Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Agarwal S, Bychkov A. Columnar cell. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidcolumnarvariant.html. Accessed April 2nd, 2025.
Definition / general
- Rare aggressive variant of papillary thyroid carcinoma
- Columnar cells with nuclear pseudostratification, scant cytoplasm and absent / minimal nuclear features of papillary thyroid carcinoma
Essential features
- Aggressive variant of papillary thyroid carcinoma with papillary structures lined by columnar cells showing prominent nuclear stratification and lacking nuclear features of papillary thyroid carcinoma
- Needs to be differentiated from metastatic colon and endometrial adenocarcinoma
Terminology
- Papillary carcinoma, columnar cell variant
ICD coding
Epidemiology
- 0.15 - 0.4% of all papillary carcinomas (Pathol Int 2018;68:641)
- Age: 32 - 90 years; usually older than patients with classic papillary thyroid carcinoma (Cancer Cytopathol 2017;125:389, Thyroid 2013;23:714, Turk Patoloji Derg 2015;31:34)
- 40 - 72% women (Mod Pathol 2011;24:739, Cancer Cytopathol 2017;125:389, Am J Transl Res 2019;11:6262)
Sites
- Lateral lobes or isthmus of thyroid gland
Clinical features
- Painless neck mass or symptomatic thyroid mass with compression symptoms or enlarged cervical lymph node (Mod Pathol 2011;24:739)
- Associated with aggressive behavior and poor prognosis when unencapsulated (Am J Transl Res 2019;11:6262, Cancer Manag Res 2018;10:465)
- Extrathyroidal extension and nodal metastases in up to 55%
- Distant metastases in up to 5%
- Local recurrence
- Advanced clinical stage (AJCC stage III or IV) at presentation
- Poorer cancer specific survival in comparison with classic papillary thyroid carcinoma
Diagnosis
- Workup is similar to any thyroid mass / nodule
- Ultrasound with fine needle aspiration cytology
- CT scan may be useful to evaluate extrathyroidal extension and lymph node metastases
- Diagnosis is made via histological examination of a resection specimen, supplemented by immunohistochemistry
- Fine needle aspiration cytology can raise a suspicion of columnar cell variant and influence surgical decision making
- Need to differentiate from adenocarcinoma metastatic to the thyroid gland
Radiology description
- Sonography: solid and hypoechoic nodules with microcalcifications; smooth margins in indolent tumors; microlobulated margins in invasive cases (Ultrasonography 2017;36:103, Korean J Radiol 2018;19:1000)
- Heterogeneously enhancing nodule on contrast enhanced computed tomographic scanning (Diagn Cytopathol 2016;44:816)
Prognostic factors
- Poorer prognosis than classic papillary thyroid carcinoma (Am J Transl Res 2019;11:6262, Cancer Manag Res 2018;10:465, Thyroid 2016;26:1)
- Studies have reported better outcome for asymptomatic patients, young patients, smaller / lower stage and circumscribed / encapsulated tumors (Korean J Radiol 2018;19:1000, Mod Pathol 2011;24:739, Cancer Manag Res 2018;10:465)
- Risk stratification as per ATA (American Thyroid Association) 2015 (Thyroid 2016;26:1)
Case reports
- 18 year old woman with mixed columnar cell and tall cell variant of papillary carcinoma (Diagn Cytopathol 2012;40:E4)
- 42 year old woman with thyroid mass (Cytopathology 2017;28:338)
- 50 year old man with colon carcinoma and 18FDG avid nodules in thyroid and neck lymph nodes (Endocr Pathol 2015;26:187)
- 58 year old woman with history of progressively increasing neck swelling (Cytojournal 2014;11:27)
- 64 year old woman with pathologic fracture of the femur neck (Pathol Res Pract 1998;194:861)
- 86 year old man with composite mucoepidermoid carcinoma and columnar cell variant of papillary thyroid carcinoma (Int J Surg Pathol 2016;24:336)
- 87 year old woman with brain metastasis (Virchows Arch 2013;462:473)
Treatment
- Based on ATA (American Thyroid Association) 2015 and NCCN guidelines, usually surgical excision (Thyroid 2016;26:1, J Natl Compr Canc Netw 2018;16:1429)
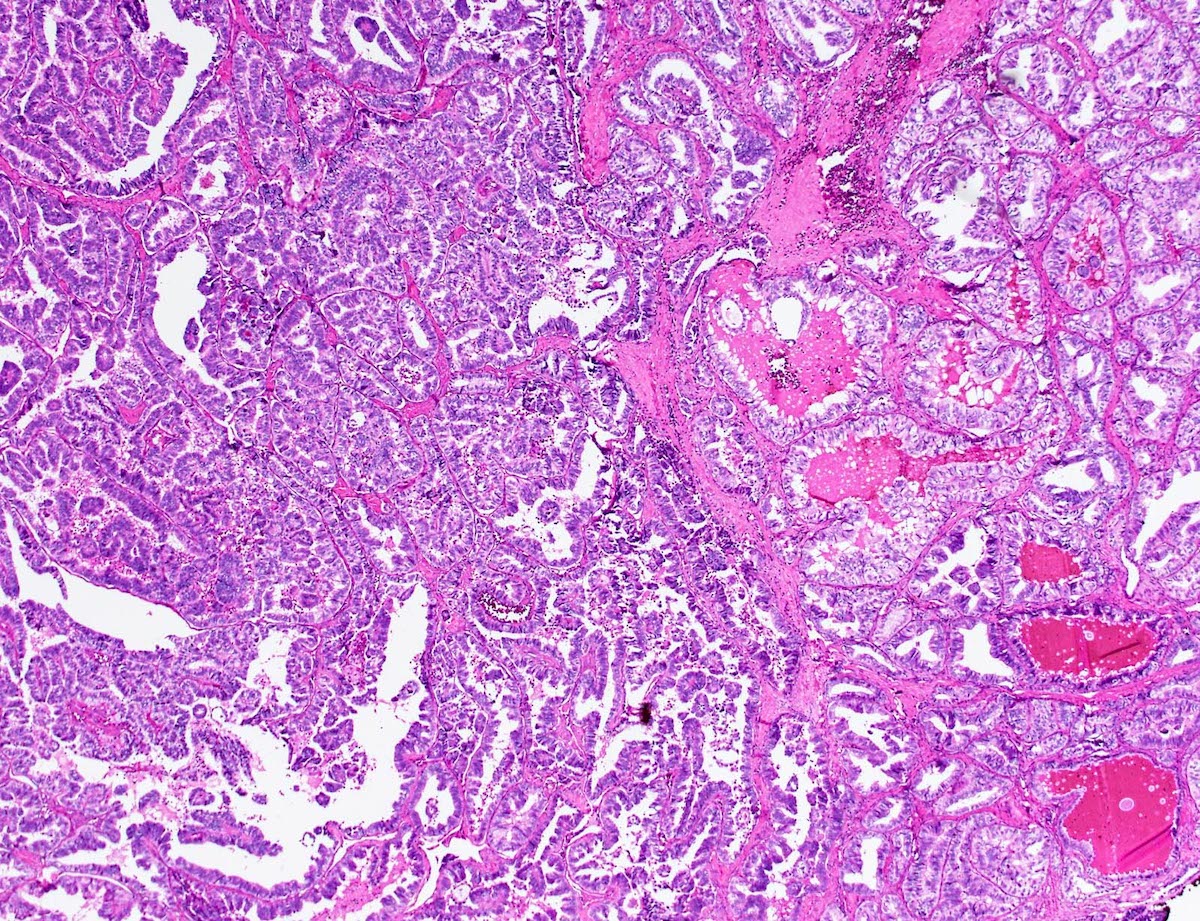
Gross description
- Solid nodule, 0.6 - 10 cm (Cancer Cytopathol 2017;125:389, Mod Pathol 2011;24:739)
- Invasive, rarely encapsulated
- Variable calcification
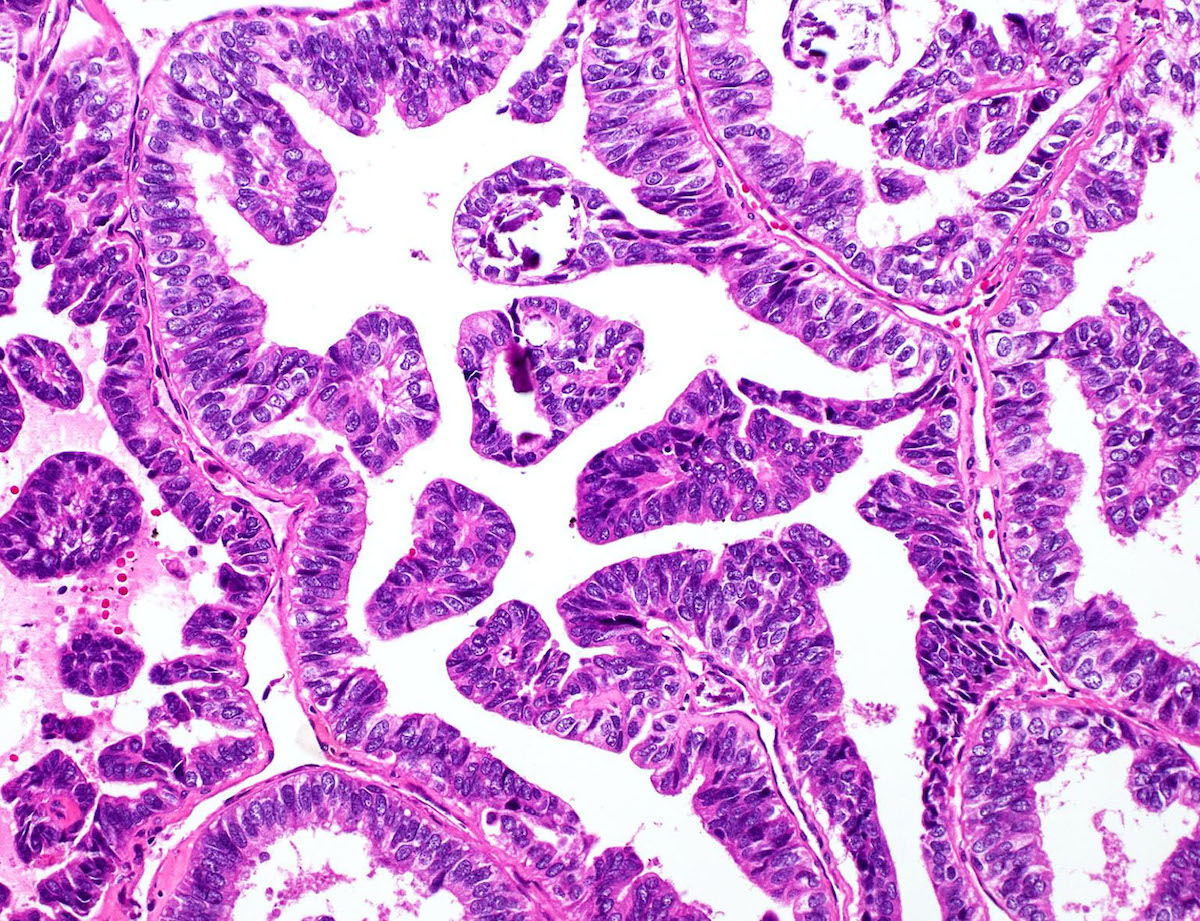
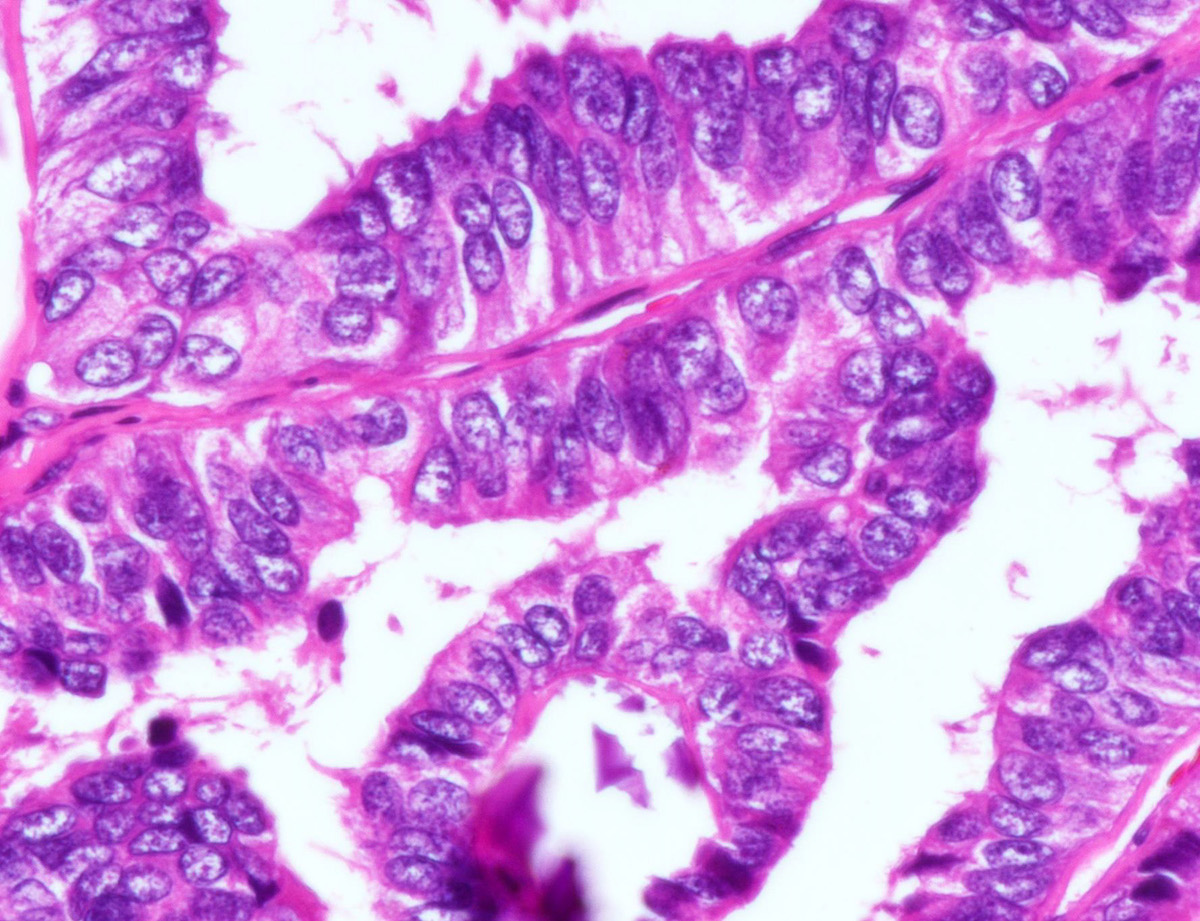
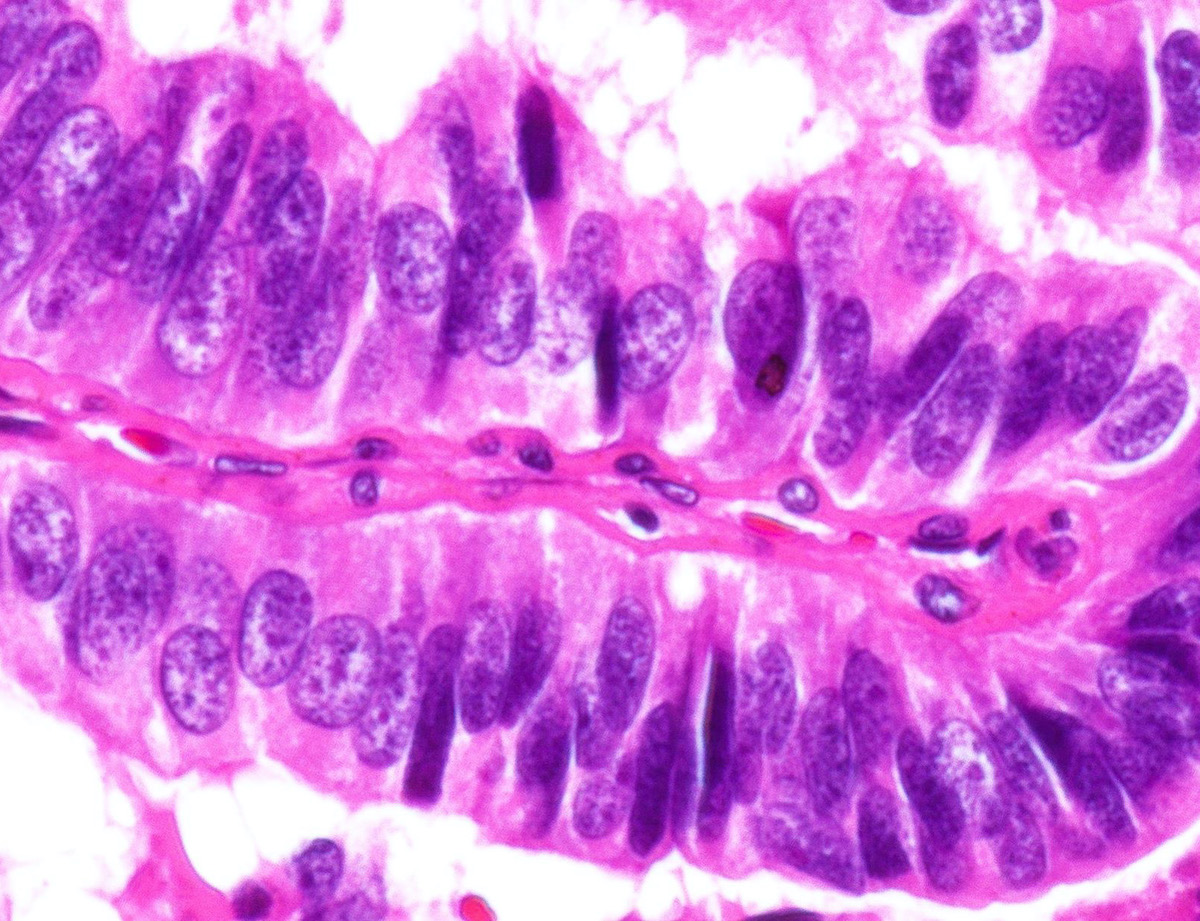
Microscopic (histologic) description
- Patterns
- Papillary is the most common (Cancer Cytopathol 2017;125:389)
- Others include trabecular, follicular, solid and cribriform (Histopathology 2018;72:40, Turk Patoloji Derg 2015;31:34, Mod Pathol 2011;24:739)
- Rare squamous morule formation or rosette-like structures (Mod Pathol 2011;24:739, Cytojournal 2014;11:27)
- Columnar cells
- Clear to pale eosinophilic cytoplasm (Mod Pathol 2011;24:739)
- Supranuclear or subnuclear cytoplasmic vacuoles resembling secretory endometrium (Histopathology 2018;72:40, Adv Anat Pathol 2018;25:172, Cancer Cytopathol 2017;125:389)
- Nuclear features
- Prominent pseudostratification (Cancer Cytopathol 2017;125:389)
- Elongated, hyperchromatic nuclei with coarse chromatin (Histopathology 2018;72:40, Adv Anat Pathol 2018;25:172, Head Neck 2011;33:1052)
- Rare or absent chromatin clearing, nuclear grooves and intranuclear inclusions
- Nuclear grooves may be prominent (Cancer Cytopathol 2017;125:389, Cytojournal 2014;11:27)
- Inconspicuous nucleoli
- Mitotic activity can be increased (Adv Anat Pathol 2018;25:172, Mod Pathol 2011;24:739)
- Variable necrosis (Mod Pathol 2011;24:739)
- Usually lacks psammoma bodies (Adv Anat Pathol 2018;25:172, Cancer Cytopathol 2017;125:389)
Microscopic (histologic) images
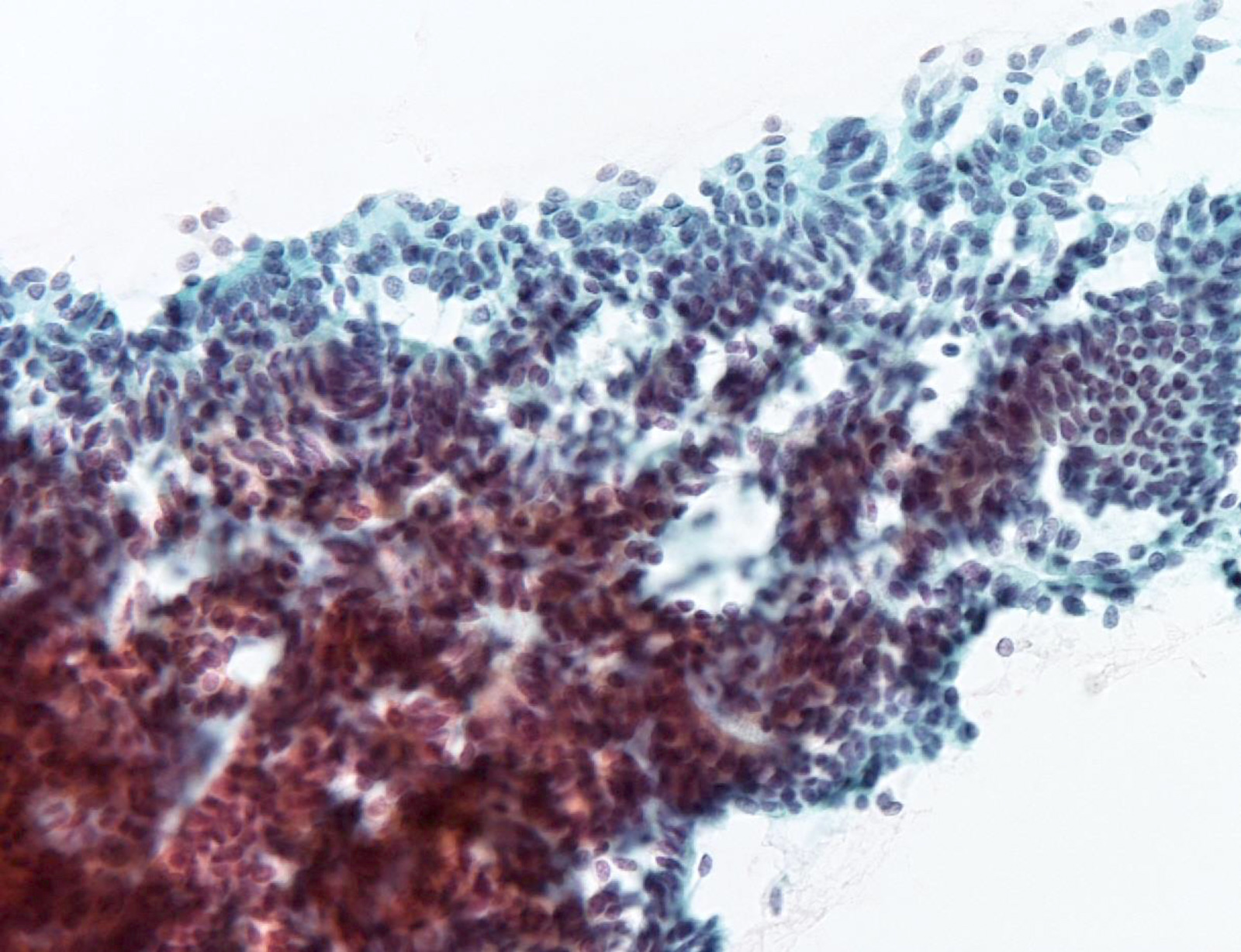
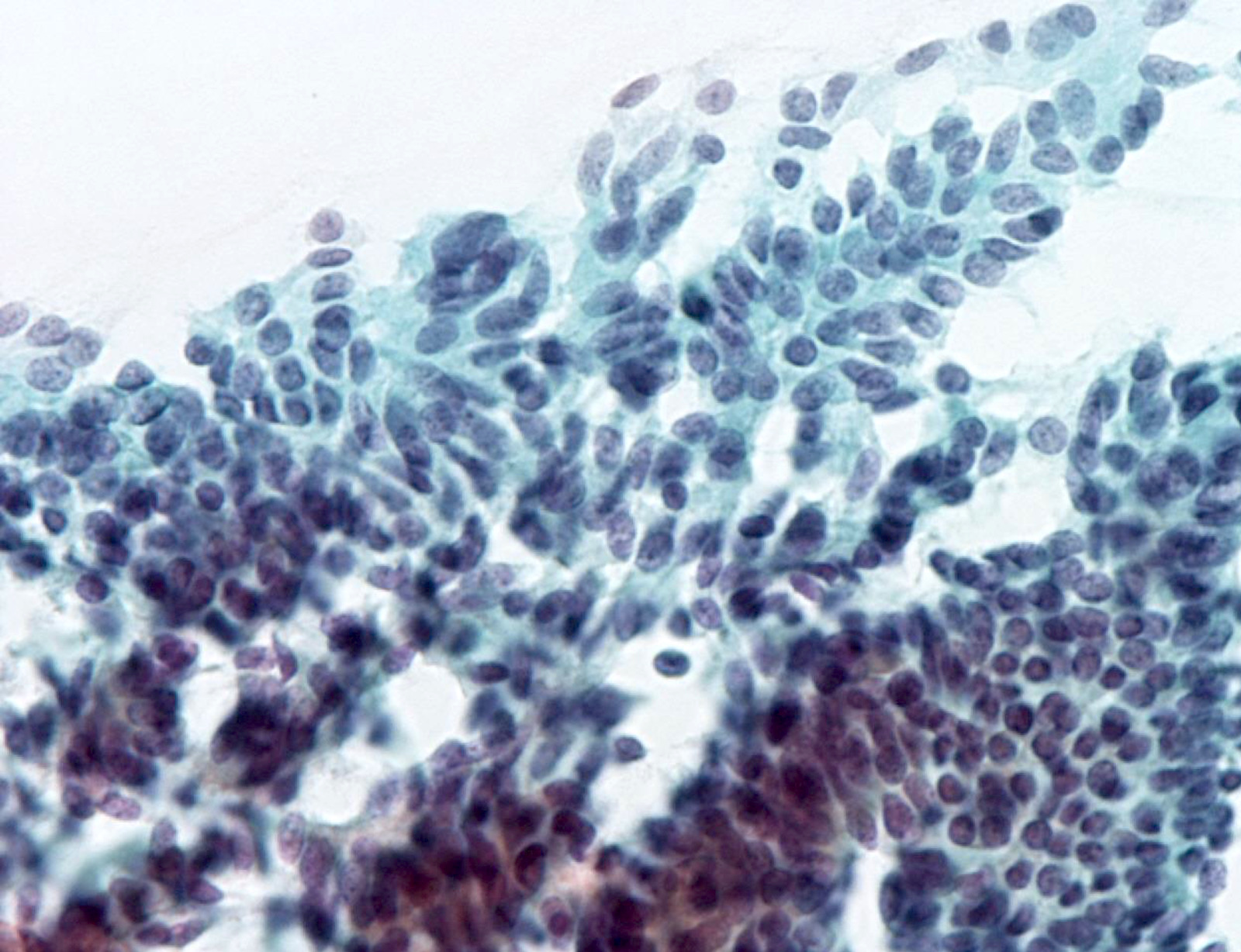
Cytology description
- Cellular aspirate with absent or scant colloid
- Patterns
- Papillary fragments with fibrovascular cores (Cancer Cytopathol 2017;125:389)
- Variable interspersed singly distributed cells
- Less common syncytial, honeycomb, microfollicular or cribriform
- Rare rosette-like structures (Cytojournal 2014;11:27, J Cytol 2017;34:183)
- Tumor cells
- Columnar and spindle shaped
- Variably vacuolated or wispy cytoplasm (Diagn Cytopathol 2012;40:E4, Cytojournal 2014;11:27)
- Elongated, hyperchromatic oval / elongated / pleomorphic nuclei
- Nuclear pseudostratification
- Rare or absent nuclear features of papillary thyroid carcinoma
- Rare cases with frequent nuclear grooves (Cancer Cytopathol 2017;125:389, Cytojournal 2014;11:27)
- Inconspicuous nucleoli
- Sometimes mitotic figures
- Most correspond to the Bethesda VI category (Cancer Cytopathol 2017;125:389)
Positive stains
- Thyroid specific: TTF1, PAX8, thyroglobulin
- Cytokeratins: AE1 / AE3, CK7
- CDX2 expression is diagnostic, reported in 10 - 66% (Thyroid 2013;23:1498, Thyroid 2013;23:714, Am J Clin Pathol 2012;137:722)
- ER in 67 - 70%, PR in 50 - 55% (Thyroid 2013;23:714, Mod Pathol 2011;24:739)
- Variable Ki67 proliferative index, up to 50% (Thyroid 2013;23:714, Mod Pathol 2011;24:739)
- Increased nuclear expression of cyclin D1
Negative stains
Molecular / cytogenetics description
- BRAF V600E mutation in 17 - 33% based on limited evidence (Thyroid 2013;23:1498, Thyroid 2013;23:714, Mod Pathol 2011;24:739)
Sample pathology report
- Thyroid, total thyroidectomy:
- Papillary thyroid carcinoma, columnar cell variant, right lobe, 5.5 cm (see synoptic report)
Differential diagnosis
- Tall cell variant of papillary thyroid carcinoma:
- Height of cells 2 - 3 times the cell width
- Oncocytic cytoplasm
- Well developed nuclear features of papillary thyroid carcinoma
- Prominent intranuclear inclusions
- Metastatic intestinal adenocarcinoma:
- Metastatic endometrial adenocarcinoma:
- Clinical history or radiology findings
- Vimentin positive
- TTF1 / PAX8 / thyroglobulin negative
- CDX2 negative
- Metastatic pulmonary adenocarcinoma:
- Clinical history or radiology findings
- PAX8 / thyroglobulin negative
- Medullary thyroid carcinoma (rare on cytology):
- Thyroglobulin negative
- Calcitonin positive
Board review style question #1
Board review style answer #1
A. TTF1+, PAX8+, CDX2+. Cells of columnar cell variant of papillary thyroid carcinoma are positive for thyroid specific markers (TTF1 / PAX8), as well as the intestinal epithelial marker CDX2.
Comment Here
Reference: Columnar cell variant
Comment Here
Reference: Columnar cell variant
Board review style question #2
Which of the following is true about columnar cell variant of papillary thyroid carcinoma?
- An indolent clinical course
- Abundant oncocytic cytoplasm
- Multiple intranuclear pseudoinclusions
- One of the most common variants of papillary thyroid carcinoma
- Morphology mimics metastatic adenocarcinoma
Board review style answer #2
E. Morphology mimics metastatic adenocarcinoma. Columnar cell variant is rare and an aggressive papillary thyroid carcinoma type, characterized by scant clear or eosinophilic cytoplasm and lack of well developed nuclear features of papillary thyroid carcinoma. Due to absence of typical nuclear features of papillary thyroid carcinoma, metastatic adenocarcinoma needs to be ruled out.
Comment Here
Reference: Columnar cell variant
Comment Here
Reference: Columnar cell variant