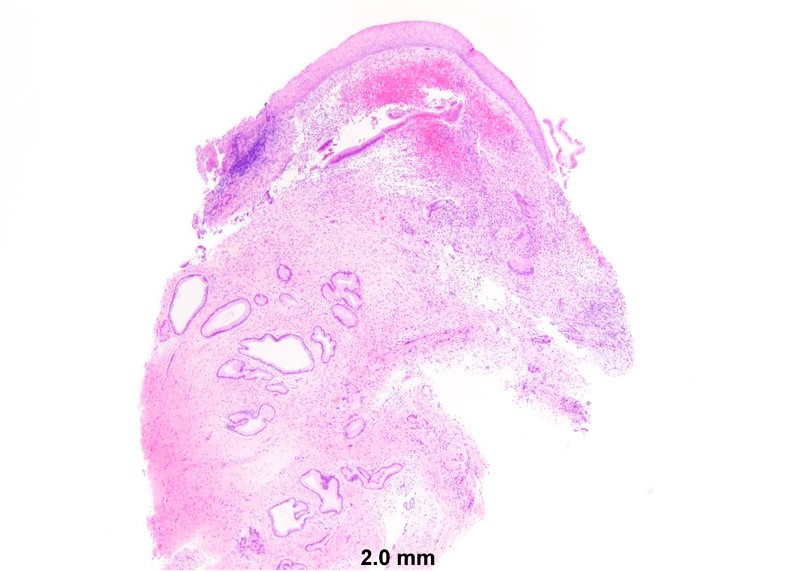
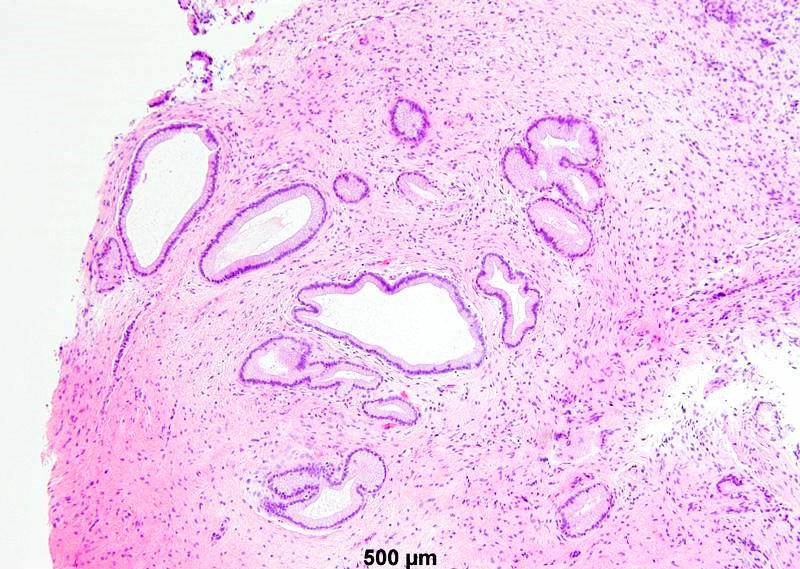
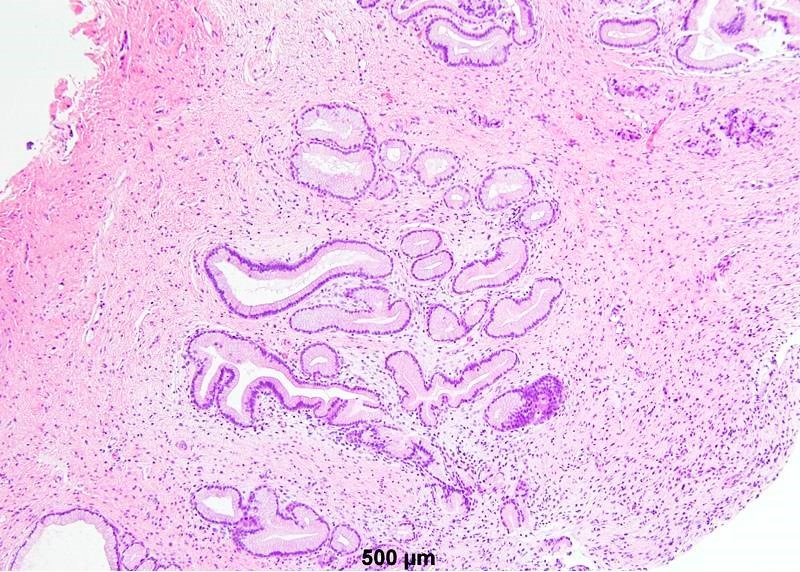
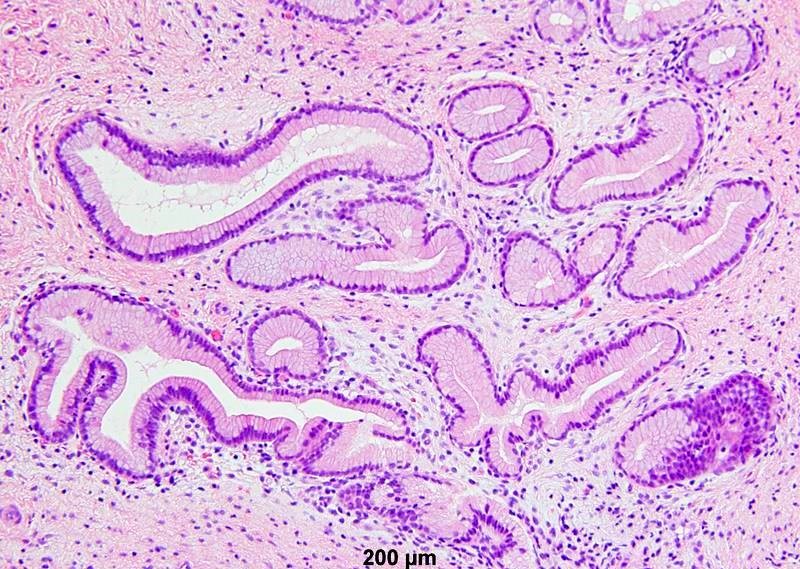
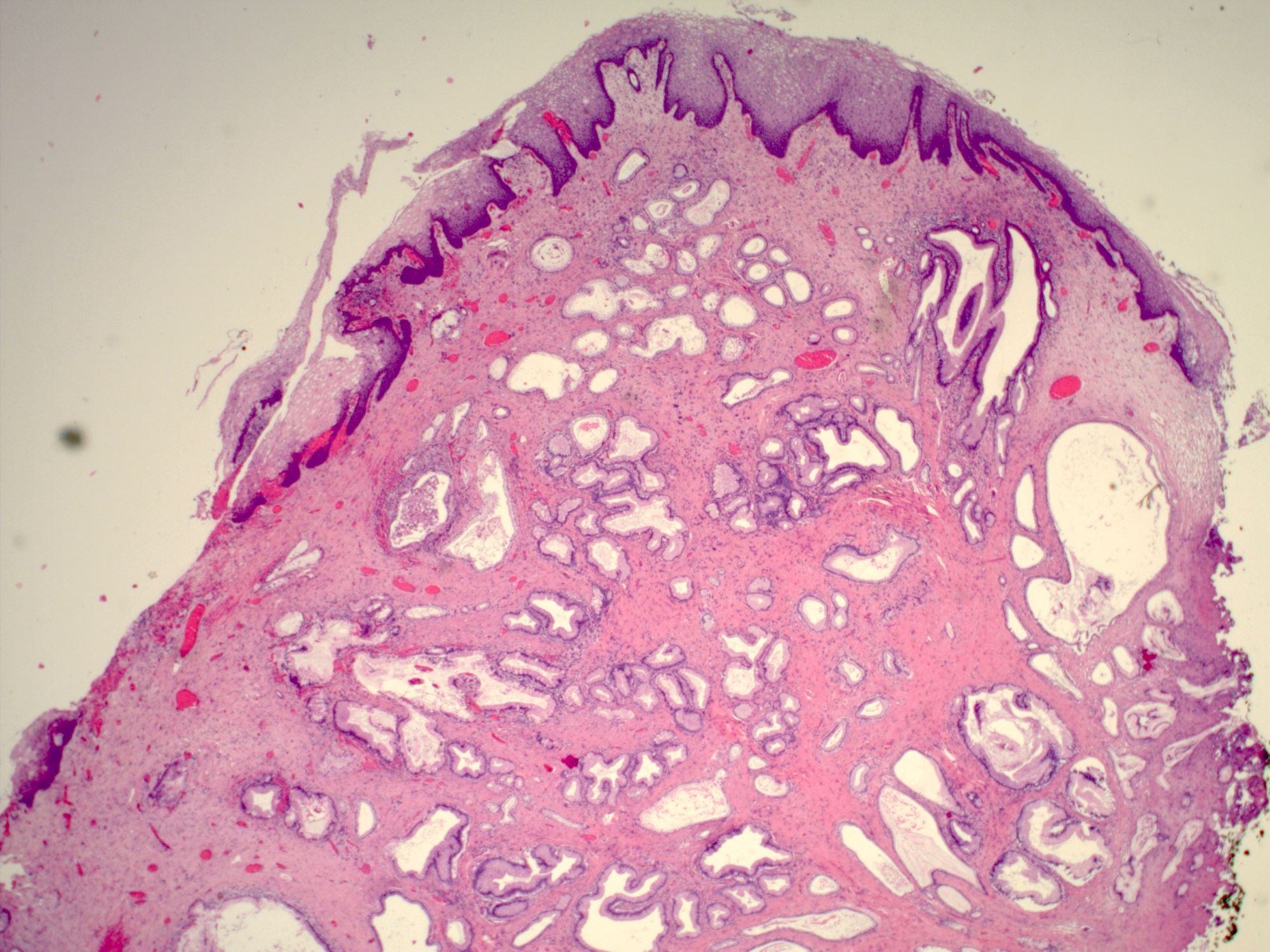
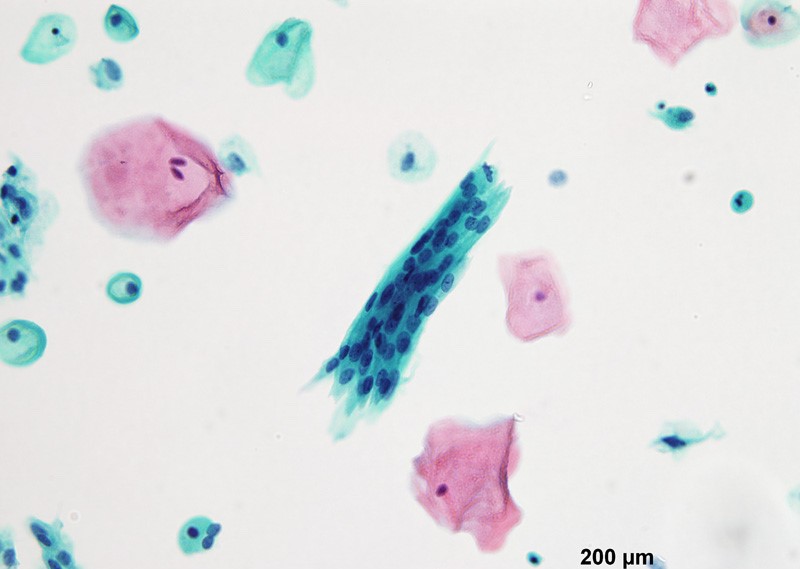
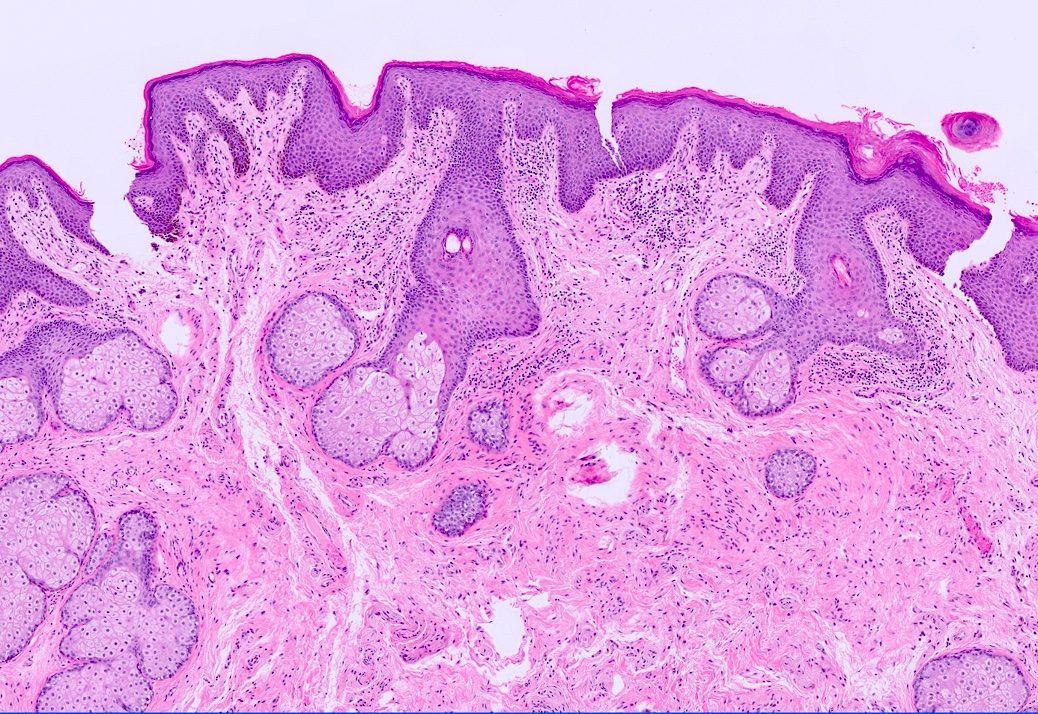
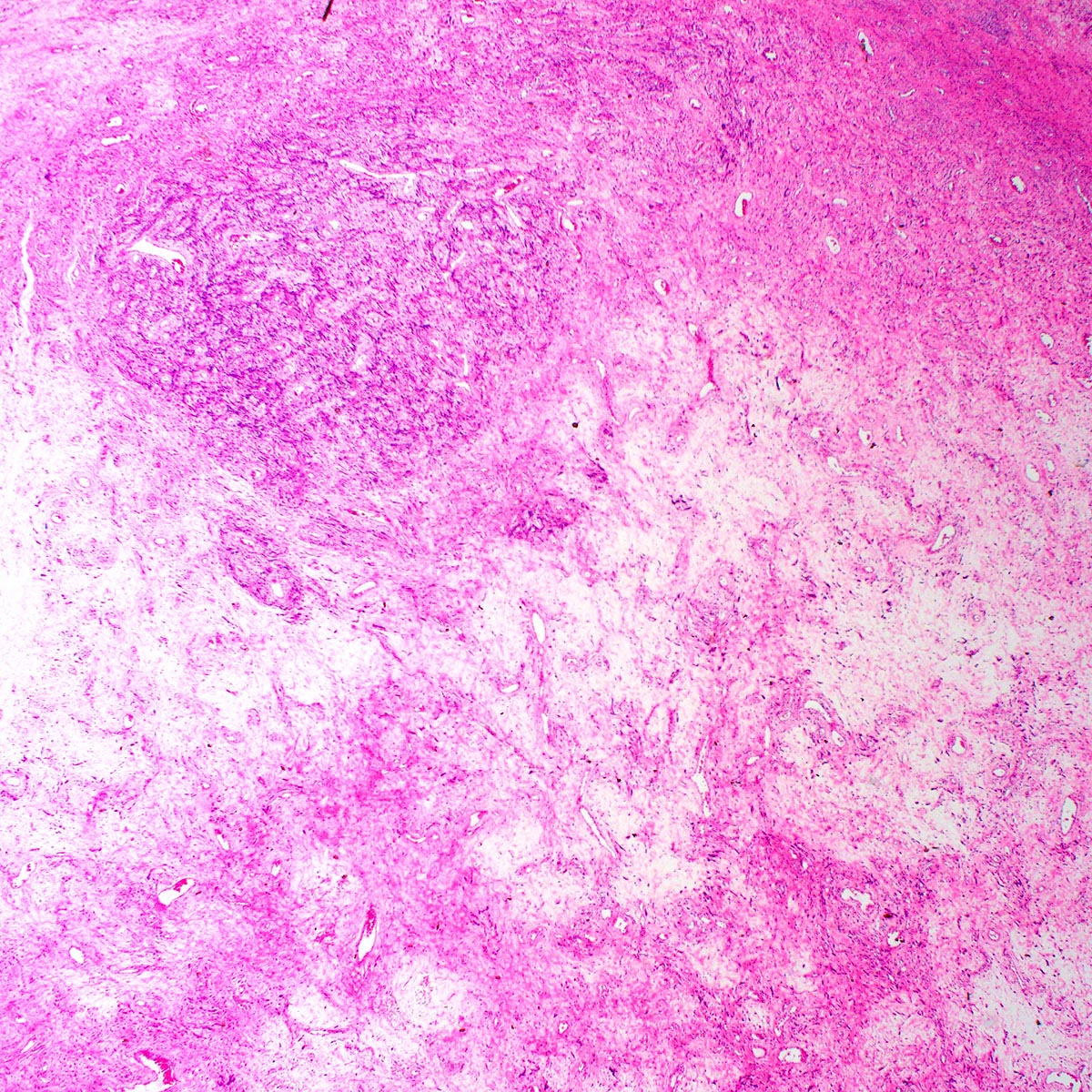
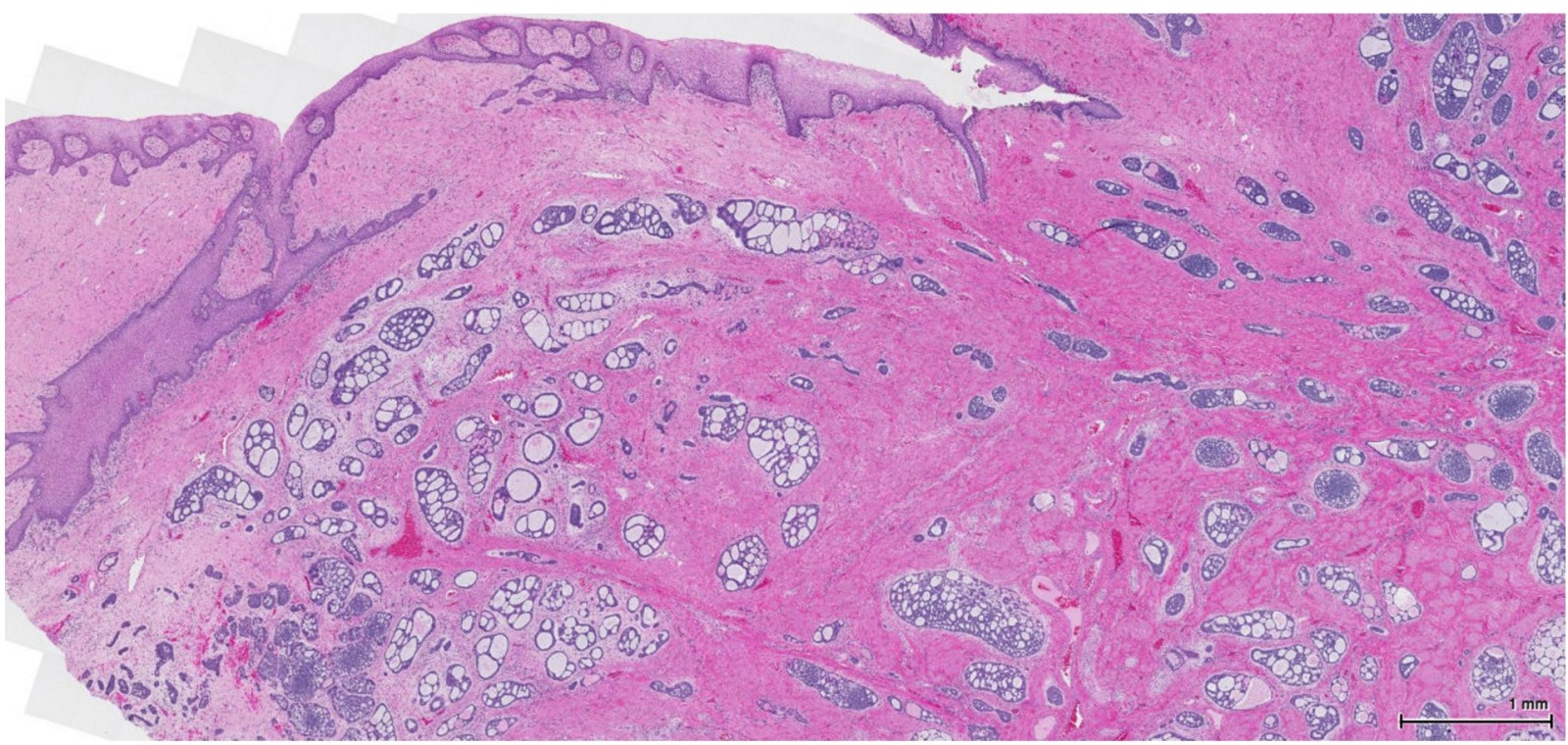
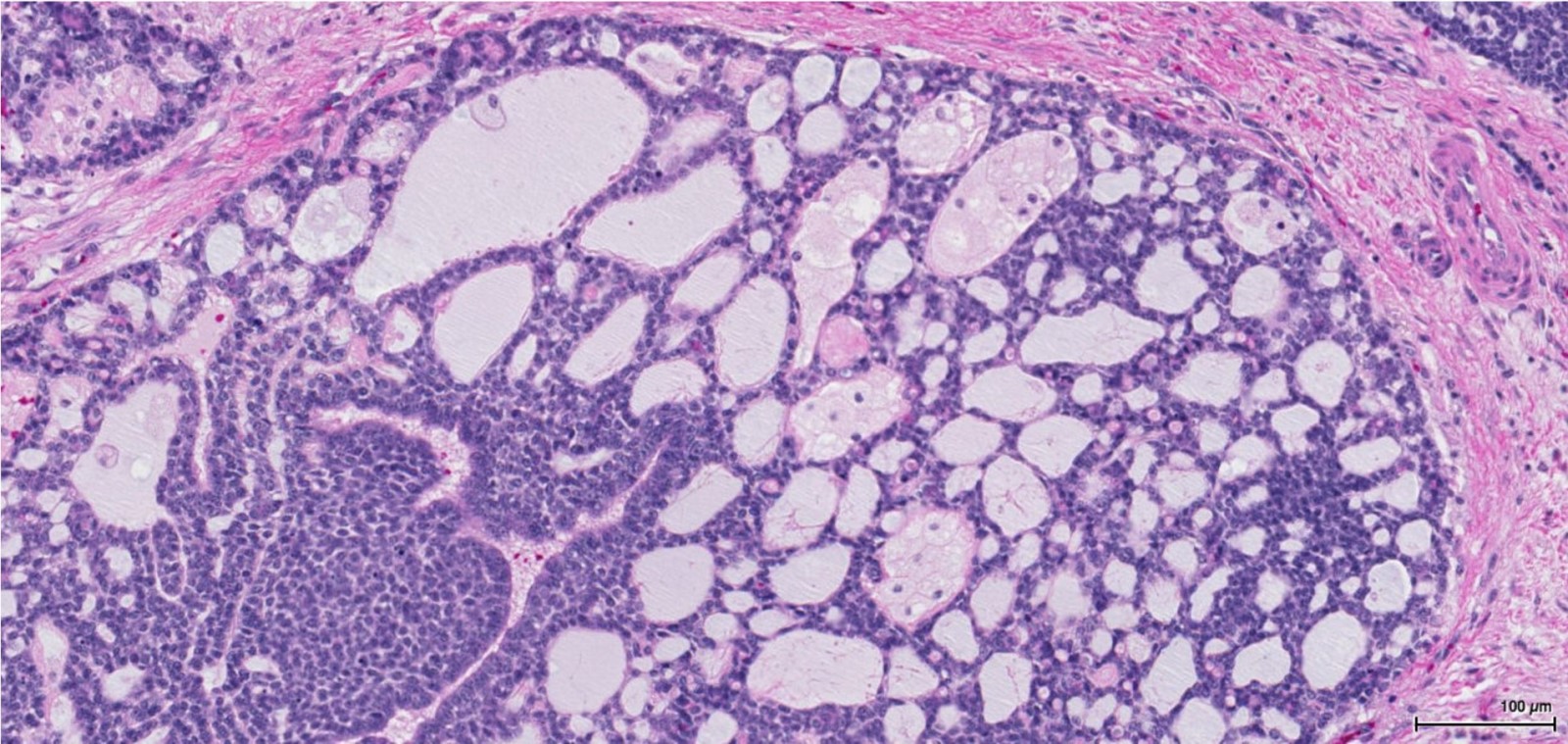
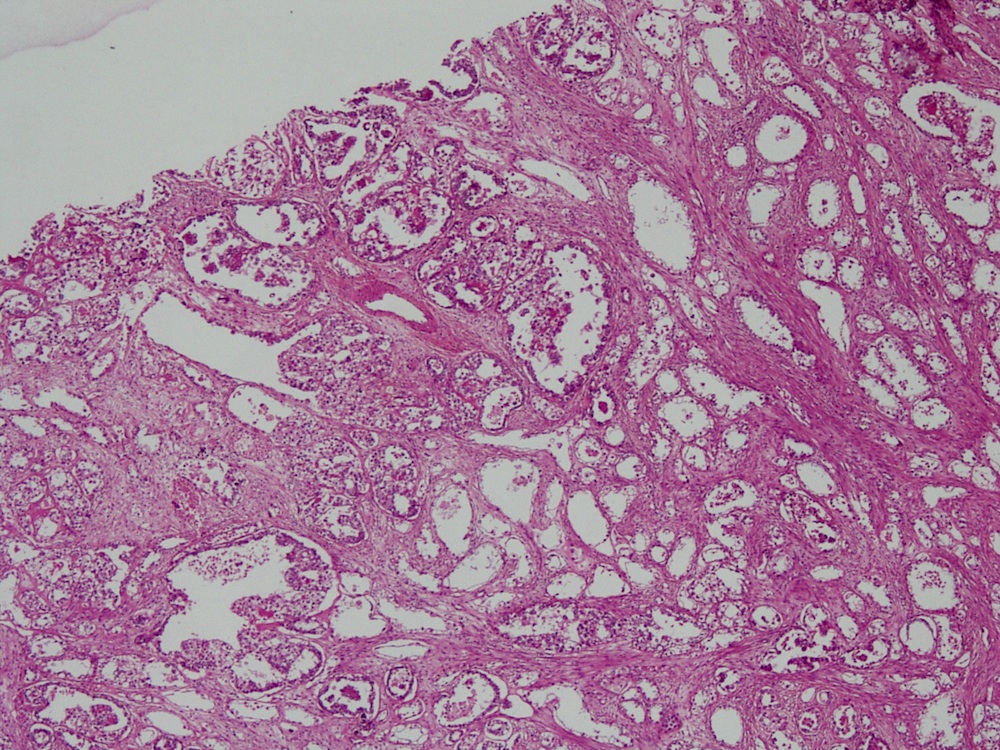
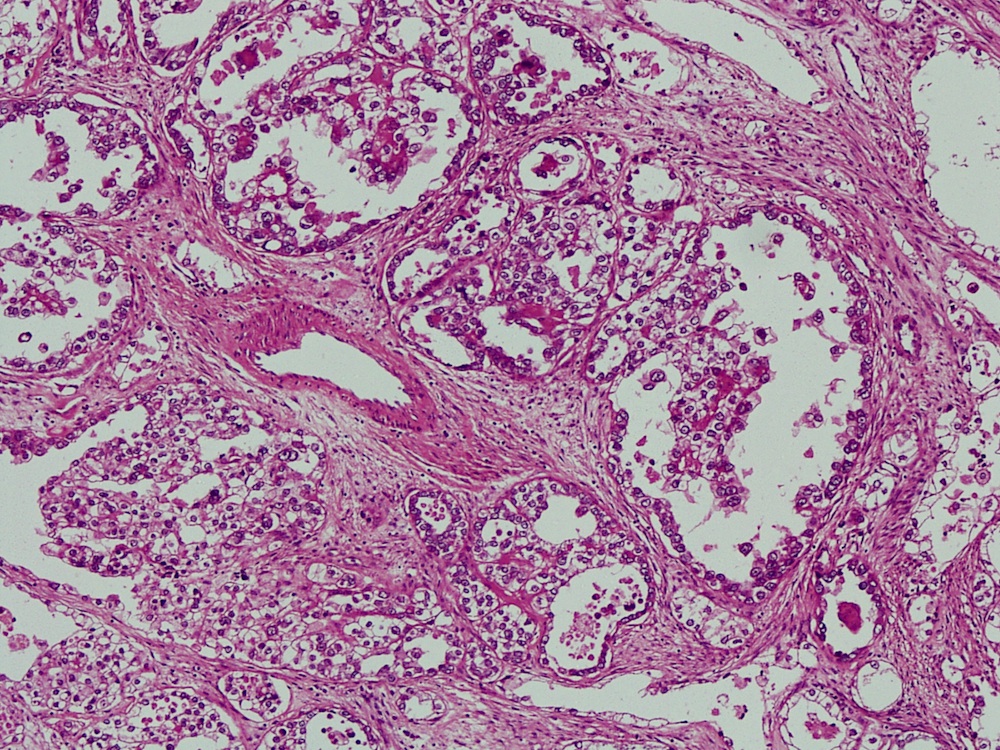
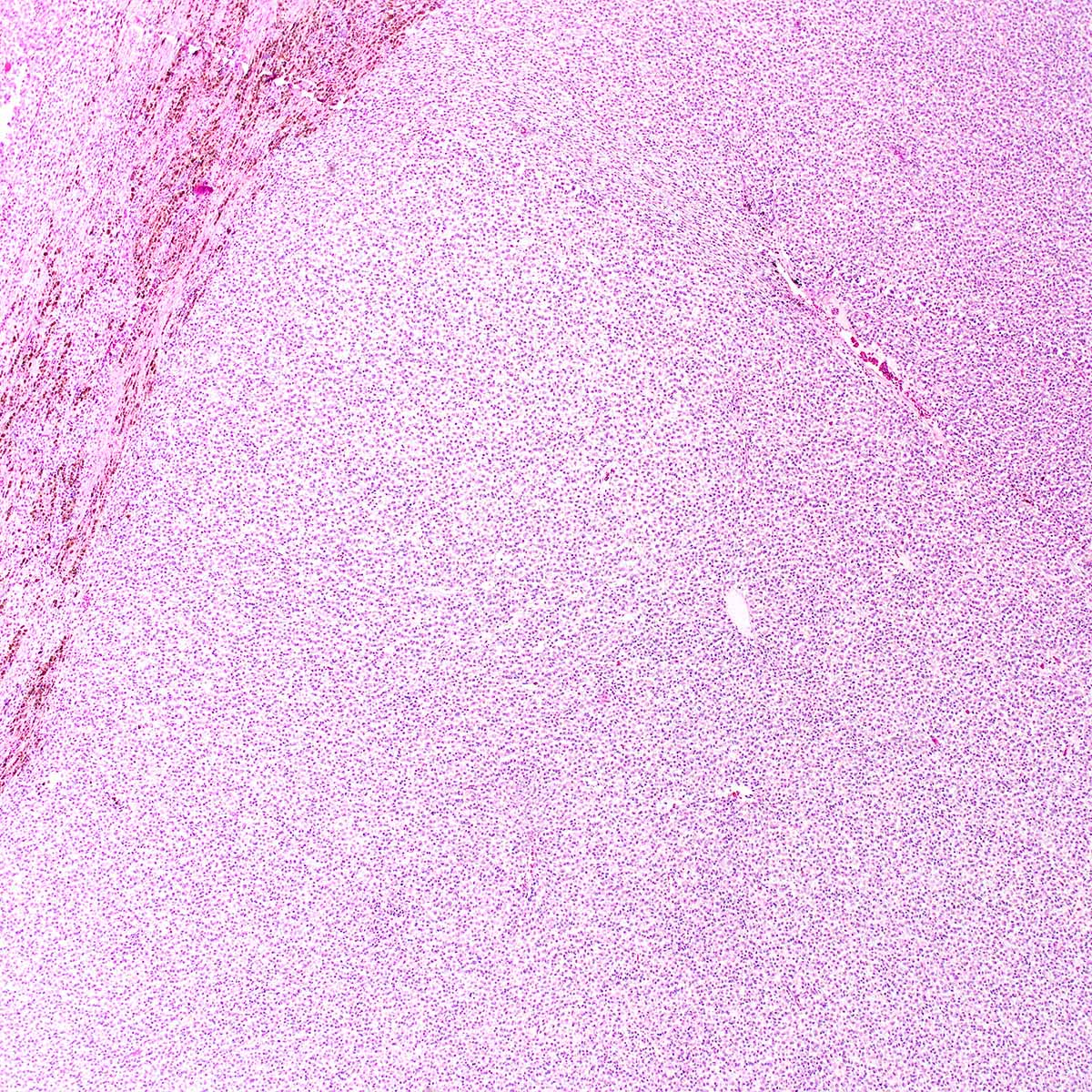
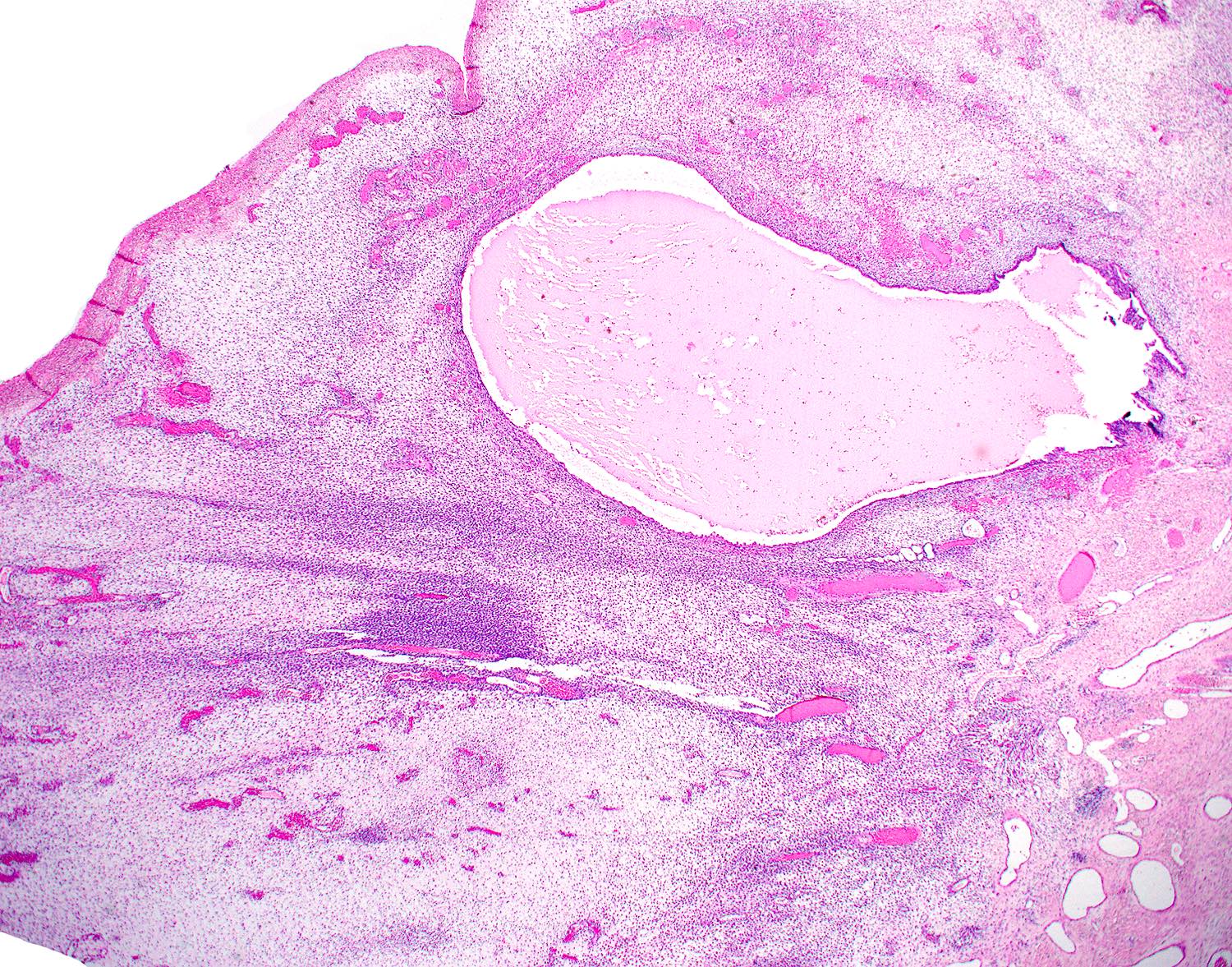
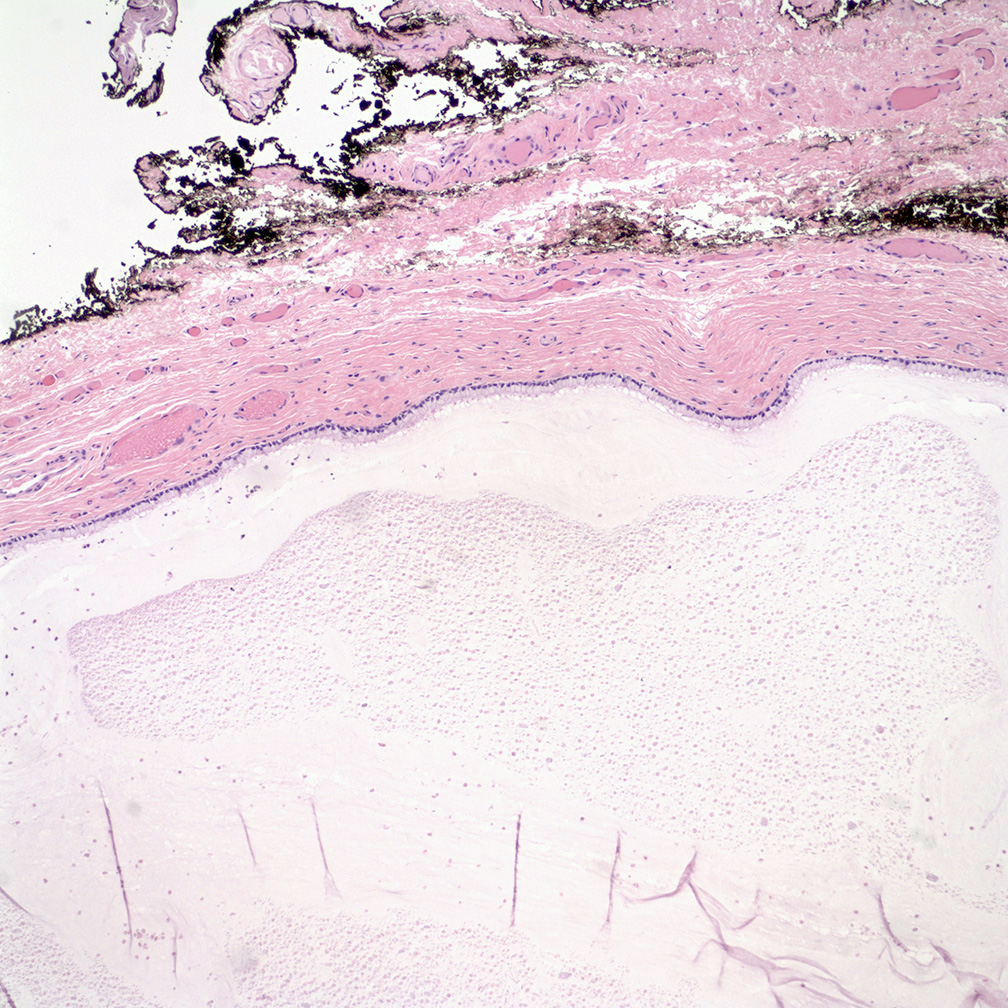
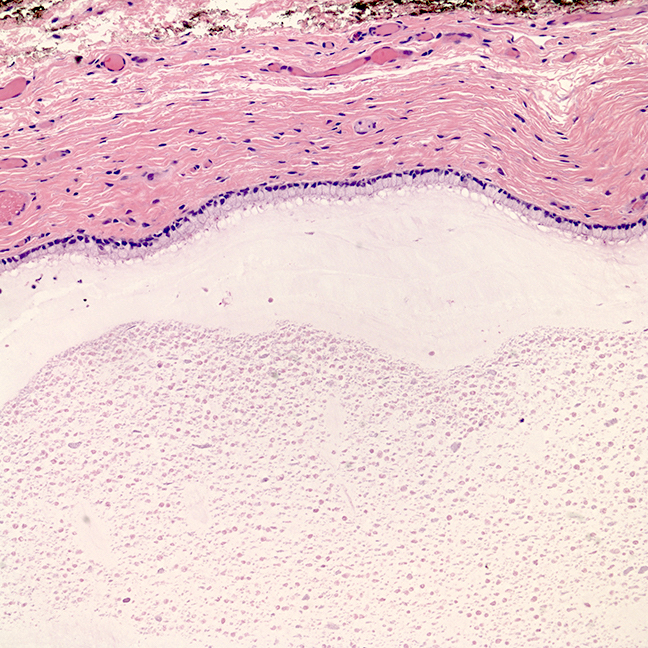
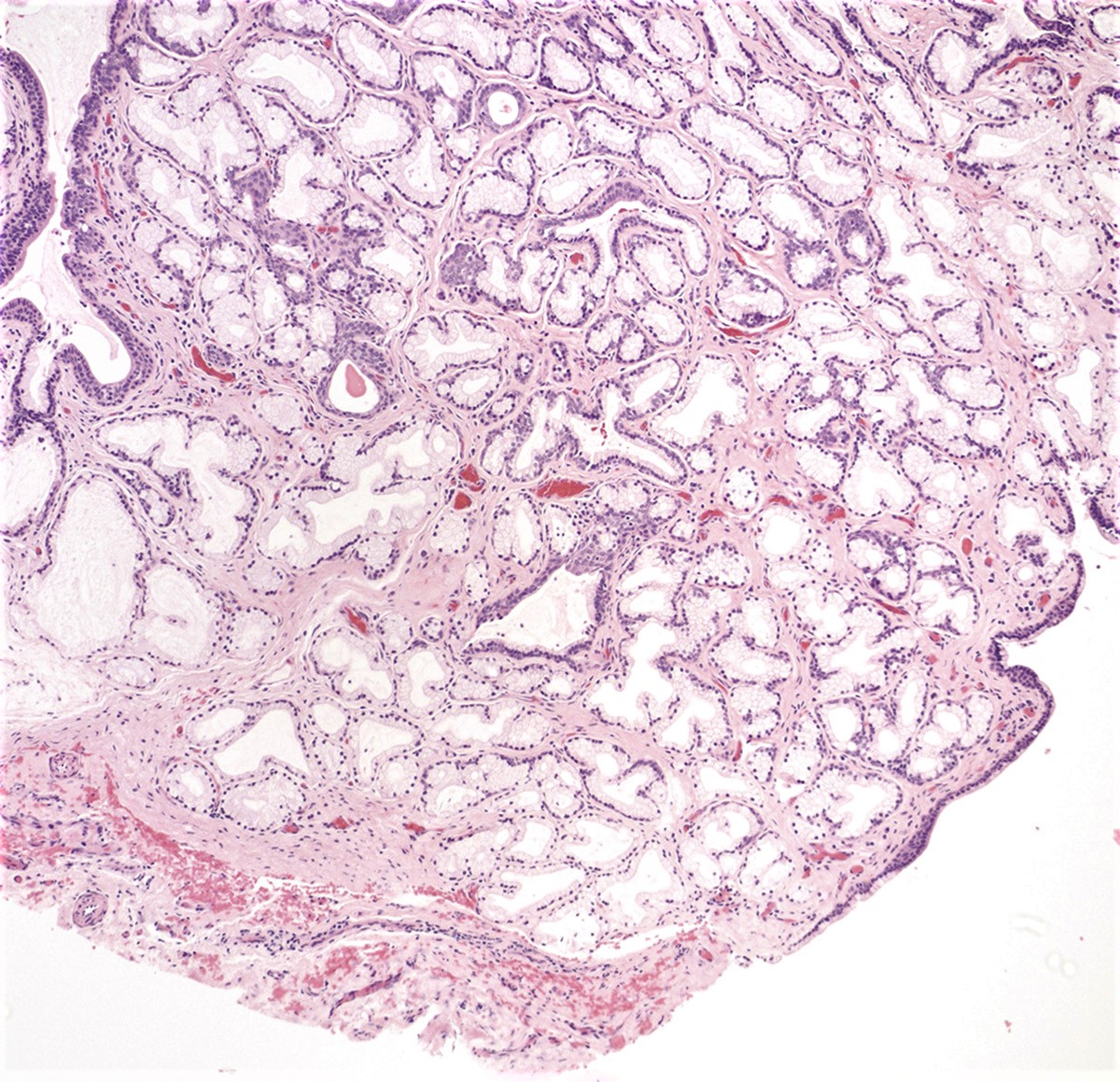
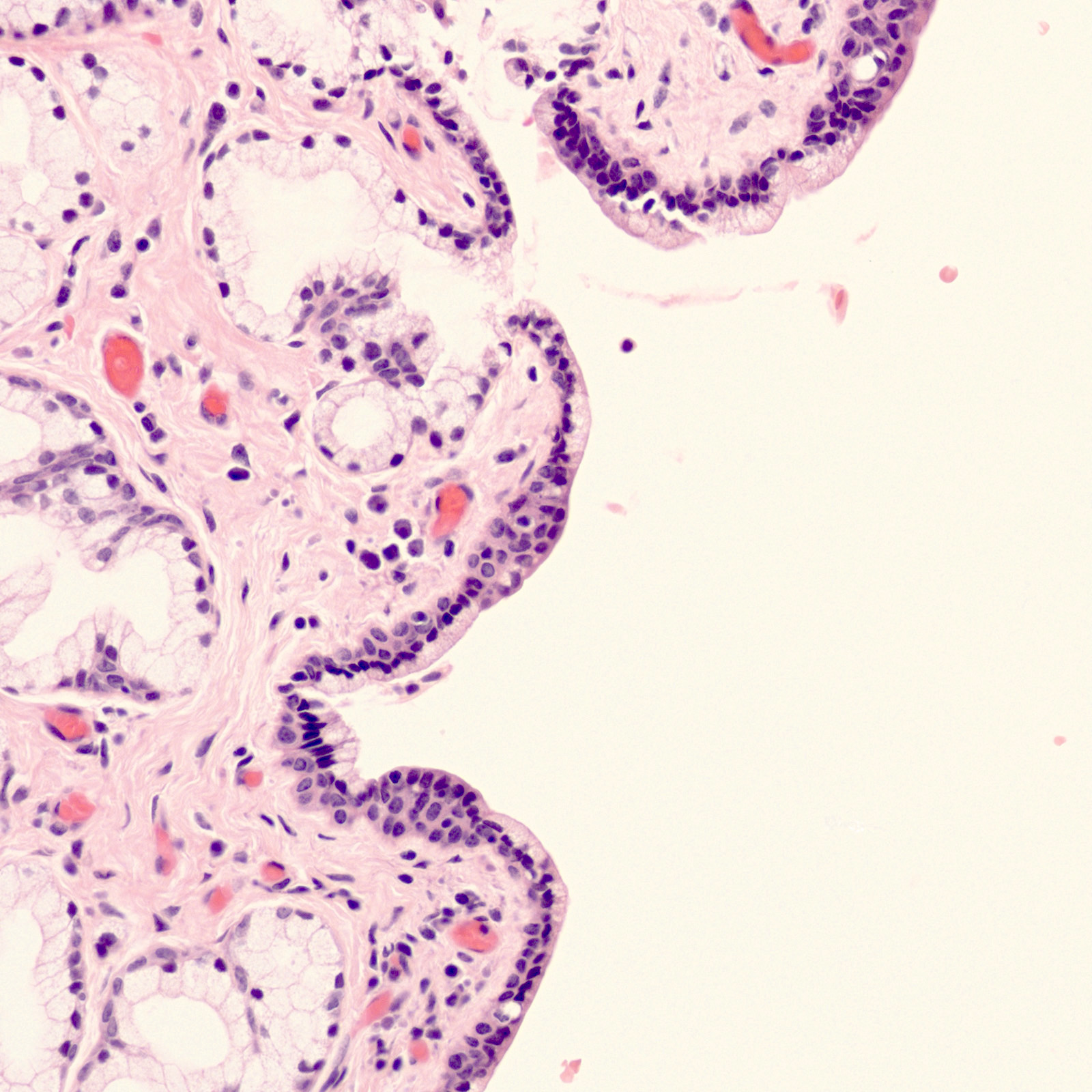
Vaginal adenosis diffuse, rare case
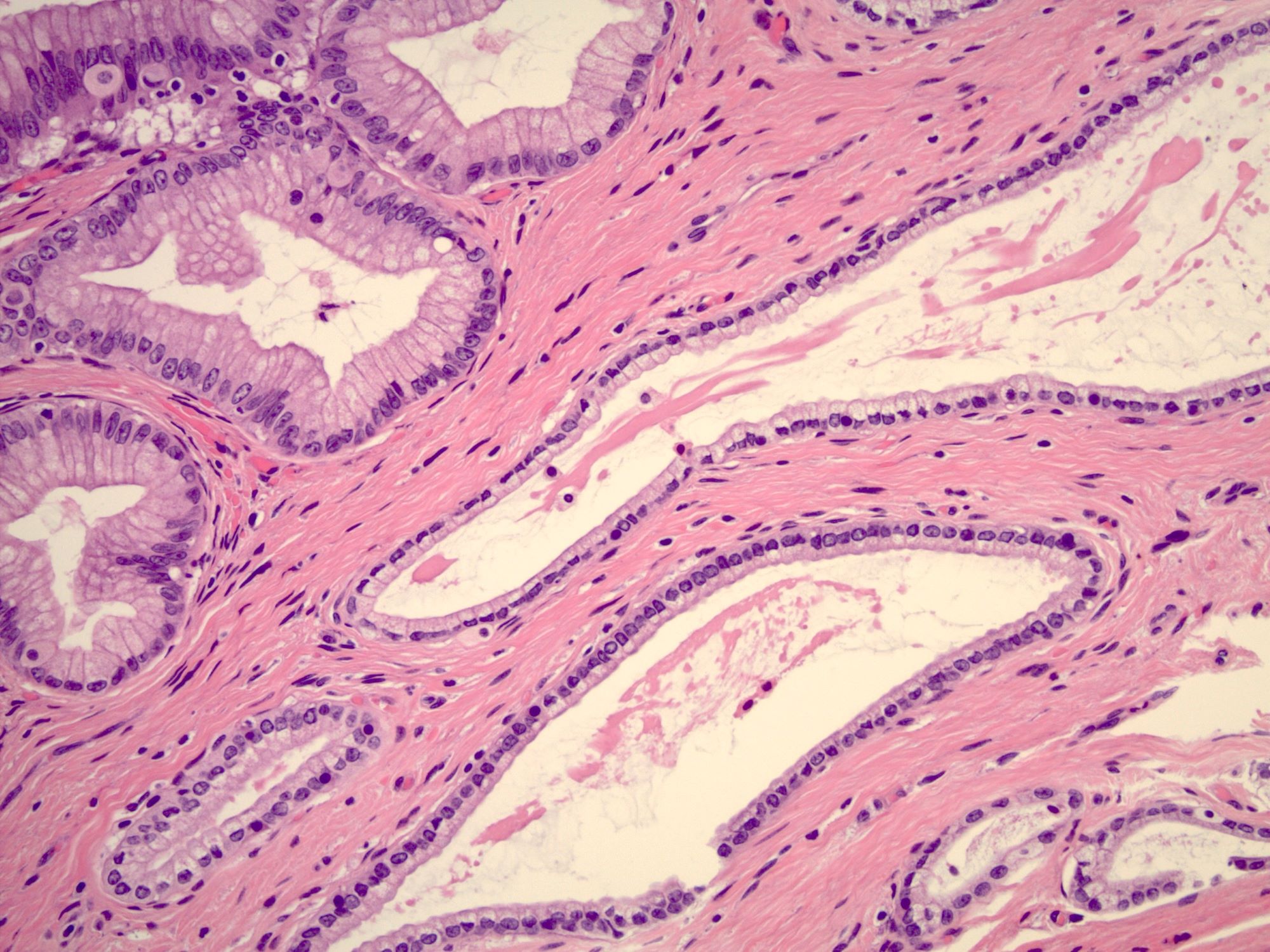
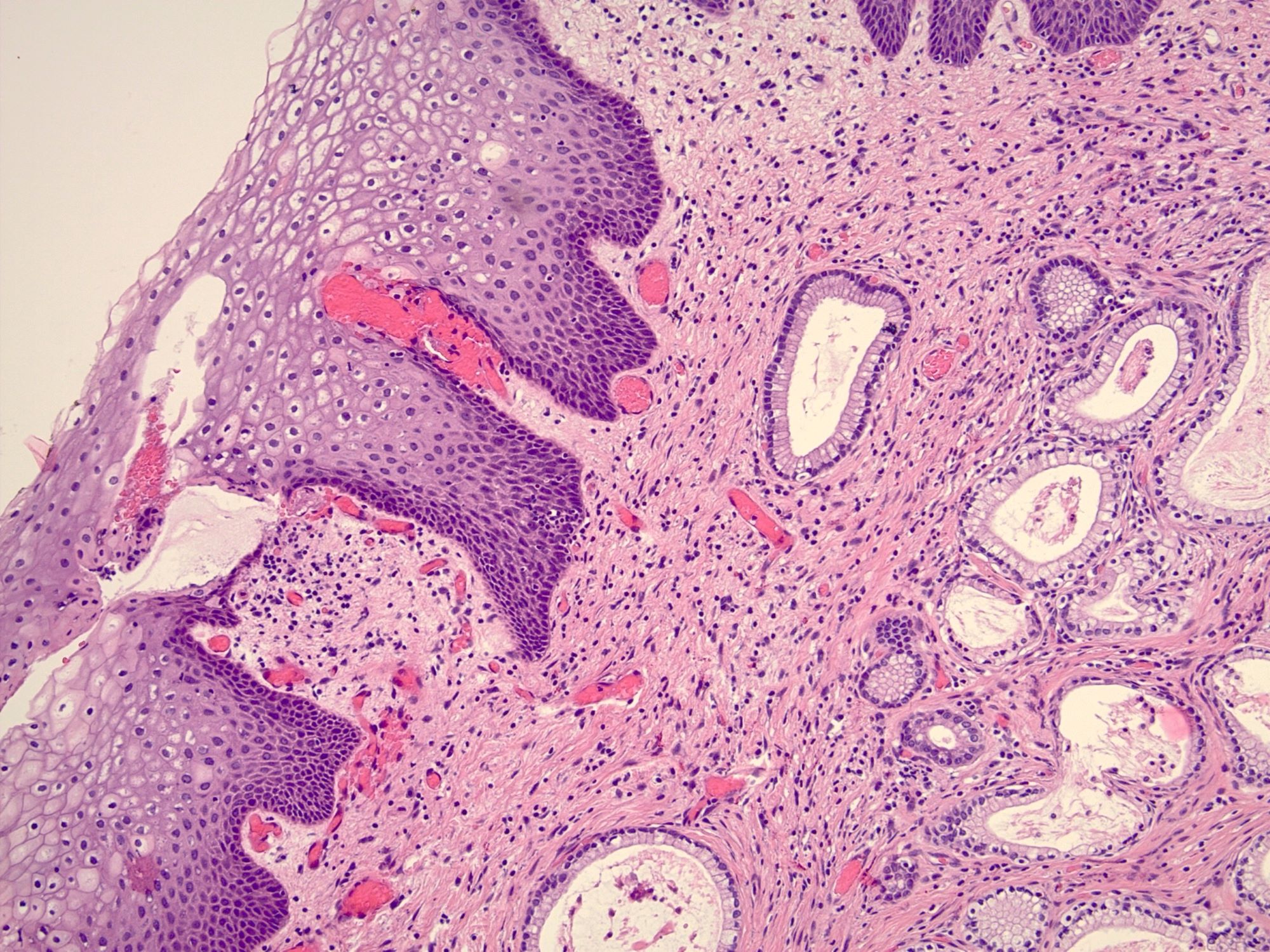
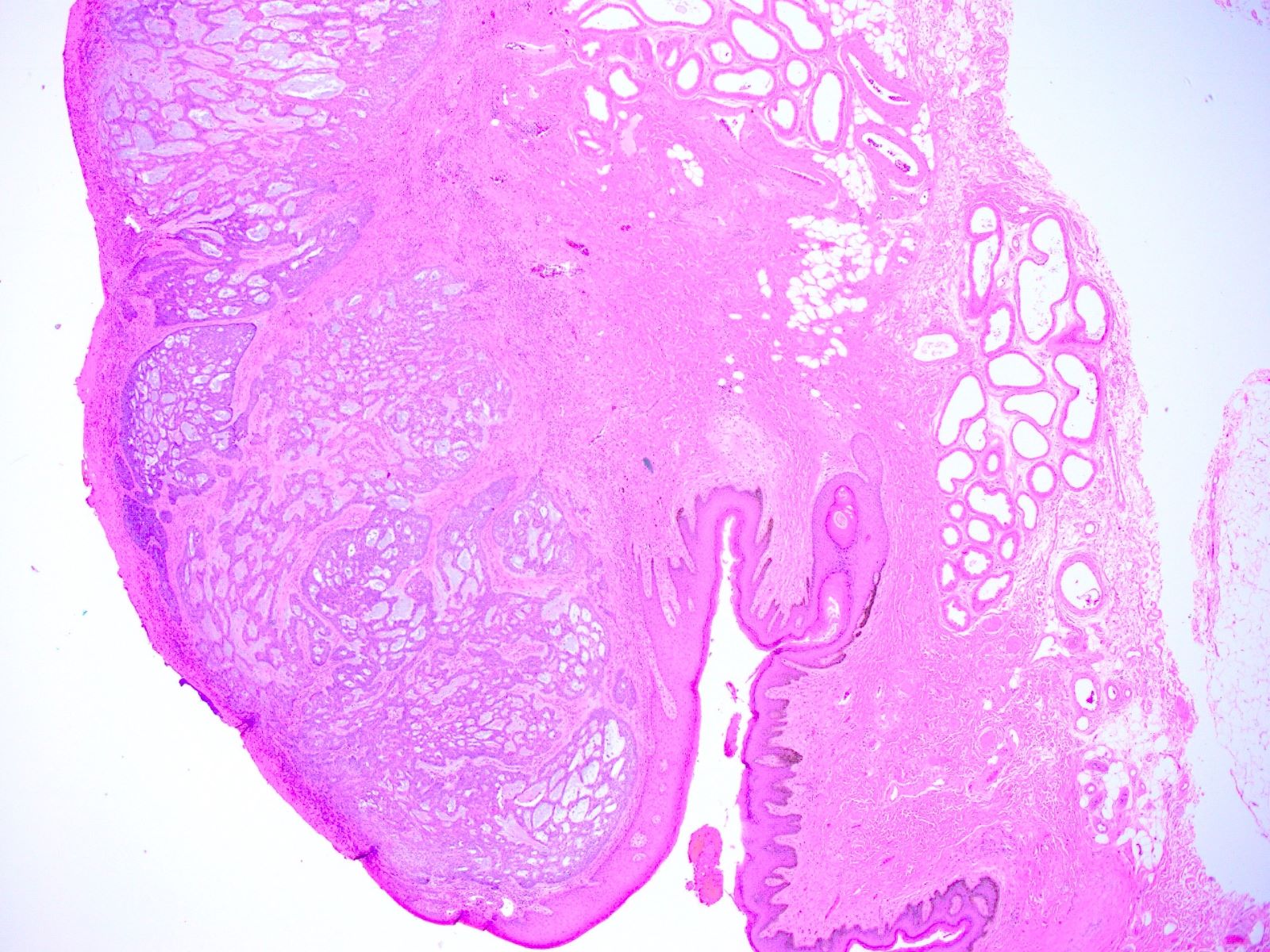
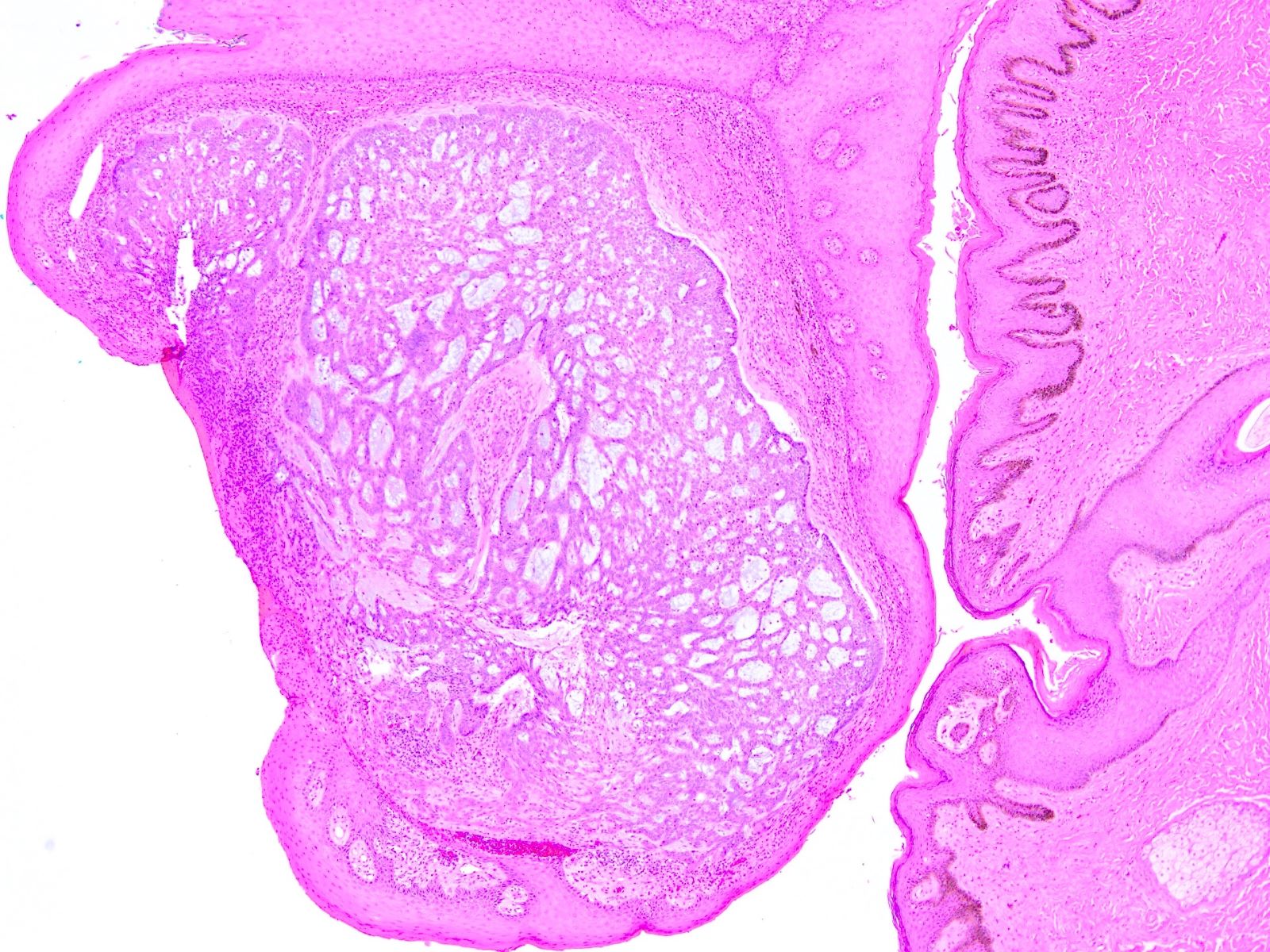
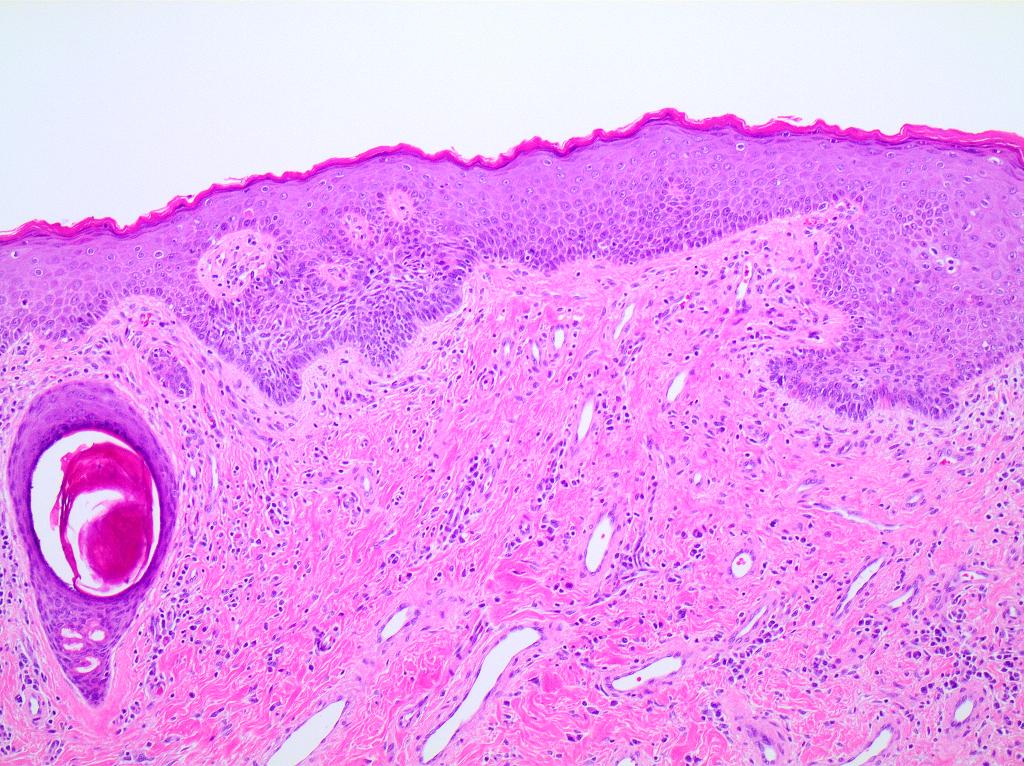
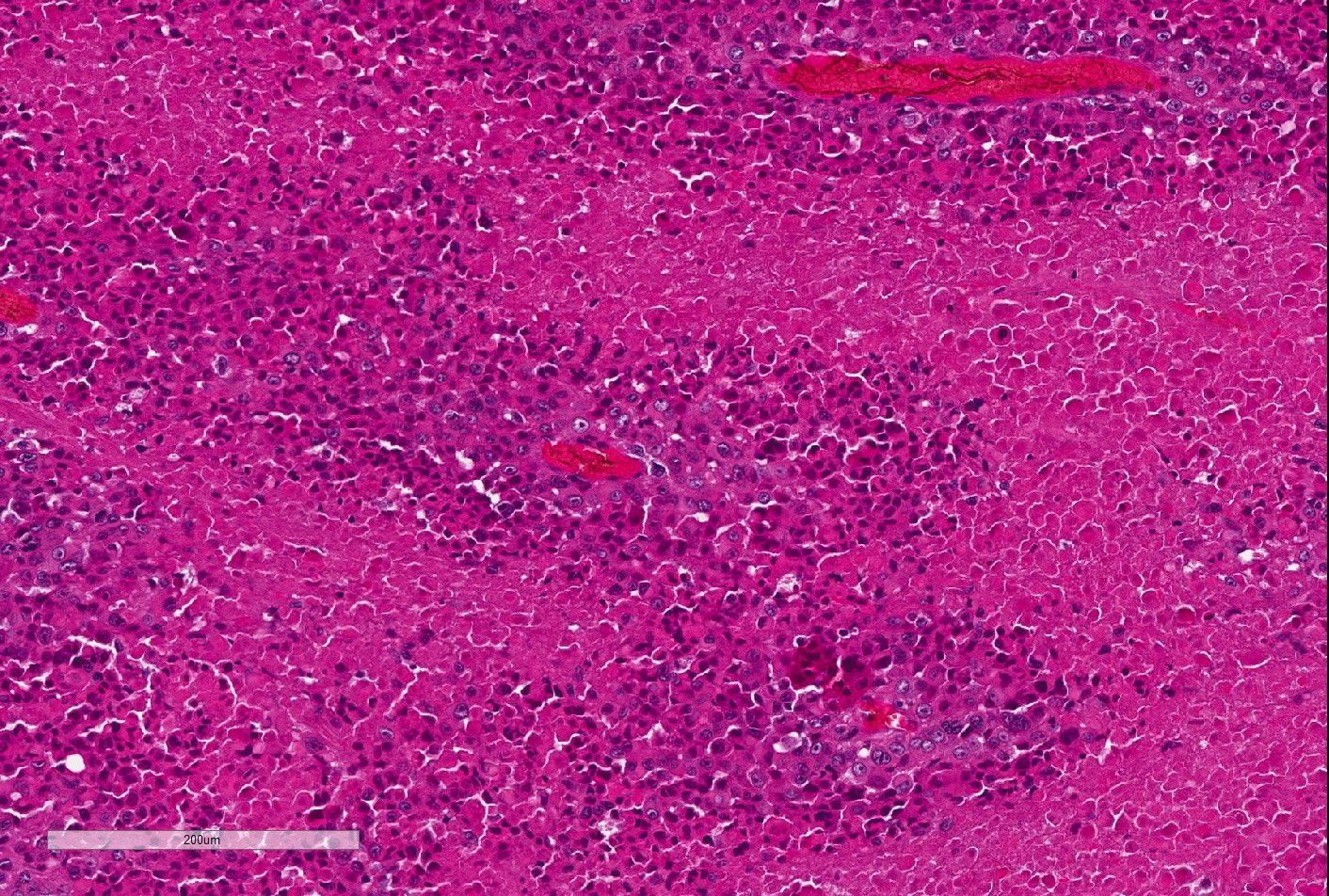
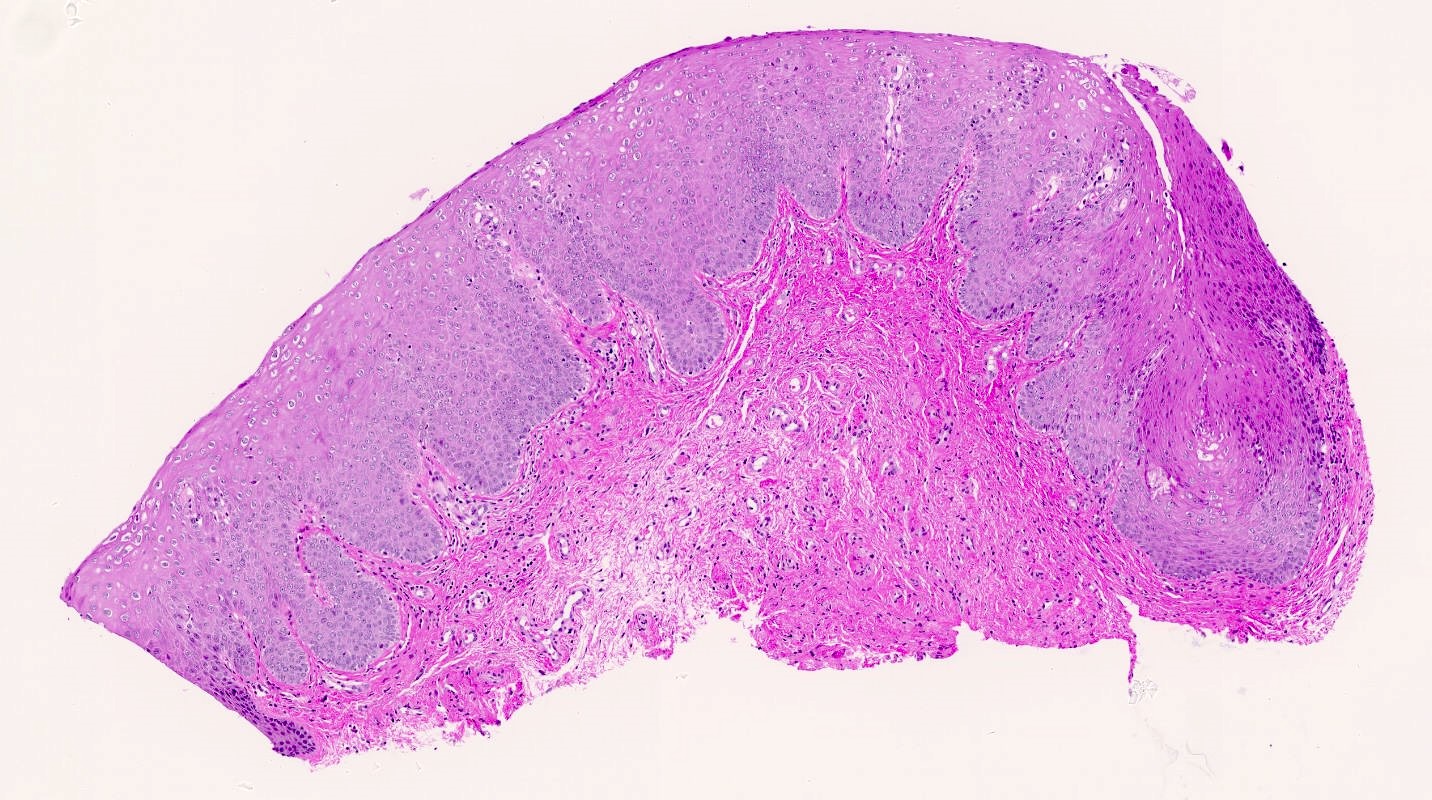
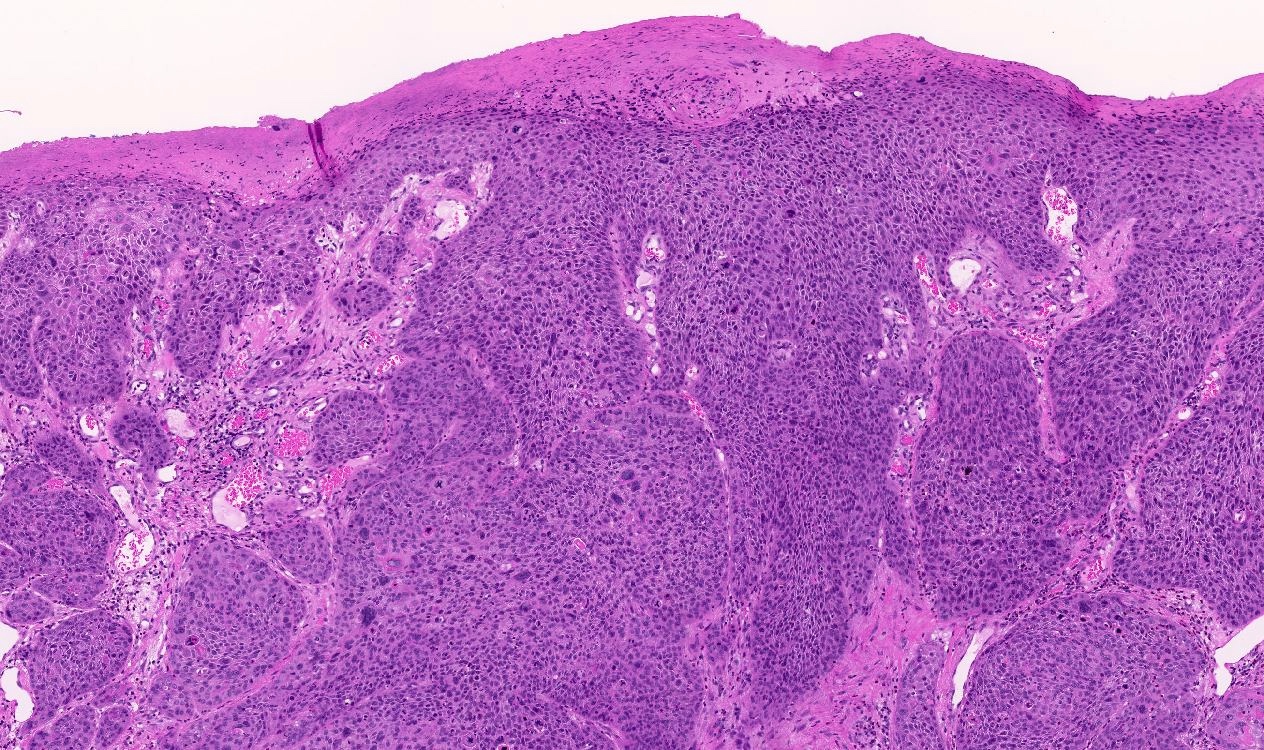
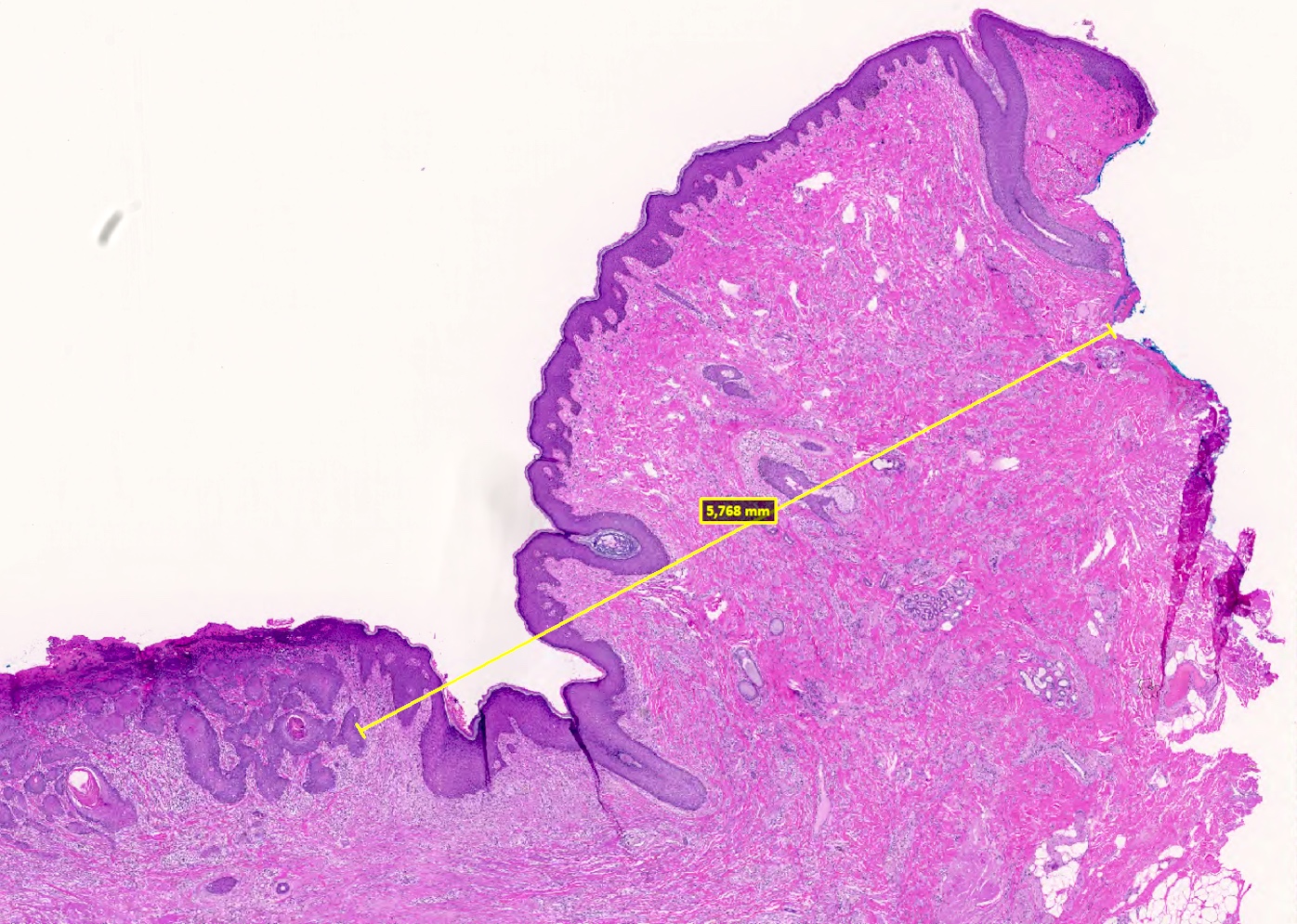
Histopathology
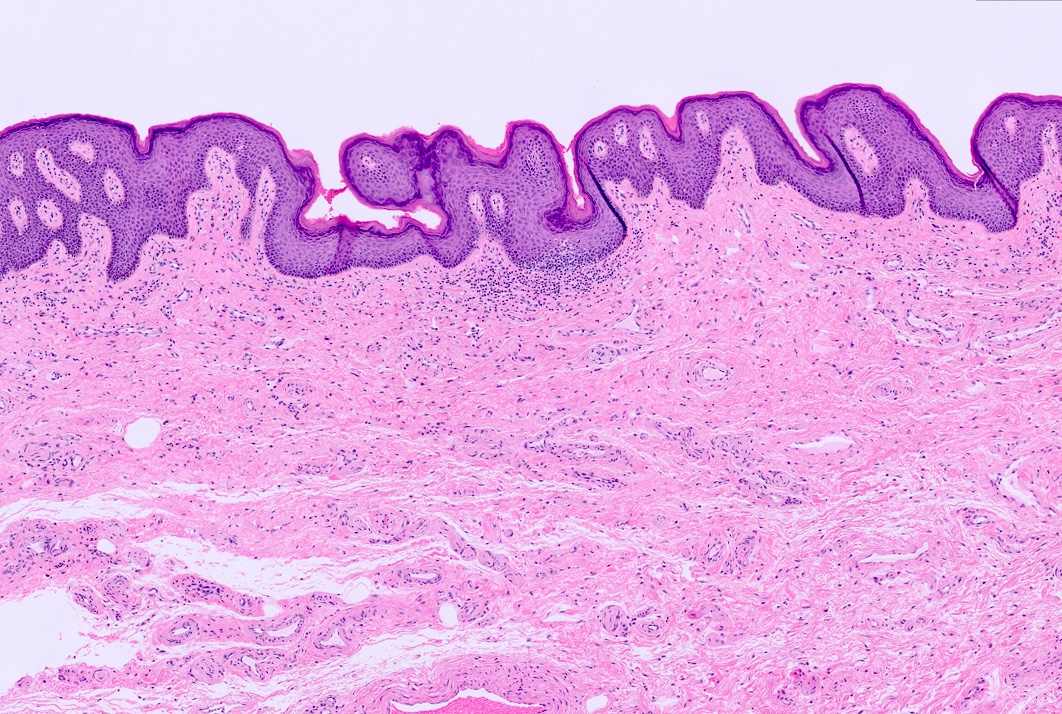
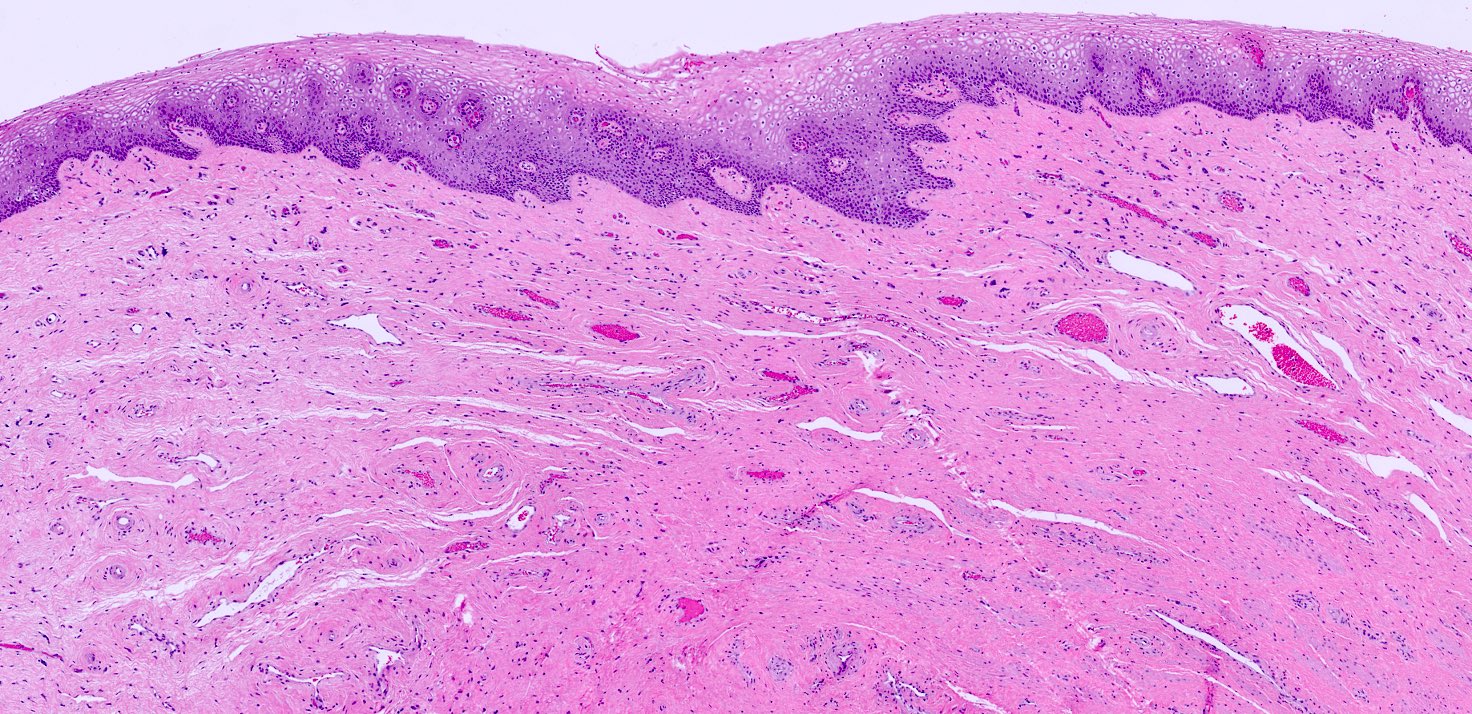
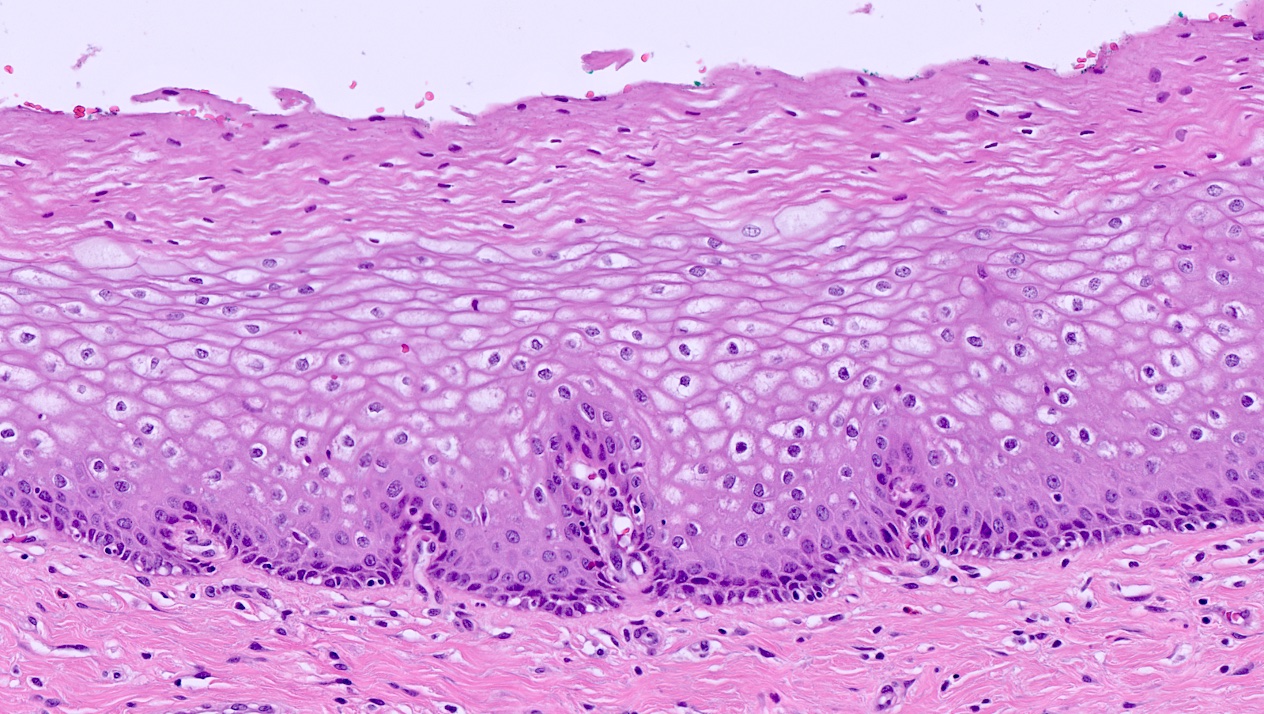
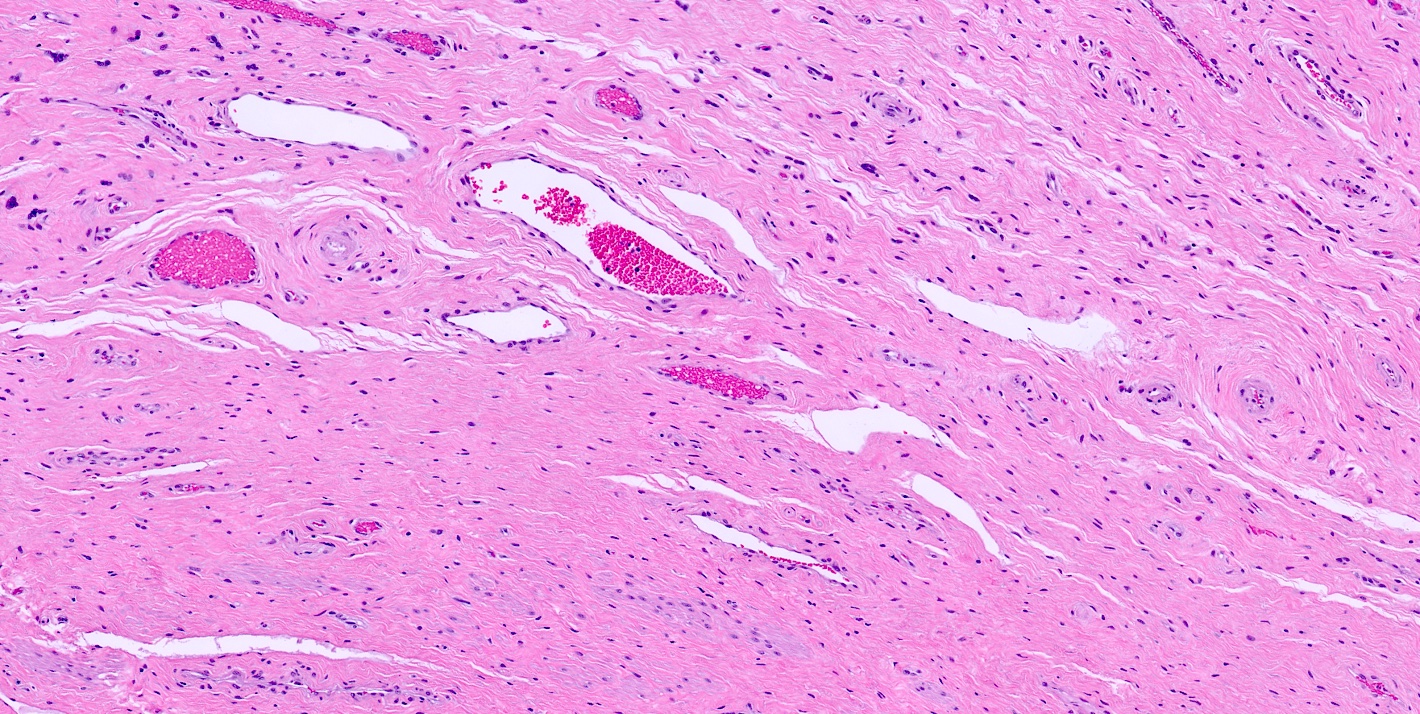
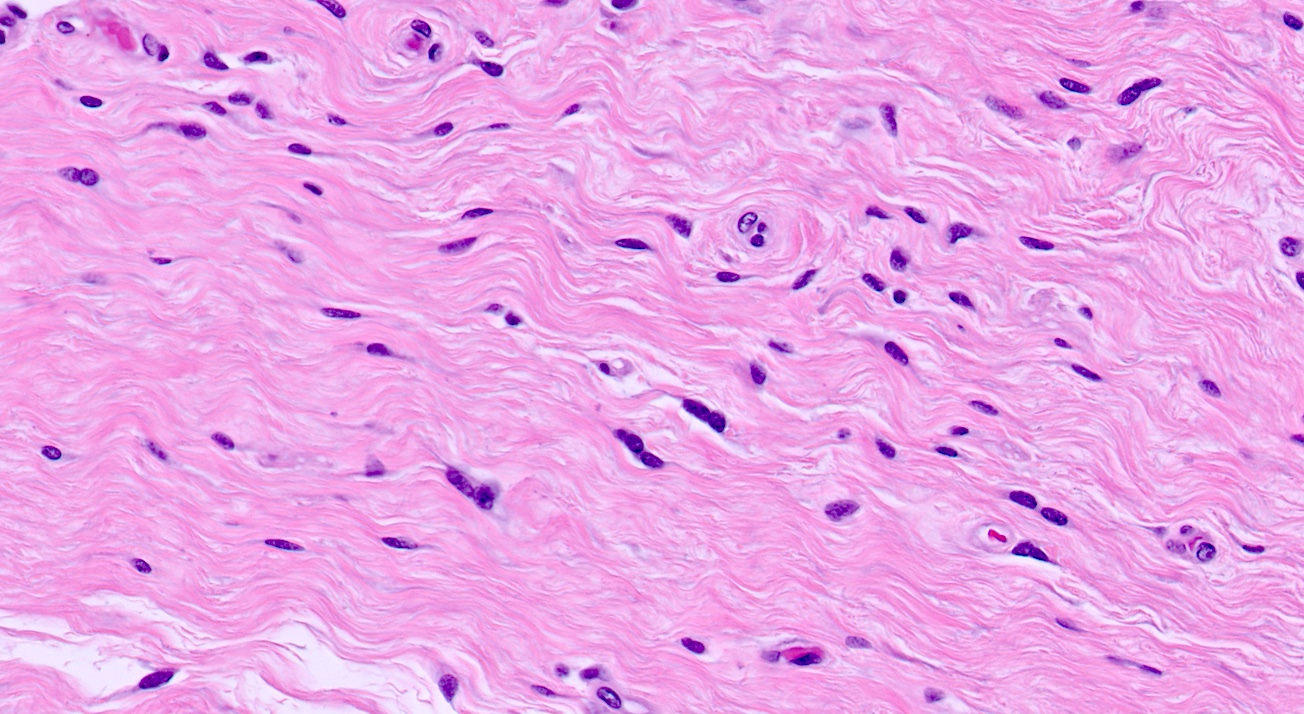
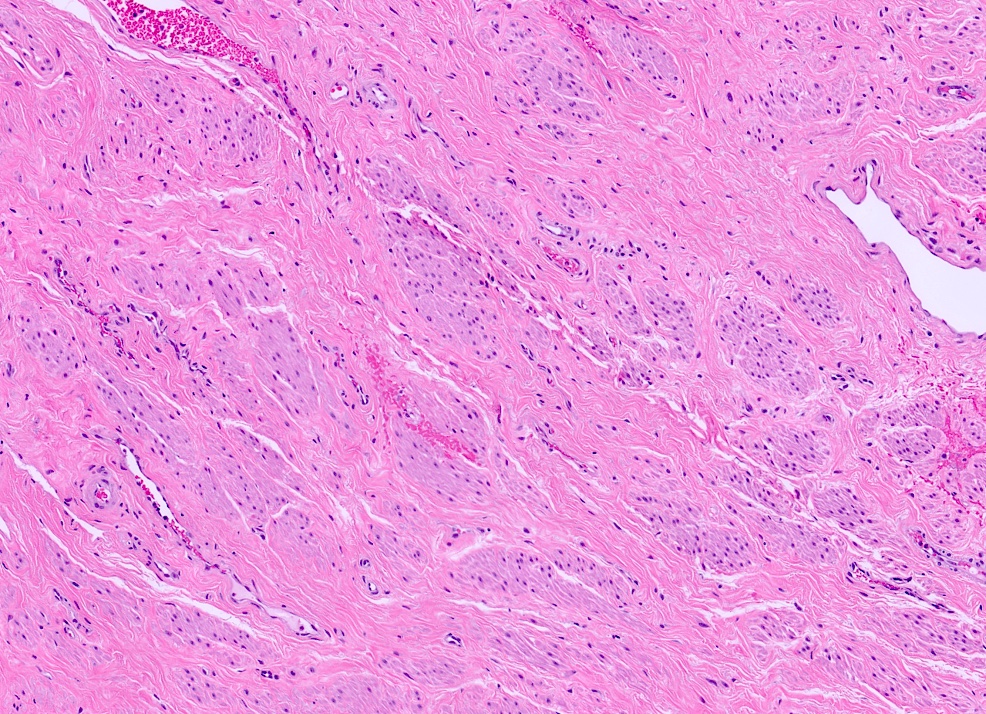
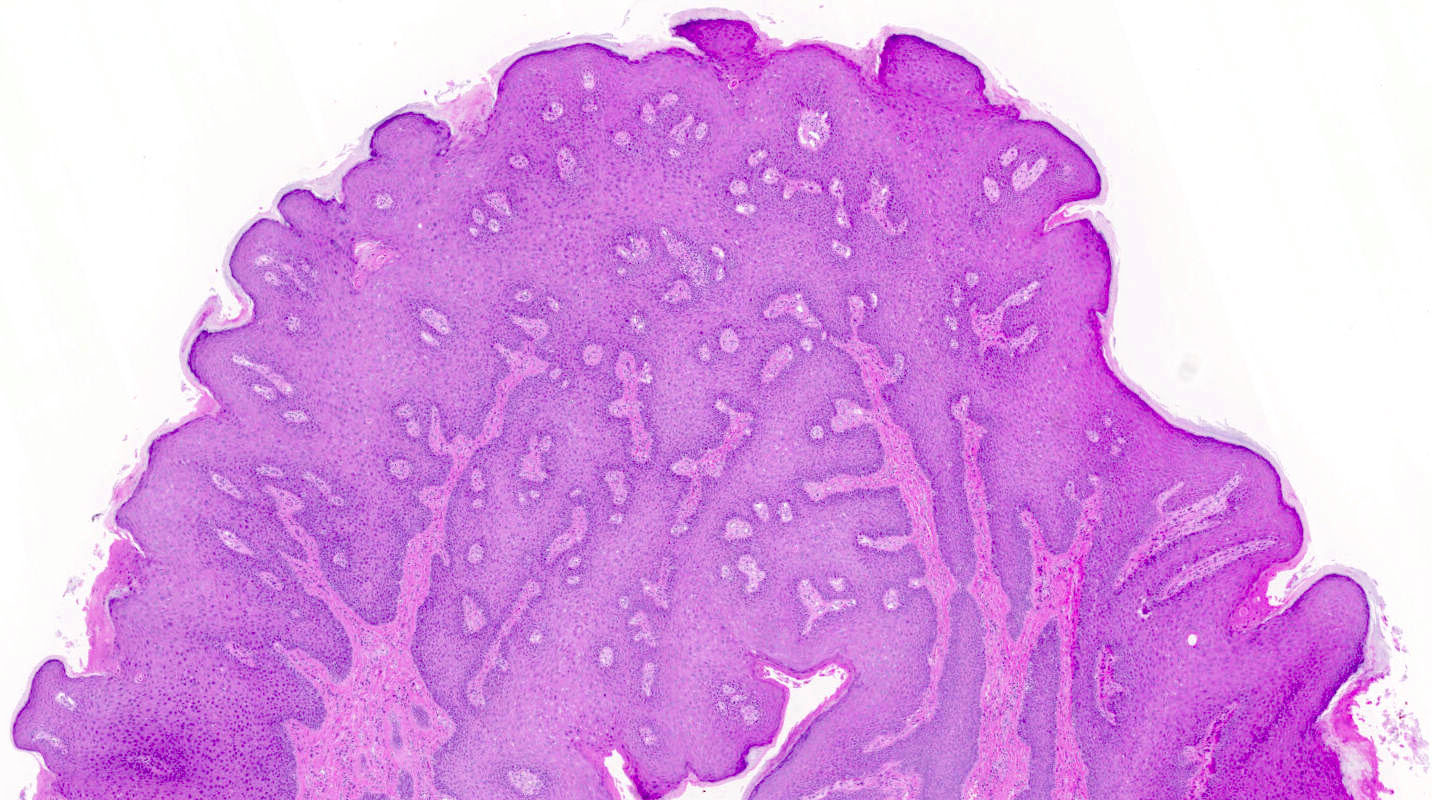
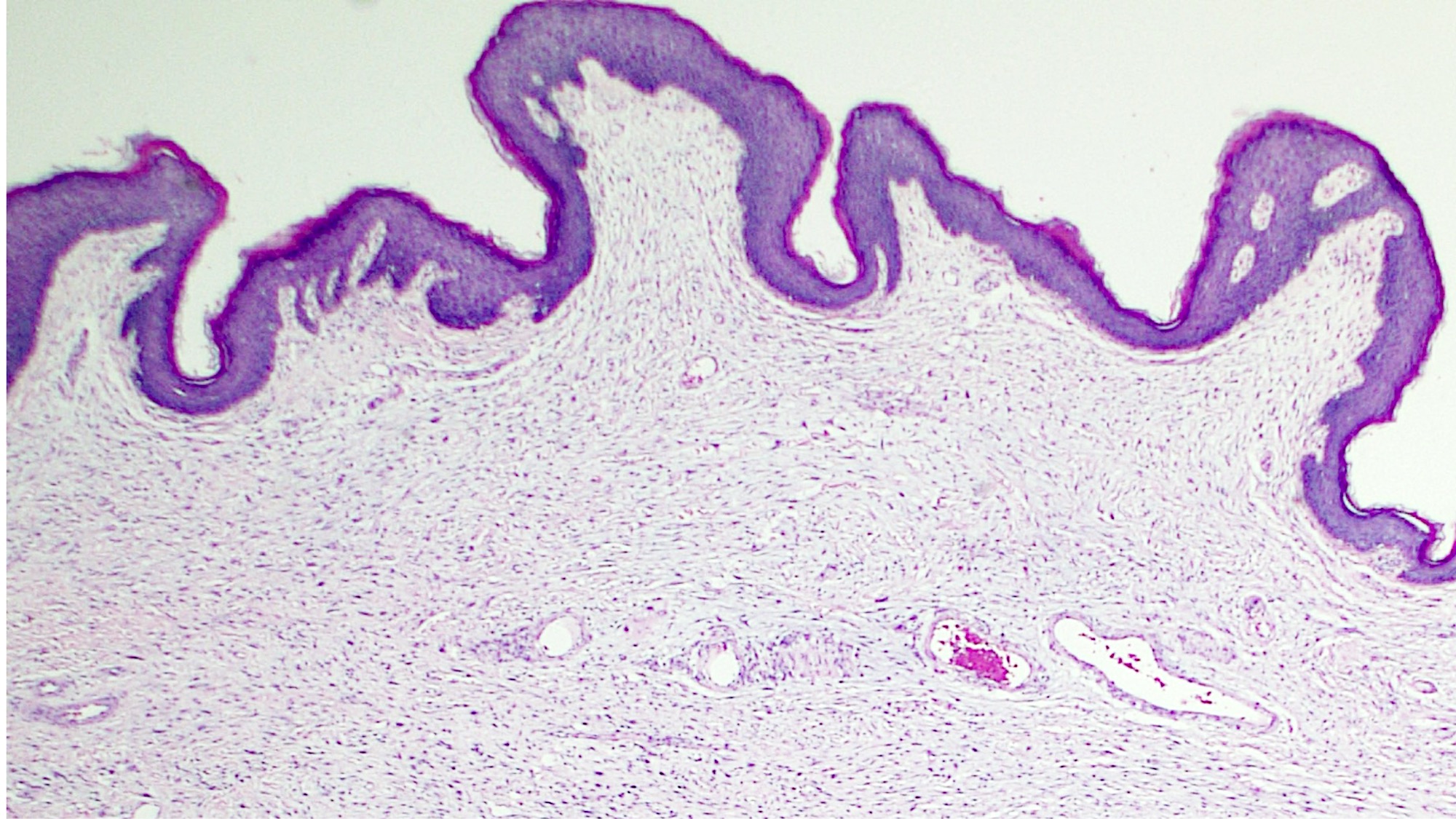
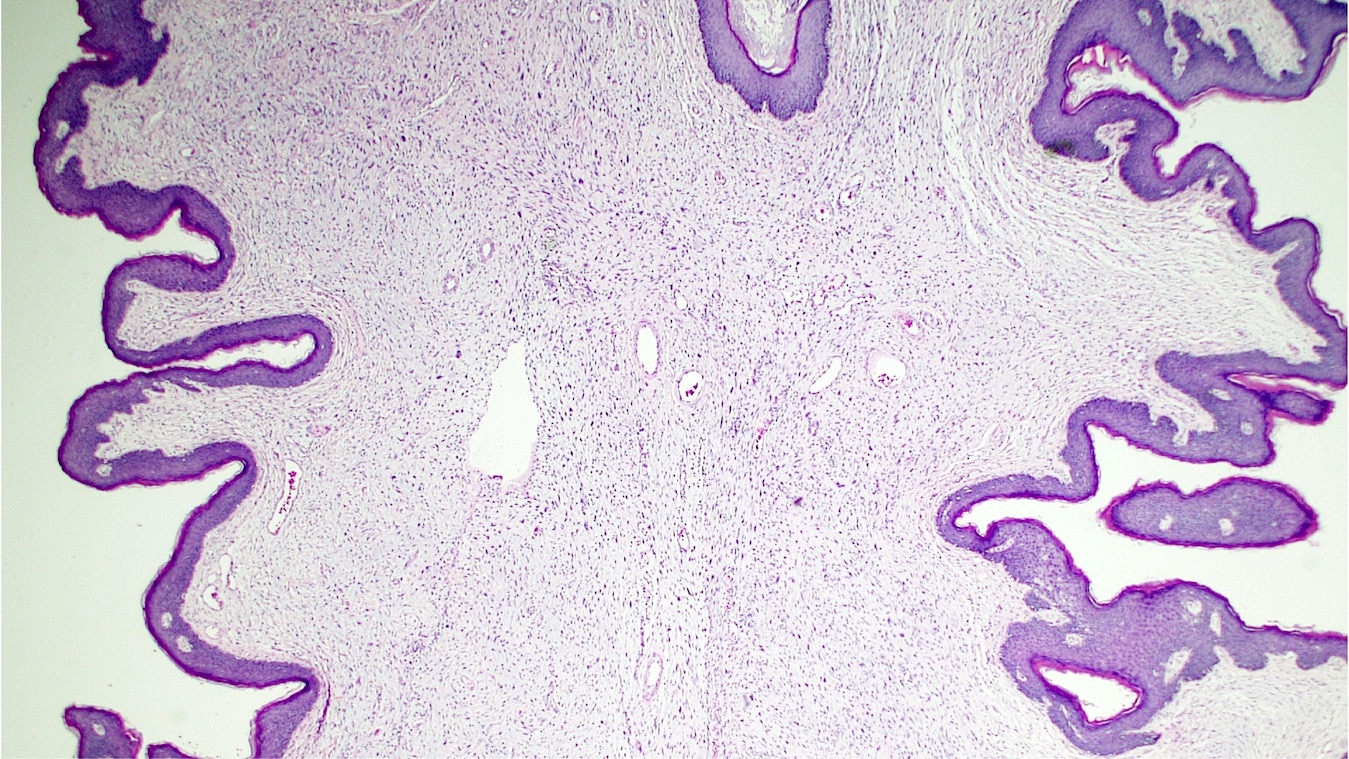
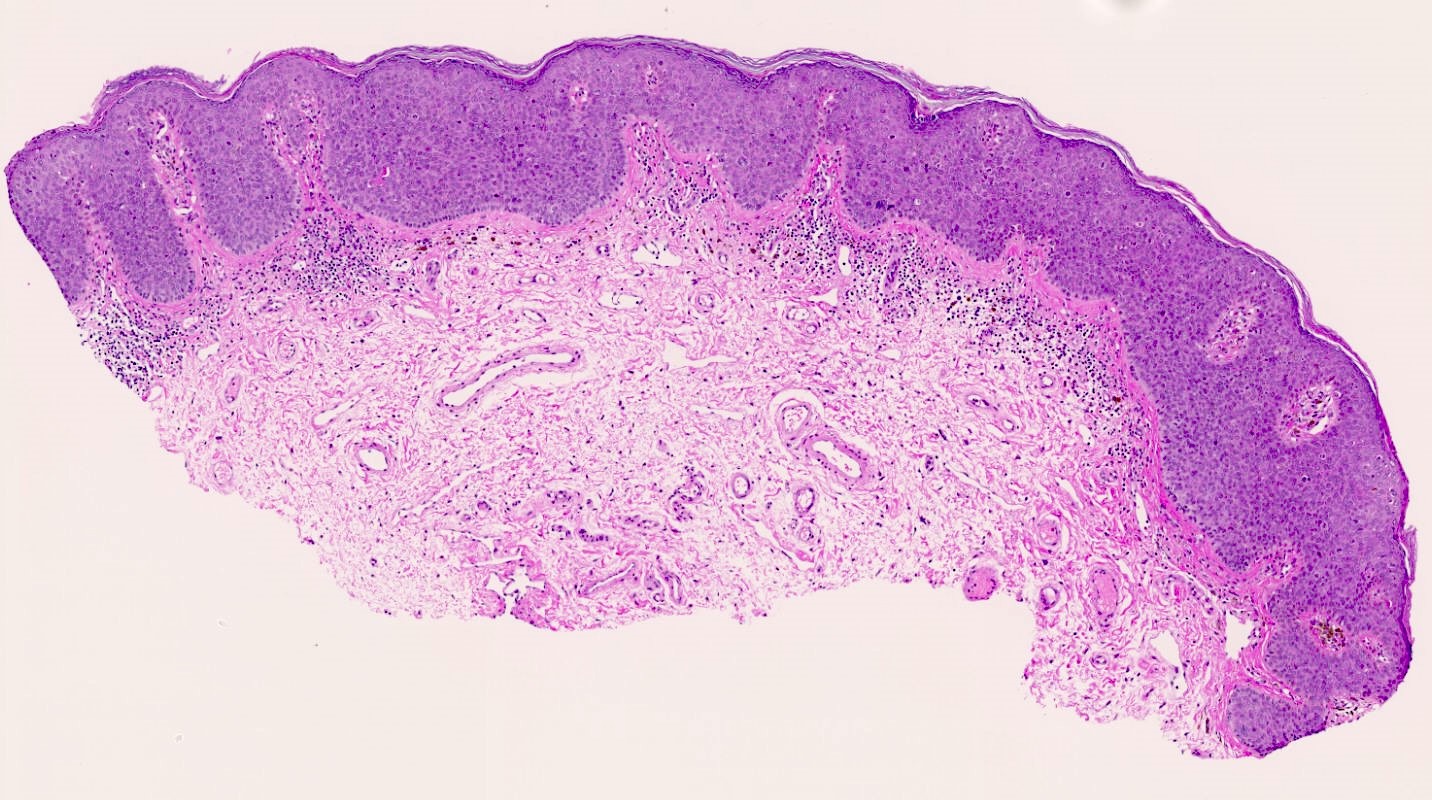
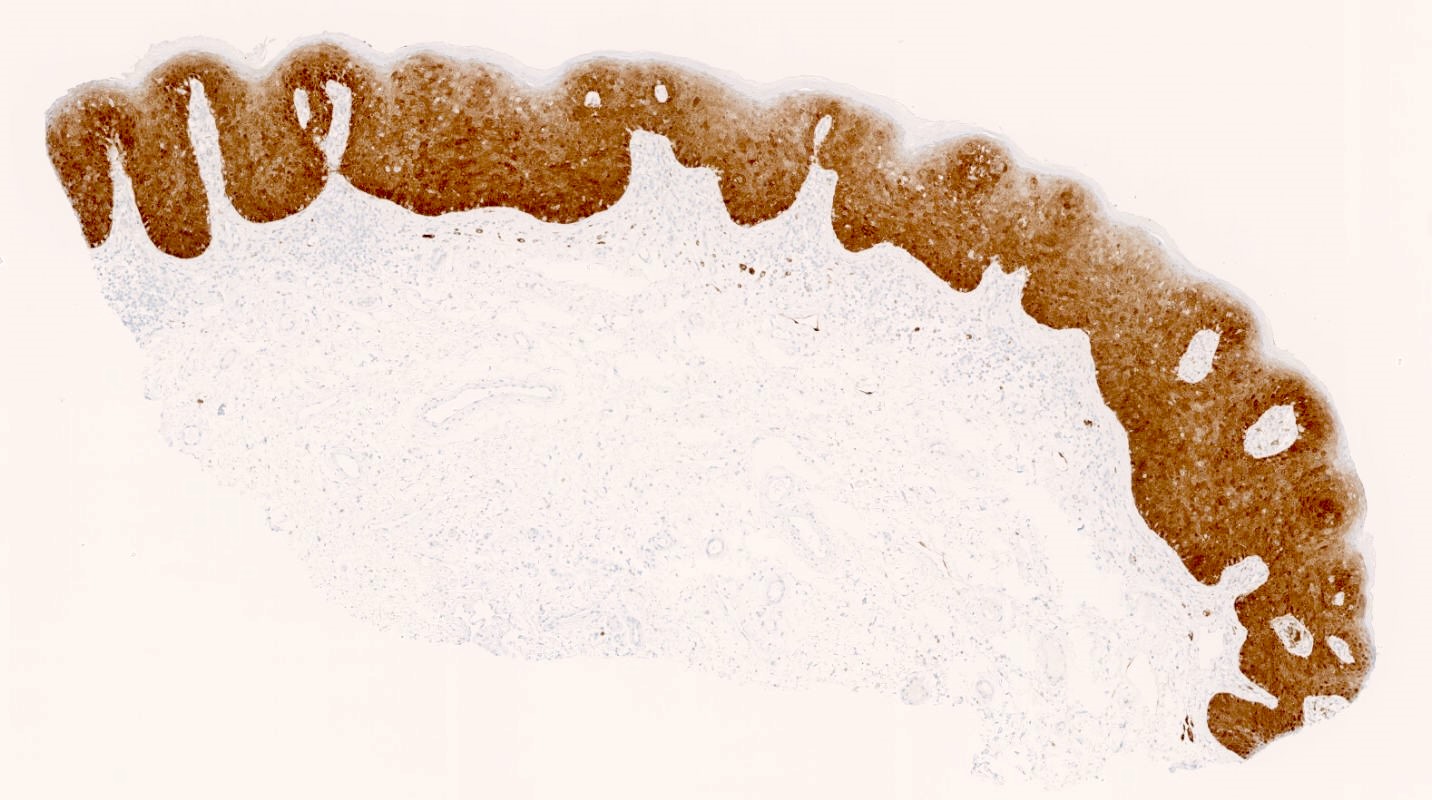
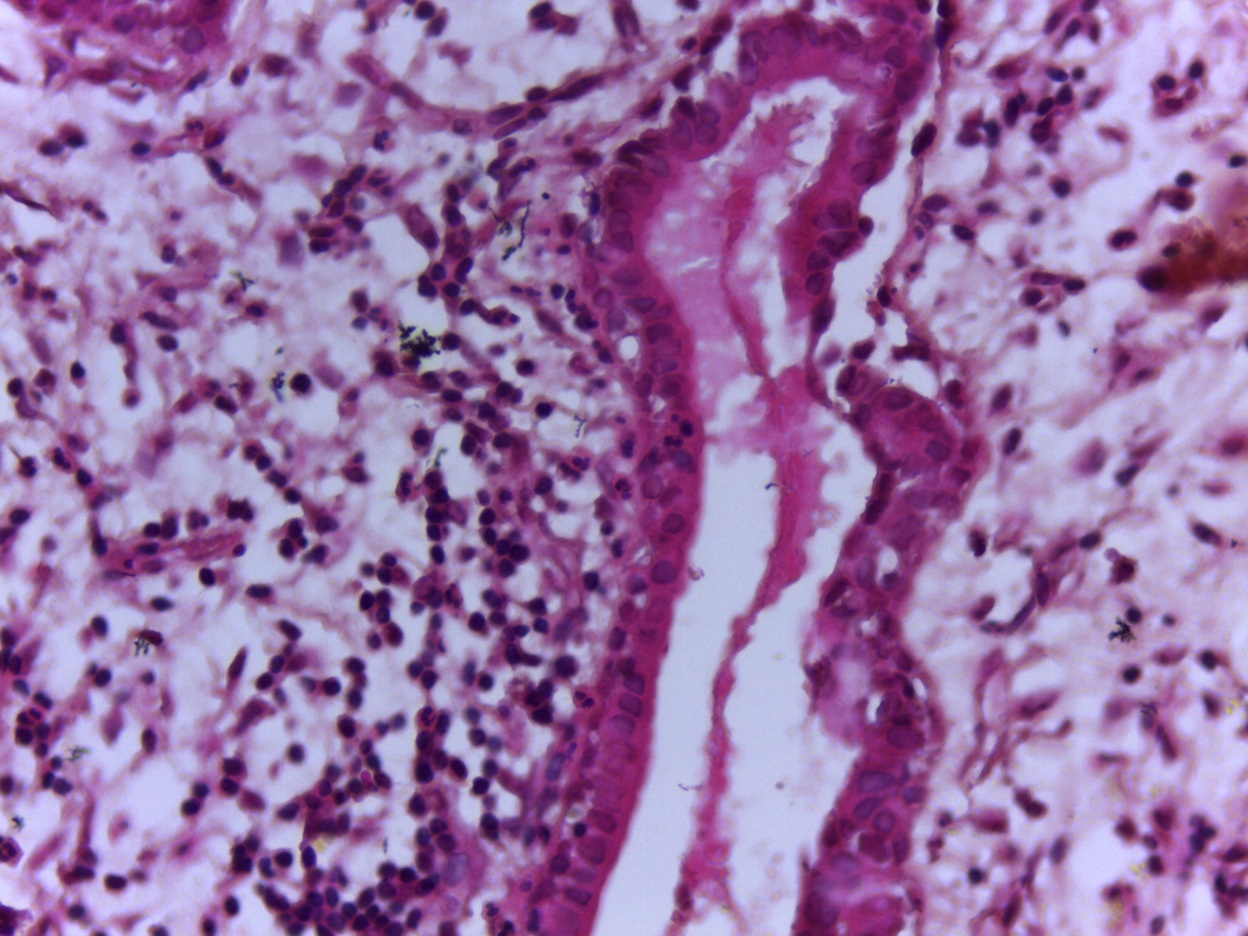
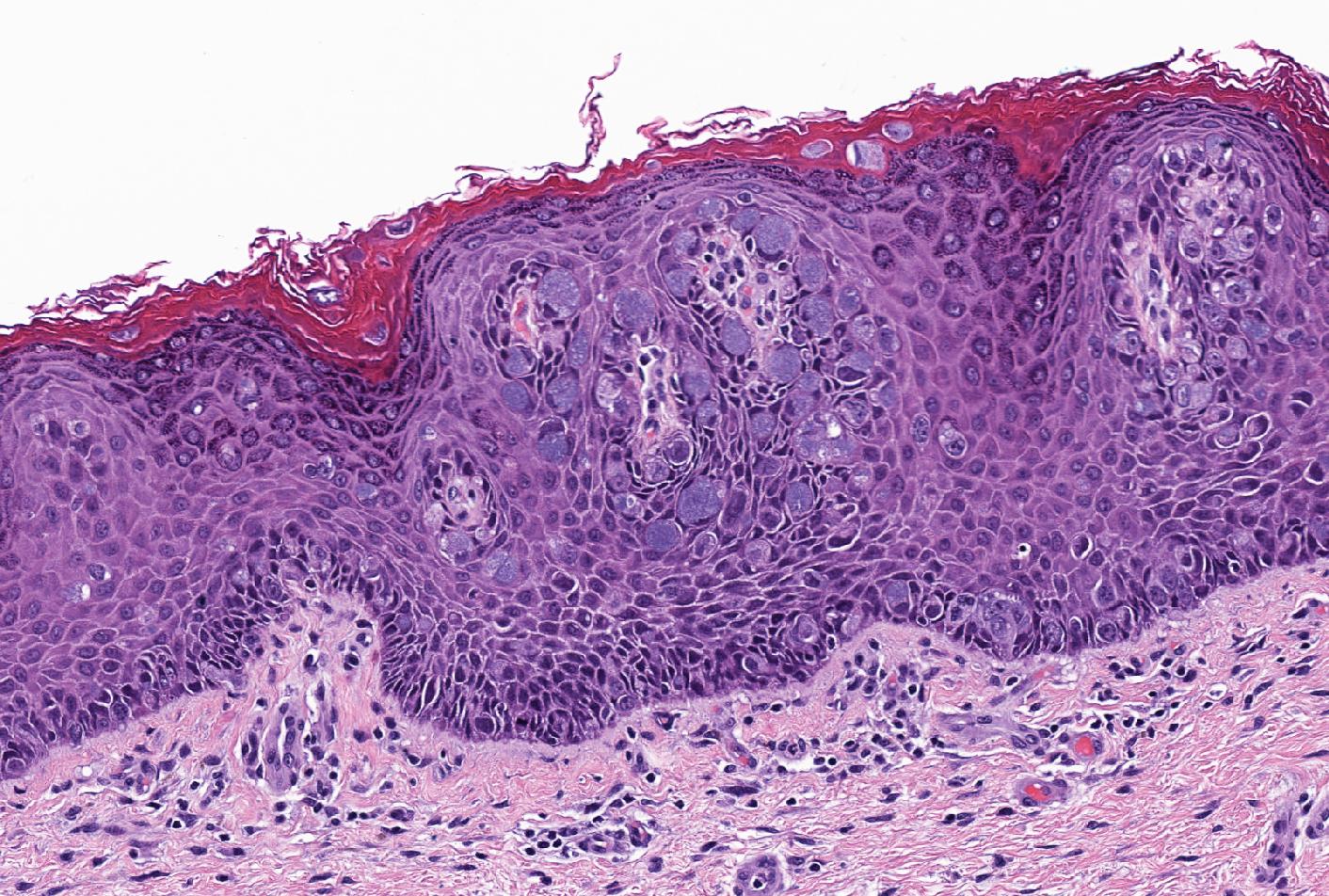
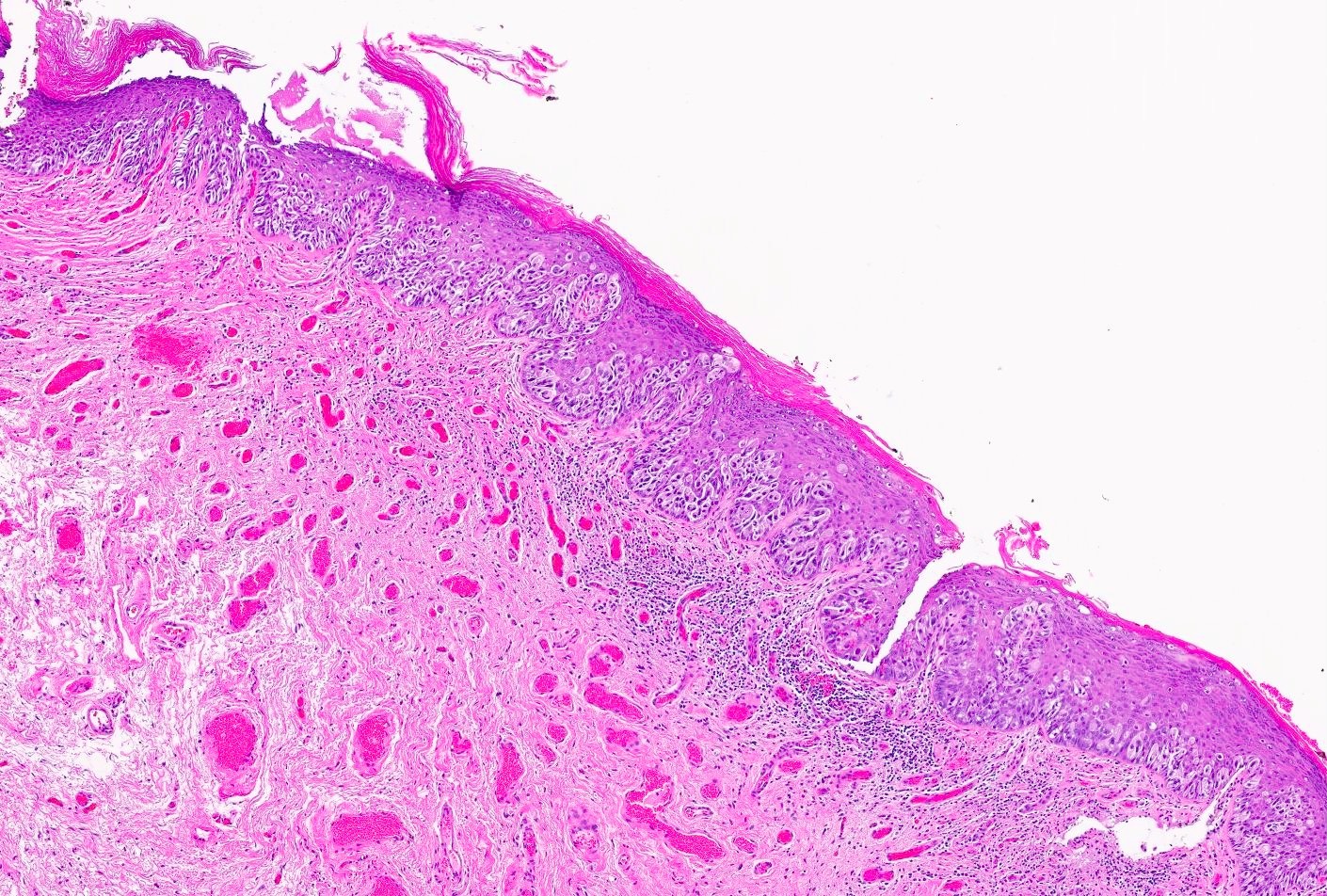
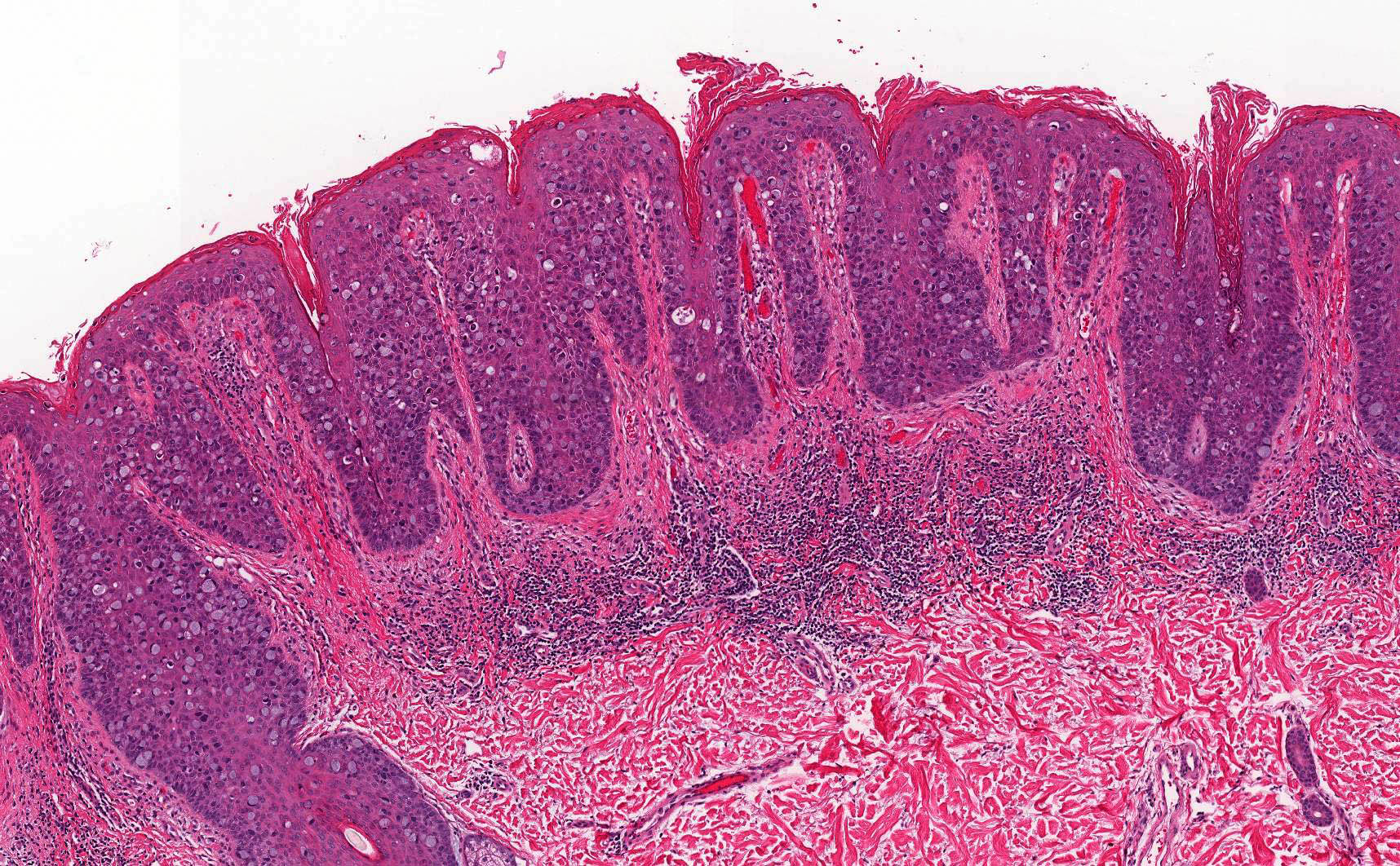
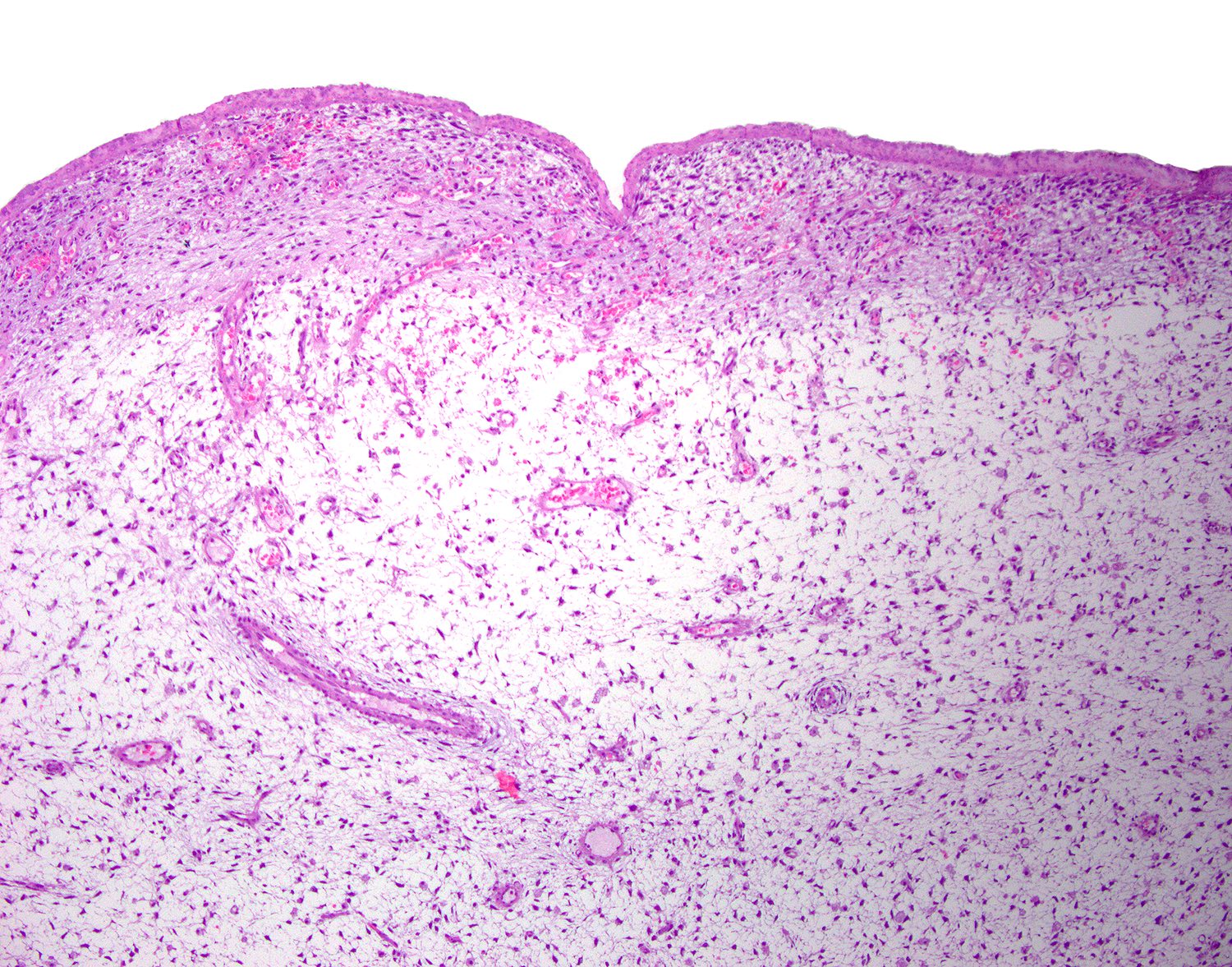
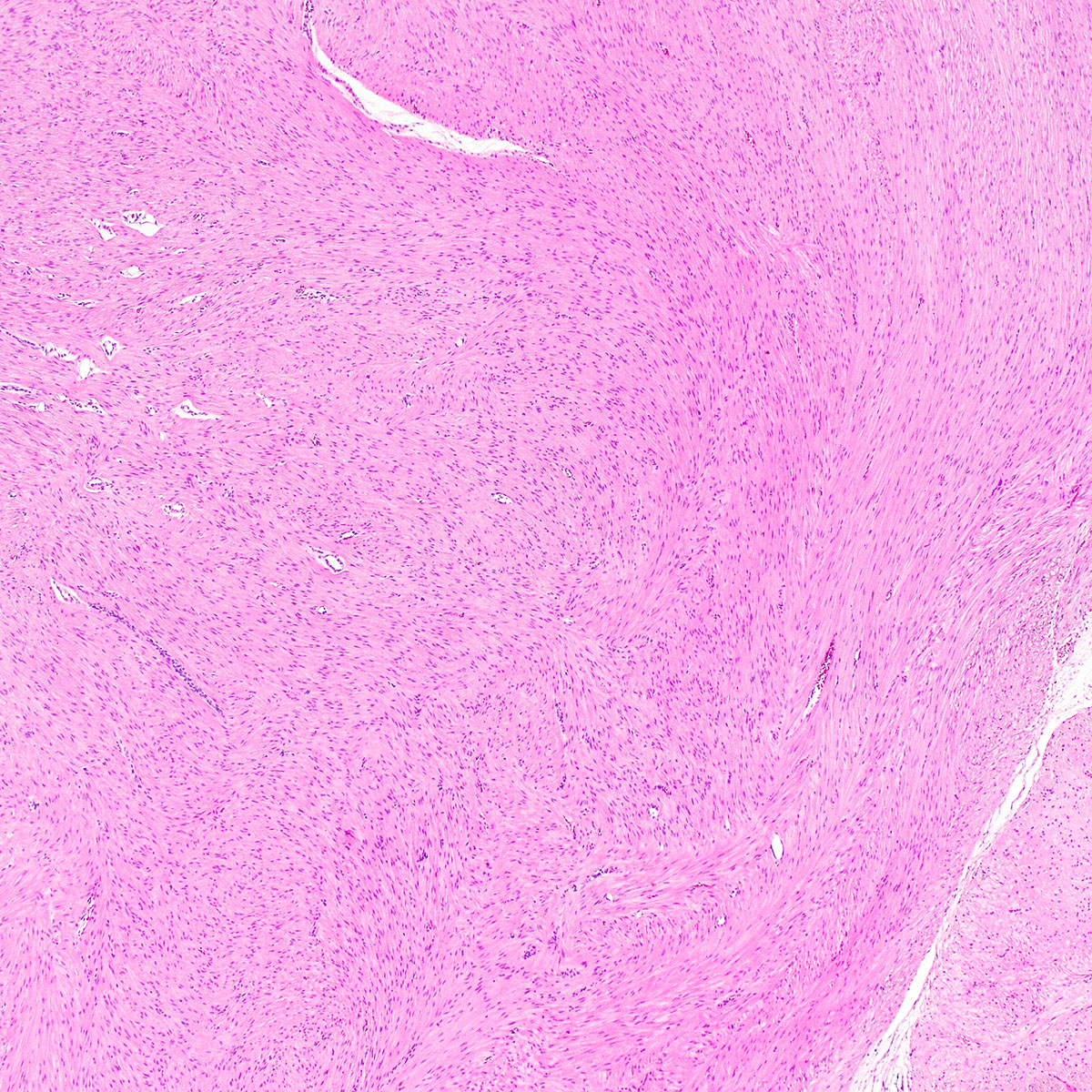
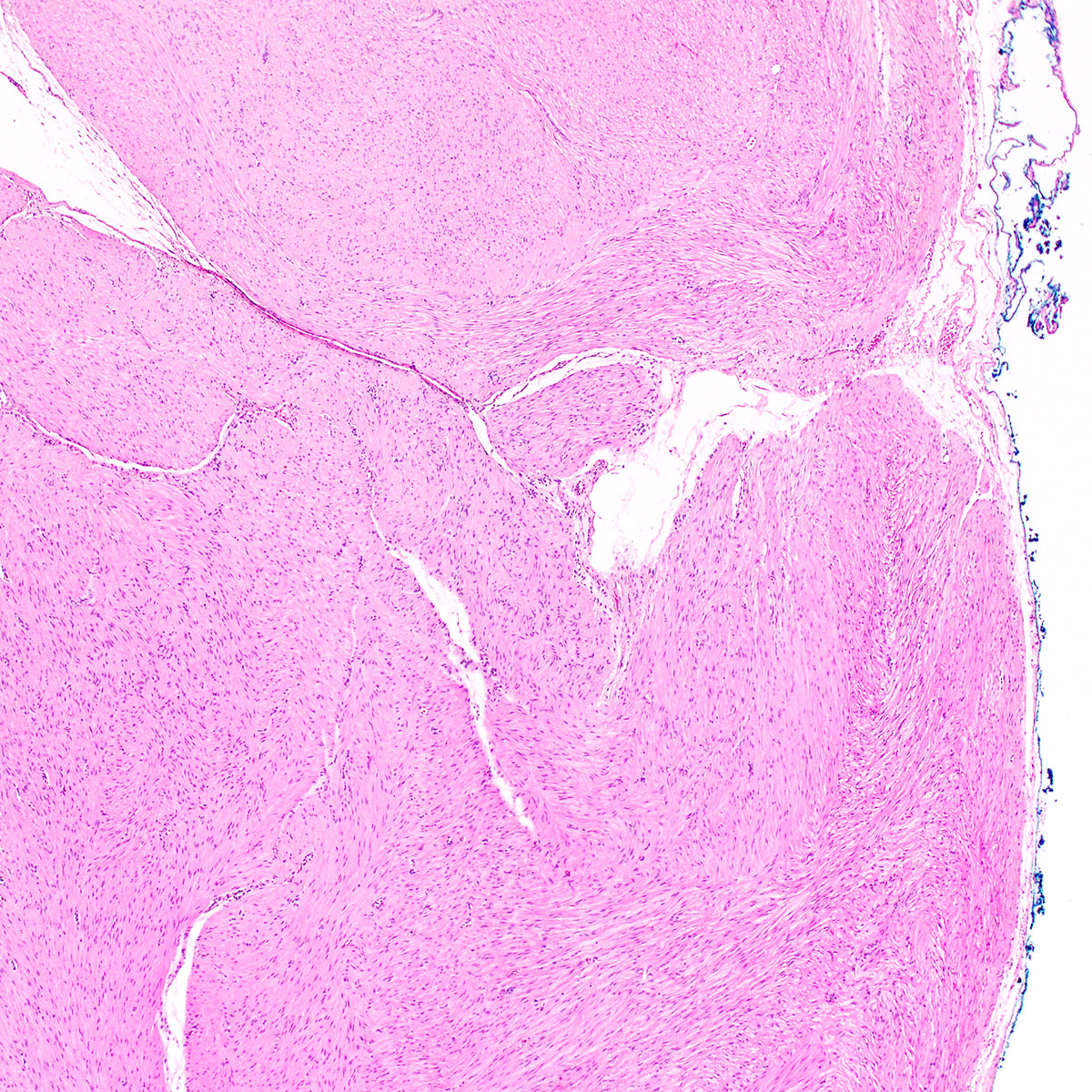
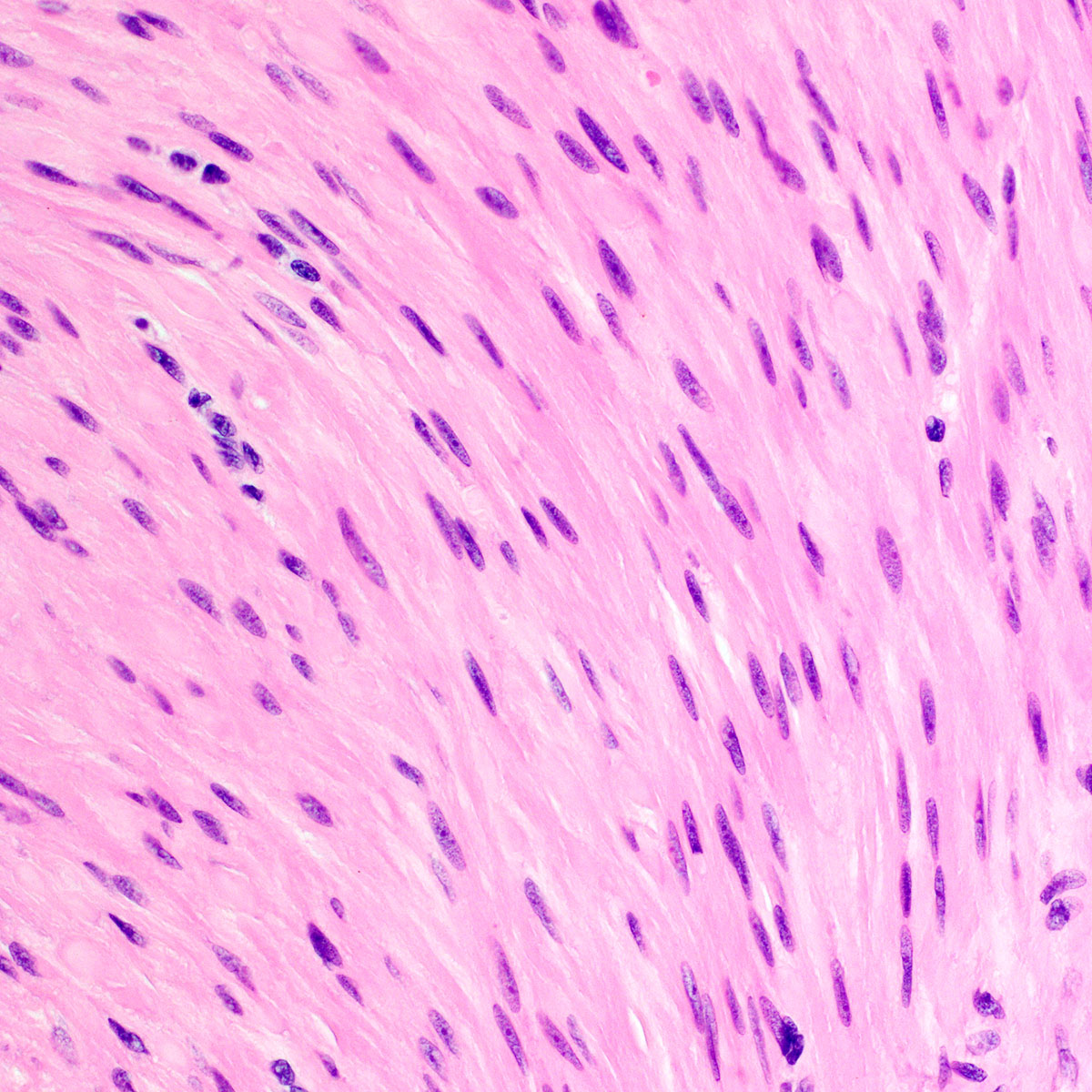
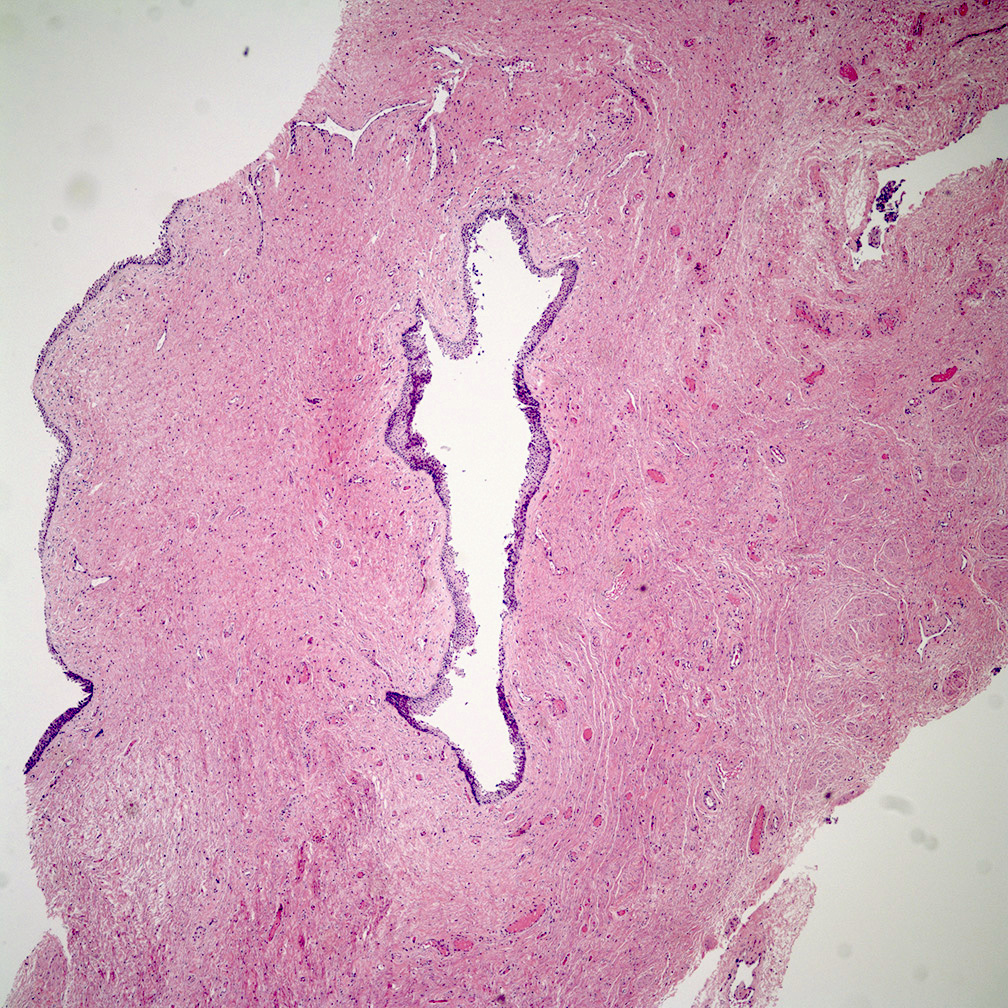
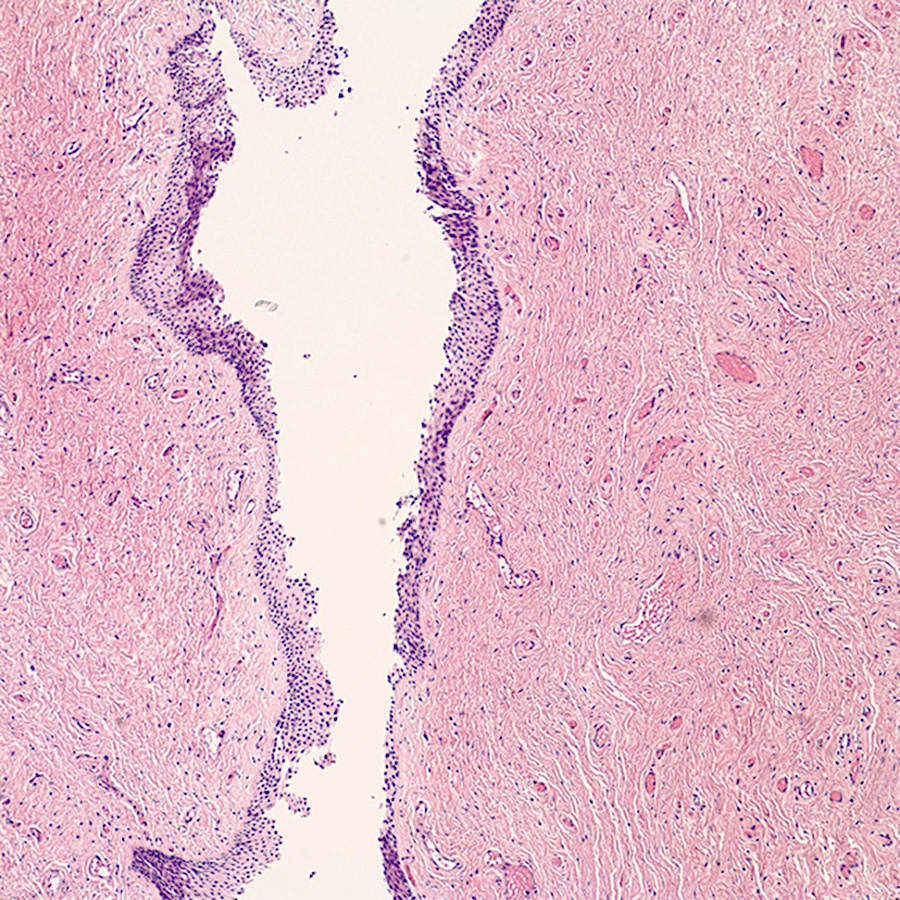
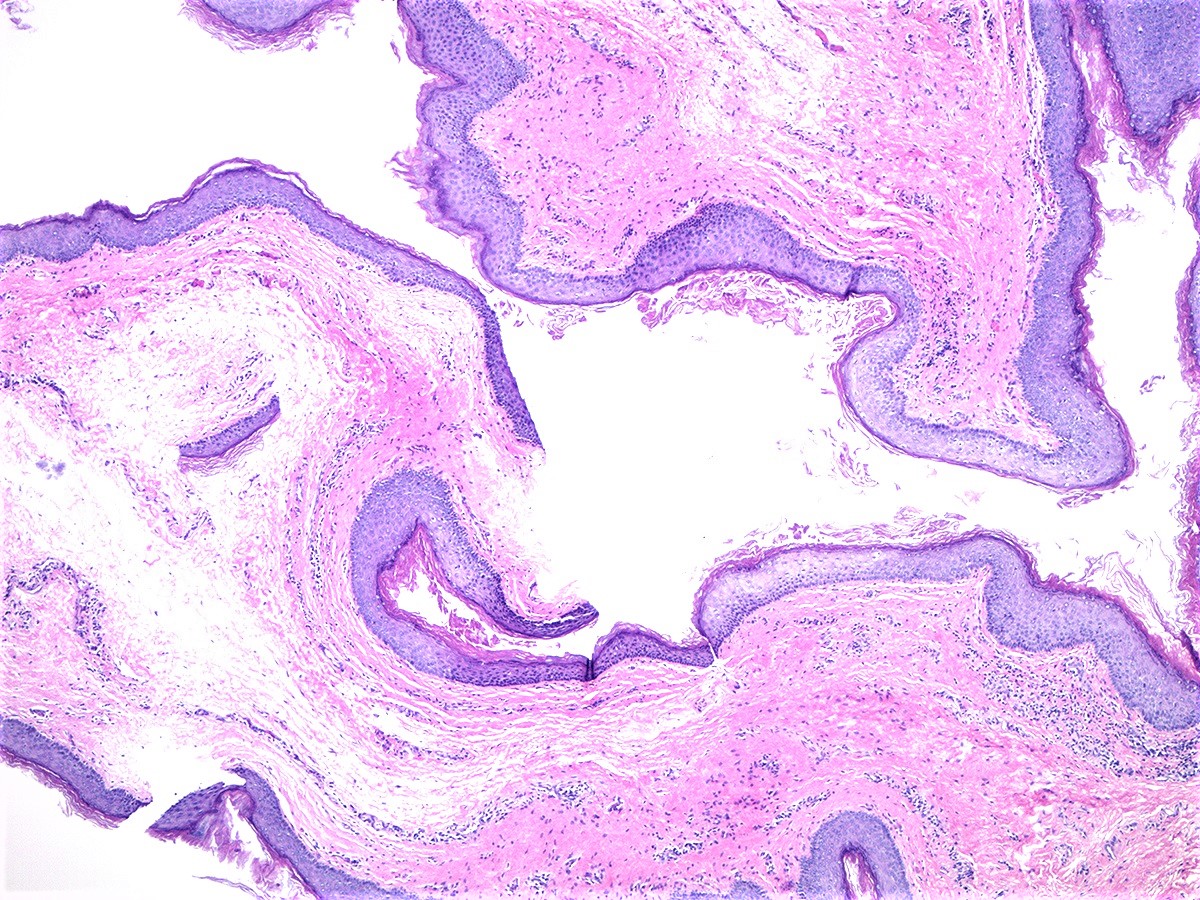
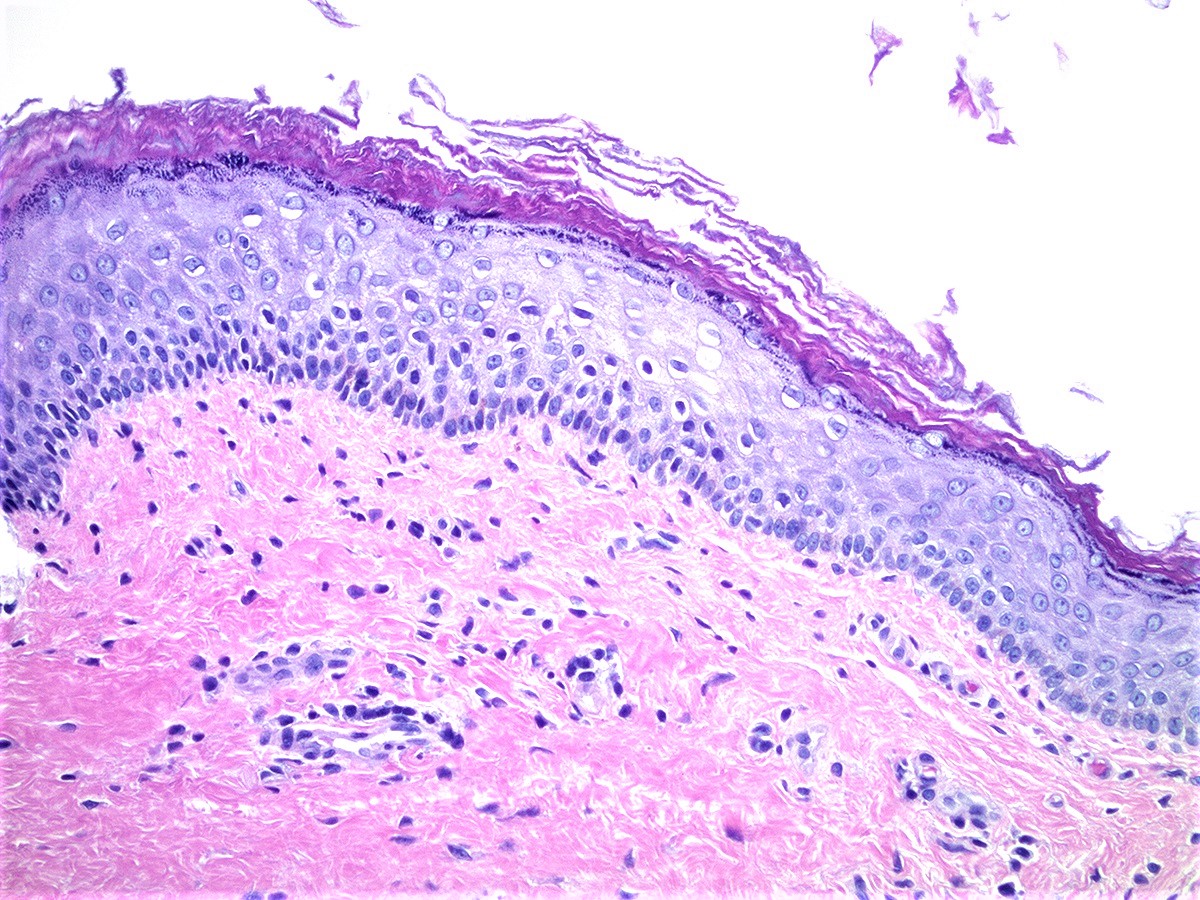
Normal histology of vagina
Anatomy of female urethra
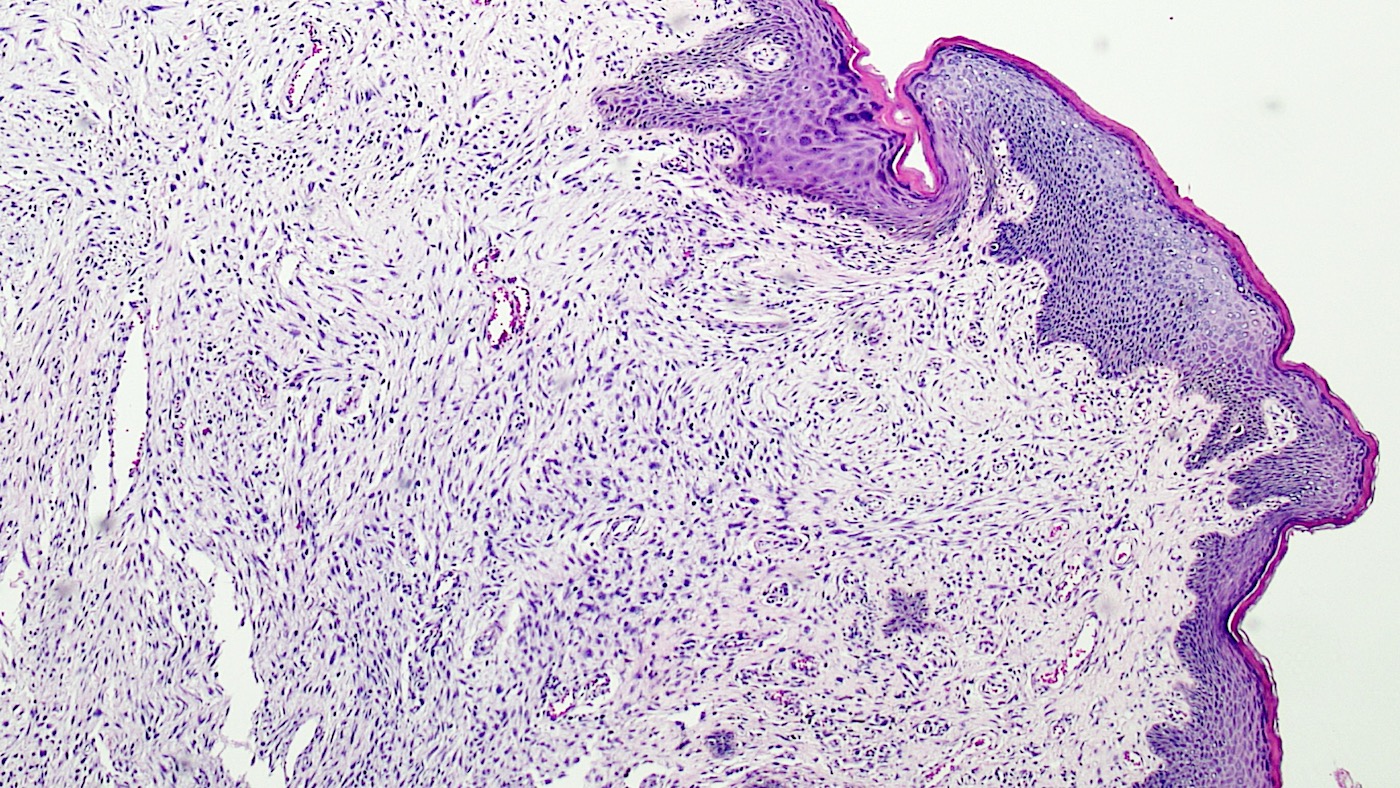
Histology of female urethra
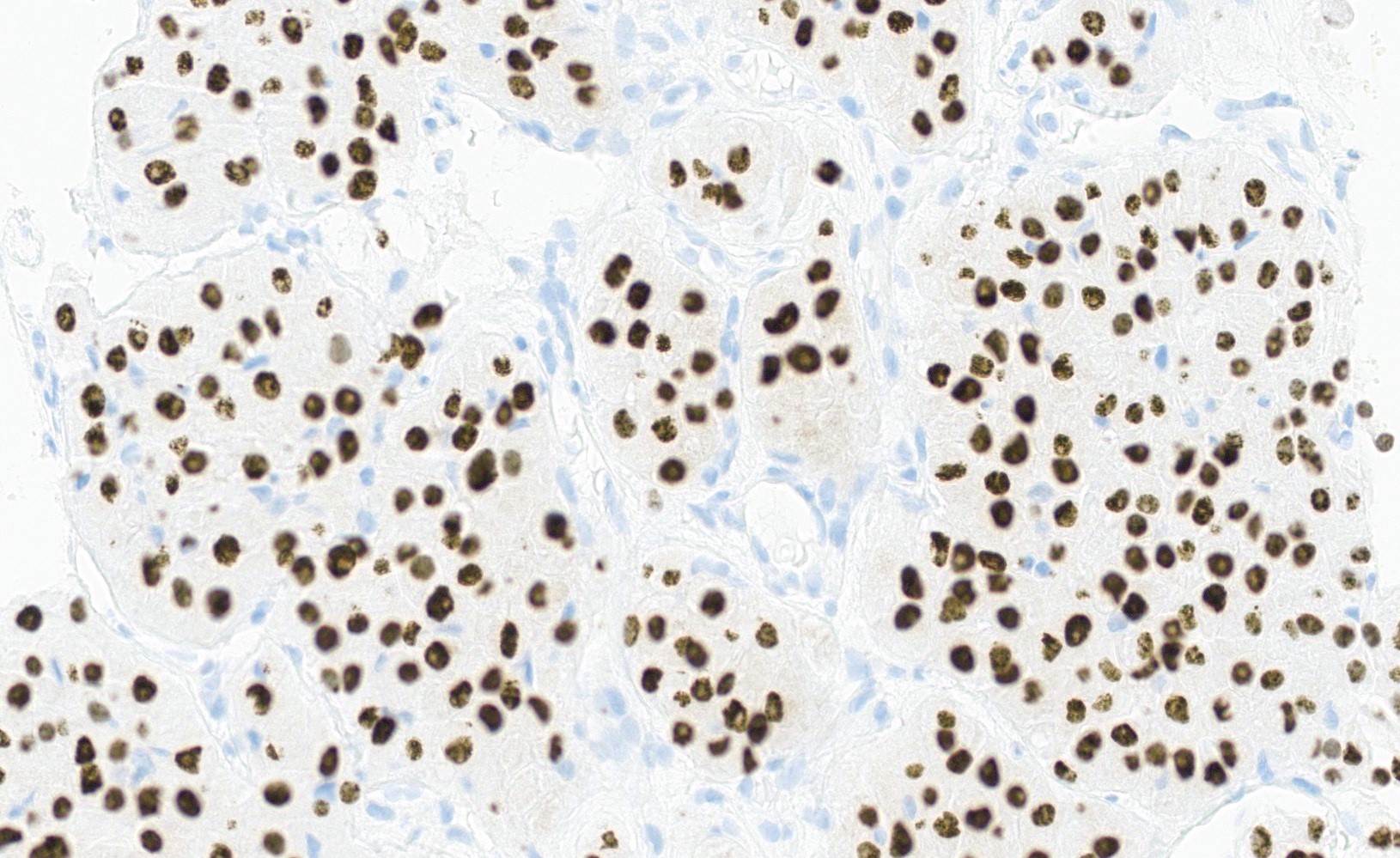
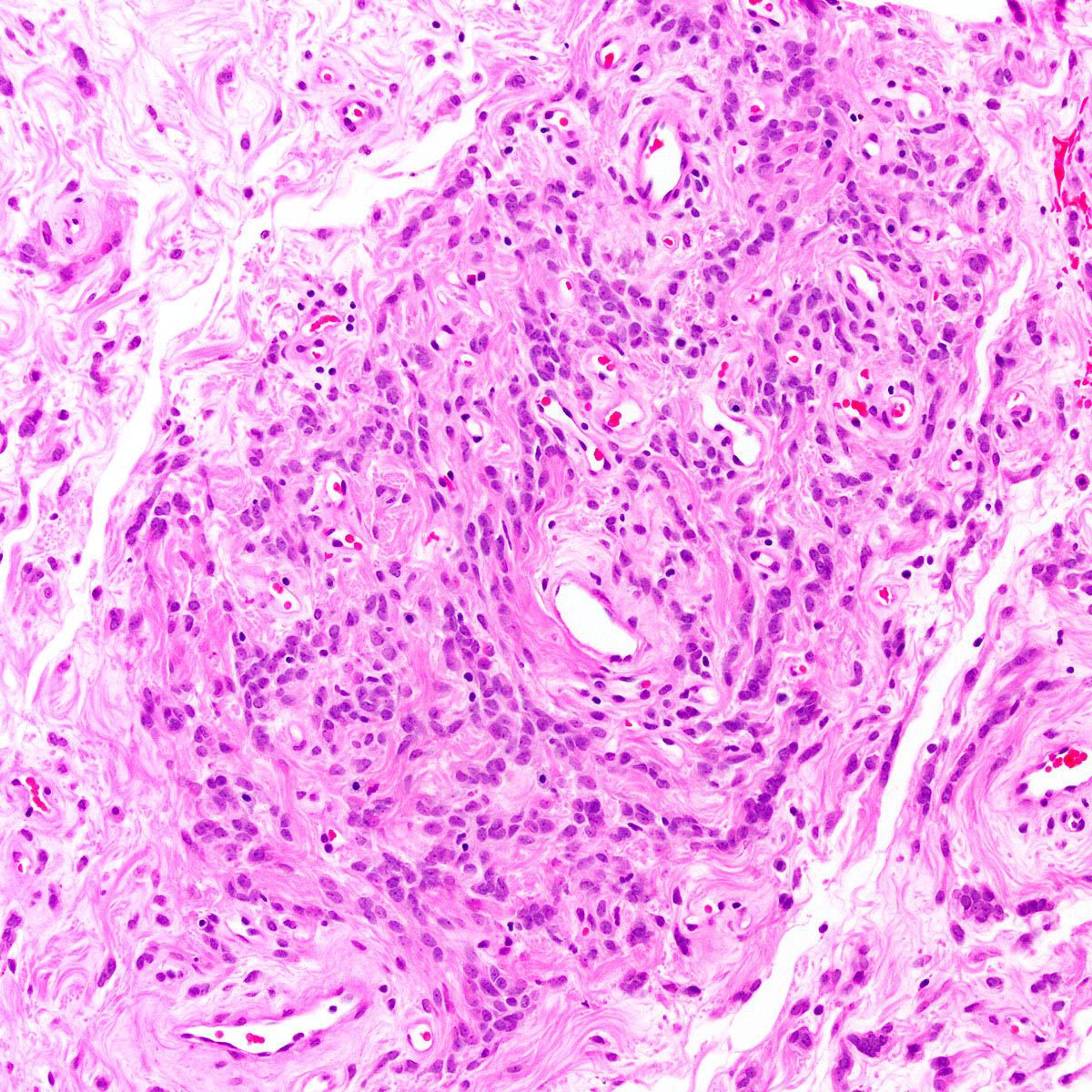
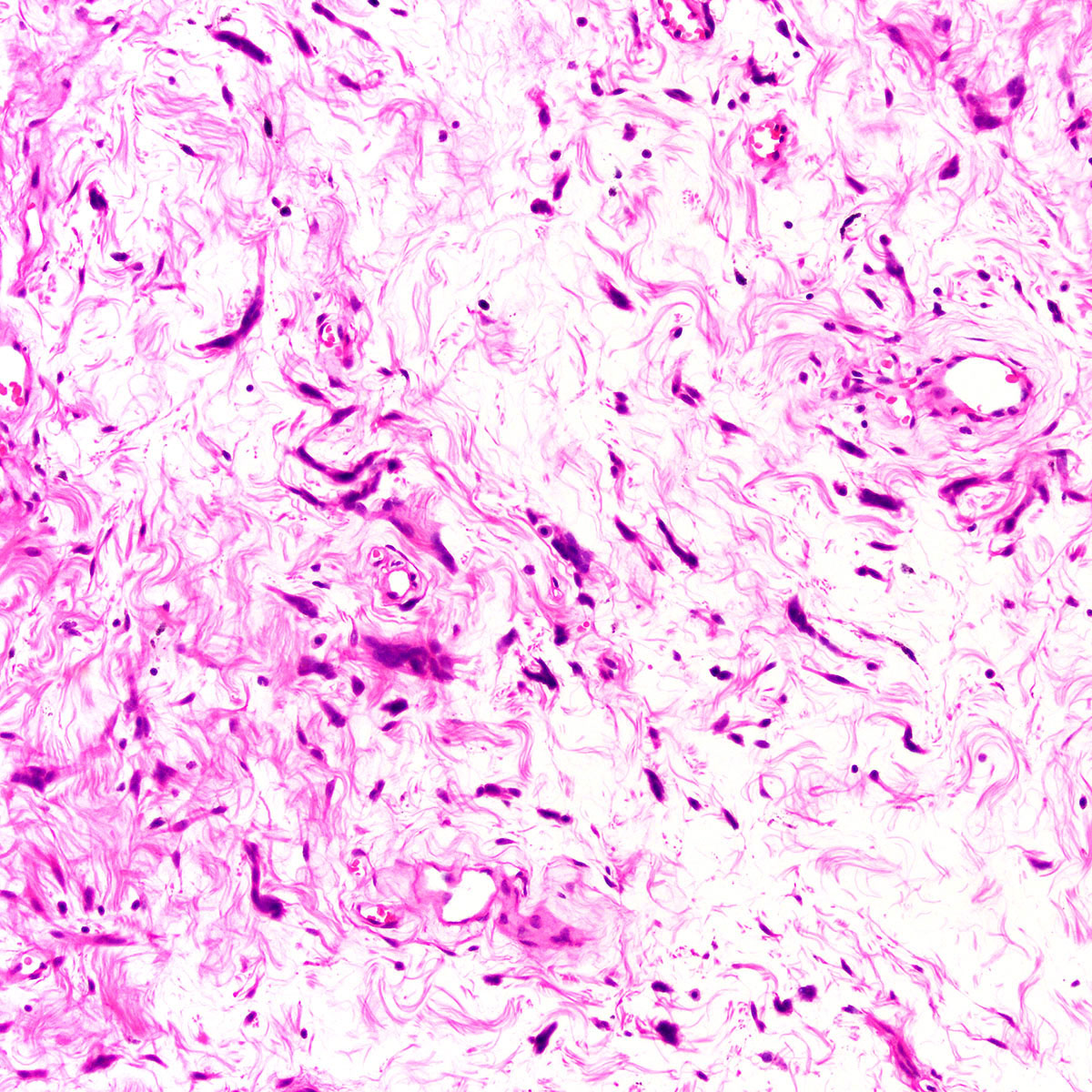
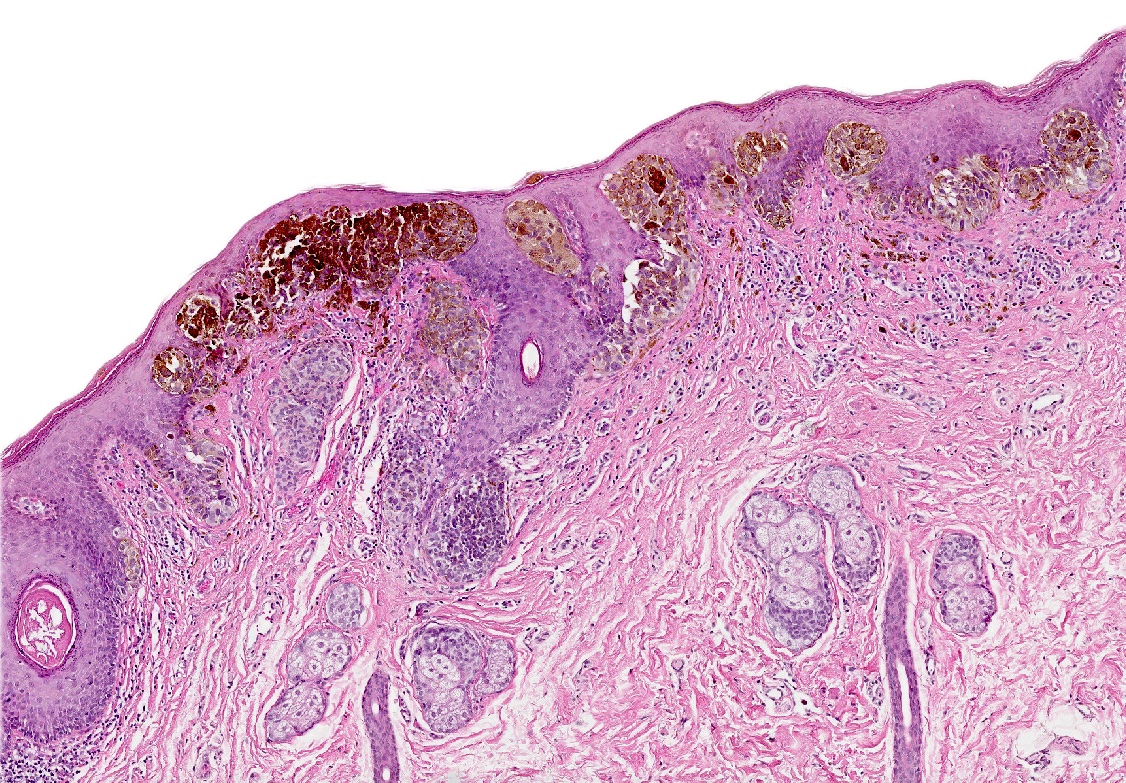
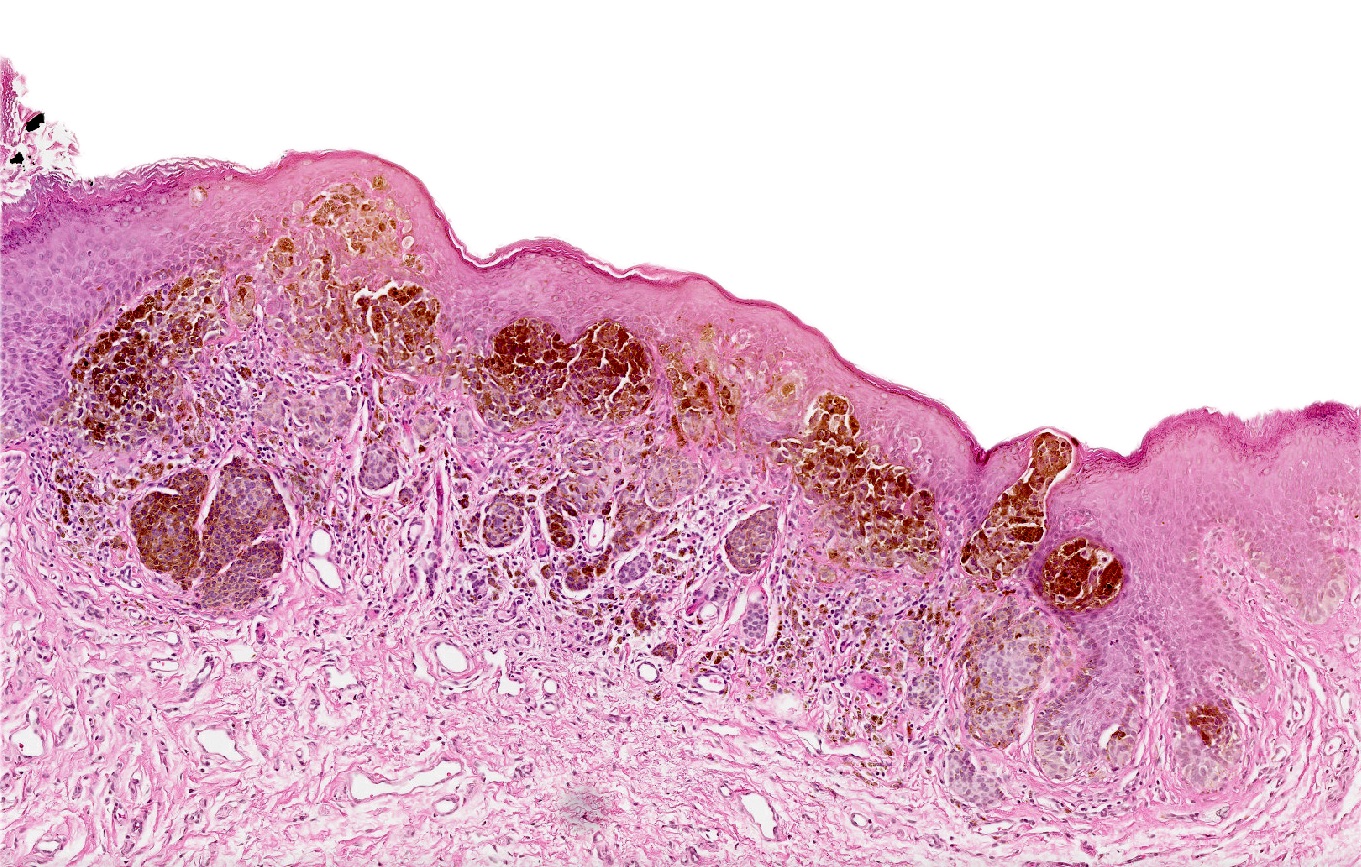
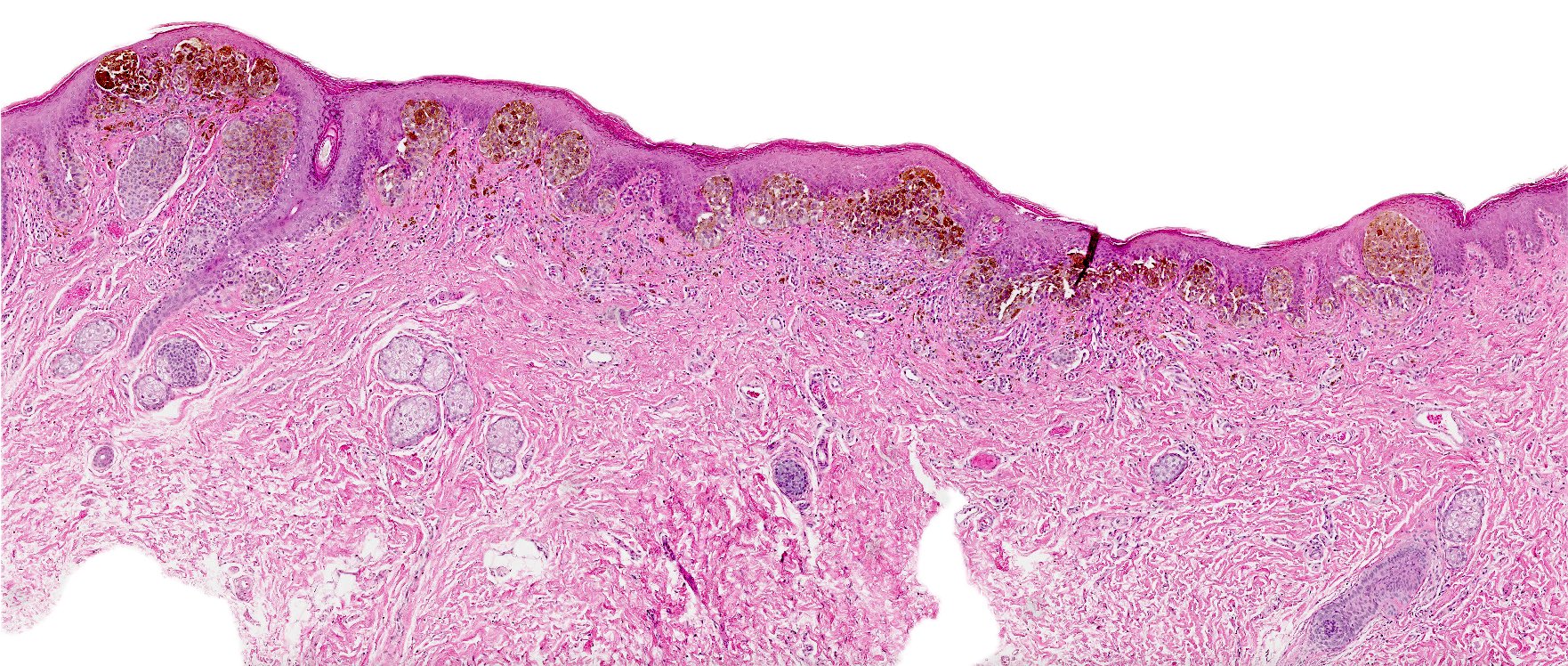
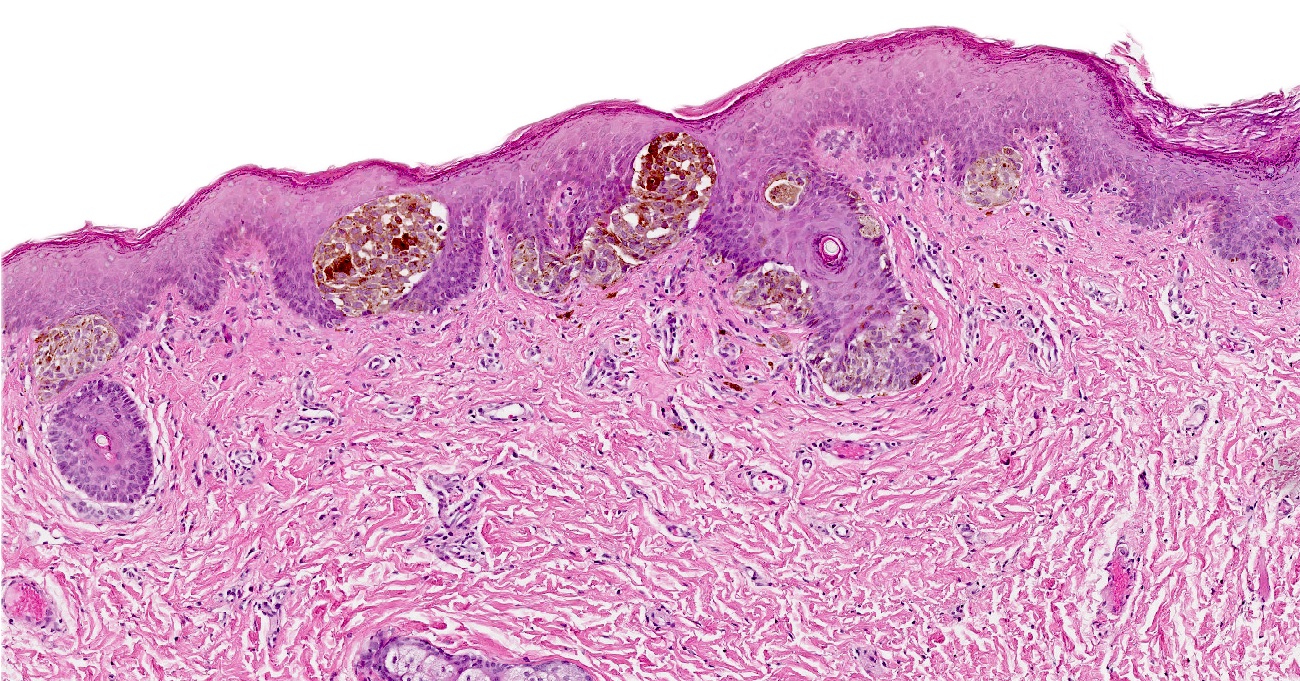
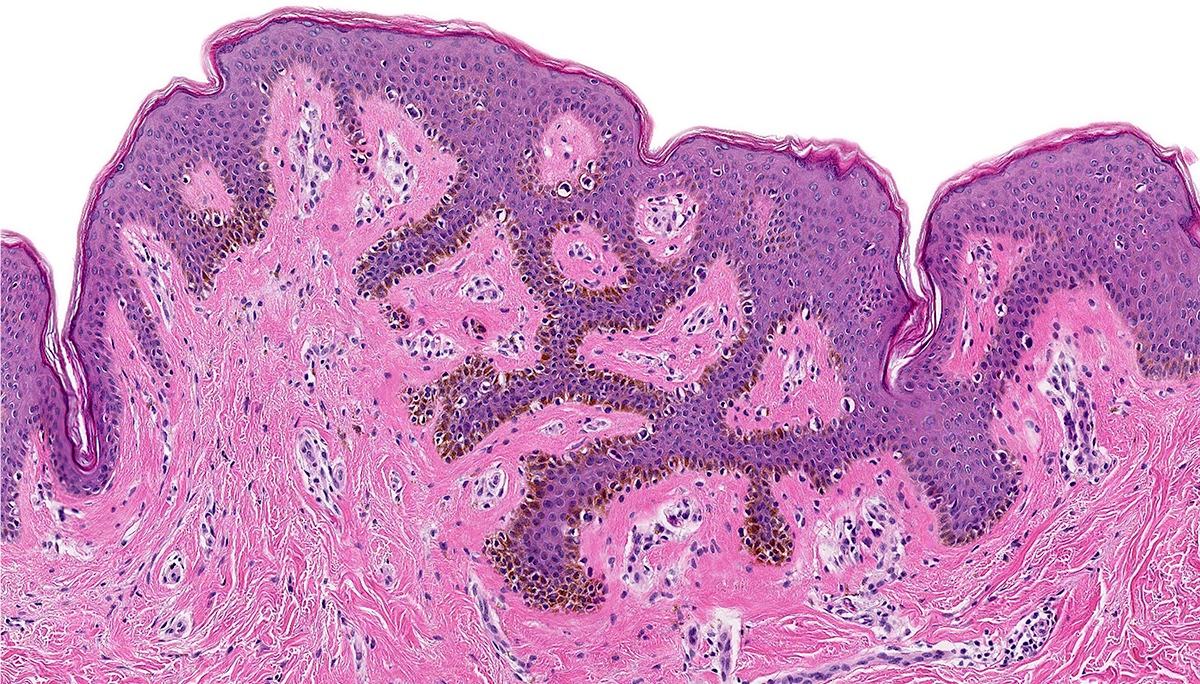
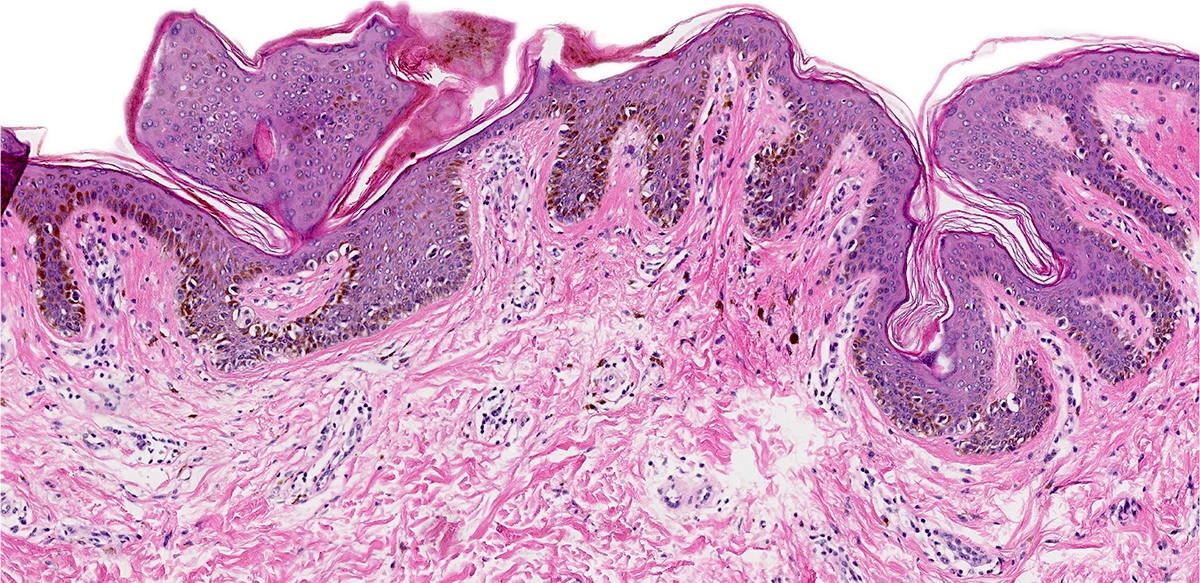
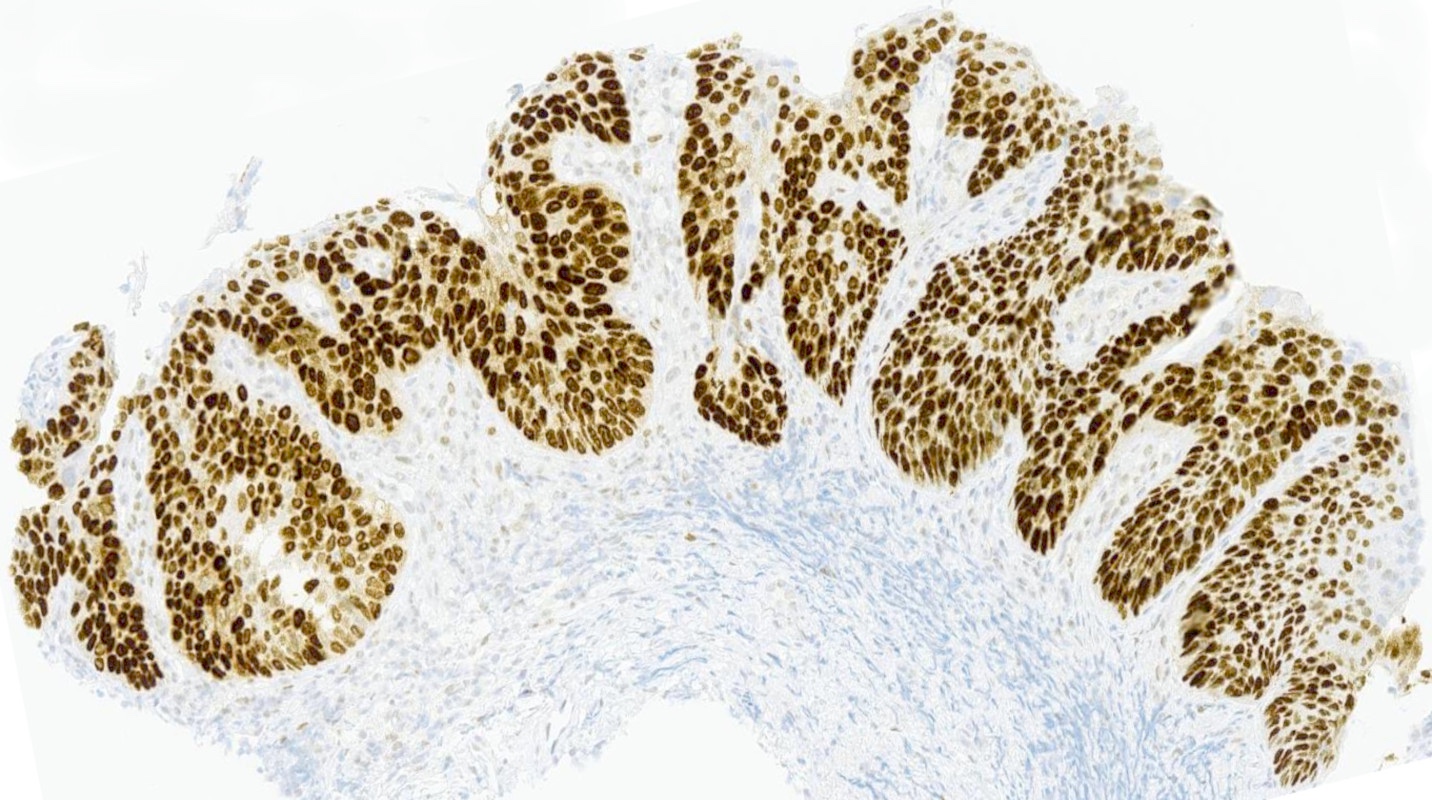
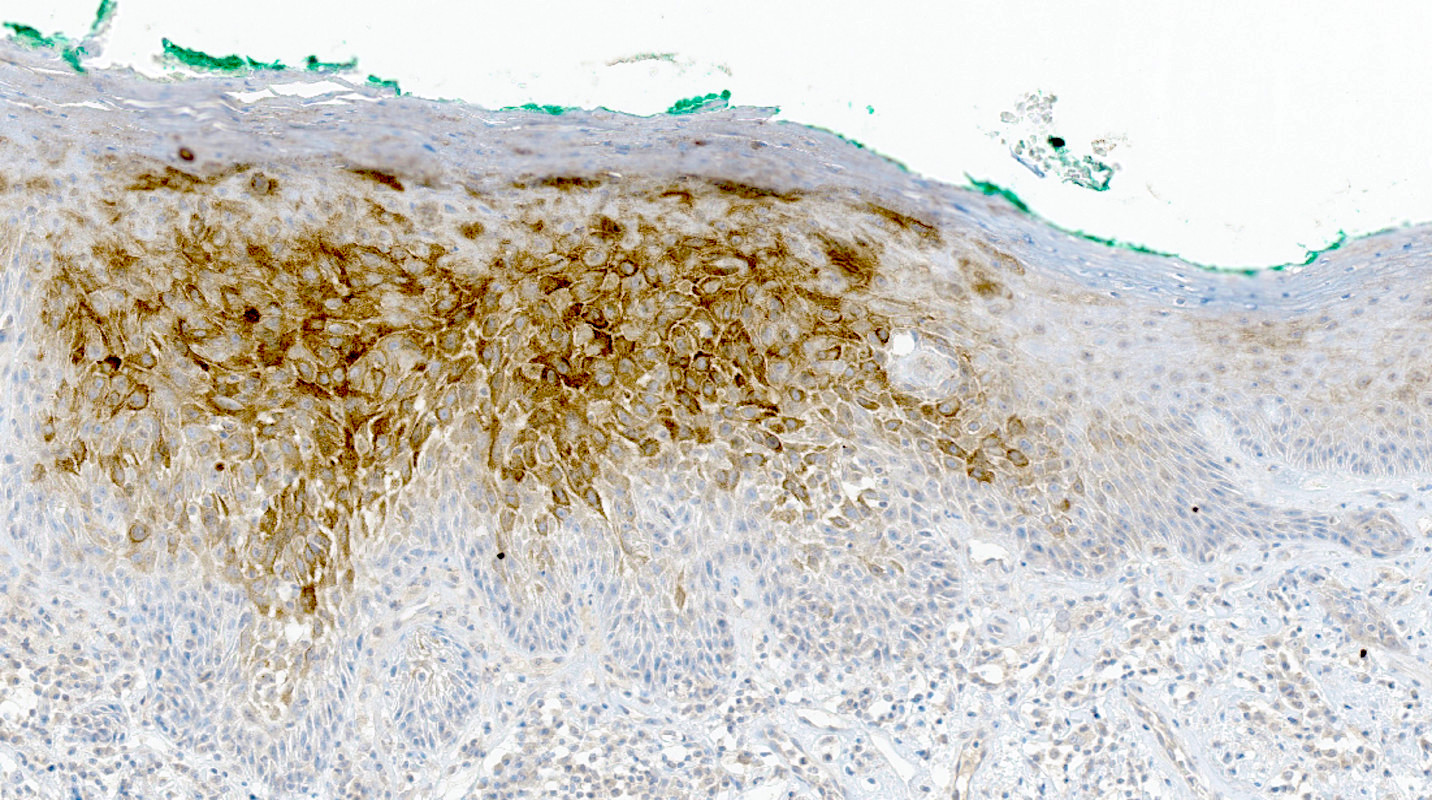
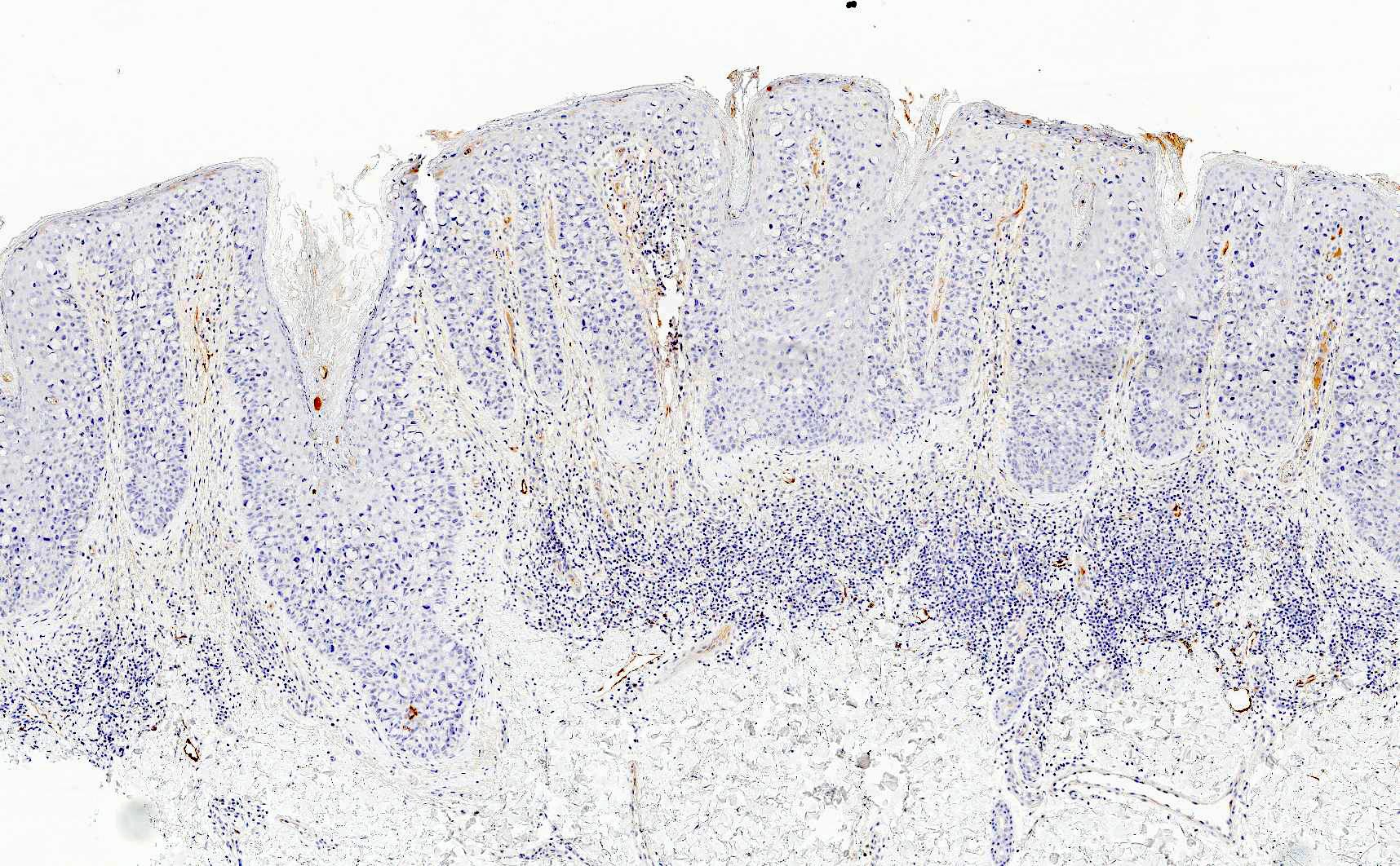
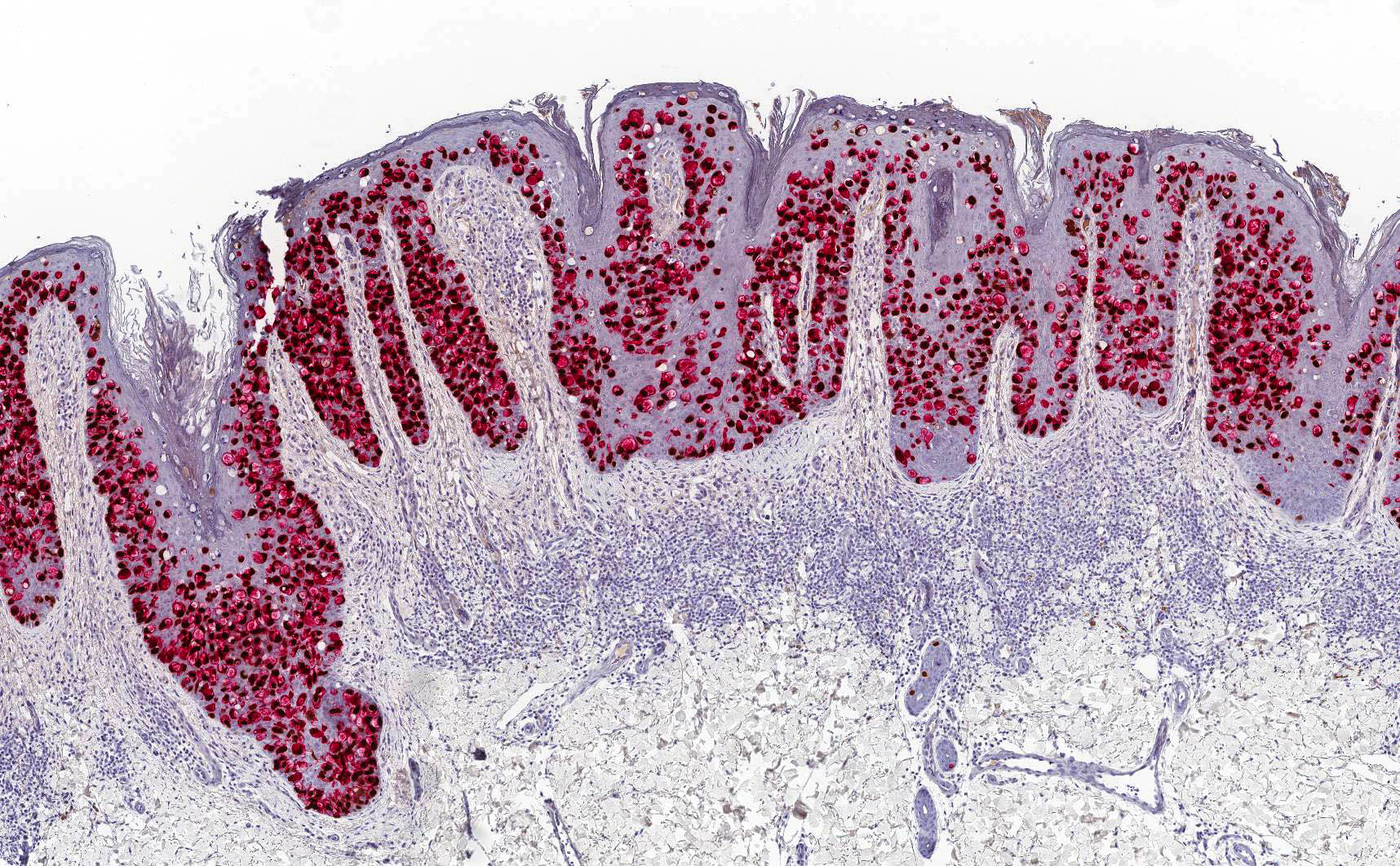
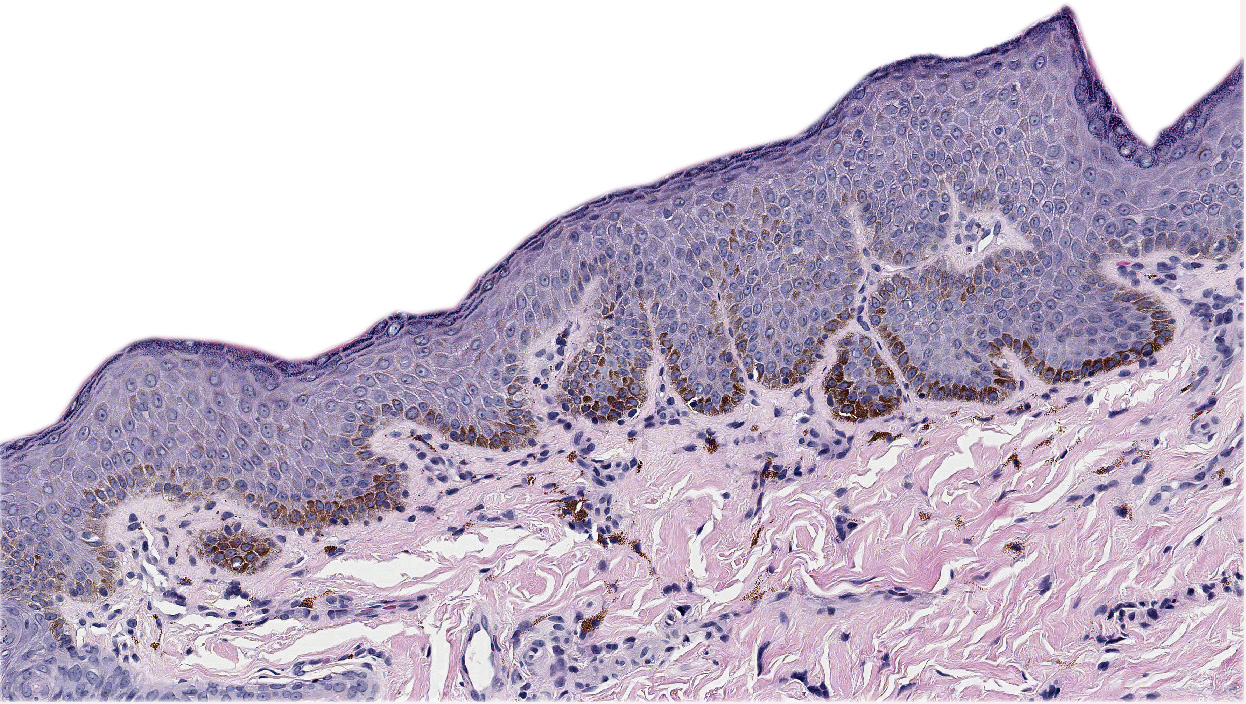
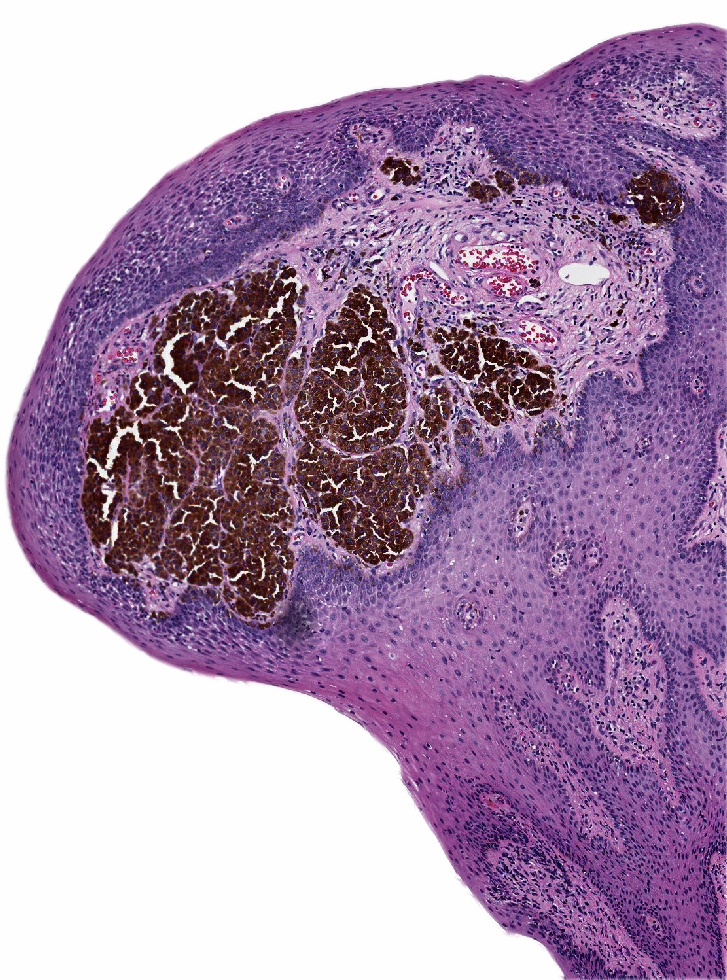
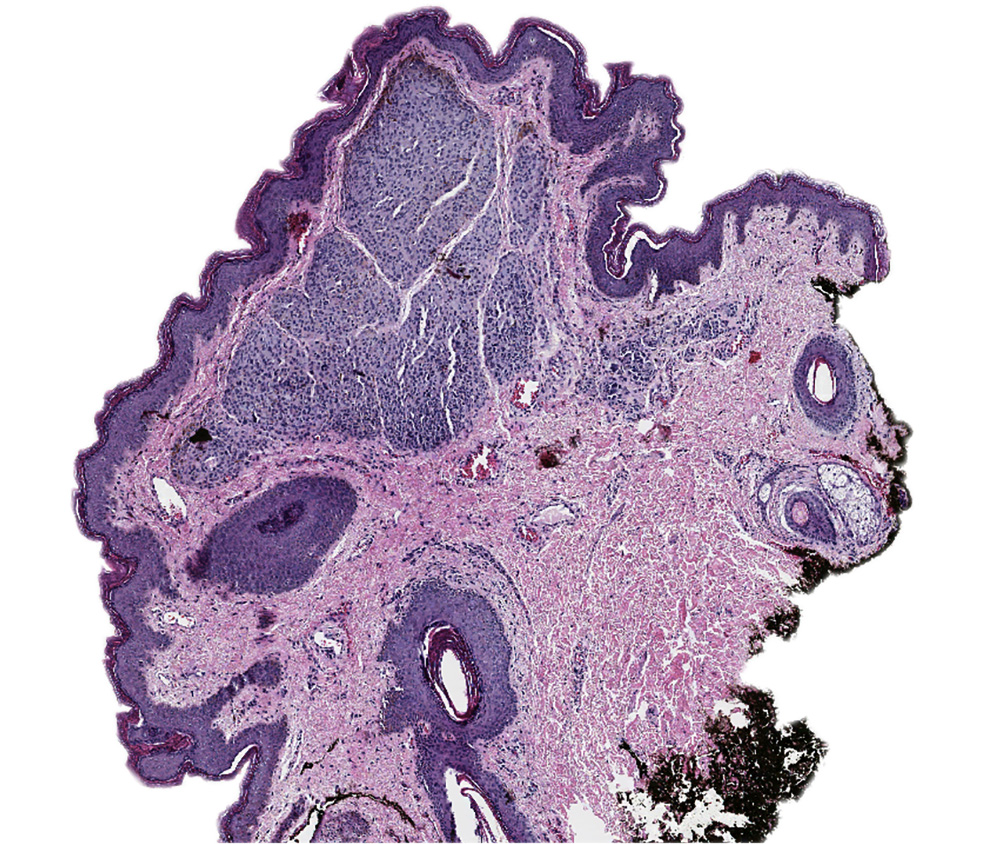
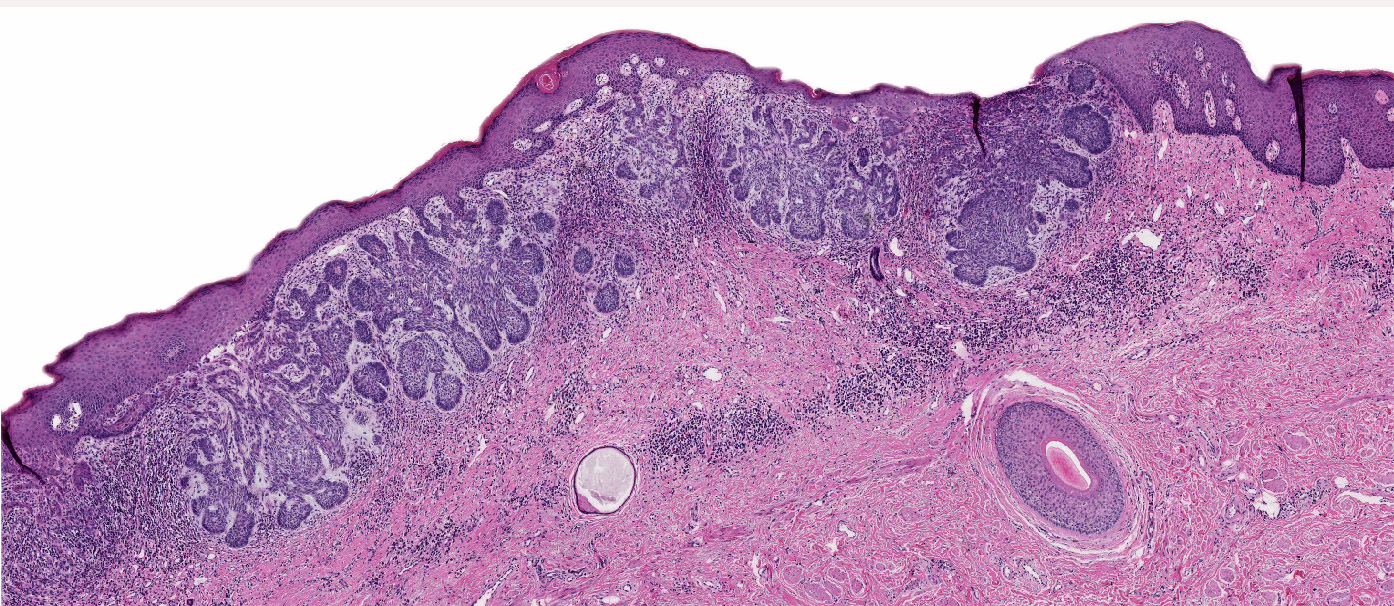
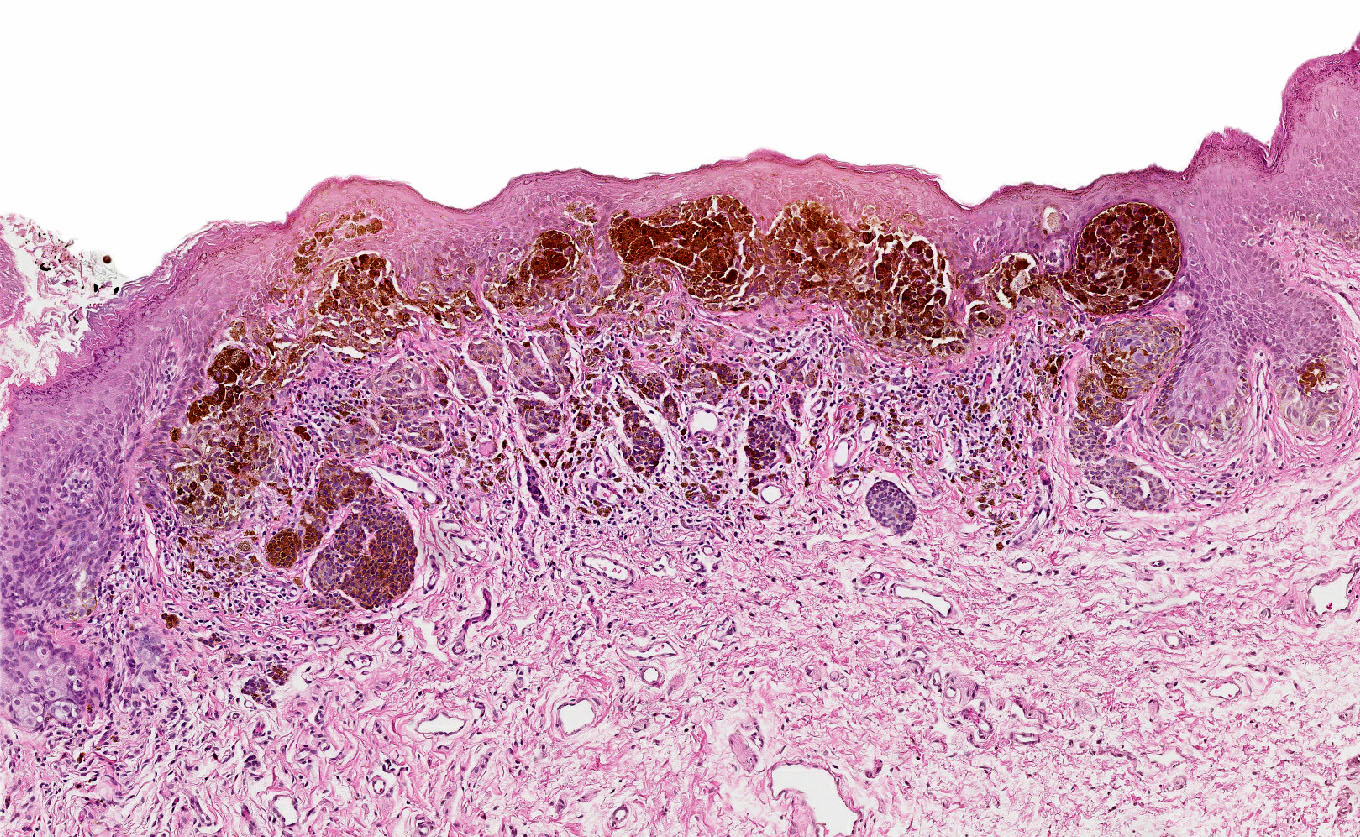
Atypical nevi and nevi of special sites by Dr. Phillip McKee
Atypical nevi and melanoma by Dr. Steven Wang
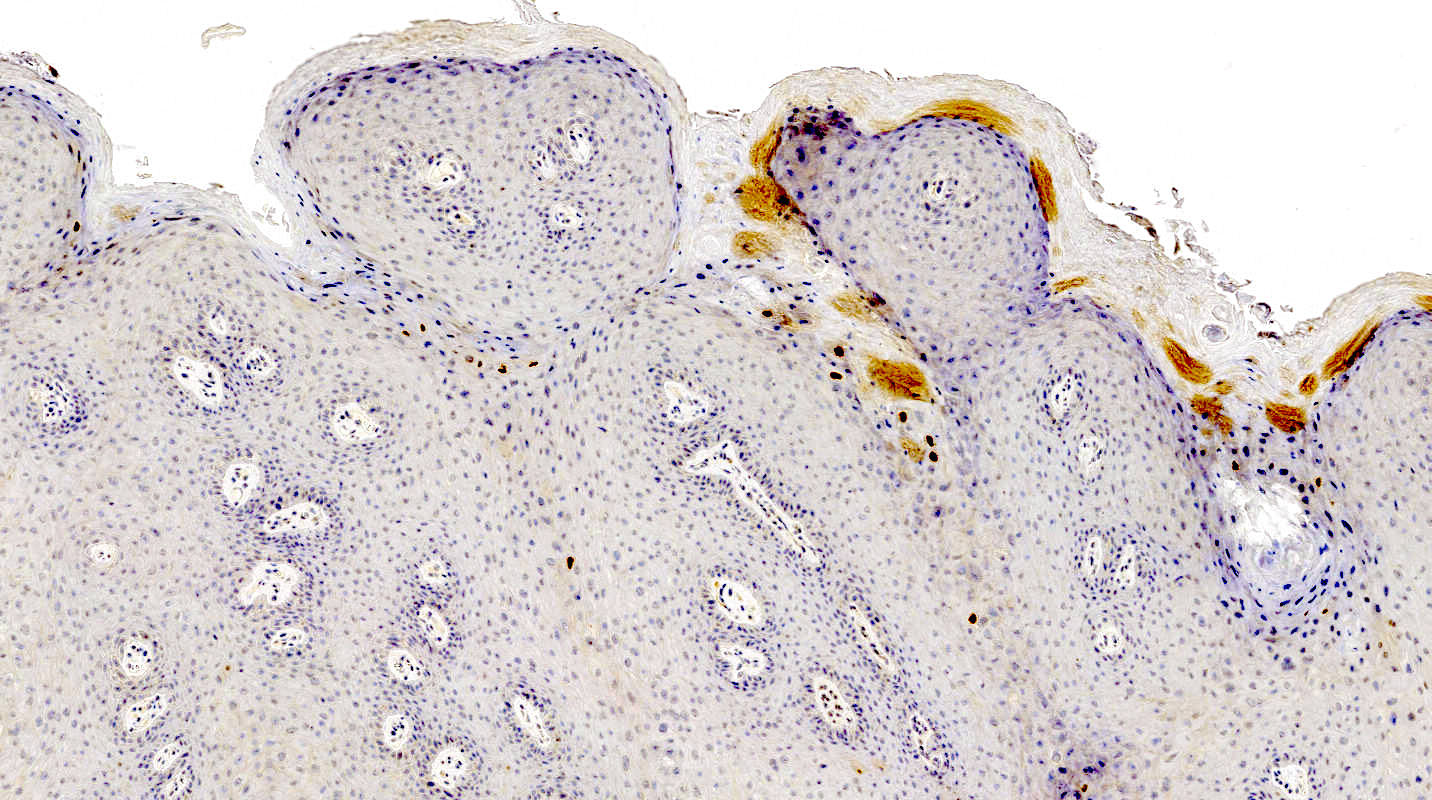
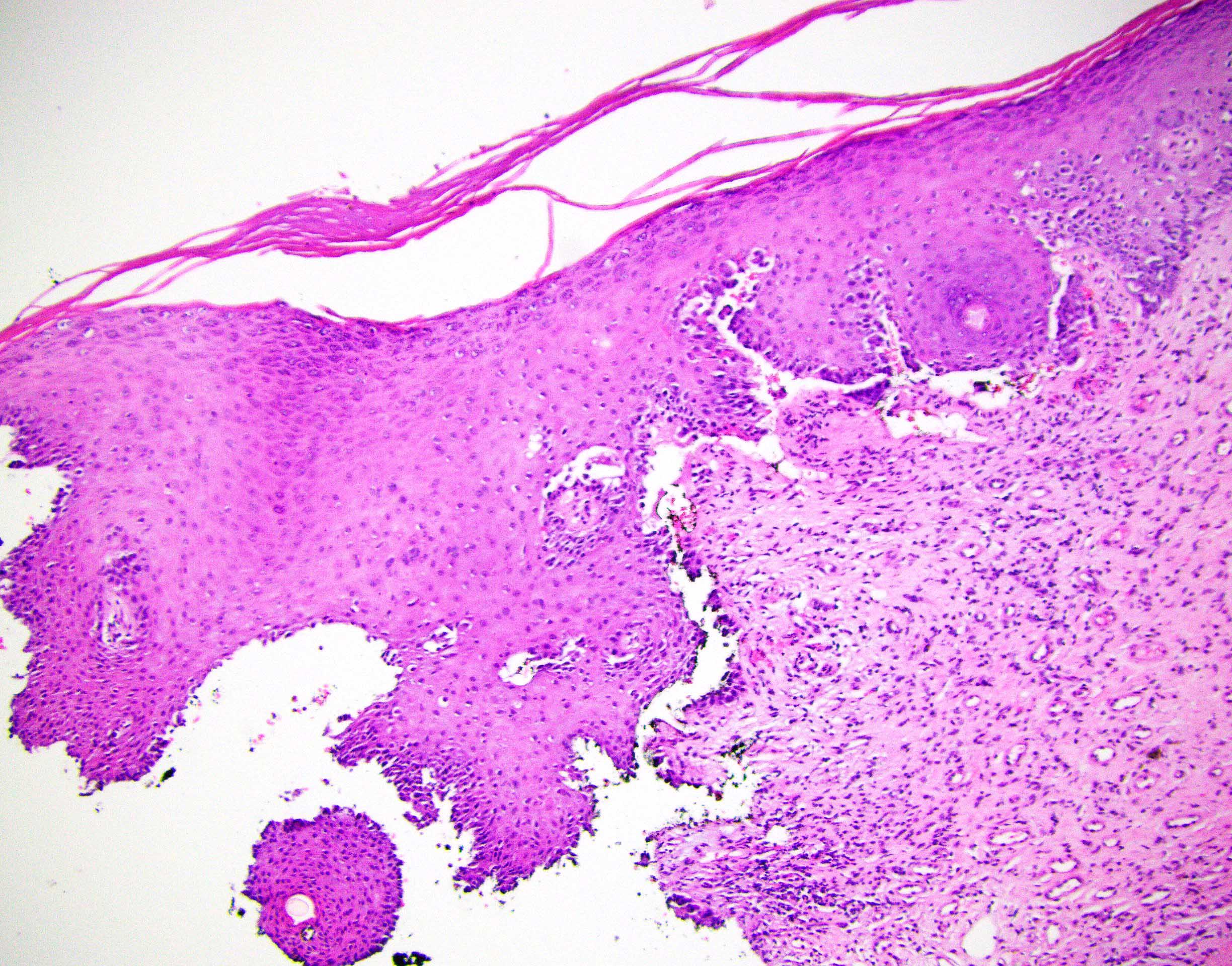
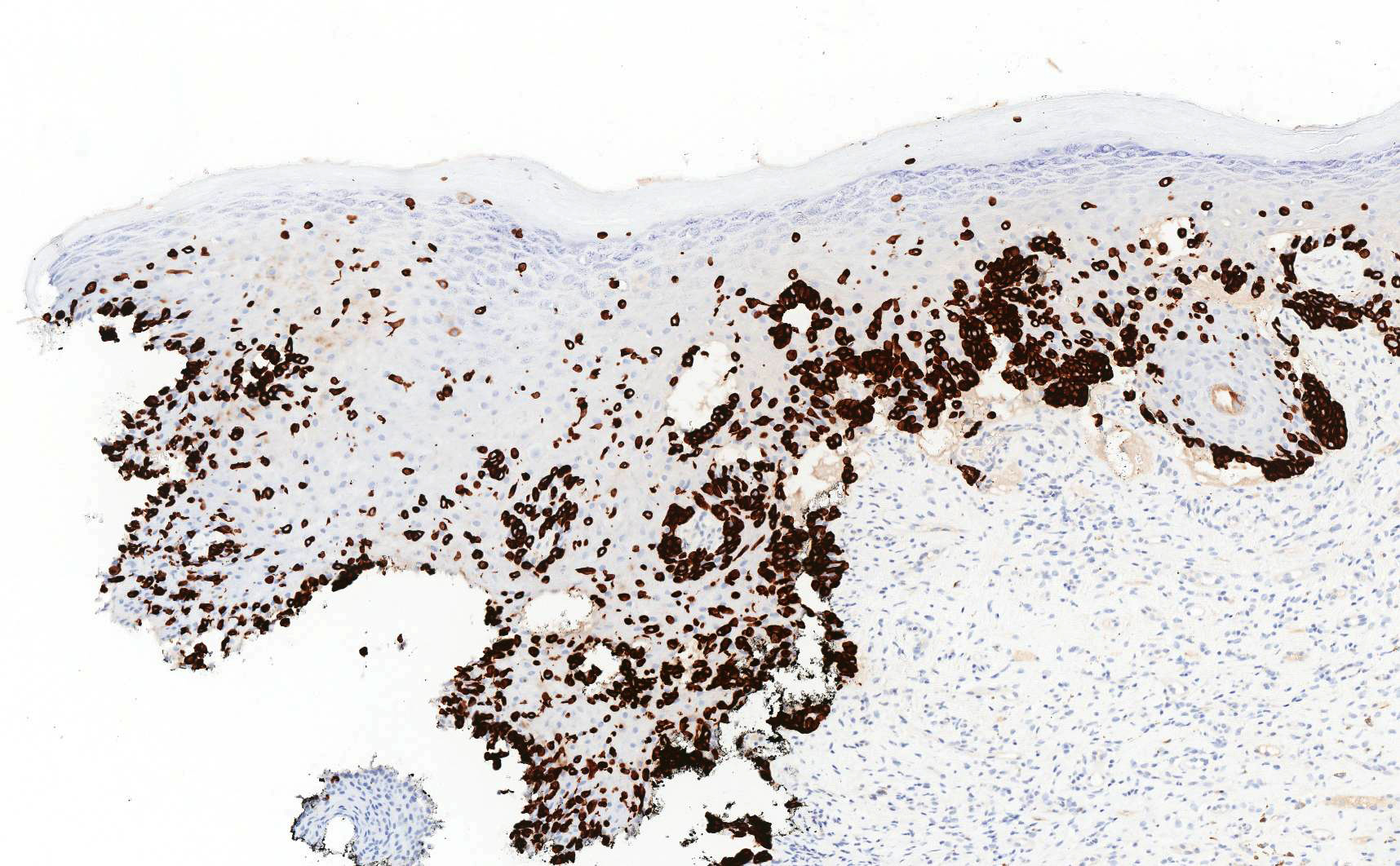
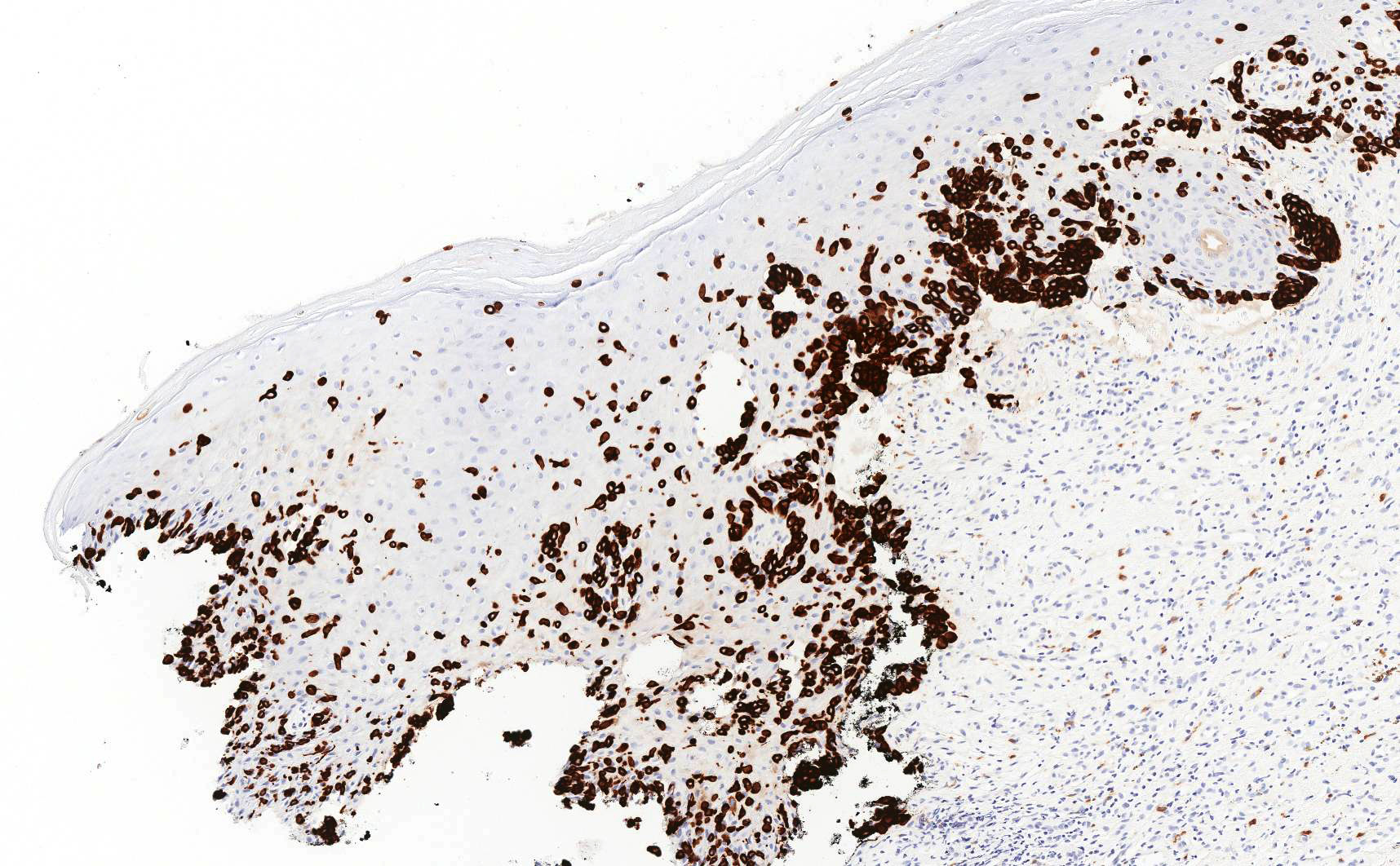
Contributed by Lucy Ma, M.D. and Priya Nagarajan, M.D., Ph.D.
BCC 101 by Dr. Jerad Gardner
Reporting BCC by Dr. Catriona McKenzie, pathCast
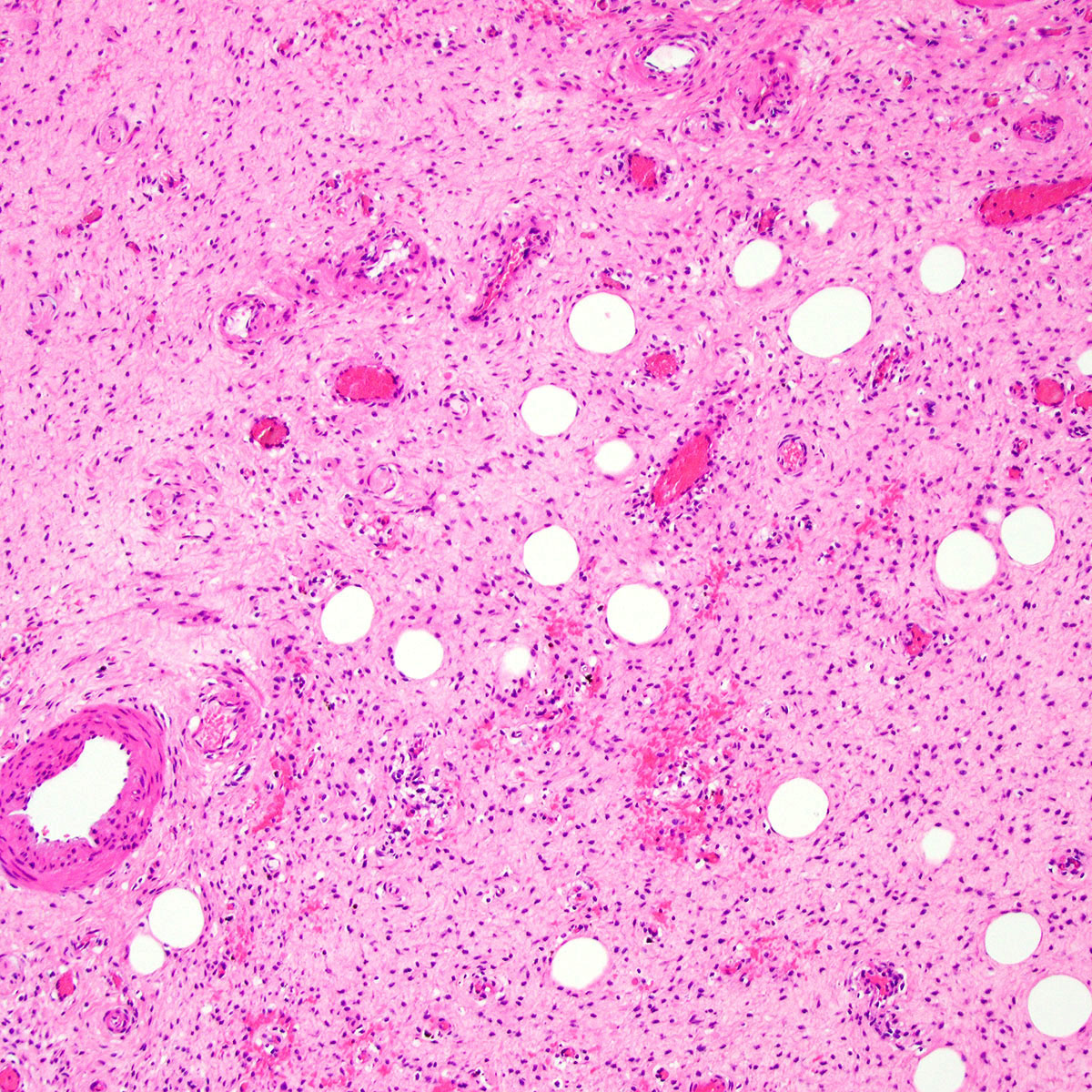
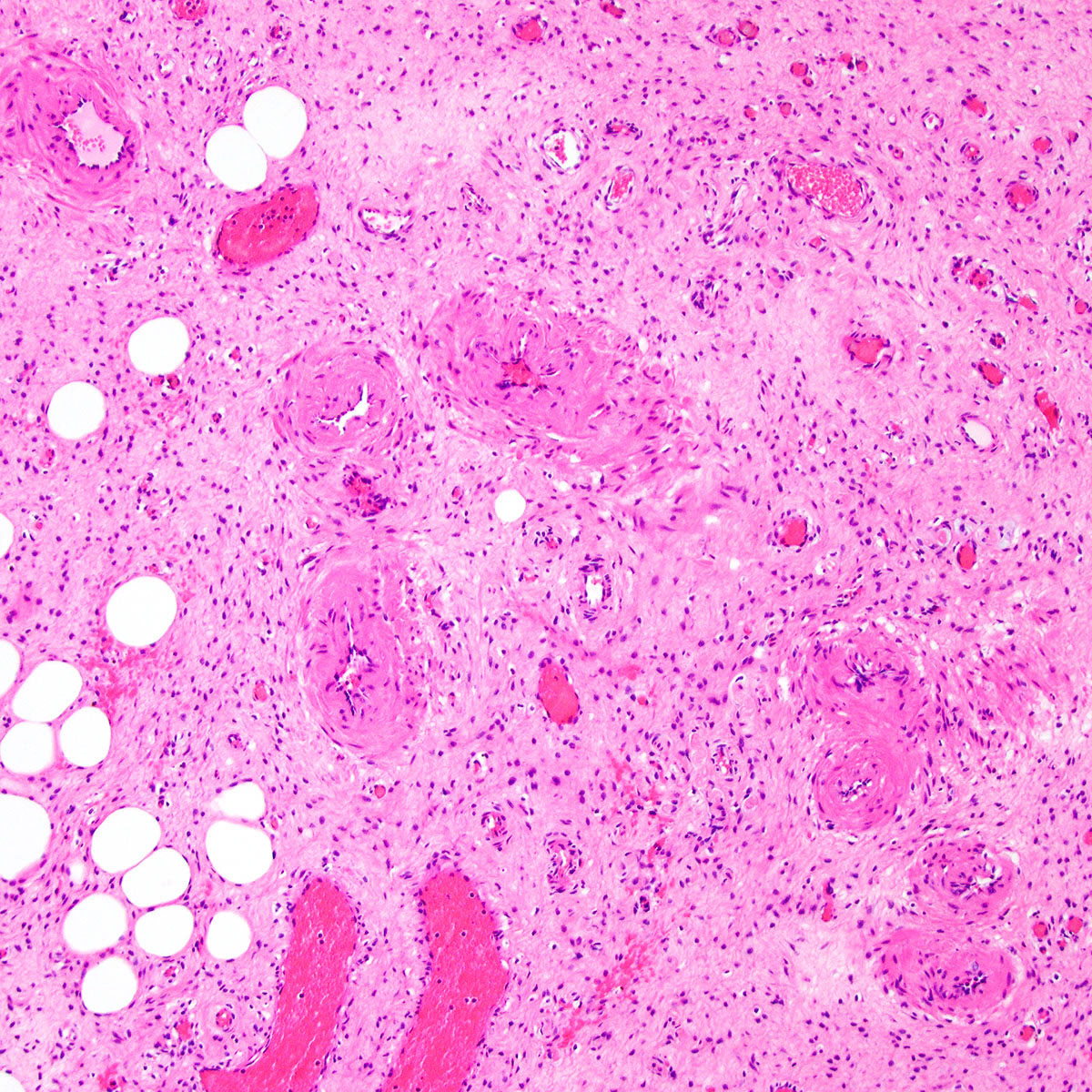
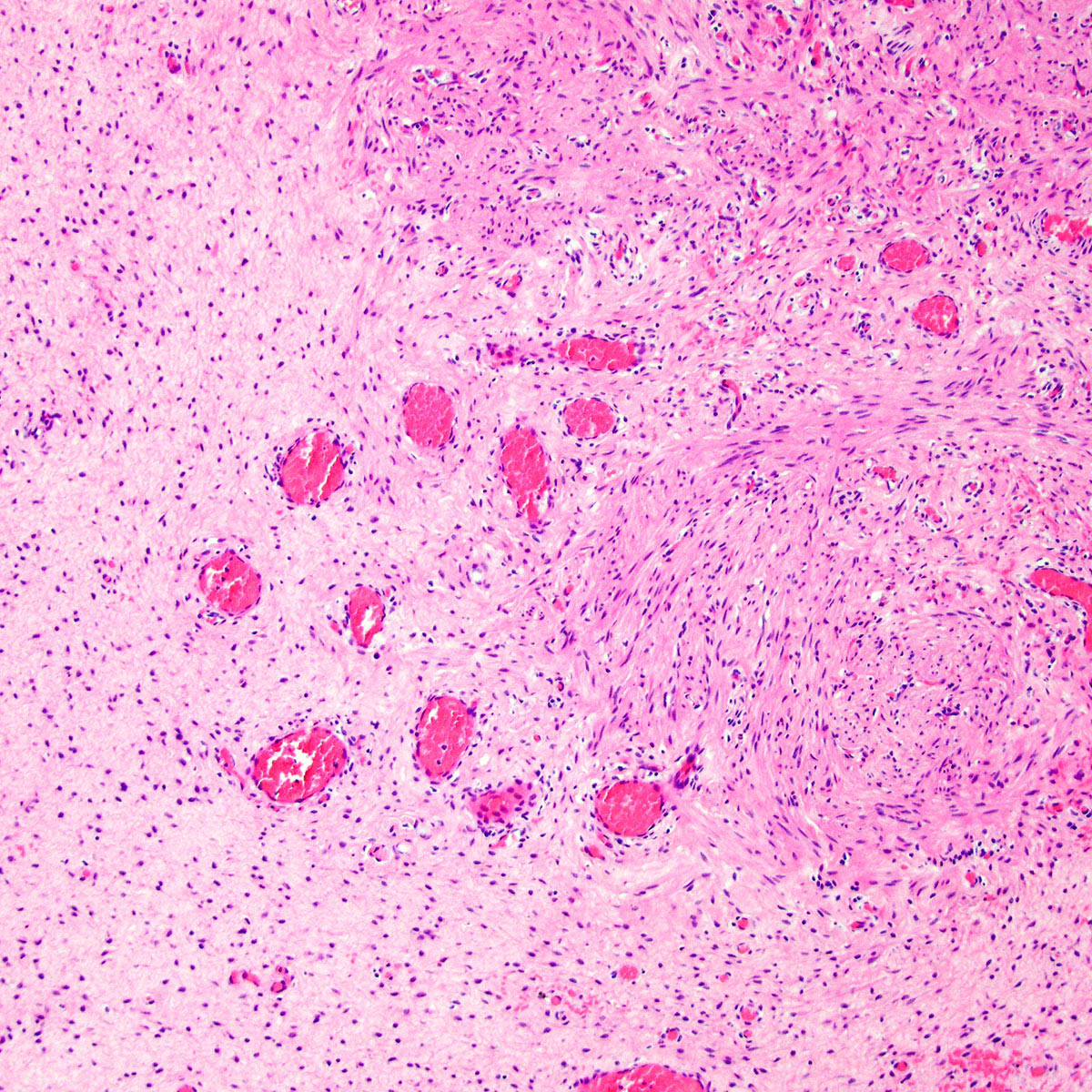
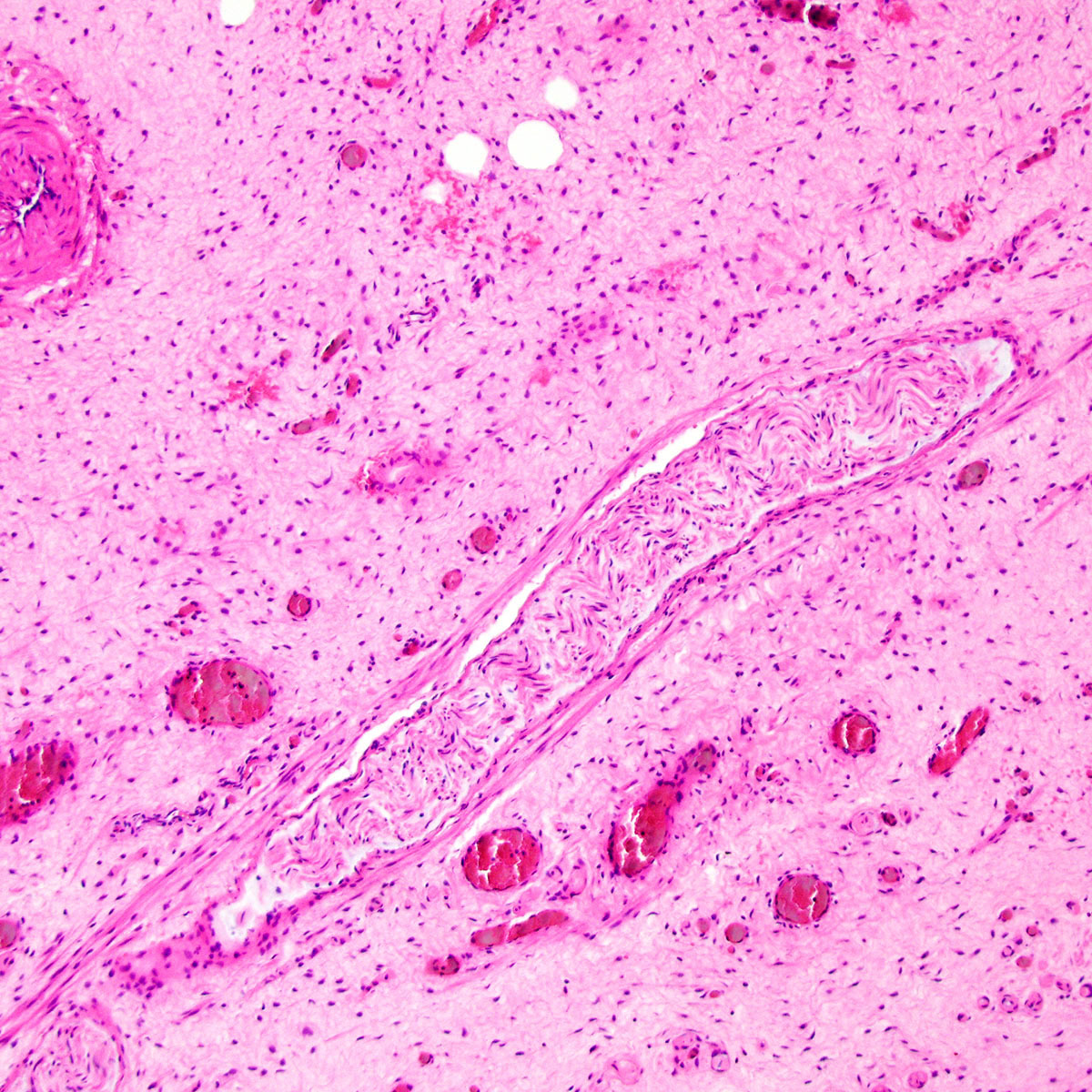
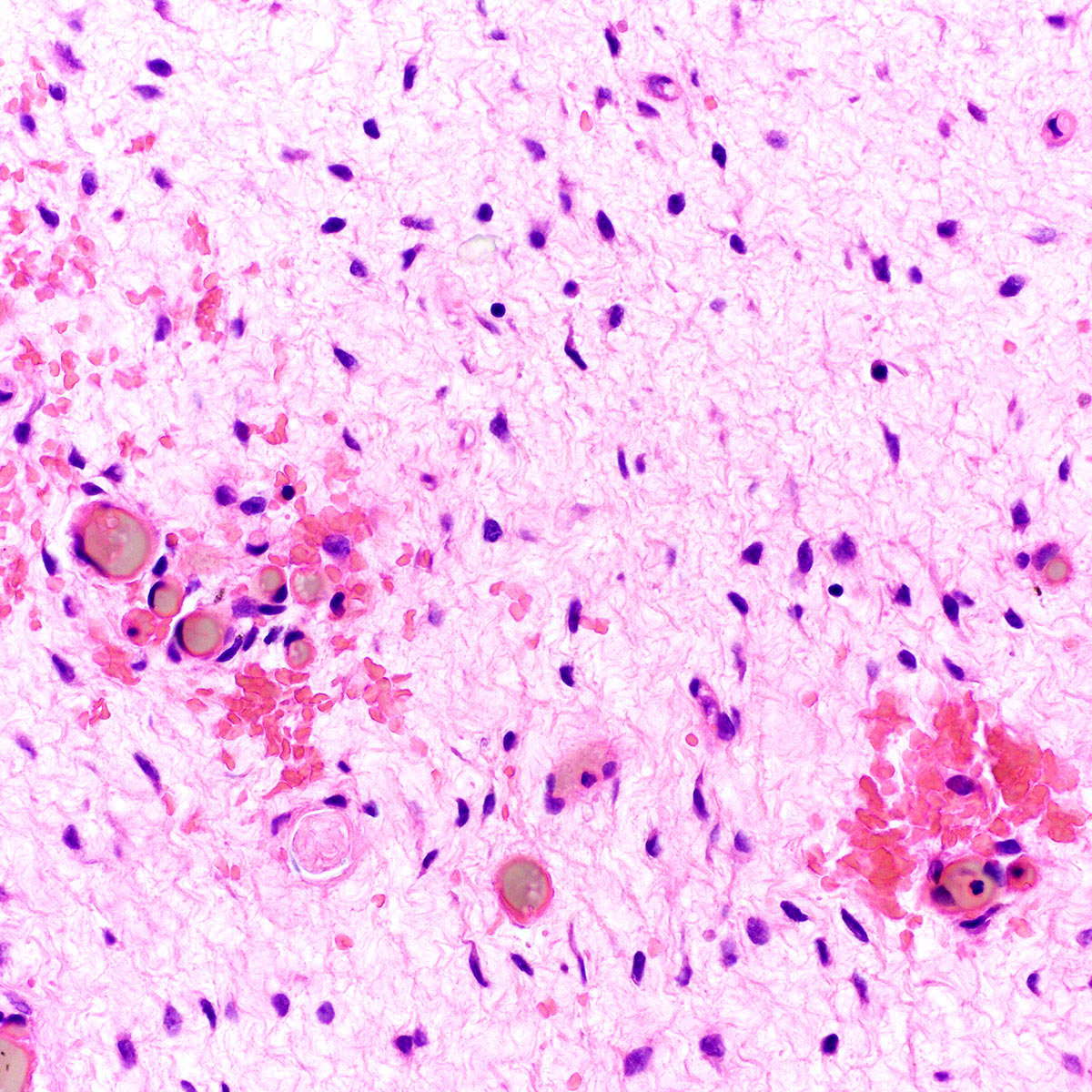
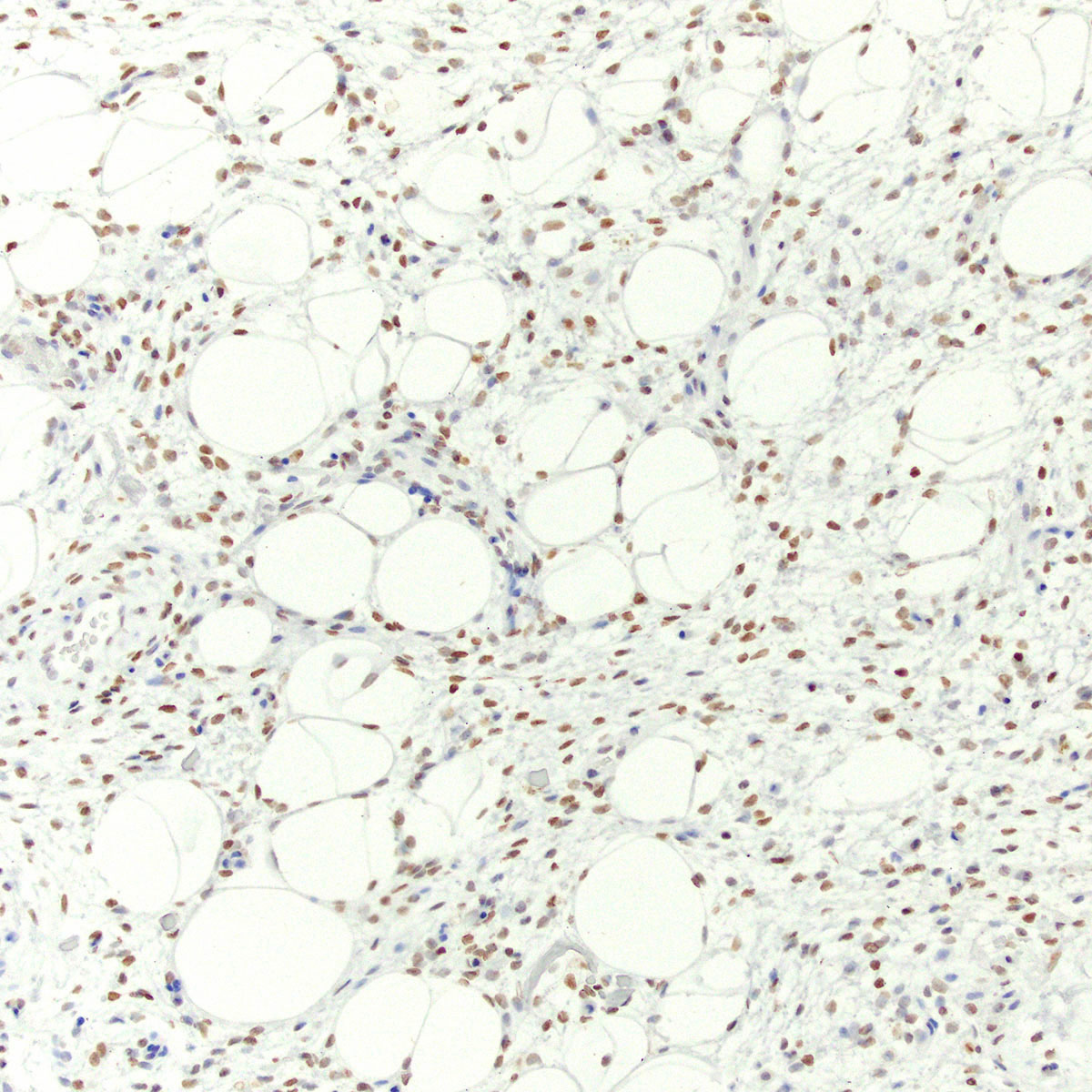
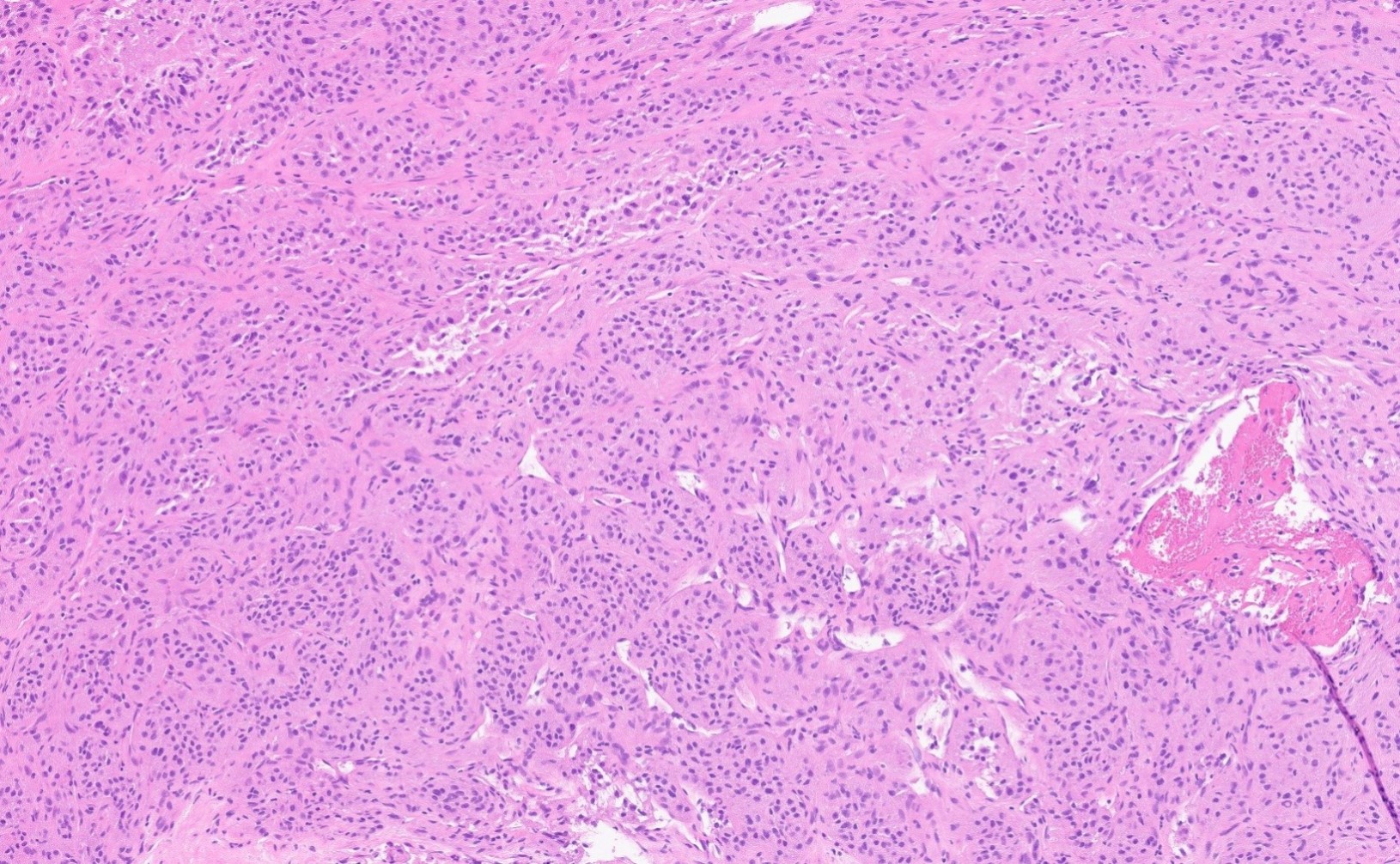
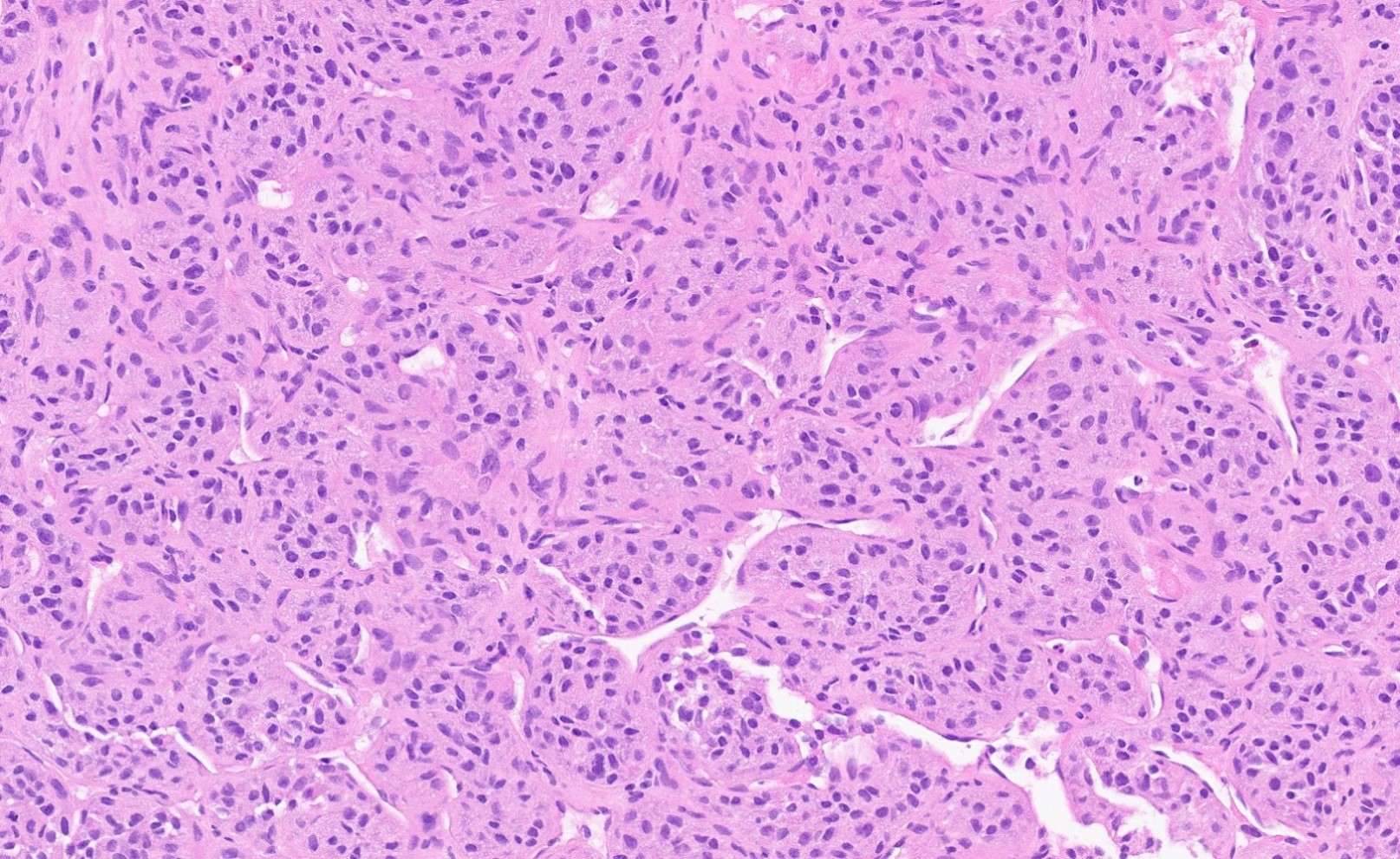
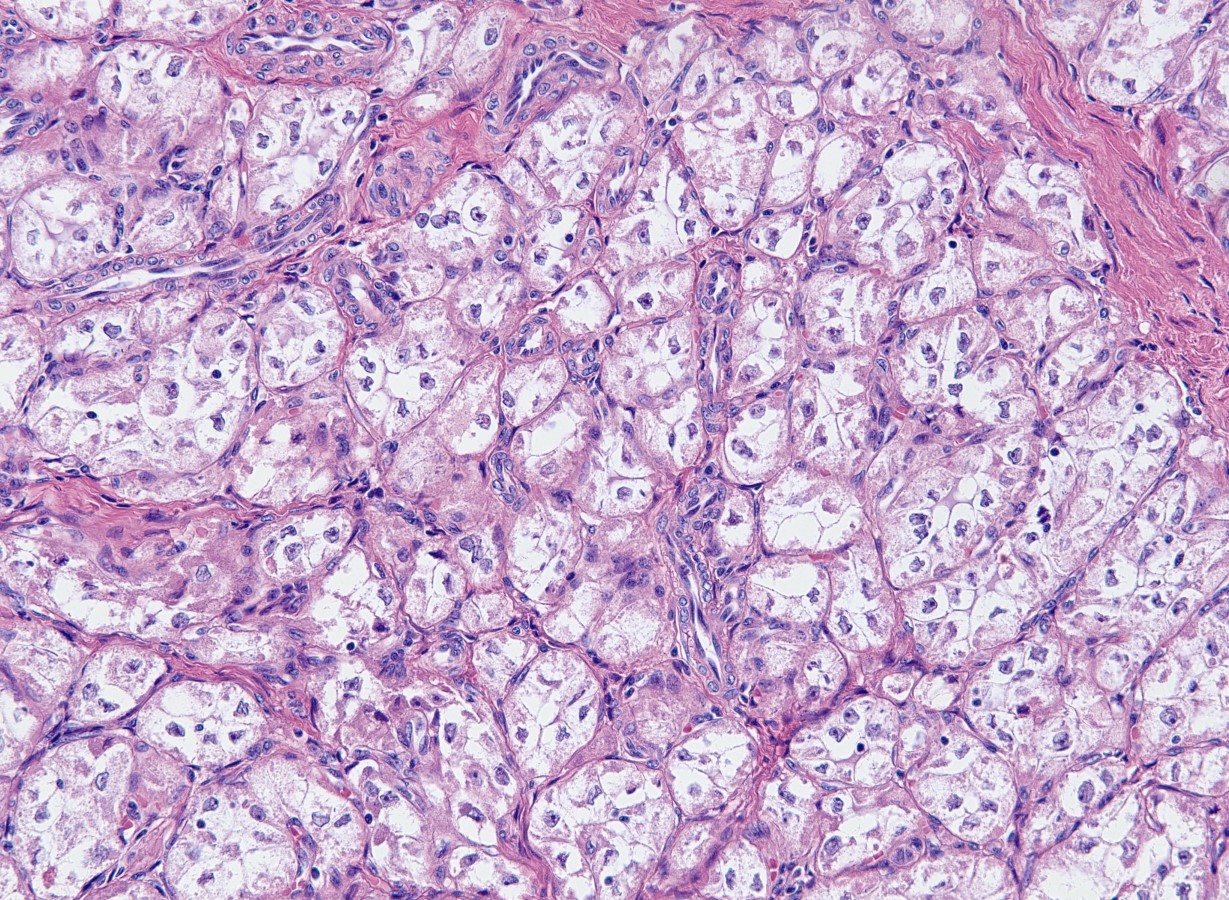
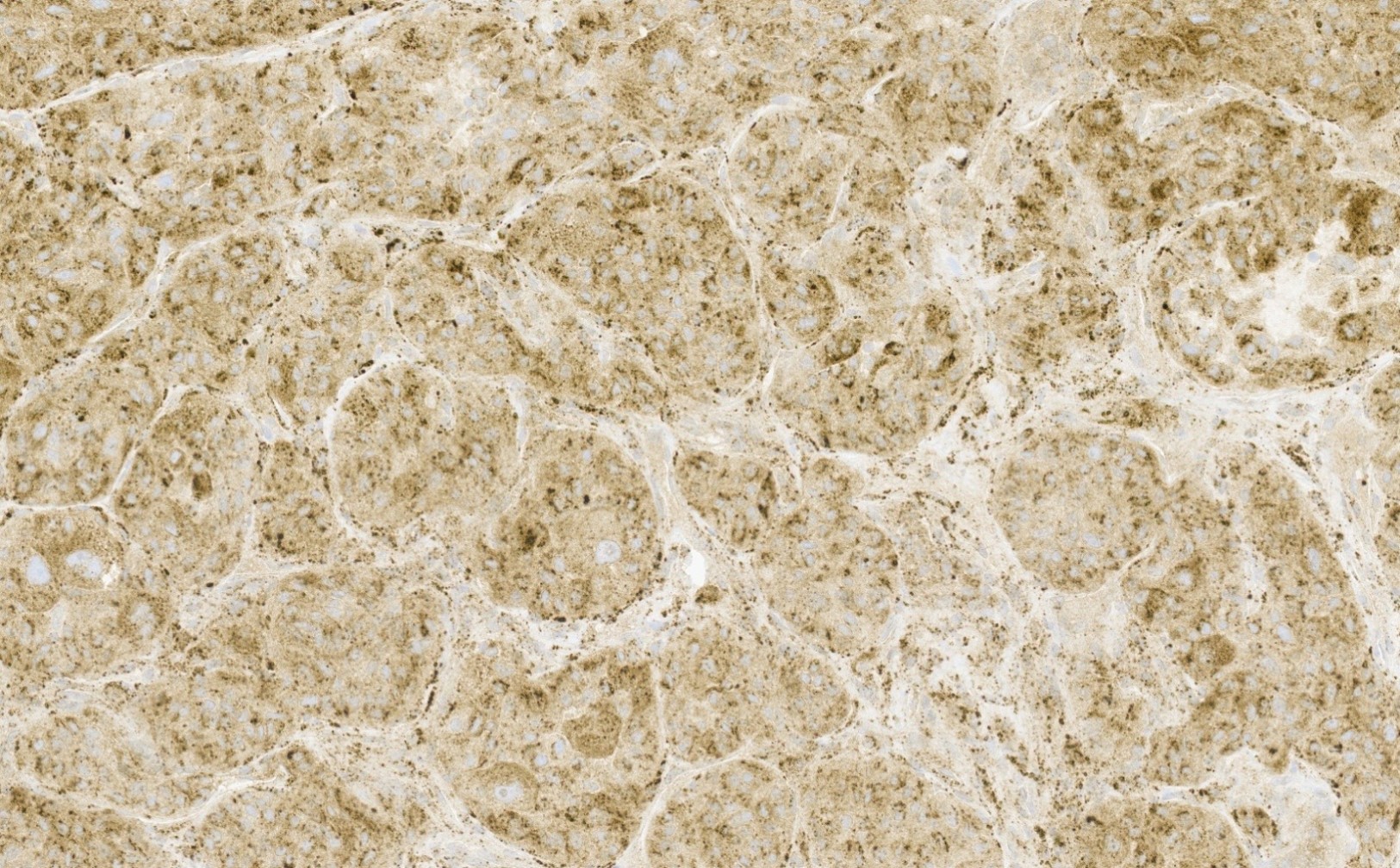
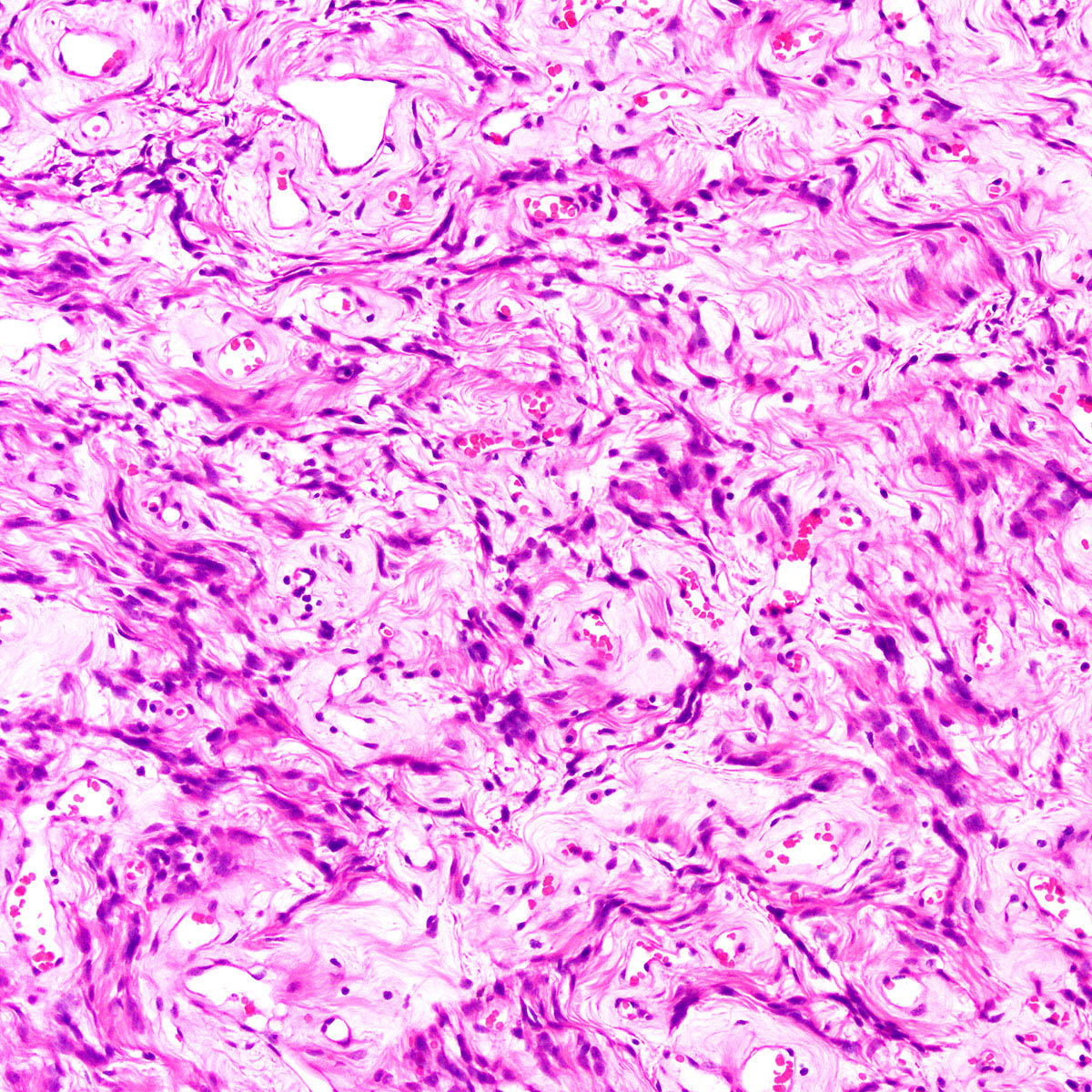
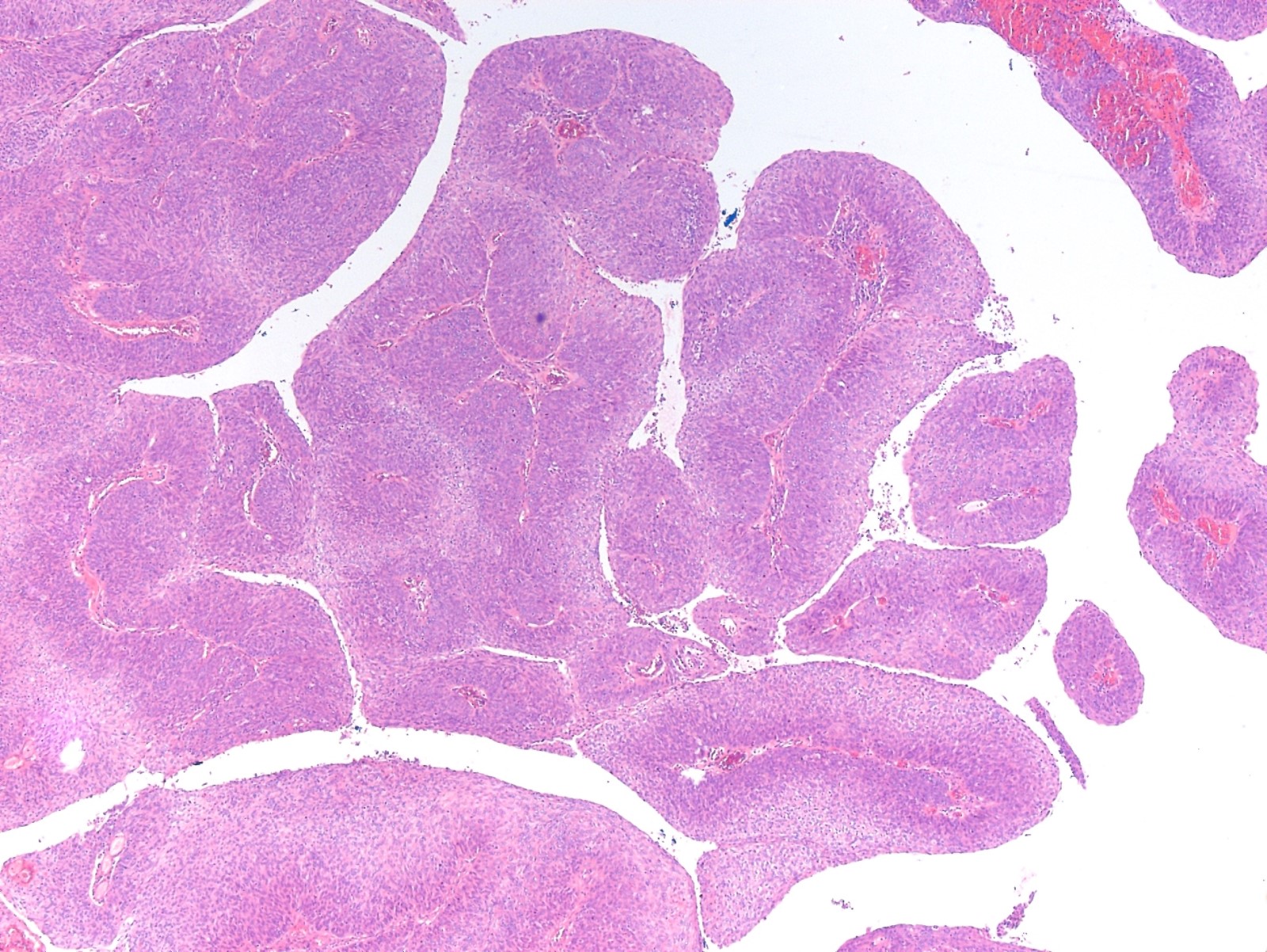
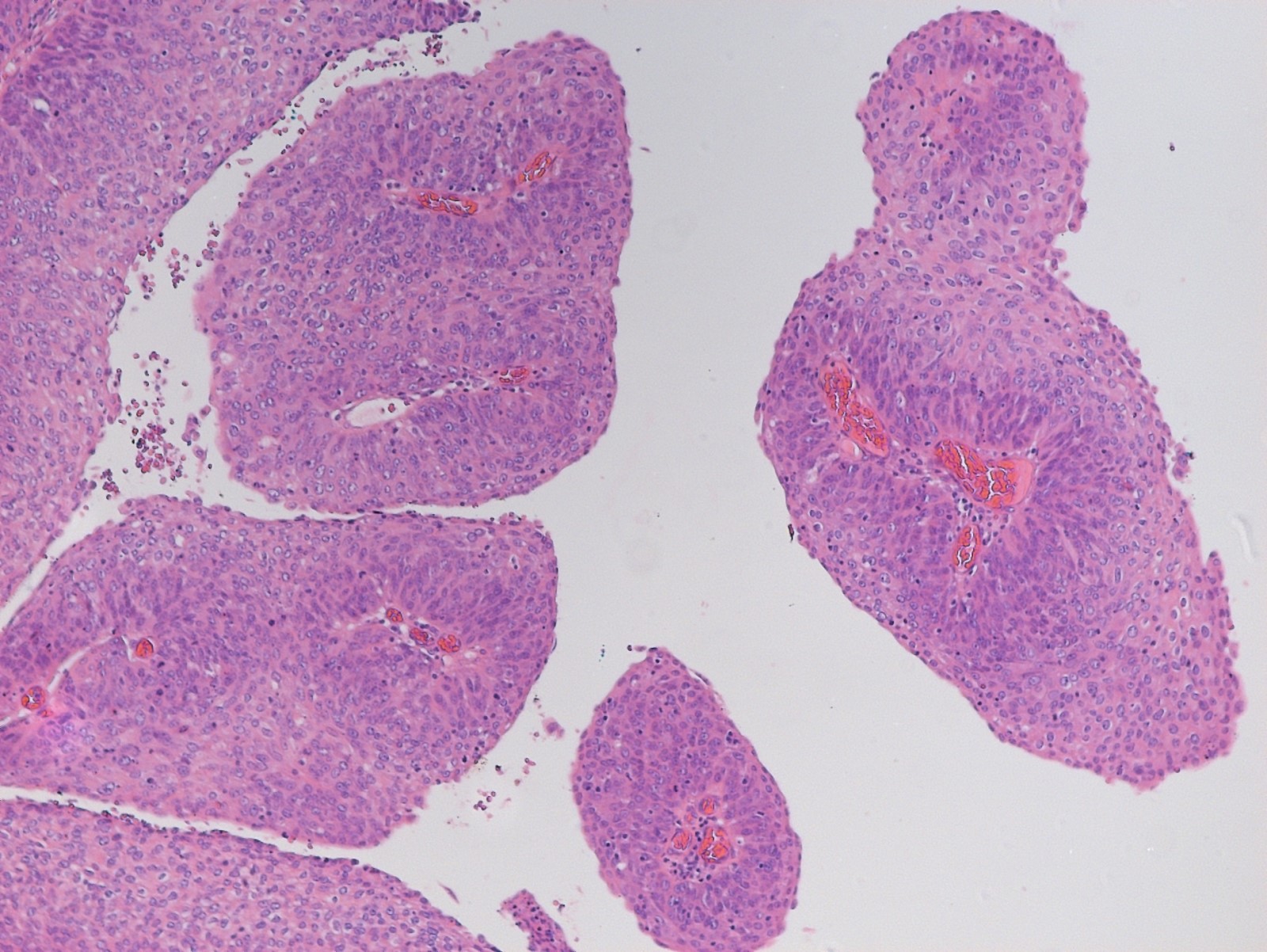
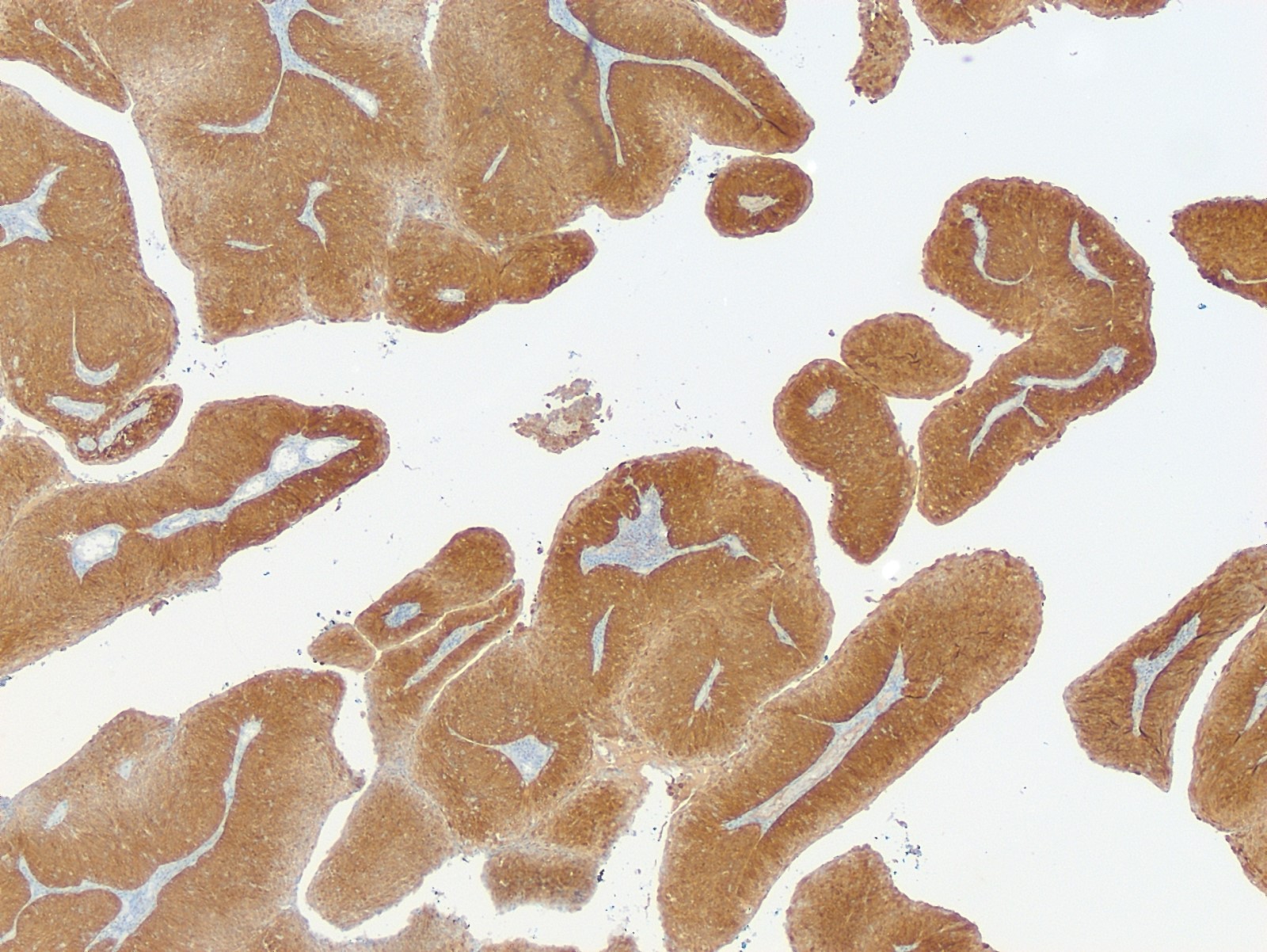
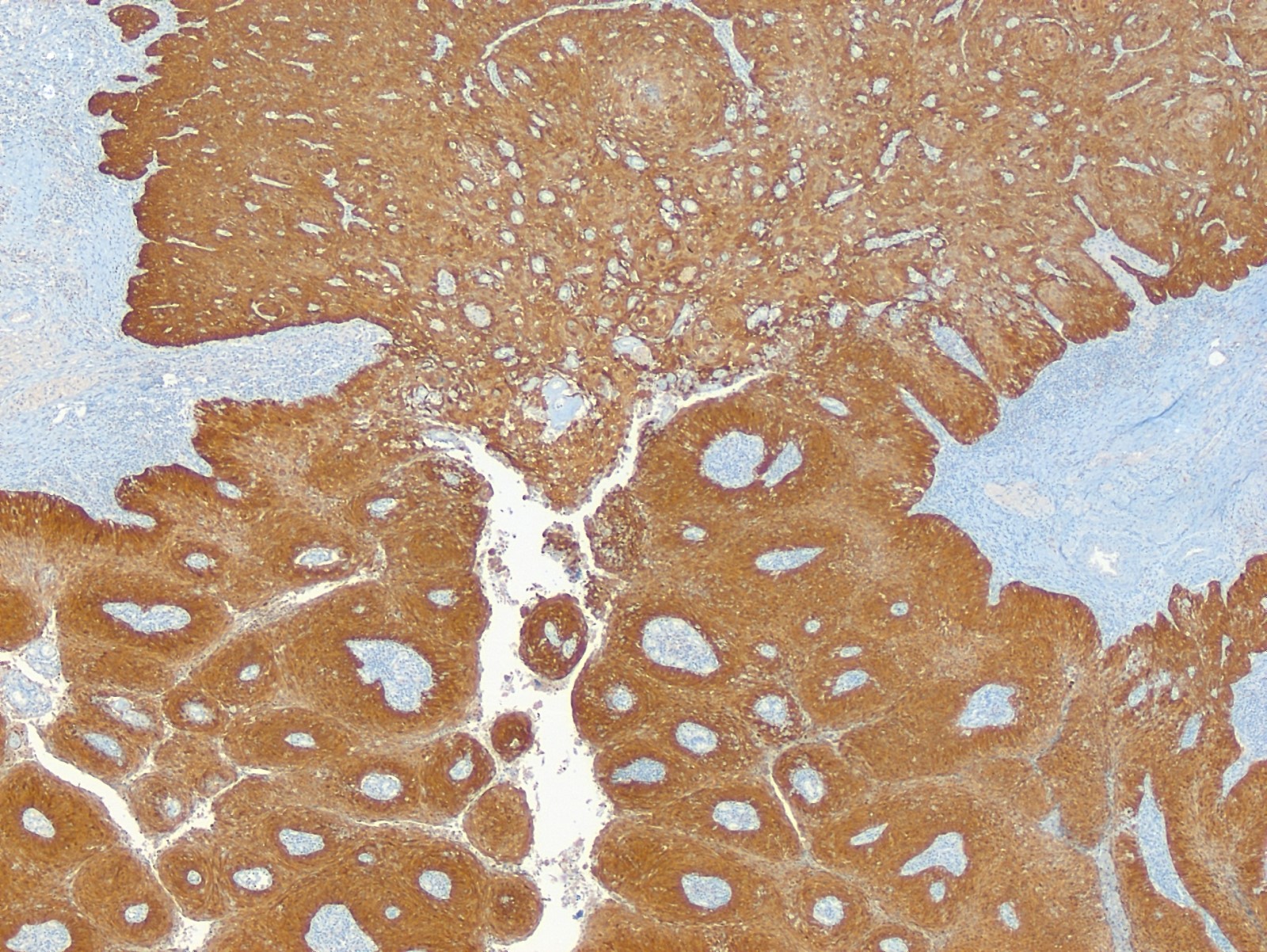
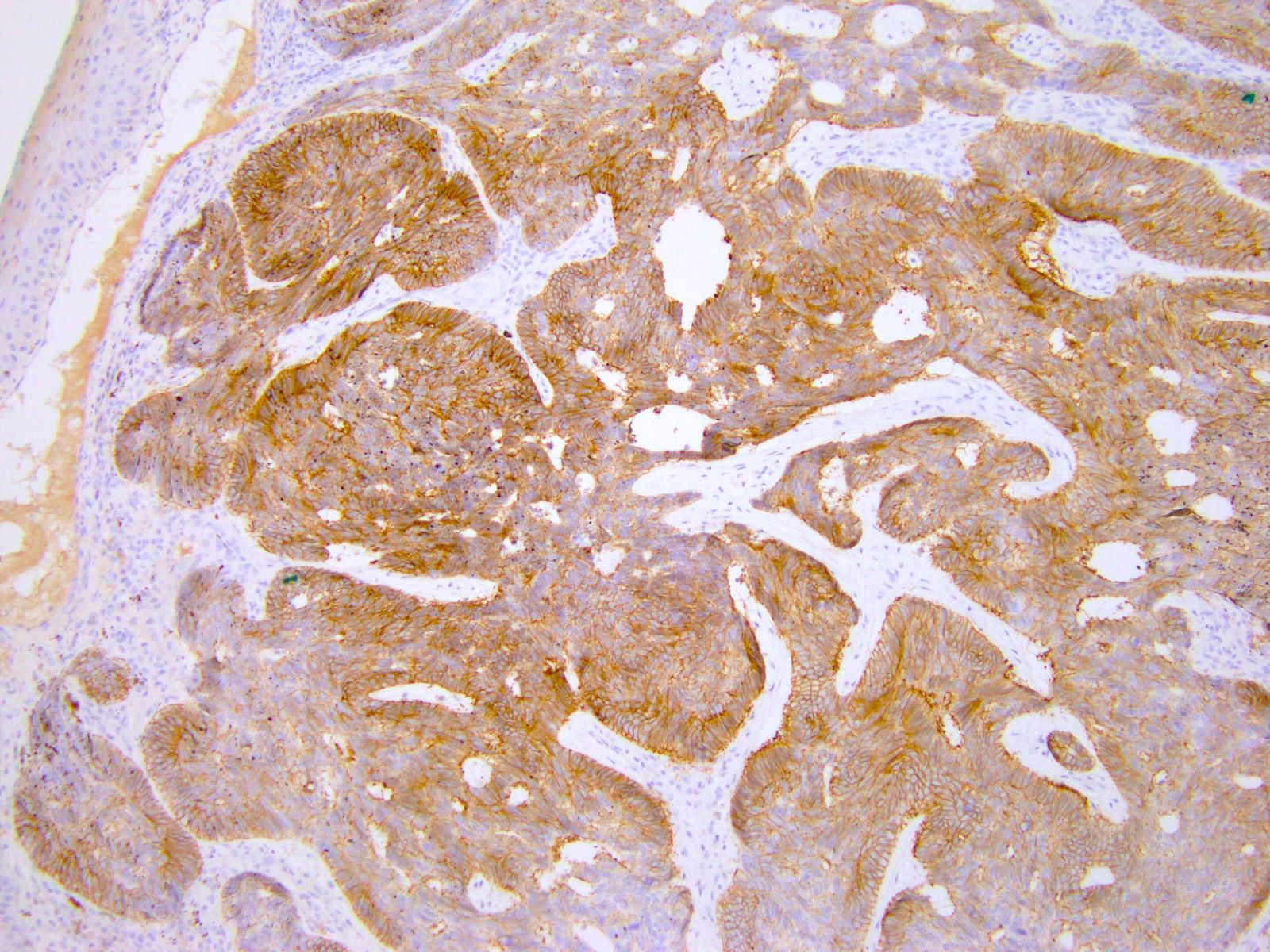
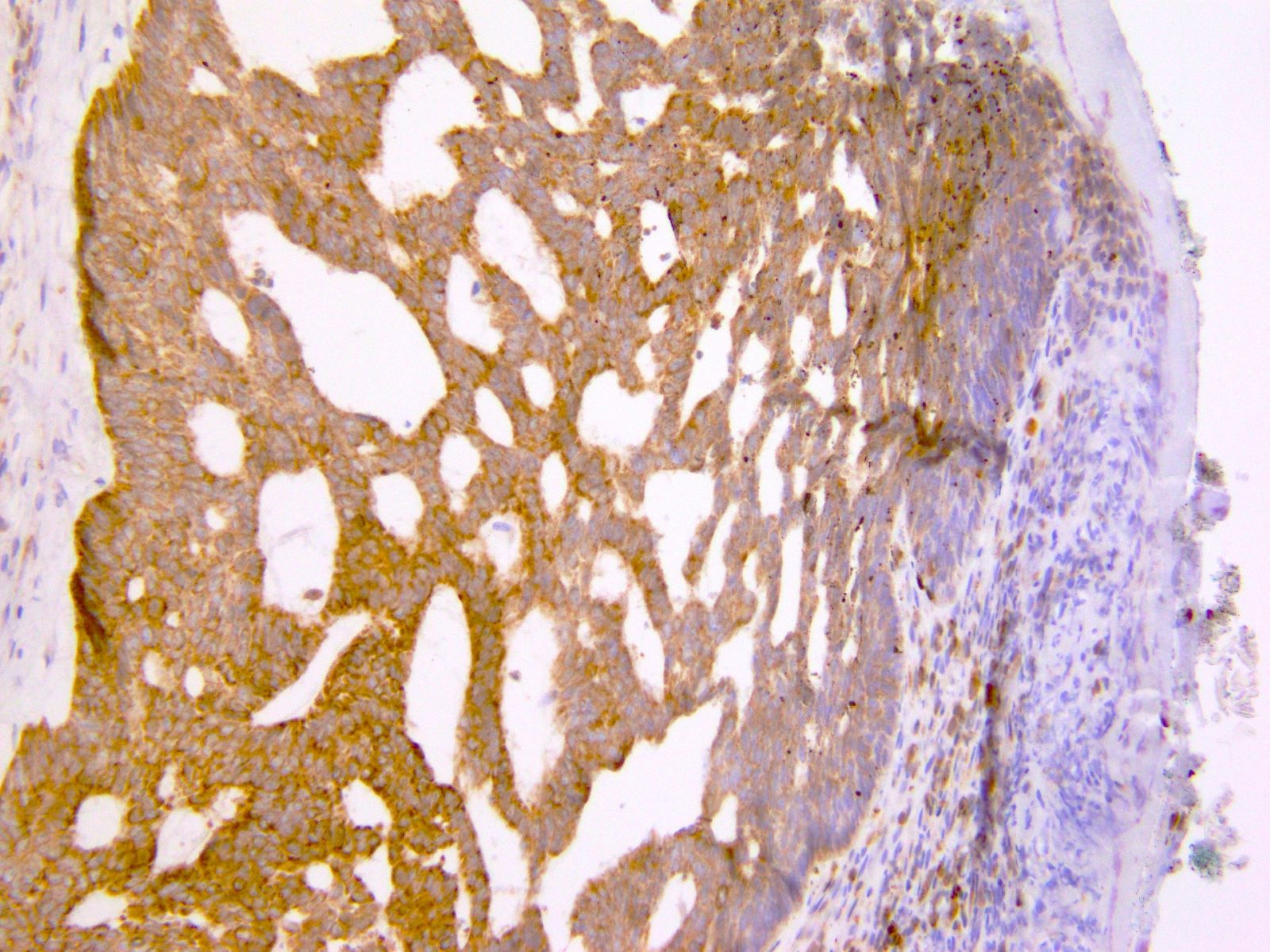
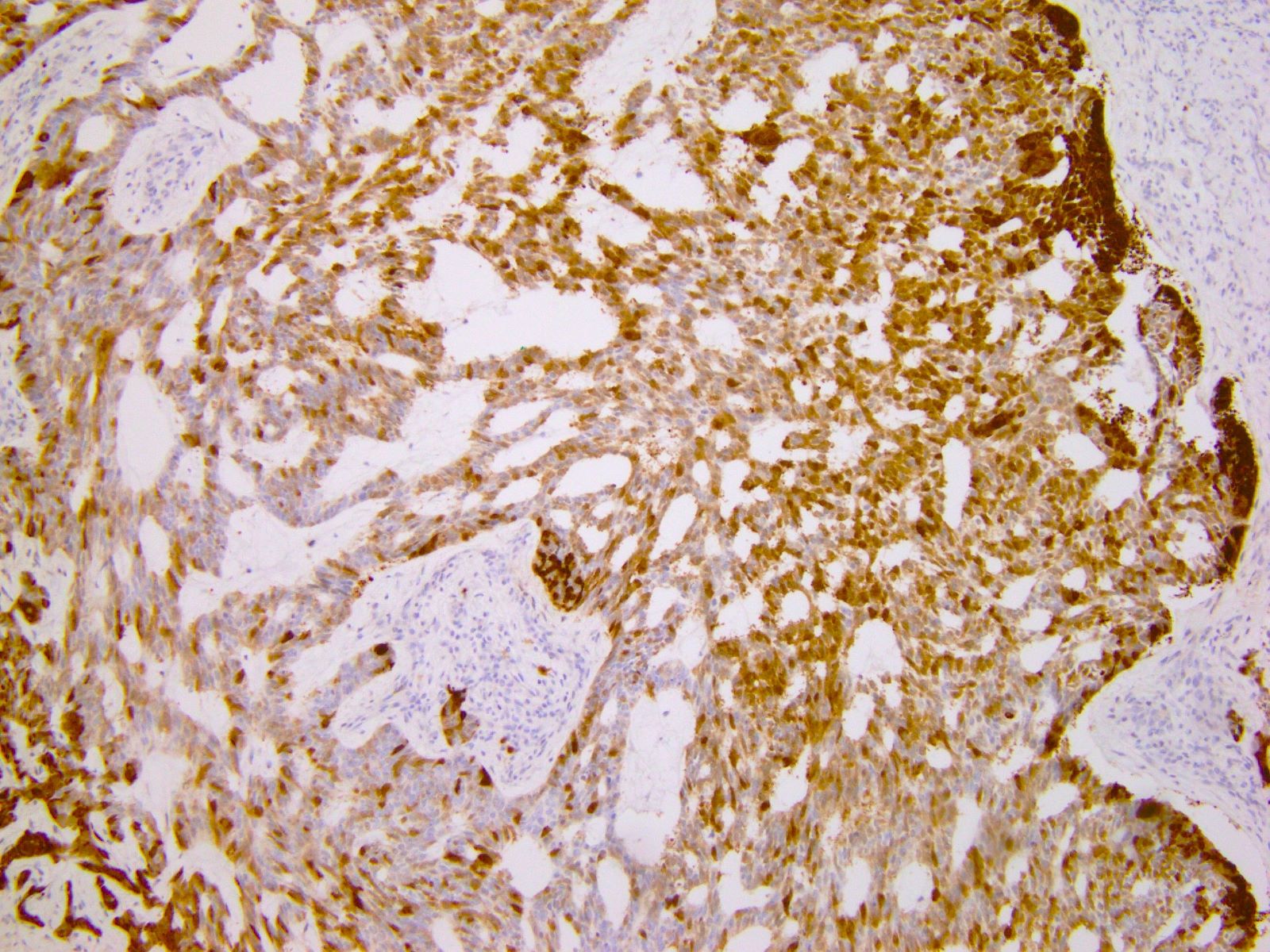
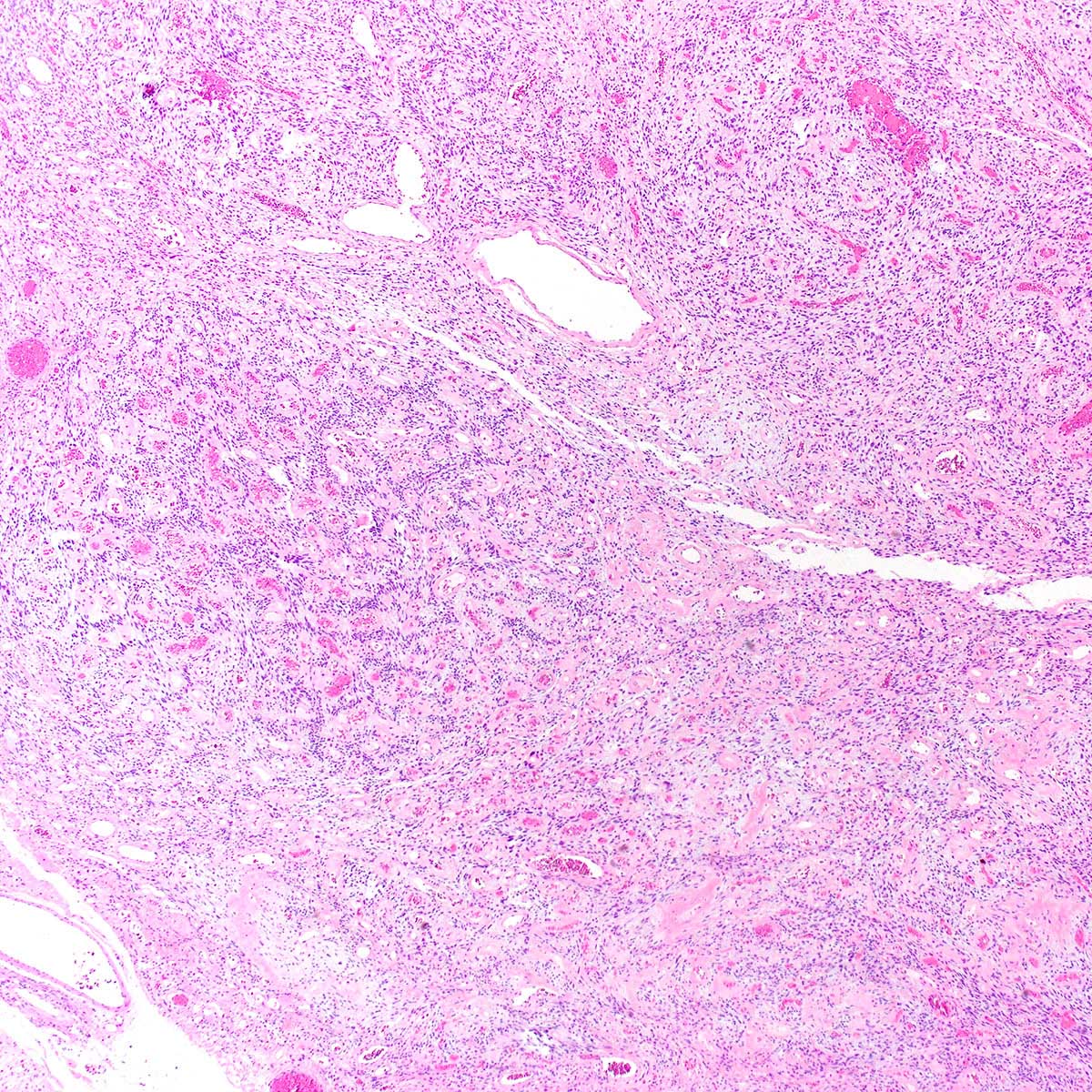
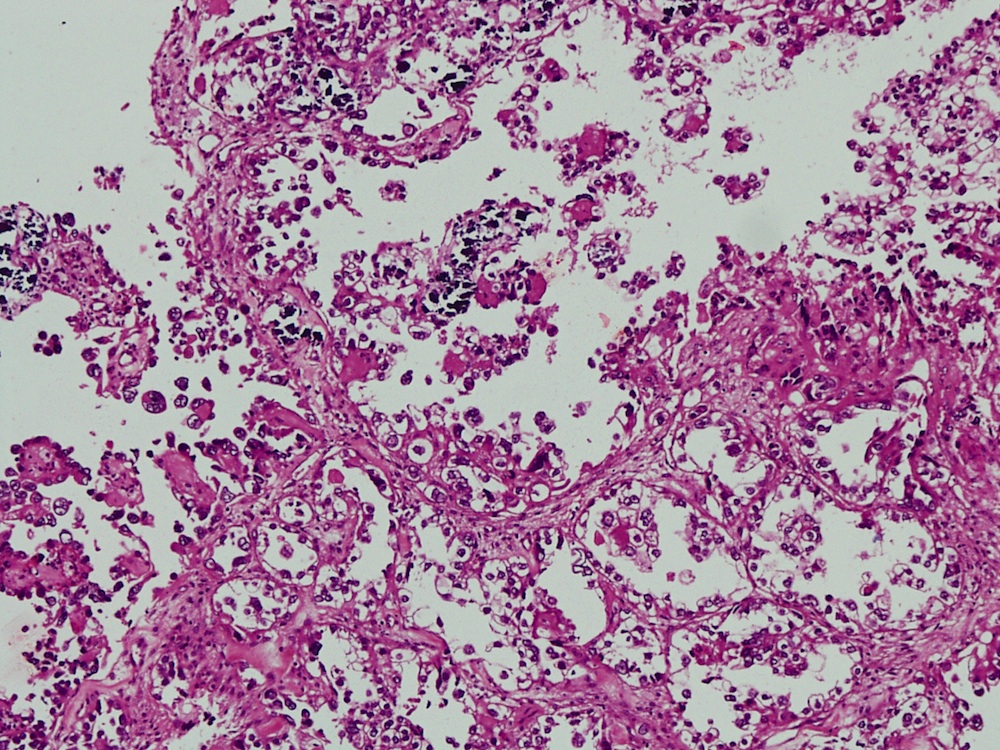
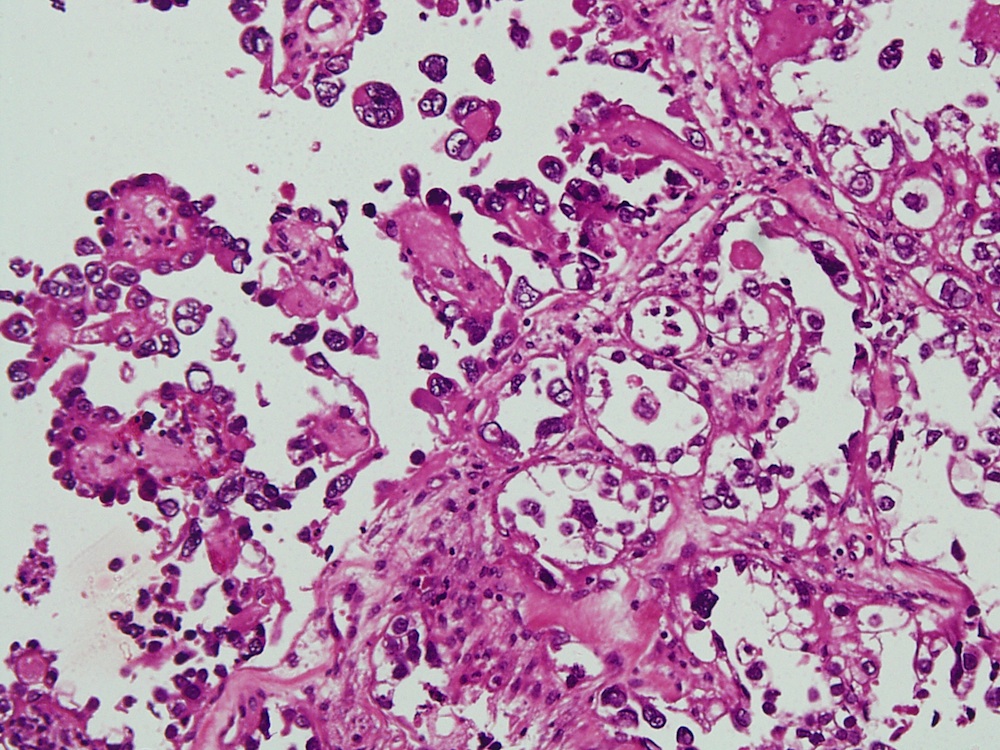
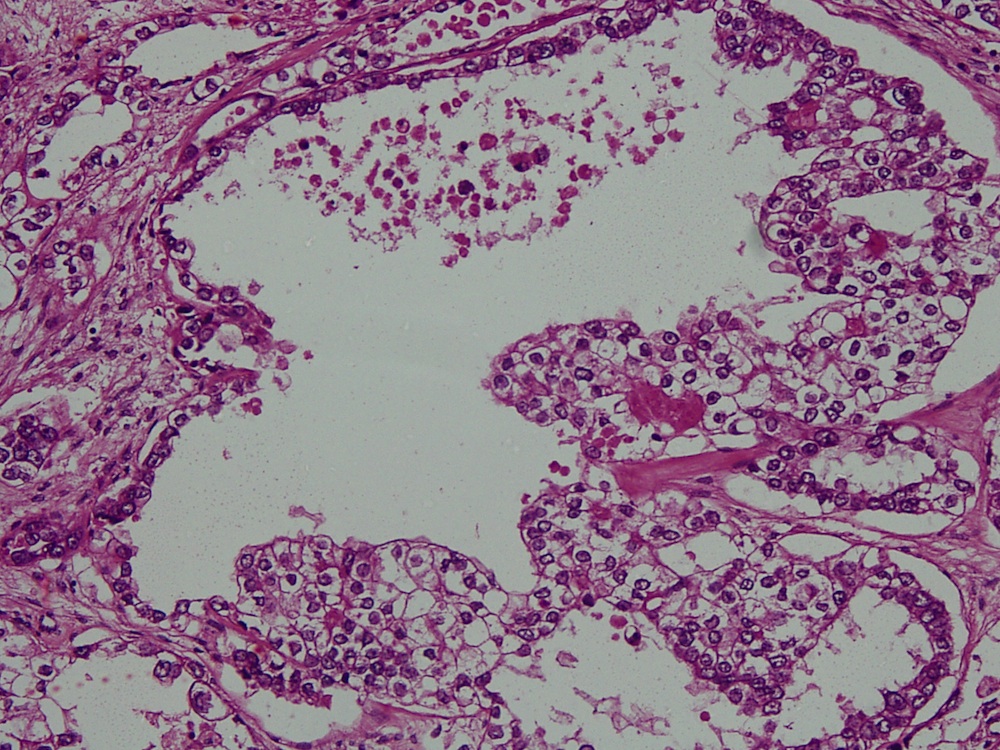
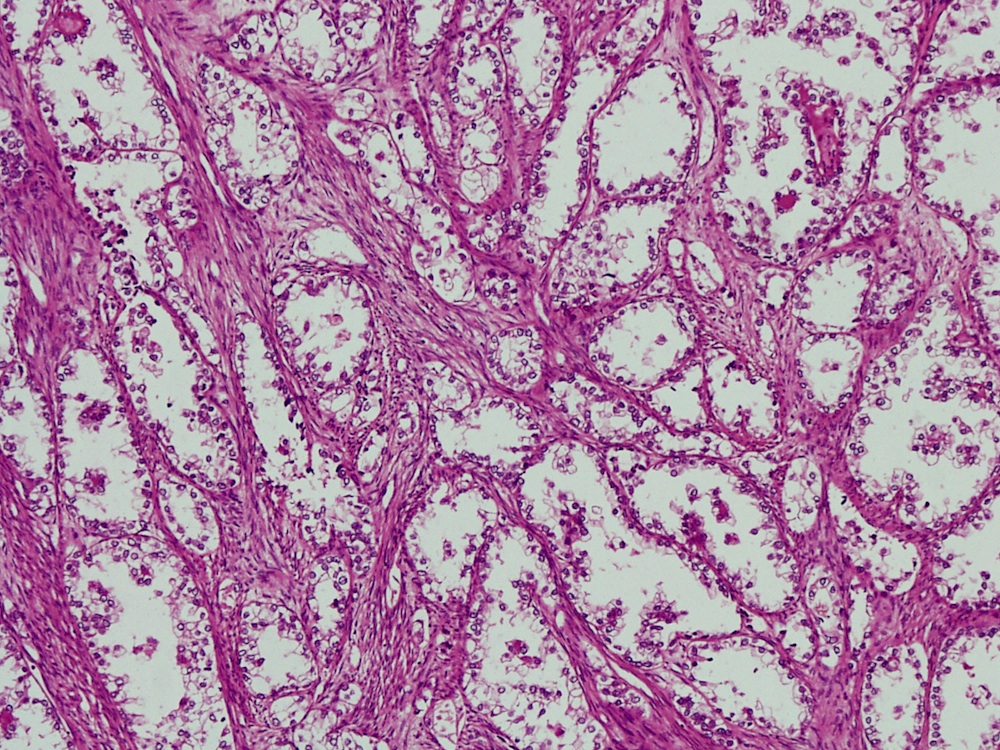
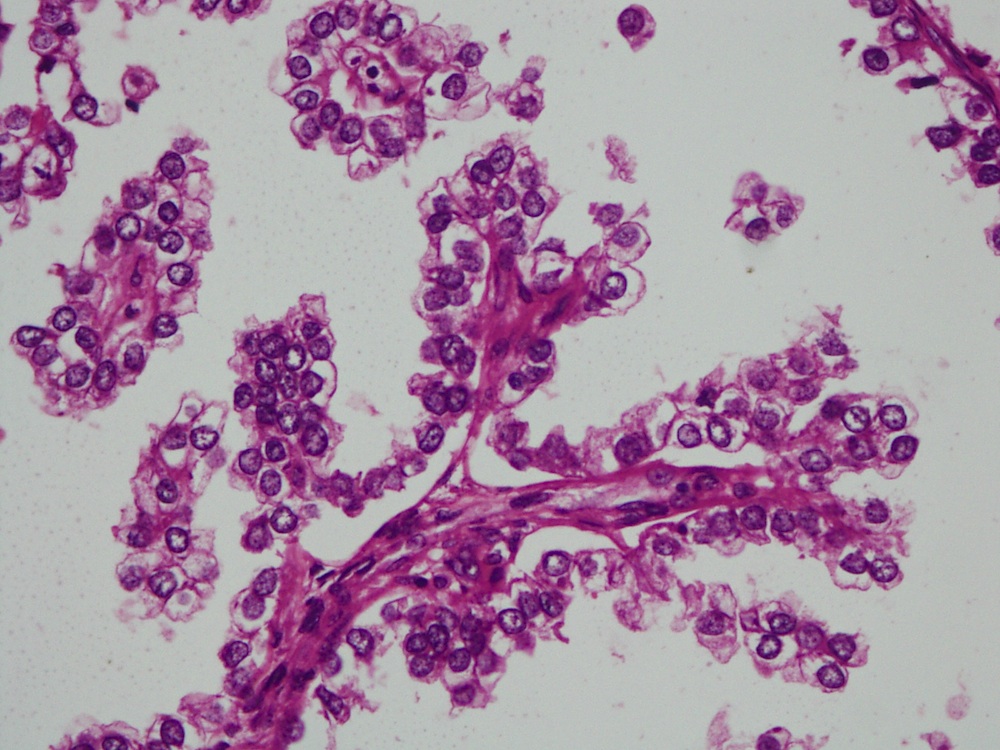
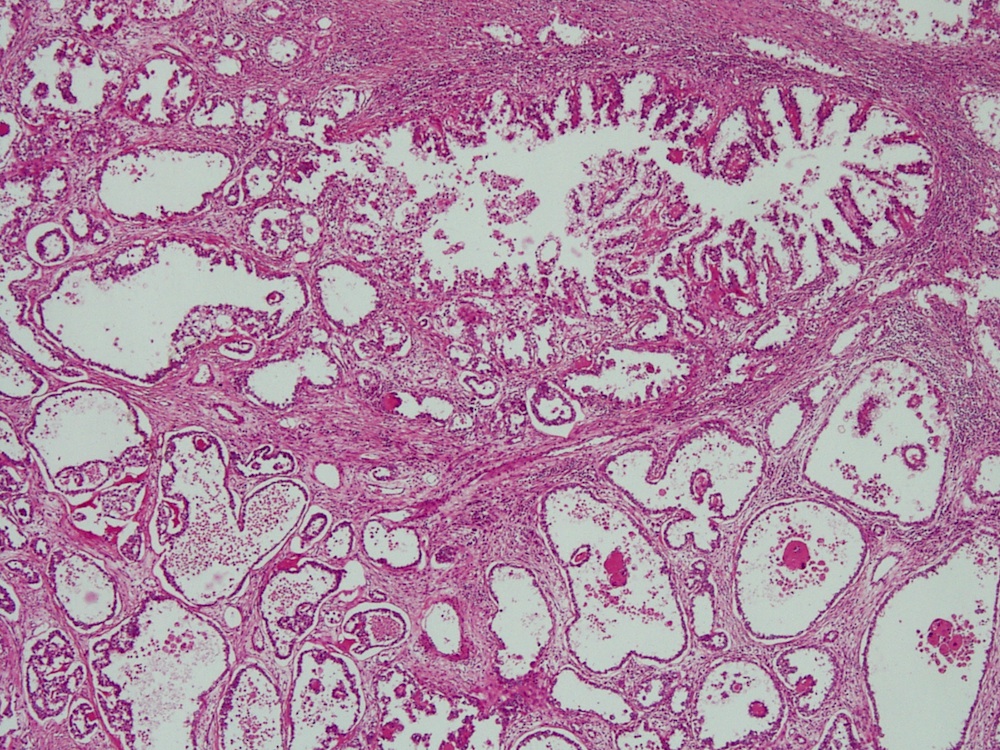
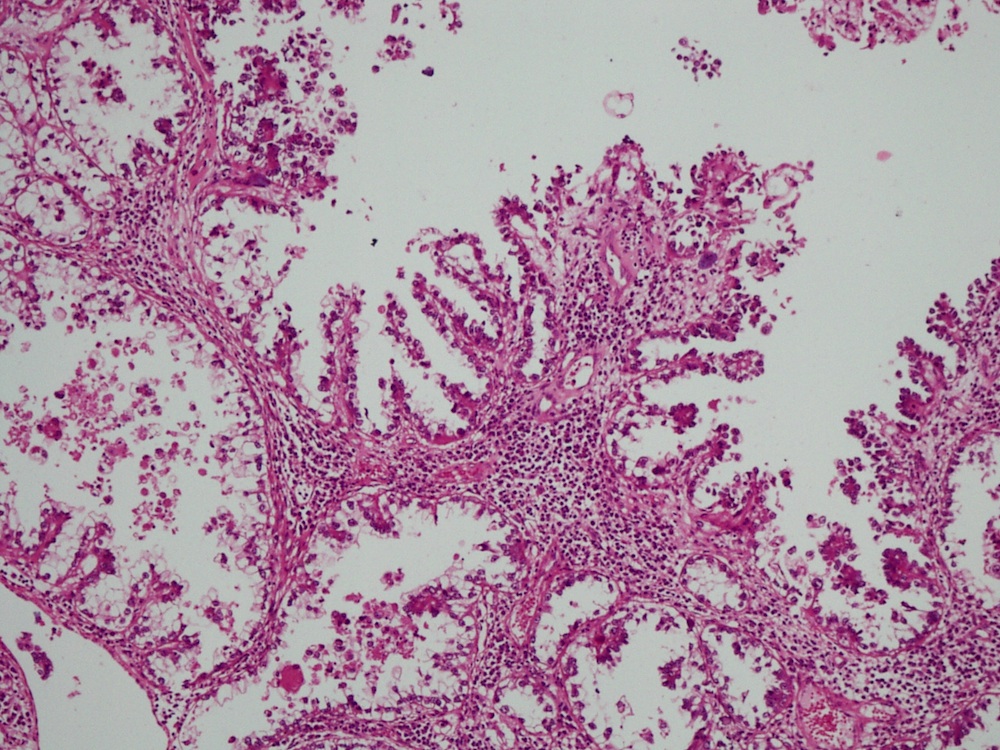
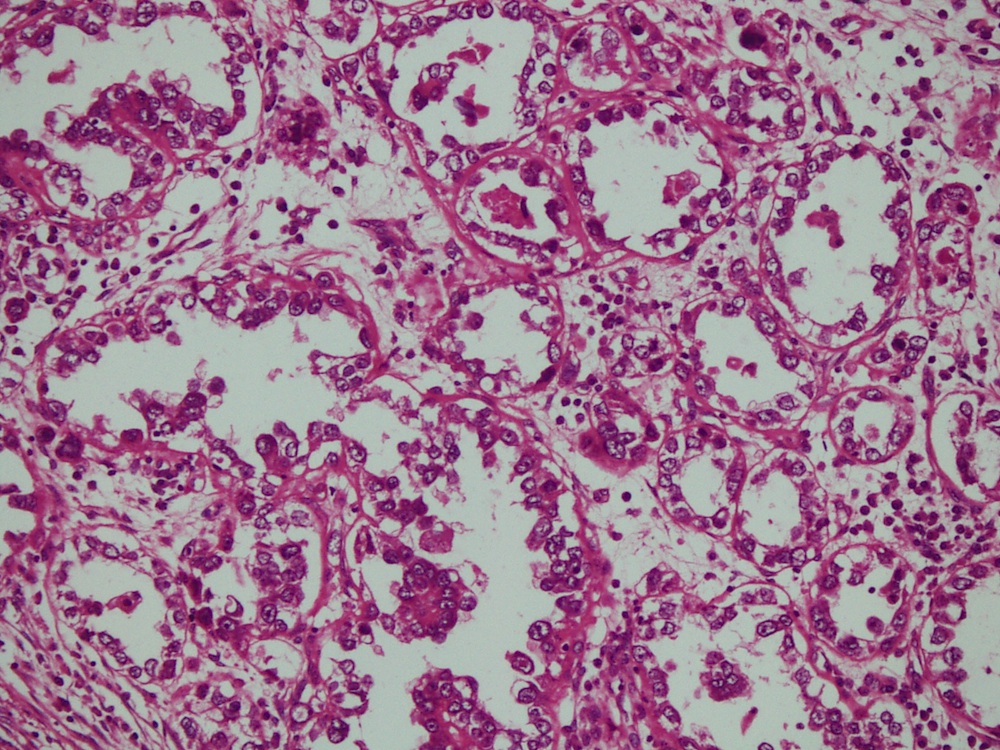
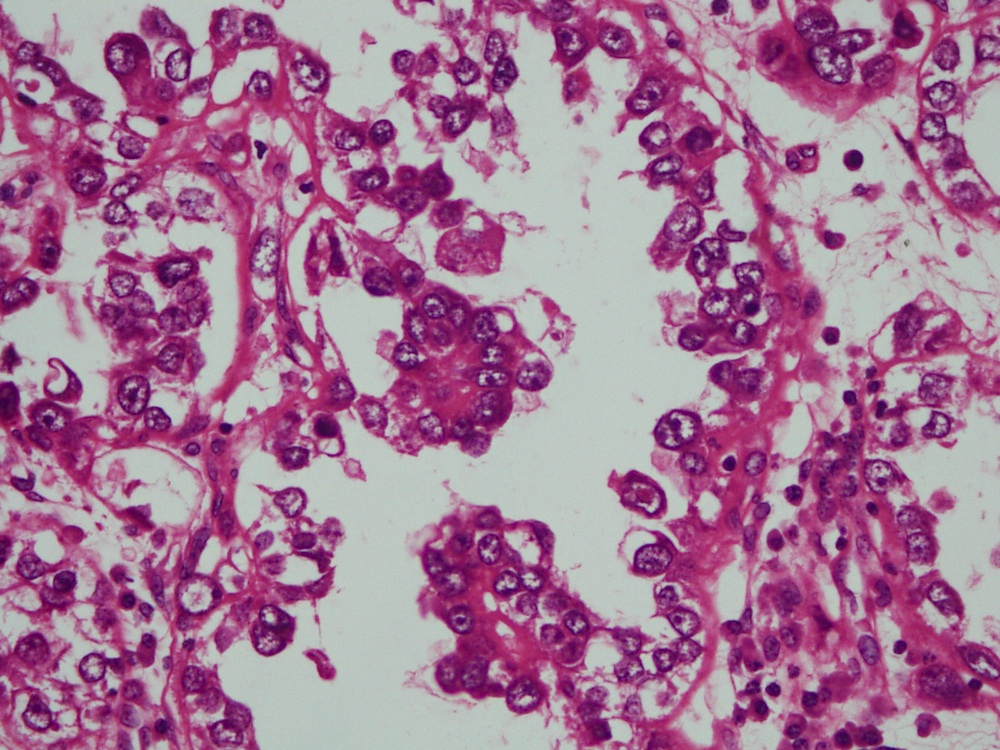
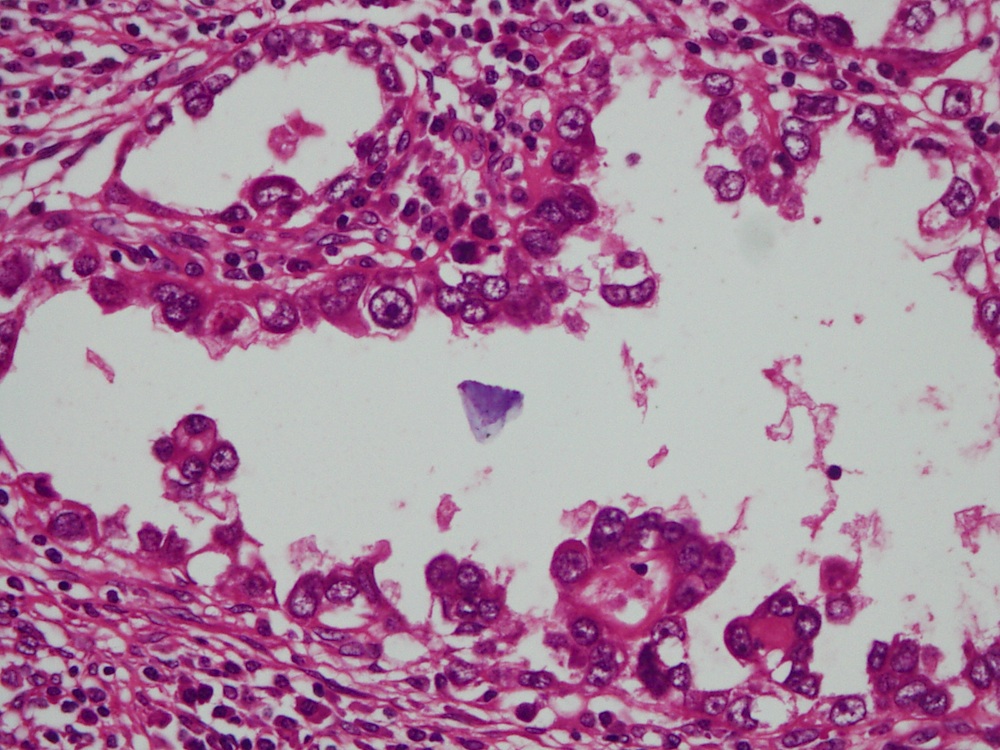
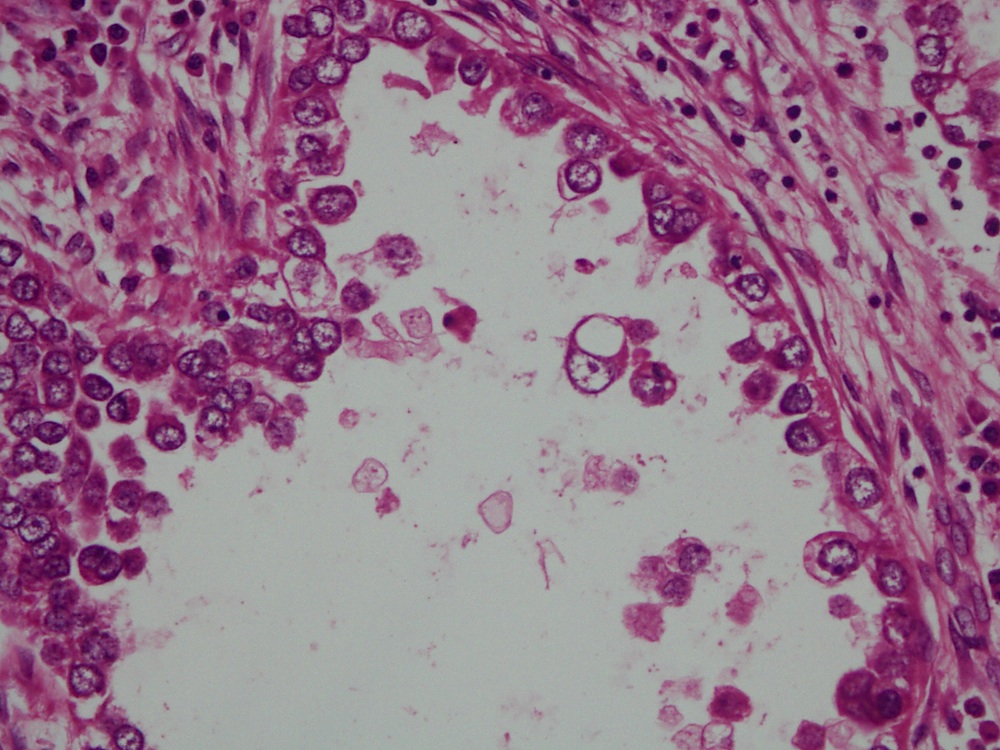
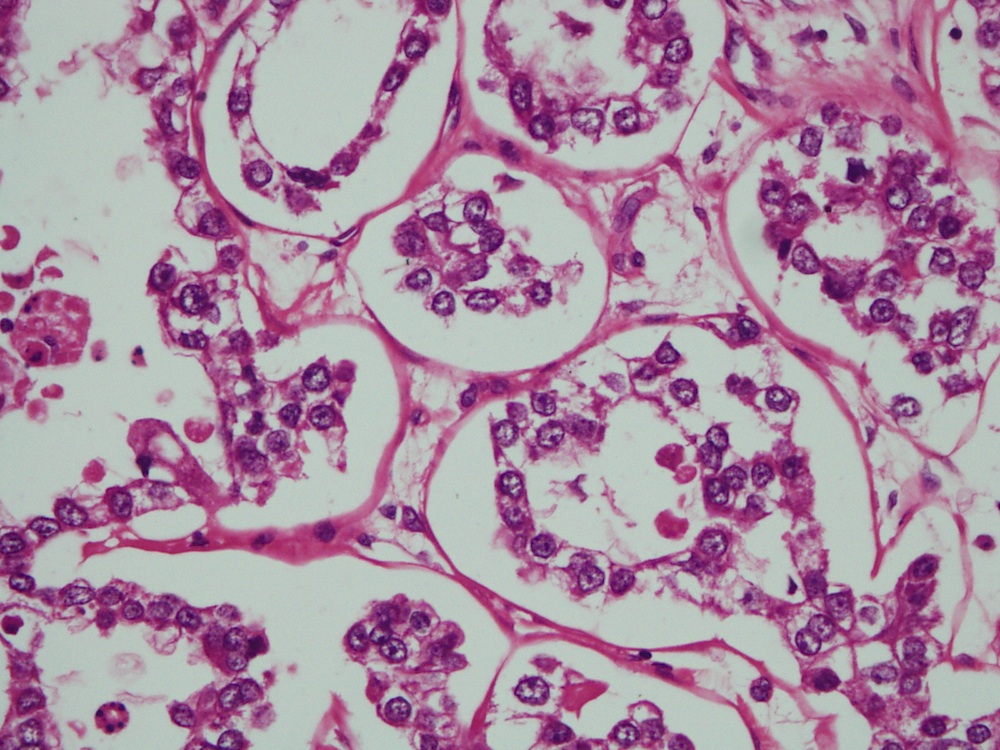
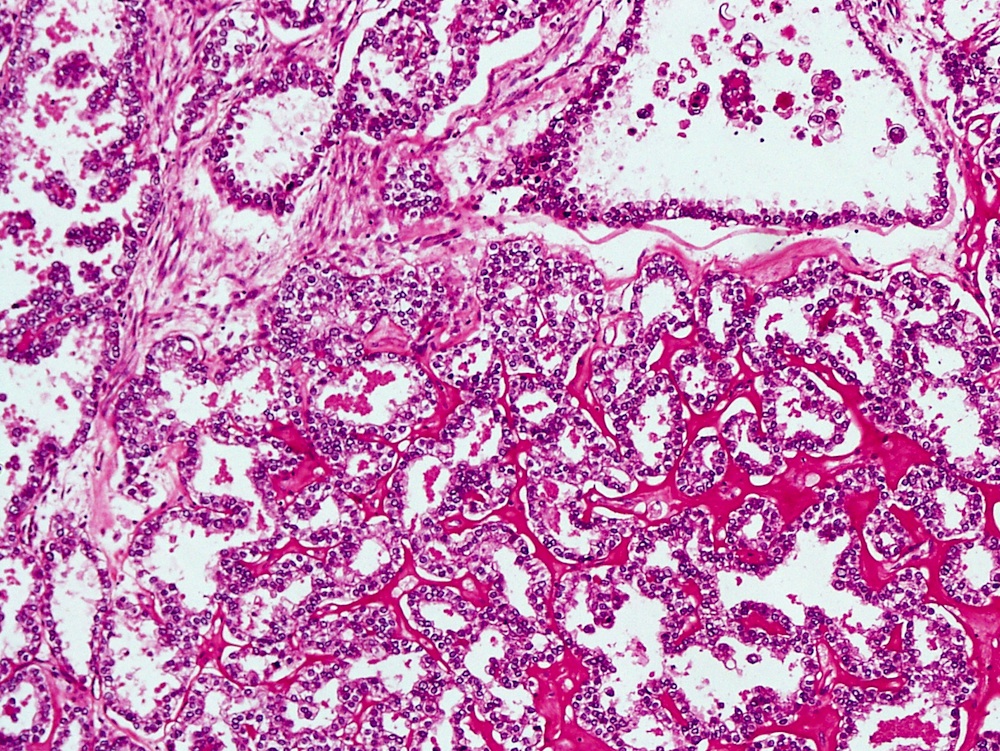
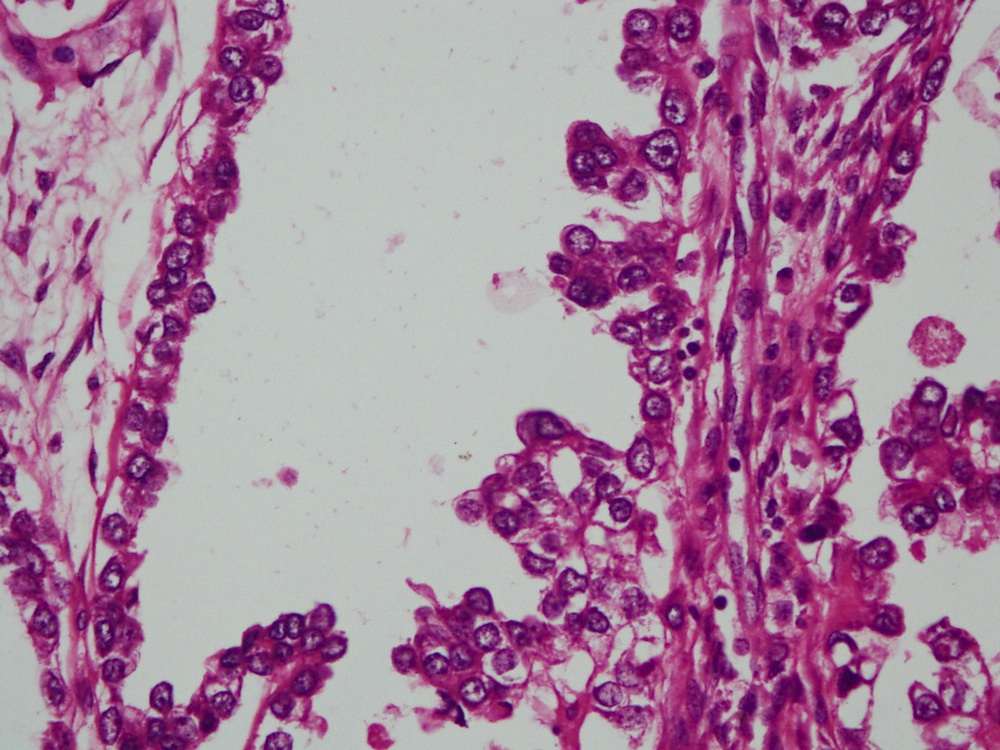
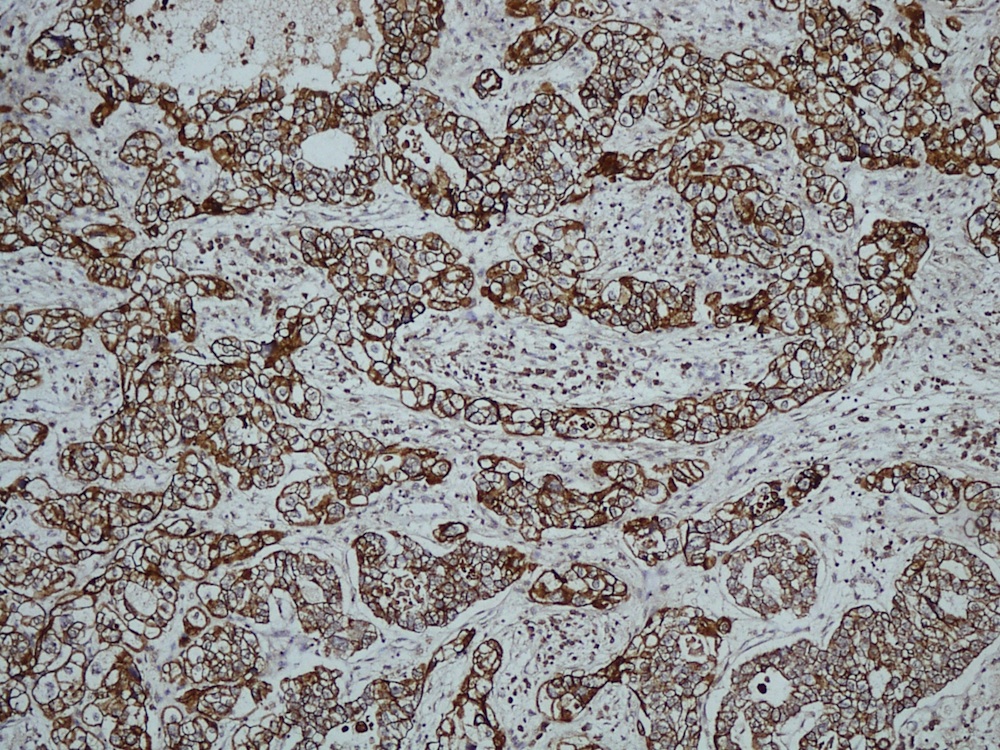
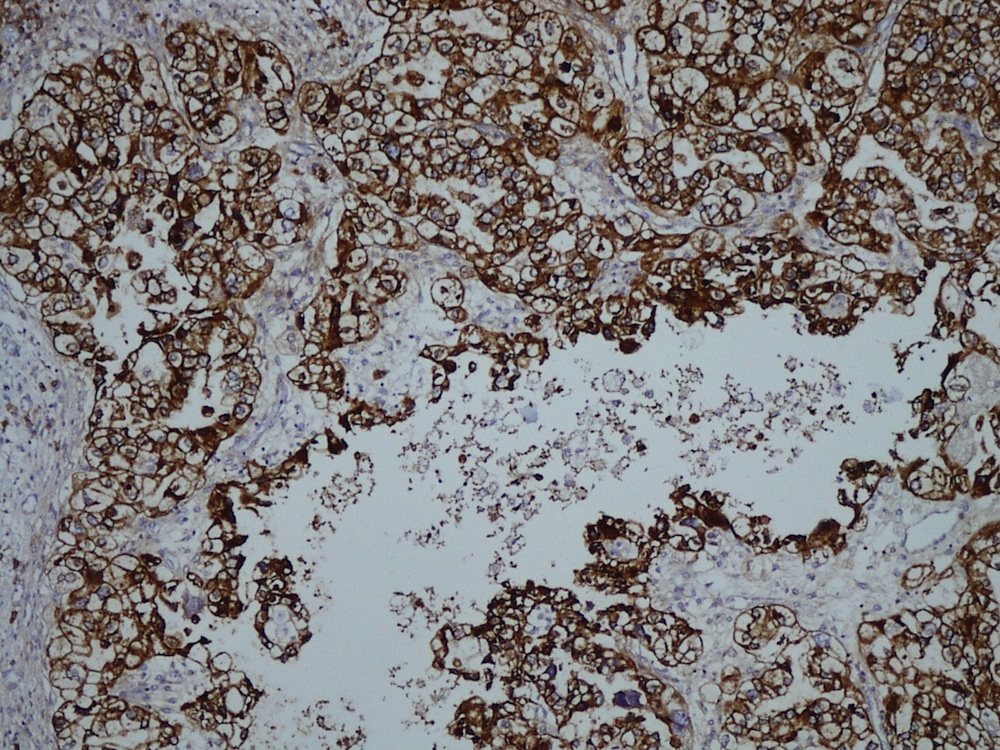
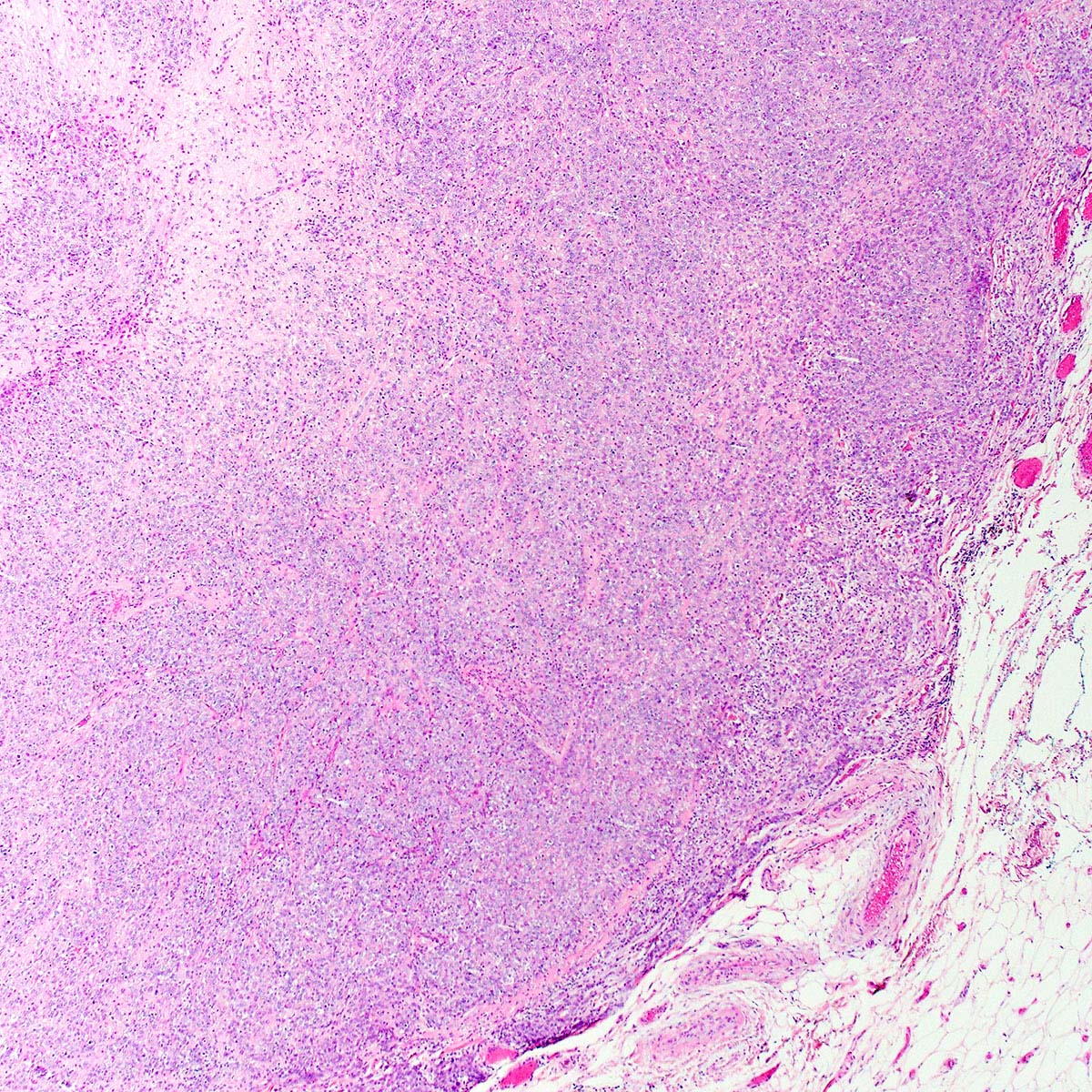
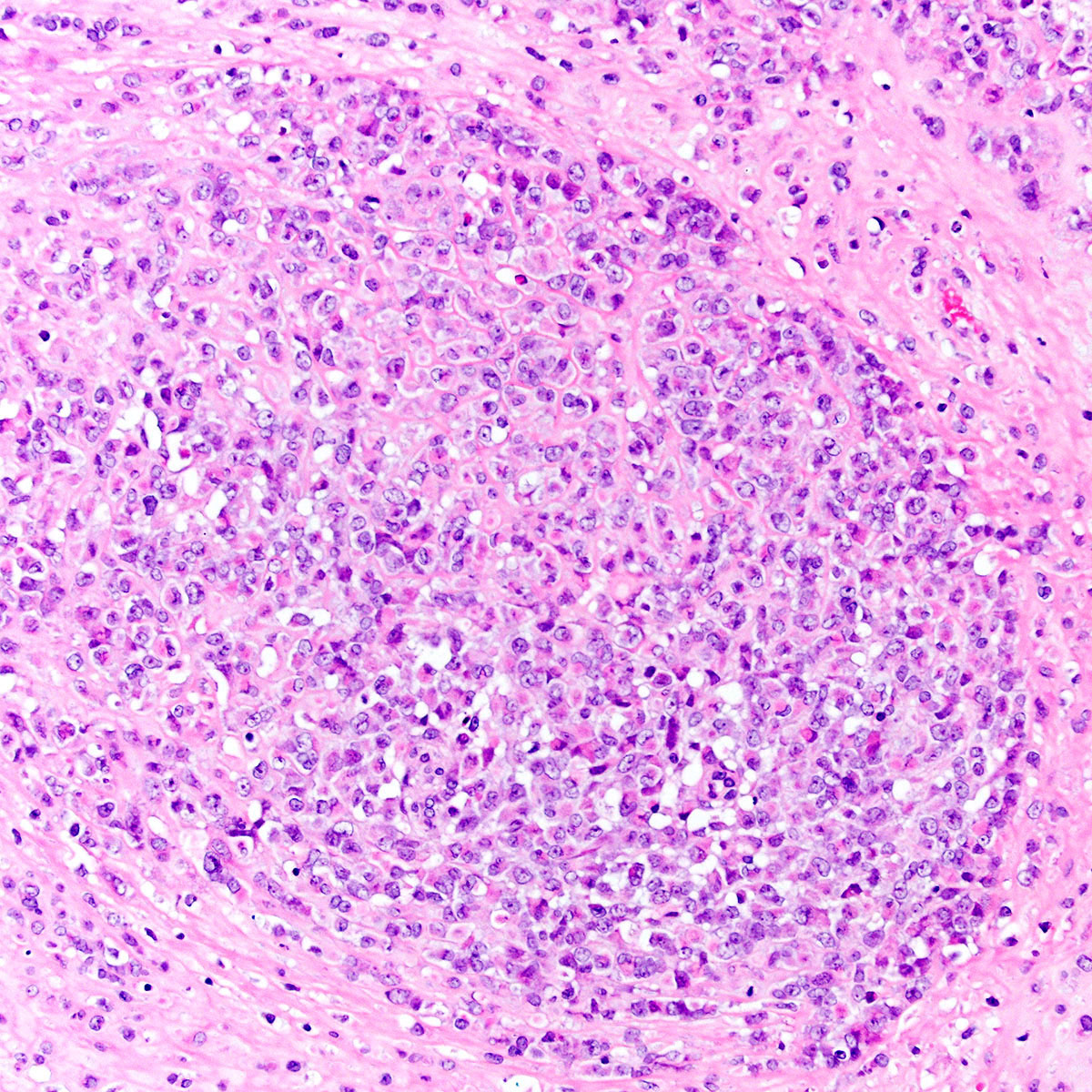
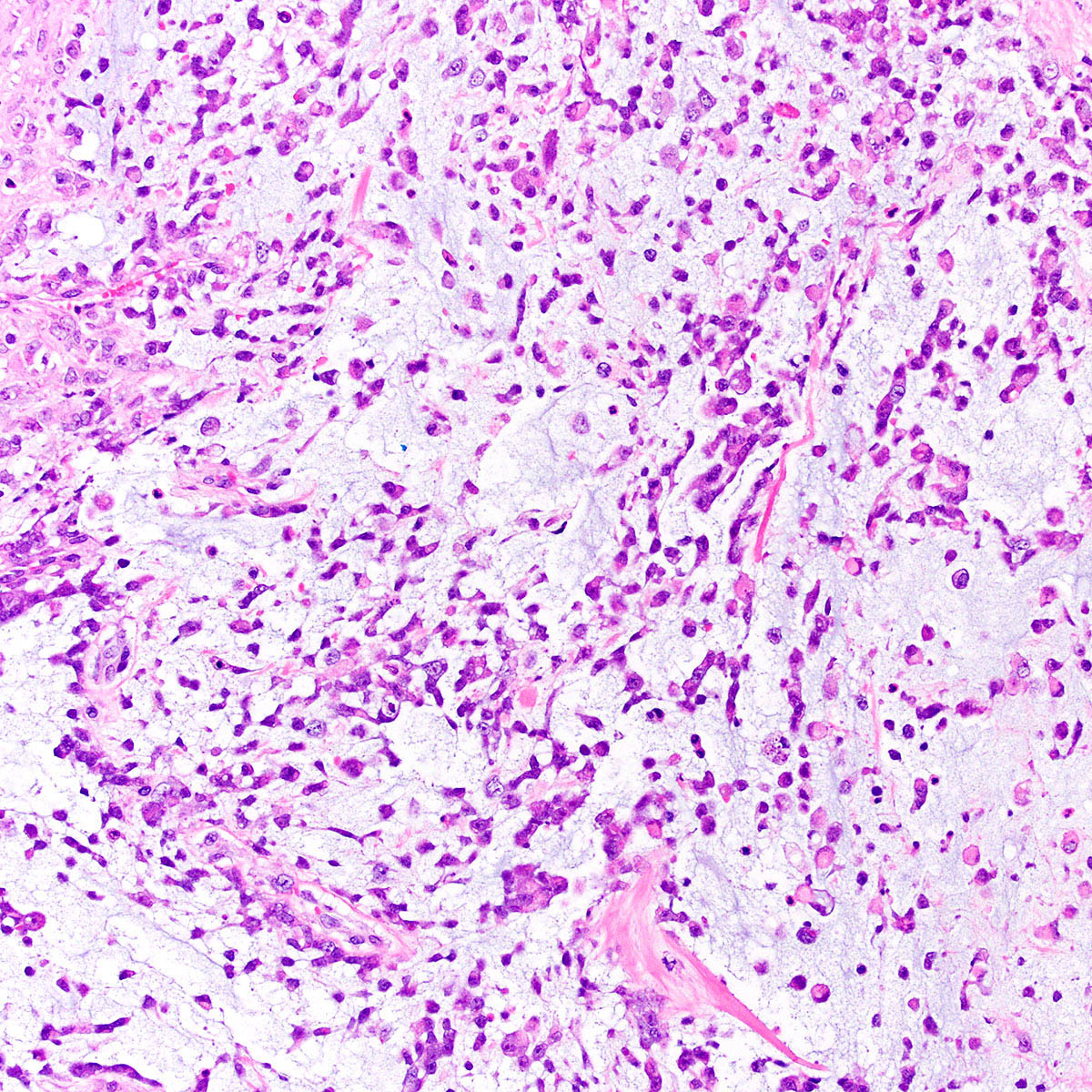
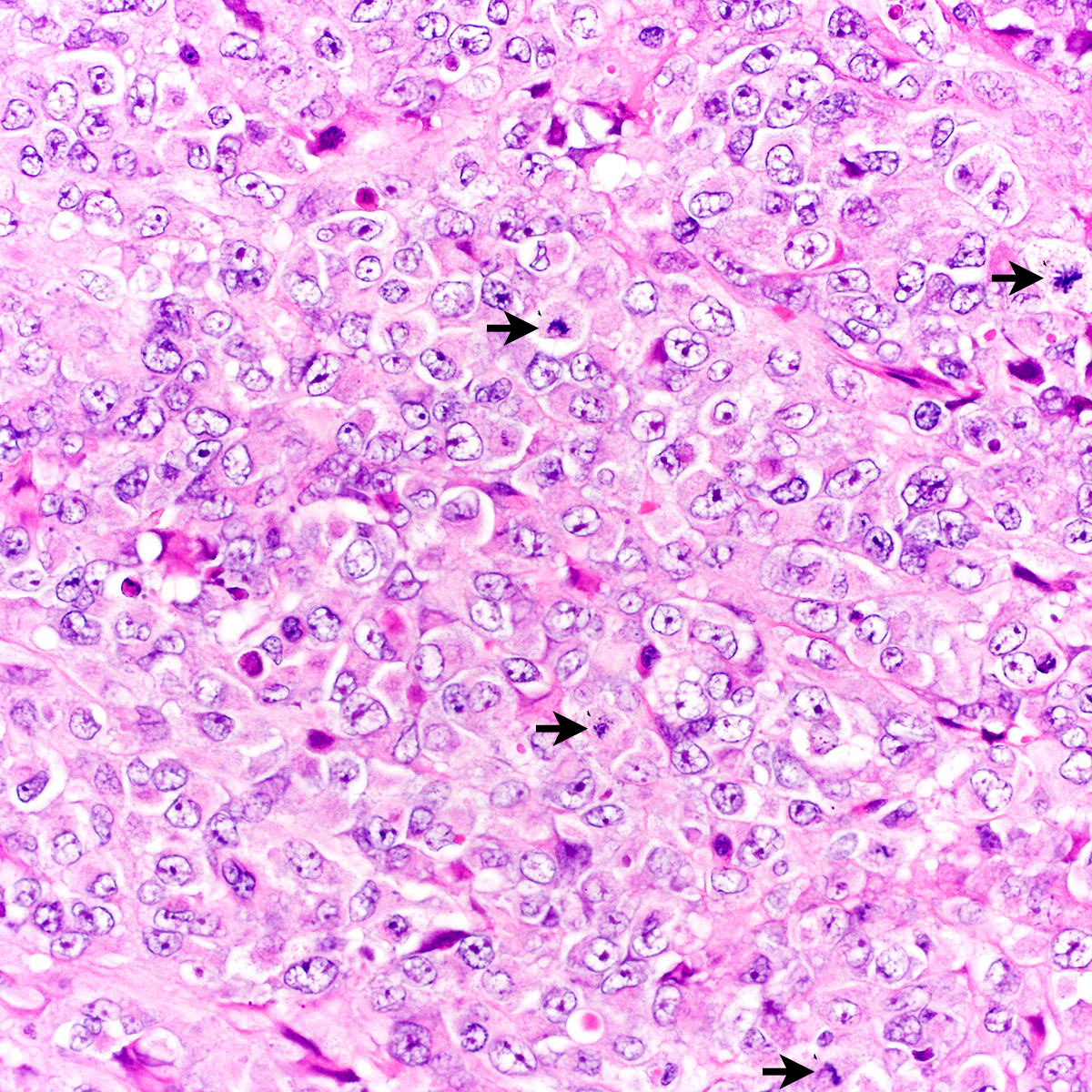
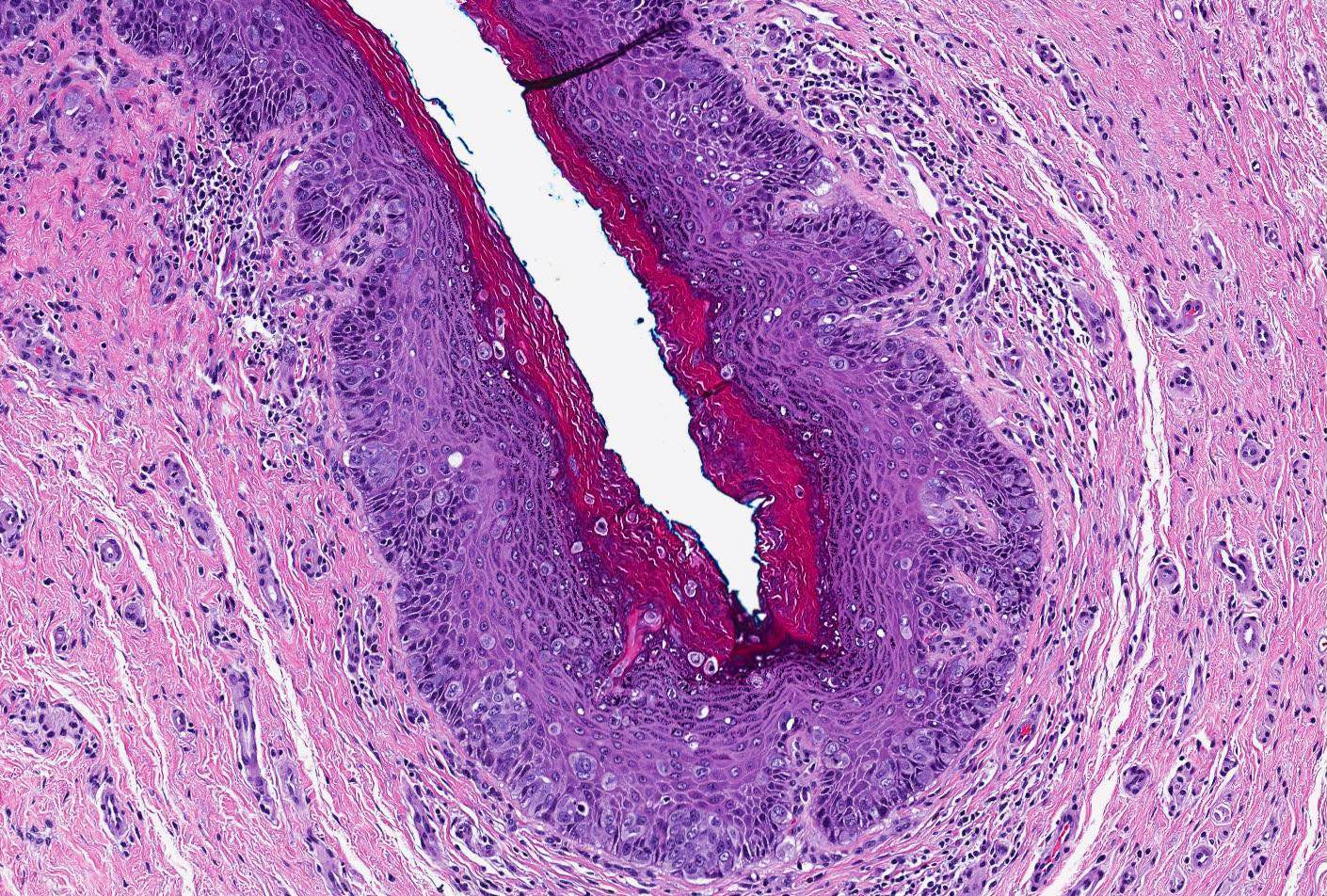
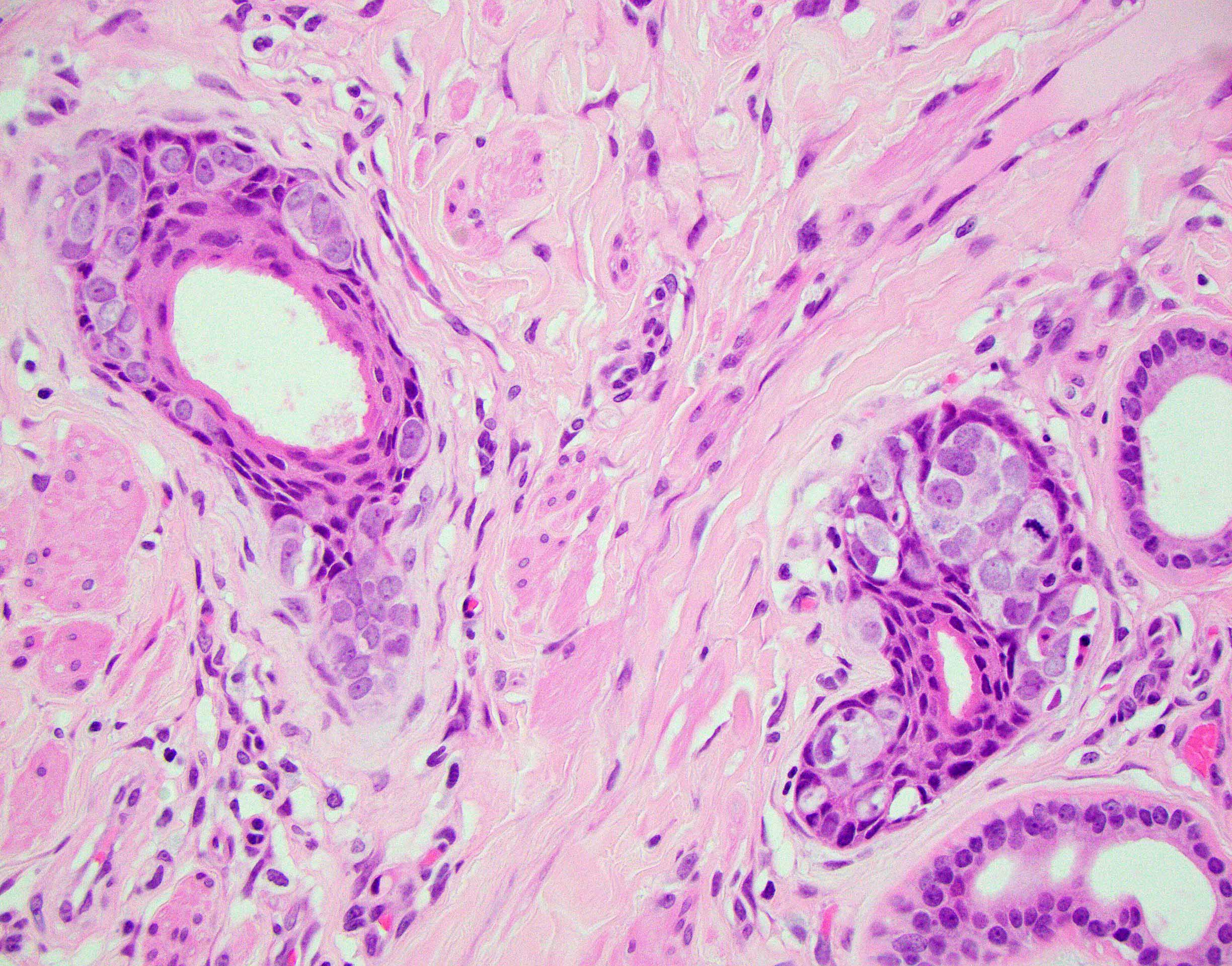
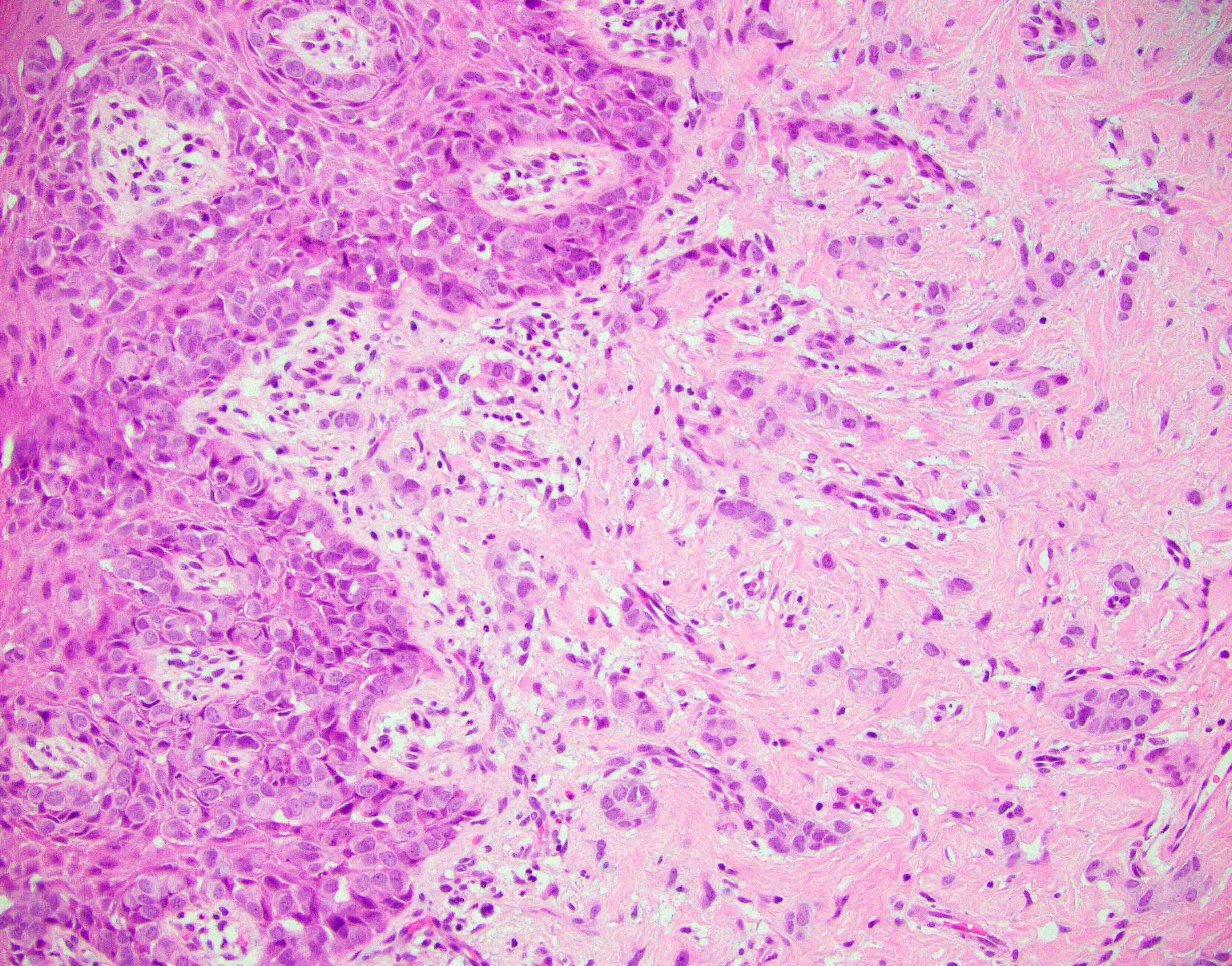
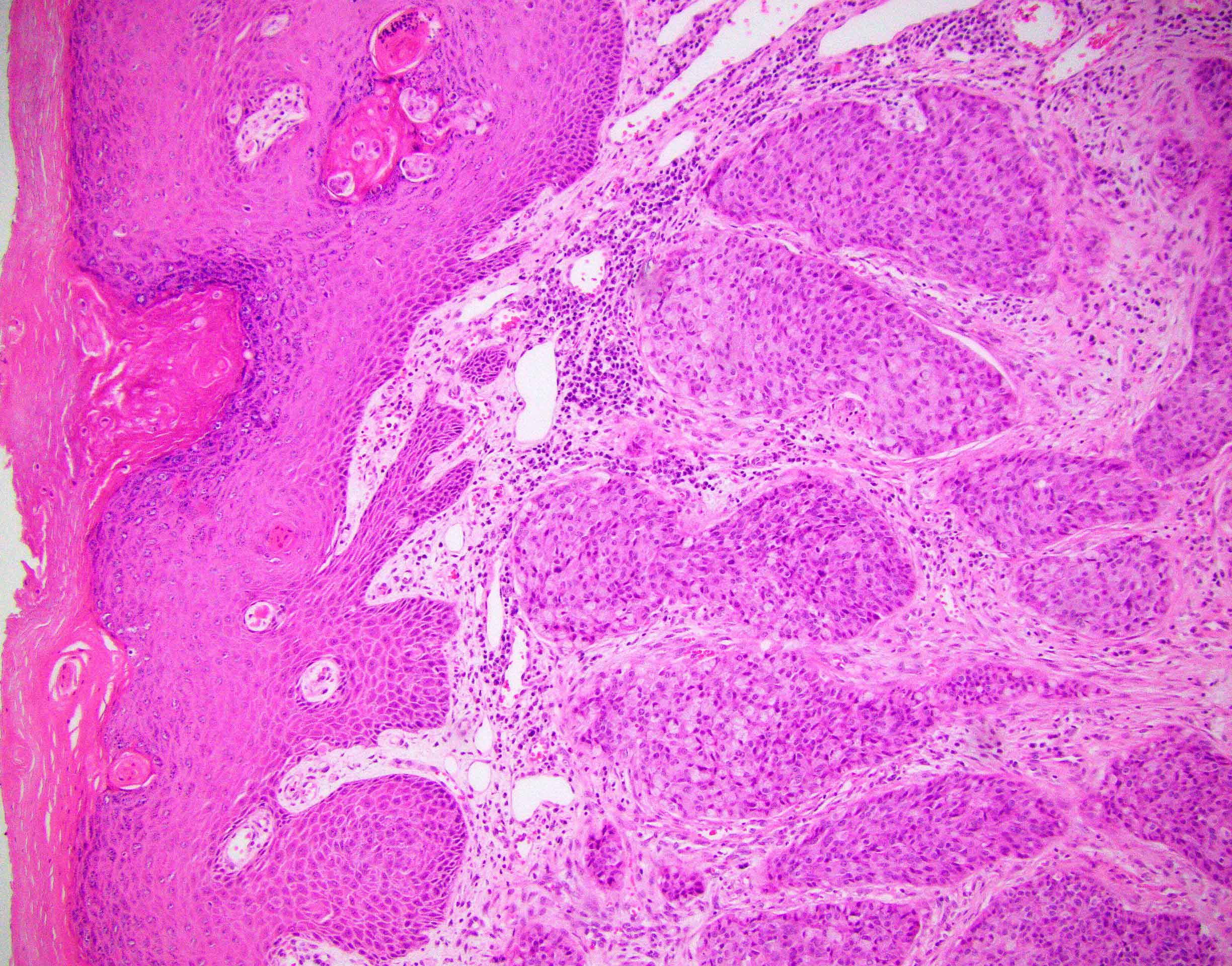
Histopathology vagina - clear cell carcinoma
Dysplastic nevus: 5 minute pathology pearls by Dr. Jerad Gardner
Dysplastic nevi by Prof. Naseem Ahmed
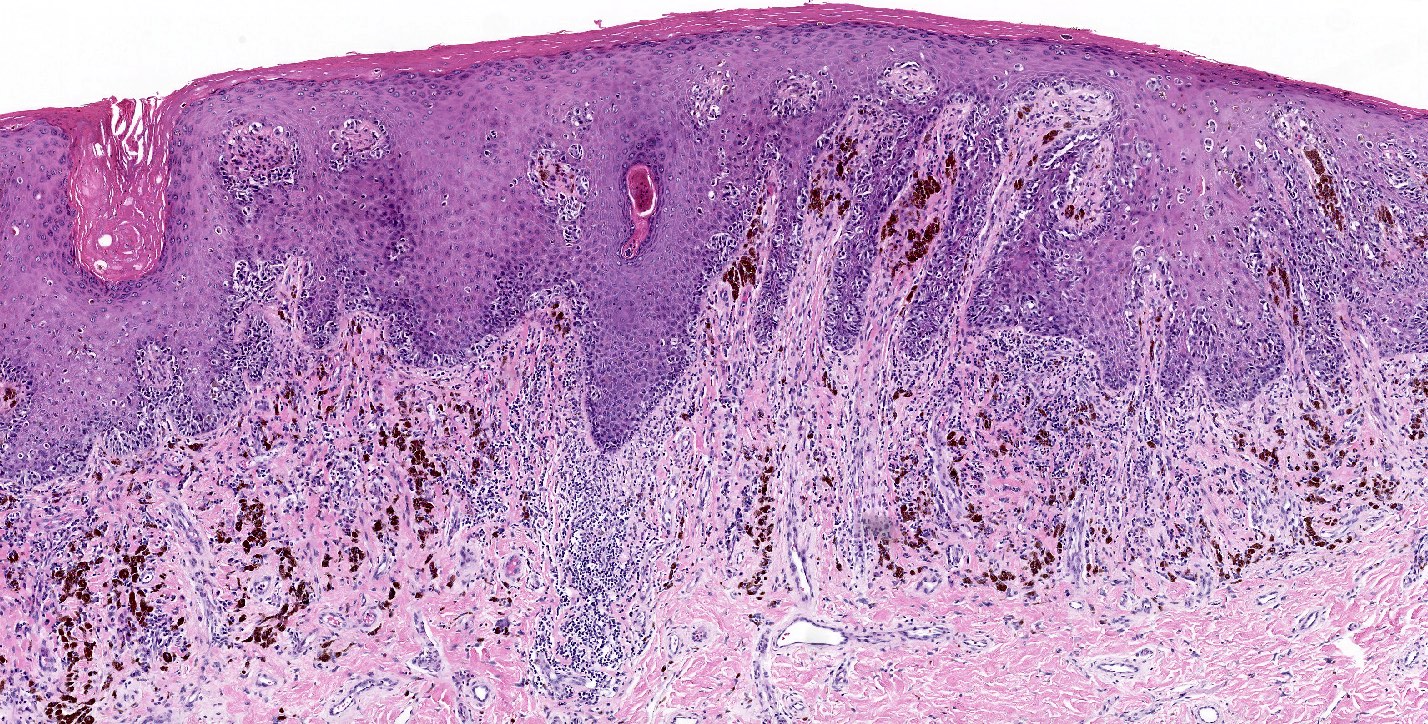
Melanoma arising in a dysplastic nevus by Drs. Philip H. Mckee and Antonina Kalmykova
Histopathology and dermoscopy of severely dysplastic nevus / in situ melanoma by Dr. Sasi Kiran Attili
Dysplastic nevus: fact or fiction by Prof. Cliff Rosendahl
Junctional dysplastic lentiginous nevus by Dr. Ian McColl
Dysplastic nevus by Dr. Sonam Kumar Pruthi
Dysplastic nevus by Audiopedia
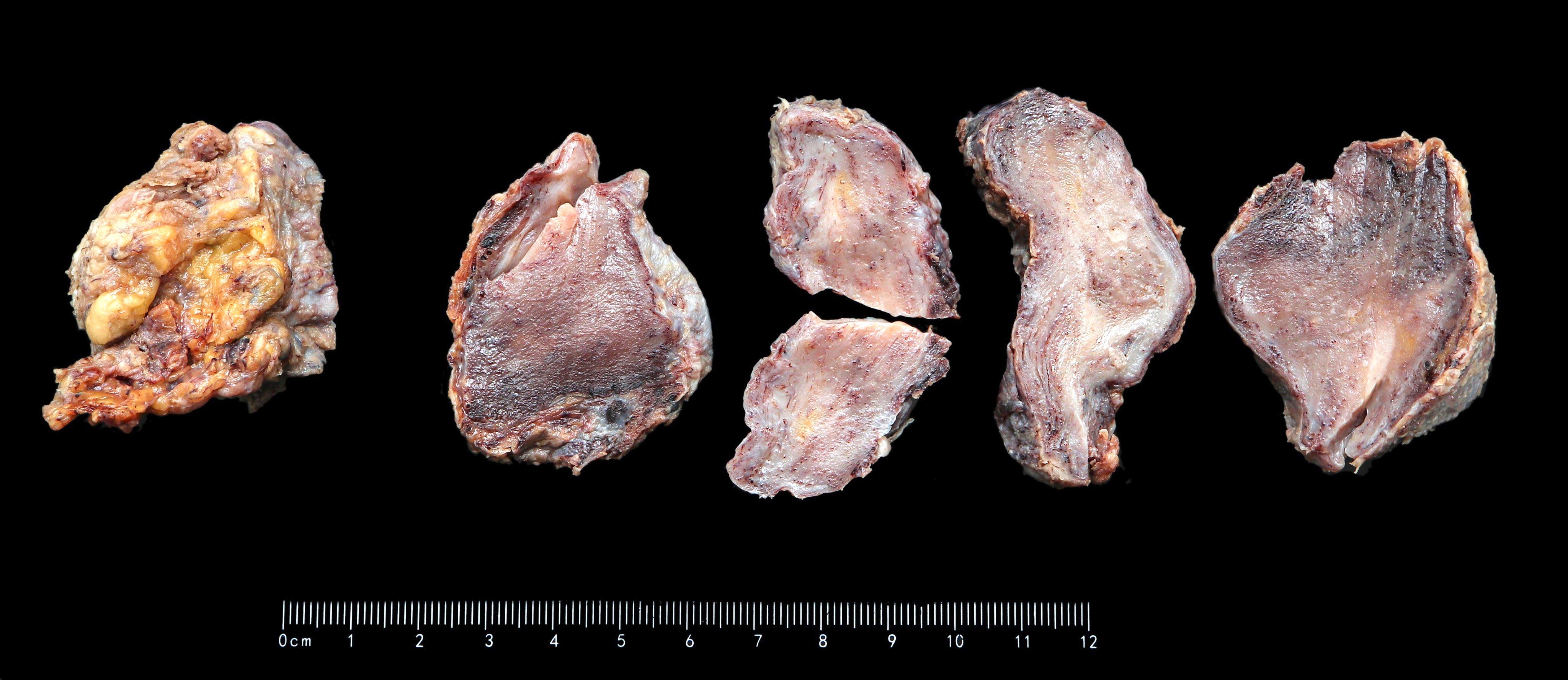
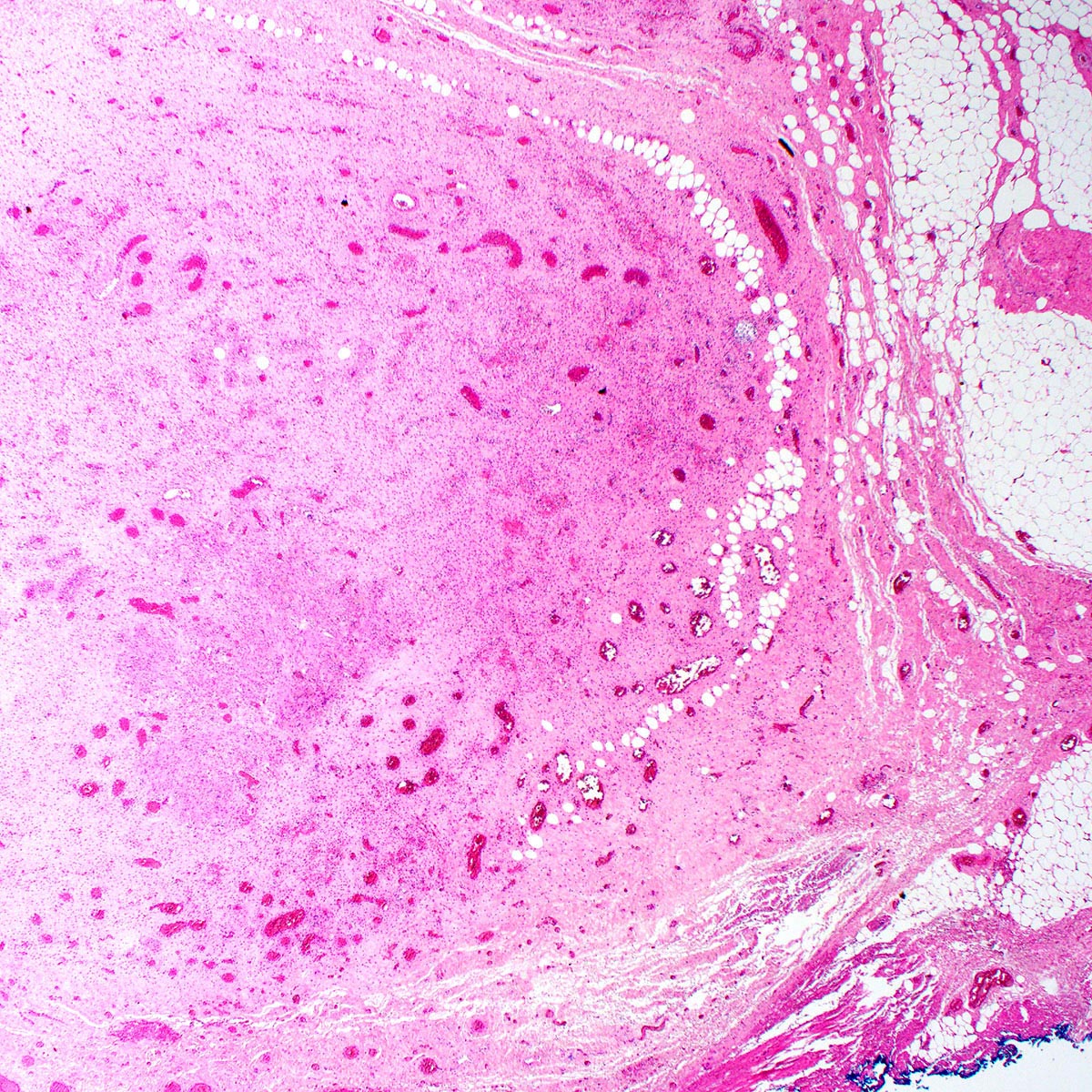
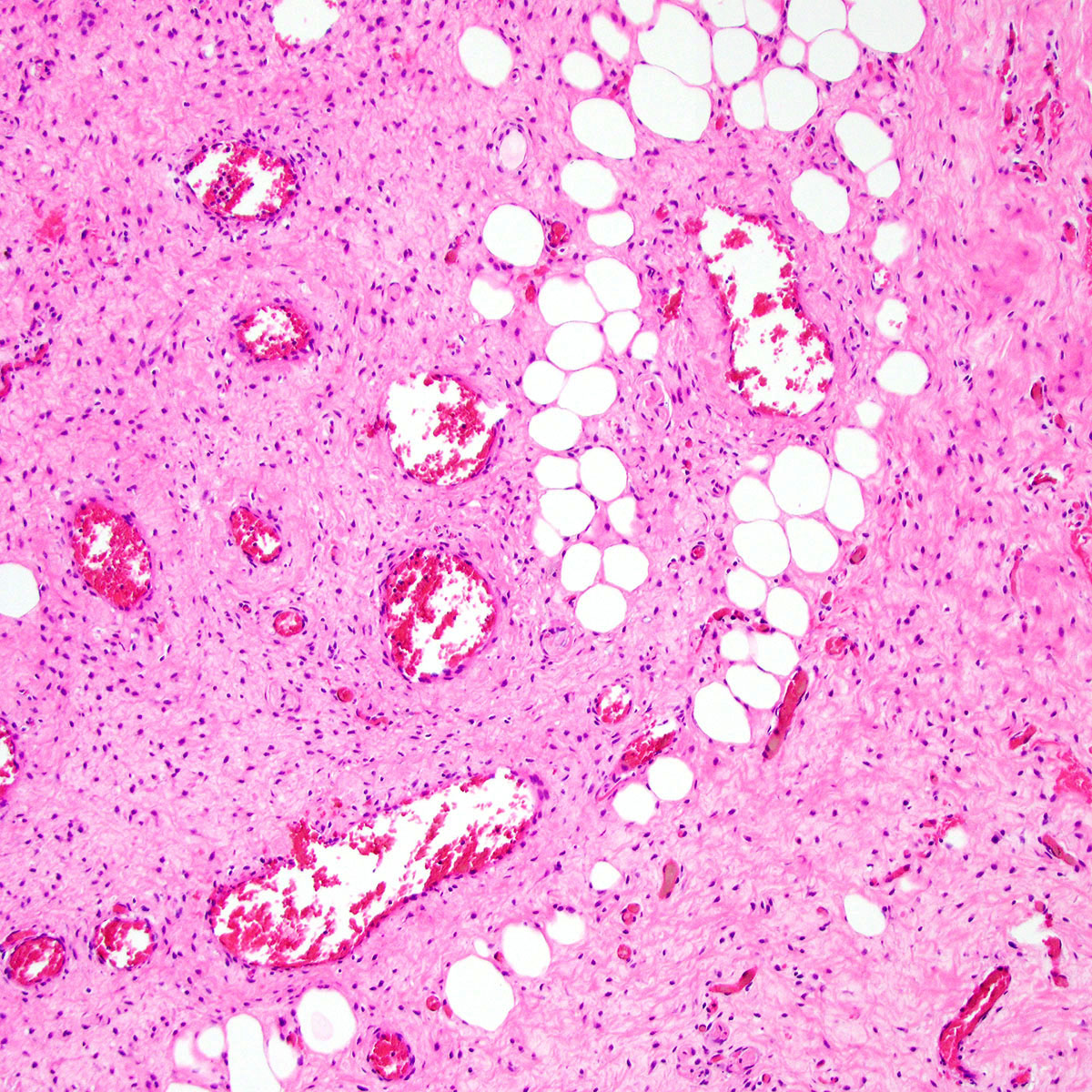
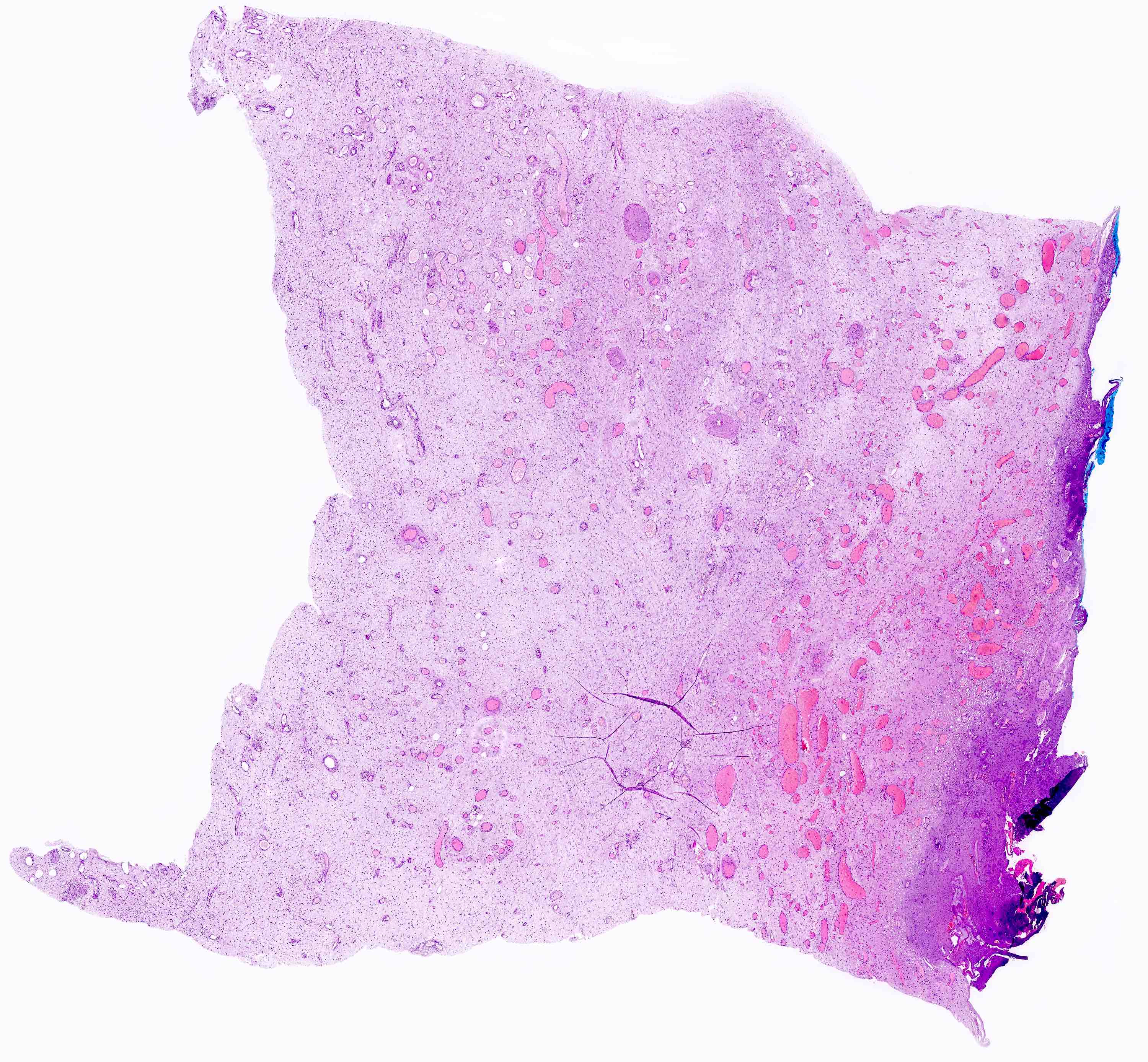
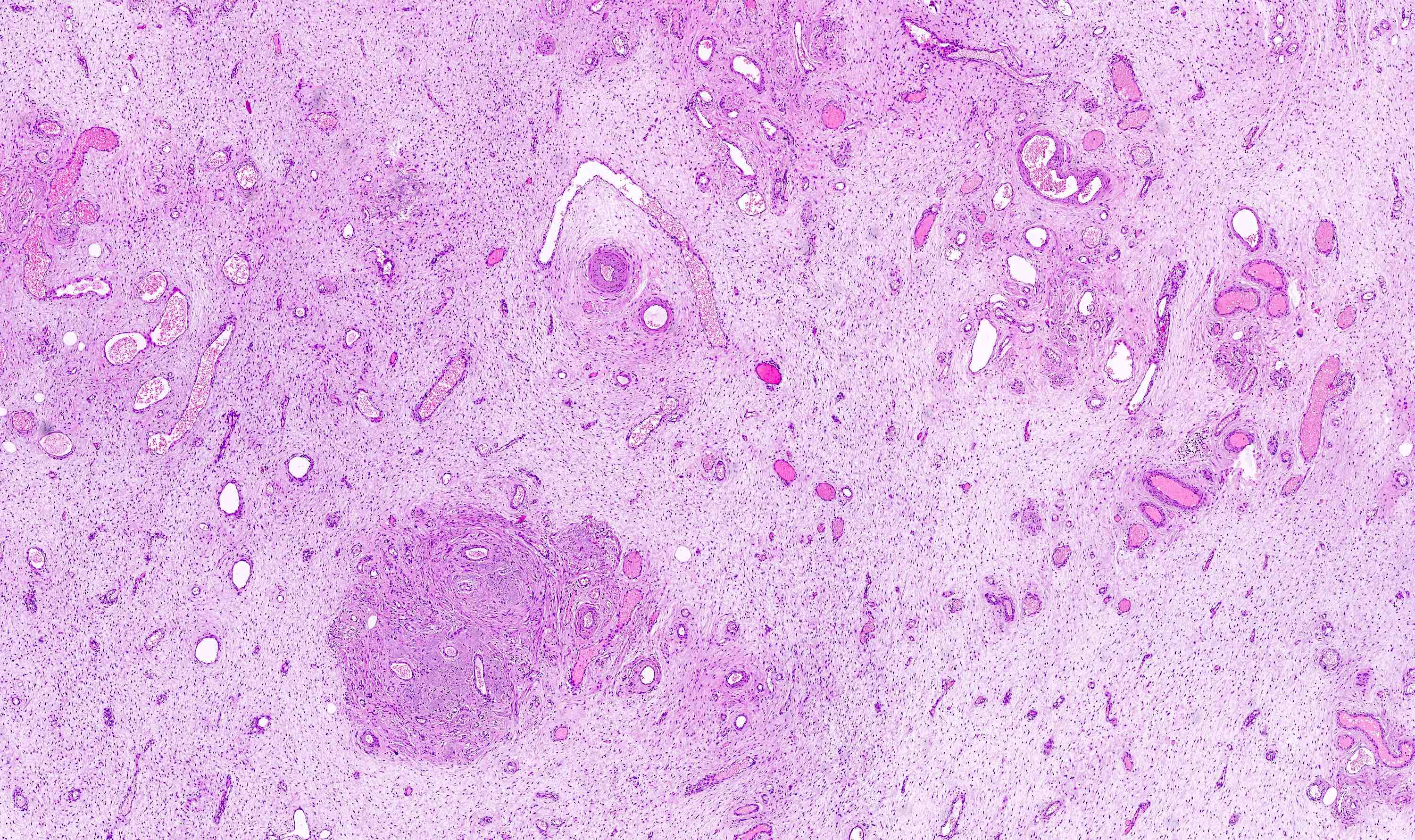
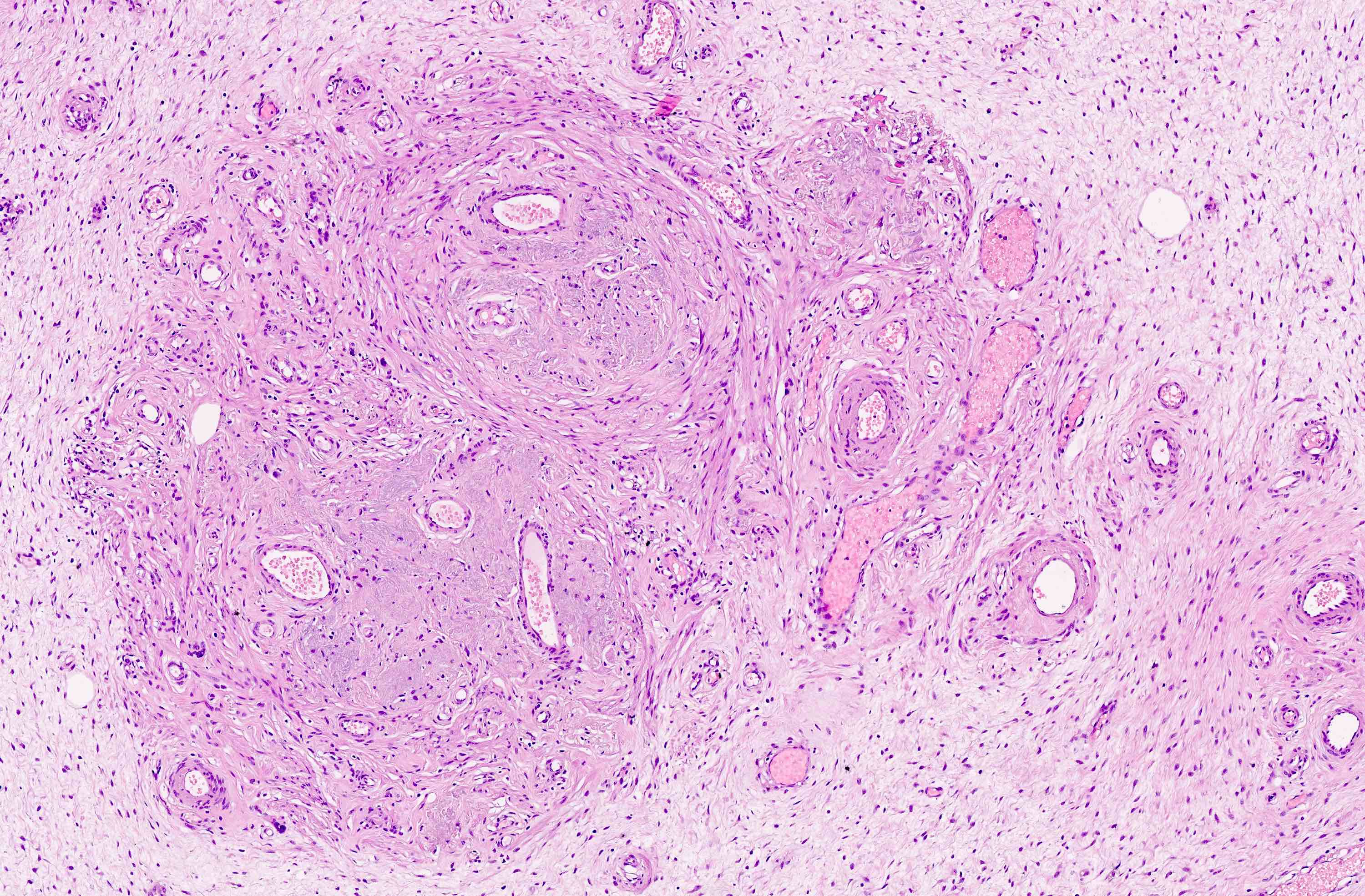
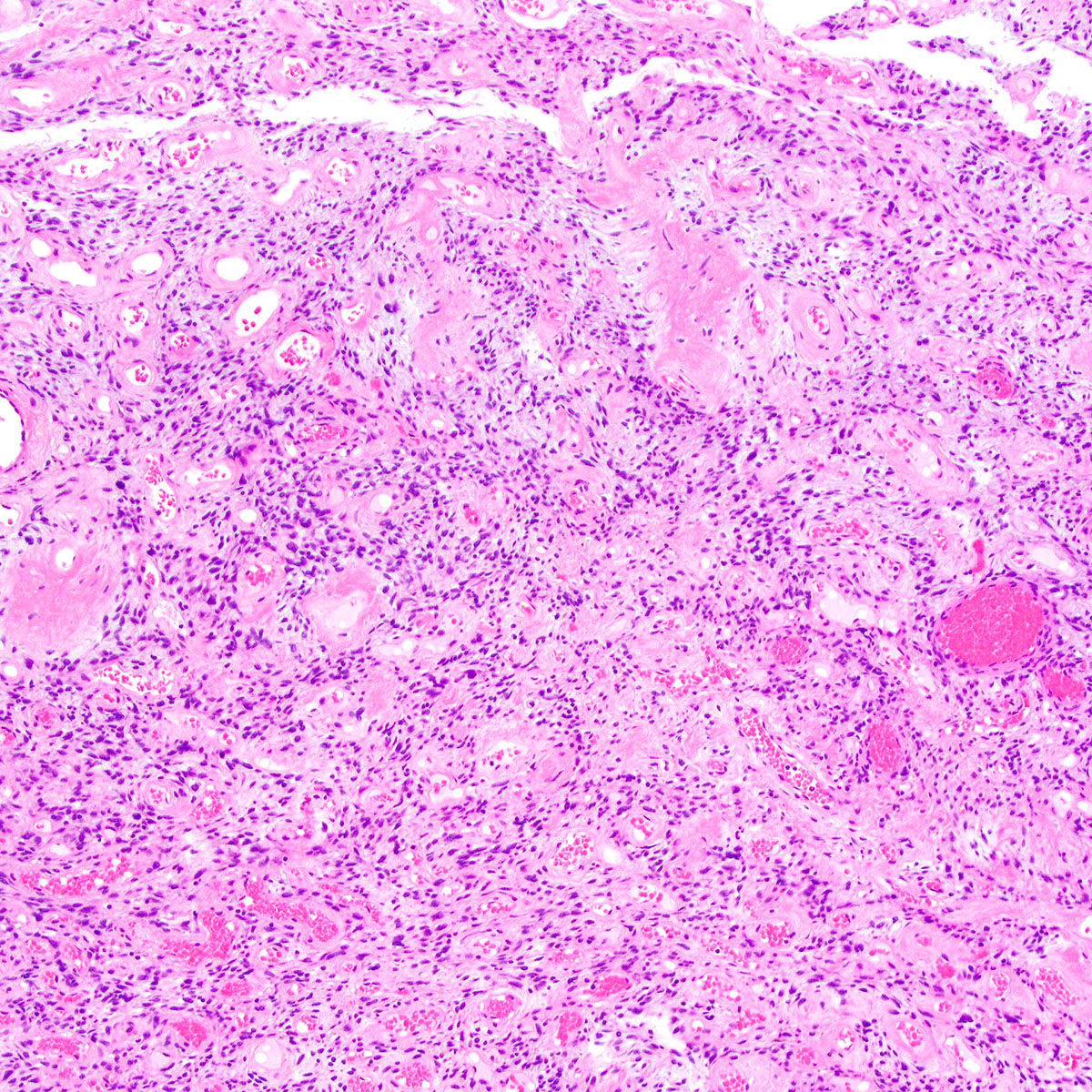
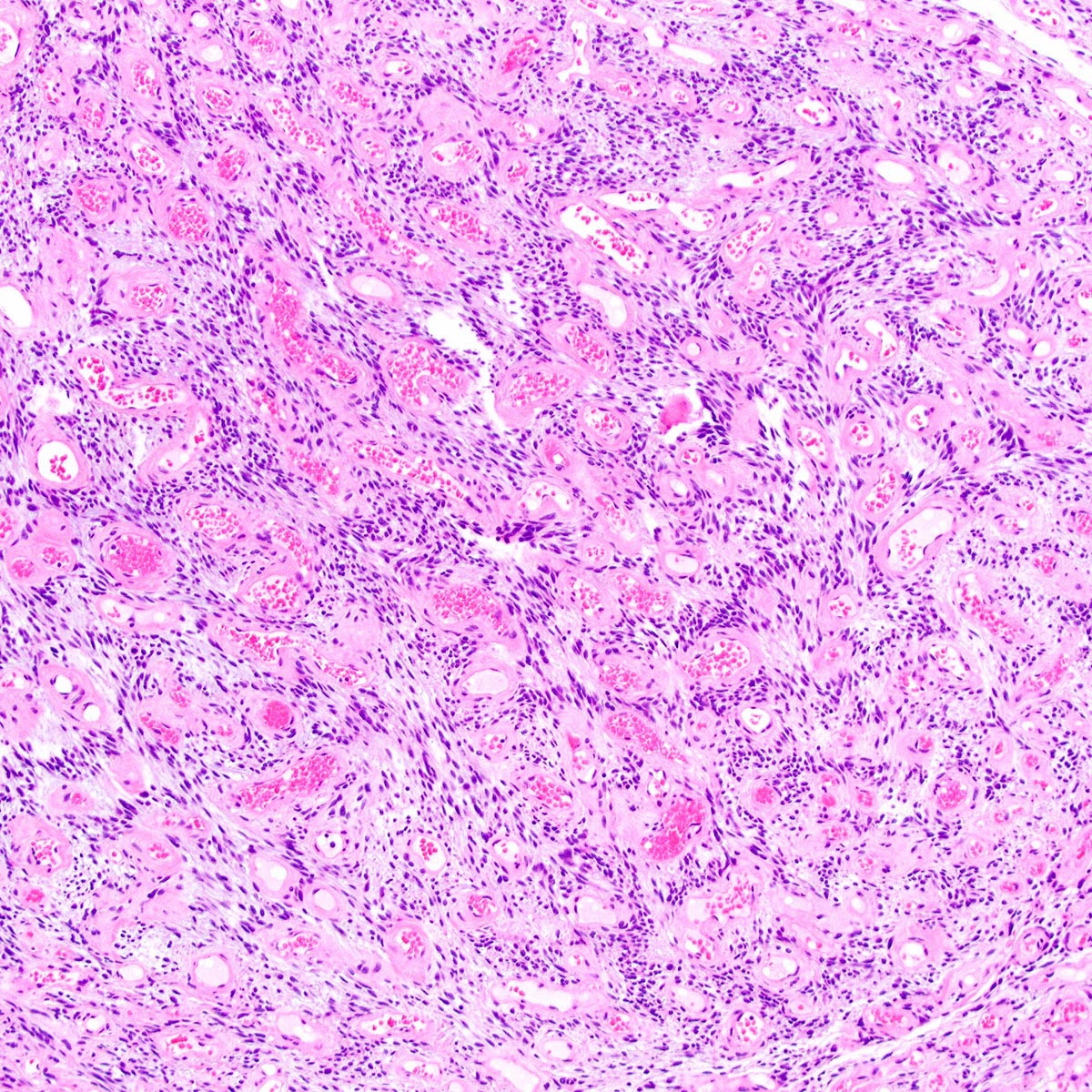
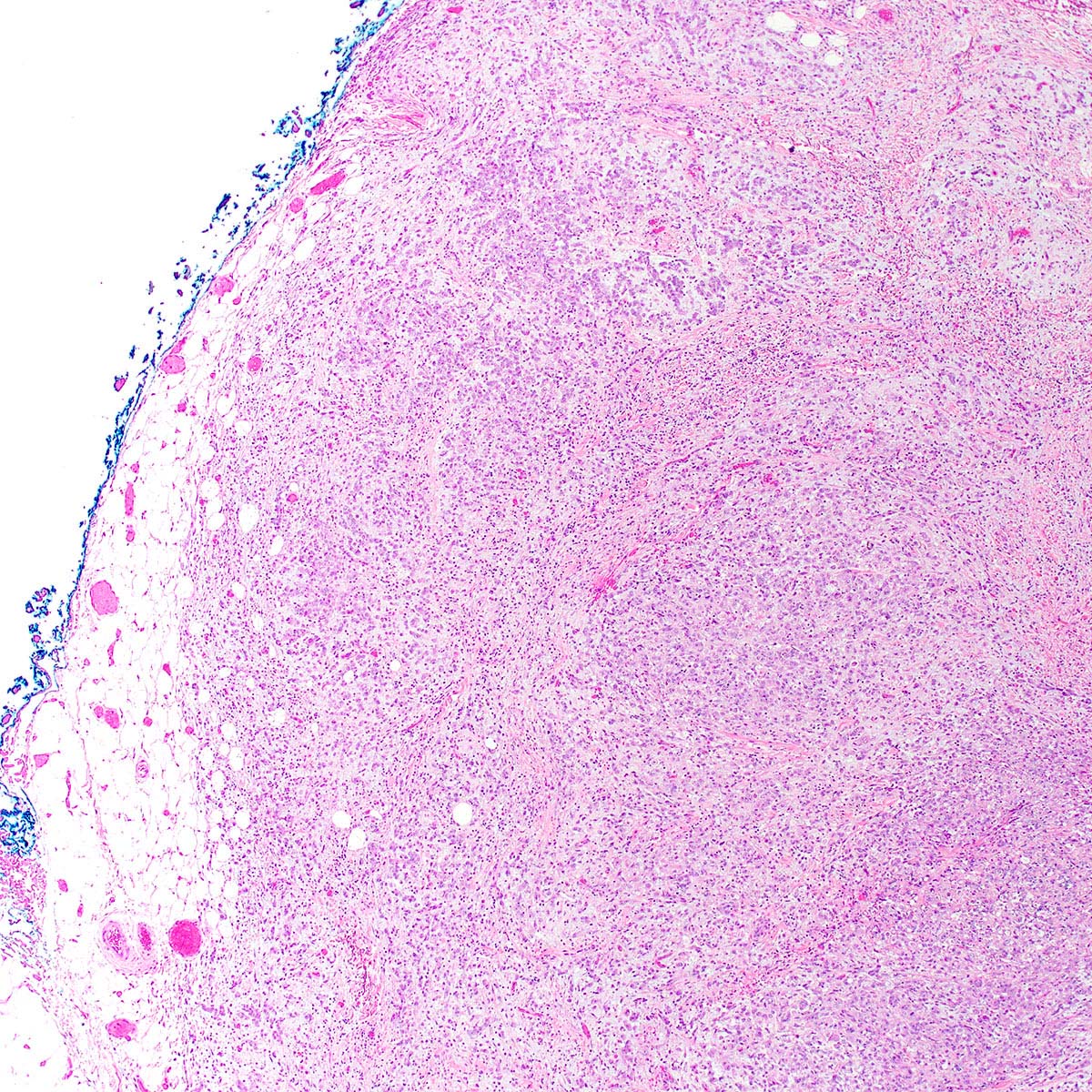
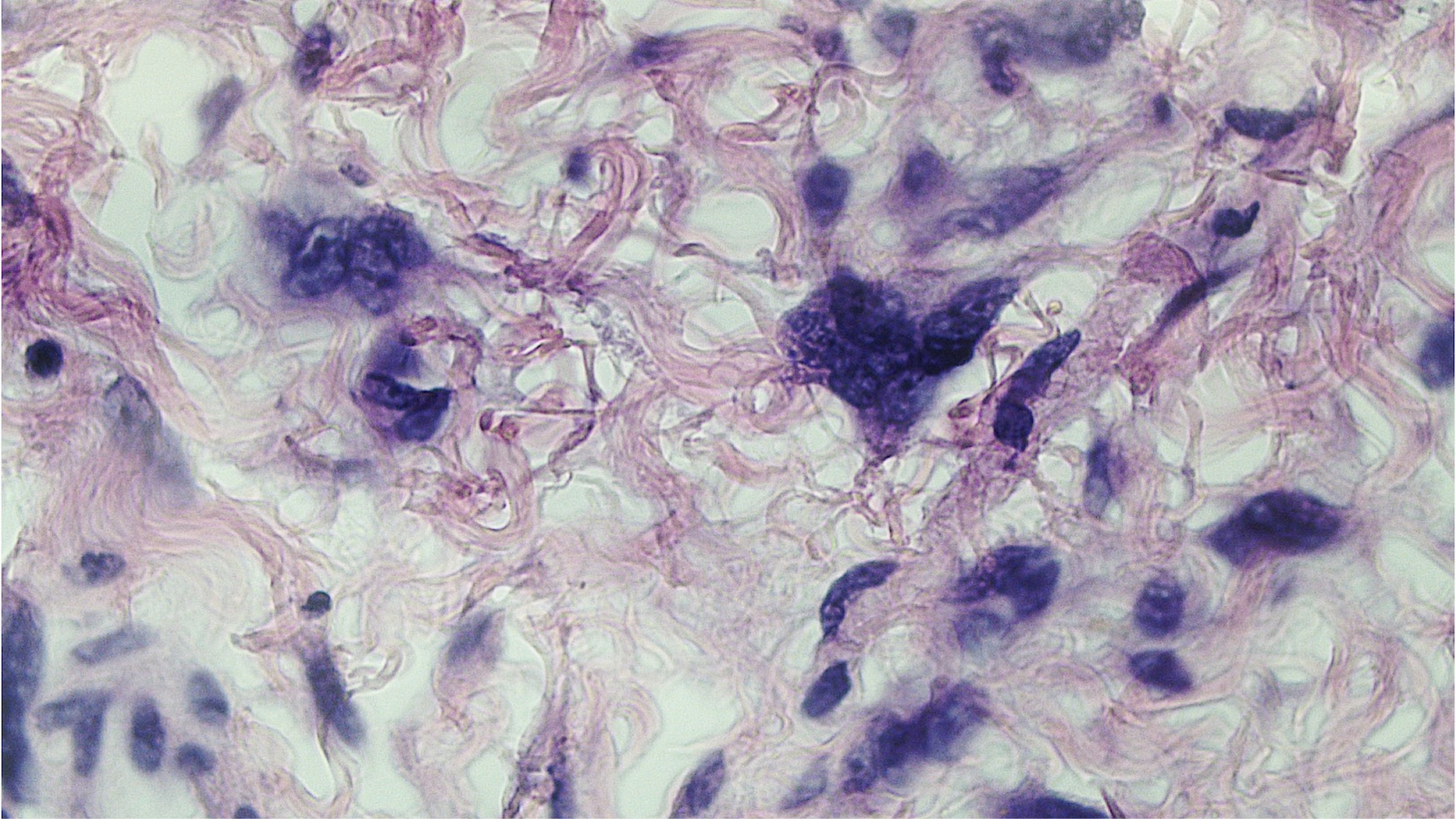
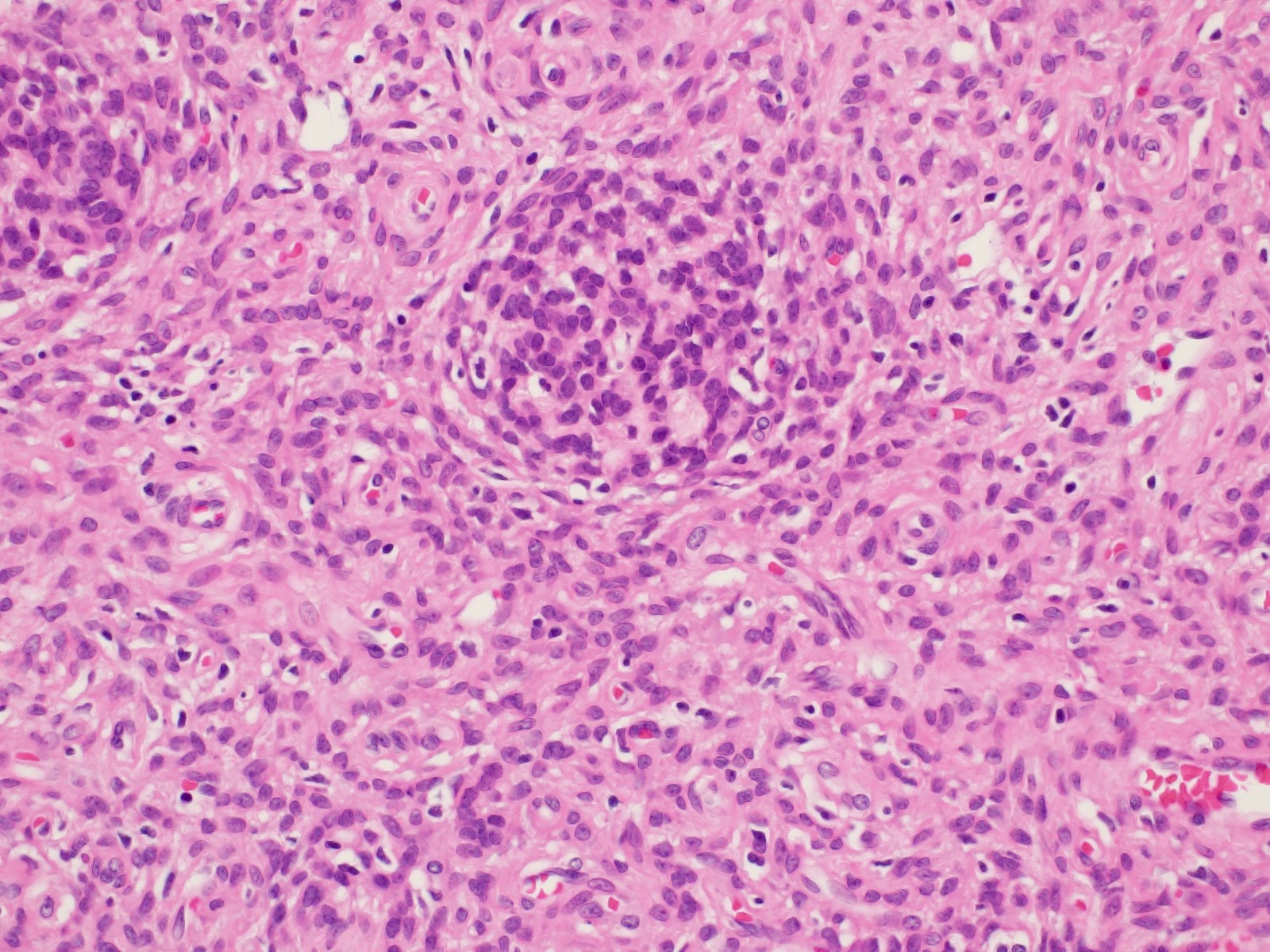
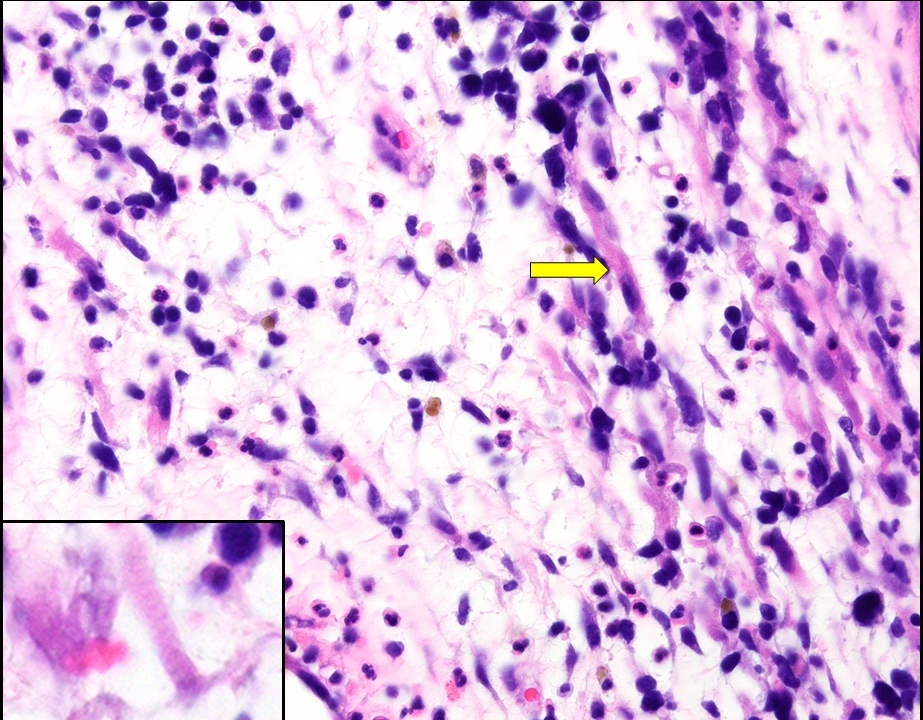
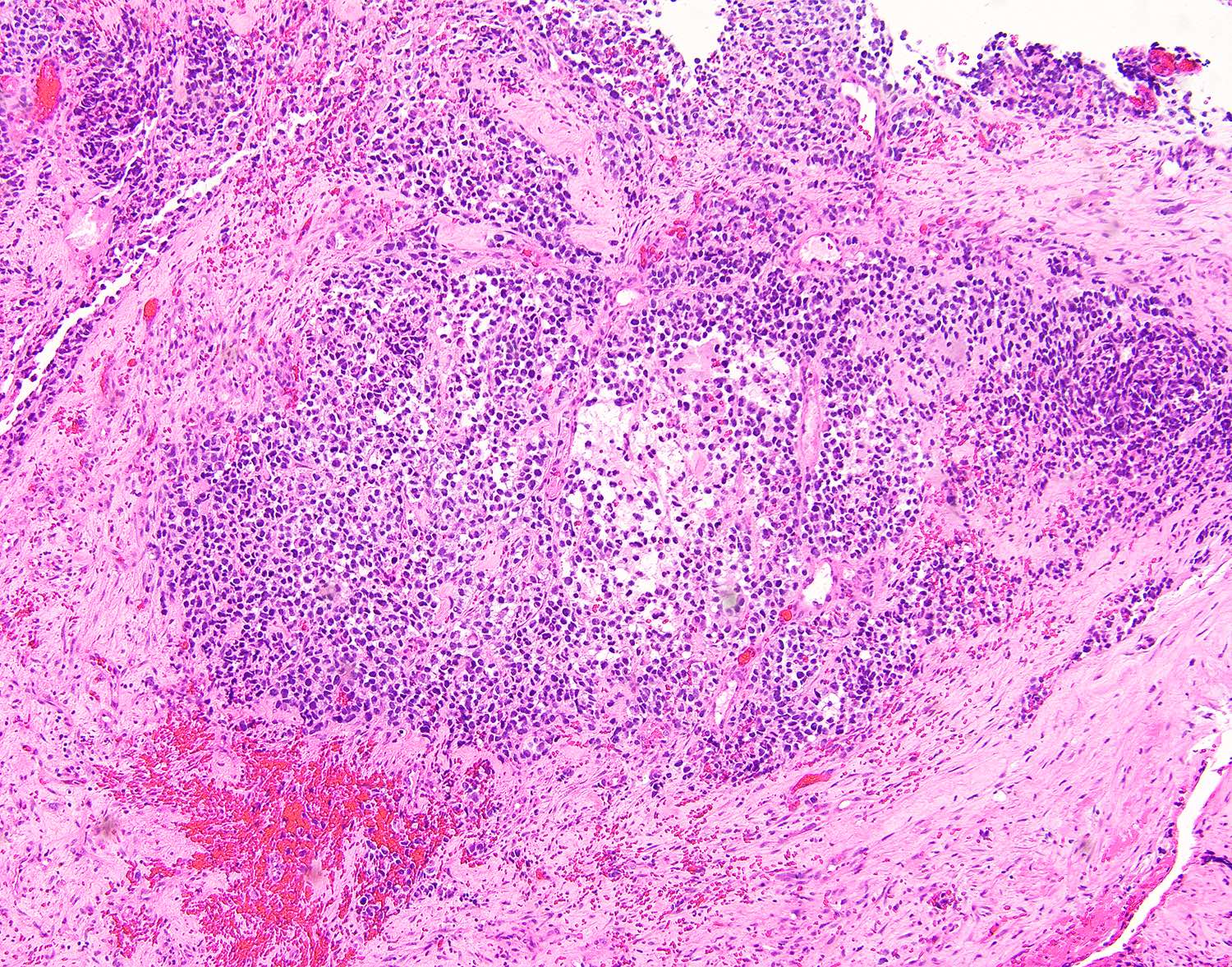
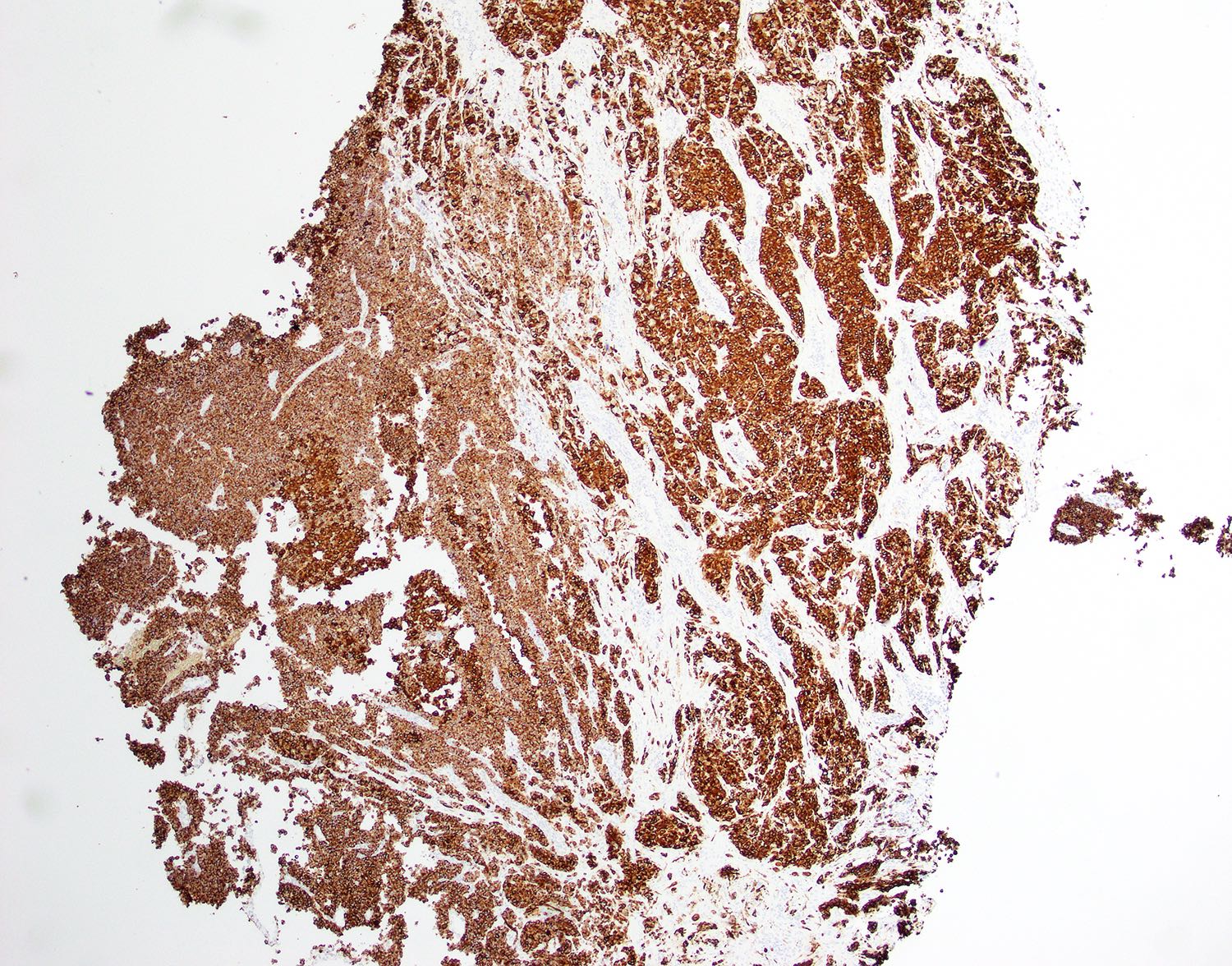
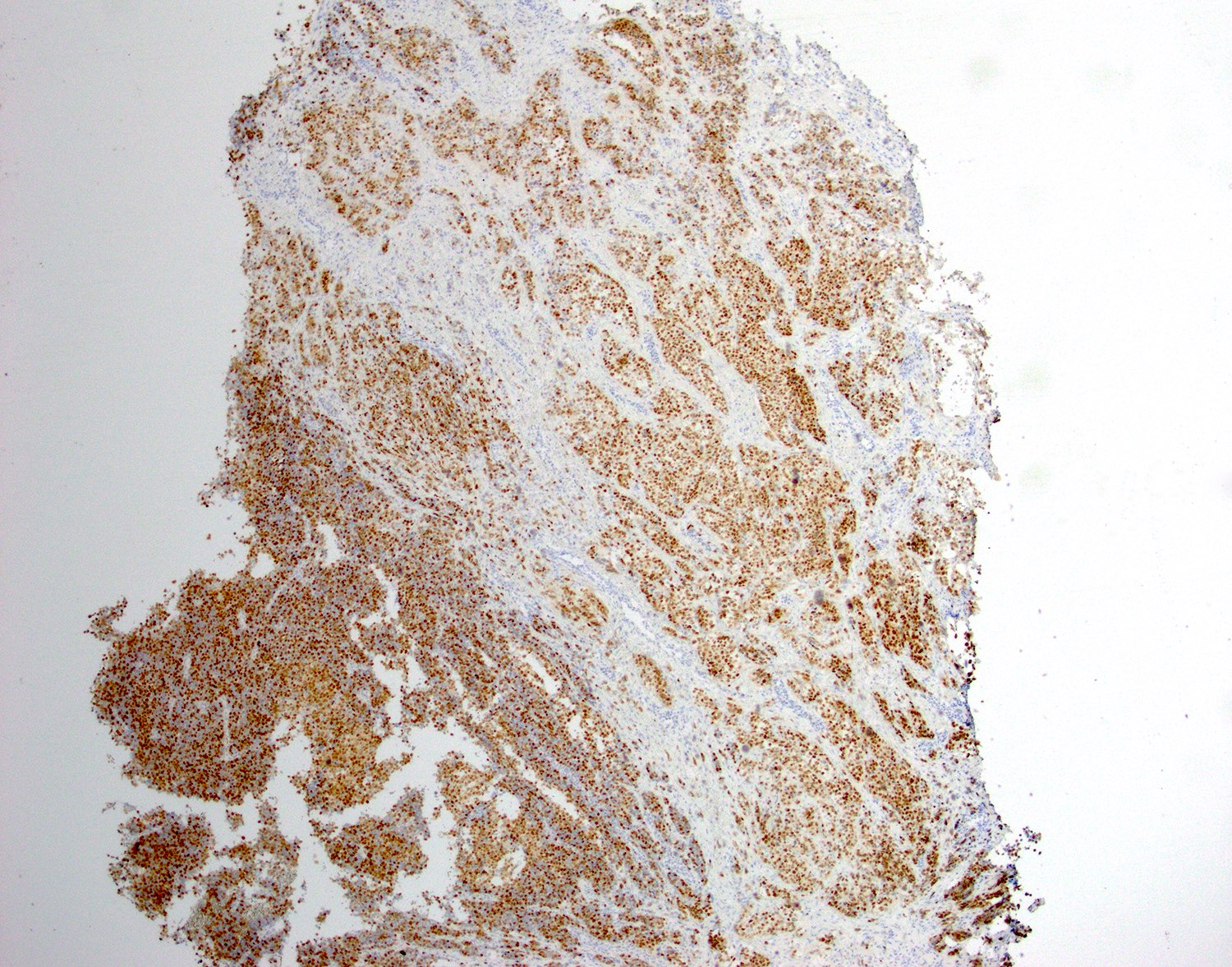
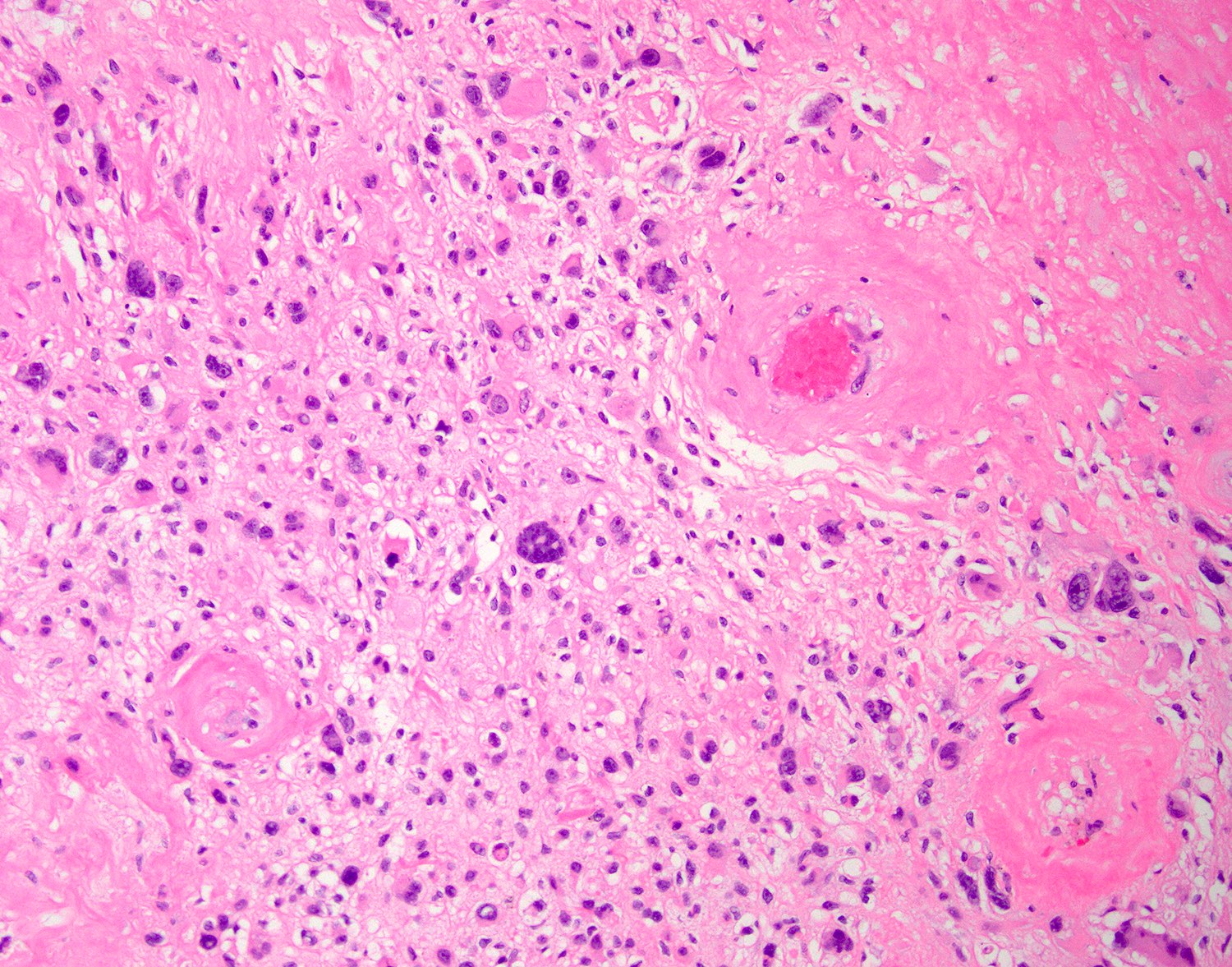
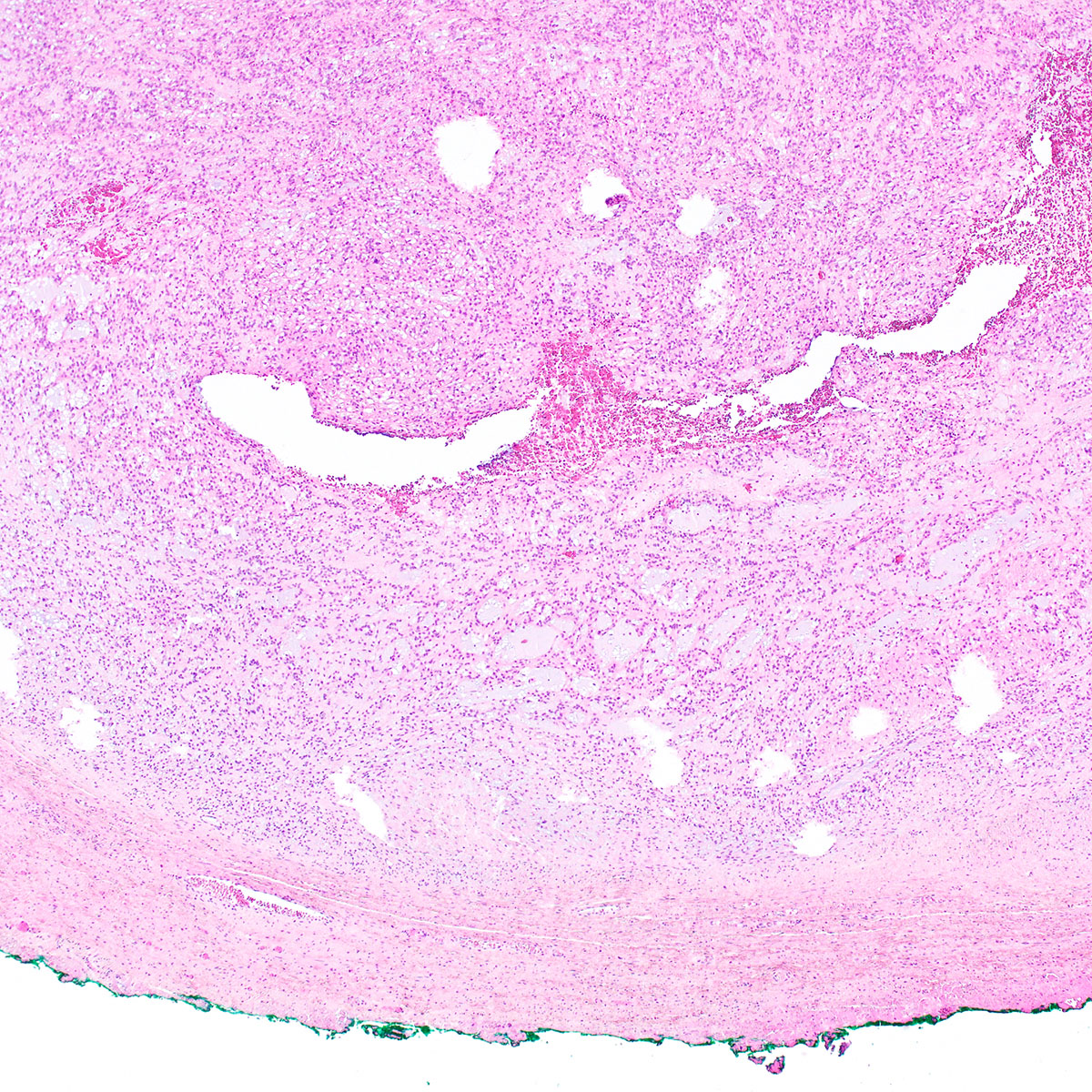
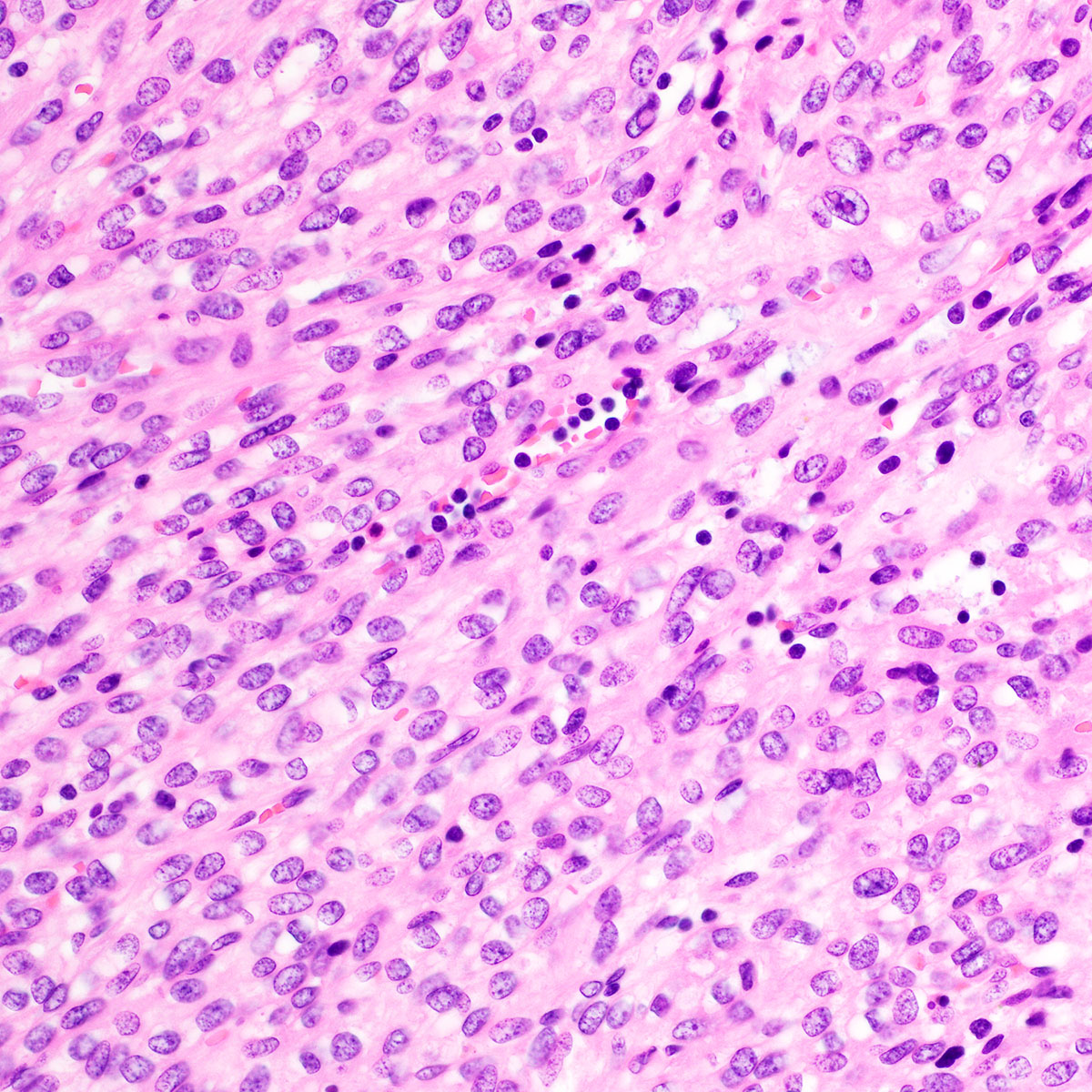
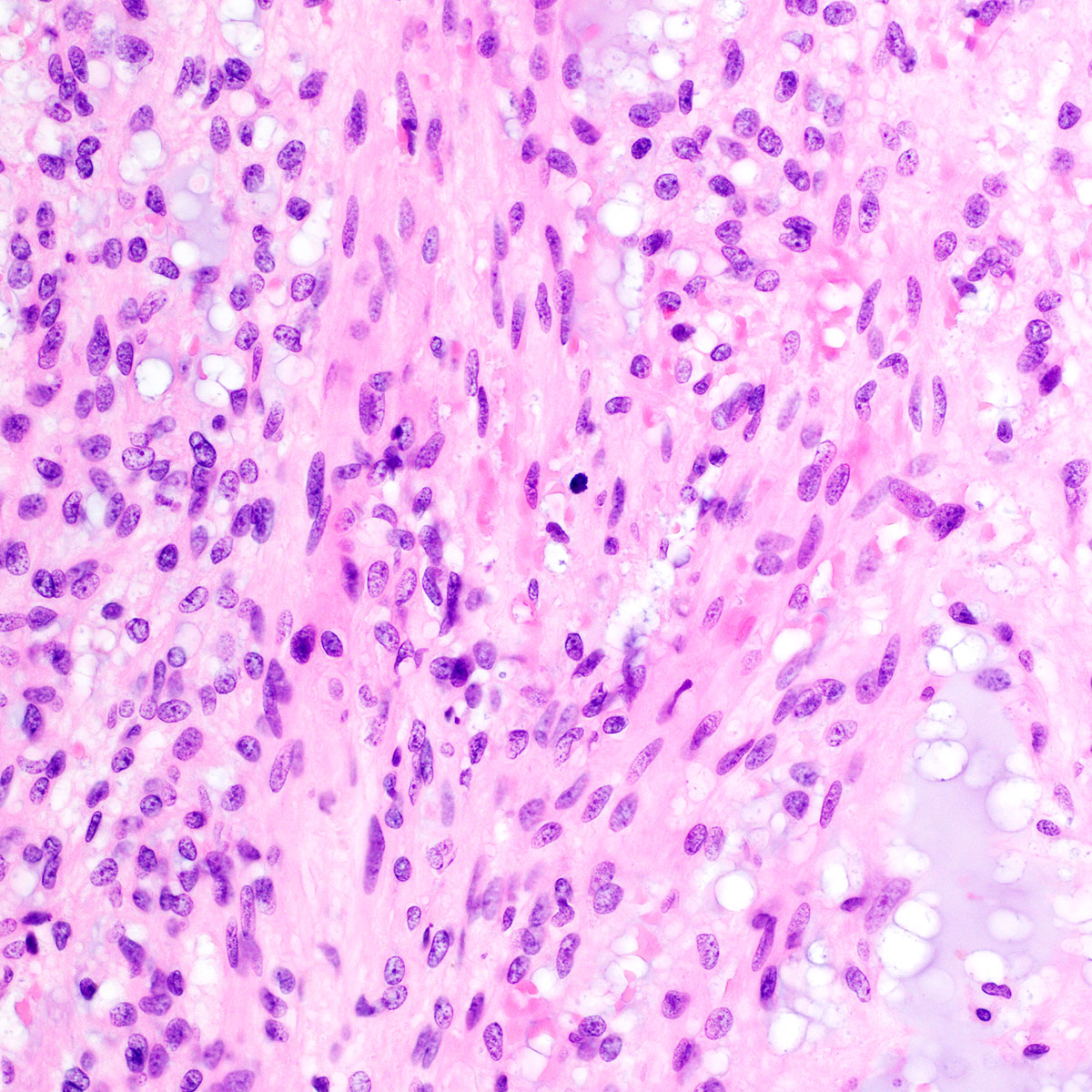
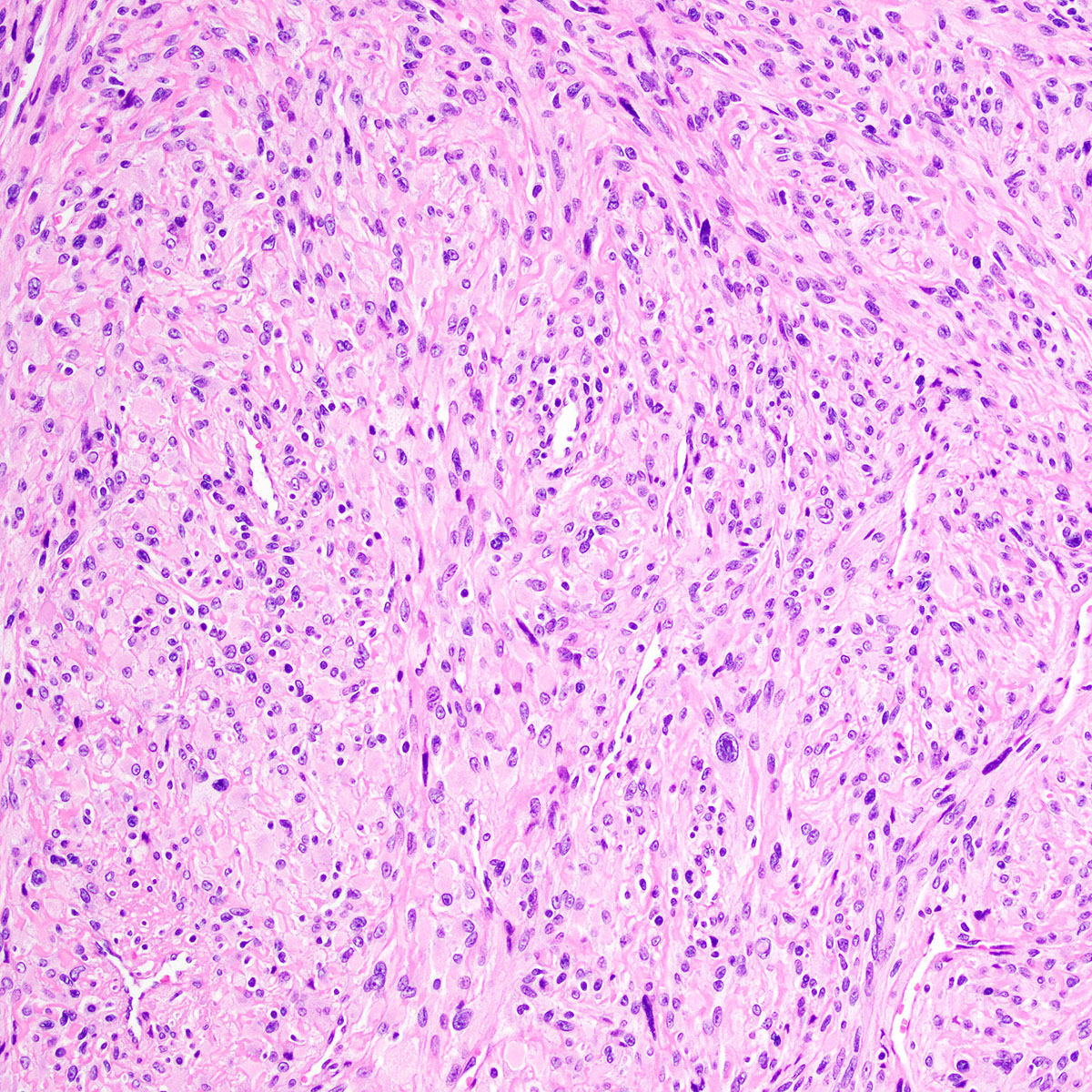
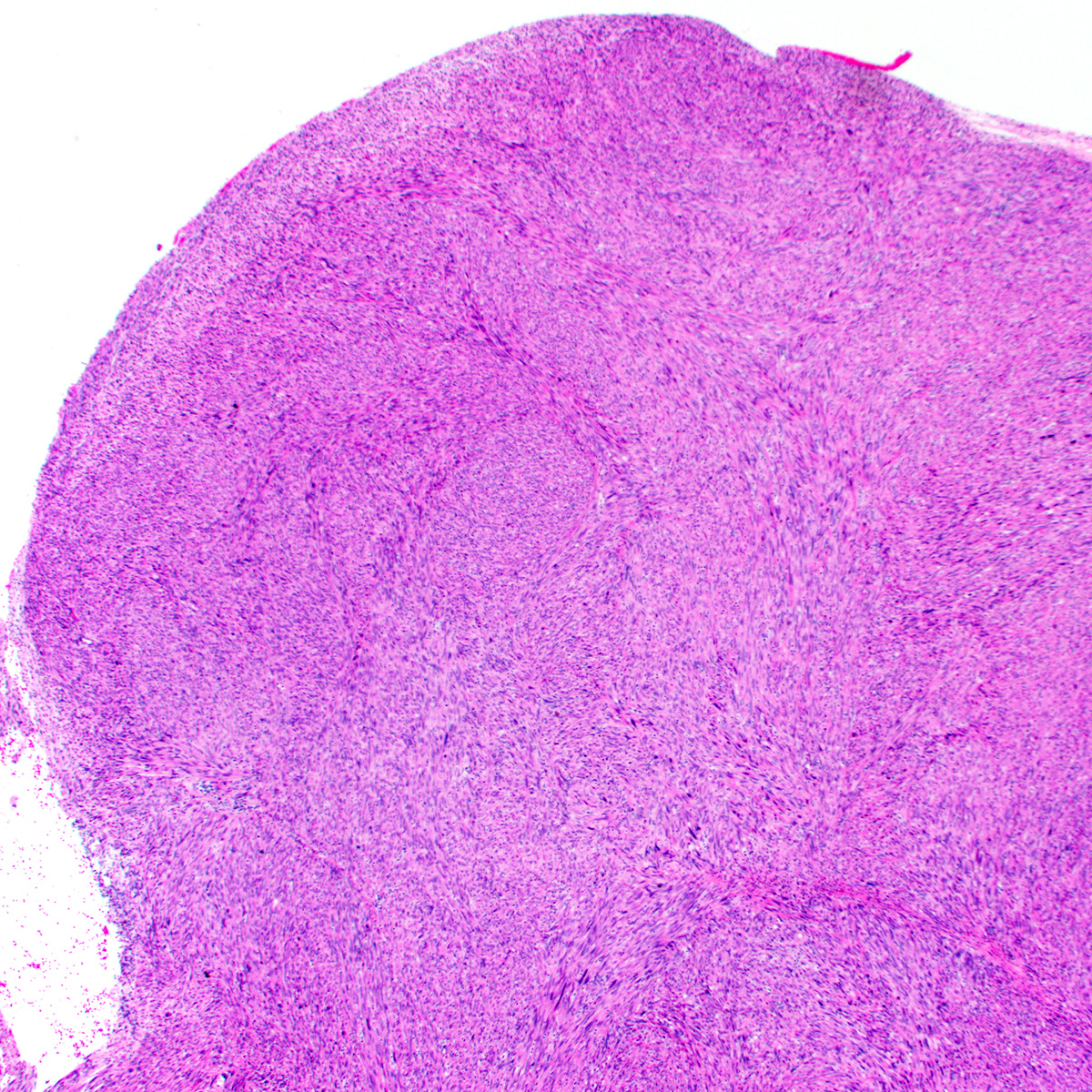
Proximal type epithelioid sarcoma of the groin
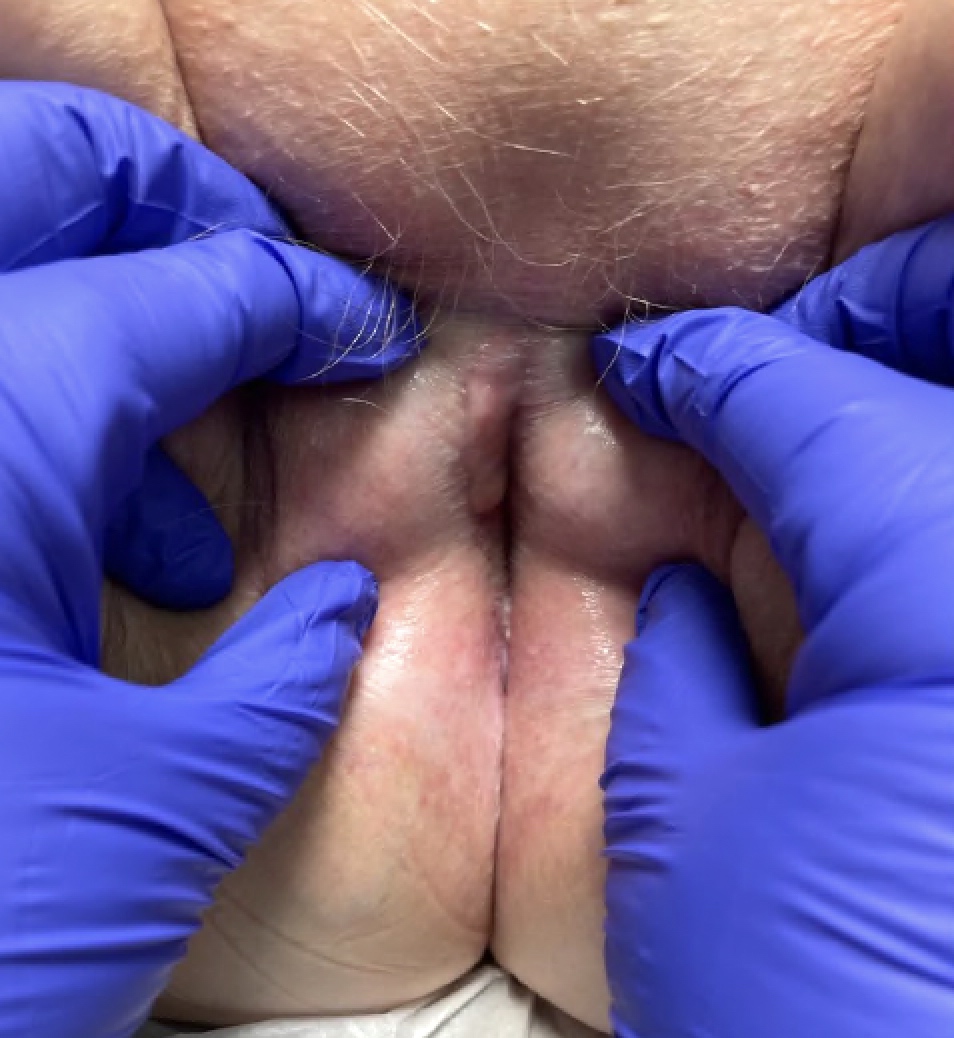
Table 1: Diagnostic criteria of vulvar erosive lichen planus by the International Society of the Study of Vulvovaginal Disease (ISSVD) (adapted from Br J Dermatol 2013;169:337)
| 3 out of 9 criteria needed for diagnosis |
| Well demarcated erosions or glazed erythema of introitus |
| Wickham striae on surrounding skin |
| Pain or burning |
| Scarring or loss of architecture |
| Vaginal inflammation |
| Involvement of other mucosal surfaces |
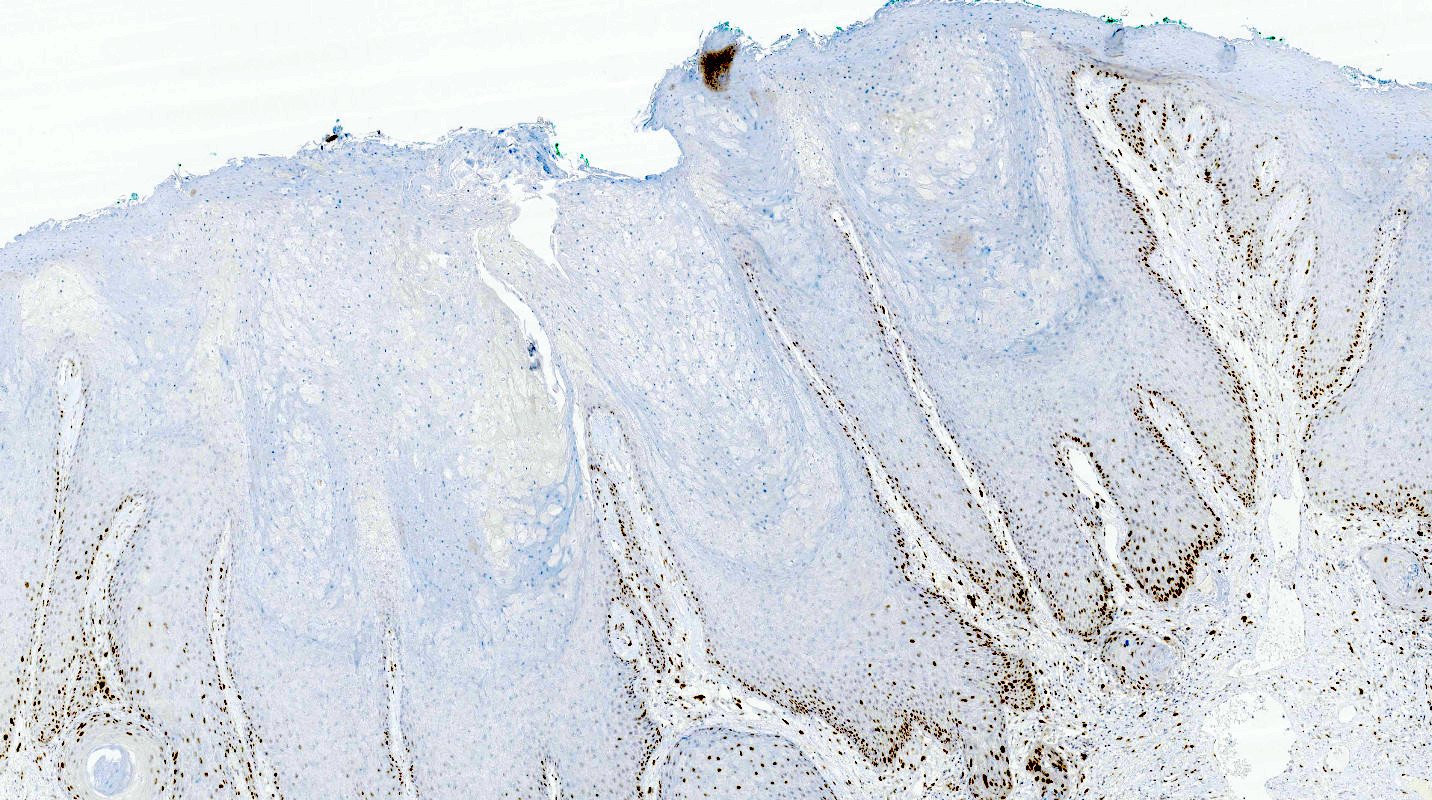
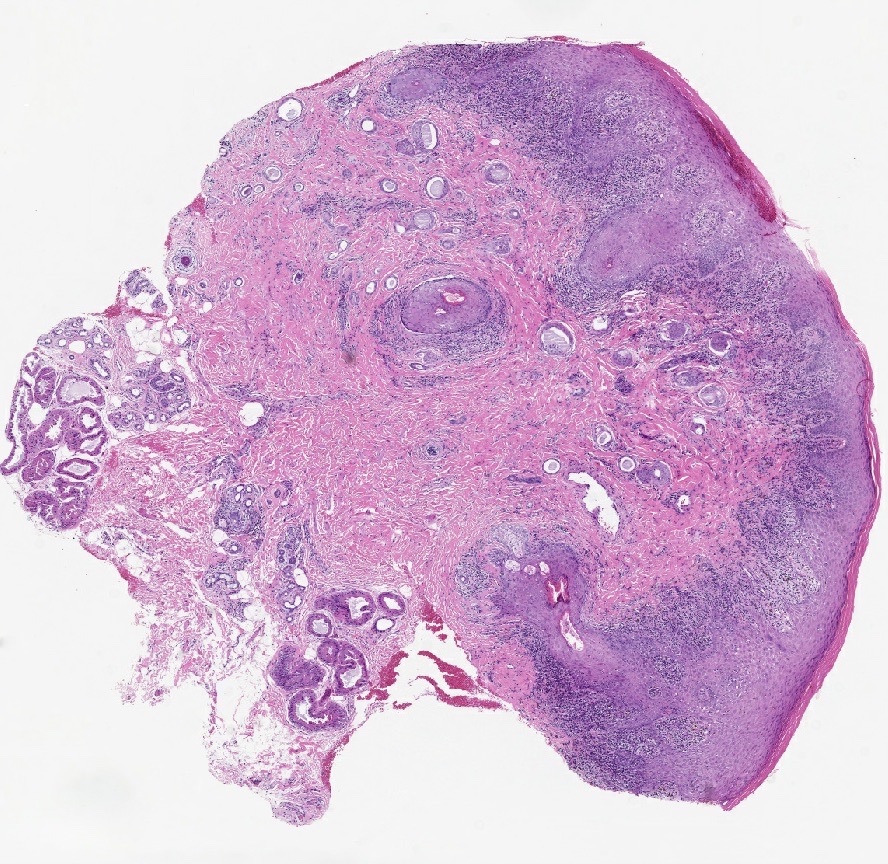
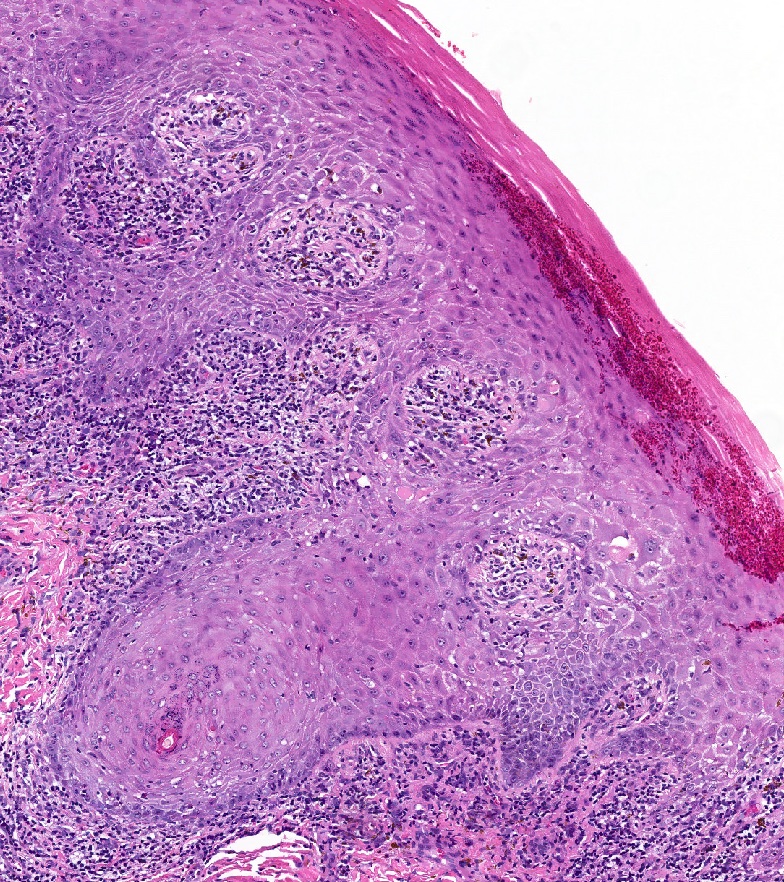
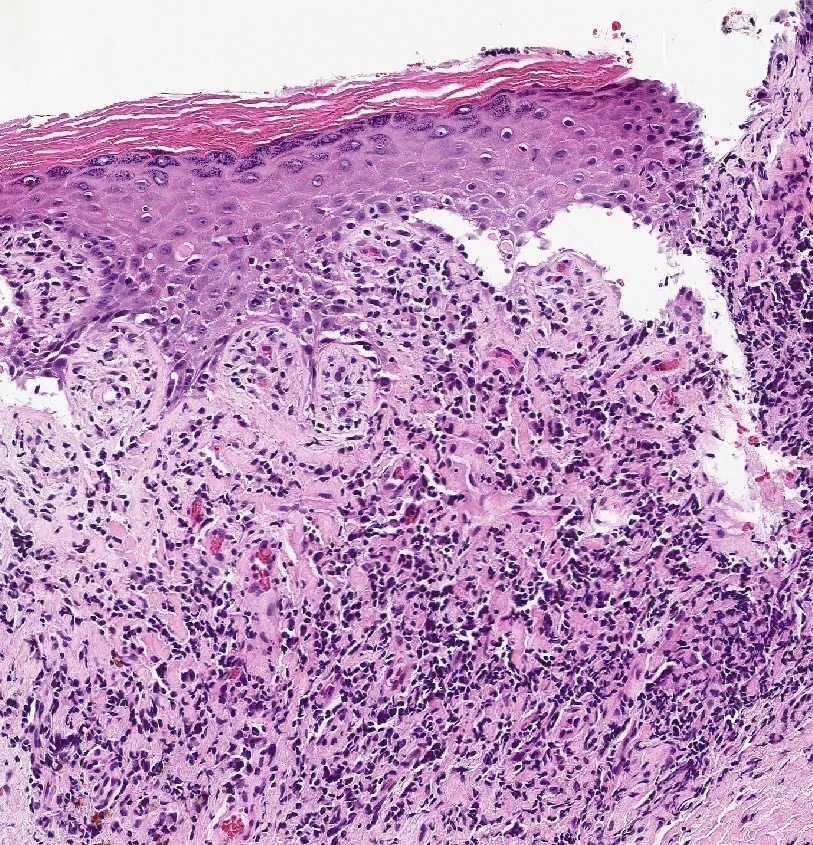
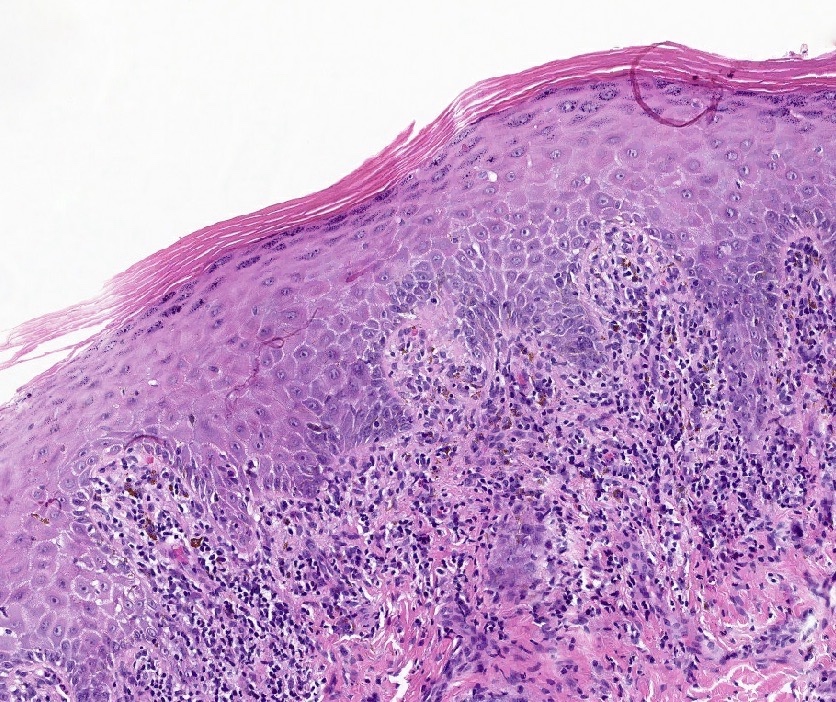
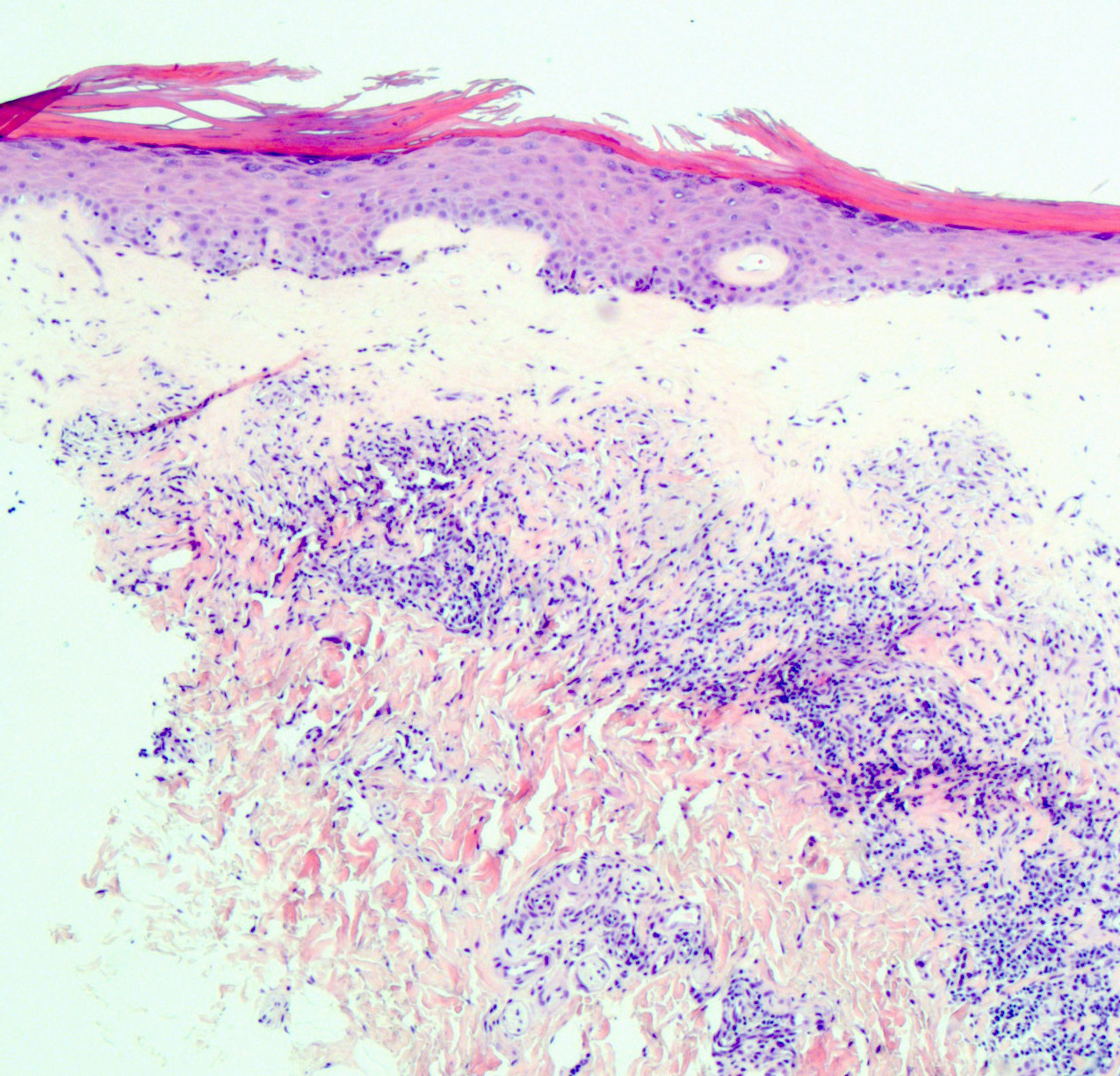
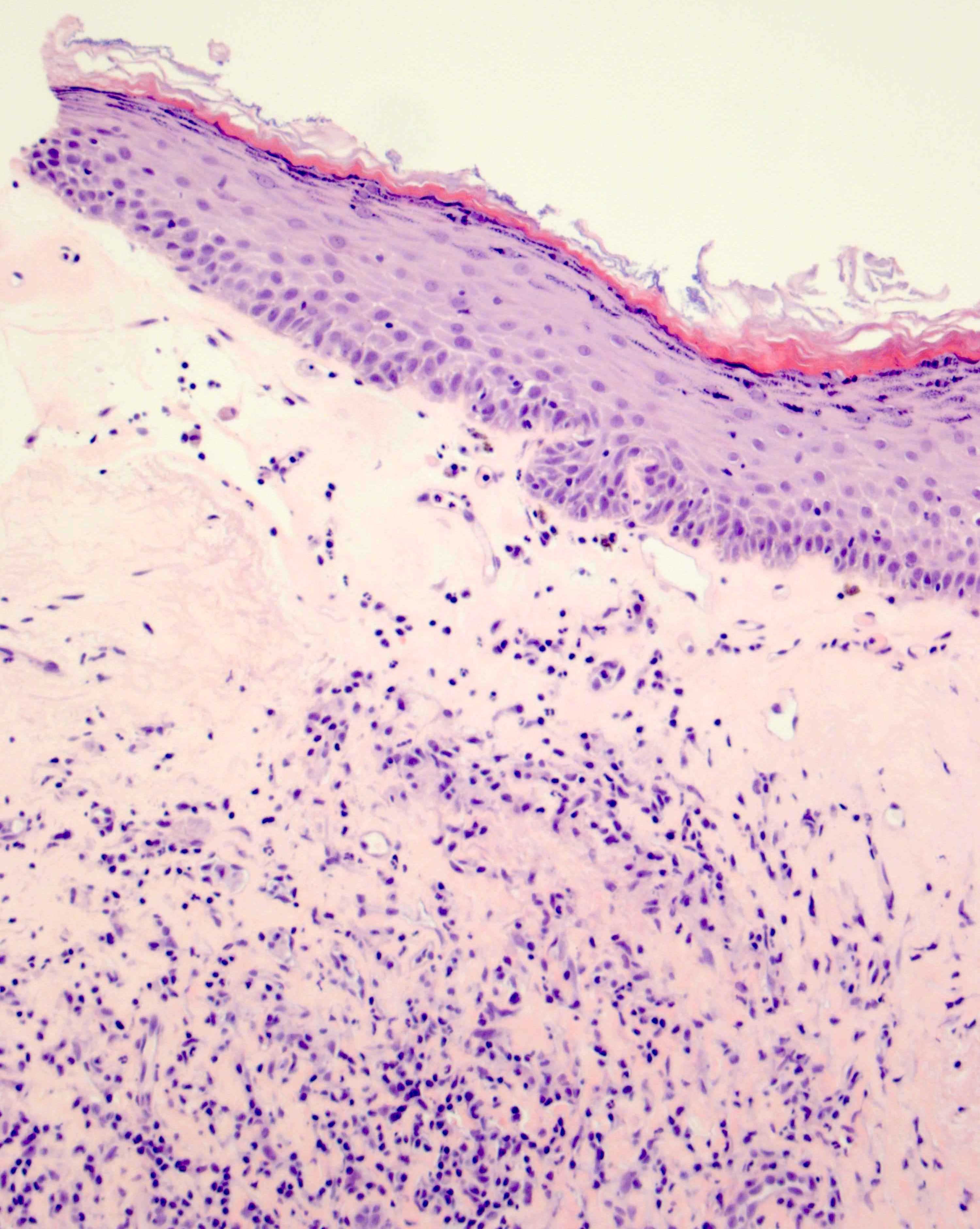
| Well defined inflammatory band in superficial connective tissue involving dermoepidermal junction |
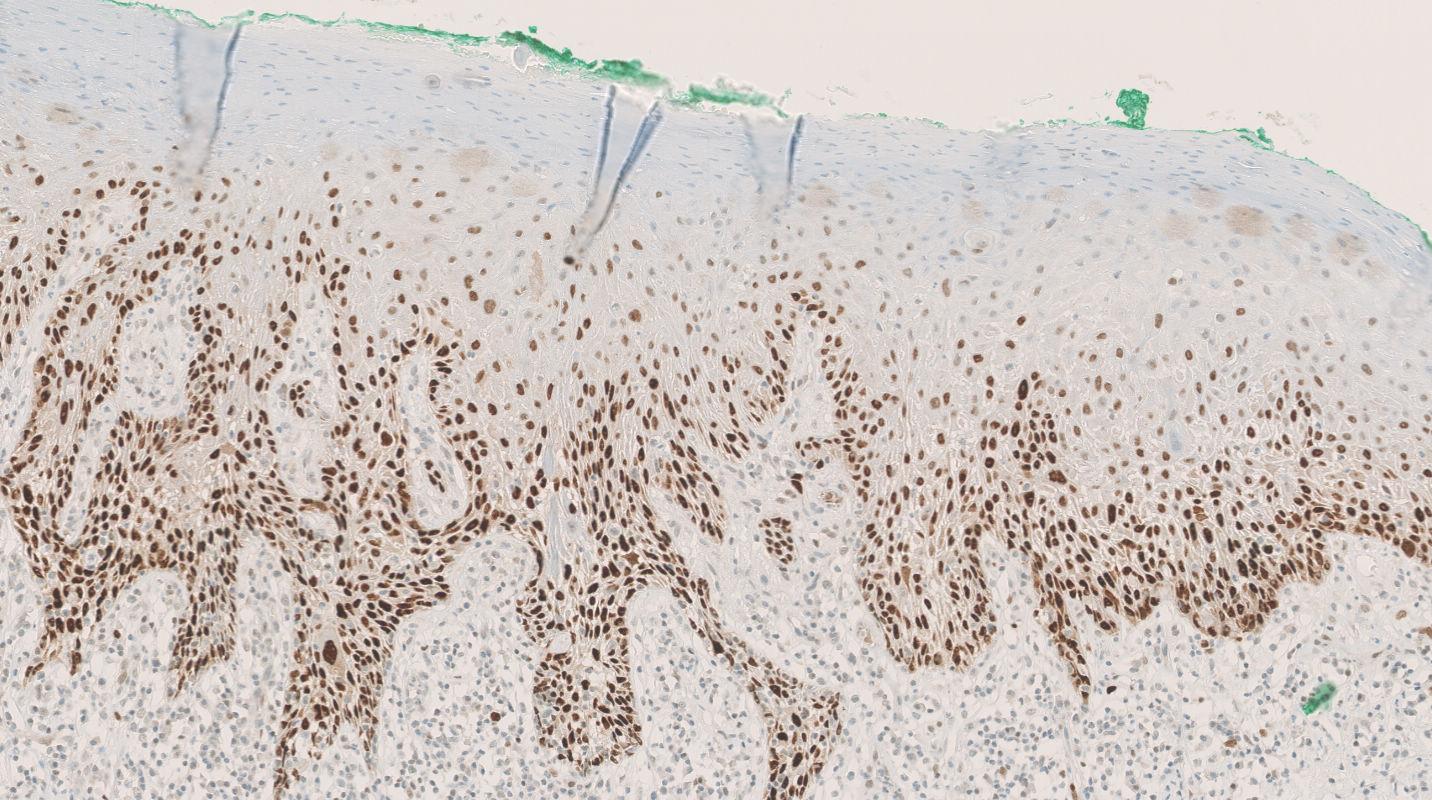
| Inflammatory band consists of predominantly lymphocytes |
| Evidence of basal cell layer degeneration (e.g., Civatte bodies, abnormal keratinocytes or basal apoptosis) |
Table 2: Summary of minimum clinicopathologic criteria to diagnose vulvar erosive lichen planus, more specific than those proposed by ISSVD (adapted from J Low Genit Tract Dis 2020;24:317)
| All 5 criteria must be present | |
| Clinical presentation (signs) | Well demarcated glazed red macule or patch located on vestibule, labia minora or vagina* |
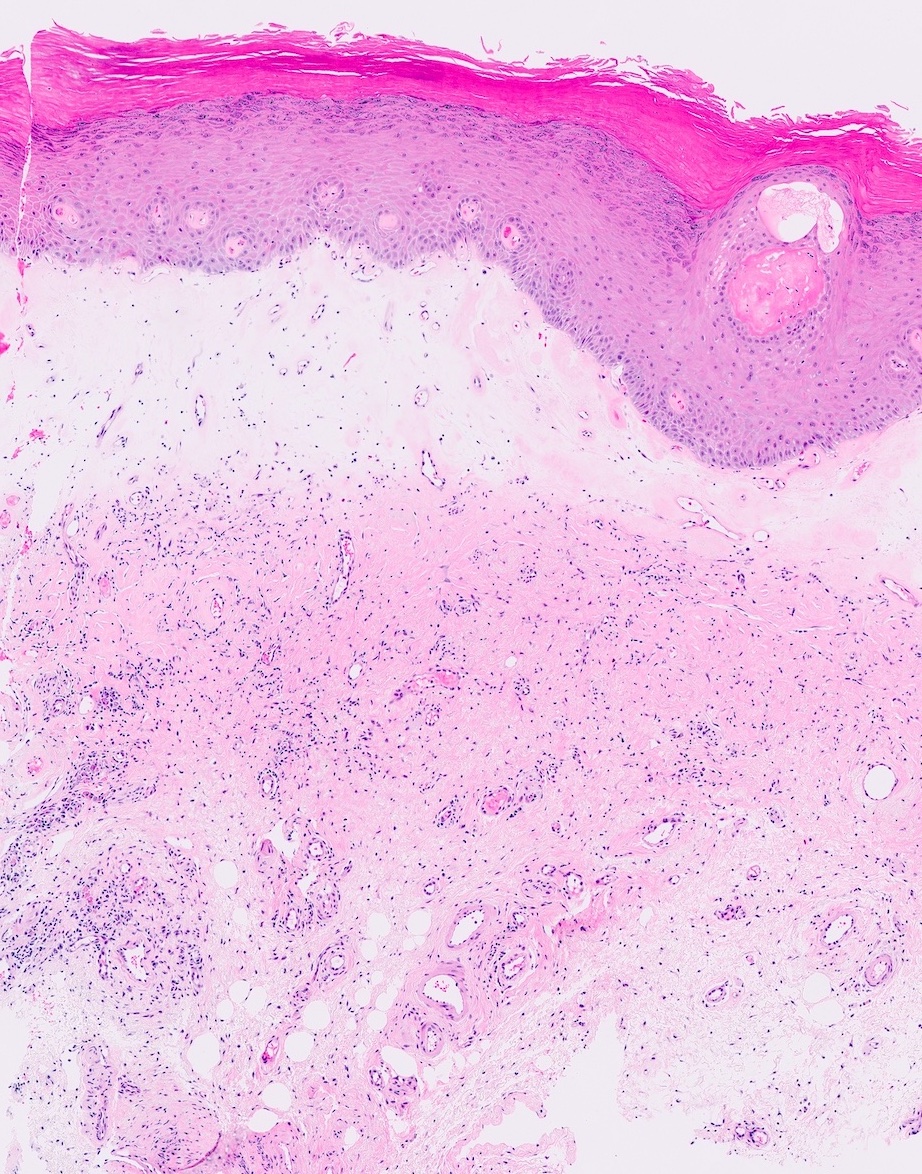
| Histopathological correlate | Nonkeratinized squamous epithelium, mucocutaneous junction or adjacent hairless skin |
| Band-like lymphocytic infiltrate abuts the epithelial layer | |
Basal layer with one of the following patterns
| |
| Sclerosis is absent | |
- *Supportive features
- Architectural changes include midline fusion or labia minora, adhesions between affected opposed structures
- Common comorbidities: lichen sclerosis (LS), other types of locations of lichen planus, systemic autoimmune diseases
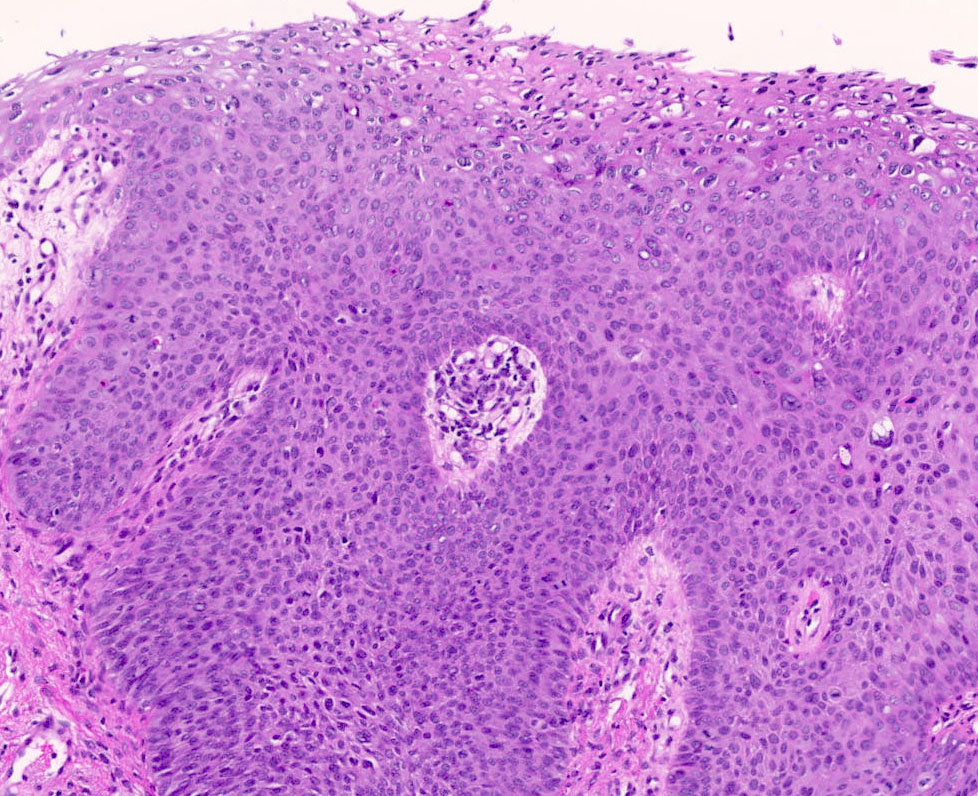
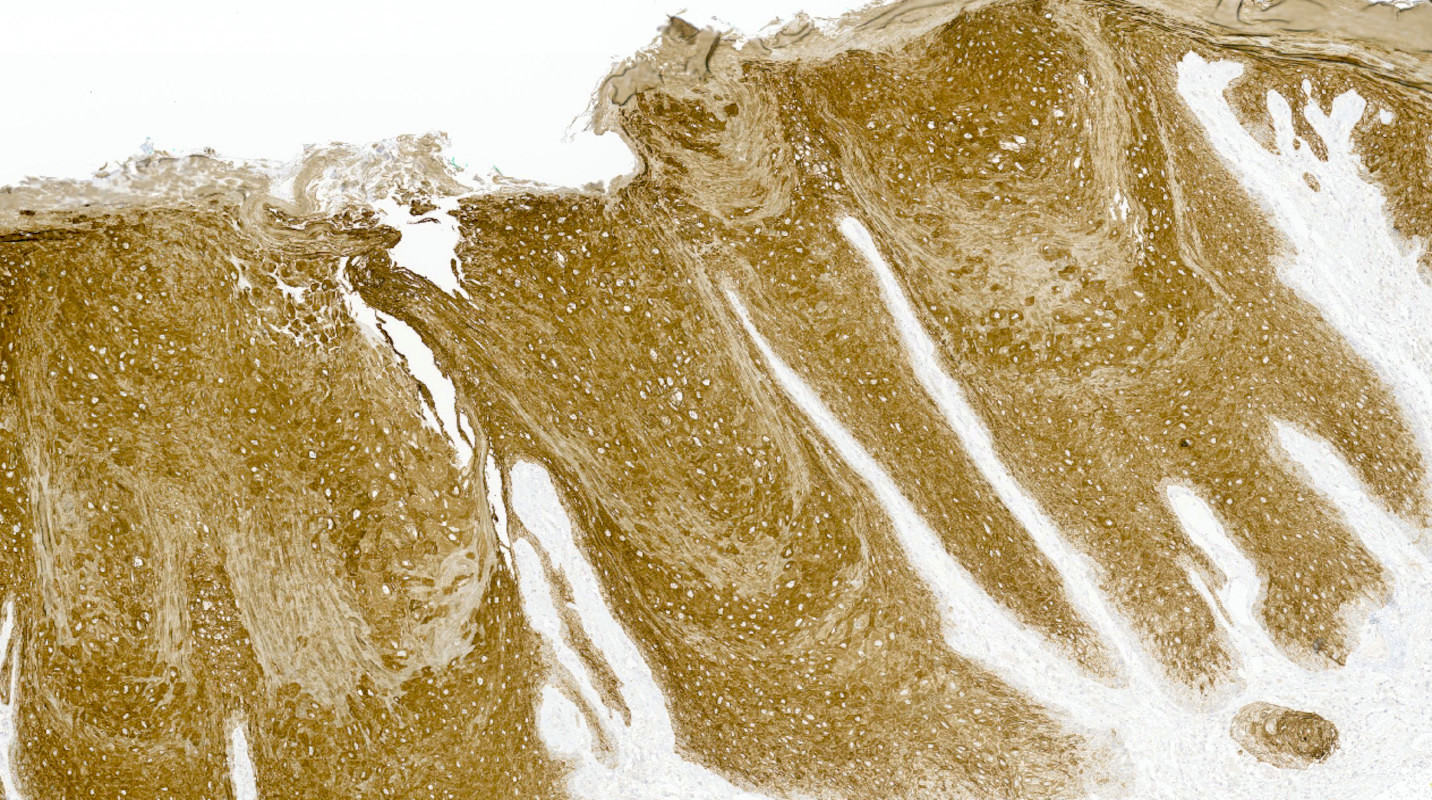
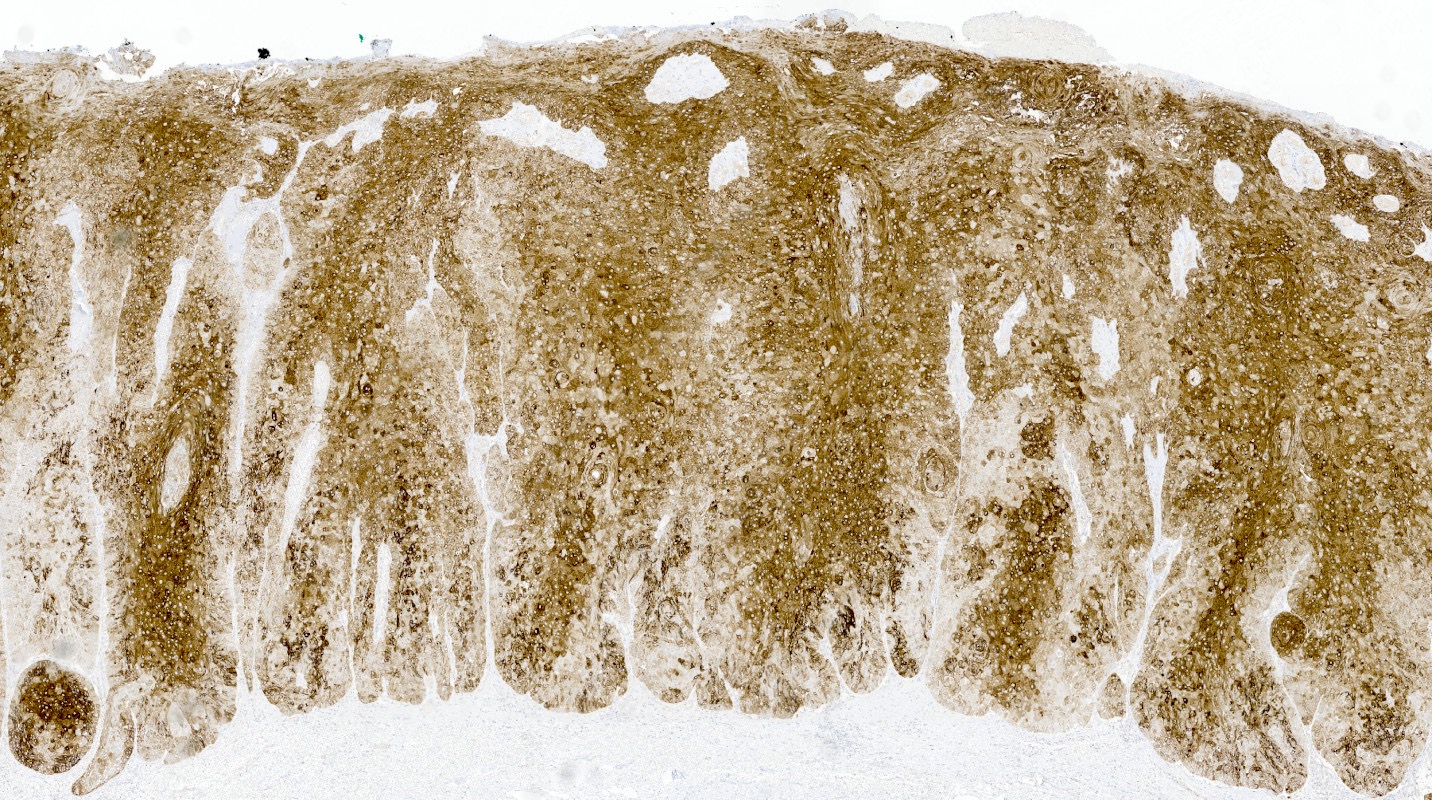
Table 3: Clinicopathologic features of classic hypertrophic lichen planus (adapted from J Low Genit Tract Dis 2020;24:317)
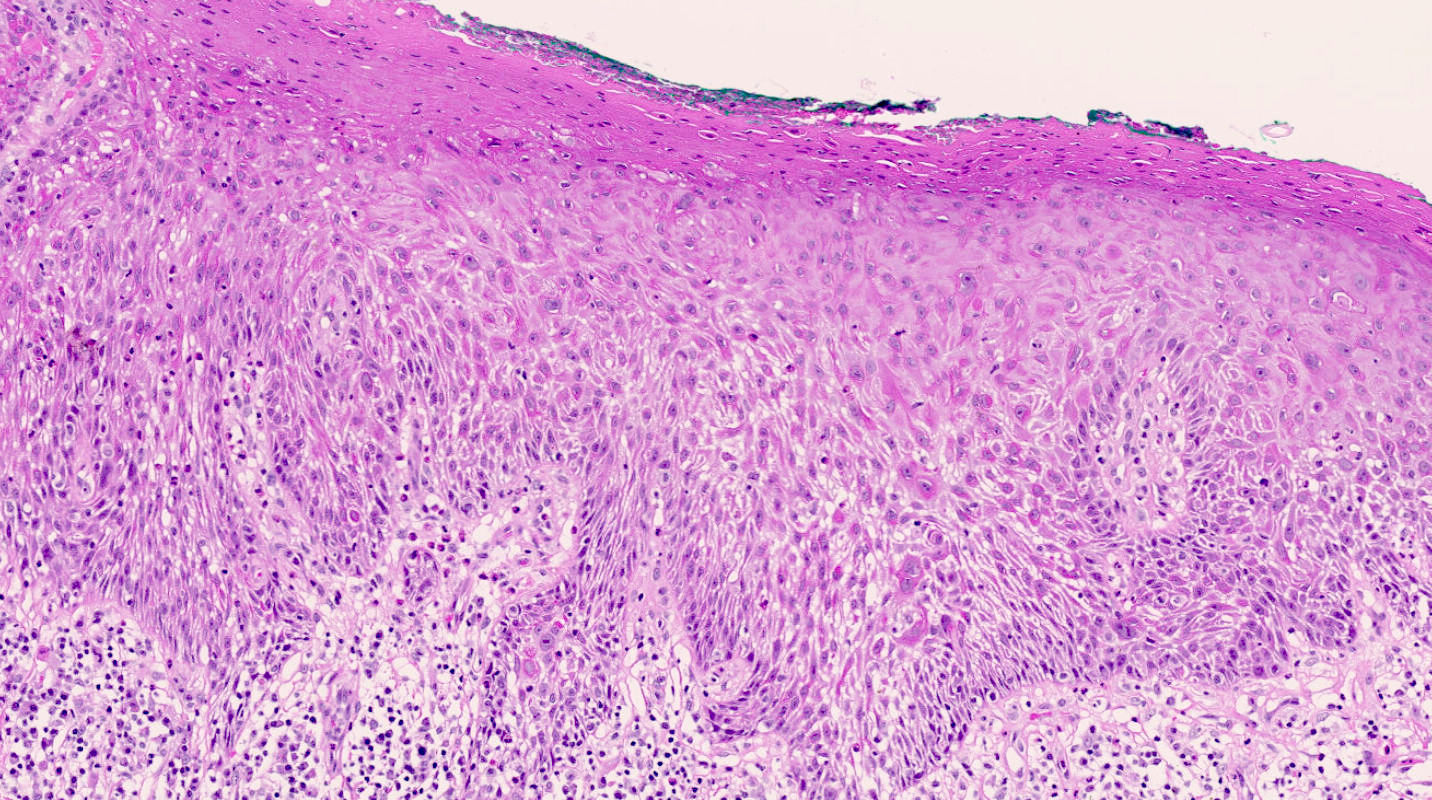
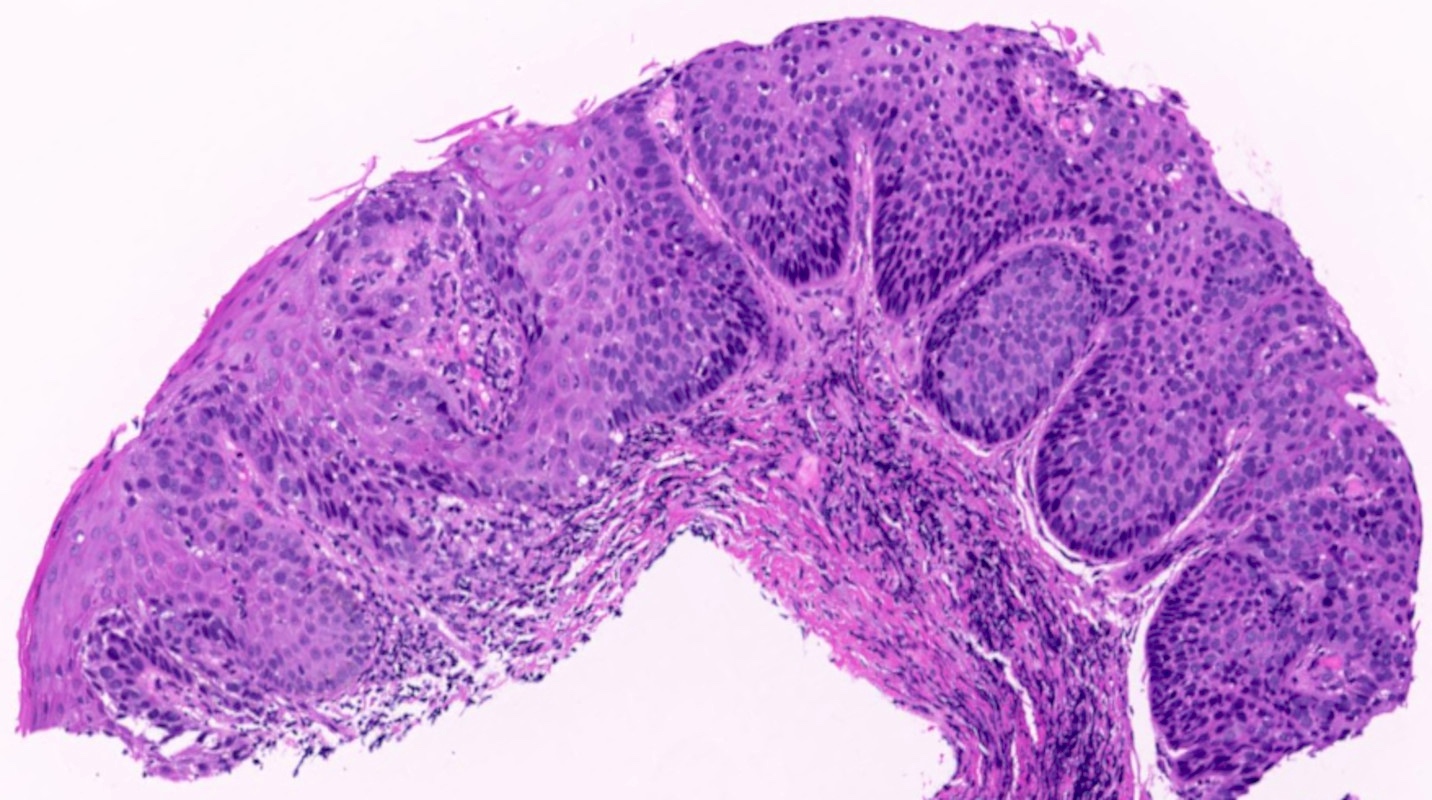
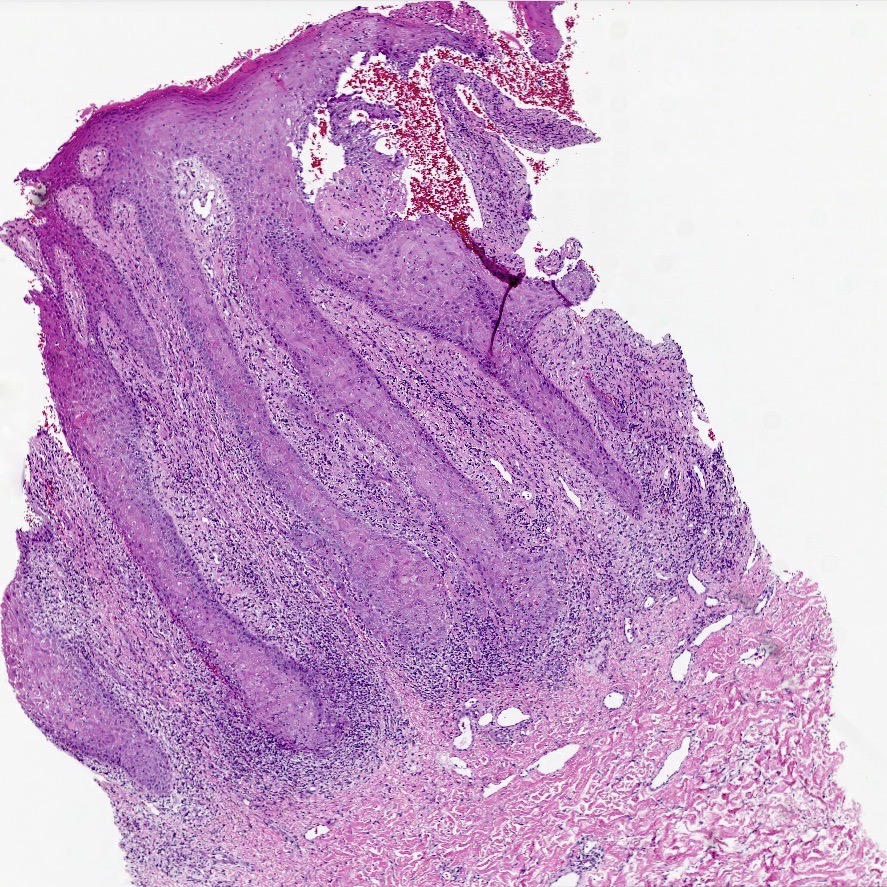
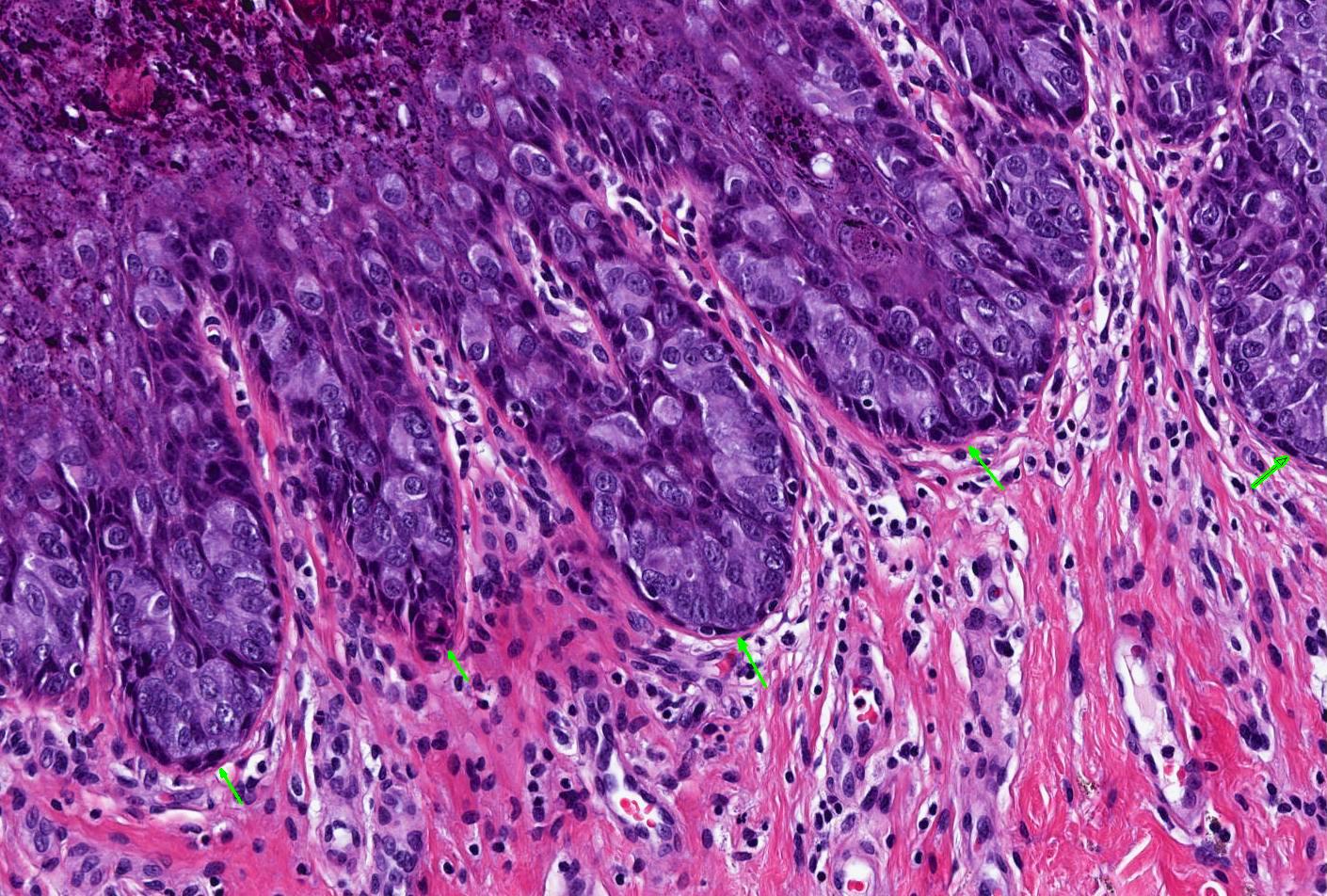
| Classic lichen planus | Hypertrophic lichen planus | |
| Clinical features | Red, gray-white or purple-brown plaque or papules on hairless or hair bearing skin | Circumferential red plaque over hairless and hair bearing skin of vulva or perianal area |
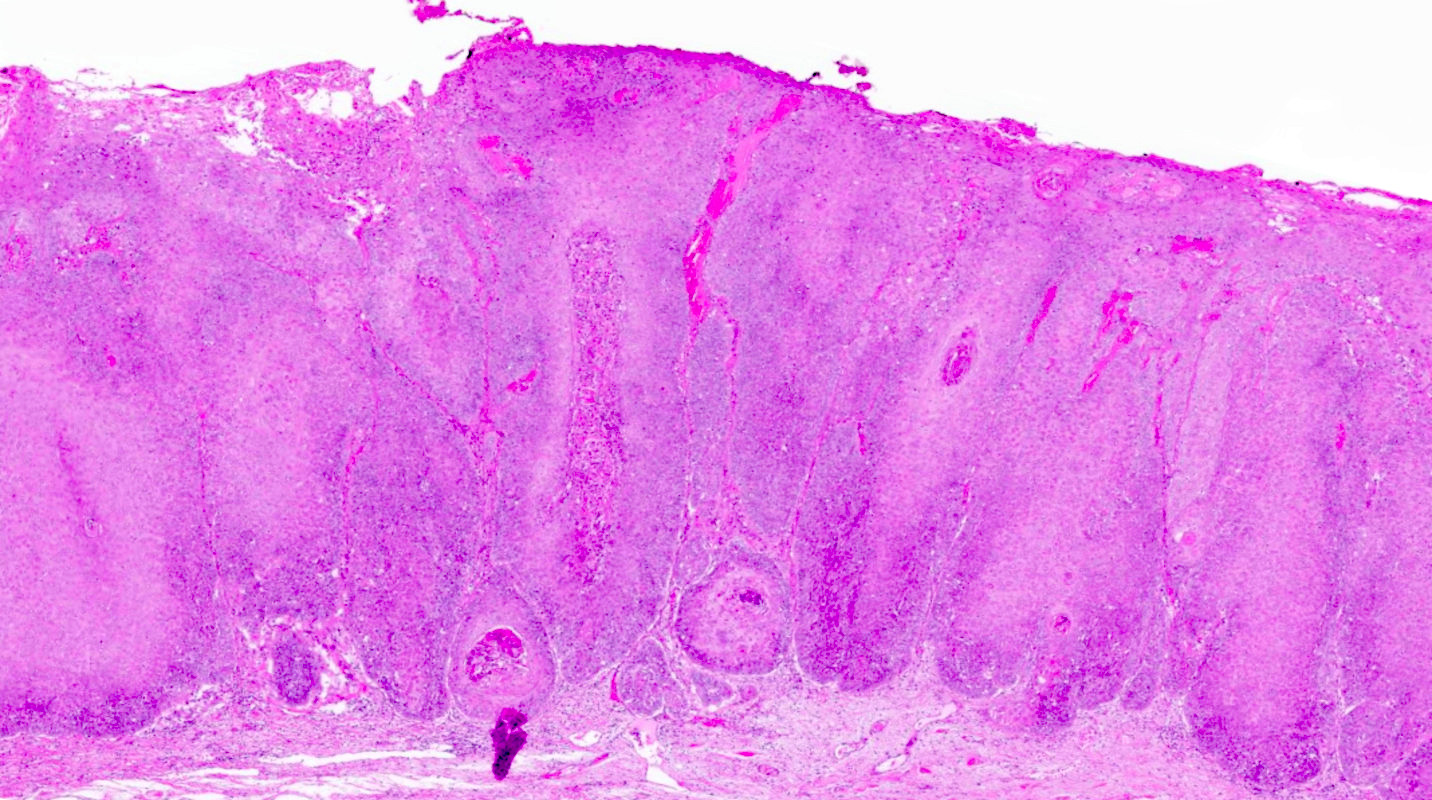
| Histopathological correlate | ||
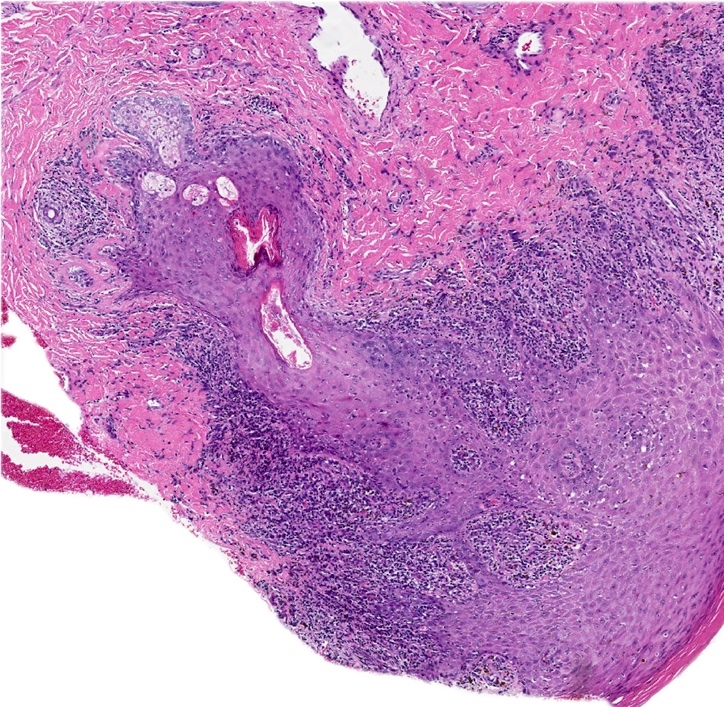
| Stratum corneum* | Hyperkeratosis | Marked hyperkeratosis |
| Granular cell layer* | Hypergranulosis | Diffuse and marked hypergranulosis |
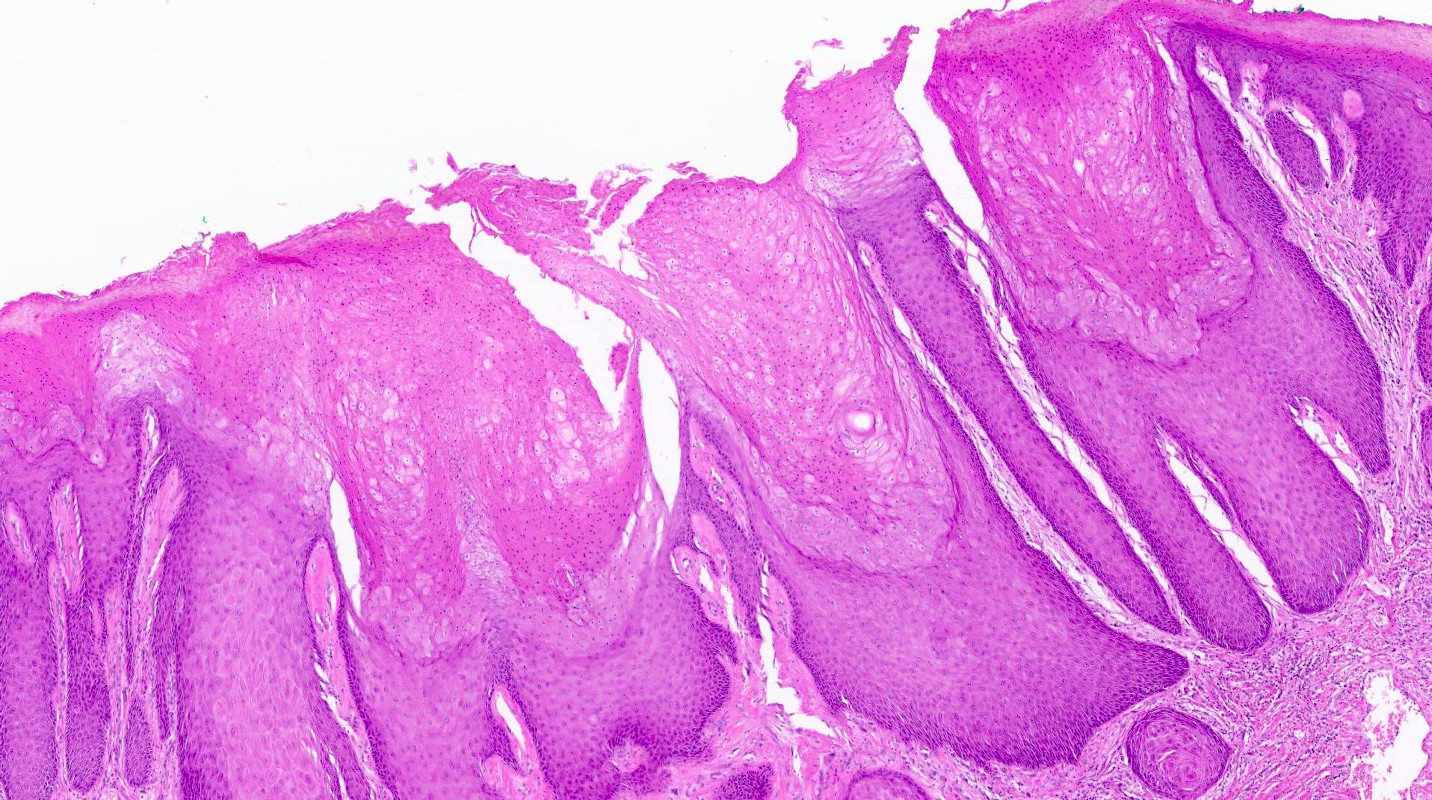
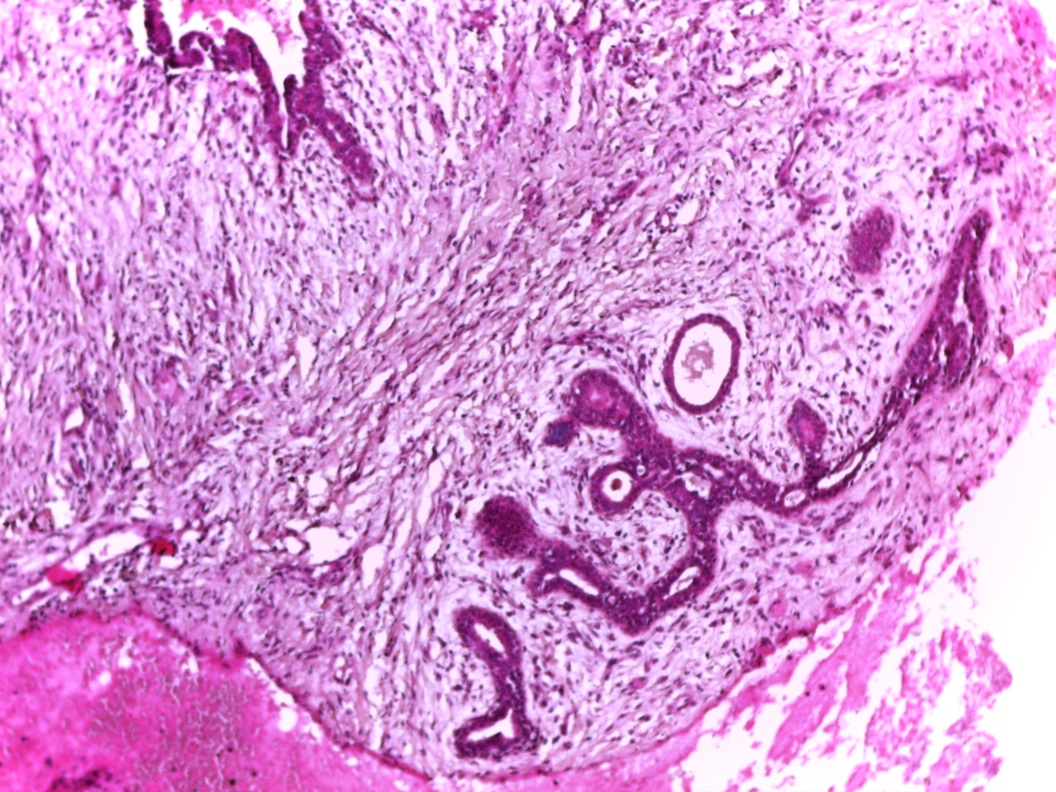
| Rete ridge morphology | Mild to moderate acanthosis with irregular rete ridges, often sawtoothed or spiky | Marked acanthosis with deep and irregular rete ridges |
| Basal layer | Apoptotic bodies, squamatization, vacuolar change Lymphocytosis | Apoptotic bodies, squamatization, vacuolar change may be confined to rete tips / basal layer above papillary processes
Lymphocytosis |
| Dermis | Band-like applied lymphocytic infiltrate | |
| Papillary dermal fibrosis | ||
- *May be altered by excoriation, especially in hypertrophic lichen planus
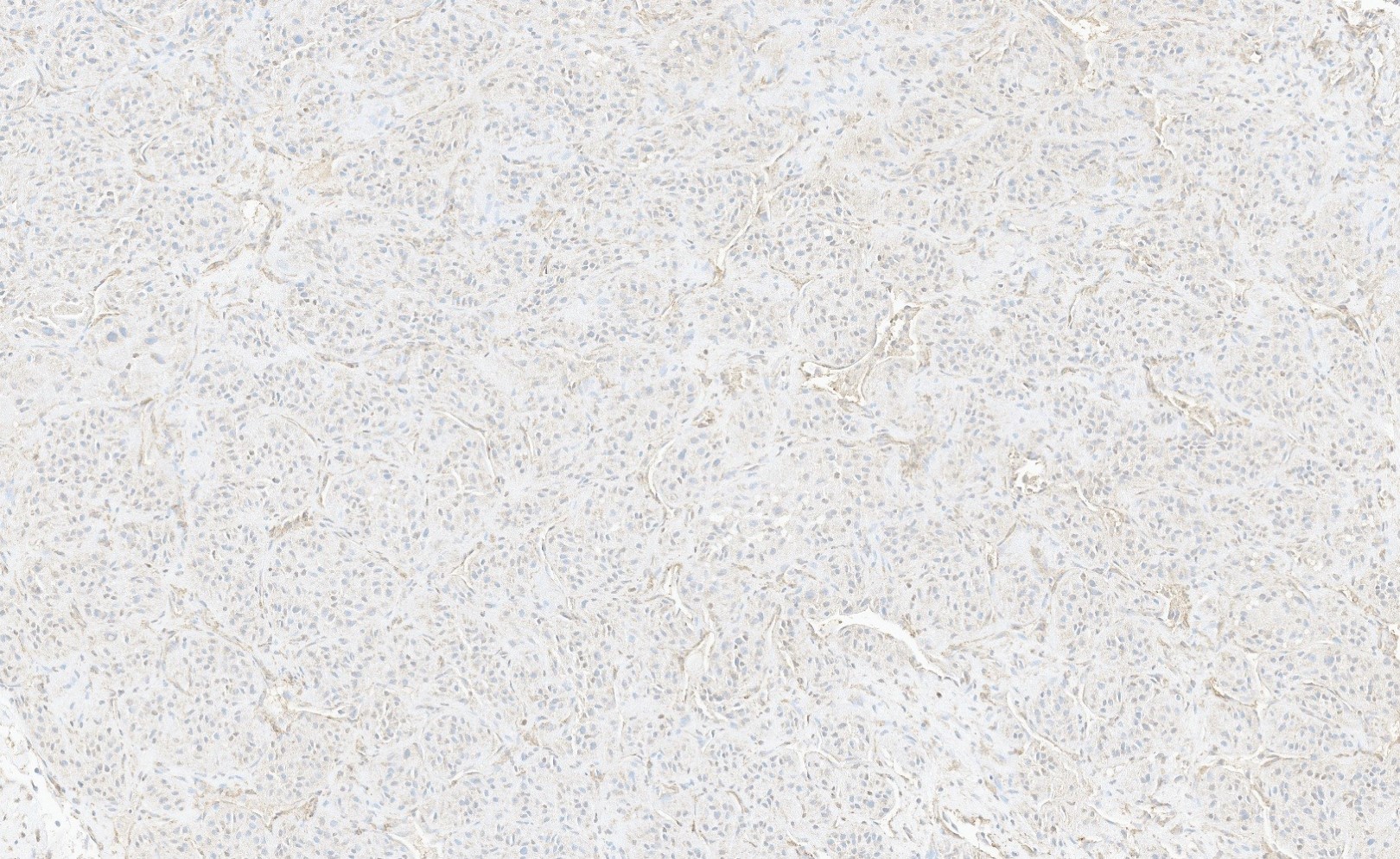
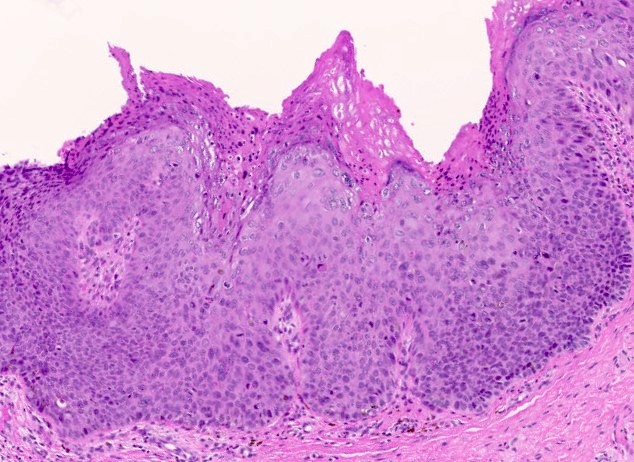
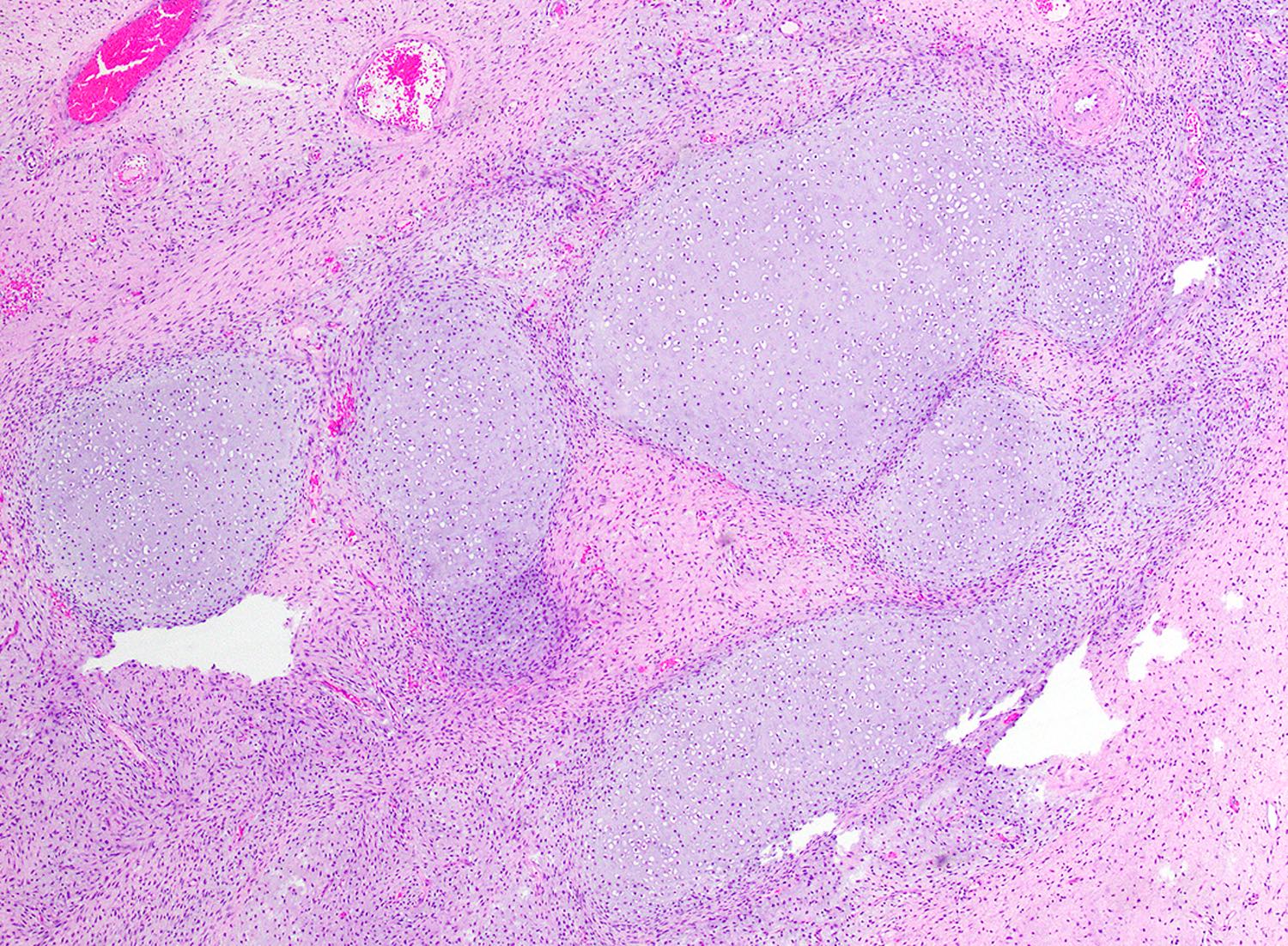
Lichen planus & hypertrophic lichen planus
Hypertrophic lichen planus: 5 minute pathology pearls
Lichen planus
Introduction to lichen sclerosus
Contributed by Anna Sarah Erem, M.D., Gulisa Turashvili, M.D., Ph.D. and Priya Nagarajan, M.D., Ph.D.
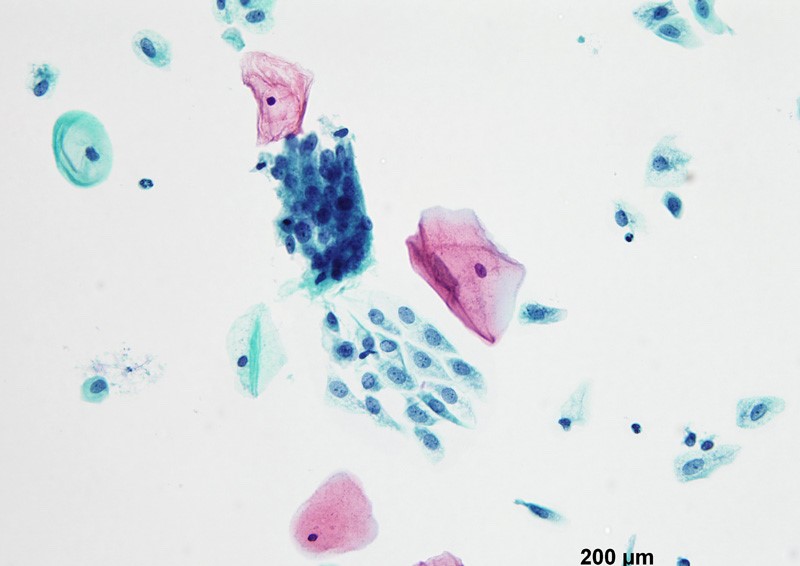
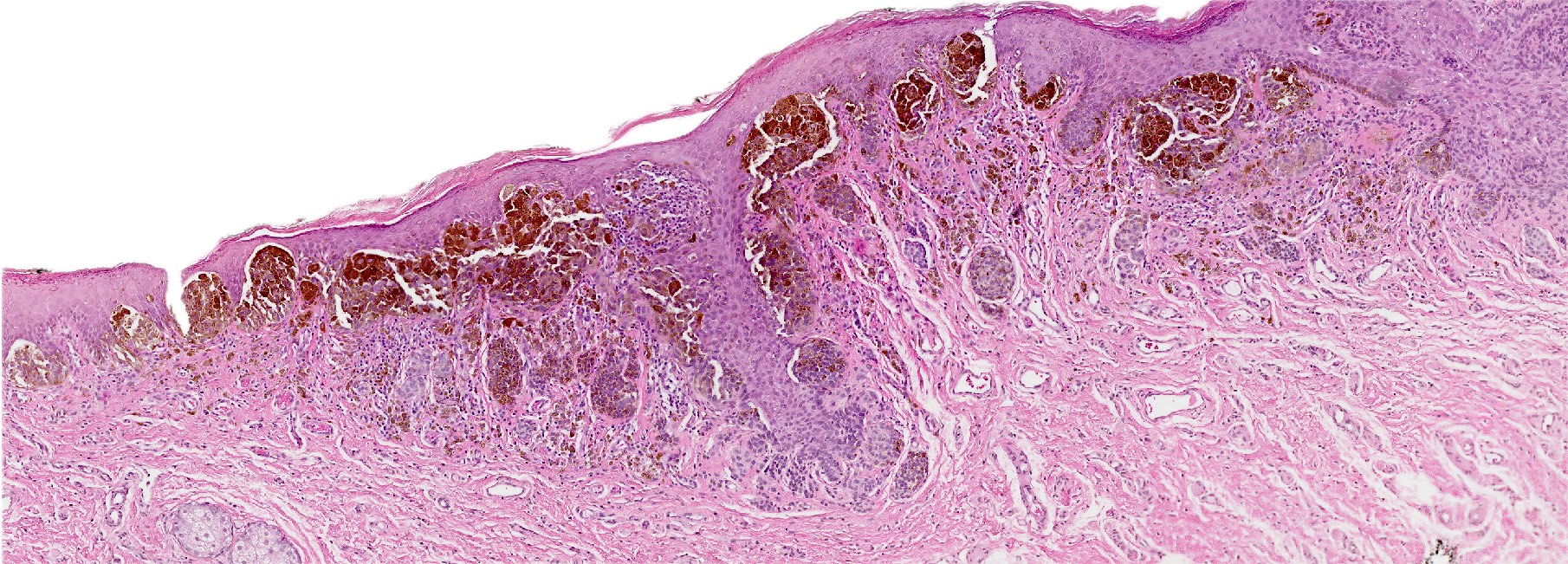
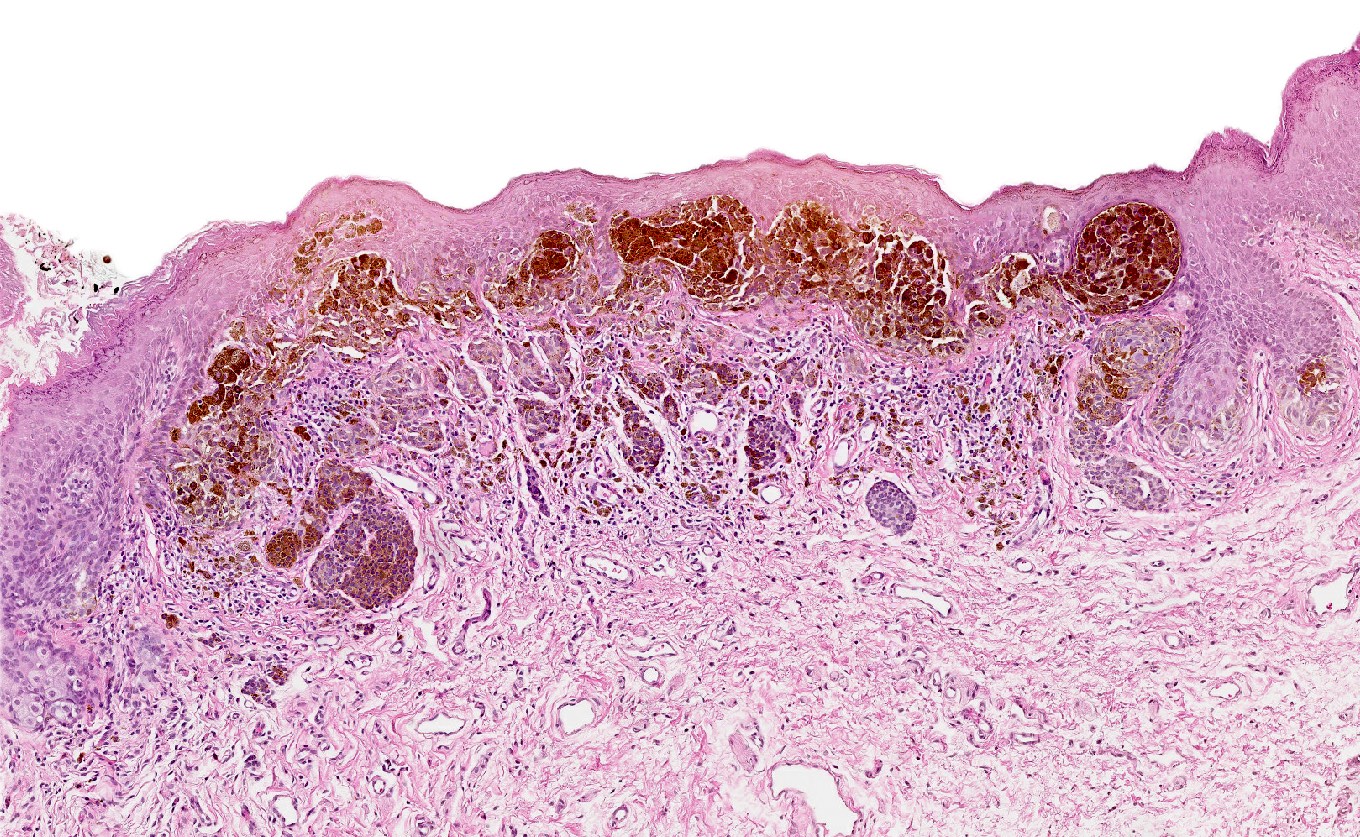
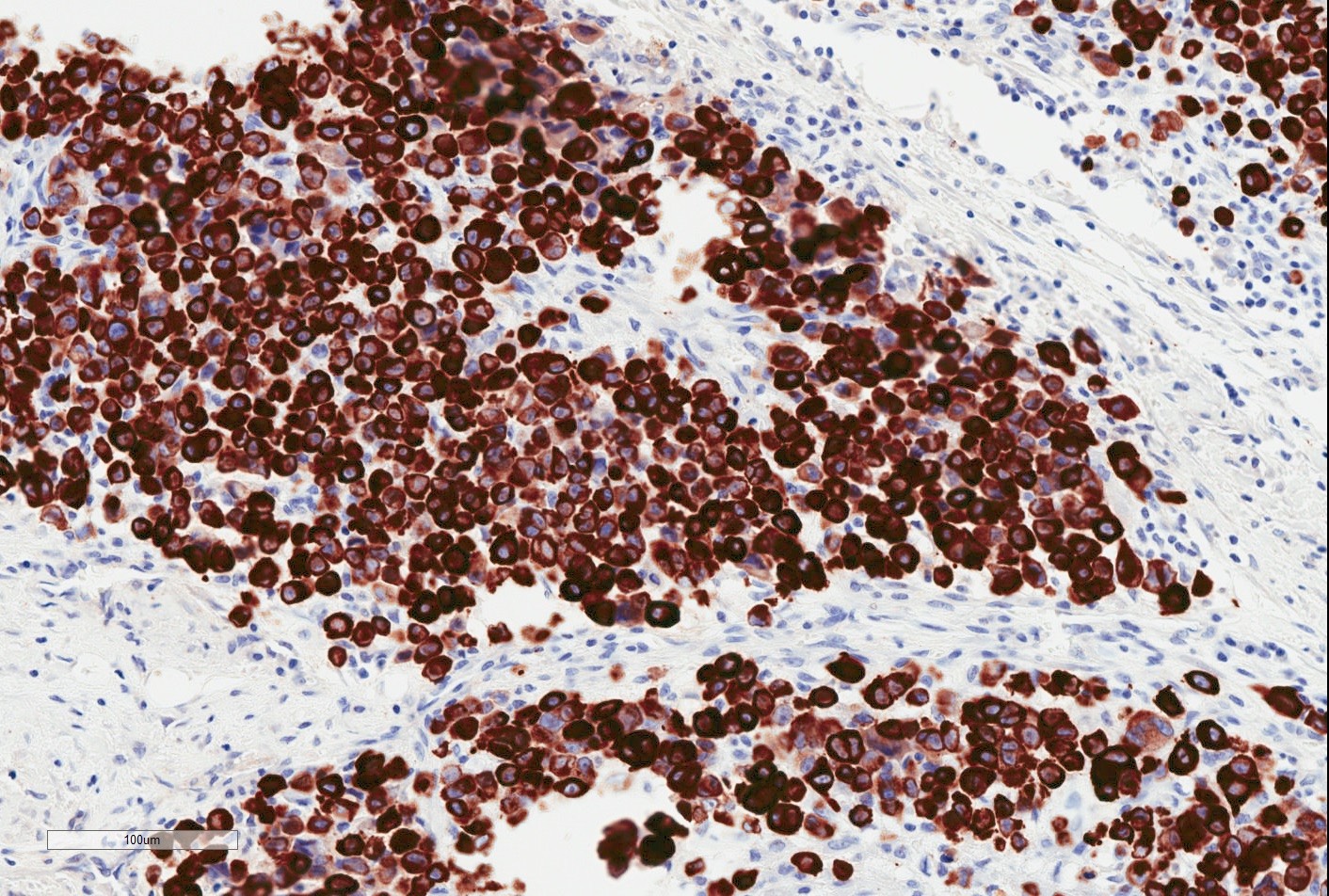
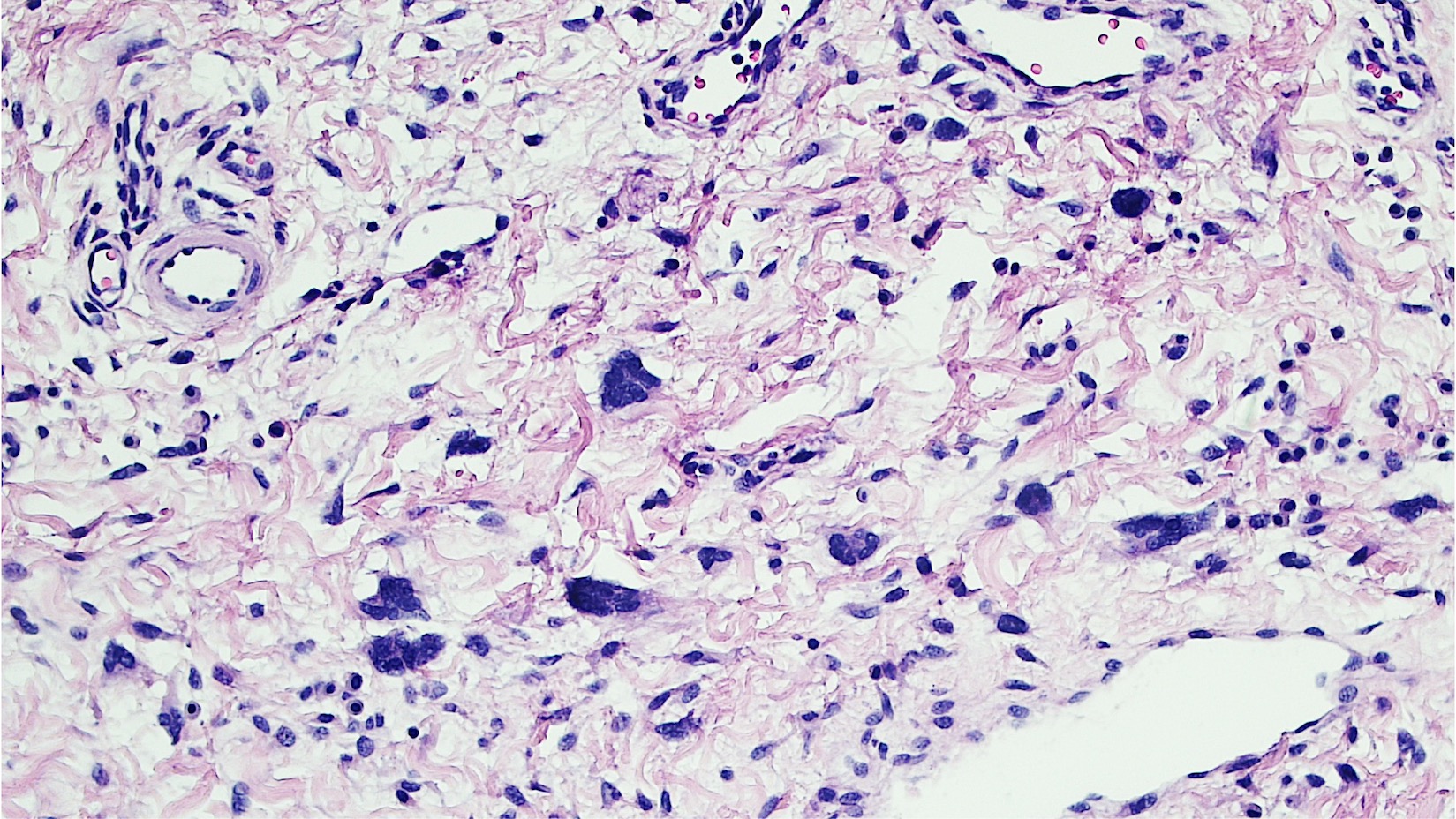
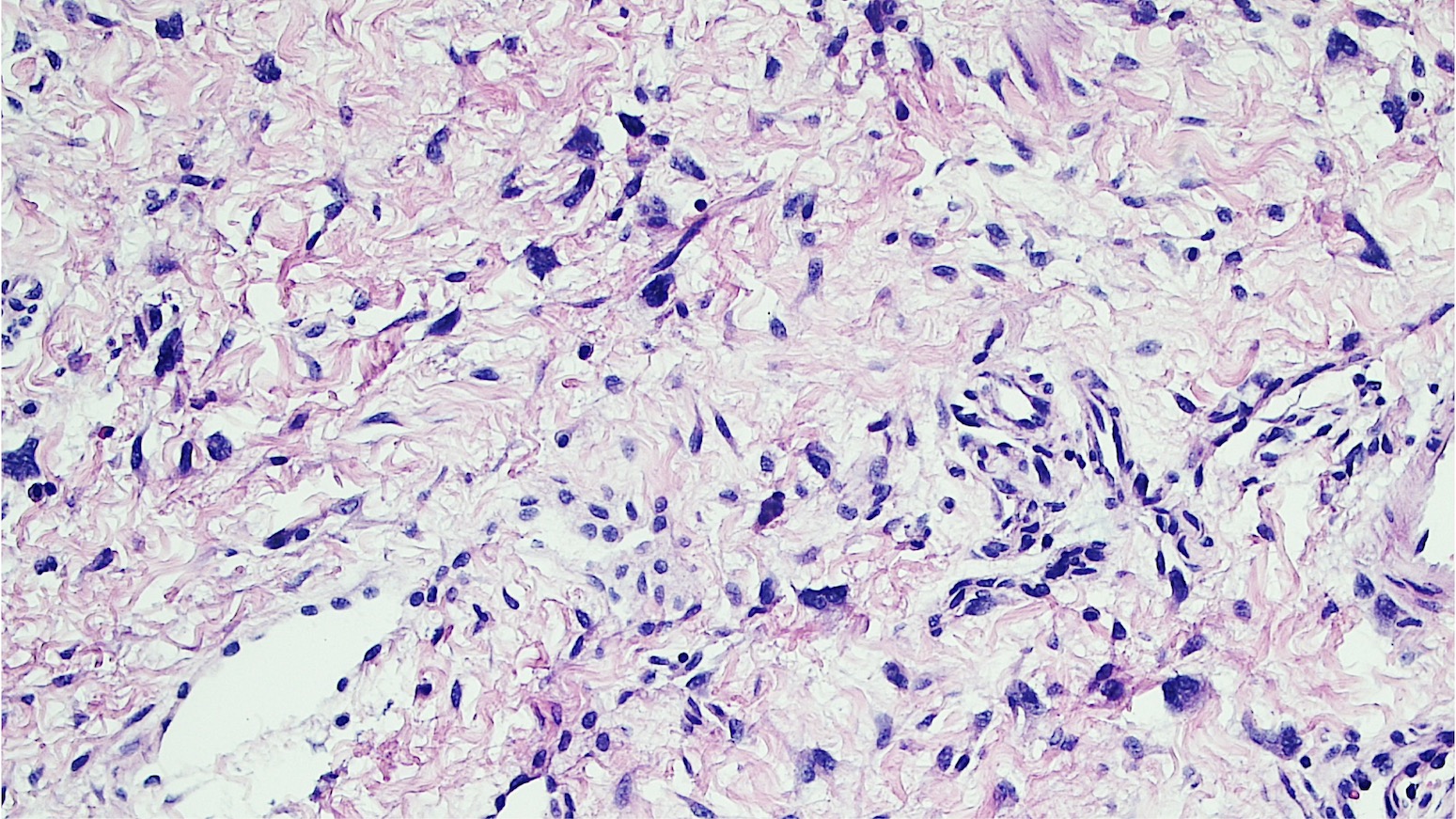
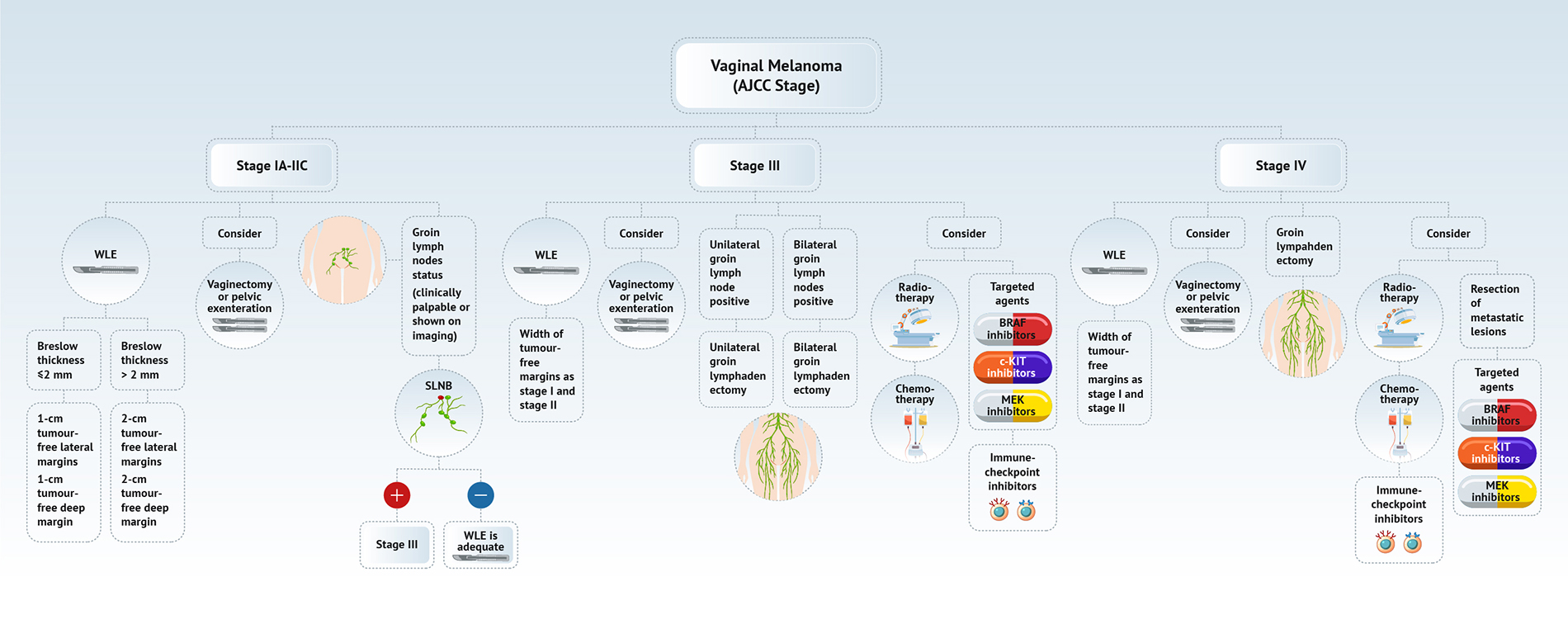
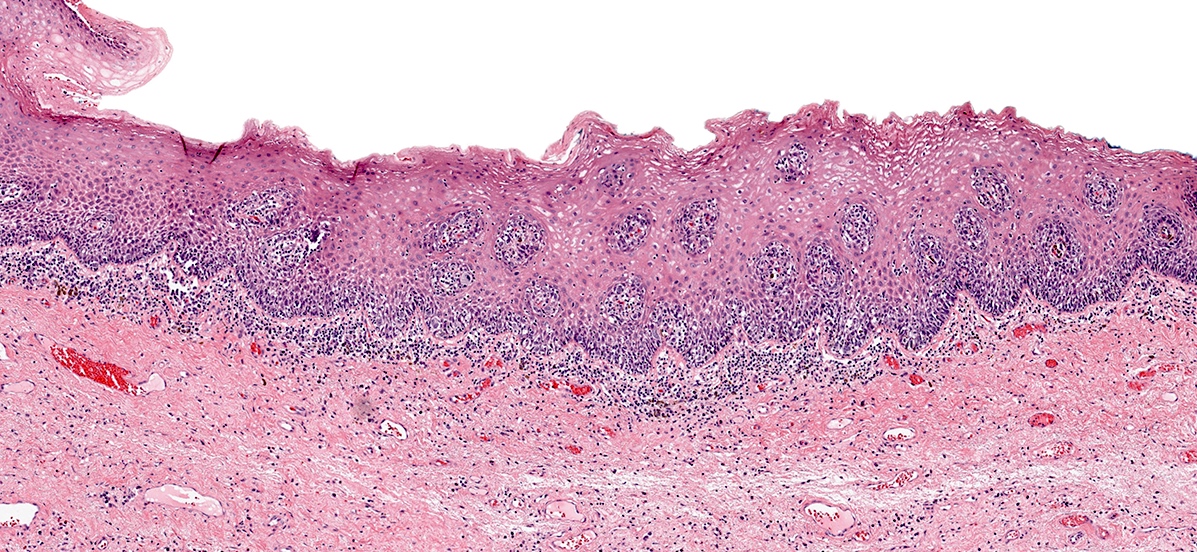
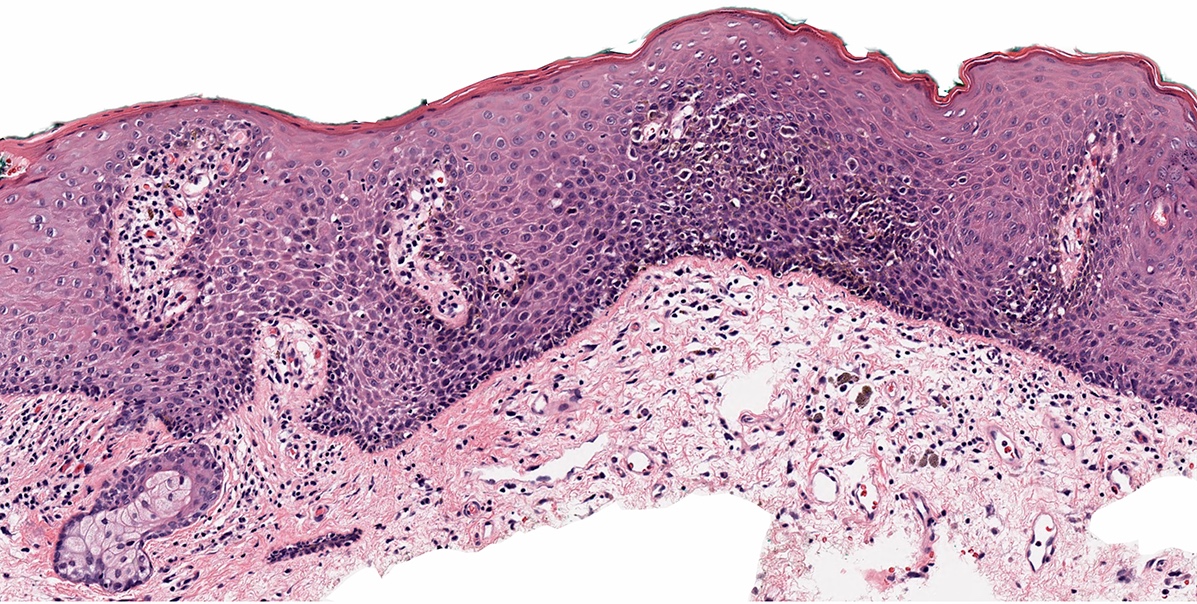
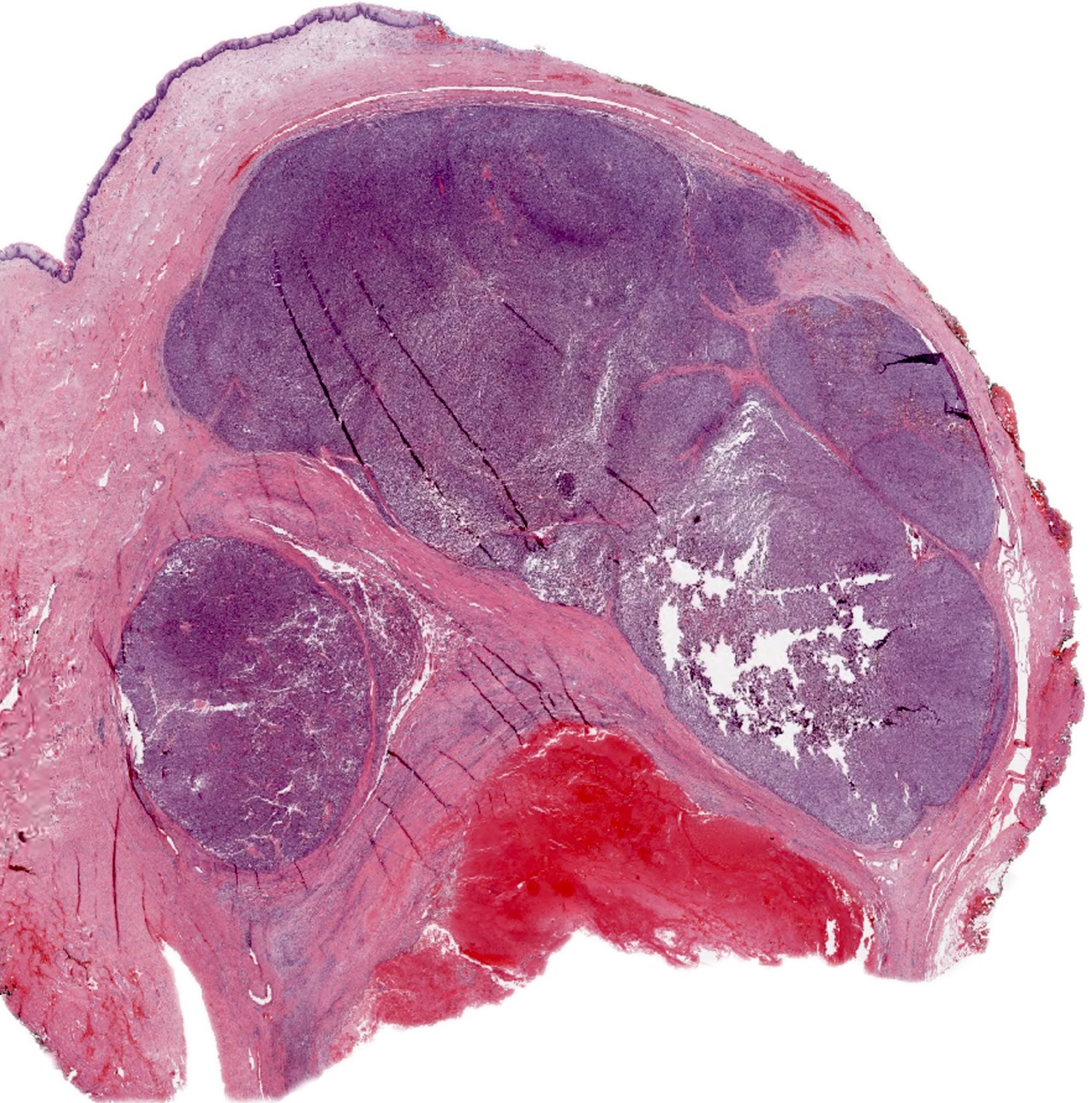
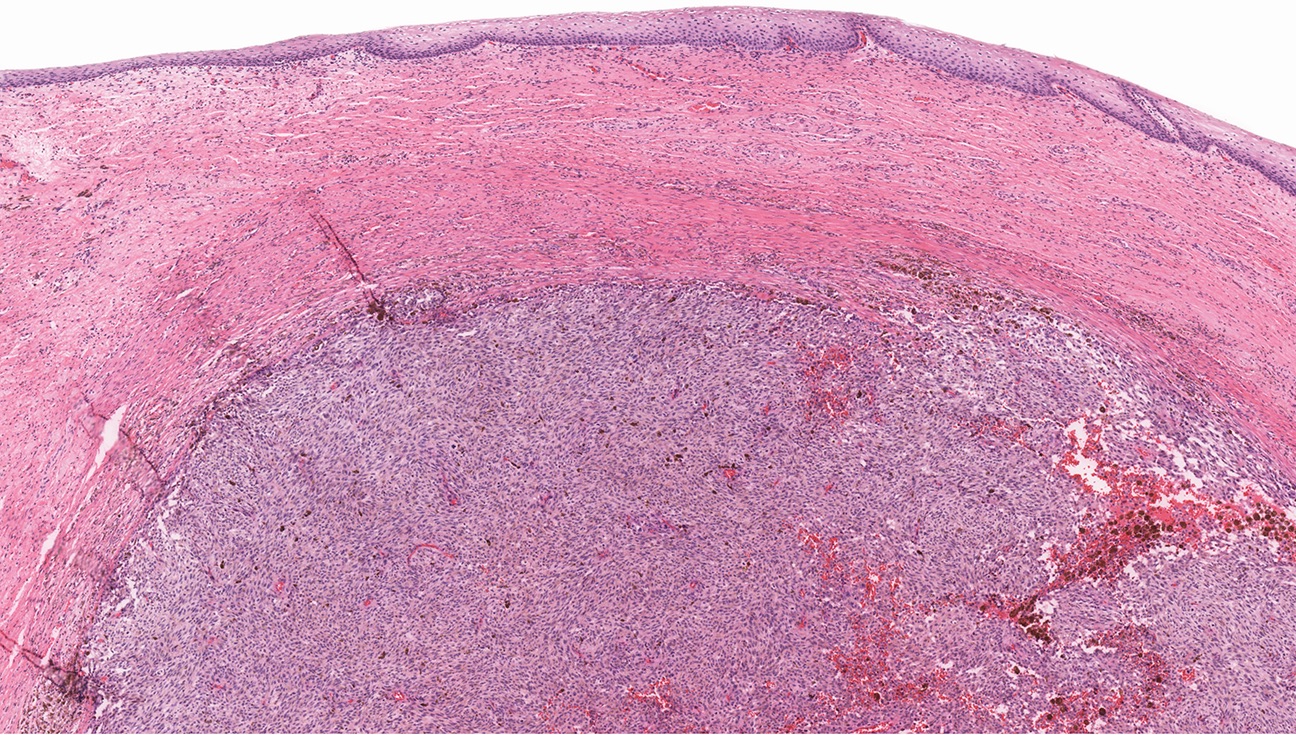
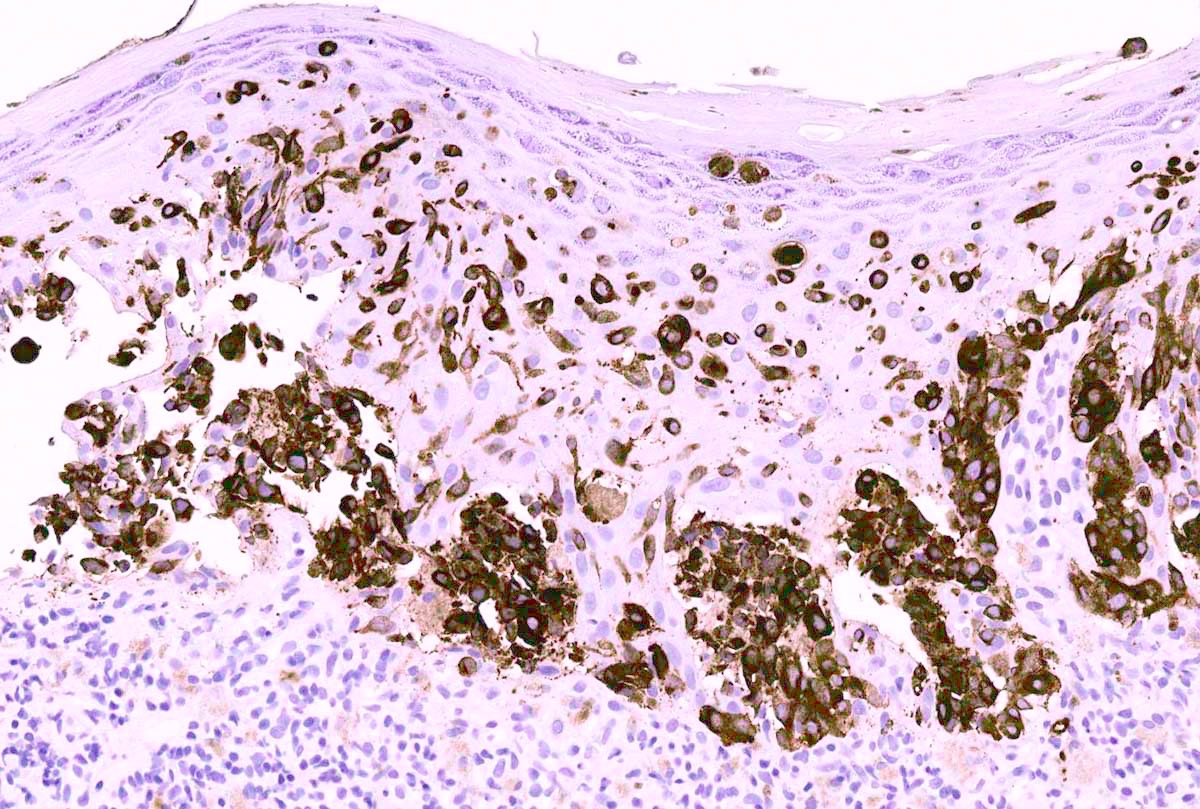
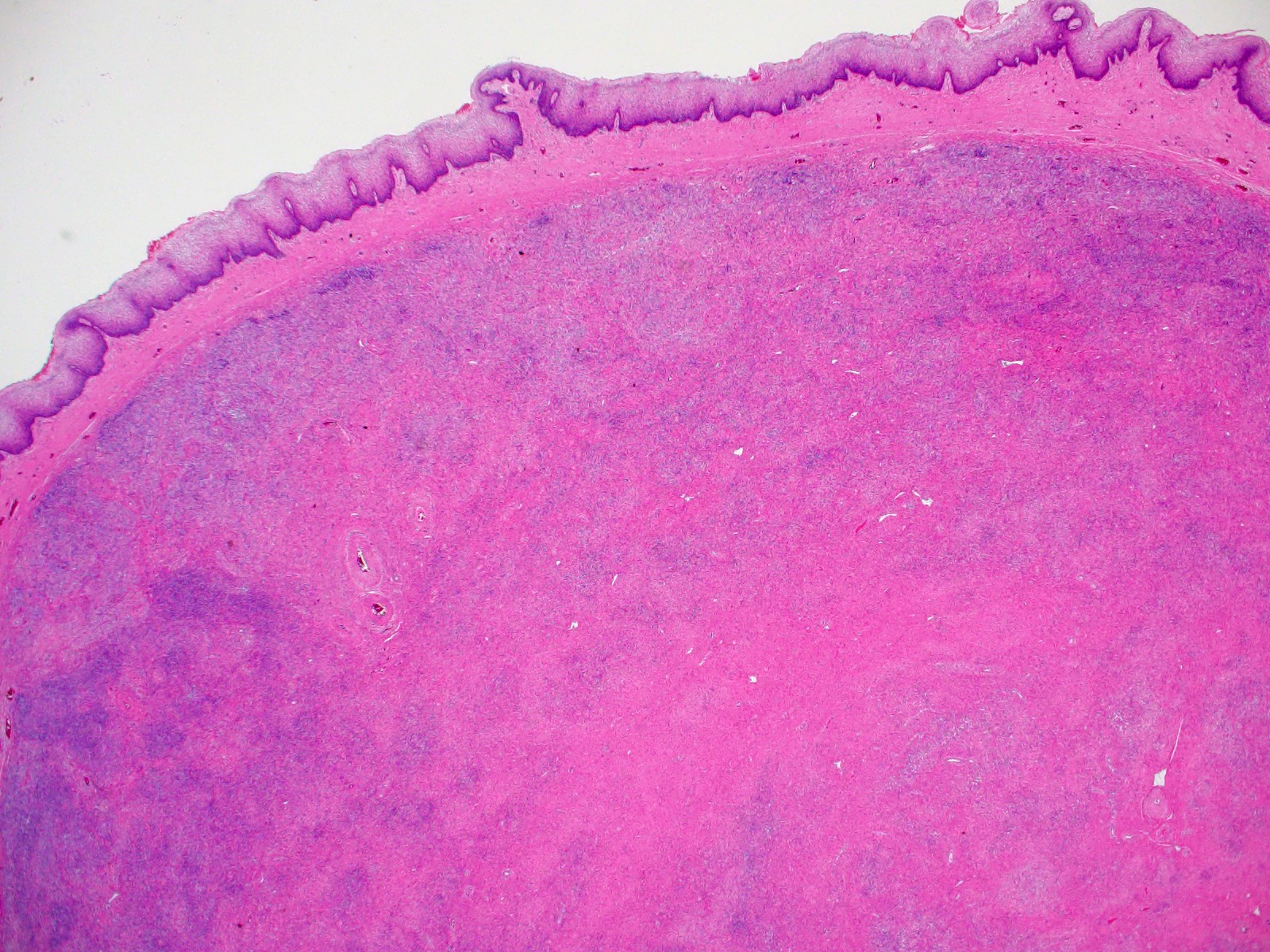
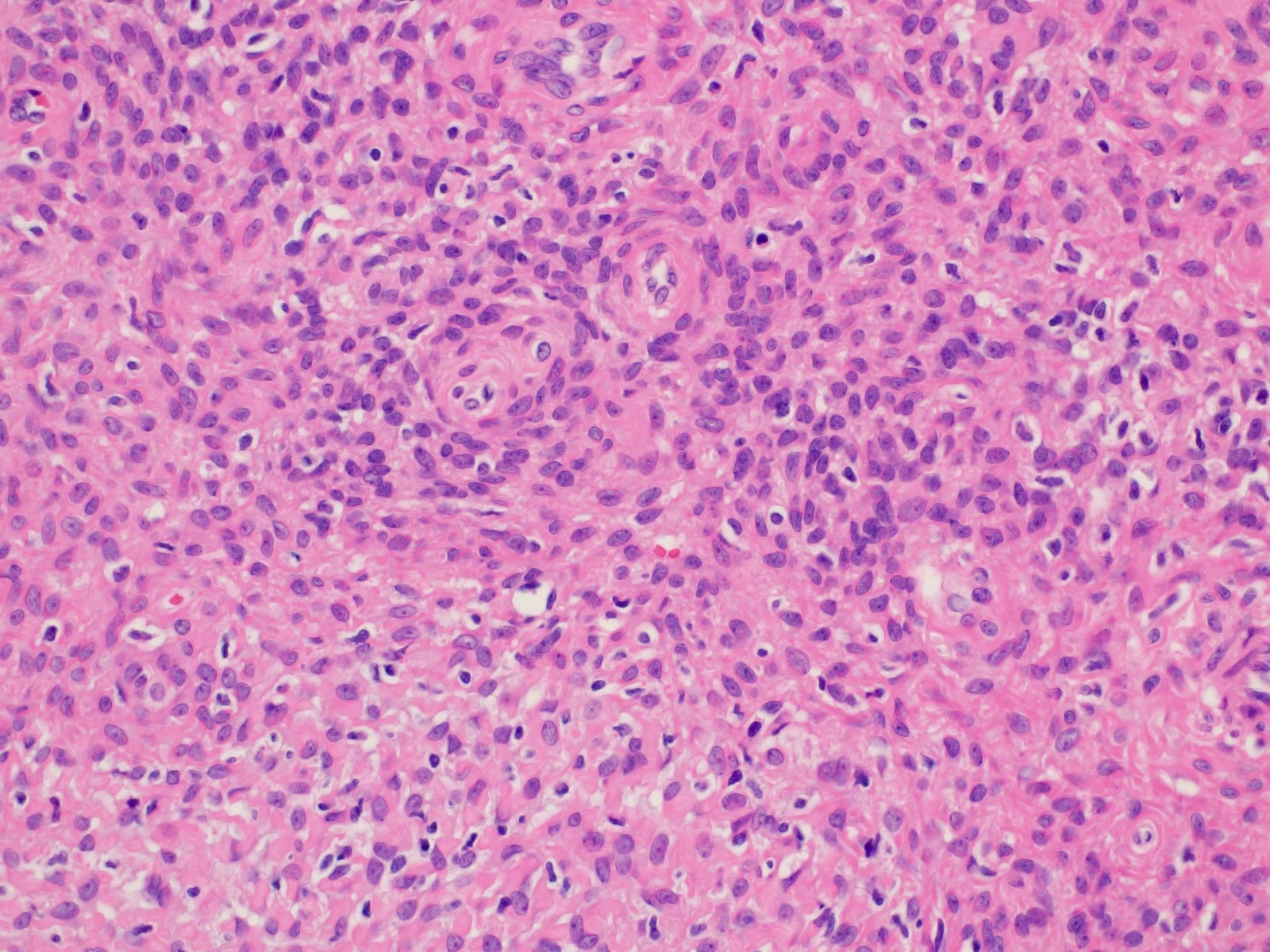
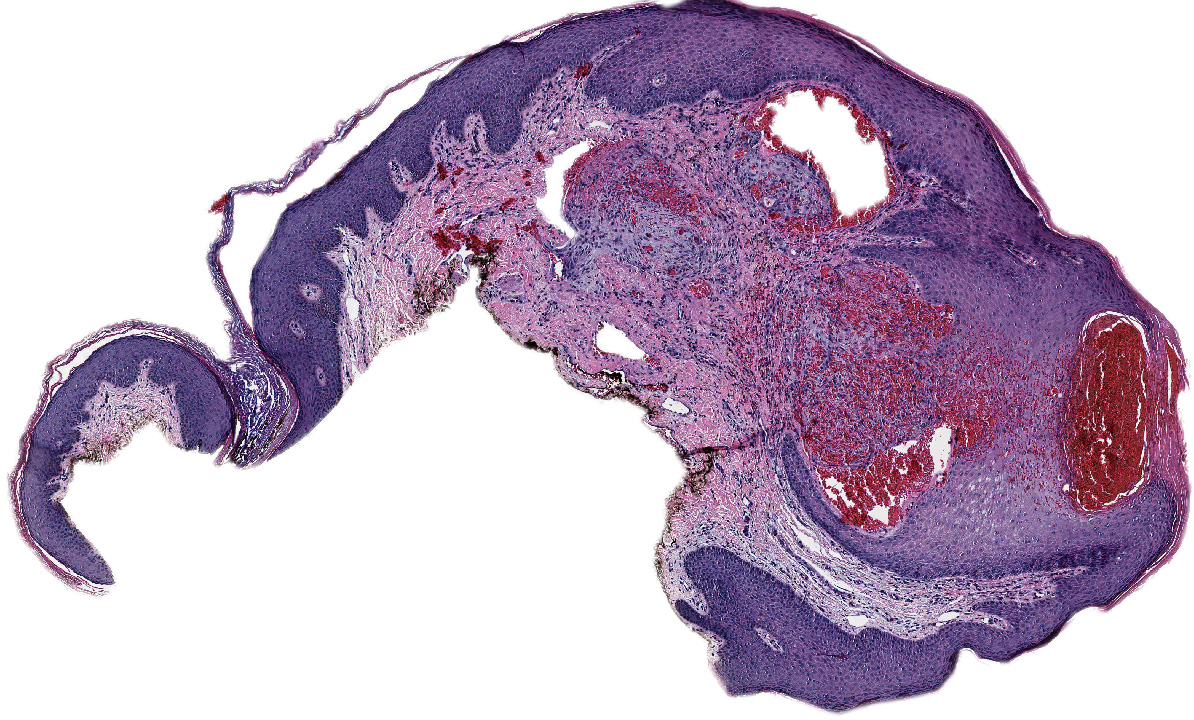
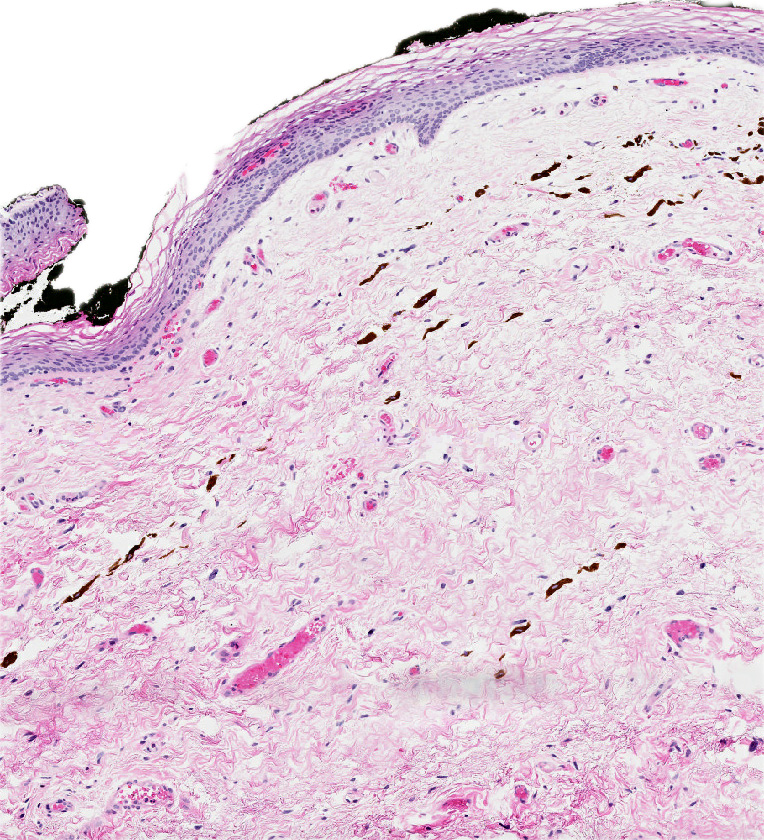
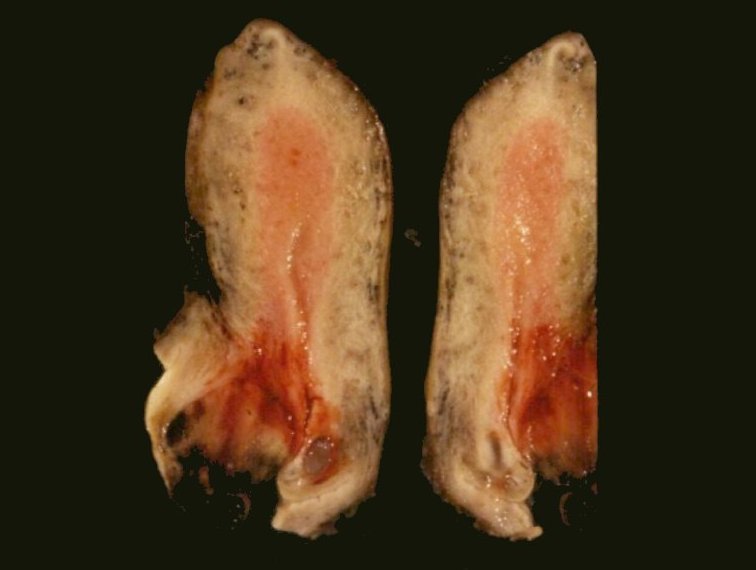
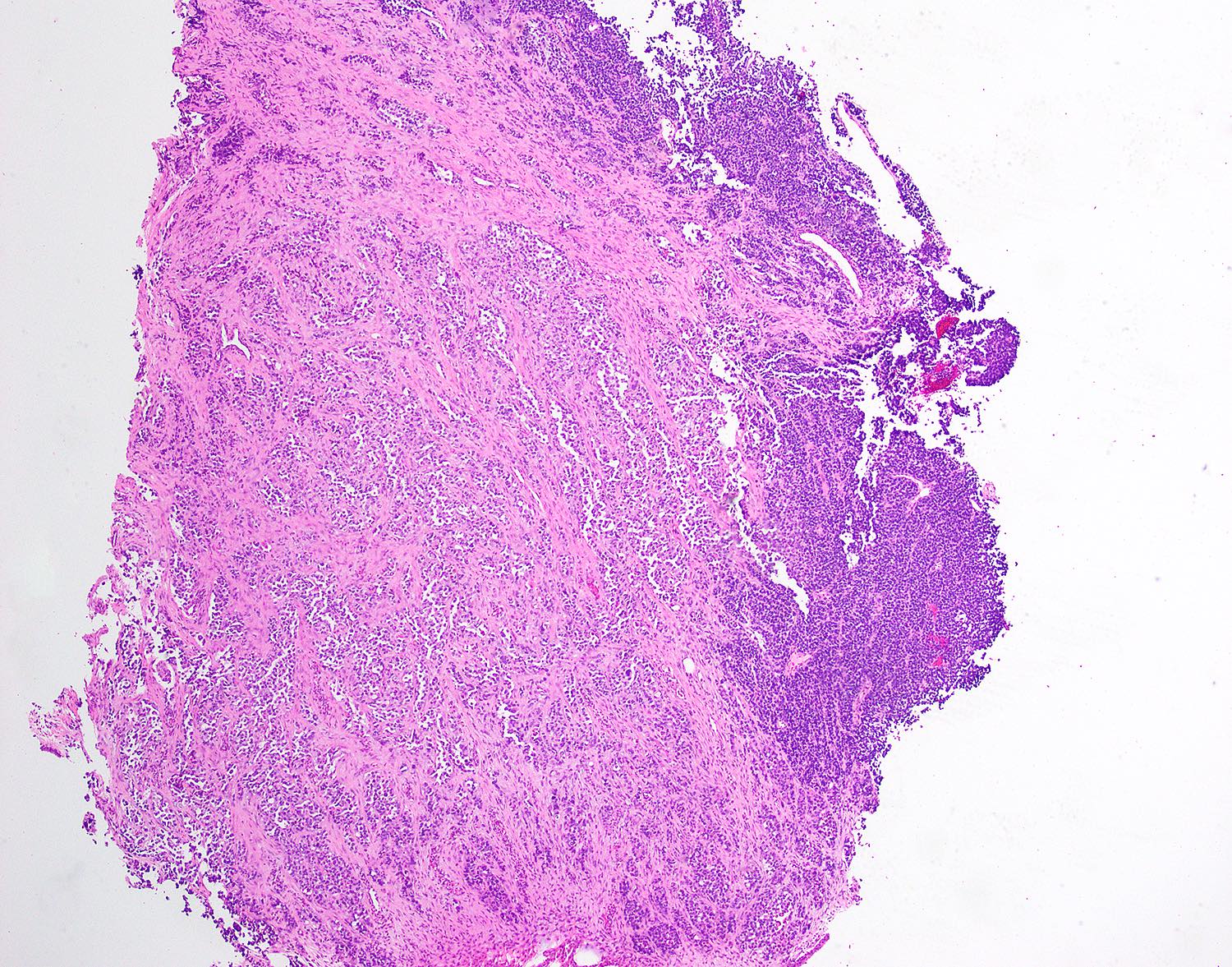
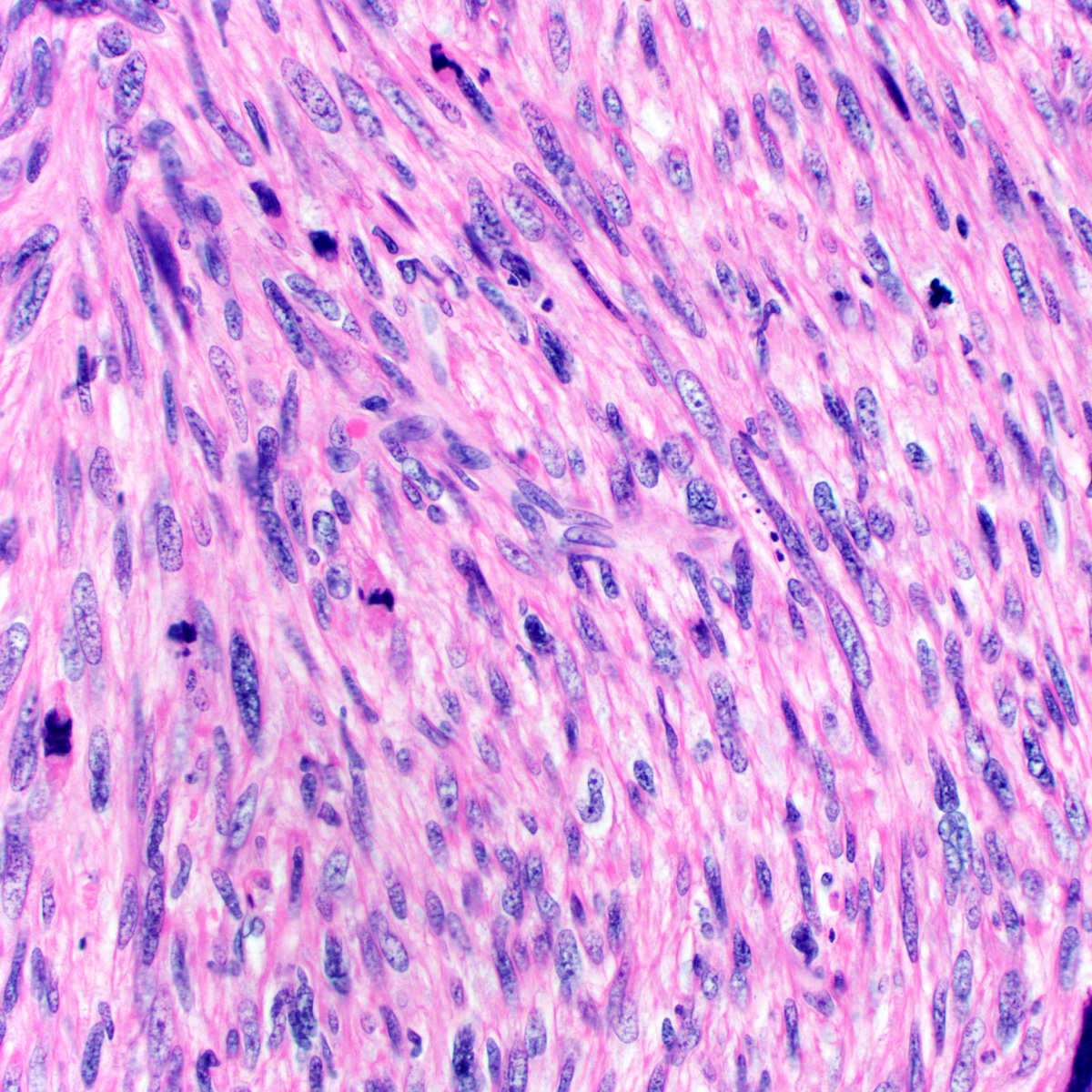
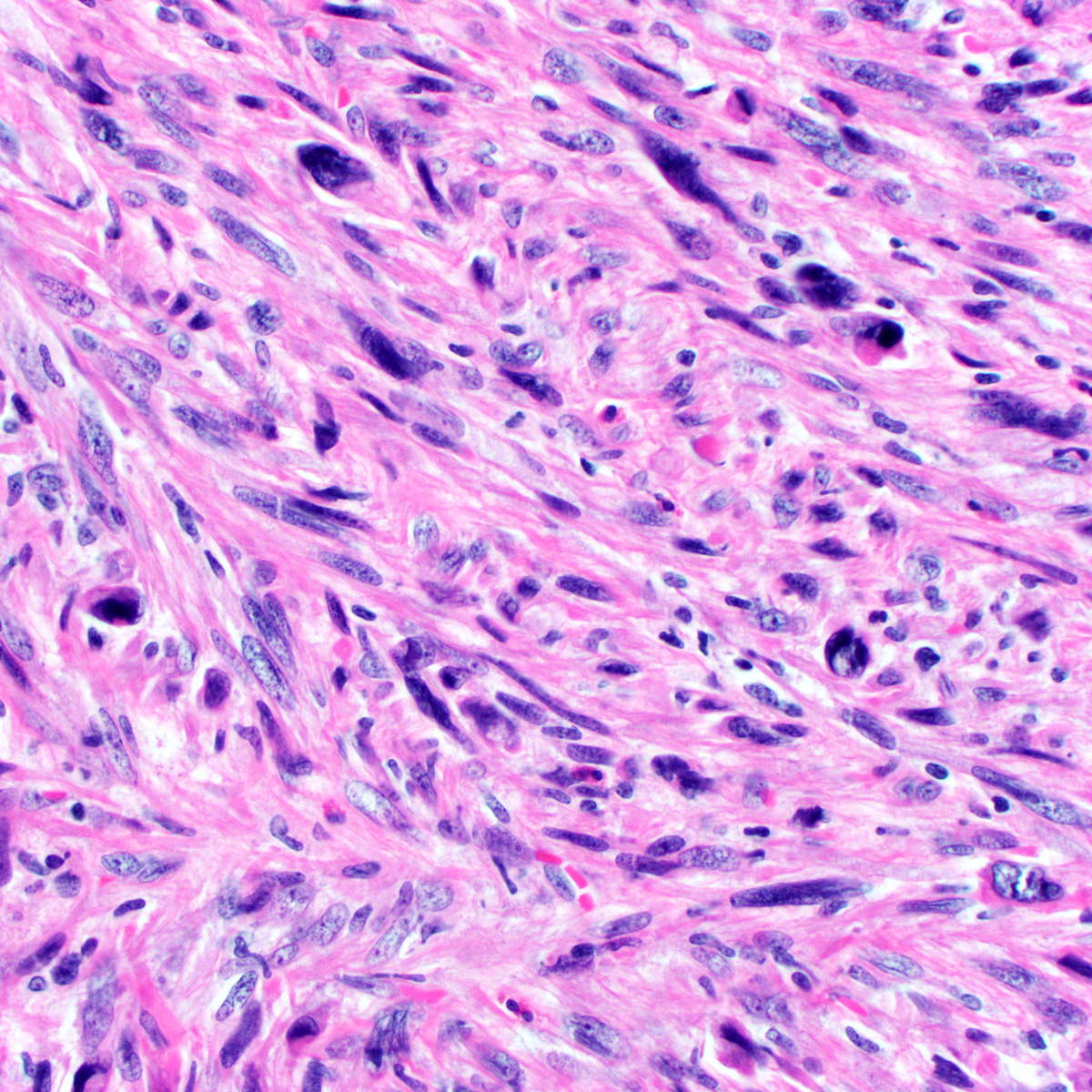
Vulvovaginal melanoma
by Dr. Lewis Hassell
Vaginal melanoma radiology
by Dr. Ayushi Gupta
Vaginal melanoma
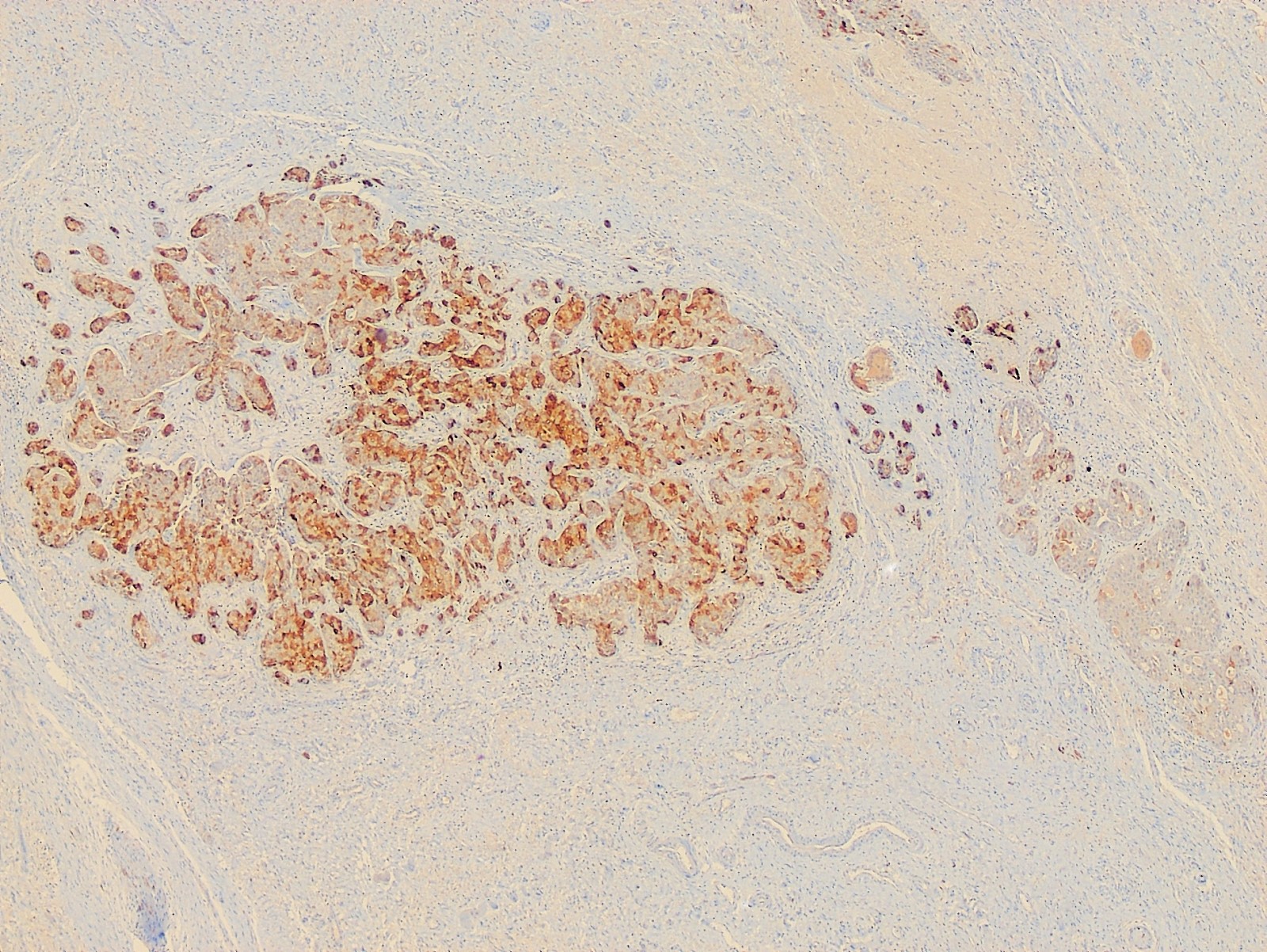
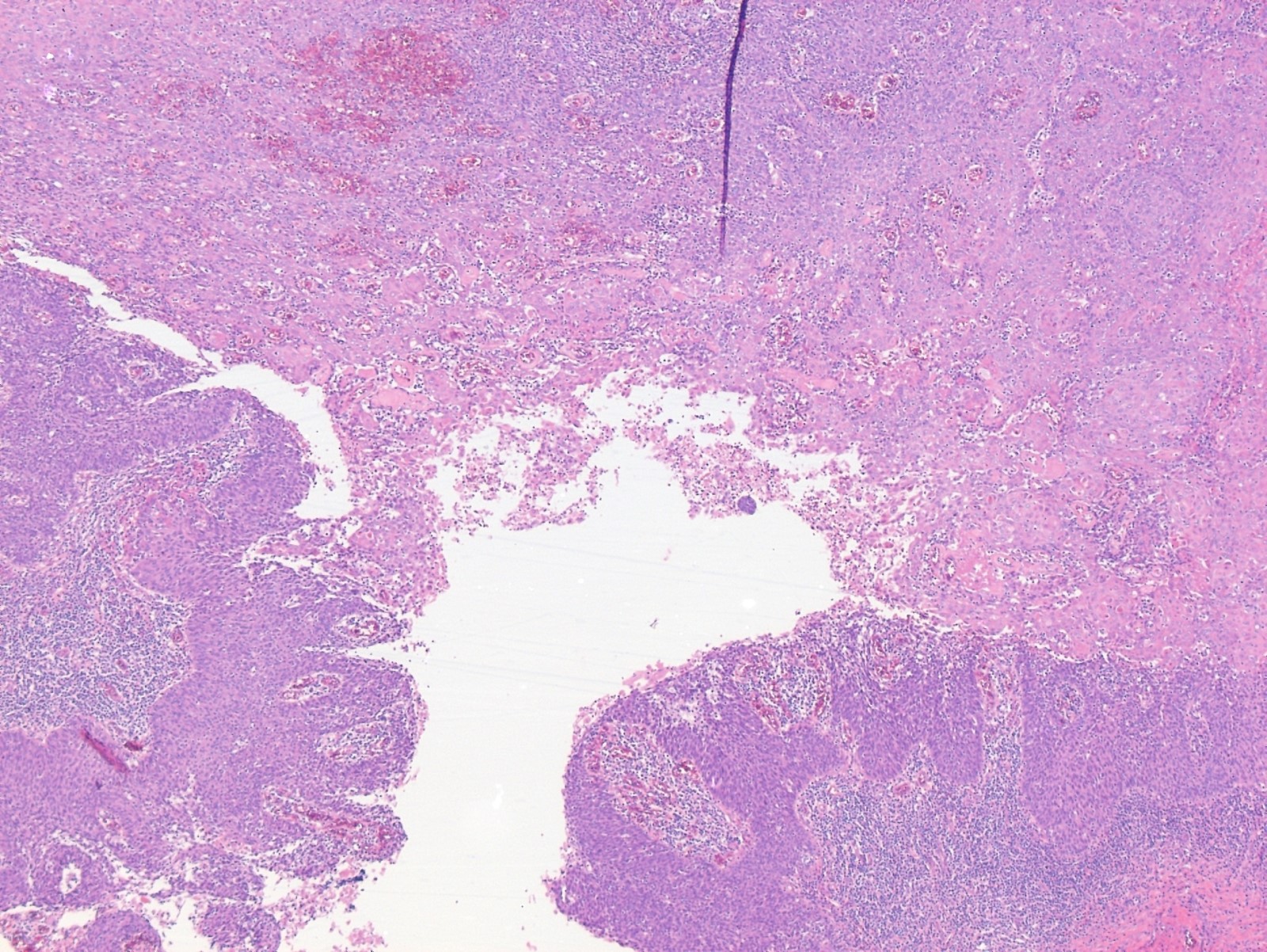
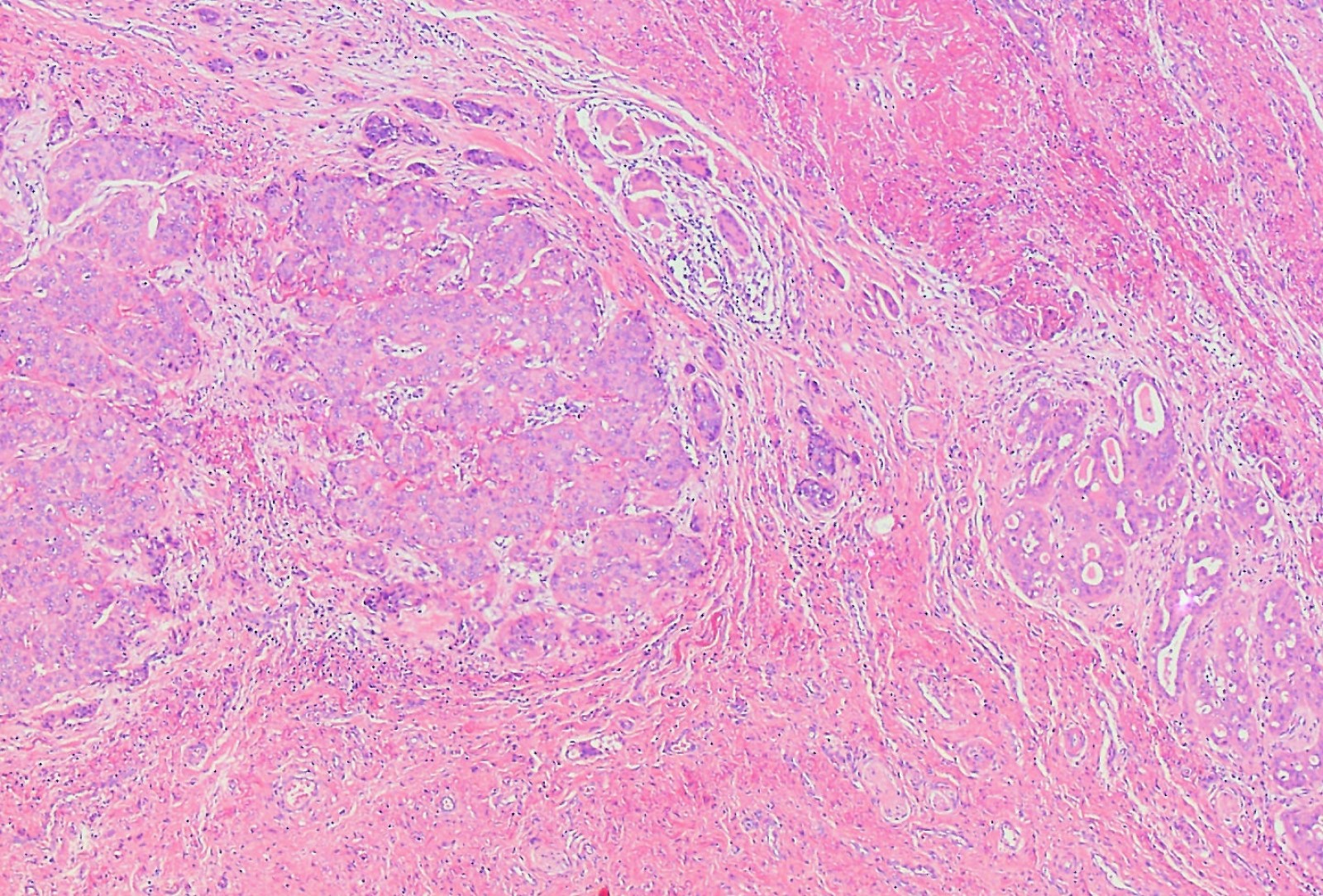
Contributed by Priya Nagarajan, M.D., Ph.D. and Lucy Ma, M.D.
Extramammary Paget disease: 5 minute pathology pearls
Paget disease versus melanoma versus squamous cell carcinoma in situ
Table 1: Features distinguishing vulvar nevi, melanosis and melanoma (adapted from J Am Acad Dermatol 2014;71:1241)
| Reassuring features suggestive of a benign process | Concerning features for possible malignancy | |
| Clinical |
|
|
| Dermoscopy |
|
|
| Reflectance confocal microscopy |
|
|
Table 2: Clinical morphology for pigmented vulvar lesions (adapted from Dermatol Ther 2010;23:449)
| Papules and macules | Patches and plaques |
| Pigmented nevi (nevocellular nevi) | Physiologic hyperpigmentation |
| Dysplastic nevi | Postinflammatory hyperpigmentation |
| Malignant melanoma | Vulvar melanosis (vulvar lentiginosis) |
| Anogenital warts | Acanthosis nigricans |
| Vulvar intraepithelial neoplasia | |
| Seborrheic keratosis | |
| Basal cell carcinoma | |
| Angiokeratoma |
Table 3: Genodermatosis syndromes with vulvar melanosis (adapted from J Am Acad Dermatol 2014;71:1241)
| Genodermatosis | Areas affected | Key features | Genetic mutation |
| Peutz-Jeghers syndrome | Oral, perianal and genital area, lips, nostrils, hands, feet | Hamartomatous polyps in the gastrointestinal tract (GIT), breast, ovarian, pancreatic and GIT cancers | STK11 |
| Carney complex | Oral and genital area, lips, eyelids, conjunctiva | Blue nevus, psammomatous melanotic schwannoma, myxomas (usually cardiac), endocrine neoplasms | PRKAR1A |
| Multiple lentigines syndrome (LEOPARD syndrome) | Face, neck, trunk, genital area | Delayed growth, sensorineural deafness, ECG abnormalities, ocular hypertelorism, pulmonic stenosis, abnormal genitalia | PTPN11, RAF1, BRAF |
| Bannayan-Riley-Ruvalcaba syndrome | Face, genital area | Macrocephaly, intellectual and motor deficiencies, joint hyperextensibility, pectus excavatum, scoliosis, intestinal hamartomatous polyposis, lipomas, hemangiomas | PTEN |
| Dowling-Degos syndrome | Axillae, neck, flexural folds, inguinal and genital area | Follicular papules, comedone-like lesions, perioral scar, reticulated hyperpigmentation, hypopigmented or erythematous macules | KRT5 |
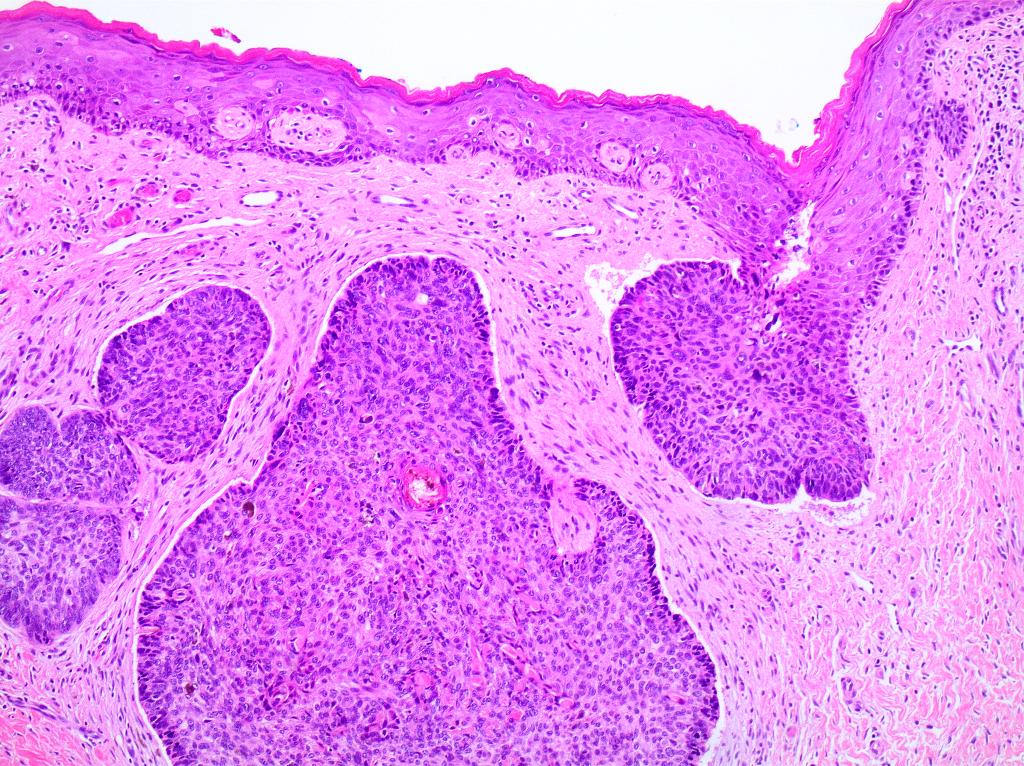
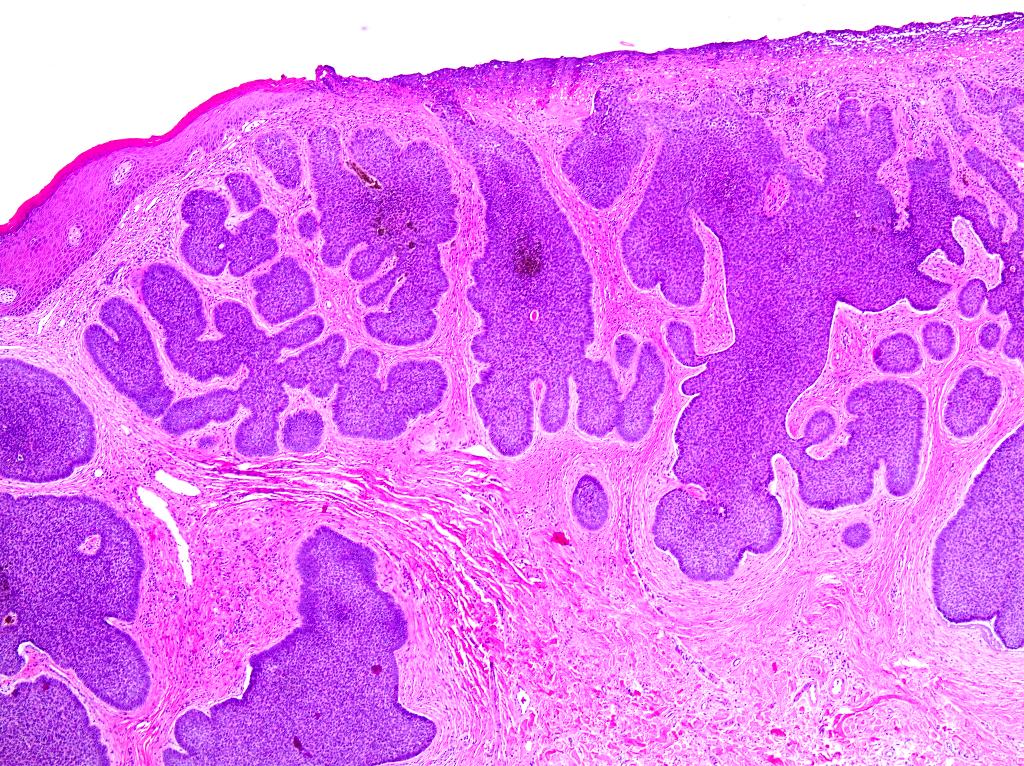
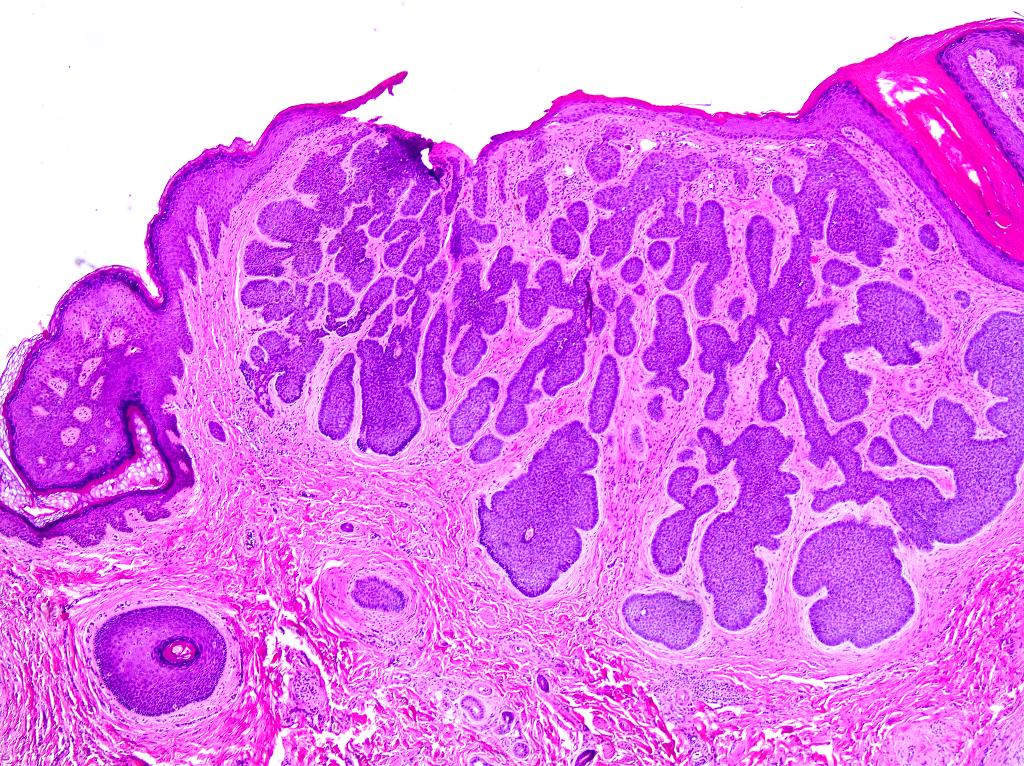
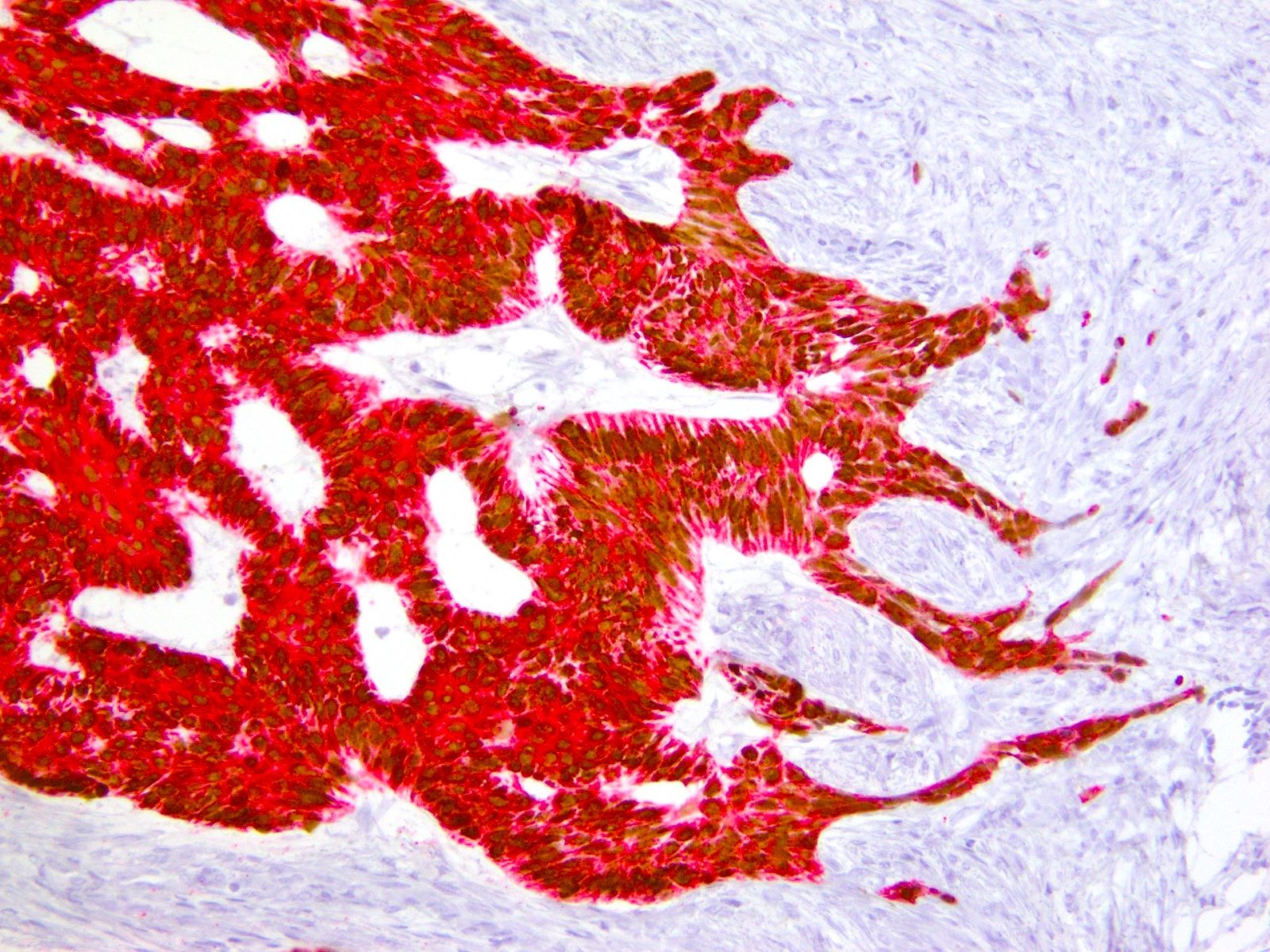
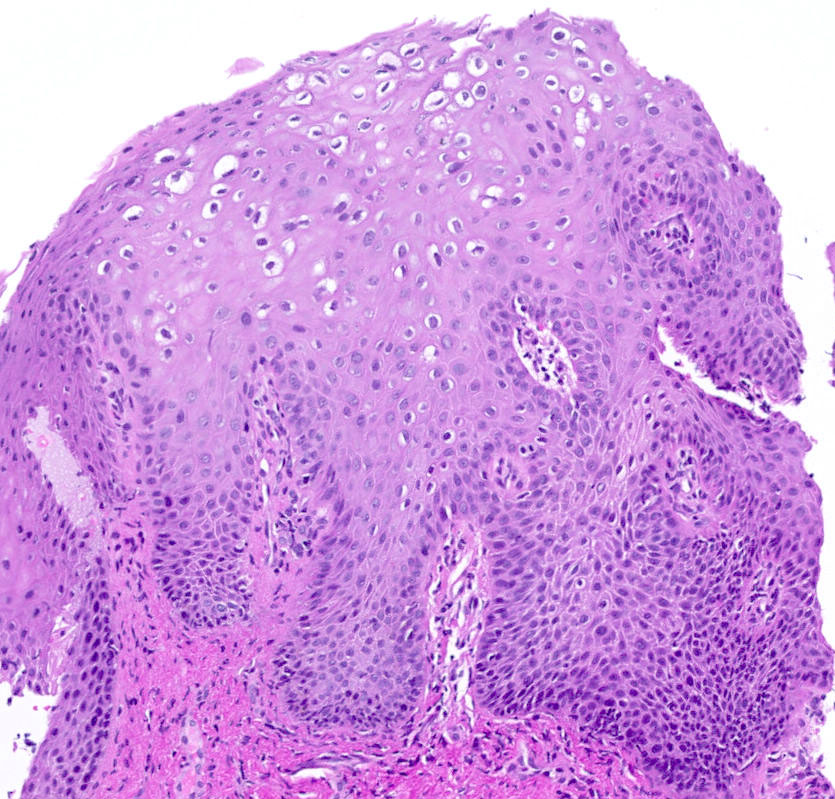
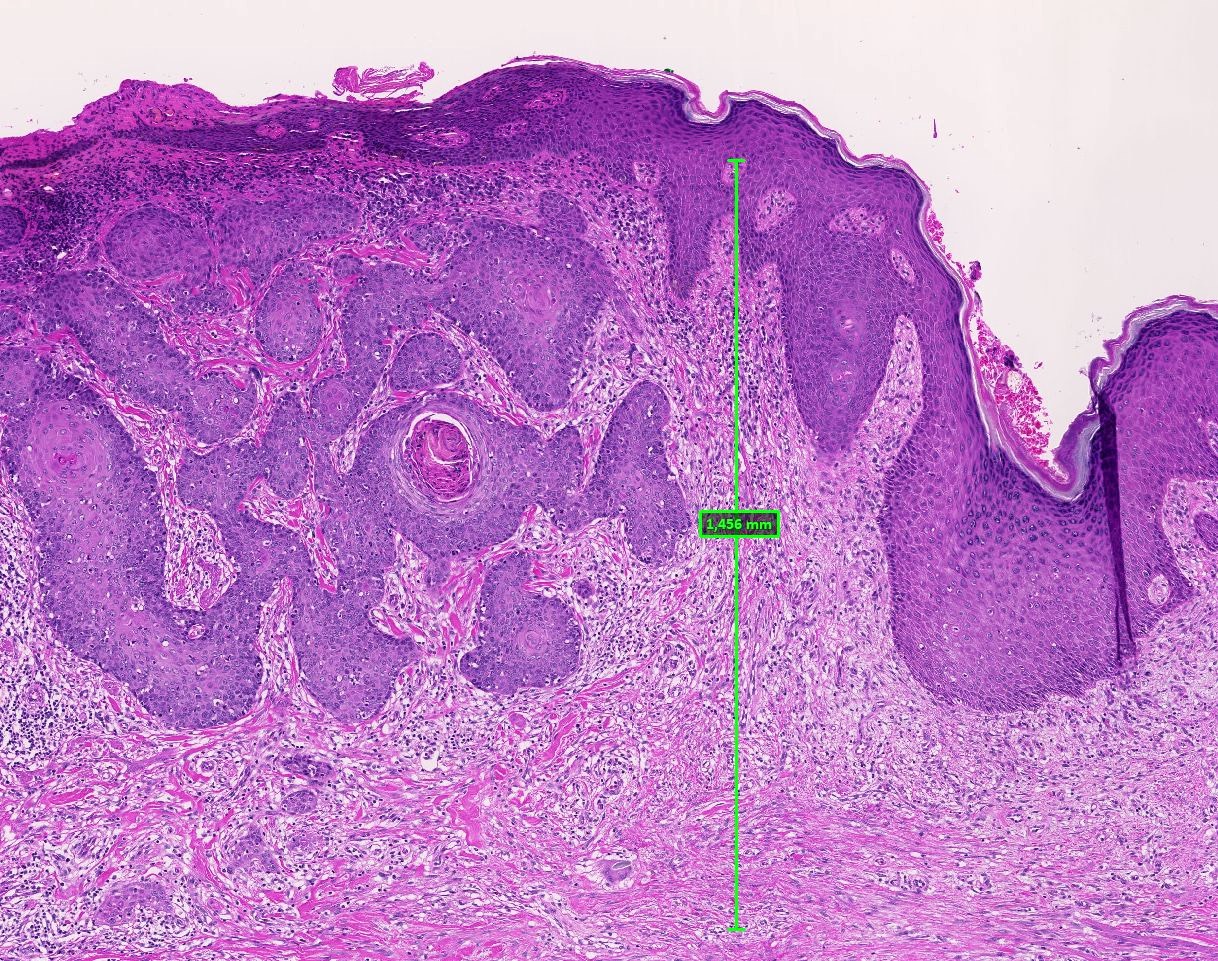
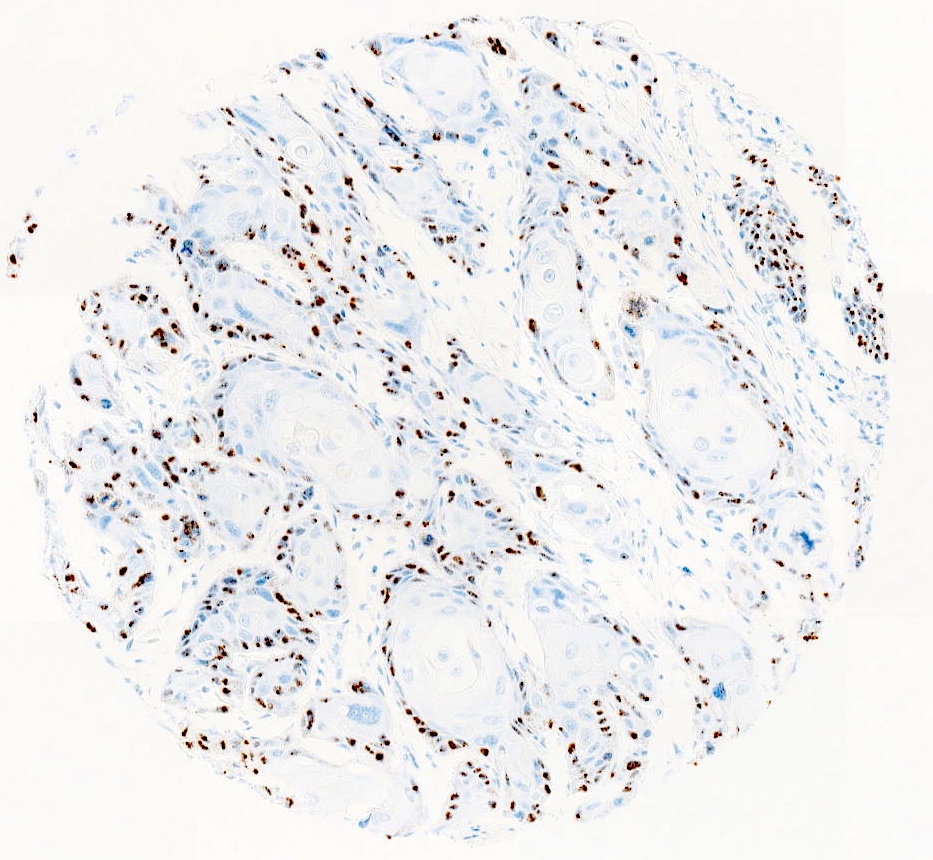
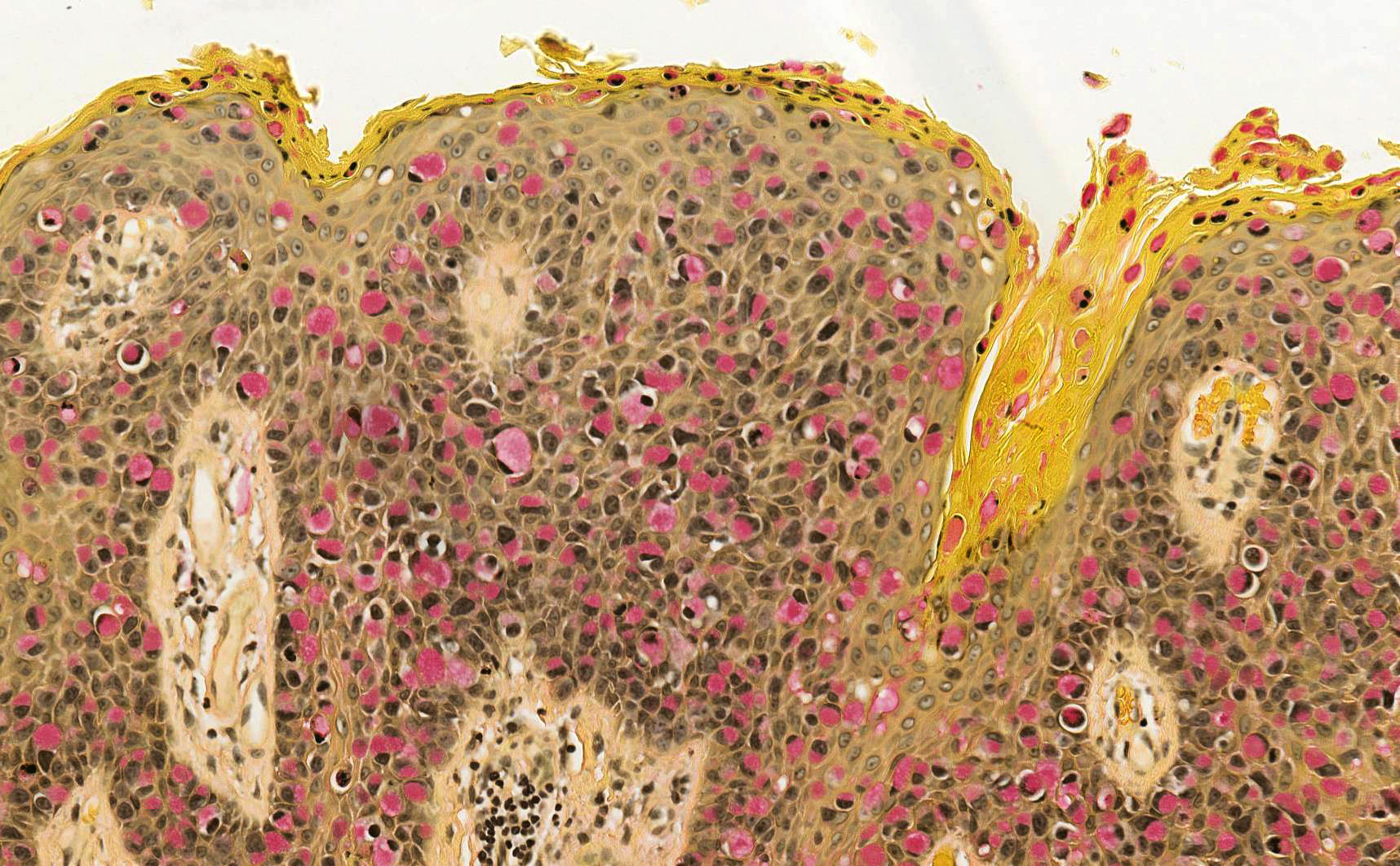
Table 4: Clinical and histologic differences between atypical genital nevus and vulvar melanoma
(adapted from Hoang: Melanocytic Lesions - A Case Based Approach, 1st Edition, 2014)
| Proposed diagnosis | Atypical genital nevus of special anatomic site | Vulvar melanoma |
| Age | Premenopausal, young adult | Postmenopausal |
| Size | > 1 cm | |
| Delineation | Well circumscribed | Infiltrative |
| Symmetry | Present | Absent |
| Lateral extension of junctional component | Focal | Present |
| Lentiginous junctional component | Focal | Present |
| Junctional nests | Dyscohesive | Confluent |
| Retraction artefact | Present | Absent |
| Ulceration | Absent or due to trauma | Often present |
| Pagetoid upward spread | Focal, central, inconspicuous | Prominent |
| Cytologic atypia | Superficial, mild - moderate | Deep, moderate to severe |
| Dermal mitosis | Rare and superficial | Conspicuous, atypical, deep |
| Dermal maturation | Present | Absent |
| Melanin pigmentation | Coarse, uniform | Fine, irregular |
| Dermal fibrosis | Broad zone of superficial coarse dermal fibrosis | Regression type |
Contributed by José Alberto Fonseca Moutinho, M.D.
Images hosted on other servers:
Angiokeratoma by Filip Sokol
Angiokeratoma by Pathology mini tutorials
Atypical nevi and nevi of special sites by Dr. Phillip McKee
Bartholin gland cyst of the vulva - histopathology
Find related Pathology books: gynecologic