Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Vithanage I, Haroon S. Giardia lamblia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelgiardiasis.html. Accessed November 29th, 2024.
Definition / general
- Protozoan disease caused by Giardia lamblia / Giardia intestinalis, a common parasite that can be detected in small bowel biopsies; it can also be detected in stool
- Clinical presentation ranges from asymptomatic shedding of giardial cysts to symptomatic giardiasis (i.e., malabsorption, chronic diarrhea)
Essential features
- Protozoan disease with asymptomatic colonization or acute or chronic diarrheal illness; can be histologically confirmed by visualization of the organisms
Terminology
- Giardia intestinalis
- Giardia duodenalis
- Giardia lamblia
- Beaver fever
ICD coding
- ICD-10: A07.1 - giardiasis (lambliasis)
Epidemiology
- Found throughout the world but less common in developed countries (Int J Parasitol 2012;42:443)
- Common in areas with poor sanitation and limited water treatment facilities (Recent Pat Inflamm Allergy Drug Discov 2019;13:134)
- Infection is more common in children than in adults
- Equal in both sexes
- Persons at increased risk are children, travelers to endemic areas, workers and children in daycare settings, individuals with immunodeficiency, cystic fibrosis patients and individuals who practice unprotected oral - anal sex (Recent Pat Inflamm Allergy Drug Discov 2019;13:134)
Sites
- Found in the small intestine, classically duodenum
- Jejunum, ileum and stomach are other possible sites (Scand J Gastroenterol 1997;32:48)
Pathophysiology
- Giardia intestinalis infection causes enterocyte damage and loss of brush border of the epithelial cells of the small intestine, which leads to shortening of microvilli and altered epithelial barrier function (Curr Top Med Chem 2018;18:1287)
- Mucosal alterations cause watery diarrhea, malabsorptive steatorrhea, nausea, abdominal pain, vomiting and weight loss
- Main consequence of Giardia colonization is nutrient malabsorption
- Most infections are asymptomatic
Etiology
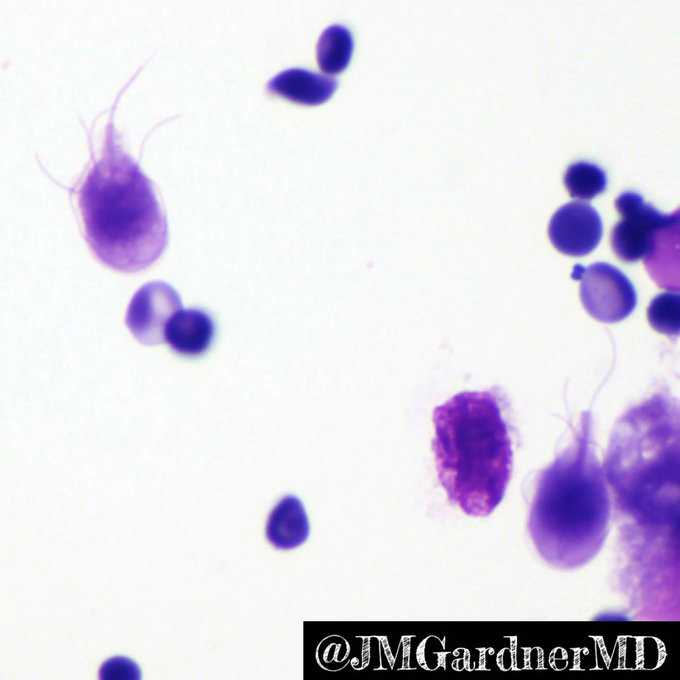
- Causative agent is flagellate protozoan Giardia intestinalis (also known as G. lamblia or G. duodenalis) (Int J Parasitol 2012;42:443)
- Giardia exists in 2 forms: trophozoites and cysts
- Trophozoites: motile, 4 pairs of flagellates, pear shaped organism
- Cysts: elliptical infective form
- Infection is transmitted through feco-oral route, frequently through ingestion of contaminated water and food or person to person transmission through contaminated surfaces or objects (Recent Pat Inflamm Allergy Drug Discov 2019;13:134)
Clinical features
- Most infections are asymptomatic
- Symptomatic infections can present as acute or chronic infection; acute infection manifests as aqueous diarrhea, nausea, vomiting and fever, whereas chronic infection is associated with loose stools, malabsorption and resultant weight loss (Int J Surg Pathol 2021;29:257)
- Main consequence of Giardia colonization is nutrient malabsorption
Diagnosis
- Diagnostic test of choice depends on clinical presentation and feasibility
- Demonstration by microscopy of Giardia trophozoites or cysts in stool specimens (sensitivity of 50 - 70%) (J Clin Diagn Res 2014;8:DC04)
- Detection of Giardia antigen in stool (sensitivity of 95 - 100%) (J Clin Diagn Res 2014;8:DC04)
- PCR assay for detecting Giardia in stool
- Histological demonstration of Giardia organisms in small intestinal biopsy; this is most important in chronic subset of patients
Laboratory
- Stool examination: detection of Giardia trophozoites or cysts in stool specimens by microscopic examination of wet mounts and concentrated samples or after preservation with polyvinyl alcohol or 10% formalin for permanent staining with trichrome or iron hematoxylin stains
- Sensitivity of stool test increases to > 90% with 3 serial specimens collected every 2 - 3 days
- Direct fluorescent antibody (DFA) test detects intact organisms
- Enzyme linked immunosorbent assay (ELISA) detects soluble antigens in the stool
- PCR assays can detect specific genes of the parasite in stool samples
- Direct aspiration of the duodenum or use of the commercially available string test (Enterotest)
- Duodenal biopsy (Recent Pat Inflamm Allergy Drug Discov 2019;13:134)
Prognostic factors
- Overall prognosis is good with treatment
- Dehydration can be life threatening for infants and pregnant women
- Chronic diarrhea might lead to rectal prolapse
- Reference: Recent Pat Inflamm Allergy Drug Discov 2019;13:134
Case reports
- 31 year old woman with skin lesions due to giardiasis treated with antiparasitic treatment (Ann Agric Environ Med 2005;12:299)
- Woman in her 40s with intestinal pseudo-obstruction caused by Giardia lamblia infection (BMJ Case Rep 2022;15:e252319)
- 66 year old man with an acute respiratory distress syndrome due to SARS-CoV-2 infection and hypereosinophilia due to giardiasis reactivation (Parasitol Int 2021;80:102241)
- 70 year old man underwent upper EUS for evaluation of pancreatic cyst; incidental finding of mucosal discoloration in the entire duodenum (Case #543)
Treatment
- Commonly treated by antibiotics such as metronidazole, tinidazole and nitazoxanide
- Symptomatic management, such as avoiding dehydration in case of extensive diarrhea (Int J Surg Pathol 2021;29:257)
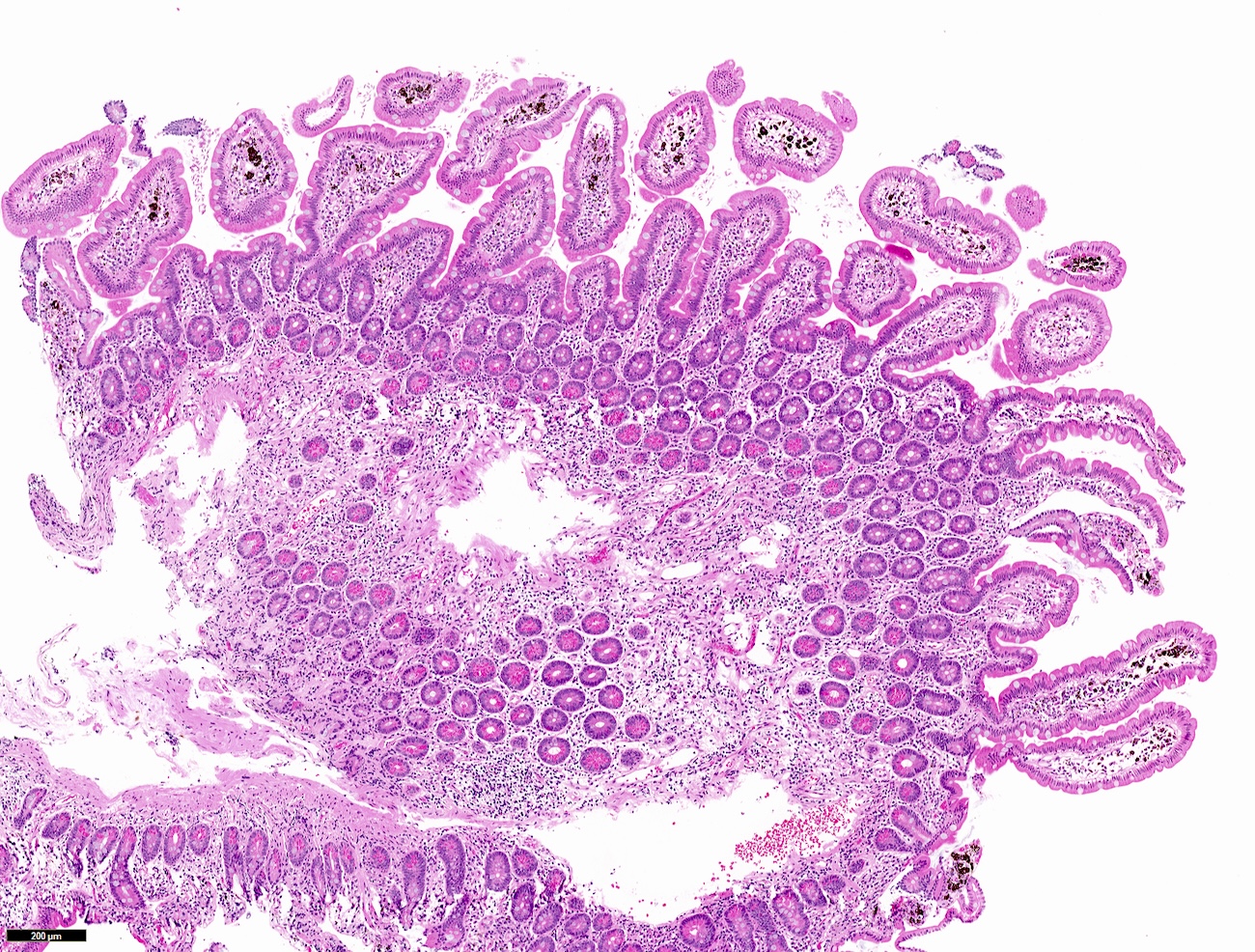
Gross description
- Mostly normal appearing mucosa
- Blunting of villi resembling celiac sprue
- Congestion, erythema, erosion, nodular mucosa, rarely polyps (Int J Surg Pathol 2021;29:257)
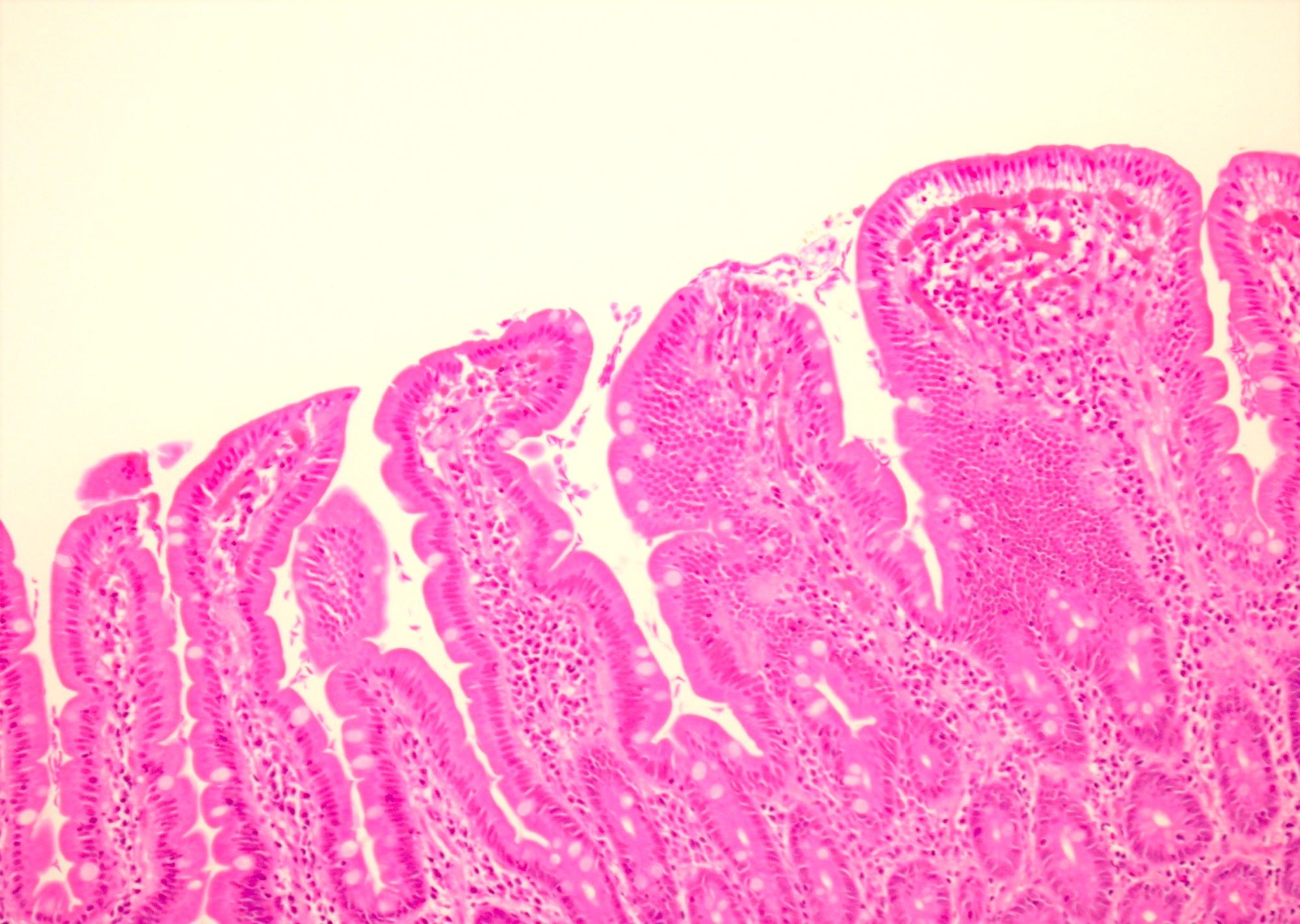
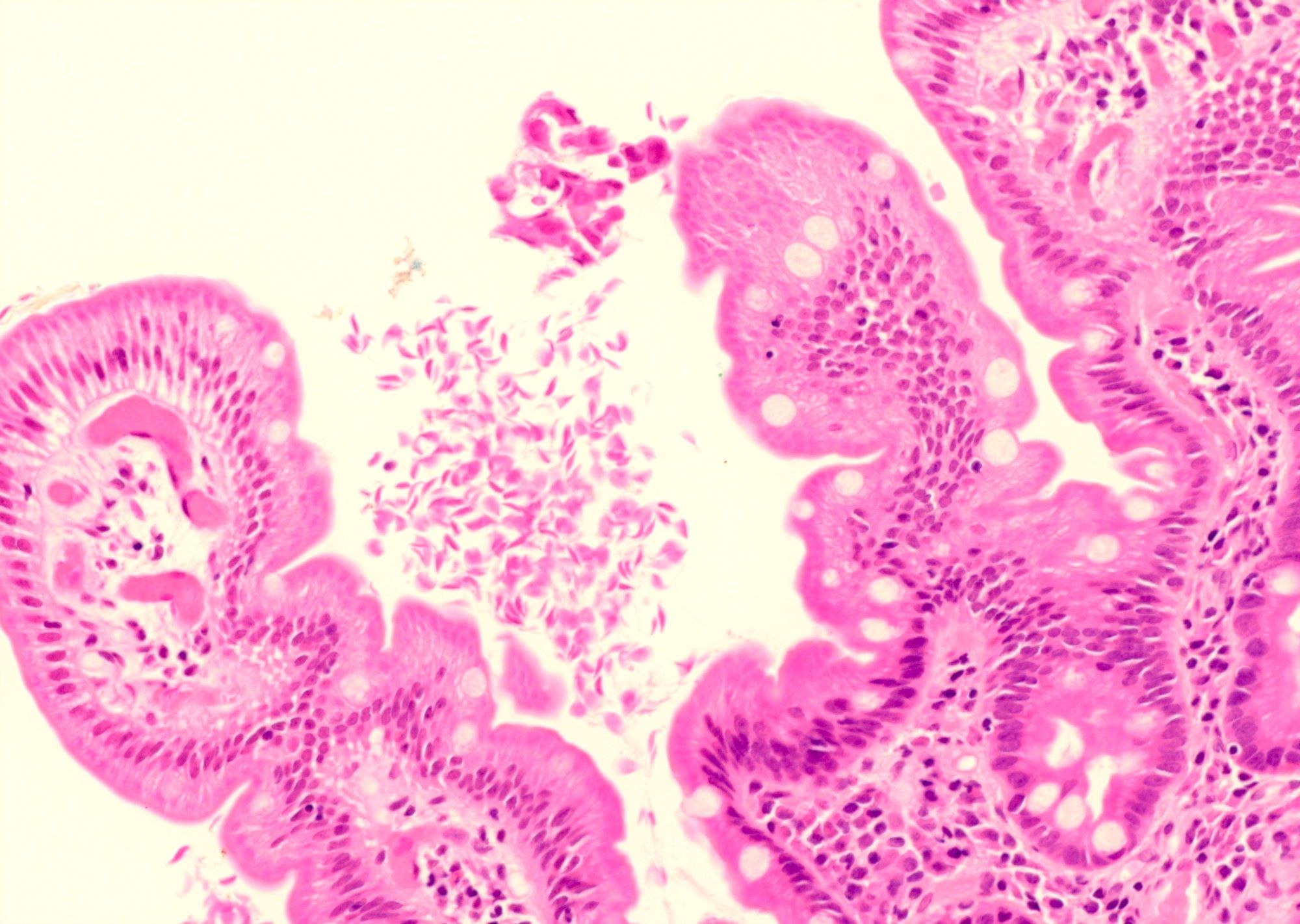
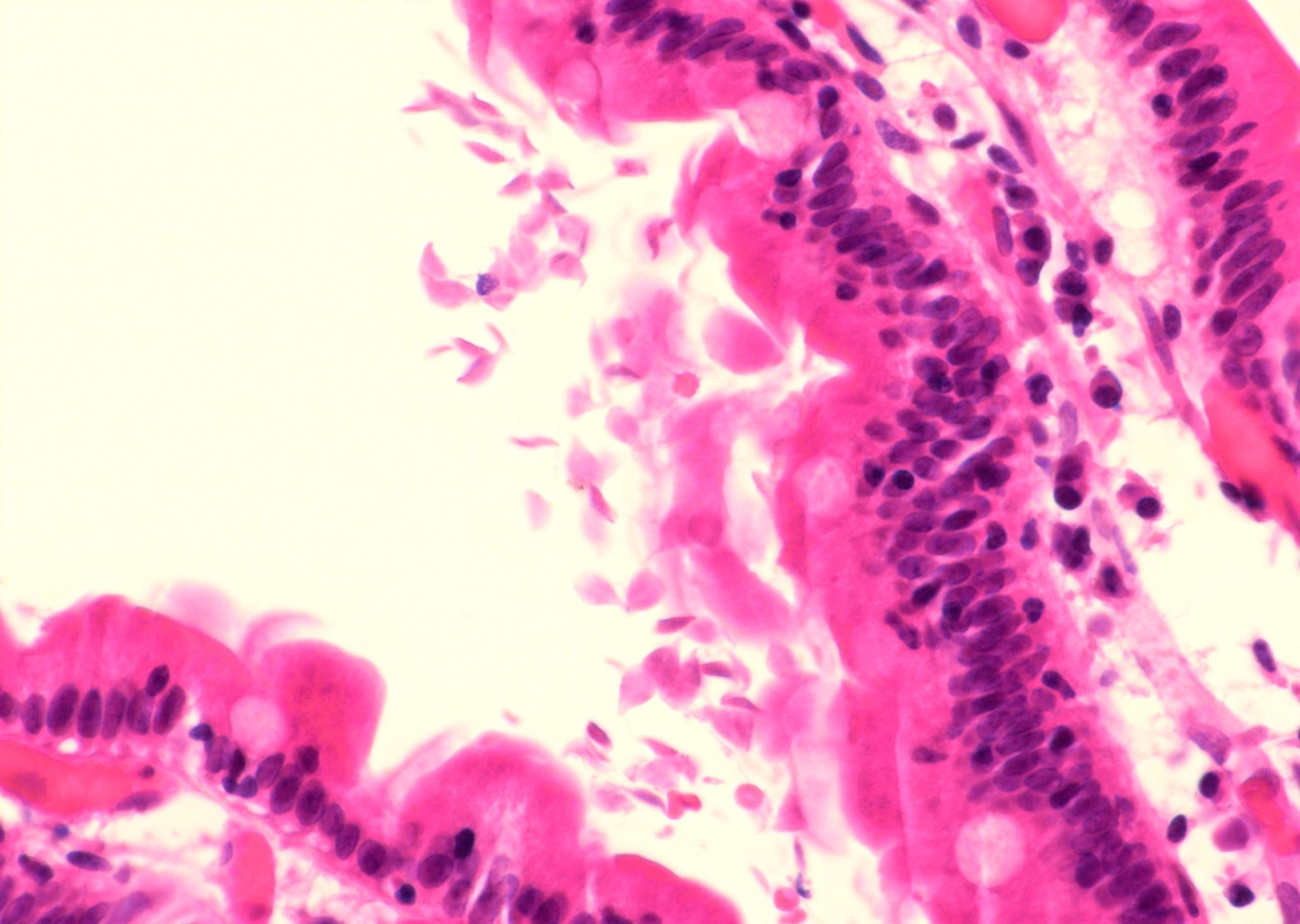
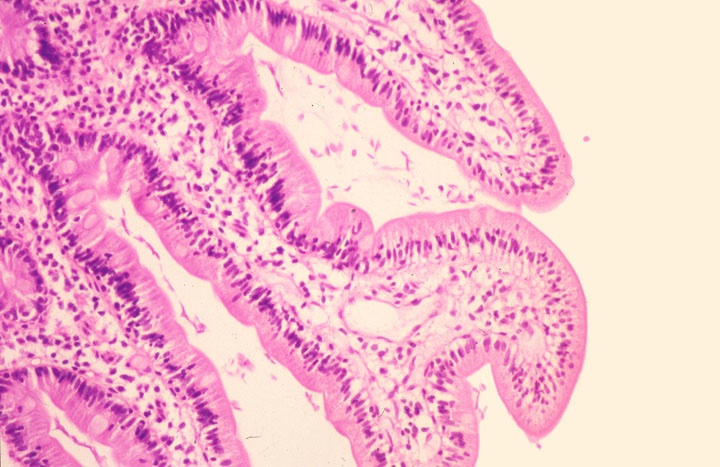
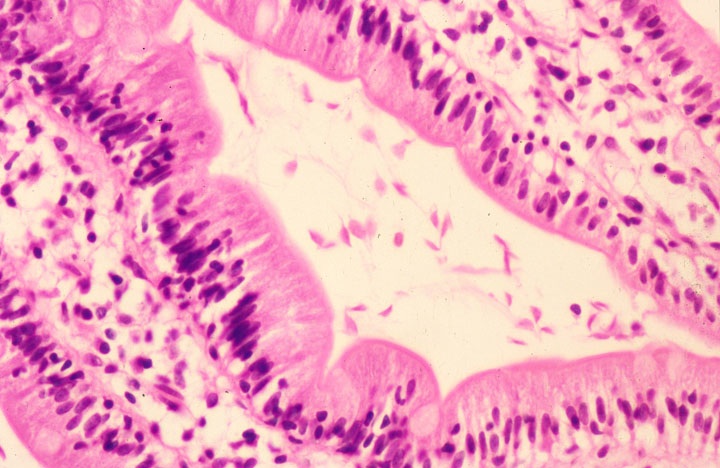
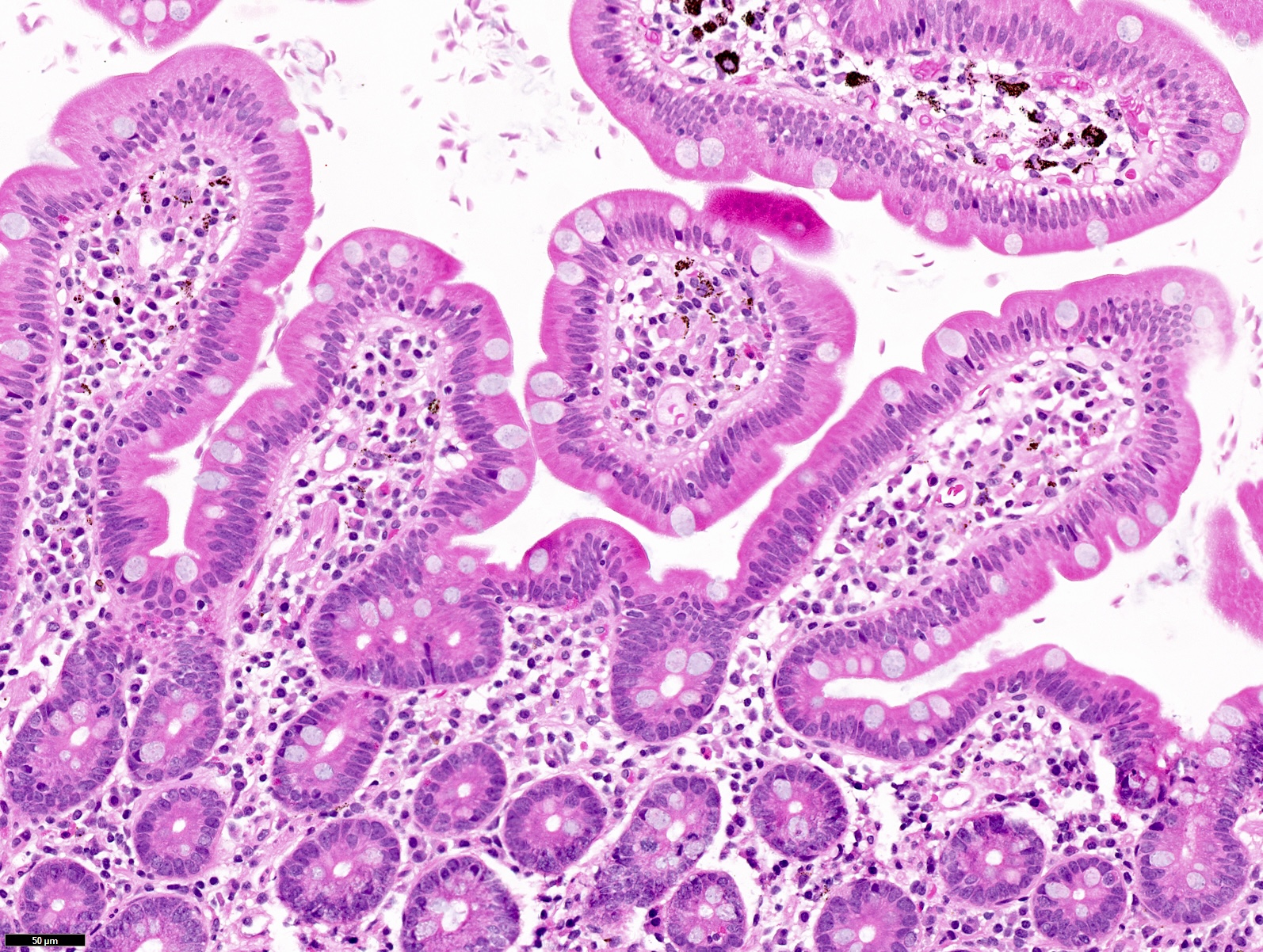
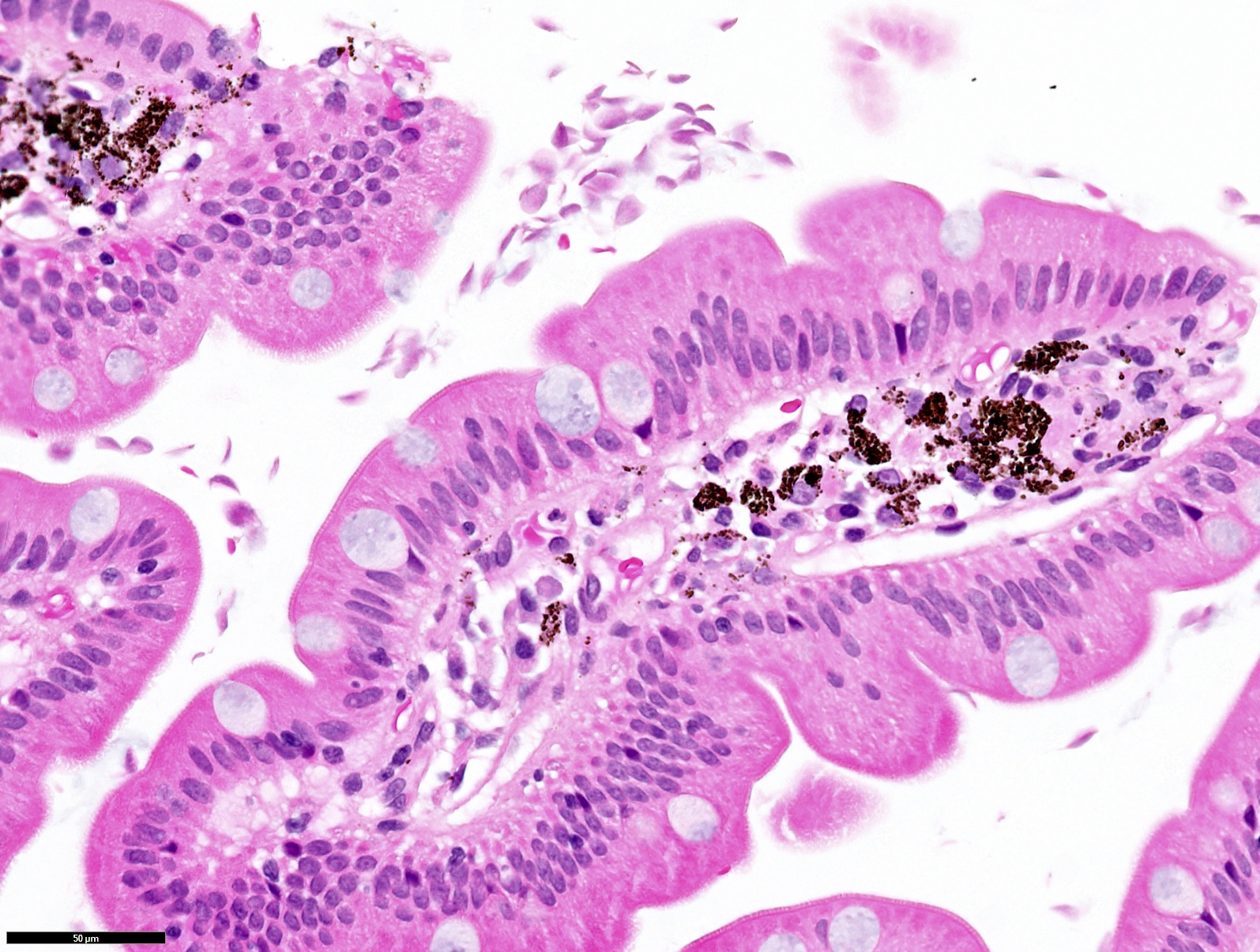
Microscopic (histologic) description
- Wide range of histological features
- Range of normal villous architecture to variable villous blunting and expansion
- Increased intraepithelial lymphocytes
- Increased inflammatory cells and prominent lymphoid aggregates in the lamina propria (Int J Surg Pathol 2021;29:257)
- Demonstration of organisms is diagnostic; they float freely in the lumen between the duodenal villi, adhere to the mucosal surface or are located in the cytoplasm of the epithelial cells but not invading (Hum Pathol 2009;40:323)
- Organisms are pear shaped or have a falling leaves appearance and are about the size of an epithelial cell nucleus (often misinterpreted as sloughed epithelial cells or luminal contents), with 2 nuclei, mostly pale eosinophilic to translucent in crescent shaped trophozoites
- If the diagnosis of giardiasis is made, the pathologist should routinely check the lamina propria for plasma cells since chronic giardiasis can be seen with CVID and a paucity of plasma cells could be a clue to this second diagnosis
Microscopic (histologic) images
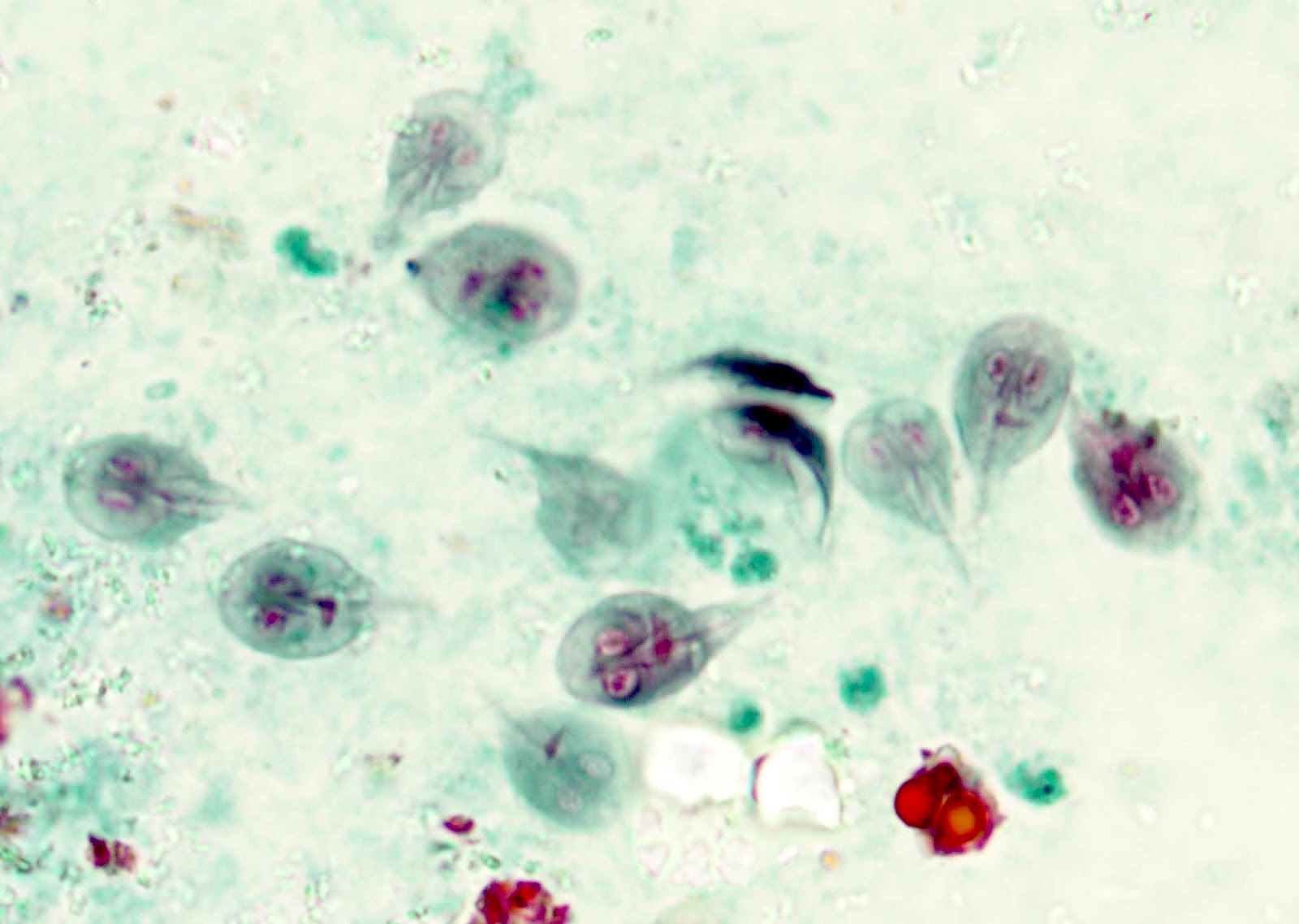
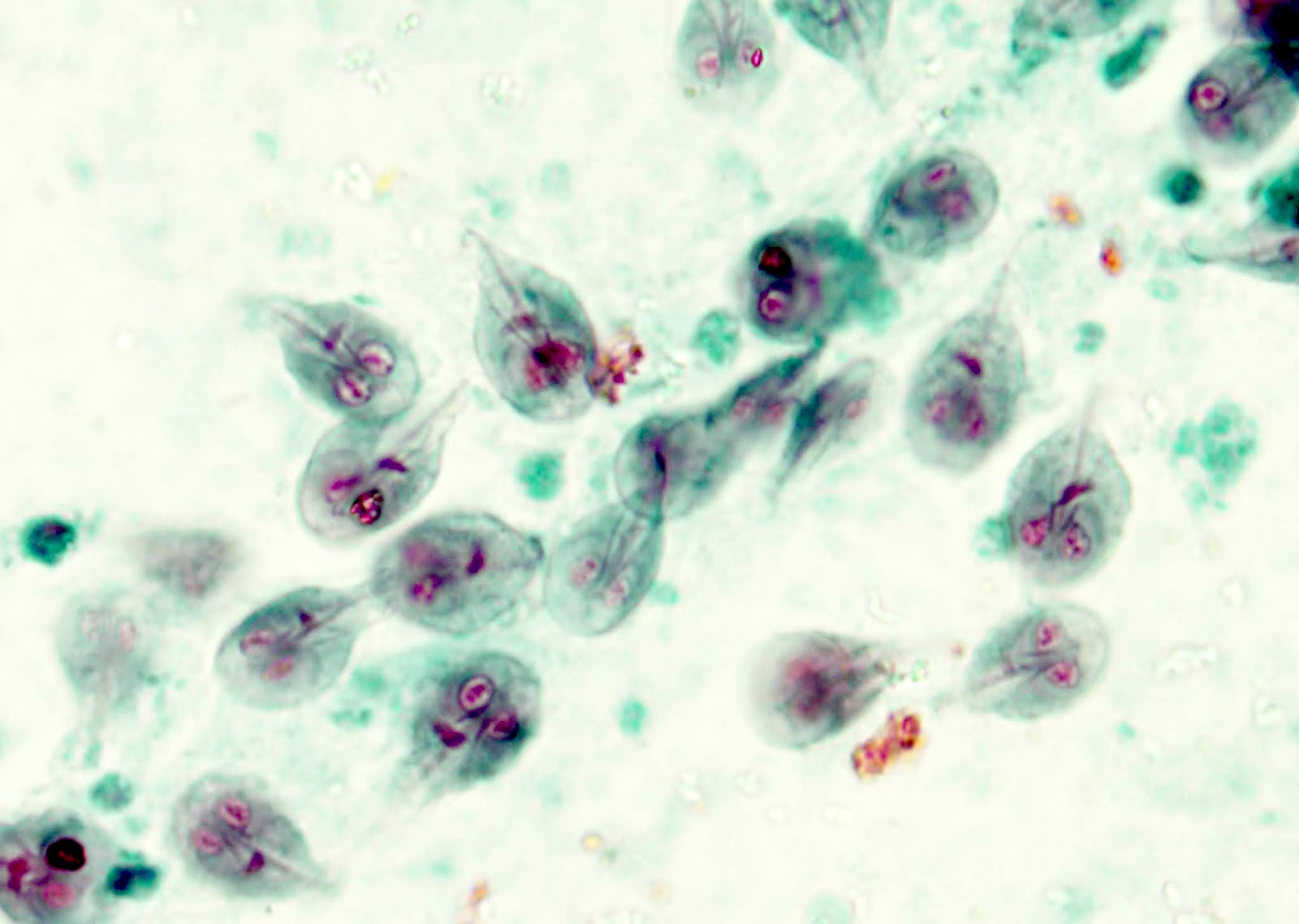
Cytology description
- Duodenal fluid aspiration cytology shows pear or teardrop shaped organisms containing multiple flagella (Am J Surg Pathol 2017;41:570)
- Brush cytology of the duodenum detected giardiasis in a few cases with negative mucosal biopsy findings along with multiple negative stool examinations
Cytology images
Positive stains
- Trichrome with iron hematoxylin counterstain; methylene blue positively stains the trophozoites; Giemsa stain
- CD117 / KIT immunostain is positive (Hum Pathol 2009;40:323)
Videos
Giardiasis tutorial
Sample pathology report
- Duodenum, biopsy:
- Multiple pear shaped microorganisms seen on villous surface, consistent with Giardia
- Increased intraepithelial lymphocyte count noted
Differential diagnosis
- Celiac disease:
- Strong morphological mimic; no Giardia organisms identified
- Normal duodenal biopsy:
- Sloughed epithelial cells and extruded mucin, common in normal duodenal biopsies, are in the differential diagnosis; however, the morphology will be different
Additional references
Board review style question #1
After a long hiking trip, most children in a large family group developed watery diarrhea, fatigue and stomach cramps along with bloating. At the hospital visit, the affected children told the doctor that they drank directly from the streams and river without the use of water purifier tablets or filters during the trip. Various tests were requested, including multiple stool samples collected over several days. Stool microscopy with direct fluorescent antibody testing (DFA) showed that the kids had giardiasis. If a duodenal biopsy is performed, which of the following is most likely to be true of the findings?
- Deeper part of the small intestinal mucosa is frequently invaded by Giardia
- Duodenal villous architecture can never be normal in this condition
- Giardia organisms are pear shaped
- Giardia organisms cannot be seen by light microscope
- Immunohistochemical studies are mandatory for diagnosis
Board review style answer #1
C. Giardia organisms are pear shaped. This is the correct answer as Giardia organisms can be described as pear shaped or as having a falling leaves appearance. Answer B is incorrect because the duodenal mucosa's villous architecture can be normal with organisms only floating on the surface in giardiasis. Answer E is incorrect because immunohistochemical studies, although utilized in some cases (such as CD117), are not mandatory in routine diagnosis of Giardia in biopsies. Answer A is incorrect because the organisms are usually found floating freely in the lumen between the duodenal villi, adhered to the mucosal surface or in the cytoplasm of the superficial epithelial cells but never in deeper parts of mucosal tissue. Answer D is incorrect because Giardia organisms are identifiable on light microscopy on routine H&E stain and are similar in size to duodenal epithelial cells (Int J Surg Pathol 2021;29:257, Hum Pathol 2009;40:323).
Comment Here
Reference: Giardia lamblia
Comment Here
Reference: Giardia lamblia
Board review style question #2
A 39 year old man presents to a general physician with malaise, episodic watery diarrhea and mild weight loss for the past 3 months. There is no significant past medical or surgical history. His vitals are stable, apart from mild tachycardia. On upper GI endoscopy, there was duodenal nodularity. Biopsy is taken with the clinical suspicion of celiac disease. The histopathological section image is given above. What is the diagnosis?
- Celiac disease
- Duodenal amebiasis
- Duodenal giardiasis
- Helicobacter pylori infection
- These are nonspecific findings
Board review style answer #2
C. Duodenal giardiasis, since the photomicrograph shows many Giardia organisms on the mucosal surface of small intestinal villi. Answer A is incorrect because in celiac disease, although the histological features can be simulated, there will be no Giardia organisms. Answer B is incorrect because in duodenal amebiasis, the morphology of the organisms is different; it is also very rare. Answer D is incorrect because in Helicobacter pylori infection, there will be V shaped / sea gull shaped or curved comma shaped tiny organisms. Answer E is incorrect because there are organisms on the surface of duodenal mucosa; therefore, these findings are not nonspecific (Int J Surg Pathol 2021;29:257).
Comment Here
Reference: Giardia lamblia
Comment Here
Reference: Giardia lamblia
Board review style question #3
In giardiasis patients, it is necessary to evaluate for which of the following additional diseases / pathologies?
- Celiac disease - look for increased intraepithelial lymphocytes and villous blunting
- Common variable immunodeficiency (CVID) - look for absence of plasma cells
- Inflammatory bowel disease - look for granulomas
- Primary melanoma - look for atypical cells
Board review style answer #3
B. Common variable immunodeficiency (CVID) - look for absence of plasma cells. Checking for plasma cells in the lamina propria is recommended in patients with giardiasis as they are often seen in patients with CVID due to chronic giardiasis. Answers A, C and D are incorrect because giardiasis is not associated with any of these options.
Comment Here
Reference: Giardia lamblia
Comment Here
Reference: Giardia lamblia