Table of Contents
Definition / general | Essential features | The Cancer Genome Atlas (TCGA) network classification | The Asian Cancer Research Group (ACRG) classification | Sites | Clinical features | Diagnosis | Prognostic factors | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Board review style question #1 | Board review style answer #1Cite this page: Fassan M. Molecular pathology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachmolecular.html. Accessed April 2nd, 2025.
Definition / general
- 2 main gastric cancer molecular classifications have been proposed by comprehensive molecular profiling, with partial overlap (Nature 2014;513:202, Nat Med 2015;21:449)
- Routine immunohistochemical analysis and in situ hybridization may be useful for tumor molecular classification (Am J Surg Pathol 2017;41:106, Virchows Arch 2018;472:369, PLoS One 2019;14:e0224812)
Essential features
- PDL1 overexpression in microsatellite instability (MSI) and Epstein-Barr virus (EBV) associated tumors (Nat Med 2018;24:1449)
- MSI tumors are susceptible to immune checkpoint blockade (World J Gastroenterol 2019;25:5773)
- EBV tumors may be identified by Epstein-Barr encoding region (EBER) in situ hybridization (Gut 2014;63:236)
- MSI tumors may be identified by mismatch repair (MMR) immunohistochemical protein analysis or microsatellite molecular testing (Ann Oncol 2019;30:1232)
- MSI tumors are frequently characterized by the hypermethylation of the MLH1 gene promoter (Cell Mol Life Sci 2018;75:4151)
The Cancer Genome Atlas (TCGA) network classification
- EBV positive tumors (~9%)
- Gastric fundus or body
- Male prevalence
- Extensive DNA promoter hypermethylation
- CDKN2A (p16INK4A) promoter hypermethylation
- PIK3CA, ARID1A and BCOR mutations
- Overexpression of PDL1 and PDL2 (assessable with IHC)
- Tumors with MSI (~22%)
- Preferred localization in the gastric antrum
- Associated with intestinal histotype
- Elderly age of onset
- More favorable prognosis than the other molecular subtypes
- MLH1 gene promoter hypermethylation
- High mutational burden
- In contrast to MSI colorectal adenocarcinoma, there is no association with BRAF mutations
- Can be part of the spectrum of inherited malignancies such as Lynch syndrome
- Genomically stable tumors (~20%)
- Distal localization
- Poorly cohesive histotype
- Younger patients in comparison to other molecular subtypes
- Worst prognosis among the 4 TCGA subtypes
- Low copy number alterations
- Low mutational burden
- ARID1, RHOA and CDH1 mutations
- CLDN18-ARHGAP26 fusions in 15%
- Tumors with chromosomal instability (CIN) (~50%)
- Frequently located at the gastroesophageal junction / cardia
- Most are classified as intestinal type
- DNA aneuploidy and highly variable chromosomal copy numbers
- Frequent mutations of the tumor suppressor TP53
- Frequent genomic amplifications of receptor tyrosine kinases (RTKs) / RAS pathway, including epidermal growth factor receptor (EGFR), ERBB2 (HER2), ERBB3, MET proto-oncogene (MET), fibroblast growth factor receptor 2 (FGFR2), vascular endothelial growth factor A (VEGFA) and KRAS
- Reference: Nature 2014;513:202
The Asian Cancer Research Group (ACRG) classification
- Microsatellite unstable (MSI) tumors (~23%)
- Preferred location in the gastric antrum
- Intestinal histology
- Often diagnosed at an early stage
- Best overall prognosis
- Silencing of MLH1 gene
- DNA methylation signature
- Presence of hypermutation
- Mutations of ARID1A, KRAS and ALK
- Alterations affecting the PI3K-PTEN-mTOR pathway
- Overexpression of PDL1 (assessable with IHC)
- Epithelial to mesenchymal-like type tumors (microsatellite stable [MSS] / EMT) (~15%)
- Poorly cohesive histotype
- Younger age at presentation compared to all other subtypes
- Higher TNM stages at presentation (III / IV)
- Higher frequency of peritoneal metastases
- Worst prognosis
- CDH1 loss of expression
- Lower number of mutation events when compared to the other MSS groups
- MSS / TP53 positive tumors (~26%)
- Intestinal histology
- Male predominance
- Frequent EBV infection
- Frequent mutations in ARID1A, PIK3CA, SMAD4 and APC
- MSS / TP53 negative tumors (~36%)
- Intestinal histology
- Male predominance
- Highest prevalence of TP53 and RHOA mutations ("TP53 negative" refers to loss of function, not presence of mutation)
- Mutations in APC, ARID1A, KRAS, PIK3CA and SMAD4
- Reference: Nat Med 2015;21:449
Sites
- EBV tumors are more common in the fundus or body (Gastroenterology 2009;137:824)
- MSI tumors are more common in the antrum (Nature 2014;513:202)
- Tumors with chromosomal instability are frequently located at the gastroesophageal junction / cardia (Nature 2014;513:202)
Clinical features
- EBV tumors are more common in men (Gastroenterology 2009;137:824)
- MSI tumors have an elderly age of onset (Cell Mol Life Sci 2018;75:4151)
- MSI tumors can be part of the spectrum of inherited malignancies such as Lynch syndrome (Cell Mol Life Sci 2018;75:4151)
- MSI tumors are often diagnosed at an early stage (Cell Mol Life Sci 2018;75:4151)
- Genomically stable tumors are characterized by an earlier age of onset in comparison to other molecular subtypes (Nature 2014;513:202)
Diagnosis
- EBV tumors may be identified by EBER in situ hybridization (Gut 2014;63:236)
- MSI tumors may be identified by MMR immunohistochemical protein analysis or microsatellite molecular testing (Ann Oncol 2019;30:1232)
- MSI tumors are frequently characterized by the hypermethylation of the MLH1 gene promoter (Cell Mol Life Sci 2018;75:4151)
- Complete loss of or clonal p53 overexpression (i.e. strong and with a diffuse pattern) is frequently observed in tumors with chromosomal instability (Am J Surg Pathol 2017;41:106, Virchows Arch 2018;472:369, PLoS One 2019;14:e0224812)
Prognostic factors
- MSI tumors have a more favorable prognosis (Cell Mol Life Sci 2018;75:4151)
- Genomically stable tumors have the worst prognosis among the 4 TCGA subtypes (Nature 2014;513:202)
Treatment
- MSI tumors are susceptible to immune checkpoint blockade (World J Gastroenterol 2019;25:5773)
- EBV positive tumors seem to benefit significantly from immune checkpoint blockade (World J Gastroenterol 2019;25:5773, Nat Med 2018;24:1449)
Microscopic (histologic) description
- Genomically stable tumors have a poorly cohesive histotype (Nature 2014;513:202)
- MSI tumors and tumors with chromosomal instability are usually characterized by an intestinal histotype (Nature 2014;513:202)
- Gastric adenocarcinoma with lymphoid stroma is usually associated with EBV infection or MSI status (Am J Surg Pathol 2018;42:453, Int J Mol Sci 2018;19:2079)
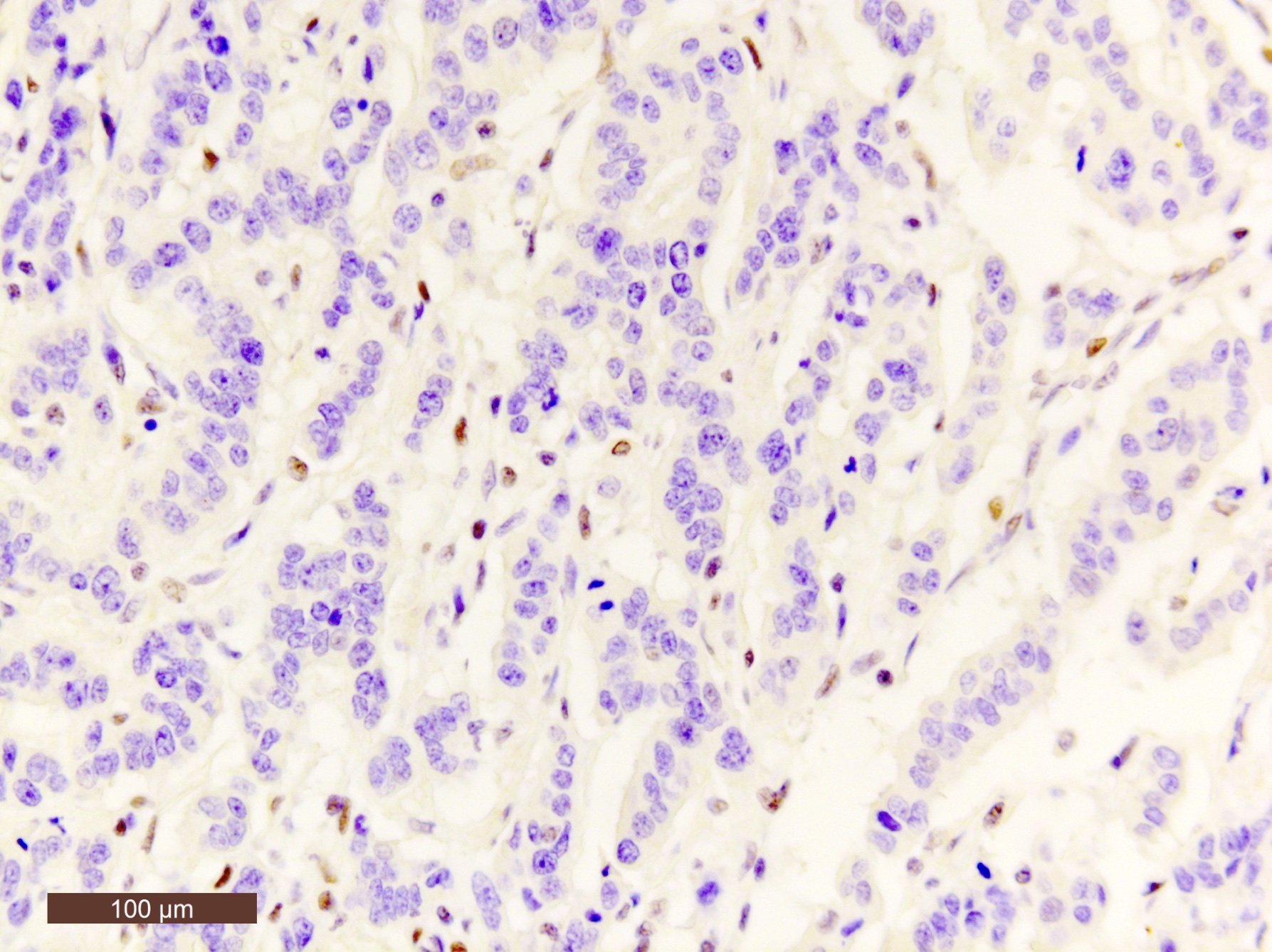
Microscopic (histologic) images
Positive stains
- EBER in situ hybridization in EBV tumors (Gut 2014;63:236)
- PDL1 overexpression in MSI and EBV associated tumors (Nat Med 2018;24:1449)
- Higher prevalence of HER2 overexpression in tumors with chromosomal instability (Nature 2014;513:202)
Negative stains
- MLH1 loss in MSI tumors (Am J Surg Pathol 2017;41:106, Virchows Arch 2018;472:369, PLoS One 2019;14:e0224812)
- E-cadherin loss in genomically stable tumors (Am J Surg Pathol 2017;41:106, Virchows Arch 2018;472:369)
Board review style question #1
Board review style answer #1
C. High mutational burden. Alterations in the DNA mismatch repair machinery results in the accumulation of frame shift mutations (either through insertions or deletions) with a subsequent increased mutational burden.
Comment Here
Reference: Molecular pathology of stomach cancer
Comment Here
Reference: Molecular pathology of stomach cancer