Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Lendel A, Zynger DL. Embryonal carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisembryonal.html. Accessed December 22nd, 2024.
Definition / general
- Pluripotent and malignant germ cell tumor (GCT) resembling undifferentiated stem cells during embryonic development
Essential features
- Pleomorphic, high grade appearing type of GCT
- Usually occurs mixed in combination with other types of testicular GCT
- Predominance in a mixed GCT is associated with a higher risk of metastases and relapse (BJU Int 2020;125:355, BMC Cancer 2020;20:728)
- Positive: OCT 3/4, CD30; negative / weak: D2-40, CD117, glypican 3
ICD coding
- ICD-O: 9070/3 - embryonal carcinoma, NOS
Epidemiology
- Testicular GCT is more common in Caucasian men than African American men (Arch Pathol Lab Med 2007;131:1267)
- Global incidence rates for testicular GCT are highest in Northern Europe and lowest in Northern and sub-Saharan African countries (Cancer Epidemiol Biomarkers Prev 2010;19:1151)
- Global incidence of testicular GCT is increasing but mortality rate is decreasing due to advances in treatment (Med Clin North Am 2018;102:251)
- Nonseminomas account for 44% of testicular GCTs (Cancer Epidemiol Biomarkers Prev 2010;19:1151, Int Rev Cell Mol Biol 2009;278:277, Acta Radiol Oncol 1984;23:239)
- Embryonal carcinoma is the most frequent tumor component of testicular mixed GCT, present in ~80 - 90% of cases (Cancer Epidemiol Biomarkers Prev 2010;19:1151, Int Rev Cell Mol Biol 2009;278:277, Acta Radiol Oncol 1984;23:239, Mod Pathol 2021;34:834, Hum Pathol 2018;82:113)
- Pure embryonal carcinoma (Arch Pathol Lab Med 2007;131:1267, Hum Pathol 2018;82:113, Cell Rep 2018;23:3392, Am J Surg Pathol 2014;38:689):
- Up to 16% of testicular GCT cases (Am J Surg Pathol 2014;38:689)
- Second most common type of testicular pure GCT
- Average age of presentation 25 - 35 years old, ~10 years younger than seminoma
- Rare in children and after 50 years of age
Sites
- Testis
- Anterior mediastinum
- Retroperitoneum
Pathophysiology
- Gain of pluripotency is likely due to polygenic factors
- Chromosome 12 aberrations have been implicated in testicular GCT, 80% of which are isochromosome 12 formation (Expert Rev Anticancer Ther 2020;20:75)
- Pluripotency may also be due to transcription factor OCT 3/4 and SOX2 overexpression (Expert Rev Anticancer Ther 2020;20:75)
- Low to intermediate amount of DNA methylation (Front Oncol 2018;8:571)
Etiology
- Multi hit hypothesis: likely multifactorial, resulting from both genetic and environmental factors (Expert Rev Anticancer Ther 2020;20:75)
- Risk factors include cryptorchidism and a personal or family history of testicular GCT
- Believed to arise through abnormal differentiation beginning in fetal life (Expert Rev Anticancer Ther 2020;20:75)
- Undergoes malignant transformation during puberty due to hormonal influence (Expert Rev Anticancer Ther 2020;20:75)
- Precursor lesion is germ cell neoplasia in situ (GCNIS)
Clinical features
- Typically presents with a unilateral, painless testicular mass (Med Clin North Am 2018;102:251)
- Dull aching sensation in lower abdomen or scrotal area can also be present
- Acute pain is less common
- Initial presentation may be due to metastatic symptoms, including lower back pain, dyspnea or hemoptysis (Med Clin North Am 2018;102:251)
- Initial metastasis to retroperitoneal lymph nodes
- Can present with infertility (Statpearls: Nonseminomatous Testicular Tumors [Accessed 19 January 2022])
Diagnosis
- Ultrasound
- Serum tumor markers
- CT imaging with contrast of chest, abdomen and pelvis to evaluate for metastasis
- Radical inguinal orchiectomy with histopathologic evaluation is necessary for definitive diagnosis
Laboratory
- Serum tumor markers should not be used as a screening tool
- Elevated serum human chorionic gonadotropin (hCG), alpha fetoprotein (AFP) and lactate dehydrogenase (LDH) may be present (J Clin Oncol 2010;28:3388)
- Current guidelines recommend measuring hCG, AFP and LDH before and after initial treatment (J Clin Oncol 2010;28:3388)
- Serum tumor markers can be used to monitor for recurrence
Radiology description
- Heterogenous and hypoechoic appearance on ultrasound; microlithiasis may be present (J Clin Ultrasound 2010;38:21)
- Testicular non(pure)seminomatous GCTs appear heterogenous on MRI, with enhancement in areas of necrosis and hemorrhage (AJR Am J Roentgenol 2007;189:W331)
- CT imaging is recommended to identify presence of metastases
- Lymph node metastases from testicular nonseminomatous GCTs appear heterogenous or cystic on CT imaging (Radiol Clin North Am 2012;50:1111)
Prognostic factors
- With surveillance, survival rate for nonseminomatous GCTs is 98.6% (Crit Rev Oncol Hematol 2007;64:182)
- More aggressive disease course with embryonal carcinoma predominance in mixed GCT (World J Urol 2017;35:1103, J Urol 2009;181:2097)
- Most important pathologic prognostic indicator in the testis is presence of lymphovascular invasion (BJU Int 2020;125:355)
- Tumor size > 4 cm is more often associated with lymphovascular invasion (Am J Clin Pathol 2016;145:341)
- Presence of discontinuous involvement of spermatic cord is predictive of advanced disease (Mod Pathol 2021 Sep 9 [Epub ahead of print])
- More likely to relapse if patient is older at presentation (Urol Oncol 2013;31:499)
- Higher likelihood of metastases and lymphovascular invasion with micropapillary growth pattern (Int J Surg Pathol 2013;21:599)
- For patients presenting with metastatic diseases treated with orchiectomy, chemotherapy and lymph node dissection, pure embryonal carcinoma had lower relapse and lower mortality rates than mixed GCTs (Urology 2018;114:133)
Case reports
- 24 year old man with endobronchial metastases (Respirol Case Rep 2020;8:e0064)
- 24 year old man with calcified solitary testicular mass on ultrasound (BMJ Case Rep 2017;2017:bcr2017220081)
- 28 year old man with extensive metastasis to the gastrointestinal system and inferior vena cava thrombosis (Indian J Pathol Microbiol 2019;62:350)
- 34 year old man with urethral metastasis (Urol Case Rep 2021;36:101572)
- 36 year old man with an intra-abdominal embryonal carcinoma in an undescended testicle (Med Pharm Rep 2020;93:213)
Treatment
- Initial management is radical inguinal orchiectomy
- No further treatment necessary in 75% of clinical stage I nonseminomatous GCT (Ann Oncol 2010;21:1296)
- If pT2 or higher, retroperitoneal lymph node dissection or chemotherapy
- If pN2 - 3, chemotherapy
- Resistant to radiation therapy (Arch Pathol Lab Med 2012;136:435)
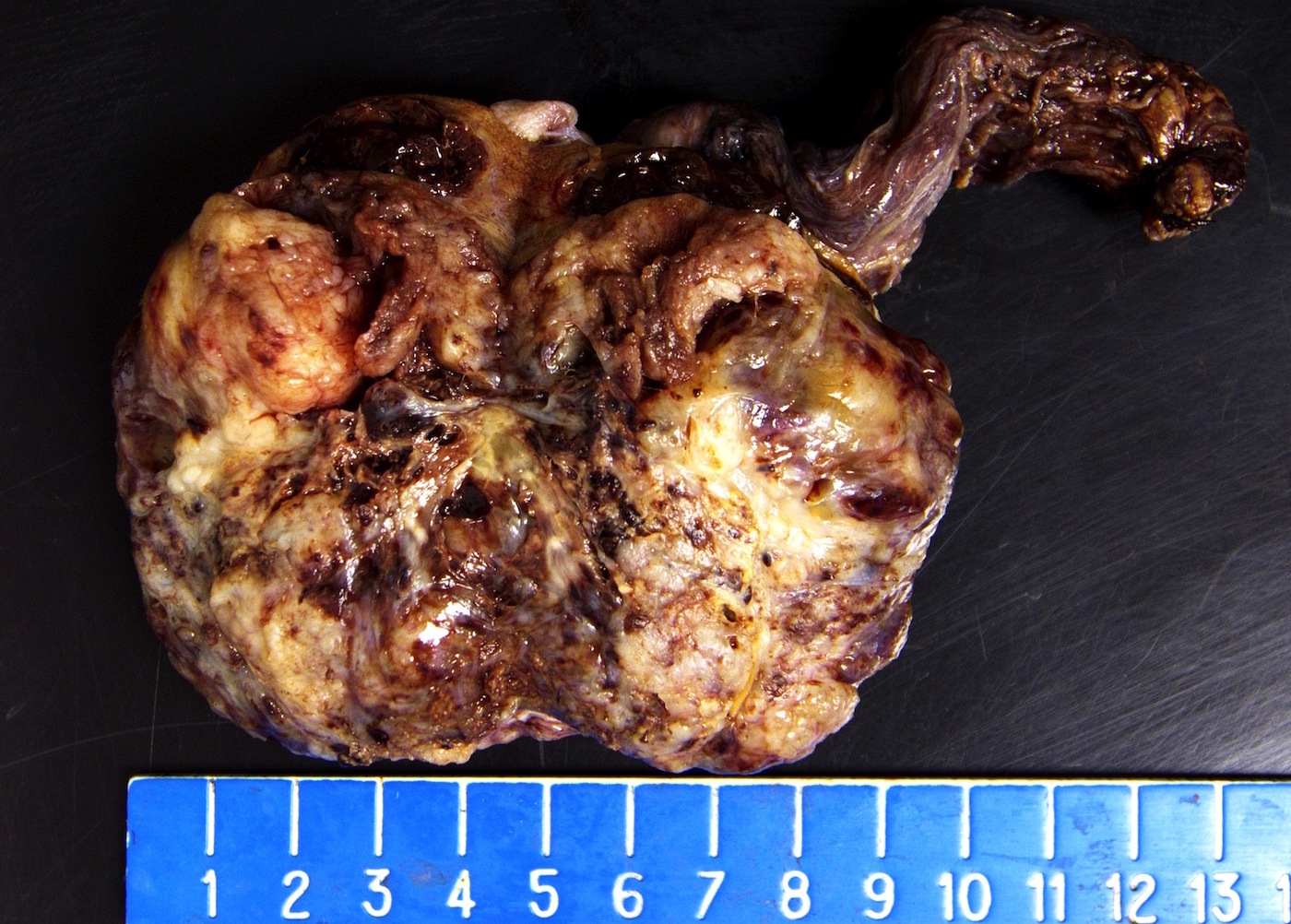
Gross description
- Gray-tan mass with hemorrhage and necrosis
Gross images
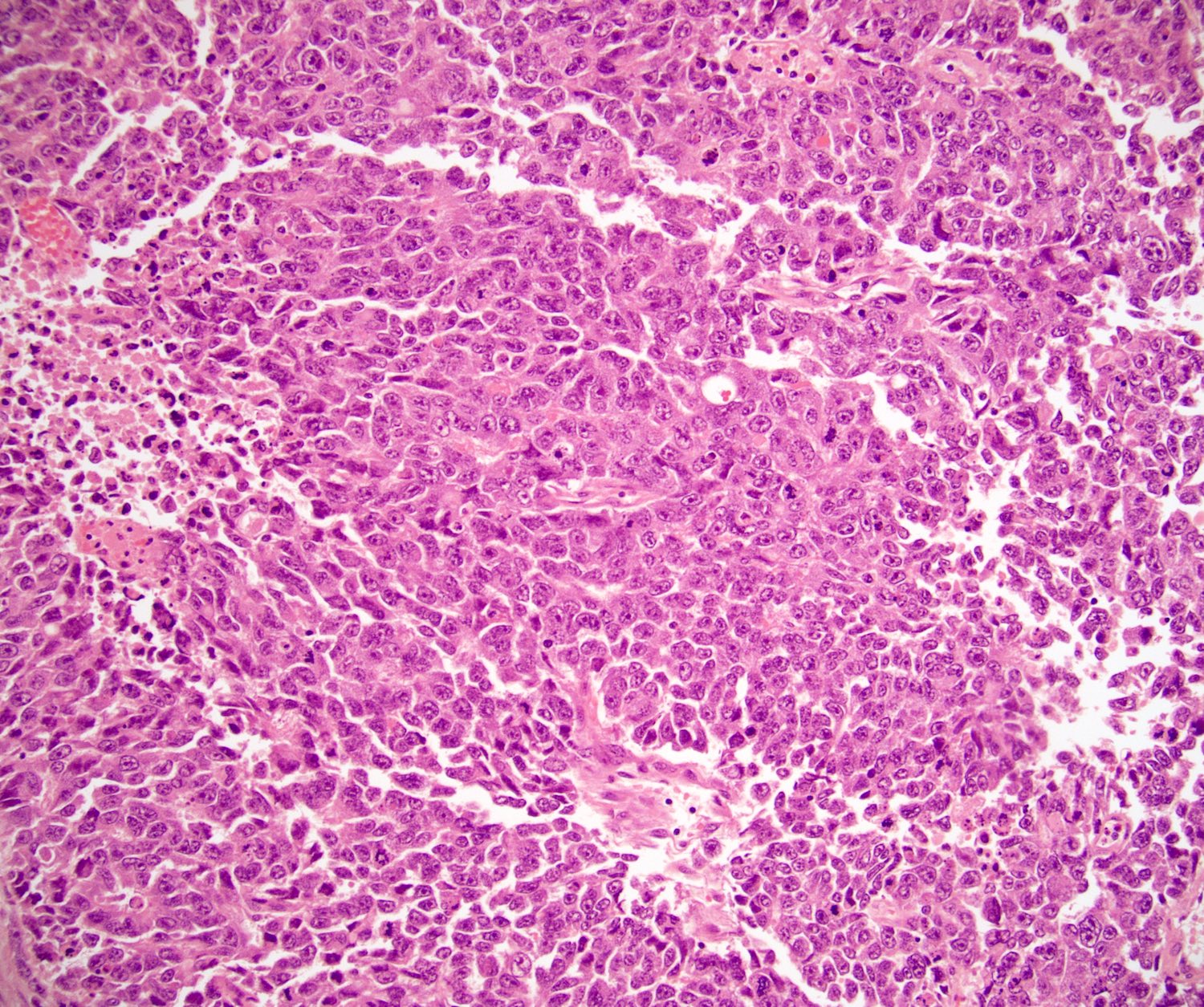
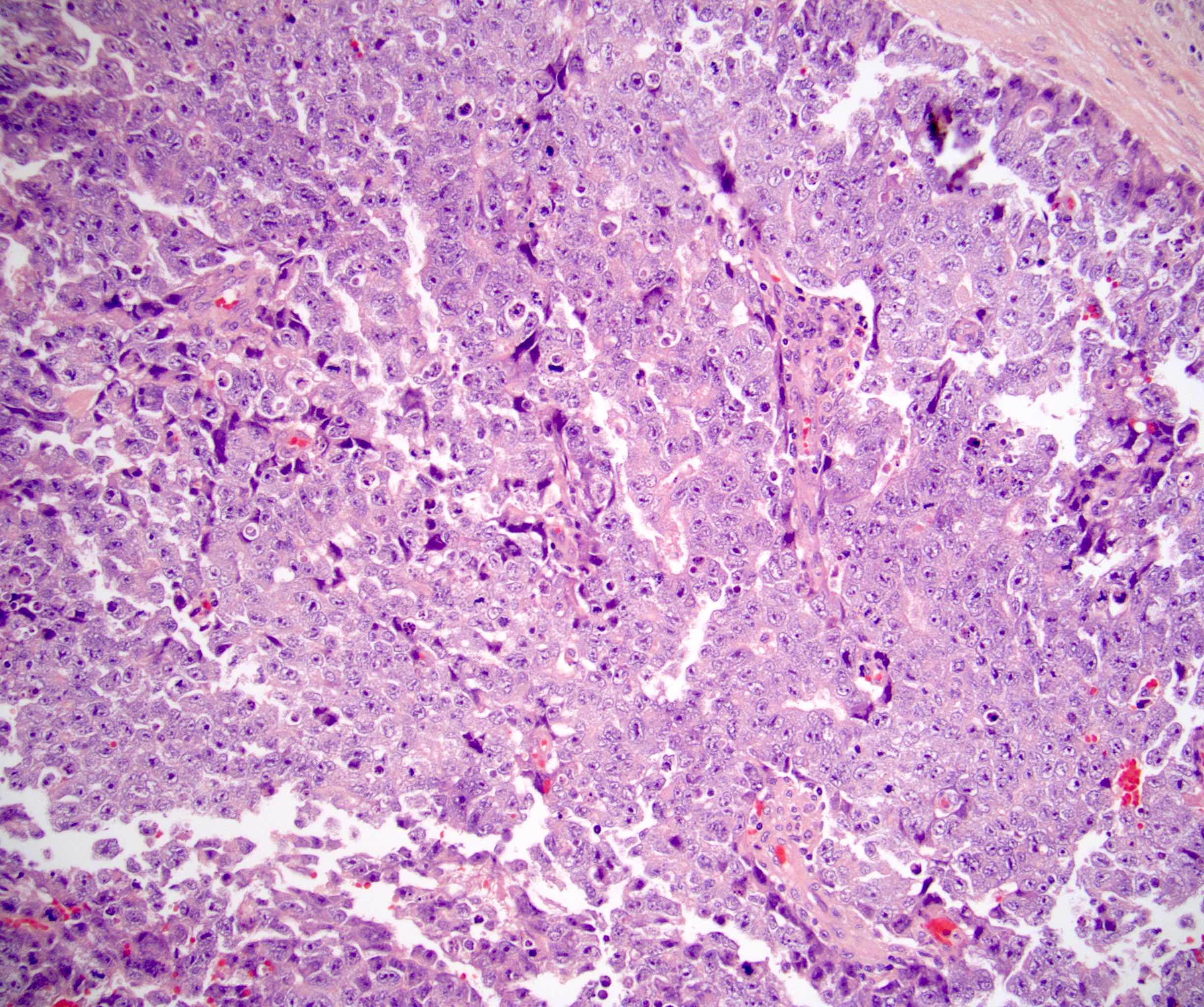
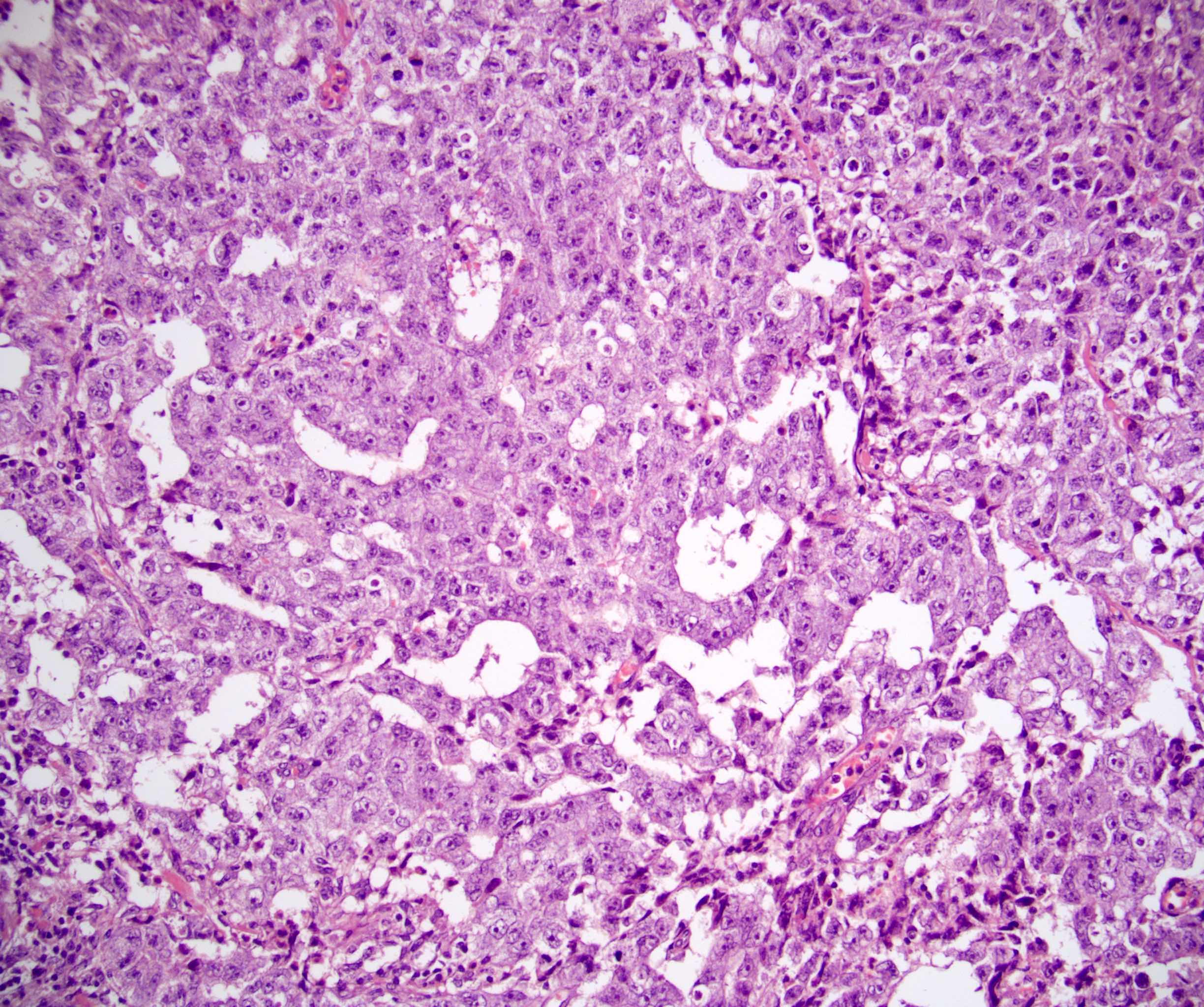
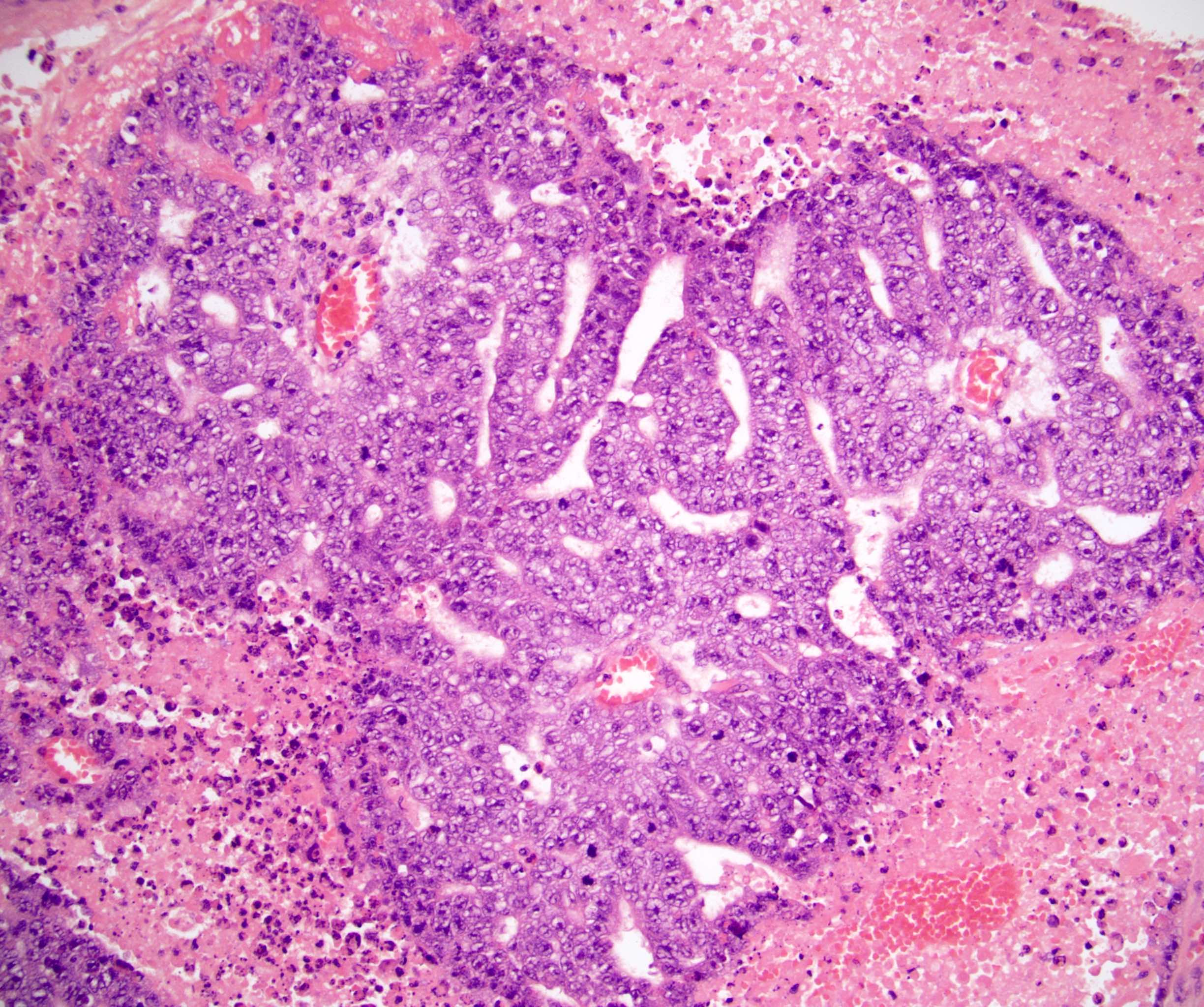
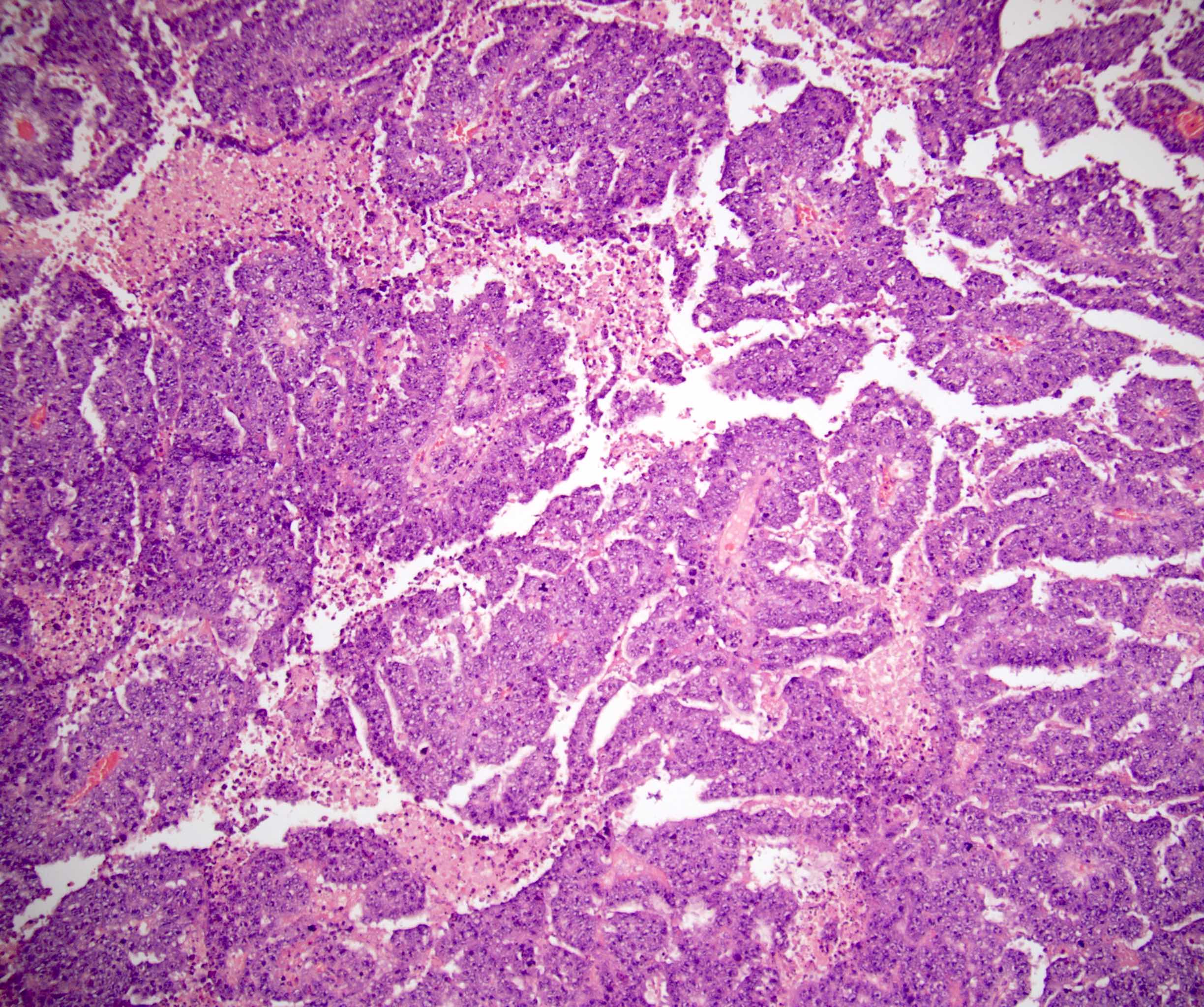
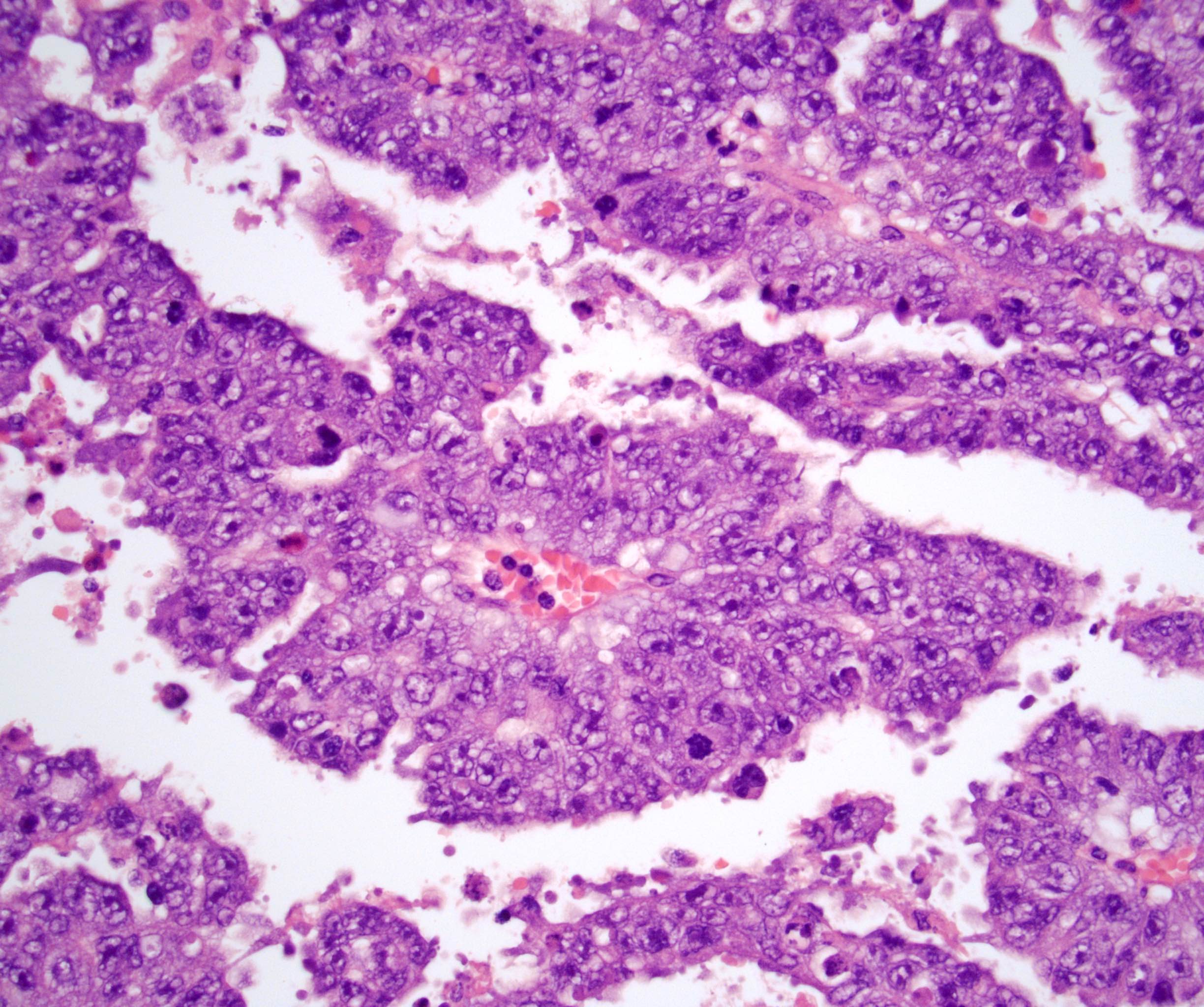
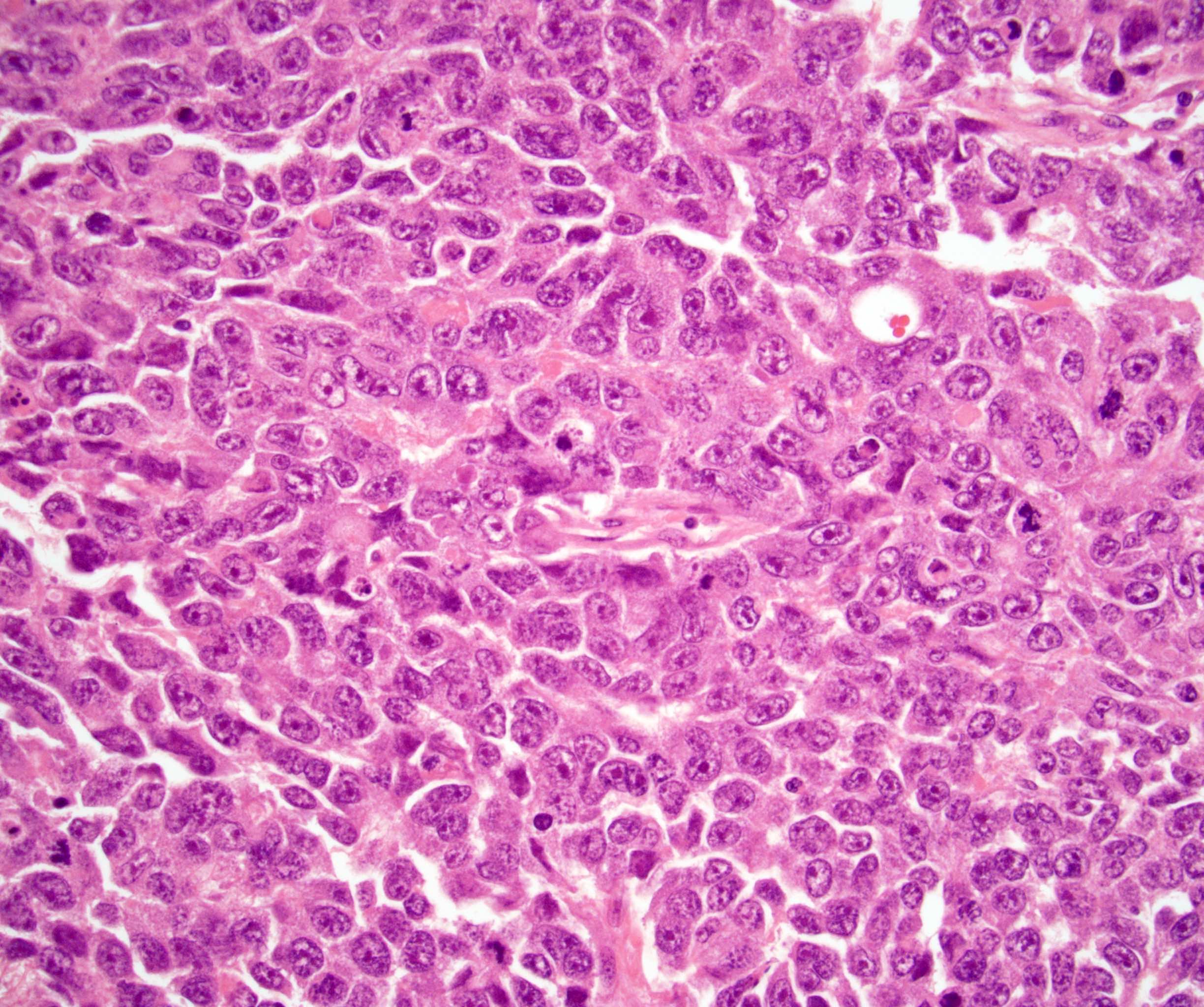
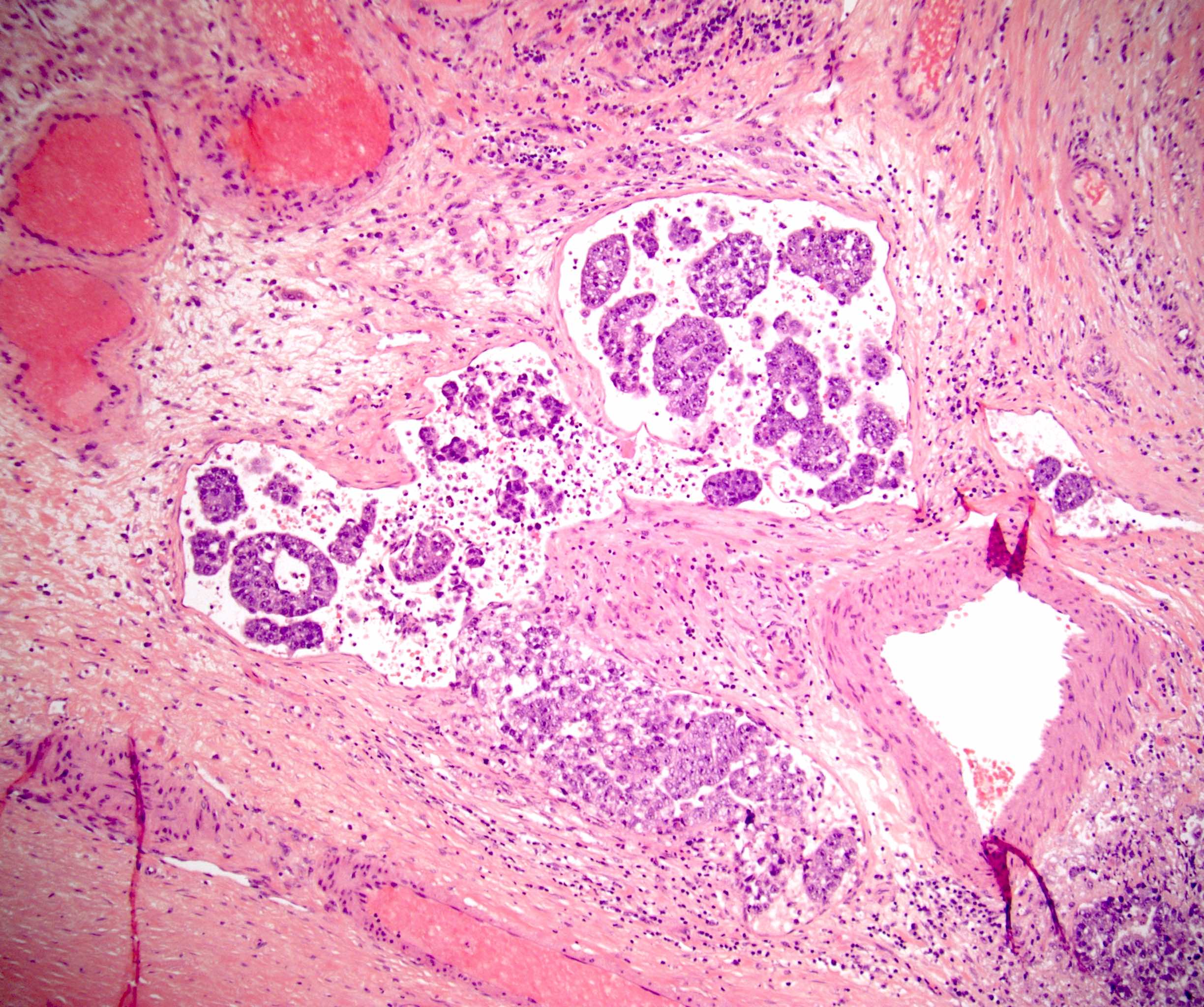
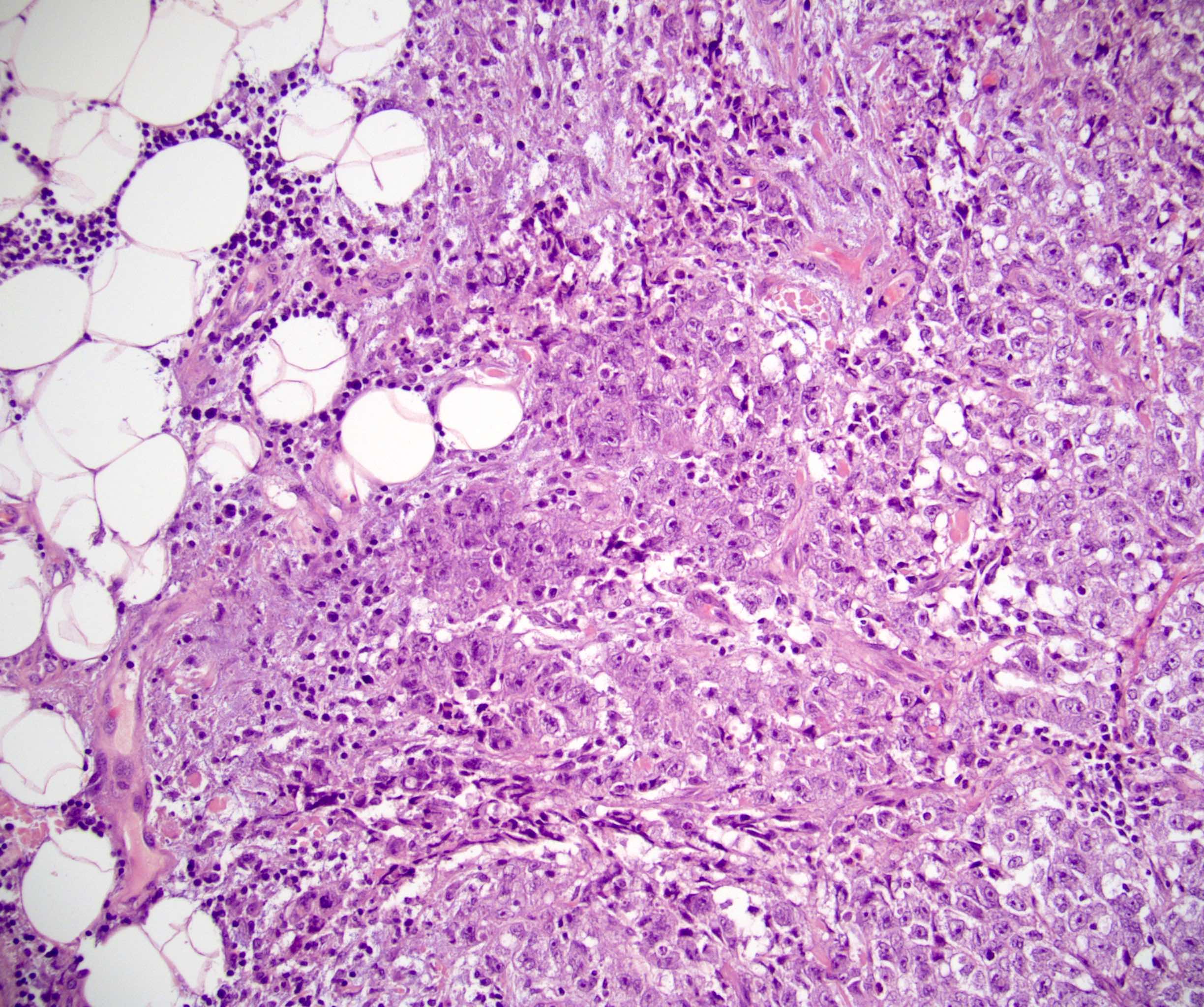
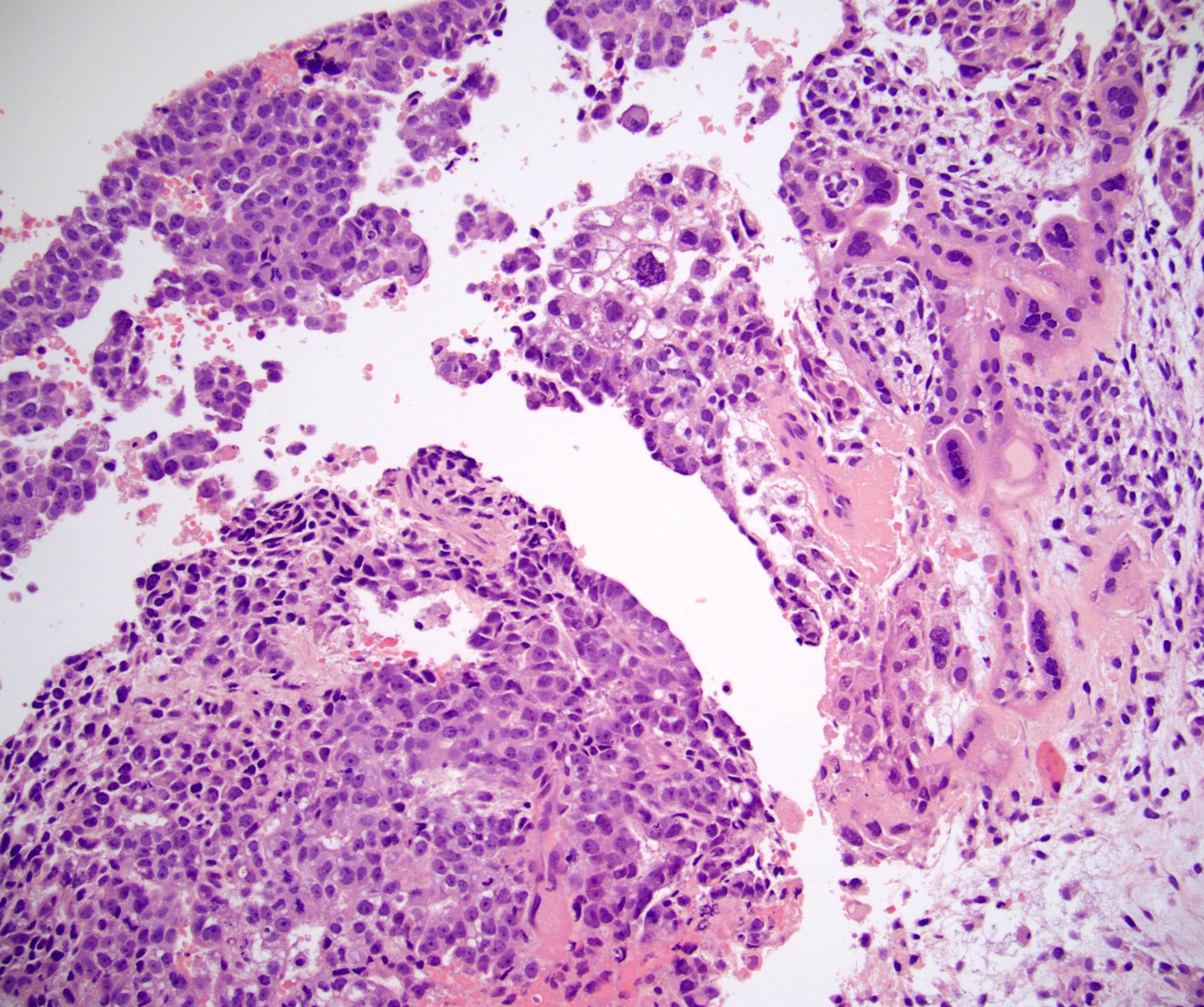
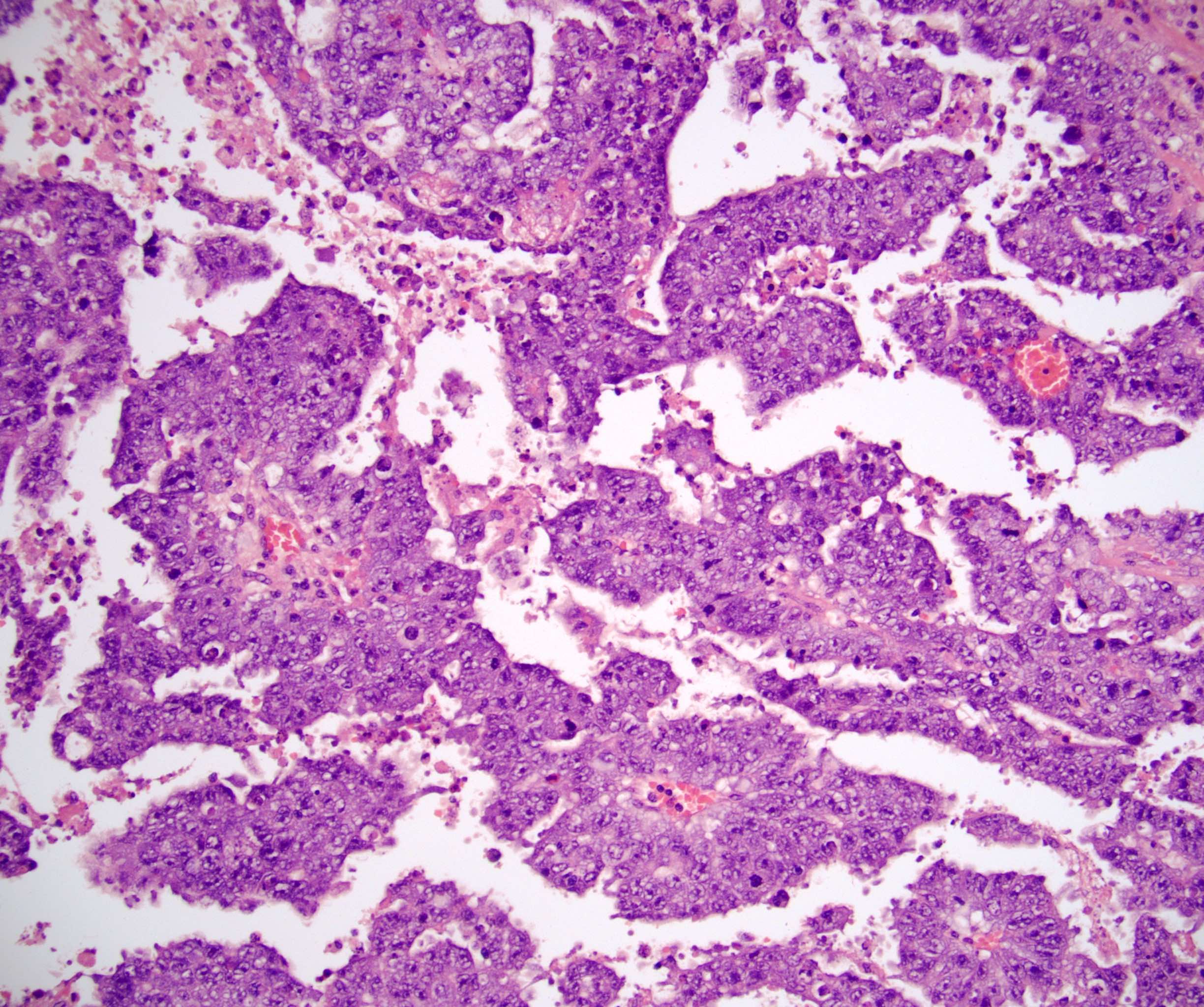
Microscopic (histologic) description
- Multiple growth patterns usually present (Am J Surg Pathol 2014;38:689)
- 3 most common growth patterns: solid (55%), glandular (17%) and papillary (11%) (Am J Surg Pathol 2014;38:689)
- Rare patterns: nested (3%), micropapillary (2%), anastomosing glandular (1%), sieve-like glandular (< 1%), pseudopapillary (< 1%), and blastocyst-like (< 1%) (Am J Surg Pathol 2014;38:689)
- Polygonal cells (Arch Pathol Lab Med 2007;131:1267)
- Cells are crowded, have indistinct distinct cell borders and appear to have overlapping nuclei
- Moderate amount of amphophilic and granular cytoplasm
- Pleomorphic, high grade nuclear features
- Mitotic figures are common
- Smudgy degenerative appearing nuclei are often seen
- Necrosis is common, both as single cell necrosis and larger foci
- Often grows admixed with yolk sac tumor and can rarely form polyembryoma-like structures, called embryoid bodies
- Residual seminiferous tubules may contain germ cell neoplasia in situ (GCNIS) or intratubular embryonal carcinoma, which entirely fills the tubule
- Lymphovascular invasion is common within embryonal carcinoma predominant GCTs, is usually best visualized at the periphery testicle and may entirely occlude vessels, mimicking nodules of tumor
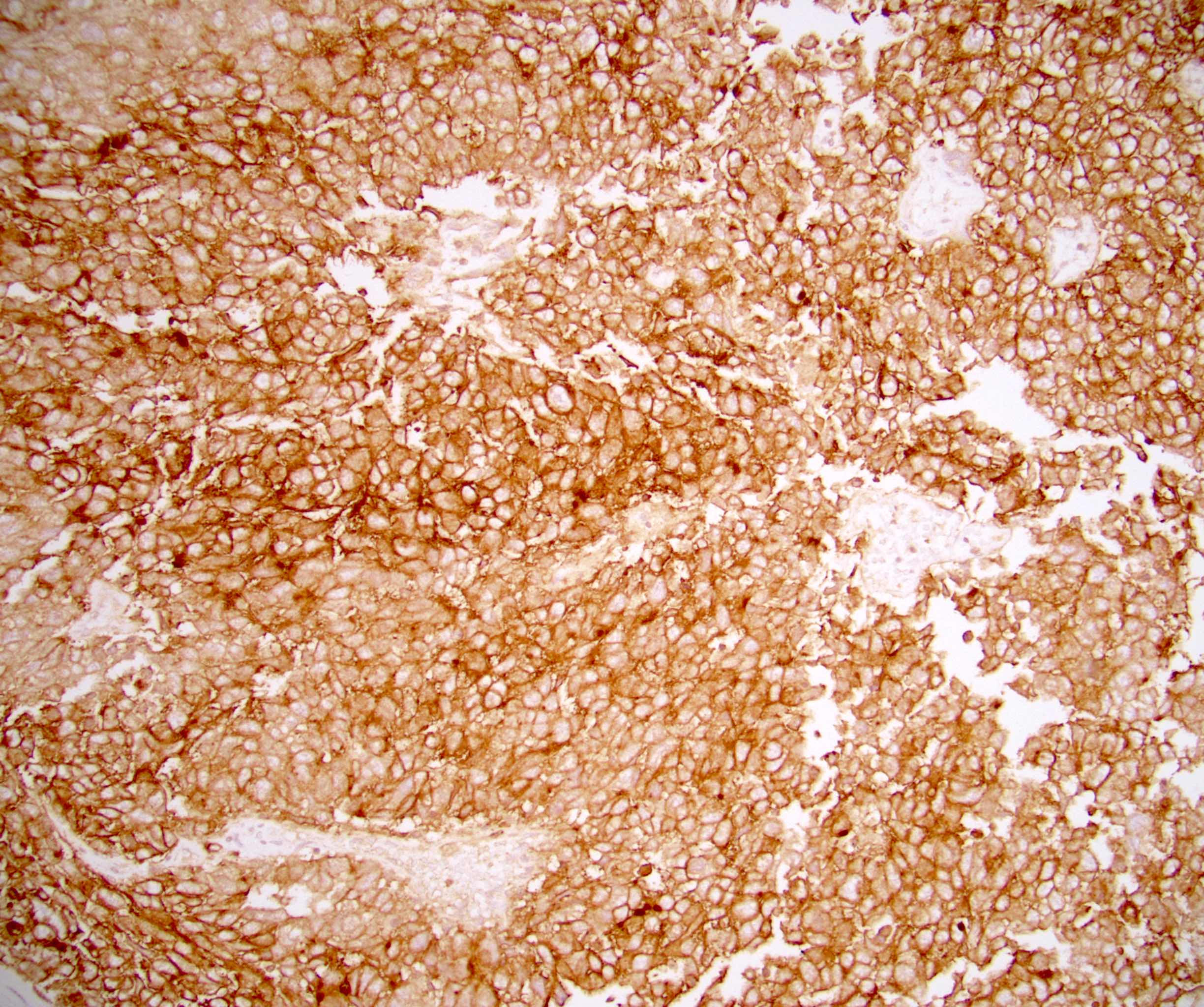
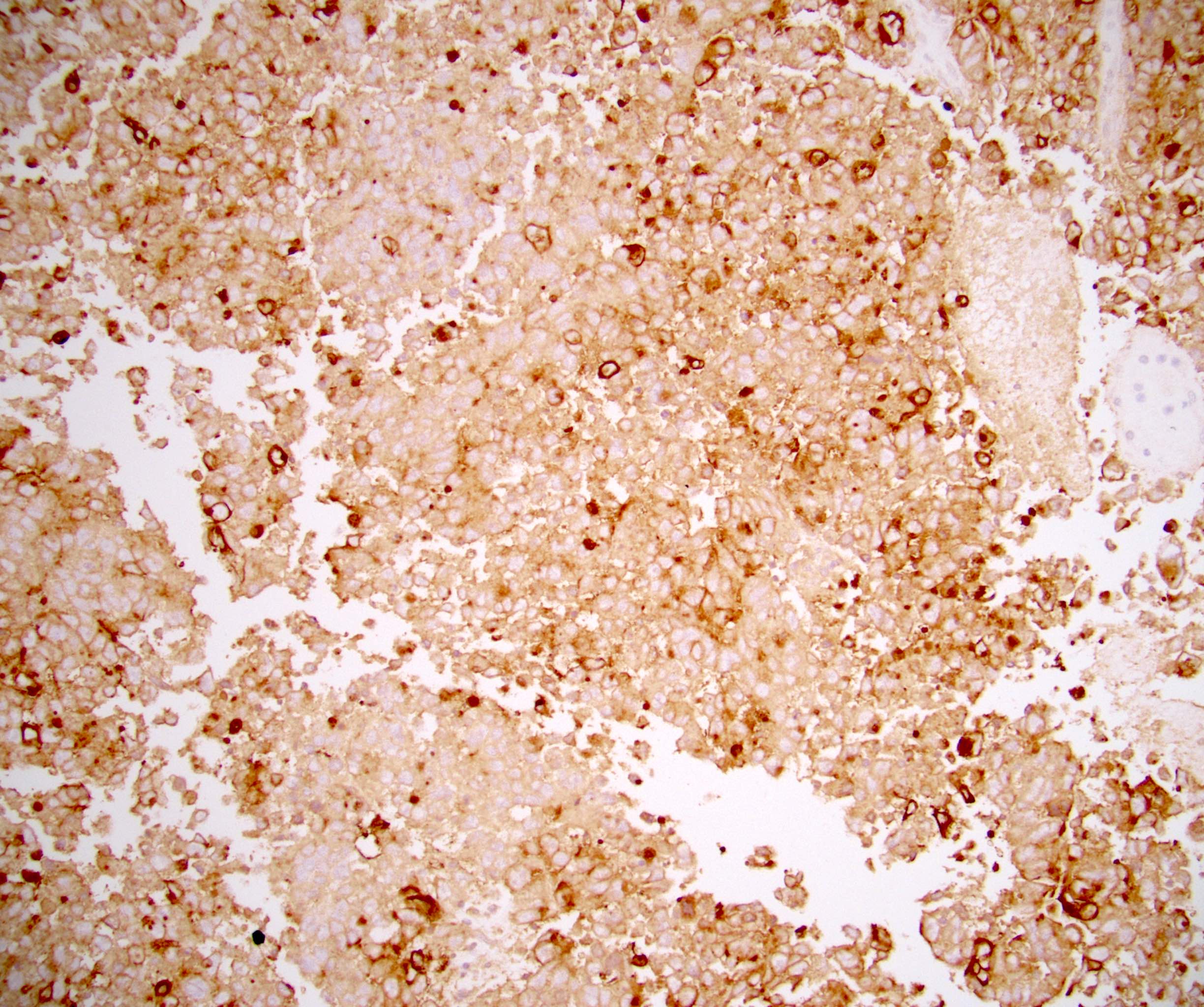
Microscopic (histologic) images
Virtual slides
Cytology description
- No role in diagnosis of primary testicular GCT
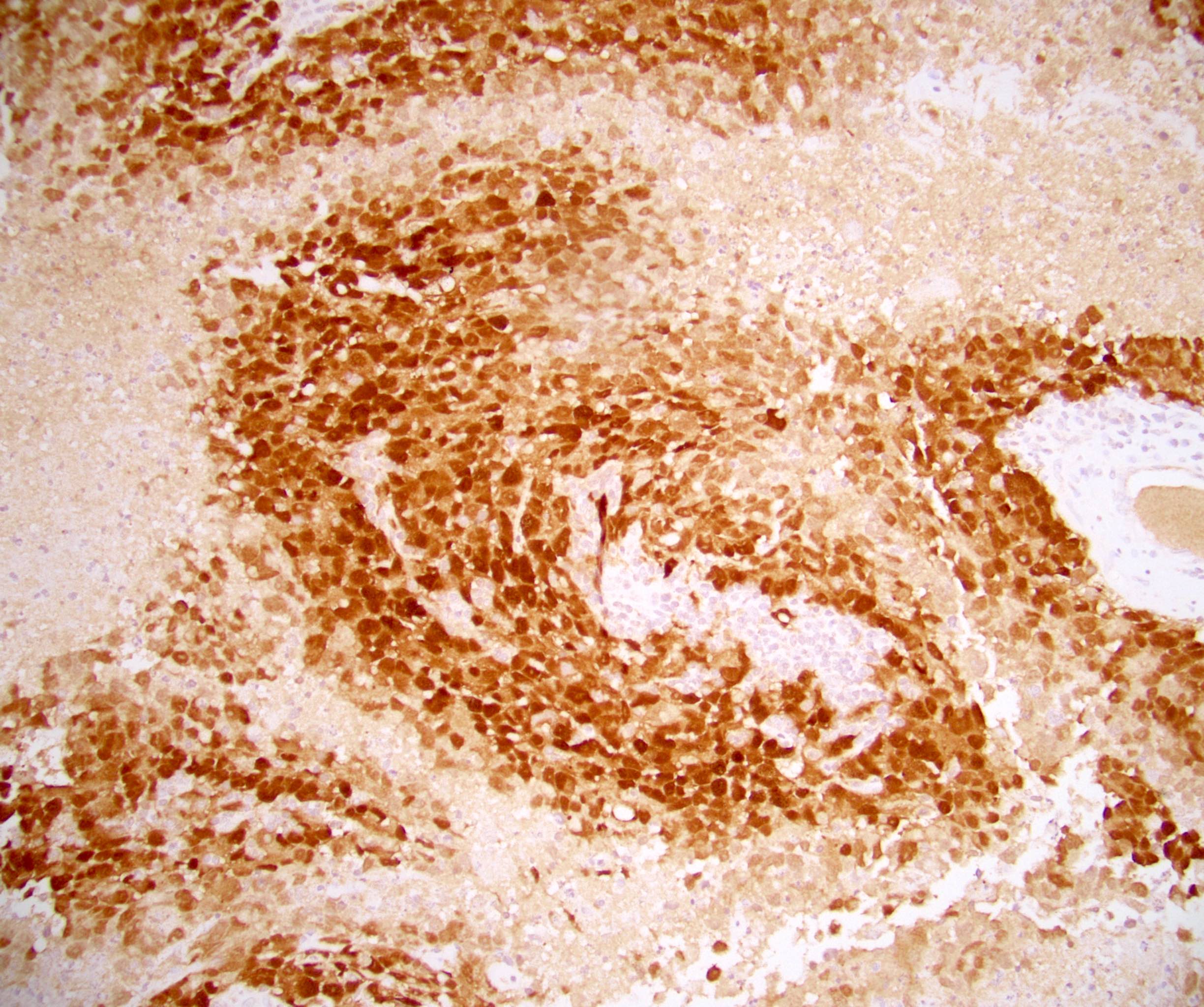
Positive stains
- OCT 3/4 (nuclear and cytoplasmic) (Cancer Res 2003;63:2244)
- CD30 (Mod Pathol 2007;20:320)
- PLAP: heterogenous (Hum Reprod Update 2006;12:303)
- SOX2 (Am J Clin Pathol 2009;131:731)
- AE1 / AE3 (Am J Clin Pathol 2000;113:583)
- SALL4 (Cancer 2009;115:2640)
Negative stains
- CD117 / KIT: patchy, weak (Int J Androl 1994;17:85)
- D2-40 / podoplanin: patchy, weak, nonmembranous (Mod Pathol 2007;20:320)
- Glypican 3: weak, focal (Virchows Arch 2006;449:308)
- AFP: 21% positive (Urology 1983;22:649, Acta Pathol Microbiol Immunol Scand A 1983;91:165)
- CK7: 52% weak (Hum Pathol 2019;84:254)
- Inhibin (Hum Pathol 2019;84:254)
- p63 (Hum Pathol 2019;84:254)
- GATA3 (Hum Pathol 2016;48:18)
- Calretinin (Int J Gynecol Pathol 2001;20:346)
- SOX17 (Am J Clin Pathol 2009;131:731)
- Beta hCG: caveat that tumors containing choriocarcinoma can have expression that diffuses into all GCT types, requiring careful interpretation and use of more specific markers (Hum Pathol 2019;84:254)
Electron microscopy description
- Long tight junctions and telolysosomes (Cancer 1986;57:257)
- No microvilli anchoring rootlets (Cancer 1986;57:257)
- Frequent desmosomes (Ultrastruct Pathol 1988;12:67)
- Electron dense extracellular lumens with microvilli (Ultrastruct Pathol 1988;12:67)
- Heterochromatin is often present (Ultrastruct Pathol 1988;12:67)
- Within the cytoplasm, glycogen, ribosomes and large numbers of mitochondria are easily visible (Ultrastruct Pathol 1988;12:67)
Molecular / cytogenetics description
- Isochromosome 12p: present in most testicular GCT components including embryonal carcinoma (Expert Rev Anticancer Ther 2020;20:75)
Sample pathology report
- Left testis, radical orchiectomy:
- Mixed germ cell tumor, teratoma (45%), embryonal carcinoma (25%), yolk sac tumor (15%), seminoma (10%) and choriocarcinoma (5%) types (see synoptic report)
- See staging information
Differential diagnosis
- Choriocarcinoma:
- Seminoma:
- Uniform cells with distinct borders and pale clear cytoplasm
- Fibrous septae with lymphocytes
- Positive: CD117 / KIT, podoplanin / D2-40, PLAP (greater reactivity than embryonal carcinoma), OCT 3/4 (both positive)
- Negative: CD30
- Yolk sac tumor:
- Variety of growth patterns, usually with flattened cells, paler eosinophilic cytoplasm, frequent hyaline globules and myxoid material and less inconspicuous mitotic figures
- Positive: glypican 3, AFP, GATA3 (weak)
- Negative: OCT 3/4, CD30
- Lymphoma:
- Typically 60 years or older
- Color Doppler ultrasound with increased blood flow (Radiographics 2015;35:400)
- Cells are round, with more uniform nuclei and dispersed chromatin
- Positive: CD45, CD20 (usually)
- Negative: SALL4, OCT 3/4, PLAP (Hum Pathol 1987;18:946)
- Carcinoma of nongerm cell origin:
- Lacks chromosomal 12p abnormalities
- Positive: site specific markers
- Negative: SALL4 (although can be expressed in certain carcinomas, such as gastric adenocarcinoma), OCT 3/4, CD30 (Am J Surg Pathol 2014;38:410, Cancer Res 2003;63:2244)
Board review style question #1
Board review style answer #1
Board review style question #2
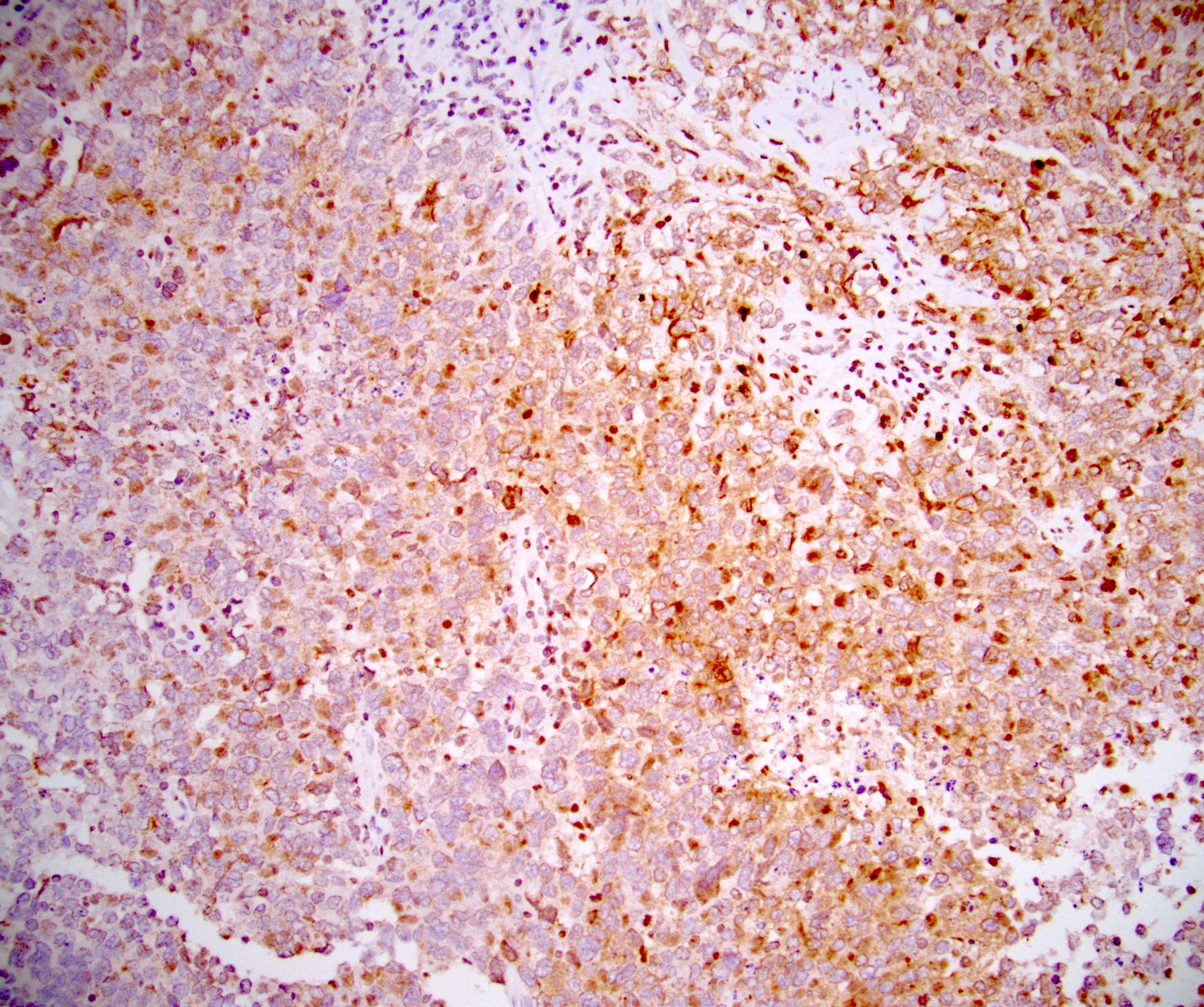
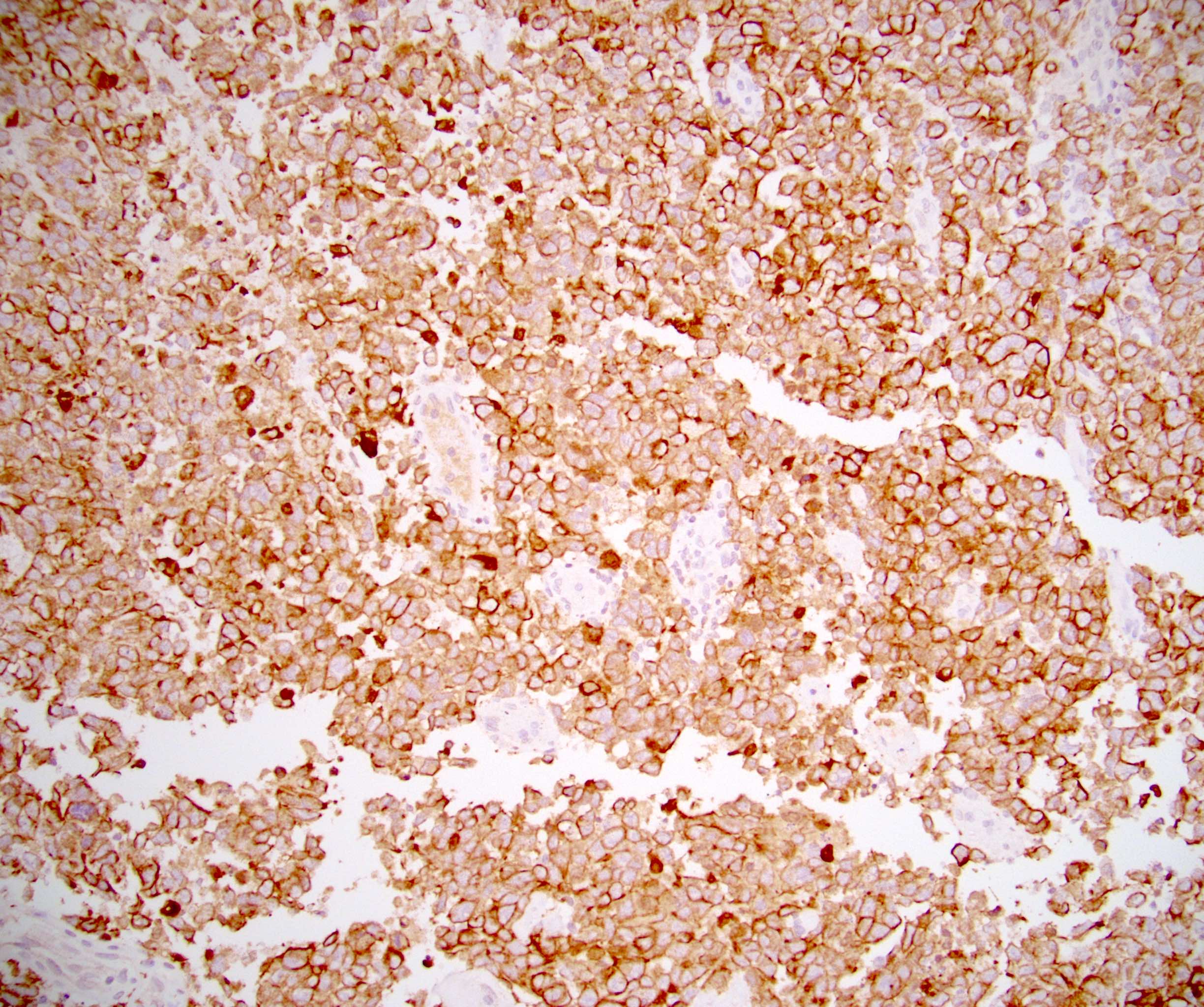
The H&E image above is a brain metastasis of testicular germ cell tumor with choriocarcinoma and embryonal carcinoma. Which of the following 2 immunostains will be positive in choriocarcinoma but weak or negative in embryonal carcinoma (one of which is shown above)?
- AFP, PLAP
- CD30, OCT 3/4
- CK7, p63
- D2-40, CD117
- SALL4, AE1 / AE3
Board review style answer #2
C. CK7, p63. CK7 (shown in the immunostain image above) is strongly and diffusely positive choriocarcinoma. CK7 is weak or negative in embryonal carcinoma. Expression for p63 is seen in mononucleated trophoblast cells in choriocarcinoma. p63 is negative in embryonal carcinoma. AFP is positive in yolk sac tumor and weak to negative in embryonal carcinoma and choriocarcinoma. PLAP is variably positive in embryonal carcinoma and negative in choriocarcinoma. CD30 and OCT 3/4 are positive in embryonal carcinoma and negative in choriocarcinoma. D2-40 and CD117 are positive in seminoma but negative in both choriocarcinoma and embryonal carcinoma. SALL4 and AE1 / AE3 are positive in both choriocarcinoma and embryonal carcinoma.
Comment Here
Reference: Embryonal carcinoma
Comment Here
Reference: Embryonal carcinoma
Board review style question #3
Board review style answer #3
A. Embryonal carcinoma. In a testicular germ cell tumor, higher percentage of embryonal carcinoma and choriocarcinoma are associated with negative outcomes, such as local and distant metastases. Increased proportions of teratoma and yolk sac tumor are associated with better outcomes. In a mixed germ cell tumor, percentage of seminoma usually does not impact prognosis or management. Spermatocytic tumor is a germ cell tumor unrelated to germ cell neoplasia in situ.
Comment Here
Reference: Embryonal carcinoma
Comment Here
Reference: Embryonal carcinoma