Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chapel DB. Smooth muscle tumors. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvaLMS.html. Accessed April 1st, 2025.
Definition / general
- Leiomyoma and leiomyosarcoma are, respectively, the most common benign and malignant mesenchymal neoplasms of the vulva and vagina
- Subset of tumors with equivocal features is diagnosed as smooth muscle tumor of uncertain malignant potential (STUMP)
Essential features
- Leiomyoma and leiomyosarcoma are, respectively, the most common benign and malignant vulvovaginal mesenchymal tumors
- The morphologic spectrum of vulvovaginal smooth muscle neoplasia mirrors that seen in the uterus, including leiomyoma variants
- Although myxoid stroma is more common in vulvovaginal smooth muscle tumors than in their uterine counterparts, conventional spindled morphology still predominates
- The diagnostic criteria for vulvovaginal leiomyosarcoma have evolved over the last 5 decades, with recent evidence suggesting that criteria for diagnosing malignancy in uterine smooth muscle tumors are also accurate in vulvovaginal tumors
- The diagnosis smooth muscle tumor of uncertain malignant potential (STUMP) is applied to tumors with worrisome morphologic features that fall short of the diagnostic threshold for leiomyosarcoma
Terminology
- For uniformity of diagnosis, smooth muscle tumor of uncertain malignant potential should be used, when applicable, in place of atypical leiomyoma or atypical smooth muscle tumor
ICD coding
Epidemiology
- Most common benign (leiomyoma) and malignant (leiomyosarcoma) vulvovaginal mesenchymal tumors (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Obstet Gynecol 1995;86:269, Am J Surg Pathol 2018;42:84)
- Age range: 15 - 87 years (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Am J Surg Pathol 2018;42:84, Hum Pathol 2020;103:83, Am J Surg Pathol 1996;20:779, Histopathology 1991;18:523)
- Most common in fourth and fifth decades
Sites
- Vagina > vulva (approximately 3:1) (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Obstet Gynecol 1995;86:269, Am J Surg Pathol 2018;42:84)
- Vagina: upper, middle and lower thirds equally affected (Obstet Gynecol 1979;53:689)
- Vulva: mons pubis and labia majora > labia minora (Obstet Gynecol 1979;53:213, Histopathology 1991;18:523)
Clinical features
- May present incidentally or as a painless or tender prolapsing mass (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Am J Surg Pathol 2018;42:84, Hum Pathol 2020;103:83, Histopathology 1991;18:523)
- Present for weeks to years before diagnosis
- Vulvar tumors often diagnosed clinically as Bartholin cyst
- Rarely, vaginal wall tumors grow posteriorly, impinging on the rectum or pouch of Douglas (Case Rep Obstet Gynecol 2017;2017:2190135)
- Fumarate hydratase (FH) deficient vulvovaginal smooth muscle tumors may be associated with hereditary leiomyomatosis renal cell carcinoma (HLRCC) syndrome (Mod Pathol 2021;34:767 - see abstract 614, page 735)
- Multiple vulvar leiomyomas (leiomyomatosis) may co-occur with multiple esophageal leiomyomas (retained FH expression, distinct from HLRCC) (Gynecol Oncol 1991;41:92)
Diagnosis
- Definitive diagnosis best made on an excision specimen
- Diagnostic core biopsy obtained in a subset (particularly in vaginal tumors) (Case Rep Obstet Gynecol 2017;2017:2190135)
Radiology description
- MRI:
- Circumscription favors benign diagnosis (Indian J Radiol Imaging 2009;19:238)
- Infiltration highly worrisome for malignancy (Taiwan J Obstet Gynecol 2020;59:314)
- May show necrosis in leiomyosarcoma (Clin Imaging 2009;33:482)
- Ultrasound principally used to characterize vaginal tumors (J Midlife Health 2019;10:204, Indian J Radiol Imaging 2009;19:238, Medicine (Baltimore) 2021;100:e24911)
- CT:
- Examination of chest, abdomen and pelvis to exclude tumor metastasis
- PET avidity may highlight primary or recurrent leiomyosarcoma (Gynecol Oncol Rep 2017;21:28, Cureus 2016;8:e550)
Radiology images
Prognostic factors
- Leiomyoma: excellent prognosis
- Negligible recurrence risk, even with positive margins (Am J Surg Pathol 2018;42:84)
- Leiomyoma variants (plexiform, cellular, with bizarre nuclei) follow benign course (Hum Pathol 2020;103:83, Histopathology 1991;18:523)
- Smooth muscle tumor of uncertain malignant potential (STUMP): intermediate prognosis
- 1 of 5 recently reported cases recurred (Hum Pathol 2020;103:83)
- Few cases and limited follow up available
- Leiomyosarcoma: guarded prognosis
- In a recent study with median follow up of 64 months (Am J Surg Pathol 2018;42:84):
- Local or distant recurrence in 12 of 15 (80%) vulvovaginal leiomyosarcomas
- Distant metastasis in 10 of 15
- Death from disease in 8 of 15
- Recurrences reported up to 10 years after diagnosis (Am J Surg Pathol 1996;20:779)
- In a recent study with median follow up of 64 months (Am J Surg Pathol 2018;42:84):
Case reports
- Leiomyoma
- 24 year old woman with a vaginal leiomyoma (Medicine (Baltimore) 2021;100:e24911)
- 36 year old woman with a vaginal leiomyoma (BMC Womens Health 2020;20:12)
- 39 year old woman with a vulvar leiomyoma BMC Womens Health 2020;20:89)
- 45 year old woman with a vulvar epithelioid leiomyoma (Medicine (Baltimore) 2019;98:e17423)
- 45 year old woman with a vaginal leiomyoma (J Midlife Health 2019;10:204)
- STUMP
- 34 year old woman with a vulvar STUMP (Gynecol Oncol Rep 2017;20:1)
- Leiomyosarcoma
- 37 year old woman with vulvar leiomyosarcoma (Cureus 2016;8:e550)
- 58 year old woman with vaginal leiomyosarcoma (Taiwan J Obstet Gynecol 2020;59:314)
- 63 year old woman with vulvar leiomyosarcoma (Oman Med J 2020;35:e153)
- 66 year old woman with vaginal leiomyosarcoma (J Gynecol Oncol 2008;19:261)
- 73 year old woman with vulvar leiomyosarcoma (Prz Menopauzalny 2020;19:184)
Treatment
- Leiomyoma
- Conservative simple excision curative
- STUMP (based on limited data)
- Complete excision with negative margins
- At least 10 mm margin has been advocated (Histopathology 2000;36:97)
- Close follow up (Int J Gynecol Pathol 2001;20:105)
- Leiomyosarcoma
- Wide local excision
- (Neo)adjuvant chemotherapy or radiation per clinical indication (Cureus 2016;8:e550, J Gynecol Oncol 2008;19:261)
- Hormonal therapy may be effective in some cases (Gynecol Oncol Rep 2017;21:28)
- Effective use of neoadjuvant GnRH analog therapy reported (Medicine (Baltimore) 2021;100:e24911)
- Long term follow up required
- Genetic counseling advised for patients with morphologic or immunohistochemical features of FH deficiency
Clinical images
Gross description
- Wide size range: 0.5 - 16 cm, with most < 5 cm (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Am J Surg Pathol 2018;42:84, Am J Surg Pathol 1996;20:779, Histopathology 1991;18:523)
- Broad size overlap between leiomyoma and leiomyosarcoma (Am J Surg Pathol 2018;42:84)
- Leiomyoma:
- Well circumscribed
- Rubbery, white-tan, whorled surface (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Hum Pathol 2020;103:83)
- Leiomyosarcoma:
- May be well or poorly circumscribed
- Soft, fleshy to variegated cut surface
- Hemorrhage and necrosis may be apparent (Am J Surg Pathol 2018;42:84)
Gross images
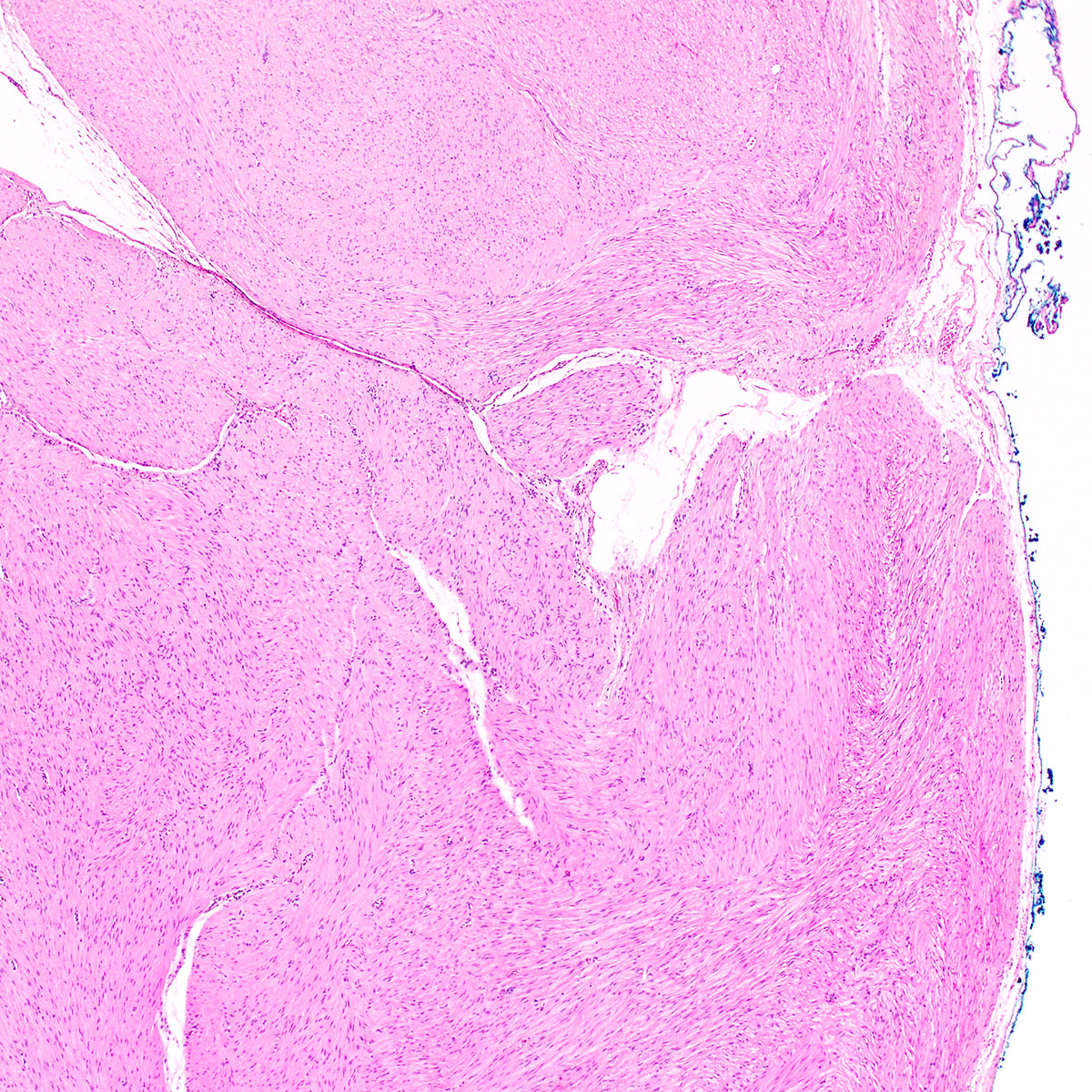
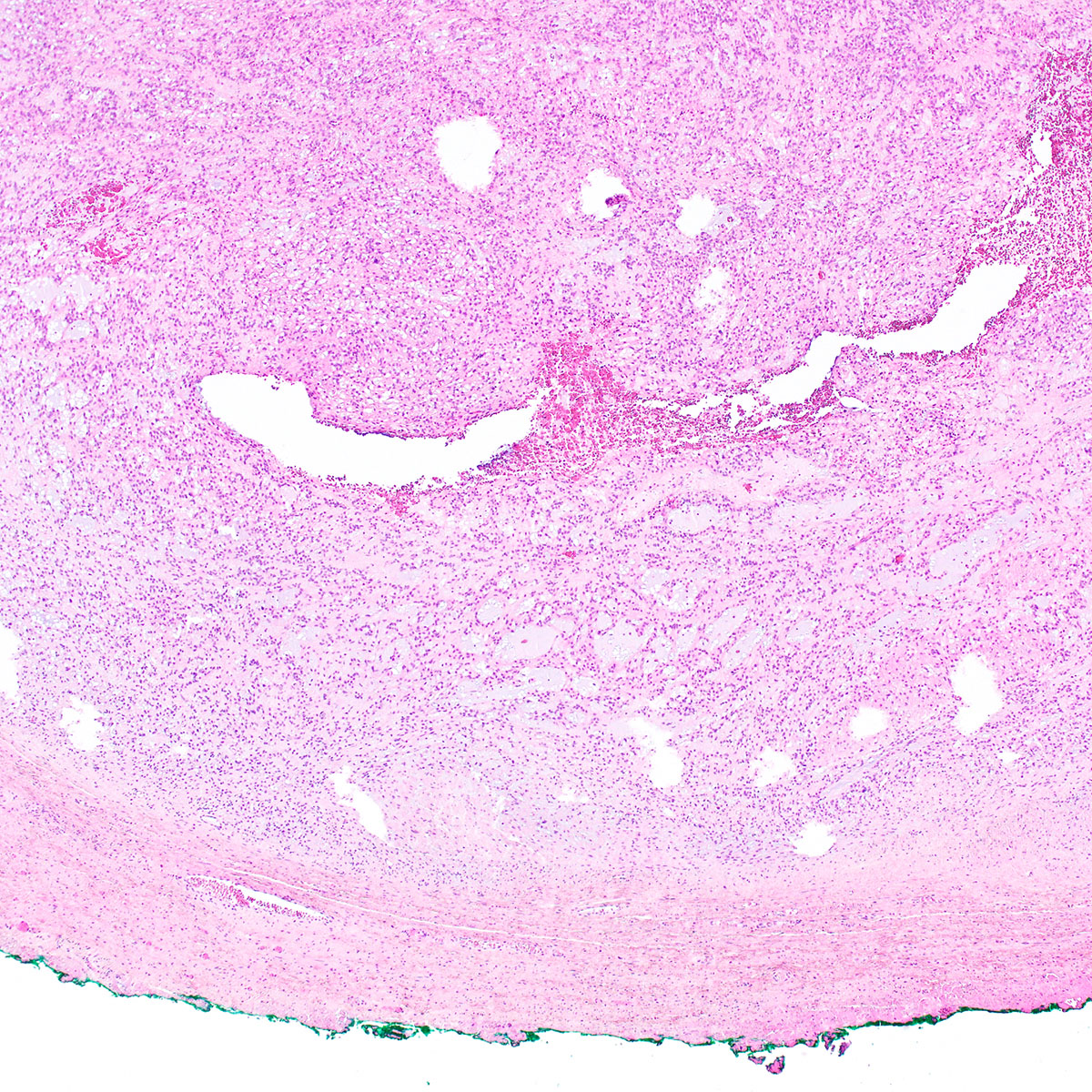
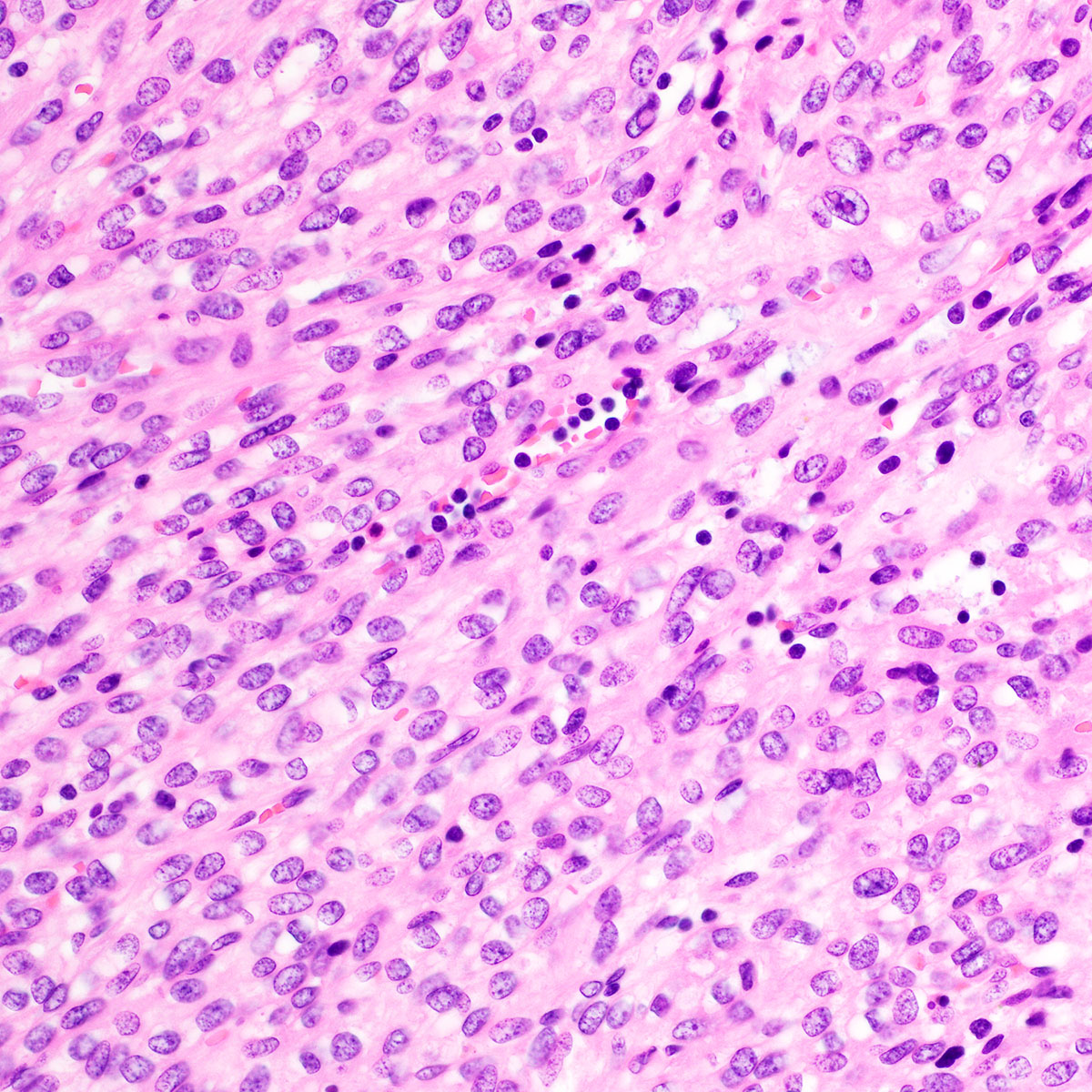
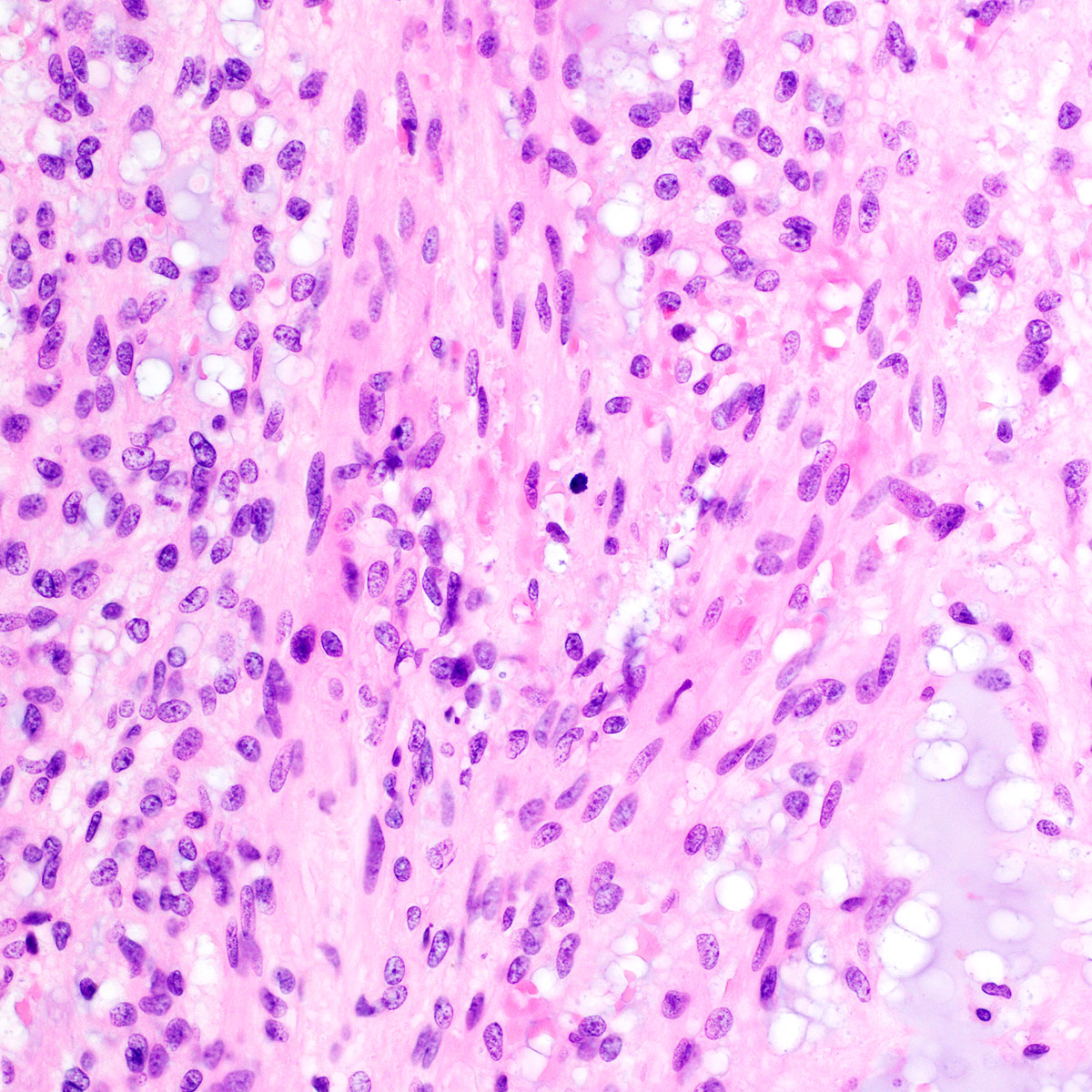
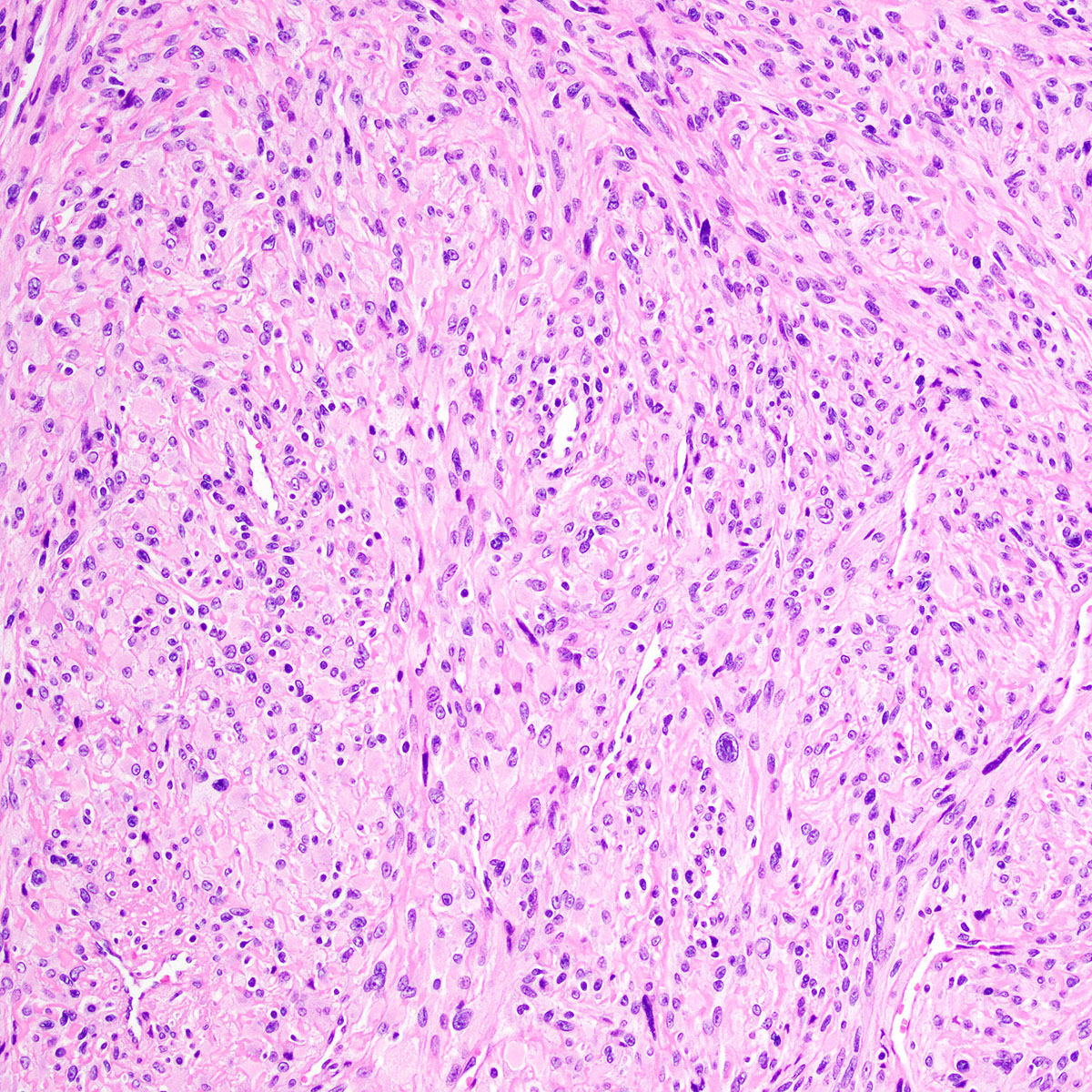
Microscopic (histologic) description
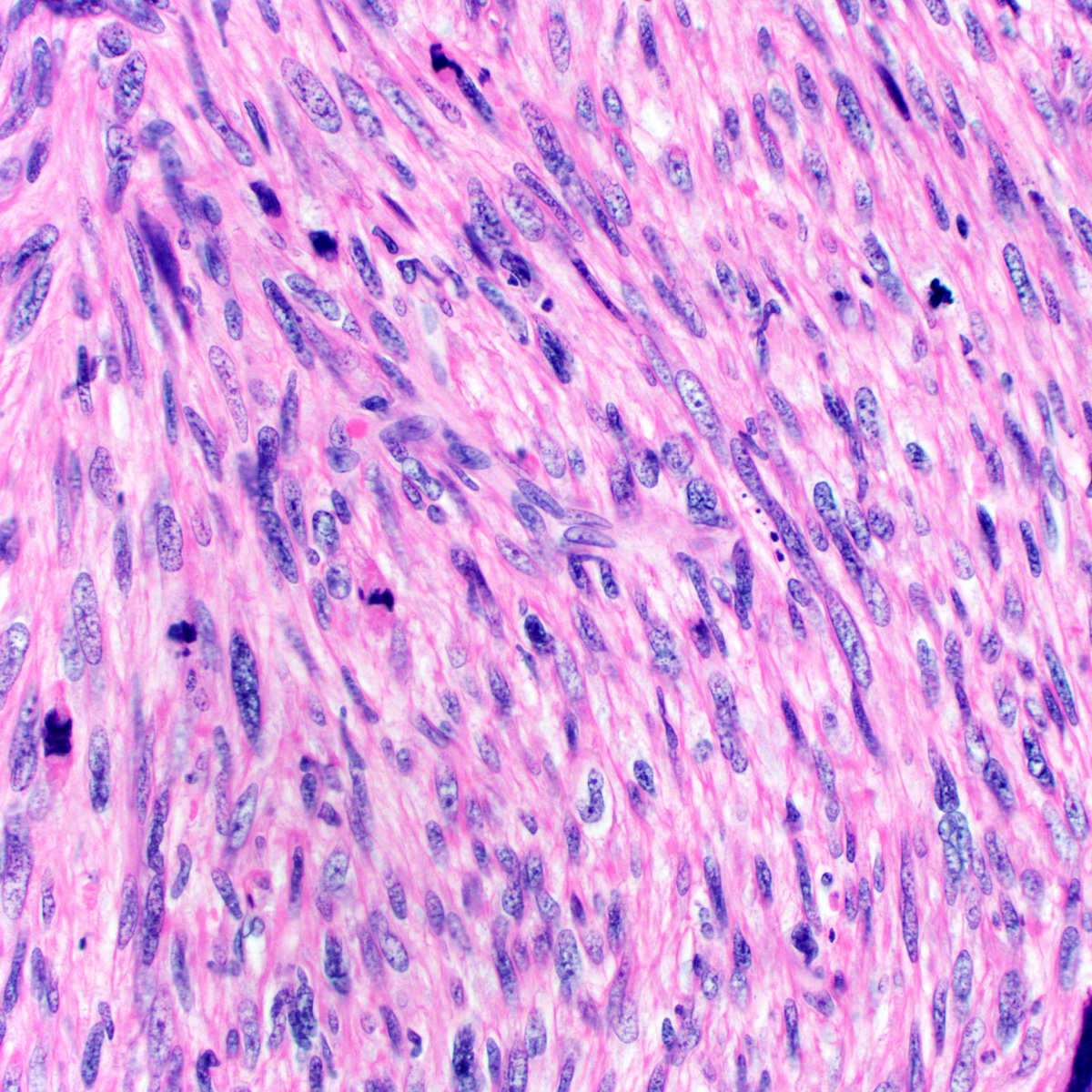
- Leiomyoma: morphologic spectrum similar to uterine smooth muscle tumors
- Spindle cell morphology most common (Am J Surg Pathol 1996;20:779, Histopathology 1991;18:523)
- Intersecting fascicles of spindle cells
- Cigar shaped nuclei
- Eosinophilic cytoplasm
- Epithelioid and myxoid morphologies well documented (Am J Surg Pathol 1996;20:779, Histopathology 1991;18:523, Medicine (Baltimore) 2019;98:e17423, Gynecol Oncol 2005;96:548)
- Myxoid change more common in vulvovaginal smooth muscle tumors than in uterine smooth muscle tumors
- Myxoid change may predominate in pregnancy (Obstet Gynecol 1979;53:213)
- Uncommon morphologic variants reported (Obstet Gynecol 1979;53:689, Obstet Gynecol 1979;53:213, Am J Surg Pathol 2018;42:84, Hum Pathol 2020;103:83, Am J Surg Pathol 1996;20:779, Histopathology 1991;18:523, Medicine (Baltimore) 2019;98:e17423, Gynecol Oncol 2005;96:548):
- Plexiform leiomyoma
- Cellular leiomyoma
- Leiomyoma with bizarre nuclei
- Fumarate hydratase (FH) deficient leiomyomas show characteristic morphologic features
- Nuclear atypia
- Orangeophilic macronucleoli with perinucleolar clearing
- Staghorn (hemangiopericytoma-like) vessels
- Alveolar pattern edema
- Chain-like nuclear arrangement
- Vaginal leiomyomas: degenerative hyalinization, calcification, hemorrhage and edema common (probably secondary traumatic changes) (Obstet Gynecol 1979;53:689)
- Spindle cell morphology most common (Am J Surg Pathol 1996;20:779, Histopathology 1991;18:523)
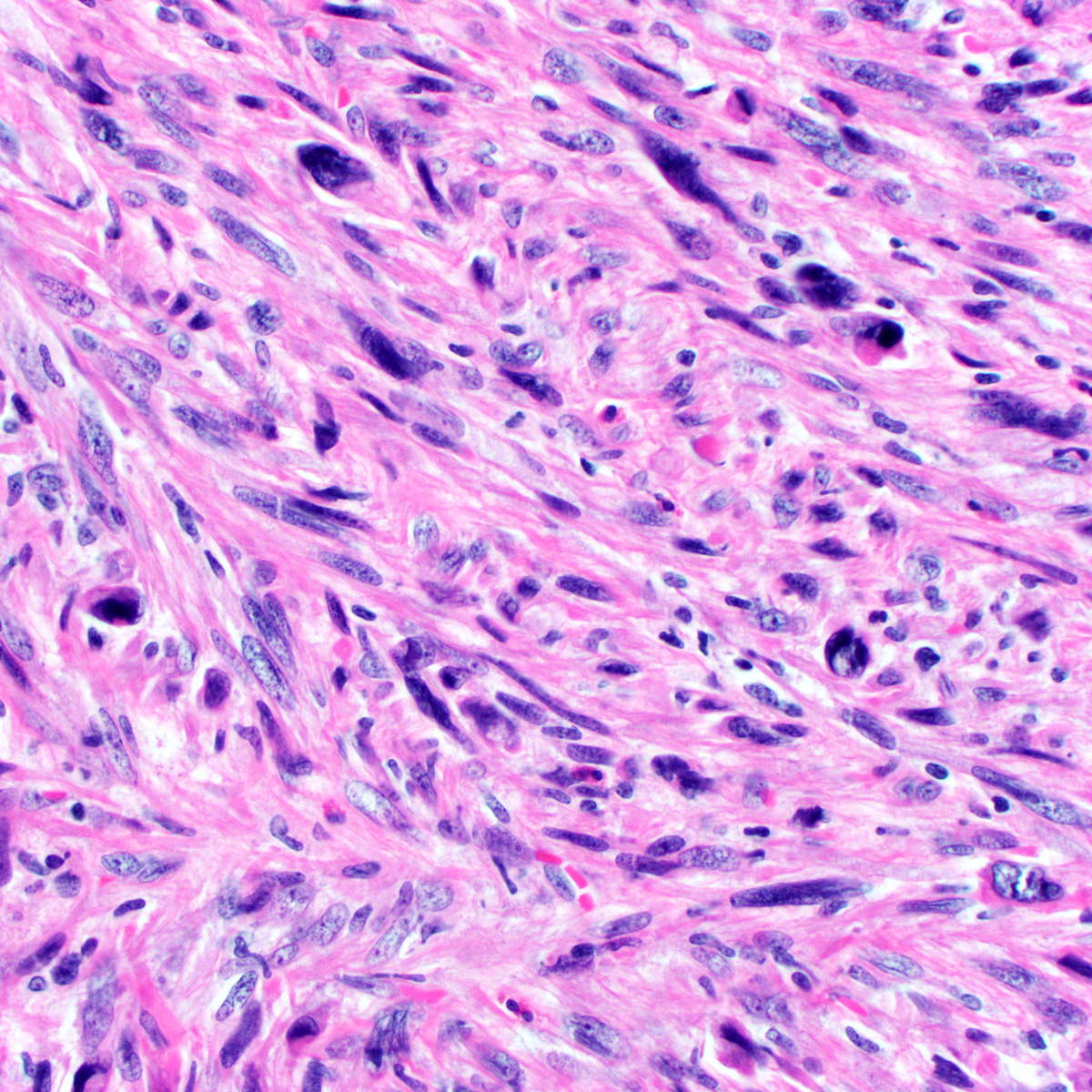
- Leiomyosarcoma: criteria for malignancy have evolved
- Original criteria for vaginal leiomyosarcoma (Obstet Gynecol 1979;53:689)
- ≥ 5 mitoses per 10 high power fields AND moderate or marked atypia OR
- Infiltrative border
- Original criteria for vulvar leiomyosarcoma (Obstet Gynecol 1979;53:213)
- ≥ 5 cm AND ≥ 5 mitoses per 10 high power fields AND infiltrative border
- Modified criteria for vulvar leiomyosarcoma (Am J Surg Pathol 1996;20:779)
- At least three of the following:
- Moderate to severe nuclear atypia
- ≥ 5 cm
- ≥ 5 mitoses per 10 high power fields
- Infiltrative border
- At least three of the following:
- Recent data suggest uterine criteria for leiomyosarcoma are applicable to vulvovaginal tumors (Am J Surg Pathol 2018;42:84, Hum Pathol 2020;103:83, Gynecol Oncol Rep 2017;20:1)
- At least two of the following:
- Moderate to severe nuclear atypia
- Mitoses ≥ 10 per 10 high power fields
- Coagulative tumor necrosis
- Uterine criteria for epithelioid and myxoid leiomyosarcoma not yet validated in vulvovaginal tumors (Medicine (Baltimore) 2019;98:e17423)
- At least two of the following:
- Original criteria for vaginal leiomyosarcoma (Obstet Gynecol 1979;53:689)
- STUMP: criteria difficult to establish, given rarity and lack of long term follow up
- Nielsen, et al., defined atypical leiomyoma by presence of two atypical features (Am J Surg Pathol 1996;20:779):
- Moderate to severe nuclear atypia
- ≥ 5 cm
- ≥ 5 mitoses per 10 high power fields
- Infiltrative border
- Nucci and Fletcher defined STUMP by presence of any of the following (Histopathology 2000;36:97):
- Infiltrative margins
- Nuclear atypia
- Any mitotic activity
- More recent data suggest that uterine criteria for STUMP may apply to vulvovaginal tumors (Hum Pathol 2020;103:83, Gynecol Oncol Rep 2017;20:1)
- Nielsen, et al., defined atypical leiomyoma by presence of two atypical features (Am J Surg Pathol 1996;20:779):
Microscopic (histologic) images
Positive stains
Negative stains
- CD34
- S100
- Cytokeratins
- Note: CAM5.2 may show cross reactivity with smooth muscle
- Myogenin
- MyoD1
- FH deficiency reported in a subset (Mod Pathol 2021;34:767 - see abstract 614, page 735)
Electron microscopy description
- Pleomorphic cells with complex cytoplasmic projections (Taiwan J Obstet Gynecol 2020;59:314)
- Well developed rough endoplasmic reticulum
- Large indented nuclei with prominent nucleoli
- Myofilaments may be rare
- Intercellular junctions absent
Electron microscopy images
Sample pathology report
- Leiomyoma:
- Right labial mass, excision:
- Leiomyoma (3 cm) (see comment)
- Margins negative
- Comment: Microscopic examination reveals a well circumscribed tumor composed of fascicles of bland spindle cells with abundant eosinophilic cytoplasm. The tumor is entirely submitted for histologic examination. No necrosis or mitoses are identified. The morphology is consistent with a leiomyoma.
- Right labial mass, excision:
- STUMP:
- Right labial mass, excision:
- Smooth muscle tumor of uncertain malignant potential (4 cm) (see comment)
- Margins negative
- Comment: Microscopic examination reveals a smooth muscle tumor, comprised of fascicles of spindle cells with moderate to focally marked nuclear atypia. Mitoses number up to 6 per 10 high power fields. There is no necrosis and the tumor is well circumscribed, without infiltration of surrounding vulvar tissues. Margins are negative (tumor approaches to within 0.3 cm of one unoriented inked margin, block A3). The morphologic findings, including nuclear atypia and increased mitoses, are worrisome but do not reach the threshold for diagnosis of leiomyosarcoma. Accordingly, this tumor is best classified as a smooth muscle tumor of uncertain malignant potential (STUMP). Recent reports indicate that vulvovaginal STUMPs have the potential for local recurrence (see reference) but specific prognostic factors are not well defined. Clinical correlation is advised and close clinical follow up is recommended (Hum Pathol 2020;103:83).
- Right labial mass, excision:
- Leiomyosarcoma:
- Right labial mass, wide local excision:
- Leiomyosarcoma (6.5 cm) (see comment)
- Comment: Microscopic examination reveals a high grade spindle cell neoplasm, composed of fascicles of atypical to focally pleomorphic cells, with conspicuous mitoses (up to 12 per 10 high power fields), including atypical forms. Tumor type coagulative necrosis is identified and there is multifocal tumor infiltration of surrounding vulvar tissues. Margins are negative (tumor approaches to within 0.4 cm of the inked lateral margin). Immunostains for SMA, desmin and caldesmon are positive, whereas CD34, S100 and CK AE1 / AE3 immunostains are negative. The findings are diagnostic of leiomyosarcoma. Correlation with clinical and radiographic findings is advised.
- Right labial mass, wide local excision:
Differential diagnosis
- Cellular angiofibroma (Am J Surg Pathol 2018;42:84):
- Angiomyofibroblastoma:
- Alternating hypo and hypercellular foci
- Short spindle to epithelioid or plasmacytoid cells, clustered around abundant small, thin walled vessels
- Aggressive angiomyxoma:
- Inflammatory myofibroblastic tumor:
- Conspicuous inflammatory infiltrate, often with plasma cells
- ALK IHC positive and rearranged by molecular testing
- Solitary fibrous tumor:
- Variable (patternless) architecture
- Alternating hypocellular and hypercellular zones
- Staghorn (HPC-like) vasculature
- Adipocytic component in a subset
- STAT6 IHC positive
- NAB2-STAT6 gene fusion
- PEComa:
- Epithelioid cells with clear to eosinophilic and granular cytoplasm
- HMB45, MelanA, PNL2, cathepsin K positive
- Melanoma:
- Myoepithelial neoplasm:
- Prominent myxoid stroma
- Coexpression of EMA, cytokeratin and S100 typical
- GFAP and p63 expressed in ~50%
- SMARCB1 / INI1 lost in ~50%
- Dermatofibrosarcoma protuberans:
- Spindle cells arranged in short storiform fascicles
- Sarcomatous transformation: increased mitoses, increased atypia, more sweeping fascicles in a herringbone pattern
- Dermal based tumor with subcutaneous infiltration (characteristic honeycomb fat trapping)
- CD34 positive
- Desmin and SMA negative
- COL1A1-PDGFRB t(17;22) fusion
Additional references
Board review style question #1
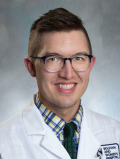
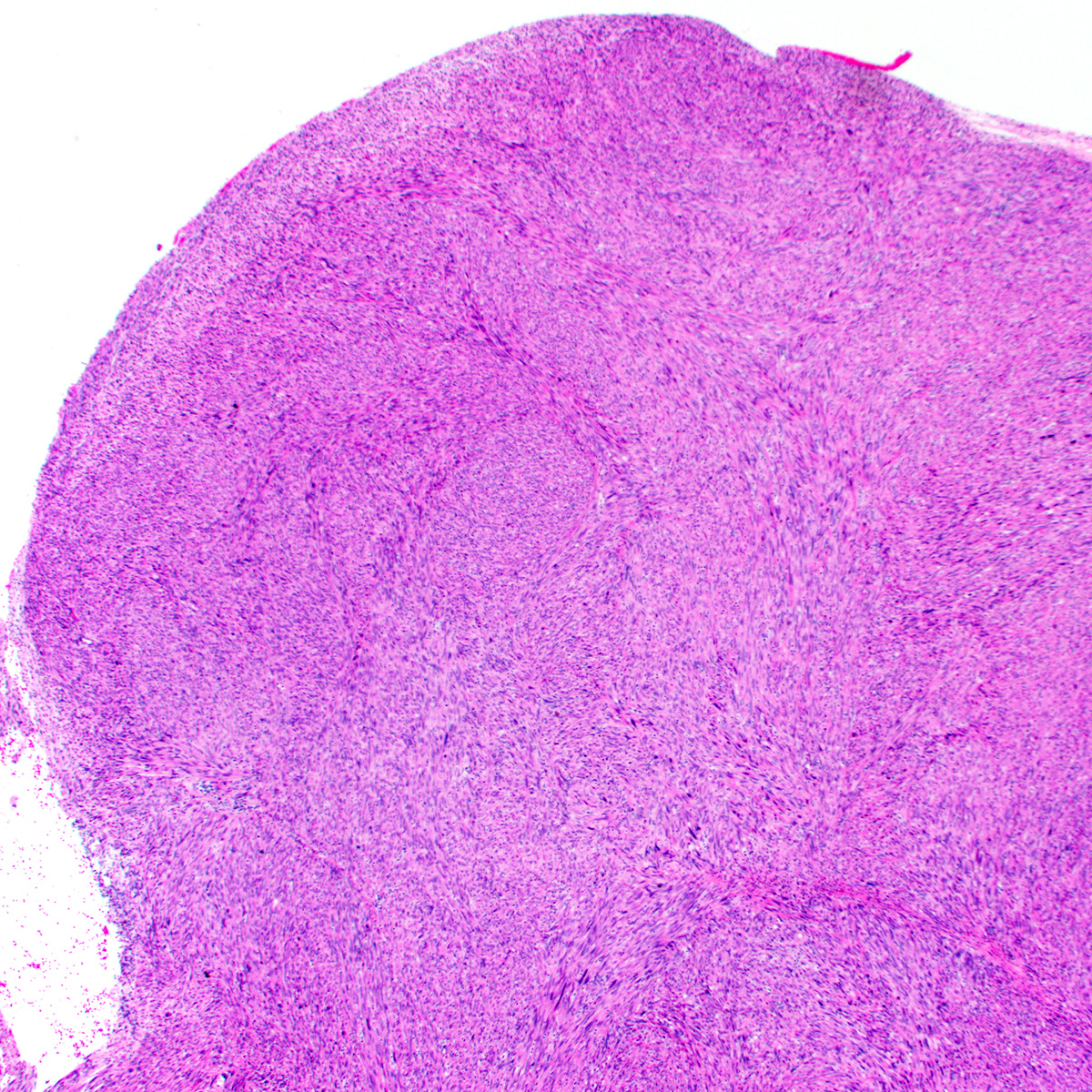
A 36 year old woman undergoes excision of a 3 cm, slow growing, painless vulvar mass. The lesion is well circumscribed and microscopic examination reveals no nuclear atypia, necrosis or mitotic activity. A representative photomicrograph is shown above. Immunostains for smooth muscle actin, desmin and caldesmon are positive. Which of the following statements is true regarding the depicted tumor?
- Approximately 50% recur after simple local excision
- CD34 immunohistochemistry is positive in > 90% of cases
- Estrogen and progesterone receptor are expressed in < 10%
- Plexiform architecture merits a malignant diagnosis
- This is the most common vulvar mesenchymal neoplasm
Board review style answer #1
E. Leiomyoma is the most common mesenchymal neoplasm of the vulva.
Comment Here
Reference: Smooth muscle tumors
Comment Here
Reference: Smooth muscle tumors
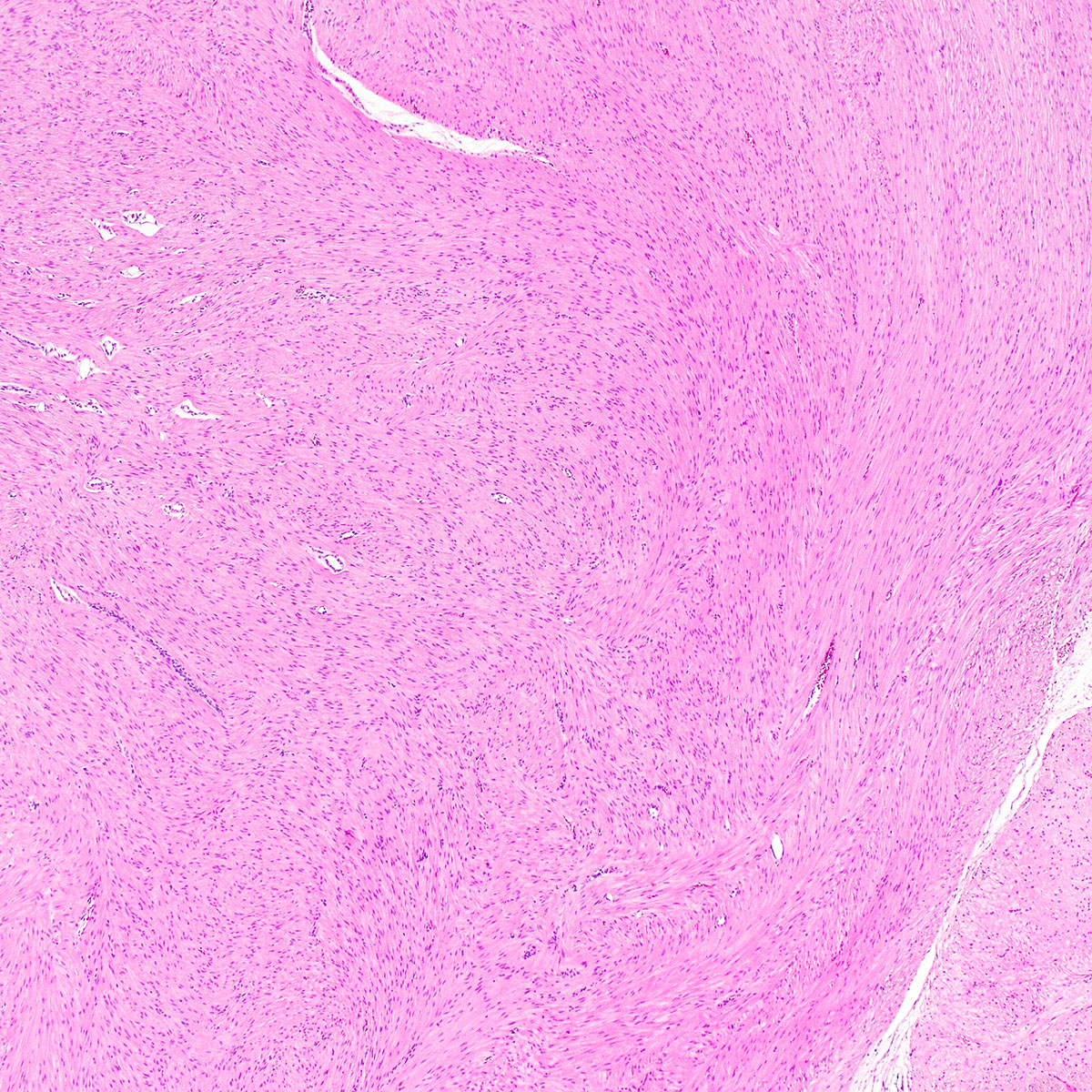
Board review style question #2
A 60 year old woman presents with vaginal bleeding and is found to have a 7 cm prolapsing mass. A preoperative MRI shows infiltration of the rectovaginal septum. A core biopsy is obtained, showing atypical spindle cells with brisk mitoses (up to 12 per 10 high power fields) and coagulative necrosis. A representative photomicrograph is shown above. Immunostains for desmin and caldesmon are positive. Which of the following statements is true regarding the depicted tumor?
- Local recurrence or distant metastasis occur in > 50%
- Most are grossly and microscopically well circumscribed
- Most cases show predominantly epithelioid morphology
- MyoD1 immunohistochemistry is strongly and diffusely positive
- Positive surgical margins are not associated with increased risk of local recurrence
Board review style answer #2
A. Primary vulvovaginal leiomyosarcoma is associated with > 50% risk of local recurrence or distant metastasis.
Comment Here
Reference: Smooth muscle tumors
Comment Here
Reference: Smooth muscle tumors