Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Erem AS, Turashvili G. Atypical melanocytic nevi of the genital type-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvaAMNGT.html. Accessed April 2nd, 2025.
Definition / general
- Rare benign melanocytic lesion, most commonly involving the vulva of young women with concerning histologic features that may overlap with melanoma but are associated with benign behavior (J Cutan Pathol 2008;35:24)
- Belongs to the general group nevi of special sites
- Commonly also part of pigmented lesions of the vulva (J Cutan Pathol 2008;35:24)
Essential features
- Nonmelanoma histologic diagnosis
Terminology
- Atypical melanocytic nevi of genital type (AMNGT)
- Atypical genital nevi (AGN)
- Nevi with site related atypia
- Nevi of special sites
ICD coding
- ICD-O
- ICD-10
- ICD-11
- EG9Y - skin disorders involving other specific body regions
- EG9Z - skin disorders involving certain specific body regions, unspecified
- Specific anatomy (use additional code, if desired)
Epidemiology
- Generally occurs in young women, with 50% of patients < 20 years old (median: 26 years; range: 6 - 54 years) (Am J Surg Pathol 2008;32:51, J Cutan Pathol 2008;35:24, J Am Acad Dermatol 2014;71:1241, Dermatology 2011;222:157)
Sites
- Most common: labia majora > labia minora > clitoris, followed by mons pubis and perineum (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51, Arch Pathol Lab Med 2011;135:317)
- More frequent on mucosal areas in children < 10 years old (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51)
- In adults, equal distribution between mucosal and hair bearing surfaces (Am J Surg Pathol 2008;32:51)
Etiology
- Largely unknown but associated with anatomic milk line, including axillae, breasts, periumbilical region and groin (Am J Surg Pathol 2008;32:51)
Clinical features
- Compared to other nevi of special sites, AMNGT may have alarming clinical features, including darker pigmentation, irregular borders and size up to 2 cm (median: 0.5 cm) (Am J Surg Pathol 2008;32:51, Hum Pathol 1998;29:S1)
- Mucosal sites most commonly present with flat lesions and demonstrate atypical foci of hyperpigmentation (Am J Surg Pathol 2008;32:51)
- See table 1
Table 1: Clinical and histologic differences between atypical genital nevus and vulvar melanoma (adapted from Hoang: Melanocytic Lesions - A Case Based Approach, 1st Edition, 2014)
| Proposed diagnosis | Atypical genital nevus of special anatomic site | Vulvar melanoma |
| Age | Premenopausal, young adult | Postmenopausal |
| Size | < 1 cm | > 1 cm |
| Delineation | Well circumscribed | Infiltrative |
| Symmetry | Present | Absent |
| Lateral extension of junctional component | Focal | Present |
| Lentiginous junctional component | Focal | Present |
| Junctional nests | Discohesive | Confluent |
| Retraction artifact | Present | Absent |
| Ulceration | Absent or due to trauma | Often present |
| Pagetoid upward spread | Focal, central, inconspicuous | Prominent |
| Cytologic atypia | Superficial, mild to moderate | Deep, moderate to severe |
| Dermal mitosis | Rare and superficial | Conspicuous, atypical, deep |
| Dermal maturation | Present | Absent |
| Melanin pigmentation | Coarse, uniform | Fine, irregular |
| Dermal fibrosis | Broad zone of superficial coarse dermal fibrosis | Regression type |
Diagnosis
- Dermoscopy for nonmodified mucous membranes is useful (Dermatol Ther 2010;23:449)
- May have any of the dermoscopic patterns seen in benign nevi
- Globular / cobblestone, homogenous, structureless or mixed patterns are most common (Dermatology 2011;222:157, Dermatology 2010;221:55)
- Shiny white streaks (SWS), inverse pigment network and atypical network can be seen in AMNGT in setting of symmetry pattern and absence of melanoma specific dermoscopic features (Dermatology 2011;222:157, Dermatology 2010;221:55)
- See table 2
- Histologic diagnosis is confirmatory
- For optimal diagnosis, lichen sclerosus should be controlled before excision of the nevus (J Am Acad Dermatol 2004;50:690, Arch Dermatol 2002;138:77)
Table 2: Distinguishing vulvar nevi, melanosis and melanoma (adapted from J Am Acad Dermatol 2014;71:1241)
| Reassuring features suggestive of a benign process | Concerning features for possible malignancy | |
| Clinical |
|
|
| Dermoscopy |
|
|
| Reflectance confocal microscopy |
|
|
Prognostic factors
- Thought to have a benign clinical course (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51)
- No recurrences noted in cases with negative margins (Hum Pathol 1998;29:S1, Am J Surg Pathol 2008;32:51)
- Limited studies show a 9% recurrence in those that have positive or uncertain margins (Am J Surg Pathol 2008;32:51)
Case reports
- 7 year old girl with a genital nevus in the background of lichen sclerosus (Am J Dermatopathol 2012;34:838)
- 12 year old girl with a new variant of site related histological atypia (Am J Dermatopathol 2011;33:611)
- 13 year old girl with an atypical melanocytic nevus of genital type (Dermatol Reports 2023;15:9667)
- 30 year old woman with atypical melanocytic nevi of genital tract (Dermatol Online J 2010;16:9)
Treatment
- Simple excision is usually sufficient
Clinical images
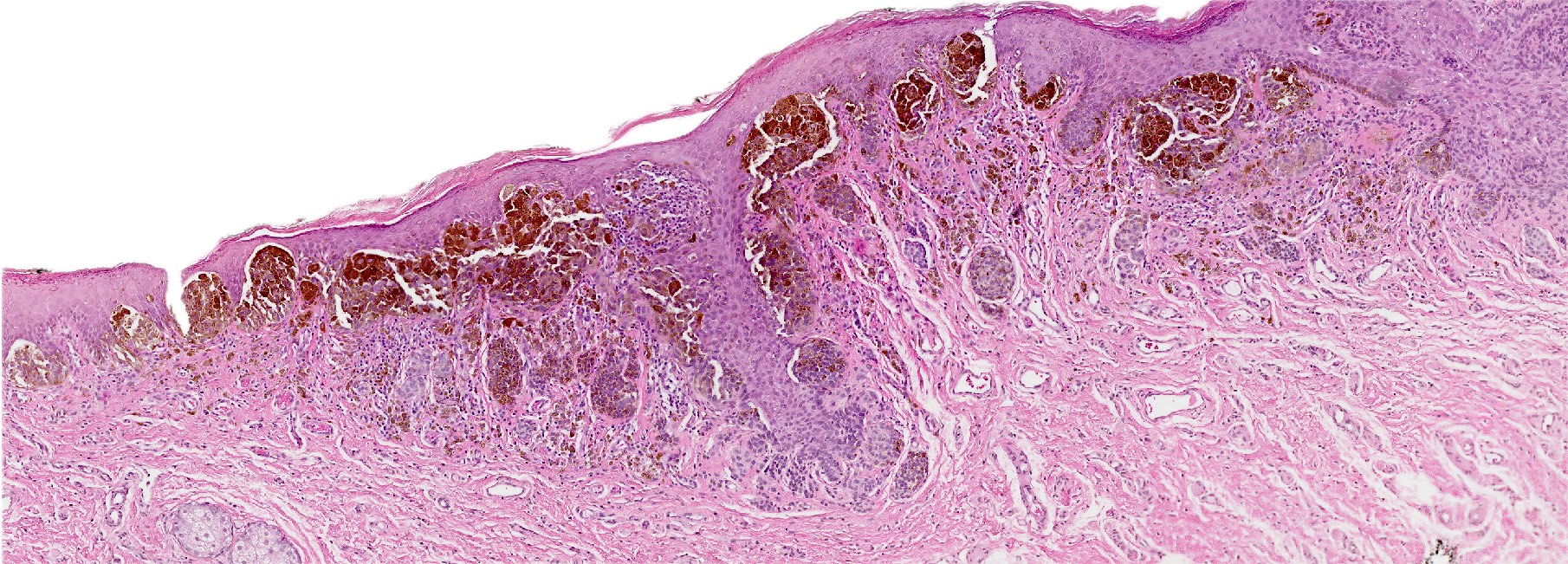
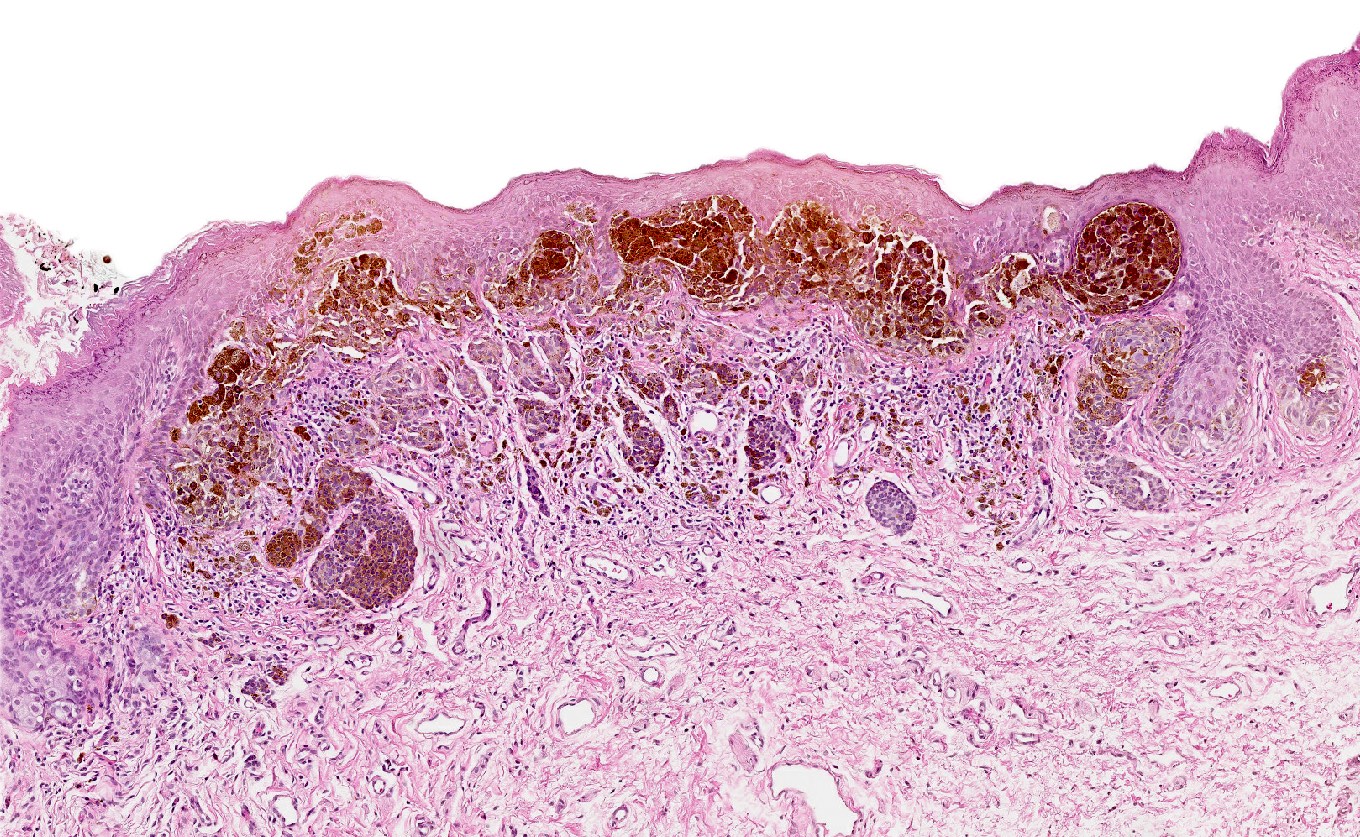
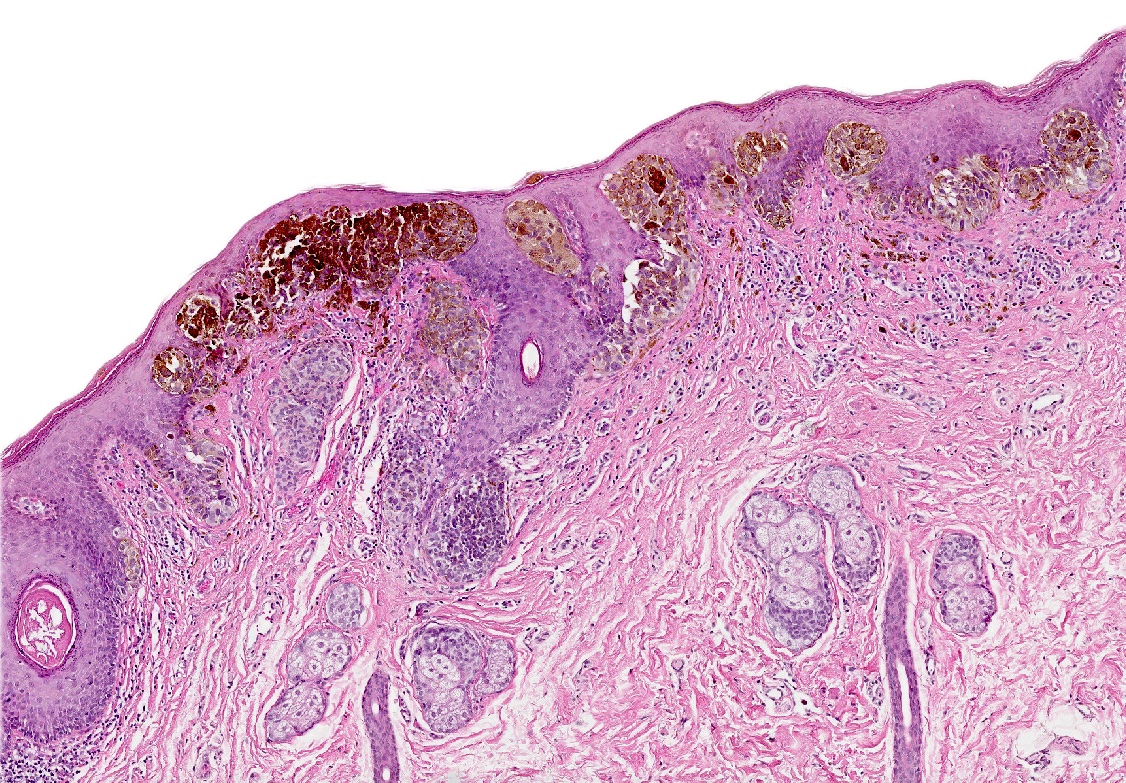
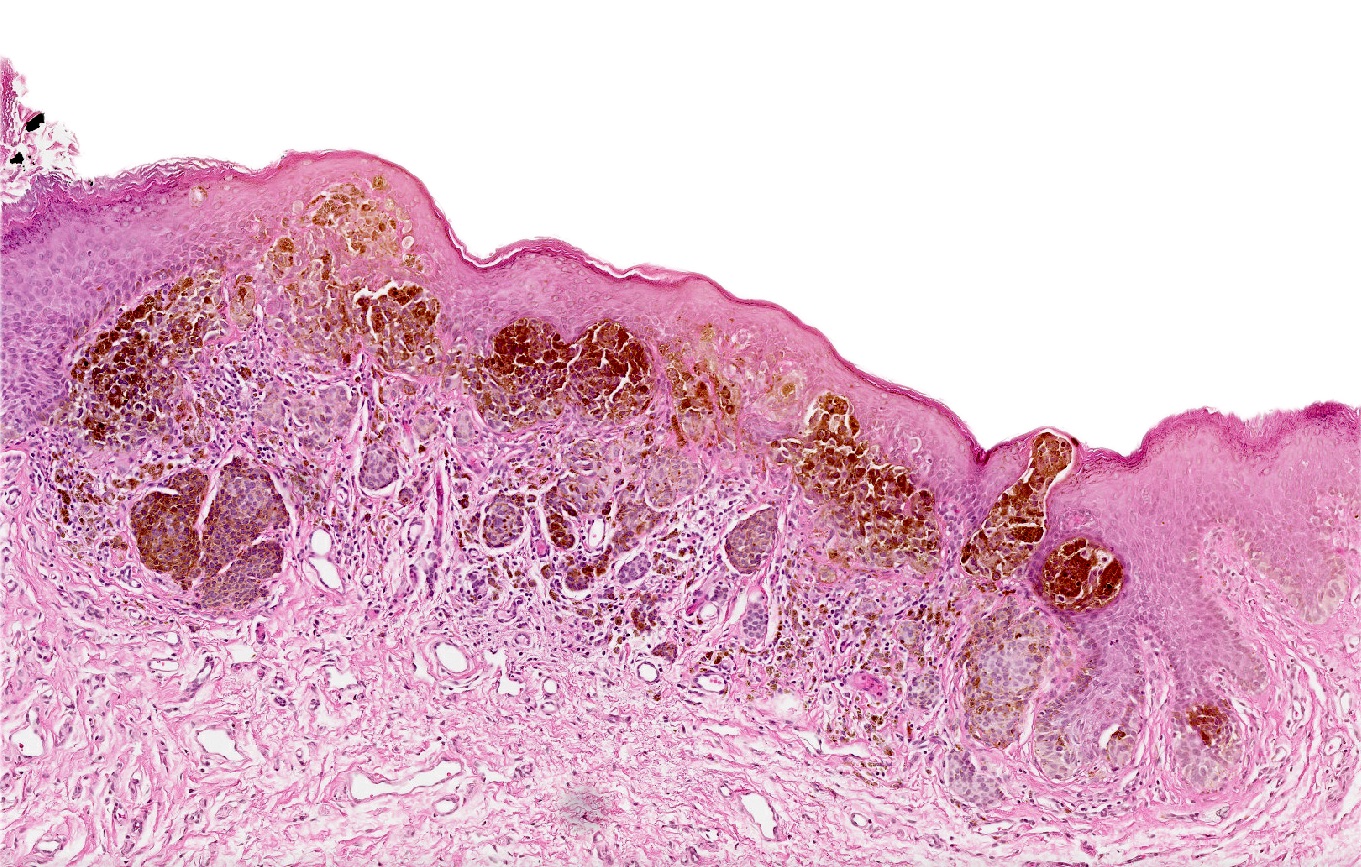
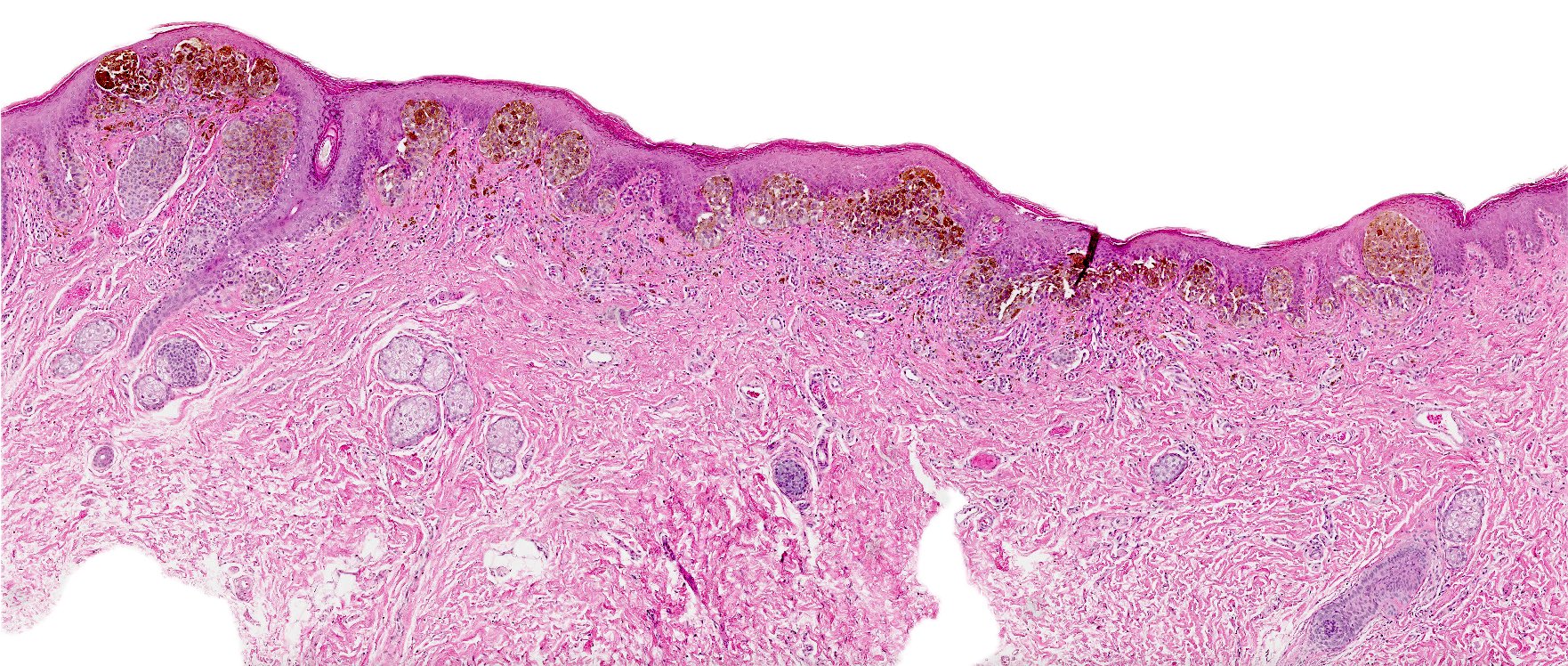
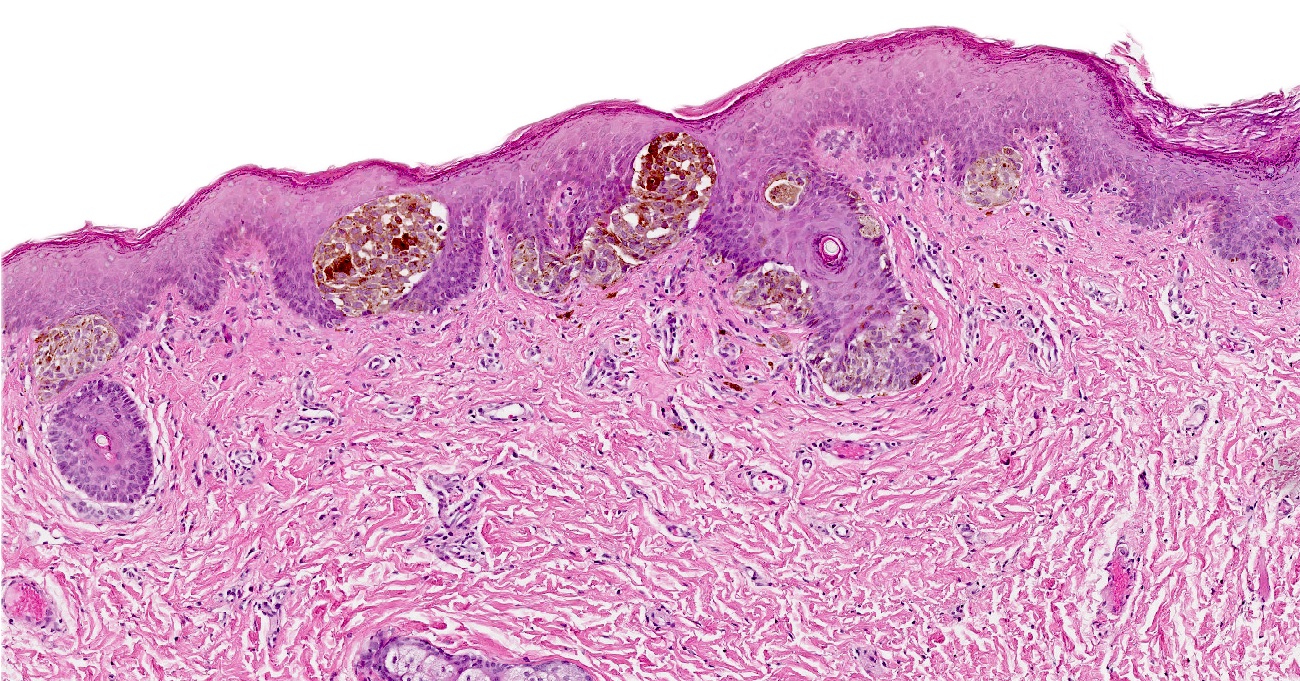
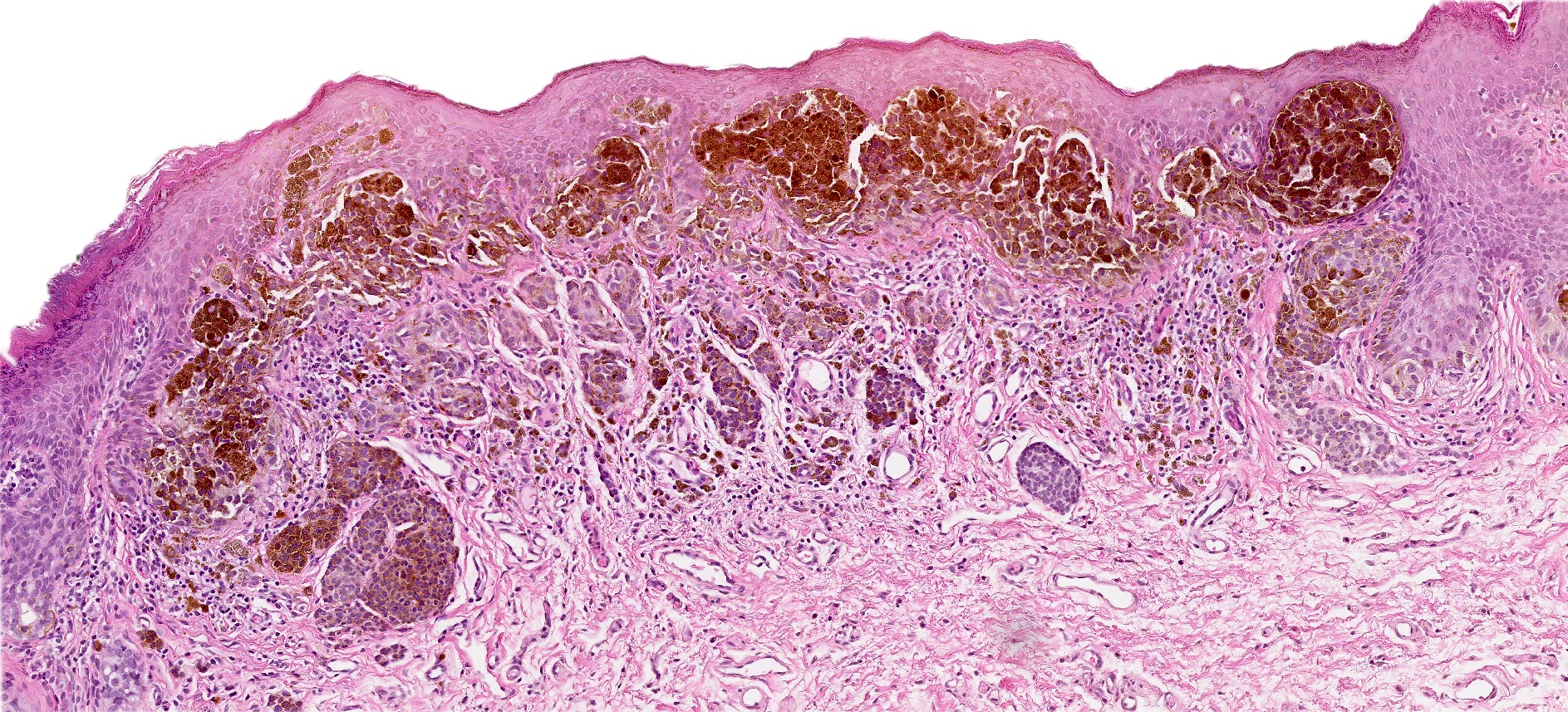
Microscopic (histologic) description
- Symmetric lesion with sharp demarcation and dermal maturation (J Cutan Pathol 2008;35:24)
- 3 histologic patterns described by Clark (Hum Pathol 1998;29:S1)
- Nested: oval, typically large nests, perpendicular or parallel to dermoepidermal junction
- Discohesive nests: nearly contiguous, forming a band that separates the epidermis from the mature dermal melanocytes
- Crowded: closely apposed, ill defined nests and single cells obscuring the dermal epidermal junction
- Usually mild to moderate uniform cytologic atypia (J Cutan Pathol 2008;35:24)
- Single cell growth with focal pagetoid spread may be present but is usually located in the center of the lesion (J Cutan Pathol 2008;35:24)
- Adnexal spread may be present (Hum Pathol 1998;29:S1)
- Dense eosinophilic fibrosis in the superficial dermis (Hum Pathol 1998;29:S1, J Cutan Pathol 2008;35:24)
- Intradermal component with maturation is often present (J Cutan Pathol 2008;35:24)
- Nevi within lichen sclerosus can appear more atypical
- See table 1
Microscopic (histologic) images
Positive stains
- Melanocytic markers
- MelanA (MART1) may help to highlight fused nests in nevi (J Cutan Pathol 2020;47:446)
- HMB45 (Ann Diagn Pathol 2023;67:152211, Biomed Rep 2016;5:327, J Am Acad Dermatol 2012;67:446)
- In common junctional and compound nevi, expressed in melanocytes at dermoepidermal junction
- Highlights a gradient or maturation (zonation) pattern (diminishing or loss of expression from top to bottom)
- Highly variable in Spitz and congenital nevi
- SOX10 highlights junctional melanocytes to help differentiate melanoma in situ from benign counterparts (Appl Immunohistochem Mol Morphol 2014;22:142)
- Ki67 proliferation rate should be low in the dermal component of genital nevi (J Am Acad Dermatol 2012;67:446)
Negative stains
- HMB45 is commonly negative in intradermal and compound nevi
- PRAME (preferentially expressed antigen in melanoma) is typically lost in nevi (J Cutan Pathol 2020;47:1123)
Molecular / cytogenetics description
- BRAF mutation is the most common alteration in melanocytic nevi of genital skin but not in vulvar melanomas (N Engl J Med 2015;373:1926, J Invest Dermatol 2016;136:1858)
- Fluorescence in situ hybridization (FISH) or comparative genomic hybridization (CGH) may be considered in very challenging cases to rule out melanoma
- Sensitivity of both tests may be lower than expected, due to decreased cellularity in vulvar lesions
- For vulvar melanomas, pTERT and CDK4 can be considered but may not be part of each FISH panel (Nat Commun 2019;10:3163, Am J Cancer Res 2020;10:4017)
Videos
Atypical nevi and nevi of special sites by Dr. Phillip McKee
Atypical nevi and melanoma by Dr. Steven Wang
Sample pathology report
- Vulva, labia minora, excisional biopsy:
- Atypical melanocytic nevus of the genital type, compound pattern, excised entirely
Differential diagnosis
- Melanoma:
- May be most challenging to differentiate from superficial spreading subtype of melanoma (SSM)
- Atypical melanocytes in the epidermis as single cells or forming nests with pagetoid spread
- Dermal component shows no maturation with cells forming sheets, nests, cords, single cells and rarely fascicles
- S100, SOX10 and nerve growth factor receptor (NGFR) are the most sensitive markers in visualization of invasive growth
- PRAME shows diffuse staining
- Melanomas of vulva usually lack BRAF mutation (Br J Dermatol 2010;162:677)
- Pigmented epithelioid melanocytoma (PEM) of the vulva:
- PEM family consists of multiple, usually slow growing, distinct histologic melanocytic entities with potential to metastasize but with a better prognosis than melanoma
- Infiltrative deep dermal tumor that may involve subcutis
- Hypercellular tumor with cells ranging from medium sized epithelioid cells to large epithelioid cells and spindled cells
- Low mitotic activity
- PRKAR1A loss in 67% of PEMs (Am J Surg Pathol 2017;41:1333, Am J Surg Pathol 2019;43:480)
- Dysplastic nevus of vulva:
- Differentiation requires clinical pathologic correlates
- Presence of junctional shoulders; extension of junctional component at least 3 rete ridges beyond the dermal component
- Superficial nests are usually very similar and may show focal bridging or coalescence of the nests
- Elongation and bridging of the rete ridges with nests
- Melanocytes may scatter suprabasally (confined to the lower epidermal layer and centrally)
- 2 tier grading of cytologic atypia is recommended by World Health Organization (WHO) classification and is largely based on nuclear features (Hum Pathol 1999;30:500)
Additional references
- WHO Classification of Tumours Editorial Board: Skin Tumours, 5th Edition, 2023, J Cutan Pathol 2008;35:889, Am J Surg Pathol 1995;19:792, Ackerman: Pathology of Malignant Melanoma, 1st Edition, 1981, McKee: Pathology of the Skin with Clinical Correlations, 3rd Edition, 2005, Busam: Pathology of Melanocytic Tumors, 1st Edition, 2018
Board review style question #1
A 28 year old woman presented to the clinic with a 0.6 cm, flat, dark brown lesion with an irregular border on the labia majora. The histologic findings of the shave biopsy demonstrated a relatively symmetric, broad melanocytic proliferation with large oval nests with retraction perpendicular to the dermal epidermal junction, focal fusion and mild cytologic atypia. Dermal maturation is evident. What is the most likely molecular alteration in this lesion?
- ALK fusion
- BRAF mutation
- Homozygous deletion of CDKN2A
- PTEN mutation
Board review style answer #1
B. BRAF mutation. The majority of atypical melanocytic nevi of genital type (AMNGT) have a driver mutation in BRAF. Answer A incorrect because ALK fusion is more characteristic of Spitz nevi. Answers C and D are incorrect because those alterations are specific to superficial spreading melanoma.
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Board review style question #2
A 16 year old girl presented with her parents to the OBGYN clinic with an irregular, dome shaped, dark pigmented papule on the mons pubis. A biopsy demonstrated large, ill defined nests with focal retraction. What is the most likely interpretation of the immunohistochemical stains for this patient's lesion?
- Diffuse expression of PRAME
- Gradient pattern of HMB45
- High Ki67 proliferation index in the dermal component
- SOX10 highlighting pagetoid and extensive lentiginous growth
Board review style answer #2
B. Gradient pattern of HMB45. The histologic features are consistent with atypical melanocytic nevi of genital type (AMNGT). Although HMB45 expression varies in nevi, the stain can be useful to highlight the maturation (zonation) pattern (diminished or loss of expression from epidermal to dermal component). Answers A, C and D are incorrect because PRAME is usually diffusely positive in melanoma, SOX10 helps to highlight the increase of melanocytes and pagetoid growth in melanoma and Ki67 is expected to be low in the dermal component of genital nevi.
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva