Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Wei S. Oncocytic (Hürthle cell) tumors. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidhurthle.html. Accessed April 1st, 2025.
Definition / general
- Follicular neoplasm with more than 75% oncocytic tumor cells
- Oncocytic appearance is due to accumulation of dysfunctional mitochondria
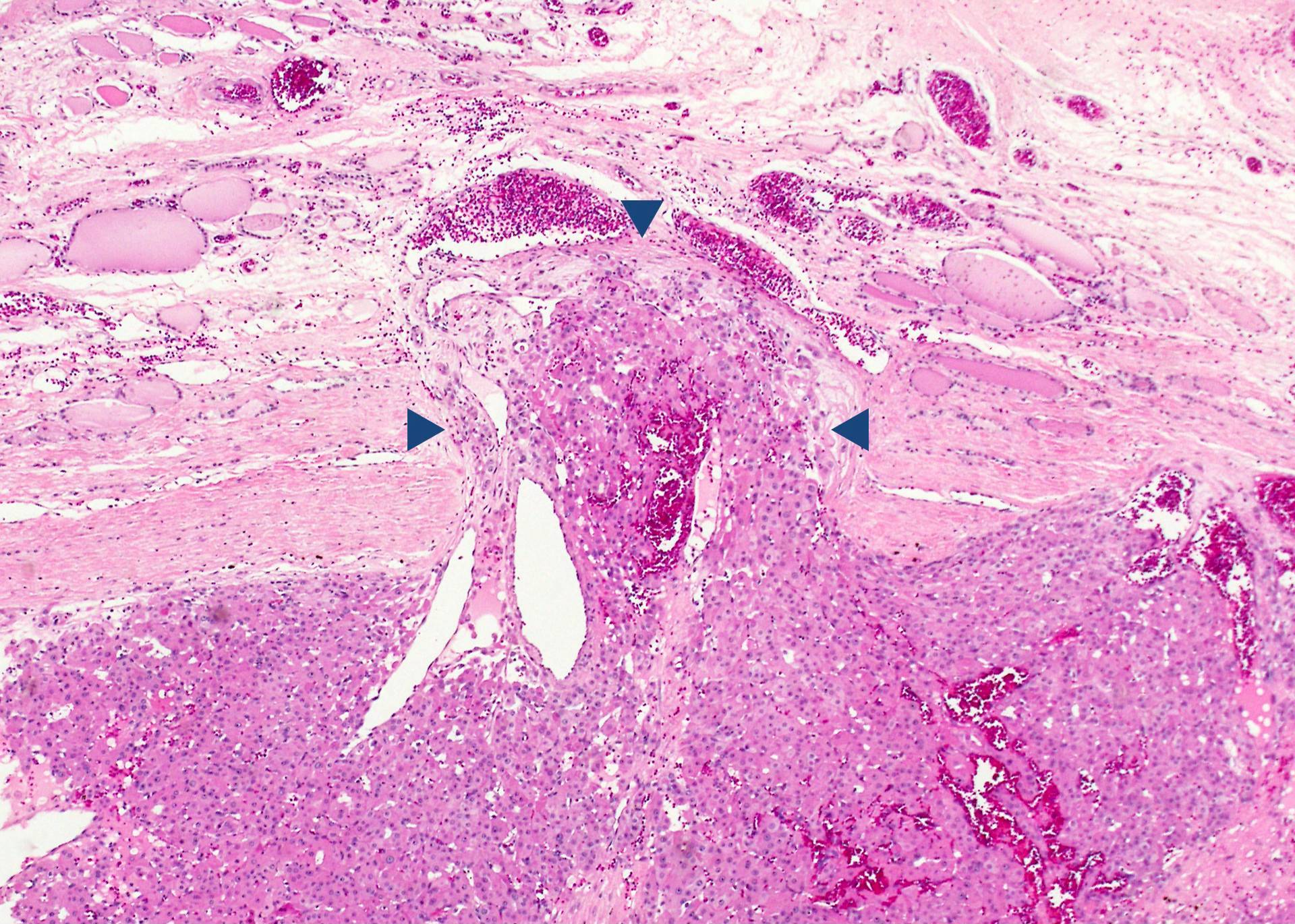
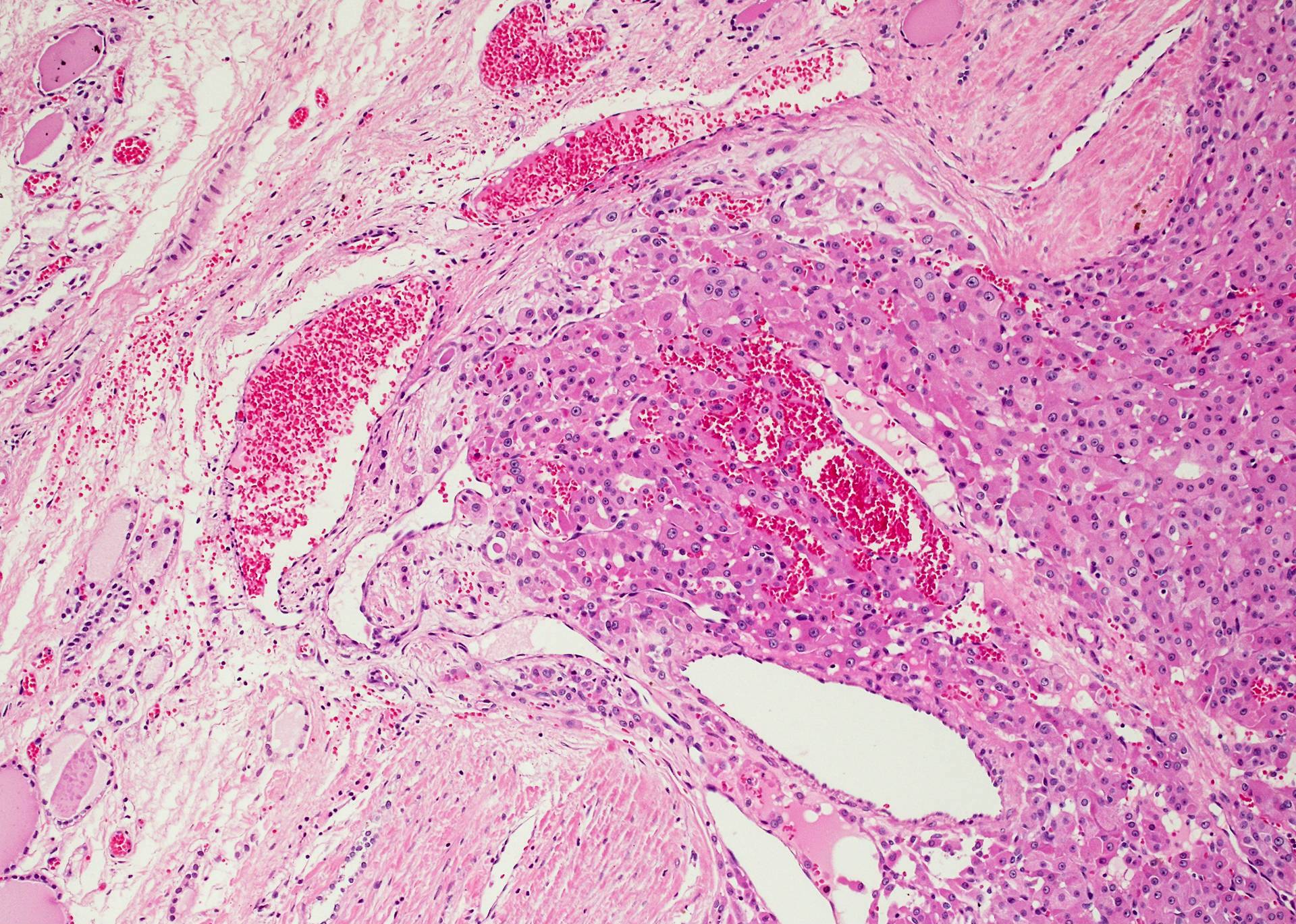
- Malignant if capsular and / or vascular invasion
- Tumor size, nuclear atypia, multinucleation, pleomorphism, mitoses or histologic pattern of the lesion are not determinants of malignancy (Arch Pathol Lab Med 2008;132:1241)
- Hematogenous metastases, 30% to lymph node (in contrast, rare in follicular carcinoma)
- No known exogenous risk factors for developing oncocytic tumors
Essential features
- Follicular neoplasm composed of more than 75% oncocytes
- Malignant if capsular and / or vascular invasion
- Malignant tumors have more aggressive behavior than conventional follicular carcinoma
Terminology
- Synonym: oncocytic cell is also called Hürthle, Askanazy and oxyphilic cells
- "Hürthle cell" is a misnomer - Dr. Hürthle originally used it to describe C cells instead of oncocytes
Epidemiology
- Carcinoma is more common in older men (mean age: 57 years)
Radiology description
- Similar to follicular adenoma / carcinoma
Prognostic factors
- Oncocytic adenoma is benign, no recurrence after excision
- Overall, oncocytic carcinoma is more aggressive than conventional follicular carcinoma, with higher frequency of extrathyroidal extension, local recurrence and metastasis to lymph nodes
- Mortality rate: 10 - 80%
- Worse prognosis: old age, tumor size > 4 cm and extensive vascular invasion
Case reports
- 21 year old man with Hürthle cell thyroid carcinoma and parathyroid carcinoma (J Clin Diagn Res 2015;9:OD08)
- 55 year old man with 3 year history of increasing neck mass (University of Pittsburgh: Neck Mass [Accessed 19 October 2017])
- 55 year old woman with phyllodes tumor metastatic to Hürthle cell adenoma (Arch Pathol Lab Med 2002;126:1233)
- 59 year old man with mixed oncocytic and mucinous secreting carcinoma (Arch Pathol Lab Med 2000;124:1547)
- 77 year old woman with metastasis to breast (Int Semin Surg Oncol 2008;5:14)
- 79 year old man with rapidly increasing lump on neck and colloid goiter 24 years ago (World J Surg Oncol 2004;2:27)
Treatment
- Adenoma: lobectomy
- Carcinoma: total thyroidectomy or radiation ablation
- Radioactive iodine: resistant compared to conventional follicular carcinoma
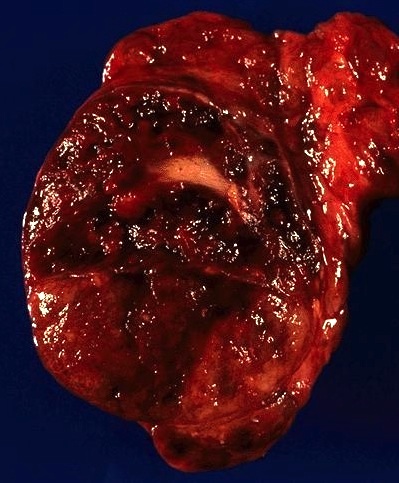
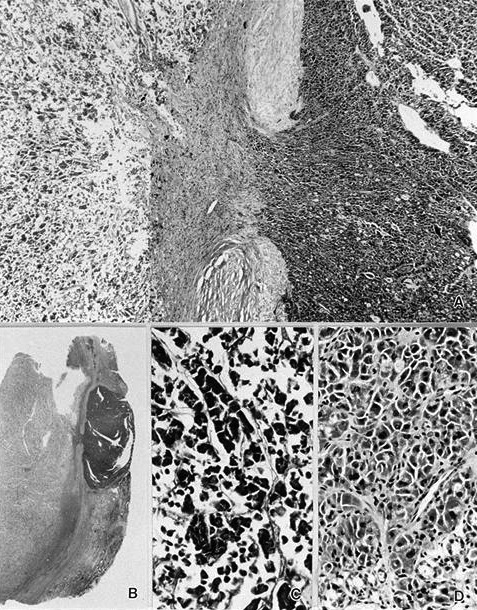
Gross description
- Most are more than 2 cm
- Prone to infarction or hemorrhage, especially after FNA or core biopsy
- Solitary, solid, bright brown to mahogany color, mostly encapsulated, lobulated, may have central scar
- Widely invasive tumors have irregular borders, may have satellite nodule / multinodular appearance
Gross images
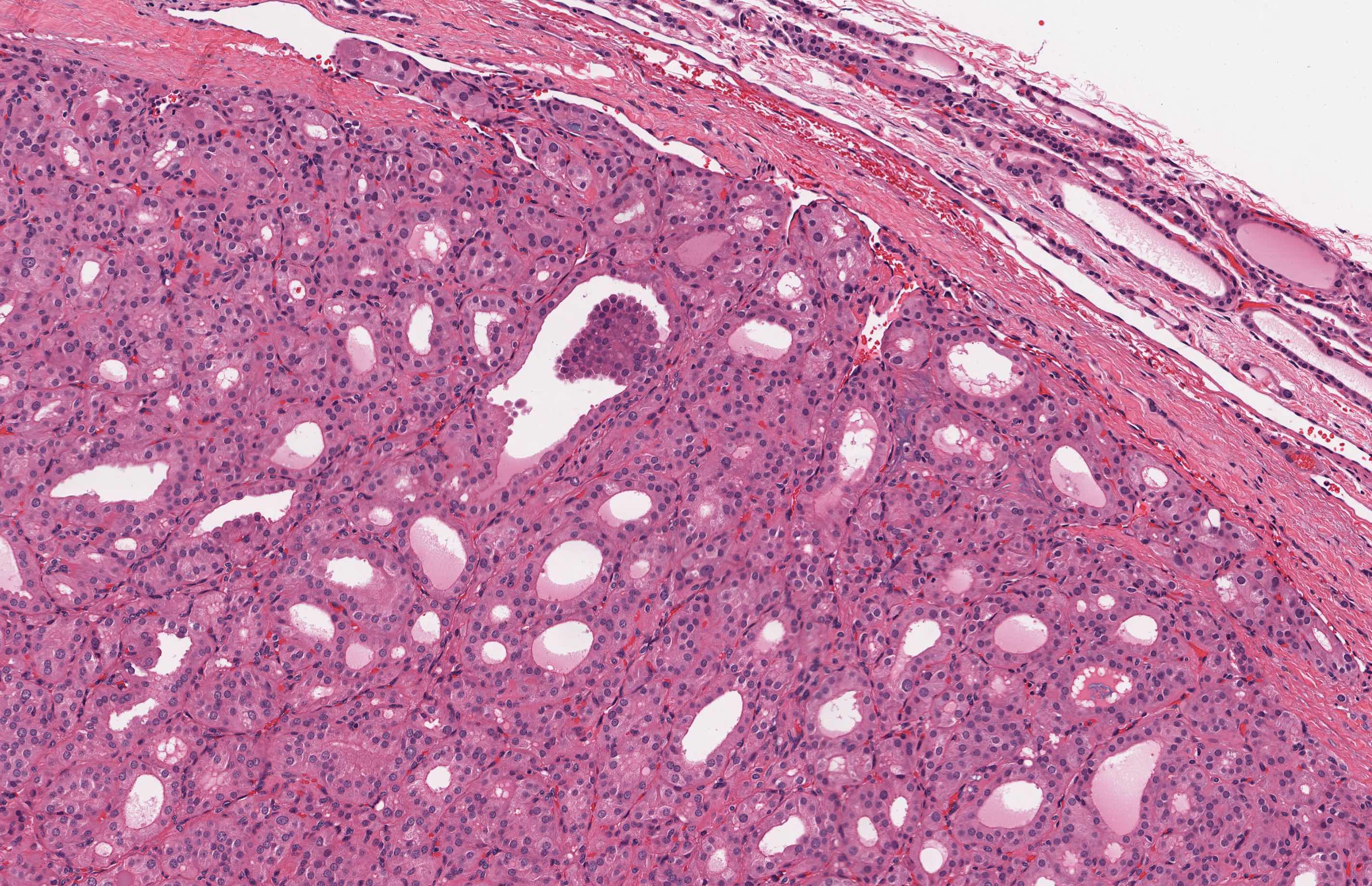
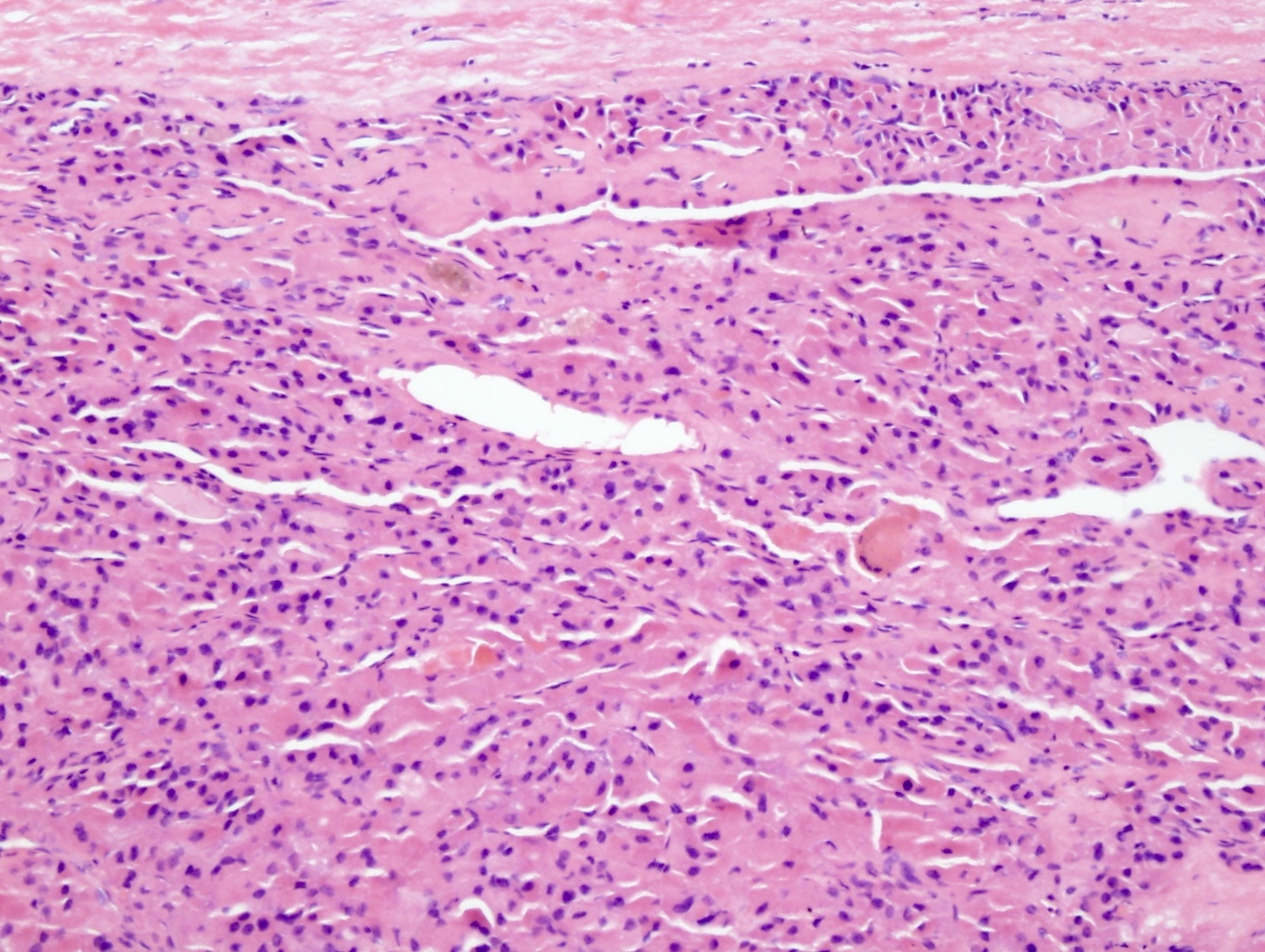
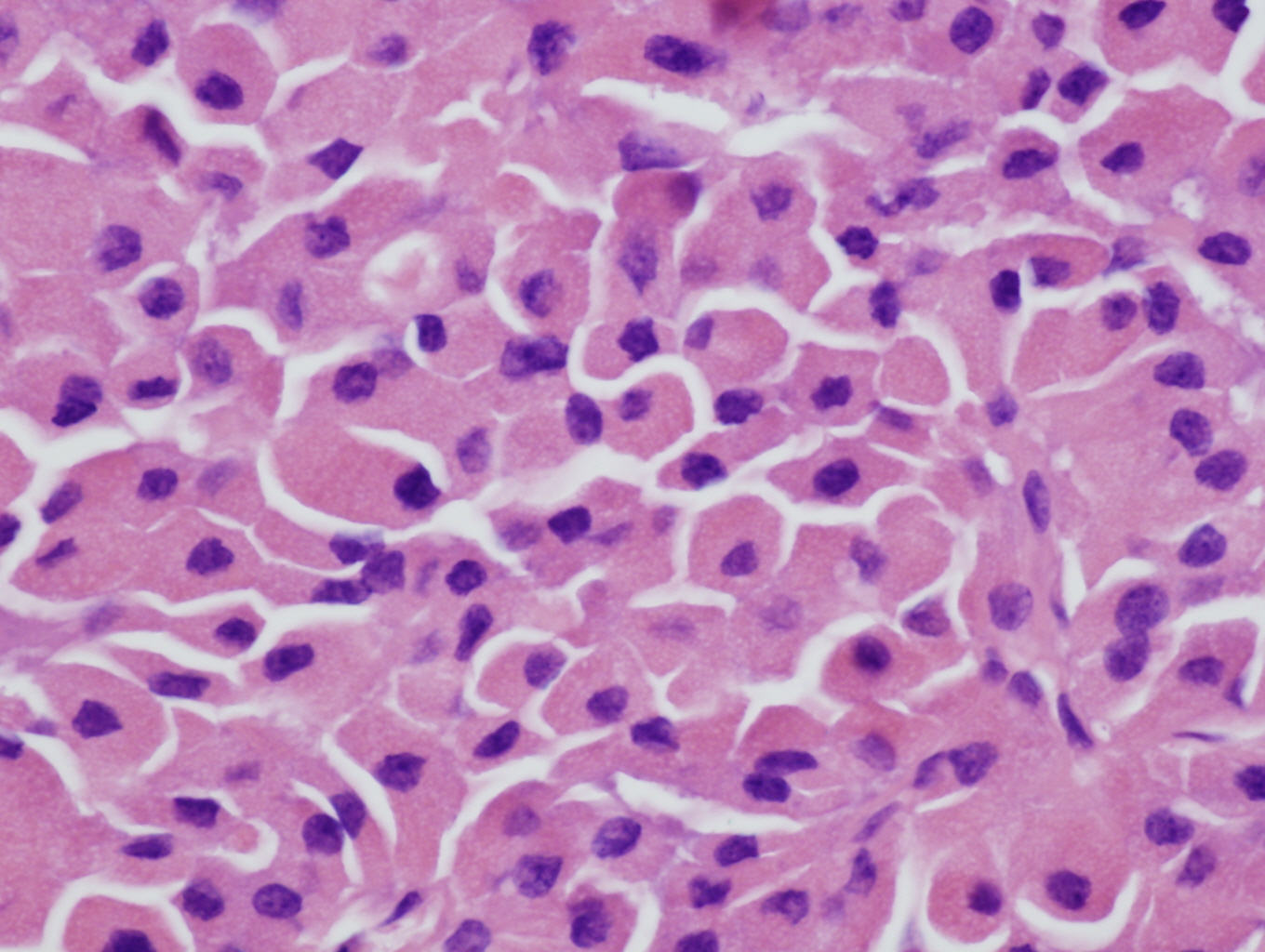
Microscopic (histologic) description
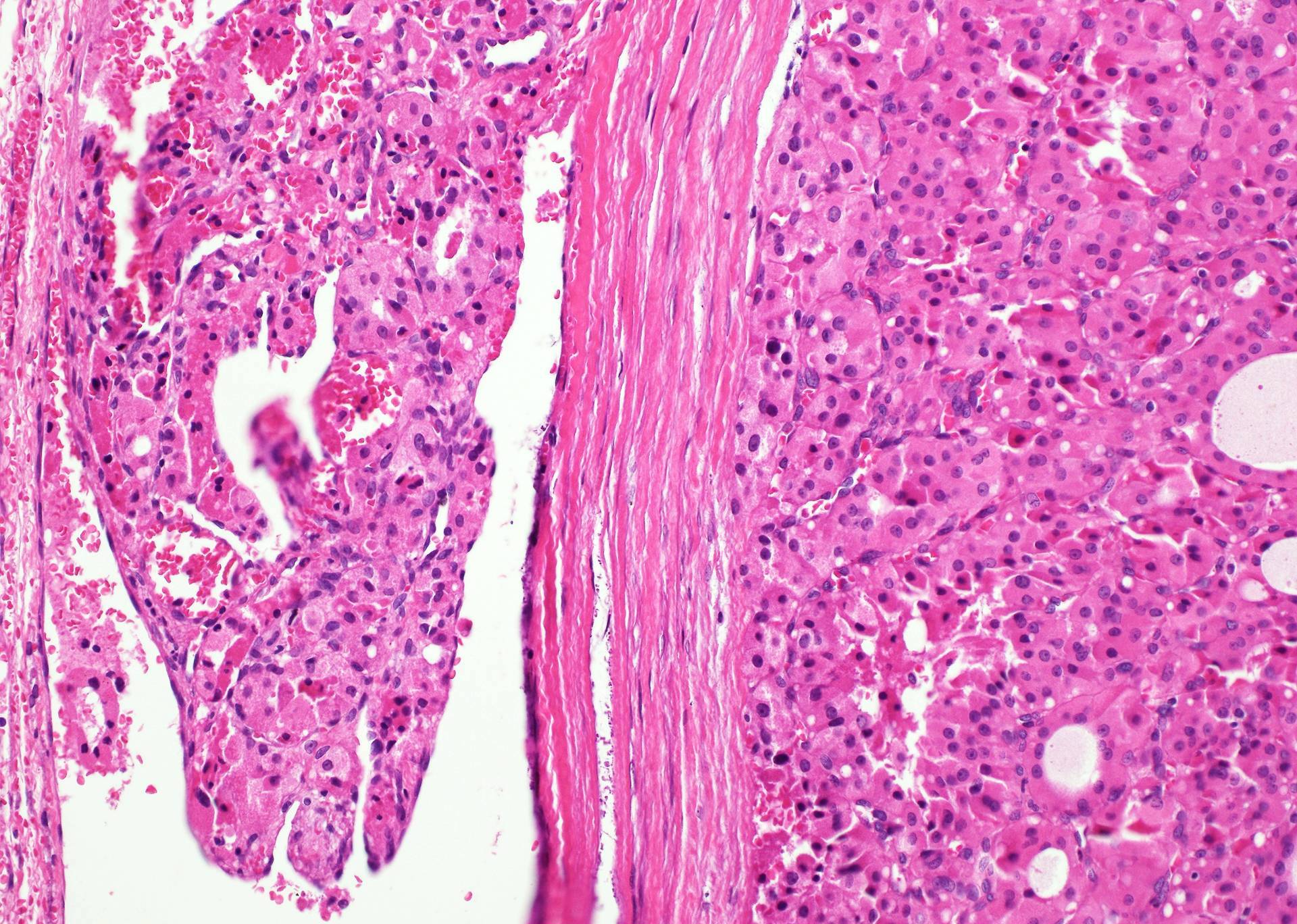
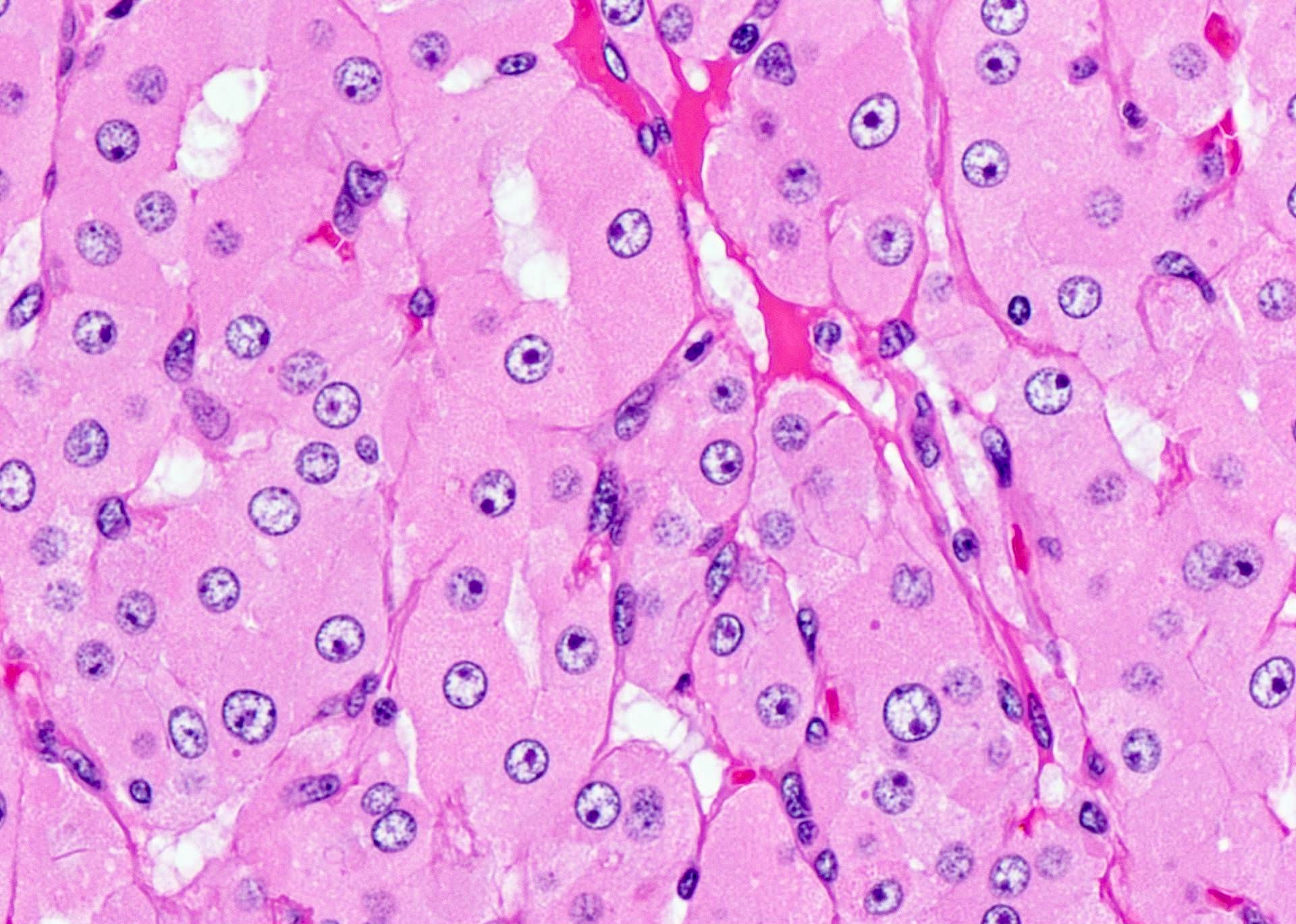
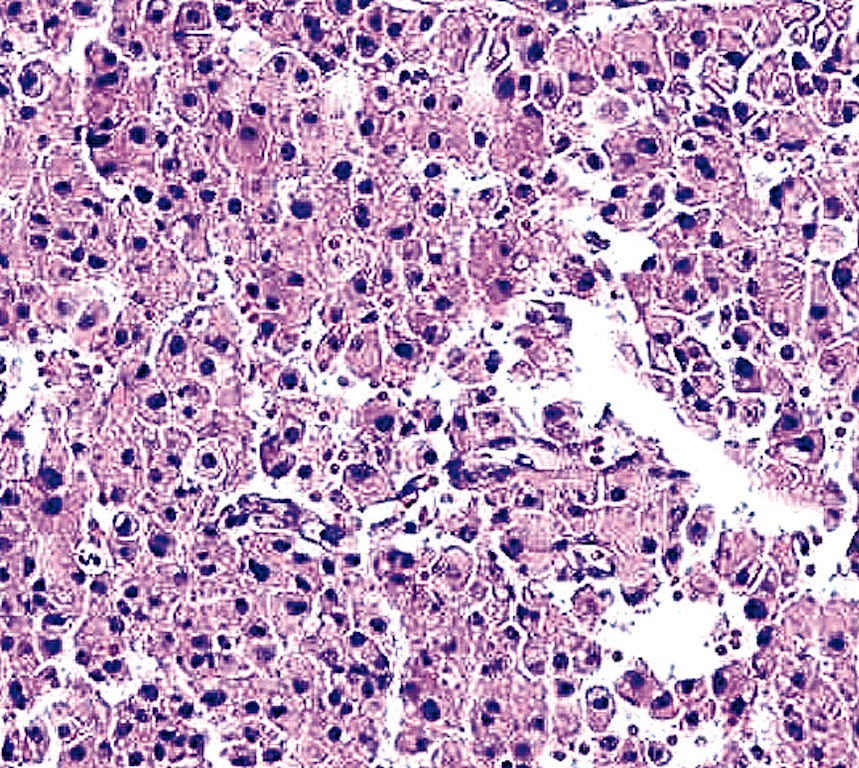
- At least 75% of tumor cells are oncocytes with large size, distinct cell borders, deeply eosinophilic and granular cytoplasm, large nucleus with prominent nucleolus, complete loss of cell polarity
- Follicular, trabecular, solid or papillary growth patterns
- Occasional nuclear grooves or nuclear pseudoinclusions
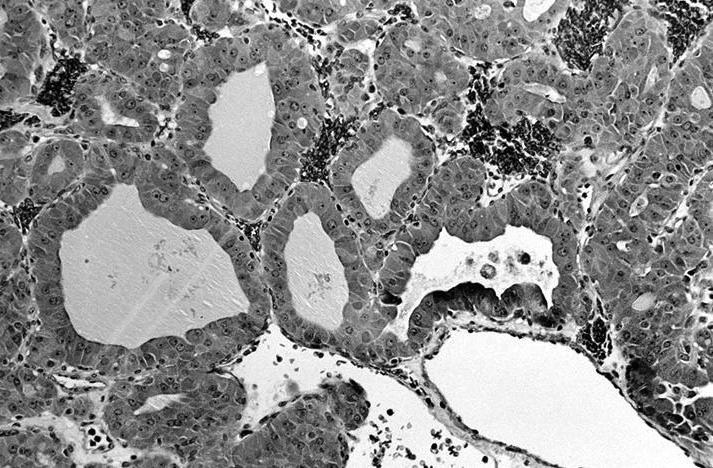
- May have psammomatous-like calcifications without lamination in the lumen of follicle (papillary carcinoma has laminated psammoma body in the stroma)
- Random nuclear atypia common but not evidence for malignancy
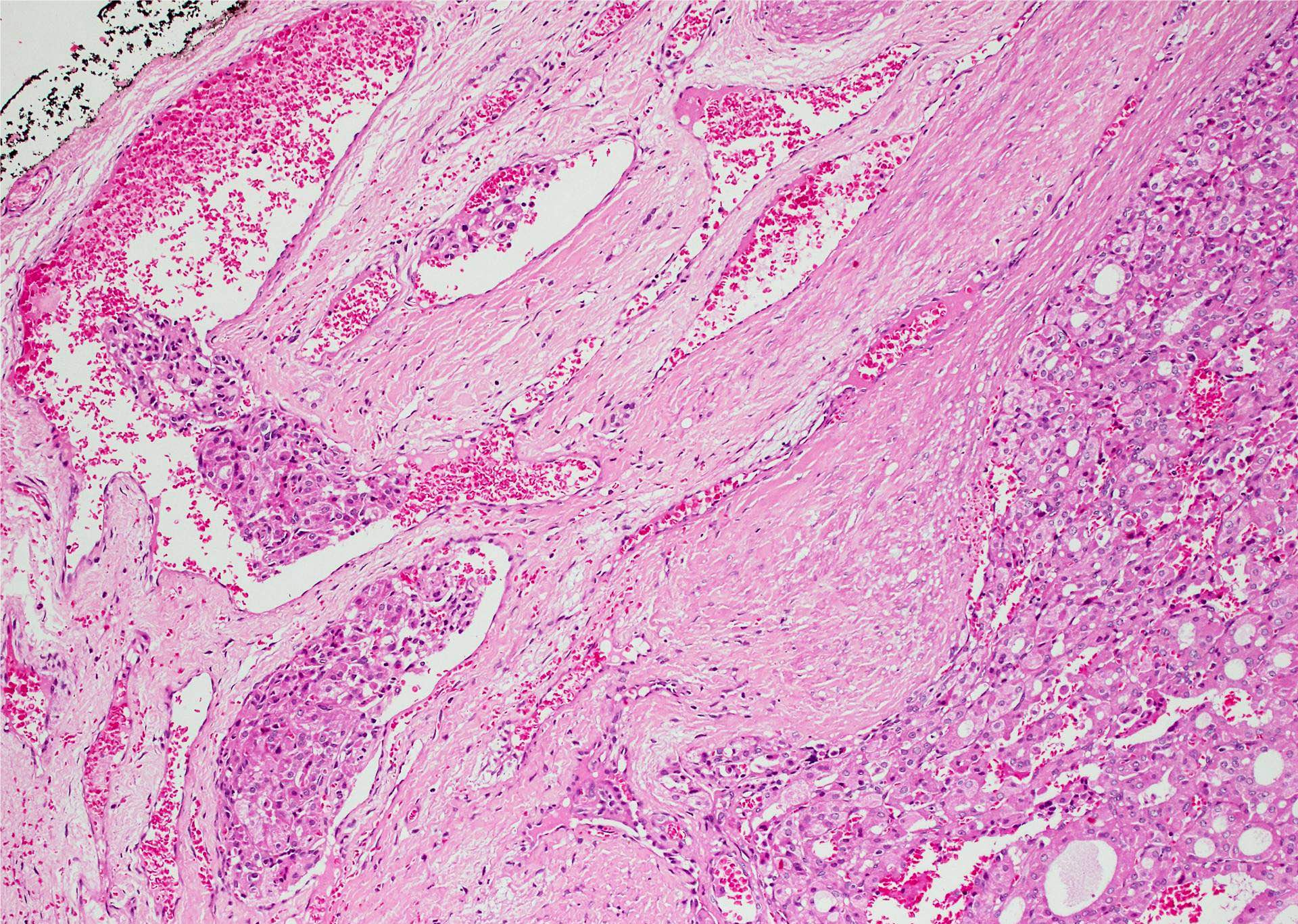
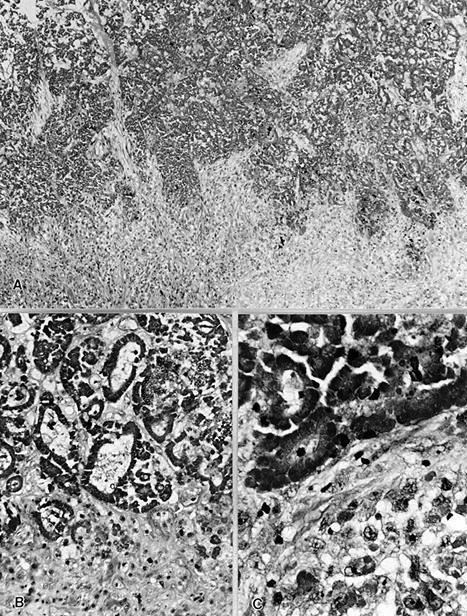
- Carcinoma tends to have:
- Thicker capsule than that of adenoma
- Solid / trabecular rather than follicular pattern of growth
- Smaller cells with high N/C ratio, increased mitotic figures
- Can have clear cell changes due to dilated mitochondria
- Poorly differentiated oncocytic carcinoma: size > 4 cm, with tumor necrosis, numerous mitoses, foci of small tumor cells
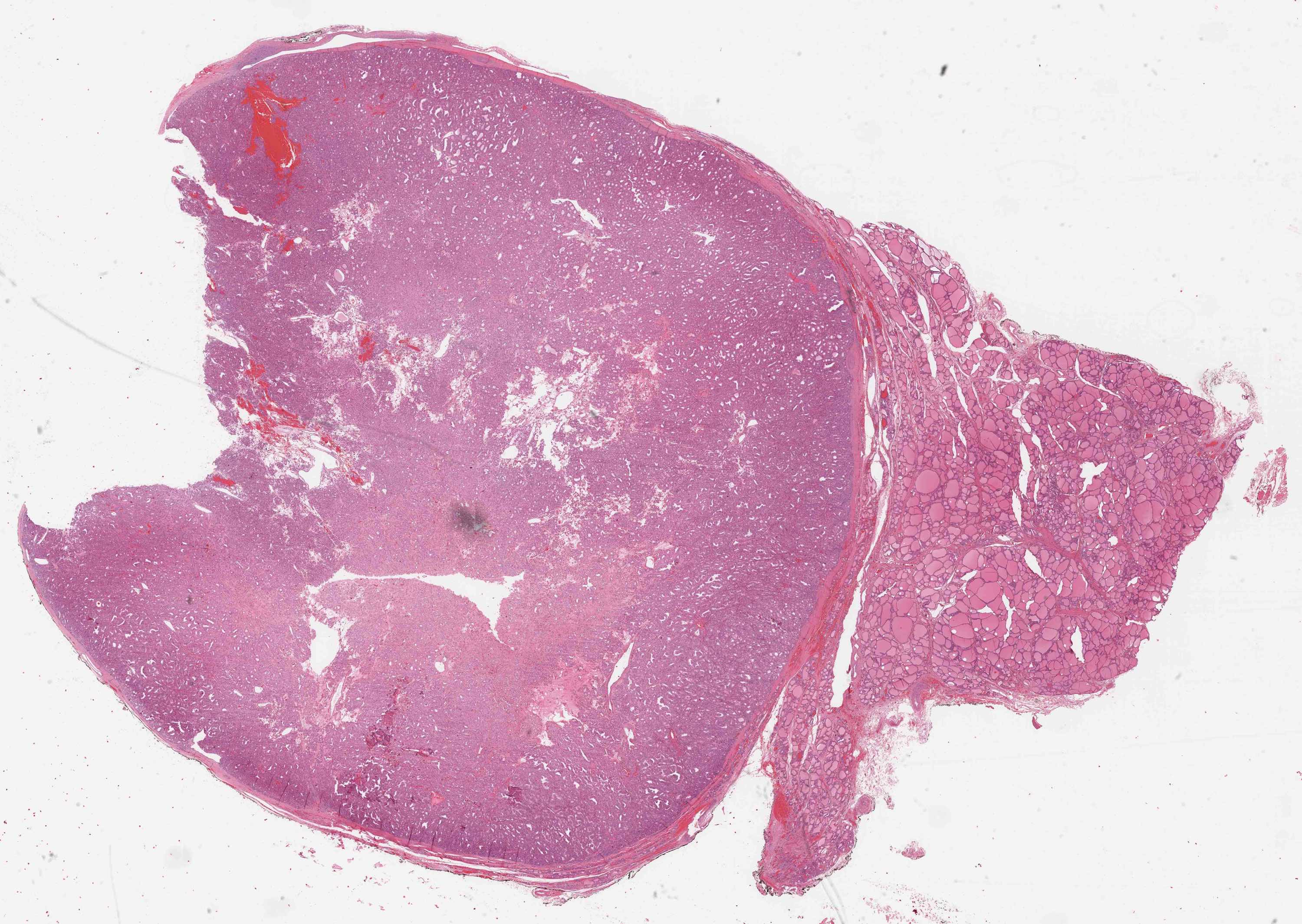
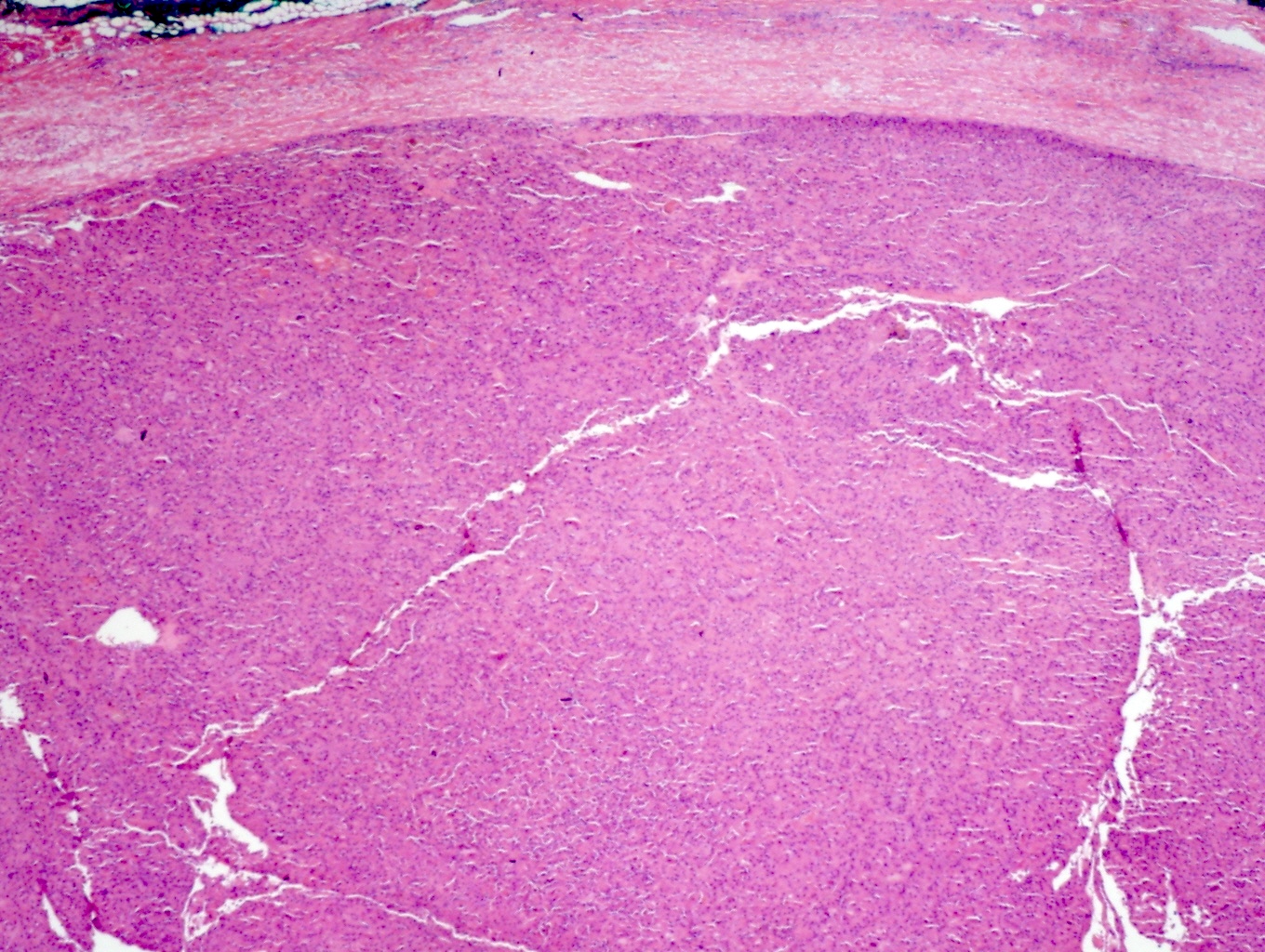
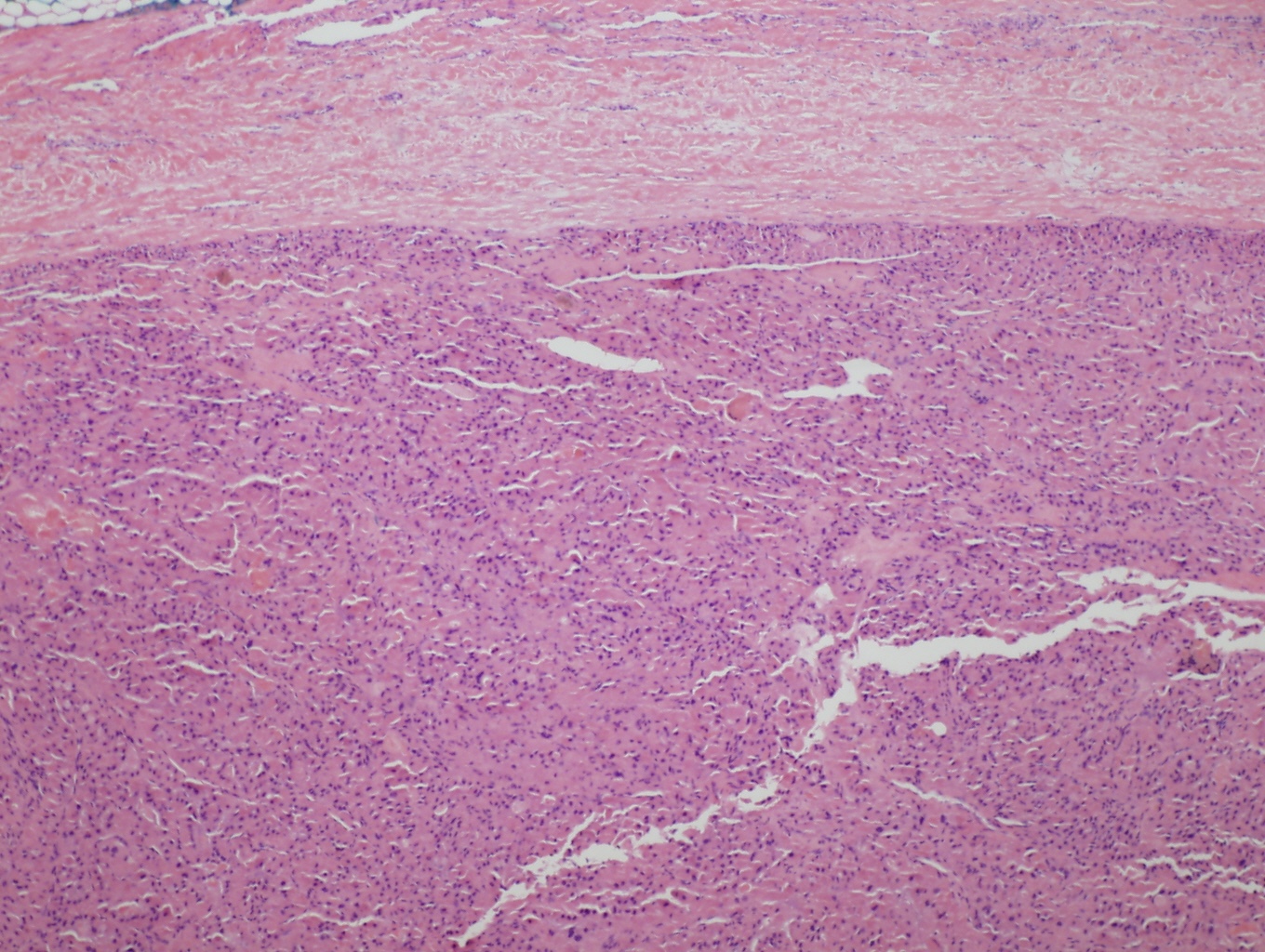
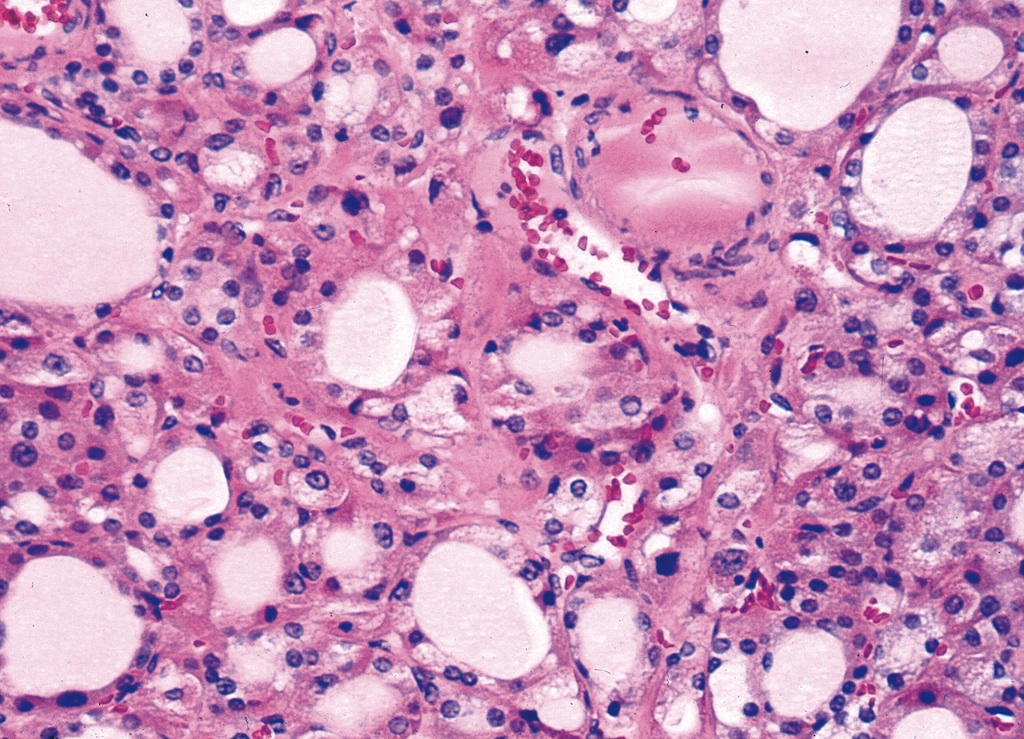
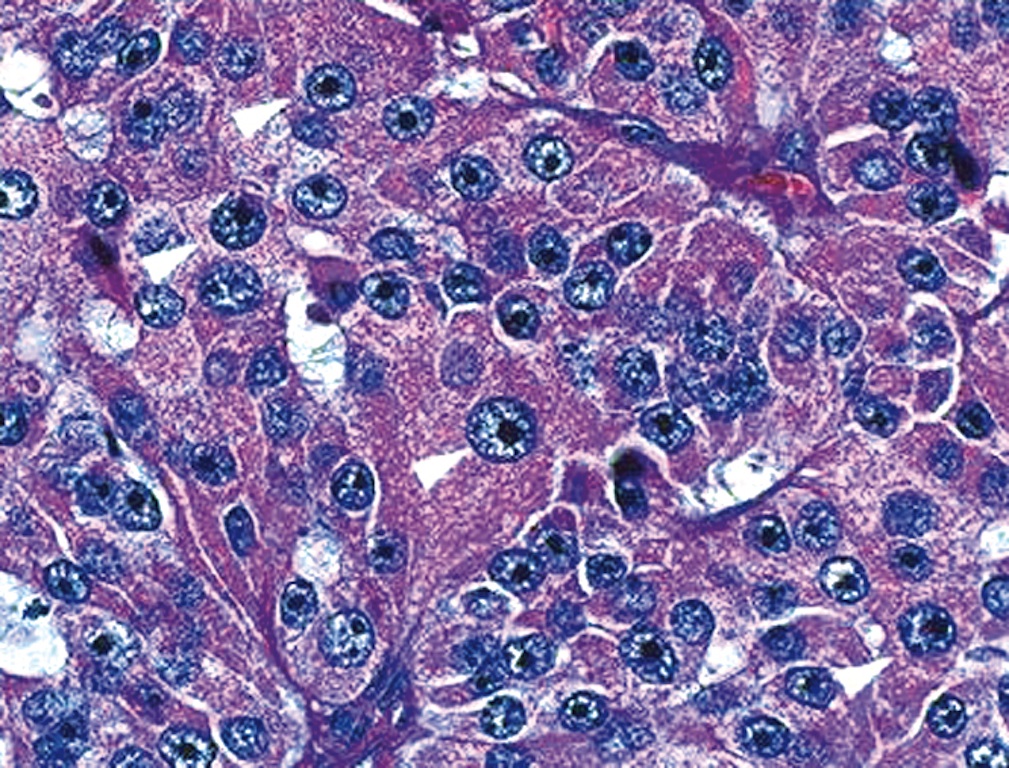
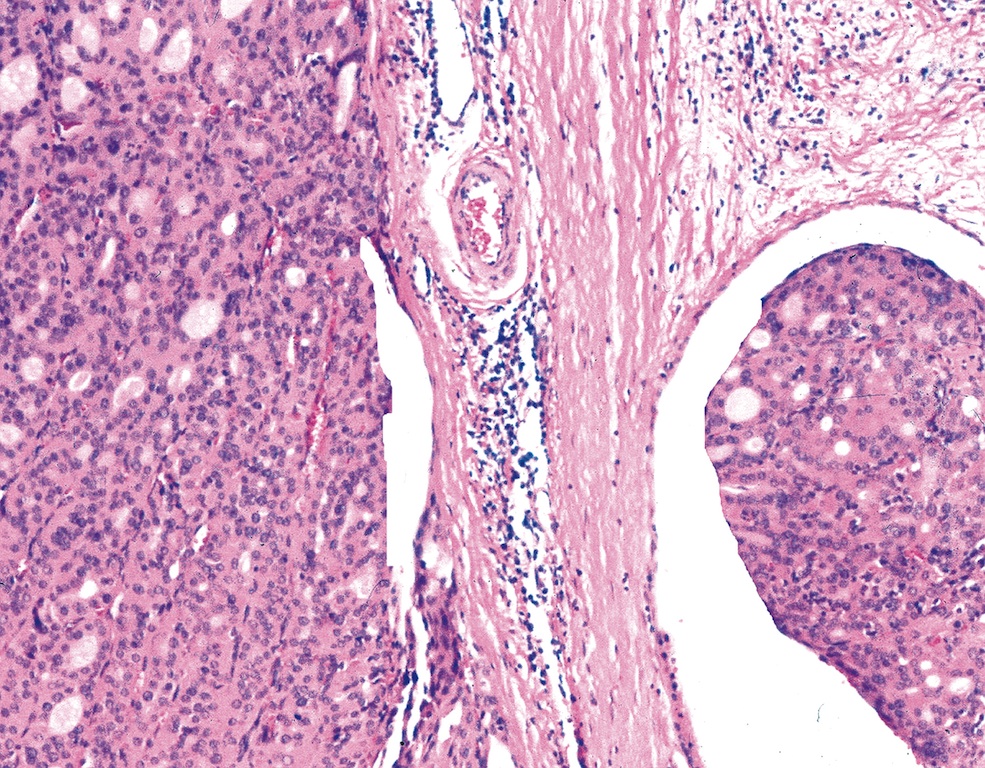
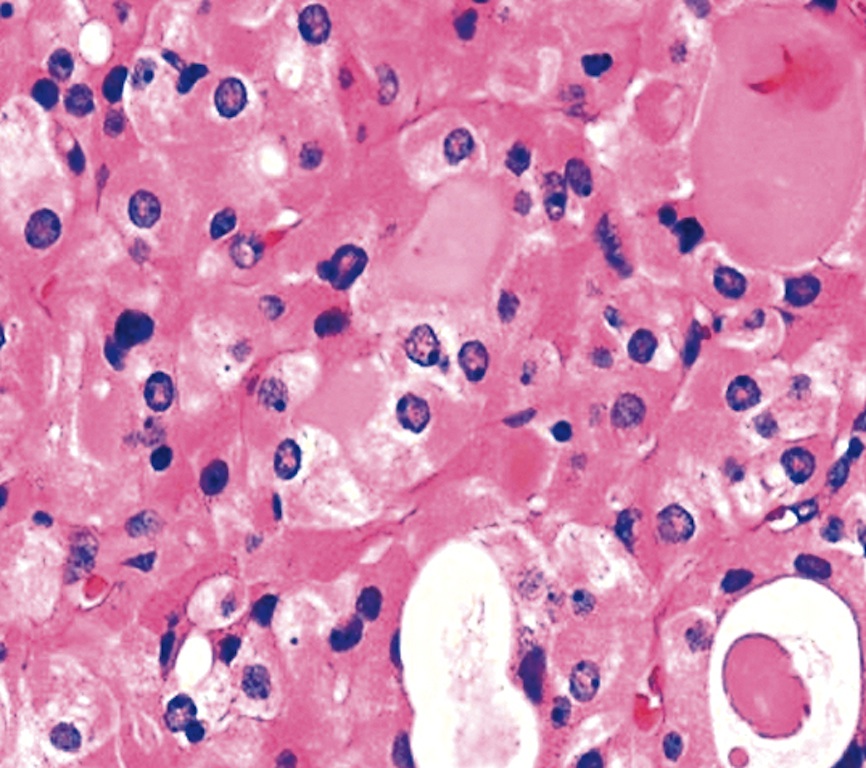
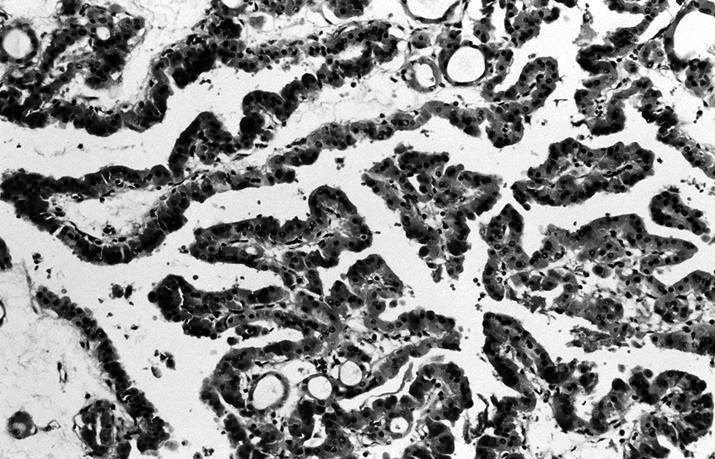
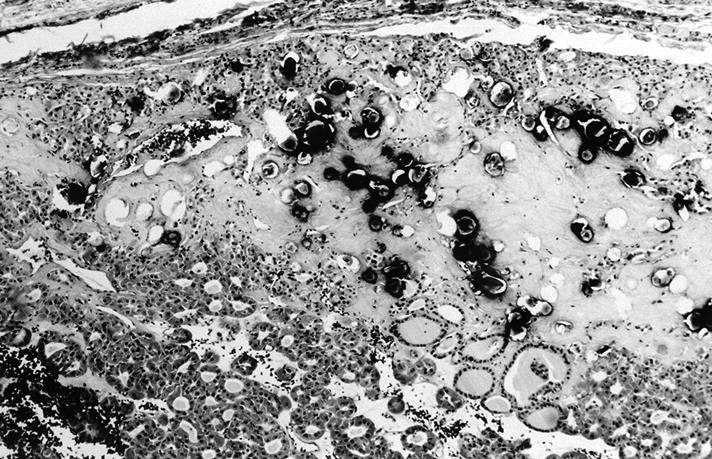
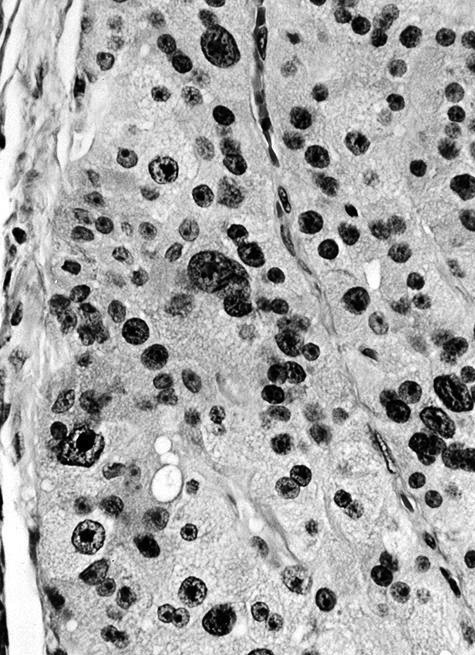
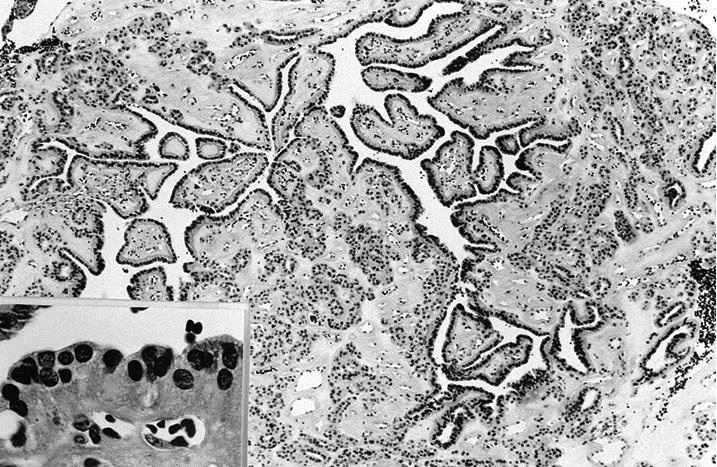
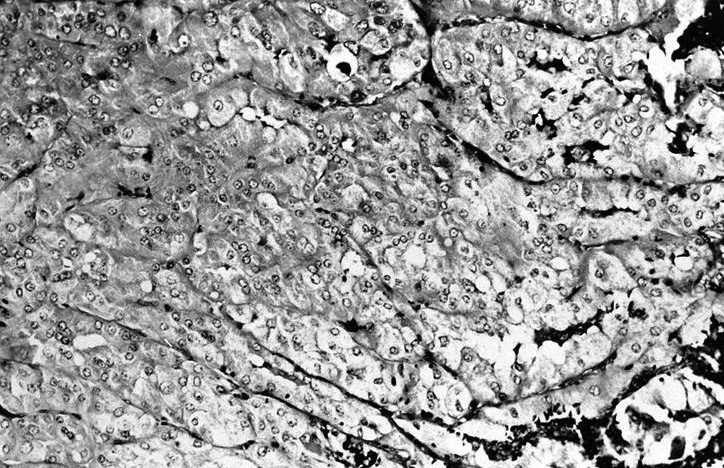
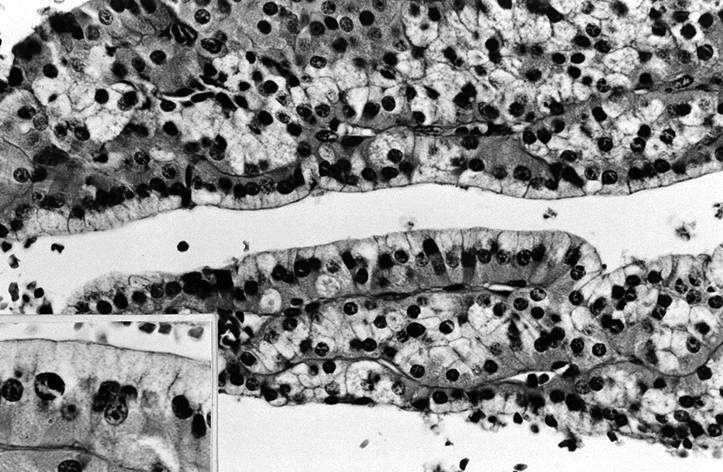
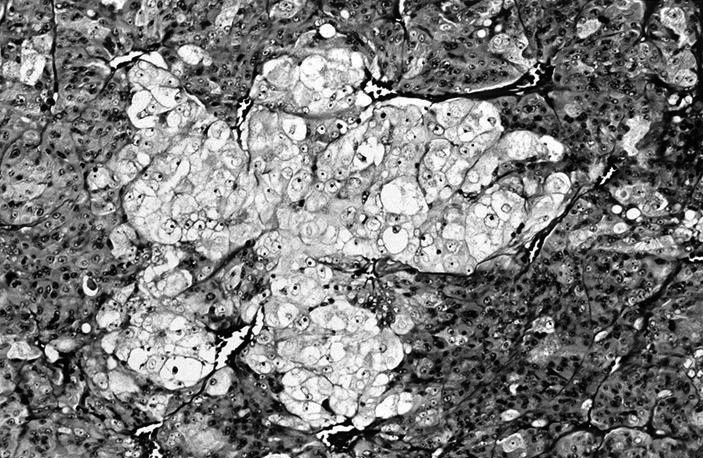
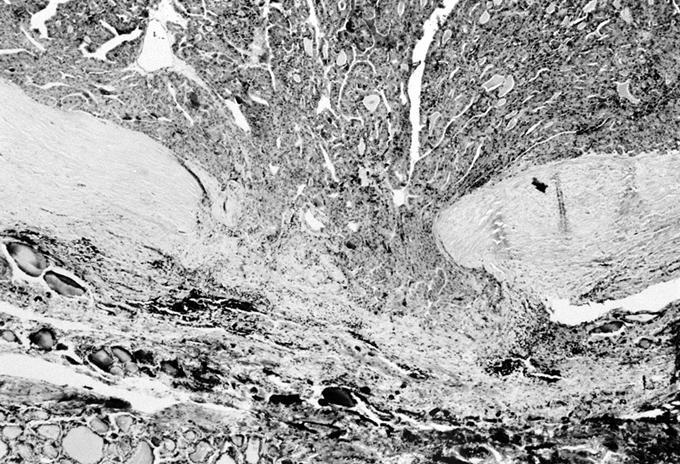
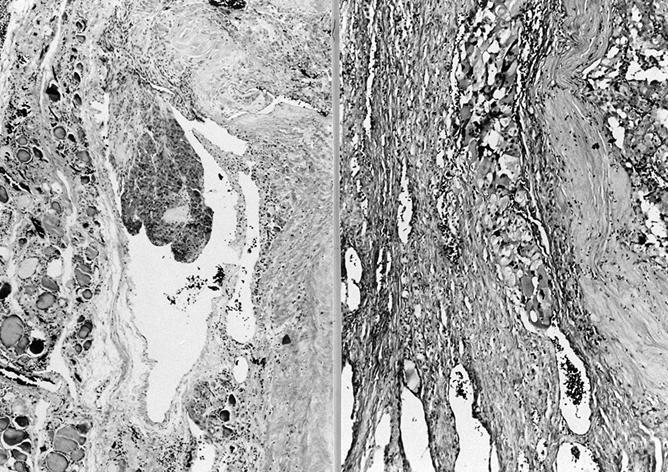
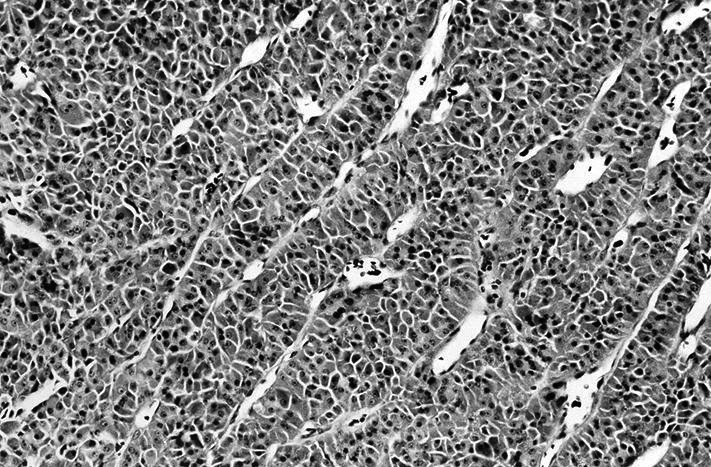
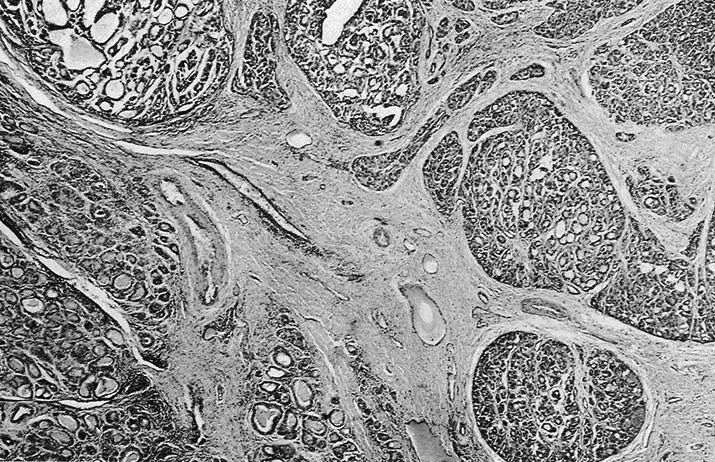
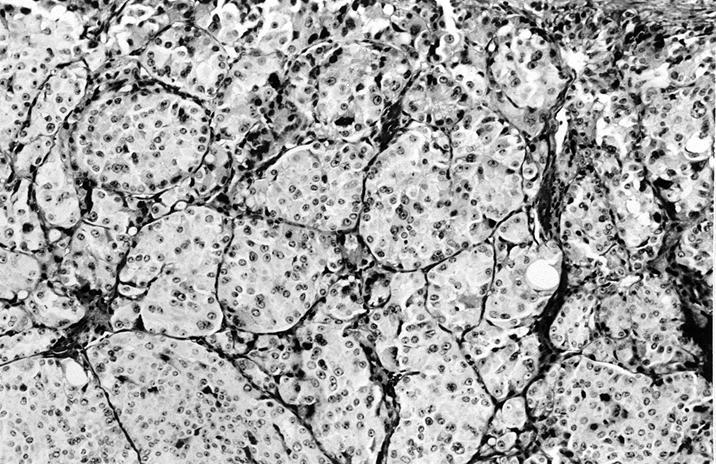
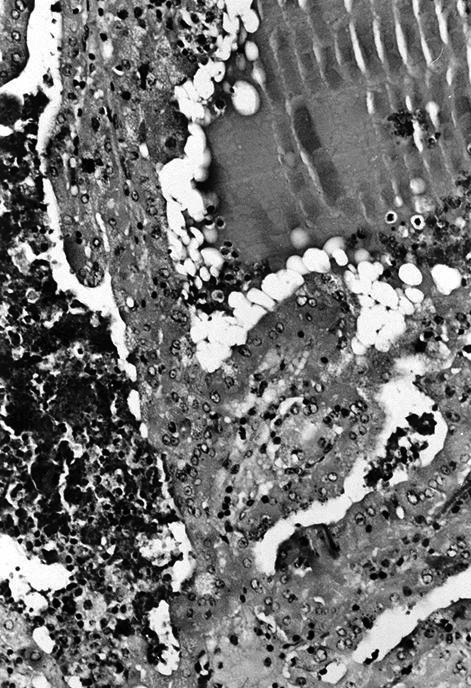
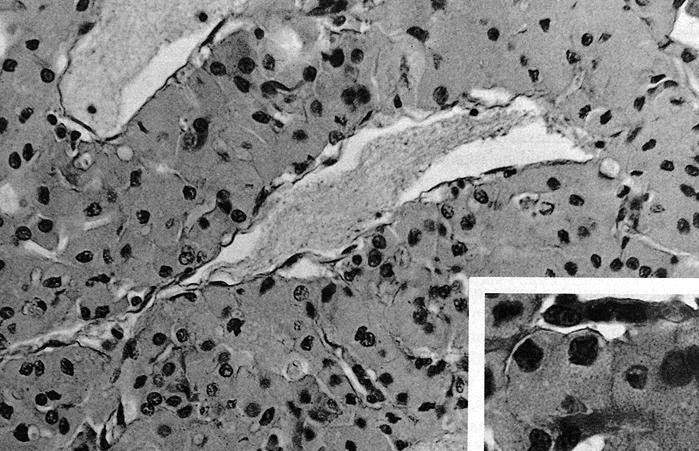
Microscopic (histologic) images
Contributed by Shuanzeng Wei, M.D., Ph.D., Andrey Bychkov, M.D., Ph.D., Grace C.H. Yang, M.D. and Mark R. Wick, M.D.
AFIP images
Adenoma:
Clear cell change:
Carcinoma:
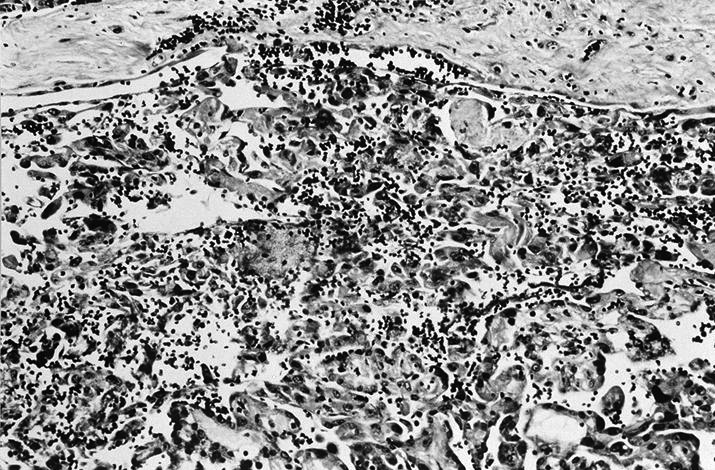
Minimally invasive Hürthle cell carcinoma:
Images hosted on other servers:
Carcinoma:




Oncocytes with abundant eosinophilic granular cytoplasm (far right image is with intraluminal calcifications)
Minimally invasive Hürthle cell carcinoma:
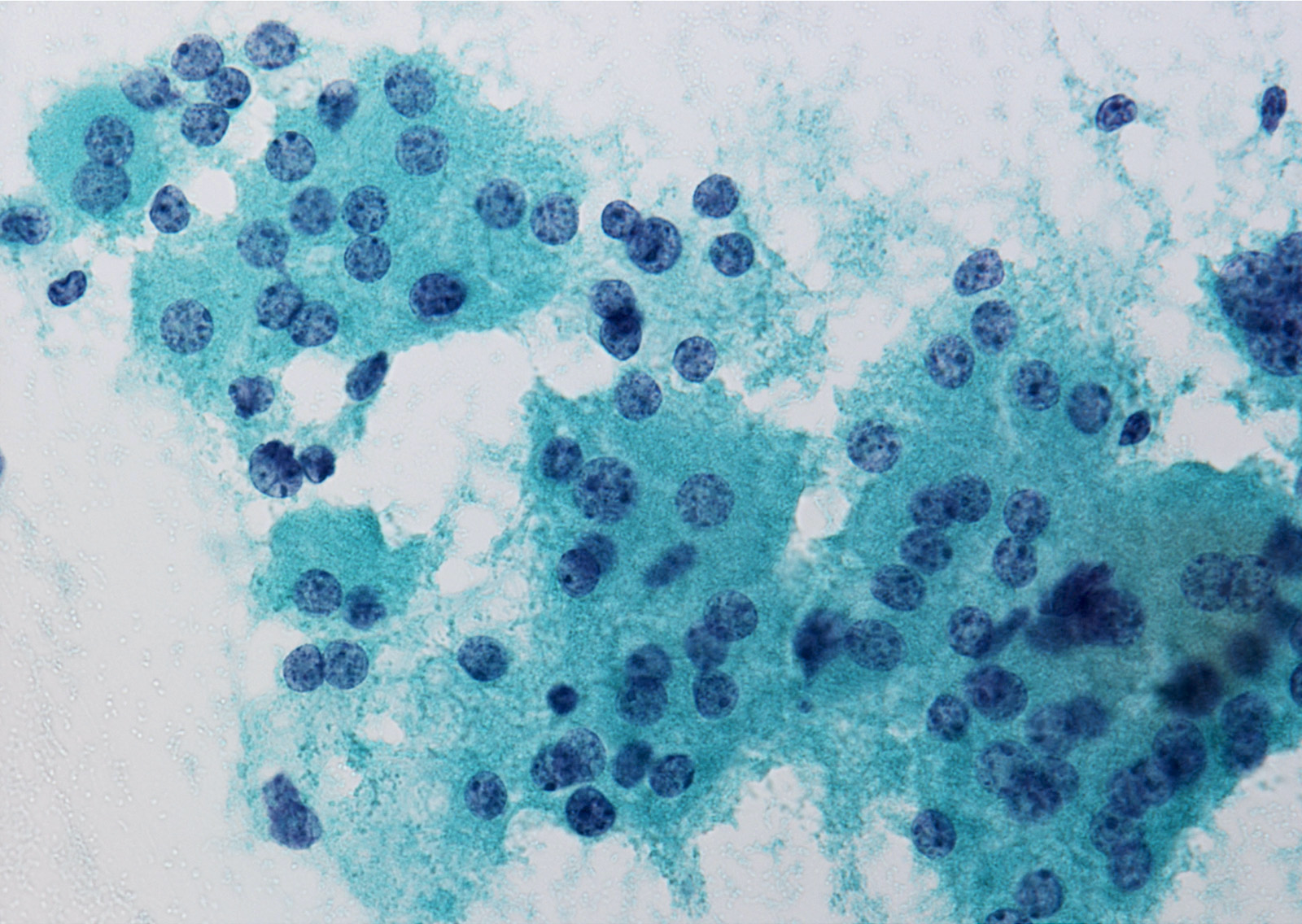
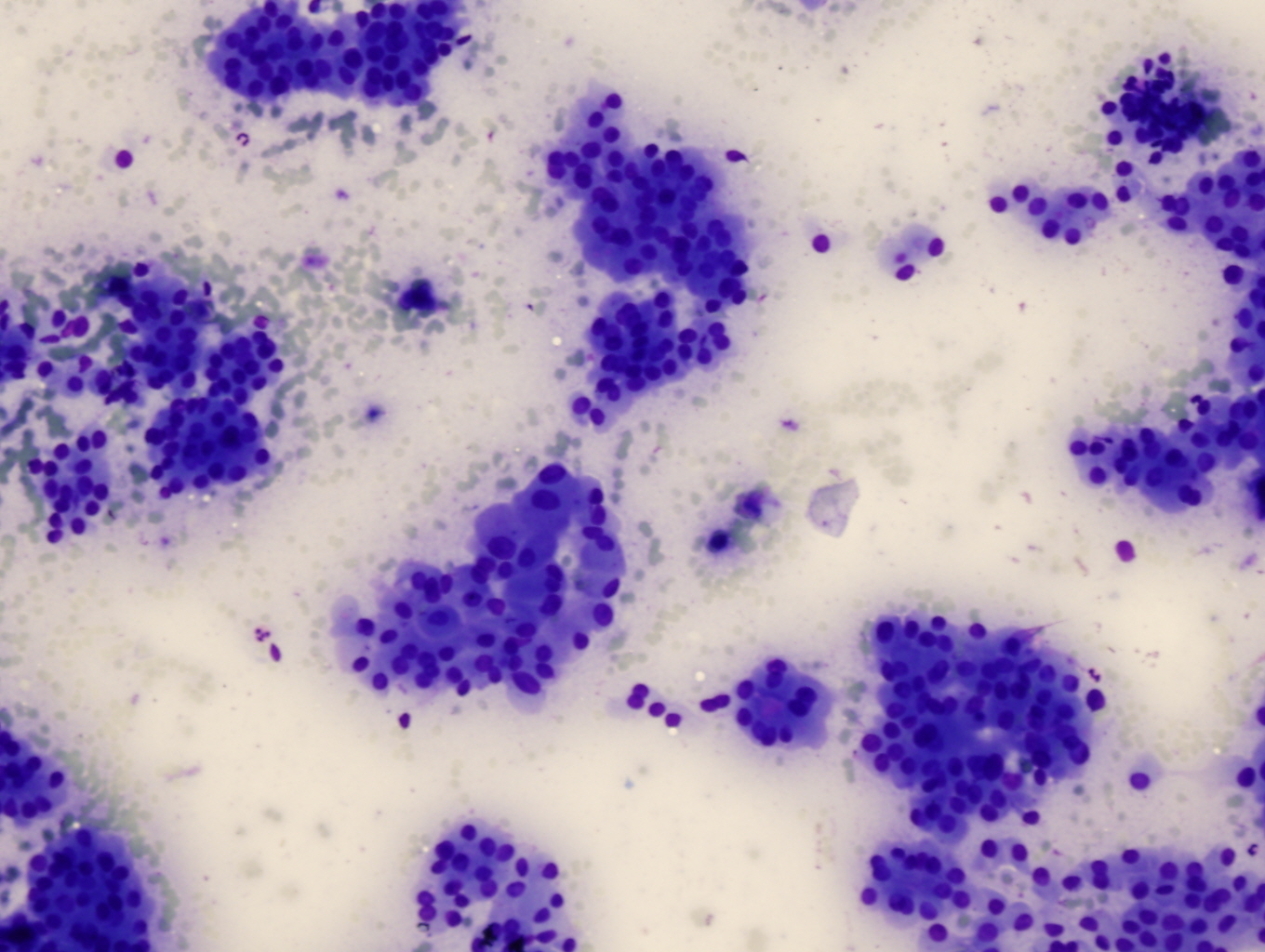
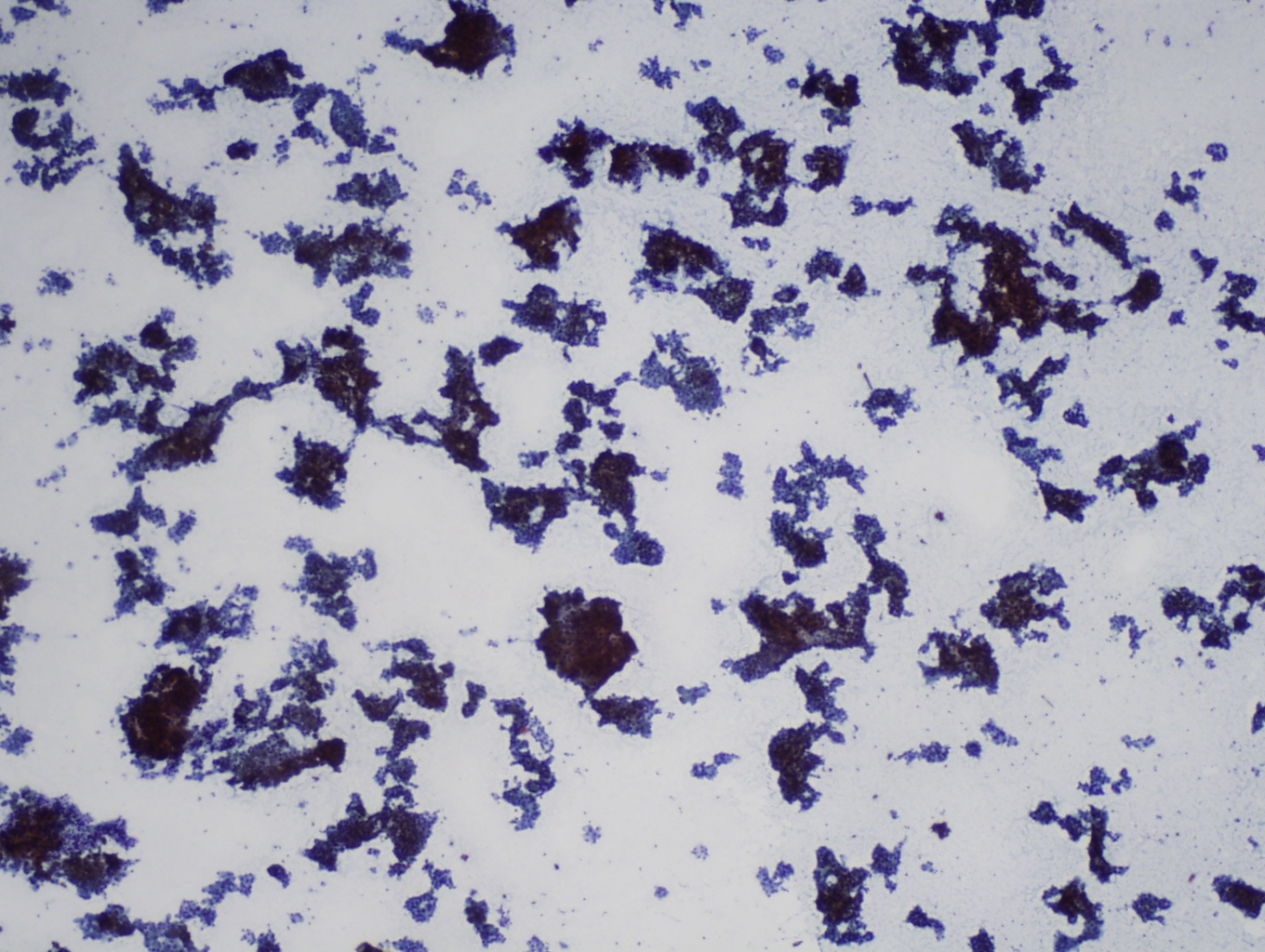
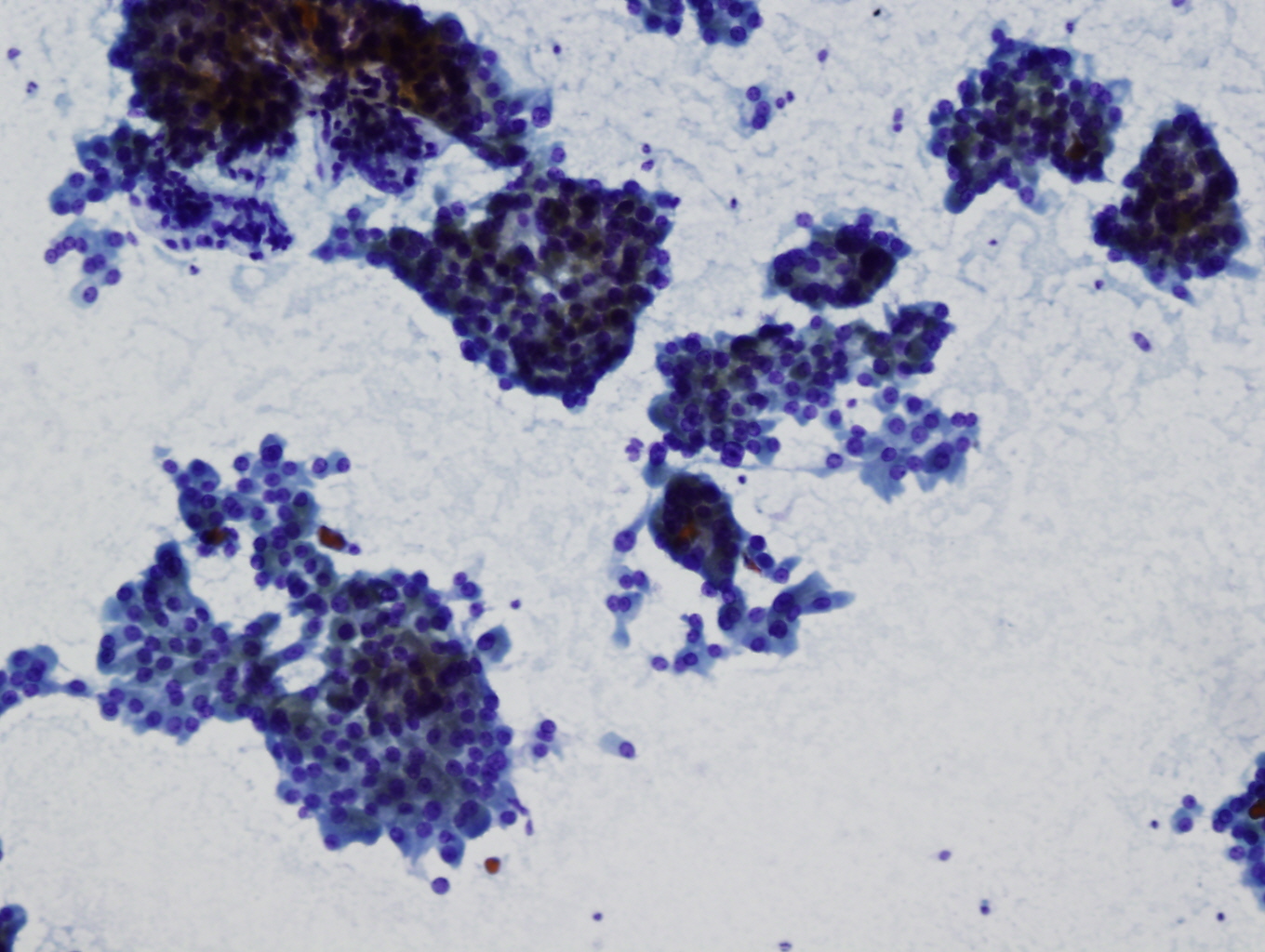
Cytology description
- Highly cellular, 75% or more Hürthle cells (abundant granular cytoplasm, round nuclei, often prominent nucleoli), often discohesive cells, some enlarged and pleomorphic with intracytoplasmic lumens (empty vacuoles with magenta [Diff Quik], green [Pap] or no material); transgressing vessels (capillaries in clusters of Hürthle cells) (Arch Pathol Lab Med 2001;125:1031)
- No colloid, lymphocytes, histiocytes, plasma cells or ordinary follicular cells
- Cannot definitively diagnose malignancy based on cytologic material (Am J Clin Pathol 1993;100:231, Acta Cytol 2008;52:659) but malignant cases tend to have small or large cell dysplasia, nuclear crowding and discohesive cells (Diagn Cytopathol 2008;36:149)
- Metastatic tumors may have bland cytologic features (Diagn Cytopathol 2007;35:439)
Cytology images
Positive stains
- Thyroglobulin (moderate), TTF1, CK7 (CK20 negative)
- Poorly differentiated oncocytic carcinoma may be negative for TTF1 and thyroglobulin
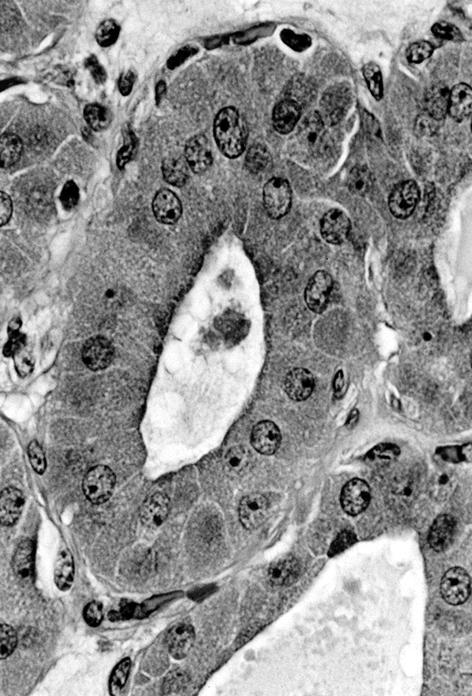
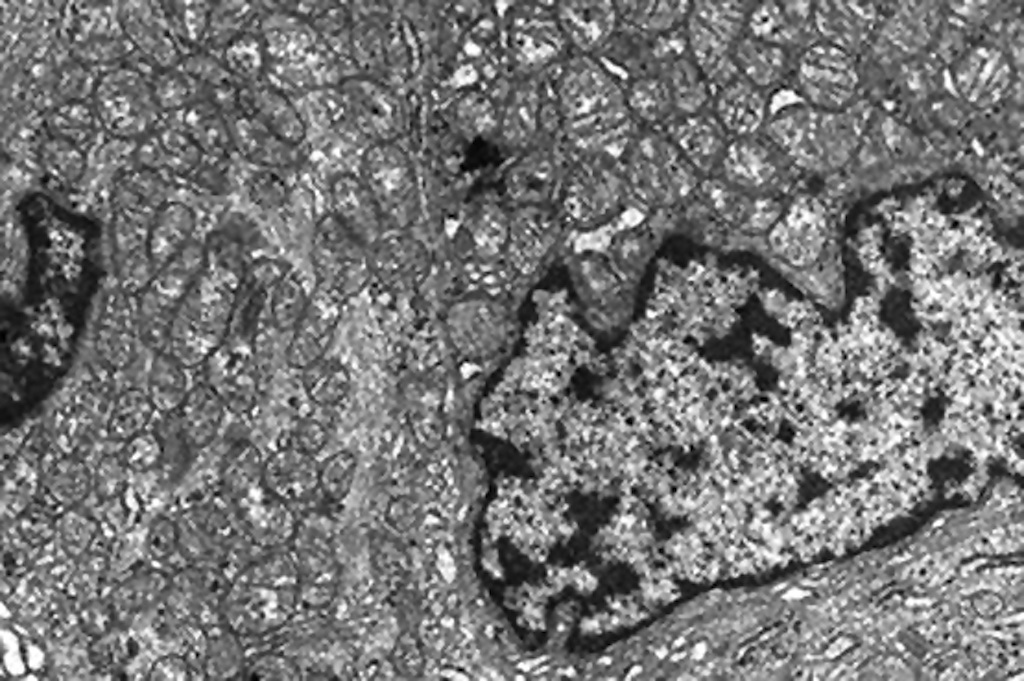
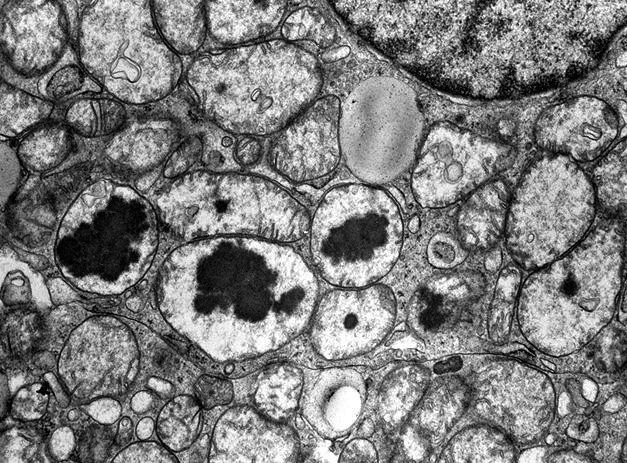
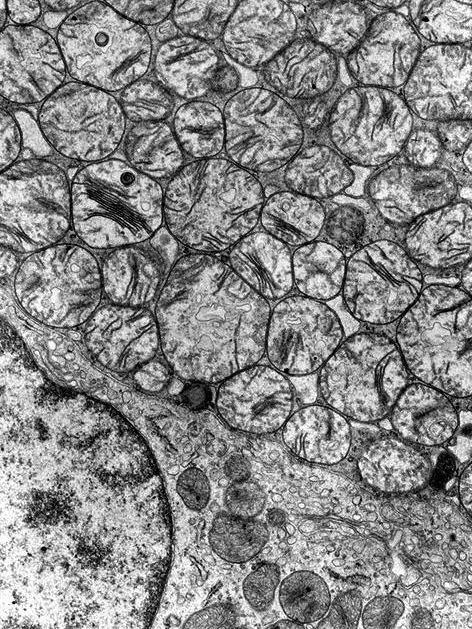
Electron microscopy description
- Numerous large mitochondria
Electron microscopy images
Molecular / cytogenetics description
- Aneuploidy is common in oncocytic tumors, including chromosome gains and losses
- Deletions or mutation of mitochondrial DNA (mtDNA) coding for oxidative phosphorylation (OXPHOS) proteins, which leads to energy production defects and compensatory mitochondrial proliferation
- PTEN and TP53 mutations (Endocr Pathol 2015;26:365)
- MEN1 loss of function mutations in 4% of patients diagnosed with oncocytic thyroid carcinoma (J Clin Endocrinol Metab 2015;100:E611)
Videos
Oncocytic lesions by Z. Baloch (2020)
Differential diagnosis
- Hashimoto thyroiditis: abundant lymphocytes without distinct nodule
- Medullary carcinoma with Hürthle cell-like cells: calcitonin+, CEA+, thyroglobulin-
- Nodular goiter with prominent oncocytic cells: abundant colloid, follicular cells and histiocytes mixed with oncocytic cells
- Papillary thyroid carcinoma, oncocytic variant, Warthin-like variant, tall cell variant: with nuclear features of papillary carcinoma
Additional references
Board review style question #1
Which statement is not true for oncocytic carcinoma?
- More aggressive compared to conventional follicular carcinoma
- More resistant to radioactive iodine compared to conventional follicular carcinoma
- Not only metastases to bone or lung; can also spread to lymph node
- Oncocytic appearance is due to accumulation of dysfunctional mitochondria
- Risk factors include iodine deficiency and irradiation exposure
Board review style answer #1
E. Risk factors include iodine deficiency and irradiation exposure. There are no known exogenous risk factors for developing oncocytic tumors.
Comment Here
Reference: Oncocytic (Hürthle cell) tumors
Comment Here
Reference: Oncocytic (Hürthle cell) tumors