Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Park BU, Zhang L. Eosinophilic gastroenterocolitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloneosinophilic.html. Accessed April 3rd, 2025.
Definition / general
- Eosinophilic gastrointestinal disorders (EGIDs) consist of eosinophilic esophagitis, eosinophilic gastritis, eosinophilic gastroenteritis, eosinophilic enteritis and eosinophilic colitis (J Allergy Clin Immunol 2004;113:11)
- However, eosinophilic esophagitis differs from eosinophilic gastroenterocolitis (EGEC) in all aspects and should be considered a different entity
- Eosinophilic gastroenterocolitis is an inflammatory disorder characterized by prominent eosinophilic infiltration of the gastrointestinal tract (stomach, duodenum, small intestine or large intestine) with no known causes of tissue eosinophilia
Essential features
- Inflammatory process characterized by the abnormal eosinophilic infiltration of different segments of the gastrointestinal tract in the absence of a known cause (drug reaction, parasitic infection, malignancy, etc.)
- Can occur throughout the gastrointestinal tract; most reported in the stomach, followed by the small intestine and colon
- Its diagnosis requires the presence of:
- Gastrointestinal symptoms
- Demonstration of gastrointestinal eosinophilia by biopsy
- Exclusion of other known causes of tissue eosinophilia
Terminology
- Allergic gastroenteritis
- Eosinophilic gastroenterocolitis
- Eosinophilic gastrointestinal disorder (includes eosinophilic esophagitis)
ICD coding
Epidemiology
- Rare disease
- Overall prevalence of eosinophilic gastroenteritis in the U.S. is 5.1/100,000 (Clin Gastroenterol Hepatol 2017;15:1733)
- Overall prevalence of eosinophilic colitis in the U.S. is 2.1/100,000 (Clin Gastroenterol Hepatol 2017;15:1733)
- In other parts of the world, such as Japan, the prevalence may be up to 5.5 times higher when compared to the U.S. (J Gastroenterol 2013;48:333)
- Disease of both adults and children
- More prevalent in the younger population (18 years or younger) (J Pediatr Gastroenterol Nutr 2016;62:36, Clin Gastroenterol Hepatol 2017;15:1733)
- However, eosinophilic colitis specifically is more prevalent in adults (> 18 years of age) (Clin Gastroenterol Hepatol 2017;15:1733)
- Predominantly affects females (J Pediatr Gastroenterol Nutr 2016;62:36, Dig Dis Sci 2016;61:2585)
- Diagnosis is commonly described in the Caucasian population but reported occurrence in all races and ethnic backgrounds
- Up to 70% of patients have personal or family history of atopic disorders (asthma, eczema or hay fever) (Paediatr Drugs 2002;4:563)
Sites
- Throughout the gastrointestinal tract: most common stomach, followed by small intestine and colon (Scott Med J 1990;35:163)
- 2 or more gastrointestinal sites of involvement are commonly seen
- Rare cases of bile duct involvement have been reported (Gut 1990;31:54)
Pathophysiology
- Although not fully understood, it likely has genetic and environmental factors
- ~10 - 70% of patients with immediate family member history (J Pediatr 2002;141:576)
- Leading key players are mast cells and eosinophils
- Immediate phase of reaction is dependent on the mast cell activation through the high affinity IgE receptor
- Late phase (non-IgE mediated) of reaction involves Th2 lymphocyte and monocytes producing cytokines and chemokines such as eotaxin 1 and interleukin 5, inducing eosinophil accumulation
- Eosinophils, when recruited in the intestinal epithelium, become cytotoxic by producing inflammatory mediators, such as eosinophil peroxidase, eosinophil derived neurotoxin, eosinophil cationic protein and major basic protein, causing destruction of the gastrointestinal epithelium and organ dysfunction (Baillieres Clin Gastroenterol 1996;10:443, N Engl J Med 1990;323:645, Clin Rev Allergy Immunol 2016;50:175)
- Eosinophil's 4 major cationic proteins (Nature 1986;321:613):
- Eosinophil peroxidase (EPO): cytotoxic effect on the epithelium, by the generation of toxic hydrogen peroxide and halide acid leading to tissue damage (J Allergy Clin Immunol 2004;113:11)
- Eosinophil derived neurotoxin (EDN): ribonuclease activity
- Eosinophil cationic protein (ECP): cytotoxic effect on the epithelium, by ion nonselective pore insertion (site of entry to other toxic molecules); also has ribonuclease activity
- Major basic protein (MBP): cytotoxic effect on the epithelium and also plays a role in the degranulation of mast cells and basophils
Etiology
- Cause is unknown
- Some research suggests allergic or immune dysregulation as many patients with eosinophilic gastrointestinal disorders (EGIDs) are also atopic (Adv Immunol 2001;78:291, Pediatr Neonatol 2011;52:272, Paediatr Perinat Epidemiol 2007;21:2)
- EGIDs can be categorized into primary versus secondary (Clin Rev Allergy Immunol 2016;50:175):
- Primary EGIDs are defined as an inflammatory process characterized by the abnormal eosinophilic infiltration of different segments of the gastrointestinal tract in the absence of a known cause (drug reaction, parasitic infection, malignancy, etc.) (J Allergy Clin Immunol 2004;113:11)
- Secondary EGIDs are due to drug reaction, parasitic infection, bacterial infection, hypereosinophilic syndrome, Churg-Strauss syndrome, celiac disease, inflammatory bowel disease, polyarteritis nodosa and other connective disorders
Clinical features
- Nondisease specific gastrointestinal symptoms:
- Abdominal pain
- Vomiting, nausea, diarrhea
- Malnutrition
- Poor growth and weight loss
- Some symptoms may be more frequently observed, depending on the depth of gastrointestinal tract wall involvement (Klein classification) (J Allergy Clin Immunol 2004;113:11, Medicine (Baltimore) 1970;49:299):
- Mucosal pattern: abdominal pain, nausea, vomiting, diarrhea, bleeding, malabsorption, weight loss
- Muscular pattern: pyloric or intestinal obstruction
- Serosal pattern: ascites with eosinophilia
- Often have a prior or concurrent history of atopy (asthma, allergic rhinitis and elevated serum IgE) (Pediatr Neonatol 2011;52:272)
- Some may present with gross or occult hematochezia, which may lead to significant anemia (Pediatr Neonatol 2011;52:272)
- Rare reported cases of EGIDs associated with pancreatitis and duodenal ulcer or perforation (World J Gastroenterol 2009;15:2156, Endoscopy 2011;43:E358)
Diagnosis
- Combination of clinical history, physical exam, endoscopy, radiology and laboratory studies are required as the diagnosis requires the presence of (Gut 1990;31:54):
- Gastrointestinal symptoms
- Demonstration of gastrointestinal eosinophilia by biopsy
- Exclusion of other known causes of tissue eosinophilia
- Endoscopy
- Spectrum of findings from normal appearing to mucosal erythema, edema, friability, granularity, ulceration, thickening of folds, mucosal nodules and whitish specks (Gastrointest Endosc 2002;56:762, Clin Rev Allergy Immunol 2016;50:175)
Laboratory
- No single laboratory test or procedure is diagnostic for EGIDs
- Maintaining a high index of suspicion is essential
- Although not specific, the following laboratory tests / findings may support the diagnosis (Clin Rev Allergy Immunol 2016;50:175):
- Allergy testing to assess allergies that may trigger the onset of symptoms; its utility remains controversial (J Gastroenterol Hepatol 2013;28:1306)
- Peripheral blood eosinophilia (seen in 20 - 80% of cases)
- Elevated erythrocyte sedimentation rate
- Iron deficiency anemia
- Elevated IgE levels
- Low serum albumin
- Fecal levels of eosinophilic cationic protein
- Serum eosinophilic cationic protein and eosinophil derived neurotoxin (Scand J Gastroenterol 2011;46:1074)
- Elevated 2 macroglobulin level (Scand J Gastroenterol 2011;46:1074)
- Stool examination (to rule out parasites)
Radiology description
- Its usefulness is limited
- Ultrasound:
- To detect the presence of bowel wall thickening, ascites or peritoneal nodules
- Reported use in follow up setting and determination of response to treatment (Ultraschall Med 2011;32:E57)
- Computerized tomography:
- May demonstrate nodular, irregular folds and thickening of the stomach and small intestines (J Comput Assist Tomogr 1999;23:417)
- Barium contrast:
- Identification of variable degree of stenosis, mucosal irregularity and thickened mucosal folds (J Clin Pathol 1986;39:1)
- Tc-99m hexamethyl propylene amine oxime (HMPAO) white blood cell scintigraphy:
- Reported uptake in areas of active eosinophilic inflammation
- Useful to determine the extent of disease and assessment of the treatment response (Clin Nucl Med 1997;22:536, Ann Nucl Med 2003;17:601)
- Ultrasound:
Radiology images
Prognostic factors
- Unknown due to the rarity of the disease but observed to be dependent on response to treatment and Klein classification of disease (Clin Gastroenterol Hepatol 2011;9:950)
- Patients have 3 different disease courses (Clin Gastroenterol Hepatol 2011;9:950):
- Single flare: more associated with serosal pattern
- Recurring course: more related to muscular pattern
- Continuous course: more associated with mucosal pattern
Case reports
- 9 year old boy with fever, melena and hematemesis (Turk Pediatri Ars 2020;55:299)
- 14 year old girl with continuous epigastralgia, vomiting and loss of appetite (Allergol Int 2017;66:621)
- 15 year old boy with a duodenal ulcer (Intern Med 2020;59:2249)
- 17 year old boy with nausea and melena for 3 - 4 days (Turk Pediatri Ars 2020;55:299)
- 28 year old man with vague abdominal pain, unintentional weight loss and progressive ascites (Am J Case Rep 2019;20:189)
- 48 year old woman with recurrent eosinophilic peritonitis (Cureus 2020;12:e9422)
- 51 year old woman with eosinophilic gastroenteritis presenting as small bowel obstruction (World J Gastroenterol 2007;13:1758)
- 54 year old man with HIV with recurrent presentations for colitis since initiating emtricitabine / tenofovir (Cureus 2018;10:e3498)
- 66 year old man with a 15 day history of persistent upper abdominal pain and distension (Clin Case Rep 2020;8:2843)
Treatment
- No established standard treatment guidelines are available due to the lack of extensive prospective studies; current treatments are based on case reports and case series
- Treatments are empiric and based on the severity of the clinical manifestation
- Avoidance of allergen or trigger
- Common issue: recurrence of symptoms with the reintroduction of the allergen, such as specific food
- Elemental diet (J Pediatr Gastroenterol Nutr 1996;23:81)
- Anti-inflammatory medication
- Systemic and topical steroids are the mainstay of therapy (Curr Allergy Asthma Rep 2005;5:259)
- Reserved for severe disease presentation or failed dietary restriction
- Serosal EGIDS often have a better response to steroids (Dig Dis Sci 2003;48:1013)
- Other steroid sparing treatment modalities: mast cell stabilizers (cromolyn sodium), mast cell secretion inhibitor (ketotifen), leukotriene receptor antagonist (montelukast), selective Th2, cytokine IL4 and IL5 inhibitors (subplatast tosilate)
- Other specific pathway targeting treatment options: anti-IgE monoclonal antibody (omalizumab), anti-IL5 antibodies (reslizumab and mepolizumab) and anti tumor necrosis factor alpha (infliximab)
- Fecal microbiota transplantation (World J Gastroenterol 2014;20:16368)
- Avoidance of allergen or trigger
Clinical images
Gross description
- Nonspecific findings on the mucosal surface, including thickened mucosa, erythema, erosion, ulceration, white plaques, edema, telangiectasia or submucosal nodules
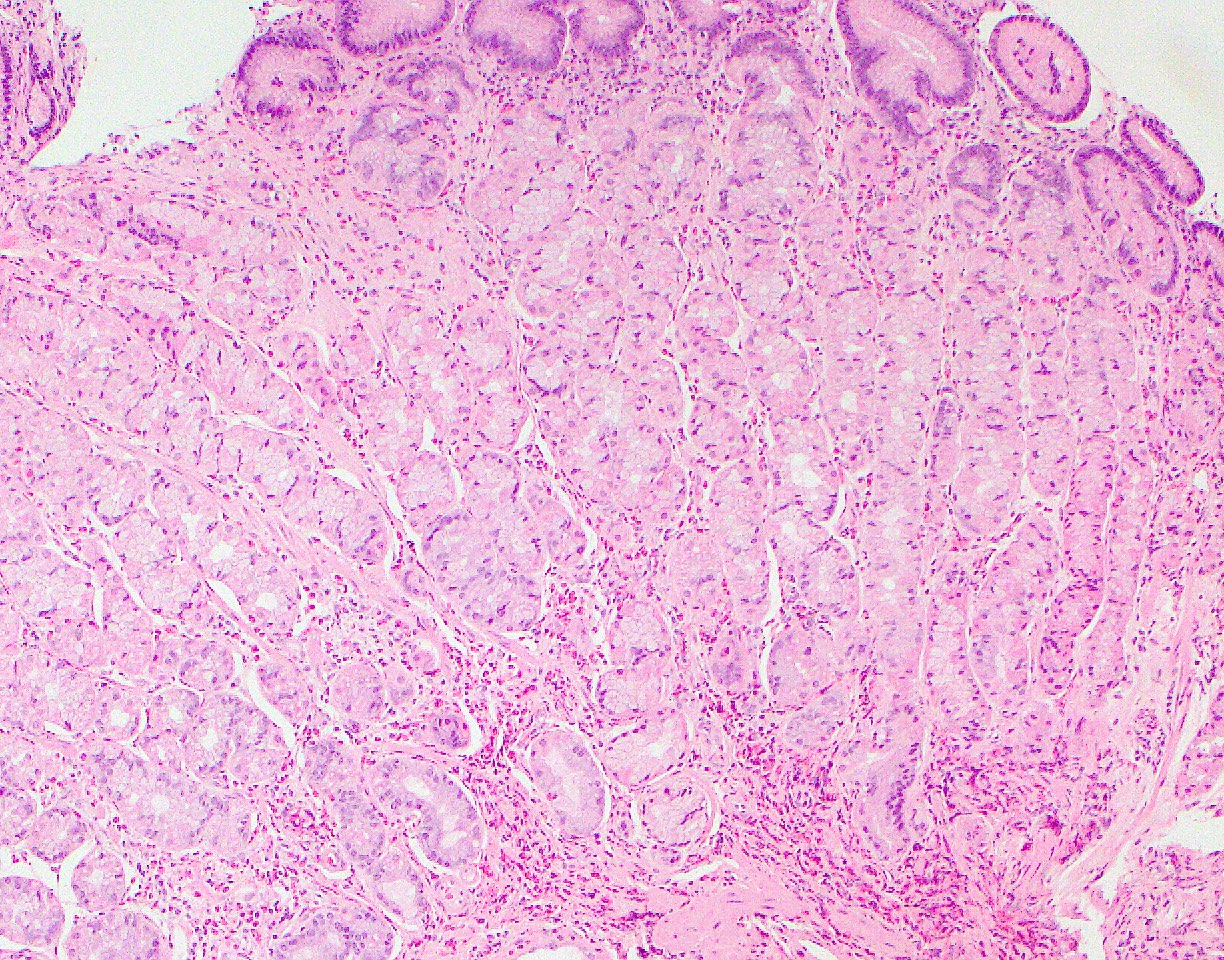
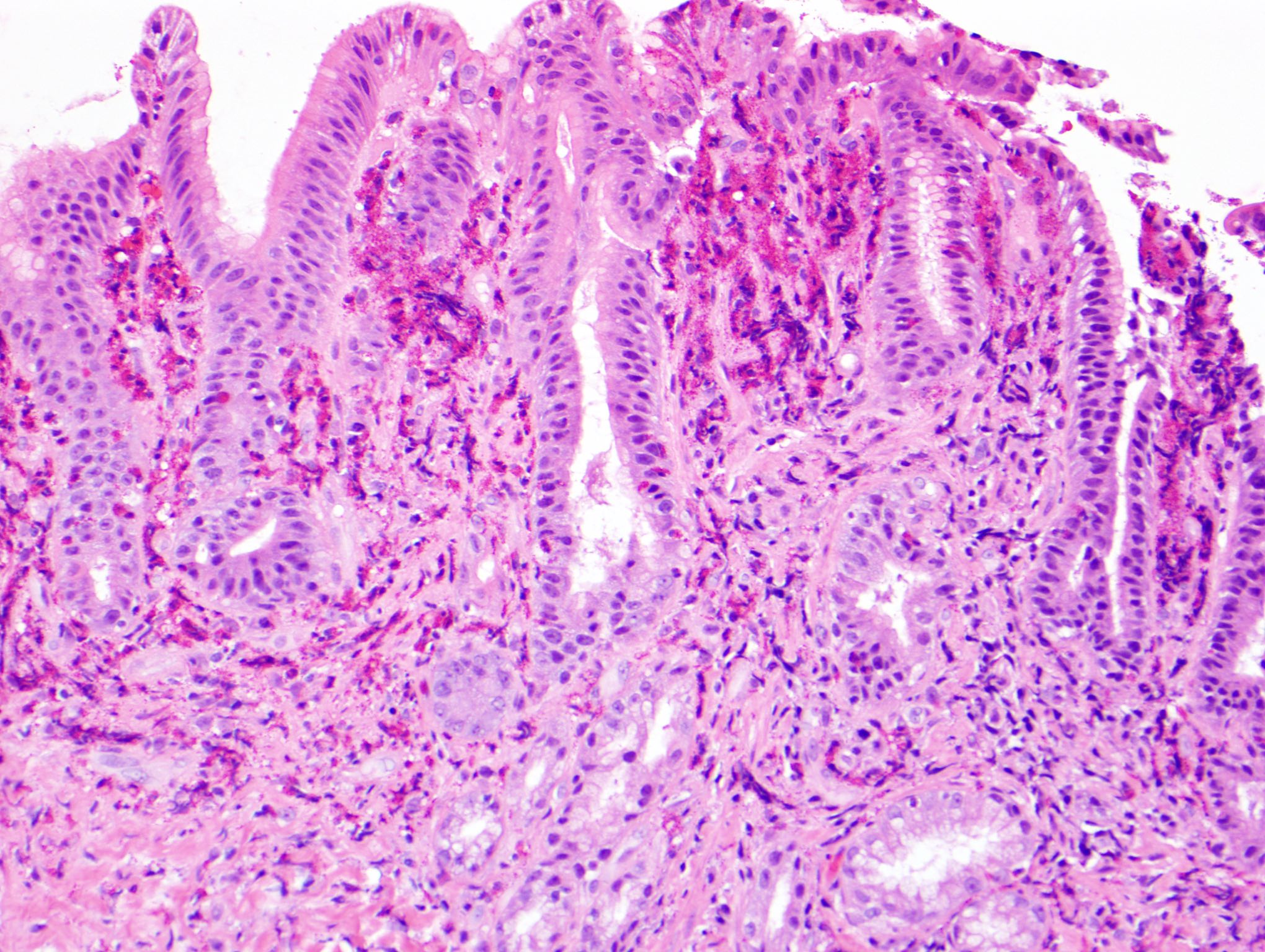
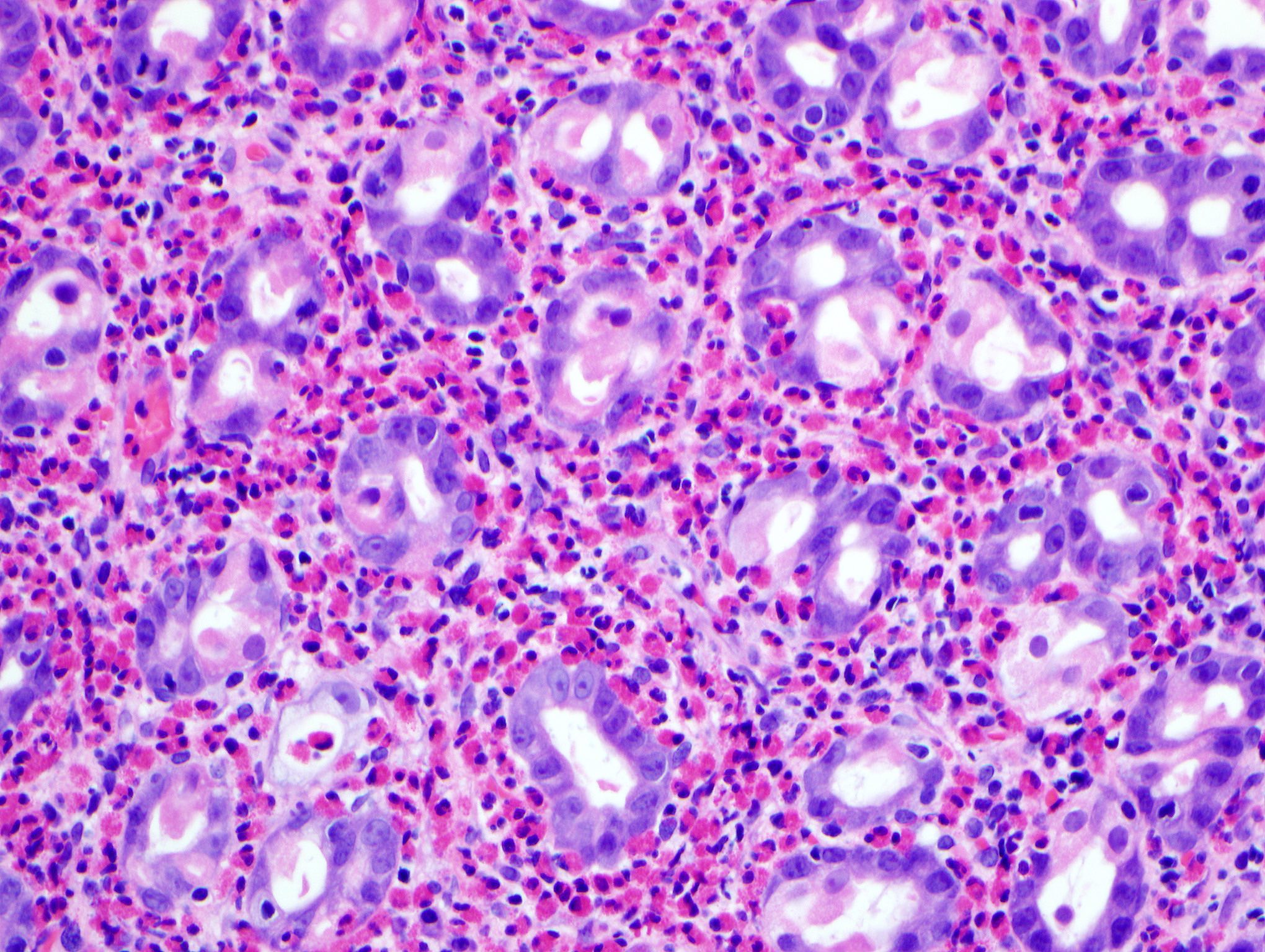
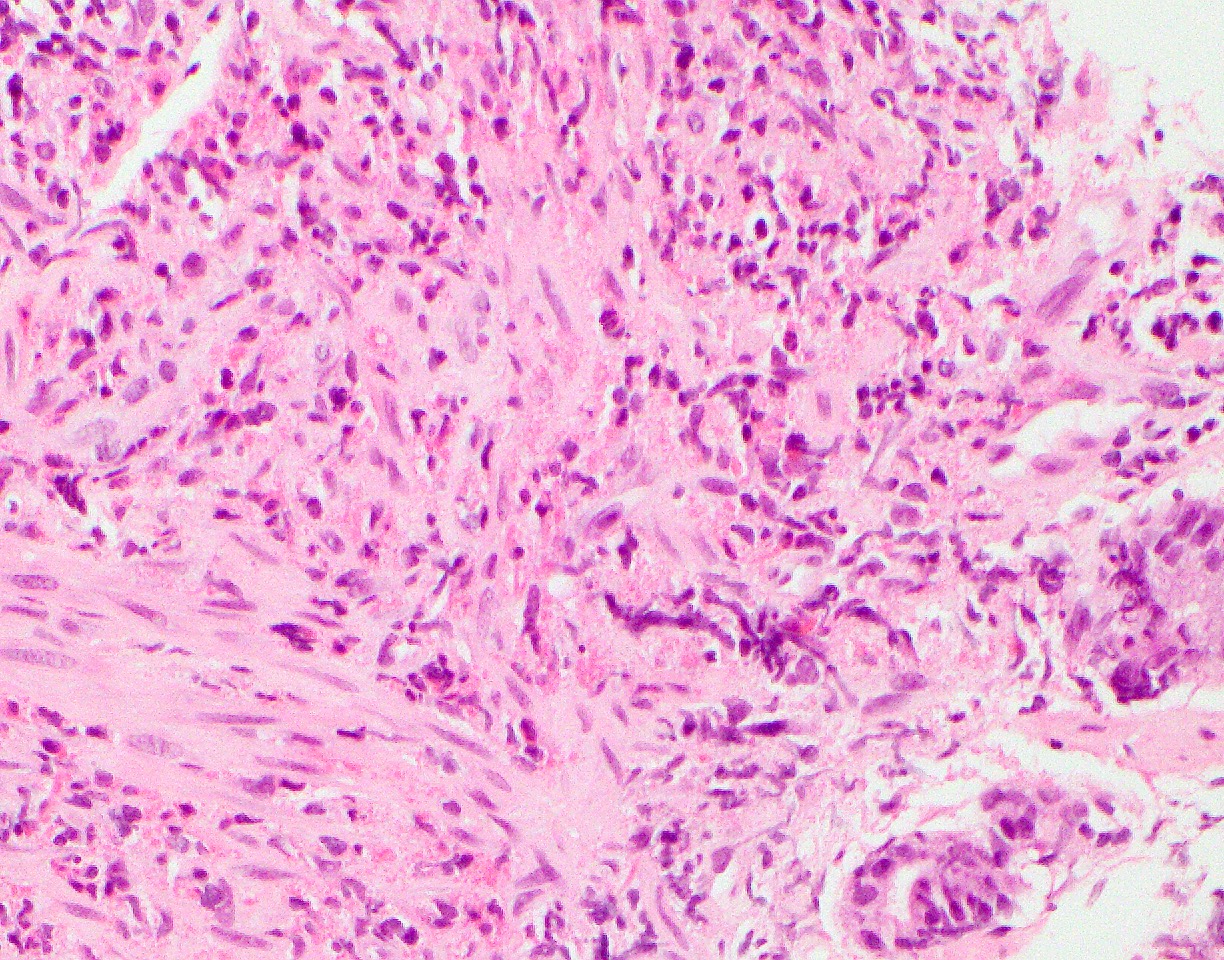
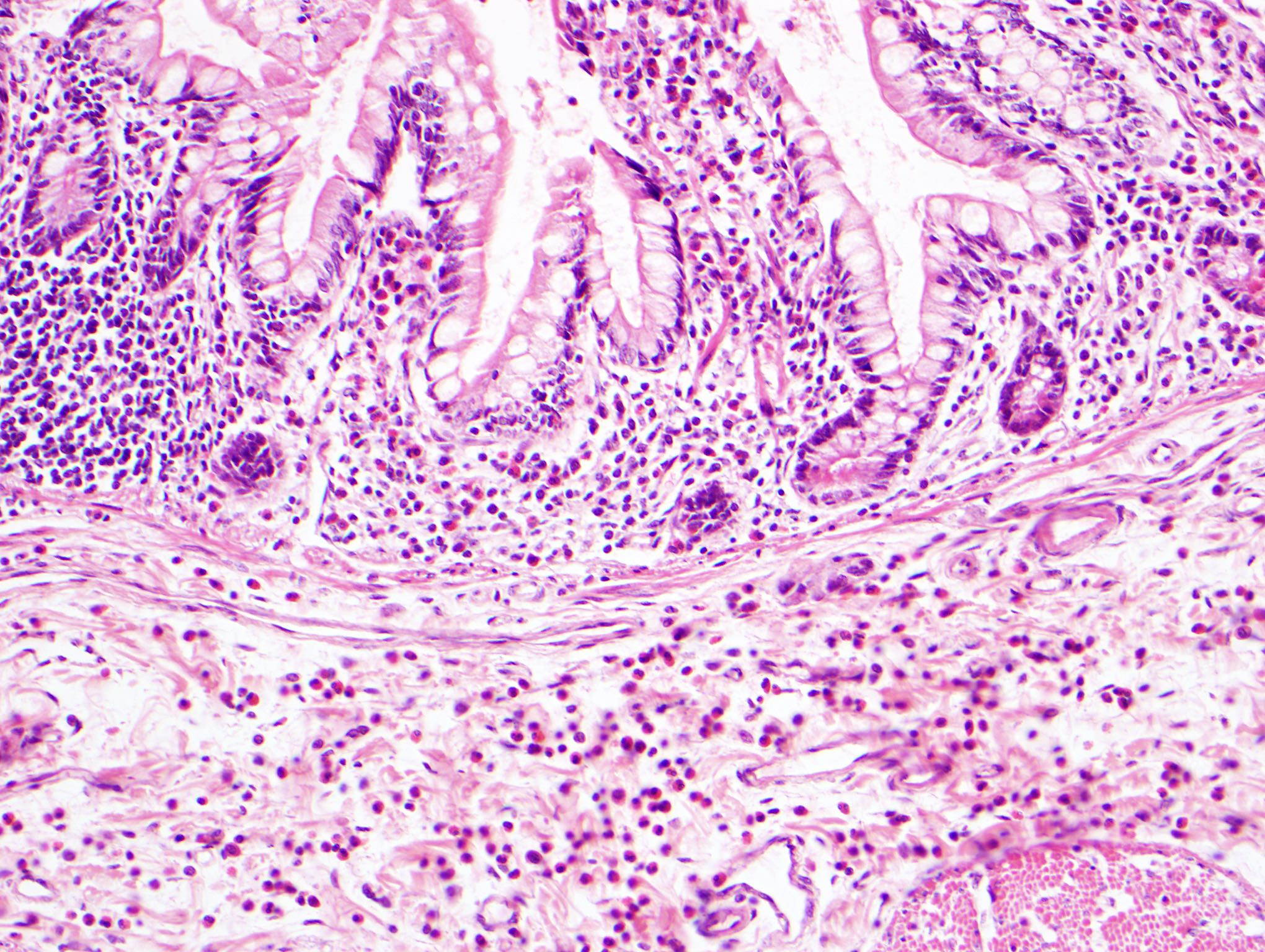
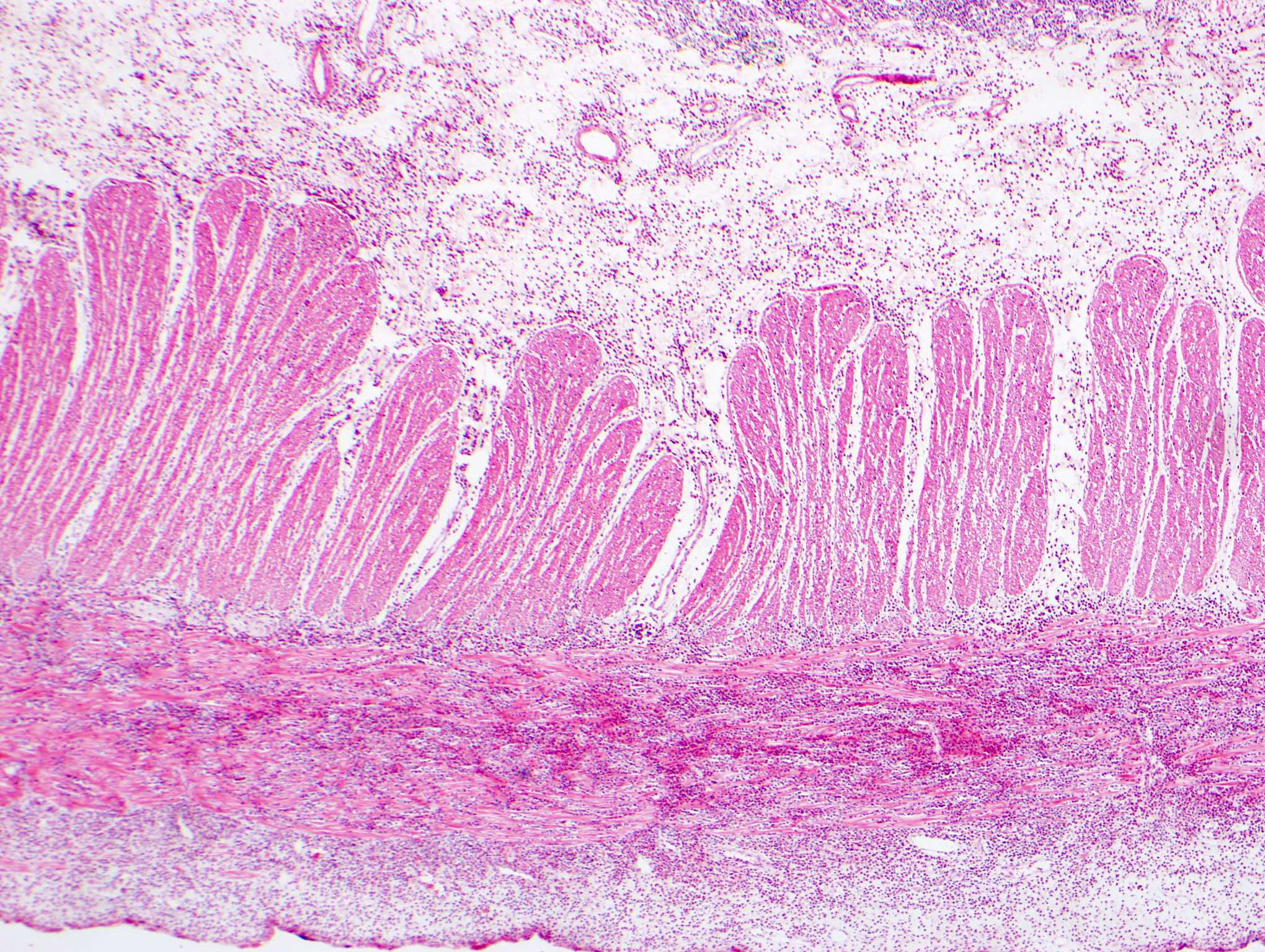
Microscopic (histologic) description
- Diagnosis requires confirmation by histopathological examination of gastric, small intestinal or large intestinal biopsies (Adv Anat Pathol 2011;18:335)
- Distribution of eosinophils may be patchy (obtaining multiple biopsy samples is helpful)
- Eosinophils are seen in the entire gastrointestinal tract except in the esophagus in a normal physiologic state; they are an essential part of the innate immune system of the digestive tract
- Ranges of normal numbers of eosinophils in different sites of the GI tract and different individuals vary significantly (J Allergy Clin Immunol 2004;113:11, Mod Pathol 1996;9:110)
- Highest concentration of eosinophils found in the cecum and appendix (up to 30/high power field) (Mod Pathol 1996;9:110, J Gastroenterol 2008;43:741)
- Lack of consensus on histological features of EGEC due to the relative rarity of the disease and variation of the numbers of eosinophils but it is characterized by prominent eosinophilic infiltration of the wall (most commonly affected sites: stomach and small intestine) (Case Rep Gastroenterol 2013;7:293)
- No established cutoff for the number of eosinophils/high power field to diagnose EGECs
- Pathologists should comment on the findings if eosinophils are more than expected
- Recently suggested cutoff numbers are shown below but they are not formal diagnostic criteria (Gastroenterol Clin North Am 2014;43:257):
- Stomach: ≥ 30 eosinophils/high power field in 5 high power fields
- Duodenum: > 52 eosinophils/high power field
- Ileum: > 56/high power field in the ileum
- Right colon: > 100/high power field
- Transverse and descending colon: > 84/high power field
- Rectosigmoid colon: > 64/high power field
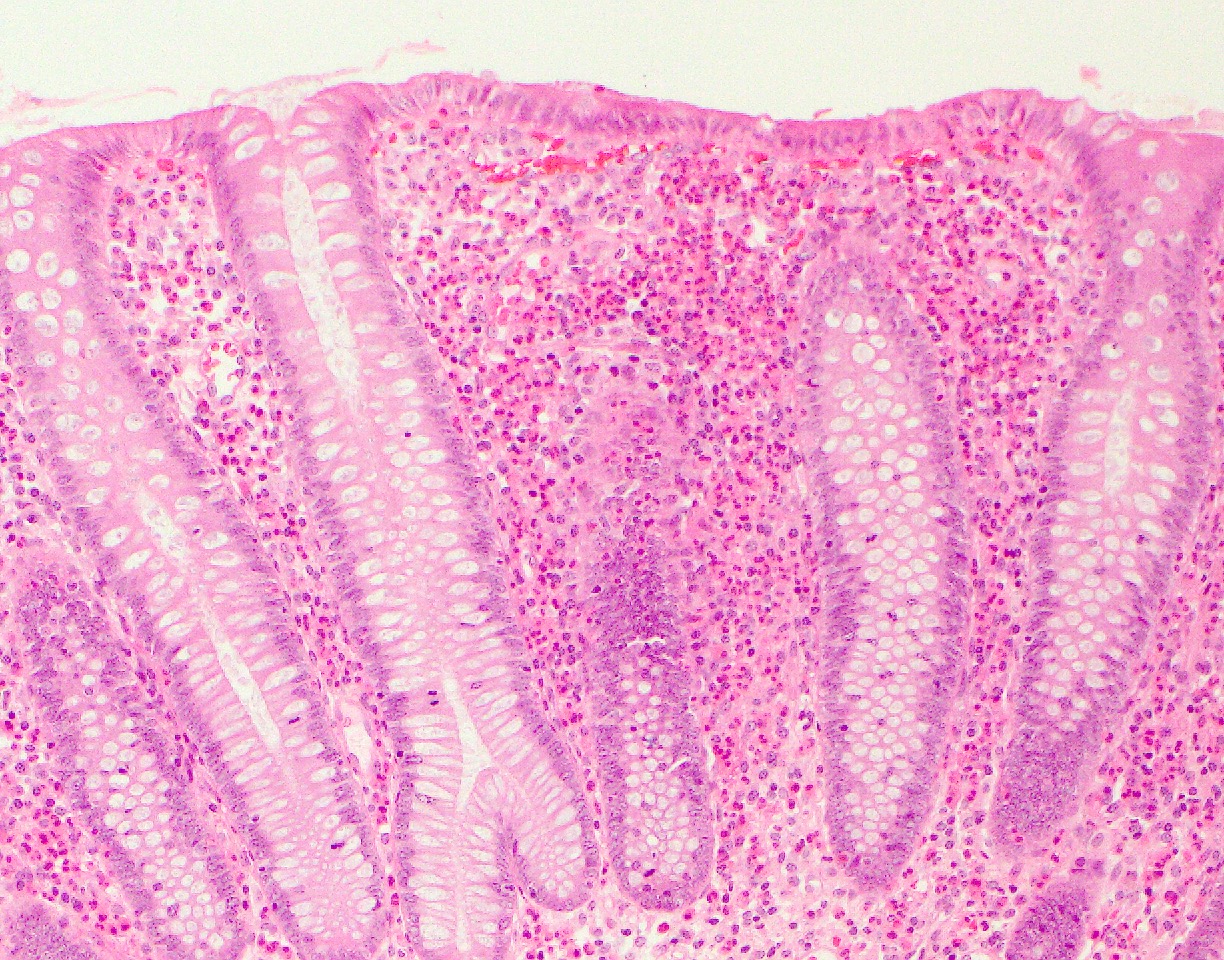
- Distribution of eosinophils is also an essential clue for EGEC irrespective of the eosinophil counts
- Presence of eosinophils within the crypts (intraepithelial eosinophils and eosinophilic crypt abscesses), clusters of eosinophils in lamina propria and eosinophils in muscularis mucosae are abnormal
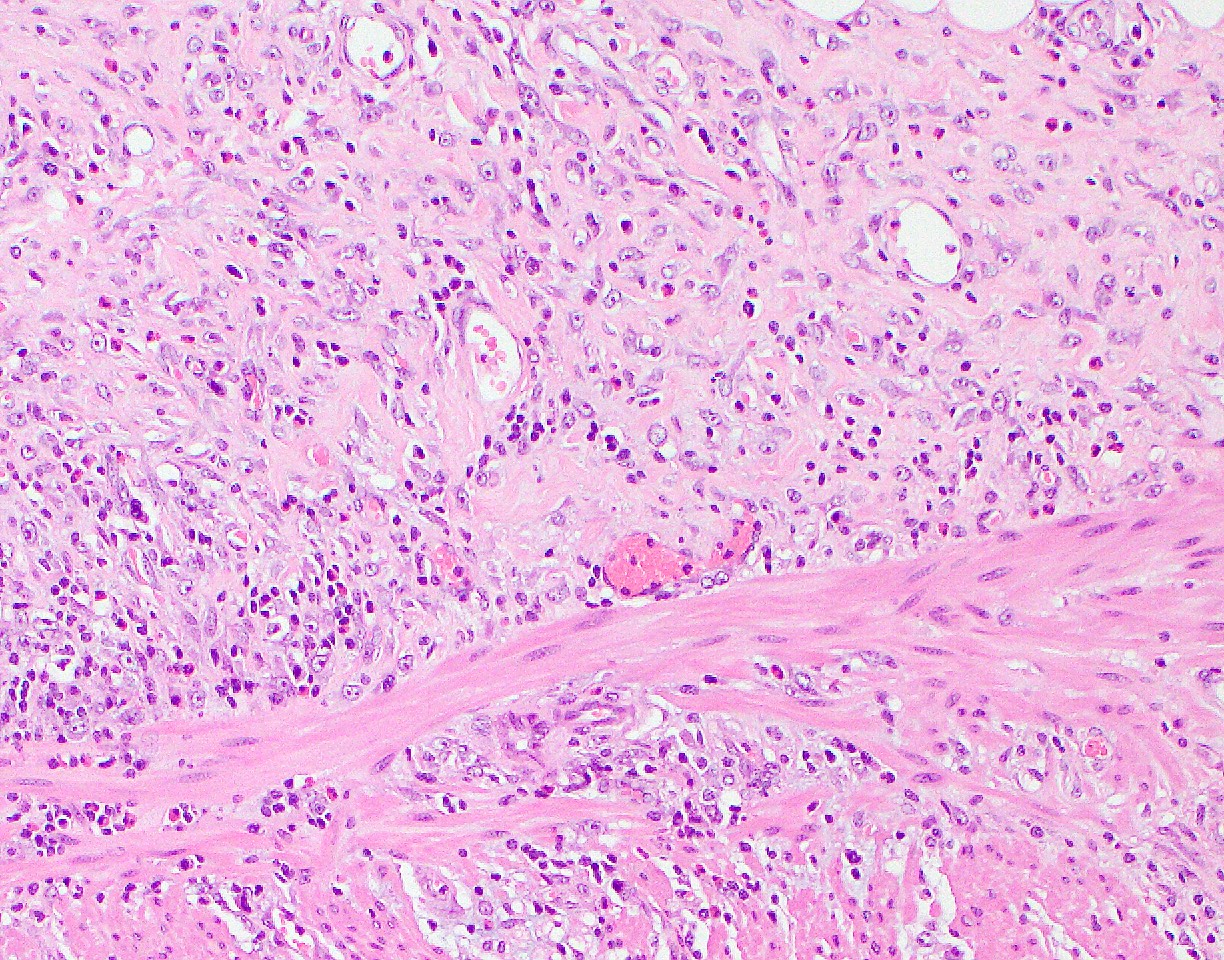
- In resection specimens, transmural eosinophilic infiltration may be present
- May accompany other inflammatory cells, especially mast cells
- Other nonspecific changes include edema, mucin depletion, erosion, reactive epithelial changes (foveolar hyperplasia and villous atrophy) and mild architectural distortion
- Areas of increased eosinophilic inflammation may show extracellular deposition of eosinophil granule constituents (Gastroenterology 1992;103:137)
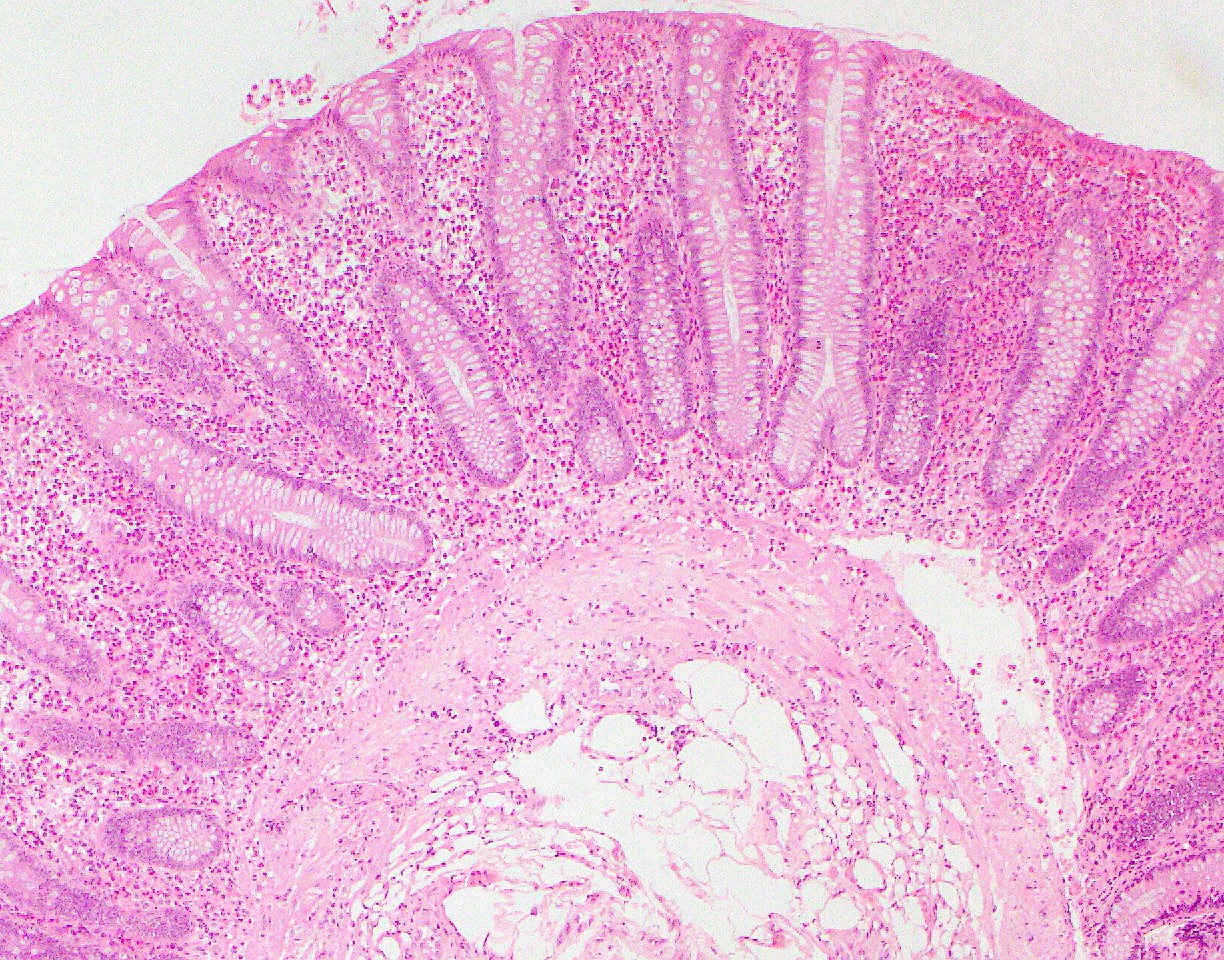
- Klein et al. classified the disease based on the location of the eosinophilic infiltration in the different layers of the intestinal wall (depth of eosinophilic infiltration) into mucosal, muscular and subserosal patterns of disease (Medicine (Baltimore) 1970;49:299)
- Mucosal:
- Most commonly reported; 57 - 100% of cases (Gut 1990;31:54, Clin Gastroenterol Hepatol 2010;8:669)
- Infiltration of the mucosa without the involvement of the muscular or serosal layers
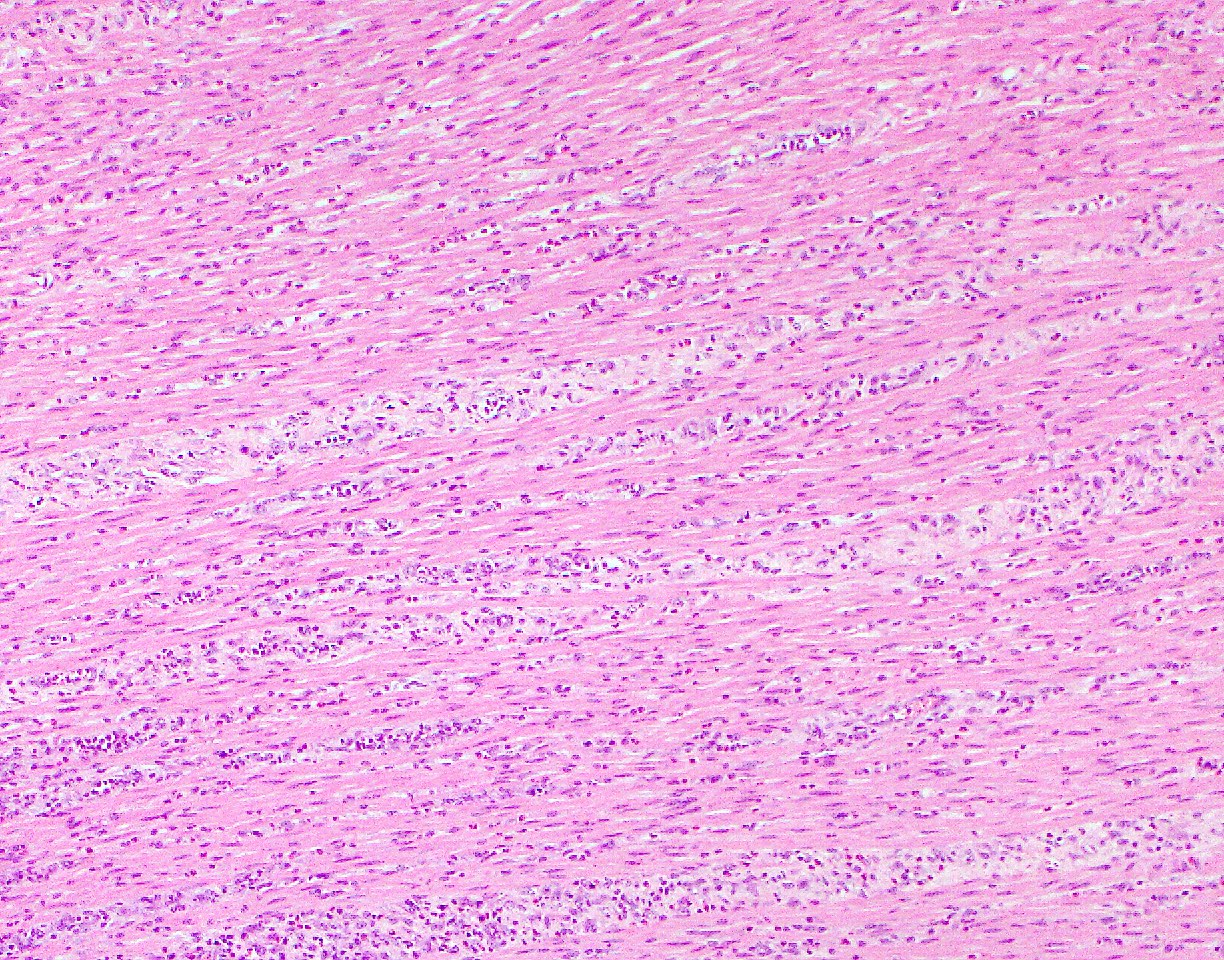
- Muscular:
- Second most commonly reported
- Infiltration of eosinophils predominantly in the muscle layer
- Causes wall thickening, which may lead to gastric outlet obstruction, intestinal obstruction or intussusception without eosinophilic ascites (World J Gastroenterol 2007;13:1758, Am Surg 1997;63:741)
- Subserosal:
- Most unusual form; estimated prevalence of up to 9% in Japan and 13% in the U.S. (Intern Med 1996;35:779)
- Infiltration of eosinophils in the serosa layer
- Hallmark of this type is ascitic fluid with eosinophilia
- Often accompanying peripheral eosinophilia, peritonitis (Medicine (Baltimore) 1970;49:299)
- May present with isolated abdominal ascites or ascites along with symptoms more characteristic of mucosal or muscular EGIDSs
- Chang et al. observed muscular and serosal types of having concomitant mucosal eosinophilic gastroenteritis, suggesting disease progression from mucosal to serosal (Clin Gastroenterol Hepatol 2010;8:669)
- Mucosal:
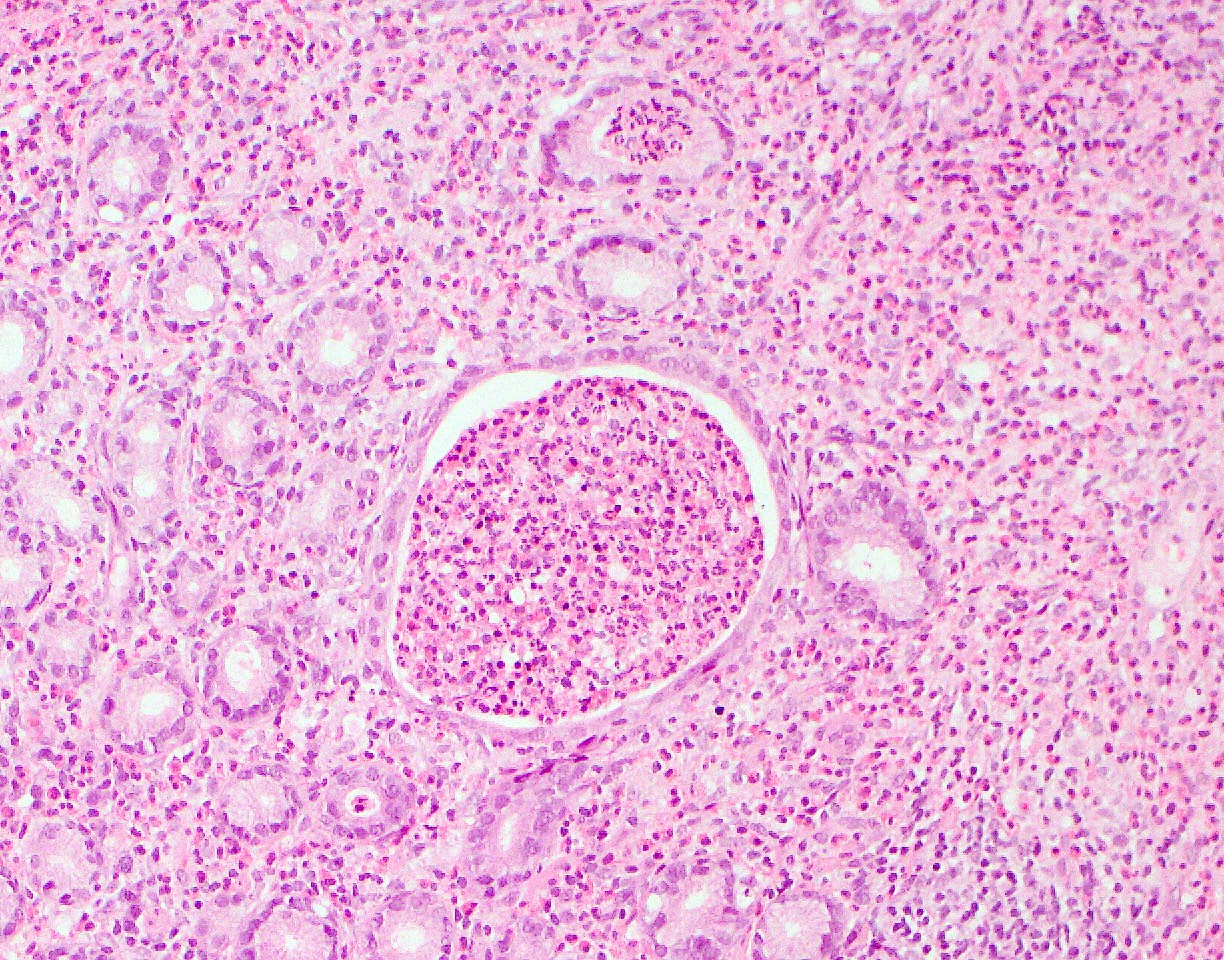
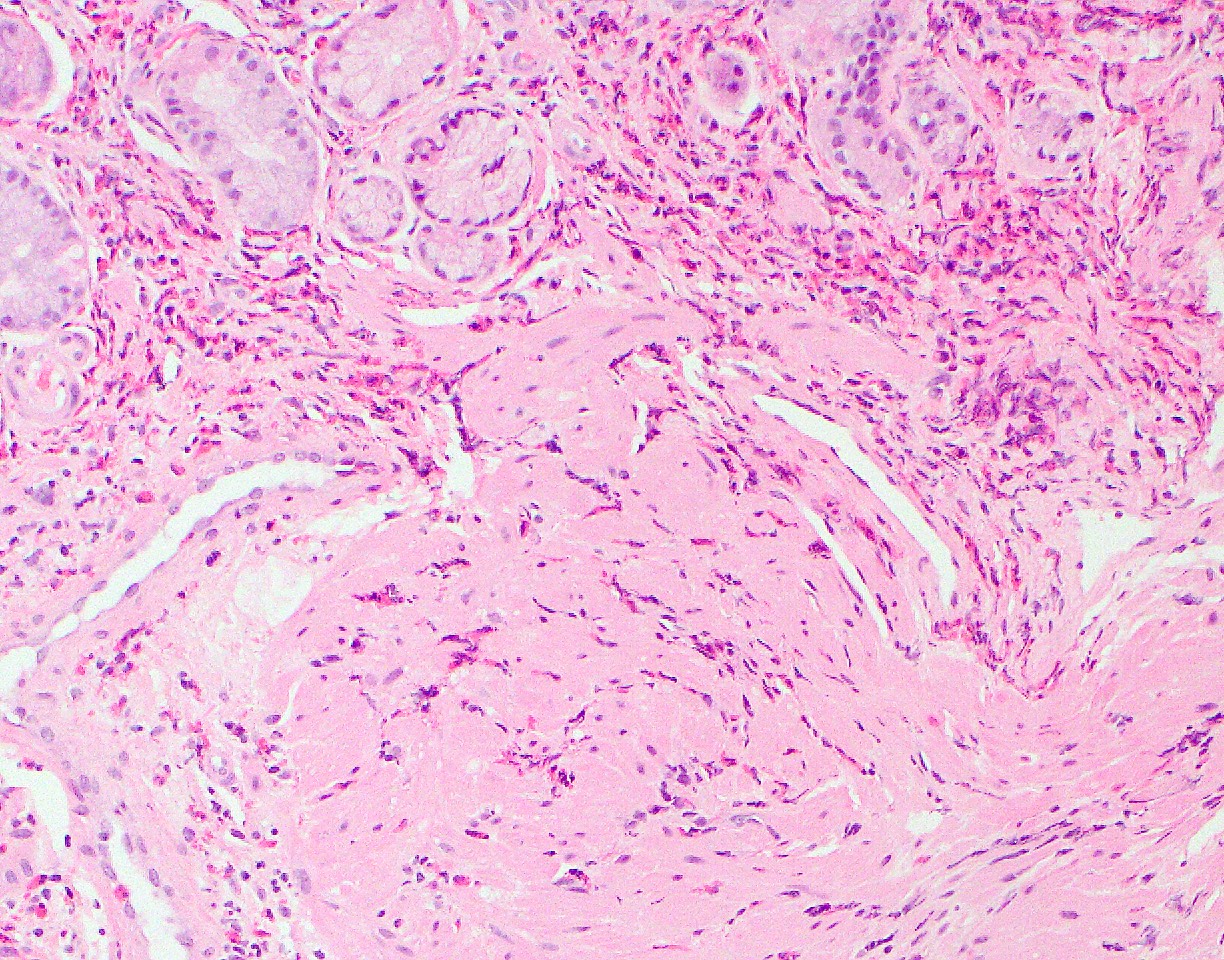
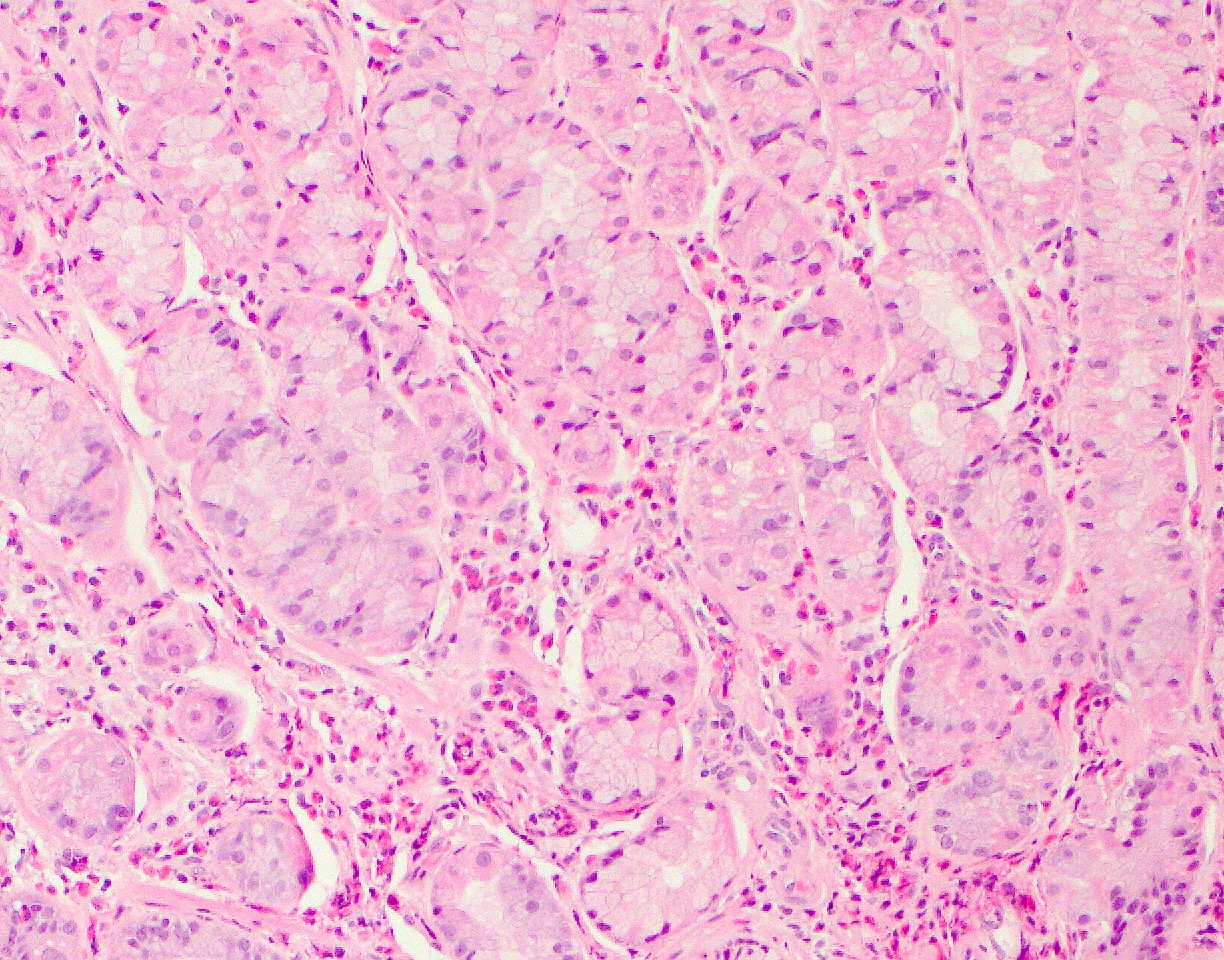
Microscopic (histologic) images
Contributed by Byoung Uk Park, M.D. and Lizhi Zhang, M.D.
Positive stains
- Major basic protein (MBP) (Allergy 2000;55:985)
Sample pathology report
- Small intestine and stomach, biopsy:
- Marked eosinophilic infiltration identified in both small bowel and gastric mucosa (see comment)
- Comment: The biopsy shows diffuse eosinophilic infiltrate (> 50/high power field) involving the mucosa and submucosa with focal intraepithelial eosinophils. No apparent microorganisms, neutrophils, vasculitis or granulomas are identified. In the appropriate clinical setting, the findings may be indicative of eosinophilic gastroenteritis. Clinical and pathologic correlation and further workup are recommended to rule out secondary causes of the observed eosinophilia.
Differential diagnosis
- Parasitic or bacterial infections:
- Enterobius (pinworms), Ancylostoma (hookworms), Ascaris, Anisakis, Eustoma, Trichuris and Schistosoma
- Toxocara canis can cause eosinophilic ascites
- Should be excluded
- H. pylori infection:
- Biopsy and silver stain to rule out H. pylori infection
- Reported cases of successful treatment of EGIDS with the eradication of H. pylori (Gut 2005;54:1822, J Clin Gastroenterol 2008;42:1063)
- Inflammatory bowel disease (Mayo Clin Proc 1997;72:117):
- May present with peripheral and intestinal eosinophilia
- Lacks the florid eosinophilia
- Hypereosinophilic syndrome:
- Rare and idiopathic condition
- Persistence (> 6 month) of marked peripheral eosinophilia (often exceeding > 1,500 eosinophils/microliter)
- Along with the presence of organ damage or dysfunction related to eosinophilic infiltration and release of mediators
- Most common presenting manifestation: dermatologic and pulmonary (J Allergy Clin Immunol 2009;124:1319)
- Vasculitis disorders (Churg-Strauss syndrome and polyarteritis nodosa):
- Eosinophilic infiltrate of the small vessels
- Peripheral eosinophilia
- Elevated markers of inflammation and autoantibodies
- Connective tissue disorders (scleroderma and dermatomyositis):
- Episodic peripheral eosinophilia and a band-like eosinophil and mast cell infiltrate of the lamina propria
- Drug hypersensitivity:
- Gastrointestinal eosinophilia has been associated with a long list of medications, such as carbamazepine, rifampicin, naproxen, NSAIDs, interferon, azathioprine, enalapril and gold compounds
- Mastocytosis and Langerhans histiocytosis:
- Gastrointestinal eosinophilia is usually seen in GI involvement by mastocytosis and Langerhans histiocytosis
- Besides eosinophils, prominent mononuclear cell infiltration with a nodular or tumefactive growth pattern is present
- Mononuclear cells may show characteristic morphologic features of either mast cells or Langerhans cells which immunohistochemical stains can confirm
Board review style question #1
Board review style answer #1
B. Eosinophils in muscularis mucosae. Prominent eosinophilic infiltration is a hallmark of eosinophilic gastroenterocolitis (EGEC), which is sensitive but not specific for diagnosing EGEC. The cutoff numbers of eosinophilic counts have not been well established. On the other hand, the abnormal distribution of eosinophils, such as muscularis mucosae, in this case, is an essential clue for EGEC.
Comment Here
Reference: Eosinophilic gastroenterocolitis
Comment Here
Reference: Eosinophilic gastroenterocolitis
Board review style question #2
Which of the following statements are true regarding the histologic finding of the above gastric biopsy?
- Although there are increased eosinophils in the lamina propria, the eosinophil count does not meet the diagnostic criteria for eosinophilic gastritis
- Diagnosis of eosinophilic gastritis should be considered but exclusion of other known causes of tissue eosinophilia is needed
- Increased eosinophils in the lamina propria are diagnostic for eosinophilic gastritis
- Observed changes are diagnostic for H. pylori infection
- Similar finding in other sites of the GI tract in this patient is unlikely
Board review style answer #2
B. Diagnosis of eosinophilic gastritis should be considered but exclusion of other known causes of tissue eosinophilia is needed. The picture shows eosinophilia in gastric mucosa, which can be due to various causes, such as eosinophilic gastroenteritis, drug effect, parasites, hypereosinophilic syndrome, etc. The cutoff numbers of eosinophilic counts have not been well established for the diagnosis of eosinophilic gastroenterocolitis. Therefore, it is a diagnosis of exclusion and other known causes of tissue eosinophilia must be ruled out with clinical correlation.
Comment Here
Reference: Eosinophilic gastroenterocolitis
Comment Here
Reference: Eosinophilic gastroenterocolitis