Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Wiedemeyer K, Chapel DB. Alveolar soft part sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixalveolarsoftpartssarcoma.html. Accessed January 1st, 2025.
Definition / general
- Alveolar soft part sarcoma (ASPS) is a morphologically distinctive neoplasm of unknown histogenesis / cell lineage, which may rarely occur in the female genital tract
- Alveolar soft part sarcoma is a high grade sarcoma by definition (no formal grading system available)
Essential features
- Rare malignant mesenchymal neoplasm exhibiting nested or solid growth patterns with pseudoalveolar spaces
- Composed of large, polygonal cells with abundant eosinophilic cytoplasm and PASD+ intracytoplasmic granules or crystals
- Harbors characteristic ASPSCR1::TFE3 gene fusion
Terminology
- Alveolar soft part sarcoma is the preferred WHO terminology
ICD coding
- ICD-O: 9581/3 - alveolar soft part sarcoma
- ICD-10: C49.9 - malignant neoplasm of connective and soft tissue, unspecified
- ICD-11: 2B5F.2 & XH8V95 - sarcoma, not elsewhere classified of other specified sites & alveolar soft part sarcoma
Epidemiology
- Alveolar soft part sarcoma of the female genital tract is rare; 50 - 60 cases published to date (Int J Womens Health 2024;16:17)
- Affects women over a wide age range (8 - 68 years), with most cases diagnosed in the third and fourth decades (Am J Surg Pathol 2017;4:622)
- Alveolar soft part sarcoma of nongenital sites also shows a ~2:1 female predilection (J Surg Oncol 2016;113:581)
Sites
- ASPS can affect any site in the female genital tract, most commonly cervix (cervix > uterine corpus > vagina) (Int J Gynecol Pathol 1995;14:283, Am J Surg Pathol 2017;4:622, Int J Gynecol Pathol 2014;33:263)
- Vulvar, perineal and adnexal tumors are very rare
- Overall, ASPS is much more common in deep soft tissues of the extremities and head and neck than in the female genital tract
Pathophysiology
- Unbalanced translocation: der(17)t(X:17)(p11;p25)
- Translocation results in fusion of ASPSCR1 (ASPL) gene on chromosome 17 to the TFE3 gene on X chromosome
- ASPSCR1 gene is joined in frame upstream of either the third or fourth exon of TFE3, yielding 2 fusion variants (type 1 and type 2) (J Clin Pathol 2006;59:1127)
Etiology
- No risk factors have been identified
- No associated germline mutations
Clinical features
- Uterine, cervical and vaginal tumors typically present with vaginal / abnormal uterine bleeding or menstrual cycle shortening (Int J Clin Exp Pathol 2017;10:9812, Int J Gynecol Pathol 1995;14:283)
- May also be discovered incidentally during pregnancy or at surgery for an unrelated cause
- Rare vulvar or perineal tumors present as a painless mass (Int J Gynecol Pathol 2014;33:263)
Diagnosis
- Characteristic histomorphology: eosinophilic, polygonal cells with a nested or solid growth pattern, delicate vasculature and intracytoplasmic PASD positive material
- TFE3 nuclear expression by immunohistochemistry
- Molecular confirmation of TFE3 rearrangement or ASPSCR1::TFE3 fusion
- Reference: JAMA Oncol 2019;5:254
Radiology description
- Hypervascular tumors with high signal intensity on T2 weighted magnetic resonance imaging
- Contrast enhanced masses on computed tomography
- Lobulated contours
- Well defined tumors of the uterine corpus or cervix (compared to more ill defined alveolar soft part sarcoma of other sites) (Korean J Pathol 2014;48:361)
Radiology images
Prognostic factors
- Prognostic information on ASPS of the female genital tract is limited by short median follow up in published studies
- ASPS of the uterine corpus, cervix or adnexa appear to have a more favorable prognosis than their soft tissue counterparts, likely reflecting early clinical detection, small size or resectability (Korean J Pathol 2014;48:361, Am J Surg Pathol 2017;4:622, Int J Gynecol Pathol 1995;14:283)
- Vulvar and vaginal tumors appear to have a prognosis more comparable to their soft tissue counterparts, with disease related mortality in ~33% of cases
Case reports
- 10 year old girl with alveolar soft part sarcoma occurring in the uterine cervix (Diagnostics (Basel) 2022;12:1102)
- 33 year old woman with alveolar soft part sarcoma of the uterine corpus (Taiwan J Obstet Gynecol 2023;62:769)
- 57 year old postmenopausal woman with uterine alveolar soft part sarcoma with pelvic lymph node metastasis (Int J Clin Exp Pathol 2012;5:715)
- 68 year old postmenopausal woman with alveolar soft part sarcoma of the uterine cervix (Int J Clin Exp Pathol 2017;10:9812)
Treatment
- Complete surgical resection is first line therapy
- Most vulvovaginal ASPS reported in the literature have been treated with adjuvant radiation and a subset with adjuvant chemotherapy, though objective data are scarce (Int J Gynecol Pathol 2014;33:263)
- Surgical staging offers little prognostic benefit (Arch Gynecol Obstet 2009;279:263)
- Given the propensity for late recurrence or metastasis, long term follow up is recommended
Gross description
- Circumscribed or infiltrative, solid, lobular mass with white to tan-gray cut surface
- Size variation in female genital tract: 0.5 - 9 cm (median: 5.5) (Int J Gynecol Pathol 2014;33:263)
- Ulceration reported in half of vaginal tumors (Int J Gynecol Pathol 1995;14:283)
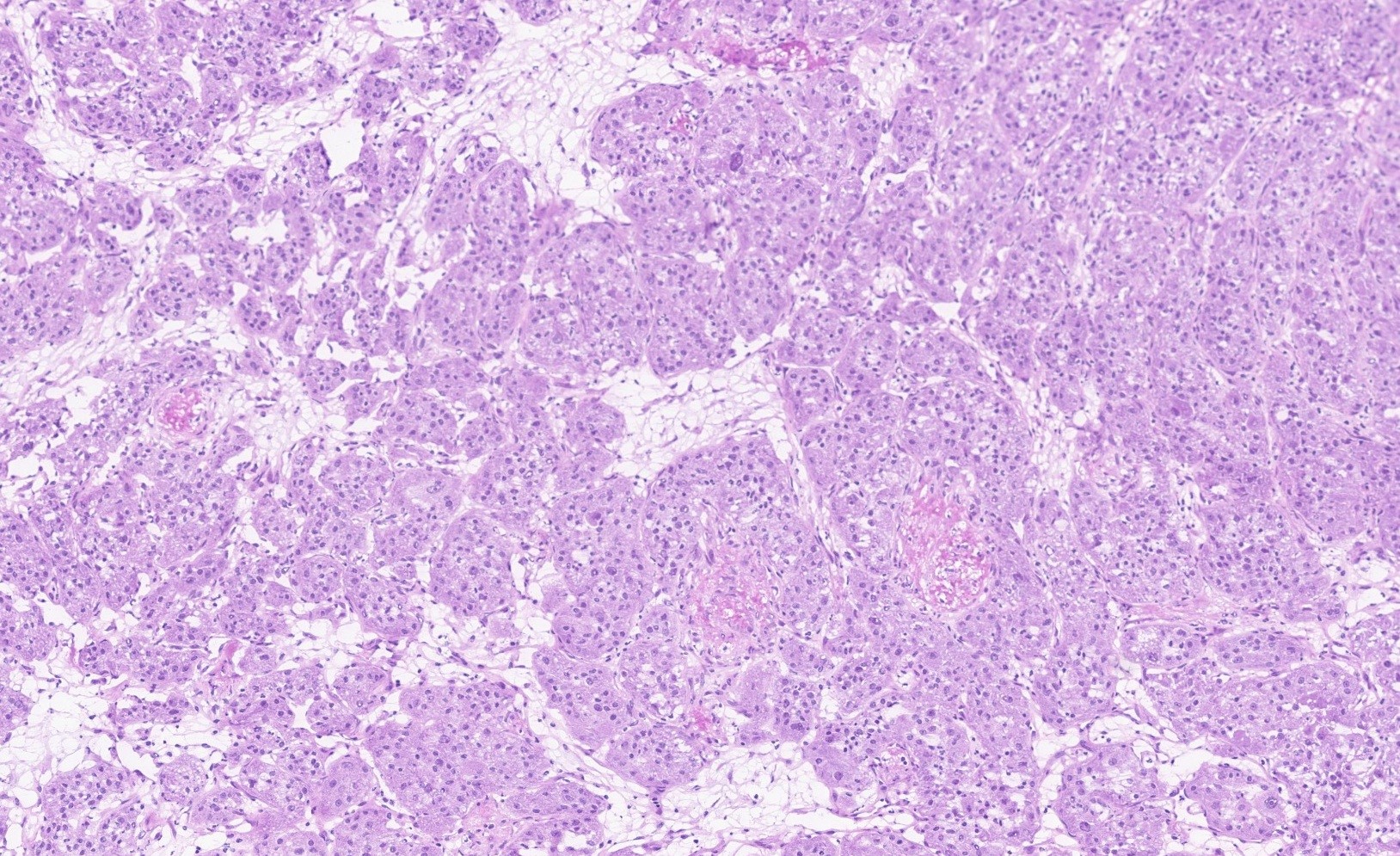
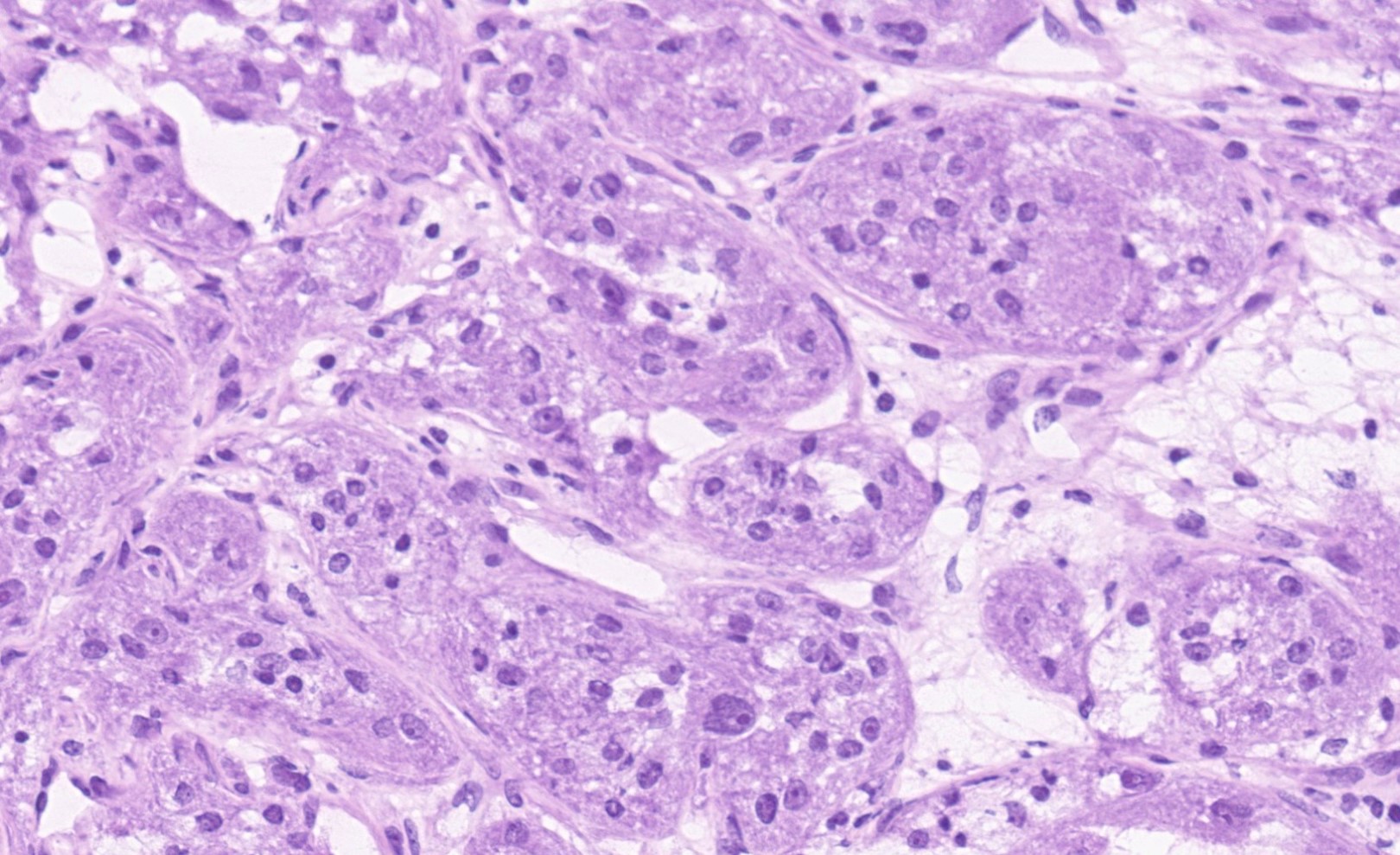
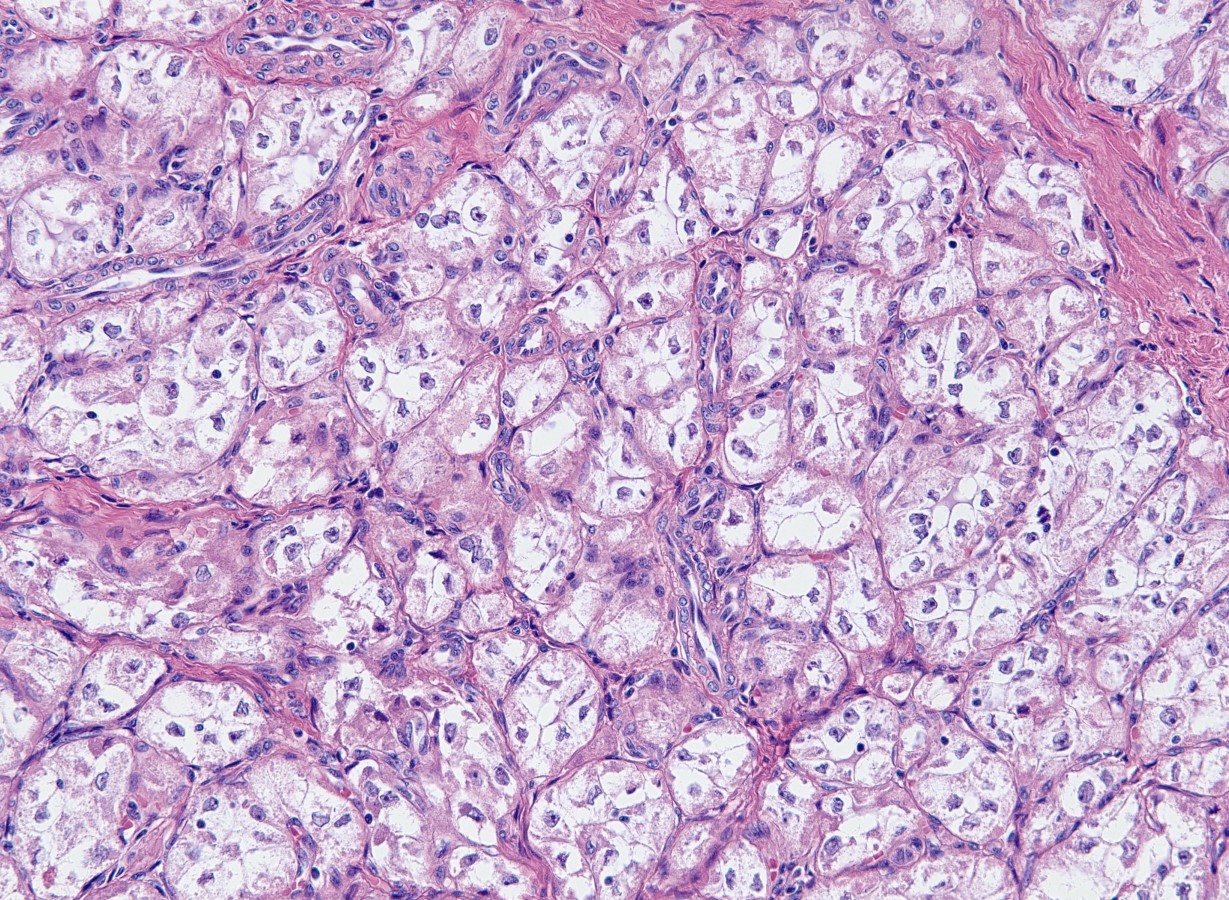
Frozen section description
- Large, round to polygonal cells with abundant eosinophilic granular cytoplasm and round, vesicular nucleus with prominent nucleolus
- Organoid / nest-like growth pattern or solid growth pattern
- Central discohesion results in characteristic pseudoalveolar-like structures
- Rich capillary network
- Reference: Cancer 2009;117:500
Frozen section images
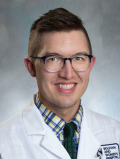
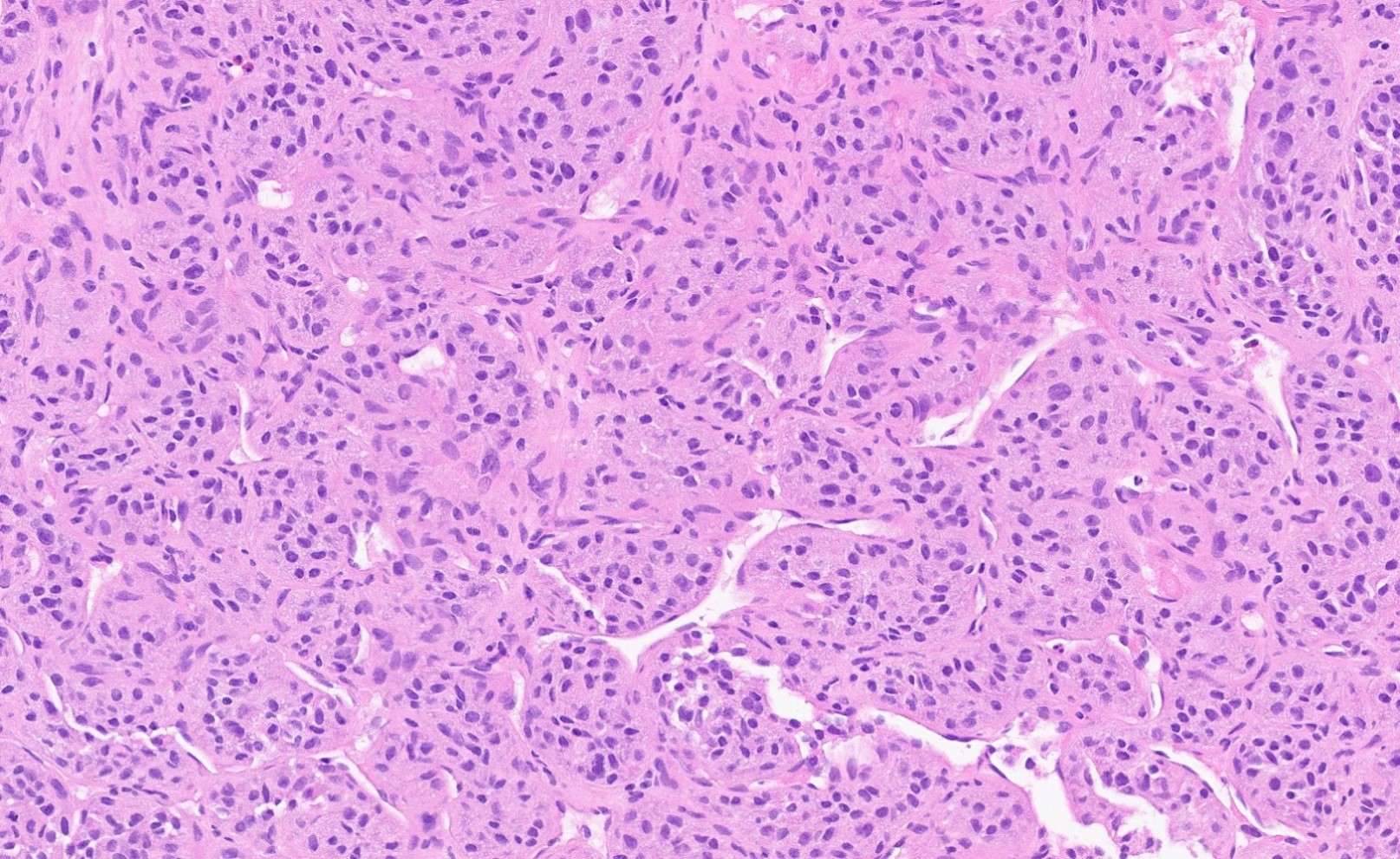
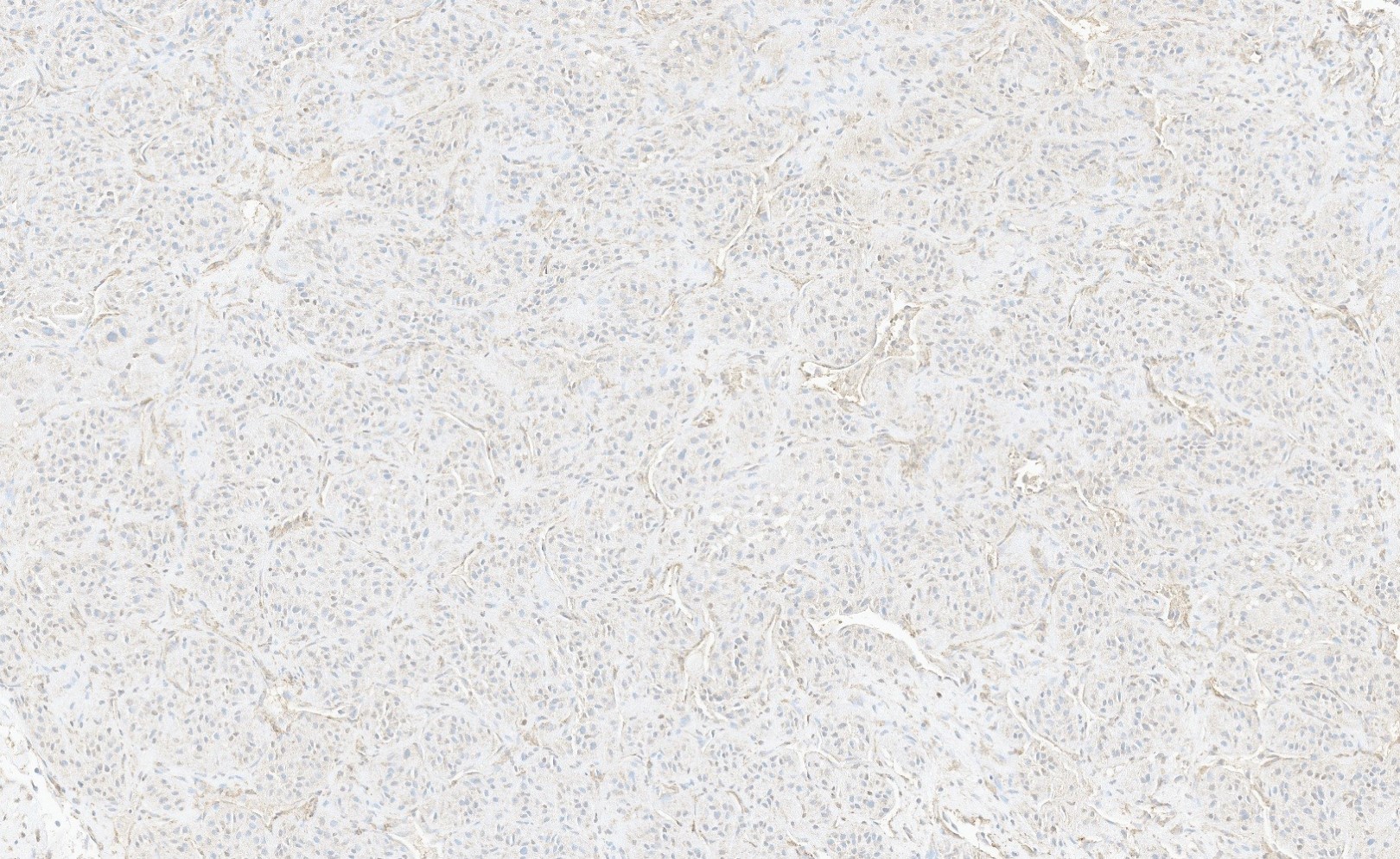
Microscopic (histologic) description
- ASPS of the female genital tract is indistinguishable from its soft tissue counterpart (Int J Gynecol Pathol 1995;14:283, Am J Surg Pathol 2017;4:622)
- Multinodular to lobular architecture with intervening fibrous septa
- Pushing or infiltrative invasion into surrounding tissues
- Well delineated tumor cell nests surrounded by thin walled vessels
- Loss of tumor cell cohesion results in pseudoalveolar pattern
- Subset show areas of solid sheet-like growth
- Tumor cells are large and polygonal with ample granular eosinophilic or clear cytoplasm and monomorphic, round to ovoid nuclei with prominent nucleoli
- Mitoses are rare (typically 0 - 1 per 10 HPF)
- Features seen in a minority of tumors: necrosis, nuclear hobnailing, nuclear pleomorphism (typically focal), bi or multinucleated tumor cells
Microscopic (histologic) images
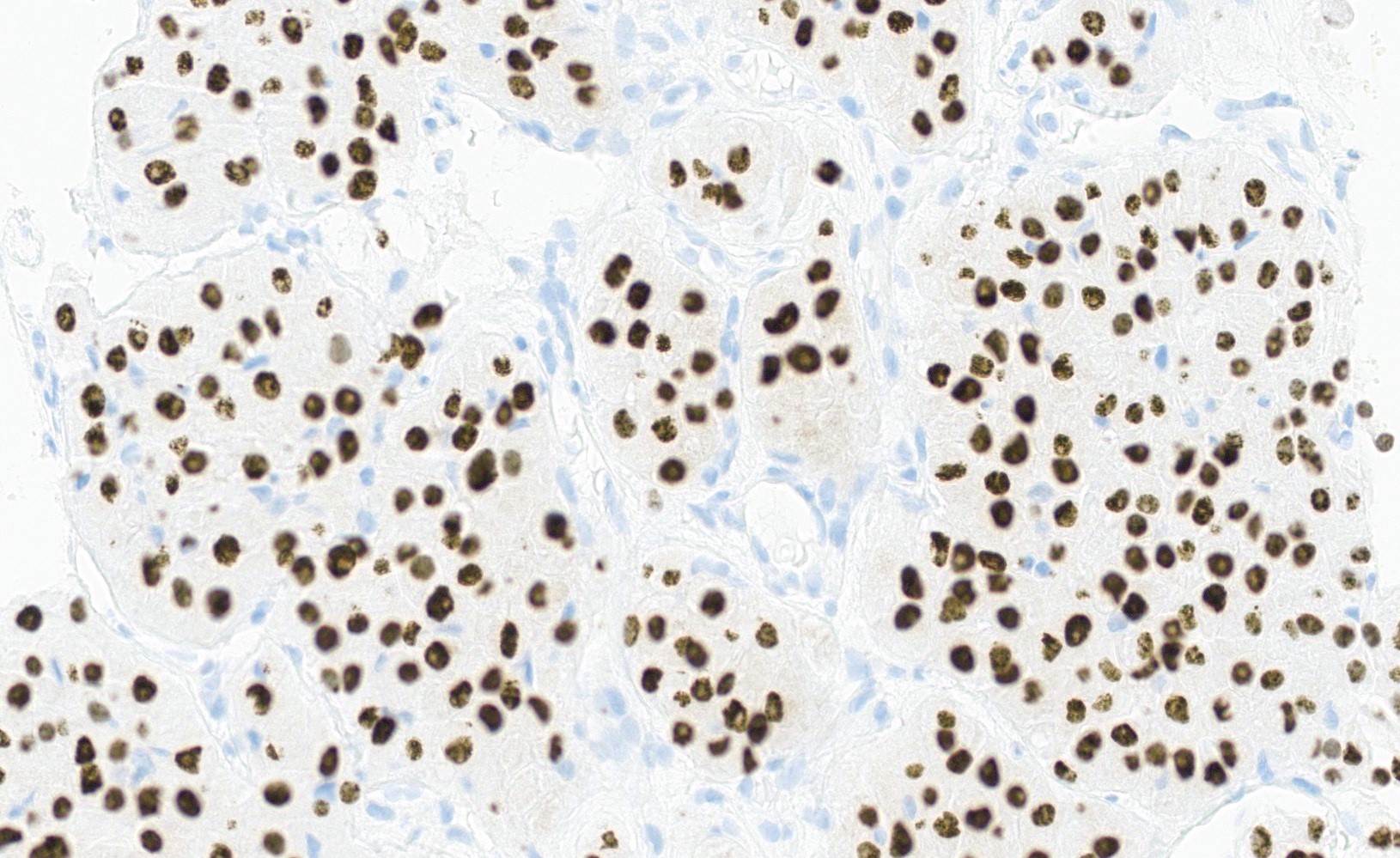
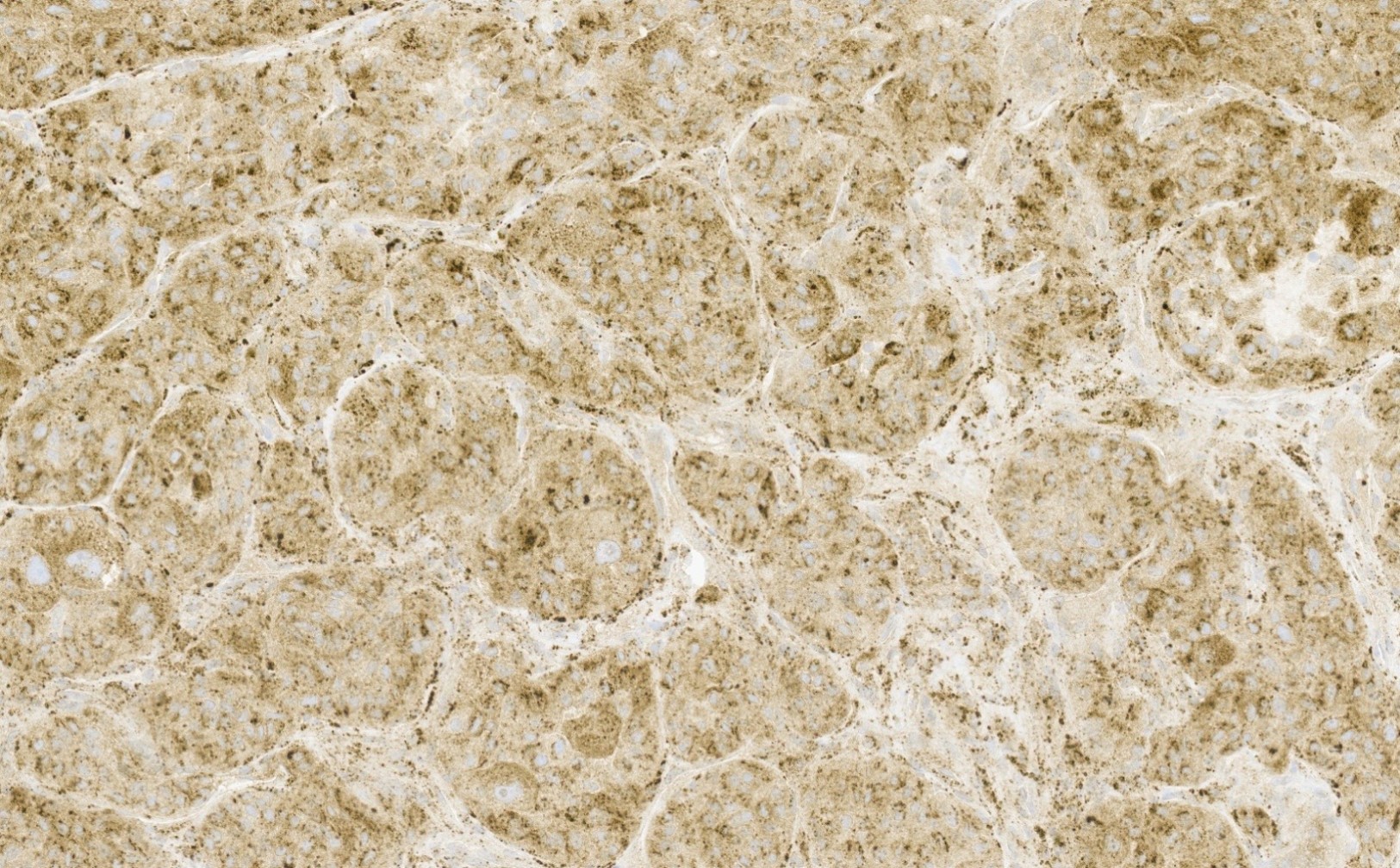
Positive stains
- TFE3 (staining percentage 100%, strong nuclear staining) (Int J Gynecol Pathol 2005;24:131, Am J Surg Pathol 2017;4:622, Int J Gynecol Pathol 2014;33:263)
- Cathepsin K (100%) (Mod Pathol 2011;24:1313)
- PASD highlights intracytoplasmic granules and crystals
- INI1 retained (positive)
- PR positive in alveolar soft part sarcomas of uterus and cervix (Diagnostics (Basel) 2022;12:1102)
Negative stains
- Muscle markers
- SMA (unspecific, weak staining possible)
- Desmin (can be focally positive [50%]) (J Clin Pathol 2006;59:1127)
- h-caldesmon
- Myogenin
- MyoD1
- Melanocytic markers
- HMB45 (rarely focal positivity) (Am J Surg Pathol 2017;4:622)
- MelanA
- MITF
- S100
- Pancytokeratin
- EMA
- PAX8
- CD34
- Inhibin
- Calretinin
- Chromogranin
- Synaptophysin
Electron microscopy description
- Intracytoplasmic rhomboid or rod shaped crystals (Arch Gynecol 1987;240:125)
Electron microscopy images
Molecular / cytogenetics description
- FISH confirms TFE3 gene rearrangement
- Reverse transcription polymerase chain reaction (PCR) can detect ASPSCR1::TFE3 fusion transcripts
- ASPSCR1::TFE3 gene fusions are characteristic for ASPS but the same fusion has been reported in a subset of PEComas (tumors with Perivascular and epithelioid cell differentiation) and a small subset of renal cell carcinomas
- References: Am J Surg Pathol 2013;37:1619, Nat Commun 2023;14:1957
Molecular / cytogenetics images
Sample pathology report
- Uterus and cervix, hysterectomy:
- Uterus:
- Proliferative endometrium, negative for hyperplasia and malignancy
- Myometrium and serosa without pathologic findings
- Cervix:
- Alveolar soft part sarcoma (see comment)
- Max tumor size: 4 cm (grossly)
- Lymphovascular invasion present
- Negative for perineural invasion
- All margins negative for tumor, closest margin: proximal (0.7 cm)
- Comment: Alveolar soft part sarcoma rarely affects the cervix or other sites of the female genital tract. It is a neoplasm of unknown differentiation but is defined as a high grade sarcoma. Molecular analysis confirmed the characteristic gene fusion involving ASPSCR1 and TFE3.
- Uterus:
Differential diagnosis
- PEComa:
- Coexpression of melanocytic (HMB45, MelanA) and myoid markers (SMA, desmin)
- May show nuclear expression of TFE3 as there are TFE3 rearranged subtypes (PSF / SFPQ::TFE3 and other TFE fusions) (Histopathology 2024;84:482, Am J Surg Pathol 2017;4:622)
- Melanoma:
- Clear cell carcinoma:
- Metastatic renal cell carcinoma:
- Paraganglioma:
- Granular cell tumor:
- Rhabdomyoma:
- Alveolar rhabdomyosarcoma:
Additional references
Board review style question #1
Board review style answer #1
D. It shows histopathologic overlap with TFE3 rearranged PEComa. The entities show considerable morphologic and genetic overlap. ASPS and TFE3 rearranged PEComa are considered 2 distinctive entities despite their known morphological overlap. Recent studies have suggested a potential histogenetic relationship between them. PEComa can be ruled out with appropriate immunohistochemical stains (MelanA, HMB45, S100). Answer A is incorrect because ASPS typically affects the soft tissue of the extremities and the head and neck area. The female genital tract, including the cervix, is a very rare site of ASPS. Answer B is incorrect because ASPS grows slowly despite of being defined as a high grade sarcoma. Answer C is incorrect because ALK rearrangements have not been described in ASPS. ASPS shows the translocation der(17)t(X;17)(p11.2;q25), resulting in ASPSCR1::TFE3 gene fusion.
Comment Here
Reference: Cervix - Alveolar soft part sarcoma
Comment Here
Reference: Cervix - Alveolar soft part sarcoma
Board review style question #2
Which statement about alveolar soft part arising in the cervix is true?
- It is diffusely positive for S100 protein, CD68 and SOX10
- It typically harbors the ASPSCR1::TFE3 fusion protein
- It typically stains negative for PASD
- It typically stains positive for myogenin and MyoD1
Board review style answer #2
B. It typically harbors the ASPSCR1::TFE3 fusion protein. Like ASPS of other sites, ASPS arising in the cervix is characterized by the translocation der(17)t(X;17)(p11.2;q25), resulting in ASPSCR1::TFE3 gene fusion; therefore, ASPS of the cervix overexpresses the fusion protein ASPSCR1::TFE3 and it stains positive for TFE3 (nuclear positivity).
Answer D is incorrect because ASPS is consistently negative for myogenin and MyoD1. These markers are positive in alveolar rhabdomyosarcoma and help distinguish this entity from ASPS.
Answer C is incorrect because PASD highlights the cytoplasmic granular and crystalline material in ASPS. It is positive in ASPS and is useful in making the diagnosis.
Answer A is incorrect because S100, CD68 and SOX10 are consistently negative in ASPS. Granular cell tumor is diffusely positive for S100 protein, CD68 and SOX10. These markers help to distinguish the entity from granular cell tumor.
Comment Here
Reference: Cervix - Alveolar soft part sarcoma
Comment Here
Reference: Cervix - Alveolar soft part sarcoma