Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Symptoms | Screening | Blood donor screening | Blood donor testing | Donor deferral | Case reports | Treatment | Clinical images | Sample assessment & plan | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gniadek TJ. Coombs test / DAT. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/transfusionmedcoombs.html. Accessed March 31st, 2025.
Definition / general
- Used to determine whether a patient’s red blood cells (RBCs) are coated with immunoglobulins or complement in vivo
- Originally described using Coombs reagent: polyclonal rabbit antihuman globulin serum
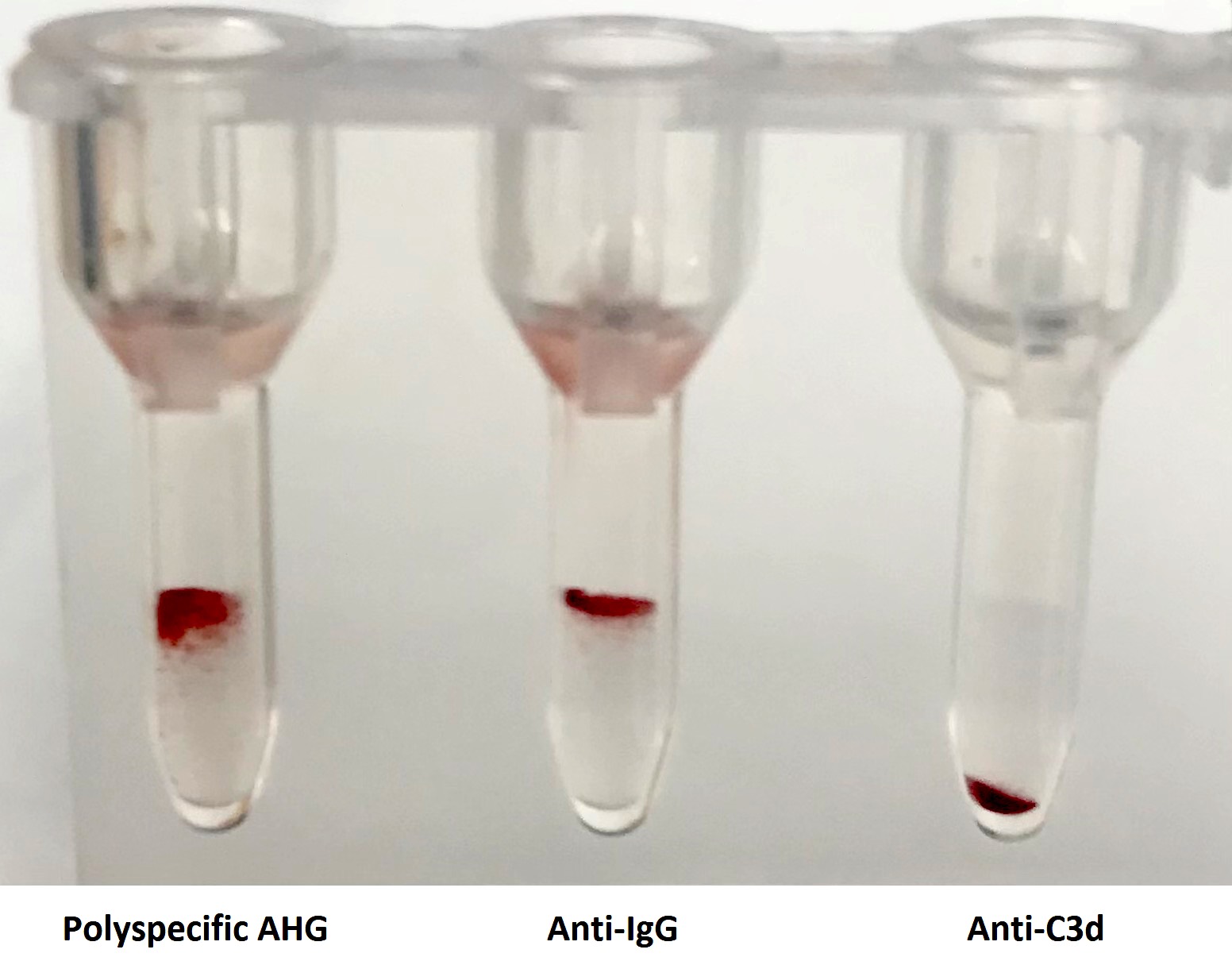
- Modern Coombs reagents include anti-immunoglobulin G (IgG) and anticomplement antibodies either mixed together into one reagent (polyspecific) or used separately (monospecific)
Essential features
- A positive Coombs test suggests that antibodies or activated complement proteins from the patient are binding to RBCs in the patient’s blood
Terminology
- Direct antiglobulin test (DAT or Coombs test): tests whether patient RBCs are coated with antibodies present in vivo
- Indirect antiglobulin test (IAT or indirect Coombs test): tests whether antibodies from a patient bind to reagent RBCs in vitro
- Autoantibody: antibody that binds patient’s own RBCs and can bind reagent / transfused RBCs as well
- Panagglutinin: a molecule (can be an IgG) that binds all RBCs tested, causing agglutination of the RBCs in tube testing
- Alloantibody: antibody that does not bind a patient’s RBCs but does bind reagent RBCs or RBCs from a donor
Pathophysiology
- Indicates whether antibodies or complement are bound to RBCs within the patient
- Polyspecific (anti-immunoglobulin and anticomplement) reagent is used in a single step screen
- If polyspecific reagent is positive, then monospecific reagents are used to determine whether the RBCs are coated with IgG or complement
- IgM antibodies often deposit complement proteins more efficiently than IgG antibodies
- IgG antibodies may or may not cause detectable complement deposition on RBCs
- Positive DAT could be due to alloantibody (alloantibody binding transfused RBCs in circulation) or autoantibody (warm or cold autoimmune hemolytic anemia as well as paroxysmal cold hemoglobinuria)
- Passenger lymphocyte syndrome: posttransplant patients can develop a positive DAT due to antibody production from donor derived lymphocytes (Blood Transfus 2015;13:423)
- Positive DAT can also be due to passively transferred antibodies, e.g. hemolytic disease of the fetus and newborn (HDFN), passive transfer of antibodies due to recent transfusion of plasma or administration of concentrated immunoglobulins (e.g. intravenous immunoglobulin (IVIG) or RhoGAM) (Transfusion 1987;27:28)
Clinical features
- Hemolysis may or may not be present in patients with a positive Coombs test
- Patients recently transfused with allogeneic RBCs who develop a positive Coombs test may have formed a RBC alloantibody
- In these cases, an eluate can be performed to determine the antigenic specificity of the antibody
- Positive Coombs test with negative eluate (i.e. no alloantibody identified in the eluate) can occur in cases of drug induced RBC antibodies (Asian J Transfus Sci 2008;2:20)
- Recently transfused patients who have antibodies against the transfused RBCs may have a negative DAT despite clear signs of hemolysis, since the transfused RBCs may have been entirely cleared from circulation prior to performing the DAT (Transfus Med Hemother 2008;35:346)
- DAT may be negative in rare cases of autoimmune hemolytic anemia (Immunohematology 1997;13:115)
- Since IgG antibody crosses the placenta, the presence of a positive DAT in cord blood suggests a maternal derived IgG that binds fetal RBCs
- This can be due to maternal alloantibodies such as anti-D but most commonly is due to maternal derived anti-A, anti-B or anti-A,B (Laeknabladid 2016;102:326)
- Maternal fetal ABO incompatibility exists in 15 - 25% of pregnancies with a 1% chance of positive cord blood DAT in these pregnancies but only ~ 23% of infants with a positive DAT will have enough hemolysis to cause clinically significant jaundice (Arch Pediatr 2011;18:279)
Symptoms
- Signs and symptoms of hemolysis may or may not be present in a patient with a positive DAT
Screening
- DAT is often performed as part of blood bank type and screen testing when the results are abnormal or when a DAT is specifically ordered by a clinician
- Prevalence of DAT positivity in hospitalized patients is high (J Clin Pathol 1979;32:1014)
- If a DAT is negative, a control reaction with check cells (abbreviated as “cc”) is performed to confirm that the Coombs reagent is working; the check cells should be positive and serve as a positive control
Blood donor screening
- Blood donors are not routinely tested with DAT
- Studies have shown approximately 0.008% of donors have a positive DAT (Asian J Transfus Sci 2019;13:70)
- Presence of a positive DAT in a blood donor may correlate with an increased risk for future diagnosis of malignancy, especially hematologic malignancies; however, larger studies are needed to confirm this finding (Transfusion 2009;49:838)
Blood donor testing
- Not routinely performed
Donor deferral
- Although there is currently no universal guideline to defer a donor who has a positive DAT, a blood donor center medical director may elect to defer the donor out of caution
Case reports
- 37 year old liver transplant recipient who developed hemolytic anemia and positive DAT in the setting of posttransplant passenger lymphocyte syndrome (Transfusion 2017;57:1262)
- 70 year old patient incompatible with a donor RBC unit in AHG phase due to the donor having a positive DAT (Transfus Apher Sci 2014;50:239)
- 72 year old man with CLL presenting with panagglutinin and positive DAT (CMAJ 2006;174:305)
Treatment
- Positive DAT without signs of hemolysis is not an indication for treatment
- In recently transfused patients, a positive DAT (especially a newly positive DAT) is an indication for performing an eluate to evaluate for the development of an alloantibody
- Alloantibodies can cause a positive DAT and positive eluate in recently transfused patients even if the serum antibody screen is negative
- If an alloantibody is identified on an eluate, then antigen negative crossmatch compatible RBCs are indicated for future transfusions
- Reference: Blood 2019;133:1821
Sample assessment & plan
- Positive DAT, negative eluate and negative antibody screen:
- Assessment: The patient is a 75 year old woman with a history of recent Bactrim use. The blood group antibody screen is negative for common clinically significant alloantibodies. The direct antiglobulin test (DAT) is positive with anti-IgG. An eluate was performed, which did not react with any of the control cells tested. Potential causes of a positive DAT with negative eluate include drug-induced RBC antibodies and hypergammaglobulinemia (Arch Pathol Lab Med 2017;141:305).
- Plan: Drug dependent RBC antibody testing is available upon request. Patients with a positive DAT should be monitored for signs and symptoms of hemolysis.
- Positive DAT due to autoantibody:
- Assessment: The patient is an 80 year old man with a history of lymphoma. The blood group antibody screen is positive at 37 °C for a panagglutinin and the direct antiglobulin test is positive using anti-IgG and anti-C3d reagents. An eluate was performed which showed reactivity against all controls cells tested. The patient has not been transfused in the past, therefore an autoabsorption was performed. Autoabsorped plasma showed no reactivity against the control cells tested, ruling out an underlying alloantibody against common clinically significant antigens. These findings are consistent with a warm autoantibody.
- Plan: The patient should be monitored for signs of hemolysis.
Differential diagnosis
- Nonantibody mediated RBC agglutination due to Wharton jelly contamination of cord blood or rouleaux
- Nonspecific antibody binding due to elevated immunoglobulin levels, secondary to antiphospholipid antibodies or infection
- Incomplete washing of RBCs, overcentrifugation or other lab error (Arch Pathol Lab Med 2017;141:305)
Additional references
Board review style question #1
A 45 year old woman with no prior history of RBC transfusion presented with anemia. The results of a patient’s direct antiglobulin (DAT) / Coombs test are shown above. An eluate was performed, which reacted with 11 of 11 control RBCs tested by indirect antiglobulin test (IAT) in gel. Which of the following is the most likely diagnosis?
- Cold agglutinin disease
- Warm autoimmune hemolytic anemia
- Hemolytic transfusion reaction
- Drug dependent RBC antibody
Board review style answer #1
Board review style question #2
Plasma from patient A was crossmatched with four randomly selected RBC units using antihuman globulin (AHG) reagent in gel: 1 of the 4 crossmatches were positive. However, patient A’s plasma did not react with any reagent screening cells or any other RBC units tested. The RBC unit that yielded the positive crossmatch with patient A’s plasma also resulted in a positive AHG crossmatch when tested with plasma from five other patients who all had negative antibody screens.
What is the most likely explanation?
What is the most likely explanation?
- Patient A has an antibody against a low frequency RBC antigen
- Patient A has an autoantibody
- The donor of the reactive RBC unit has an alloantibody
- The donor of the reactive RBC unit has a warm autoantibody
Board review style answer #2
D. The donor of the reactive RBC unit has a warm autoantibody
Comment Here
Reference: Coombs test / DAT
Comment Here
Reference: Coombs test / DAT