Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shah MD, Zynger D. Regressed germ cell tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisregressedgct.html. Accessed April 2nd, 2025.
Definition / general
- Testicular germ cell tumor presenting with spontaneous complete or partial regression (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303, Case Rep Oncol 2017;10:846)
Essential features
- Testicular germ cell tumor presenting with spontaneous complete or partial regression (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303, Case Rep Oncol 2017;10:846)
- Presents as metastasis, residual testicular germ cell tumor or both (BJU Int 2004;94:74, Case Rep Oncol 2017;10:846, Am J Surg Pathol 2006;30:858)
- Histologic features of testicular tumor regression include fibrous scar and germ cell neoplasia in situ (J Ultrasound Med 2003;22:515, Am J Surg Pathol 2006;30:858)
- Most commonly associated with pure seminoma in metastasis and residual testicular tumor (Am J Surg Pathol 2006;30:858, J Urol 2009;182:2303)
Terminology
- Regressed germ cell tumor
- Burned out germ cell tumor
- Burnt out germ cell tumor
Epidemiology
- 3% of all testicular tumors (J Ultrasound Med 2003;22:515)
- Median age of diagnosis is between 28 and 32 (range 17 - 67 years) (Am J Surg Pathol 2006;30:858, J Urol 2009;182:2303)
- 10% of retroperitoneal germ cell tumors have a regressed testicular primary (J Ultrasound Med 2003;22:515)
Sites
- Retroperitoneal metastasis is most common (Am J Surg Pathol 2006;30:858)
- Metastasis to liver, lung, bone and brain has been reported (Case Rep Urol 2015;2015:835962)
Pathophysiology
- Poorly understood (J Ultrasound Med 2003;22:515)
- Proposed mechanisms (J Ultrasound Med 2003;22:515, BJU Int 2004;94:74, Case Rep Oncol 2017;10:846):
- Immune modulated regression
- Ischemic regression
Clinical features
- Metastatic symptoms are the most common initial presentation: extragonadal mass, abdominal pain, back pain, lymphadenopathy, weight loss and fever (Am J Surg Pathol 2006;30:858, J Ultrasound Med 2003;22:515, J Urol 1996;156:85)
- Less common presentations include: testicular mass, elevated serum tumor markers (AFP, beta hCG and LDH) and testicular pain (J Ultrasound Med 2003;22:515, Am J Surg Pathol 2006;30:858)
Diagnosis
- Discovered most commonly as metastatic disease in the absence of palpable testicular mass (J Ultrasound Med 2003;22:515, J Urol 1996;156:85)
- Sonographic evidence of testicular abnormality (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303)
- Extragonadal germ cell tumor identified (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303)
- Histopathologic features of tumor regression within testis (Am J Surg Pathol 2006;30:858, Am J Pathol 1961;38:207)
Radiology description
- Sonographic features of tumor regression (J Ultrasound Med 2003;22:515, Am J Surg Pathol 2006;30:858, J Urol 2009;182:2303):
- Macrolithiasis (> 0.2 cm) or microlithiasis (< 0.2 cm)
- Loss of testicular homogeneity
- Nonspecific hyperechoic or hypoechoic lesions
- Testicular atrophy
- Computed tomographic (CT) features of metastasis (J Ultrasound Med 2003;22:515):
- Lymphadenopathy
- Extragonadal mass
Radiology images
Prognostic factors
- Posttreatment disease free survival rate: 29% at 5 years and 12% at 10 years (J Urol 2009;182:2303)
- No difference in prognosis between complete and partial regression (J Urol 2009;182:2303)
- In context of regressed germ cell tumor with metastasis, pure seminoma has a more favorable prognosis (J Urol 2009;182:2303)
- No data is available comparing prognosis of regressed versus nonregressed testicular germ cell tumors
Case reports
- 24 year old man with brain metastasis (Cureus 2016;8:e551)
- 43 year old man with retroperitoneal seminoma (Rom J Morphol Embryol 2011;52:193)
- 45 year old man with retroperitoneal metastasis (Int J Health Sci (Qassim) 2018;12:94)
- 54 year old man with pancreatic choriocarcinoma (Mod Pathol 2004;17:1573)
- 54 year old man with pulmonary choriocarcinoma (Intern Med 2016;55:1481)
Treatment
- Combination systemic chemotherapy is mainstay of treatment for metastasis (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303)
- Can be combined with radiotherapy for seminoma
- Radical orchiectomy for abnormal sonographic features (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303)
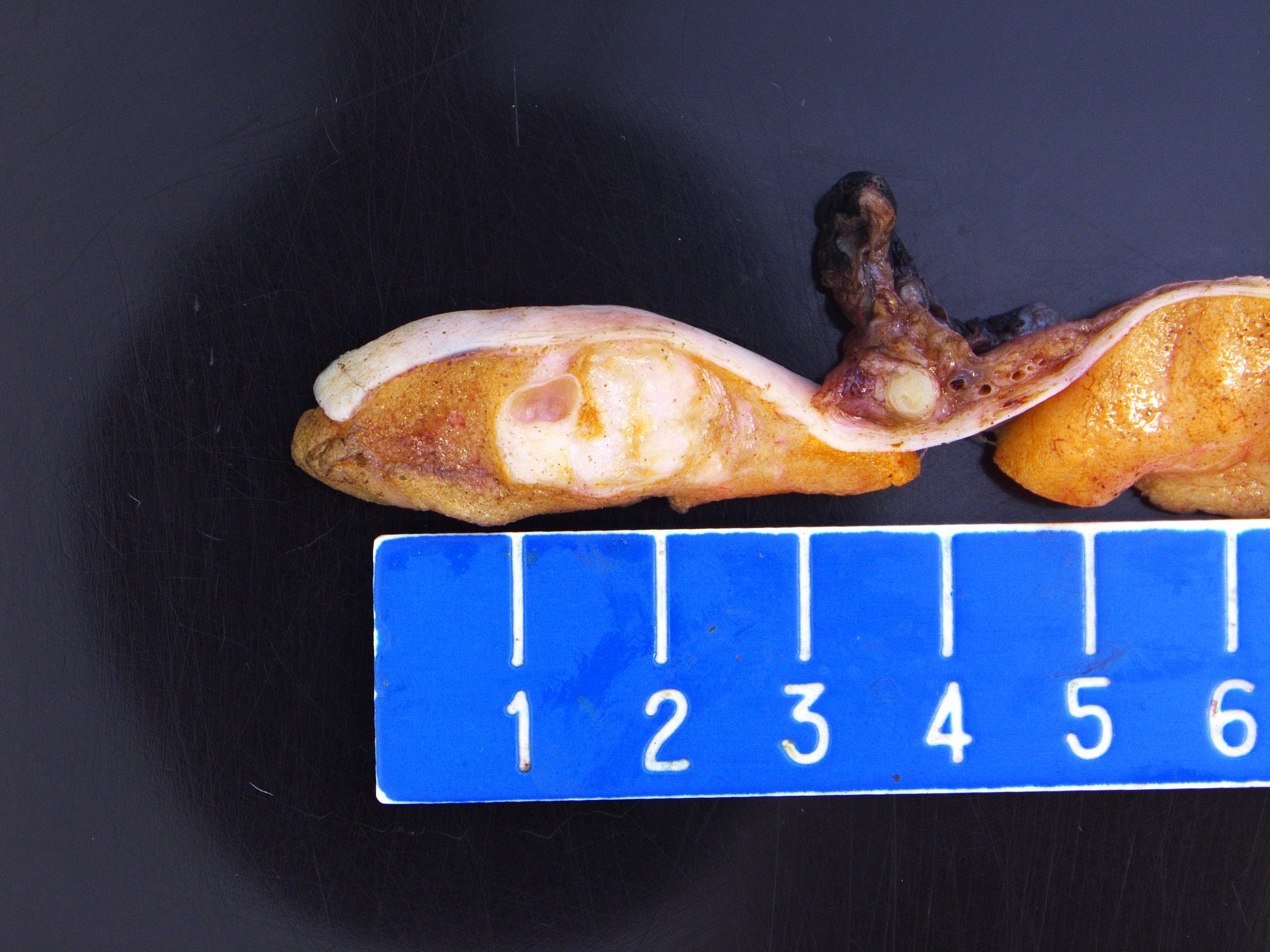
Gross description
- Fibrous scar displacing normal testicular parenchyma (J Ultrasound Med 2003;22:515, J Urol 2009;182:2303)
- Scars appear white to tan in color (Am J Surg Pathol 2006;30:858)
- Scars can appear as well demarcated nodular foci or stellate lesions (Am J Surg Pathol 2006;30:858)
Gross images
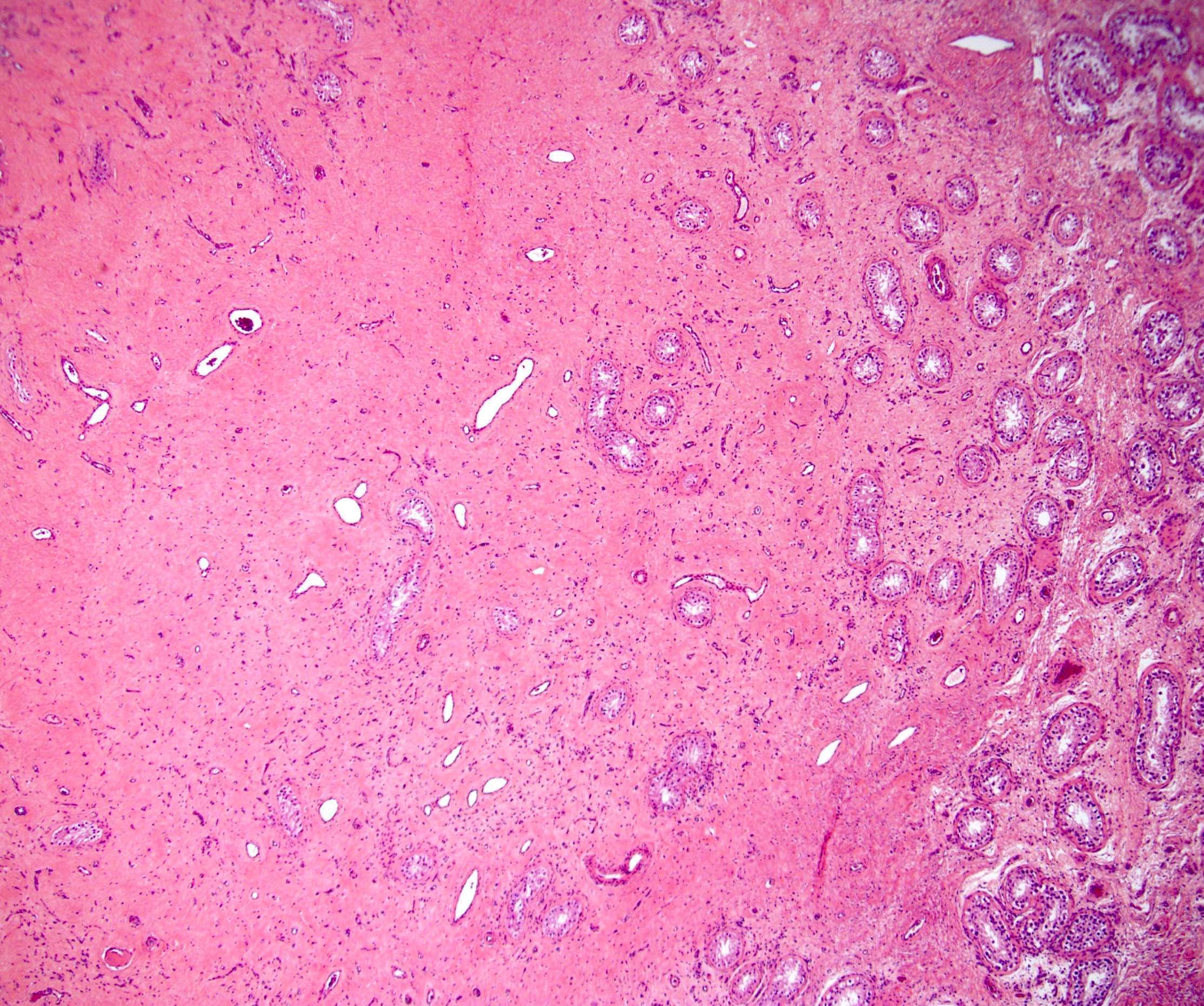
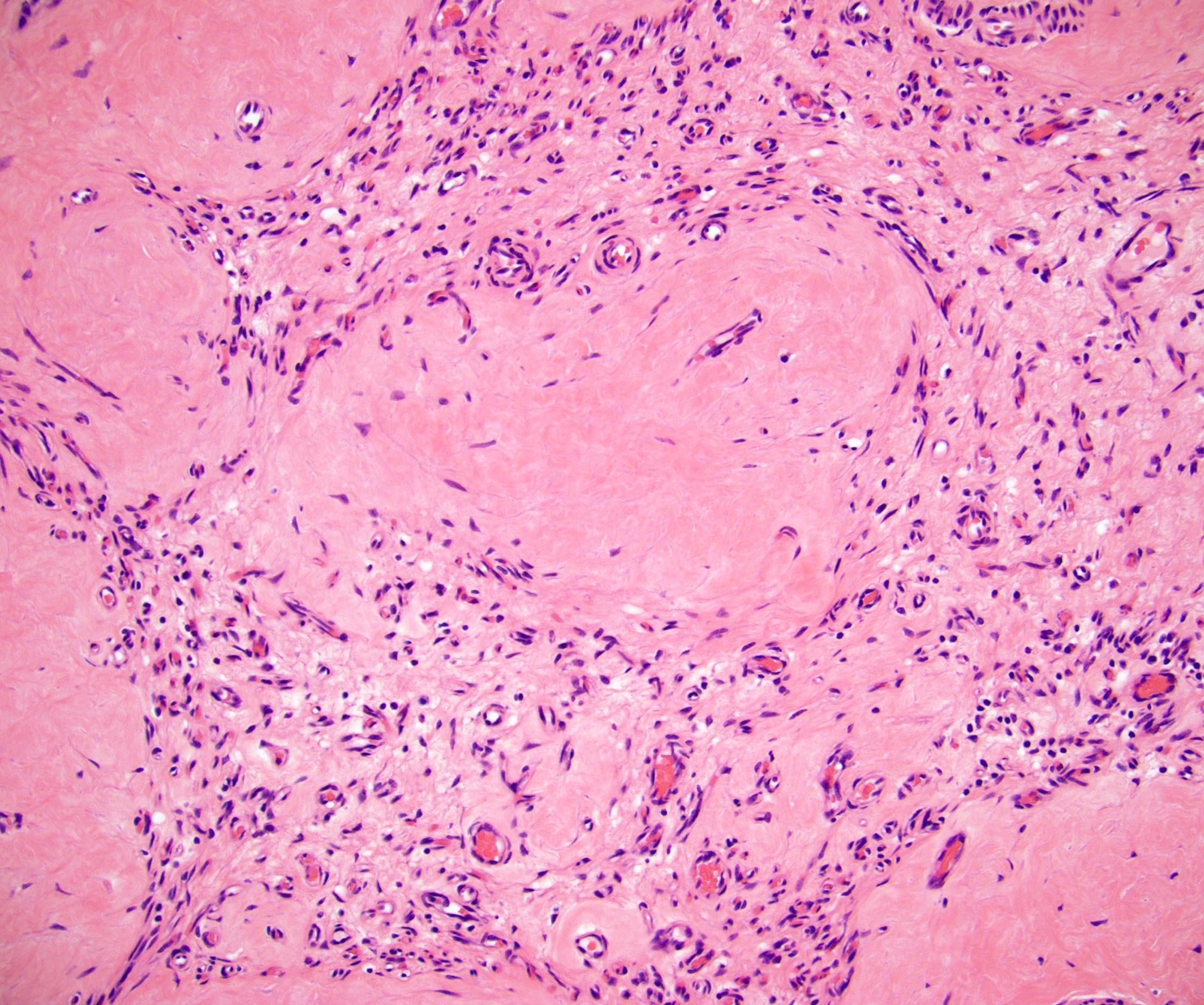
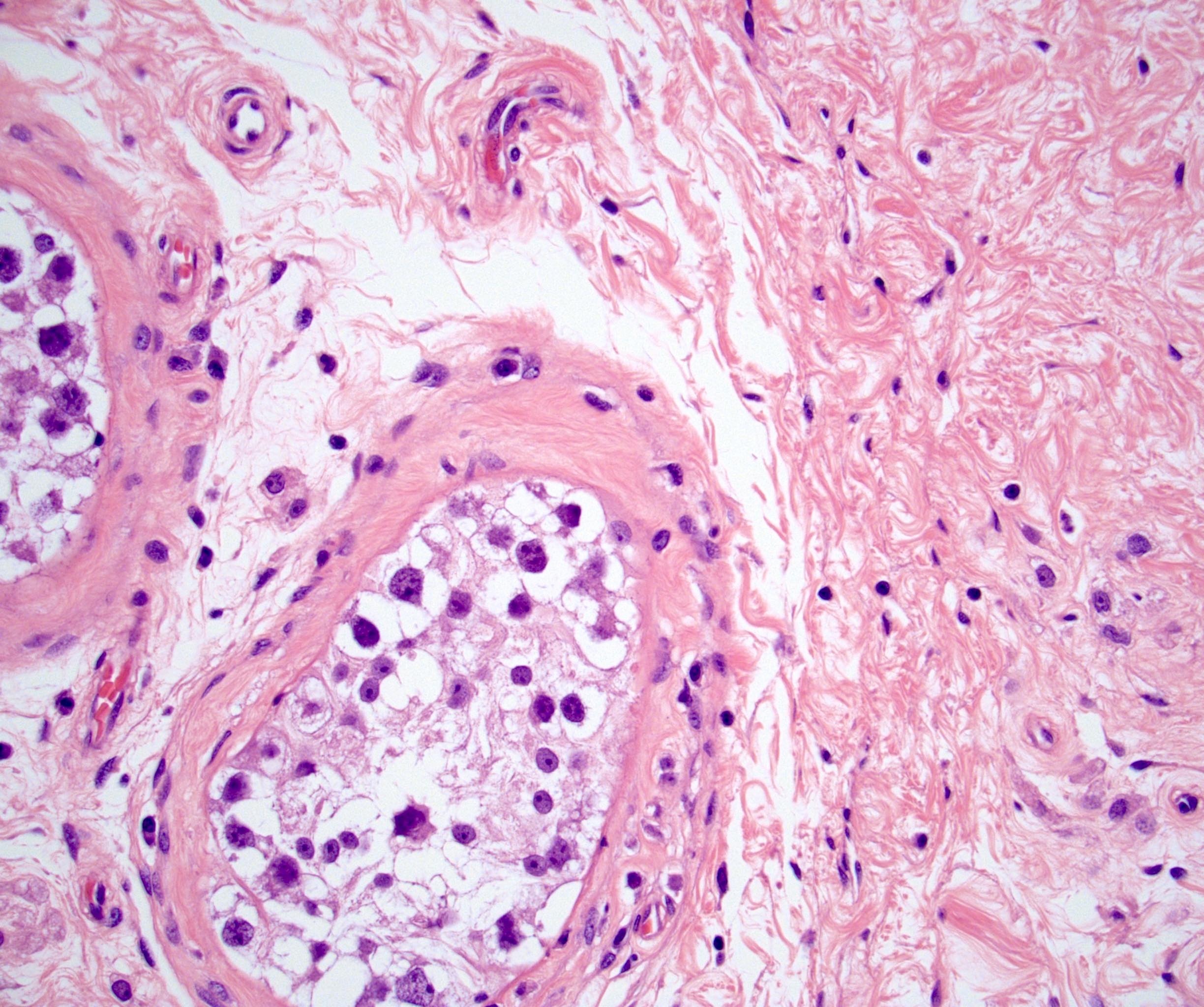
Microscopic (histologic) description
- Intratesticular fibrous scar (Am J Surg Pathol 2006;30:858, Am J Pathol 1961;38:207):
- Acellular collagenous tissue with numerous small interspersed vessels
- Foamy or hemosiderin laden macrophages
- Lymphoplasmacytic infiltrate
- May have necrosis or intratubular calcification (microlithiasis)
- Residual germ cell tumor may be present if regression is incomplete
- Pure seminoma most common (Am J Surg Pathol 2006;30:858, J Urol 2009;182:2303)
- Testicular parenchyma (Am J Surg Pathol 2006;30:858):
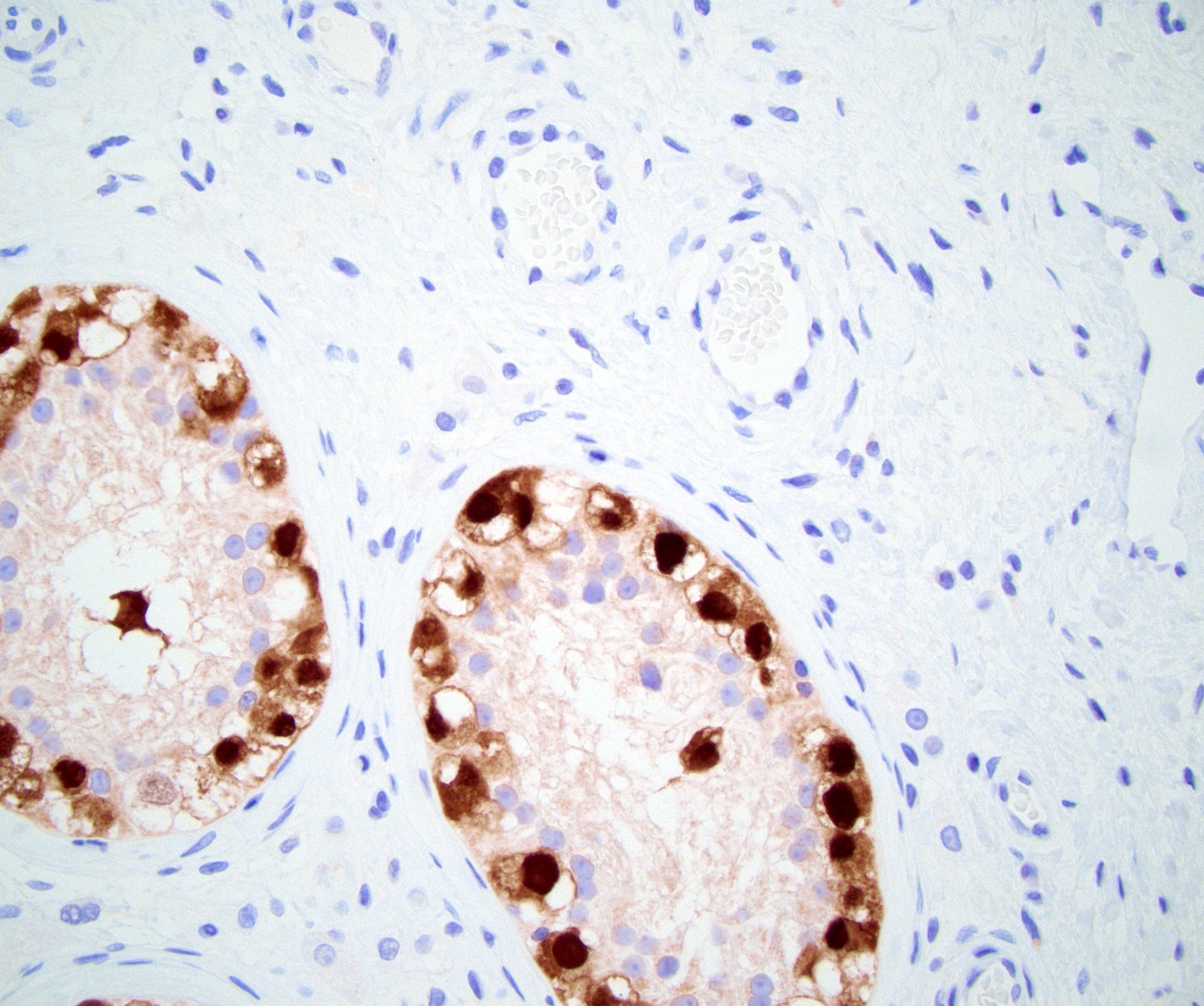
- Germ cell neoplasia in situ (50% of cases)
- Remaining parenchyma may be atrophic with:
- Shrunken seminiferous tubules with decreased spermatogenesis
- Sertoli cell only lined tubules
- Thickened peritubular basement membrane
Microscopic (histologic) images
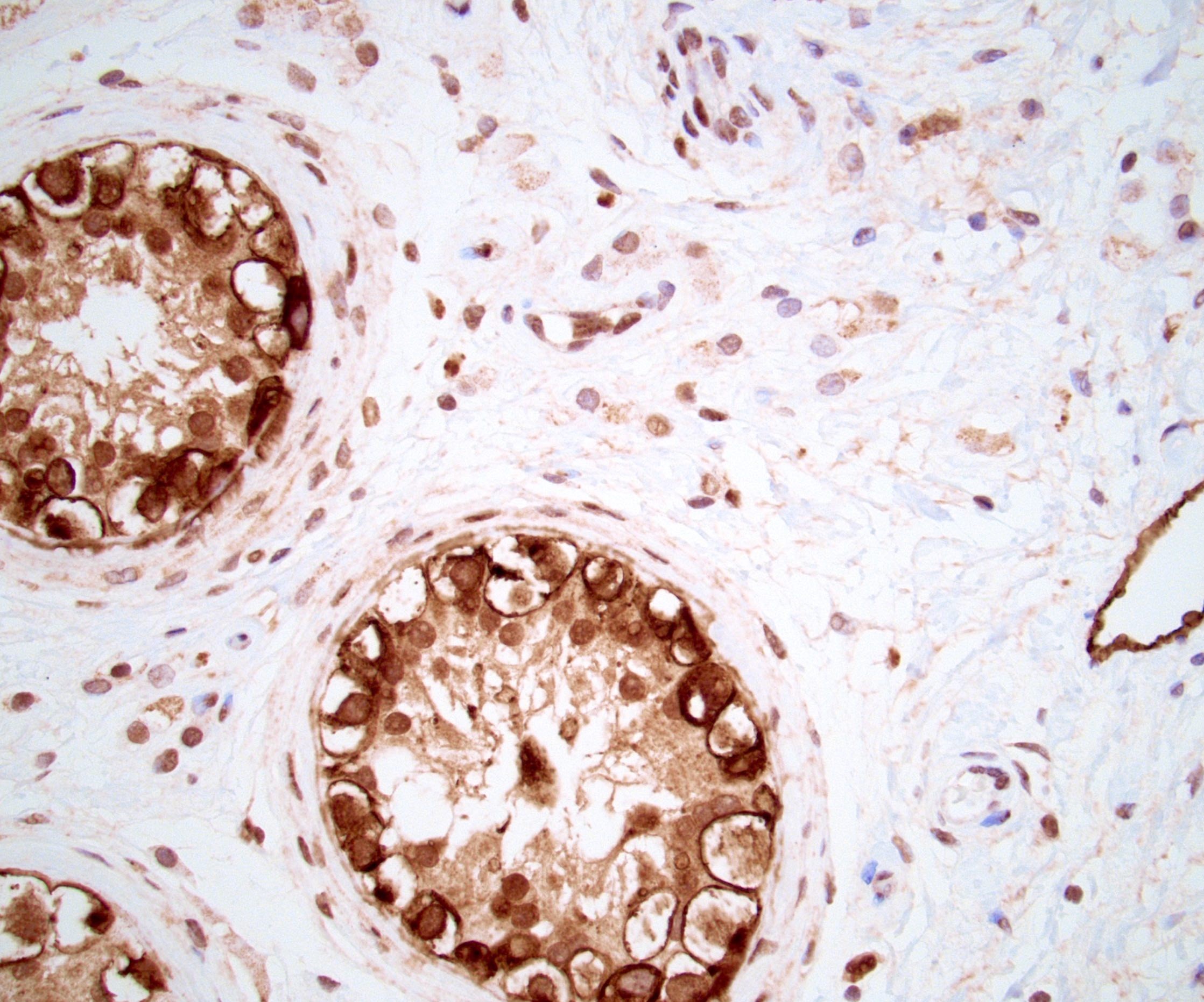
Positive stains
- Germ cell neoplasia in situ / seminoma: SALL4, OCT3 / 4, CD117 (c-kit), PLAP, D2-40 (podoplanin)
- Embryonal carcinoma: SALL4, AE1 / AE3, CD30, OCT3 / 4, PLAP (variable)
- Yok sac tumor: SALL4, AE1 / AE3, glypican 3, AFP
- Choriocarcinoma: SALL4, AE1 / AE3, CK7, hCG, glypican 3
Negative stains
Molecular / cytogenetics description
- Identification of isochromosome 12p by FISH can confirm a testicular germ cell tumor metastasis although immunohistochemistry is more commonly used and has wider availability
Sample pathology report
- Left testicle and spermatic cord, radical inguinal orchiectomy:
- Scar (1.5 cm) and germ cell neoplasia in situ, consistent with regressed germ cell tumor (see synoptic report, pTis NX)
- Comment: the germ cell neoplasia in situ expresses OCT3/4, D2-40, CD117 and PLAP
Differential diagnosis
- Nonneoplastic scar:
- Testicular atrophy:
- Treatment effect:
- History of chemotherapy for germ cell tumor
Board review style question #1
Board review style answer #1
Board review style question #2
What is the most common tumor subtype in a partially regressed testicular germ cell tumor?
- Choriocarcinoma
- Embryonal carcinoma
- Seminoma
- Teratoma
- Yolk sac tumor
Board review style answer #2