Table of Contents
Definition / general | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Gordetsky J, Rane S. Mesothelioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testismesotheliomamalignant.html. Accessed April 2nd, 2025.
Definition / general
- Malignant tumor of mesenchymal origin arising from the serosal membrane of the tunica vaginalis
- Usually aggressive, similar to peritoneal cavity tumor (Am J SurgPathol 1995;19:815)
Epidemiology
- Extremely rare ( < 1% of all mesotheliomas)
- Typically middle aged to elderly men (mean age 53, range 12-76 years) but also children (Am J Surg Pathol 1995;19:815, J Urol 1997;158:198)
- Most patients > 50 years old; < 10% cases < 25 years
- ~1/3 associated with asbestos exposure (Am J SurgPathol 2001;25:1304, Cancer 1998;83:2437, Urol Oncol 2006;24:36)
Sites
- Rarely arises from the tunica vaginalis (0.3 - 5% of all tumors), often in relation to the epididymis, testis or spermatic cord
- More commonly arises in pleura (68 - 85%) and peritoneum (9 - 24%) (Arch Pathol Lab Med 2012;136:113)
Pathophysiology
- Originates from tunica vaginalis, which derives from invagination of the peritoneum into the scrotum
Etiology
- Exposure to asbestos (Orphanet J Rare Dis 2008;3:34), trauma, herniorrhaphy and longstanding hydrocele have all been implicated as predisposing factors (Arch Pathol Lab Med 2012;136:113)
- Variable latency period from initial asbestos exposure to clinical diagnosis
Clinical features
- Usually present with hydrocele - insidious, painless swelling of scrotum
- Most cases are unilateral; bilateral tumors are rare, ~4% of cases (Cancer 1998;83:2437)
- Other presentations include inguinal hernia, epididymitis or testicular mass
- Poor prognosis, even with negative resection margins
- Mean disease specific survival of 23 months, range of 2 to 64 months (Arch Pathol Lab Med 2012;136:113)
Radiology description
- Scrotal ultrasonography usually reveals hydrocele with thickened wall and hypoechoic nodule over epididymis / tunica vaginalis, or a solid paratesticular mass (Urology 2012;80:e3) Ultrasound reveals hydrocele with thickened wall with hypoechoic nodule over epididymis / tunica vaginalis
Radiology images
Prognostic factors
- Extent of disease at presentation is important prognostic factor (Cancer 1998;83:2437); metastases at presentation is associated with worse prognosis
- Complete / adequate excision improves disease free survival; lower recurrence rate after radical orchiectomy (~10%) versus simple hydrocele sac excision (~30%) (Cancer 1998;83:2437)
- Better outcome in younger patients
- Well differentiated papillary mesothelioma has better prognosis than undifferentiated spindle cell mesothelioma
- Other prognostic factors include tumor size, lymph node metastases, invasion into adjacent structures, degree of differentiation
Case reports
- 36 year old man with no history of hydrocele, trauma or exposure to asbestos (Urology 2012;80:e3)
- 53 year old man (World J Surg Oncol 2012;10:238)
- 57 year old man with mesothelioma of tunica vaginalis of "uncertain malignant potential" (Diagn Pathol 2011;6:78)
- 59 year old man (Case #148)
- 64 year old man with malignant mesothelioma of tunica vaginalis testis (Pathol Int 2004;54:930)
- 65 year old man without asbestos exposure (Cases J 2008;1:310)
- 70 year old man with well differentiated papillary mesothelioma of tunica vaginalis (Pathol Res Pract 2010;206:105)
- Malignant mesothelioma of tunica vaginalis testis (Cancer 1998;83:2437)
Treatment
- Radical orchiectomy is standard treatment
- If treated with transcrotal surgery, subsequent hemiscrotectomy or hemiscrotal irradiation is often recommended
- Retroperitoneal lymph node dissection is recommended only if pre-op workup reveals suspicious nodes
- Well differentiated papillary mesothelioma may be treated with only surgery
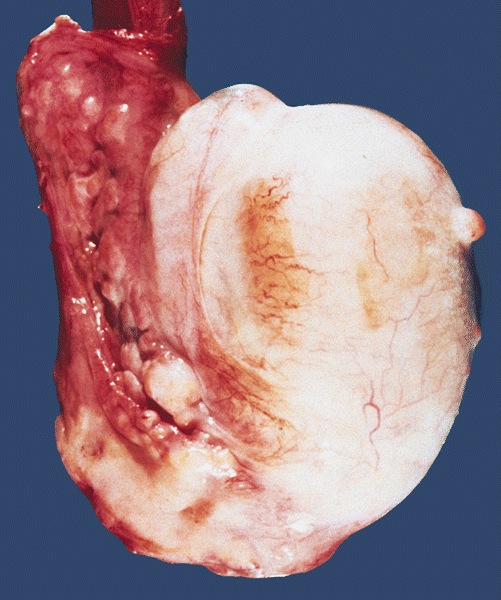
Gross description
- Multiple nodules within hydrocele sac, frequently associated with mass infiltrating spermatic cord, epididymis or testis
- May be a solitary nodule
- Hydrocele sac is thick walled, often containing hemorrhagic fluid and papillary excrescences
- Less often, mesothelioma creeps along tunica without forming a mass-like lesion
Gross images
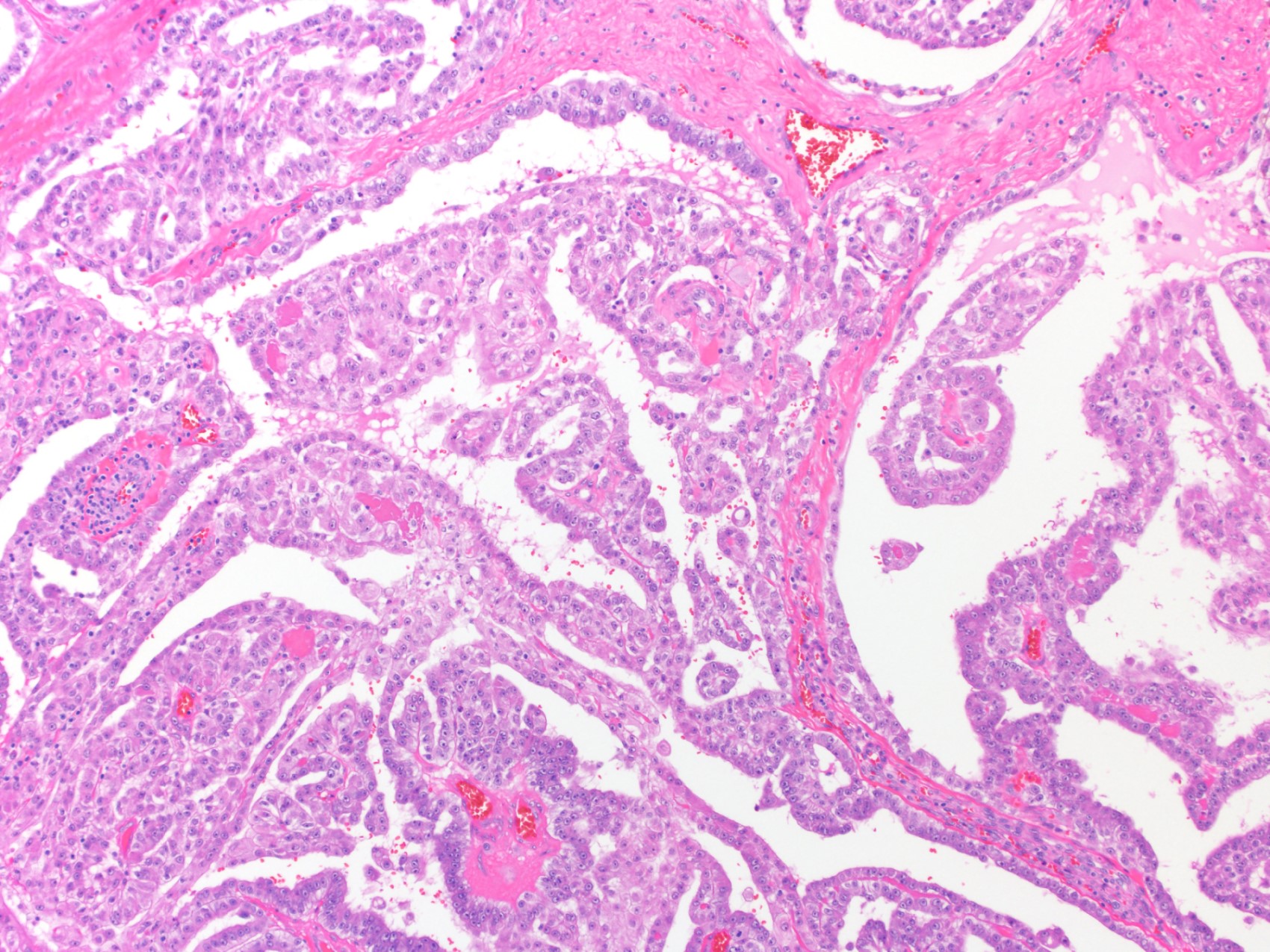
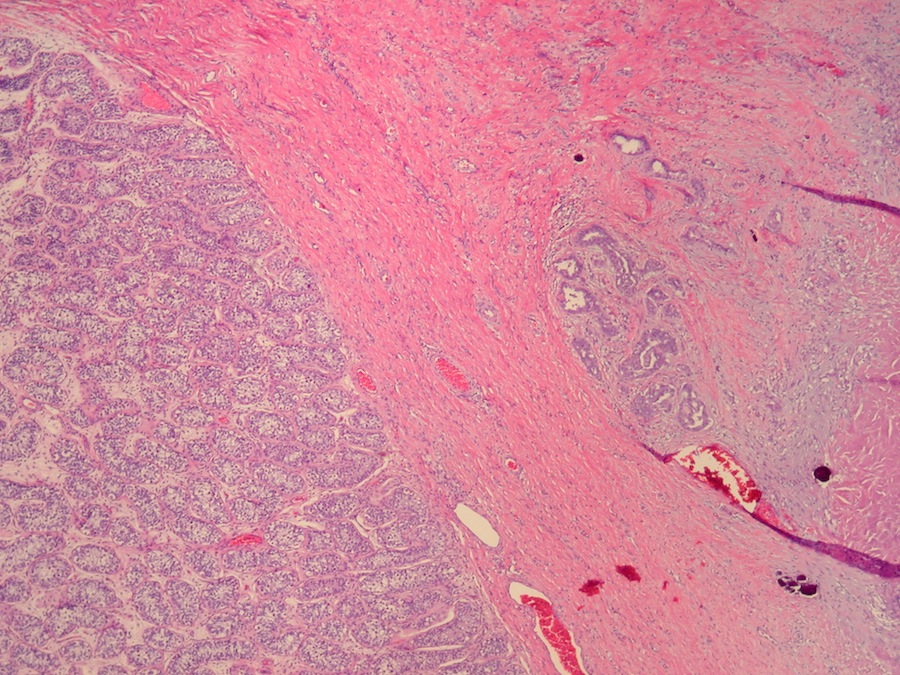
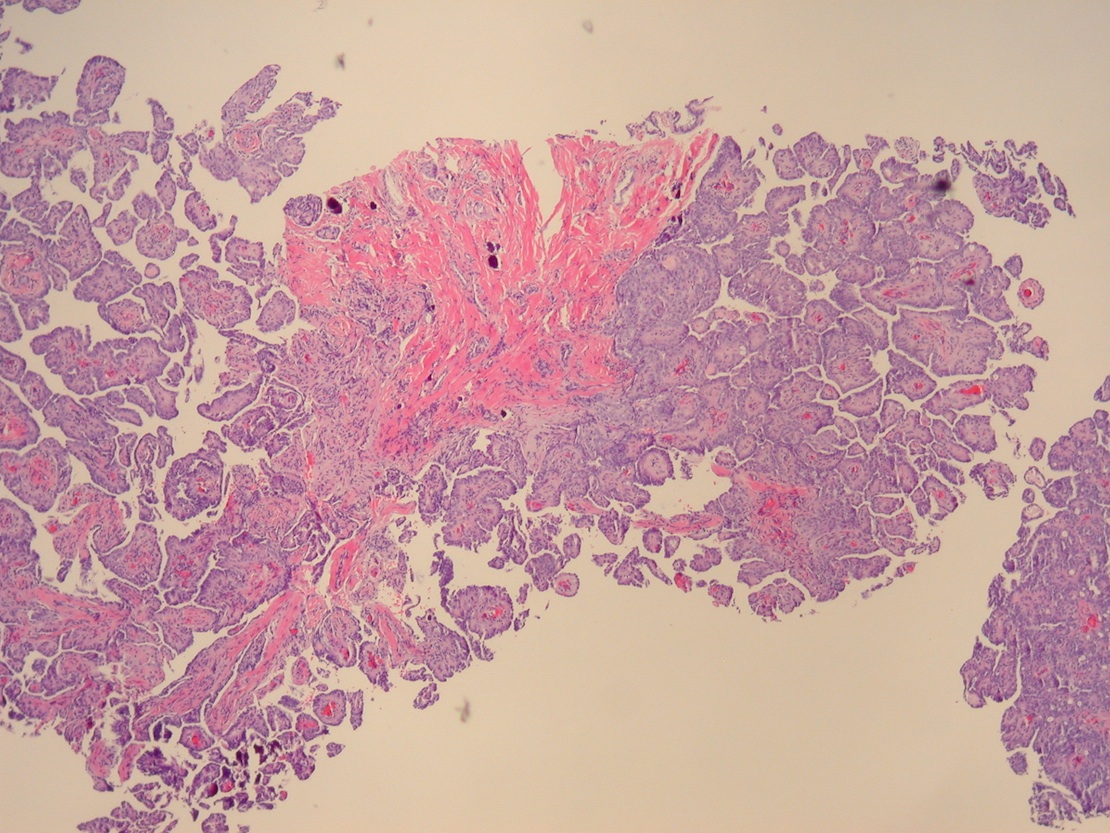
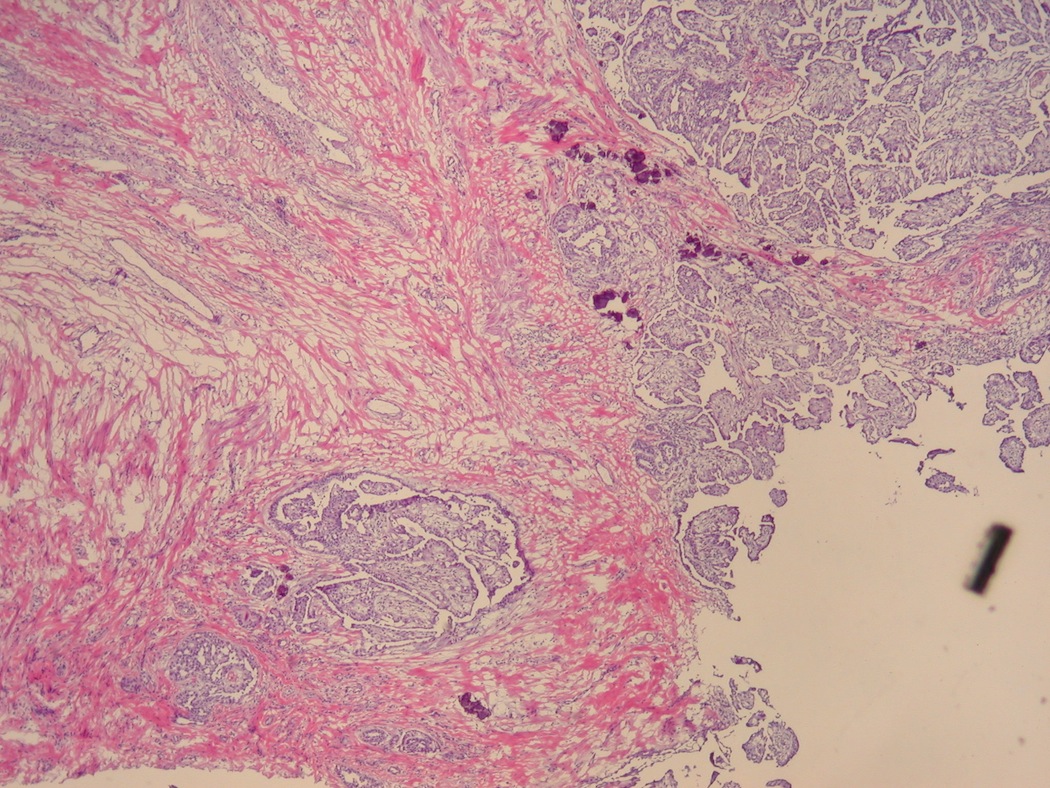
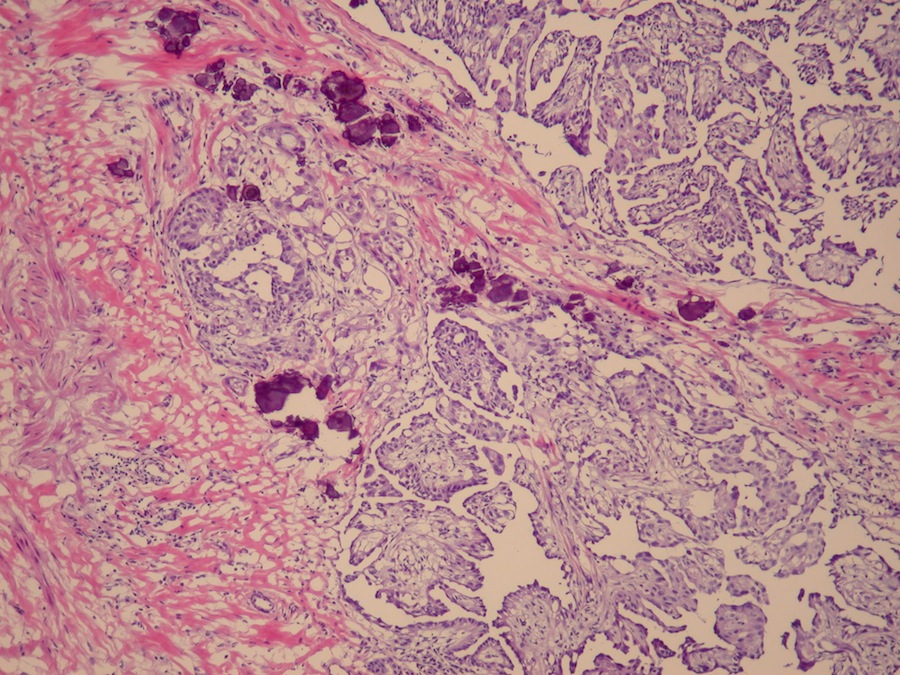
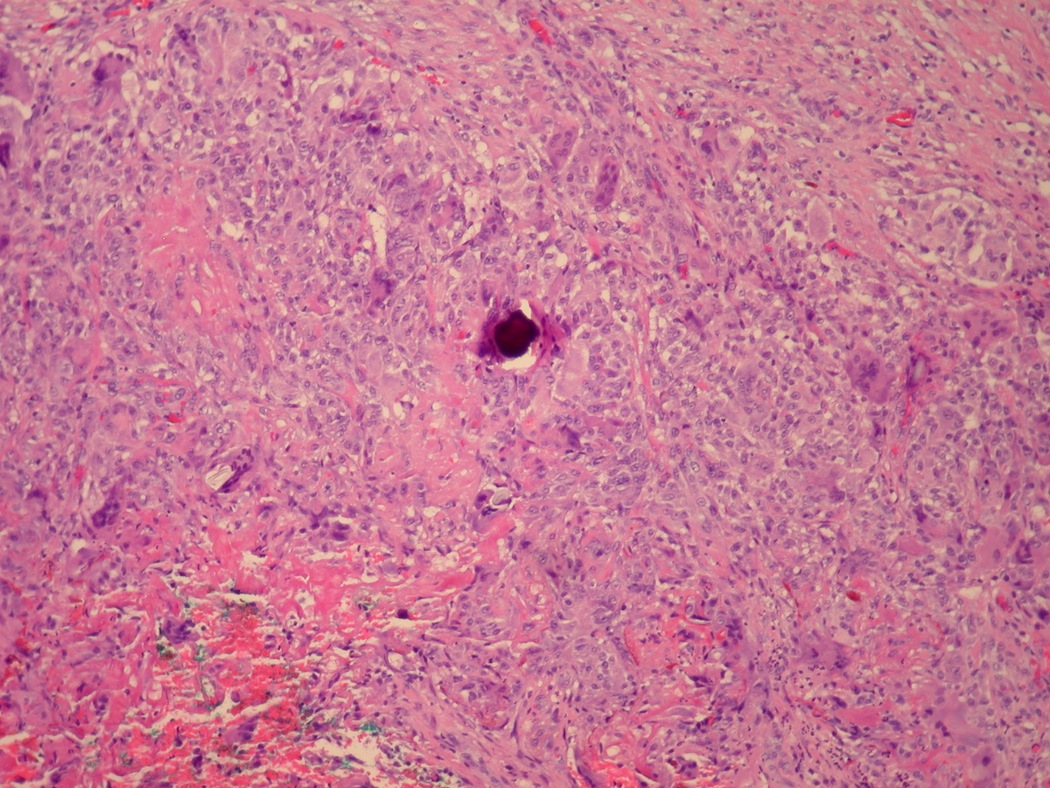
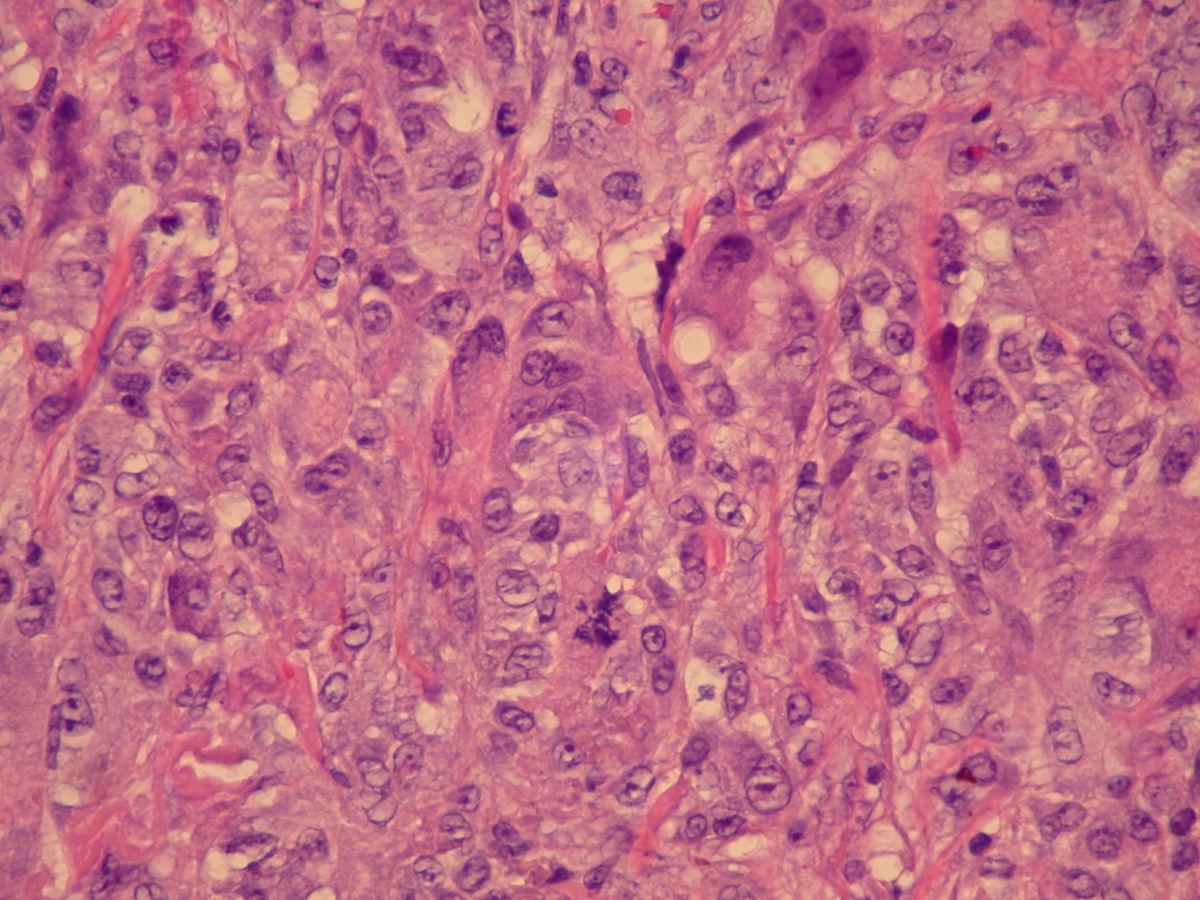
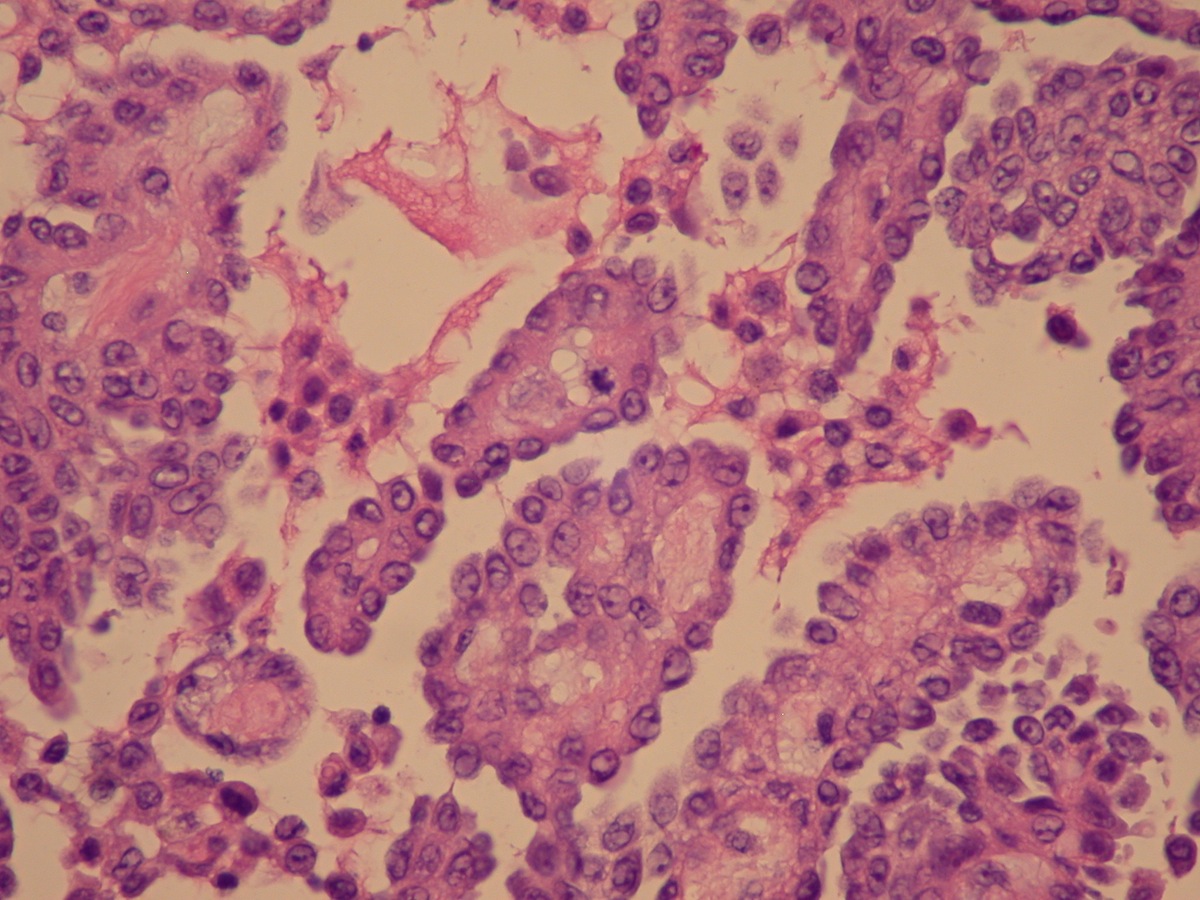
Microscopic (histologic) description
- Same as mesothelioma at other sites
- Either epithelial (60 - 70%), spindle cell (least common) or biphasic type (30 - 40%)
- Epithelial type has epithelioid cells arising from the tunica vaginalis with papillary, tubular, adenomatoid or solid architectural patterns
- Biphasic type has fascicles of spindle cells with scanty stroma, often merging with epithelial cells
- In well differentiated tumors, neoplastic cells are typically cuboidal with scant to moderate amounts of eosinophilic cytoplasm and bland cytologic features
- Tumors may also appear poorly differentiated
- Papillae have thick, hyalinized fibrovascular cores lined by a single layer of atypical mesothelium
- Stroma may be desmoplastic or show necrosis
- Variable psammoma bodies
Microscopic (histologic) images
Contributed by Jennifer Gordetsky, M.D.
Case #261
Images hosted on other servers:
Cytology description
- Moderately cellular smears; well differentiated tumors have papillary clusters of epithelial cells with minimal atypia
Positive stains
- AE1 / AE3,
EMA,
calretinin,
D2-40,
CK5 /
6
- Thrombomodulin. vimentin, WT1, EMA, CK7 (Am J Surg Pathol 2006;30:1)
Negative stains
Electron microscopy description
- Cells show epithelial and mesenchymal differentiation
- Epithelial cells joined by intercellular junctions, including desmosomes and junctional complexes, with lumen formation
- Numerous cytoplasmic filaments including tonofibrils; cytoplasmic glycogen is also present
- Long, slender microvilli are typically seen on the surface of the tumor cells as well as in intracellular and intercellular lumina
- Microvilli length to diameter ratio > 10 (Ulbright: AFIP Series 3, Vol 25)
Molecular / cytogenetics description
- Poorly characterized - mesotheliomas harbor multiple cytogenetic abnormalities with no specific diagnostic characteristics
- Losses of chromosomal regions in 1p, 3p, 6q, 9q, 8p, 14q and 22q and gains in 5p, 6p, 8q, 15q, 17q, 20 and monosomy 22 have been reported (Arch Pathol Lab Med 2012;136:113)
Differential diagnosis
- Adenomatid tumor
- Florid mesothelial hyperplasia
- Germ cell tumor
- Pleomorphic sarcoma
- Adenocarcinoma of rete testis, epididymis
- Metastatic adenocarcinoma
- Serous papillary tumor
- Well differentiated papillary mesothelioma: no atypia or invasion