Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Bell P, Findeis-Hosey J. GIST. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachGIST.html. Accessed March 27th, 2025.
Definition / general
- Most common mesenchymal tumor of the gastrointestinal tract
- Arises from the interstitial cells of Cajal within the myenteric plexus of the muscularis propria
- Micro / mini / subclinical GIST: minute growths (1 - 10 mm) of interstitial cells of Cajal / GIST-like cells (Am J Pathol 2002;160:1567)
- Extragastrointestinal GIST: GIST arising outside of the gastrointestinal tract (omentum, mesentery, retroperitoneum or pleura)
Essential features
- Most common in stomach
- Most due to mutations in proto-oncogene KIT (exon 11)
- 3 histologic types: spindle, epithelioid and mixed
- Prognosis: depends on tumor size, mitotic rate and site of origin
- Treatment: surgical excision or imatinib
Terminology
- Gastrointestinal stromal tumor (GIST)
- Historic terms:
- Gastrointestinal smooth muscle tumor
- Gastrointestinal autonomic nerve tumor
- Leiomyoblastoma
- Smooth muscle tumor of uncertain malignant potential
- Gastrointestinal pacemaker cell tumor
ICD coding
Epidemiology
- M:F = 1:1, no clear sex predilection
- Mean age at diagnosis: 60 - 65 years old
- Annual incidence: 11 - 18 per million (World J Gastroenterol 2006;12:2223, Eur J Cancer 2005;41:2868, Cancer 2005;103:821, APMIS 2010;118:648)
Sites
- Can occur anywhere along the tubular gastrointestinal tract
- Stomach (60%) > jejunum and ileum (30%) > duodenum (4 - 5%) > rectum (4%) > colon and appendix (1 - 2%) > esophagus (< 1%) (Semin Diagn Pathol 2006;23:70)
Pathophysiology
- Activating mutations in the proto-oncogene KIT (~75%) (Science 1998;279:577) or platelet derived growth factor receptor-α (PDGFR-α) (~10%) (Science 2003;299:708)
- Leads to constitutive phosphorylation of the receptor tyrosine kinase and activation of downstream pathways → cell proliferation and survival
- KIT and PDGFRA mutations are mutually exclusive in GIST
- Succinate dehydrogenase deficient GIST (Am J Surg Pathol 2010;34:636)
- Young adults (before age 40)
- 1 - 2% of all GIST in pediatric patients (J Pediatr Hematol Oncol 2005;27:179, Cancer Res 2007;67:9084)
- Female preponderance (> 2:1)
- Almost exclusively in stomach (predilection for distal stomach and antrum)
- Pathophysiology:
- SDH is an enzyme complex in the electron transport chain and Krebs (citric acid) cycle, composed of 4 subunits (SDHA, SDHB, SDHC, SDHD)
- In the Krebs cycle, SDH catalyzes oxidation of succinate to fumarate
- Mutations in 1 of the subunits (most commonly SDHA) results in succinate accumulation, increased transcription of HIF1α-regulated genes and decreased DNA methylation
- Loss of SDHB immunoexpression
- Young adults (before age 40)
- Recently identified, less well understood mutations
- NF1 mutation
- Mutations in the RAS / RAF / MEK pathway (ex. ETV1 transcription factor associated with GIST formation)
Etiology
- Unknown at this time
- Most are sporadic
- Small percentage are familial
Clinical features
- SDH deficient GIST
- Carney triad: GIST, pulmonary chondroma, paraganglioma
- Nonhereditary
- SDHC promoter hypermethylation
- Small percentage have germline SDH mutations
- Carney-Stratakis syndrome: GIST and paraganglioma
- Hereditary, autosomal dominant
- Germline mutations in SDHB, SDHC or SDHD subunit
- Carney triad: GIST, pulmonary chondroma, paraganglioma
- Neurofibromatosis (NF): 7% of patients with NF1 develop 1 or more GIST, usually in small bowel (Am J Surg Pathol 2005;29:1170, Am J Surg Pathol 2006;30:90, Hum Mol Genet 2006;15:1015)
- Familial: germline mutations in KIT or PDGFRα autosomal dominant
- Immunopositive for SDHB
Diagnosis
- Patients most commonly present with gastrointestinal bleeding or abdominal pain
- May be an incidental finding during radiologic or endoscopic workup for other clinical issues
- Endoscopy show as a subepithelial lesion
- Definitive diagnosis cannot be made without histologic examination
Laboratory
- No significant laboratory findings
Radiology description
- Radiologic findings are variable, depending on size and time of presentation
- CT usually shows a solid, heterogeneous mass (reflecting the presence of hemorrhage or cystic degeneration)
- Endoscopic ultrasound reveals a hypoechoic solid mass
Prognostic factors
- GIST can have clinically malignant behavior
- 25% of gastric GIST act malignant (Am J Surg Pathol 2005;29:52) versus 35 - 40% of small intestinal GIST (Am J Surg Pathol 2006;30:477)
- Prognosis depends upon tumor size, mitotic rate and site of origin (Semin Diagn Pathol 2006;23:70)
- Intraoperative tumor rupture is also associated with poorer prognosis
- Compete surgical resection: improved local recurrence rate and overall survival
- Incomplete resection particularly in the area of the rectum, is associated with a higher risk of recurrence
- 60 - 80% of patients with SDH deficient GIST developed distant metastasis; however, the NIH risk stratification criteria may not be appropriate for this subtype (Am J Surg Pathol 2016;40:1616)
Gastric GIST: risk of disease progression (Semin Diagn Pathol 2006;23:70)
| Size | ≤ 5 mitoses per 50 HPF | > 5 mitoses per 50 HPF |
| > 10 cm | Moderate | High |
| > 5 to ≤ 10 cm | Low | High |
| > 2 to ≤ 5 cm | Very low | Moderate |
| ≤ 2 cm | No | No |
Case reports
- 18 year old man with a large gastric wall mass (Pediatr Dev Pathol 2019;22:492)
- 25 year old man complaining of abdominal pain is found to have a 4 cm gastric mass, which is resected (Case of the Month #523)
- 65 year old man with a 7.5 cm posterior gastric wall mass (SAGE Open Med Case Rep 2017 Dec 21 [Epub ahead of print])
- 70 year old man status post gastrectomy for gastric carcinoma with incidentally discovered nodules on gross examination (Gastrointest Tumors 2019;5:63)
- 77 year old man with 2 submucosal tumors in the stomach and duodenum (Intern Med 2018;57:1719)
Treatment
- Most GIST are treated with surgical resection
- Imatinib mesylate (Gleevec): tyrosine kinase inhibitor of KIT and PDGFRα
- Metastatic / recurrent GIST
- Sunitinib malate (Sutent): a tyrosine kinase inhibitor of KIT, PDGFRα, VEGFR
- Imatinib resistant GIST
- SDH deficient tumors are less responsive to tyrosine kinase inhibitor
Gross description
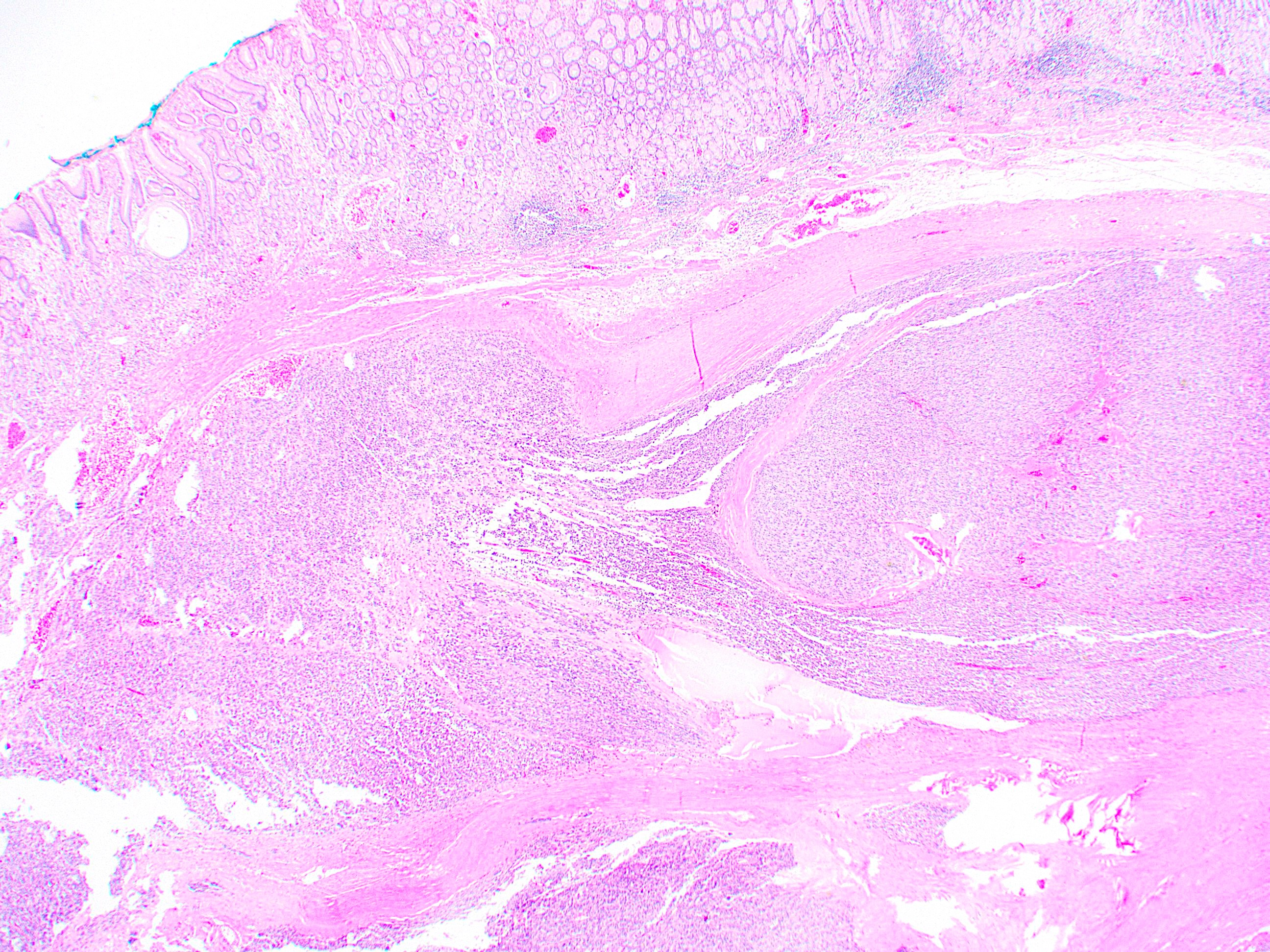
- Well circumscribed, intramural lesion, centered within the muscularis propria
- Fleshy, tan-pink cut surfaces, which may show hemorrhage or cystic degeneration
- Mean size 6 cm (0.4 - 40 cm) (Am J Surg Pathol 2005;29:52)
Frozen section description
- Spindle cell neoplasm
Frozen section images
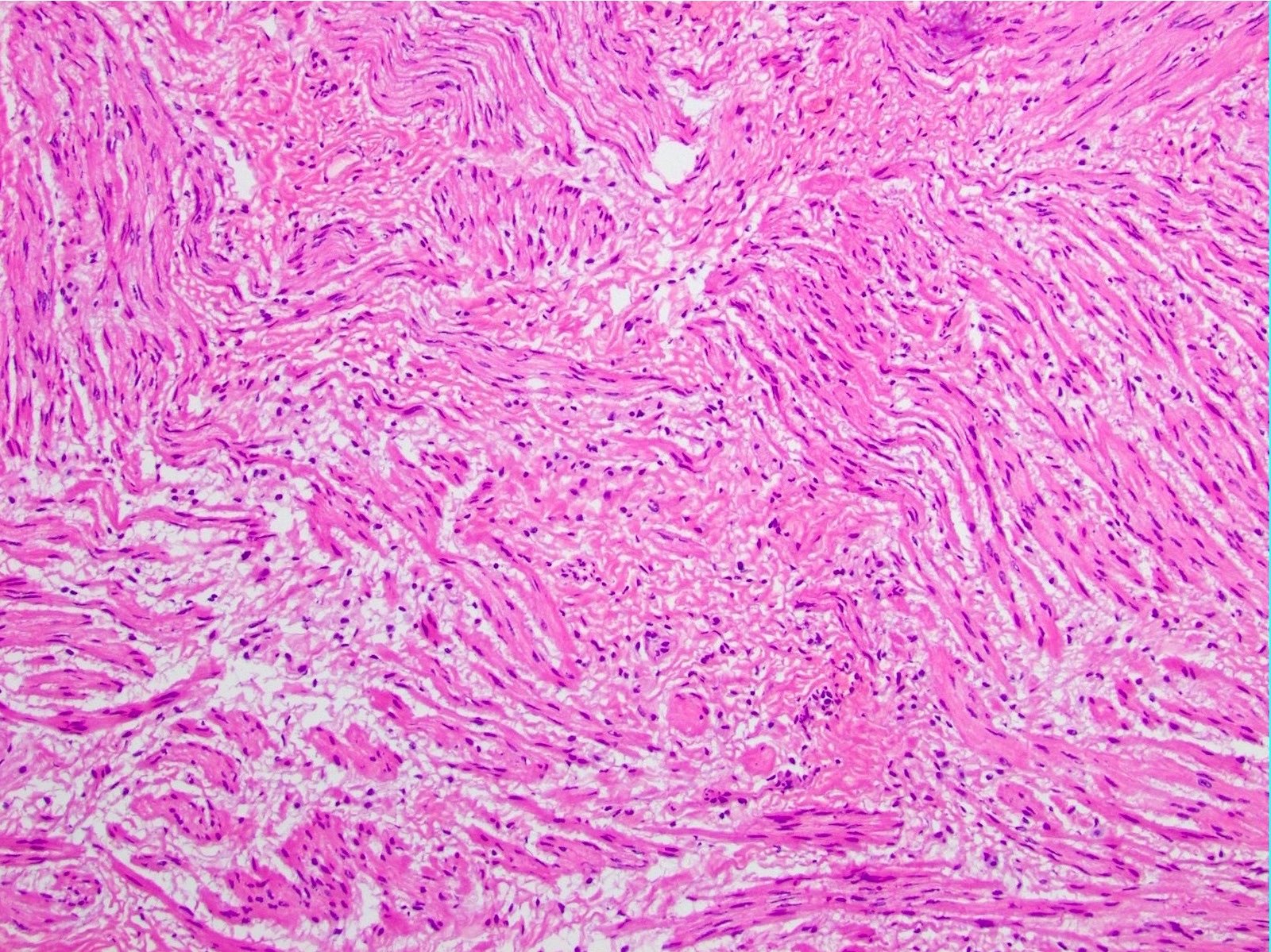
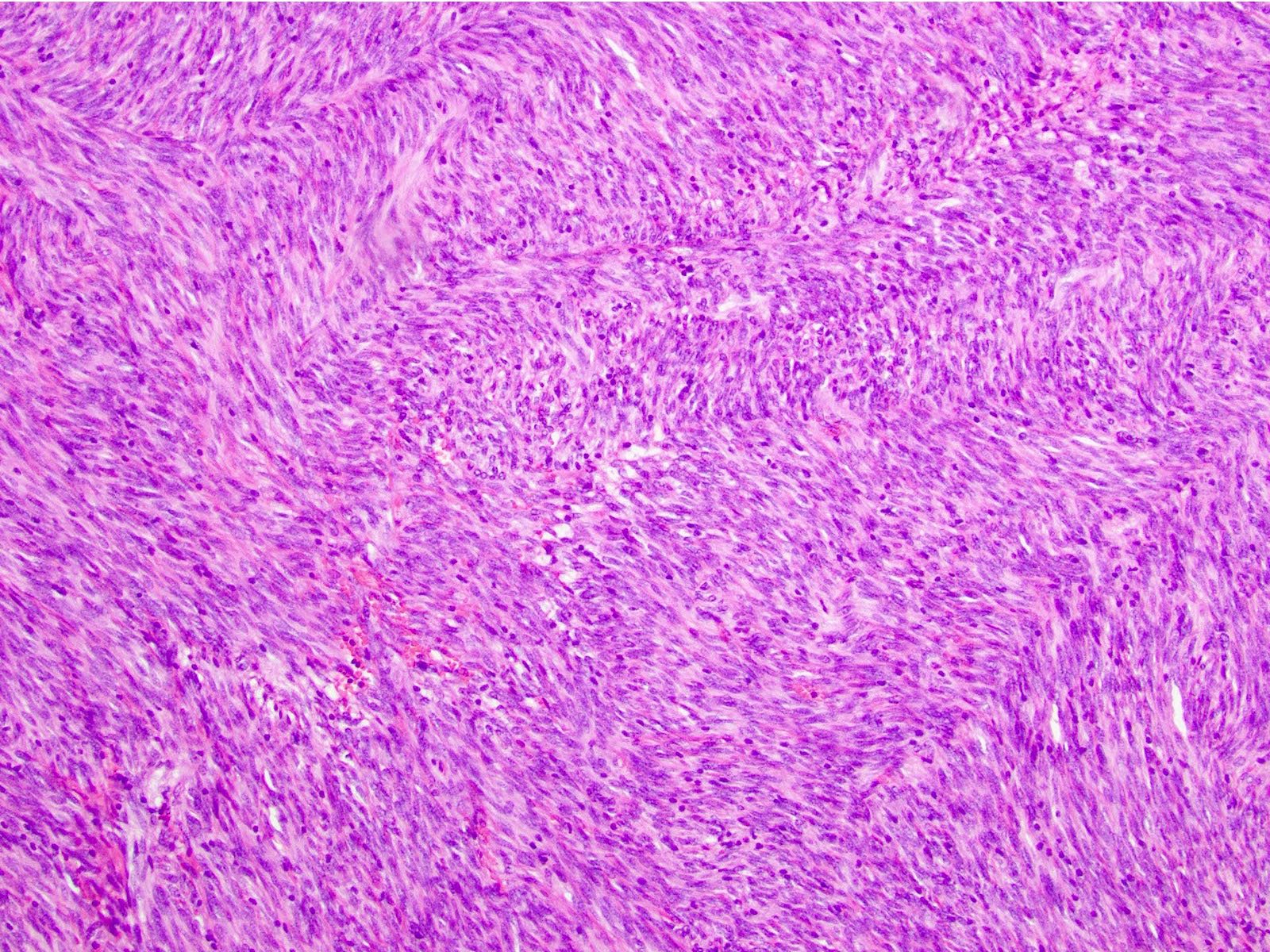
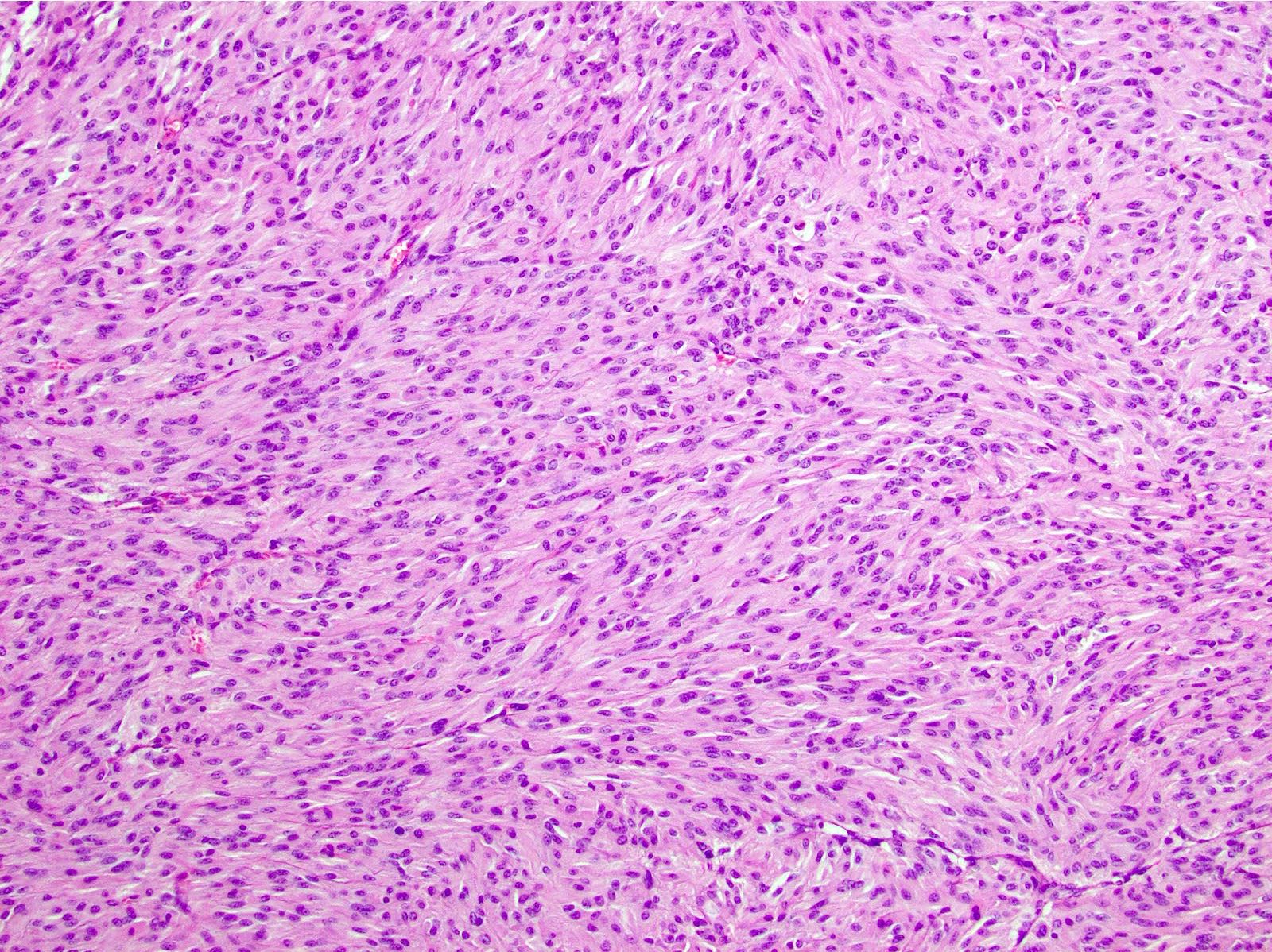
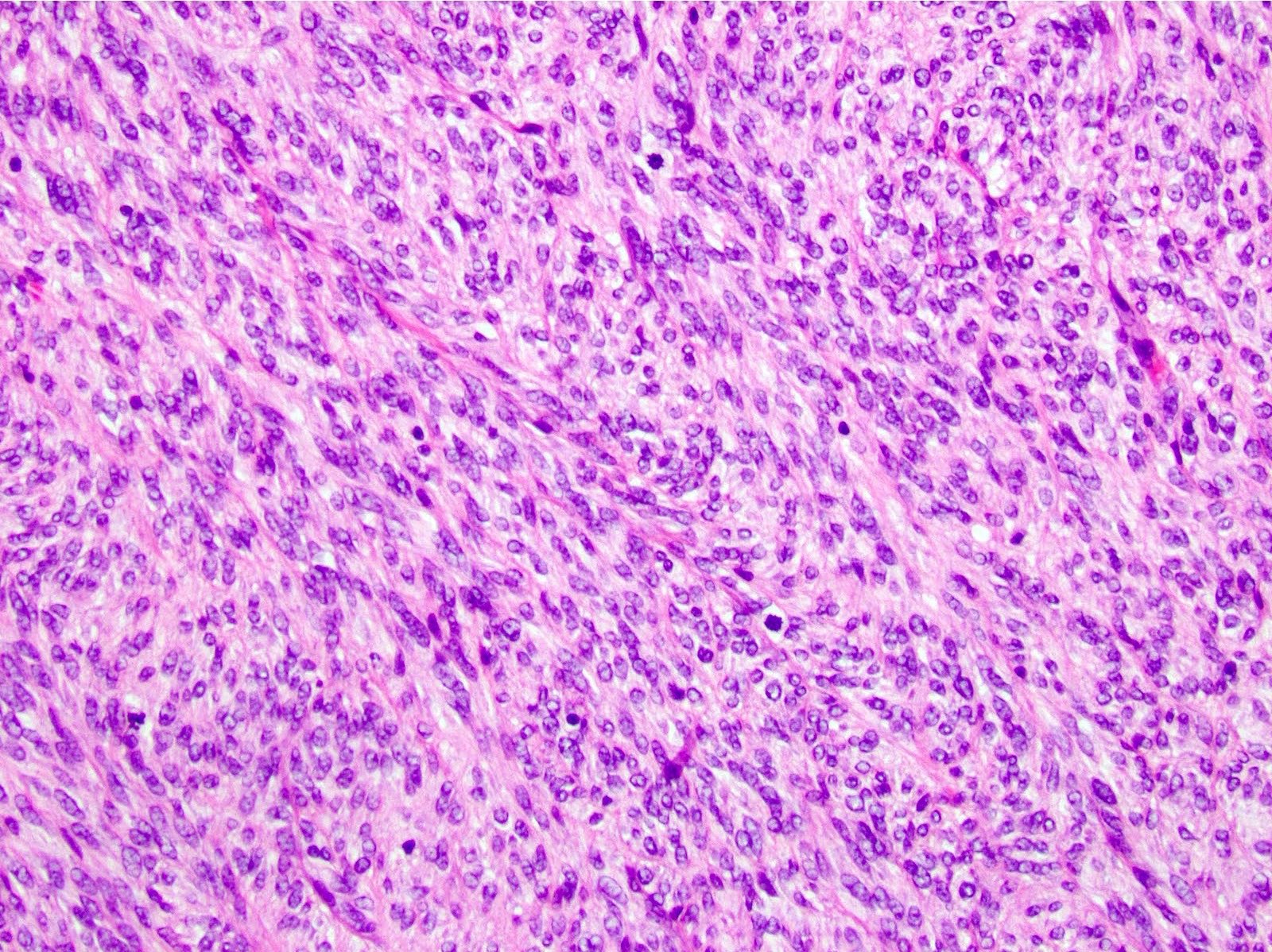
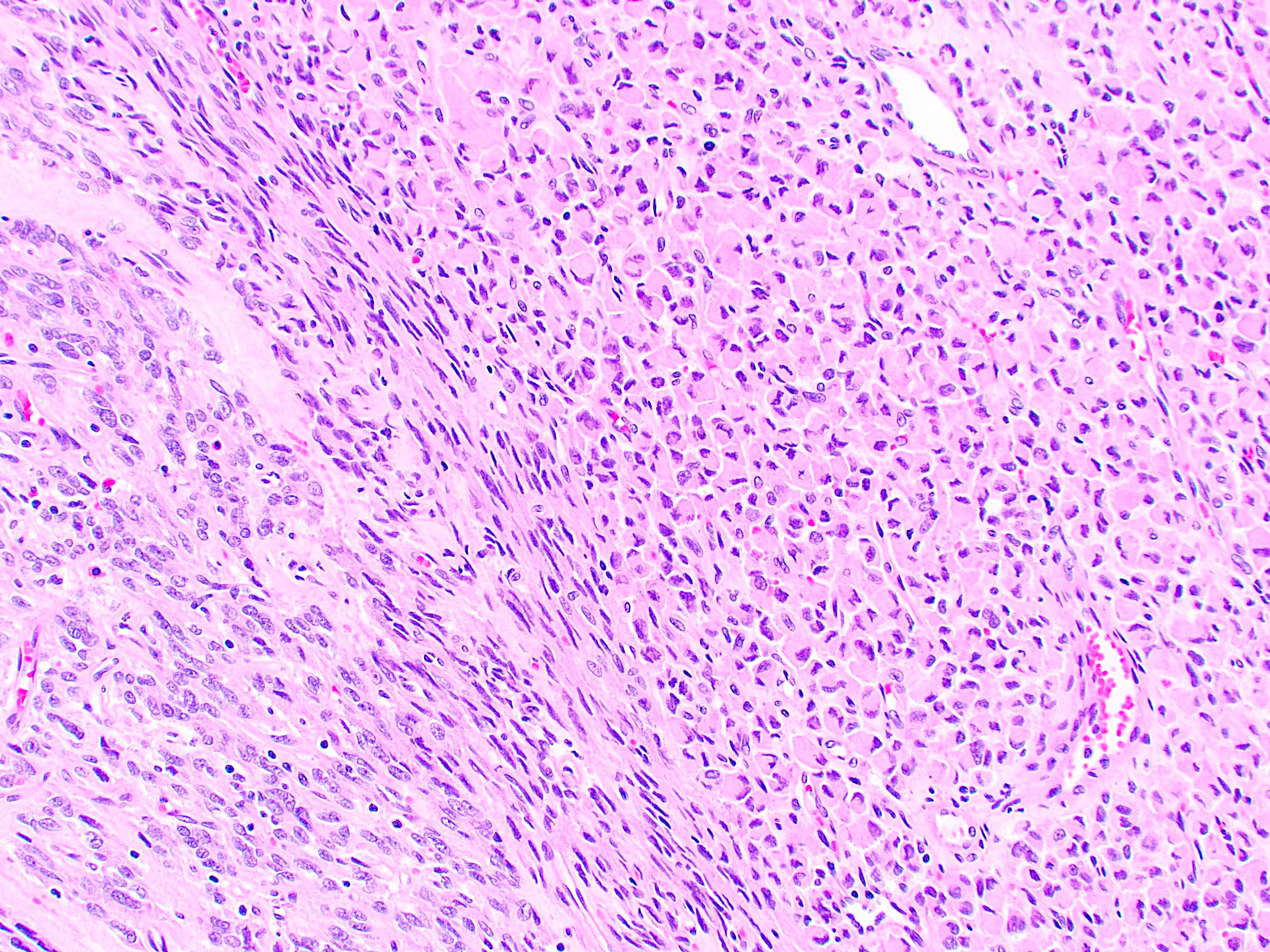
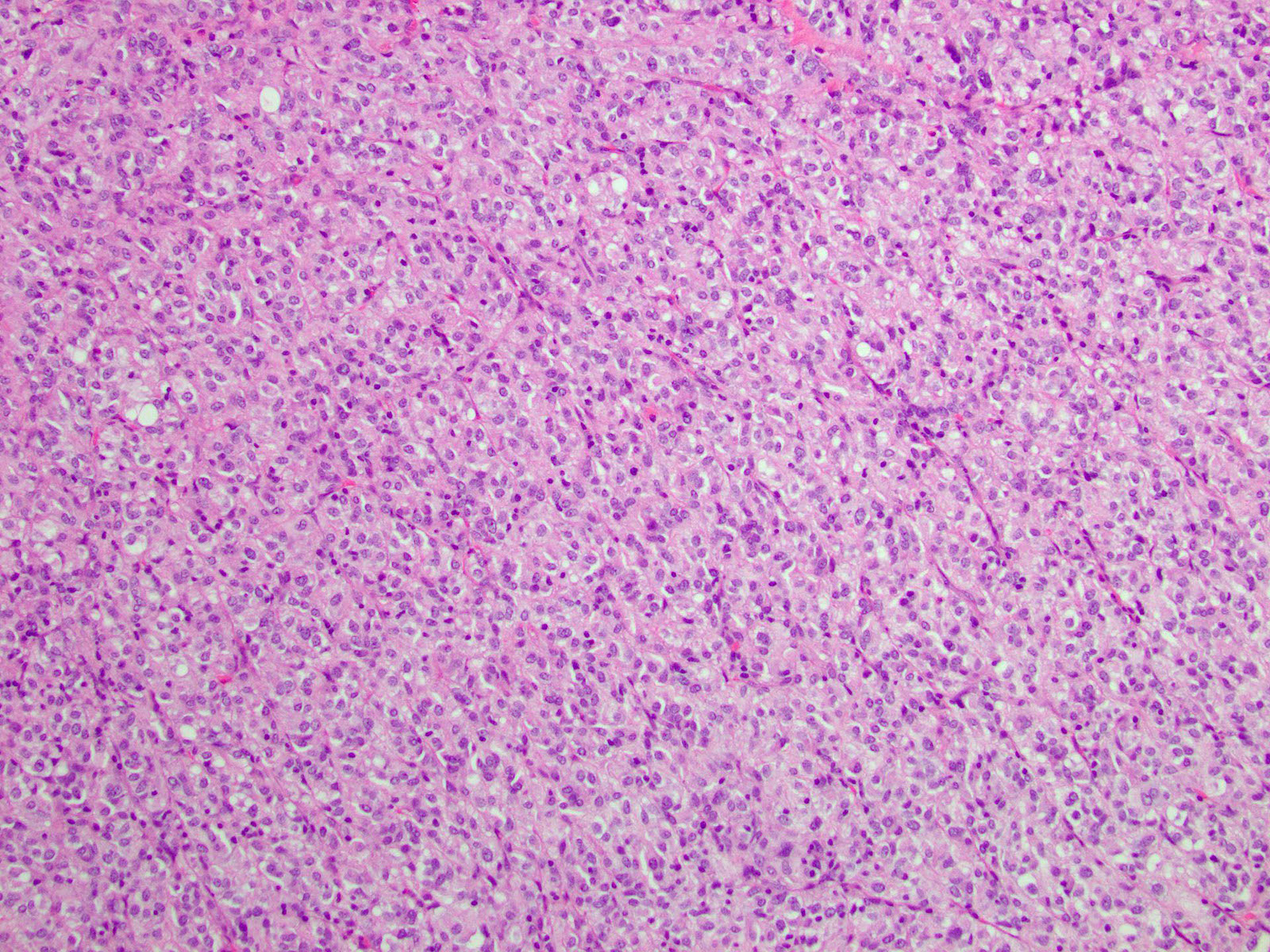
Microscopic (histologic) description
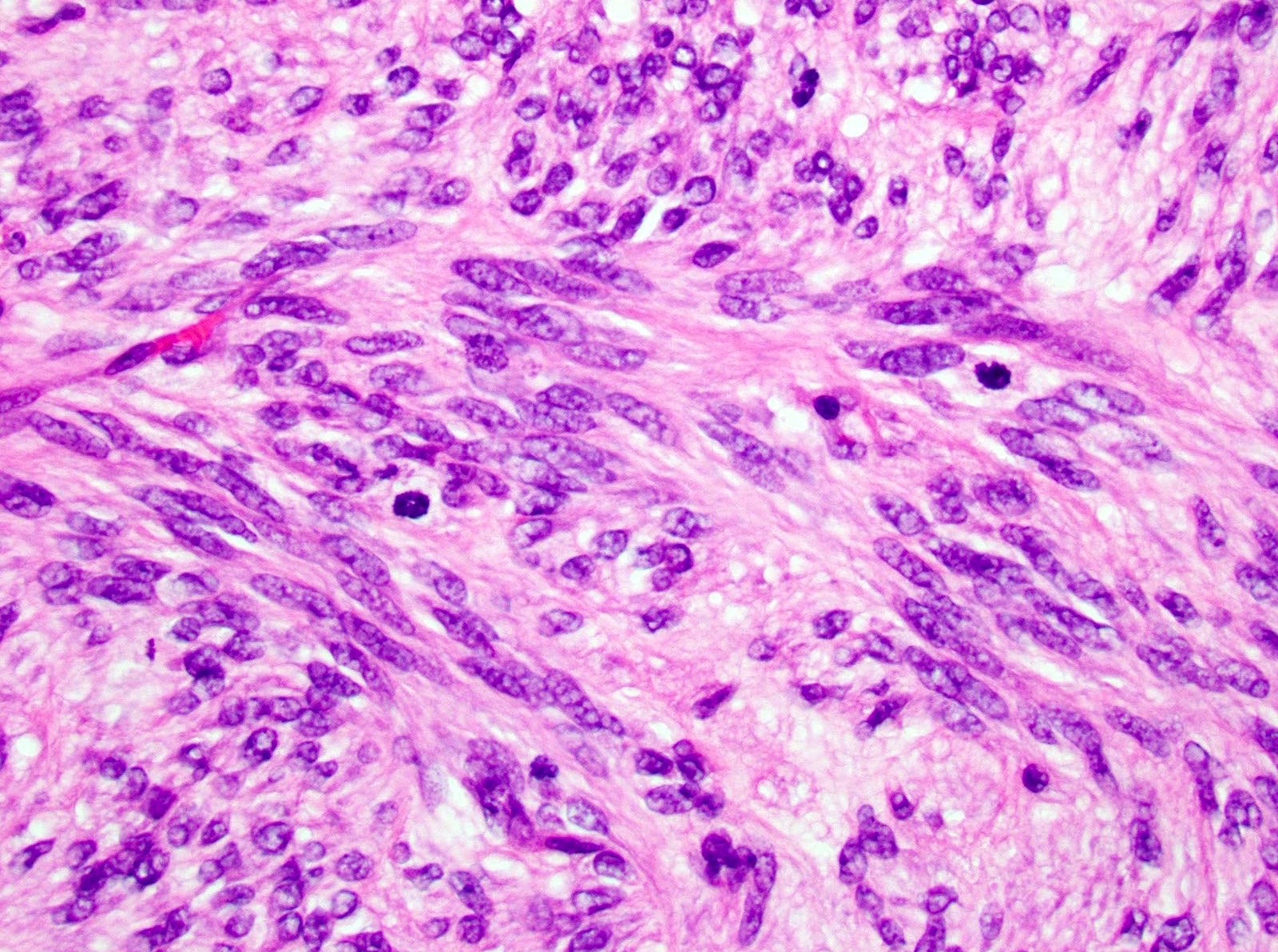
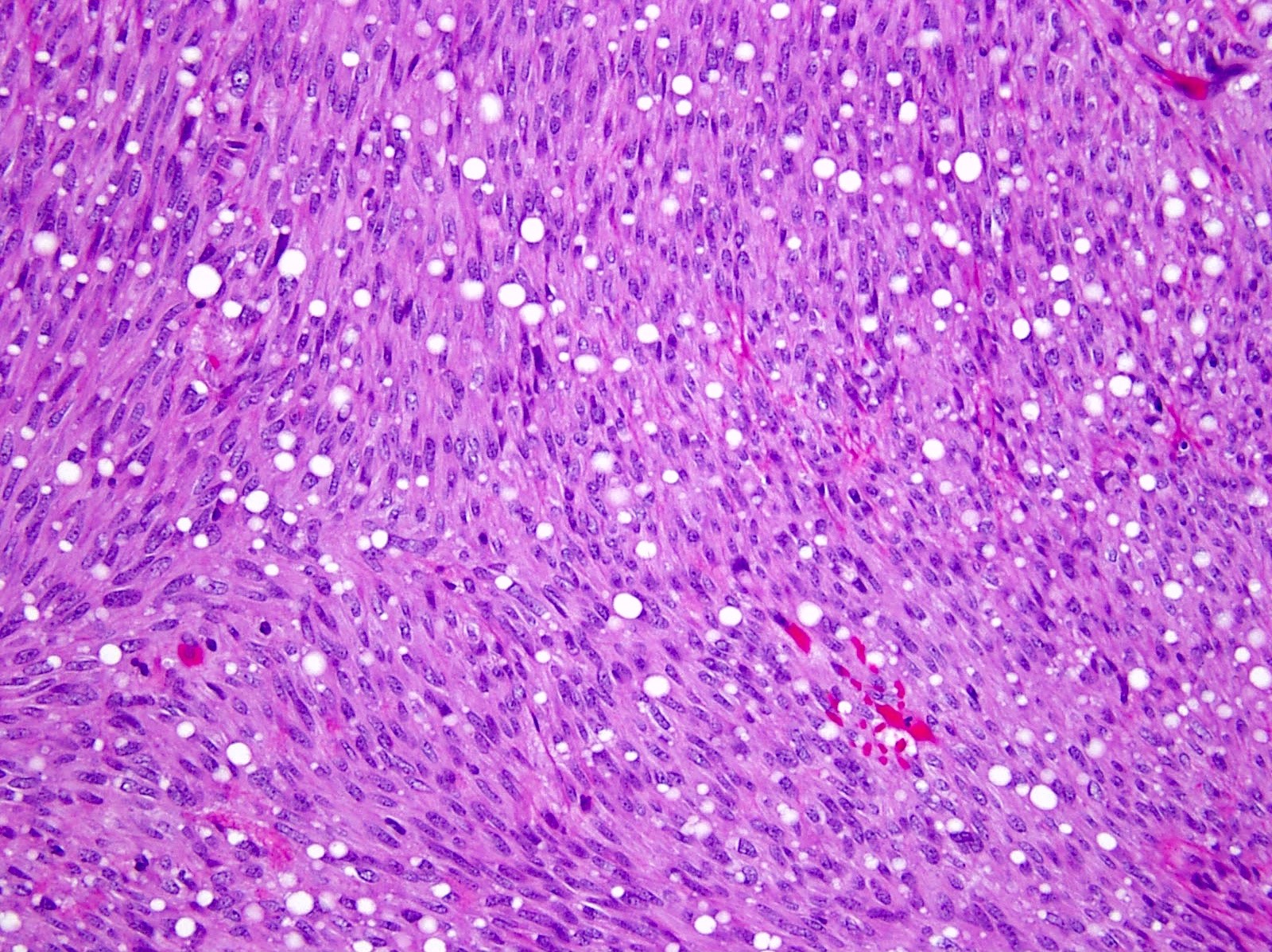
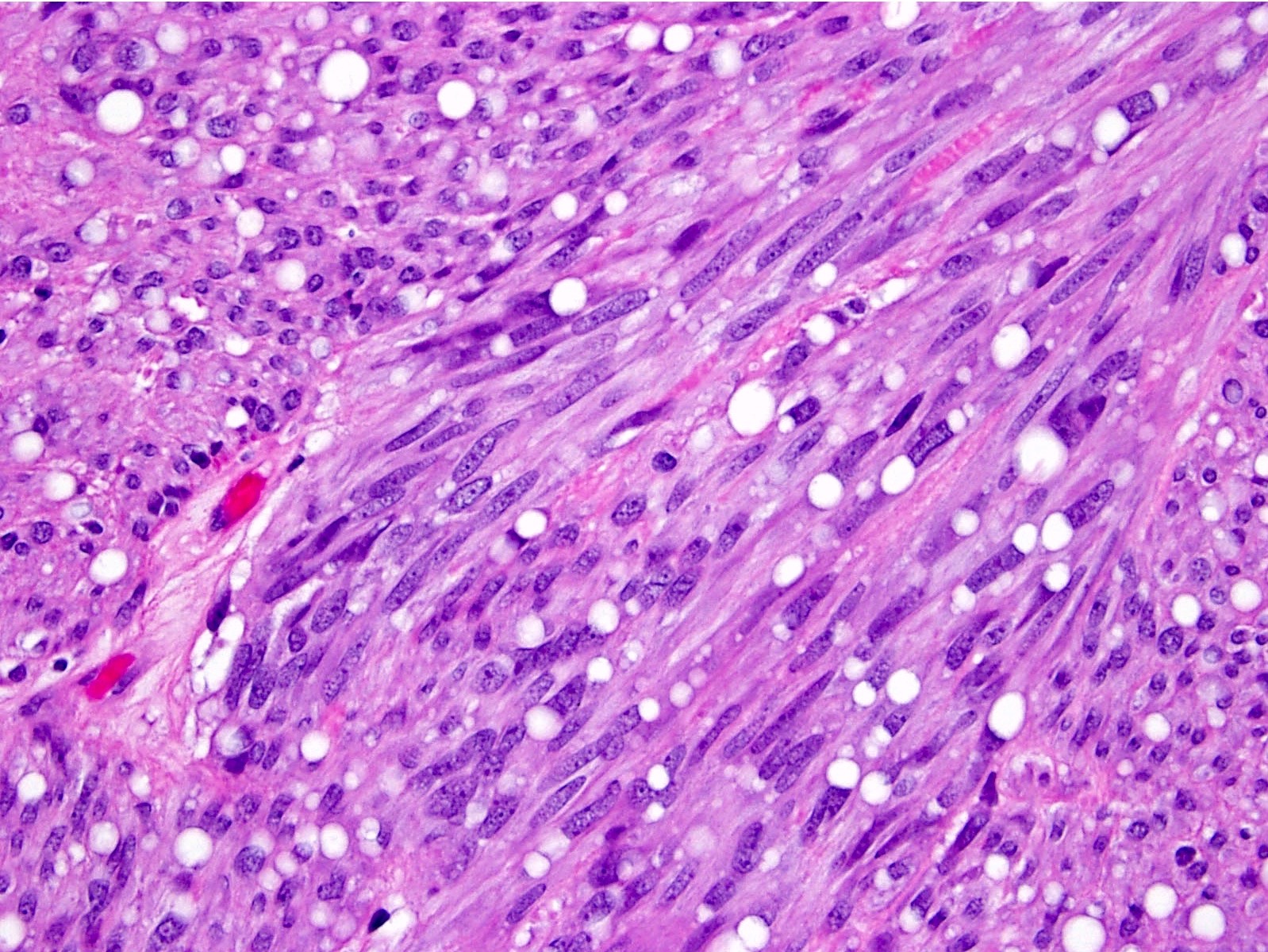
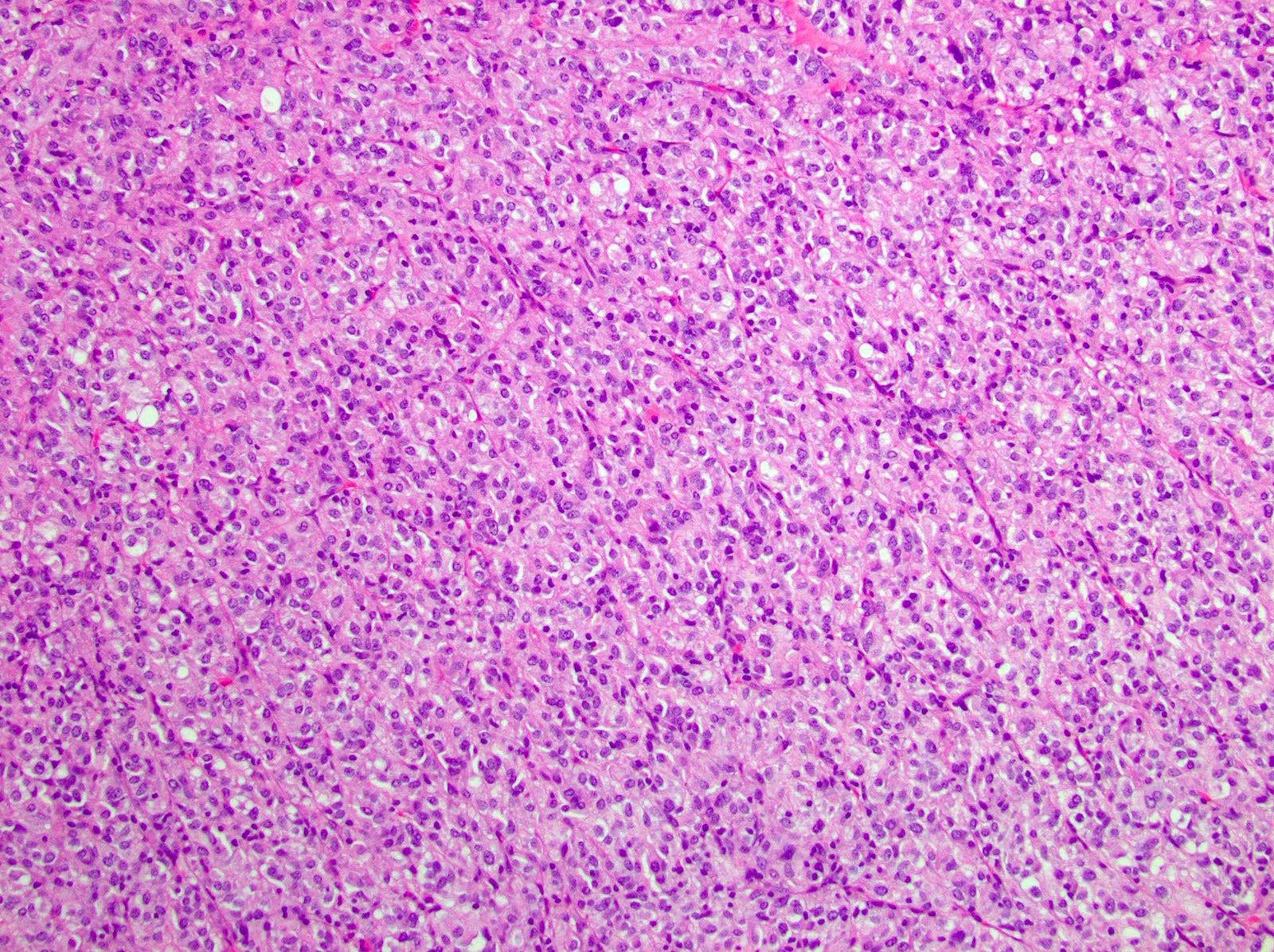
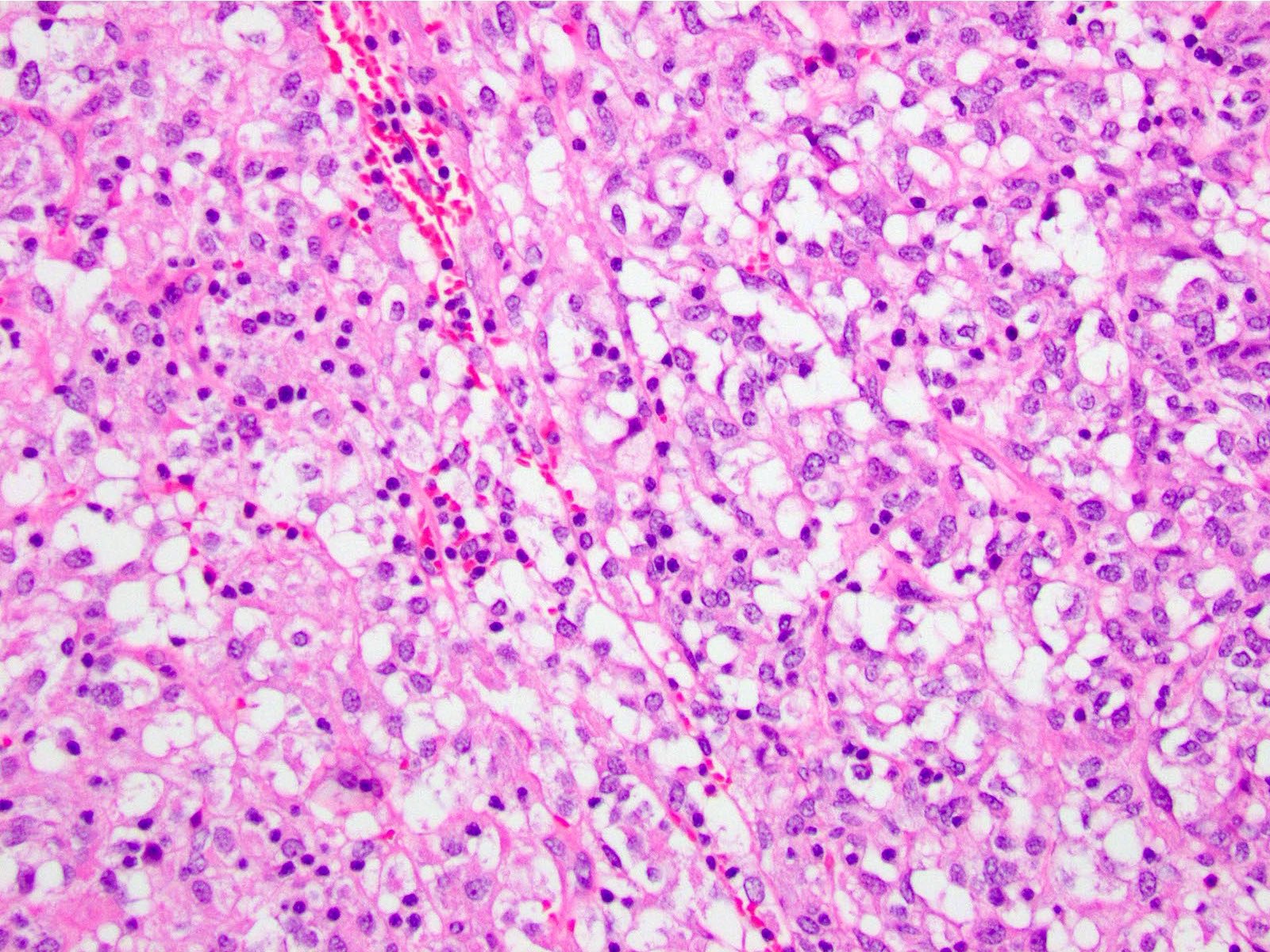
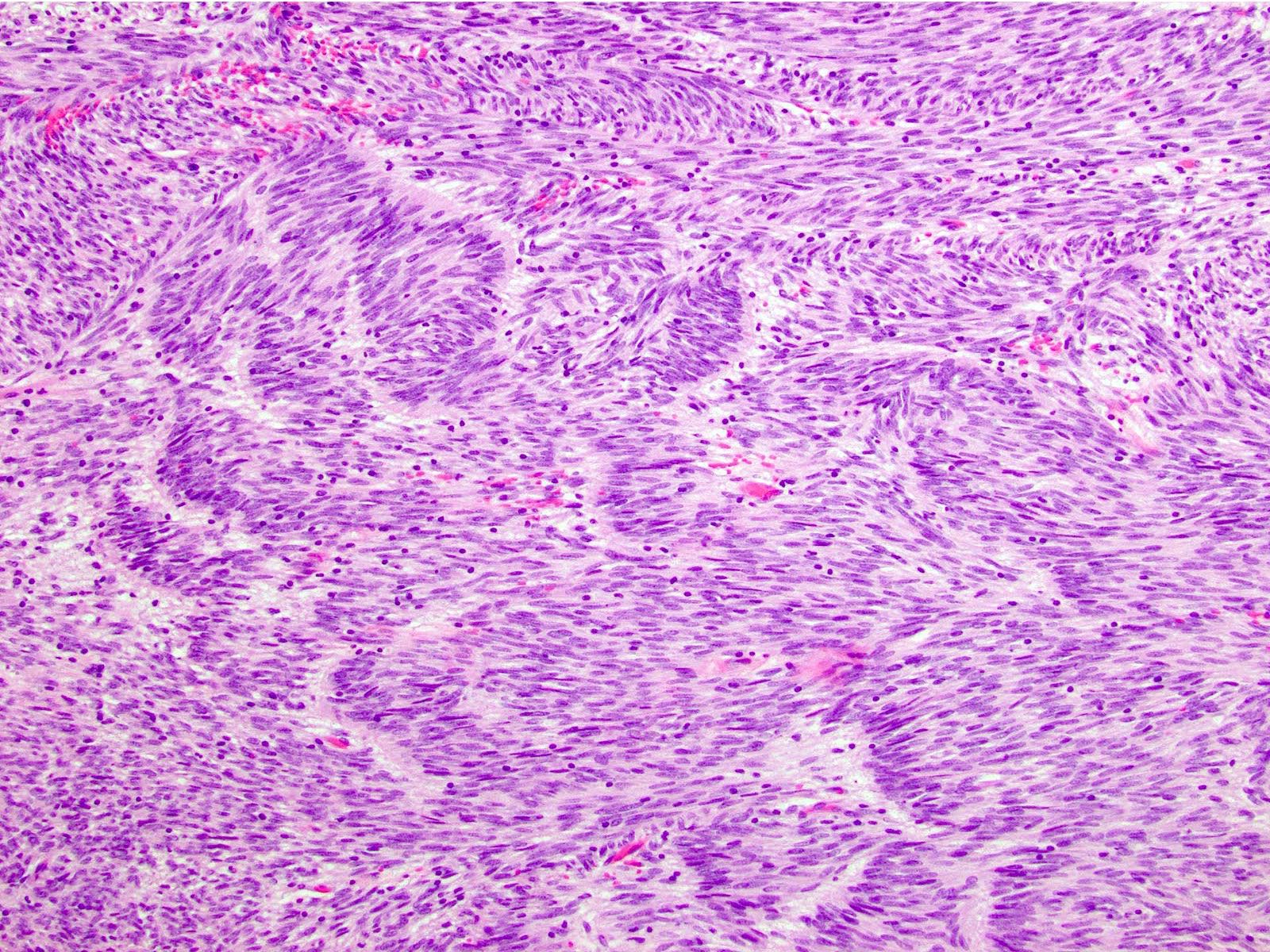
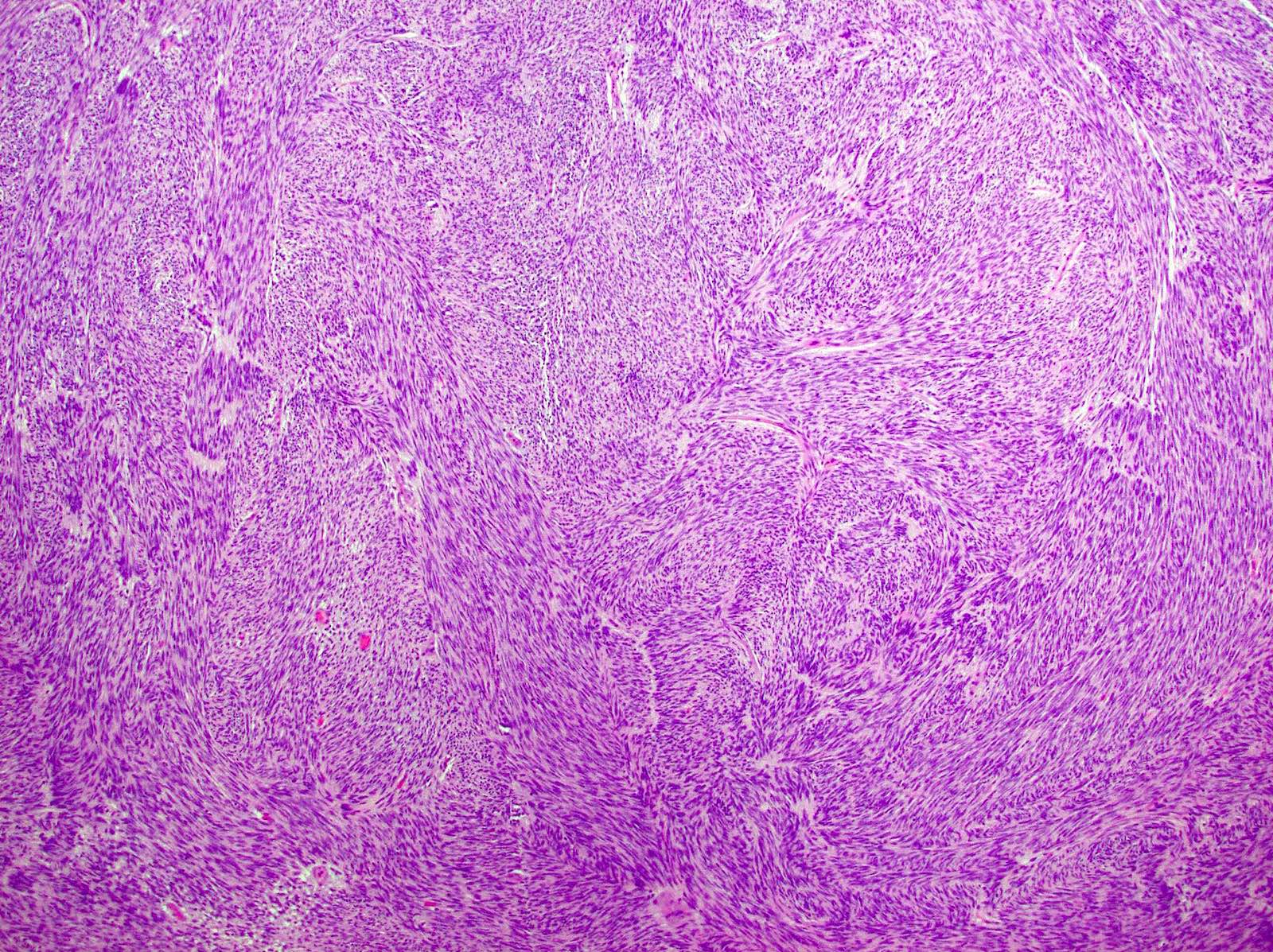
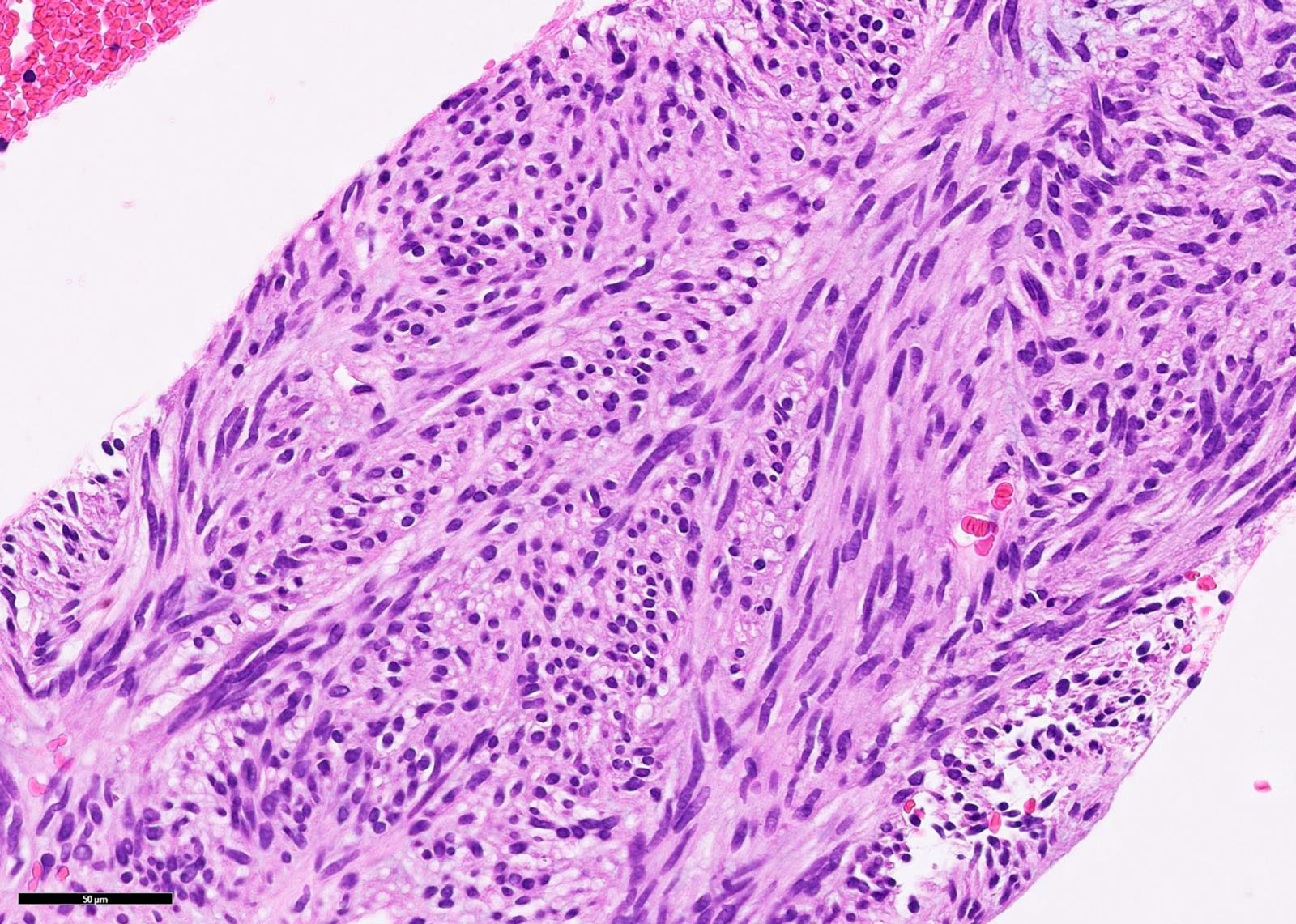
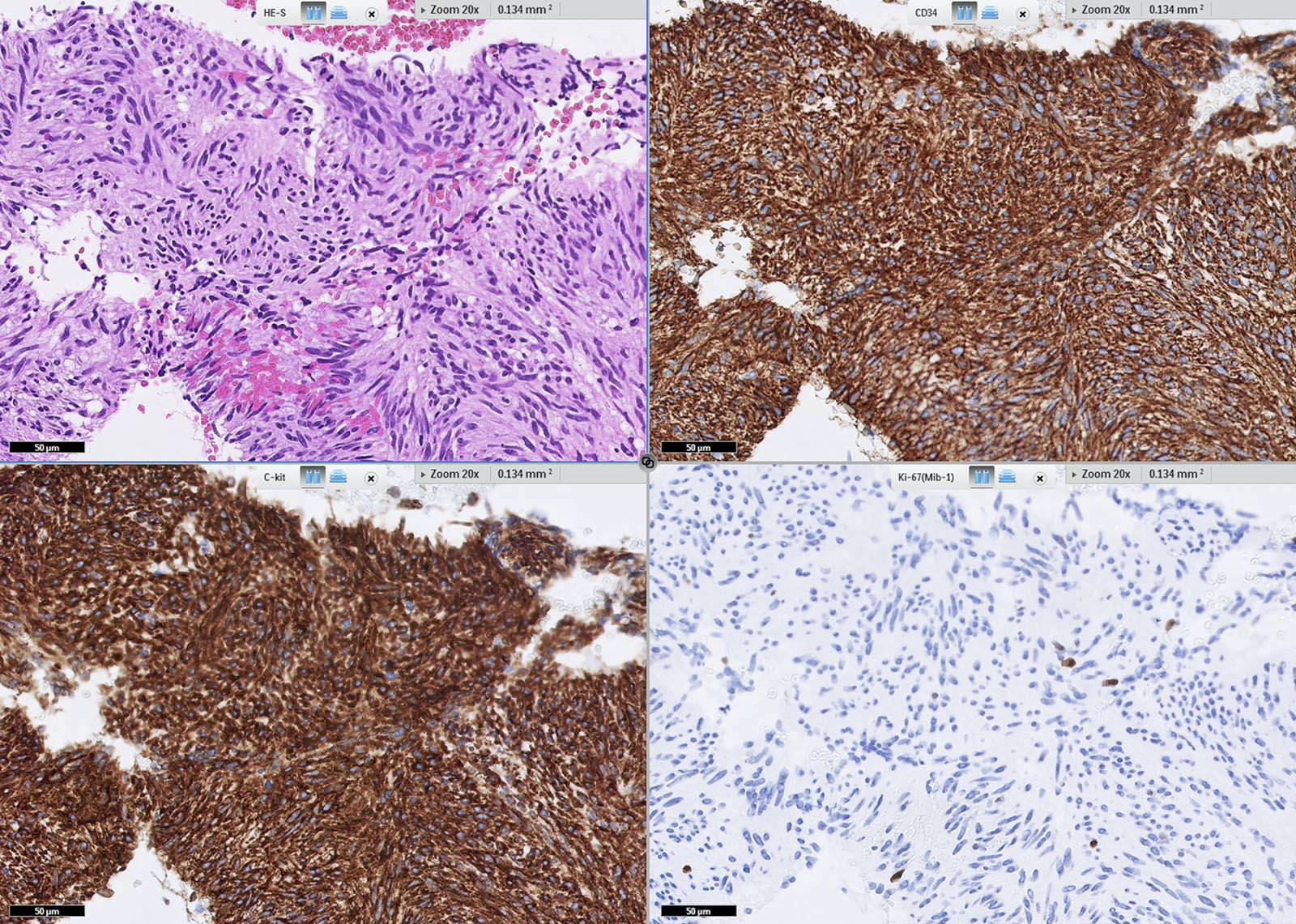
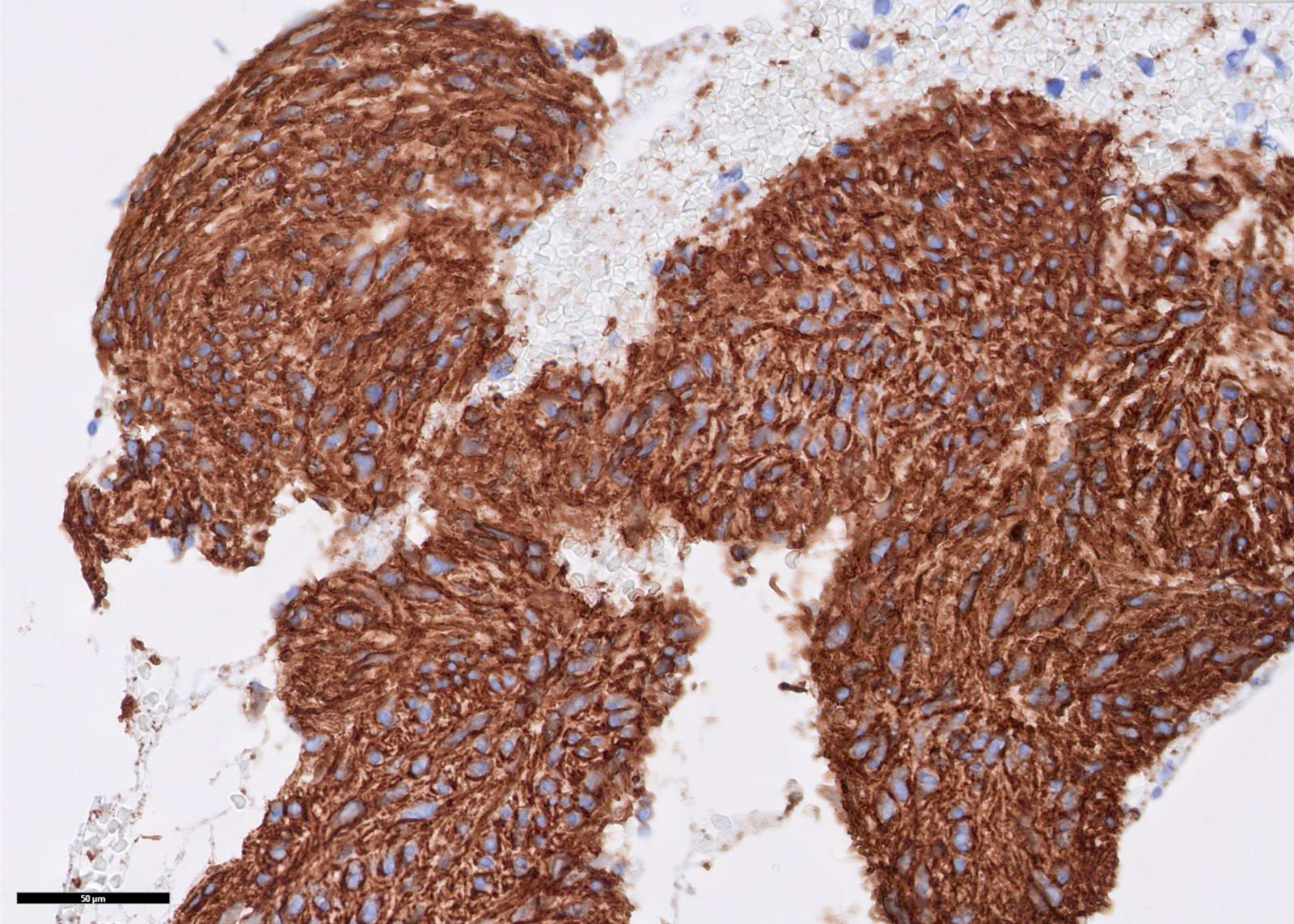
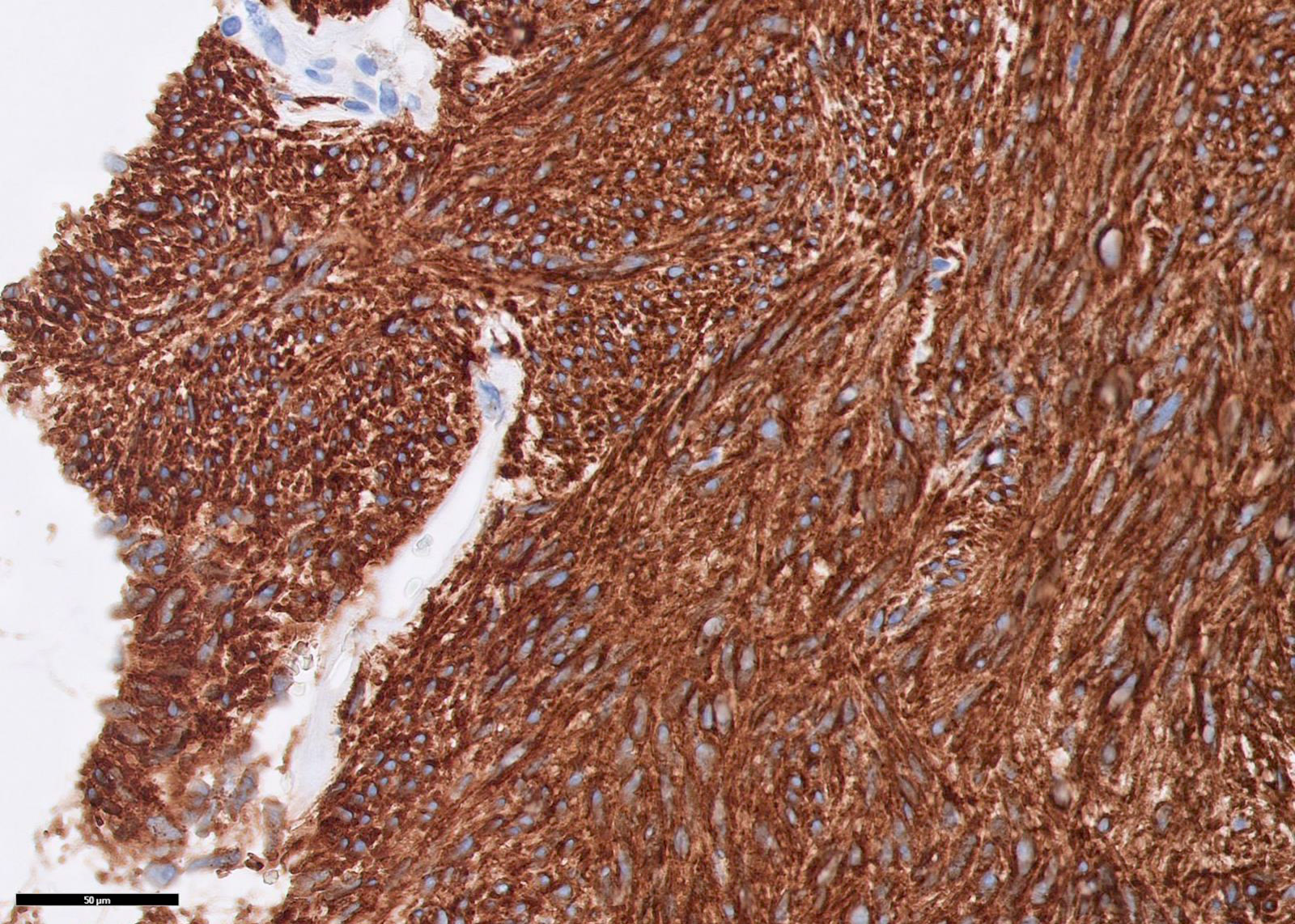
- 3 morphologic types: spindle (70%), epithelioid (20%), mixed (10%) (WHO Classification of Tumours Editorial Board: Digestive System Tumours (Medicine), 5th Edition, 2019)
- Spindle:
- Bland spindle cells with faintly eosinophilic cytoplasm in a syncytial pattern; elongated nuclei with inconspicuous nucleoli; artifactual paranuclear vacuoles common in stomach GIST"
- Subtypes: sclerosing, palisaded, vacuolated, diffuse hypercellular, sarcomatoid features with significant nuclear atypia and mitotic activity
- Epithelioid:
- Round cells with clear to eosinophilic cytoplasm in sheets or nests; increased tendency for pleomorphism versus spindle type
- Subtypes: sclerosing, discohesive, hypercellular, sarcomatous with significant atypia and mitotic activity
- Mixed:
- Tumor is composed of cells with spindle and epithelioid morphology
- Spindle:
- SDH deficient: epithelioid or mixed epithelioid / spindle cell morphology, multinodular pattern, minimal nuclear pleomorphism, occasional atypical mitoses
- Dedifferentiated: anaplastic appearance with an unusual phenotype (may lose expression of KIT or may aberrantly express other markers such as cytokeratin)
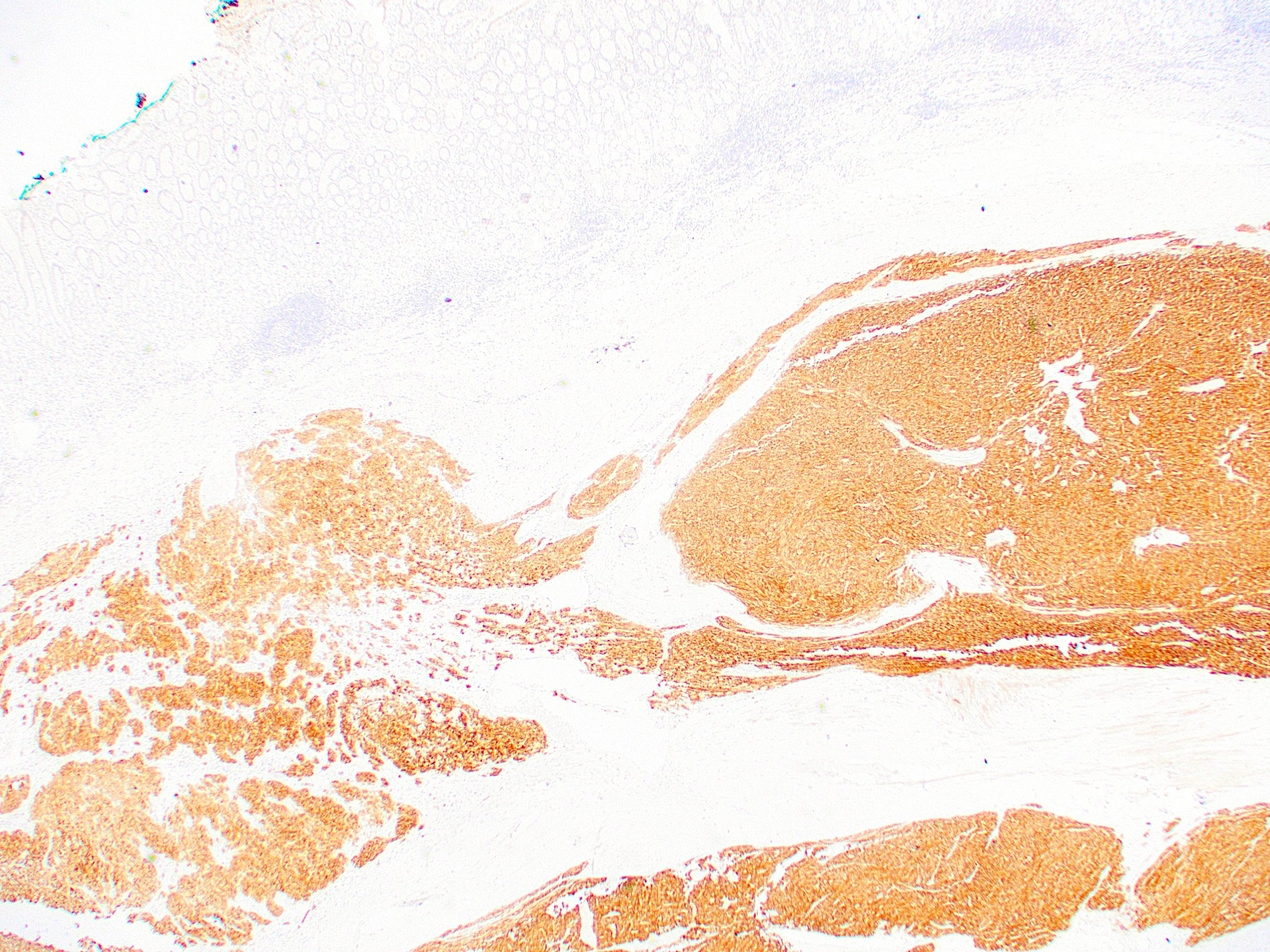
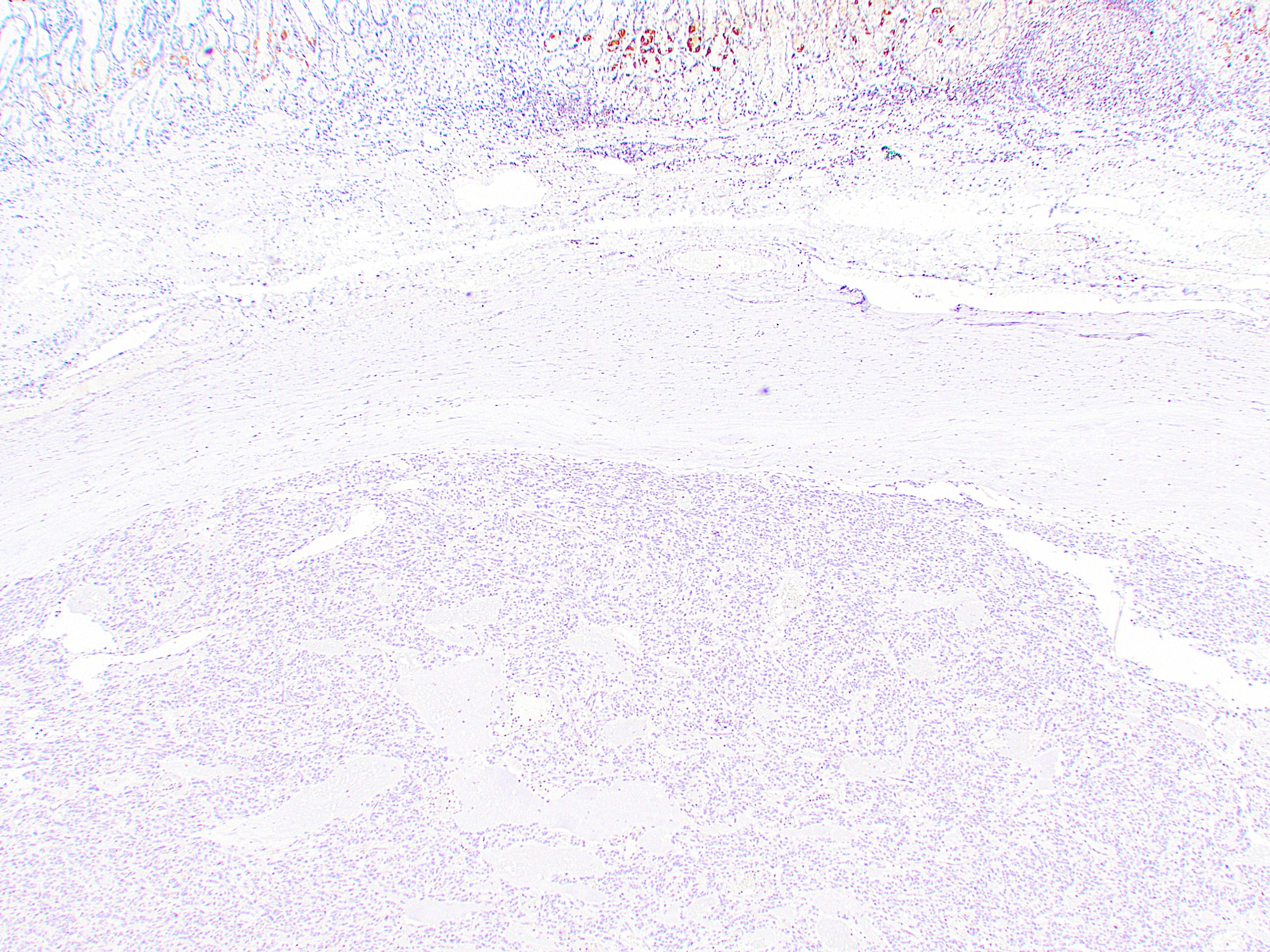
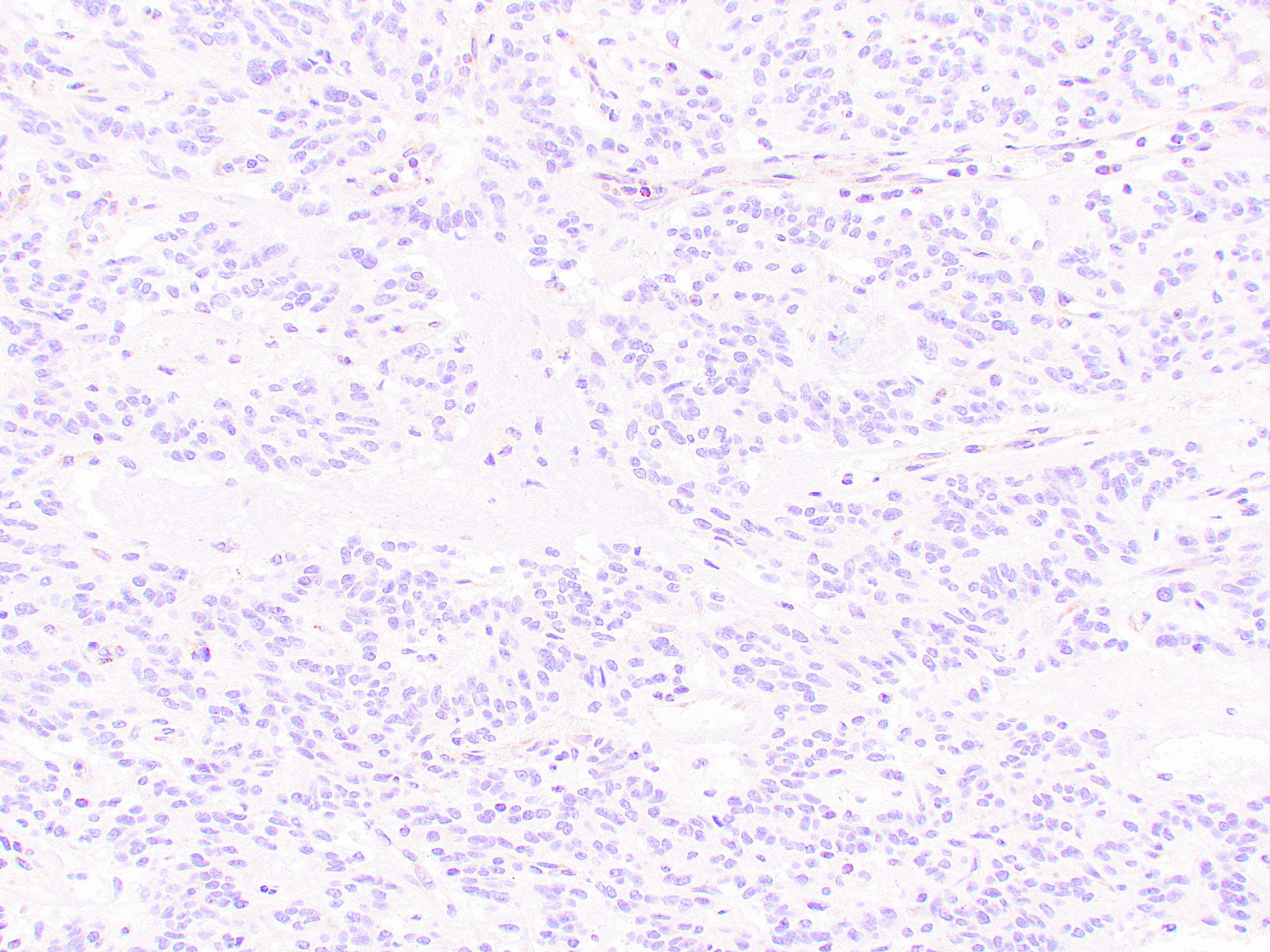
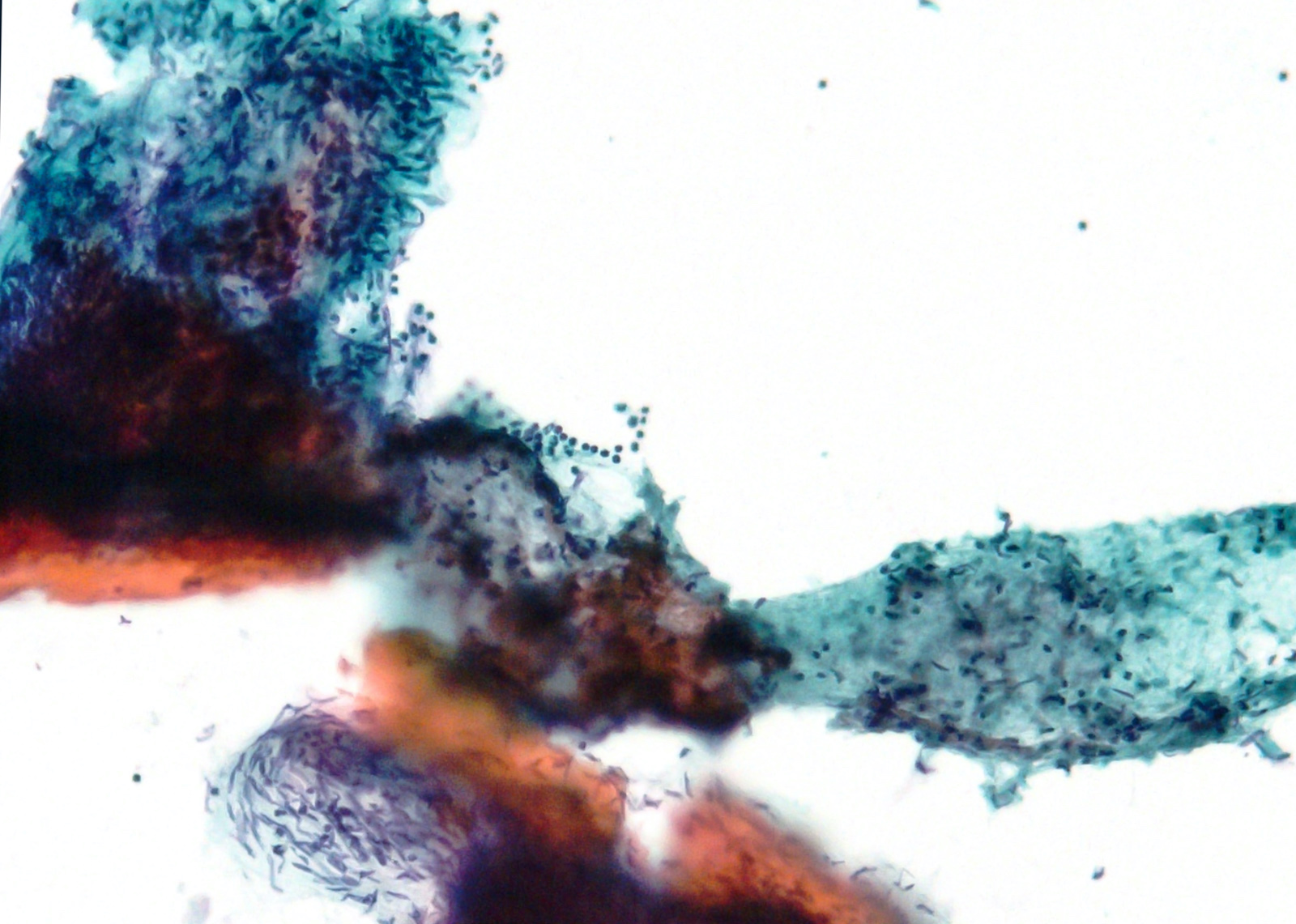
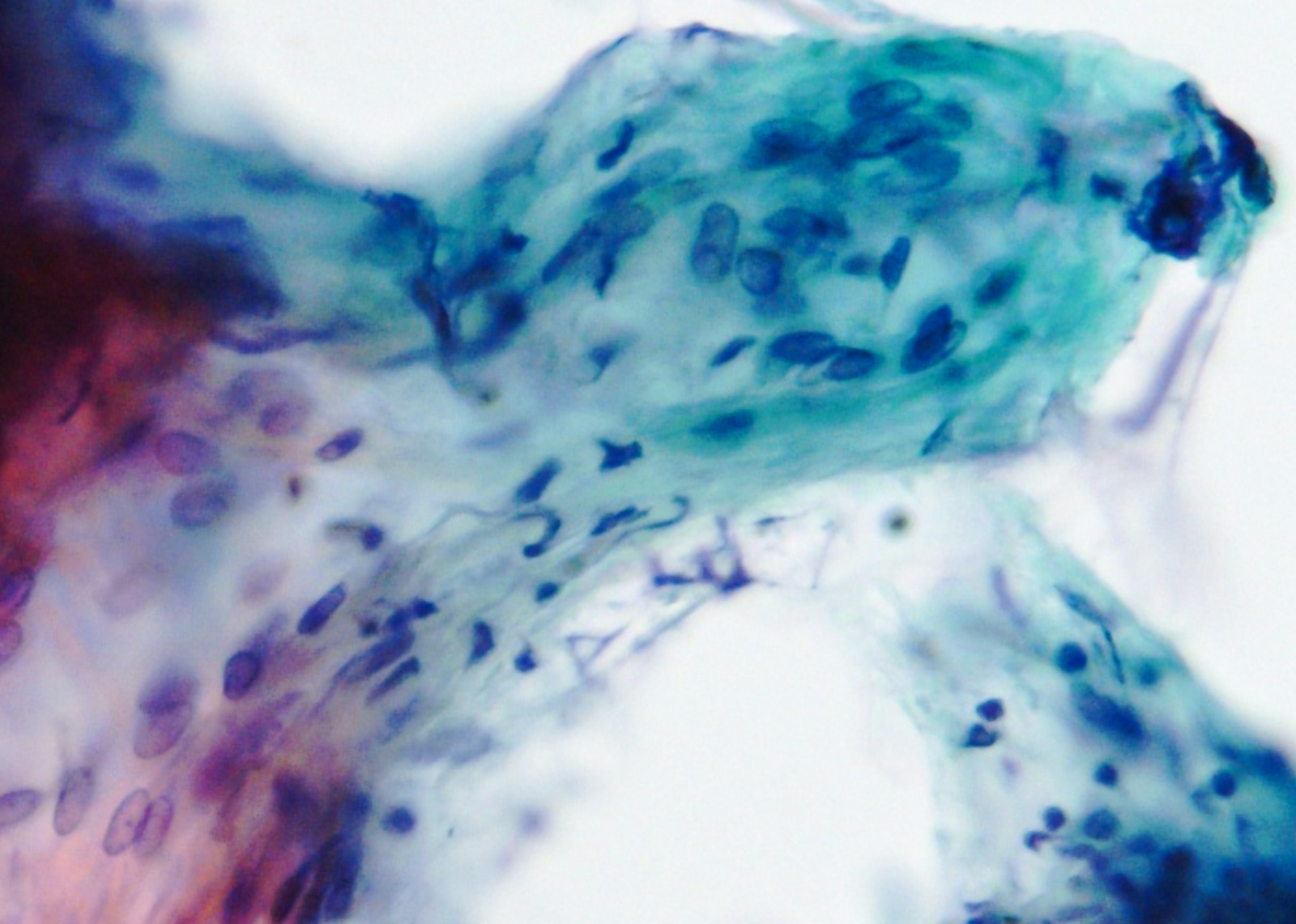
Microscopic (histologic) images
Contributed by Phoenix D. Bell, M.S., M.D. and Jennifer Findeis-Hosey, M.D.
Contributed by Andrey Bychkov, M.D., Ph.D.
Contributed by Raul S. Gonzalez, M.D. (Case #523)
Cytology description
- Endoscopic ultrasound guided fine needle aspiration may lend a preliminary diagnosis
- Bland spindle to epithelioid cells arranged in fascicles
Positive stains
- DOG1, ANO1 98% (Am J Pathol 2004;165:107)
- c-KIT / CD117 95% (Am J Surg Pathol 2009;33:1401)
- Membranous, diffusely cytoplasmic or concentrated in a dot-like perinuclear pattern
- CD34 82% (Am J Surg Pathol 2005;29:52) versus 40% in small intestinal GIST (Am J Surg Pathol 2006;30:477)
- SMA 18% (Am J Surg Pathol 2005;29:52) versus 34% in small intestinal GIST (Am J Surg Pathol 2006;30:477)
Molecular / cytogenetics description
- See Pathophysiology
Sample pathology report
- Stomach, fundus, partial gastrectomy:
- Gastrointestinal stromal tumor (GIST), mixed spindle cell and epithelioid type (see synoptic report)
Differential diagnosis
Additional references
Board review style question #1
Board review style answer #1
D. The image shows cells with round nuclei, abundant eosinophilic cytoplasm, inconspicuous nucleoli and minimal pleomorphism, representative of an epithelioid type GIST. This subtype is commonly seen in patients with an SDH deficient GIST, which are most often due to mutations in the SDHA subunit; however, rare mutations in the other subunits have also been identified. The majority of GIST result from mutations in the KIT (75%) or PDGFR-α (10%) proto-oncogenes. They are usually found in the stomach and are composed of a spindle, versus epithelioid, population. More recently, there have been reports suggesting patients with neurofibromatosis 1 (NF1) mutations are predisposed to GIST development.
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Board review style question #2
- A 60 year old man presents with abdominal pain and a CT reveals a mass within the gastrointestinal system, which is resected. Histopathologic examination reveals a submucosal mass composed of spindle cells with lightly eosinophilic cytoplasm arranged in a syncytial pattern. The pathologic diagnosis is a GIST, spindle cell type. Which of the following answer choices correlates with the most favorable prognosis for this patient?
- KIT mutation present
- Mass 11 cm in greatest dimension
- Mass located in the jejunum
- Mitotic rate ≥ 5 per 50 HPF
- R1 resection
Board review style answer #2
A. The main prognostic factors associated with GIST are mitotic rate, tumor size and tumor location. The extent of surgical resection and the presence of a KIT mutation also affect prognosis. GIST findings suggesting a more favorable prognosis include: stomach location, tumor size ≤ 2 cm, mitotic rate < 5 per 50 HPF, R0 (a resection with negative margins) and the presence of a KIT mutation.
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Board review style question #3
- Which of the following is true about succinate dehydrogenase deficient gastrointestinal stromal tumors (SDH deficient GISTs)?
- They almost always arise in the colon
- They are negative for KIT by immunohistochemistry
- They have a very poor prognosis
- They sometimes metastasize to lymph nodes
Board review style answer #3
D. They sometimes metastasize to lymph nodes. SDH deficient GISTs may metastasize to lymph nodes, which almost never happens in GISTs that arise through other molecular pathways. Despite this behavior, they have a relatively good prognosis. SDH deficient GISTs almost always arise in the stomach, not the colon. They are positive for KIT and DOG1 by immunohistochemistry, facilitating the diagnosis of GIST. They have a moderate prognosis, and patients often have a protracted clinical course with metastases to lymph nodes and distant organs.
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)