Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Florianova L, Pusztaszeri M. Tall cell. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidtallcellvariant.html. Accessed April 2nd, 2025.
Definition / general
- Papillary thyroid carcinoma (PTC) variant characterized by presence of ≥ 30% of tall cells (2 - 3 times taller than wide) with abundant granular eosinophilic (oncocytic-like) cytoplasm and the typical nuclear changes of PTC
- Variable diagnostic criteria over time with significant interobserver variability (Thyroid 2017;27:1498)
- Often underrecognized (Thyroid 2008;18:1179, Thyroid 2007;17:655)
- First described in 1976 (Cleve Clin Q 1976;43:207)
Essential features
- The most common aggressive variant of papillary thyroid carcinoma, characterized by tall cells occupying ≥ 30% tumor and well developed papillary thyroid carcinoma nuclear features
- Usually requires more aggressive treatment and closer disease surveillance
- BRAF V600E mutation present in most cases
- Papillary thyroid carcinomas with tall cell features (≥ 10% tall cells) have worse prognosis than those without tall cells; more than 10% tall cells in a tumor should be reported in final pathology reports
Terminology
- 2017 WHO classification of tumors of endocrine organs requires ≥ 30% of tall tumor cells to define this variant
- Variable diagnostic criteria over time
- WHO 2017 (current): 2 - 3x height / width cells occupying ≥ 30% tumor
- WHO 2004 (outdated): 3x height / width cells occupying ≥ 50% tumor
- If tall cell features are > 10% but < 30%, the tumor should be designated as PTC with tall cell features (Endocr Relat Cancer 2015;22:419)
ICD coding
Epidemiology
- 5 - 10% of PTCs (World J Surg 2008;32:1535)
- Usually older age patients; exceedingly rare in the pediatric population
- F > M (Oncotarget 2016;7:40792, Thyroid 2007;17:655, Laryngoscope 2008;118:32)
Sites
- Thyroid
- Exceedingly rare at other sites, e.g. ectopic thyroid tissue in thyroglossal duct (see case reports below)
Pathophysiology
- Clonal neoplastic proliferation of thyroid follicular cells, usually with a specific driver mutation (see molecular / cytogenetics description below)
Etiology
- Sporadic in most cases
- Shared risk factors with most other variants of PTC
- Ionizing radiation and pre-existing benign thyroid disease
Clinical features
- Asymptomatic or enlarging neck mass
- May present as an incidental thyroid nodule
- Local symptoms (dysphagia, hoarseness, stridor) may be present for more advanced cases with vocal cord paralysis or tracheal compression
- Thyroid function tests at the time of diagnosis are typically normal
Diagnosis
- Gold standard for the diagnosis of the tall cell variant is histopathologic evaluation of thyroid resection specimens
- Nevertheless, tall cell features may be recognized on fine needle aspiration cytology
Laboratory
- Persistent or recurrent disease can be monitored by serum thyroglobulin (J Clin Endocrinol Metab 2003;88:3668)
Radiology description
- Cold nodules on thyroid scanning
- Highly suspicious nodule on thyroid ultrasound in most cases
- Markedly hypoechoic solid nodule with microcalcifications and ill defined spiculated or microlobulated margins (Front Endocrinol (Lausanne) 2018;9:223, Ultrasonography 2017;36:103, J Ultrasound Med 2011;30:853)
- Extrathyroidal extension and metastatic lymph nodes are commonly seen
Prognostic factors
- Even without extrathyroidal extension, tall cell variant was shown to have a more aggressive behavior than classic PTC independent of age, gender and tumor size (Thyroid 2007;17:655)
- Often but not always larger tumor size, more frequent extrathyroidal extension and lymph node involvement as well as a higher stage at presentation than classic PTC (Thyroid 2007;17:655, Laryngoscope 2008;118:32, Hum Pathol 2007;38:212, Oncol Lett 2017;13:3501, Oncotarget 2017;8:6222, Oncotarget 2016;7:40792)
- Higher recurrence rate, increased tumor related mortality and more frequent distant metastases compared with classic PTC (Thyroid 2007;17:655, Laryngoscope 2008;118:32, Oncol Lett 2017;13:3501, Oncotarget 2017;8:6222, Oncotarget 2016;7:40792)
- Accounts for ~20% of radioiodine refractory thyroid carcinomas (Thyroid 2008;18:1179, Cancer 2008;113:48)
- Risk of dedifferentiation into poorly differentiated or anaplastic thyroid carcinoma (tall cell PTC often seen as a component of these tumors) (Mod Pathol 1991;4:637)
- The tall cell variant of papillary microcarcinoma (< 1 cm) is also associated with aggressive features at presentation and should be differentiated from other papillary thyroid microcarcinomas (Thyroid 2013;23:1525, Thyroid 2007;17:655)
Case reports
- 40 year old woman with tall cell PTC in struma ovarii (J Cancer Res Ther 2013;9:119)
- 51 year old man with hemoptysis, shortness of breath and stridor (Case Rep Endocrinol 2017;2017:4581626)
- 62 year old man with a metastasis to the pancreas (JOP 2006;7:417)
- 72 year old man with a combined tall cell and Hürthle cell thyroid carcinoma (Arch Pathol Lab Med 2001;125:541)
- 75 year old woman with a brain metastasis at initial presentation (Head Neck Oncol 2009;1:23)
- 77 year old woman with tall cell PTC arising in a thyroglossal duct cyst Ann Med Surg (Lond) 2015;4:129)
- 80 year old woman with a squamous cell carcinoma arising in a tall cell PTC (J Clin Pathol 2005;58:662)
- Man with a thyroid carcinoma with mixed tall cell and columnar cell features (Am J Clin Pathol 1990;94:442)
Treatment
- Total thyroidectomy in most cases
- With or without neck lymph node dissection with or without radioiodine therapy in selected cases
- BRAF targeted therapy may be beneficial in selected advanced cases (J Endocr Soc 2017;1:285, Lancet Oncol 2016;17:e468)
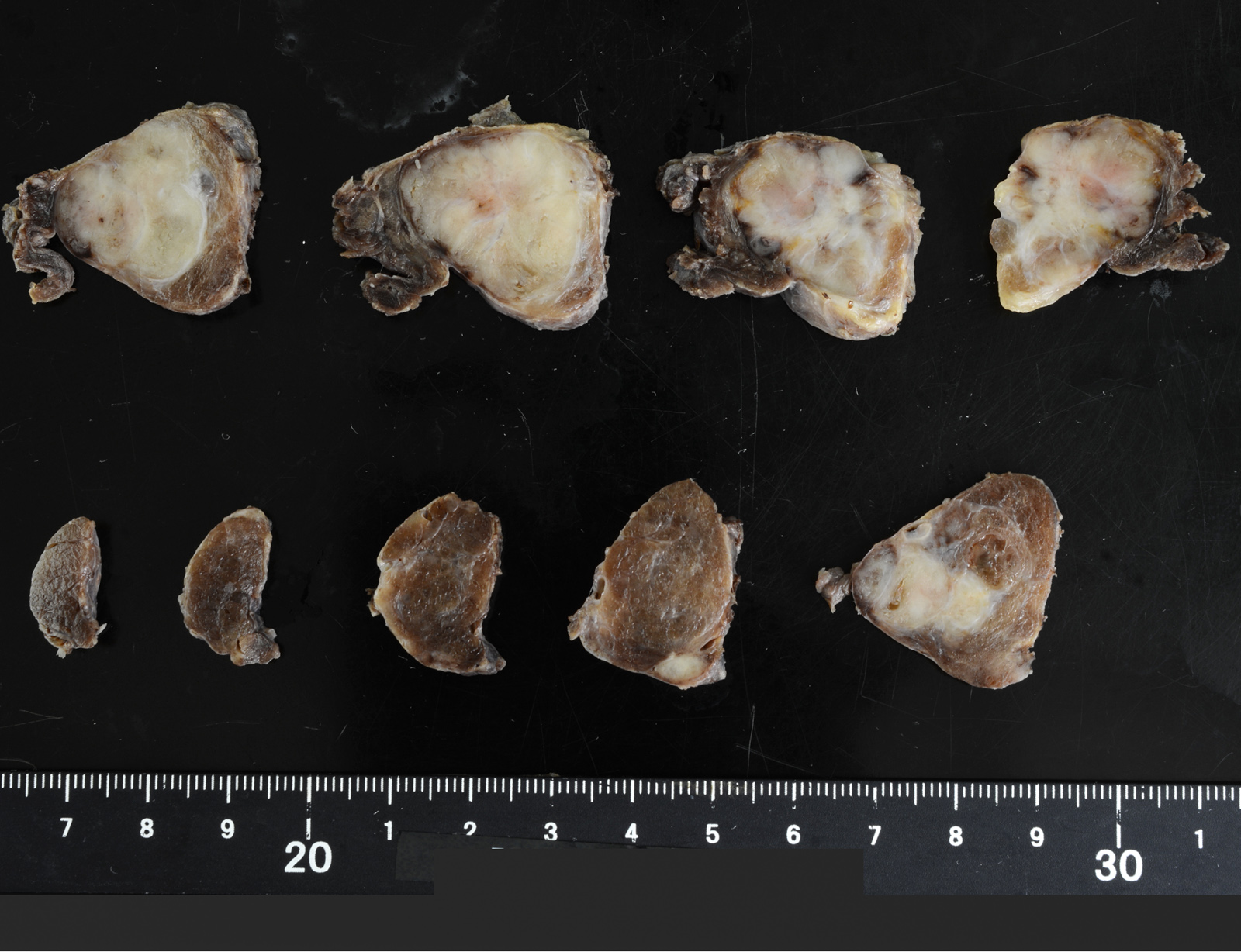
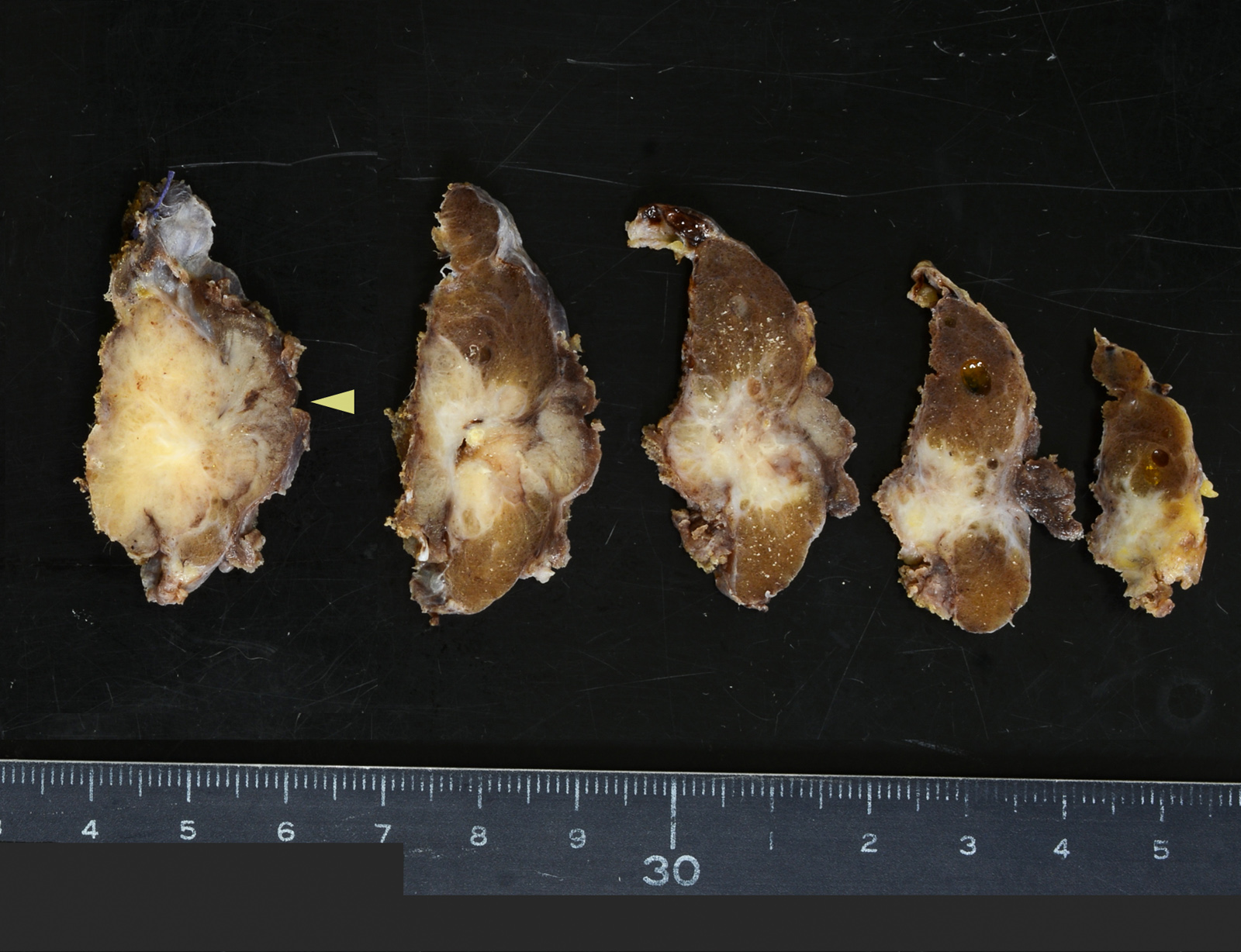
Gross description
- Tend to be large (> 5 cm)
- Extrathyroidal extension may be grossly apparent
Frozen section description
- Frozen section is usually not indicated
- Standard of care is to perform preoperative fine needle aspiration to establish the diagnosis of PTC and to determine the most appropriate surgical procedure
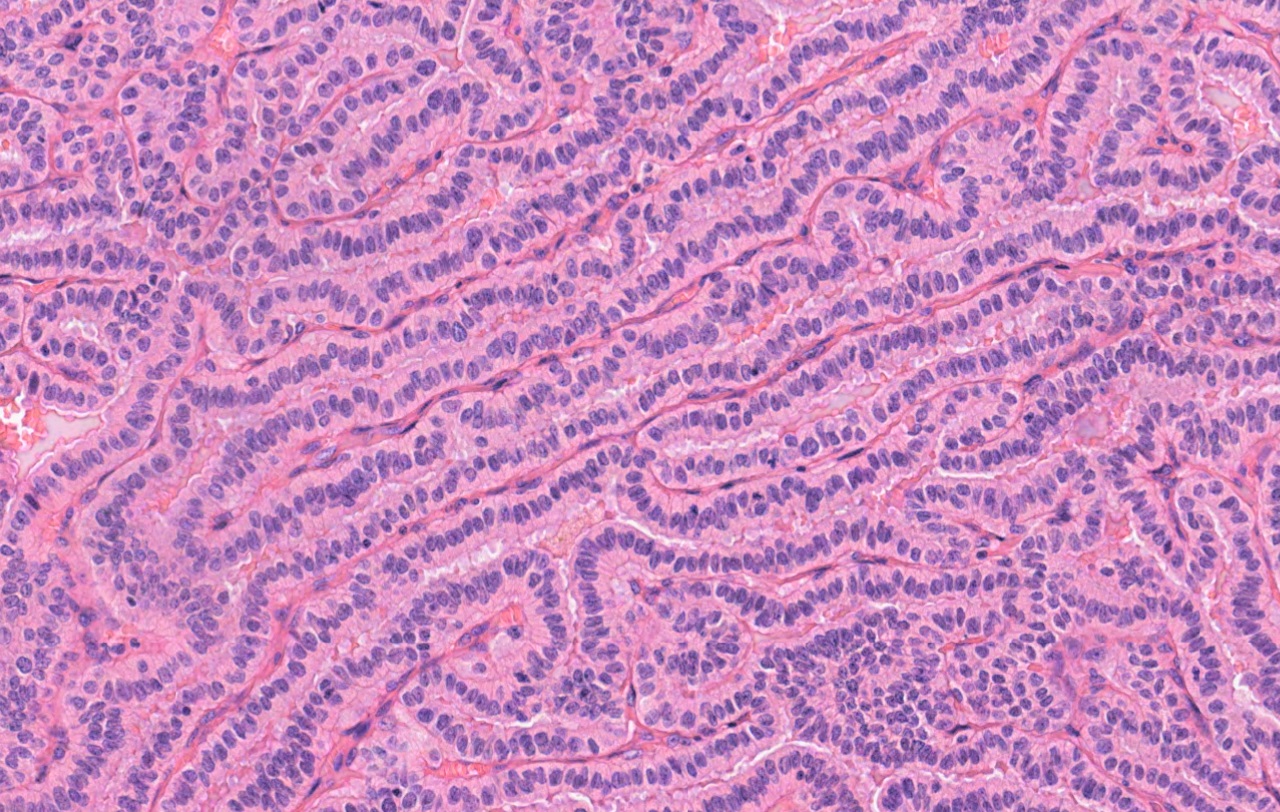
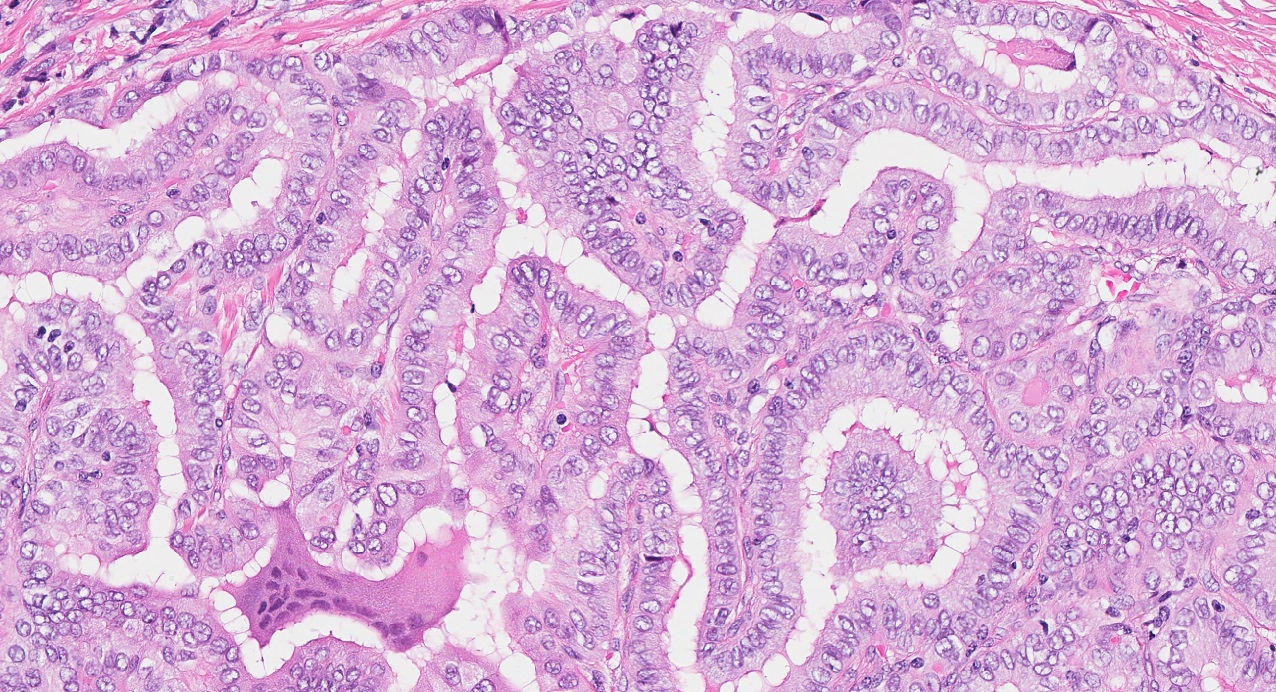
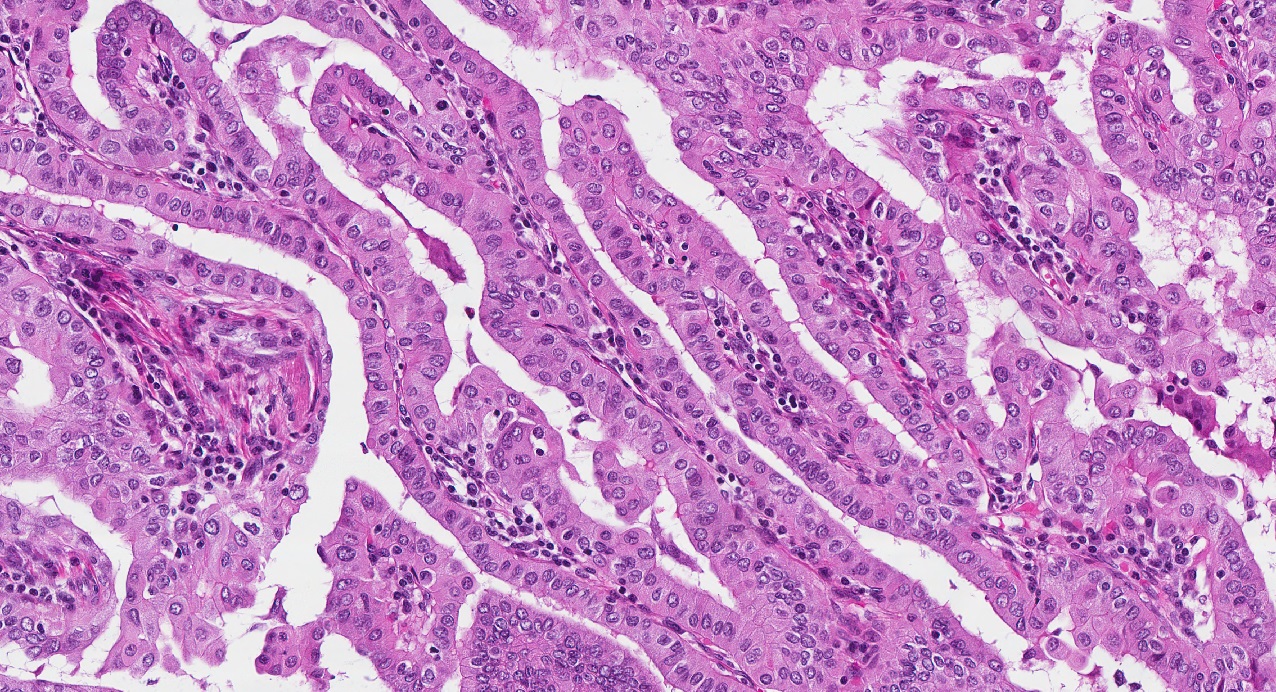
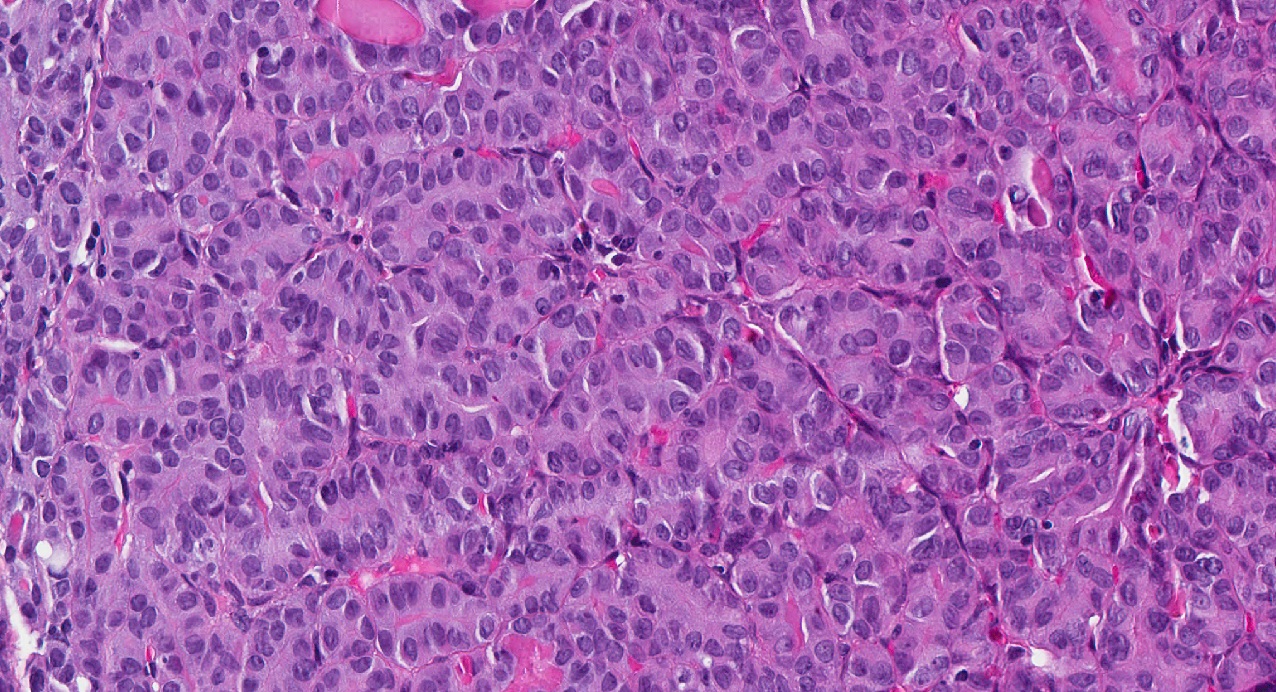
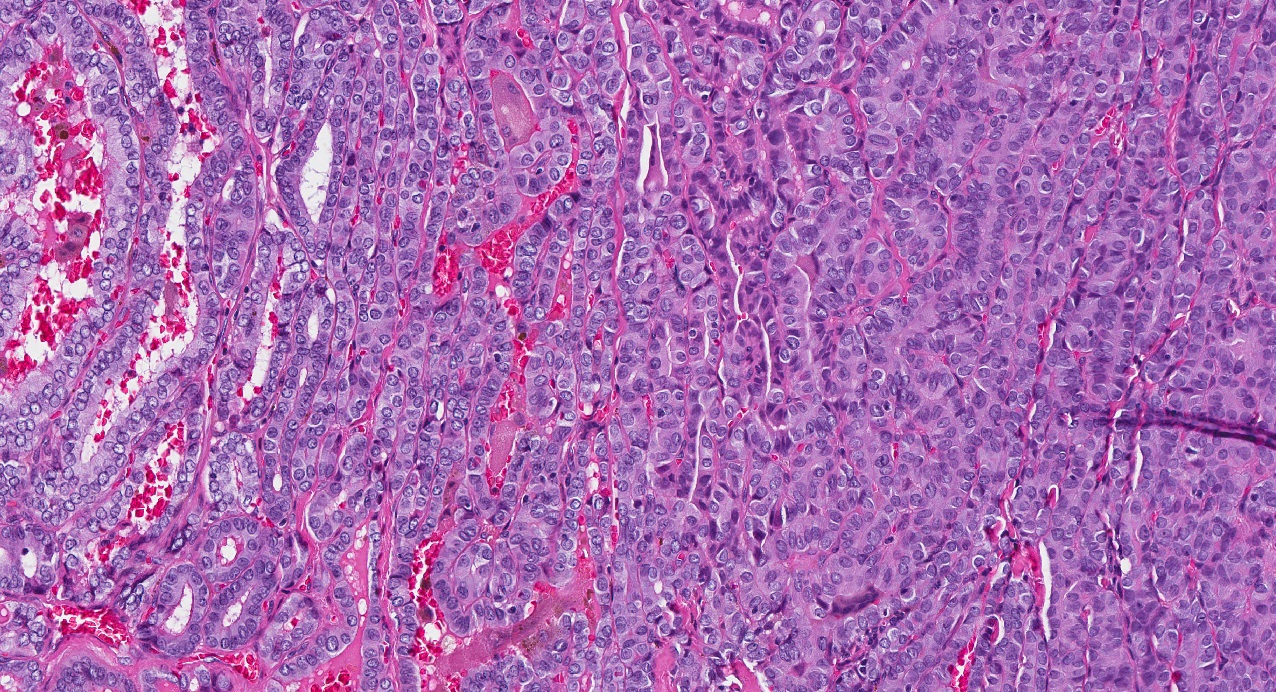
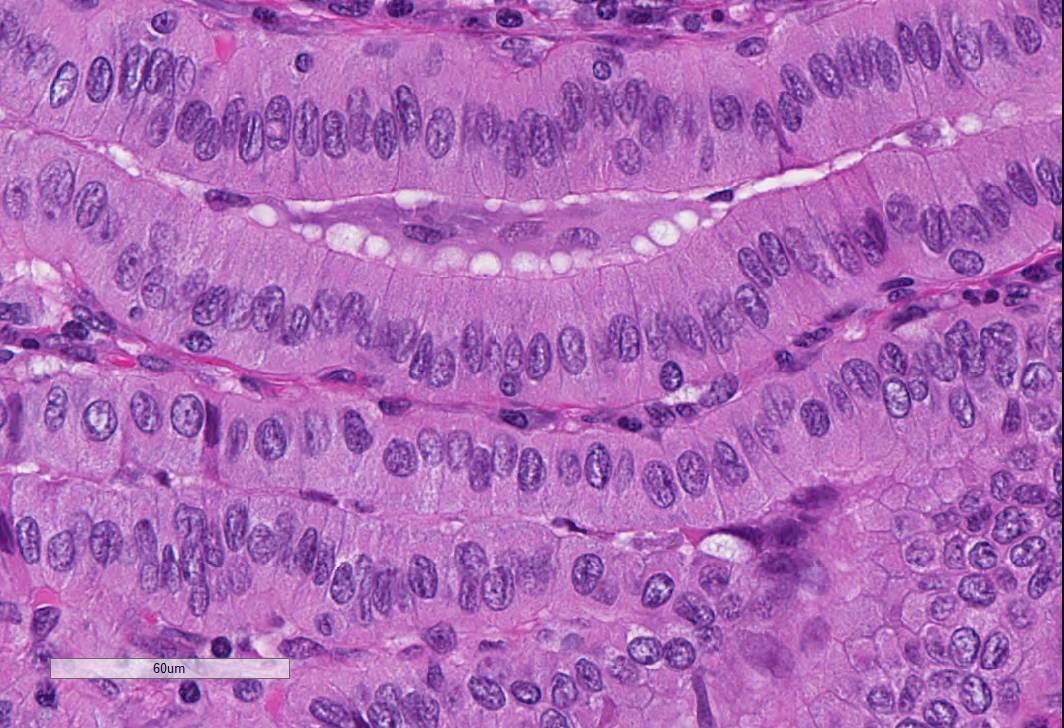
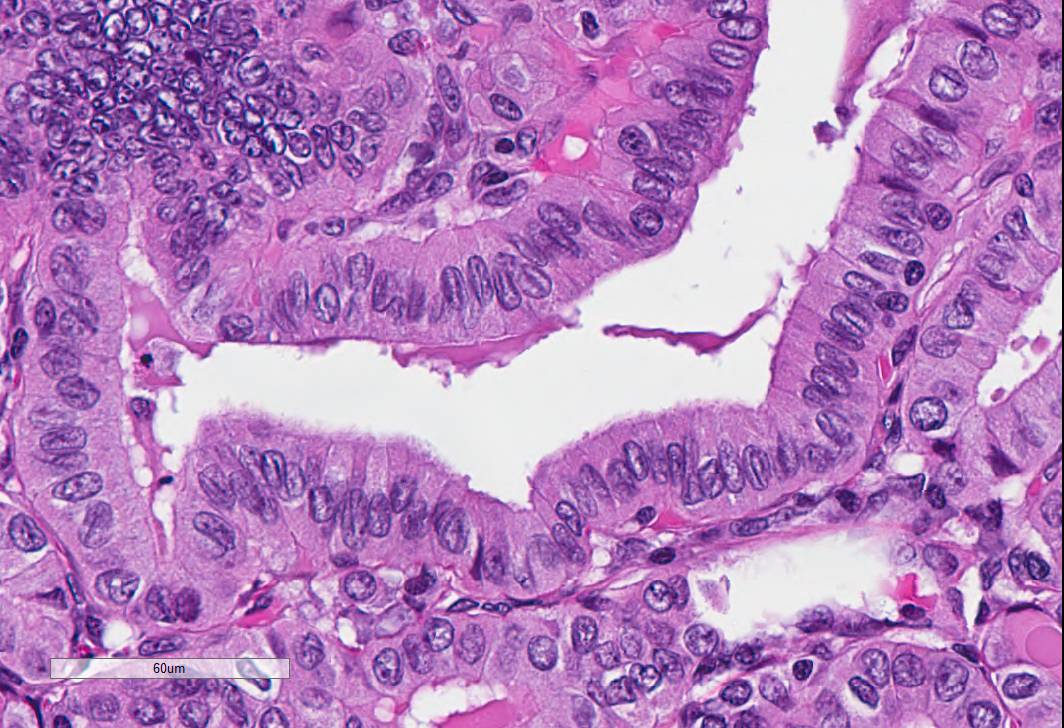
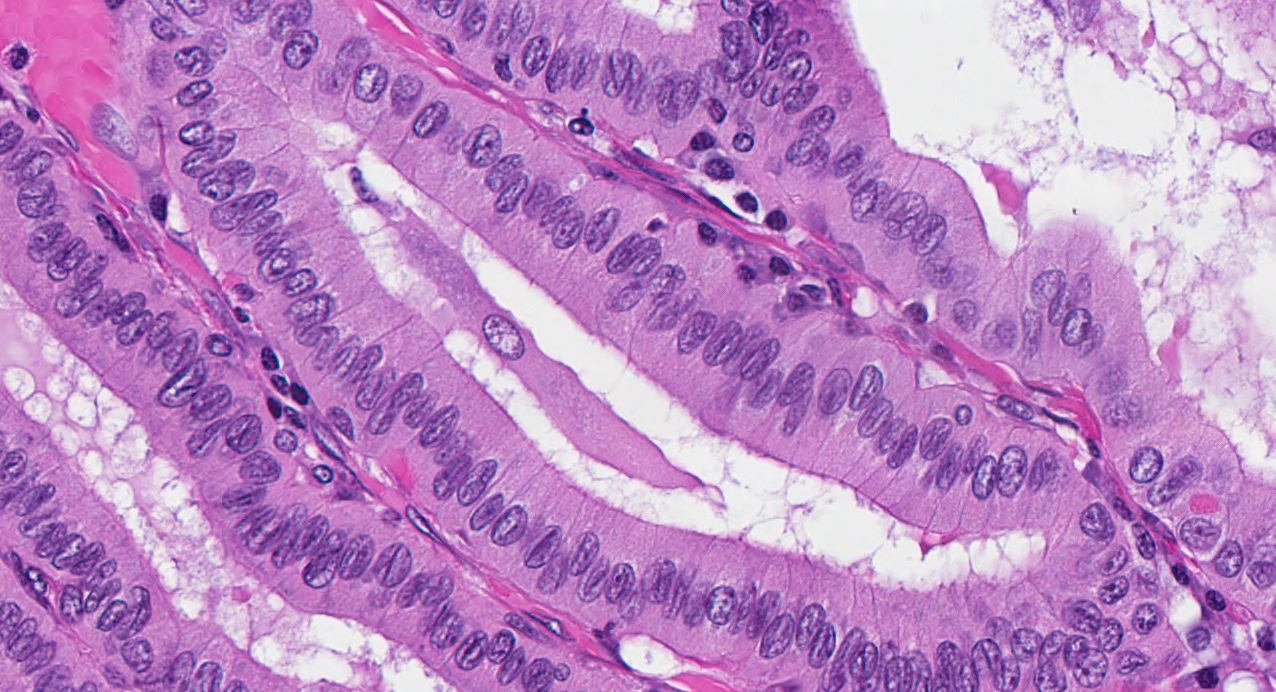
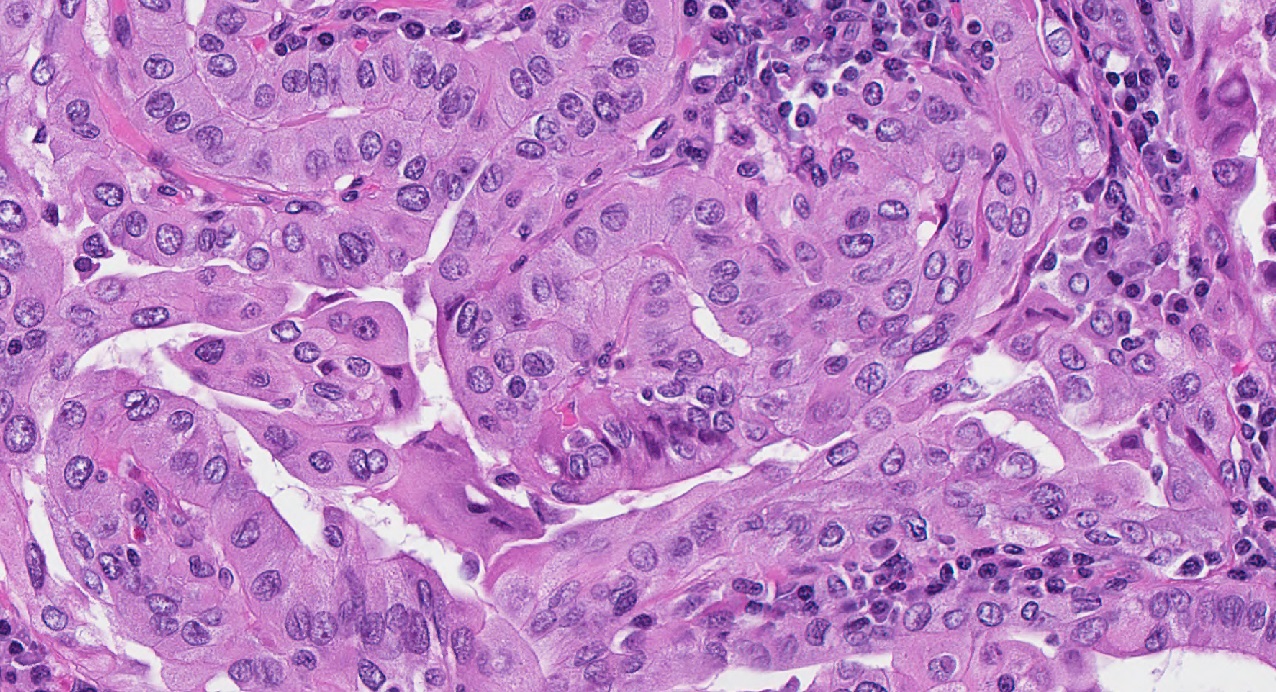
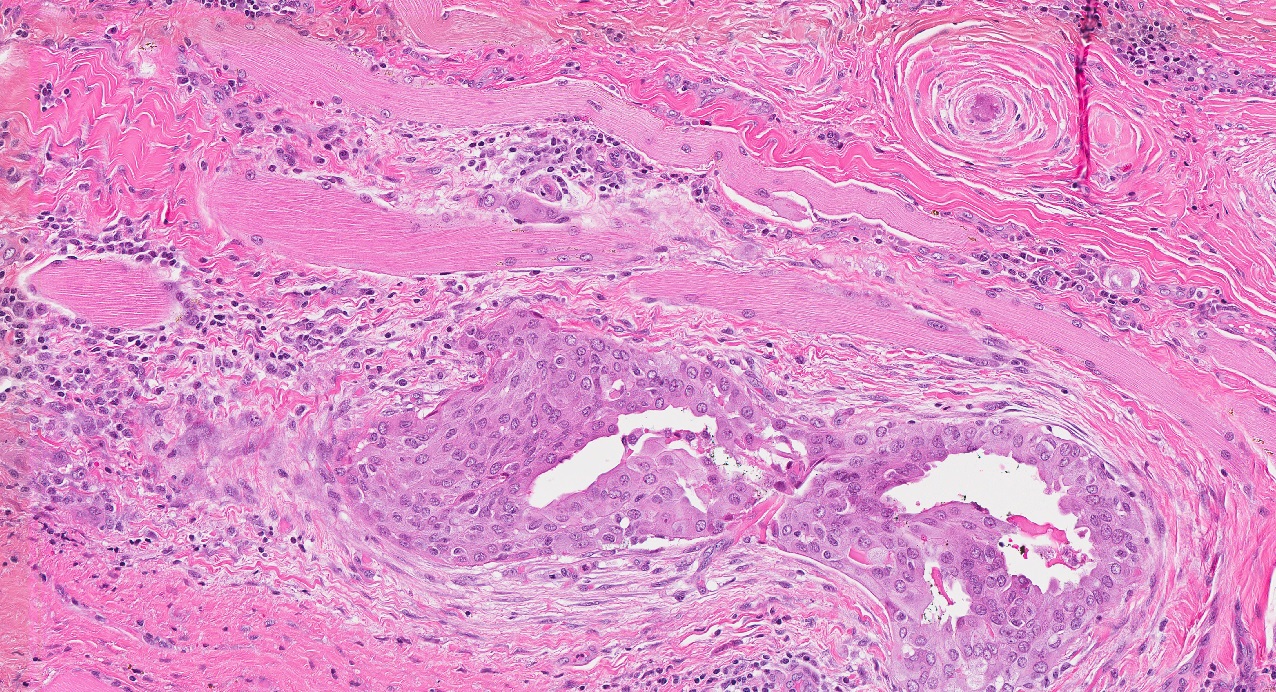
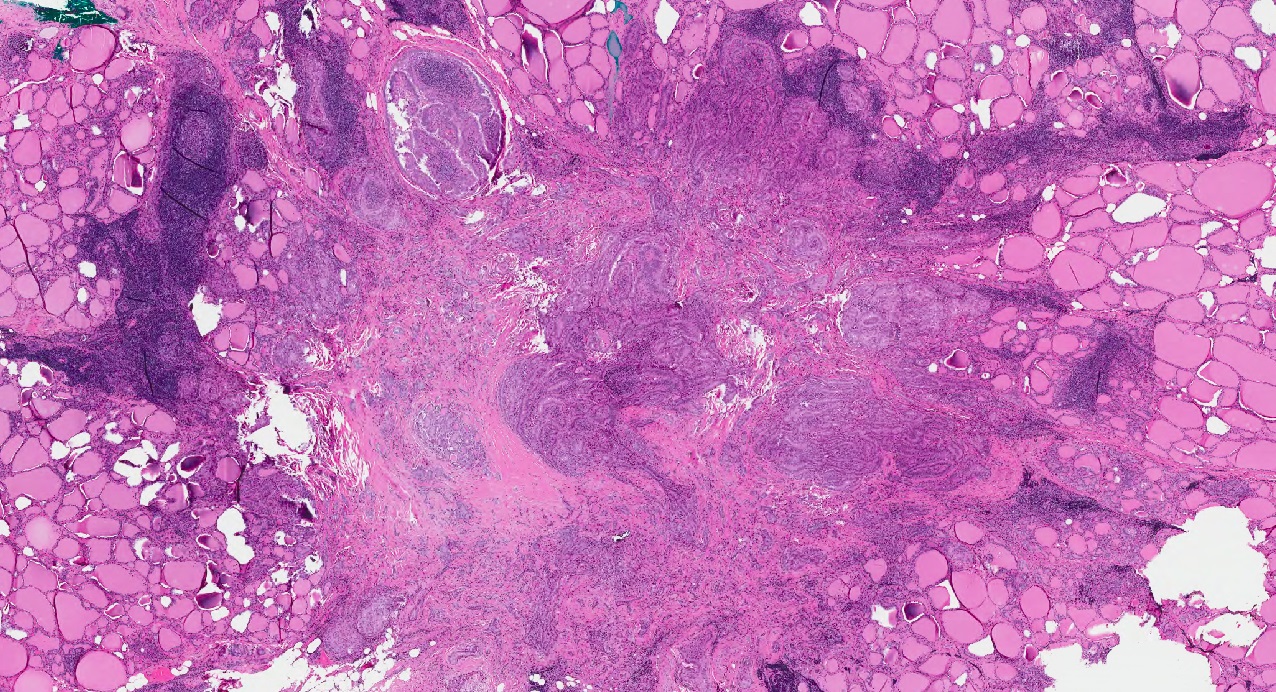
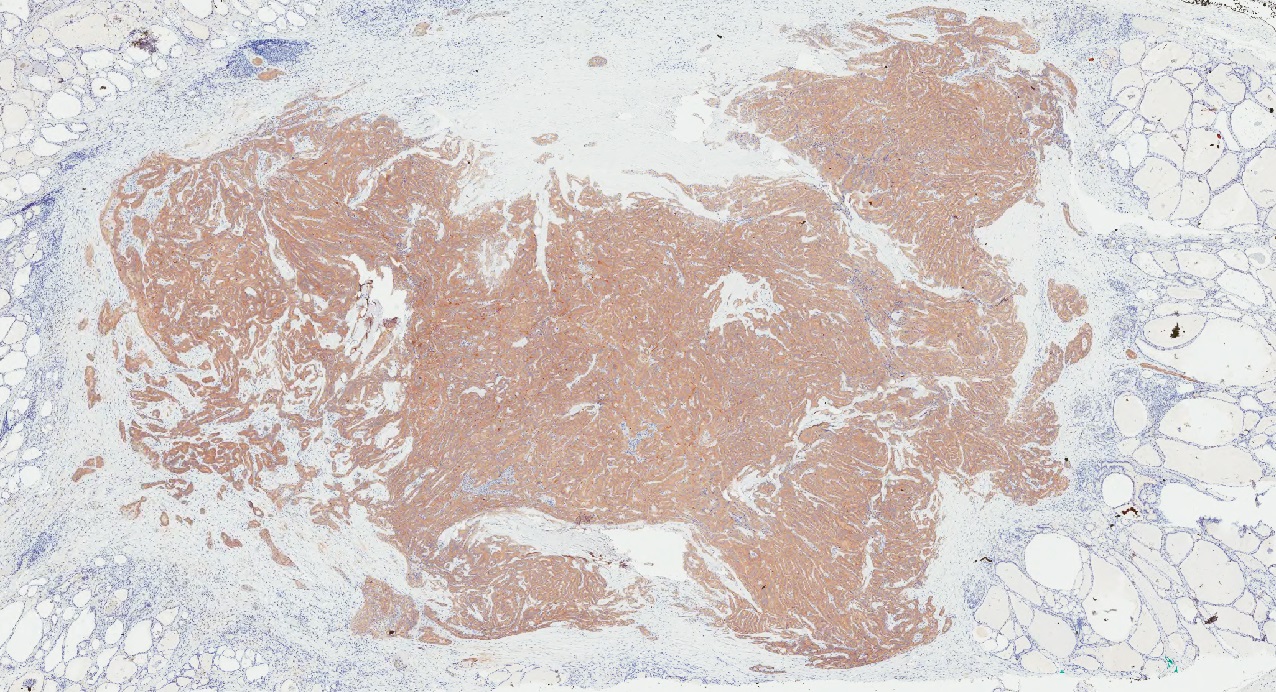
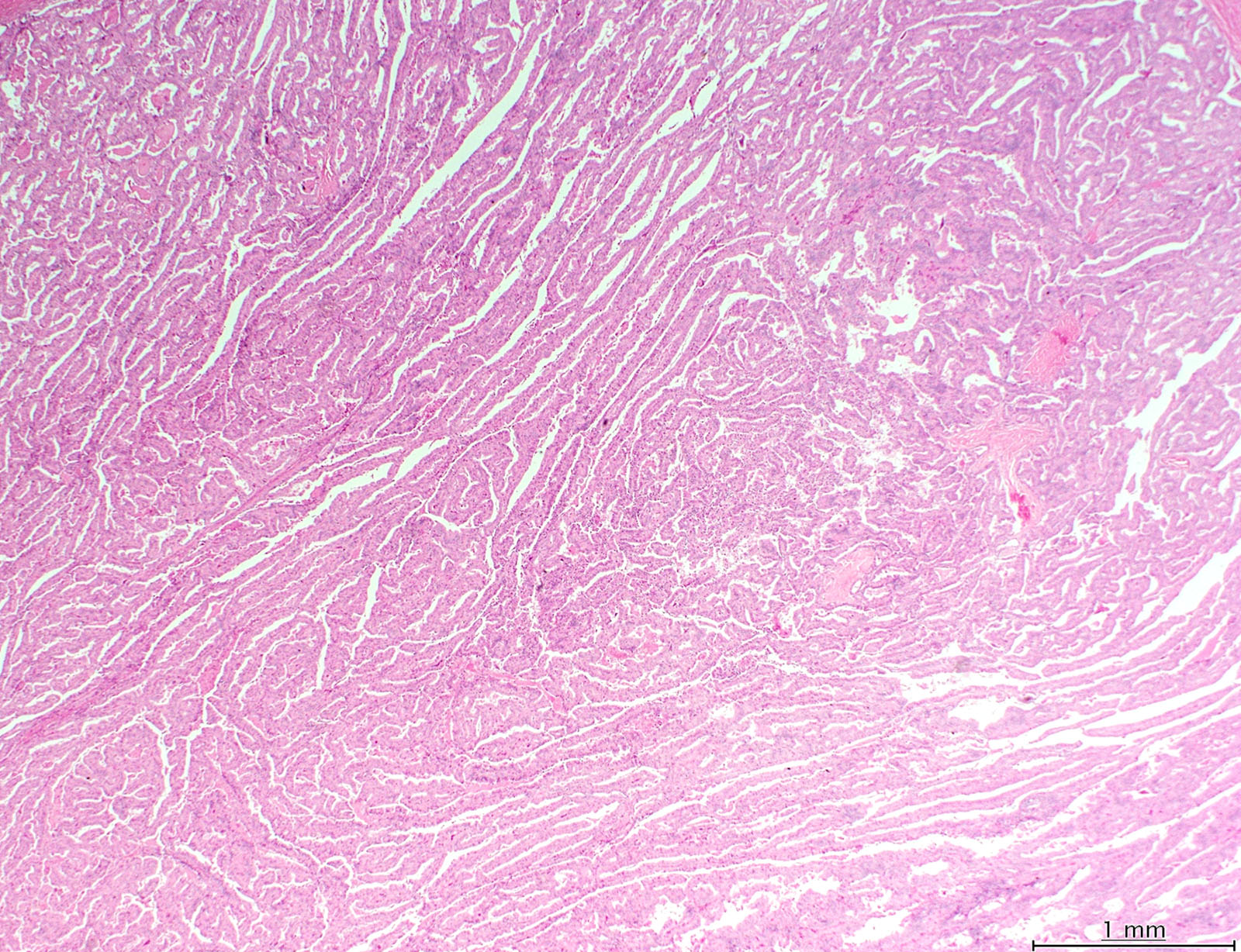
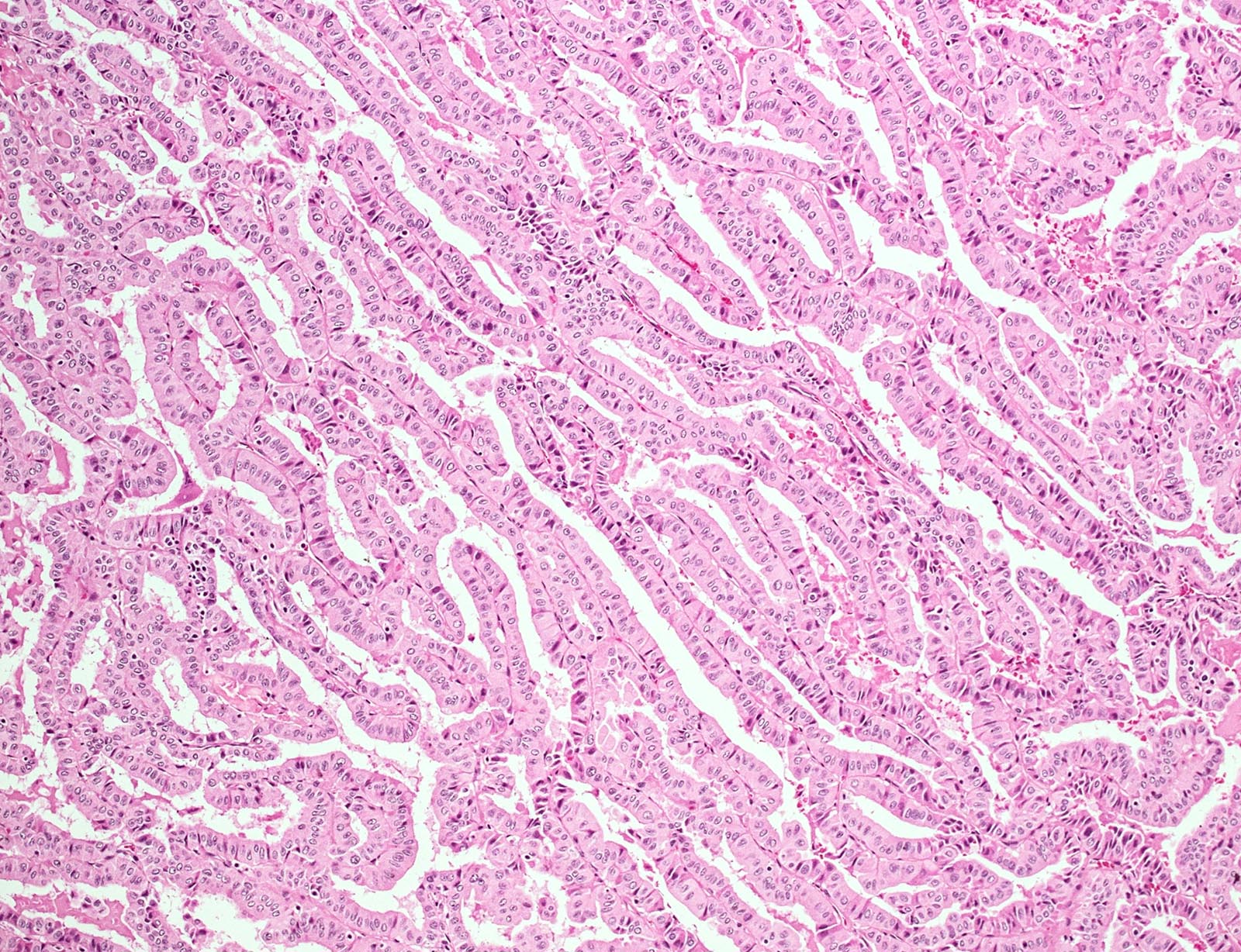
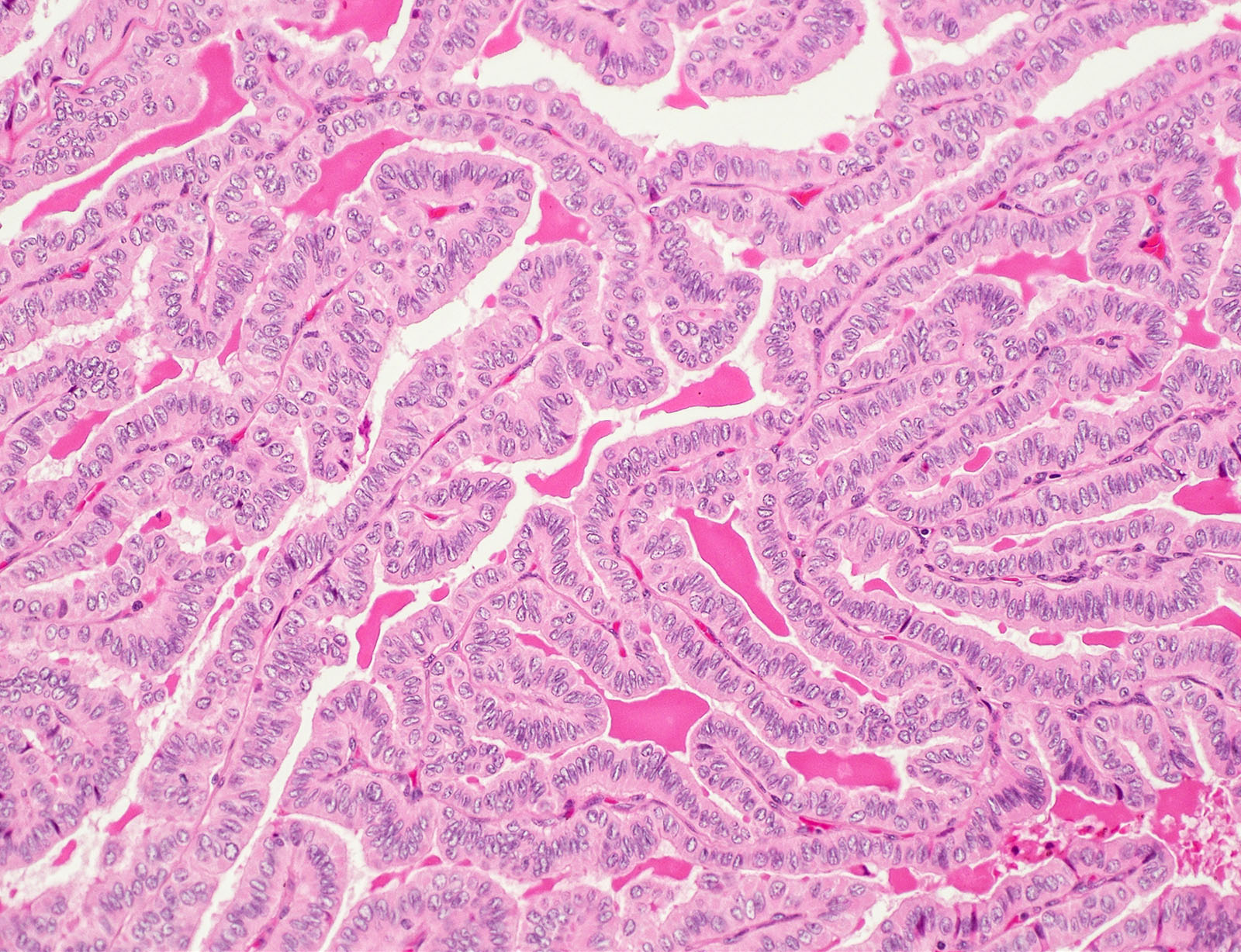
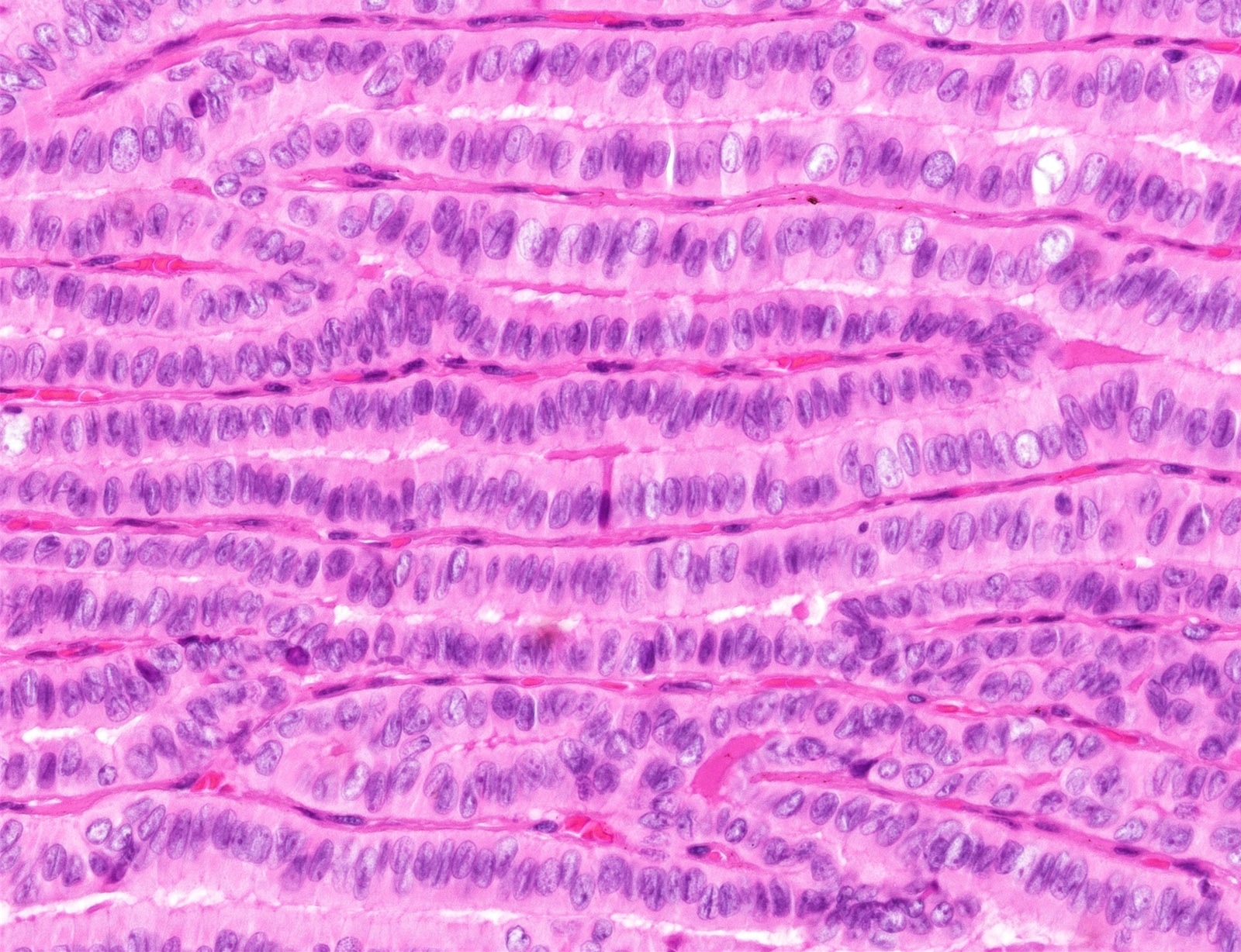
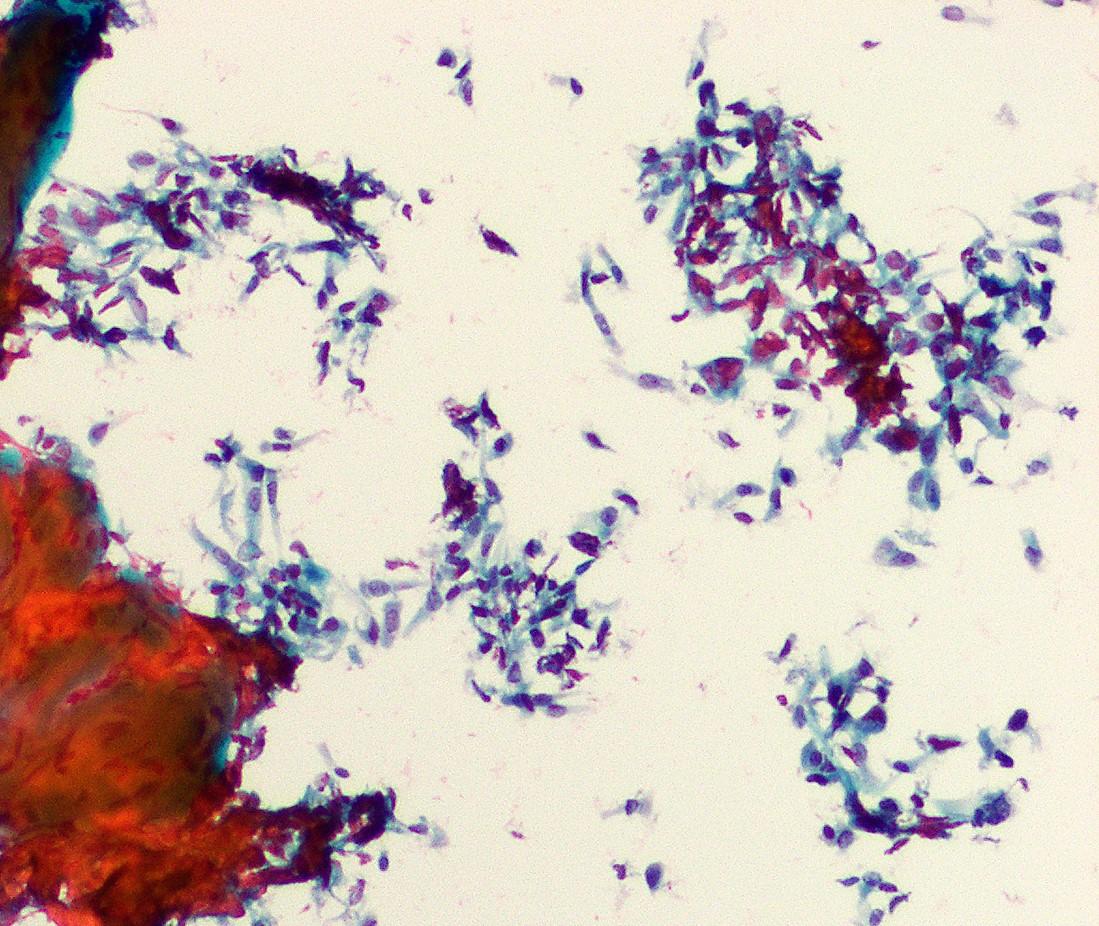
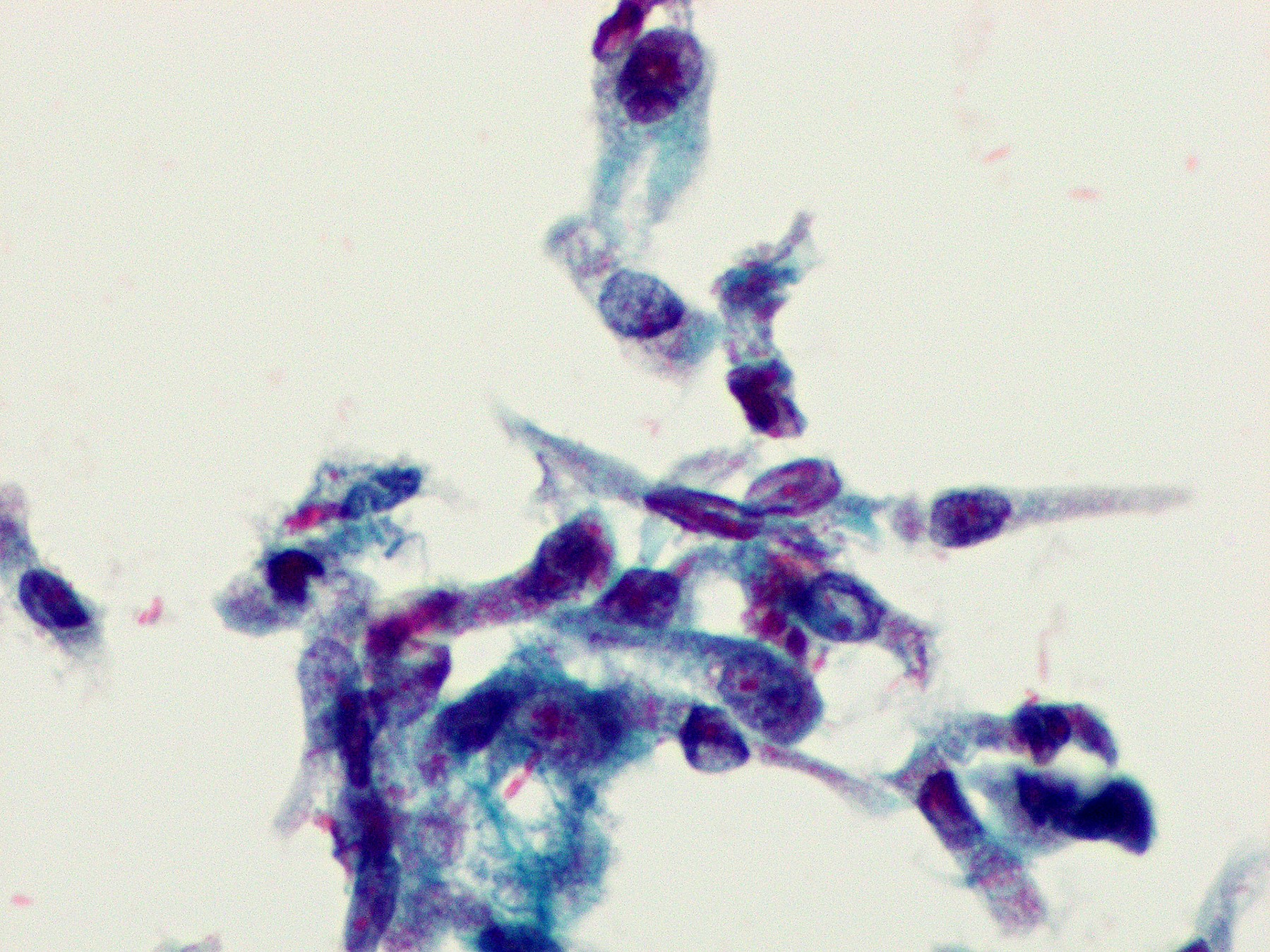
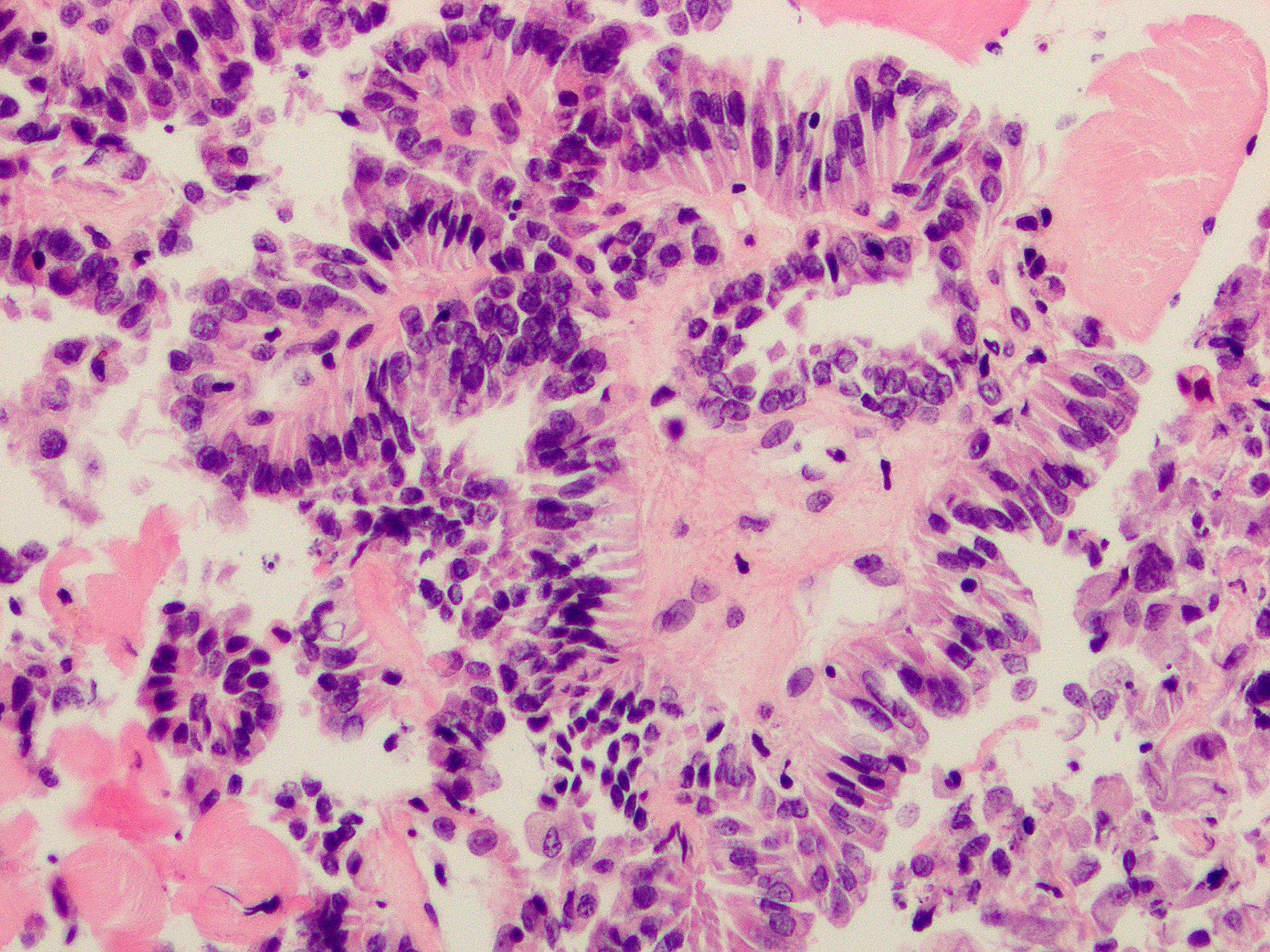
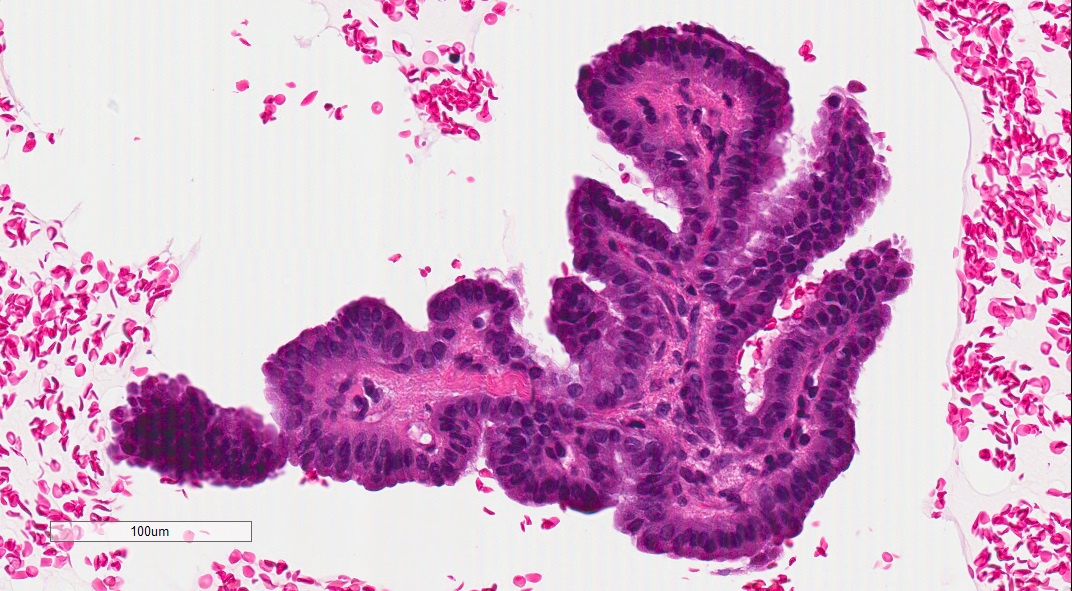
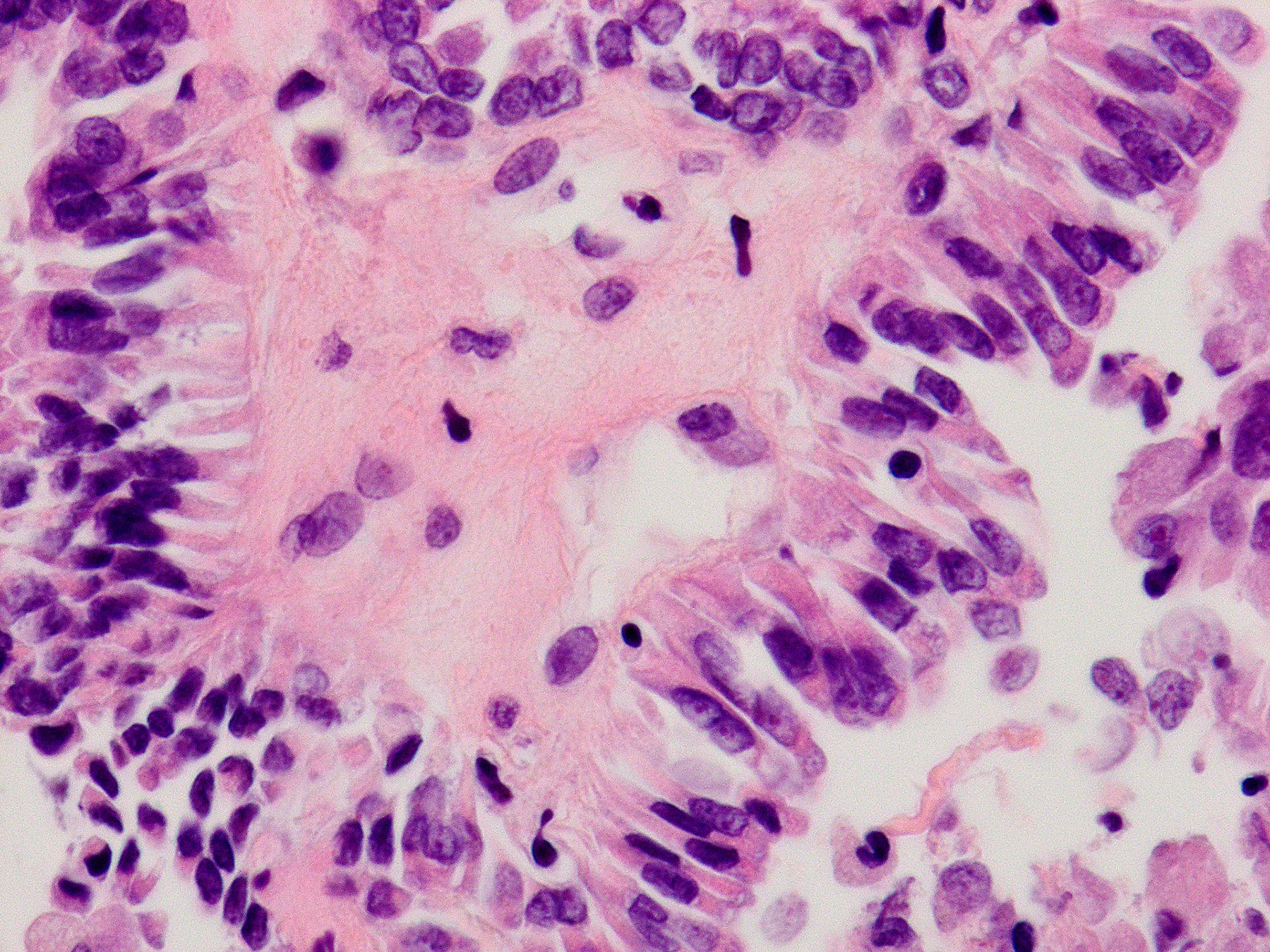
Microscopic (histologic) description
- Usually unencapsulated and infiltrative
- Growth patterns
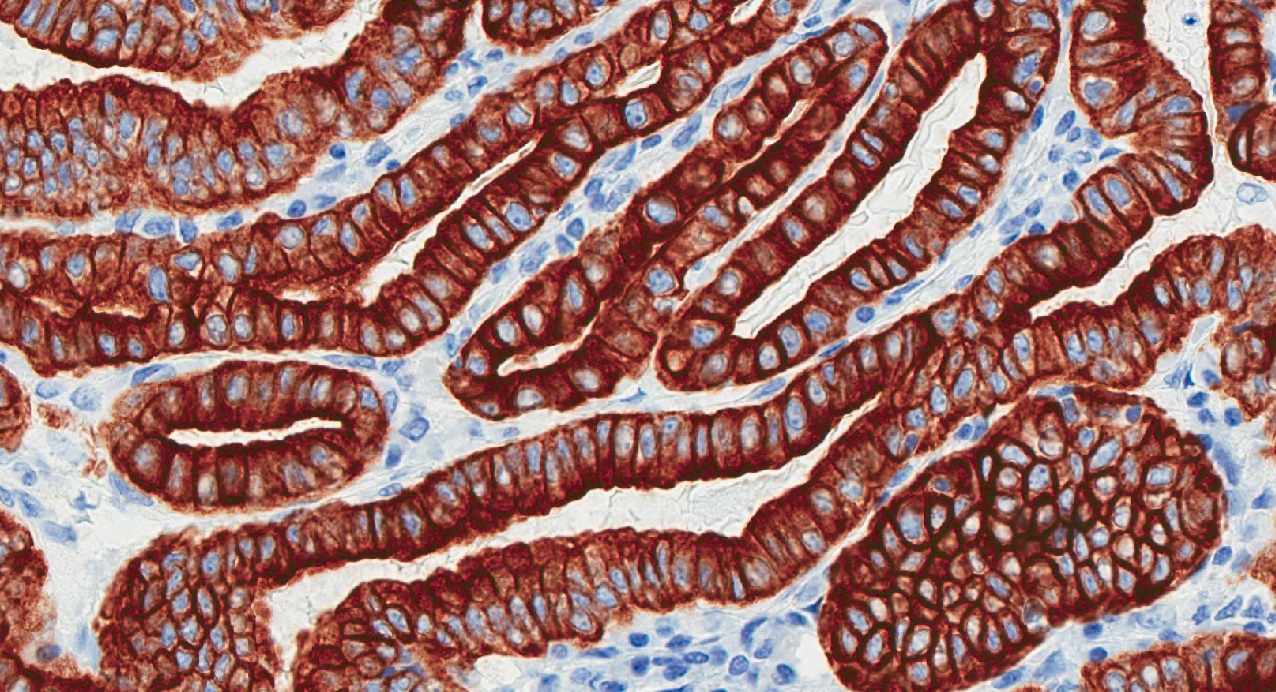
- Papillary is the most common
- Trabecular (due to closely packed papillae) and follicular
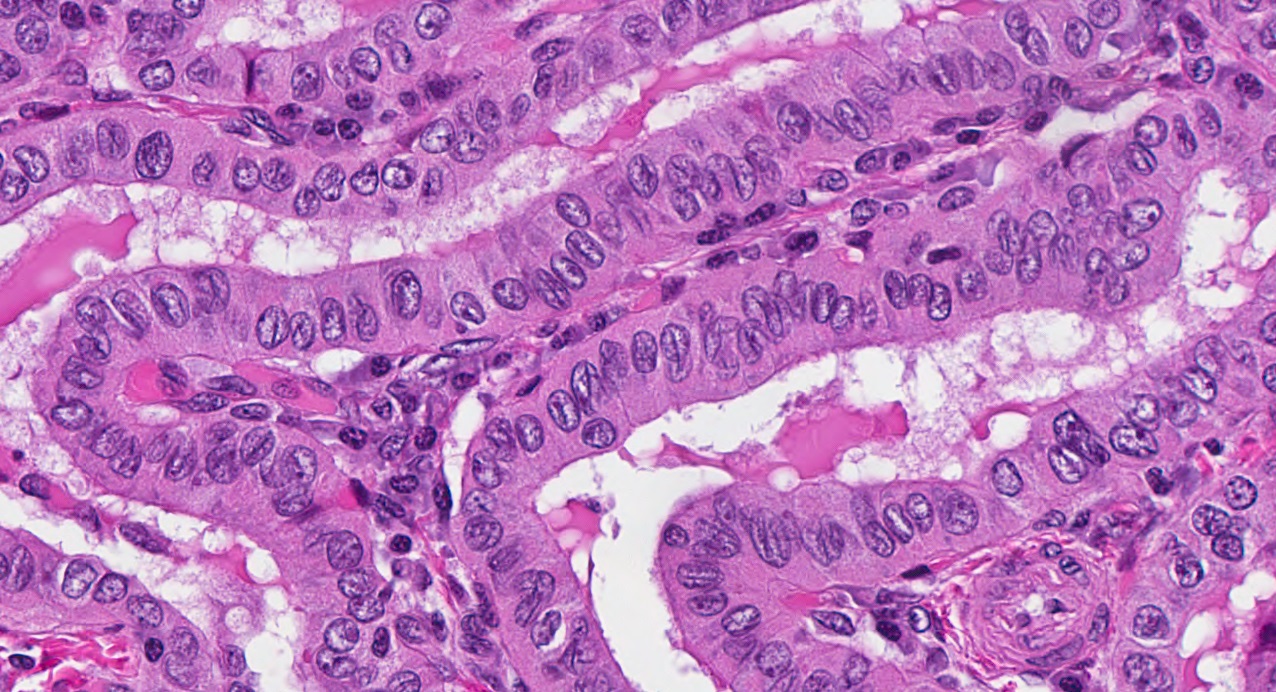
- Areas of tram track or railroad track-like appearance on lower power
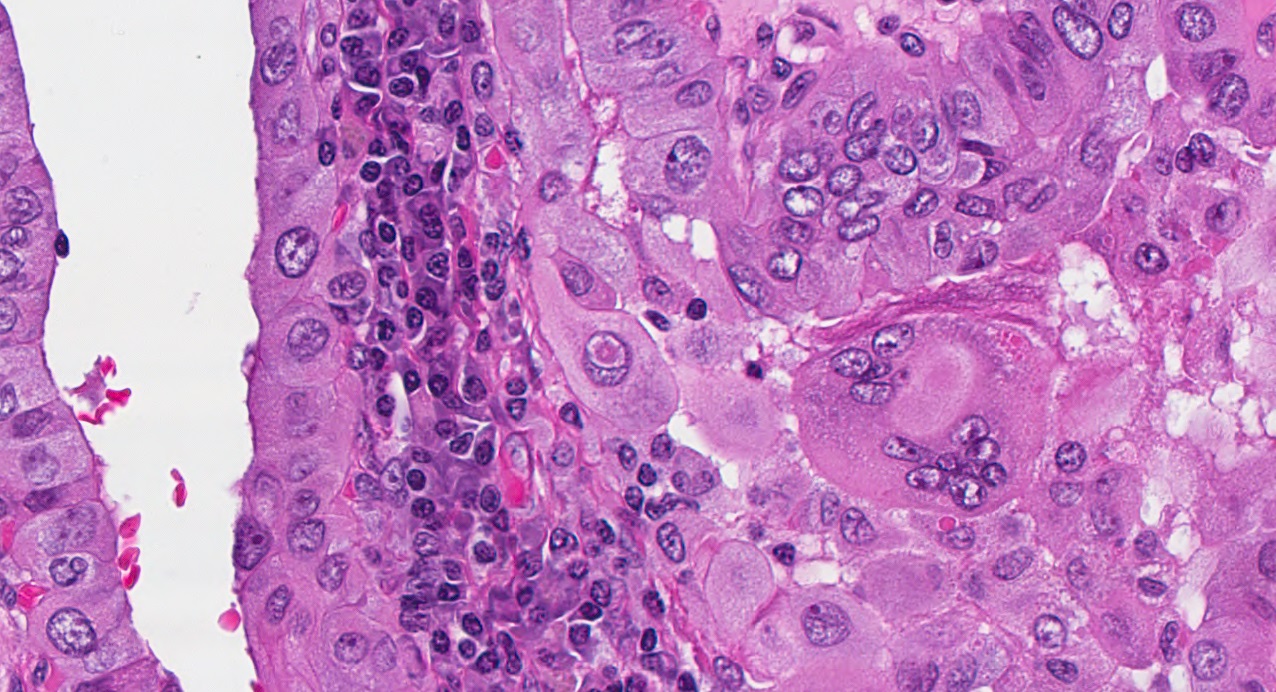
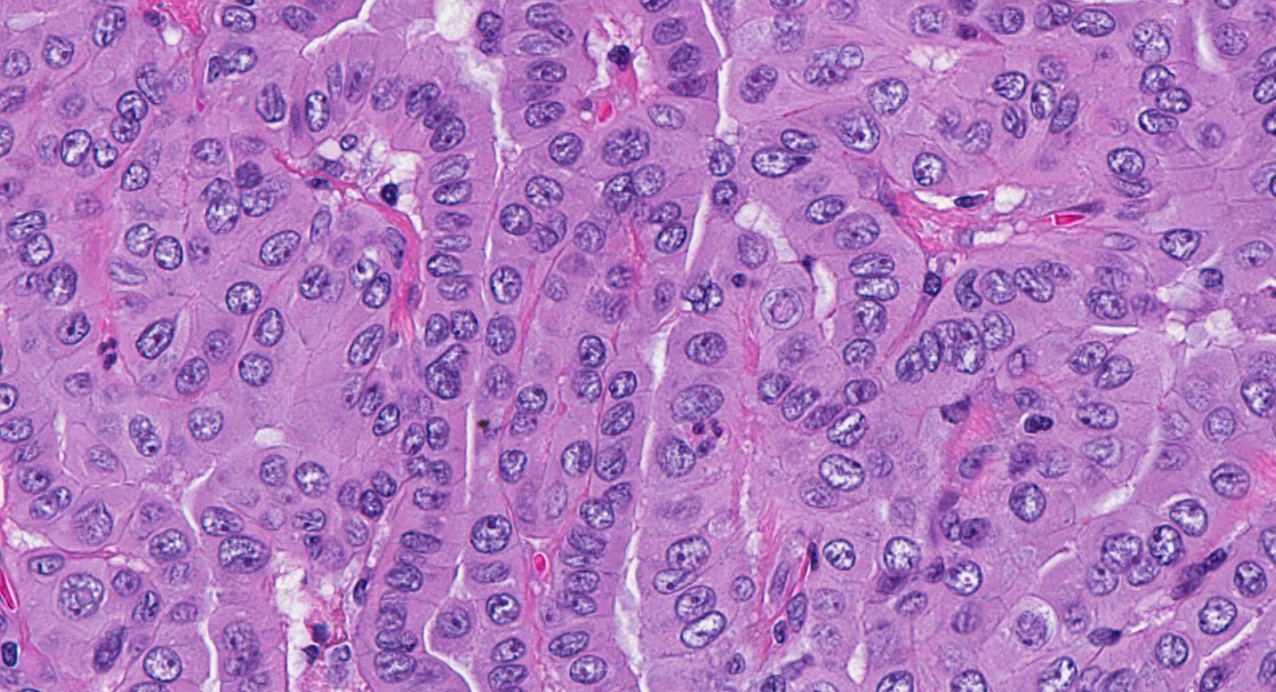
- Intricate, well formed, long papillae lined by single layer of tall columnar cells (cell height is 2 - 3 times their width)
- Depending on the plane of sectioning, cells may appear wide rather than tall
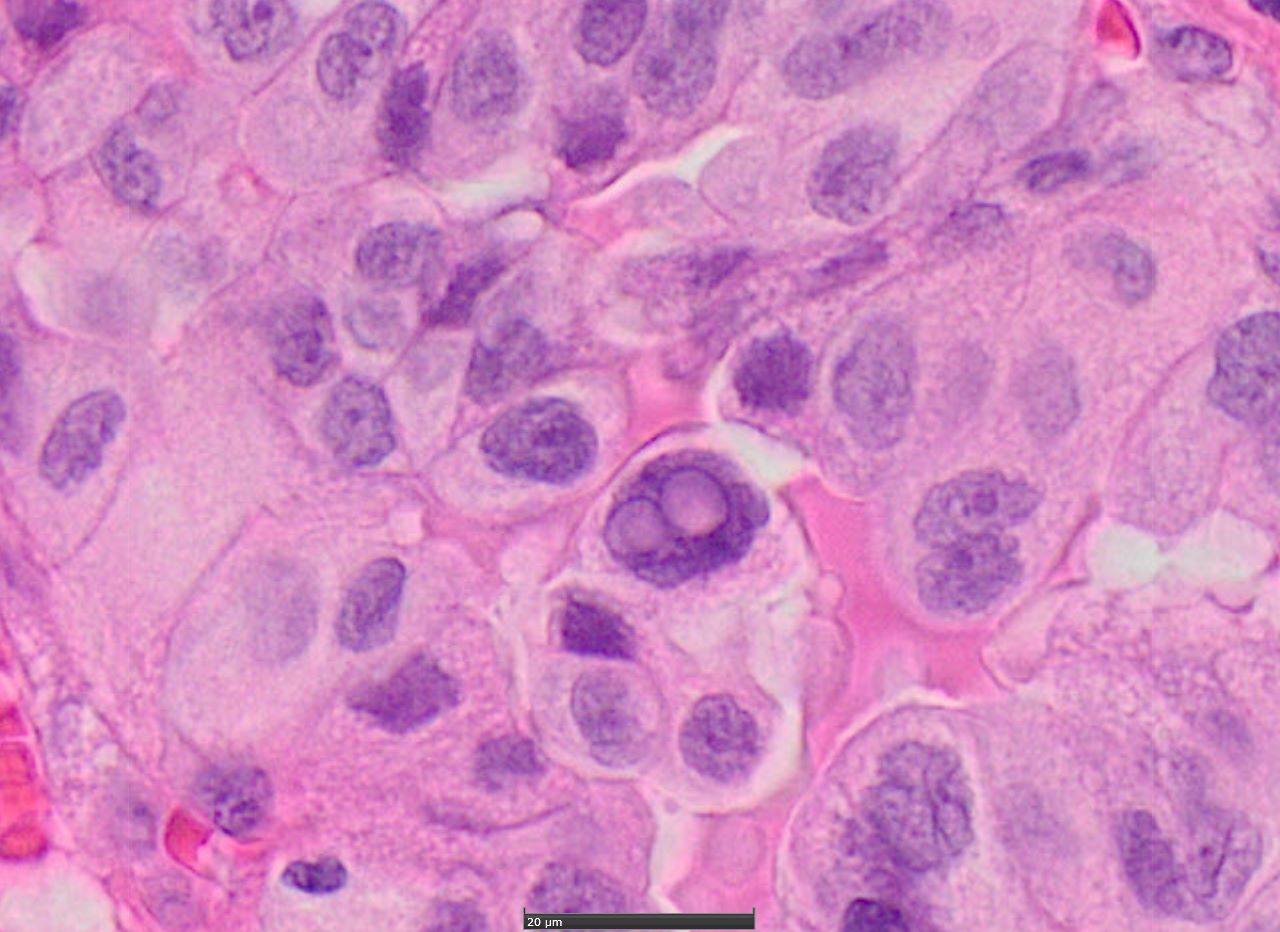
- Well developed and easily identifiable nuclear features of PTC: enlarged nuclei with numerous grooves and pseudoinclusions
- Sharply delineated cell borders with intensely eosinophilic and finely granular cytoplasm
- Tall cell features / pattern are frequently seen in the areas of extrathyroidal invasion of PTC
- Psammoma bodies uncommon
- Absent features: nuclear stratification, squamoid morules
- May exhibit prominent vascular invasion, mitotic activity
- Often found as a well differentiated component within anaplastic (undifferentiated) carcinomas and poorly differentiated thyroid carcinomas (Thyroid 2011;21:493)
- May be associated with lymphocytic thyroiditis
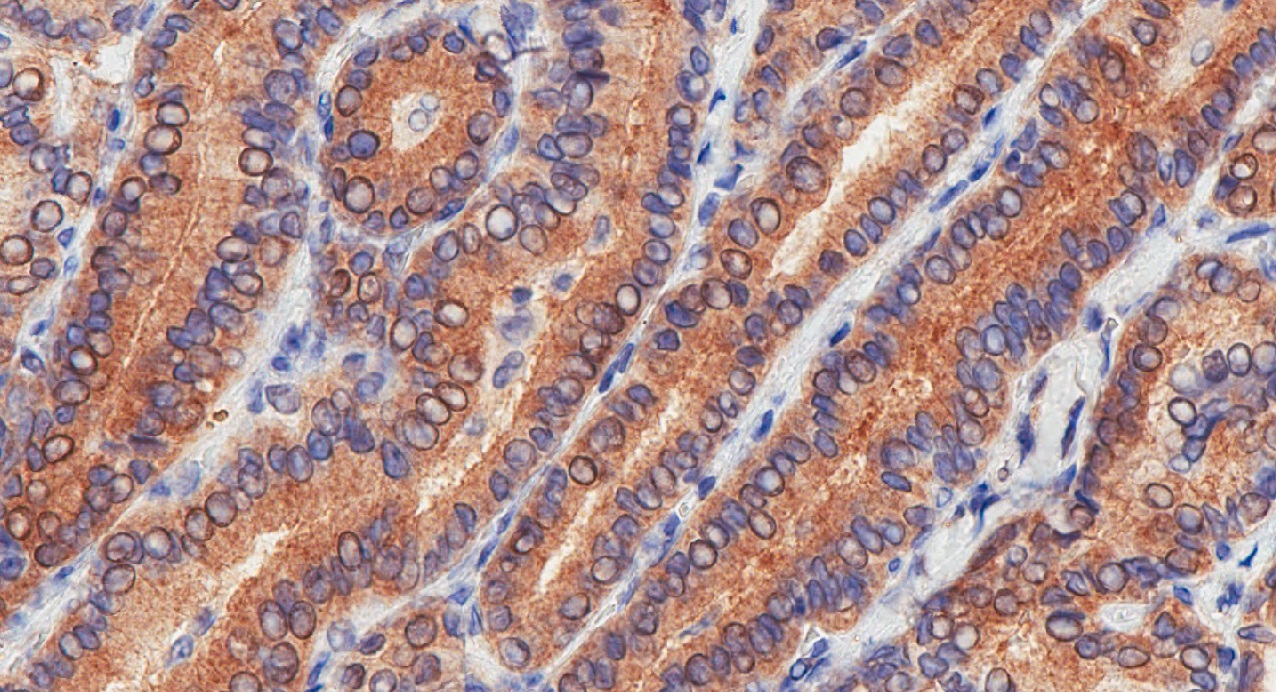
Microscopic (histologic) images
Contributed by Livia Florianova, M.D., M.Sc. and Marc Pusztaszeri, M.D.
Contributed by Andrey Bychkov, M.D., Ph.D.
Virtual slides
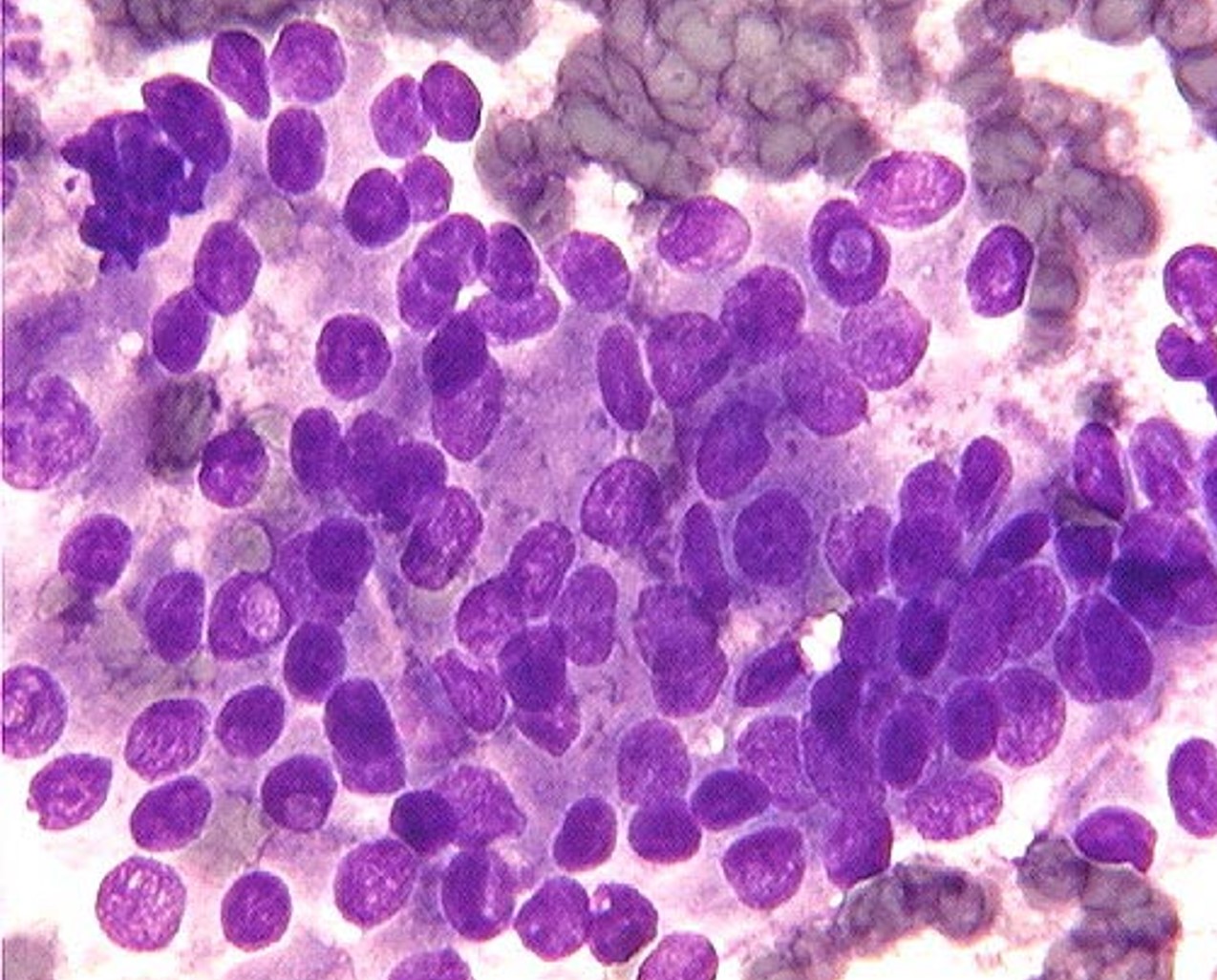
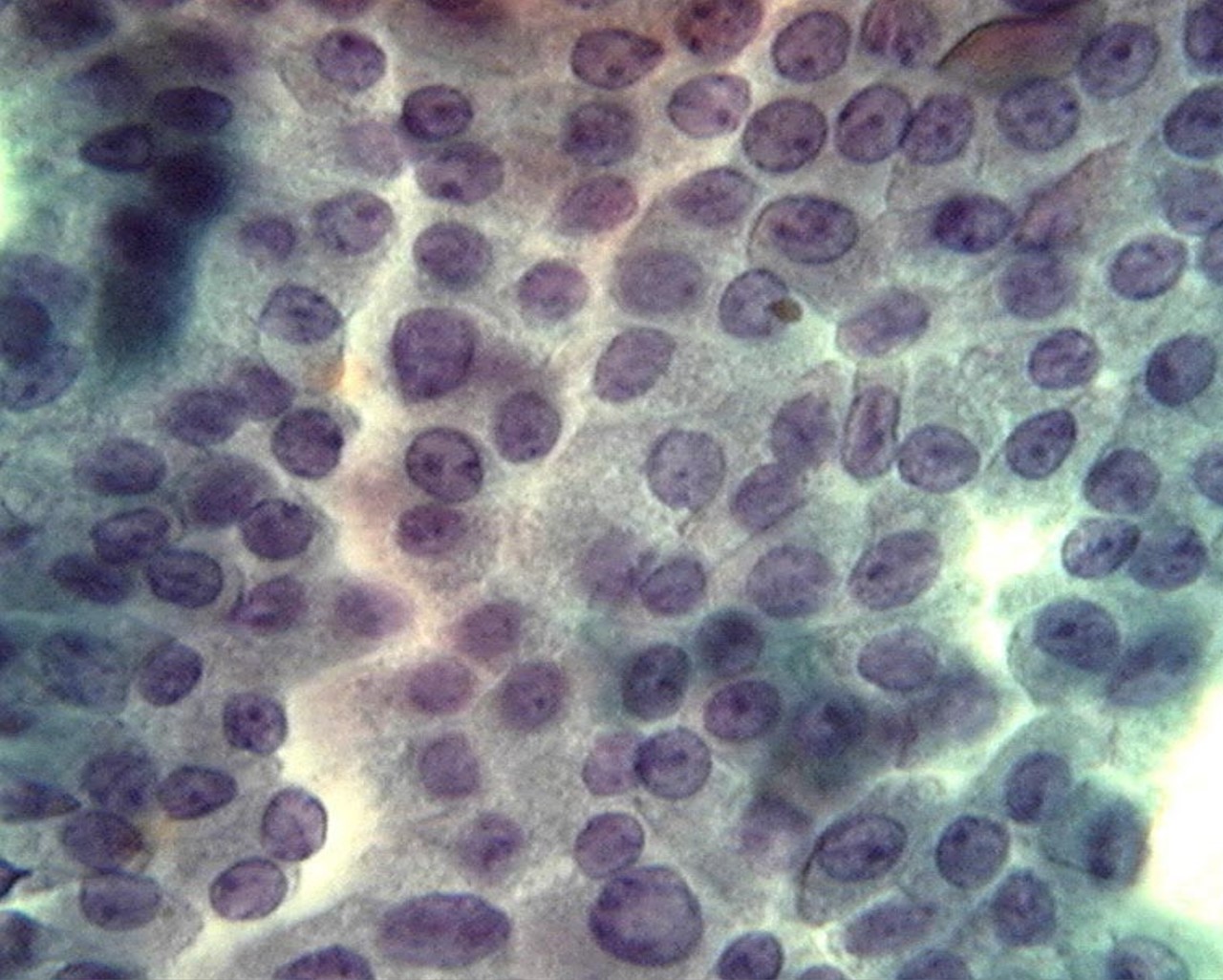
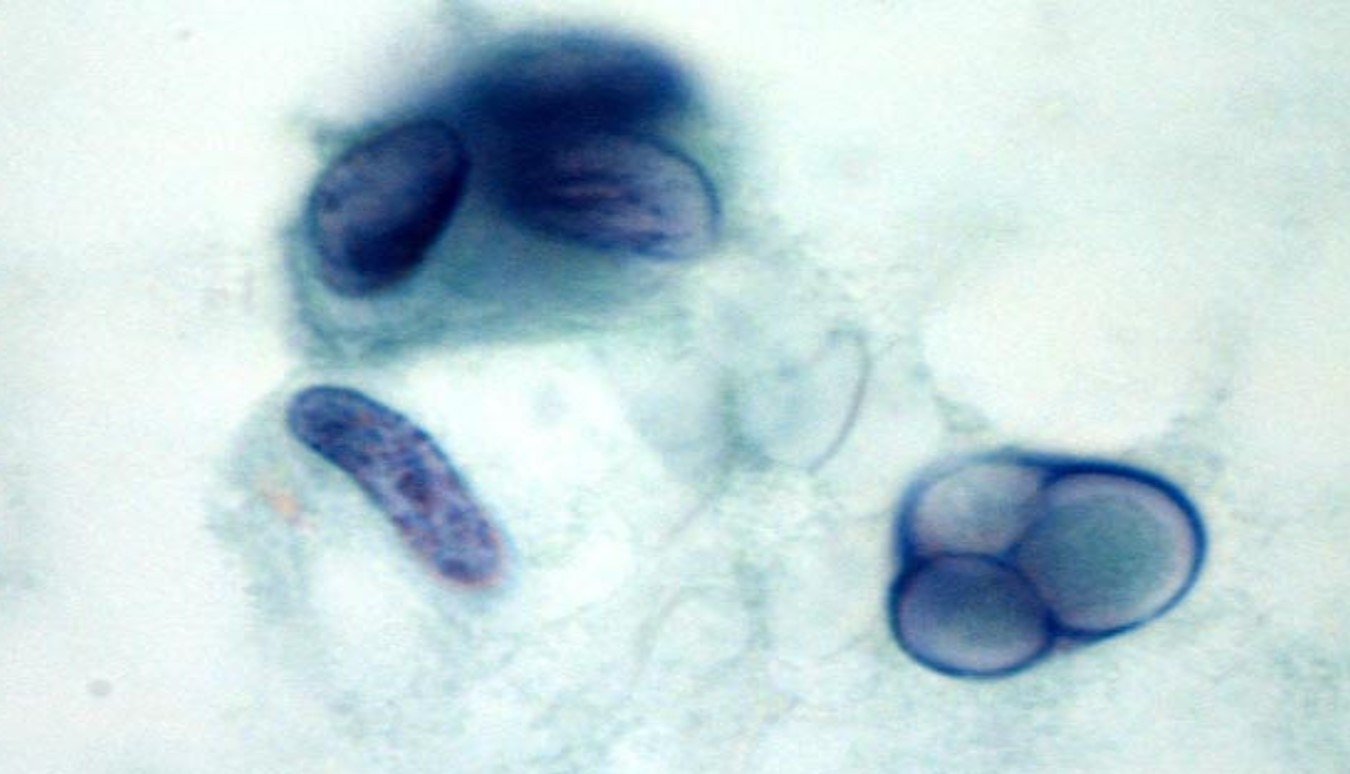
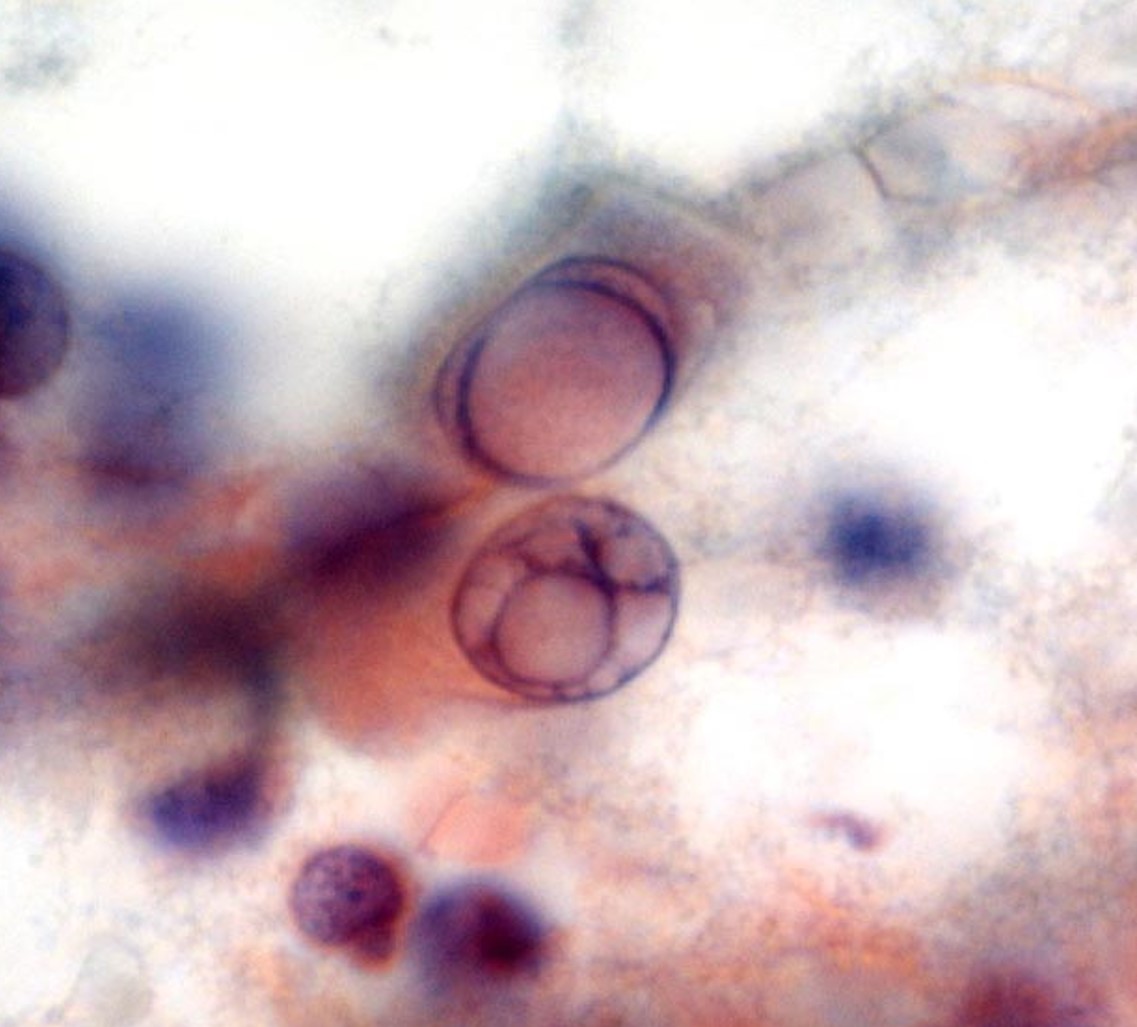
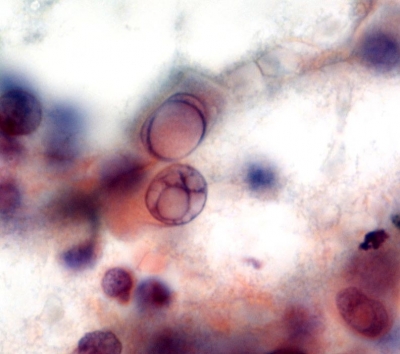
Cytology description
- Tall cell features may be recognized by cytology (see below) but a definitive diagnosis of a tall cell variant requires histologic evaluation (see definition)
- Tall / polygonal cells whose height is 2 - 3 times their width (Diagn Cytopathol 2019;47:452)
- Well defined granular eosinophilic or dense cytoplasm
- Nuclei with grooves and pseudoinclusions which can resemble soap bubbles due to multiple pseudoinclusions in the same nucleus (Diagn Cytopathol 2002;27:143, Diagn Cytopathol 2019;47:452)
- Palisaded arrangement and solid clusters
- Cells at the periphery of clusters show a tapering cytoplasmic tail to the outside (cytoplasmic elongation or tadpole cell-like)
- Individual detached cells may show a spindle-like shape or tombstone appearance (both luminal and basal cell borders are horizontal) (Diagn Cytopathol 2019;47:452)
- Lymphocytes may also be present (Acta Cytol 2004;48:325, Diagn Cytopathol 2019;47:452)
Cytology images
Positive stains
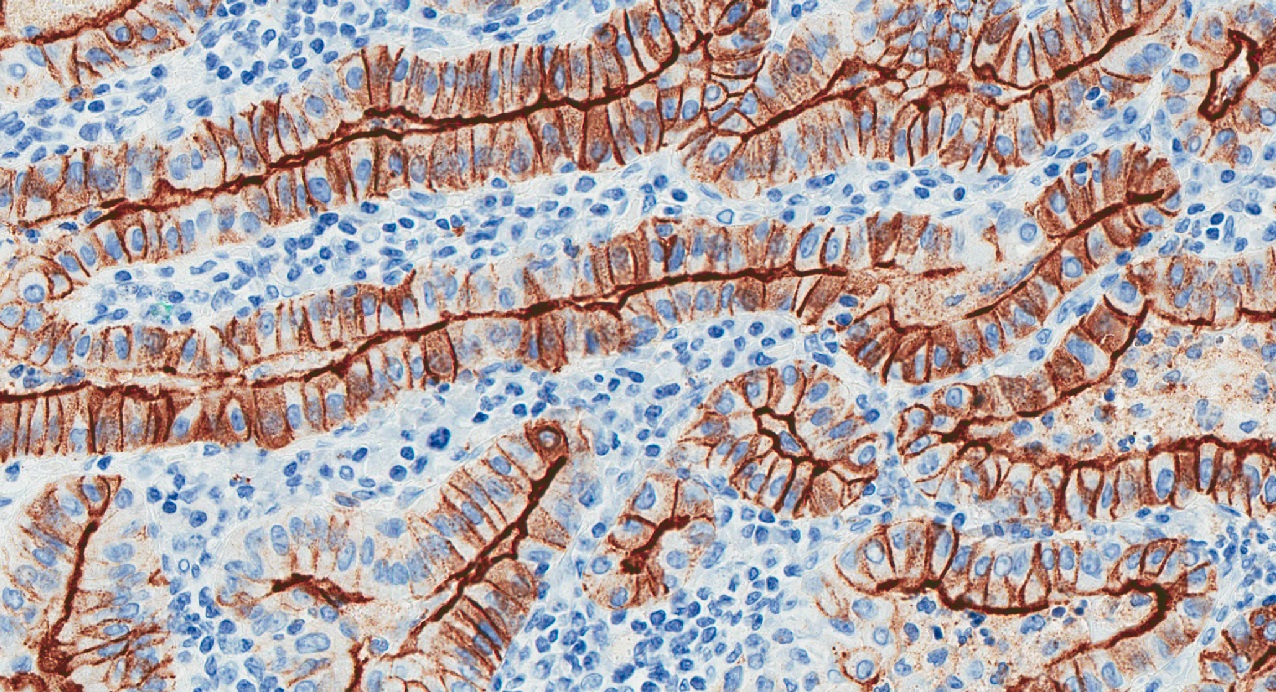
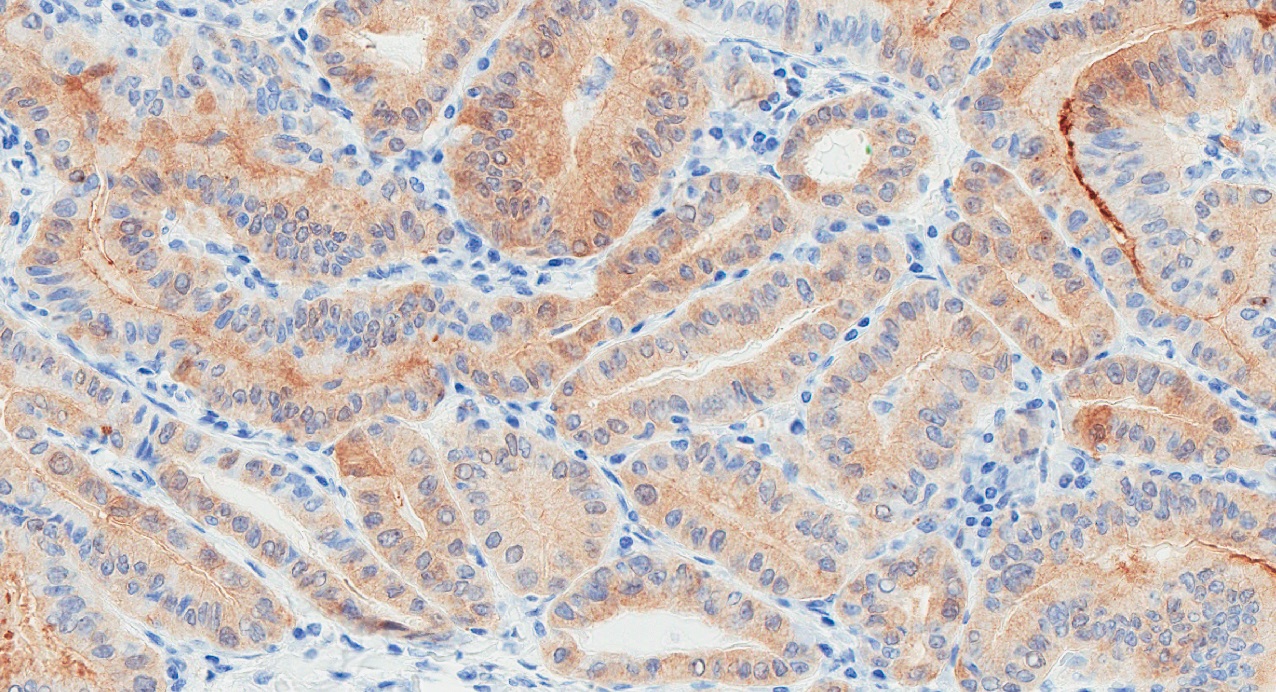
- Thyroid specific: Thyroglobulin, TTF1, PAX8
- Cytokeratins: CK19, broad spectrum cytokeratins (AE1 / AE3)
- HBME, galectin3
- BRAF V600E by mutation specific antibody (VE1)
- May be positive for napsin A (DDx with metastatic lung carcinoma) (Hum Pathol 2010;41:20, Endocr Pathol 2020;31:39)
Negative stains
Electron microscopy description
- Intranuclear cytoplasmic inclusions and abundant mitochondria in cytoplasm (Ultrastruct Pathol 1985;8:131)
Molecular / cytogenetics description
- Highest mutation density (DNA copy number alterations) of all PTC variants (Cell 2014;159:676)
- BRAF V600E mutation in ~80% of cases (Oncogene 2004;23:7436, Endocr Relat Cancer 2005;12:245, J Clin Endocrinol Metab 2003;88:5399)
- Higher frequency of TERT promoter mutations than in classic PTC (5 - 30% versus 10%) (Endocr Relat Cancer 2013;20:60)
- RAS mutations have not been identified
Videos
High grade and poorly differentiated and anaplastic thyroid carcinoma
Ultrasound of tall cell variant of PTC
Sample pathology report
- Thyroid, left lobe, fine needle aspiration:
- Satisfactory for evaluation
- Malignant (Bethesda diagnostic category VI)
- Papillary thyroid carcinoma, favor tall cell variant
- Thyroid, left lobe, left hemithyroidectomy:
- Papillary thyroid carcinoma, classic type with tall cell features (20%) (see synoptic report)
- Thyroid, total thyroidectomy:
- Papillary thyroid carcinoma, tall cell variant (see synoptic report)
Differential diagnosis
- Other papillary thyroid carcinoma variants:
- Classic variant with tall cell features:
- < 30% of tall cell component
- Columnar cell variant:
- Nuclear stratification, rare nuclear pseudoinclusions, absence of eosinophilic cytoplasm and distinct cell borders
- Often CDX2 positive
- Warthin-like variant:
- Dense lymphocytic infiltration within vascular cores of stroma, rarely infiltrative
- Oncocytic variant:
- No or only rare tall cells, lack of distinct cell borders, prominent nucleoli
- Classic variant with tall cell features:
- Breast tall cell carcinoma with reversed polarity (very rare):
- Focal positivity for GATA3, GCDFP-15 and mammaglobin
- TTF1, thyroglobulin and BRAF V600E consistently negative (Mod Pathol 2018;31:1367, Am J Surg Pathol 2017;41:887, Histopathology 2018;73:339)
Board review style question #1
Which of the following statements concerning the tall cell variant of papillary thyroid carcinoma is correct?
- It usually has an indolent clinical course
- Most cases are associated with a RAS mutation
- Patients are usually older adults
- The tumor is positive for TTF1, synaptophysin and calcitonin
- Tumor cells are stratified and only focal areas show characteristic papillary thyroid carcinoma nuclear features
Board review style answer #1
Board review style question #2
Which of the following diagnostic features are associated with the tall cell variant of papillary thyroid carcinoma?
- A dense lymphocytic infiltration of tumor stroma
- Cells with granular eosinophilic cytoplasm and nuclei with a soap bubble appearance on cytology
- Focal positivity for GATA3
- Infrequent nuclear grooves and pseudoinclusions
- High nucleus to cytoplasm ratio
Board review style answer #2
B. Cells with granular eosinophilic cytoplasm and nuclei with a soap bubble appearance on cytology
Comment Here
Reference: Papillary carcinoma, tall cell variant
Comment Here
Reference: Papillary carcinoma, tall cell variant