Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Berg K, Longacre TA. Dysplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachdysplasia.html. Accessed March 31st, 2025.
Definition / general
- Gastric dysplasia is a precursor lesion to gastric adenocarcinoma; it can be flat, polypoid (adenoma) or arise on the surface of an existing nondysplastic polyp
Essential features
- Gastric dysplasia is a precursor lesion to gastric adenocarcinoma
- Classified into low and high grade
- Histologic subtypes include intestinal, foveolar, crypt, tubule neck and serrated type dysplasia
- Isolated lesions may be treated with endoscopic submucosal resection or dissection
Terminology
- High grade dysplasia may be diagnosed as noninvasive carcinoma in Japan (Am J Surg Pathol 1999;23:511)
- Alternate / historic name for intestinal dysplasia is adenomatous dysplasia
- Alternate / historic names for foveolar dysplasia are type II dysplasia and hyperplastic dysplasia
ICD coding
- ICD-10: D00 - carcinoma in situ of oral cavity, esophagus and stomach
Epidemiology
- Male predominant
- Higher incidence in Asia, Eastern Europe and South America
- Risk factors include Helicobacter infection
Sites
- Stomach
Pathophysiology
- Most common cause of gastric dysplasia is Helicobacter pylori infection, which results in chronic active gastritis, atrophy and intestinal metaplasia
Etiology
- Helicobacter infection is the most common cause worldwide (Gastroenterology 1997;113:S56)
- Smoking, radiation exposure and occupation in rubber manufacturing
Clinical features
- Predominantly asymptomatic, although larger lesions may cause bleeding or anemia
- Can present as a flat, ulcerated or polypoid lesion on endoscopy
Diagnosis
- Diagnosed by upper endoscopy with biopsy
Prognostic factors
- High grade dysplasia is associated with a much higher rate of progression to adenocarcinoma (Gut 2003;52:1111)
Case reports
- 26 year old man and 74 year old woman with tubule neck dysplasia (Pathology 2006;38:468)
- 62 year old woman with original diagnosis of low grade gastric dysplasia progressing to early gastric carcinoma (Medicine (Baltimore) 2019;98:e15686)
- 81 year old man with high grade gastric intestinal dysplasia (Cureus 2020;12:e7427)
Treatment
- Treated with endoscopic submucosal resection or endoscopic submucosal dissection
Microscopic (histologic) description
- Gastric dysplasia is divided into several subtypes
- Intestinal and foveolar type are the most common
- Crypt dysplasia and serrated dysplasia are more recently described but are recognized subtypes in the World Health Organization gastrointestinal book
- Tubule neck or globoid dysplasia is the rare precursor lesion to poorly cohesive gastric carcinoma
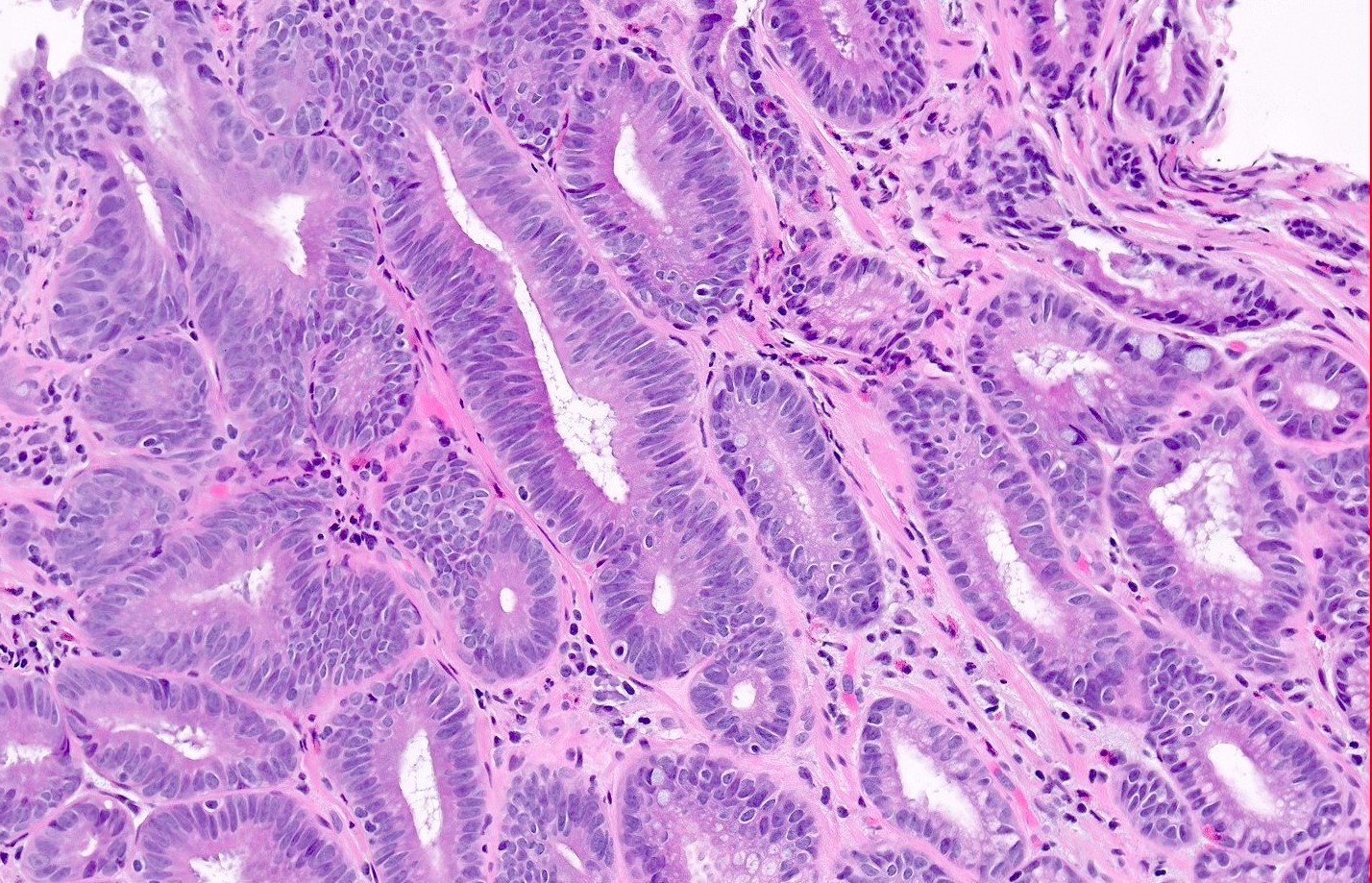
- Intestinal type dysplasia:
- Similar morphology to colorectal adenomas
- Tubular architecture
- Cells have elongated nuclei with clumped chromatin, hyperchromasia and pseudostratification
- Frequently admixed goblet cells and Paneth cells
- Often arising in a background of intestinal metaplasia
- High grade intestinal dysplasia shows loss of polarity, nuclear rounding, anisonucleosis, vesicular chromatin and increased N/C ratios
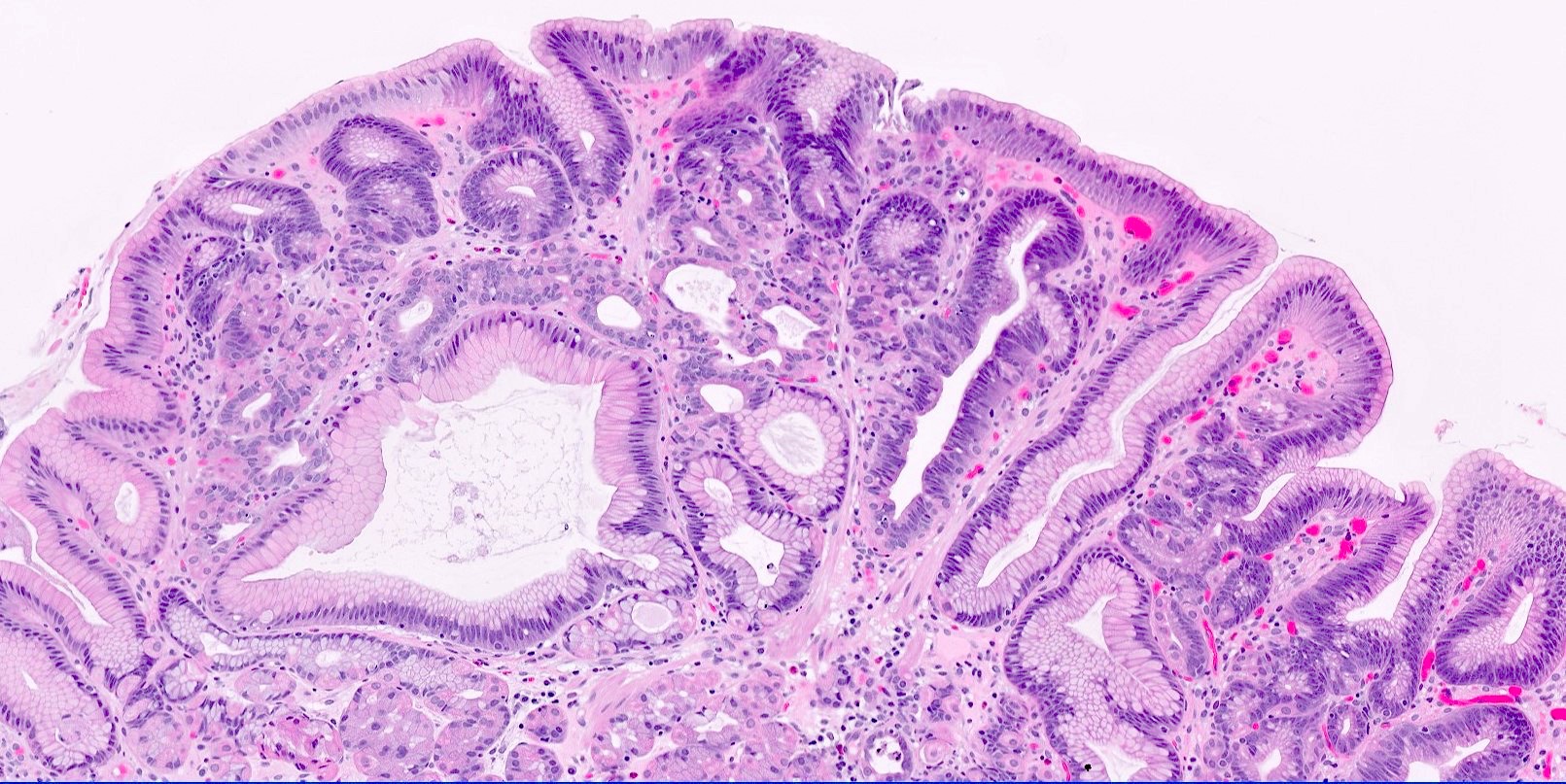
- Foveolar type dysplasia:
- Surface involvement with irregular branching
- Cuboidal to columnar cells with hyperchromatic oval nuclei and pale cytoplasm
- High grade foveolar dysplasia shows loss of polarity, increased N/C ratios, vesicular chromatin and prominent nucleoli
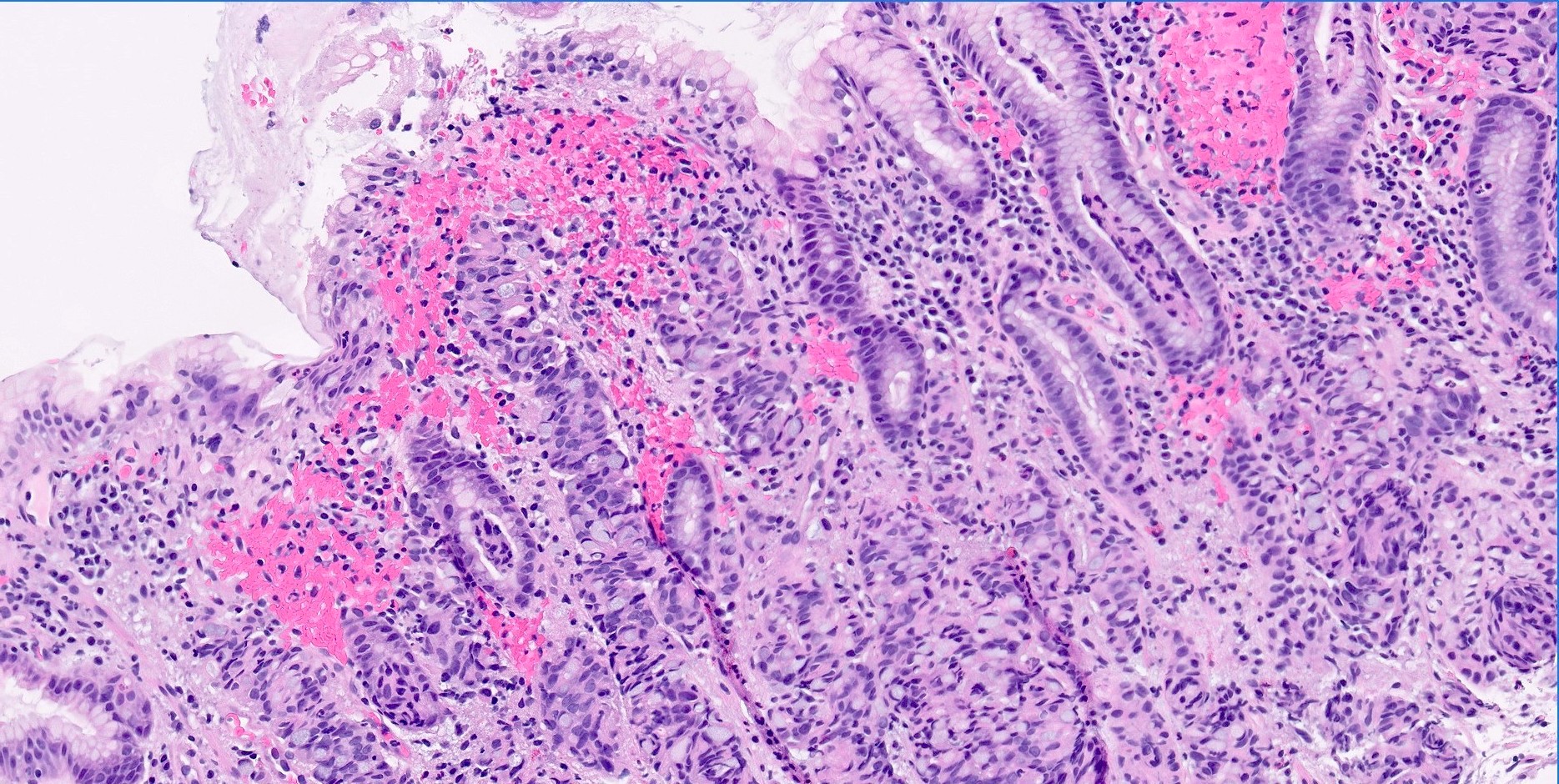
- Tubule neck dysplasia or globoid dysplasia:
- Rare precursor lesion to poorly cohesive (signet ring) gastric carcinoma
- Increased cellularity in the gastric neck region
- Enlarged clear cells with vacuolated cytoplasm and similar appearance to signet ring cells
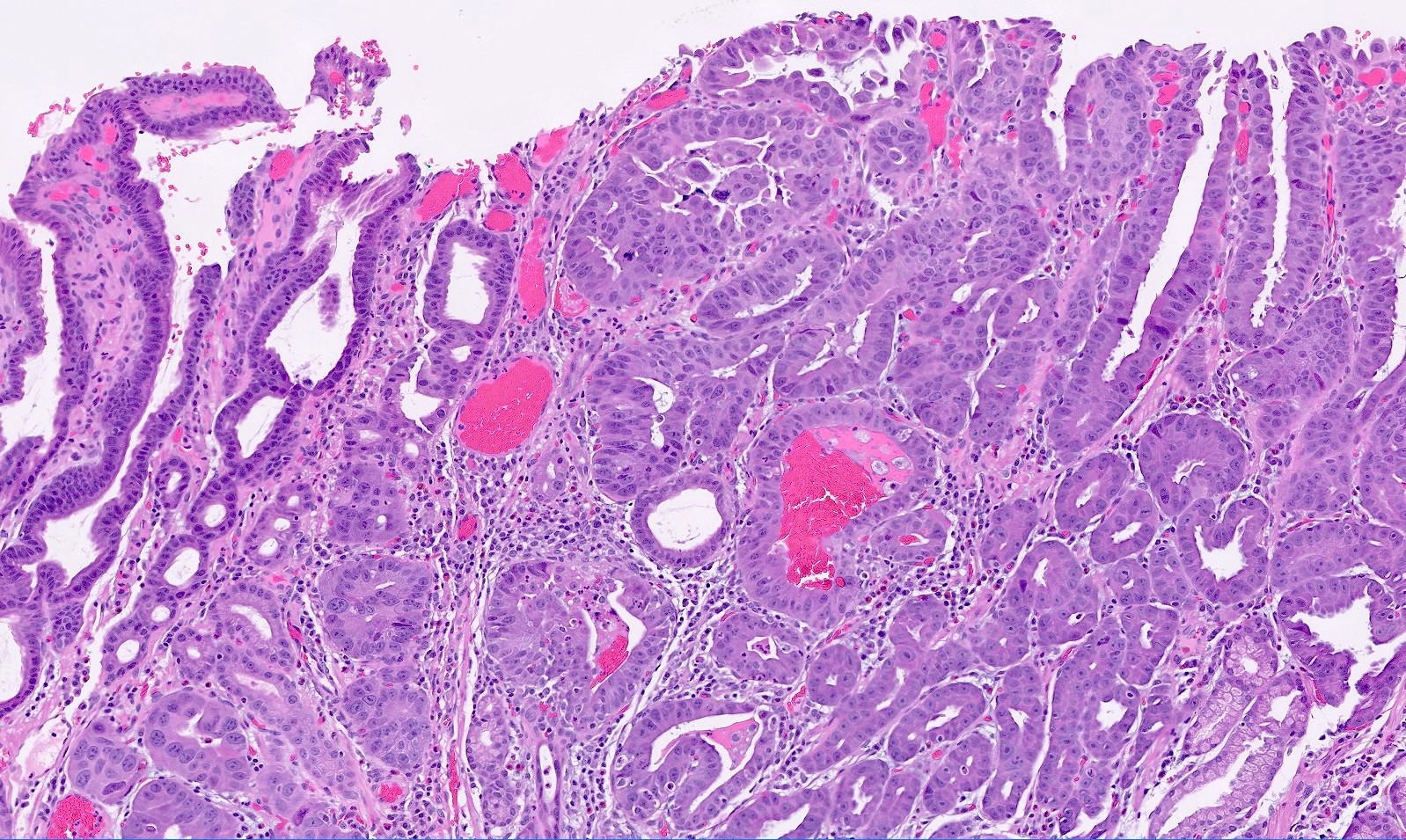
- Crypt dysplasia or pit dysplasia:
- Marked cytologic atypia characterized by nuclear pleomorphism, increased N/C ratio, irregular nuclear contours and hyperchromasia that is limited to the gastric crypts / pits and does not reach the surface (Histopathology 2016;68:843)
- Serrated dysplasia:
- Rare polyp similar to the colorectal traditional serrated adenoma (Histol Histopathol 2013;28:453)
- Characterized by stratified pencillate nuclei and abundant eosinophilic cytoplasm with slit-like serrations
Microscopic (histologic) images
Positive stains
- MUC2 in intestinal type dysplasia (Am J Surg Pathol 2008;32:524)
- MUC5AC in foveolar type dysplasia (Am J Surg Pathol 2008;32:524)
- p53 overexpression or loss of expression in high grade dysplasia and crypt / pit dysplasia (Gut 1994;35:1697, Histopathology 2016;68:843)
Molecular / cytogenetics description
- p53 is the most common mutation in high grade dysplasia (Gastric Cancer 2014;17:442)
Sample pathology report
- Stomach, biopsy:
- Low grade dysplasia, intestinal type (see comment)
- Comment: Background of intestinal metaplasia. Negative for Helicobacter organisms by immunohistochemistry.
Differential diagnosis
- Reactive atypia (due to reactive / chemical type injury, ulceration):
- Uniform nuclear enlargement with visible nucleoli
- No nuclear crowding
- Surrounding inflammation
- Chemotherapy and radiation therapy atypia:
- History of treatment
- Pleomorphic nuclei but maintained N/C ratios
Additional references
Board review style question #1
Which of the following is the most common risk factor for gastric dysplasia?
- Alcohol use
- Helicobacter infection
- Radiation exposure
- Smoking
Board review style answer #1
Board review style question #2
Board review style answer #2