Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Laboratory | Radiology description | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Videos | Differential diagnosisCite this page: Bychkov A. Parathyroid tissue. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidparathyroidtissue.html. Accessed April 3rd, 2025.
Definition / general
- Caused by aberrant migration of parathyroid (PT) glands during embryogenesis
- First described by Lahey in 1926 (J Surg Oncol 1984;27:271)
- May undergo same pathologic processes as PT glands (Mod Pathol 1989;2:652, Int Surg 1997;82:87), usually functioning adenoma or hyperplasia
- Intrathyroidal PT glands are rare, but intrathyroidal PT tissue is not
- A survey of the thyroids of 350 infants and children suggests that the presence of thymus and PT tissue within the thyroid is so common as to be classified as normal (J Anat 1976;122:77)
Terminology
- Definition: intrathyroidal PT gland (true intrathyroidal PT gland) is a PT gland, normal or abnormal, situated totally within the thyroid, surrounded on all aspects by thyroid parenchyma and with no capsule
- This entity must be clearly distinguished from subcapsular / intracapsular PT gland and those glands located in crevices in the thyroid (Ann Surg 1976;183:271, World J Surg 1987;11:110)
Epidemiology
- Intrathyroidal PT tissue was found in 2% - 3% of total thyroidectomy cases (Laryngoscope 1999;109:1238, Arch Otolaryngol Head Neck Surg 2007;133:1105)
- The incidence of true functioning intrathyroidal PT glands is < 1% of all hyperparathyroidism cases in large series (Otolaryngol Head Neck Surg 2011;144:867, Surgery 2012;152:1193); an additional 1% - 2% are intrathyroidal PT glands of subcapsular location
- F:M = 3:1, mean age is 54 years (Surgery 2012;152:1193)
- Adenoma > Hyperplasia > Carcinoma
- 400+ cases of intrathyroidal PT adenoma have been described in series and case reports, but < 10 cases of intrathyroidal PT carcinoma
- Intrathyroidal PT tissue was found in 3% of infants on routine sections, 70% on step sections (J Anat 1976;122:77)
Sites
- Superior vs. Inferior = 3:1
- R:L = 3:2
Pathophysiology / etiology
- A primordium of the superior PT glands (derived from 4th branchial pouch) may become trapped within the thyroid as the lateral and medial lobes fuse, resulting in an intrathyroidal superior PT gland (Ann Surg 1976;183:271)
- The inferior PT glands (derived from 3rd branchial pouch) are pulled by the thymus during its descent, and, because of migrating a longer distance, they have an increased chance of becoming entrapped during the fusion of the thyroid lobes (Am J Surg 1992;164:496, Am J Surg 2006;191:418)
Clinical features
- 30% are asymptomatic (Surgery 2012;152:1193)
- Hyperparathyroidism is seen in functioning lesions (adenoma, hyperplasia)
- May cause failure in surgical treatment of hyperparathyroidism (World J Surg 1987;11:110)
- Conversely, excision during thyroidectomy of intrathyroid PT glands may cause hypoparathyroidism (J Surg Oncol 1984;27:271)
Laboratory
- May cause high PTH serum levels, hypercalcemia or hyperphosphatemia in functioning lesions (adenoma, hyperplasia)
- PTH immunoassay in FNA aspiration fluid shows higher level than in serum
Radiology description
- Detect with 99m Technetium-sestamibi scintigraphy (MIBI scan), MIBI-CT (see Video below)
- US: the most characteristic feature of intrathyroidal PT adenoma is a hyperechoic line on the ventral surface of the PT gland (Endocr J 2011;58:989)
Case reports
- Nontumor:
- 6 year old boy with intrathyroidal thymic tissue surrounding an intrathyroidal parathyroid gland (Thyroid 2008;18:1125)
- 29 year old woman with ectopic intrathyroidal nonfunctioning parathyroid cyst (Endocr Pract 2007;13:56)
- 41 year old woman with intrathyroidal parathyroid hyperplasia (J Surg Case Rep 2013 May 8;2013(5))
- 52 year old woman with intrathyroidal supernumerary parathyroid gland (Nephrol Dial Transplant 2007;22:293)
- 74 year old man with intrathyroidal parathyroid gland (Endocr Pract 2008;14:80)
- Bilateral intrathyroidal hyperplastic parathyroid glands (J Surg Oncol 1984;27:271)
- Amyloid goiter associated with intrathyroid parathyroid and lymphoepithelial cyst (Endocr Pathol 2009;20:243)
- Ectopic intrathyroidal parathyroid gland and papillary microcarcinoma of the thyroid (Histopathology 2004;44:300)
- Intrathyroid parathyroid gland and neonatal primary hyperparathyroidism (J Pediatr Surg 2000;35:1517)
- Adenoma:
- 19 year old woman with giant intrathyroidal parathyroid adenoma (J Emerg Trauma Shock 2012;5:196)
- 22 year old woman with intrathyroidal parathyroid adenoma mimicking lymphocytic thyroiditis (Diagn Cytopathol 1999;21:276)
- 24 year old woman with primary hyperparathyroidism (Endocrinol Diabetes Metab Case Rep 2013;2013:130019)
- 44 year old woman with primary hyperparathyroidism due to intrathyroidal parathyroid adenoma (BMJ Case Rep 2012 Jun 8;2012)
- 48 year old woman with ectopic intrathyroid parathyroid adenoma (Med Ultrason 2011;13:241)
- Intrathyroid parathyroid adenoma (Diagn Cytopathol 2006;34:790)
- Carcinoma:
- 40 year old man with intrathyroid parathyroid carcinoma with intrathyroidal metastasis (Jpn J Clin Oncol 2011;41:1142)
- 51 year old woman with intrathyroidal parathyroid carcinoma (Case Rep Pathol 2013;2013:198643)
- 63 year old woman with intrathyroidal parathyroid carcinoma (Diagn Pathol 2008;3:46)
- 67 year old woman with intrathyroidal parathyroid carcinoma as cause of hypercalcemia (Endocr Pract 2007;13:176)
Treatment
- Surgical excision
- Thyroid lobectomy for a missing PT tumor is the most common approach (J R Soc Med 1981;74:49)
- Alternatively, thyroidotomy is performed over the lower third of the thyroid only if (a) a lower gland is missing, (b) the ipsilateral thymus is examined and removed, and (c) 3 other glands have been found (Otolaryngol Head Neck Surg 2011;144:867)
- Careful search for hidden subcapsular PT glands is mandatory to avoid unnecessary thyroid surgery
- Draining and ethanol ablation of a cyst
Clinical images
Gross description
- Yellowish tan soft nodule, completely enveloped by the thyroid
- 5 mm to 4 cm in size, rarely occupying the whole lobe; mean weight 300 - 400 mg (Surgery 2012;152:1193)
- The corresponding normal PT gland is missing
- Adenoma may have degenerating cystic center (intrathyroidal PT cyst)
Gross images
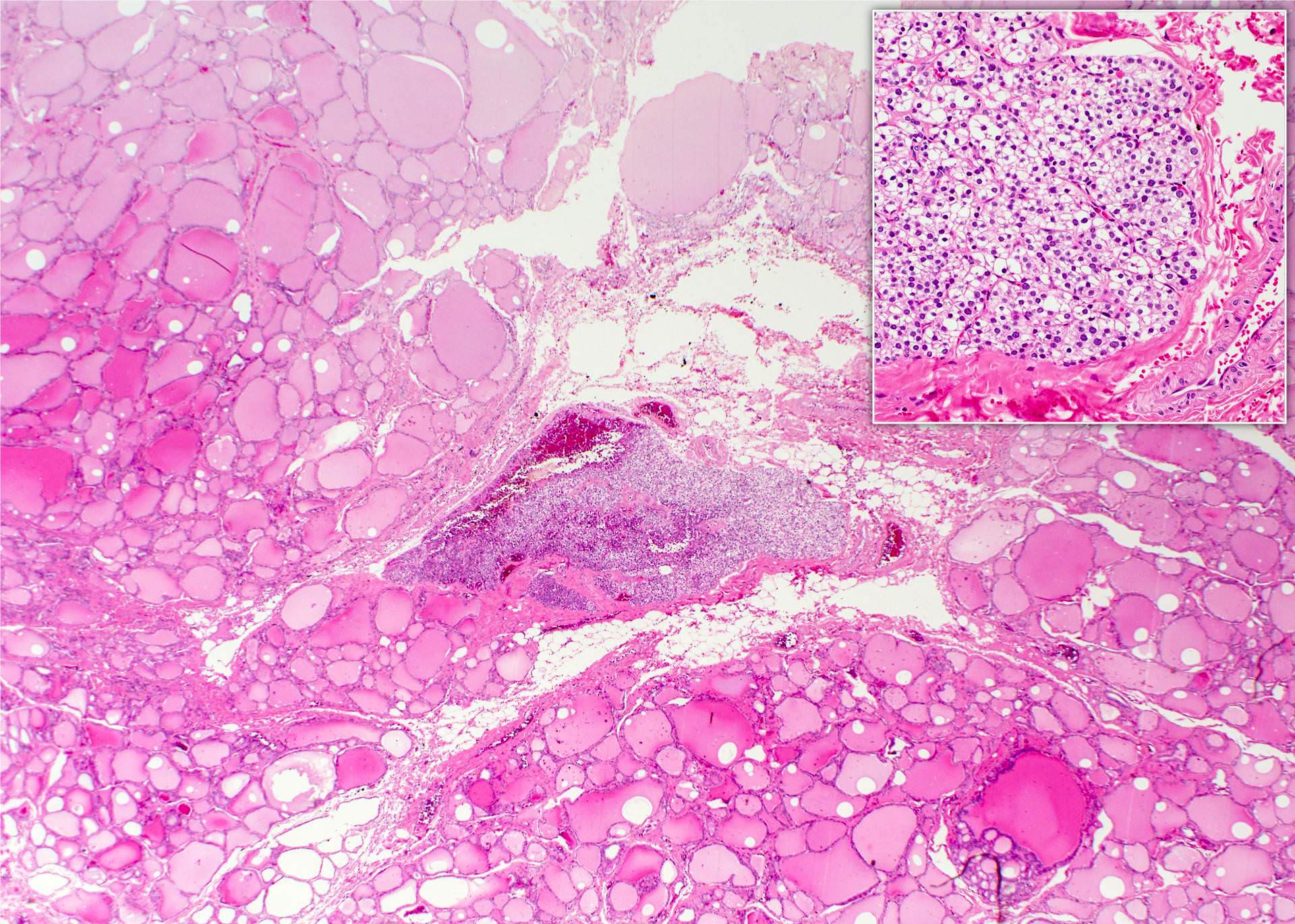
Microscopic (histologic) description
- Incidental intrathyroidal PT tissue / gland has a typical histology of PT
- Ectopic PT gland is completely encased by thyroid parenchyma
- Adenoma may consist of any PT cell population and repeats the composition of orthotopic PT adenoma, with a lack of fatty tissue and peripheral rim of compressed PT parenchyma
- Carcinoma is diagnosed by the presence of invasion or metastasis
Microscopic (histologic) images
Cytology description
- Monotonous cell population of chief cells appeared as discohesive naked nuclei with coarse granular chromatin mimicking lymphocytes (Surgical Pathology Clinics 2014;7:515)
- The cytoplasmic feature unique to PT is the perinuclear oil vacuoles of chief cells, which can be seen on Diff-Quik stain in ~13% of cases (Yang: Thyroid Fine Needle Aspiration, 2013)
- Stippled nuclear chromatin (Cytojournal 2006;3:6)
- Abundant capillaries with attached epithelial cells corresponded to the highly vascular parenchyma (Diagn Cytopathol 1999;21:276)
- The distinction of the different PT lesions including hyperplasia, adenoma and carcinoma cannot be made solely on the basis of cytologic features
- PT adenoma aspirate may contain microfollicular, trabecular, or papillary arrangements, colloid-like secretions, and macrophages similar to thyroid (Yang: Thyroid Fine Needle Aspiration, 2013)
Positive stains
Negative stains
Electron microscopy description
- EM can identify hidden chief cells in "pure" oxyphilic adenoma, explaining PTH production
Videos
Sestamibi Scans and How to See Your Parathyroid Glands
Differential diagnosis
- Chief cell intrathyroidal PT adenoma
- Thyroid follicular adenoma: less vasculature, larger nuclei, colloid with birefringent oxalate crystals and scalloping
- Intrathyroidal PT chief cell hyperplasia
- Lymphocytic thyroiditis (Cancer 2007;111:130)
- Intrathyroidal PT adenoma should be differentiated from thyroid tumors: naked nuclei on FNA, often has an admixture of different PT cell types (chief, oxyphil and clear cells), may have a rim of compressed benign PT tissue at the periphery, PTH+ / TTF1-
- Oncocytic / oxyphilic intrathyroidal PT adenoma
- Thyroid Hürthle cell adenoma: large nuclei, more often prominent nucleoli, indistinct cell membrane (Diagn Cytopathol 2004;31:276, Diagn Cytopathol 2010;38:833)
- Thyroid medullary carcinoma: infiltrative growth with sclerosis and prominent amyloid deposition
- Water clear-cell intrathyroidal PT adenoma
- Thyroid clear cell adenoma