Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Han L, Garcia R, Busca A, Parra-Herran C. Endometriosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarynontumorendometriosis.html. Accessed December 27th, 2024.
Definition / general
- Presence of endometrial tissue outside of endometrium and myometrium, consisting of both endometrial glands and stroma
Essential features
- Ectopically located endometrial tissue consisting of at least 2 of the following: endometrial type glands, endometrial type stroma or evidence of chronic hemorrhage
- Endometriosis is associated with ovarian clear cell carcinoma and endometrioid carcinoma and shares similar molecular alterations
- Endometriosis in patients without cancer harbors oncogenic mutations in ARID1A, PIK3CA, KRAS and PPP2R1A, suggesting a neoplastic nature in some cases (N Engl J Med 2017;376:1835)
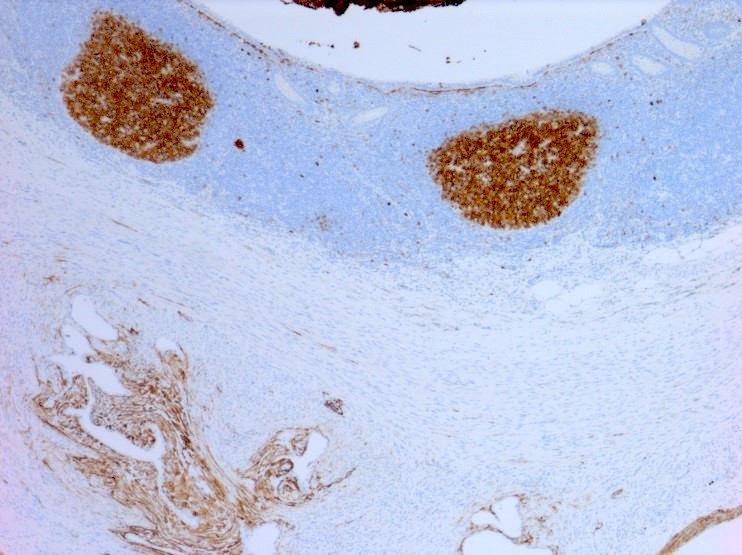
- CD10 immunohistochemistry can be used to confirm the presence of endometrial stroma
Terminology
- Endometriotic cyst / endometrioma: cystic form of endometriosis
- Atypical endometriosis: endometriosis with cytologic atypia or crowded glands lined by atypical epithelium resembling endometrial atypical hyperplasia (Adv Anat Pathol 2007;14:241)
ICD coding
- ICD-10: N80 - endometriosis of uterus
- N80.0 - endometriosis of uterus
- N80.1 - endometriosis of ovary
- N80.2 - endometriosis of fallopian tube
- N80.3 - endometriosis of pelvic peritoneum
- N80.4 - endometriosis of rectovaginal septum and vagina
- N80.5 - endometriosis of intestine
- N80.6 - endometriosis in cutaneous scar
- N80.8 - other endometriosis
- N80.9 - endometriosis, unspecified
Epidemiology
- Affects 5 - 15% women of reproductive age
- Peak incidence: 30 - 45 years of age
- Estrogen dependent; can rarely affect individuals assigned male at birth taking large doses of estrogen (Fertil Steril 2012;98:511)
Sites
- Ovary (67%) > anterior and posterior cul de sac > posterior broad ligaments, uterosacral ligaments > uterus > fallopian tubes > sigmoid colon and appendix > round ligaments (Eur J Obstet Gynecol Reprod Biol 2018;230:36)
- Also seen in bladder and cervix
- Rarely in remote sites such as lung, regional lymph nodes or skin
Pathophysiology
- Retrograde menstruation hypothesis: endometrial lining cells travel backwards through fallopian tubes during menses to reach peritoneal cavity, proliferate and cause chronic inflammation with formation of adhesions (Nat Rev Endocrinol 2014;10:261)
- Coelomic metaplasia hypothesis: metaplastic transformation of coelomic cells lining the pelvic peritoneum (J Lab Physicians 2010;2:1)
- Induction hypothesis: a combination of the first 2 theories (N Engl J Med 1993;328:1759)
- Development of malignant neoplasm occurs in < 1% of cases; 75% of malignant neoplasms arise in ovarian endometriosis (J Lab Physicians 2010;2:1)
Etiology
- Organochlorine pollutant exposure (Environ Int 2017;108:195)
Clinical features
- Pelvic pain (Arch Gynecol Obstet 2015;292:1295)
- Dyspareunia
- Dysmenorrhea
- Infertility
- Rarely, infection or rupture of an endometriotic cyst with ascites or hemoperitoneum
Diagnosis
- Laparoscopy required for definitive diagnosis, although ~50% laparoscopic biopsy specimens contain microscopic endometriosis (Am J Obstet Gynecol 2001;184:1407)
- Endometriosis in pelvis categorized as superficial peritoneal, ovarian and deeply infiltrating
Radiology description
- Ultrasound is mostly used for ovarian endometriotic cysts
- Typically multilocular cysts with septations and hyperechoic mural nodules (Radiology 1999;210:739)
Prognostic factors
- Risk of development of malignant neoplasm is estimated at 1% for premenopausal women and up to 2.5% for postmenopausal women
- ~75% neoplasms complicating endometriosis arise within the ovary; most common extraovarian site is rectovaginal septum
- Increased risk of endometrioid carcinoma followed by clear cell carcinoma (Clin Chim Acta 2019;493:63)
- Other associated neoplasms include seromucinous neoplasms (mainly borderline), endometrioid adenofibromas and borderline neoplasms, adenosarcomas and endometrial stromal sarcomas (Histopathology 2020;76:76)
- Women with carcinoma arising in endometriosis tend to be premenopausal, obese and with history of unopposed estrogens (Gynecol Oncol 2000;79:18)
- Endometriosis associated carcinomas (other than clear cell) tend to be lower grade and stage than similar ovarian carcinoma without associated endometriosis (Gynecol Oncol 2001;83:100)
Case reports
- 32 year old woman with ruptured endometrioma (J Med Case Rep 2022;16:161)
- 35 year old woman presenting with hematuria and abdominal pain (BMJ Case Rep 2018;11:e226927)
- 37 year old woman with history of pelvic surgery presenting with pelvic pain (Medicine (Baltimore) 2018;97:e0376)
- 37 year old woman with decidualized ovarian endometrioma in pregnancy (J Ovarian Res 2022;15:33)
- 40 year old woman with elevated CA125 and pelvic mass (Medicine (Baltimore) 2019;98:e15741)
- 42 year old woman with supernumerary ovary on rectosigmoid colon with associated endometriosis (Obstet Gynecol Sci 2018;61:702)
- 49 year old Japanese woman with abnormal vaginal bleeding and adenocarcinoma diagnosed by cervical cytology (J Obstet Gynaecol Res 2020;46:536)
- 55 year old woman with peritoneal endometriosis and smooth muscle metaplasia (Int J Clin Exp Pathol 2015;8:3370)
- 62 year old woman presenting with hematuria (Pathology 2017;49:441)
Treatment
- Pain treated with NSAIDs, hormonal contraceptives, GnRH analogues and aromatase inhibitors (Arch Gynecol Obstet 2015;292:1295)
- Surgical resection
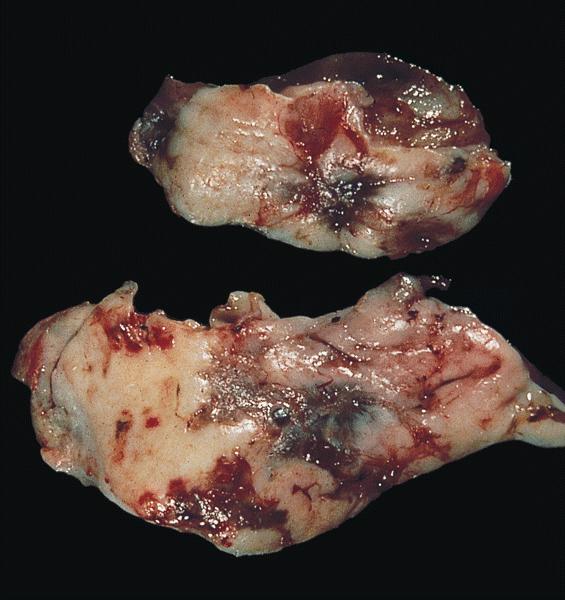
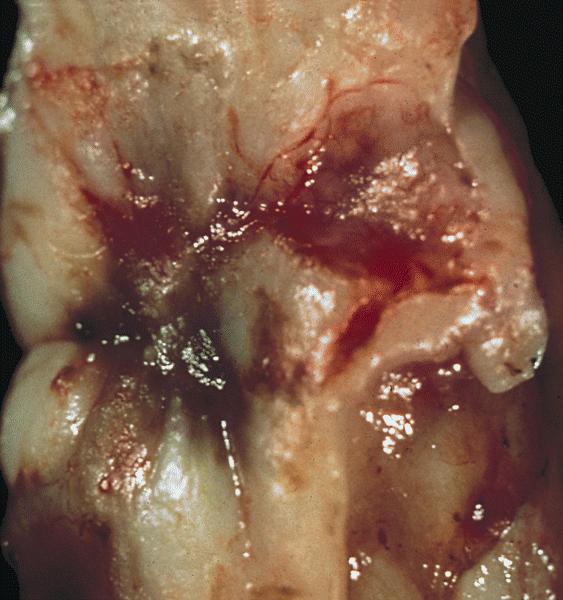
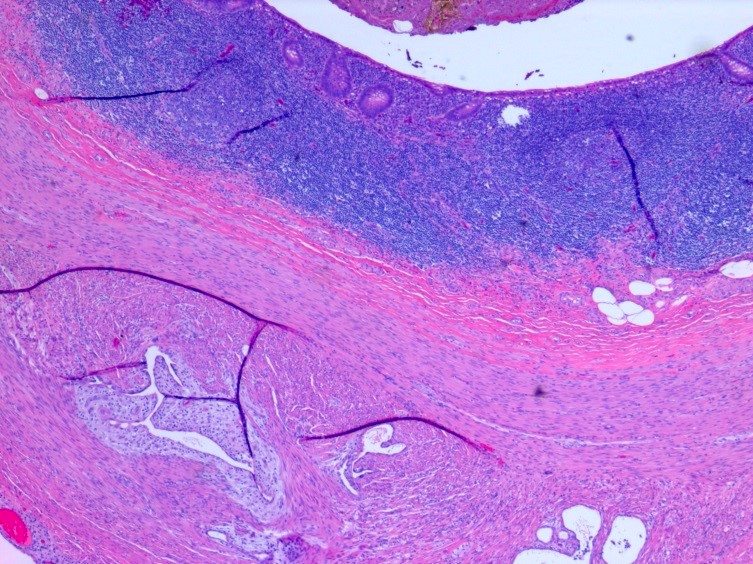
Gross description
- Ovarian endometriotic cysts (endometriomas) have fibrotic walls, a smooth lining and dark brown cyst contents (chocolate cyst), often adherent to adjacent organs
- Polypoid endometriosis has a polypoid configuration that raises the differential diagnosis of a neoplasm on gross and intraoperative examination (Am J Surg Pathol 2004;28:285)
- Red, brown, white plaques, sometimes with a gelatinous appearance (Arch Gynecol Obstet 2015;292:1295, Taiwan J Obstet Gynecol 2019;58:328)
Gross images
Frozen section description
- Presence of endometrial glands or endometrial stroma (Taiwan J Obstet Gynecol 2019;58:328)
- Sometimes only macrophages and hemosiderin are present (diagnose as consistent with clinical impression of endometriosis, as other causes are possible)
- Can be associated with fibrous adhesions
- Negative for neoplastic features such as glandular complexity
Frozen section images
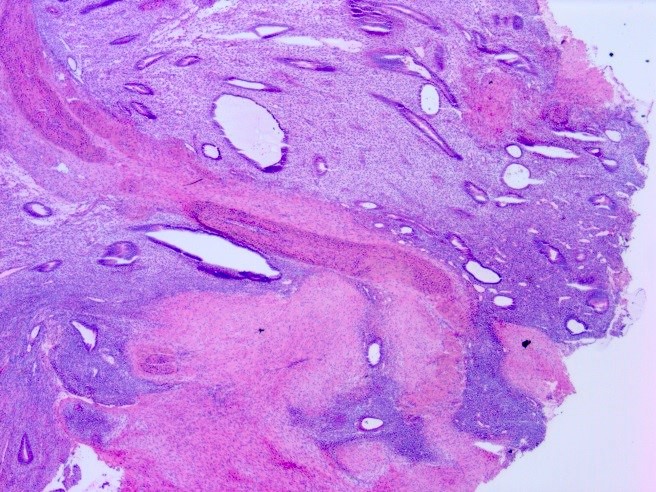
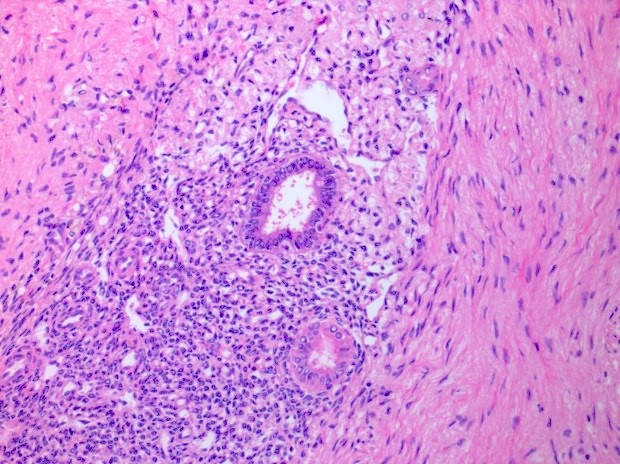
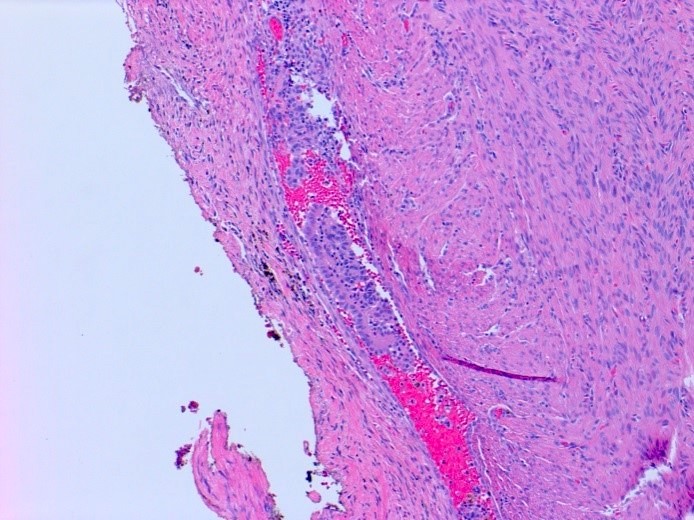
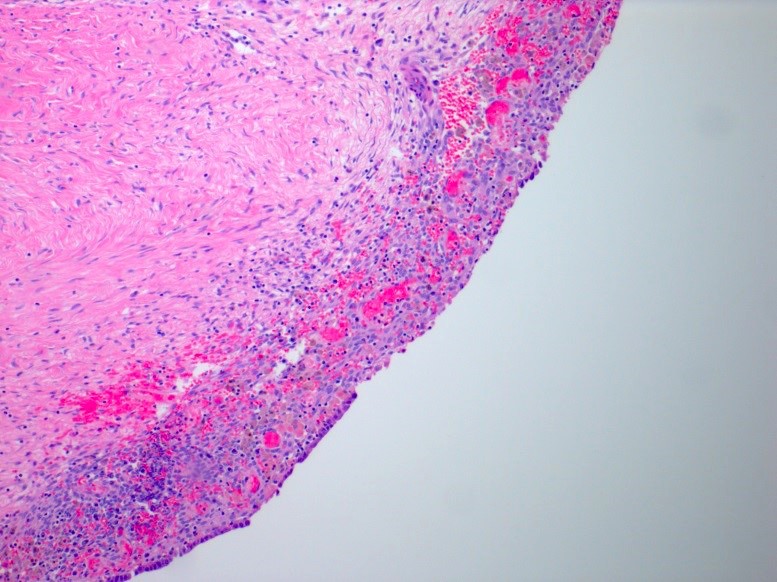
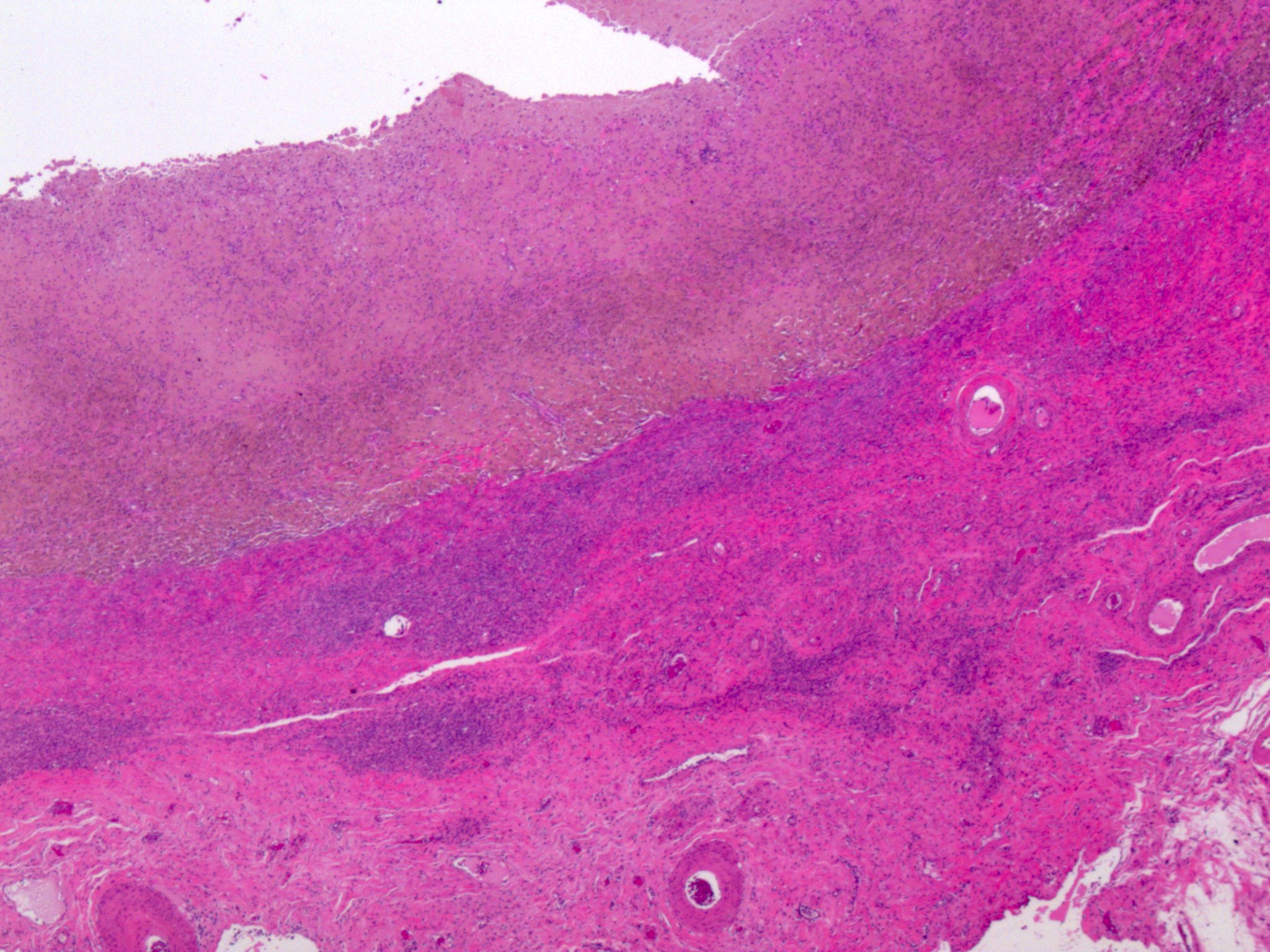
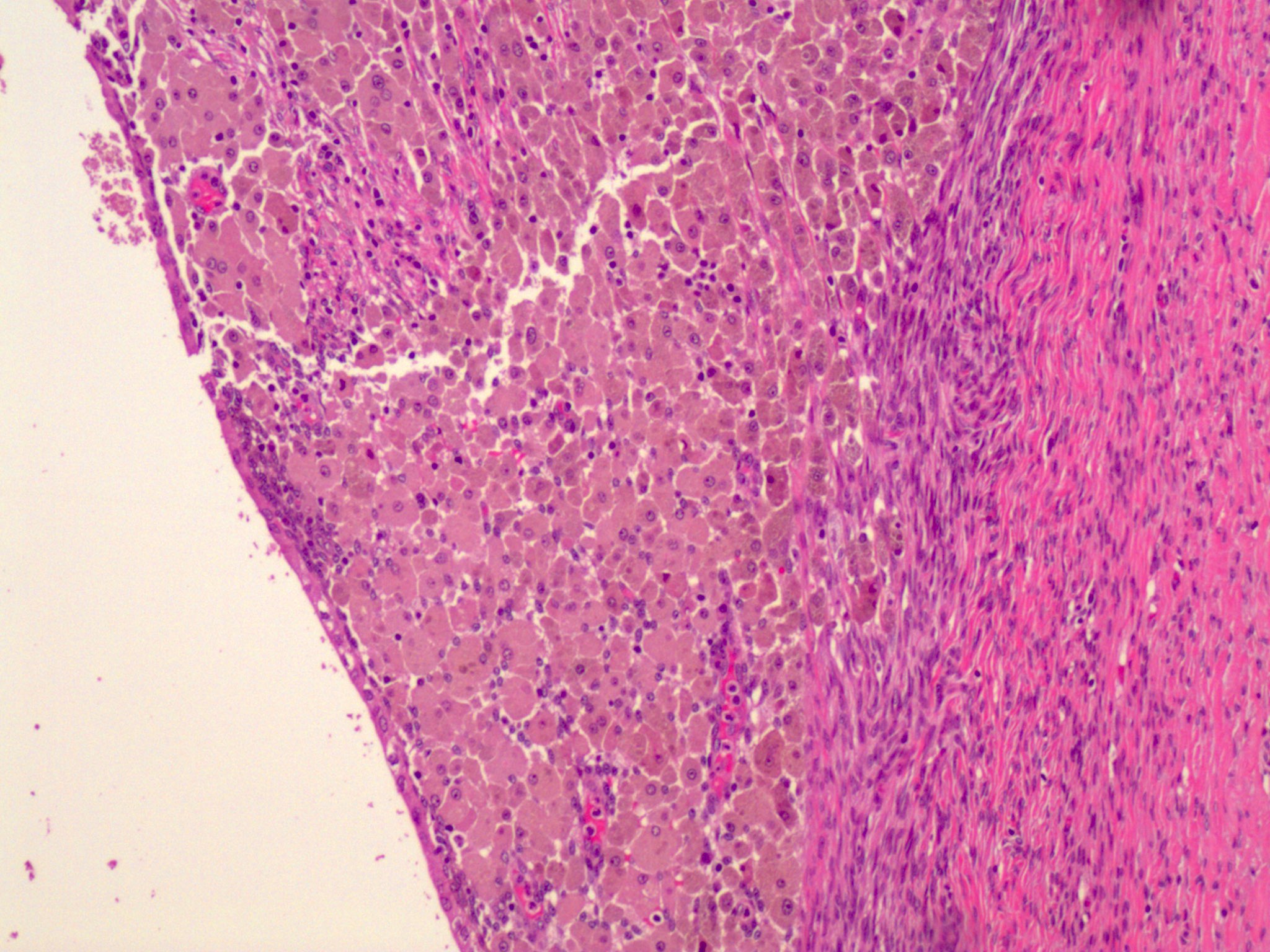
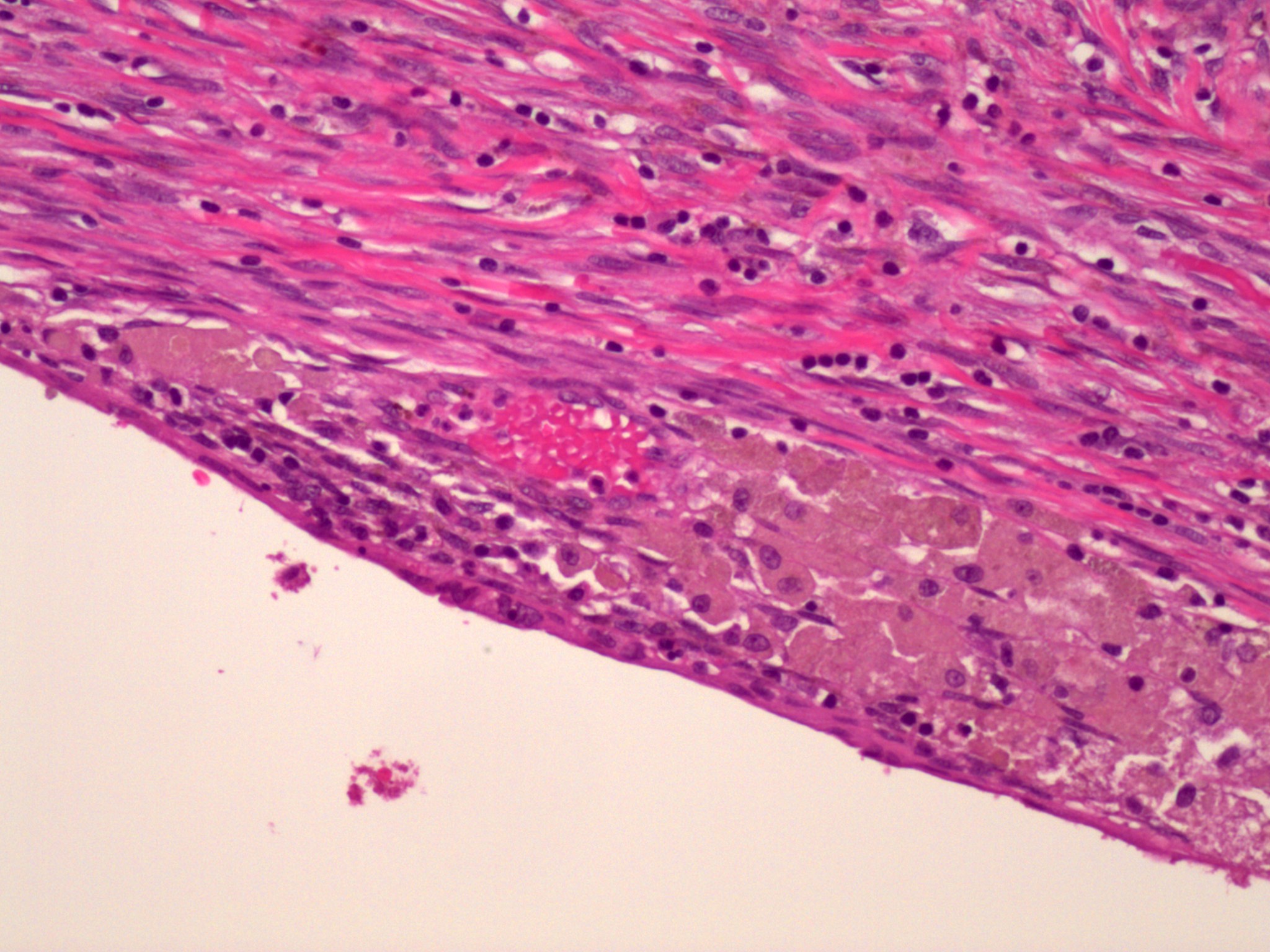
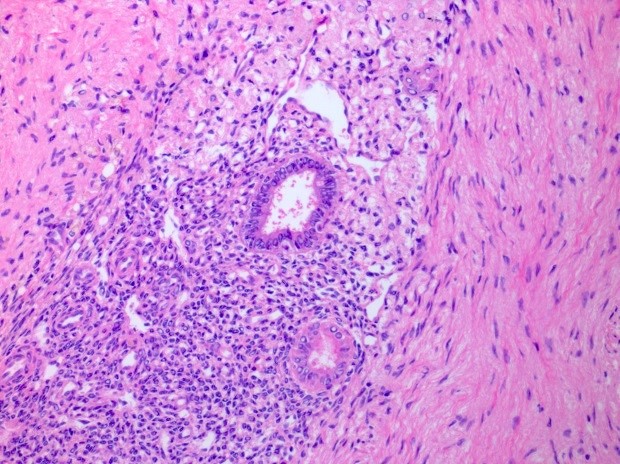
Microscopic (histologic) description
- At least 2 of the following 3 features
- Endometrial type glands
- Müllerian type epithelium (can be atrophic to cycling endometrium)
- Can show degenerative atypia (enlarged smudgy nuclei) or metaplasia
- Endometrial type stroma
- Often contains fine capillary network
- May undergo smooth muscle metaplasia, fibrosis (longstanding), decidual change
- May be myxoid (particularly in pregnancy)
- Stroma may be the only identifiable component (stromal endometriosis)
- Evidence of chronic hemorrhage (hemosiderin laden or foamy macrophages)
- Endometrial type glands
- Other rare findings
- Necrotic pseudoxanthomatous nodules: central necrosis surrounded by histiocytes and outer fibrous zone
- Liesegang rings: eosinophilic acellular rings within necrotic tissue (Histopathology 2020;76:76)
- Burnt out endometriosis: this term has been proposed for changes suggestive of endometriosis, such as central necrosis with surrounding fibrosis and pseudoxanthoma cells but lacking confirmatory features as listed above
- Atypical endometriosis: this has been reported in 1.7 - 4.4% of endometriotic lesions and is considered the precursor lesion for endometriosis associated carcinomas (clear cell or endometrioid); may be in continuity with these tumors
- Includes crowded glands lined by atypical epithelium resembling endometrial atypical hyperplasia; nuclear atypia is typically moderate or severe, with hobnailing (Histopathology 1997;30:249, Case Rep Oncol 2013;6:480, Int J Gynecol Pathol 2023 Mar 13 [Epub ahead of print])
- Is associated with synchronous / subsequent neoplasia in 25% of cases and harbors genomic alterations seen in endometriosis associated tumors (Int J Gynecol Pathol 2023 Mar 13 [Epub ahead of print])
Microscopic (histologic) images
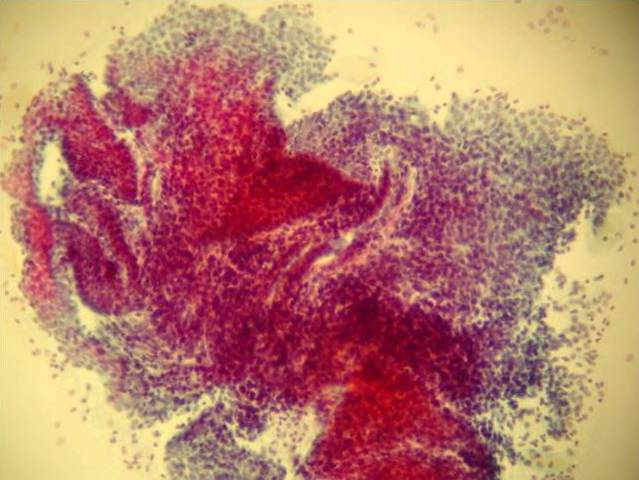
Cytology description
- Reported in peritoneal fluid and fine needle aspiration of scar tissue following gynecologic procedure (e.g., Caesarean section) (J Cytol 2017;34:61)
- Variably sized, 3 dimensional spherules with periphery of polygonal endometrial cells with larger, hyperchromatic nuclei and moderate amount of cytoplasm, often with a center of stromal cells with hyperchromatic nuclei, scant cytoplasm and indistinct cytoplasmic borders (Cancer Cytopathol 2013;121:582)
- May have admixed hemosiderin laden macrophages
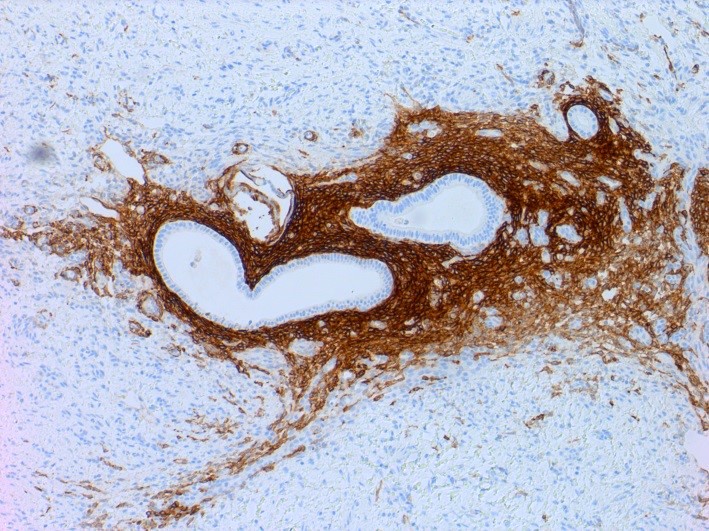
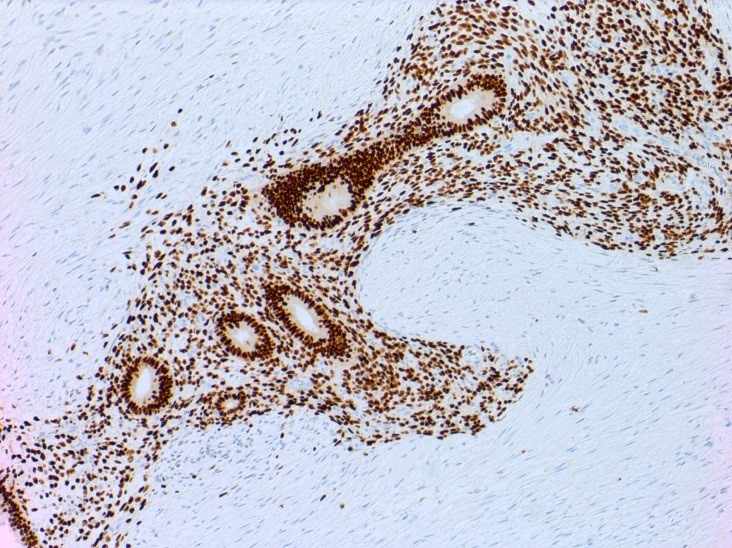
Positive stains
- CD10 is positive in endometrial stroma
- ER, PR and PAX2 are often positive in endometrial glands and stroma (Am J Surg Pathol 2013;37:1342)
Molecular / cytogenetics description
- Endometriosis and synchronous carcinoma share similar genetic alterations including ARID1A, PTEN and PIK3CA
- Mutations in ARID1A, a tumor suppressor gene, identified in up to 57% of ovarian endometrioid carcinoma and up to 30% of clear cell carcinoma
- Multiple studies suggest ARID1A mutation occurs at early stage of canceration of endometriosis (Oncol Rep 2016;35:607)
- Endometriosis occurring distant from ARID1A deficient carcinomas are more likely to retain ARID1A expression
- Other associated genetic alterations include loss of BAF250a, ER and PR and upregulation of hepatocyte nuclear factor - beta and SKP2
- In one study, loss of DNA mismatch repair protein expression was found in 10% of patients with endometriosis associated ovarian carcinoma (Int J Gynecol Pathol 2012;31:524)
Videos
Causes, symptoms, diagnosis, treatment, pathology
Histopathology - ovary
Sample pathology report
- Uterus, hysterectomy:
- Proliferative endometrium negative for hyperplasia or malignancy
- Unremarkable cervix
- Myometrium with leiomyomata
- Uterine serosa with multifocal endometriosis
- Right ureterosacral peritoneum, excision:
- Fibrous tissue with focal endometrial type stroma and hemorrhage, suggestive of endometriosis
Differential diagnosis
- Endocervicosis:
- Glandular component is endocervical mucinous type, no endometrial stroma, no hemorrhage
- Endosalpingiosis:
- Glandular component is tubal (ciliated with peg / intercalated) cells, no endometrial stroma, no hemorrhage
- Adenomyosis:
- Endometrial glands and stroma in myometrium
- Endometrioid adenocarcinoma:
- Complex glandular growth and cytologic atypia
- Metastatic carcinoma:
- Morphology varies by site of origin; however, no endometrial stroma
- Other features of neoplasm present, including crowded irregular glands, nuclear atypia or elevated mitotic activity
Additional references
Board review style question #1
A 39 year old woman presents with pelvic pain and menorrhagia. Hysterectomy was performed and the histologic findings shown in this photomicrograph were present on the serosal surface and right ovary. What malignant neoplasm is most associated with the lesion?
- Clear cell sarcoma
- Endometrial stromal sarcoma
- High grade serous carcinoma
- Immature teratoma
- Ovarian endometrioid carcinoma
Board review style answer #1
E. Ovarian endometrioid carcinoma. Endometriosis can be associated with endometrioid and clear cell carcinoma, with the greatest association identified in the former neoplasm. Rare endometrial stromal sarcomas and adenosarcomas have also been reported to arise in association with endometriosis. Answer D is incorrect because there is no reported association between germ cell tumors and endometriosis. Answer C is incorrect because there is no reported association between high grade serous carcinoma and endometriosis. Answer A is incorrect because there is no reported association between clear cell sarcoma and endometriosis. Answer B is incorrect because even though some cases of adenosarcomas have been reported to arise in association with endometriosis, the association is less frequent than endometrioid carcinoma.
Comment Here
Reference: Endometriosis
Comment Here
Reference: Endometriosis
Board review style question #2
Which of the following genes is most commonly altered in endometriosis associated carcinomas?
- ARID1A
- BRAF
- CDKN2A (p16)
- PTEN
- TP53
Board review style answer #2
A. ARID1A. Of the 5 genes listed, mutations in tumor suppressor gene ARID1A are most commonly identified in endometriosis and endometriosis associated carcinomas. Many studies suggest that loss of ARID1A expression is an early driver mutation. Other common molecular alterations include mutations in PTEN, PIK3CA, KRAS and to a lesser extent, microsatellite instability with MMR protein loss. Answer D is incorrect because PTEN mutations are less frequent. Answers E and C are incorrect because TP53 and CDKN2A mutations are rare. Answer B is incorrect because BRAF mutations are not associated with endometriosis.
Comment Here
Reference: Endometriosis
Comment Here
Reference: Endometriosis