Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Postchemotherapy / radiation therapy changes | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sheganoski T, Huber AR. Reactive (chemical) gastropathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachchemical.html. Accessed March 31st, 2025.
Definition / general
- Gastric mucosal pattern of injury induced by endogenous (bile / pancreatic reflux) or exogenous (chronic use of nonsteroidal anti-inflammatory drugs [NSAIDs], acetylsalicylic acid, ethanol or chemotherapeutics) agents (Pathologe 2001;22:44)
- Second most common diagnosis on gastric biopsy (Arch Pathol Lab Med 2007;131:86)
Essential features
- Gastric epithelial pattern of injury in response to an endogenous or exogenous irritant
- Histology is characterized by foveolar hyperplasia, mucin depletion in surface epithelial cells and lamina propria expansion by fibromuscular and capillary hyperplasia
- No prominent inflammatory cells on histology
Terminology
- Other names used today (or historically) pathologists may be more familiar with:
- Chemical gastritis
- (Bile) reflux gastritis
- Reactive gastritis
- Type C gastritis
- References: J Clin Pathol 1990;43:303, Aliment Pharmacol Ther 2012;36:736, Pathol Res Pract 2014;210:847
ICD coding
- ICD-10: K31.9 - disease of stomach and duodenum, unspecified
Epidemiology
- No known geographic variation in the United States
- Slight female predominance
- Highest prevalence in African Americans > Hispanics > Caucasians
- Often seen in those with reflux esophagitis, Barrett esophagus and lymphocytic esophagitis
- References: Aliment Pharmacol Ther 2012;36:736, Gastrointest Tumors 2021;8:115
Sites
- Gastric surface epithelium
- Antral mucosa > oxyntic mucosa, typically
Pathophysiology
- Insult to gastric surface epithelium results in excessive cellular exfoliation, leading to foveolar hyperplasia
- NSAID induced:
- Permeation of gastric cell membranes, due to their nature as weak organic acids, allows direct access to mucosal lining
- Inhibition of cyclooxygenase enzymes prevents synthesis of prostaglandin from arachidonic acid and production of leukotrienes
- Disruption of cellular proliferative / reparative processes, microcirculation and growth factor expression
- Reduced secretion of bicarbonate and mucin results in diminished hydrophobic nature of gastric surface mucous gel layer
- References: Arch Pathol Lab Med 2007;131:86, Mediators Inflamm 2013;2013:258209
- Bile reflux induced:
- Often a sequela of partial gastrectomy
- Increased gastric pH from bile acids plus bacterial contamination evoke cytolysis and alter the structure / function of gastric mucosa
- Associated with increased levels of conjugated bile acids
- References: Sci Rep 2020;10:11601, Gastrointest Tumors 2021;8:115, Arch Pathol Lab Med 2007;131:86
Etiology
- Most commonly caused by NSAID use, followed by chronic bile reflux (Gastrointest Tumors 2021;8:115)
- Alcohol, iron salts, other agents (alendronate, sodium phosphate, etc.) (UpToDate: Etiology-Based Classification of Gastropathy and Gastritis [Accessed 23 May 2022])
Clinical features
- Potential indigestion, epigastric discomfort, diarrhea, bloating, nausea, vomiting
- May be asymptomatic
- Minor correlation with chronic inactive gastritis, Helicobacter negative chronic active gastritis and intestinal metaplasia
- Patients with reactive gastropathy are more likely to have duodenal peptic injury and intraepithelial lymphocytosis
- Other significant associations: H. pylori gastritis, active ileitis, focal active colitis and collagenous colitis (Aliment Pharmacol Ther 2012;36:736)
- High rates of concurrent conditions in certain ethnic groups: Hispanics - diabetes, African Americans - hypertension, Caucasians - tobacco / alcohol use (Gastrointest Tumors 2021;8:115)
Postchemotherapy / radiation therapy changes
- Occur in 8% of patients with chemoradiation therapy for esophageal carcinoma, may be confused with dysplasia
- Also occurs after hepatic artery infusion chemotherapy (Am J Surg Pathol 1983;7:261, Mod Pathol 2001;14:389)
Diagnosis
- Endoscopic observation of mucosal erythema or friability
- Endoscopic biopsies of gastric antrum or corpus
- Definitive diagnosis via identification of histopathologic criteria (Pathol Res Pract 2014;210:847)
Prognostic factors
- Prognosis is good and recurrence rate is generally low with removal of offending agent
- If gastropathy is sequela of gastrectomy, it may contribute to pathogenesis of stump carcinoma / remnant gastric cancer (Eur J Gastroenterol Hepatol 2003;15:35)
Case reports
- 29 year old man misdiagnosed with biliary reflux gastritis (World J Gastroenterol 2015;21:3425)
- 50 year old man with bile reflux gastritis cystica profunda (Medicine (Baltimore) 2019;98:e15295)
- 54 year old man with gastropathy from home remedy for rheumatoid arthritis (Eur J Gastroenterol Hepatol 2003;15:35)
Treatment
- Removal of offending agent
- Prevention via combination therapy of NSAIDs with gastroprotective agent(s) or alternative use of selective COX2 inhibitors (Mediators Inflamm 2013;2013:258209)
Clinical images
Gross description
- Generally soft tissue fragments from endoscopic biopsy (Rom J Morphol Embryol 2005;46:269)
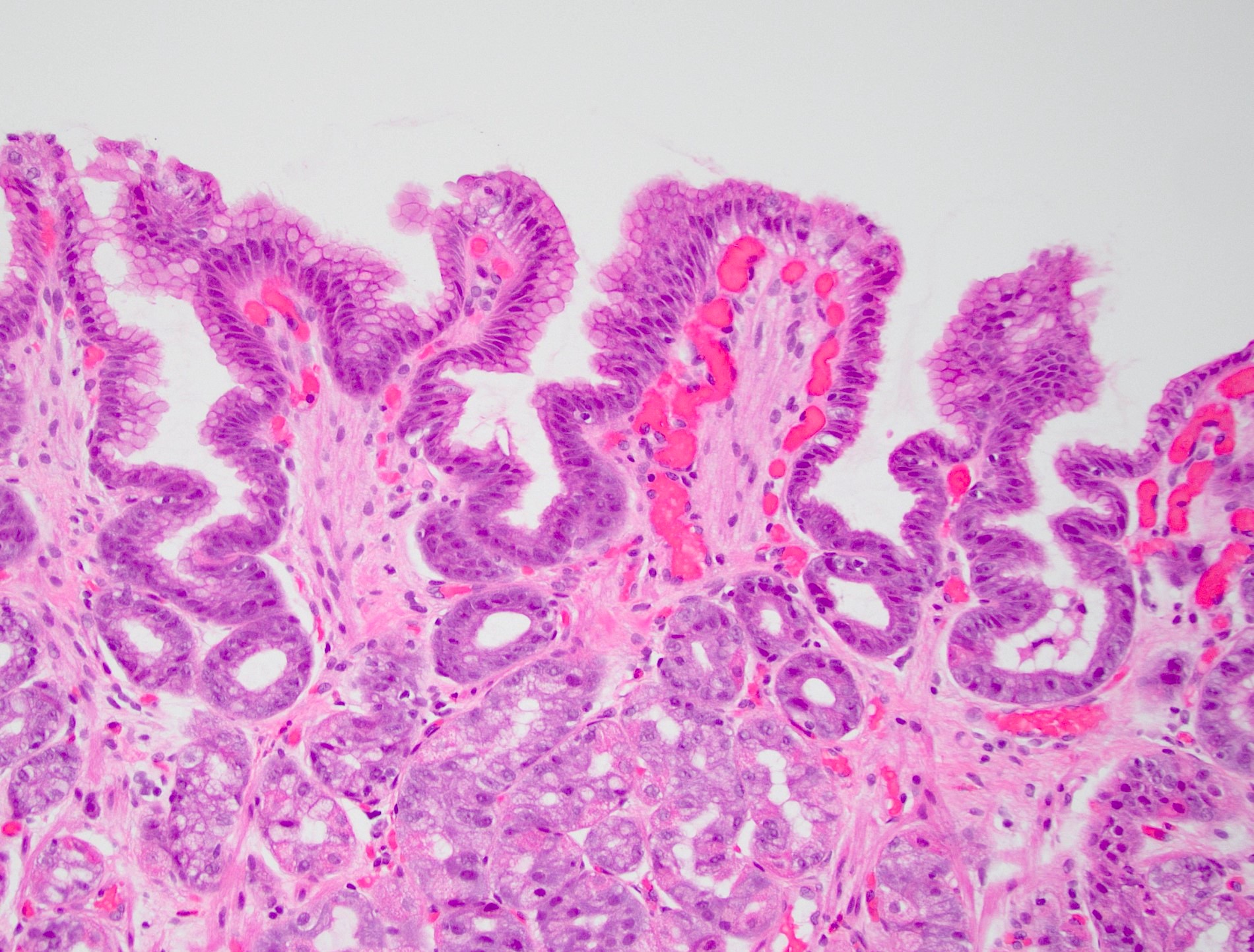
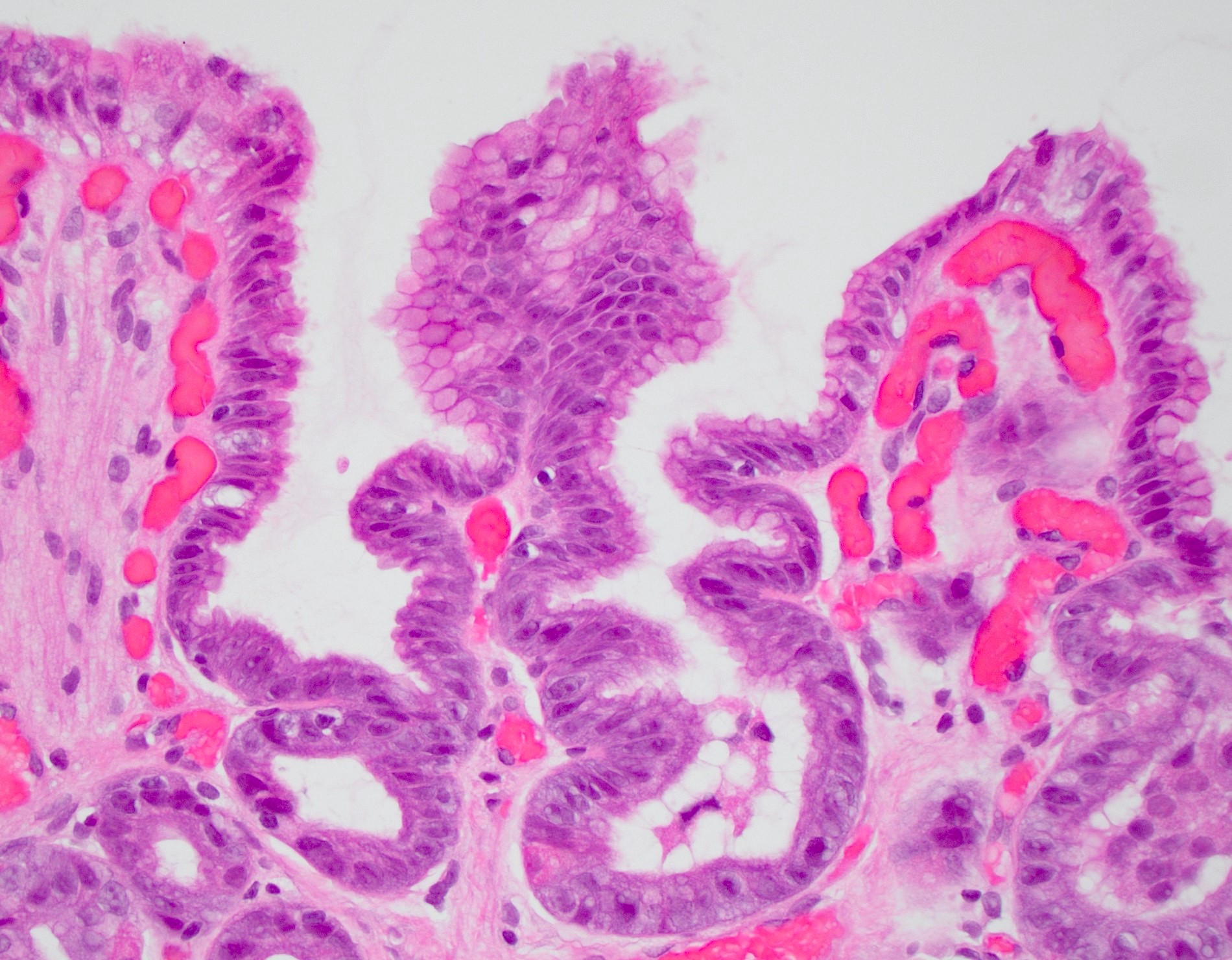
Microscopic (histologic) description
- Lack of significant edema or inflammation
- Foveolar hyperplasia: tortuosity / corkscrew appearance with a minimum twofold elongation of gastric cardiac foveolae and pits
- Mucin poor columnar cells with enlarged, hyperchromatic nuclei
- Lamina propria expansion with fibromuscular proliferation and congested, ectatic capillaries
- Chemotherapy related changes
- More epithelial damage and apoptosis but often no effect (Arch Pathol Lab Med 1991;115:807)
- May have large hyperchromatic nuclei that can mimic virally infected cells or bizarre nuclear atypia
- May see reduction in tumor cellularity, increase in dense fibrosis, formation of large mucin pools with lymphocytes and macrophages
- No atypical mitoses, no cytoplasmic eosinophilia, no vacuolization, no intestinal metaplasia, no irregular glandular microcystic change
- In signet ring carcinomas, see smaller intracytoplasmic mucin vacuoles
- Radiation related changes
- Ectatic vessels and lamina propria fibrosis
- References: Gastrointest Tumors 2021;8:115, J Clin Pathol 2002;55:352, Arch Pathol Lab Med 2007;131:86
Microscopic (histologic) images
Negative stains
- Complete or patchy loss of apical MUC1 expression (Arch Pathol Lab Med 2007;131:86)
- Negative H. pylori staining (Aliment Pharmacol Ther 2012;36:736)
Videos
Gastritis versus gastropathy
Sample pathology report
- Stomach, antrum, biopsy:
- Reactive (chemical) gastropathy
- No Helicobacter organisms identified on routine H&E stained sections
Differential diagnosis
- Low grade dysplasia:
- Hyperchromatic nuclei with pencillate nuclei
- Mitotic figures at the surface of the epithelium
- Abrupt transition from benign to dysplastic epithelium
- H. pylori gastritis:
- Chronic inflammation with plasma cells in the lamina propria
- Active (neutrophilic) inflammation
- Gastric antral vascular ectasia:
- Fibrin thrombi in vessels is the hallmark
- Reference: Semin Diagn Pathol 2005;22:273
Board review style question #1
A 48 year old woman with rheumatoid arthritis presents with dyspepsia and bloating. Endoscopy shows erythematous mucosa. Histopathology is significant for serrated gastric pits, foveolar hyperplasia, paucity of mucin in surface epithelial cells and ectatic superficial capillaries (see image). What is the diagnosis?
- Gastric antral vascular ectasia
- H. pylori gastritis
- Low grade dysplasia
- Reactive gastropathy
Board review style answer #1
D. Reactive gastropathy. Histology of low grade dysplasia includes intestinal metaplasia, mucosal atrophy and pencillate, hyperchromatic nuclei within tall columnar epithelium. Gastric vascular ectasia will also have distended capillaries but with fibrin thrombi and without foveolar hyperplasia. Histology of H. pylori gastritis should emphasize more inflammation, especially epithelial neutrophils and plasma cells in the lamina propria.
Comment Here
Reference: Reactive (chemical) gastropathy
Comment Here
Reference: Reactive (chemical) gastropathy
Board review style question #2
A patient suffers severe reflux following sleeve gastrectomy and is diagnosed with a gastric injury pattern characterized by papillary foveolar extension, expanded lamina propria lacking inflammation and mucin depleted superficial cells. What condition does this potentially predispose her to?
- Gastric mucosal atrophy
- Gastric outlet obstruction
- Gastric ulcer
- Remnant gastric cancer
Board review style answer #2
D. Remnant gastric cancer. The other answer options are more closely associated with chronic gastritis. The described histology is classic for reactive (chemical) gastropathy, which can contribute to the pathogenesis of stump / remnant gastric cancer.
Comment Here
Reference: Reactive (chemical) gastropathy
Comment Here
Reference: Reactive (chemical) gastropathy