Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Symptoms | Screening | Blood donor screening | Blood donor testing | Donor deferral | Laboratory | Case reports | Sample assessment and plan | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Goel A, Gupta R. Antibody identification & panel interpretation . PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/transmedantibody.html. Accessed April 1st, 2025.
Definition / general
- Identification of antibodies formed as a result of immune response against red blood cell (RBC) antigen(s) that are not present in the patient (alloantibodies) or have developed against the patient's own red cell antigens (autoantibodies)
- Follows a positive antibody screen, which is an essential part of pretransfusion compatibility testing and standard prenatal testing of pregnant women (Acta Inform Med 2023;31:121)
Essential features
- Antibody screening and identification helps in determining the presence of atypical red cell antibodies of likely clinical significance and to enable the blood center to select compatible units, should transfusion be required (Acta Inform Med 2023;31:121)
- If the antibody screen comes out to be positive, further testing is required to identify the antibody or antibodies giving a positive reaction with screening reagent red cells
- It is one of the principal tools for preventing potential hemolytic transfusion reactions and investigating causes of immune hemolytic anemias (Asian J Transfus Sci 2019;13:34)
- Positive antibody screen result also helps in notifying the clinician of the probable delay in issuing compatible blood to the patient (Transfus Med 2013;23:3)
Terminology
- Identification of irregular antibodies or unexpected antibodies
Pathophysiology
- Unexpected antibodies can be
- Immune alloantibodies: by far the most common; produced in response to RBC stimulation through transfusion, transplantation or pregnancy (Asian J Transfus Sci 2019;13:34)
- Naturally occurring: produced naturally without any exposure to foreign RBC antigen (anti-M, anti-Leb) but due to exposure to pollen, fungus or bacteria (Cent Eur J Immunol 2018;43:466)
- Passively acquired: transmitted via plasma derivatives, such as intravenous immunoglobulin (IVIG), RhIG (Asian J Transfus Sci 2019;13:34)
- Autoantibodies: produced against one's own RBC antigens
Diagrams / tables
Clinical features
- Detailed clinical history regarding
- Race: RBC antigen profiles differ in different races (Asian J Transfus Sci 2022;16:167)
- For example, the frequency of antigen Mi(a) is very low in most populations as compared to Chinese and South East Asian people (Indian J Med Res 2016;143:633)
- Transfusion, pregnancy and any organ transplant surgery (Asian J Transfus Sci 2019;13:34)
- These conditions may expose an individual to foreign red cells which is the usual cause of red cell immunization; patients who have never been pregnant or received transfusion, rarely have clinically significant alloantibodies though naturally occurring antibodies may be present
- Medications and IV solutions
- Drugs like Daratumumab, commonly used for multiple myeloma, interact with RBCs causing a positive DAT (direct antiglobulin test) and interferes with pretransfusion testing (J Blood Med 2021;12:327)
- Infections
- Infections with Mycoplasma pneumoniae are often associated with anti-I
- Viral infections in children may result in formation of autoantibodies with anti-P specificity which may give a positive antibody screen
- Autoimmune disorders
- Autoimmune disorders like systemic lupus erythematosus (SLE) may result in formation of warm autoantibodies with a positive DAT (direct antiglobulin test) along with a positive antibody screen (Indian J Med Res 2016;143:633)
- Autoimmune disorders like systemic lupus erythematosus (SLE) may result in formation of warm autoantibodies with a positive DAT (direct antiglobulin test) along with a positive antibody screen (Indian J Med Res 2016;143:633)
- Race: RBC antigen profiles differ in different races (Asian J Transfus Sci 2022;16:167)
Symptoms
- Healthy blood donors: asymptomatic; 0.2 - 2% individuals have detectable unexpected RBC antibodies picked up during routine antibody screening (Asian J Transfus Sci 2018;12:17, Indian J Med Res 2020;152:280, Asian J Transfus Sci 2019;13:34)
- Before transfusion: patient samples show cross match incompatibility with multiple donor units and a positive antibody screen in pretransfusion testing
- After transfusion: acute / delayed hemolytic transfusion reaction
- Hemolytic disease of the fetus / newborn
Screening
- Antibody screening is the first step done for detecting presence of alloantibodies before identification; it simply tells about the presence or absence of alloantibody, whereas antibody identification helps to identify the particular alloantibody
- Mandatory part of pretransfusion compatibility testing (Acta Inform Med 2023;31:121)
- Principle: based on indirect antiglobulin test where patient serum / plasma is mixed with reagent red cells / screen cells in presence of anti-IgG / C3 (antihuman globulin [AHG]) (Acta Inform Med 2023;31:121)
- Screen cells: set of 2 or preferably 3 cell suspension with O blood group and known and unique antigenic profile (lot specific); together should cover all significant antigens including D, C, c, E, e, K, k, Fya, Fyb, Jka, Jkb, Lea, Leb, P1, M, N, S and s
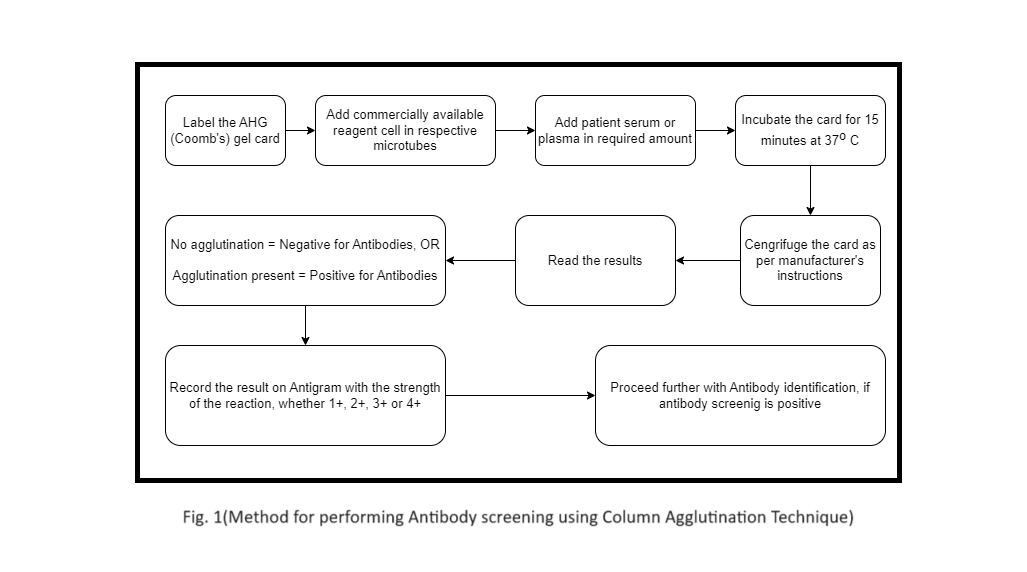
- May be done by conventional tube technique, column agglutination technique or using solid phase red cell adherence assay
- Methodology: see Diagrams / tables
- Direct antiglobulin test (DAT) and autocontrol (mixing patients' serum with own red cells) are always done in parallel to rule out presence of autoantibody
- If the result is positive with any of the panel cells, antibody identification is the next step (Asian J Transfus Sci 2019;13:34)
- Interpretation: a positive reaction is indicated by agglutination or hemolysis
- Phase of reaction
- Immediate spin phase: IgM (anti-N, anti-I, anti-P1)
- AHG phase: IgG (Rh, Kell, Duffy, Kidd)
- Phase of reactivity can help to determine whether the antibody is cold reacting (i.e., IgM type) or warm reacting (i.e, IgG type)
- Positive autocontrol: autoantibody or recent transfusion (alloantibody coating circulating donor RBCs)
- True agglutination versus rouleaux: rouleaux will be seen in all cells and can be dispersed by adding a few drops of saline
- Phase of reaction
- Note: a negative screen does not always rule out an alloantibody since the specific antigen may not be expressed on any of the panel cells
Blood donor screening
- All blood donors are screened for the presence of any unexpected antibody using a set of 2 or 3 reagent red cells
Blood donor testing
- Testing of all blood donors is mandatory for unexpected alloantibodies
Donor deferral
- Blood units that are antibody screen positive have their plasma and platelets excluded from the inventory but packed red cells can be used for transfusion
- Donors are recalled and counseled regarding the presence of the unexpected antibody
- They are given a detailed report indicating the antibody present and advised to show it in case they themselves require a blood transfusion in the future; this will help the blood center find compatible units
- Reference: Hematology 2012;17:302
Laboratory
- Antibody identification
- Performed after positive antibody screen (Asian J Transfus Sci 2019;13:34)
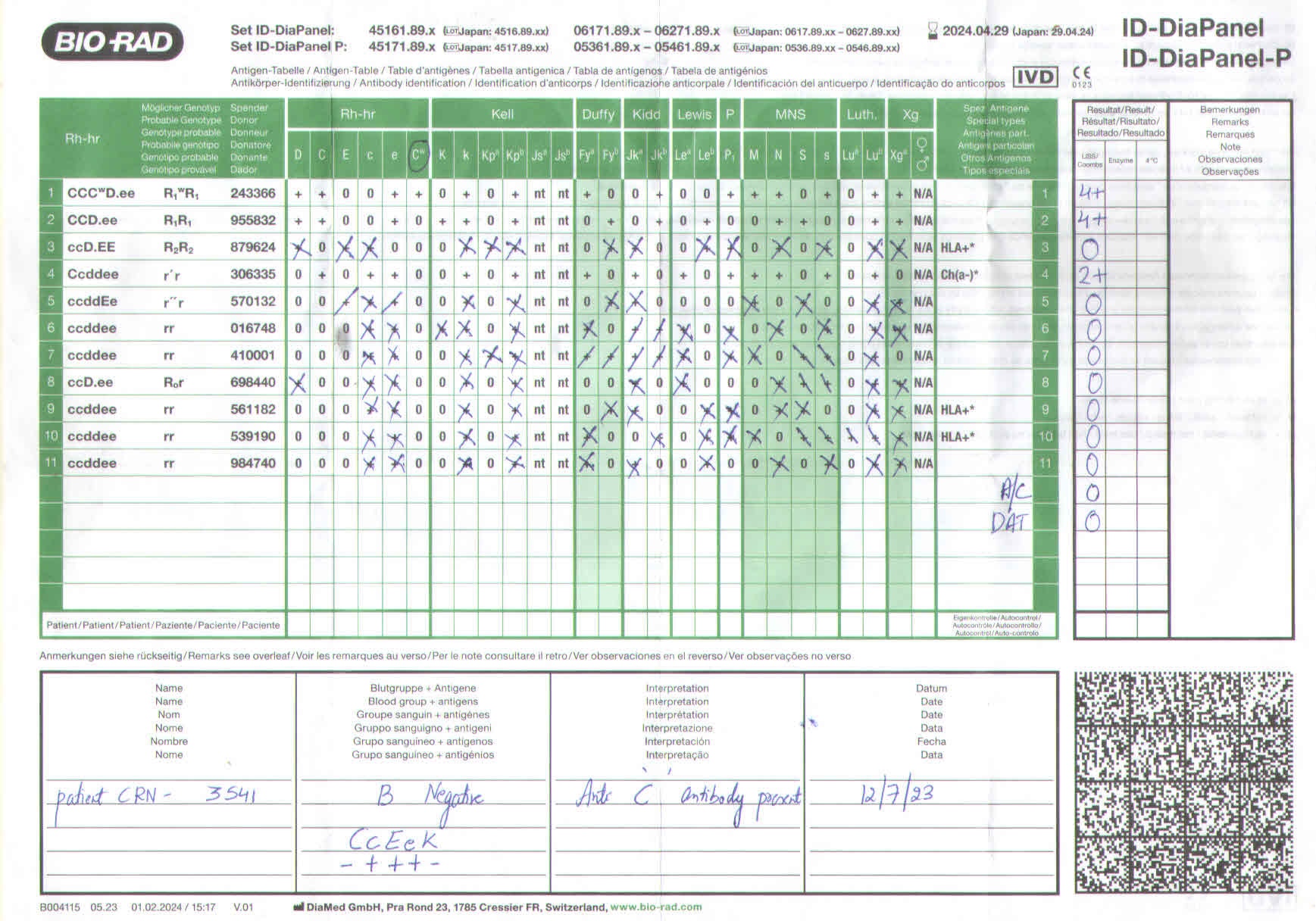
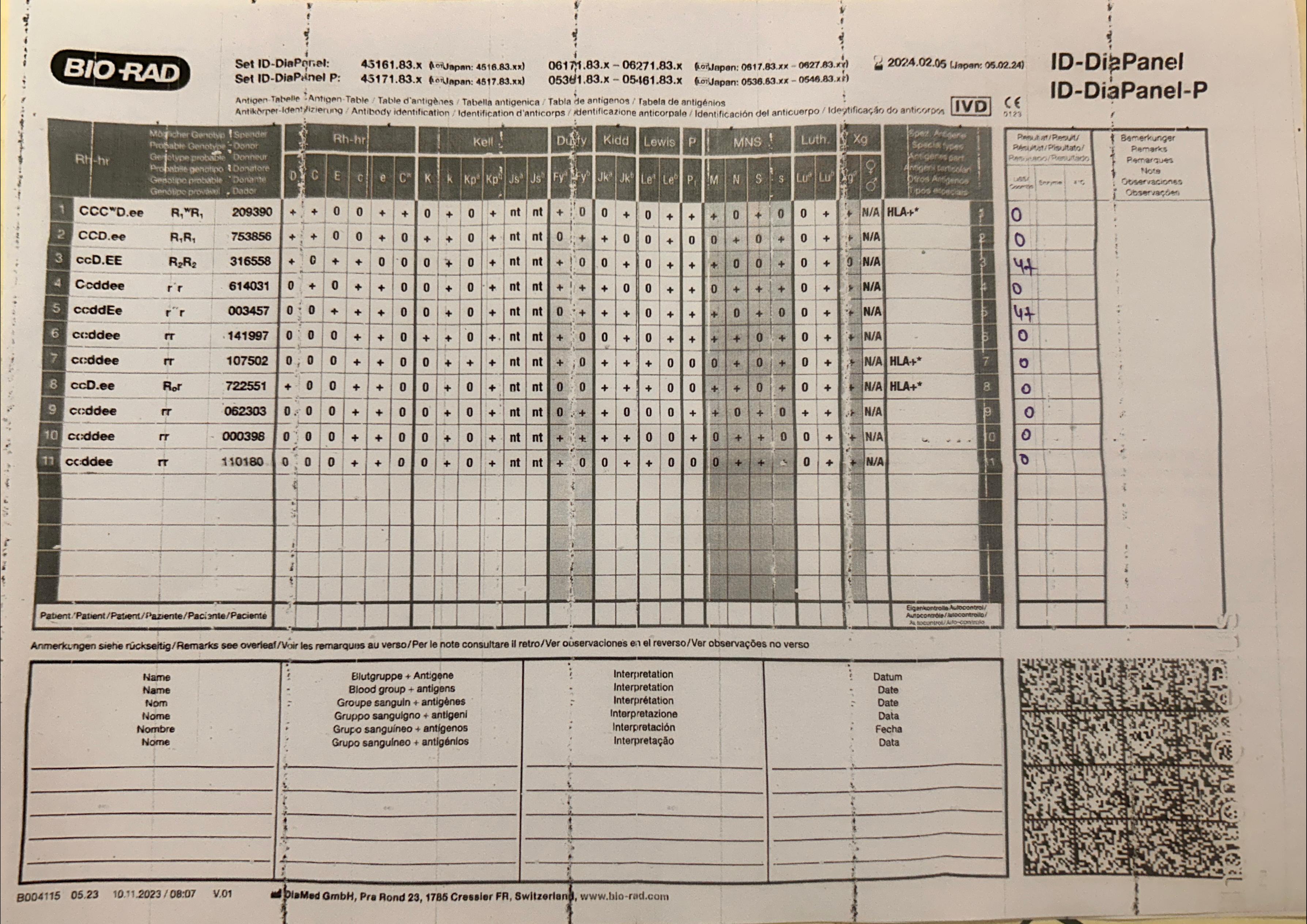
- Principle: serum or plasma is tested against an extended panel of 11, 15, 16 or 20 reagent red cells of known antigen profile (lot specific)
- Panel should be diverse to include variable expression of clinically significant antigens
- Profile sheet specifying the different antigens present on the cells or antigram is provided with the panel (see Diagrams / tables)
- Methodology: basic methodology is the same as antibody screen (see Diagrams / tables), the only difference being the number of cell suspensions used in the panel (2 - 3 in screen versus 11 - 20 in identification)
- Interpreting the antigram
- Results with all panel cells are recorded on the antigram and the antibody is identified using the following steps
- Ruling out / exclusion: cells with a negative reaction to all tested phases are used to rule out the presence of antigens
- Respective antigens on these sets of cells can be eliminated as a possible cause of antibody reactions; cells that are heterozygous should not be crossed to avoid excluding a weak antibody reaction
- Matching the pattern: the next step is to look at the reactions that are positive and match the pattern; in case of a single antibody, all cells possessing that antigen will show a positive reaction
- Rule of 3: presence of at least 3 antigen positive red cells that produce a reaction and 3 antigen negative red cells that do not produce a reaction will result in accurate identification of the antibody (p value < 0.05)
- Strength and phase of reaction: identifying the phase at which reaction occurs (immediate spin [IS] versus 37 °C or AHG) and strength of reaction also helps in identifying the antibody; presence of different reaction strengths with different cells may be due to presence of more than one antibody or dosage phenomenon (stronger reaction with antigen homozygous cells as compared to heterozygous cells)
- Ruling out / exclusion: cells with a negative reaction to all tested phases are used to rule out the presence of antigens
- Results with all panel cells are recorded on the antigram and the antibody is identified using the following steps
- Additional tests: required when the identification panel does not yield specific results
- Selected cell panels: additional panels with different antigen combinations as needed for further characterization
- Enzymes: RBCs are treated with enzymes like ficin, papain, bromelain to alter the expression of antigens (some enhanced while others inactivated); comparing reactions of treated versus untreated cells with serum can help pinpoint the alloantibody
- Neutralization: certain substances will result in binding and inactivation of the antibody in the test serum (e.g., saliva for anti-Lewis, hydatid cyst fluid for anti-P1); a positive reaction before neutralization and a negative reaction with the same test cells postneutralization will clearly indicate the presence of specific antibody that was neutralized
- Use of dithiothreitol (DTT)
- DTT breaks the disulfide bonds in IgM antibodies and inactivates them, thus helping in identifying the presence of any IgG alloantibody
- It also breaks the CD38 disulfide bonds on the red cells thus preventing daratumumab from binding to red cells; so it helps in identifying alloantibodies in patients being treated with daratumumab
Case reports
- 32 hour old, full term girl with progressive anemia and hyperbilirubinemia having maternal anti-M alloantibody (Asian J Transfus Sci 2022;16:144)
- 3 day old boy with hyperbilirubinemia having anti-Jka antibody (Indian J Hematol Blood Transfus 2016;32:497)
- 26 year old pregnant woman with multiple Rh alloantibodies (Asian J Transfus Sci 2021;15:109)
- 53 year old man who developed acute hemolytic transfusion reaction due to anti-c antibodies (Asian J Transfus Sci 2015;9:213)
Sample assessment and plan
- Assessment:
- Patient is a 27 year old, gravida 2 para 1, Rh negative woman with anti-D antibodies during 28th week of pregnancy with titers of 1:32
- Follow up visit at 32 weeks shows increased anti-D titers to 1:128
- Fetal middle cerebral artery (MCA) indicates increased peak systolic velocity suggestive of anemia
- First child was Rh positive and required phototherapy for neonatal jaundice
- Plan:
- Antenatal management
- Regular antenatal care with monitoring for hemolytic disease of the fetus and newborn (HDFN)
- Intrauterine transfusion may be considered if fetal anemia worsens on MCA Doppler
- Elective cesarean at 37 weeks if fetal distress is present
- Postnatal management
- Initial assessment: blood type, DAT, total bilirubin, reticulocyte count
- Phototherapy to manage hyperbilirubinemia
- Intravenous Rh immunoglobulin to reduce hemolysis
- Monitoring of bilirubin levels every 6 hours
- Double volume exchange transfusion should be considered in case of worsening hyperbilirubinemia and progressive anemia
- Baby should be discharged when bilirubin levels are < 10 mg/dL, hemoglobin is stable without transfusion requirement and the baby is gaining weight
- Weekly outpatient follow up
- Antenatal management
Additional references
Board review style question #1
A 58 year old man presents to the hospital for knee replacement surgery. The patient has a history of blood transfusion a few years ago following a road traffic accident. A type and screen sample (ethylenediaminetetraacetic acid [EDTA] anticoagulant) is submitted to the blood bank. Blood group is reported as O positive and antibody screen is positive. Antibody identification is performed using the 11 cell panel shown above. Which antibody is present in the patient's sample?
- Anti-C antibody
- Anti-D antibody
- Anti-E antibody
- Anti-K antibody
Board review style answer #1
C. Anti-E antibody is present in the given sample. Only 2 cells (3 and 6) show reaction; all other cells are negative. The pattern of reactivity matches with anti-E antibody. Answer A is incorrect because the negative reaction in cells 1, 2 and 11 helps to rule out anti-C antibody. Answer B is incorrect because anti-D antibody is ruled out as cells 1, 2, 4 and 11 did not show a reaction though D antigen is present. Answer D is incorrect because anti-K antibody is ruled out as cells 1 and 7 did not show a reaction though K antigen is present.
Comment Here
Reference: Antibody identification & panel interpretation
Comment Here
Reference: Antibody identification & panel interpretation
Board review style question #2
A 60 year old man with a history of myelodysplastic syndrome presents with fatigue and pallor. He has received multiple transfusions in the past and has developed alloantibodies. His blood group is O positive. Antibody screening is done using a 3 cell panel that is positive (3+) in the first 2 cells. What is the best strategy to ensure that he receives compatible blood?
- Perform antibody identification and administer antigen negative blood
- Transfuse autologous blood
- Transfuse O negative blood only
- Transfuse O positive blood only
Board review style answer #2
A. Perform antibody identification and administer antigen negative blood. Antibody identification should be done for this patient to identify the alloantibodies present. Once alloantibodies are identified, corresponding antigen negative units should be transfused into this patient. Answer B is incorrect because autologous blood cannot be transfused as the patient is suffering from myelodysplastic syndrome and requires frequent transfusions. Answers C and D are incorrect because transfusing O positive or O negative blood without performing antibody identification and antigen matching may result in acute or delayed hemolytic transfusion reaction.
Comment Here
Reference: Antibody identification & panel interpretation
Comment Here
Reference: Antibody identification & panel interpretation