Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yakoub M, Sharma D. Portal hypertensive gastropathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachportalhypertensivegastropathy.html. Accessed January 10th, 2025.
Definition / general
- Portal hypertensive gastropathy (PHG) refers to the pathologic effects of increased portal venous pressure on the mucosal surface of the stomach
Essential features
- Portal hypertensive gastropathy is mainly a clinical and endoscopic diagnosis; histologic findings should be correlated with the clinical diagnosis
- Histologic features are nonspecific and show congested capillaries and venules in the gastric mucosa, mainly in the body and fundus, without significant inflammation or fibrin thrombi
Terminology
- Congestive gastropathy: historic term first described by McCormack et al. in 1985 (Gut 1985;26:1226)
ICD coding
- ICD-10: K31.89 - other diseases of stomach and duodenum
Epidemiology
- 20 - 98% prevalence in patients with liver cirrhosis (Gastroenterology 2000;119:181)
- Wide range of prevalence is related to the variability of the characterization criteria of the disease
- Risk factors:
- Schistosomiasis
- Heart failure
Sites
- Most commonly in proximal stomach (fundus and body of the stomach) (Gastroenterology 1991;101:472)
- Gastric antrum is typically spared
Pathophysiology
- Poorly understood
- Portal hypertension: increased pressure in high resistance venous system
- Backing up of blood in the collateral circulation of the gastrointestinal tract, including the proximal stomach (venous congestion and bleeding)
- Vascular and mucosal changes in the stomach
- Additional theories include mucosal injury, hypoxia, cytokine production and inflammation (Gastroenterology 1992;102:2066)
Etiology
- Portal hypertension:
- Increased sinusoidal and portal venous pressure (cirrhosis)
- Presinusoidal diseases, like portal vein thrombosis and veno-occlusive disorders
- Postsinusoidal etiology, like heart failure
- No well documented correlation between severity of portal hypertension and development of portal hypertensive gastropathy (Gastroenterology 1992;102:994)
Clinical features
- Patients with portal hypertensive gastropathy usually present with chronic gastrointestinal bleeding that can result in iron deficiency anemia (Gastroenterology 2000;119:181)
- Acute gastrointestinal bleeding is less common
- Portal hypertensive gastropathy can be associated with esophageal varices
- Classification systems are based on endoscopic findings
- 2 category classification system (see esophagogastroduodenoscopy [EGD] findings under Diagnosis) (J Hepatol 2000;33:846)
Diagnosis
- Clinical: association with cirrhosis
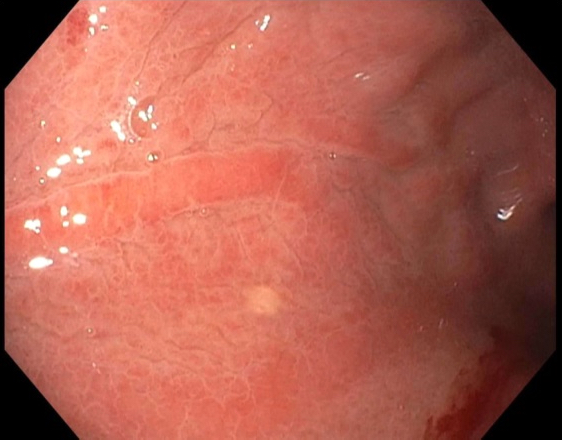
- Upper gastrointestinal endoscopy (i.e., EGD) findings:
- Mild cases: snake skin, mosaic-like pattern of stomach mucosa
- Severe cases: bulging red to brown marks
- Specificity of endoscopic findings for portal hypertensive gastropathy diagnosis were reported as follows (World J Gastrointest Endosc 2013;5:323):
- Mosaic-like pattern: 100% sensitivity and 92% specificity
- Red point lesions: 48% sensitivity and 91% specificity
- Cherry red spots: 39% sensitivity and 96% specificity
- Confluent red marks: 22% sensitivity and 100% specificity
- Capsule endoscopy:
- 74% sensitivity and 83% specificity compared to EGD (Hepatology 2008;47:1595)
- Radiologic findings (double contrast upper gastrointestinal imaging study):
- Poorly studied and nonspecific
- Thickened nodular folds in gastric fundus or body (AJR Am J Roentgenol 2000;175:1609)
Radiology description
- See Diagnosis
Prognostic factors
- Poor prognosis is associated with severe cases presenting with acute bleeding
- Rarely fatal bleeding has been reported (J Clin Diagn Res 2016;10:HD01)
- Cirrhotic patients with severe portal hypertensive gastropathy associated with higher portal pressure had worse prognosis than patients with mild portal hypertensive gastropathy (Dig Dis Sci 2010;55:3561)
Case reports
- 24 year old man with end stage renal disease (ESRD) and recurrent pleuritic chest pain (J Renal Inj Prev 2016;5:48)
- 26 year old man with Cohen syndrome and large volume hematemesis (Case Reports Hepatol 2020;2020:8893713)
- 53 year old man who died as a result of acute gastric bleeding (J Clin Diagn Res 2016;10:HD01)
- 76 year old woman with chronic gastrointestinal bleeding (Mayo Clin Proc 1994;69:1195)
Treatment
- Iron supplementation for chronic gastrointestinal bleeding
- Beta blockers and octreotide to decrease portal blood pressure
- Transjugular intrahepatic portosystemic shunt (TIPS) procedure (Hepatology 1995;21:1011)
- Endoscopic therapy (sclerotherapy or coagulation therapy):
- Limited data on efficacy: bleeding is usually diffuse (World J Gastrointest Endosc 2022;14:163)
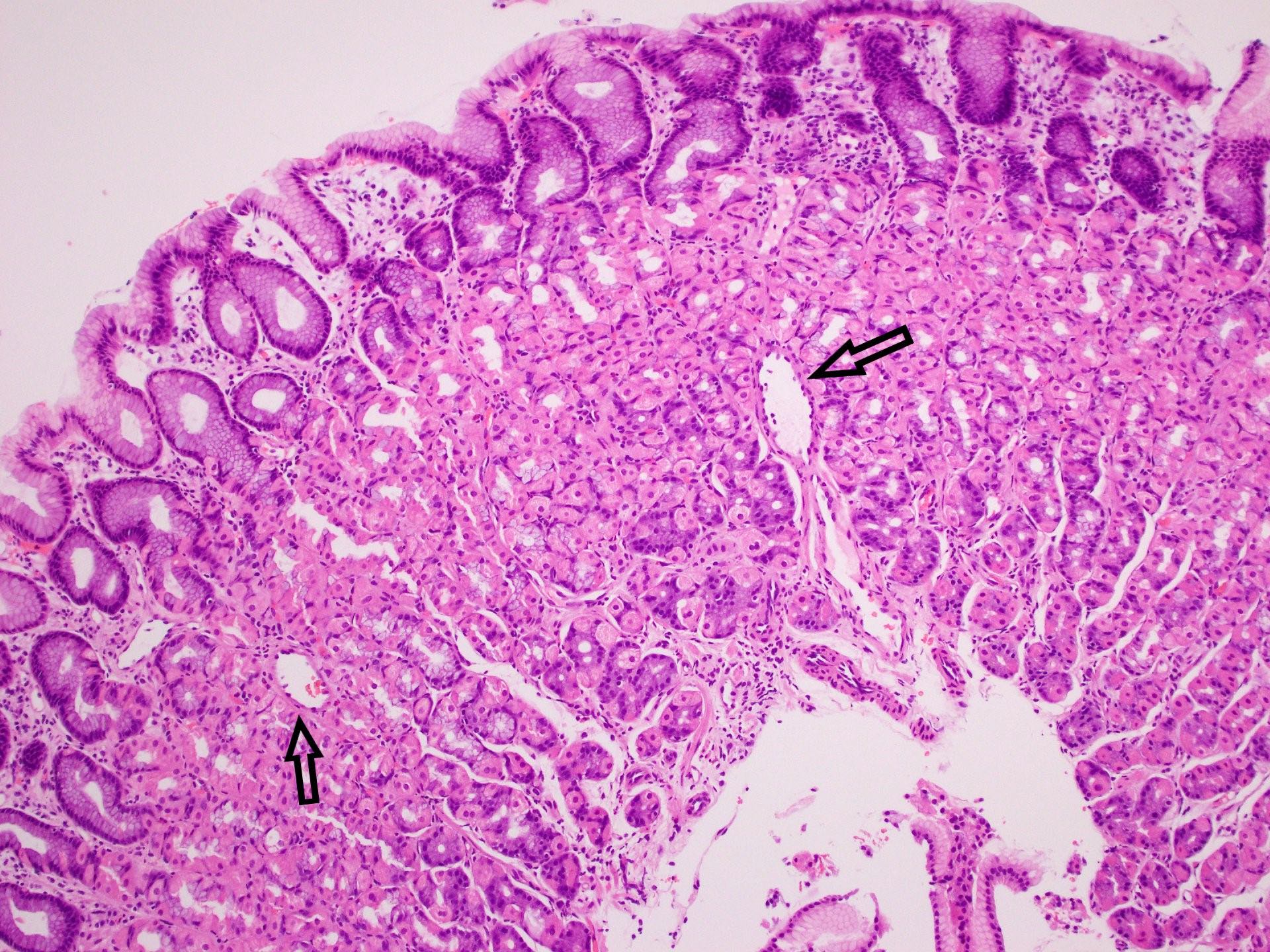
Microscopic (histologic) description
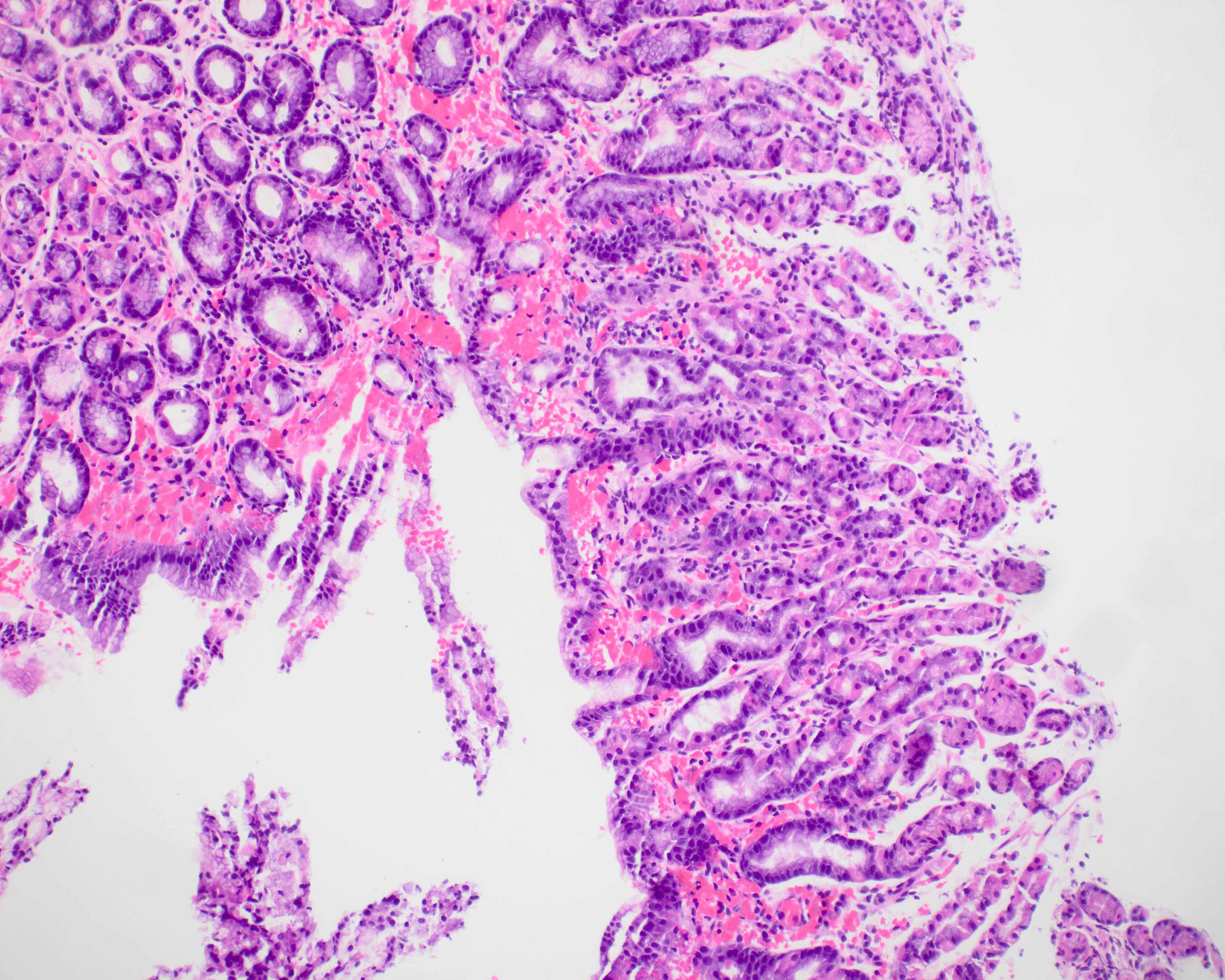
- No specific histologic diagnostic criteria for portal hypertensive gastropathy
- Histologic diagnosis is correlated with clinical history (portal hypertension) and endoscopic findings
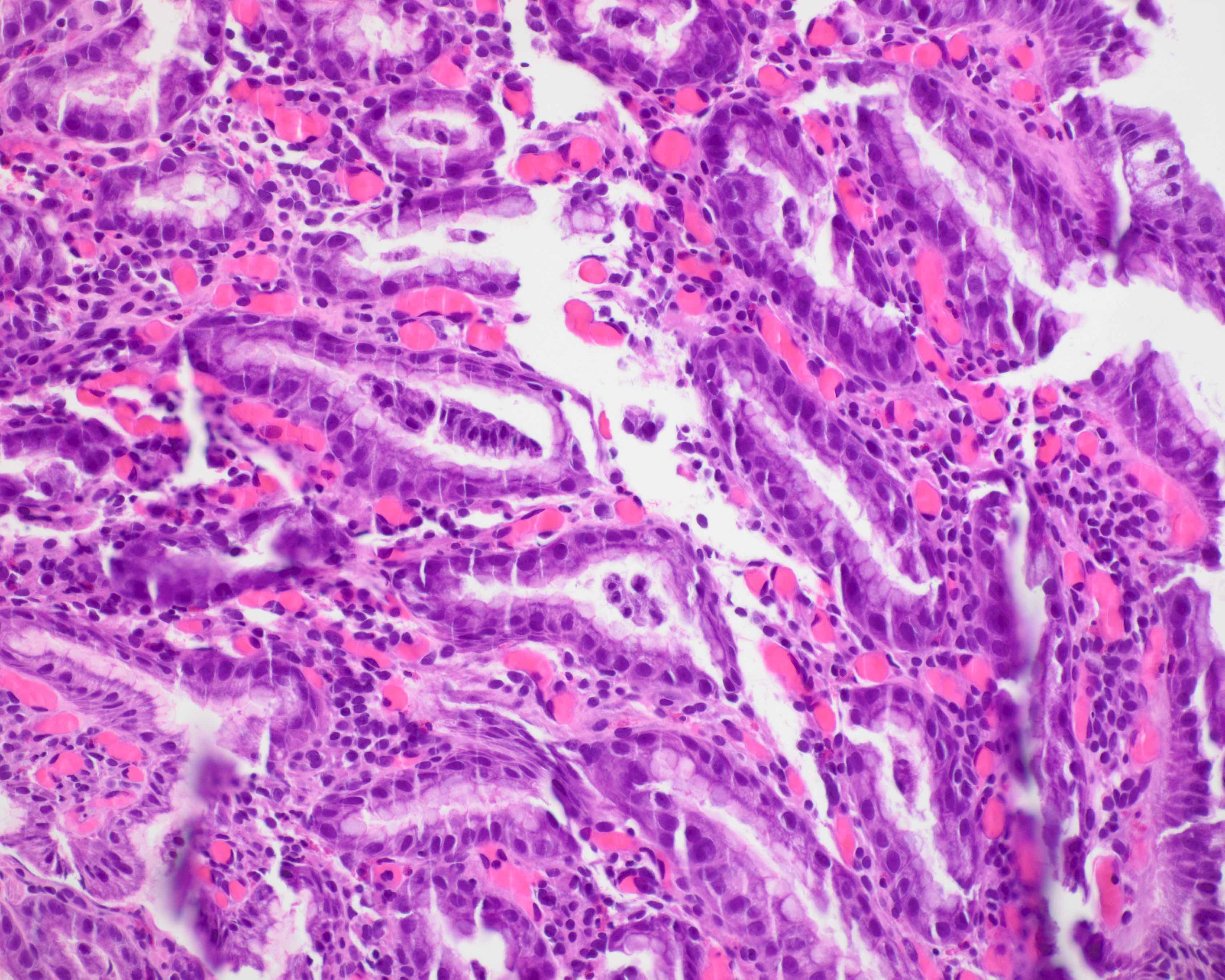
- Prominent congested blood vessels (capillaries and venules) in the lamina propria
- Lamina propria edema or fibrosis
- Congested, dilated and tortuous mucosal and submucosal venules (Gut 1985;26:1226)
- Features of reactive gastropathy can be seen
- The above features can only be seen in the submucosa; with variable degrees, a normal gastric biopsy does not exclude the clinical diagnosis of portal hypertensive gastropathy (Am J Clin Pathol 2022;158:632)
- Absence of significant inflammation and fibrin thrombi
Microscopic (histologic) images
Sample pathology report
- Stomach, biopsy:
- Portal hypertensive gastropathy (see comment)
- Comment: Mild reactive gastropathy with mucosal congestion and dilated vessels within lamina propria is consistent with portal hypertensive gastropathy.
- Negative for intestinal metaplasia, dysplasia or malignancy.
Differential diagnosis
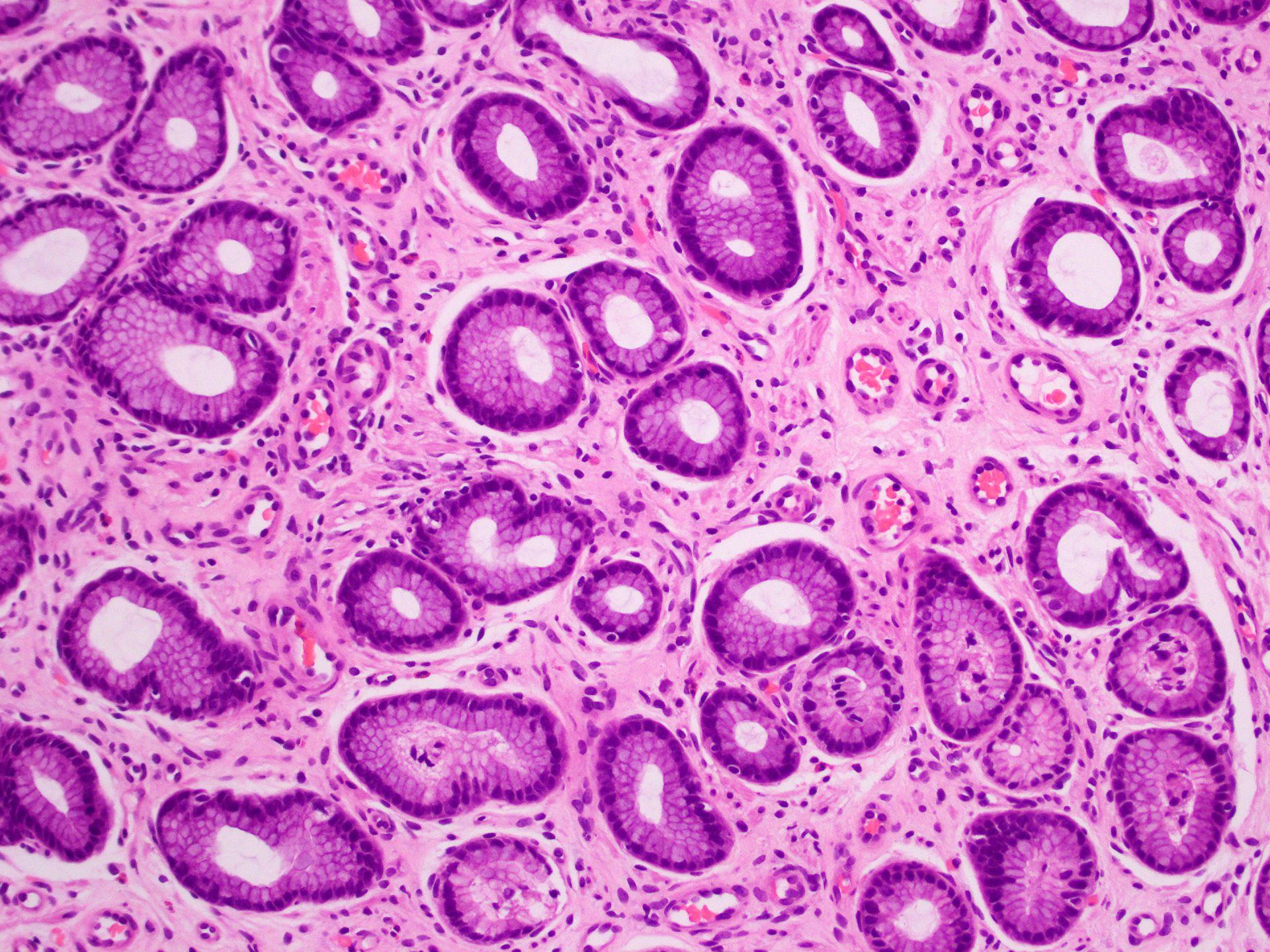
- Gastric antral vascular ectasia (GAVE):
- Usually located in distal stomach (antrum)
- Watermelon stomach on endoscopy
- Vascular ectasia, fibromuscular proliferation and fibrin thrombi
Additional references
Board review style question #1
A 58 year old man with a history of hepatitis C cirrhosis and prior bleeding varices presented with chronic chest pain, dyspepsia and anemia. Esophagogastroduodenoscopy (EGD) showed mucosal red spots in the stomach fundus. Which of the following histologic features is expected to be noted on biopsy?
- Active chronic inflammation
- Congested capillaries in the lamina propria without significant inflammation
- Ectatic blood vessels and fibrin thrombi
- Extensive intestinal metaplasia
Board review style answer #1
B. Congested capillaries in the lamina propria without significant inflammation. The clinical history suggests portal hypertension (cirrhosis and bleeding varices), which raises concern of portal hypertensive gastropathy. EGD findings show mucosal red spots or mosaic pattern that support the diagnosis.
Comment Here
Reference: Portal hypertensive gastropathy
Comment Here
Reference: Portal hypertensive gastropathy
Board review style question #2
The figure above is from a stomach biopsy in a 63 year old woman with history of recurrent deep vein thrombosis. Esophagogastroduodenoscopy (EGD) shows mosaic-like pattern of the stomach mucosa without bleeding. Which of the following is a possible etiology of the endoscopic findings?
- Atrophic gastritis
- Chronic hypertension
- Inflammatory bowel disease
- Portal vein thrombosis
Board review style answer #2
D. Portal vein thrombosis. The patient history and the EGD findings of the stomach suggest portal hypertension due to veno-occlusive disorder. Portal vein thrombosis can result in backing up of collateral circulation in the upper gastrointestinal tract causing portal hypertensive gastropathy. The biopsy of the stomach shows diffuse congestion of mucosal capillaries, supporting portal hypertensive gastropathy.
Comment Here
Reference: Portal hypertensive gastropathy
Comment Here
Reference: Portal hypertensive gastropathy