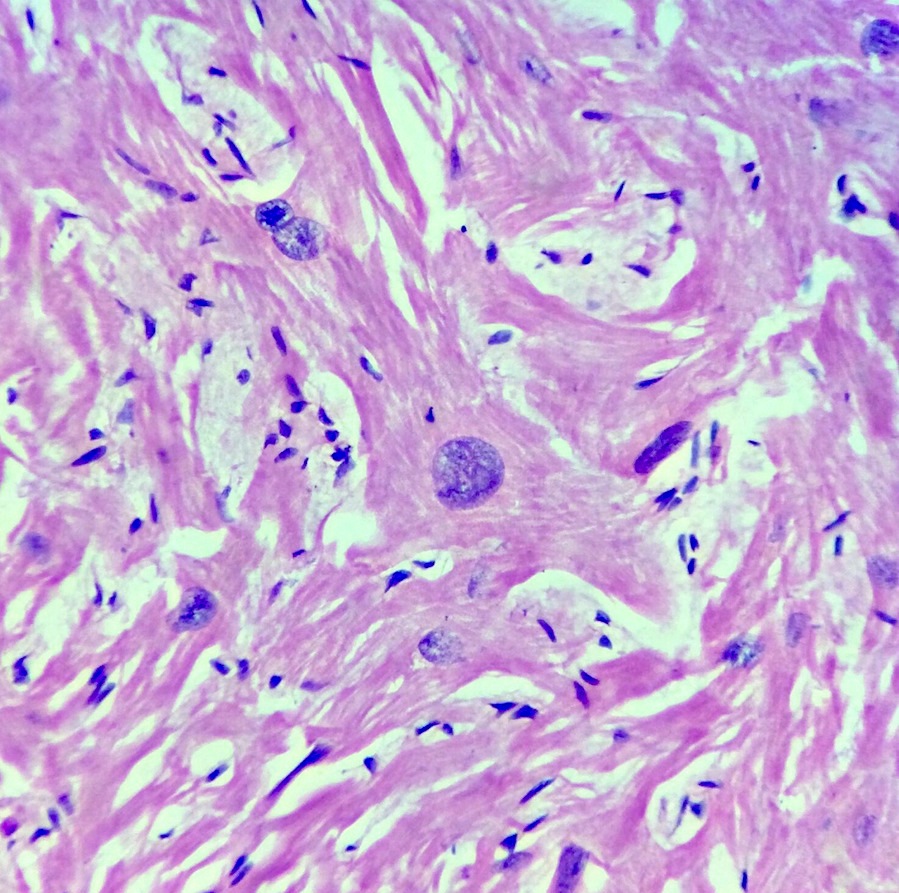
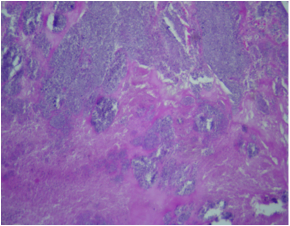
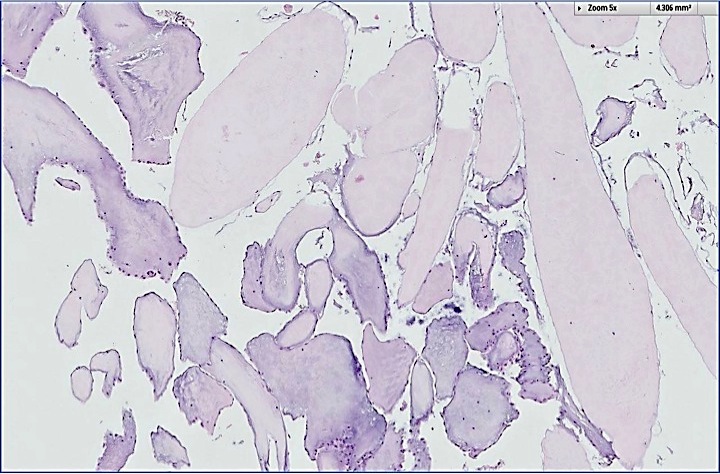
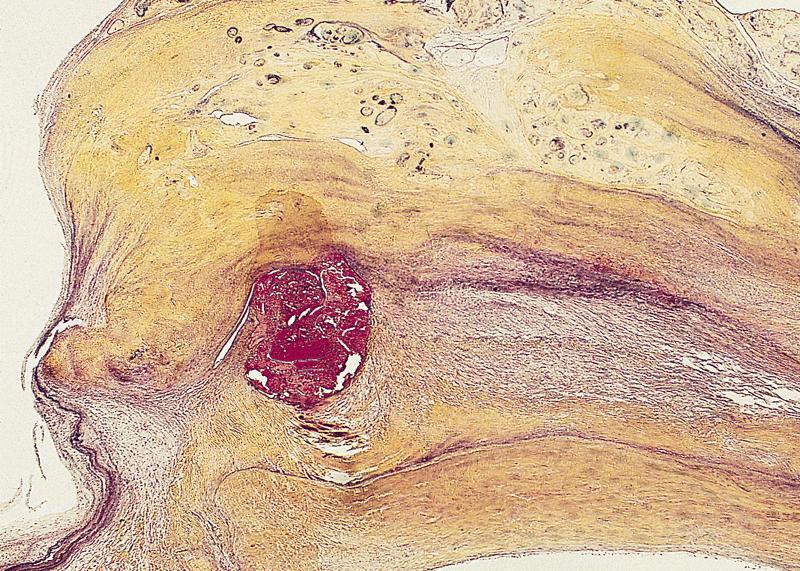
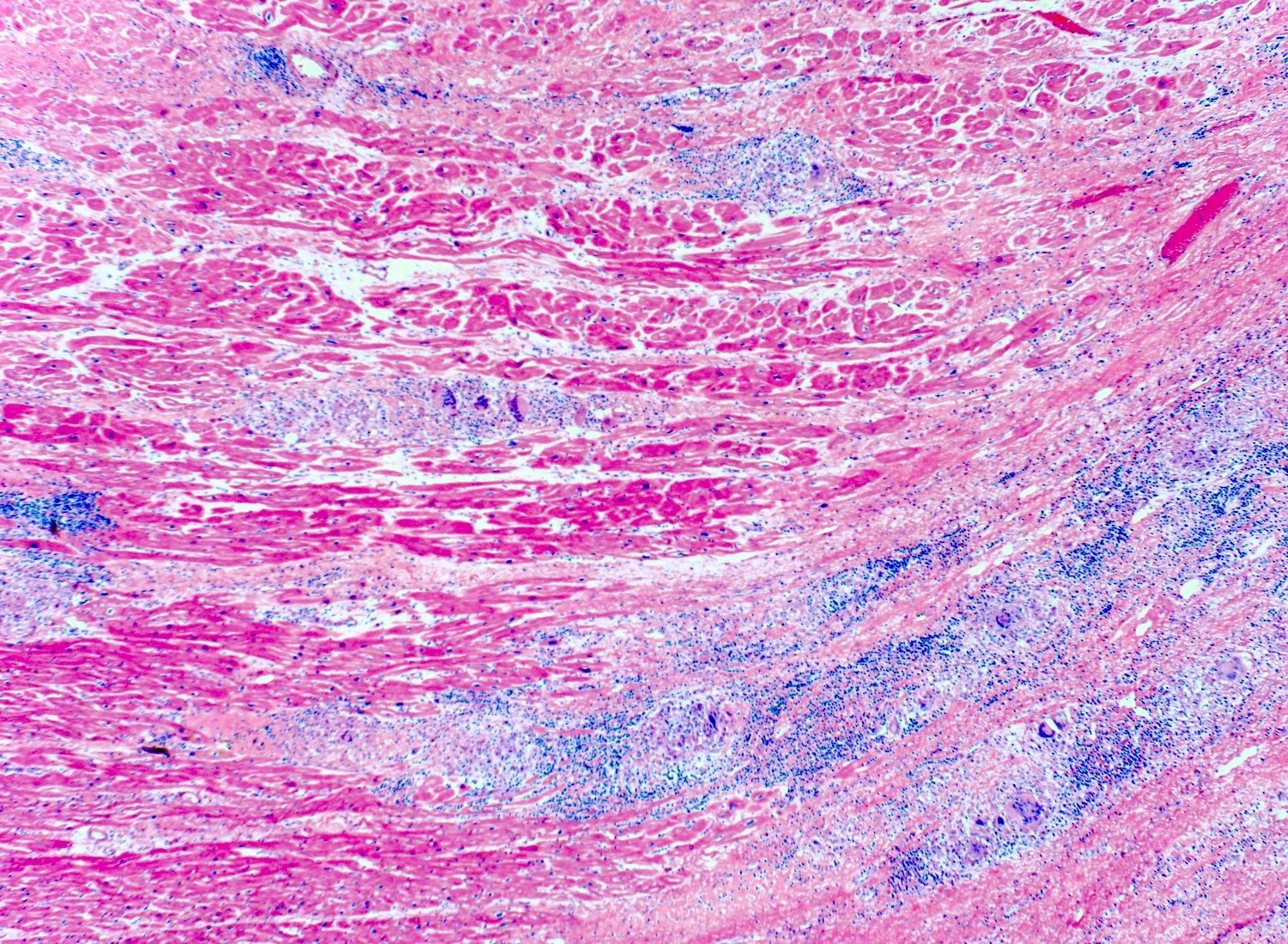
Microscopic (histologic) description
- International Society for Heart and Lung Transplantation (ISHLT) 2004 standardized endomyocardial biopsy grading (J Heart Lung Transplant 2005;24:1710):
- Grade 0R (no rejection): no evidence of cellular infiltration or myocyte damage
- Grade 1R (mild): interstitial or perivascular infiltrate with or without 1 focus of myocyte damage
- Grade 2R (moderate): ≥ 2 foci of infiltrate with associated myocyte damage
- Grade 3R (severe): diffuse infiltrate with multifocal myocyte damage variable edema, vasculitis and interstitial hemorrhage
- Inflammatory infiltrate: lymphocytes variable macrophages and eosinophils
- Neutrophils generally absent except in severe cases
- Presence of plasma cells suggests an alternative etiology
- Inflammatory infiltrate is usually proportionally greater than the degree of myocyte damage
- Myocyte damage and encroachment of inflammatory cells (→ irregular myocyte borders and distorted myocardial architecture)
- Mild: myocytolysis (sarcoplasmic / nuclear clearing, nuclear enlargement, prominent nucleoli)
- Severe: contraction band or coagulation necrosis
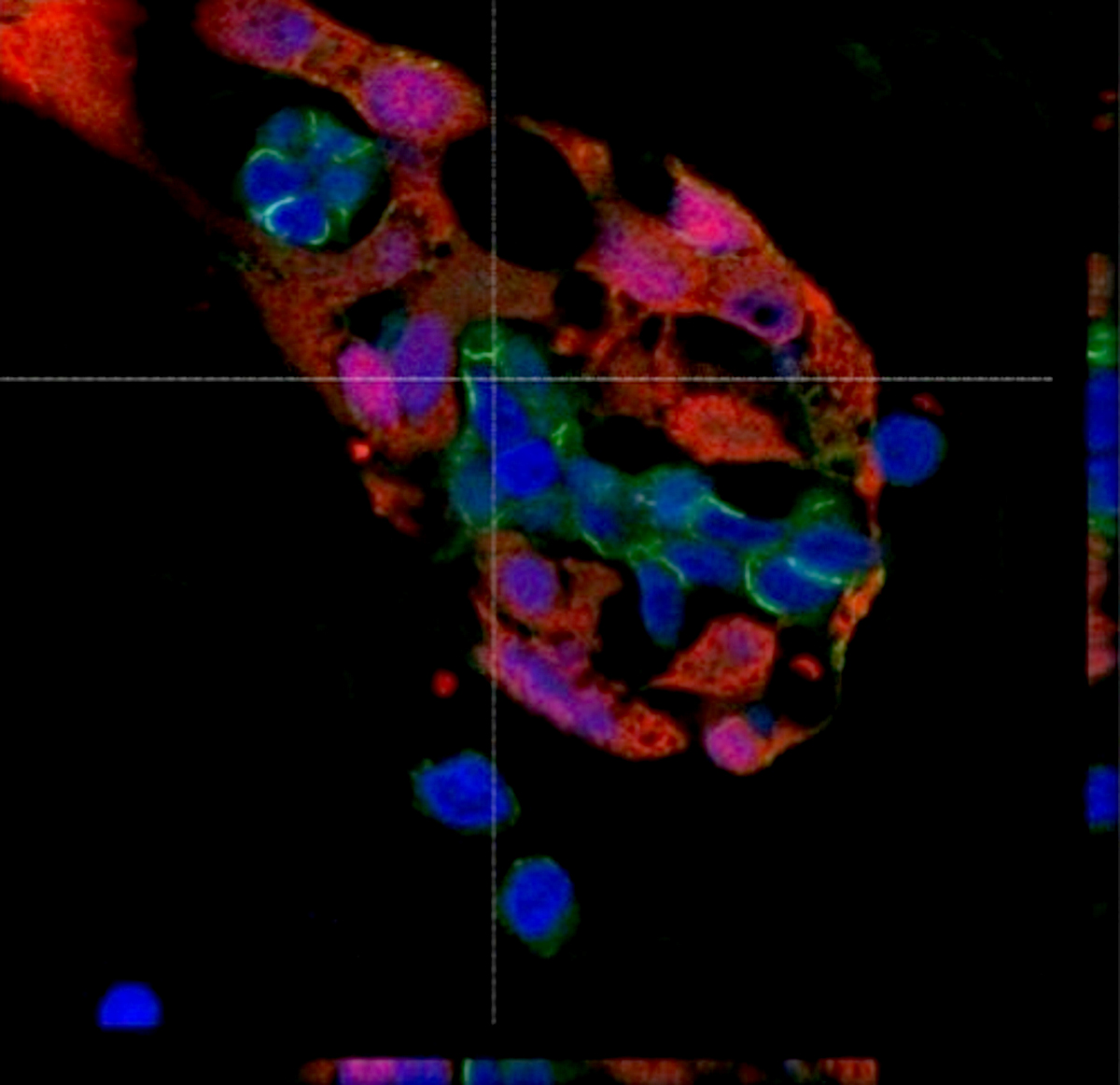
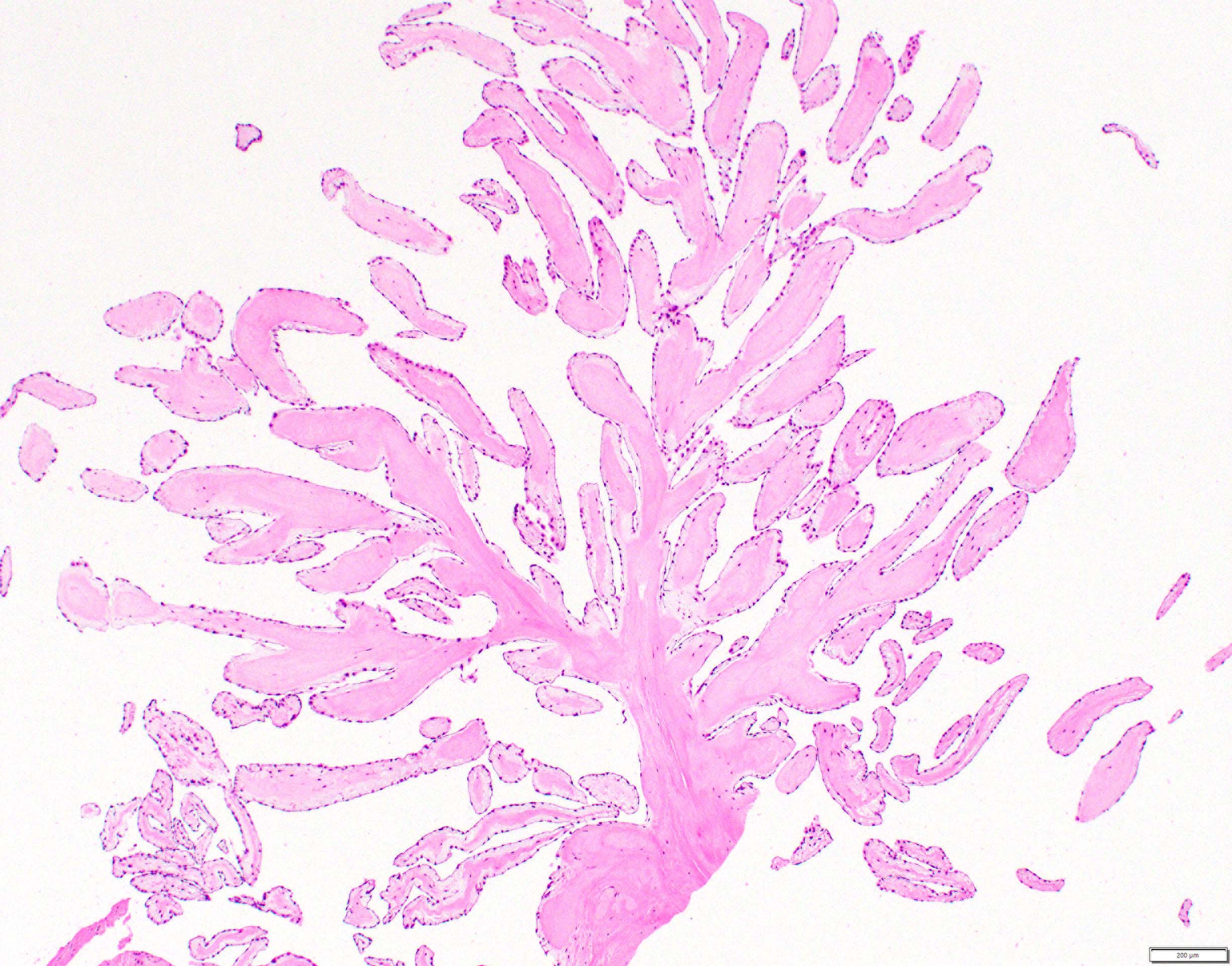
Microscopic (histologic) images
Virtual slides
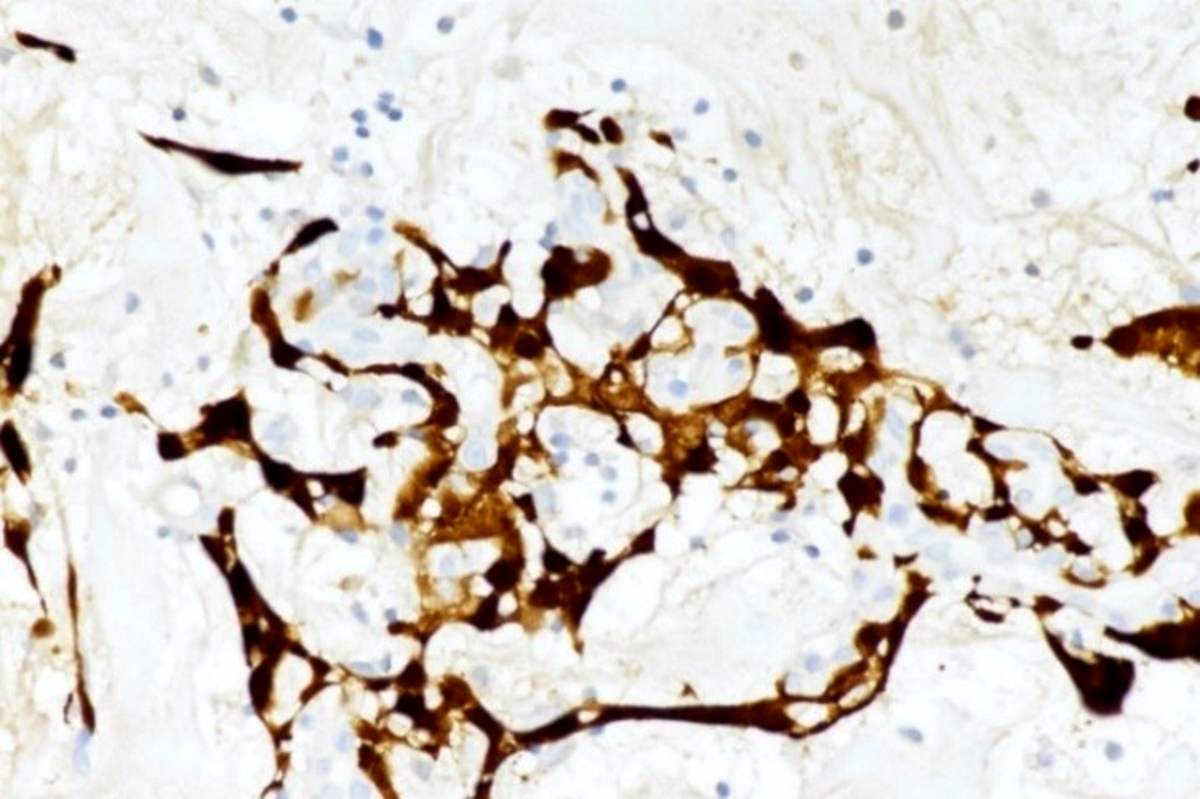
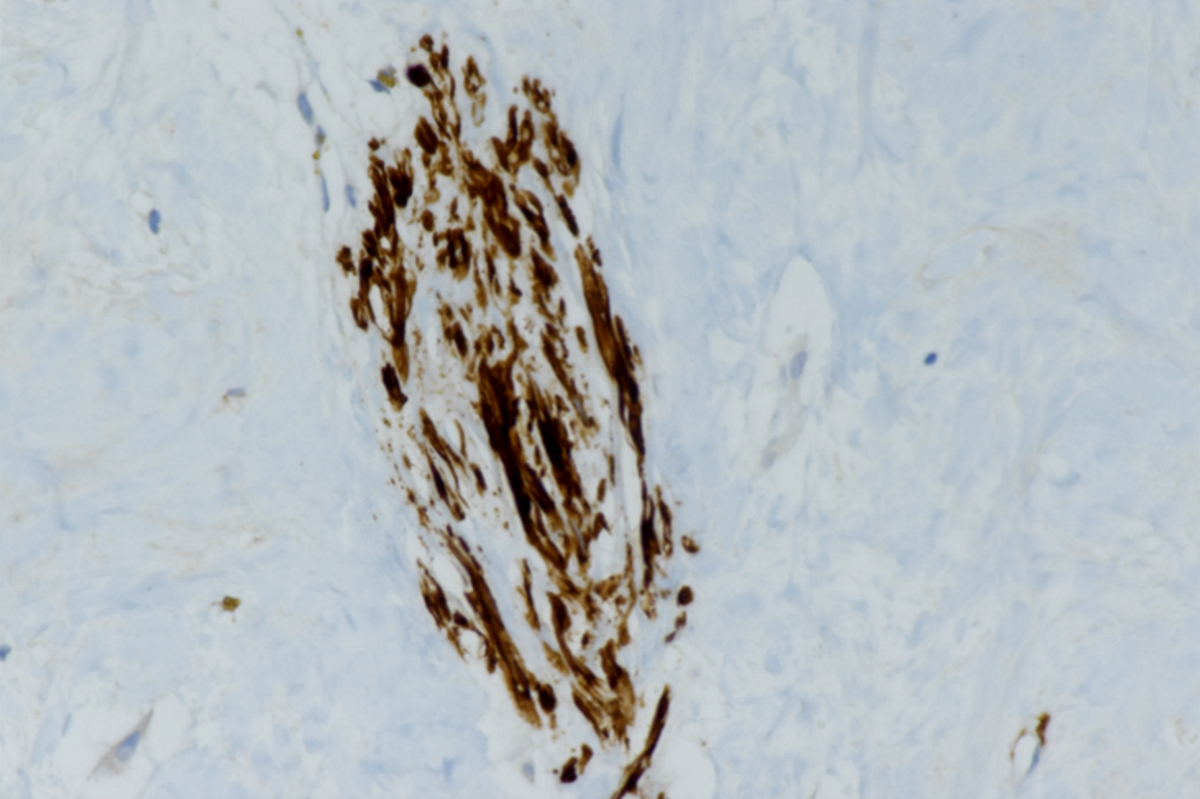
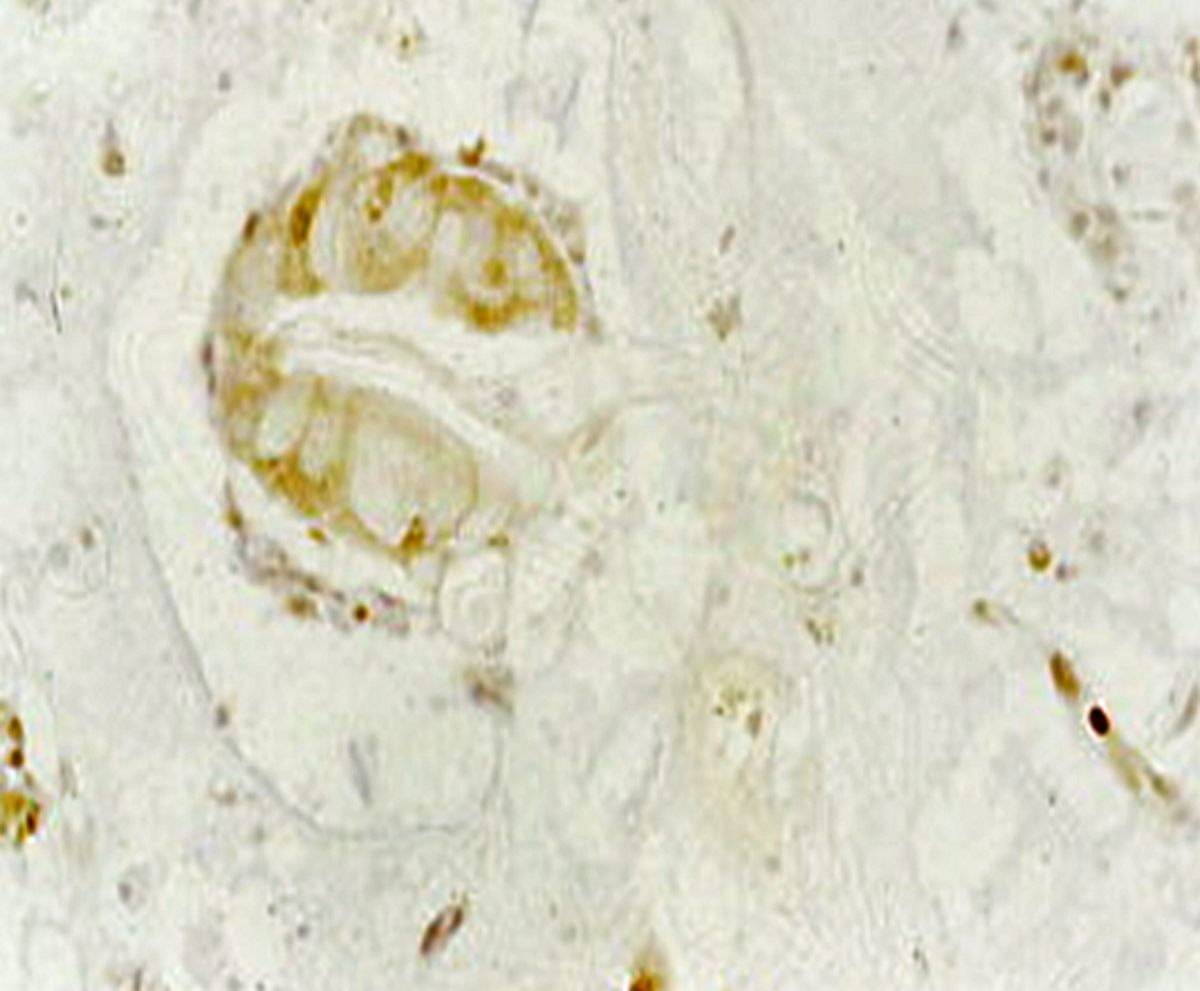
Positive stains
- CD3, CD4 and CD8 positive T lymphocytes within inflammatory infiltrate
- Increased intercellular adhesion molecules with high MHC class II expression on cardiac myocytes (Ludhwani: StatPearls, 2019)
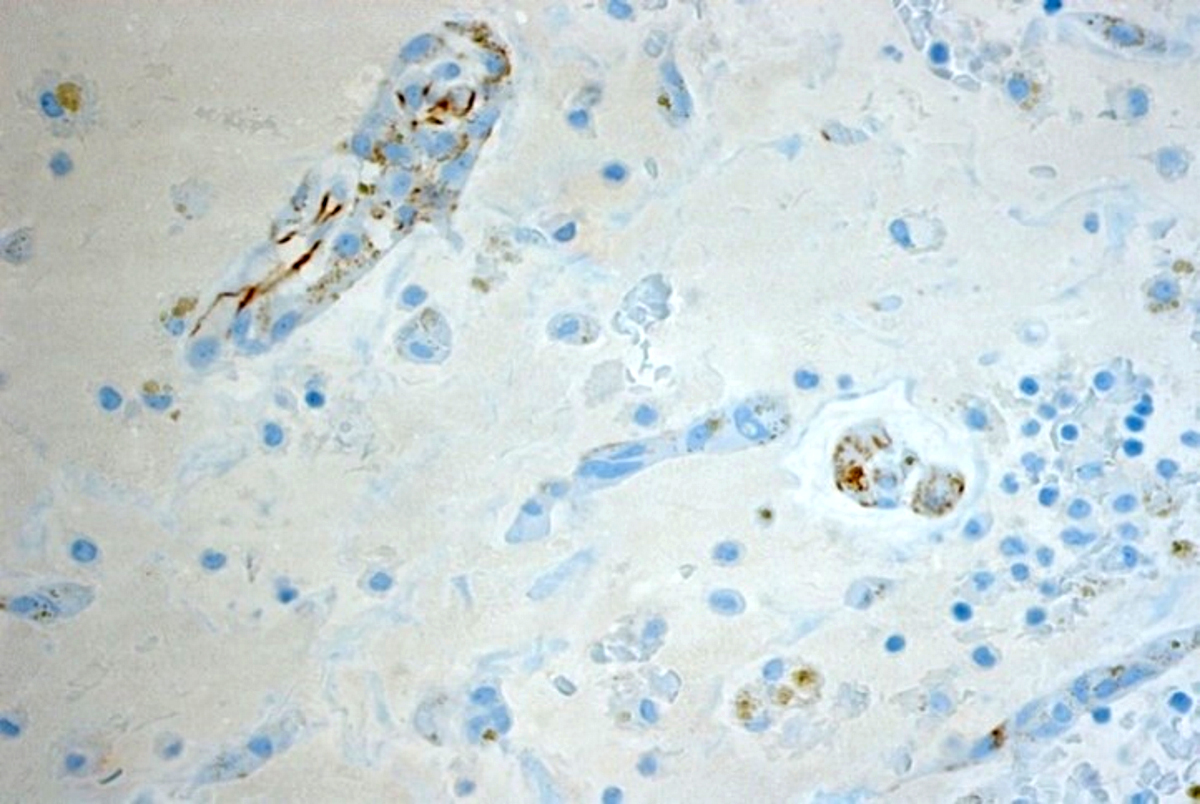
Negative stains
- Lack of C4d deposition on capillary endothelium on stain or immunofluorescence (presence is typical of antibody mediated rejection)
- Can have mixed humoral and cellular acute rejection, so should assess endomyocardial biopsies for both (Arch Pathol Lab Med 2016;140:910)
Sample pathology report
- Heart, endomyocardial biopsy:
- Multifocal moderate acute cellular allograft rejection with associated multifocal myocyte necrosis (ISHLT Grade 2R; 1990 Grade 3A)
- pAMR 0: No significant evidence of antibody mediated rejection on immunohistology.
- Quilty effect: Moderate focal endocardial inflammatory cell aggregate with myocardial encroachment.
Differential diagnosis
- Ischemic injury (e.g., perioperative ischemia or allograft coronary disease)
- Infiltrate is predominantly neutrophils and macrophages rather than lymphocytes (Arch Pathol Lab Med 2007;131:1169)
- If perioperative: proportionally greater myocyte damage than inflammatory infiltrate
- If allograft coronary disease: secondary myocardial changes (myocyte vacuolization or microinfarcts)
- Acute antibody mediated rejection: positive immunofluorescence for immunoglobulins, complement and CD68 staining for macrophages (J Heart Lung Transplant 2005;24:1710)
- Quilty lesions: extends to endocardium and may involve B lymphocytes (Ludhwani: StatPearls, 2019)
- Infection (e.g. cytomegalovirus, myocarditis, toxoplasmosis, disseminated aspergillosis): demonstration of infectious entity on endomyocardial biopsy
- Sarcoidosis: noncaseating granulomas (Chest 1986;90:528)
- Giant cell myocarditis: inflammatory cell infiltrate with multinucleated giant cells (CD68+), nonnecrotizing granulomas and eosinophils (Arch Pathol Lab Med 2016;140:1429)
- Prior biopsy site: biopsy will feature a lesion in several stages of healing, including thrombus, granulation tissue and perimyocytic fibrosis
- Cardiac allograft vasculopathy: presence of angiographic evidence supporting cardiac allograft vasculopathy (Croat Med J 2014;55:562)
- Posttransplant lymphoproliferative disease: EBV seroconversion or reactivation of anti-EBV IgM with constitutional symptoms (J Cardiovasc Pharmacol Ther 2006;11:77)
Board review style question #1
A 42 year old black man underwent an orthotopic heart transplantation 4 months ago following viral myocarditis induced dilated cardiomyopathy in which he received a heart from a 19 year old Hispanic male. A routine posttransplant surveillance endomyocardial biopsy demonstrated mild interstitial inflammatory cell infiltrate with one small focus of myocyte damage. There was no evidence of myocyte necrosis. At that time, the patient was completely asymptomatic and reported no history of complications from his heart transplant. Which of the following is a significant risk factor in the development of this patient's disease?
- Donor Hispanic race
- Donor young age
- Recipient black race
- Sex matched transplantation
Board review style answer #1
C. Recipient black race. This patient has acute cellular rejection following his orthotopic heart transplantation. Given the brief histological description of his endomyocardial biopsy, this patient has an International Society for Heart and Lung Transplantation acute cellular rejection grade of 1R. Acute cellular rejection has a peak incidence 3 - 6 months after transplantation, which aligns with this patient's current presentation. Recipient black race is associated with an increased risk / incidence of acute cellular rejection. A sex mismatched transplantation, recipient (or donor) female sex and a pediatric donor would also increase the risk / incidence of acute cellular rejection, not the inverse as presented in the answer choices for this case. Donor race has not been demonstrated to have an impact on the risk or incidence of acute cellular rejection.
Comment Here
Reference: Acute cellular rejection
Comment Here
Reference: Acute cellular rejection
Board review style question #2
A 20 year old man received an orthotopic heart transplant 3 months ago for restrictive cardiomyopathy. He attended his first followup visit but was unable to return to clinic for any subsequent appointments. He presented urgently today with concerns that, for the last few weeks, he has been experiencing progressive exertional dyspnea and intermittent palpitations. He also reports that he needed to use 4 to 5 pillows last night to sleep, as he felt as if he couldn't breathe well while lying flat. These symptoms have never happened before. His physician obtained an endomyocardial biopsy and a representative section (H&E) is shown above. Which of the following statements about this disease is true?
- Condition is mediated by B cells, which extend into the endocardium
- High dose IV corticosteroids are the first line therapy for this condition
- Invasive coronary angiography with assessment of cardiac allograft function is required to make the diagnosis
- Myocardial inflammatory infiltrate is predominantly composed of neutrophils
- Positive immunofluorescence for endothelial C4d is characteristic of the disease
Board review style answer #2
B. High dose IV corticosteroids are the first line therapy for this condition. This patient has an International Society for Heart and Lung Transplantation grade 3R acute cellular rejection following his orthotopic heart transplantation. The endomyocardial biopsy demonstrates a diffuse inflammatory infiltrate with multifocal myocyte damage, myocardial edema and interstitial hemorrhage, consistent with an International Society for Heart and Lung Transplantation grade of 3R. In acute cellular rejection, the first line therapy is high-dose IV corticosteroids. Positive immunofluorescence for C4d is characteristic of acute humoral rejection, not acute cellular rejection. Coronary angiography is used to diagnose cardiac allograft vasculopathy; in acute cellular rejection, endomyocardial biopsy is the gold standard for diagnosis. The inflammatory infiltrate in acute cellular rejection is T lymphocyte predominant and occurs primarily within the myocardium. A neutrophilic infiltrate is associated with ischemic injury while a B lymphocyte mediated process in the endocardium is consistent with a quilty lesion.
Comment Here
Reference: Acute cellular rejection
Comment Here
Reference: Acute cellular rejection
Amyloidosis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Amyloid infiltration of the myocardium
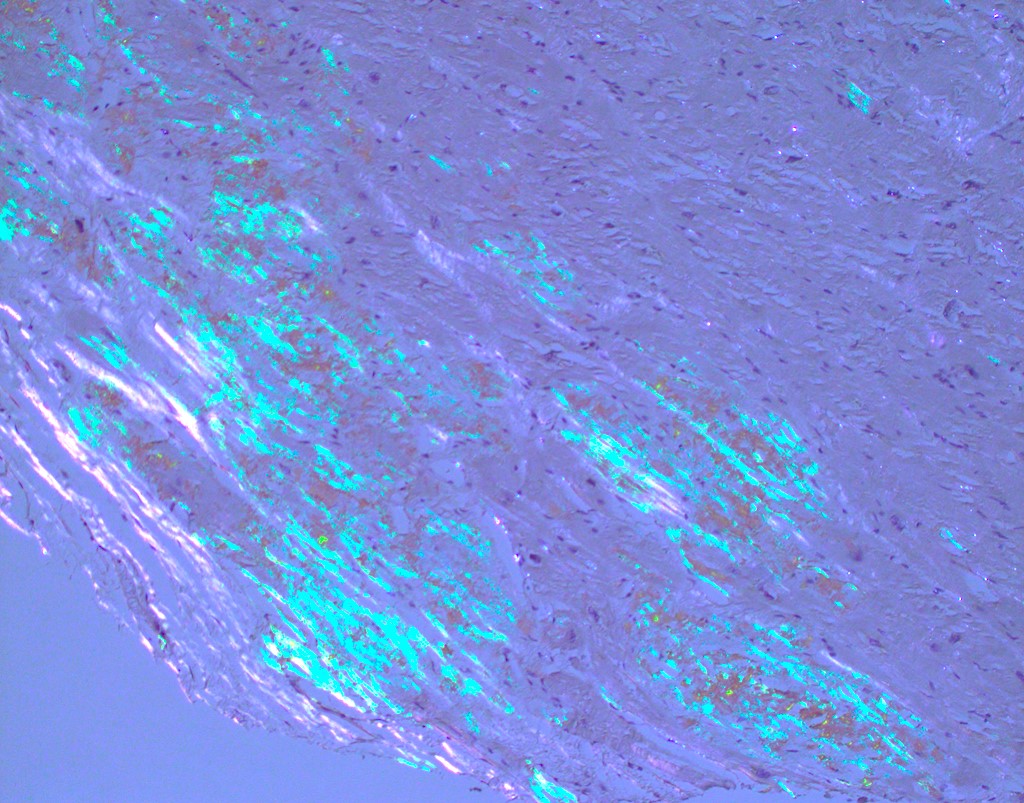
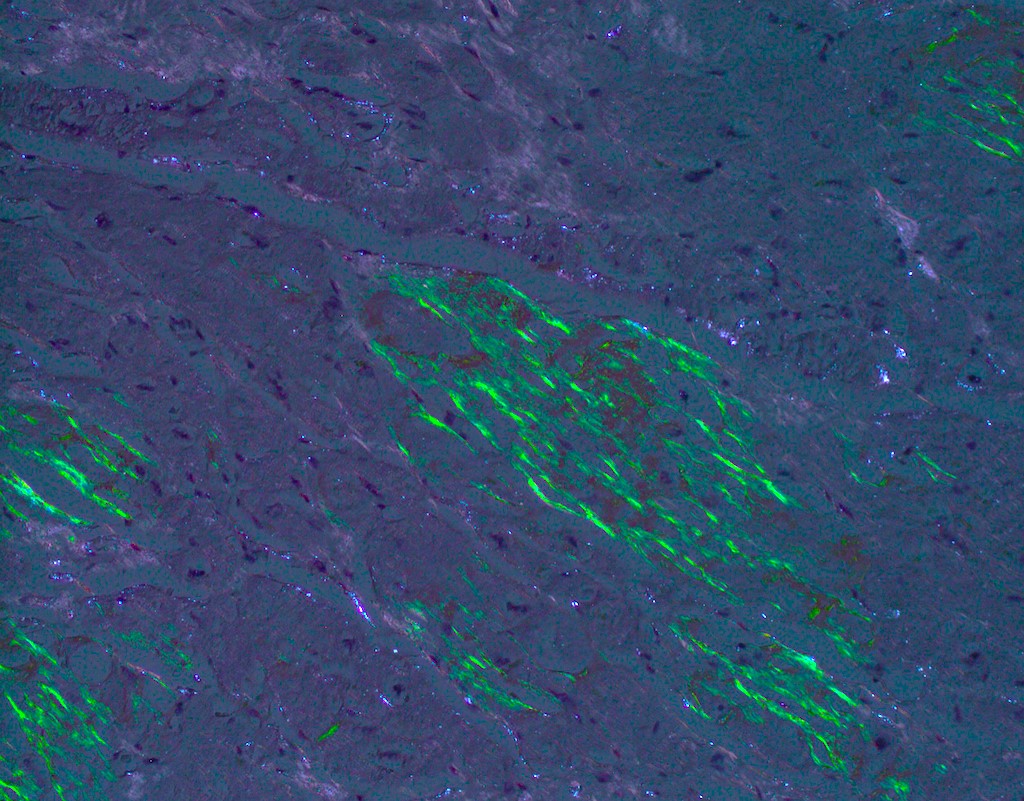
- Multiple types are named after the precursor protein of amyloid deposit; however, they are all characterized by the deposition of an eosinophilic amorphous material that stains bright red with Congo red and shows an apple green birefringence upon polarization
Essential features
- Heterogenous group of diseases caused by deposition of amyloid, an abnormal protein with a beta pleated structure composed of haphazardly arranged nonbranching fibrils measuring 8 - 10 nm in diameter
- Light microscopy shows amorphous eosinophilic deposits that show apple green birefringence under polarized light
- Main cardiac forms are transthyretin amyloidosis (including wild type and hereditary subtypes) and light chain amyloidosis
- Endomyocardial biopsy and histological analysis is the gold standard for diagnosis but less invasive techniques such as echocardiography, cardiac magnetic resonance imaging (CMR) and cardiac nuclear imaging can raise index of suspicion for this diagnosis
Terminology
- 2 main types (95% of cardiac amyloidosis cases)
- Transthyretin amyloidosis (ATTR amyloidosis)
- Wild type (wtATTR) subtype (previously senile systemic amyloidosis)
- Hereditary (hATTR) subtype
- Light chain amyloidosis (AL amyloidosis), also known as primary systemic amyloidosis (Clin Cardiol 2021;44:322)
- Transthyretin amyloidosis (ATTR amyloidosis)
- Rare types of cardiac amyloidosis include
- Serum amyloid A amyloidosis (AA)
- Hereditary apoprotein A1 (AApoA1)
- Apoprotein A4 (AApoA4) amyloidosis
ICD coding
- ICD-10
- ICD-11
- 5D00.0 - AL amyloidosis
- 5D00.1 - AA amyloidosis
- 5D00.2 - hereditary amyloidosis
- 5D00.20 - hereditary ATTR amyloidosis
- 5D00.21 - nonneuropathic heredofamilial amyloidosis
- 5D00.2Y - other specified hereditary amyloidosis
- 5D00.2Z - hereditary amyloidosis, unspecified
- 5D00.3 - dialysis associated amyloidosis
- 2A83.5 - monoclonal immunoglobulin deposition disease
- 2A83.50 - heavy chain deposition disease
- 2A83.51 - light and heavy chain deposition disease
- 2A83.52 - light chain deposition disease
- 5D00.Y - other specified amyloidosis
- 5D00.Z - amyloidosis, unspecified
Epidemiology
- Wild type transthyretin amyloidosis (wtATTR amyloidosis)
- Prevalence unknown
- Age: > 60 years
- Males: 90%
- Hereditary transthyretin amyloidosis (hATTR amyloidosis)
- Autosomal dominant, variable penetrance
- Prevalence unknown (> 120 gene variants associated with hATTR; some more prevalent in specific regions or ethnic groups and others more widely distributed) (Curr Med Res Opin 2013;29:63)
- Age: > 50 years but can be seen ranging from 30 years
- Males: 76 - 86%
- Light chain amyloidosis (AL amyloidosis)
- Rare, annual incidence 1/100,000 people in the U.S.
- Age: > 40 years
- Males: 60% (Clin Cardiol 2021;44:322)
Sites
- Amyloid can deposit in any cardiac structures: endocardium, valves, myocardium, epicardium, parietal pericardium (Clin Cardiol 2021;44:322)
- Commonly causes concentric biventricular hypertrophy, biatrial enlargement and atrial septal thickening, valvular thickening
Pathophysiology
- Extracellular (predominantly) tissue deposition of amyloid, composed of both fibril and nonfibril components
- Fibrils make up ~95% of deposits and are soluble polymers that undergo conformational change into an antiparallel beta pleated sheet configuration; this renders them insoluble and causes autoaggregation into highly ordered fibrils
- Nonfibril components make up ~5% of deposits and include serum amyloid P component (SAP), apolipoprotein E (ApoE) and glycosaminoglycans
- Infiltration of cardiac structures causes changes in calcium transport, receptor modulation, cellular metabolism and cardiomyocyte edema
- Damage via cardiomyocyte necrosis and interstitial fibrosis
- Unique to AL amyloidosis, circulating light chain toxicity is directly myotoxic (Clin Cardiol 2021;44:322)
Etiology
- Acquired or hereditary
- Wild type ATTR - precursor protein is structurally normal transthyretin (TTR)
- Mechanism of pathogenic deposition of this normally structured protein is unclear
- Hereditary ATTR - precursor protein is mutated TTR (point mutation)
- Mutated transthyretin tetrads are unstable, misfolded and prone to deposit
- Most common variants associated with cardiac involvement are Val122Ile (most common in the U.S.), Val130Met (most common globally) and Thr60A1a
- Light chain amyloidosis - precursor protein is misfolded immunoglobulin light chains
- Associated with plasma cell dyscrasias (monoclonal gammopathy of uncertain significance [MGUS], multiple myeloma, B cell lymphoma, others)
- Wild type ATTR - precursor protein is structurally normal transthyretin (TTR)
- References: Clin Cardiol 2021;44:322, UpToDate: Cardiac Amyloidosis [Accessed 16 November 2023]
Clinical features
- Presents as restrictive cardiomyopathy / diastolic dysfunction (HFpEF) with right heart failure
- Patients with symptoms of dyspnea, lower extremity edema, hepatic congestion, ascites, presyncope or syncope
- ATTRwt
- More conduction issues than hATTR, such as atrial fibrillation, first and second degree heart blocks
- Typically an isolated cardiomyopathy (J Am Coll Cardiol 2016;68:1323)
- Can be associated with carpal tunnel syndrome or lumbar spinal stenosis (ESC Heart Fail 2019;6:1128)
- hATTR
- Atrial and ventricular arrhythmias, heart blocks
- Val30Met variant often requires pacemaker (Circulation 2020;142:e7)
- Cardiac predominant, neuropathy predominant or mixed
- Can be associated with neuropathic, renal, ophthalmologic or musculoskeletal (MSK) involvement (Clin Cardiol 2021;44:322)
- AL amyloidosis
- 50 - 70% of systemic AL amyloidosis cases have cardiac infiltration and this is the main prognostic determinant
- Right sided HFpEF more severe than ATTR types (Curr Oncol Rep 2017;19:46)
- Usually sinus rhythm but can also have arrhythmias and heart blocks
- Vascular involvement is not uncommon
- Multiorgan complex: nephrotic syndrome, hepatic, neuropathic, MSK, macroglossia (Clin Cardiol 2021;44:322)
Diagnosis
- General approach: EKG, echocardiogram, cardiac MRI (CMR), serum studies (see Laboratory)
- If monoclonal protein is identified, then tissue biopsy is pursued
- AL amyloidosis
- Noncardiac biopsy with amyloid of AL type and CMR consistent with cardiac amyloidosis is sufficient to diagnose the majority of cardiac AL amyloidosis cases
- Negative findings on tissue biopsy of noncardiac organs do not rule out cardiac amyloidosis
- ATTR amyloidosis
- May or may not have monoclonal protein identified (can be present in up to 40% of ATTR cases) (Clin Cardiol 2021;44:322)
- Technetium pyrophosphate scintigraphy (PYP scan): cardiac nuclear imaging to detect cardiac transthyretin
- Endomyocardial biopsy, followed by immunohistochemistry or mass spectrometry to type the specific amyloid protein
- Genetic testing after ATTR is proven via positive scintigraphy or cardiac biopsy to differentiate between ATTRwt and hATTR
- In cases of hATTR, it may be recommended for other family members to consider genetic testing
Laboratory
- AL specific biomarkers
- Identification of a monoclonal protein via serum and urinary free light chain (FLC) measurements and immunofixation electrophoresis (IFE)
- Serum kappa / lambda FLC ratio analysis
- 90% of untreated AL cases have abnormal ratio ( 1.65) (J Am Coll Cardiol 2016;68:1323)
- Note: FLC and IFE are sometimes raised in ATTRwt and in cases of MGUS, hence not specific markers of AL
- Nonspecific serum biomarkers
- B type natriuretic peptide (BNP) and N terminal proBNP (NT-proBNP) disproportionately high in cardiac amyloidosis due to direct compression of cardiomyocytes and stress caused by raised filling pressures (J Am Coll Cardiol 2016;68:1323)
- Cardiac troponin T (cTnT) reflects cardiomyocyte death and is useful as a negative prognostic indicator (BMC Cardiovasc Disord 2018;18:221)
Radiology description
- Echocardiogram: relative apical sparing of longitudinal strain, ventricular hypertrophy, biatrial dilation, thickened cardiac valves, diastolic > systolic dysfunction
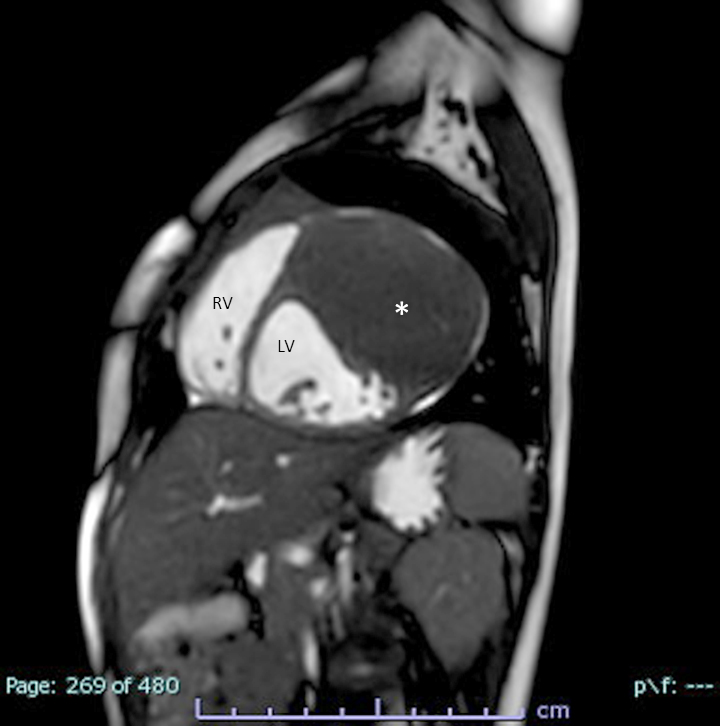
- CMR: diffuse subendocardial pattern of late gadolinium enhancement (LGE) is pathognomonic (95% specificity), although transmural LGE is most common (Clin Cardiol 2021;44:322)
- Diffuse transmural: ATTR > AL
- Subendocardial: AL > ATTR
- Technetium pyrophosphate scintigraphy (PYP scan): cardiac nuclear imaging study that detects cardiac transthyretin can identify early deposition prior to onset of clinical disease and can prognosticate in some cases
Radiology images
Prognostic factors
- Chronic and progressive condition
- AL amyloidosis: extent of cardiac involvement is most important predictor of survival
- ATTR amyloidosis: heart to contralateral (H/CL) ratio ≥ 1.6, calculated on PYP scintigraphy, is associated with significantly worse outcome over 5 years (Clin Cardiol 2021;44:322)
- Staging system incorporating NT-proBNP, cTnT and serum FLC (J Clin Oncol 2012;30:989)
- Stages I through IV, with higher stage conferring increased mortality
Case reports
- 50 year old woman diagnosed with AL amyloidosis demonstrated long term pathological response to chemotherapy and was able to withdraw from the heart transplant list (Eur Heart J Case Rep 2022;6:ytac130)
- 73 year old woman presented with cardiogenic shock and was subsequently diagnosed with cardiac amyloidosis with scintigraphy and endomyocardial biopsy (World J Clin Cases 2019;7:742)
- 84 year old man with new onset signs and symptoms of heart failure, diagnosed with wild type transthyretin amyloidosis (Cureus 2023;15:e33364)
Treatment
- AL amyloidosis: stem cell transplants, chemotherapy, proteasome inhibitors
- Chemotherapy care standard: cyclophosphamide, bortezomib and dexamethasone (CyBorD) and addition of daratumumab based on recent phase 3 study ANDROMEDA (Blood 2020;136:71)
- ATTR amyloidosis: goal is transthyretin stabilization and deposit removal
- Stabilizing: tafamidis and diflusinal
- Removal: doxycycline and tauroursodeoxycholic acid (Rev Esp Cardiol (Engl Ed) 2017;70:991)
- hATTR: gene silencer patisiran targets TTR mRNA to decrease liver production (Neurodegener Dis Manag 2019;9:5)
- Caution with traditional heart failure therapies
- Typical heart failure drugs such as ACEinh, ARBs, beta blockers, calcium channel blockers are detrimental in cardiac amyloidosis
- Low sodium diet, fluid restriction, loop diuretics and aldosterone inhibitors are recommended for volume management
- Transplant is the definitive treatment option
- AL amyloid: cardiac transplant
- ATTR amyloidosis: both cardiac and liver transplants needed
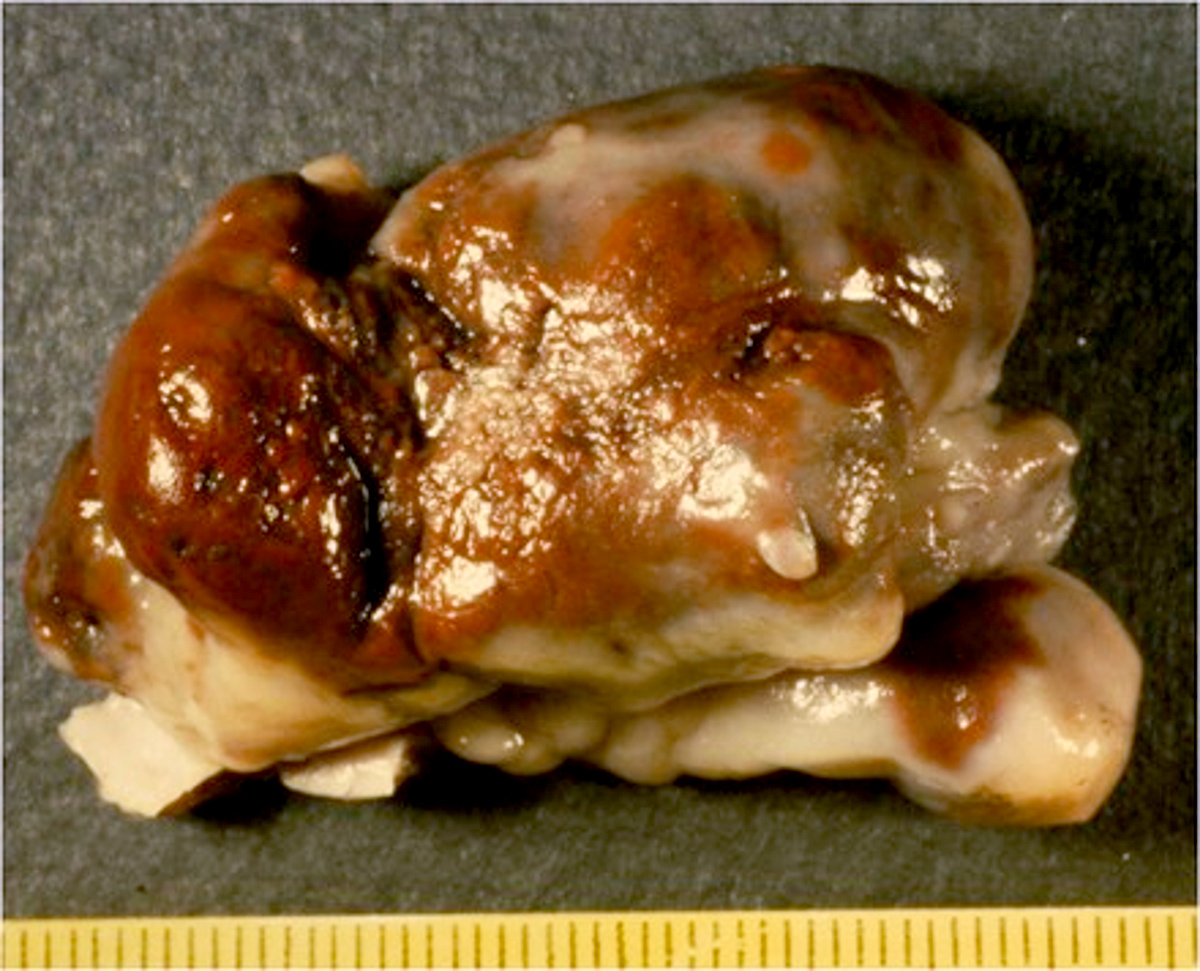
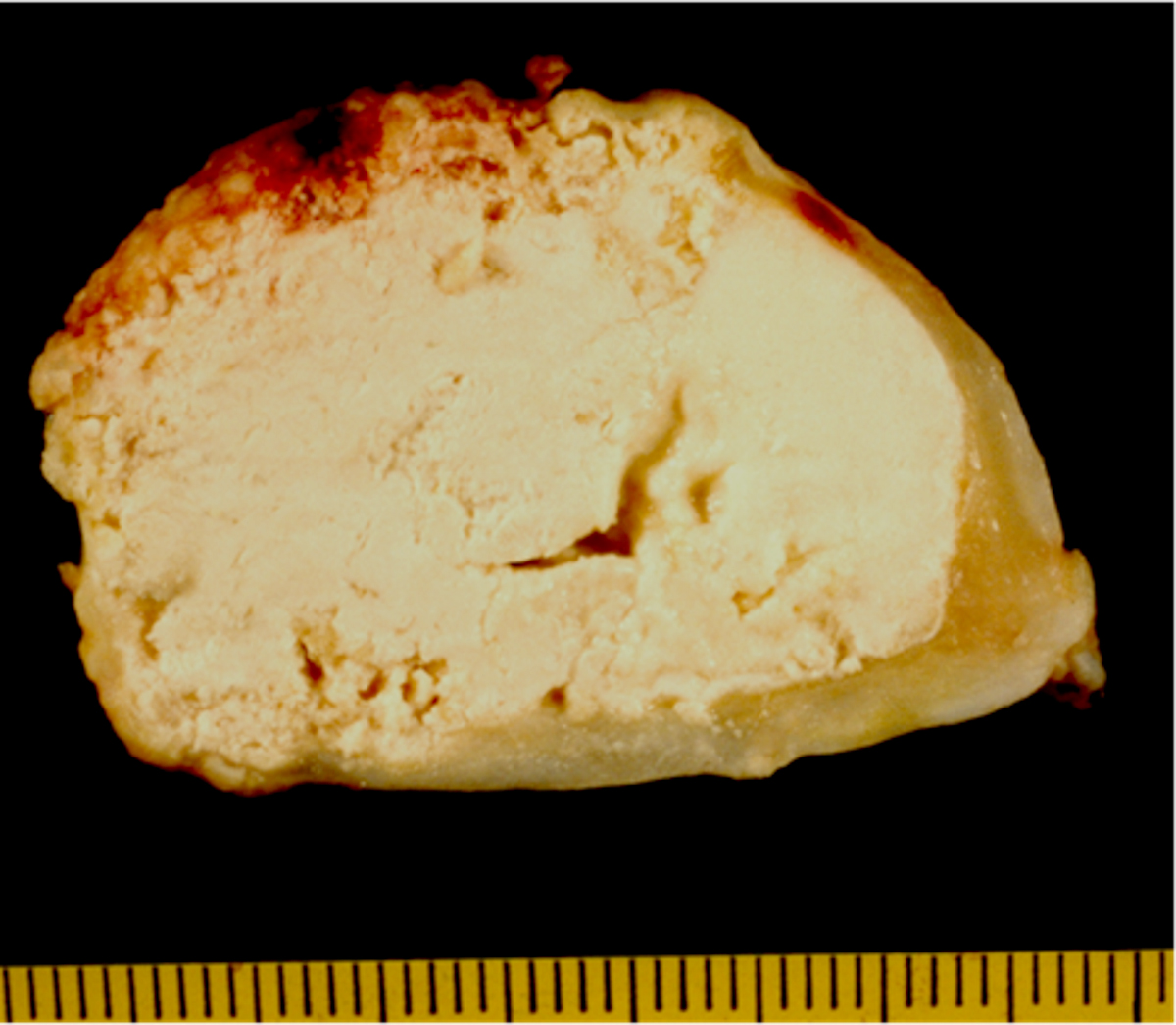
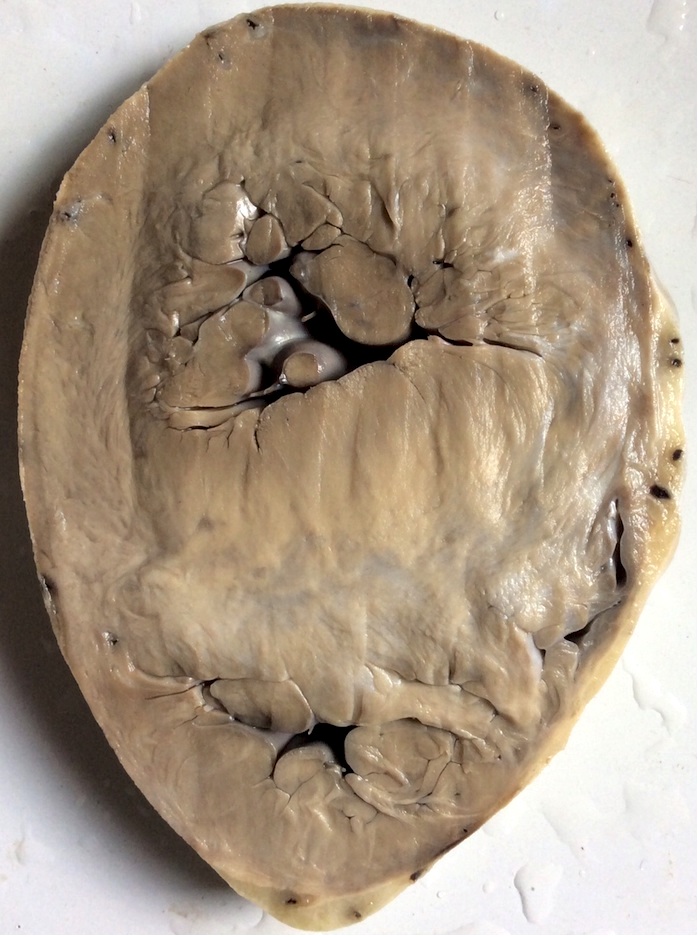
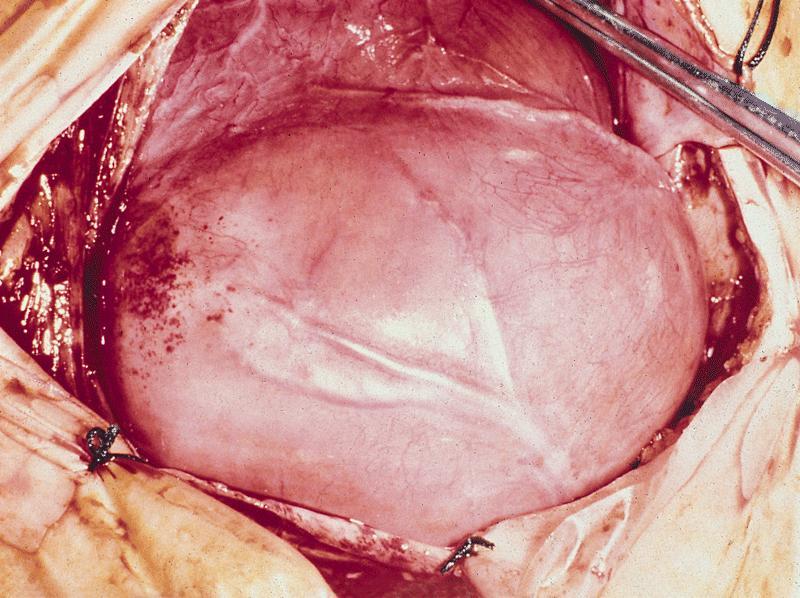
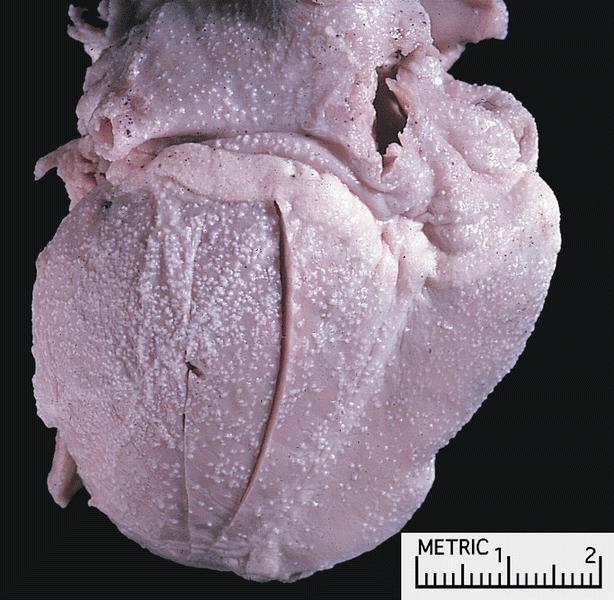
Gross description
- Amyloid deposits are most commonly seen in myocardium and also in atria, pericardium, endocardium and microvasculature, giving the myocardium a waxy pale appearance
- Myocardium is thickened, firm and rubbery in consistency
- Endocardial deposits may cause lining of heart to look gritty or sandpaper-like
- More than half of myocardium is involved in AL type
- Intracardiac thrombus formation is frequently seen
- Reference: J Clin Pathol 2005;58:125
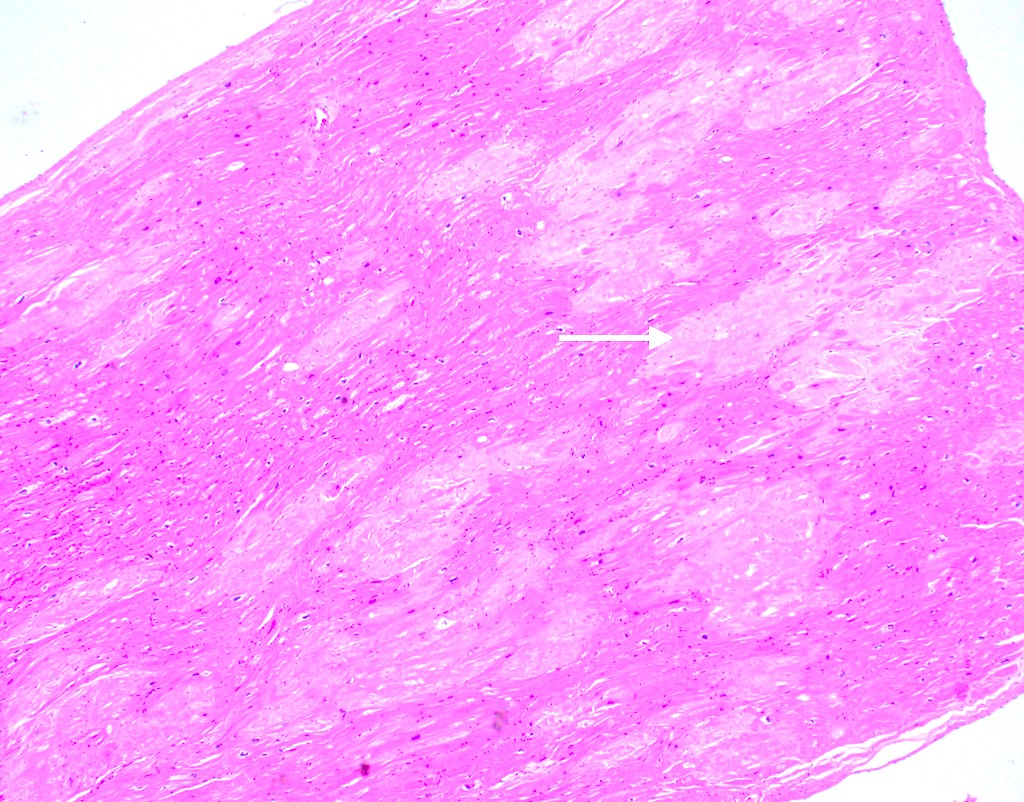
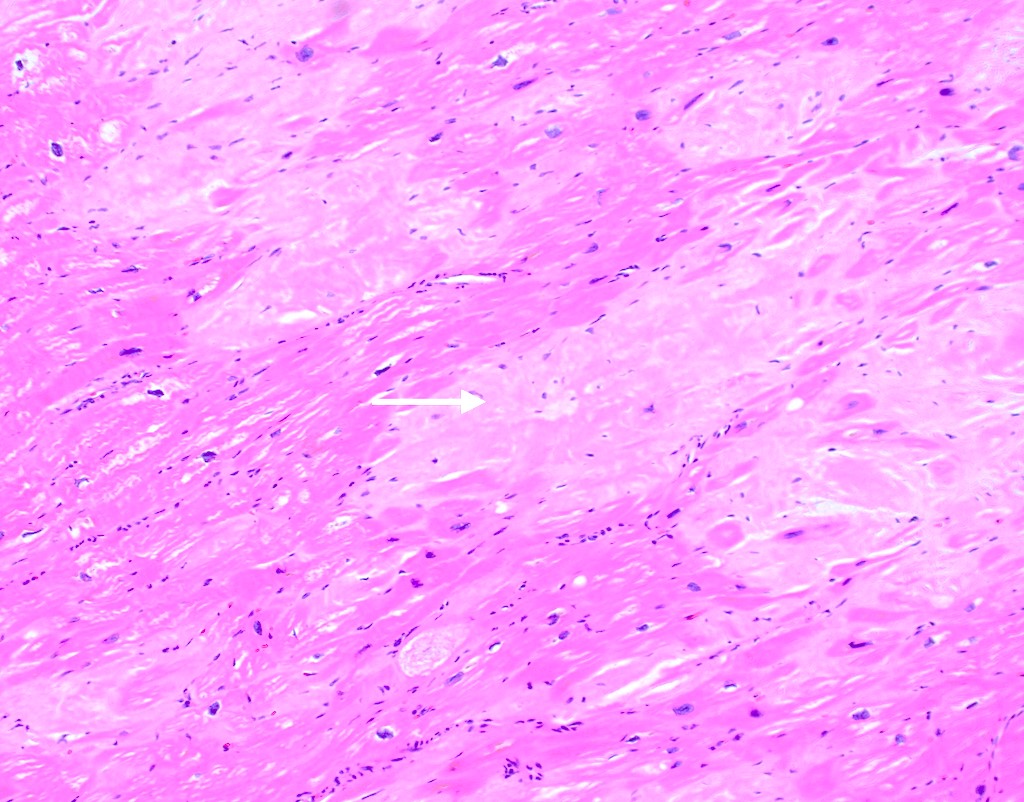
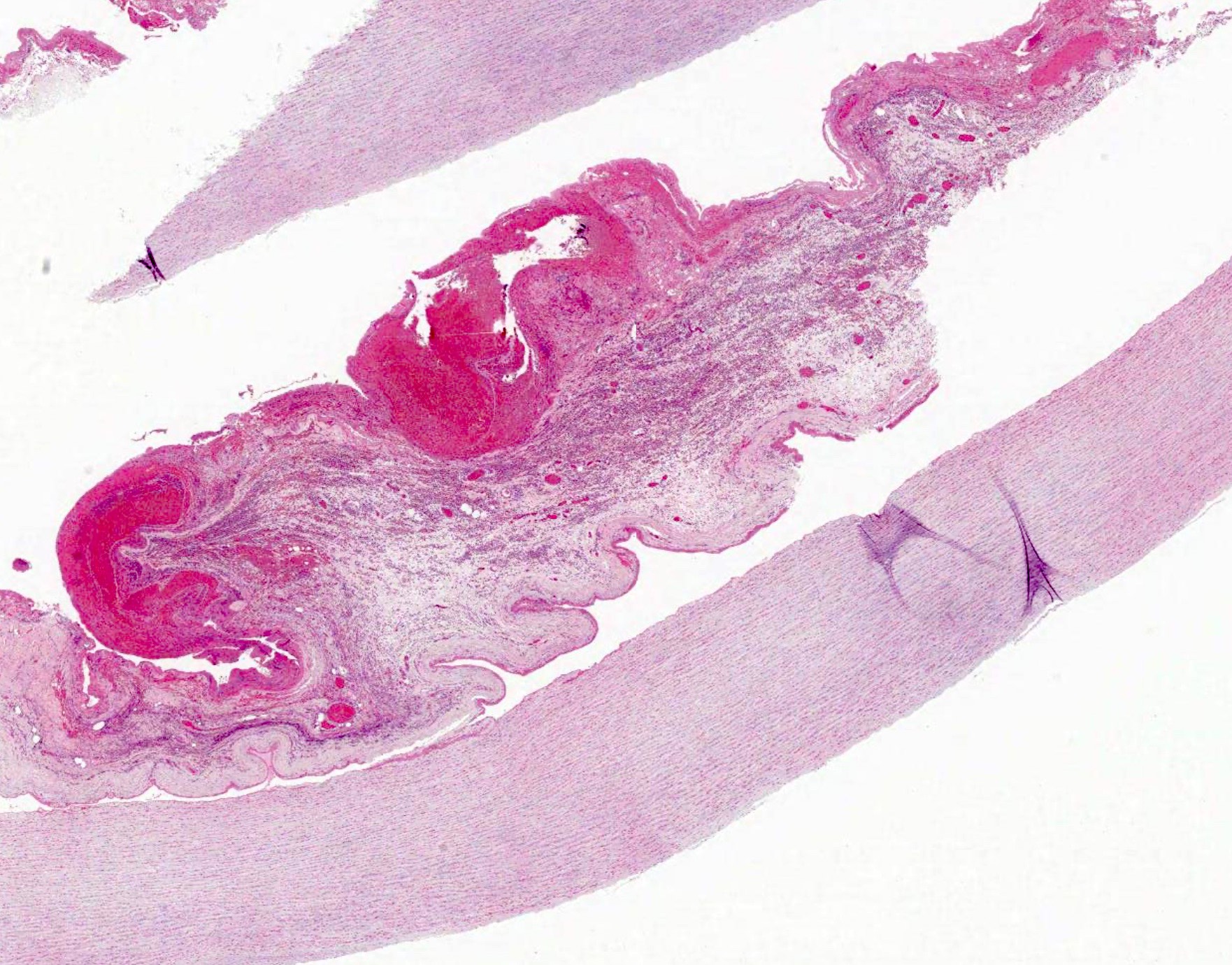
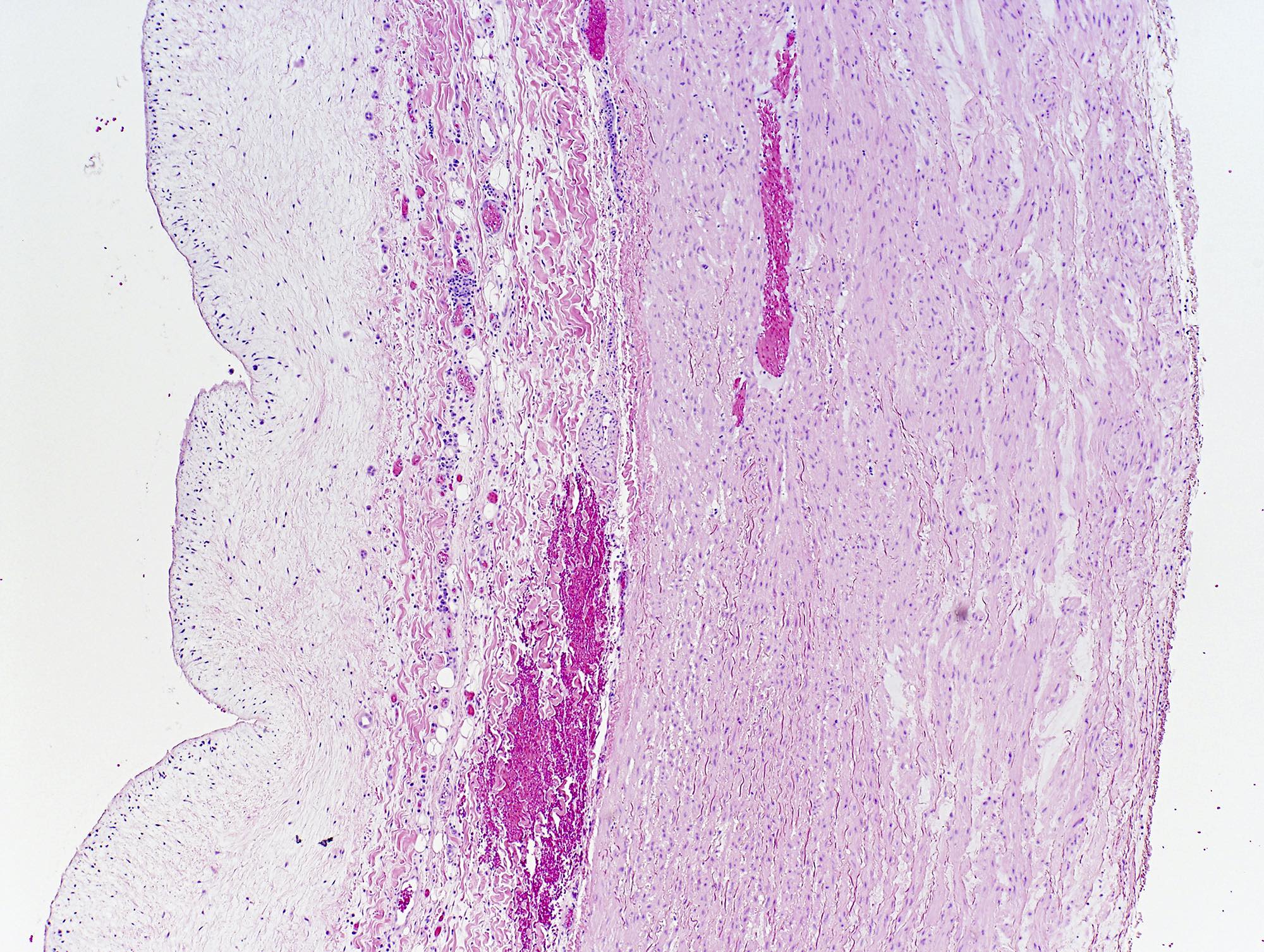
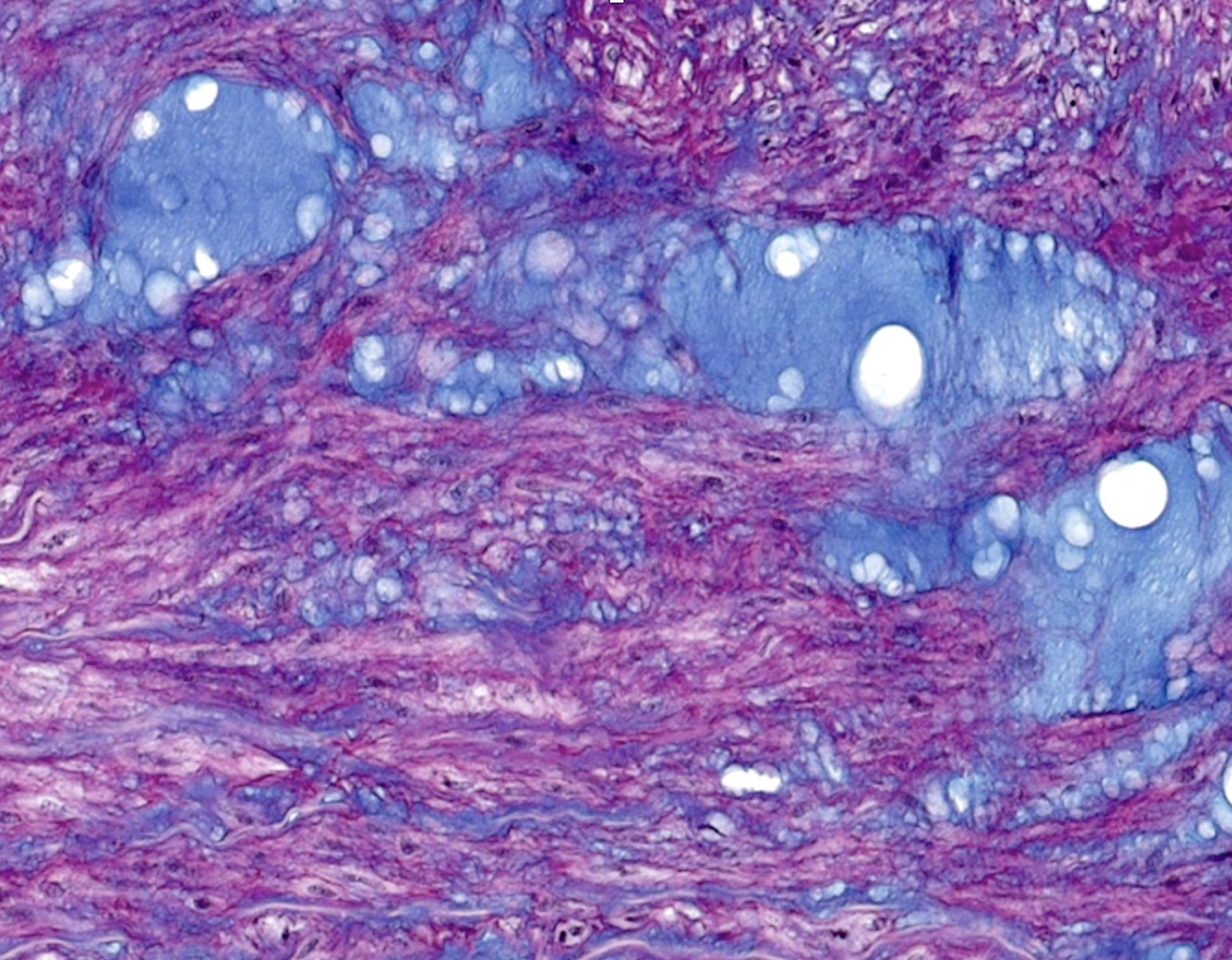
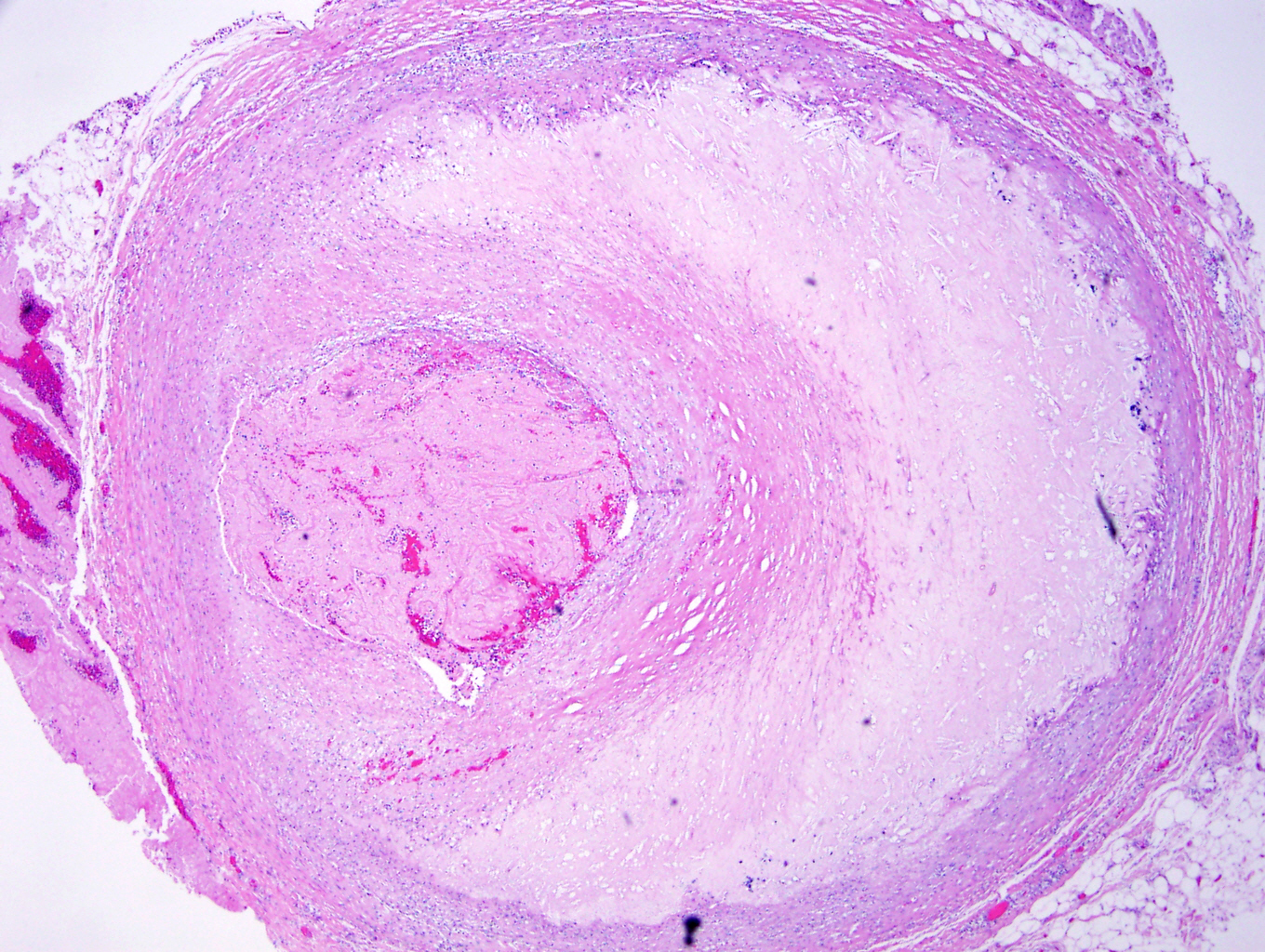
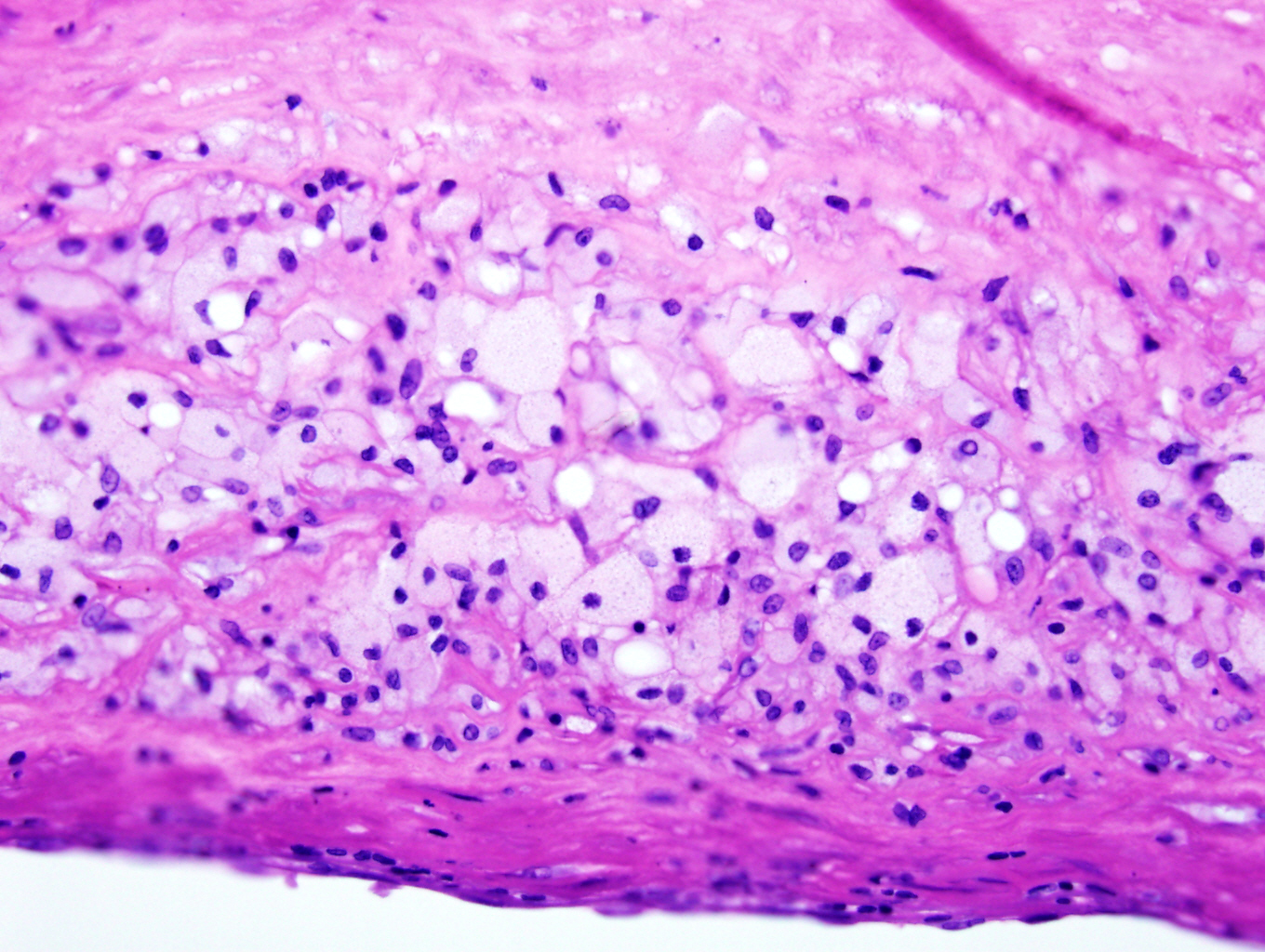
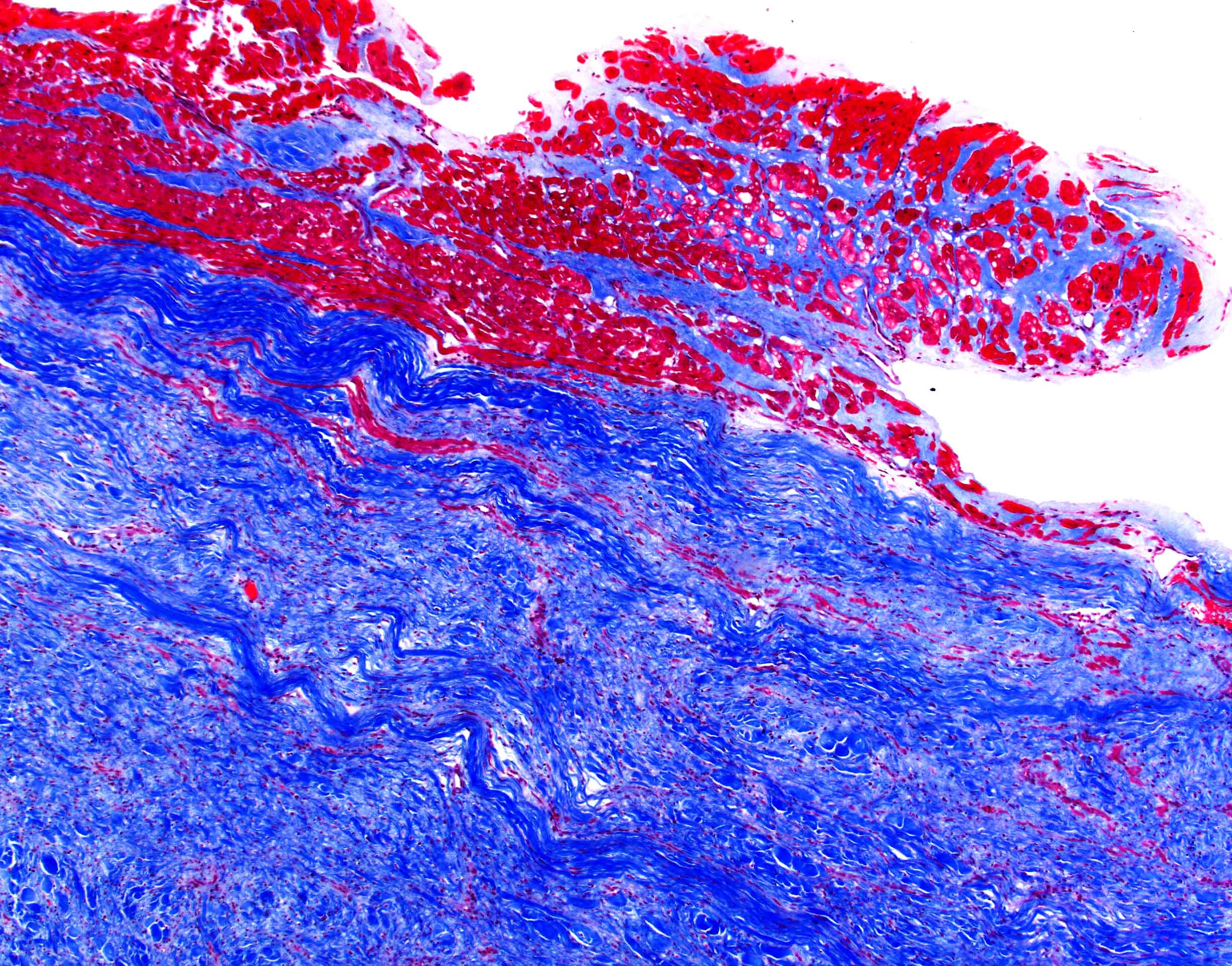
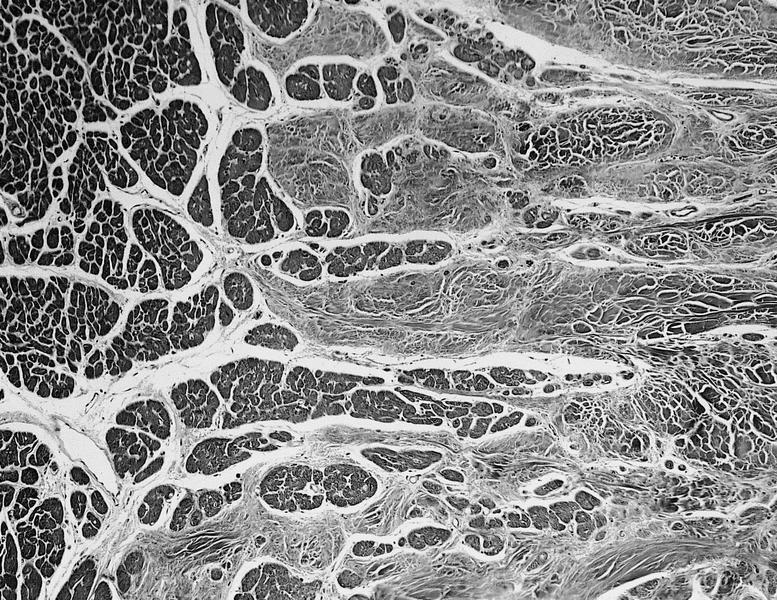
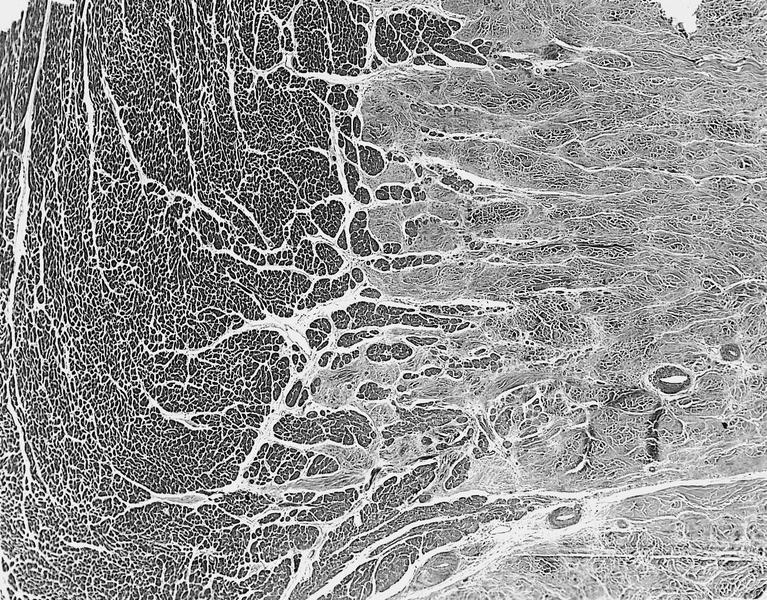
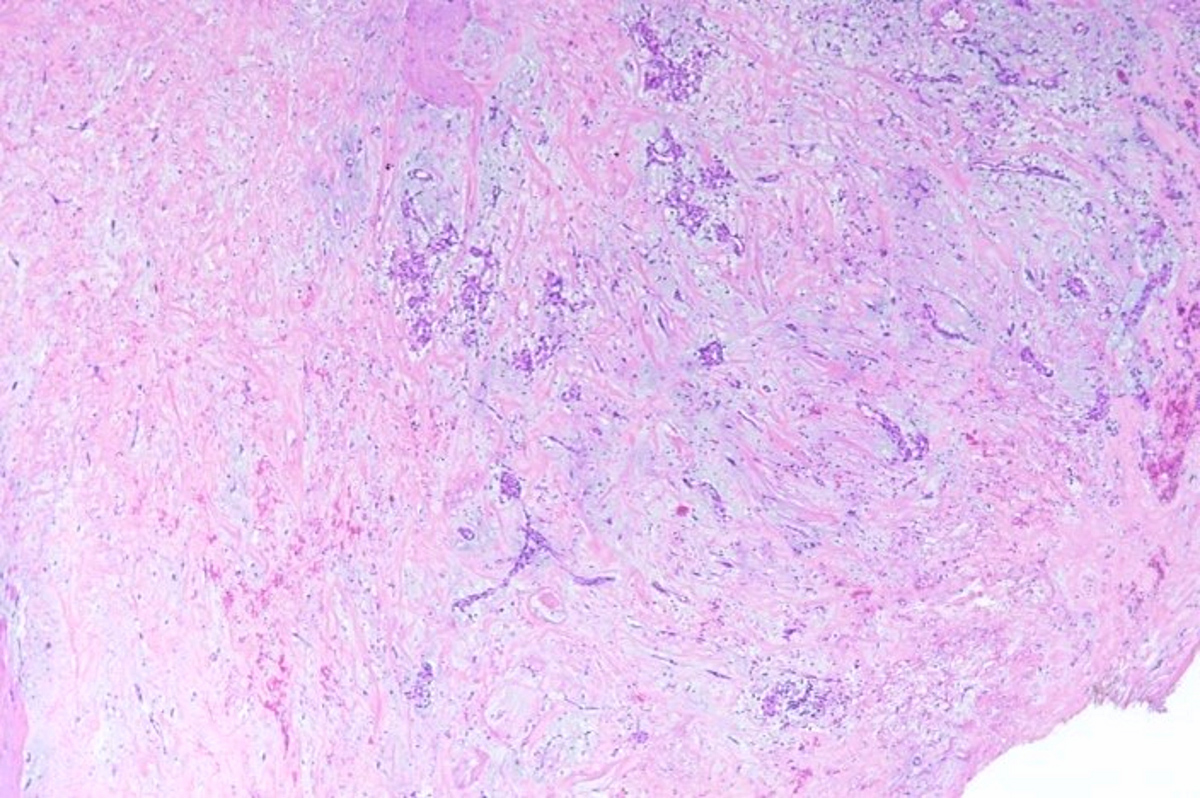
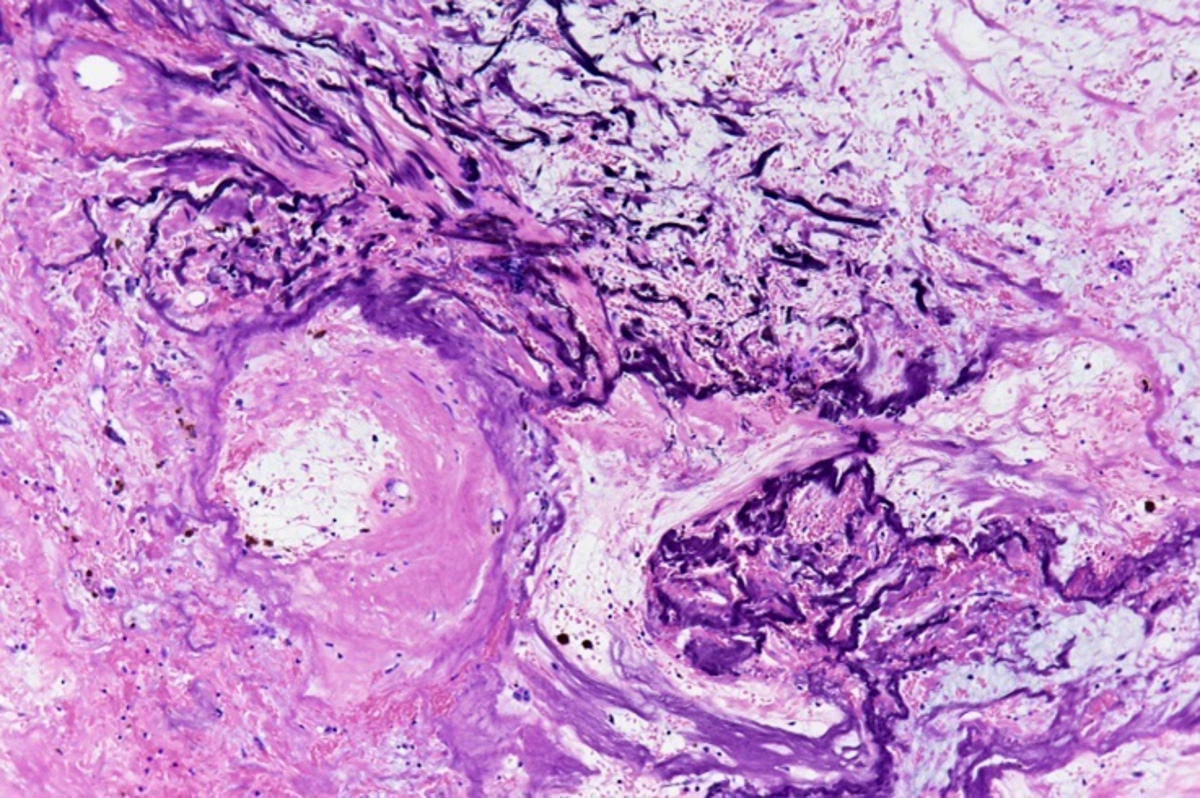
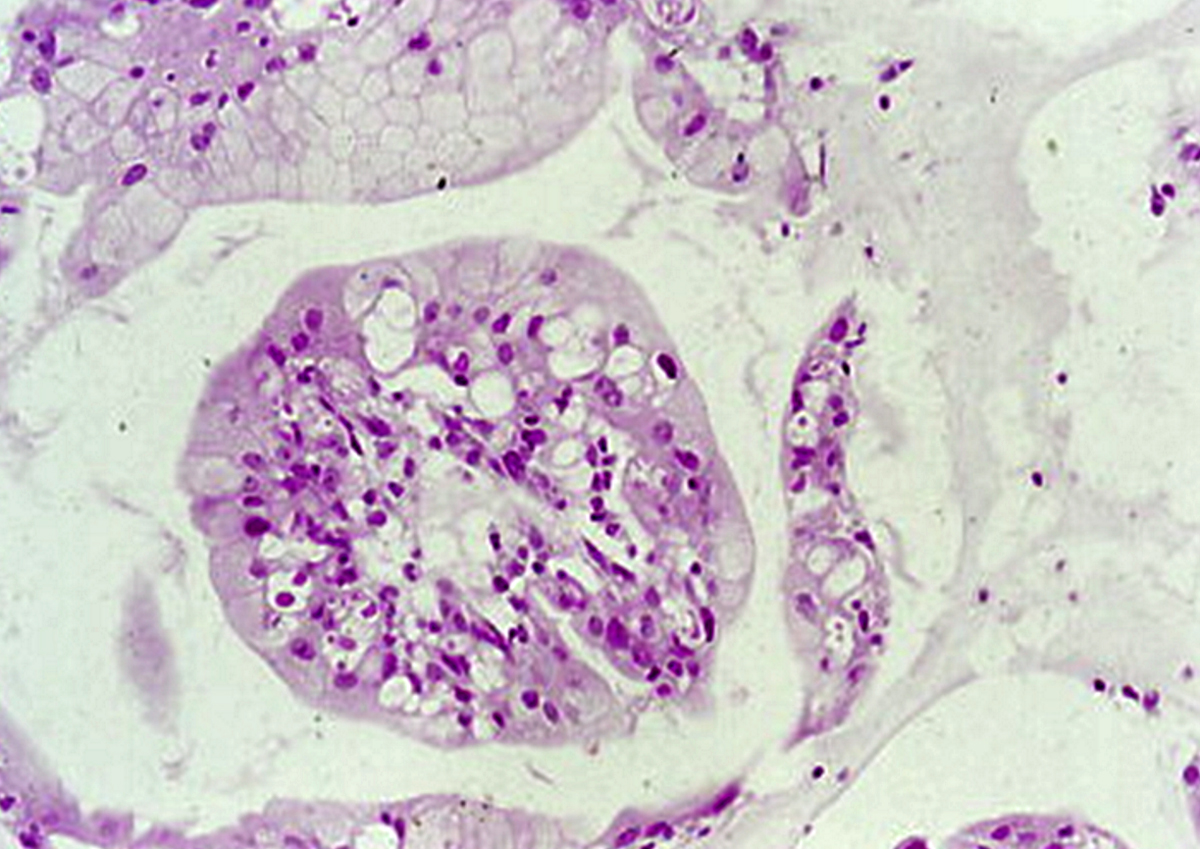
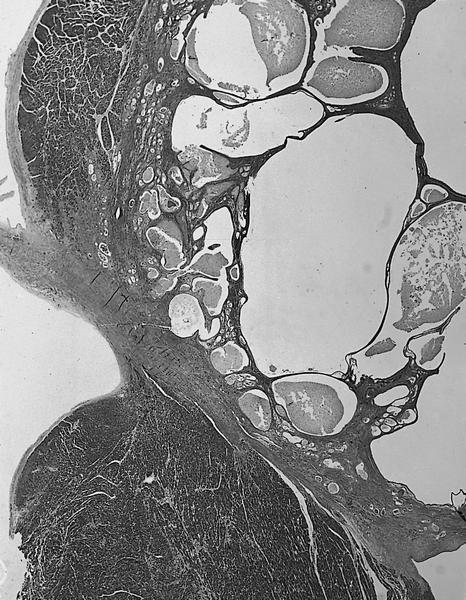
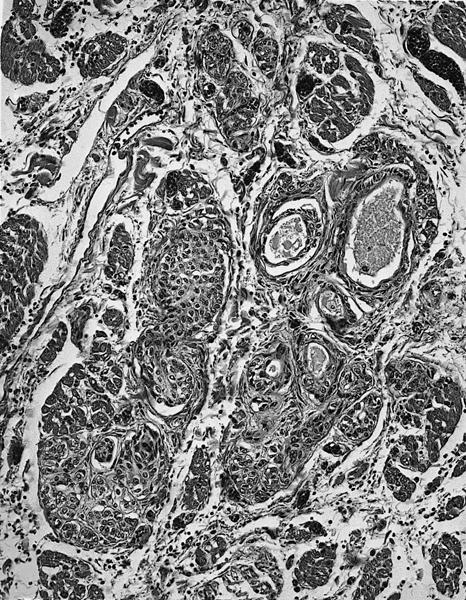
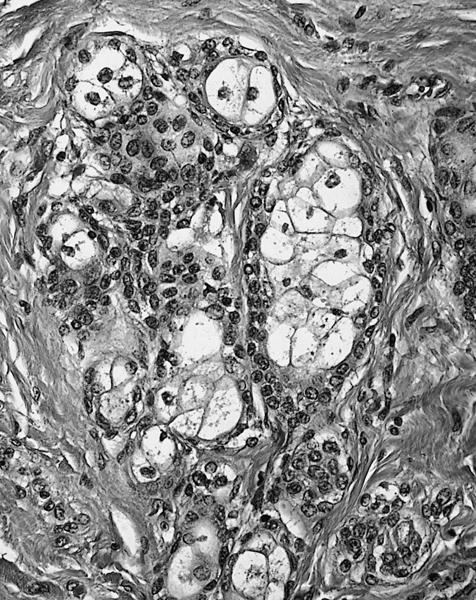
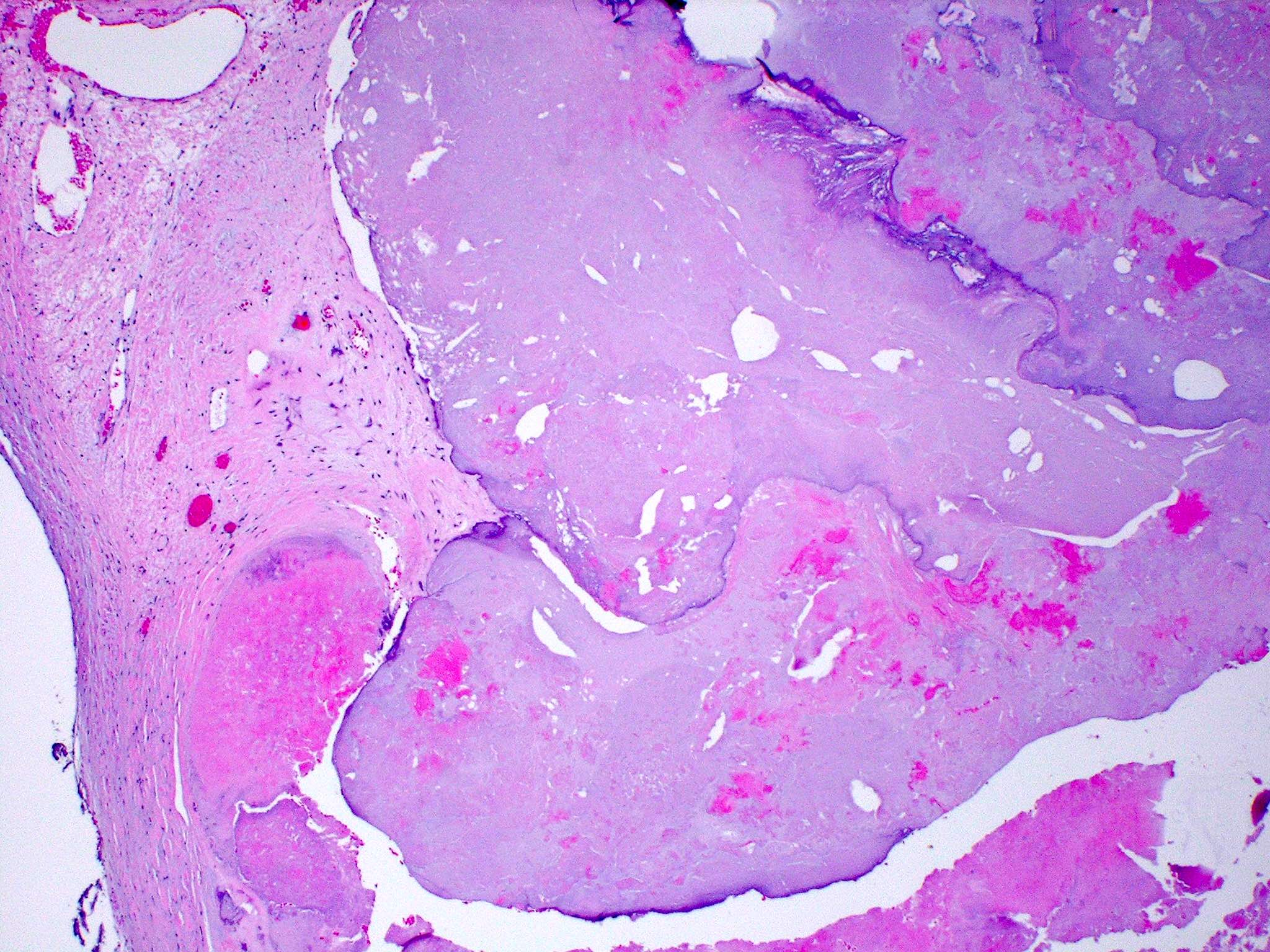
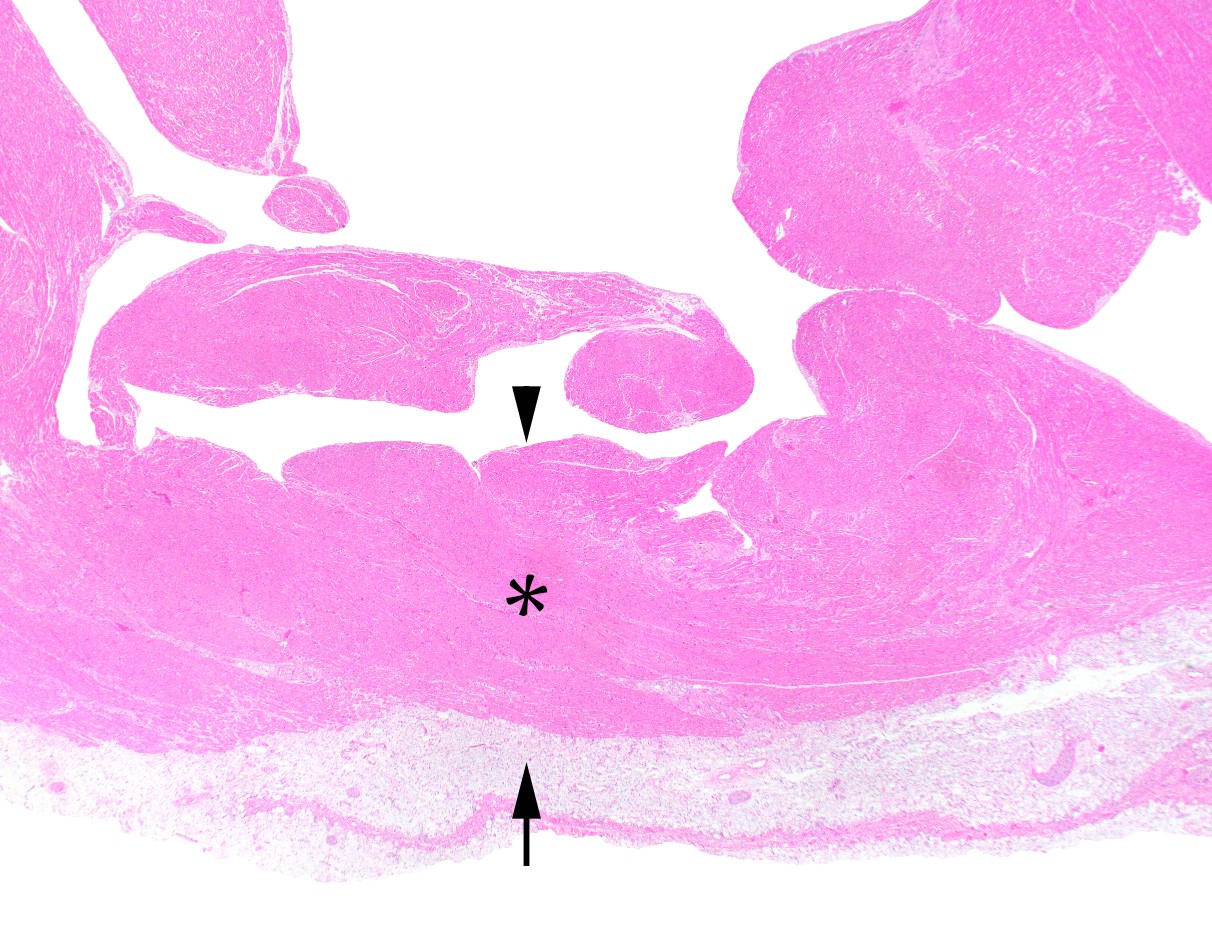
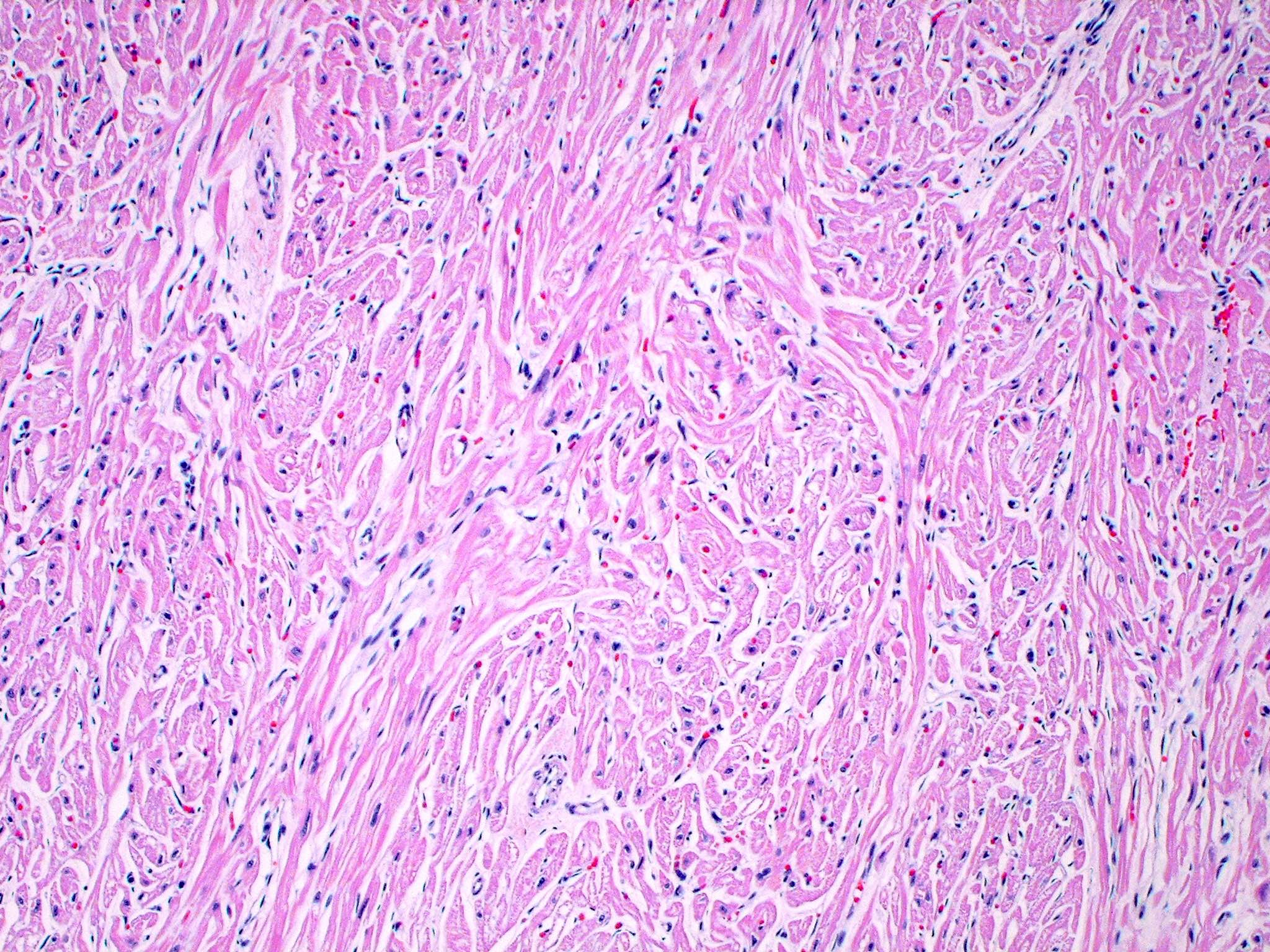
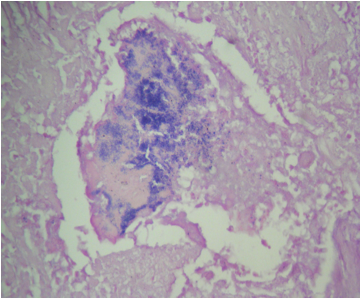
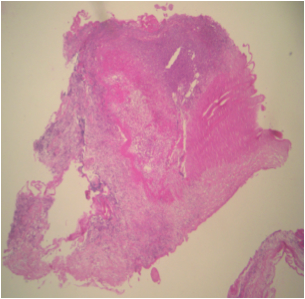
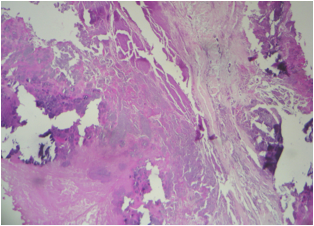
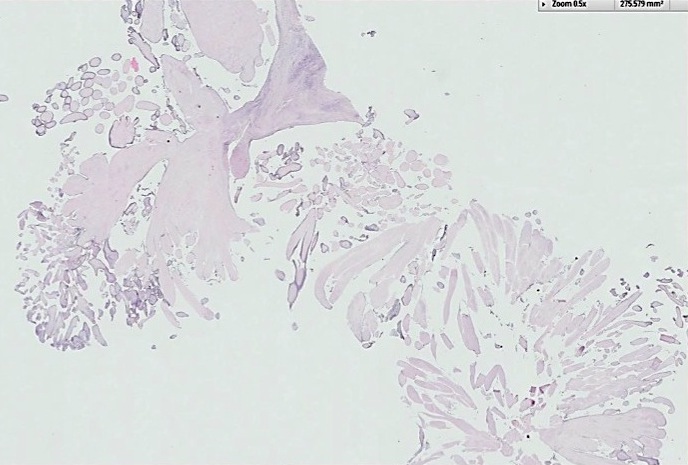
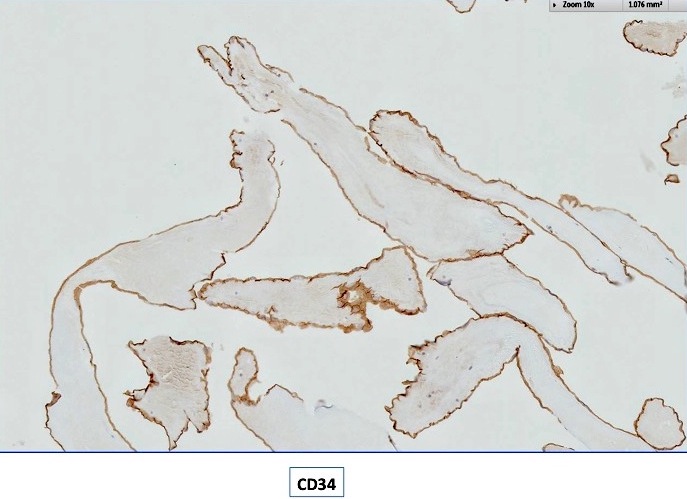
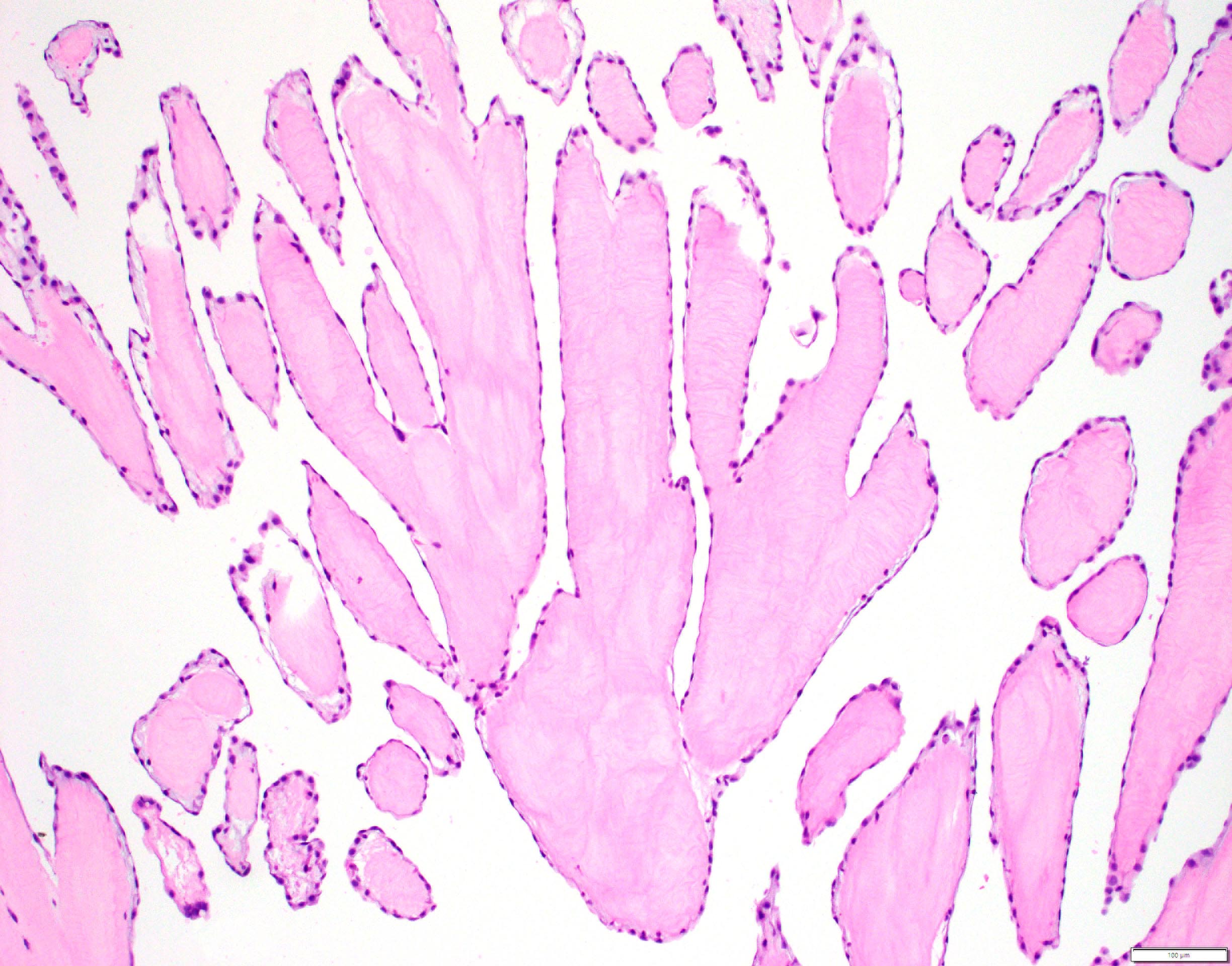
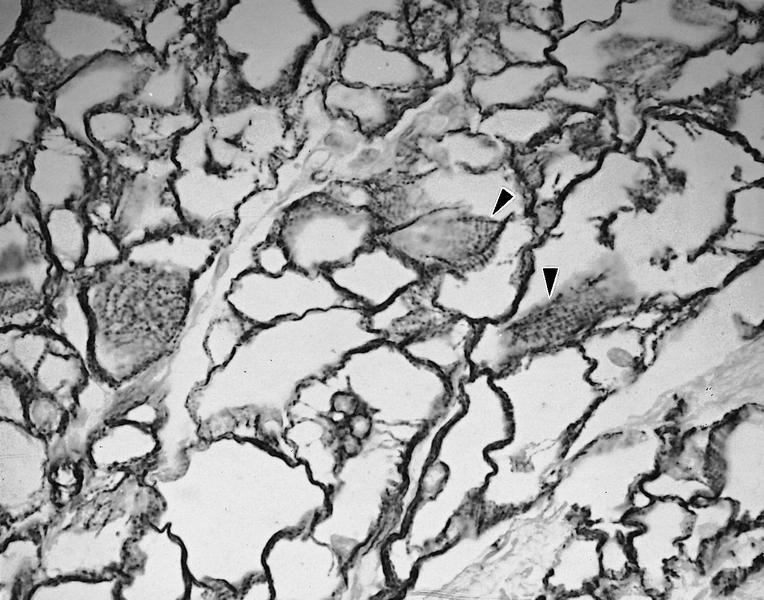
Microscopic (histologic) description
- Amorphous and homogenous, with pale eosinophilic areas / hyaline deposits seen predominantly in the extracellular space
- Cardiac amyloidosis is a myocardial and a vascular / microvascular disease (Front Cardiovasc Med 2022;9:1081098)
- Myocardial interstitial patterns: 2 main patterns that can also be mixed
- Pericellular: amyloid distributed around individual cardiomyocytes, varied thickness and extent of involvement, produces lace-like aspect
- Nodular / replacement: nodular or micronodular aggregates distort architecture and replace myocardium
- Vascular / microvascular patterns
- Arteries and veins, epicardial and intramyocardial sites, more extensive involvement in mural vessels
- Deposits can partially or fully involve vessel circumference, can be localized to wall layers (intima, media) or involve full wall and can cause varying degrees of stenosis to the point of obstruction
- Capillary networks may show reduced density
- Deposits are also seen in subendocardium as nodular aggregates with or without fibrosis, as well as in the epicardial tissue (Front Cardiovasc Med 2022;9:1081098)
- Myocardial interstitial patterns: 2 main patterns that can also be mixed
- Disease specific patterns of deposition
- AL amyloidosis: usually diffuse pericellular infiltration with deposition in small blood vessels
- ATTR amyloidosis: usually nodular
- Atrophy of surrounding myocytes and fibrosis of the conduction system have been noted in relation to amyloid deposition
Microscopic (histologic) images
Cytology description
- Limited value in routine smears
Immunofluorescence description
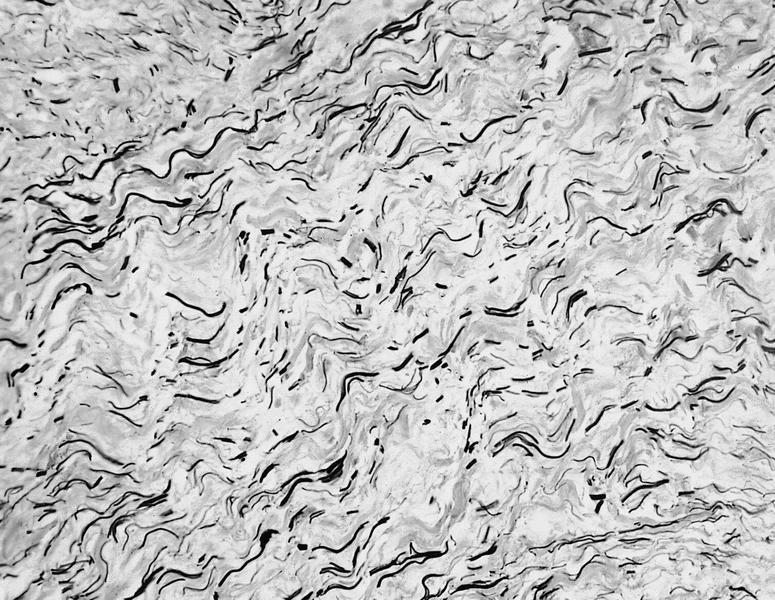
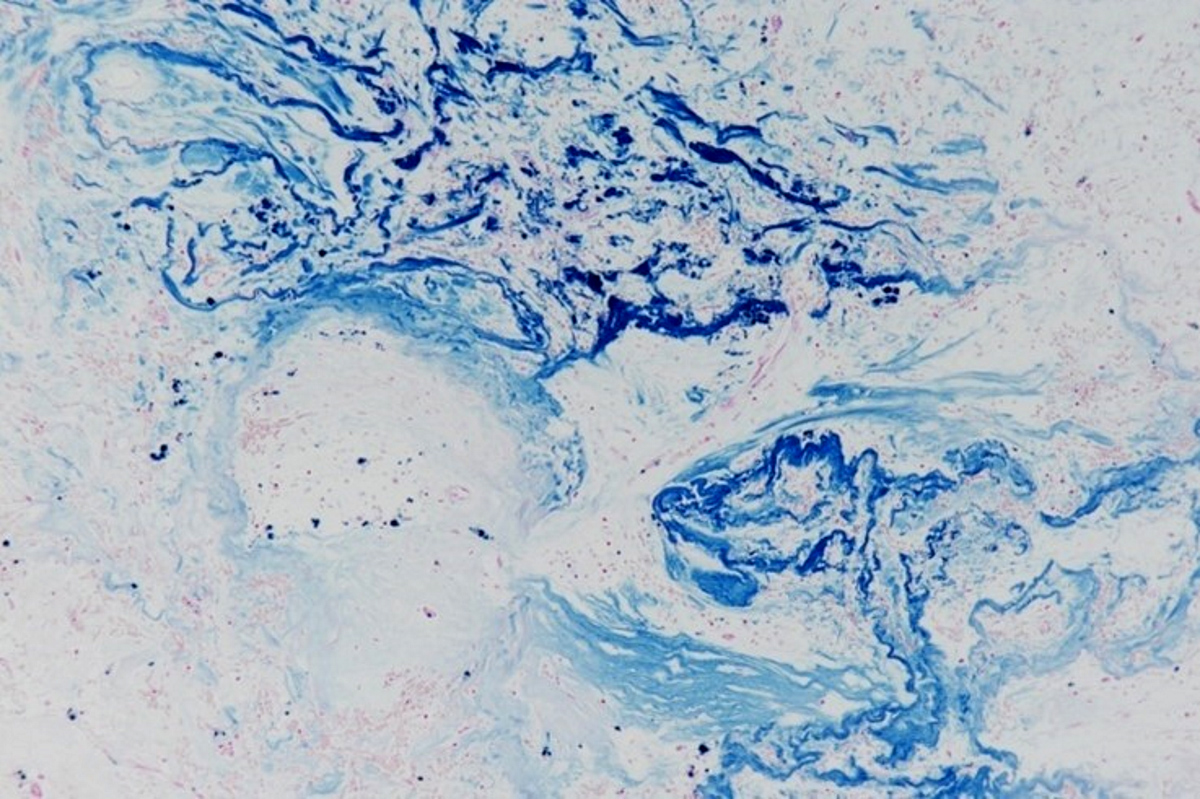
Positive stains
- Congo red on 8 - 10 micron sections: apple green birefringence under polarized light
- High sensitivity and specificity rate on endomyocardial biopsy
- Caveat: systemic AL amyloidosis may stain weakly or even negative
- Crystal violet: purple metachromatic staining
- Infrequently used - thioflavin T: yellow-green fluorescence
- Infrequently used - sulfated Alcian blue: amyloid stains a turquoise / green color
- Special note: pitfalls of Congo red staining
- Proper equipment is necessary to improve sensitivity (Diagn Pathol 2019;14:57)
- Use a mechanical rotating stage to view slides at variable angles
- Avoid plastic coverslips as they interfere with ability to perform crossed polarized light examination
- When a sample is deemed negative or equivocal, follow previously published modifications such as using polar mounting media or omitting the alcohol differentiation step
- Use proper stain free optics (such as a metallurgical microscope) and avoid use of polarizer with built in compensator
- Proper equipment is necessary to improve sensitivity (Diagn Pathol 2019;14:57)
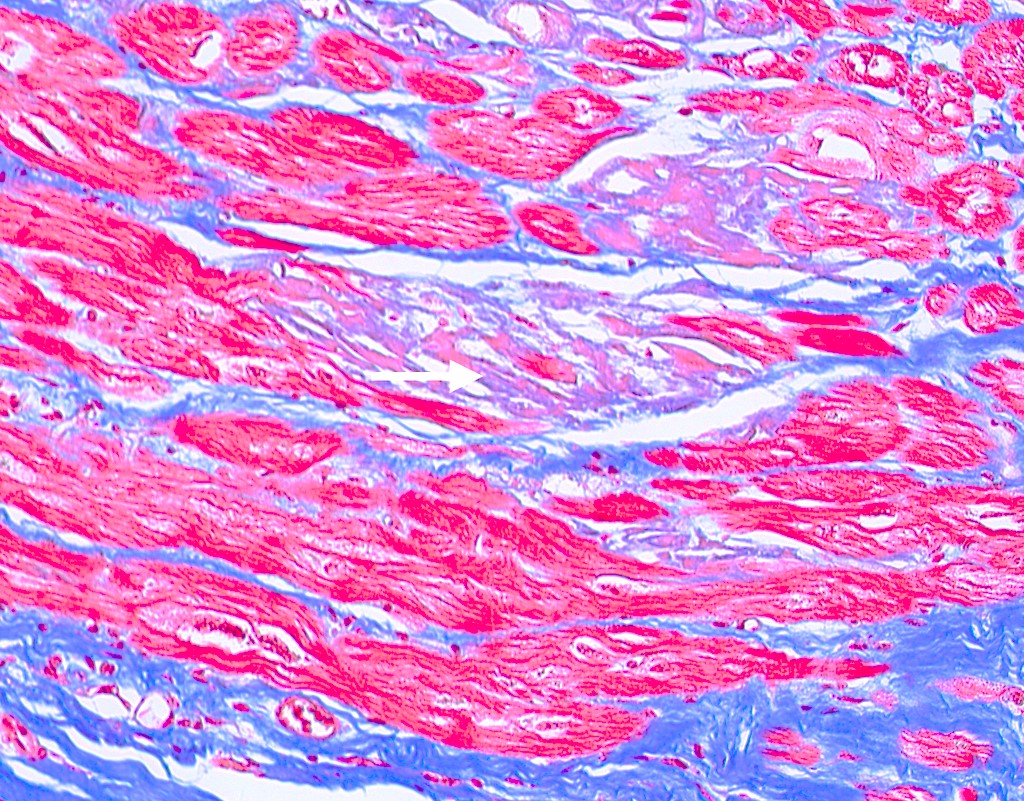
Negative stains
- Trichrome: pale blue staining but no deep blue staining (differentiates from collagen deposition, which stains brilliant blue)
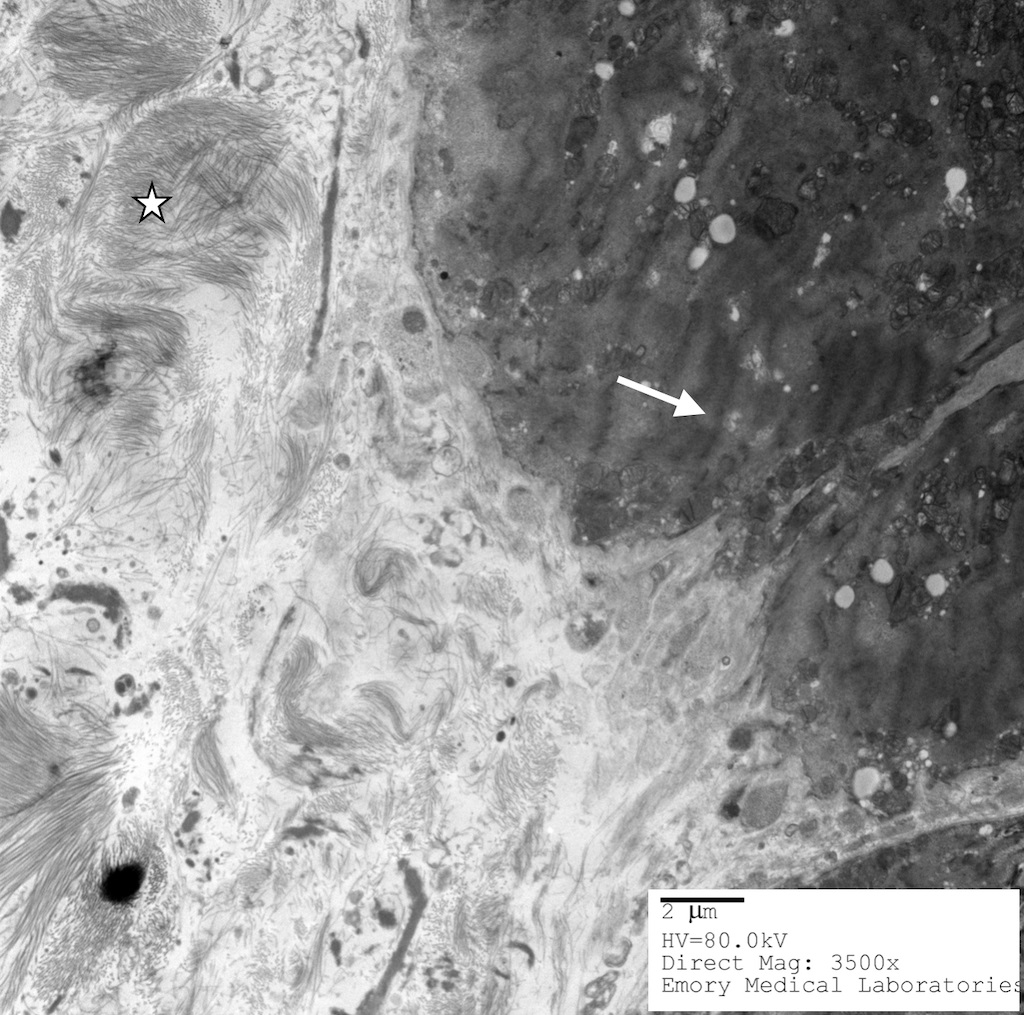
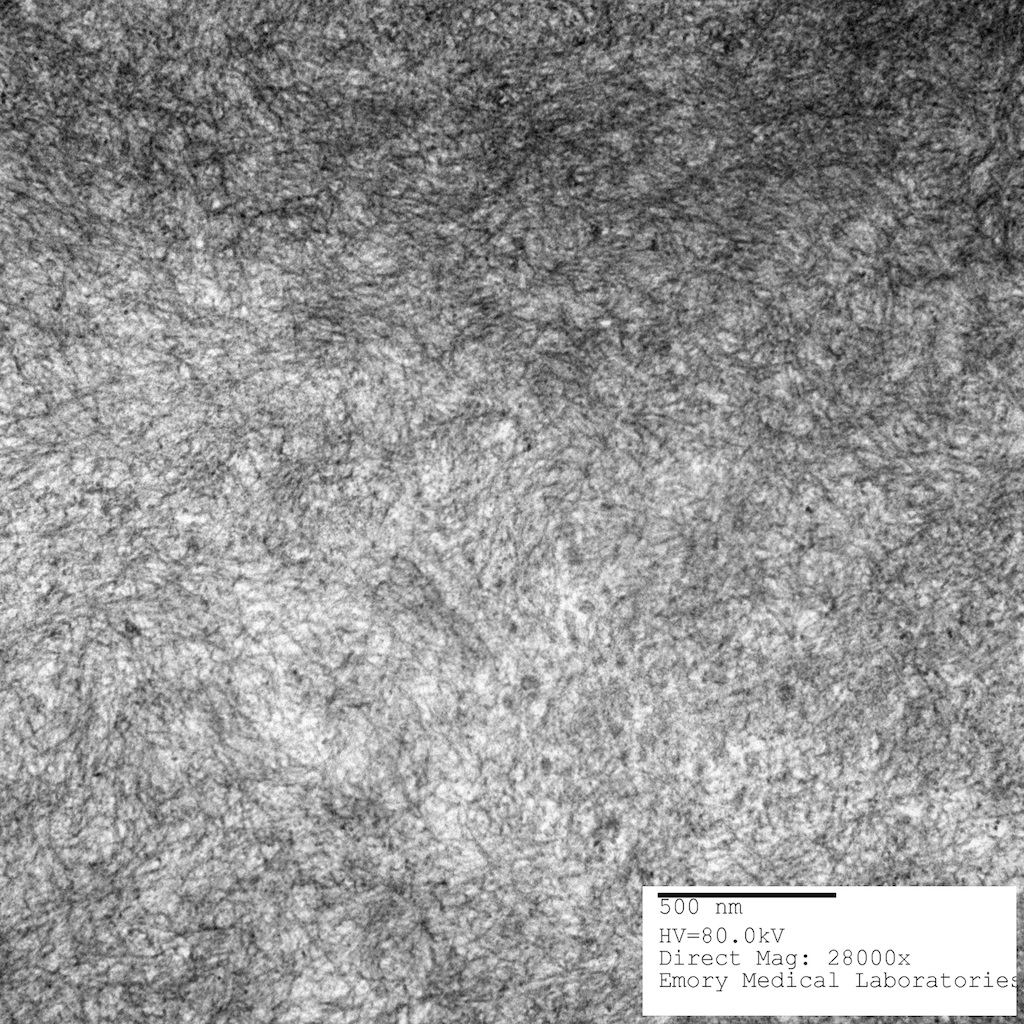
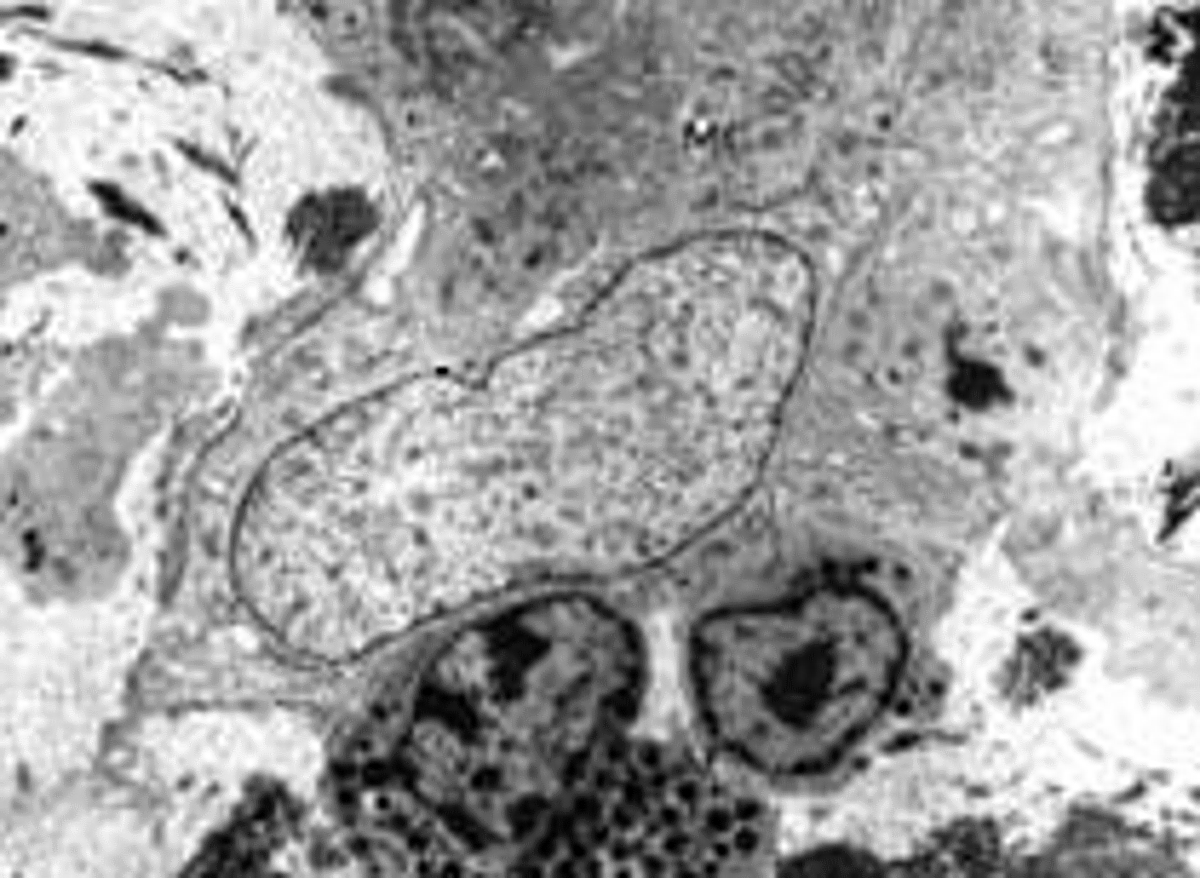
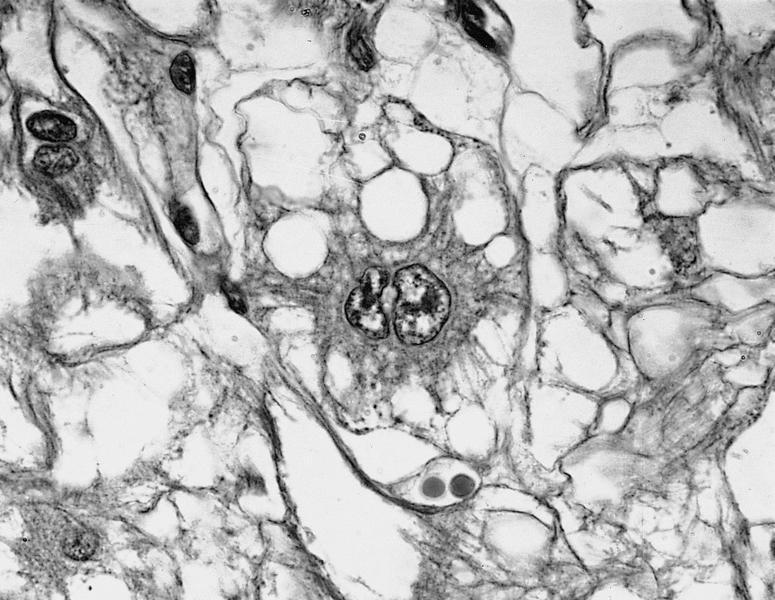
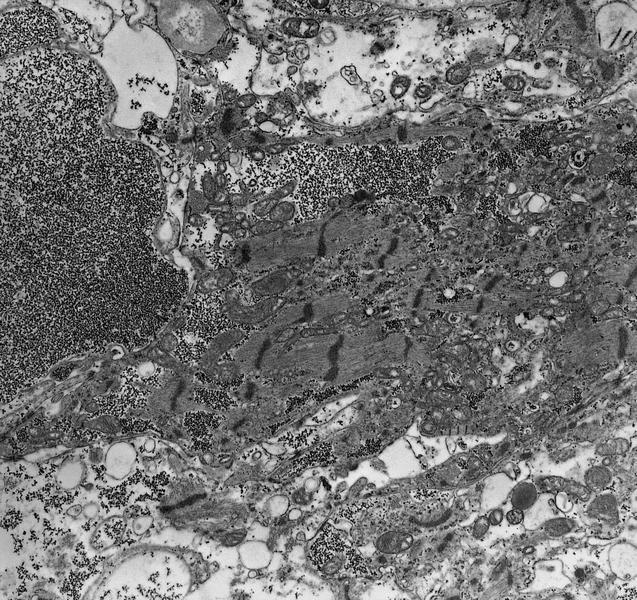
Electron microscopy description
- Electron microscopy is highly specific but has poor sensitivity due to the patchy nature of disease and magnification levels of electron microscopy
- Straight, unbranching fibrils 8 - 10 nm in width
- Composed of protofilaments at higher resolution
- In the myocardium, pericellular encasement nonbranching fibrils are found adjacent to the basement membrane; associated focal increase in mitochondria
- Can detect amyloid even when histochemical stains (Congo red) are negative (J Clin Pathol 2005;58:125)
Electron microscopy images
Molecular / cytogenetics description
- Mass spectrometry with laser microdissection - gold standard to identify precursor protein and amyloidosis type (even over immunohistochemistry, immunofluorescence and immunoelectron microscopy discussed above)
Sample pathology report
- Cardiac, core biopsy of left ventricular apex:
- Myocardium with extensive amyloid deposition in the interstitium with mild interstitial fibrosis
- Special studies: strongly positive on Congo red stain with apple green birefringence under polarized light; strongly positive crystal violet stain with purple metachromatic staining
Differential diagnosis
- Other disease processes that present with LV hypertrophy, such as
- Ischemic cardiomyopathy with fibrosis:
- Hypertrophic cardiomyopathy:
- Myocardium has a glistening leiomyoma-like appearance
- Myocytes display bizarre Y shaped forms into characteristic whorled appearance
- Often associated with family history of sudden cardiac death
- LVH secondary to hypertension:
- Most commonly concentric (less commonly eccentric) thickening of the left ventricular wall without outflow tract obstruction
- Boxcar nuclei on microscopy: enlarged nuclei with squaring of the nuclear edges
- Anderson-Fabry disease (Fabry disease):
- Rare
- Reduced concentration of serum alpha galactosidase A level or its activity is diagnostic
- Deficiency causes intracellular accumulation of galabiosylceramide and digalactosyl ceramide in myocardium (as well as in skin, vessels, kidney, eyes, ganglion cells)
- In prehypertrophy stage, the myocytes have perinuclear glycosphingolipid engorged vacuoles, which increase with extent of hypertrophy; this finally ends in necrosis and moderate fibrosis, intraluminal vessels are narrowed and thickened
Additional references
Board review style question #1
A cardiac biopsy demonstrates negative Congo red staining and there is a well founded morphologic suspicion for cardiac amyloidosis. What is the next best step?
- Abdominal fat pad biopsy
- Crystal violet stain
- Provide the negative diagnosis and suggest alternative diagnoses
- Repeat Congo red stain on 2 more sections
Board review style answer #1
D. Repeat Congo red (CR) stain on 2 more sections. Repeat the CR stain on 2 or more 8 - 10 micron sections in order to exclude technical problems. Use a rotating stage to evaluate various angles, avoid plastic coverslips and use proper optics (avoid polarizer with built in compensator). If CR stain is still negative, then proceed to crystal violet stain (answer B) (Diagn Pathol 2019;14:57). In practice, a repeat CR stain and crystal violet stain may be done simultaneously. Answer A is incorrect, as the patient has undergone a cardiac biopsy. An abdominal fat pad biopsy, even if positive for amyloidosis, is not diagnostic of cardiac amyloidosis. Answer C is incorrect because in a patient with a high index of suspicion and a negative CR stain, the stain should be double checked or repeated to control for possible technical errors.
Comment Here
Reference: Cardiac amyloidosis
Comment Here
Reference: Cardiac amyloidosis
Board review style question #2
What is the gold standard to identify amyloid subtype and precursor protein?
- Electron microscopy
- Immunofluorescence studies
- Immunohistochemistry
- Mass spectrometry
Board review style answer #2
D. Mass spectrometry. Mass spectrometry is the gold standard for identifying amyloid subtypes and precursor proteins. Answers A - C are incorrect as these methods are not the gold standard. Note that formalin fixed and paraffin embedded (FFPE) specimens can be used for a complete examination and characterizations (suitable for histologic, histochemical, immunohistochemical investigations, as well as molecular analysis). Frozen sections are only needed at centers that traditionally use immunofluorescence for amyloid typing (Front Cardiovasc Med 2022;9:1081098, Biomedicines 2022;10:3054).
Comment Here
Reference: Cardiac amyloidosis
Comment Here
Reference: Cardiac amyloidosis
Anomalous coronary artery
Table of Contents
Definition / general | Epidemiology | Pathophysiology | Clinical features | Diagrams / tables | Diagnosis | Radiology description | Case reports | Treatment | Clinical images | Gross description | Additional referencesDefinition / general
- A coronary anomaly is defined as any coronary pattern with a feature (number of ostia, proximal course, termination, etc.) "rarely" encountered in the general population
Epidemiology
- Coronary anomalies affect 1% of the general population
- Necropsies yield an even lower incidence (0.3%)
- According to the Sudden Death Committee of the American Heart Association, coronary anomalies cause 19% of deaths in athletes (Circulation 1996;94:850)
- Burke et. al. reported that in 14 to 40 year olds, coronary anomalies are involved in 12% of sports related sudden cardiac deaths versus 1.2% of non sports related deaths (Am Heart J 1991;121:568)
Pathophysiology
- Anomaly: right and left coronary arteries both originate from the same sinus of valsalva
- Normally, the coronary ostia are round to oval in shape but in this anomaly, the coronary artery has an acute takeoff angle that makes the ostium slit like in shape
- With increased cardiac output (e.g., exercise), the aorta dilates and upon aortic wall stretching, this slit like ostium becomes severely narrowed
- Anomaly: high takeoff of coronary arteries
- Normally, the coronary ostia are located within the sinuses of Valsalva which permits maximal opportunity for coronary artery diastolic filling
- Location of the ostia in the tubular portion of the aorta (i.e., high takeoff position) may be associated with decreased coronary perfusion
Clinical features
- Signs / symptoms: chest pain, sudden death, cardiomyopathy, syncope, dyspnea, ventricular fibrillation, myocardial infarction
Diagnosis
- Thallium exercise stress test may be used for diagnosis but is not sufficiently sensitive to show myocardial perfusion defects
Radiology description
- Coronary angiography and transesophageal echocardiography are useful
- Contrast enhanced electron beam tomography: offers excellent spatial resolution and identifies most anomalies of coronary vessels but it uses ionizing radiation and potentially nephrotoxic or allergenic contrast agent
- MRI: avoids radiation and contrast agents and yields excellent images in determining coronary origination, especially in patients with congenital defects
- Its greatest limitation is in determining the distal coronary course
- Hence it is less helpful in evaluating fistulas, coronary origination outside the normal sinuses (e.g. from a ventricle or pulmonary artery) and collateral vessels, and visualization of the posterior descending branch
Case reports
- 5 year old girl with anomalous origin of left coronary artery (Clinics (Sao Paulo) 2010;65:1215)
- 56 year old man with anomalous origin of right coronary artery (Internet Journal of Cardiology 2006;5(1))
- 71 year old man with myocardial ischemia caused by an anomalous circumflex coronary artery (Rev Esp Cardiol 2002;55:200)
- 73 year old man with myocardial ischemia caused by a coronary anomaly (Tex Heart Inst J 2004;31:273)
Treatment
- If diagnosed antemortem, surgery is the treatment of choice in most cases
- Takeuchi procedure: used to correct the infantile form of anomalous origin of coronaries by creating a communication between the aorta and the left coronary ostium through the pulmonary artery using tubular material (graft) (J Cardiothorac Surg 2008;3:33)
- Usually, this technique is performed when direct implantation of the anomalous artery into the aorta is difficult due to unfavorable conditions
- In the adult form, ligation of the origin of the coronary artery at the pulmonary artery is performed in a combined manner so that flow is either restored or persists through a connection with either the internal thoracic artery or a saphenous vein graft from the ascending aorta
Clinical images
Gross description
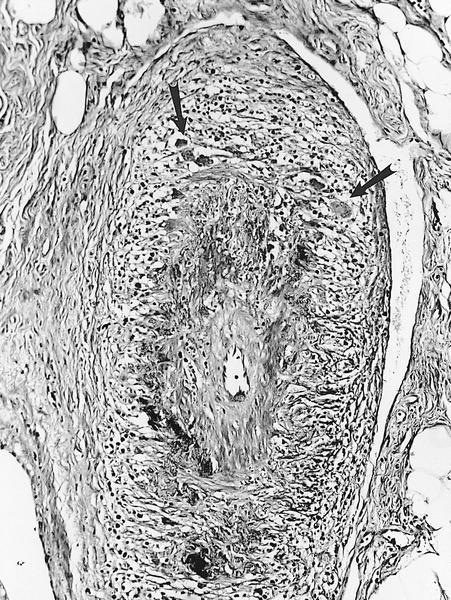
- Myocardial bridges ("tunneled" epicardial coronary artery)
- The coronary arteries which normally course over the epicardial surface of the heart may dip into the myocardium to travel for varying lengths and then reappear on the heart surface
- The muscle overlying the intramyocardial segment of the epicardial coronary artery is termed a "myocardial bridge" and the artery coursing within the myocardium is called a "tunneled" artery
- Congenital coronary artery aneurysms are found most commonly in the right coronary artery
- Abnormal flow patterns within the aneurysm may lead to thrombus formation with subsequent vessel occlusion, distal thromboembolization and myocardial infarction
Antibody mediated rejection (pending)
[Pending]
Aortic aneurysms
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Progressive, irreversible, localized dilatation of the aortic wall (involving all 3 layers) exceeding the expected aortic diameter by > 1.5 fold
Essential features
- Majority of cases are asymptomatic until rupture, which is fatal (> 80% estimated mortality) (J Vasc Surg 2018;68:612)
- Aneurysm size and growth rate are the best predictors of risk of rupture (Gen Thorac Cardiovasc Surg 2019;67:1)
- Intervention is recommended for diameter > 5.0 - 5.5 cm or growth > 0.5 cm/year
- Risk factors include male sex, advanced age, smoking, hypertension, atherosclerosis, bicuspid aortic valve (BAV) and connective tissue syndromes (Circ Res 2019;124:607)
- Characteristic histologic findings include disruption of elastic lamellae, loss of smooth muscle cells, inflammation infiltration, increased proteolysis of extracellular matrix (Cardiovasc Pathol 2016;25:247)
Terminology
- Thoracic aortic aneurysm (TAA): aortic aneurysm (AA) located within the chest cavity
- Abdominal aortic aneurysm (AAA): aortic aneurysm located within abdominal cavity
- Pseudoaneurysm: false aneurysm; a rupture of the arterial wall contained by the tunica adventitia or a blood clot
- Aortic root dilation / aortic root aneurysm: aortic aneurysm located at the aortic root
- Aortic dissection: tear of the inner layer of the aortic wall, can involve multiple layers
- Ectasia: dilatation of the aorta that does not measure > 1.5 times the diameter of normal aorta
ICD coding
- ICD-10
- I71 - aortic aneurysm and dissection
- I71.0 - dissection of aorta
- I71.1 - thoracic aortic aneurysm, ruptured
- I71.2 - thoracic aortic aneurysm, without rupture
- I71.3 - abdominal aortic aneurysm, ruptured
- I71.4 - abdominal aortic aneurysm, without rupture
- I71.5 - thoracoabdominal aortic aneurysm, ruptured
- I71.6 - thoracoabdominal aortic aneurysm, without rupture
- I71.8 - aortic aneurysm of unspecified site, ruptured
- I71.9 - aortic aneurysm of unspecified site, without rupture
- A52.01 - syphilitic aneurysm of aorta
- S25.09 - other specified injury of thoracic aorta
- S35.09 - other injury of abdominal aorta
- I71 - aortic aneurysm and dissection
Epidemiology
- It is estimated that 1 - 2% of the population have an AA, increasing to 10% of individuals older than 65 years (Cardiovasc Pathol 2016;25:432)
- According to the Centers for Disease Control and Prevention (CDC), AA rupture accounted for 9,317 deaths in 2020
- There is higher prevalence in men, White populations, individuals with hypertension, with tobacco use, with advanced age (Circulation 2009;119:2202, J Vasc Surg 2010;52:539)
- TAA frequently occurs as a manifestation of connective tissue disorders (Marfan, Loeys-Dietz, Ehlers-Danlos, familial TAA)
- AAAs are often associated with atherosclerosis (Circulation 2010;121:e266)
Sites
- Thoracic aortic aneurysm
- Sinus of Valsalva
- Aortic root
- Ascending aorta
- Aortic arch
- Descending aorta
- Combined
- Abdominal aortic aneurysm: most common
- Suprarenal aorta
- Infrarenal aorta
- Combined
- Integrated (with iliac arteries)
- Thoracoabdominal aortic aneurysm
- Type I (from left subclavian artery [LSA] to celiac artery [CA])
- Type II (from LSA to iliac bifurcation [IB])
- Type III (from sixth intercostal space to IB)
- Type IV (from subdiaphragmatic segment to IB)
- Type V (from sixth intercostal space to renal artery [RA])
- Reference: Semin Vasc Surg 2021;34:18
Pathophysiology
- Medial degeneration, led by 3 interconnected processes (Cardiovasc Pathol 2016;25:432)
- Excessive extracellular matrix (ECM) degradation
- Disruption of elastin and collagen homeostasis
- Increase in matrix metalloproteinase activity leading to extensive proteolysis
- Inflammation
- Inflammatory cell infiltration and activation of proteases (Circ Res 2019;124:607)
- Neovascularization
- Smooth muscle cell (SMC) apoptosis
- Significant loss or disorganization of smooth muscle cells within the intima media
- Excessive extracellular matrix (ECM) degradation
- Degradation of the aortic wall → weakening of the aortic wall → dilation of the aorta → increased aortic wall stress → further wall weakening and risk of rupture
Etiology
- Degenerative (Vasc Med 2022;27:88)
- Hypertension and atherosclerosis accelerate medial degeneration
- Smoking and hypercholesterolemia
- Familial / genetic
- Marfan, Ehlers-Danlos, Loeys-Dietz and familial TAA
- Anatomic
- Bicuspid aortic valve (BAV)
- Infectious
- Hematogenous spread of infectious microemboli, preexisting intimal defect infection or direct inoculation of the aortic wall (Anesthesiol Clin 2022;40:671)
- Staphylococcus and Streptococcus, fungal infections, syphilis
- Hematogenous spread of infectious microemboli, preexisting intimal defect infection or direct inoculation of the aortic wall (Anesthesiol Clin 2022;40:671)
- Inflammatory
- Giant cell arteritis, Takayasu arteritis, Kawasaki disease, Behçet syndrome (Anesthesiol Clin 2022;40:671)
- Others
- Trauma
- Dissection
- Angioplasty
- Drug eluting stents
Clinical features
- Risk factors: smoking, older age, male sex, family history of AA, hypertension, atherosclerosis, connective tissue syndromes (Cardiovasc Pathol 2016;25:432)
- Most cases are asymptomatic until rupture
- Can present as nonpositional angina pectoris, back pain, diffuse abdominal pain, tenderness on palpation, abdominal bruit or edema (Anesthesiol Clin 2022;40:671)
- Symptomatic AAs are at an increased risk of rupture
- Ruptured AA can cause severe / diffuse abdominal pain, dyspnea, shock and a palpable / pulsatile abdominal mass
- Median yearly growth rate of AAs is 0.1 - 0.4 cm/year (J Transl Int Med 2016;4:35)
- Diameter has an exponential effect on risk of rupture
Diagnosis
- Computed tomography (CT) is the gold standard for evaluation of AA size and morphology (Circulation 2022;146:e334)
- Ultrasound (US) is the main screening, diagnostic and monitoring tool (Br J Radiol 2018;91:20170306)
- U.S. Preventive Services Task Force (USPSTF) recommends US screening for men 65 - 75 years who ever smoked (Ann Vasc Surg 2019;54:298)
- CT scan with contrast is preferred for intervention planning
- Magnetic resonance imaging (MRI) used as alternative during pregnancy
Radiology description
- Chest radiographs: widening of the mediastinum or bulging of the ascending aorta (J Vasc Interv Radiol 2008;19:S2)
- Ultrasound: dilatation of the aorta of > 1.5 times the normal diameter (J Vasc Interv Radiol 2008;19:S2)
- CT / MRI: dilatation of the aortic lumen; the walls may be thin or thickened by the presence of a mural thrombus (Emerg Med Clin North Am 2021;39:745)
Radiology images
Prognostic factors
- Without intervention, AA will continue to expand and eventually rupture
- Without immediate intervention, rupture is fatal
- Mortality rate of surgical rupture repair is estimated to be 43 - 46% (J Vasc Surg 2021;73:39)
- Risk factors for dissection / rupture (PLoS One 2022;17:e0270585, Bioengineering (Basel) 2020;7:79, Gen Thorac Cardiovasc Surg 2019;67:1)
- > 5 - 7 cm diameter
- Rapid growth rate: > 0.5 cm in 6 months
- Longer aneurysm segment
- Diastolic pressure > 105 mmHg
- High peak wall stress (hypertension, atherosclerosis)
- Asymmetry
- Tobacco / cocaine use
- Connective tissue disorder: Marfan, Ehlers-Danlos, bicuspid aortic valve
- Vascular inflammation: giant cell arteritis, Takayasu arteritis, syphilis
- Family history of AA or aortic dissection
- Symptomatic aneurysm
- Advanced age
Case reports
- 25 year old man with Marfan syndrome and giant aortic root aneurysm (J Invasive Cardiol 2021;33:E231)
- 37 year old man with large thoracic aortic aneurysm (Vasc Health Risk Manag 2022;18:1)
- 58 year old man with mycotic abdominal aortic aneurysm (J Med Case Rep 2022;16:44)
- 79 year old man with 10 cm abdominal aortic aneurysm (Perm J 2019;23:18.218)
- 84 year old woman with thoracic aortic aneurysm (BMC Gastroenterol 2020;20:63)
Treatment
- American College of Cardiology (ACC) / American Heart Association (AHA) guidelines (2022) recommends repair for AA ≥ 5.0 - 5.4 cm and surveillance for smaller diameter lesions (Circulation 2022;146:e334)
- Intervention: endovascular aneurysm repair versus open surgical repair
- Earlier intervention may be recommended (Trends Cardiovasc Med 2020;30:500)
- Growth rate: > 0.5 cm in 6 months
- Connective tissue syndromes / vascular inflammation
- Family history of aortic dissection
- Women
- Cross sectional aortic area/height ratio > 10 cm2/m
- Earlier intervention may be recommended (Trends Cardiovasc Med 2020;30:500)
- Society for Vascular Surgery (2018) recommended surveillance (J Vasc Surg 2018;67:2)
- > 2.5 - 2.9 cm: rescreen after 10 years
- 3.0 - 3.9 cm: 3 year interval
- 4.0 - 4.9 cm: 1 year interval
- 5.0 - 5.4 cm: 6 month interval
- Intervention: endovascular aneurysm repair versus open surgical repair
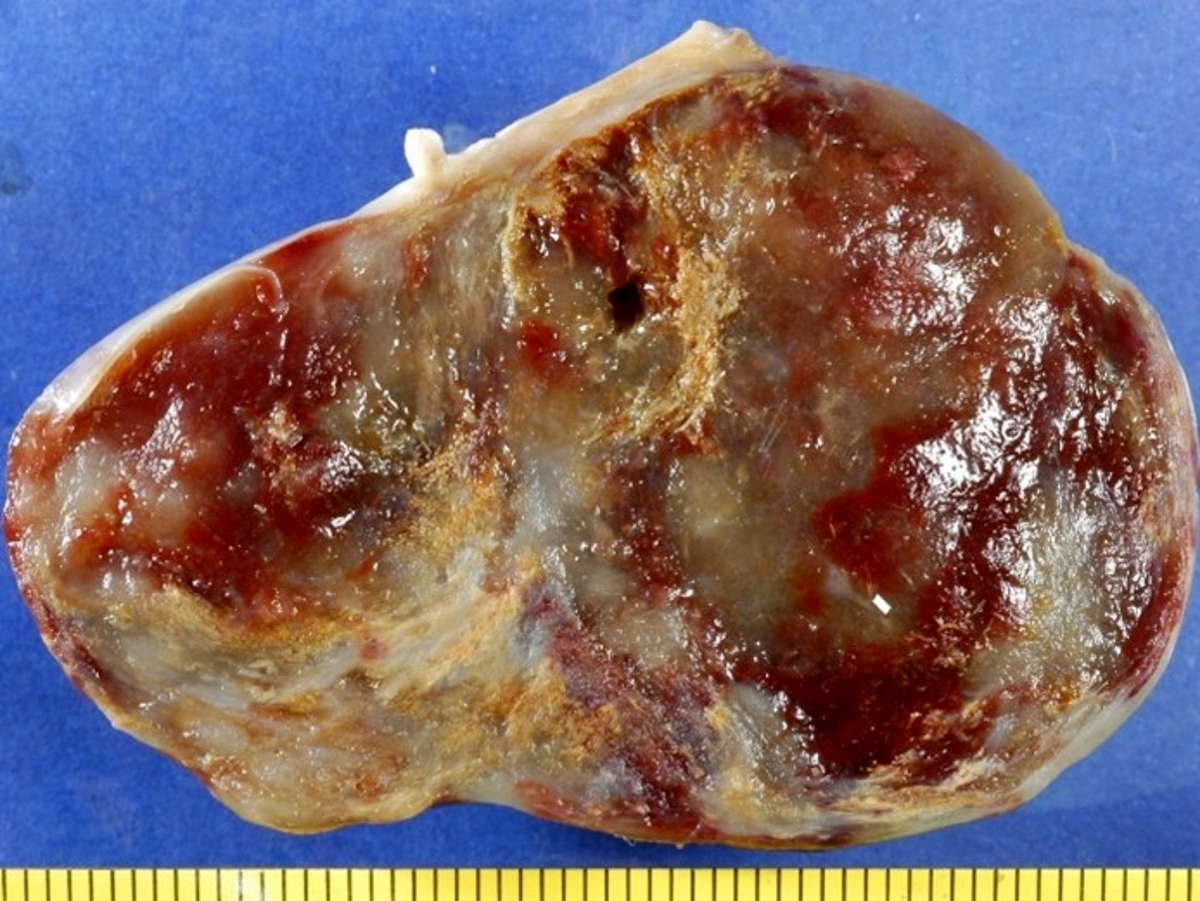
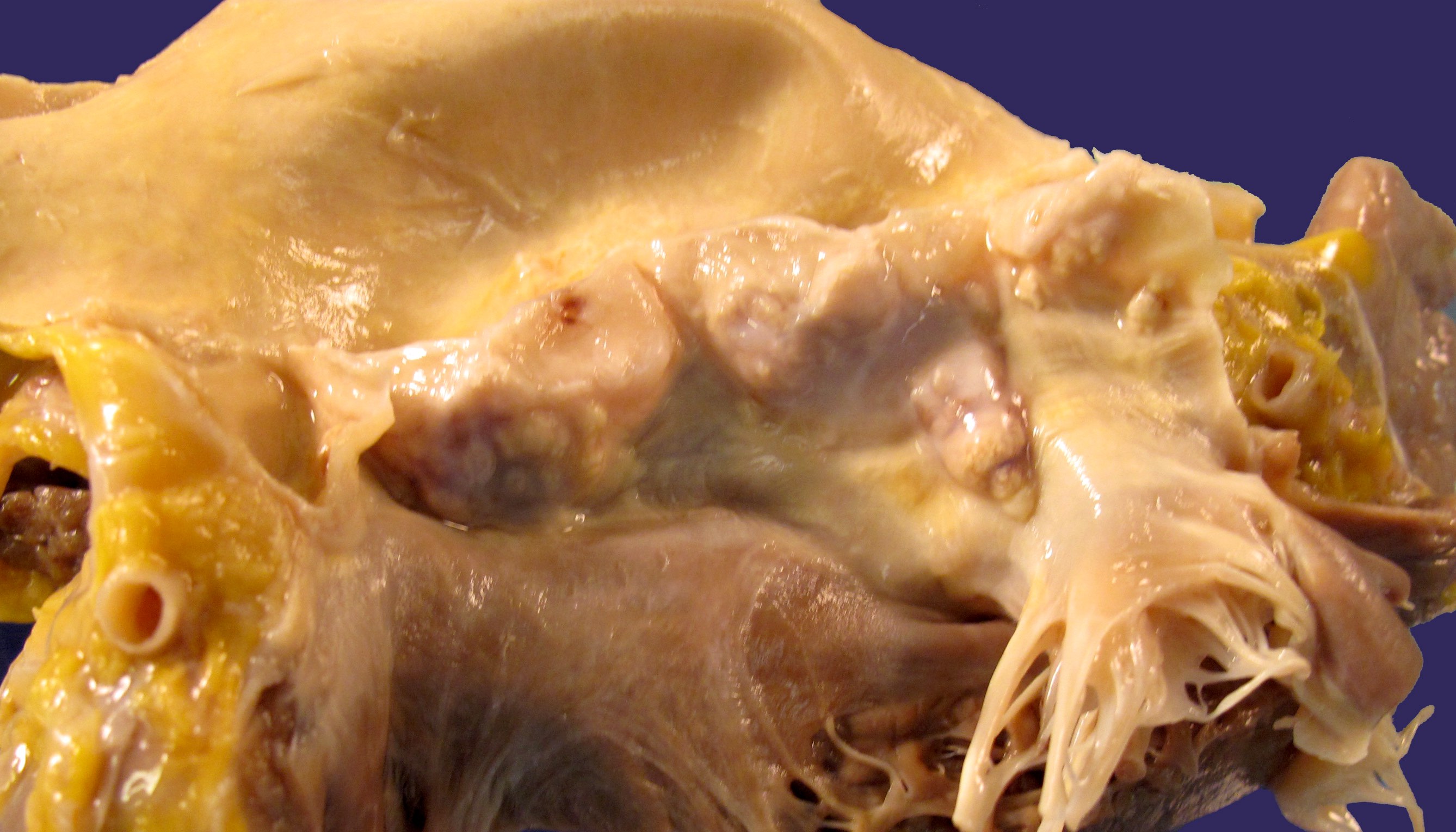
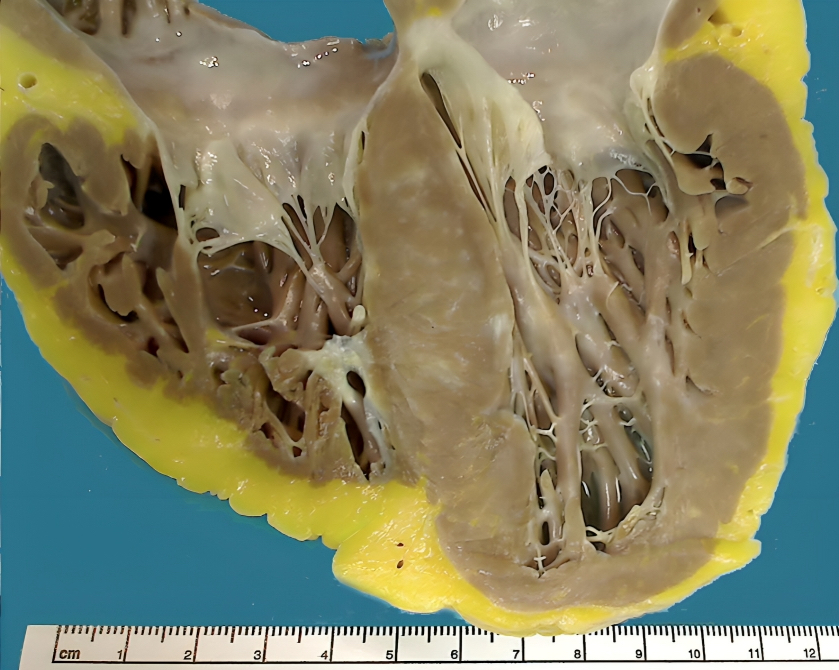
Gross description
- Aortic aneurysms are defined as a focal dilatation of at least 50% of the normal arterial diameter
- AAA typically > 3 - 3.5 cm (J Am Coll Cardiol 2022;80:e223)
- TAA typically > 4.0 - 5.0 cm (J Am Coll Cardiol 2022;80:e223)
Gross images
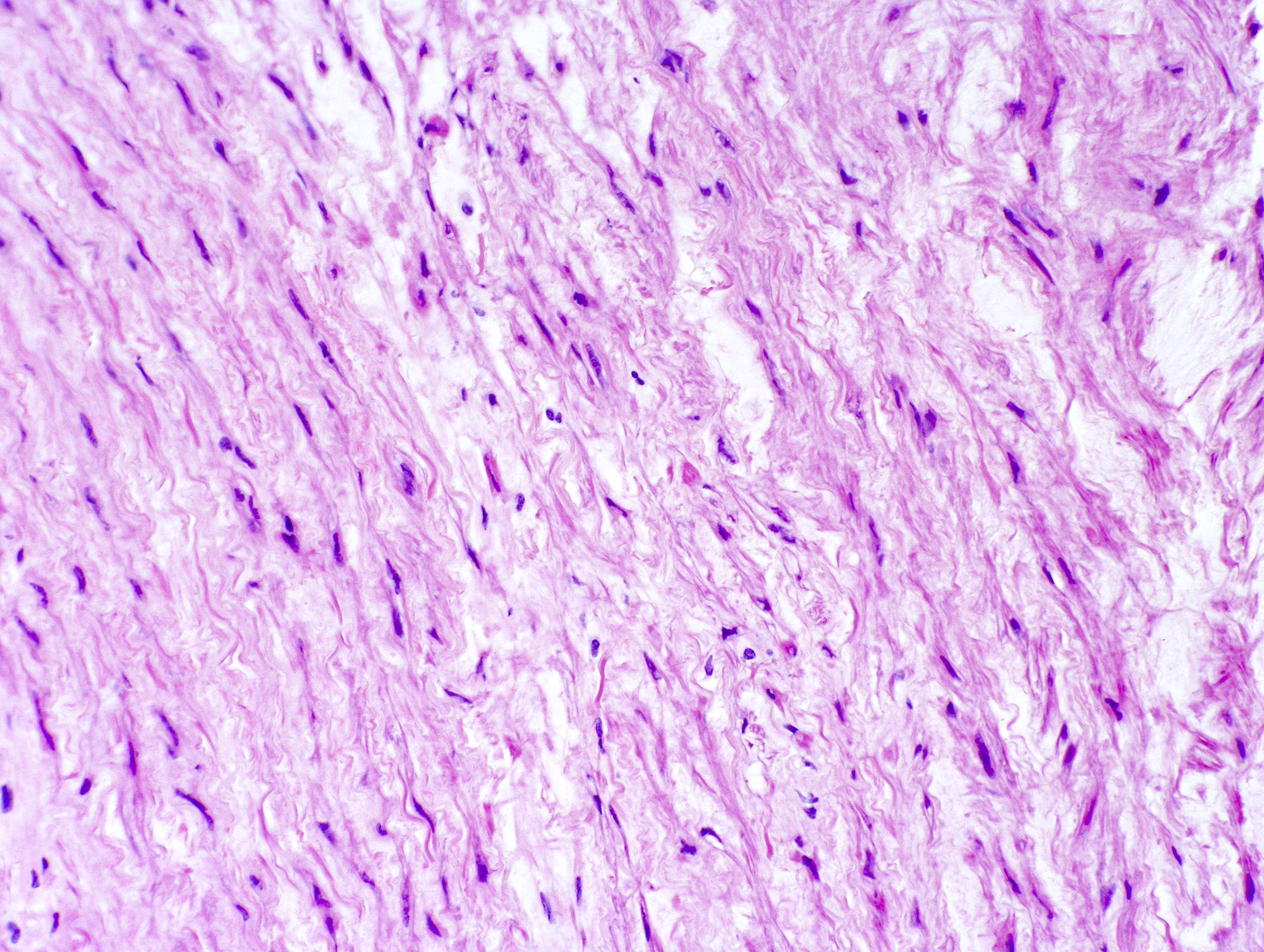
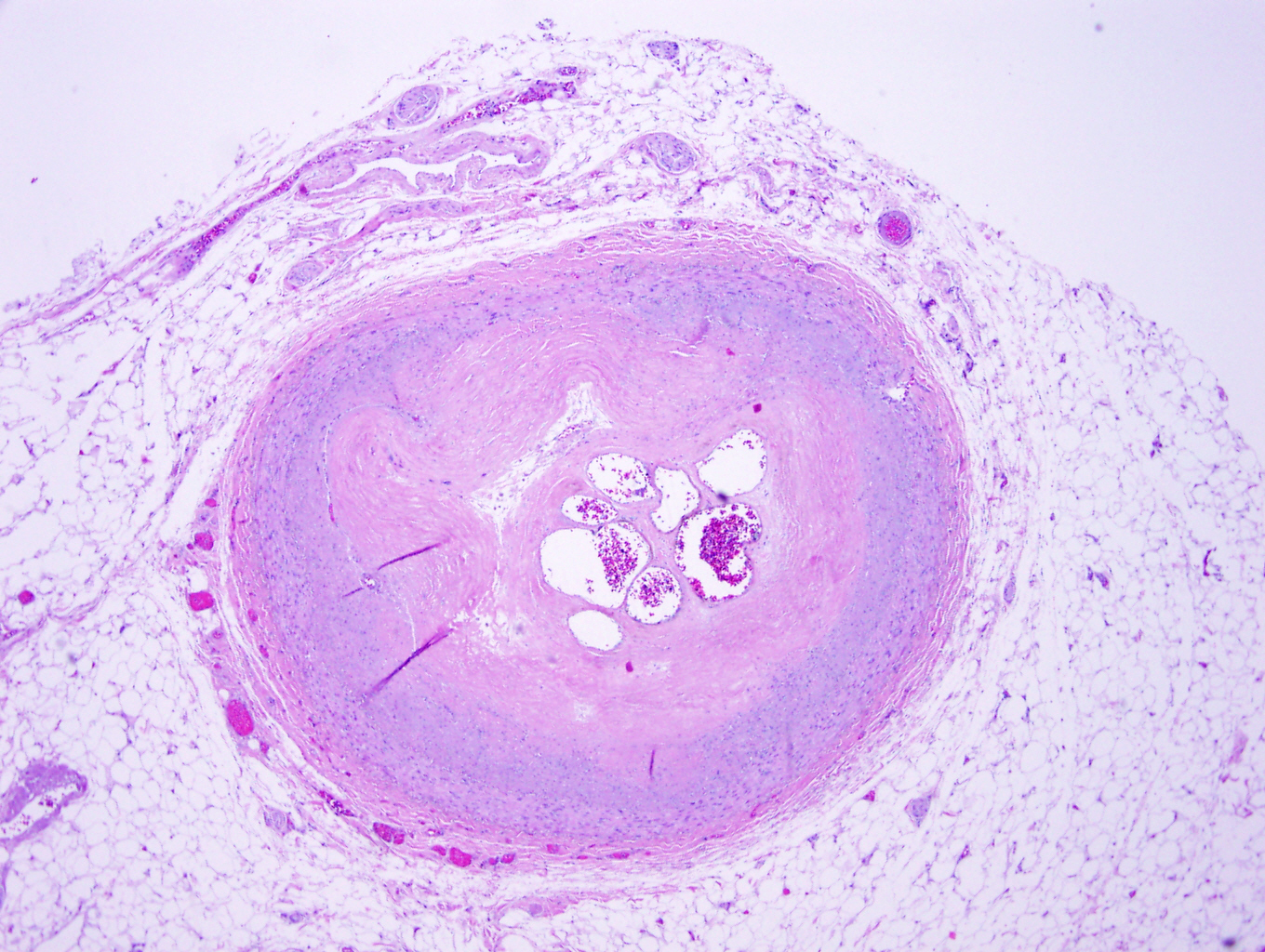
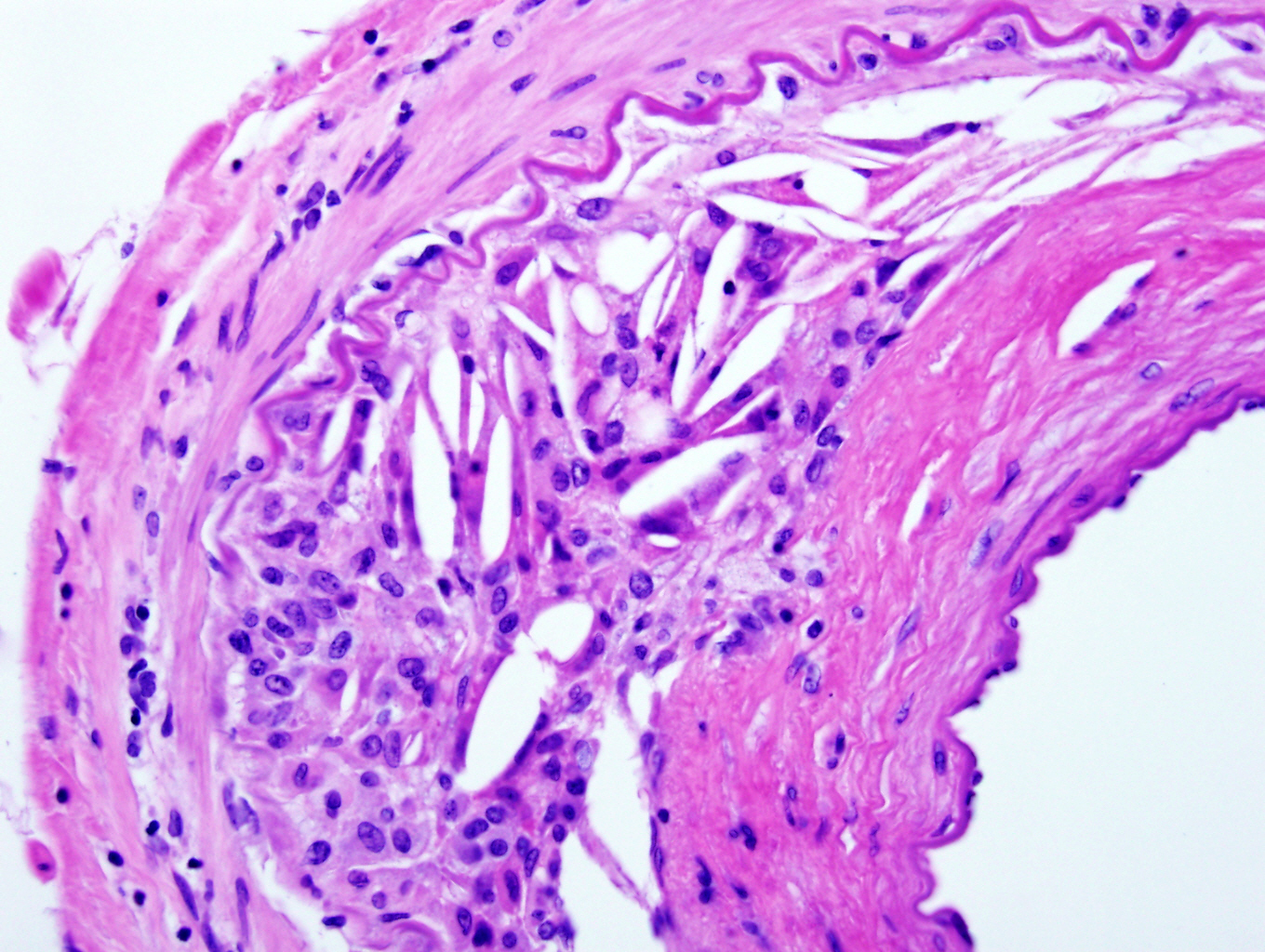
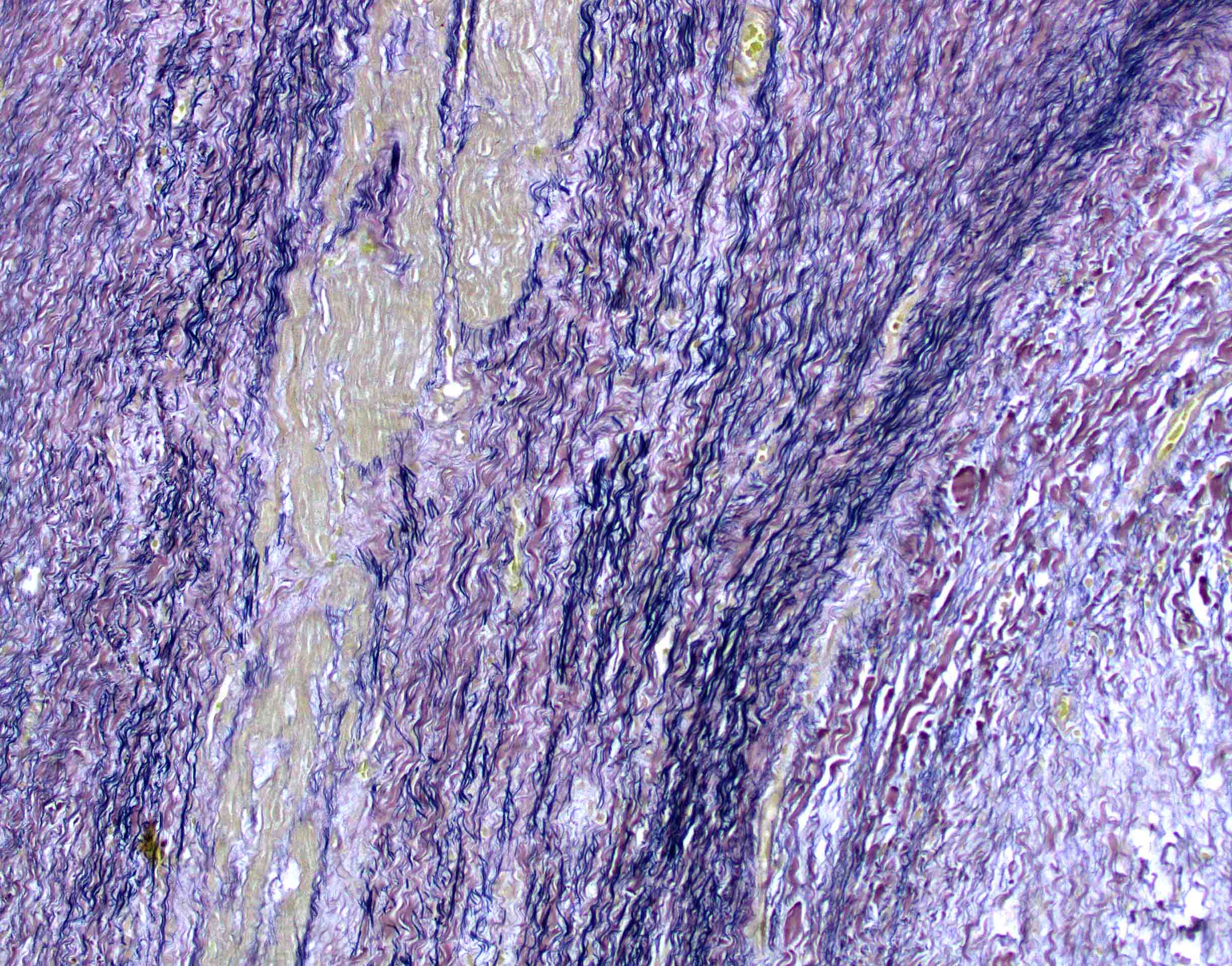
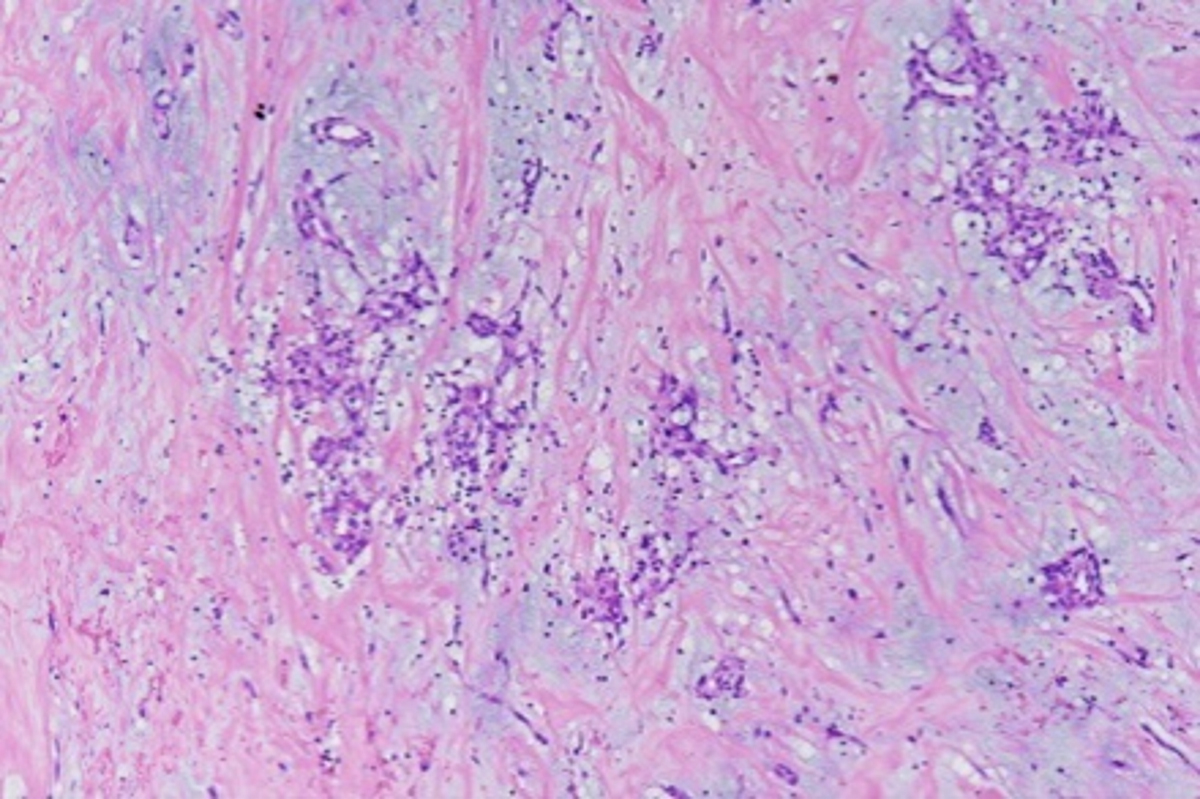
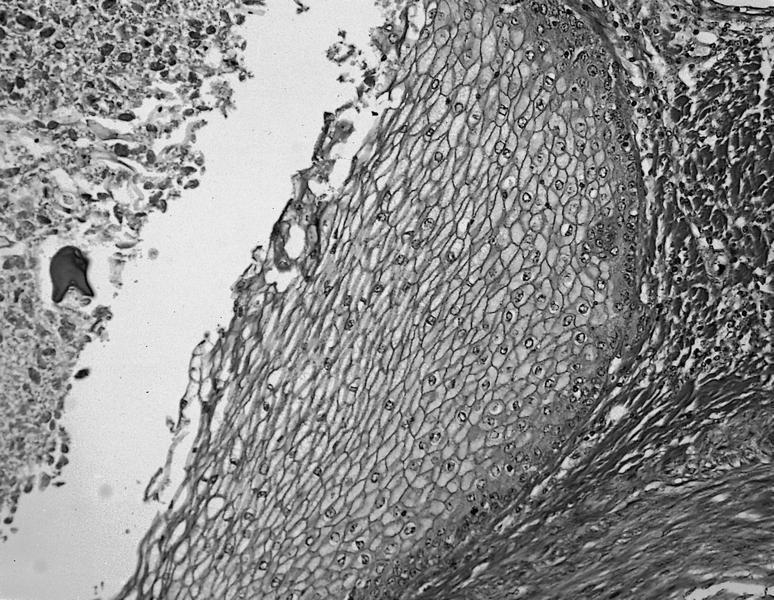
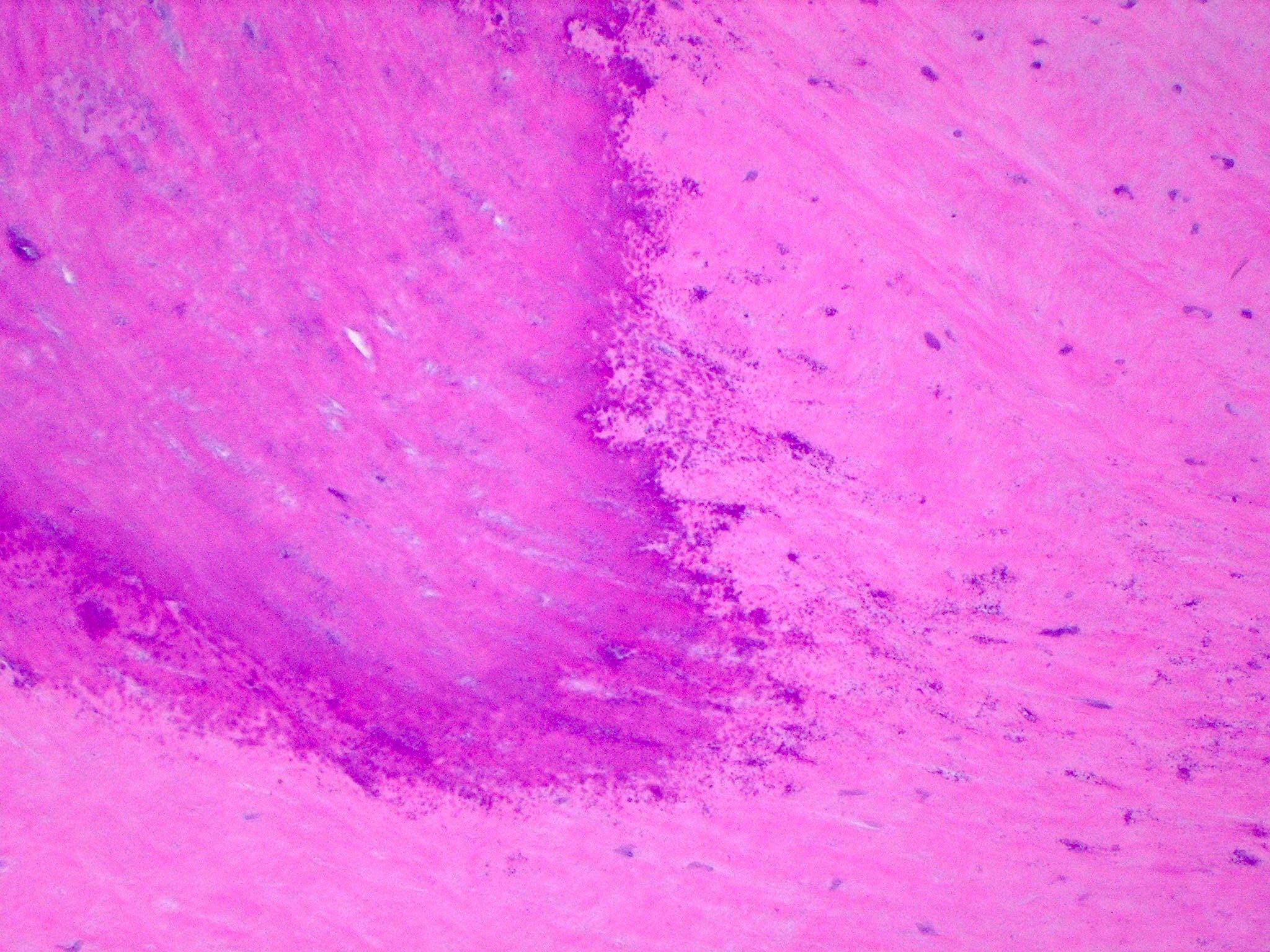
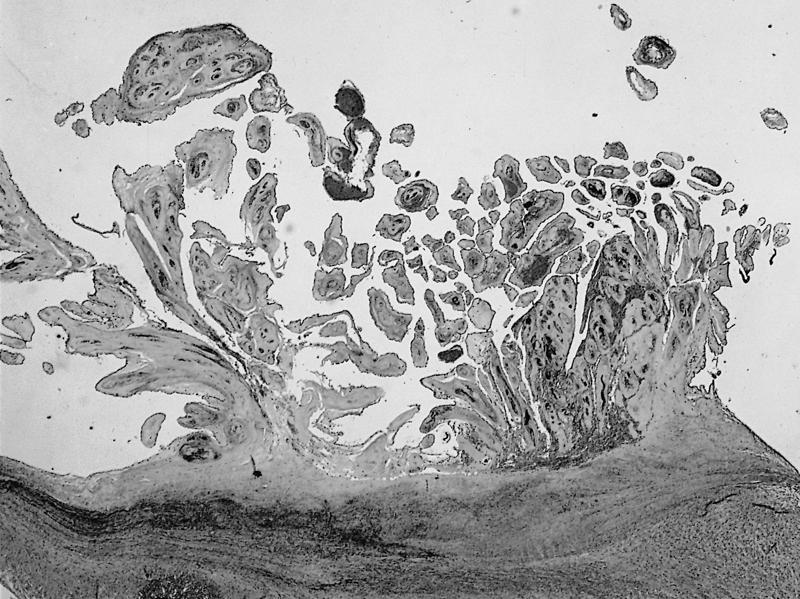
Microscopic (histologic) description
- Medial degeneration (Histopathology 1990;16:557)
- Loss / disorganization of elastic lamellae
- Loss of smooth muscle cells
- Mucoid extracellular matrix accumulation (MEMA)
- Medial fibrosis
- Border between tunica media and tunica intima may be obscured
- Inflammatory reaction (JVS Vasc Sci 2021;2:260)
- Lymphocyte and macrophage infiltration
- Medial neovascularization
- Increased proteolysis
- Increasing proteoglycan deposition
- Atherosclerotic lesions (Cardiovasc Pathol 2015;24:267)
- Lipid deposits, foam cells, cholesterol clefts, eosinophilic debris, calcifications or neovascularization
- Increase of various matrix metalloproteinases (MMPs) and cadherin (Histopathology 1990;16:557)
- Increased collagenase / elastase activity
- There may be luminal fibrin thrombus present (Cardiovasc Pathol 2015;24:267)
Microscopic (histologic) images
Sample pathology report
- Pathology is usually not included for diagnosis and diagnosis does not need to be reported but can be included in the microscopic description
- Abdominal aorta, endovascular aneurysm repair (EVAR):
- Abdominal aortic aneurysm (6.2 cm) (see comment)
- Comment: Microscopic examination reveals multifocal, extensive intralamellar and translamellar MEMA (mucoid extracellular matrix accumulation). There is also extensive elastic fiber disorganization and elastic fiber fragmentation along the tunica media. Morphologic findings, including frequent, band-like smooth muscle nuclei loss and extensive smooth muscle disorganization along the tunica media, are worrisome and along with the rest of the findings, reach the threshold for classification of severe medial degeneration.
- Abdominal aorta, endovascular aneurysm repair (EVAR):
Differential diagnosis
- Aortic dissection:
- There is a distinct intimal wall tear as well as separation of the arterial layers
- Pseudoaneurysm:
- Local hematoma in vessel not containing any layer of the vessel wall
- Myocardial infarction:
- Electrocardiogram (ECG) changes, elevated cardiac enzymes, ischemic changes in myocardium
- Acute cholecystitis:
- Imaging US / CT can show gallstones, edema and fat stranding surrounding gallbladder
- Gastritis and peptic ulcer disease:
- Abdominal pain usually related to positional changes and eating habits
- Pancreatitis:
- Elevated amylase / lipase levels, CT shows pancreatic edema / fat stranding, duct changes
- Bowel obstruction / ischemic bowel:
- Imaging will show bowel obstruction or reduced flow to the bowel
- Appendicitis:
- Presents with fever, McBurney point tenderness
- CT shows enlarged appendix with inflammatory signs
- Musculoskeletal pain:
- Associated with point tenderness and does not radiate
- Pulmonary embolism:
- Imaging shows central filling defect
- Pain tends to be pleuritic
Additional references
Board review style question #1
A 70 year old man dies after the sudden onset of back pain. The autopsy pathologist (gross image shown above) notes severe medial degeneration when examining a section of the suprarenal aorta. What specific change is most likely to also be seen in this tissue sample?
- Fibrinoid necrosis of vessel walls
- Inflammation limited to the adventitia with scarring
- Significant loss of smooth muscle cells
- Well formed granulomas with eosinophilic presence
Board review style answer #1
C. Significant loss of smooth muscle cells. Significant loss of smooth muscle cells is a characteristic process of medial degeneration in aortic aneurysm. Answer A is incorrect because fibrinoid necrosis can be seen in necrotizing vasculitis. Answer D is incorrect because granulomas with eosinophilic infiltrate can be seen in eosinophilic granulomatosis with polyangiitis. Answer B is incorrect because inflammation limited to the adventitia with scarring is more commonly seen in atherosclerosis.
Comment Here
Reference: Aortic aneurysms
Comment Here
Reference: Aortic aneurysms
Board review style question #2
A 55 year old man is seen for follow up imaging for a 4.2 cm thoracic aortic aneurysm found 4 months ago. Computed tomography (CT) with contrast shows a focal dilation along the descending aorta, measuring 4.9 cm. What is the most recommended next step for this patient's management?
- Elective aortic aneurysm repair
- Follow up CT in 6 months
- Follow up ultrasound in 6 months
- Follow up ultrasound in 12 months
Board review style answer #2
A. Elective aortic aneurysm repair. Although the diameter of the aneurysm has not reached > 5.0 cm (general threshold recommended by American College of Cardiology [ACC] / American Heart Association [AHA] guidelines 2022 for intervention), the aneurysm has grown > 0.5 cm in 6 months. Thus, this patient's aneurysm growth rate meets the guidelines for recommending intervention. Answers B and C are incorrect because although screening every 6 months is recommended for men with AAA of diameter 4.0 - 4.9 cm, according to ACC / AHA guidelines 2022 for intervention, a repair is recommended for an AAA that has grown > 0.5 cm in 6 months as there is an increased risk of rupture. Answer D is incorrect because this is the surveillance recommendation for patients with AAA with a diameter of 3.0 - 3.9 cm, whereas this patient requires repair due to the risk of rupture.
Comment Here
Reference: Aortic aneurysms
Comment Here
Reference: Aortic aneurysms
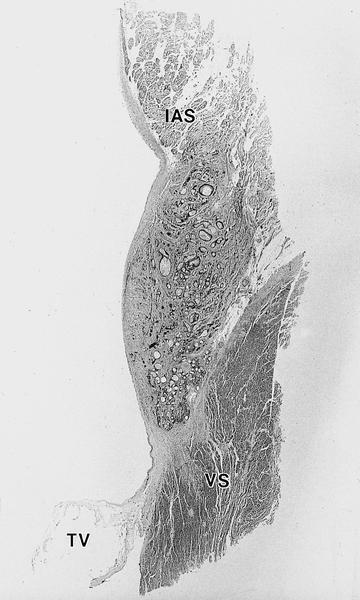
Arrhythmogenic right ventricular cardiomyopathy
Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a primary heart muscle disease characterized by progressive myocardial atrophy of the right ventricle, with transmural fatty or fibrofatty replacement, either segmental or diffuse, accounting for electrical instability at risk of life threatening ventricular arrhythmias
Terminology
- Also known as arrhythmogenic right ventricular dysplasia
Epidemiology
- Incidence varies between 1 in 1,000 and 1 in 5,000
Sites
- Right ventricular free wall
Pathophysiology
- ARVC is an acquired, nonischemic atrophy of the right ventricular myocardium
- Dystrophic theory: the fibrofatty infiltration is viewed as a healing phenomenon in the setting of chronic myocarditis
- Genetic factors: genetic predisposition to viral infection triggering an immune response, with a selective involvement of the right ventricle
Etiology
- Genetic
- Inherited in an autosomal dominant pattern, with variable expression
- Point mutations in genes coding for desmosomal proteins are the main causatives for the development of this disease
Clinical features
- Most common symptom is palpitations
- Palpitations can occur at rest but are often triggered by physical activity
- They may be associated with chest pain, light headedness or blackouts
- ARVC is also a recognised cause of sudden cardiac death
Diagnosis
- ECG:
- Right ventricular outflow tract (RVOT) tachycardia is the most common VT seen in individuals with ARVD
- In this case, the ECG shows a left bundle branch block (LBBB) morphology with an inferior axis
- Signal averaged ECG (SAECG) is used to detect late potentials and epsilon waves in individuals with ARVD
- Echocardiography may reveal an enlarged, hypokinetic right ventricle with a paper thin RV free wall
- The dilatation of the RV will cause dilatation of the tricuspid valve annulus, with subsequent tricuspid regurgitation
- Paradoxical septal motion may also be present
- Cardiac MRI: to detect fatty infiltration of the RV free wall
- Right ventricular angiography is considered the gold standard for the diagnosis of ARVD
- Findings include akinetic or dyskinetic bulging localized to the infundibular, apical and subtricuspid regions of the RV; these findings are 90% specific
- Transvenous biopsy of the right ventricle can be highly specific for ARVD
Case reports
- 42 year old woman with arrhythmogenic right ventricular cardiomyopathy without arrhythmias (Diagn Pathol 2012;7:67)
- 72 year old man with late presentation of arrhythmogenic right ventricular cardiomyopathy (J Med Case Rep 2009;3:7235)
Treatment
- Medication including beta blockers, sotalol and amiodarone can be used to reduce palpitations and abnormal rhythms
- Ablation therapy
- Implantable cardiac defibrillator (ICD)
Clinical images
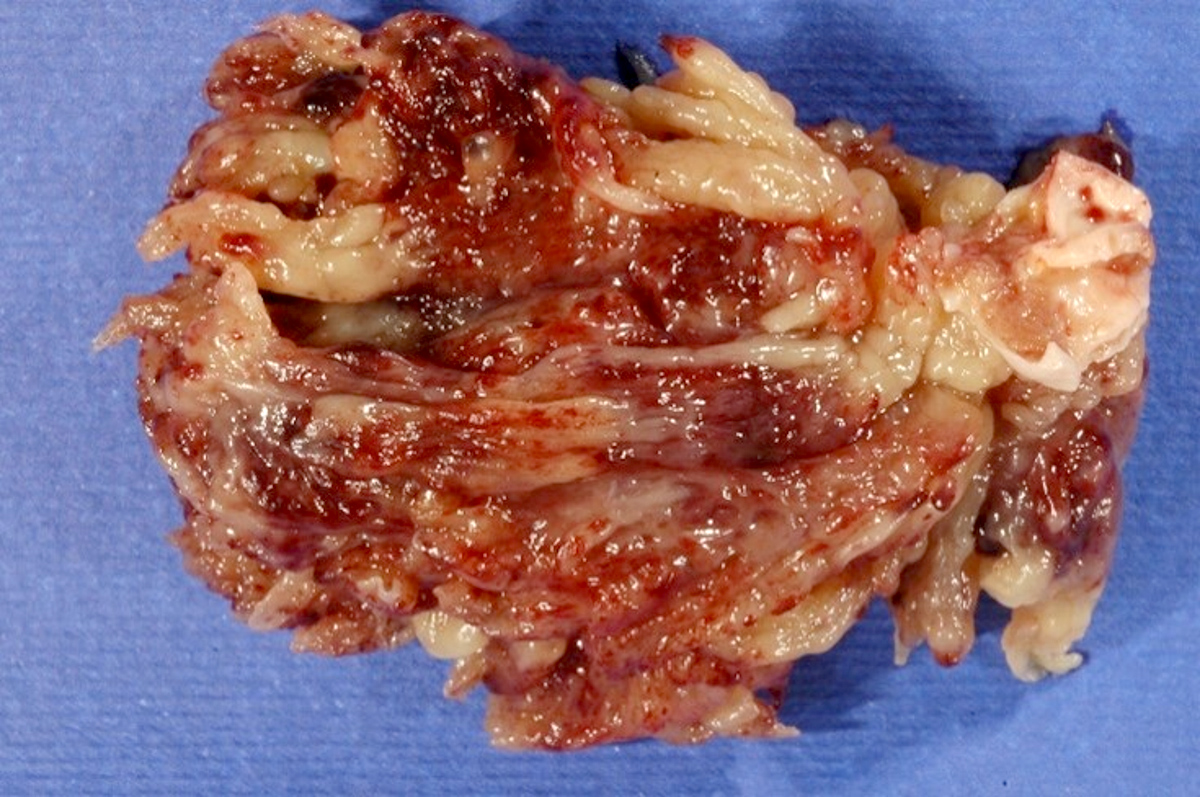
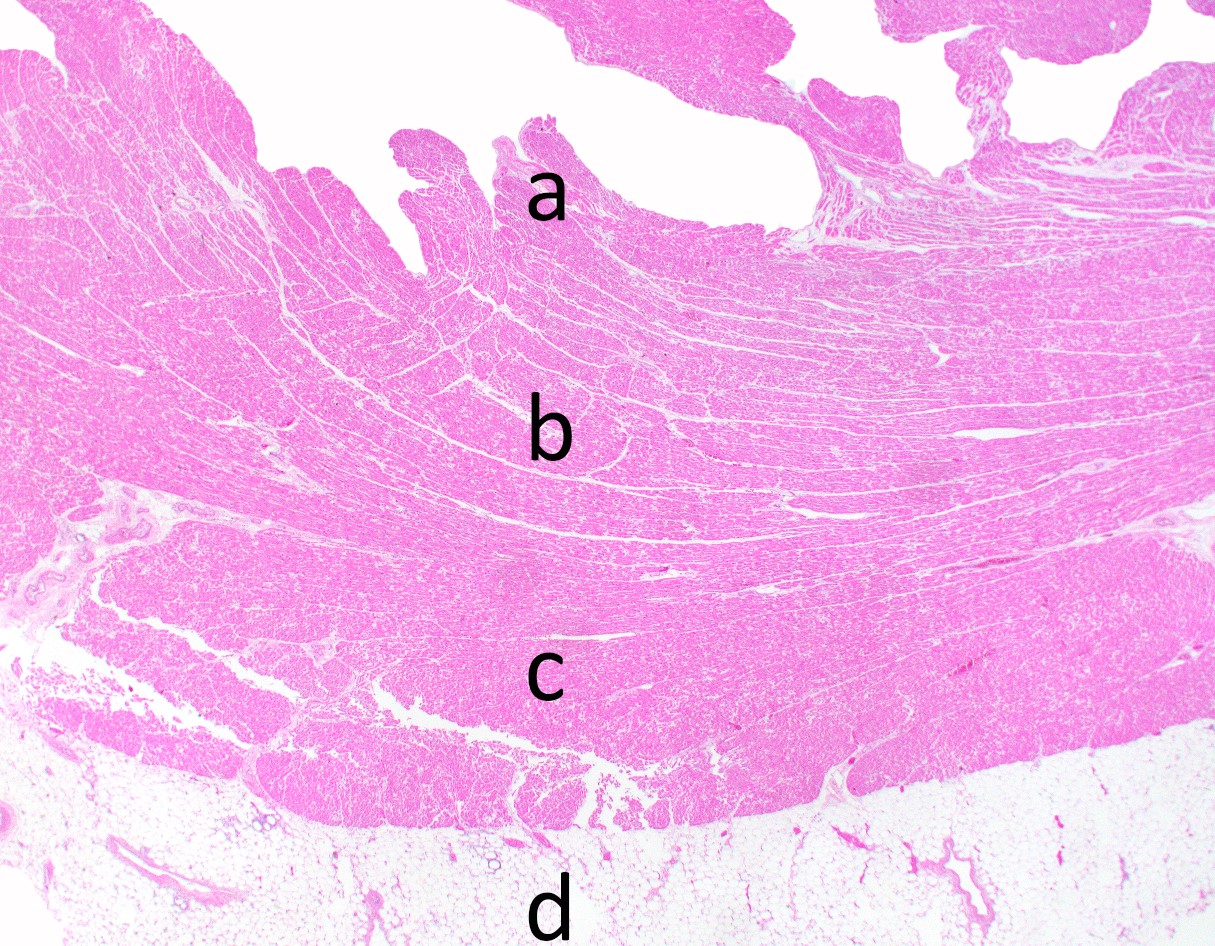
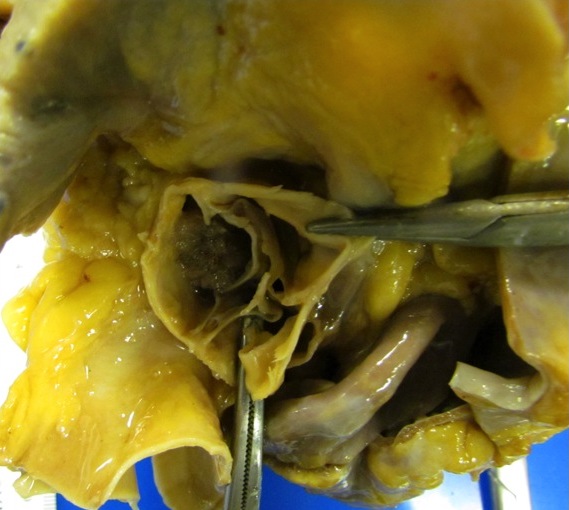
Gross description
- The heart weight is usually normal and does not exceed 400 g
- The right side of the heart appears yellowish or whitish due to fatty or fibrofatty infiltration of the underlying myocardium
- The right ventricular inflow outflow tract appear lardaceous / fatty
- The right ventricular free wall appears parchment like when held against a light source
- The changes may be focal in 20% and diffuse in 80% of cases
- Aneurysms of the right ventricular free wall, whether single or multiple, are considered a pathognomonic feature
- Right ventricular enlargement (mild, moderate or severe) is a constant feature
- The left ventricle and the ventricular septum are grossly normal in most cases, a paradox which explains why these hearts are able to withstand the cardiac output of a strenuous exercise performance and at the same time are electrically vulnerable because of fibrofatty infiltration of the right ventricle
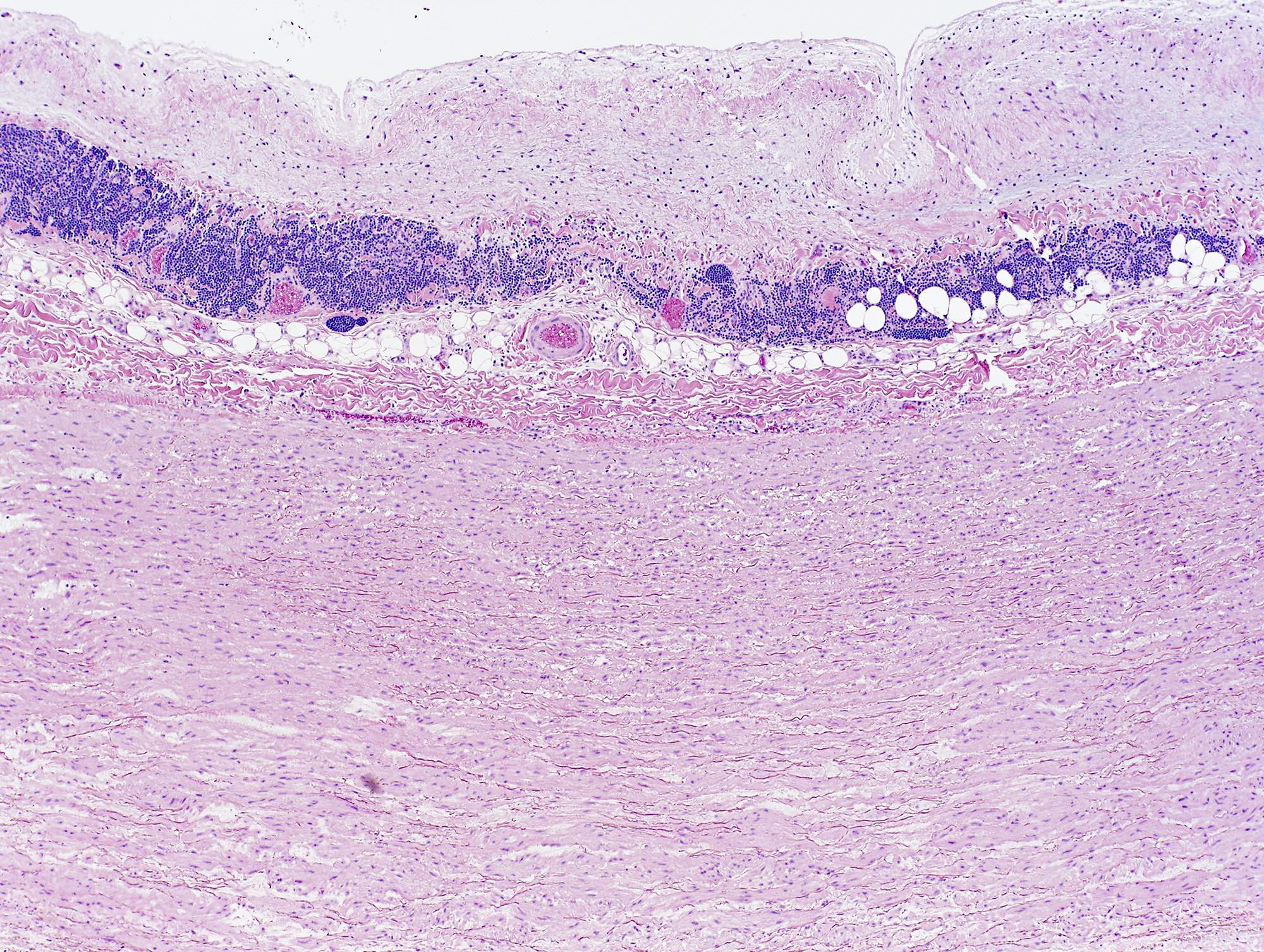
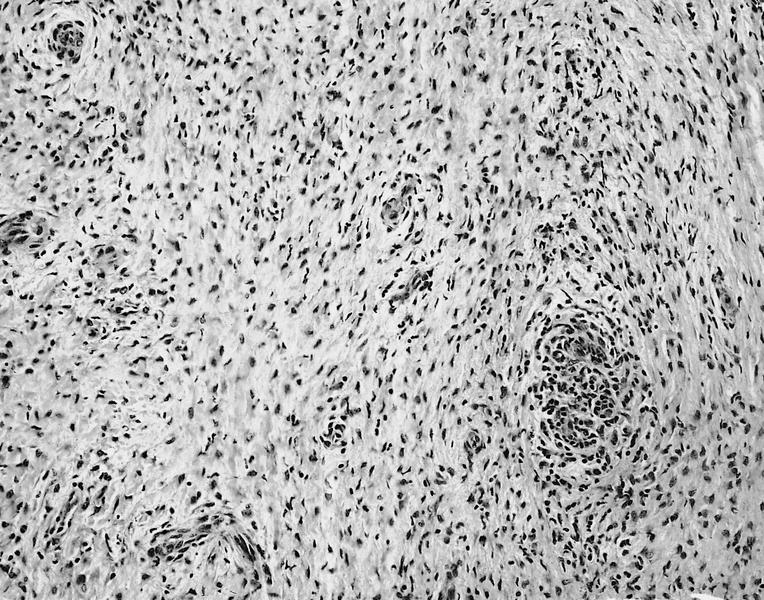
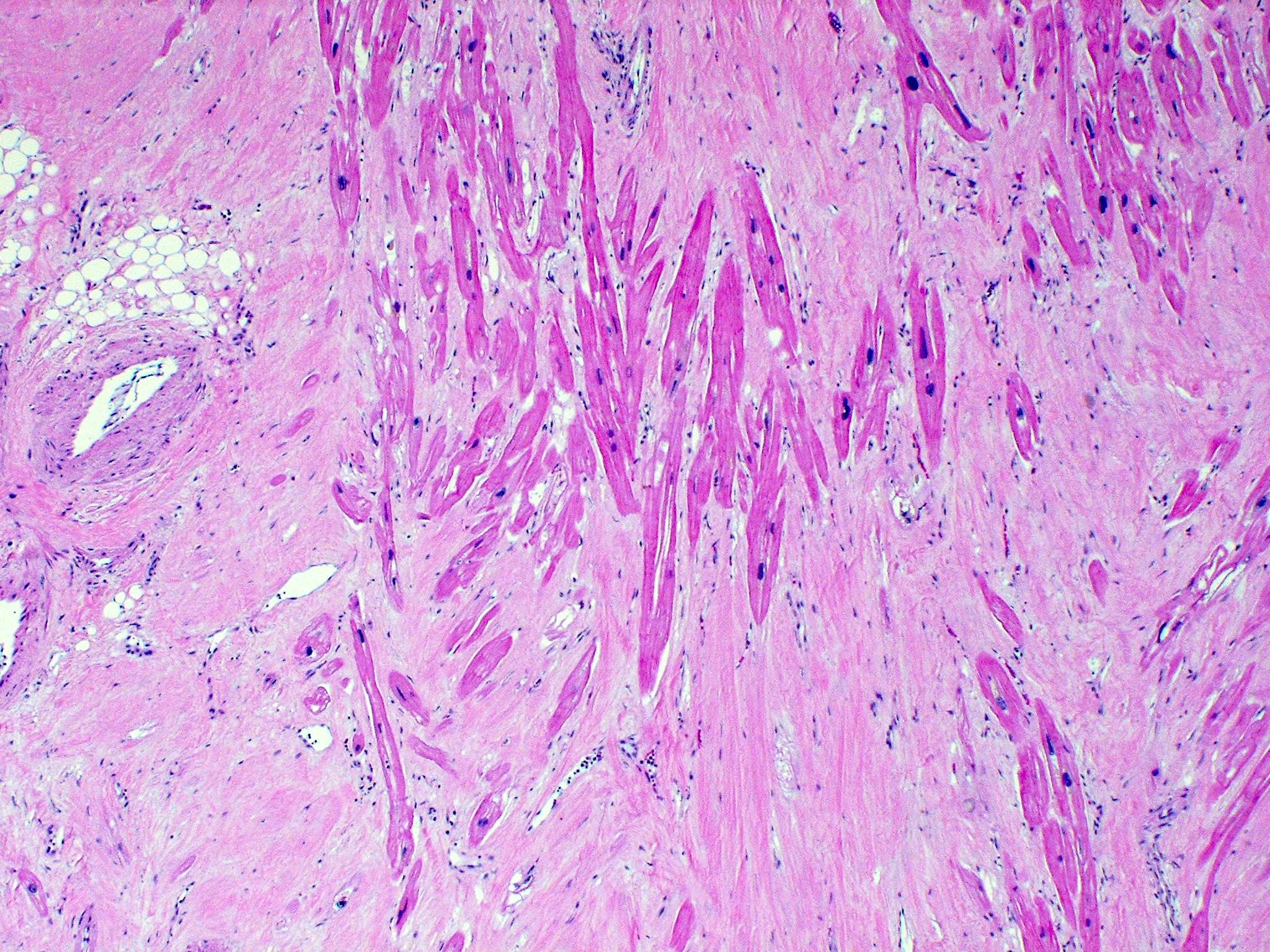
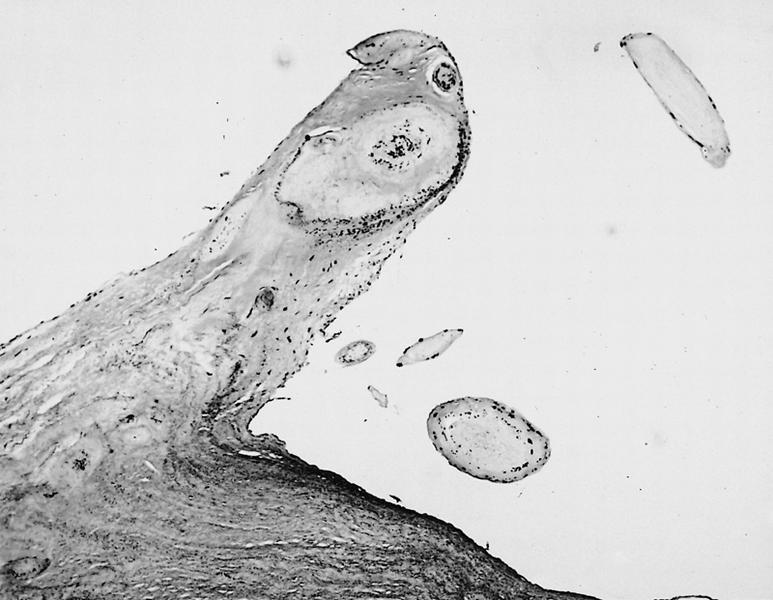
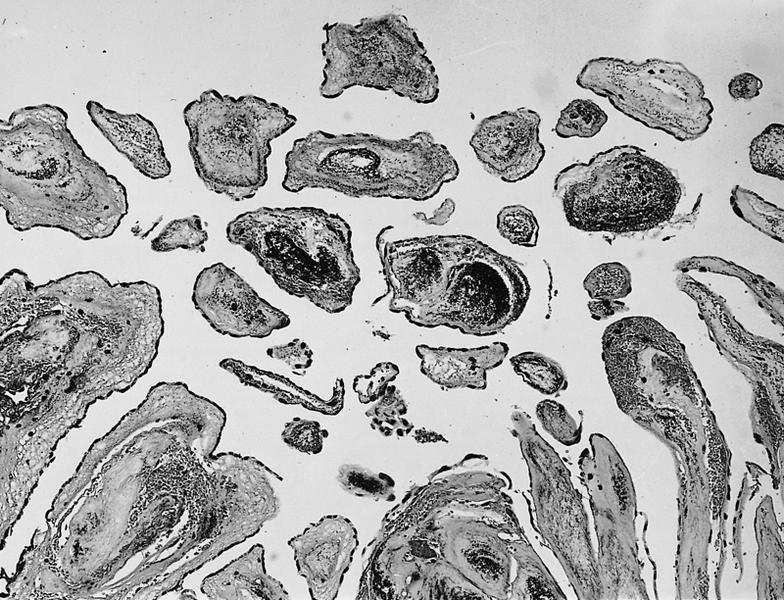
Microscopic (histologic) description
- Histology of the free wall of the right ventricle shows disappearance of the myocardium with transmural fibrofatty replacement
- The pathologic process starts from the subepicardium and extend to the endocardium as a wave front phenomenon
- Patchy myocarditis with myocyte death and round cell inflammatory infiltrates may be seen
Microscopic (histologic) images
Differential diagnosis
- Acquired heart disease:
- Bundle branch re-entrant tachycardia
- Pulmonary hypertension
- Right ventricular infarction
- Tricuspid valve disease
- Congenital heart disease:
- Atrial septal defect
- Ebstein anomaly
- Partial anomalous venous return
- Repaired tetralogy of Fallot
- Uhl anomaly
- Miscellaneous:
- Idiopathic RVOT tachycardia
- Pre-excited AV re-entry tachycardia
- Sarcoidosis
Additional references
Atherosclerotic coronary artery disease
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Progressive luminal narrowing of coronary arteries caused by development of atheromatous plaque composed of lipids, inflammatory cells and connective tissue
Essential features
- Development of atherosclerosis follows a predictable path from initiation phase to progression and development of lipid rich atheromatous plaque to complications leading to ischemic events
- Numerous risk factors for the development of coronary artery disease are common among patients, including obesity, smoking, dyslipidemia and hypertension
- Typical atherosclerotic plaque shows a well formed necrotic core and overlying fibrous cap; smooth muscle cells, macrophages, lymphocytes, connective tissue components and calcification are variably present
Terminology
- Coronary artery disease, cardiovascular disease, myocardial ischemia, ischemic heart disease
ICD coding
Epidemiology
- Subclinical lesions may develop before adolescence; clinical manifestations commonly occur in middle aged and older adults (Diabetes Care 2014;37:2632)
- Studies suggest higher prevalence in women and higher mortality in men (Atherosclerosis 2015;241:211)
- Individuals with obesity, diabetes and hypertension
- Tobacco use
- Physical inactivity
Sites
- Coronary arteries
- Similar changes can be identified in arteries throughout the body, especially at branch points and in areas with turbulent blood flow
Pathophysiology
- Divided in 3 phases (Nat Rev Dis Primers 2019;5:56)
- Initiation:
- Deposit of cholesterol rich, low density lipoprotein (LDL) particles in the intima (fatty streak)
- Endothelial activation secondary to proinflammatory signals and mechanical stress
- Binding of LDL particles to subendothelial proteoglycans
- Aggregates engorged by smooth muscle cells (SMCs) and macrophages
- Progression:
- Recruitment of leukocytes and SMC production of extracellular matrix molecules contribute to thickening of the intimal layer
- SMCs and macrophages die, forming a necrotic lipid rich core
- Variable accumulation of calcium, large mineralization decreases risk of thrombotic event
- Complication:
- Plaque rupture: thrombus formation in plaques with large lipid core and thin fibrous cap
- Plaque erosion: plaques with rich extracellular matrix, little lipid content and thin friable fibrous cap
- Buried caps are evidence of prior rupture and healing
- Initiation:
Etiology
- At least 164 genetic risk loci have been identified (Cardiovasc Res 2018;114:1241)
- Elevated low density lipoproteins (Eur Heart J 2017;38:2459)
- Cigarette smoking (Curr Med Chem 2014;21:3936)
- Diabetes mellitus and insulin resistance (metabolic) syndrome (Endocr Rev 2019;40:1447)
- Elevated triglycerides (Arch Cardiovasc Dis 2021;114:132)
- Conditions associated with proinflammatory profile, such as systemic lupus erythematous, rheumatoid arthritis, celiac disease (Curr Opin Rheumatol 2018;30:441, Clin Rev Allergy Immunol 2020;58:1, Mayo Clin Proc 2021;96:666)
- Lifestyle and environmental factors (Eur J Prev Cardiol 2020;27:394):
- Sedentarism
- Poor diet
- Psychosocial stress
- Sleep deprivation and noise
- Certain infections (Curr Cardiol Rep 2021;23:52)
Clinical features
- Most cases remain asymptomatic for decades
- Symptoms relate to a reduction in blood flow caused by the luminal stenosis or to thrombotic obstruction (i.e. acute coronary syndrome, myocardial infarction)
- Clinical presentation can be acute or chronic and depends on the organ / body part involved
- Renovascular hypertension and reduced renal function are manifestations of atherosclerosis involving renal arteries
- References: BMC Med 2021;19:258, J Clin Med 2021;10:4664, Atherosclerosis 2021;335:31, Am J Kidney Dis 2021 Aug 9 [Epub ahead of print]
Diagnosis
- Multiple diagnostic criteria are available for symptomatic atherosclerotic lesions, depending on arterial vessel involved
- Stress tests can reveal decreased blood flow in coronary circulation
- Coronary angiography for diagnosis and therapy
- Evidence of atherosclerosis screening by imaging is limited (J Gen Intern Med 2012;27:220)
Radiology description
- Invasive angiography is gold standard to evaluate luminal stenosis
- Plaque visualization is possible with ultrasonography (US), doppler US, CT angiogram, MRI, optical coherence tomography, intravascular US (Am J Med 2009;122:S15)
- Fluorodeoxyglucose (FDG) PET evaluates plaque metabolism (Am J Med 2009;122:S15)
Radiology images
Prognostic factors
- Myocardial infarction, aortic dissection, abdominal aortic aneurysm and other major cardiovascular events are associated with increased mortality rates
Case reports
- 37 year old woman with heterozygous factor V Leiden mutation developed rapidly progressive angina within a month (Turk Kardiyol Dern Ars 2019;47:148)
- 53 year old man with extensive atherosclerotic lesions, Tangier disease and Leriche syndrome (J Atheroscler Thromb 2018;25:1076)
- 72 year old man with a history of coronary atherosclerosis developed left subclavian artery thrombosis compromising left internal mammary artery blood flow (Cureus 2020;12:e11524)
Treatment
- Goal is to decrease progression of atherosclerotic plaque or complications
- Low density lipoprotein cholesterol (LDL C) lowering therapy (statins)
- Antithrombotic therapy (aspirin)
- Treatment of hypertension
- Glycemic control
- Exercise
- Nutrition
- Smoking cessation
- Reference: Circulation 2019;140:e596
Gross description
- Fatty streaks are flat yellow discoloration in the intima surface
- Early plaque is raised yellow, well defined lesion, focal in distribution and irregular in shape
- Complicated plaques show ulcers, protrusions and thrombus (PLoS One 2017;12:e0186630, Arterioscler Thromb Vasc Biol 2000;20:1177)
Gross images
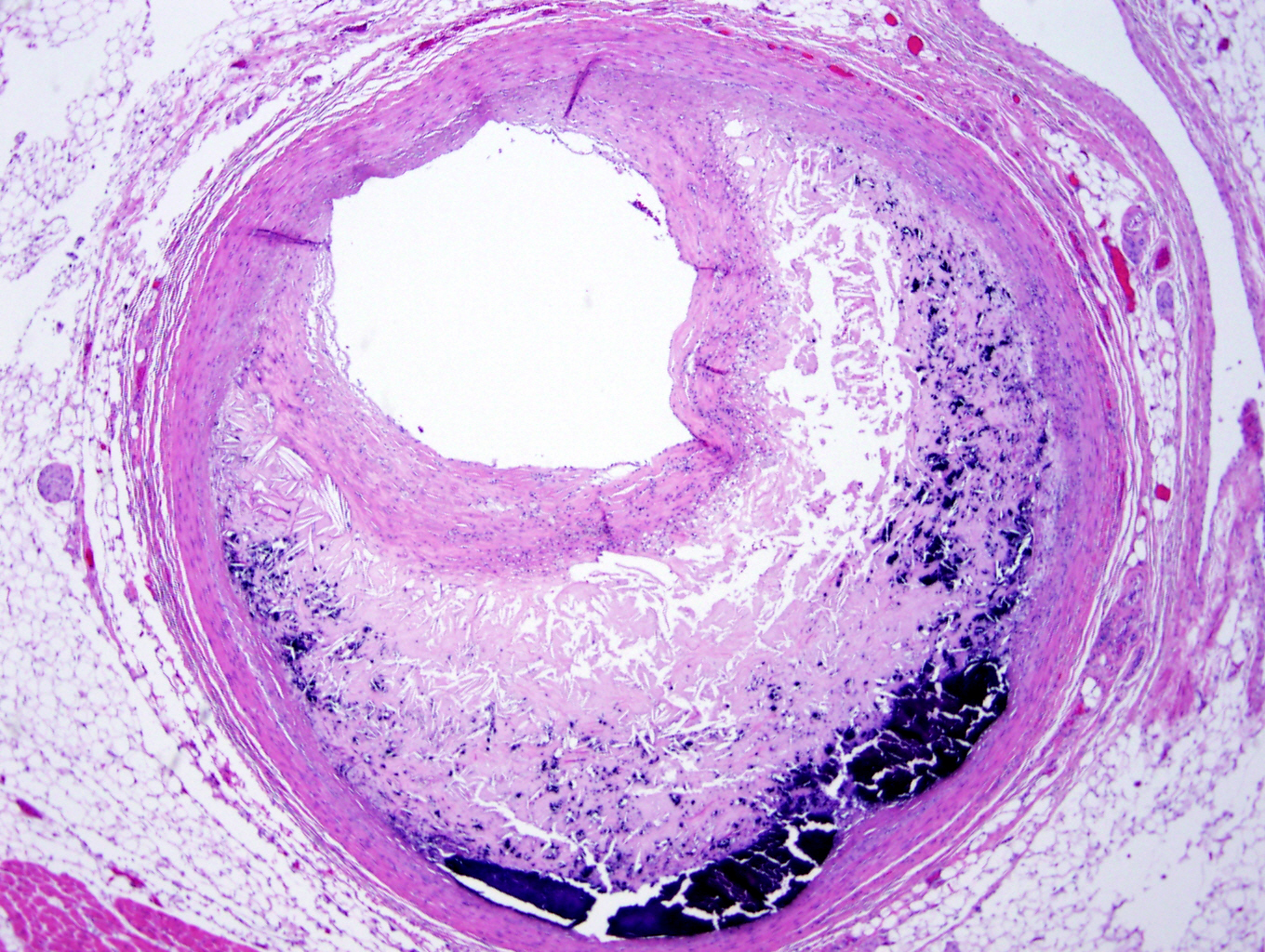
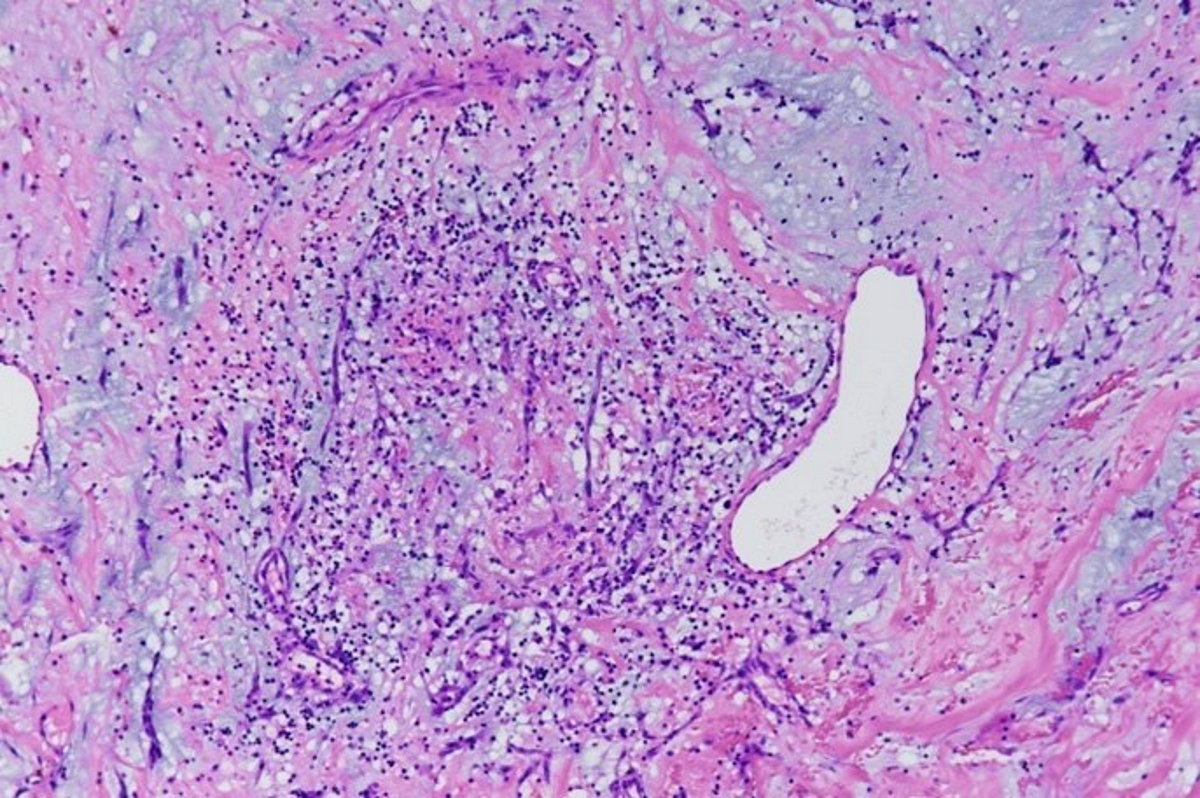
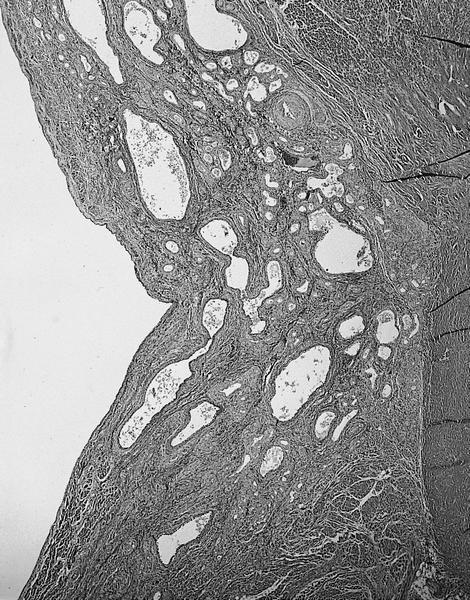
Microscopic (histologic) description
- Fatty streak: subendothelial accumulation of foam cells without necrotic core or fibrous cap
- Fibrous cap atheroma (Am J Med 2009;122:S3):
- Well formed necrotic core with overlying fibrous cap; smooth muscle cells, macrophages, lymphocytes and connective tissue components may be present
- With rupture: luminal thrombus communicates with underlying necrotic core
- With erosion: luminal thrombosis; no communication of thrombosis with necrotic core
- Fibrocalcific plaque: collagen rich plaque, contains large areas of calcification with few inflammatory cells, necrotic core may be present
Microscopic (histologic) images
Sample pathology report
- Coronary arteries are not received as an anatomic pathology specimen unless part of a heart explant or autopsy case
- Heart, explant:
- Ischemic heart disease characterized by multifocal macroscopic and microscopic infarctions (weeks to months old) and severe calcific coronary artery disease
Differential diagnosis
- Coronary artery dissection or aneurysm:
- Can be seen in conjunction with coronary artery disease
- Diagnosis requires changes in vascular anatomy (separation of vessel layers in dissection and dilation of vessel in aneurysm)
- Mönckeberg medial calcific sclerosis:
- Ring-like calcification of medial layer
- Other features of atheromatous plaque are absent
- Vasculitic process:
- Often shows destruction of vessel by inflammatory infiltrate
Board review style question #1
A 75 year old man presents with acute chest pain, shortness of breath and EKG changes concerning for acute myocardial infarction. At autopsy, the above finding is identified when examining the coronary arteries. Which of the following is a risk factor for this finding?
- Coronary artery plaque with thick fibrous cap
- Lipid rich coronary artery plaque with thin fibrous cap
- Low blood triglyceride level
- Patient is a nonsmoker
Board review style answer #1
B. Lipid rich coronary artery plaque with thin fibrous cap
Comment Here
Reference: Atherosclerotic coronary artery disease
Comment Here
Reference: Atherosclerotic coronary artery disease
Board review style question #2
An adolescent male dies and undergoes autopsy. The autopsy pathologist notes some changes associated with atherosclerosis. The most likely finding to be identified at this age is
- Accumulation of calcium in vessel walls
- Fatty streak formation
- Lipid rich atheromatous plaques
- Vascular intimal thickening
Board review style answer #2
Cardiac fibroma
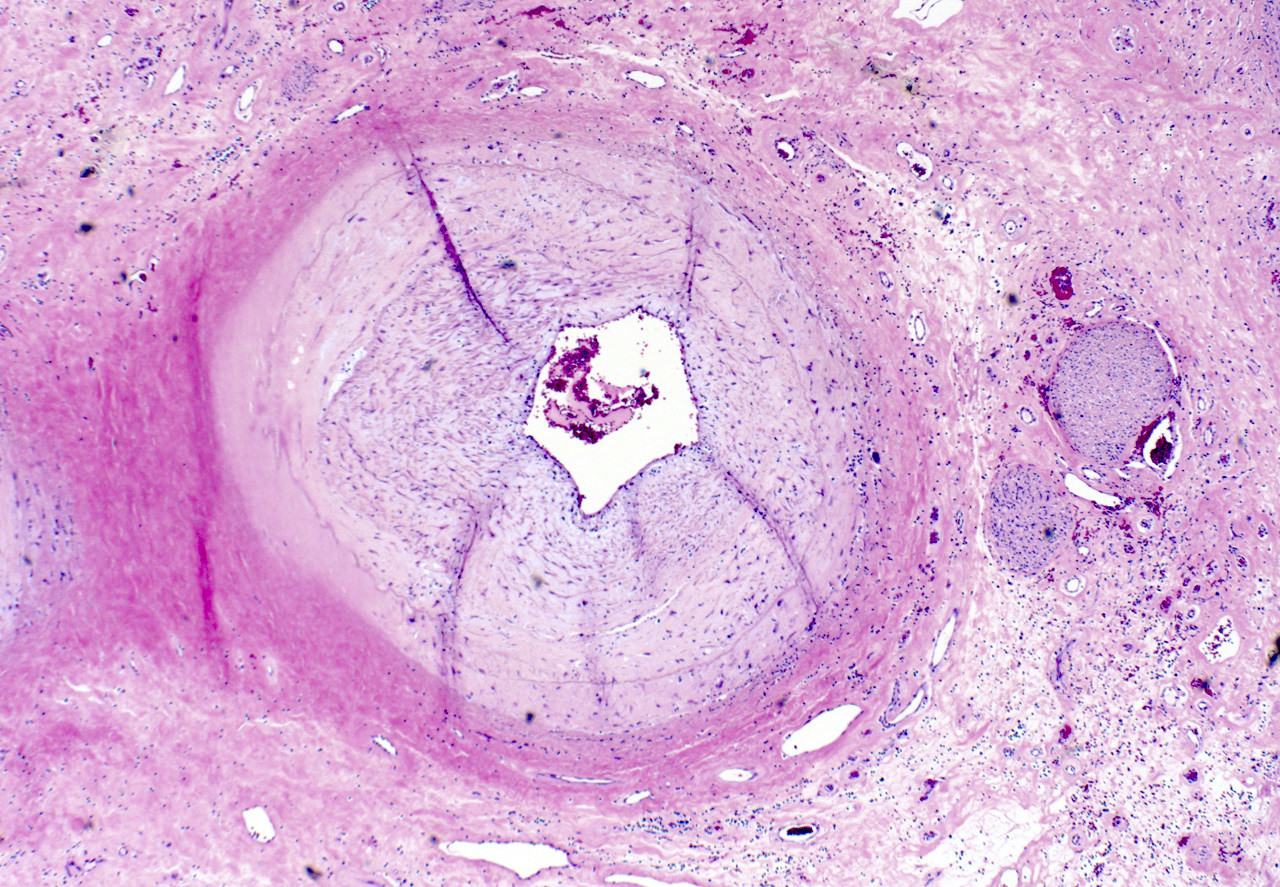
Table of Contents
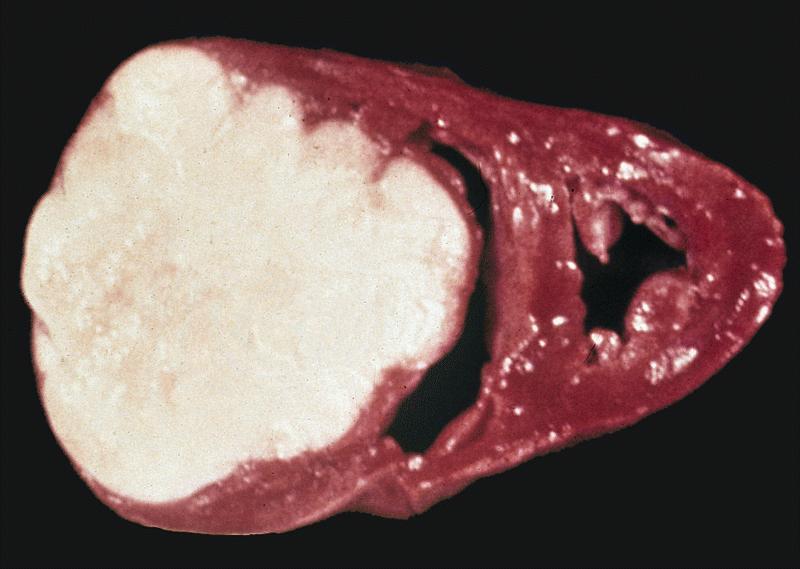
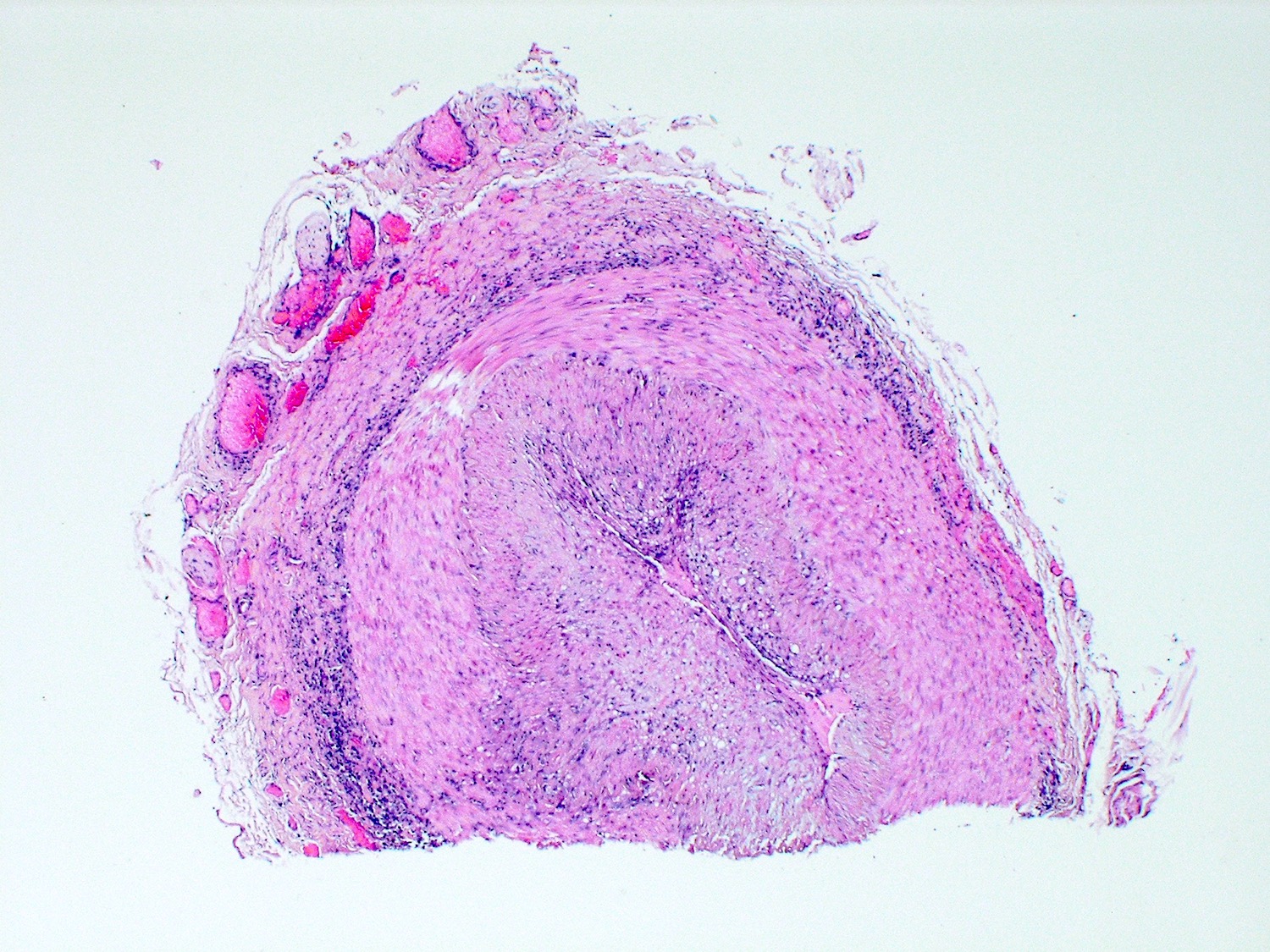
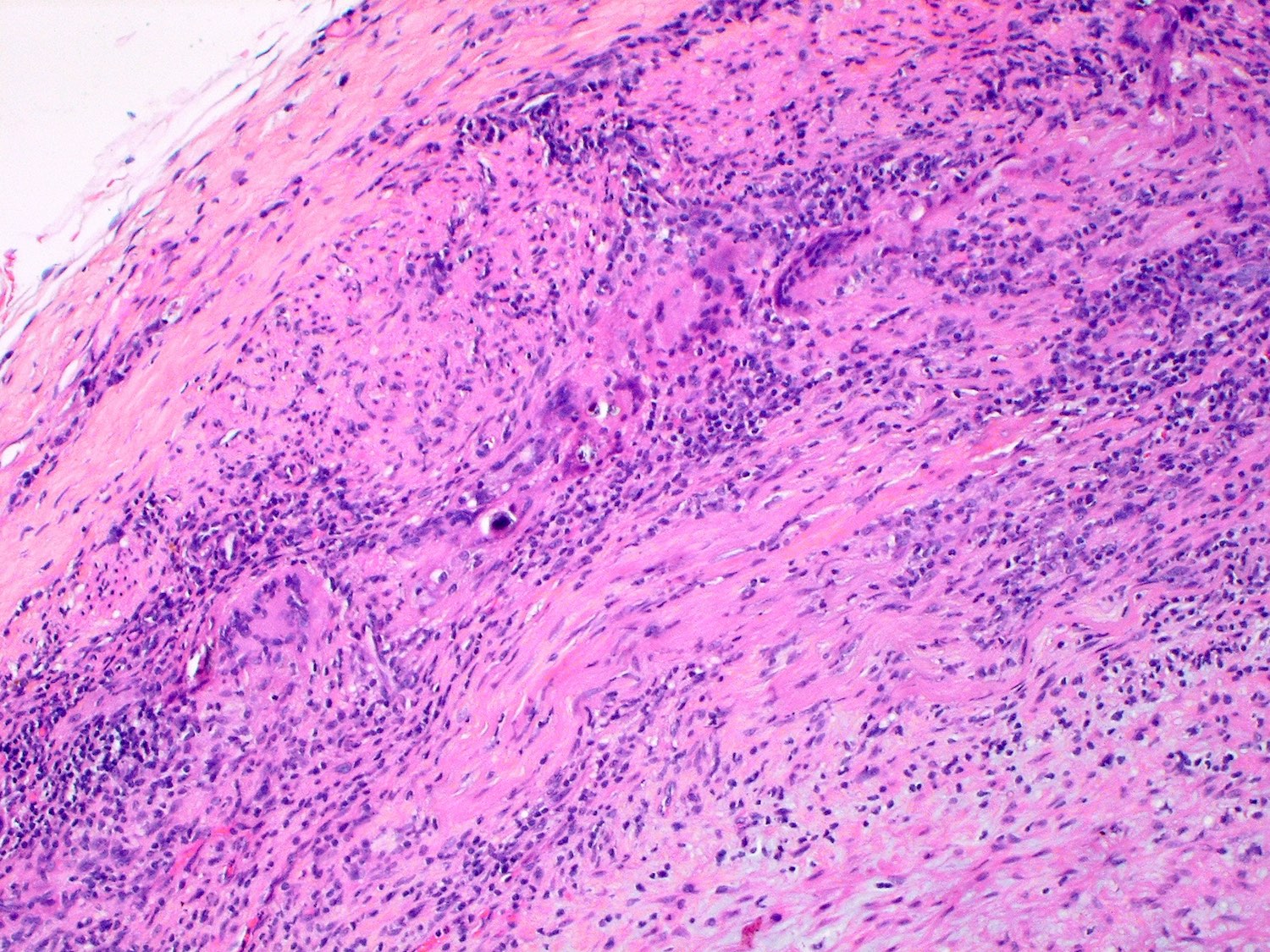
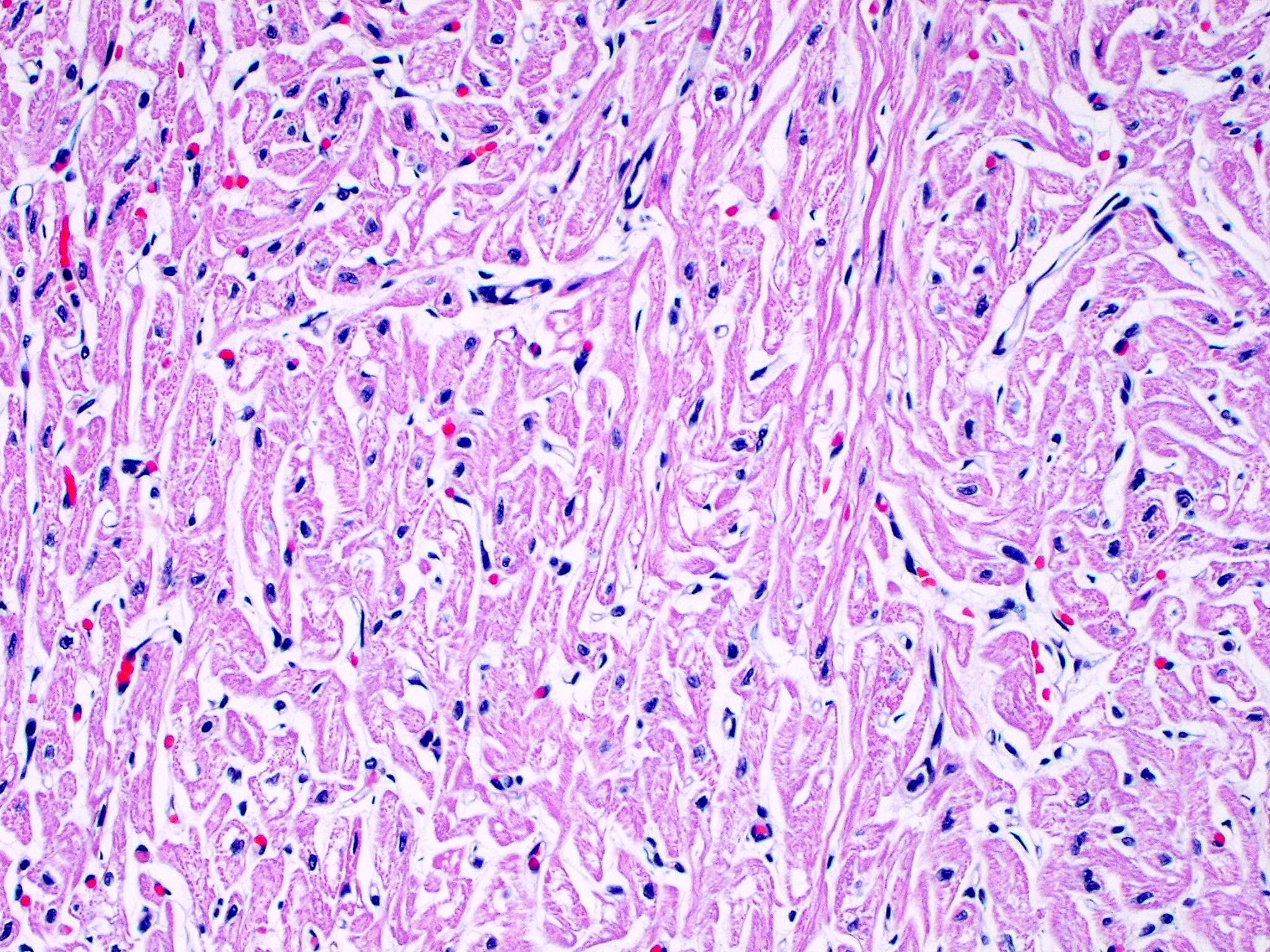
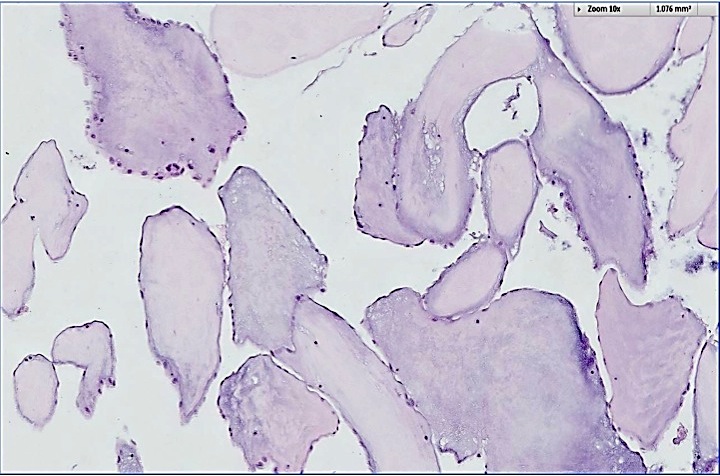
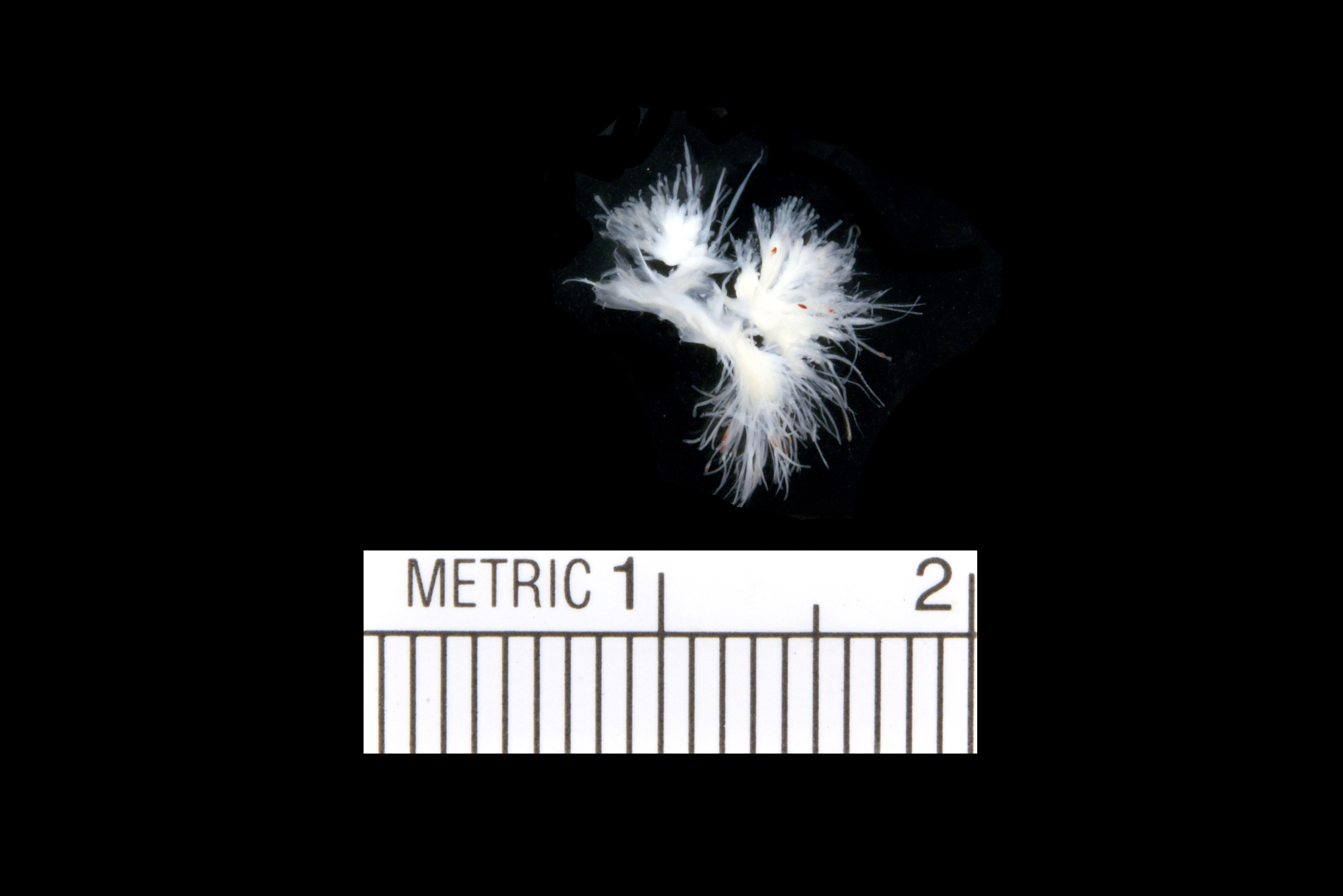
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Cardiac fibroma is rare but is also the second most common cardiac tumor in children and may occur in association with basal cell nevus syndrome (BCNS), also known as Gorlin syndrome (Eur J Cardiothorac Surg 1997;12:730, JACC Clin Electrophysiol 2019;5:563, J Thorac Cardiovasc Surg 1994;108:862, Am J Cardiol 2022;182:95)
- Usually arises within the ventricle or ventricular septum and can cause heart failure due to obstruction of blood flow or sudden death from ventricular arrhythmia (JACC Clin Electrophysiol 2019;5:563)
Essential features
- Second most common primary cardiac tumor in children (34%) but also occurs in adolescents and adults (~40%) (J Thorac Cardiovasc Surg 1994;108:862)
- Solid, unencapsulated tumor arising predominantly from the ventricles
- Microscopically consists of bland fibroblasts, varying amounts of collagen and immature mesenchymal cells with little or no atypia and interdigitating / entrapped myocardium (particularly toward the tumor - normal myocardium interface) (JACC Clin Electrophysiol 2019;5:563)
- Known association with BCNS (Gorlin syndrome)
- Complete surgical resection may cure ventricular arrhythmias but incomplete removal may result in persistence of arrhythmias (JACC Clin Electrophysiol 2019;5:563)
ICD coding
Epidemiology
- Second most common primary cardiac tumor in children (34%) (J Am Coll Cardiol 2011;58:1903)
- Majority of patients are Age range: newborn to 62 years old (J Am Coll Cardiol 2011;58:1903, Cardiovasc Pathol 2022;56:107381, Eur J Med Res 2012;17:5)
- No sex or race predilection reported (J Am Coll Cardiol 2011;58:1903, Cardiovasc Pathol 2022;56:107381)
Sites
- Predominantly affects the ventricles (JACC Clin Electrophysiol 2019;5:563):
- Left ventricle: up to 90%
- Right ventricle: 7%
- Interventricular septum: 3%
- Could also involve the right atrium, left and right ventricular outflow tracts and main pulmonary artery: 1 - 7% (Cardiovasc Pathol 2022;56:107381)
- Size range: 0.5 - 17 cm (Cardiovasc Pathol 2022;56:107381, JACC Clin Electrophysiol 2019;5:563)
Pathophysiology
- Multinodular architecture of cardiac fibromas suggests a multifocal origin of the tumor arising from proliferation of scattered resident stromal fibroblasts / myofibroblasts interspersed between cardiomyocytes from multiple foci, with progressive nodular growth and subsequent formation of a larger and more compact solid tumor mass (JACC Clin Electrophysiol 2019;5:563)
- Prominent multilobulation observed in some of these tumors is also consistent with this hypothesis
Etiology
- Poorly understood; often congenital (Eur J Med Res 2012;17:5)
- Isolated deletions and translocations involving chromosome 9 suggests potential role of a critical region in chromosome 9 regardless of syndromic association (JACC Clin Electrophysiol 2019;5:563)
- PTCH1 gene, which is involved in Gorlin syndrome, has been localized to chromosome 9q22.3 (Lancet 1992;339:581, Cell 1996;87:553)
Clinical features
- Children present with arrhythmia (32%), murmur (20%) and abnormal chest Xray (20%) (J Am Coll Cardiol 2011;58:1903)
- Heart failure, arrhythmias, sudden death and chest pain (J Thorac Cardiovasc Surg 1994;108:862)
- Ventricular tachycardia occurs in 64% of children with fibroma (J Am Coll Cardiol 2011;58:1903, JACC Clin Electrophysiol 2019;5:563)
- Possibly asymptomatic
Diagnosis
- Patient work up often follows clinical presentation
- Echocardiography (echogenic or complex echogenicity) (J Thorac Cardiovasc Surg 1994;108:862)
- MRI (see Radiology description)
- ECG may reveal ventricular tachycardia (J Am Coll Cardiol 2011;58:1903)
Laboratory
- No laboratory findings specific to cardiac fibromas have been reported
Radiology description
- Cardiomegaly, calcifications on chest Xray (J Thorac Cardiovasc Surg 1994;108:862)
- Homogenous or heterogenous enhancement on CT (J Thorac Cardiovasc Surg 1994;108:862)
- MRI (J Am Coll Cardiol 2011;58:1044):
- Intramyocardial location involving the ventricular septum or free wall
- Well defined borders with a thin rim of myocardium
- Strong hyperenhancement on myocardial delayed enhancement (MDE) imaging, with or without hypoenhancing core
- Hypointense on first pass perfusion (FPP) or magnetic resonance angiogram
- Heterogeneous appearance on T1 and T2 weighted turbo spin echo (TSE) sequences with variable areas of slightly hypointense or hyperintense areas
Prognostic factors
- Unfavorable prognostic factors:
- Younger age at diagnosis: worse survival; higher incidence of fatal arrhythmias in children Eur J Med Res 2012;17:5, JACC Clin Electrophysiol 2019;5:563)
- Involvement of interventricular septum: worse survival (Eur J Med Res 2012;17:5)
- Larger tumor volume index: postoperative regional wall motion abnormality (Circ Cardiovasc Imaging 2021;14:e011748)
- Diffuse myocyte interdigitation: sustained arrhythmia (JACC Clin Electrophysiol 2019;5:563)
- Postoperative mitral regurgitation (Circ Cardiovasc Imaging 2021;14:e011748)
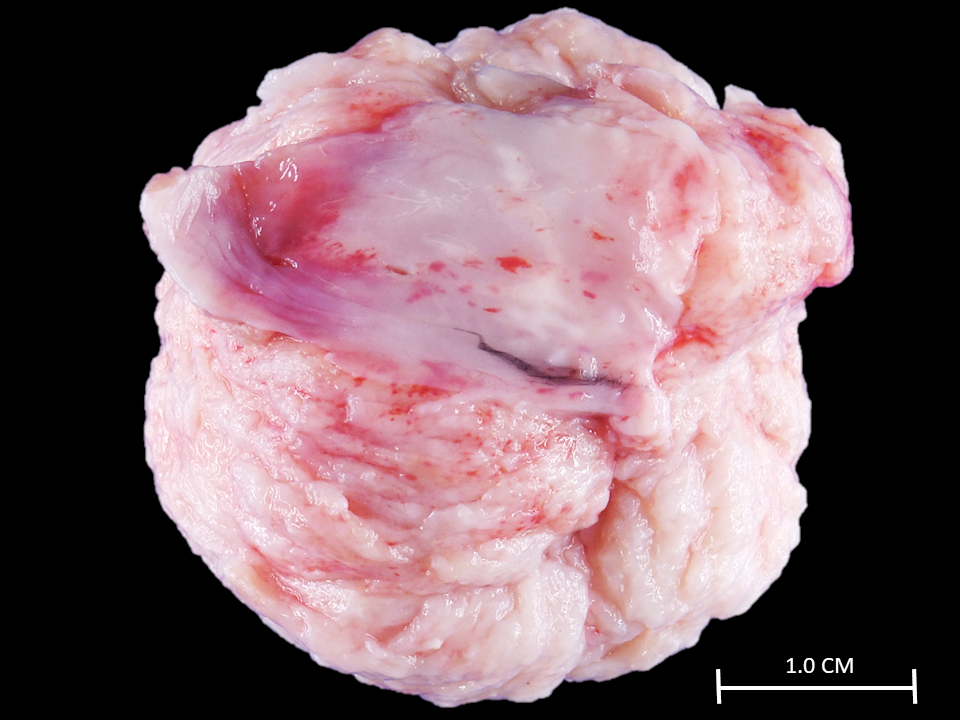
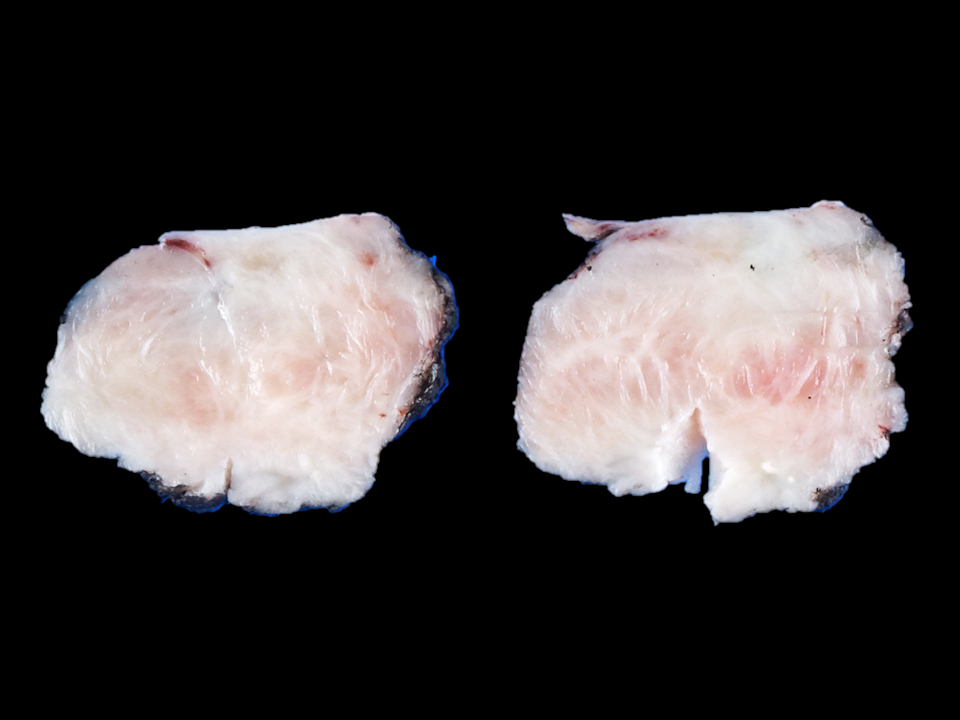
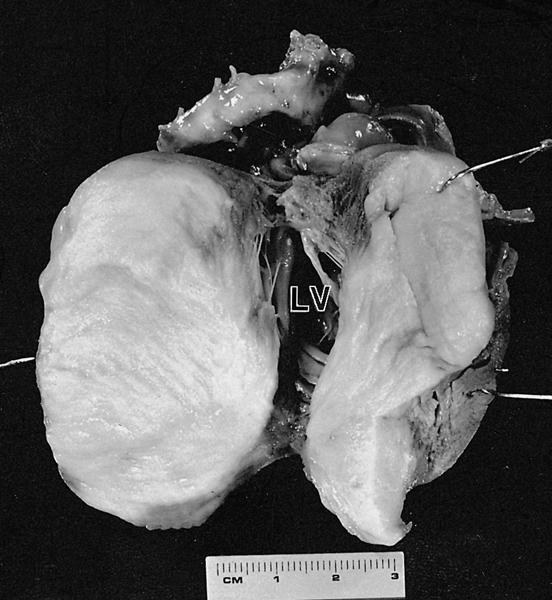
Case reports
- 3 month old girl with a fibroma in the right ventricle (Cardiol Young 2020;30:129)
- 5 month old girl with a fibroma in the right ventricle (J Cardiothorac Surg 2017;12:49)
- 14 year old man with a fibroma in the left ventricle (Innovations (Phila) 2020;15:283)
- 40 year old man with a fibroma in the right atrium (Ann Card Anaesth 2018;21:65)
- 46 year old woman with a fibroma in the left ventricle (Eur Heart J Case Rep 2020;4:1)
Treatment
- Surgical resection / excision has been shown to cure arrhythmias (J Am Coll Cardiol 2011;58:1903, JACC Clin Electrophysiol 2019;5:563)
- Heart transplants are sometimes considered and performed, particularly for large tumors that are not amenable to surgical removal (J Thorac Cardiovasc Surg 1993;106:1208, J Heart Lung Transplant 1995;14:382)
Gross description
- Tumors are often large and multinodular and may include attenuated epicardial tissue on the surface
- May be singular or multilobulated (Cardiovasc Pathol 2022;56:107381)
- Depending on the surgical approach, the tumor may be received intact or in multiple pieces
- Cut surfaces are grayish white to light beige, whorled to trabeculated, with rubbery to firm consistency (J Thorac Cardiovasc Surg 1994;108:862, Eur J Med Res 2012;17:5, Circ Cardiovasc Imaging 2021;14:e011748, JACC Clin Electrophysiol 2019;5:563)
- Tumor is almost always unencapsulated and adherent to surrounding myocardium (JACC Clin Electrophysiol 2019;5:563)
- Entrapped or interdigitating strands of myocardium are sometimes visible on closer examination (JACC Clin Electrophysiol 2019;5:563)
Gross images
Frozen section description
- Intraoperative frozen sections are usually not performed on cardiac fibromas unless there are concerns for malignancy on imaging
Microscopic (histologic) description
- Bland spindle cell / fibroblastic proliferation with abundant collagen, sometimes immature mesenchymal cells, with little or no atypia (Eur J Med Res 2012;17:5)
- Cellularity tends to decrease while collagen increases with age (JACC Clin Electrophysiol 2019;5:563)
- Occasional findings within the tumor include calcification, aggregates of lymphocytes and histiocytes, prominent elastic fibers, extramedullary hematopoiesis, necrosis and ossification (J Thorac Cardiovasc Surg 1994;108:862, JACC Clin Electrophysiol 2019;5:563)
- Tumor may infiltrate into surrounding myocardium; isolated islands of entrapped myocardium may also be seen
- Increased mitotic activity or atypia is usually not observed
Microscopic (histologic) images
Contributed by Chrystalle Katte Carreon, M.D.
AFIP images
Positive stains
- Smooth muscle actin and vimentin (Cardiovasc Pathol 2022;56:107381)
- CD31 and CD34 highlights scattered vascular channels (Cardiovasc Pathol 2022;56:107381)
- Trichrome stain highlights collagen bundles (JACC Clin Electrophysiol 2019;5:563)
- Elastic stain highlights abundant elastic fibers (Case Rep Cardiol 2015;2015:713702)
Negative stains
- AE1 / AE3, desmin, myoglobin, ALK, S100, calretinin or STAT6 (J Am Coll Cardiol 2011;58:1903)
- In contrast to the tumor, entrapped myocardium is positive for desmin (JACC Clin Electrophysiol 2019;5:563)
Electron microscopy description
- Fibroblasts with abundant, rough endoplasmic reticulum
- Intercellular space contains collagen fibers that are regularly banded and arranged in whorls, clustered elastic fibers and ground substance (J Thorac Cardiovasc Surg 1993;106:1208)
Molecular / cytogenetics description
- Cytogenetics: deletions in chromosomes 9 and 3 (Cancer Genet Cytogenet 1996;87:34, Cardiol Young 2003;13:101, Cardiovasc Pathol 2008;17:93, JACC Clin Electrophysiol 2019;5:563)
- Isolated translocations, t(4;13), t(5:11) and t(1;9), are reported (JACC Clin Electrophysiol 2019;5:563)
- FISH: homozygous and heterozygous loss of the PTCH1 locus (Cardiovasc Pathol 2008;17:93)
- High resolution microarray analysis showed losses of somatic copy numbers on chromosome 9q21.33 to q22.33, encompassing the PTCH1 locus as well (Cancer Genet 2015;208:615)
Sample pathology report
- Heart, left ventricular mass, resection:
- Cardiac fibroma (4.5 cm) (see comment)
- Comment: Immunohistochemical stain for desmin shows entrapment of cardiomyocytes within the tumor.
Differential diagnosis
- Inflammatory myofibroblastic tumor:
- Denser proliferation of myofibroblastic cells within an inflammatory background, mostly consisting of plasma cells and lymphocytes
- Cytoplasmic staining for ALK correlates with ALK gene rearrangement, seen in up to 60% of cases
- Variable staining for SMA and desmin
- Focal cytokeratin staining may be observed; immunostain positive (Cardiovasc Pathol 2022;56:107381)
- Fibrosarcoma:
- Mitotically active, with prominent cellular atypia
- Solitary fibrous tumor:
- Scar:
- Lacks a mass-like growth
- Often associated with chronic ischemic change in surrounding myocardium
Board review style question #1
Board review style answer #1
D. Prominent calcifications. Other microscopic features that may be observed in cardiac fibromas include dystrophic calcifications, lymphocytic infiltrate and extramedullary hematopoiesis, among others. High grade features are absent.
Comment Here
Reference: Cardiac fibroma
Comment Here
Reference: Cardiac fibroma
Board review style question #2
Cardiac fibromas may be a manifestation of which of the following syndromes?
- Carney complex
- Gorlin syndrome
- Holt-Oram syndrome
- Tuberous sclerosis
Board review style answer #2
B. Gorlin syndrome, also known as basal cell nevus syndrome (BCNS), is caused by mutations in a tumor suppressor gene called PTCH1. This gene is located on chromosome 9. Mutations in this gene may increase the risk for other tumors, including keratocystic odontogenic tumors, medulloblastomas and ovarian fibromas.
Comment Here
Reference: Cardiac fibroma
Comment Here
Reference: Cardiac fibroma
Cardiac myxoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Cardiac myxoma is a rare and benign tumor, distinct from soft tissue myxoma, most often occurring as a solitary, sporadic, pedunculated mass in the left atrium; approximately 10% occur in the context of Carney syndrome
Essential features
- Most common primary tumors of the heart, usually single in sporadic forms and mainly located in the left atrium
- In rare familial forms are related to Carney complex (see below) and there may be multiple and often relapsing tumors
- May mimic malignant neoplasia because of frequent embolism, systemic or obstructive symptoms
- May cause sudden death, usually due to mitral valve obstruction
- Histologic features include polygonal (lepidic) myxoma cells, either single or forming cords, nests and perivascular cuffs, a myxoid stroma and the absence of necrosis, mitotic activity and significant cell atypia
- Excellent prognosis but treatment requires complete surgical resection to avoid / prevent relapse and embolic or systemic symptoms
Terminology
- Recommended: cardiac myxoma
- Unusual components (i.e. glands, lymphoid proliferation, thymic rests) may be noted if present
ICD coding
Epidemiology
- Although rare, they represent the most common (~50% and up to 78% in surgical series) primary tumors of the heart; their incidence ranges between 0.0017% and 0.03% in autopsy series (J Thorac Oncol 2016;11:441)
- F:M = 1.8:1
- Mean age 50 years; most patients in 30 - 60 year range
- Rarely reported in pediatric age or as a part of a genetic disease (i.e. Carney complex) in young patients without sex predilection (Eur J Endocrinol 2021;184:R99)
Sites
- Intracardiac (J Thorac Oncol 2016;11:441)
- 90% occur in atria, 75% on left side and localized to the interatrial septum, close to fossa ovalis
- 90% are solitary and pedunculated tumors
- Can be found in any other cardiac chamber (right atrium, ventricles and valves)
Pathophysiology
- Uncertain origin and histopathogenesis
- Main hypothesis suggests an origin from multipotent mesenchymal cells, the rarely reported gland component representing entrapped foregut rests (European Heart Journal 2020,41:4332, Stem Cells Int 2016,2016:2059584, Am Heart J 2000;140:134)
- Controversial role of HSV infection (Cardiovasc Pathol 2017;27:31, Am J Pathol 2003;163:2407)
- Highly vascular tumors (sometimes supplied by neovascularization from coronary artery)
- Produce growth factors, matrix metalloproteases and cytokines, including vascular endothelial growth factor (VEGF), inflammatory cytokines, interleukin 6 (Heart Vessels 2018,33:1403, Am J Pathol 2005,166:1619)
- 90% are sporadic
- 10% are familial with autosomal dominant transmission (Carney syndrome)
- Autosomal dominant disease caused by mutations in protein kinase A regulatory subunit 1 alpha (PRKAR1A)
- Characterized by multiple cardiac and extracardiac (skin) myxomas, spotty skin pigmentation, endocrine overactivity, schwannomas, epithelioid blue nevus (Circ J 2005,69:994, Nat Genet 2000,26:89, Orphanet J Rare Dis 2006;1:21, Eur J Endocrinol 2021;184:R99)
- In Carney syndrome, myxomas:
- Occur in younger patients (mean 24 years), more often in men (66%)
- Often multiple (50%)
- Greater recurrence risk (Cardiovasc Pathol 2020;49:107231)
- More frequently located in the cardiac ventricles as compared with sporadic cases (13% versus 2%)
Clinical features
- Symptoms depend on size and location
- Most common presenting symptom is systemic embolism (30 - 50% of cases), which causes syncope, dyspnea, neurologic symptoms or ischemic limb pain; rarely, complete tumor embolization occurs (J Cardiovasc Echogr 2020,30:S45, Lancet Oncol 2005,6:219, Tex Heart Inst J 2005,32:238)
- Nonspecific constitutional symptoms and signs are present in 90% of cases; fever / malaise may be associated with elevated sIL6 mediating acute phase response (Neuropathology 2021;41:49)
- Pedunculated tumors may move through atrioventricular valve at systole with a "wrecking ball" effect and cause valve obstruction, syncope and even sudden death (Cardiovasc Pathol 2020;49:107244)
- In a few cases, cardiac myxoma is asymptomatic and may be incidentally diagnosed, in vivo (usually by echocardiography) or at autopsy
Diagnosis
- Diagnosis of cardiac myxoma requires histology
- Usually done on surgically excised tumors, although endomyocardial biopsy may be performed in cases with atypical presentation (Cardiovasc Pathol 2012;21:245)
Laboratory
- Elevated erythrocyte sedimentation rate (ESR), C reactive protein, sIL6 and serum gamma globulin levels can be found but have limited specificity
Radiology description
- Echocardiography is the main tool for in vivo diagnosis of cardiac masses, including myxomas
- Shows lucencies and cystic areas due to hemorrhage (Echo Res Pract 2016;3:R65)
- Cardiac MRI provides accurate assessment of location, attachment site and functional impact of cardiac myxomas (Radiol Clin North Am 2021;59:231)
Radiology images
Prognostic factors
- Typically benign tumors but possible local (after incomplete resection) or distant (due to tumor embolization) recurrence (Lancet Oncol 2005,6:219)
- If untreated, cardiac myxomas may cause systemic embolism and cerebrovascular accidents or valve obstruction and congestive heart failure
- Embolic phenomena (sometimes mimicking metastasis) might be related to overexpression of matrix metalloproteinase (MMP) (Heart Vessels 2018,33:1403, Am J Pathol 2005,166:1619)
- Greater recurrence risk in myxomas associated with Carney syndrome
- If untreated, cardiac myxomas may cause systemic embolism and cerebrovascular accidents or valve obstruction and congestive heart failure
Case reports
- 23, 55 and 57 year old men and a 45 year old woman with glandular cardiac myxoma in the left or right atrium (Virchows Arch 2003;443:618)
- 31 year old man with left atrial myxoma embolization causing ischemic stroke (Stroke 2021;52:e10)
- 43 year old man with a left ventricle myxoma and infective endocarditis (Tex Heart Inst J 2019;46:215)
- 55 year old woman with EBV positive atypical lymphoid proliferation in a left atrial myxoma (Cardiovasc Pathol 2013,22:e5)
- 69 year old man with a right atrial lithomyxoma showing extramedullary hematopoiesis (Heart 2002;88:10)
Treatment
- Radical excision; minimally invasive surgery (right lateral minithoracotomy) may be effective (Heart Lung Circ 2019;28:327)
- Rare recurrences following incomplete excision or in Carney complex (J Med Case Rep 2014,8:134)
Gross description
- Variable size, 1- 15 cm, sessile or pedunculated; 41% have surface thrombus
- Gross features: smooth, oval and lobulated or villous, friable and soft or gelatinous-like mass (J Thorac Oncol 2016;11:441)
- Rarely flat and sessile because of massive embolization
- Occasionally presents as calcified, stone-like mass (lithomyxoma) due to repeated hemorrhage
- Rarely grows on both sides of fossa ovalis
- Hemorrhagic areas are frequent, no necrosis
Gross images
Microscopic (histologic) description
- Diagnostic criteria: neoplastic (lepidic) cells within myxoid stroma
- Complex structures resembling cords, nests or rings around blood vessels
- These structures are composed of polygonal / stellate myxoma (lepidic) cells with abundant eosinophilic cytoplasm, indistinct cell borders, oval nucleus with open chromatin and indistinct nucleolus
- Abundant mucopolysaccharide (myxoid) ground substance containing chondroitin sulfate and hyaluronic acid
- Usually present: inflammatory cells and hemorrhage with hemosiderin deposits; often smooth muscle cells within the myxoid stroma
- Neither frank mitotic activity nor necrosis in the lepidic cells of myxoma
- Variable fibrosis (41%), calcification (20%), Gandy-Gamna bodies (17%, identical to those in spleen of sickle cell anemia patients), ossification (8%), extramedullary hematopoiesis (7%, more common in children)
- Rarely, glandular structures with mucin forming glands, lymphoid proliferations mimicking lymphoma (see case report) or thymic rests or thymoma (Virchows Arch 2003;443:618, Am J Surg Pathol 2005;29:1208)
Microscopic (histologic) images
Positive stains
- Calretinin (strong, diffuse, cytoplasmic and nuclear staining), S100, CD31 variable, CD34 variable (Heart Vessels 2018,33:1403)
- Rarely present glandular components are keratin positive (Virchows Arch 2003;443:618)
- Smooth muscle cells are alpha SMA (1A4) positive
Negative stains
- CD68 (except for associated inflammatory elements), cytokeratins (except for rare glandular elements)
Electron microscopy description
- Lepidic cells of myxoma show features of immature mesenchymal cells and are associated with endothelial and smooth muscle cells (Ultrastruct Pathol 2013;37:77)
- Lepidic cells have abundant smooth and rough endoplasmic reticulum, free ribosomes, polyribosomes, lysosomes and pinocyticvesicles, also numerous filaments and frequent iron deposits (Hum Pathol 1973;4:111)
Electron microscopy images
Molecular / cytogenetics description
- Expression of matrix metalloprotease (MMP) and its inhibitor (TIMP) is likely related to embolic potential (Heart Vessels 2018,33:1403, Am J Pathol 2005,166:1619)
- Carney complex is caused by heterozygous mutation of the PRKAR1A gene on chromosome 17q24, coding for the regulatory subunit type I alpha of the protein kinase A (PKA, cyclic adenosine monophosphate [cAMP] dependent protein kinase) enzyme
- PRKAR1A gene is a tumor suppressor gene
- Mutation induces haploinsufficiency, causing predisposition to tumorigenesis (OMIM: Protein Kinase, cAMP-dependent, Regulatory, Type I, Alpha; PRKAR1A [Accessed 26 April 2021])
Sample pathology report
- Left atrium, excision:
- Cardiac myxoma (see comment)
- Comment: There is a proliferation of polygonal (lepidic) cells, forming cords and nests, surrounding a central vessel or scattered within a myxoid stroma. By immunohistochemistry, the tumor cells show cytoplasmic expression of calretinin and S100, whereas they are negative for SMA, desmin and cytokeratins. Hemorrhage, calcifications and lymphoid infiltrates are abundant; glandular structures are rare. This constellation of morphological and immunohistochemical features strongly supports the diagnosis of cardiac myxoma. It may recur unless completely excised. It has embolic potential.
Differential diagnosis
- Thrombus:
- No cell nests, cords or rings
- Calretinin negative
- Metastatic carcinoma:
- Cell atypia and mitoses are present in glandular structures of metastatic adenocarcinoma
- Cardiac myxoma may have glandular structures but no mitosis or marked cell atypia is detected
- Sarcomas:
- May show prominent myxoid stroma (myxofibrosarcoma, myxoid leiomyosarcoma, myxoid liposarcoma, etc.)
- Have mitoses, cell atypia and necrosis
- Immunophenotype is usually not consistent with cardiac myxomas (J Thorac Oncol 2016;11:441)
- Papillary fibroelastoma:
- On valve cusps and is constituted by avascular papillary fronds with a fibroelastotic core and lined by endothelial cells
- Shows CD31, CD34 and factor VIII related antigen immunoreactivity
- Calretinin and S100 negative
Additional references
Board review style question #1
Board review style answer #1
A. Diagnostic criteria are based on the presence of myxoid stroma and lepidic cells
The diagnosis of cardiac myxoma, which is distinctive from soft tissue myxomas, requires the presence of the typical lepidic myxoma cells that are polygonal cells with no or mild atypia and abundant eosinophilic cytoplasm. They are arranged as single cells, nests or cordons, often around vessels, within an abundant myxoid stroma. Other findings are leukocytic infiltrates, hemorrhage, calcifications, osseous metaplasia, thymic rests or glandular structures. Most patients are between 30 and 60 years of age (mean age 50 years); cardiac myxoma can be found in younger patients and in children in rare cases, in particular in patients with Carney complex
Most cases are in the left atrium: 90% occur in atria, 75% on left side and localized to the interatrial septum and close to fossa ovalis but cardiac myxoma can be localized to any other cardiac chamber (right atrium, ventricles and valves) (J Pediatr 2013;162:964).
Comment Here
Reference: Cardiac myxoma
The diagnosis of cardiac myxoma, which is distinctive from soft tissue myxomas, requires the presence of the typical lepidic myxoma cells that are polygonal cells with no or mild atypia and abundant eosinophilic cytoplasm. They are arranged as single cells, nests or cordons, often around vessels, within an abundant myxoid stroma. Other findings are leukocytic infiltrates, hemorrhage, calcifications, osseous metaplasia, thymic rests or glandular structures. Most patients are between 30 and 60 years of age (mean age 50 years); cardiac myxoma can be found in younger patients and in children in rare cases, in particular in patients with Carney complex
Most cases are in the left atrium: 90% occur in atria, 75% on left side and localized to the interatrial septum and close to fossa ovalis but cardiac myxoma can be localized to any other cardiac chamber (right atrium, ventricles and valves) (J Pediatr 2013;162:964).
Comment Here
Reference: Cardiac myxoma
Board review style question #2
In a patient presenting with a stroke, a cardiac mass of the left atrium is shown by echocardiography. At surgery, a left atrial mass with villous projection is excised. Histology does not show necrosis or mitotic activity of the myxoid mass; calretinin is strongly expressed by the tumor cells. Which of the following is most likely the correct diagnosis?
- Cardiac myxoma
- Leiomyosarcoma
- Metastatic carcinoma
- Mesothelioma
Board review style answer #2
A. Cardiac myxoma
Cardiac myxomas are more frequently found in the left atrium and may frequently embolize, even causing stroke. Treatment requires complete surgical resection to avoid relapse and embolic or systemic symptoms. The presence of a myxoid tumor in a cardiac chamber requires histology for differential diagnosis from malignant tumors, including sarcomas, which exhibit mitotic activity, marked cell atypia, necrosis and a different immunophenotypes. Cardiac myxomas are strongly immunoreactive for calretinin and do not show significant cell atypia, necrosis or mitotic activity.
Comment Here
Reference: Cardiac myxoma
Cardiac myxomas are more frequently found in the left atrium and may frequently embolize, even causing stroke. Treatment requires complete surgical resection to avoid relapse and embolic or systemic symptoms. The presence of a myxoid tumor in a cardiac chamber requires histology for differential diagnosis from malignant tumors, including sarcomas, which exhibit mitotic activity, marked cell atypia, necrosis and a different immunophenotypes. Cardiac myxomas are strongly immunoreactive for calretinin and do not show significant cell atypia, necrosis or mitotic activity.
Comment Here
Reference: Cardiac myxoma
Chambers
Table of Contents
Epidemiology | Etiology | Radiology description | Gross description | Gross images | Additional referencesEpidemiology
- About 1% of all children are born with congenital heart disease
Etiology
- Multifactorial inheritance involving both genetic and environmental causes
- Maternal factors:
- Antiseizure medications
- Lithium to treat depression
- Phenylketonuria
- Insulin dependent diabetes
- Rubella
- Genetic syndromes:
- Down syndrome (trisomy 21)
- Trisomy 18 and trisomy 13
- Turner syndrome
- Cri-du-chat syndrome
- Wolf-Hirshhorn syndrome
- DiGeorge syndrome (22q11)
- Single gene defects:
- Marfan syndrome
- Smith-Lemli-Opitz syndrome
- Ellis-van Creveld syndrome
- Holt-Oram syndrome
- Noonan syndrome
- Mucopolysaccharidoses
- Goldenhar syndrome (hemifacial microsomia)
- William syndrome
- VACTERL association (tracheal and esophageal malformations associated with vertebral, anorectal, cardiac, renal and limb abnormalities)
Radiology description
- Chest radiography is a useful adjunct in the evaluation of any congenital heart defect, including tricuspid atresia
- The radiographic features are also useful in evaluating the pulmonary blood flow and categorizing them into pulmonary oligemia and pulmonary plethora groups
- These echocardiographic features are best demonstrated in the apical and subcostal 4 chamber views
- The size of the left atrium and the size and function of the left ventricle can be assessed with M-mode echocardiography
- Repeated measurements during follow-up are useful in evaluating left ventricular function
Gross description
- Right atrium:
- The right auricle is separated from the right atrium by a shallow posterior vertical indentation on the right atrium (i.e. the sulcus terminalis) and internally, by a vertical crest, the crista terminalis
- The inner wall of the right atrium is composed of a smooth posterior portion (into which the vena cavae and coronary sinus drain) and a ridgelike muscular anterior portion separated by the crista terminalis
- The thebesian valve is located at the orifice of the coronary sinus
- The limbus of the fossa ovalis is located on the medial wall of the right atrium and circumscribes the septum primum of the fossa ovalis anteriorly, posteriorly and superiorly
- Congenital anomalies:
- Tricuspid atresia: the eustachian and thebesian valves may be so enlarged that they physically separate the right atrium into 2 distinct sections
- Juxtaposition of both atrial appendages
- Malpositioning of both appendages
- Left atrium:
- The 4 pulmonary veins drain into the left atrium
- The flap valve of the fossa ovalis is located on the septal surface of the left atrium
- The appendage of the left atrium is consistently narrow and long
- Recognition of this appendage is the most reliable way to differentiate the left atrium from the right atrium
- Right ventricle:
- The right ventricle receives blood across the tricuspid valve, which is located in the anterolateral (sinus) portion of the right ventricle and discharges blood into the pulmonary artery across the pulmonic (semilunar) valve located in the outflow tract (infundibulum)
- The inflow tract (sinus) and outflow tract (infundibulum) of the right ventricle are widely separated
- Internally, the sinus area and infundibulum contain coarse trabeculations
- The septal portion of the right ventricle has 3 components:
- The inflow tract, which supports the tricuspid valve
- The trabecular wall, which typifies the internal appearance of the right ventricle
- The outflow tract, which itself is subdivided into 3 components, namely the conal septum, septal band division and trabecular septum
- Lateral to the conal septum, the parietal extension of the infundibular septum and the infundibular fold comprise the crista supraventricularis
- The tricuspid valve is supported by a large anterior papillary muscle, which arises from the anterior free wall and the moderator band, and by several small posterior papillary muscles, which attach posteriorly to the septal band
- Congenital anomalies:
- Malposition of the conal septum can cause double outlet right ventricle
- Ventricular septal defects (VSDs) commonly occur in the area between the sinus and the outlet tract of the right ventricle
- Left ventricle:
- The left ventricle receives blood from the left atrium via the mitral (bicuspid) valve and ejects blood across the aortic valve into the aorta
- The left ventricle can be divided into 2 primary portions, namely, the large sinus portion containing the mitral valve and the small outflow tract that supports the aortic (semilunar) valve
- Inflow and outflow portions are closely juxtaposed, unlike in the right ventricle, in which the tricuspid and pulmonic valves are widely separated
- The free wall and apical half of the septum contain fine internal trabeculations
- The septal surface is divided into a trabeculated portion (sinus) and a smooth portion (outflow)
- The sinus area just beneath the mitral valve is the inlet septum; the remainder of the sinus area is termed the trabecular septum
- The outflow tract is located anterior to the anterior mitral leaflet and is part of the atrioventricular (AV) septum
- Both the right half of the anterior mitral valve leaflet and the right aortic cusp attach to the septum
- The left half of the anterior mitral leaflet is in direct fibrous contact with the aortic valve at the aortic-mitral annulus
- The conal septum of the right ventricle is positioned opposite the aortic valve
- The mitral valve is supported by 2 large papillary muscles (anterolateral, posteromedial) attached to the free wall
- The anterior papillary muscle is attached to the anterior portion of the left ventricular wall, and the posterior papillary muscle arises more posteriorly from the ventricle's inferior wall
Additional references
Chronic allograft vasculopathy
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Diffuse, concentric hyperplasia of the coronary vasculature after orthotopic heart transplantation, resulting in progressive luminal narrowing, ischemic injury and allograft failure
Essential features
- Long term complication after heart transplantation
- Invasive coronary angiography is diagnostic
- Concentric intimal hyperplasia of the epicardial arteries / veins and medial disease of the intramyocardial microvasculature
ICD coding
Epidemiology
- Long term complication after orthotopic heart transplant causing over 10% mortality at 3 years and affecting 47% of patients within 10 years
- Increased incidence / risk:
- Donor factors: older age (≥ 50 year old), white race, male sex, elevated weight (≥ 85 kg) and history of hypertension, diabetes or tobacco use (Ann Thorac Surg 2010;90:168)
- Recipient factors: dyslipidemia, glucose intolerance, increased hsCRP and CMV IgG/IgM positivity (Transplant Proc 2008;40:3056, J Am Coll Cardiol 2004;43:1034, Transplantation 2003;76:1470, J Heart Lung Transplant 2007;26:324, J Am Coll Cardiol 2003;42:477)
- Increasing time after transplant (J Heart Lung Transplant 2017;36:1037)
- Earlier onset (within 5 years):
- Donor factors: hypertension and male
- Recipient factors: male, black race and pretransplant coronary artery disease (J Heart Lung Transplant 1998;17:744)
- Greater number of HLA-DR mismatches
- Increased transplant center volume (J Heart Lung Transplant 2007;26:769)
Sites
- Allograft epicardial and intramyocardial arteries and veins (Circulation 1997;96:2069)
- Sparing of recipient vessels (Can J Surg 2005;48:319)
Pathophysiology
- Host allorecognition of donor HLA on coronary endothelium → T cell activation → altered cytokine expression → endothelial activation, vascular smooth muscle proliferation and extracellular matrix deposition → intimal (epicardial) or medial (microvasculature) thickening and vasculopathy (Circulation 2007;116:1274)
- Formation of anti HLA or anti endothelial antibodies → increased risk of chronic allograft vasculopathy and cardiovascular mortality (J Heart Lung Transplant 2006;25:1277, J Heart Lung Transplant 2010;29:717, Circulation 1989;80:III122)
- Nonimmunological factors (e.g., coronary artery disease, tobacco use) → endothelial dysfunction and vascular inflammation → enhanced graft immunogenicity (Croat Med J 2014;55:562)
Etiology
- Interplay between immunologic (cellular / antibody mediated rejection and HLA matching) and nonimmunologic (e.g., recipient hyperlipidemia, donor hypertension) factors
Clinical features
- Rarely present with angina due to allograft denervation
- Arrhythmia, diaphoresis, exertional dyspnea, gastrointestinal distress, progressive heart failure, sudden cardiac death or syncope (Croat Med J 2014;55:562)
Diagnosis
- Concentric intimal hyperplasia of the left anterior descending artery (> 70% stenosis on angiography with clinically demonstrated allograft dysfunction; International Society for Heart and Lung Transplantation grade CAV 3)
- Multifocal mild acute cellular allograft rejection with focal myocyte necrosis (International Society for Heart and Lung Transplantation grade 1R; 1990 grade 2)
- pAMR 0: no significant evidence of antibody mediated rejection on immunohistology
- Quilty effect: moderate focal endocardial inflammatory cell aggregate with myocardial encroachment
- Clinical information
- Cardiac allograft vasculopathy status post orthotopic heart transplant
Radiology description
- Coronary angiography: diffuse, longitudinal and concentric luminal narrowing of primary or branch vessels (J Heart Lung Transplant 2010;29:717)
- Intravascular ultrasound: increased maximal intimal thickness of the coronary arteries, predominantly left anterior descending (J Am Coll Cardiol 2005;45:1532)
Radiology images
Prognostic factors
- Favorable: late onset (J Heart Lung Transplant 2010;29:717)
- Poor: stenotic microvasculopathy with minimal intimal thickening on intravascular ultrasound of ≥ 0.5 mm and abnormal dobutamine stress echocardiography within first year (Circulation 2007;116:1274, Circulation 2009;120:1561, Circulation 1999;100:509, Cardiovasc Revasc Med 2019 Jan 25 [Epub ahead of print])
Case reports
- 27 year old woman with pregnancy related HLA-II sensitization (Transplant Proc 2013;45:800)
- 32 year old man with Danon disease requiring repeat transplantation (Rev Cardiovasc Med 2018;19:69)
- 40 year old man with total vascular scaffold resorption following treatment for advanced disease (JACC Cardiovasc Interv 2017;10:1270)
- 43 year old woman with early disease (Case Rep Med 2012;2012:734074)
- 58 year old man treated with a drug eluting stent (Heart 2005 Feb;91:e11)
Treatment
- Preventative therapy: statins and posttransplantation immunosuppressants
- Palliative therapy: percutaneous coronary intervention and coronary artery bypass (Catheter Cardiovasc Interv 2018;92:E527)
- Repeat transplantation is the only definitive treatment (Croat Med J 2014;55:562)
Gross description
- Thickened intramural arteries on the ventricular cut surface (Arch Pathol Lab Med 2007;131:1169)
- Gross luminal narrowing of the epicardial coronary arteries
- Focal areas of myocardial scarring (J Heart Lung Transplant 2011;30:1044)
Microscopic (histologic) description
- Endomyocardial biopsy of intramyocardial arteries (J Heart Lung Transplant 2011;30:1044):
- Concentric fibromuscular intimal and medial thickening with luminal stenosis
- Subendothelial lymphocytic accumulation
- Perivascular fibrosis
- Epicardial artery and vein sections (Catheter Cardiovasc Interv 2018;92:E527):
- Concentric intimal thickening (proliferation of smooth muscle cells and myofibroblasts) along vessel length with luminal stenosis
- Variable mononuclear inflammatory infiltrate (T lymphocytes, macrophages and foam cells) in the intima, media, or adventitia
- May have fibrinoid necrosis of the media and damage to the inner elastic lamina
- Myocardial sections (Arch Pathol Lab Med 2007;131:1169):
- Bilateral, patchy ischemic injury (acute and healing) with myocytolysis, coagulative necrosis and interstitial fibrosis
- May have coincident atheromatous plaques, usually eccentric and proximal
Microscopic (histologic) images
Immunofluorescence description
- CD11c and IgM/IgG IF usually absent (Circulation 2015;131:1608)
Positive stains
- CD3 (Leu4) and CD68 may be positive particularly in subendothelium (Catheter Cardiovasc Interv 2018;92:E527)
Negative stains
- C4d deposition absent around interstitial capillaries
Sample pathology report
- Given the histological heterogeneity of chronic allograft vasculopathy, this is a diagnosis made clinically rather than microscopically. The ISHLT grading guidelines rely upon coronary angiography (demonstrating luminal narrowing of primary vessels) and assessment of allograft function (i.e. ultrasound or echo). While this entity does have distinct microscopic features, it is usually not included in a pathology report line diagnosis.
Differential diagnosis
- Acute cellular rejection:
- Presence of a mononuclear inflammatory infiltrate but lacks angiographic evidence supporting chronic allograft vasculopathy (J Heart Lung Transplant 2009;28:320)
- Acute antibody mediated rejection:
- Positive immunofluorescence for immunoglobulins, complement and CD68 staining for macrophages (J Heart Lung Transplant 2005;24:1710)
- Posttransplant lymphoproliferative disease:
- EBV seroconversion or reactivation of anti-EBV IgM with constitutional symptoms (J Heart Lung Transplant 2005;24:1710)
- Infectious myocarditis:
- Demonstration of infectious entity on endomyocardial biopsy
- Coronary artery vasospasm:
- Resolved with intracoronary nitroglycerin (Croat Med J 2014;55:562)
- Atherosclerotic coronary artery disease:
- Slow progression of focal lesions limited to the arteries (Circ Res 2006;99:801)
Board review style question #1
A 34 year old Hispanic man underwent an orthotopic heart transplantation six years ago following intractable idiopathic restrictive cardiomyopathy where he received a heart from a 25 year old white woman. Routine posttransplant endomyocardial biopsies showed no histological evidence of rejection but surveillance coronary angiography and intravascular ultrasound recently revealed diffuse, circumferential thickening of the left anterior descending artery with significant intimal thickening and 70% luminal stenosis. The patient has no history of dyslipidemia, diabetes or CMV infection. Which of the following is a significant risk factor in the development of this patient's disease?
- Absence of histological evidence of rejection
- Donor female sex
- Donor white race
- Donor young age
- Recipient CMV IgG/IgM seronegativity
Board review style answer #1
C. This patient has chronic allograft vasculopathy as indicated by diffuse concentric intimal hyperplasia and 70% stenosis of a single primary vessel (left anterior descending) on angiography. White race of the donor is associated with an increased incidence of cardiac allograft vasculopathy in the recipient. Recipient CMV IgG/IgM seropositivity, not seronegativity, is also associated with an increased risk of disease. Absence of histological evidence of rejection has no effect on incidence and may be reflective of sampling error (i.e., biopsies did not capture diseased microvasculature). Donor old age and male sex, not young age and female sex, are risk factors for the development of cardiac allograft vasculopathy.
Comment Here
Reference: Chronic allograft vasculopathy
Comment Here
Reference: Chronic allograft vasculopathy
Board review style question #2
A 51 year old woman received an orthotopic heart transplant four years ago due to end stage dilated cardiomyopathy. One year ago, she began experiencing mild exertional dyspnea. At that time, invasive angiography demonstrated 60% stenosis and diffuse narrowing of the left circumflex artery. Over time, the patient developed progressive heart failure and required a repeat transplantation. A representative section of her explanted heart is shown above.
Which of the following statements about this disease is true?
- Although donor vasculature is affected, recipient vasculature is spared
- Characteristic mononuclear inflammatory infiltrate is limited to the adventitia
- Concentric intimal thickening and luminal stenosis is found in epicardial arteries but not epicardial veins
- Development of the disease is closely associated with EBV seroconversion or reactivation of anti-EBV IgM
- Positive immunofluorescence for IgG, IgM or IgA is diagnostic of the disease
Board review style answer #2
A. This patient has chronic allograft vasculopathy as indicated by diffuse concentric intimal hyperplasia and 60% stenosis of a single primary vessel (left main coronary artery) on angiography. The patient's biopsy also shows severe intimal hyperplasia with marked luminal stenosis. In this disease, the donor coronary vasculature is affected while the recipient vasculature is spared. EBV seroconversion or reactivation is more associated with posttransplant lymphoproliferative disease. While acute antibody mediated rejection events (indicated by immunofluorescence in choice B) may occur in the context of cardiac allograft vasculopathy, it is not diagnostic. The inflammatory infiltrate seen in the disease may occur in any layer of the vessel and concentric intimal thickening may occur in both epicardial arteries and veins.
Comment Here
Reference: Chronic allograft vasculopathy
Comment Here
Reference: Chronic allograft vasculopathy
Conduction tissue
Table of Contents
Definition / general | Gross description | Diagrams / tables | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- The specialized tissues of the heart (neuromyocardial cells) that initiate and conduct the cardiac impulse consist of:
- Sinus node (SA node, sinoauricular node, node of Keith-Hack)
- Atrioventricular junctional area, including the AV node (node of Twara) and His bundle
- Bundle branches (branching portion of AV bundle, bifurcation, ventricular conduction tissue) and Purkinje fibers
Gross description
- Sinus node:
- An oval shaped, elongated mass 10-20 mm long and up to 5 mm thick
- The "head" of the node extends toward the interatrial groove while its "tail" extends toward the orifice of the inferior vena cava
- In most hearts, it is located in the subepicardial region (less than 1 mm from the epicardial surface) at the lateral junction of the superior vena cava and right atrium
- Supplying the sinus node is a prominent artery ("sinus node artery") arising from the right coronary artery in 55 - 60% of cases and from the left circumflex coronary artery in 40 - 45%
- Atrioventricular (AV) node:
- Situated in the inferomedial right atrium and forms the top of the only normal electrical connection between atria and ventricles
- Blood supply is from the right coronary artery in 90% of cases, the left circumflex in the remainder
- His-Purkinje System:
- Located at the crest of the interventricular septum
- The AV node terminates in the top of the His bundle which then branches into a left and right bundle branch
- The right bundle branch is a cord-like structure insulated from surrounding myocardium for most of its length
- When it reaches the right ventricular apex it makes its initial electrical contact with myocardial cells of the anterior papillary muscle
- In contrast, the left bundle branch is usually a fan-like structure, dividing soon after its origin into anterior and posterior fascicles
- These fascicles then further ramify into the rest of the Purkinje network
- Blood supply is almost entirely from the left anterior descending artery
- The proximal His bundle may have dual supply, from both right and left coronary arteries
Diagrams / tables
Microscopic (histologic) description
-
Sinus node:
- Cells include nodal cells, transitional cells and atrial muscle cells
- Nodal cells (P cells) are small ovoid, pale staining and poorly striated compared with the general myocardial cells
- The nodal cells are grouped together in interconnecting fascicles placed in a background of fibrous matrix
- Nodal cells are thought to be the source of normal impulse formation in the sinus node
- In the infant sinus node, the nodal cells predominate relative to the fibrous matrix; in contrast, in the adult sinus node, the fibrous tissue is predominant with the nodal cells scattered within the connective tissue
- Transitional cells (T cells) are elongated with characteristics intermediate between the packed nodal cells and the individual atrial myocardial cells
- Transitional cells are located at the margins of the node where the nodal cells become contiguous with atrial myocardium
Microscopic (histologic) images
Additional references
Connective tissue diseases
Table of Contents
Definition / general | Epidemiology | Sites | Diagrams / tables | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- Systemic autoimmune inflammatory conditions frequently involving the blood vessels and heart
Epidemiology
- Echocardiographic and autopsy studies show valvular abnormalities in up to 70% of patients with systemic autoimmune disease, although far fewer patients have symptoms
- In seronegative spondyloarthropathies, aortic root or left sided valvular insufficiency is noted in up to 100% of cases in autopsy series
Sites
- Mitral valve is most frequently affected, followed by the aortic, tricuspid, and pulmonic valves, in descending order of involvement
Pathophysiology
- The mechanisms of antiphospholipid antibody associated valvular dysfunction are unknown, but several have been suggested:
- Immune complexes may injure the valvular endothelium
- Disruption of phospholipid interaction between endothelial cells and platelets
- Capillaries within the valvular endothelium may be damaged
- Any of these processes may lead to subsequent thrombotic and fibrotic changes of the valve
Etiology
- See Cleve Clin J Med 2004;71:881 - Table 1
Clinical features
- Valvular disease associated with autoimmune diseases is most often clinically quiescent but a few patients develop rapid, progressive valvular incompetence
Diagnosis
- Cardiac involvement can be the first presentation of systemic autoimmune disease
Laboratory
- Neither serologic nor acute phase reactant monitoring or sequential imaging is completely reliable to detect recurrent or ongoing inflammation
- If elevation of acute phase reactants is associated with aortitis preoperatively, this may be useful to follow, with the caveat that normal levels of acute phase reactants do not exclude active progressive vascular inflammation
Radiology description
- Serial imaging by magnetic resonance angiography with edema weighted images may be helpful in detecting wall thickening or "edema," but these findings do not always indicate active inflammation
- Conversely, inflammation can exist or progress without visible changes on imaging
Case reports
- 22 year old woman with SLE and valvular masses (Journal of the Saudi Heart Association 2013;25:130)
- Valvular lesions in patients with systemic lupus erythematosus and antiphospholipid syndrome (Rev Port Cardiol 2012;31:295)
Treatment
- Bacterial endocarditis prophylaxis should be considered for these patients with valvular heart disease following American Heart Association guidelines (AHA: Prevention of infective (bacterial) endocarditis (2017))
- Patients with SLE who have persistent antiphospholipid antibodies (measured in the same laboratory at least twice, at least 6 weeks apart) without the clinical syndrome do not require treatment, but often are given low dose aspirin (81 mg / day)
Gross description
- Rheumatoid arthritis:
- Fibrosis, thickening and calcific changes detected most commonly at the base of the valve and in the valve ring
- SLE:
- Most common is nonspecific thickening of the mitral and aortic valves
- Owing to this thickening, the valve cusps may not close properly
- The most characteristic valvular abnormality is Libman-Sacks endocarditis: noninfectious verrucous valvular vegetations, most commonly on the mitral valve but often on multiple valves
- The verrucae are most often found in the recess between the ventricle wall and posterior valve leaflet but can involve either surface of the valve, the commissures and the rings and, less commonly, the chordae, papillary muscles and endocardium
- Healing of these verrucous lesions results in scarring and shortening of leaflets with valvular insufficiency
- Antiphospholipid Antibody Syndrome (APLA syndrome):
- Both primary and secondary APLA syndrome are associated with an increased prevalence of cardiovascular abnormalities, e.g. nonspecific thickening of valve leaflets, thrombotic valvular vegetations, free floating thrombi and valvular insufficiency
- Ankylosing spondylitis:
- Aortic root dilation, valvular fibrosis with retraction of the cusp bases and inward rolling of the cusp margins
- Additionally, mitral insufficiency may occur as a result of subaortic fibrosis of the anterior valve leaflet
Microscopic (histologic) description
- SLE: microscopic appearance may vary with hematoxylin bodies, immunoglobulin deposits, fibrin and granular material
Coronary vessels
Table of Contents
Gross description | Diagrams / tables | Microscopic (histologic) description | Microscopic (histologic) images | Electron microscopy images | Additional referencesGross description
- As the left and right coronary arteries run on the surface of the heart, they can be called epicardial coronary arteries
- The coronary arteries that run deep within the myocardium are referred to as subendocardial
- The coronary arteries are classified as "end circulation", since it is the only source of blood supply to the myocardium
- Two coronary arteries originate from the left side of the heart at the aortic root; the left posterior aortic sinus and anterior aortic sinus give rise to the left and right coronary arteries, respectively
- The third sinus, the right posterior aortic sinus, typically does not give rise to a vessel
- Left coronary artery:
- The left coronary artery distributes blood to the left side of the heart, the left atrium and ventricle, and the interventricular septum
- The circumflex artery arises from the left coronary artery and fuses with the small branches of the right coronary artery
- The larger anterior interventricular artery, also known as the left anterior descending artery (LAD), is the second major branch arising from the left coronary artery
- It follows the anterior interventricular sulcus around the pulmonary trunk
- Along the way it gives rise to numerous smaller branches that interconnect with the branches of the posterior interventricular artery, forming anastomoses
- Right coronary artery:
- The right coronary artery distributes blood to the right atrium, portions of both ventricles, and the heart conduction system
- Normally, one or more marginal arteries arise from the right coronary artery inferior to the right atrium
- The marginal arteries supply blood to the superficial portions of the right ventricle
- On the posterior surface of the heart, the right coronary artery gives rise to the posterior interventricular artery, also known as the posterior descending artery
- It runs along the posterior portion of the interventricular sulcus toward the apex of the heart, giving rise to branches that supply the interventricular septum and portions of both ventricles
- Coronary artery dominance:
- The artery that supplies the posterior descending artery or AV nodal artery determines the coronary dominance
- If the posterior descending artery is supplied by the right coronary artery (RCA), then the coronary circulation can be classified as "right-dominant"
- If the posterior descending artery is supplied by the circumflex artery (CX), a branch of the left artery, then the coronary circulation can be classified as "left-dominant"
- If the posterior descending artery is supplied by both the right coronary artery and the circumflex artery, then the coronary circulation can be classified as "co-dominant"
- Approximately 70% of the general population are right-dominant, 20% are co-dominant, and 10% are left-dominant
Diagrams / tables
Microscopic (histologic) description
- Blood vessels basically contain three layers, whose thickness varies greatly depending upon the size and type of vessel (from outer to inner):
- Tunica adventitia: outermost collagen and elastin rich layer; also has small 'vasa vasorum' as the large arteries need their own blood supply
- Tunica media is broad and elastic with concentric fenestrated sheets of elastin, and collagen and only relatively few smooth muscle fibers
- Tunica intima is made up of an epithelium, which is a single layer of flattened epithelial cells, together with a supporting layer of elastin rich collagen; this layer also has fibroblasts and 'myointimal cells' that accumulate lipid with aging
- Arteries are classified into three types according to their size:
- Large or elastic arteries
- Medium (or muscular or distributive) arteries
- Small arteries or arterioles, which are less than 0.5 mm in diameter
- Venules:
- Have a clear tunica intima layer, without any elastic fibers, and a tunica media with one or two layers of muscle fibers
- The tunica adventitia fuses with surrounding tissue
- Vein:
- Has a wall similar to arteries but with a thinner tunica media
- Typically wall is much thinner than diameter of the lumen
- With such relatively thin walls, veins tend to appear flattened or collapsed in cross section in postmortem histological preparations (in contrast to arteries, which tend to appear more round)
Additional references
COVID myocarditis (pending)
[Pending]
Cystic tumor of the atrioventricular node
Table of Contents
Definition / general | Case reports | Radiology images | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Differential diagnosisDefinition / general
- Also called cystic tumor of AV node or mesothelioma of AV node but does not appear to have mesothelial origin
- Rare; usually identified at autopsy
- May be congenital rests of endodermal origin (Arch Pathol Lab Med 1990;114:1057) or ultimobranchial heterotopia identical to solid cell nests of thyroid (Am J Clin Pathol 2005;123:369)
- Associated with other congenital anomalies
- Often causes heart block and sudden death
- Mean age 38 years, 75% female
- Should examine conduction system in all patients with sudden death, particularly if a history of arrhythmia or heart block
Case reports
- 7 year old boy with rare cause of sudden cardiac death (Arch Pathol Lab Med 2001;125:573)
- 24 year old woman with sudden cardiac death (Am J Forensic Med Pathol 2005;26:349)
- Patient with mesothelioma of the atrioventricular node (Am J Clin Pathol 1975;63:377)
- Patient with unusual site for the AV node tumor (Cardiovasc Pathol 1999;8:325)
- Patient with congenital cystic tumors of the atrioventricular node (Cardiovasc Pathol 1999;8:233)
- Patient with with atrioventricular nodal tumor associated with polyendocrine anomalies (Pathol Res Pract 1996;192:54)
Treatment
- Pacemaker implantation, anti-arrhythmic drugs, possibly surgical excision (Heart 2000;83:E6)
Gross description
- May not be visible due to small size (2 to 20 mm)
- Multicystic lesion in area of atrioventricular node and membranous septum
Gross images
Microscopic (histologic) description
- Must sample conduction system
- Solid and cystic areas lined by nonciliated, epithelial appearing cuboidal cells (main cells), mixed with occasional clear cells (neuroendocrine or C cells)
- Lumina contains PAS+ diastase resistant material which may calcify
- May have inflammatory cells and fibrosis
- No smooth muscle, no mitotic figures, no atypia
Microscopic (histologic) images
Positive stains
Negative stains
Electron microscopy description
- Cells form solid nests with well formed basement membranes, cytoplasmic tonofilaments and desmosomes or glandular structures with desmosomes, electron dense material and short microvilli
Differential diagnosis
- Bronchogenic cyst: solitary, grossly visible, on epicardial surface, smooth muscle present
- Mesothelial cyst: larger, unilocular, on surface of heart
- Teratoma: has neural or other ectodermal structures (Pediatr Pathol 1994;14:913)
Degenerative valve disease
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Diagnosis | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Degenerative valve disease is a term used to describe deterioration of the valve over time, which leads to either stenosis or regurgitation from the valve (J Am Coll Cardiol 2006;47:1707)
Essential features
- Degenerative mitral valve disease is more common than aortic valve disease
- Degeneration happens over time due to multiple pathophysiologies
- Diagnosis is made clinically
- Aortic valve often needs replacement whereas mitral valve can be repaired
Terminology
- Calcific aortic stenosis
- Mitral annular calcification, mitral degenerative disease
- Mitral valve prolapse (Barlow syndrome), floppy valve disease, balloon mitral valve
ICD coding
- ICD-10: I35.9 - nonrheumatic aortic valve disorder, unspecified
Epidemiology
- Calcific aortic stenosis is seen in ~9 million people worldwide
- Calcific aortic stenosis is highly age related; an increasing trend is noted in developed countries (Nat Rev Cardiol 2021;18:853)
- Degenerative mitral valve disease is seen in ~24 million people (Nat Rev Cardiol 2021;18:853)
Sites
- Aortic and mitral valves
Pathophysiology
- In calcific aortic stenosis, prior injury due to hyperlipidemia, hypertension, inflammation and other factors precede calcification of the valve
- This leads to the release of VEGF, leading to angiogenesis and collagen X which leads to calcification of the valve
- These valves contain abnormal cells which resemble osteoblasts, which synthesize bone matrix and deposit calcium (J Cardiol 2018;71:215)
- In degenerative mitral stenosis, calcific deposits develop in the peripheral fibrous ring (annulus), which are stony hard, irregular ulcerated nodules which appear behind the leaflets
- In degenerative mitral valve prolapse, there are portions of the leaflets that become thick, redundant and rubbery
- Over time, the chordae tendineae become thinner and rupture, leaving the annulus dilated; this rupture allows the valves to become floppy and prolapse into the atrium during systole
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Etiology
- Old age is the most common cause of degenerative valve disease
- Early occurrence of degeneration can occur if the patient has a prior valve disease (Int J Stroke 2018;13:612)
Diagrams / tables
Diagnosis
- Many patients are not diagnosed until they develop symptoms
- Auscultation during routine checkup plays an important role in diagnosis
- Following auscultation, patients can undergo echocardiography for definite diagnosis
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Radiology description
- Calcified aortic valve
- Late in the disease, chest radiograph might reveal aortic calcifications and enlargement of the heart along with pulmonary congestion and alveolar edema
- On echocardiogram, severity is determined by various factors
- Mild aortic stenosis: jet velocity of 2.6 - 2.9 m/s and aortic valve area of > 1.5 cm
- Moderate aortic stenosis: jet velocity of 3 - 4 m/s and aortic valve area of 1 - 1.5 cm
- Severe aortic stenosis: jet velocity of > 4 m/s and aortic valve area of < 1 cm (Radiopaedia: Aortic Valve Stenosis [Accessed 19 January 2023])
- Mitral valve prolapse
- On echocardiography, the coaptation (closing of the valves) line lies behind the annular plane (Radiopaedia: Mitral Valve Prolapse [Accessed 7 April 2023])
- Mitral annular calcification
- On a frontal chest radiograph, calcification can be observed in the expected location of the mitral valve
- CT scan is more sensitive for detection of calcification on the annulus but it is subject to degree of motion artifact (Radiopaedia: Mitral Annular Calcification [Accessed 19 January 2023])
Case reports
- 39 year old man with epilepsy, hypertension and a 1 month history of worsening shortness of breath was diagnosed with pulmonary edema (BMJ Case Rep 2019;12:e228414)
- 50 year old man with a history of atrial fibrillation, hypertension, diverticulitis and asthma presented with fatigue and moderate exertional dyspnea (Autops Case Rep 2018;8:e2018058)
- 55 year old man with a history of erosive, seropositive rheumatoid arthritis and interstitial lung disease presented with shortness of breath (Front Cardiovasc Med 2017;4:14)
Treatment
- In severe aortic valve stenosis, transcatheter aortic valve replacement offers a better survival rate; percutaneous balloon valvotomy can also serve as a treatment option for poor surgical candidates
- In mitral valve disease, transcatheter mitral valve repair is considered better than open heart surgery due to the low risk associated with it (Mayo Clin Proc 2010;85:483)
Gross description
- Calcified aortic valve
- Heaped up calcified cusps that prevent valve opening is hallmark
- In the early stages, calcification begins in the valvular fibrosa at the point of maximal cusp flexion
- Gradual narrowing of the orifice is noted
- Mitral annular calcification
- Calcific deposits are seen as irregular, stony hard and ulcerated nodules
- Mitral valve prolapse
- The leaflets appear enlarged, rubbery and thick with the connecting chordae tendineae appearing as thin, elongated or sometimes even ruptured
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Gross images
Microscopic (histologic) description
- Calcified aortic valve
- Large nodular calcific deposits obstructing the functional valve area
- Mitral valve prolapse
- Outer collagenous layer appears weakened, whereas the middle spongiosa layer appears thicker due to deposition of myxomatous material
- Over time, there is more deposition of myxomatous material leading to rupture of the chordae tendineae
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Microscopic (histologic) images
Sample pathology report
- Mitral valve, repair:
- Fibromyxoid valvular degeneration
Differential diagnosis
- Bicuspid aortic valve:
- Congenital disease
- On gross appearance, aortic valve presents with 2 cusps compared to a normal valve of 3 cusps
- Rheumatic heart valve:
- Acute rheumatic fever
- On gross examination, there are small vegetations on involved valves, typically mitral and aortic valves
- On microscopic examination, Aschoff bodies (collections of lymphocytes, plasma cells and activated macrophages) can be seen in any part of the heart, including valves and myocardium
- Chronic rheumatic fever
- On gross examination, valves exhibit leaflet thickening, commissural fusion and shortening along with fusion of the chordae tendineae
- On microscopic examination, the valves exhibit fibrosis and calcifications
- Acute rheumatic fever
- Infectious endocarditis:
- On gross appearance of both acute and subacute infectious endocarditis, friable and bulky vegetations are seen on the valve
- On microscopic examination, the vegetations consist of fibrin, inflammatory cells and microorganisms
- In subacute infectious endocarditis, granulation tissue may be present; fibrosis and calcification occurs over time
Board review style question #1
Which specific degenerative valve disease is the most common worldwide?
- Bicuspid aortic valve
- Calcific aortic stenosis
- Degenerative mitral valve
- Myxomatous mitral valve degeneration
Board review style answer #1
C. Degenerative mitral valve. Degenerative mitral valve disease is the most common, occurring in ~24 million people worldwide compared with 9 million with calcific aortic stenosis, which is the second most common.
Comment Here
Reference: Degenerative valve disease
Comment Here
Reference: Degenerative valve disease
Board review style question #2
What test is used for definitive diagnosis of degenerative mitral valve?
- Chest MRI
- Chest ultrasonography
- Echocardiogram
- Physical examination
Board review style answer #2
C. Echocardiogram. Patients undergo auscultation at regular intervals to confirm the diagnosis, whereas a definitive diagnosis can be made with an echocardiogram once the diagnosis has been established.
Comment Here
Reference: Degenerative valve disease
Comment Here
Reference: Degenerative valve disease
Drug induced valvular heart disease
Table of Contents
Definition / general | Sites | Pathophysiology | Diagrams / tables | Etiology | Diagnosis | Radiology description | Prognostic factors | Case reports | Gross description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Drug induced valvular heart disease (DIVHD) was first described in the 1960s (Heart 2013;99:7), often due to fenfluramine (Wikipedia: Fenfluramine [Accessed 2 March 2018]), phentermine (Wikipedia: Phentermine [Accessed 2 March 2018]) and benfluorex (Wikipedia: Benfluorex [Accessed 2 March 2018])
- DIHVD is defined echocardiographically as abnormal thickening of valve leaflets or cusps, resulting in a restrictive motion in the absence of carcinoid syndrome, left ventricular remodelling (due to ischemic valve involvement), rheumatic heart disease, Libman-Sacks endocarditis and congenital abnormalities
Sites
- Most frequently affects the aortic and the mitral valves
Pathophysiology
- The serotonin 2B (5-HT2B) receptor is the culprit receptor
- Stimulation of this receptor leads to the upregulation of target genes involved in the proliferation and stimulation of valvular interstitial cells through different intracellular pathways
- These involve G protein mediated activation of protein kinase C, Src protein and extracellular regulated kinases 1 and 2 (ERK 1/2)
- Transforming growth factor b (TGF-b) receptor activation is also involved in this process
- Although both fenfluramine and phentermine lack 5-HT2B agonistic properties, norfenfluramine, the primary metabolite of fenfluramine and a metabolite of benfluorex, is a potent 5-HT2B agonist
- 5-HT2B agonist effect is also found for pergolide, cabergoline, MDMA, ergotamine and methylergonovine, a metabolite of methysergide
- The net valvulopathic effect is dependent on the 5-HT2B activity of the parent drug, and on the pharmacodynamic effects of their metabolites (Heart 2013;99:7)
Diagrams / tables
Etiology
- Ergot alkaloids (such as methysergide and ergotamine)
- Ergot derived dopaminergic agonists (such as pergolide and cabergoline)
- Drugs metabolized into norfenfluramine (such as fenfluramine, dexfenfluramine and benfluorex)
- Drugs for Parkinson disease, hyperprolactinemia
- 3,4 methylendioxymetamphetamine (MDMA, 'Ecstasy'), guanfacine, oxymetazoline, quinidine, xylometazoline and fenoldapam
Diagnosis
- Echocardiography, with high spatial and temporal resolution, is the standard approach used in the diagnosis of DIVHD
Radiology description
- Echo:
- In mitral disease, both the leaflets and the subvalvular apparatus may be affected
- The leaflets are thickened, show reduced mobility and are more retracted towards the apex during systole (leaflet tenting) resulting in valve regurgitation
- An affected aortic valve is characterised by systolic doming of the thickened leaflets with reduced mobility and incomplete diastolic coaptation which causes regurgitation
- Score 1 to 4: from very likely to unlikely
- Proven restrictive valvular heard disease (confirmed with histopathology and / or regression after interruption of ergot treatment)
- Important restrictive valve disease (regurgitation > 2/4) or restrictive tricuspid disease, even with regurgitation less than 2/4
- Mild to moderate (regurgitation
- No restrictive valve dysfunction
Prognostic factors
- Older age
- Higher diastolic blood pressure
- Drug dosage
- Duration
- Severity of valvular abnormalities
Case reports
- 52 year old woman with methysergide induced heart disease (Circulation 1977;56:889)
- Serotonergic drugs and valvular heart disease (Expert Opin Drug Saf 2009;8:317)
- Benfluorex and drug induced valvular heart disease (Eur J Echocardiogr 2011;12:263)
Gross description
- In mitral and tricuspid valve disease, a prominent subvalvular disease with thickening and shortening of the chordae tendinae and leaflet tethering with malcoaptation contributes to the regurgitation
- For the aortic valve, cusp thickening with doming and regurgitation is typically present without aortic root dilatation
- Macroscopically, the valves and tendinous chords are both thickened and shortened and may have a shiny white appearance
- Thickening of the valvular surface and subvalvular apparatus occurs by formation of fibromyxoid plaques
- Calcification is not usually part of this process
Microscopic (histologic) images
Differential diagnosis
- Other causes of restrictive valve motion need to be ruled out when diagnosing DIVHD:
- Left ventricle remodelling (i.e. ischemic MR)
- Rheumatic VHD: absence of commissural fusion and calcifications are helpful in differentiating when concomitant valve obstruction is absent
- Carcinoid VHD
- Libman-Sacks (antiphospholipid syndrome) endocarditis
- Congenital abnormalities
Additional references
Embryology
Definition / general
- Heart develops from the embryonic mesodermal germ layer cells that differentiates into mesothelium, endothelium and myocardium
- Mesothelial pericardium forms the outer lining of the heart
- The inner lining of the heart develops from endothelium
Embryonic heart:
- On either side of the neural plate, a horseshoe shaped area develops as the cardiogenic region
- This is formed from cardiac myoblasts and blood islands
- By day 19, an endocardial tube begins to develop in each side of this region
- The two endocardial merge to form the tubular heart, also called the primitive heart tube, that loops and septates into the four chambers and paired arterial trunks that form the adult, human heart
- The tubular heart quickly differentiates into the truncus arteriosus, bulbus cordis, primitive ventricle, primitive atrium and the sinus venosus
- The truncus arteriosus splits into the ascending aorta and pulmonary artery
- The bulbus cordis forms part of the ventricles
- The sinus venosus connects to the fetal circulation
Cardiac looping:
- As the heart tube loops, the cephalic end of the heart tube bends ventrally, caudally and slightly to the right
- The bulboventricular sulcus becomes visible from the outside, and from the inside a primitive interventricular foramen forms
- The internal fold formed by the bulboventricular sulcus is known as the bulboventricular fold
- The bulboventricular segment of the heart is now U shaped
- The bulbus cordis forms the right arm of the U shaped heart tube and the primitive ventricle forms the left arm
- This looping of the bulboventricular segment causes the atrium and sinus venosus to become dorsal to the heart loop
- At this stage, the paired sinus venosus extends laterally and gives rise to the sinus horns
- The following veins drain into the sinus venosus on each side:
- The common cardinal vein, which drains from the anterior cardinal vein (draining the cranial part of the embryo)
- The posterior cardinal vein (draining the caudal part of the embryo)
- The umbilical vein (connecting the heart to the primitive placenta)
- The vitelline vein (draining the yolk sac, gastrointestinal system and the portal circulation)
- As the cardiac looping progresses, the paired atria form a common chamber and move into the pericardial sac
- The atrium now occupies a more dorsal and cranial position and the common atrioventricular junction becomes the atrioventricular canal, connecting the left side of the common atrium to the primitive ventricle
- The primitive ventricle will develop into the left ventricle and the proximal portion of the bulbus cordis will form the right ventricle
- The distal part of the bulbus cordis will form the outflow tract of both ventricles, and the truncus arteriosus will form the roots of both great vessels
Atrioventricular canal:
- Atrioventricular valves form during the 5 to 8 week of development
- Initially, endocardial cushion tissue forms bulges at the atrioventricular junction
- These two masses will meet in the middle, thus dividing the common atrioventricular canal into right and left atrioventricular orifices
- The formation of the atrioventricular valve starts when the atria and inlet portion of the ventricle enlarge, but the atrioventricular junction (or canal) lags behind
- This process causes the sulcus tissue to invaginate into the ventricular cavity, forming a hanging flap
- The endocardial cushion tissue is located at the tip of this flap, which is formed from three layers—the outer layer from atrial tissue, the inner layer from ventricular tissue and the middle layer from invaginated sulcus tissue
Atria and atrial septum:
- The trabeculated portions (appendages) of the right and left atria are from the primitive atria, whereas the smooth walled posterior portions of the left and right atria originate from the incorporation of venous blood vessels
- The posterior aspect of the left atrium is formed by the incorporation of the pulmonary veins, but the posterior smooth portion of the right atrium is derived from the sinus venosus
- The two sinus horns are initially paired structures; later, they fuse to give a transverse sinus venosus
- The sinoatrial junction will become guarded by two valve-like structures, resulting from the invagination of the atrial wall at the right and left sinoatrial junction
- The right and left sinoatrial valves join at the top, forming the septum spurium
- Atrial septation starts when the common atrium becomes indented externally by the bulbus cordis and truncus arteriosus
- This indentation will correspond internally with a thin sickle shaped membrane developing in the common atrium on day 35, which divides the atrium into right and left chambers, called the septum primum
- The orifice connecting the two atria is called the ostium primum
- As the superior and inferior endocardial cushions fuse, dividing the atrioventricular canal into a right and left orifice, the concave lower edge of the septum primum fuses with it, obliterating the ostium primum
- However, just before this happens, fenestrations appear in the posterosuperior part of the septum forming the ostium secundum, thus maintaining a communication between the two atria
Ventricles
-
Muscular interventricular septum:
- On approximately day 30, a muscular fold extending from the anterior wall of the ventricles to the floor appears at the middle of the ventricle near the apex and grows toward the atrioventricular valves with a concave ridge
- In addition, trabeculations from the inlet region coalesce to form a septum, which grows into the ventricular cavity at a slightly different plane than that of the primary septum
- This is the inlet interventricular septum, which is in the same plane of that of the atrial septum
- The point of contact between these two septa will cause the edge of the primary septum to protrude slightly into the right ventricular cavity, forming the trabecular septomarginalis
- The fusion of these two septa forms the bulk of the muscular interventricular septum
- In 1942, Kramer suggested that there are three embryological areas: the conus, the truncus, and the pulmonary arterial segments
- The aortopulmonary septum is formed by ridges separating the fourth (future aortic arch) and the sixth (future pulmonary arteries) aortic arches
- The truncus ridges are formed in the area where the semilunar valves are destined to be formed, thus forming the septum between the ascending aorta and the main pulmonary artery
- The conus ridges form just below the semilunar valves and from the septation between the right and left ventricular outflow tracts
- At first, the sinus venosus communicates with the common atrium
- At 8 weeks, the distal end of the left cardinal vein degenerates, and the more proximal portion forms the common connection between left brachiocephalic vein and right anterior cardinal vein or right brachiocephalic vein, thus forming the superior vena cava
- The left posterior cardinal vein also degenerates, and the left sinus horn becomes the coronary sinus
- The right vitelline vein becomes the inferior vena cava, and the right posterior cardinal vein becomes the azygos vein
- The left umbilical vein degenerates and the right umbilical vein connects to the vitelline system through the ductus venosus
Cardiac outflow tract:
Systemic venous system:
Videos
Additional references
Features to report
Table of Contents
Definition / generalDefinition / general
Click here to see Editors note
* Mandatory to report for accreditation purposes by American College of Surgeons Committee on Cancer
Recommended but not required:
- * Specimen type
- * Tumor site
- * Tumor size (greatest dimension)
- * Histologic tumor
- * Histologic grade
- * Extent of invasion, as appropriate
- * Margins, as appropriate
* Mandatory to report for accreditation purposes by American College of Surgeons Committee on Cancer
Recommended but not required:
- Additional tumor dimensions
- Additional pathologic findings
Fibromuscular dysplasia
Table of Contents
Definition / general | Sites | Etiology | Clinical features | Radiology description | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Fibromuscular dysplasia (FMD) is a vascular disease affecting small to medium sized vessels
- It is a noninflammatory, nonatherosclerotic condition occurring more frequently in younger individuals and women
Sites
- Renal artery involvement is most common (60 - 75%), followed by cervicocranial arteries (25 - 30%), visceral arteries (9%) and arteries in extremities (5%)
Etiology
- Rushton et. al. suggested it may be autosomal dominant with variable penetrance (Arch Intern Med 1980;140:233)
- Associated with hormonal factors, ergotamine preparations, methysergide, rubella syndrome
- Also heterozygous alpha-1-antitrypsin deficiency, pheochromocytoma, neurofibromatosis
- Ehlers-Danlos syndrome , Alport syndrome Type IV, cystic medial necrosis, coarctation of the aorta
Clinical features
- Symptoms occur when lesions are tightly stenotic producing hypoperfusion, if an associated aneurysm ruptures, if lesions embolize, thrombose or dissect
- Presenting symptoms include hypertension, headache, altered mentation, tinnitus, vertigo, neck pain
- Also transient ischemic attack, cerebral infarction, subarachnoid hemorrhage, syncope, Horner syndrome, cranial nerve palsies
- Deterioration of renal function is rare in fibromuscular dysplasia but common in atherosclerosis
- Overall, medial fibroplasia is the most common type of fibromuscular dysplasia, but in children, intimal fibroplasia is most common
Radiology description
- Angiographically a smooth focal stenosis (concentric band) or a long smooth (tubular) stenosis may be present
- "String of beads" describes its angiographic appearance, where the "bead" diameter is larger than the proximal vessel in medial fibroplasias
- Perimedial fibroplasia may also appear as arterial beading on an angiogram
- However, unlike medial fibroplasia, the caliber of the beads does not exceed that of the proximal artery and the beads are usually less numerous
- This dysplastic lesion results in severe stenosis and may be associated with collateral circulation
- Medial hyperplasia appears as a concentric, smooth stenosis on an angiogram, making it difficult to differentiate from intimal fibroplasia; sites of vessel involvement are similar to medial fibroplasia but do not affect branches of renal artery as often
Case reports
- Concomitant carotid, mesenteric and renal artery stenosis due to primary intimal fibroplasia (J Urol 1983;129:798)
- Woman with diffuse intimal fibromuscular dysplasia with multiorgan failure (Arch Intern Med 1996;156:2611)
Treatment
- Medical management to treat hypertension
- Antiplatelet agents
- Smoking cessation or other risk factor modification
- Endovascular therapy or surgery indicated if:
- Hypertension is poorly controlled despite maximum doses of three antihypertensive medications
- Patient is unable to tolerate medications or is noncompliant
- As an alternative to lifelong medication in this relatively young population
Gross description
- Medial fibroplasia:
- Involves distal 2/3 of main renal artery, occasionally extending into its branches
- Also commonly encountered in internal carotid artery at C1 and C2 vertebrae, compared to atherosclerosis which typically occurs at carotid bifurcation
Microscopic (histologic) description
- In 1971, a classification system to describe FMD of renal artery was proposed by Harrison and McCormack (Mayo Clin Proc 1971;46:161) based on dominant arterial wall layer involved:
- Intimal fibroplasia
- Medial dysplasia
- Adventitial (periarterial) fibroplasias
- Intimal fibroplasia:
- Circumferential or eccentric deposition of collagen in intima but no lipid or inflammatory component
- Internal elastic lamina is identifiable but may be fragmented or duplicated
- This appearance may be mimicked by endarteritis due to inflammation or trauma
- Can occur as a generalized disorder involving renal, carotid, upper and lower extremity and mesenteric vasculature simultaneously mimicking a multisystem disease such as necrotizing vasculitis
- Medial dysplasia:
- Divided into medial fibroplasia, perimedial fibroplasia, medial hyperplasia
- Medial fibroplasia:
- A subtype of medial FMD, histologic finding in 75 - 80% of all cases of FMD
- Alternating areas of thinned media and thickened fibromuscular ridges containing collagen
- Some areas of internal elastic membrane are lost
- Perimedial fibroplasia:
- 10 - 15% of all lesions, found in young girls
- Extensive collagen deposition located in outer half of media and can replace it entirely, but does not extend beyond external elastic lamina
- Medial hyperplasia:
- True smooth muscle hyperplasia without fibrosis
- Found in 1 - 2% of all lesions
- Medial fibroplasia:
- Adventitial fibroplasias:
- Rarely seen (Dense collagen replaces fibrous tissue of adventitia and may extend into surrounding tissue
- The other arterial layers and elastic laminae remain intact
Differential diagnosis
- Intimal fibroplasia: necrotizing vasculitis
- Medial fibroplasia: atherosclerosis
Additional references
General (transplant)
Table of Contents
Definition / general | Epidemiology | Pathophysiology | Etiology | Diagnosis | Prognostic factors | Microscopic (histologic) description | Differential diagnosis | Additional referencesDefinition / general
- First human heart transplantation was performed in 1967 (S Afr Med J 2011;101:97)
- Heart transplantation remains the most effective therapy for end stage heart disease of coronary and noncoronary etiology
Epidemiology
- More than 73,000 heart transplants have been performed worldwide to date
Pathophysiology
- Donor heart dysfunction results from the "catecholamine storm" (hypertension, tachycardia and intense vasoconstriction) that produces an increase in myocardial oxygen demand and potential myocardial ischemia
- These phenomena may mediate myofibrillar degeneration, a process characterized by injury and death of myofibers in a hypercontracted state
- After dissipation of this intense sympathetic activity, there is loss of sympathetic tone with a massive reduction in systemic vascular resistance, which may contribute to a second phase of potential myocardial injury, precipitated by abnormal myocardial loading conditions and impaired coronary perfusion
- Myocardial injury interacts with other factors such as older donor age and longer ischemic time, increasing the probability of postoperative primary graft dysfunction
Etiology
- Risk factors for graft failure:
- Older donor age
- Donor left ventricular (LV) dysfunction
- Longer ischemic time
- Size mismatch (smaller donor to a larger recipient)
- Indications include coronary heart disease, non ischemic cardiomyopathies, congenital heart disease
Diagnosis
- Endomyocardial biopsy (EMB) remains the gold standard for rejection surveillance in the heart transplant patient
Prognostic factors
- 10 year survival rate after cardiac transplantation currently approaches 50% and more in high volume centers
Microscopic (histologic) description
- Quilty lesions, also known as endocardial lymphocytic infiltrates, are collections of predominantly T lymphocytes with admixed B cells, occasional macrophages and plasma cells seen in the endocardium of transplanted hearts that vary in size from 0.007 to 1.89 mm
- Acute cellular rejection consists of a mononuclear inflammatory infiltrate that is predominantly a T cell mediated response directed against the cardiac allograft
- The grades proposed in the ISHLT-WF1990 were mainly based on the amount of inflammatory infiltrate and the presence of myocyte damage
-
1990 Grading System of the International Society of Heart and Lung Transplantation for Acute Cellular Rejection:
- Grade 0 (no acute rejection)
- Grade 1A (focal, mild acute rejection)
- Grade 1B (diffuse, mild acute rejection)
- Grade 2 (focal, moderate acute rejection)
- Grade 3A (multifocal moderate rejection)
- Grade 3B (diffuse, borderline severe acute rejection)
- Grade 4 (severe acute rejection)
- 2004 Grading System of the International Society of Heart and Lung Transplantation for Acute Cellular Rejection:
- Grade 0R (no acute cellular rejection)
- Grade 1R (mild, low grade, acute cellular rejection): interstitial and/or perivascular infiltrate with up to 1 focus of myocyte damage
- Grade 2R (moderate, intermediate grade, acute cellular rejection): 2 or more foci of infiltrate with associated myocyte damage
- Grade 3R (severe, high grade, acute cellular rejection): diffuse infiltrate with multifocal myocyte damage +/- edema, +/- hemorrhage +/- vasculitis
Differential diagnosis
- Ischemic injury:
- Should be differentiated from cellular rejection
- The extent of myocyte necrosis is usually out of proportion to the inflammatory infiltrate in ischemic injury, with the infiltrates consisting mostly of neutrophils and macrophages
- In cellular rejection, the infiltrates are predominantly lymphocytic
- Previous biopsy site:
- Will show several stages of healing
- Recent biopsy sites will show thrombus and granulation tissue
- Late findings include fibrosis with entrapped myocytes that often exhibit disarray and a variable amount of mononuclear cell infiltrate
- Old biopsy sites present as endocardial scars
Additional references
Giant cell arteritis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Giant cell arteritis (GCA) is a systemic inflammatory disorder characterized by granuloma formation in medium and large sized arteries, occurring most frequently in adults (StatPearls: Giant Cell Arteritis (Temporal Arteritis) [Accessed 24 May 2024])
- Very frequently it coexists with polymyalgia rheumatica
Essential features
- Commonly presents in older patients above age 50, mostly women, with new onset headache
- Most common in Scandinavian countries
- Timely diagnosis is essential to prevent irreversible vision loss
- Transmural inflammation of the vessel wall with giant cells is the main histological finding
- Important stains include elastic stain, CD68 and CD3
Terminology
- Horton arteritis
- Granulomatous arteritis
- Temporal arteritis
- Arteritis of the aged
- Cranial arteritis (StatPearls: Giant Cell Arteritis (Temporal Arteritis) [Accessed 24 May 2024])
ICD coding
Epidemiology
- Average age of diagnosis is 79 years
- F:M = 2.5:1
- Highest incidence in Scandinavia (6 times higher compared to Asia) and lowest in Asia
- Haplotype variations in certain MHC class II alleles with HLA-DRB1*04 being most common (Arthritis Res Ther 2021;23:82)
- Infectious diseases may lead to immune mediated hypersensitivity and play a role in the pathogenesis of the condition
Sites
- Medium vessel arteritis involving temporal artery, occipital artery and intraorbital blood vessels (ophthalmic and posterior ciliary)
- Large vessel arteritis involving the thoracic aorta, carotid arteries, subclavian and axillary artery (Circ Res 2023;132:238)
Pathophysiology
- Predominantly Th1 mediated immune response with significant expression of IFN gamma
- Initial endothelial injury results in activation of dendritic cells
- Activated dendritic cells release chemokines attracting CD4+ T cells and macrophages into the arterial wall
- Dendritic cells also release chemokines like IL16 and IL18, which cause T cell activation and interferon gamma release
- IFN gamma causes the characteristic chronic inflammation with formation of granulomas
- IFN gamma is also responsible for activation of mononuclear macrophages that tend to release enzymes called matrix metalloproteinase, resulting in breakdown of matrix proteins in the vessel wall and disruption of internal elastic lamina
- Role of IL6 in causing CD4+ helper T cell differentiation leading to development of Th17 cells while suppressing the T regulatory cells (StatPearls: Giant Cell Arteritis (Temporal Arteritis) [Accessed 24 May 2024])
Etiology
- Systemic inflammation largely driven by IL6 is a core feature of GCA
- Haplotype variations in MHC class II alleles (most commonly HLA-DRB1*04) seem to be a common finding among patients with this condition (Arthritis Res Ther 2021;23:82)
Clinical features
- Cranial involvement can present as
- New onset headache in the temporal region (most common presenting complaint)
- Scalp tenderness and visual disturbances
- Jaw and tongue claudication
- Transient visual disturbances
- Extracranial involvement can present as
- Limb claudication
- Vascular bruits
- Systemic symptoms like fatigue, weight loss, fever and flu-like symptoms
- Complications that can result without timely treatment include
- Ischemic optic neuropathy
- Central retinal artery occlusion
- Cerebrovascular accidents (transient ischemic attack or stroke)
- Aortic aneurysm and dissection (Rheumatology (Oxford) 2020;59:iii5)
Diagnosis
- Physical examination findings
- Temporal arteries may be thickened and tender on palpation
- Absent or diminished pulses
- Laboratory findings
- Raised erythrocyte sedimentation rate (ESR) or C reactive protein (CRP)
- Radiology
- Color Doppler ultrasound of temporal arteries
- Magnetic resonance imaging (MRI) or computed tomography (CT) angiography
- Pathology
- Temporal artery biopsy is gold standard (Rheumatology (Oxford) 2020;59:iii5)
Laboratory
- Raised ESR or CRP
Radiology description
- Doppler ultrasound findings
- Hypoechoic and diffuse thickening of arterial wall
- Halo sign: indicator of the thickness of the vessel wall caused by inflammation and considered a pathognomonic sign of GCA on ultrasound
- Reference: Ultrasound Med Biol 2021;47:201
Prognostic factors
- Factors associated with decreased risk of permanent blindness
- Fever
- Rheumatic symptoms
- Factors associated with increased risk of permanent blindness
- Age
- History of transient ischemic visual symptoms
- Jaw claudication (J Rheumatol 2016;43:1393)
Case reports
- 69 year old man with giant cell arteritis and the simultaneous onset of multiple intracranial vascular occlusions (Surg Neurol Int 2022;13:21)
- 73 year old man with an unusual presentation for giant cell arteritis (Pract Neurol 2021;21:228)
- 78 year old woman with giant cell arteritis who developed scalp necrosis (J Am Acad Dermatol 2009;61:701)
Treatment
- Corticosteroids are the mainstay of treatment, especially to prevent blindness
- Dosage: 1 mg/kg per day or 40 - 60 mg per day in divided doses for initial 4 weeks followed by gradual tapering as condition improves
- Steroid sparing agents like methotrexate, azathioprine and sulfasalazine
- Addition of a disease modifying antirheumatic drug (DMARD) may be needed in some cases (Dtsch Arztebl Int 2013;110:376)
Gross description
- Thickened, nodular and rubbery wall in the segment of the muscular artery involved
- Grossing should be done thoroughly to account for the possibility of skip lesions
- Submit whole specimen in 2 - 3 mm cross sections
- Reference: Rheumatology (Oxford) 2020;59:iii5
Microscopic (histologic) description
- The following findings are observed classically
- Multifocal segmental destructive arteritis involving all 3 layers of vessel wall
- Transmural inflammation with marked disruption of internal elastic membrane
- Granulomatous inflammation with giant cells at the intima - media junction (J Autoimmun 2016;69:94)
- More intense inflammatory infiltrate with a larger concentration of giant cells is seen during active disease while scant giant cells are seen during the inactive phase (Surg Neurol Int 2022;13:21)
- Transmural inflammatory infiltrate consisting of CD4+ T cells, macrophages, a few eosinophils and neutrophils seen in the highest concentration between the adventitia and media
- Intimal fibrosis and remodeling of blood vessels (Front Immunol 2021;12:623716)
- Other patterns of inflammation called restricted inflammation include small vessel vasculitis, vasa vasorum vasculitis and inflammation limited to adventitia
Microscopic (histologic) images
Positive stains
- Elastic stain shows fragmentation of elastic fibers in vessel wall
- CD68 and CD3 highlight macrophages and T lymphocytes respectively
Sample pathology report
- Left temporal artery, biopsy:
- Histological findings consistent with giant cell arteritis involving the temporal artery (see comment)
- Comment: There is transmural inflammation of the involved vessel with focal lymphocytic and macrophagic infiltrate and occasional giant cells. Disruption of the internal elastic membrane has been demonstrated with the elastic stain, further supporting the diagnosis.
- Gross description: Specimen A is received in formalin in a container and labeled with the patient's name and specimen number and designated left temporal artery. The specimen consists of a tan, tubular structure consistent with a muscular artery that measures 1.2 cm in length and is notably thick and nodular. The specimen is serially cross sectioned at 3 mm intervals, placed between sponges and submitted entirely in 1 cassette.
Differential diagnosis
- Vasculitides like Takayasu arteritis or granulomatosis with polyangitis:
- Histological findings lack granulomatous chronic inflammation and can include fibrinoid necrosis with neutrophilic infiltration
- Antineutrophil cytoplasmic antibodies (ANCA) titers are normal in GCA
- Varicella zoster virus infection:
- Biopsy would show inflammation without granulomas
- Systemic amyloidosis:
- Histological findings include amorphous, homogenous pale eosinophilic areas or hyaline deposits predominantly in the extracellular space that stain positive with Congo red stain
- Lymphoma:
- Biopsy will reveal atypical lymphoid cells with possible clonal proliferation
- Immunohistochemistry will reveal specific markers for specific lymphoma subtypes
- Reference: Front Immunol 2021;12:623716
Board review style question #1
Which of the following histopathological features is characteristic of giant cell arteritis (GCA) and distinguishes it from other vasculitides?
- Extensive eosinophilic infiltrates within vessel walls
- Fibrinoid necrosis with neutrophilic infiltration
- Granulomatous inflammation with giant cells at the intima - media junction
- Homogenous, pale eosinophilic areas
Board review style answer #1
C. Granulomatous inflammation with giant cells at the intima - media junction. The hallmark histopathological feature of GCA is granulomatous inflammation with giant cells at the intima - media junction. Answer A is incorrect because eosinophilic infiltrates within vessel walls are commonly seen in eosinophilic granulomatosis with polyangiitis. Answer B is incorrect because, in contrast, fibrinoid necrosis with neutrophilic infiltration is characteristic of granulomatosis with polyangiitis. Answer D is incorrect because homogenous, pale eosinophilic areas are suggestive of systemic amyloidosis.
Comment Here
Reference: Giant cell arteritis
Comment Here
Reference: Giant cell arteritis
Board review style question #2
Board review style answer #2
A. Chronic inflammation with multinucleated giant cells are the hallmark pathognomonic feature in H&E stained sections of biopsies in GCA.
Answer D is incorrect because intimal fibrosis can also be seen in GCA but it is not prominent in this image. Answers B and C are incorrect because duplication of elastic lamina and fragmentation of elastic fibers can be appreciated with the use of special elastic stain and not on routine H&E sections.
Comment Here
Reference: Giant cell arteritis
Comment Here
Reference: Giant cell arteritis
Histology
Table of Contents
Definition / general | Essential features | Physiology | Clinical features | Laboratory | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Electron microscopy description | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Specialized muscle cells, namely cardiomyocytes, allow for synchronized contractions to facilitate the pumping of blood throughout the body
Essential features
- Heart wall consists of 3 layers: endocardium, myocardium and epicardium
- Variation in the relative thickness of each of these layers exists between ventricles and atria, and between left and right sided chambers
- Myocardium is primarily composed of cardiac myocytes: specialized striated muscle cells organized in fascicles and bands
Physiology
- Heart serves as a pump that drives 2 parallel vascular circuits:
- Systemic circuit:
- Blood is ejected from the left ventricle through the aortic valve during systole at a normal pressure of 120 mmHg
- Blood travels through the ascending aorta, aortic arch and descending aorta; it then progresses through peripheral arteries, arterioles and eventually the systemic capillary beds, before entering the venous return
- Systemic venous blood returns to the right atrium from the superior and inferior vena cava at a pressure of < 5 mmHg
- Pulmonic circuit:
- Spontaneous contraction of the right atrium moves deoxygenated blood through the tricuspid valve to the right ventricle
- Ventricular contraction (systole) moves blood from the ventricle through the pulmonic valve to the pulmonary artery at a normal pressure of 25 mmHg
- Blood travels through the arteries and arterioles of the lung before reaching the alveolar capillaries
- Newly oxygenated blood returns to the left atrium via 4 pulmonic veins at a normal pressure of approximately 10 mmHg
- Left atrial contraction moves blood through the mitral valve into the left ventricle
- Coronary circulation
- The subendocardium is the last layer in the cardiac wall to receive blood flow from the coronary arteries and is most prone to ischemic injury
- Systemic circuit:
- The cardiac conduction system allows for coordinated atrioventricular contraction via the conduction of electrical impulses by specialized myocardial cells (J Interv Card Electrophysiol 2016;46:9)
- Sinoatrial (SA) node:
- Pacemaker of the heart located near the sinotubular junction, where the superior vena cava meets the right atrium
- Depolarization of the sinoatrial node cells allows for conduction of the electrical impulse through the conduction tracts within the wall of the right atrium:
- Posterior tract (Thorel tract)
- Middle tract (Wenckebach tract)
- Anterior tract (Bachmann bundle): extends to left atrium
- Depolarization also facilitates atrial contraction
- Atrioventricular (AV) node:
- Receives impulses from the sinoatrial nodal tracts, in order to propagate electrical cardiac impulse and facilitate ventricular contraction
- Located in the right atrium, in the space between the ostium of the coronary sinus, septal leaflet of the tricuspid valve and tendon of Todaro (Koch triangle) (Koch triangle)
- Bundle of His:
- Located in the membranous septum that separates the right atrium from the left ventricle
- Relays electrical impulses to the left and right bundle branches of the ventricular (muscular) septum
- Sinoatrial (SA) node:
Clinical features
- Clinical evaluation of cardiac structure and function is multifaceted and may include:
- Imaging:
- Echocardiogram
- Stress echocardiogram
- Xray / computerized tomography
- Cardiac MRI
- Coronary artery angiography
- Testing:
- Electrocardiogram
- Biopsy (see below)
- Serology (see Laboratory section)
- Imaging:
- Common cardiac pathology specimens include:
- Endomyocardial biopsy (J Clin Pathol 2006;59:121):
- Interventionalist uses a bioptome via an endovascular procedure, to sample endocardium and myocardium from the right ventricular septum
- Most common indication for endomyocardial biopsy is in the setting of transplant rejection monitoring
- In the appropriate clinical context, biopsies may also be used for the evaluation of heart disease, especially if there is concern for myocarditis, amyloidosis, hemochromatosis, drug toxicity or storage disorders
- Septal myectomy:
- Surgeon enters the left ventricle, either through the aortic valve (after aortotomy) or through the apical ventricular wall (ventriculotomy)
- Endocardium and myocardium are shaved for evaluation of septal abnormalities seen on echocardiogram
- Most common indication / etiology is hypertrophic cardiomyopathy but in the right demographic ruling out amyloidosis or storage disease is prudent
- Apical core resection: full thickness ventricular wall excision, allowing for placement of a ventricular assist device
- Atriotomy: normally excised for access to the heart chambers in a valve replacement procedure
- Atrial appendage: may be excised during procedures to replace heart valves, to reduce stroke risk in atrial fibrillation or for coronary artery bypass (Eur J Cardiothorac Surg 2018;53:i33)
- Orthotopic heart transplant
- Autopsy
- Endomyocardial biopsy (J Clin Pathol 2006;59:121):
Laboratory
- Serologic markers of acute coronary syndrome (UpToDate: Biomarkers of Myocardial Injury Other Than Troponin [Accessed 15 January 2021]):
- Troponin I / troponin T:
- Normal proteins present in myocardium which are released into systemic circulation following myocyte injury
- May remain elevated for up to 10 - 14 days post insult
- Creatinine kinase (CK / CK-MB):
- Enzyme that is present in both cardiac and skeletal muscle
- Elevations begin 4 - 6 hours post insult and resolve within 36 - 48 hours
- Isoenzyme CK-MB is proportionally greater in cardiac muscle but is present in larger absolute quantities in skeletal muscle
- Formerly the preferred test of choice, now replaced by troponin due to its higher specificity for cardiac injury than CK-MB
- Myoglobin:
- Heme complexed protein that is present in wide range of cell types and is released in response to damage
- Low specificity makes this an antiquated test that should rarely be employed
- Lactate dehydrogenase:
- Legacy test, no longer in use
- Troponin I / troponin T:
- Serologic markers of heart failure (UpToDate: Natriuretic Peptide Measurement in Heart Failure [Accessed 15 January 2021]):
- Brain natriuretic peptide (BNP, proBNP, NT proBNP)
- Three distinct proteins / cleavage products initially found in brain but also present in ventricular myocytes
- Released in response to increased ventricular pressure
- Elevated BNP is highly sensitive but not very specific for heart failure
- Atrial natriuretic peptide (ANP)
- Protein present in atrial myocytes
- Released in response to dilation of atria due to increased volumes
- Brain natriuretic peptide (BNP, proBNP, NT proBNP)
Gross description
- Isolated myocardial specimens:
- Endocardium: thin, shiny, translucent layer without fibrotic (tan-white) thickening
- Myocardium: uniform tan-brown to red striated tissue with firm but pliable texture
- No areas of gray-brown mottling and no areas of dense fibrosis
- Epicardium: thin, shiny and translucent without fibrosis; epicardial fat may be present
- Explant and autopsy specimens:
- Evaluation of the surgical or autopsy specimen should be conducted with a systematic approach (Allen: Moss & Adams' Heart Disease in Infants, Children, and Adolescents, 8th Edition, 2012)
- In addition to review of clinical history, gross evaluation should include the following:
- Position in the thoracic cavity
- Sidedness (situs)
- Evaluation of systemic connections and epicardial surface
- Coronary artery distribution and patency
- Inspection of endocardium and myocardium via short axis sectioning and opening of chambers along lines of blood flow
- Inspection for septal defects
- Evaluation of semilunar and atrioventricular valves
- Determination of atrioventricular concordance
- Measurement of heart weight, wall thickness and chamber dimension (at midventricular level)
Gross images
Microscopic (histologic) description
- Endocardium (innermost layer):
- Thin tissue which lines all 4 chambers of the heart
- Consists of 3 layers: endothelium, subendothelium and elastic layer
- Endothelium is a thin single cell layer that is continuous with the endothelial lining of the systemic vasculature
- Subendothelial layer may have variable thickness; it is most prominent in the left atrium
- Elastic layer is the thickest layer of the endocardium and shows prominent elastic fibers admixed with smooth muscle cells
- Myocardium (middle layer):
- Organized in 3 layers / regions:
- Subepicardial (superficial)
- Middle
- Subendocardial (deep)
- Cardiac myocytes:
- Striated involuntary muscle cells measuring approximately 10 - 20 micrometers in diameter (3 - 5 red blood cells thick)
- Components:
- Sarcolemma: thin cell membrane
- Nucleus: small, round and basophilic, approximately the size of 1 red blood cell
- Sarcoplasm:
- Contains longitudinal myofibers composed of myofilaments, giving it the striated appearance
- Myofilaments (actin and myosin) are arranged in a staggered pattern to form the sarcomere, the contractile unit of the myocyte
- Interstitium:
- Composed of fibroblasts, extracellular matrix, adipocytes and scattered inflammatory cells
- Penetrating capillaries and arterioles originating from the epicardial coronary arteries are present throughout the interstitium and supply blood and oxygen to the cardiac myocytes, in an epicardial to subendocardial distribution
- Organized in 3 layers / regions:
- Epicardium (outermost layer) (Prog Cardiovasc Dis 2017;59:327):
- Composed of mesothelial cells that are part of the innermost layer of pericardium (visceral pericardium), along with subjacent fibroconnective and vascular tissue
- Benign fibrotic thickening may occur over the anterior surface of the heart giving rise to the soldier's patch
- Epicardial fat may also be considered part of the epicardial layer
- Reference: Buja: Cardiovascular Pathology, 4th Edition, 2015
Microscopic (histologic) images
Immunohistochemistry & special stains
- Immunohistochemical stain targeting skeletal muscle will also stain cardiac myocytes
- IHC: actin, desmin, vimentin (Cytobios 1986;45:195)
- Special stains may be used in evaluation of normal myocardium:
- Congo red in the evaluation for amyloid (apple green birefringence) (Hum Pathol 2014;45:1766)
- Sulfated Alcian blue in the evaluation for amyloid (sea foam green) (J Clin Pathol 1976;29:22)
- Prussian blue in the evaluation for iron (Rev Esp Patol 2019;52:45)
- Masson trichrome in the evaluation for interstitial fibrosis (Circulation 2018;138:1224)
Electron microscopy description
- Sarcomere (Environ Health Perspect 1978;26:159):
- Composed of myofilaments arranged in a staggered pattern (alternatively actin and myosin)
- Bound by perpendicular electron dense Z bands
- Contraction pulls Z bands closer and relaxation allows for them to move further apart
- Orderly spacing of parallel myofilaments
- Nucleus:
- Fine chromatin with single nucleolus
- Mitochondria:
- Circular to ovoid structures of relatively uniform size with prominent layered cristae
- Intercalated disk:
- Jagged electron dense line representing cell - cell junctions between myocytes
- Lipofuscin:
- Radio dense material associated with age related changes
- Often perinuclear in distribution
Board review style question #1
Board review style answer #1
Board review style question #2
Which structure is referred to as the pacemaker of the heart?
- Atrioventricular node
- Bachmann bundle
- Bundle of His
- Sinoatrial node
Board review style answer #2
Hypertrophic cardiomyopathy
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Disease inherited in an autosomal dominant pattern involving sarcomere proteins (Eur J Heart Fail 2020;22:228)
- Consists of left ventricular hypertrophy, fibrosis and hypercontractility (Eur J Heart Fail 2020;22:228)
Essential features
- Genetic disorder that consists of left ventricular hypertrophy and hypercontractility
- Hallmarks of histological diagnosis include myocyte hypertrophy, fibrosis and disarray
- Mechanisms of hypertrophic cardiomyopathy (HCM) consist of left ventricular hypertrophy, which leads to increased muscle mass that the existing vasculature cannot support
- Hypertrophy may be symmetric or asymmetric; asymmetric is more commonly seen and is found at the septum
Terminology
- Hypertrophic obstructive cardiomyopathy
- Asymmetric septal hypertrophy
ICD coding
Epidemiology
- Previously thought to be a disease only of youth but average age at diagnosis is increasing (Circ Heart Fail 2020;13:e007230)
- Can present from infancy to seventh decade of life (Int J Cardiol Heart Vasc 2020;27:100503)
- M:F = ~3:2 (Circ Heart Fail 2020;13:e007230)
- 20 million people are thought to be suffering from hypertrophic cardiomyopathy worldwide (JACC Heart Fail 2018;6:376)
Sites
- Primarily affects the left ventricle of the heart
Pathophysiology
- Mechanisms of hypertrophic cardiomyopathy consist of left ventricular hypertrophy, which leads to increased muscle mass that the existing vasculature cannot support
- Lumen of the coronary arteries also narrows due to wall hardening
- All of these phenomena lead to myocardial ischemia (Int J Cardiol Heart Vasc 2020;27:100503)
- Left ventricular hypertrophy causes decreased compliance and outflow obstruction (Eur J Heart Fail 2020;22:228)
Etiology
- More than 400 different known mutations (mostly missense) in 9 different genes
- Most common are mutations affecting cardiac beta myosin heavy chain (MYH7) and myosin binding protein C (MYBPC) (Eur J Heart Fail 2020;22:228)
- May be associated with phenotypic variations like Fabry disease and Friedreich ataxia (Int J Cardiol Heart Vasc 2020;27:100503)
Clinical features
- Common symptoms include chest pain and breathlessness upon exertion; exercise capacity decreases (Eur J Heart Fail 2020;22:228)
- Sudden cardiac death can occur in younger patients who have few or no symptoms (Int J Cardiol Heart Vasc 2020;27:100503)
- On physical exam, findings may include systolic thrill at left sternal border, pulsus paradoxus, elevated "a" wave on JVP and a B4 on auscultation (Int J Cardiol Heart Vasc 2020;27:100503)
Diagnosis
- Transthoracic echocardiography (Int J Cardiol Heart Vasc 2020;27:100503)
- Cardiac magnetic resonance (CMR) is used if assessment is difficult using echocardiography (Int J Cardiol Heart Vasc 2020;27:100503)
- Genetic testing and DNA analysis may also be performed (Int J Cardiol Heart Vasc 2020;27:100503)
Laboratory
- Cardiac enzymes such as creatinine phosphokinase and troponins
- In one study, 42 out of 98 HCM patients had a minimum serum high sensitivity cardiac troponin T (hs-cTnT) level of 14 ng/L (J Cardiol 2014;63:140)
- Mean hs-cTnT level was 12.37 ng/L
- Thus, hs-cTnT was elevated in a significant number of HCM patients
- In another study, abnormal creatine kinase MB elevation was seen in 64% of HCM patients (Circ J 2016;80:218)
Radiology description
- EKG shows ST segment and T wave changes (Int J Cardiol Heart Vasc 2020;27:100503)
- Transthoracic echocardiography should show ventricular wall thickness ≥ 15 mm in at least one segment or alternatively, ≥ 13 mm in someone with a first degree relative who has HCM (Int J Cardiol Heart Vasc 2020;27:100503)
- Cardiac magnetic resonance imaging may highlight myocardial fibrosis after paramagnetic contrast is used (Int J Cardiol Heart Vasc 2020;27:100503)
Prognostic factors
- Left ventricular mass index can foretell if major cardiac events, such as mortality, transplantation or arrhythmias, will occur and myocardial fibrosis predicts arrhythmias in people with HCM (Int J Cardiovasc Imaging 2021;37:2027)
- FT (feature tracking) strain analysis also gives information on ventricular dysfunction and risk stratification (Int J Cardiovasc Imaging 2021;37:2027)
- Nonobstructive HCM usually has a good prognosis
- If it has been present long term, it may evolve into dilated cardiomyopathy
- Obstructive HCM can lead to pulmonary congestion and heart failure
- Rarely, arrhythmias may also occur (Int J Cardiol Heart Vasc 2020;27:100503)
Case reports
- 39 year old man with sudden cardiac death (Transplant Proc 2022;54:2703)
- 43 year old man with an apical left ventricular aneurysm and midhypertrophic cardiomyopathy obstruction and a 63 year old man with apical hypertrophic cardiomyopathy (J Cardiothorac Surg 2021;16:360)
- 57 year old man with chest pain and T wave inversions (Eur Heart J Case Rep 2020;5:ytaa493)
Treatment
- Beta blockers and nondihydropyridine calcium channel blockers are used to reduce left ventricular outflow tract (LVOT) obstruction (Eur J Heart Fail 2020;22:228)
- Arrhythmias are treated with sotalol, amiodarone and disopyramide
- Catheter / surgical ablation may be performed for atrial fibrillation (Eur J Heart Fail 2020;22:228)
- Septal myectomy and alcohol septal ablation (ASA) are useful for obstructive HCM if the patient is refractory to drugs (Eur J Heart Fail 2020;22:228)
- Heart transplantation is indicated when HCM has reached the end stage and there is severe left ventricular or diastolic dysfunction (Int J Cardiol Heart Vasc 2020;27:100503)
- Future of treatment may involve genome editing (Eur J Heart Fail 2020;22:228)
Gross description
- Main gross findings include left ventricular hypertrophy; asymmetric hypertrophy is more common than symmetric and is found at the septum (Int J Mol Sci 2024;25:1275)
- There may also be subaortic mitral valve fibrosis (Int J Mol Sci 2024;25:1275)
- If the HCM has been progressing, dilation of ventricle can occur (Int J Mol Sci 2024;25:1275)
- White scars due to fibrous tissue buildup can be observed in ventricles (Int J Mol Sci 2024;25:1275)
Gross images
Microscopic (histologic) description
- Hallmarks of histological diagnosis include myocyte hypertrophy, fibrosis and disarray (Int J Mol Sci 2024;25:1275)
- Cells are abnormally branched with hyperchromatic and enlarged nuclei (Int J Mol Sci 2024;25:1275)
- Fibrosis is present interstitially between myocytes, around capillaries in a perivascular pattern or forms scar / replacement tissue after myocyte death (Int J Mol Sci 2024;25:1275)
Microscopic (histologic) images
Contributed by Aliya N. Husain, M.D. and Saranya Singaravel, M.B.B.S.
Positive stains
- The following stains have been used but are not needed for diagnosis
Negative stains
Electron microscopy description
- Electron microscopy showed a profound disruption in mitochondrial ultrastructure, in which a subset of interfibrillar mitochondria were swollen with disorganized and reduced cristae density (Circulation 2021;144:1714)
- Mitochondrial morphology is disturbed; interfibrillar mitochondria are inflated and cristae are decreased (Circulation 2021;144:1714)
Molecular / cytogenetics description
- MYH7 codes for beta myosin heavy chain and MYBPC3 codes for myosin binding protein C
- These genes are both responsible for HCM pathogenesis
- MYH7 gene involves p.Arg403Glu (p.R403Q) mutation (Circ Res 2021;128:1533)
Videos
Hypertrophic cardiomyopathy
by Dr. Yuichi J. Shimada
Sample pathology report
- Heart, resection for transplantation:
- Hypertrophic cardiomyopathy (750 g) (see comment)
- Comment: The left ventricle displays extensive myocyte hypertrophy and disarray with areas of replacement fibrosis.
Differential diagnosis
- Hypertension and aortic stenosis:
- Both lead to left ventricular hypertrophy (Glob Cardiol Sci Pract 2018;2018:20)
- Fabry disease:
- Causes concentric right ventricular hypertrophy (Glob Cardiol Sci Pract 2018;2018:20)
- Amyloidosis:
- Apple green birefringence on Congo red staining (Glob Cardiol Sci Pract 2018;2018:20)
- Mitochondrial disease:
- Ragged red fibers stain red with Gomori trichrome stain (Glob Cardiol Sci Pract 2018;2018:20)
Board review style question #1
Which of the following is true regarding the gross image shown above?
- Disease is inherited in an autosomal recessive pattern
- Hallmarks of histological diagnosis include myocyte hypertrophy, fibrosis and disarray
- Mainstay of diagnosis is magnetic resonance imaging
- Severe coronary atherosclerosis is the underlying etiology
Board review style answer #1
B. Hallmarks of histological diagnosis include myocyte hypertrophy, fibrosis and disarray. The gross picture shows hypertrophic cardiomyopathy and the listed features should be present if we look at the tissue sample under a microscope. Answer A is incorrect because this disease is autosomal dominant. Answer C is incorrect because echocardiography is usually used to diagnose hypertrophic cardiomyopathy. Answer D is incorrect because the pattern of hypertrophy and fibrosis does not fit ischemic heart disease.
Comment Here
Reference: Hypertrophic cardiomyopathy
Comment Here
Reference: Hypertrophic cardiomyopathy
Board review style question #2
A 23 year old man with a family history of cardiomyopathy fell unconscious and died on the way to the hospital. His ambulatory EKG showed ST segment and T wave changes. Upon autopsy, his heart showed myocyte disarray and fibrosis. Which of the following mutations is his condition caused by?
- Mutations affecting cardiac beta myosin heavy chain (MYH7) and myosin binding protein C (MYBPC)
- Mutations in genes encoding for pore forming alpha subunits (KCNQ1, KCNH2) of potassium channels
- Mutations in HCN4 gene
- Mutations in SCN5A gene
Board review style answer #2
A. Mutations affecting cardiac beta myosin heavy chain (MYH7) and myosin binding protein C (MYBPC). The diagnosis is hypertrophic cardiomyopathy; cardiac beta myosin heavy chain (MYH7) and myosin binding protein C (MYBPC) are mutated in this disease. Answer B is incorrect because the genetic mutations in potassium channels cause long QT syndrome, which would show QT interval prolongation on ECG. Answer D is incorrect because SCN5A gene mutations cause Brugada syndrome and would show ST segment elevation in the right precordial leads. Answer C is incorrect because HCN4 gene is mutated in idiopathic sick sinus syndrome which would have showed prolonged QRS intervals.
Comment Here
Reference: Hypertrophic cardiomyopathy
Comment Here
Reference: Hypertrophic cardiomyopathy
Idiopathic restrictive cardiomyopathy
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Differential diagnosis | Additional referencesDefinition / general
- Rare heart muscle disease with altered hemodynamic pattern and myocardial compliance, resulting in a restrictive filling pattern and diastolic ventricular dysfunction with normal or near normal systolic function and ventricular wall thickness
- Abnormal morphology may or may not be present
- It is a diagnosis of exclusion and no evidence of infiltrative, pericardial or endocardial disease should be present
- Accounts for 3% - 5% of cardiomyopathies
Essential features
- Restrictive filling pattern
- Mutations in sarcomeric protein genes
- Diagnosis of exclusion
Terminology
- Also known as primary restrictive cardiomyopathy
Epidemiology
- Restrictive cardiomyopathy is the least common type of cardiomyopathy
- Exact prevalence is not known
- Slightly more common in women (F:M ratio, 1.5:1)
- More common in adults but can occur in any age group
- Prognosis is particularly poor in children and two year survival is less than 50%
Pathophysiology
- Mutations in sarcomeric proteins such as cTnI (a troponin subunit) increase the Ca2+ sensitivity of cardiac myofilaments, increasing the contractility and producing diastolic dysfunction
Etiology
- Etiology of primary restrictive cardiomyopathy is not clear
- Mutations have been identified in the sarcomeric protein genes such as cardiac troponin I, troponin T2, beta myosin heavy chain and alpha cardiac actin
- Autosomal dominant inheritance pattern is seen
- Familial cases have been documented
- Cases of restrictive and hypertrophic cardiomyopathy have been seen in the same family and may represent 2 different phenotypes of the same basic sarcomeric disease
- Mutations in the desmin gene have also been identified - restrictive phenotype is typically accompanied by atrioventricular blocks
Clinical features
- Most common presentation is congestive heart failure and patients may require transplantation
- Atrial fibrillation is very common; also elevated systemic and pulmonary venous pressures
- Jugular venous pressure may be increased
- Left ventricular impulse is usually normal and palpable
- Third heart sound may be audible due to rapid ventricular filling
- Systolic murmurs of mitral and tricuspid regurgitation may also be auscultated
Diagnosis
- Diagnostic right and left heart catheterization is an important diagnostic modality
- Pressures in all the chambers and cardiac output are measured according to the Fick method
- Dip plateau morphology in the LV diastolic pressure tracing is characteristic
- ECG is invariably abnormal but is nonspecific
- Predominant rhythm is atrial fibrillation with premature beats and conduction delay
- QRS voltage is normal
Laboratory
- Diagnosis can be established on right ventricular endomyocardial biopsy
- One biopsy fragment may be fixed in glutaraldehyde for electron microscopic evaluation
Radiology description
- Biatrial enlargement with pulmonary venous congestion and pleural effusions
Radiology images
Case reports
- Report of seven cases (PDF file - Acta Pediátr Mex 2014;35:87)
Treatment
- Heart failure is managed medically
- In cases with atrial fibrillation, antiarrythmics are useful
- In severe cases, heart transplant may be considered
Gross description
- Gross examination of the heart shows biatrial dilatation due to increased filling pressures
- Ventricles are relatively normal sized
- Ventricular cavity is normal
- Ventricular wall is abnormal, with a rubbery texture
- Thickening of the endocardium may be observed
Gross images
Microscopic (histologic) description
- Microscopic changes are nonspecific and include myocyte hypertrophy, focal or diffuse perimyocytic fibrosis and focal myofiber disarray
Microscopic (histologic) images
Positive stains
- Masson's trichrome may be useful to demonstrate the perimyocytic fibrosis
Electron microscopy description
- Diffuse fibrosis of the perimyocyte produces a characteristic lattice of collagen surrounding every myocyte
- Patients with desmin cardiomyopathy show granulofilamentous intracytoplasmic material
Differential diagnosis
- Constrictive pericarditis (J Am Coll Cardiol 2016;67:2061)
- Obliterative endomyocardial disease
- Specific cardiomyopathies such as amyloidosis and hemochromatosis
Additional references
Infective endocarditis
Table of Contents
Definition / general | Epidemiology | Sites | Etiology | Pathophysiology | Causative organisms | Classification | Clinical features | Diagnosis | Diagrams / tables | Investigation | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Histochemical stains | Immunohistochemistry & special stains | Molecular / cytogenetics description | Complications and their mechanism | Additional referencesDefinition / general
- First described by William Osler in 1885
- Defined as an infection on endothelial surfaces of heart which includes:
- Mural endocardium
- Valves and their apparatuses
- Prosthetic or implanted components, including valves, homografts, pacemakers, intracardiac cardioverter defibrillators and their leads
- Ventricular assist devices
- Surgical shunts and septal defect occluders
- Endovascular devices or clips
Epidemiology
- Population based incidence is 4 -10 per 100,000 per year, slightly higher rate in men
- Mortality estimated at 1 per 100,000 per year, greater in intravenous drug abuse (IVDA)
- Endocarditis accounts for ~0.75 admissions per 1000 per year in large community hospitals (eMedicine: Pathology of Infectious Endocarditis [Accessed February 28, 2018])
Sites
- Endocardial surface of valve, endocardium of cardiac chamber
- In the presence of a ventricular septal defect (VSD), vegetations can be found on the right ventricular side of the VSD, on the tricuspid valve or where the jet impinges on the right ventricular wall
- Vegetations found in coarctation usually occur distal to the obstruction
Etiology
- Risk factors:
- Pre existing structural heart disease: rheumatic heart disease (RHD), hypertrophic cardiomyopathy (HCM), subaortic stenosis, ventricular aneurysm
- Degenerative valve disease: mitral valve prolapse, bicuspid aotic valve, calcific aortic valve disease
- Cardiac interventions: prosthetic valve, pacemaker, defibrillator, IVDA (right sided endocarditis), indwelling catheter
- Congenital heart disease: small ventricular septal defect, bicuspid aortic valve, coarctation of aorta, patent ductus arteriosus
- Uncommon with large VSD, mitral stenosis, atrial septal defect
Pathophysiology
- Experimental evidence indicates that 2 factors are needed to establish endocardial infection:
- Endothelial denudation over valve cusp with platelet deposition (thrombus)
- Episode of bacteremia
- Endothelial damage can be due to aberrant jet streams and turbulent flow in the setting of diseased cardiac valves and septal defects or direct trauma from intravascular devices
- A platelet / fibrin clot is formed over the exposed underlying extracellular matrix as the reparative process ensues
- If transient bacteremia occurs before a protective layer of endothelium forms, colonization of the fibrin may develop and progress to an infected vegetation
- Organism proliferates within the thrombus, forming infective vegetations, which elicits inflammatory response resulting in erosion or perforation of the valve cusps, leading to valvular aneurysms, perforations and incompetence, damage to the conduction pathway (if in the septal area), or rupture of a sinus of Valsalva (if in the aortic area)
- Prolonged antibiotic treatment is needed to sterilize the vegetations
- Endocarditis on a prosthetic valve usually begins in the valve ring and may protrude into the valve orifice causing obstruction and regurgitation
- Annular abscesses around the sewing ring of the valve are common, leading to dehiscence of sutures and paraprosthetic leaks
- Organisms which can bind via receptors to fibronectin, other subendothelial components or to platelets are the most virulent
- Healing process depends on the degree of valve damage in the initial acute phase
- Over time, vegetation decreases in size and organizes as a fibrous nodule which may calcify
- Cusp fibrosis leads to cusp thickening and retraction
Causative organisms
- Streptococci:
- 50% - 80% of infective endocarditis (IE) cases
- S. viridans (e.g. S. anguis, S. milleri, S. mutans, S. mitior), normally found in the upper aerodigestive tract, may disseminate during tonsillectomy, dental extraction, dental cleaning etc. resulting in bacteremia
- Staphylococci:
- 20% - 30% of subacute cases of IE and 50% of acute cases
- S. aureus and S. epidermidis
- Common in patients with indwelling central venous catheters, IVDA, diabetes, chronic hemodialysis and prosthetic valve endocarditis
- Staphylococcal endocarditis can affect functionally normal native valves and cause extensive tissue damage and septic emboli
- Prosthetic valve endocardits is mainly due to coagulase negative staphylococci
- Enterococci: 5% - 15% of IE cases; e.g.: S. faecalis, S. bovis, S. faecium
- HACEK organisms: Haemophilus parainfluenza, Haemophilus aphrophilus, Actinobacillus (Haemophilus) actinomycetemcomitans, Cardiobacterium hominis, Eikenella species, and Kingella species
- Less common organisms: Candida, Aspergillus, Histoplasma, and Brucella (common in IVDA, alcoholics, and patients with prosthetic heart valves)
Classification
- Older classification was based on course of untreated disease: acute, subacute, chronic
- Newer classification system is based on causative organism
- Also classify based on native valve or prosthetic valve endocarditis
Clinical features
- Vague constitutional symptoms such as fever, rigors, night sweats, anorexia, weight loss, arthralgia
- Development of new murmur or change in nature of an existing murmur (a regurgitant murmur may disappear or worsen)
- Skin lesions
- Osler nodes: tender lesions found on finger pulps and thenar / hypothenar eminences
- Janeway lesions: transient, nontender macular papules on palms or soles
- Splinter hemorrhages
- Petechiae (embolic or vasculitic)
- Clubbing: in long standing disease
- Eyes: Roth spots (boat shaped hemorrhages with pale centers, in retina) and conjunctival splinter hemorrhages
- Neurological:
- Confusion, hemiplegia and sensory dysfunction due to emboli
- Subarachnoid hematoma due to rupture of mycotic aneurysm
- Renal:
- Infarction causes loin pain and hematuria
- Immune complex deposition may cause glomerulonephritis
- Splenomegaly and splenic infarction due to emboli
Diagnosis
- Requires (a) 2 major criteria or (b) 1 major and 2 minor criteria or (c) 5 minor criteria (see Table below)
- These are associated with a 99% specificity for diagnosis in follow up studies
Investigation
- Blood count: normochromic normocytic anemia is usual, while neutrophil leucocytosis is common
- ESR: may be raised
- Renal and liver function test: levels of creatinine may be raised; levels of liver enzymes may be raised in a hepatocellular (nonobstructive) pattern
- CRP: increases acutely in bacterial infection
- Urine microscopy: microscopic hematuria is common in early disease
- Culture: all skin lesions, drip sites or other foci of infection should be cultured
- Electrocardiography (ECG): ECG regularly (daily if aortic or septal root abscess is suspected)
- Culture negative endocarditis:
- In up to 10% of cases of IE diagnosed by clinical criteria, blood cultures may be negative
- This is due to either subtherapeutic antibiotic therapy or an organism whose growth requirements make in vitro growth difficult
- Gram negative organisms of the HAECK group, Brucella, Fungi, Coxiella, Chlamydia are more likely in these cases
- In these cases, diagnosis is best obtained by serology or broad range PCR
Case reports
- 67 year old man with fungal endocarditis of the mitral valve (Clin Cardiol 2000;23:55)
- Fungal endocarditis: an autopsy study (Asian Cardiovasc Thorac Ann 2004;12:95)
- Cardiac valves in patients with Q fever endocarditis (J Infect Dis 2003;187:1097)
Treatment
- Blind treatment with antibiotics should not be undertaken since it will delay diagnosis and identification of the causal organism
- Antibiotics should not be initiated before three sets of blood cultures have been taken
- Current guidelines on antibiotic prophylaxis:
- American Heart Association (2007): changes past recommendation; now, no antibiotic prophylaxis after GI or GU procedures in group A patients (prosthesis, congenital heart disease, previous history of IE) (AHA: Prevention of Infective Endocarditis [Accessed 28 February 2018], Prophylaxis Against Infective Endocarditis, London: National Institute for Health and Clinical Excellence (UK) 2008 )
Gross description
- Vegetations are seen attached to atrial aspect of AV valves and ventricular aspect of semilunar valves in relation to the line of apposition
- Large vegetations may extend into adjacent parts of cusp or leaflets, chordae tendinae or sinus of valsalva
- Largest vegetation is seen in fungal infections
- Colour varies from red to pink to yellow and may be soft or friable or firm
- Surface is smooth, often irregular granular
- Lesions may calcify with time after antibiotic treatment
Microscopic (histologic) description
- Two features always present are inflammation and surface thrombus
- Depending on the duration of the infection and treatment, the inflammation may be primarily neutrophilic or mostly lymphohistiocytic
- Fresh vegetations contain platelets and fibrin with a rich infiltrate of neutrophils
- Colonies of embedded organisms may be seen
- Organizing and organized thrombi with fibrosis are common in lesions that have been present for weeks or more
- In chronic lesions, vegetations may show varying degrees of organization, vascularization and calcification
- Care must be taken to distinguish between irregularly sized granules of calcium and viable bacteria
- Numerous giant cells with lymphocytes are a feature of Coxiella burnetti (Q fever) endocarditis
Microscopic (histologic) images
Histochemical stains
- Gram stain, Methanemine silver stain (GMS), PAS
- Combination of these identifies fungal spores and hyphae and may show cocci with altered staining characteristics
- Giemsa and Machiavello stains: for suspected Rickettsial infections
Immunohistochemistry & special stains
- Useful in culture negative endocarditis, due to fastidious microbes like Coxiella and Legionella
Molecular / cytogenetics description
- Polymerase chain reaction (PCR) to detect fastidious bacteria in culture negative cases; specific organisms that have been tested in this way include Rickettsia (Coxiella, Bartonella, T whipplei)
Complications and their mechanism
- Cardiac failure: volume overload due to regurgitant lesions, infarcts
- Systemic infarcts: emboli
- Systemic abscess: infected emboli
- Aneurysms: infected emboli
- Renal failure: emboli, immune mediated glomerulonephritis
Infective myocarditis
Table of Contents
Definition / general | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory / cardiac testing | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Diagrams / tables | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Molecular / cytogenetics description | Additional referencesDefinition / general
- The term 'myocarditis' was first introduced by Corvisart
- It is defined by WHO / International Society and Federation of Cardiology (ISFC) as an inflammatory disease of the heart muscle, diagnosed by established histological, immunological and immunohistochemical criteria
Epidemiology
- Postmortem data identify myocarditis in 8.6% to 12% of cases of sudden death in young adults
- The Myocarditis Treatment Trial reported the incidence of biopsy proven myocarditis in patients with unexplained heart failure to be 9.6%
Pathophysiology
- Murine models of enteroviral myocarditis suggest viral myocarditis is characterized by 3 phases
- Acute: entry of virus into myocytes, mediated through specific receptors such as the transmembrane coxsackievirus and adenovirus receptors (CAR)
- Subacute: acute injury of the myocytes, induced by virus replication leading to myocyte necrosis
- This exposes the intracellular antigens (e.g. cardiac myosin) and activates the host immune system
- The first phase is virus induced myocyte injury; the second phase is autoimmune mediated injury due to activated virus specific T cells which may target host organs by molecular mimicry
- The immune response declines with virus elimination; ventricular function usually recovers without sequelae or it may persist leading to the
- Chronic phase, characterized by myocardial remodeling and development of dilated cardiomyopathy (DCM)
Etiology
- Parvovirus B19, Coxsackie B virus, human herpesvirus 6 (HHV6) type B, adenovirus (Arch Cardiovasc Dis 2009;102:559 - Table 1)
Clinical features
- Highly nonspecific
- Patient may be asymptomatic or present with signs / symptoms of myocardial infarction or cardiac failure, including chest pain and cardiac arrhythmias
Diagnosis
- Endomyocardial biopsy is the gold standard to diagnose myocarditis
- As myocarditis is a focal disease, four to five biopsy samples obtained in more than one area of the right ventricular (RV) septum should be analysed using light microscopic examination and immunohistochemical assays
Laboratory / cardiac testing
- Leukocytosis and increased CRP levels but normal values do not exclude myocarditis
- Cardiac biomarkers such as troponins and creatine kinase lack specificity but may help to confirm the diagnosis of myocarditis
- Higher levels of troponin T may have prognostic value
- Serology of infective organisms is helpful
- Interpretation of antibody assays is complicated by other confounders such as reactivation or reinfection (e.g. HSV) or by cross reactions (e.g. EBV or enterovirus)
- ECG: widely used as screening tool despite low sensitivity
- Findings vary from nonspecific T wave and ST segment changes to ST segment elevation mimicking an acute myocardial infarction
- Atrial or ventricular conduction delays, supraventricular and ventricular arrhythmias can occur in patients with myocarditis
- The presence of Q waves or a new left bundle branch block (LBBB) are associated with higher rates of cardiac death or heart transplantation
Radiology description
- Chest Xray: cardiomegaly due to chamber dilation or pericardial effusion; may show pulmonary venous congestion, interstitial infiltrates, pleural effusions
- Echocardiography:
- Evaluates cardiac chamber size and wall thickness
- Assess systolic and diastolic function
- Rule out other causes of cardiac failure such as valvular heart disease or other cardiomyopathies (hypertrophic or restrictive cardiomyopathy)
- Before an endomyocardial biopsy (EMB) procedure, echo is needed to exclude pericardial effusion and intracavitary thrombi
- Cardiovascular MRI: edema in T2 weighted imaging indicates acute myocardial inflammation
- Myocardial early gadolinium enhancement: T1 weighted segmented inversion recovery gradient echo sequence shows a difference in signal intensity between diseased and healthy myocardial regions with Gd-DTPA accumulation in late gadolinium enhancement (LGE) imaging
- Combination of these findings is currently regarded as the most sensitive and specific noninvasive approach to diagnose myocarditis
Radiology images
Prognostic factors
- Depends on clinical presentation, clinical parameters and EMB findings
- Patients with acute myocarditis and preserved left ventricular ejection fraction (LVEF) have a good prognosis with a high rate of spontaneous improvement without sequelae
- Patients with fulminant viral myocarditis and hemodynamic compromise at presentation have an excellent long term prognosis and are more likely to experience complete recovery if aggressive treatment or mechanical circulatory support is initiated early during the fulminant phase
Case reports
- 14 year old boy with family history of dilated cardiomyopathy induced by viral myocarditis (Case Reports in Cardiology 2012;2012)
- 15 year old boy with myocarditis mimicking acute coronary syndrome following influenza B virus infection (Cases J 2009;2:6809)
- 19 year old woman with viral myocarditis (Mayo Clin Proc 2009;84:1001)
- 23 year old man with idiopathic acute myocarditis during treatment for controlled malaria infection (Malar J 2014;13:38)
- 27 year old man with parvovirus B19 associated fulminant myocarditis successfully treated with immunosuppressive and antiviral therapy (Antivir Ther 2010;15:681)
- 34 year old man with acute myocarditis from coxsackie infection, mimicking subendocardial ischemia (Hellenic J Cardiol 2009;50:147)
- 46 year old woman with fulminant myocarditis (Rev Port Cardiol 2012;31:503)
- Two cases of dengue myocarditis (Infection 2013;41:709)
Treatment
- As no pathogen specific therapy of viral myocarditis has been shown to improve survival, treatment is symptomatic and based on clinical presentation
Diagrams / tables
Gross description
- Findings are nonspecific and include normal or dilated chambers
- May have softening and pallor of ventricles
- May have pericardial effusion and pericarditis with viral or bacterial myocarditis
- Late stages may show fibrosis that is focal or diffuse but the distribution is often random (see the image below), in contrast to the subendocardial fibrosis typically seen in ischemia
Microscopic (histologic) description
- Dallas criteria:
- Acute myocarditis: lymphocytic infiltrates in association with myocyte necrosis
- Borderline myocarditis: inflammatory infiltrates without evidence of myocyte necrosis
- Due to high interobserver variability, IHC is increasingly used for diagnosis
Microscopic (histologic) images
Immunohistochemistry & special stains
- CD3 for T cells
- CD68/PGM1 for activated macrophages
- HLA-DR to assess HLA class II
- EMB is considered to be inflamed by immunohistochemical detection of focal or diffuse mononuclear infiltrates (T lymphocytes and macrophages) with 14 cells / mm2, in addition to enhanced expression of HLA class II antigen
Molecular / cytogenetics description
- Nested PCR / real time PCR in EMB
- In situ hybridization techniques for identification of replicating viral genomes
Lambl excrescence
Table of Contents
Definition / general | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- Also called valvular strands
- Common finding in elderly patients
- Small filiform / papillary processes that are age-related; may be organized mural thrombi at site of minor endothelial damage
- Associated with stroke, particularly among younger patients (Stroke 1997;28:2185)
- Aortic/pulmonic valves: most common at nodules of Aranti, along lines of closure and free cuspal edges
- Tricuspid/mitral valves: at site of valve closure on atrial surface
Clinical images
Microscopic (histologic) description
- Connective tissue / fibrin covered by endothelium
Microscopic (histologic) images
Additional references
Left ventricular assist device (LVAD)
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Laboratory | Prognostic factors | Case reports | Treatment | Gross images | Videos | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Left ventricular assist device (LVAD) is a mechanical pump flow device that helps the left ventricle pump blood to the rest of the body in patients with heart failure, which affects > 6 million Americans (Circulation 2020;141:e139)
- LVADs are standard of care for medically refractory stage D heart failure as either bridge to transplant or destination therapy (long term or indefinite therapy)
Essential features
- Serves as a bridge for patients waiting for a heart transplant
- LVADs not only improve survival but also quality of life; patients experience a significant reduction in New York Heart Association functional class (N Engl J Med 2019;380:1618)
- LVADs improve survival and quality of life for patients with stage D heart failure, defined as the presence of refractory symptoms after optimal medical, surgical and device therapies (J Card Fail 2015;21:519)
- First generation LVADs were based on pulsatile flow
- Subsequent LVADs use continuous flow instead of pulsatile flow, which allows for engineering modifications including smaller size and improved long term survival (J Heart Lung Transplant 2013;32:141, N Engl J Med 2009;361:2241)
Terminology
- Durable mechanical circulatory support device (MCS)
- HeartMate II™ (HMII), HeartMate 3™ (HM3)
- Other ventricular assist devices (VAD)
- Right ventricular assist device (RVAD)
- Biventricular assist device (BiVAD); when both LVAD and RVAD are implemented
ICD coding
- ICD-10: Z95.811 - presence of heart assist device
Epidemiology
- Between June 2006 and December 2018, nearly 25,000 adult patients received mechanical circulatory support devices; > 2,000 LVADs are still being implanted annually
- > 580,000 individuals have stage D heart failure in the U.S. with a 1 year survival rate ranging from 6% to 25% (N Engl J Med 2001;345:1435)
- Men are more likely to receive LVADs due to the increased risk of developing heart failure (BMJ Glob Health 2017;2:e000298)
- 52% of LVAD recipients are in some form of cardiogenic shock during time of implantation (J Am Coll Cardiol 2022;79:1092)
- Heart transplant waitlist mortality decreased from 14.6 deaths per 100 waitlist years in 2005 to 9.7 deaths in 2015, due to improvements in medical therapy guidelines, organ donor systems and continuous flow LVADs used as a bridge to transplant (Am J Transplant 2018;18:291)
Sites
- Heart: left ventricle
- Left ventricular core (base of the heart)
Pathophysiology
- Patients with heart failure present with low or reduced ejection fraction (HFrEF: EF < 40%) and also systolic heart failure (Eur Heart J 2016;37:2129)
- HFrEF hearts undergo eccentric remodeling accompanied with ventricular chamber dilatation, volume overload and activation of the renal angiotensin system (Cardiovasc Diagn Ther 2021;11:263)
- Patients may present with preserved ejection fraction (HFpEF: EF > 50%) and also diastolic heart failure or mid range ejection fraction (HFmrEF: EF 40 - 49%) (Eur Heart J 2016;37:2129)
- HFpEF hearts show concentric remodeling accompanied with ventricular hypertrophy, impaired ventricular relaxation or filling, increased ventricular stiffness and elevated filling pressure (Cardiovasc Diagn Ther 2021;11:263)
Etiology
- Common etiologies associated with HFrEF / systolic dysfunction patients include coronary heart disease (myocardial infarction), valvular heart disease volume overload (aortic stenosis, mitral regurgitation) or uncontrolled hypertension, arrhythmias, inflammatory diseases, idiopathic cardiomyopathy and alcoholic / toxic cardiomyopathy (Cardiovasc Diagn Ther 2021;11:263)
- Common etiologies associated with HFpEF / diastolic dysfunction include obesity, hypertension, atrial fibrillation, diabetes mellitus, volume overload / pressure overload, hypertrophic cardiomyopathy, restrictive cardiomyopathy, amyloid (Cardiovasc Diagn Ther 2021;11:263)
Clinical features
- Complications after LVAD implantation include (J Am Heart Assoc 2022;11:e027251, J Clin Med 2022;11:2575)
- Bleeding (Ann Thorac Surg 2021;111:778)
- Common in the beginning of the postoperative period (0 - 90 days)
- Nearly 33% of patients experience 1 episode of bleeding within 1 year of operation; gastrointestinal (GI) bleeding is most common, occurring in 60% of LVAD patients (Hematology Am Soc Hematol Educ Program 2019;2019:88)
- Infection (Am J Cardiol 2018;122:1021, J Heart Lung Transplant 2019;38:721)
- Common where driveline exits the abdominal wall
- ~40% of patients experience major infection
- Correct driveline management can mitigate infection
- Most VAD specific infections are localized to the driveline
- VAD specific infections may affect the LVAD pump, cannula or pocket
- VAD related infections include endocarditis, bloodstream infections and mediastinitis from sternal wound or pocket infection
- Non‐VAD infections include pneumonia, urinary tract infection, cholecystitis and Clostridium difficile infection
- Thrombosis (typically around the inflow cannula) (ASAIO J 2016;62:375, N Engl J Med 2019;380:1618)
- Continuous innovations lower the risk of thrombosis / need for LVAD exchange (HM3 design associated with less friction, increased intrinsic pulsatility, decreased shear stress and stasis of blood)
- MOMENTUM 3 (multicenter study of MagLev technology in patients undergoing mechanical circulatory support therapy with HeartMate 3) trial compared HM3 to the HMII, incidence of LVAD thrombosis at 2 years was 1.4% in HM3 versus 13.9% in HMII, p < 0.001
- < 10% of patients experience pump thrombosis
- Neurologic events / strokes (N Engl J Med 2017;376:451, Circ Heart Fail 2012;5:241)
- Both ischemic and hemorrhagic strokes range from 5% to 30%
- ~13% of patients experience a stroke within 1 year of implantation (J Am Coll Cardiol 2022;79:1092)
- Ischemic strokes are likely caused by thromboembolism
- Hemorrhagic strokes can occur from elevated blood pressure (BP), high velocity intracranial flow or hemorrhagic conversion from thromboembolic strokes
- Right heart failure (J Am Coll Cardiol 2021;78:2294, J Heart Lung Transplant 2017;36:50)
- Occurs in 53% of patients
- Divided into 3 phases
- Early acute: RVAD is necessary at the time of LVAD implantation
- Early postimplant: RVAD is necessary within 30 days of LVAD implantation
- Late stage: RVAD is necessary after 30 days of LVAD implantation
- Bleeding (Ann Thorac Surg 2021;111:778)
Laboratory
- Divide into routine monitoring and labs to assess complications
- Recommended tests
- Technical: power source maintenance (batteries, power module), daily self test, dressing changes
- Hematocrit and hemoglobin to assess bleeding
- Lactate dehydrogenase (LDH)
- Haptoglobin
- Free hemoglobin
- Coagulation tests (e.g., complete blood count [CBC])
- Electrocardiogram (EKG): assess for arrhythmia
- Computed tomography (CT): assess for deep space soft tissue infection
- Reference: J Clin Med 2023;12:5216
Prognostic factors
- Landmark REMATCH (randomized evaluation of mechanical assistance for the treatment of congestive heart failure) trial, 1 year survival with the first generation pulsatile HeartMate XVE LVAD was 52% compared with 25% in the medical therapy group (P = 0.002) (N Engl J Med 2001;345:1435)
- MOMENTUM 3 trial demonstrated survival with HM3 LVAD reached 79% at 2 years (N Engl J Med 2019;380:1618)
- Survival (data from 2015 - 2019) (JACC Heart Fail 2022;10:948)
- 1 year survival: 82.3%
- 2 year survival: 73.1%
- Median survival duration: > 4.5 years
- Unfavorable risk factors (J Am Coll Cardiol 2022;79:1092)
- Old age
- Obesity
- Poor nutritional status
- Previous cardiac surgery
- Lower serum sodium
- Higher blood urea nitrogen (BUN)
- Small left ventricular size
- Right atrial pressure to pulmonary capillary wedge pressure ratio > 0.6
Case reports
- 31 year old man with COVID-19 contracted after implantation of LVAD led to right ventricular failure and inotrope necessity (J Card Surg 2021;36:3405)
- 41 year old man with sternal osteomyelitis and bacteremia status post-LVAD implantation (Clin Pract Cases Emerg Med 2023;7:89)
- 63 year old man with antiphospholipid syndrome; successful LVAD implantation (Int J Artif Organs 2022;45:235)
Treatment
- Medication: warfarin (to achieve an international normalized ratio of 2.0 - 3.0), aspirin (81 - 325 mg daily) (J Am Coll Cardiol 2022;79:1092)
Gross images
Videos
Overview of the HeartMate II
Sample pathology report
- Left ventricular apex, VAD core, excision:
- Replacement fibrosis consistent with healed ischemic injury (see comment)
- Myocyte hypertrophy, mild to focally moderate
- Interstitial fibrosis, mild
- Endocardial fibrosis, mild
- Myocyte vacuolization suggestive of chronic ischemic injury, focal
- Comment: No histologic evidence of amyloid, myocarditis, granulomatous inflammation, myocyte disarray, extensive adipocytic infiltration, iron deposition or acute infarction.
- LVAD:
- Inflow cannula: a 5.5 x 5.0 cm gray metal medical device with connected outflow cannula tubes is present protruding from the apex of the heart; the device is inscribed with manufacturer number "X"
- Outflow cannula: a 19.4 cm in length by 1.6 cm in width outflow cannula consisting of ribbed Dacron material is present; there is a 13.7 cm in length by 1.5 cm in width ribbed impression overlying the right aspect of the heart, consistent with the outflow tract
Board review style question #1
Board review style answer #1
A. Bleeding is the most common complication in LVAD patients. ~60% of patients experience GI bleeding. Answer C is incorrect because pump thrombosis is a less common complication (~14%). Answer D is incorrect because strokes are also a less common complication (~12 - 28%). Answer B is incorrect because infection is the second most common complication (~40%).
Comment Here
Reference: Left ventricular assist device (LVAD)
Comment Here
Reference: Left ventricular assist device (LVAD)
Board review style question #2
A 26 year old White man recently received a left ventricular assist device (LVAD) implantation after suffering from sudden heart failure. The patient reported that he had been keeping a healthy diet ever since he suffered a non-ST elevation myocardial infarction at age 19. Which of the following factors heavily contributed to the development of stage D heart failure in the patient?
- Age
- Gender
- Nutrition
- Previous cardiac surgery
Board review style answer #2
D. Previous cardiac surgery. Patients who underwent previous cardiac surgery are more susceptible to heart failure than those without a previous history. Answer A is incorrect because the patient is relatively young. Answer B is incorrect because at a young age, gender does not seem to be a contributing factor. Answer C is incorrect because the patient had been eating properly.
Comment Here
Reference: Left ventricular assist device (LVAD)
Comment Here
Reference: Left ventricular assist device (LVAD)
Nonatherosclerotic coronary artery disease
Table of Contents
Epidemiology | Etiology | Pathophysiology of specific conditions | Diagnosis | Case reports | Clinical images | Gross description | Micro description - coronary arteritis | Differential diagnosis | Additional referencesEpidemiology
- 4 - 7% with acute myocardial infarction have nonatherosclerotic coronary artery disease
Etiology
- Various disorders, other than atherosclerotic CAD, can reduce or interrupt coronary blood flow
- Congenital coronary artery anomalies: ostial lesions, passage of a major artery between the walls of the pulmonary trunk and aorta, origin of a major artery from the pulmonary trunk, myocardial "bridges"
- Coronary aneurysm: congenital or due to angioplasty, arteritis (including syphilis), atherectomy, atherosclerosis, dissection (spontaneous or secondary), laser procedures, mucocutaneous lymph node syndrome, mycotic emboli, trauma
- Coronary arteritis: due to ankylosing spondylitis, Burger disease (thromboangiitis obliterans), giant cell arteritis, infective endocarditis, leprosy, mucocutaneous lymph node syndrome, polyarteritis nodosa, rheumatoid arthritis, rheumatic fever, Salmonella, syphilis, systemic lupus erythematosus, Takayasu disease, tuberculosis, typhus, granulomatosis with polyangiitis (Wegener's)
- Coronary artery dissection: primary, due to coronary angiography, cardiac surgery, chest trauma, postpartum women (spontaneous); or secondary due to extension from aortic root dissection
- Coronary artery thrombosis without underlying atherosclerotic plaque (thrombosis in situ): due to leukemia, polycythemia vera, primary thrombocytosis, sickle cell anemia, thrombocytopenia purpura
- Coronary emboli: natural causes, iatrogenic causes, and "paradoxical" causes
- Coronary fistula
- Coronary ostia: high take off position
- Dynamic changes in wall of otherwise normal artery (spasm)
- Encroachment of lumen by disease of arterial wall or adjacent tissues (external narrowing): sinus of valsalva aneurysms and epicardial tumor metastases
- Fixed luminal obstructions (internal narrowing / ostial narrowing):
- Aneurysm, saccular, of aorta
- Aortic dissection extending into coronary ostium (right ostium more common than left)
- Aortic valve surgery with or without coronary artery canulation
- Embolus, causing occlusion
- Fibromuscular hyperplasia associated with methysergide therapy
- Nonatheromatous, calcific protrusion from sinotubular junction into right or left ostium
- Obliteration of ostium due to adhesion of free edge of aortic cusp to aortic wall above coronary ostium
- Occlusive fibroelastois
- Ostial valve like ridges
- Supravalvular aortic stenosis with severe intimal thickening
- Syphilis
- Takayasu disease
- Intimal fibrous proliferation: due to cardiac transplantation, fibromuscular hyperplasia of renal arteries, mediastinal irradiation, methysergide, ostial cannulation during cardiac surgery or following aortic valve repIacement, percutaneous balloon angioplasty
- Myocardial oxygen demand supply disproportion: due to carbon monoxide poisoning, prolonged shock
- Substance abuse (cocaine): coronary artery vasoconstriction due to intranasal cocaine
- Systemic metabolic disorders: Fabry disease, homocystinuria, Hunter and Hurler diseases, primary oxalosis, Sandhoff disease
- Trauma: coronary angiography (embolus, inadvertent ligation, intimal dissection, laceration), nonpenetrating blunt chest wall injury (steering wheel injury), penetration trauma (laceration from stab wound or bullet)
- Intramural coronary artery disease (small vessel disease): due to amyloid heart disease, cardiac transplantation, collagen vascular disorders (scleroderma, SLE), diabetes mellitus, hypertrophic cardiomyopathy, metabolism abnormalities, neuromuscular disorders (Friedreich ataxia, progressive muscular dystrophy), polyarteritis nodosa, rheumatoid arthritis
Pathophysiology of specific conditions
- Origin of both right and left coronary arteries from the same sinus of valsalva:
- Normally, the coronary ostia are round to oval in shape, but in this anomaly, the coronary artery has an acute takeoff angle that makes the ostium slit like in shape
- With increased cardiac output (e.g., exercise), the aorta dilates, and upon aortic wall stretching this slit like ostium becomes severely narrowed
- High take off of coronary arteries:
- Normally, the coronary ostia are located within the sinuses of Valsalva, which permits maximal opportunity for coronary artery diastolic filling
- Location of the ostia in the tubular portion of the aorta (i.e., high takeoff position) may be associated with decreased coronary perfusion
Diagnosis
- Angina pectoris or acute MI in patient Br Heart J 1992;68:601)
- Asymptomatic older patients with these anomalies are usually discovered by abnormal electrocardiogram, precordial murmur or sudden death
- Coronary arterial emboli are clinically suspected due to severe chest pain (acute MI) during cardiac catheterization or cardiac surgery or if these conditions are present: active infective endocarditis, atrial fibrillation, cardiac tumor, dilated cardiomyopathy, left ventricular aneurysm, native left sided valve stenosis, prosthetic left sided valve
Case reports
- 31 year old woman with acute myocardial infarction due to polyarteritis nodosa (Korean Circ J 2010;40:197)
- 33 year old man and 37 year old woman with non atherosclerotic coronary artery aneurysms (Heart 1997;78:613)
Clinical images
Gross description
Myocardial bridges ("tunneled" epicardial coronary artery):
- Coronary arteries which normally course over the epicardial surface of the heart may dip into the myocardium to travel for varying lengths and then reappear on the heart's surface
- The muscle overlying the intramyocardial segment of the epicardial coronary artery is termed a "myocardial bridge"; the artery coursing within the myocardium is called a "tunneled" artery
- Congenital coronary artery aneurysms are found most commonly in the right coronary artery
- Abnormal flow patterns within the aneurysm may lead to thrombus formation with subsequent vessel occlusion, distal thromboembolization and myocardial infarction
Micro description - coronary arteritis
- Baroldi considers these findings as signs of coronary arteritis: (Baroldi G: Diseases of the coronary arteries, Cardiovascular Pathology, 3rd Edition, 2001)
- Focal artery necrosis with or without calclfication
- Acute coronary artery thrombosis or recanalized thrombus unassociated with underlying atherosclerotic plaque
- Rupture of the vessel wall unassociated with trauma or an interventional procedure
- Coronary artery wall thickening with secondary luminal narrowing
- Wall thinning with aneurysm formation
Differential diagnosis
Noninfective endocarditis
Table of Contents
Definition / general | Terminology | Diagrams / tables | Epidemiology | Sites | Pathophysiology | Risk Factors | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- First described by Zeigler in 1888, who called it "thromboendocarditis"
- In 1936, Gross and Friedberg coined the term "nonbacterial thrombotic endocarditis" (NBTE)
- Defined as vegetations on the valve surface, rich in fibrin and platelet aggregates but devoid of inflammation or infective organisms
Terminology
- Also called marantic endocarditis
Diagrams / tables
Epidemiology
- NBTE is uncommon but underestimated as symptoms are often attributed to other diseases
Sites
- Cardiac valves and endocardial surface
Pathophysiology
- Thrombotic endocarditis develops due to endothelial damage and subsequent exposure of the subendothelial connective tissue to circulating platelets
- The factors involved in pathogenesis can be divided into initiating NBTE and subsequent development of vegetation
- Factors implicated in initiation are: (a) immune complexes, (b) hypoxia, (c) hypercoagulability and (d) carcinomatosis
- Immune complexes: Libman-Sacks endocarditis is the prototype
- Hypoxia: studied by Nakanishi et al. in a rodent model (Virchows Arch 1998;433:375)
- Hypercoagubility: Trousseau first noted the association between thrombosis and malignancy
- Histological evidence of disseminated intravascular coagulopathy (DIC) has been found in 50% patients with NBTE
- Carcinomatosis: mucin producing adenocarcinoma from the gut, lung and ovary and acute promyelocytic leukemia are commonly associated with NBTE
Risk Factors
- Advanced stage malignancy: solid organ or hematological
- Chronic diseases: tuberculosis, uremia, AIDS
- Connective tissue disorders with hypercoaguable state: SLE patients with APLA positive
- Trauma from indwelling pulmonary catheter or central venous catheter, snake bite, late effect of radiation therapy
Clinical features
- There are no pathognomonic signs and symptoms that allow for the confident diagnosis of NBTE
- Patients can present with:
- Cardiac failure
- Secondary to valvular dysfunction (most commonly mitral regurgitation), leading to dyspnea, orthopnea, paroxysmal nocturnal dyspnea, peripheral edema, lethargy
- Cerebrovascular embolism
- Focal weakness or numbness, visual loss, dysphasia, dysarthria, dysphagia, memory loss
- Systemic thromboembolism
- Pain, coldness and numbness of the peripheries, or acute abdominal syndromes with pain and vomiting
- Secondary infective endocarditis
- Fever, weight loss, night sweats, lethargy, chest pain
- Cardiac failure
Diagnosis
- Requires a high degree of clinical suspicion in a patient treated for infective endocarditis (IE) and not clinically improving
- Mckay and Wahler proposed a triad for diagnosis of NBTE:
- Presence of a disease process known to be associated with NBTE
- Presence of heart murmur and
- Evidence of multiple systemic emboli
- Main differential diagnosis is Infective endocarditis - distinction is important
Laboratory
- Exclude DIC: full blood count, prothrombin time, partial thromboplastin time, fibrinogen, thrombin time, D dimers and cross linked fibrin degradation products
- These may be normal, but in the presence of risk factors, an abnormal result should alert the physician to a diagnosis of NBTE
- Multiple blood cultures to rule out any infective cause
- Immunological assays for antiphospholipid syndrome (APS)
- Polymerase chain reaction (PCR) for rapid and reliable detection of culture negative endocarditis by fastidious organisms
Radiology description
- Transoesophageal echo (TEE) has a higher sensitivity (90%) than transthoracic echo (TTE), especially for vegetations of Cardiac MRI using TrueFISP gradient echo sequence allows the morphology of small heart structures such as valves to be examined in detail (J Comput Assist Tomogr 1996;20:613)
- Diffusion weighted MRI (DWI) can differentiate cardioembolic stroke caused by infective endocarditis from that of NBTE due to the lack of a cellular component in NBTE emboli
Prognostic factors
- Dependent on underlying disease activity and associated renal and myocardial dysfunction
Case reports
- Young woman (J Heart Valve Dis 2009;18:159)
- 43 year old woman with Libman-Sacks endocarditis in systemic lupus erythematosus (J Gen Intern Med 2008;23:883)
- 55 year old woman (J R Soc Med 2005;98:24)
- Extensive nonbacterial thrombotic endocarditis isolated to the tricuspid valve in primary antiphospholipid syndrome (J Am Soc Echocardiogr 2010;23:107)
- Nonbacterial thrombotic endocarditis in three members of a family (N Engl J Med 1997;336:1677)
Treatment
- Treatment is difficult - correction of the underlying cause is of paramount importance
- In patients with potentially curable cancer, coagulopathy should be corrected and, if there is no contraindication, these patients should be anticoagulated with heparin
- There are no guidelines for surgical intervention in patients with NBTE - decision is based upon individual case
Clinical images
Gross description
- NBTE vegetations are typically small, friable, white or tan masses, Vary from tiny lesions to large and exuberant masses
- Based on morphology, Allen and Sirota proposed a macroscopic classification of NBTE:
- Type 1:
- Small,
- Type 2:
- Large, > 3mm univerrucal, adherent to the valve
- Type 3:
- Small, 1 - 3mm multiverrucal, friable
- Type 1:
Gross images
Microscopic (histologic) description
- NBTE consists of degenerating platelets interwoven with strands of fibrin and forming a bland, featureless eosinophilic mass except for a few trapped leucocytes
- Three stages have been described in the evolution of NBTE vegetations: (eMedicine: Libman-Sacks Endocarditis Workup [Accessed 28 February 2018])
- Active verrucae: Consist of clumps of fibrin on and within the valvular leaflet tissue which is focally necrotic, with plasma cells and lymphocytes
- Combined active and healed lesions: Contain vascularized, fibrous tissue adjacent to fibrinous and necrotic areas
- Healed lesions: Consist of dense, vascularized, fibrous tissue
Differential diagnosis
Noninfective myocarditis
Table of Contents
Definition / general | Terminology | Epidemiology | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Additional referencesDefinition / general
- Myocarditis is an inflammatory disease of the myocardium caused by different infectious and noninfectious triggers
- Non infectious types include lymphocytic, eosinophilic and giant cell myocarditis (GCM)
Terminology
- GCM has been termed idiopathic GCM, pernicious myocarditis, Fiedler myocarditis, acute idiopathic interstitial myocarditis, giant cell granulomatous myocarditis, and granulomatous myocarditis
Epidemiology
- Incidence difficult to determine as most cases are believed to be subclinical or underdiagnosed
Pathophysiology
- Most cases of lymphocytic myocarditis are idiopathic
- A primary autoimmune etiology has been suggested for GCM, based on the antimyosin GCM Lewis rat model and a high prevalence of associated autoimmune disorders, especially inflammatory bowel disease
Clinical features
- Asymptomatic or nonspecific symptoms of chest pain, fever, sweats, chills, dyspnea
- Palpitations, syncope or sudden cardiac death may develop because of underlying ventricular arrhythmias or atrioventricular block
- In necrotizing eosinophilic myocarditis (NEC), a previously healthy patient experiences a rapid, acute progression to systolic failure and hemodynamic compromise which is usually fatal
Diagnosis
Radiology description
- Features are similar to those described in infective myocarditis
Radiology images
Prognostic factors
- Most patients recover spontaneously with no known sequela
- A small percentage of patients, mostly children and young adults, present with fulminant disease at onset and may progress rapidly to sudden death
Case reports
- 15 year old adolescent with eosinophilic myocarditis (Cardiol Young 2013;23:277)
- 30 year old man with recurrent lymphocytic myocarditis and ulcerative colitis (Eur J Med Res 2014;19:11)
- 47 year old man with acute myocarditis and successful clearance of human parainfluenza virus type 2 viraemia (J Clin Virol 2013;56:37)
- 54 year old man with acute eosinophilic myocarditis mimicking myocardial infarction (Tex Heart Inst J 2009;36:355)
- 72 year old man with idiopathic giant cell myocarditis (Indian J Pathol Microbiol 2003;46:241)
- 76 year old man with eosinophilic myocarditis (BMC Res Notes 2013;6:538)
- Three cases of sudden death occurring in systemic sarcoidosis with myocardial involvement (N Z Med J 1989;102:501)
Treatment
- Treatment of myocarditis includes supportive therapy for symptoms of acute heart failure and withdrawal of the offending agent, if applicable
Gross description
- Cardiac hypertrophy may be present with associated ventricular dilation
- The affected myocardium may appear pale, sometimes with hemorrhagic foci
Microscopic (histologic) description
- Lymphocytic myocarditis:
- A focal or diffuse lymphohistiocytic infiltrate (mostly T cell type) within myocardial fibers
- Myocyte necrosis is typically present; interstitial fibrosis of varying degree is commonly seen
- Presence of edema should not be used as a criterion for diagnosis of myocarditis
- Giant cell myocarditis:
- Diffuse infiltration of myocardium by a heterogeneous infiltrate composed of abundant lymphocytes, eosinophils, plasma cells and scattered prominent giant cells
- There are no well defined granulomas
- It has a more fulminant course (J Card Fail 2002;8:74, Semin Arthritis Rheum 2000;30:1)
- Eosinophilic myocarditis:
- Mixed inflammatory cell infiltrate consisting of many eosinophils with histiocytes, lymphocytes and plasma cells; myocardial necrosis is not common and interstitial fibrosis is typically absent or minimal
- Eosinophilic myocarditis associated with hypereosinophilic syndrome is characterized by peripheral eosinophilia greater than 1,500 / μL over 6 months, without a known cause and with an indolent course (Can J Cardiol 2006;22:1233)
- Hypersensitivity myocarditis (HSM):
- Due to drug exposure; less necrosis, more prominent perivascular infiltrate, vasculitis and liver involvement
- Necrotising eosinophilic myocarditis:
- Extensive myocardial necrosis due to release of major basic protein from degranulated eosinophils
- Sarcoid myocarditis:
- Noncaseating granulomas on endomyocardial biopsy performed in a patient with a dilated cardiomyopathy is virtually pathognomonic (J Am Coll Cardiol 2003;41:322, Prog Cardiovasc Dis 2010;52:336)
Microscopic (histologic) images
Additional references
Noninfective pericarditis
Table of Contents
Definition / general | Terminology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Prognosis | Gross description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Pericarditis is an inflammation of the pericardium characterized by chest pain, pericardial friction rub and serial ECG changes
Terminology
- Idiopathic pericarditis
- Acute pericarditis
- Chronic pericarditis
- Chronic effusive pericarditis and chronic constrictive pericarditis
- Recurrent pericarditis
Pathophysiology
- The acute inflammatory response in pericarditis can produce either serous or purulent fluid or a dense fibrinous material
- Neoplastic, tuberculous, and purulent pericarditis may be associated with large effusions that are hemorrhagic and exudative
- Prolonged pericarditis may result in persistent accumulation of pericardial fluid which may form a thick coating that surrounds the myocardium causing constrictive pericarditis
Etiology
- Idiopathic: No identifiable etiology found after routine testing
- Specific causes:
- Immunologic conditions including systemic lupus erythematosus (more common among women) or rheumatic fever
- Myocardial infarction (Dressler syndrome)
- Trauma to the heart, e.g. puncture, resulting in infection or inflammation
- Uremia (uremic pericarditis)
- Malignancy (as a paraneoplastic phenomenon)
- Side effect of medication, e.g. isoniazid, cyclosporine, hydralazine, warfarin, heparin
- Radiation induced
- Aortic dissection
- Tetracyclines
- Postpericardiotomy syndrome: usually after CABG surgery
Clinical features
- Chest pain, usually precordial or retrosternal
- Low grade intermittent fever
- Dyspnea / tachypnea
- Cough and dysphagia
- Malignancy associated pericarditis: fever, night sweats, and weight loss are common
Diagnosis
- Initial evaluation includes a clinical history and physical examination, ECG, echocardiography, chest radiography, lab studies
- 12 lead electrocardiogram shows diffuse, nonspecific, concave, ST segment elevation in all leads except aVR and V1; also PR segment depression is possible in any lead except aVR; sinus tachycardia and low voltage QRS complexes may be seen if subsymptomatic levels of pericardial effusion
- The PR depression is often seen early in the process as the thin atria are affected more easily than the ventricles by the inflammatory process of the pericardium
Laboratory
- Increased urea (BUN) or increased blood creatinine in uremic pericarditis
- Troponin (I, T), CK-MB, myoglobin, and LDH1 (Lactase Dehydrogenase isotype 1) may be normal or elevated
Case reports
- 54 year old man with constrictive pericarditis after renal transplant (J Med Case Rep 2014;8:8)
- 83 year old man with complicated pericarditis (Proceedings of UCLA Healthcare 2011;15)
Treatment
- Aspirin, or other nonsteroidal anti-inflammatory drugs (NSAIDs)
- Pericardiocentesis to treat pericardial effusion / tamponade
- Antibiotics to treat tuberculosis or other bacterial causes
- Steroids are not recommended because they increase the risk of recurrent pericarditis
- Pericardiectomy in rare cases
Prognosis
- Generally, acute pericarditis is benign and self limiting
- Complications include tamponade, constriction, or recurrence
- Nearly 50% will have recurrence
Gross description
- Epicardial surface appears roughened compared to its normal glistening appearance; this is due to strands of pink-tan fibrin
Differential diagnosis
- Myocardial infarction
Additional references
Papillary fibroelastoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Papillary fibroelastoma is a benign papillary growth of endocardium and avascular fibroelastic tissue
- Usually benign and discovered incidentally but can embolize to distal sites
Essential features
- Papillary fibroelastoma is the most common cardiac tumor
- Benign behavior but may result in morbidity / mortality from downstream (thrombo) embolization
- Associated with KRAS mutations in up to 80% of lesions
Terminology
- Fibroelastic papilloma (not recommended)
- Cardiac papilloma (not recommended)
- Giant Lambl excrescence (not recommended)
ICD coding
Epidemiology
- Most common cardiac tumor (J Am Coll Cardiol 2018;72:202)
- Typical patient:
- 60 - 70 years but has been seen in all ages
- M = F
- Risk factors:
- Damaged endothelium (prior radiation therapy, cardiac surgery, structural heart disease resulting in hemodynamic alterations) (Hum Pathol 2002;33:1165, J Am Soc Echocardiogr 2010;23:595)
Sites
- May arise on any endocardial lined surface (e.g. valves, chamber walls)
Etiology
- Debated: reactive versus neoplastic
- Associated with injured endocardium, both iatrogenic and intrinsic, suggesting a reactive phenomenon (Hum Pathol 2002;33:1165, J Am Soc Echocardiogr 2010;23:595)
- KRAS mutations documented in 33 - 80% of lesions, implying a neoplastic origin (J Pathol Clin Res 2017;3:100, Am J Surg Pathol 2020;44:626)
Clinical features
- Considerable variation to clinical presentation
- Most commonly asymptomatic and diagnosed incidentally on routine imaging or at the time of cardiac surgery for an alternate indication
- May present with syncope, myocardial infarction or sudden death
- Stroke / ischemia occurs in 33% diagnosed on imaging (J Am Coll Cardiol 2015;65:2420)
- Embolism thought to be secondary to tumor fragmentation or from thrombi formed on the surface of the lesion
- Higher incidence in individuals with prior cardiac surgery, thoracic radiation or underlying structural heart disease / cardiomyopathy
Diagnosis
- Imaging is the most classic means of diagnosis
- Echocardiography is common due to ubiquitous nature of the modality
- CT also useful as it provides high spatial resolution
Radiology description
- Characteristic appearance on imaging (J Am Coll Cardiol 2018;72:202)
- All modalities:
- Mobile, frond-like lesion on stalk
- Special considerations:
- Echocardiogram: speckled appearance with stippling at tumor edge
- Magnetic resonance: may show some T2 hyperintensity but enhancement is uncommon
Prognostic factors
- Excellent prognosis with surgical removal
- 5 year survival significantly worse without resection (J Am Coll Cardiol 2015;65:2420)
Case reports
- 55 year old man with exertional dyspnea and palpitations (Cardiol Res 2019;10:378)
- 58 year old woman with multiple systemic infarcts (Cureus 2019;11:e4798)
- 71 year old woman with stroke (Proc (Bayl Univ Med Cent) 2019;32:247)
Treatment
- Surgical resection is recommended
- Anticoagulation may be considered in patients who are not surgical candidates (Am Heart J 2003;146:404)
Gross description
- Arborizing, thin strands of tan-white tissue, usually arising from a common stalk
- Likened to a sea anemone
- Fronds may not be apparent unless tumor is placed in an aqueous medium
Gross images
Microscopic (histologic) description
- Multiple, branching fronds of paucicellular, avascular fibroelastic tissue lined by a single layer of endocardium
- Has multiple branching fronds by definition
- Differential diagnosis: Lambl excrescences are microscopically identical but are simple, nonbranching projections of fibroelastic tissue
- May show hydropic change
- Histologic characteristics do not appear to correlate with KRAS mutation status
Microscopic (histologic) images
Positive stains
- Elastic fibers: Verhoeff van Gieson (VVG) or other elastic stain highlights elastic core of fronds
Negative stains
Molecular / cytogenetics description
- KRAS mutations identified in up to 80% (J Pathol Clin Res 2017;3:100, Am J Surg Pathol 2020;44:626)
Videos
Resection of large aortic valve papillary fibroelastoma
Sample pathology report
- Heart, aortic valve, excision:
- Papillary fibroelastoma (evaluated with elastic stain)
Differential diagnosis
- Lambl excrescence:
- Similar histology but lacks complex architecture and anastomosing fronds
- Only occurs on the closing edge of valves
- Cardiac myxoma:
- May show similar gross features (particularly when papillary fibroelastoma is collapsed)
- Contains lepidic or myxoma cells that are calretinin positive
- Valvular vegetation:
- May show similar gross features
- Infectious vegetation shows mixed inflammation with or without microorganisms
- Nonbacterial thrombotic endocarditis is a sterile vegetation consisting predominantly of fibrin and blood products
Additional references
Board review style question #1
Board review style answer #1
D. Thoracic irradiation. Endocardial injury is associated with the development of papillary fibroelastomas. Damage may be from iatrogenic causes (e.g. thoracic irradiation, prior cardiac surgery) or from hemodynamic changes secondary to intrinsic structural heart disease. Chemotherapies and antibiotics have not been associated with papillary fibroelastoma development. IVC filters do not contact the heart.
Comment Here
Reference: Papillary fibroelastoma
Comment Here
Reference: Papillary fibroelastoma
Board review style question #2
A 63 year old woman experienced multiple transient ischemic attacks and was subsequently found to have a large, mobile cardiac mass attached to her aortic valve by a stalk on echocardiography. Why would her cardiologist recommend surgical excision?
- Definitive diagnosis and triage to chemotherapeutic regimen
- Genetic testing for identification of at risk family members
- Potential for malignant transformation
- Risk of thrombus formation with subsequent thromboembolization
Board review style answer #2
D. Risk of thrombus formation with subsequent thromboembolization. Papillary fibroelastomas undergo surgical excision because of their (thrombo) embolic potential. The most common mechanism is thought to be related to thrombus formation with subsequent embolization; however, portions of the tumor may fragment and result in downstream ischemia. They have not been documented to show malignant transformation and surgical resection is considered curative without need for subsequent chemotherapy. They are not thought to be hereditary in origin.
Comment Here
Reference: Papillary fibroelastoma
Comment Here
Reference: Papillary fibroelastoma
Primary and secondary dilated cardiomyopathy
Table of Contents
Definition / general | Epidemiology | Etiology | Clinical features | Laboratory | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Additional referencesDefinition / general
- Dilated cardiomyopathy (DCM) is characterized by a poorly contracting dilated left ventricle with a normal or reduced left ventricular wall thickness
Epidemiology
- DCM is the most common cause of congestive cardiac failure (CCF), with an estimated prevalence of at least 36.5 per 100,000 persons in the USA
- It occurs more frequently in men than women and is most common between ages 20 and 60 years
Etiology
- In most cases, no definite cause is identifiable
- Most prevalent toxic cause is alcohol
- Single gene mutations involve:
- Structural proteins: dystrophin, metavinculin, lamin
- Mitochondrial DNA
- Coronary artery disease
- Infections: coxsackievirus, adenovirus, parvovirus, HIV, bacterial, fungal rickettsial, myobacterial and parasitic (Chagas disease)
- Nutritional deficiency: carnitine selenium deficiencies
- Cardiotoxins (anthracycline)
- Puerperium
- Metals (cobalt, lead, mercury, arsenic)
- Autoimmune and systemic disorders
- Pheochromocytoma
Clinical features
- Shortness of breath, syncope, angina
Laboratory
- Complete blood count
- Metabolic panel
- Thyroid function tests
- Cardiac biomarkers
- B type natriuretic peptide assay
- Chest radiography
- Echocardiography
- Cardiac magnetic resonance imaging (MRI)
- Electrocardiography (ECG)
Case reports
- 36 year old man with dilated cardiomyopathy secondary to hypothyroidism (J Cardiovasc Ultrasound 2014;22:32)
- 39 year old woman with alcoholic cardiomyopathy (The Internet Journal of Cardiology 2000;10(1))
Treatment
- Essentially the same as treatment of chronic heart failure (CHF)
Gross description
- The heart assumes a globular shape and there is pronounced ventricular chamber dilatation, diffuse endocardial thickening and atrial enlargement, often with thrombi in the appendages
Microscopic (histologic) description
- Increase in myocyte nuclear size
- Myofibrillary loss within myocyte
- Focal myocyte death
- Increase in interstitial T lymphocytes / macrophages
- Interstitial fibrosis
- The individual myocytes are increased in length rather than in width, lose the normal number of intracellular contractile myofibrils and appear empty and vacuolated
- The myocyte nuclei increase in size because of the synthesis of DNA and become polyploid
- Death of individual myocytes occurs both by apoptosis and necrosis
- Fibrosis characteristically is interstitial and begins to surround and isolate individual myocytes
- The number of macrophages and T lymphocytes in the interstitial spaces is often increased compared with normal hearts
Microscopic (histologic) images
Molecular / cytogenetics description
- The pattern of inheritance of familial DCM (FDCM) is variable and includes autosomal dominant, X linked, autosomal recessive and mitochondrial
- Autosomal forms of FDCM are the most frequent
- Pure DCM phenotype: mutations of genes encoding cardiac actin, desmin, d-sarcoglycan, b-sarcoglycan, cardiac troponin T, tropomyosin
- DCM with cardiac conduction system disease: lamin A/C gene
- Autosomal dominant Emery-Dreifuss muscular dystrophy
- The X linked forms of DCM includes X linked dilated cardiomyopathy and Barth syndrome
- Caused by mutations in the dystrophin gene
- X linked dilated cardiomyopathy (XLCM) occurs in males during adolescence or early adulthood and has a rapidly progressive clinical course
- Female carriers develop a mild form of DCM with onset in middle age
- Creatine kinase levels are elevated but without clinical signs of skeletal myopathy
- The infantile form of X linked DCM or Barth syndrome typically presents
in male infants
- It is characterised by neutropenia, 3-methylglutaconic aciduria, growth retardation and mitochondrial dysfunction
- The cardiac manifestations include left ventricular dilatation, endocardial fibroelastosis or a dilated hypertrophied left ventricle
- Mutations in the gene G4.5, which encodes the protein tafazzin, cause Barth syndrome
Additional references
Prosthetic valves
Table of Contents
Definition / general | Radiology images | Case reports | Treatment | Complications | Gross description | Diagrams / tables | Gross images | Microscopic (histologic) images | Additional referencesDefinition / general
- Prosthetic cardiac devices improve survival and greatly increase the quality of life in most patients
Radiology images
Case reports
- 30 year old woman with prosthetic heart valve thrombosis, anticoagulation and pregnancy (Neth Heart J 2007;15:306)
- 47 year old woman with mitral valve sparing procedures and prosthetic heart valve failure (Can J Cardiol 2009;25:e86)
- 65 year old man and 59 and 60 year old women with thrombolytics and left sided prosthetic valve thrombosis (Tex Heart Inst J 1998;25:130)
Treatment
- The American Heart Association / American College of Cardiology (AHA/ACC) task force recommends bioprostheses for those over 65 undergoing aortic valve replacement (see table below)
- For younger patients undergoing aortic valve replacement, a modern bileaflet mechanical valve appears to be optimal
Complications
- Common prosthesis associated complications are:
- Thrombosis, thromboembolism
- Infection on annulus or biological tissues
- Structural or nonstructural dysfunction
- All mechanical prostheses have an absolute requirement for anticoagulant treatment
- Thromboembolism has been reported to occur at a higher rate with Starr-Edwards versus Bjork-Shiley valves
- Bileaflet prostheses such as the St. Jude valve appear to have the lowest risk of thromboembolism
- Rates of thromboembolism are higher following mitral valve replacement than following aortic valve replacement
Gross description
- Mechanical prostheses
- Ball valves
- Disc valves
- Bileaflet valves
- Biological prosthetic valves
- An autologous or autogeneous valve
- Autograft valve
- Homograft (or allograft) valve
- Heterograft (or xenograft) valve
- Bovine pericardial valves
- See Heart 2002;87:583 for a full description of these valves
- Gross findings to be recorded from an explanted prosthetic valve: see table below
Diagrams / tables
Gross images
Microscopic (histologic) images
Additional references
Rhabdomyoma
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Differential diagnosis | Additional referencesDefinition / general
- 50 - 90% of primary heart tumors in children
- Usually discovered in patients less than 1 year of age, rarely in fetuses (Ital Heart J 2002;3:48)
- May obstruct valvular orifice or cardiac chamber; may present with sudden cardiac death (Pediatr Dev Pathol 2007;10:129)
- Not a true neoplasm, but a hamartoma or malformation due to mutation in TSC1 and TSC2 genes
- 50% of patients have tuberous sclerosis; sporadic cases are occasionally associated with congenital heart disease
Case reports
- 2 year old boy with tuberous sclerosis (Arch Pathol Lab Med 2002;126:1559)
- 13 year old boy with diffuse rhabdomyomatosis (Arch Pathol Lab Med 1977;101:78)
Treatment
- Many tumors regress spontaneously
- Excision if left ventricular outflow tract obstruction or refractory arrhythmia
Gross description
- Small, firm, gray-white, well circumscribed myocardial masses (often multiple) that protrude into ventricles
- Average size is 3 - 4 cm, up to 10 cm, particularly in sporadic cases
- Rhabdomyomatosis: numerous miliary nodules less than 1 mm
Gross images
Microscopic (histologic) description
- Clear cells and large, rounded, polygonal cells ("spider cells") with glycogen vacuoles separated by strands of cytoplasm extending between cell membrane and nucleus
- No mitotic activity
- Adult tumors: more cellular with smaller cells, few spider cells and more cellular proliferation (Hum Pathol 2002;33:1092)
Microscopic (histologic) images
Positive stains
Negative stains
Electron microscopy description
- Altered myocytes with abundant glycogen, small and sparse mitochondria
- Cellular junctions resembling intercalated disks are extensive and randomly distributed, not just at poles of cell as in normal myocytes (Hum Pathol 1977;8:700)
Electron microscopy images
Differential diagnosis
- Glycogen storage disease: no well formed nodules, cells have intercalated disks at poles by EM
- Granular cell tumor: epicardial, no vacuoles, no myofibers, S100+, desmin-, myoglobin-
- Histiocytoid myopathy: small tumor nodules, finely granular cells, no large vacuoles, no spider cells; a variant of rhabdomyomatosis
- Lipoma: usually epicardial, no myofibers, no glycogen
Additional references
Sarcoidosis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Cardiac sarcoidosis is a type of infiltrative cardiomyopathy and a potential cause of heart failure
Essential features
- Nonnecrotizing granulomata are classic
- Presents with symptoms of cardiac dysfunction (arrhythmias, conduction disturbances)
- Often clinically silent and subsequently diagnosed on explant hearts or autopsy
Epidemiology
- Occurs in approximately 5% of patients with systemic or pulmonary manifestations of sarcoidosis (Clin Chest Med 2015;36:657)
- U.S. autopsy studies revealed cardiac manifestations in 20 - 29% of patients with systemic sarcoidosis
- Average age at presentation: 50 years old (Circulation 2015;131:624)
Sites
- Myocardium is most frequently involved
- Involvement of pericardium and endocardium usually results from extension of myocardial disease (Semin Respir Crit Care Med 2014;35:372)
Pathophysiology
- Not fully understood; some consider as spectrum of autoimmune etiology
- Nonnecrotizing granulomata are classic
- Often presents initially with local inflammation, which then progresses to fibrotic scarring; however, disease progression is highly variable (Intern Med 2014;53:1595)
Etiology
- Not fully known; however, mycobacteria, propionibacteria, Borellia, Rickettsia and herpes have been suggested as possible antigens leading to granuloma formation (Postgrad Med J 2014;90:582, Dis Mon 2009;55:649)
Clinical features
- Atrioventricular (AV) block
- Supraventricular and ventricular arrythmias
- Heart failure
- Sudden cardiac death
- Hypercalcemia
- Acute coronary syndrome, rarely (Clin Cardiol 2009;32:E68)
Diagnosis
- Electrocardiogram (ECG): PR lengthening, T wave abnormalities, Q waves
- Echocardiograms: decreased left ventricular ejection fraction, ventricular aneurysm, regional wall motion abnormality, basal septal thinning (Heart Rhythm 2014;11:1305)
- Cardiac imaging (see Radiology description)
Laboratory
- Elevated erythrocyte sedimentation rate
- Increased levels of angiotensin converting enzyme (Indian Pacing Electrophysiol J 2020;20:184)
- Hypercalcemia
- Increased levels of IL12, IL10, IL6 and interferon gamma (Front Immunol 2020;11:1443)
Radiology description
- Cardiovascular magnetic resonance imaging (CMR): multifocal areas of late gadolinium enhancement (LGE), midmyocardial and subepicardial LGE, extension of LGE from the left ventricle to the right ventricle (JACC Cardiovasc Imaging 2013;6:501, Curr Opin Pulm Med 2009;15:507)
- Fluorodeoxyglucose (FDG) PET may reveal FDG uptake, which is a nonspecific finding that indicates inflammation
Prognostic factors
- Prognosis is poor if complicated by heart failure
- In the U.S., 13 - 25% of deaths from sarcoidosis have been attributed to cardiac sarcoidosis (Sarcoidosis Vasc Diffuse Lung Dis 2002;19:220)
- 5 year estimate of event free survival is 70 - 80% (J Am Heart Assoc 2021;10:e019415)
- Patients with right ventricular involvement have a worse prognosis
Case reports
- 40 year old woman with dyspnea on exertion in the setting of heart failure (Cureus 2021;13:e18685)
- 49 year old woman with dyspnea and negative CMR (HeartRhythm Case Rep 2021;7:139)
- 54 year old man with fatigue and ventricular tachycardia on ECG (CASE (Phila) 2021;5:213)
- 56 year old woman with exertional chest pressure and dyspnea initially diagnosed as giant cell myocarditis (Eur Heart J Case Rep 2021;5:ytab042)
- 58 year old man currently being treated with ixekizumab for psoriasis presents with acute onset heart failure (CJC Open 2020;3:118)
Treatment
- Management largely involves treatment of underlying cardiac dysfunction and prevention of cardiovascular disease
- Patients may be candidates for cardiac transplant, pacemaker or implantable cardioverter defibrillator
- Heart failure medications and antiarrhythmics are often indicated
- Patients with evidence of current myocardial inflammation and cardiac dysfunction may be eligible for immunosuppressive medications (Chest 2012;141:154)
- Corticosteroids are the mainstay of treatment
- Methotrexate has also been suggested (J Am Heart Assoc 2019;8:e010952)
Gross description
- Diffuse myocardial infiltrates with irregular borders, which can vary from yellow to white / gray (Arch Pathol Lab Med 2010;134:1039)
- There may be ventricular dilation and aneurysms present (Virchows Arch 2011;458:671)
- If present, fibrosis may be focal or diffuse and is usually most prominent in the basal septum and left ventricular free wall
- Pericardial thickening
Microscopic (histologic) description
- Nonnecrotizing granulomas and multinucleated giant cells in transmural or focal distribution (Clin Cardiol 2018;41:1386)
- Giant cell inclusions may be present
- Schaumann bodies: oval, concentrically laminated intracytoplasmic inclusions
- Asteroid bodies: stellate shaped with cytoplasmic clearing
- Giant cell inclusions may be present
- Transmural or focal interstitial fibrosis (Arch Pathol Lab Med 2010;134:1039)
- Small coronary arteries may be involved
Sample pathology report
- Heart, left ventricle, endomyocardial biopsy:
- Cardiac sarcoidosis (see comment)
- Comment: Biopsy contains several well formed granulomas with multinucleated giant cells containing intracytoplasmic inclusions. Moderate fibrosis is present. Microscopic appearance consistent with clinical diagnosis of cardiac sarcoidosis.
Differential diagnosis
- Foreign body granulomas:
- Granulomas are not well formed
- Polarized light reveals foreign material
- Giant cell myocarditis:
- Not associated with systemic disease
- Granulomas are not well formed
- Eosinophils
- Fibrosis not seen acutely
- Fungal / mycobacterial infections:
- Lyme carditis:
- Transmural lymphocytic inflammation
- No granulomas
- Other symptoms of systemic lyme disease present
Board review style question #1
A 40 year old woman presented with dyspnea on exertion and several pulmonary nodules seen on a prior abdominal CT scan. Additional CT scan of the chest showed cardiomegaly and subsequent endomyocardial biopsy revealed the histology seen above. What is the diagnosis?
- Amyloidosis
- Giant cell myocarditis
- Hemochromatosis
- Sarcoidosis
Board review style answer #1
D. Sarcoidosis. This patient has nonnecrotizing granulomas on cardiac biopsy. In the setting of pulmonary nodules on prior imaging, this most likely represents sarcoidosis with cardiac involvement. Her shortness of breath may represent development of heart failure.
Comment Here
Reference: Sarcoidosis
Comment Here
Reference: Sarcoidosis
Board review style question #2
A 28 year old woman with no significant medical history presents with dizziness. On further questioning, the patient describes a sensation of blacking out. Electrocardiogram (ECG) is performed and reveals sinus rhythm with PR prolongation. Chest Xray reveals bilateral lung opacities. What is the diagnosis?
- Coronary artery disease
- Hyperthyroidism
- Sarcoidosis
- Viral myocarditis
Board review style answer #2
C. Sarcoidosis. This patient likely has presyncope due to conduction abnormalities, as evidenced by atrioventricular (AV) block on ECG. In the setting of lung opacities on chest Xray and with no other explanation for AV block in this young patient who is otherwise healthy, this is most likely due to sarcoidosis with cardiac involvement.
Comment Here
Reference: Sarcoidosis
Comment Here
Reference: Sarcoidosis
Syphilis
Table of Contents
Definition / general | Pathophysiology | Clinical features | Diagnosis | Complications | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- Due to spirochete, Treponema pallidum
- Rare in developed and developing countries
- Male:female is 2:1 to 4:1
- Affects aortic valve and ascending aorta
Pathophysiology
- Treponema pallida reach cardiovascular system a short time after initial infection but it takes 2 - 20 years for clinical manifestations to develop
- Manifestations are more common in patients with insufficient treatment in early stages of infection than in those who had late treatment
- In cardiovascular syphilis, the vasa vasorum of the ascending aorta shows dense inflammation mainly confined to the adventitia and the media
- This leads to infiltration and replacement of the elastic layer and muscle fibers by fibrous tissue, causing the aortic wall to become weak and dilatable; due to inflammation of the wall of the proximal aorta, the coronary artery orifices become narrowed or blocked and the aortic valve becomes involved, giving rise to aortic incompetence rather than aortic stenosis
- Aortic incompetence and coronary stenosis are due to the mesaortitis of the proximal portion of the aorta; the various changes in the syphilitic heart (ischemia, fibrosis, hypertrophy, dilatation, cardiac degeneration, angina pectoris) are end results of aortitis which increases the heart's workload and diminishes its blood supply
- The aortic arch is the most common site for aneurysmal dilatation
- Syphilis may also involve other large arteries, cerebral vessels or myocardium
Clinical features
- Substernal oppression or "burning", precordial anxiety, pain or distress
- Dyspnea, paroxysmal or nocturnal
- Mild diastolic hypertension in young
- Palpable and visible pulsation in suprasternal notch
Diagnosis
- Ejection murmur and aortic diastolic murmur
- Characteristic loud "tambour like" (booming and ringing quality like a drum) second sound is the most significant sign of syphilitic aortitis
Complications
- Aortic aneurysm, aortic regurgitation and coronary ostia stenosis
Laboratory
- Non treponemal tests are less sensitive (71 - 73%): VDRL test and rapid plasma reagin (RPR) test
- Treponema specific tests are more sensitive (94 - 96%): TPHA, micro hemagglutination test, flourescent treponemal antibody absorption test
Radiology description
- Chest X ray: irregular dilatation and linear calcification of ascending aorta
- CT angiogram is best imaging study to define the size and anatomy of the aneurysm, but in the setting of an aneurysm, the echocardiogram and coronary angiogram are mandatory to exclude aortic regurgitation and coronary flow limiting lesions
Prognostic factors
- Prognosis depends on age, sex, occupation, stage of infection, site and extent of lesion, nature of lesion (progressive or stationary), response to treatment, cardiac efficiency, presence of complications
- The prognosis is better in patients with uncomplicated aortitis than in those with aortic insufficiency, aneurysmal dilatation or myocardial degeneration
- Once the aorta is damaged or it has damaged the heart, antisyphilitic treatment may at best arrest the advance of the disease, increase life expectancy and ease symptoms
Case reports
- 40 year old man and 75 year old woman (Med J Aust 2006;184:241)
- 46 year old man with bilateral ostial coronary lesion (Rev Bras Cir Cardiovasc 2008;23:129)
- 51 year old woman with palpitations and visible neck pulsations (Br J Cardiol 2011;18:94)
Treatment
- Intravenous penicillin
- Prednisolone to prevent a Jarisch-Herxheimer reaction (Wikipedia: Jarisch-Herxheimer reaction [Accessed 2 March 2018])
Clinical images
Gross description
- Aorta intima has irregular wrinkling, fine or coarse, with irregularities of surface produced by scattered inflammatory fibrosis, producing the characteristic tree bark appearance
Microscopic (histologic) description
- Perivascular inflammation around vasa vasoram causing obliterative endarteritis which begins in adventitia but extends into media by formation of capillaries
- Inflammation is mainly lymphocytes and plasma cells
- Resultant fibrosis leads to retraction of media and wrinkling and furrowing of intima
Additional references
Takotsubo cardiomyopathy
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Takotsubo cardiomyopathy is a process of acute myocardial injury which occurs in the setting of excessive catecholamines and is sometimes associated with an identifiable physical or emotional stressor
- Characterized by balloon-like deformation of the ventricular myocardium, which produces profound but potentially short lived functional impairment
- Risk of severe complications is greatest in the acute setting but may persist chronically even after recovery
Essential features
- Ventricular wall motion abnormality in a regional ballooning pattern
- Evidence of reversible ischemic damage without widespread cell death
- Leading hypothesis suggests process is catecholamine mediated
- Clinical presentation mimics acute coronary syndrome
- Absence of severe coronary artery disease or thrombus on imaging
- Usually self limiting and reversible but carries risk of severe complications
Terminology
- Broken heart syndrome
- Stress cardiomyopathy
- Apical ballooning syndrome
- Happy heart syndrome
- Ampulla cardiomyopathy
Epidemiology
- 1 - 3 % of all people presenting with acute coronary syndrome, 5 - 6% of all female patients presenting with acute coronary syndrome (Eur Heart J 2018;39:2032)
- F > M (90% female)
- Average age: 66.8 years old
- Commonly have comorbid psychiatric or neurological disorder (N Engl J Med 2015;373:929)
Sites
- Left ventricular myocardium
- Apical (81.7%) > midventricular (14.6%) > basal (2.2%) > focal (1.5%) (N Engl J Med 2015;373:929)
Pathophysiology
- Catecholamine hypothesis:
- Sudden extreme stress (emotional or physical) → increase in circulating catecholamines → multivessel coronary vasospasm → acute cardiac dysfunction (Heart 2017;103:1461)
- Physical stressors capable of inducing catecholamine excess include thyrotoxicosis, pheochromocytoma and acute subarachnoid hemorrhage with sympathetic storm
- Multiple mechanisms of damage to cardiomyocytes:
- Vasoconstriction of coronary microvasculature leading to ischemia
- Catecholamine toxicity of cardiomyocytes
- Interstitial mononuclear inflammatory response (Eur Heart J 2018;39:2032)
- Cardiomyocyte damage → characteristic ballooning of ventricular walls:
- High level of wall motion abnormality
- Large area of ballooning relative to troponin levels suggests stretch and nonapoptotic myocardial injury (Heart 2018;104:96)
- Localization to ventricular myocardium may be related to apical - basal gradient of sympathetic innervation and beta adrenergic receptor density (Eur Heart J 2018;39:2032)
Etiology
- Classically associated with an emotional or physical stressor
- Stressor not always identifiable
- Emotional stressor can be negative (e.g. loss of a loved one) or positive (e.g. very happy events)
- Physical stressor can be related to pre-existing medical conditions (e.g. acute critical illness, respiratory failure) or iatrogenic (e.g. surgery, exercise tests)
- Loss of sympatholytic estrogens thought to play a role in predisposing postmenopausal women to this condition (Heart 2017;103:1461)
Clinical features
- Mimics acute coronary syndrome
- Acute chest pain (60 - 100%) > dyspnea > syncope (Herz 2010;35:240)
- Sinus tachycardia
- Reduced left ventricular ejection fraction (LVEF) with recovery of systolic LV function over time (N Engl J Med 2015;373:929)
- Symptoms rapidly improving within several hours after admission (Eur Heart J 2007;28:2456)
- Associated conditions: any cause of high catecholamine levels
Diagnosis
- Echocardiographic findings: left ventricular wall motion abnormalities (see Radiology description)
- Coronary angiography: absence of coronary artery disease or thrombus
- Presence of incidental coronary artery disease (10 - 15%) does not preclude diagnosis; this can lead to misclassification as coronary artery disease (N Engl J Med 2015;373:929)
- New ECG abnormalities: ST elevation or T wave inversion (Herz 2010;35:240)
- Postmortem gross examination may reveal ventricular ballooning with or without wall rupture (Forensic Sci Med Pathol 2019 Nov 9 [Epub ahead of print])
- Pathologic examination generally does not play a major role in diagnosis
Laboratory
- Elevated myocardial injury markers (creatine kinase, creatine kinase MB, troponin)
- Elevation less than expected for extent of wall motion abnormality (Heart 2017;103:1461)
- Mean troponin elevation similar to that seen in acute coronary syndrome (N Engl J Med 2015;373:929)
- Serum cardiac brain natriuretic peptides (BNP) elevated compared with patients with acute coronary syndrome
- 4 circulating miRNAs identified as possible biomarkers (Heart 2017;103:1461)
Radiology description
- Coronary angiography: normal and unobstructed coronary arteries
- Left ventriculography: 4 different wall motion patterns identified
- Apical, midventricular, basal and focal (see Radiology images) (Heart 2017;103:1461)
- Echocardiography: wall motion abnormality of left ventricular midsegments with or without apical involvement; severely reduced LV function
- Cardiac MRI: wall motion abnormality (Herz 2010;35:240)
Radiology images
Prognostic factors
- Complete functional recovery expected within 12 ± 3 days but chronic complications are possible (Eur Heart J 2007;28:2456)
- Complications = major cardiac / cerebrovascular events
- Rate is 9.9% per patient year (N Engl J Med 2015;373:929)
- Frequent: acute heart failure, LV outflow tract obstruction, cardiogenic shock, mitral regurgitation
- Moderate: Afib, LV thrombus, cardiac arrest, AV block
- Rate is 9.9% per patient year (N Engl J Med 2015;373:929)
- Rare: tachyarrhythmia, bradyarrhythmia, torsades de pointes, death, Vtach or Vfib, acute ventricular septal defect (VSD) (Eur Heart J 2018;39:2047)
- Unfavorable prognostic factors (re: in hospital complications):
- Older age
- Male
- Physical stressor
- Lower LVEF at admission
- Higher neutrophil / lymphocyte ratio at admission
- Higher WBCs / mean platelet volume ratio at admission (Clinical Cardiology 2020;43:1294)
- Higher troponins
- Acute neuro or psychiatric disease (N Engl J Med 2015;373:929)
- Presence of atrial fibrillation (JAMA Cardiol 2016;1:335)
- Mortality = 5.6% per patient year, similar to ST elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI) (Int J Cardiol 2015;185:282)
Case reports
- 27 year old man with iatrogenic epinephrine overdose induced cardiomyopathy (Proc (Bayl Univ Med Cent) 2019;32:567)
- 57 year old woman develops cardiomyopathy in the setting of COVID-19 infection (BMJ Case Rep 2020;13:e236811)
- 66 year old woman with cardiomyopathy associated heart failure as the presenting symptom of a pheochromocytoma (Tex Heart Inst J 2019;46:124)
- 73 year old woman with mild traumatic brain injury presenting in cardiogenic shock (Neurocrit Care 2017;26:284)
- 80 year old woman with exertional chest pain and vomiting in the absence of an identifiable stressor (Cureus 2019;11:e5749)
- 85 year old woman with acute chest pain in the setting of severe anxiety (QJM 2020;113:488)
Treatment
- Supportive care during acute phase and treatment of any complications, such as heart failure or arrhythmia
- ACE inhibitors and angiotensin II receptor blockers (ARBs) associated with improved survival at 1 year (N Engl J Med 2015;373:929)
- No evidence for improved survival benefit with beta blockers
Gross description
- Apical biventricular ballooning
- Death associated with Takotsubo cardiomyopathy is often due to complications, such as cardiac wall rupture, which are notable on gross examination (Forensic Sci Med Pathol 2019 Nov 9 [Epub ahead of print])
Microscopic (histologic) description
- Acute phase (day of admission)
- Hypertrophied myocytes (> 20 μm)
- Intracytoplasmic glycogen + PAS staining
- Recovery phase (12 ± 3 days after admission)
- Reduced PAS staining (Eur Heart J 2007;28:2456)
Immunofluorescence description
- Intracellular proteins show diminished density and disrupted intracellular organization during the acute phase of illness
- Alpha actinin
- N terminal dystrophin
- C terminal dystrophin
- Connexin 43
- Titin (T12, Tz1) (Eur Heart J 2007;28:2456)
- Cardiomyocytes demonstrate more normal cross striated and homogenous staining after recovery of contractile function (Eur Heart J 2007;28:2456)
Immunofluorescence images
Positive stains
- Cardiomyocyte staining is well described but not commonly used in diagnostic practice
- Alpha actinin:
- Acute: located in border areas of myocytes
- Recovered: regular distribution
- Actin:
- Acute: reduced in amount, displaced to border of myocytes
- Recovered: regular distribution
- Dystrophin (amino terminal):
- Acute: reduced
- Recovered: regular distribution
- Dystrophin (carboxy terminal):
- Acute: regular distribution
- Recovered: regular distribution
- Connexin 43:
- Acute: myocardial organization disturbed, profound loss of gap junctions
- Recovered: reorganization of cell - cell contact
- Titin:
- Acute: missing from some myocytes, abnormal punctate pattern
- Recovered: most myocytes showed recovery of regular cross striated pattern
- Fibronectin:
- Acute: widened interstitial space with large amounts of fibronectin between cells
- Recovered: reduced from acute but still increased compared with controls
- Collagen 1:
- Acute: increased in amount
- Recovered: reduced from acute but still increased compared with controls
- CD68 (macrophages):
- Acute: multiple extracellular clusters
- Recovered: multiple extracellular clusters
- CD3 (T lymphocytes):
- Acute: increased number
- Recovered: reduced to normal
- Ubiquitin:
- Acute: several ubiquitin positive cells detected but no large accumulations of ubiquitin protein complexes
- Recovered: same as above (Eur Heart J 2007;28:2456)
Negative stains
- Complement 9
- TUNEL (Eur Heart J 2007;28:2456)
Electron microscopy description
- Acute phase (day of admission)
- Heterogenous vacuoles (varying contents: cellular debris, myelin bodies)
- Enlarged myocytes
- Cytoskeletal and contractile proteins dissolved
- Contractile material mostly seen around edges of myocytes
- Sporadic contraction bands
- Abnormalities in size and shape of clustered mitochondria
- Rounded / oval nuclei
- Interstitial space = widened, containing fibrotic material
- Recovery phase (12 ± 3 days after admission)
- Normal size myocytes
- Fewer, smaller vacuoles
- Regular composition of myocardium
- Intracellular structures nearly normal (Eur Heart J 2007;28:2456)
Molecular / cytogenetics description
- Adrenergic receptor polymorphisms are potentially relevant (Eur Heart J 2018;39:2032)
Videos
Illustrated walkthrough of the essential features of Takotsubo cardiomyopathy
Ventricular angiography video showing the 4 main subtypes of Takotsubo cardiomyopathy
Sample pathology report
- Heart, left ventricle, endomyocardial biopsy:
- Takotsubo cardiomyopathy (see comment)
- Comment: Microscopic examination reveals hypertrophied myocytes with vacuolar degeneration as well as rare contraction bands. PAS staining shows intracellular accumulation of glycogen. Moderate cellular infiltration observed in the interstitium. No necrosis identified. Microscopic appearance consistent with clinical diagnosis of Takotsubo cardiomyopathy in the acute phase, with symptom onset 2 days prior to biopsy.
Differential diagnosis
- Myocardial infarction:
- Positive history of coronary artery disease
- Coronary angiography: significant vessel occlusion
- BNP moderately elevated
- Acute myopericarditis:
- Preceding flu-like symptoms
- Leukocytosis
- Positive viral serology
- Angina:
- Positive history of coronary artery disease
- Improves with nitroglycerin and is relieved by rest
- Anxiety / panic attack:
- ECG normal (with or without sinus tachycardia)
- Cardiac biomarkers normal
Board review style question #1
A 68 year old woman experiences acute onset chest pain and dyspnea upon receiving news that she is being evicted from her home. Cardiac imaging (shown above) suggests Takotsubo cardiomyopathy. Which of the following is most likely to be seen on biopsy of the affected myocardium?
- Abundant inflammatory cell infiltrate
- Atherosclerotic plaque in microvessels
- Coagulative necrosis of the cardiac apex
- Myocyte hypertrophy
Board review style answer #1
D. Myocyte hypertrophy. Takotsubo cardiomyopathy is characterized by ischemic damage to the ventricular myocardium, which leads to myocyte hypertrophy, resolving in a matter of days to weeks. In the absence of complications, necrosis is not usually seen. Atherosclerotic plaques are not usually seen in Takotsubo cardiomyopathy and if present are regarded as incidental findings. Some inflammatory cells could be seen but would not be the characteristic finding.
The picture (taken through ventriculography) shows ballooning at the apex of the heart, which is the most common pattern seen in Takotsubo cardiomyopathy.
Comment Here
Reference: Takotsubo cardiomyopathy
The picture (taken through ventriculography) shows ballooning at the apex of the heart, which is the most common pattern seen in Takotsubo cardiomyopathy.
Comment Here
Reference: Takotsubo cardiomyopathy
Board review style question #2
A 72 year old woman presents with acute onset chest pain and dyspnea. Cardiac enzymes are elevated and ECG shows a new ST elevation. Cardiac imaging reveals an enlarged, balloon-like left ventricle which fails to contract during systole. However, coronary angiography reveals no evidence of coronary artery disease or thrombus. The patient improves clinically with minimal supportive care over the next 2 weeks and is discharged to her home. What is the most likely diagnosis?
- Dressler syndrome
- Hypertrophic cardiomyopathy
- Takotsubo cardiomyopathy
- Viral myocarditis
Board review style answer #2
C. Takotsubo cardiomyopathy classically mimics acute coronary syndrome's presentation. Unobstructed coronary arteries, however, point towards Takotsubo cardiomyopathy. The ballooning appearance on echocardiography or ventriculography, as well as her relatively rapid recovery, are characteristic of Takotsubo cardiomyopathy.
Comment Here
Reference: Takotsubo cardiomyopathy
Comment Here
Reference: Takotsubo cardiomyopathy
Tetralogy of Fallot (pending)
[Pending]
VACTERL association
Table of Contents
Definition / general | Essential features | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Differential diagnosis | Additional referencesDefinition / general
- Refers to the co-occurrence of birth defects including Vertebral anomalies, Anal atresia, Cardiac defects, Tracheoesophageal fistula or Esophageal atresia, Renal or radial anomalies and Limb defects
- Called an association rather than a syndrome because the defects are not pathogenetically related and tend to occur in a non random manner
- Linda Quan and David Smith first described VATER association, including only Vertebral, Anal, TracheoEsophageal features and Radial dysplasia in 1972; years later, when it was found that cardiac and renal abnormalities were common in the association, the acronym was changed to VACTERL (J Med Genet 2006;43:545)
Essential features
- Typically defined by the presence of at least three of the congenital malformations at below: (Orphanet J Rare Dis 2011;6:56)
- Vertebral anomalies
- Anal atresia
- Cardiac defects
- Tracheoesophageal fistula
- Esophageal atresia
- Renal or radial anomalies
- Limb defects
Epidemiology
- Most cases are sporadic; however, some families have several involved members
- The incidence is approximately 1 in 10,000 to 40,000 live born infants (Orphanet J Rare Dis 2011;6:56)
- Seen more frequently in infants born to diabetic mothers
- Associated with chromosomal defects such as Trisomy 18
Pathophysiology
- VACTERL association specifically refers to the abnormalities in structures derived from the embryonic mesoderm
Etiology
- In general, the etiology of "associations" is not defined
- No specific genetic or chromosome problem has been identified with this association, and it is most likely caused by multiple factors (Am J Med Genet 2002;110:320)
Clinical features
- Vertebral anomalies usually consist of hypoplastic vertebra or hemivertebra (80% of patients)
- Anal atresia or imperforate anus (55%)
- Congenital heart disease including ventricular septal defect, atrial septal defects and tetralogy of Fallot (up to 75%)
- Esophageal atresia with tracheoesophageal fistula (70%)
- Renal defects including incomplete formation of one or both kidneys or urologic abnormalities such as obstruction of outflow of urine or severe reflux (50%)
- Limb defects include a displaced or hypoplastic thumb, polydactyly, syndactyly and forearm defects such as radial aplasia (70%)
- In addition, up to 35% of patients have a single umbilical artery
- Features secondary to VACTERL components include ambiguous genitalia, abdominal wall defects, diaphragmatic hernia, intestinal and respiratory anomalies and oligohydramnios sequence defects
Diagnosis
- Based upon complete physical exam and a variety of specialized tests for its major and minor features
Prognostic factors
- Some affected infants do not survive
- Many babies with VACTERL are born small and have difficulty gaining weight, but they do tend to have normal development and normal intelligence
- Later in life, vertebral abnormalities may put the child at risk for developing scoliosis
- Renal problems can cause kidney failure early in life and may require kidney transplant
Treatment
- Many problems can be corrected surgically before any damage can occur
Differential diagnosis
- CHARGE syndrome
- Deletion 22q11.2 syndrome
- Fanconi anemia
- MURCS association
- Oculo-auriculo-vertebral syndrome
- Opitz G / BBB syndrome
- Pallister-Hall syndrome
- VACTERL with hydrocephalus
Additional references
Valves
Table of Contents
Definition / general | Diagrams / tables | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Electron microscopy description | Electron microscopy images | Additional referencesDefinition / general
- The four heart valves (tricuspid, pulmonic, mitral, aortic) enable blood to flow in a unidirectional way
- They open and close over three billion times during a normal life
- Between 1 and 20 liters per minute of blood flows through the valves during rest, exercise or other conditions
- Each heart valve is composed of different structures, with different histological profiles to provide optimal function for varied roles in the cardiac cycle
Diagrams / tables
Gross description
-
Tricuspid valve (Valve atrioventricularis dexter):
- Composed of an anterior, anterosuperior, ventral or mural leaflet (Cuspid anterior); a posterior, inferior or dorsal leaflet (Cuspis posterior) and a septal or medial leaflet (Cuspis septalis)
- It is positioned between the right atrium and the right ventricle and builds a structural unit with the annulus, chordae tendinae and the papillary muscles
- The three leaflets of the tricuspid valve differ in size
- The mural or anterior leaflet is the largest; it stretches from the infundibular area downwards to the inferolateral wall of the right ventricle
- The septal or medial leaflet is attached to both the membranous and muscular portions of the ventricular septum
- The posterior leaflet is the smallest and attached to the tricuspid ring along its posteroinferior border
- Sometimes, four leaflets can be identified - the posterior leaflet can be divided or an additional leaflet is positioned between the posterior and the septal one
- The free margins of the leaflets show an arcade-like composition and terminate into the chordae tendinae
- Similar to the mitral valve leaflets, closure of the tricuspid valve is achieved by a plane of attachment of the leaflets to each other, by which the subvalvular apparatus prevent the leaflets from passing into the atrium
- The tricuspid leaflets differ from the mitral leaflets in being thinner, more translucent, and less easily separated into well defined leaflets
- The tricuspid orifice is larger than the mitral valve orifice
- Connects the Conus arteriosus (infundibulum) of the right ventricular outflow tract and the truncus pulmonalis of the pulmonary artery
- The root consist of the sinus (sinus trunci pulmonalis), the annulus, the commissures, the leaflets and the sinotubular junction
- The aortic and pulmonary leaflet show similar histological characteristics
- The pulmonary leaflets are thinner and the noduli of Arantii is smaller compared with the aortic leaflets
- Pulmonary valve leaflets consist of the hinge, the belly, the coapting surface and the lannula with the noduli of Arantii
- The belly, which forms the main area of one leaflet, is almost transparent in its center
- In the zone of the hinge area, the leaflets are attached to the pulmonary annulus
- The mitral valve is composed of the annulus, 2 leaflets, the chordae tendinae and the papillary muscles
- The annulus is the opening area of the mitral valve, composed anteriorly of a fibrous component which is localized between the two fibrous trigones, the trigonum fibrosum dextrum (the central part of the skeleton of the heart) and the trigonum fibrosum sinistrum
- The anterior leaflet is the larger of the two leaflets, and is divided into the zone of attachment to the annulus, the 'translucent' zone and the 'rough' zone, where the chordae tendinae are attached to the ventricular side of the leaflet and into the free margin
- The posterior leaflet is divided into three parts: posteromedial or right, intermediate and anterolateral or left
- Although the posterior leaflet is attached to almost two thirds of the circumference, and its area is significantly larger than the area of the anterior leaflets, it participates to a lesser extent in closure of the mitral orifice
- Both leaflets meet each other at the two commissures (posteromedial and anterolateral)
- On the leaflets, the majority of the chordae insert either at the free margin or behind the free margin at the ventricular side (rough zone)
- The aortic root is composed of the annulus, commissures, interleaflet triangles (trigones), sinuses of Valsalva, sinotubular junction and 3 leaflets (Ann Cardiothorac Surg 2013;2:53)
- Supports the aortic valve and forms the anatomic boundary between the left ventricle and the aorta
- Commissure:
- Apex of the crown-like annulus where the two leaflets are attached to the aortic wall at the height of the sinotubular junction
- The commissure between the right and left coronary leaflets is positioned anteriorly and is more or less opposite to the corresponding commissure of the pulmonary valve
- The commissures have a fibrous structure and suspend the valve leaflets
- Leaflets:
- Originally named according to their anatomical position as anterior and posterior right and left leaflet (British Terminology Anatomical System) or anterior and right and left posterior leaflet (International Terminology Nomenclatura Anatomica)
- In the 1950s, surgeons adopted the simpler terminology of non coronary leaflet, right coronary leaflet and left coronary leaflet, based on their relationship to the coronary ostia
- The triangle between the right and non-coronary sinuses is in direct continuity with the membranous septum proximally
- The bundle of His, coming from the anterior extension of the AV node, penetrates through the central fibrous body just below the inferior margin of the membranous ventricular septum at the crest of the muscular ventricular septum under this triangle; it is closely related to the septal leaflet of the tricuspid valve
- Aortic valve leaflet consist of four components: hinge, belly, coapting surface, lannula with the noduli of Arantii
Pulmonary / pulmonic valve:
Mitral valve (Valva atrioventricularis sinistra OR valva bicuspidalis OR valva mitralis)
Aortic valve (Valva Aortae)
Gross images
Microscopic (histologic) description
-
Tricuspid valve:
- The leaflets are composed of a fiber skeleton and an endocardial surface
- The atrial layer of the endocardium shows a smooth surface, and is a monolayer of endothelium
- These cells are interconnected in various fashions
- They show either a straight border interlocked with each other, or 'roof tile'-like overlaps
- The endothelium is underlined by a basal membrane, composed of an osmiophilic lamina densa and an osmiophobic lamina rara
- The lamina spongiosa is composed of loosely arranged layer of connective tissue
- The lamina fibrosa is composed of dense collagenous fibers which form a solid plane
- Light microscopy shows five layers between the ventricular and arterial endocardial layers of the leaflet: lamina ventricularis, lamina radialis, lamina spongiosa, lamina fibrosa and lamina arterialis
- Lamina ventricularis: layer under the ventricular endothelium; composed of a tight network of reticular fibers with only rare thin collagenous fibers and elastic fibers; thickness is 21 to 48 mm
- Lamina radialis: next layer; incorporates radial oriented collagenous and elastic fibers with some reticular fibers in between; proceeds into the endocardium and the subendocardial layer of the ventricle; thickness is 58 to 108 mm
- Lamina spongiosa: composed of loosely arranged reticular fibers with bundles of collagenous and some elastic fibers; many of the collagenous fibers radiate from the lamina radialis and lamina fibrosa into this layer, which sometimes make it difficult to identify; thickness is 40 to 300 mm
- Lamina fibrosa: circular arranged collagen fibers connected to the annulus; thickness is 80 to 170 mm
- Lamina arterialis: layer under the endothelium at the arterial side; composed of a thin layer of reticular fibers and is not always present in light microscopic sections
- Leaflets are composed of a fibrous skeleton with an endocardial surface
- The atrial layer has a smooth endocardial cell layer
- On the anterior leaflet, this smooth endocardial layer is also present on the ventricular side
- Leaflets are covered by a continuous layer of endothelial cells with a smooth surface on the ventricular side and numerous ridges on the arterial side
- The arrangement of the endothelial cells is across, not in line with the direction of flow
- The cells are joined to one another by junctions similar to those present on endothelial cells elsewhere in the vascular system
- Between the ventricular and aortic surfaces, there are up to five layers of connective tissue: lamina ventricularis, lamina radialis, lamina spongiosa, lamina fibrosa and lamina arterialis (nomenclature of Gross and Kugel)
- Within the connective tissue, the elastic and collagen fibers are mechanically coupled to each other in a well defined honeycomb or sponge-like structure
- The arterial layer contains coarse bundles of circumferential collagen fibers, which form the macroscopic folds parallel to the free edge of the leaflets
- It is this arrangement of fibers that transfers the load of the leaflets to the wall of the aortic root
- Between the extracellular components reside interstitial cells designated myofibroblasts, with characteristics of fibroblasts and smooth muscle cells
Pulmonary valve:
Mitral valve:
Aortic valve:
Microscopic (histologic) images
Electron microscopy description
- Electron microscopy demonstrates that endothelial cell layers are bordered by a basal membrane
- Endothelial cells either interdigitate or overlap
- They are further characterized by pinocytic vesicles, indicating an active transport system
- In the subendothelial reticular tissue, collagenous fibrils are scanty, but fibroblasts are common
- The lamina fibrosa consists of tight bundles of collagenous fibrils
- Fibroblasts lying among these fibrils show multiple long processes
Electron microscopy images
Additional references
Recent Heart & vascular pathology Pathology books
Find related Pathology books: cardiovascular, lung, mediastinum/serosa, forensic, pediatric