Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aljuboori O, Garcia-Buitrago MT. Hyperplastic polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachhyperplastic.html. Accessed March 28th, 2025.
Definition / general
- The second most common gastric epithelial polyp encountered during endoscopy
- Usually a solitary polyp, commonly found in gastric antrum
- Associated with autoimmune type gastritis, Helicobacter pylori gastritis, postsurgery and bile reflux gastritis (Am J Surg Pathol 2001;25:500, Am J Surg Pathol 2010;34:1591)
- Usually < 1 cm, more than 50% are < 0.5 cm; large polyps up to 12 cm can occur and mimic malignancy
- Dysplasia is more likely when > 1 cm and > 2.5 cm (Gut Liver 2009;3:271, GE Port J Gastroenterol 2021;28:328)
- Resembles other GI dysplasia, either low grade or high grade
Essential features
- Surface epithelium derived polyp
- Elongated and architecturally distorted, irregular foveolar epithelium with cystic dilatations
- Corkscrew appearance can occur
- Lamina propria shows edema, congestion, variable acute and chronic inflammation
- Smooth muscle strands can be seen extending from muscularis mucosae towards surface
- Thick walled vessels may be present towards the base of the polyp
Terminology
- Synonyms: regenerative polyp and hyperplasiogenous polyp (Tohoku J Exp Med 1984;142:125)
ICD coding
- ICD-10: K31.7 - polyp of stomach and duodenum
Epidemiology
- Second most common gastric polyp in adults, accounting for 17% of gastric polyps (Histopathology 2021;78:106, Am J Gastroenterol 2009;104:1524)
- This could be due to increasing use of proton pump inhibitors and detection of fundic gland polyps (World J Gastroenterol 2016;22:8883, Dig Dis Sci 2009;54:1839, Arq Gastroenterol 2007;44:14)
- Most common polyp among children, representing 42% of gastric polyps (Histopathology 2021;78:106)
- M = F; age range: 20 - 80 years, peaks in sixth and seventh decades (World J Gastroenterol 2016;22:8883)
- Usually solitary, can be multiple in 20% of cases, commonly in atrophic gastritis (Histopathology 2021;78:106, Diagn Histopathol 2021;27:75)
- If multiple, must rule out juvenile polyposis, Peutz-Jeghers or familial adenomatous polyposis (FAP) syndromes (Surg Pathol Clin 2020;13:431)
- > 50 polyps suggests gastric polyposis syndrome, an entity not well established by diagnostic criteria (J Clin Diagn Res 2012;6:1428)
- Dysplasia occurs in 2 - 19% (Int J Surg Pathol 2016;24:704, GE Port J Gastroenterol 2021;28:328)
- Risk increases with age and polyp size
- Polyps > 1 - 2.5 cm, presence of intestinal metaplasia and pedunculated in shape and age, particularly if > 50 years
- Carcinoma reported in 0.6 - 2.1% (Int J Surg Pathol 2016;24:704, GE Port J Gastroenterol 2021;28:328)
Sites
- Common site is gastric antrum but can occur anywhere in the stomach; recently body of the stomach has become more common due to autoimmune gastritis and the increased use of proton pump inhibitors (Am J Gastroenterol 2009;104:1524, Int J Mol Sci 2021;22:6548)
- Hyperplastic polyps in pyloric and prepyloric regions may have features of prolapse associated polyps
- Hyperplastic polyps at gastroesophageal junction are associated with Barrett esophagus in 33% of cases (Am J Surg Pathol 2011;35:1038)
Pathophysiology
- Excessive proliferation of foveolar cells lining the surface and pits accompanied by increased exfoliation in response to longstanding mucosal injury (World J Gastroenterol 2016;22:8883, Surg Pathol Clin 2020;13:431)
Etiology
- Associated with underlying gastritis
- Helicobacter pylori associated chronic gastritis (25%) (Histopathology 2021;78:106)
- Reactive gastropathy (chemicals, drugs, bile reflux) (21%) (Histopathology 2021;78:106)
- Autoimmune gastritis (12%) (World J Gastroenterol 2016;22:8883)
- Association with gastric antral vascular ectasia and cytomegalovirus gastritis has also been reported (Histopathology 2021;78:106)
- Helicobacter pylori CagA protein expression can lead to development of hyperplastic polyps (Am J Gastroenterol 2009;104:1524, Proc Natl Acad Sci USA 2008;105:1003)
- CagA can cause aberrant activation of human oncoprotein SHP2 in stomach (Proc Natl Acad Sci USA 2008;105:1003)
Clinical features
- Mean age: 65 years
- In the last decade, patients aged 45 - 59 had twice as many gastric polyps as 10 years ago (World J Gastroenterol 2016;22:8883)
- Dyspepsia, heartburn and abdominal pain; patients may have anemia due to upper gastrointestinal bleeding (Dig Dis Sci 2007;52:105)
- Obstructive symptoms if near pylorus or gastroesophageal junction
Diagnosis
- Histopathology
Case reports
- 55 year old woman with malignant transformation of gastric hyperplastic polyp (BMC Gastroenterol 2016;16:130)
- 60 year old man with a history of hematemesis and epigastric pain who was found to have a giant gastric hyperplastic polyp (Radiol Case Rep 2021;17:355)
- 70 year old woman with melena found to have a adenocarcinoma arising in a hyperplastic polyp (AIM Clinical Cases 2022;1:e210041)
- 75 year old man with abdominal pain and constipation found to have inverted hyperplastic polyp (Exp Ther Med 2022;25:6)
Treatment
- Management of hyperplastic polyps is determined by the size and presence or absence of dysplasia
- Endoscopic mucosal resection for polyps > 1 cm or symptomatic, with annual follow up if dysplasia is found (Histopathology 2021;78:106)
- Since dysplasia suggests background chronic mucosal injury, close follow up is needed to rule out dysplasia elsewhere in stomach (Gastroenterol Rep (Oxf) 2016;4:158)
- Eradication of H. pylori infection; 71% regress after resolution of H. pylori infection (StatPearls: Gastric Polyp [Accessed 24 August 2023], Ann Intern Med 1998;129:712, Eur J Gastroenterol Hepatol 1999;11:727)
- 50% recur after resection by endoscopy
Gross description
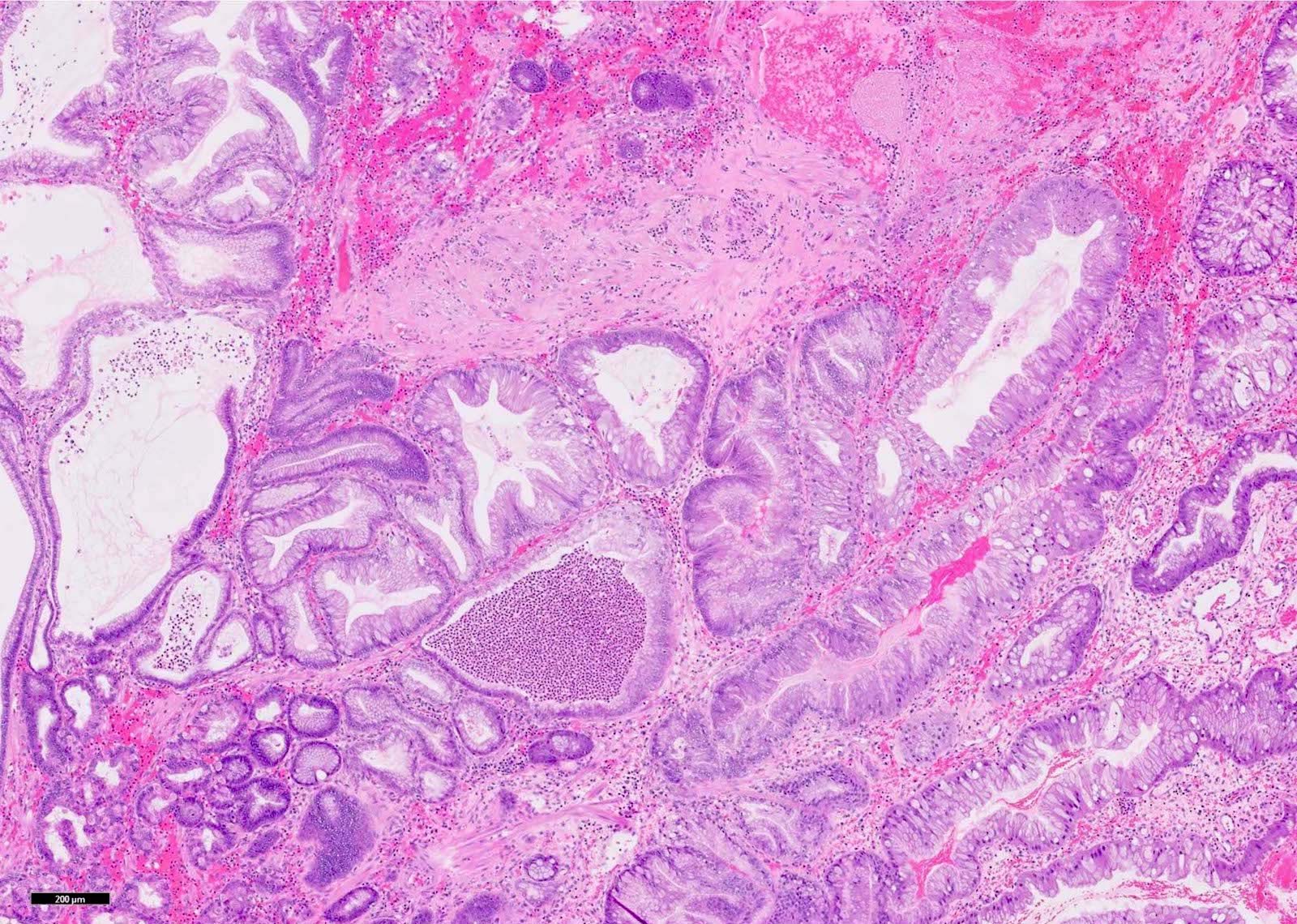
- Broad based polyp with smooth lobulated contour (Surg Pathol Clin 2020;13:431)
- Surface erosion may occur in large polyps
- Should be submitted entirely to rule out dysplasia or malignancy
Microscopic (histologic) description
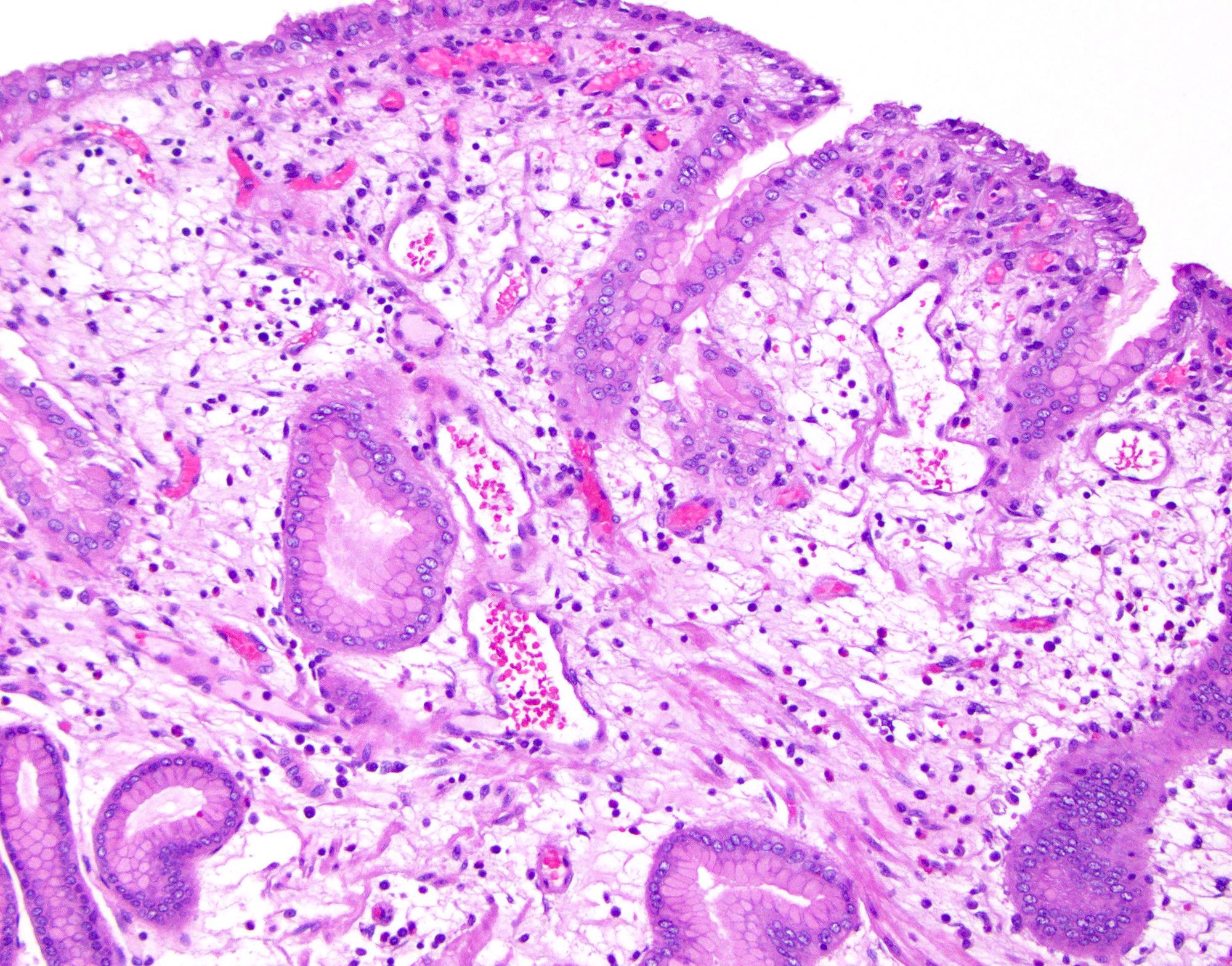
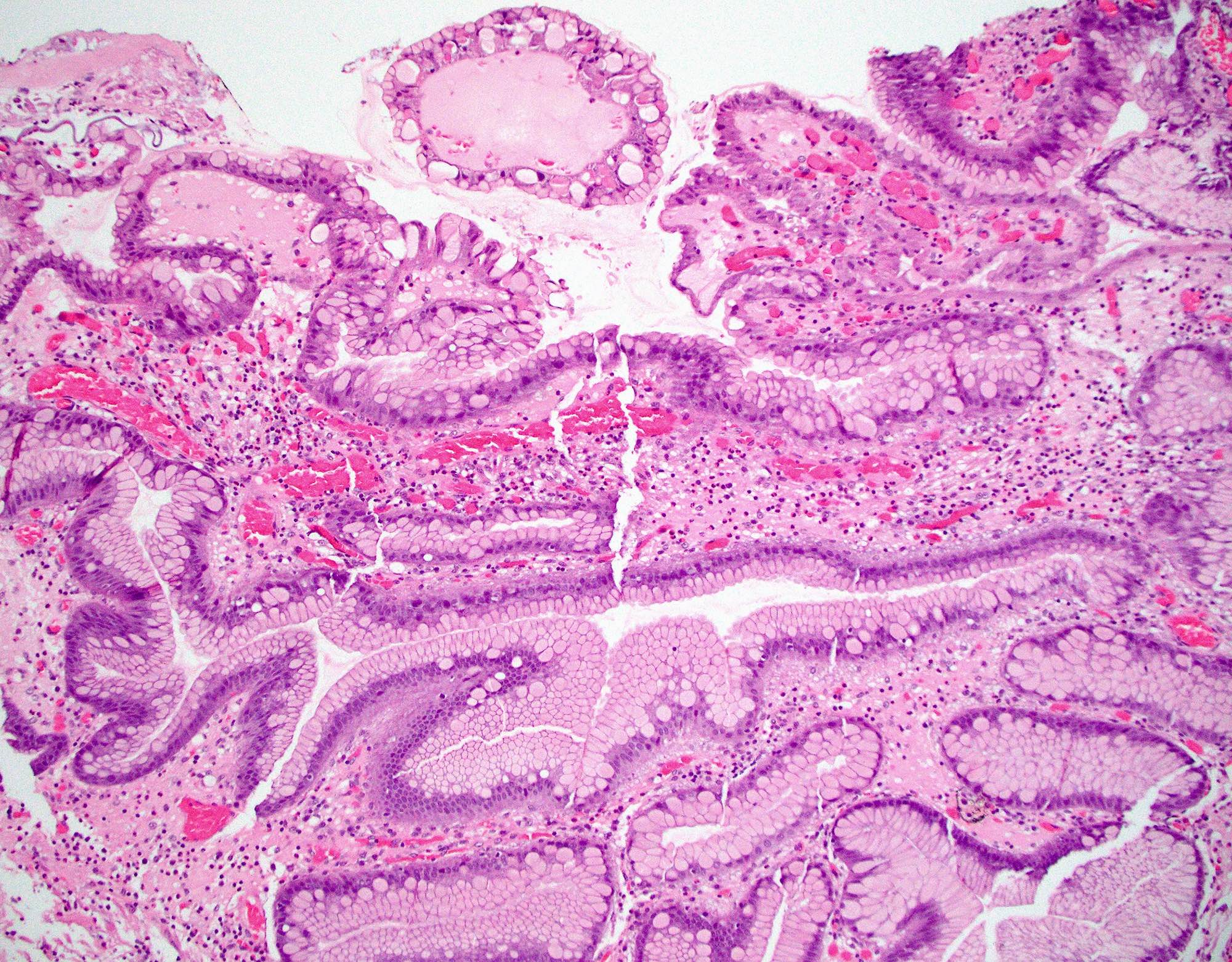
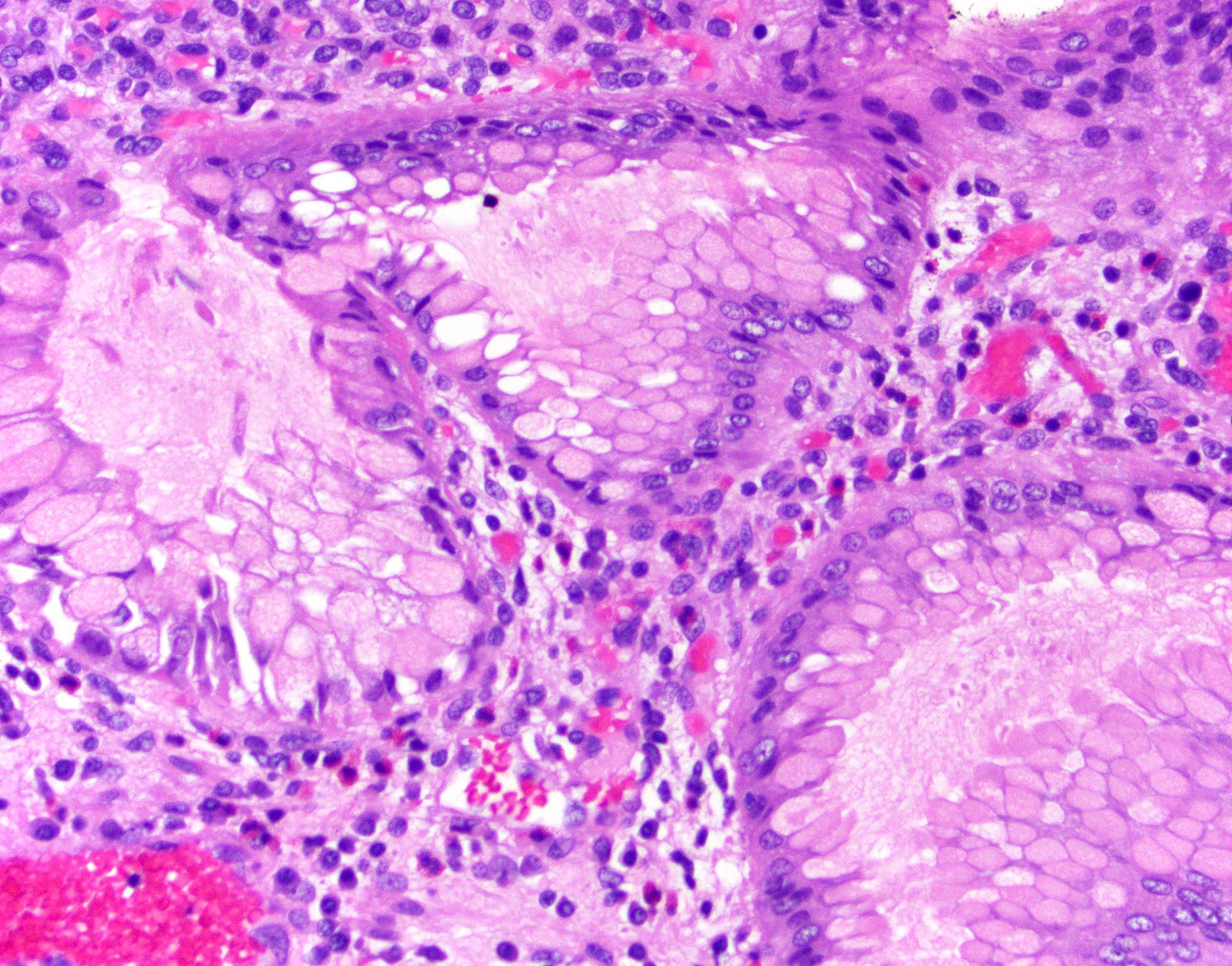
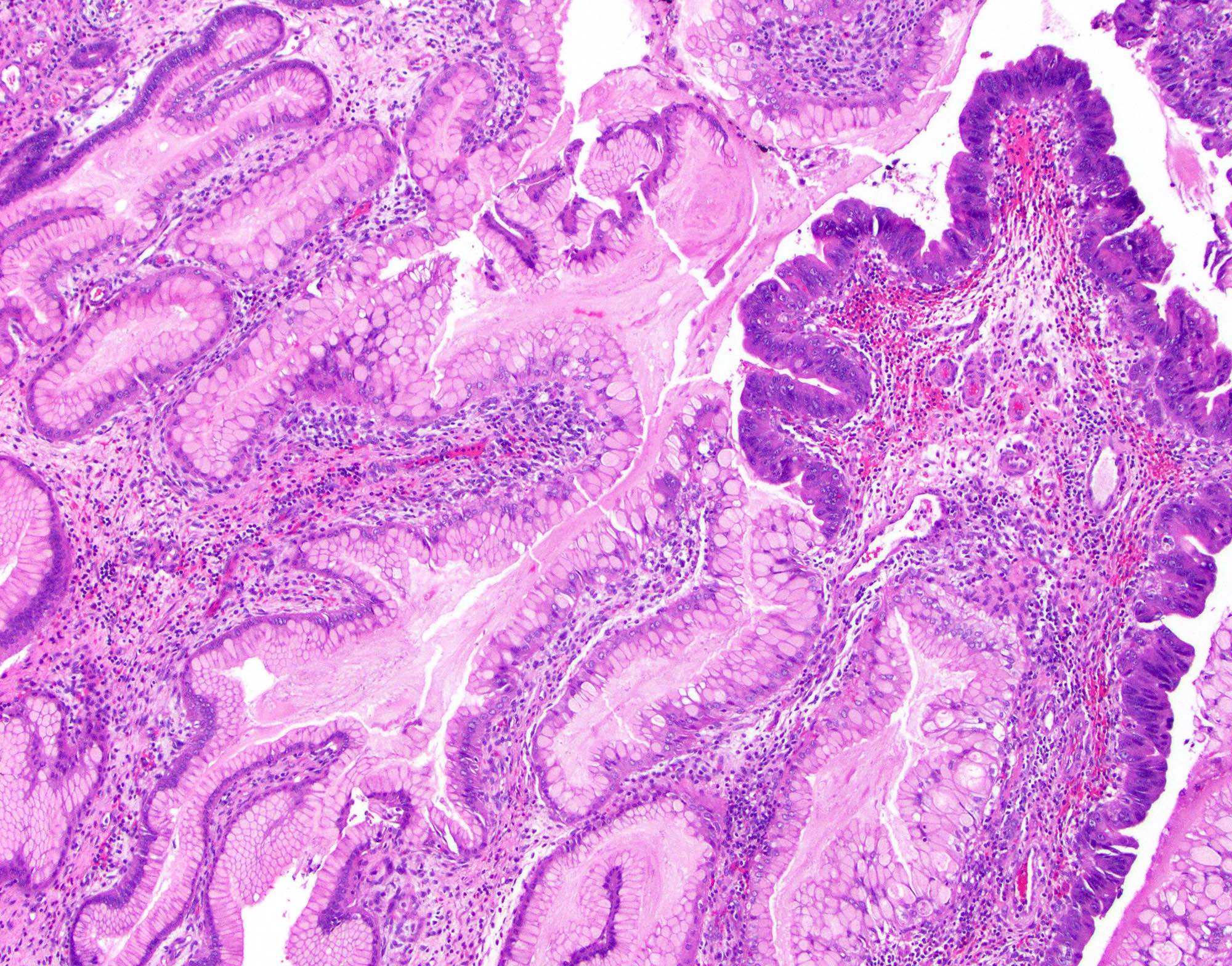
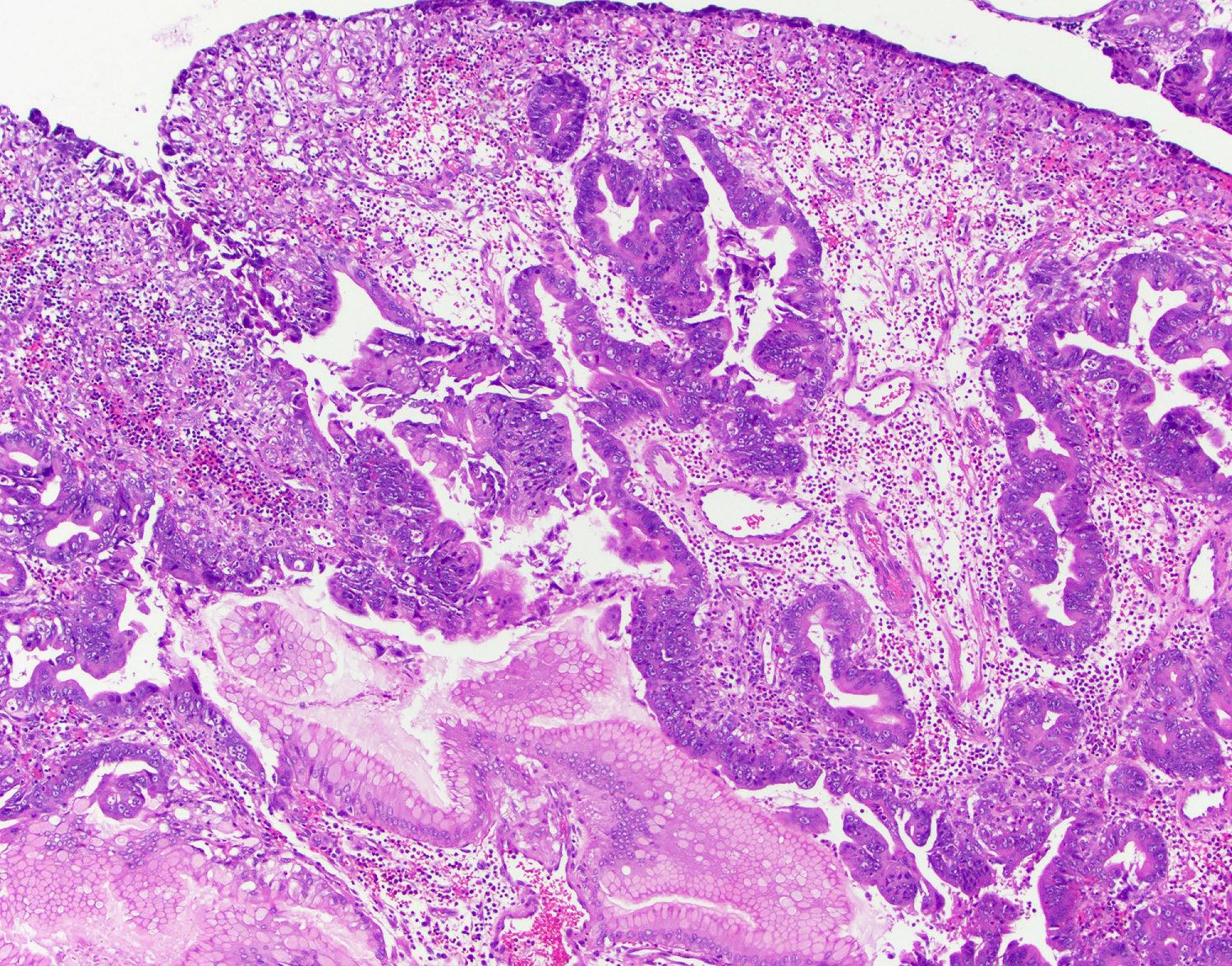
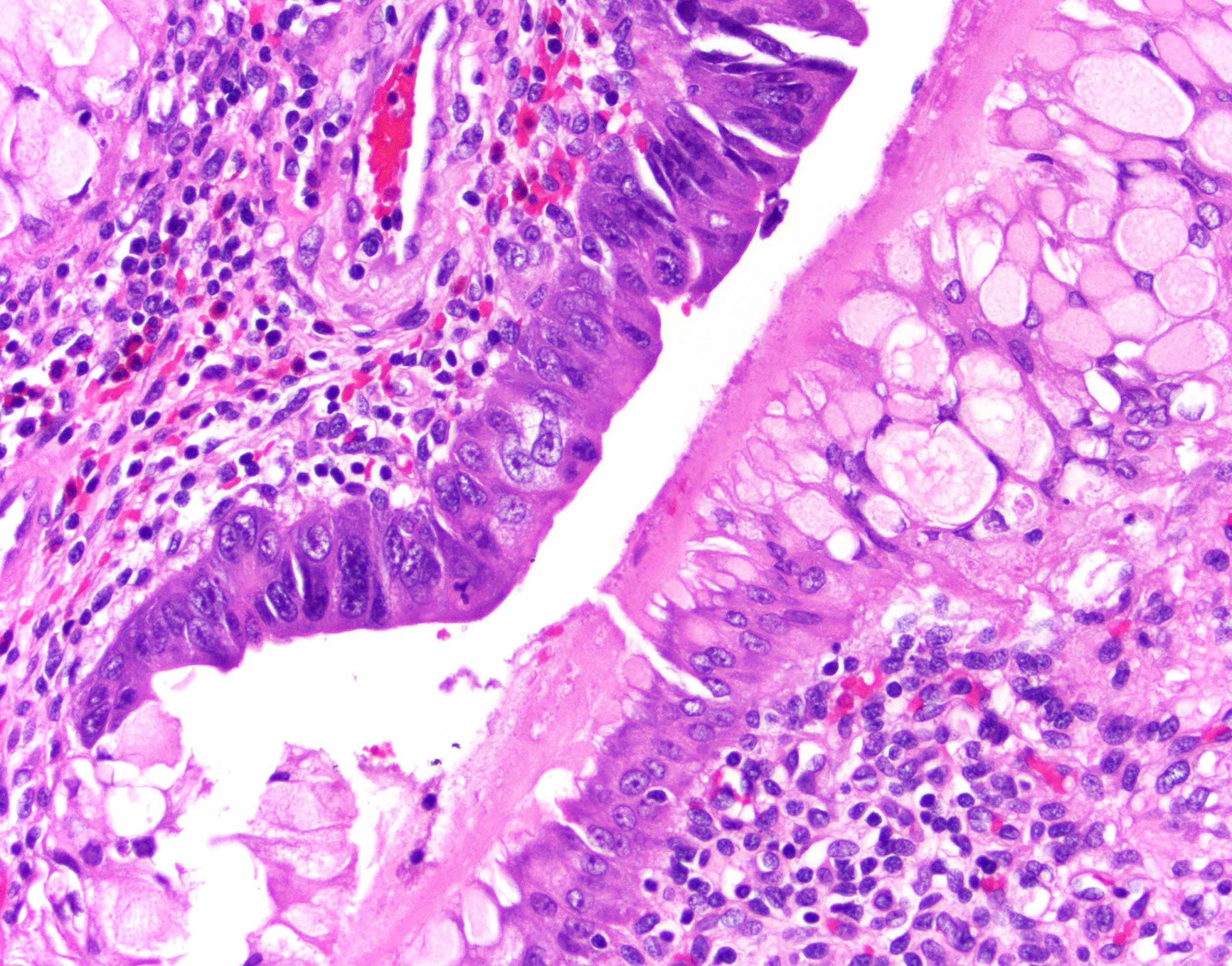
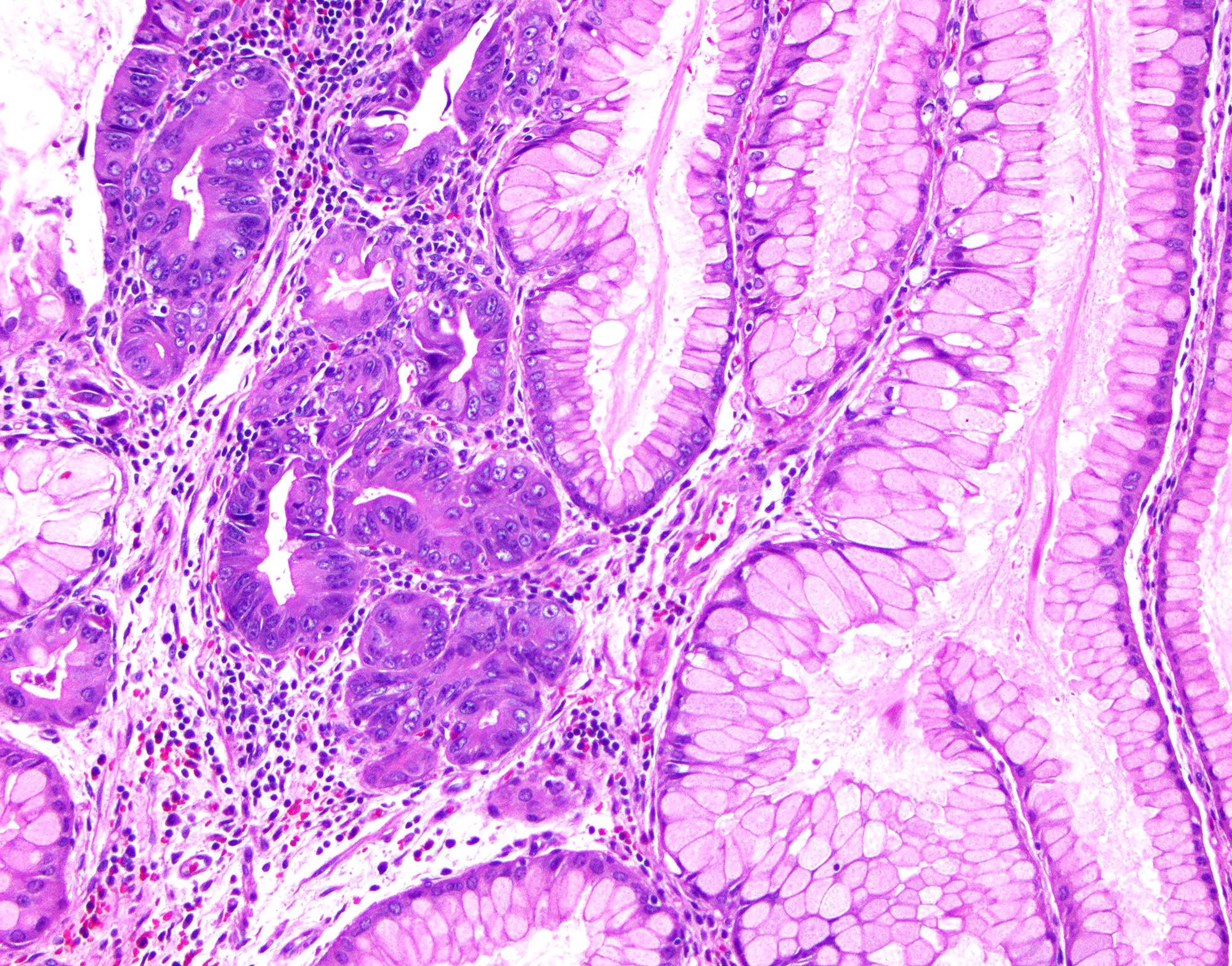
- Elongated, architecturally distorted, irregular pits with outpouchings, cystic dilation and papillary formation
- Foveolar epithelium with apical neutral mucin cap
- Can show overt hypertrophic features with the formation of clustered pseudogoblet cells or even pseudo-signet ring cells, especially in damaged areas
- Edematous lamina propria with lymphocytes, plasma cells and eosinophils
- Erosion areas can also show neutrophils
- Helicobacter pylori associated polyps: more likely show lymphoplasmacytic inflammation in lamina propria and neutrophils in the epithelium (Int J Surg Pathol 2016;24:704)
- Smooth muscle strands can extend from muscularis mucosae to the surface
- Thick walled blood vessels can be seen at the base
- Intestinal metaplasia can be seen
- Regenerative epithelial changes with focal mucin depletion, prominent nucleoli and hyperchromasia
- Ulcerated areas can display increased mitotic activity in epithelium and granulation tissue with reactive fibroblasts and endothelial cells
- Dysplasia is rare (4%); may be intestinal, foveolar or mixed (Histopathology 2021;78:106)
- High grade dysplasia: complex architecture with cribriform formation or budding, back to back arrangement of glands
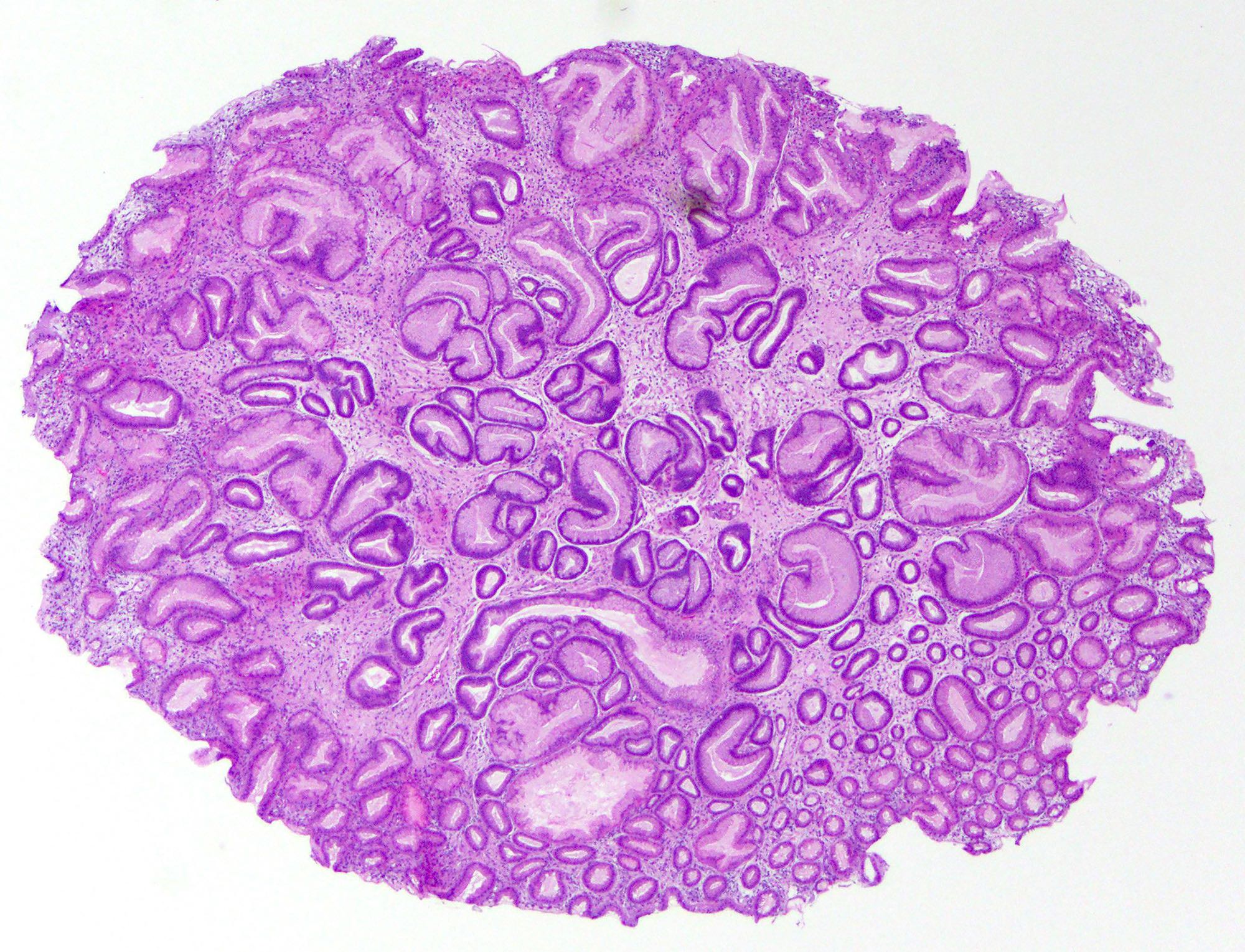
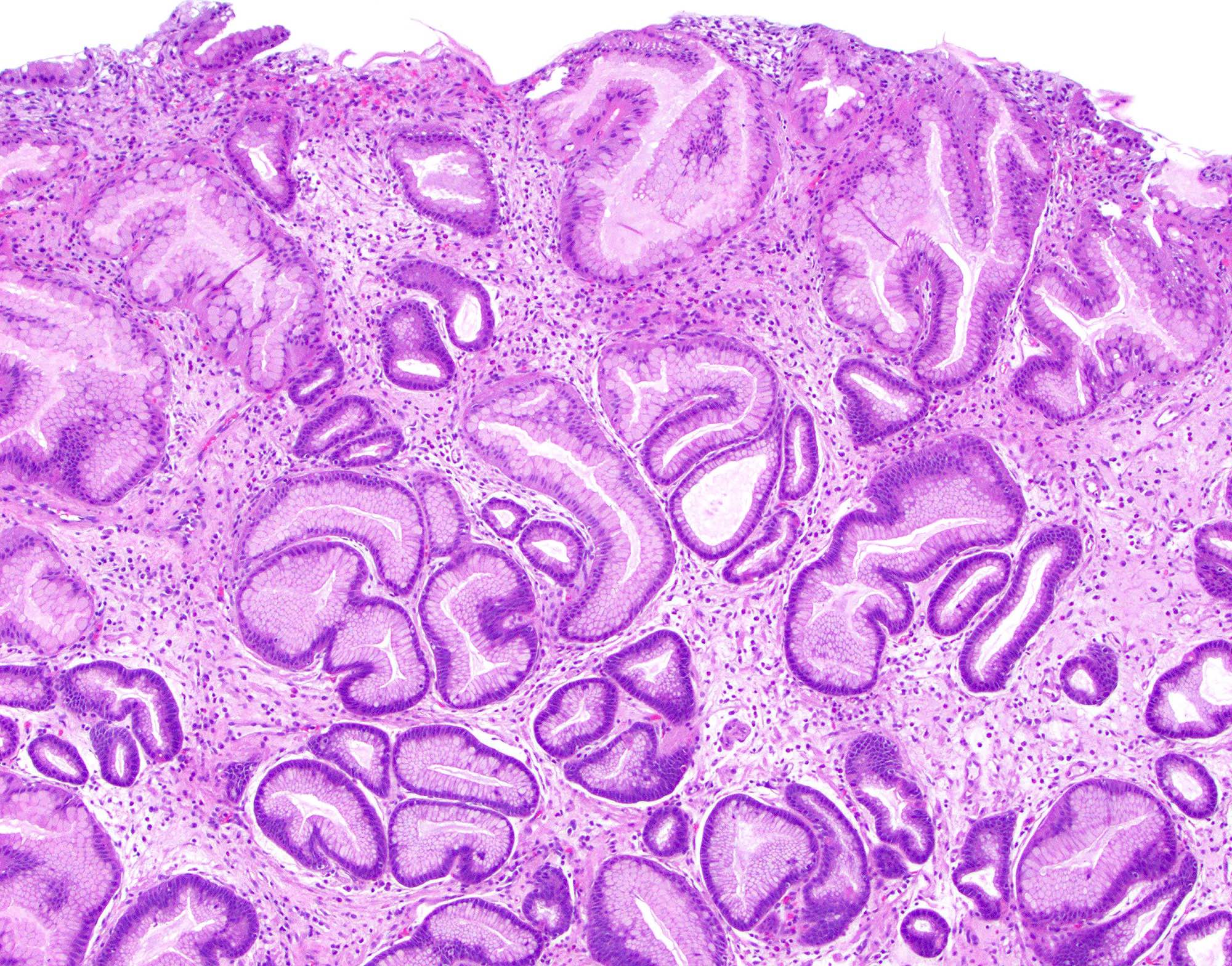
Microscopic (histologic) images
Contributed by Monica T. Garcia-Buitrago, M.D., Omar Aljuboori, M.B.B.S. and Andrey Bychkov, M.D., Ph.D.
Molecular / cytogenetics description
- Genetic alterations identified in large dysplastic hyperplastic polyps, including loss of MGMT expression, APC or CTNNB1 and TP53; less frequently KRAS or BRAF alterations (Virchows Arch 2019;475:383, Exp Mol Pathol 2015;99:468)
Sample pathology report
- Stomach, esophagogastroduodenoscopy:
- Gastric hyperplastic polyp (see comment)
- Comment: Large gastric hyperplastic polyps typically arise in a background of damaged mucosa and are frequently associated with Helicobacter pylori or autoimmune gastritis. Follow up sampling of the flat mucosa from both the antrum and body / fundus in such patients may provide information on the setting in which the polyp has arisen.
Differential diagnosis
- Polypoid gastritis:
- Normal architecture, no smooth muscle wisps
- Polypoid foveolar hyperplasia:
- No cystic dilation, no smooth muscle wisps
- Gastritis cystica profunda:
- Entrapped, distorted, dilated glands in muscularis
- Fundic gland polyp:
- Distorted glands and cysts lined by parietal and chief cells
- Ménétrier disease:
- Affects gastric body only; foveolar hyperplasia, atrophy of glands, adjacent epithelium normal
- Cronkhite-Canada syndrome:
- Affects entire stomach; foveolar hyperplasia, atrophy of glands, adjacent epithelium shows atrophy of glands and microcystic change
- Juvenile polyposis:
- Adjacent mucosa is normal as opposed to hyperplastic polyp, which often has chronic gastritis
- Peutz-Jeghers polyposis:
- Autosomal dominant inherited disorder with multiple hamartomatous polyps and mucocutaneous hyperpigmentation
- Pyloric adenoma:
- Closely packed tubular glands lined by cuboidal to low columnar epithelium with ground glass cytoplasm, bland nuclei and no well formed apical mucin cap
- Inflammatory fibroid polyp:
- Submucosal lesion composed of spindle and stellate stromal cells
- Dysplasia must be differentiated from regenerative change:
- Dysplasia is present at the surface; regenerative change shows surface maturation and atypia like changes only in the proliferative zones, not at the surface
- Dysplasia is typically abrupt
- Dysplasia has architecturally complex patterns (cribriform, budding and branching)
- Dysplasia has nuclear pleomorphism, elongation and hyperchromasia without prominent nucleoli
- Regenerative epithelium shows gradual change, lacks complex patterns, has hyperchromasia but with ovoid nuclei and prominent nucleoli
Board review style question #1
Which Helicobacter pylori protein is associated with a role in the development of gastric neoplasia?
- CagA
- PAR1
- SHP2
- SRC
Board review style answer #1
A. CagA. CagA in Helicobacter pylori can cause aberrant activation of SHP2, a human oncoprotein, in the stomach (Proc Natl Acad Sci USA 2008;105:1003). Answer B is incorrect because PAR1 is a human kinase inhibited by CagA. Answer C is incorrect because SHP2 is a human oncoprotein, not a Helicobacter pylori protein. Answer D is incorrect because SRC is a human tyrosine kinase that mediates CagA phosphorylation and cytoskeletal rearrangements.
Comment Here
Reference: Hyperplastic polyp
Comment Here
Reference: Hyperplastic polyp
Board review style question #2
Board review style answer #2
B. Hyperplastic polyp. Gastric polyp showing elongated, tortuous and dilated gastric pits and edematous lamina propria (Surg Pathol Clin 2020;13:431). Answer A is incorrect because the polyp shows dilated pits lined by foveolar epithelium, not oxyntic epithelium. Answer C is incorrect because the polyp shows cystically dilated pits. Answer D is incorrect because the polyp has abnormal architecture and does not show predominant plasmacytic and neutrophilic inflammation.
Comment Here
Reference: Hyperplastic polyp
Comment Here
Reference: Hyperplastic polyp