Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sanguedolce F. Hydrocele. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testishydrocele.html. Accessed April 2nd, 2025.
Definition / general
- Accumulation of serous fluid between visceral and parietal layers of tunica vaginalis
Essential features
- Accumulation of serous fluid between visceral and parietal layers of tunica vaginalis
- Idiopathic or associated with nonneoplastic or neoplastic lesions
- Note: thorough macroscopic examination and extensive sampling are needed to rule out mesothelioma (Singapore Med J 2015;56:e53)
Epidemiology
- Prevalence: 6% children, 1% adult men
- Any age
- Reference: Acta Medica (Hradec Kralove) 2020;63:57
Sites
- Scrotum
- Rarely, the hydrocele sac may extend beyond the scrotum to the abdomen via the inguinal canal (abdominoscrotal hydrocele) (Urol Case Rep 2020;32:101254)
Pathophysiology
| Persistent communication with the peritoneal cavity | No | Yes |
| Etiology | Defective closure at both proximal and distal ends of processus vaginalis | Defective closure of the distal end of tunica vaginalis |
| Macroscopic differential diagnosis | Inguinal lymphadenopathy, hernia, tumor of the spermatic cord |
Etiology
- Mostly idiopathic, putative causes: excessive secretion or decreased reabsorption of fluid by parietal mesothelial cells, congenital lack of efferent lymphatics
- Association with inguinal hernia, scrotal trauma, inflammation (epididymoorchitis) or tumors of the testis / paratestis (BJU Int 2011;107:1852)
- Filarial hydrocele (StatPearls: Filarial Hydrocele [Accessed 2 February 2023]):
- Late and chronic manifestation of filariasis
- Very common in endemic areas (tropical and subtropical countries)
- Due to parasite induced blockage and dysfunction of the lymphatic vessels
Clinical features
- Painless scrotal swelling, feeling of heaviness (BJU Int 2011;107:1852)
Diagnosis
- Usually diagnosed by physical examination and transillumination
Radiology description
- Simple fluid collection at ultrasound; may contain septations, calcifications or cholesterol (Radiographics 2009;29:2017)
- Avascular at Doppler evaluation
- MRI: low signal on T1, high signal on T2 weighted images
Case reports
- 18 year old man with an asymptomatic palpable mass in the left testis growing into the lower abdomen (Pan Afr Med J 2018;31:213)
- 63 year old man with giant hemorrhagic hydrocele (Urol Case Rep 2018;18:44)
- 80 year old man with longstanding hydrocele and eggshell peripheral calcifications (BMJ Case Rep 2020;13:e232827)
Treatment
- Spontaneous resolution in most cases
- Some cases require surgical treatment
- Follow up due to possible recurrences (Cheng: Urologic Surgical Pathology, 4th Edition, 2019)
Gross description
- Usually unilocular, can be multicameral (Nistal: Atlas of Peculiar and Common Testicular and Paratesticular Tumors, 1st Edition, 2020)
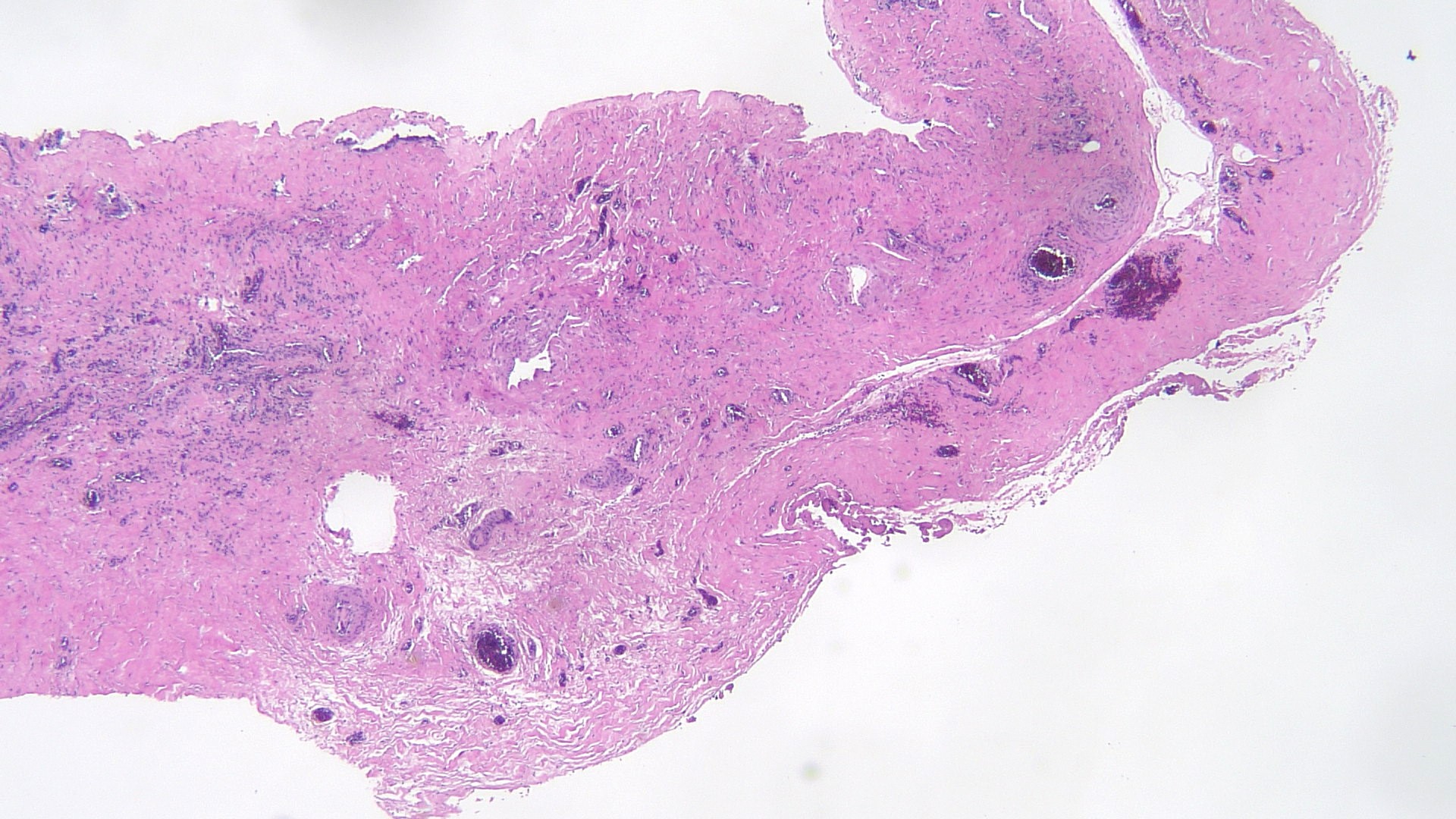
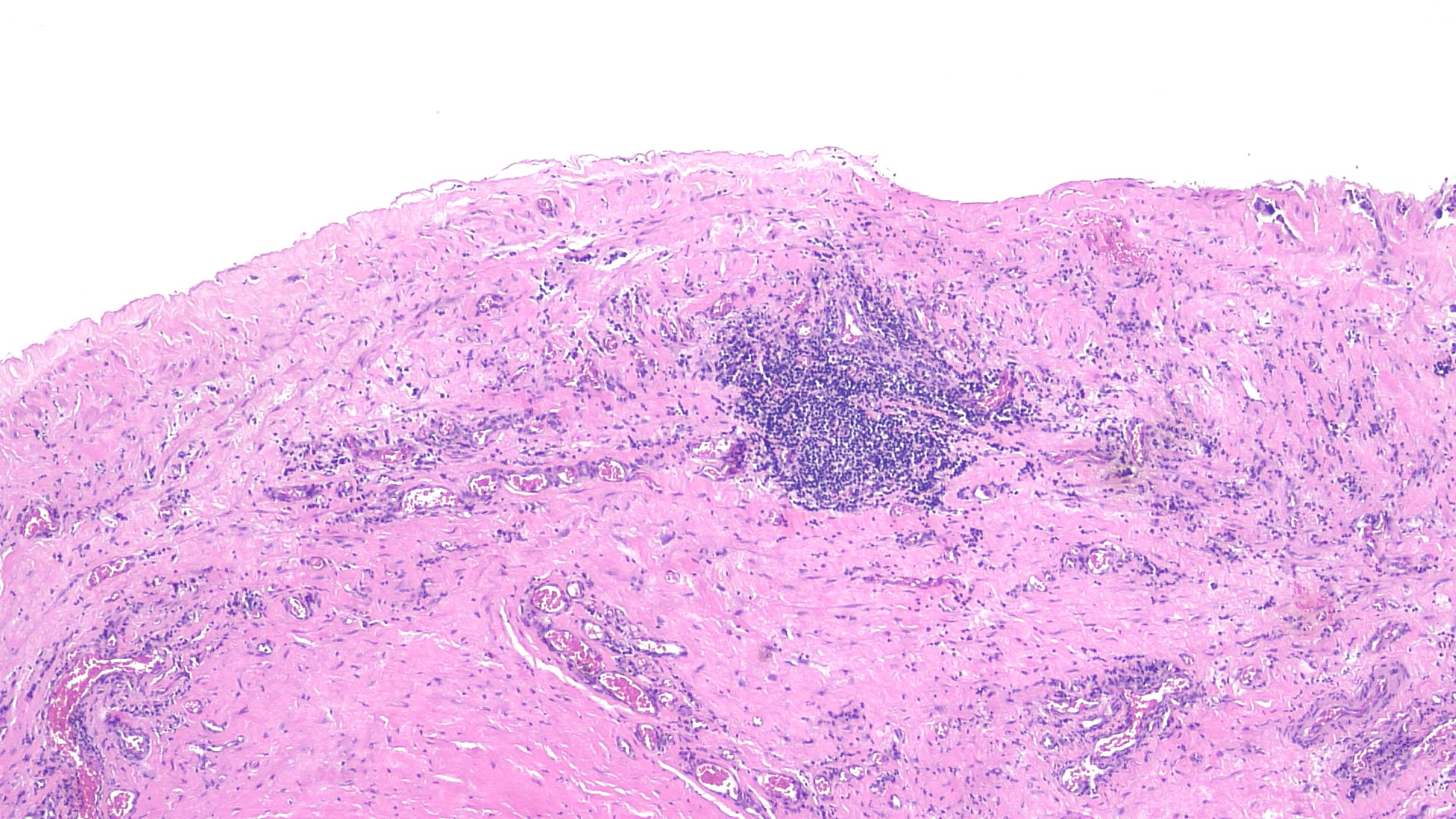
Microscopic (histologic) description
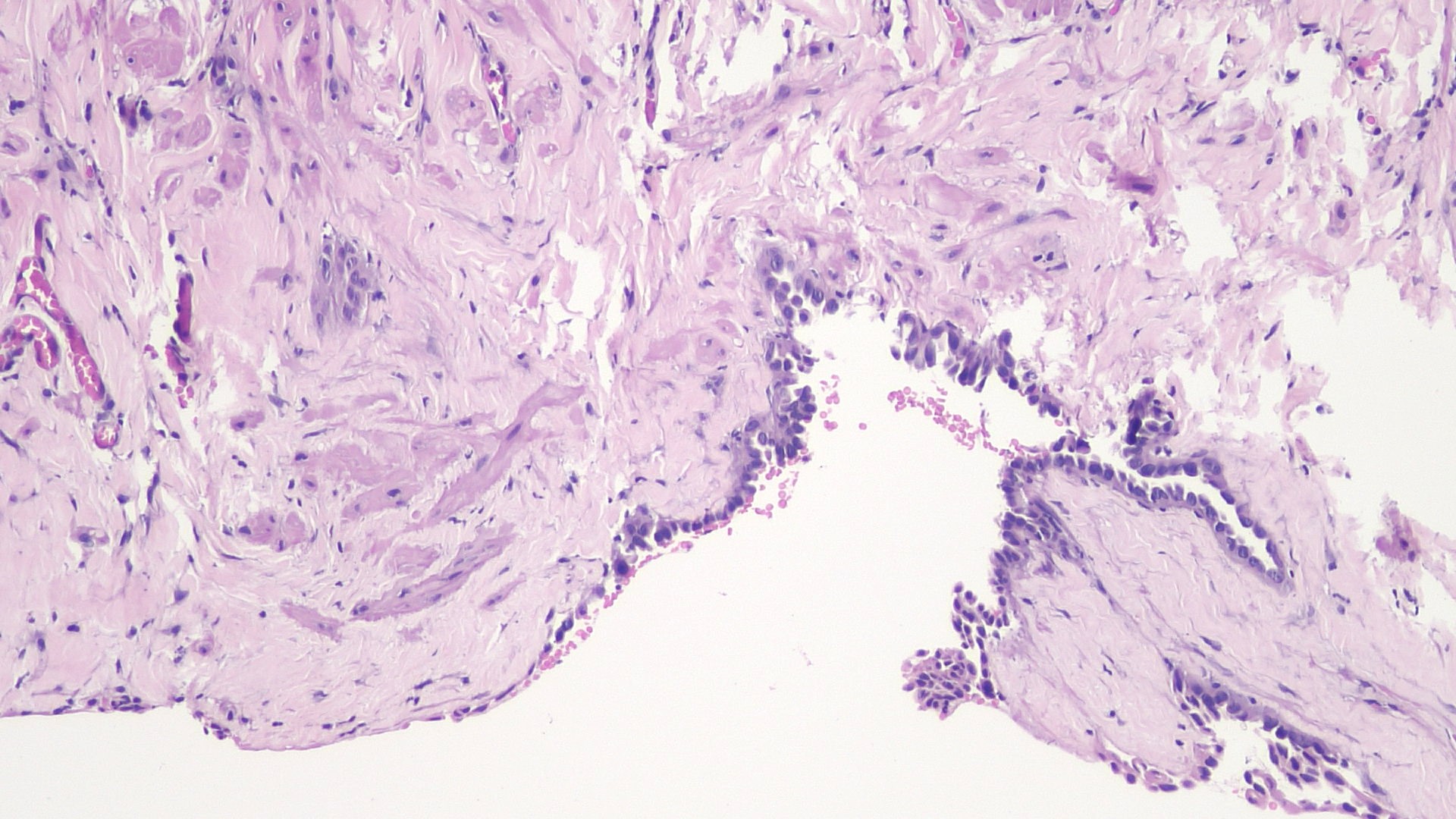
- Loose connective tissue lined by a single layer of cuboidal or flattened mesothelial cells
- Lining may show mesothelial hyperplasia (both solid and papillary), squamous metaplasia or prominent atypia
- Usually clear luminal fluid
- Fibrinous exudate, chronic inflammatory infiltrate and fibrosis in longstanding cases, due to infection or hemorrhage (Cheng: Urologic Surgical Pathology, 4th Edition, 2019)
- Occasional presence of florid nodular collections of histiocytes and aggregates of incidental benign small blue cells of possible rete epithelial origin (Hum Pathol 2010;41:88, Am J Surg Pathol 2016;40:1507)
Microscopic (histologic) images
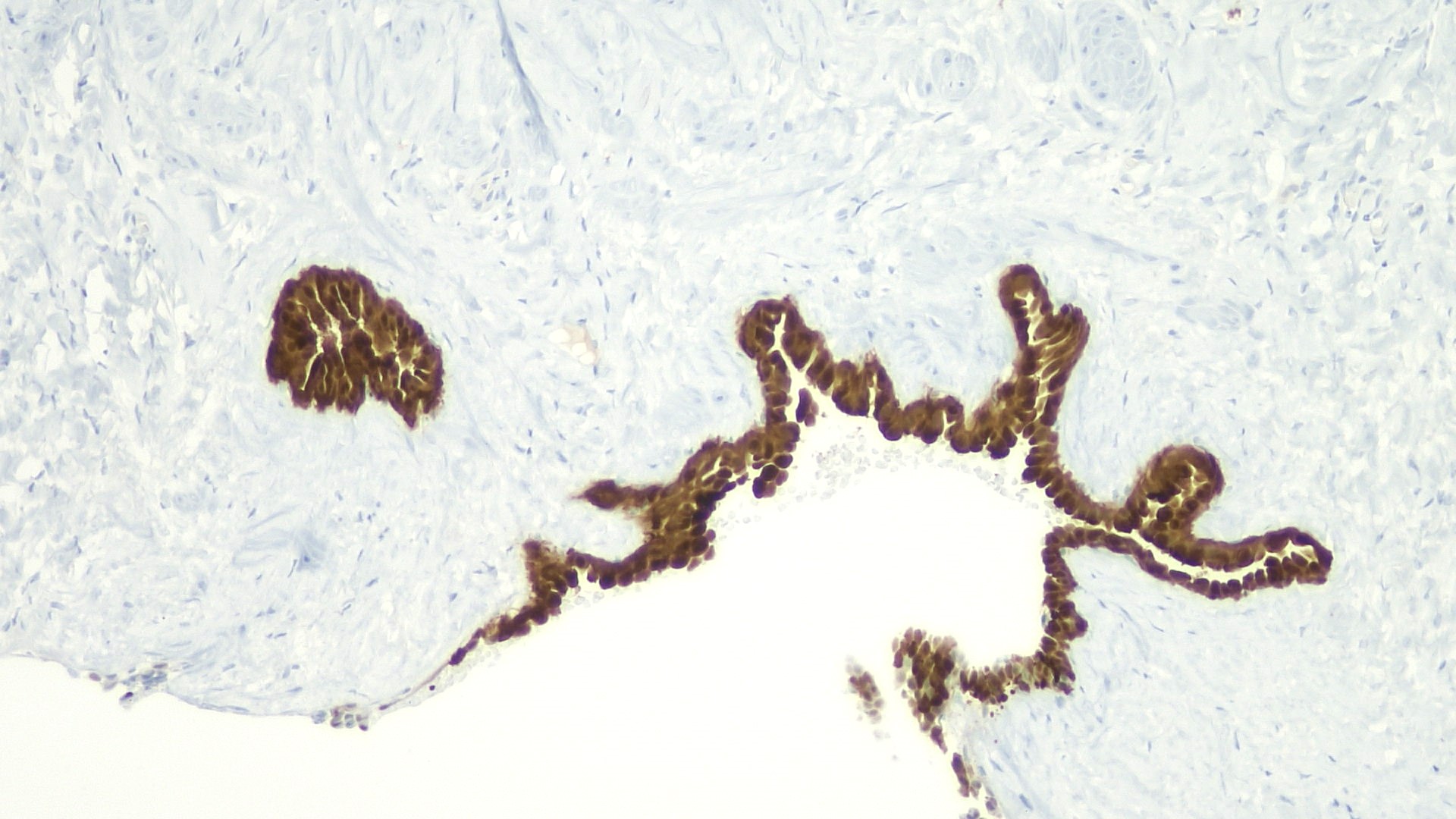
Positive stains
- Calretinin, BAP1, MOC31 (Raspollini: Uropathology, 1st Edition, 2020)
- Other mesothelial markers: pancytokeratin, CAM 5.2, WT1, D2-40 (podoplanin)
Sample pathology report
- Left testis, hydrocelectomy:
- Hydrocele
Differential diagnosis
- Testis tumor:
- Solid mass at transillumination
- Mesothelioma:
- Thickened tunica vaginalis and small papillary projections at ultrasound (Arch Pathol Lab Med 2012;136:113)
- Extensive growth in tunica with infiltration into underlying connective tissue; frank cytologic atypia (Hum Pathol 2019;92:48)
- Positive for calretinin and D2-40
- Negative for BAP1 and MOC31
- Spermatocele:
- Cystic dilatation of the epididymis, efferent ductule or proximal rete testis
- Negative for mesothelial markers
- Spermatozoa and proteinaceous fluid in the lumen
- Often ciliated epithelial lining
Board review style question #1
Board review style answer #1
C. Mesothelial cells. Since hydrocele is defined as an accumulation of serous fluid between visceral and parietal layers of tunica vaginalis, its lining is provided by mesothelial cells.
Comment Here
Reference: Hydrocele
Comment Here
Reference: Hydrocele
Board review style question #2
Which microscopic findings can occur in a hydrocele?
- Acute inflammation, mucinous metaplasia
- Chronic inflammation, fibrosis, squamous metaplasia
- Clear cell hyperplasia
- Psammoma bodies
Board review style answer #2
B. Chronic inflammation, fibrosis, squamous metaplasia. Longstanding hydrocele may be complicated by inflammation and hemorrhage, resulting in abnormal findings involving both the lining cells and the connective tissue.
Comment Here
Reference: Hydrocele
Comment Here
Reference: Hydrocele