Table of Contents
Definition / general | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Endoscopy findings | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Flow cytometry description | Videos | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shlyakhova N, Lu Y. Graft versus host disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachGVHD.html. Accessed April 2nd, 2025.
Definition / general
- Donor lymphocytes attack and damage recipient tissue after allogeneic transplant (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- Initially divided into acute ( < 100 days posttransplant) and chronic ( > 100 days posttransplant)
- Newer definition is based on the clinicopathologic correlation (NIH consensus development project, Biol Blood Marrow Transplant 2006;12:31)
Sites
- Most commonly affected site in GI tract is small bowel, followed by esophagus, stomach, colon or liver
- Any site can be affected from oral mucosa to anus
- Best diagnostic sites: duodenum and colon (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
Pathophysiology
- T cells of the donor attack the recipient tissue via cytokine release (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016, Am J Surg Pathol 2006;30:444)
Etiology
- Hematopoietic cell transplant (HCT) is one of the most common causes (40 - 80%) that lead to GVHD
- Solid organ transplant: small bowel transplant (5%) and other solid organs (1%) of all cases (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- Blood transfusion is a rare cause that occurs in immunosuppressed patients (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
Clinical features
- Acute GVHD: rash, abdominal cramps with diarrhea, rising serum bilirubin within first 100 days following transplantation (UpToDate: Clinical Manifestations, Diagnosis and Grading of Acute Graft Versus Host Disease [Accessed 1 August 2018])
- Nausea, vomiting, anorexia related to gastric pain, dyspepsia with or without diarrhea, GI bleeding (Am J Surg Pathol 2006;30:444)
Diagnosis
- Histologic criteria (grading) originally described in 1975 by Lerner et al. includes 4 histological grades for the GI biopsies (Transplant Proc 1974;6:367, Ann Intern Med 1994;120:143):
Organ Involvement Grade Skin Liver Gut I Epidermal, basal cell, vacuolar degeneration < 25% small interlobular bile ducts abnormal (degeneration or necrosis) Single cell necrosis of epithelial cells II Grade I changes plus "eosinophilic bodies" 25% to 50% bile ducts abnormal Necrosis and loss of glands III Grade II changes plus separation of the dermal epidermal junction 50% to 75% bile ducts abnormal Focal microscopic mucosal denudation IV Frank epidermal denudation > 75% bile ducts abnormal Diffuse mucosal denudation
- Currently, NIH consensus criteria incorporate timing of the presentation and clinical findings in addition to histologic criteria:
- Classic acute GVHD: cases present within 100 days of HCT and display features of acute GVHD; diagnostic and distinctive features of chronic GVHD are absent
- Persistent, recurrent, late onset acute GVHD: cases present greater than 100 days post-HCT with features of acute GVHD; diagnostic and distinctive features of chronic GVHD are absent
- Classic chronic GVHD: cases may present at any time post-HCT; diagnostic and distinctive features of chronic GVHD are present and there are no features of acute GVHD
- Overlap syndrome: cases may present at any time post-HCT with features of both chronic GVHD and acute GVHD; on occasion, this is colloquially referred to as "acute on chronic" GVHD (UpToDate: Clinical Manifestations, Diagnosis and Grading of Acute Graft Versus Host Disease [Accessed 1 August 2018])
- Diagnosis of chronic GVHD requires the presence of at least one diagnostic clinical sign of chronic GVHD or the presence of at least one distinctive manifestation confirmed by pertinent biopsy or other relevant tests in the same or another organ
- Other possible diagnoses for clinical symptoms must be excluded
- No time limit is set for the diagnosis of chronic GVHD (UpToDate: Clinical Manifestations, Diagnosis and Grading of Acute Graft Versus Host Disease [Accessed 1 August 2018])
- Pathology report recommendation:
- All pathology reports should report both histologic features and a final diagnosis
- Final diagnosis integrates the histopathologic results and the clinical context and is summarized in 1 of 4 categories:
- No GVHD
- Possible GVHD
- Consistent with GVHD (equivalent to "favor," "suggestive of" or "probable")
- Definite, unequivocal GVHD (Biol Blood Marrow Transplant 2006;12:31 )
Endoscopy findings
- Wildly variable with up to 40% normal appearing mucosa having histologic appearance of GVHD (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- None specific with 30 - 80% patients demonstrating GVHD after normal endoscopy (Am J Surg Pathol 2006;30:444)
- Presence of esophageal webs and scleroderma-like changes often constitutes chronic GVHD (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
Prognostic factors
- 50% of patients develop clinical problems - biggest cause of morbidity and mortality in long term hematopoietic cell transplant (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- Histologic grading (1 - 4) does not correlate with clinical outcome (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
Case reports
- 44 year old woman with fulminant gastrointestinal graft versus host disease with cytomegalovirus infection (World J Gastroenterol 2013;19:597)
Treatment
- Steroids, mycophenolate mofetil, tacrolimus, cyclosporine, infliximab, daclizumab
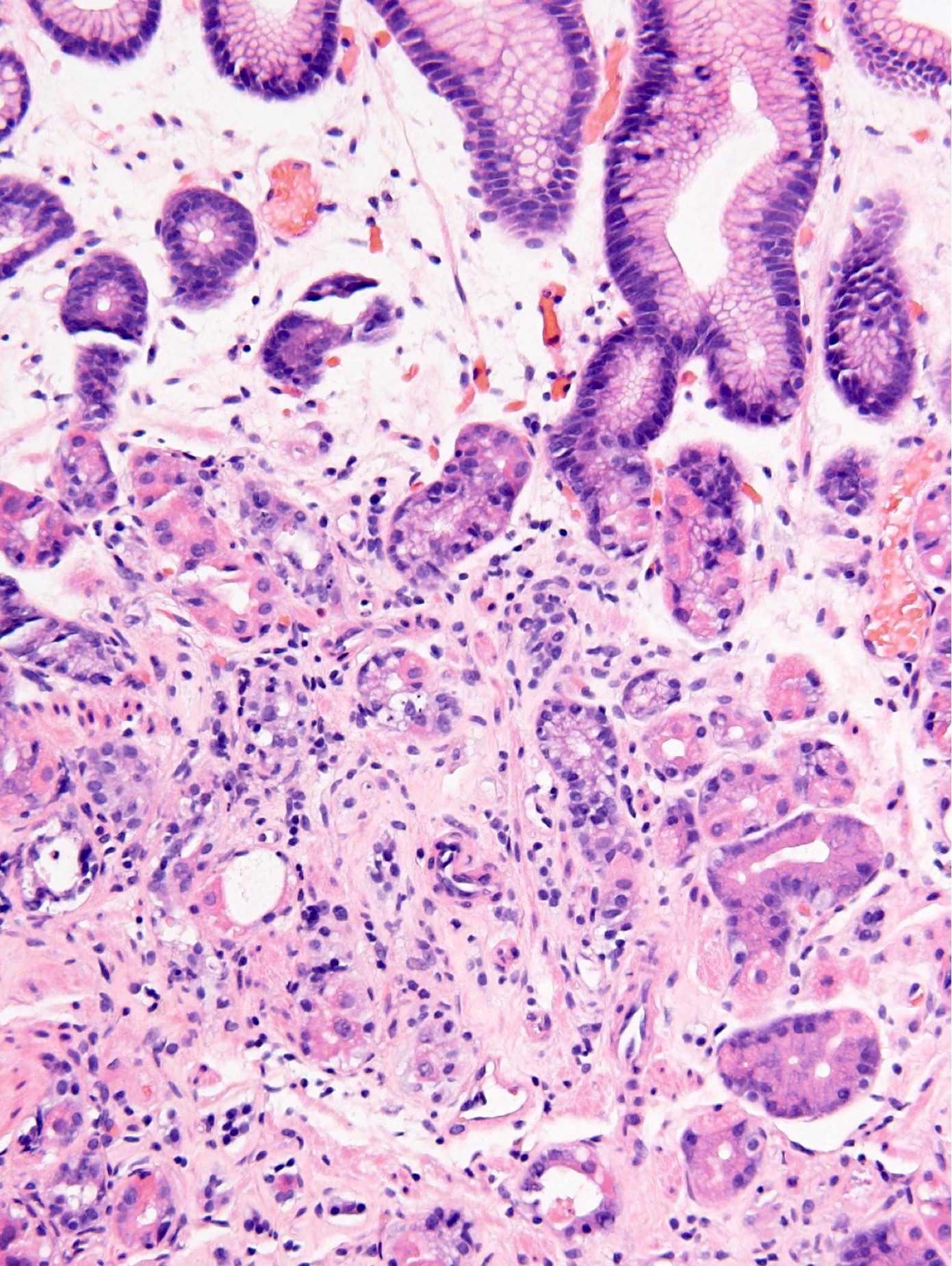
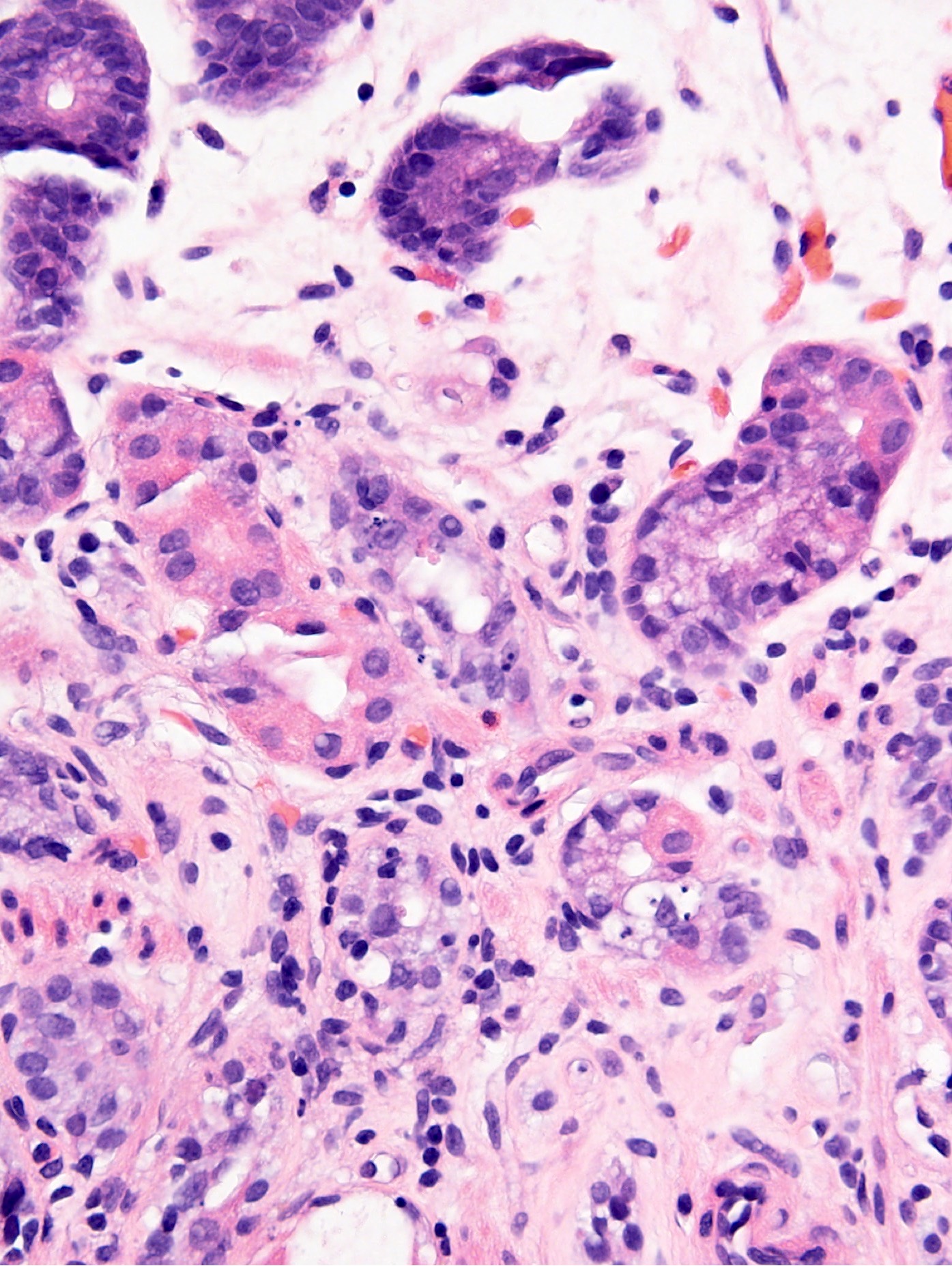
Microscopic (histologic) description
- Predominant pattern of injury: inflammatory
- Predominant compartment: epithelial, glandular
- Apoptosis is the main feature of GVHD although not specific
- Few lymphocytes or eosinophils could be present in the crypts
- Paucity of the inflammation in the lamina propria
- Mucosa may be completely denuded
- May have severe gland or crypt distortion mimicking IBD (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- Gastric endocrine cells are generally resistant to GVHD in the GI tract and could be mistaken for an infiltrating adenocarcinoma in a single cell pattern in a biopsy specimen (Odze and Goldblum: Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2014)
- Active GVHD: > 1 apoptotic figure in crypts per biopsy piece
- Chronic: destruction of glands, ulceration or submucosal fibrosis reflects long standing disease but are not specific for chronic GVHD (Biol Blood Marrow Transplant 2006;12:31)
- Different institutions use different diagnostic threshold for GVHD; for some, finding a single epithelial apoptotic body in the gastric biopsy is considered a diagnostic finding in the gastric biopsy performed for GVHD (Am J Surg Pathol 2006;30:444)
- Chronic features such as: fibrosis / stenosis, Paneth cell metaplasia and crypt distortion all can occur in acute GVHD (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
Microscopic (histologic) images
Flow cytometry description
- Activated peripheral blood T cells may reflect acute GVHD (Blood 2012;120:691)
Videos
Chronic graft versus host disease and the gastrointestinal tract
Differential diagnosis
- Chemotherapy effect (conditioning): wait 21 days to differentiate (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- Infections: CMV, adenovirus, cryptosporidiosis (apoptosis induction)
- PMNs - bacterial infection (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
- Mycophenolate mofetil effect: look for dilated crypts filled with eosinophils to differentiate (Greenson: Diagnostic Pathology - Gastrointestinal, 2nd Edition, 2016)
Additional references
Board review style question #1
What is the differential diagnosis for gastrointestinal GVHD?
- Chemotherapy
- CMV infection
- Cryptosporidiosis
- H. pylori infection
- Mycophenolate mofetil treatment
- NSAIDs
- Oral sodium phosphate bowel preparation
- All of the above
Board review style answer #1
Board review style question #2
What type of cell is generally resistant to GVHD in the GI tract and could be mistaken for an infiltrating adenocarcinoma in a single cell pattern in a biopsy specimen?
- Esophageal mucosa squamous cells
- Gastric endocrine cells
- Gastric glandular cells
- Goblet cells
- Paneth cells
- None of the above
- All of the above
Board review style answer #2