Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Lai JK, Pusztaszeri M. Cribriform-morular thyroid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidcribriformmorular.html. Accessed April 1st, 2025.
Definition / general
- Uncommon thyroid carcinoma of uncertain histogenesis characterized by a complex architecture, primarily cribriform with squamoid morules and absent / scant colloid formation
- Cribriform-morular thyroid carcinoma (CMTC) was traditionally considered as a variant of papillary thyroid carcinoma (PTC); recent studies, however, showed that CMTC constitutes a clinicopathologically distinct category of thyroid carcinoma driven by Wnt / beta catenin pathway activation (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Relat Cancer 2017;24:R109)
Essential features
- Histologic features include areas of cribriform, papillary, trabecular and solid growth with squamoid morules and absent / scant colloid formation
- Classical nuclear features of papillary thyroid carcinoma (nuclear enlargement, elongation, overlapping, grooves, membrane irregularity, pseudoinclusions, clearing, chromatic marginalization) are often rare or absent (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168)
- Almost all cases have genetic alterations in the Wnt / beta catenin pathway with APC mutations being the most common and found in both the familial and sporadic setting (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Pathol 2022;33:27)
- Germline APC gene mutation in cases of familial adenomatous polyposis (FAP)
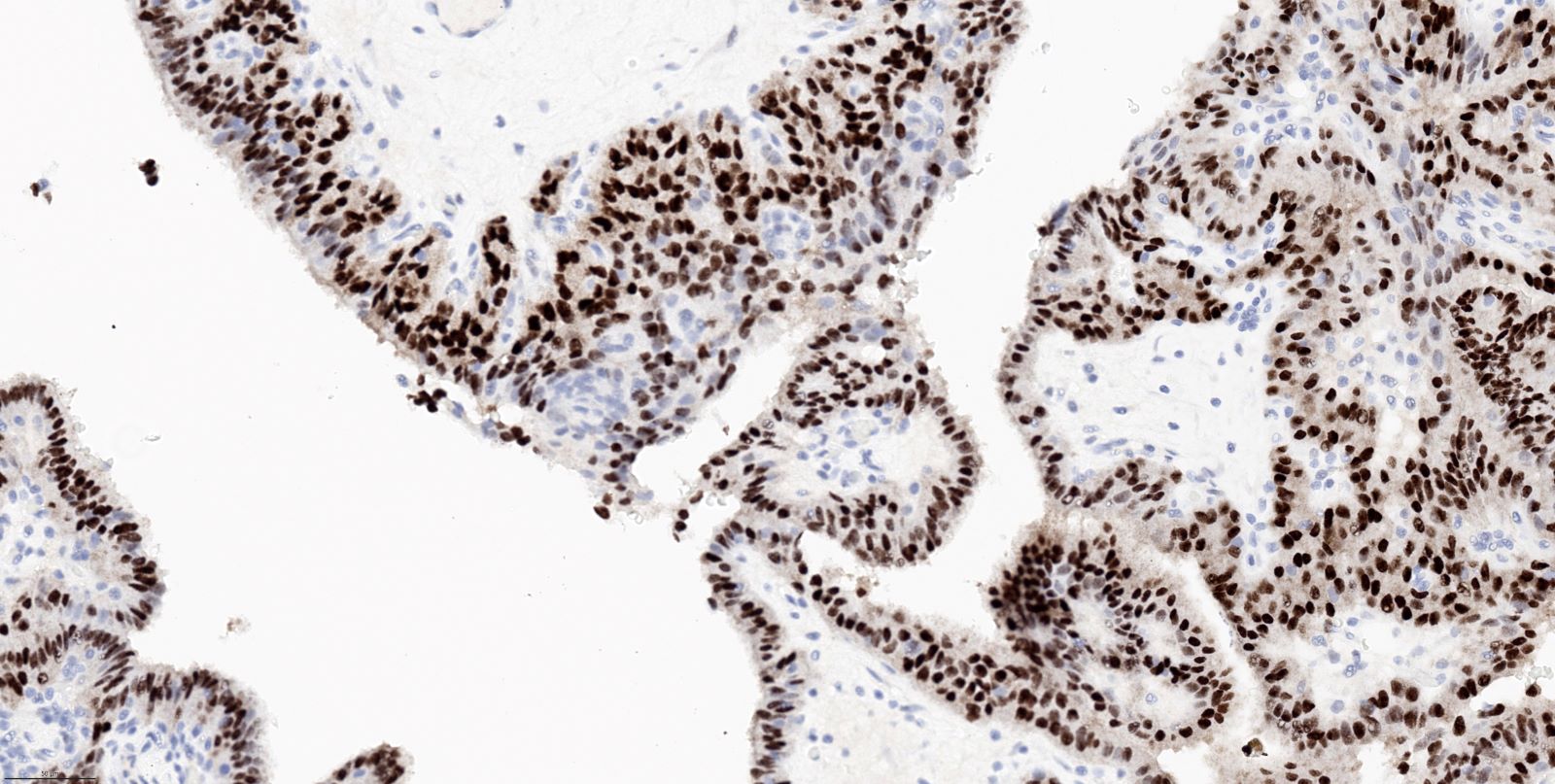
- Diffuse nuclear and cytoplasmic positivity for beta catenin is the hallmark of CMTC in both FAP associated or non-FAP associated cases (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Pathol 2022;33:27)
- Diagnosis of CMTC should alert the pathologist and clinician for a possible diagnosis of FAP and initiation of genetic screening (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168)
Terminology
- Previously known as cribriform-morular variant of papillary thyroid carcinoma (not recommended) (Endocr Pathol 2022;33:27)
ICD coding
- ICD-O: 8201/3 - cribriform carcinoma, NOS
- ICD-11: 2D10.Y & XH1YZ3 - other specified malignant neoplasms of thyroid gland & cribriform carcinoma, NOS
Epidemiology
- Almost exclusively in women; mean age is 26 - 33 years (range of 8 - 61; median is 24 - 30) (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Relat Cancer 2017;24:R109)
- Frequently associated (up to 53%) with FAP or Gardner syndrome (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Relat Cancer 2017;24:R109)
Sites
- Thyroid
Pathophysiology
- Germline mutation in APC gene is seen in cases of FAP with thyroid tumors
- Somatic mutations that result in activation of the Wnt / beta catenin signaling pathway can also lead to CMTC (Endocr Pathol 2022;33:27)
- APC protein is a tumor suppressor that normally promotes degradation of beta catenin; in cases of APC protein mutation, the Wnt / beta catenin signaling pathway is constitutively activated, thus leading to uncontrolled proliferation and loss of cellular differentiation (see Diagrams)
- Due to distinct clinicopathological, immunohistochemical profile and genetics, CMTC is no longer considered as a subtype of papillary thyroid carcinoma in the 2022 WHO classification of thyroid tumors (Endocr Pathol 2022;33:27)
- Complete lack of colloid in CMTC; absent PAX8 and thyroglobulin immunoreactivity suggest it is not a follicular cell derived tumor but rather a tumor of uncertain histogenesis (Endocr Pathol 2021;32:327)
- Squamoid morules typically coexpress CK5 and CD5, which suggests a thymic / ultimobranchial pouch related differentiation (Endocr Pathol 2021;32:327)
Etiology
- Genetic alterations in the Wnt / beta catenin pathway
- APC mutations are the most common genetic alteration and can be found in both familial and sporadic forms
- Some cases may develop after external radiotherapy to the neck (J Clin Lab Anal 2023;37:e24819)
Diagrams / tables
Clinical features
- Generally euthyroid
- Thyroid enlargement or mass noted during physical examination
- Incidental discovery during ultrasonography (Endocr Pathol 2014;25:302)
- CMTC often precedes by several years the development of polyposis coli
- Generally, FAP associated CMTC occurs in younger patients and is multifocal, whereas sporadic CMTC presents as a solitary thyroid nodule (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Pathol 2022;33:27)
Diagnosis
- Diagnosis may be done or suggested either preoperatively using thyroid FNA or (more commonly) postoperatively with histologic evaluation and immunohistochemical confirmation
Laboratory
- Serum thyroglobulin are normal or slightly elevated (J Med Ultrason (2001) 2015;42:83)
- Because CMTC frequently does not express thyroglobulin, the use of serum thyroglobulin as a tumor marker in the follow up of patients may be unreliable (Endocr Pathol 2017;28:49)
Radiology description
- Sonography findings are similar to follicular tumor or nodular goiter, rather than papillary thyroid carcinoma (J Med Ultrason (2001) 2015;42:83)
- Sonographic findings include smooth or focal jagged margin, hypoechoic nodule, lateral shadow, posterior acoustic enhancement, poor marginal and internal vascularity and no microcalcification (J Med Ultrason (2001) 2015;42:83)
- Most cases do not have features of malignancy on sonography (Thyroid 2013;23:45)
Radiology images
Prognostic factors
- Generally indolent clinical course with good prognosis but some aggressive cases have been reported
- Lymph node metastases at presentation: 5 - 12% of cases (Endocr Relat Cancer 2017;24:R109, Mod Pathol 2018;31:1168)
- Distant metastases: 3 - 6% of cases (Endocr Relat Cancer 2017;24:R109, Mod Pathol 2018;31:1168)
- Overall mortality: 2% (Endocr Relat Cancer 2017;24:R109)
- High proliferative index, poorly differentiated features, TERT promoter mutations suggest aggressive features with poor outcome (Int J Surg Pathol 2013;21:379, Endocr Pathol 2017;28:49)
- CMTC can show a high Ki67 labeling index, despite its excellent prognosis (Ki67 labeling index ranges from 4.8 to 36.4% [mean of 15.2%]) (Pathobiology 2019;86:248)
Case reports
- 15 year old girl who underwent external radiotherapy to the neck for Hodgkin disease and developed CMTC 5 years after radiotherapy (J Clin Lab Anal 2023;37:e24819)
- 19 year old woman, with a 3.7 cm thyroid mass (Case #528)
- 19 year old woman with right sided neck swelling (Case #470)
- 20 year old woman with thyroid carcinoma (Acta Biomed 2021;92:e2021153)
- 22 year old woman with an incidental neck lump (Endocr Pathol 2014;25:302)
- 22 year old woman with no history of FAP (Fam Cancer 2020;19:15)
- 28 year old woman with FAP and lung lesions (Pathol Int 2018;68:700)
- 42 year old man with FAP and lung and brain lesions (Am J Clin Pathol 2009;131:134)
Treatment
- Lobectomy is recommended for non-FAP associated CMTC and total thyroidectomy for FAP associated CMTC (Endocr J 2011;58:685, Pathol Res Pract 2015;211:712)
- Extensive lymph node dissection is not necessary because nodal metastases are rare (Endocr J 2011;58:685, Pathol Res Pract 2015;211:712)
- Lack of follicular cell differentiation raises the possibility that these tumors may not benefit from radioactive iodine (RAI) related adjuvant therapies
- Cases with recurrences or distant metastases may respond to lenvatinib (Thyroid 2019;29:1511)
- Clinicians should be alerted to exclude FAP since this diagnosis is the first indicator of FAP syndrome in 25% of cases
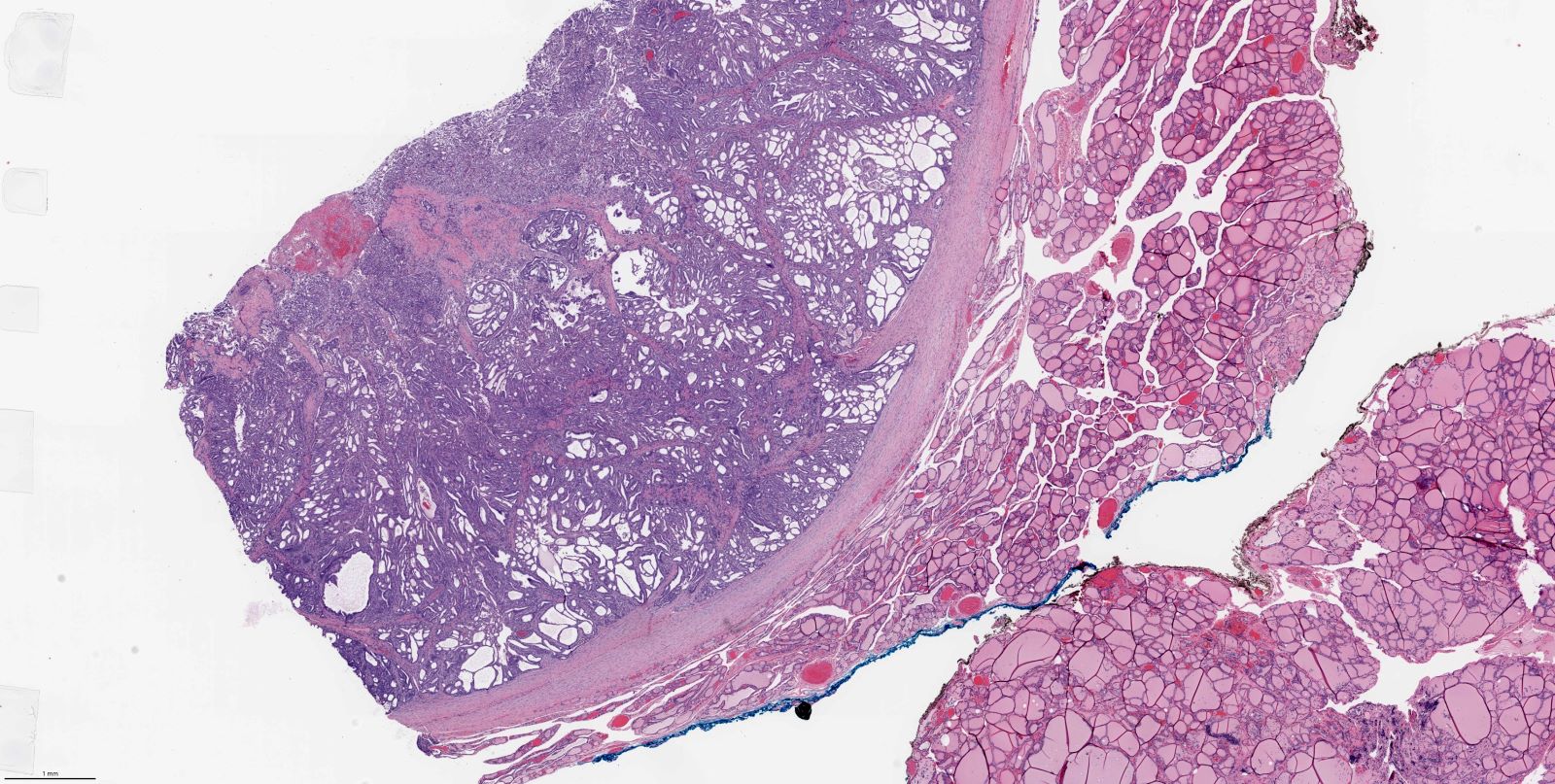
Gross description
- Multifocal lesions throughout the entire thyroid in syndromic patients (Arch Pathol Lab Med 2019;143:1382)
- Well circumscribed, solid with cystic areas and white lesions (Arch Pathol Lab Med 2019;143:1382)
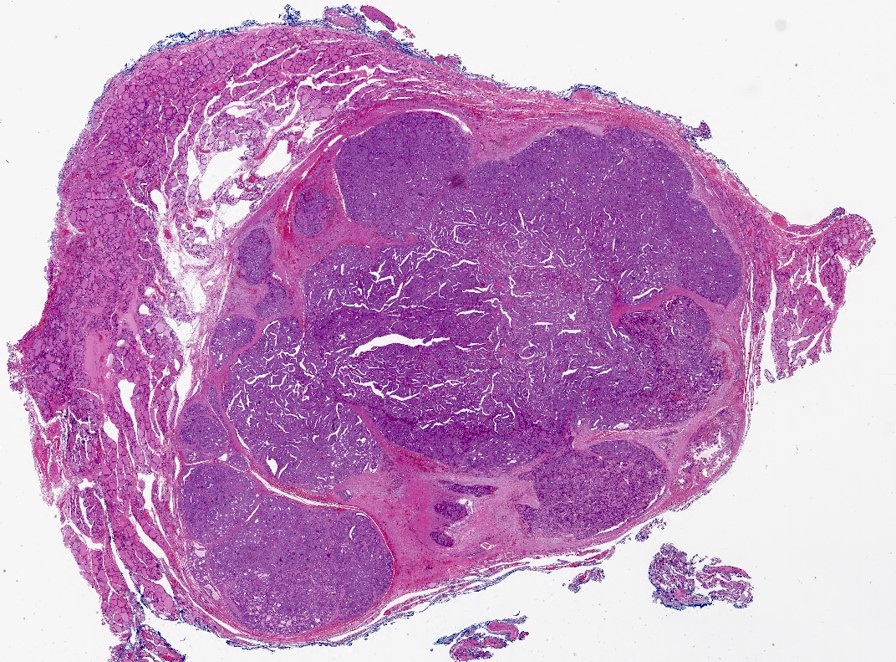
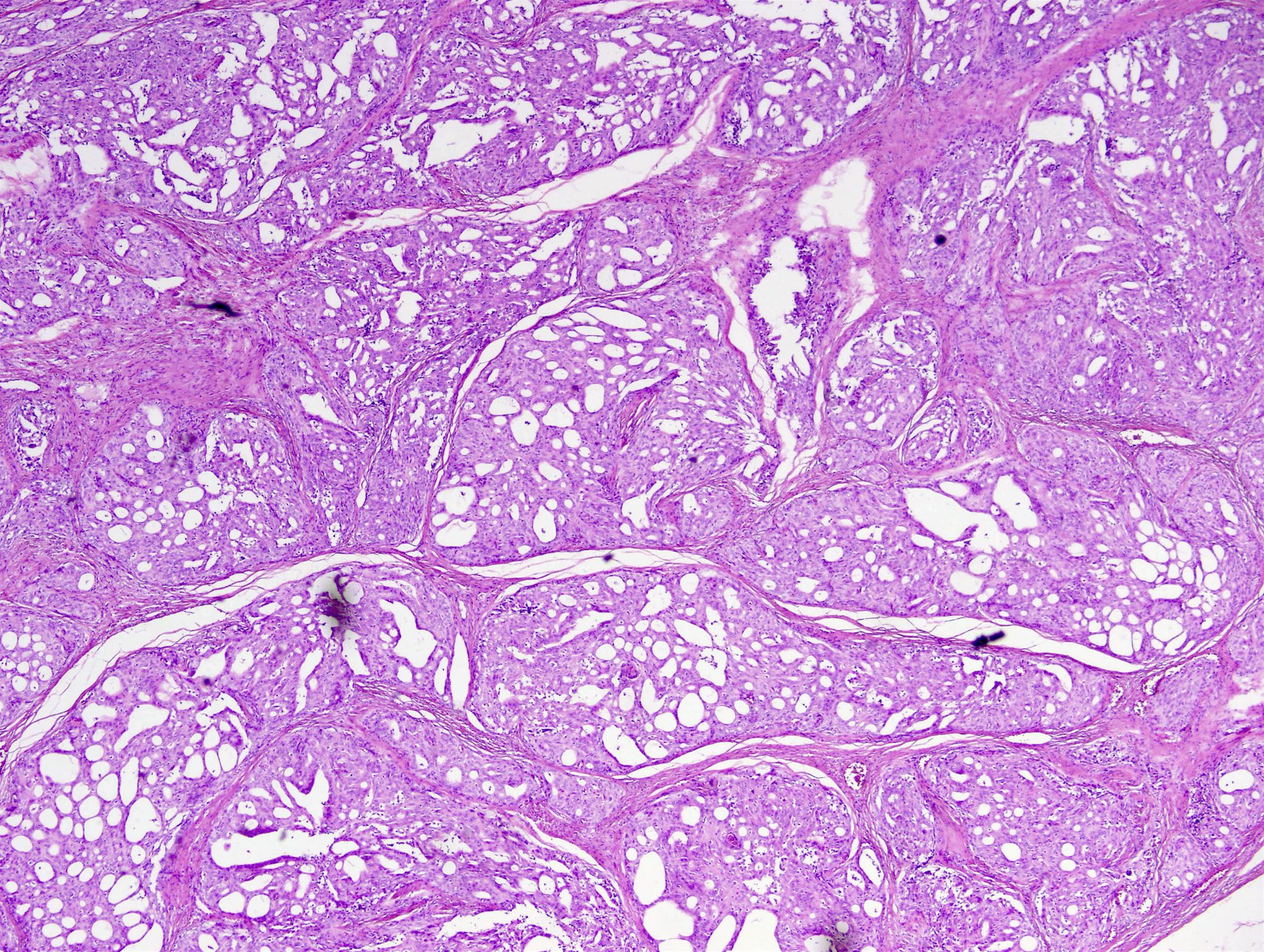
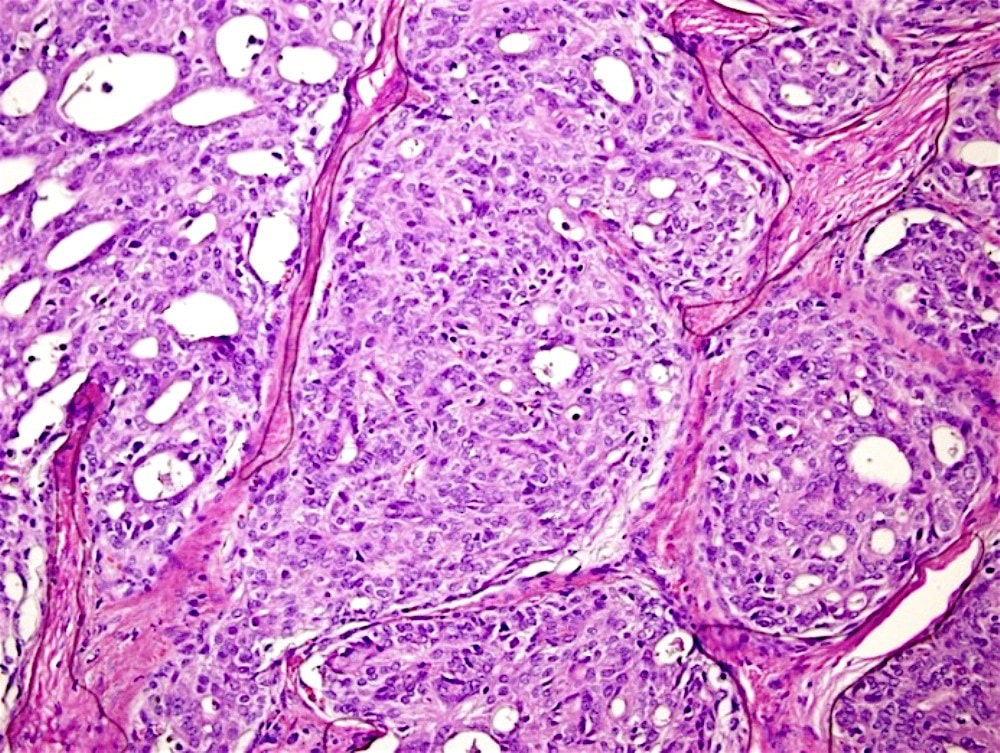
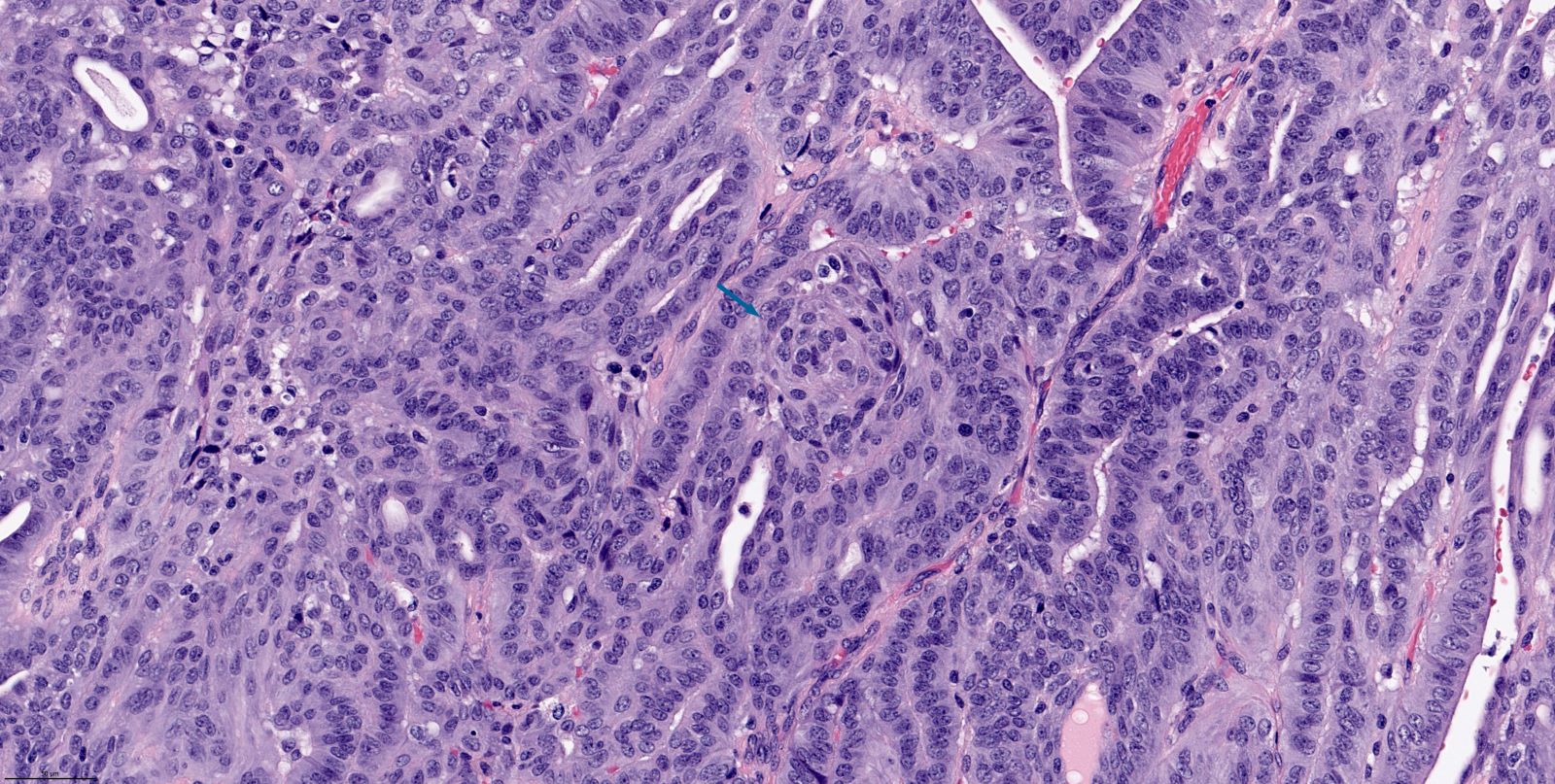
Microscopic (histologic) description
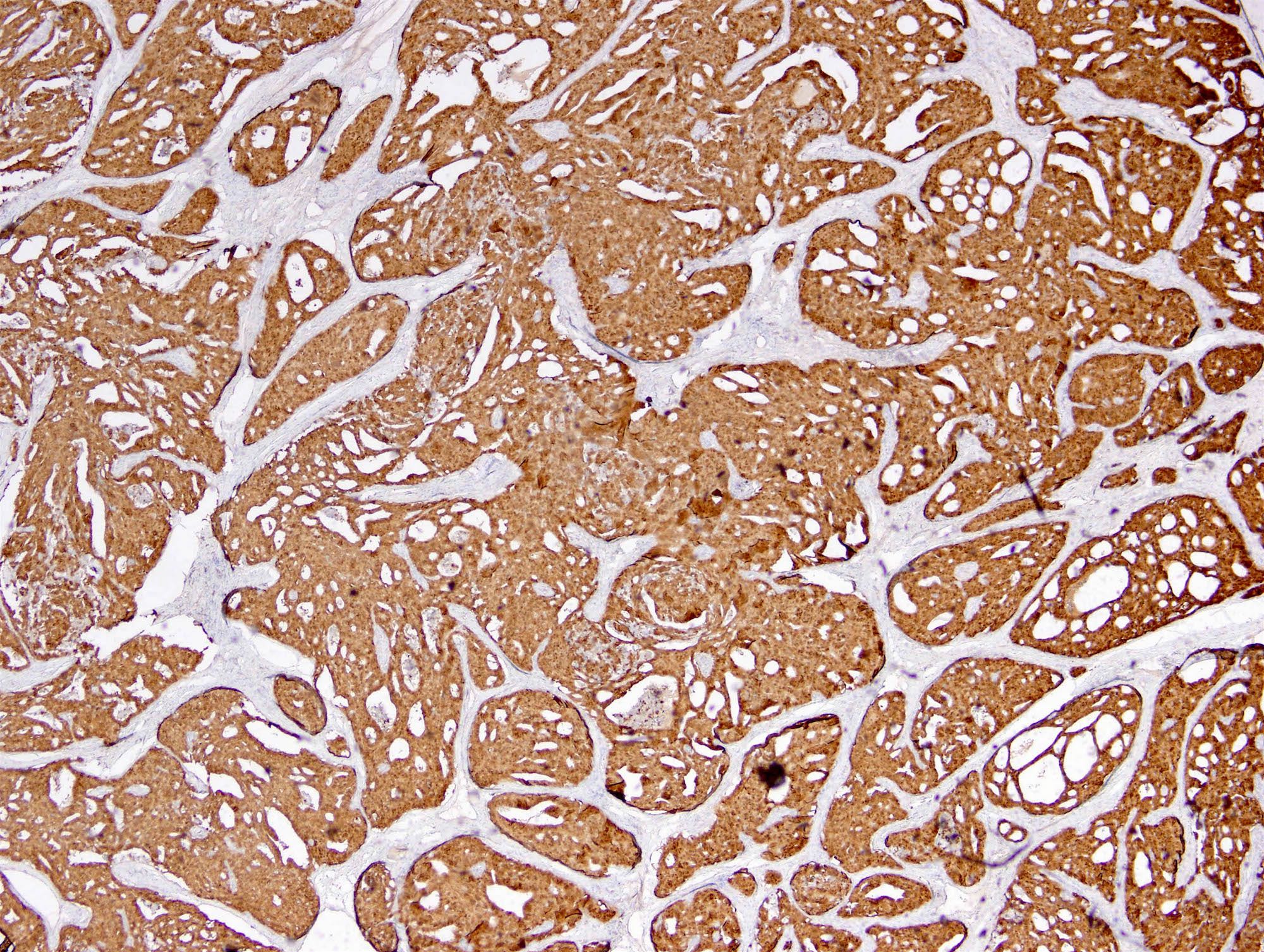
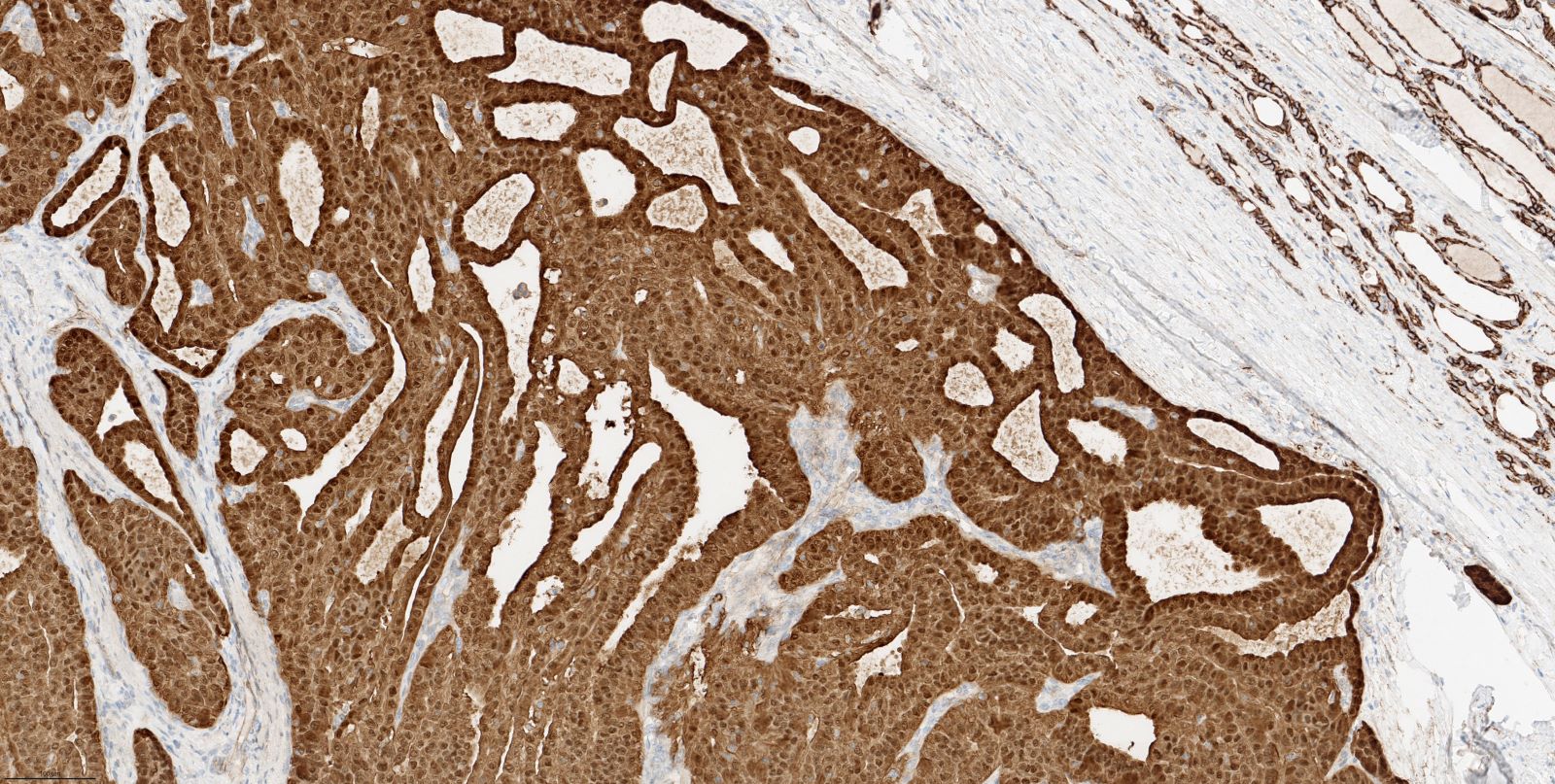
- Lesion is well circumscribed and encapsulated
- Fibrous septa separating the tumor into multiple lobules
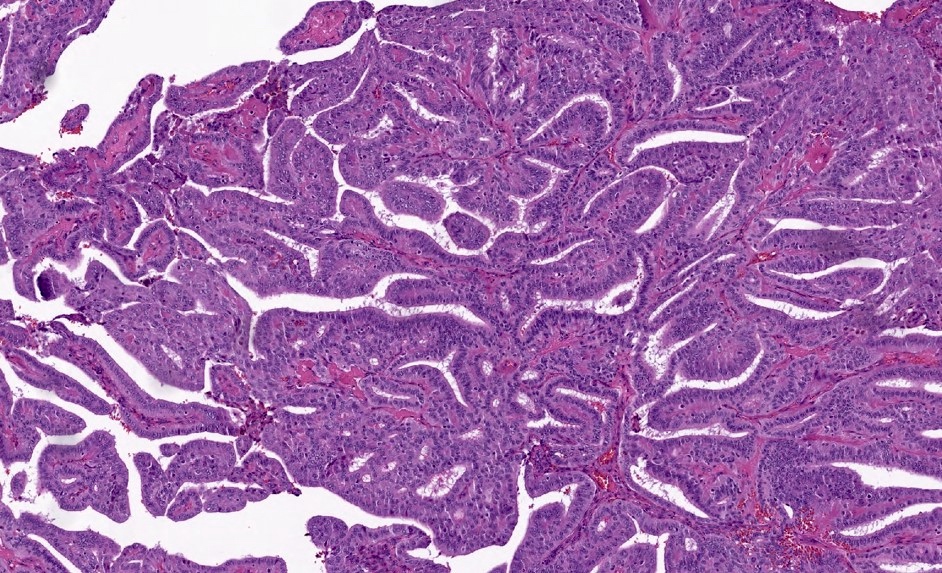
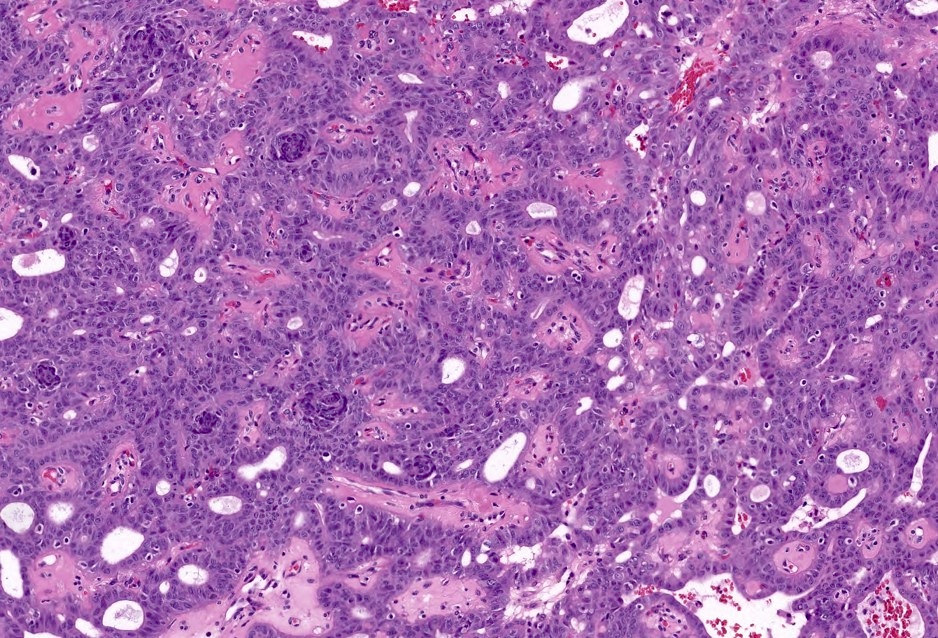
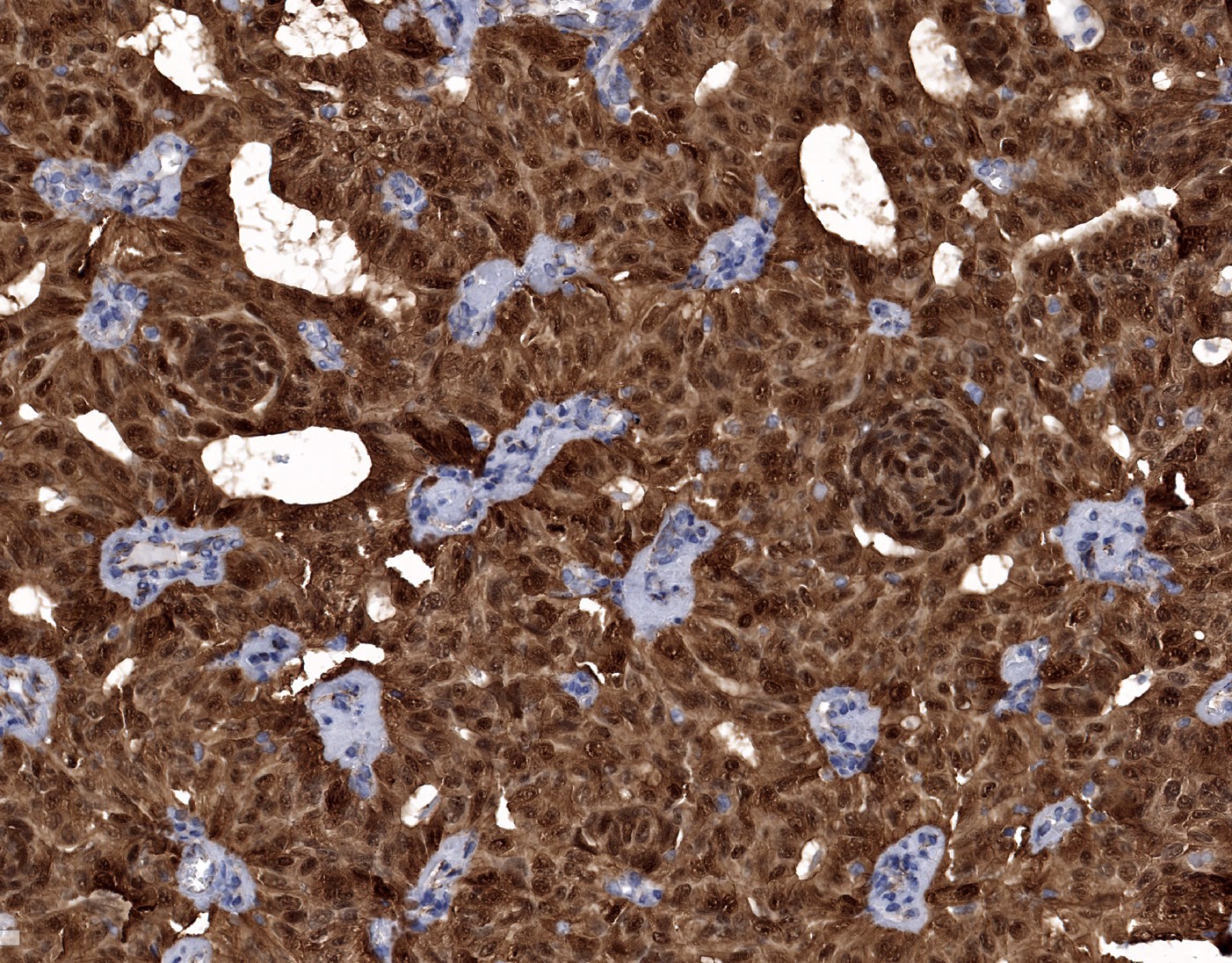
- Common growth patterns: cribriform, follicular, papillary, trabecular and solid
- Tubular follicles without colloid
- Papillary or pseudopapillary structures lined with tall or pseudostratified columnar cells
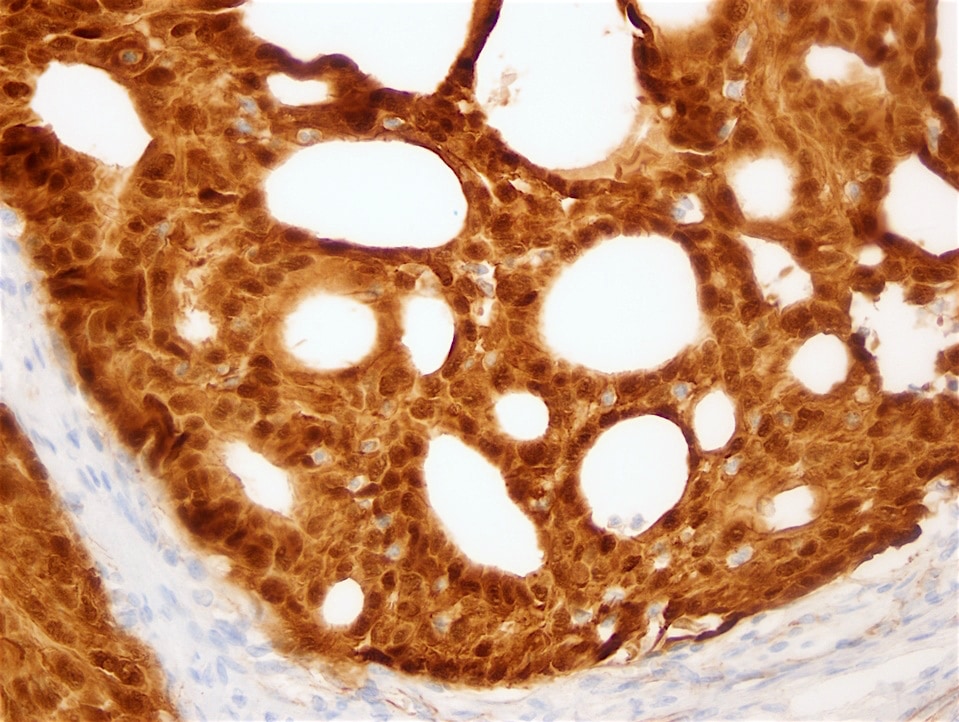
- Cribriform architecture with anastomosing bars and arches without intervening fibrous stroma
- Hyperchromatic nuclei with occasional papillary thyroid carcinoma nuclear features, such as nuclear overlap, grooves, pseudoinclusions and clearing
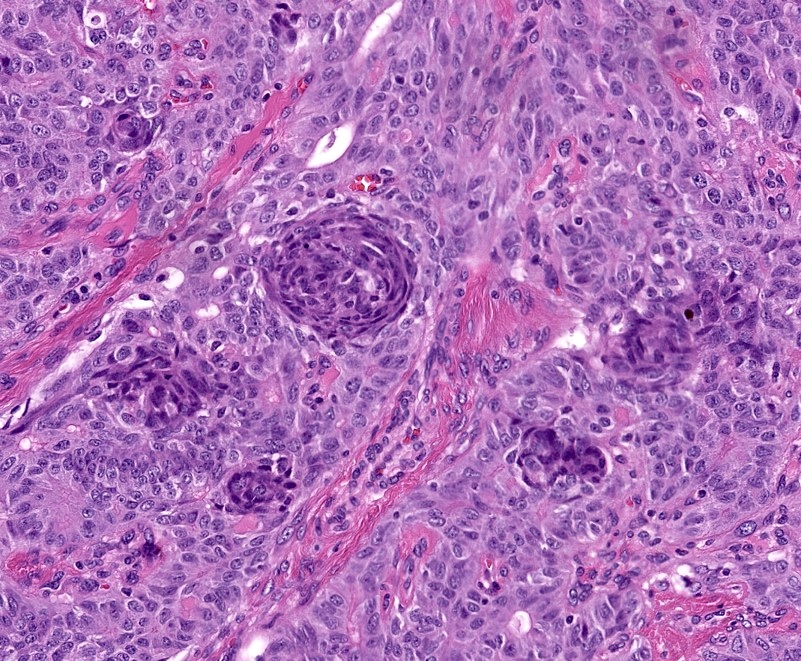
- Distinctive squamoid morules composed of whorls of spindle to ovoid cells with nuclear clearing and lacking keratinization
- These morules may be rare and difficult to find in some cases
- Psammoma bodies are rare (Endocr Relat Cancer 2017;24:R109)
- Capsular invasion (30%), angioinvasion (40%) and extrathyroidal extension in a subset of cases (Mod Pathol 2018;31:1168)
- Aggressive features include neuroendocrine differentiation, necrosis and high mitotic activity (Mod Pathol 2018;31:1168, Am J Clin Pathol 2009;131:134, Pathol Int 2018;68:700)
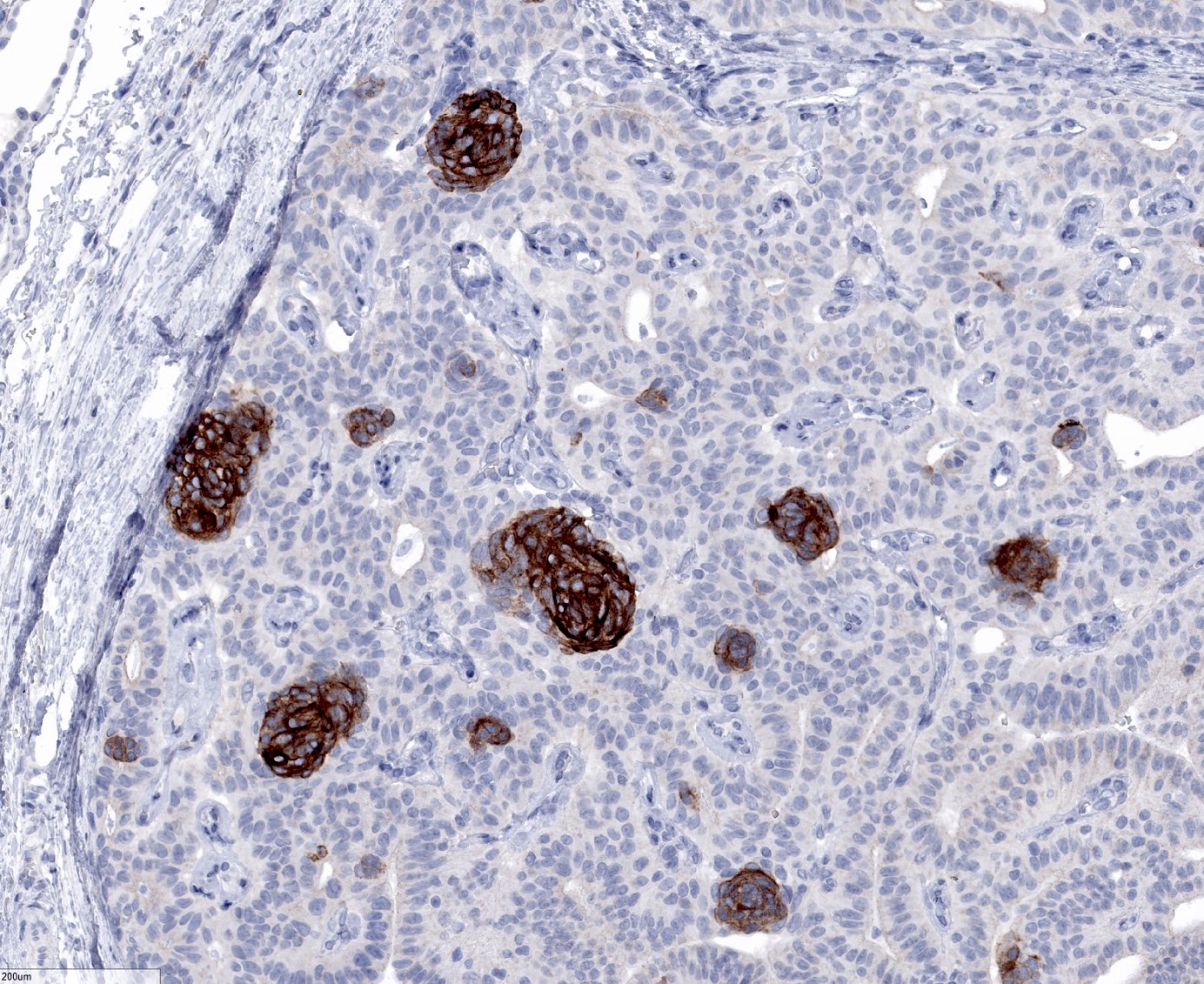
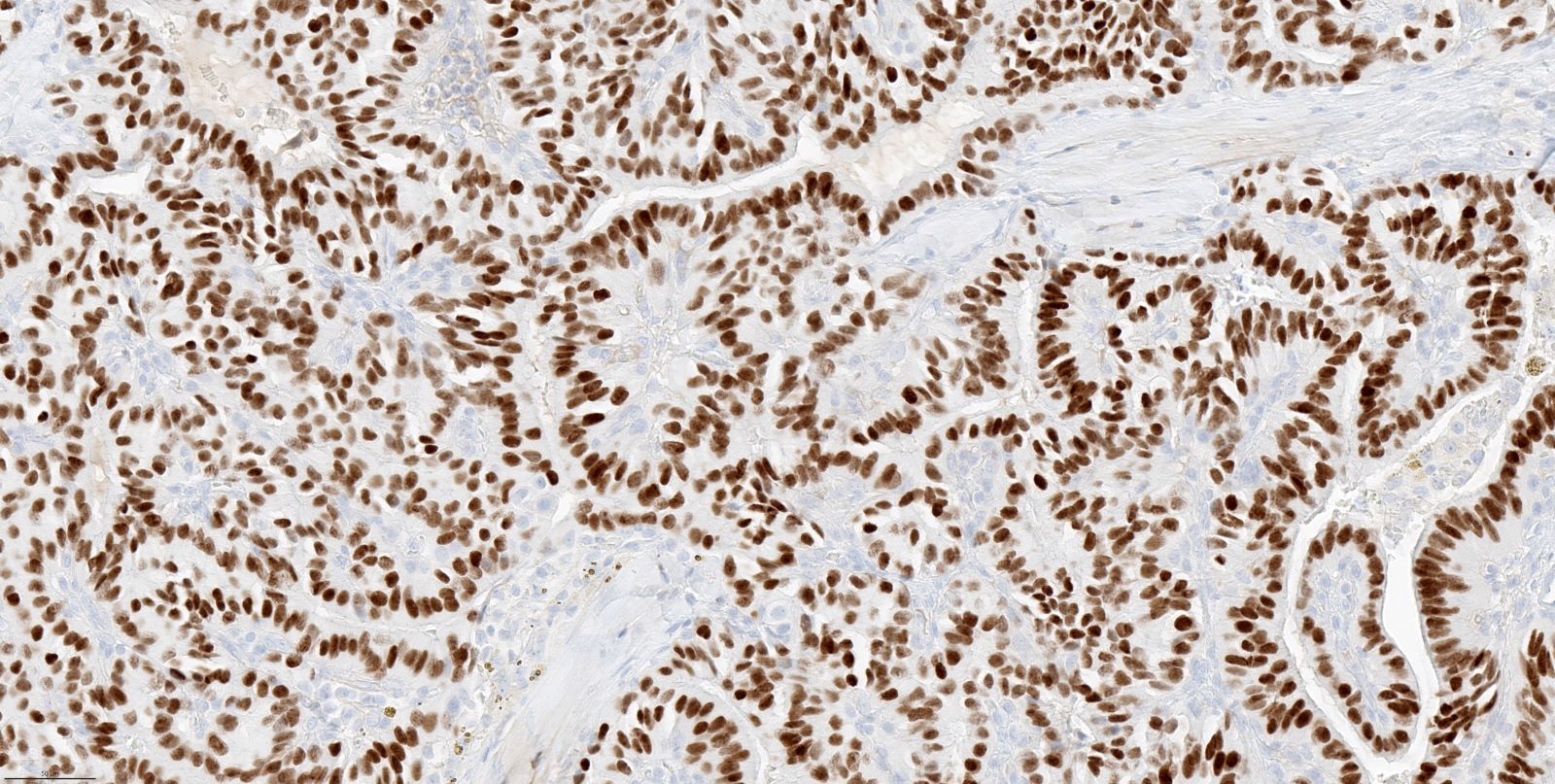
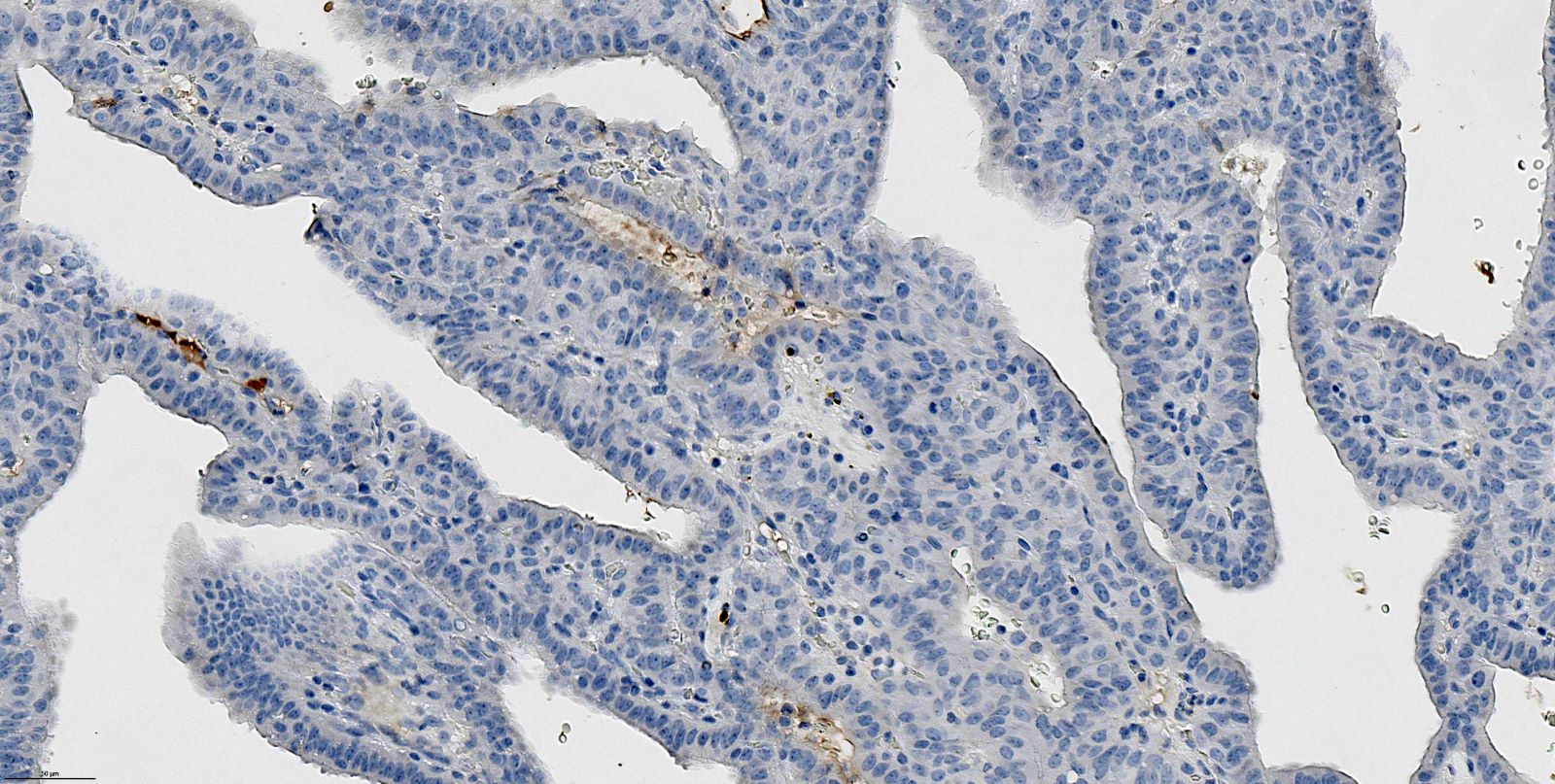
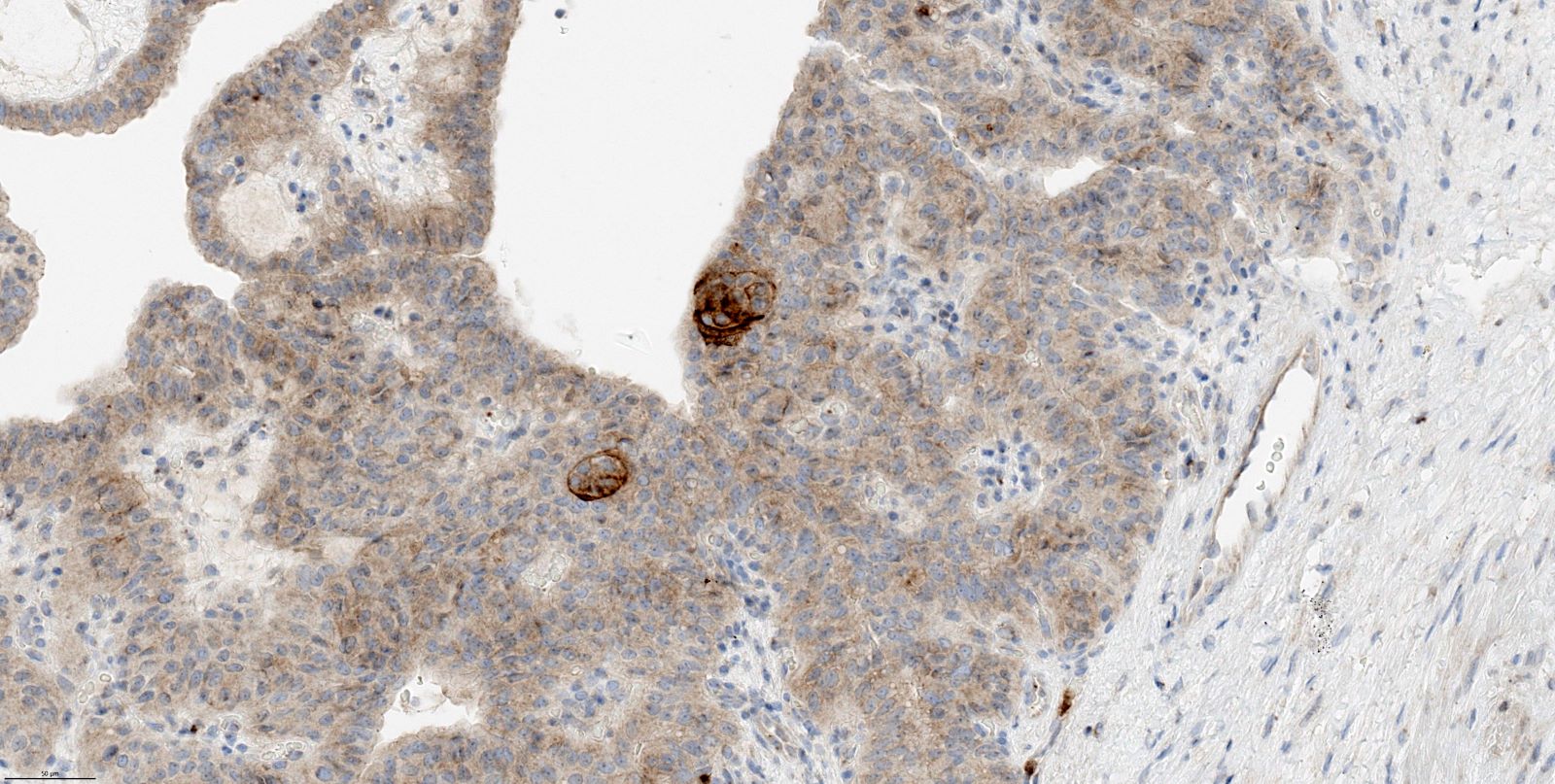
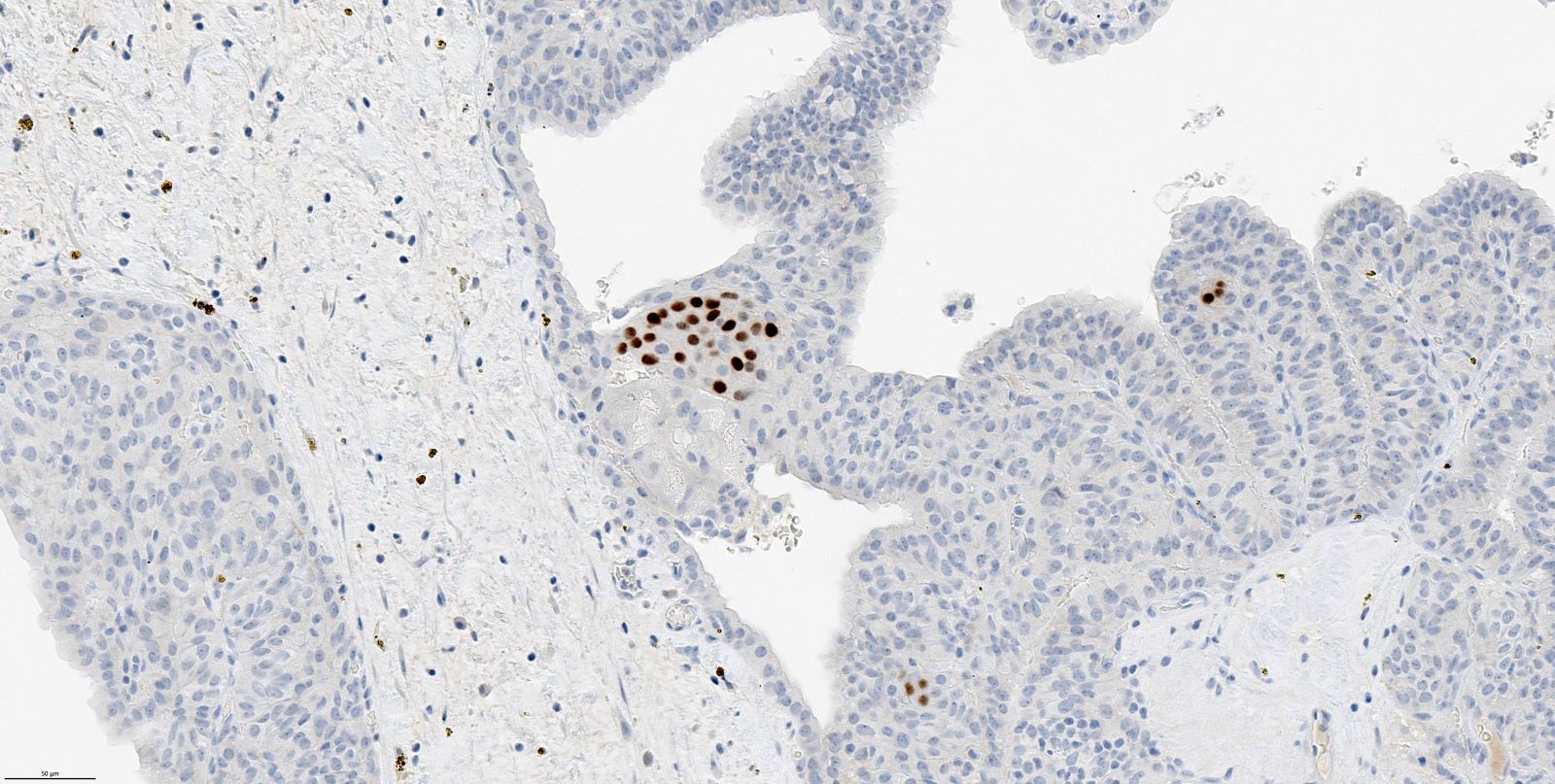
Microscopic (histologic) images
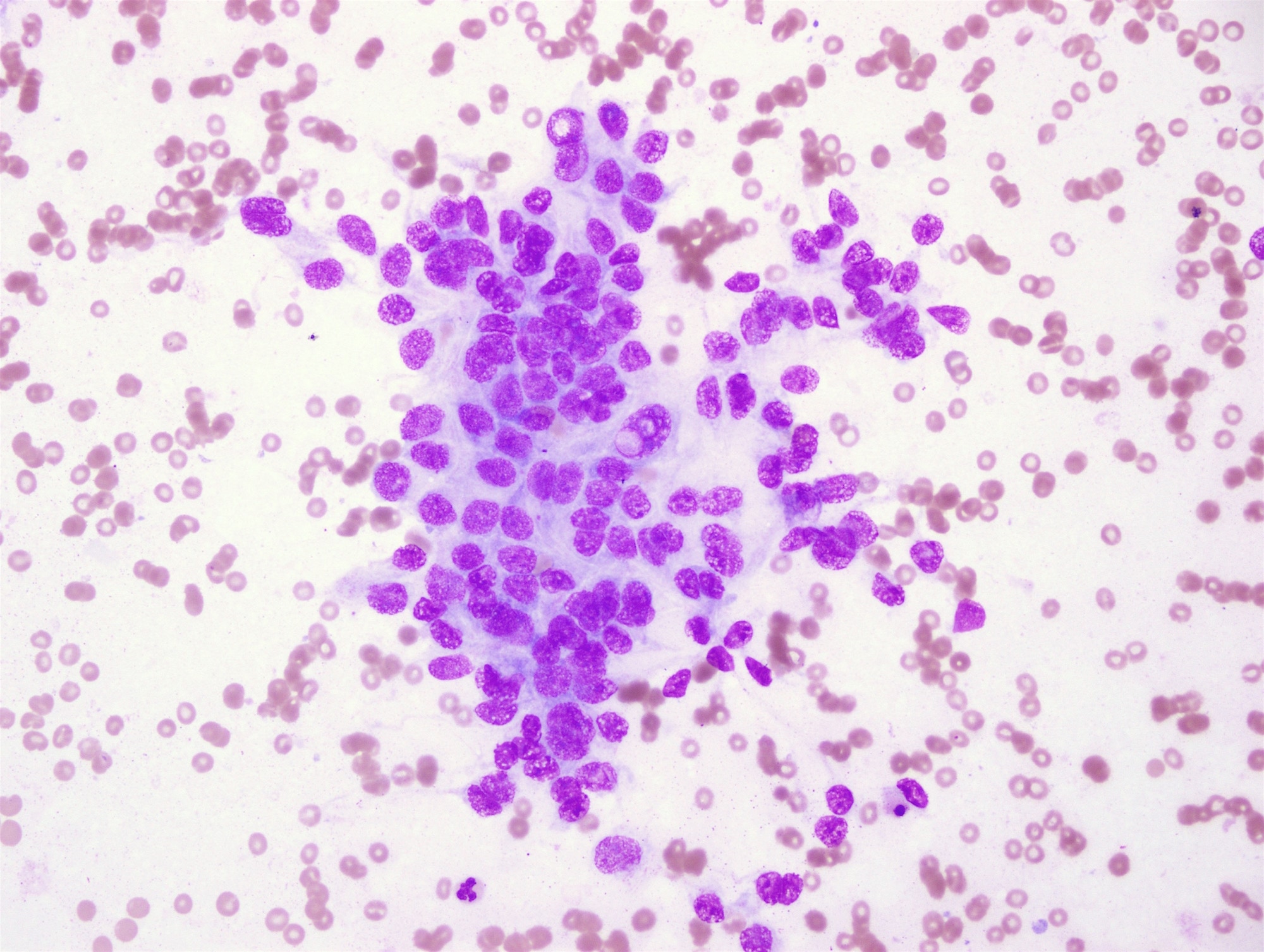
Cytology description
- Smears are hypercellular (Diagn Cytopathol 2010;38:890)
- Colloid is absent (Diagn Cytopathol 2010;38:890)
- Tall, columnar neoplastic cells with a papillary-like arrangement (Diagn Cytopathol 2010;38:890)
- Round to oval slit-like empty spaces formed by spindle to ovoid cells within cell clusters are present (cribriform pattern) (Acta Cytol 2013;57:127)
- Cell clusters with eddy formation (morules) are present (Acta Cytol 2013;57:127, Diagn Cytopathol 2010;38:890)
- Spindle shaped tumor cells are present in the background (Diagn Cytopathol 2010;38:890)
- Pale staining nuclei with thickened nuclear membranes is present focally (Diagn Cytopathol 2010;38:890)
- Nuclear grooves are present but intranuclear pseudoinclusions are less common than in the conventional papillary thyroid carcinoma (Diagn Cytopathol 2010;38:890)
- Cell block, if available, is extremely valuable to perform confirmatory immunostains including beta catenin (see below)
Cytology images
Positive stains
- Cribriform component: beta catenin (nuclear and cytoplasmic), LEF1, TTF1, CK, EMA, estrogen, progesterone (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168)
- Morular component: CDX2, CD10, CD5, CK5, BCL2, cyclin D1, Galectin3, CA 19-9 (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168)
Negative stains
- Cribriform component: CK20, calcitonin, WT1, thyroglobulin, PAX8, HBME1 (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168)
- Morular component: 34 beta E12, CK7, CK20, p63, p40, thyroglobulin, TTF1, PAX8, CEA, estrogen, progesterone (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168)
Electron microscopy description
- Numerous microfilaments ~100 nm long at the nuclear clearing area of the morular regions (Ultrastruct Pathol 2004;28:97)
Molecular / cytogenetics description
- Almost all cases have genetic alterations in the Wnt / beta catenin pathway with APC mutations being the most common and found in both the familial and sporadic setting (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Pathol 2022;33:27)
- Mutations in other genes involved in the Wnt / beta catenin pathway such as CTNNB1 have also been detected (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Pathol 2022;33:27)
- BRAF mutations are absent (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Endocr Pathol 2022;33:27)
- Other uncommon associated molecular alterations include RET / PTC rearrangements, mutations in PIK3CA or RAS genes
- TERT mutation may be associated with poor outcome (Endocr Pathol 2021;32:327, Mod Pathol 2018;31:1168, Thyroid 2014;24:1184)
Sample pathology report
- Left thyroid lobe, resection:
- Cribriform-morular thyroid carcinoma, pathologic stage: pT2, N0 (see comment)
- Tumor size: 2.0 cm
- Microscopic extrathyroidal extension: not identified
- Margins: < 1 mm
- Lymphovascular invasion: identified
- Perineural invasion: not identified
- Ancillary studies: BRAF V600E immunostain is negative; beta catenin immunostain is positive (cytoplasmic and nuclear)
- Lymph nodes:
- Number identified: 1
- Number involved: 0
- Intrathyroidal parathyroid identified
- Comment: Cribriform-morular thyroid carcinoma is frequently associated (up to 53%) with FAP or Gardner syndrome. Genetic testing is recommended.
- Cribriform-morular thyroid carcinoma, pathologic stage: pT2, N0 (see comment)
Differential diagnosis
- Papillary thyroid carcinoma subtypes:
- Columnar cell:
- CMTC has darker nuclear chromatin, solid areas, tall cells with marked pseudostratification
- Columnar cell papillary thyroid carcinoma displays supranuclear and subnuclear cytoplasmic vacuoles
- Thyroglobulin, TTF1 and PAX8 positive
- CDX2 positive in up to 50% of cases (note: CMTC is also CDX2 positive in the morular component)
- Tall cell:
- Basal nuclei
- Positive for thyroglobulin, TTF1, PAX8, HBME1 and BRAF V600E (90% of cases)
- Conventional:
- Prominent papillary thyroid carcinoma nuclear features and colloid
- Positive for thyroglobulin, TTF1, PAX8, HBME1 and BRAF V600E (40 - 60% of cases)
- Columnar cell:
- Poorly differentiated thyroid carcinoma:
- CMTC displays CD10 positive morulae, lower mitotic activity and is negative for thyroglobulin and PAX8
- Hyalinizing trabecular tumor:
- CMTC can have areas of trabecular growth
- Positive for thyroglobulin, TTF1 and PAX8
- Positive for Ki67 with a membranous pattern of staining (using MIB1 antibody at room temperature)
- Metastatic breast carcinoma:
- Metastatic colon cancer:
Board review style question #1
A 26 year old woman presented with multiple thyroid lesions. After a thyroidectomy, the histological features were consistent with the diagnosis of cribriform-morular thyroid carcinoma. Further clinical surveillance includes monitoring for which of the following associated neoplasms?
- Cardiac myxoma
- Colorectal carcinoma
- Pheochromocytoma
- Pleuropulmonary blastoma
- Trichilemmomas
Board review style answer #1
B. Colorectal carcinoma. Familial adenomatous polyposis (FAP) is a related to germline mutation of APC tumor suppressor gene, which strongly predisposes to colorectal carcinoma. Cribriform-morular thyroid carcinoma is associated with FAP as well. Other syndromes associated with thyroid pathologies include DICER1 syndrome (pleuropulmonary blastoma and multinodular goiter), Carney complex (cardiac myxoma and thyroid follicular adenoma / carcinoma), Cowden disease (trichilemmomas and follicular adenoma / carcinoma), MEN 2A / B (pheochromocytoma and C cell hyperplasia / medullary thyroid carcinoma).
Comment Here
Reference: Cribriform-morular thyroid carcinoma
Comment Here
Reference: Cribriform-morular thyroid carcinoma
Board review style question #2
What is the beta catenin immunohistochemical staining pattern in cribriform-morular thyroid carcinoma (CMTC)?
- Diffuse cytoplasmic and nuclear positivity
- Loss of nuclear staining
- Membranous, cytoplasmic and Golgi staining
- Stippled nuclear staining
- Strong membranous staining
Board review style answer #2
A. Diffuse cytoplasmic and nuclear positivity. CMTC is associated with FAP and driven by Wnt / beta catenin pathway activation. The hallmark immunoreactivity of CMTC is diffuse nuclear and cytoplasmic positivity for beta catenin due to decreased proteasomal degradation of beta catenin following mutation of the APC tumor suppressor gene.
Comment Here
Reference: Cribriform-morular thyroid carcinoma
Comment Here
Reference: Cribriform-morular thyroid carcinoma
Board review style question #3
Which of the following statements about cribriform-morular thyroid carcinoma is true?
- It does not occur in a familial setting
- It is a subtype (variant) of papillary thyroid carcinoma
- It typically is negative for thyroglobulin and PAX8
- No distinct mutations are commonly identified
Board review style answer #3
C. It typically is negative for thyroglobulin and PAX8. Answer A is incorrect because they may be familial. Answer B is incorrect because the tumors are no longer considered a variant of papillary thyroid carcinoma. Answer D is incorrect because up to 53% of cases occur in the setting of germline APC mutation (familial adenomatous polyposis) and sporadic cases often harbor molecular alterations of the WNT / beta catenin pathway.
Comment Here
Reference: Cribriform-morular thyroid carcinoma
Comment Here
Reference: Cribriform-morular thyroid carcinoma