Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Morrow M, Gonzalez RS. Collagenous gastritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachcollagenous.html. Accessed March 31st, 2025.
Definition / general
- Poorly understood disease manifesting as thickened subepithelial collagen in the stomach
Essential features
- An extremely rare disease characterized by the presence of a band of increased subepithelial collagen in the stomach, with associated chronic inflammation in the lamina propria
- Often subtyped into pediatric and adult versions
- No standard therapy
ICD coding
- ICD-10: K52.89 - Other specified noninfective gastroenteritis and colitis
Epidemiology
- Extremely rare, with only 60 cases reported since it was first described in 1989 (World J Gastrointest Endosc 2015;7:265)
- Slight female predominance, occurring in all ages, but age at presentation centers around young adults (J Nat Sci Biol Med 2018;9:285)
Sites
- Pediatric patients possibly more likely to have body / fundus predominant disease versus antrum in adults (Mod Pathol 2015;28:533)
Pathophysiology
- Poorly understood etiology / pathophysiology
Clinical features
- Associated with celiac disease, collagenous colitis, collagenous sprue and other autoimmune disease (Arch Pathol Lab Med 2001;125:1579)
- Most common clinical symptoms include abdominal pain, anemia, diarrhea, nausea / vomiting, GI bleeding and weight loss
- Through limited case reports, the disease has been phenotyped into adult and pediatric types but many patients may not fit either category (Am J Surg Pathol 2001;25:1174)
- Pediatric type classically presents with upper GI symptoms including abdominal pain and anemia, which are a result of the disease process
- Adult type is characterized by accompanying collagenous colitis, related to underlying autoimmune processes or celiac disease
Diagnosis
- Established by gastric biopsy
Case reports
- 12 year old girl with abdominal pain and low ferritin (Rev Esp Enferm Dig 2015;107:313)
- 21 year old woman with gastritis after Helicobacter pylori eradication (ACG Case Rep J 2017;4:e69)
- 26 year old woman with a past medical history of gastroesophageal reflux disease and scleroderma presenting with abdominal pain and diarrhea (Gastroenterology Res 2017;10:126)
- 47 year old woman with systemic lupus erythromatosis presenting with mild anemia and dyspepsia (J Med Case Rep 2014;8:278)
Treatment
- No standard therapy has been defined
Clinical images
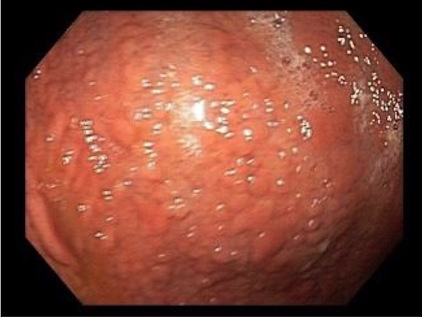
Gross description
- Nodularity of the gastric corpus is the characteristic endoscopic finding but is not seen in all cases (World J Gastrointest Endosc 2015;7:265)
- Depressed mucosa between the nodules shows atrophy and deposition of subepithelial collagen, whereas the nodular lesions themselves show unaffected mucosa (Dig Dis Sci 2007;52:995)
- Other mucosal findings include erythema, erosions and exudate
- Occasionally there are no findings (akin to collagenous colitis)
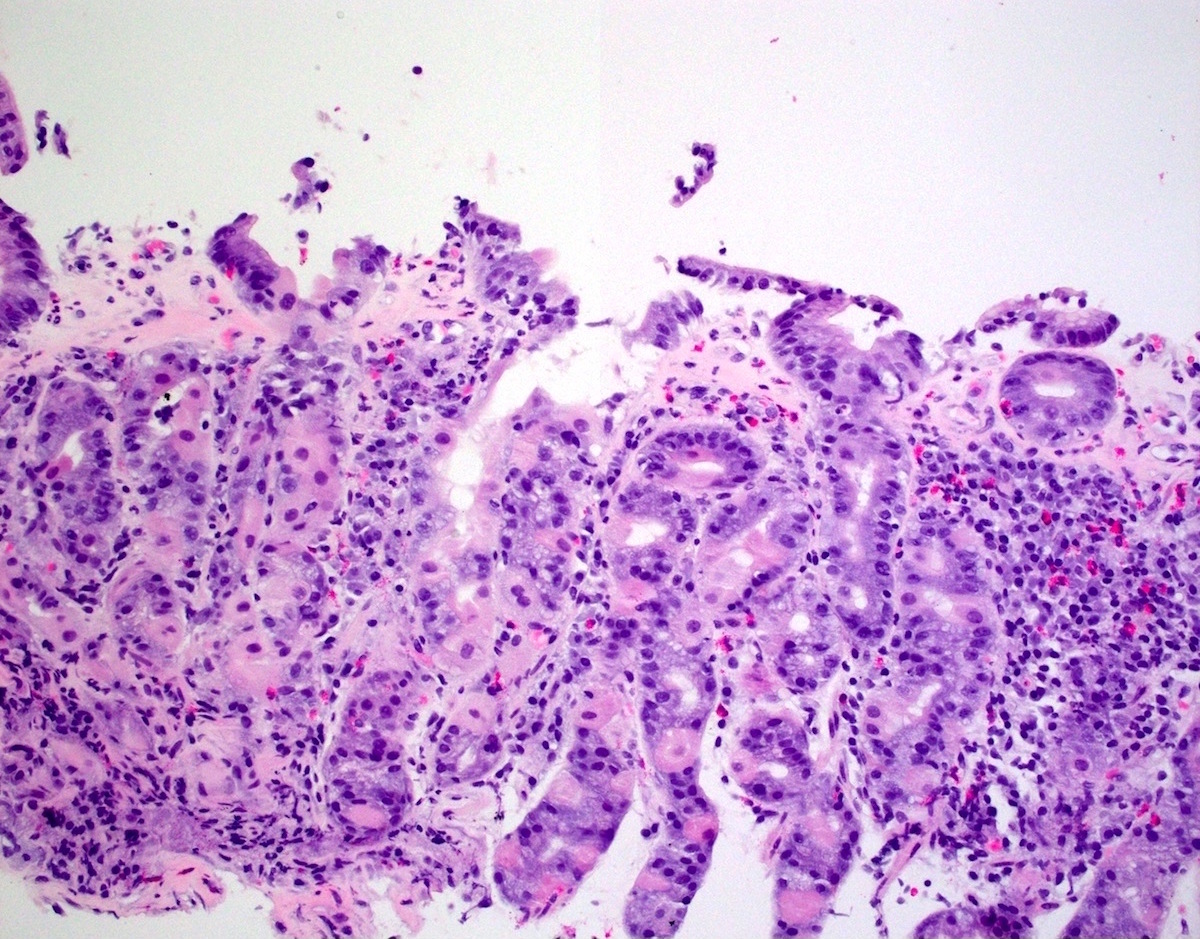
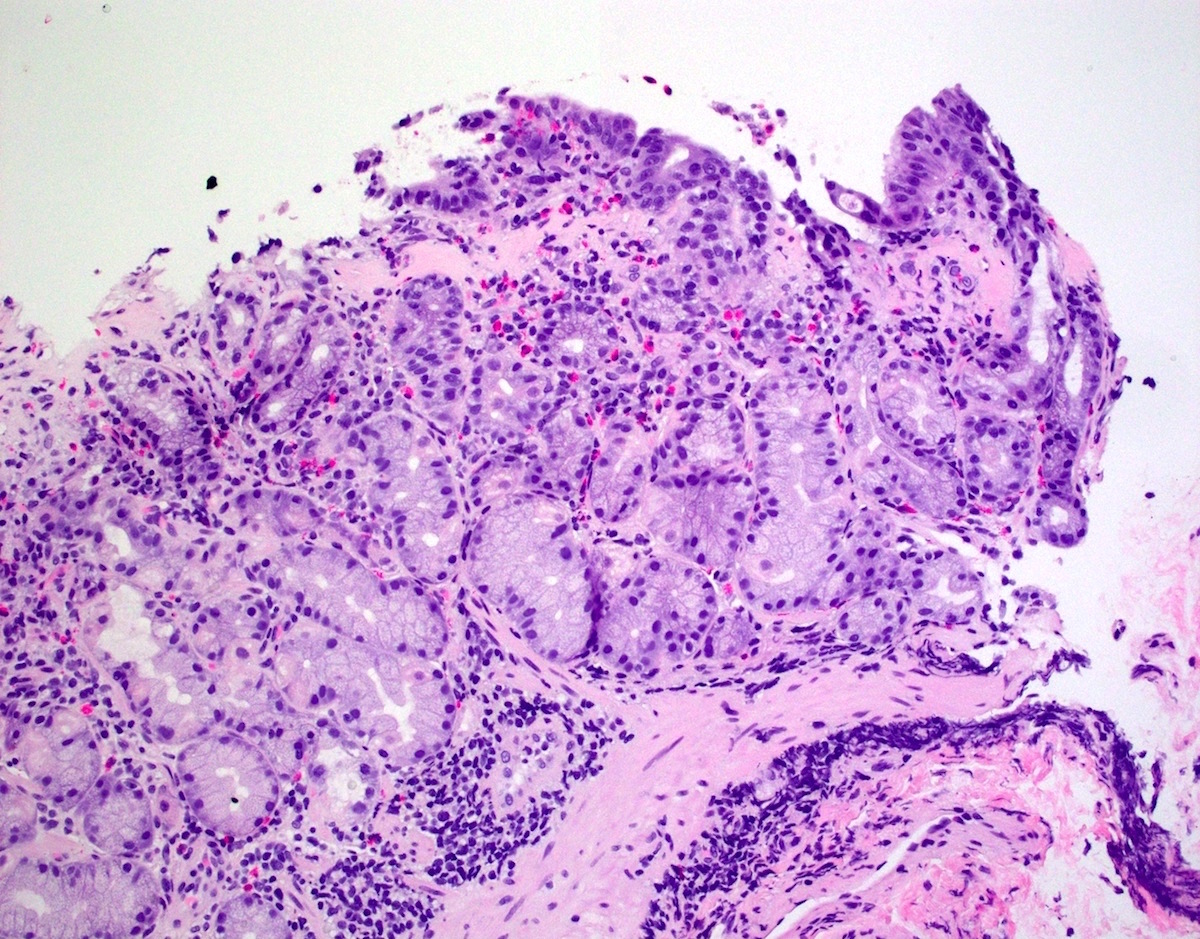
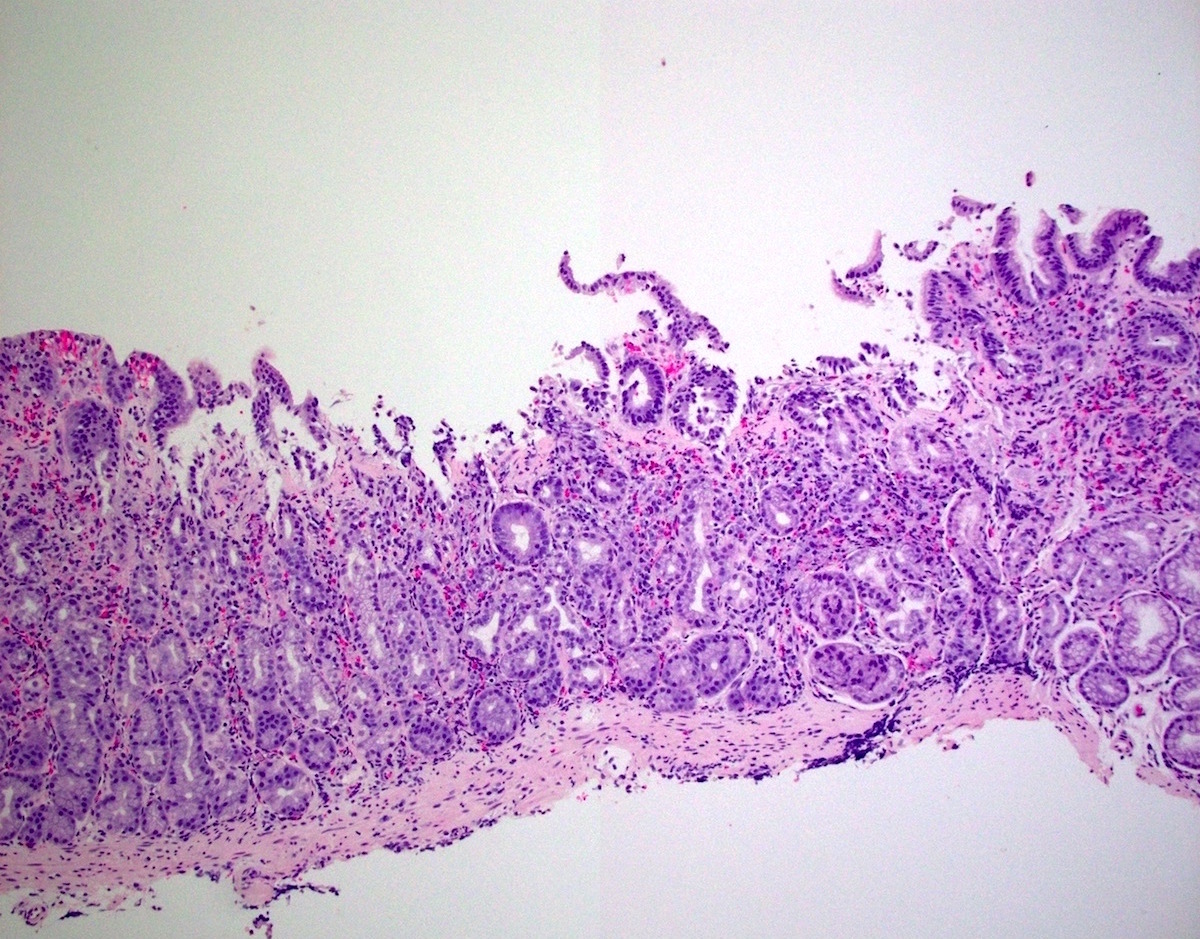
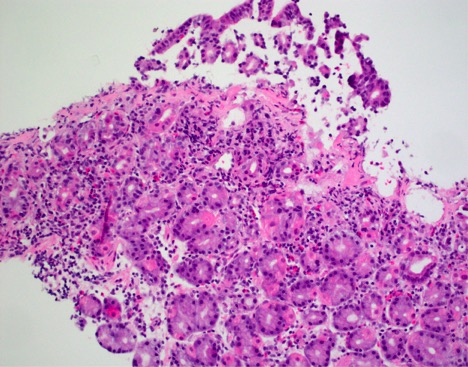
Microscopic (histologic) description
- Patchy increased subepithelial collagen, having a thickness ≥ 10 µm
- Maximum thickness on average ranges from 15 to 115 μm, mean 55.1 μm (Mod Pathol 2015;28:533)
- Often associated with the entrapment of red blood cells, inflammatory cells and superficial capillaries (Am J Surg Pathol 2001;25:1174)
- Associated with the denudation or separation of the surface gastric epithelium
- Increased chronic inflammatory infiltrate of the lamina propria including increased eosinophils and many times neutrophils
- Increased intraepithelial lymphocytes, but fewer than in lymphocytic gastritis
- Histologic features may persist for years (Mod Pathol 2015;28:533)
Microscopic (histologic) images
Contributed by Matthew Morrow, M.D.
Images hosted on other servers:
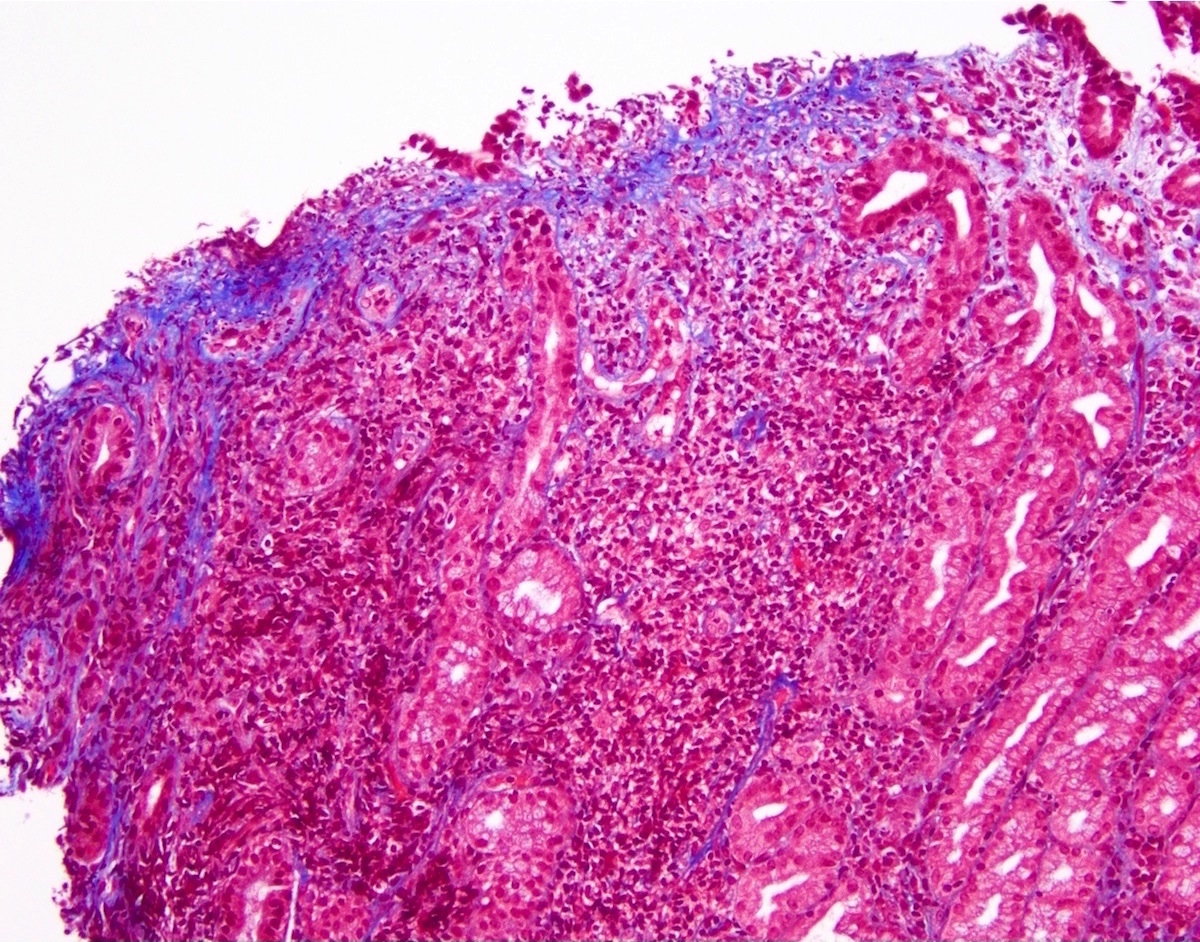
Positive stains
- Masson trichrome stain highlights the thickened subepithelial layer of collagen
Negative stains
Sample pathology report
- Stomach, antrum, biopsy:
- Collagenous gastritis (see comment)
- Comment: A trichrome special stain highlights a thickened basement membrane.
Differential diagnosis
- Amyloid deposition:
- Positive for Congo red
- Autoimmune gastritis or radiation therapy effect:
- May show diffuse collagen deposition, not specifically located in a subepithelial location
- Scleroderma:
- Fibrosis at all levels of the mucosa and possibly also deep to the mucosa (Ital J Anat Embryol 2010;115:115)
- Tangential sectioning of normal subepithelial collagen:
- Other features (e.g. increased inflammation) not seen
- May need to correlate with clinical presentation
Additional references
Board review style question #1
- A 10 year old boy presents with chronic abdominal pain and anemia. The following is a biopsy from the stomach. Which of the following statements is true?
- Immunosuppression is standard therapy
- The absence of both HLA-DQ2 and HLA-DQ8 haplotypes essentially excludes the diagnosis
- The histologic features may persist for years
- The pediatric type of the disease is classically characterized by accompanying collagenous colitis
Board review style answer #1
C. The histologic features may persist for years. In one study, of the patients who had follow up biopsies, 75% had persistent histologic features, sometimes lasting up to 10 years (Mod Pathol 2015;28:533).
Comment Here
Reference: Collagenous gastritis
Comment Here
Reference: Collagenous gastritis
Board review style question #2
- Which of the following statements about collagenous gastritis is true?
- An increase in collagen is seen in the deep lamina propria and bowel wall
- If nodular gastric mucosa is seen, for diagnosis of this entity it is best to biopsy at the tips of the nodules
- It can be associated with celiac disease
- It is mainly a disease of the elderly
Board review style answer #2
C. Collagenous gastritis can be associated with celiac disease
Comment Here
Reference: Collagenous gastritis
Comment Here
Reference: Collagenous gastritis