Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Diagrams / tables | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khanlari M, Miranda RN. Primary follicular lymphoma-testis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomafolliculartesticular.html. Accessed December 26th, 2024.
Definition / general
- Primary follicular lymphoma of testis (PFLT) in children and adolescents is a subset of extranodal follicular lymphoma (FL)
- Lymphoma composed of follicle center B cells that arise in testis
- Follicular lymphoma involving testis as manifestation of systemic disease is excluded
- Not recognized as specific variant in 2017 World Health Organization classification
Essential features
- Localized disease limited to the testis
- Favorable course despite its aggressive histology
- Systemic relapses are uncommon
Terminology
- Primary follicular large cell lymphoma (Arch Pathol Lab Med 2001;125:551)
Epidemiology
- Primary non-Hodgkin lymphoma (NHL) of testis: 1% of all cases of non-Hodgkin lymphoma
- Primary follicular lymphoma of testis is rare
- Limited to single case reports or small case series
- Most cases series are in children and young adults
- Less common in adults
- In adults non-Hodgkin lymphoma of the testis is mostly diffuse large B cell lymphoma (DLBCL)
- Reference: Am J Surg Pathol 2007;31:1050
Sites
- Testis
Pathophysiology / etiology
- Poorly understood
- Tumor seems to lack protection against apoptosis (J Clin Pathol 2002;55:684)
Diagrams / tables
Clinical features:
| Nodal follicular lymphoma | Testicular follicular lymphoma | |
| Age (median) | Adults and elder (sixth decade) | Children and young adults |
| Gender (M:F) | Men and women | Men only |
| Affected sites | Lymph nodes with extranodal spread | Testicle and adnexa |
| Symptoms | Generalized lymphadenopathy | Painless mass |
| Stage (Ann Arbor) | High (III - IV) in most cases | IE |
Pathologic features:
| Nodal follicular lymphoma | Testicular follicular lymphoma | |
| Gross appearance | Discrete mass or complete effacement | Discrete mass or diffuse involvement |
| Histologic grade | Grades 1 - 3 | Grade 3 |
Immunophenotype:
| Nodal follicular lymphoma | Testicular follicular lymphoma | |
| CD10 | Variable | Variable |
| BCL2 | Usually positive | Negative |
Molecular features:
| Nodal follicular lymphoma | Testicular follicular lymphoma | |
| IGH-BCL2 | Present, up to 90% | Negative |
Clinical features
- Painless discrete mass or diffuse testicular enlargement
- May be mistaken with hydrocele (Cancer 1999;85:1626)
- No peripheral lymphadenopathy
- No hepatosplenomegaly
- No B symptoms
- Reported cases are predominantly at clinical stage of IE
Radiology description
- Ultrasonography:
- Hypoechoic areas
- Variably hypervascular
Prognostic factors
- Excellent prognosis for children and young adults with stage IE disease
- Enrollment in Children’s Oncology Group may be important for developing future advances in treatment
- Small number of adult cases with generally short follow up
- However, a favorable clinical outcome is observed (Am J Surg Pathol 2007;31:1050)
- Reference: J Pediatr Hematol Oncol 2004;26:104
Case reports
- 3 year old boy with a case of follicular lymphoma of the testis (J Pediatr Hematol Oncol 2004;26:104)
- 4 year old boy presenting with left testis swelling without other signs and symptoms (J Clin Pathol 2002;55:684)
- 90 year old man presented with a left scrotal mass (J Med Case Rep 2012;6:24)
Treatment
- Resection
- With or without subsequent chemotherapy
Gross description
- Discrete mass or diffuse involvement of testis
- Fleshy tan or pink distinct nodule
- Either poorly or well demarcated
- 1.2 - 4.0 cm
- Reference: J Pediatr Hematol Oncol 2012;34:68
Frozen section description
- Same criteria applied in microscopic evaluation
- When possible, spare tissue for cytogenetic analysis, flow cytometry immunophenotype; preparation of imprints is recommended
Microscopic (histologic) description
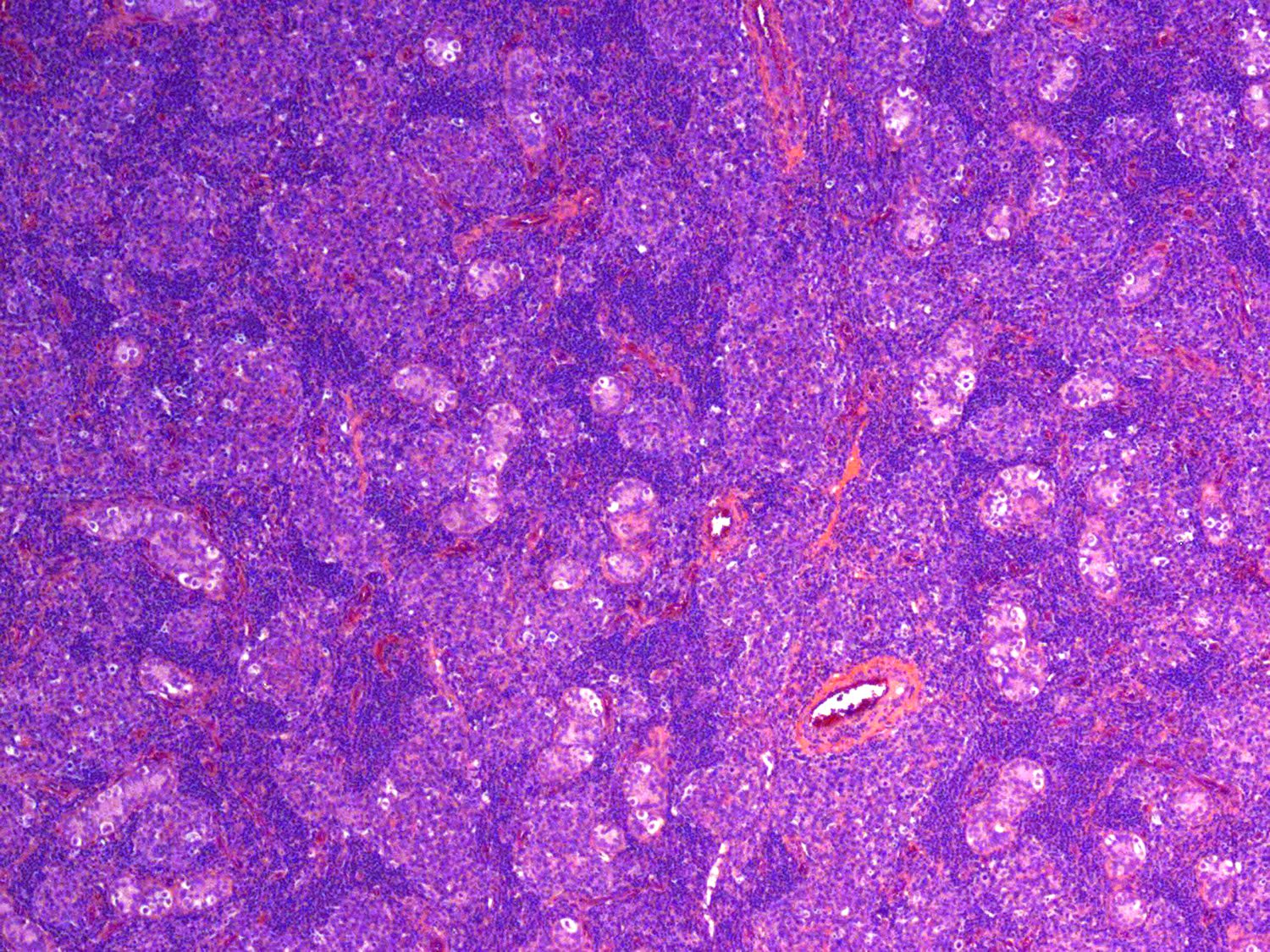
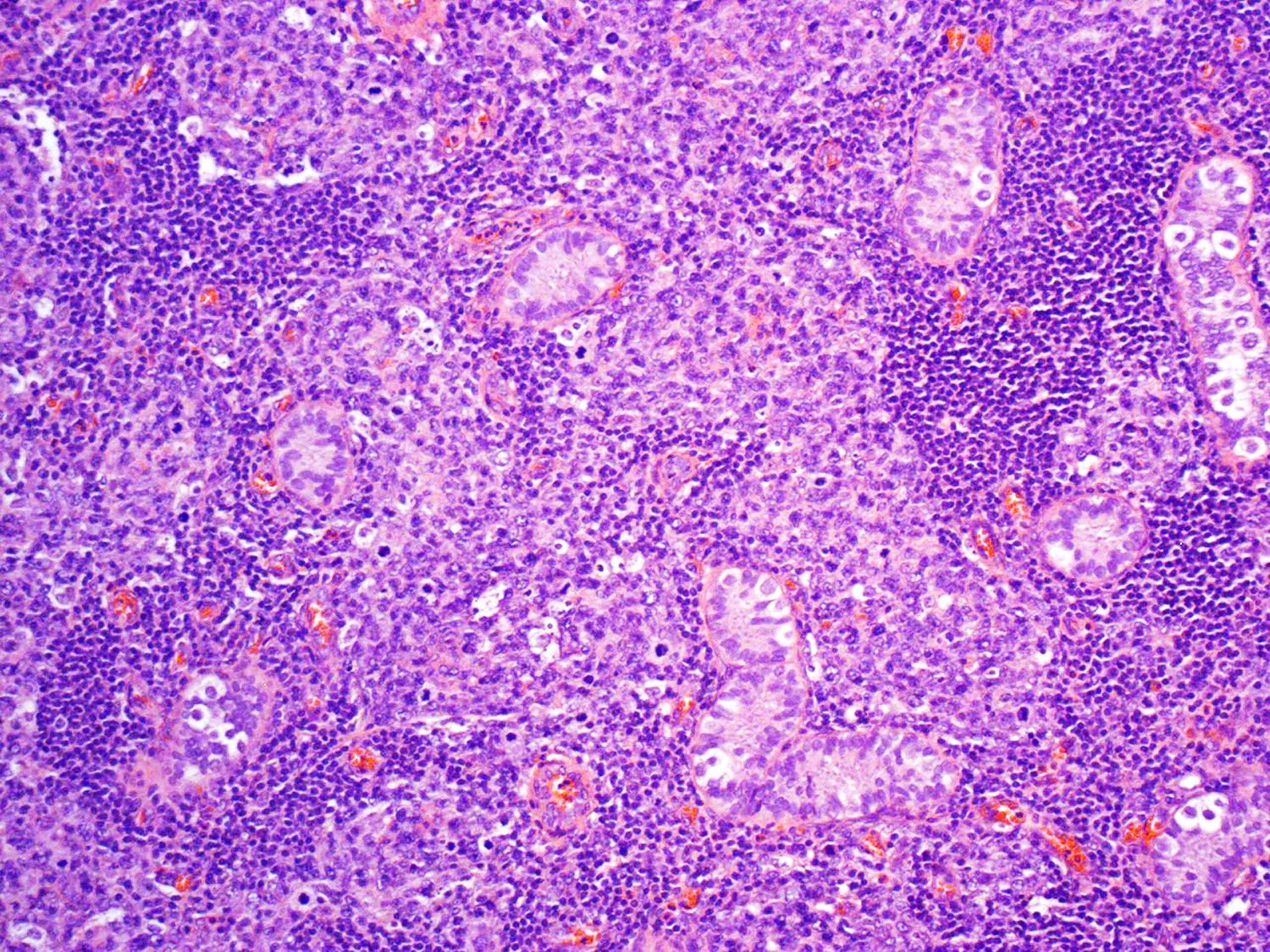
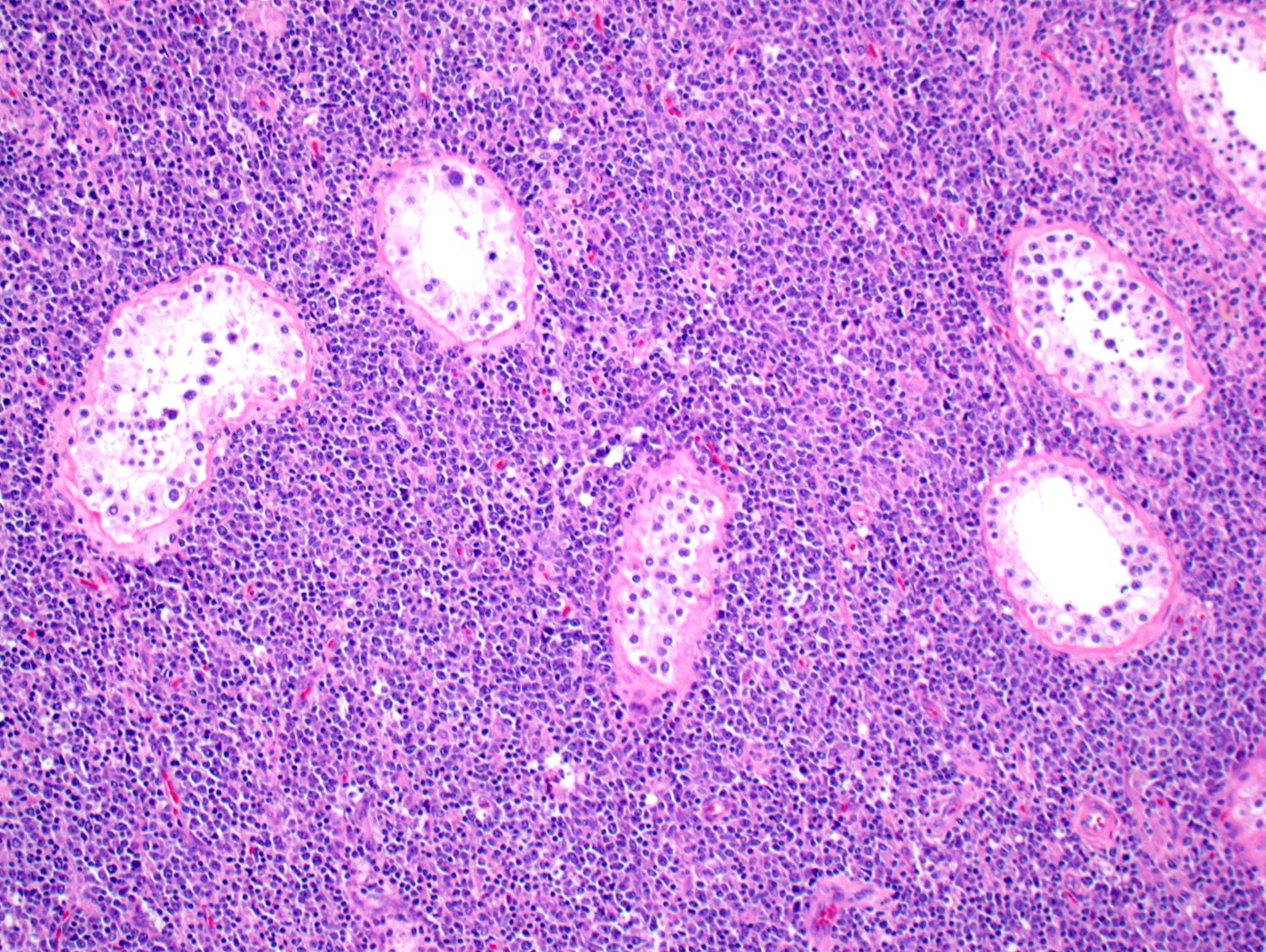
- Nodular pattern consistent with follicular lymphoma
- Follicular lymphoma involves mainly testicular parenchyma and secondarily adnexa
- Neoplastic follicles grow between tubuli
- May completely replace testicular parenchyma
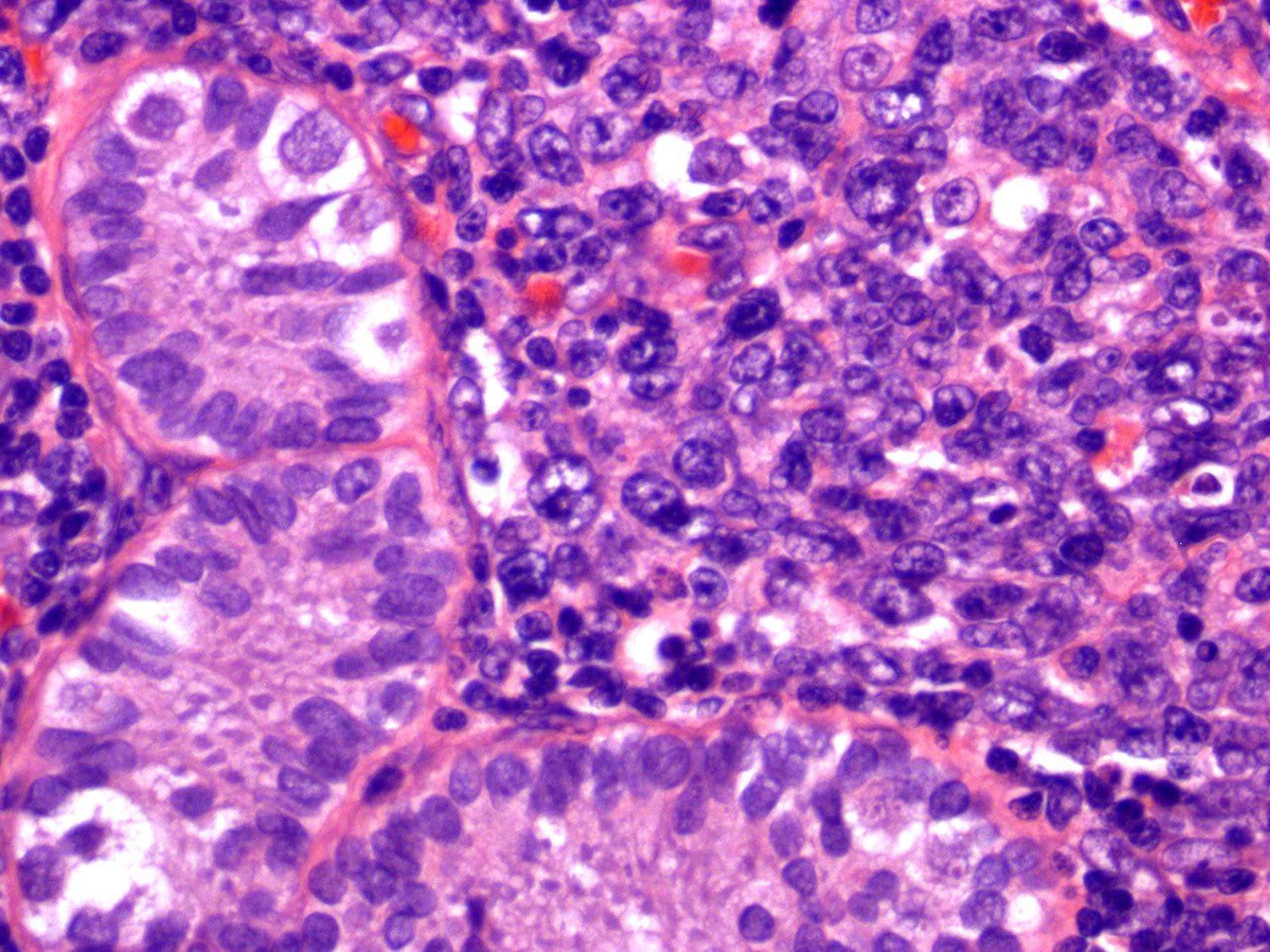
- Reported cases are predominantly grade 3A
- Large lymphocytes (centroblasts) predominate
- Some small cleaved lymphocytes (centrocytes) are admixed
- Occasionally, focal areas of diffuse growth support focal diffuse large B cell lymphoma
- Prominent interstitial fibrosis (Am J Surg Pathol 2007;31:1050)
- Mantle zone usually attenuated or lost around neoplastic follicles
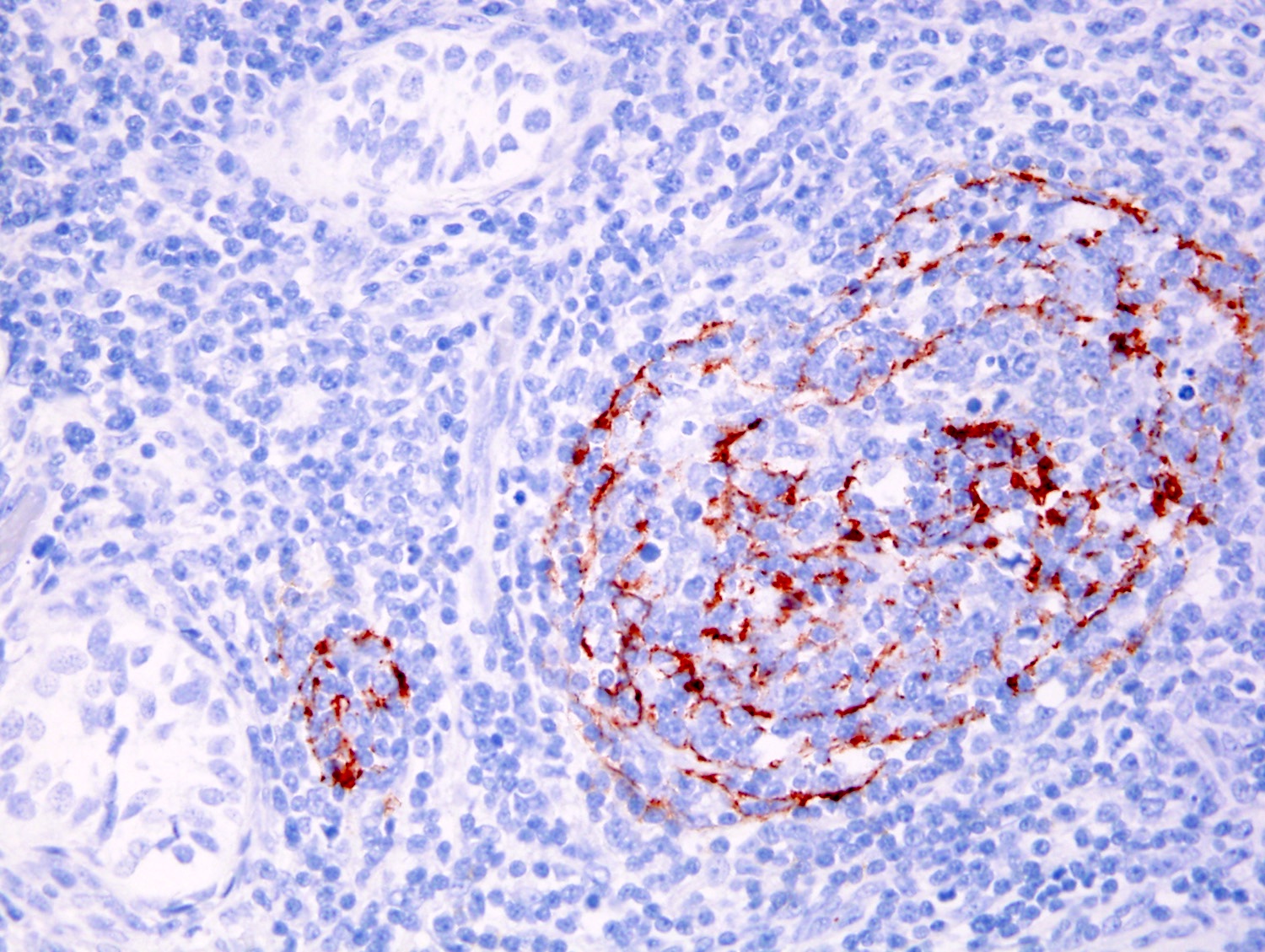
Microscopic (histologic) images
Cytology description
- Majority of cells: large noncleaved cells (centroblasts)
- Multilobated large cells
- May be an admixture of centroblasts and small centrocytes
- Reference: Hum Pathol 2012;43:1514
Positive stains
- Pan-B cell antigens
- Monotypic surface Ig
- CD10 (variable) and BCL6 protein (variable)
- Weakly expressed by cells in the interfollicular region
- Ki67 / MIB1: high proliferation rate
- p53 protein: often positive in primary follicular lymphoma of testis of adults
- Reference: Arch Pathol Lab Med 2001;125:428
Negative stains
- Epstein-Barr virus (EBER)
- IRF4, MYC, BCL2, cytokeratins and PLAP
- Reference: Arch Pathol Lab Med 2001;125:428
Molecular / cytogenetics description
- Monoclonal IGH rearrangements
- IGH-BCL2 fusion is uncommon based on PCR and FISH
- With or without BCL6 translocations (Cancer 1999;85:1626)
Sample pathology report
- Right testicular tumor, orchiectomy:
- Follicular lymphoma with a follicular pattern, grade 3A, with prominent sclerosis (see comment)
- Comment: Histologic sections demonstrate testicular parenchyma almost completely involved by malignant lymphoma. The lymphoma consists of numerous neoplastic follicles, that are composed of large noncleaved cells (centroblasts) that average > 15 per high power field, admixed with small cleaved lymphocytes (centrocytes) supporting a diagnosis of follicular lymphoma grade 3A. The neoplastic cells surround and invade seminiferous tubulei displacing germ cells and Sertoli cells. Tumor cells inside of the seminiferous tubulei are also seen. Mitoses are easily found. Small areas of infarction are seen in the testicular parenchyma. The noninvolved testicular parenchyma is morphologically unremarkable.
- Immunophenotypic studies show that the tumor cells are positive for CD10, CD20, CD45 (LCA) and BCL6 (less than 10%). The aberrant cells are negative for CD3, CD5, MUM1 and BCL2. CD21 highlights residual follicular dendritic cell networks in a subset of the neoplastic follicles. The proliferation index as determined by Ki67 is approximately 60%.
- Fluorescence in situ hybridization (FISH) performed in the laboratory of cytogenetics did not detect rearrangement of the MYC gene. However, extra copies of the MYC gene consistent with an aneuploid cell population were detected.
- FISH studies failed to detect the presence of of t(14;18) or IGH-BCL2 fusion.
Differential diagnosis
- Diffuse large B cell lymphoma (DLBCL):
- Diffuse large B cell lymphoma is most common lymphoma involving testis
- Primary follicular lymphoma of testis can be grade 3 and predominantly diffuse
- Features supporting diffuse large B cell lymphoma over extranodal follicular lymphoma
- Diffuse large B cell lymphoma is most common lymphoma involving testis
- Reactive follicular hyperplasia:
Additional references
Board review style question #1
Which of the following extranodal follicular lymphomas is predominantly high grade?
- Ocular adnexa
- Small intestine
- Stomach
- Testis
Board review style answer #1
Board review style question #2
A 26 year old man has presented with a testicular mass without any previous history of infection or autoimmune disease. Monoclonal IGH rearrangement is detected on the fresh tissue submitted at the time of excision. Which of the following options is most likely correct about this patient or patient's pathology sample?
- IGH-BCL2 rearrangement is detected in cytogenetic studies
- Lymphoma has high grade feature
- Patient has generalized lymphadenopathy
- Patient's prognosis is poor despite therapy
Board review style answer #2