Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Demko N, Florianova L, Pusztaszeri M. Microcarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidmicrocarcinomavariant.html. Accessed March 30th, 2025.
Definition / general
- Papillary thyroid carcinoma (PTC) of ≤ 1 cm
- 2017 World Health Organization definition based only on tumor size (irrespective of it being incidental or not)
Essential features
- The most common variant of papillary thyroid carcinoma in the United States
- The majority are indolent but some can exhibit malignant behavior
- No definite biological or clinical parameters currently exist to distinguish indolent from potentially aggressive papillary thyroid microcarcinoma
- Active surveillance may be considered as an alternative to surgery for a select group of patients with low risk tumors
Terminology
- Synonym: papillary microtumor
- Formerly called occult sclerosing carcinoma, occult papillary carcinoma and nonencapsulated sclerosing tumor
ICD coding
Epidemiology
- Very common (~30 - 40% of all papillary thyroid carcinomas)
- Incidental finding in 7 - 17% of surgical thyroidectomies performed for benign or malignant thyroid lesions (J Postgrad Med 2007;53:23, BMC Cancer 2015;15:330)
- Incidental finding in 6 - 36% of autopsies in adults who died of nonendocrine related causes (Cancer 1985;56:531, Am J Clin Pathol 1988;90:72)
- No strong sex predilection (as compared with other thyroid diseases) (BMC Cancer 2015;15:330, Adv Anat Pathol 2006;13:69)
- Predominantly adult patients without a specific age category (BMC Cancer 2015;15:330)
Sites
- Thyroid
- Exceedingly rare at other sites (see Case reports below)
Pathophysiology
- Clonal neoplastic proliferation of thyroid follicular cells, usually with a specific driver mutation (see Molecular / cytogenetics description below)
Etiology
- Shared risk factors with most other variants of papillary thyroid carcinoma
- Ionizing radiation
- Pre-existing benign thyroid disease (Adv Anat Pathol 2006;13:69)
- Higher body mass index (BMI) in women only (Eur J Endocrinol 2013;168:879)
Clinical features
- Usually an incidental finding in a thyroid removed for other reasons or at autopsy (Adv Anat Pathol 2006;13:69)
- Increasingly identified by more sensitive imaging techniques, especially ultrasonography (Surg Clin North Am 2004;84:973, Nat Clin Pract Endocrinol Metab 2007;3:240)
- May be an occult primary tumor identified following diagnosis of cervical lymph node metastasis (Int J Clin Exp Pathol 2014;7:5210)
- Familial form (~6% of cases): often multifocal and bilateral with lymphovascular invasion and lymph node metastases (Endocr Relat Cancer 2016;23:R577, Ann Surg Treat Res 2017;92:129)
Diagnosis
- Histopathologic evaluation of thyroid resection specimens
- Fine needle aspiration cytology (FNAC)
Laboratory
- Recurrent disease (especially after total thyroidectomy) may be monitored by recombinant human TSH (rhTSH) stimulated serum thyroglobulin measurement, with or without neck ultrasound (J Clin Endocrinol Metab 2003;88:3668)
Radiology description
- On ultrasonography: irregular nodule shape, aspect ratio (anteroposterior to transverse diameter of the nodule) of ≥ 1, unclear nodule boundary, blurred margins, internal heterogeneous hypoechogenicity, microcalcifications (Oncol Lett 2016;12:2451)
Prognostic factors
- Excellent prognosis overall
- Most represent a nonprogressive, clinically innocuous disease (self limiting cancer)
- 10 year active surveillance trials showed size enlargement in 7 - 8% and lymph node metastases in 1 - 4% (Eur J Surg Oncol 2018;44:307)
- Small proportion have an aggressive clinical behavior; these represent early stages of papillary thyroid carcinoma that would eventually present as larger tumors
- Meta analysis of 11 studies showed means of 7.2% for microscopic extrathyroidal extension, 28% for lymph node metastases, 0.7% for distant metastases, 5% for tumor recurrence and 0.3% for tumor related death (Endocr Pract 2007;13:498)
- No definite biological or clinical parameters currently exist to distinguish low risk indolent from potentially aggressive tumors
- Meta analysis of 17 studies revealed that recurrence was associated with younger age (< 45 years), tumor multifocality and lymph node metastasis at presentation, whereas no association with gender, tumor size and extrathyroidal extension was found (Eur J Endocrinol 2008;159:659)
- BRAF V600E mutation may be associated with aggressive disease but, as an isolated element, cannot identify cases that will spread locoregionally or to distant sites (Ann Surg Oncol 2009;16:240, Eur J Cancer 2020;124:161)
- Coexistence of BRAF with other oncogenic mutations (PIK3CA, AKT1, TERT promoter or TP53) mutations may indicate a less favorable outcome (Thyroid 2016;26:1)
Case reports
- 44 year old woman with a midline neck mass (J Med Case Rep 2008;2:42)
- 59 year old man with seizures and dysphagia (Ann R Coll Surg Engl 2020;102:e107)
- 2 cases with suggestion of partial regression (Ann Diagn Pathol 2007;11:97)
Treatment
- No consensus on treatment but generally similar to thyroid carcinomas > 1 cm, depending on the lymph node status and other clinical factors
- Thyroid lobectomy alone is sufficient treatment for small, unifocal, intrathyroidal carcinomas in the absence of prior head and neck radiation, familial thyroid carcinoma or clinically detectable cervical nodal or distant metastases (Thyroid 2016;26:1)
- Active surveillance may be considered as an alternative to surgery in selected patients with low risk tumors without clinically evident lymph nodes metastases or local invasion (Eur J Surg Oncol 2018;44:307, Cancer 2017;123:372, Thyroid 2016;26:1)
- Diagnosis of incidental papillary thyroid microcarcinoma in thyroid resection specimens is not, by itself, an indication for additional treatment (i.e. surgery, radioactive iodine)
Gross description
- White-gray fibrotic nodule with irregular contours or an ill defined light brown nodule, measuring ≤ 1 cm
- Multifocality in 20 - 46% (World J Clin Cases 2020;8:1350, Adv Anat Pathol 2006;13:69)
- Due to their small size, these lesions can be easily missed on gross examination and are often identified only microscopically
Frozen section description
- Frozen section is usually not indicated
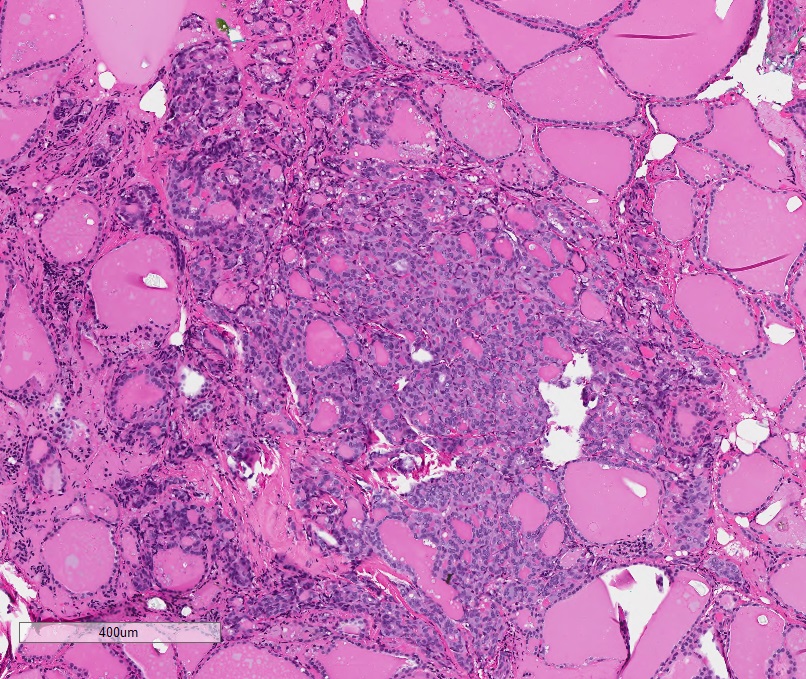
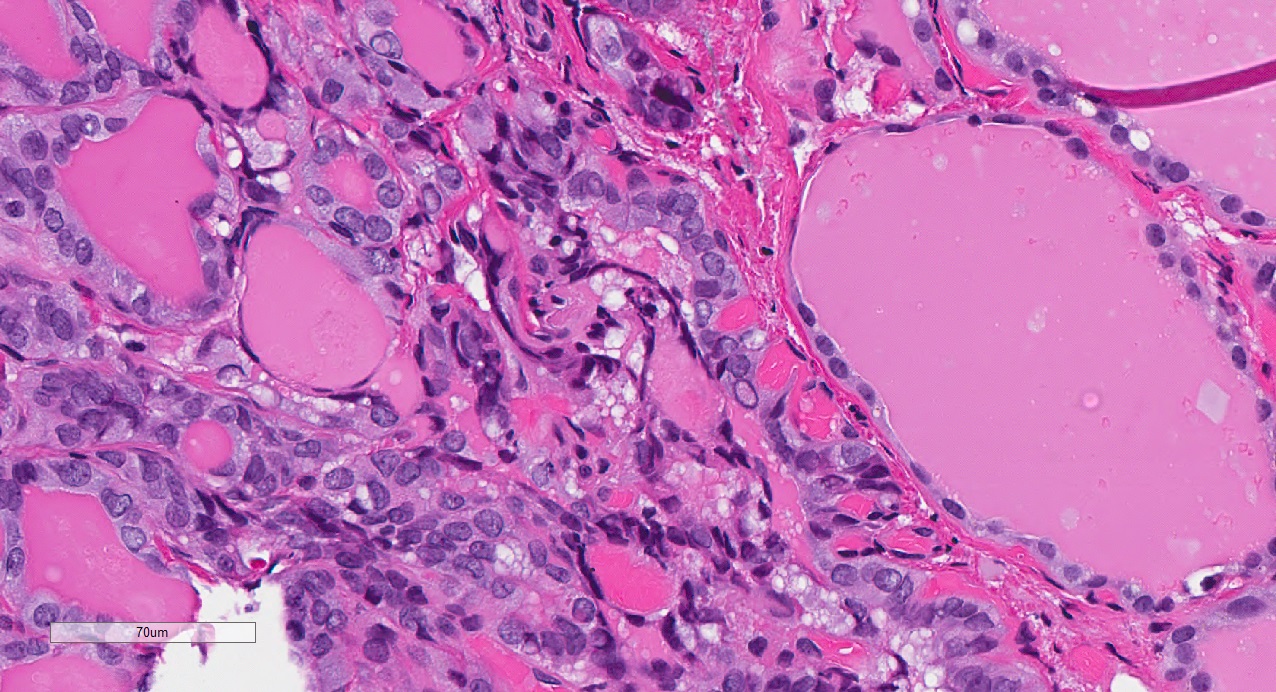
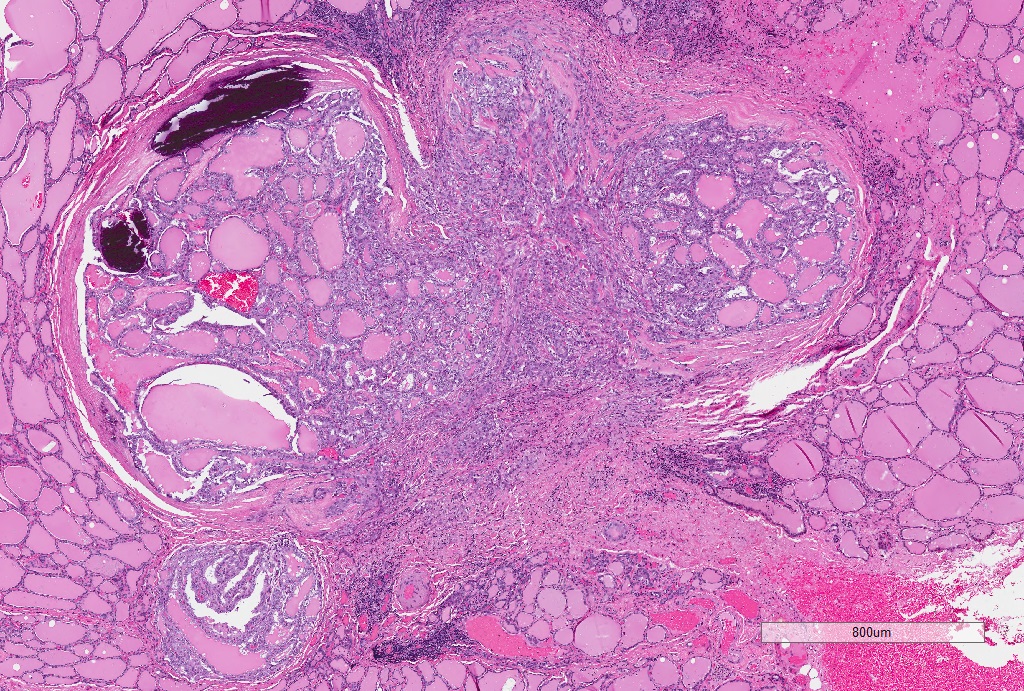
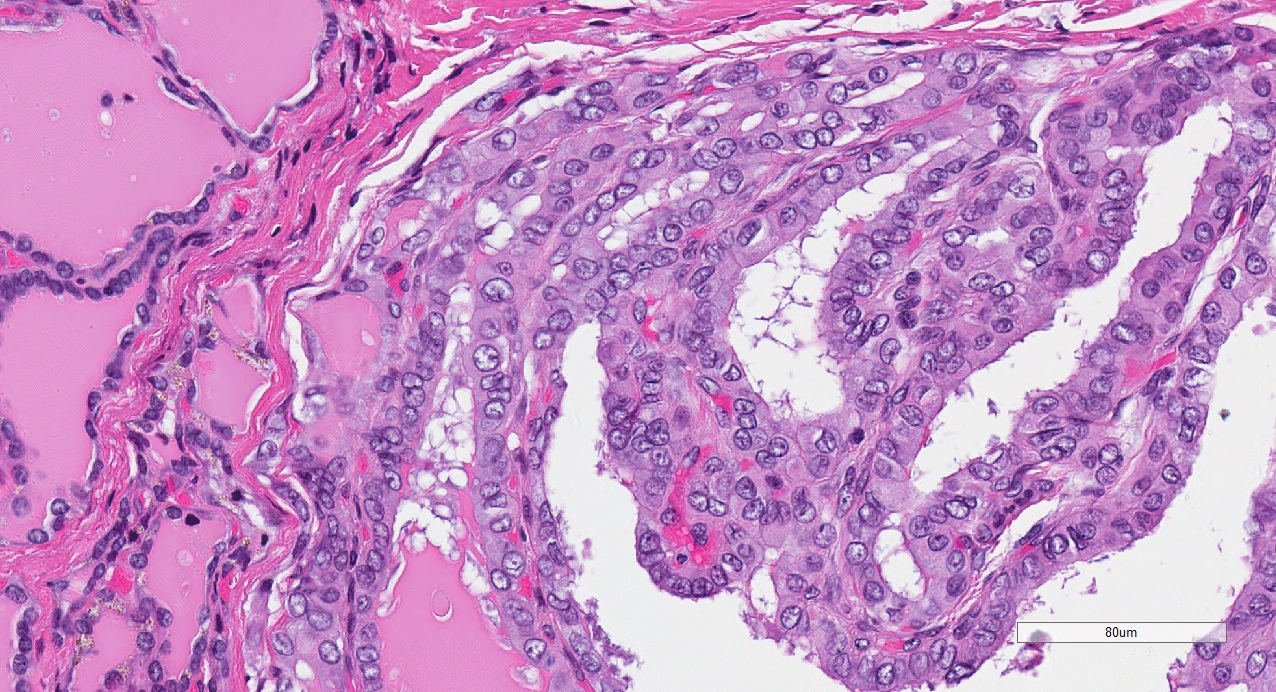
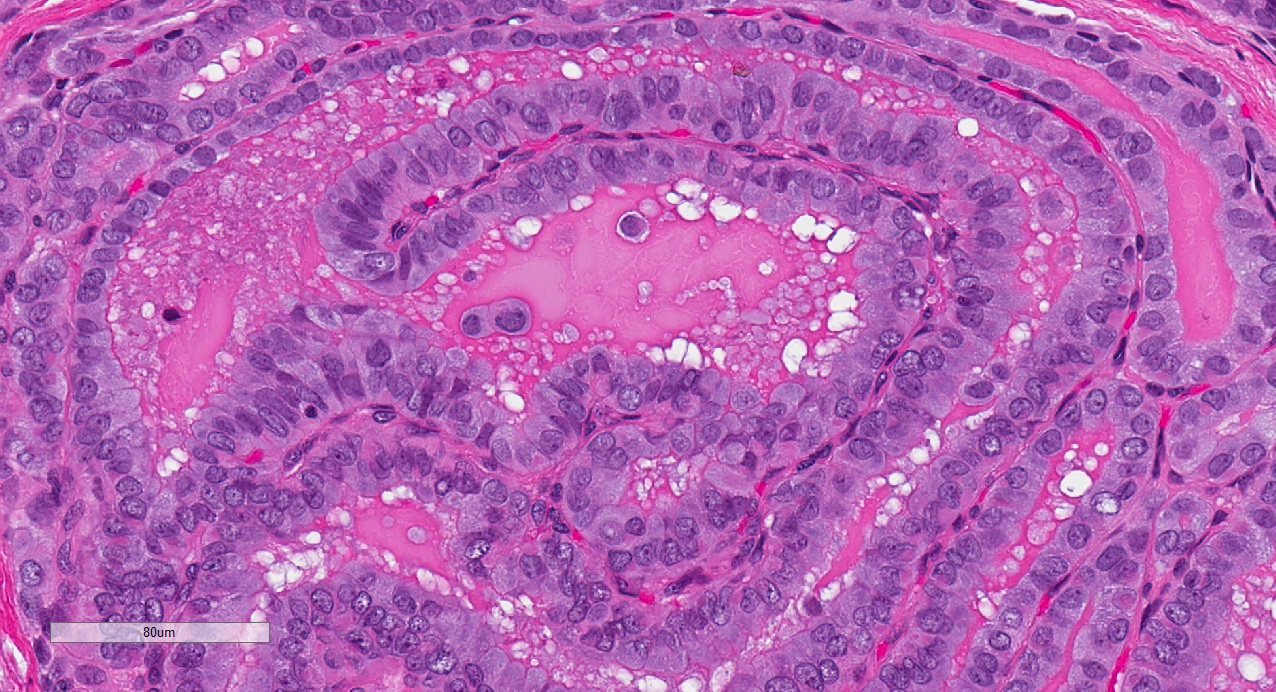
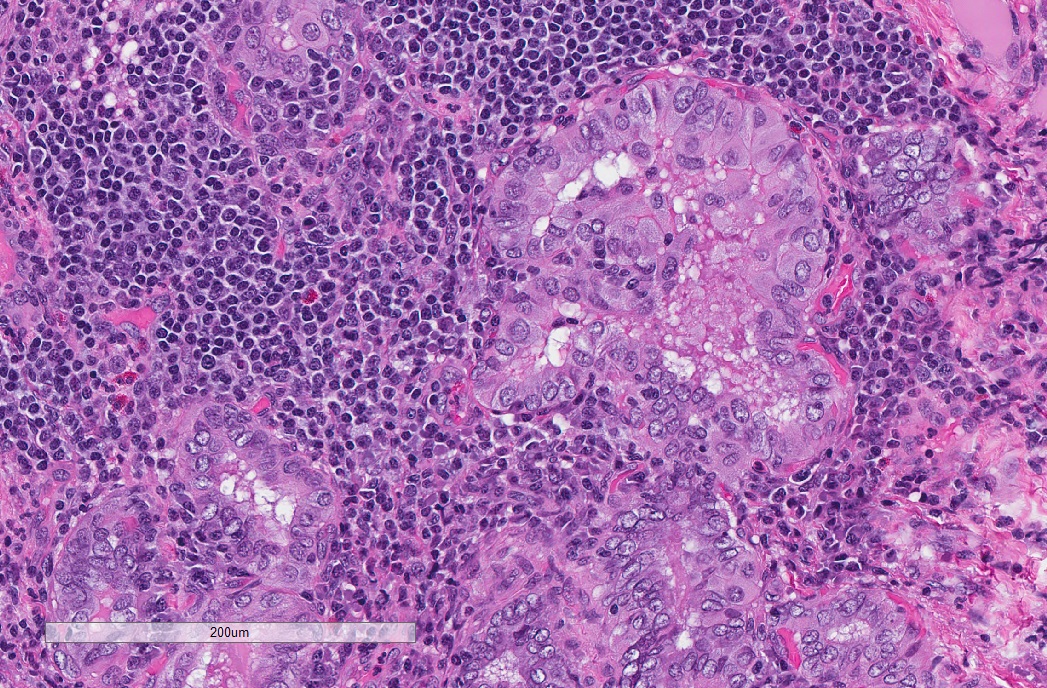
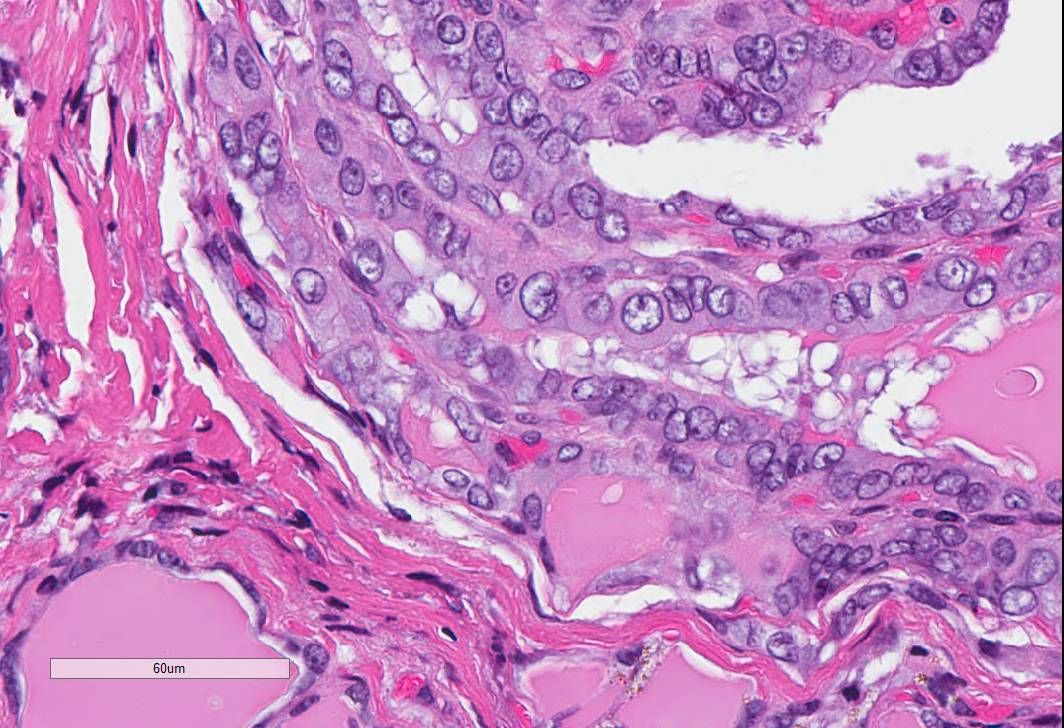
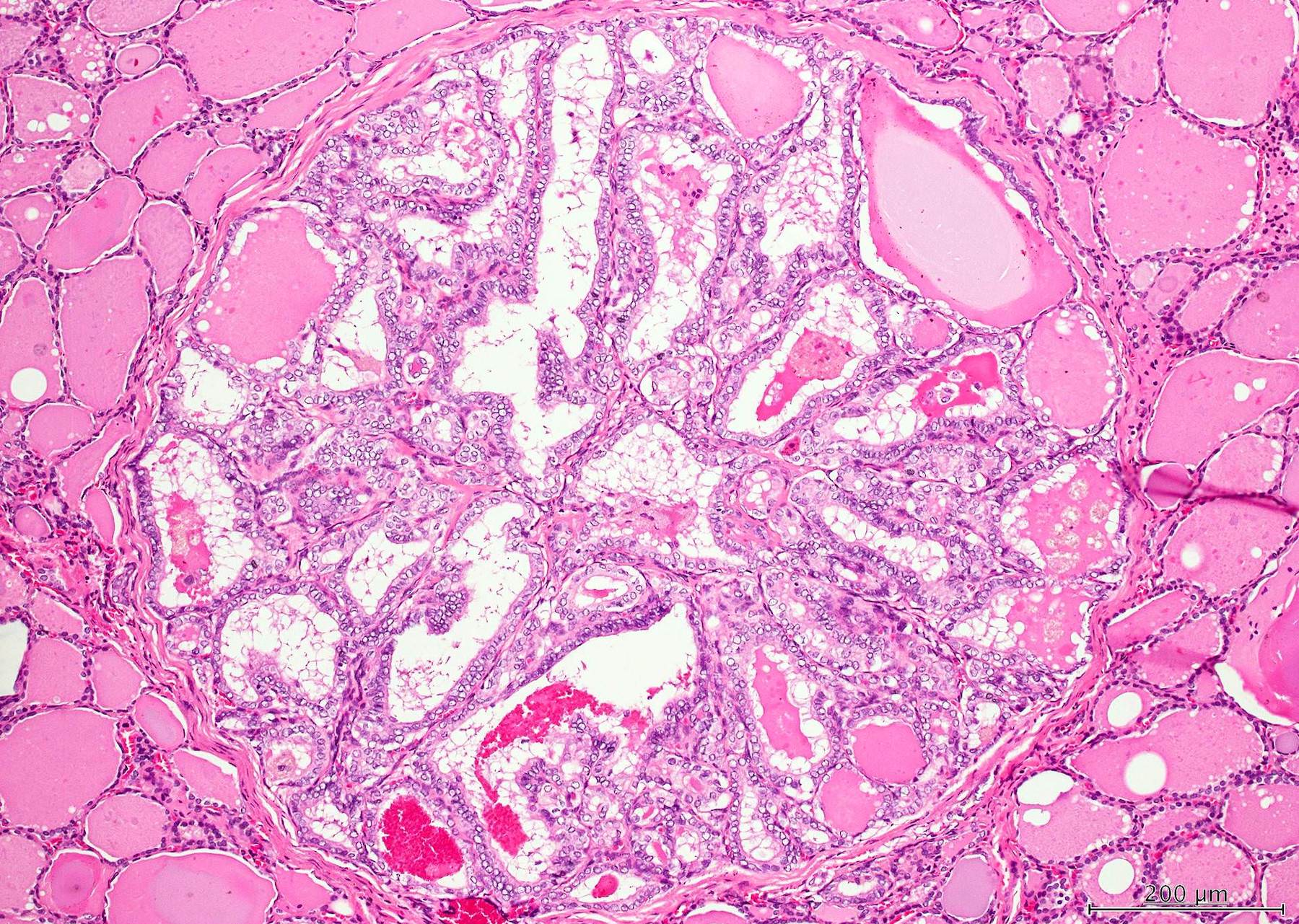
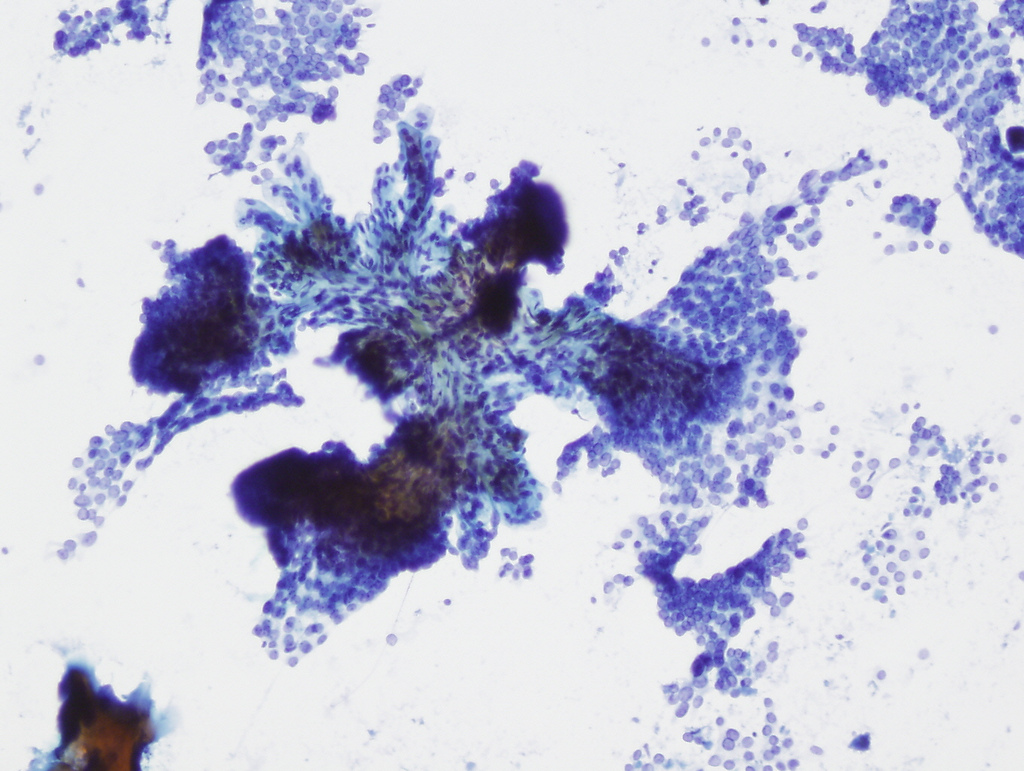
Microscopic (histologic) description
- Defined solely by the ≤ 1 cm size criterion; does not have a unique morphology
- Overall varied architectural patterns with characteristic nuclear features of papillary thyroid carcinoma
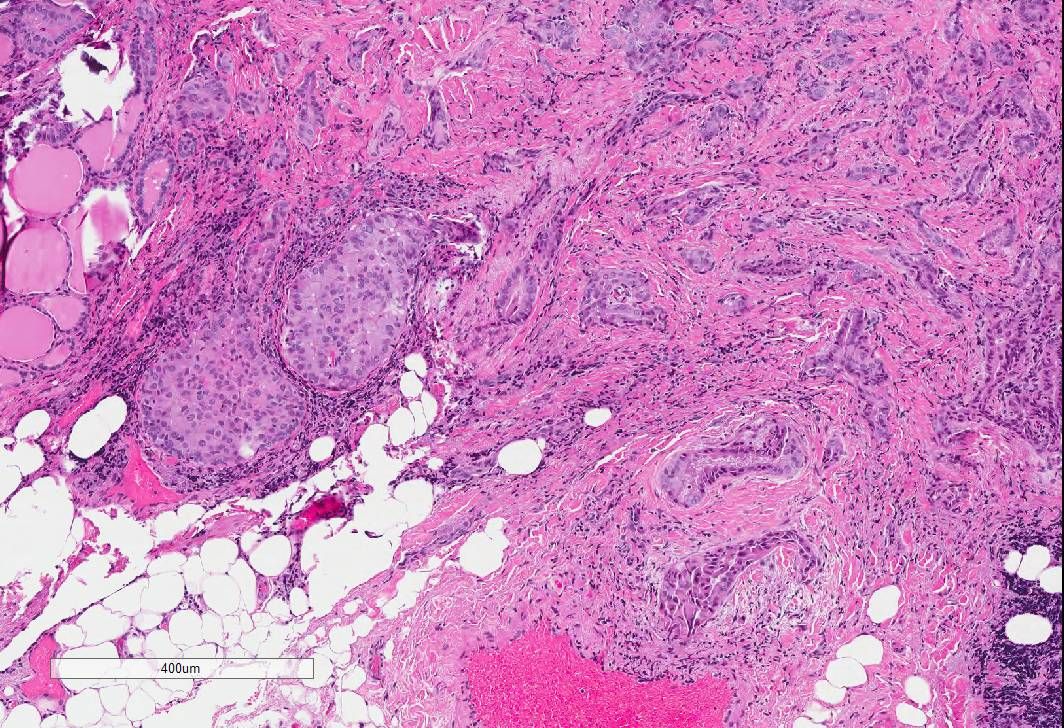
- Typically shows an irregular stellate or scar-like configuration
- May be nonencapsulated or encapsulated, with or without a sclerotic rim
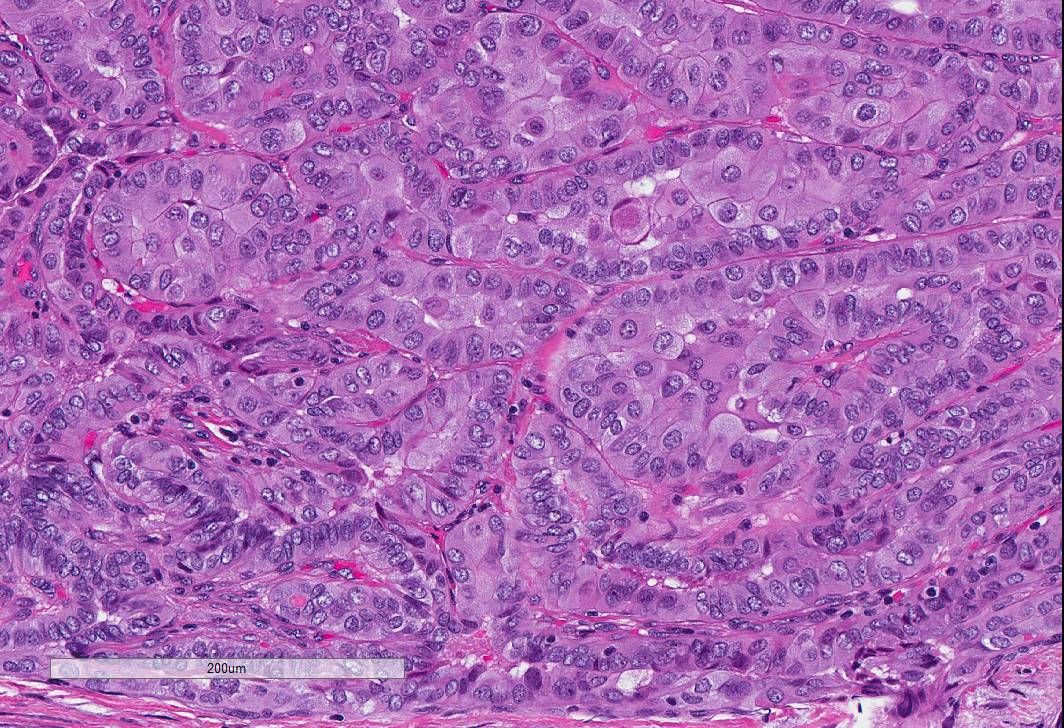
- Composed of papillary or follicular structures or a mixture of both
- Follicular pattern more common than a pure papillary (classical) pattern (Adv Anat Pathol 2006;13:69)
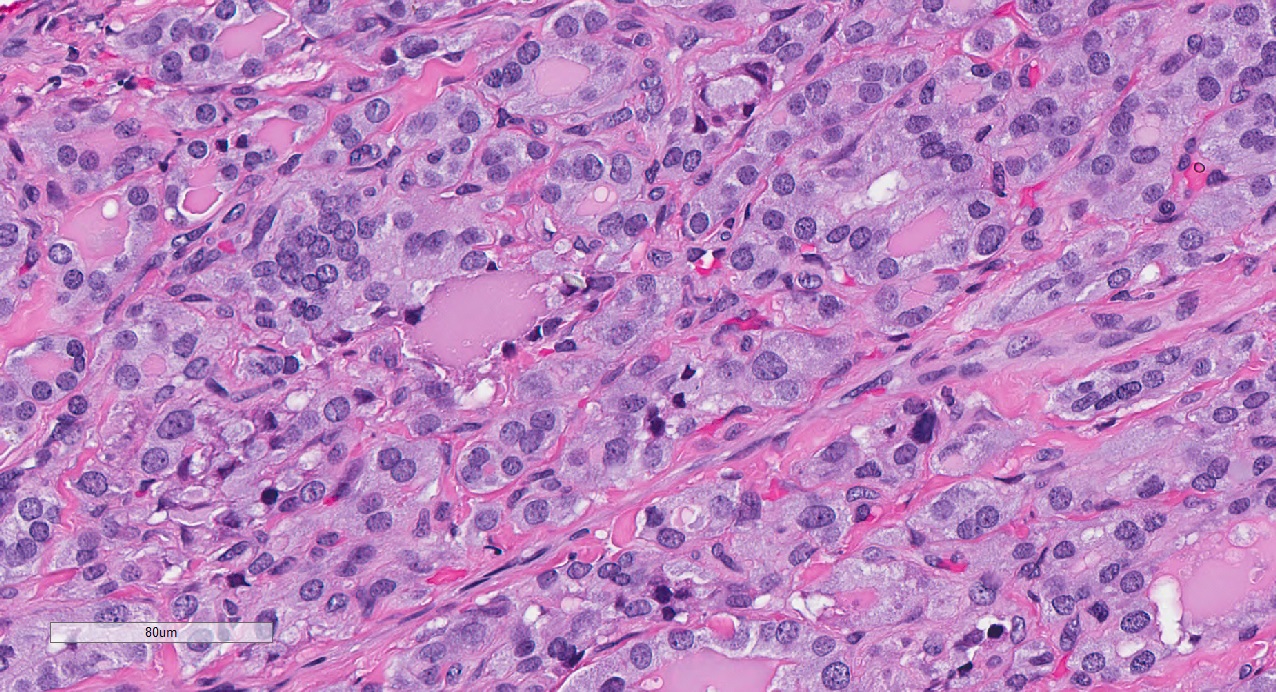
- Characteristic nuclear attributes are present at high power: nuclear enlargement and overlapping, chromatin clearing, irregular nuclear contour, nuclear grooves and nuclear pseudoinclusions
- May show cytologic or architectural features of several variants, including follicular or tall cell
- Does not usually require subclassification
- However, the tall cell variant should be recognized since it is associated with aggressive features (Oncol Lett 2017;13:3501, Thyroid 2013;23:1525)
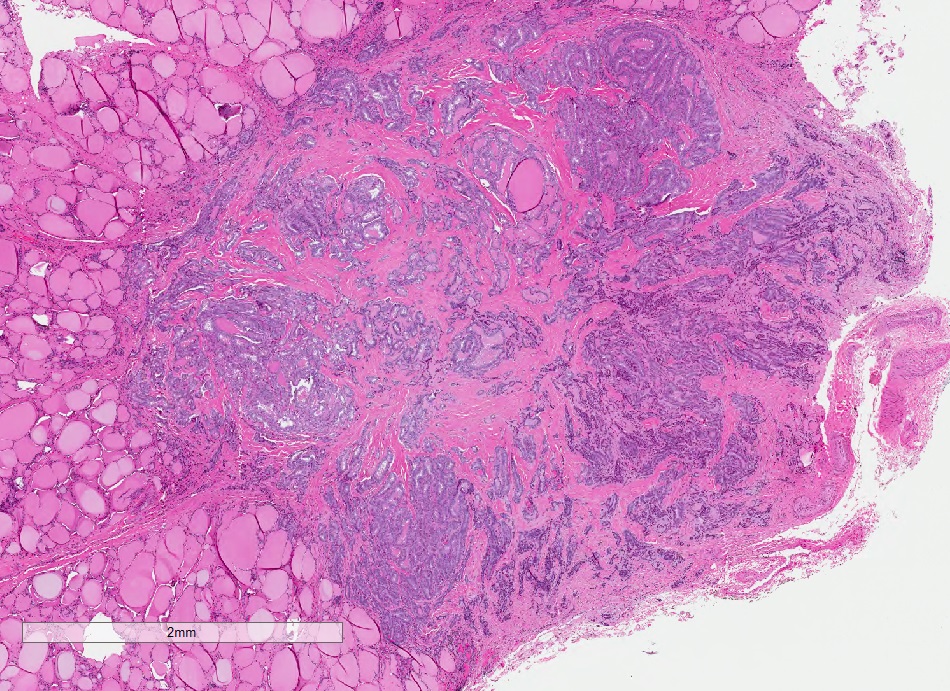
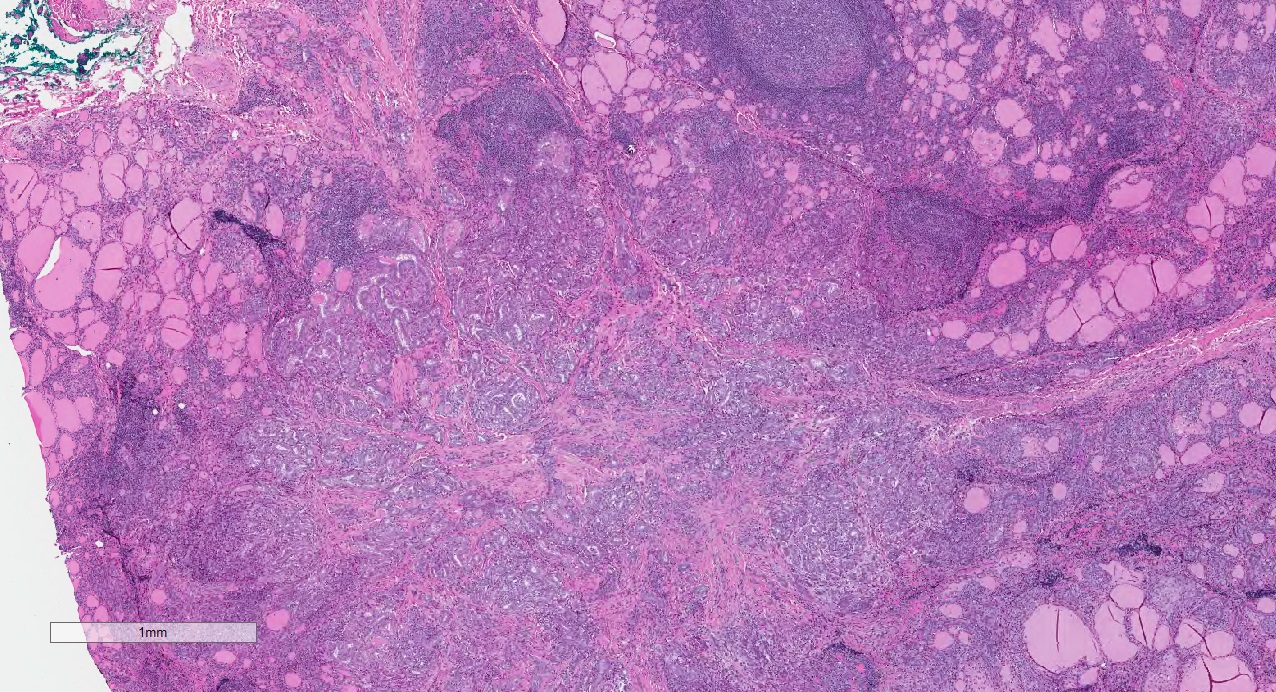
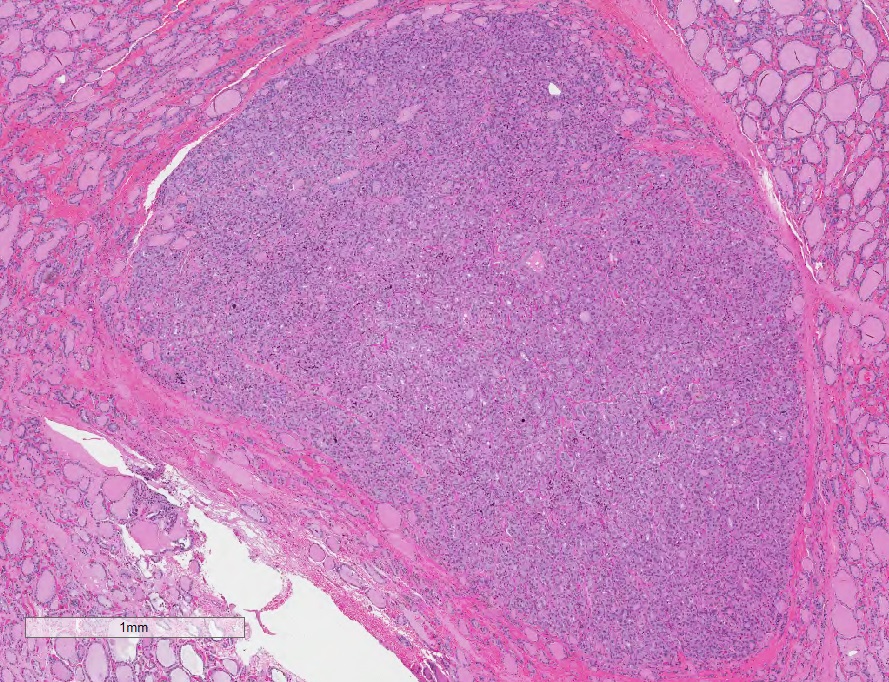
Microscopic (histologic) images
Contributed by Nadine Demko, M.D.C.M., M.Sc., Livia Florianova, M.D., M.Sc. and Marc Pusztaszeri, M.D.
Contributed by Andrey Bychkov, M.D., Ph.D.
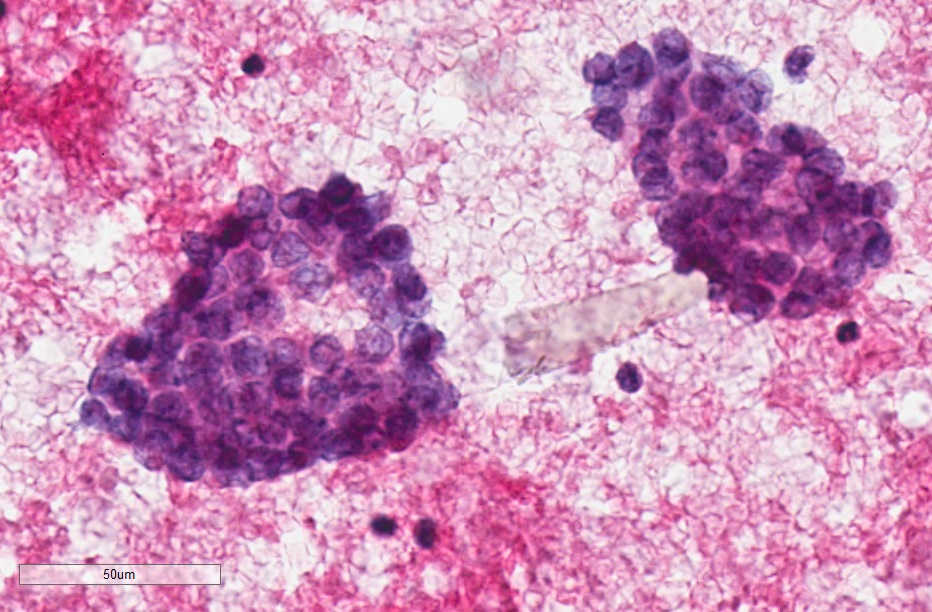
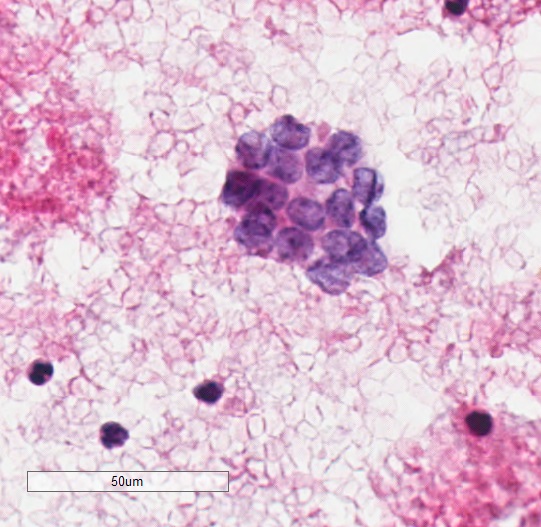
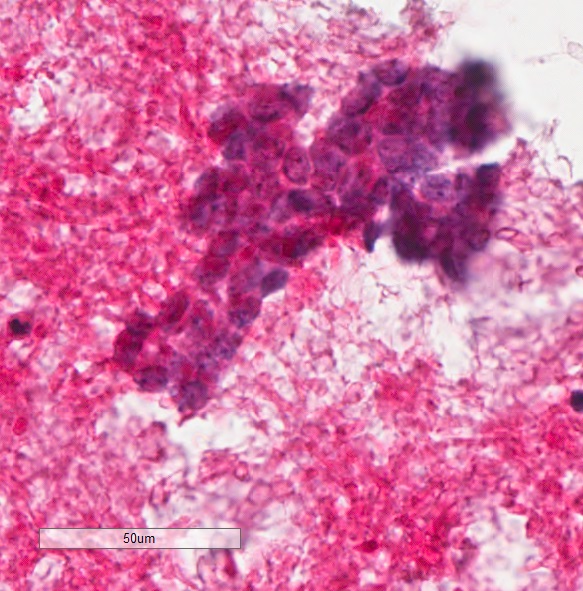
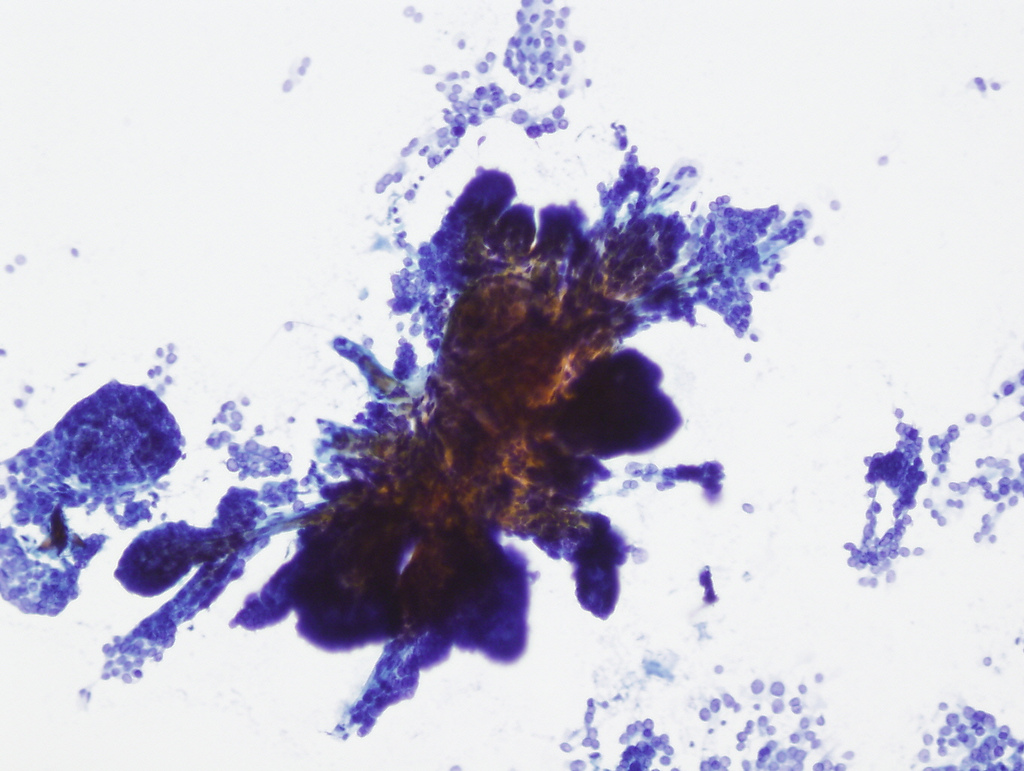
Cytology description
- Usually incidental and is not sampled by fine needle aspiration cytology
- However, some of these lesions undergo fine needle aspiration cytology because of suspicious radiology findings (multifocality, calcification, etc.) or in patients with a history of radiation to the head and neck region to establish the diagnosis and to determine the most appropriate management
- May be accidentally sampled during the aspiration of other clinically significant thyroid nodules (Acta Cytol 2001;45:341)
- Cytologic features are essentially the same as for papillary thyroid carcinoma (Int J Surg Pathol 2002;10:133, Acta Cytol 2001;45:341)
Cytology images
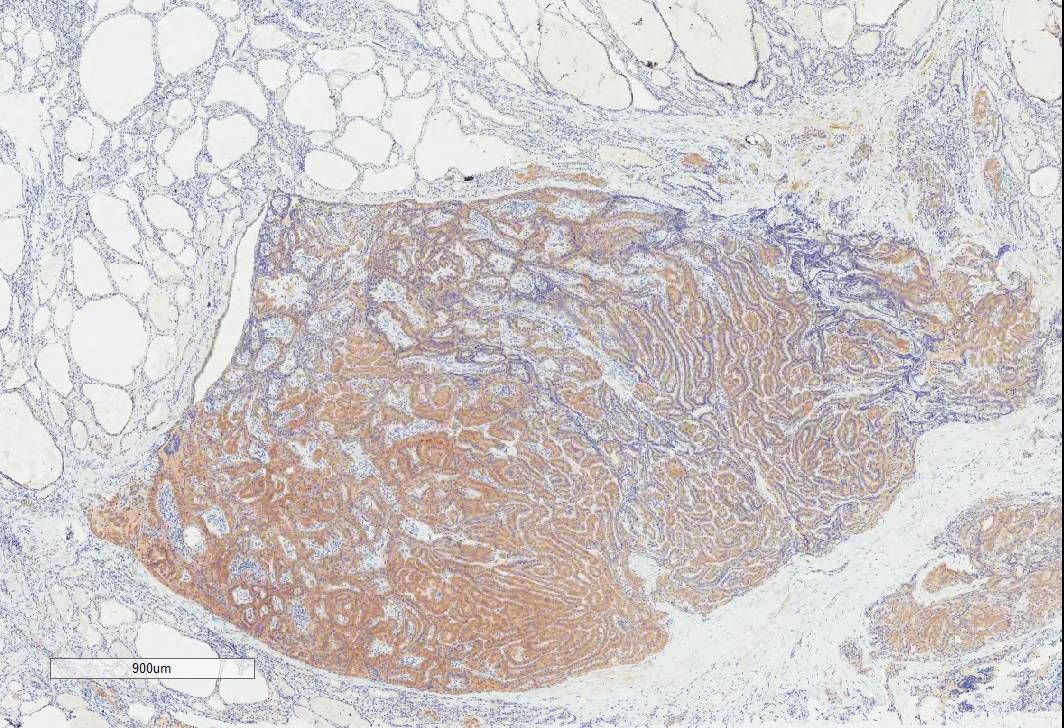
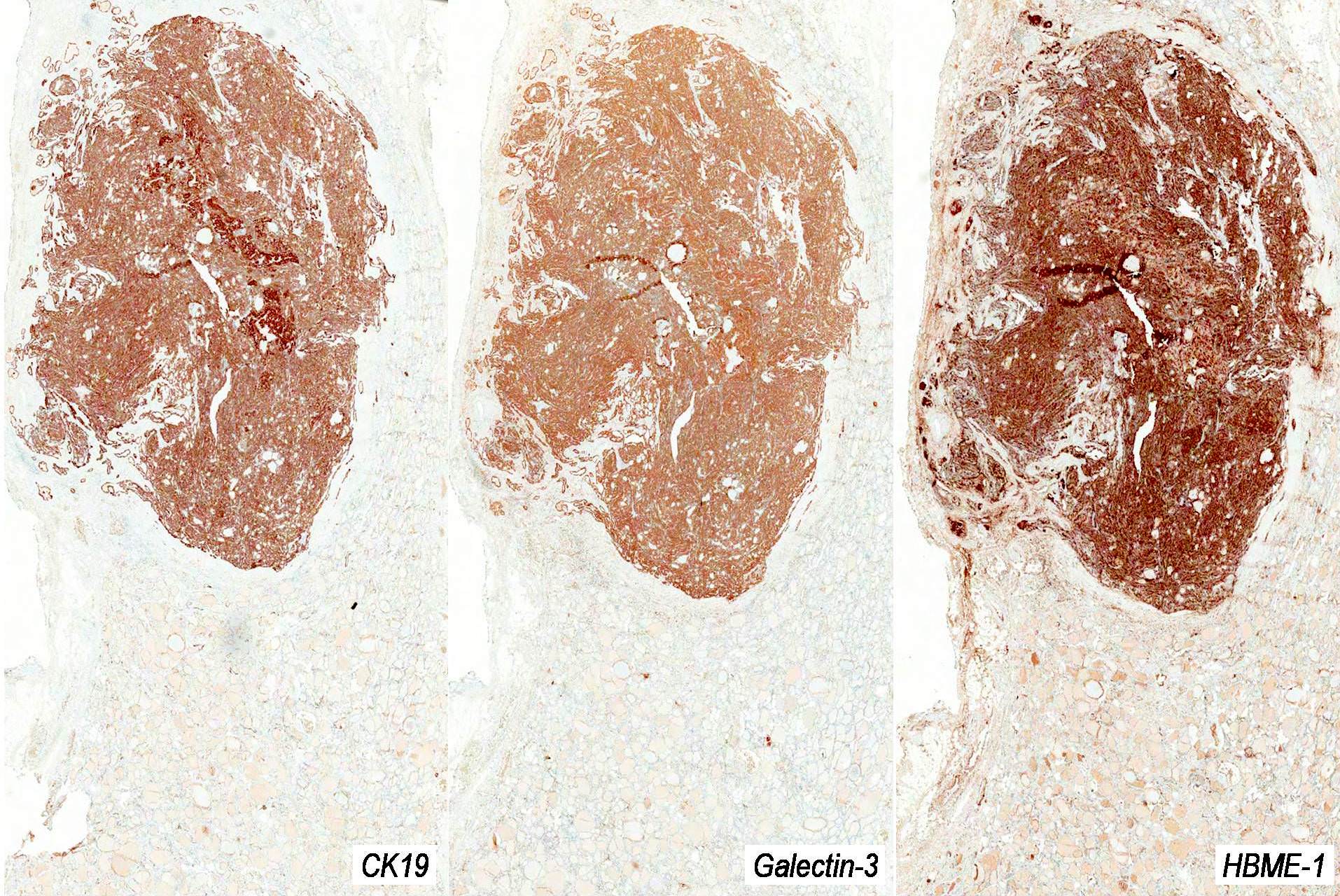
Positive stains
- Same as for papillary thyroid carcinoma > 1 cm
- Thyroglobulin, TTF1, PAX8 and low molecular weight cytokeratins (including CK19), broad spectrum cytokeratins (AE1 / AE3, MNF116), HBME, galectin3 (Mod Pathol 2006;19:1631, Head Neck 2010;32:38, Arch Pathol Lab Med 2015;139:67)
- BRAF V600E in some cases (Arch Pathol Lab Med 2015;139:67)
Negative stains
Molecular / cytogenetics description
- Similar mutations as papillary thyroid carcinoma > 1 cm
- BRAF V600E mutation in 30 - 67% (Thyroid 2016;26:1)
Videos
Active surveillance
Sample pathology report
- Thyroid, right lobe, right hemithyroidectomy:
- Incidental papillary thyroid microcarcinoma, 3 mm, negative for lymphatic invasion and extrathyroidal extension; resection margin negative
- Thyroid, total thyroidectomy:
- Papillary thyroid microcarcinomas, x 5, bilateral, measuring up to 8 mm, negative for lymphatic invasion and extrathyroidal extension; resection margin negative
Differential diagnosis
- Reactive nuclear changes in chronic lymphocytic thyroiditis:
- Usually associated with a lymphoplasmacytic infiltrate and not associated with sclerosis
- Hyperplastic ultimobranchial body rests / solid cell nests:
- Positive for p63 and negative for thyroglobulin and TTF1
- Nonneoplastic follicles entrapped in areas with post-FNAC changes / needle tract:
- Fibrosis and chronic inflammation may cause reactive changes in the nuclei
Board review style question #1
Which of the following statements about papillary thyroid microcarcinoma (shown in the image) is correct?
- Can always be diagnosed on cytology alone
- Can contain tall cell features
- More likely to show a pure papillary rather than follicular architecture
- Must be incidental and measure ≤ 1 cm
- Requires a total thyroidectomy
Board review style answer #1
B. Can contain tall cell features. Papillary thyroid microcarcinoma may show features of other variants including tall cell. Tall cell features should be recognized and reported since they are associated with more aggressive behavior. The other answer choices are incorrect because the 2017 World Health Organization definition is based only on tumor size (irrespective of it being incidental or not), the final size is most often determined on a surgical resection specimen (though it may also be estimated by ultrasound), follicular architectural pattern is more common than pure papillary (classical) pattern and may be managed by a lobectomy or active surveillance.
Comment Here
Reference: Papillary thyroid microcarcinoma (PTMC)
Comment Here
Reference: Papillary thyroid microcarcinoma (PTMC)
Board review style question #2
Which of the following immunostains is usually not expressed in papillary thyroid microcarcinoma?
- BRAF V600E
- CK19
- Galectin3
- HBME
- p63
Board review style answer #2
E. p63. Papillary thyroid microcarcinoma is usually negative for p63, in contrast to the mimicker solid cell nests which are usually positive for p63. HBME, galectin3 and CK19 are expressed in most and can be used to support the diagnosis. BRAF V600E immunostain is often expressed and can be used as a reliable surrogate marker for the corresponding BRAF V600E gene mutation, present in 30 - 67%.
Comment Here
Reference: Papillary thyroid microcarcinoma (PTMC)
Comment Here
Reference: Papillary thyroid microcarcinoma (PTMC)