Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Dall C, Zynger DL. Teratoma with somatic type malignancy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisteratocarcinoma.html. Accessed April 2nd, 2025.
Definition / general
- Testicular germ cell tumor with an area of pure somatic type malignancy that arises from germ cell tumor progenitor cells and occupies ≥ 0.5 cm (approximately ≥ 1 microscopic field using 4x objective)
Essential features
- Identified within primary testicular tumor or at a metastatic site
- Rhabdomyosarcoma, adenocarcinoma, embryonic type neuroectodermal tumor and sarcoma, NOS are the most frequent histologies (Histopathology 2022;81:84, Am J Surg Pathol 2022;46:11)
- Varying morphologies, including neuroglial, neuroendocrine carcinoma and neuroblastoma, may make diagnosis difficult (Histopathology 2022;81:84)
- Must be distinguished from sarcomatoid or glandular yolk sac tumor, which represent up to 60% of postchemotherapy sarcomatous tumors (Am J Surg Pathol 2015;39:251)
Terminology
- Current terminology: teratoma with somatic type malignancy
- Previous terminology: teratoma with malignant transformation, teratoma with somatic malignancy
- Currently recommended that embryonic type neuroectodermal tumor should replace primitive neuroectodermal tumor (PNET) when referring to a teratoma with this type of somatic malignancy because although it resembles CNS PNET, it lacks EWSR1 rearrangement (Am J Surg Pathol 2021;45:1299)
ICD coding
- ICD-O: 9084/3 - teratoma with malignant transformation
- ICD-11: 2C80.Y & XH33E8 - other specified malignant neoplasms of testis & teratoma with malignant transformation
Epidemiology
- 3 - 6% of testicular germ cell tumors (Cancer 1985;56:860, Cancer 1984;54:1824, J Urol 1994;152:1144, Histopathology 2022;81:84)
- Median age of diagnosis within testis: 26 years (range: 17 - 55) (Am J Surg Pathol 2022;46:11)
- Median age of diagnosis at metastatic site: 39 years (range: 23 - 62) (Am J Surg Pathol 2022;46:11)
Sites
- Testis
- Metastatic locations (e.g., retroperitoneum, lungs)
Pathophysiology
- 3 proposed origins of somatic type malignancy (Eur Urol 2007;51:1306):
- Mature teratoma
- Embryonal carcinoma
- Yolk sac tumor (Am J Surg Pathol 2015;39:251, Am J Surg Pathol 2021;45:463)
Clinical features
- More commonly found as metastasis, rather than at initial diagnosis confined to the testis
- Most frequently identified after chemotherapy (J Urol 2014;192:1403, Am J Surg Pathol 2022;46:11)
Diagnosis
- Found as metastatic disease, within the testis or both (J Urol 1998;159:133)
- Histologic features and immunohistochemistry determine type of somatic malignancy
Radiology description
- Imaging may suggest specific somatic malignancy in germ cell tumors (Eur J Radiol 2009;69:230)
- Ossified lymph nodes and soft tissue reported in osteosarcoma
- Peritoneal carcinoma seen in adenocarcinoma
- Septal thickening and opacifications reported in a case of bronchoalveolar carcinoma
Prognostic factors
- If confined to the testis without synchronous metastasis, somatic malignancy does not appear to confer a worse prognosis Am J Surg Pathol 2022;46:11)
- Presence in a metastatic site is associated with poor survival (median survival: 44 months) Am J Surg Pathol 2022;46:11)
- Median time from initial diagnosis of testicular germ cell tumor and diagnosis of somatic malignancy at metastatic site: 70 months (range: 0 - 384 months) Am J Surg Pathol 2022;46:11)
Case reports
- 32 year old man with angiosarcoma (Int J Surg Pathol 2022;30:462)
- 37 year old man with neuroendocrine carcinoma (Case Rep Oncol 2022;15:191)
- 40 year old man with rhabdomyosarcoma (Urol Case Rep 2020;33:101385)
- 50 year old man with sarcoma, NOS (Front Oncol 2021;11:633543)
Treatment
- Surgical resection is the mainstay of treatment
- Chemotherapy is based on histologic subtype of malignant transformation (J Clin Oncol 2003;21:4285)
- Radical surgery is often utilized for advanced disease (J Urol 1998;159:133)
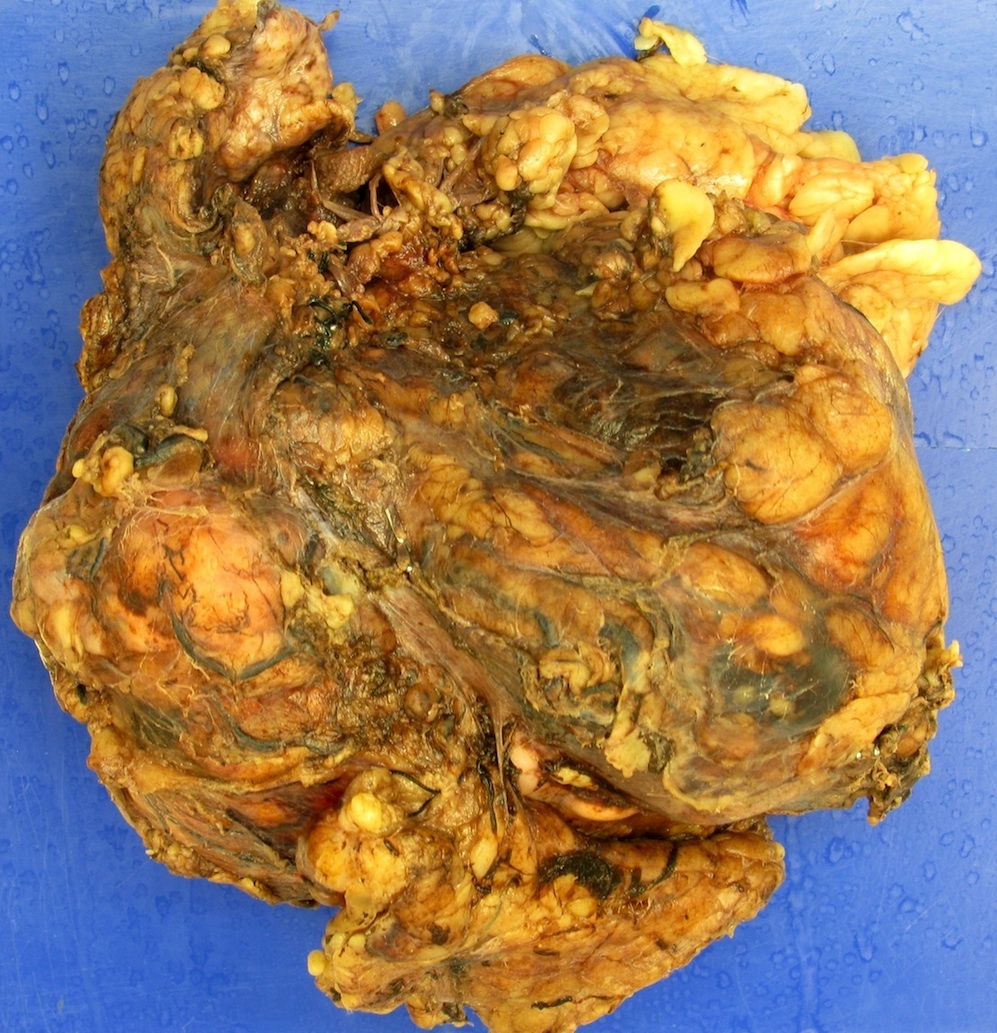
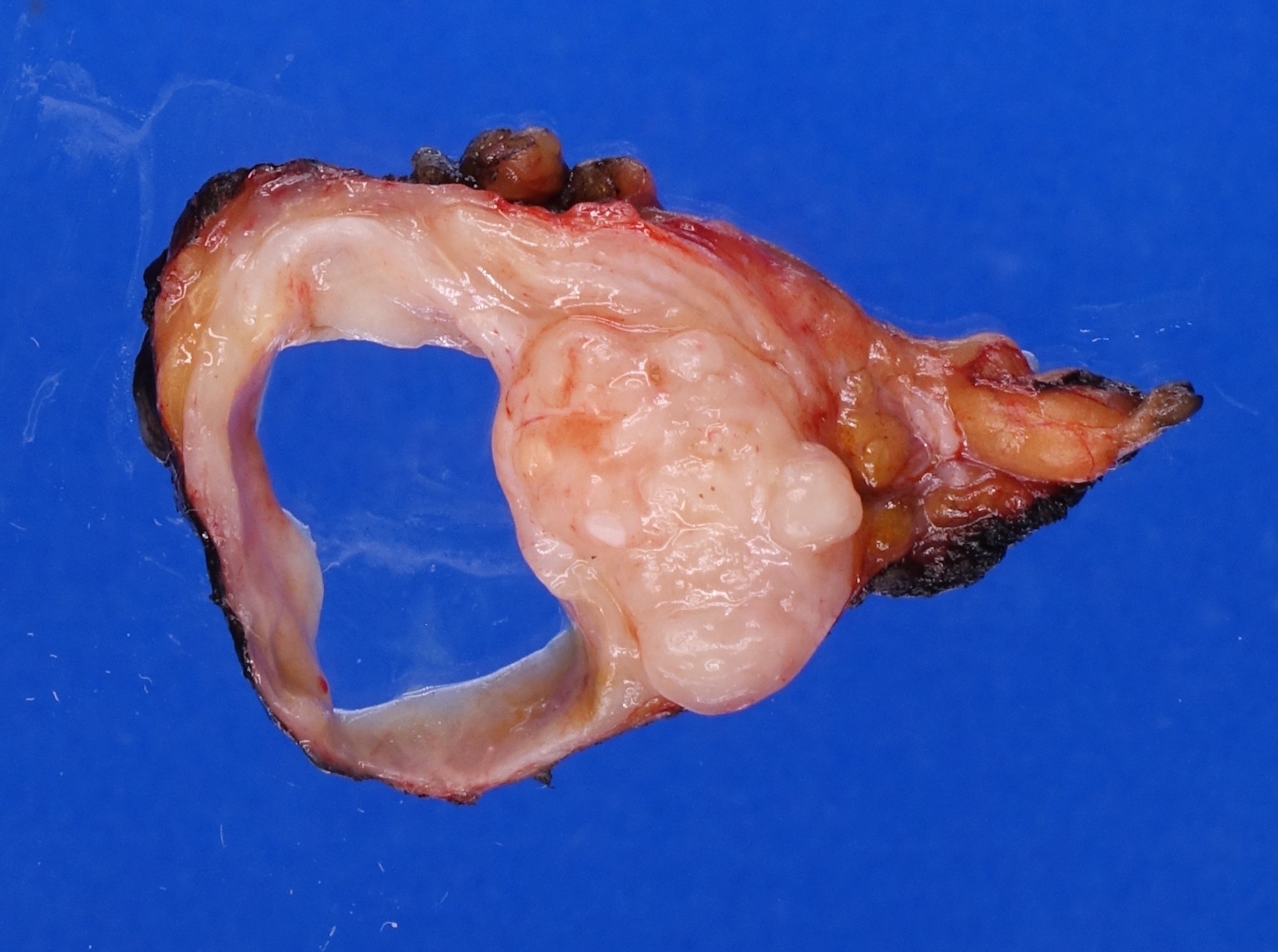
Gross description
- No gross findings have been reported in large cases series (Histopathology 2022;81:84, Am J Surg Pathol 2022;46:11)
Gross images
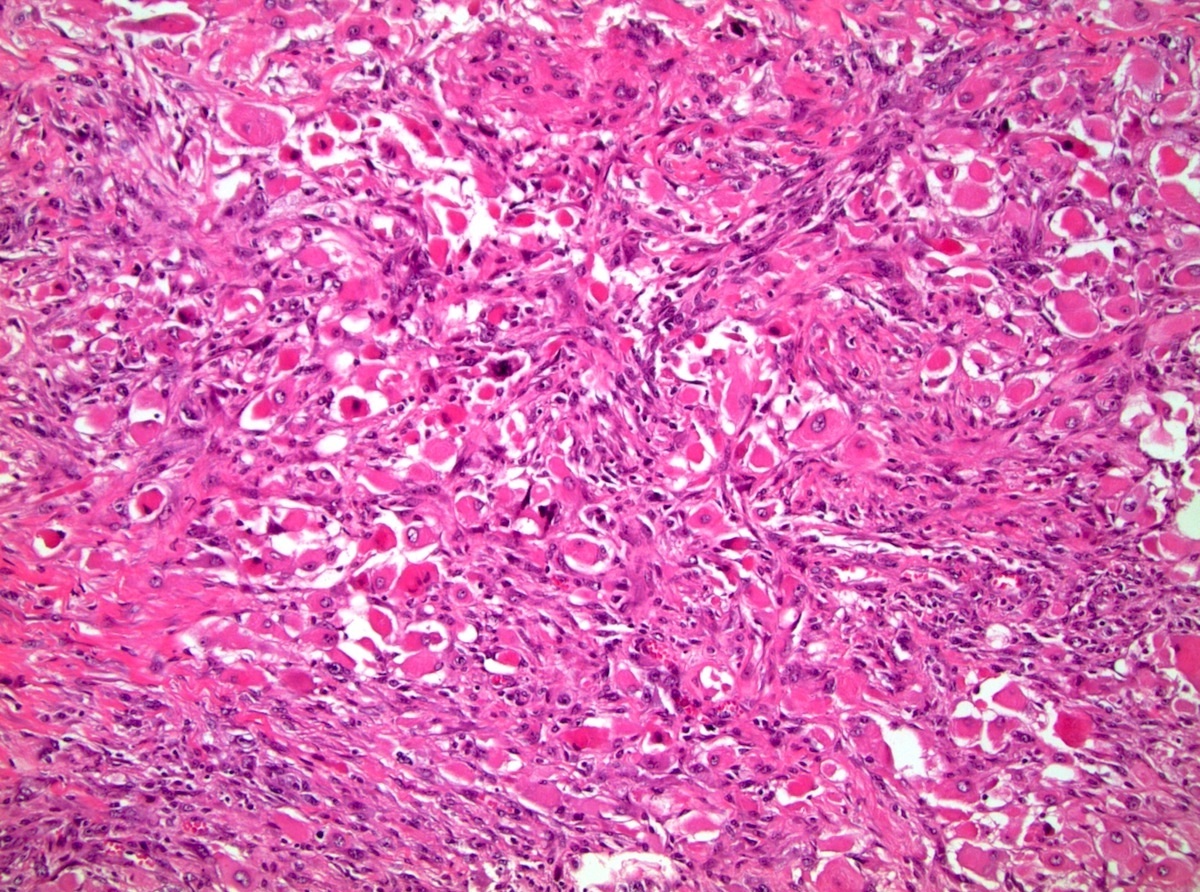
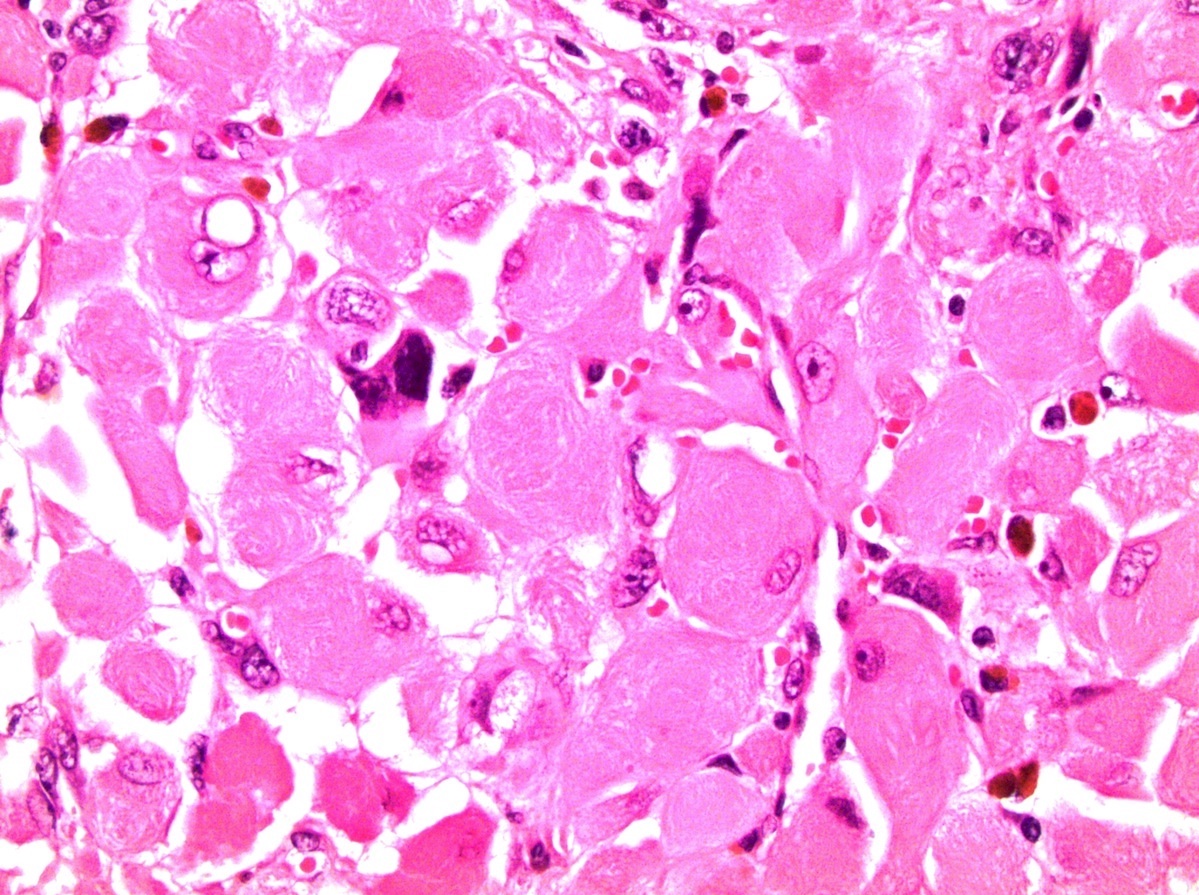
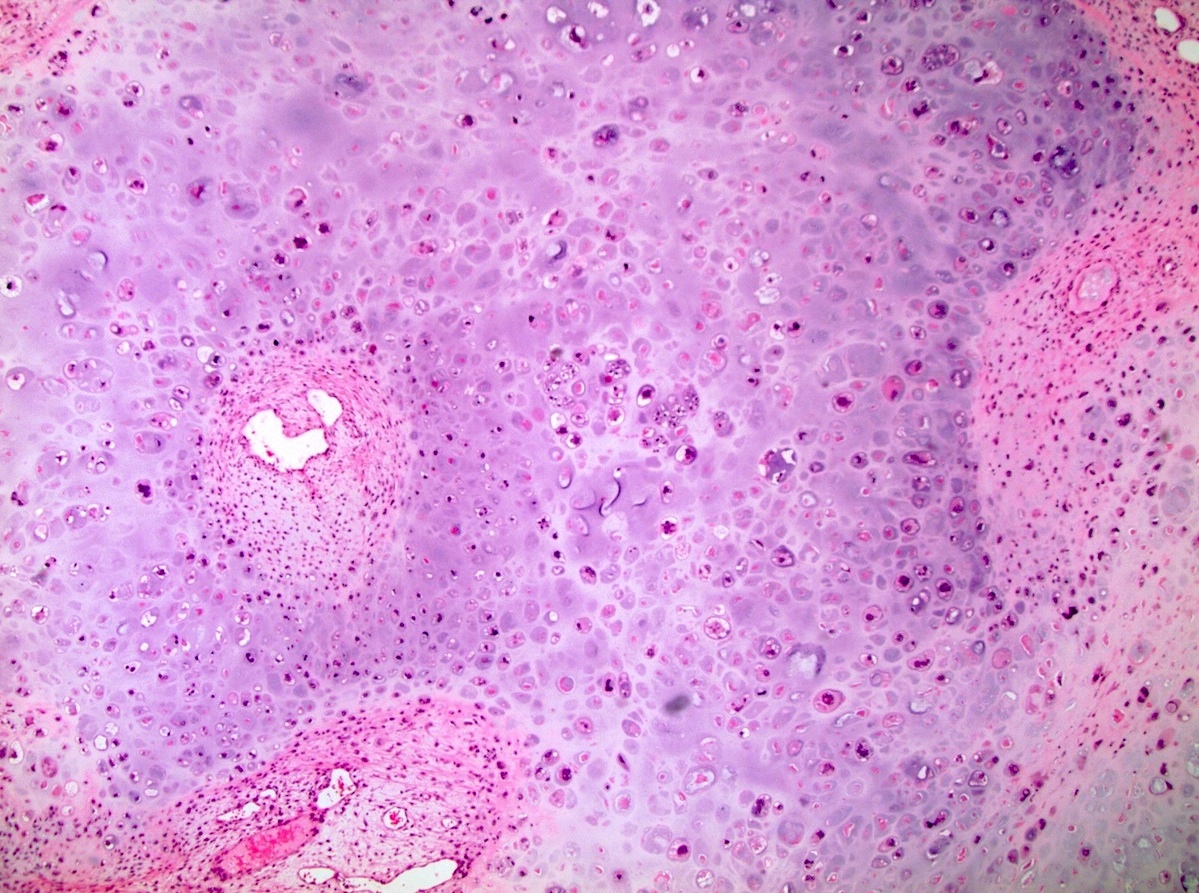
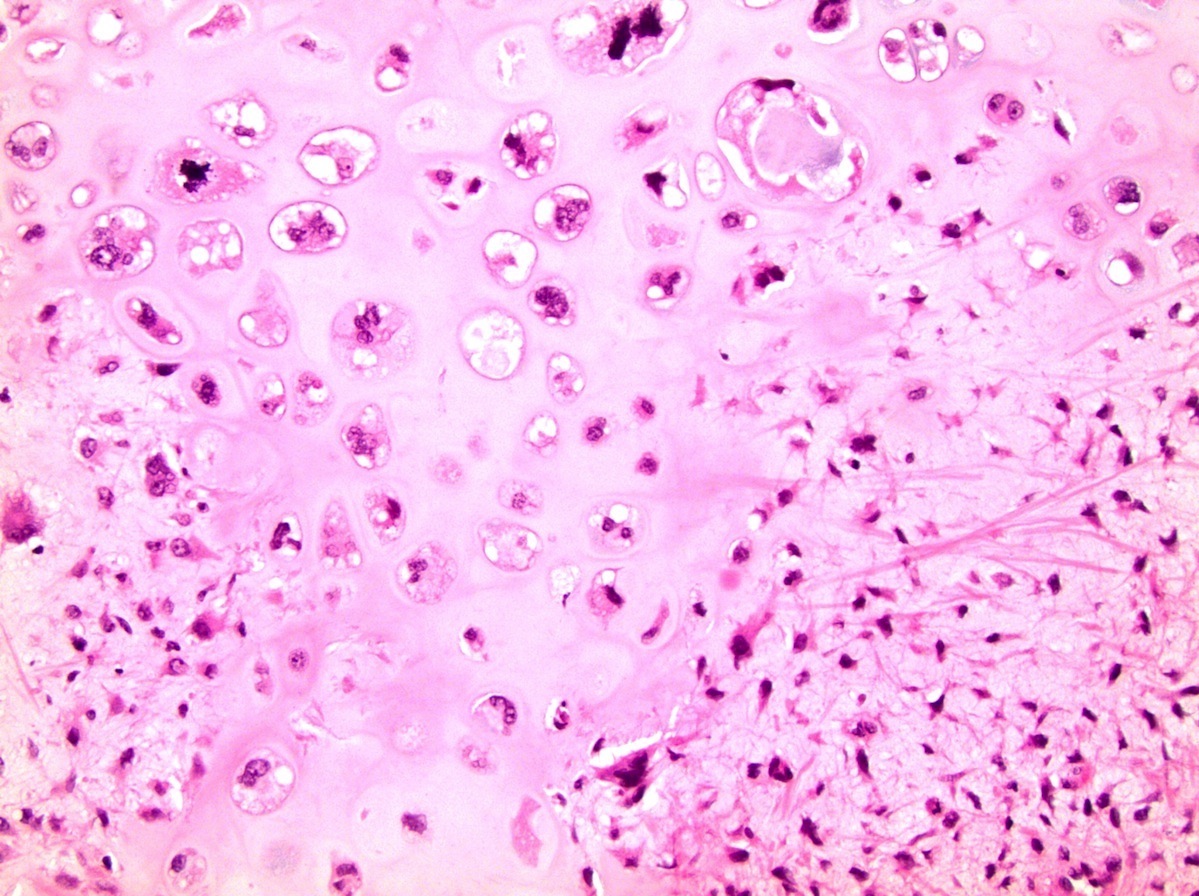
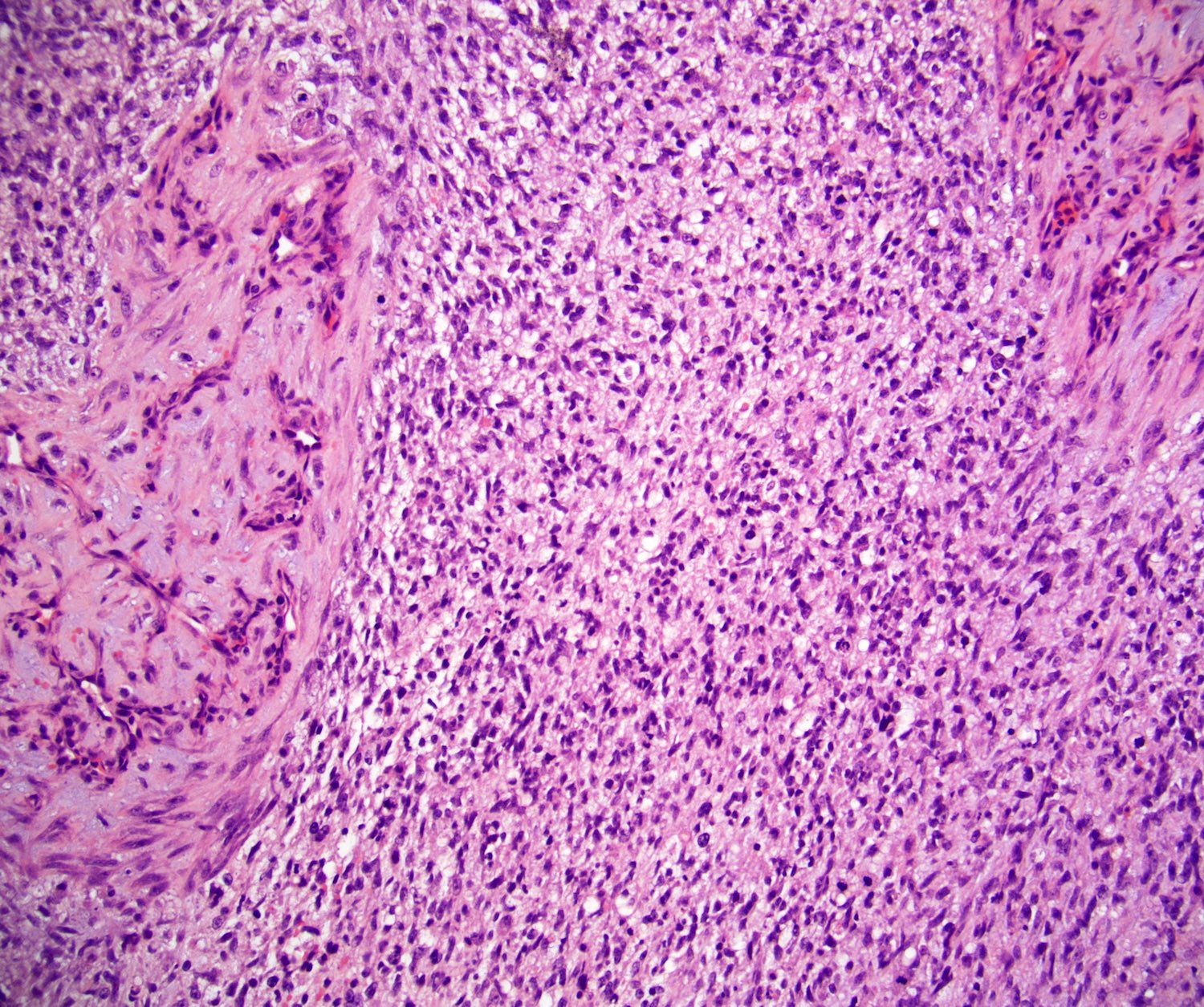
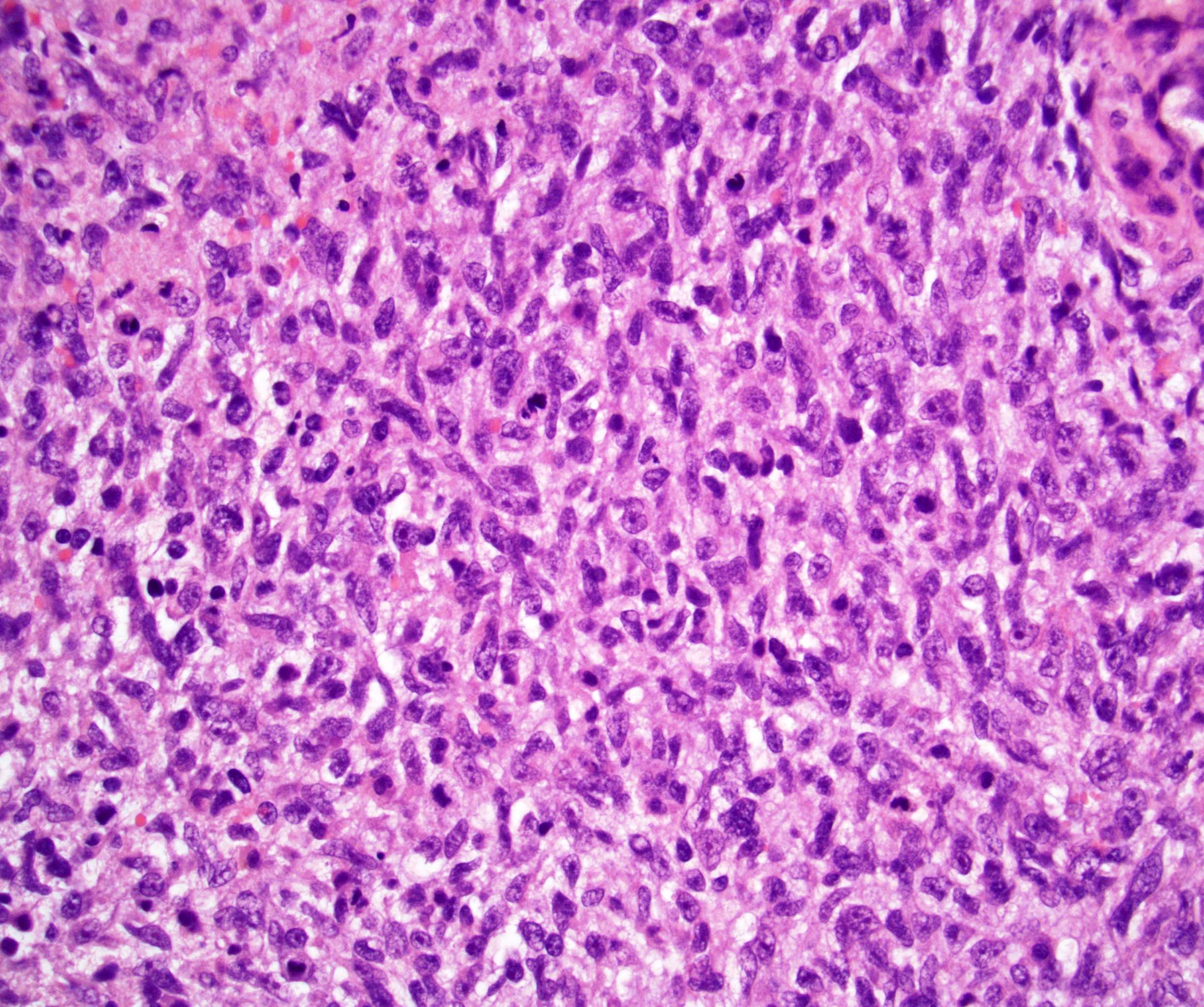
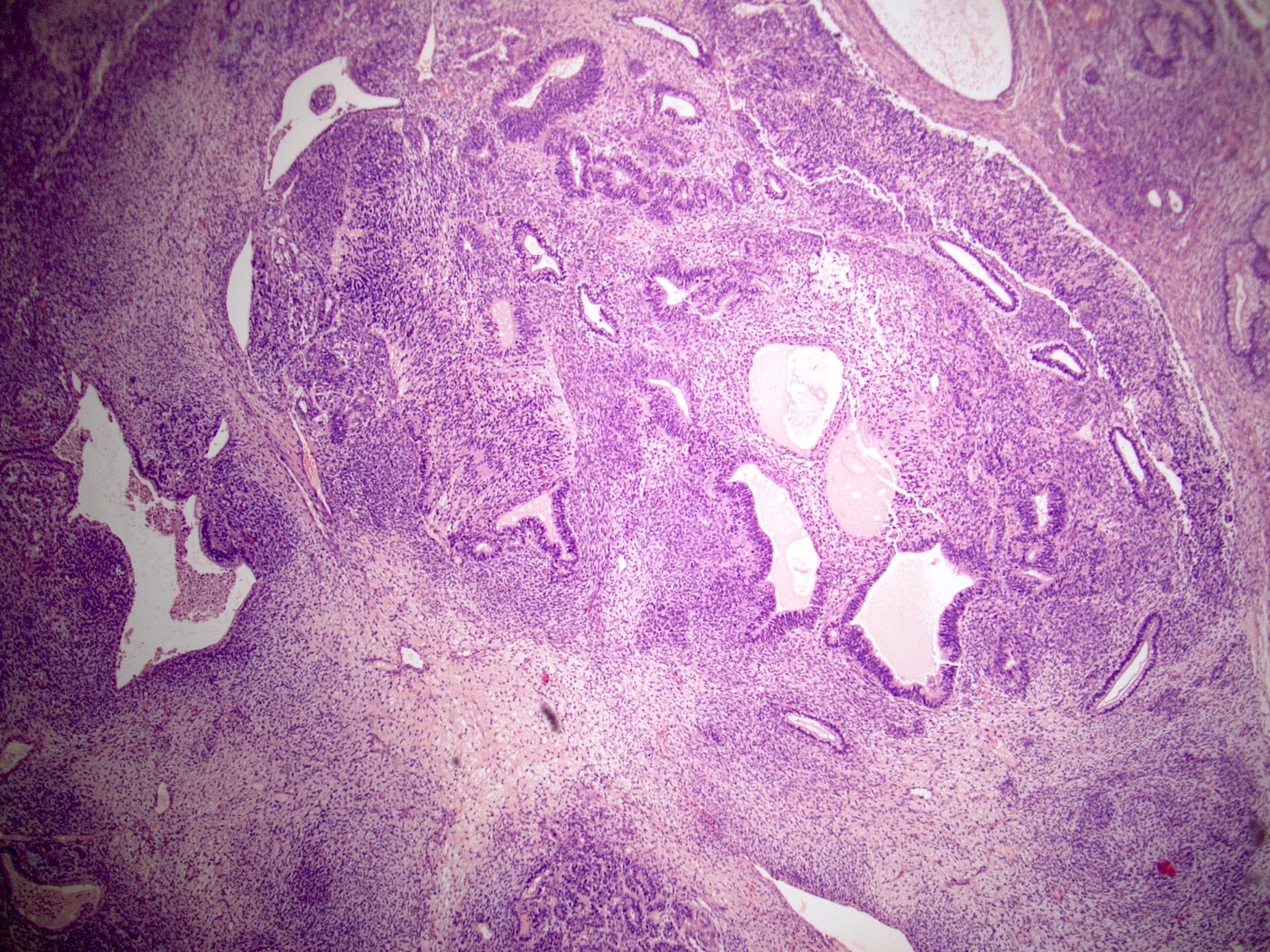
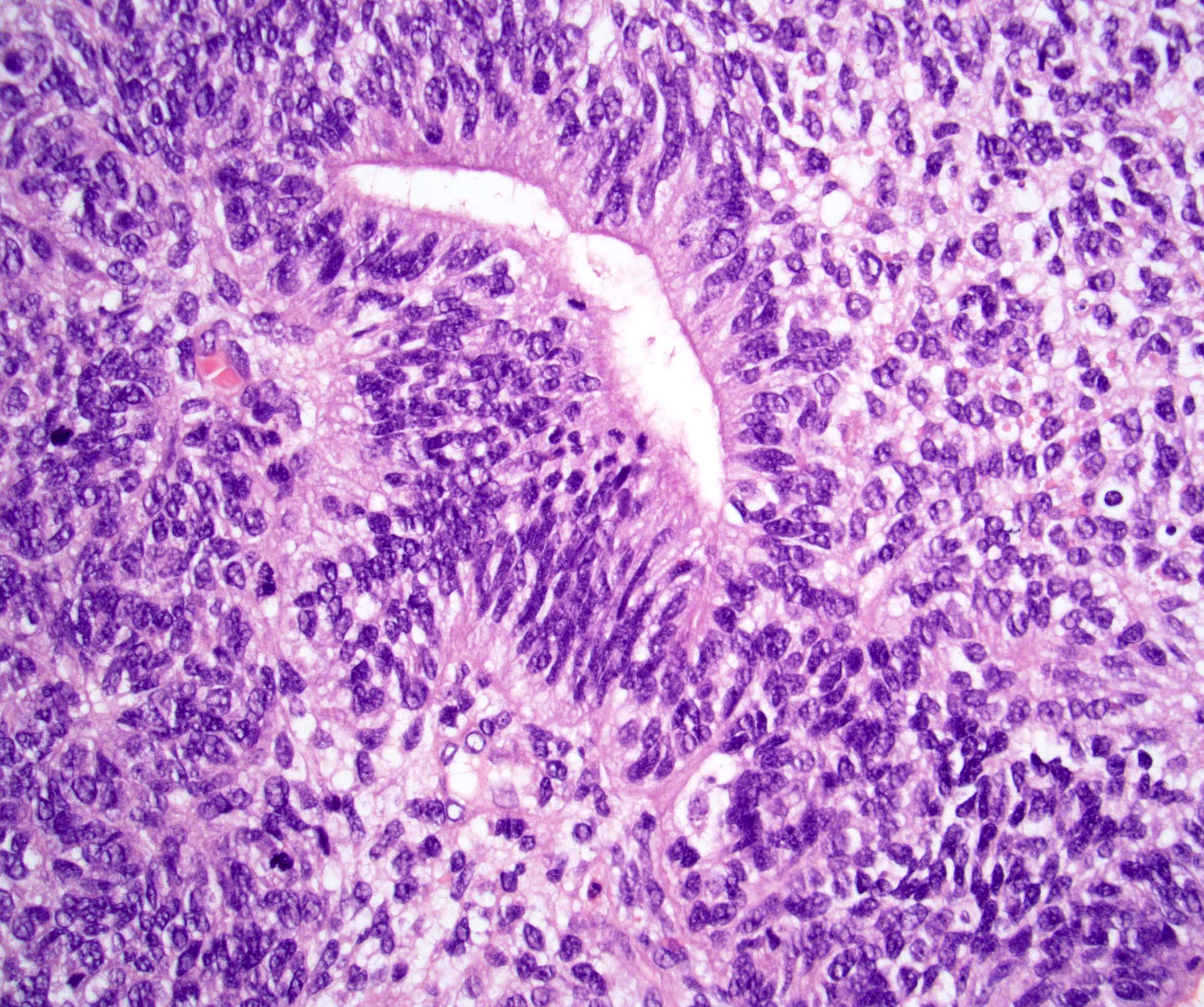
Microscopic (histologic) description
- Expansile and infiltrative pure area of atypical mesenchymal or epithelial cells that occupies ≥ 0.5 cm
- 4 most common histologies (Am J Surg Pathol 2022;46:11, Histopathology 2022;81:84):
- Rhabdomyosarcoma
- Adenocarcinoma
- Embryonic type neuroectodermal tumor
- Sarcoma, NOS
- Embryonic type neuroectodermal tumor appears as immature neuroectodermal elements
- Neuroglial tumors have CNS-like morphology similar to astrocytoma, glioma, glioblastoma and gliosarcoma (Am J Surg Pathol 2019;43:422)
- Nephroblastoma-like histology has been described
Microscopic (histologic) images
Positive stains
- Sarcoma:
- Desmin, myogenin, vimentin depending on type of sarcoma
- GPC3 (92% in rhabdomyosarcoma, variable to negative in other types of sarcoma) (Am J Surg Pathol 2014;38:1396)
- Adenocarcinoma:
- Cytokeratin, EMA (81%) (Virchows Arch 2012;461:27, Am J Surg Pathol 2014;38:1396)
- BerEP4 (91%), MOC31 (92%) (Am J Surg Pathol 2014;38:1396)
- CDX2 (63%) (Am J Surg Pathol 2014;38:1396)
- Embryonic type neuroectodermal tumor:
- Undifferentiated components: SOX11, synaptophysin (Arch Pathol Lab Med 2021;145:953)
- Differentiated components: S100, GFAP (Arch Pathol Lab Med 2021;145:953)
- Neuroglial:
- GFAP, ATRX (retained) (Am J Surg Pathol 2019;43:422)
Negative stains
- Sarcoma:
- SALL4 (0%) (Am J Surg Pathol 2014;38:1396)
- AFP (0%) (Am J Surg Pathol 2014;38:1396)
- Adenocarcinoma:
- CK7 (43%) (Am J Surg Pathol 2014;38:1396)
- SALL4 (36%) (Am J Surg Pathol 2014;38:1396)
- GPC3 (7%), AFP (4%) (Am J Surg Pathol 2014;38:1396)
- TTF1 (0%) (Am J Surg Pathol 2014;38:1396)
- Embryonic type neuroectodermal tumor:
- Undifferentiated components: S100, GFAP (Arch Pathol Lab Med 2021;145:953)
- Differentiated components: chromogranin, SOX11 (Arch Pathol Lab Med 2021;145:953)
- Neuroglial:
- IDH1 pR132H (wildtype), BRAF p.V600E (Am J Surg Pathol 2019;43:422)
Molecular / cytogenetics description
- 12p gain or i(12p) is usually present (Histopathology 2022;81:84, Am J Surg Pathol 2012;36:1849)
- Clonal relationship to the associated teratoma (Am J Surg Pathol 2012;36:1849)
Sample pathology report
- Right testis, radial orchiectomy:
- Mixed germ cell tumor, embryonal carcinoma (75%), yolk sac tumor (10%), teratoma (10%), teratoma with somatic malignancy composed of embryonic type neuroectodermal tumor (5%) (see synoptic report)
- Left lung, wedge resection:
- Metastatic rhabdomyosarcoma, 3.2 cm (see comment)
- Comment: The patient has a history of a mixed testicular germ cell tumor. The current tumor is consistent with testicular origin (teratoma with somatic malignancy).
Differential diagnosis
- Metastasis of non-germ cell tumor (primary sarcoma or carcinoma):
- History of primary sarcoma or carcinoma
- Both primary sarcoma / carcinoma and somatic malignancies of sarcoma / carcinoma are usually SALL4 negative so this cannot be used to discriminate
- Lack 12p abnormality
- Teratoma without somatic type malignancy:
- Malignant appearing somatic cells occupy < 0.5 cm
- Yolk sac tumor (glandular or sarcomatoid):
- Mimics adenocarcinoma and sarcoma
- Should be considered before a postchemotherapy diagnosis of sarcoma as the somatic type is rendered (Am J Surg Pathol 2015;39:251)
- Sarcomatoid yolk sac tumor: GPC3 (100%), AE1 / AE3 (100%), SALL4 (60%), AFP (0%) (Am J Surg Pathol 2014;38:1396)
- Glandular yolk sac tumor: GPC3 (86%), EMA (71%), SALL4 (71%), AFP 71%, CK7 (14%) (Am J Surg Pathol 2014;38:1396)
- Choriocarcinoma:
- Cytotrophoblasts mimic squamous cell carcinoma
- βhCG positive
- Embryonal tumor with multilayered rosettes, C19MC altered:
- Mimics embryonic type neuroectodermal tumor
- C19MC amplification
- Lack 12p abnormality
- Ewing sarcoma
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
- A 43 year old man with a history of testicular mixed germ cell tumor treated with orchiectomy and chemotherapy is found to have an undifferentiated mesenchymal tumor. Which finding would best support this tumor being teratoma with somatic type malignancy?
- Isochromosome 12p
- MYC amplification
- TERT promoter mutation
- Expression of ERG
Board review style answer #2