Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Benign metastasizing leiomyoma | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alran L, Rychlik A, Croce S. Leiomyoma-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusleiomyoma.html. Accessed December 4th, 2024.
Definition / general
- Most common uterine tumor (Mod Pathol 2016;29:S104)
- Benign mesenchymal tumor derived from smooth muscle
Essential features
- Benign mesenchymal tumor derived from smooth muscle
- 90% of leiomyomas are the conventional type:
- Conventional / usual leiomyoma:
- Monotonous spindle cells with indistinct borders arranged in intersecting fascicles
- Mitoses: rare (in general < 5/10 high power fields)
- Subtypes:
- Cellular
- Leiomyoma with bizarre nuclei
- Fumarate hydratase (FH) deficient
- Mitotically active
- Hydropic
- Apoplectic
- Lipoleiomyoma
- Epithelioid
- Myxoid
- Dissecting leiomyoma
- Diffuse leiomyomatosis
- Conventional / usual leiomyoma:
Epidemiology
- All ages, especially in fifth decade; third decade for fumarate hydratase deficient leiomyoma
- More common (up to 80%) in African American women
- References: Best Pract Res Clin Obstet Gynaecol 2008;22:571, BJOG 2017;124:1501
Sites
- Uterine corpus
- Less common in vulva, vagina, cervix, broad ligament, ovary
Pathophysiology
- Leiomyomas have a clonal origin
- Several alterations identified (Table 1) (Clin Obstet Gynecol 2016;59:25)
- Risk decreased by oral contraceptives
- May occur in hereditary leiomyomatosis and renal cancer syndrome (HLRCC) and Alport syndrome
Etiology
- Mitotically active leiomyoma: associated ischemia or hormonal stimulation (endogenous or exogenous) (Am J Surg Pathol 2016;40:563)
- Apoplectic leiomyoma: progesterone (or analogues) exposure (contraception or pregnancy and postpartum)
Diagrams / tables
Contributed by Sabrina Croce, M.D., Ph.D.
Table 2: differential diagnosis in uterine spindle cell smooth muscle lesions
| | | | |
| - | + | ≥ 10 | Leiomyosarcoma |
| + | + | ≥ 10 | |
| + | + | < 10 | |
| - | - | > 15** | Smooth muscle tumor of uncertain malignant potential (STUMP) |
| - | + | < 10 | |
| + | - | < 10 | |
| - | - | ≥ 6 and ≤ 15** | Mitotically active leiomyoma |
| * Mitoses/mm2 (mitoses/10 HPF of 0.55 mm in diameter) | |||
| ** > 15 or ≥ 15, cutoff value varies according to the references | |||
Table 3: differential diagnosis in uterine myxoid smooth muscle lesions
| | | | |
| Infiltrative borders | - | - | 1 or more of these criteria:
|
| Atypia | - | - | |
| Tumor cell necrosis | - | - | |
| Mitoses* | - | 1 | |
| * Mitoses/mm2 (mitoses/10 HPF of 0.55 mm in diameter) | |||
Table 4: differential diagnosis in uterine epithelioid smooth muscle lesions
| | | | |
| Atypia | - | - | 1 or more of these criteria:
|
| Tumor cell necrosis | - | - | |
| Mitoses* | < 2 | ≥ 2 and < 4 | |
| * Mitoses/mm2 (mitoses/10 HPF of 0.55 mm in diameter) | |||
Clinical features
- 25% symptomatic; remainder asymptomatic
- Symptoms depend on size and location
- Menorrhagia and pelvic pain in 33% of patients
- Reference: Nat Rev Dis Primers 2016;2:16043
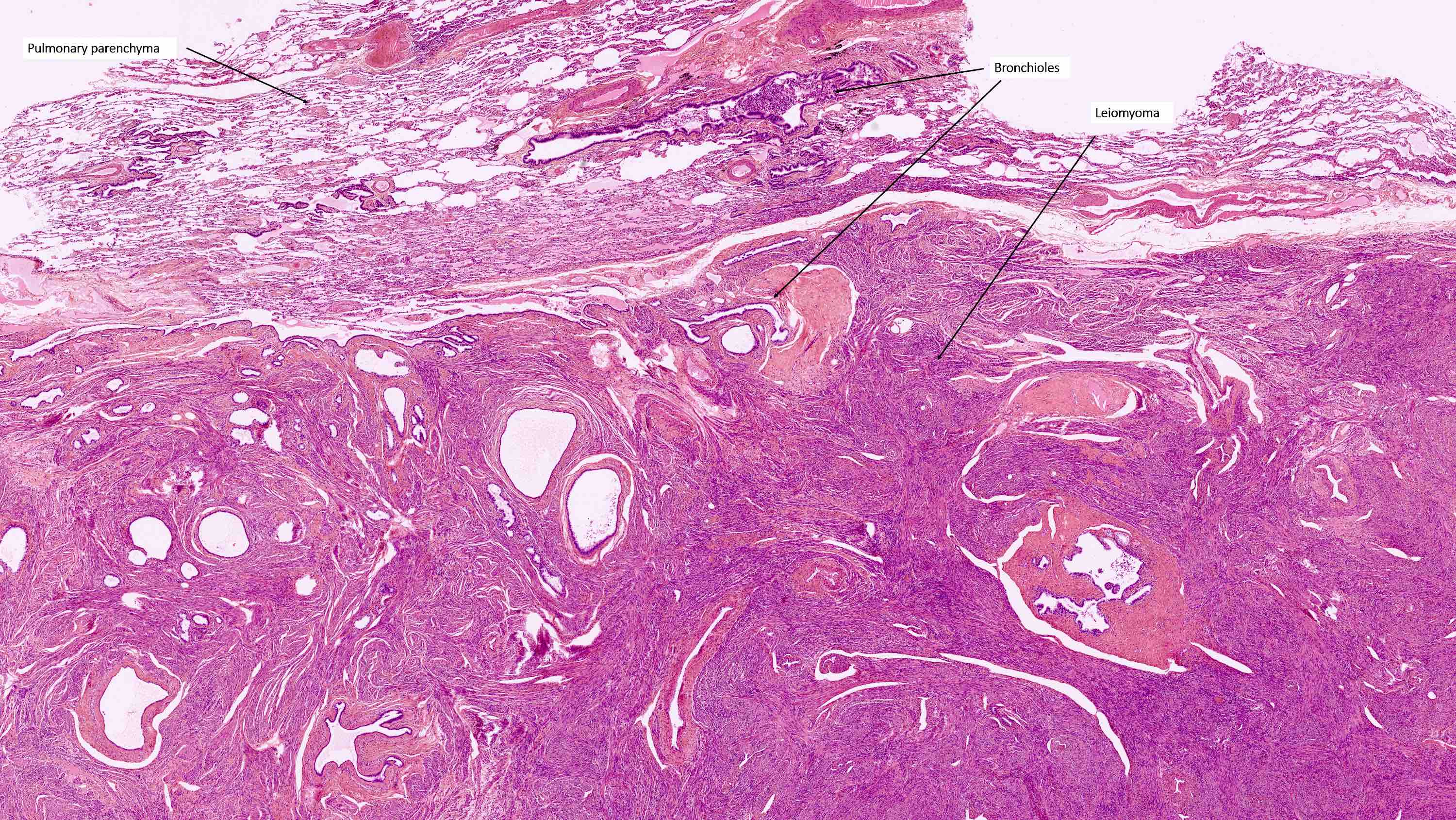
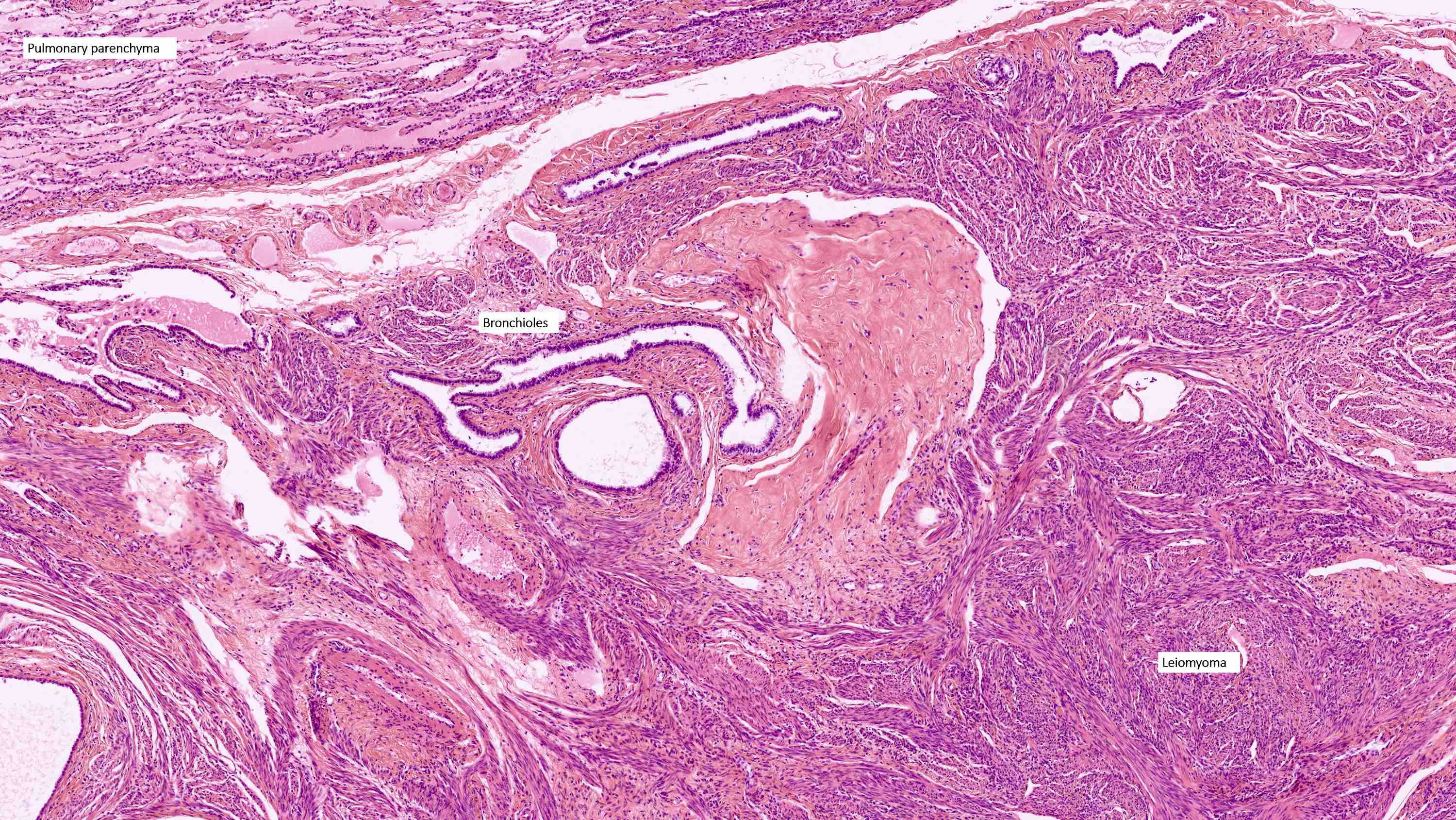
Benign metastasizing leiomyoma
- Rare, benign appearing smooth muscle tumor in lung; may represent hematogenous spread of a uterine leiomyoma or a metastasis of a well differentiated leiomyosarcoma of low malignant potential (Mod Pathol 2006;19:130)
- Usually women 36 - 64 years, mean 44 years, with history of uterine leiomyoma
- Lung is most common site, sparing bronchus and pleura; also reported in lymph nodes, retroperitoneum, skin, bone, spine, skull base, heart
- Usually multiple nodules, up to a few centimeters in size
- Lesions tend to regress during pregnancy or after oophorectomy and stabilize or grow slowly in postmenopausal women
- Usually asymptomatic but may present with dyspnea, cough, hemoptysis, chest pain
- Chest Xray: diffuse, bilateral nodular opacities; rarely associated with miliary pattern, cavitary lesions, multiloculated cysts, interstitial lung disease (J Thorac Dis 2014;6:E92)
- Surveillance acceptable treatment for indolent, asymptomatic disease
Diagnosis
- Can be established by resection of the whole uterus (hysterectomy), by resection of the leiomyoma if accessible by curetting (if submucosal) or by myomectomy (if subserosal)
- Ultrasound or magnetic resonance imaging (MRI) (guided core biopsy of the leiomyoma is a promising new procedure (Int J Gynecol Cancer 2020;30:A113)
Prognostic factors
- Uterine leiomyomas are benign tumors that may recur, especially after myomectomy
- Fumarate hydratase deficient leiomyomas:
- Recur more frequently
- Genetic counseling should be recommended
Case reports
- 32 year old woman with enlarged uterus with hypervascular lesions likely representing fibroids (Case #508)
- 32 year old woman with uterine leiomyoma with high stage renal carcinoma in a context of HLRCC syndrome (Am J Surg Pathol 2011;35:1235)
- 32 year old woman with pulmonary benign metastasizing leiomyoma (J Thorac Dis 2014;6:E92)
- 52 and 56 year old women with benign metastasizing leiomyoma (Case Rep Oncol Med 2014;2014:842801)
- 58 year old woman with uterine leiomyomas and osteoclast giant cells (Int J Gynecol Pathol 2016;35:30)
Treatment
- Asymptomatic: does not require therapy
- Symptomatic leiomyoma:
- Surgery (hysterectomy or myomectomy)
- Hysteroscopic resection
- Medical treatment - progestins / levonorgestrel intrauterine system, gonadotropin releasing hormone (GnRH) analogs or aromatase inhibitors
- Ulipristal acetate; widely used in conservative treatment of uterine leiomyomas but rejected by the FDA due to risk of liver toxicity
- Interventional treatments - uterine artery embolization or radiofrequency myolysis
- Reference: J Obstet Gynaecol Can 2015;37:157
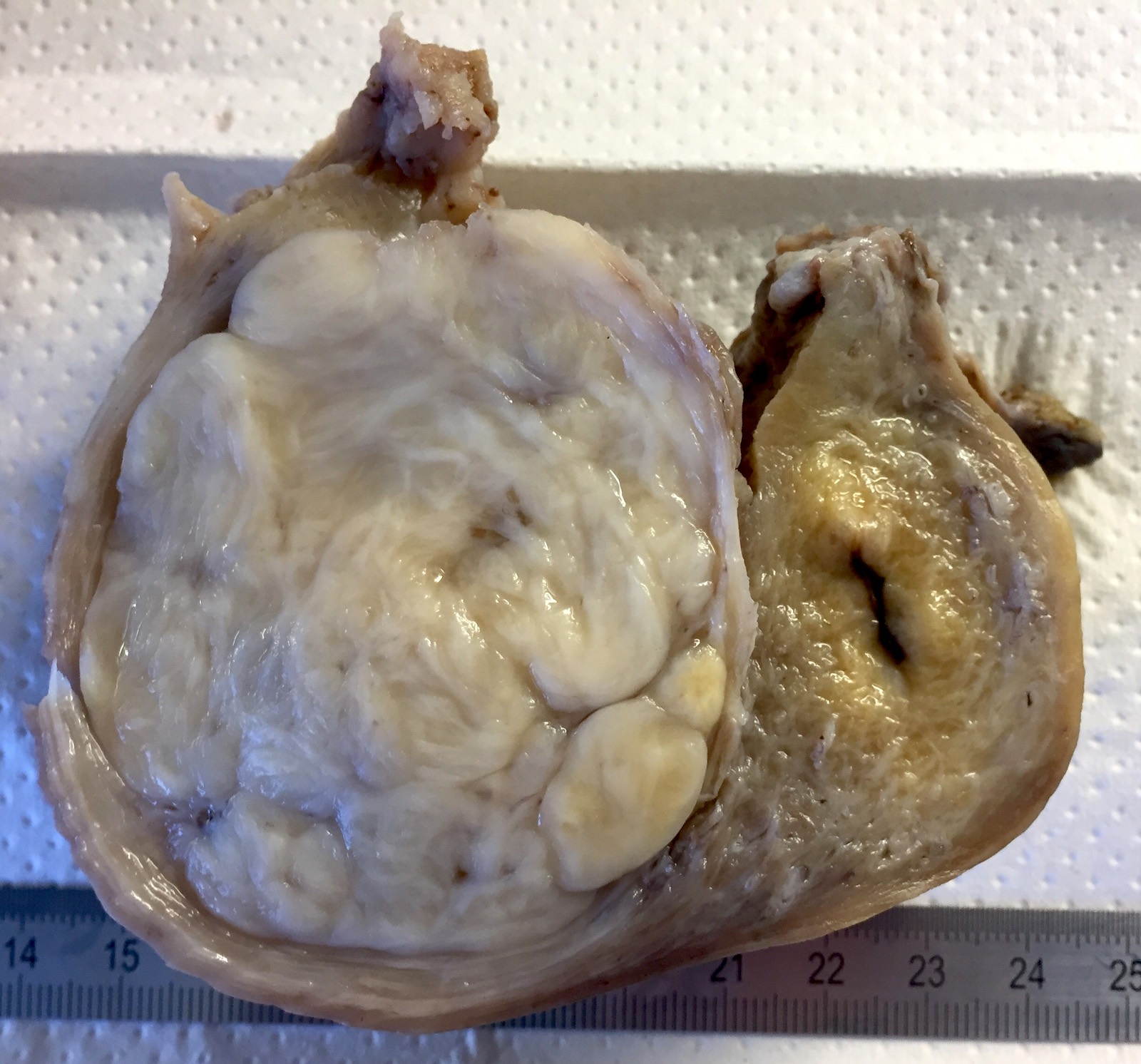
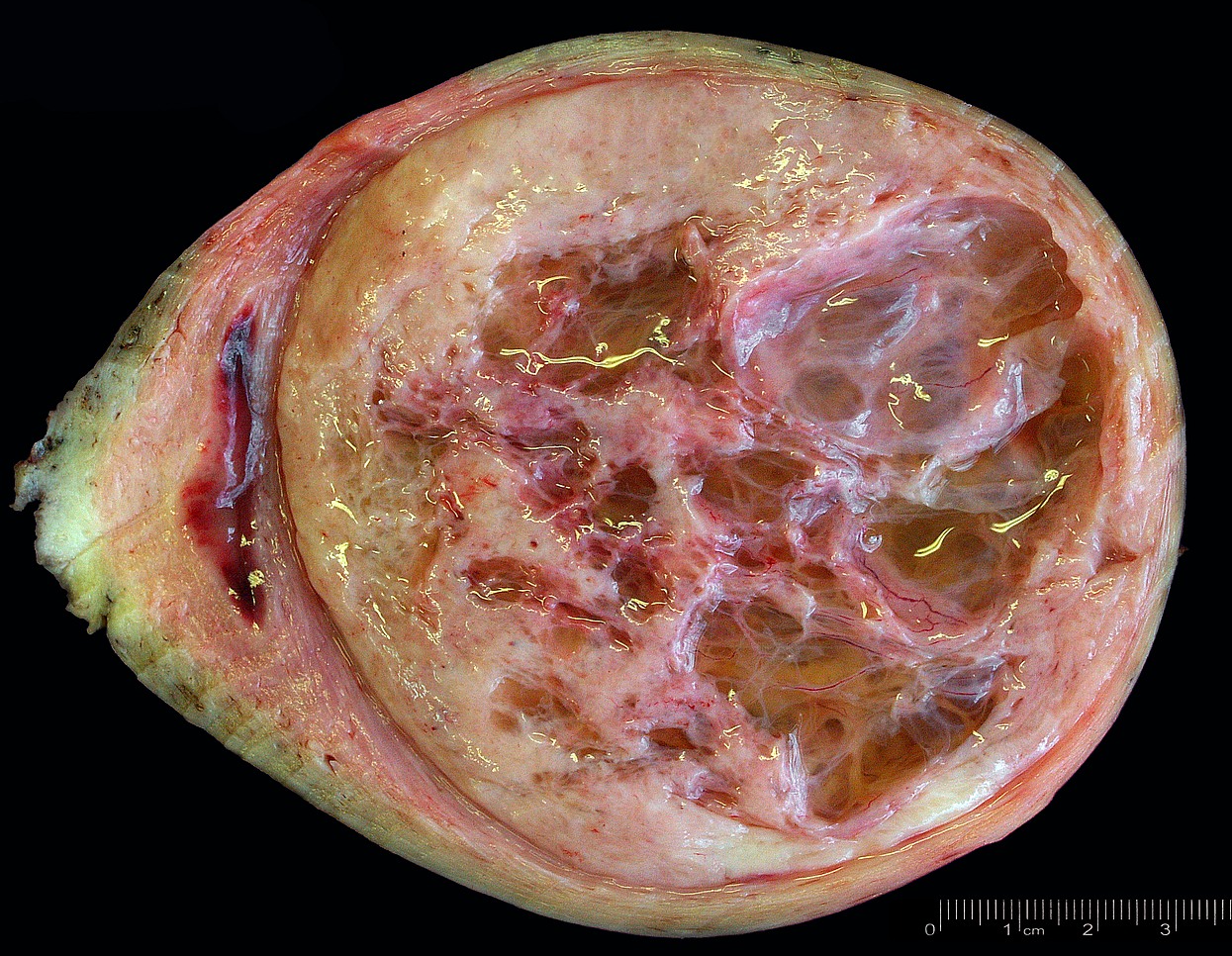
Gross description
- Location in the uterus: intramural, submucosal and subserosal
- Often multiple
- Typically well circumscribed but nonencapsulated
- On cut surface: white or tan-white, whorled, firm, bulging
- Hemorrhage and infarction can be present in large tumors
- Calcifications can be present
- Apoplectic change (foci of hemorrhage) associated with progesterone therapy
- Extensive sampling (to exclude malignancy)
- Especially in leiomyomas that lack the classic gross appearance
- Myxoid areas to exclude myxoid leiomyosarcoma
- Reference: Mod Pathol 2016;29:S104
Gross images
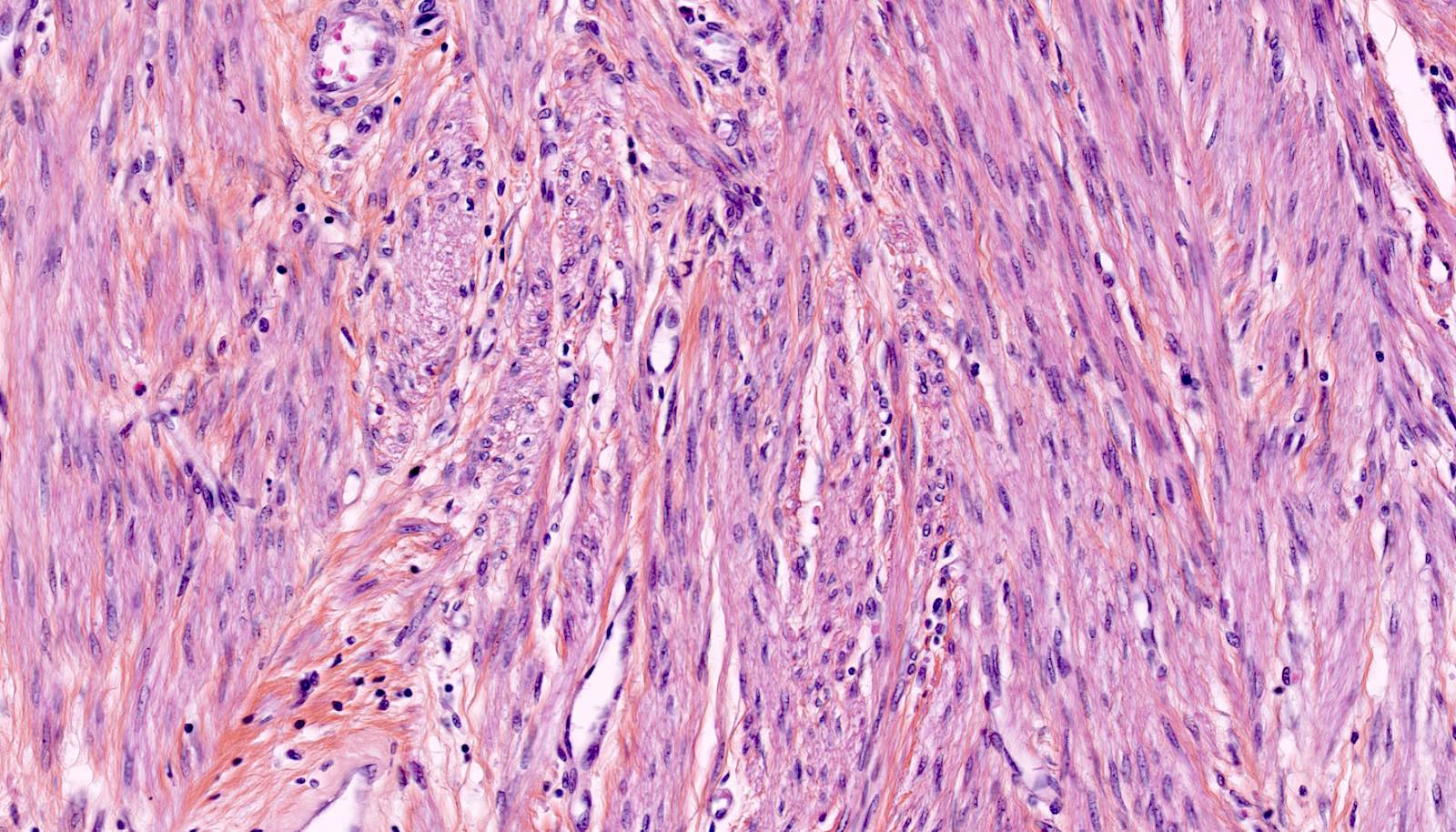
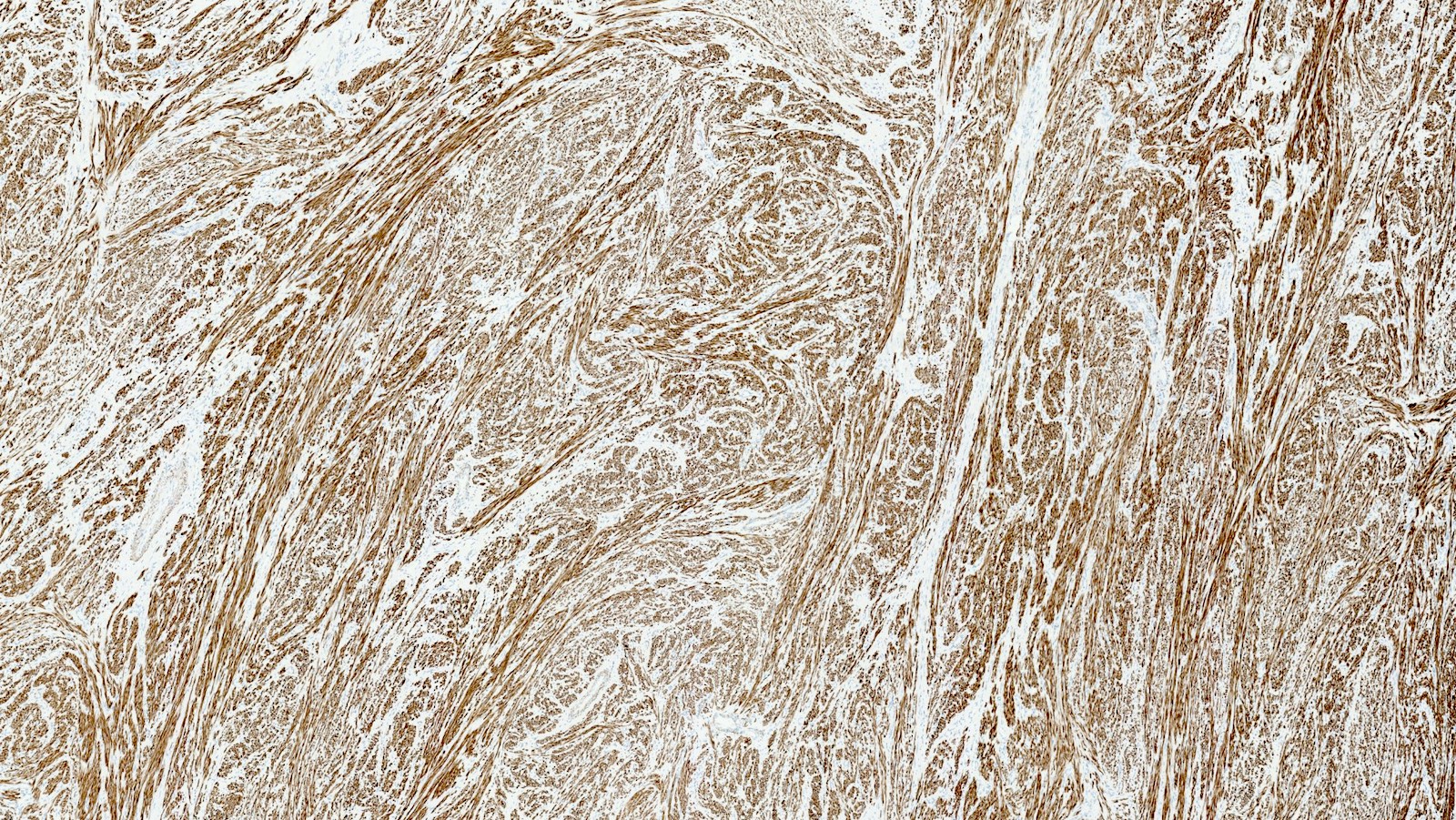
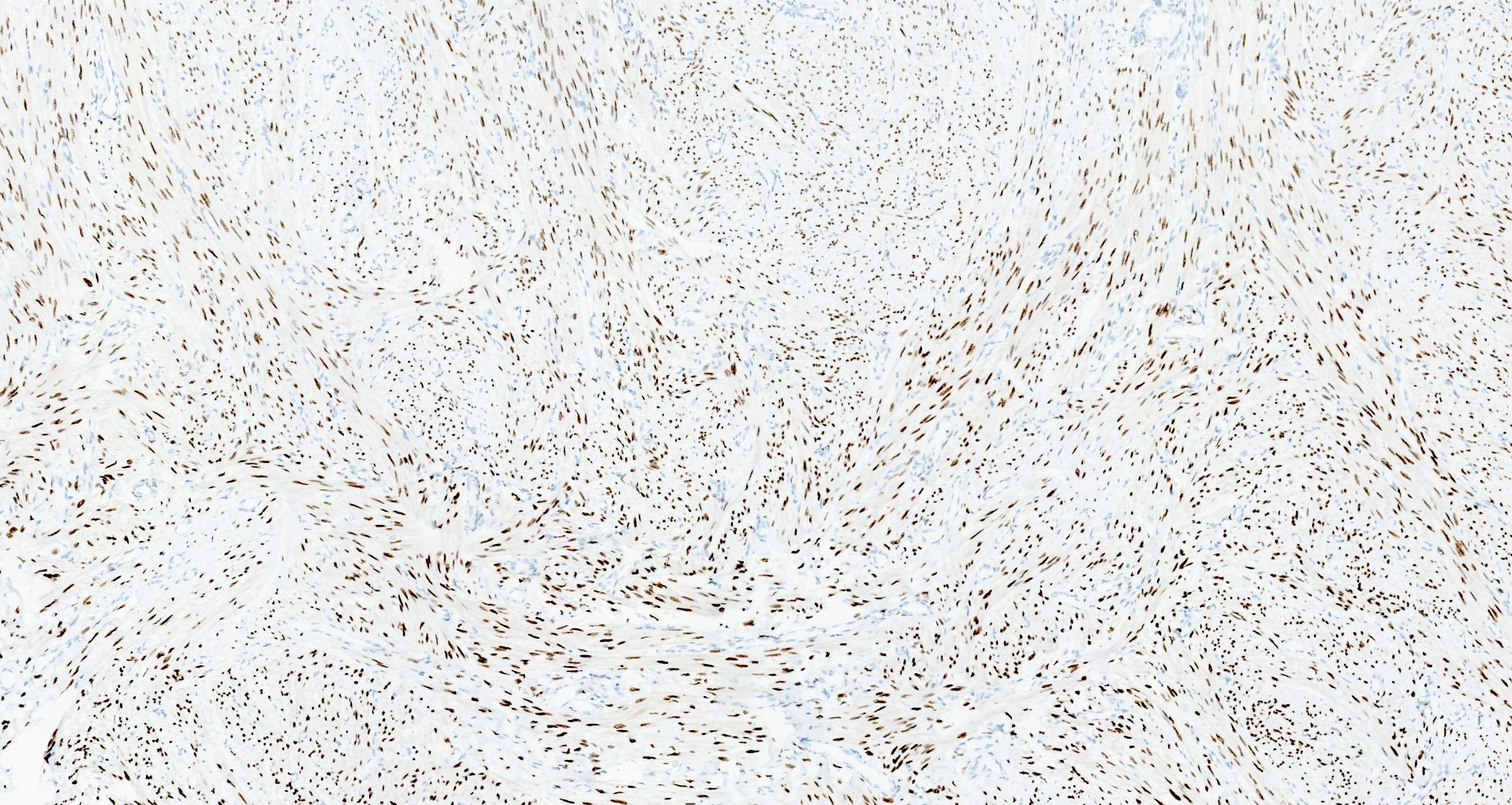
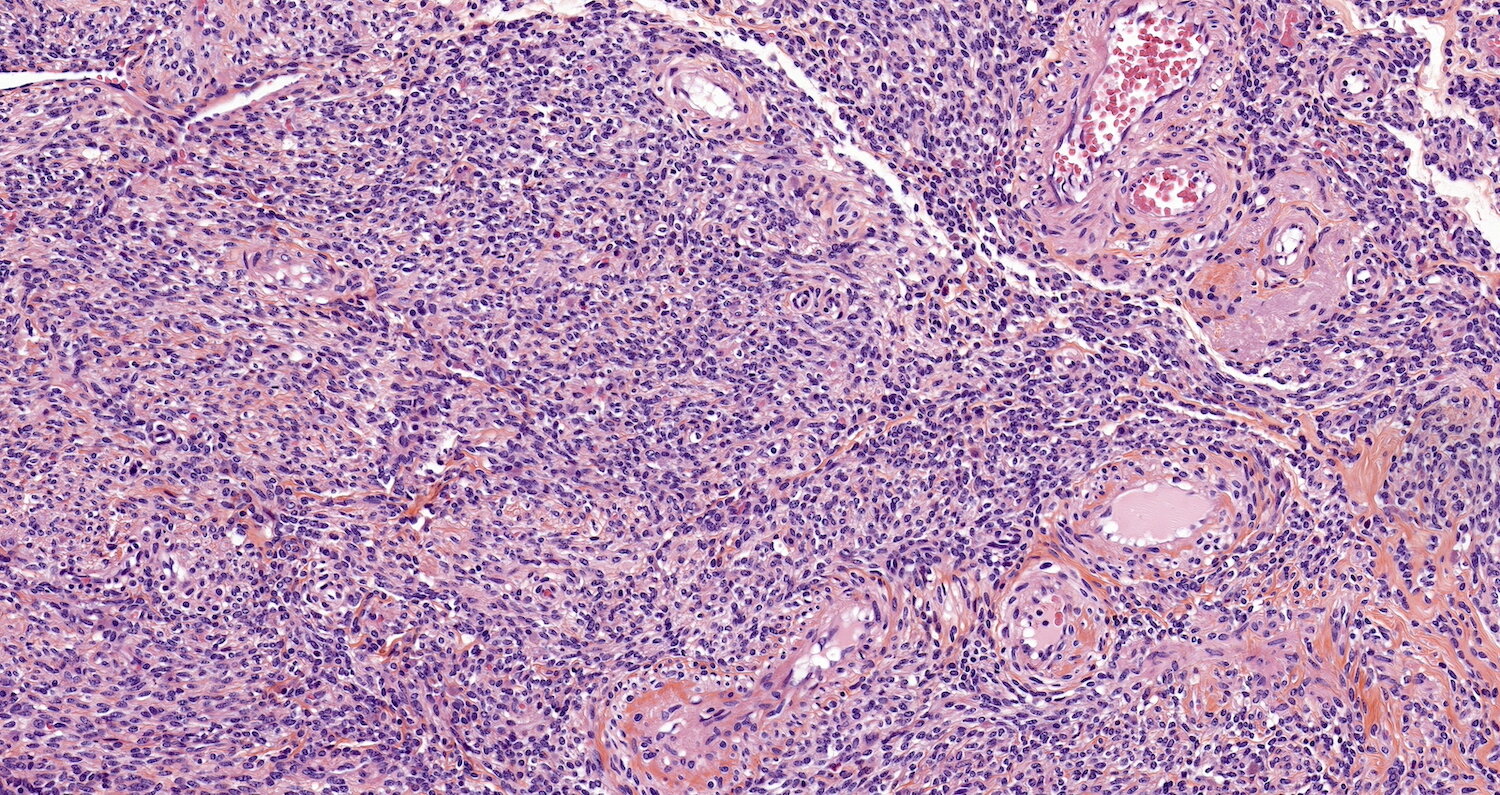
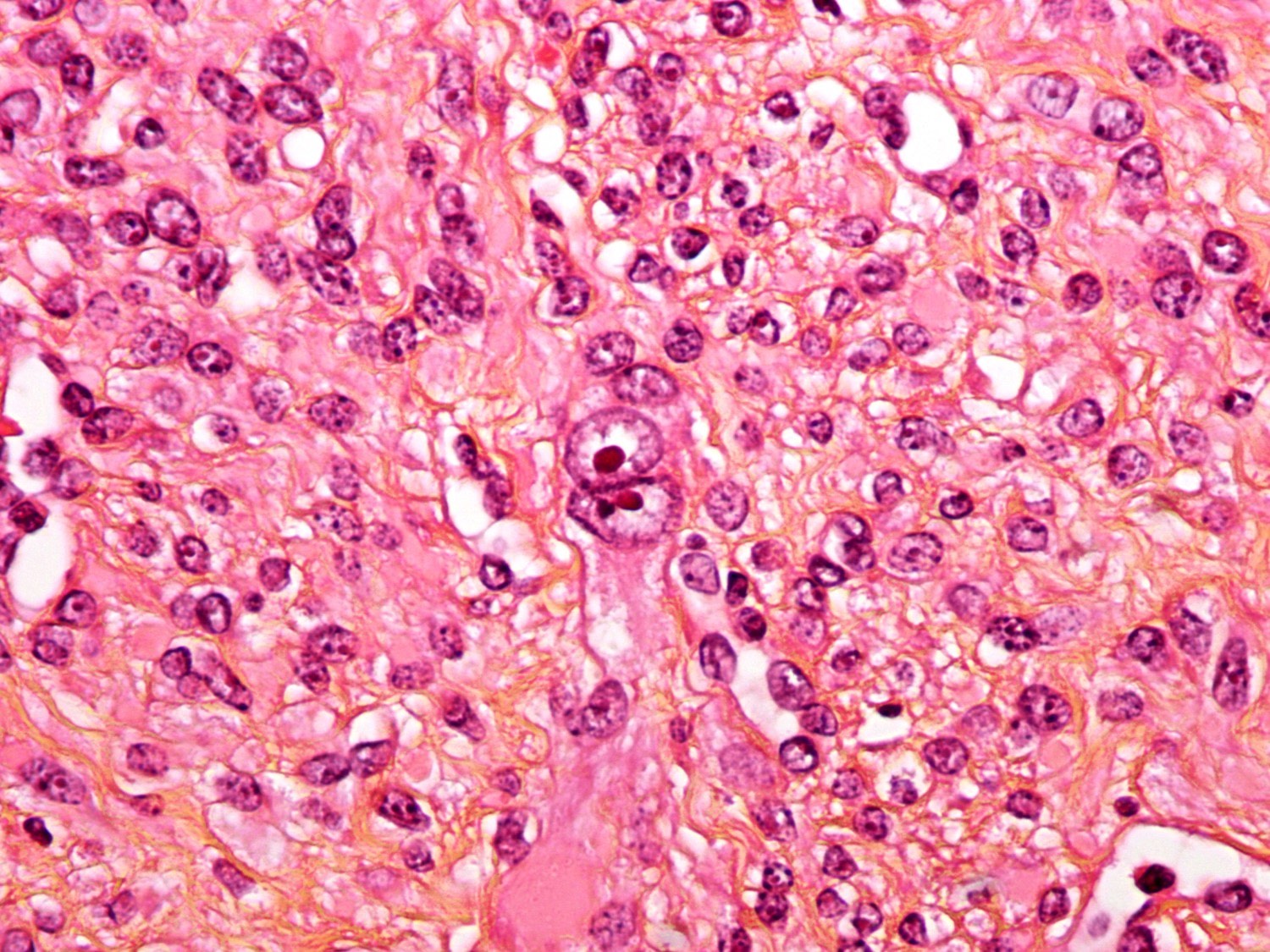
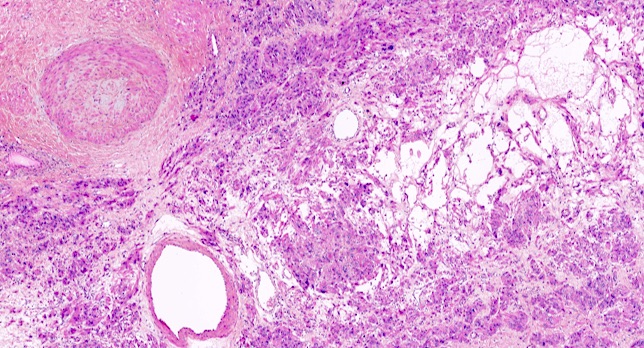
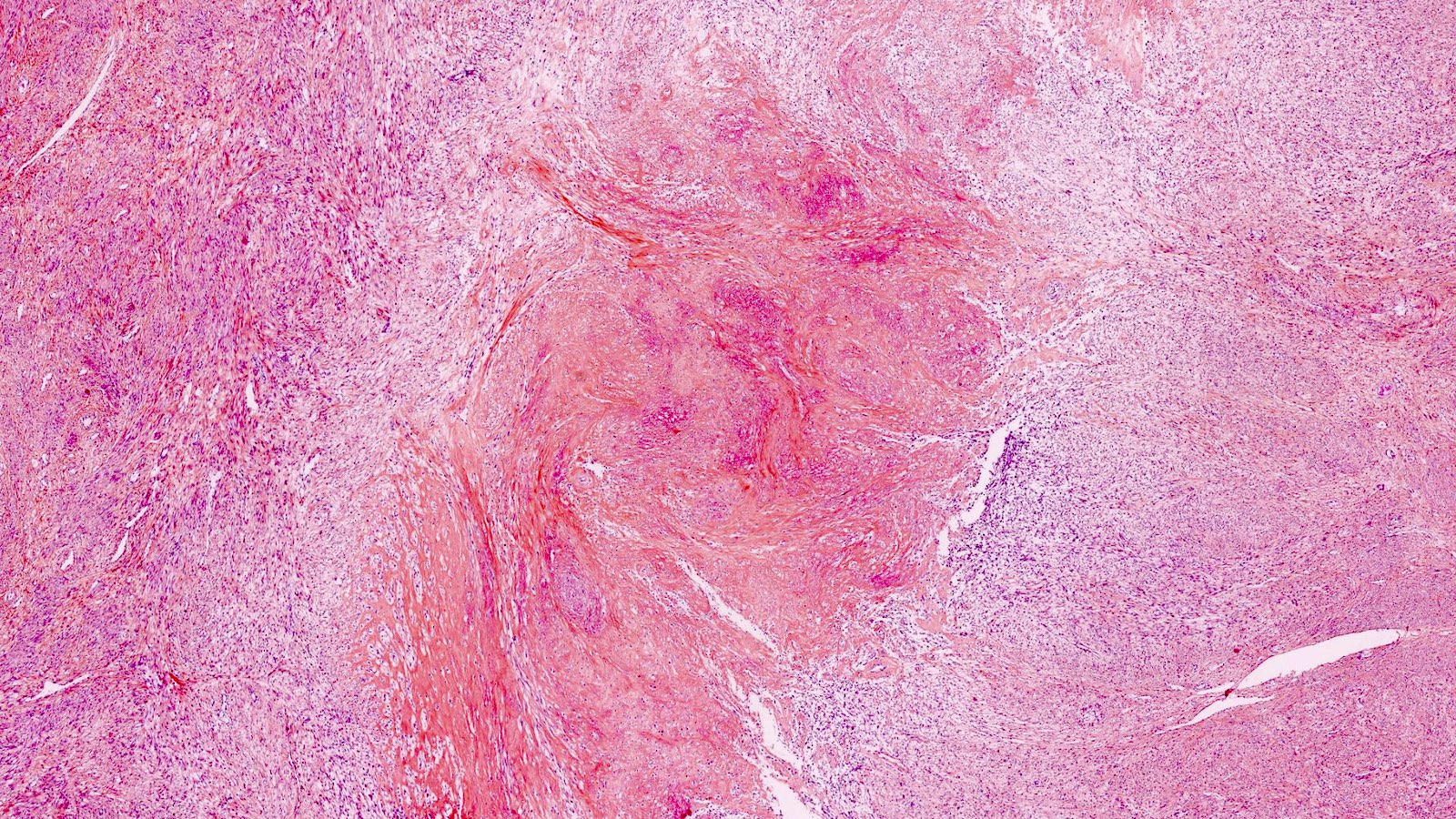
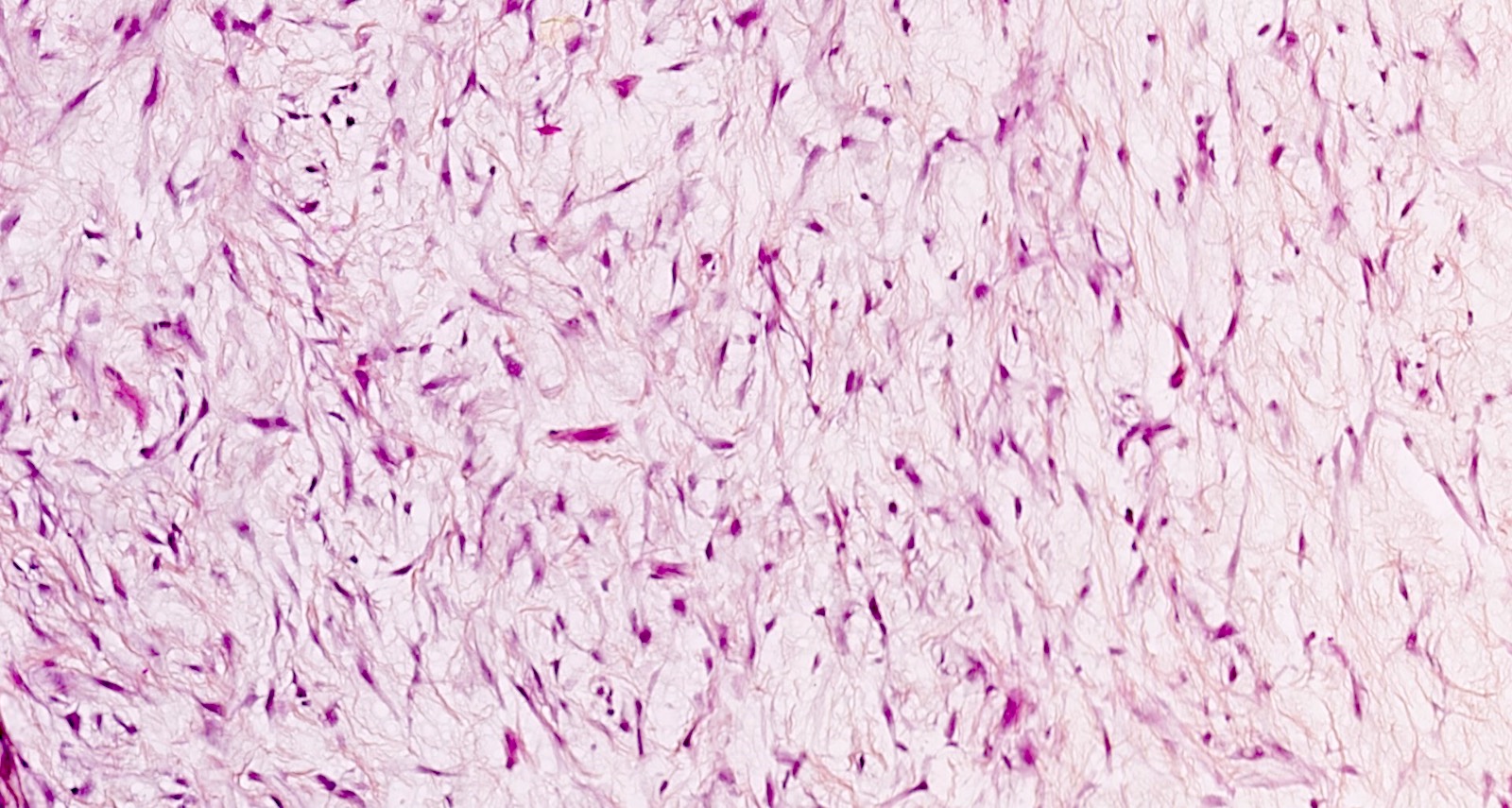
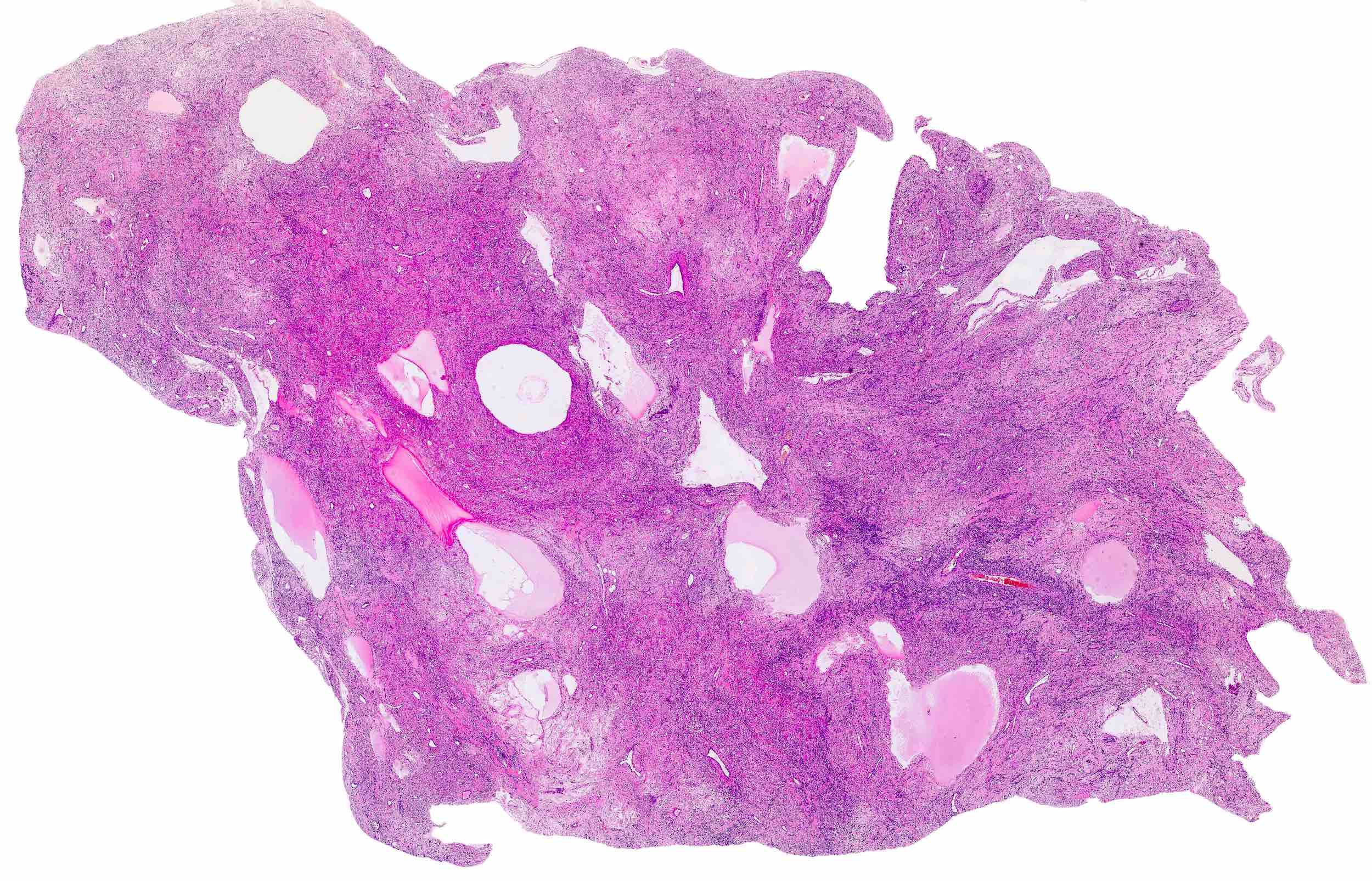
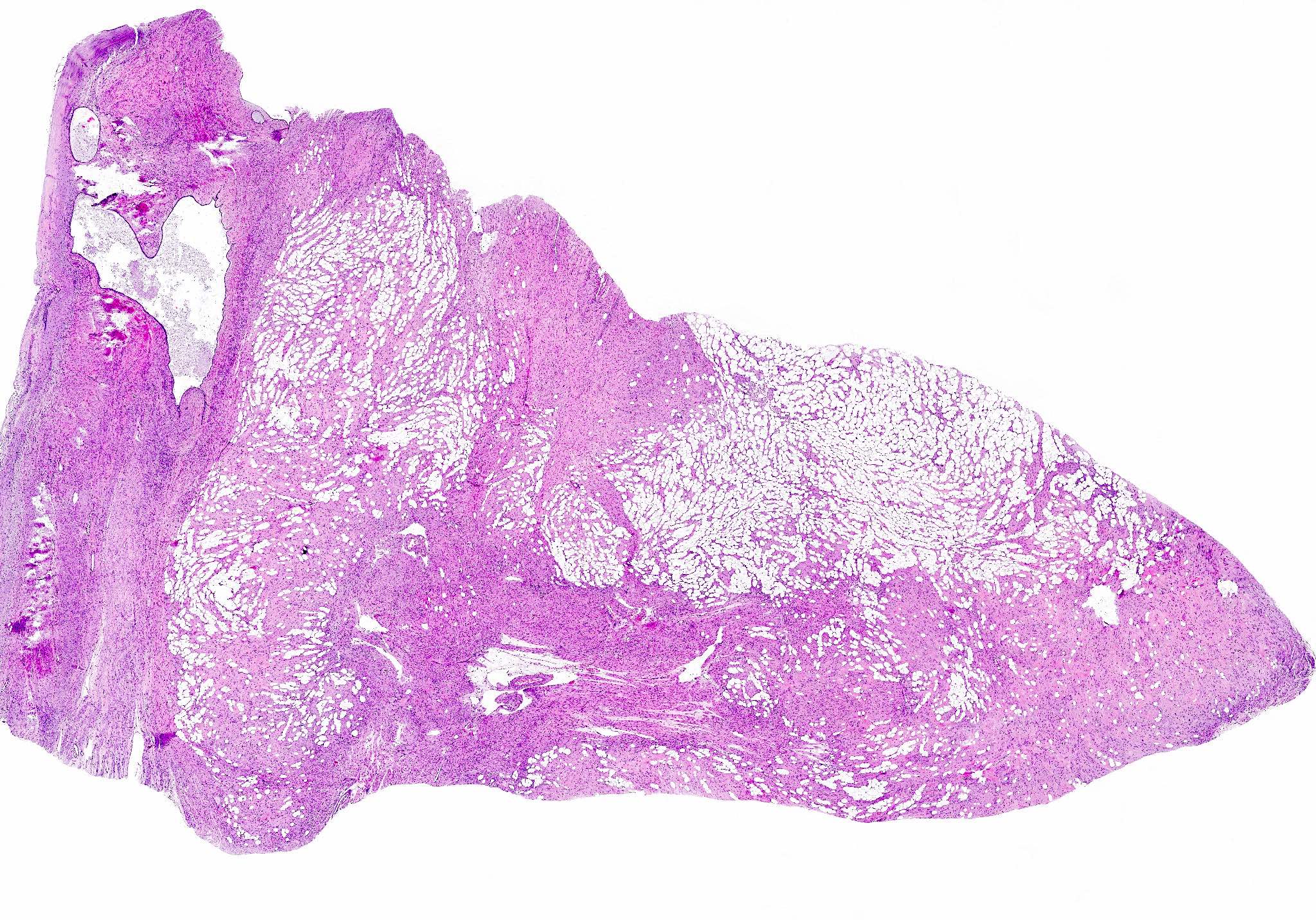
Microscopic (histologic) description
- Conventional / usual leiomyoma (spindle):
- Well defined borders
- Normocellular
- Intersecting fascicles of monotonous spindle cells with indistinct borders, eosinophilic cytoplasm, cigar shaped nuclei (with tapered ends) and small nucleoli
- Atypia: absent or mild
- Mitoses: rare (in general < 5/10 high power fields)
- Blood vessels with thick walls
- With or without infarct type necrosis, hyalinization, calcification, cystic change
- Subtypes:
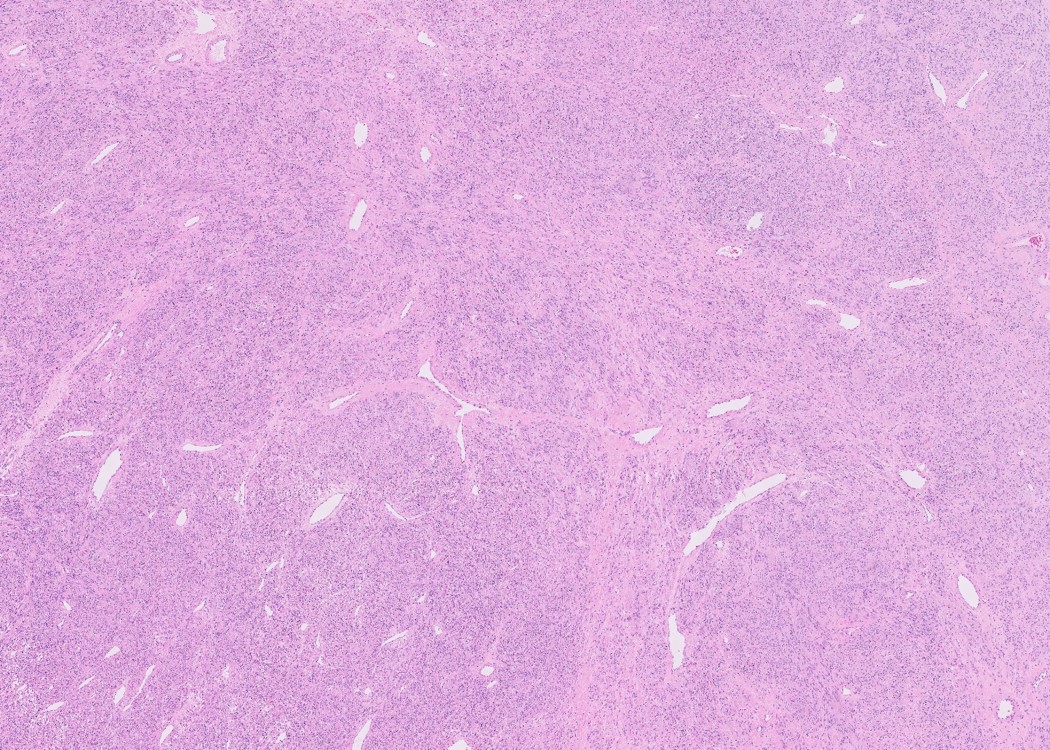
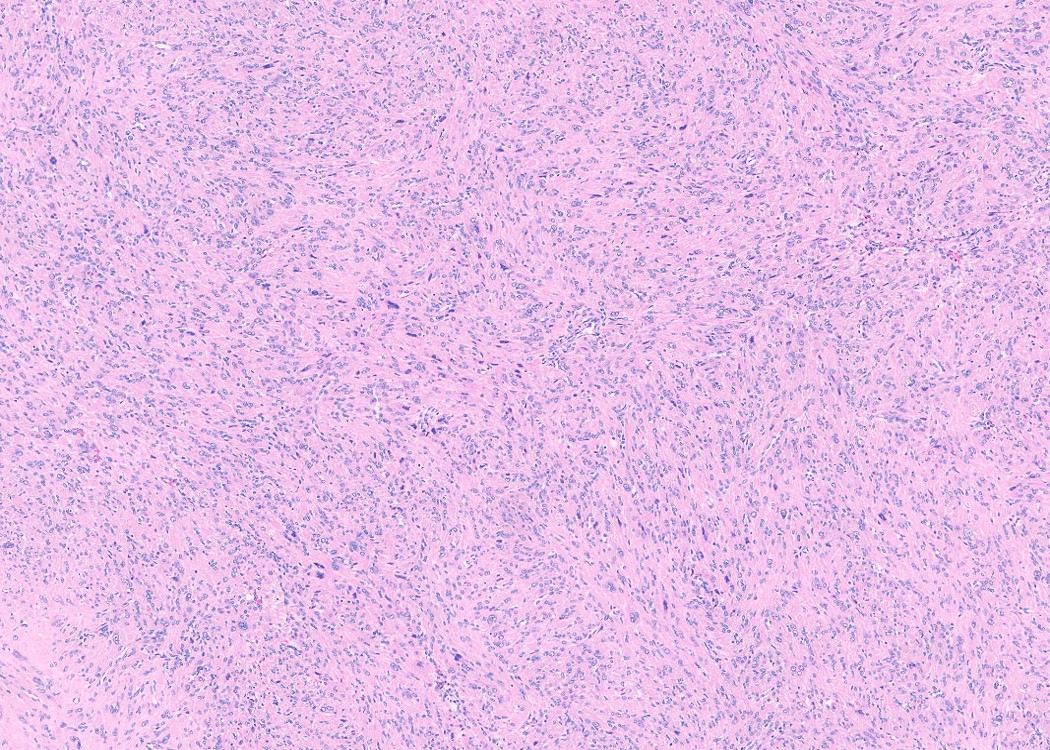
- Cellular
- Increased cellularity (more cellular than background myometrium)
- Scant cytoplasm without increased mitotic activity and atypia
- May have irregular borders
- Highly cellular leiomyoma is not a WHO diagnosis
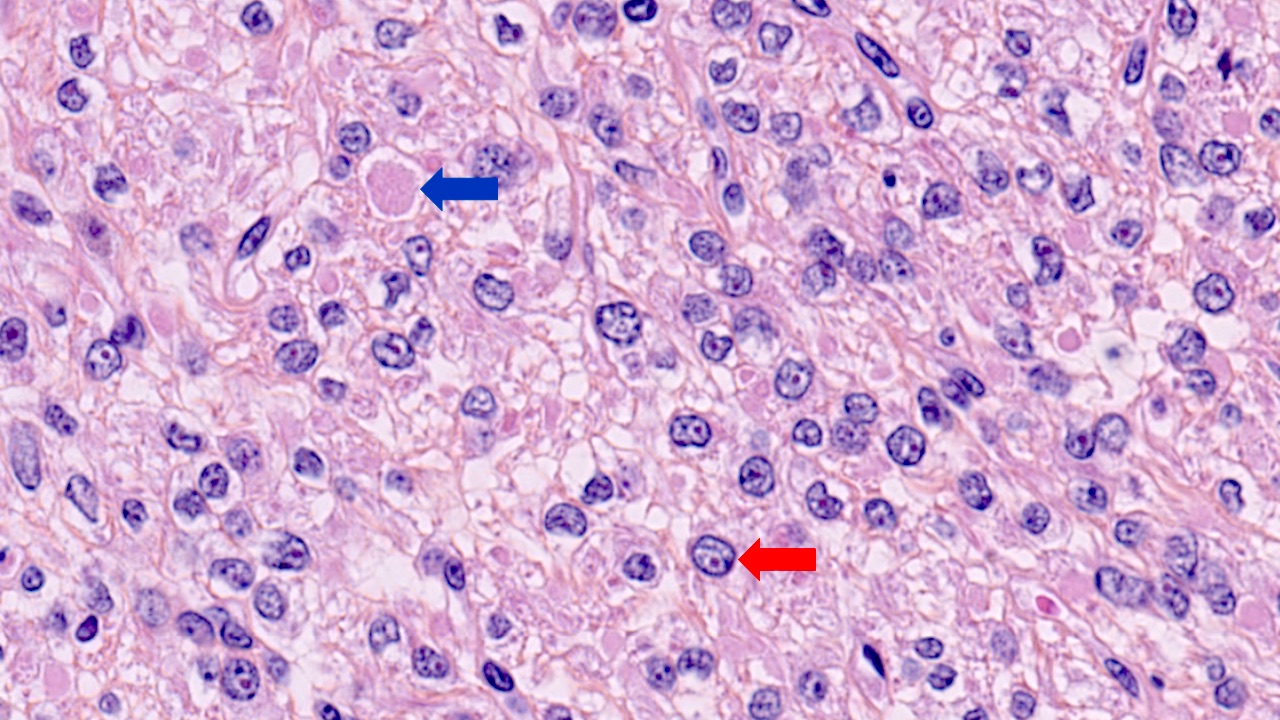
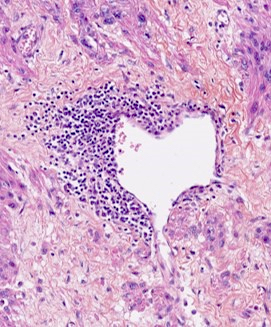
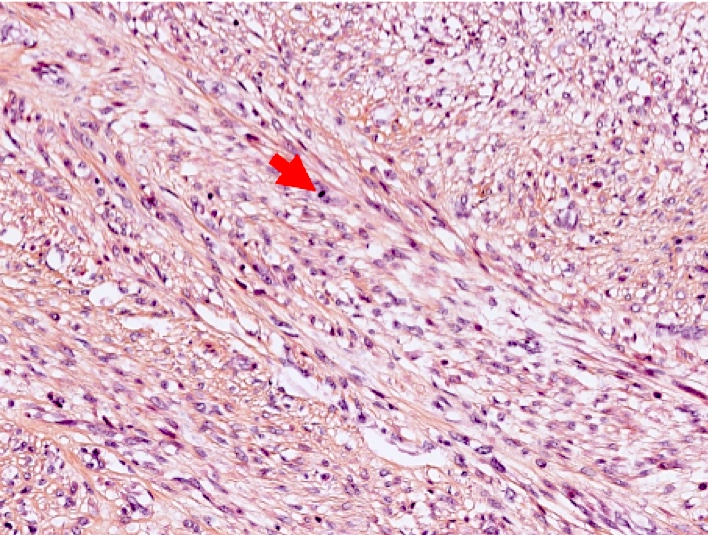
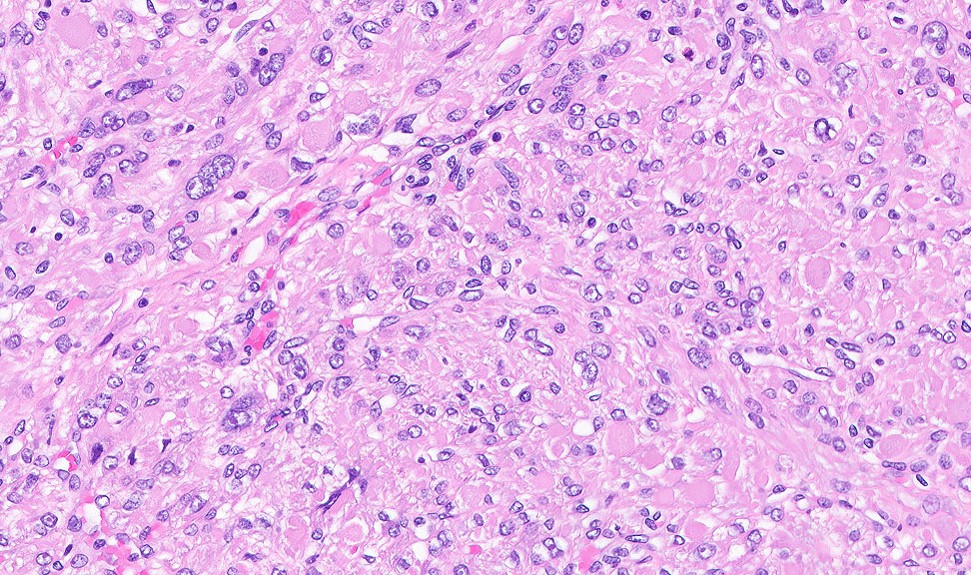
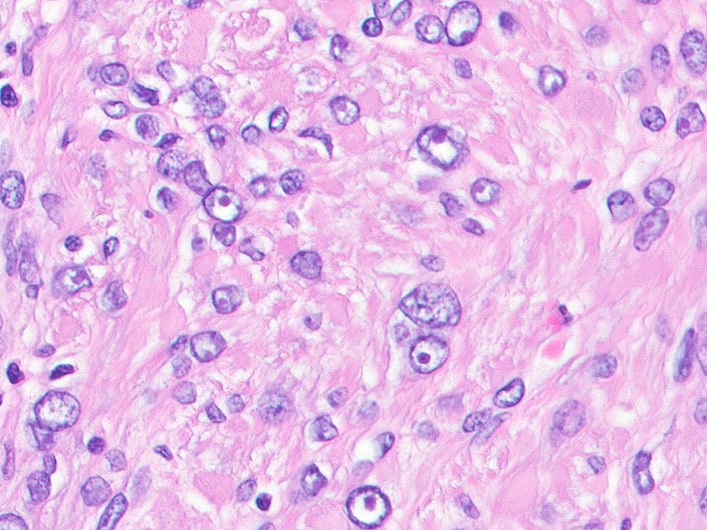
- Leiomyoma with bizarre nuclei:
- Bizarrely shaped, hyperchromatic, multilobulated nuclei with nuclear pseudoinclusions
- Arranged in a multifocal to diffuse distribution in a background of a typical leiomyoma (Am J Surg Pathol 2014;38:1330, Mod Pathol 2017;30:1476, Am J Surg Pathol 2016;40:923, Cancer 2014;120:3165, Am J Surg Pathol 1997;21:1261)
- Alveolar edema, staghorn vessels
- Low mitotic activity (< 5 mitoses/10 high power fields)
- Absence of tumor cell necrosis
- Vasculature variable (staghorn vessels, thick walled vessels, fibrinoid necrosis of vessel walls, luminal vascular obliteration)
- Diagnostic key: intermixed normal spindled smooth muscle cells
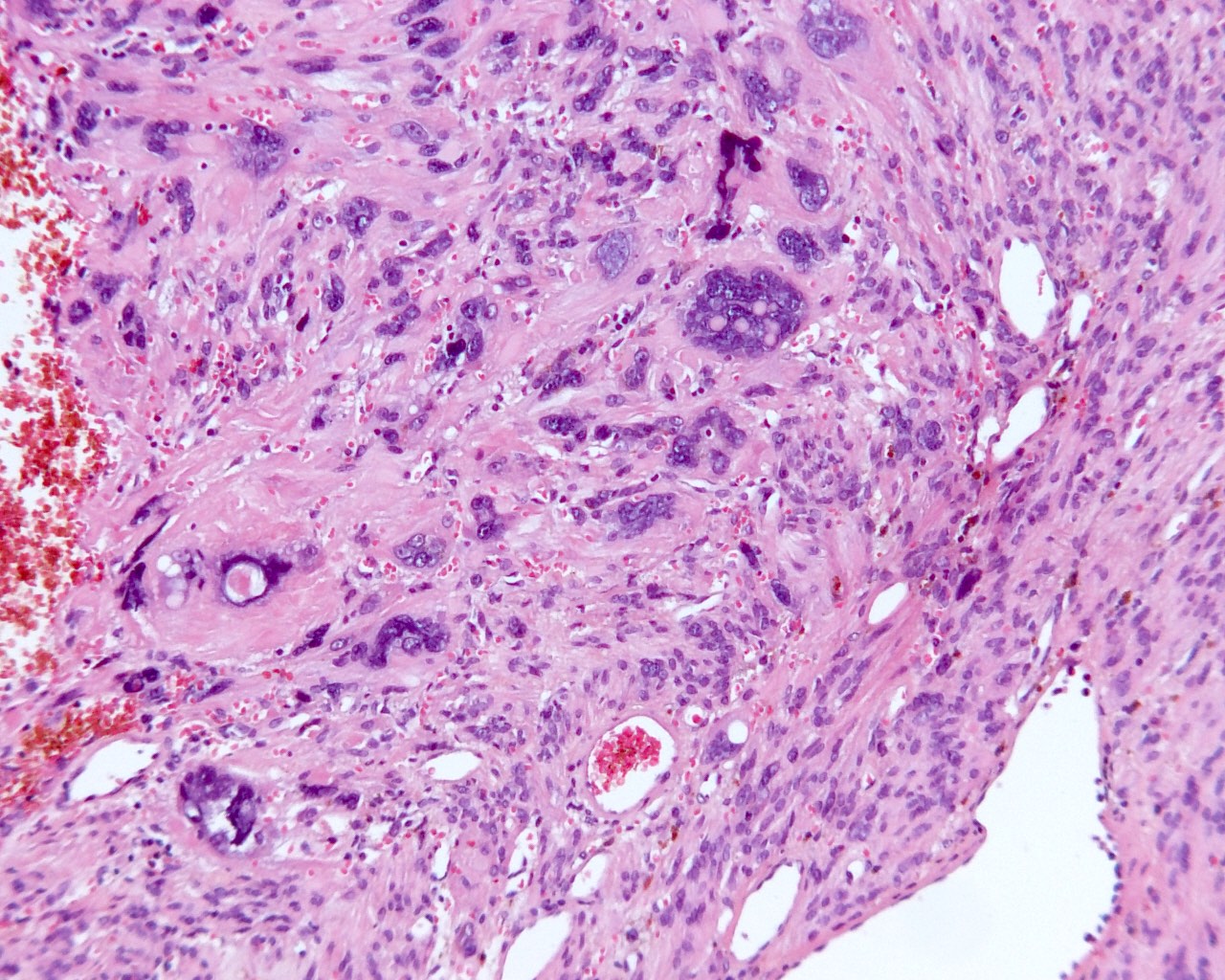
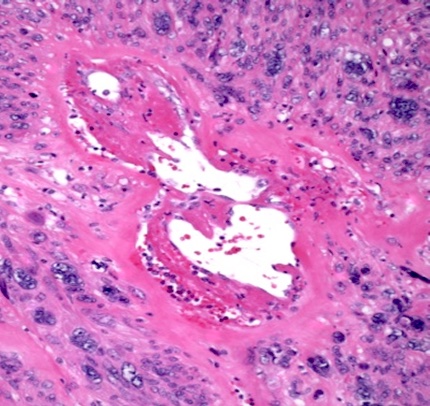
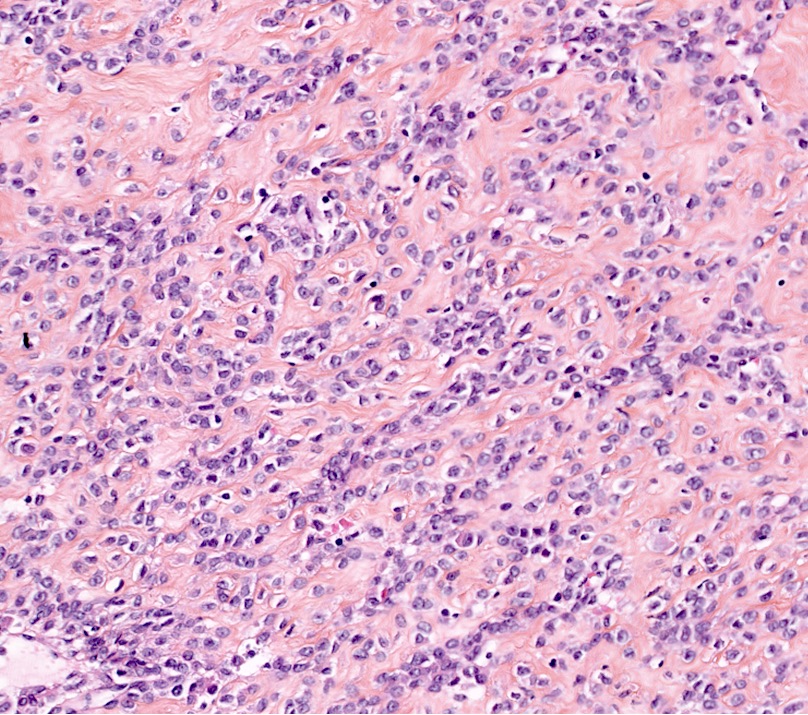
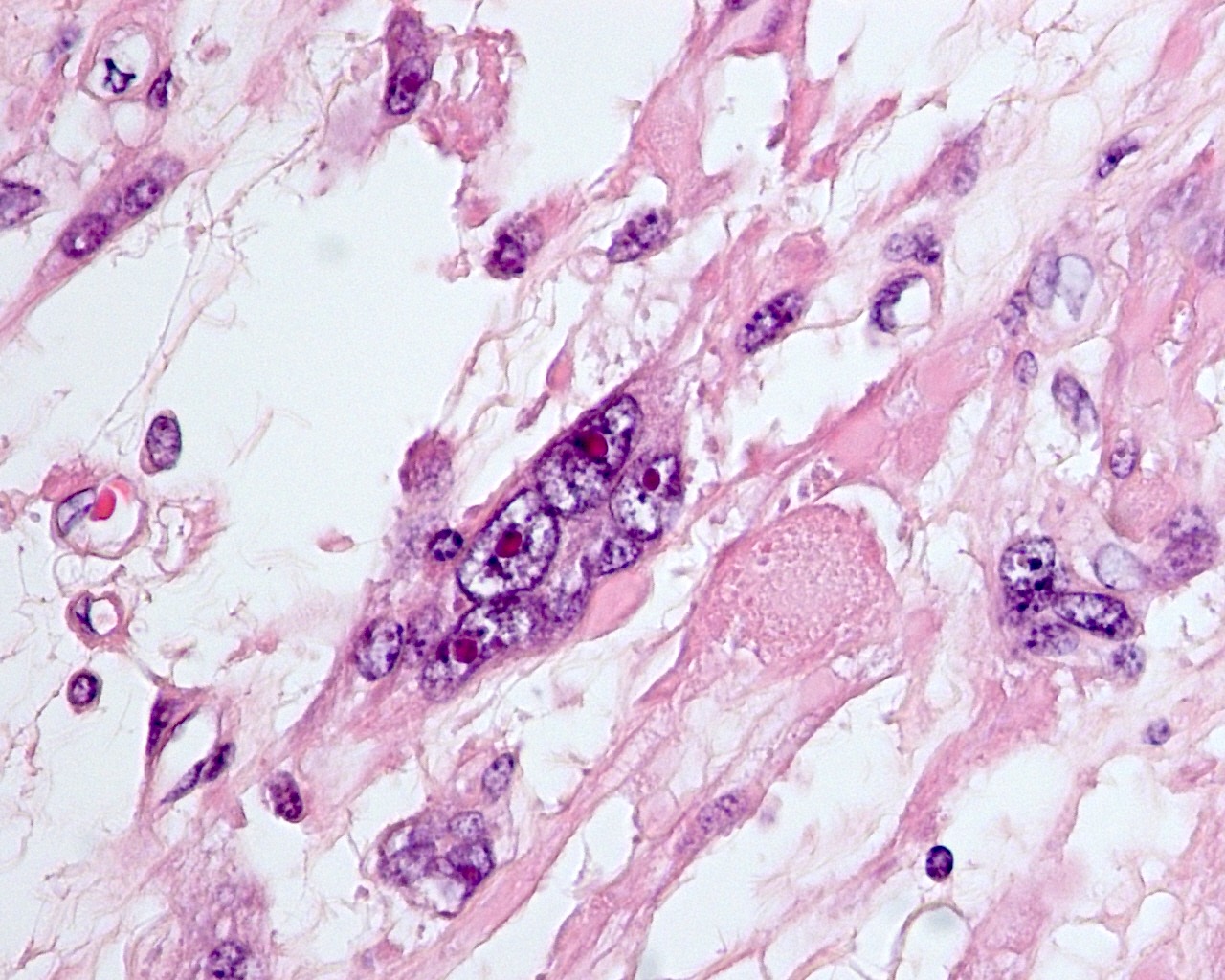
- Fumarate hydratase deficient leiomyoma:
- Alveolar edema
- Staghorn or hemangiopericytoma-like vessels
- Chain-like growth of tumor cells
- Spindle or epithelioid cells with ovoid nuclei and prominent eosinophilic nucleoli surrounded by perinucleolar halos
- Rhabdoid / eosinophilic cytoplasmic inclusions
- May include multinucleated cells and cells with bizarre nuclei
- Mitotically active:
- Spindle cell leiomyoma without atypia or tumor cell necrosis
- Increased mitotic activity (the mitotic cutoff varies according to the authors 6 - 14 mitoses/10 high power fields or 6 - 15 mitoses/10 high power fields)
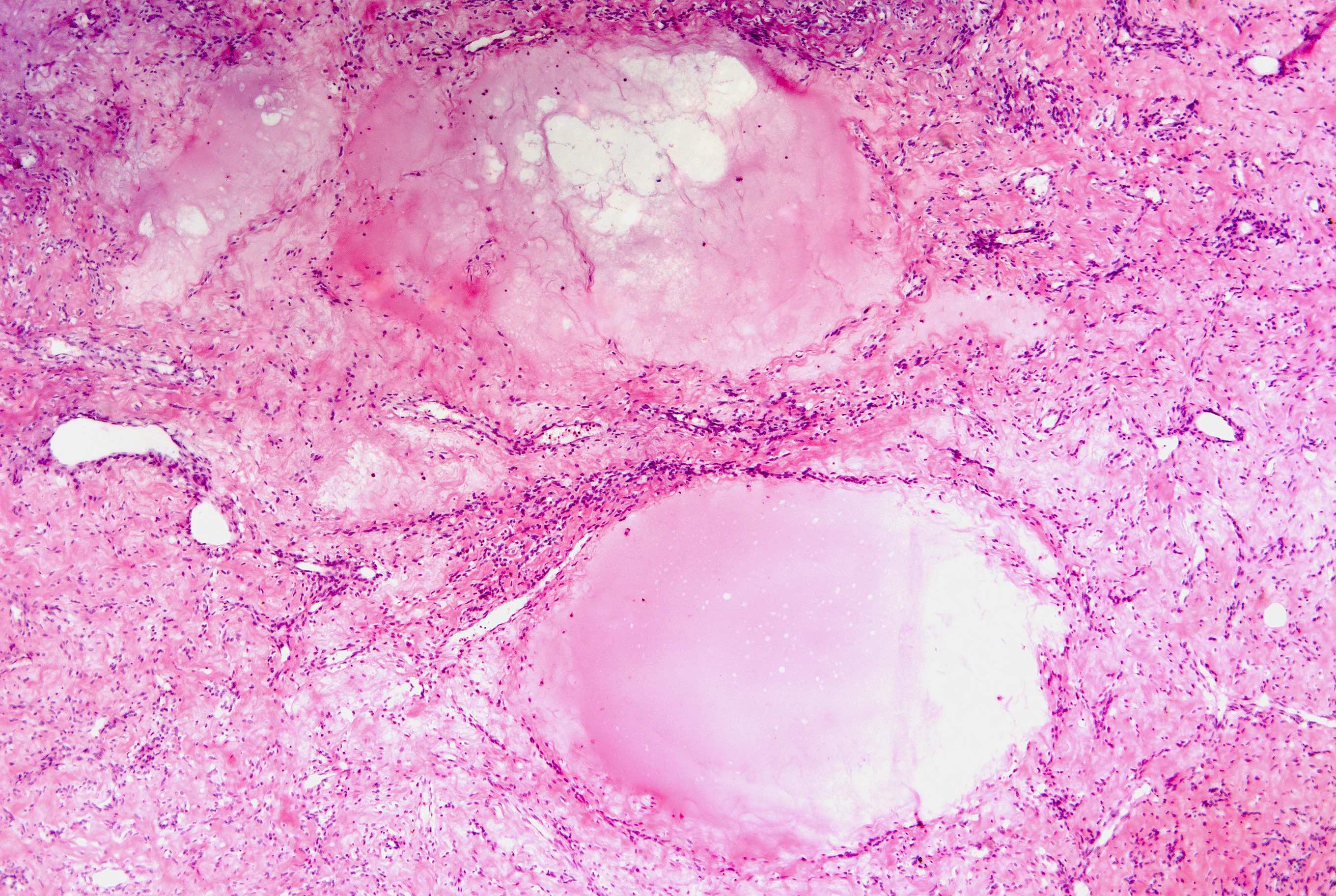
- Hydropic:
- Tumor cells separated by watery or eosinophilic and proteinaceous fluid, resulting in a trabecular, nested architecture
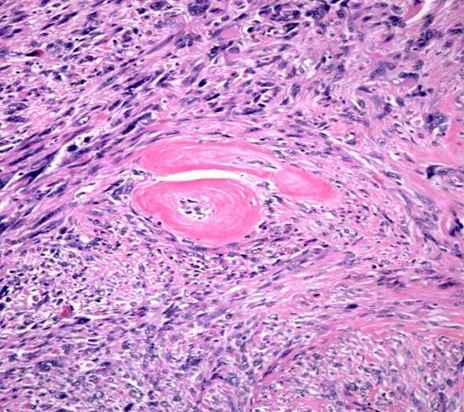
- Apoplectic:
- Central zone of hemorrhage and necrosis with increased mitotic activity in its periphery or myxoid changes (zonation phenomenon)
- Usual appearance away from the central necrosis
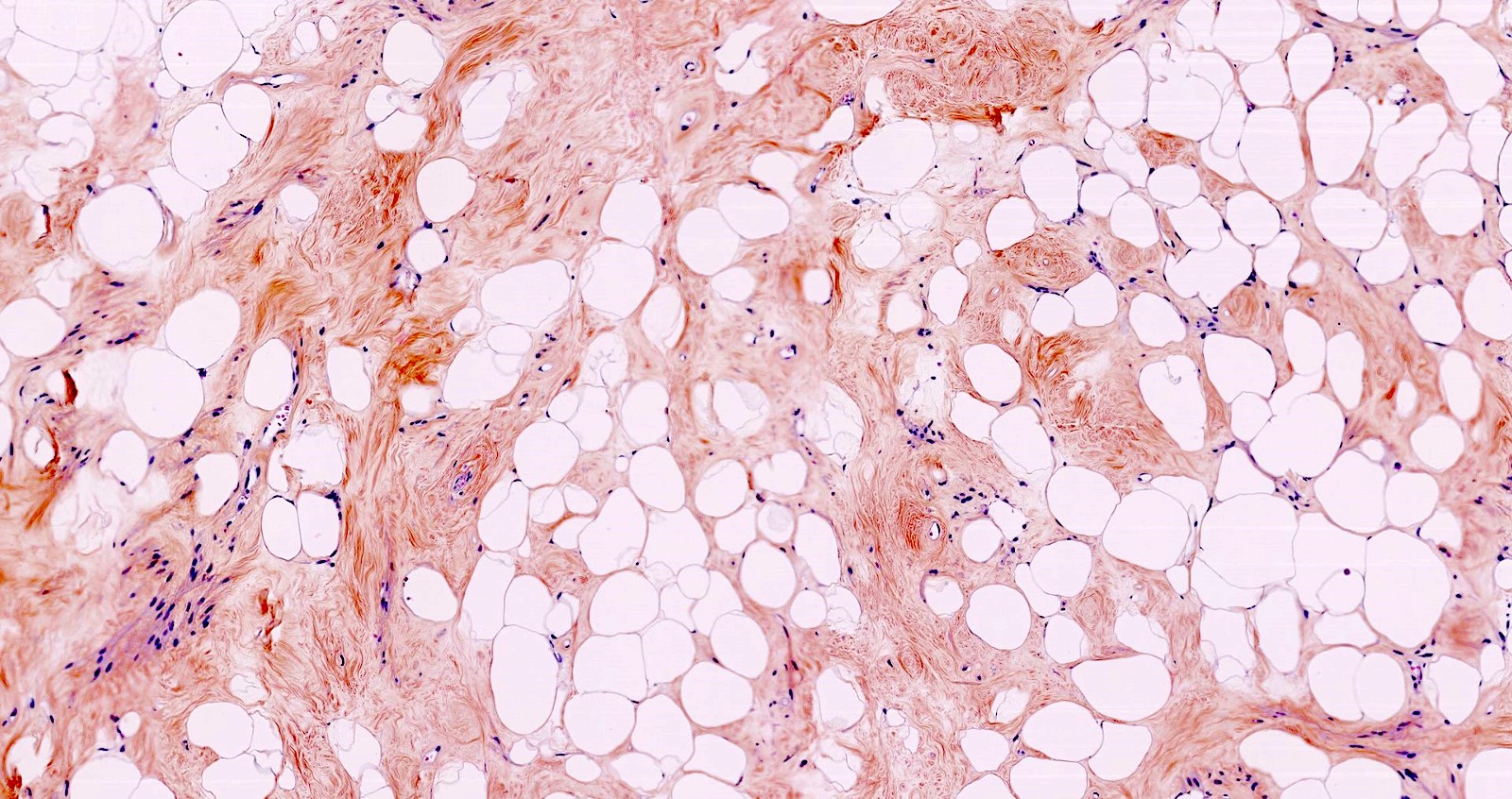
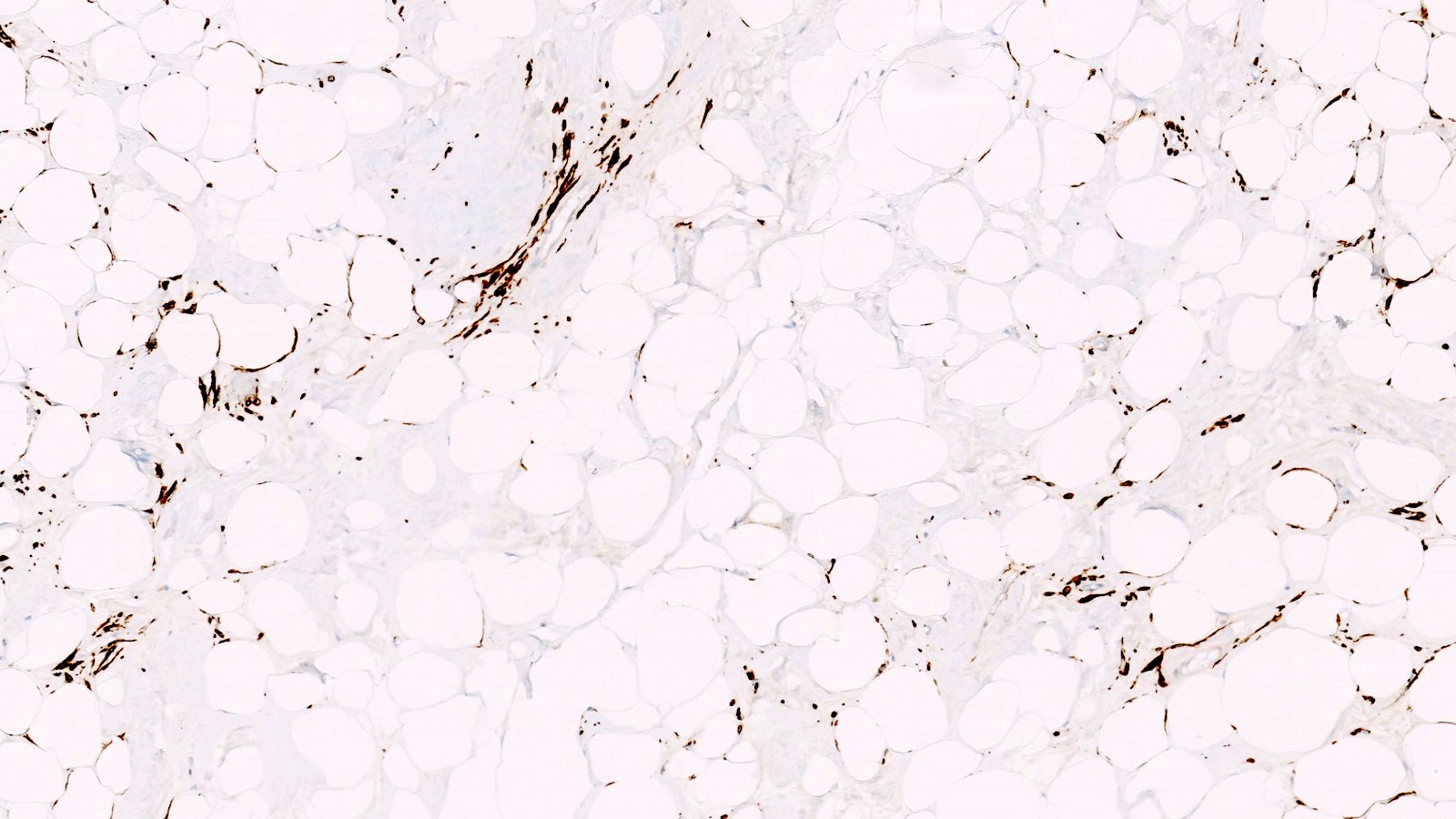
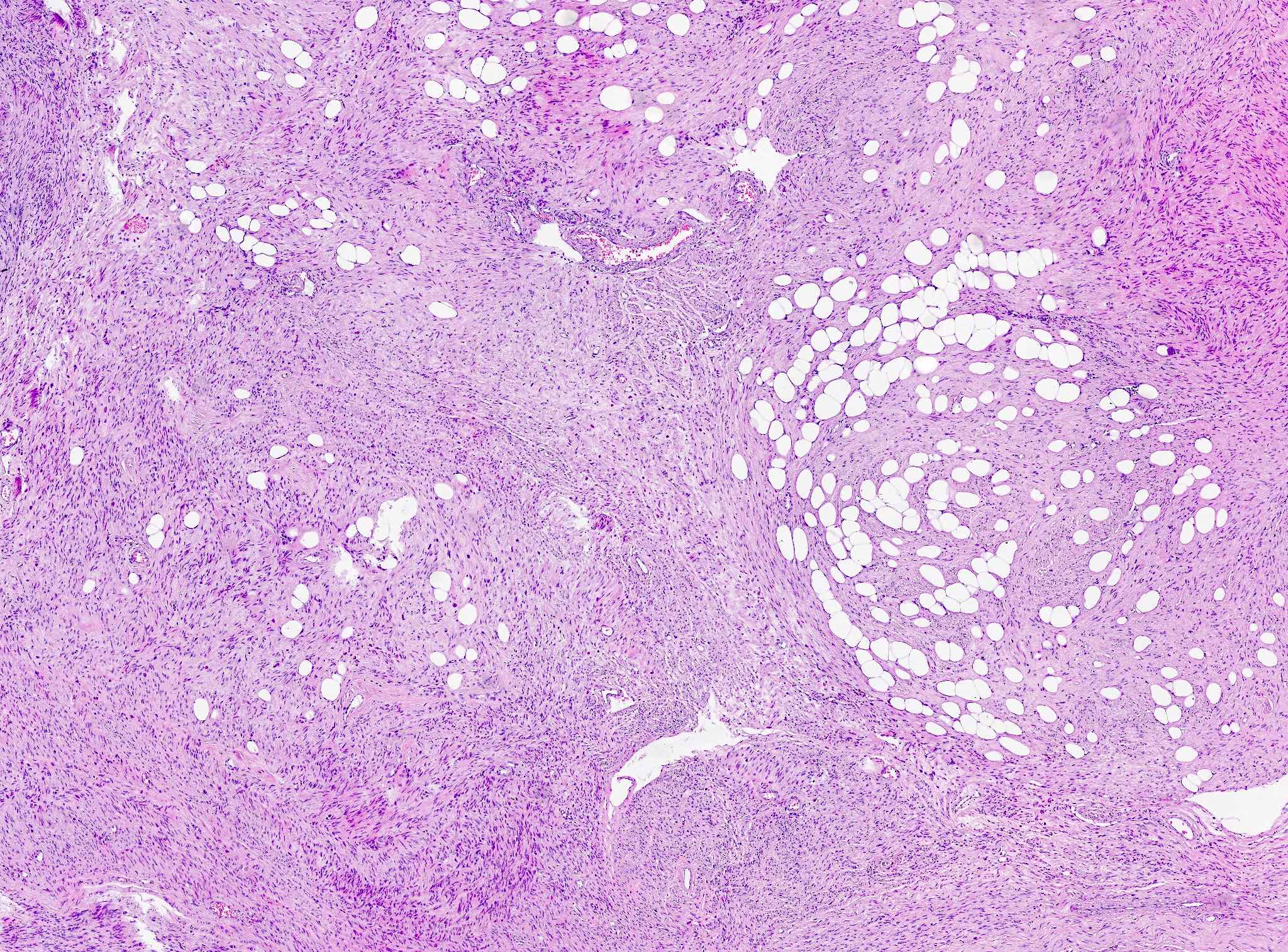
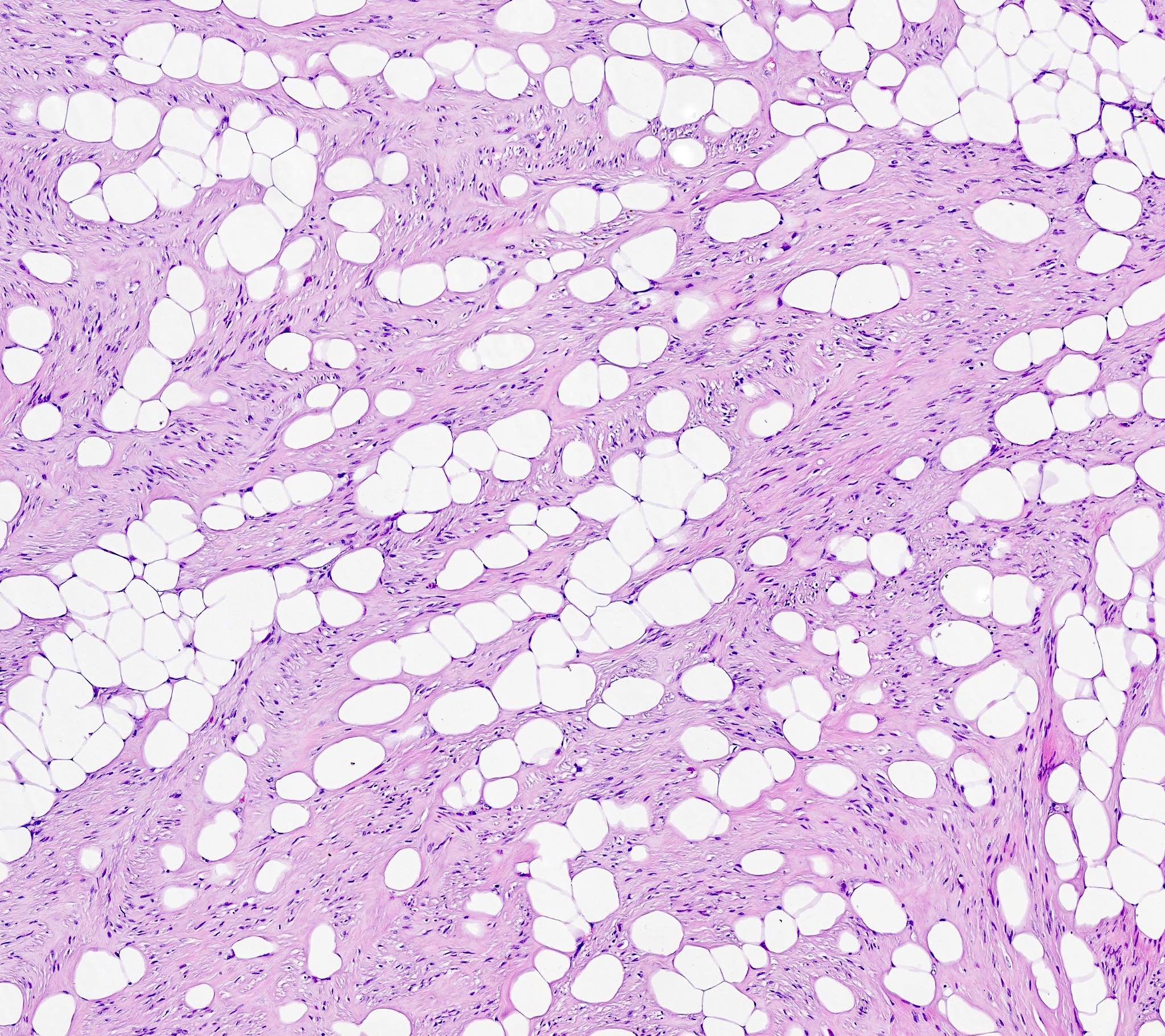
- Lipoleiomyoma:
- Tumor composed of smooth muscle cells mixed with mature adipocytes (variable quantity)
- Epithelioid:
- Round or polygonal cells with eosinophilic or clear cytoplasm (in general, ≥ 50% of tumor cells)
- Nested or trabecular architecture
- No cytologic atypia or tumor cell necrosis
- Mitotic count is < 2 mitoses/10 high power fields
- Myxoid:
- Hypocellular tumor
- Cells separated by myxoid matrix composed of glycosaminoglycans (Alcian blue+) occupying ≥ 50% of the overall tumor volume
- Well circumscribed borders (most important criteria)
- No cytologic atypia, mitoses or tumor cell necrosis
- Dissecting leiomyoma:
- Nodules of smooth muscle cells dissecting the myometrium; occasionally hydropic changes and intravenous extension can be seen
- Called cotyledonoid leiomyoma if extends outside the uterus
- Diffuse leiomyomatosis:
- Diffuse, poorly circumscribed, innumerable tumor nodules in the myometrium
- No atypia and tumor cell necrosis
- Low mitotic count
- Cellular
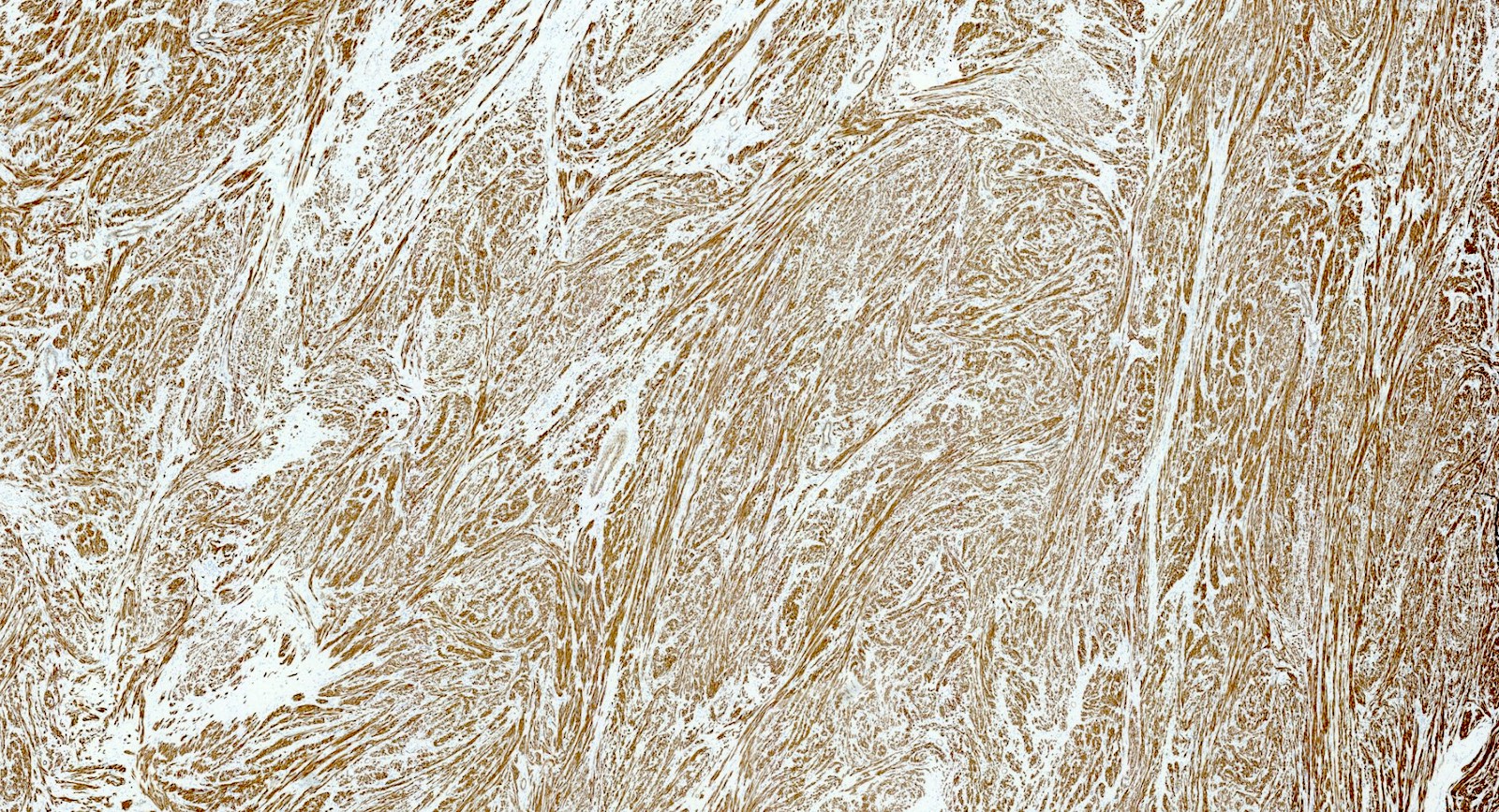
Microscopic (histologic) images
Contributed by Sabrina Croce, M.D., Ph.D., Kristina Doytcheva, M.D., Jennifer A. Bennett, M.D. (Case #508) and @Andrew_Fltv on Twitter
Virtual slides
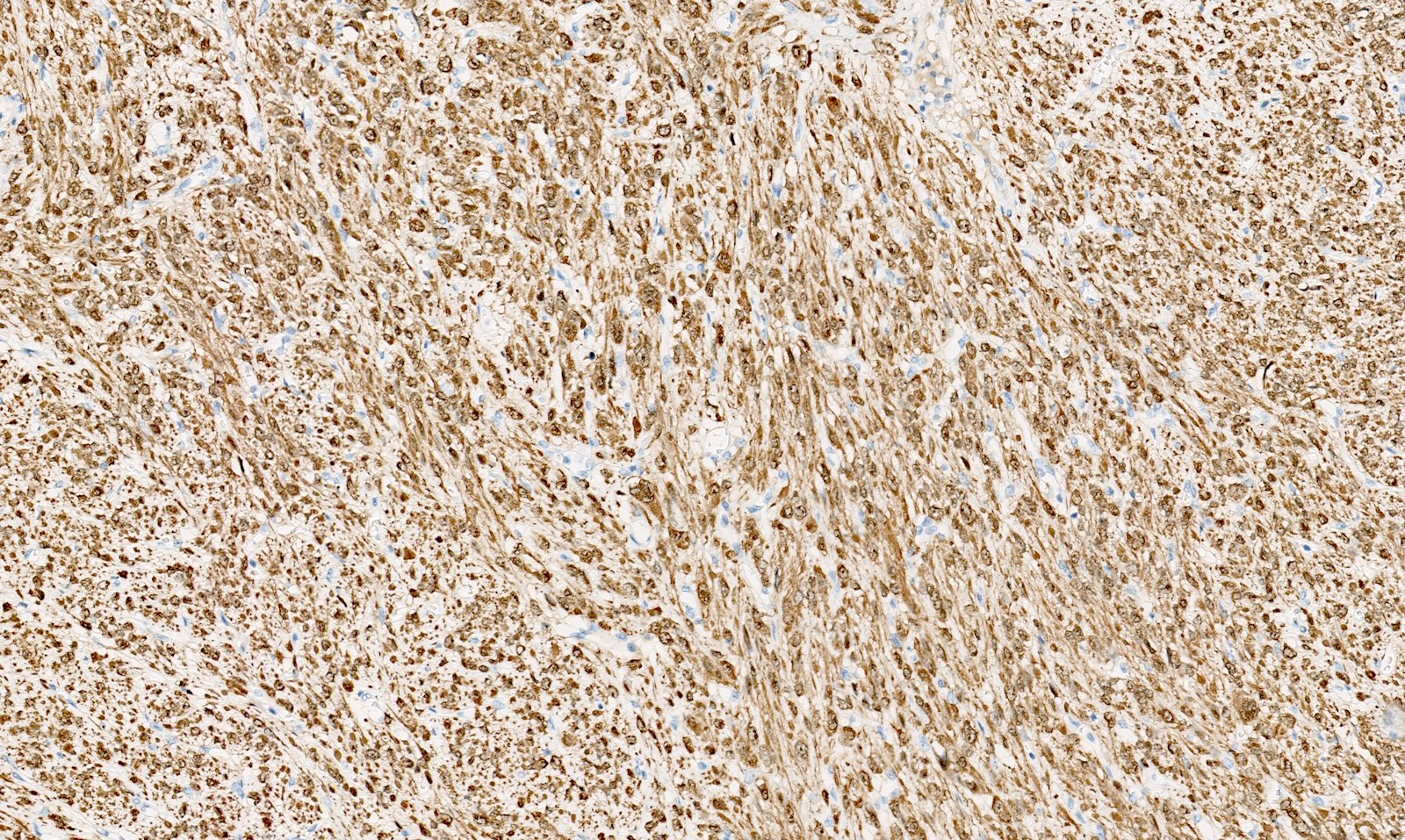
Positive stains
- Desmin
- h-caldesmon
- Smooth muscle actin
- Transgelin
- Smooth muscle markers can be weak in epithelioid and myxoid leiomyomas
- Estrogen and progesterone receptors
- WT1
- Up to 40% of leiomyomas are CD10 positive (especially cellular leiomyomas) (Am J Surg Pathol 2002;26:403)
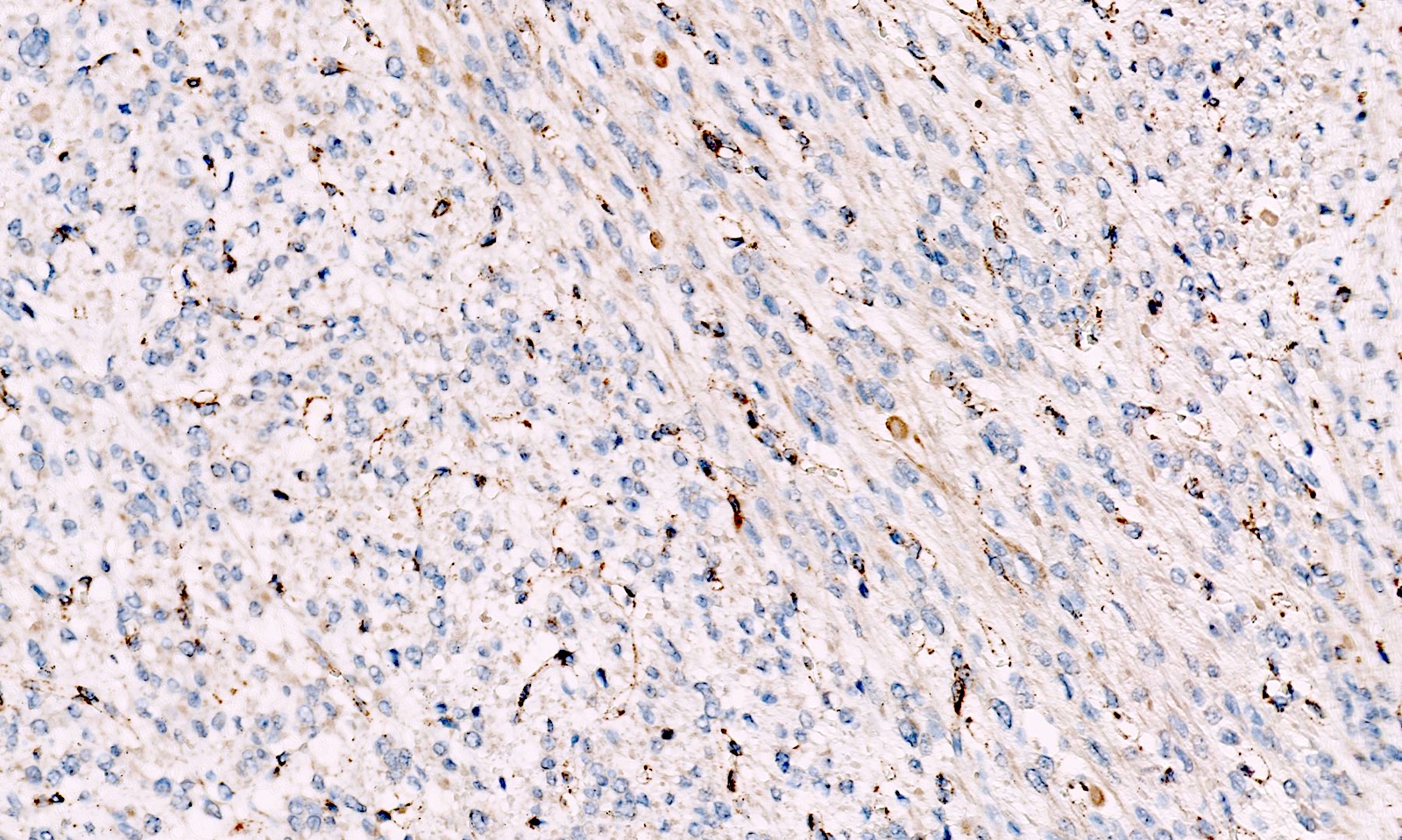
- FH loss of expression and 2SC positivity may be useful to identify fumarate hydratase deficient leiomyoma (Am J Surg Pathol 2016;40:599, Mod Pathol 2014;27:1020)
- FH loss of expression is specific of FH deficient leiomyoma but its sensitivity is low with different results across different leiomyomas of the same patient; for these reasons, the clinical value of FH staining is limited (Am J Surg Pathol 2015;39:1529, Am J Surg Pathol 2019;43:1170, Genes Chromosomes Cancer 2021;60:210)
- 2SC nuclear staining has been reported in FH deficient leiomyomas but is not widely commercially available and experience is limited (Am J Surg Pathol 2014;38:627, Am J Surg Pathol 2015;39:1529, Mod Pathol 2014;27:1020, Genes Chromosomes Cancer 2020 Oct 24 [Epub ahead of print])
Negative stains
Molecular / cytogenetics description
- About 70% of conventional leiomyomas harbor MED12 mutations and nearly 40% HMGA2 / HMGA1 rearrangements, COL4A5 / COL4A6 deletions or FH mutations (Fertil Steril 2014;102:621, Mol Cancer 2017;16:101)
- Other less frequent alterations include 7q22 deletion involving CUX1 gene, 22q deletion with DEPDC5 gene and 1p deletion with NPHP4 gene (Genes Chromosomes Cancer 2013;52:11, Proc Natl Acad Sci U S A 2016;113:1315, N Engl J Med 2013;369:43, Am J Obstet Gynecol 2014;210:572.e1, Cancer Genet Cytogenet 2009;193:54)
- In leiomyomas with bizarre nuclei, the genomic profiles and genomic index can be more complex compared with that of classic leiomyoma (Mod Pathol 2016;29:1262):
- At a molecular level, leiomyomas with bizarre nuclei are separated in 2 subtypes: FH abnormal and TP53 and RB1 abnormal (Mod Pathol 2017;30:1476, Mol Cancer 2017;16:101)
- Bi-allelic inactivation of FH has been described in up to 33% of leiomyomas with bizarre nuclei (Mol Cancer 2017;16:101)
- For FH deficient leiomyomas, the FH mutation may be somatic or germline (Am J Surg Pathol 2016;40:1661, Mod Pathol 2014;27:1020, Am J Surg Pathol 2019;43:639, Genes Chromosomes Cancer 2021;60:210)
- TPCN2-YAP1 fusion (Genes Chromosomes Cancer 2020 Jul 17 [Epub ahead of print])
Sample pathology report
- Uterus, total hysterectomy:
- Conventional leiomyoma: 5.0 cm (see comment)
- Comment: Microscopic examination reveals a smooth muscle tumor composed of spindle, cigar shaped cells arranged in fascicular pattern without cytologic atypia and tumor cell necrosis. Mitoses are rare (4 mitoses/10 high power fields). Tumor borders are well circumscribed. By immunohistochemistry the tumor cells are positive for desmin, h-caldesmon, ER and PR.
Differential diagnosis
- Smooth muscle tumor of uncertain malignant potential (STUMP):
- Uterine spindle cell STUMP:
- Only 1 morphologic criteria of malignancy (Table 2)
- Myxoid STUMP:
- Mitoses: 1/10 high power fields in the absence of cytologic atypia and tumor cell necrosis (Table 3)
- Epithelioid STUMP:
- Mitoses: ≥ 2/10 high power fields) and < 4/10 high power fields in the absence of cytologic atypia and tumor cell necrosis (Table 4)
- Uterine spindle cell STUMP:
- Leiomyosarcoma:
- Uterine spindle cell leiomyosarcoma (Table 2):
- 2 or more morphologic criteria of malignancy:
- Cytologic atypia
- Tumor cell necrosis
- Mitoses: ≥ 10/10 high power fields
- 2 or more morphologic criteria of malignancy:
- Myxoid leiomyosarcoma (Table 3):
- 1 or more morphologic criteria of malignancy:
- Mitoses: ≥ 2/10 high power fields
- Cytologic atypia
- Tumor cell necrosis
- 1 or more morphologic criteria of malignancy:
- Epithelioid leiomyosarcoma (Table 4):
- 1 or more morphologic criteria of malignancy:
- Mitoses: ≥ 4/10 high power fields
- Tumor cell necrosis
- Cytologic atypia
- 1 or more morphologic criteria of malignancy:
- Uterine spindle cell leiomyosarcoma (Table 2):
- Endometrial stromal nodule (Mod Pathol 2016;29:S104):
- Endometrial stromal nodule versus highly cellular leiomyoma:
- Diffuse arteriolar vascularization
- Absence of thick vessels at the center of the lesion
- Absence of fascicular growth
- Immunohistochemistry:
- Weak to absent smooth muscle marker staining
- CD10 (not specific): can help if diffuse and strong in absence of smooth muscle markers
- JAZF1, PHF1, EPC1, MEAF6, MBTD1 or EZHIP fusions (Genes Chromosomes Cancer 2021;60:160)
- Endometrial stromal nodule with smooth muscle metaplasia:
- Smooth muscle metaplasia in endometrial stromal nodule can be present but is typically a minor component of the tumor
- Endometrial stromal nodule versus highly cellular leiomyoma:
- PEComa versus epithelioid leiomyoma (Genes Chromosomes Cancer 2020 Oct 24 [Epub ahead of print], Am J Surg Pathol 2018;42:1370):
- Thin and delicate vasculature
- Nested and trabecular architecture
- Clear to eosinophilic granular cytoplasm with round nuclei
- Immunohistochemistry: at least 2 melanocytic markers expressed, preferably HMB45 and MelanA (or cathepsin K, PNL2)
- Molecular:
- TSC1 or TSC2 alterations (Am J Surg Pathol 2015;39:813, Oncology 2020;98:905, Genes Chromosomes Cancer 2021;60:168)
- TFE3 fusions (Am J Surg Pathol 2015;39:394, Am J Surg Pathol 2012;36:783, Genes Chromosomes Cancer 2021;60:168)
- Inflammatory myofibroblastic tumor versus myxoid leiomyoma (Int J Gynecol Pathol 2021;40:28, Am J Surg Pathol 2020;44:1441, Mod Pathol 2017;30:1489):
- Presence of lymphoplasmacytic inflammation
- Spindle, myofibroblastic cells embedded in myxoid stroma
- Tissue culture-like pattern
- Immunohistochemistry:
- ALK positive
- Smooth muscle markers not useful: positive in both
- ALK rearrangements / fusions
Additional references
Board review style question #1
A 23 year old woman with multiple recurrent leiomyomas is diagnosed with a FH deficient leiomyoma. Which of the following is true?
- FH deficiency is a risk factor for uterine leiomyosarcoma
- Staghorn vessels, alveolar oedema, macronuclei with perinucleolar halos and cytoplasmic eosinophilic globules are typical morphologic features of FH deficient leiomyoma
- Bizarre nuclei and FH deficient leiomyoma are mutually exclusive
- All FH deficient leiomyomas are 2SC positive and FH negative
- All FH deficient leiomyomas are associated with a germline mutation
Board review style answer #1
B. Staghorn vessels, alveolar oedema, macronuclei with perinucleolar halos and cytoplasmic eosinophilic globules are typical morphologic features of FH deficient leiomyoma
Comment Here
Reference: Leiomyoma-general
Comment Here
Reference: Leiomyoma-general
Board review style question #2
A 44 year old woman presents with 4 cm leiomyoma with bizarre nuclei. Which of the following is true?
- The presence of atypia alone is a sufficient criterion warrant the diagnosis of leiomyosarcoma
- Significant number of leiomyomas with bizarre nuclei harbor FH biallelic inactivation
- Leiomyomas with bizarre nuclei are malignant
- p16 staining is a reliable marker of leiomyomas with bizarre nuclei
- Arteriolarization of vessels is a typical feature of bizarre nuclei leiomyoma
Board review style answer #2
B. Significant number of leiomyomas with bizarre nuclei harbor FH biallelic inactivation
Comment Here
Reference: Leiomyoma-general
Comment Here
Reference: Leiomyoma-general