Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ardighieri L, Ayhan A, Strickland AL. Uterine tumors resembling ovarian sex cord tumors. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusutrosct.html. Accessed December 26th, 2024.
Definition / general
- Rare neoplasms that resemble ovarian sex cord tumors, without a component of recognizable endometrial stroma
Essential features
- Rare uterine tumor of uncertain histogenesis; morphologically shows overlap with ovarian sex cord tumors, affecting perimenopausal or menopausal women (mean age is 52)
- Absence of JAZF1::SUZ12 fusion (JAZF1::JJAZ1) and PHF1 gene rearrangements distinguish these neoplasms from endometrial stromal tumors
- Low malignant potential (~5% recurrence risk or rare metastasis); however, most cases are benign
- Currently within the mesenchymal category in the WHO classification of tumors of the uterine corpus
Terminology
- Uterine tumor resembling ovarian sex cord tumor (UTROSCT), endometrial stromal tumor resembling ovarian sex cord tumor
ICD coding
- ICD-O: 8590/1 - uterine tumor resembling ovarian sex cord tumor
- ICD-11: 2F76 & XH8CW8 - neoplasms of uncertain behavior of female genital organs & uterine tumor resembling ovarian sex cord tumor
Epidemiology
- Usually perimenopausal or menopausal women; age range is 21 - 84 years, mean age is 52 (Am J Surg Pathol 2023;47:234)
- Rare, < 1% of uterine mesenchymal tumors
- Accounts for < 0.5% of all uterine malignancies and 10 - 15% of mesenchymal uterine malignancies (Crum: High Yield Pathology - Gynecologic and Obstetric Pathology, 1st Edition, 2016)
Sites
- Corpus, mostly intramural, less frequently submucosal or subserosal or polypoid / intracavitary
- Rarely endocervix (Int J Gynecol Pathol 2003;22:297)
Pathophysiology
- Postulated theories include (Int J Gynecol Pathol 2016;35:301)
- Derivation from ovarian sex cord cells which have been displaced during embryogenesis
- Derivation from uncommitted mesenchymal stem cells
- Derivation from pluripotent endometrial stromal cells
- Molecular evidence suggests that derivation may not be from endometrial stroma (Am J Surg Pathol 2009;33:1206)
- Overgrowth of sex cord elements within endometrial stromal neoplasm or adenosarcoma (however, note that these tumors do not have the cytogenetic abnormalities found in stromal neoplasms)
Etiology
- Tumors of unknown histogenesis
Clinical features
- Abnormal bleeding, pelvic pain, enlarged uterus, mass sensation
- Occasionally found incidentally (Int J Gynecol Pathol 2008;27:229)
- Endometrial sampling may not reveal the diagnosis (Crum: High Yield Pathology - Gynecologic and Obstetric Pathology, 1st Edition, 2016)
Diagnosis
- Based on histomorphologic features including a predominant pattern of the cords, nests and trabeculae resembling sex cord tumors of the ovary and immunophenotype, characterized by coexpression of epithelial, smooth muscle, sex cord markers and steroid receptors
- Imaging studies are not diagnostic; histopathology is the gold standard (Arch Pathol Lab Med 2013;137:1832)
Radiology description
- They can be diagnosed with ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI)
- No specific image findings (Oncol Lett 2016;11:1496)
- At transvaginal pelvic ultrasound, they may be seen in a normal or enlarged uterus and may appear as myometrial masses, with myomatous features or as masses protruding in the endometrial cavity, suggesting a polypoid lesion
- UTROSCT reported to exhibit high signal intensity on MRI diffusion weighted images in contrast to generally low signal associated with leiomyoma (Magn Reson Med Sci 2019;18:113)
Prognostic factors
- Most tumors exhibit benign behavior
- However, they are considered to have uncertain malignant potential because of a low rate of recurrence and rare metastases (lymph nodes, epiploic appendix, omentum, small bowel, subcutaneous) (Int J Clin Exp Pathol 2015;8:4158, Int J Clin Exp Pathol 2014;7:1051, Cesk Patol 2014;50:46, Int J Gynecol Pathol 2008;27:58)
- No definitive prognostic morphologic features have been identified (Histopathology 2017;71:751, Eur J Obstet Gynecol Reprod Biol 2014;181:163)
Case reports
- 22 year old woman (nulligravida) with UTROSCT (Gynecol Endocrinol 2015;31:856)
- 51 year old woman with UTROSCT with aggressive histologic features harboring a GREB1::NCOA2 fusion (Int J Gynecol Pathol 2023;42:54)
- 57 year old woman with UTROSCT with sarcomatous features, treated with extended radical surgery without recurrence (Medicine (Baltimore) 2020;99:e19166)
- 62 year old woman with UTROSCT after receiving tamoxifen for breast carcinoma for 3 years (Pathol Res Pract 2019;215:1089)
- 3 cases manifesting classical histomorphological features of UTROSCT alongside diverse immunohistochemical findings (Ann Diagn Pathol 2010;14:432)
Treatment
- Hysterectomy with or without bilateral salpingo-oopherectomy considered the standard treatment (Eur J Obstet Gynecol Reprod Biol 2014;181:163)
- Conservative surgery: uterine sparing organ preserving surgery, especially for young patients who desire fertility preservation (Gynecol Oncol Rep 2017;19:53, Obstet Gynecol Sci 2015;58:418)
- Cases reported with postoperative conceptions during follow up: Oncol Lett 2016;11:1496, Case Rep Obstet Gynecol 2016;2016:5736865, Gynecol Endocrinol 2015;31:856
- Such cases should have long term follow up
- Some patients receive chemotherapy or pelvic radiation because of extrauterine extension (to parametrium and ovarian hilum) and positive surgical margins or in the setting of locoregional / distant recurrent disease (Gynecol Oncol Rep 2015;15:22)
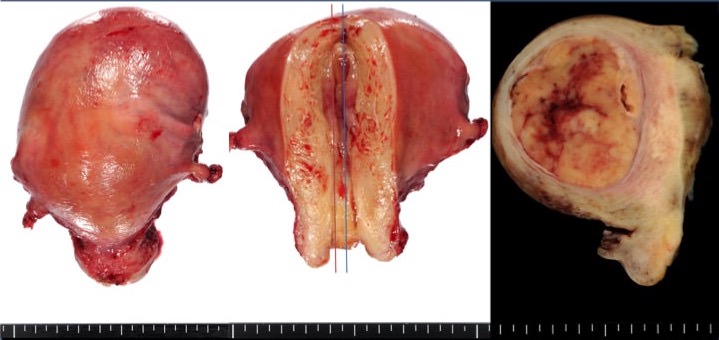
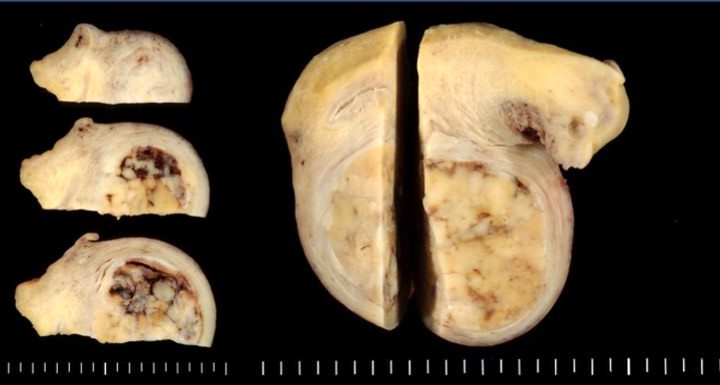
Gross description
- Intramural / submucosal / subserosal nodules or polypoid tumors growing in the endometrial cavity
- Mainly solid, round, well circumscribed masses
- Average of 6 cm; ranging from 2 to 24 cm
- Yellow, tan, grayish white surface; firm to soft to rubbery consistency
- Cut surface grayish yellow to white
- Rarely predominantly cystic
- Hemorrhage can be seen; necrosis unusual
- Reference: Crum: High Yield Pathology - Gynecologic and Obstetric Pathology, 1st Edition, 2016
Frozen section description
- Typically similar morphology as permanent sections (see Microscopic (histologic) description); maintain differential when signing out the frozen section
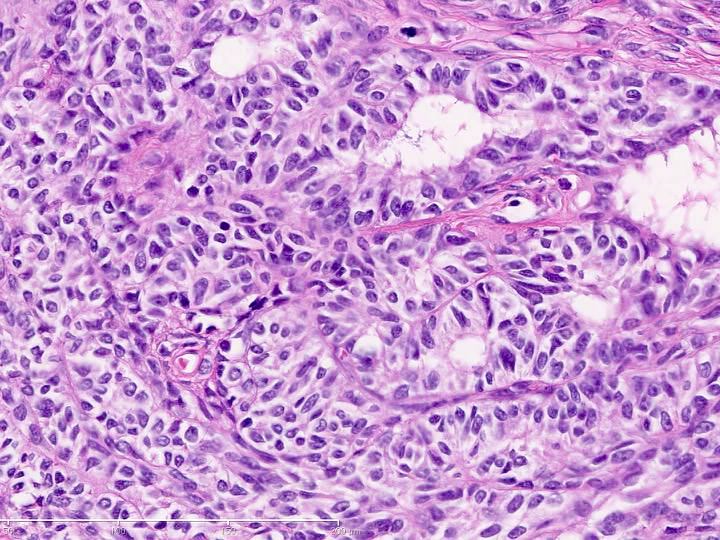
Microscopic (histologic) description
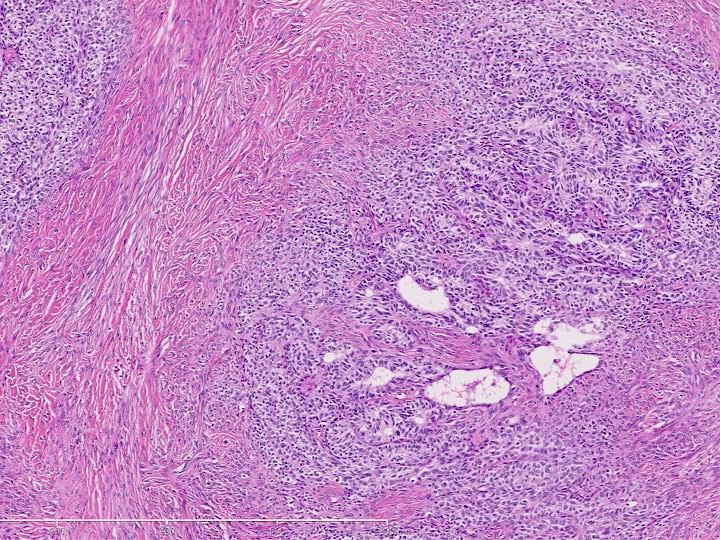
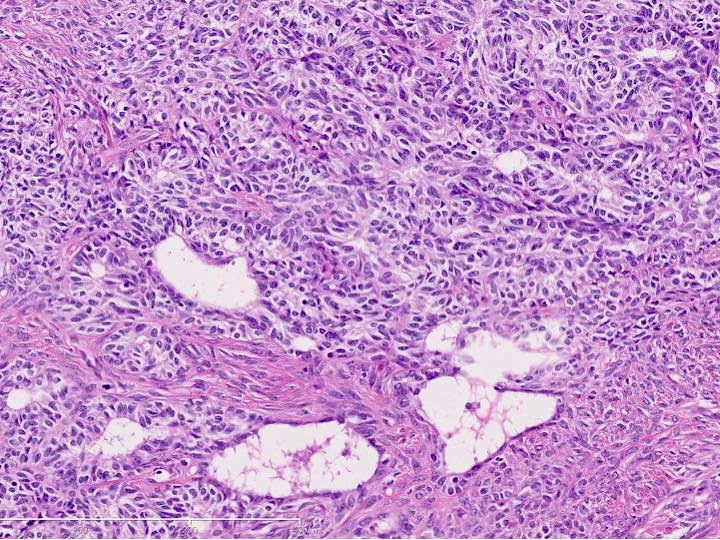
- Usually well circumscribed but unencapsulated; may have a pseudoinfiltrative appearance due to incorporated smooth muscle bundles; true myometrial invasion is rare
- Organized in sheets, cords, nests, trabeculae, hollow or solid tubules with repetitive pattern of cord-like / tubular growth; more rarely has retiform or glomeruloid appearance or papillae and solid pattern predominance
- Neoplastic cells are small, round to ovoid with monotonous nuclei, inconspicuous nucleoli, mild nuclear hyperchromasia, rare nuclear grooves, with usually minimal cytologic atypia and low mitotic activity
- Call-Exner-like bodies may be rarely present
- Scant intervening stroma (hyalinized, fibroblastic or edematous)
- In some tumors, endometrial stromal type cells or benign appearing smooth muscle may be present; rare findings are a sparse lymphocytic infiltrate accompanied by foamy histiocytes, a few multinucleated giant cells, hemosiderin deposition or cholesterol crystals
- Occasionally vascular invasion, heterologous elements and necrosis
- Reference: Crum: High Yield Pathology - Gynecologic and Obstetric Pathology, 1st Edition, 2016
Microscopic (histologic) images
Cytology description
- Cells resembling epithelial cells, with scant cytoplasm or abundant eosinophilic / clear (including vacuolated) / foamy cytoplasm, reminiscent of Sertoli cell or granulosa cell tumors (Diagn Cytopathol 2019;47:603)
- Can show rhabdoid features with abundant eosinophilic cytoplasm and eccentric nuclei (J Clin Pathol 2007;60:1148)
- Minimal atypia; rare mitoses (ranging from < 1 - 5/10 high power fields)
- Ovoid and small nuclei with irregular contours (sometimes grooved)
- Finely distributed chromatin with small to indistinct nucleoli
- Leydig-like cells may be present
Positive stains
- Ovarian sex cord markers: calretinin (positive in 95.8% of cases), WT1 (83.3%), CD99, MelanA (85%), CD56, FOXL2, SF1 (Ultrastruct Pathol 2010;34:16, Mod Pathol 2006;19:17)
- Epithelial markers: KL1, CK AE1 / AE3 (50%), CAM5.2 (Am J Surg Pathol 2010;34:1749)
- Smooth muscle markers: h-caldesmon, smooth muscle myosin heavy chain and histone deacetylase 8 (66.6%) (Am J Surg Pathol 2010;34:1749)
- CD10 (60%), ER and PR (and less commonly AR) may be positive (J Clin Pathol 2007;60:1148)
- Vimentin, BCL2 (Int J Clin Exp Pathol 2014;7:1051)
Negative stains
- HMB45 (Int J Clin Exp Pathol 2014;7:1051)
- Chromogranin (J Clin Pathol 2007;60:1148)
- CD34 (Int J Clin Exp Pathol 2014;7:1051)
- Ovarian sex cord marker: inhibin (48%) (Ultrastruct Pathol 2010;34:16, Mod Pathol 2006;19:17)
- Epithelial marker: EMA (34.4% focal) (Am J Surg Pathol 2010;34:1749)
- Smooth muscle markers: smooth muscle actin (40.8%), desmin (25.3%) (Am J Surg Pathol 2010;34:1749)
- CD117 (weak, 33.3%), S100 (18.2%) in occasional tumors (Am J Surg Pathol 2010;34:1749)
Electron microscopy description
- Cell junctions, desmosome-like junctions, tonofilaments, lumina formation, microvilli (indicative of epithelial differentiation)
- Sex cord like features (nuclear indentation, abundant intracellular filaments, endoplasmic reticulum [granulosa cells], intracytoplasmic lipid droplets)
- No dense bodies, subplasmalemmal densities or pinocytotic vesicles (indicating no smooth muscle differentiation)
- Reference: Ultrastruct Pathol 2010;34:16
Molecular / cytogenetics description
- No JAZF1::SUZ12 fusion seen in endometrial stromal tumors or PHF1 gene rearrangements (Am J Surg Pathol 2009;33:1206)
- No DICER1 or FOXL2 mutations (Int J Gynecol Pathol 2016;35:301)
- Presence of t(X;6)(p22.3;q23.1) and t(4;18)(q21.1;q21.3) in a single case (Diagn Mol Pathol 2003;12:174)
- Focal amplification on chromosome 17q11.2 including the SUZ12 gene in a single UTROSCT (Am J Surg Pathol 2009;33:1206)
- NCOA1-3 rearrangements and NCOA2/3 gene fusions have been reported with regularity (Am J Surg Pathol 2020;44:30)
Sample pathology report
- Uterus, hysterectomy:
- Uterine neoplasm most consistent with uterine tumor resembling ovarian sex cord tumor (see comment)
- Comment: Within the uterine corpus is an intramural mass that histologically demonstrates sheets of bland cells with scant to abundant cytoplasm and ovoid nuclei. Minimal cytologic atypia is appreciated, very low mitotic activity is present (1 per 10 high power fields) and no necrosis is seen. The lesion is positive for calretinin, WT1 and inhibin, while negative for HMB45 and CD34. The morphology and immunoprofile are supportive of a diagnosis of uterine tumor resembling ovarian sex cord tumor, a rare uterine neoplasm of unknown etiology.
Differential diagnosis
- Endometrial stromal tumor with sex cord-like elements:
- Has irregularly distributed sex cord elements and endometrial stromal component is prominent
- 60% contain JAZF1::SUZ12 gene fusion (not present in UTROSCT) and sex cord-like areas should be negative for sex cord markers (Am J Surg Pathol 2009;33:1206, Nucci: Diagnostic Pathology - Gynecological, 1st Edition, 2014)
- Leiomyomas, including epithelioid and plexiform, vascular leiomyoma with plexiform pattern and leiomyoma with tubules (Ann Diagn Pathol 2010;14:355, Int Semin Surg Oncol 2008;5:15):
- Prominent thick walled blood vessels, frequent and diffuse smooth muscle markers
- Metastatic ovarian sex cord stromal tumor:
- Presence of ovarian sex cord tumor and EMA negativity in ovarian SCT
- (Epithelioid) leiomyosarcoma:
- Has severe cytologic atypia, high mitotic activity (over 10/10 high power fields) and necrosis
- Adenosarcoma:
- No sex cord elements
- Endometrioid carcinoma (spindled and corded pattern):
- Has conventional endometrial carcinoma areas and may show a high degree of cytologic atypia (Nucci: Diagnostic Pathology - Gynecological, 1st Edition, 2014)
- Nuclear beta catenin positivity (Histol Histopathol 2009;24:149)
- PEComa:
Additional references
- Am J Clin Pathol 1976;66:512, Hum Pathol 1986;17:91, Am J Surg Pathol 1998;22:1078, Hum Pathol 1999;30:671, Virchows Arch 2001;439:97, Ann Diagn Pathol 2014;18:329, Kurman: WHO Classification of Tumors of the Female Reproductive Organs, 4th Edition, 2014, WHO Classification of Tumours: Female Genital Tumours, 5th Edition, 2020
Board review style question #1
The typical morphology of uterine tumors resembling ovarian sex cord tumors (UTROSCT) includes which of the following features?
- Cords
- High mitotic activity
- Necrosis
- Severe cytologic atypia
Board review style answer #1
A. Cords. UTROSCT contains morphology organized in sex cord structures, including sheets, cords, nests, trabeculae and tubules. Answers B, C and D are incorrect because high mitotic activity, necrosis and severe cytologic atypia are not typically seen in UTROSCT cases.
Comment Here
Reference: Uterine tumors resembling ovarian sex cord tumors
Comment Here
Reference: Uterine tumors resembling ovarian sex cord tumors
Board review style question #2
Board review style answer #2
B. Calretinin+, WT1+, HMB45-. The typical immunoprofile for uterine tumor resembling ovarian sex cord tumor (UTROSCT) is positivity for sex cord markers and negativity for melanoma markers like HMB45. Answers A and D are incorrect because chromogranin, CD34 and CD10 would all be negative in this entity and are not helpful for the diagnosis of UTROSCT. Answer C is incorrect because calretinin would be positive in this entity.
Comment Here
Reference: Uterine tumors resembling ovarian sex cord tumors
Comment Here
Reference: Uterine tumors resembling ovarian sex cord tumors