Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Pusztaszeri M. Differentiated high grade thyroid carcinoma / high grade differentiated thyroid carcinoma (HGDTC). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroiddifferentiatedHGcarcinomas.html. Accessed April 1st, 2025.
Definition / general
- Malignant follicular cell derived thyroid neoplasm that retains the distinctive architectural and cytomorphological features of differentiated thyroid carcinoma (DTC) (including papillary thyroid carcinoma [PTC], follicular thyroid carcinoma [FTC] and oncocytic thyroid carcinoma [OTC]) except for the presence of ≥ 5 mitoses/2 mm2 or tumor necrosis
- Biologic features and prognoses are
- Intermediate between the favorable outcome of DTC and the very poor outcome of anaplastic thyroid carcinoma (ATC)
- Similar to poorly differentiated thyroid carcinoma (PDTC) (classified as per Turin criteria)
Essential features
- Differentiated high grade thyroid carcinoma (DHGTC) is a new diagnostic entity most recently defined in the 2022 WHO Classification of Endocrine and Neuroendocrine Tumors (Endocr Pathol 2022;33:27)
- DHGTC follows the definition of poorly differentiated thyroid carcinoma (PDTC) proposed by the Memorial Sloan Kettering Cancer Center (MSKCC) in 2006, which differs from the diagnostic criteria of PDTC proposed by the Turin consensus and restricts PDTC to mitotically active or necrotic tumor with solid / trabecular / insular growth pattern that lacks nuclear features of papillary thyroid carcinoma (Cancer 2006;106:1286)
- Diagnostic concept of DHGTC captures a subset of aggressive thyroid carcinoma that was previously classified as regular papillary thyroid carcinoma, follicular thyroid carcinoma or oncocytic thyroid carcinoma that otherwise do not meet the Turin criteria for PDTC and fall short of meeting criteria for anaplastic thyroid carcinoma
Terminology
- High grade differentiated thyroid carcinoma, papillary thyroid carcinoma (PTC) with high grade features, high grade PTC, high grade follicular carcinoma, follicular carcinoma with high grade features, PDTC on the basis of MSKCC criteria
ICD coding
- ICD-10: C73 - malignant neoplasm of thyroid gland
Epidemiology
- Uncommon and underrecognized tumor representing < 3% of all thyroid cancers (Hum Pathol 2024;144:53, Endocr Pathol 2023;34:34)
- However, incidence may vary around the world, perhaps due to geographic or environmental influences
- Most common in the sixth to eighth decades of life (mean age: 63.3; range: 3 - 90) (Hum Pathol 2024;144:53)
- Typically occurs a decade later than differentiated thyroid carcinoma
- Slightly more common in women; F:M = 1.1 - 2.1:1 (Hum Pathol 2024;144:53)
Sites
- Usually thyroid gland
- May rarely develop from ectopic thyroid tissue (e.g., mediastinum, thyroglossal duct cysts, ovary, etc.)
- Progression to DHGTC may occur in lymph node metastases or at other metastatic sites
Pathophysiology
- Arises following synchronous or metachronous progression of differentiated thyroid carcinoma (mainly papillary thyroid carcinoma), of which it retains the driving molecular signatures (mainly BRAF V600E mutation) and typically gains additional mutations, such as TERT promoter, TP53 and PI3K (Hum Pathol 2024;144:53, Endocr Pathol 2023;34:34, Adv Anat Pathol 2023;30:3)
Etiology
- Not well characterized
Diagrams / tables
Clinical features
- Typically presents as a large solitary mass that has grown over several months
- May develop as rapidly growing masses in the background of multinodular goiter
- At presentation, often (but not always) associated with locally advanced disease, including gross extrathyroidal extension
- Distant metastasis identified in up to 25% of patients at presentation but with time, there is increased incidence (40 - 70%) of distant metastasis, the most common sites being lung, bone and brain (Histopathology 2022;80:322, Cureus 2022;14:e32177)
- Accounts for half of radioactive iodine (RAI) refractory FDG avid thyroid carcinoma cases
Diagnosis
- Workup is similar to any thyroid mass / nodule
- Ultrasound with fine needle aspiration cytology
- CT scan may be useful to evaluate extrathyroidal extension and lymph node metastases
- Because of the lack of criteria with high specificity and sensitivity, the preoperative diagnosis of DHGTC is hardly ever made or suggested on cytology
- Variable cytologic appearance and categorization according to the Bethesda system are expected depending on the underlying well differentiated thyroid carcinoma (papillary thyroid carcinoma, follicular thyroid carcinoma, oncocytic follicular thyroid carcinoma [OFTC]); most cases are classified as Bethesda VI or Bethesda V, since most cases are high grade papillary thyroid carcinoma
- Molecular testing of cytologic aspirates may assist in preoperative diagnosis
- Definitive diagnosis is made via histological examination of a resection specimen, supplemented by immunohistochemistry
- References: Cureus 2022;14:e32177, Hum Pathol 2024;144:53
Laboratory
- Patients are euthyroid
Radiology description
- Ultrasonography
- Usually described as solid, heterogeneous and hypoechoic with irregular and indistinct borders
- Most common Thyroid Imaging Reporting and Data System (TIRADS) scores are 4 and 5 (Hum Pathol 2024;144:53)
- 18F fluorodeoxyglucose positron tomography (PET / CT 18F FDG) may show an hypermetabolic mass (Diagnostics (Basel) 2020;11:4, Indian J Nucl Med 2011;26:196)
Prognostic factors
- Established adverse prognostic factors include larger tumor size, age over 45, extrathyroidal extension and distant metastasis
- On multivariate analysis, independent adverse prognostic factors for disease specific survival may be older age, extensive necrosis and lack of encapsulation (Histopathology 2022;80:322)
- Independent adverse factors for distant metastasis free survival include older age, male sex and vascular invasion (Histopathology 2022;80:322)
- Independent adverse factors for locoregional recurrence free survival are older age, extensive necrosis, high N stage and positive margins (Histopathology 2022;80:322)
- Disease specific survival of DHGTC may be worse compared with those with PDTC (Histopathology 2022;80:322)
- In a recent study of cases meeting PDTC or DHGTC criteria, long term survival was poor, with 3 year, 5 year, 10 year and 20 year overall survival rates of 88%, 75%, 54% and 28% respectively and disease specific survival rates of 89%, 76%, 60% and 35%, respectively (Histopathology 2022;80:322)
- TP53, PTEN and TERT promoter mutations are associated with adverse prognosis in DHGTC (Histopathology 2022;80:322)
- Noninvasive DHGTC
- Rare but recognized occurrence
- Characterized by a tumor fulfilling all criteria for DHGTC but without evidence of invasive growth (after evaluation of the whole capsule / tumor interface)
- Usually has indolent biologic behavior, although some metastatic cases and fatal cases have been reported (Histopathology 2022;80:322, Mod Pathol 2000;13:861, Int J Surg Pathol 2014;22:749)
Case reports
- 43 year old woman with DHGTC and NRAS mutation, presenting with metastatic follicular component to the bone and papillary component to lymph nodes (Cureus 2022;14:e32177)
- 62 year old man with distant metastases to the left sixth rib, iliac crest and vertebrae ( J Clin Images Med Case Rep 2023;4:2730)
Treatment
- Standardized management strategies are not well defined
- Standard clinical management includes total thyroidectomy with consideration of lateral neck dissection (in the setting of clinically or radiographically abnormal nodes) (Endocr Pathol 2023;34:34)
- Adjuvant therapy and external beam radiation can be considered for advanced or refractory disease on a case by case basis (Endocr Pathol 2023;34:34)
- Targeted therapeutics should be considered since many cases of DHGTC (at least 50%) have targetable driver mutations, including BRAF V600E mutation or RET or NTRK rearrangements (Endocr Pathol 2023;34:34)
- Tyrosine kinase inhibitors lenvatinib and sorafenib have been used in patients with radioiodine resistant / refractory carcinoma; dabrafenib and trametinib in BRAF V600E mutant tumors; selpercatinib and pralsetinib in RET rearranged tumors; and larotrectinib and entrectinib in NTRK rearranged tumors
- Postoperative radioactive iodine (RAI): DHGTC is enriched with RAI refractory FDG avid thyroid carcinoma (~50% of cases); therefore, management and surveillance with fluorodeoxyglucose positron emission tomography (FDG PET) is recommended by the American Thyroid Association (Endocr Pathol 2023;34:34)
- Similarly, as this lesion may produce less thyroglobulin given its relatively diminished maturation, serum thyroglobulin measurements may be an inaccurate method of surveilling these patients for disease recurrence (Histopathology 2022;80:322, Endocr Pathol 2023;34:34)
Gross description
- Typically, overtly infiltrative with extrathyroidal extension but may rarely appear partially or even totally encapsulated (Hum Pathol 2024;144:53, Endocr Pathol 2023;34:34)
- Varies in size between 2 and 13 cm but most are large tumors > 4 cm (average: 5 cm) (Hum Pathol 2024;144:53, Endocr Pathol 2023;34:34)
- Foci of hemorrhage and tumor necrosis may be seen macroscopically (Hum Pathol 2024;144:53, Endocr Pathol 2023;34:34)
- ~30 - 50% are associated with easily identifiable lymph node metastases
Frozen section description
- Usually not performed
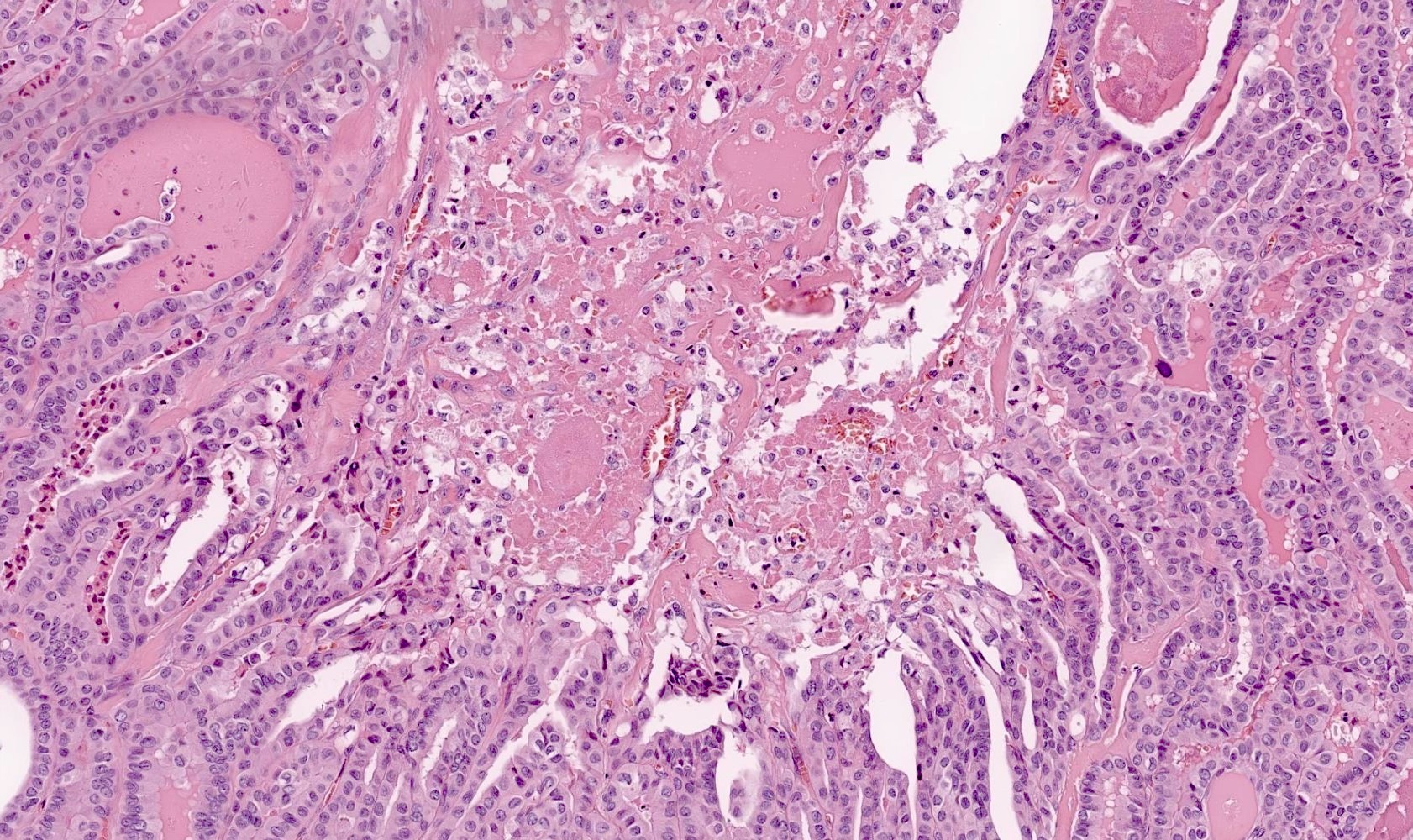
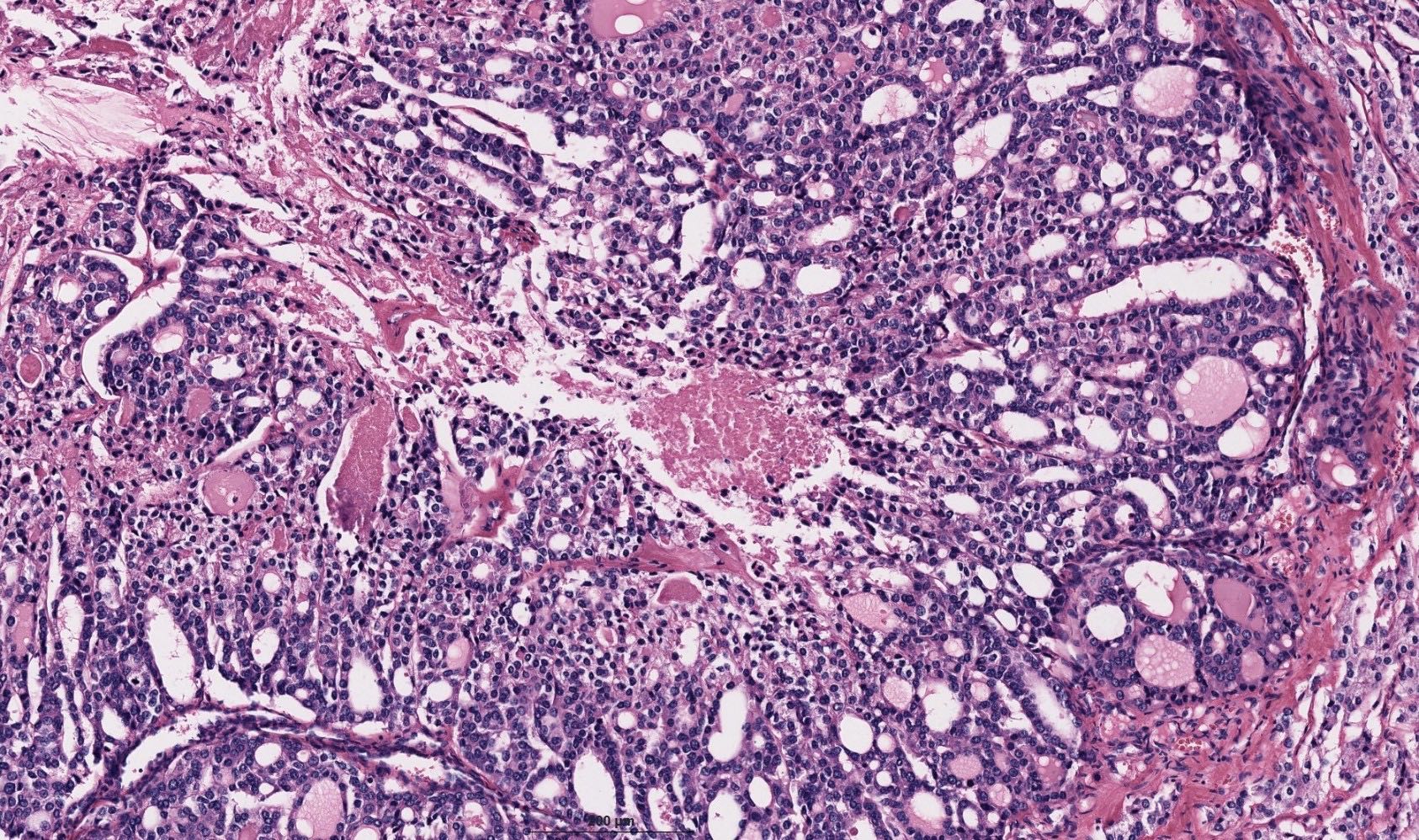
Microscopic (histologic) description
- Overall cytomorphology and growth patterns depend on the underlying differentiated thyroid carcinoma and should be subclassified according to the dominant subtype, as follows
- High grade papillary thyroid carcinoma (PTC)
- Most common histology of DHGTC (> 80%) (Histopathology 2022;80:322)
- Commonly associated with aggressive PTCs, including tall cell, columnar cell and hobnail subtypes
- Can also be seen in classical PTC and follicular variant of PTC (infiltrative or encapsulated)
- High grade PTC can show transition to PDTC (based on the Turin criteria) or to anaplastic thyroid carcinoma
- If the tumor shows dominant solid / trabecular / insular growth patterns but retains diagnostic nuclear features of PTC, the tumor is still classified as high grade PTC
- High grade follicular thyroid carcinoma (FTC) (< 10% of DHGTC)
- Usually widely invasive FTC or tumors with extensive angioinvasion (> 4 vessels)
- High grade FTC can show transition to PDTC (based on the Turin criteria) or to anaplastic thyroid carcinoma
- If the tumor shows dominant solid / trabecular / insular growth patterns, the tumor is better classified as PDTC
- High grade oncocytic thyroid carcinoma (OTC) (< 10% of DHGTC)
- Uncommon and restricted to OTC that shows follicular architecture
- OTC tends to have dominant solid, trabecular and insular growth patterns; in such cases, the tumor is better classified as PDTC
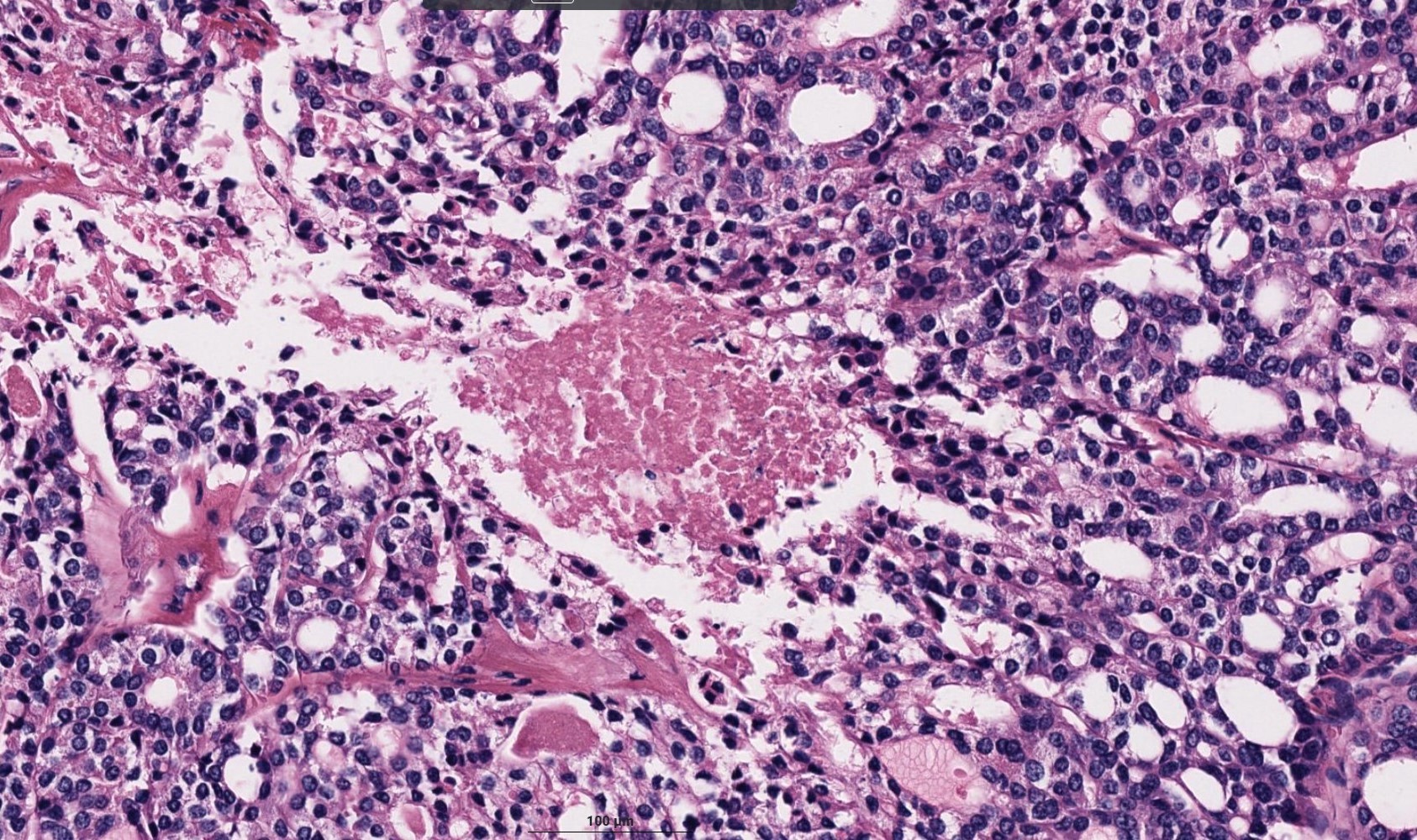
- Mitotic activity
- Increased mitotic activity (≥ 5 per 2 mm2) is one of the hallmark of DHGTC
- Atypical mitoses may be found
- Mitotic count to be performed in the hotspot with the highest mitotic activity
- If there are areas of increased mitotic activity but they fall short of ≥ 5 per 2 mm2, additional sampling is recommended
- Tumor necrosis
- Tumor necrosis is the other hallmark of DHGTC
- Represents coagulative type necrosis characterized by karyorrhectic nuclear debris or ghost contours of dead tumor cells
- May be focal or extensive, sometimes comedo-like (Histopathology 2022;80:322)
- Must be distinguished from infarct type necrosis secondary to FNAB, which is often accompanied by fibrosis, granulation tissue, histiocytes, hemosiderin, calcification or cholesterol clefts or regressive changes in oncocytic tumors (Hum Pathol 2024;144:53, Endocr Pathol 2023;34:34)
Microscopic (histologic) images
Virtual slides
Cytology description
- Due to its rarity, reports on the cytological features of DHGTC are limited
- Because of the lack of criteria with high specificity and sensitivity, the preoperative diagnosis of DHGTC is hardly ever made or suggested on cytology
- Variable cytologic appearance and categorization according to the Bethesda system are expected depending on the underlying well differentiated thyroid carcinoma (papillary thyroid carcinoma, follicular thyroid carcinoma, oncocytic thyroid carcinoma)
- Since most cases are high grade papillary thyroid carcinoma, most cases were classified as Bethesda VI or Bethesda V (Hum Pathol 2024;144:53)
- However, ~30 - 35% are classified as Bethesda IV (Hum Pathol 2024;144:53)
- Necrosis and mitotic figures may or may not be identified
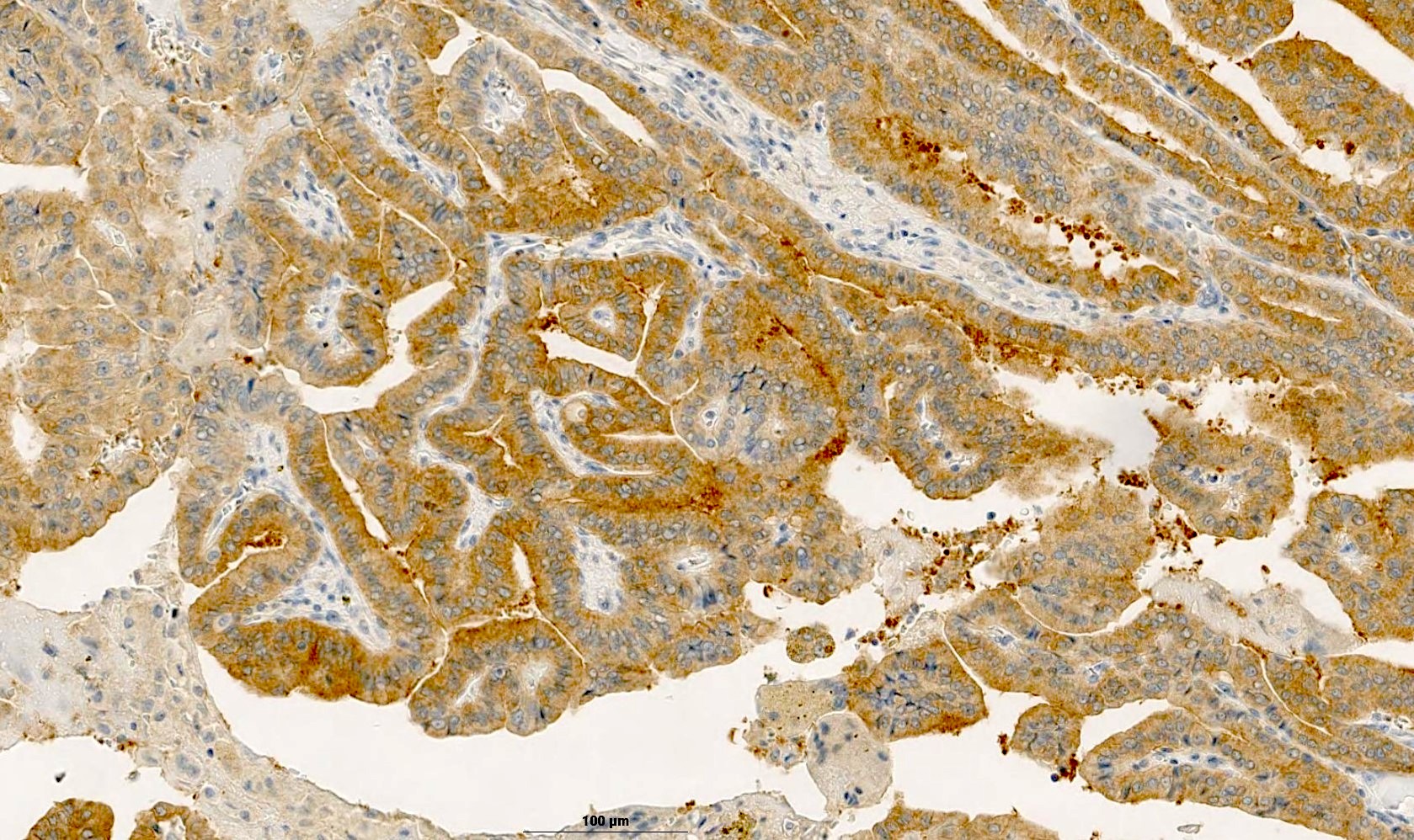
Positive stains
- Thyroglobulin (tends to be weak and focal with dot-like reactivity), TTF1, PAX8, CK7
- BRAF V600E (VE1): positive in up to 80 - 90% of cases (high grade papillary thyroid carcinoma)
- Ki67: ranges from 1 to 30% (Hum Pathol 2024;144:53)
Negative stains
Molecular / cytogenetics description
- Molecularly heterogeneous group of tumors
- Molecular profile of DHGTC follows the BRAF::RAS mutation driver dichotomy of differentiated thyroid carcinoma
- In contrast to PDTC, DHGTC is enriched with BRAF V600E mutations (81%), given the high frequency of high grade papillary thyroid carcinoma in this group (Endocr Pathol 2023;34:34, Histopathology 2022;80:322)
- ~25% of high grade papillary thyroid carcinoma cases harbor oncogenic fusions, including ETV6::NTRK3, AGK::BRAF, CCDC30::ROS1 (Endocr Pathol 2023;34:34, Histopathology 2022;80:322)
- RAS mutations, in particular NRAS mutations, are the second most common mutations in DHGTC and correlate with a high grade follicular thyroid carcinoma phenotype (Endocr Pathol 2023;34:34, Histopathology 2022;80:322)
- DHGTC has an increasing frequency of additional molecular alterations, including TERT promoter mutations (39 - 44%), TP53 (8 - 43%), E1F1AX (6 - 11%) (Endocr Pathol 2023;34:34. Histopathology 2022;80:322)
- PIK3CA (2 - 6%) and PTEN mutations (3%) can coexist with RAS mutation and correlate with a high grade follicular thyroid carcinoma phenotype (Endocr Pathol 2023;34:34, Histopathology 2022;80:322)
Molecular / cytogenetics images
- See Diagrams
Videos
Special types of thyroid cancer with Dr. Virginia LiVolsi
Poorly differentiated carcinoma of the thyroid with Dr. Margaret Brandwein
What is new in the WHO 2022 in thyroid pathology
Sample pathology report
- Thyroid, total thyroidectomy:
- Differentiated high grade thyroid carcinoma, papillary subtype, 5.5 cm in the left lobe (see synoptic report)
- Thyroid, left hemithyroidectomy:
- Differentiated high grade thyroid carcinoma, follicular subtype, 5 cm (see synoptic report)
- Thyroid, right hemithyroidectomy:
- Differentiated high grade thyroid carcinoma, oncocytic subtype, 6 cm (see synoptic report)
Differential diagnosis
- Classic papillary thyroid carcinoma (PTC) and PTC subtypes:
- No high grade features (i.e., mitotic activity [≥ 5 per 2 mm2]) or presence of tumor necrosis
- Follicular thyroid carcinoma:
- No high grade features (i.e., mitotic activity [≥ 5 per 2 mm2]) or presence of tumor necrosis
- Poorly differentiated thyroid (insular) carcinoma:
- Shares increased mitotic activity (≥ 5 per 2 mm2) or presence of tumor necrosis
- Solid / trabecular / insular growth patterns
- No nuclear features of PTC but may have convoluted nuclei (Am J Surg Pathol 2007;31:1256)
- Anaplastic thyroid carcinoma (ATC):
- Small percentage of DHGTC cases may progress to ATC at primary site, recurrence or metastasis
- ATC shows loss of follicular cell differentiation by histology and immunohistochemistry, such as loss of thyroglobulin and TTF1 expression
- Medullary thyroid carcinoma:
- Absence of colloid
- No nuclear features of PTC; salt and pepper chromatin
- Immunoreactivity for calcitonin, CEA, synaptophysin, chromogranin and INSM1
- Absence of immunoreactivity for thyroglobulin and PAX8
- Parathyroid carcinoma:
- Clinicoradiological context
- Immunoreactivity for PTH, GATA3, synaptophysin, chromogranin and INSM1
- Absence of immunoreactivity for thyroglobulin, TTF1 and PAX8
- Metastases to the thyroid gland:
- Clinicoradiological context
- Absence of immunoreactivity for thyroglobulin
- Absence of immunoreactivity for TTF1 (except lung) and PAX8 (except renal and upper Müllerian origin tumors)
- NUT carcinoma:
- Positive for NUT by immunohistochemistry or for NUTM1 fusion
- Can be positive for TTF1 and PAX8 in about 33% to > 50% of cases (Am J Surg Pathol 2022;46:1706, Histopathology 2024 May 6 [Epub ahead of print])
Additional references
Board review style question #1
What is the main difference between poorly differentiated thyroid carcinoma (PDTC) and differentiated high grade thyroid carcinoma (DHGTC)?
- Increased mitotic activity
- Presence of necrosis
- Presence of RAS mutations
- Presence of solid / trabecular / insular architecture and absence of nuclear features of papillary thyroid carcinoma
- Presence of TERT promoter mutations
Board review style answer #1
D. Presence of solid / trabecular / insular architecture and absence of nuclear features of papillary thyroid carcinoma (PTC). Although PDTC may have convoluted nuclei, nuclear features of PTC is a rule out criterion for the diagnosis of PDTC according to the Turin criteria. In contrast, any nuclear features (including follicular neoplasm-like or papillary-like) and any growth pattern are allowed in DHGTC. Answers A, B, C and E are incorrect because PDTC and DHGTC can both have tumor necrosis or increased mitotic activity, RAS mutations and TERT promoter mutations; however, in contrast to PDTC, DHGTC is enriched with BRAF V600E mutations (81%), given the high frequency of high grade PTC in this group.
Comment Here
Reference: Differentiated high grade thyroid carcinoma / high grade differentiated thyroid carcinoma (HGDTC)
Comment Here
Reference: Differentiated high grade thyroid carcinoma / high grade differentiated thyroid carcinoma (HGDTC)
Board review style question #2
Which of the following statements about differentiated high grade thyroid carcinoma (DHGTC) is correct?
- DHGTC is typically classified as Bethesda IV (follicular neoplasm) on cytology
- Most common subtype of DHGTC is high grade papillary carcinoma
- Most cases of DHGTC respond well to postoperative radioactive iodine (RAI)
- Prognosis of DHGTC is better than poorly differentiated thyroid carcinoma (PDTC)
Board review style answer #2
B. Most common subtype of DHGTC is high grade papillary carcinoma. The most common subtype of DHGTC is high grade papillary thyroid carcinoma (PTC) (> 80%). Oncocytic thyroid carcinoma (OTC) and follicular thyroid carcinoma (FTC) are both uncommon. Answer A is incorrect because most cases of DHGTC are high grade PTC (especially aggressive subtypes), so the majority of them can be classified as Bethesda V or VI on cytology. About 30 - 35% are classified as Bethesda IV, corresponding mainly to high grade FTC and high grade OTC. Necrosis and mitotic figures may or may not be present on cytology. Answer C is incorrect because DHGTC is enriched with RAI refractory FDG avid thyroid carcinoma (~50% of cases). Answer D is incorrect because DHGTC is enriched with RAI refractory FDG avid thyroid carcinoma (~50% of cases). Answer D is incorrect because the prognosis of DHGTC is similar or even worse than poorly differentiated thyroid carcinoma (PDTC).
Comment Here
Reference: Differentiated high grade thyroid carcinoma / high grade differentiated thyroid carcinoma (HGDTC)
Comment Here
Reference: Differentiated high grade thyroid carcinoma / high grade differentiated thyroid carcinoma (HGDTC)