Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Agarwal S, Bychkov A. Oncocytic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidoncocytic.html. Accessed April 1st, 2025.
Definition / general
- Rare type of papillary carcinoma (PTC) characterized by nuclear features of papillary carcinoma and oncocytic / oxyphilic / Hürthle cell like cytoplasm (mitochondria-rich)
- Oncocytic changes can be seen in other thyroid cancer (Hürthle cell carcinoma, medullary carcinoma) and in other variants of papillary carcinoma (tall cell variant, Warthin-like variant)
Essential features
- Papillary carcinoma with oncocytic cytoplasm
- Abundant altered mitochondria on ultrastructural examination
- Must differentiate from other oncocytic thyroid tumors, especially tall cell papillary thyroid carcinoma
Terminology
- Papillary carcinoma, oxyphilic variant
- Papillary carcinoma, Hürthle cell variant
ICD coding
Epidemiology
- Less than 10% of all papillary carcinomas (Ann Otol Rhinol Laryngol 2009;118:374, Thyroid 2018;28:1462)
- < 0.5% when purely oncocytic without admixture of other patterns (Oncotarget 2017;8:77075, Lloyd: WHO Classification of Tumours of Endocrine Organs, 4th Edition, 2017)
- Age: 20 - 76 years, usually older than patients with conventional papillary carcinoma (Thyroid 2018;28:1462, Ann Otol Rhinol Laryngol 2009;118:374, Oncotarget 2017;8:77075, Eur J Nucl Med Mol Imaging 2019;46:2526)
- 74 - 86% women (Thyroid 2018;28:1462, Ann Otol Rhinol Laryngol 2009;118:374, Oncotarget 2017;8:77075)
Sites
- Either lobe or isthmus of thyroid gland, also in ectopic thyroid tissue, e.g., thyroglossal cyst or struma ovarii
Pathophysiology
- Increasing accumulation of somatic mitochondrial DNA mutations, upregulation of energy pathways (pyruvate synthesis, Krebs cycle, electron transport chain) and mitochondrial related pathways (Mitochondrion 2019;46:123)
Clinical features
- Painless neck swelling or enlarged cervical lymph node
- Associated with lymphocytic / Hashimoto thyroiditis in 38 - 91% (Thyroid 2018;28:1462, Am J Clin Pathol 1995;103:280)
Diagnosis
- Preoperative fine needle aspiration cytology
- Histopathological examination of tumor post resection
Radiology description
- Similar to classic papillary carcinoma on ultrasound
- Well lobulated with peripheral calcifications or macrocalcification (J Ultrasound Med 2015;34:1)
- Lacks microcalcification (Front Endocrinol (Lausanne) 2018;9:223)
Prognostic factors
- Recent series showed that prognosis is similar to classical papillary carcinoma, although earlier reports raised concern about poorer prognosis (Braz J Otorhinolaryngol 2013;79:738, Oncotarget 2017;8:77075, Thyroid 2018;28:1462, Eur J Nucl Med Mol Imaging 2019;46:2526, Ann Otol Rhinol Laryngol 2009;118:374, Clin Endocrinol (Oxf) 2016;85:797)
- Radioactive iodine resistance has been reported (Arch Pathol Lab Med 2008;132:1241)
- Risk stratification as per American Thyroid Association 2015 guidelines (Thyroid 2016;26:1)
Case reports
- 28 year old woman with lymphocytic thyroiditis (Asian Journal of Oncology 2016;02:85)
- 60 year old man with lymph node metastases (Pathology 2015;47:S81)
- 64 year old woman with multifocal involvement (Türk Onkoloji Dergisi 2010;25:161)
- 70 year old woman with brain metastasis (Virchows Arch 2013;462:473)
Treatment
- Usually surgical excision per American Thyroid Association and The National Comprehensive Cancer Network guidelines (Thyroid 2016;26:1, J Natl Compr Canc Netw 2018;16:1429)
Gross description
- Mean size 2.0 - 2.8 cm (Thyroid 2018;28:1462, Eur J Nucl Med Mol Imaging 2019;46:2526)
- Solid, firm nodule
- Brown in color similar to Hürthle cell tumors
- Variable calcification and encapsulation
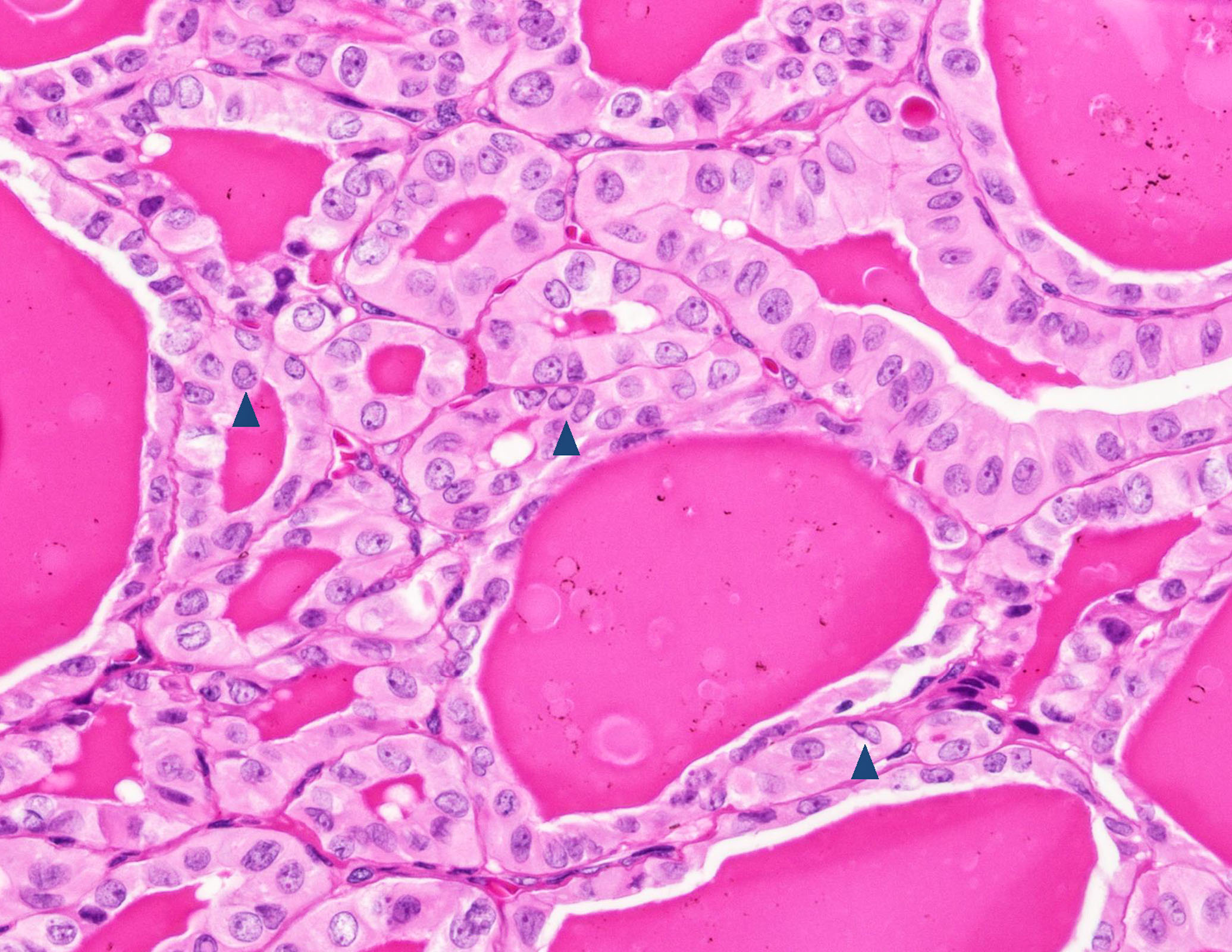
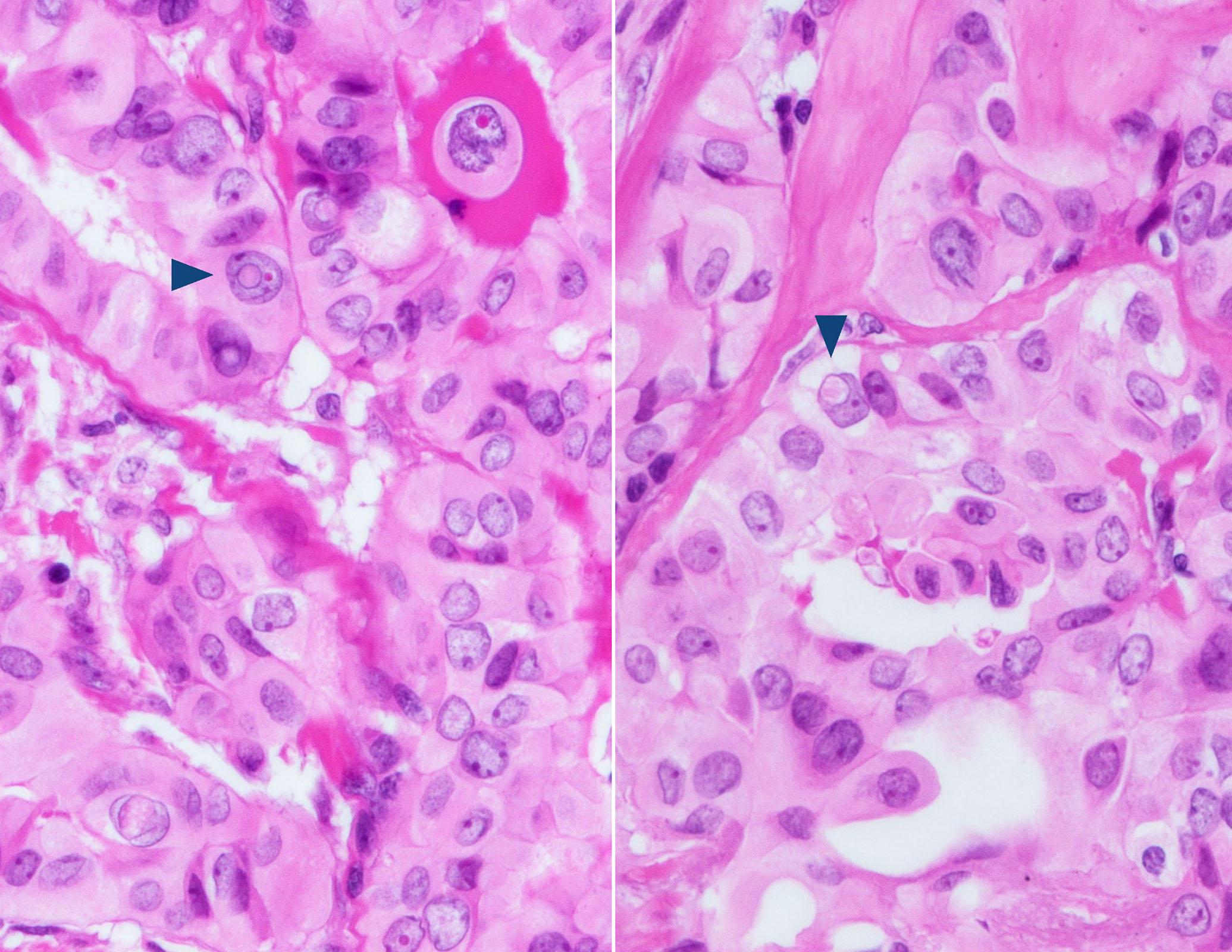
Microscopic (histologic) description
- Usually papillary, can be follicular, rarely solid (Nikiforov: Diagnostic Pathology and Molecular Genetics of the Thyroid, 3rd Edition, 2019, Clin Endocrinol (Oxf) 2016;85:797, Acta Cytol 2019:1)
- Composed of oncocytic (oxyphilic, Hürthle) cells
- Polygonal cells with well defined cell borders
- Abundant, dense eosinophilic, granular cytoplasm
- Can be discohesive, similar to Hürthle cell tumors (adenoma / carcinoma)
- Nuclear features
- Nuclear enlargement, round to oval nuclei
- Nuclear membrane with irregular contour, nuclear grooves, frequent intranuclear pseudoinclusions
- Chromatin clearing / chromatin margination / Orphan-Annie nuclei / ground glass nuclei
- Prominent nucleoli, may be hidden due to above nuclear changes
- Nuclear overlapping is uncommon (Acta Cytol 2019:1)
- Ideally should be purely oncocytic, however cut off of for proportion of oncocytic cells is not established
- Psammoma bodies may be found
Microscopic (histologic) images
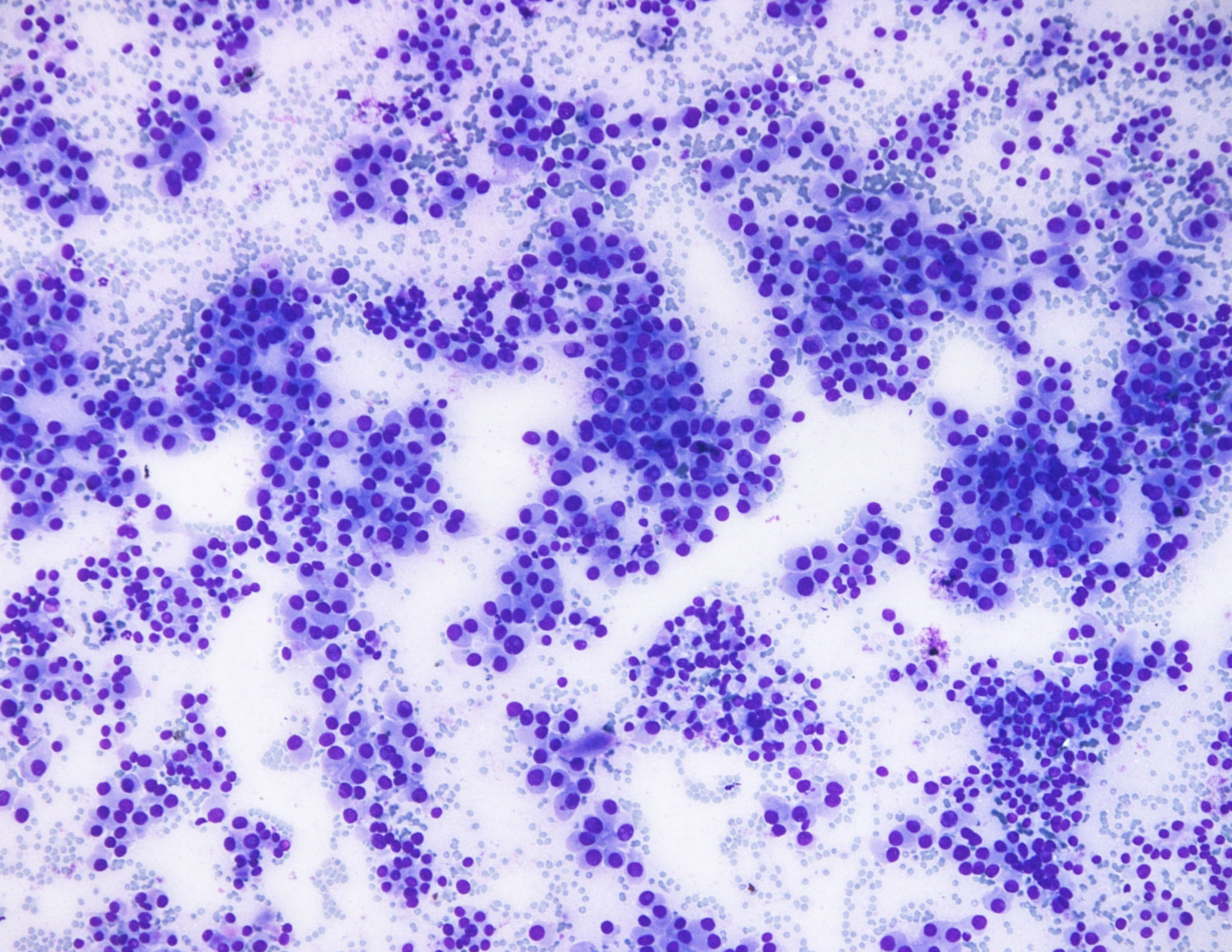
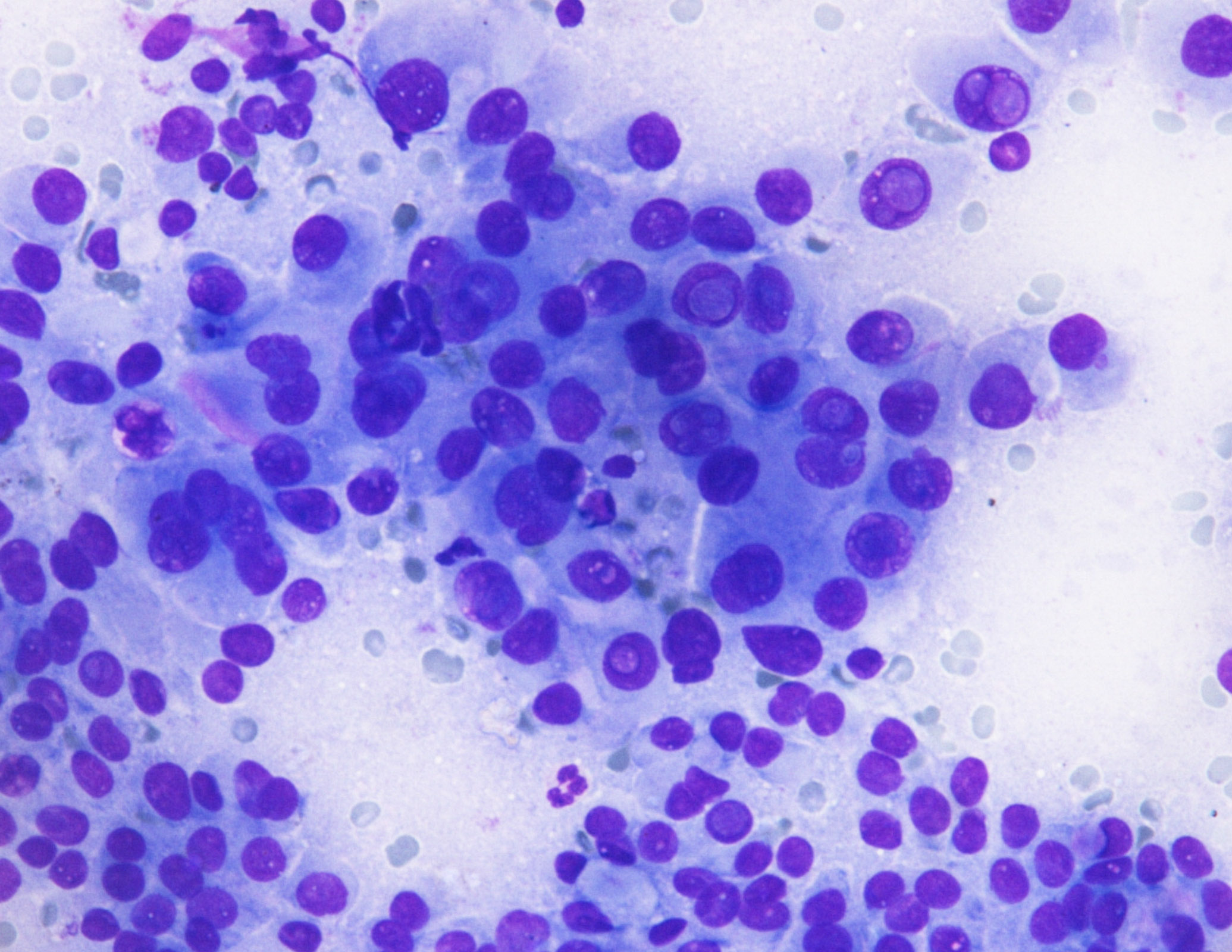
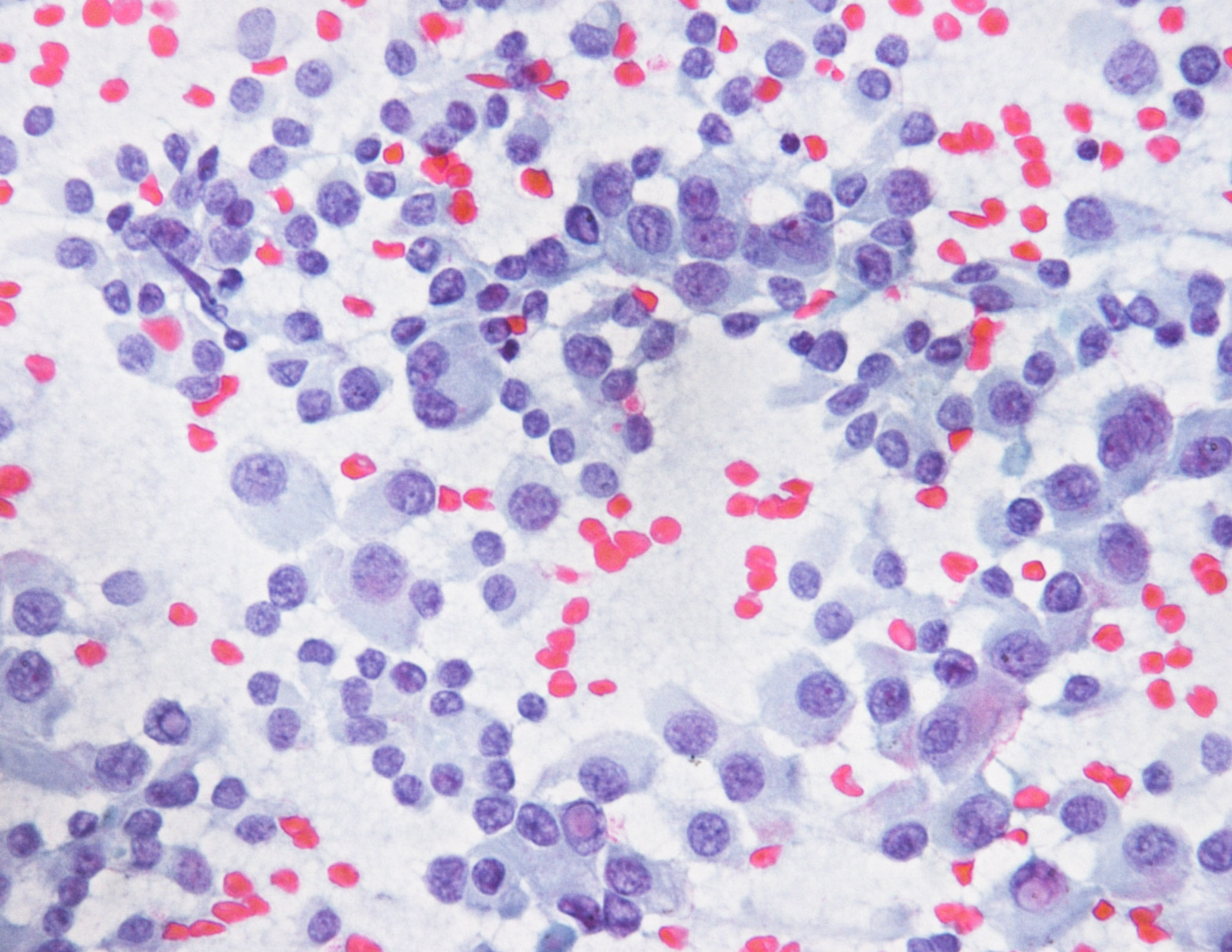
Cytology description
- Cellular aspirate
- Monotonous population of polygonal cells arranged as sheets, clusters, papillae or single
- More than 75% of cells have oncocytic changes of dense cytoplasm and well defined cell borders (Acta Cytol 2019:1)
- Nuclear enlargement, fine powdery chromatin, nuclear grooves, prominent intranuclear pseudoinclusions
Cytology images
Positive stains
- Thyroid specific: TTF1, PAX8, thyroglobulin
- Cytokeratins: AE1/AE3, CK7, CK19
- HBME, galectin3 (Virchows Arch 2004;445:183)
- Hürthle cells frequently demonstrate unusual staining pattern (lower intensity for TTF1/PAX8, abnormal positivity of cytoplasmic markers) compared to nononcocytic thyroid tumors due to abundant intracellular biotin
Negative stains
Electron microscopy description
- Dark and clear cells, both having abundant abnormal mitochondria (more so in dark cells), displaying stacks of parallel cristae, filamentous bundles and woolly densities (Ultrastruct Pathol 1985;8:269, Ultrastruct Pathol 1985;8:131)
- Small dense bodies (Ultrastruct Pathol 1985;8:269, Ultrastruct Pathol 1985;8:131)
- Indented nuclei (Ultrastruct Pathol 1985;8:269, Ultrastruct Pathol 1985;8:131)
- Intact autophagosomes (Mitochondrion 2019;46:123)
Molecular / cytogenetics description
- Mitochondrial DNA mutations, especially complex I genes of the oxidative phosphorylation, are characteristic (Mitochondrion 2019;46:123, Biochim Biophys Acta 2011;1807:633, BMC Cancer 2012;12:53)
- BRAFV600E mutation in about half of cases in limited series (J Pathol 2004;202:247)
- High prevalence of RET⁄PTC in early studies is currently debated (Nikiforov: Diagnostic Pathology and Molecular Genetics of the Thyroid, 3rd Edition, 2019)
- Somatic and germline mutations of GRIM-19 involved in mitochondrial metabolism (Br J Cancer 2005;92:1892)
Sample pathology report
- Thyroid, total thyroidectomy:
- Papillary thyroid carcinoma, oncocytic variant, left lobe, 1.5 cm (see synoptic report)
Differential diagnosis
- Tall cell variant of papillary thyroid carcinoma:
- Height of cells 2 to 3 times the cell width, has adverse prognosis
- Warthin-like variant of papillary thyroid carcinoma:
- Dense lymphoplasmacytic rich infiltrate within the vascular cores
- Hürthle cell adenoma:
- Encapsulated oncocytic tumor, round nuclei, prominent centrally placed nucleoli, cells lack well developed nuclear features of papillary thyroid carcinoma
- Hürthle cell carcinoma:
- Encapsulated oncocytic tumor with capsular or vascular invasion, round nuclei, prominent centrally placed nucleoli
- Cells lack well developed nuclear features of papillary thyroid carcinoma
- Oncocytic variant of poorly differentiated thyroid carcinoma:
- Increased mitotic activity of ≥ 3 mitoses per 10 high powered field, necrosis, lack of nuclear features of papillary thyroid carcinoma
- Oncocytic variant of medullary thyroid carcinoma:
- Stippled chromatin, amyloid, calcitonin immunoreactivity, scattered enlarged hyperchromatic nuclei, secretory granules on ultrastructural examination
- Nodular / adenomatous hyperplasia with oncocytic metaplasia:
- Develops in a background of lymphocytic / Hashimoto thyroiditis / adenomatous goiter, cells lack fully developed nuclear features of papillary carcinoma
Board review style question #1
Board review style answer #1
A. Abnormal mitochondria. This is oncocytic variant of papillary thyroid carcinoma. The cells of have abundant abnormal mitochondria, displaying stacks of parallel cristae, filamentous bundles and woolly densities.
Comment Here
Reference: Oncocytic
Comment Here
Reference: Oncocytic
Board review style question #2
- Oncocytic variant of papillary thyroid carcinoma is typically associated with which of the following molecular alterations?
- BRAFV600E mutation
- Mitochondrial DNA mutations
- PAX8/PPARγ translocation
- RAS mutations
- TERT promoter mutations
Board review style answer #2
B. Mitochondrial DNA mutations. Oncocytic papillary thyroid carcinomas show accumulation of mitochondrial DNA mutations. BRAFV600E mutation can be found in oncocytic papillary thyroid carcinoma but is much more prevalent in tall cell variant of papillary thyroid carcinoma. PAX8/ PPARγ translocation and RAS mutations are usually associated with follicular variant of papillary thyroid carcinoma. TERT promoter mutations have been reported to occur with increasing frequency in cases with de-differentiation.
Comment Here
Reference: Oncocytic
Comment Here
Reference: Oncocytic