Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Valencia A, Gordetsky JB, Craig JC. Well differentiated papillary mesothelial tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testismesothelioma.html. Accessed April 2nd, 2025.
Definition / general
- Well differentiated papillary mesothelial tumor is a neoplasm of uncertain malignant potential that originates from the mesothelium of the pleura, peritoneum or tunica vaginalis
Essential features
- Mesothelial tumor without significant cytologic atypia (Ann Diagn Pathol 2019;38:43, Ann Surg Oncol 2019;26:852)
- Composed entirely of papillary structures and tubules lined by a single layer of bland cuboidal cells with no identifiable invasion
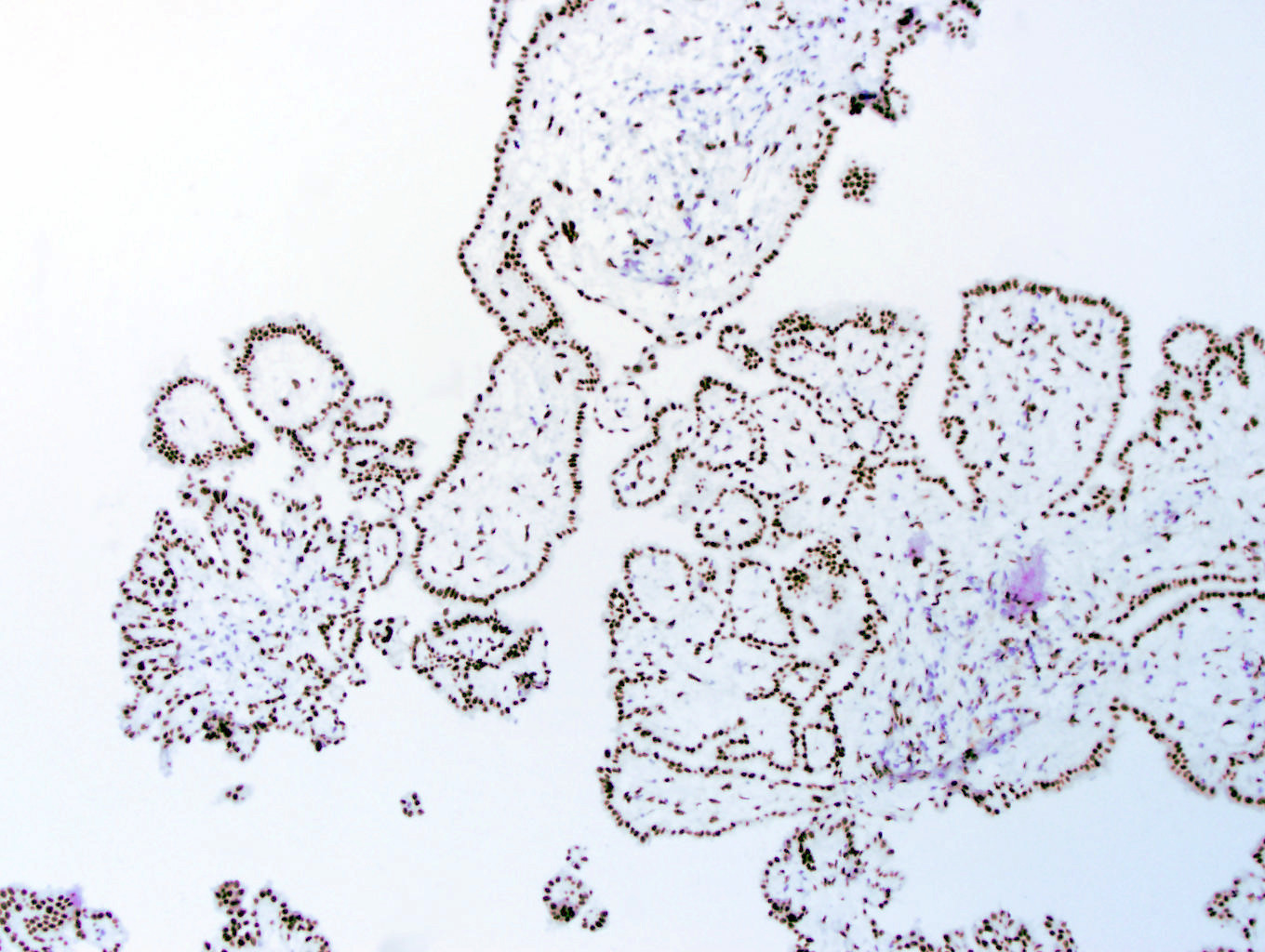
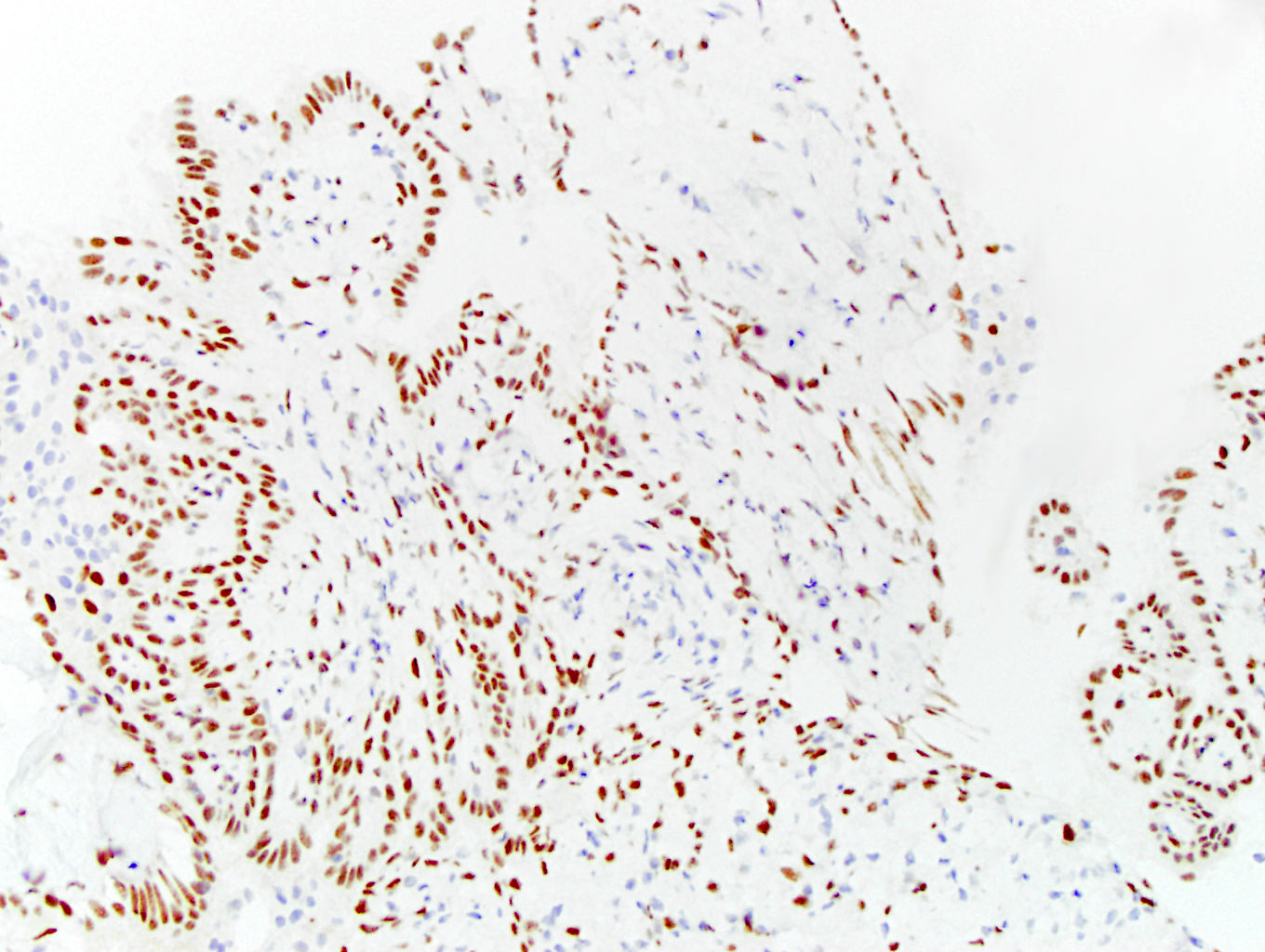
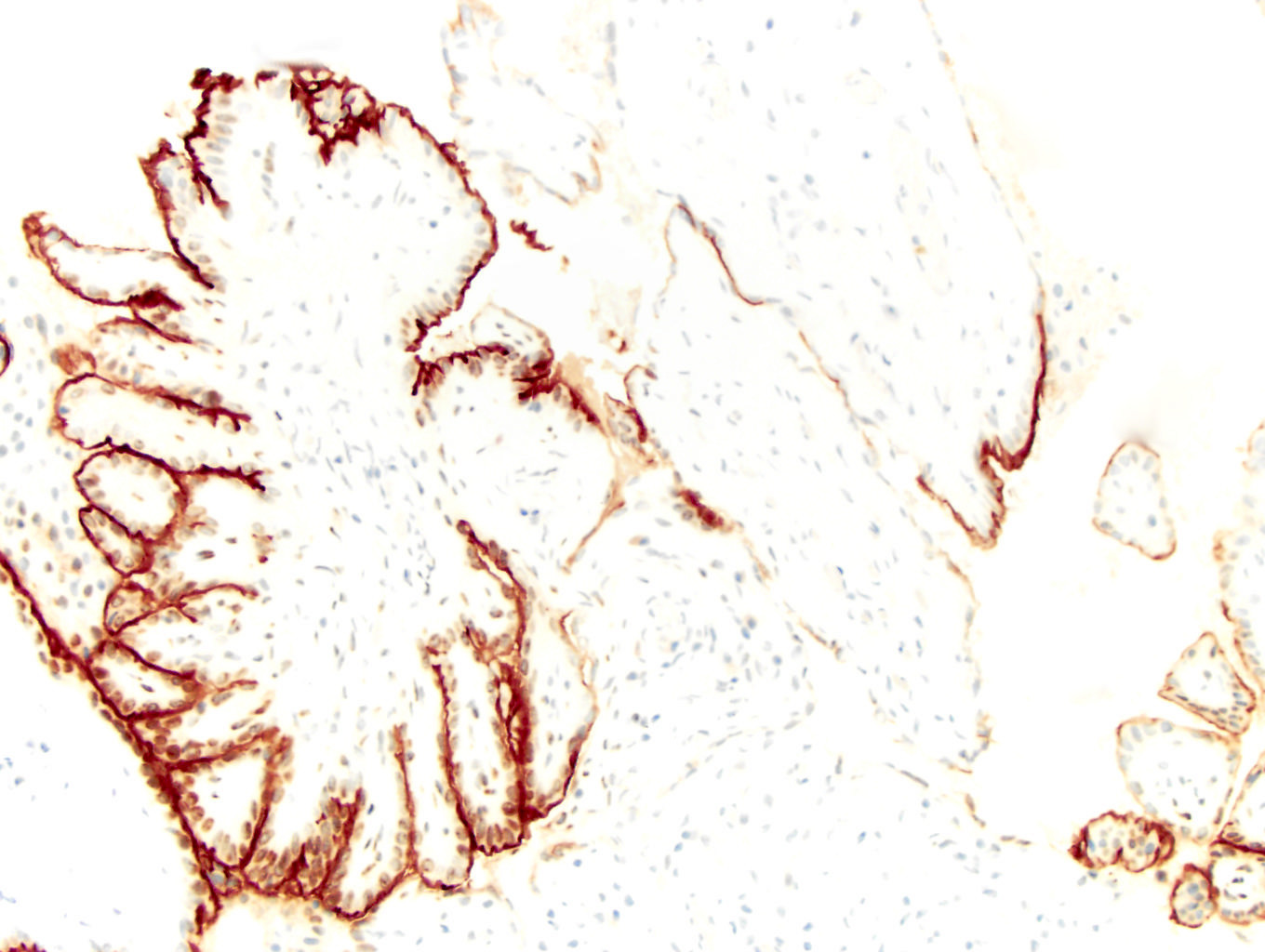
- Positive staining for mesothelial markers (calretinin, WT1)
- BAP1 and MTAP immunohistochemical staining should be retained
Terminology
- Well differentiated papillary mesothelioma (Eur Urol 2022;82:458)
Epidemiology
- Tumors arising from tunica vaginalis are rare and comprise < 1% of mesotheliomas (Mod Pathol 2022;35:1327)
- Age range is 18 - 70 years
Sites
- Peritoneum
- Tunica vaginalis
- Pleura
- Pericardium
- References: Mod Pathol 2022;35:1327
Pathophysiology
- Unknown
Etiology
- Unknown
Clinical features
- Pleural cases are often symptomatic and associated with a pleural effusion (Mod Pathol 2022;35:1327)
- Peritoneal cases are typically identified incidentally during surgery (Mod Pathol 2022;35:1327)
- Cases involving the tunica vaginalis are associated with hydrocele and testicular pain (Mod Pathol 2022;35:1327, Clin Genitourin Cancer 2016;14:e435, Can Urol Assoc J 2018;12:E425)
Diagnosis
- Histologic diagnosis is required
Radiology description
- No specific imaging findings (Radiographics 2023;43:e220128, Adv Anat Pathol 2023;30:280)
- There may be no imaging abnormalities (Radiographics 2023;43:e220128)
- Sometimes there may be small peritoneal nodules, a single nodule or scattered areas of peritoneal thickening (Radiographics 2023;43:e220128)
- Calcifications may be present (Radiographics 2023;43:e220128)
Prognostic factors
- This tumor is likely benign in nature but is often morphologically identical to mesothelioma in situ, which may explain the rare reports of recurrence as mesothelioma (Am J Surg Pathol 2023;47:611)
Case reports
- 18 year old man with hydrocele (J Clin Pathol 1992;45:1029)
- 35 year old man with bilateral hydroceles (Urol Oncol 2006;24:36)
- 47 year old man with a testicular tumor found after an episode of acute epididymitis (Int J Surg Pathol 2023;31:1126)
- 48 year old man without asbestos exposure (Korean J Pathol 2014;48:225)
- 55 year old man with chronic testicular pain, epididymitis and a hydrocele (Int J Surg Pathol 2023;31:1126)
Treatment
- Complete excision
Gross description
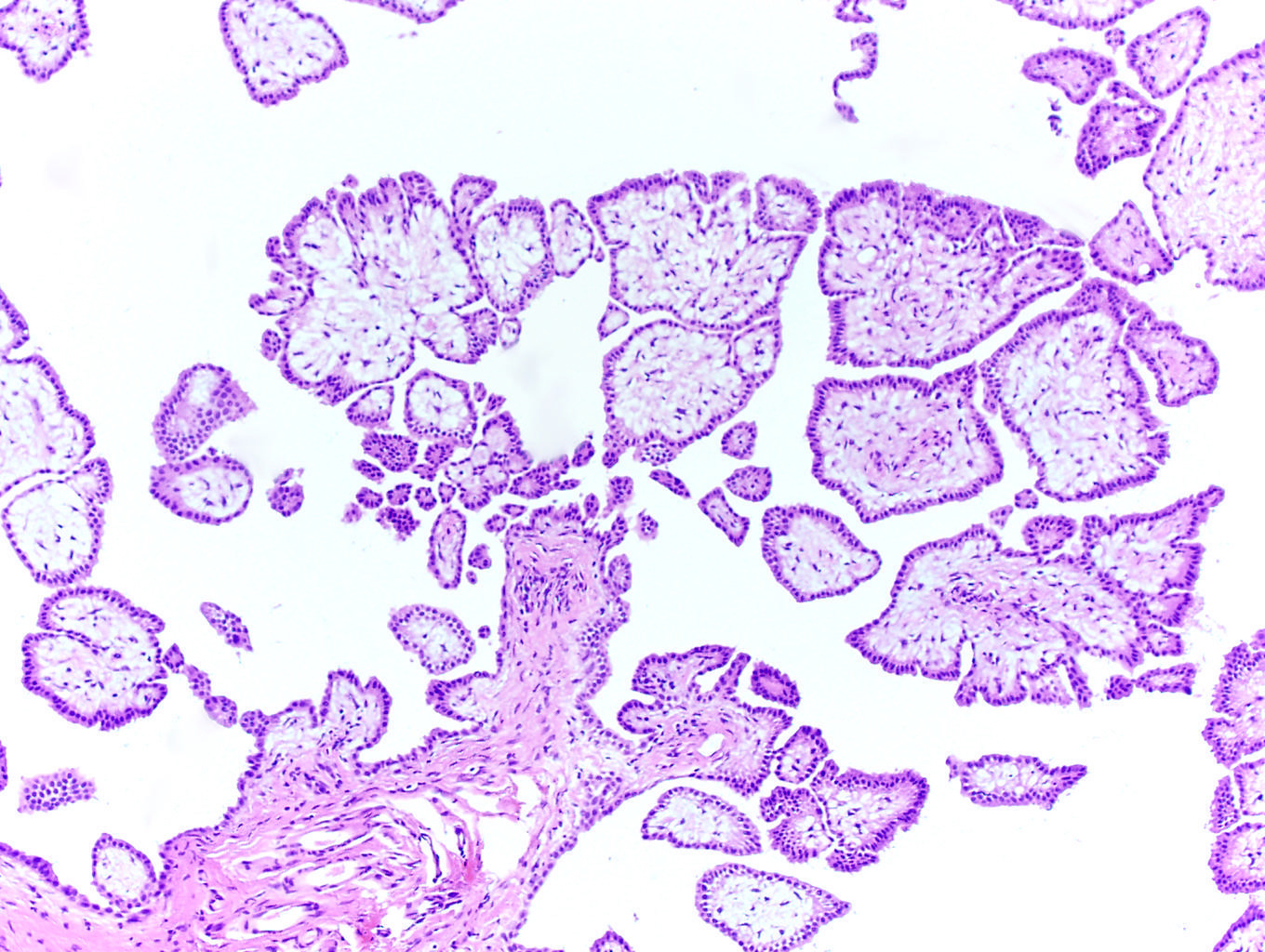
- Peritoneal surfaces with small nodules or papillary excrescences, single to innumerable (Mod Pathol 2022;35:1327)
Frozen section description
- These tumors are often found incidentally during other procedures, prompting frozen section evaluation
- Expanded papillary structures with edema or myxoid change, lined by a single layer of bland mesothelial cells
- Invasion should be excluded
- Reference: Int J Surg Pathol 2021;29:844
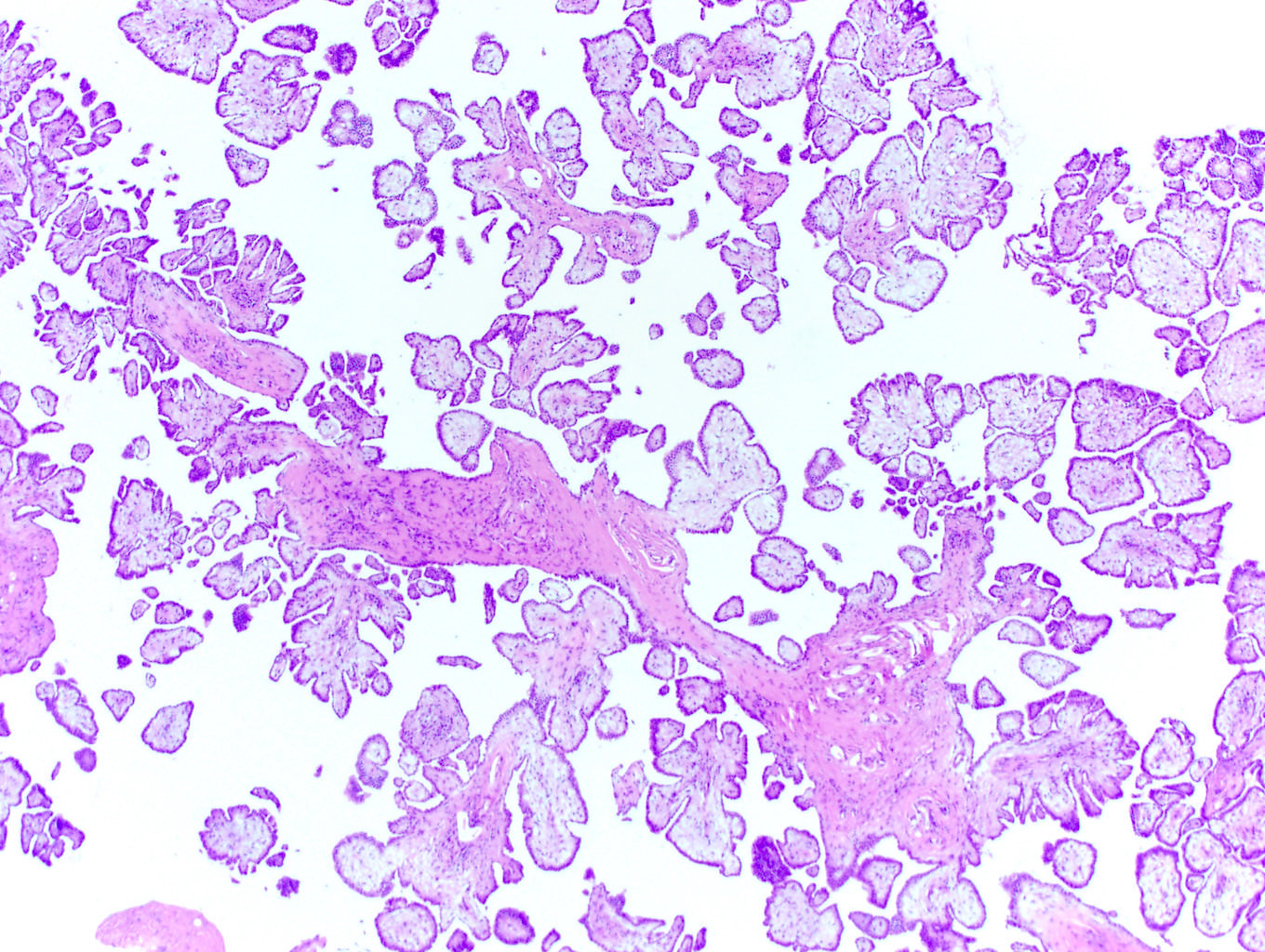
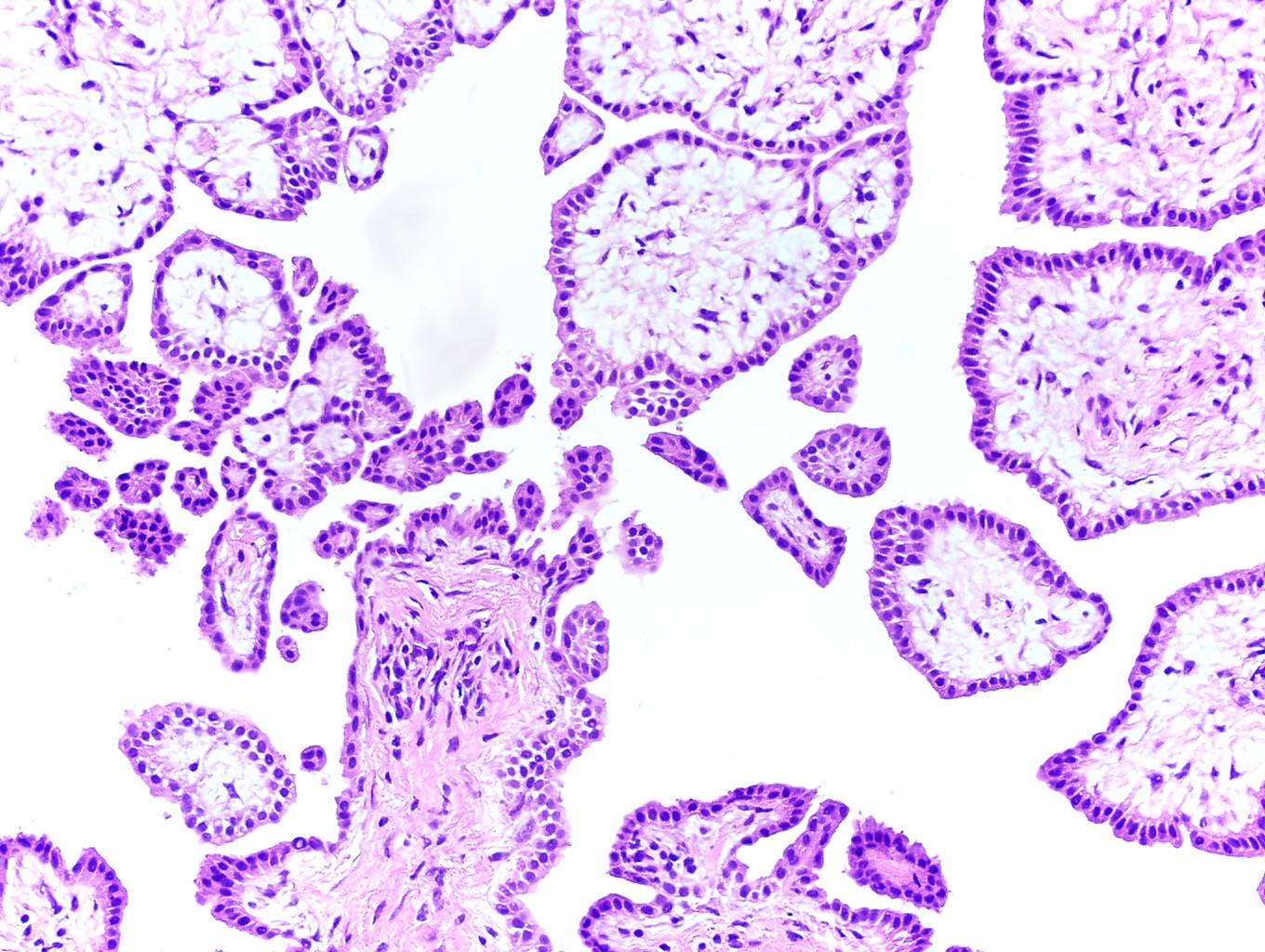
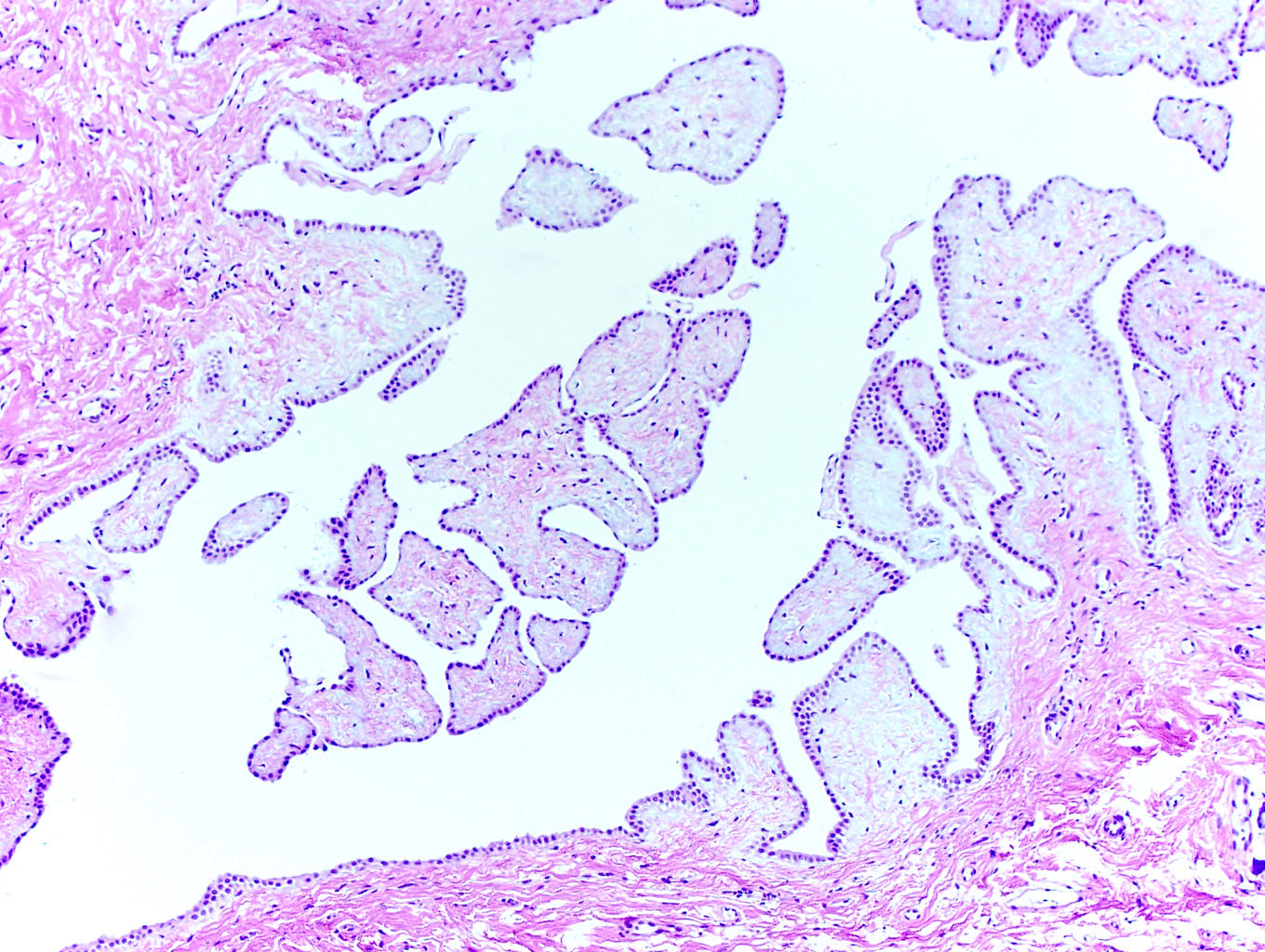
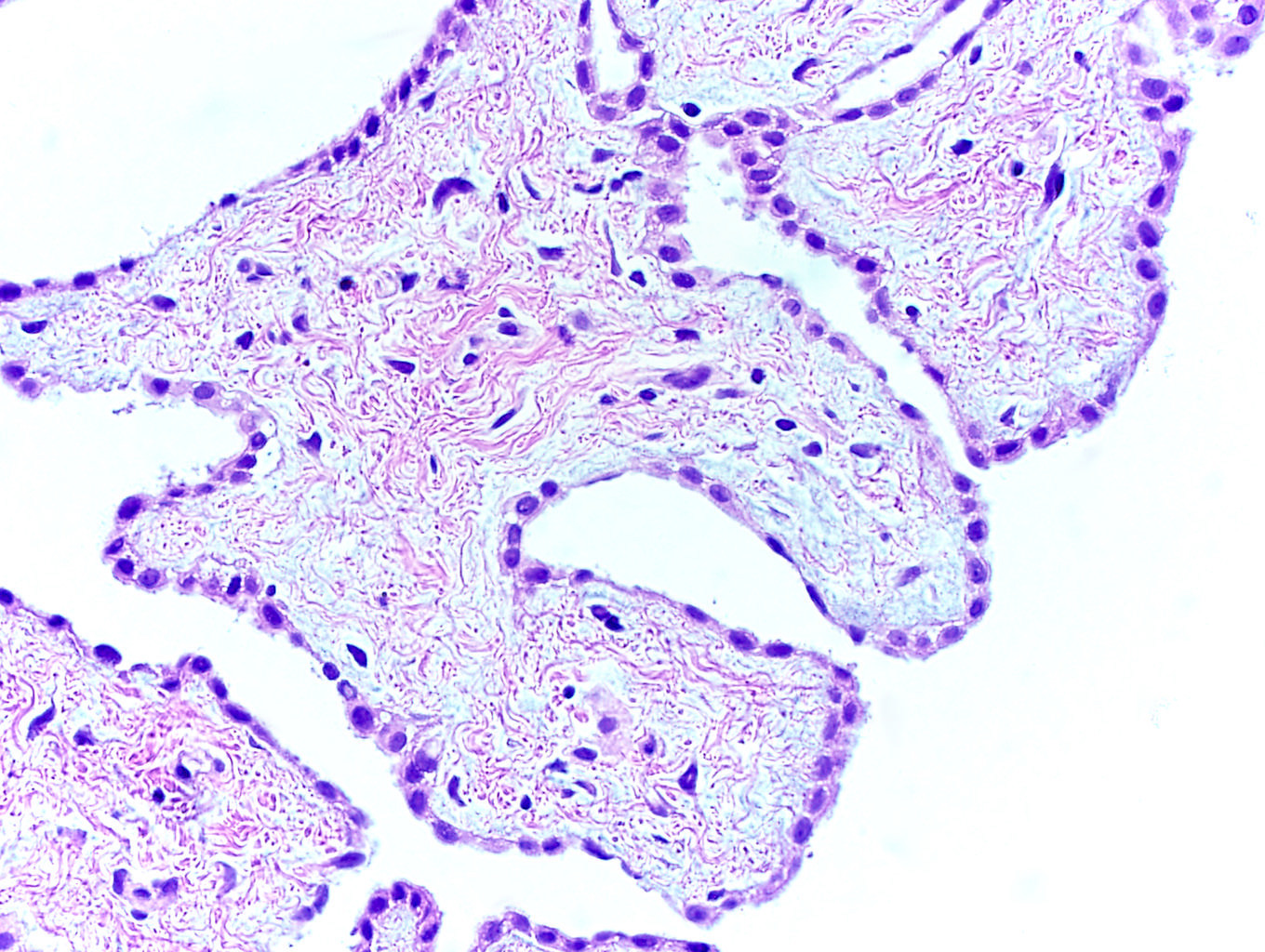
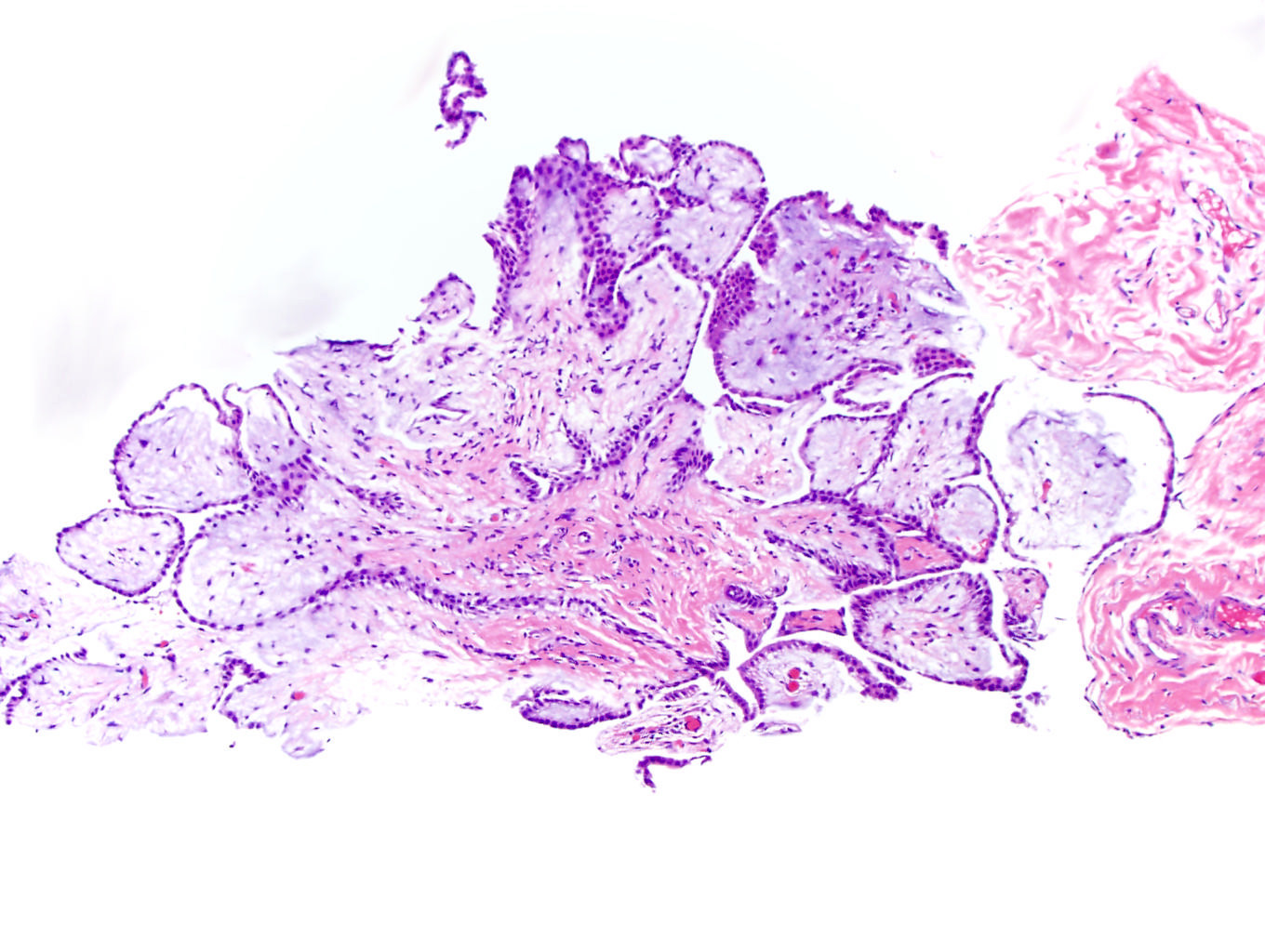
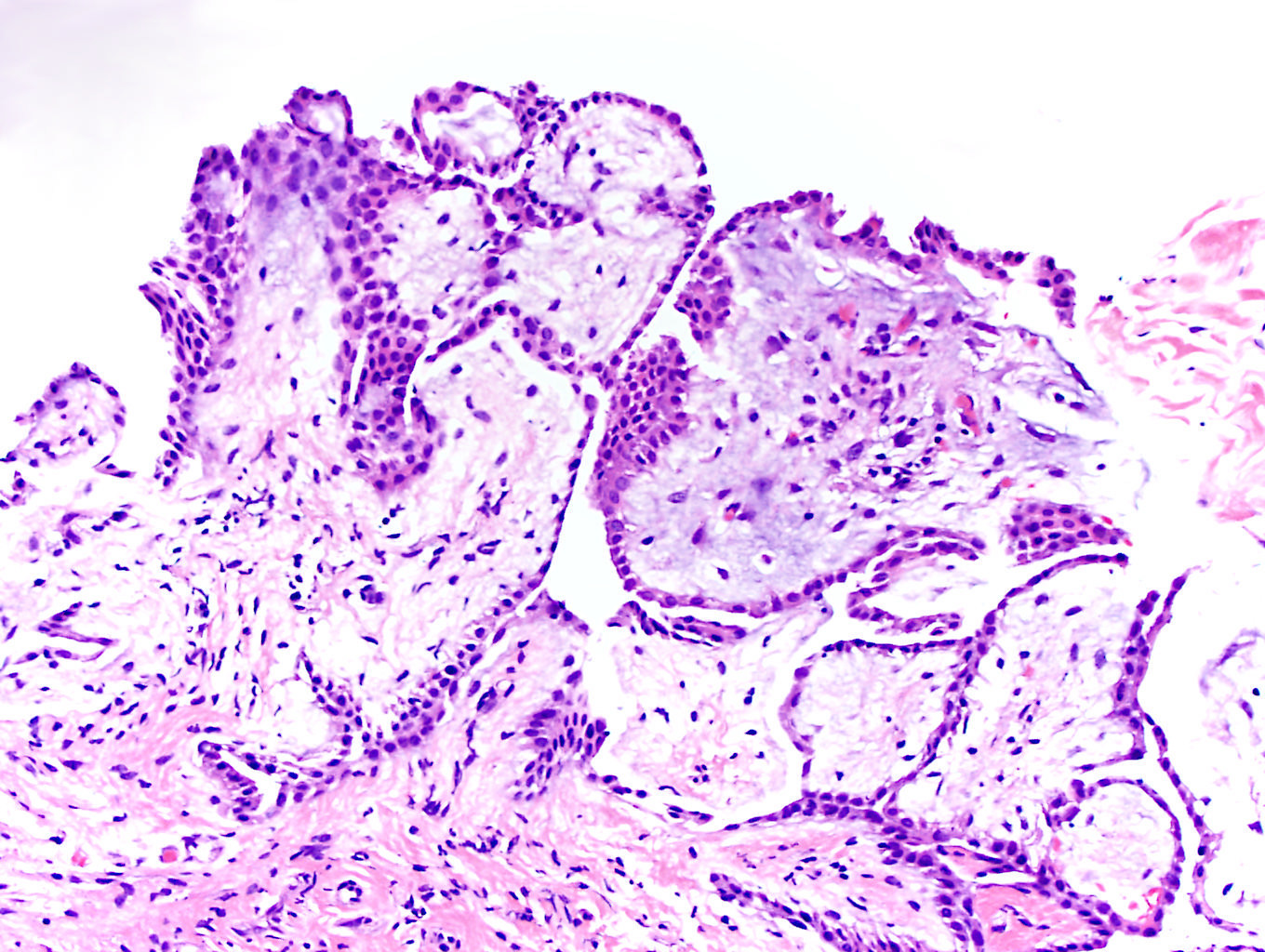
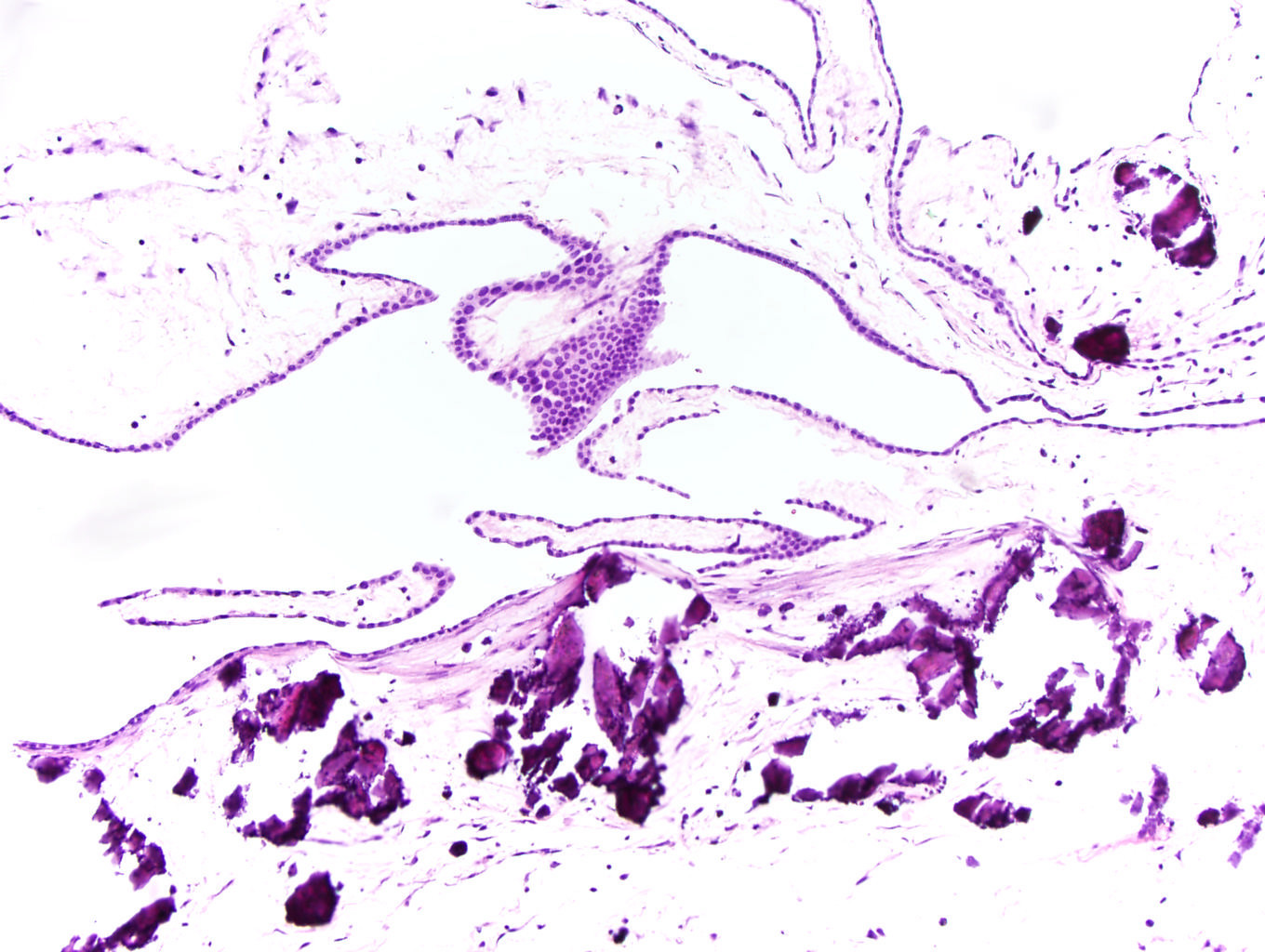
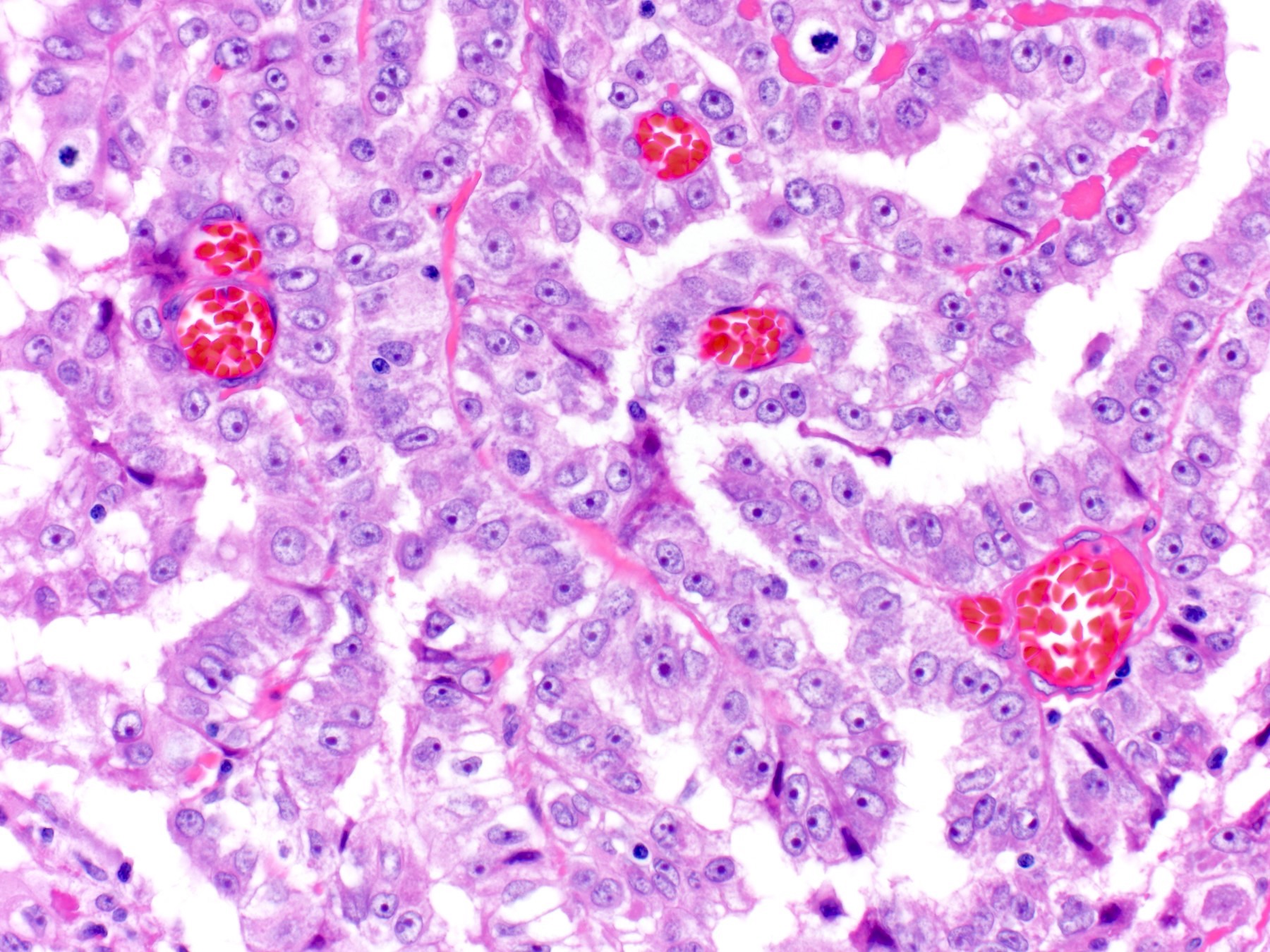
Microscopic (histologic) description
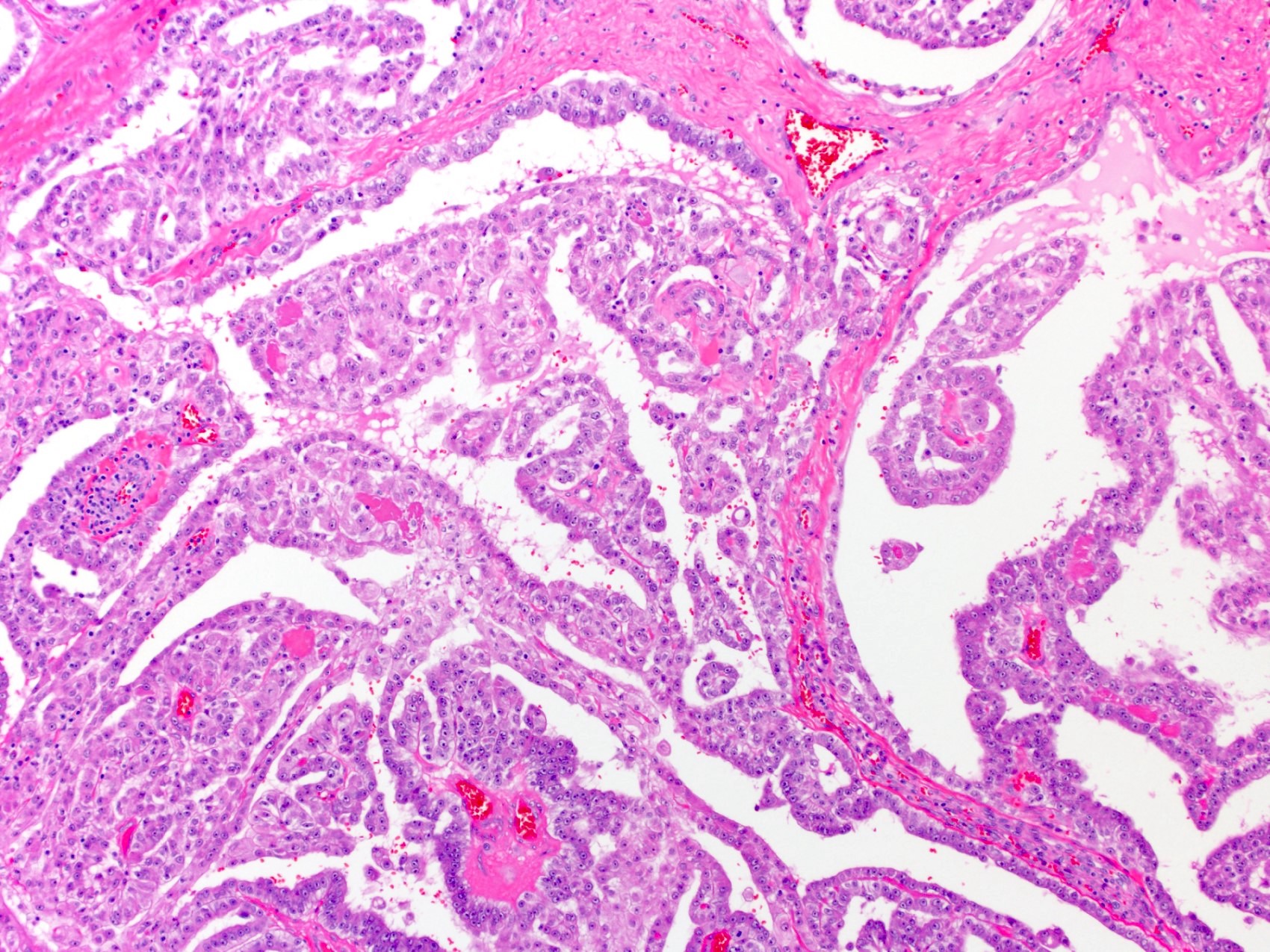
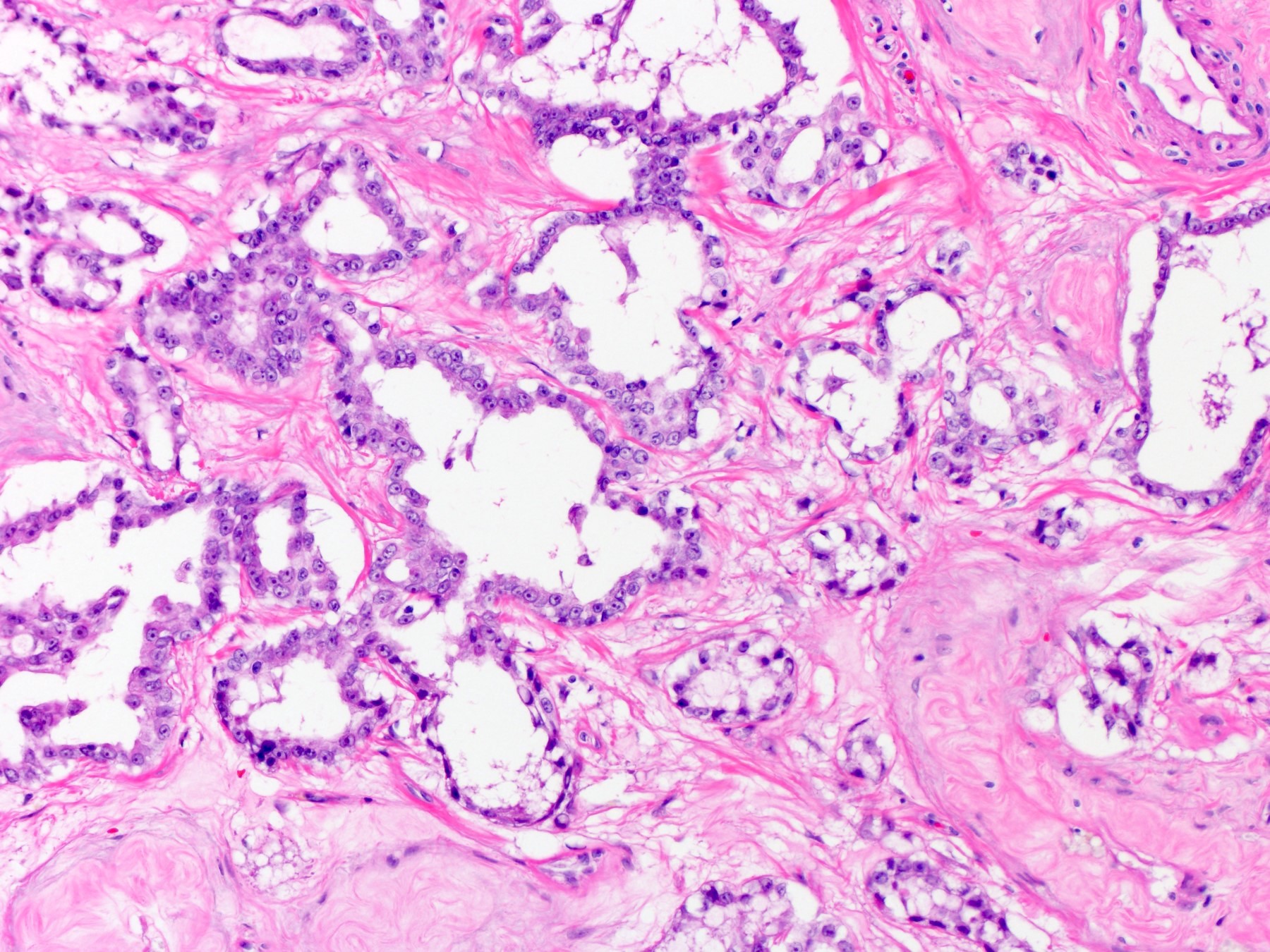
- Papillary structures with expansile cores showing myxoid features
- Papillary structures are lined by a bland simple layer of flattened to cuboidal cells
- Fibrovascular cores generally lack inflammation and psammoma bodies
- Occasional gland-like or tubulocystic areas may be seen
- There should be a lack of stromal invasion, significant atypia and mitotic activity (Mod Pathol 2022;35:1327)
Microscopic (histologic) images
Virtual slides
Cytology description
- Clusters of uniform mesothelial cells without atypia
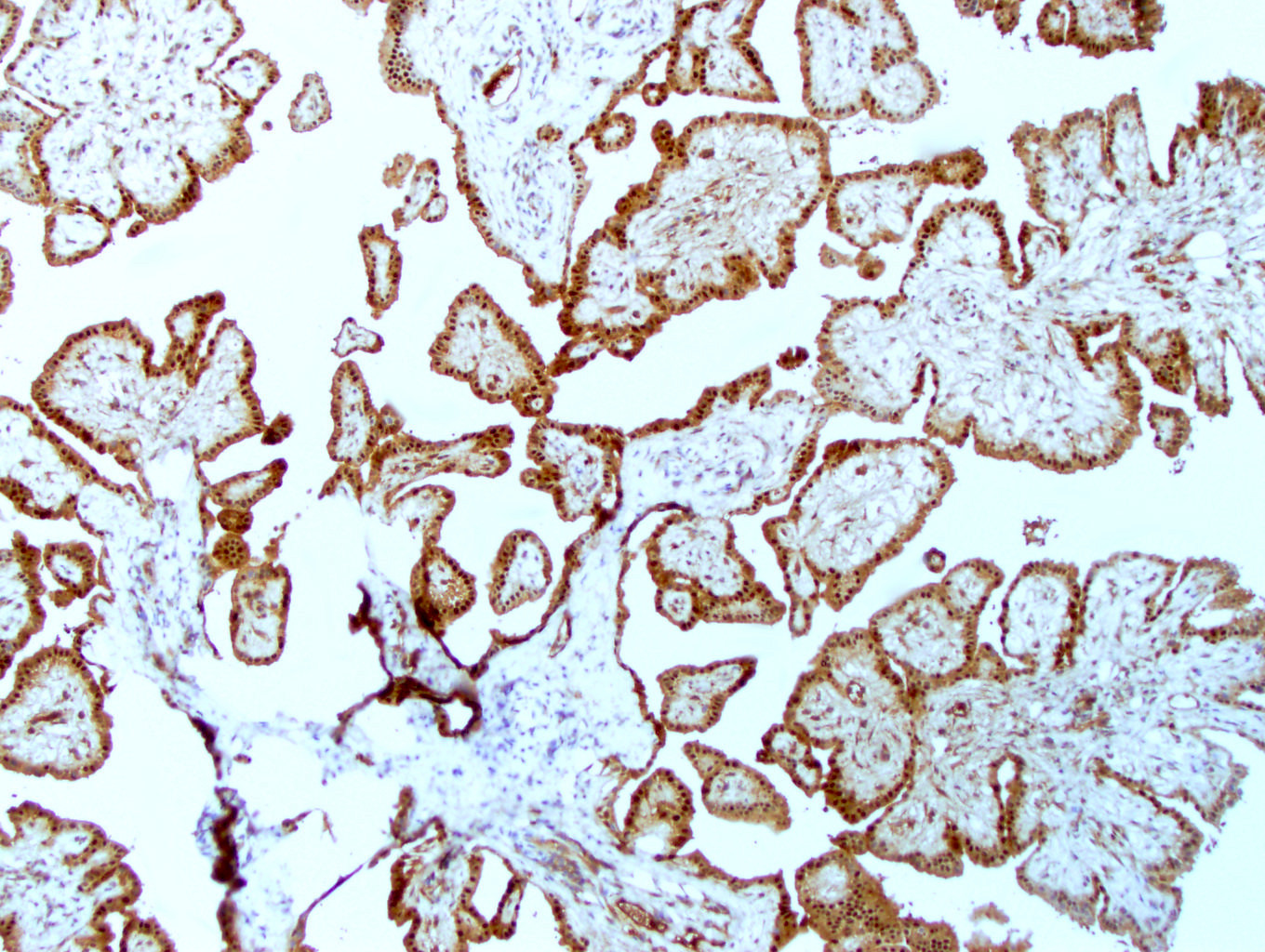
Positive stains
- MTAP retained (Mod Pathol 2020;33:245)
- BAP1 retained (Am J Surg Pathol 2018;42:256)
- PAX8 may have aberrant expression (pitfall) (94%) (Hum Pathol 2018;72:160)
- WT1
- D2-40
- CK5/6
- Calretinin
Molecular / cytogenetics description
- Still being studied, information based on small series
- 2 cases of CDC42 missense mutations (Mod Pathol 2019;32:88)
- 8 cases of TRAF7 missense mutations localized at the C terminus of the protein (Mod Pathol 2019;32:88)
- 5 cases of recurrent missense mutations of EHD1, ATM, FBXO10, SH2D2A, CDH5, MAGED1 and TP73 (Cancers (Basel) 2020;12:1568)
Sample pathology report
- Scrotum, hydrocelectomy:
- Well differentiated mesothelial tumor
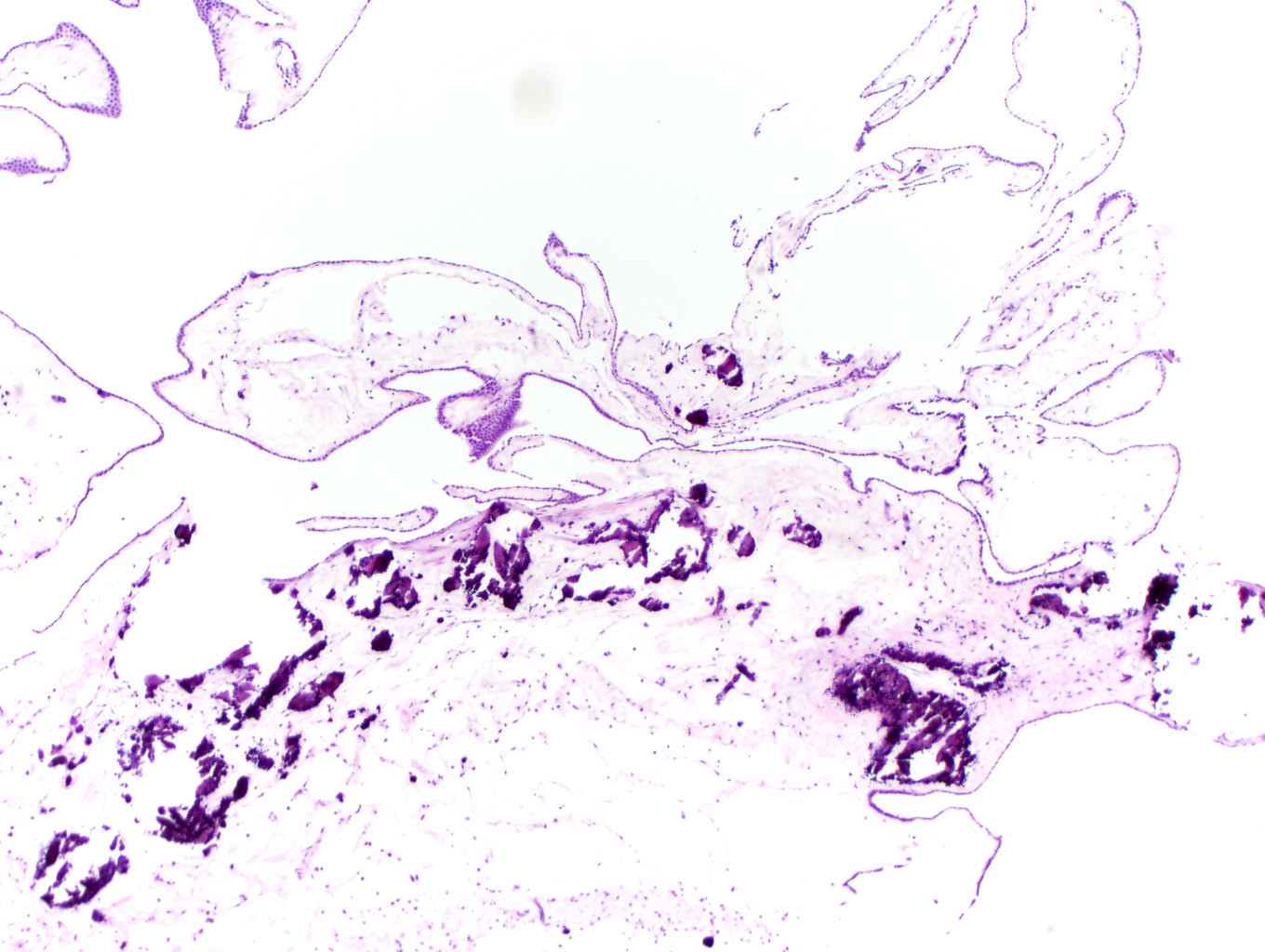
Differential diagnosis
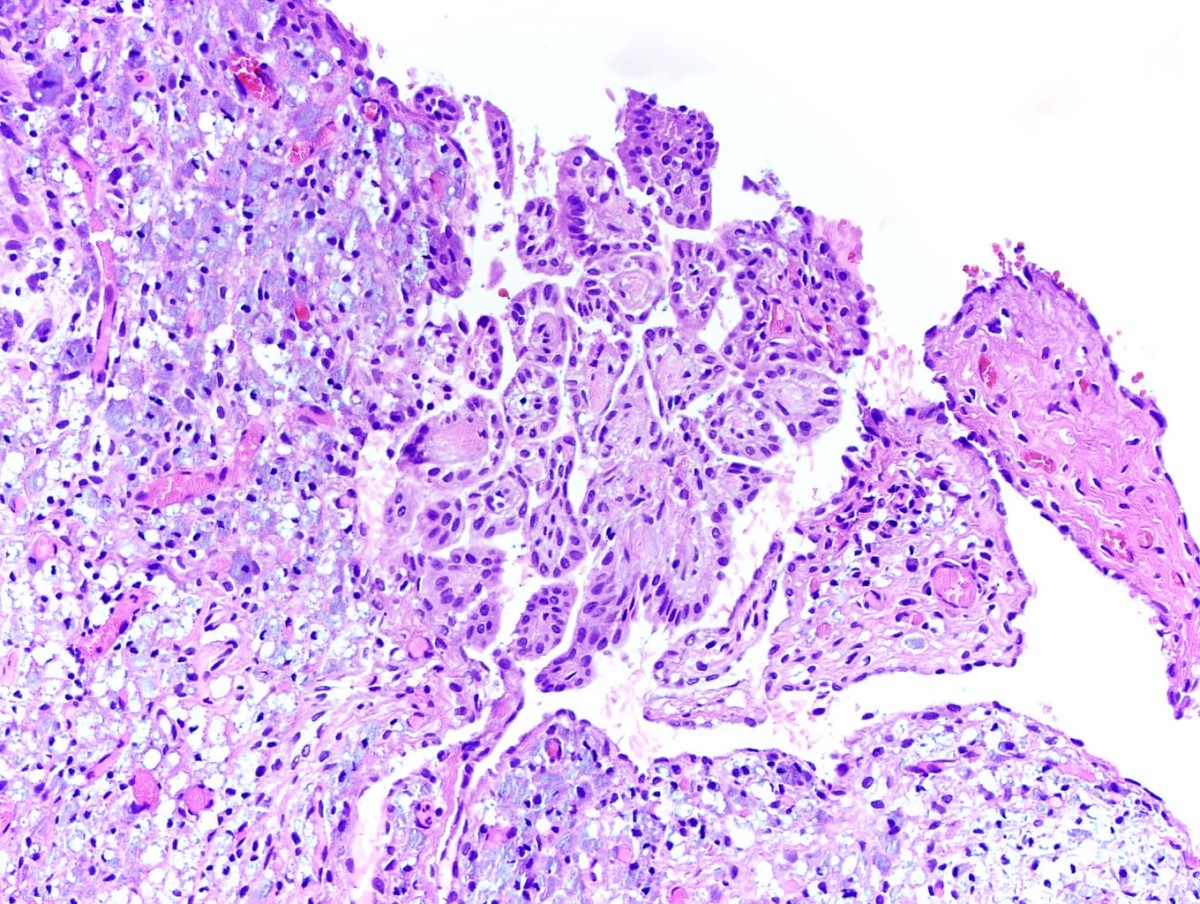
- Mesothelioma:
- Cytologic atypia, mitoses and invasion
- Loss of BAP1
- Mesothelioma in situ:
- Cytologic atypia and mitoses
- Loss of BAP1
- Invasion will not be present
- Serous cystadenoma:
- May have similar morphologic features
- Negative for calretinin, D2-40
- Serous borderline tumors:
- Architectural complexity of papillae or epithelial proliferation
- Negative for calretinin, D2-40
- Low grade serous cystadenocarcinoma:
- Invasion is present
- Negative for calretinin, D2-40
- Adenomatoid tumor:
- Tubules, cysts and cords without papillae
- Infiltrative growth is common
- Also mesothelial in origin; both express CK5/6, WT1, calretinin, D2-40
Board review style question #1
Board review style answer #1
B. BAP1 retained, MTAP retained, calretinin+, WT1+. These images show a well differentiated mesothelial tumor, which should have retained BAP1 and MTAP. Mesothelial markers will be positive.
Answer A is incorrect because while a well differentiated mesothelial tumor will express mesothelial markers, BAP1 should be retained.
Answer C is incorrect because mesothelial tumors will express both CK5/6 and D2-40.
Answer D is incorrect because this immunophenotype is more in keeping with an ovarian type serous tumor.
Comment Here
Reference: Well differentiated papillary mesothelial tumor
Comment Here
Reference: Well differentiated papillary mesothelial tumor
Board review style question #2
A patient presents with scrotal swelling that has been persistent over the last few years. An orchiectomy is done. Which of the following immunophenotypes would favor a mesothelioma over a well differentiated papillary mesothelial tumor?
- BAP1 loss, calretinin+, WT1+
- BAP1 retained, MTAP retained, calretinin+, WT1+
- Cytokeratin 5/6-, D2-40+
- p53 null, AE1 / AE3+, PAX8+
Board review style answer #2
A. BAP1 loss, calretinin+, WT1+. These images show a tumor with significant cytologic atypia and invasion into the testis. This is a mesothelioma of the tunica vaginalis. Mesotheliomas will express mesothelial markers and have BAP1 loss.
Answer B is incorrect because this immunophenotype is in keeping with a benign mesothelial lesion.
Answer C is incorrect because mesothelial tumors will express both CK5/6 and D2-40.
Answer D is incorrect because this immunophenotype is more in keeping with an ovarian type serous tumor.
Comment Here
Reference: Well differentiated papillary mesothelial tumor
Comment Here
Reference: Well differentiated papillary mesothelial tumor