Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Pusztaszeri M. Solid / trabecular. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidsolidvariant.html. Accessed April 2nd, 2025.
Definition / general
- Uncommon papillary thyroid carcinoma (PTC) subtype in which > 50% of tumor has solid, trabecular or insular growth but lacks diagnostic features of a higher grade tumor (high grade PTC or poorly differentiated thyroid carcinoma)
- Literature on the prognosis and outcomes of solid / trabecular subtype of PTC (S / T PTC) is sparse and conflicting, with some studies reporting it as a clinically aggressive subtype while others did not
Essential features
- Rare form of PTC, accounting for 1 - 3% of all PTC subtypes in adults
- Proportion of solid component needed to render the diagnosis of (S / T PTC) has been inconsistent in the literature
- 3rd edition of the WHO classification of endocrine tumors required all or nearly all of a tumor to show solid, trabecular or insular growth, whereas the 4th edition established a cutoff of > 50%
- This variation in the proportion of solid component might contribute to the conflicting results regarding the aggressiveness of this subtype, along with other confounding factors including variability in the assessment / diagnosis of nuclear features of PTC, mitotic activity or necrosis and tumor encapsulation / invasiveness
- Therefore, a diagnosis of S / T PTC, regardless of the diagnostic criteria used (i.e., % of solid component), should not automatically trigger a more aggressive treatment approach and other clinicopathological features including encapsulation / invasiveness should be considered as well
Terminology
- Paraganglioma-like variant or Chernobyl variant
ICD coding
Epidemiology
- Rare: 1 - 3% of all PTC subtypes in adults (Ann Diagn Pathol 2021;52:151737)
- Female predominance (F:M = 2 - 9:1), similar to classic PTC (Head Neck 2018;40:1588, Histopathology 2022;81:171, Ann Diagn Pathol 2021;52:151737)
- Mean age of 45 - 48 years (range: 7 - 85), similar to classic PTC (ANZ J Surg 2014;84:380, Histopathology 2022;81:171, Ann Diagn Pathol 2021;52:151737)
- More common in young patients and in patients with a history of exposure to ionizing radiation
- S / T PTC was reported in ~34% of children with PTC after the Chernobyl disaster (Endocr Pathol 2006;17:307, Endocr J 2020;67:241, Ann Diagn Pathol 2021;52:151737)
Sites
- Thyroid gland
Pathophysiology
- S / T PTC is a heterogeneous group of tumors associated with different etiologies (sporadic and radiation induced) and molecular pathways
Etiology
- May be radiation induced or not
- Higher radiation doses associated with higher frequency of S / T PTC and diffuse sclerosing PTC subtypes as well as histologic features of cancer aggressiveness, including lymph vascular invasion, intrathyroidal infiltration and multifocality (Cancer 1994;74:748)
Clinical features
- Not well established, usually similar to classic PTC
- See Case reports for various clinical presentations
Diagnosis
- Workup is similar to any thyroid mass / nodule
- Ultrasound with fine needle aspiration cytology
- Computed tomography (CT) scan may be useful to evaluate extrathyroidal extension and lymph node metastases
- Because of the lack of criteria with high specificity and sensitivity, the preoperative diagnosis of S / T PTC is hardly ever made or suggested on cytology
- However, most cases of S / T PTC are diagnosed as malignant or suspicious for malignancy (PTC or FVPTC) by fine needle aspiration biopsy (FNAB)
- Molecular testing of cytologic aspirates may assist in preoperative diagnosis
- Definitive diagnosis is made via histological examination of a resection specimen, supplemented by immunohistochemistry
Radiology description
- Ultrasonography
- Usually well defined solid nodules with hypoechoic rim (Cancer Cytopathol 2015;123:71)
- Tumors with well defined borders with hypoechoic rim correlate with totally encapsulated tumors on histology, which are associated with indolent behavior in the absence of invasion (Cancer Cytopathol 2015;123:71)
- May have irregular borders (J Clin Endocrinol Metab 2023;108:e1186)
- Rarely, knobby or lobulated nodule or conglomeration of nodules replacing a lobe (Cancer Cytopathol 2015;123:71)
- Calcifications (central or coarse) may be present (J Clin Endocrinol Metab 2023;108:e1186, Cancer Cytopathol 2015;123:71)
- Diagnosed as high or intermediate suspicion nodules using ultrasound (US) based on the Korean Thyroid Image Reporting and Data System (Korean J Radiol 2016;17:811)
- 18F fluorodeoxyglucose positron tomography (PET / CT 18F FDG) may show an hypermetabolic mass (Diagnostics (Basel) 2020;11:4, Indian J Nucl Med 2011;26:196)
Radiology images
Prognostic factors
- Literature on the prognosis / outcomes of S / T PTC is sparse and conflicting, with some studies reporting it as a clinically aggressive subtype, while others showed that S / T PTC may not be clinically aggressive (Clin Endocrinol (Oxf) 2023;99:335, Histopathology 2022;81:171)
- These conflicting results may be due to the fact that S / T PTC is a rare variant with diagnostic criteria that have changed over time
- Other confounding factors including variability in the assessment / diagnosis of nuclear features of PTC, mitotic activity or necrosis and encapsulation / invasiveness
- Systematic review with meta analysis of 205 cases (with several potential confounding factors) concluded that S / T PTC is an aggressive subtype with higher tumor recurrence and mortality rates (Head Neck 2018;40:1588)
- Different clinicopathologic features of S / T PTC appear to influence prognosis
- When stringently selected to exclude differentiated high grade thyroid carcinomas, S / T PTC appear to follow an indolent clinical course characterized by a low risk of nodal metastasis (18%) and a very indolent clinical course with a 10 year disease specific survival of 96% and 10 year relapse free survival of 87% (Histopathology 2022;81:171)
- Determining factor for nodal metastasis and disease free survival is the encapsulation / infiltration status rather than the solid / trabecular percentage (Histopathology 2022;81:171)
- Encapsulated noninvasive tumors follow an indolent course with a very low risk of nodal metastasis and recurrence (Histopathology 2022;81:171)
- In contrast, infiltrative S / T PTC had a significantly higher rate of nodal metastasis (33 - 56%) and 10 year recurrence (14 - 26%) (Histopathology 2022;81:171)
- Post-Chernobyl radiation induced cases is a distinct subgroup associated with higher frequency of lymph node metastases, angioinvasion, extrathyroidal invasion (Cancer 1994;74:748)
- However, among children and young adults with post-Chernobyl PTCs, many of which had S / T PTC, the mortality overall remained at a very low level (< 1%) during the first 10 years of follow up (Cancer 1994;74:748)
- Reported rate of distant metastasis varies from 4% to 25% (13.5% in the meta analysis by Vuongg et al.) (Head Neck 2018;40:1588)
Case reports
- 14 year old girl with multiple cervical lymphadenopathies (BMJ Case Rep 2013;2013:bcr2013010001)
- 21 year old man with Hashimoto thyroiditis with challenging cytological features (BMJ Case Rep 2019;12:e226153)
- 22 year old woman with Turner syndrome with chronic thyroiditis (Front Oncol 2023;13:1150002)
- 47 year old woman with multinodular goiter and S / T PTC with novel BRAF VK600-1E mutation (Hum Pathol 2005;36:694)
- 61 year old woman with focal differentiated high grade thyroid carcinoma on histology (Ecancermedicalscience 2023;17:1587)
- 64 year old man with S / T PTC diagnosed by cytology and BRAF mutational analysis (Cytojournal 2008;5:2)
- 67 year old man with a 4.7 cm adrenal incidentaloma as the initial manifestation of a S / T PTC (AACE Clin Case Rep 2022;8:131)
Treatment
- Similar to classic PTC
- Management of S / T PTC may include total thyroidectomy, bilateral neck dissection (in cases with cervical lymphadenopathy) and postoperative radioiodine ablation (BMJ Case Rep 2013;2013:bcr2013010001, Ann Diagn Pathol 2021;52:151737)
- Diagnosis of S / T PTC, regardless of the diagnostic criteria used, should not automatically trigger a more aggressive treatment approach and other clinicopathological features including invasiveness should be considered as well (Histopathology 2022;81:171)
Gross description
- Size ranges from 0.1 cm to 11 cm (Ann Diagn Pathol 2021;52:151737)
- Multifocal involvement in 39.3% of cases (Ann Diagn Pathol 2021;52:151737)
- Often well circumscribed white-tan nodule in the thyroid gland
- Infiltrative nodules and nests may be found (Histopathology 2022;81:171)
- Generally no necrosis or hemorrhage (Ann Diagn Pathol 2021;52:151737, Endocr J 2020;67:241)
- Cystic changes may be present (Diagnostics (Basel) 2020;11:4)
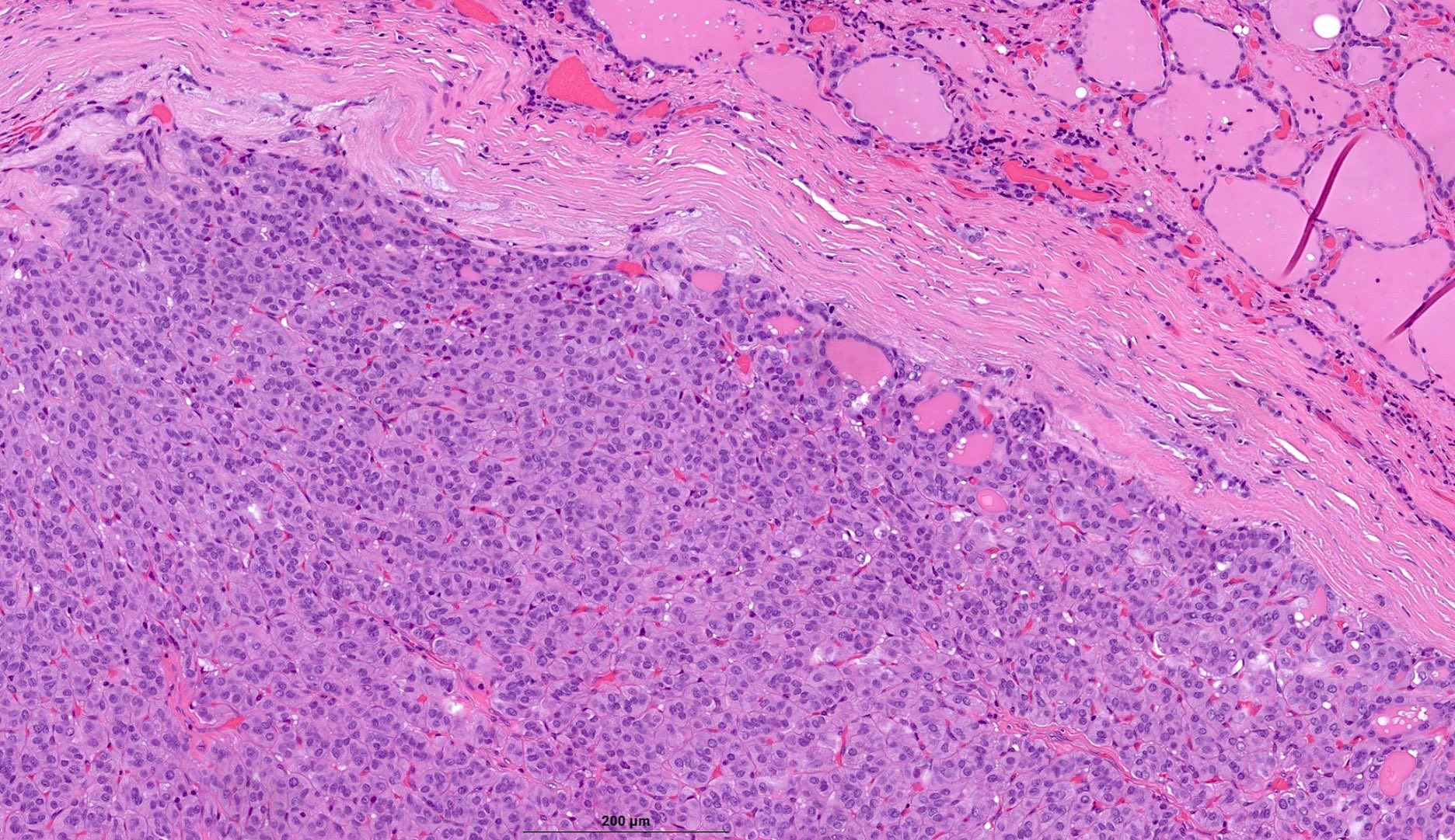
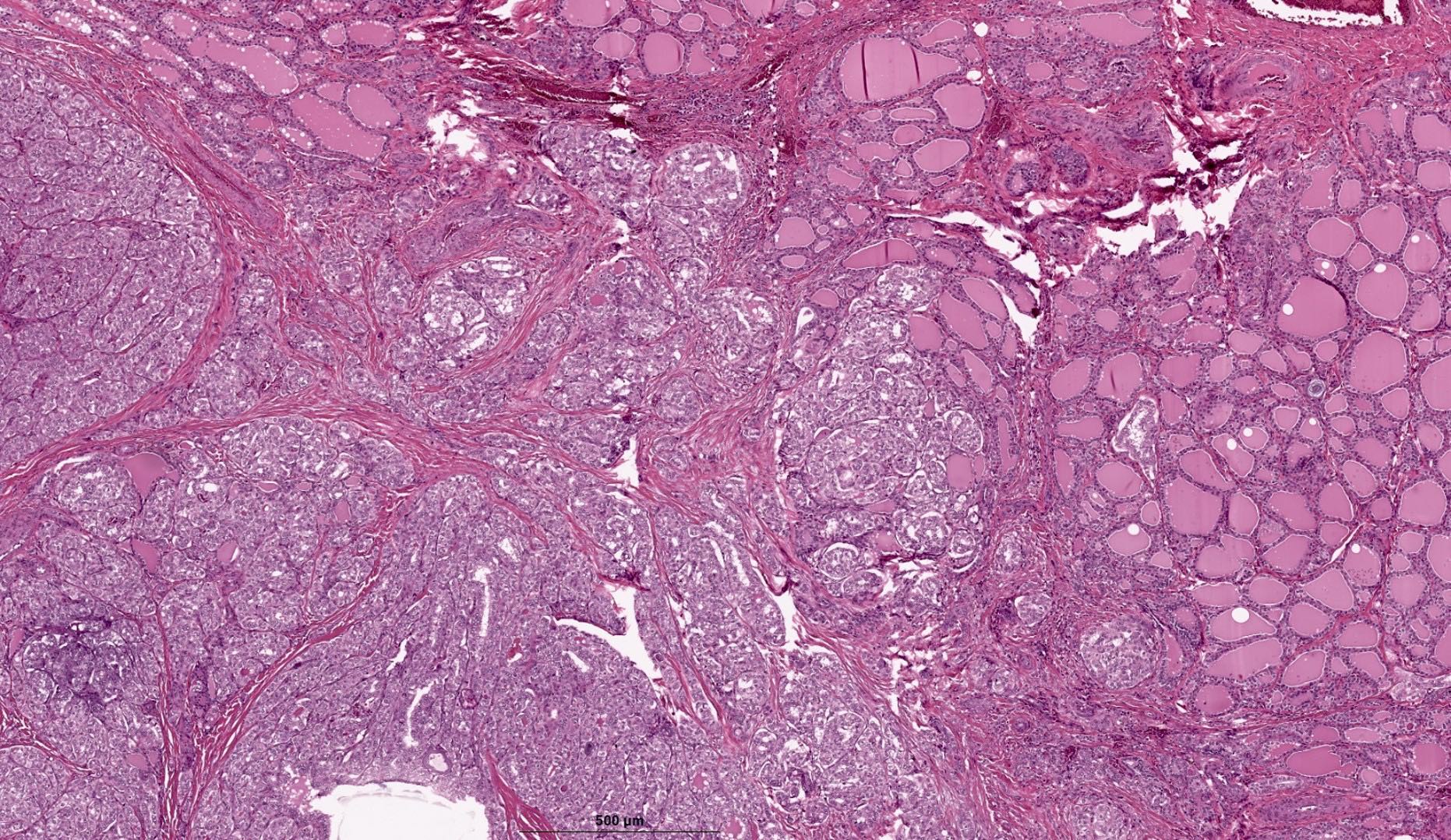
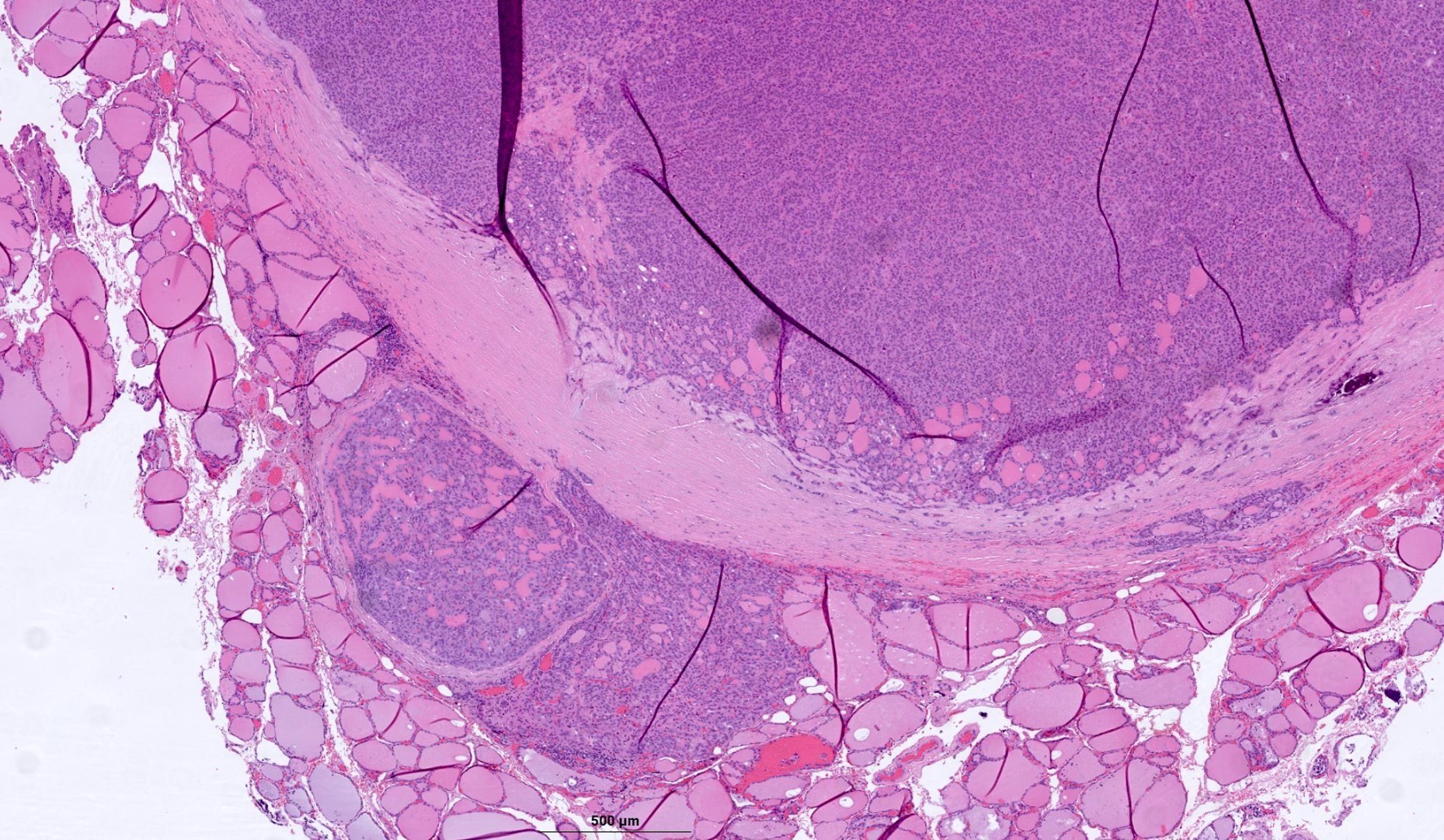
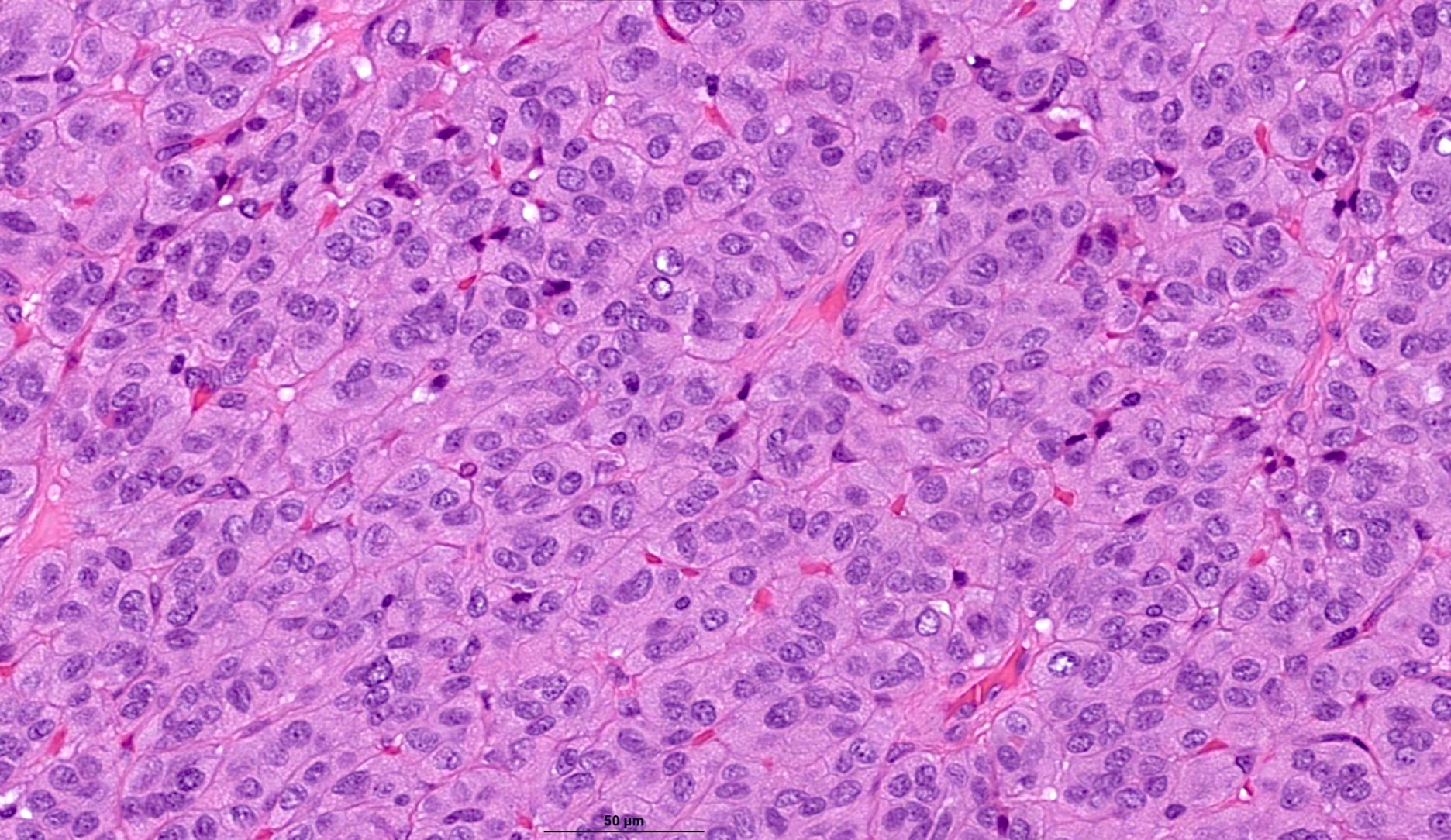
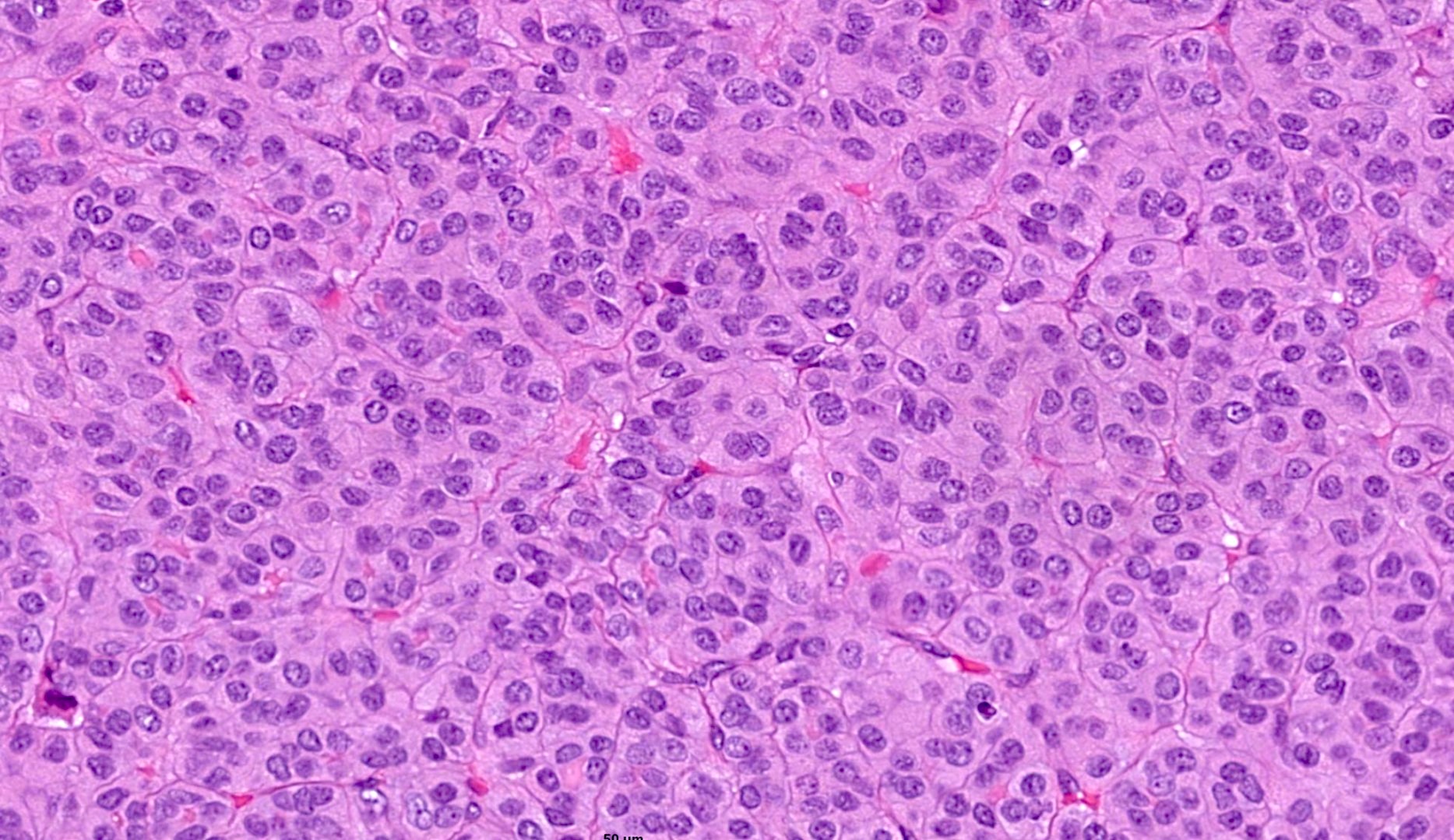
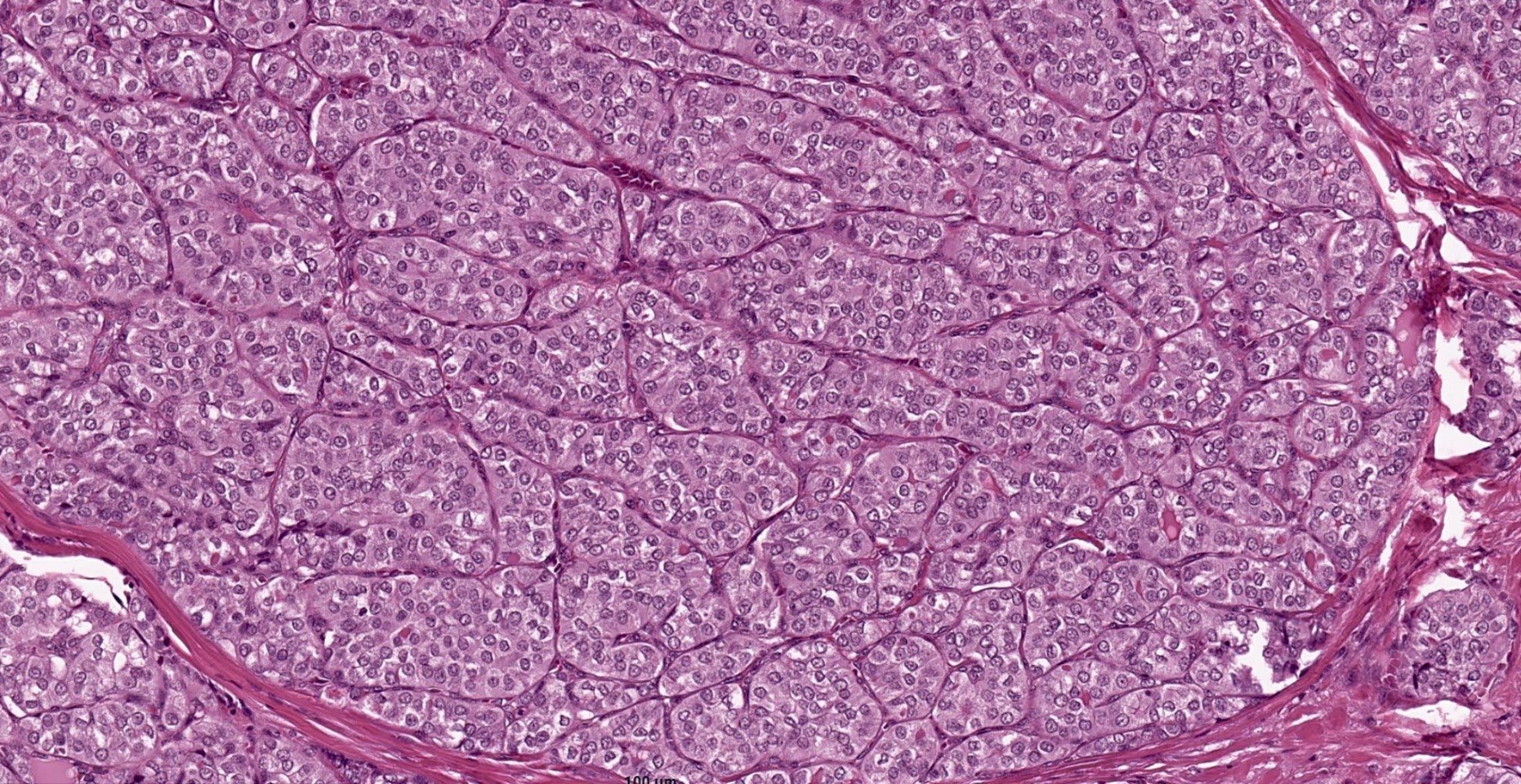
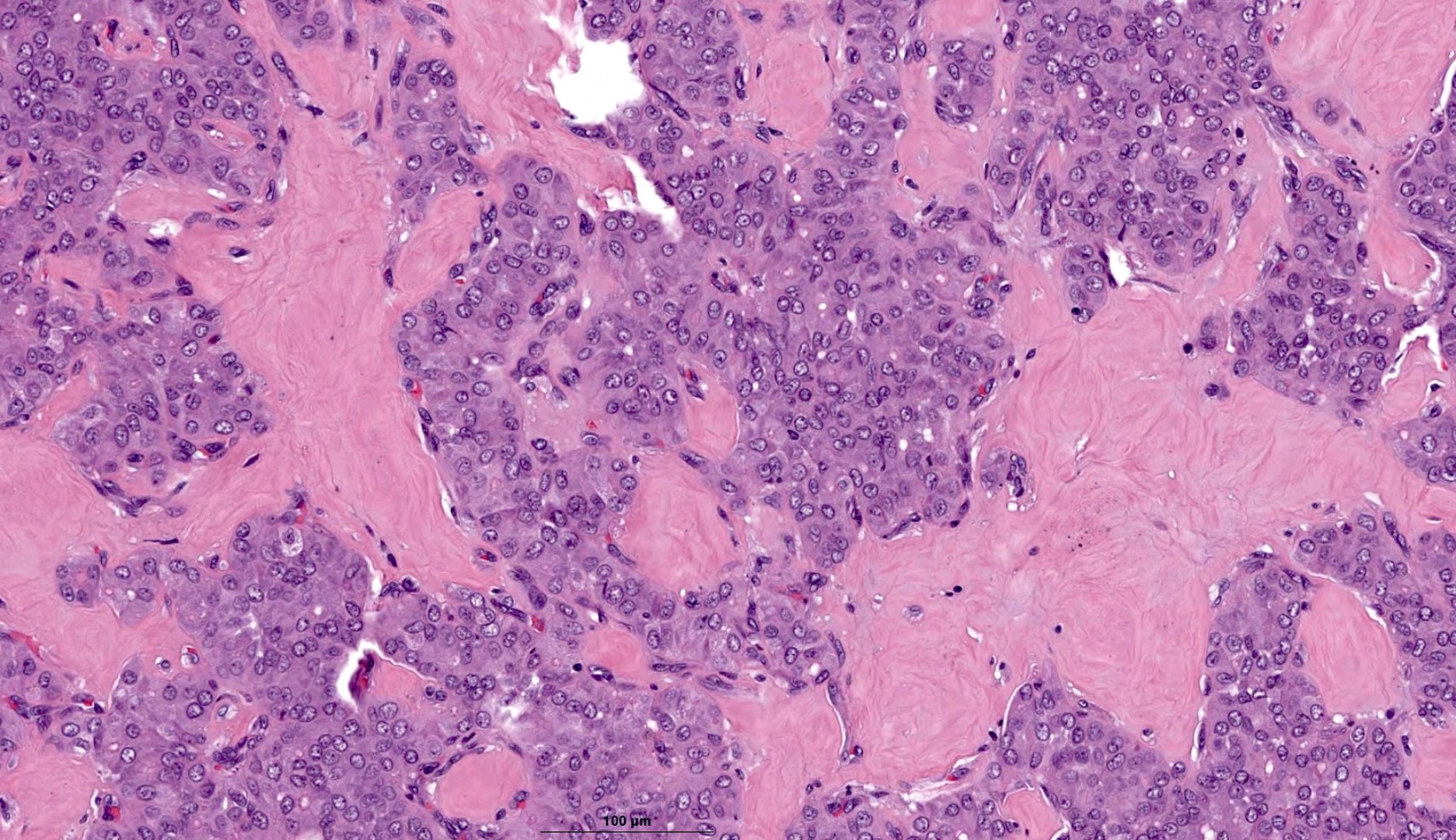
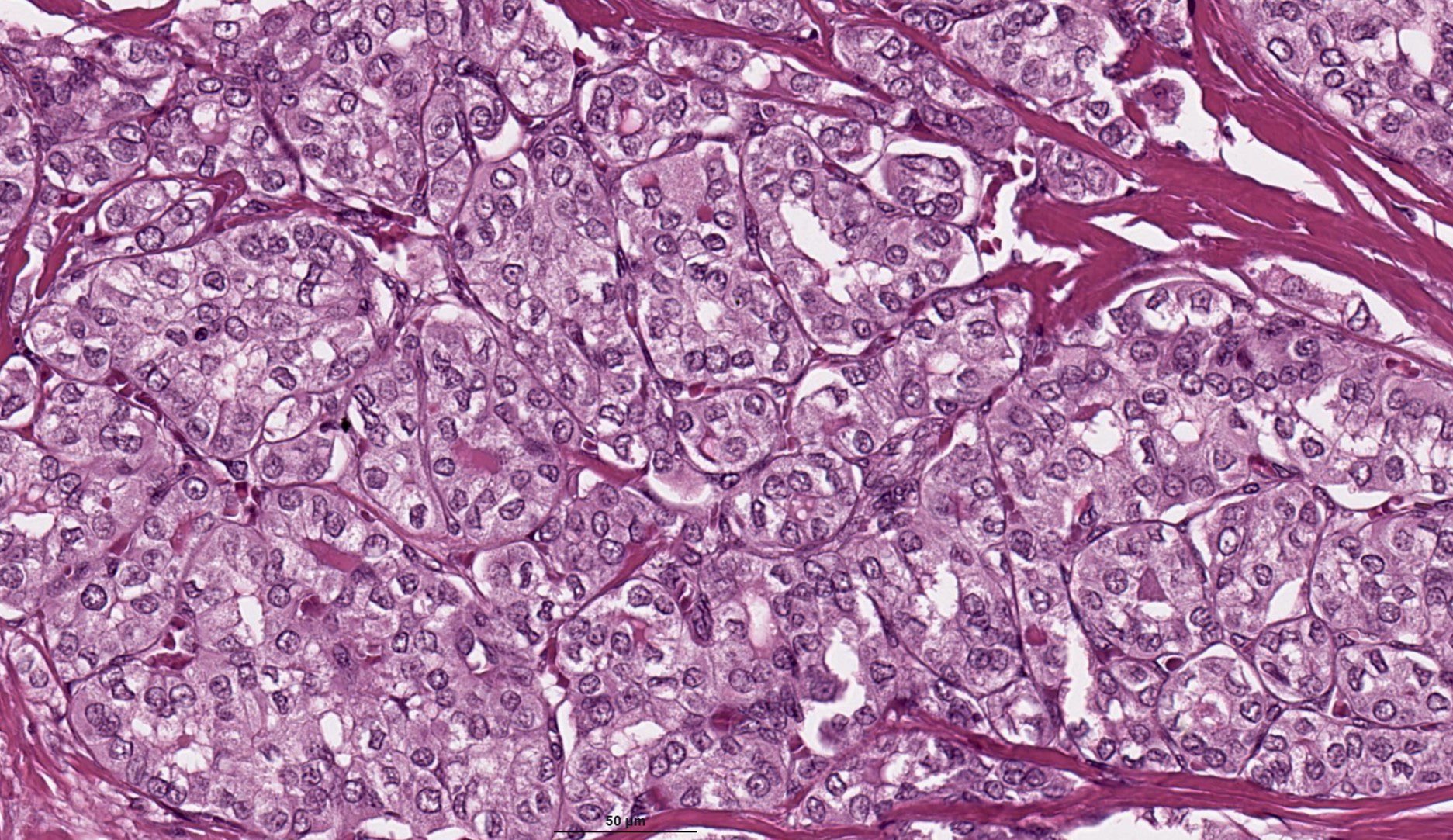
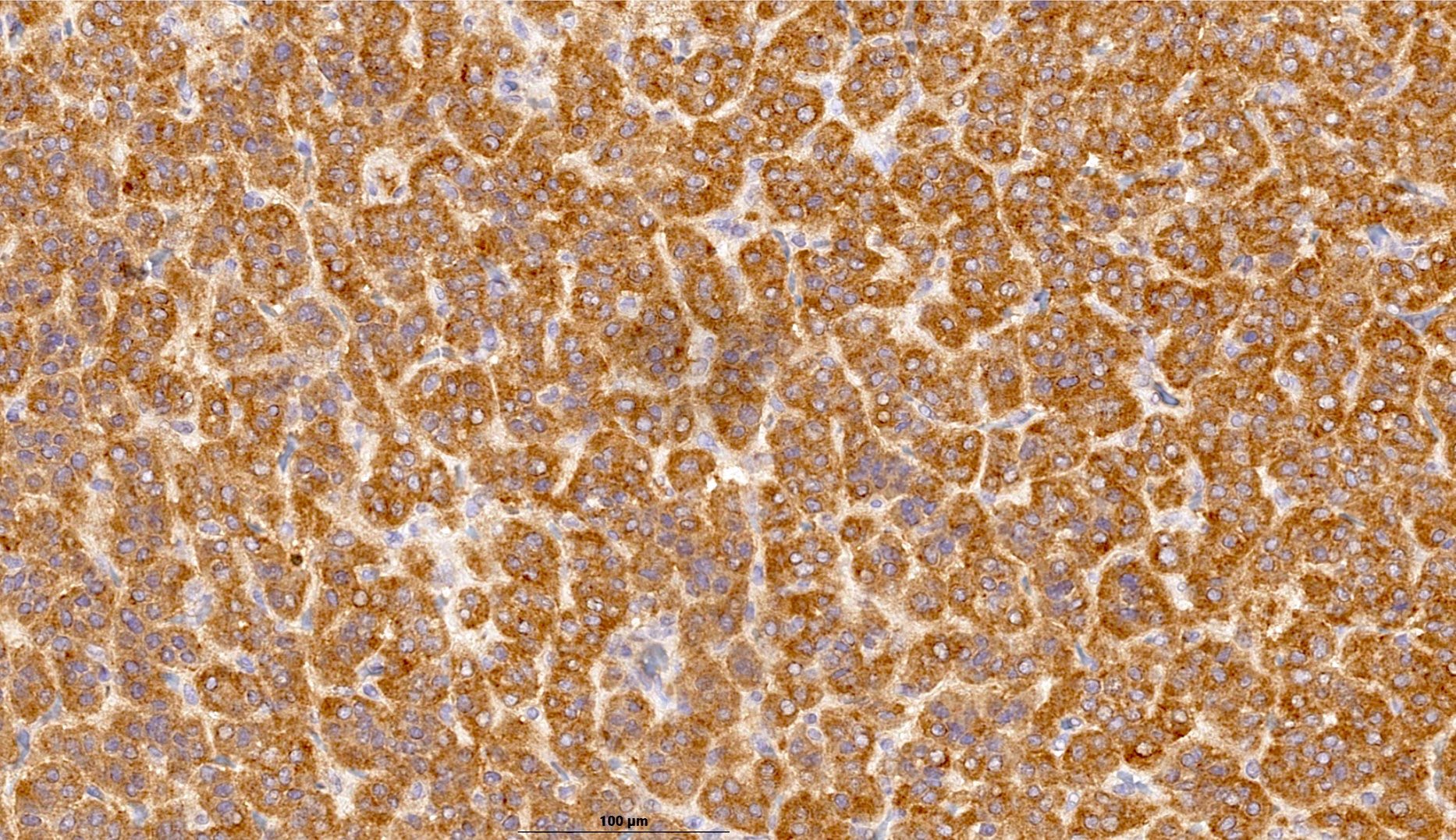
Microscopic (histologic) description
- ~67% of tumors are encapsulated while 33% of tumors are invasive; among encapsulated tumors, about half of them lack invasion (either capsular or vascular) (Histopathology 2022;81:171, Ann Diagn Pathol 2021;52:151737)
- > 50% of tumor has solid, trabecular or insular growth but lacks diagnostic features of a higher grade tumor (high grade PTC or poorly differentiated thyroid carcinoma)
- Other growth patterns may be seen as minor components, including follicular and papillary architecture (Histopathology 2022;81:171)
- Tight microfollicles (with or without colloid) and larger colloid filled follicles may be identified
- Abortive papillae or well formed papillae can be seen
- Nuclear features of PTC are present but may be less obvious than in classic PTC
- Stromal component may vary from thin fibrous strands to thick fibrous bands
- Solid nests may be separated by thin fibrovascular stroma, creating insular or nested / organoid pattern of growth
- No increase in mitotic activity (< 5 mitoses per 10 high power fields [HPF]) and no tumor necrosis
- Psammomatous calcifications in 17.9% of tumors (Ann Diagn Pathol 2021;52:151737)
- Vascular invasion and extrathyroidal extension can be encountered in 25 - 40% and 14 - 30% of cases, respectively (Histopathology 2022;81:171, Ann Diagn Pathol 2021;52:151737)
- Nodal metastases are detected in ~7 - 18% of cases at the time of initial surgery (Histopathology 2022;81:171, Ann Diagn Pathol 2021;52:151737)
Microscopic (histologic) images
Contributed by Marc Pusztaszeri, M.D. (source: World Tumor Registry)
Cytology description
- Due to its rarity, reports on the cytological features of S / T PTC are limited
- Because of the lack of criteria with high specificity and sensitivity, the preoperative diagnosis of S / T PTC is hardly ever made or suggested on cytology
- However, most cases of S / T PTC are diagnosed as malignant or suspicious for malignancy (PTC or FVPTC) by FNAB (Cancer Cytopathol 2015;123:71)
- Common cytologic patterns described in the literature include trabeculae, cohesive solid nests, syncytial fragments and 3 dimensional clusters; other possible patterns include microfollicles and scattered single cells (dyshesive) (Cancer Cytopathol 2015;123:71, Ecancermedicalscience 2023;17:1587)
- Predominant microfollicular pattern may be seen, which causes difficulty in distinguishing this subtype from the follicular variant of PTC or NIFTP; accordingly, some of these cases are diagnosed as Bethesda IV (Cancer Cytopathol 2015;123:71, Ecancermedicalscience 2023;17:1587, Acta Cytol 2018;62:371)
- Nuclear crowding, overlapping, grooving, intranuclear pseudoinclusions and chromatin clearing are seen to a variable extent in S / T PTC (Ecancermedicalscience 2023;17:1587)
- However, in some cases, the nuclei might appear round and darker than those of conventional PTC
Cytology images
Images hosted on other servers:
Positive stains
- Thyroglobulin (may be very focal or limited in extent), TTF1, PAX8, CK7
- Galectin3, CK19 and HBME1: less often expressed than in classical PTC (Endocr J 2020;67:241)
- Ki67: usually < 10% (Endocr J 2020;67:241)
- RAS Q61R (33%) (Histopathology 2022;81:171)
- BRAF V600E (VE1) (11%) (Histopathology 2022;81:171)
Negative stains
Electron microscopy description
- Solid / trabecular areas share similar ultrastructural features with poorly differentiated carcinomas (Ultrastruct Pathol 2001;25:13)
Molecular / cytogenetics description
- Molecularly heterogeneous group of tumors
- RET::PTC3 (NCO4::RET) is strongly associated with pediatric cases that developed after radiation exposure (80% of cases)
- RET::PTC1 (CCDC6::RET) and ETV6::NTRK3 may be seen in adult cases with or without radiation exposure
- RAS mutations are associated with encapsulated lesions (54%) and an absence of nodal metastasis (Histopathology 2022;81:171)
- BRAF V600E mutations are uncommon in the encapsulated form (7%) while they are relatively more common in invasive forms (19%) (Histopathology 2022;81:171)
- Noncanonical BRAF mutations have been reported in S / T PTC; a triplet deletion of the BRAF gene leading to the replacement of a valine and a lysine by a glutamate (BRAF V600E + K601) has been reported only in S / T PTC (Endocr Pathol 2009;20:122, Cytojournal 2008;5:2, Hum Pathol 2005;36:694)
- TERT promoter mutation is found in ~12% of S / T PTC cases (Eur J Endocrinol 2015;172:403, PLoS One 2016;11:e0153319)
- ROS1 gene fusion was identified in a single case of S / T PTC with a locally aggressive presentation (Thyroid 2016;26:794)
Molecular / cytogenetics images
Videos
Special types of thyroid cancer with Dr. Virginia LiVolsi
Sample pathology report
- Thyroid, right hemithyroidectomy:
- Solid / trabecular papillary thyroid carcinoma, encapsulated, 2.9 cm (see synoptic report and comment)
- Comment: In the absence of high grade features or invasion, the solid / trabecular subtype of PTC follows an indolent clinical course and should not warrant aggressive management (Histopathology 2022;81:171).
Differential diagnosis
- Poorly differentiated thyroid (insular) carcinoma:
- Rare tumor type in children, adolescents and young adults, which are typically characterized by DICER1 mutation (Mod Pathol 2020;33:1264)
- Shares growth patterns with S / T PTC
- No nuclear features of PTC
- Presence of at least 1 of following: convoluted nuclei, ≥ 3 mitotic figures/10 HPF, tumor necrosis (Am J Surg Pathol 2007;31:1256)
- Differentiated high grade thyroid carcinoma:
- Increased mitotic activity (≥ 5 per 10 HPF) or presence of tumor necrosis
- Follicular or papillary architecture
- Medullary thyroid carcinoma:
- Absence of colloid filled follicles
- No nuclear features of PTC; salt and pepper chromatin
- Immunoreactivity for calcitonin, CEA, synaptophysin, chromogranin and INSM1
- Absence of immunoreactivity for thyroglobulin and PAX8
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP):
- Up to 30% solid / trabecular component is allowed in NIFTP
- Follicular thyroid carcinoma with a solid growth pattern:
- No nuclear features of PTC
- Paraganglioma:
- No nuclear features of PTC
- Immunoreactivity for synaptophysin, chromogranin, INSM1 and S100 in sustentacular cells
- Absence of immunoreactivity for cytokeratins, thyroglobulin, TTF1, PAX8
- Hyalinizing trabecular tumor:
- Absence of colloid filled follicles
- Elongated / polygonal cells
- Prominent intratrabecular and intracytoplasmic hyalinization
- Pale yellow cytoplasmic bodies
- Aberrant cytoplasmic reactivity with Ki67 (using MIB1 clone at room temperature)
Additional references
Board review style question #1
Which statement is correct about solid / trabecular papillary thyroid carcinoma (S / T PTC)?
- Aggressive subtype of PTC associated with a poor prognosis
- Common subtype of PTC
- More common in the elderly than in children and young adults
- Requires all or nearly all of the tumor to have a solid / trabecular / insular growth pattern for the diagnosis
- RET::PTC3 (NCO4::RET) is strongly associated with pediatric cases that developed after radiation exposure
Board review style answer #1
E. RET::PTC3 (NCO4::RET) is strongly associated with pediatric cases that developed after radiation exposure (80% of cases). S / T PTC is a molecularly heterogeneous group of tumors. RET::PTC1 (CCDC6::RET) and ETV6::NTRK3 may be seen in adult cases with or without radiation exposure. In sporadic cases, RAS mutation is associated with encapsulated tumors and an absence of nodal metastasis, while BRAF V600E mutation is associated with infiltrative tumors. Answer B is incorrect because S / T PTC accounts only for 1 - 3% of all PTCs in adults. Answer C is incorrect because S / T PTC is more common in children and young adults where it is commonly associated with ionizing radiation (e.g., following the Chernobyl disaster). Answer D is incorrect because while the diagnostic criteria have varied over time, the latest WHO 2022 classification requires > 50% of solid, trabecular or insular growth pattern for a PTC to be classified as S / T PTC, in the absence of high grade features. Answer A is incorrect because literature on the prognosis / outcomes of S / T PTC is sparse and conflicting, with some studies reporting it as a clinically aggressive subtype, while others showed that S / T PTC may not be clinically aggressive.
Comment Here
Reference: Solid / trabecular papillary thyroid carcinoma
Comment Here
Reference: Solid / trabecular papillary thyroid carcinoma
Board review style question #2
Board review style answer #2
C. > 50%. The presence of at least 50% of solid / trabecular component is required to diagnose a tumor as PTC solid / trabecular subtype according to the latest WHO classification in 2022. The 3rd edition of the WHO classification of endocrine tumors required all or nearly all of a tumor to show solid, trabecular or insular growth, whereas the 4th edition established a cutoff of > 50%. Answer E is incorrect because the WHO criteria for S / T PTC was updated to an established cutoff of > 50% as noted in the 4th edition of WHO released in 2022. Answer D is incorrect because the threshold for diagnosing S / T PTC does not have to be greater than 70% but rather greater than 50%. Answers A and B are incorrect because these percentages are too low and have not been used as a diagnostic cutoff for S / T PTC.
Comment Here
Reference: Solid / trabecular papillary thyroid carcinoma
Comment Here
Reference: Solid / trabecular papillary thyroid carcinoma