Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kaur G, Vyas M. Diffuse type. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachdiffuse.html. Accessed April 2nd, 2025.
Definition / general
- Diffuse type gastric adenocarcinoma - carcinoma composed of poorly differentiated / signet ring cells, present as scattered individual cells or clusters
- This type of carcinoma is associated with aggressive behavior (rapid invasion, chemoresistance, peritoneal metastasis) and poor prognosis
Essential features
- Diffuse type gastric carcinoma is an aggressive form of gastric cancer that varies from the intestinal type in many aspects
- It can be seen in sporadic and familial settings
- Mutations in the CDH1 gene are most commonly implicated and can be germline in familial settings
- Diffuse type carcinoma is composed of poorly cohesive cells that can be either signet ring cell type or non signet ring cell (poorly differentiated) type
- This an aggressive neoplasm characterized by early spread via lymphatic dissemination and by local extension into neighboring organs or as peritoneal carcinomatosis
Terminology
- Official WHO term is poorly cohesive carcinoma
- Other terms: Lauren diffuse type, linitis plastica, signet ring cell gastric adenocarcinoma
ICD coding
- ICD-10: C16.9 - malignant neoplasm of stomach, unspecified
Epidemiology
- Incidence of diffuse type gastric adenocarcinoma is increasing worldwide but is slightly less than intestinal type (Eur J Cancer 2020;130:23)
- Diffuse type is more uniformly distributed geographically but with an increasing incidence in the U.S. and in Europe (Oncol Lett 2019;18:674)
- More common in younger patients: mean age 48 years
- No sex predilection seen; M = F (Oncol Lett 2019;18:674)
- While diffuse type gastric carcinomas can be seen in sporadic settings, a significant proportion of cases are seen in the context of hereditary diffuse gastric cancer (HDGC) syndrome
- Patients with hereditary diffuse gastric cancer are also predisposed to lobular breast cancer
Pathophysiology
- Majority of gastric carcinomas of diffuse type may develop from the ECL cells secondary to long term hyperstimulation with gastrin (Int J Mol Sci 2018;19:4109)
- Underlying genetic alterations maybe germline or biallelic somatic mutations
- Mutations in CDH1 gene are most commonly implicated; pathogenic germline mutations in this gene are responsible for HDGC
- E-cadherin is a calcium dependent adhesion molecule that interacts with beta catenin to maintain the structure of epithelium
- When a patient with germline E-cadherin gene (CDH1) mutation acquires a second hit, whether by loss of heterozygosity or promoter methylation or somatic mutation, it results in development of gastric carcinomas of diffuse type at an early age (Int J Mol Sci 2018;19:4109)
- CDH1 mutations seem to be the most frequent abnormality; other adhesion molecules could be involved in fewer cases, such as somatic mutations of beta catenin / APC genes or dysregulation of the Wnt / beta catenin pathway (World J Gastroenterol 2015;21:11428)
- Other genes responsible for HDGC include CTNNA1, PALB2, BRCA2, etc., each described in a handful of cases
Etiology
- Diffuse type gastric carcinoma originates from the gastric mucosa and in sporadic cases is usually associated with gastritis (Oncol Lett 2016;11:2959)
- HDGC may have minimal or no background gastritis and may have early precursor components (described below)
Clinical features
- Potential symptoms include indigestion, nausea or vomiting, dysphagia, postprandial fullness, loss of appetite, melena, hematemesis, weight loss (Front Surg 2017;4:42)
- May cause pathologic peritoneal and pleural effusions, obstruction of the gastric outlet
Diagnosis
- Endoscopy shows flat or depressed lesions with an ill defined border (Gut Liver 2017;11:807)
- In some cases, thickened folds may be a clue to the underlying abnormality
- Very early lesions may only show some pale discoloration or even grossly normal mucosa
- Chromoendoscopy increases the yield of detection of early lesions
- Biopsy
- Chest radiograph to evaluate for metastatic lesions
- CT scan or MRI of the chest, abdomen and pelvis
Laboratory
- Complete blood cell count can identify anemia
- Carcinoembryonic antigen is increased in 45 - 50% of cases (eMedicine: Gastric Cancer [Accessed 26 June 2020])
- Cancer antigen (CA) 19-9 is elevated in about 20% of cases (eMedicine: Gastric Cancer [Accessed 26 June 2020])
Radiology description
- Thickening of the gastric wall
- Gastric outlet obstruction
Prognostic factors
- Advanced stage diffuse type adenocarcinoma has poor prognosis
- Diffuse type gastric carcinoma spreads early via lymphatic dissemination and by local extension into neighboring organs or as peritoneal carcinomatosis
- Lymph node metastasis is an important prognostic factor
- High CA19-9 is associated with poor survival (Eur J Med Res 2011;16:29)
Case reports
- 10 year old boy with diffuse type gastric adenocarcinoma (Rev Gastroenterol Peru 2017;37:187)
- 22 year old woman with HDGC associated with E-cadherin germline mutation (Hawaii J Med Public Health 2014;73:204)
- 53 year old woman with synchronous occurrence of hereditary gastric adenocarcinoma, gastrointestinal stromal tumor and esophageal small cell and squamous carcinoma in situ (BMC Cancer 2017;17:720)
- 59 year old man with multiple gastrointestinal cancers (Indian J Surg Oncol 2018;9:633)
Treatment
- In early gastric cancer, minimally invasive procedures such as wedge resection or advanced endoscopic techniques may constitute an equally radical treatment method (Prz Gastroenterol 2018;13:200)
- Gastrectomy and lymphadenectomy for more advanced lesions
- Chemotherapy including 5-fluorouracil (5-FU), platinum, taxanes, irinotecan and anthracycline; these drugs may be administered separately, using double or triple drug regimens in combination with epirubicin or docetaxel (Prz Gastroenterol 2018;13:200)
- For patients with a germline mutation, a prophylactic gastrectomy is offered as the modality of choice
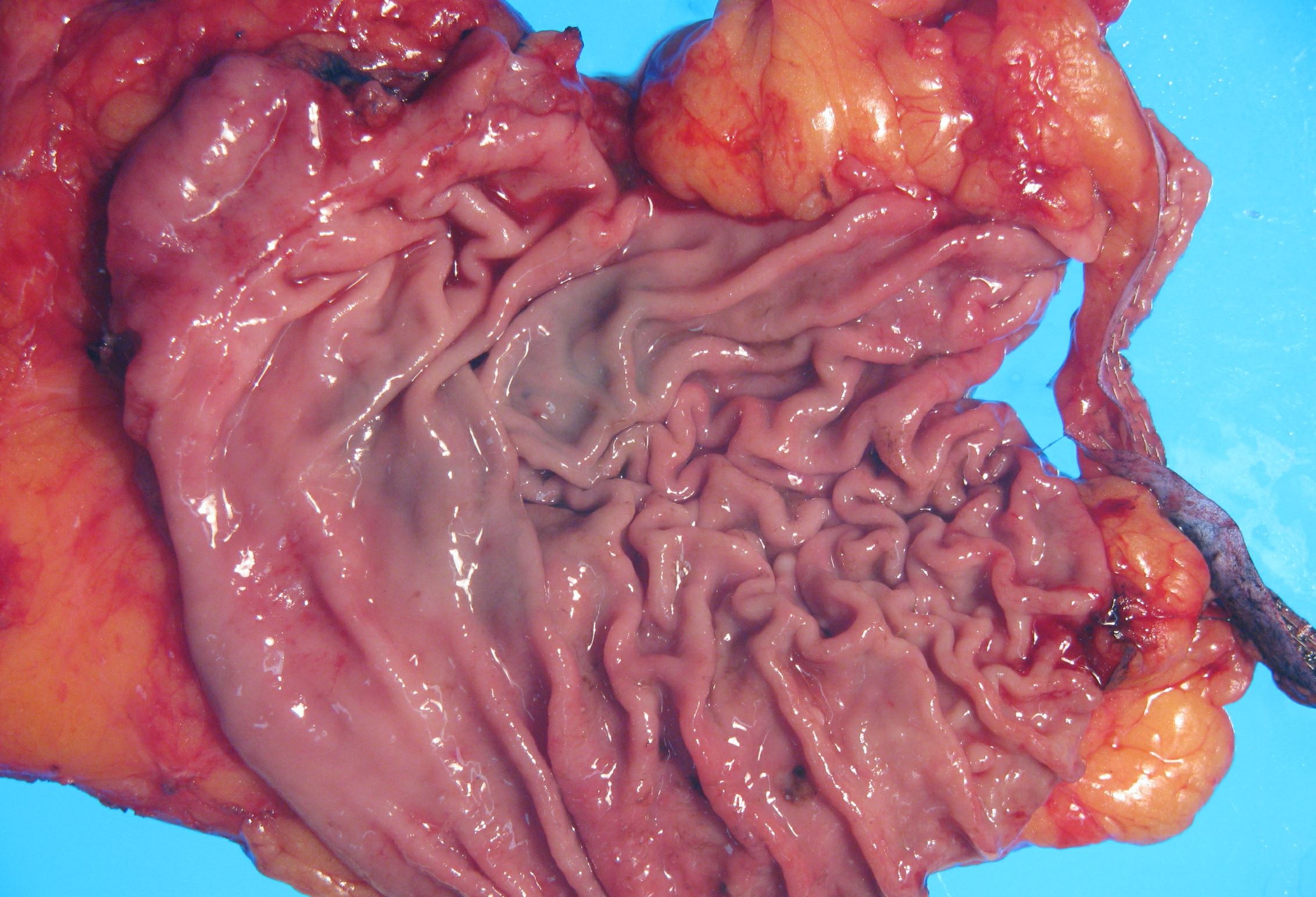
Gross description
- Very early stage lesions, typically in context of prophylactic gastrectomy, may not produce any visible abnormalities / lesions (Front Pharmacol 2018;9:1421)
- More advanced lesions may present as thickening, ulceration or just rigid, leather bottle-like stomach (linitis plastica) due to extensive infiltration by the malignancy; may cause pyloric obstruction (Int J Mol Sci 2018;19:4109)
- Gastric carcinoma of diffuse type typically invades the submucosa at an early phase and the tumor cells often spread in the upper layers of the stomach wall instead of growing as a tumor protruding into the lumen
- Therefore, diffuse gastric carcinomas may be easily overseen at early phases even at endoscopy
Gross images
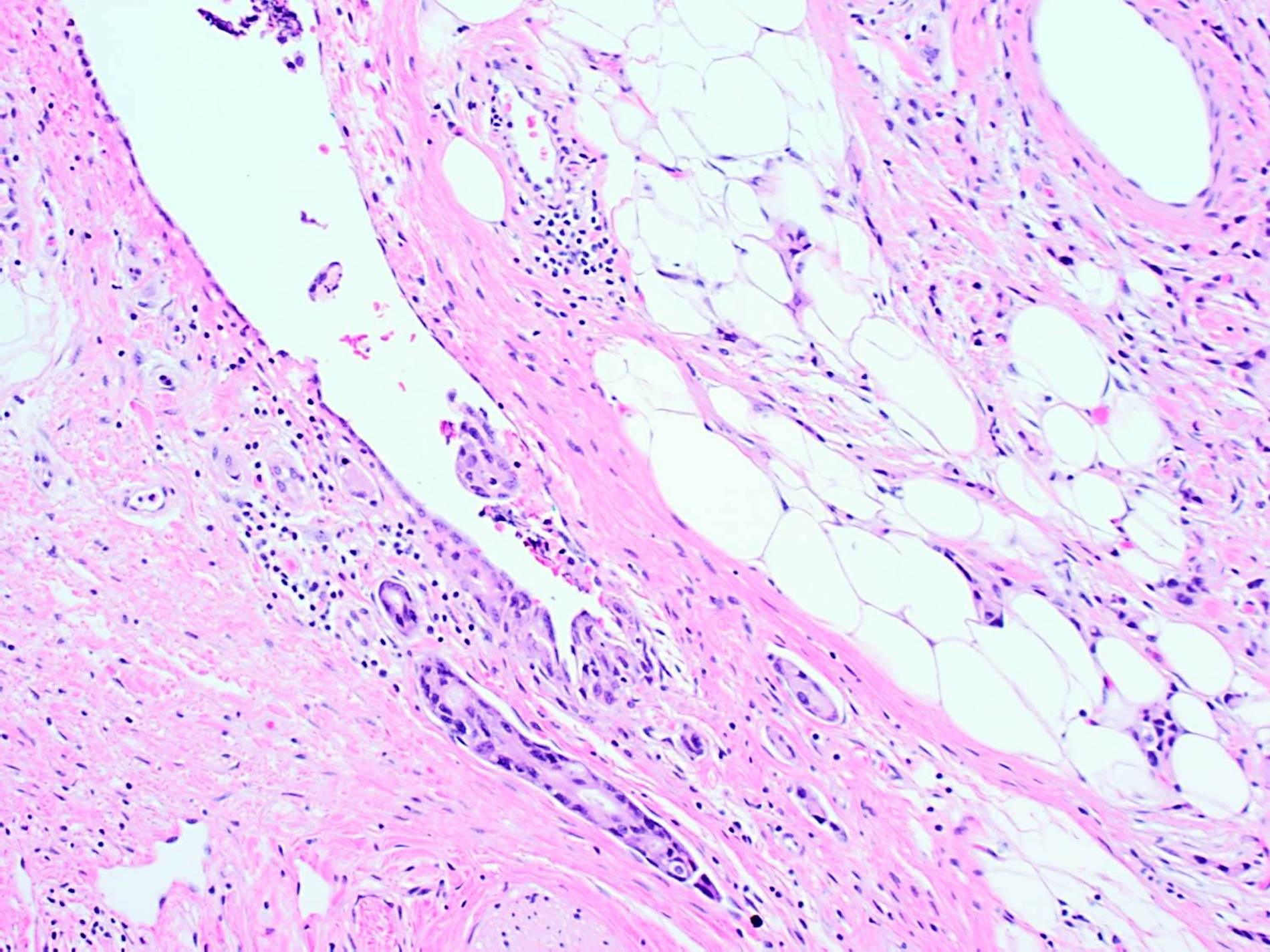
Frozen section description
- Intraoperative consultation is frequently sought for evaluation of margin status at the time of gastrectomy
- Carcinoma can be present at the margin in the form of small foci and lack significant tissue reaction or inflammation, making frozen section diagnosis extremely challenging
- Additionally, detached signet ring cells can be seen as an artifact in the gastric mucosa, making interpretation even more difficult (J Med Genet 2015;52:361)
- Due to their diffuse morphology, the tumor cells may be indistinct and difficult to distinguish from inflammatory or stromal cells (Virchows Arch 2020 Mar 25 [Epub ahead of print])
- Helpful features are the presence of cells with a single distinct cytoplasmic mucin vacuole, focal gland formation and perineural invasion
- Other helpful features are irregular nuclear contours, large nuclear size with many nuclei > 4x the size of a small lymphocyte, disruption / obliteration of normal structures and the presence of mitotic figures
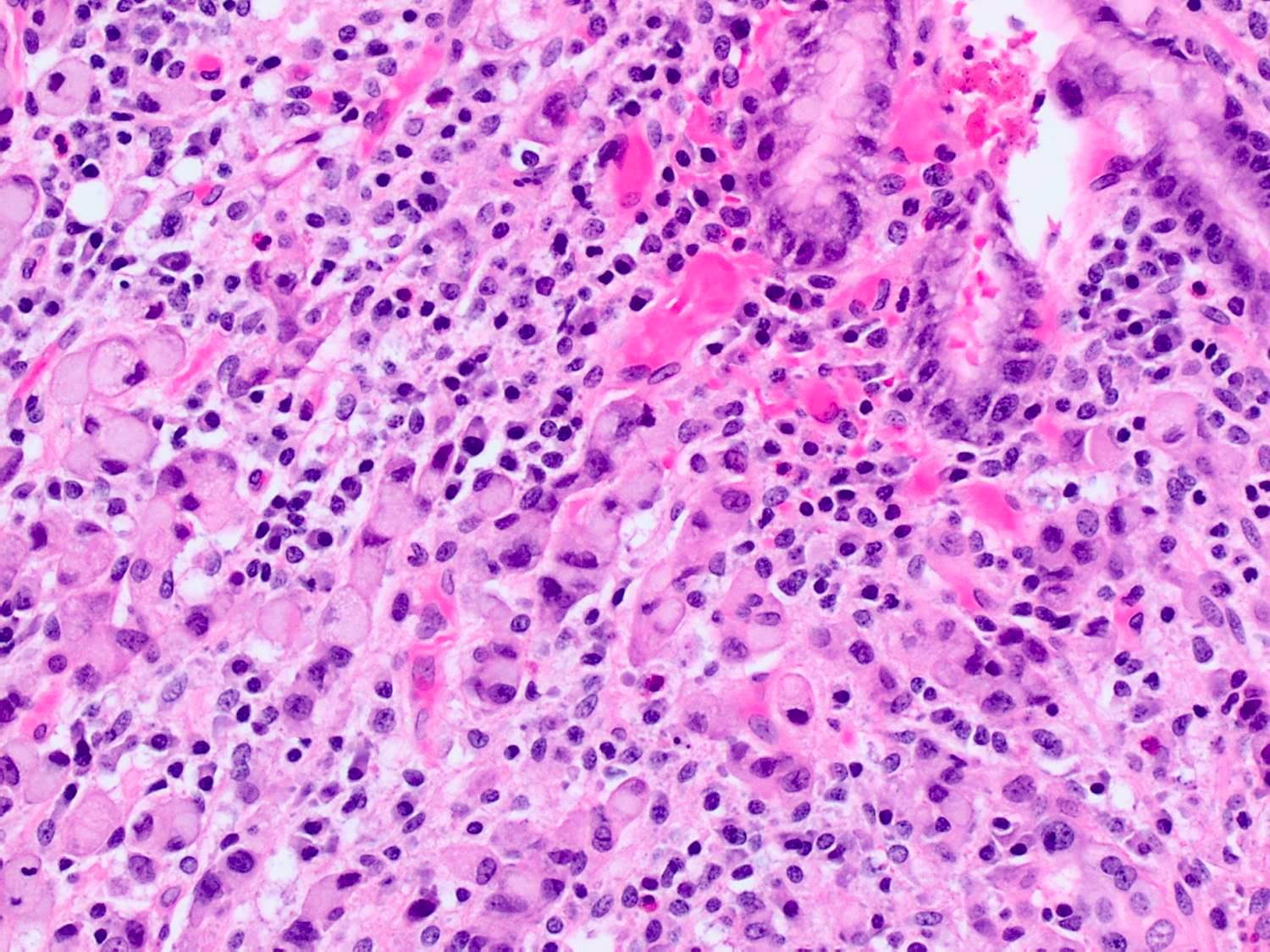
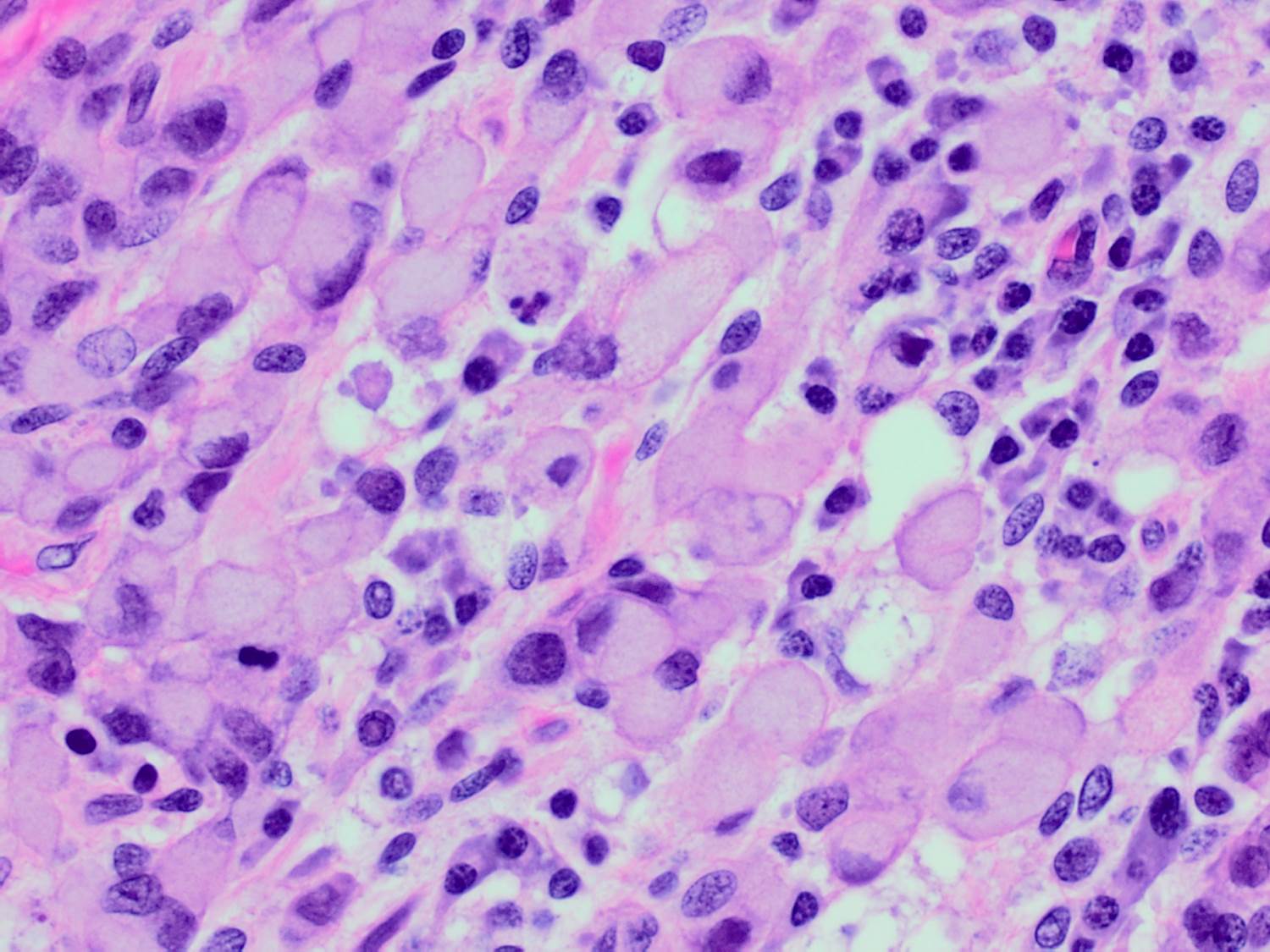
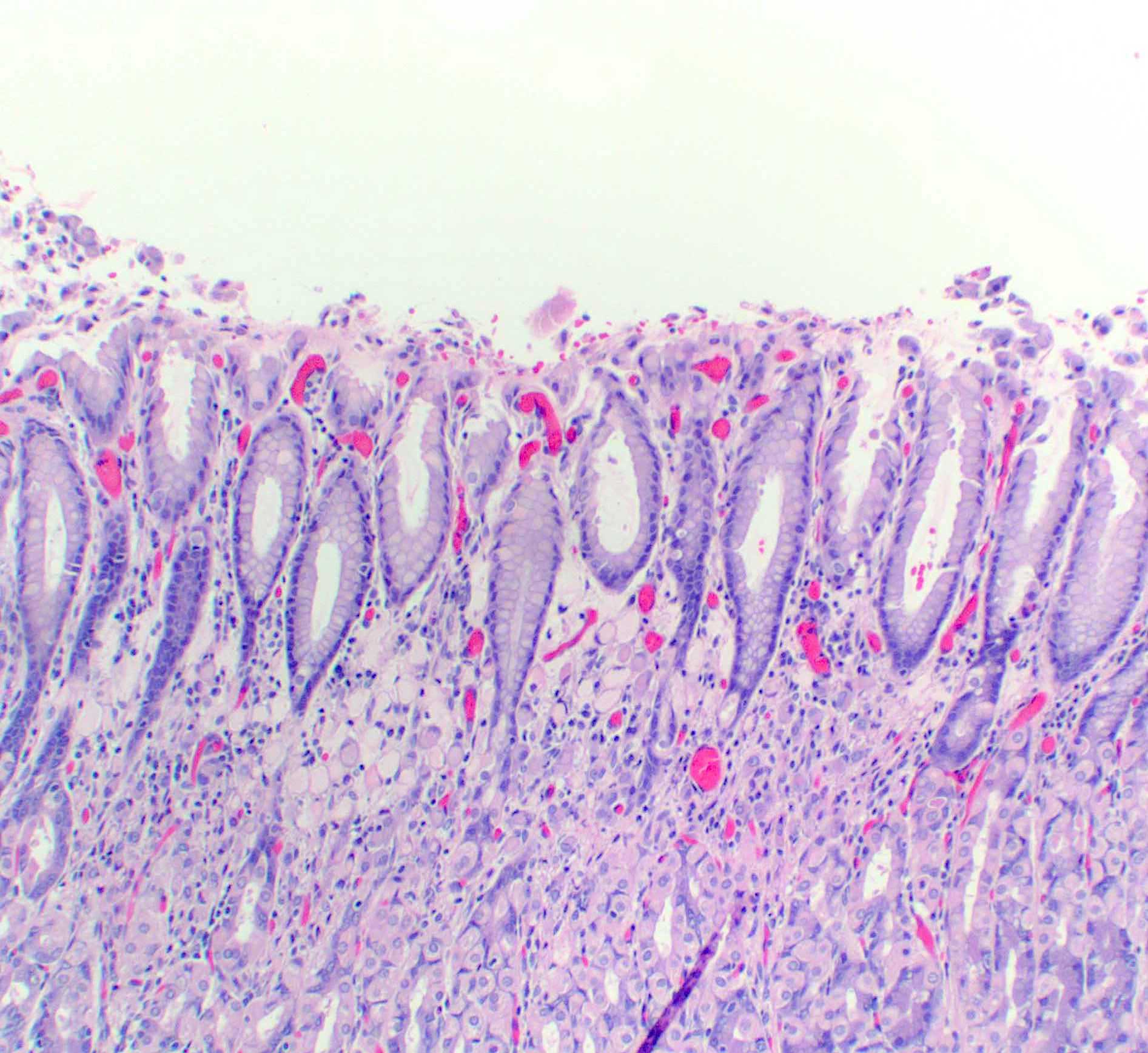
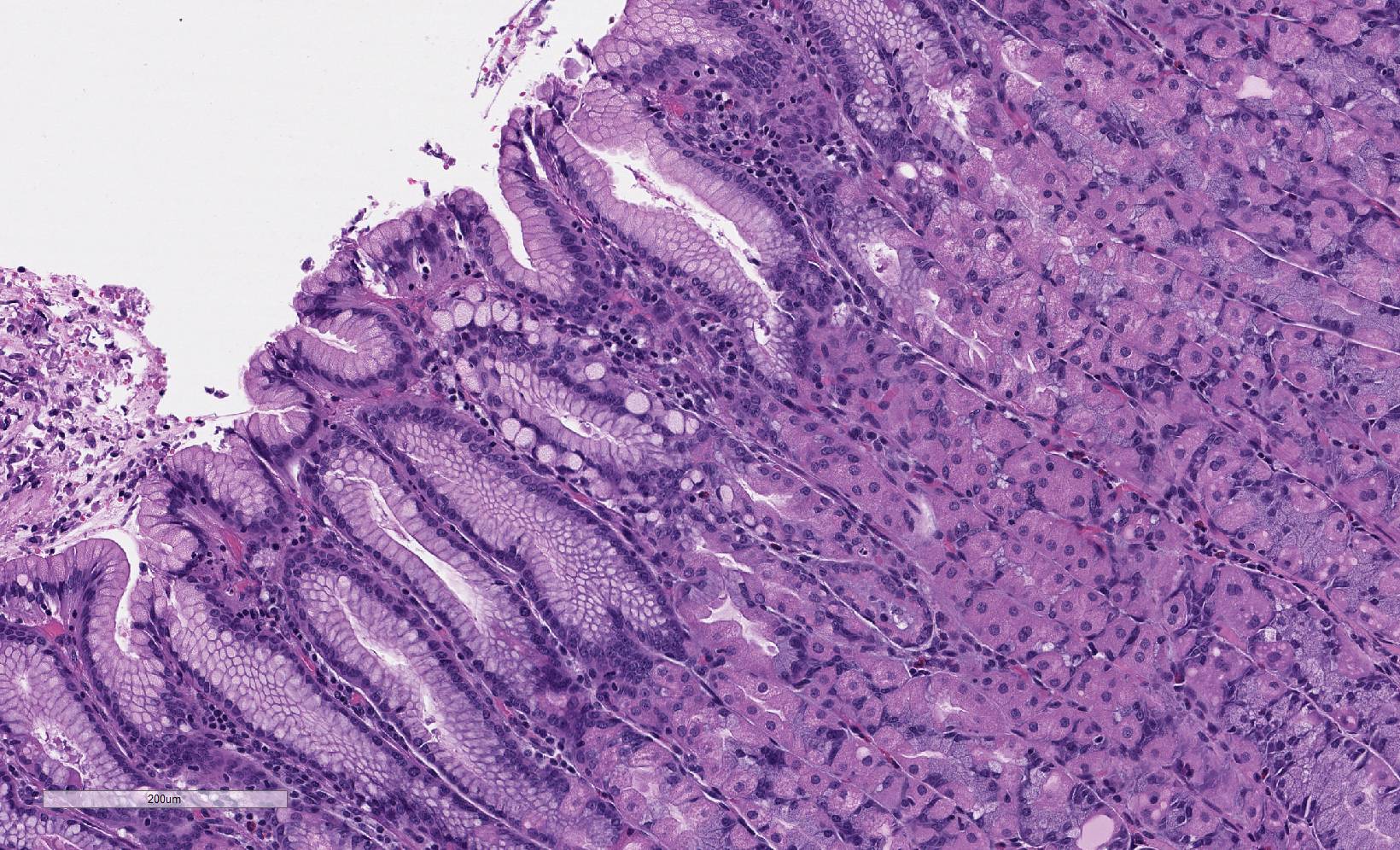
Microscopic (histologic) description
- Neoplastic cells that are isolated or arranged in small aggregates without well formed glands
- Poorly cohesive carcinomas can be either signet ring cell type or non signet ring cell (poorly differentiated) type
- Signet ring cell carcinoma (SRCC) is composed predominantly or exclusively of signet ring cells, which are characterized by a central, optically clear, globoid droplet of cytoplasmic mucin with an eccentrically placed nucleus
- Signet ring cells may form a lace-like glandular or delicate microtrabecular pattern
- Other cellular subtypes include tumors composed of neoplastic cells resembling histiocytes or lymphocytes
- Others have deeply eosinophilic cytoplasm, bizarre pleomorphic nuclei
- 2 types of precursor lesions are described in the context of HDGC (but not sporadic cases) (Front Pharmacol 2018;9:1421):
- In situ SRCC: signet ring cells are confined within the epithelium of glands / foveolae without breaking the basement membrane
- Pagetoid SRCC: signet ring cells spread below the preserved epithelium of glands / foveolae without breaking the basement membrane
- Early lesions arise in the region of mucous neck cells of the gastric glands and are limited to the lamina propria; they may lack any tissue or inflammatory response
- 3 cell types have been described in the carcinomas seen in patients with HDGC - small SRCC, large SRCC and poorly differentiated cells
- Advanced SRCC in patients with HDGC resemble sporadic SRCC microscopically
- There is marked desmoplasia, in particular when infiltrating into the submucosa or beyond
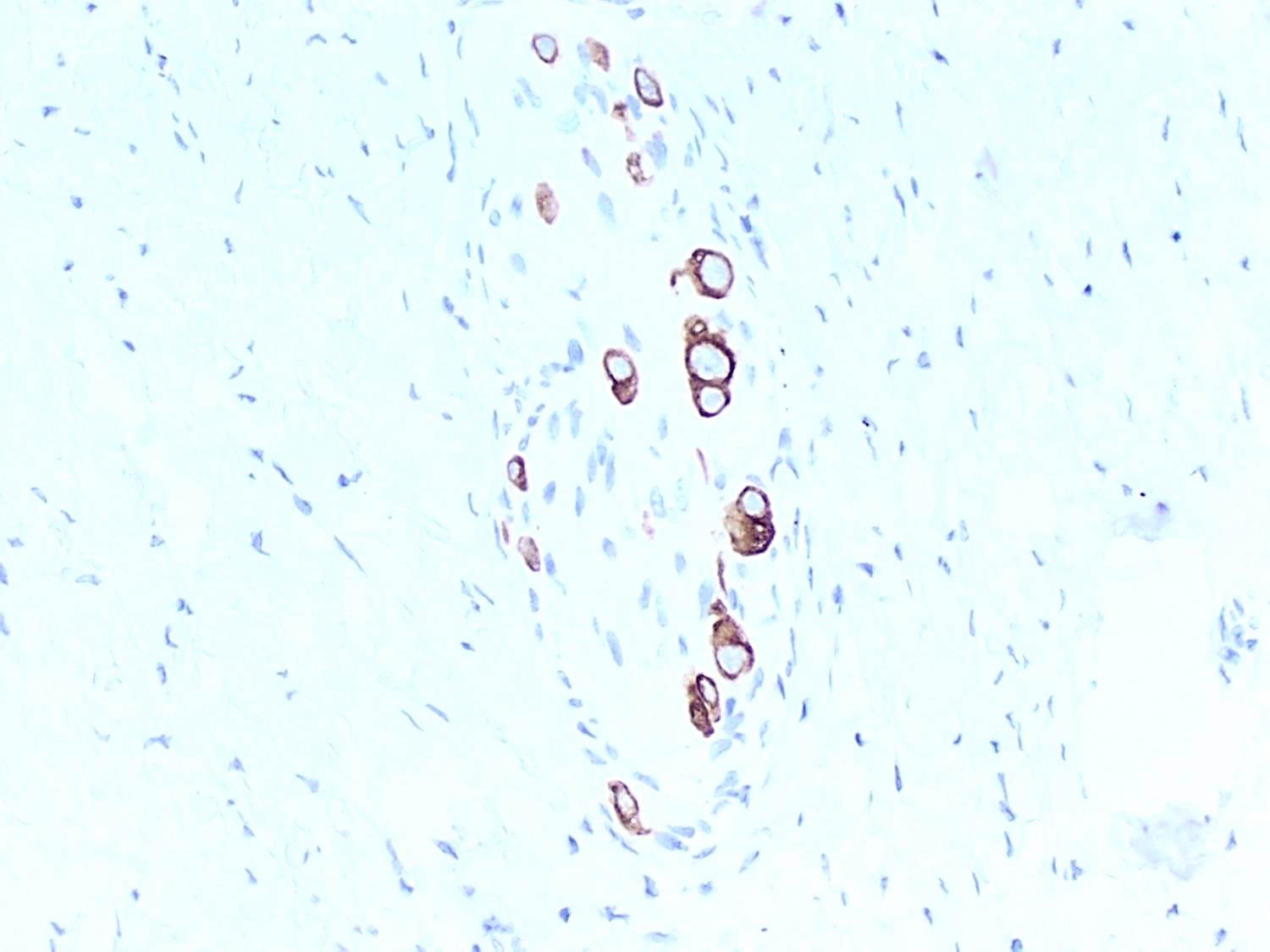
Microscopic (histologic) images
Cytology description
- Single atypical cells or clusters of cells forming a vague gland (Front Pharmacol 2018;9:1421):
- Malignant cells with eccentric nuclei
- Intracytoplasmic mucin can be identified
- Atypical naked nuclei
Positive stains
- PAS stain is positive due to the presence of neutral mucin in malignant cells (Indian J Med Paediatr Oncol 2013;34:229)
- Cytokeratin AE1 / AE3, mucicarmine, Alcian blue - PAS, CEA, EMA, keratin, villin
Negative stains
- E-cadherin: complete absence of membranous staining
- Aberrant staining patterns: dotted staining (due to staining of nonfunctional residual domains in proteins), cytoplasmic staining and reduced membranous staining (Int J Clin Exp Pathol 2017;10:8980)
- TTF1, p53
Molecular / cytogenetics description
- Mutations in CDH1 gene leading to reduced E-cadherin expression (J Gastrointest Oncol 2012;3:251)
- Activated ErbB2 / ErbB3 complex in signet ring cell carcinoma binds PI3K leading to phosphorylation of tyrosine residues and activation of downstream pathways including p38 MAP kinase (World J Gastroenterol 2015;21:11428)
- Activation of p38 MAP kinase lead to loss of cell to cell contact by disruption of adherent junctions
- MUC4 has been reported to increase activation of the ErbB2 / ErbB3 complex
- MUC4 belongs to the family of mucins that are normally expressed in gastric mucosae (MUC1, MUC5AC, MUC6) or expressed de novo in gastric cancer (MUC2, MUC4)
- Among the molecular subtypes of gastric carcinoma (based on the TGCA data), the genomically stable category is enriched in diffuse type phenotype associated with CDH1 mutations (Nat Rev Dis Primers 2017;3:17036)
Sample pathology report
- Stomach, total gastrectomy:
- Poorly differentiated adenocarcinoma, diffuse type (tumor size), with invasion into the submucosa
- Surgical margins are negative for adenocarcinoma
- Five (0/5) benign reactive lymph nodes
- See synoptic report and comment
Differential diagnosis
- Lymphoma with artifactual signet ring cells due to cytoplasmic shrinkage (Arch Pathol Lab Med 1997;121:623):
- CD20 positive in lymphoma
- Cytokeratin AE1 / AE3 positive in diffuse gastric carcinoma
- Metastases from breast (lobular carcinoma) (Arch Pathol Lab Med 2001;125:567):
- Both have signet ring cell morphology and negative E-cadherin stain
- GATA3 / ER positive in breast primary and negative in gastric carcinoma
- Reactive epithelial atypia / pseudo signet ring cells associated with tissue injury or otherwise:
- Histology of the background tissue may offer clues; detached cells floating on surface or in a space with inflammatory cells should be interpreted with caution, as they often represent pseudo signet ring cells
- E-cadherin stain will show membranous positivity in reactive epithelial atypia and may exhibit aberrant expression in true signet ring cells
- Xanthoma:
Board review style question #1
A 56 year old woman presents with nausea, vomiting and 4 months of weight loss. Endoscopy is performed and shows an erythematous area with ill defined borders. Biopsy is performed and shows poorly differentiated adenocarcinoma with signet ring type morphology. What is the most likely gene mutated in this malignancy?
- CDH1
- FAP
- HER2
- PTEN
Board review style answer #1
Board review style question #2
A 30 year old woman is found to have a germline CDH1 mutation and undergoes a prophylactic gastrectomy. Which other malignancy is she at a higher risk of developing?
- Clear cell renal cell carcinoma
- Lobular carcinoma of breast
- Melanoma
- Osteosarcoma
Board review style answer #2
B. Lobular carcinoma of breast
Comment Here
Reference: Diffuse (poorly cohesive) type adenocarcinoma
Comment Here
Reference: Diffuse (poorly cohesive) type adenocarcinoma