Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Electron microscopy description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Storozuk T, Setia N. Helicobacter pylori. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachhelicobacter.html. Accessed March 30th, 2025.
Definition / general
- Helicobacter pylori gastritis is the most frequent and treatable form of gastritis, affecting more than half the world's population
Essential features
- Most patients are asymptomatic or have mild self limited dyspeptic symptoms but some present with abdominal pain with or without peptic ulcer disease
- H. pylori organisms are Gram negative, helical or spiral shaped and flagellate
- Diagnostic tests include invasive tests such as biopsy urease test, histology or bacterial culture and sensitivity test or noninvasive tests such as urea breath test, stool antigen test and serology
- Chronic active gastritis with superficial band of lymphoplasmacytic cells with or without neutrophils is the most common histologic pattern of H. pylori gastritis
- Bismuth quadruple, levofloxacin triple or rifabutin triple therapies are used for treatment
- Upfront H. pylori testing is not recommended; GIPS recommendations for utility of ancillary stains when evaluating gastric biopsies for H. pylori should be followed (Am J Surg Pathol 2013;37:e12)
- Complications of H. pylori gastritis include gastroduodenal ulcers, atrophy, intestinal metaplasia, gastric cancer and mucosa associated lymphoid tissue (MALT) lymphoma
Terminology
- Superficial gastritis
- Type B (bacterial) gastritis
ICD coding
- ICD-10: B96.81 - Helicobacter pylori (H. pylori) as the cause of diseases classified elsewhere
Epidemiology
- More than half the world's population is infected (Gastroenterology 2017;153:420)
- Africa has the highest pooled prevalence (70.1%); Northern America (37.1%) and Oceania (24.4%) have the lowest prevalence
- H. pylori prevalence differs by ethnicity in the U.S.:
- Non-Hispanic whites: 18.4 - 26.2%
- Nonwhites: 34.5 - 61.6%
- Native American / Alaskan Native: 75.0%
- H. pylori prevalence reflects the level of urbanization, sanitation, access to clean water and varied socioeconomic status
- In children, the most frequent transmission route is from mother to child (Adv Exp Med Biol 2019;1149:107)
Sites
- Organisms colonize the antrum first by binding to gastric mucins (TFF1) in a pH dependent manner; the organisms have affinity for gastric mucous cells but do not attach to small intestinal or other gastric epithelial cell types (Gastroenterology 2008;135:2043, J Clin Pathol 1994;47:699, Proc Natl Acad Sci U S A 1993;90:2035)
- Ideal pH for bacteria survival: 4 - 8
- Ideal pH for bacterial growth: 6 - 8 (World J Gastroenterol 2017;23:4867)
Pathophysiology
- Major virulence factors: CagA (cytotoxin associated gene A) and its pathogenicity island (Cag PAI) and VacA (vacuolating cytotoxin A)
- CagA and Cag PAI:
- Translocates to the host cytoplasm and binds to the inner surface of the cell membrane
- Major effects: disrupts tight junctions, provokes proinflammatory and mitogenic response
- VacA:
- Cytochrome c release and activation of proapoptotic factor leading to apoptosis
- CagA and Cag PAI:
- Gastric inflammation is a result of H. pylori infection mediated upregulation of cytokines; most significant are:
- CagA PAI mediated induction of NFκB and IL8 secretion
- Reactive oxygen species and reactive nitrogen species produced by host gastric epithelial cells
- Reference: Cancer Lett 2014;345:196
Etiology
- Pathogenic species in humans:
- Helicobacter pylori, Helicobacter heilmannii
- Taxonomy:
- Campylobacterales (order); Helicobacteraceae (family); Helicobacter (genus)
- Characteristic features:
- Gram negative
- Helical or spiral shaped
- Flagellate
- 3 physiologic states or forms of H. pylori:
- Vegetative / proliferative: S shaped, culturable and viable, capable of replication
- Dormant: C / U shaped, reversible state, not obviously viable but culturable, transformation induced at low pH (< 6)
- Coccoid: nonviable
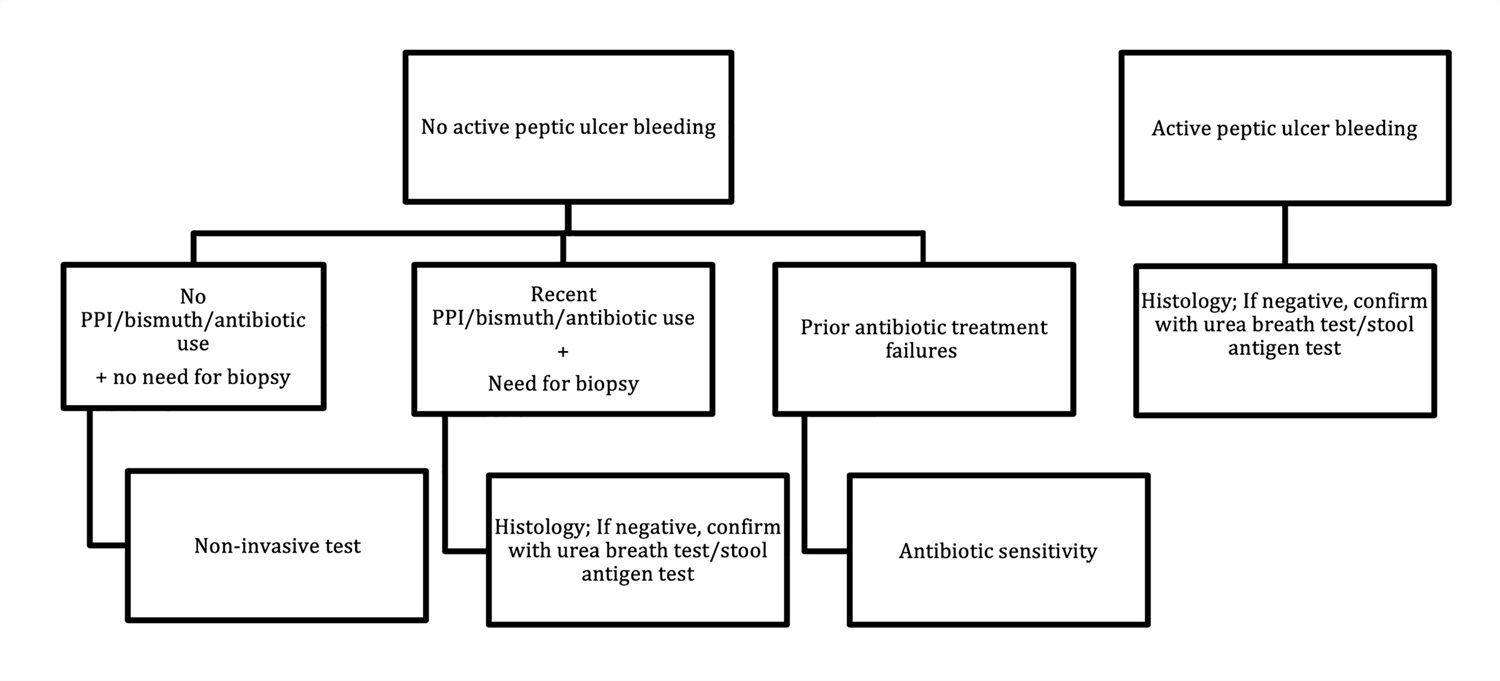
Diagrams / tables
Clinical features
- Asymptomatic or mild self limited dyspeptic symptoms with transient hypochlorhydria - acute gastritis
- Abdominal pain seen with chronic gastritis with or without peptic ulcer disease
- Extragastrointestinal manifestations: iron deficiency anemia, idiopathic thrombocytopenic purpura, vitamin B12 deficiency
Diagnosis
- Diagnostic test of choice based on active bleeding due to suspected peptic ulcer, use of proton pump inhibitor therapy [PPI], antibiotics and bismuth
- Proposed algorithm (see Diagrams / tables)
Laboratory
- Invasive (endoscopic) and noninvasive techniques:
- Endoscopic diagnosis:
- Biopsy urease test: sensitivity and specificity, 90% and 95%
- Histology: sensitivity and specificity, 95% and 98%
- Bacterial culture and sensitivity test: high specificity, low sensitivity as H. pylori is difficult to culture
- Noninvasive testing:
- Urea breath test: sensitivity and specificity, 88 - 95% and 95 - 100%
- Stool antigen test: sensitivity and specificity, 94% and 97%
- Serology: sensitivity and specificity, 85% and 79%
- Endoscopic diagnosis:
- Eradication confirmation recommended; tests recommended: urea breath test, stool antigen testing or endoscopy based testing
- Other infrequently used tests:
- 13C urea assay: serodiagnostic test using a 13C urea assay
- Polymerase chain reaction: used to detect low bacterial loads and identify specific mutations associated with antimicrobial resistance
- Reference: UpToDate: Bacteriology and epidemiology of Helicobacter pylori infection [Accessed 17 August 2020]
Radiology description
- Not indicated; historically, presence of thickened gastric folds was the best radiographic criterion (Radiology 1995;195:763)
Prognostic factors
- ~20% of cases not cured with first course of treatment and need retreatment
- Complications of H. pylori gastritis: gastroduodenal ulcers, atrophy, intestinal metaplasia, gastric cancer, MALT lymphoma
Case reports
- 12 year old girl with refractory iron deficiency anemia and H. pylori associated lymphocytic gastritis (J Pediatr Hematol Oncol 2013;35:321)
- 14 year old girl with H. pylori gastritis and associated gastric low grade mucosa associated lymphoid lymphoma treated only for the H. pylori infection, resulting in complete resolution of her lymphoproliferative disease (Gastroenterology 1995;109:973)
- 23 year old man with subacute combined degeneration of the spinal cord, low serum vitamin B12, anti-intrinsic factor antibodies and H. pylori gastritis (BMJ Case Rep 2013;2013:bcr201320038)
- 66 year old man with reflux esophagitis and Russell body gastritis (Dig Liver Dis 2015;47:526)
Treatment
- Bismuth quadruple (PPI, bismuth subcitrate, tetracycline and metronidazole) or levofloxacin triple (PPI, levofloxacin, amoxicillin), rifabutin triple (PPI, rifabutin and amoxicillin) (Am J Gastroenterol 2017;112:212)
- Decision made based on risk factors for macrolide resistance and the presence of a penicillin allergy
Clinical images
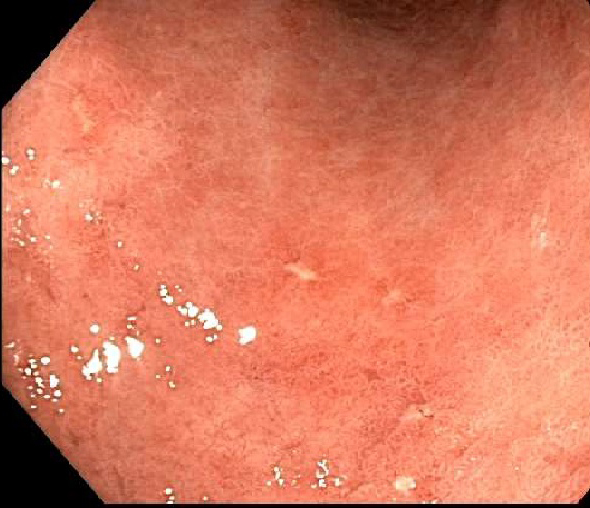
Gross description
- Endoscopic appearance:
- ~50%: normal
- Others: mucosal erythema, friable gastric mucosa, diffuse antral nodularity and erosions (World J Gastroenterol 2015;21:11221)
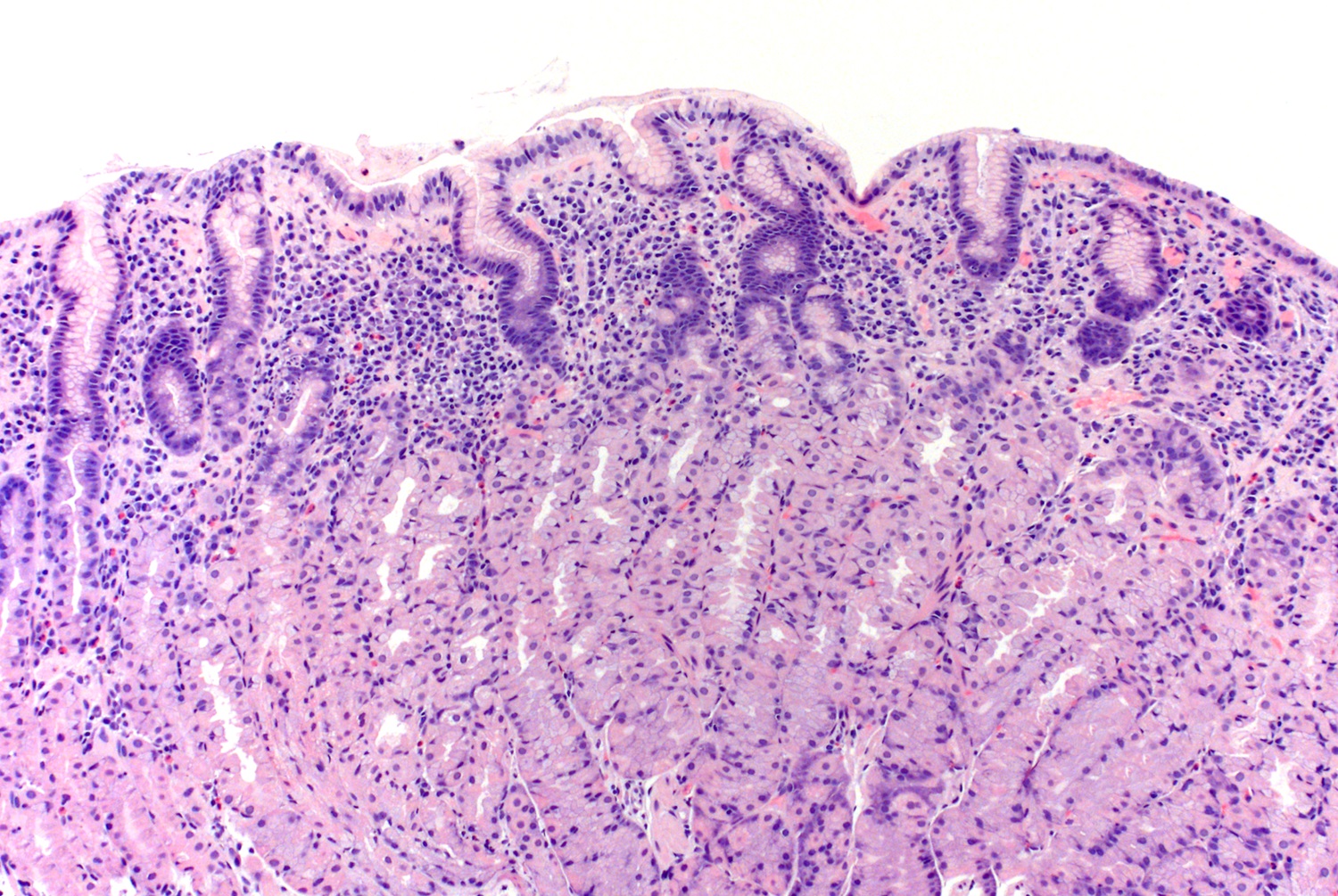
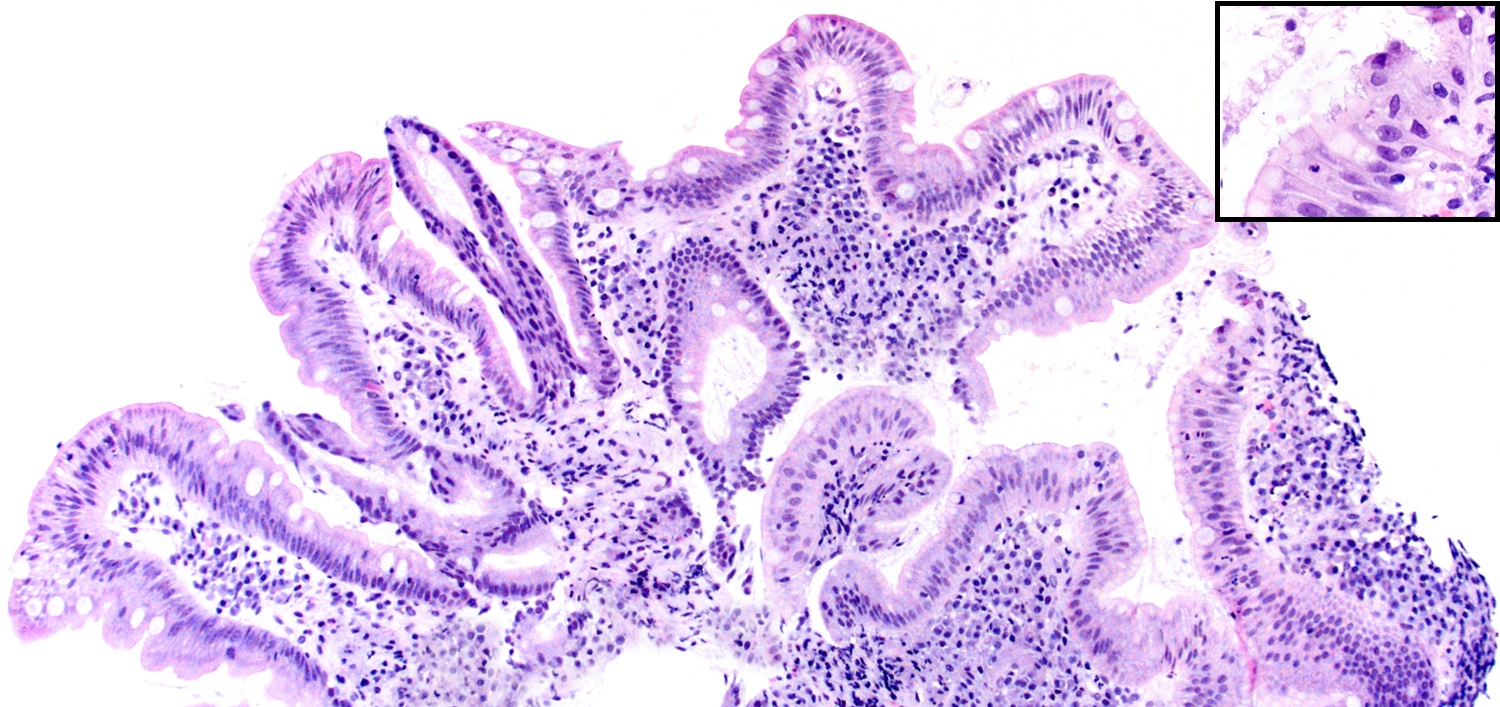
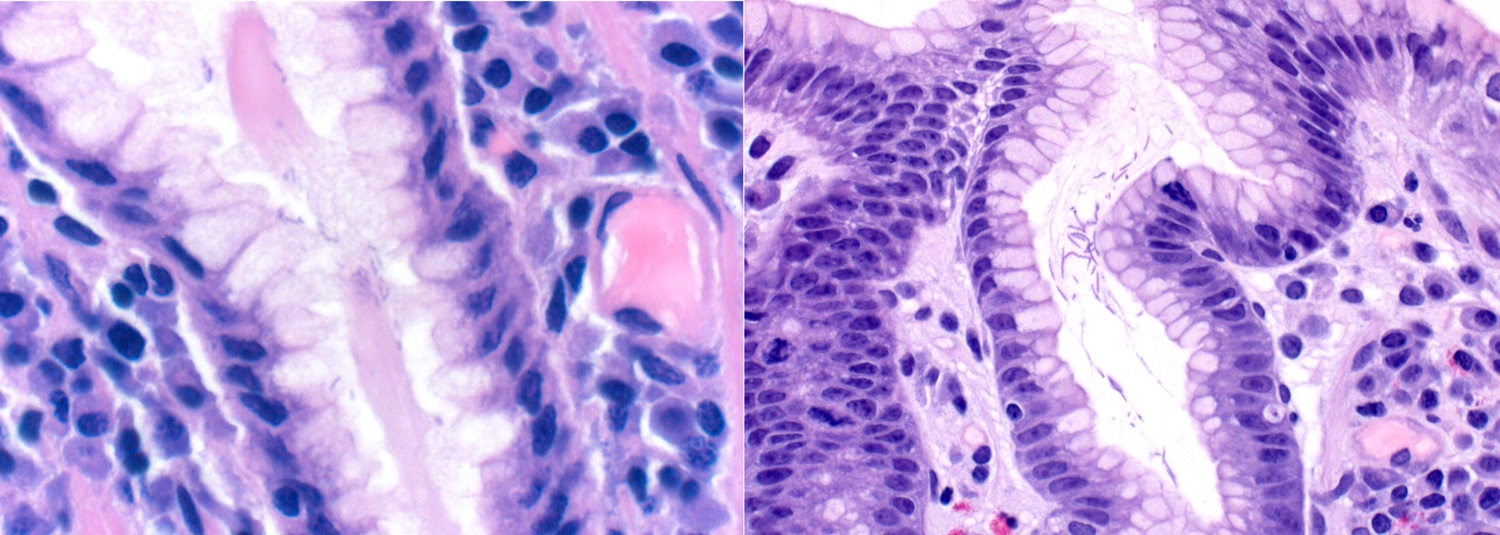
Microscopic (histologic) description
- Chronic antral gastritis: infiltration of lamina propria by plasma cells, lymphocytes and a small number of eosinophils seen as a superficial band of inflammation
- Active chronic antral gastritis: when the above is associated with neutrophils; this should prompt a search for organisms
- Lymphoid follicles in antral mucosa are common but nonspecific
- Variation in histologic patterns:
- May present as corpus predominant gastritis or pangastritis
- Duodenum may show foveolar metaplasia and duodenitis, with or without H. pylori organisms
- Use of PPIs facilitates proximal migration of the organisms to the oxyntic mucosa; the organisms also migrate deeper into the oxyntic glands
- May be associated with hyperplastic polyps; eradication of H. pylori is recommended in patients with hyperplastic polyps (Ann Intern Med 1998;129:712)
- An acute gastritis - initial transient stage followed by either resolution or onset of chronic gastritis
- Coccoid morphology of H. pylori is found most often in patients with recent PPI use or eradication therapy; this morphology of H. pylori has a diameter that is one half to one third the length of spiral forms (Am J Clin Pathol 2002;118:719)
- Sequalae of H. pylori gastritis:
- Atrophic antral and corpus gastritis
- H. pylori related gastric ulcers: associated with pangastritis
- H. pylori related duodenal ulcers: associated with antral gastritis, usually seen in the first part of duodenum, distal to the pylorus
- Intestinal metaplasia often involving the incisura or the antrum
- Lymphocytic gastritis
- Histologic features with regression of H. pylori gastritis:
- Neutrophils disappear
- Regression of chronic inflammation over several years
- Slow decrease in the number of lymphoid follicles
- Sydney classification (Am J Surg Pathol 1996;20:1161):
- Not used in routine practice
- Records five histologic variables: chronic inflammation, activity, atrophy, intestinal metaplasia and H. pylori density; makes recommendations for obtaining optimal biopsy samples
Microscopic (histologic) images
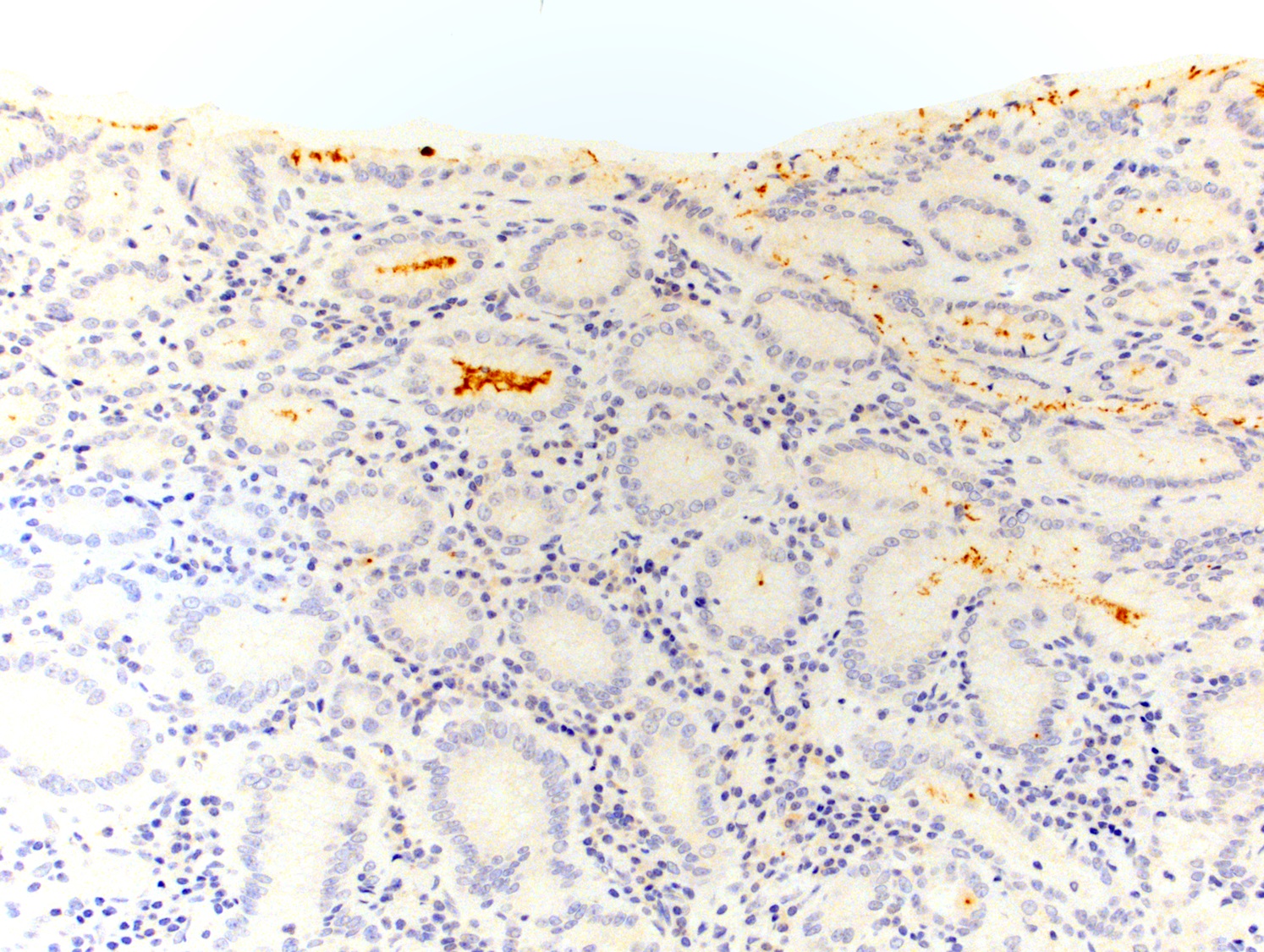
Positive stains
- Easily recognized on routine H&E stain, upfront H. pylori immunohistochemistry not recommended (Am J Surg Pathol 2013;37:e12)
- Immunohistochemistry and special stains: histochemical stains do not distinguish H. pylori from other bacteria and immunohistochemical antibodies against H. pylori cross react with H. heilmanni
- Immunohistochemistry: most common, associated with low false positive rare, also stains coccoid forms
- Silver based stains: Warthin-Starry, Steiner, El-Zimaity dual stain, Genta
- Nonsilver based stains: Diff-Quik, Giemsa, Leung Alcian yellow
- Gastrointestinal Pathology Society (GIPS) offers recommendations for ancillary stains in detecting H. pylori when evaluating gastric biopsies (Am J Surg Pathol 2013;37:e12)
Electron microscopy description
- On scanning electron microscopy, the bacterium shows a helical bacillary morphology with a minor axis / major axis ratio of ≤ 1 / 1.2
- Coccoid form is spherical with a smooth surface and minor axis / major axis ratio > 1 / 1.2 (Microbiol Immunol 2018;62:221)
Videos
Histopathology, H. pylori gastritis
Basic pathogenesis of H. pylori infection
Sample pathology report
- Stomach, upper gastrointestinal biopsies:
- Active antral / body H. pylori gastritis (see comment)
- Comment: There is no intestinal metaplasia or dysplasia in these biopsies.
Differential diagnosis
- Non-H. pylori chronic gastritis (J Gastroenterol 2010;45:131, Virchows Arch 2018;473:533):
- No organisms seen on H. pylori immunostain
- Helicobacter heilmannii gastritis (J Clin Pathol 2001;54:774):
- H. heilmannii organisms are twice as long and considerably thicker than H. pylori organisms, with a corkscrew shape
Board review style question #1
A 55 year old man presents with abdominal pain and vomiting; imaging shows pneumoperitoneum and posterior duodenal wall perforation for which an exploratory laparotomy with antrectomy, proximal duodenectomy, Roux-en-Y gastrojejunostomy and truncal vagotomy is performed. The section of the gastric wall showed a dense band of superficial gastritis in the gastric antrum and body mucosa (as shown above) with several spiral shaped organisms in the gastric mucin. Which of the following is true about this gastritis?
- A corpus restricted chronic gastritis is a typical presentation of H. pylori gastritis
- A focally enhanced chronic active gastritis is a typical biopsy finding in H. pylori gastritis
- H. pylori organisms are twice as long and considerably thicker than H. heilmannii organisms
- It is associated with a risk of peptic ulcer disease, primary gastric lymphoma and gastric carcinoma
- The treatment of H. pylori gastritis is optional as the infection is asymptomatic in the vast majority of infected individuals
Board review style answer #1
D. H. pylori infection is associated with complications including gastroduodenal ulcers, atrophy, intestinal metaplasia, gastric cancer and mucosa associated lymphoid tissue (MALT) lymphoma. Choice A: a corpus restricted chronic gastritis is a typical presentation of autoimmune gastritis whereas an antral predominant gastritis is the most common pattern of H. pylori gastritis in the western world. Choice B: a superficial chronic active gastritis with a dense band of lymphoplasmacytic inflammation is typical for H. pylori gastritis. A focally enhanced chronic active gastritis is typical of Crohn's gastritis, especially when the findings are discrete and intense. Choice C: H. heilmannii organisms are twice as long and considerably thicker than H. pylori organisms. Choice E: according to AGA recommendations, all patients with a positive test of active infection with H. pylori should be offered treatment (Am J Gastroenterol 2018;113:1102).
Comment Here
Reference: Helicobacter pylori
Comment Here
Reference: Helicobacter pylori
Board review style question #2
In patients with active peptic ulcer bleeding, what is the best method to diagnose H. pylori infection?
- Bacterial culture
- Breath test
- Histology
- Serology
- Stool Antigen
Board review style answer #2
Board review style question #3
H. pylori immunohistochemistry may be used to help in diagnosis of H. pylori gastritis in which of the following scenarios?
- Active chronic antral gastritis when no organisms are identified on H&E
- For confirmation of H. pylori organisms that are clearly identifiable on H&E
- In every case to rule out H. pylori infection in symptomatic patients
- To distinguish between H. pylori and H. heilmannii organisms
- When the clinician requests to rule out H. pylori despite no other histologic features
Board review style answer #3
A. Active chronic antral gastritis when no organisms are identified on H&E
Comment Here
Reference: Helicobacter pylori
Comment Here
Reference: Helicobacter pylori