Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Lechner A, Parra-Herran C. Mixed tumor of vagina. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vaginaspindlecellep.html. Accessed January 1st, 2025.
Definition / general
- First described by Brown in 1953 (Am J Clin Pathol 1953;23:237)
- Rare; only ~60 reported cases
- Of unclear histogenesis
Essential features
- Rare, benign tumor commonly of the lower posterior vaginal wall (near hymenal ring)
- Well circumscribed, unencapsulated, detached from overlying epithelium
- Predominantly bland spindle cells (cytokeratin+, SMA+, S100-) with sparsely admixed glands / squamous islands
- Recurrence following complete excision is rare
Terminology
- Mixed tumor of vagina is the term currently endorsed by the World Health Organization classification of female genital tract tumors
- The term spindle cell epithelioma (SCE) is not recommended
Epidemiology
- Middle aged women (mean 40; range 20 - 80) (Am J Surg Pathol 1993;17:509, Pathol Res Pract 2012;208:424, Eur J Obstet Gynecol Reprod Biol 1996;69:143, Am J Surg Pathol 1981;5:413)
- 1 familial case (2 sisters) has been reported (Gynecol Oncol 1979;8:21)
Sites
- Most commonly within the posterior vaginal wall near the hymenal ring (Am J Surg Pathol 1993;17:509)
Pathophysiology
- Unlike mixed tumors of other anatomic sites (e.g., pleomorphic adenoma), the spindle cell component of SCE shows ultrastructural and immunohistochemical evidence of epithelial differentiation (Am J Surg Pathol 1993;17:509, Pathol Res Pract 2012;208:424, Mod Pathol 2004;17:1243)
- Müllerian origin versus urogenital sinus origin is debated
- High frequency of CD10, BCL2, ER, PR positivity favors Müllerian (Pathol Res Pract 2012;208:424)
- Propensity for hymenal ring favors urogenital sinus (Int J Gynecol Cancer 2003;13:543)
- CD34 and WT1 expression argue for a common progenitor cell with the capacity for multiple pathways of differentiation (Arch Pathol Lab Med 2001;125:547, Int J Surg Pathol 2015;23:677)
Clinical features
- Often discovered incidentally
- Well defined, may be pedunculated / polypoid or intramural (Int J Gynecol Cancer 2003;13:543, Clin Imaging 2018;50:181)
- May be perceived as a cyst (Int J Surg Pathol 2015;23:677)
Diagnosis
- Diagnosis is made by histopathologic examination, either via biopsy or excision of the lesion
Radiology description
- Ovoid, well circumscribed
- T1 isointense, T2 hyperintense relative to adjacent vaginal wall; homogenous enhancement and restricted diffusion (Clin Imaging 2018;50:181)
Prognostic factors
- Benign
- May recur with incomplete excision (Gynecol Oncol 1991;40:84)
Case reports
- 20 year old woman with a perineal itching sensation and posterior vaginal wall mass on MRI (J Korean Med Sci 2002;17:845)
- 28 year old woman with a mass protruding from the vagina (Ann Saudi Med 2002;22:202)
- 45 year old woman with a clinical diagnosis of vaginal wall leiomyoma (J Clin Diagn Res 2013;7:1743)
Treatment
- Local excision
Gross description
- 1 - 6 cm in size (Am J Surg Pathol 1993;17:509)
- Intramural without connection to mucosa
- Well circumscribed, unencapsulated (Am J Surg Pathol 1993;17:509)
- Soft to rubbery consistency
- Tan-white, homogenous cut surface with or without grossly visible cysts (Int J Gynecol Cancer 2003;13:543)
Microscopic (histologic) description
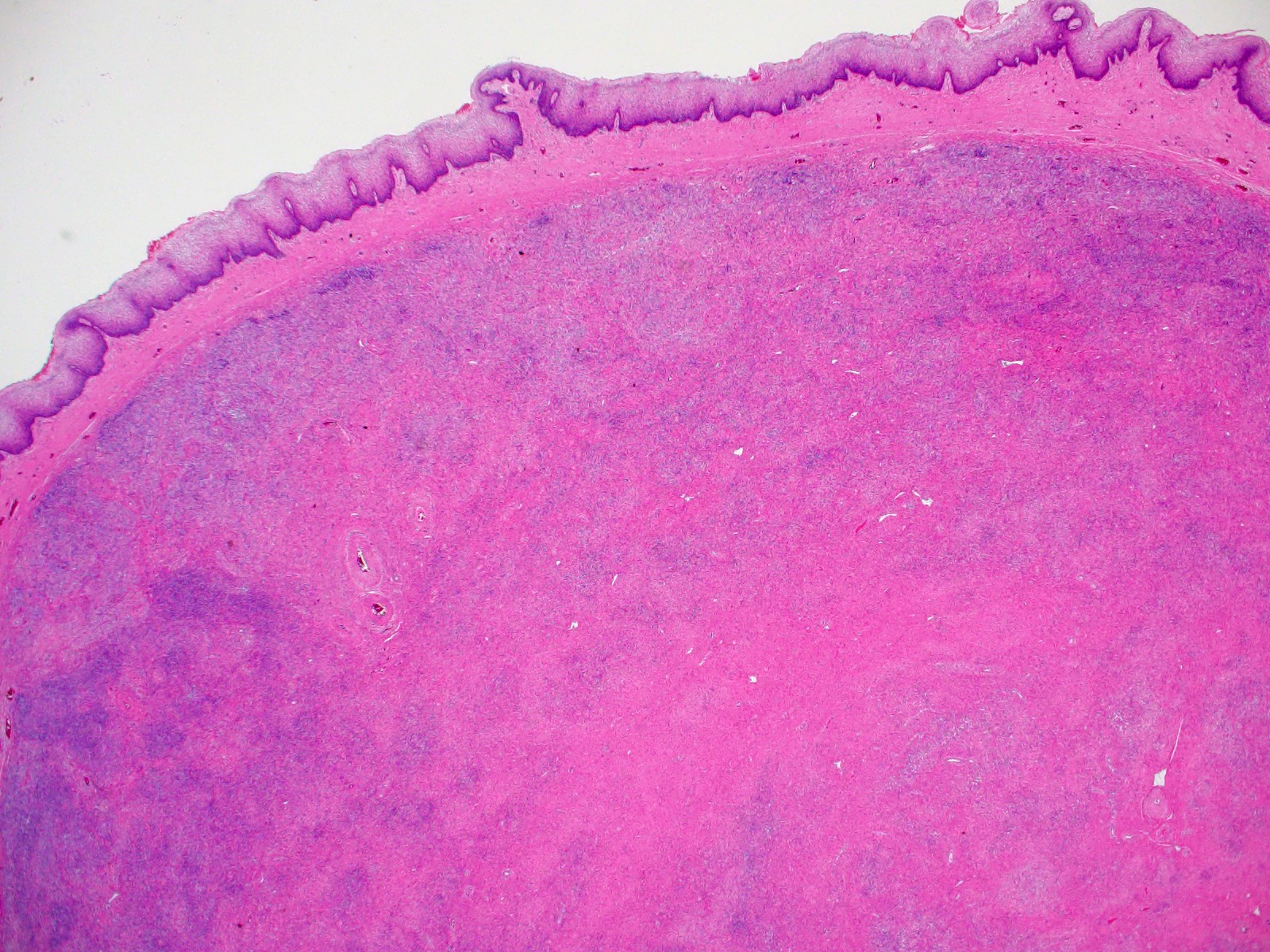
- Well circumscribed but unencapsulated with a pushing border
- Located just deep (< 3 mm) to the vaginal mucosa but without connection to overlying epithelium (seen as a Grenz-like zone of loose connective tissue in between)
- Biphasic population of predominantly spindle cells with a minor squamous or glandular component and numerous small vessels (Am J Surg Pathol 1993;17:509)
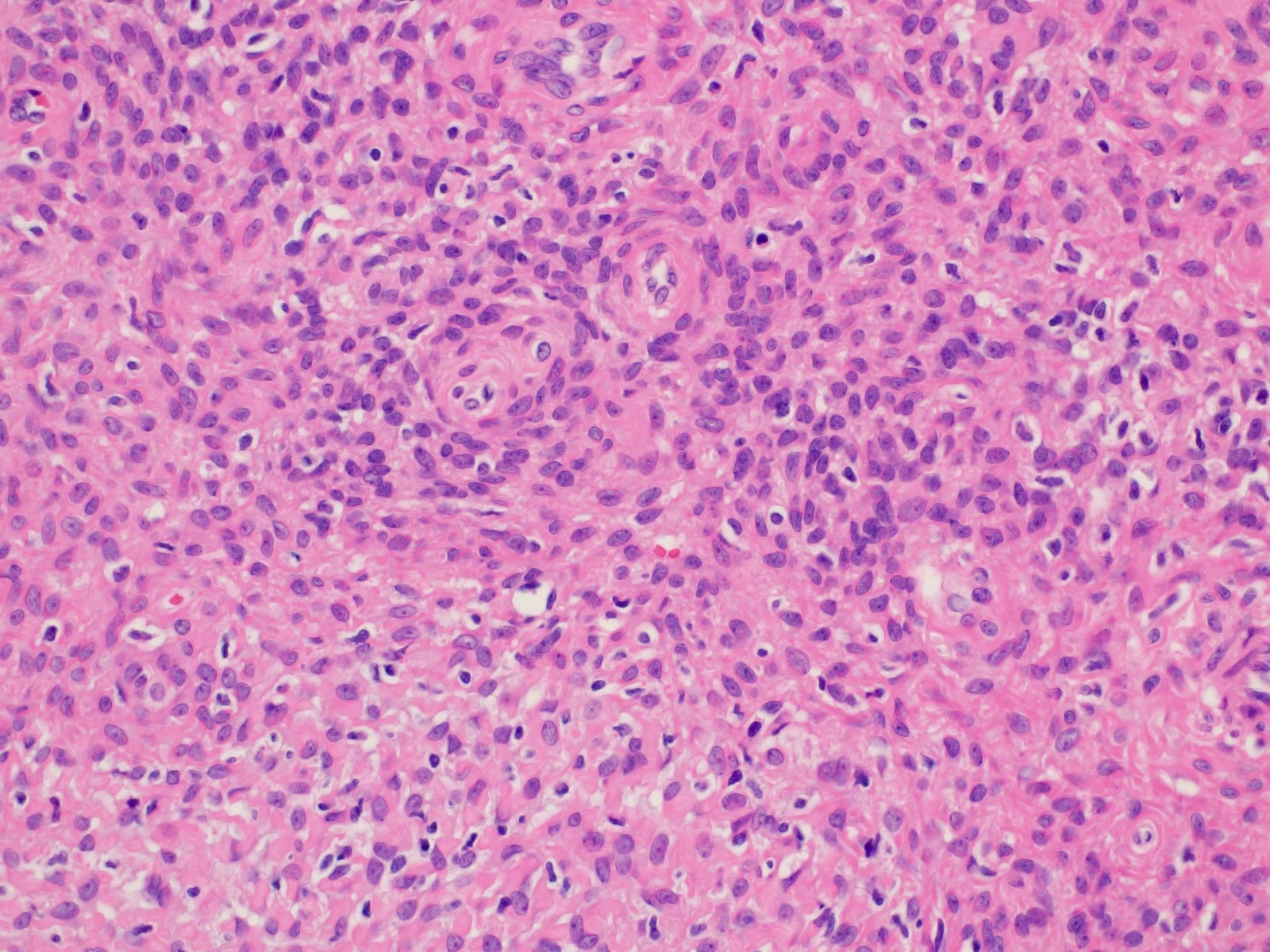
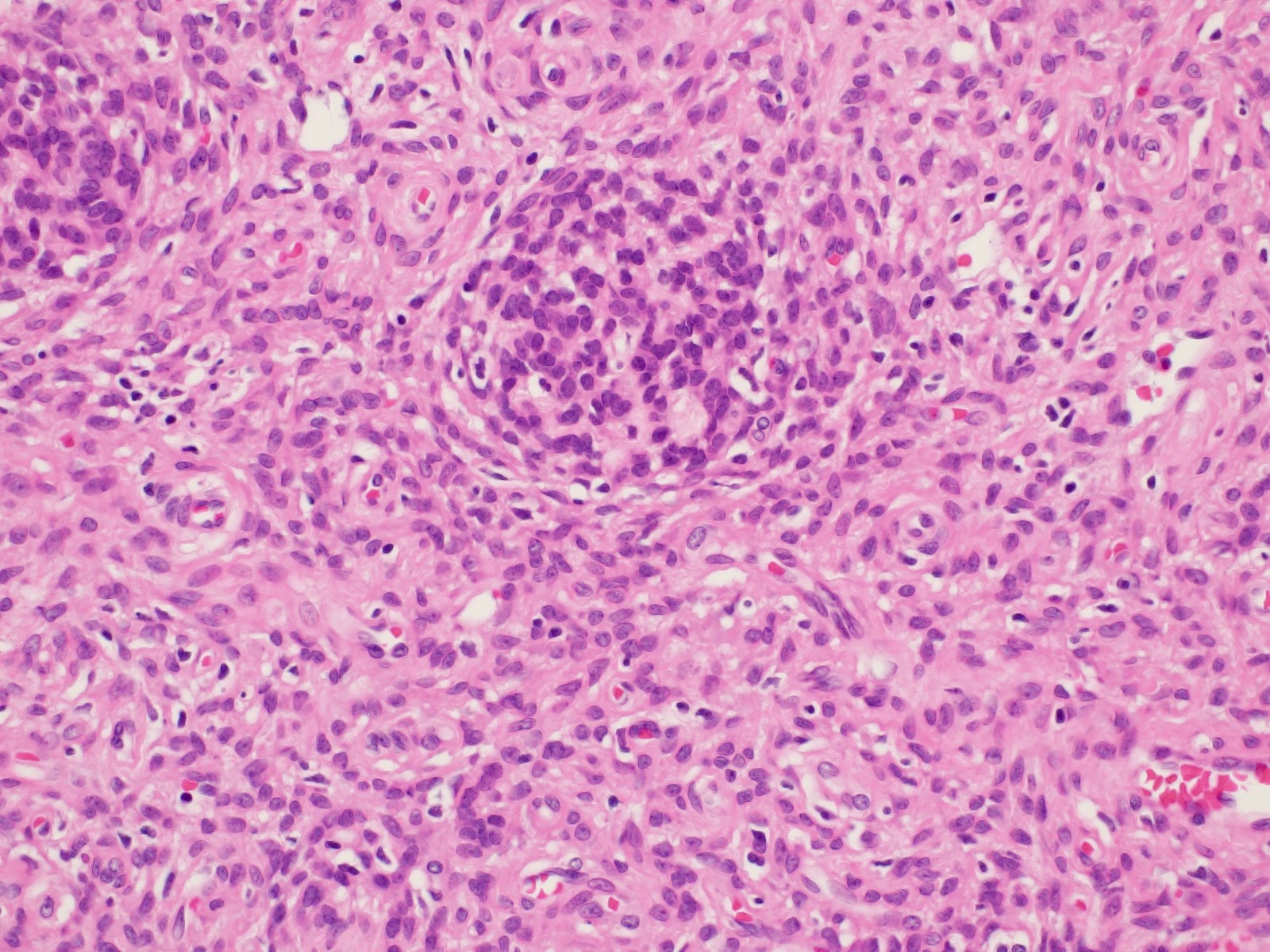
- Spindle cell (major) component:
- Variably cellular spindle cell component
- Hypocellular areas of fibroblastic type cells
- Bland cytology, minimal mitotic activity
- Cytoplasm is usually indistinct but can appear eosinophilic
- Condensed extracellular matrix forms eosinophilic hyaline globules
- Glandular / squamoid (minor) component:
- More often seen at the periphery of the lesion
- Simple glands lined by cuboidal to columnar epithelium
- Glandular epithelium may resemble endocervical epithelium with intracytoplasmic mucin
- Squamous metaplasia is common, resulting in nests / morules and cords of plump squamous cells with glycogenated cytoplasm (Am J Surg Pathol 1993;17:509, Pathol Res Pract 2012;208:424)
Microscopic (histologic) images
Positive stains
- Spindle and epithelial components show unique staining (Mod Pathol 2004;17:1243):
- Spindle cells: cytokeratin, vimentin, SMA, desmin, CD10, CD34, BCL2, ER, PR
- Epithelial cells: cytokeratin, EMA, ER, PR, PAS (diastase sensitive) (Am J Surg Pathol 1993;17:509)
- Spindle cells show variable staining for caldesmon
- Both epithelial and spindle cells are frequently CK7+ / CK20-
- WT1 and calretinin expression has been reported (Int J Surg Pathol 2015;23:677)
Negative stains
Electron microscopy description
- Spindle cells show prominent tonofilaments with associated desmosomes (Am J Surg Pathol 1993;17:509)
- Myoepithelial features (dense myofibrils, pinocytotic vesicles, basal laminar investitures) are not seen
Sample pathology report
- Vagina, local excision:
- Benign mixed tumor of vagina, 1.5 cm, margins are uninvolved by tumor (see comment)
- Comment: Immunostaining shows AE1 / AE3, CD10, SMA positivity in lesional cells. S100 and SOX10 are negative. The cytomorphology and immunohistochemical profile are consistent with the above diagnosis.
Differential diagnosis
- Carcinosarcoma of vagina:
- Infiltrative border
- Overtly sarcomatous mesenchymal component
- Malignant glandular component (usually high grade morphologically)
- Müllerian adenosarcoma:
- Cambium layer
- Mitotic activity (≥ 2 per 10 high power fields)
- Leaf-like (phyllodes-like) architecture
- Periglandular stromal condensation
- Atypical / frankly malignant spindle cell component
- Tubulosquamous polyp:
- Anatomically more superior
- Thought to arise from mesonephric rests
- Epithelial elements with squamoid and glandular appearance are discrete but are not associated with a surrounding spindle cell population
- GATA3+ and NKX3.1+ epithelium, CD10- and cytokeratin- stroma (Am J Surg Pathol 2007;31:1013)
- Metastatic endometrial stromal sarcoma:
- Infiltrative border
- Usually epithelial elements are absent
- Previous history of the disease
- Metastatic / primary spindle cell carcinoma:
- Infiltrative border and marked atypia
- Overlying mucosal dysplasia or better differentiated squamous cell carcinoma components (if primary)
- Synovial sarcoma:
- Infiltrative border
- SS18::SSX+ (Am J Surg Pathol 2020;44:922)
Board review style question #1
A 31 year old woman presents with a 2 cm solid mass protruding from the vagina. A local resection is performed and shows a submucosal, well circumscribed but unencapsulated lesion composed of predominantly bland spindle cells with sparse glands and squamous metaplasia (see image shown above). Electron microscopy of the spindle cells shows abundant tonofilaments and desmosomes but no pinocytotic vesicles. Which of the following is true regarding these spindle cells?
- They are derived from mesonephric rests
- They are derived from normal myoepithelial cells found in the vagina
- They are likely keratin+, CD10+ and SMA+
- They are the malignant component of this biphasic tumor
Board review style answer #1
C. They are likely keratin+, CD10+ and SMA+. This lesion represents a benign spindle cell epithelioma (mixed tumor of vagina). Electron microscopy of the spindle cells of this lesion shows epithelial cell features and a lack of contractile elements. A differential diagnosis of this lesion is a tubulosquamous polyp, which is thought to be derived from mesonephric rests. Myoepithelium does not normally occur in the vagina; a multipotent progenitor cell is thought to give rise to this lesion.
Comment Here
Reference: Mixed tumor of vagina
Comment Here
Reference: Mixed tumor of vagina