Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | History / evolution | ABC toolbox | Drivers | Approaches related to surgery | Overarching approaches | Ongoing interventions | Case reports | Sample assessment & plan | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Onyenekwu CP, George MR. Patient blood management. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/transfusionmedicinepatientbloodmanagement.html. Accessed April 1st, 2025.
Definition / general
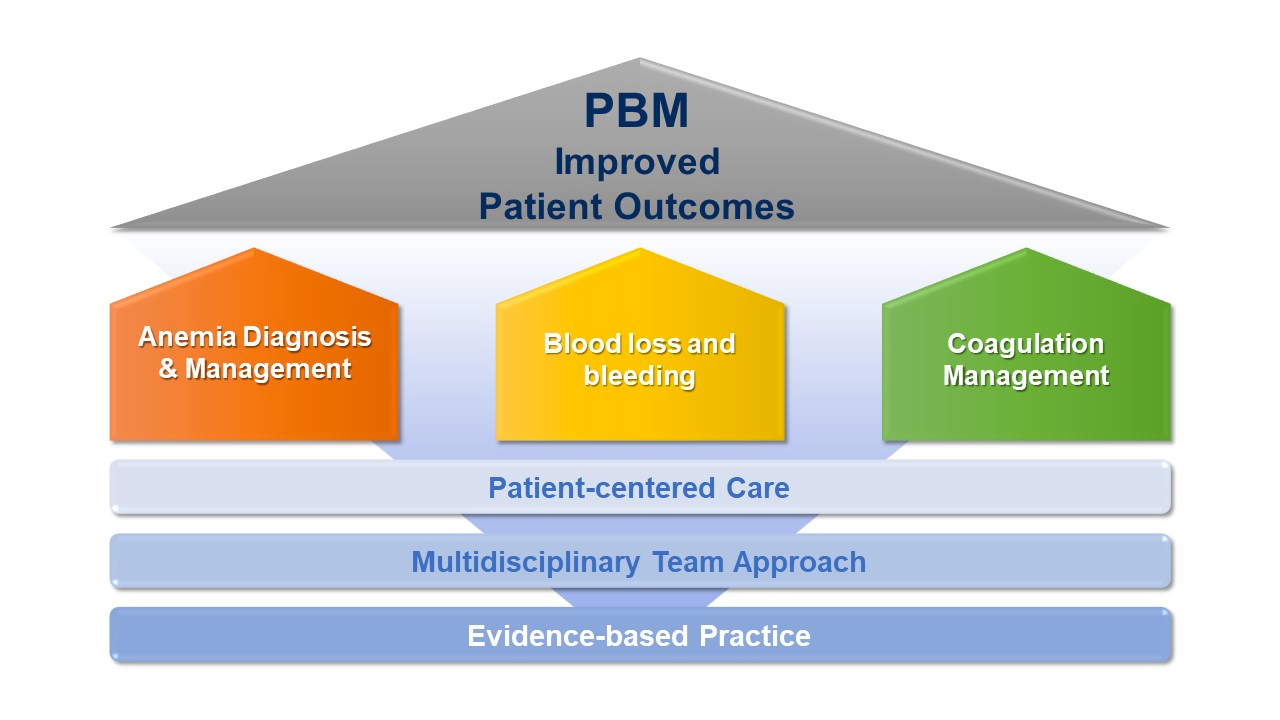
- Multidisciplinary approach targeted toward optimization of patient care while employing the best available evidence in patients requiring blood transfusion (AABB: Technical Manual of the American Association of Blood Banks, 20th Edition, 2020)
- Peer developed definition by representatives of various patient blood management (PBM) organizations: "a patient centered, systematic, evidence based approach to improve patient outcomes by managing and preserving a patient's own blood, while promoting patient safety and empowerment" (Anesth Analg 2022;135:476)
Essential features
- Revolves around quality of care improvement, patient safety and transfusion economics
- Involves a transdisciplinary and multistrategic approach
- Blood conservation
- Optimization of red cell mass
- Incorporating patient oriented decision making
- Evidence based practice to achieve improved patient outcomes
- Applied to both surgical and nonsurgical patients
- Surgical patient blood management addresses perioperative and intraoperative care
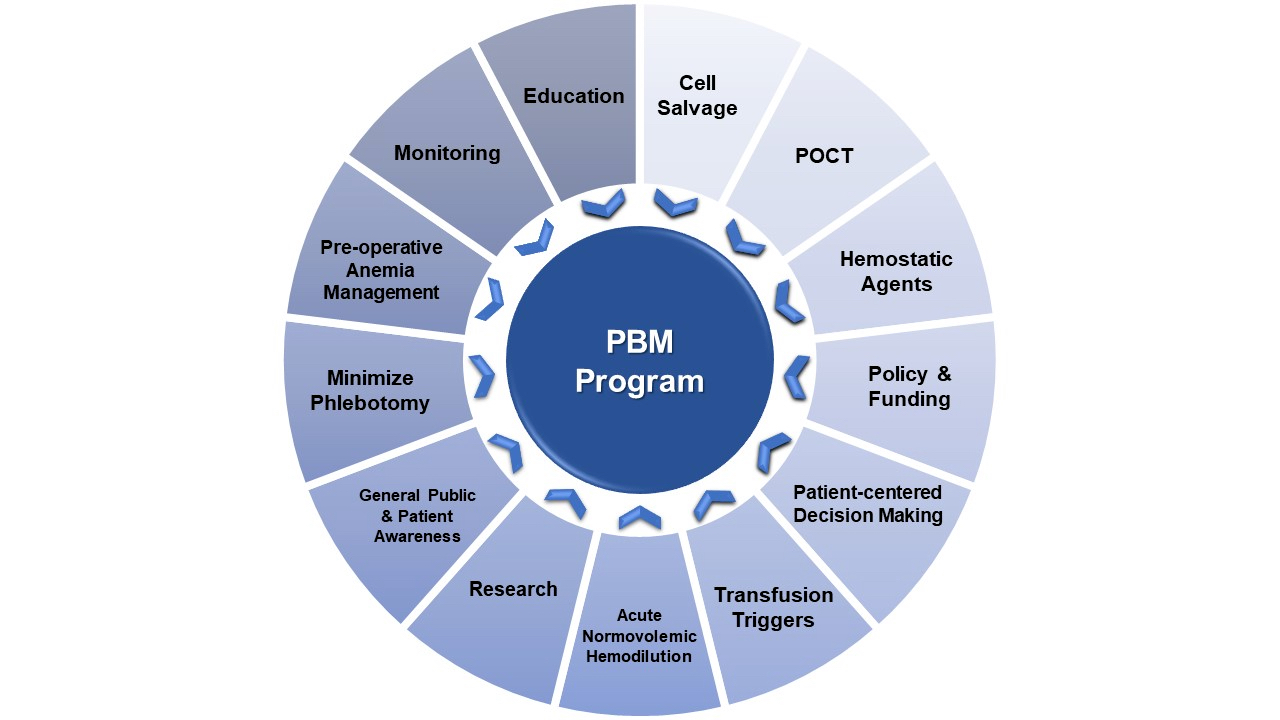
- A strong PBM program requires
- Adequate funding and resources
- Education and strategic involvement of healthcare providers
- Ongoing research
- Continuous monitoring and feedback
- Use of appropriate quality indicators
- Public and patient awareness
Terminology
- Patient blood management (PBM)
- Blood management (no longer recommended)
- Association for the Advancement of Blood and Biotherapies (formerly the American Association of Blood Banks) (AABB)
- Bloodless medicine and surgery (BMS)
- Society for the Advancement of Patient Blood Management (SABM)
- International Foundation of Patient Blood Management (IFPBM)
History / evolution
- Advent of allogeneic transfusion in the early twentieth century decreased emphasis on anemia and bleeding prevention
- Bloodless surgery evolved in the latter half of the twentieth century, starting with intricate cardiovascular surgeries with minimization of allogeneic transfusion based on patient and available evidence (Ann Thorac Surg 1998;65:125)
- Terminologies adopted over time include
- Bloodless medicine and surgery
- Blood conservation
- Blood management
- Patient blood management was coined in 2005 (Anesth Analg 2022;135:476, Blood Transfus 2019;17:191, Transfus Apher Sci 2002;27:29, J Australas Ass Blood Conserv 2005;2:3)
ABC toolbox
- ABC toolbox of PBM from the IFPBM SABM workgroup summarizes practical principles of PBM to target 3 areas (Anesth Analg 2020;131:74)
- Anemia and iron deficiency
- Blood loss and bleeding
- Coagulopathy management
Drivers
- Increasing demand for quality improvement in healthcare
- Transfusion associated risks
- Economic benefits of decreased transfusion
- Advancement of evidence based practice
- Patient centered care, autonomy and satisfaction
- Excessive use of blood and blood components
- Increasing frequency of blood shortage (AABB: Technical Manual of the American Association of Blood Banks, 20th Edition, 2020)
Overarching approaches
- PBM program oversees staff education on
- Minimizing phlebotomy blood loss
- Increased use of POCT and microvolume sampling
- Use of noninvasive laboratory measurements such as hemoglobin when appropriate
- PBM program liaises with the laboratory to review test ordering patterns and the frequency of inadequate specimens to decrease irrelevant tests and the need for sample recollections (SABM: Administrative and Clinical Standards for Patient Blood Management Programs, 5th Edition, 2019)
- Transfusion triggers
- Packed red blood cells (pRBCs) (Choosing Wisely: A Watershed Moment in Health Care [Accessed 21 June 2023])
- Do not transfuse more units of RBCs or other components than absolutely necessary
- Restrictive threshold (7.0 - 8.0 g/dL) should be used for most stable patients without evidence of impaired tissue oxygenation
- Threshold of 8.0 g/dL is appropriate for patients with pre-existing cardiovascular disease
- Transfusion decisions should be influenced by clinical symptoms and hemoglobin
- Single unit red cell transfusions should be the starting point for nonbleeding, hospitalized patients
- Additional units should only be given after reassessment of clinical symptoms and lab values
- Do not transfuse RBCs for iron deficiency without hemodynamic instability
- Better options include oral or intravenous iron supplementation
- Do not perform serial blood counts on clinically stable patients
- Multiple blood draws can cause iatrogenic anemia and promote unnecessary transfusions
- Do not transfuse O negative blood except to O negative patients in emergencies for women of childbearing potential with unknown blood group
- Do not transfuse more units of RBCs or other components than absolutely necessary
- Plasma (FFP, thawed plasma, PF24, etc.) (Society of Hospital Medicine: Anemia Prevention and Management Program Implementation Guide, 2015)
- Do not transfuse plasma to correct coagulopathy in nonbleeding patients
- Do not routinely use blood products to reverse vitamin K antagonists (VKA); e.g., warfarin
- Reversal of VKA should be based on the international normalized ratio (INR) plus bleeding risks and urgency of reversal
- INR < 4.5 without bleeding
- Hold warfarin if not emergent
- Oral or IV vitamin K (5 - 10 mg)
- 4 factor prothrombin complex concentrate (4F PCC), a hemostatic concentrate of at least 4 coagulation factors (factors II, VII, IX and X), for reversal < 2 hours
- Plasma (15 mL/kg) if 4F PCC is not available
- INR 4.5 - 10 without bleeding
- Hold warfarin
- IV vitamin K (5 - 10 mg) for more rapid reversal
- 4F PCC for reversal < 2 hours
- Plasma (15 - 30 mL/kg) if 4F PCC is not available
- INR > 10 without bleeding
- Hold warfarin
- IV vitamin K (5 - 10 mg)
- 4F PCC for reversal < 2 hours
- Plasma (20 - 30 mL/kg) if 4F PCC is not available
- Serious life threatening bleeding at any INR
- IV vitamin K 10 mg
- 4F PCC for reversal < 2 hours
- Plasma (20 - 30 mL/kg) if 4F PCC is not available
- Platelets (Choosing Wisely: A Watershed Moment in Health Care [Accessed 21 June 2023], Ann Intern Med 2015;162:205)
- Do not transfuse platelets without laboratory guidance outside of fixed ratio massive transfusions
- Prophylactic transfusion for a platelet count of < 10 x 109 cells/L to reduce risk of spontaneous bleeding
- Single apheresis platelet unit or equivalent
- Half doses may be equally effective, especially in times of inventory shortage
- Prophylactic transfusion for a platelet count of < 20 x 109 cells/L for elective placement of central venous catheter
- Prophylactic transfusion for elective diagnostic lumbar puncture with a platelet count < 50 x 109 cells/L
- Prophylactic transfusion for major elective nonneuraxial surgery with a platelet count < 50 x 109 cells/L
- No indication for prophylactic transfusion for patients who are nonthrombocytopenic undergoing cardiac surgery with cardiac bypass
- Not enough evidence for or against transfusion for patients on antiplatelet therapy with intracranial hemorrhage
- Packed red blood cells (pRBCs) (Choosing Wisely: A Watershed Moment in Health Care [Accessed 21 June 2023])
Ongoing interventions
- Education
- Identify key stakeholders (physicians, nurses, administrators, laboratorians, phlebotomists)
- Chief medical officer: administrative / resource support
- Chief quality / safety officer: administrative / resource support
- Chief executive / financial officer: resource allocation
- Anesthesiology: optimization of pre / peri / postoperative hemostasis and hemoglobin
- Surgery: surgical techniques to minimize/manage bleeding
- Hematology oncology: optimize hemostasis in patients with cancer and hematologic disorders
- Clinical laboratory: appropriate laboratory utilization
- Blood bank: blood product stewardship
- Pharmacy: role in appropriate use of pharmacologic interventions that decrease blood usage (vitamin K, parental iron, tranexamic acid)
- Information technology: make changes in electronic medical record (EMR) such as computerized provider order entry (CPOE) and best practice alerts
- Identify key stakeholders (physicians, nurses, administrators, laboratorians, phlebotomists)
- Monitoring
- Determine what data is available from the EMR versus the blood bank computer system
- Pharmacy is a source of data on iron use and adjuvant medications to optimize hemostasis
- Determine if information obtained electronically is reliable for if additional chart search is necessary
- EMR interventions
- Clinical decision support (CDS)
- Reduction of errors and adverse events
- Promotion of best practices
- Quality and safety
- Appropriate utilization
- Cost reduction
- Cost profile improvement
- Use evidence based recommendations (J Am Med Inform Assoc 2018;25:1556)
- Computerized provider order entry (CPOE): embed best practices into EMR
- Alerts: automatic message to communicate essential information to provider at time of order
- May feature best practice guidelines or prompting questioning of order
- Passive alert: information is presented but does not interrupt the user workflow, no user interaction required
- May lead to alert fatigue and providers ignoring the messaging
- Overrides may pose dangers
- Hard stop: user is either prevented from taking an action altogether or allowed to proceed only with the external override of a third party
- Soft stop: user is allowed to proceed against the recommendations presented in the alert as long as an active acknowledgement reason is entered
- Clinical decision support (CDS)
Case reports
- 101,794 patients ages 18 years and older involved in a patient blood management monitoring and feedback program (Transfusion 2015;55;2807)
- Impact of a patient blood management monitoring and feedback program on allogeneic blood transfusions and related costs with 213,882 adult patients (Anaesthesia 2019;74:1534)
Sample assessment & plan
- Assessment: A 68 year old woman who observes a vegan diet has a past medical history significant for obesity and osteoarthritis. She is referred by her primary care physician to the orthopedic surgery clinic for a 3 year history of worsening right knee pain. On assessment for a right total knee replacement, her complete blood count showed a hemoglobin of 9.8 mg/dL (12 - 16 g/dL), mean corpuscular volume (MCV) of 72 fL (79 - 98 fL), mean corpuscular hemoglobin concentration (MCHC) of 28 g/dL (32 - 36 g/dL) and red cell distribution width (RDW) of 17.1% (11.1 - 14.9%). Iron studies showed a low serum iron and ferritin with an increased transferrin iron binding capacity. Vitamin B12 and folate levels were within normal limits.
- Right knee osteoarthritis
- Obesity
- Iron deficiency anemia
- Plan:
- Schedule for right total knee replacement in 8 weeks
- Stool for occult blood, ova and parasites (negative results)
- Commence trial of oral iron therapy for 4 weeks
- Repeat hemoglobin and iron studies in 4 weeks
- Repeat tests at the 4 week follow up visit showed a hemoglobin of 11.2 g/dL, the surgeon deemed this adequate response with no plan to use adjuvant erythropoietic agents
- Follow up assessment and plan:
- Resolve anemia
- Continue oral iron therapy
- Repeat hemoglobin 1 day prior to planned surgery: 12.5 g/dL
- Proceed with surgery as planned; administer intraoperative fibrinolytic / hemostatic agents
- Patient underwent knee replacement surgery without administration of intraoperative tranexamic acid and use of topical hemostatic agents. She had a moderate amount of intraoperative blood loss with a postoperative hemoglobin of 10.3 mg/dL. She was, however, stable and was discharged to a rehabilitation facility.
- Postoperative plan:
- Continue oral iron therapy and rehabilitation therapy
- Follow up in 4 weeks at anemia clinic
Additional references
Board review style question #1
You are the Medical Director of Transfusion Medicine at your hospital. You are currently working with Information Technology to implement some updates to the clinical decision support in your electronic medical records (EMR) for the ordering of blood products. Which best practice recommendations would you embed in the orders for packed red blood cells (pRBCs)?
- 1 unit pRBCs are not normally recommended; 2 should always be given
- Additional units of pRBCs should be given without checking hemoglobin (Hb) in stable patients to avoid unnecessary blood draws and iatrogenic anemia
- pRBC transfusion is not recommended in hemodynamically unstable cardiac patients with evidence of impaired tissue oxygenation until Hb < 7.0 g/dL
- pRBC transfusion is recommended in hemodynamically stable patients with evidence of impaired tissue oxygenation and Hb < 7.0 g/dL
Board review style answer #1
D. pRBC transfusion is recommended in hemodynamically stable patients with evidence of impaired tissue oxygenation and Hb < 7.0 g/dL. Answers A and B are incorrect because 1 unit pRBC transfusion is recommended for most indications and stable patients, followed by rechecking of hemoglobin for transfusion response. Answer C is incorrect because for patients who are hemodynamically unstable and have pre-existing cardiovascular disease, the hemoglobin threshold for transfusion is often higher at 8.0 g/dL rather than the more restrictive < 7.0 g/dL.
Comment Here
Reference: Patient blood management
Comment Here
Reference: Patient blood management
Board review style question #2
A patient is scheduled to undergo an elective central venous catheter insertion. The patient is not taking anticoagulants and has a reasonable hemoglobin level of 12.2 g/dL. What is the recommended platelet count transfusion threshold in this scenario?
- < 10 x 109 cells/L
- < 20 x 109 cells/L
- < 50 x 109 cells/L
- < 100 x 109 cells/L
Board review style answer #2
B. < 20 x 109 cells/L. Insertion of a central venous catheter and otherwise stable patient carries a recommendation for a platelet transfusion threshold of at least 20 x 109 cells/L. Answers A and C are incorrect because prophylactic platelet transfusion is recommended to avoid spontaneous bleeding in patients with a platelet count of < 10 x 109 cells/L and for patients who are to undergo lumbar puncture with platelet count of < 50 x 109 cells/L, respectively. Additionally, patients about to undergo neuroaxial surgical procedures should be transfused for platelet count < 50 x 109 cells/L. Answer D is incorrect because it refers to the older recommendation of transfusing for a platelet count of < 100 x 109 cells/L for patients undergoing any sort of neurosurgery; however, there is not much high quality evidence to support that practice.
Comment Here
Reference: Patient blood management
Comment Here
Reference: Patient blood management
Board review style question #3
A 40 year old woman with a history of heavy menstrual bleeding due to uterine fibroids is scheduled for elective hysterectomy. Her hemoglobin is 9.7 g/dL and her iron studies are consistent with iron deficiency anemia. She is otherwise healthy. Which of the following interventions is most likely to decrease the likelihood of allogeneic transfusion during her surgery?
- Acute normovolemic hemodilution during the surgery
- Preoperative anemia clinic management with correction of iron deficiency scheduled well in advance of her date of surgery
- Provider education with best practice guideline alerts in the EMR regarding appropriate hemoglobin thresholds for pRBC transfusion
- Use of point of care devices such as thromboelastography during surgery to assess clot formation in real time
Board review style answer #3
B. Preoperative anemia clinic management with correction of iron deficiency scheduled well in advance of her date of surgery. In advance of elective hysterectomy, optimization of hemoglobin with iron therapy would be the most appropriate PBM intervention and is very achievable if the surgery is scheduled several weeks in advance. Answer A is incorrect because acute normovolemic hemodilution is not normally used during procedures such as hysterectomy, which are not usually associated with multiple unit red blood cell loss. Answer C is incorrect since best practice alerts may be helpful in the stable in patient setting but are less likely to be helpful to aid decision making during surgeries. Answer D is incorrect because point of care devices such as thromboelastography are typically employed during high blood loss cases such as cardiothoracic surgery, trauma or liver transplant. They are not typically employed during routine hysterectomy cases.
Comment Here
Reference: Patient blood management
Comment Here
Reference: Patient blood management