Superpage
Superpage Topics
Accessory tragi
Anatomy, histology & grossing
Ceruminous adenocarcinoma
Ceruminous adenoma
Cholesteatoma
Chondrodermatitis nodularis chronica helicis
Congential - other
Endolymphatic sac tumor
Exostosis
Infectious / inflammatory
Inflammatory aural / otic polyp
Keloid
Middle ear adenocarcinoma (pending)
Middle ear neuroendocrine tumor
Middle ear papilloma (pending)
Middle ear paraganglioma
Otosclerosis
Squamous cell carcinoma of middle ear
Squamous cell carcinoma of the external auditory canal
WHO classificationAccessory tragi
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Accessory tragus is a benign congenital anomaly of the external ear that often appears as a skin colored papule located in the preauricular region (An Bras Dermatol 2015;90:519)
Essential features
- Accessory tragi are usually located near the tragus
- May have associated renal (hydronephrosis, horseshoe kidney) and cardiac abnormalities and associations with some congenital syndromes
- Important distinguishing feature of accessory tragi is the presence of a cartilaginous core but this may not always be present
Terminology
- Heterotrophic tragi, supernumerary tragi (Can Fam Physician 2012;58:772)
- Often inaccurately labeled as preauricular skin tags, accessory auricle, polyotia, rudimentary ear or supernumerary pinna (Can Fam Physician 2012;58:772)
- Cervical tragus (if it is located on the neck) (Arch Surg 1982;117:968)
ICD coding
Epidemiology
- Congenital malformation (BMJ Case Rep 2013;2013:bcr2013008645)
- No sex predilection
- Most cases are sporadic but familial cases have been documented (BMJ Case Rep 2013;2013:bcr2013008645)
- Estimated prevalence is 1.7:1,000 (BMJ Case Rep 2013;2013:bcr2013008645)
Sites
- Accessory tragi are usually located near the tragus (Ann Dermatol 2010;22:61)
- May less commonly present on the cheek from tragus to angle of mouth, along the anterior edge of the sternocleidomastoid muscle, in the nasal vestibule, on the glabella or the suprasternal area (Ann Dermatol 2010;22:61)
Pathophysiology
- Auricle is formed from fusions between the first and second branchial arches; accessory tragus results from incomplete fusion between the arches
- As the mandible grows, the auricle ascends from the lower lateral neck to the side of the head; therefore, accessory tragi may occur along this migratory line due to their origin from the mandibular branchial arch (BMJ Case Rep 2013;2013:bcr2013008645)
- During development, the auricle ascends from the lower lateral neck to the side of the head; accessory tragi may occur anywhere along this migratory line (BMJ Case Rep 2013;2013:bcr2013008645)
Clinical features
- Usually unilateral but can be bilateral (6% of cases) or multiple (An Bras Dermatol 2015;90:519)
- May be pedunculated or sessile and soft or firm depending on presence of cartilage (An Bras Dermatol 2015;90:519, Ann Dermatol 2010;22:61)
- Papule is typically 3 - 5 mm in size (Ann Dermatol 2010;22:61)
- May be covered in vellus hair (Ann Dermatol 2010;22:61)
- Can be associated with hearing impairments (Can Fam Physician 2012;58:772, BMJ Case Rep 2013;2013:bcr2013008645)
- May have associated renal (hydronephrosis, horseshoe kidney) and cardiac abnormalities (BMJ Case Rep 2013;2013:bcr2013008645)
- Usually isolated; few reports on familial accessory tragi and cases with other associated anomalies of the first and second branchial arches
- Has associations with Delleman syndrome, Goldenhar syndrome, Haberland syndrome and Townes-Brocks syndrome, Treacher-Collins syndrome, VACTERL syndrome, Wolf-Hirschhorn syndrome and Down syndrome (Int J Dermatol 2014;53:1442, BMJ Case Rep 2013;2013:bcr2013008645)
- These associations are more common when there are multiple lesions
Diagnosis
- Diagnosis is based off clinical presentation and patient history (BMJ Case Rep 2013;2013:bcr2013008645)
- Histological evaluation can confirm clinical diagnosis (BMJ Case Rep 2013;2013:bcr2013008645)
Prognostic factors
- Benign defect; excellent prognosis (BMJ Case Rep 2013;2013:bcr2013008645)
Case reports
- 1 day old girl with accessory tragus located on nasal vestibule (Ann Dermatol 2010;22:61)
- 21 month old girl with accessory tragus in the middle ear (Int J Pediatr Otorhinolaryngol 2010;74:1338)
- 3 year old boy with postauricular mass (Cureus 2021;13:e13645)
- 21 year old man with pedunculated cervical mass (Iran J Otorhinolaryngol 2022;34:121)
- 48 year old woman with trichofolliculoma mimicking accessory tragus (J Audiol Otol 2020;24:99)
Treatment
- Clinically insignificant; reassurance is reasonable (BMJ Case Rep 2013;2013:bcr2013008645)
- Surgical excision can be performed for cosmesis or if local irritation occurs (BMJ Case Rep 2013;2013:bcr2013008645)
- Incomplete surgical excision may leave an exposed cartilaginous fragment, potentially leading to chondrodermatitis (BMJ Case Rep 2013;2013:bcr2013008645)
- Unclear guidelines on screening for hearing, renal and cardiac abnormalities (Can Fam Physician 2012;58:772)
Gross description
- Sessile or pedunculated papule, often covered with fine hair
- 3 - 5 mm in size
- Smooth surface
- Soft or firm depending on amount of cartilage
- Skin colored
- Reference: Int J Dermatol 2014;53:1442
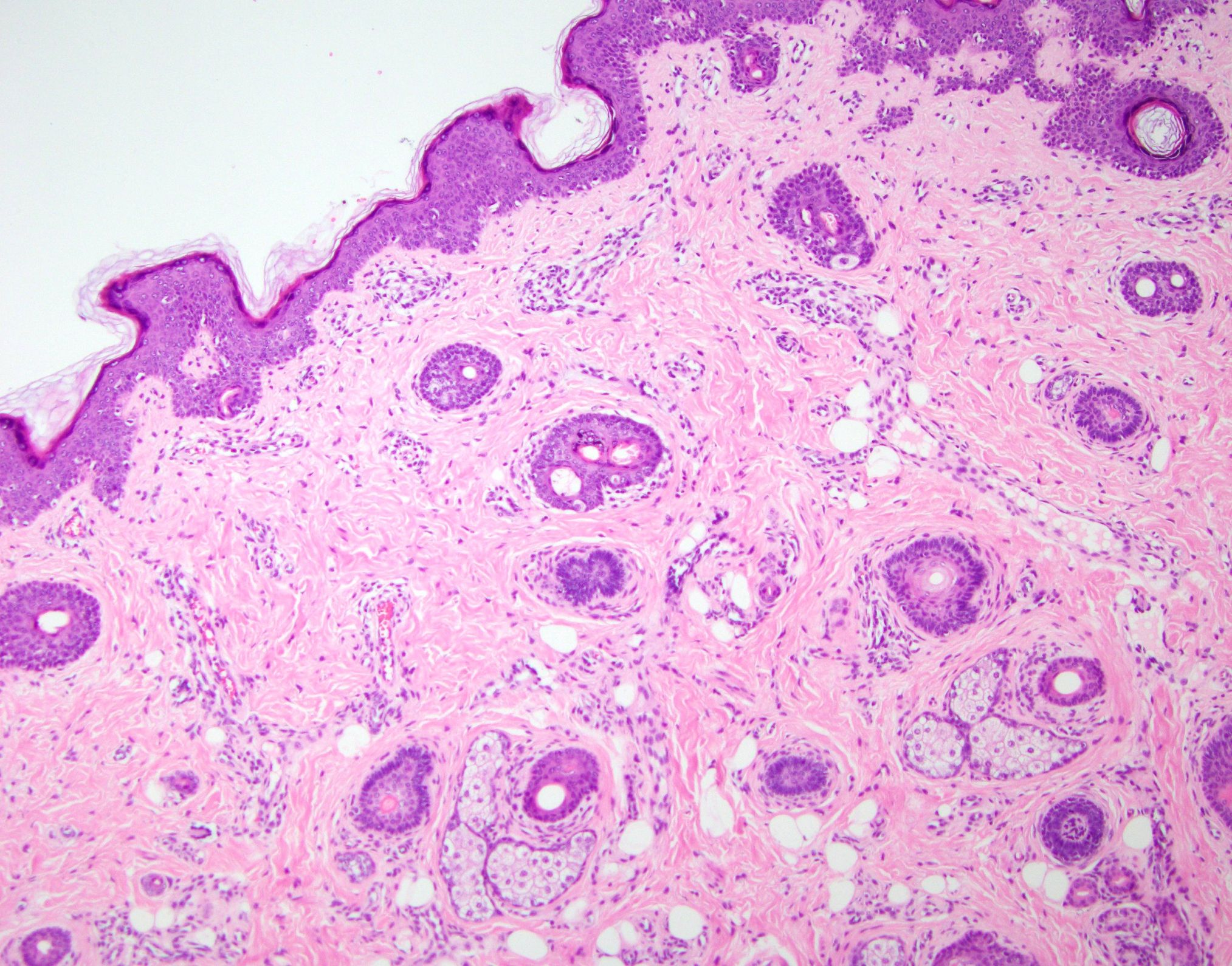
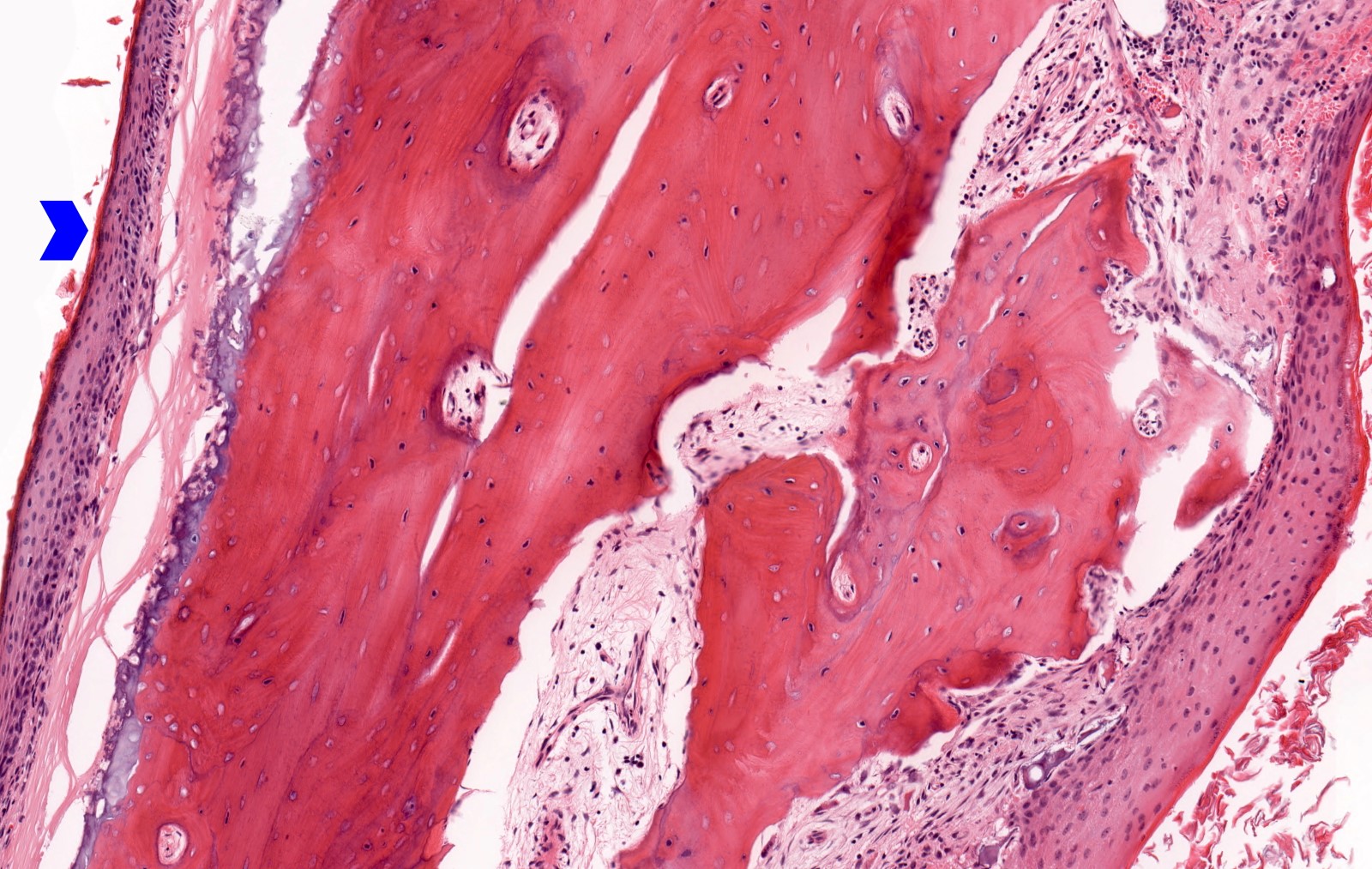
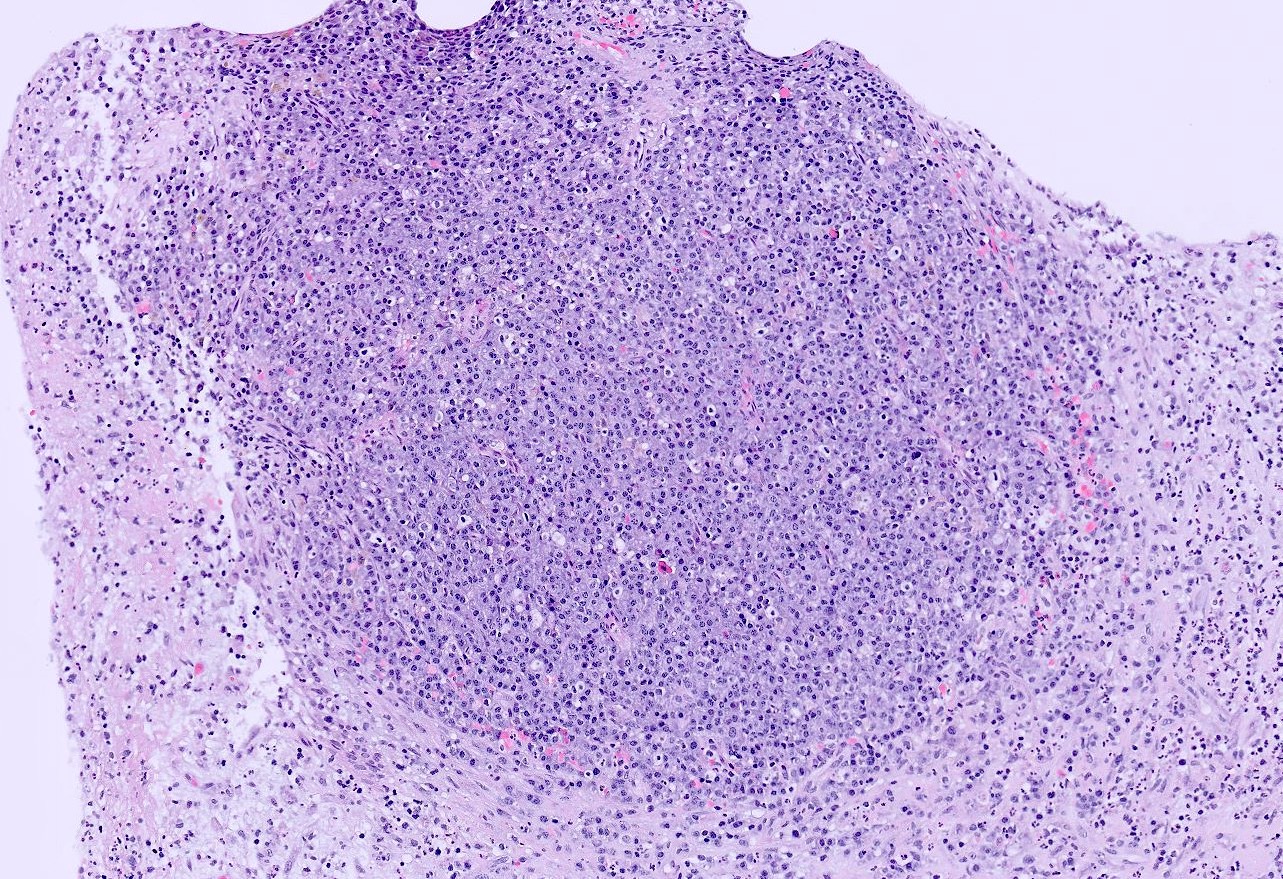
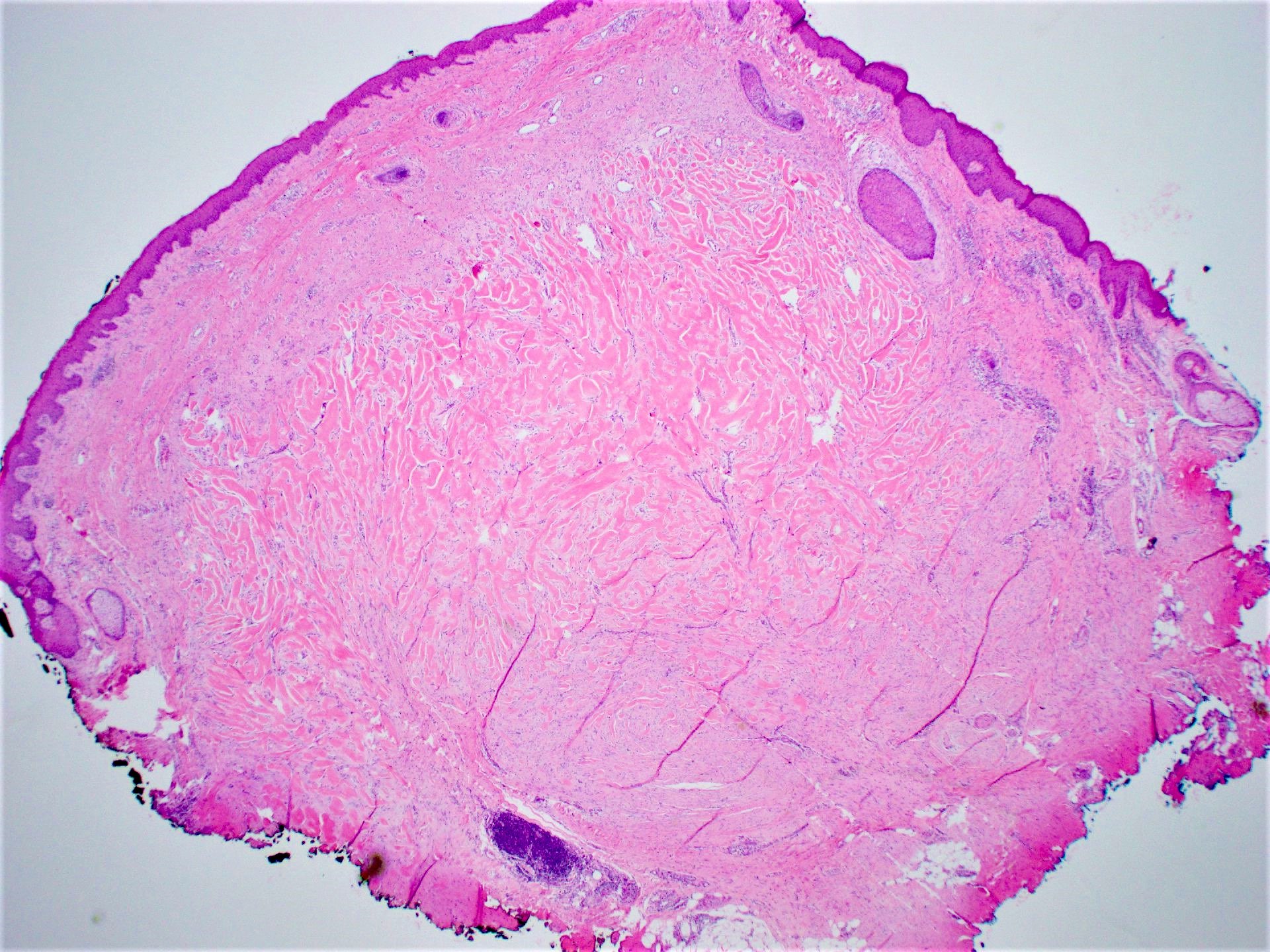
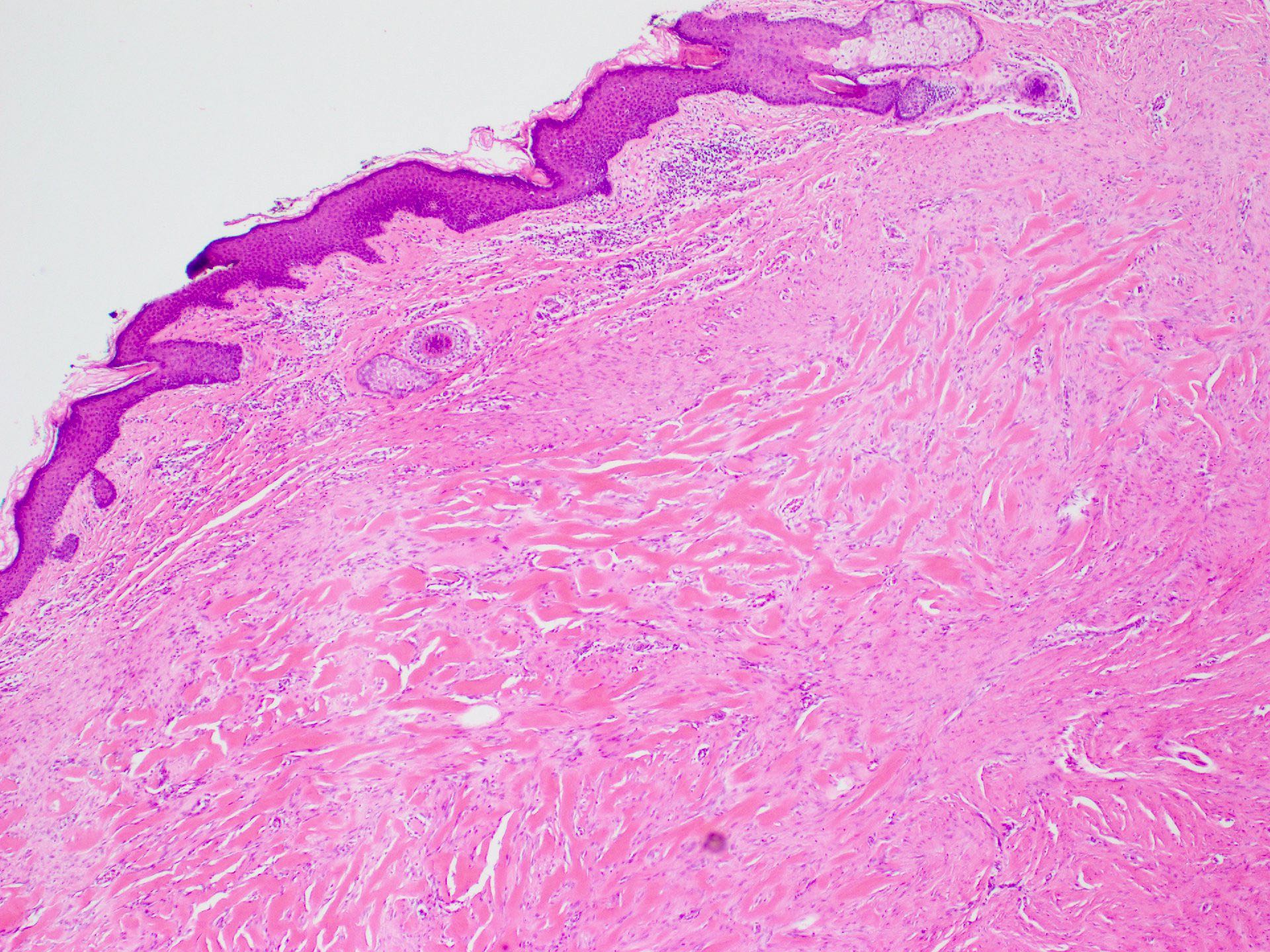
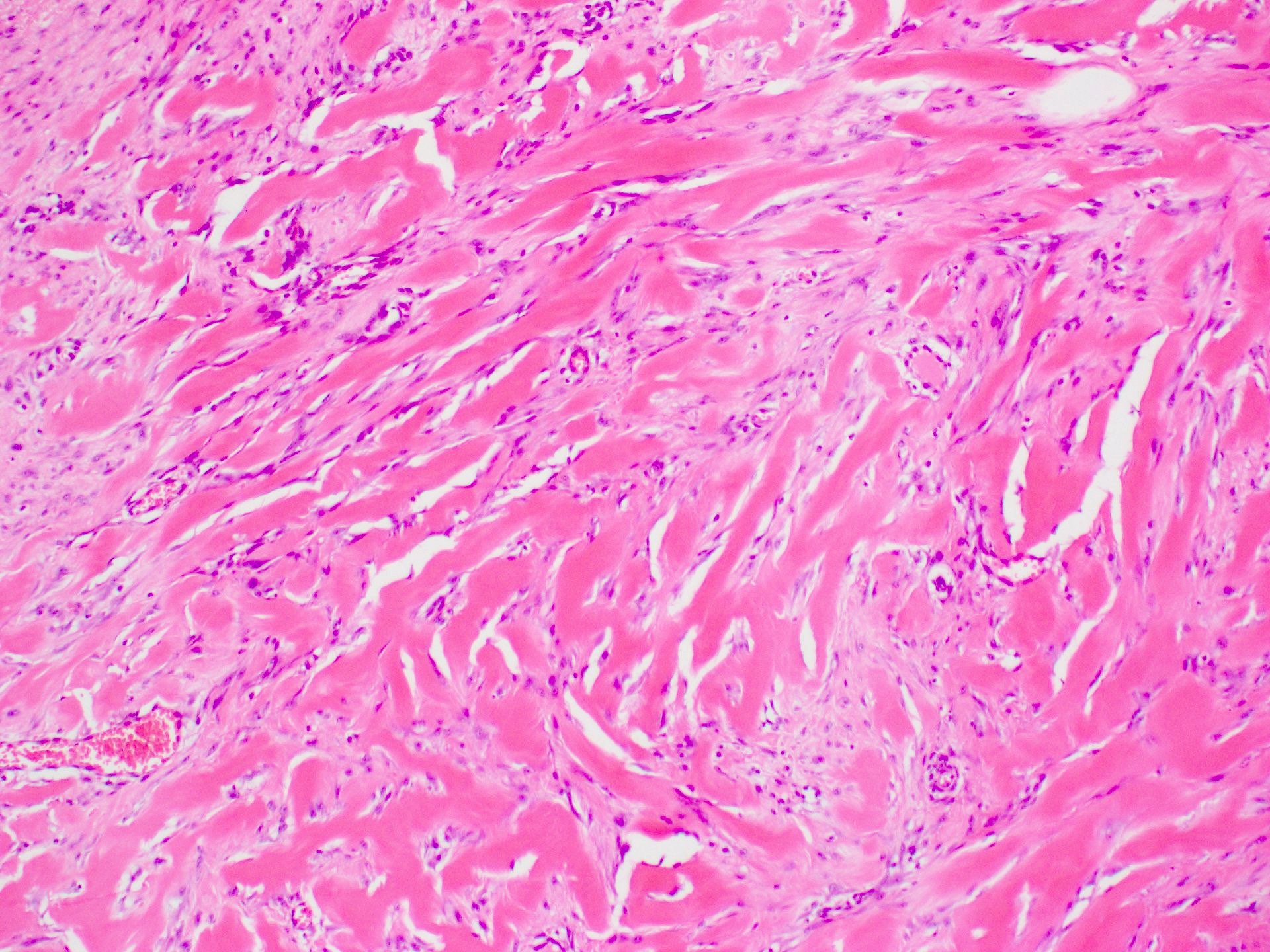
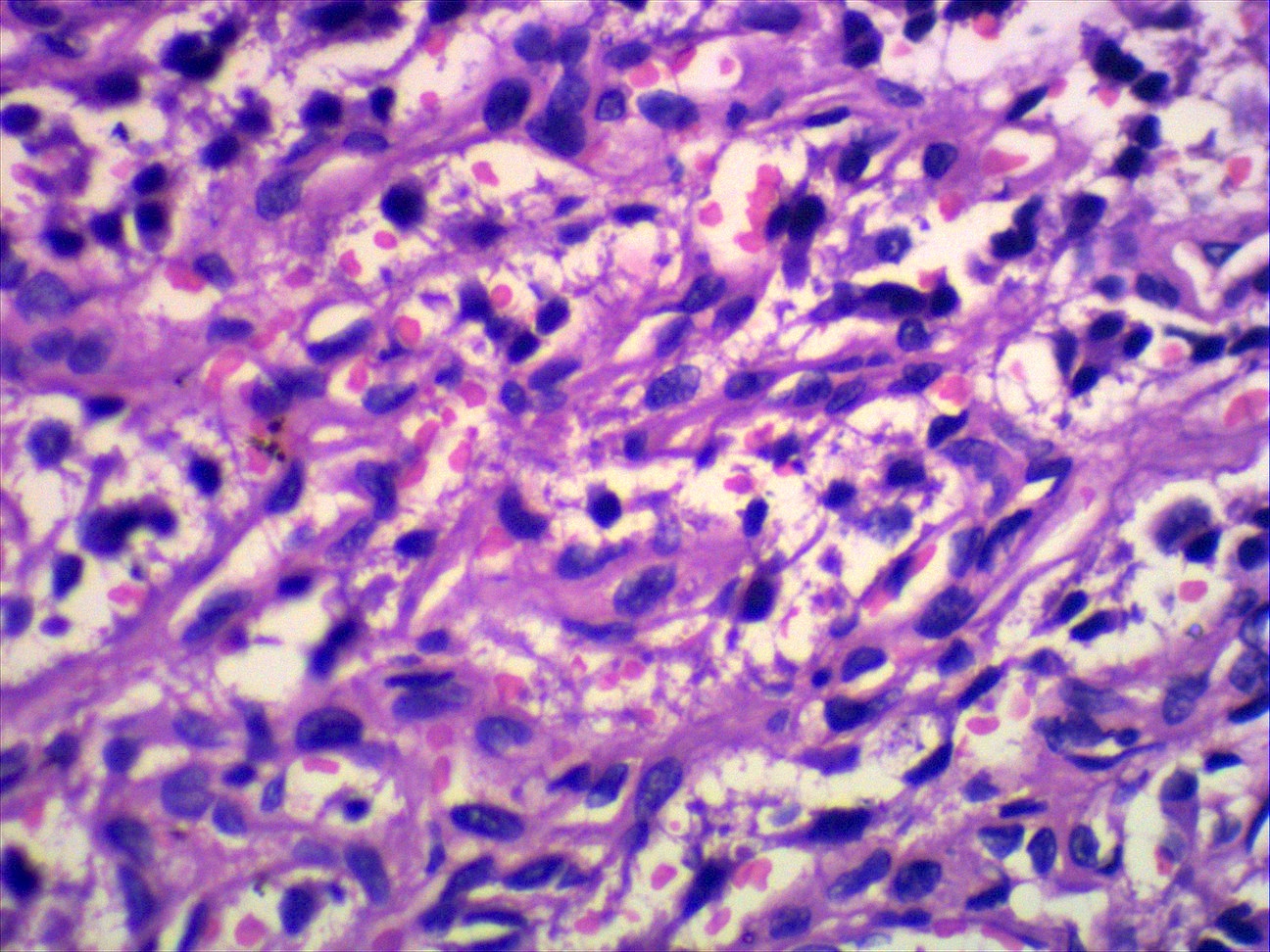
Microscopic (histologic) description
- Mild orthokeratosis over the epidermis (BMJ Case Rep 2013;2013:bcr2013008645)
- Prominent connective tissue structure in subcutaneous fat (BMJ Case Rep 2013;2013:bcr2013008645, Ann Dermatol 2010;22:61)
- Numerous vellus hair follicles and sebaceous glands present in the papillary dermis (BMJ Case Rep 2013;2013:bcr2013008645)
- Fibrovascular tissue with fat lobules (Ann Dermatol 2010;22:61)
- May be sessile or pedunculated polyp (Ann Dermatol 2010;22:61)
- With or without central cartilage surrounded by adipose tissue (Ann Dermatol 2010;22:61)
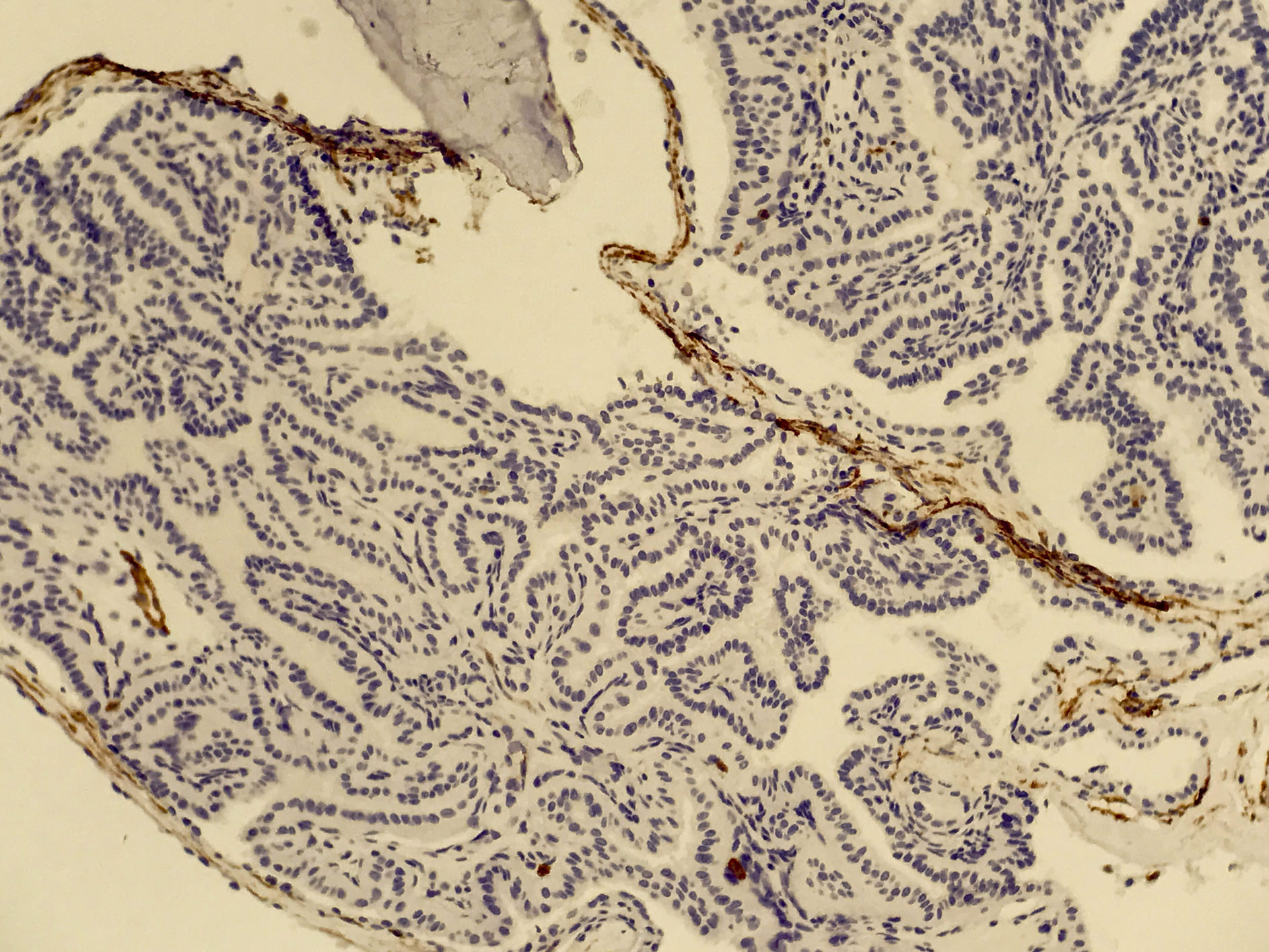
Microscopic (histologic) images
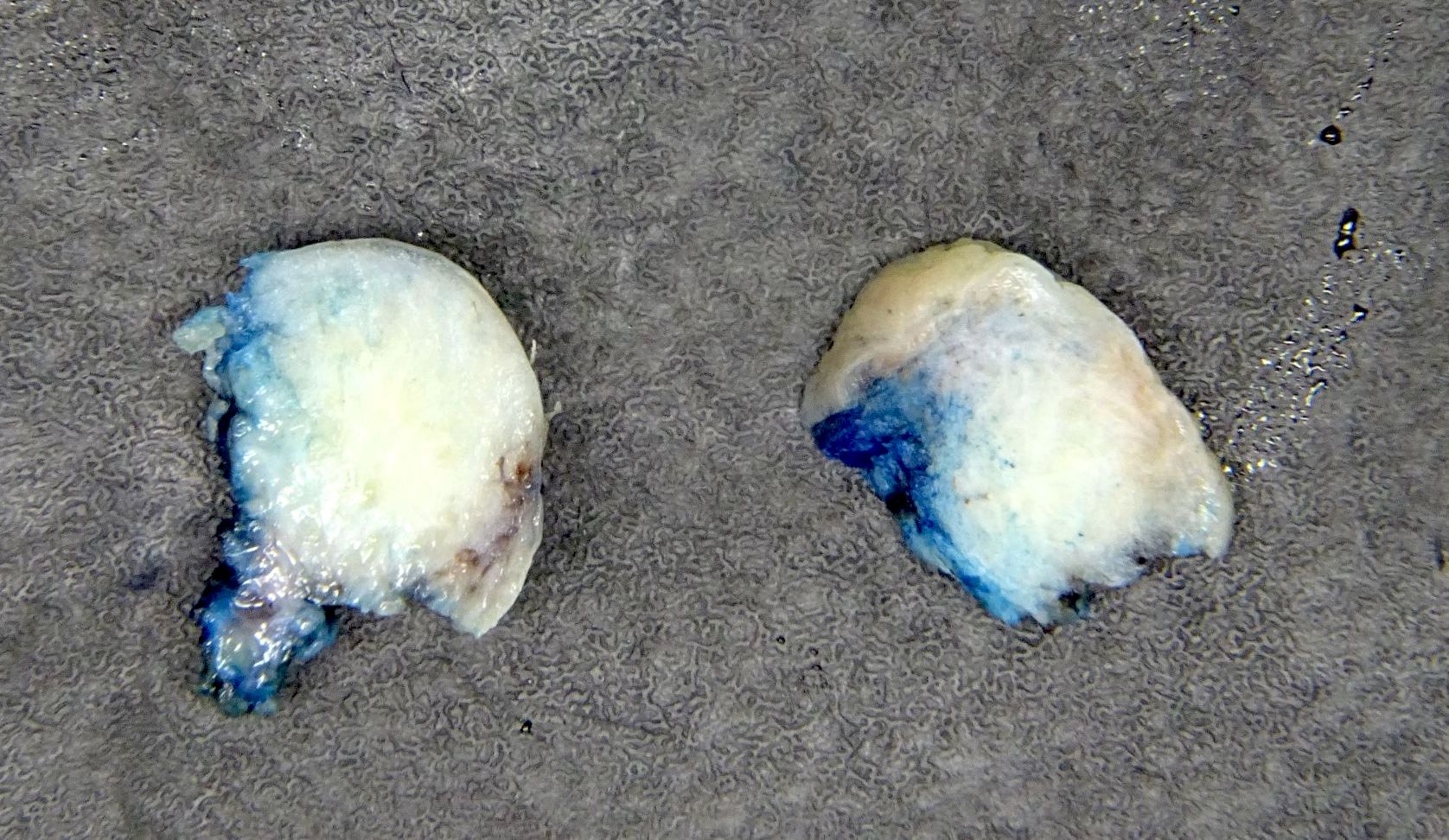
Contributed by Sepideh Nikki Asadbeigi, M.D.
Videos
Dr. Michael Lee explains the major histological features of an accessory tragus
Sample pathology report
- Skin, left ear, excision:
- Accessory tragus (see comment)
- Microscopic description: The sections reveal a pedunculated lesion covered by slightly acanthotic epidermis. At the core of the lesion, there is fibroadipose mature tissue with some adnexal structures and a fragment of cartilage. Atypia was not identified.
Differential diagnosis
- Hair follicle nevus (An Bras Dermatol 2015;90:519)
- Connective tissue framework in subcutaneous fat and numerous hair follicles are found in both entities
- Accessory tragus is differentiated by the presence of more abundant subcutaneous adipose
- Potential presence of a cartilaginous component in accessory tragus will also help distinguish between them
- Location on the anterior ear is more suggestive of accessory tragus
- Trichofolliculoma (An Bras Dermatol 2015;90:519)
- Connective tissue framework in subcutaneous fat and numerous hair follicles are found in both entities
- Will contain a central cyst and radiating hair follicles
- Potential presence of a cartilaginous component in accessory tragus will also help distinguish between them
- Auricular fistulas (Can Fam Physician 2012;58:772)
- Both may be present at birth
- These will usually present as depression or pits around the helix of ear, not a nodule anterior to the ear
- Congenital branchial cysts (Can Fam Physician 2012;58:772)
- Both may be congenital
- These are located more commonly on upper lateral aspect of neck
- Congenital branchial cysts often grow slowly over time
- When excised, may drain clear or mucinous fluid mixed with granular cellular debris
- Epidermoid cysts (Can Fam Physician 2012;58:772)
- Usually not congenital
- Can become inflamed or infected
- May express keratinized substance with cheesy consistency when excised
- True preauricular skin tag (Can Fam Physician 2012;58:772)
- Not present at birth
- Will never contain cartilage
Board review style question #1
Board review style answer #1
A. Presence of a cartilaginous core. An accessory tragus is characterized by the presence of a cartilaginous core, which is a remnant of the normal auricular cartilage. In contrast, a hair follicle nevus lacks a cartilaginous component. This histological distinction helps differentiate between the 2 entities but may not always be present in an accessory tragus. Answers B, C and D are incorrect because a dense connective tissue framework, sebaceous glands and well developed hair follicles can all be found in both entities.
Comment Here
Reference: Accessory tragi
Comment Here
Reference: Accessory tragi
Anatomy, histology & grossing
Table of Contents
Definition / general | External ear - anatomy | External ear - histology | Middle ear - anatomy | Middle ear - histology | Inner ear - anatomy | Inner ear - histology | GrossingDefinition / general
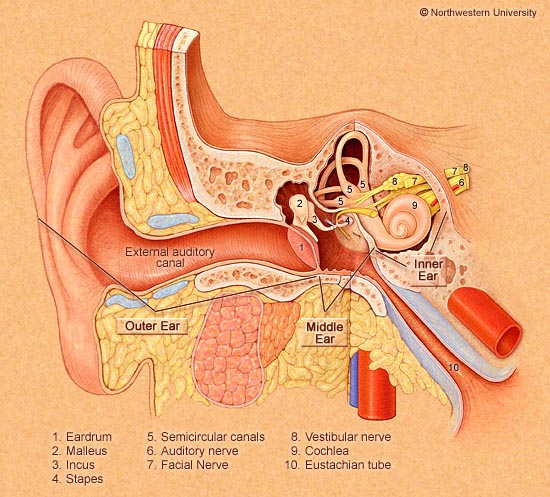
- Sense organ for hearing and balance
- Divided into external ear, middle ear and temporal bone and inner ear
- External ear conducts sound vibrations to tympanic membrane; middle ear conducts sound to auditory portion of inner ear
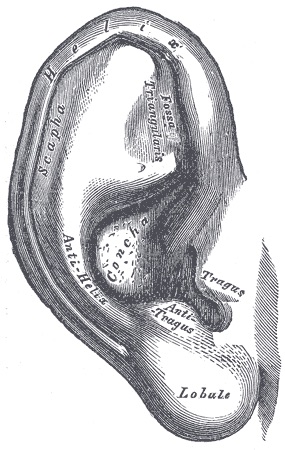
External ear - anatomy
- Consists of pinna (auricle) leading into external auditory canal which ends at tympanic membrane
- Pinna: develops from fusion of auricular hillocks, themselves from first and second branchial areas; helix is prominent rim; antihelix is prominence that is parallel with and in front of helix
- External auditory canal: S shaped passage, 2.5 cm long, develops from remnant of first branchial groove; has outer cartilaginous portion and inner osseous portion
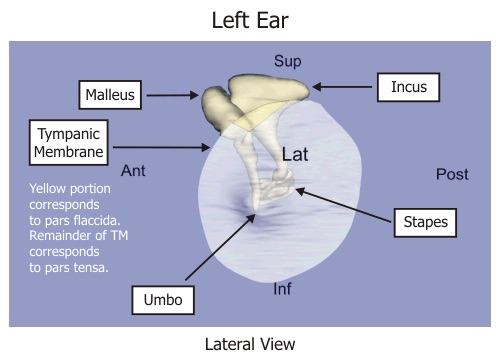
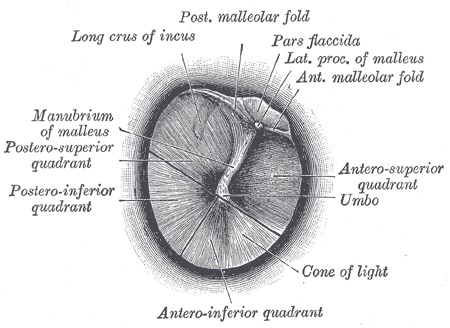
- Tympanic membrane: develops from first and second branchial pouches and first branchial groove
Diagrams / tables:
Images hosted on other servers:
External ear - histology
- Pinna: resembles skin elsewhere with keratinized, stratified squamous epithelium, dermal adnexal structures, subcutaneous fibroconnective tissue, fat and elastic fibrocartilage which provides support
- External auditory canal: lined by thin keratinized stratified squamous epithelium covering scant fibrous stroma along entire canal and covering external tympanic membrane
- Outer third contains ceruminous glands (modified apocrine glands) deep within dermis that produce cerumen; glands are in clusters of cuboidal cells with intensely eosinophilic cytoplasm with apical snouts and containing golden yellow, granular pigment and secretory droplets along luminal border; glands are surrounded by myoepithelial cells; outer canal contains cartilage not bone
- Inner two thirds has very thin epidermis which lacks rete pegs, no / reduced number of ceruminous glands and dermal adnexa; contains bone not cartilage
- Cerumen: watery fluid devoid of lipids; drains from glands into ducts which open into hair sacs of ear canal hairs; fluid mixes with sebaceous gland secretions to produce cerumen (wax)
- Tympanic cavity: thin fibrous structure lined by attenuated keratinizing squamous epithelium on external canal side
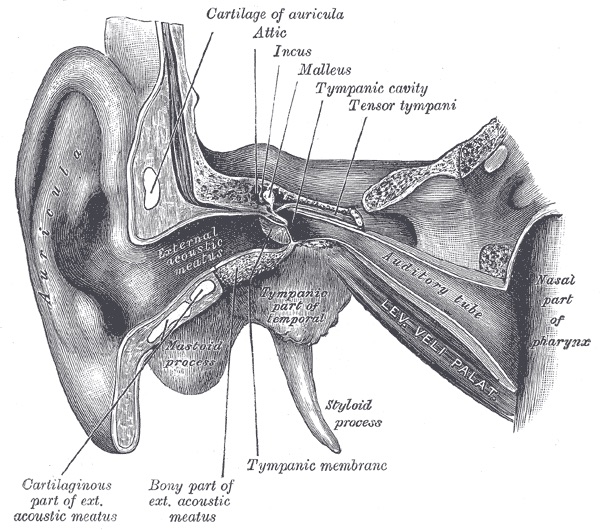
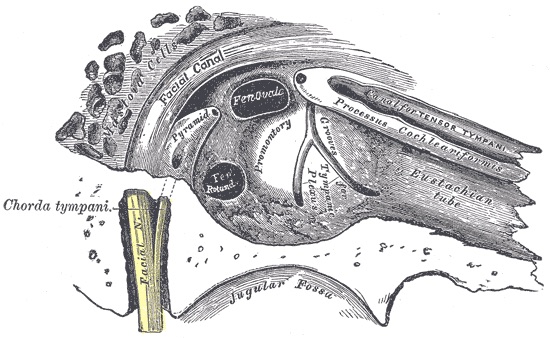
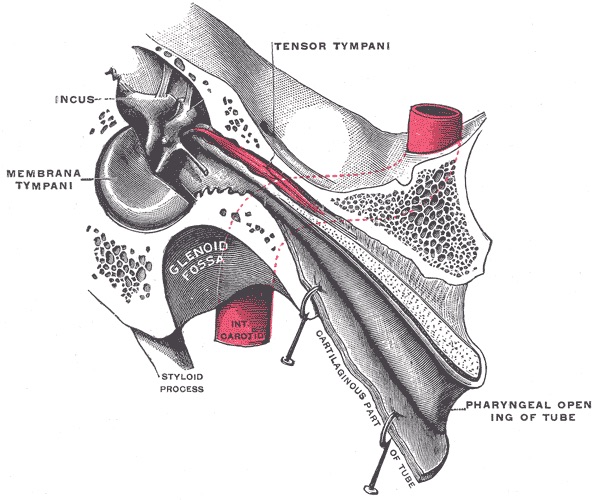
Middle ear - anatomy
- Also called tympanic cavity
- Filled with air (via eustachian tube); contains chain of movable bones which convey vibrations communicated to tympanic membrane across the middle ear cavity to the internal ear
- Lateral aspect is tympanic membrane and squamous portion of temporal bone
- Medial aspect is petrous portion of temporal bone
- Superior aspect is tegmen tympani, a thin plate of bone separating middle ear space from cranial cavity
- Inferior aspect is thin plate of bone separating tympanic cavity from superior bulb of internal jugular vein
- Anterior aspect is thin plate of bone separating tympanic cavity from carotid canal containing internal carotid artery
- Posterior aspect is petrous portion of temporal bone containing mastoid air cells and mastoid antrum
- Develops from invagination of first branchial pouch (pharyngotympanic tube) from primitive pharynx
- Contains auditory ossicles (malleus, incus, stapes), eustachian tube, tympanic cavity, epitympanic recess, mastoid cavity, chorda tympani of facial nerve (cranial nerve VII)
- Malleus and incus develop from mesoderm of first branchial arch (Meckel cartilage), stapes develops from mesoderm of second branchial arch (Reichert cartilage)
- Connects to pharynx through Eustachian tube
- Connects with mastoid cavity through contiguous pneumatic spaces
Diagrams / tables:
Images hosted on other servers:
Middle ear - histology
- Eustachian tube: respiratory epithelium that becomes pseudostratified as it approaches nasopharynx; lymphoid component, prominent in children, is called Gerlach tubal tonsil; no glands
- Tympanic membrane: thin fibrous structure lined by flat, single layer of cuboidal epithelium on middle ear side
- Mastoid: flat, single, cuboidal epithelium
- Ossicles: typical synovial joints
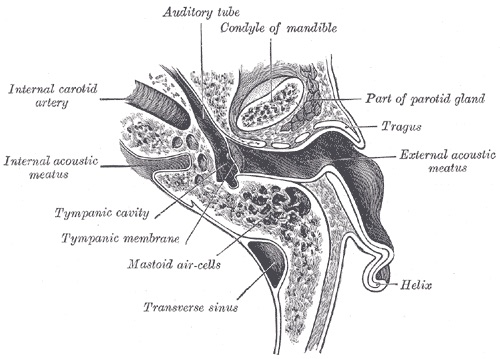
Inner ear - anatomy
- Located in medial (petrous) portion of temporal bone
- Contains cochlea (sense organ for hearing) and vestibular labyrinth (sense organ for balance with membranous and osseous portions) and internal auditory canal (contains vestibulocochlear nerve, CN VIII)
- Vestibular labyrinth contains semicircular canals, includes blind endolymphatic sac, located in petrous bone
- Endolymphatic sac is connected to utricle and saccule by endolymphatic duct which passes along petrous bone
- Develops before middle and external ear at end of first month of gestation
- References: Wikipedia: Cochlea [Accessed 4 January 2019]
Diagrams / tables:
Images hosted on other servers:
Inner ear - histology
- Vestibular labyrinth is lined by flat to low columnar epithelium overlying vascular stroma
Grossing
- Orientation is essential; may need to consult with surgeon, particularly if middle ear or inner ear tissue is present
- Must determine surgical resection margins
- Extensive decalcification may be needed
- Stapes: orient for embedding after decalcification to reveal outline of entire ossicle
Ceruminous adenocarcinoma
Table of Contents
Definition / general | Treatment | Case reports | Microscopic (histologic) description | Differential diagnosisDefinition / general
- Usually men, ages 30 - 59 years but wide age range
- Associated with local pain
- Tends to recur locally; only rarely metastasizes to regional lymph nodes and lung
- Adenoid cystic carcinoma subtypes (Eur Arch Otorhinolaryngol 1993;250:240) usually have relatively good 5 year survival, but poor 10 and 20 year survival
Treatment
- En bloc resection
- More radical surgery if middle ear or temporal bone involvement
- Radiation therapy
Case reports
- 38 year old man with ceruminous gland adenoid cystic carcinoma with contralateral metastasis to the brain (Arch Pathol Lab Med 2002;126:87)
- 54 year old man with ceruminous gland adenocarcinoma (Cancer 1978;41:545)
- 57 year old man with recurrent ceruminous adenocarcinoma of the external auditory canal (ORL J Otorhinolaryngol Relat Spec 2003;65:300)
- Patient with adenocarcinoma of ceruminous glands (Acta Morphol Hung 1991;39:157)
Microscopic (histologic) description
- Loss of glandular double cell layer as only luminal epithelial cells are present
- Pleomorphism, nuclear anaplasia, mitotic activity and invasive growth are evident except in well differentiated tumors which may resemble adenomas except for invasive growth
- Variants include adenoid cystic carcinoma and mucoepidermoid carcinoma
Differential diagnosis
- Direct extension of parotid gland tumors
- Dermal eccrine cylindroma
- Paraganglioma of middle ear
Ceruminous adenoma
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosis | Additional referencesDefinition / general
- Arise from cerumen secreting modified apocrine glands of external auditory canal
- Uncommon in general but most common external auditory canal tumor in outer portion where ceruminal glands exist
- Slightly more common in men, mean age 52 - 54 years, range 12 - 85 years
- Location of tumor (parotid gland, middle ear, external auditory canal) is important because treatment differs
- Term ceruminoma is obsolete
- Symptoms: slow growing external auditory canal mass or blockage with conductive hearing loss
Case reports
- 37 year old woman with expansion of an ceruminous adenoma into the middle ear (Laryngorhinootologie 2006;85:444)
Treatment
- Complete surgical excision
- Recurrences are due to incomplete excision
Gross description
- Skin covered, circumscribed, polypoid or rounded mass, gray-white-pink, 0.4 to 2 cm
- Usually not ulcerated
- Specimens are usually received by pathologist in small fragments without obvious surface epithelium
Microscopic (histologic) description
- Unencapsulated but well circumscribed glandular proliferations in cribriform, solid, cystic or papillary patterns
- Glands composed of inner cuboidal or columnar cells with eosinophilic cytoplasm and apical snouts (decapitation type secretion) and outer spindled myoepithelial cells with hyperchromatic nuclei
- Inner cells contain yellow-brown granular cerumen pigment
- Hyalinized stroma present
- No prominent pleomorphism or mitotic figures, no invasion or necrosis
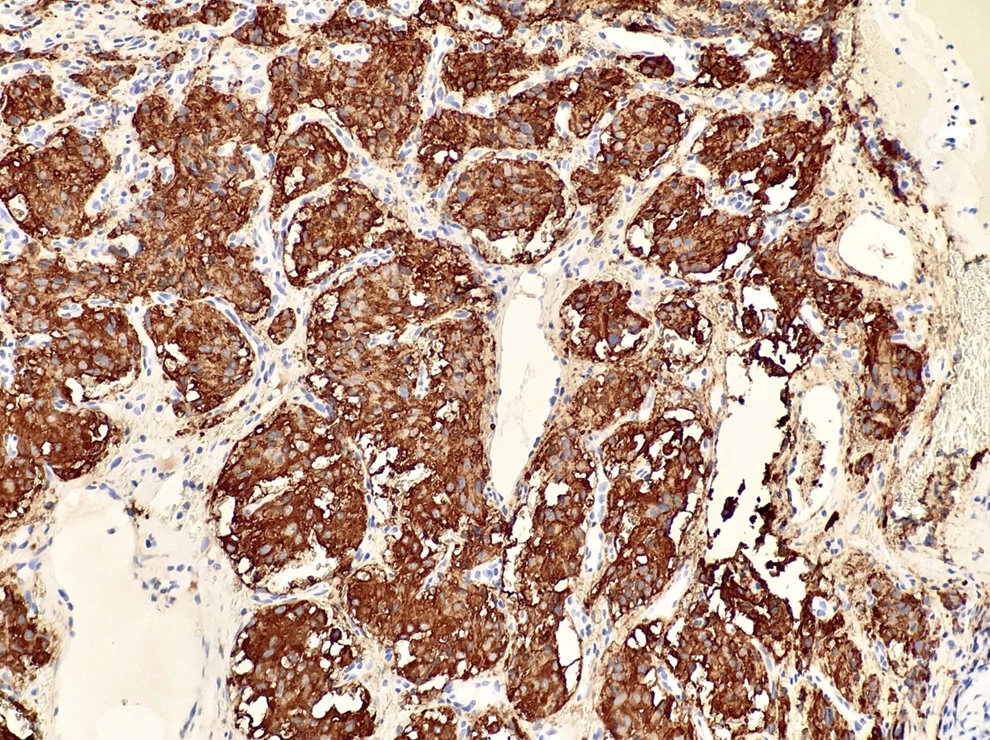
Microscopic (histologic) images
Positive stains
Differential diagnosis
- Ceruminal adenocarcinoma:
- More infiltrative; perineural invasion, irregular gland formation, pleomorphism with prominent nucleoli, increased mitotic figures including atypical mitotic figures, tumor necrosis
- Usually no ceruminous granules
- Middle ear adenoma
- Paraganglioma:
- Nested pattern of paraganglia cells supported by sustentacular cells
- Chromogranin+, S100+
- Parotid gland tumor
Additional references
Cholesteatoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Classification | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
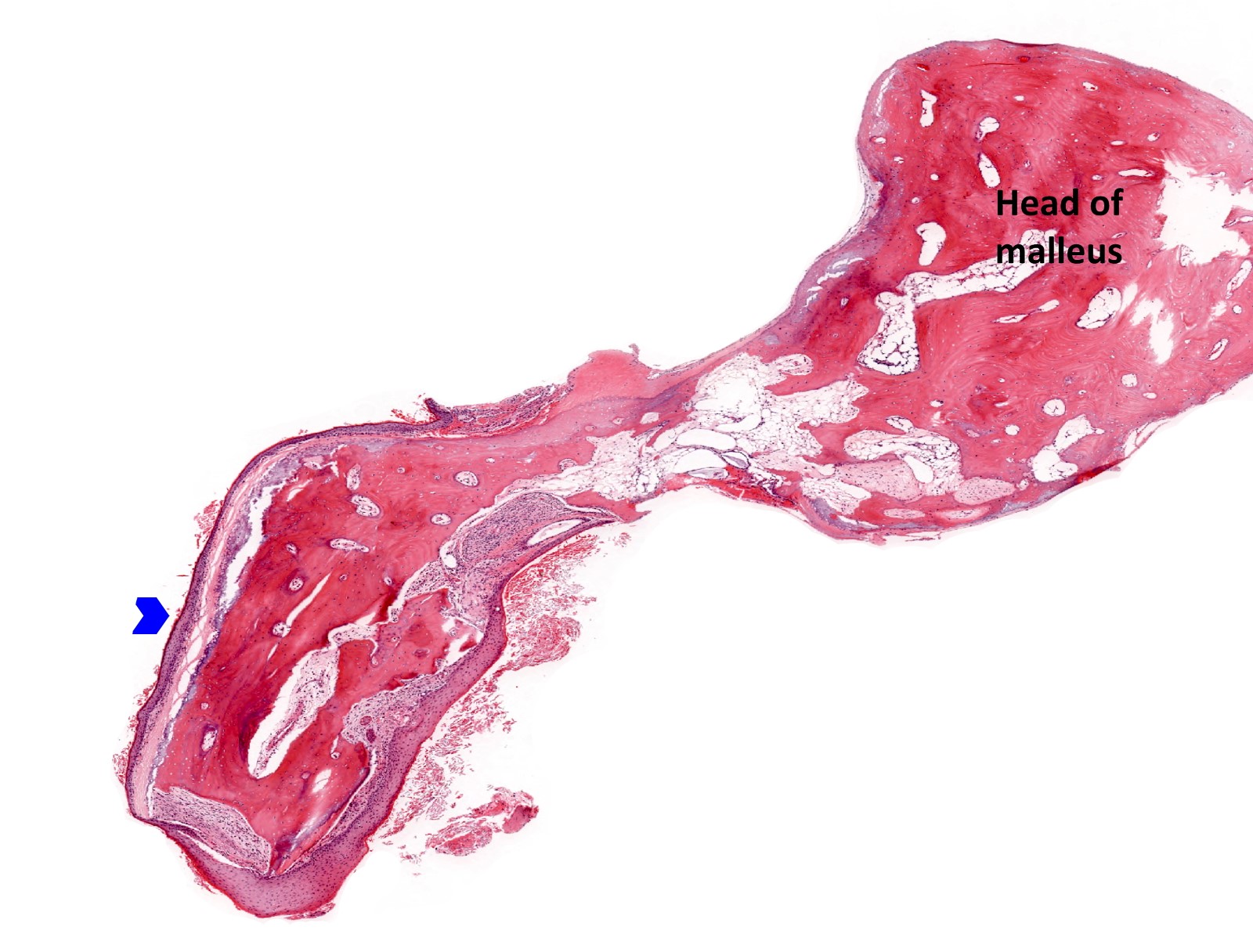
- Cholesteatoma is a benign, nonneoplastic destructive lesion in the middle ear or mastoid, most commonly unilateral
- Accumulation of keratinizing stratified squamous epithelium and keratinous debris, with stromal fibrosis and associated inflammatory reaction, leads to destruction of adjacent structures (e.g., bone) including components of ossicular chain, eventually producing clinical symptoms
Essential features
- Located in middle ear or mastoid, may involve medial external canal
- Cystic strips of nonneoplastic, nondysplastic keratinizing squamous epithelium, with a prominent granular layer, keratin debris and background stromal inflammation
- History of chronic otitis media is present in most
- 2 general forms: congenital and acquired; acquired cholesteatoma is more common than congenital cholesteatoma
- Clinical findings include expansile pearly cyst within the middle ear or mastoid cavity
- Pathophysiology is likely multifactorial and remains controversial
- Treatment is surgical but may recur locally
- Untreated cholesteatoma progresses, can become infected and can lead to conductive hearing loss and serious intracranial complications
Terminology
- Cholesteatoma (chole = cholesterol, steat = fat, oma = benign tumor) is a misnomer, as the lesion is nonneoplastic and diagnostic microscopic features do not include cholesterol or fat
- Less frequently used terms for middle ear cholesteatoma: epidermal cyst, epidermoid cysts or epidermal inclusion cyst
- Also known as keratoma, although this term can be confused with keratosis obturans, which is an external auditory canal lesion and is not typically osteolytic
- Middle ear atelectasis and retraction pockets are not considered cholesteatomas as long as they do not retain keratin debris (Otol Neurotol 2019;40:63)
ICD coding
- ICD-10: H60.41 - cholesteatoma of right external ear
Epidemiology
- Annual incidence ranges between 3 - 14 per 100,000 children and 9.2 - 13 per 100,000 adults, with slight male predilection (M:F = 1.4:1) (Acta Otolaryngol 1999;119:568, Eur Arch Otorhinolaryngol 2004;261:6)
- Incidence and detection of congenital cholesteatoma is on the rise, possibly due to technological advances (Eur Ann Otorhinolaryngol Head Neck Dis 2010;127:143)
- Due to treatment advances in otic pathology, acquired cholesteatoma is decreasing due to adequate treatment of otitis media (Eur Ann Otorhinolaryngol Head Neck Dis 2010;127:143)
- Conditions involving cleft palate or ear anomalies show increased tendency for cholesteatoma formation (Auris Nasus Larynx 2014;41:101, Int J Pediatr Otorhinolaryngol 2013;77:1403)
- Association with allergic rhinitis (Laryngoscope 2018;128:547)
Sites
- Usually the middle ear is affected with potential destruction of surrounding structures, including bone, ossicular chain, erosion into external ear, inner ear and cranial cavity
- Congenital cholesteatoma tends to arise in the superior anterior middle ear, possibly in area of tensor tympani (Eur Arch Otorhinolaryngol 2020;277:987, Head Neck Pathol 2022;16:224)
- Acquired cholesteatoma tends to arise in the superior posterior middle ear, posterior epitympanic (pars flaccida) or posterior mesotympanic (posterior superior quadrant of the pars tensa) (Braz J Otorhinolaryngol 2017;83:126)
- External ear cholesteatoma has been rarely reported and remains controversial and difficult to distinguish from keratosis obturans (J Am Acad Dermatol 2011;65:e88, Otol Neurotol 2013;34:91, Otolaryngol Head Neck Surg 2015;152:326)
Pathophysiology
- Pathophysiology of congenital and acquired cholesteatoma remains controversial
- Congenital:
- Epidermoid formation suggested as etiology; pathophysiology of cholesteatoma formation is unknown (Head Neck Pathol 2018;12:419, Pediatr Ann 2016;45:e167)
- Tensor tympani tendon suggested as etiology; pathophysiology of cholesteatoma formation is unknown (Head Neck Pathol 2022;16:224)
- Acquired (Otolaryngol Clin North Am 2006;39:1143, J Laryngol Otol 2007;121:1013, Otolaryngol Head Neck Surg 2009;140:884, J Laryngol Otol 1989;103:149, Laryngoscope 2015;125:234):
- Mechanism by which the epithelium enters the middle ear is probably via a combination of 1 or more of the proposed mechanisms below:
- Retraction theory: retraction pockets of pars flaccida (or pars tensa or both) is caused by negative pressure of the middle ear leading to cholesteatoma; during these processes, an inclusion of keratinized squamous epithelium may occur, leading in a few cases to cholesteatoma formation
- Migration theory: migration of squamous epithelium from the external surface of tympanic membrane or external canal, through a traumatic or iatrogenic defect
- Squamous metaplasia: still others believe cholesteatoma is due to middle ear metaplasia, essentially due to chronic irritation
- Basal cell hyperplasia (papillary ingrowth) theory: formation of keratin filled microcysts in the basal layer of the epithelium
- Mechanism by which the epithelium enters the middle ear is probably via a combination of 1 or more of the proposed mechanisms below:
Etiology
- Congenital cholesteatoma:
- Persistent epidermoids (Head Neck Pathol 2018;12:419, Pediatr Ann 2016;45:e167):
- Most commonly accepted etiology is an embryologic defect known as persistent epidermoids (squamous epithelium present in the fetus in middle ear mucosa adjacent to the tympanic membrane), that fail to resorb
- These structures are found on the lateral anterior superior surface of the middle ear in the temporal bones after 15 week gestation and typically disappear during the first postpartum year
- If epidermoid formations fail to resorb, they presumably continue to grow and develop into congenital cholesteatomas
- Tensor tympani tendon (Head Neck Pathol 2022;16:224):
- Histologic examination confirmed the connection between the cholesteatomatous sac and tensor tympani tendon; one group correlated imaging, intraoperative findings and histology, proposing that the tensor tympani tendon could be the primary site from which congenital cholesteatoma originates
- Persistent epidermoids (Head Neck Pathol 2018;12:419, Pediatr Ann 2016;45:e167):
- Acquired cholesteatoma can be due to recurrent otitis media, traumatic or iatrogenic tympanic membrane perforation
Clinical features
- Congenital cholesteatomas:
- Clinical appearance: white or yellow mass, may have foul odor
- Most commonly unilateral
- Age: infancy and early childhood
- Gender predilection: none
- Most common location: anterior superior quadrant of the middle ear
- Status of tympanic membrane: intact
- Otorrhea: absent
- History of otologic surgery: none
- History of otitis media: possible
- Symptoms: many asymptomatic; may vary depending on extent of disease
- Conductive hearing loss: possible
- Acquired cholesteatomas:
- Clinical appearance: white or yellow mass, may have foul odor
- Most commonly unilateral, bilateral in ~15 - 17% (Braz J Otorhinolaryngol 2017;83:126)
- Age: any, most commonly adults
- Gender predilection: slight male
- Most common location: posterior superior
- Status of tympanic membrane: intact or disrupted
- Otorrhea: present or absent
- History of otologic surgery: yes
- History of otitis media: yes, prevalence of cholesteatoma in patients with chronic otitis media 20 - 25%
- Symptoms: otalgia, conductive hearing loss, vertigo, tinnitus; may vary depending on disease extent
Classification
- Cholesteatoma is separated into 2 types: congenital and acquired
- Acquired cholesteatoma comprises the majority of cases (95 - 98%)
- One additional type, unclassifiable cholesteatoma, has been suggested, although it remains controversial
- Congenital cholesteatoma:
- Rare, 2 - 5% of cholesteatoma cases
- Presumed to be present at birth and diagnosed in childhood
- Etiology and pathophysiology debated
- Most commonly used criteria for distinction from acquired (Levenson's criteria) (Otolaryngol Clin North Am 1989;22:941):
- White mass in middle ear cavity, medial to an intact tympanic membrane
- Normal pars flaccida and pars tensa of the tympanic membrane
- No past history of otorrhea and perforations
- No prior otologic surgery
- Past history of otitis media should not be an exclusion criterion
- Acquired cholesteatoma:
- Primary acquired (PAC): usually arises in the setting of retraction of the tympanic membrane (TM), as a result of otitis media or chronic eustachian tube dysfunction; negative middle ear pressure due to eustachian tube dysfunction, poor pneumatization of the mastoid, inflammation or TM atrophy leads to TM retraction
- Arises as a diverticulum from the pars flaccida > pars tensa
- Invagination is the most accepted theory of PAC
- Progressive retraction forms a pocket resulting in disrupted normal epithelial migration and drainage of keratin debris
- As this process progresses, a cholesteatoma forms
- Secondary acquired (SA): occurs in the setting of TM perforation, with subsequent epithelial migration
- TM perforation is associated with inflammation and eustachian tube dysfunction
- Results in proliferation of keratinizing epithelium
- External canal cholesteatoma (ECC):
- ECC as a third type of acquired cholesteatoma remains controversial
- Generally occurs in older aged individuals
- Present with otorrhea and unilateral chronic pain
- Does not produce a conductive hearing loss
- Probably arises as result of a minor trauma in external ear canal, inducing an osseous defect secondary to periostitis and osteonecrosis
- Surrounding squamous epithelium will then invaginate and proliferate within the affected bone and squamous keratinized material will accumulate in the external ear canal
- Tympanic membrane generally intact
- Primary acquired (PAC): usually arises in the setting of retraction of the tympanic membrane (TM), as a result of otitis media or chronic eustachian tube dysfunction; negative middle ear pressure due to eustachian tube dysfunction, poor pneumatization of the mastoid, inflammation or TM atrophy leads to TM retraction
- Unclassified cholesteatoma:
- Cholesteatoma whose origin cannot be accurately determined; difficult to establish confidently whether the cholesteatoma is congenital or acquired
- Distinction supported by The European Academy of Otology and Neurotology and Japan Otological Society (EAONO / JOS)
Diagnosis
- Clinical symptoms (see Clinical features)
- Detailed otoscopic examination findings: most commonly pearly white masses (intact) or white-yellow debris in the middle ear
- Clinical findings during operative exploration
- Imaging measures, such as high resolution computed tomography (HRCT) and in some cases, non echo planar diffusion weighted magnetic resonance imaging (MRI)
- Pure tone and speech audiogram essential
- Histopathology additionally supports the diagnosis
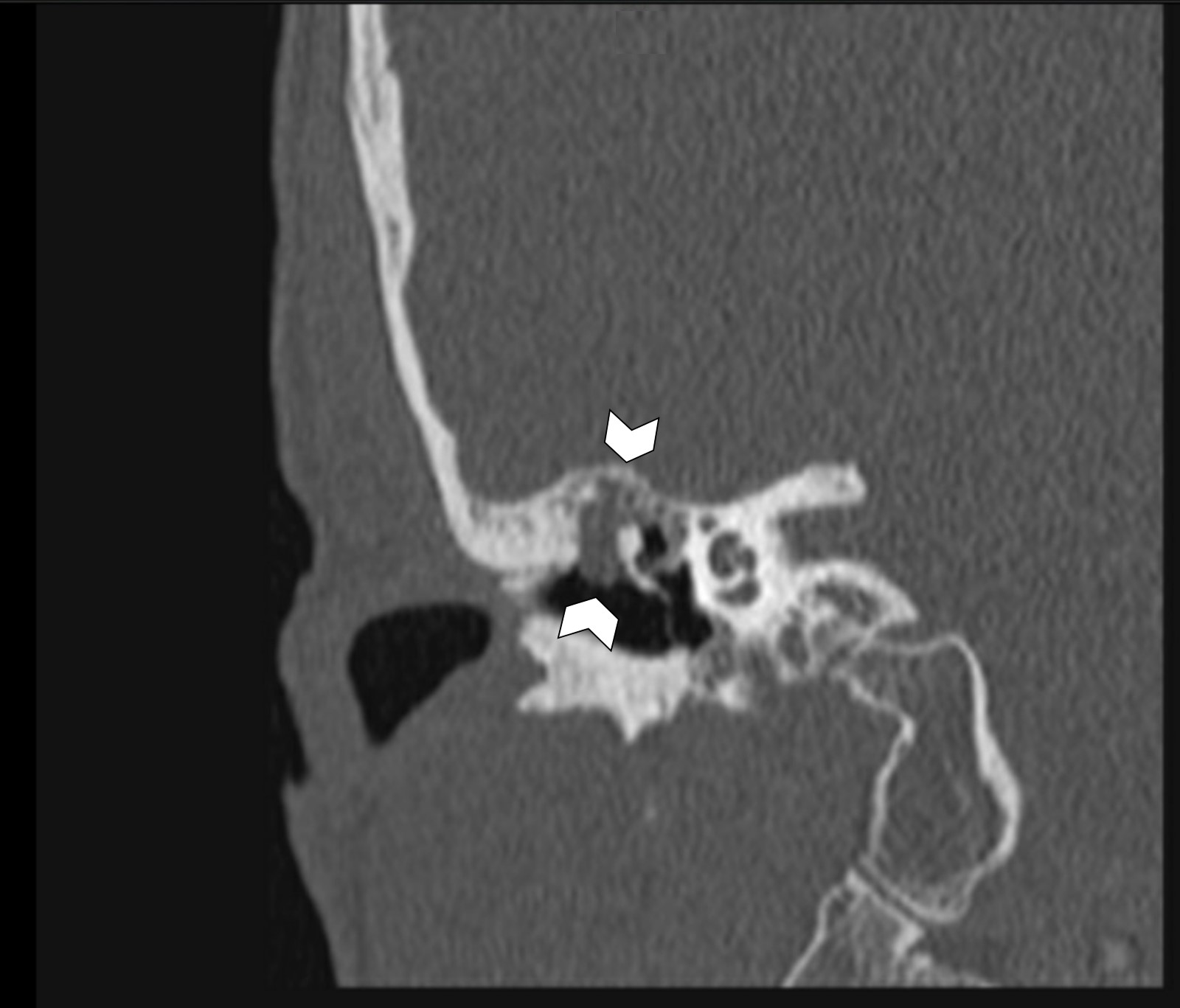
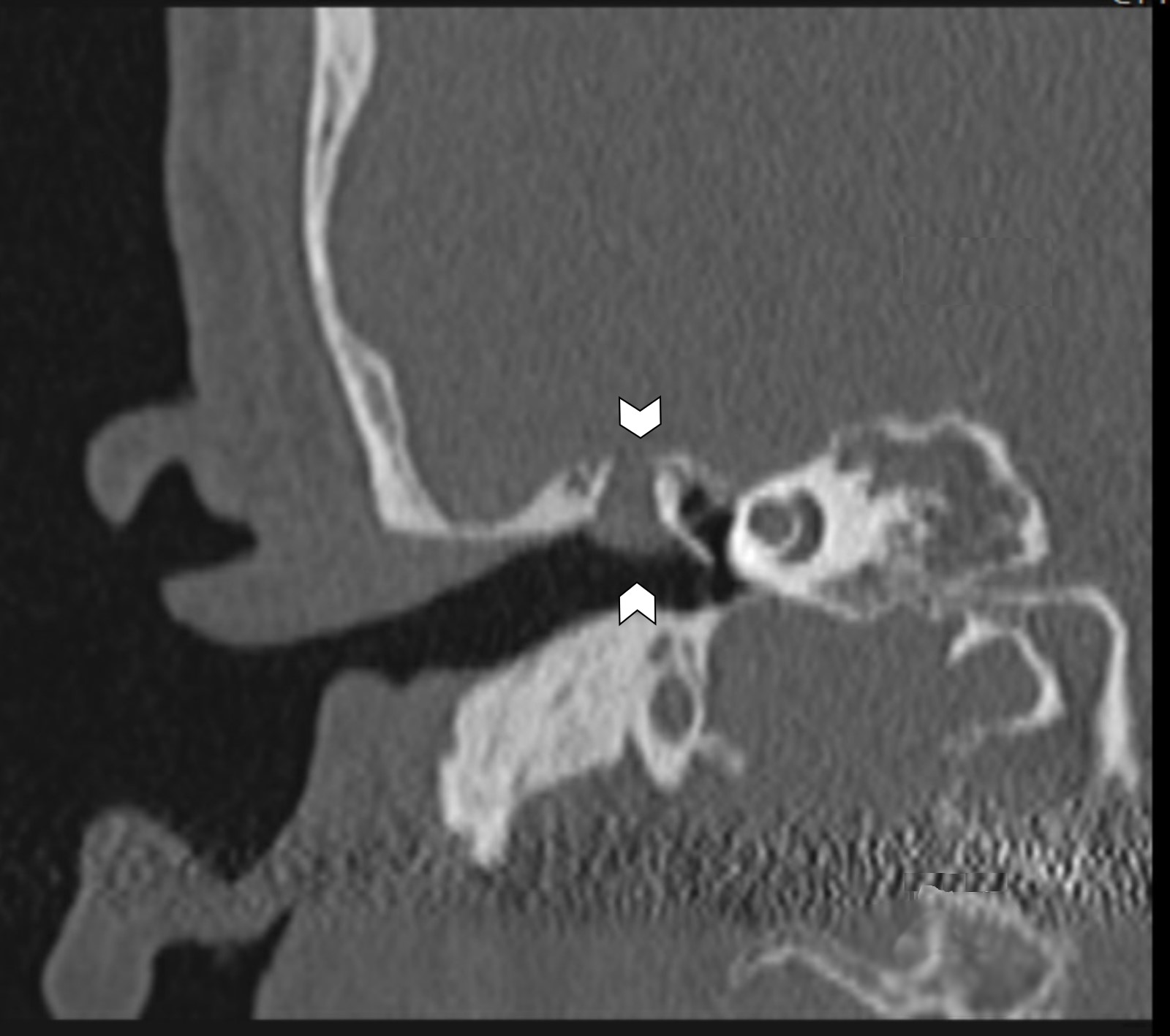
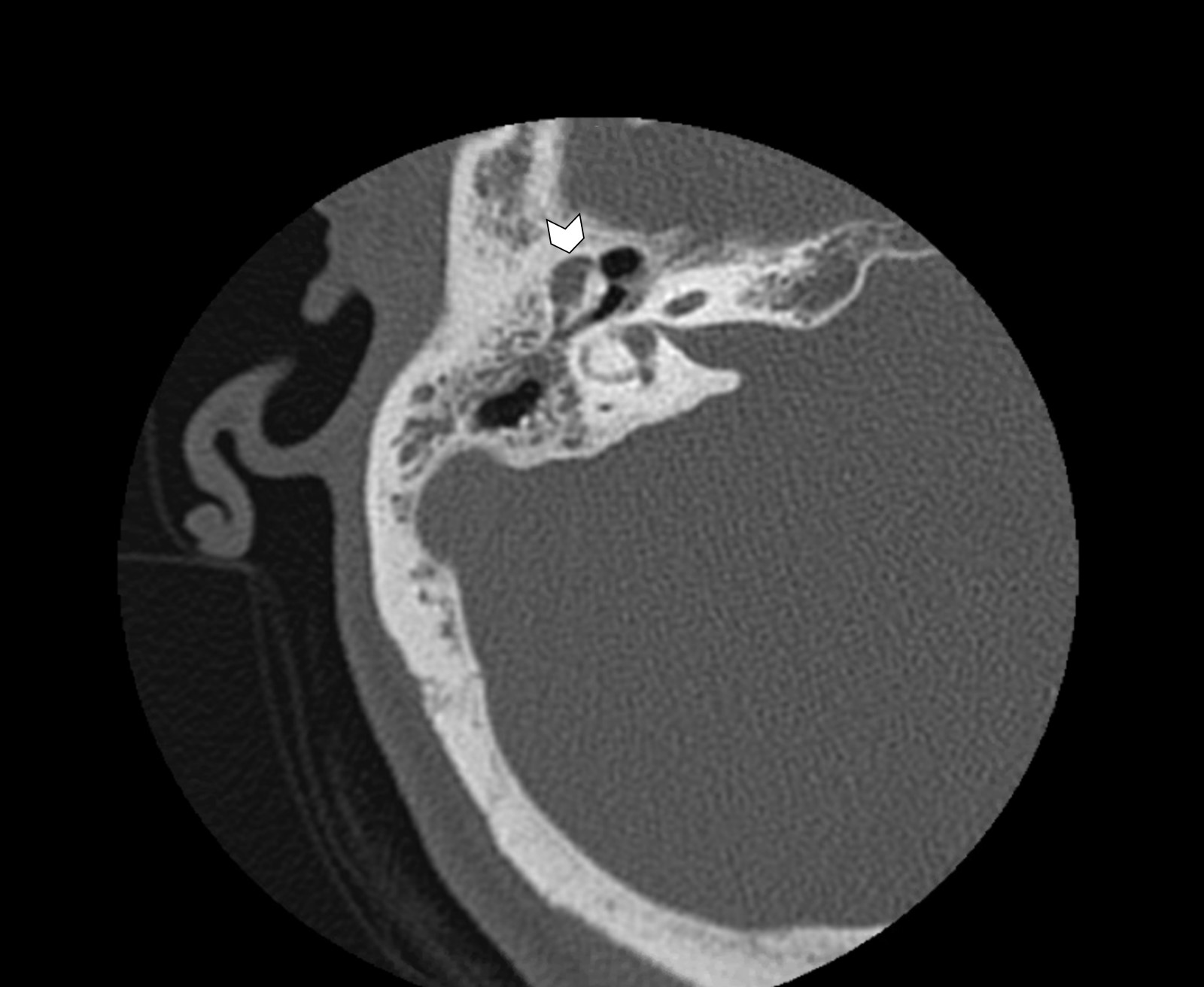
Radiology description
- Radiology essential to identify landmarks and the extent of disease in the preoperative and follow up setting
- CT and MRI are complementary studies for cholesteatoma
- High resolution CT highlights abnormalities of the thin and complex bony structures, provides precise localization of the opacity and assessment of postsurgical or congenital additional temporal bone anomalies
- Sharply demarcated, nonenhancing mass in Prussak space, with retraction of the tympanic membrane and erosion of the ossicles is common
- Likelihood of cholesteatoma increases when the soft tissue opacity is nondependent
- Blunting or erosion of the scutum is a common finding (bony prominence in the lateral portion of the middle ear and superior portion of the external auditory canal)
- CT has high sensitivity but low specificity for cholesteatoma and is not capable of differentiating between granulation, fibrous tissue, fluid and cholesteatoma (Pol J Radiol 2022;87:e51)
- MRI displays spatial relationships and has the ability to differentiate soft tissues and fluid in the middle ear and mastoid; specifically, non echo planar based, diffusion weighted MRI has been shown to have a high reliability in detecting cholesteatoma, particularly recurrence (Pol J Radiol 2022;87:e51)
Prognostic factors
- Hearing loss and tinnitus are the most reported postoperative complaints
- Prognosis and potential for complications influenced by elements such as (Eur Arch Otorhinolaryngol 2022 Apr 10 [Epub ahead of print]):
- Ossicular chain status
- Ossicular chain reconstruction
- Extension of cholesteatoma
- Labyrinthine fistula (abnormal communication between the inner ear and the middle / mastoid cavity) (Front Neurol 2022;13:804915)
- Infection or abscess
- Cranial nerve dysfunction:
- Facial paralysis (Acta Otolaryngol 2022;142:30)
- Loss of taste (Otol Neurotol 2022;43:e582)
- Residual disease: cholesteatoma extension to the sinus tympani or widespread in the mastoid, as well as absence of the stapes superstructure, were predictive of residual disease (Braz J Otorhinolaryngol 2020;86:201, Otol Neurotol 2022;43:472)
- Recurrence (Int Arch Otorhinolaryngol 2020;24:e18, J Laryngol Otol 2022;136:119):
- 15 - 20% in adults
- 35 - 40% in children
- Young age and low tegmen is associated with increased risk
- Discharging ear in preoperative state
- Marked ossicular chain erosion or destruction
- Polypoid mucosal disease or extensive disease and mastoid involvement
- Chronic otorrhoea and reperforation are most common signs of late recurrences
- Squamous cell carcinoma, arising in association with cholesteatoma, remains a controversial topic and would be regarded as exceptionally rare (J Neurol Surg Rep 2022;83:e13)
Case reports
- 23 year old man with a parotid gland cholesteatoma (SAGE Open Med Case Rep 2017;5:2050313X17749083)
- 25 year old woman with progressive hearing loss and blocked sensation in left ear for 1.5 months and past history of myringoplasty (Iran J Otorhinolaryngol 2019;31:311)
- 45 year old woman with 8 months of left ear pain and swelling (J Clin Diagn Res 2017;11:ED08)
- 56 year old man with cholesteatoma originating in the sella turcica (Medicine (Baltimore) 2016;95:e2938)
- 67 year old man with temporomandibular joint symptoms as first manifestation of external auditory canal cholesteatoma (Ann Med Surg (Lond) 2022;74:103287)
- 82 year old diabetic woman with sphenoid sinus cholesteatoma (Clin Med Insights Case Rep 2019;12:1179547619835182)
Treatment
- Treatment of cholesteatoma is surgical
- Surgical objectives: total removal of disease and optimal hearing restoration
- Complete removal is essential to minimize risk of residual pathology and prevent recurrent disease (Otol Neurotol 2019;40:63)
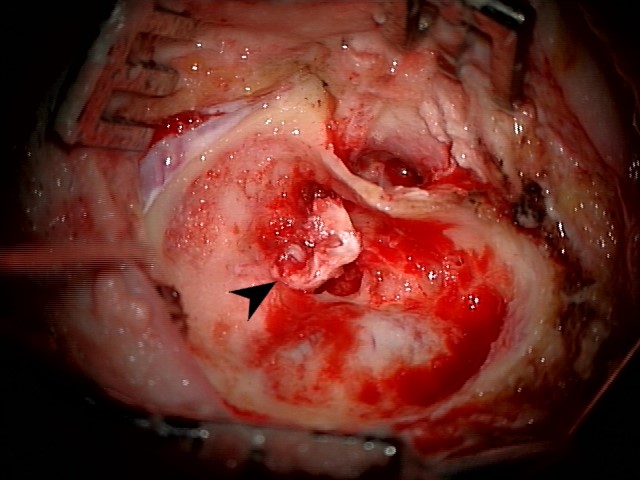
Clinical images
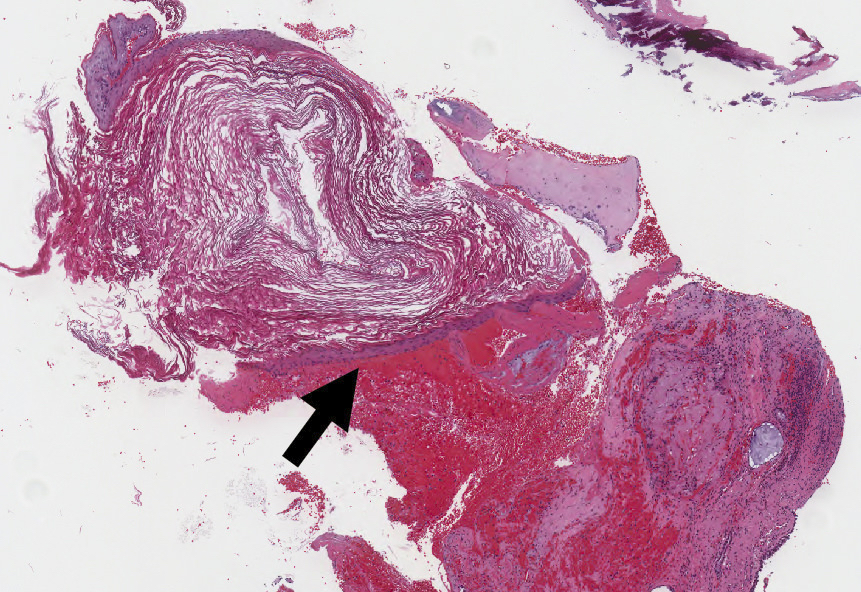
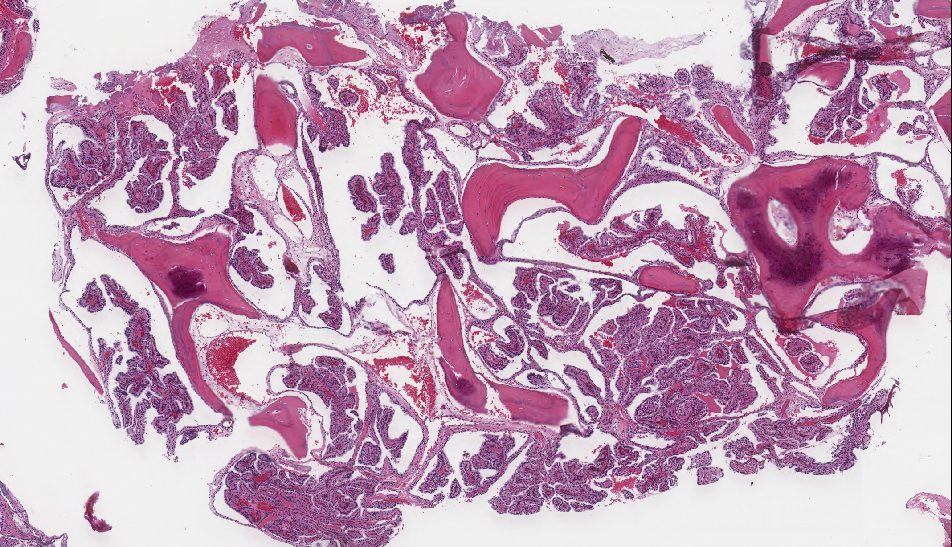
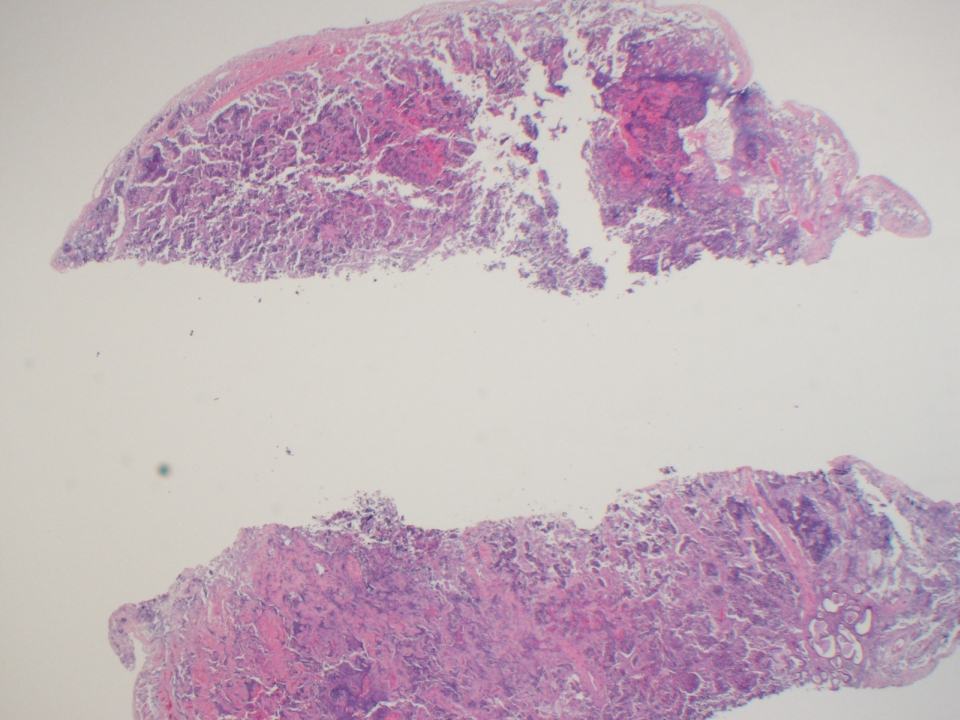
Gross description
- Cholesteatoma rarely intact after surgical removal
- Surgical specimens usually consist of multiple, irregular, gray-white to yellow fragments
- Innumerable minute, detached white flakes (keratin debris) within specimen container
- Possible minute bone fragments
- All tissue should be submitted for histologic examination to definitively confirm the diagnosis
Frozen section description
- Abundant detached anucleate keratin, keratinizing stratified squamous epithelium and inflamed fibrous connective tissue stroma components appear similar to that identified in routine processing
Frozen section images
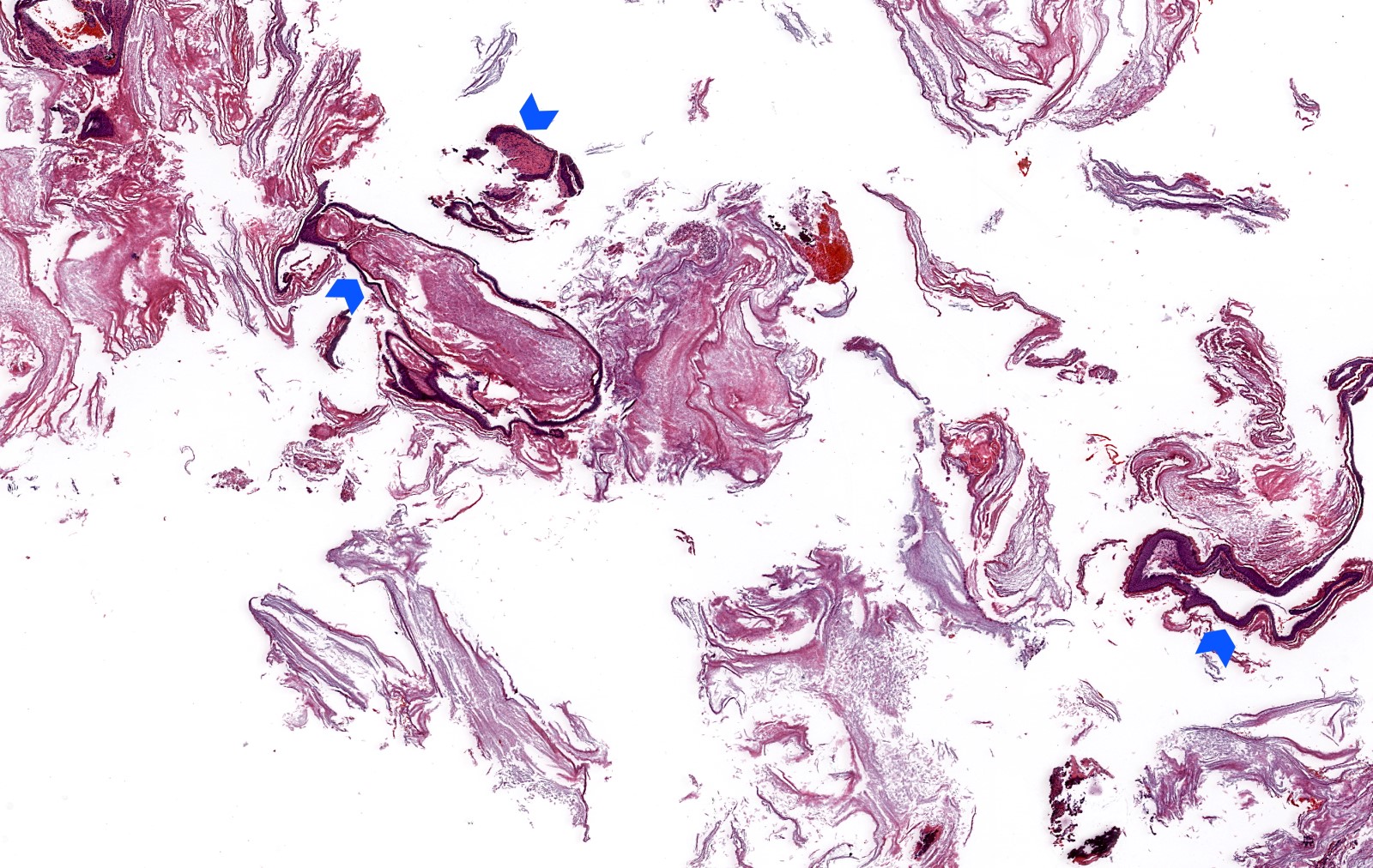
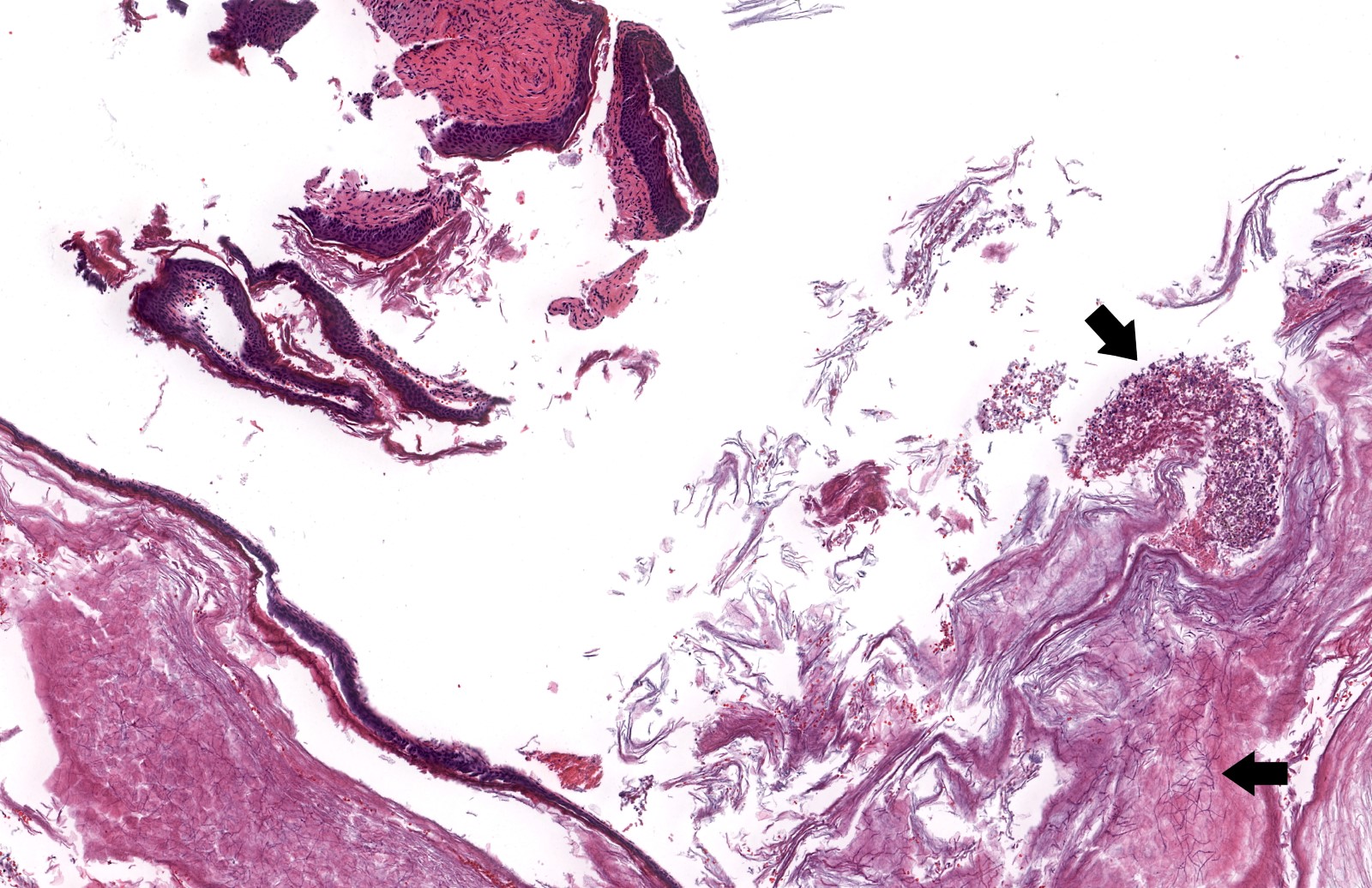
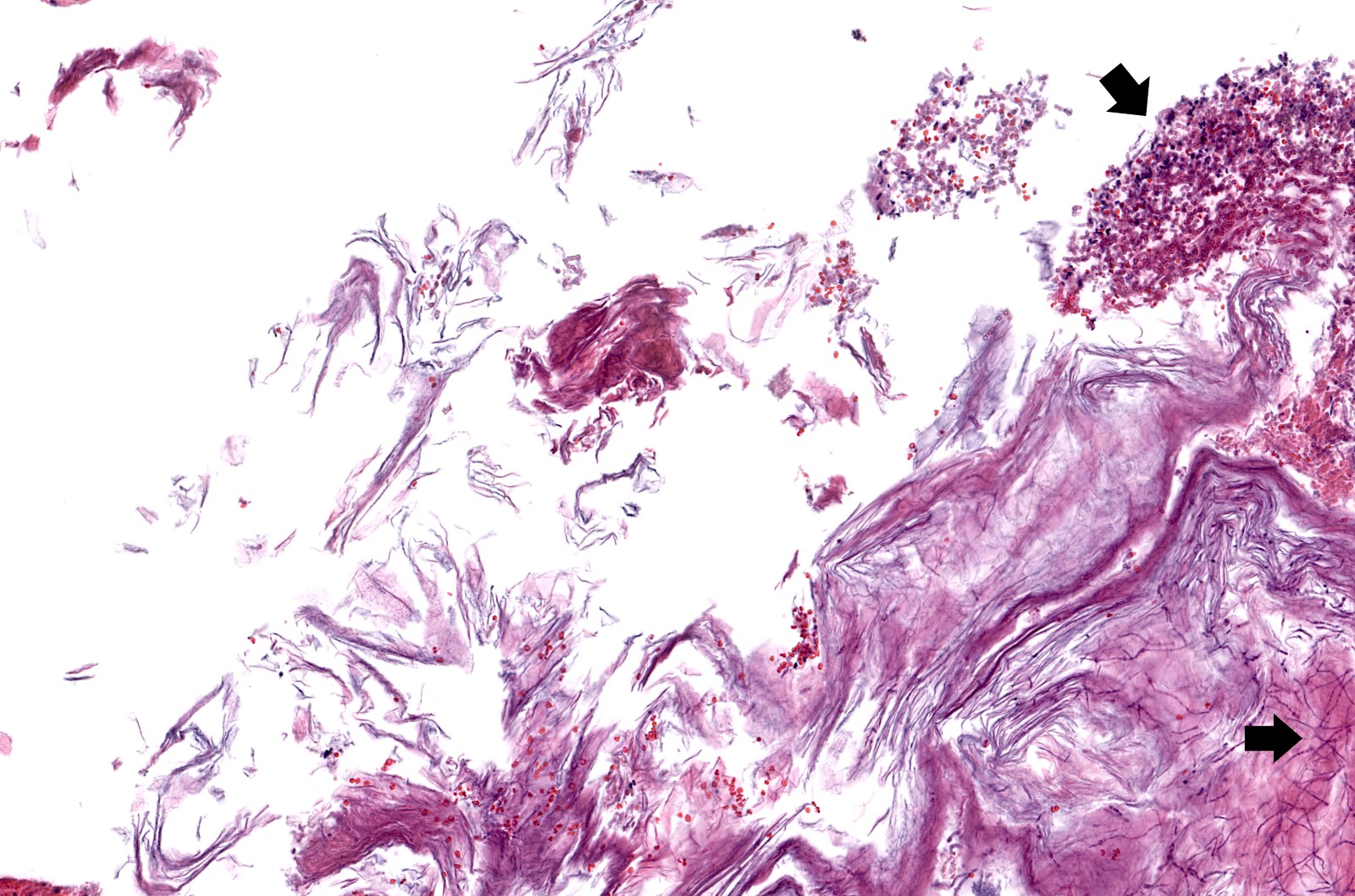
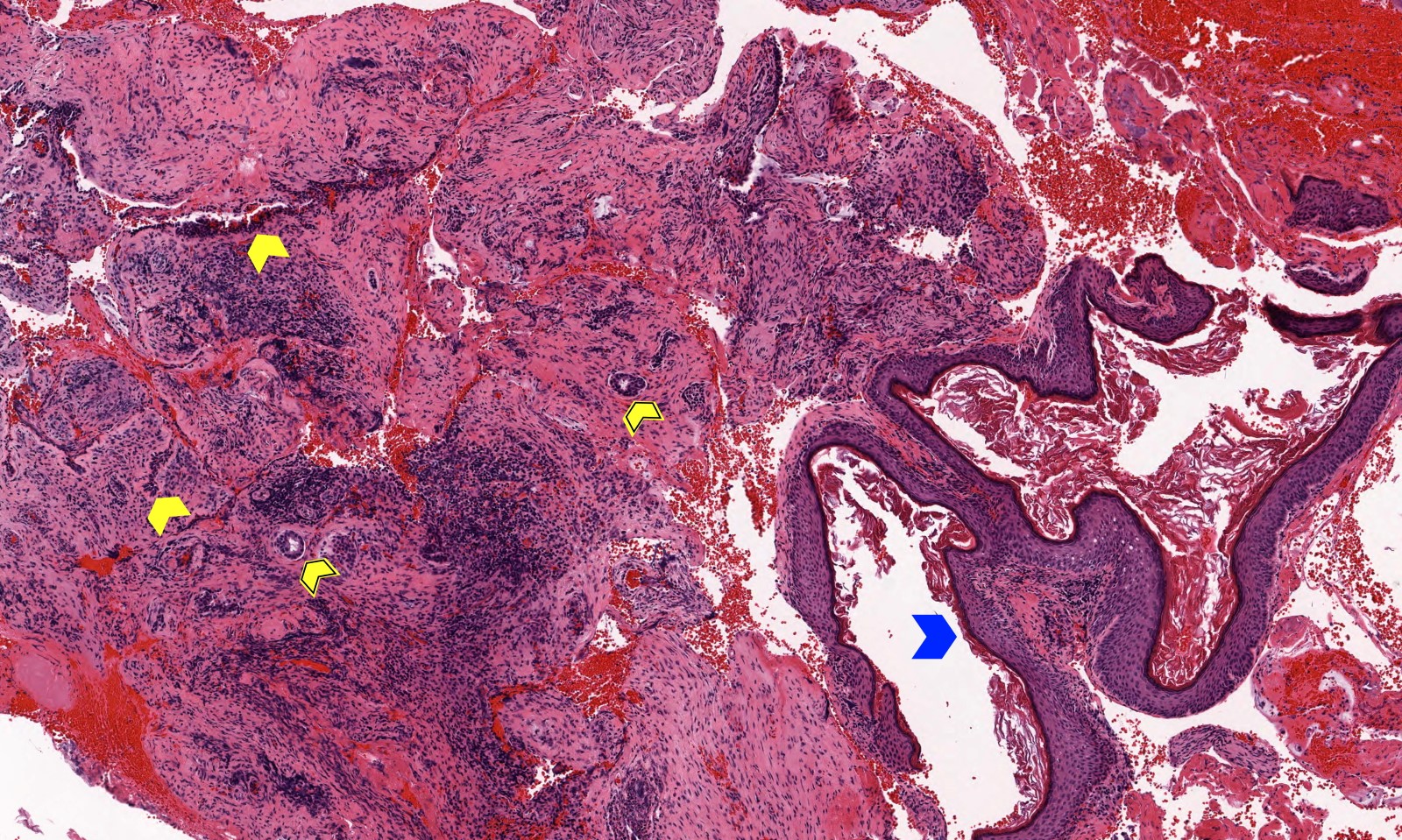
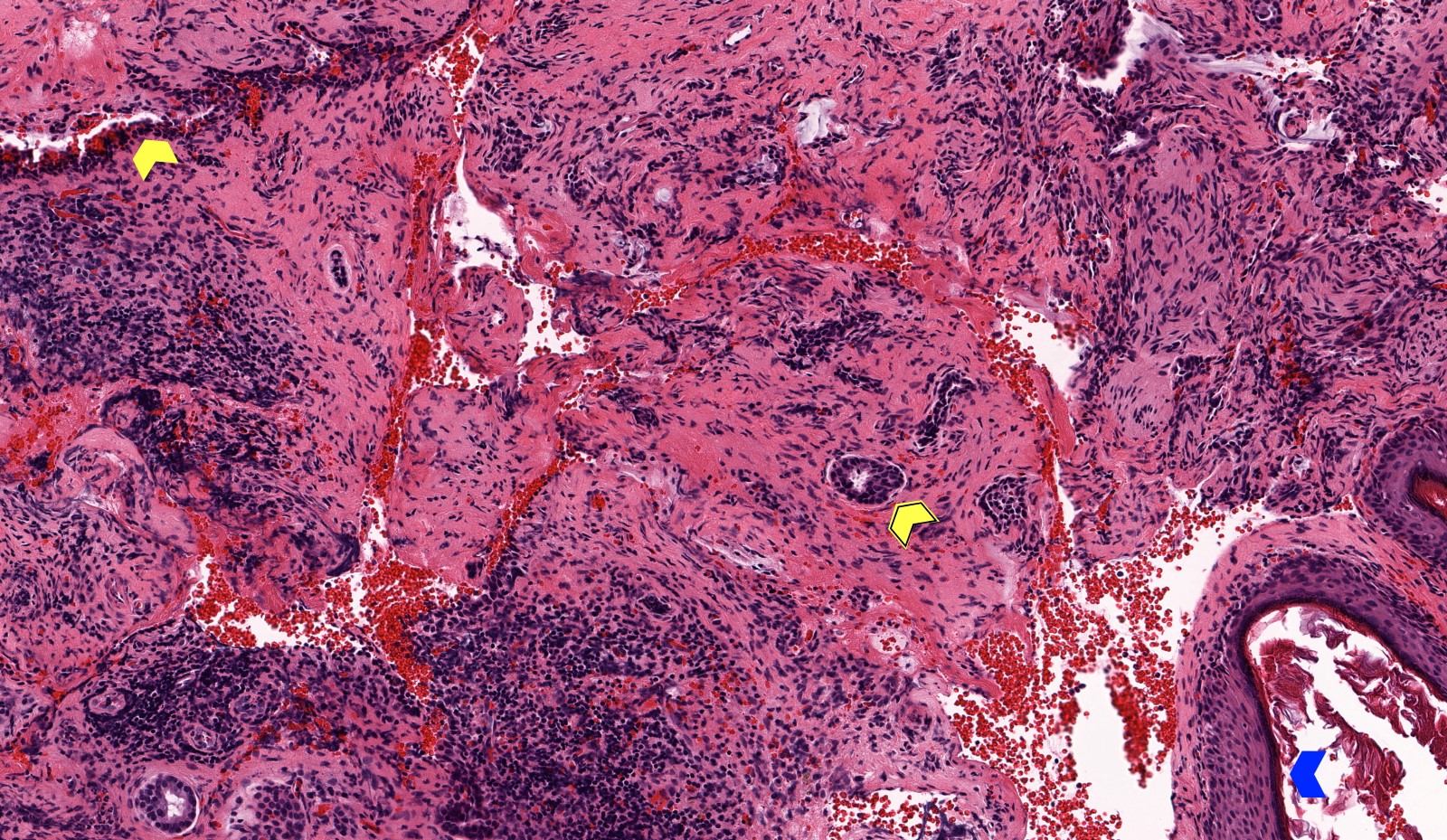
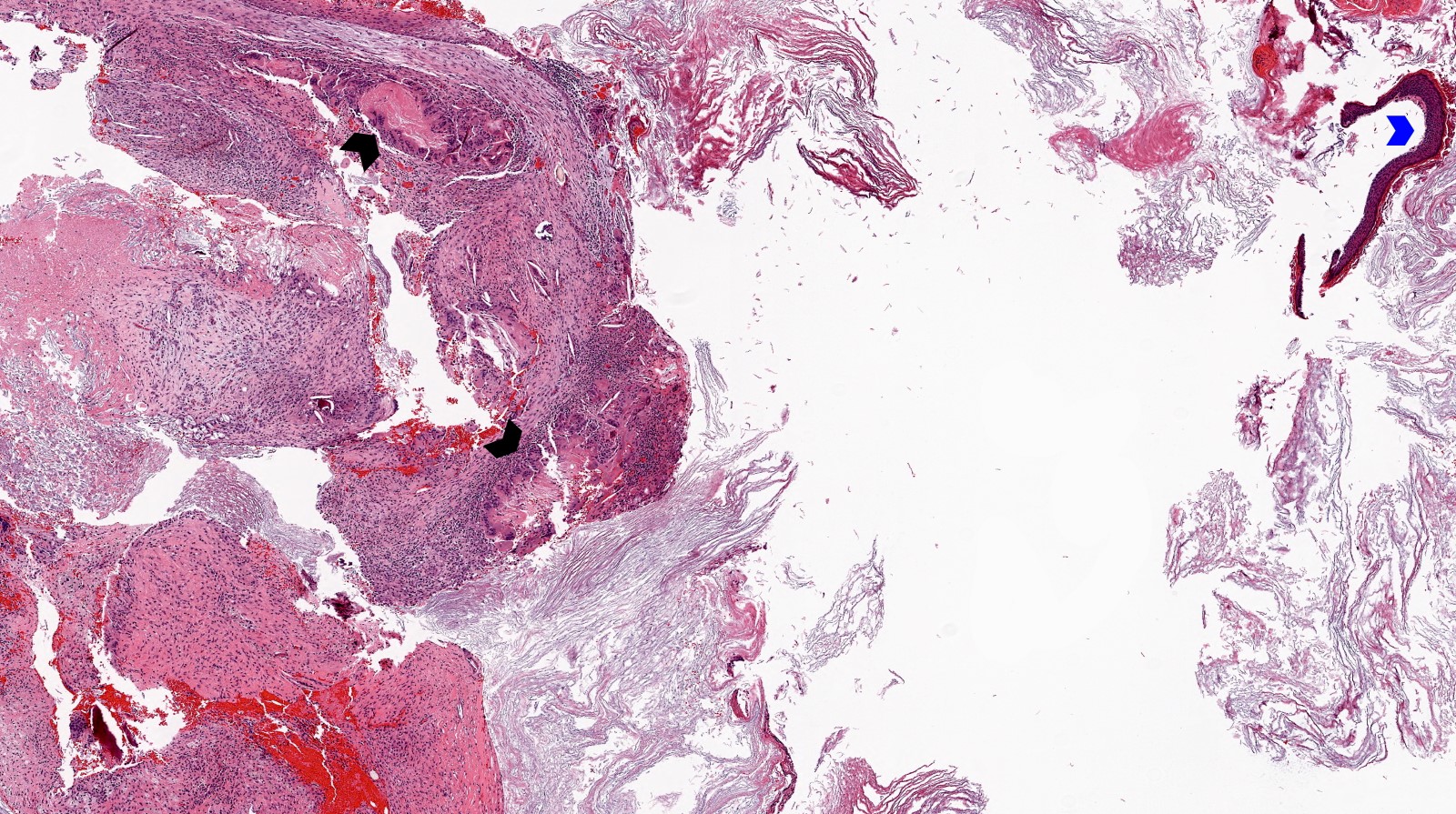
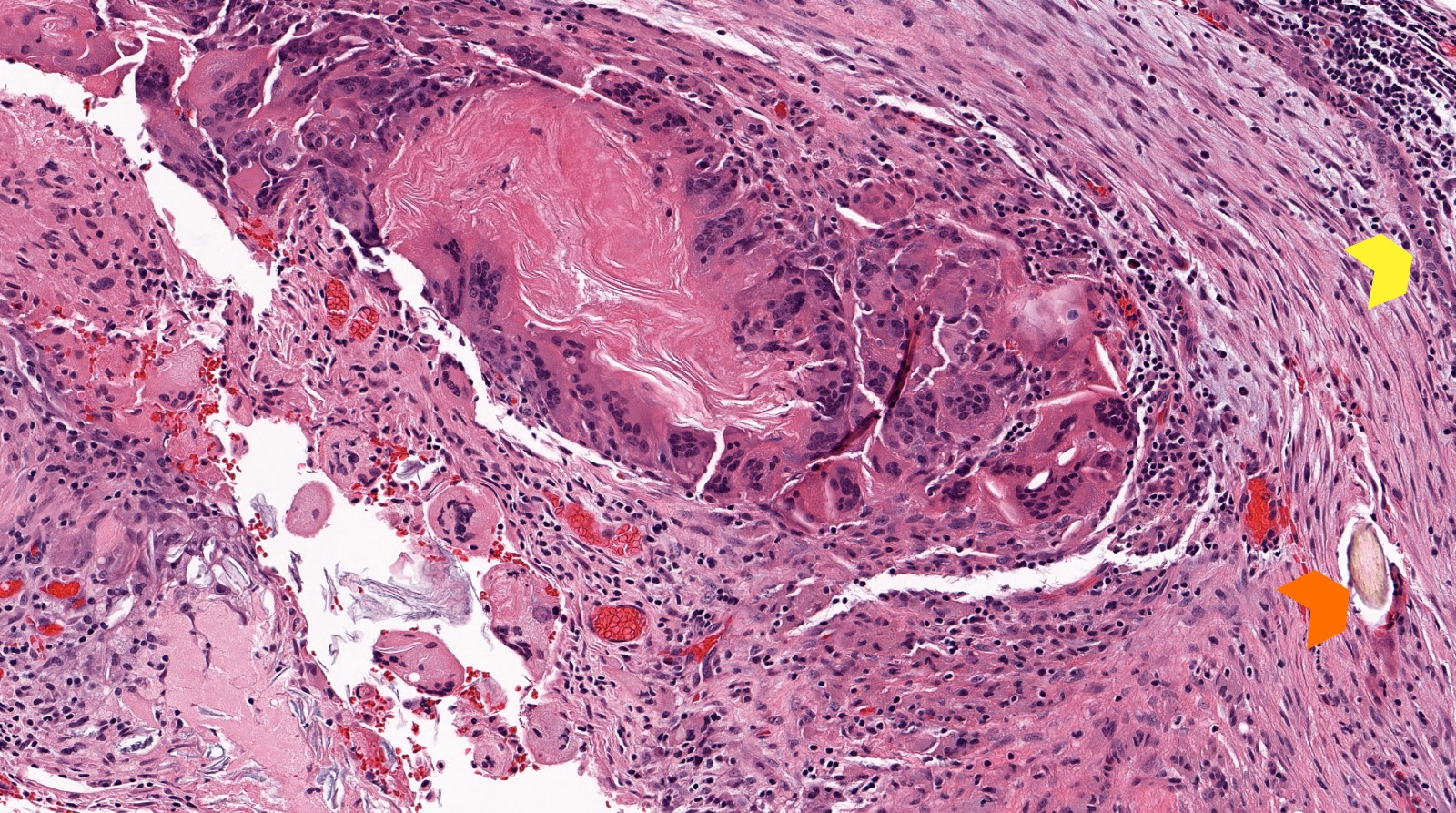
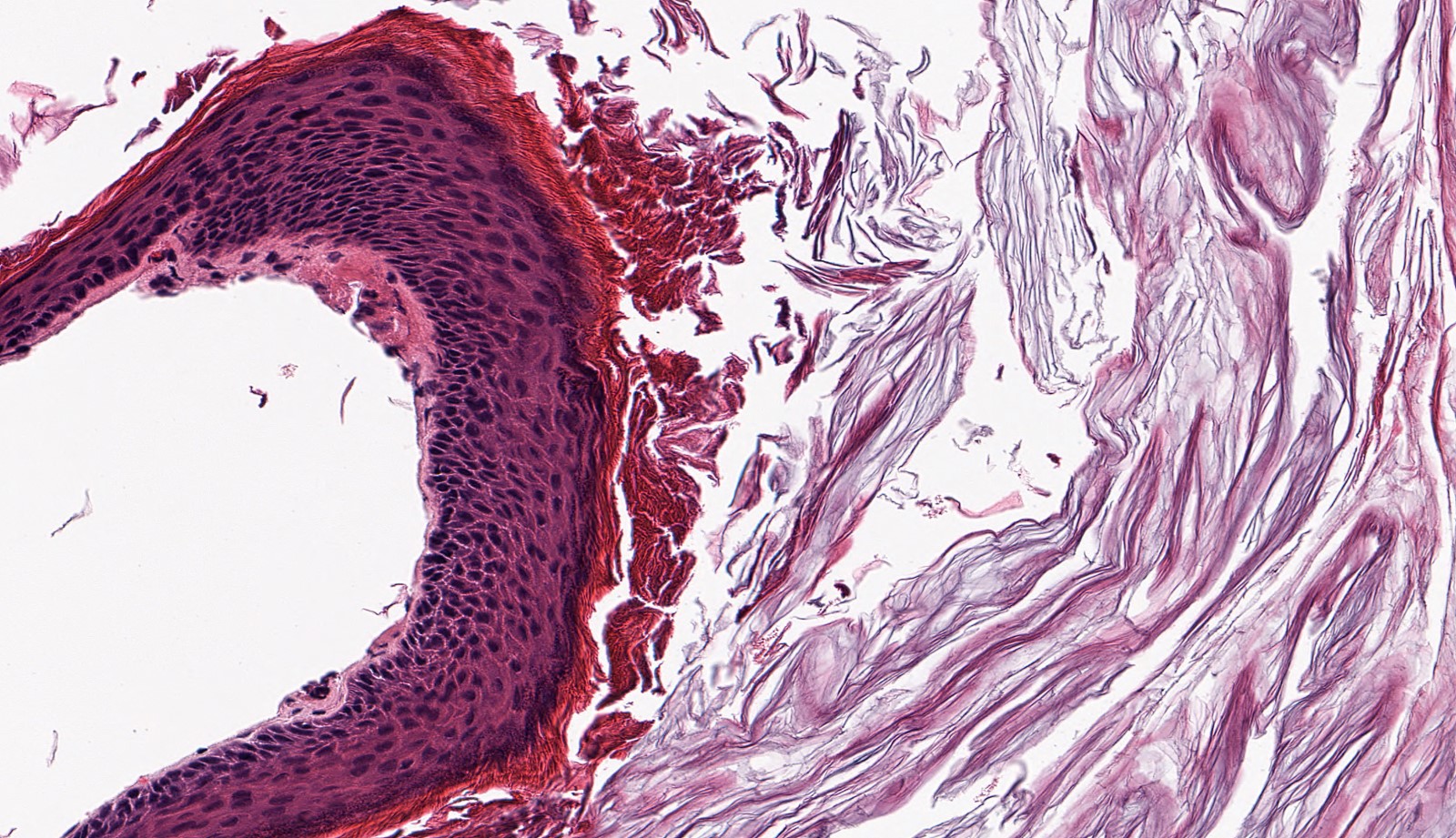
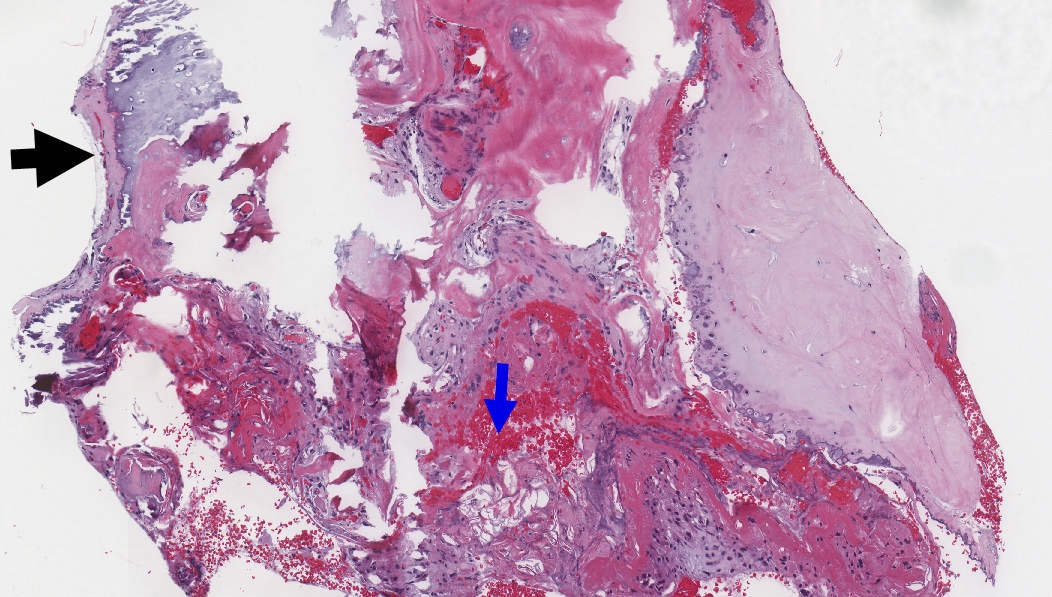
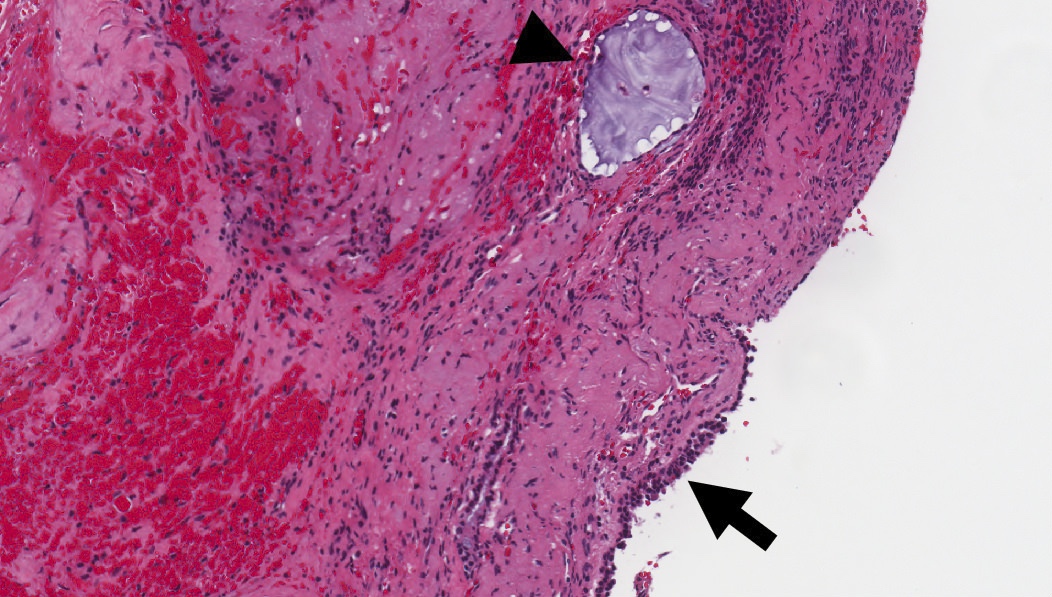
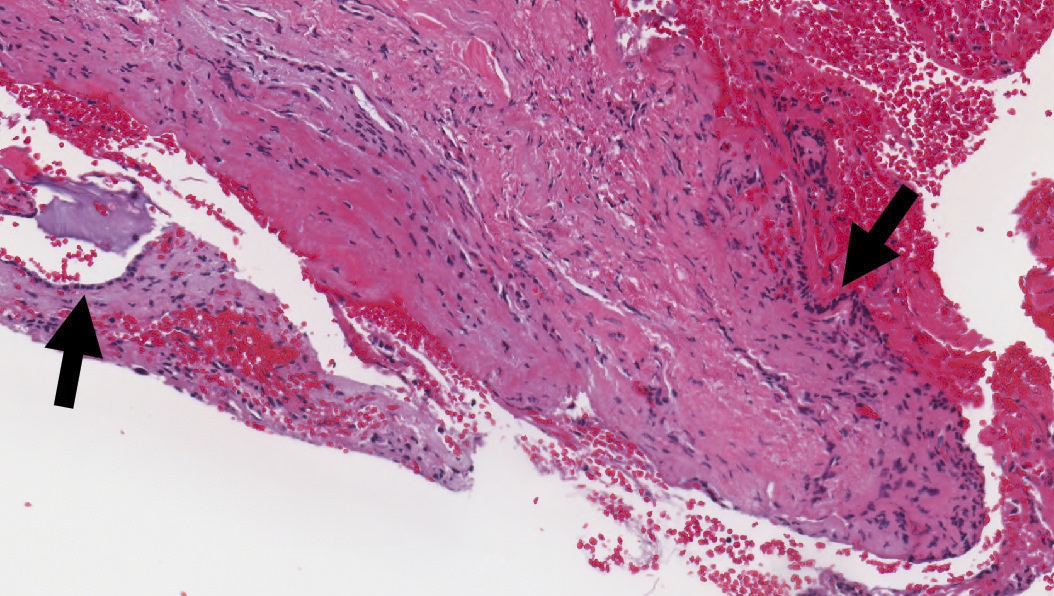
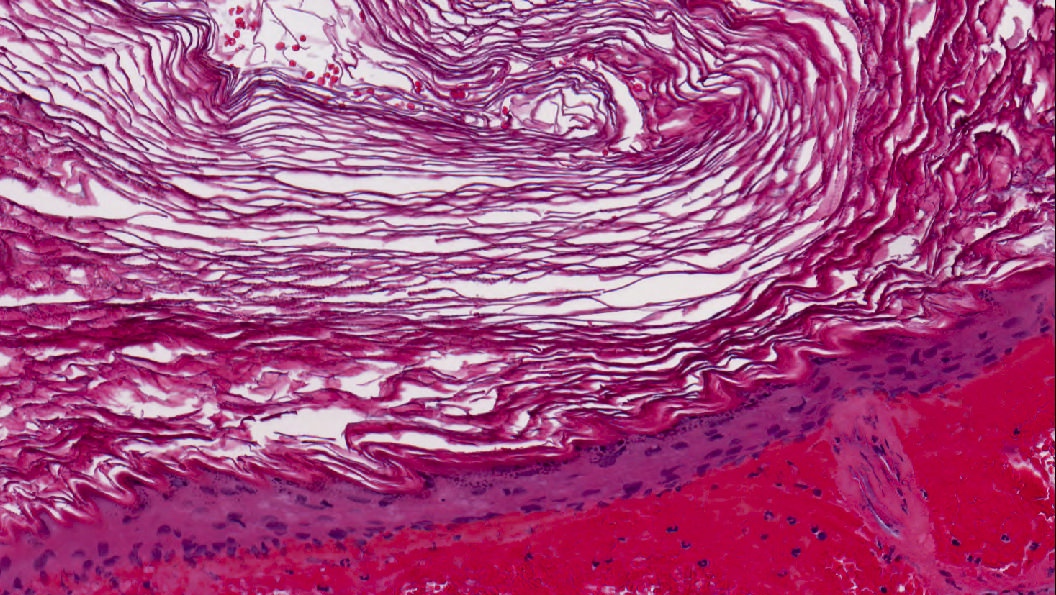
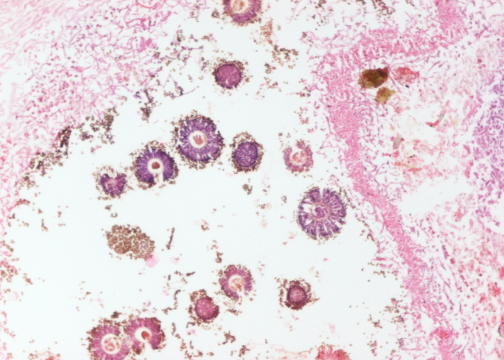
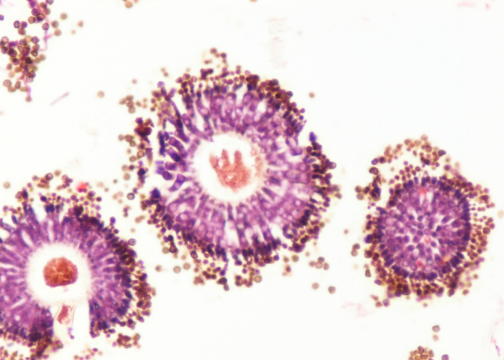
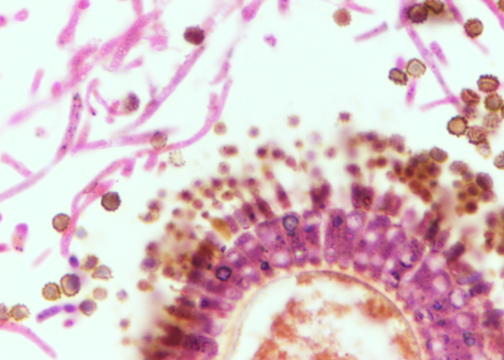
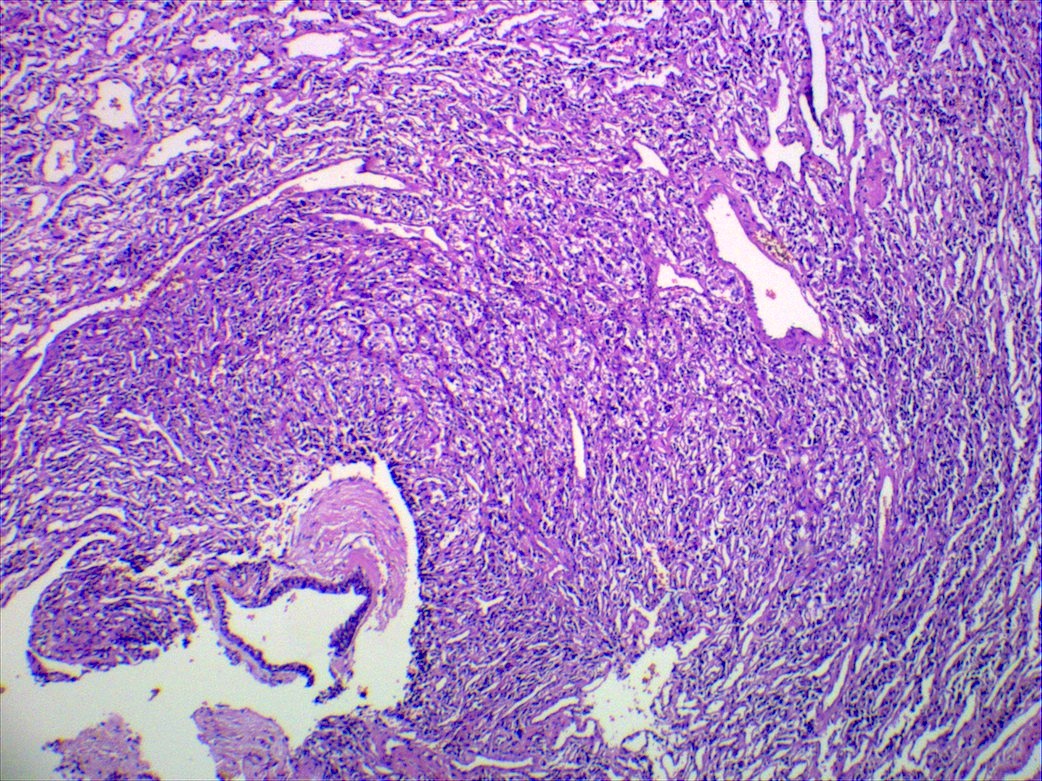
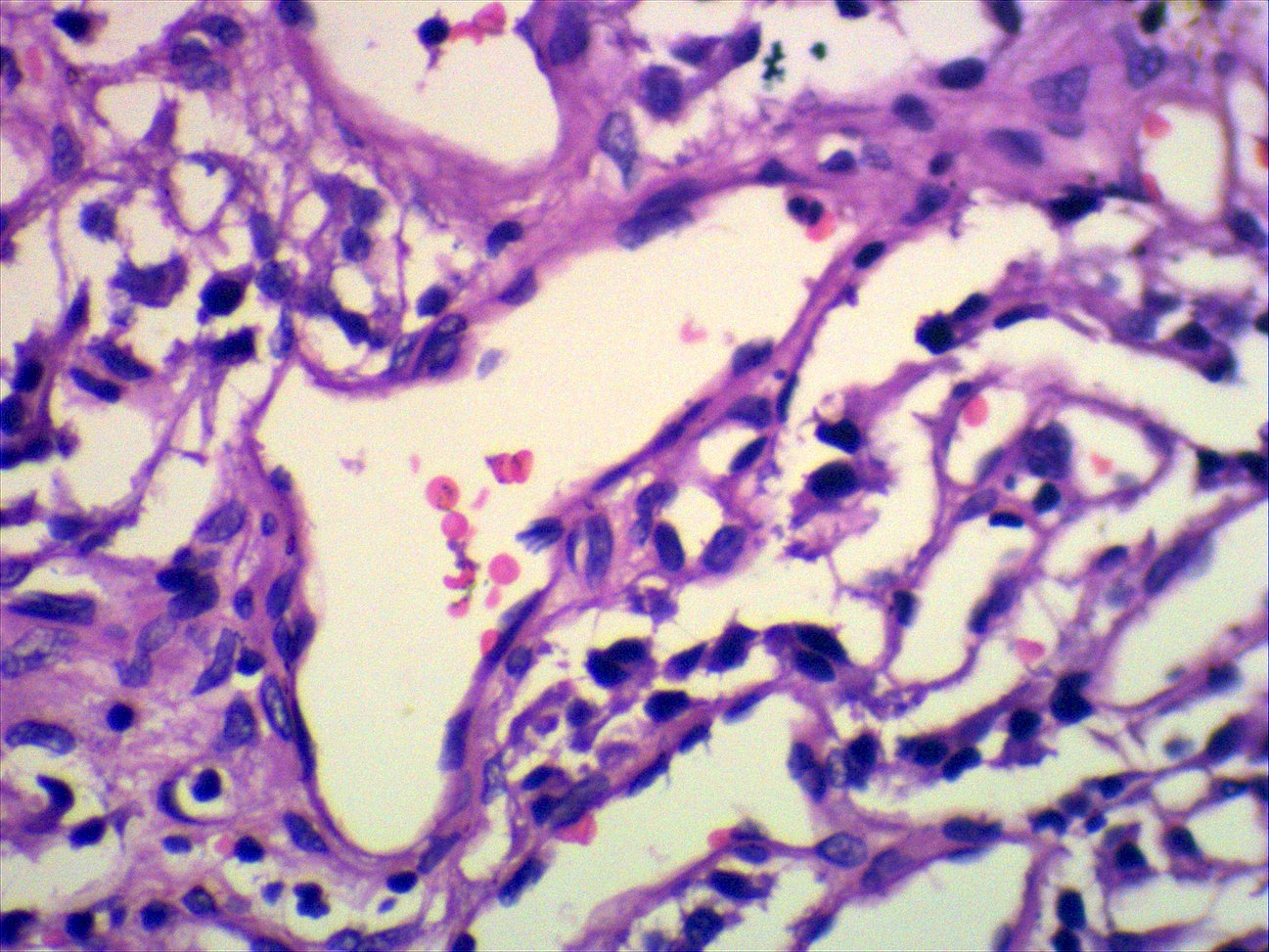
Microscopic (histologic) description
- Normal histology of the middle ear epithelium includes cuboidal or columnar glandular epithelium
- If the specimen unequivocally originates from the middle ear, then any squamous epithelium is abnormal
- Diagnosis rests on the presence of 3 key components:
- Keratinous material (anucleate keratin squamous)
- Clinically, commonly referred to as cyst content
- Abundant detached anucleate keratin, can be laminated or disorganized aggregates
- May show bacteria or fungal overgrowth
- Note: the presence of keratin debris alone is not diagnostic of a cholesteatoma and should be interpreted with caution
- Keratinizing stratified squamous epithelium
- Also known as matrix (clinically synonymous term)
- Prominent granular layer and absent rete pegs
- Cellular maturation and lack of any significant atypia
- Inflamed fibrous connective tissue stroma
- Also known as perimatrix (clinically synonymous term)
- May be middle ear mucosa included
- Infiltrate is usually comprised of lymphocytes, plasma cells, histiocytes and mast cells
- Foreign body type giant cells to keratin debris common
- Cholesterol clefts may be seen
- Keratinous material (anucleate keratin squamous)
- Incidental findings possible:
- Cholesterol granuloma, otic polyp, tympanosclerosis, acquired encephalocele and paraganglioma
- Reference: Head Neck Pathol 2018;12:419
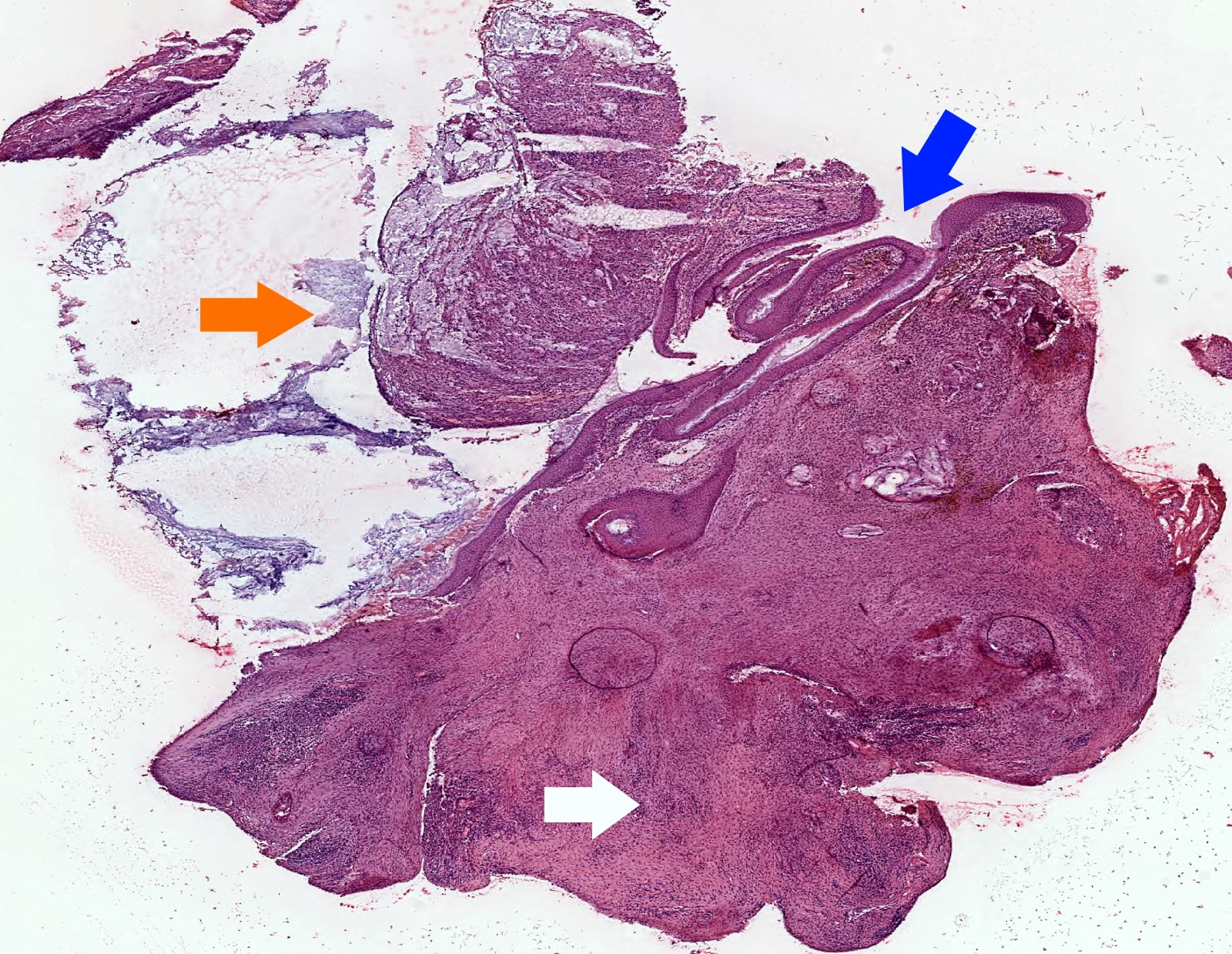
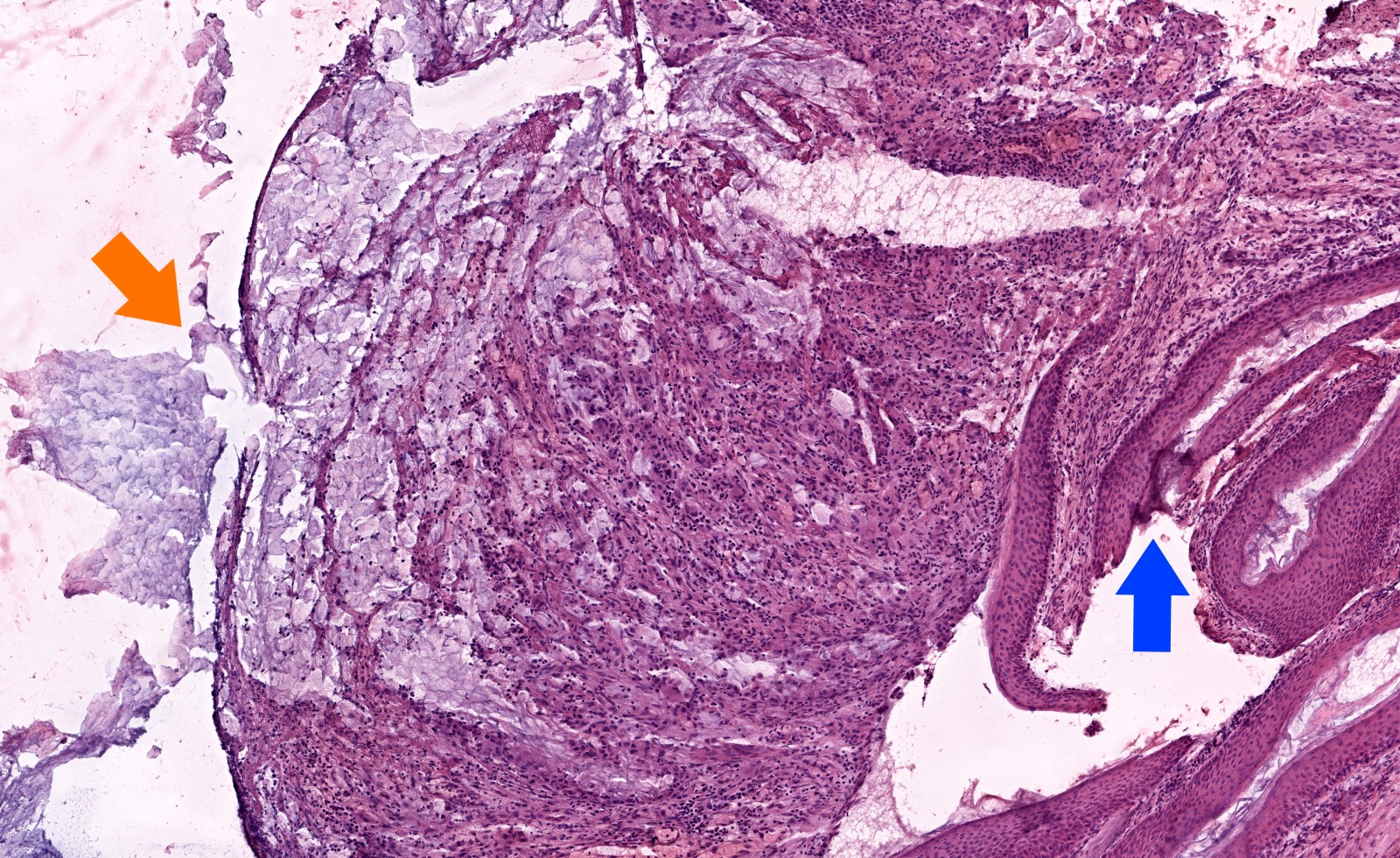
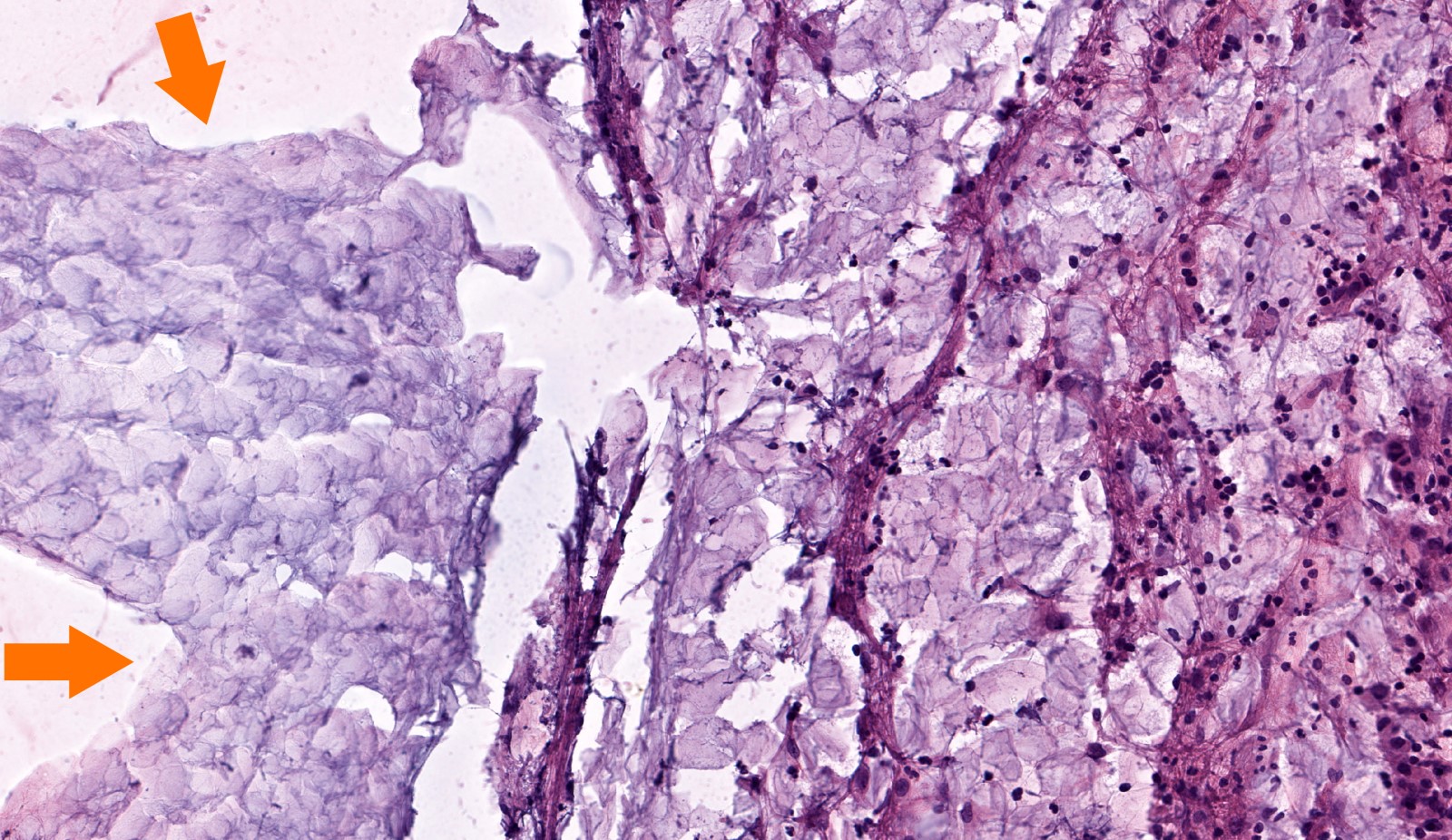
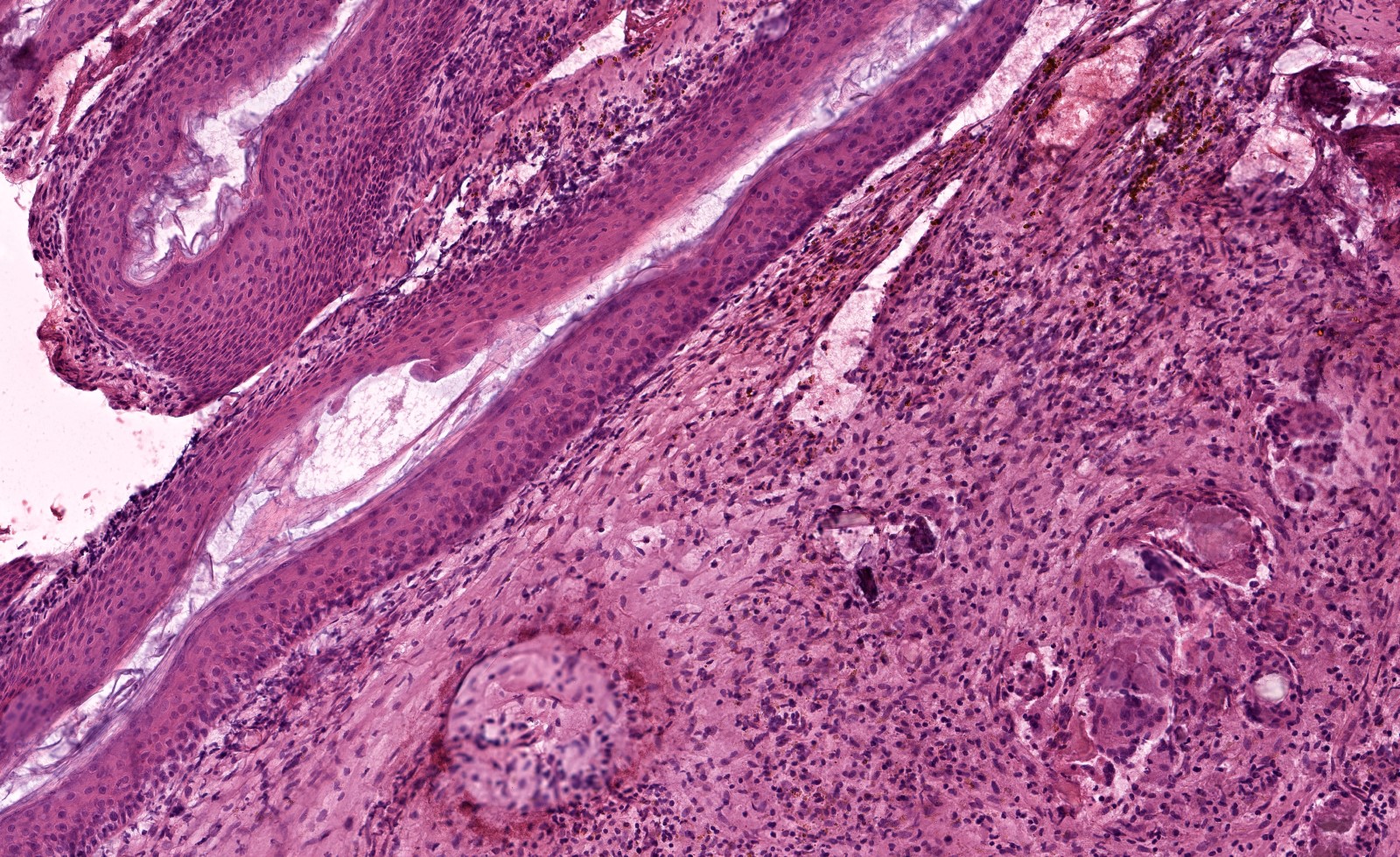
Microscopic (histologic) images
Contributed by Kelly Magliocca D.D.S., M.P.H.
Positive stains
- No specific immunohistochemistry required for cholesteatoma
- Squamous epithelium expected to be immunoreactive for cytokeratins, p63 and p40
- GMS fungal stain may highlight yeasts and fungal elements in keratinous debris
- References: J Assoc Res Otolaryngol 2018;19:223, Front Microbiol 2021;12:761111
Videos
Primary and secondary acquired cholesteatoma
Sample pathology report
- Left middle ear and mastoid contents:
- Cholesteatoma
- Middle ear mucosa with acute and chronic inflammation
Differential diagnosis
- Cholesterol granuloma:
- Elongated clefts (spaces) in tissue remaining after cholesterol crystals are dissolved in processing
- Clefts are associated with an adjacent or surrounding foreign body type giant cell reaction
- Rich granulation type inflammatory infiltrate, including hemosiderin laden macrophages
- Otic (aural) polyp:
- Polypoid chronic inflammation and granulation tissue only
- Lacking keratinizing squamous epithelial proliferation
- Lacking anucleate squames
- Chronic otitis media:
- Lacks the proliferative squamous epithelium or the anucleate squames
- Keratosis obturans:
- Accumulation of keratin debris within the medial aspect of the external auditory canal
- May show bony erosion
- More commonly bilateral
- Tympanic membrane intact
- Microscopically some cases may be identical to cholesteatoma, though if middle ear is preserved, no middle ear mucosa will be seen microscopically
- Squamous cell carcinoma:
- Lack of epithelial cell maturation or polarity, atypical mitosis, pleomorphism, dyskeratosis or individual cell keratinization
Additional references
Board review style question #1
Board review style answer #1
C. Matrix. Matrix, perimatrix and cystic contents are terms that are more commonly used clinically and refer to the keratinizing squamous epithelium, connective tissue wall and keratin debris, respectively.
Comment Here
Reference: Cholesteatoma
Comment Here
Reference: Cholesteatoma
Board review style question #2
How does congenital cholesteatoma typically present?
- White-yellow mass in anterior superior quadrant of the middle ear, disrupted tympanic membrane, slowly progressive sensorineural hearing loss
- White-yellow mass in anterior superior quadrant of the middle ear, intact tympanic membrane, slowly progressive conductive hearing loss
- White-yellow mass in posterior superior retraction pocket, disrupted tympanic membrane, slowly progressive sensorineural hearing loss
- White-yellow mass in posterior superior retraction pocket, intact tympanic membrane, slowly progressive conductive hearing loss
Board review style answer #2
B. White-yellow mass in anterior superior quadrant of the middle ear, intact tympanic membrane, slowly progressive conductive hearing loss. Congenital cholesteatoma usually arises in the middle ear, most commonly in the absence of otorrhea, related to an intact tympanic membrane. Most patients are asymptomatic, although this, in addition to other symptoms, depends on the extent of disease. Over time, patients will develop conductive hearing loss related to cholesteatoma formation.
Comment Here
Reference: Cholesteatoma
Comment Here
Reference: Cholesteatoma
Chondrodermatitis nodularis chronica helicis
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Also called Winkler's disease
- Idiopathic, nonneoplastic ulcerative lesion of auricle
- Usually men ages 40+; uncommon in women
- Symptoms: appears spontaneously; unilateral, painful nodule
Treatment
- Wedge or cartilage excision, glucocorticoid injection
- Frequently recurs
Gross description
- Dome shaped nodule, 0.3 - 1.8 cm, with crusty scale covering central area of ulceration
Microscopic (histologic) description
- Central ulceration of epidermis with adjacent acanthosis, hyperkeratosis, parakeratosis and pseudoepitheliomatous hyperplasia
- Base of ulcer has granulation tissue that usually involves perichondrium and cartilage
- Usually nerve hyperplasia identified with S100 (J Am Acad Dermatol 2006;55:844)
- May have foci of fibrinoid necrosis
- No dermal adnexa at site of lesion
Microscopic (histologic) images
Differential diagnosis
- Clinically resembles carcinoma
- Vascular proliferation may resemble a glomus tumor
Congential - other
Definition / general
- Congenital anomalies of the ear are common (1 per 6,000 births); higher incidence in Japanese and Navajo Indians
- More common in males
- 90% are unilateral
- Either isolated or with other abnormalities
- Cosmetic or functional
- Anotia: complete absence of external ear
- Microtia: mild to severe deformity; associated with other defects
Accessory tragi
- See Accessory tragi
Heterotopia / choristoma
Definition / general
Case reports
Radiology images
Images hosted on other servers:
Additional references
- WHO classification includes salivary gland choristoma and glial choristoma
- Heterotopia: mass of tissue normal to the site in abnormal location
- Choristoma: mass of tissue foreign to the site
- Hamartoma: mass of tissue normal to site in haphazard arrangement
- Middle ear choristomas include salivary gland tissue and neuroglial tissue
- Salivary gland choristomas usually occur in women, associated with facial nerve and ossicle anomalies, suggesting a second branchial arch developmental anomaly; have mucinous and serous elements similar to submandibular and sublingual glands
- Neuroglial choristomas are often actually an acquired encephalocele with herniation of brain into middle ear and mastoid; treatment is surgical, although tissue may adhere to facial nerve; determine relationship to CNS structures at operation or radiographically, not by histology (Laryngoscope 2000;110:1731, Ann Diagn Pathol 2004;8:252)
- Cartilaginous choristoma of external ear canal: may be relatively common (Otolaryngol Head Neck Surg 2005;133:786)
Case reports
- 14 year old girl with salivary gland choristoma of the middle ear (Laryngoscope 2006;116:1033)
- 50 year old man with glial choristoma of middle ear and mastoid bone (J Korean Med Sci 2004;19:155)
- Patient with salivary gland choristoma of the middle ear (Arch Pathol Lab Med 1982;106:39)
Radiology images
Images hosted on other servers:
Additional references
Endolymphatic sac tumor
Table of Contents
Definition / general | Terminology | Radiology description | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Differential diagnosis | Additional referencesDefinition / general
- Uncommon, associated with von Hippel-Lindau syndrome (11% have these tumors) and female adnexal tumor of presumed wolffian origin (Am J Surg Pathol 1994;18:1254); also somatic mutations of VHL gene in non VHL patients (Cancer Res 2000;60:5963)
- Most arise within intraosseous portion of the endolymphatic duct / sac, with precursor lesions present in VHL patients (Cancer Res 2005;65:10847)
- Median age 30s, range of 11 - 71 years
- Symptoms: early sensorineural hearing loss, tinnitus and episodic vertigo
Terminology
- The 2017 WHO now separates aggressive papillary tumor from endolymphatic sac tumor
- Also called papillary adenoma of endolymphatic sac / temporal bone, adenocarcinoma of temporal bone / mastoid, low grade adenocarcinoma of probable endolymphatic sac origin, Heffner tumor
Radiology description
- Tumor in posterior medial petrous ridge of temporal bone (site of endolymphatic sac)
Case reports
- 20 year old woman with endolymphatic sac tumor associated with von Hippel-Lindau disease (Mod Path 2001;14:727)
- 32 year old woman with papillary neoplasm of the endolymphatic sac associated with Hippel-Lindau disease (J Clin Pathol 1994;47:959)
- 42 year old woman with endolymphatic sac tumor associated with von Hippel-Lindau disease (Arch Pathol Lab Med 2003;127:1387)
- 77 year old man with aspirated cyst (Mod Pathol 2001;14:920)
- Patient with mutation of von Hippel-Lindau tumor suppressor gene in a sporadic endolymphatic sac tumor (Hum Pathol 2001;32:1272)
- Patients with low grade papillary adenomatous tumors of the temporal bone (Mod Pathol 1995;8:603)
Treatment
- Radical surgery including mastoidectomy and temporal bone resection with possible loss of cranial nerves
- Tumor grows slowly with only one reported metastasis (J Neurosurg Spine 2005;3:68) but may recur with inadequate excision
- Is infiltrative, destructive and may cause death
- Bleeds profusely at surgery
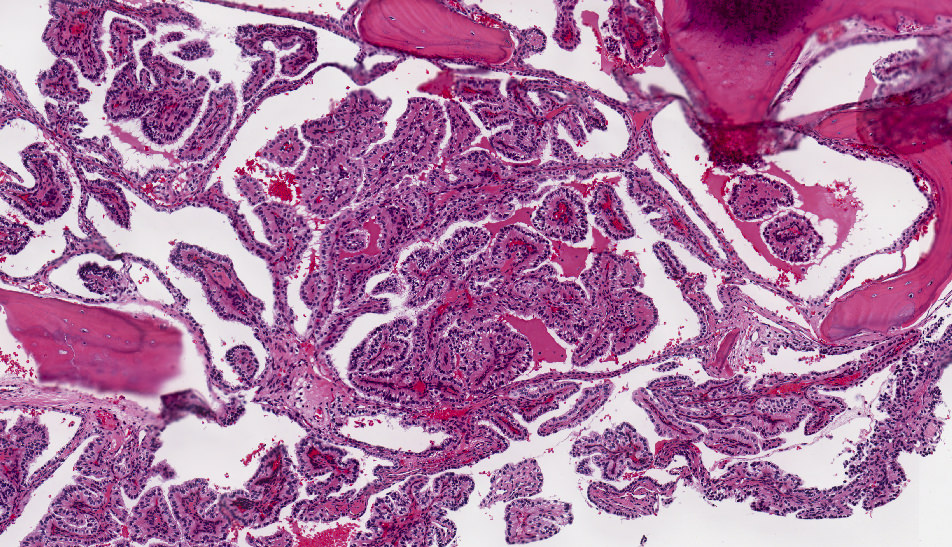
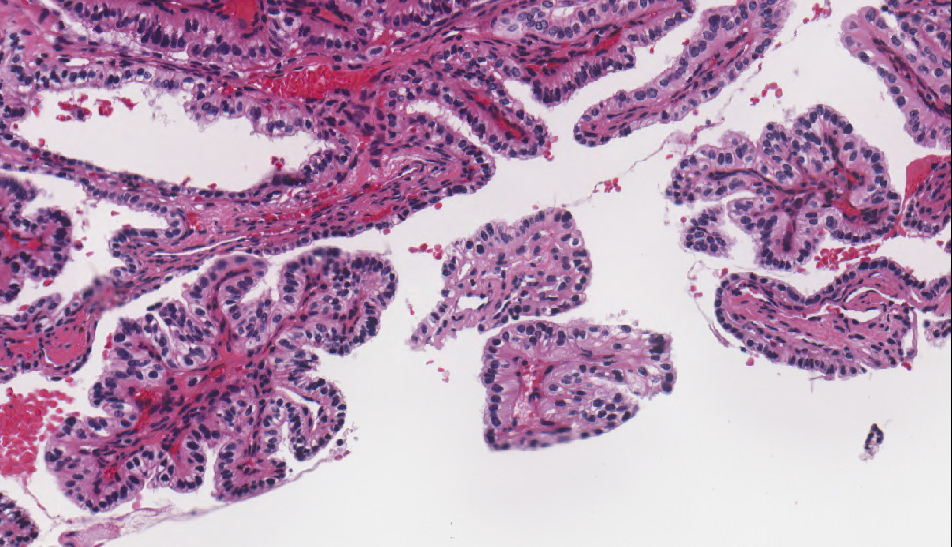
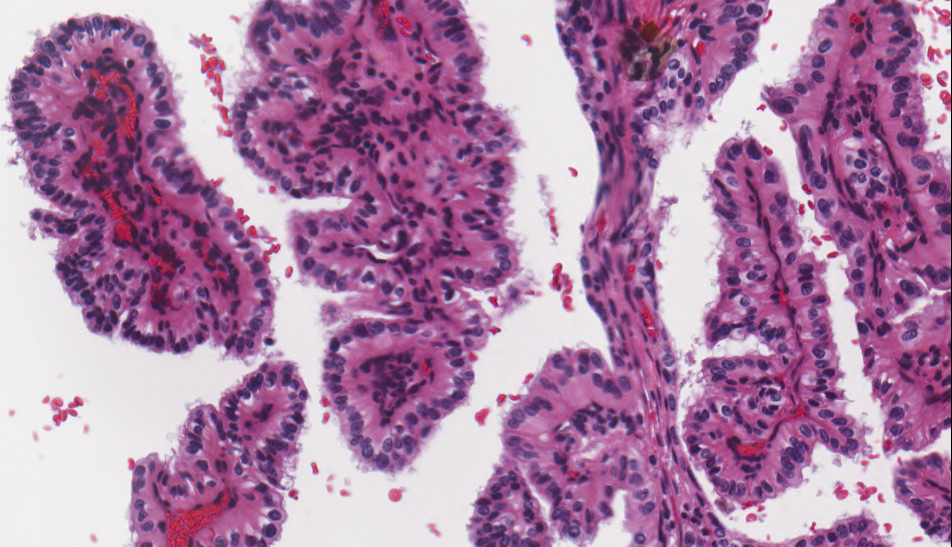
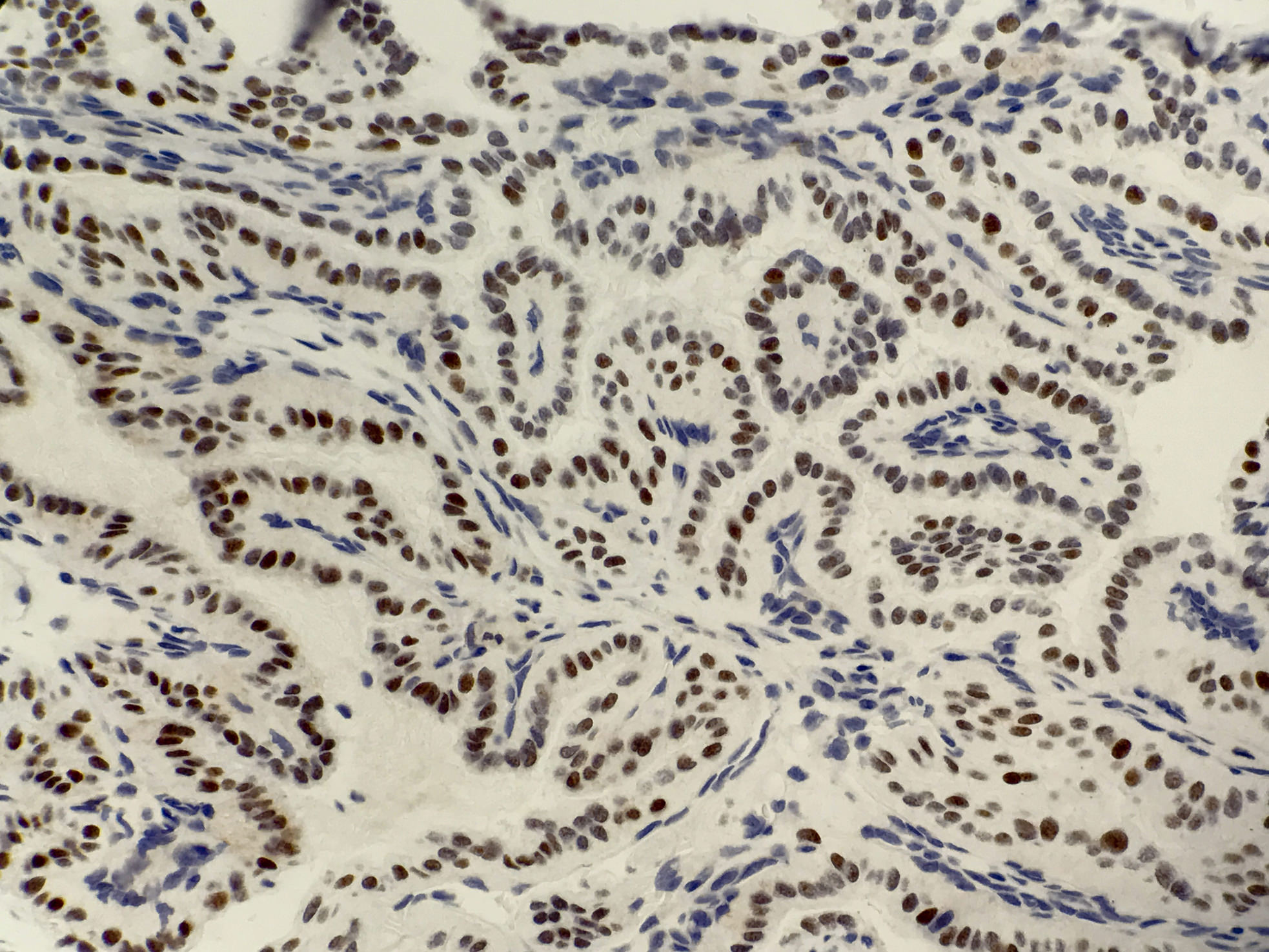
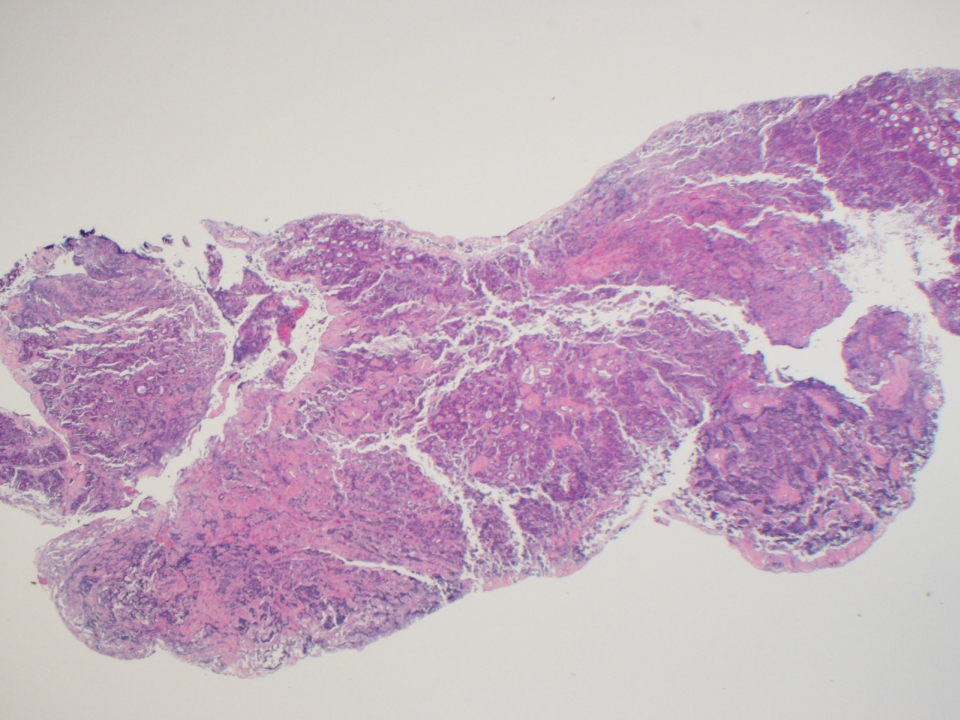
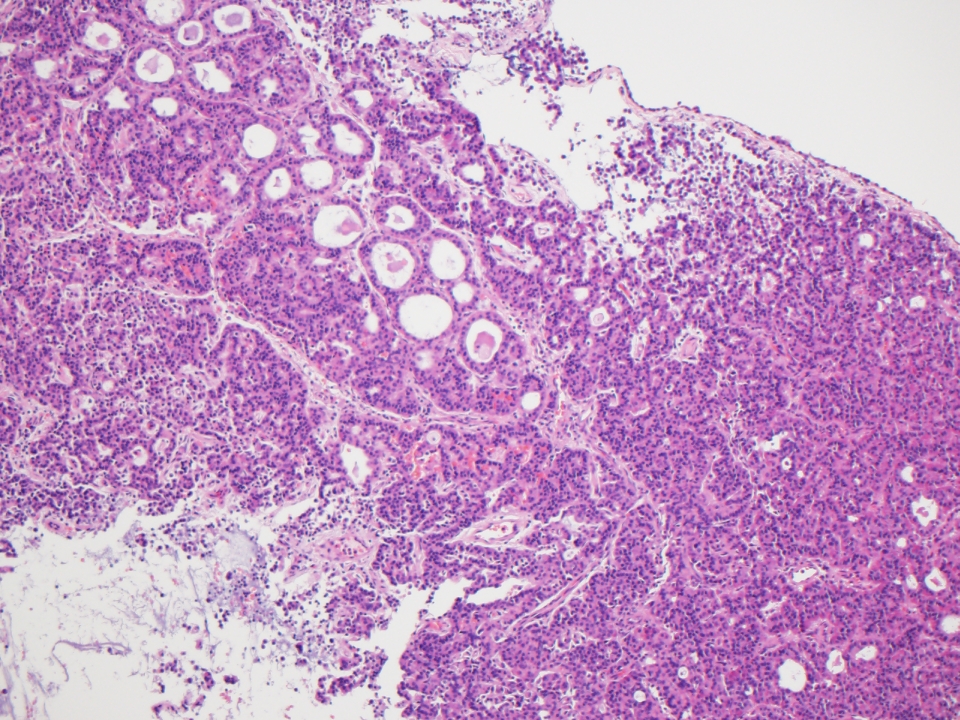
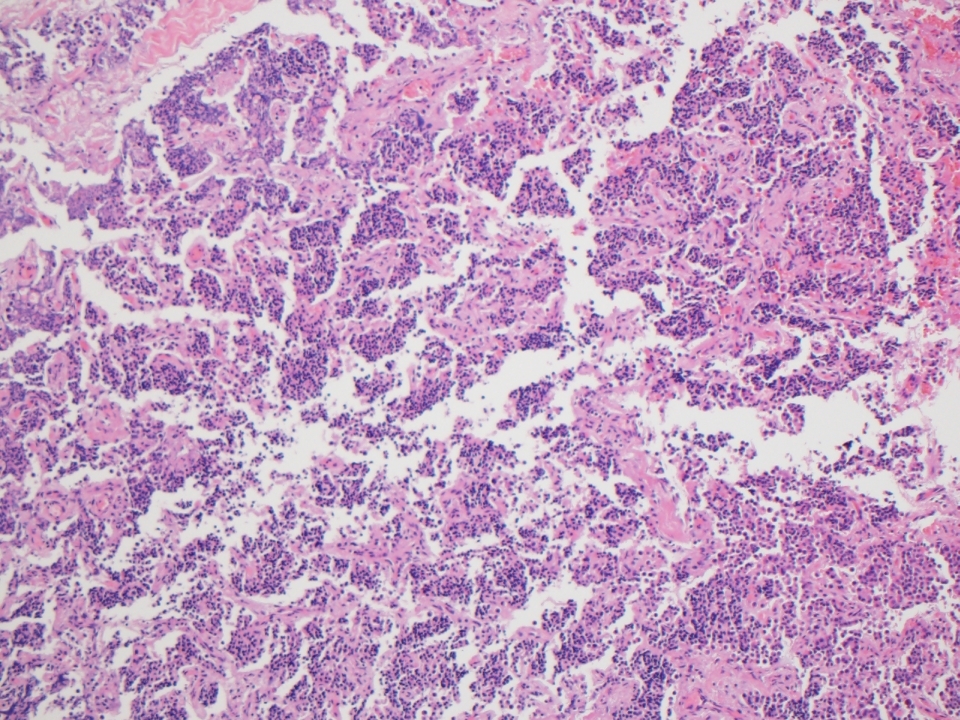
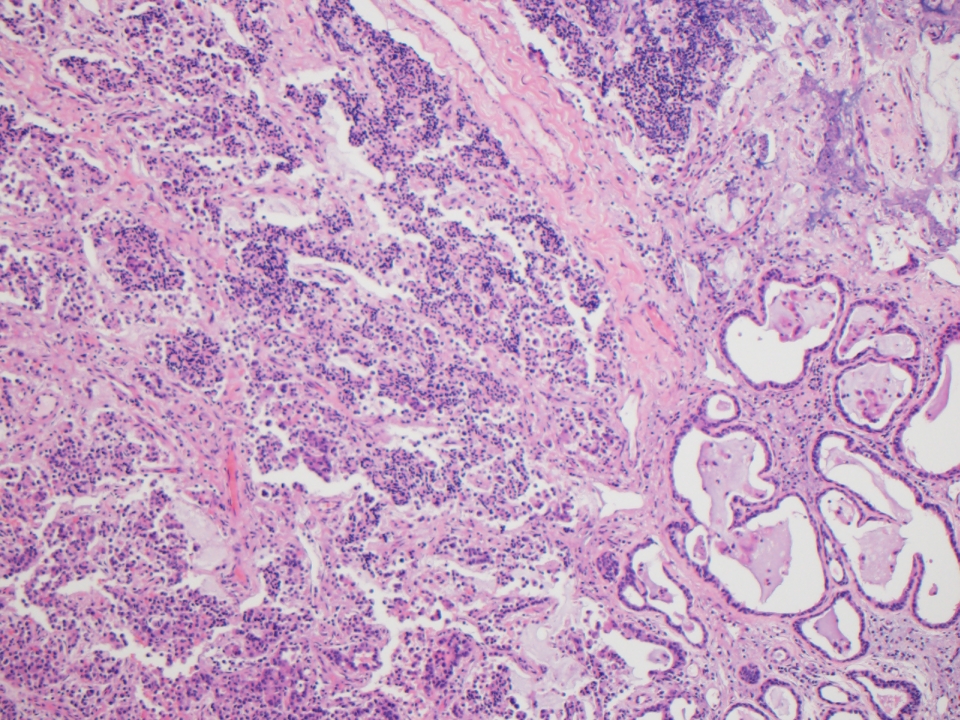
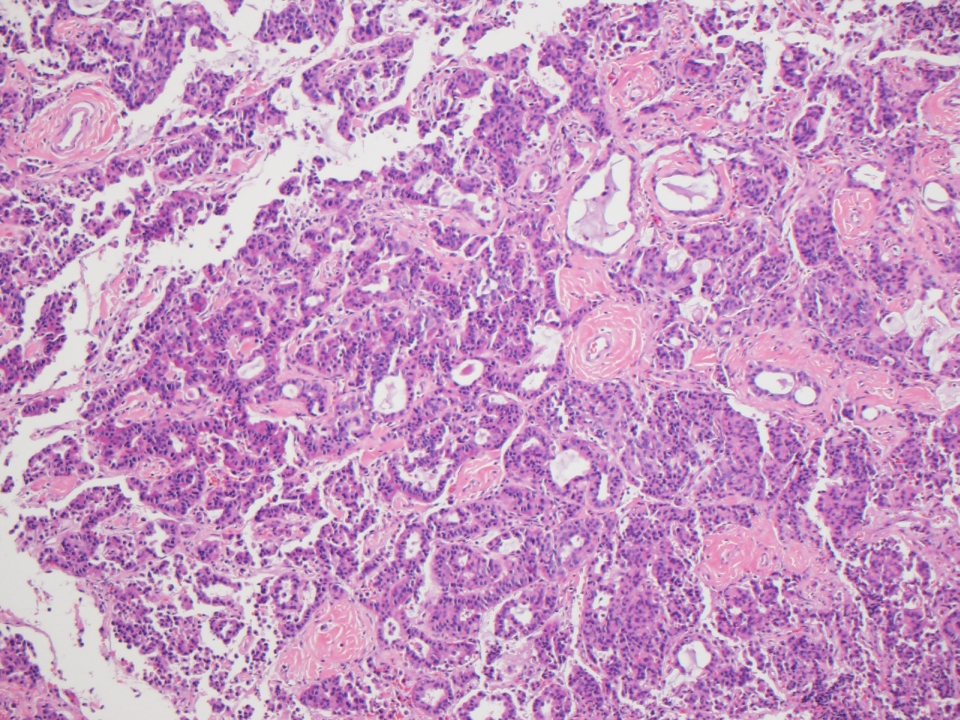
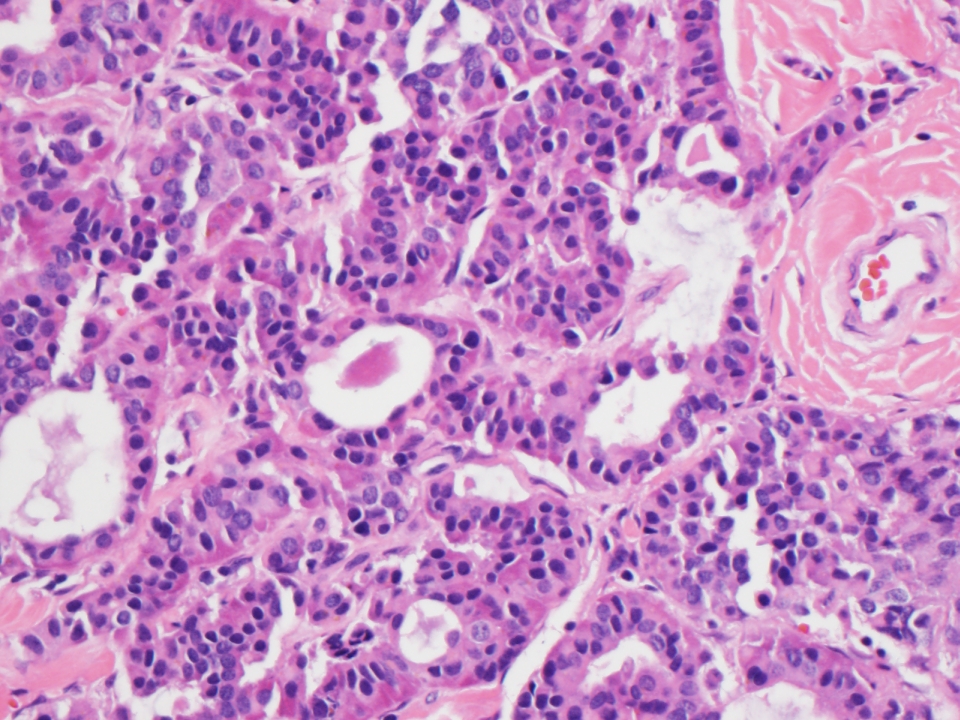
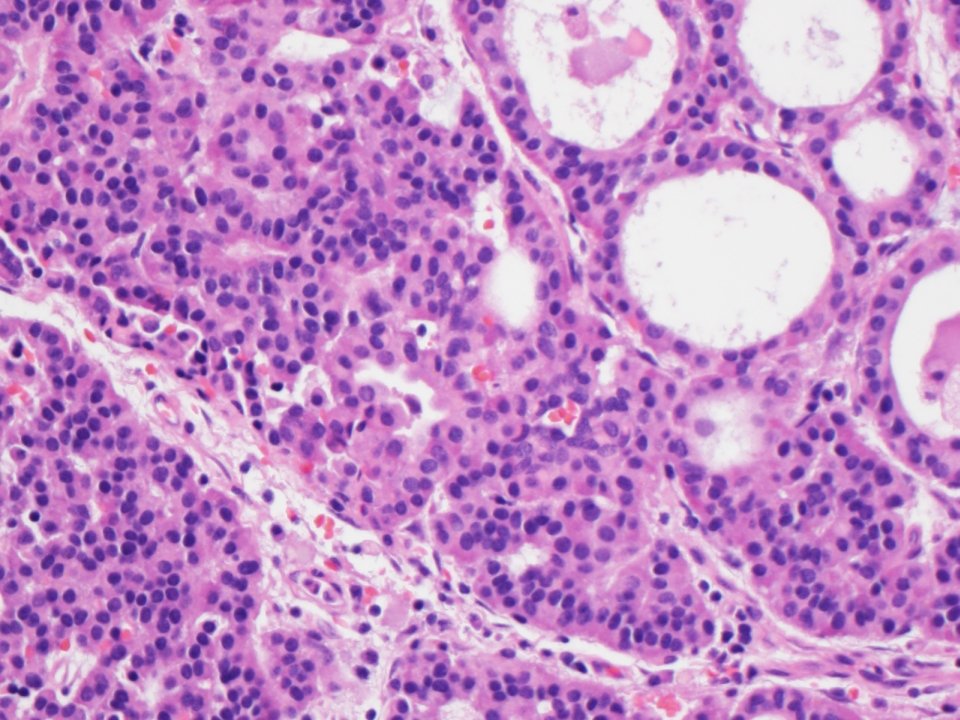
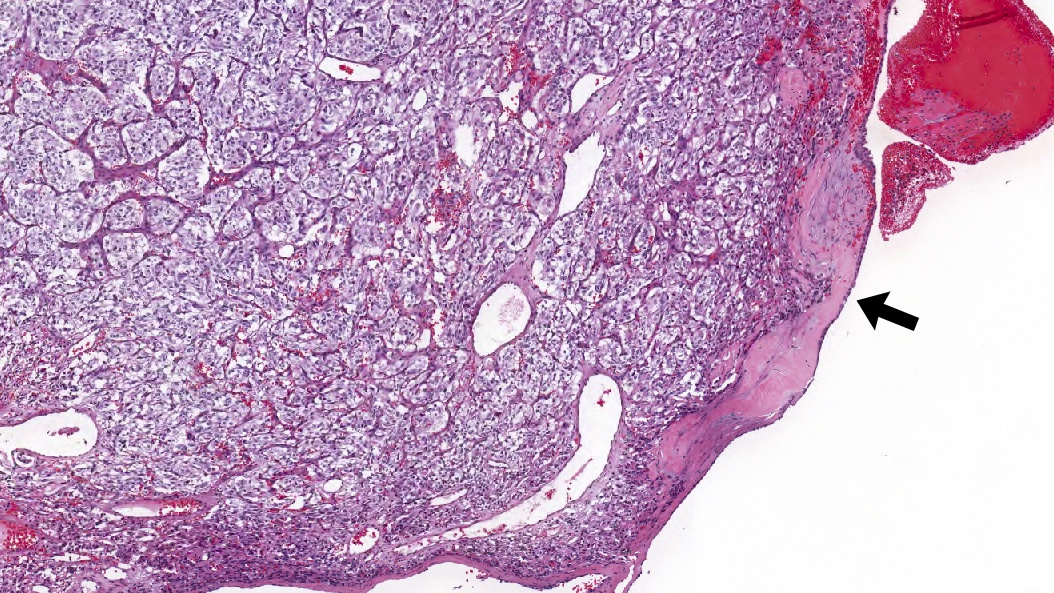
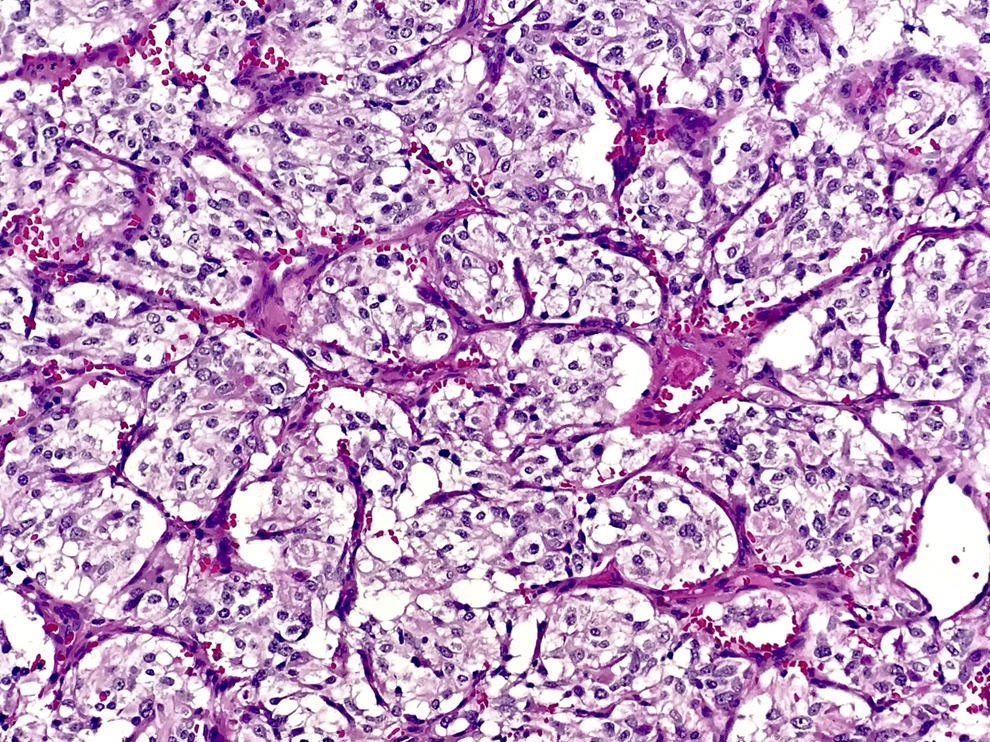
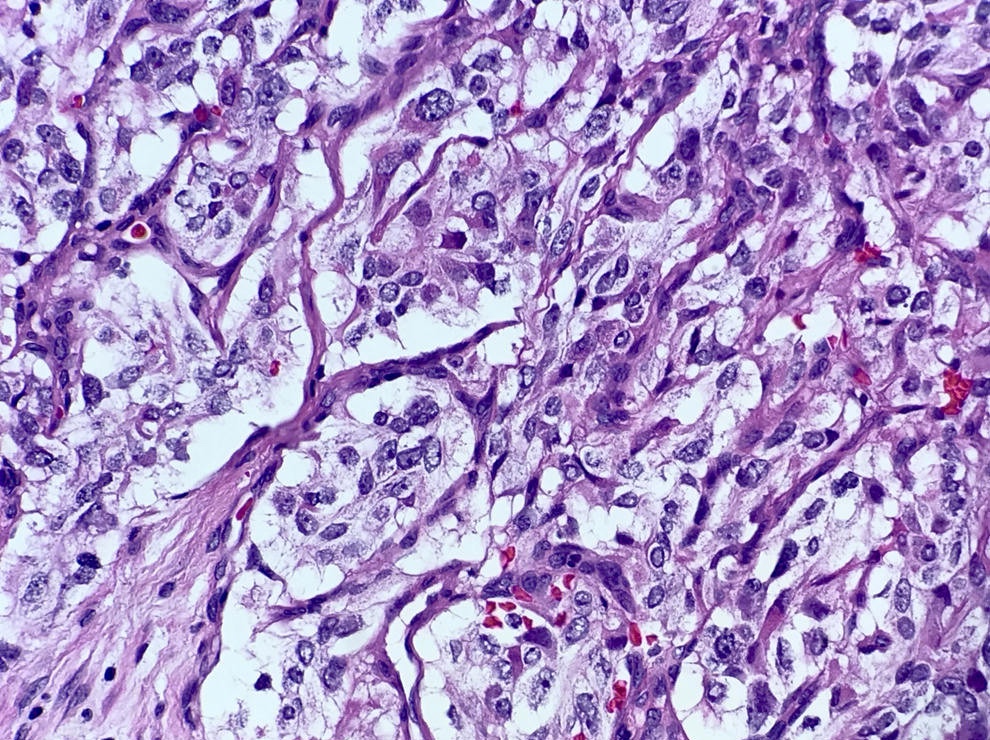
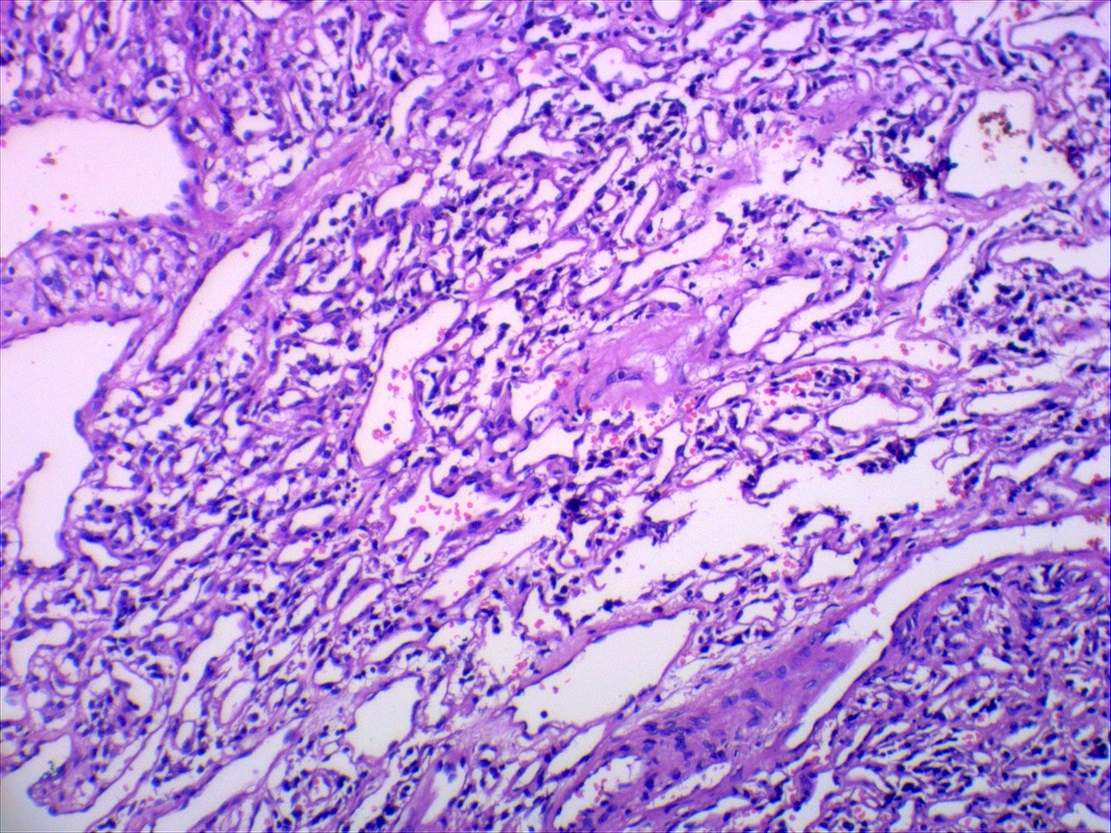
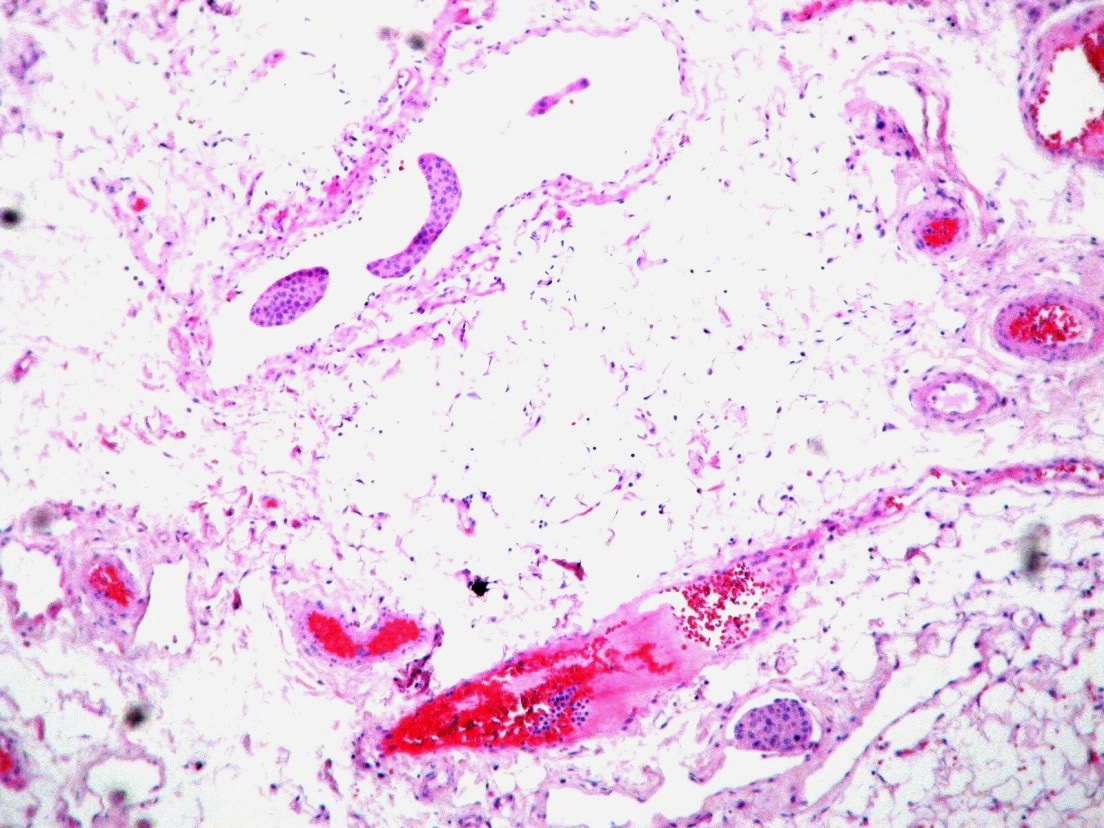
Microscopic (histologic) description
- Simple papillary structures composed of single layer of columnar to cuboidal epithelium, often with distinct cell boundaries
- May have apparent myoepithelial layer that actually is flattened stroma; epithelial cells have pale-clear cytoplasm, uniform central or luminal nuclei
- Often granulation tissue reaction with small vascular spaces and mixed inflammatory infiltrate is present next to tumor cells
- Occasional thyroid like hypercellular areas with cystic glandular spaces containing colloid like material
- May have areas of recent hemorrhage with cholesterol clefts
- Minimal pleomorphism
- No / rare mitotic figures or necrosis
- Resembles choroid plexus papilloma
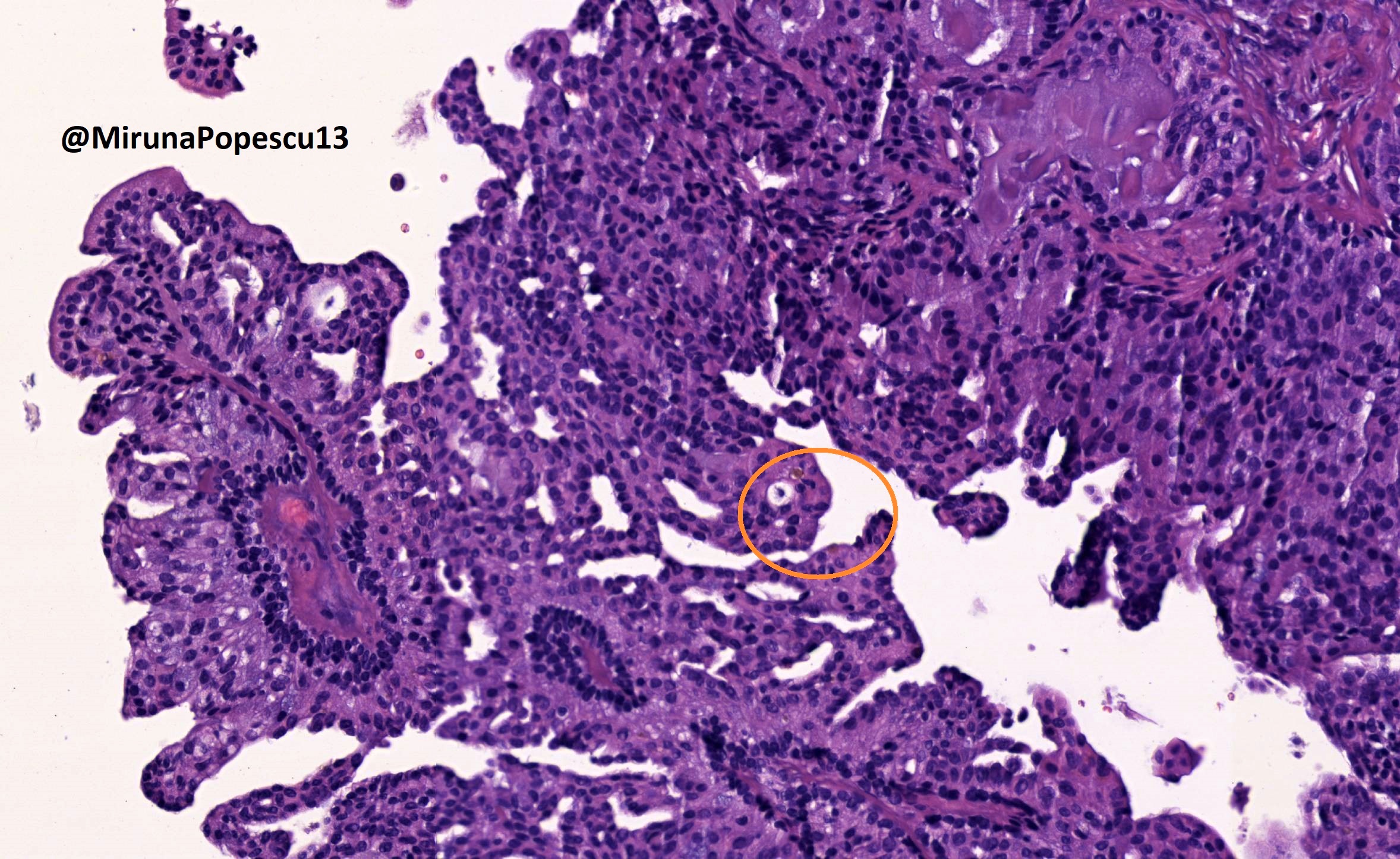
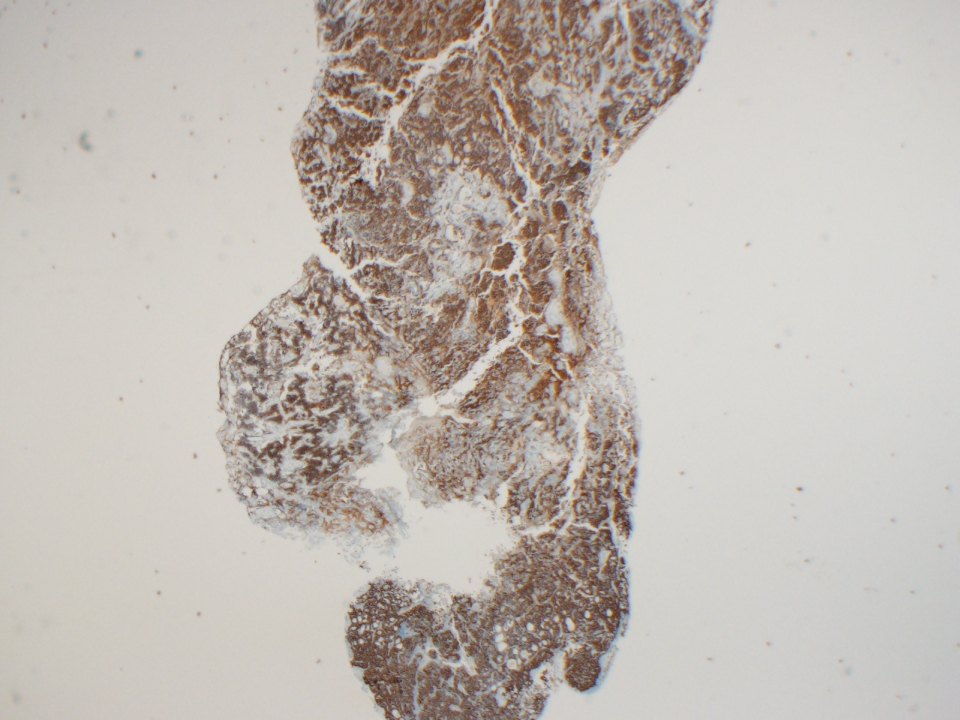
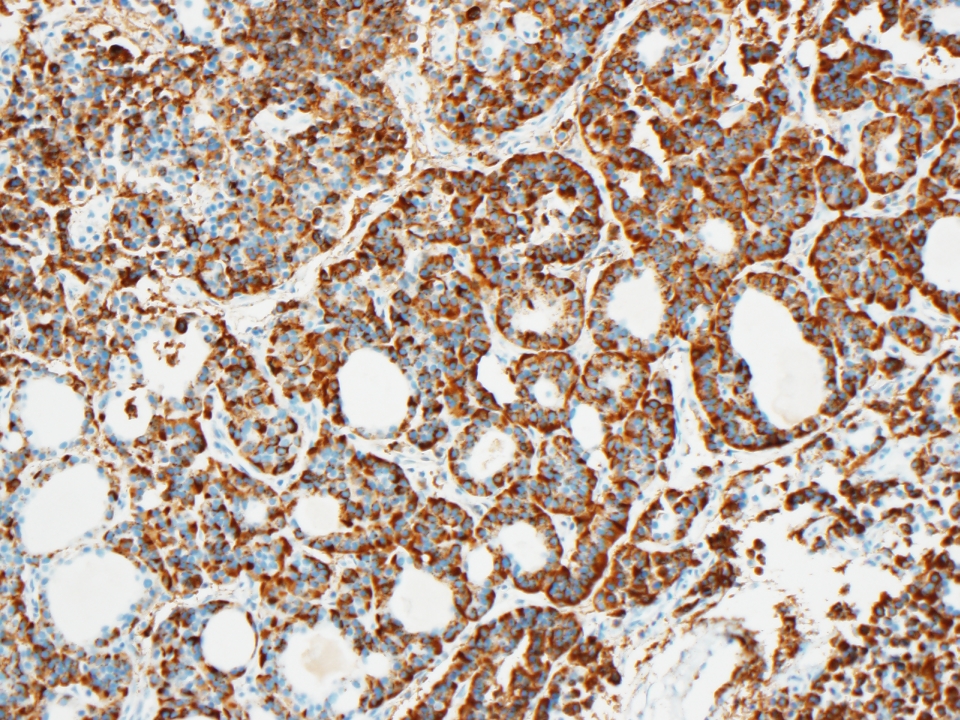
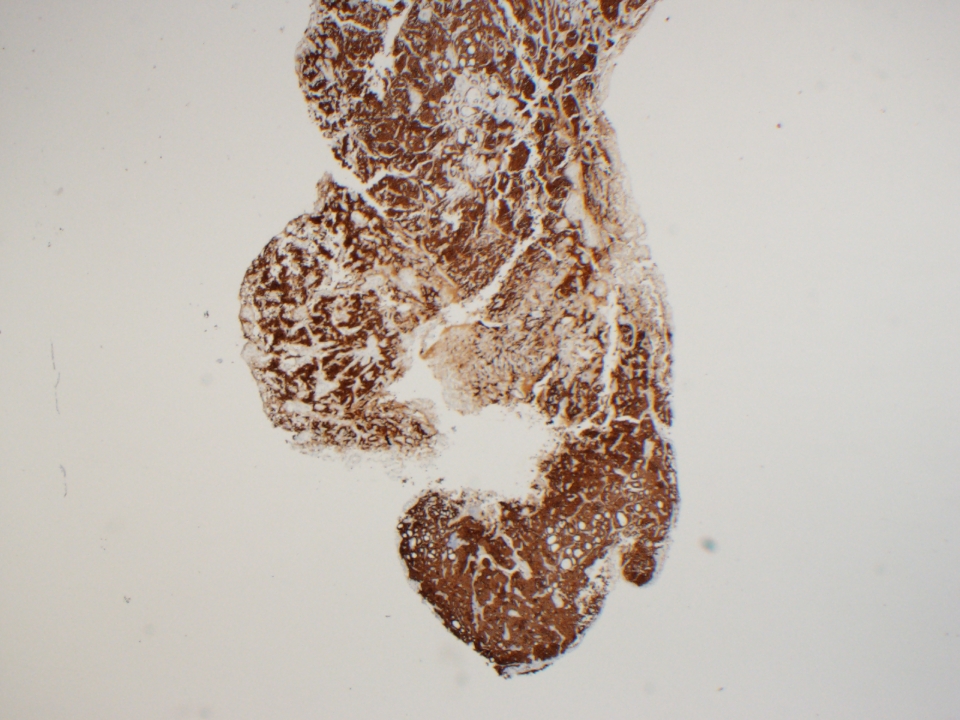
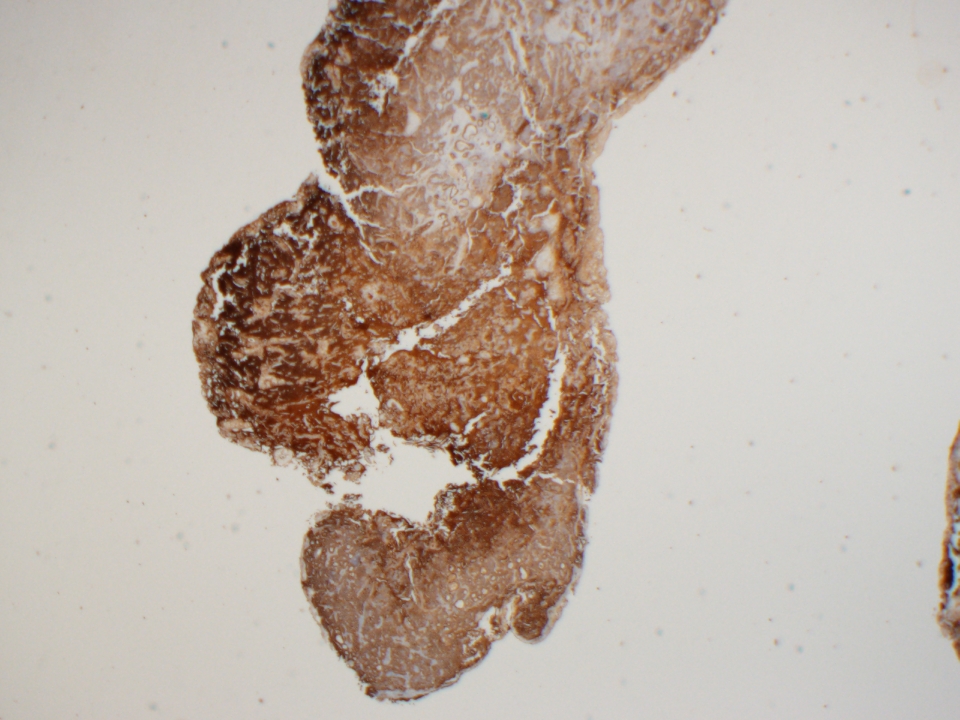
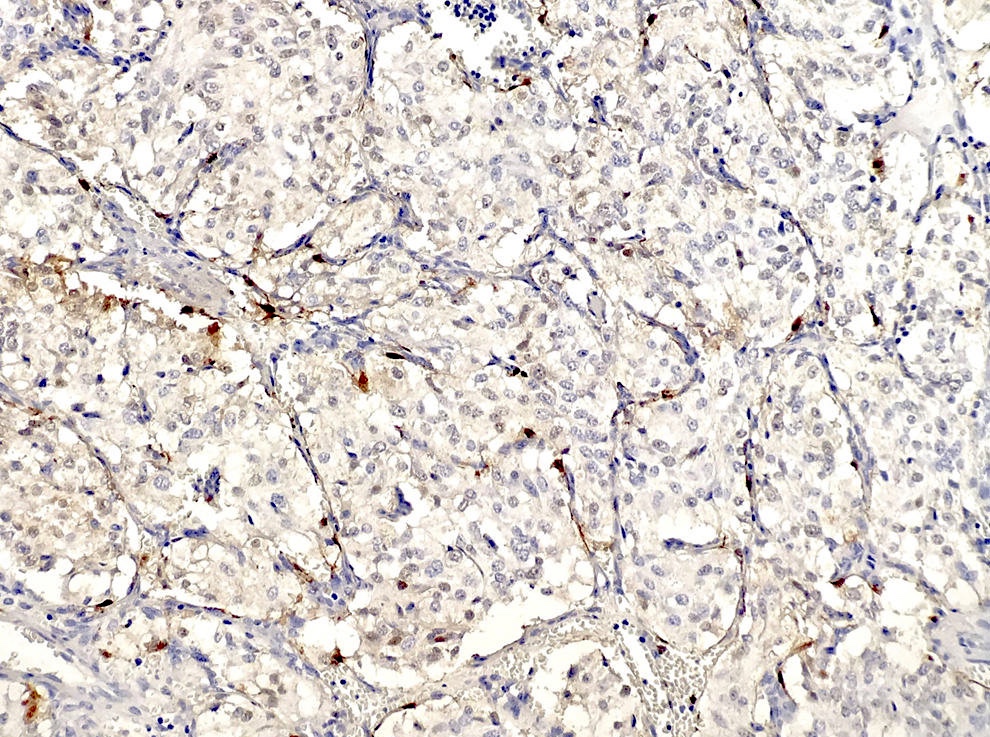
Microscopic (histologic) images
Contributed by Kelly Magliocca D.D.S., M.P.H.
Images hosted on other servers:
Cytology description
- Rare epithelial cell clusters, some with papillary features
- Foamy macrophages
- Epithelial cells have eosinophilic and focally vacuolated cytoplasm, some with pigmented granules resembling hemosiderin, well defined cell borders, bland nuclei
Positive stains
Negative stains
Electron microscopy description
- Intercellular junctional complexes, microvilli, basement membrane, rough ER, glycogen, secretory granules
Differential diagnosis
- Choroid plexus papilloma-carcinoma: originates within brain ventricles, S100+
- Jugulotympanic paraganglioma: vascular, but not papillary cystic, "zellballen", keratin negative
- Metastatic renal cell carcinoma: S100-, GFAP-, synaptophysin-, kidney tumor present on CT
- Metastatic thyroid carcinoma: thyroglobulin+, characteristic nuclear features
- Middle ear adenoma: not papillary, doesn't invade or destroy bone
Additional references
Exostosis
Table of Contents
Definition / general | Treatment | Gross description | Differential diagnosis | Additional referencesDefinition / general
- Also called surfer's ear
- Reactive, localized overgrowth of bone with a broad base
- Called osteoma if pedunculated
- Arises from wall of external auditory canal
- Usually multiple and bilateral; asymptomatic until large enough to block external auditory canal
- Highest incidence in cold water swimmers and surfers in Australia and New Zealand (J Laryngol Otol 2004;118:348)
Treatment
- Medical (for external otitis, antibiotics and aspiration), transmeatal surgical excision if medical treatment fails and patient is symptomatic (ORL J Otorhinolaryngol Relat Spec 2003;65:189)
Gross description
- Broad based, mound like bony proliferation resembling normal cortical bone (however pathologist usually only gets fragments)
- No bone marrow spaces
- Bone is covered by periosteum with overlying thin skin
Differential diagnosis
- Osteoma: uncommon in ear
Additional references
Infectious / inflammatory
Table of Contents
Idiopathic cystic chondromalacia of auricular cartilage | Meniere disease | Necrotizing malignant external otitis | Otitis media | Otomycosis | Relapsing polychondritisIdiopathic cystic chondromalacia of auricular cartilage
Definition / general
Case reports
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
Additional references
- Also called auricular or endochondral pseudocyst
- Benign cystic degeneration of auricular cartilage of unknown cause
- Usually men age 20 - 40 years
- Unilateral swelling of cartilage over weeks to years, most commonly on scaphoid fossa of auricle
- May be due to minor trauma
Case reports
- 32 year old man with auricular swelling (J Clin Pathol 1994;47:961)
Treatment
- Excision
Microscopic (histologic) description
- Fluid filled distended mass composed of cyst like wall with fibrous and granulation tissue lining but no epithelium
- Cyst contains 1 - 2 mm rim of cartilage
- Cyst fluid resembles olive oil
- No / mild atypia
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
- Chondrodermatitis nodularis helicis chronicus
- Relapsing polychondritis
- Subperichondrial hematoma
Additional references
Meniere disease
Definition / general
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Additional references
- Also called endolymphatic hydrops
- Idiopathic disorder of inner ear associated with episodic attacks of vertigo, fluctuating sensorineural hearing loss, tinnitus and sensation of aural fullness
- Incidence varies from 7.5 per 100,000 in France to 157 per 100,000 in England
- 60% women, peaks in 40s to 60s but wide age range
- Rarely occurs in children (J Laryngol Otol 2006;120:343)
- Associated with HLA B8 / DR3
- May be due to accumulation of endolymph in membranous labyrinth, perhaps due to inadequate absorption by endolymphatic sac
Treatment
- Dietary modification, intermittent dehydration, diuretics, vasodilators in increase microcirculation of ear
- 60 - 80% improve
- Surgery includes shunting and decompression of endolymphatic sac, labyrinthectomy, sectioning of vestibular nerve (Laryngoscope 2005;115:1454)
Microscopic (histologic) description
- Initially involves cochlear duct and saccule
- Later entire endolymphatic system with dilation, rupture and collapse of membranous labyrinth with possible fistula
- May have severe atrophic changes with loss of cochlear neurons
Microscopic (histologic) images
Images hosted on other servers:
Additional references
Necrotizing malignant external otitis
Definition / general
Treatment
Case reports
Gross description
Microscopic (histologic) description
Positive stains
Differential diagnosis
Additional references
- Potentially fatal external otitis due to Pseudomonas aeruginosa (Ann Otolaryngol Chir Cervicofac 2000;117:291), Aspergillus or other fungal infection
- Usually older patients, often with diabetes, chronic debilitation or immunodeficiency; also undernourished African infants (Rev Laryngol Otol Rhinol 2002;123:225)
- Initially affects external auditory canal with symptoms of acute otitis externa; later pain, purulent otorrhea and swelling; may progress to cellulitis, chondritis, osteomyelitis, involve middle ear space or base of skull and cause cranial nerve palsies, meningitis, venous thrombosis or brain abscess (Rev Stomatol Chir Maxillofac 2006;107:167)
- Up to 75% mortality if treatment is delayed
- Due to tissue ischemia (from above primary pathologic state) plus neutrophilic migratory defect plus virulence of Pseudomonas
Treatment
- Antibiotics, surgical debridement, hyperbaric oxygen (HNO 2003;51:315)
Case reports
- Female patient with calcium oxalate crystal deposition in necrotizing otomycosis caused by Aspergillus niger (Mod Pathol 1993;6:493)
- Patient with necrotizing otitis externa caused by Stenotrophomonas maltophilia (Hautarzt 2003;54:1080)
- 47 year old man with necrotizing external otitis in a patient caused by Klebsiella pneumoniae (Eur Arch Otorhinolaryngol 2006;263:344)
- 58 year old man with necrotizing otitis externa caused byStaphylococcus epidermidis (Eur Arch Otorhinolaryngol 1999;256:439)
Gross description
- Ulcerated skin near osseous portion of external auditory canal, often with abundant necrotic and granulation tissue
Microscopic (histologic) description
- Epithelium is necrotic or ulcerated with pseudoepitheliomatous hyperplasia, marked mixed inflammatory infiltrate in subcutaneous tissue, necrotizing vasculitis
- Necrotic bone and cartilage with heavy inflammatory infiltrate in viable bone
- Variable sequestra of nonviable bone or cartilage
Positive stains
- Gram stain (Gram negative rods)
Differential diagnosis
Additional references
Otitis media
Definition / general
Treatment
Gross description
Microscopic (histologic) description
Differential diagnosis
Additional references
- Acute or chronic infectious disease of middle ear
- Usually childhood disease caused by Streptococcus pneumoniae or Haemophilus influenzae; also coinfection by viruses (Pediatr Infect Dis J 2004;23:1142, Clin Infect Dis 2006;43:1417)
- Rarely caused by fungi or pneumocystis in HIV+ patients
- Hyperemic, opaque and bulging tympanic membrane with limited mobility; may have purulent otorrhea
- Infection probably occurs post pharyngitis via eustachian tube
- Severe cases are associated with destruction of ossicles
- Tympanosclerosis: dystrophic calcification of tympanic membrane or middle ear associated with recurrent cases of otitis media, occurs in 3 - 33% of cases; may be reversible in children, usually irreversible in adults and associated with conductive hearing loss
Treatment
- Antibiotics or observation (Pediatr Infect Dis J 2006;25:1102, Lancet 2006;368:1429)
- Complications of mastoiditis, labyrinthitis, meningitis or abscess are now rare
Gross description
- Not a common specimen but may have small fragments of soft / rubbery granulation tissue
Microscopic (histologic) description
- Acute and chronic inflammatory cells, haphazard glandular metaplasia with cilia, fibrosis, hemorrhage, foci of calcification (tympanosclerosis), cholesterol granulomas and reactive bone formation (Laryngoscope 1982;92:273)
- Cholesterol granulomas: foreign body granulomas in response to cholesterol crystals from rupture of red blood cells and breakdown of lipid bilayer in cell membrane, prominent cholesterol clefts; associated with interference to drainage or ventilation of middle ear space; not related to cholesteatomas
Differential diagnosis
- Middle ear adenoma:
- Regular, not haphazard glands, no cilia
Additional references
Otomycosis
Relapsing polychondritis
Definition / general
Laboratory
Treatment
Microscopic (histologic) description
Positive stains
Additional references
- Also called polychondropathia
- Uncommon systemic episodic or relapsing disease with progressive degeneration of cartilage throughout the body
- Probable autoimmune process (antibodies to type II collagen) associated with other autoimmune disorders
- Whites, no gender preference, usually symptomatic in 40s to 60s although affects all ages
- 90% have involvement of auricular cartilage, usually bilateral, with swelling, erythema and tenderness
- Earlobes are typically spared
- Variable relapsing of disease
- May cause cauliflower ear and saddle node deformities
- Clinical diagnosis requires 3 of the following
- Recurrent chondritis of both auricles
- Nonerosive inflammatory arthritis
- Chondritis of nasal cartilage
- Ocular inflammation including conjunctivitis, keratitis, scleritis, episcleritis or uveitis
- Chondritis of upper respiratory tract including larynx or tracheal cartilage
- Cochlear or vestibular damage with sensorineural hearing loss, tinnitus or vertigo
Laboratory
- Nonspecific elevated sedimentation rate, mild leukocytosis, normochromic normocytic anemia; variable elevated ANCA
- Prognosis varies from prolonged course to aggressive and fulminant disease leading to death from respiratory tract or cardiovascular involvement (aortic insufficiency)
Treatment
- Responds to steroids or dapsone (this also confirms diagnosis)
- Advanced cases require immunosuppressive agents
Microscopic (histologic) description
- Mixed inflammatory infiltrate (lymphocytes, plasma cells, neutrophils, occasional eosinophils) extending into cartilage with blurring of interface between cartilage and adjacent soft tissue
- Cartilage shows loss of normal basophilia, loss of chondrocytes and destruction of lacunar architecture at advancing edge of inflammation with cartilage replaced by fibrous tissue
Positive stains
- Granular deposition of IgG and C3 in perichondrial fibrous tissue (Hum Pathol 1980;11:19)
Additional references
Inflammatory aural / otic polyp
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Proliferation of granulation tissue with chronic inflammatory cells in response to a longstanding inflammatory process usually lacking epithelial proliferation
- Commonly associated with cholesteatoma (80% of cases)
Essential features
- Proliferation of granulation tissue with chronic inflammatory cells in response to a longstanding inflammatory process
- Associated with cholesteatoma in 80% of cases
- More common in children but occurs in all ages
- May perforate tympanic membrane and appear to originate from the external auditory canal; with time, may destroy ossicles
- The otologic tissue specimen submitted as polyp should be evaluated with the knowledge of the spectrum of diseases known to clinically mimic aural polyp disease (see Diagrams / tables)
Terminology
- Aural polyp
- Otic polyp
- Inflammatory aural polyp
ICD coding
Epidemiology
- Uncommon lesion that usually affects young ages
- M:F = 2:1
- May perforate tympanic membrane and appear to originate from the external auditory canal; with time, may destroy ossicles
- More common in children but occurs in all ages
- Usually associated with cholesteatoma (in at least 80% of cases) (Indian J Otolaryngol Head Neck Surg 2018;70:505)
- May be associated with chronic otitis media (Acta Otorrinolaringol Esp 2003;54:161)
Sites
- Usually arises from the middle ear
- May extend into the external auditory canal if tympanic membrane perforated
Pathophysiology
- Complex interplay of inflammatory processes, tissue remodeling and cellular proliferation within the ear canal or middle ear
- Chronic inflammation and irritation of the mucosal lining of the ear, often secondary to conditions such as chronic otitis media or repeated trauma, lead to the accumulation of inflammatory cells, cytokines and growth factors within the affected tissues; this triggers a cascade of cellular responses, including fibroblast activation, angiogenesis and tissue remodeling, which contribute to the development of otic polyps
Etiology
- Chronic otitis media with or without cholesteatoma may be associated with the formation of an aural polyp, which is usually confined to the middle ear and external auditory canal (EAC) but may sometimes protrude outside the EAC
Clinical features
- The most common symptoms of an aural polyp are otorrhea, diminished hearing and a visible mass in the ear; otalgia and bleeding or sensation of mass are far less common
- In longstanding cases, partial or complete destruction of the ossicles may occur
- Usually confined to the middle ear and external auditory canal (EAC) but may sometimes protrude outside the EAC
- Commonly unilateral, bilateral cases can occur
- May rarely occur in association with aspirin exacerbated respiratory disease (AERD), formerly Samter triad (rhinosinusitis with polyposis, asthma and nonsteroidal anti-inflammatory drug [NSAID] intolerance) (Otol Neurotol 2012;33:774, Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- Aural polyps in association with AERD / Samter triad are often bilateral (Head Neck Pathol 2018;12:328)
Diagnosis
- High resolution computed tomography (HRCT) shows loss of pneumatization of mastoid air cells
- In large polyps completely obstructing the external ear, radiographic studies are an invaluable aid in identifying the origin of the polyp
- Key histologic findings: a well circumscribed mass with granulation tissue, mixed inflammation and abundant plasma cells
Radiology description
- See Diagnosis
Prognostic factors
- In the absence of an infectious cause, local surgical excision is curative
- Recurrence is more common in the setting of AERD / Samter triad
Case reports
- 39 year old man with a history of human immunodeficiency virus (HIV) and bilateral aural polyps (J Laryngol Otol 2002;116:288)
- 52 year old woman with a history of chronic rhinosinusitis with sinonasal polyps found to have bilateral aural polyps (Int J Otolaryngol 2009;2009:464958)
- 57 year old woman with a history of AERD / Samter triad and bilateral otorrhea (Otol Neurotol 2012;33:774)
Treatment
- Surgical excision
- Possibly mastoid exploration
Gross description
- Polypoid, soft to rubbery, tan-white to pink-red lesion
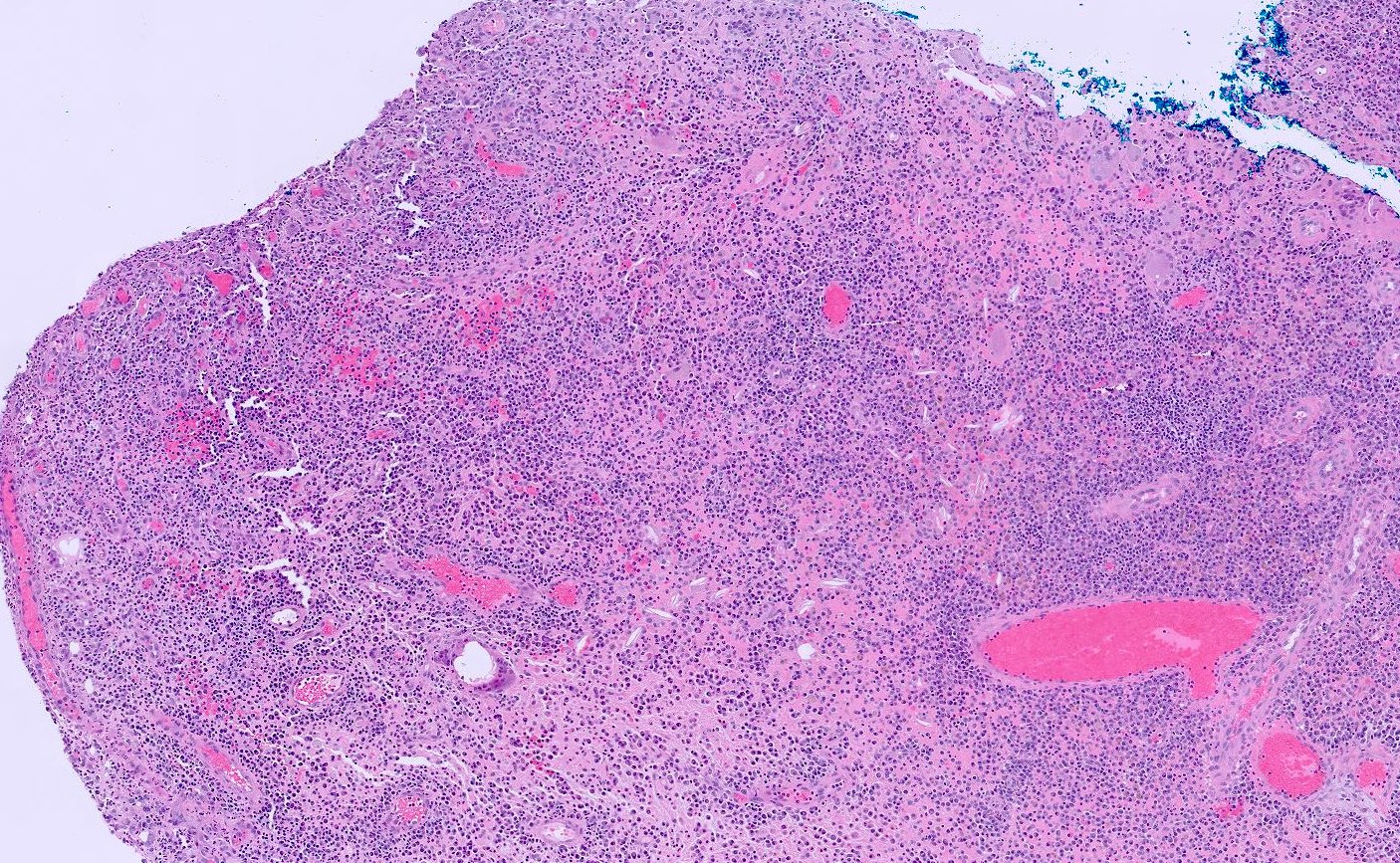
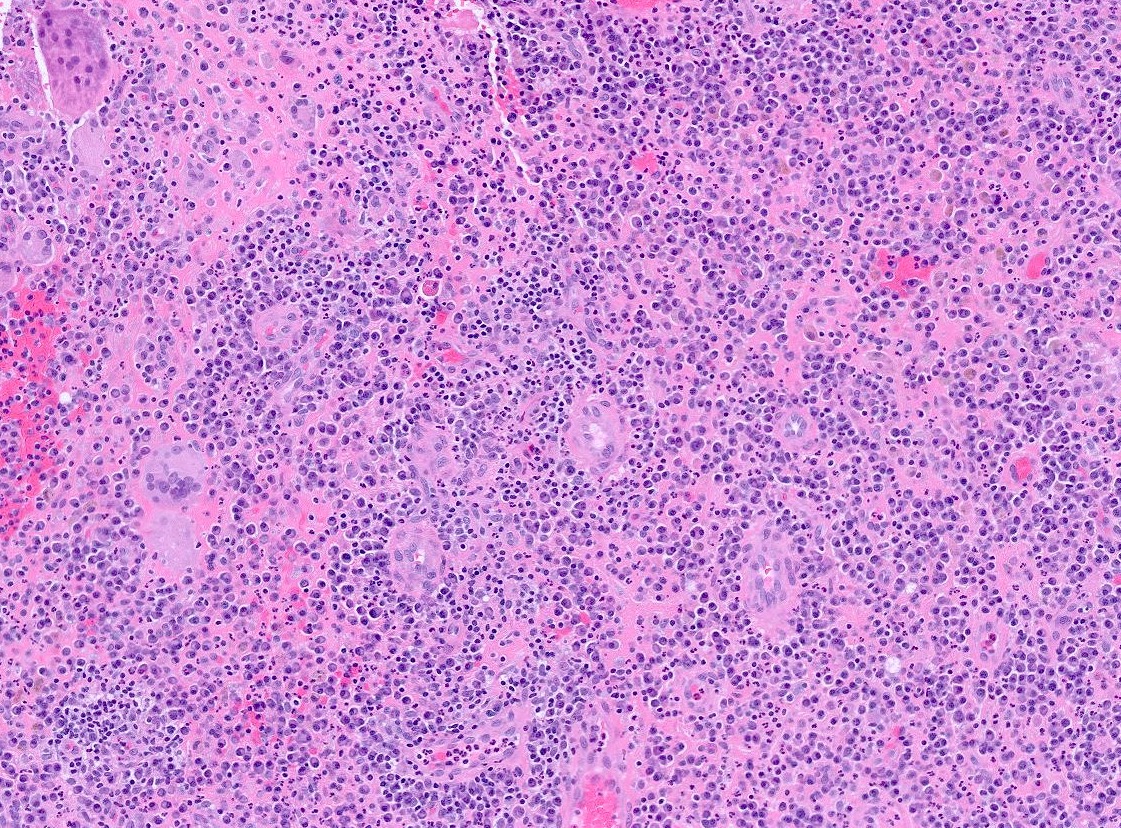
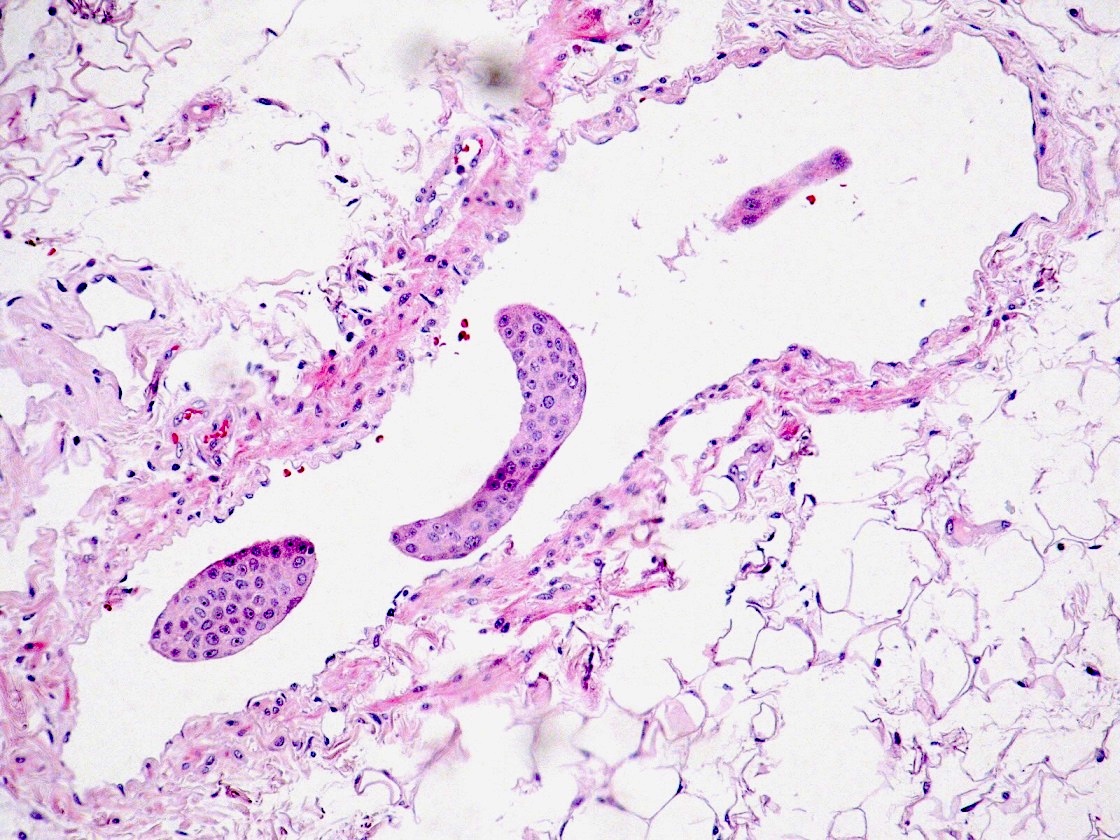
Microscopic (histologic) description
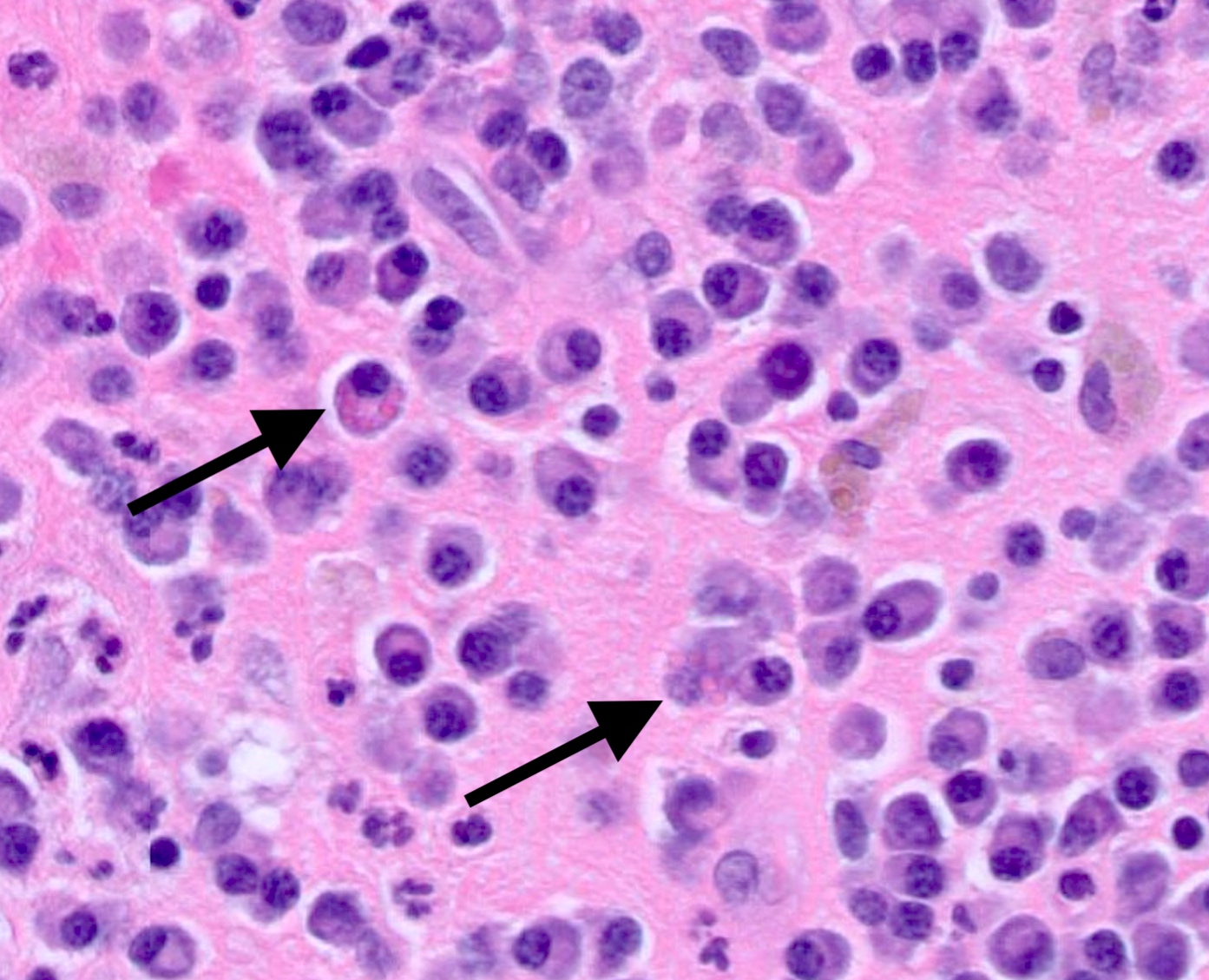
- Cellular polypoid mass primarily consisting of a chronic inflammatory cell infiltrate, including mature lymphocytes, plasma cells, histiocytes and eosinophils
- Relative to the plasma cells, Russell bodies or Mott cells containing large eosinophilic immunoglobules can be seen and are indicative of a benign plasma cell proliferation
- Polymorphonuclear leukocytes may be present
- Stroma includes granulation tissue varying in appearance from edematous and richly vascularized to fibrous with a decreased vascular component
- Multinucleated giant cells may be present
- Cholesterol granulomas and calcific debris (tympanosclerosis) may be present
- When the epithelium is present, it appears as pseudostratified columnar or cuboidal cells with or without cilia and may demonstrate squamous metaplasia (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- Finding of granulation tissue reaction and keratin in an aural polyp is a good predictor for the presence of a cholesteatoma or cholesteatomatous chronic otitis media (Acta Otorrinolaringol Esp 2003;54:161)
Microscopic (histologic) images
Positive stains
- Nonspecific
- Cytokeratin positive in epithelial cells within the otic polyp
Negative stains
- Special stains for microorganisms (fungi, spirochetes, mycobacteria, protozoa and parasites) are negative but are indicated to rule out an infectious cause
Videos
Infected aural polyp ear wax removal
Sample pathology report
- Soft tissue, middle ear, left, biopsy:
- Inflammatory aural / otic polyp
- Soft tissue, middle ear, left, polypectomy:
- Otic polyp
- No malignancy identified
Differential diagnosis
- Paraganglioma:
- Well differentiated nonepithelial neoplasm
- Found in the middle ear in 30% of cases
- Histologically, classic organoid (zellballen) or nesting pattern oval chief cells
- Uniform nuclei with dispersed chromatin
- Expresses neuroendocrine markers but negative for cytokeratins
- Cholesteatoma:
- Chronic inflammation without a polypoid mass
- Keratinizing squamous epithelium with keratin debris
- Prominent granular layer and inflammation
- Langerhans cell histiocytosis:
- Middle ear neuroendocrine tumor:
- Rare, benign middle ear epithelial neoplasm
- Tumor is white, gray or red-brown, with soft or rubbery consistency
- Histologically, the tumor exhibits cuboidal to columnar cells with distinct cell borders and eosinophilic cytoplasm
- Neoplastic cells coexpress keratins (AE1 / AE3, CAM5.2) and neuroendocrine markers
- Plasmacytoma:
- Similar dense plasma cell component
- Not commonly found in the middle ear
- Monoclonal by immunocytochemistry or in situ hybridization of kappa or lambda light chains
- Does not contain mature plasma cells or Russell bodies
Board review style question #1
Which of the following statements regarding otic polyps is true?
- Composed primarily of keratinized squamous epithelium
- Often associated with a history of cholesteatoma
- They commonly arise from the tympanic membrane
- Typically present with sudden sensorineural hearing loss
- Usually become malignant if untreated
Board review style answer #1
B. Often associated with a history of cholesteatoma. Otic polyps are associated with cholesteatoma in 80% of cases.
Answer C is incorrect because otic polyps commonly arise from the mucosa of the middle ear or external auditory canal, rather than the tympanic membrane itself.
Answer E is incorrect because otic polyps are typically benign growths composed of granulation tissue, inflammatory cells and sometimes hypertrophic mucosa. Malignant transformation has not been reported in the literature.
Answer D is incorrect because otic polyps may lead to conductive hearing loss due to obstruction of the external auditory canal or middle ear space. Sudden sensorineural hearing loss is not a typical presentation of otic polyps.
Answer A is incorrect because otic polyps are primarily composed of granulation tissue, which consists of fibroblasts, blood vessels and inflammatory cells, such as lymphocytes and plasma cells. Keratinized squamous epithelium is not a predominant component of otic polyps.
Comment Here
Reference: Inflammatory aural / otic polyp
Comment Here
Reference: Inflammatory aural / otic polyp
Board review style question #2
A 55 year old woman presents with recurrent episodes of unilateral otorrhea, hearing loss and a sensation of fullness in the affected ear. Examination reveals a pink, fleshy mass protruding into the external auditory canal. Histopathological examination demonstrates hyperplastic squamous epithelium and numerous dilated vessels infiltrated by chronic inflammatory cells. Which of the following is the most likely diagnosis?
- Cerumen impaction
- Cholesteatoma
- Otic polyp
- Otitis externa
- Squamous cell carcinoma
Board review style answer #2
C. Otic polyp. It arises from the middle ear but may extend into the external auditory canal if perforated. The mass appears fleshy and is composed of granulation tissue, mixed inflammation and abundant plasma cells.
Answer E is incorrect because squamous cell carcinoma typically presents as a nonhealing ulcer often associated with bleeding, pain and hearing loss.
Answer A is incorrect because while cerumen impaction can cause symptoms such as hearing loss and fullness in the ear, it typically does not present as a fleshy mass. Additionally, cerumen impaction does not demonstrate the histopathological findings described in the question stem, such as hyperplastic squamous epithelium and dilated vessels infiltrated by chronic inflammatory cells.
Answer B is incorrect because cholesteatoma is a benign but locally destructive growth of keratinizing squamous epithelium with keratin debris and inflammation. It is typically not described as a fleshy mass.
Answer D is incorrect because otitis externa, also known as swimmer's ear, refers to inflammation of the external auditory canal. While otitis externa can present with otorrhea, hearing loss and a sensation of fullness in the ear, it typically does not manifest as a fleshy mass.
Comment Here
Reference: Inflammatory aural / otic polyp
Comment Here
Reference: Inflammatory aural / otic polyp
Keloid
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Abnormal proliferation of scar tissue that extends beyond the boundaries of the initial injury and does not regress (Sci Rep 2021;11:9390)
- Forms at the site of cutaneous injury (often minor) (Sci Rep 2021;11:9390)
Essential features
- Excessive scar tissue that extends beyond the boundaries of the initial injury
- Very common in dark skinned people (Fitzpatrick skin types 4 - 6) (Cureus 2022;14:e23503)
- Recurrence after excision is common (Burns Trauma 2020;8:tkaa031)
- Characteristic broad, pink bands of collagen (keloidal collagen)
Terminology
- Keloid / keloid scar
- Keloid is Greek for crab claw
- Not to be confused with hypertrophic scar, which is confined to the limits of the injury (Exp Dermatol 2021;30:146)
Epidemiology
- Any age but most are in patients 10 - 30 years old (Front Cell Dev Biol 2020;8:360)
- 15 times more common in Asian, Hispanic and African populations (J Clin Aesthet Dermatol 2021;14:S24)
- Among keloids in the head and neck, 70% occur on the ear / earlobe (Facial Plast Surg Aesthet Med 2021;23:59)
- Common in young African women after ear piercing
- Unique to humans (Adv Wound Care (New Rochelle) 2019;8:77)
- First recorded in the Smith papyrus from Egypt around 1700 B.C. (Exp Dermatol 2021;30:146)
Sites
- Sites of previous surgery, trauma or burns
- Common sites: anterior chest, shoulders, upper back, back of neck, cheeks and earlobes (Clujul Med 2013;86:313)
Pathophysiology
- Exact pathogenesis of keloids and hypertrophic scar formation is unknown
- Keloids and hypertrophic scars are an abnormal response to trauma
- Wounds more likely to undergo keloid formation include wounds healing by secondary intention, wounds with prolonged inflammation (foreign body, infection, burn, earring site) and sites of repeated trauma (Clujul Med 2013;86:313)
- Hypothesized pathogenesis involves excessive and prolonged inflammation leading to dysregulated normal healing with excessive production of collagen, elastin and extracellular matrix (Scars Burn Heal 2021;7:2059513120980320)
- Fibroblasts and mast cells are increased (Scars Burn Heal 2021;7:2059513120980320)
- Growth factors and cytokines such as TGF beta, TNF alpha, interleukins are increased in keloids (Scars Burn Heal 2021;7:2059513120980320)
- Keloids have higher collagenase activity, type III collagen, chondroitin 4 sulphate and glycosaminoglycans than normal scars (Exp Dermatol 2021;30:146)
- Inconsistent genetic associations have been found linked to certain HLA subtypes and blood group A (Téot: Textbook on Scar Management, 1st Edition, 2020)
Etiology
- May develop after minor injuries, trauma, burns, insect bites, surgery, cryotherapy, topical treatments (e.g., imiquimod), acne, infections (e.g., shingles) and immunization (Int J Mol Sci 2017;18:606)
- May arise months or years after injury (Am Fam Physician 2009;80:253)
Clinical features
- Patients usually present with cosmetic concerns but may present with itch or pain (J Clin Aesthet Dermatol 2021;14:S24)
- Red to purple, firm, smooth and raised area with no hair
- Grows slowly, over months to years
- Characteristically grow laterally beyond the border of the original wound (Burns Trauma 2019;7:39)
- Clinical overlap can make distinction from hypertrophic scars and other mimics difficult (Exp Dermatol 2021;30:146)
- Risk factors include
- Age: Fitzpatrick skin types 4 - 6 (Cureus 2022;14:e23503)
- Body region (see Sites) (Facial Plast Surg Aesthet Med 2021;23:59)
- Family history
- Previous history or multiple keloids
- History of only minor injury preceding onset of the scar
- Local tension on the skin
- Pregnancy
- Hypertension
- Rare syndromes (e.g., Noonan syndrome)
- No useful biomarkers exist to predict risk
Diagnosis
- Can usually be diagnosed by visual inspection, palpation and history (Burns Trauma 2019;7:39)
- May mimic a tumor and therefore imaging (ultrasound, CT or MRI) may help define extent and nature but there are no imaging modalities that can accurately identify keloids (Burns Trauma 2019;7:39)
- Ultrasound elastography may be helpful as keloids and hypertrophic scars are harder than the surrounding tissues
- Ultrasound may also assess effect of treatment
Radiology description
- Ultrasound: hypoechoic dermal based lesion
Prognostic factors
- Keloid is biologically harmless with no risk of malignant transformation (Sci Rep 2021;11:9390)
- Most eventually stop growing and remain stable or even involute slightly (J Plast Reconstr Aesthet Surg 2014;67:87)
- Persistence and recurrence are common (Semin Plast Surg 2021;35:145)
- May lead to aesthetic issues and serious adverse psychosocial outcomes (G Ital Dermatol Venereol 2019;154:148)
- May undergo suppuration, in which cystic cavities in keloids result in acute inflammatory flares and oozing (Int J Dermatol 2021;60:1392)
Case reports
- 10 year old child with meatoplasty keloid (J Laryngol Otol 2006;120:594)
- 30 year old woman with keloids in stretch marks (Clin Case Rep 2022;10:e6723)
- 32 year old man developed keloids following cupping therapy (Plast Reconstr Surg Glob Open 2022;10:e4669)
- 47 year old woman with extensive keloid scarring from pemphigus vulgaris (Clin Case Rep 2022;10:e6424)
- 70 year old woman with spontaneous keloids (Cureus 2022;14:e23227)
Treatment
- Multiple treatment options exist and there is considerable variability in practice
- Optimal treatment will vary depending on the age of the patient (pediatric versus adult) and body site
- An escalating treatment algorithm may be followed (Burns Trauma 2019;7:39)
- Treatment options include
- Emollients and regular massage
- Occlusive dressing
- Compression
- Fixation for lesions on a joint
- Local corticosteroid
- Steroid tape / plaster
- Steroid injections: intralesional steroids (e.g., triamcinolone acetonide)
- Surgical excision
- Recurrence following excision alone 45 - 100%; the new keloid may be larger than the original (Burns Trauma 2020;8:tkaa031)
- Excision may be combined with other modalities including steroids, imiquimod, bleomycin, cryotherapy or radiotherapy and recurrence rates are lower (Dermatol Ther 2022;35:e15425)
- Radiotherapy (Front Med (Lausanne) 2022;9:1043840)
- Laser therapy is not effective as recurrence rates are very high
- Other injectables: 5FU, interferon
- Oral medicines if large or multiple keloids
Gross description
- Polypoid, covered by thin, hairless skin
- Can be small (< 2 cm) up to very large
Gross images
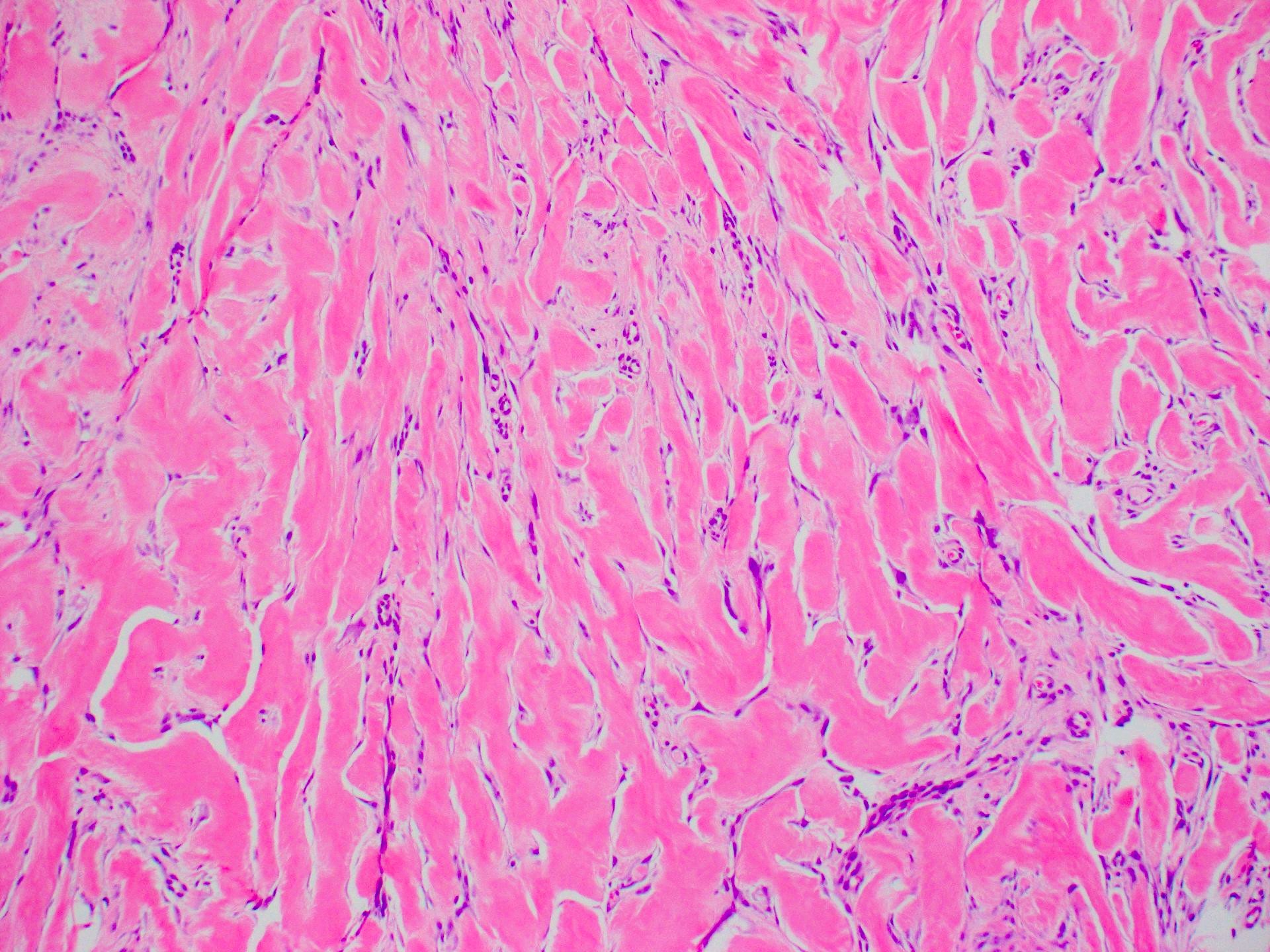
Microscopic (histologic) description
- Lesion of the deep dermis; sparing of papillary dermis (Am J Dermatopathol 2004;26:379)
- Characteristic long, broad, closely packed collagen bundles that stain uniformly eosinophilic (keloidal collagen) arranged in haphazard fascicles (Scars Burn Heal 2021;7:2059513120980320)
- Fibroblasts are increased compared to normal skin (Front Cell Dev Biol 2020;8:360)
- May appear edematous due to increased dermal mucosubstances (J Zhejiang Univ Sci B 2022;23:699)
- Tongue-like advancing edge (Front Cell Dev Biol 2020;8:360)
- Epidermis may be normal, thin or thick (most) and may be affected by secondary changes (such as hypertrophy and inflammation due to irritation / scratching) (Front Cell Dev Biol 2020;8:360)
- Lesion replaces adnexal structures (i.e., hair follicles and sweat glands) (Histol Histopathol 2015;30:1033)
- Fewer capillaries and blood vessels than surrounding skin (J Plast Surg Hand Surg 2010;44:272)
- Tend to have marked inflammation in the dermis at the leading edge of growing keloids (Scars Burn Heal 2021;7:2059513120980320)
- Overlap with hypertrophic scar and therefore correlation with the clinical features is recommended
Microscopic (histologic) images
Virtual slides
Videos
Keloid scar:
5 minute pathology pearls
by Dr. Jerad Gardner
Sample pathology report
- Skin sternum, excision:
- Dermal scar with keloidal type collagen (see comment)
- Comment: The histological features are consistent with keloid or hypertrophic scar; correlation with the clinical features is recommended.
Differential diagnosis
- Hypertrophic scar:
- Confined to the area of injury without lateral extension
- Histological overlap: tends to have more delicate fibrillar collagen and no abundant mucosubstances
- Does not recur; clinical correlation may be required to help distinction from keloid
- Dermatofibroma, particularly keloidal dermatofibroma:
- More cellular; typically lacks keloidal collagen
- No history of preceding trauma
- Dermatofibrosarcoma protuberans:
- No history of preceding incisions / surgery at the site
- Pseudoepitheliomatous hyperplasia of the overlying epidermis
- Storiform pattern
- More cellular
- Cytological atypia present but may be subtle
- Lacks keloidal collagen
- Infiltrative edges
- Extension into subcutaneous tissue
- Morphea / scleroderma:
- Involves full thickness of dermis
- Architecture of dermis largely intact
- Collagen is thickened and hypereosinophilic but does not form intersecting bands
- Perivascular inflammatory infiltrate of lymphocytes, plasma cells and macrophages in early lesions
- Does not have increased ground substance
- Desmoplastic melanoma:
- Poorly circumscribed with deep infiltration
- Elongated spindle cells surrounded by collagen bundles; also scattered hyperchromatic or multinucleated cells with bizarre nuclei
- May have small foci of lymphoid aggregates
- May be pure or combined with classic melanoma
Additional references
Board review style question #1
Which of the following is true of keloid?
- Hypertrophic scar is synonymous with keloid scar
- Keloids are more common in Asian and African populations
- Recurrence after surgical excision is uncommon
- Thick collagen bundles are unique to keloid
Board review style answer #1
B. Keloids are more common in Asian and African populations. Keloids are up to 15 times more common in Asians, Hispanics and Africans. Answer A is incorrect because hypertrophic scars overlap histologically with keloid but are a separate clinical entity; clinical correlation may be required to separate them. Answer C is incorrect because recurrence occurs in up to half following simple excision. Answer D is incorrect because keloidal collagen is characteristic of keloid but can be seen to a lesser extent in hypertrophic scars.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid
Board review style question #2
Board review style answer #2
C. Keloid. The image shows the classic and characteristic appearance of keloidal collagen. Answer A is incorrect because while dermatofibroma can be similar in appearance, it is typically more cellular and is most common on the legs. Answer B is incorrect because while hypertrophic scars can overlap in histological appearance with keloid, they are generally more cellular and have less keloidal collagen. Clinical history helps to make the diagnosis as Asian individuals have a much higher risk, keloids are most common in young people (10 - 30 years old) and the earlobe is a typical site. Answer D is incorrect because while scleroderma / morphea can mimic keloid on a small biopsy, the collagen pattern is different (being more ordered and almost acellular) and the clinical history is not suggestive.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid
Middle ear adenocarcinoma (pending)
[Pending]
Middle ear neuroendocrine tumor
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Differential diagnosis | Additional referencesDefinition / general
- Rare, benign glandular neoplasm originating from middle ear mucosa
- First described in 1976 (Laryngoscope 1976;86:1123, Clin Otolaryngol Allied Sci 1976;1:17)
- Neuroendocrine and epithelial differentiation; also called carcinoid tumor or amphicrine tumor (Ultrastruct Pathol 2001;25:73)
- Rosai believes they form a continuum with carcinoid tumor and could be considered adenocarcinoid tumors
- No gender preference, usually 20's to 40's, but wide age range
- Affects all sites in middle ear
- Occasionally perforates tympanic membrane and extends into external auditory canal
- Not associated with chronic otitis media or cholesteatoma
- Excellent prognosis; rarely is locally aggressive, invades vital structures, has regional metastases (Laryngoscope 2005;115:1660) or causes death
Case reports
- 21 year old man and 34 year old woman with carcinoid tumors of the middle ear (Am J Clin Pathol 1987;87:592)
- 27 year old man and 42 year old woman with middle ear adenoma (J Clin Pathol 1991;44:652)
- 63 year old woman with 1 cm middle ear mass (Case #376)
Treatment
- Complete surgical excision
- Mastoidectomy may be necessary for large lesions
- Recurs with inadequate excision
Gross description
- Gray-white to red-brown, firm/rubbery masses
- Relatively well circumscribed
- Not encapsulated
- No hemorrhage, mean 0.8 cm
Microscopic (histologic) description
- Variable patterns (sheets, solid, trabecular, cystic, cribriform, glandular, NOT papillary) of glands or tubules composed of uniform single layer of cuboidal or columnar cells with variable eosinophilic cytoplasm and round/oval hyperchromatic nuclei, eccentric nucleoli (if present)
- May appear plasmacytoid, may have significant pleomorphism
- May produce PAS+ mucin
- Sparse fibrous or myxoid stroma
- No/rare mitotic figures, no necrosis
- May have neuroendocrine differentiation morphologically and immunohistochemically
Microscopic (histologic) images
Positive stains
- Keratin (90%), CK7 (90%), chromogranin (88%), CAM5.2 (81%), mucin (intraluminal), lysozyme, neuron specific enolase (50%), synaptophysin (31%), serotonin (25%), S100 (15%), CK20 (6%, focal)
Negative stains
- Actin
Electron microscopy description
- Desmosomes and microvilli
- Often membrane bound dense core granules
- May have glandular differentiation (Am J Clin Pathol 1985;84:541)
Differential diagnosis
- Acoustic neuroma
- Glandular metaplasia: focal or haphazard in background of chronic otitis media
- Jugulotympanic paraganglioma: zellballen surrounded by S100+ sustentacular cells
- Meningioma
- Middle ear adenocarcinoma: marked pleomorphism, mitotic activity, necrosis, invasion of bone and soft tissue
Additional references
Middle ear papilloma (pending)
[Pending]
Middle ear paraganglioma
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Additional referencesDefinition / general
- Also called glomus jugulare tumor or glomus tympanicum tumor
- Most common tumor of middle ear
- Usually women, ages 40 - 69 years
- 85% arise in jugular bulb causing mass in middle ear or external auditory canal; 12% arise from tympanic branch of glossopharyngeal nerve (Jacobson nerve) causing middle ear mass; 3% arise from posterior auricular branch of vagus nerve (Arnold nerve) causing external auditory canal mass
- Usually causes conductive hearing loss
- May be locally invasive into temporal bone and mastoid; may cause cranial nerve palsies, cerebellar dysfunction, dysphagia, hoarseness
- Tumors are fed by branches of nearby large arteries; may bleed profusely at biopsy
- Histology usually benign but this does not predict behavior
- Rarely are malignant histologically (necrosis, mitotic activity, vascular invasion) with metastases to cervical lymph nodes, lung, liver (J Laryngol Otol 2000;114:17)
Case reports
- 45 year old man with middle ear mass (Case of the Week #349)
- Patient with tumor with regional metastases and spinal metastases 10 - 13 years after presentation (Arch Pathol Lab Med 1990;114:976)
Treatment
- Complete excision (may be difficult) with possible preoperative embolization or radiation therapy (reduces vascularity, promotes fibrosis)
- 50% recur locally
Gross description
- Polypoid, red, friable
Microscopic (histologic) description
- Classic organoid (zellballen) or nesting pattern of paragangliomas with central round / oval chief cells containing abundant eosinophilic granular or vacuolated cytoplasm, uniform nuclei with dispersed chromatin
- Sustentacular cells (spindled, basophilic, difficult to see with H&E) are present at periphery of nests
- Prominent fibrovascular stroma separates nests
- May have pleomorphism but this does not predict malignant behavior; occasional dense fibrous stroma or apparent infiltrative growth
- Rare mitotic figures or necrosis
- No glandular or alveolar differentiation
Microscopic (histologic) images
Positive stains
- Chromogranin and synaptophysin (chief cells), S100 (sustentacular cells)
- Reticulin (stains stroma and delineates nesting pattern, particularly helpful with crushed specimens), variable vimentin (both cell types)
Electron microscopy description
- Neurosecretory granules
Molecular / cytogenetics description
- Germline mutations for succinate dehydrogenase gene subunits if multiple tumors (Diagn Mol Pathol 2005;14:109)
Differential diagnosis
- Acoustic neuroma
- Carcinoma
- Melanoma
- Meningioma
- Middle ear adenoma
- Other neuroendocrine tumors
Additional references
Otosclerosis
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) description | Additional referencesDefinition / general
- Disorder of bone remodeling affecting bony labyrinth and stapes footplate
- Does not appear to occur outside temporal bone (Am J Otol 1999;20:162)
- Causes fixation of stapes footplate in oval window and inability to transmit sound waves manifesting as conductive hearing loss
- Usually women; 50% have family history; begins in teenagers and slowly progresses
- More common in whites than blacks, Asians or Native Americans
- Associated with measles virus (Ann Otol Rhinol Laryngol 2001;110:897)
- 85% bilateral
Treatment
- Stapedectomy (correction of fixation of footplate of stapes)
Gross description
- Specimens are usually head and crura of stapes which are not affected by disease
Microscopic (histologic) description
- Initially bone resorption and replacement by cellular fibrovascular tissue around blood vessels; then immature bone is deposited with continuous resorption and remodeling; over time, bone is deposited with increased collagen and reduced ground substance resulting in densely sclerotic bone with prominent cement lines
Squamous cell carcinoma of middle ear
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Microscopic (histologic) description | Differential diagnosis | Additional referencesDefinition / general
- Rare; usually age 50s and 60s
- Usually > 20 year history of chronic otitis media or radiation therapy for intracranial tumor or middle ear inflammation
- 25% have associated cholesteatomas
- Symptoms: long standing chronic otitis media with sudden onset of pain, otorrhea, hemorrhage
- 5 year survival: 39%; 10 year survival: 21%; usually no metastatic disease
Case reports
- 71 year old man with primary squamous cell carcinoma of middle ear invading cochlea (Ann Otol Rhinol Laryngol 1983;92:290)
Treatment
- Radical surgery with radiation therapy, chemotherapy for advanced disease
Gross description
- Tumor fills middle ear spaces, may invade walls of mastoid air cells, bone adjacent to carotid canal, internal auditory meatus, Eustachian tube and external auditory canal
Microscopic (histologic) description
- Resembles squamous cell carcinomas at other sites, well to poorly differentiated
- Infiltrative malignant cells with keratinization, intercellular bridges
Differential diagnosis
- Cholesteatoma: no atypia
- Direct invasion from nasopharynx, skin, external ear, parotid gland
- Metastases: need good history to rule out
Additional references
Squamous cell carcinoma of the external auditory canal
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Differential diagnosis | Additional referencesDefinition / general
- 15% of primary cutaneous carcinomas of external ear and auditory canal
- Usually age 60+ years
- Poor prognostic factors: > 2 cm, depth > 4 mm, poorly differentiated tumors, perineural invasion, development within a scar, previously treated squamous cell carcinoma at the site, immunosuppression, location within inner portion of canal with deep involvement of temporal bone
- Tumor spread: tumors of helix spread along helix, to antihelix, to posterior surface of ear; tumors of antihelix spread concentrically; tumors of posterior surface spread to helix; tumors of canal tend to invade bone, may destroy tympanic membrane and penetrate middle ear
- Adenoid squamous carcinoma:
- Unusual variant
- Also called pseudoglandular or acantholytic
- Often face and scalp in sun exposed areas, particularly periauricular area
- Due to a desmosomal defect that causes lack of cell adhesion (acantholysis)
Case reports
- 65 year old woman with pigmented squamous cell carcinoma with dendritic melanocyte colonization in the external auditory canal (Pathol Int 1999;49:909)
- 69 year old man with bilateral squamous cell carcinoma of the external auditory canals (Laryngoscope 2002;112:1003)
- 72 year old man with bilateral auditory canal squamous cell carcinoma (HNO 2006;54:41)
- 89 year old man with angiolymphoid hyperplasia with eosinophilia associated to a squamous cell carcinoma of the ear (Dermatol Surg 2004;30:1367)
- Squamous cell carcinoma in situ of external auditory canal (J Laryngol Otol 2006;120:684)
Treatment
- Complete excision (mastoidectomy or temporal bone resection for canal tumors), possibly radiation therapy
- Tumors of external ear have low recurrence rate (Dermatol Surg 2005;31:1423)
- Canal tumors often recur (19%) or metastasize (11%); death may occur due to intracranial extension
Gross description
- Polypoid, firm / rubbery nodules, frequent ulceration
Microscopic (histologic) description
- Well differentiated:
- Most common, composed of infiltrating nests of cells with keratin pearls or individual cell keratinization and intercellular bridges
- Variable nuclear atypia
- Frequent mitotic activity with atypical forms; invasion may be superficial with irregular budding of basal epithelium or irregular tongues of tumor projecting downward
- Moderated differentiated:
- Scattered individually keratinized cells; no keratin pearls
- Poorly differentiated:
- No obvious keratinization but squamous epithelial dysplasia, pavement-like cellular pattern, foci with intercellular bridges
- Spindle cell variant:
- Infiltrating tumor with interlacing bundles or fascicular growth
- Spindled and epithelioid cells with amphophilic or eosinophilic cytoplasm, pleomorphic and hyperchromatic nuclei, increased N/C ratios, frequent mitotic activity with atypical forms
- Often surface ulceration, surface epithelial dysplasia and differentiated squamous cell carcinoma
- May produce chondroid or osteoid matrix
- Adenoid squamous carcinoma:
- Pseudoglandular appearance due to tumor cell acantholysis in center of tumor nests
- Usually dysplastic surface epithelium
Negative stains
- Adenoid squamous carcinoma: mucin
Differential diagnosis
- Irritated seborrheic keratosis
- Malignant fibrous histiocytoma
- Melanoma
- Pseudoepitheliomatous hyperplasia (Laryngoscope 1998;108:620)
- Adenocarcinoma
- Adenosquamous carcinoma
- Vascular tumors
Additional references
WHO classification
WHO (2022)
Tumors of the external auditory canal
Tumors of the middle and inner ear
- Squamous cell carcinoma
- Ceruminous adenocarcinoma
- Ceruminous adenoma
- Cystic chondromalacia
- Chondrodermatitis nodularis chronica helicis
- Exostosis (osteoma)
Tumors of the middle and inner ear
Additional references
Recent Ear Pathology books
Find related Pathology books: head & neck/endocrine