Table of Contents
Definition / general | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Electron microscopy description | Differential diagnosisCite this page: Rane S. Leiomyosarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisleiomyosarcoma.html. Accessed April 1st, 2025.
Definition / general
- Malignant mesenchymal tumor with smooth muscle differentiation
Epidemiology
- Second most common malignant mesenchymal tumor of paratestis, after liposarcoma (Urol Oncol 2014;32:52)
- 10 - 30% of paratesticular sarcomas are leiomyosarcomas (Int Braz J Urol 2006;32:66, Urol Int 2009;82:448, Urol Oncol 2014;32:52)
- 5 year and 10 year disease specific survival rates are 77% and 66% (Urol Oncol 2014;32:52)
- After 4 year follow up, 30% had metastases (lymph nodes, lungs, liver) (all grade 3 tumors) (Am J Surg Pathol 2001;25:1143)
- Median age is 64 years, range 17 - 92 years (Am J Surg Pathol 2001;25:1143, Urology 2002;60:1112)
Sites
- Spermatic cord is most common paratesticular site (Am J Surg Pathol 2001;25:1143)
- Other sites include epididymis and scrotal sac (Can Urol Assoc J 2011;5:E121)
Pathophysiology
- Hypothesized to arise from cremasteric muscle, vas deferens or contractile cells of other structures such as tunica or blood vessels (Urology 2002;60:1112)
- Paratesticular tumors belong to "deep type" of leiomyosarcoma
- No recurrent genetic abnormality has been documented
- Tumor spreads via lymphatic and hematogenous metastases or by local extension
- Lymphatic spread is to regional lymph nodes: external iliac, hypogastric, common iliac, retroperitoneal (J Urol 1970;103:628)
- Lung is most common site for hematogenous spread
Clinical features
- Typically presents with painless, slow growing mass (at least a few months) in scrotal sac
- Rarely presents with sudden increase in size of long standing mass
- Aggressive tumors may invade dartos muscle and overlying skin, causing a fungating mass
Laboratory
- Normal serum tumor markers (LDH, β-HCG, α-fetoprotein) helps exclude a germ cell tumor
Radiology description
- Sonography shows a mass with mixed echogenicity and increased vascularity (World J Radiol 2011;3:114)
- Color Doppler ultrasonography reveals irregular vascularity, more dominant in periphery, similar to malignant tumors
- CT usually shows absence of fat (absence of foci with negative Hounsfield units)
- Variable degree of hydrocele may be present
Radiology images
Prognostic factors
- Similar to sarcoma: tumor size, tumor grade, presence of necrosis, mitotic count, completion of resection, local recurrence, distant metastases
- Specific prognostic criteria not well established due to rarity of tumor
- FNCLCC grading (recommended over NIH system) gives points for:
- Differentiation: 1, well differentiated leiomyosarcoma; 2, conventional leiomyosarcoma; 3, poorly differentiated / pleomorphic / epithelioid leiomyosarcoma
- Mitotic count: 1, 0 - 9 per 10 high powered fields; 2, 10 - 19 per 10 high powered fields; 3, 20 or more per 10 high powered fields
- Necrosis: 0, none; 1, less than or equal to 50%; 2, greater than 50%
- Grade 1 is 2 - 3 points, grade 2 is 4 - 5 points and grade 3 is 6 - 8 points
Case reports
- Infant with testicular leiomyosarcoma (J Pediatr Surg 2004;39:e16)
- 18 year old man with epithelioid tumor (Urol J 2004;1:215)
- 45 year old man with rapidly enlarging, painless testicular swelling (Case #254)
- 50 year old man successfully treated with orchiectomy and chemotherapy (Cancer Res Treat 2012;44:210)
- 53 year old man (Asian J Androl 2013;15:843)
- 58 and 75 year old men with leiomyosarcoma of epididymis (Can Urol Assoc J 2011;5:E121)
- 65 year old man (Med Princ Pract 2002;11:157)
Treatment
- Radical orchidectomy for resectable tumors
- Simple excision is insufficient as residual disease was found in 27% of cases that underwent repeat wide excision (J Urol 1981;126:611)
- Uncertain role of adjuvant radiation or chemotherapy; some authors recommend adjuvant therapy in high grade / high risk tumors and others recommend adjuvant radiotherapy for all grades to reduce local recurrence (Cancer 1996;77:1873, J Urol 1991;146:342)
- Prophylactic retroperitoneal lymph node dissection may be performed but no survival benefit has been documented, so dissection recommended only if nodes are suspicious for involvement (J Urol 1970;103:628)
- Single or multiagent chemotherapy with anthracyclines and if osfamides or gemcitabine for nonoperable or metastatic tumors
Gross description
- Tumor typically located outside tunica albuginea, may be centered on epididymis or spermatic cord
- Cut surface is usually firm, gray white
- Grossly identifiable necrotic and hemorrhagic areas may be seen
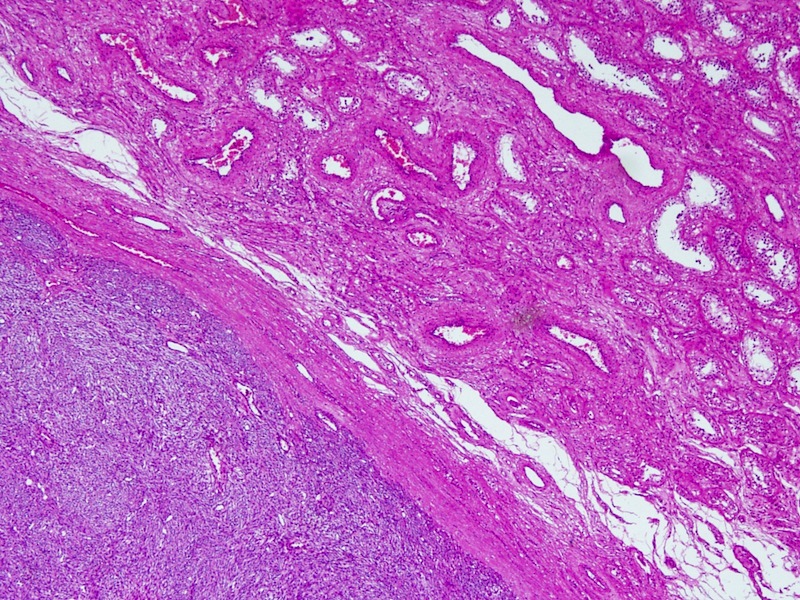
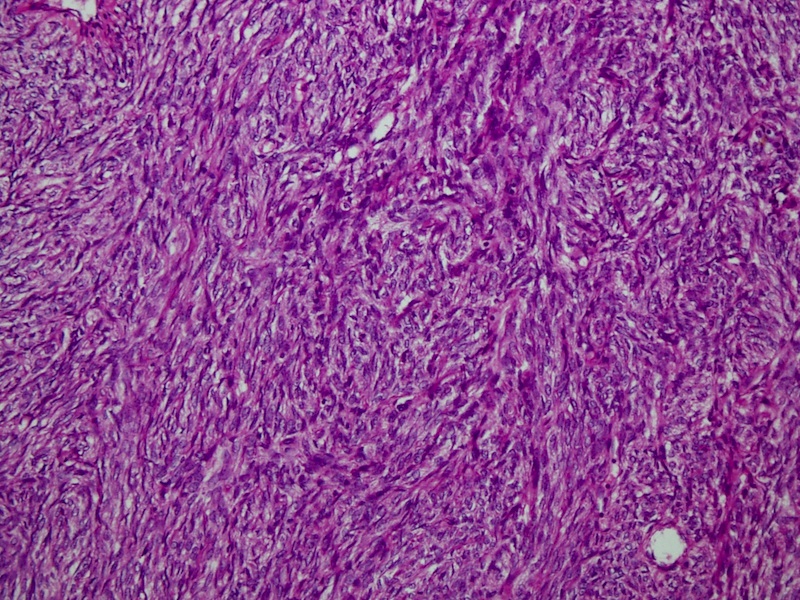
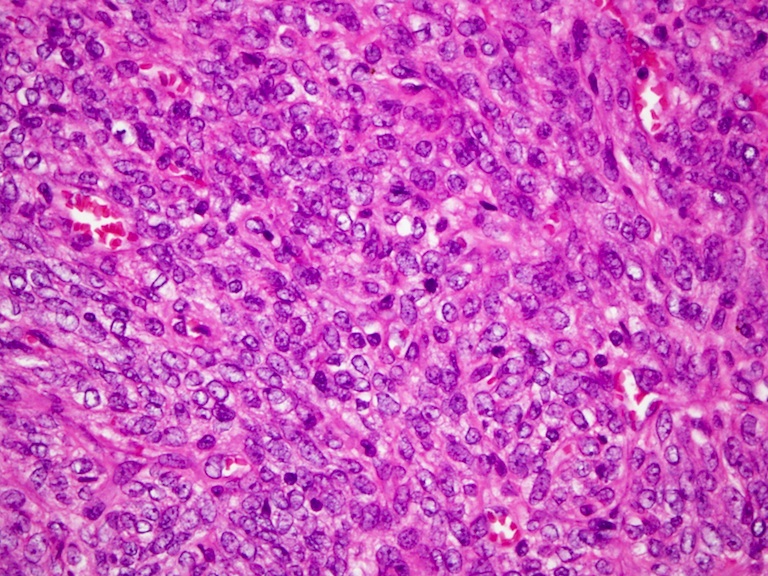
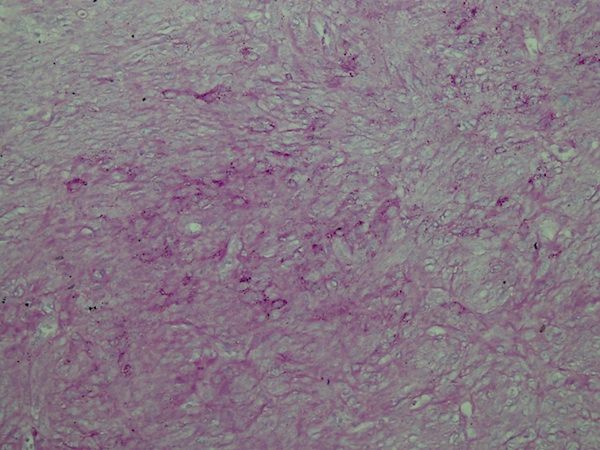
Microscopic (histologic) description
- Interlacing fascicles of spindle shaped cells with eosinophilic cytoplasm and cigar shaped nuclei
- Mitotic activity is usually seen; necrosis may be seen
- At least mild atypia; more undifferentiated cases have marked cellular atypia
- Variably scattered mast cells, inflammatory cells, hyalinization
- Histological variants:
- Epithelioid
- Dedifferentiated / pleomorphic
- Discrete transition to more pleomorphic tumor (reminiscent of malignant fibrous histiocytoma) without any smooth muscle differentiation
- Dedifferentiated areas are usually negative for all myogenic markers
- Heterologous osseous or chondro-osseous elements may be seen rarely
- With osteoclast-like giant cells (Urol Int 1996;56:259)
- Myxoid (Am J Surg Pathol 2000;24:927)
- Inflammatory
Microscopic (histologic) images
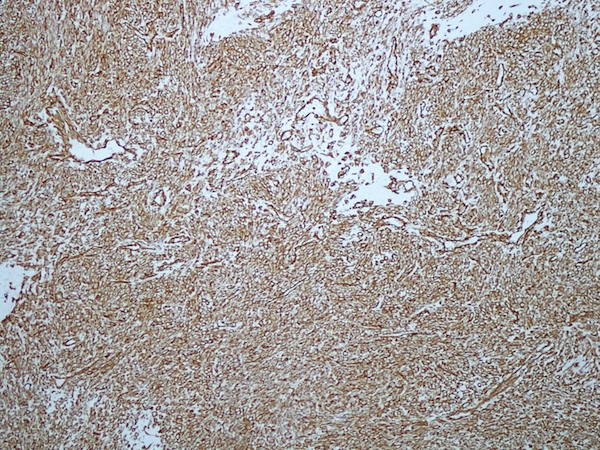
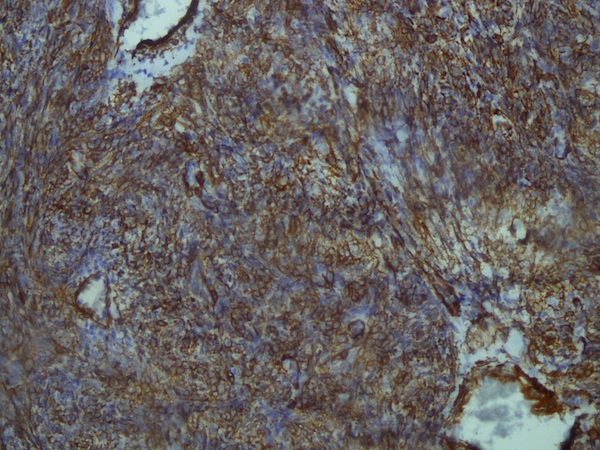
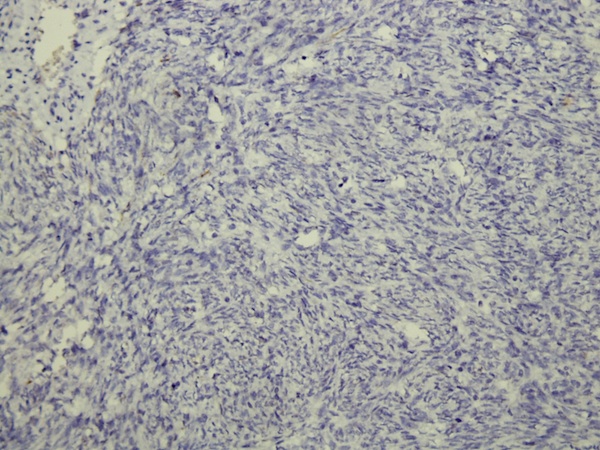
Immunohistochemistry & special stains
- Positive:
- Variable:
- Negative / focal rare cells:
Electron microscopy description
- 7 nm microfilaments, regular dense bodies, micropinocytotic vesicles, glycogen pools (Ann Diagn Pathol 2003;7:60)
Differential diagnosis
- Dedifferentiated liposarcoma with smooth muscle differentiation
- More typical liposarcomatous areas
- Fibromatosis: tapered nuclei
- Leiomyoma
- No appreciable mitotic activity or necrosis but nuclear atypia may be present
- Scrotal smooth muscle tumors should be classified as potentially malignant if any mitotic activity is seen (Ann Diagn Pathol 2003;7:60)
- Malignant peripheral nerve sheath tumor
- Mesothelioma
- Associated with hydrocele, asbestos exposure; infiltrative margins; usually keratin+, desmin-
- Solitary fibrous tumor
- Disorganized spindle cells, diffusely CD34+ and desmin-
- Spindle cell rhabdomyosarcoma
- Usually occurs in children
- Myogenin+, MyoD1+