Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Tekin B, Jimenez RE. Adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisreteadeno.html. Accessed November 28th, 2024.
Definition / general
- Rare malignant neoplasm originating from the epithelium of rete testis and associated with an aggressive clinical behavior
- Given its rarity, varied histologic presentations and nonspecific immunoprofile, primary adenocarcinoma of collecting ducts and rete testis is a diagnosis of exclusion
Essential features
- Primary adenocarcinoma of collecting ducts and rete testis is a rare aggressive neoplasm originating from the epithelium of rete testis
- Diagnosis of exclusion, with the differential diagnosis including mesothelioma, metastatic adenocarcinoma and germ cell tumors, among other entities
- On histopathologic examination, a mixture of different architectural patterns is commonly seen, such as complex tubulopapillary, glandular, solid and cribriform
- Cytokeratin 7, cytokeratin AE1 / AE3 and epithelial membrane antigen are positive in the majority of the cases, whereas CD30, inhibin, OCT 3/4 and SALL4 are negative
Terminology
- Not used anymore: papillary adenocarcinoma of the rete testis, carcinoma of the rete testis
ICD coding
Epidemiology
- Extremely rare, with fewer than 100 cases reported in the literature
- More common in elderly Caucasian males (mean age of 54 years); however, anecdotal reports in young adults (Am J Surg Pathol 2021;45:1720)
Sites
- Primary involvement of the testicular hilum
- Secondary involvement of adjacent anatomic structures by direct extension
- Some studies documented a slight right side predominance (Am J Surg Pathol 2021;45:1720, Urology 1995;46:468)
- Satellite nodules on the spermatic cord are seen in a subset of patients (Mod Pathol 2005;18:S131)
Pathophysiology
- Anecdotal cases with a history of adenomatous hyperplasia of the rete testis and subsequent development of adenocarcinoma, as well as cases with coexistent adenomatous hyperplasia and adenocarcinoma, have been reported (J Urol 1997;158:1525, Diagn Pathol 2013;8:105)
- However, more studies are needed to definitively establish a stepwise progression from normal rete testis to adenomatous hyperplasia and subsequent occurrence of primary adenocarcinoma
Etiology
- Adenocarcinoma of the rete testis has been reported in mice with in utero exposure to diethylstilbestrol; however, no such association has been described in humans (Cancer Res 1985;45:5145, Am J Surg Pathol 2019;43:670)
- Prior trauma, chronic epididymitis, cryptorchidism or inguinal hernia have been documented; however, a definitive etiologic association has not been established (Am J Surg Pathol 2021;45:1720, J Urol 2003;170:1304)
- Hydrocele was described in ~33% of cases, with many patients presenting with a working diagnosis of hydrocele and undergoing ipsilateral hydrocelectomy (Urology 1995;46:468, Mod Pathol 2005;18:S131, Am J Surg Pathol 2019;43:670)
Clinical features
- Nonspecific clinical presentation
- Majority of patients present with a scrotal mass, accompanied by pain in ~20% of the cases (Am J Surg Pathol 2019;43:670)
- Occasionally detected incidentally, following trauma (Histopathology 2022;81:77)
- Initial signs of presentation can be due to tumor metastases (e.g., groin mass, lumbar pain) (Urology 1995;46:468)
Diagnosis
- Testicular, paratesticular and metastatic tumors need to be ruled out before arriving at a diagnosis of primary rete testis adenocarcinoma; as such, it represents a diagnosis of exclusion
- Currently accepted diagnostic criteria for primary adenocarcinoma of the rete testis have been revised from Nochomovitz and Orenstein and include the following:
- Testicular hilar localization
- Absence of morphologically similar extrascrotal tumor as a possible primary site
- Morphology incompatible with other types of testicular or paratesticular neoplasms
- Supportive immunohistochemical findings and immunohistochemical exclusion of other entities, especially mesothelioma and papillary serous carcinoma (Am J Surg Pathol 2021;45:1720, Mod Pathol 2005;18:S131, Am J Surg Pathol 1984;8:625)
- Demonstration of transition from normal to neoplastic rete epithelium is a desirable criterion but frequently not identifiable since the normal anatomy tends to be obliterated by the neoplastic process (Am J Surg Pathol 2021;45:1720)
- Application of these strict criteria led to exclusion or reclassification of many cases that were initially reported as primary rete testis adenocarcinoma in the literature (Am J Surg Pathol 2019;43:670)
Laboratory
- Alkaline phosphatase (ALP), alpha fetoprotein (AFP), CA-125, CA 19-9, carcinoembryonic antigen (CEA), β human chorionic gonadotropin, (βhCG) levels are generally normal
- Anecdotal reports of elevated CA 19-9 and CEA (Urology 1995;46:468, Int Cancer Conf J 2017;6:84, Int Cancer Conf J 2020;9:240)
Radiology description
- Rationale for imaging is threefold:
- Exclusion of an extrascrotal tumor as a possible primary site
- Visualization of the scrotal tumor
- Staging
- Ultrasound may show an ill defined, hypoechoic, heterogeneous mass and increased vascularization (Urol Case Rep 2017;16:72, Oncol Lett 2014;7:455)
- Intrascrotal calcification may be present on radiographs (Urology 1995;46:468)
- Potentially improved utility of CT / PET compared to conventional CT in detecting metastases (Urology 2011;77:334)
Prognostic factors
- Predictors associated with a favorable outcome:
- Tumor size < 5 cm (Urology 1995;46:468)
- Tumors confined to the testis (Urology 1995;46:468, Am J Surg Pathol 2019;43:670)
Case reports
- 44 year old man with left scrotal swelling (Int Cancer Conf J 2020;9:240)
- 59 year old man with swelling of the left scrotum (Int Cancer Conf J 2017;6:84)
- 66 year old man with a left sided painful testicular mass (Urol Case Rep 2017;16:72)
Treatment
- Treatment options for primary rete testis adenocarcinoma are not standardized
- Treatment consists of radical orchiectomy with or without retroperitoneal lymph node dissection, in combination with adjuvant chemotherapy or radiotherapy
- Resistance to conventional chemotherapy regimens is a frequent problem (Histopathology 2022;81:77)
Gross description
- Epicenter of the mass at the testicular hilum, with variable involvement of the testicular parenchyma, spermatic cord or overlying skin by way of direct extension
- Ill defined, firm tumors ranging from 2 - 13 cm in greatest dimension
- Cut surface tan, yellow or white; solid to cystic, with focally hemorrhagic areas
- References: Am J Surg Pathol 2019;43:670, Am J Surg Pathol 2021;45:1720
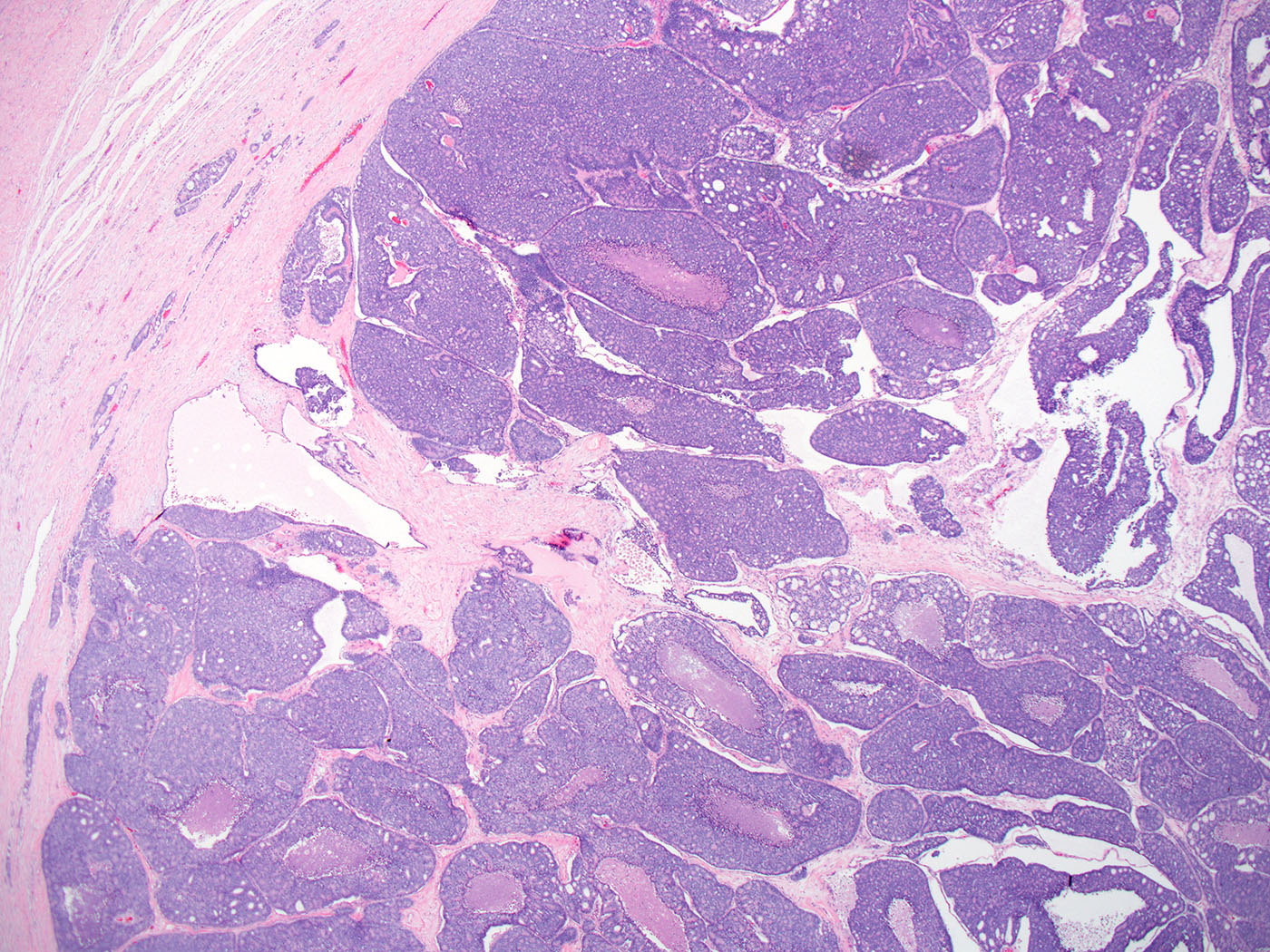
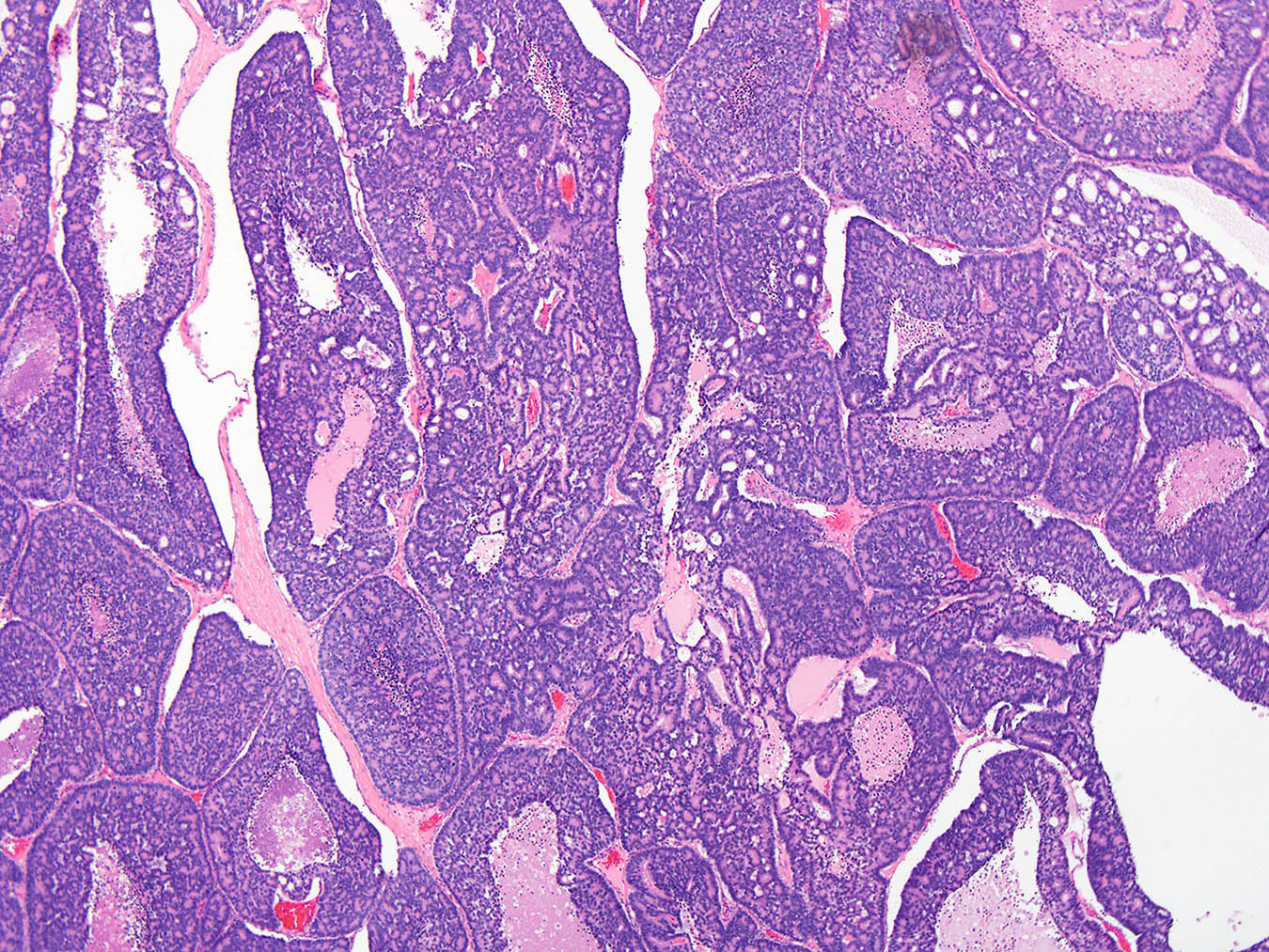
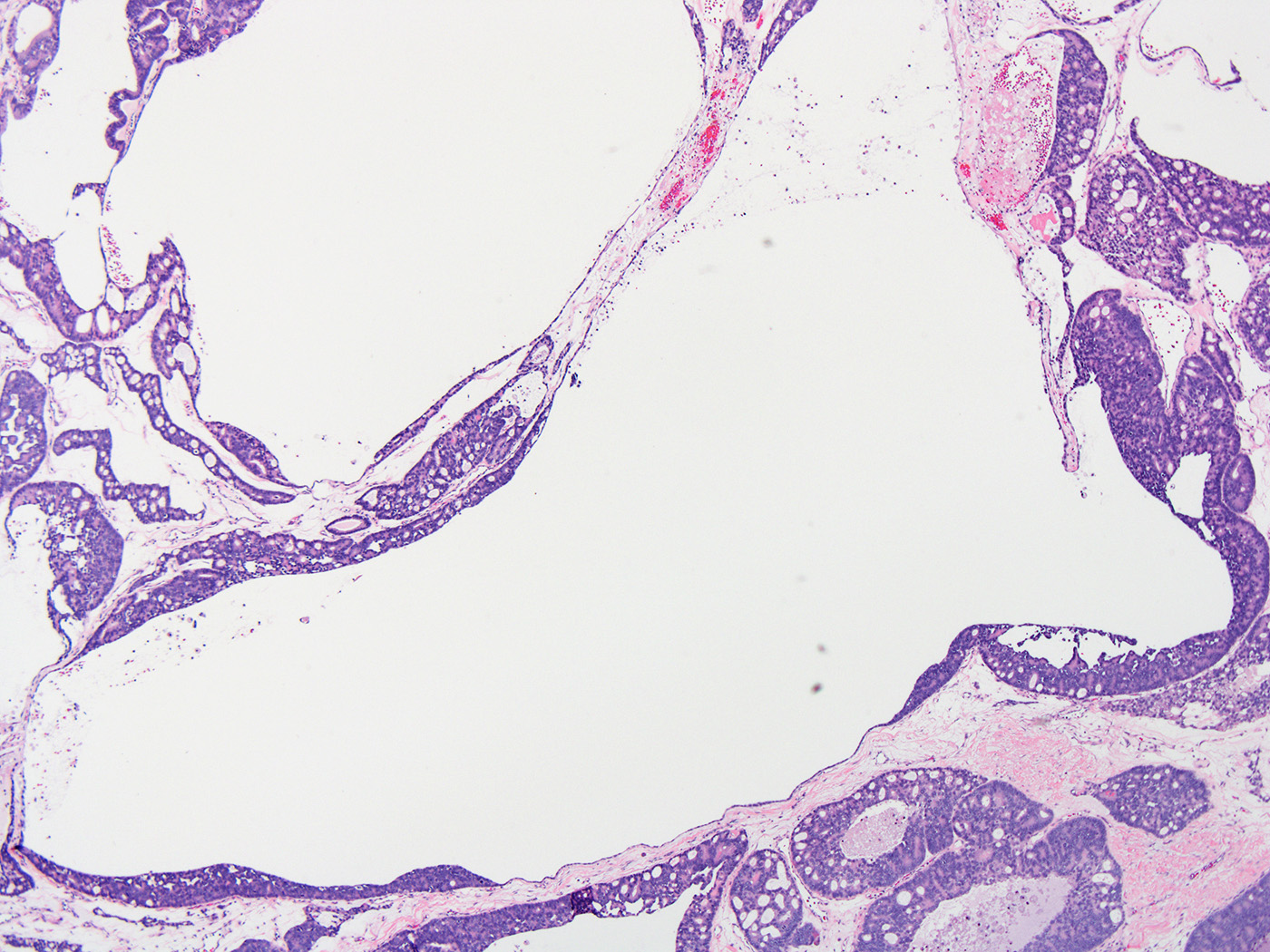
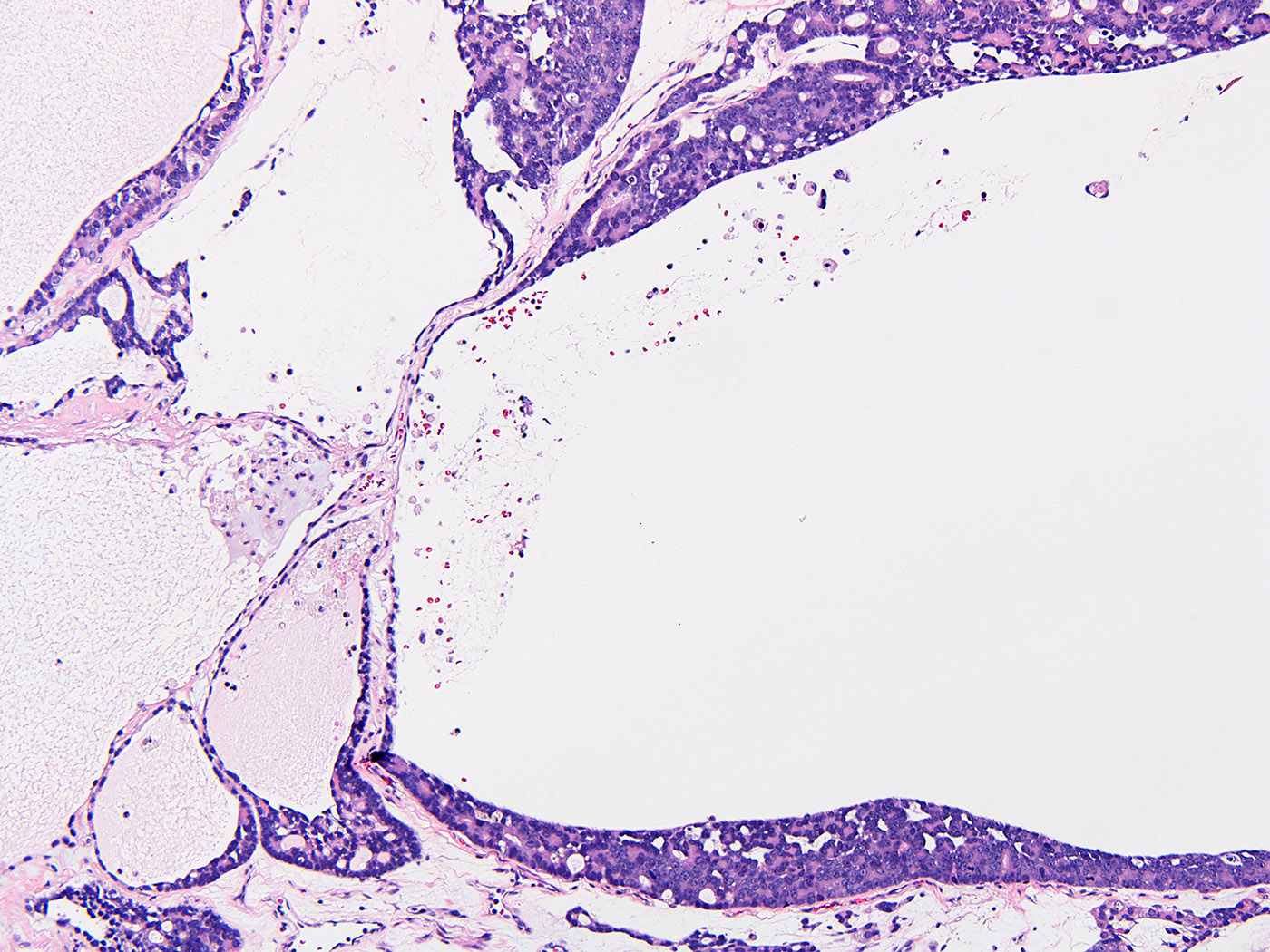
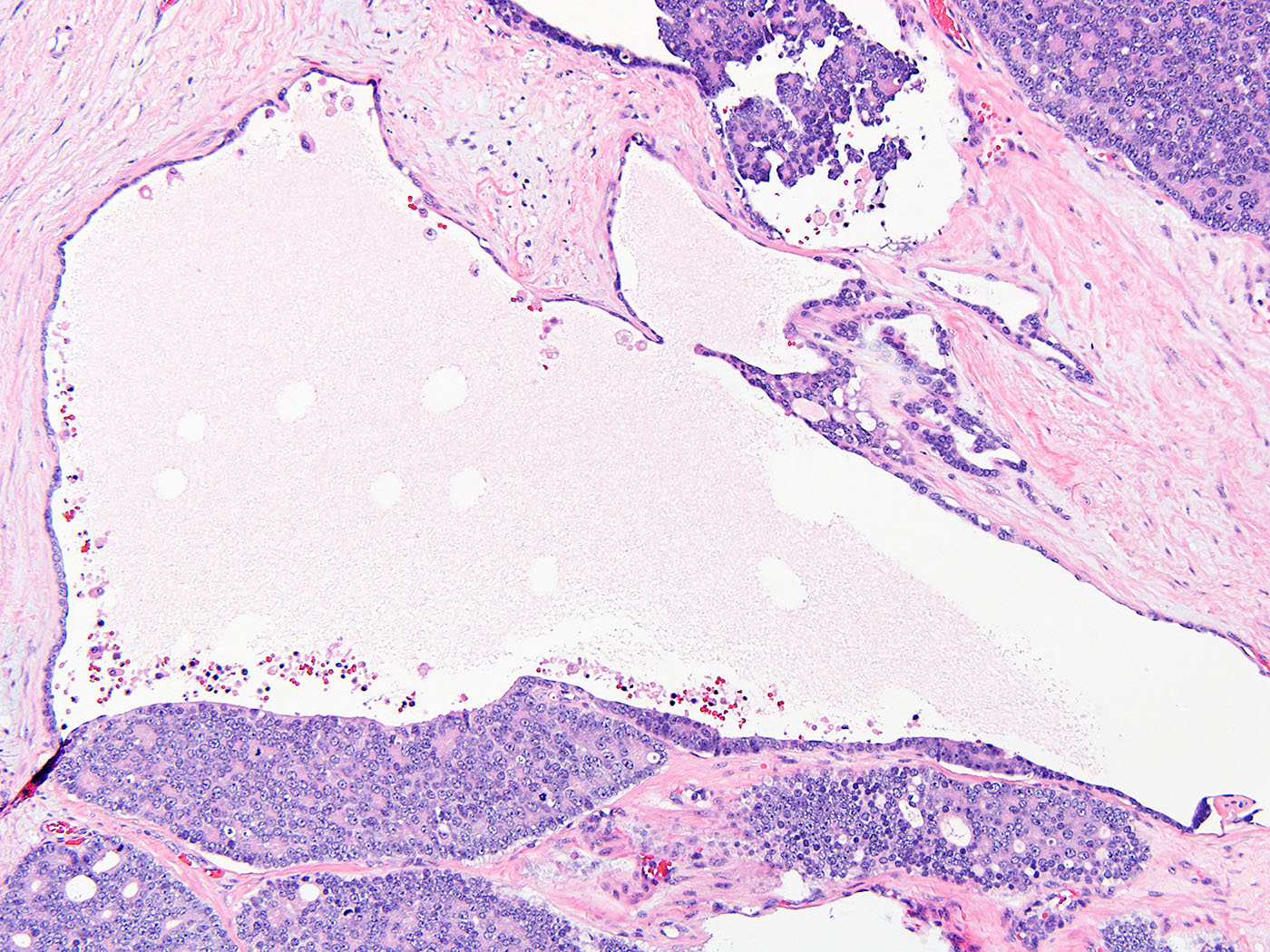
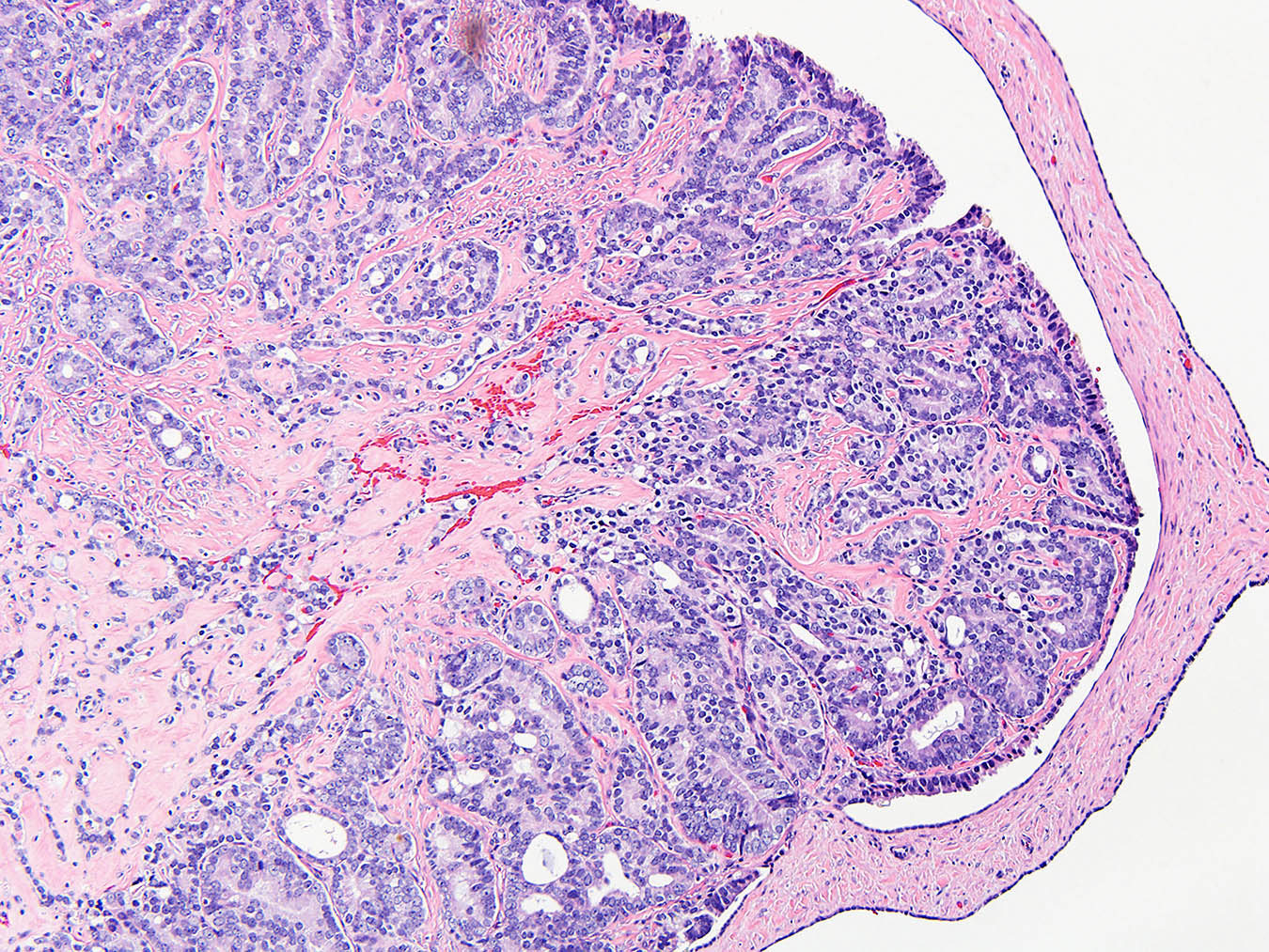
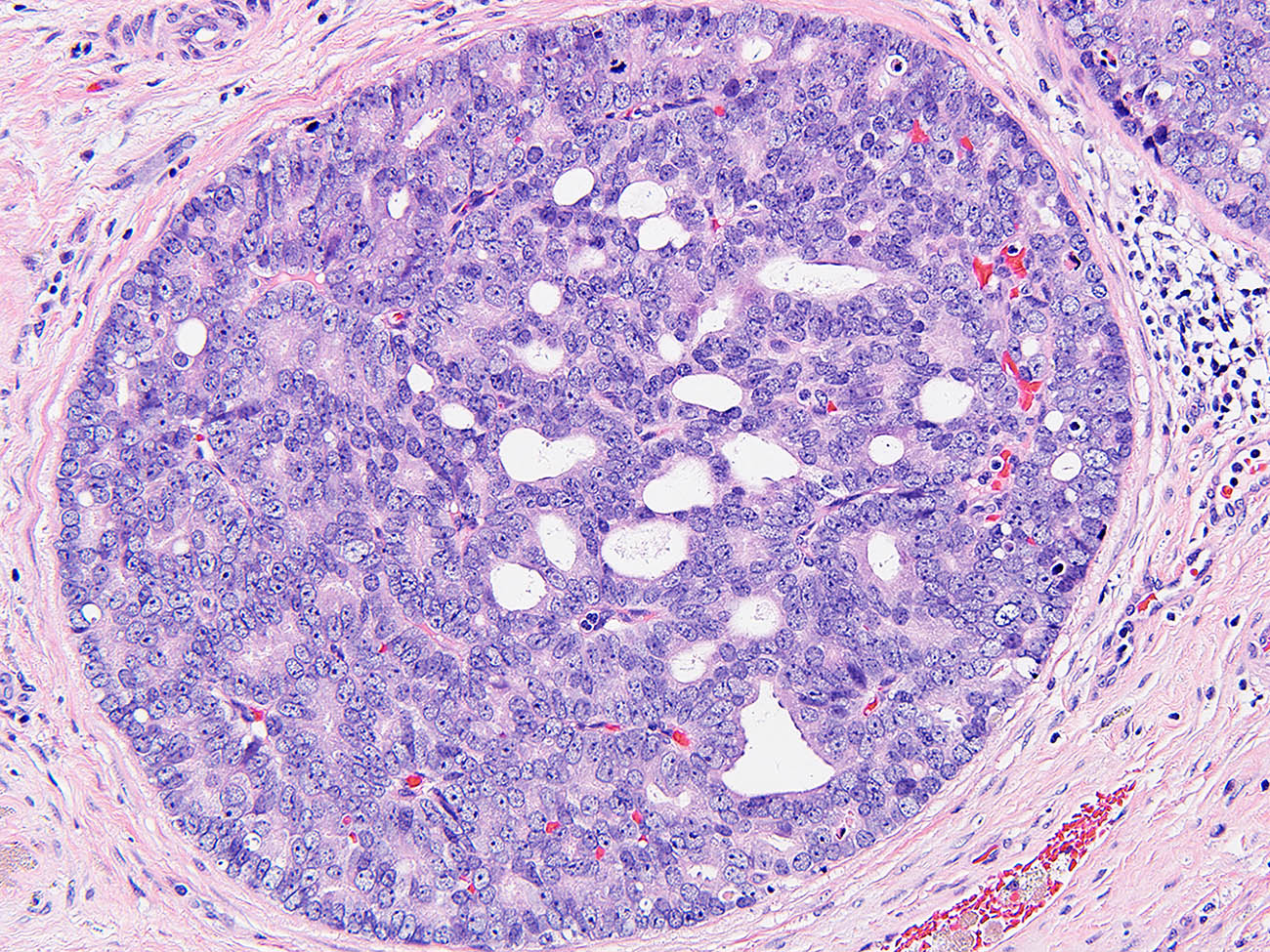
Microscopic (histologic) description
- Invasive growth pattern with extensive intrarete proliferation and extension beyond the rete testis
- Architecture: a mixture of architectural patterns among different cases and within the same case, including but not limited to (Am J Surg Pathol 2021;45:1720, Am J Surg Pathol 2019;43:670):
- Complex tubulopapillary
- Glandular
- Solid
- Cribriform
- Glomeruloid
- Retiform
- Sertoliform
- Kaposiform
- Micropapillary
- Nested
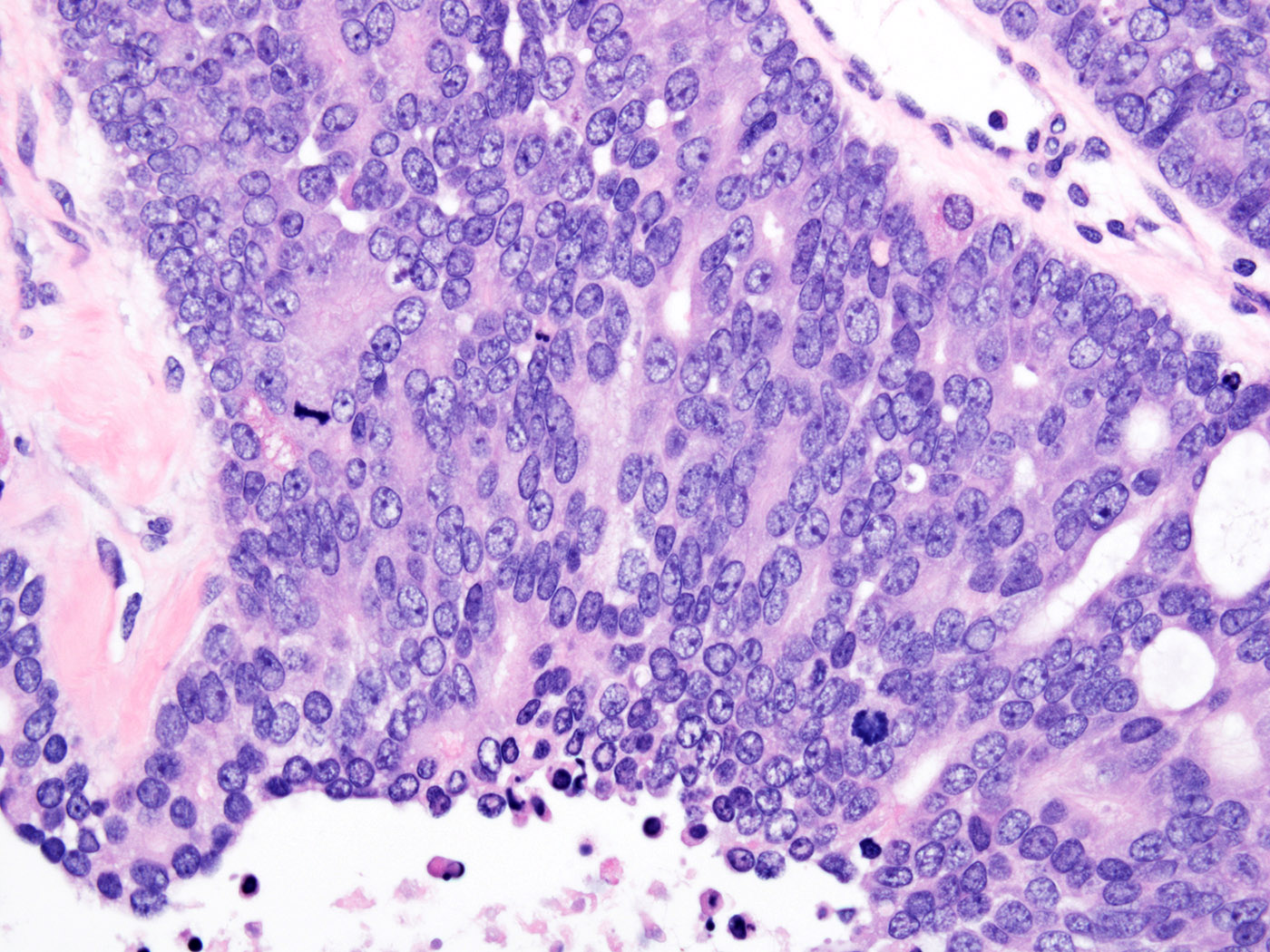
- Cytomorphology (Histopathology 2022;81:77):
- Epithelioid or biphasic (epithelioid and sarcomatoid) (J Nat Sci Biol Med 2015;6:211)
- Cuboidal to columnar cells with marked nuclear atypia, pleomorphism and prominent nucleoli
- High mitotic activity, with atypical mitoses
- Cytoplasm varies from pale to eosinophilic
- Desmoplastic stroma is a common finding
- Psammomatous calcifications and tumor necrosis may be observed (Urology 1995;46:468)
- Areas of gradual transition from normal rete testis lining to dysplastic and malignant epithelium, if present, lend support to a primary rete testis origin
Microscopic (histologic) images
Positive stains
- CK7, CK AE1 / AE3, epithelial membrane antigen (EMA) and vimentin positive in > 80% of cases
- CD10 (Mod Pathol 2005;18:S131, Indian J Pathol Microbiol 2015;58:232)
- BerEP4, CK5/6, MOC31 and PAX8 positive in > 50% of cases (Am J Surg Pathol 2021;45:1720, Diagn Pathol 2013;8:105, Am J Surg Pathol 2019;43:670, Histopathology 2022;81:77)
- Calretinin and WT1 variably positive (J Cutan Pathol 2006;33:181)
- In a series of 5 cases, calretinin was positive in 2 cases (40%) (Am J Surg Pathol 2019;43:670)
- In a recent series, nuclear WT1 was positive in 7/9 and 6/7 cases tested (78 - 86%) (Am J Surg Pathol 2021;45:1720, Histopathology 2022;81:77)
Negative stains
- CD30, inhibin, NKX3.1, OCT 3/4, PSA, PSAP and SALL4 consistently negative (Am J Surg Pathol 2021;45:1720, Am J Surg Pathol 2019;43:670, Histopathology 2022;81:77)
- CK20 rarely positive (Urol Case Rep 2017;16:72, Int J Urol 2006;13:1532)
Electron microscopy description
- Glandular spaces with amorphous, electron dense material
- Luminal spaces lined by epithelial cells with ovoid nuclei exhibiting smooth contours, dispersed heterochromatin and prominent nucleoli
- Nuclear indentations were described (Am J Surg Pathol 1988;12:492, Indian J Cancer 2002;39:106)
- Lipid droplets and bundles of intermediate cytoplasmic filaments in a subset of neoplastic cells (J Cutan Pathol 2006;33:181, Indian J Cancer 2002;39:106, Cancer 1989;64:770)
Molecular / cytogenetics description
- Acosta et al. described genomic alterations in a series of 8 cases using massively parallel DNA sequencing (Histopathology 2022;81:77)
- Pathogenic variants were noted in 6 cases:
- 3 cases harbored CDKN2A variants
- Authors also described variants in AKT1, RB1, NF2, SETD2 and TP53 genes
Sample pathology report
- Testicle, left, orchiectomy:
- Adenocarcinoma, involving the rete testis, most consistent with a primary rete testis adenocarcinoma, 2.5 cm (see comment)
- Surgical margins negative for carcinoma
- Comment: The sections show a high grade cellular proliferation with an invasive growth pattern, centered in and around the rete testis. A mixture of architectural patterns is noted, including complex tubulopapillary, glandular, cribriform and solid areas. Focally, a transition between the surface epithelium of the rete testis and the invasive component is appreciable. The cytomorphology is notable for cuboidal to columnar cells with marked nuclear atypia, pleomorphism and prominent nucleoli. Immunohistochemically, the tumor cells are reactive for BerEP4, CK7 and EMA and negative for CDX2, inhibin, NKX3.1, OCT 3/4, PSA and TTF1. These findings argue against a germ cell tumor or mesothelioma and favor a primary tumor over a metastatic process. Based on this constellation of findings, the most likely possibility is that this is a primary rete testis adenocarcinoma; however, a metastatic process cannot be completely ruled out and thus another primary process should be clinically excluded.
Differential diagnosis
- Transition between normal and neoplastic rete testis epithelium, if present, favors a diagnosis of primary rete testis adenocarcinoma over the following entities in the differential diagnosis:
- Mesothelioma:
- Significant overlap in histopathologic findings
- Multifocal enveloping of the tunica vaginalis; this is in contrast to the rete testis centered, usually solitary tumor in primary rete testis adenocarcinoma
- Generally less prominent nuclear atypia
- Positive immunostaining for calretinin and WT1 combined with negative staining for CEA and BerEP4 favors a diagnosis of mesothelioma, although primary rete testis adenocarcinomas show immunoreactivity for calretinin and WT1 in a subset of cases (see Positive stains above) (Mod Pathol 2005;18:S131)
- Metastatic adenocarcinoma:
- Should be excluded before a diagnosis of primary rete testis adenocarcinoma is rendered
- More frequently shows bilateral or multifocal involvement
- Classically exhibits an interstitial growth pattern, as opposed to originating from the rete testis (Mod Pathol 2005;18:S131)
- Germ cell tumors:
- Generally younger patient population and associated with increased serum markers
- OCT 3/4 and SALL4 positive (Am J Surg Pathol 2019;43:670)
- Epididymal carcinoma:
- More likely to show cuboidal cells having clear to eosinophilic cytoplasm in a tubular pattern
- May not be possible to distinguish in advanced tumors where anatomic landmarks have been obliterated (Am J Surg Pathol 1997;21:1474)
- Malignant Sertoli cell tumor:
- Originates from the testicular parenchyma (Mod Pathol 2005;18:S131)
- Inhibin positive (Am J Surg Pathol 2019;43:670)
- Ovarian type epithelial tumors of the paratesticular region
- Mesothelioma:
Additional references
Board review style question #1
A 68 year old man presents with a 4.7 cm nodule centered around the testicular hilum, with invasion into the testicular parenchyma. Cut surface is heterogeneous, with solid, cystic and hemorrhagic areas. Histologic examination reveals a mixture of architectural patterns, including glandular, cribriform and solid areas. The cells exhibit nuclear pleomorphism, prominent nucleoli and high mitotic activity (see figures above). Clinicoradiologic examination fails to identify any extrascrotal tumors. Based on the constellation of findings, the man is diagnosed with primary adenocarcinoma of rete testis. Regarding this entity, which of the following statements is true?
- CK7, CK AE1 / AE3 and EMA are positive in the majority of the cases
- It frequently shows immunoreactivity for CD30, OCT 3/4 and SALL4
- Many patients are asymptomatic and these tumors are usually detected incidentally on imaging studies
- These tumors typically follow an indolent course, without metastases
- This entity is typically associated with increased levels of alpha fetoprotein and βhCG
Board review style answer #1
A. CK7, CK AE1 / AE3 and EMA are positive in the majority of the cases
Comment Here
Reference: Adenocarcinoma of collecting ducts and rete testis
Comment Here
Reference: Adenocarcinoma of collecting ducts and rete testis