Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Diagrams / tables | Symptoms | Blood donor screening | Blood donor symptoms | Blood donor testing | Donor deferral | Laboratory | Case reports | Clinical images | Sample assessment & plan | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Swenson E. Hemovigilance. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/transfusionmedhemovigilance.html. Accessed April 1st, 2025.
Definition / general
- Hemovigilance is the comprehensive surveillance for complications resulting from blood donation or blood product transfusion, the evaluation of the complication data and the resulting quality improvement practices that are instituted
Essential features
- Hemovigilance encompasses monitoring blood donor and blood product recipients for adverse events, collecting and compiling that data, then using that data to improve blood donation and blood product transfusion processes and procedures to decrease risk
- Internationally, hemovigilance systems can be comprised of nationally implemented and run programs with mandatory or voluntary reporting compared with hemovigilance systems that are made up of networks of public and private entities with voluntary reporting of adverse events
- In the United States, hemovigilance definitions are standardized through the Center for Disease Control's National Healthcare Safety Network Hemovigilance Module; 12 transfusion reaction entities are defined (case definition) and further classified based on severity and imputability (CDC: National Healthcare Safety Network Biovigilance Component Hemovigilance Module Surveillance Protocol [Accessed 23 December 2024])
Terminology
- Hemovigilance: surveillance of the whole transfusion chain, including blood donation to blood transfusion, to minimize adverse events or reactions in donors and recipients and promote safe and effective use of blood components
- Biovigilance: encompasses principles of hemovigilance (blood recipients and blood donor) but also includes tissues, organs and cellular therapy (CT) components
- Imputability: the degree to which the adverse reaction was caused by transfusion
Clinical features
- Historical perspective
- Many international hemovigilance systems were established to monitor and mitigate transfusion transmitted viral infections, including transfusion transmitted HIV, hepatitis B and hepatitis C
- Goals of hemovigilance
- Continuous quality improvement of the transfusion chain through corrective and preventive actions to improve donor and patient safety
- Benefits of hemovigilance
- Improved donor safety with a reduction in the rate and severity of complications
- Increased public confidence in blood donor system and retention of donors
- Reduction in adverse events for patients, improved medical outcomes and reduced medicolegal incidences
- Early identification and mitigation of infectious and noninfectious risks
- Requirements for an effective hemovigilance system
- Sustainable national system that is integrated into the transfusion chain regionally and includes standardized definitions, traceability and confidentiality
- Timely reporting of adverse events
- Reporting of demographic and blood product utilization data
- Mechanisms to monitor the implementation of corrective and preventive actions in a timely manner and to demonstrate improved safety and clinical outcomes
- Models for hemovigilance
- Models for each country will depend on the healthcare and blood donor network systems
- Centralized and decentralized
- Active versus passive surveillance
- Active: proactive and targeted search for adverse events
- Passive: reporting of adverse events as they are recognized based on a retrospective approach
- 12% of patients with coronavirus disease 2019 (COVID-19) who received COVID-19 convalescent plasma (CCP) were found to meet diagnostic criteria for transfusion associated circulatory overload (TACO) at a single institution that implemented an active surveillance protocol to monitor for CCP related adverse events (Transfusion 2022;62:28)
- Voluntary versus mandatory reporting
- International hemovigilance
- Examples of early hemovigilance systems
- Japan: in 1993, the Japanese Red Cross Society was the first hemovigilance system that began collecting adverse event and infectious disease transmission data at a national level (Japanese Red Cross Society: Haemovigilance Information [Accessed 6 December 2024])
- United Kingdom: established the Serious Hazards of Transfusion (SHOT) in 1996 (Br J Haematol 2013;163:303)
- Data collected through SHOT showed that there was an association between transfusion related acute lung injury (TRALI) and plasma and platelet units donated by females (Transfusion 2015;55:164, Serious Hazards of Transfusion: TRALI Tables [Accessed 6 December 2024])
- Current hemovigilance systems are comprised of nationally organized systems or hemovigilance systems that are a network of public and private organizations working together
- In 2014, the Association for the Advancement of Blood & Biotherapies (AABB) and International Society of Blood Transfusion (ISBT) published the first internationally harmonized standard definitions related to blood transfusions (Vox Sang 2016;110:185)
- Examples of early hemovigilance systems
- Hemovigilance in U.S.
- Hemovigilance in the United States is coordinated by the collaboration of public and private entities; there is no formal national hemovigilance program with required adverse event reporting
- In 2010, the CDC's National Healthcare Safety Network (NHSN) hemovigilance module began national hemovigilance data collection (Transfusion 2015;55:703)
- NHSN hemovigilance module relies on voluntary passive reporting of transfusion associated adverse events
- Passive reporting of transfusion reactions underestimated the rate of TACO in a single institution (Vox Sang 2015;108:387)
- The CDC National Healthcare Safety Network has defined 12 transfusion reaction categories (CDC: National Healthcare Safety Network Biovigilance Component Hemovigilance Module Surveillance Protocol [Accessed 6 December 2024])
- TACO
- TRALI type I
- Transfusion associated dyspnea (TAD)
- Allergic reaction (when severe, life threatening or fatal)
- Hypotensive transfusion reaction
- Febrile nonhemolytic transfusion reaction (FNHTR)
- Acute hemolytic transfusion reaction (AHTR)
- Delayed hemolytic transfusion reaction (DHTR)
- Delayed serologic transfusion reaction (DSTR)
- Transfusion associated graft versus host disease (TA GVHD)
- Posttransfusion purpura (PTP)
- Transfusion transmitted infection (TTI)
- Other or unknown
- Future directions of hemovigilance systems
- Digitally enabled hemovigilance
- Using artificial intelligence or algorithms built into electronic medical records (EHR) may help identify signs and symptoms of transfusion related adverse events in real time
- Baseline of passively reported suspected transfusion reactions was 0.34% and increased to 1.3% at a single institution that implemented a digitally enabled hemovigilance system with a hemovigilance unit (a 524% increase) (Transfusion 2022;62:1010)
- Digitally enabled hemovigilance
- Reference: WHO: A Guide to Establishing a National Haemovigilance System [Accessed 6 December 2024]
Diagrams / tables
NHSN hemovigilance module adverse reaction codes, severity codes and imputability
| Case definition | Severity | Imputability |
| Definitive: the adverse reaction fulfills all of the case definition criteria | Nonsevere: medical intervention (e.g., symptomatic treatment) is required but there is minimal risk of permanent damage to the transfusion recipient | Definite: there is conclusive evidence that the reaction can be attributed to the transfusion |
| Probable: the adverse reaction meets some of the clinical signs and symptoms or radiologic, laboratory evidence or available information but does not meet all definitive case definition criteria | Severe: inpatient hospitalization or prolonged hospitalization is directly attributable to the transfusion reaction, persistent or significant disability or incapacity of the patient as a result of the reaction or a medical or surgical intervention is necessary to preclude permanent damage or impairment of a body function | Probable: there are other potential causes present that could explain the recipient's symptoms but transfusion is the most likely cause of the reaction |
| Possible: the reported clinical signs or symptoms, radiologic or laboratory evidence and available information are not sufficient to meet definitive or probable case definition criteria | Life threatening: major intervention was required after the transfusion reaction (e.g., vasopressors, intubation, transfer to intensive care) to prevent death | Possible: there are other potential causes that are most likely; however, transfusion cannot be ruled out |
| Death: the recipient died as a result of the transfusion reaction | Doubtful: there is evidence clearing in favor of a cause other than the transfusion but transfusion cannot be excluded | |
| Not determined: the severity of the adverse reaction is unknown or not stated | Ruled out: there is conclusive evidence beyond reasonable doubt of a cause other than the transfusion | |
| Not determined: the relationship between the reaction and transfusion is unknown or not stated |
Symptoms
- In blood product recipients (CDC: National Healthcare Safety Network Biovigilance Component Hemovigilance Module Surveillance Protocol [Accessed 6 December 2024])
- Information capture includes blood product recipient vital signs at discrete intervals (pretransfusion, 15 minutes into the transfusion and posttransfusion) as well as signs and symptoms of an adverse event
- The most common adverse events are allergic reactions and febrile nonhemolytic transfusion reactions (Transfusion 2021;61:1424)
- The most common causes of transfusion related death are TRALI and TACO (Transfusion 2021;61:1424)
- Signs and symptoms of transfusion associated adverse events
- Fever, ≥ 1 °C / 1.8 °F rise in temperature to ≥ 38 °C / 100.4 °F
- Chills or rigors
- Headache
- Loss of consciousness
- Respiratory distress (wheezing, coughing, hypoxia, dyspnea, cyanosis, decreased oxygen saturation (SpO2) < 90% on room air, tachypnea)
- Bronchospasm or stridor
- Pulmonary edema
- Evidence of cardiovascular system changes (elevated central venous pressure, evidence of left heart failure, widened pulse pressure, jugular venous distention, peripheral edema, enlarged cardiac silhouette)
- Evidence of fluid overload
- Hypertension
- Hypotension (drop in systolic BP of ≥ 30 mmHg and systolic BP ≤ 80 mmHg)
- Tachycardia
- Abdominal, chest, flank or back pain
- Pain at infusion site
- Skin manifestations, such as rash, flushing, urticaria, pruritus
- Edema of conjunctiva, periorbital region, lips, tongue, uvula or angioedema
- Jaundice or hemoglobinuria
- Nausea / vomiting
- Abnormal bleeding, epistaxis
- Disseminated intravascular coagulation
- Oliguria / anuria
- Marrow aplasia or pancytopenia
- Thrombocytopenia
- Other
Blood donor screening
Blood donor symptoms
- In blood donors (AABB: Donor Hemovigilance [Accessed 6 December 2024])
- Information capture includes blood donor vital signs at discrete intervals (predonation and postdonation) as well as signs and symptoms of an adverse event
- The most common donor adverse events are presyncopal reactions and small hematomas
- Signs and symptoms of donor related adverse events
- Vasovagal
- Prefaint (presyncopal), no loss of consciousness
- Loss of consciousness
- Local injury related to needle
- Hematoma / bruise
- Nerve irritation
- Arterial puncture
- Painful arm
- Delayed bleeding
- Infection
- Major blood vessel injury
- Injury
- Major injury
- Minor injury
- Apheresis related
- Citrate
- Hemolysis
- Air embolus
- Infiltration
- Allergic
- Local
- Systemic
- Anaphylactic
- Major cardiovascular event
- Angina pectoris within 24 hours
- Cardiac arrest
- Cerebrovascular accident
- Myocardial infarction within 24 hours
- Transient ischemic attack (TIA) within 24 hours
- Other
- Vasovagal
- See Donor reactions
Blood donor testing
Donor deferral
Laboratory
- Transfusion reaction workups require the implicated blood product unit as well as a posttransfusion sample to be returned to the blood bank (Cohn: Technical Manual, 20th Edition, 2020)
- Blood bank performs the following
- Clerical check of the component bag, label, paperwork and patient sample
- Repeat ABO testing of the posttransfusion sample
- Evaluate the pretransfusion and posttransfusion specimens for visual hemolysis
- Perform direct antiglobulin test (DAT) on posttransfusion sample
- Clerical check of the component bag, label, paperwork and patient sample
- Blood bank performs the following
Case reports
- 23 year old splenectomized woman with transfusion transmitted malaria (Plasmodium knowlesi) (Malar J 2016;15:357)
- 40 year old woman with transfusion transmitted CMV as complication of liposuction in the Dominican Republic (BMJ Case Rep 2021;14:e236892)
- 3 female solid organ transplant recipients in their 40s and 50s with eastern equine encephalitis virus (EEEV) infection from a single organ donor (Clin Infect Dis 2019;69:450)
- 59 year old man with COVID-19 infection developed TRALI after COVID-19 convalescent plasma transfusion (J Int Med Res 2021;49:3000605211032814)
Sample assessment & plan
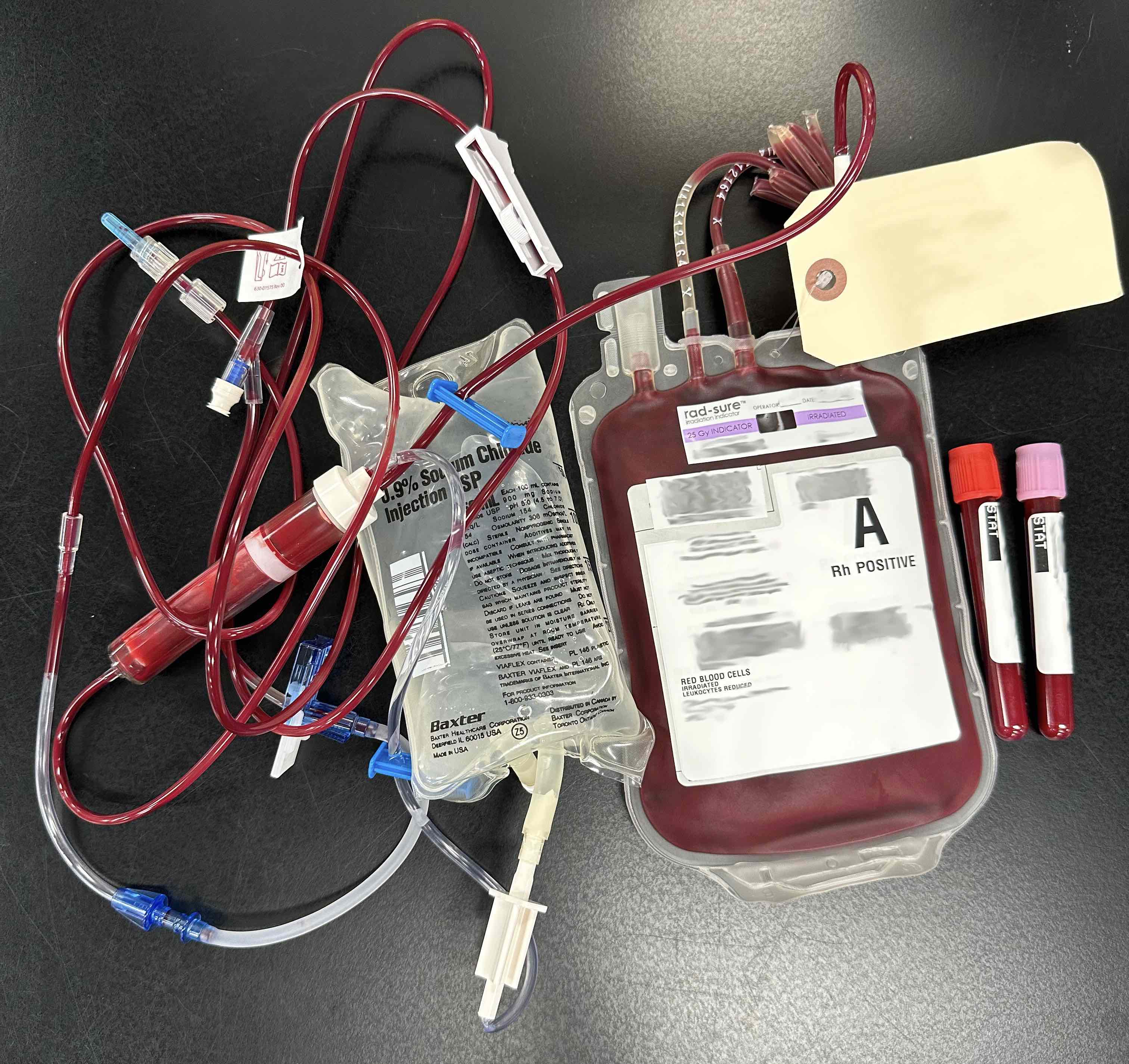
- Assessment: Patient is a 48 year old woman (A RhD positive, antibody screen negative) with a history of type II diabetes, end stage renal disease on dialysis and idiopathic cardiomyopathy with a left ventricular ejection fraction of 17%. She presents with a hemoglobin of 5.8 g/dL, fatigue and shortness of breath. She is transfused 2 units of A RhD positive red blood cells. During transfusion of the second unit she develops hypertension to 210/90, tachycardia to 112 bpm and desaturates to 89% O2 saturation on room air. A chest Xray is performed and shows bilateral pulmonary edema. The transfusion reaction workup shows clerical check correct, no evidence of hemolysis and polyspecific direct antiglobulin test (DAT) is negative (see clinical image). The patient is placed on supplemental oxygen via nasal cannula and respiratory status improves after dialysis.
- Plan: The patient presentation and laboratory workup are consistent with a diagnosis of TACO, severity is nonsevere, imputability is probable.
- Recommend judicious transfusion and we suggest transfusing at a slow rate in the future if the clinical situation allows (e.g., 1 mL/kg/hr).
Additional references
Board review style question #1
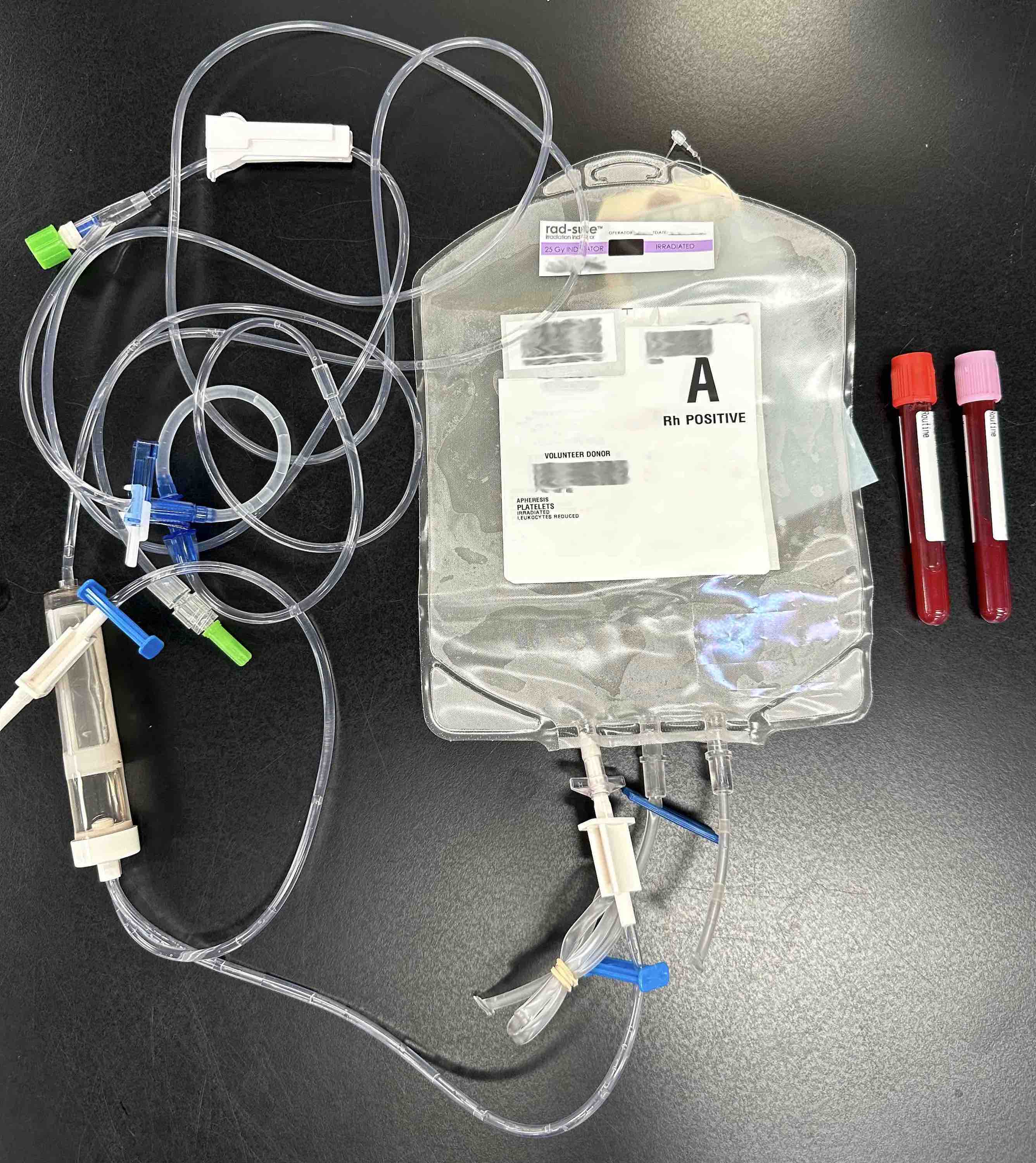
A 56 year old woman with a refractory / recurrent plasma cell neoplasm and multiple allergies to medications has received multiple transfusions of red blood cell and platelet units over years. She has had multiple mild allergic transfusion reactions, which the clinical team treated with Benadryl and steroids. She presents to the outpatient infusion clinic for a platelet transfusion (see image above). Premedication is not administered. 15 minutes into the platelet transfusion, she develops hives, itching, chest tightness, difficulty breathing, throat swelling, oxygen desaturation to 78% on room air and hypotension with blood pressure of 78/52. A code is called, epinephrine is administered, the patient is intubated and admitted to the medical intensive care unit. What is the case definition, severity and imputability of this transfusion reaction?
- Case definition: definitive; severity: life threatening; imputability: definite
- Case definition: definitive; severity: nonsevere; imputability: definite
- Case definition: possible; severity: nonsevere; imputability: definite
- Case definition: possible; severity: severe; imputability: probable
- Case definition: probable; severity: severe; imputability: probable
Board review style answer #1
A. Case definition: definitive; severity: life threatening; imputability: definite. The case definition is definitive for transfusion reaction as the patient presented with 2 or more of the diagnostic criteria during the transfusion. The patient had hypotension, respiratory distress, itching and hives. The severity is life threatening as the patient required intubation and admission to the intensive care unit. The imputability is definite as the reaction occurred during the transfusion and no other risk factors were noted. Answers B - E are incorrect because they did not list the correct case definition, severity or imputability.
Comment Here
Reference: Hemovigilance
Comment Here
Reference: Hemovigilance
Board review style question #2
Which transfusion adverse event was mitigated after collection of hemovigilance data through the United Kingdom's Serious Hazards of Transfusion (SHOT)?
- Allergic reaction
- Febrile nonhemolytic transfusion reaction (FNHTR)
- Transfusion associated circulatory overload (TACO)
- Transfusion associated graft versus host disease (TA GVHD)
- Transfusion related acute lung injury (TRALI)
Board review style answer #2
E. Transfusion related acute lung injury (TRALI). Hemovigilance data collected through the United Kingdom's Serious Hazards of Transfusion (SHOT) found an association between TRALI and plasma and platelet products donated by female patients. Low risk TRALI donor strategies, including collecting plasma from men and never pregnant women, were instituted in the early 2000s. In a meta analysis, patient populations prone to develop TRALI were found to have a significant reduction in TRALI risk (OR, 0.51; 95% CI, 0.29 - 0.90). Answer A is incorrect because premedication is not supported for the prevention of an allergic reaction. If allergic reactions are severe and recurrent, washing of red blood cell units may be considered. Answer B is incorrect because febrile nonhemolytic transfusion reaction incidence has decreased with universal leukoreduction. Answer C is incorrect because transfusion associated circulatory overload can possibly be mitigated by slow transfusion rate (1 mL/kg/hr) but data is lacking. Answer D is incorrect because transfusion associated graft versus host disease can be mitigated with irradiation and pathogen inactivation technologies (Transfusion 2015;55:164, J Hosp Med 2020 Nov;15:684, Transfusion 2004;44:25, Transfusion 2004;44:16, Transfusion 2018 ;58:1506).
Comment Here
Reference: Hemovigilance
Comment Here
Reference: Hemovigilance