Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Huvila J, Gilks CB. Bartholin gland carcinoma-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvabartholinglandcarc.html. Accessed December 26th, 2024.
Definition / general
- Rare carcinoma arising from the Bartholin gland
- These can be squamous cell carcinoma, adenocarcinoma, adenoid cystic carcinoma or other rare variants
Essential features
- Carcinoma arising from Bartholin gland
- Wide range of histologic types can be encountered but most are squamous cell carcinoma, adenocarcinoma or adenoid cystic carcinoma
- Overlying epithelium should be uninvolved, i.e. exclude downgrowth of an overlying vulvar squamous cell carcinoma or Paget disease
- Exclude metastasis to Bartholin gland from a genital or extragenital site
ICD coding
- ICD-11: 2C70.Z & XH74S1 - malignant neoplasms of vulva, unspecified and adenocarcinoma, NOS
Epidemiology
- Bartholin gland carcinomas arise in middle aged and elderly women and account for approximately 5% of vulvar malignancies (Surg Oncol 2013;22:117)
Sites
- Diagnosis of Bartholin gland carcinoma can only be made if the anatomical location of the tumor is compatible with origin from Bartholin gland, i.e. posterolateral on the vulva (posterior to the labium major), without involvement of overlying squamous epithelium
Etiology
- There is a strong causal association between human papillomavirus (HPV) and squamous cell carcinoma of Bartholin gland (Int J Gynecol Pathol 2019;38:189, Histopathology 2000;37:87, Am J Pathol 1993;142:925)
Clinical features
- Painless mass in the region of Bartholin gland in an elderly woman
- May be mistaken for a Bartholin gland cyst or abscess
Diagnosis
- Biopsy of a mass in the region of Bartholin gland
Radiology description
- Ultrasound: echogenic mass that may contain calcifications (Crit Rev Oncol Hematol 2017;117:1)
- MRI: solid, isodense to skeletal muscle (Surg Oncol 2013;22:117)
- CT scan: may detect nodal spread (Surg Oncol 2013;22:117)
- Imaging can be used to help exclude a primary tumor elsewhere that has metastasized to the Bartholin gland
Prognostic factors
- Tumor size and stage are the most important, with prognosis similar to that of vulvar squamous cell carcinoma (Surg Oncol 2013;22:117, J Clin Oncol 2008;26:884)
- Overall prognosis is favorable, especially for tumors localized to the vulva, without nodal metastasis
Case reports
- 33 year old woman with adenoid cystic carcinoma of the Bartholin gland (Case Rep Obstet Gynecol 2019;2019:1784949)
- 44 and 51 year old women with Bartholin gland epithelial myoepithelial carcinoma (Int J Gynecol Pathol 2009;28:286)
- 49 year old woman with adenoid cystic carcinoma of the Bartholin gland (Oncol Lett 2014;8:849)
- 49 year old woman with Merkel cell carcinoma of the Bartholin gland (Gynecol Oncol 2005;97:928)
- 49 year old woman with primary adenocarcinoma of the Bartholin gland (J Obstet Gynaecol 2015;35:536)
- 51 year old woman with adenoid cystic carcinoma of the Bartholin gland (Eur J Gynaecol Oncol 2013;34:487)
- 61 year old woman with adenoid cystic carcinoma of the Bartholin gland (Pathol Res Pract 2020;216:152968)
- 64 year old woman with adenoid cystic carcinoma of the Bartholin gland (Tokai J Exp Clin Med 2019;44:68)
- 66 year old women with Bartholin gland squamous cell carcinoma (J Obstet Gynaecol 2012;32:318)
Treatment
- Surgical excision, (vulvectomy with unilateral or bilateral lymphadenectomy) often with adjuvant radiotherapy administered (similar to treatment of vulvar squamous cell carcinoma)
Gross description
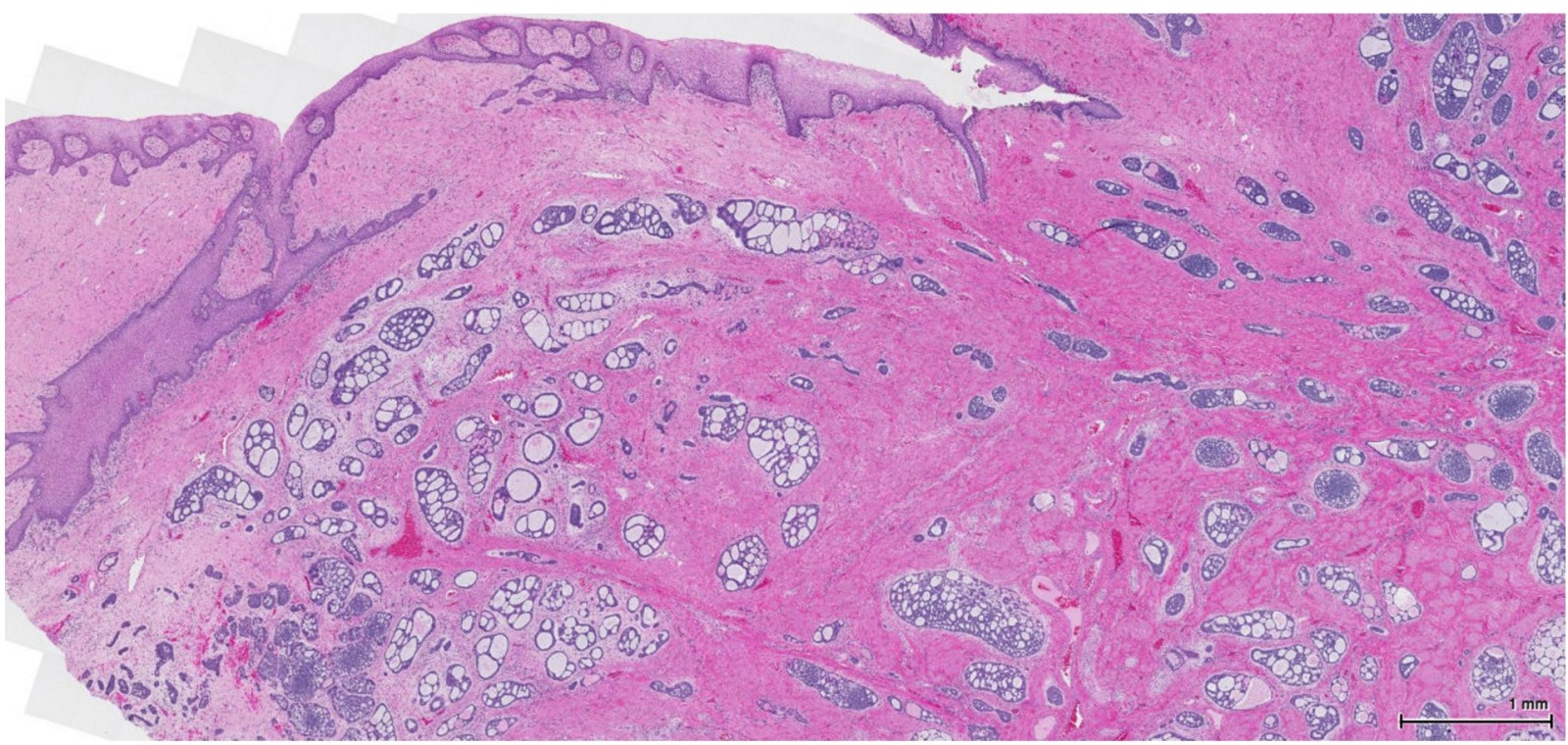
- Firm, irregularly shaped, unencapsulated mass deep to the vulvar skin
Frozen section description
- Frozen section findings are not specific and are dependent on the tumor histologic type (e.g. squamous cell carcinoma, adenocarcinoma, adenoid cystic carcinoma)
- Frozen section is typically not required as diagnosis will have been made based on preoperative biopsy
Microscopic (histologic) description
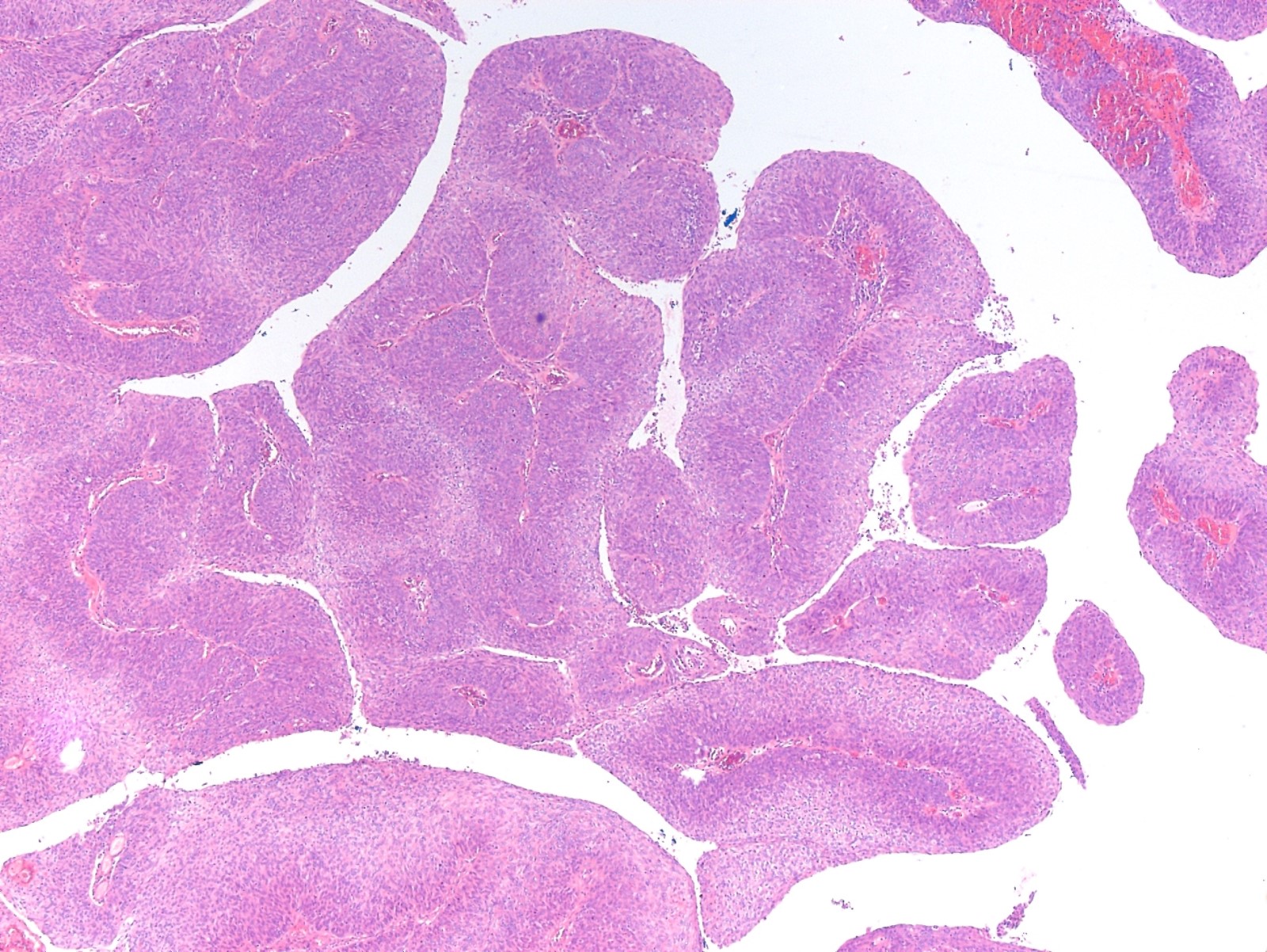
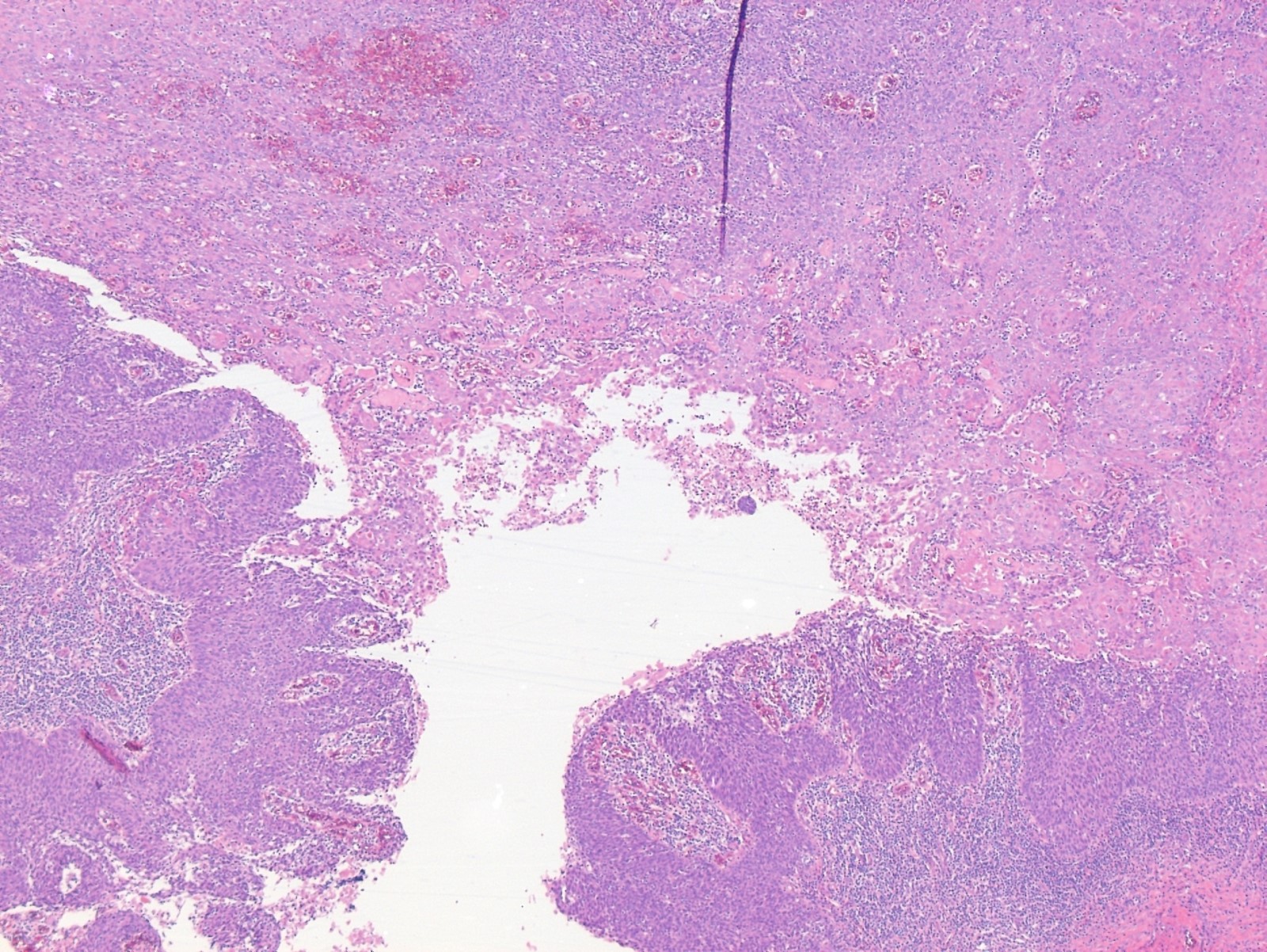
- Approximately 85 - 90% of Bartholin gland carcinomas are squamous cell carcinomas, approximately 10% adenocarcinomas and < 5% adenoid cystic carcinomas (Gynecol Oncol 2001;82:247, Int J Gynecol Cancer 2016;26:785, Int J Gynecol Pathol 2019;38:189)
- Additionally, several rare to exceedingly rare histological subtypes have been described, such as transitional cell carcinoma, neuroendocrine carcinoma, epithelial myoepithelial carcinoma, Merkel cell carcinoma and lymphoepithelioma-like carcinoma (Crit Rev Oncol Hematol 2017;117:1)
- Histopathologic diagnostic criteria include the following (Obstet Gynecol 1972;39:489):
- Tumor involves the anatomic region of the Bartholin gland and is histologically compatible with origin from the Bartholin gland
- Areas of apparent transition from normal Bartholin gland elements to neoplastic ones are present
- There is no evidence of primary tumor elsewhere
- Histological features
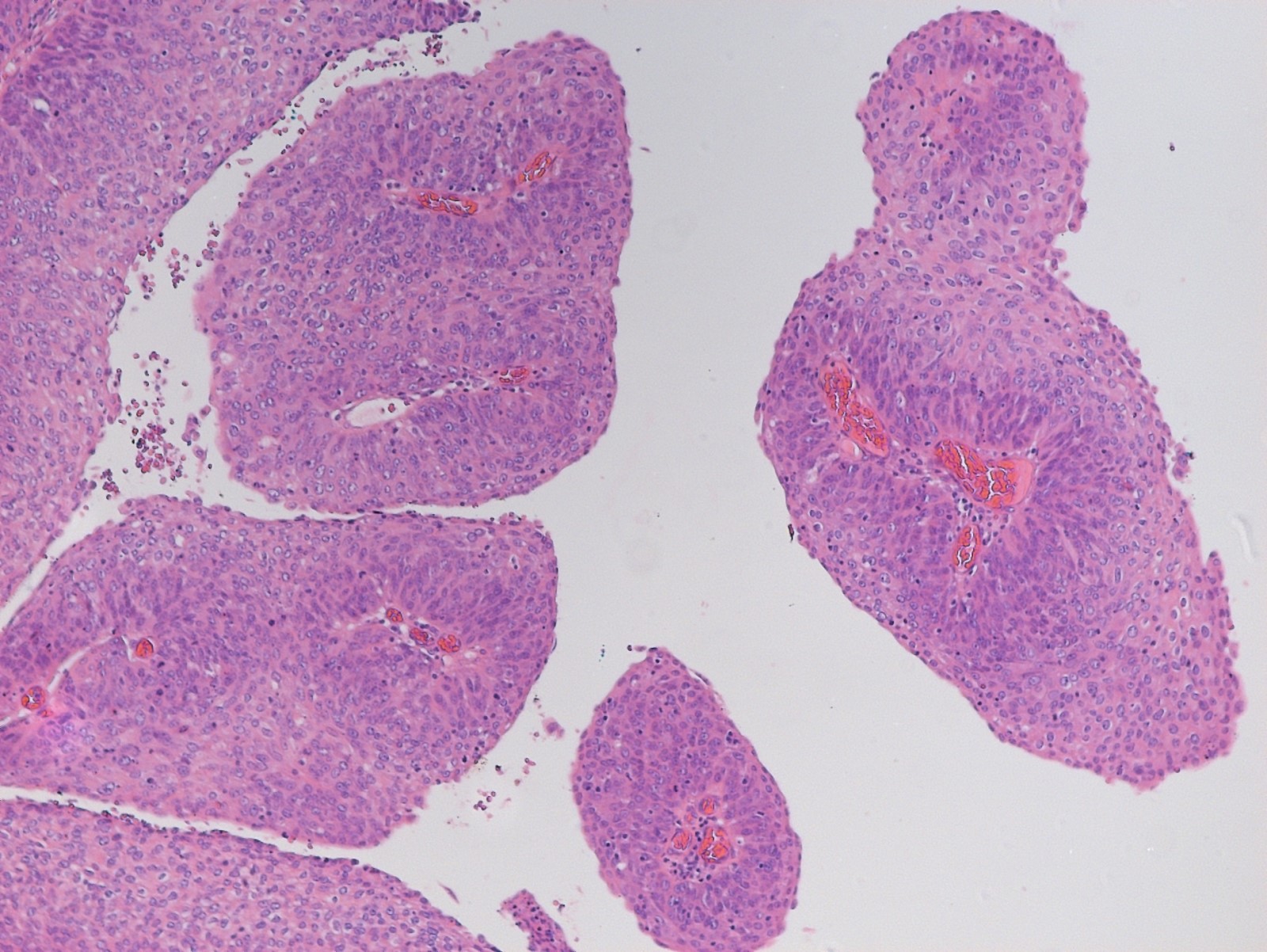
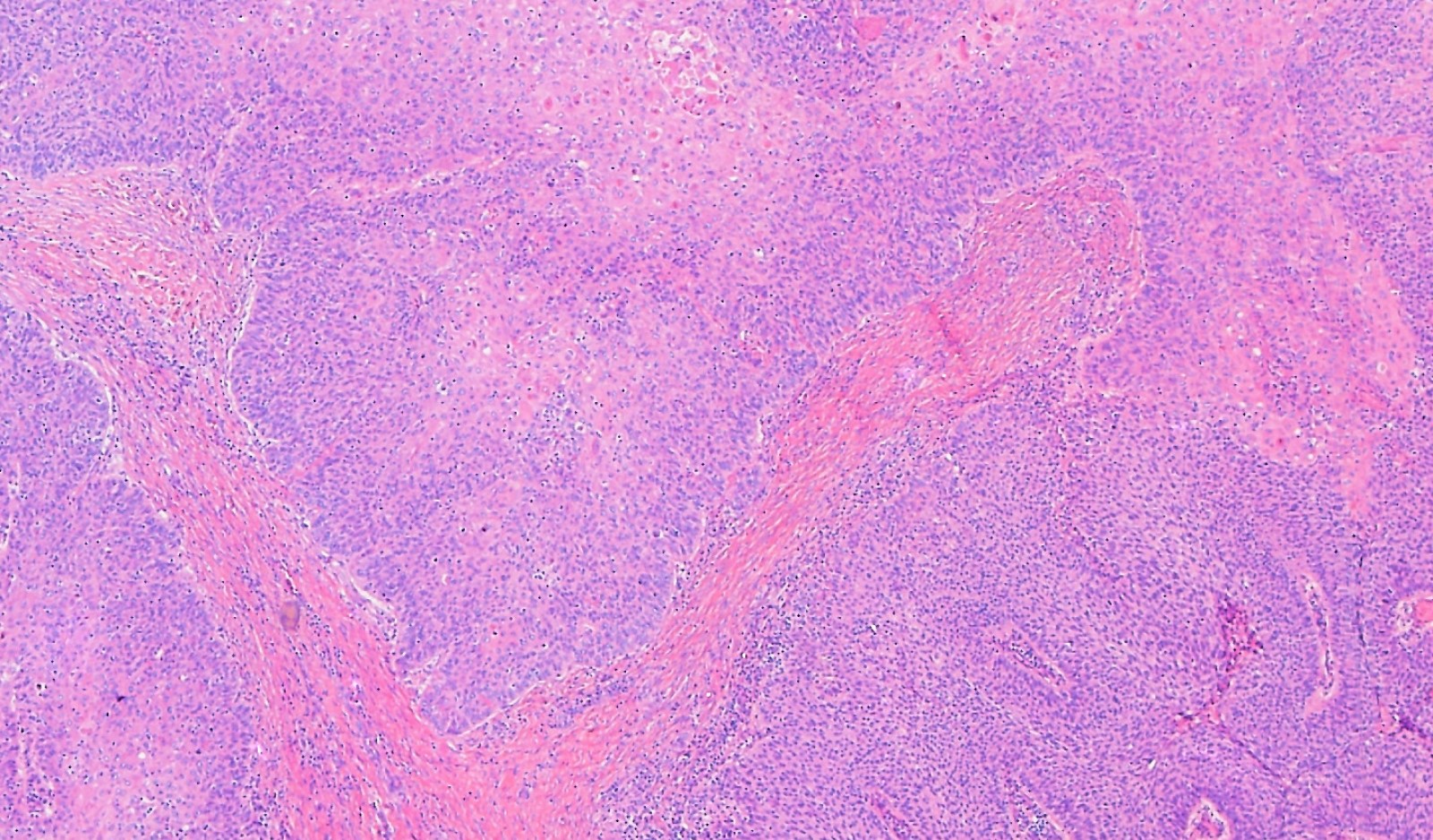
- Squamous cell carcinoma:
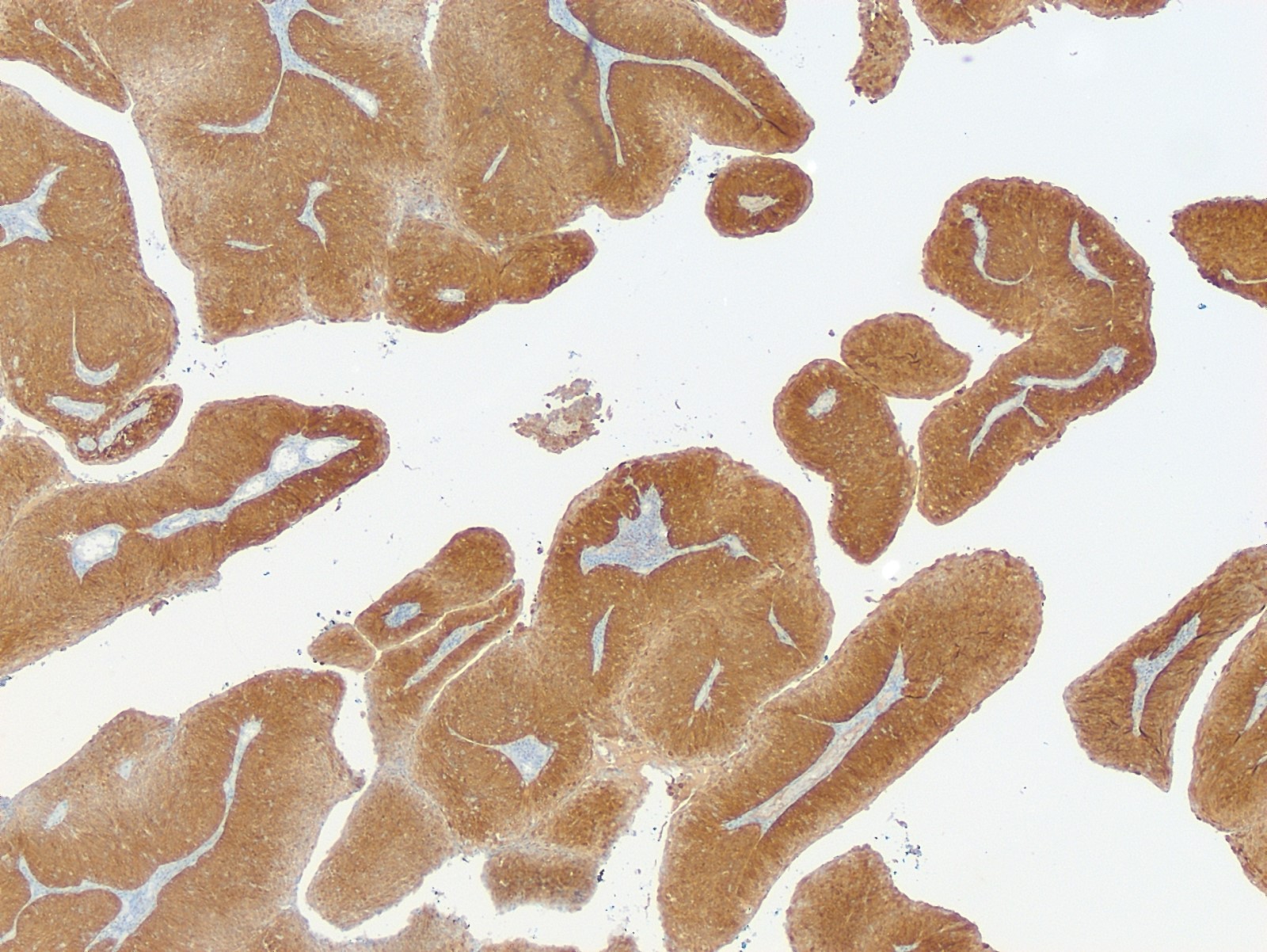
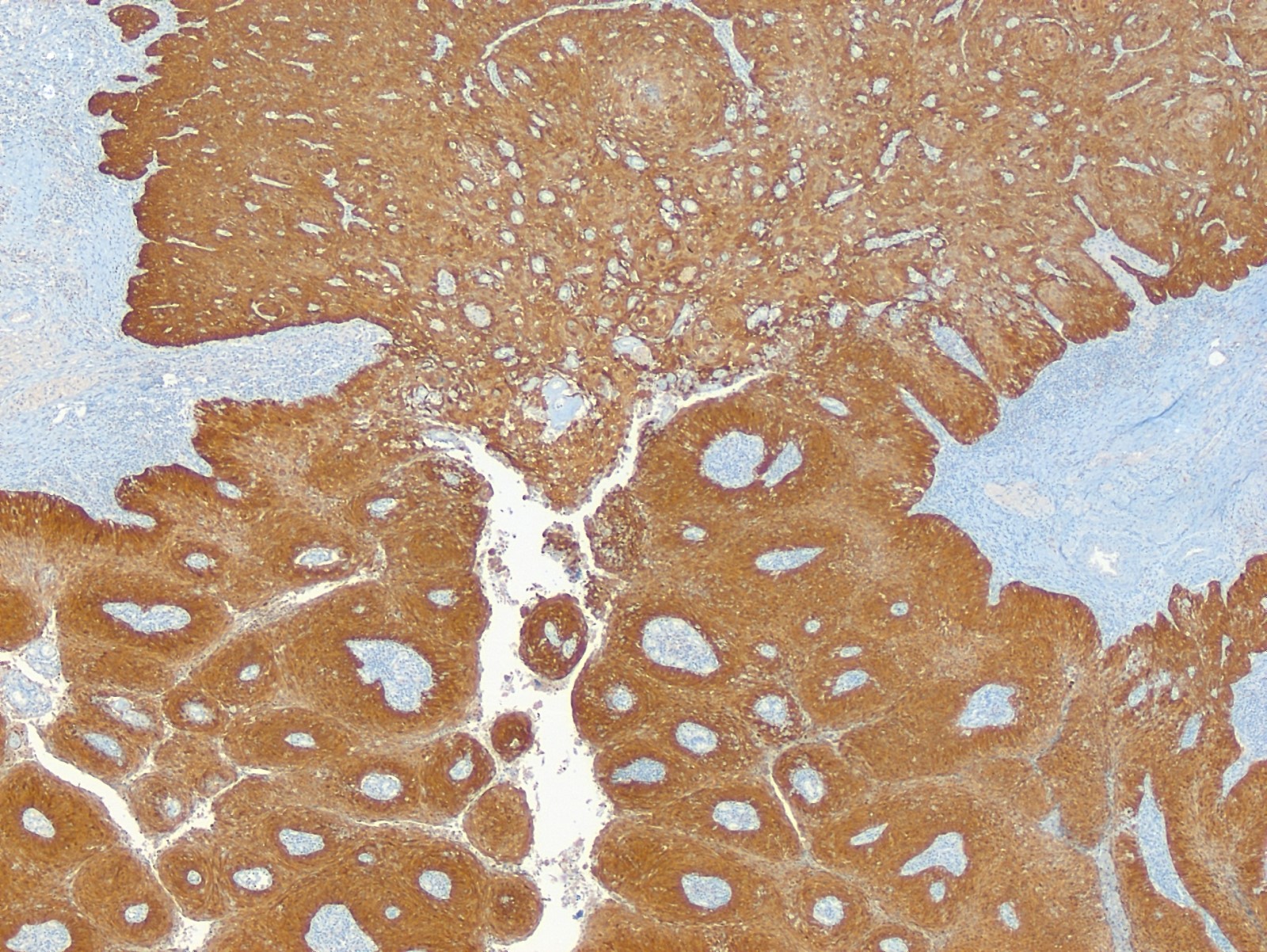
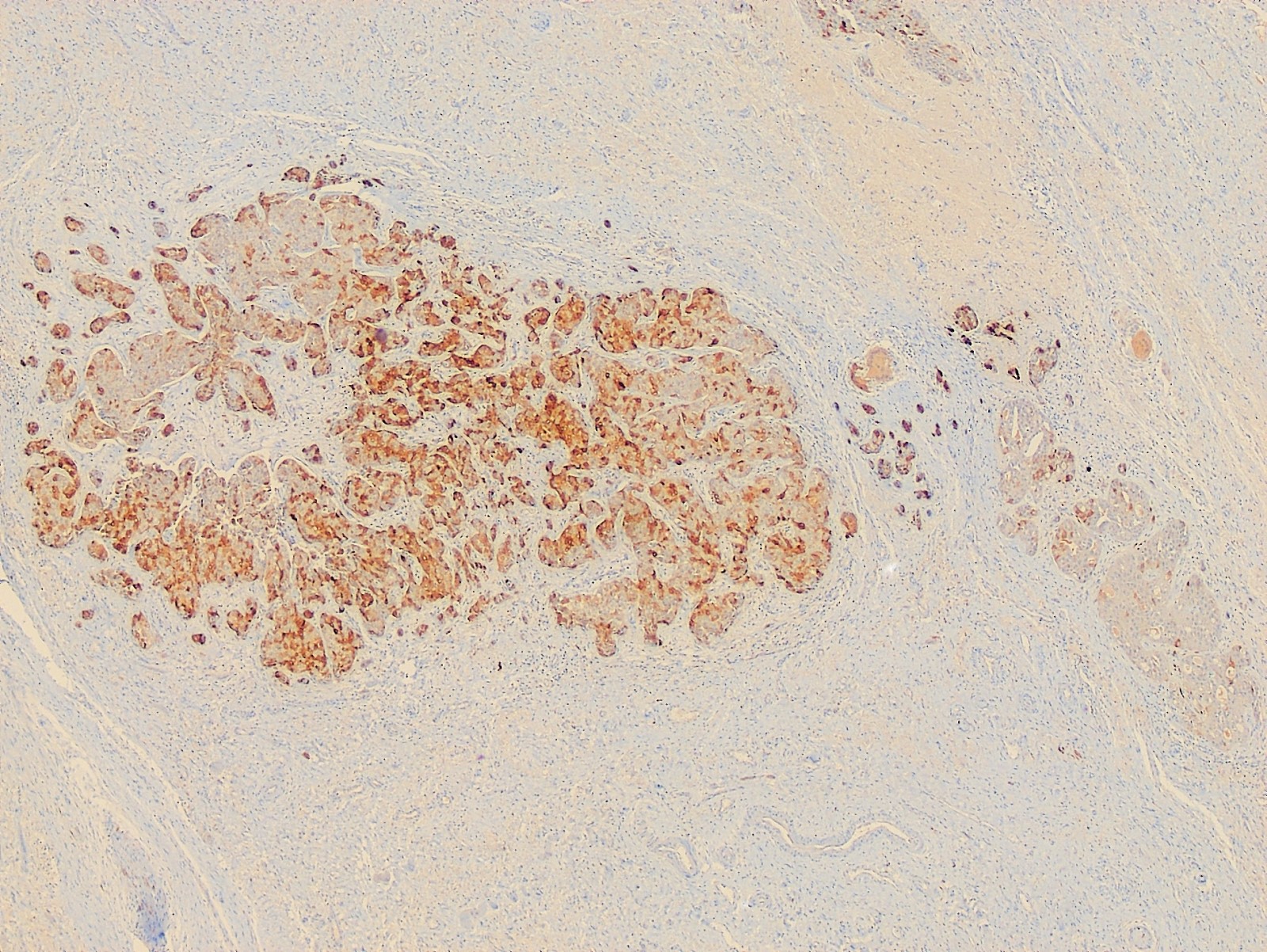
- Usually human papillomavirus (HPV) associated and has positive p16 immunostaining (Am J Pathol 1993;142:925, Int J Gynecol Pathol 2019;38:189)
- Morphology is identical to more common HPV associated squamous cell carcinomas of cervix, vagina or vulva
- Adenocarcinomas:
- Nonspecific features (adenocarcinoma NOS) are most common
- May show mucinous differentiation or other growth patterns
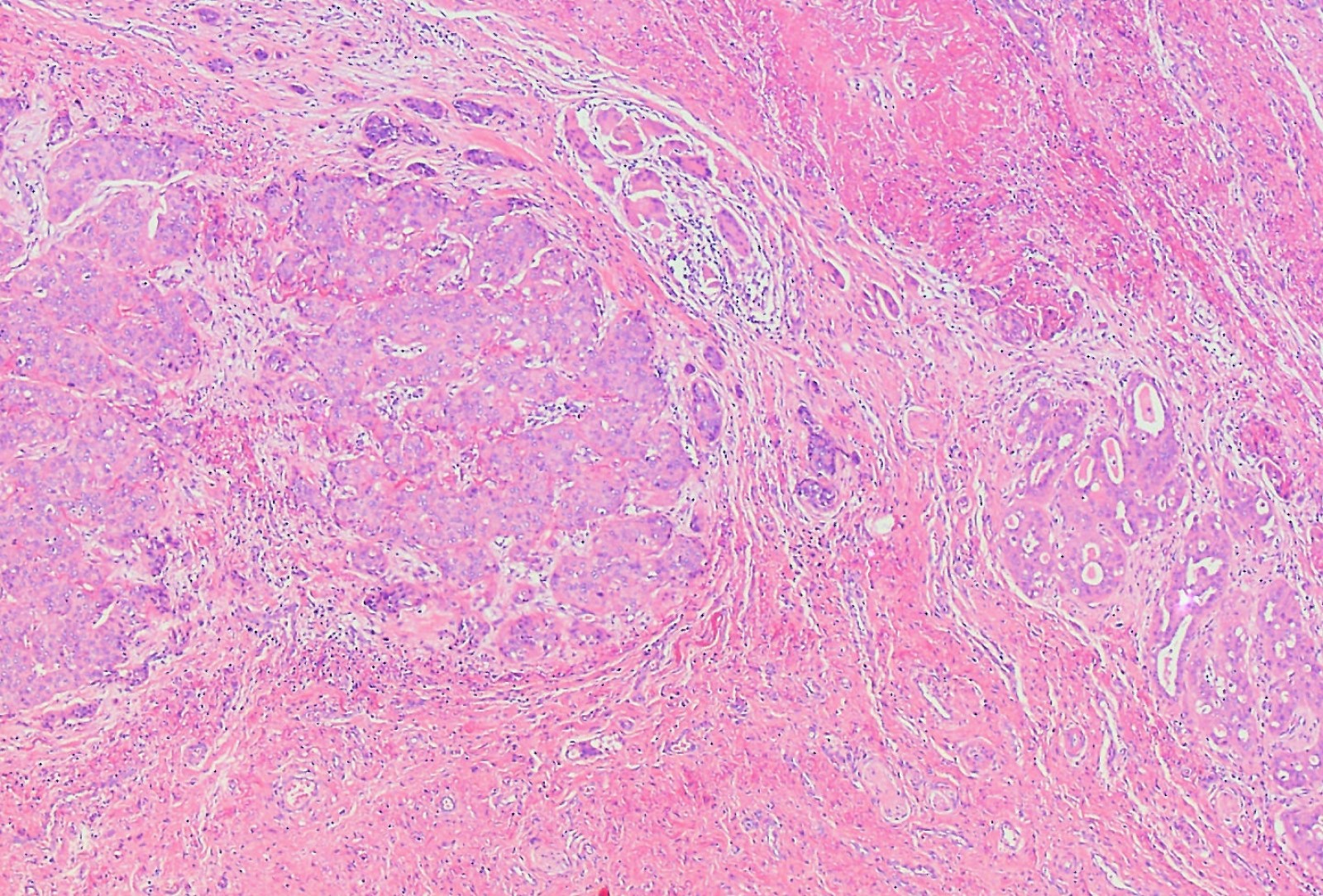
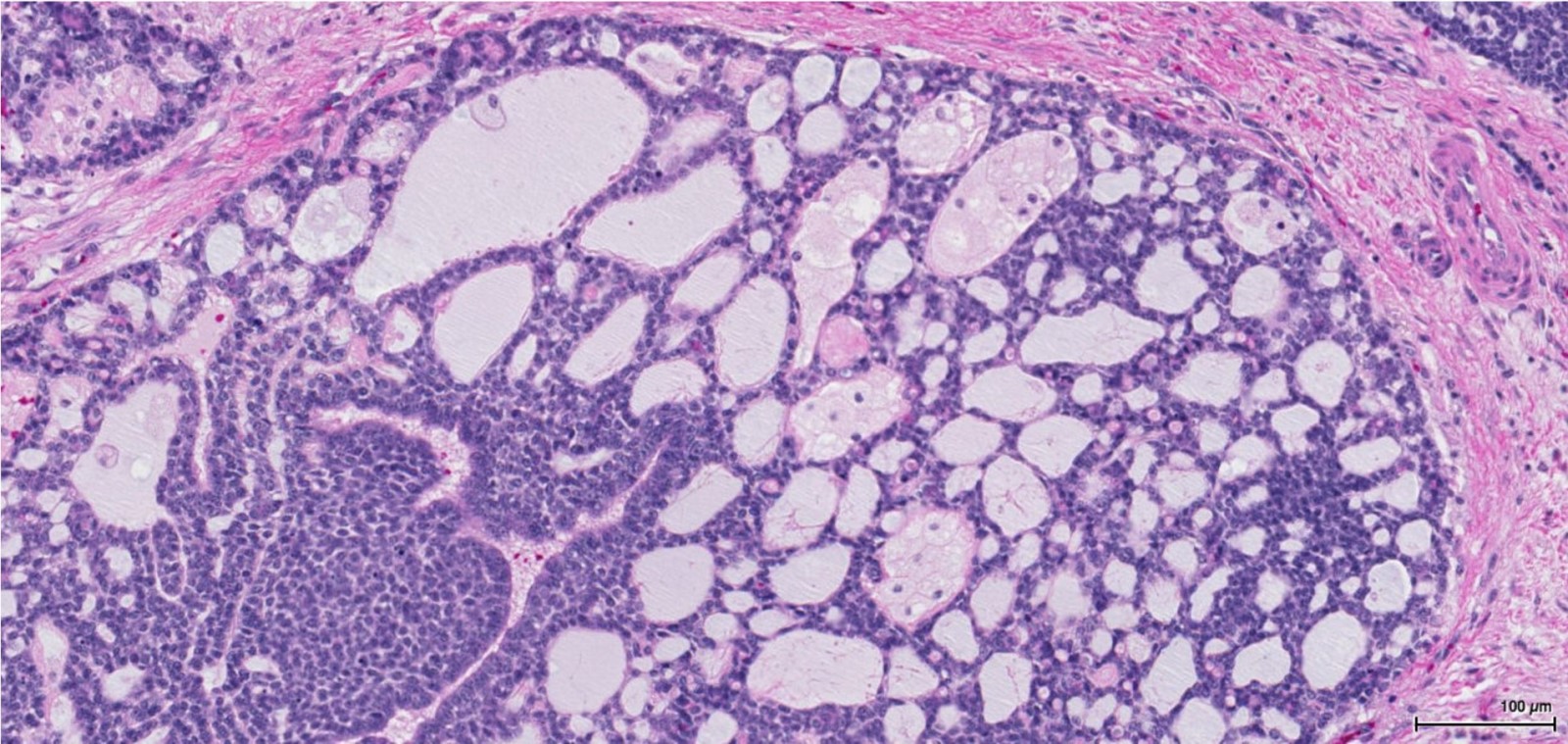
- Adenoid cystic carcinoma:
- Morphology is identical to the adenoid cystic carcinoma of salivary gland or lung
- Low grade cells arranged in cribriform pattern; luminal spaces contain mucin or basement membrane material
- Tendency for extensive perineural invasion (Tokai J Exp Clin Med 2019;44:68, Crit Rev Oncol Hematol 2017;117:1)
- Squamous cell carcinoma:
Microscopic (histologic) images
Cytology description
- Cytological examination is typically not used in diagnosis
- It may be used to confirm lymph node metastasis
- Cytological features reflect the histologic type of the carcinoma
Positive stains
Negative stains
- Adenocarcinoma:
- p16- or weak focal positivity (Am J Pathol 1993;142:925, Int J Gynecol Pathol 2019;38:189)
Molecular / cytogenetics description
- Adenoid cystic carcinomas show chromosomal rearrangements involving NFIB (also seen in adenoid cystic carcinomas arising at other anatomic sites) in most cases (Int J Gynecol Pathol 2017;36:289)
Sample pathology report
- Vulva, biopsy:
- Invasive squamous cell carcinoma, consistent with Bartholin gland carcinoma (see comment)
- Comment: This squamous cell carcinoma shows strong diffuse p16 immunoreactivity, consistent with it being associated with high risk human papillomavirus. The clinical setting, i.e. location of the tumor mass and uninvolved overlying vulvar skin, is noted. While the histologic type of this tumor is compatible with it being a primary Bartholin gland carcinoma and there are adjacent benign Bartholin gland acini in this biopsy, clinical correlation is required to exclude a metastatic squamous cell carcinoma from another site.
Differential diagnosis
- Vulvar squamous cell carcinoma:
- Involvement of overlying squamous epithelium
- Invasive Paget disease:
- Epidermocentric with extensive involvement of overlying squamous epithelium
- Mammary-like adenocarcinoma of the vulva:
- Associated benign mammary acini and ducts
- Location away from Bartholin gland
- Expression of breast cancer biomarkers (Breast J 2020;26:1242, Histopathology 2017;71:446)
- Bartholin gland cyst or abscess:
- Simple cyst lined by benign mucinous or squamous epithelium (Case Rep Obstet Gynecol 2018;2018:5256876)
Board review style question #1
- Which of the following is true about squamous cell carcinoma of the Bartholin gland?
- Has a significantly worse prognosis than other vulvar squamous cell carcinomas
- Is often associated with human papillomavirus infection
- Is the second most common histological subtype of Bartholin gland carcinoma after adenocarcinoma
- Often presents with a painful mass similar to Bartholin gland abscess
Board review style answer #1
B. Is often associated with human papillomavirus infection
Comment Here
Reference: Bartholin gland carcinoma-vulva
Comment Here
Reference: Bartholin gland carcinoma-vulva