Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Florianova L, Pusztaszeri M. Diffuse sclerosing. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroiddiffusesclerosing.html. Accessed April 2nd, 2025.
Definition / general
- Papillary thyroid carcinoma (PTC) variant characterized by diffuse involvement of one or both thyroid lobes with dense sclerosis, abundant psammoma bodies, solid foci with associated squamous metaplasia, chronic lymphocytic thyroiditis background and extensive lymphatic invasion
- First described in 1985 by Vickery et al. (Semin Diagn Pathol 1985;2:90)
Essential features
- Diffuse sclerosing variant of PTC (DSV PTC) is an uncommon variant of PTC highly prevalent in female pediatric / young patients and in patients with history of radiation exposure
- Characterized by diffuse involvement of thyroid lobes, extensive lymphatic invasion, sclerosis, abundant psammoma bodies, squamous metaplasia and background thyroiditis
- Has distinct clinical, pathological and molecular profiles when compared with conventional PTC
- Aggressive subtype of PTC associated with frequent extrathyroidal extension, cervical lymph node metastasis, greater incidence of distant metastasis (5 - 15%) and more frequent recurrence than conventional PTC, however, mortality rates are similar to classic PTC
ICD coding
Epidemiology
- Rare: 0.7 - 2% of all PTC (World J Surg 2009;33:958, Endocr Pathol 2005;16:323, Ann Surg Oncol 2006;13:176, Crit Rev Oncol Hematol 2015;94:64)
- F > M (4 - 5:1) (Ann Surg Oncol 2006;13:176, World J Surg 2009;33:958, J Surg Oncol 2004;86:44)
- Presents more frequently in the second or third decade of life with a mean age of 30 at presentation, which is 10 - 15 years earlier than conventional PTC (Ann Surg Oncol 2006;13:176, J Clin Endocrinol Metab 2016;101:4603, Endocr Pathol 2005;16:331, Crit Rev Oncol Hematol 2015;94:64)
Sites
- Thyroid, usually diffusely involving both lobes
- Sometimes can present as a single nodule (Am J Surg Pathol 1989;13:1041)
Pathophysiology
- Clonal neoplastic proliferation of thyroid follicular cells, usually with a specific driver mutation, mainly RET / PTC rearrangements resulting in the activation of the RAS / RAF / MAPK pathway (see Molecular / cytogenetics description below)
Etiology
- Sporadic in most cases
- Can occur in patients with a history of radiation exposure (Thyroid 2012;22:1016, Crit Rev Oncol Hematol 2015;94:64)
Clinical features
- Diffuse involvement of one or both thyroid lobes, usually without forming a dominant mass (Crit Rev Oncol Hematol 2015;94:64)
- Hard ("woody") thyroid gland, which may mimic Riedel thyroiditis (Case Rep Endocrinol 2015;2015:686085)
- May be associated with hyperthyroidism or hypothyroidism (Endocr Pathol 2005;16:331)
- Possible local compression symptoms such as dysphagia, hoarseness and dysphonia (Crit Rev Oncol Hematol 2015;94:64, Endocr Pathol 2005;16:331)
- Frequently enlarged cervical lymph nodes, including lateral
Diagnosis
- Workup is similar to any thyroid mass / nodule
- Ultrasound with fine needle aspiration cytology
- CT scan may be useful to evaluate extrathyroidal extension and lymph node metastases
- Diagnosis is made via histological examination of a resection specimen
- Fine needle aspiration cytology can raise a suspicion of DSV PTC and influence surgical decision making
Laboratory
- Commonly elevated antithyroglobulin, antimicrosomal and antithyroid peroxidase antibodies, perhaps due to destruction of normal thyroid follicles by tumor and exposure of cryptic antigens
- May mimic Hashimoto thyroiditis clinically, which is also a frequent association (30 - 75%) (World J Surg 2009;33:958, Cytopathology 2014;25:199, World J Surg 2015;39:1728)
Radiology description
- Most cases show diffuse, scattered microcalcifications ("snowstorm appearance") with or without associated suspicious masses and underlying heterogeneous hypoechogenicity (Clin Radiol 2007;62:382)
- Ultrasound features correlate with numerous psammoma bodies and lymphocytic infiltration on histology (Korean J Radiol 2010;11:579)
- Cervical lymphadenopathy is frequently present at the time of the ultrasound examination (Korean J Radiol 2010;11:579)
Prognostic factors
- Associated with higher rates of extrathyroidal extension (40 - 77%), lymph node metastases (68 - 86%) and distant metastases (11.6%, usually in lungs) at presentation compared with conventional PTC (J Surg Oncol 2004;86:44, Thyroid 2016;26:1285, J Clin Endocrinol Metab 2016;101:4603, Eur J Endocrinol 2017;176:433
- Associated with a shorter disease free survival; however, the overall mortality rate is similar to that of conventional PTC with disease specific survival of 95% and 93% at 5 and 10 years, respectively (possibly due to younger patient age and aggressive initial treatment) (Ann Surg Oncol 2006;13:176, Endocr Pathol 2005;16:331, World J Surg 2009;33:958, World J Surg 2015;39:1728)
- Risk stratification as per ATA (American Thyroid Association) 2015 (Thyroid 2016;26:1)
Case reports
- 11 year old girl with thyroid enlargement, hyperthyroidism and antibodies to thyroglobulin and thyroid peroxidase (Arch Pathol Lab Med 2005;129:e159)
- 18 year old woman with goiter (Ulster Med J 2007;76:113)
- 22 year old woman with diffuse thyroid calcifications (Medicine (Baltimore) 2016;95:e3141)
- 44 year old woman with a neck mass, sore throat, hoarseness and intermittent dysphagia (Case Rep Endocrinol 2015;2015:686085)
- 53 year old man with multiple brain metastases (Endocr Pathol 2000;11:97)
- 58 year old woman with hypertension and rheumatoid arthritis (Case #439)
Treatment
- This diagnosis should trigger aggressive therapeutic management in an effort to achieve a possibly excellent long term clinical outcome (Endocr Pathol 2005;16:331)
- Common treatment strategies are initial total thyroidectomy with neck dissection followed by radioiodine treatment, TSH suppression and a long term follow up (World J Surg 2009;33:958, J Surg Oncol 2004;86:44, J Clin Endocrinol Metab 2016;101:4603)
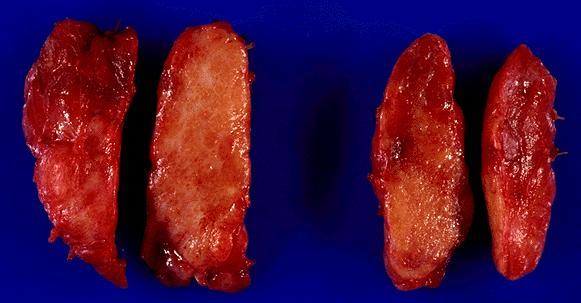
Gross description
- Diffuse enlargement of one or both thyroid lobes (Crit Rev Oncol Hematol 2015;94:64)
- Usually without a discrete tumor mass or alternatively with one or multiple ill defined masses recognizable on gross examination (Crit Rev Oncol Hematol 2015;94:64)
- The cut surface shows a patchy, reticulated white-gray appearance with a gritty consistency due to presence of innumerable psammoma bodies (Crit Rev Oncol Hematol 2015;94:64)
Gross images
Frozen section description
- Frozen section is usually not indicated
- Standard of care is to perform preoperative fine needle aspiration to establish the diagnosis of PTC and to determine the most appropriate surgical procedure
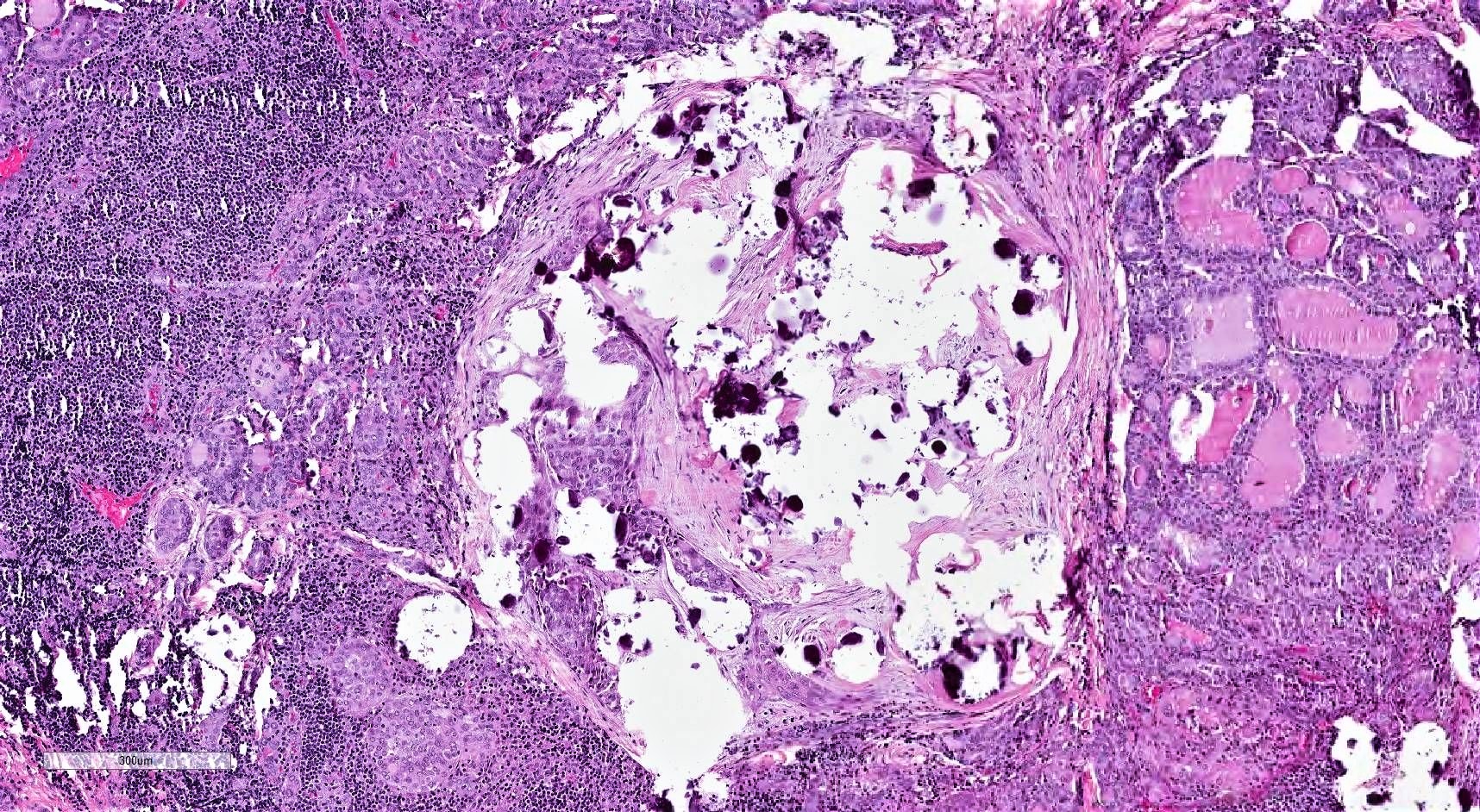
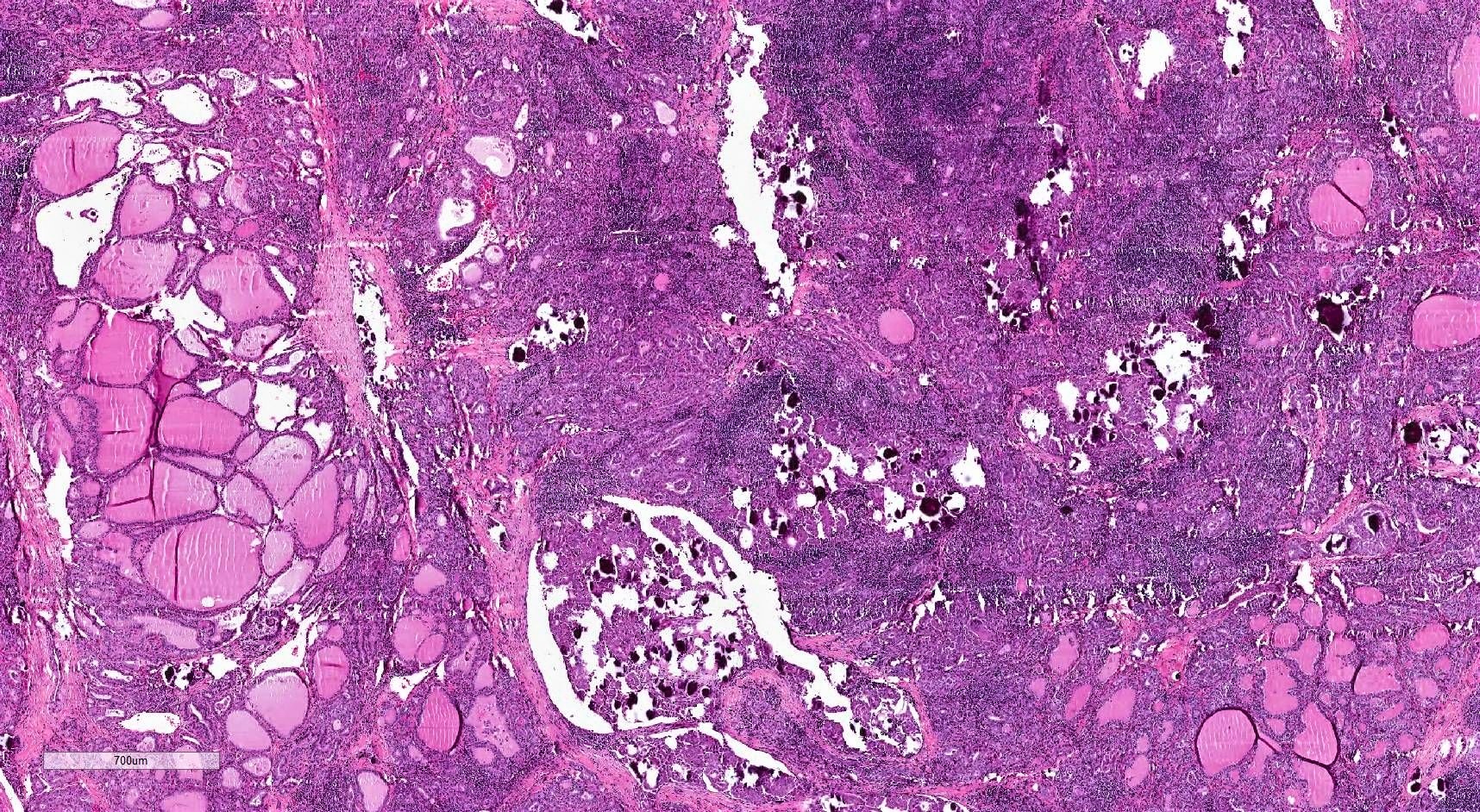
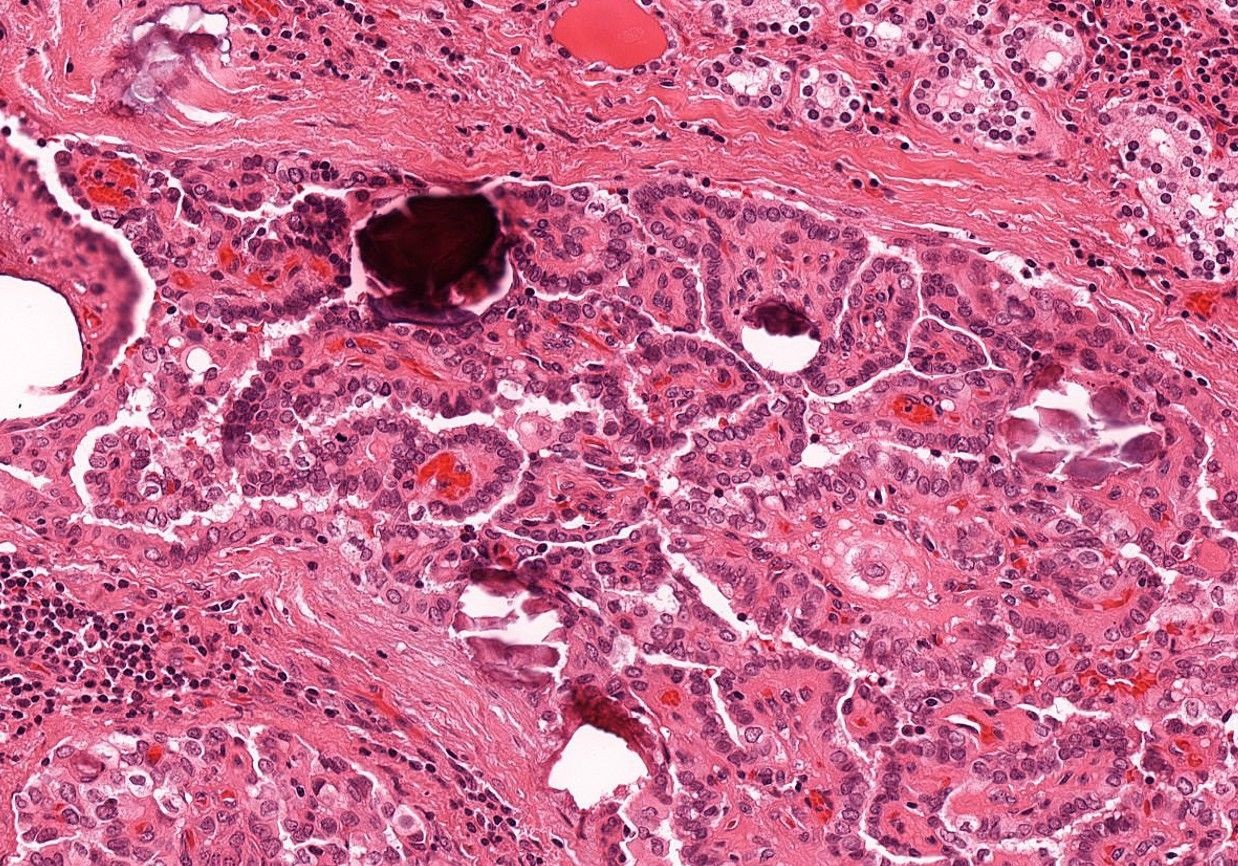
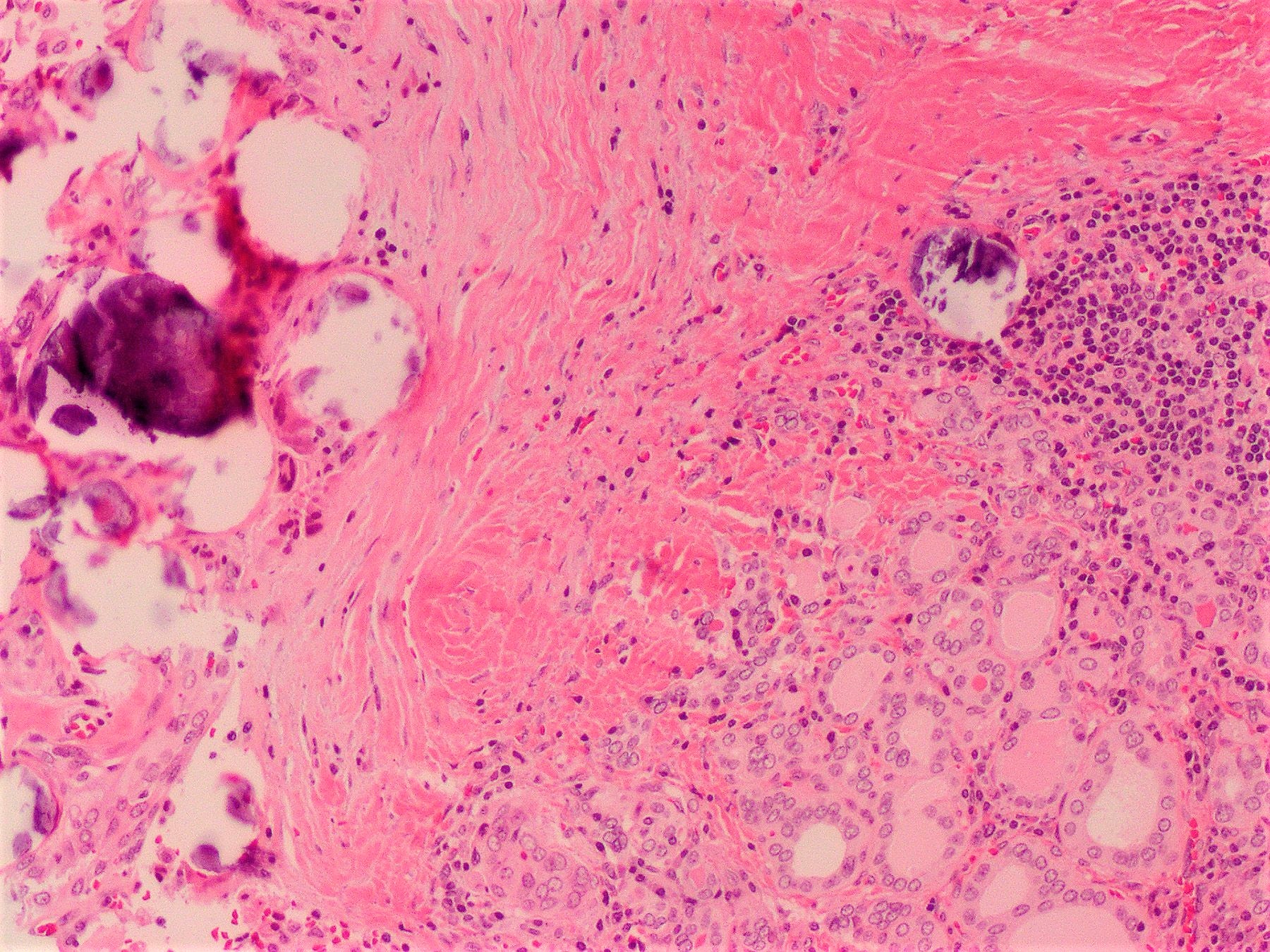
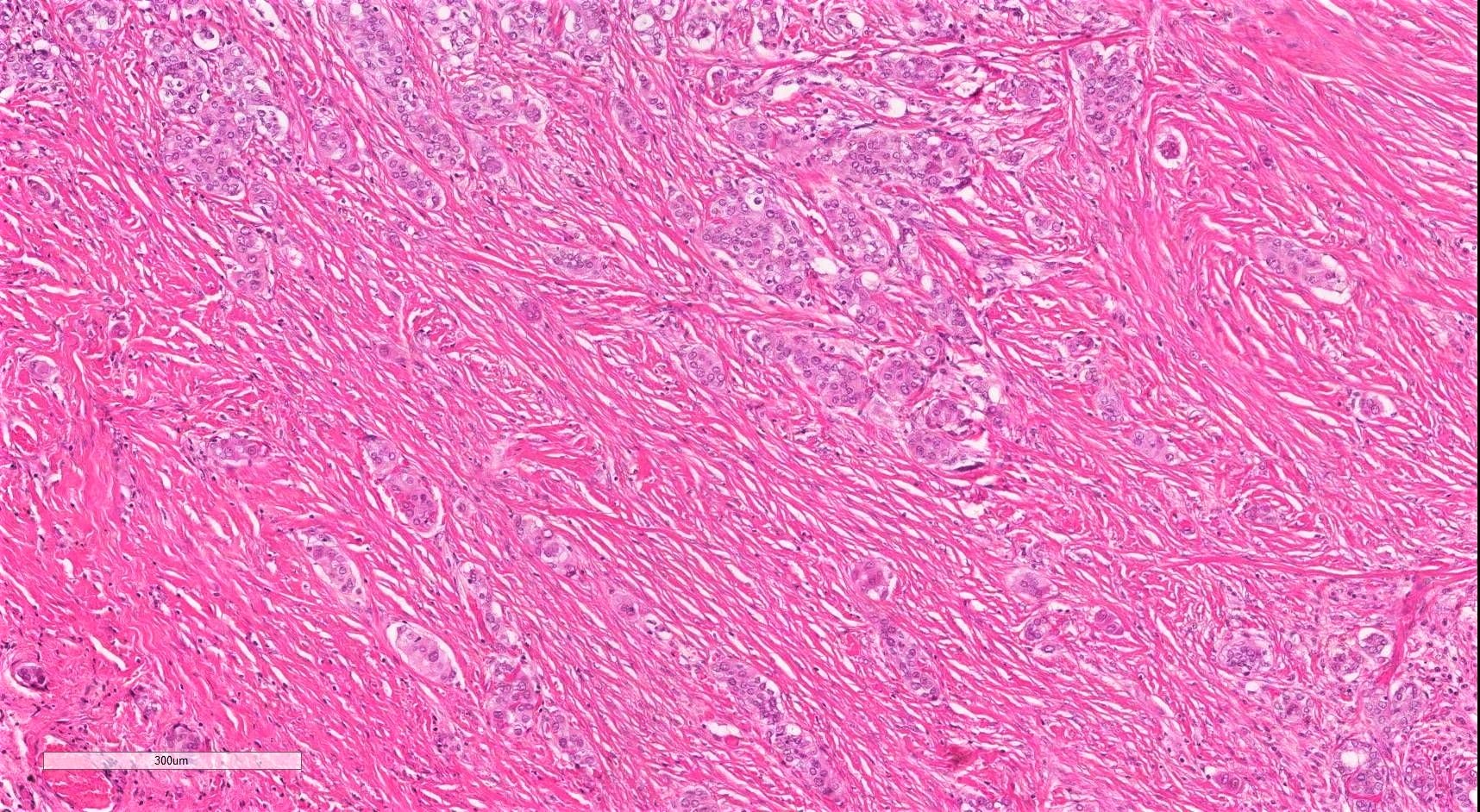
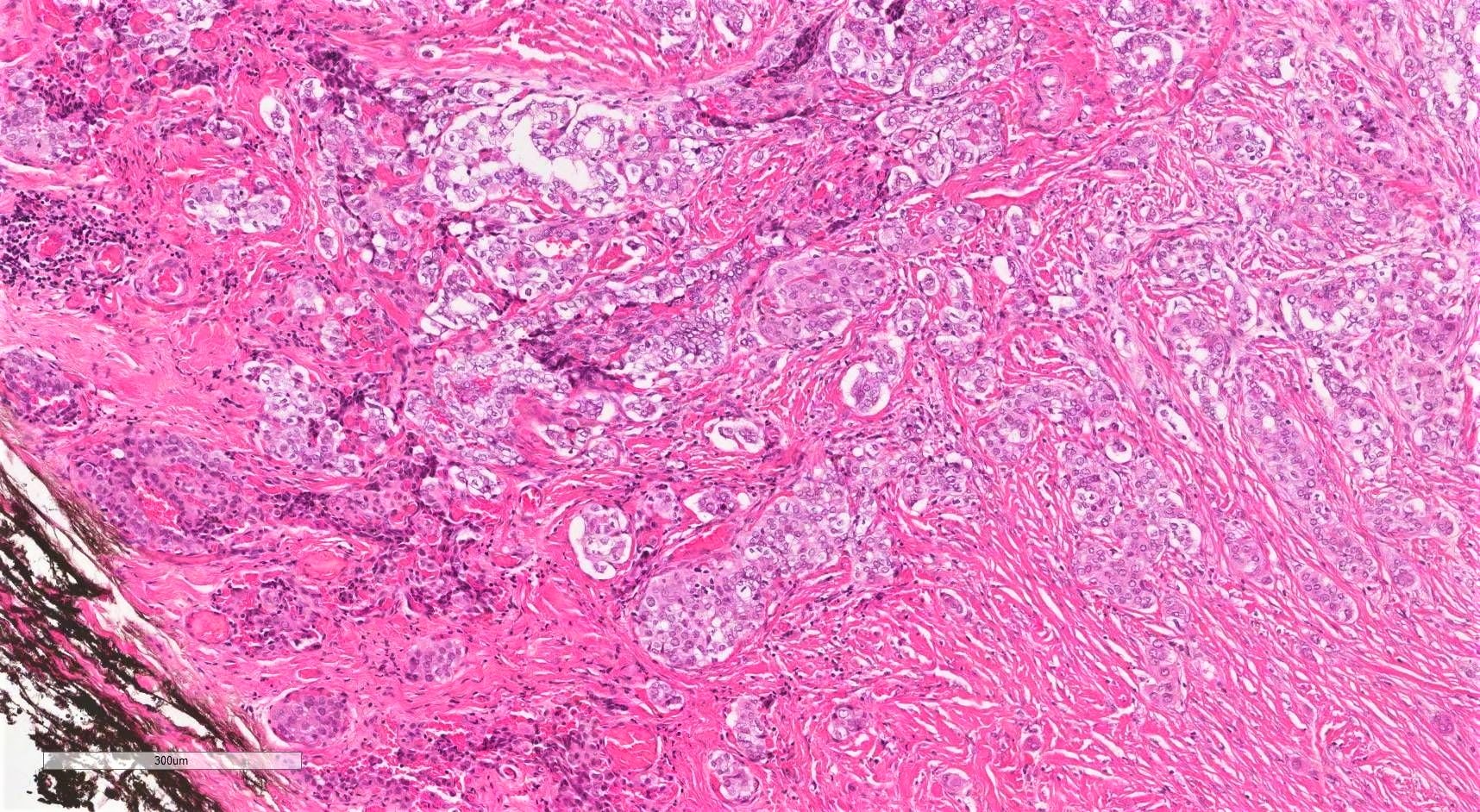
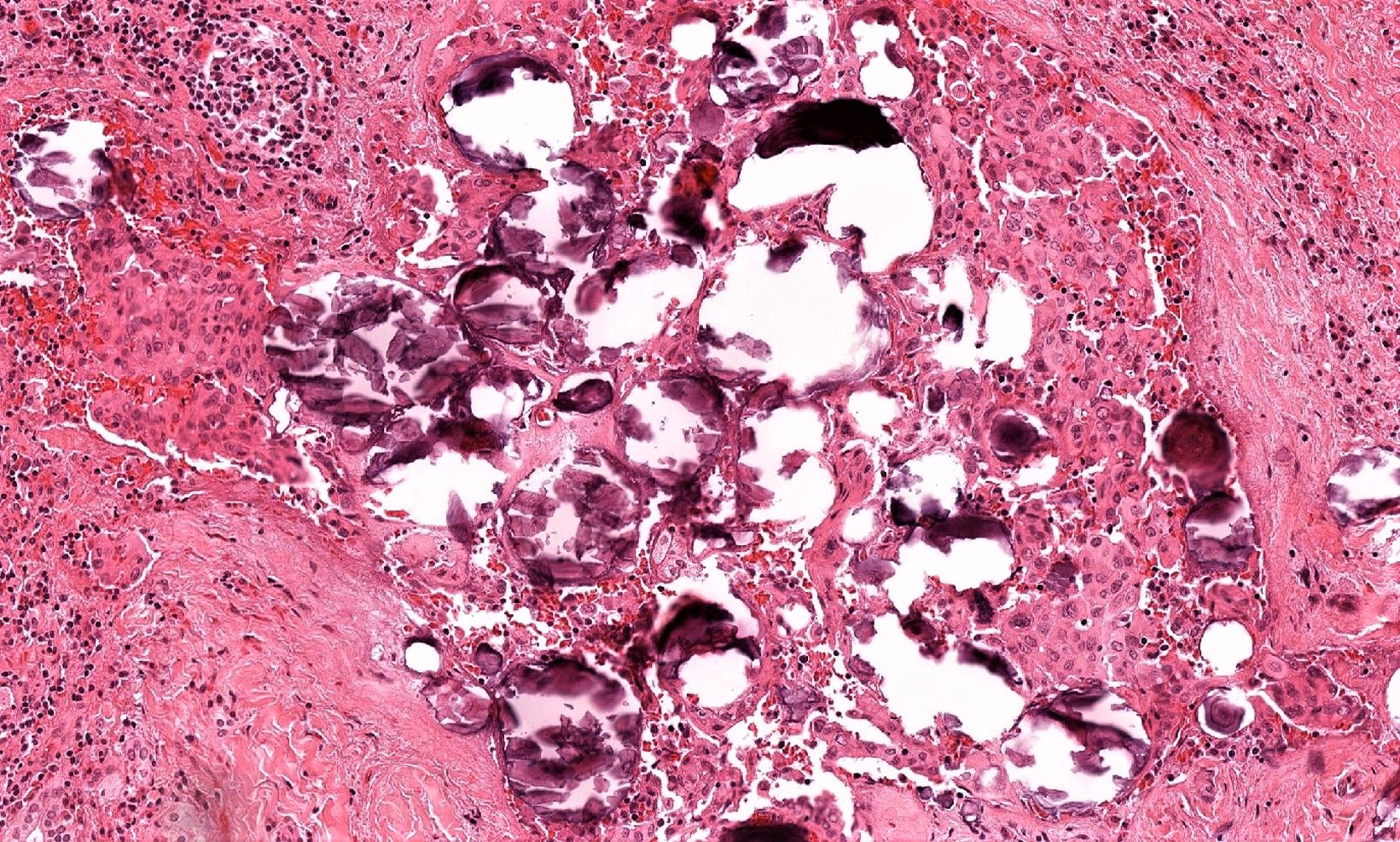
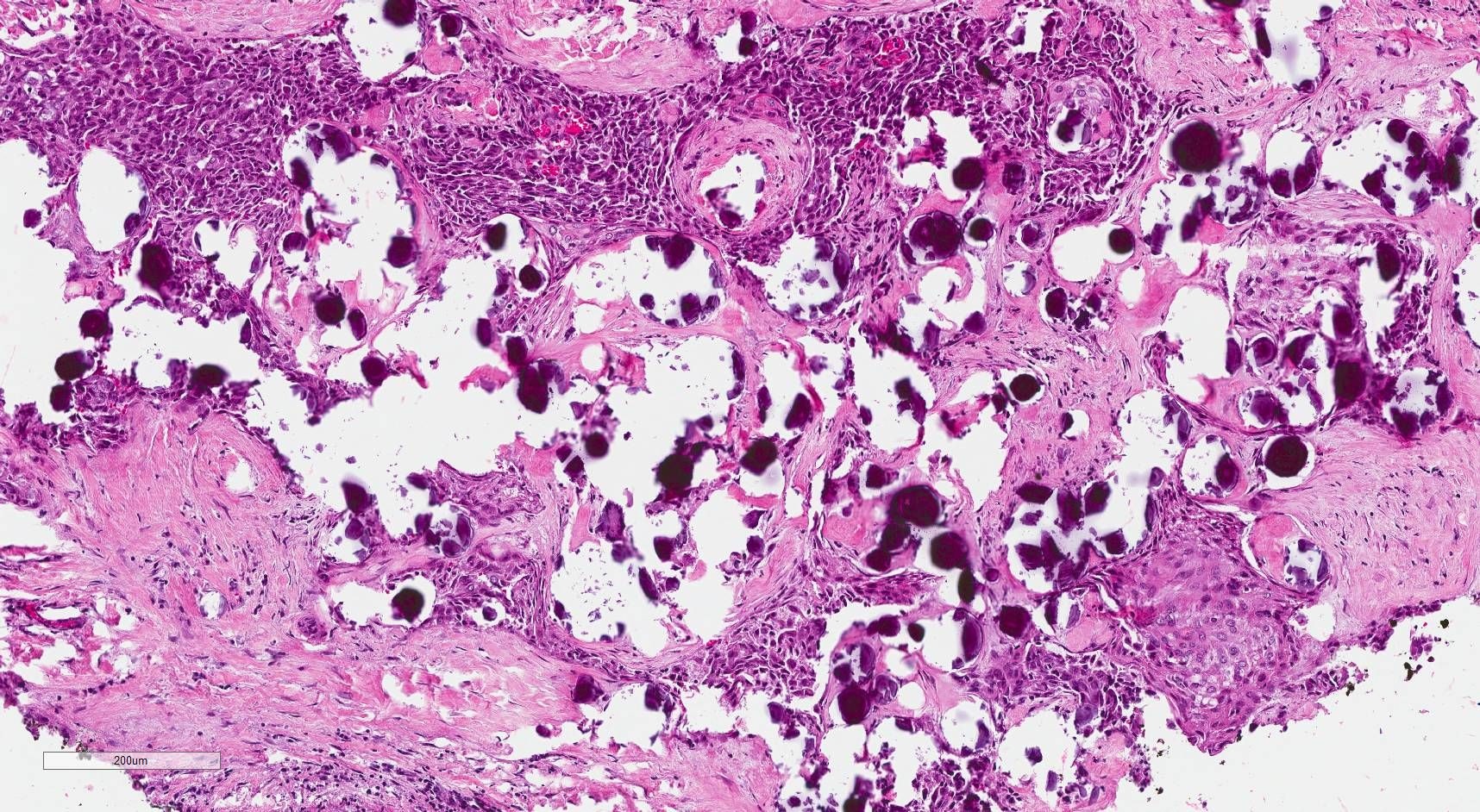
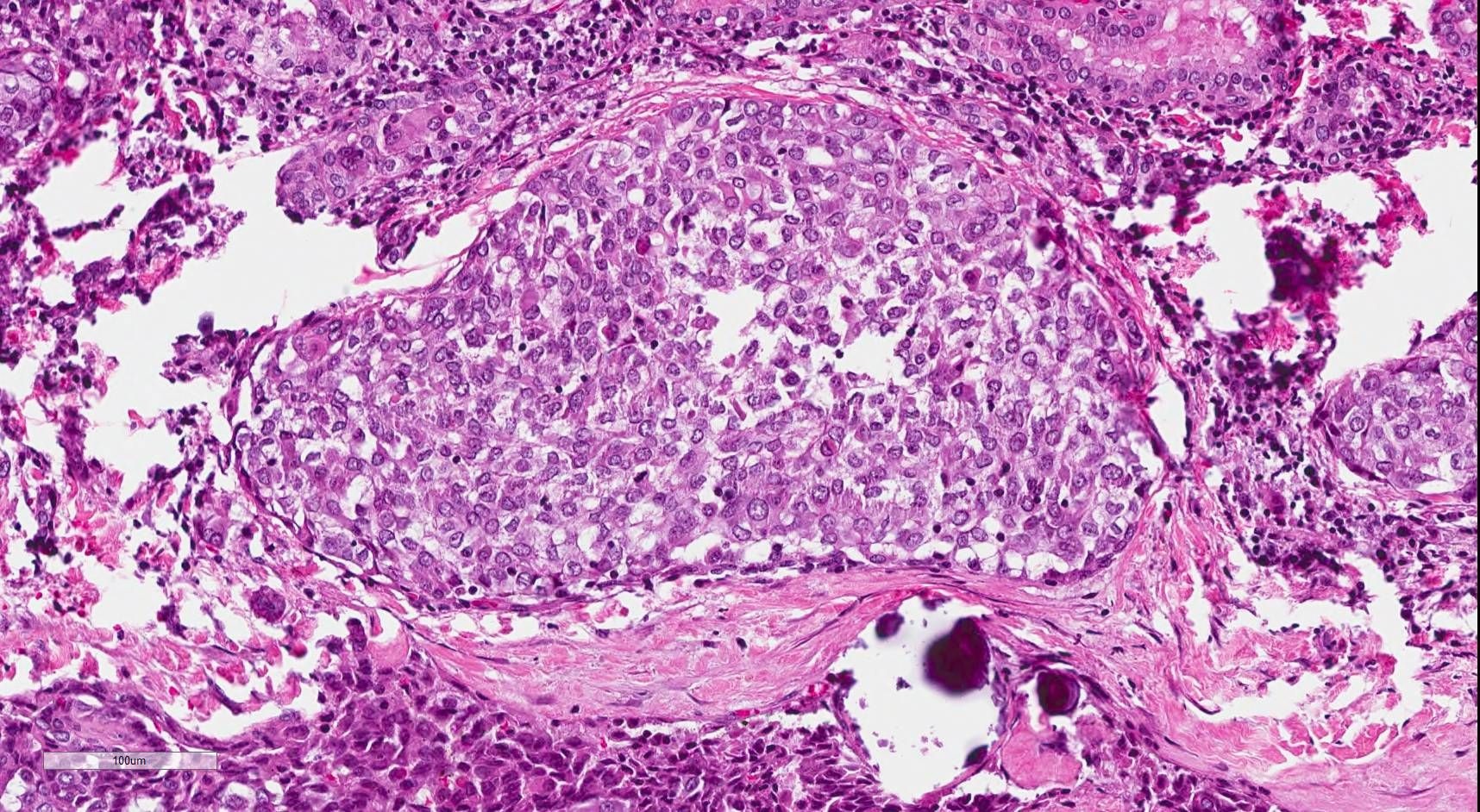
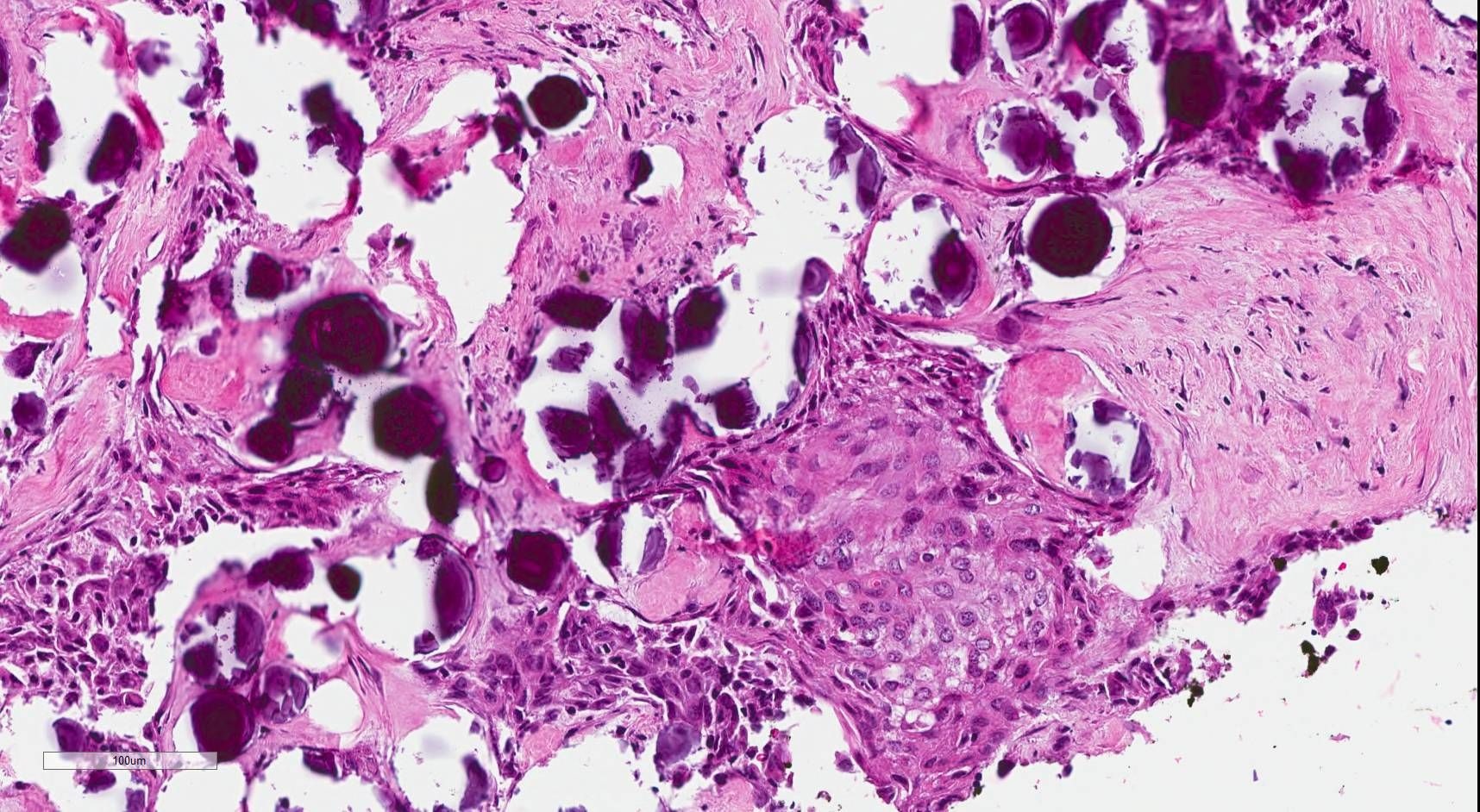
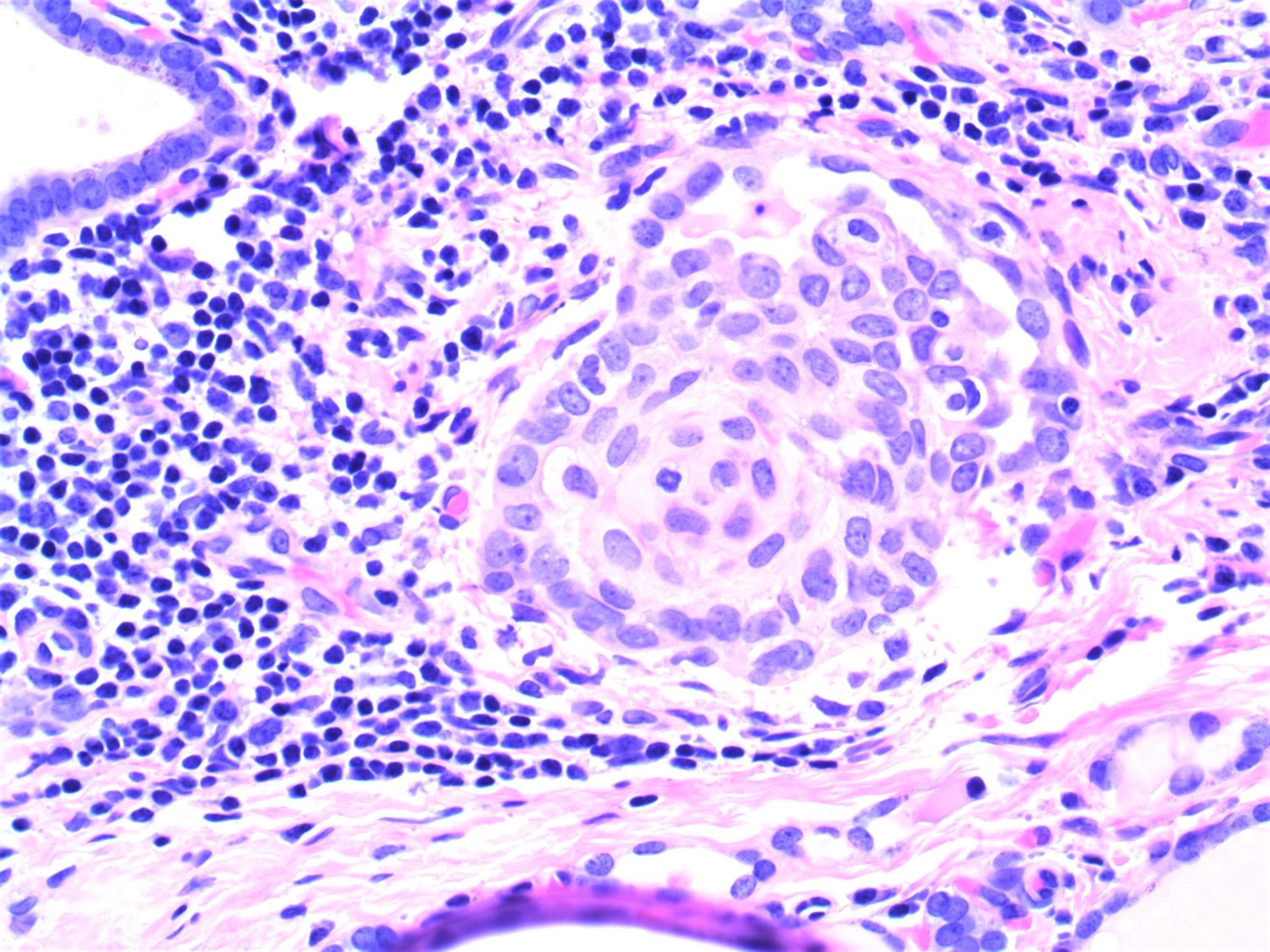
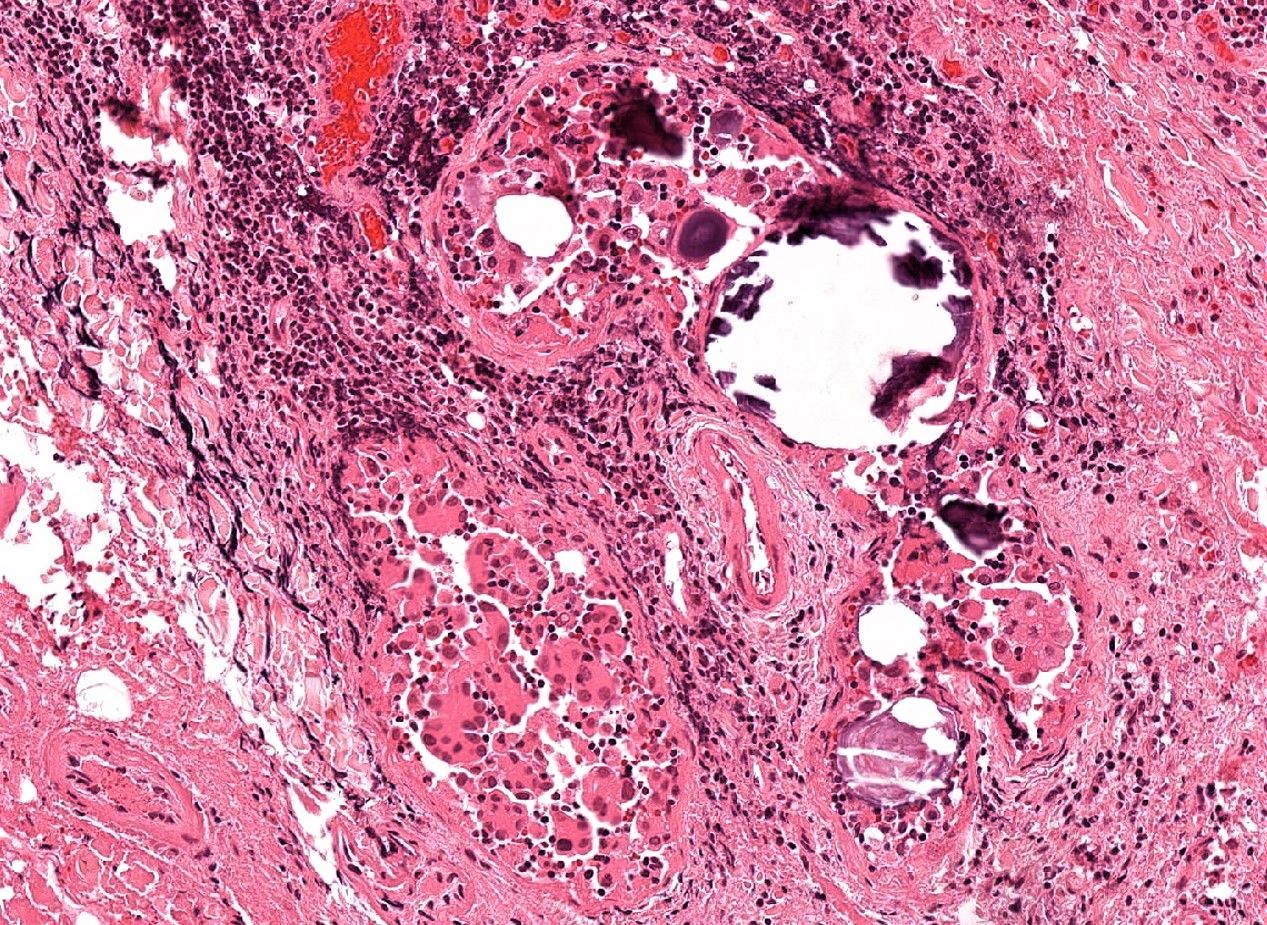
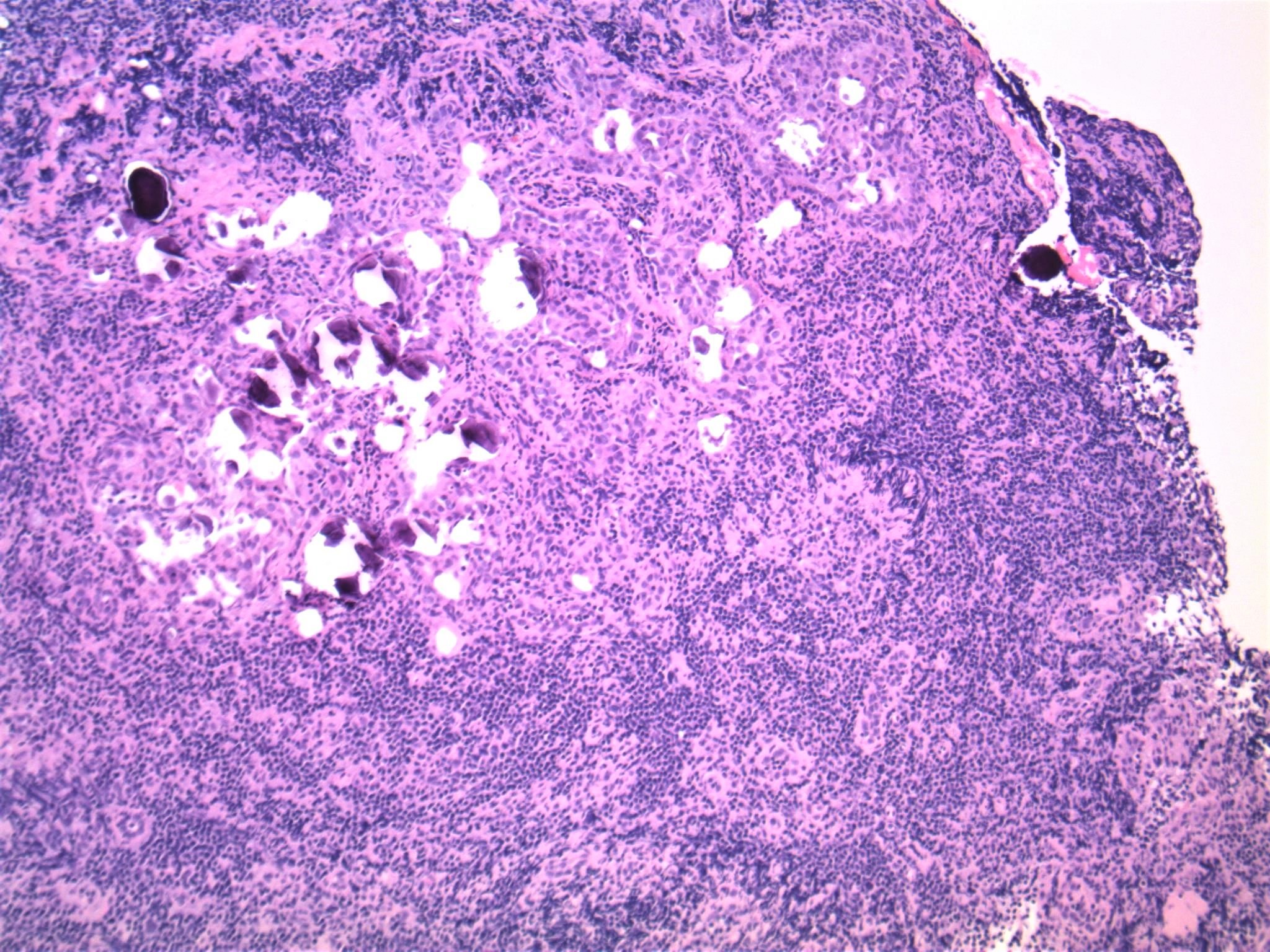
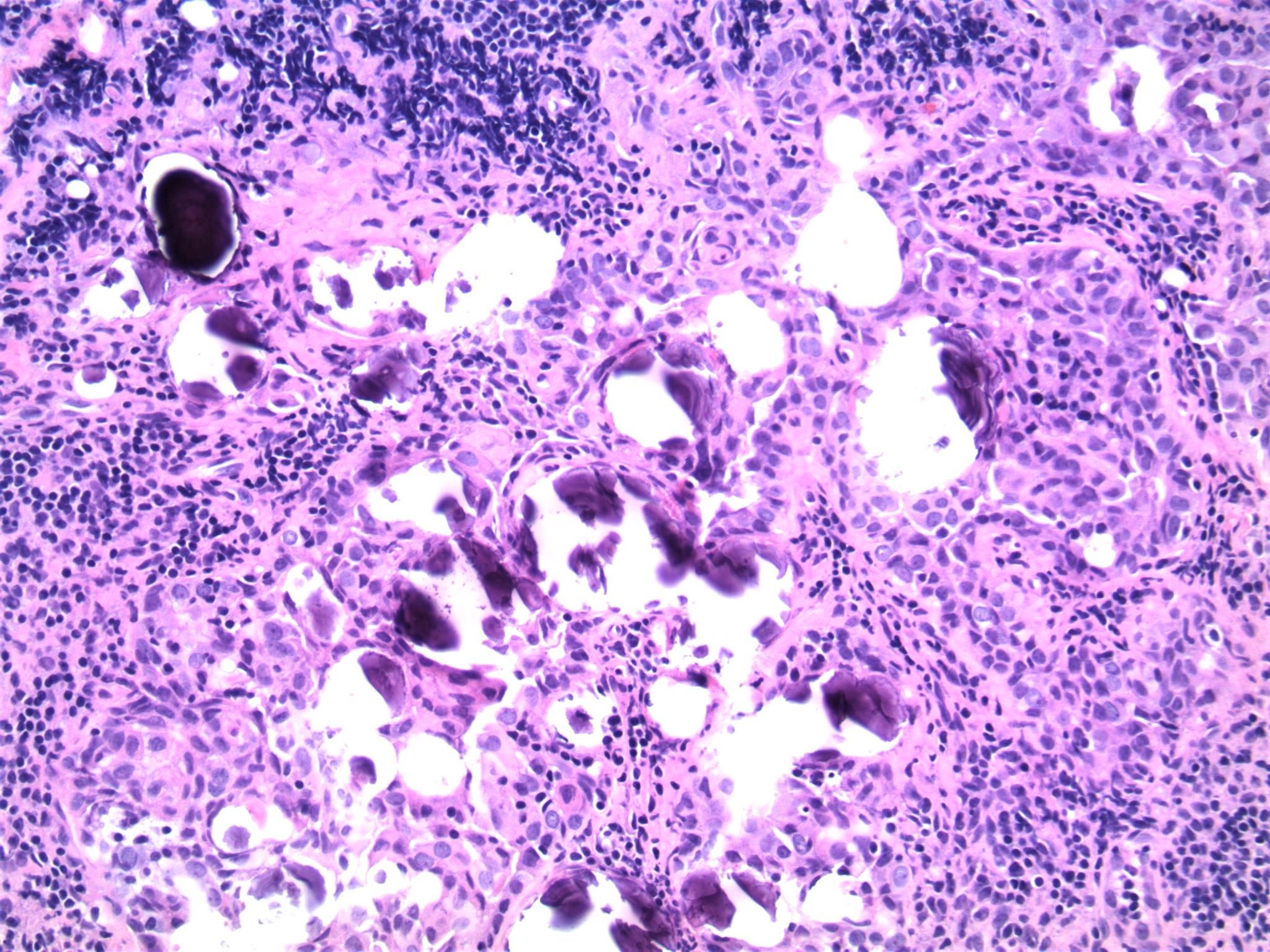
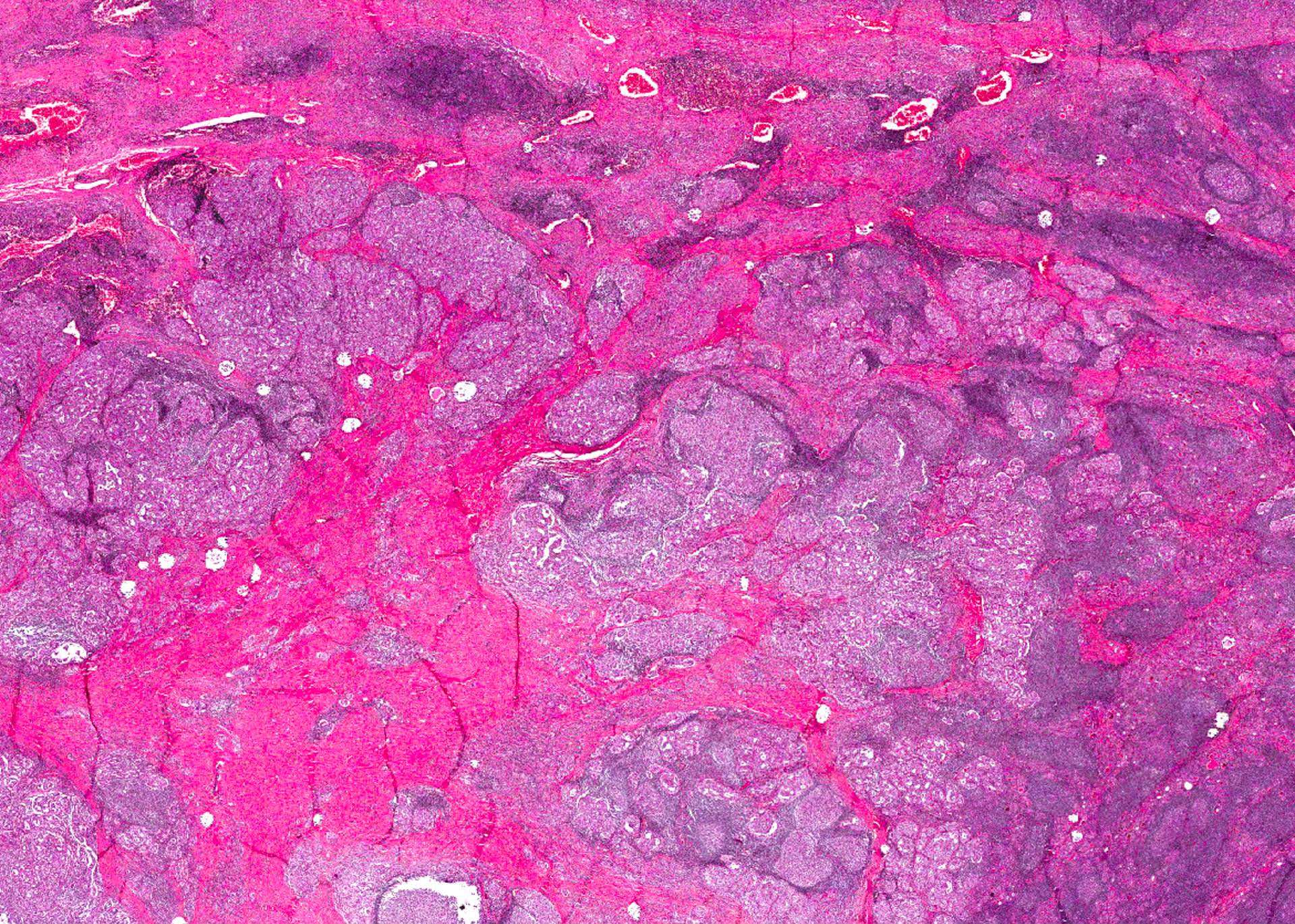
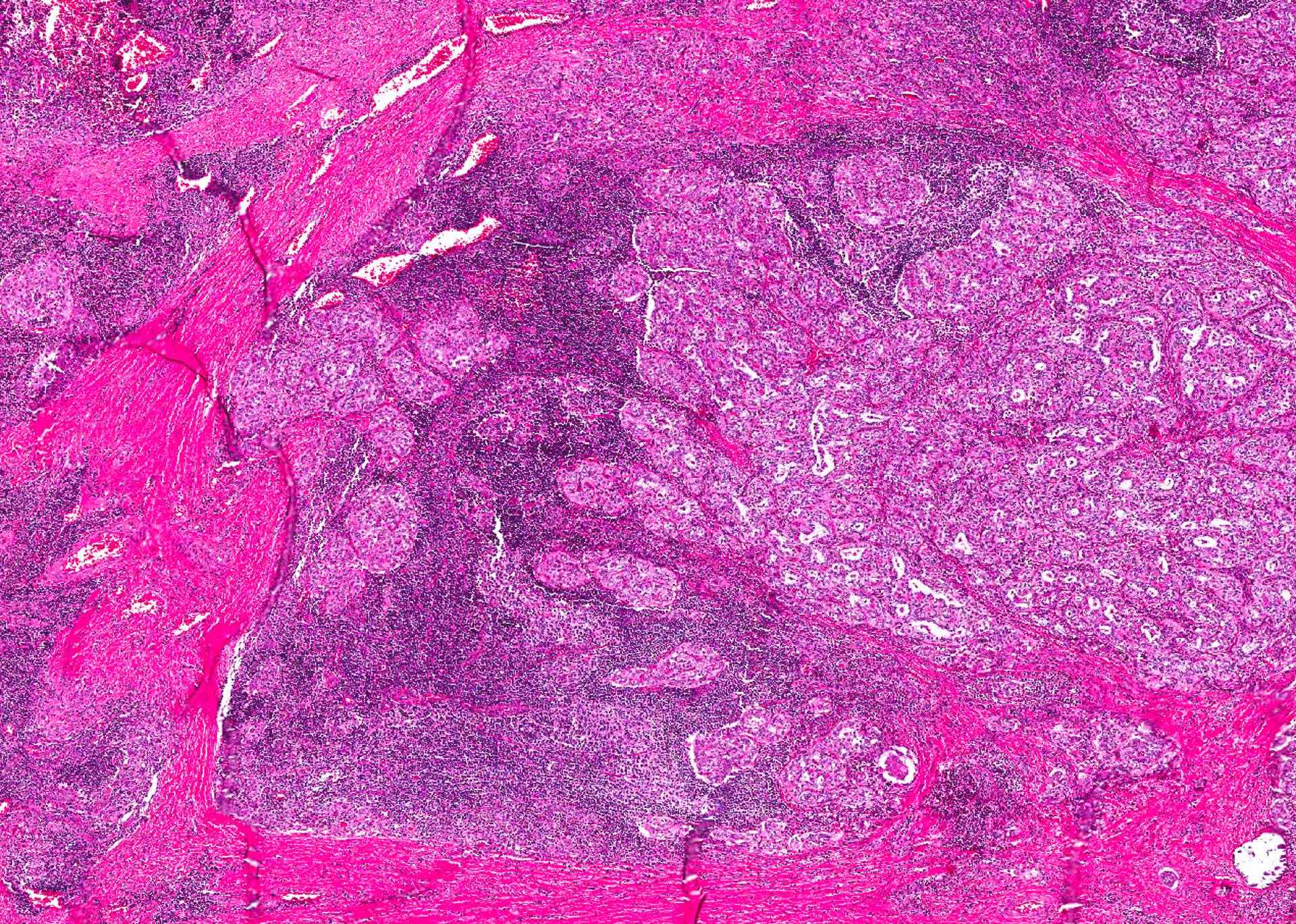
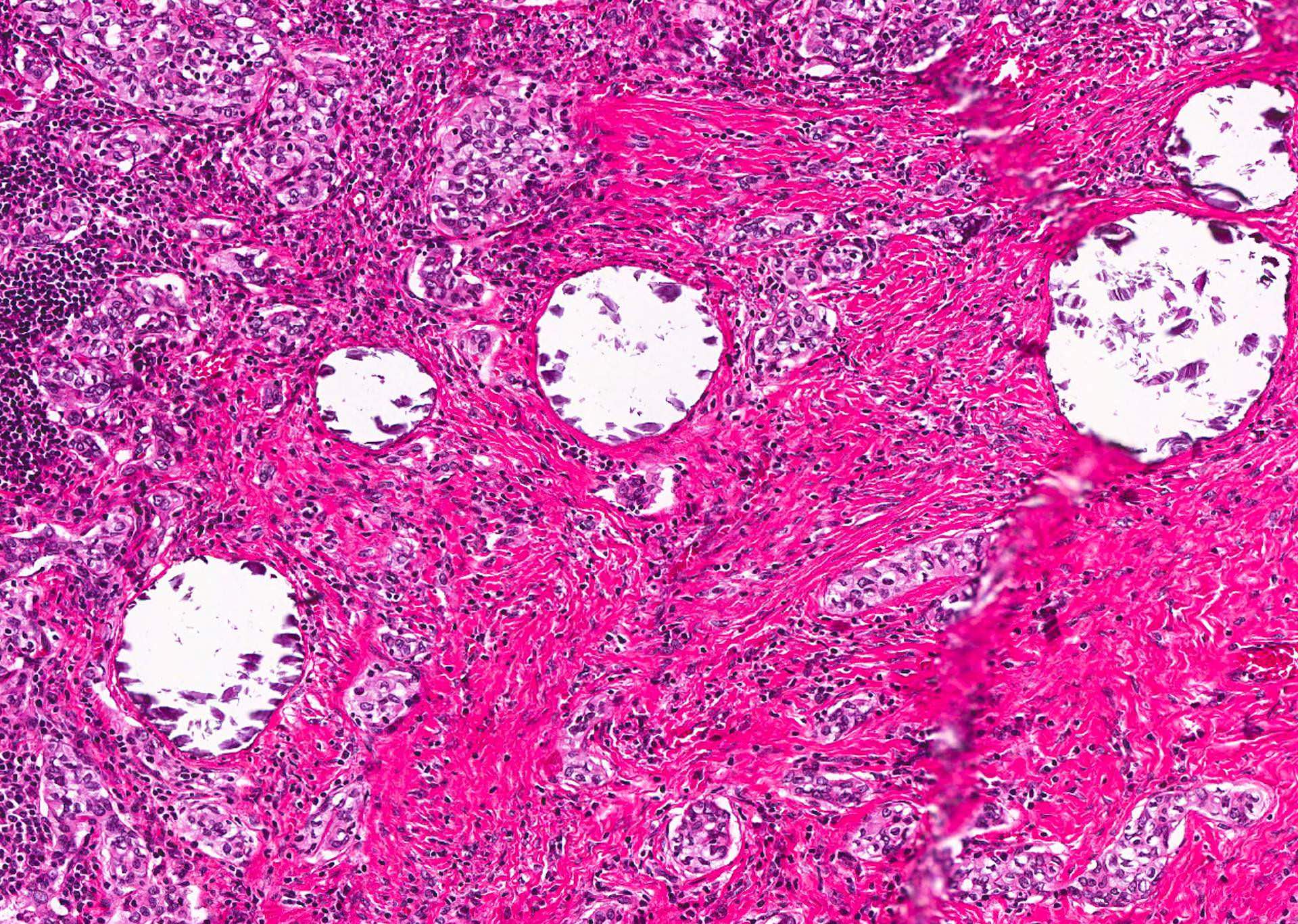
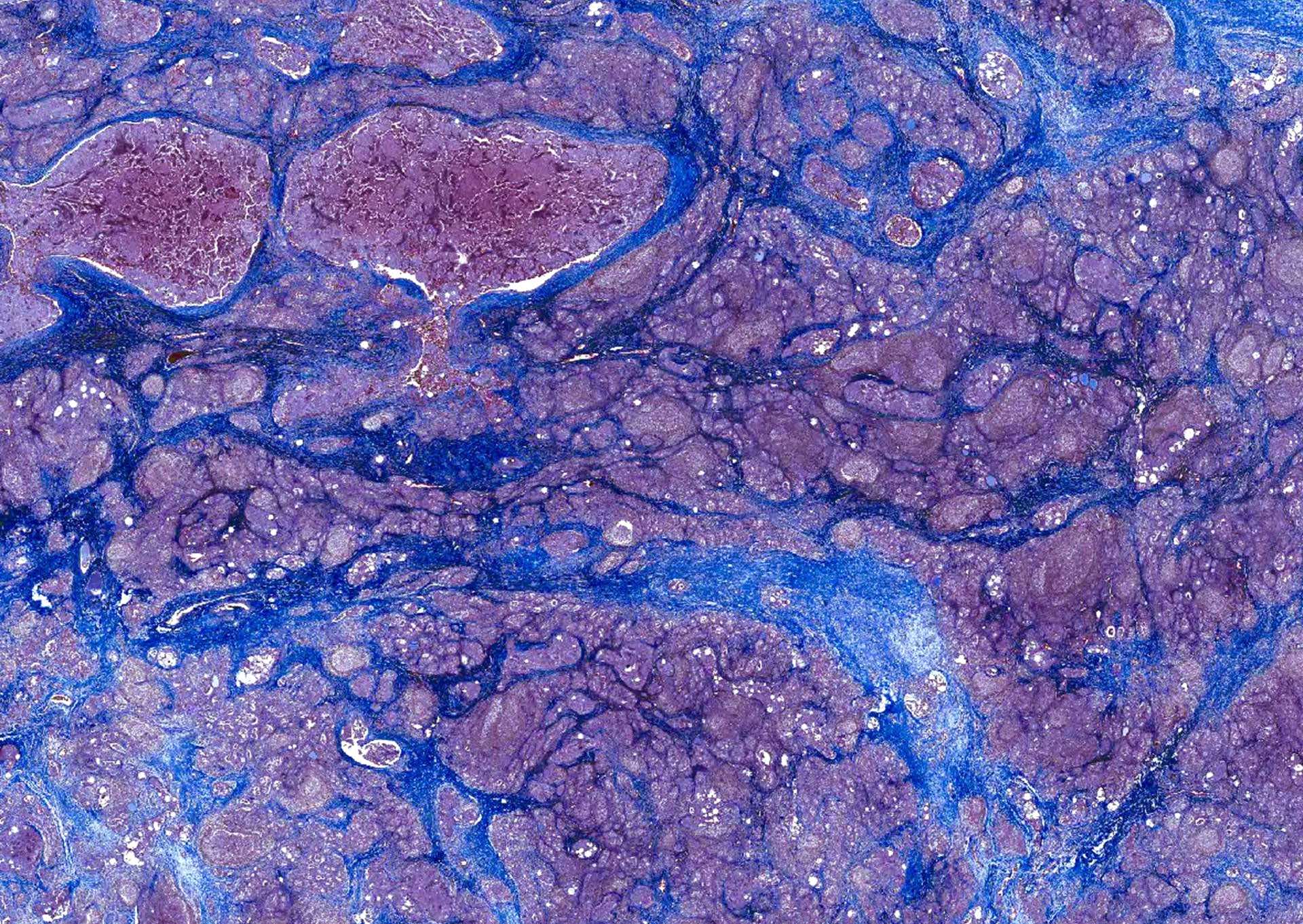
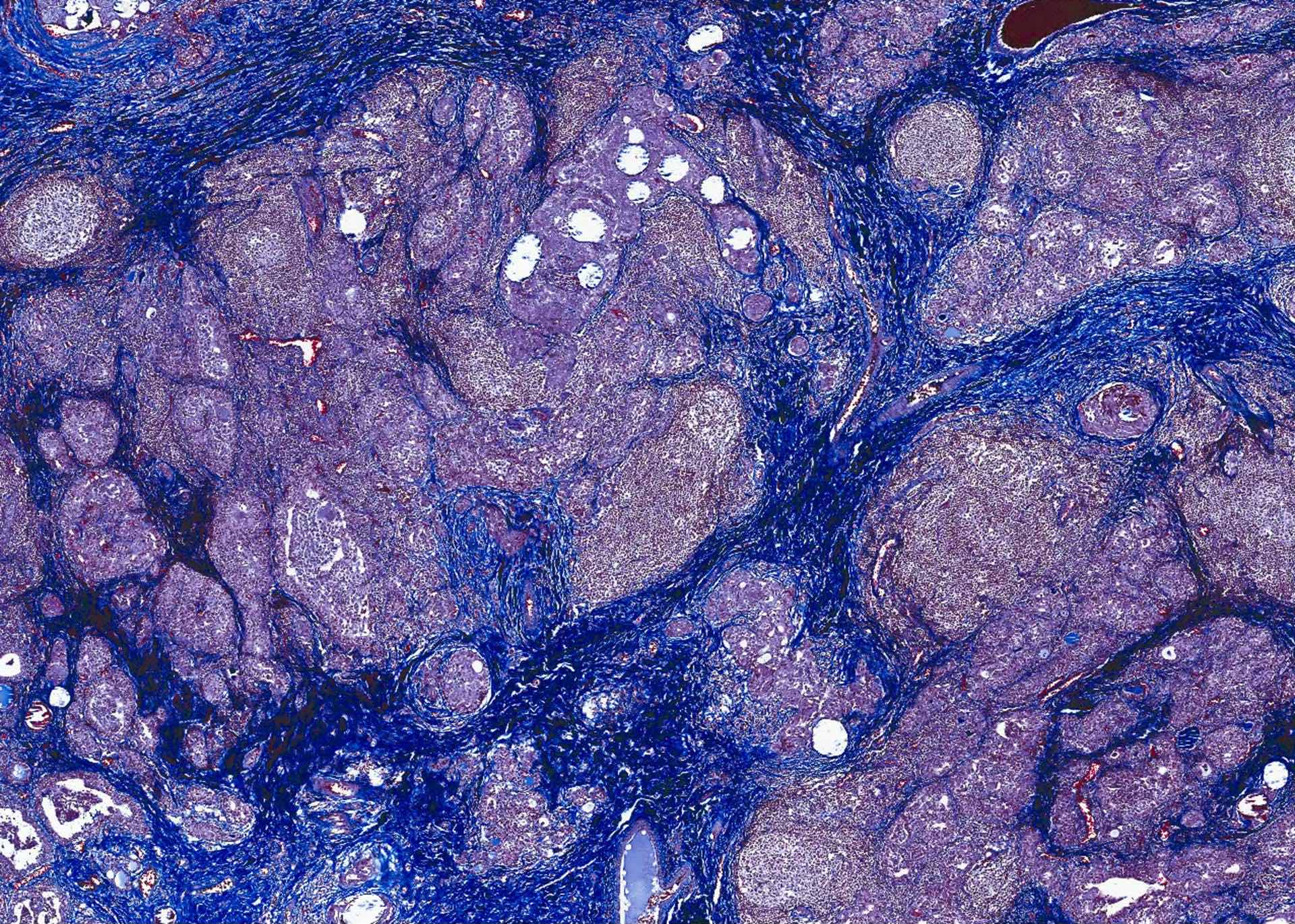
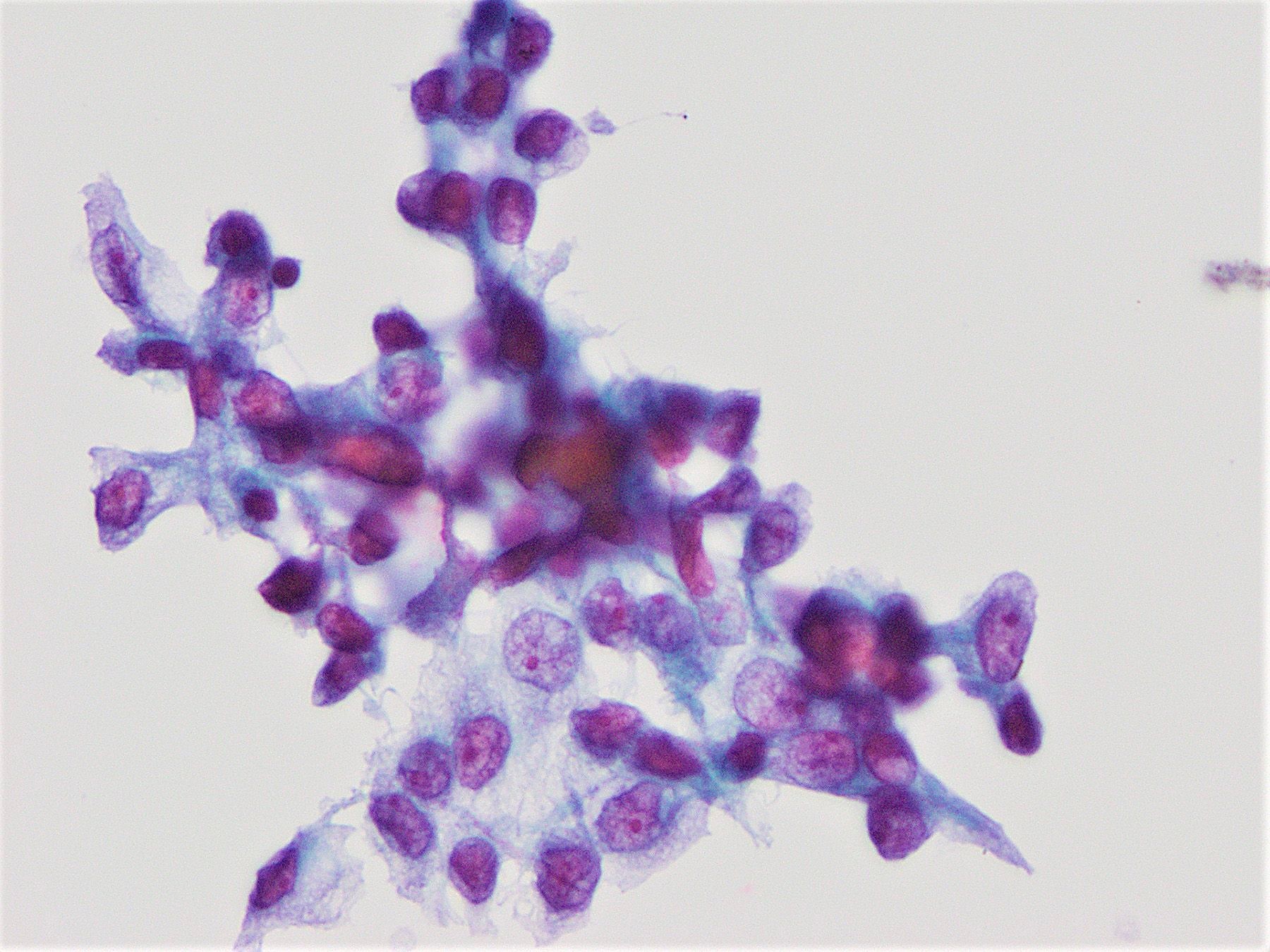
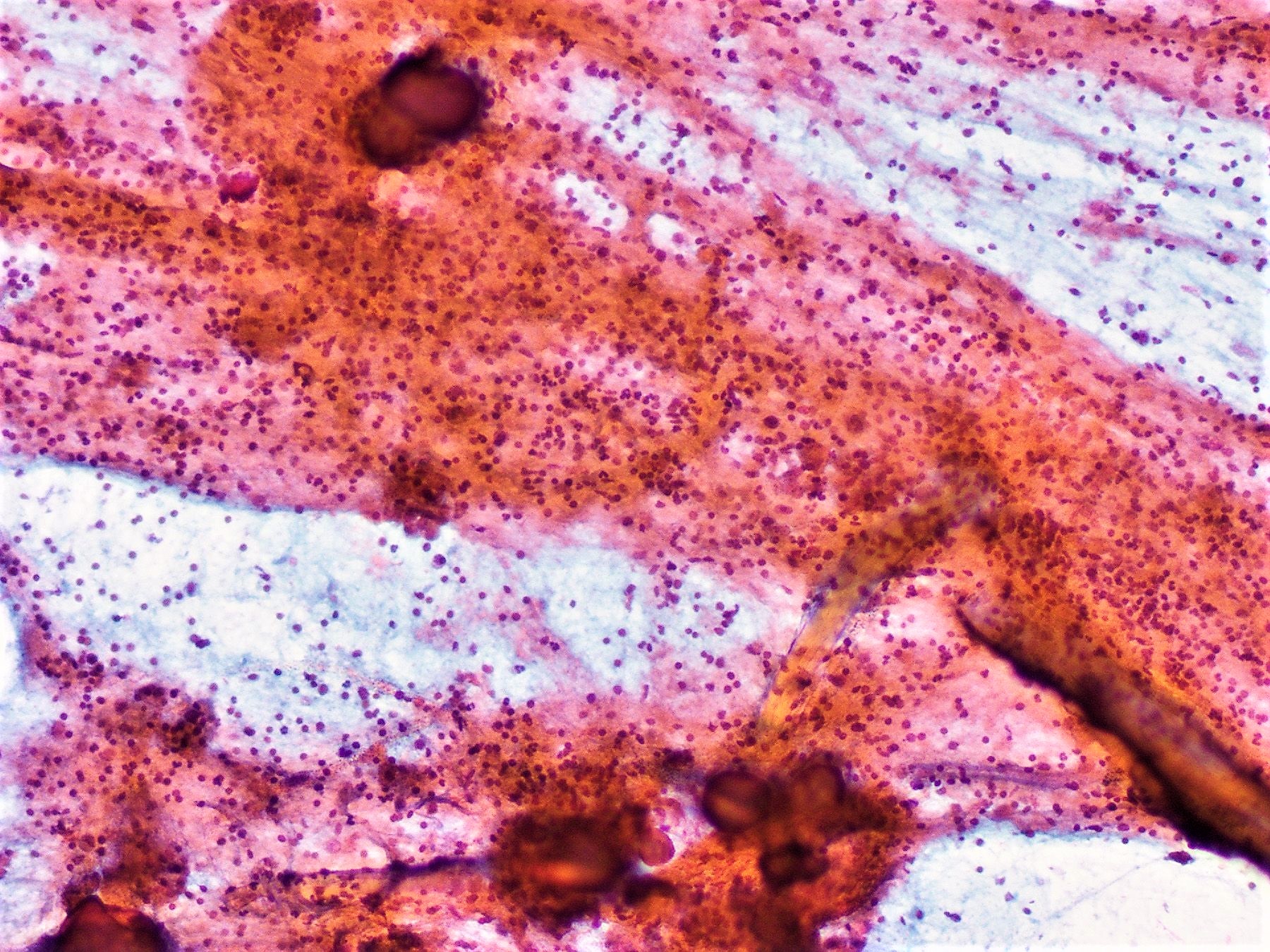
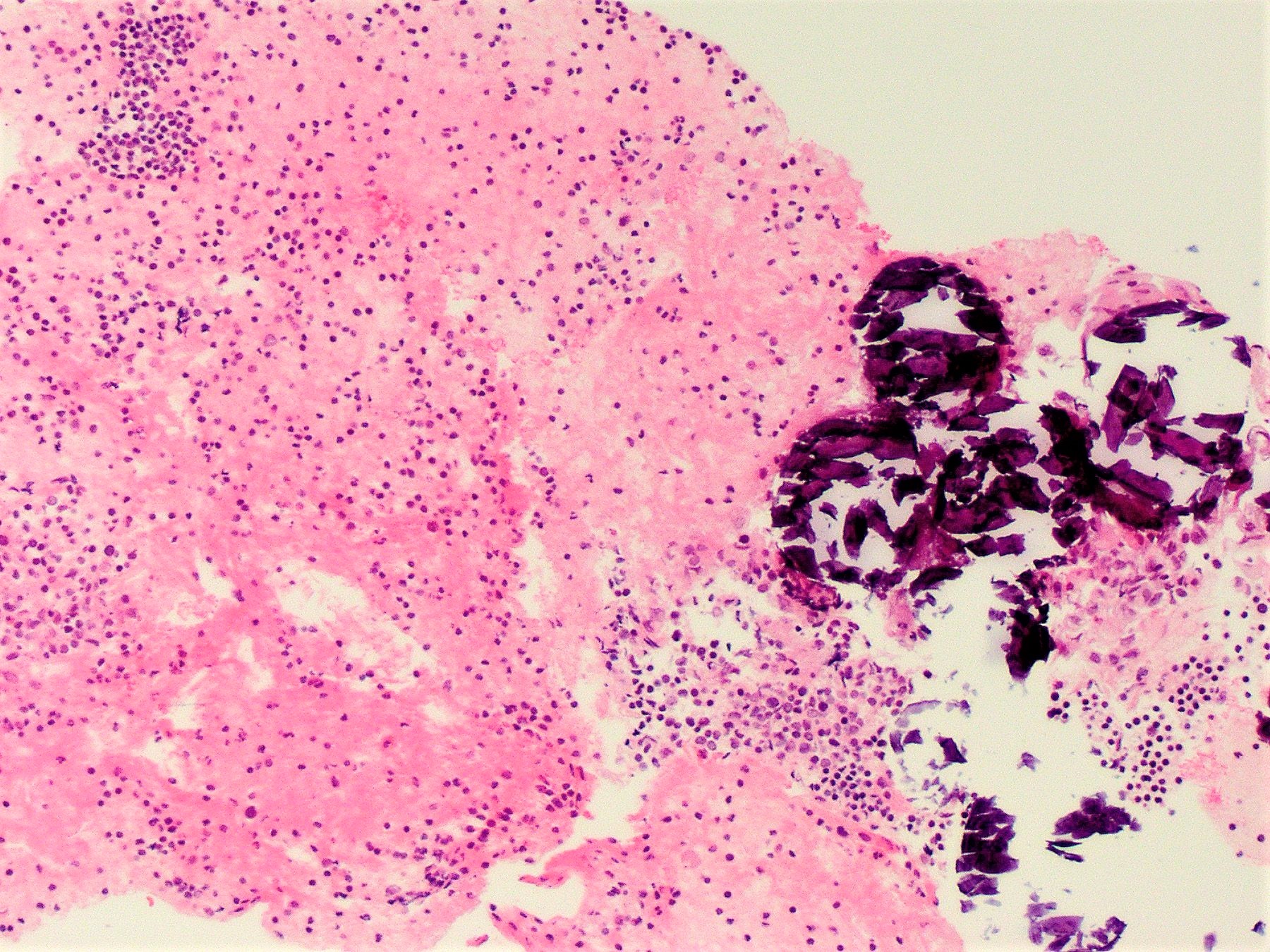
Microscopic (histologic) description
- Infiltrative growth with diffuse involvement of one or both lobes (papillary, solid or follicular pattern) (Endocr Pathol 2005;16:331, Crit Rev Oncol Hematol 2015;94:64)
- Tumor foci within large distended lymphatics throughout
- Numerous psammoma bodies frequently arranged in large clusters (Endocr Pathol 2005;16:331, Crit Rev Oncol Hematol 2015;94:64)
- Dense fibrosis
- Extensive lymphocytic infiltration and a background of chronic lymphocytic thyroiditis
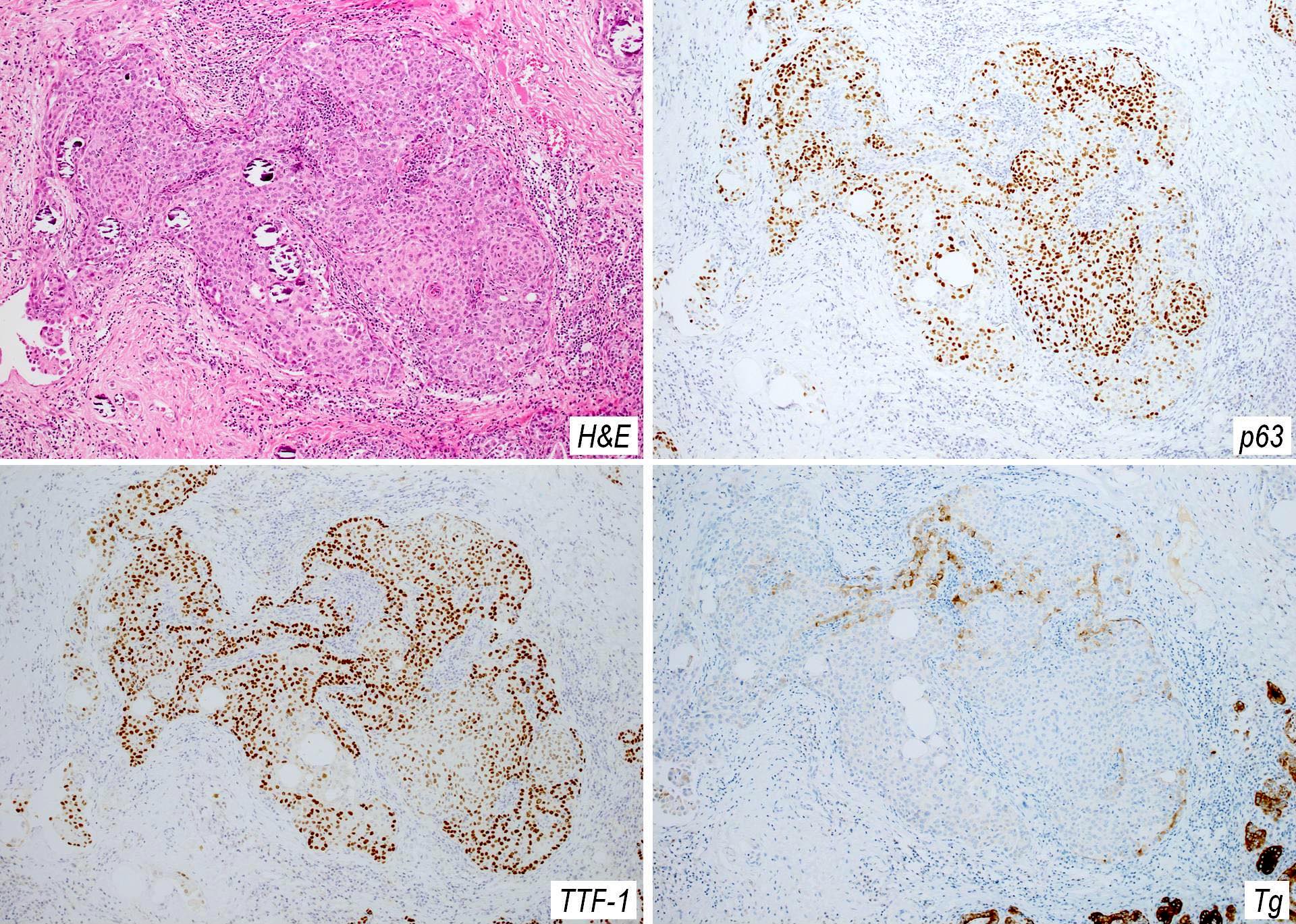
- Foci of squamous metaplasia in solid patterned areas (squamous morules) (Endocr Pathol 2005;16:331, Crit Rev Oncol Hematol 2015;94:64)
- Diagnostic nuclear features of PTC can be identified in nonsquamous areas
- Extrathyroidal extension is common (Endocr Pathol 2005;16:331, Crit Rev Oncol Hematol 2015;94:64)
- Lymph node metastases in ~ 80%, often affecting several levels of lymph nodes bilaterally (Endocr Pathol 2005;16:331)
Microscopic (histologic) images
Contributed by Livia Florianova, M.D., M.Sc. and Marc Pusztaszeri, M.D.
Contributed by Andrey Bychkov, M.D., Ph.D.
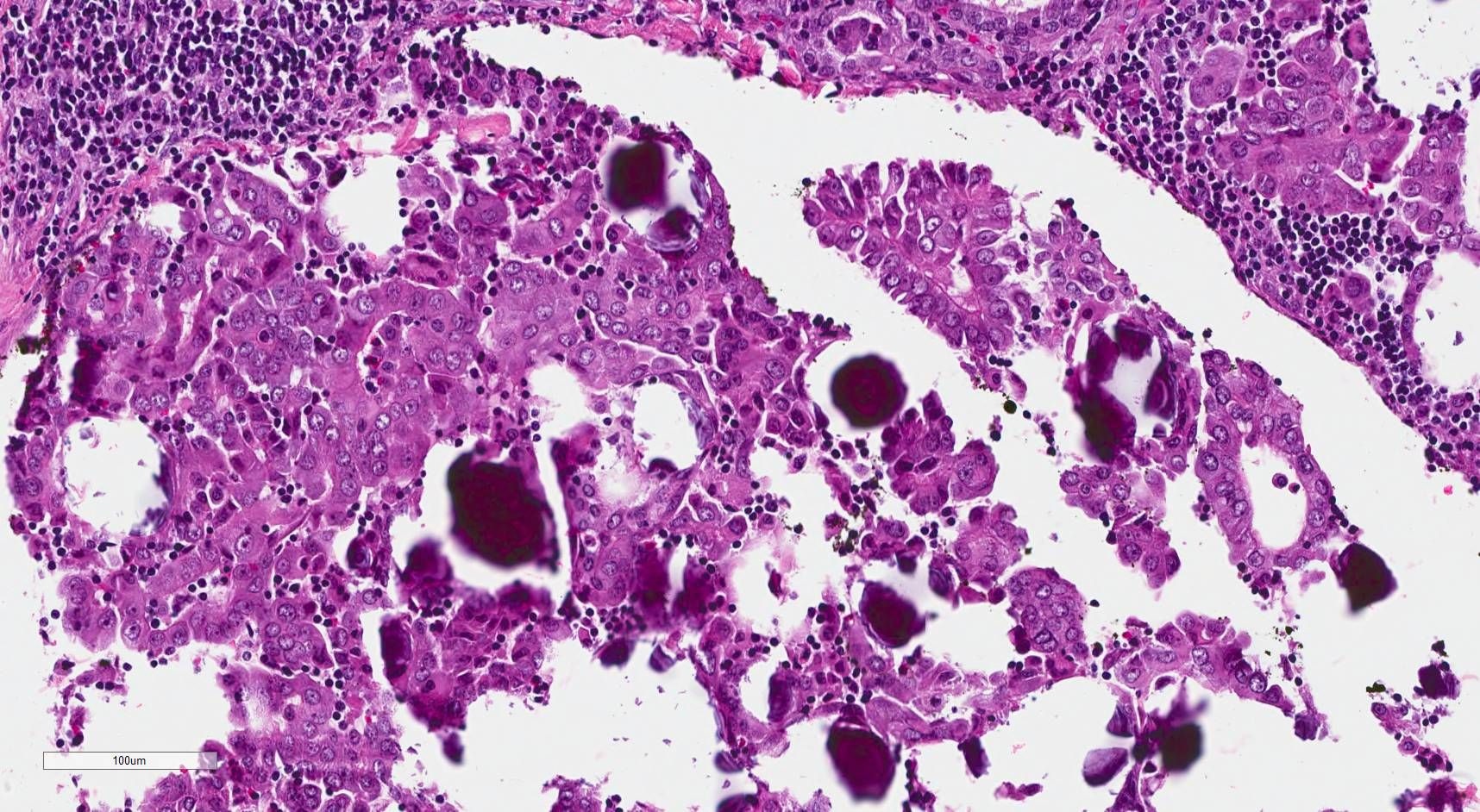
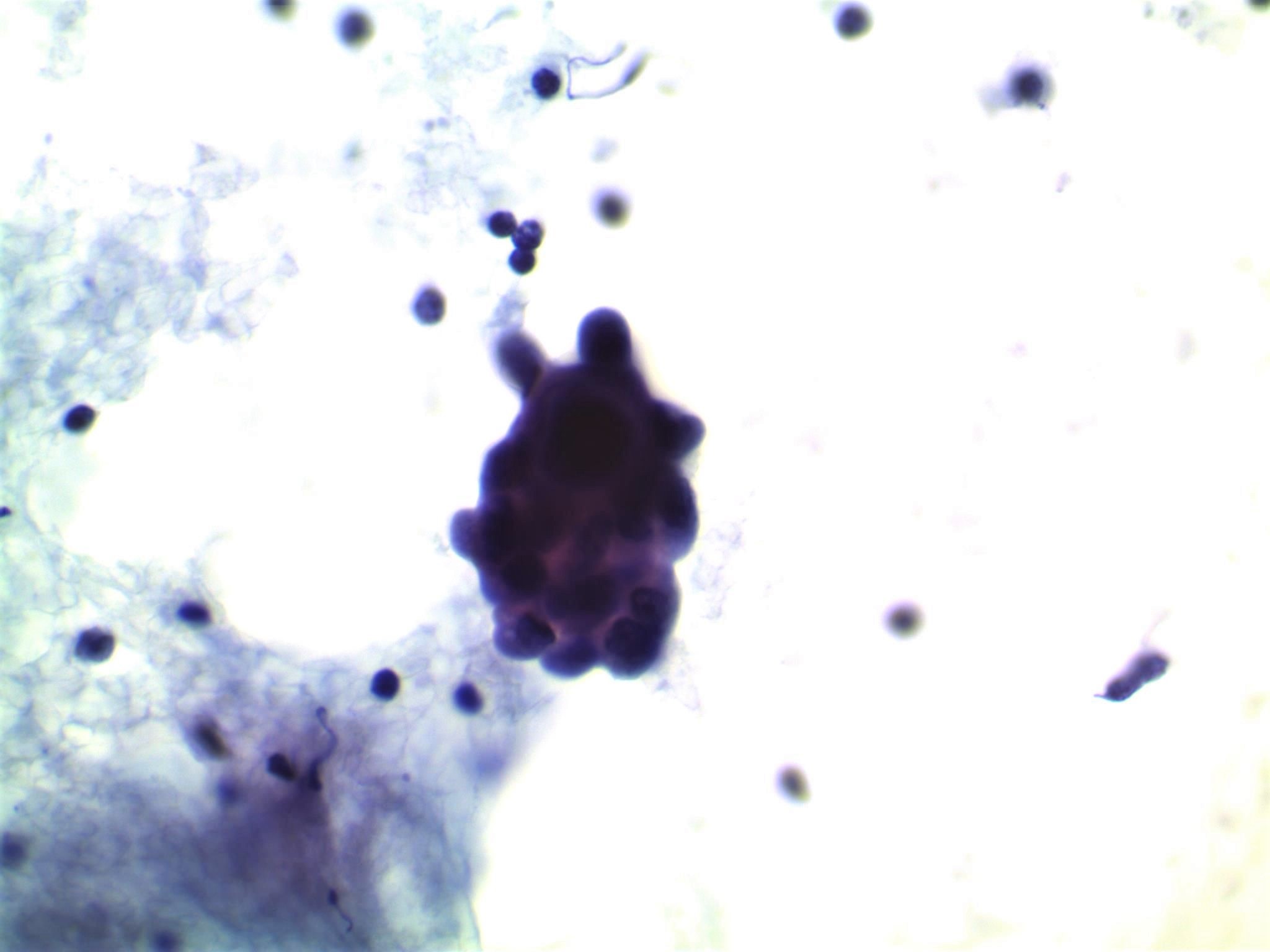
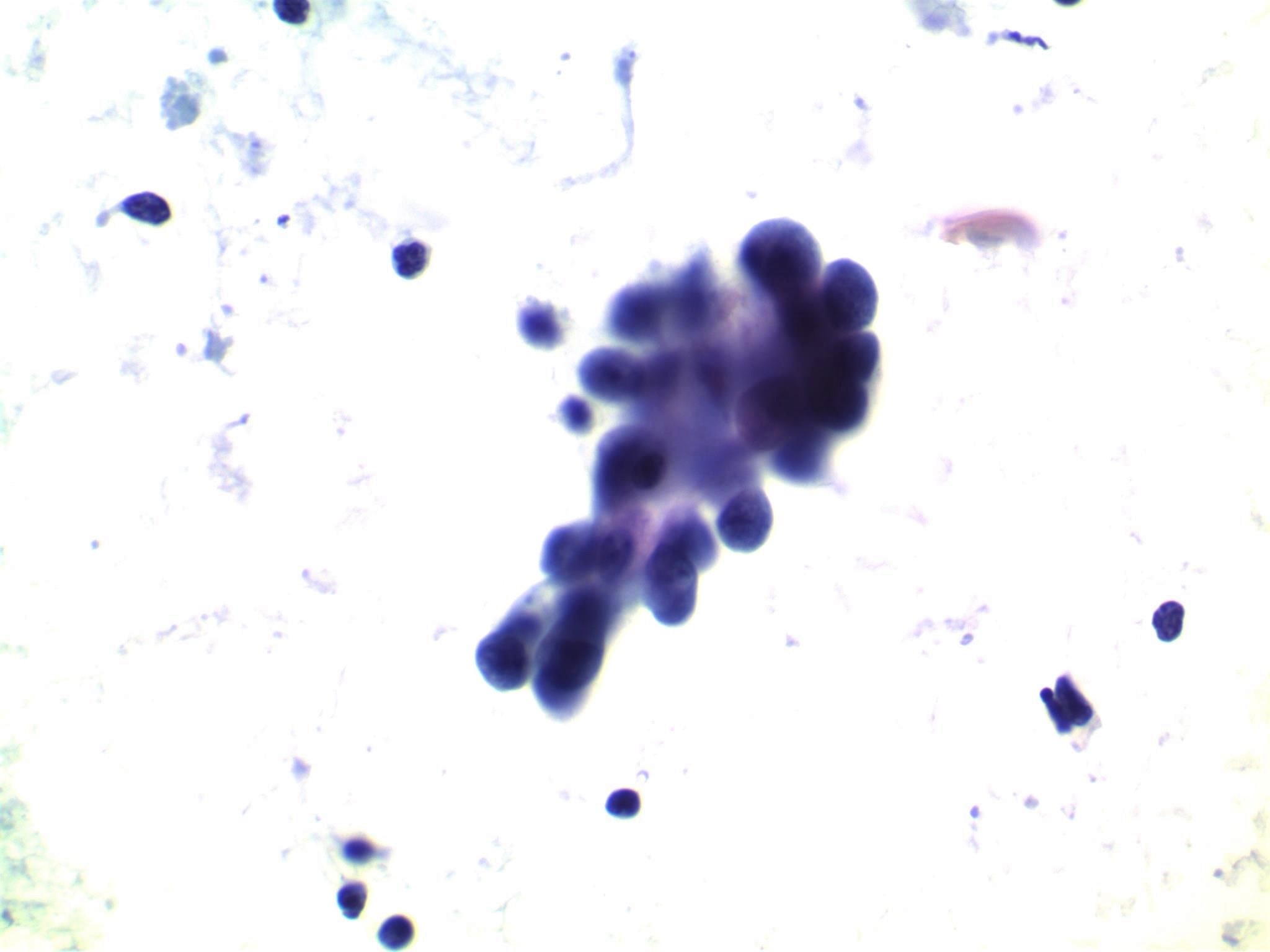
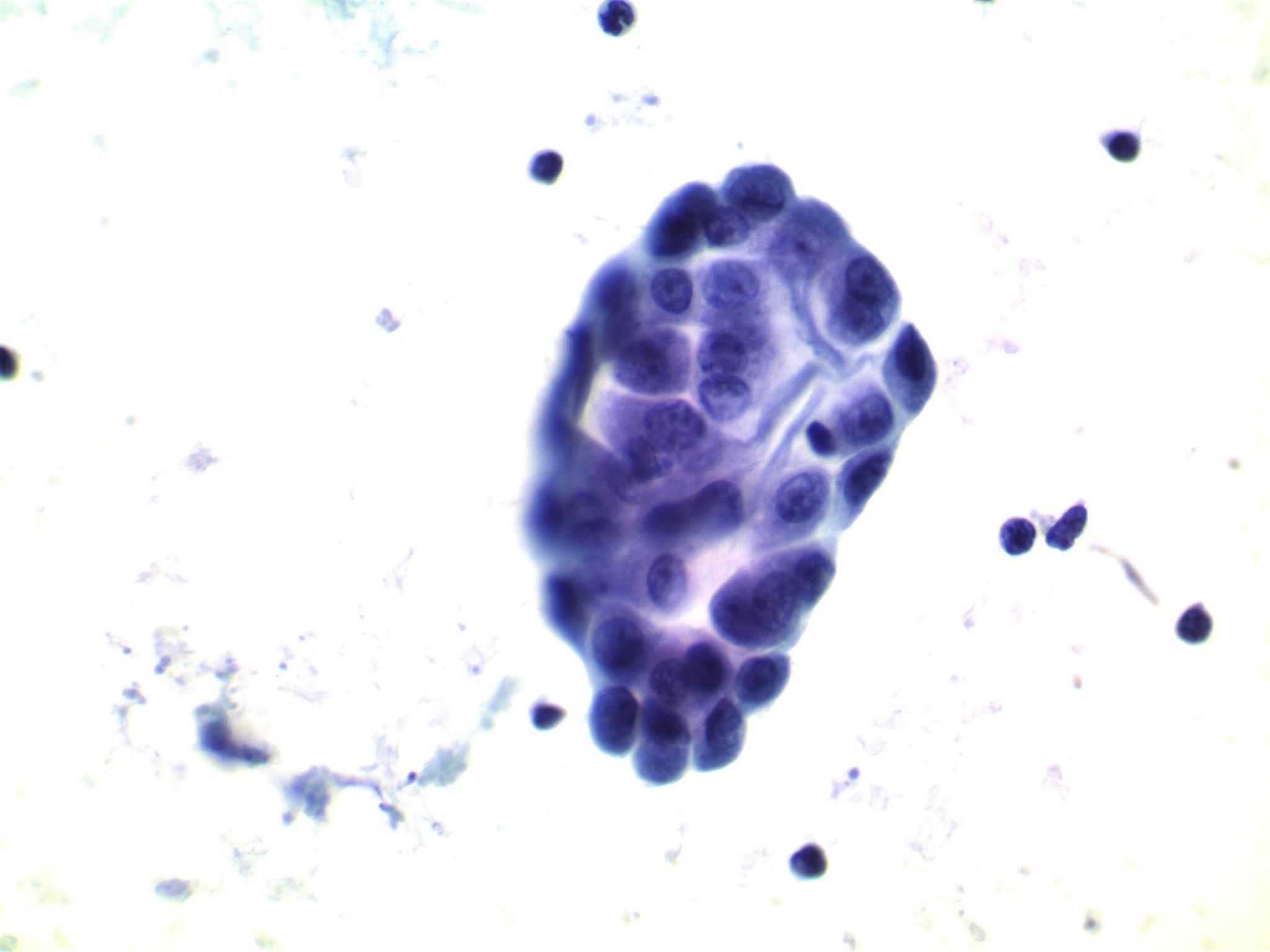
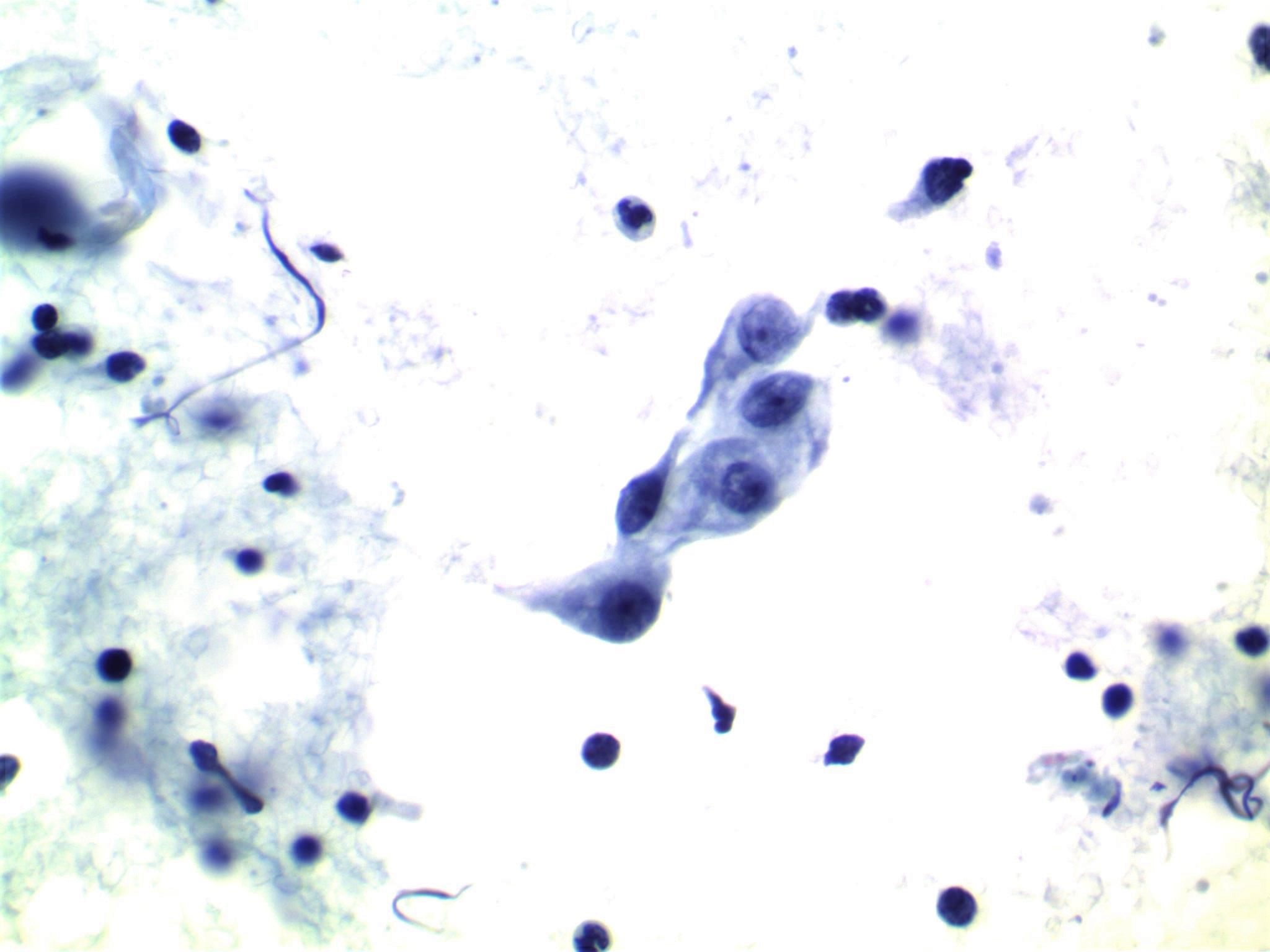
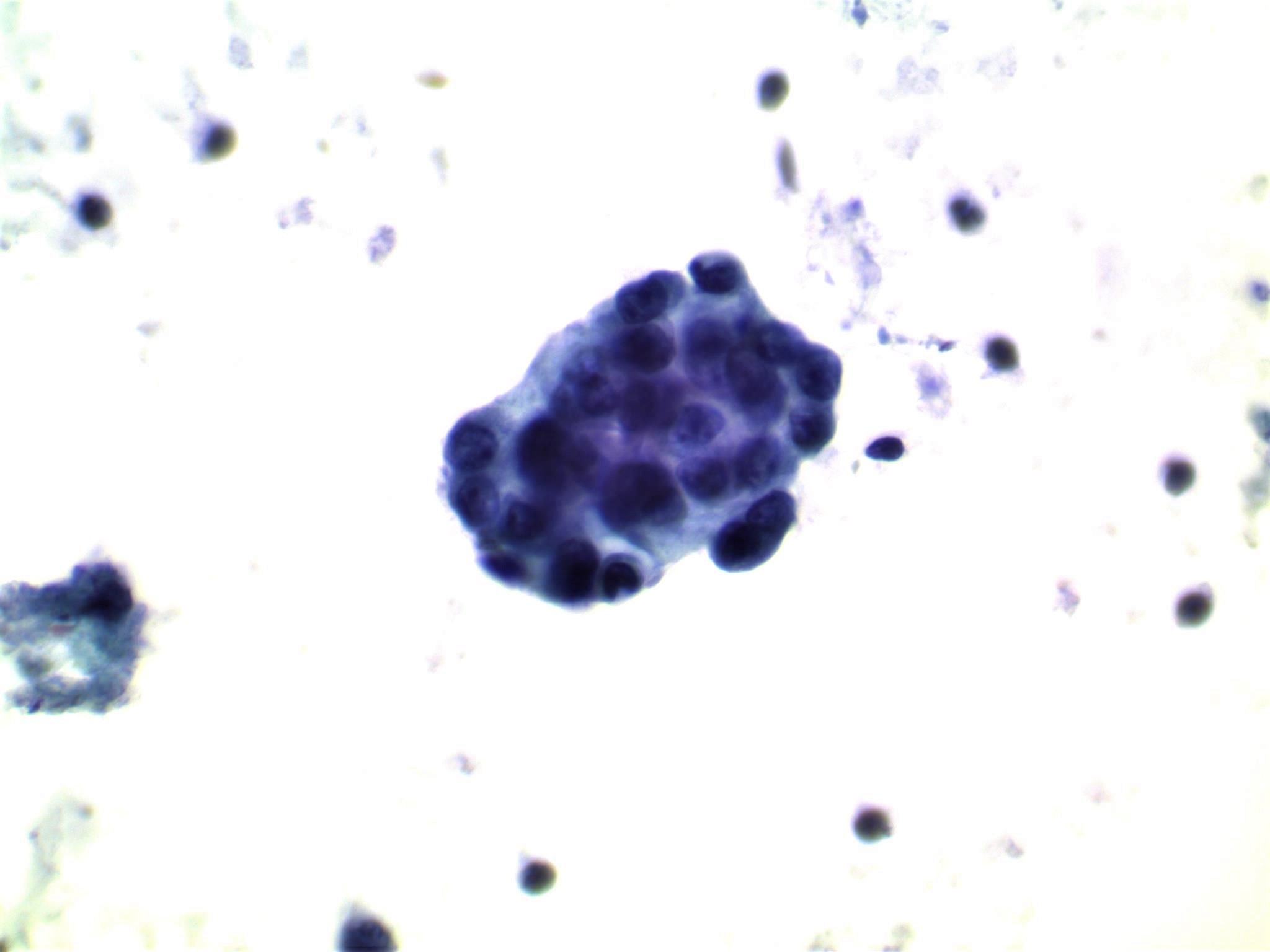
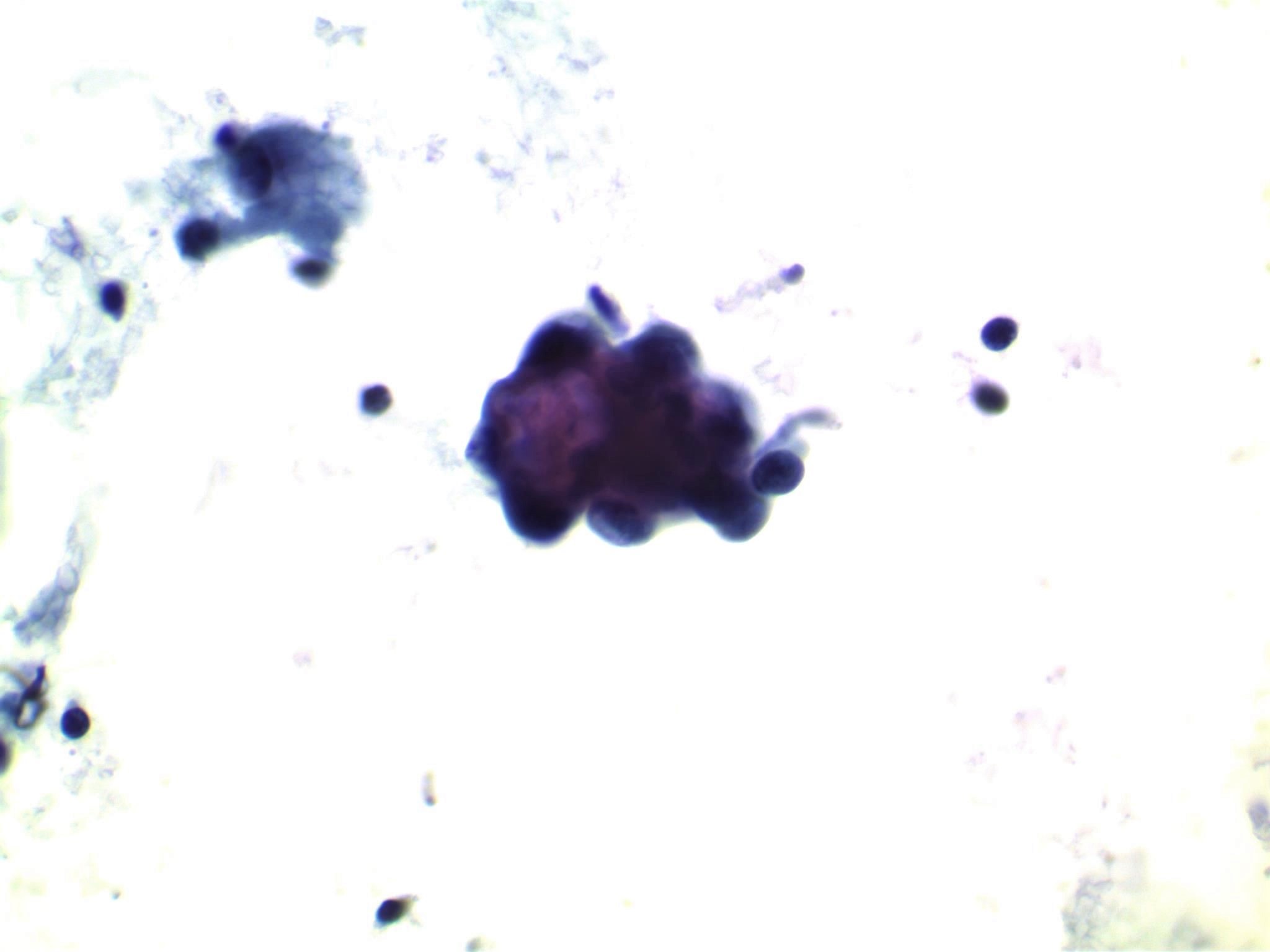
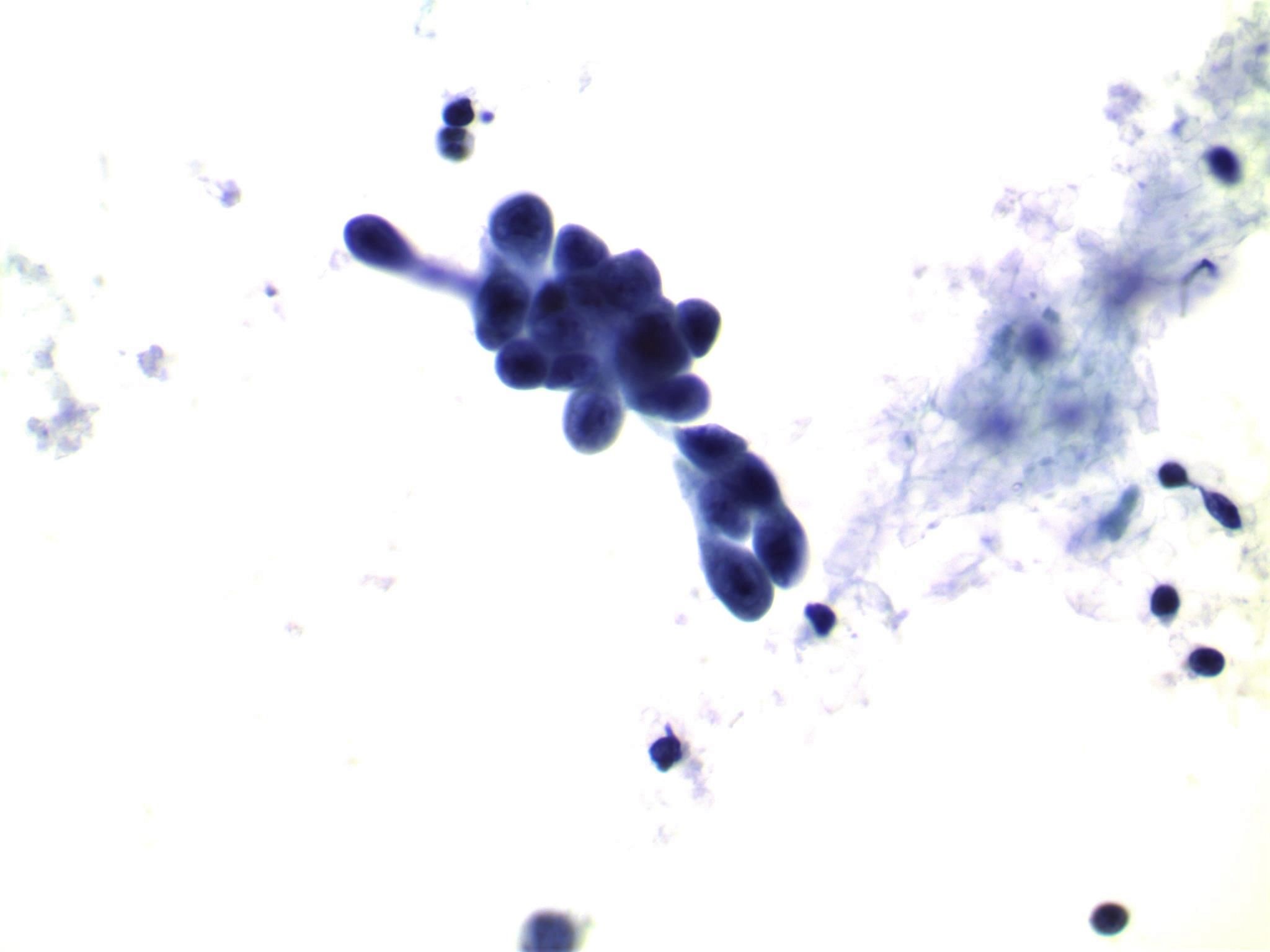
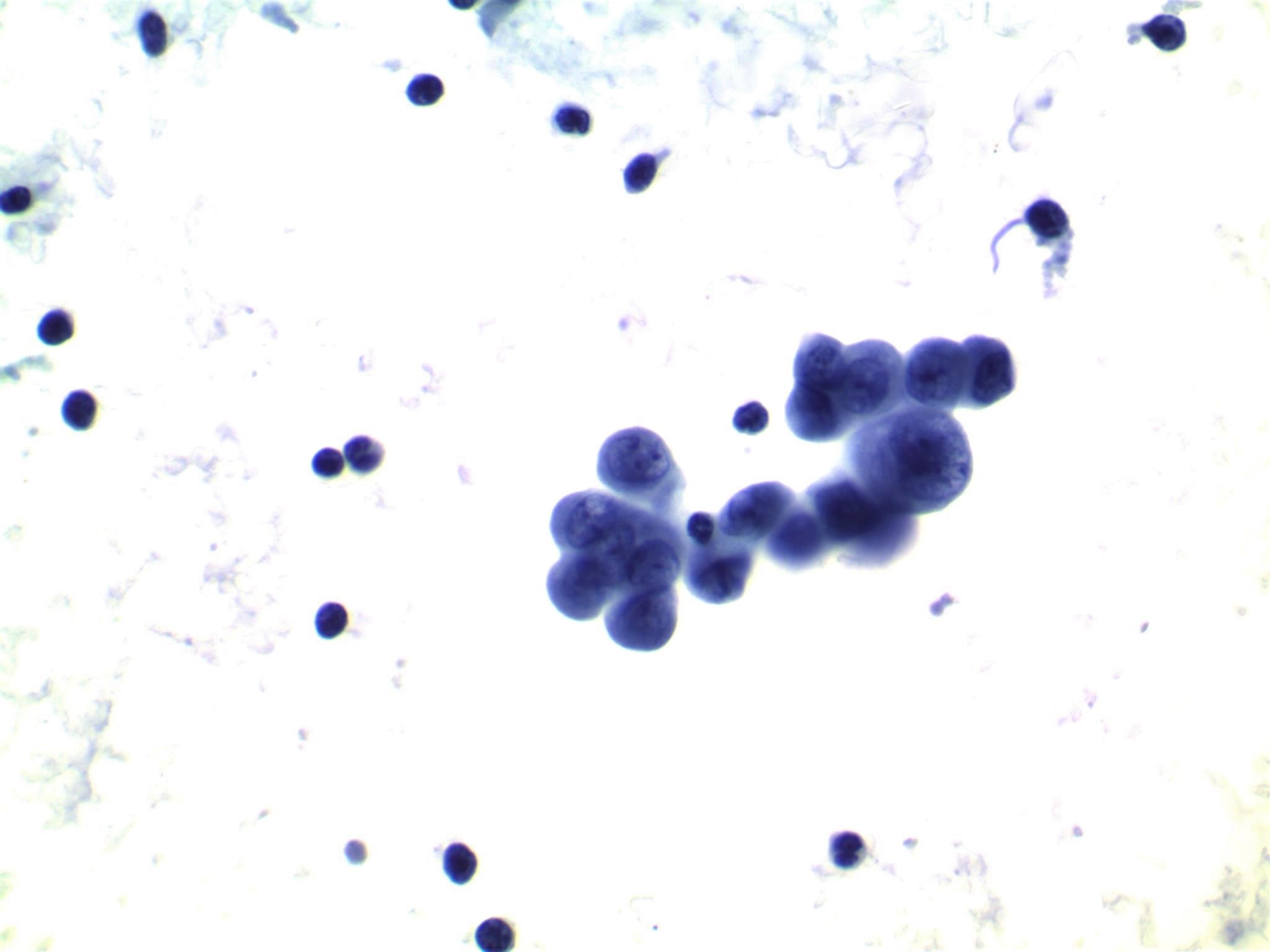
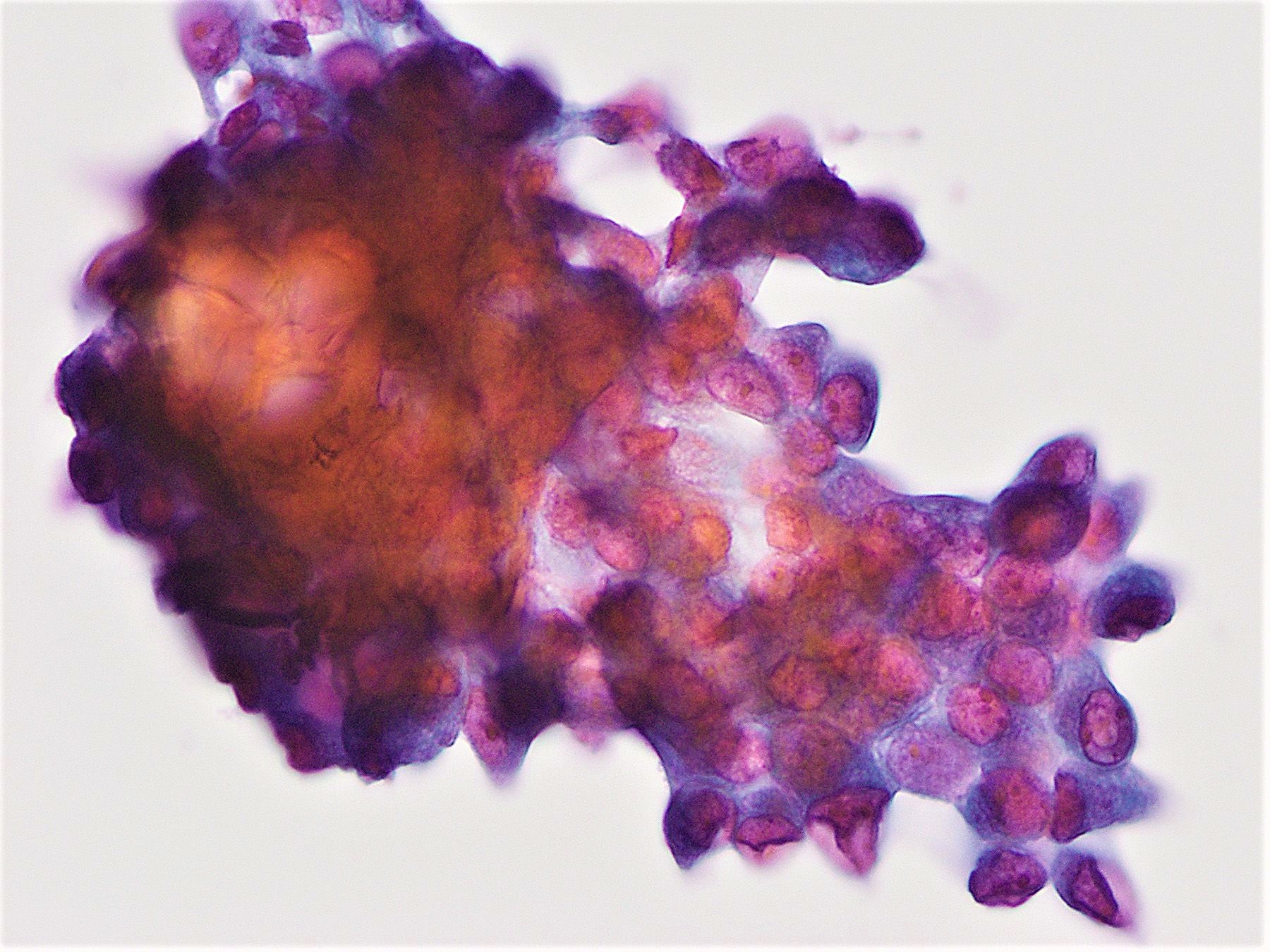
Cytology description
- Moderately to highly cellular with scant or absent colloid
- Neoplastic cells are often arranged in 3 dimensional ball-like clusters from which protruding hobnail cells can be frequently observed (Cytopathology 2014;25:199)
- In contrast to conventional PTC, there is less chromatin pallor (slightly coarser chromatin) and fewer nuclear grooves and nuclear pseudoinclusions (Cytopathology 2014;25:199)
- Squamous metaplastic changes: flat, polygonal shaped cells with sharply demarcated cell membranes, fitting together like jigsaw pieces (without overt keratinization) (Cytopathology 2014;25:199)
- Numerous lymphocytes and psammoma bodies present in the background (Cytopathology 2014;25:199)
- Cytological differential diagnosis includes chronic lymphocytic thyroiditis, PTC Warthin-like variant and lymphoma
Cytology images
Contributed by Livia Florianova, M.D., M.Sc., Marc Pusztaszeri, M.D. and Manon Auger, M.D.C.M.
Positive stains
- CK19, thyroglobulin and TTF1 expression in both papillary carcinoma and squamous metaplasia cells (Endocr Pathol 2005;16:331)
- p63 reactivity in squamous metaplastic cells (Crit Rev Oncol Hematol 2015;94:64)
- May be Napsin A positive and PAX8 negative (potential pitfalls) (Auris Nasus Larynx 2019 [Epub ahead of print], Endocr Pathol 2020;31:39)
Negative stains
Molecular / cytogenetics description
- RET / PTC rearrangements are common (~ 60%), including RET / PTC1 (28 - 46%) and RET / PTC3 (14 - 16%) (Eur J Endocrinol 2017;176:433, Mod Pathol 2007;20:779, Histopathology 2016;69:45)
- RET / PTC3 rearrangement is associated with advanced stage at diagnosis and poor clinical outcome (Histopathology 2016;69:45)
- Overall, BRAF mutations are uncommon (0 - 24%) (Mod Pathol 2007;20:779, Am J Surg Pathol 2012;36:844, Histopathology 2016;69:45)
- In contrast, the prevalence of BRAF mutation is higher in Korea (50 - 61%) (Pathology 2006;38:201, Thyroid 2013;23:1423)
- RAS mutations have not been found (Br J Cancer 2000;82:315)
- ALK translocations may be more common in DSV PTC (13%) compared with other PTC variants (2%) (Am J Surg Pathol 2015;39:652, Eur J Endocrinol 2017;176:433)
Sample pathology report
- Thyroid, left lobe, fine needle aspiration:
- Satisfactory for evaluation
- Malignant (Bethesda Diagnostic Category VI)
- Papillary thyroid carcinoma, favor diffuse sclerosing variant
- Thyroid, total thyroidectomy:
- Papillary thyroid carcinoma, diffuse sclerosing variant (see synoptic report)
Differential diagnosis
- Chronic lymphocytic thyroiditis (with squamous metaplasia)
- No psammoma bodies
- Reactive atypia; no well developed nuclear features of PTC
- No solid clusters
- No lymphovascular invasion or metastasis, unless it is associated with PTC
- PTC Warthin-like variant
- Usually one tumor mass instead of multiple tumor foci diffusely involving one or both thyroid lobes
- Oncocytic tumor cells
- Usually no solid clusters, psammoma bodies or squamous metaplasia
Board review style question #1
Which of the following statements is true about the diffuse sclerosing variant of papillary thyroid carcinoma (PTC)?
- Extrathyroidal extension and lymph node metastasis are usually not detected
- Not considered an aggressive type of papillary thyroid carcinoma
- Patients are usually older than those with classical papillary thyroid carcinoma
- Presents as a solitary thyroid nodule in which calcifications are infrequent
- Shows a high 10 year disease specific survival
Board review style answer #1
E. Shows a high 10 year disease specific survival. Despite being an aggressive variant of PTC with some adverse prognostic features, mortality rates are similar to those of classical PTC with 93% disease specific survival at 10 years.
Comment Here
Reference: Papillary thyroid carcinoma, diffuse sclerosing variant
Comment Here
Reference: Papillary thyroid carcinoma, diffuse sclerosing variant
Board review style question #2
Board review style answer #2
E. RET / PTC rearrangement. RET / PTC rearrangements are common (~ 60%), including RET / PTC1 (28 - 46%) and RET / PTC3 (14 - 16%). Overall, BRAF V600E is uncommon (0 - 24%), except in Korea (50 - 61%). ALK translocation is also uncommon (13%). RAS mutation and ETV6 / NTRK rearrangement have not been reported in diffuse sclerosing variant of papillary thyroid carcinoma.
Comment Here
Reference: Papillary thyroid carcinoma, diffuse sclerosing variant
Comment Here
Reference: Papillary thyroid carcinoma, diffuse sclerosing variant