Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Diagnosis | Case reports | Treatment | Cytology description | Cytology images | Videos | Sample cytology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Suzuki A, Bychkov A. Follicular neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidfollicularneoplasm.html. Accessed March 30th, 2025.
Definition / general
- Bethesda category IV, "follicular neoplasm / suspicious for a follicular neoplasm (FN / SFN)" is used for cases with a cellular aspirate comprised of follicular cells showing cell crowding or microfollicle formation (Thyroid 2017;27:1341)
- Cases cytologically suspected for follicular adenoma and follicular carcinoma are included
- Final diagnosis is based on tissue histology because capsular or vascular invasion are essential criteria
- Follicular patterned lesions (nodular goiter, follicular adenoma, follicular variant of papillary carcinoma, follicular carcinoma and noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP)) have overlapping cytomorphologic features and cannot be accurately distinguished by fine needle aspiration alone
- Some definitions and criteria for this category were slightly modified in the latest edition of the Bethesda system to accommodate a new entity: noninvasive follicular thyroid neoplasm with papillary-like nuclear features (Cancer 2007;111:306)
- Criteria: cases with mild nuclear atypia (papillary carcinoma-like changes) were included in follicular neoplasm / suspicious for a follicular neoplasm
- Reporting: recommended to mention the possibility of noninvasive follicular thyroid neoplasm with papillary-like nuclear features in the note (to avoid overtreatment)
Essential features
- Includes cases with most of the follicular cells are arranged in cell crowding or microfollicle formation
- Frequency 2.3 - 2.9%, resection rate 41.8 - 45.0%, risk of malignancy 25 - 40%
- Most common histopathological diagnosis is follicular adenoma, followed by adenomatous nodule, follicular variant of papillary carcinoma and follicular carcinoma (Diagn Cytopathol 2018;46:148)
- Impossible to distinguish follicular adenoma from follicular carcinoma by fine needle aspiration cytology
Terminology
- Laboratory should choose one preferable term and use it exclusively for this category
- Term "suspicious for a follicular neoplasm" may be more convenient than "follicular neoplasm" because some nodular goiter cases are included in this category
Clinical features
- Frequency: 2.3 - 2.9% (Cytojournal 2018;15:4)
- Resection rate: 41.8 - 45.0% (Arch Pathol Lab Med 2013;137:1664)
- Rate of neoplastic lesion after resection: 65 - 85%
- Risk of malignancy: 25 - 40% (Ali: The Bethesda System for Reporting Thyroid Cytopathology - Definitions, Criteria, and Explanatory Notes, 2nd Edition, 2018, BMJ 1993;306:469)
- 27 - 68%: interpreted histologically as papillary carcinoma, usually follicular variant
- Risk of malignancy decreased to 10 - 40% when noninvasive follicular thyroid neoplasm with papillary-like nuclear features is implicated (Thyroid 2017;27:1341)
Diagnosis
- Cellular aspirate comprised of follicular cells; most are arranged in an altered architectural pattern characterized by significant cell crowding or microfollicle formation
- Sparsely cellular aspirates are excluded from this category and could be interpreted as atypia of undetermined significance or follicular lesion of undetermined significance (AUS / FLUS)
- Cases that demonstrate suspicious or definitive nuclear features for papillary carcinoma are excluded from this category and should be classified as suspicious for malignancy or malignant, respectively
- Follicular patterned aspirates with mild nuclear changes (swelling, contour irregularity or chromatin clearing) can be classified as follicular neoplasm / suspicious for a follicular neoplasm if true papillae and intranuclear cytoplasmic inclusions are absent
- Invasive follicular variant of papillary carcinoma or noninvasive follicular thyroid neoplasm with papillary-like nuclear features can be represented in this category (Cancer Cytopathol 2016;124:767, Hum Pathol 2016;54:134)
Case reports
- 21 year old man with multifocal follicular thyroid carcinoma following radiotherapy for Hodgkin disease (Postgrad Med J 1982;58:180)
- 30 year old woman with mucin producing microfollicular adenoma of the thyroid (J Clin Pathol 1985;38:277)
- 39 year old woman with follicular thyroid adenoma showing numerous intracytoplasmic lumina mimicking yellow bodies (Cytopathology 2016;27:495)
- 45 year old man with follicular thyroid carcinoma and clinical hyperthyroidism showing due to functioning metastases (Can Med Assoc J 1975;112:724)
- 75 year old woman with follicular carcinoma of the thyroid metastasizing to the breast (J Natl Med Assoc 1980;72:1101)
Treatment
- Diagnostic thyroid lobectomy (Thyroid 2016;26:1)
- Molecular testing may guide treatment
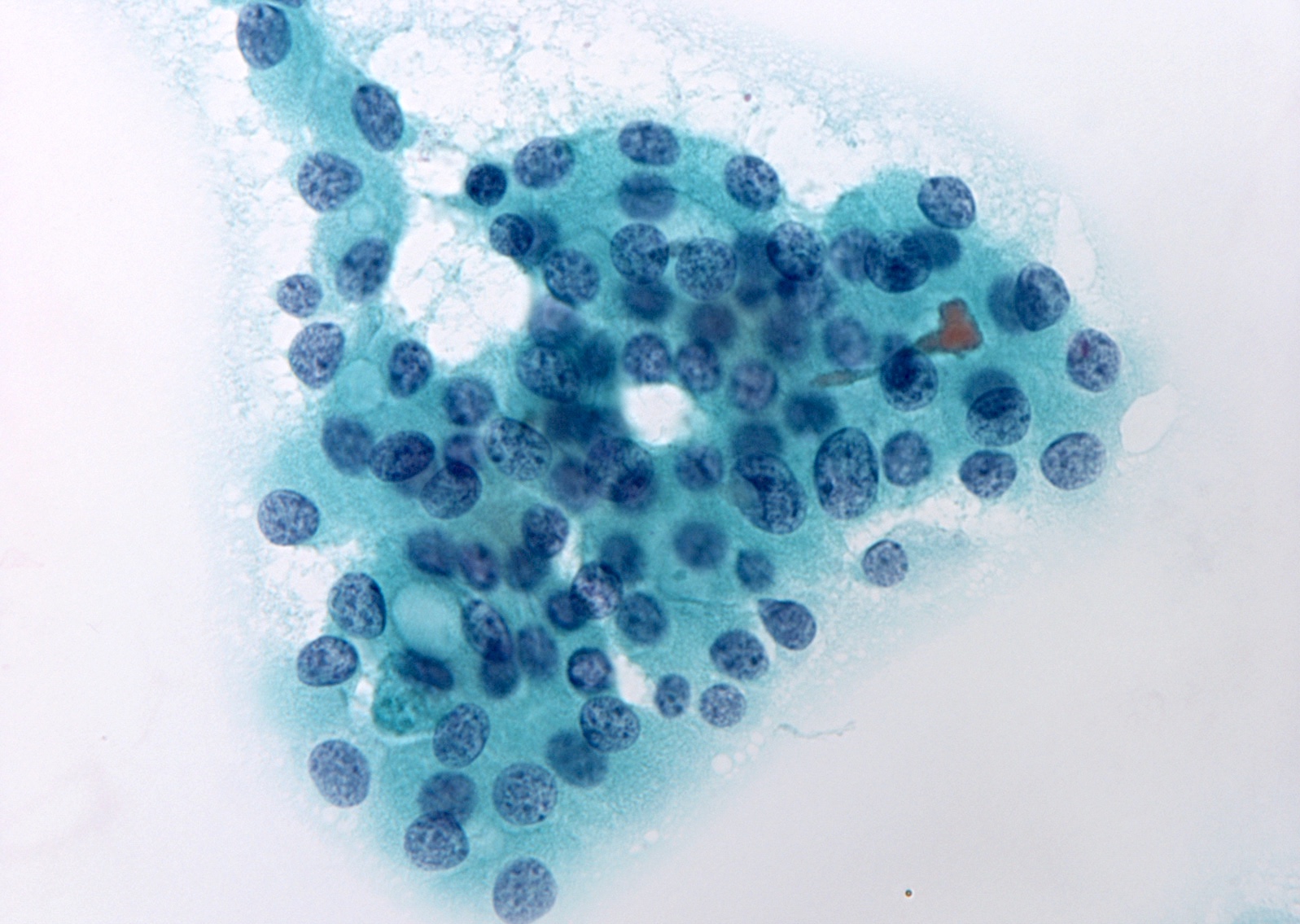
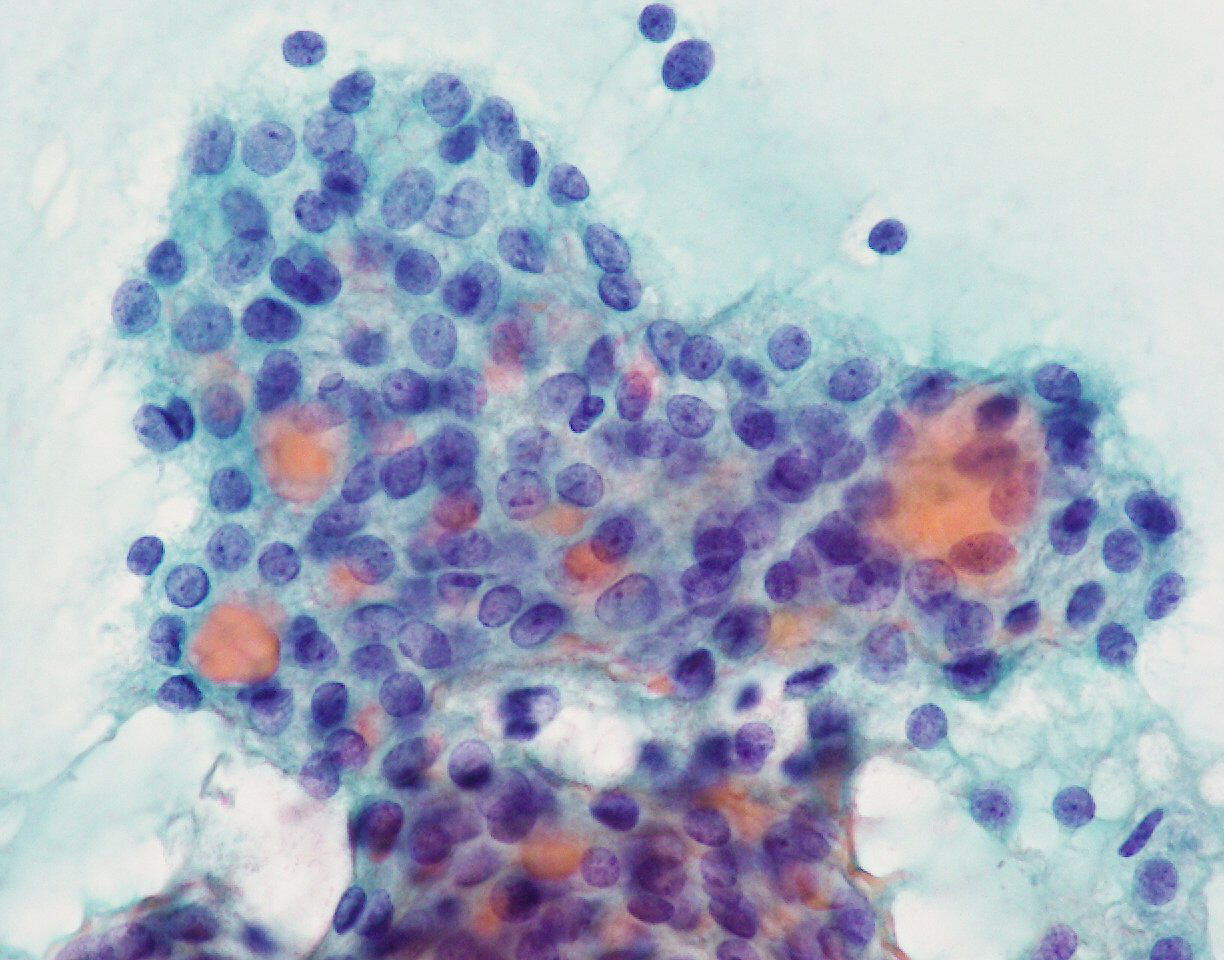
Cytology description
- Moderate or marked cellularity
- Atypical follicular cell architecture (cell crowding, microfollicles, trabecular and dispersed isolated cells)
- Microfollicle is a flat group of < 15 follicular cells arranged in a circle that is at least two thirds complete (Am J Clin Pathol 2008;130:736)
- Follicular cells are normal sized or enlarged and relatively uniform, with scant or moderate amount of cytoplasm
- Nuclei are usually round and slightly hyperchromatic, with inconspicuous nucleoli
- Some nuclear atypia may be seen, either enlarged, variably sized nuclei and prominent nucleoli or enlarged nuclei with nuclear contour irregularity and mild or focal chromatin clearing
- Colloid is scant or absent but a small amount of inspissated colloid may be present within the microfollicle
- Foamy histiocytes are not common unless the neoplasm is large
- Hürthle cell predominant cases should be classified as follicular neoplasm, Hürthle cell type or suspicious for a follicular neoplasm, Hürthle cell type
Cytology images
Videos
Head and tail of the Bethesda system for thyroid
Thyroid cancer: fine needle aspiration, malignant or indeterminate results
Sample cytology report
- Dx / category: follicular neoplasm
- Cellular aspirate of follicular cells with a predominantly microfollicular architecture, scattered isolated cells and scant colloid.
- Dx / category: suspicious for a follicular neoplasm
- Although the architectural features suggest a follicular neoplasm, some nuclear features raise the possibility of an invasive follicular variant of papillary carcinoma or noninvasive follicular thyroid neoplasm with papillary-like nuclear features; distinction between these entities is not cytologically possible.
- Dx / category: suspicious for a follicular neoplasm
- Cellular aspirate composed predominantly of crowded uniform cells without colloid. Features suggest a follicular neoplasm but the possibility of a parathyroid lesion cannot be excluded. Correlation with clinical, serologic and radiologic findings should be considered.
Differential diagnosis
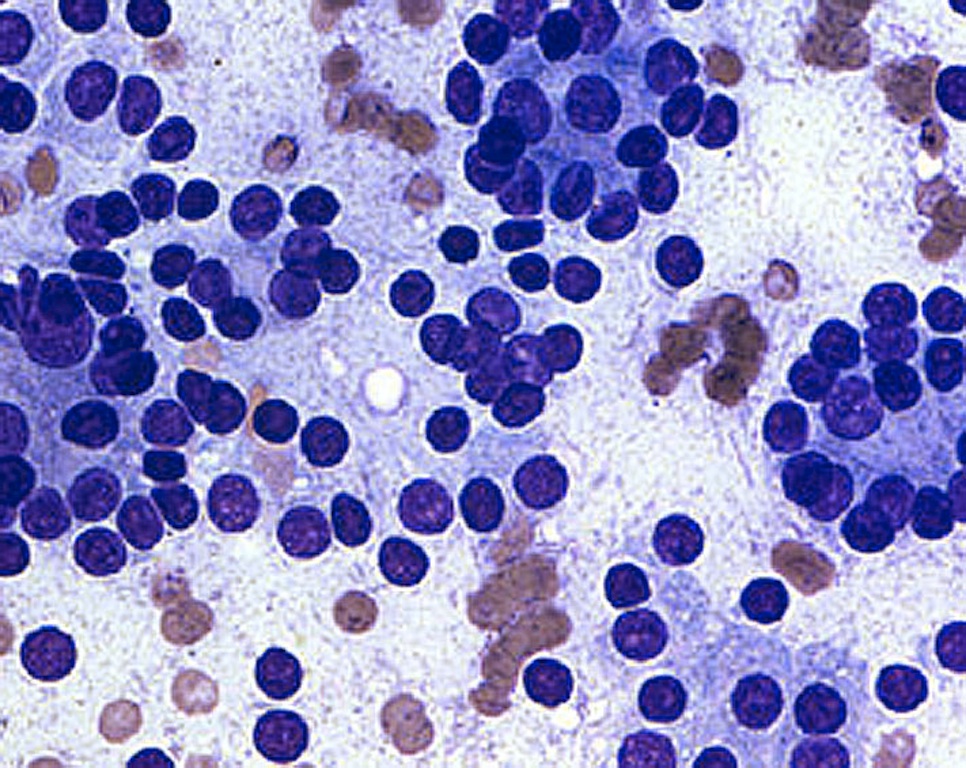
- Invasive follicular variant of papillary carcinoma or noninvasive follicular thyroid neoplasm with papillary-like nuclear features:
- Microfollicles but nuclear irregularity (grooves, chromatin clearing, pseudoinclusions) are present
- Parathyroid adenoma:
- Trabecular or microfollicular pattern but nuclei showing salt and pepper chromatin
- When located within the thyroid parenchyma and aspirated as a thyroid nodule, fine needle aspiration may be misdiagnosed as follicular neoplasm (Diagn Cytopathol 2009;37:407)
Board review style question #1
Which lesion is not included in follicular neoplasm / suspicious for a follicular neoplasm category?
- Conventional papillary carcinoma
- Follicular carcinoma
- Invasive follicular variant of papillary carcinoma
- Nodular goiter
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features
Board review style answer #1
A. Conventional papillary carcinoma. Lesions included in this category are follicular patterned lesions. Conventional papillary carcinoma is a papillary lesion with remarkable nuclear morphology.
Comment Here
Reference: Follicular neoplasm
Comment Here
Reference: Follicular neoplasm
Board review style question #2
Which histological diagnosis is most likely to correspond with this cytologic aspirate?
- Conventional papillary carcinoma
- Follicular adenoma or follicular carcinoma
- Invasive follicular variant of papillary carcinoma or noninvasive follicular thyroid neoplasm with papillary-like nuclear features
- Nodular goiter
- Parathyroid adenoma
Board review style answer #2
C. Invasive follicular variant of papillary carcinoma or noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Although the architectural features suggest a follicular neoplasm, the nuclei show grooves and powdery chromatin indicating papillary carcinoma
Comment Here
Reference: Follicular neoplasm
Comment Here
Reference: Follicular neoplasm